- Research article
- Open access
- Published: 14 December 2020

Non-communicable diseases among adolescents: current status, determinants, interventions and policies
- N. Akseer ORCID: orcid.org/0000-0002-1229-2640 1 , 2 ,
- S. Mehta 1 ,
- J. Wigle 1 , 2 ,
- R. Chera 1 ,
- Z. J. Brickman 1 ,
- S. Al-Gashm 1 ,
- B. Sorichetti 1 , 2 ,
- A. Vandermorris 1 , 3 ,
- D. B. Hipgrave 4 ,
- N. Schwalbe 5 &
- Z. A. Bhutta 1 , 2 , 6
BMC Public Health volume 20 , Article number: 1908 ( 2020 ) Cite this article
35k Accesses
66 Citations
7 Altmetric
Metrics details
Addressing non-communicable disease (NCDs) is a global priority in the Sustainable Development Goals, especially for adolescents. However, existing literature on NCD burden, risk factors and determinants, and effective interventions and policies for targeting these diseases in adolescents, is limited. This study develops an evidence-based conceptual framework, and highlights pathways between risk factors and interventions to NCD development during adolescence (ages 10–19 years) and continuing into adulthood. Additionally, the epidemiologic profile of key NCD risk factors and outcomes among adolescents and preventative NCD policies/laws/legislations are examined, and a multivariable analysis is conducted to explore the determinants of NCDs among adolescents and adults.
We reviewed literature to develop an adolescent-specific conceptual framework for NCDs. Global data repositories were searched from Jan-July 2018 for data on NCD-related risk factors, outcomes, and policy data for 194 countries from 1990 to 2016. Disability-Adjusted Life Years were used to assess disease burden. A hierarchical modeling approach and ordinary least squares regression was used to explore the basic and underlying causes of NCD burden.
Mental health disorders are the most common NCDs found in adolescents. Adverse behaviours and lifestyle factors, specifically smoking, alcohol and drug use, poor diet and metabolic syndrome, are key risk factors for NCD development in adolescence. Across countries, laws and policies for preventing NCD-related risk factors exist, however those targeting contraceptive use, drug harm reduction, mental health and nutrition are generally limited. Many effective interventions for NCD prevention exist but must be implemented at scale through multisectoral action utilizing diverse delivery mechanisms. Multivariable analyses showed that structural/macro, community and household factors have significant associations with NCD burden among adolescents and adults.
Conclusions
Multi-sectoral efforts are needed to target NCD risk factors among adolescents to mitigate disease burden and adverse outcomes in adulthood. Findings could guide policy and programming to reduce NCD burden in the sustainable development era.
Peer Review reports
The global burden of non-communicable diseases (NCDs) is a growing public health crisis that requires attention and action from the international community [ 1 ]. As the leading cause of mortality, this class of diseases is responsible for 38 million of 57 million annual deaths, with 85% of these deaths occurring in low- and middle-income countries (LMICs) [ 2 ]. However, the discussion on efforts to address NCDs to-date has focused on the adult population, with adolescents largely overlooked [ 3 ]. Since NCDs are often considered ‘lifestyle illnesses’ and the youth population is commonly thought of as healthy, modest efforts have been made to assess their health, disease prevention and lifestyle modification. Yet, adolescents experience a substantial share of the global NCD burden [ 4 , 5 ].
Extensive research has shown that NCDs are primarily attributed to underlying and modifiable risk factors that often emerge during these earlier years [ 5 , 6 , 7 ]. It is estimated that approximately 70% of premature deaths occurring during adulthood are the result of health-related behaviours that are initiated in childhood and adolescence [ 3 , 8 ]. Such risk factors, including overweight and obesity, physical inactivity, substance use and poor nutrition, substantially contribute to disease development and poor health in later life [ 8 ]. For example, the prevalence of overweight and obesity increases drastically during mid-adolescence and into adulthood [ 9 ]. Overweight and obesity during childhood and adolescence represents a significant risk for premature mortality and physical morbidity later in life, including cardiovascular disease, asthma, and certain types of cancers [ 10 ]. Drug and substance use also represent a threat for multiple health outcomes, including poor mental health [ 11 ]. Since health behaviours and risk exposures that emerge during adolescence underpin health and well-being across the life-course and also affect pregnancy outcomes, investments must be made in the health of current and future generations. In fact, the 2016 Lancet Commission on Adolescent Health and Well-being recommended investment in dominant NCD-related health behaviours among adolescents as a means of preventing future disease development [ 12 ].
Addressing NCDs has emerged as a global priority in the Sustainable Development Goals (target 3.4) [ 13 ] and the focus of a third UN high-level meeting [ 14 ], and includes the establishment and promotion of cost-effective interventions to prevent and address NCDs [ 15 ]. However, existing literature provides patchy insight into the current state of NCD-related lifestyle and behavioral risk factors among young people. In fact, to-date, there is no systematic assessment of the NCD burden, risk factors and determinants of NCDs, and effective interventions and policies for targeting these diseases in this population. Further, recent and ongoing efforts by the World Health Organization have involved the establishment of several global strategies, policies, laws and legislations to reduce the harmful use of alcohol [ 16 ], increase monitoring and decrease tobacco use [ 17 ], as well as to address childhood obesity [ 18 ]. However, limited evidence is available on the monitoring and evaluation, and effective implementation of these NCD-related efforts.
We conducted a comprehensive assessment of NCDs among adolescents, with the specific objective to: 1) develop an evidence-based conceptual framework explaining the determinants, pathways and interventions for NCDs among this age group and in later life; 2) describe the age- and sex-specific burden of major NCDs and risk factors among adolescents, globally and by geographical region; 3) examine major risk factors for adolescent NCDs and their role in adulthood NCD burden; 4) synthesize and summarize available evidence on effective interventions and delivery platforms to reduce the burden of NCDs among adolescents; 5) explore the availability of related laws and policies to reduce NCDs among adolescents globally and by geographical region; and 6) conduct multivariable assessment of key distal and intermediary contextual determinants of NCD morbidity and mortality among adolescents and, separately, the effect of these factors on adulthood NCD burden.
We used a life-course approach and socio-ecological model to inform the development of a conceptual framework illustrating factors affecting NCDs in adolescence and in later life. We explored online databases for information pertaining to the burden of NCDs among adolescents, their determinants and risk factors, and relevant policies/interventions for NCDs in this population. Details are included in the Technical Additional file 1 .
The proposed conceptual framework integrated several existing models and frameworks, including the WHO global monitoring framework [ 19 ], NCD framework for action/monitoring [ 20 ], socio-ecological models of adolescent health and development [ 2 , 21 ] and key frameworks and determinants of adolescent health outlined in the 2012 and 2016 Lancet series on adolescent health [ 3 , 20 , 22 ]. The layout of the conceptual framework was adapted from the model on the life course approach to NCD prevention by WHO [ 20 ] and the multi-sectoral nutrition conceptual framework [ 23 , 24 ]. An iterative process was conducted to identify, integrate and synthesize the concepts, development and structure of the conceptual framework.
Similar approaches were used to collect information on effective NCD-related interventions and laws/legislations/policies available for the prevention of these diseases during adolescence and in later life. The WHO Maternal, Newborn, Child and Adolescent Health (MNCAH) policy indicator database [ 25 ] contains data on eleven adolescent NCD-related risk and health outcome policies, laws and regulations from 104 low and middle income countries (LMICs) globally. We obtained and analyzed this data; details in the Technical Additional file 1 .
We obtained national estimates on health and contextual indicators related to NCD development in adolescents and adults through a review of global data repositories performed from Jan 1st 2018 to July 6, 2018. We focused on 194 countries and assembled panel datasets from 1990 to 2015; we focused on this period for quantitative analysis to evaluate change and distribution across the Millennium Development Goal (MDG) period. Key areas of interest included distal factors (conflict, governance, population density, environment, urbanization, national wealth, health spending, telecommunications, infrastructure), factors intermediary to NCD outcomes (income inequality, women’s empowerment, health care services, youth empowerment, socioeconomic status), and proximal factors (i.e. behavioural, biological, nutritional and environmental risk factors). Primary data sources included the Global Health Observatory Data Repository [ 26 ], the State of the World’s Children global statistics database [ 27 ], the World Bank database [ 28 ], the United Nations Statistics Division [ 29 ] and the 2015 Global Burden of Disease (GBD) study housed at the Institute for Health Metrics and Evaluation (IHME) [ 30 ]. Estimates were obtained directly from the respective sources for each indicator without any manipulation. A summary of the hierarchical levels, domains and indicators with sources linked to NCD outcomes among adolescents and later adulthood in this study are included in the appendix (Additional file 1 ).
The major non-communicable diseases among adolescents were identified using disability-adjusted life years (DALY) data from the GBD. We constructed ranked estimates using national cause-specific DALYs across the six WHO regions (i. African region; ii. region of the Americas; iii. Eastern Mediterranean region; iv. European region; v. South East Asia region, and vi. Western Pacific region), two adolescent age categories (10–14 years, 15–19 years of age) and by sex. We also tabulated the NCD DALYS in late adolescence to adulthood (age 15–49 years, 50–69 years) that are attributable to lifestyle and behavioral risk factors that begin in the critical adolescence period.
We conducted two sets of multivariable analyses to understand the major contextual, social, economic and environmental determinants of NCD-related mortality and morbidity among 1) adolescents and 2) adults. This country-level ecological analysis used data for 195 countries obtained from the GBD data repository for the year 2015. For the adolescent model, the primary outcome was the country’s NCD DALY rates among 10–19 year old regressed onto a series of fixed-effect covariates. For the adult model, the outcome was country-level NCD DALY rates among 25–59 year olds which was regressed onto a series of contextual, social, economic and environmental factors. We could not run regression models of panel data or change from 1990 to 2015 since many countries did not have reliable estimates for key covariate indicators in 1990. We used a hierarchical modeling approach [ 20 ] with structural, national, community, household and individual level covariate indicators mapped to the respective levels described above (Additional file 1 ). We selected largely distal and intermediary factors that could have a differential impact on proximal risk factors of NCD development in adolescence and in later adulthood. Ordinary least squares regression models were fitted, and crude and standardized beta coefficients were estimated. Variables with skewed distributions were transformed appropriately to stabilize variance for regression analysis. Variables associated with the outcome at p < 0.20 in bivariate analysis were entered into multivariable model selection algorithms. Elastic net regression was used to select statistically significant variables ( p < 0.15) in multivariable analysis at each level due to the large number of correlated predictors. Collinearity was assessed using variance inflation factors, and residual plots, influence/deviance statistics, AIC/BIC and adjusted R2 were consulted to assess model fit. Type 1 error rate was retained at 0.05 and analyses were conducted using SAS version 9.4 and RStudio Version 1.1.423.
Conceptual framework
Our novel evidence-based conceptual framework (Fig. 1 ) represents a comprehensive and integrated approach to understanding the complex pathways through which risk and protective factors contribute to NCDs among adolescents and in later life. The framework provides a depiction of four key components: i) societal determinants; ii) individual predisposing factors across the adolescent and young adulthood stages of the life course; iii) top NCD conditions among adolescents and in later adulthood; and iv) select evidence-based policies, laws and interventions for this population. Key definitions, pathways and relationships of the NCD conceptual framework are detailed in Table 1 [ 31 , 32 , 33 , 34 , 35 , 37 ].
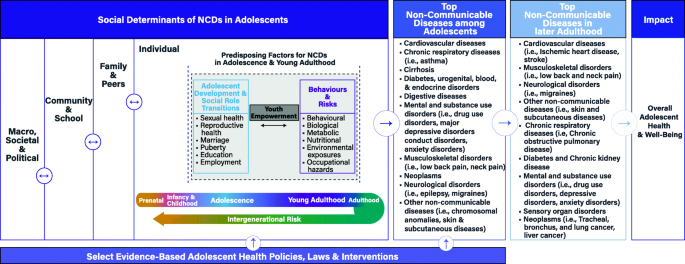
Conceptual framework on NCDs among adolescents
Burden and trends of NCD outcomes in adolescents
We explored the current burden of NCDs among adolescents by age and sex (Table 2 ), as well as by WHO region (Additional file 1 ). A large share of the burden of NCDs among 10–19 year olds is due to mental illnesses. Conduct disorder accounts for the most NCD DALYs (2595,245) among adolescents aged 10–14, representing 8% of the total NCD burden in this age group. In addition, anxiety disorders (2,100,974; 6%) and major depressive disorder (1,472,928; 4%) were the 3rd and 6th highest ranked NCD cause of DALYs among 10–14 year-olds, respectively. In 15–19 year olds, major depressive disorder is the top NCD cause of DALYs (3646,293), representing 8% of the total NCD burden in this age group. Comparable to the 10–14-year-old age group, anxiety disorders (2,510,537; 6%) and conduct disorder (1874,317; 4%) ranked 3rd and 7th, respectively, in the rank of top 10 NCDs with the highest DALY burden (Table 2 ).
DALYs due to NCD causes also vary by sex (Table 2 ). In 10–14 year olds, conduct disorder contributes the most NCD DALYs for males (1638,150; 9%), followed by asthma (1204,058), anxiety disorders (838,606), migraine (773,026) and acne vulgaris (722,333). In females of the same age, migraine contributes the greatest burden of disease (1273,422; 8%), followed by anxiety disorders (1262,368), asthma (1117,023), conduct disorder (957,096) and major depressive disorder (825,013). In 15–19 year olds, major depressive disorder contributes the most NCD DALYs for both males (1,588,775) and females (2,057,518); however, it does represent a greater proportion of all DALYs in females (9%) than in males (7%) in this age group. Overall, in both adolescent age groups, conduct disorder plays a larger role in males than females, and anxiety disorders and major depressive disorders play a larger role in females.
Across global regions, conduct disorder persists as the leading NCD among males 10–14 years of age (Additional file 1 ). In females of the same age, migraines are the most prominent NCD in the Eastern Mediterranean and South East Asia regions, anxiety disorders are the most prominent in the Americas and European and Western Pacific regions, and asthma is the most prominent NCD among girls in Africa. Among males 15–19 years of age, major depressive disorder is the leading NCD in Africa, the Americas, the Eastern Mediterranean, and South East Asia, whereas low back pain and acne vulgaris are the leading NCDs in Europe and in the Western Pacific respectively. Similarly, among females 15–19 years of age, depression contributes the most NCD DALYs in four of the six regions (Africa, Europe, Americas, Western Pacific), whereas migraine leads in the Eastern Mediterranean and South East Asia regions (Additional file 1 ).
Burden, Behavioural, and socioeconomic risk factors
Select behavioural, lifestyle and socioeconomic risk factors for NCDs from adolescence into adulthood in regions around the world are highlighted in Table 3 . With regards to lifestyle and behavioural factors, the prevalence of alcohol drinking among 15–19 year olds is more common among boys than girls, and is highest in regions of the Americas and Europe (> 50%). Similarly, tobacco use among young adolescents is higher among males compared to females, and ranges from 12 to 2% across regions. Insufficient physical activity is pervasive in almost 80% or more of adolescents aged 11–17 years across all regions and both sexes. The prevalence of overweight children and adolescents under 20 years of age is higher among males compared to females across all regions, the region with largest rate for both genders was the Americas with more than a third of the under 20 population being classified as overweight. Obesity in children and adolescents under 20 years of age is also higher among males and is highest in the regions of Middle East and North Africa and Europe. Youth literacy rates are high (almost 90% or more) in most regions but lag behind in Africa and South Asia. Secondary school enrollment rates are also consistent across most regions (70% or more) except for Eastern and Southern Africa and South Asia regions. Youth literacy and secondary school enrollment rates are similar between genders and this similarity is synonymous across all regions. Unemployment among youth 15–24 years is highest (28%+) in the MENA region followed by the Americas (18.5%) and Europe regions (18.5%).Breastfeeding patterns have been linked to overweight, type 2 diabetes, and possibly high blood pressure and cholesterol in childhood and adolescence, and even into adulthood [ 39 , 40 ]. About 50% of South Asia and Eastern and Southern Africa exclusively breastfeeds child younger than 6 months, while only 28 to 39% of those in other regions practice exclusive breastfeeding. Sanitation is part of the broad set of environmental factors that directly and indirectly influence risk of NCDs in childhood and adolescence. Poor sanitation can result in, for instance, diarrhea, which can impact nutrient absorption and disease burden. It’s also linked to individual and social perceptions about health and wellbeing, which can influence an adolescent’ mental health [ 36 , 41 ]. Access to improved water (53–62%) and improved sanitation (27–30%) facilities is notably lower in Africa while all other regions have > 80% availability.
Death and disability are associated with risk factors that begin in adolescence, although causality cannot be inferred from these data (Additional file 1 ). The top causes of premature death among 15–49 year olds are related to high body mass index (e.g. higher body adiposity), high blood pressure, high plasma blood glucose (diabetes), high cholesterol, smoking, drug and alcohol use, diets low in fruits and whole grains, and air pollution. These top factors were not different between sexes. These important risk factors even remained as the top contributors of later adulthood (50–69 years) disease-related disability and death (Additional file 1 ).
Multivariable determinants of NCDs among adolescents and adults
In our analysis of correlates of NCD DALYS among adolescents, at the distal level, macro factors such as indicators of conflict and humanitarian crises (e.g. refugee populations, p < 0.0001), and state governance (effectiveness [ p < 0.0001], corruption [ p < 0.0001]) were independently associated with higher NCD burden (Table 4 ). Across a range of statistically significant national structural factors at the intermediate I level, urbanization (R2 = 14%, p < 0.0001), GDP per capita (R2 = 11%, p < 0.0001), and total health expenditure per capita (R2 = 12%, p < 0.0001) were more strongly related to the outcome. At the intermediate II level, other indicators of household socioeconomic status, youth literacy and fertility rates, proxies of women’s empowerment, income inequities, and availability of human resources for health were all statistically significant correlates of adolescent NCDs. In multivariable analyses, a final joint model explained about 62% of the variance in adolescent NCD DALYs worldwide. This included a series of distal and intermediate factors such as the total refugee populations in a country, effective state governance, urbanization, access to electricity, population density, total health expenditure per capita, adolescent fertility, and a proxy of female gender empowerment (secondary school gender parity index) (Table 4 ).
Our model of correlates of NCD DALYs among adult populations is displayed in Table 5 . Distal level macro factors associated with the burden of NCDs among adults in bivariate analyses were government effectiveness [ p = 0.0003] and corruption [ p = 0.0119]). At the intermediate I level, access to electricity (R2 = 5%, p < 0.0001), mobile cellular subscriptions (R2 = 15%, p < 0.0001), GDP per capita (R2 = 9%, p < 0.0001), and total health expenditure per capita (R2 = 8%, p < 0.0001) were strongly related to NCD burden among adults. The final adjusted model for adult populations included the distal and intermediate factors of corruption in state governance, urbanization, access to electricity, GDP per capita, secondary enrolment ratio, physician density per 1000 population as well as proxies for female gender empowerment (secondary and tertiary school gender parity indexes) (Table 5 ). It should be noted, however, that this adult model only explained about 31% of the variance in adulthood NCD suggesting that many other proximal factors may be at play (e.g. lifestyle - smoking, drinking, drug use, diet) which were not captured in our models. The higher % variance explained in the adolescent model vs adult model suggests NCDs in adolescence are particularly vulnerable to broader macro and societal factors that are evaluated in this analysis.
National Policies, Laws and Legislations for NCD prevention
The availability of policies and laws targeting NCD-related lifestyle and behavioral risk factors among adolescents varied substantially across regions (Additional file 1 ). Across countries in the African region, the majority perform well with available national policies and strategies for sexual/reproductive health/family planning (95%), violence (85%) and mental health (82%), nutritional interventions (80%), alcohol use prevention (79%), tobacco control activities (79%), and injury prevention (71%). Similar patterns are observed in the South–East Asian region. Both regions are lacking in policies where laws and regulations allow minors to seek contraceptive services and emergency contraception without parental/caregiver consent and seek harm reduction interventions for injectable drug use. Policies which exempt adolescents aged 15–19 years from user fees in the public sector are more common in South-East Asia (71% of countries) and are lacking in Africa (21%) (Fig. 2 ). Across other regions (Additional file 1 ), the Western Pacific region specifically lacked in policies on mental health and nutritional interventions. In the Eastern Mediterranean, less than 45% of countries had adolescent-specific policies on alcohol use and injury/violence prevention. Among Eastern Mediterranean region countries with available data, none had available national laws and regulations permitting adolescents to seek contraceptive services or emergency contraception, and for harm reduction interventions for illicit drug users. In fact, these were lacking in all regions. However, not all countries in these regions participated in the surveys, and sample sizes vary by region and within region by policy type.
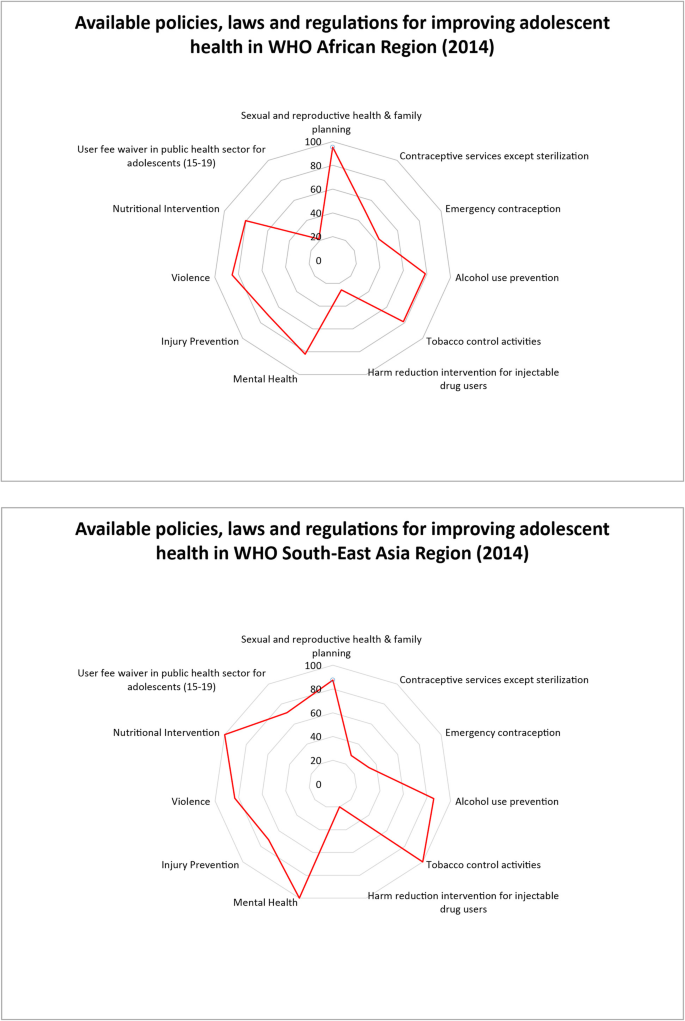
Policies, laws and regulations for adolescent NCD prevention in Africa and South East Asia
Evidence-based interventions and delivery platforms for NCD prevention
Evidence-based interventions for adolescent populations that specifically target their modifiable risk factors for NCDs in adolescent and later life, can be broadly categorized into those delivered through community-based, school-based, peer-based, and family-based platforms. Varying in their degrees of effectiveness and implementation in high-income countries (HICs) versus low-and-middle income countries (LMICs), these interventions have been used to address NCD risk factors and promote protective factors among adolescents. We detail effective interventions for NCD prevention and reduction among adolescents [ 11 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 ], and provide a project-specific overview in the appendix (Additional file 1 ).
Implementing evidence-based initiatives as part of a multi-level, multi-component and inter-sectoral approach can enhance their effectiveness by providing holistic and sustainable solutions [ 12 ]. For instance, interventions incorporating policy measures, environmental changes for promoting physical activity, and education on healthy diet and physical education simultaneously have been more effective in addressing obesity among adolescents compared to individual interventions [ 109 ]. Another example is cash incentive programs, which seek to improve school retention, while addressing issues of poverty, by providing payment incentives to students and their parents. These programs have been effective in improving educational attainment and decreased aggression, crime rates, alcohol and tobacco use, unwanted pregnancies, and mental health symptoms and disorders. Moreover, these have achieved long-term impact post-intervention, that last between 1 and 15 years [ 105 , 110 , 111 , 112 ]. Lastly, mass media and social marketing interventions that target adolescents, their families, and broader communities, have been effective in altering social norms and have served as a platform for grassroots movements by empowering adolescents and broader communities [ 12 , 113 ]. Recent advances in digital technology such as widespread availability and use of mobile phones, social media and online games may also serve as valuable intervention platforms for adolescents. Overall, efforts aimed at improving NCDs among adolescents and in later life should consider taking on holistic solutions that seek to build capacity within individual sectors while enhancing coordination across sectors.
We conducted a comprehensive review of NCD burden and determinants among adolescents, and also derived an evidence-based conceptual framework for tracking pathways to NCD development. We noted that NCDs are a prevailing public health concern among adolescents globally, among which, mental health conditions including depression and conduct disorders are leading disorders among both males and females. Proximal behavioral and lifestyle risk factors are important to disease burden among adolescents, and our analyses show that much of the burden of NCDs in adulthood are related to these modifiable factors that start in adolescence. Most notably, poor diets, smoking, alcohol use, drug use, and indicators of metabolic syndrome (high blood pressure, high cholesterol, diabetes) are the largest contributors to adulthood NCDs and the risks of each of these typically begin in adolescence. Our statistical model also demonstrates that these proximal factors are influenced by broader community and macro factors including social equality, youth empowerment, economic growth and health expenditure, infrastructure and state development, and good governance and security/stability. We also found that, globally, there is momentum towards implementing NCD specific policies/laws/legislations at the national level, but that there is a general lack of policies and laws allowing minors to seek contraceptive services and emergency contraception without consent, and to seek harm reduction interventions for injectable drug use. Additionally, mental health and nutrition related policies exist only variably across geographic regions.
Another consideration are the commercial determinants of health, which refer to consumption of commercial products such as processed food, tobacco, and alcohol, and the vested interests of corporations to encourage their use [ 114 ]. The commercial drivers of ill health are related to the lifestyle risk factors presented in our work as the tobacco, alcohol, and processed food and beverage industries influence consumption of products related to poor diets, smoking, and alcohol use, which in turn impact adolescent NCD burden [ 6 , 115 ]. The global food industry has been identified as the leading driver of NCD epidemics related to diet [ 116 ]. The commercial determinants of health fall under the larger macro, societal and political social determinants of NCDs in adolescents, and they modify the behaviours of individuals in meaningful ways.
Our conceptual framework allows for the visualization of the diverse and complex web of pathways that shape NCDs among young people and in later life. In addition, it identifies critical windows or time periods for intervention, as well as the types of interventions that are necessary to mitigate and address the current and future burden. This conceptual framework could also be used to guide and strengthen the monitoring and evaluation of NCDs among adolescents that is urgently needed. Research on NCDs among adolescents has substantially focused on their engagement in key risk and protective behaviours [ 5 , 12 ]. However, this study emphasizes that a paradigm shift is needed in order to recognize the critical role of underlying structural and societal determinants of health on NCDs among adolescents.
Key global and regional trends among adolescents highlight the significant burden of NCDs with a particular emphasis on mental illnesses such as conduct and major depressive disorders. This burden persists despite many countries globally, including 82% of countries in the African region, reporting the introduction of mental health policies. These trends may indicate weak implementation of key policies, funding, and political will to address NCDs among young people in many LMICs.
Risk and protective factors for NCDs among adolescents, including tobacco smoking, use of alcohol, physical inactivity, unemployment, and overweight, vary widely by region and sex. These findings align with previous empirical research on the burden of disease, risk and health behaviours among adolescent populations [ 5 ]. It also emphasizes the need to reduce the current burden of NCDs among young people, and prevent the heavy adult mortality and morbidity burden associated with risk factors for NCDs acquired in early life [ 5 ]. The diverse trends and inequities highlight the need to develop regional- and country-specific policies and programs to target key contributors to the NCD burden according to need.
Macro and societal factors across the life-course play a critical role on the burden of current and future NCDs among young people. Basic security, humanitarian issues and effective governance represent significant underlying structural determinants that shape both intermediate and proximal factors. Furthermore, infrastructure (e.g., urbanization and access to electricity), access to resources, health spending, human resources for health, gender equity and youth empowerment represent key intermediary influences that contribute significantly to NCDs among adolescents. These findings challenge the dominant perspective that individual and lifestyle risk and protective factors represent the primary contributors to NCDs, and emphasize the importance of underlying macro-level determinants. Other studies have also noted that broader social and economic determinants of health are linked to mortality, morbidity, and risk and protective factors among adolescents [ 12 ]. A paradigm shift in the conceptualization of NCDs and risk factors is therefore critical to developing effective interventions and policies to prevent and mitigate the increasing burden among adolescents. Investments in and emphasis on using multi-level and cross-sectoral interventions and policies that address these diverse influences must be prioritized by countries globally to achieve improvements in NCDs among adolescents. For example, current and future efforts to reduce the risk factors associated with NCDs could be focused on developing primary health-care hubs at the lowest possible level of the health-care system with essential infrastructure and human resources [ 6 ]. Health services that include NCD management and screening in community health units in villages have reported benefits in Ethiopia, Malawi, Namibia, Rwanda, and Uganda [ 117 , 118 ]. These initiatives have trained community health workers to deliver integrated programs for multiple conditions at the community level and to address the needs of women and children which has resulted in improved health outcomes [ 117 , 118 ]. Another focal point in the efforts to combat NCDs is the synergistic effort to reduce health inequalities and improve the equity of government health expenditure by financing universal health coverage [ 119 ]. Rwanda has used funding from HIV programs to expand health insurance coverage for poor sections of the population to improve access to health services, including those for NCDs [ 119 ]. While there is limited information to differentiate between the initiatives focused on adolescent or adult populations specifically, our results are congruent with the current focus on reducing NCD rates by means of supporting the improvement of state governance and increasing health expenditure to decrease health, gender, and socioeconomic inequalities. Urbanization and improved country development are suggestive of overall economic development and can be signals of improved access to health services for the management and treatment of NCDs.
Our work found that policies/laws/legislations targeting NCD risk factors among adolescents generally appear to exist in many countries, but actual implementation and impact data on these NCD policies and laws is limited. Although the MNCAH policy indicator dashboard provides information on the availability of policies or laws on NCDs by region and country, it lacks detailed information on implementation and monitoring and evaluation for impact. There is a strong need for the latter in particular as it’s needed to ensure and improve the quality and sustainability of programs, interventions, and policies targeting NCD risk factors. Tracking and holding countries accountable to their commitments for preventing NCDs is also critical, and can be initiated through preparing a core set of NCD monitoring indicators that can be used to evaluate and inform programs and policies that target NCD risk factors and health outcomes.
Our study is unique in that it used robust statistical modelling methods to explore the contributions of underlying distal, intermediate and proximal determinants in shaping the burden of NCDs among young people and adults. However, a few limitations should be noted. Firstly, our analysis was ecological (country-level) and thus results may be prone to the ecological fallacy. The sample size ( n = 194) was not large but our final models were sufficiently powered with the number of covariates included. Our cross-sectional analysis could not infer temporality and associations do not necessarily suggest causality. Several important indicators (e.g. information on peer, family, and community social support systems, interpersonal relationships) and nutrient deficiency (e.g. anemia) and dietary intake did not have adequate available data for analysis and thus their effect should not be understated. For instance, while IHME databases have indicators on prevalence/incidence for dietary iron deficiency and hemoglobinopathies and hemolytic anemias for adolescents, estimates for many LMICs is missing or incomplete, and therefore we could not use this data in our analysis. Moreover, data used in this study are from publicly available sources such as the Global Health Observatory Data Repository and the World Bank database, and thus analyses and inference are limited to the quality of these data repositories. These sources often rely on survey datasets and other administrative sources that have known challenges in LMICs [ 120 ], and estimates may be modeled or direct estimates. However these estimates are amongst the best available globally and inferences will be meaningful, nonetheless must be interpreted with caution. The WHO MNCAH policy dashboard collects data only on existence of policies and thus the analysis in this study may not be representative of the country’s actual policy implementation impact.
Efforts to prevent the burden of NCDs among adolescents and in later adult life represents an area that necessitates further research, investment and intervention. Key stakeholders, including State and non-State actors, working to improve adolescent health should address under-researched and under-funded areas that represent critical determinants of NCD burden and illness in many LMICs [ 106 ]. Evidence from this study can be used to re-frame the current situation of NCDs in adolescents, highlighting their pathways/determinants and existence (or lack thereof) of interventions/strategies for countering the diseases. Our findings can be used by UN bodies, government/policy-makers, development partners, and academia to target areas of concern for intervention and for identifying future research priorities. The critical role of structural and societal determinants on NCDs in this population must be recognized, including national governance and youth empowerment. Efforts to address these underlying influences require interventions and policies that span multiple sectors and determinants.
The findings of this study demonstrate the importance of adopting a more holistic approach to the prevention and reduction of NCD burden among adolescents, globally. The development and implementation of this approach requires a multilevel design that applies a life course perspective and addresses determinants across individual, community, national and societal levels. In addition, cross-sectoral collaboration is critical to ensuring effective development and implementation of policies to prevent NCDs among young people.
Availability of data and materials
The datasets analyzed during the current study are available in the Global Health Observatory Data Repository, https://www.who.int/gho/en/ , the State of the World’s Children global statistics database, https://data.unicef.org/resources/state-worlds-children-2017-statistical-tables/ , the World Bank database, https://data.worldbank.org/ , the United Nations Statistics Division, http://www.un.org/en/development/desa/publications/world-population-prospects-2015-revision.html , and the 2015Global Burden of Disease (GBD) study housed at the Institute for Health Metrics and Evaluation (IHME), http://www.healthdata.org/gbd .
Abbreviations
Disability-adjusted life years
Global burden of disease
Institute for health metrics and evaluation
Low and middle income country
Maternal, newborn, child, and adolescent health
Non-communicable disease
World Health Organization. Preventing Chronic Diseases - A Vital Investment: WHO Global Report. Geneva: World Health Organization; 2005.
World Health Organization. Health for the world’s adolescents: a second chance in the second decade. Geneva: World Health Organization; 2014.
Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: A foundation for future health. Lancet. 2012;379(9826):1630–40.
Article PubMed Google Scholar
NCD Alliance. A focus on children and non-communicable diseases (NCDs). 2011.
Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. 2011;377(9783):2093–102.
Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–47.
Delisle H. Programming of chronic disease by impaired fetal nutrition: evidence and implications for research and intervention strategies. 2002.
World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–81.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35(7):891–8.
Article CAS Google Scholar
Lassi ZS, Salam RA, Das JK, Wazny K, Bhutta ZA. An unfinished agenda on adolescent health: opportunities for interventions. Semin Perinatol. 2015;39(5):353–60.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78.
Article PubMed PubMed Central Google Scholar
Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME, et al. NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. 2018;392(10152):1072–88.
Article Google Scholar
WHO. Third UN High-level Meeting on Non-communicable Diseases New York. 2018;(September).
World Health Organization. ‘BEST BUYS’ and other recommended interventions for the prevention and control of noncommunicable diseases. 2017;18.
World Health Organization. Globbal Strategy to Reduce the Harmful Use of Alcohol. Geneva: World Health Organization; 2010.
World Health Organization. WHO Report on Global Tobacco Epidemic 2017: Global strategy to reduce the harmful use of alcohol. Geneva: World Health Organization; 2017.
World Health Organization. Taking Action on Childhood Obesity. Geneva: World Health Organization; 2018.
World Health Organization. NCD Global Monitoring Framework. Geneva: World Health Organization; 2013.
Pushka P. The vision and road map for addressing NCDs. In: International Conference on Healthy Lifestyles and NCDs in the Arab World and the Middle-East. Riyadh, KSA; 2012.
Blum RW, Astone NM, Decker MR, Mouli VC. A conceptual framework for early adolescence: a platform for research. Int J Adolesc Med Health. 2014;26(3):321–31.
Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–52.
USAID. Multi-Sectoral Nutrition Strategy 2014-2015. 2014.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51.
World Health Organization. Global Maternal, Newborn, Child and Adolescent Health Policy Indicator Database. 2014.
World Health Organization. Global Health Observatory Data Repository. 2016.
UNICEF. The State of the World’s Children. Statistical Tables. 2017:2017.
The World Bank. Unemployment, youth total (% of total labor force ages 15–24) (modeled ILO estimate). International Labour Organization, ILOSTAT database. Data retrieved in November 2017. 2017.
United Nations, Department of Economic and Social Affairs PD. World Population Prospects: The 2015 Revision. 2015.
Institute for Health Metrics and Evaluation. GBD Arrow Diagram. Seattle: Institute for Health Metrics and Evaluation; 2015.
Elgar FJ, Pförtner TK, Moor I, De Clercq B, Stevens GWJM, Currie C. Socioeconomic inequalities in adolescent health 2002-2010: a time-series analysis of 34 countries participating in the health behaviour in school-aged children study. Lancet. 2015;385(9982):2088–95.
Elgar FJ, Craig W, Boyce W, Morgan A, Vella-Zarb R. Income inequality and school bullying: multilevel study of adolescents in 37 countries. J Adolesc Health. 2009;45(4):351–9.
Miyamoto K, Chevalier A. Education and health. In: Improving health and SOcial Cohension through education. Paris: OECD Publishing; 2010. p. 111–79.
Google Scholar
Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369(9569):1302–13.
Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. 2010;376(9745):959–74.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afi R, Allen NB, et al. Our future : a Lancet commission on adolescent health and wellbeing. 2016;6736(16).
International Labour Organization. Global Employment Trends for Youth 2013: A generation at risk. Geneva; 2013.
World Bank Group. GNI per capita, Atlas method (current US$). World Bank national accounts data, and OECD National Accounts data files. 2018.
Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–90.
Kelishadi R, Farajian S. The protective effects of breastfeeding on chronic non-communicable diseases in adulthood: A review of evidence. Adv Biomed Res. 2014;3:3 Available from: https://pubmed.ncbi.nlm.nih.gov/24600594 .
Brumana L, Arroyo A, Schwalbe NR, Lehtimaki S, Hipgrave DB. Maternal and child health services and an integrated, life-cycle approach to the prevention of non-communicable diseases. BMJ Glob Heal. 2017;2(3):e000295 Available from: https://pubmed.ncbi.nlm.nih.gov/29082005 .
Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–44.
Amaugo LG, Papadopoulos C, Ochieng BMN, Ali N. The effectiveness of HIV/AIDS school-based sexual health education programmes in Nigeria: a systematic review. Health Educ Res. 2014;29(4):633–48.
Blank L, Baxter SK, Payne N, Guillaume LR, Squires H. Systematic review and narrative synthesis of the effectiveness of contraceptive service interventions for young people, delivered in health care settings. Health Educ Res. 2012;27(6):1102–19.
Fonner VA, Armstrong KS, Kennedy CE, O'Reilly KR, Sweat MD. School based sex education and HIV prevention in low- and middle-income countries: A systematic review and meta-analysis. PLoS One. 2014;9(3):e89692.
Harrison A, Newell M-L, Imrie J, Hoddinott G. HIV prevention for south African youth: which interventions work? A systematic review of current evidence. BMC Public Health. 2010;10(1):102.
A MKSRG. The efficacy of interventions to reduce adolescent childbearing in low- and middle-income countries: a systematic review. TT -Stud Fam Plann. 2013;44(4):369–88.
Paul-Ebhohimhen VA, Poobalan A, Van Teijlingen ER. A systematic review of school-based sexual health interventions to prevent STI/HIV in sub-Saharan Africa. BMC Public Health. 2008;8.
Speizer IS, Magnani RJ, Colvin CE. The effectiveness of adolescent reproductive health interventions in developing countries: a review of the evidence. J Adolesc Health. 2003;33(5):324–48.
Hawkins JD, Catalano RF, Kosterman R, Abbott R, Hill KG. Preventing adolescent health-risk behaviors by strengthening protection during childhood. Arch Pediatr Adolesc Med. 1999;153(3):226–34.
Article CAS PubMed Google Scholar
Hawkins JD, Guo J, Hill KG, Battin-Pearson S, Abbott RD. Long-term effects of the Seattle social development intervention on school bonding trajectories. Appl Dev Sci. 2001;5(4):214–24.
Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood. Arch Pediatr Adolesc Med. 2005;159(1):25–31.
Carson KV, Brinn MP, Labiszewski NA, Esterman AJ, Chang AB, Smith BJ. Community interventions for preventing smoking in young people. Cochrane Database Syst Rev. 2000;7:2–4.
Hawkins JD, Kosterman R, Catalano RF, Hill KG. & Abbott RD. effects of social development intervention in childhood 15 years later. Arch Pediatr Adolesc Med. 2008;162(12):1133–41.
Lonczak HS, Abbott RD, Hawkins JD, Kosterman R, Catalano RF. Effects of the Seattle social development project on sexual behavior, pregnancy, birth, and sexually transmitted disease outcomes by age 21 years. Arch Pediatr Adolesc Med. 2002;156(5):438.
Cusimano MD, Sameem M. The effectiveness of middle and high school-based suicide prevention programmes for adolescents: a systematic review. Inj Prev. 2011;17(1):43–9.
Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386–405.
Katz C, Bolton SL, Katz LY, Isaak C, Tilston-Jones T, Sareen J. A systematic review of school-based suicide prevention programs. Depress Anxiety. 2013;30(10):1030–45.
PubMed Google Scholar
Klimes-Dougan B, Klingbeil DA, Meller SJ. The impact of universal suicide-prevention programs on the help-seeking attitudes and behaviors of youths. Crisis. 2013;34(2):82–97.
Robinson J, Cox G, Malone A, Williamson M, Baldwin G, Fletcher K, et al. A systematic review of school-based interventions aimed at preventing, treating, and responding to suicide- related behavior in young people. Crisis. 2013;34(3):164–82.
World Health Organization. Adolescent mental health: mapping actions of nongovernmental organizations and other international development organizations. Geneva; 2012.
Mason-jones AJ, Crisp C, Momberg M, Koech J, Koker P De, Mathews C. A systematic review of the role of school-based healthcare in adolescent sexual , reproductive , and mental health A systematic review of the role of school-based healthcare in adolescent sexual , reproductive , and mental health. 2012;.
Owen J, Carroll C, Cooke J, Formby E, Hayter M, Hirst J, et al. School-linked sexual health services for young people (SSHYP): A survey and systematic review concerning current models, effectiveness, cost-effectiveness and research opportunities. Health Technol Assess. 2010;14(30):1–228, iii-iv.
Foxcroft DR, Tsertsvadze A. Universal family-based prevention programs for alcohol misuse in young people. Cochrane Libr. 2011.
Binagwaho A, Wagner CM, Gatera M, Karema C, Nutt CT, Ngabo F. Achieving high coverage in Rwanda’s national human papillomavirus vaccination programme. Bull World Health Organ. 2012:623–8.
LaMontagne DS, Barge S, Thi Le N, Mugisha E, Penny ME, Gandhi S, Janmohamed A, Kumakech E, Mosquiera NR, Nguyen NQ, Paul P, Tang Y, Minh TH, Uttekar BP, Jumaan AO. Human papillomavirus vaccine delivery strategies that achieved high coverage in low- and middle-income countries. Bull World Health Organ. 2011;89(11):821–30.
Ladner J, Besson MH, Rodrigues M, Audureau E, Saba J. Performance of 21 HPV vaccination programs implemented in low and middle-income countries , 2009–2013. BMC Public Health. 2014;14:1–11.
Haider R. Adolescent nutrition: a review of the situation in selected south-east Asian countries. New Delhi; 2006.
Catalano RF, Fagan AA, Gavin LE, Greenberg MT, Irwin CE, Ross DA, et al. Worldwide application of prevention science in adolescent health. Lancet. 2012;379(9826):1653–64.
Botvin GJ, Griffin KW, Nichols TD. Preventing youth violence and delinquency through a universal school-based prevention approach. Prev Sci. 2006;7(4):403–8.
Botvin GJ, Griffin KW. Life skills training: empirical findings and future directions. J Prim Prev. 2004;25(2):211–32.
DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Iii EWH, et al. Efficacy of an HIV prevention intervention. J Am Med Assoc. 2004;292(2):171–9.
Elliot DS. Blueprints for violence prevention. Boulder; 1998.
Faggiano F, Vigna-Taglianti F, Burkhart G, Bohrn K, Cuomo L, Gregori D, et al. The effectiveness of a school-based substance abuse prevention program: 18-month follow-up of the EU-dap cluster randomized controlled trial. Drug Alcohol Depend. 2010;108(1–2):56–64.
Gottschalk LB, Ortayli N. Interventions to improve adolescents’ contraceptive behaviors in low- and middle-income countries: a review of the evidence base. Contraception. 2014;90(3):211–25.
Griffin KW, Botvin GJ, Nichols TR. Long-term follow-up effects of a school-based drug abuse prevention program on adolescent risky driving. Prev Sci. 2004;5(3):207–12.
Fenton KA, Johnson AM, Mcmanus S, Erens B. Series editors measuring sexual behaviour : methodological challenges in survey research. Sex transm Inf. 2001:84–92.
Kirby D, Obasi A, Laris BA. The effectiveness of sex education and HIV education interventions in schools in developing countries. World Heaolth Organ Tech Rep Ser. 2006;938(103):317–41.
Campbell FA, Ramey CT, Miller-johnson S. Early childhood education : young adult outcomes from the abecedarian project Elizabeth Pungello and Joseph sparling. Appl Dev Sci. 2002;6(1):42–57.
Fagan AA, Catalano RF. What works in youth violence prevention: a review of the literature. Res Soc Work Pract. 2013;23(2):141–56.
Gates S, Mccambridge J, Smith LA, Foxcroft D. Interventions for prevention of drug use by young people delivered in non-school settings. Cochrane Database Syst Rev. 2009;1.
Kumpfer KL, Alvarado R, Whiteside HO. Family-based interventions for substance use and misuse prevention. Subst Use Misuse. 2003;38(11–13):1759–87 1916.
Controlled R, Olds D, Henderson CR, Cole R, Eckenrode J, Kitzman H, et al. Long-term Effects of Nurse Home Visitation on Children ’ s Criminal and Antisocial Behavior. 2014;280(14).
Olds DL, Kitzman H, Cole R, Robinson J, Sidora K, Luckey DW, Henderson CR, Hanks C, Bondy J, Holmberg J. Effects of nurse home-visiting on maternal life course and child development: age 6 follow-up results of a randomized trial. Pediatrics. 2004;114(6):1550–9.
Olds DL, Robinson J, O’Brien R, Luckey DW, Pettitt LM, Henderson CR, Ng RK, Sheff KL, Korfmacher J, Hiatt S, Talmi A. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002;110(3):486–96.
Martineau F, Tyner E, Lorenc T, Petticrew M, Lock K. Population-level interventions to reduce alcohol-related harm: an overview of systematic reviews. Prev Med (Baltim). 2013;57(4):278–96.
Reynolds AJ, Temple JA, Ou S-R, Robertson DL, Mersky JP, Topitzes JW, et al. Effects of a school-based, early childhood intervention on adult health and well-being. Arch Pediatr Adolesc Med. 2007;161(8):730.
Reynolds AJ, Temple JA, Robertson DL, Mann EA. Long-term effects of an early childhood intervention on educational achievement and juvenile arrest: A 15-year follow-up of low-income children in public schools. JAMA. 2001;285(18):2339–46.
Schinke SP, Schwinn TM, Noia J, Cole KC. Reducing the risks of alcohol use among urban youth: three-year effects of a computer-based intervention with and without parent involvement. J Stud Alcohol. 2004;65(4):443–9.
Schweinhart LJ, Barnes HV, Weikhart DP. Significant benefits: The High/Scope Perry preschool study through age 27. In: Child Welfare: Major Themes in Health and Social Welfare. London; New York: Routledge; 2005. p. 9–29.
Schwinn TM, Schinke SP. Preventing alcohol use among late adolescent urban youth: 6-year results from a computer-based intervention. J Stud Alcohol Drugs. 2010;71(4):535–8.
Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. J Consult Clin Psychol. 2009;77(4):620–32.
Thomas RE, Baker PR, Thomas BC, Lorenzetti DL. Family-based programmes for preventing smoking by children and adolescents. Cochrane Database Syst Rev. 2015;2015(2):CD004493.
Trickett EJ, Beehler S. The ecology of multilevel interventions to reduce social inequalities in health. Am Behav Sci. 2013;57(8):1227–46.
Gavin LE, Catalano RF, David-Ferdon C, Gloppen KM, Markham CM. A review of positive youth development programs that promote adolescent sexual and reproductive health. J Adolesc Health. 2010;46(3 SUPPL):S75–91.
Faggiano F, Minozzi S, Versino E, Buscemi D, Faggiano F, Minozzi S, et al. Universal school-based prevention for illicit drug use ( review ). Cochrane Database Syst Rev. 2016;3(12):1–67.
Thomas RE, Lorenzetti DL, Spragins W. Systematic review of mentoring to prevent or reduce tobacco use by adolescents. Acad Pediatr. 2013;13(4):300–7.
Sethi, D., Hughes, K., Bellis, M., Mitis, F., & Racioppi F. European report on preventing violence and knife crime among young people. 2010.
Ellsberg M, Arango DJ, Morton M, Gennari F, Kiplesund S, Contreras M, et al. Prevention of violence against women and girls: what does the evidence say? Lancet. 2015;385(9977):1555–66.
Brittain AW, Williams JR, Zapata LB, Pazol K, Romero LM, Weik TS. Youth-friendly family planning Services for Young People: a systematic review. Am J Prev Med. 2015;49(2):S73–84.
Hale DR, Fitzgerald-Yau N, Viner R. A systematic review of effective interventions for reducing multiple health risk behaviors in adolescence. Am J Public Health. 2014;104(5):e19–41.
World Health Organization. Violence prevention: the evidence. Geneva; 2010.
Pettifor A, MacPhail C, Nguyen N. & RM. can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS Behav. 2012;16(7):1729–38.
Wamoyi J, Mshana G, Mongi A, et al. A review of interventions addressing structural drivers of adolescents’ sexual and reproductive health vulnerability in sub-Saharan Africa: implications for sexual health programming. Reprod Heal. 2014;11:88.
Baird SJ, Garfein RS, McIntosh CT, Özler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–9.
Zuurmond MA, Geary RS, Ross DA. The effectiveness of youth centers in increasing use of sexual and reproductive health services: a systematic review. Stud Fam Plan. 2012;43(4):239–54.
Lundgren R, Amin A. Addressing intimate partner violence and sexual violence among adolescents: emerging evidence of effectiveness. J Adolesc Health. 2015;56(1):S42–50.
Allen-Meares P, Montgomery KL, Kim JS. School-based social work interventions: a cross-national systematic review. Soc Work (United States). 2013;58(3):253–62.
Pearson N, Braithwaite R, Biddle S. The effectiveness of interventions to increase physical activity among adolescent girls: a meta-analysis. Acad Pediatr. 2015;15(1):9–18.
Duflo, E., Dupas, P., Kremer, M., & Sinei S. Education and HIV/AIDS prevention: evidence from a randomized evaluation in Western Kenya. 2006. (World Bank Policy Research Working Paper). Report No.: 4024.
Fiszbein, A. & Schady N. Conditional Cash Transfers: Reducing Present and Future Poverty. 2009.
Baird SJ, Garfein RS, McIntosh CT, Özler B. The short-term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Econ. 2010;19(S1):55068.
Moyer-Gusé E. Toward a theory of entertainment persuasion: explaining the persuasive effects of entertainment-education messages. Commun Theory. 2008;18(3):407–25.
Buse K, Tanaka S, Hawkes S. Healthy people and healthy profits? Elaborating a conceptual framework for governing the commercial determinants of non-communicable diseases and identifying options for reducing risk exposure. Glob Health. 2017;13(1):1–12.
Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381(9867):670–9.
United Nations. Human Rights Council, 26th Session AI 3. Grover A. Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health. United Nations; 2014 p. A/HRC/26/31.
Atun R, Jaffar S, Nishtar S, Knaul FM, Barreto ML, Nyirenda M, et al. Improving responsiveness of health systems to non-communicable diseases. Lancet. 2013;381(9867):690–7.
Celletti F, Wright A, Palen J, Frehywot S, Markus A, Greenberg A, et al. Can the deployment of community health workers for the delivery of HIV services represent an effective and sustainable response to health workforce shortages? Results of a multicountry study. AIDS. 2010;24(Suppl 1):S45–57.
Kalk A, Groos N, Karasi JC, Girrbach E. Health systems strengthening through insurance subsidies: the GFATM experience in Rwanda. Trop Med Int Heal. 2010;15(1):94–7.
Harrison K, Rahimi N, Carolina D-HM. Factors limiting data quality in the expanded programme on immunization in low and middle-income countries: a scoping review. Vaccine. 2020;38(30):4652–63 Available from: http://www.sciencedirect.com/science/article/pii/S0264410X20304011 .
Download references
Acknowledgements
We would like to acknowledge the support of Hana Tasic, research assistant in the Centre for Global Child Health, Hospital for Sick Children, for her editorial review of this paper.
This study was funded by UNICEF and the Centre for Global Child Health at the Hospital for Sick Children. The funder commissioned the review, but had no role in the research process, methods or inferences from the analyses.
Author information
Authors and affiliations.
Centre for Global Child Health, Hospital for Sick Children, Toronto, ON, M5G 0A4, Canada
N. Akseer, S. Mehta, J. Wigle, R. Chera, Z. J. Brickman, S. Al-Gashm, B. Sorichetti, A. Vandermorris & Z. A. Bhutta
Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
N. Akseer, J. Wigle, B. Sorichetti & Z. A. Bhutta
Division of Adolescent Medicine, Hospital for Sick Children, Toronto, Canada
A. Vandermorris
UNICEF, New York, USA
D. B. Hipgrave
Spark Consulting, New York, USA
N. Schwalbe
Center of Excellence in Women and Child Health, the Aga Khan University, Karachi, Pakistan
Z. A. Bhutta
You can also search for this author in PubMed Google Scholar
Contributions
NA conceptualized the study, designed the analytic plan, conducted statistical analysis, drafted sections of the manuscript, critically reviewed the manuscript and approved the final manuscript as submitted. RC conducted the policy analysis, ZB drafted study tables, BS conducted statistical analysis and SAG drafted the section on evidence-based interventions. SM, JW, RC, BS, ZB and SAG drafted sections of manuscript, conducted data extraction, critically reviewed the manuscript and approved the final manuscript as submitted. AV supported development of the conceptual framework, critically reviewed the manuscript and approved the final manuscript as submitted. DH and NS reviewed and revised the study protocol, critically reviewed the manuscript and approved the final manuscript as submitted. ZAB provided overall technical oversight, reviewed and revised the study protocol, critically reviewed the manuscript and approved the final manuscript as submitted. All authors read and approved the final manuscript.
Corresponding author
Correspondence to N. Akseer .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1.
: Hierarchical levels, domains, and indicators related to NCDs among adolescents and later adulthood used for multivariable statistical modeling. Appendix 2 : Top NCD DALYs in adolescents across WHO regions. Appendix 3 : Youth and adulthood DALYS related to NCD risk factors that begin in adolescence. Appendix 4 : Top NCD DALYS for health outcomes in adults aged 15–49 and 50–69 years. Appendix 5 : Policies, laws and regulations for adolescent NCD prevention in the Eastern Mediterranean, the Americas, Europe, and the Western Pacific. Appendix 6 : Policies, laws and regulations indicator breakdown for all regions by country. Appendix 7 : Evidence-based NCD health interventions for adolescents and lifestyle factors among adolescents to prevent adulthood NCDs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Akseer, N., Mehta, S., Wigle, J. et al. Non-communicable diseases among adolescents: current status, determinants, interventions and policies. BMC Public Health 20 , 1908 (2020). https://doi.org/10.1186/s12889-020-09988-5
Download citation
Received : 09 April 2020
Accepted : 30 November 2020
Published : 14 December 2020
DOI : https://doi.org/10.1186/s12889-020-09988-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents
- Non-communicable diseases
- Determinants
- Risk factors
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Health topics /
- Noncommunicable diseases
Noncommunicable diseases (NCDs), including heart disease, stroke, cancer, diabetes and chronic lung disease, are collectively responsible for 74% of all deaths worldwide. More than three-quarters of all NCD deaths, and 86% of the 17 million people who died prematurely, or before reaching 70 years of age, occur in low- and middle-income countries.
NCDs share five major risk factors: tobacco use, physical inactivity, the harmful use of alcohol, unhealthy diets and air pollution.
The epidemic of NCDs poses devastating health consequences for individuals, families and communities, and threatens to overwhelm health systems. The socioeconomic costs associated with NCDs make the prevention and control of these diseases a major development imperative for the 21st century.
WHO’s mission is to provide leadership and the evidence base for international action on surveillance, prevention and control of NCDs. Urgent government action is needed to meet global targets to reduce the burden of NCDs.
One of the most important ways of reducing deaths from noncommunicable diseases (NCDs) is to control the risk factors that lead to their development. These include reducing the use of tobacco and the harmful use of alcohol, maintaining an active lifestyle and consuming a healthy diet, and improving air quality. Actions towards these goals are cost-effective ways for countries to reduce the number of NCD deaths. Tackling these risk factors can not only save lives, but also provide a huge economic boost for countries.
Beyond prevention, management of NCDs is critical. This includes detection, screening and treatment of the diseases, as well as palliative care for those in need. The vast majority of premature deaths from NCDs occur in low- and middle-income countries, where universal health coverage or access to health care services is often limited. The development and promotion of universal health coverage is therefore essential in tackling NCDs and working to reduce the number of preventable global deaths.
Surveillance of NCDs is another vital action for providing the information needed for policy and programme development for NCD prevention and control. Tracking and reporting on NCD related global targets and indicators to understand progress in NCD prevention and control are key activities. Accurate data from countries are vital to reverse the global rise in death and disability from NCDs, to support evidence-based decision making, and to help monitor and evaluate the progress being made.
The WHO Department of Noncommunicable Diseases is responsible for global leadership, coordination, guidance and technical support to reduce premature mortality and morbidity from NCDs. In 2019, the World Health Assembly extended the WHO Global action plan for the prevention and control of NCDs 2013–2020 to 2030. It called for the development of an Implementation Roadmap 2023–2030 to accelerate progress on preventing and controlling NCDs. The Implementation Roadmap supports actions to achieve a set of 9 global targets with the greatest impact towards prevention and management of NCDs.
Noncommunicable diseases are recognized as a major global challenge in the United Nations 2030 Agenda for Sustainable Development. The Agenda sets the target of reducing premature deaths from NCDs by one third by 2030. WHO plays a key leadership role in the coordination and promotion of the global fight against NCDs and the achievement of the Sustainable Development Goals target 3.4.
- NCD data portal
- Global health observatory (GHO)
- NCD microdata repository
- Global NCD compact 2020–2030
- Global Group of Heads of State and Government for the Prevention and Control of NCDs
- High-level policy expert group of the SIDS ministerial conference on NCDs and mental health
- WHA53.17: Prevention and control of noncommunicable diseases
- WHA56.1: WHO Framework convention on tobacco control
- WHA61.14: Prevention and control of noncommunicable diseases: implementation of the global strategy
- Noncommunicable Diseases, Rehabilitation and Disability
- Global Noncommunicable Diseases Platform
Nearly 1.8 billion adults at risk of disease from not doing enough physical activity
WHO 5-year milestone report on global trans fat elimination illustrates latest progress up to 2023
New report maps efforts to improve adolescent health and well-being
COVID-19 eliminated a decade of progress in global level of life expectancy
Latest publications

WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention:...
In 2022, cervical cancer was the fourth most commonly occurring cancer among women globally and also the fourth leading cause of cancer deaths among...

Global strategy and action plan on oral health 2023–2030
This document incorporates all key policy documents that inform and define the renewed global oral health agenda towards 2030: the resolution on oral health...

Tackling NCDs: best buys and other recommended interventions for the prevention and control of noncommunicable...
This document provides an updated list of “best buys” and other recommended interventions to address noncommunicable diseases (NCDs). It is...

Global oral health status report: towards universal health coverage for oral health by 2030: regional...
This regional summary draws on the WHO Global oral health status report, published in 2022, which provides a comprehensive overview of the global oral...
Integrated management of NCDs
Strengthening NCD integration in humanitarian emergencies
Management of noncommunicable diseases
Preventing noncommunicable diseases
India: Bringing primary health care to remote populations in Chhattisgarh
Donors making a difference for universal health coverage
How we work: collaborating centres across Europe
Journalism Training on Noncommunicable Diseases (NCDs) in Athens, Greece, 16 - 18 October 2023
Infographics

Core projects under the CureALL framework of the Global Initiative for Childhood Cancers

Access education resources

Set of nine voluntary global NCD targets for 2025

Global monitoring framework

Noncommunicable Diseases (NCDs) Hard Talks webinar: Toxic air is fueling NCDs - Why don't we act?

WHO press conference on global health issues - 5 July 2023
Who press conference on global health issues - 21 june 2023.

LIVE: Countdown to 2023: WHO Report on Global Trans Fat Elimination 2022
International dialogue on sustainable financing for NCDs and mental health
H20 Summit: “The Future of Global Health Diplomacy in a Changing World”
4th meeting of the Strategic and Technical Advisory Group on the Prevention and Control of Noncommunicable Diseases (STAG-NCD)
Adolescent obesity management guidelines: sixth Guideline Development Group meeting
Country profiles
Related health topics
Air pollution
Cardiovascular diseases
Chronic respiratory diseases
Healthy diet
Palliative care
Physical activity
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 09 January 2024
An evidence gap map of interventions for noncommunicable diseases and risk factors among children and adolescents
- Rehana A. Salam 1 ,
- Maryam Hameed Khan ORCID: orcid.org/0000-0002-1197-8165 2 ,
- Syed Saqlain Ali Meerza ORCID: orcid.org/0000-0002-8966-5353 2 ,
- Jai K. Das 2 ,
- Laura Lewis-Watts 3 &
- Zulfiqar A. Bhutta ORCID: orcid.org/0000-0003-0637-599X 3
Nature Medicine volume 30 , pages 290–301 ( 2024 ) Cite this article
1129 Accesses
1 Citations
12 Altmetric
Metrics details
- Risk factors
Substance misuse, obesity, mental health conditions, type 1 diabetes, cancers, and cardiovascular and chronic respiratory diseases together account for 41% of disability-adjusted life years linked to noncommunicable diseases (NCDs) among children and adolescents worldwide. However, the evidence on risk factors and interventions for this age group is scarce. Here we searched four databases to generate an evidence gap map of existing interventions and research gaps for these risk factors and NCDs. We mapped 159 reviews with 2,611 primary studies; most (96.2%) were conducted in high-income countries, and only 100 studies (3.8%) were from low- and middle-income countries (LMICs). The efficacy of therapeutic interventions on biomarkers and adverse events for NCDs appears to be well evidenced. Interventions for mental health conditions appear to be moderately evidenced, while interventions for obesity and substance misuse appear to be moderate to very low evidenced. Priority areas for future research include evaluating digital health platforms to support primary NCD prevention and management, and evaluating the impact of policy changes on the prevalence of obesity and substance misuse. Our findings highlight the wide disparity of evidence between high-income countries and LMICs. There is an urgent need for increased, targeted financing to address the research gaps in LMICs.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

The FRESHAIR4Life study: Global implementation research on non-communicable disease prevention targeting adolescents’ exposure to tobacco and air pollution in disadvantaged populations
Global population attributable fraction of potentially modifiable risk factors for mental disorders: a meta-umbrella systematic review
Public health primary prevention implemented by clinical high-risk services for psychosis
Data availability.
All reviews included in this evidence gap map were identified via PubMed, Cochrane, Embase and Campbell Collaboration. The data analyzed in the paper were extracted from published reviews and papers and are available within the manuscript, Supplementary Information and extended data figures. The full database (including initial search results and screening) can be accessed upon reasonable request from the corresponding author, as this is contained within Covidence, EPPI-Reviewer and Excel spreadsheets (data extracted from the included reviews and primary studies). There is no restriction to the availability of the data or the timeline for availability. For inquiries regarding data access or any additional information about the data, please contact the corresponding author. Source data are provided with this paper.
Mokdad, A. H. et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 387 , 2383–2401 (2016).
Article PubMed Google Scholar
Hanson, M. A. & Gluckman, P. D. Early developmental conditioning of later health and disease: physiology or pathophysiology? Physiol. Rev. 94 , 1027–1076 (2014).
Article CAS PubMed PubMed Central Google Scholar
Kelishadi, R. et al. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull. World Health Organ. 85 , 19–26 (2007).
Article PubMed PubMed Central Google Scholar
Akseer, N. et al. Non-communicable diseases among adolescents: current status, determinants, interventions and policies. BMC Public Health 20 , 1–20 (2020).
Article Google Scholar
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1204–1222 (2020).
Murray, C. J. et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1223–1249 (2020).
Global Status Report on Noncommunicable Diseases 2014 (WHO, 2014).
Motlagh M.E. et al. Methodology and early findings of the fifth survey of childhood and adolescence surveillance and prevention of adult noncommunicable disease: the CASPIAN-V study. Int. J. Prev. Med. 8 , 77 (2017).
Cappa, C., Wardlaw, T., Langevin-Falcon, C. & Diers, J. Progress for children: a report card on adolescents. Lancet 379 , 2323–2325 (2012).
Sawyer, S. M. et al. Adolescence: a foundation for future health. Lancet 379 , 1630–1640 (2012).
Brumana, L., Arroyo, A., Schwalbe, N. R., Lehtimaki, S. & Hipgrave, D. B. Maternal and child health services and an integrated, life-cycle approach to the prevention of non-communicable diseases. BMJ Glob. Health 2 , e000295 (2017).
Global Indicator Framework for the Sustainable Development Goals and Targets of the 2030 Agenda for Sustainable Development (Affairs UNDoEaS, 2020); https://unstats.un.org/sdgs/indicators/indicators-list/
Fullman, N. et al. Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: an analysis from the Global Burden of Disease Study 2016. Lancet 390 , 1423–1459 (2017).
Goal 3: Ensure Healthy Lives and Promote Well-Being for All at All Ages (United Nations, 2016); https://www.un.org/sustainabledevelopment/health/
Haregu, T. N. et al. A scoping review of non-communicable disease research capacity strengthening initiatives in low and middle-income countries. Glob. Health Res. Policy 4 , 31 (2019).
Snilstveit, B., Vojtkova, M., Bhavsar, A., Stevenson, J. & Gaarder, M. Evidence & gap maps: a tool for promoting evidence informed policy and strategic research agendas. J. Clin. Epidemiol. 79 , 120–129 (2016).
White, H. et al. Guidance for producing a Campbell evidence and gap map. Campbell Syst. Rev. 16 , e1125 (2020).
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019). Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020; https://vizhub.healthdata.org/gbd-compare/
Boumparis, N. et al. Short-and long-term effects of digital prevention and treatment interventions for cannabis use reduction: a systematic review and meta-analysis. Drug Alcohol Depend. 200 , 82–94 (2019).
Carson‐Chahhoud, K. V. et al. Mass media interventions for preventing smoking in young people. Cochrane Database Sys. Rev. 6 , CD001006 (2017).
Gilligan, C. et al. Family‐based prevention programmes for alcohol use in young people. Cochrane Database Syst. Rev. 3 , CD012287 (2019).
Hefler, M., Liberato, S.C. & Thomas, D. P. Incentives for preventing smoking in children and adolescents. Cochrane Database Syst. Rev . 6 , CD008645 (2017).
Langford, R. et al. The World Health Organization’s Health Promoting Schools framework: a Cochrane systematic review and meta-analysis. BMC Public Health 15 , 130 1–5 (2015).
MacArthur, G. et al. Individual‐, family‐, and school‐level interventions targeting multiple risk behaviours in young people. Cochrane Database Syst. Rev. 10 , CD009927 (2018).
MacArthur, G. J., Harrison, S., Caldwell, D. M., Hickman, M. & Campbell, R. Peer‐led interventions to prevent tobacco, alcohol and/or drug use among young people aged 11–21 years: a systematic review and meta‐analysis. Addiction 111 , 391–407 (2016).
Minozzi, S., Amato, L., Bellisario, C. & Davoli, M. Detoxification treatments for opiate dependent adolescents. Cochrane Database Syst. Rev. 4 , CD006749 (2014).
Selph, S. et al. Primary care-relevant interventions for tobacco and nicotine use prevention and cessation in children and adolescents: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 323 , 1599–1608 (2020).
Steele, D. W. et al. Brief behavioral interventions for substance use in adolescents: a meta-analysis. Pediatrics 146 , e20200351 (2020).
Taylor, G. M. et al. Internet‐based interventions for smoking cessation. Cochrane Database Syst. Rev. 9 , CD007078 (2017).
Wolfenden, L. et al. Strategies for enhancing the implementation of school‐based policies or practices targeting risk factors for chronic disease. Cochrane Database Syst. Rev. 11 , CD011677 (2017).
Axon, E. et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst. Rev. 11 , CD012436 (2016).
Ells, L. J. et al. Surgery for the treatment of obesity in children and adolescents. Cochrane Database Syst. Rev. 6 , CD011740 (2015).
Fowler, L. A. et al. Harnessing technological solutions for childhood obesity prevention and treatment: a systematic review and meta-analysis of current applications. Int. J. Obes. 45 , 957–981 (2021).
Li, P., Fan, C., Lu, Y. & Qi, K. Effects of calcium supplementation on body weight: a meta-analysis. Am. J. Clin. Nutr. 104 , 1263–1273 (2016).
Article CAS PubMed Google Scholar
Loveman, E. et al. Parent-only interventions for childhood overweight or obesity in children aged 5 to 11 years. Cochrane Database Syst . Rev. 12 , CD012008 (2015).
McGavock, J. et al. Layperson-led vs professional-led behavioral interventions for weight loss in pediatric obesity: a systematic review and meta-analysis. JAMA Netw. Open 3 , e2010364 (2020).
Mohammadi, H. et al. Effects of pro-/synbiotic supplementation on anthropometric and metabolic indices in overweight or obese children and adolescents: a systematic review and meta-analysis. Complement. Ther. Med. 44 , 269–276 (2019).
Morgan, E. H., Schoonees, A., Sriram, U., Faure, M., Seguin-Fowler, R. A. Caregiver involvement in interventions for improving children’s dietary intake and physical activity behaviors. Cochrane Database Syst. Rev. 1 , CD012547 (2020).
Oliveira, C. B. et al. Effects of active video games on children and adolescents: a systematic review with meta‐analysis. Scand. J. Med. Sci. Sports 30 , 4–12 (2020).
Salam, R. A. et al. Effects of lifestyle modification interventions to prevent and manage child and adolescent obesity: a systematic review and meta-analysis. Nutrients 12 , 2208 (2020).
Schroeder, K., McCormick, R., Perez, A. & Lipman, T. H. The role and impact of community health workers in childhood obesity interventions: a systematic review and meta‐analysis. Obes. Rev. 19 , 1371–1384 (2018).
Yavuz, H. M., van Ijzendoorn, M. H., Mesman, J. & van der Veek, S. Interventions aimed at reducing obesity in early childhood: a meta‐analysis of programs that involve parents. J. Child Psychol. Psychiatry 56 , 677–692 (2015).
Abraham, O. et al. Investigating serious games that incorporate medication use for patients: systematic literature review. JMIR Serious Games 8 , e16096 (2020).
Absil, H., Baudet, L., Robert, A. & Lysy, P. A. Benefits of physical activity in children and adolescents with type 1 diabetes: a systematic review. Diabetes Res. Clin. Pract. 156 , 107810 (2019).
Abualula, N. A., Jacobsen, K. H., Milligan, R. A., Rodan, M. F. & Conn, V. S. Evaluating diabetes educational interventions with a skill development component in adolescents with type 1 diabetes: a systematic review focusing on quality of life. Diabetes Educ. 42 , 515–528 (2016).
Al Khalifah, R. A., Alnhdi, A., Alghar, H., Alanazi, M. & Florez, I. D. The effect of adding metformin to insulin therapy for type 1 diabetes mellitus children: a systematic review and meta‐analysis. Pediatr. Diabetes 18 , 664–673 (2017).
Aljawarneh, Y. M., Al-Qaissi, N. M. & Ghunaim, H. Y. Psychological interventions for adherence, metabolic control, and coping with stress in adolescents with type 1 diabetes: a systematic review. World J. Pediatr. 16 , 456–470 (2020).
Aljawarneh, Y. M., Wardell, D. W., Wood, G. L. & Rozmus, C. L. A systematic review of physical activity and exercise on physiological and biochemical outcomes in children and adolescents with type 1 diabetes. J. Nurs. Scholarsh. 51 , 337–345 (2019).
Alotaibi, A., Al Khalifah, R. & McAssey, K. The efficacy and safety of insulin pump therapy with predictive low glucose suspend feature in decreasing hypoglycemia in children with type 1 diabetes mellitus: a systematic review and meta‐analysis. Pediatr. Diabetes 21 , 1256–1267 (2020).
Campbell, F. et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst. Rev. 4 , CD009794 (2016).
Cherubini, V. et al. Effectiveness of ketoacidosis prevention campaigns at diagnosis of type 1 diabetes in children: a systematic review and meta-analysis. Diabetes Res. Clin. Pract. 175 , 108838 (2021).
Chin‐Jung, L., Hsiao‐Yean, C., Yeu‐Hui, C., Kuan‐Chia, L. & Hui‐Chuan, H. Effects of mobile health interventions on improving glycemic stability and quality of life in patients with type 1 diabetes: a meta‐analysis. Res. Nurs. Health 44 , 187–200 (2021).
Clar, C., Waugh, N. & Thomas, S. Routine hospital admission versus out-patient or home care in children at diagnosis of type 1 diabetes mellitus. Cochrane Database Syst. Rev . 3 , CD004099 (2003).
Dos Santos, T. J., Campos, J. D., Argente, J. & Rodríguez-Artalejo, F. Effectiveness and equity of continuous subcutaneous insulin infusions in pediatric type 1 diabetes: a systematic review and meta-analysis of the literature. Diabetes Res. Clin. Pract. 172 , 108643 (2021).
Dovc, K. et al. Free-living use of artificial pancreas for children with type 1 diabetes: systematic review. Diabetes Mellit. 21 , 206–216 (2018).
Hasan, I., Chowdhury, A. A., Haque, M. I. & Patterson, C. C. Changes in glycated hemoglobin, diabetes knowledge, quality of life, and anxiety in children and adolescents with type 1 diabetes attending summer camps: a systematic review and meta‐analysis. Pediatr. Diabetes 22 , 124–131 (2021).
Knox, E. C., Quirk, H., Glazebrook, C., Randell, T. & Blake, H. Impact of technology-based interventions for children and young people with type 1 diabetes on key diabetes self-management behaviours and prerequisites: a systematic review. BMC Endocr. Disord. 19 , 7 1–4 (2019).
Langendam, M. et al. Continuous glucose monitoring systems for type 1 diabetes mellitus. Cochrane Database Syst. Rev. 1 , CD008101 (2012).
Nørgaard, K., Sukumar, N., Rafnsson, S. B. & Saravanan, P. Efficacy and safety of rapid-acting insulin analogs in special populations with type 1 diabetes or gestational diabetes: systematic review and meta-analysis. Diabetes Ther. 9 , 891–917 (2018).
Schultz, A. T. & Smaldone, A. Components of interventions that improve transitions to adult care for adolescents with type 1 diabetes. J. Adolesc. Health 60 , 133–146 (2017).
Viana, L. V., Gomes, M. B., Zajdenverg, L., Pavin, E. J. & Azevedo, M. J. Brazilian Type 1 Diabetes Study Group (BrazDiab1SG). Interventions to improve patients’ compliance with therapies aimed at lowering glycated hemoglobin (HbA1c) in type 1 diabetes: systematic review and meta-analyses of randomized controlled clinical trials of psychological, telecare, and educational interventions. Trials 17 , 94. 1–2 (2016).
Zhao, X., Huang, H. & Zheng, S. Effectiveness of internet and phone‐based interventions on diabetes management of children and adolescents with type 1 diabetes: a systematic review. Worldviews Evid. Based Nurs. 18 , 217–225 (2021).
Barlow, J., Bennett, C., Midgley, N., Larkin, S. K. & Wei, Y. Parent–infant psychotherapy for improving parental and infant mental health: a systematic review. Campbell Syst. Rev. 6 , 1−223 (2015).
Barlow, J., Bergman, H., Kornør, H., Wei, Y. & Bennett, C. Group-based parent training programmes for improving emotional and behavioural adjustment in young children. Cochrane Database Syst. Rev. 8 , CD003680 (2016).
Bergman, H. et al. Client feedback in psychological therapy for children and adolescents with mental health problems. Cochrane Database Syst. Rev . 8 , CD011729 (2018).
Blake, M. J., Sheeber, L. B., Youssef, G. J., Raniti, M. B. & Allen, N. B. Systematic review and meta-analysis of adolescent cognitive–behavioral sleep interventions. Clin. Child Fam. Psychol. Rev. 20 , 227–249 (2017).
Buchanan-Pascall, S., Gray, K. M., Gordon, M. & Melvin, G. A. Systematic review and meta-analysis of parent group interventions for primary school children aged 4–12 years with externalizing and/or internalizing problems. Child Psychiatry Hum. Dev. 49 , 244–267 (2018).
Caldwell, D. M. et al. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry 6 , 1011–1020 (2019).
Datta, S. S., Daruvala, R. & Kumar, A. Psychological interventions for psychosis in adolescents. Cochrane Database Syst. Rev. 7, CD009533 (2020).
Fisher, C. A., Skocic, S., Rutherford, K. A. & Hetrick, S. E. Family therapy approaches for anorexia nervosa. Cochrane Database Syst. Rev. 10 , CD004780 (2019).
Gan, J., Galer, P., Ma, D., Chen, C. & Xiong, T. The effect of vitamin D supplementation on attention-deficit/hyperactivity disorder: a systematic review and meta-analysis of randomized controlled trials. J. Child Adolesc. Psychopharmacol. 29 , 670–687 (2019).
Hetrick, S. E., Cox, G. R., Witt, K. G., Bir, J. J. & Merry, S. N. Cognitive behavioural therapy (CBT), third-wave CBT and interpersonal therapy (IPT) based interventions for preventing depression in children and adolescents. Cochrane Database Syst. Rev. 8 , CD003380 (2016).
James, A. C., Reardon. T., Soler, A., James, G. & Creswell, C. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst. Rev. 11 , CD013162 (2020).
Jochim, J., Rifkin-Zybutz, R. P., Geddes, J. & Cipriani, A. Valproate for acute mania. Cochrane Database Syst. Rev. 10 , CD004052 (2019).
Kortekaas-Rijlaarsdam, A. F., Luman, M., Sonuga-Barke, E. & Oosterlaan, J. Does methylphenidate improve academic performance? A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 28 , 155–164 (2019).
Krause, M. et al. Efficacy, acceptability, and tolerability of antipsychotics in children and adolescents with schizophrenia: a network meta-analysis. Eur. Neuropsychopharmacol. 28 , 659–674 (2018).
Li, J. et al. Optimal approaches for preventing depressive symptoms in children and adolescents based on the psychosocial interventions: a Bayesian network meta-analysis. J. Affect. Disord. 280 , 364–372 (2021).
Locher, C. et al. Efficacy and safety of selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors, and placebo for common psychiatric disorders among children and adolescents: a systematic review and meta-analysis. JAMA Psychiatry 74 , 1011–1020 (2017).
Loy, J. H., Merry, S. N., Hetrick, S. E. & Stasiak K. Atypical antipsychotics for disruptive behaviour disorders in children and youths. Cochrane Database Syst. Rev. 8 , CD008559 (2017).
Papola, D. et al. Psychological and social interventions for the prevention of mental disorders in people living in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst. Rev. 9 , CD012417 (2020).
Punja S. et al. Amphetamines for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database Syst. Rev. 2 , CD009996 (2016).
Radovic, S., Gordon, M. S. & Melvin, G. A. Should we recommend exercise to adolescents with depressive symptoms? A meta‐analysis. J. Paediatr. Child Health 53 , 214–220 (2017).
Reid, J. E. et al. Cognitive behavioural therapy with exposure and response prevention in the treatment of obsessive–compulsive disorder: a systematic review and meta-analysis of randomised controlled trials. Compr. Psychiatry 106 , 152223 (2021).
Storebø, O. J. et al. Social skills training for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst. Rev. 6 , CD008223 (2019).
Tchanturia, K., Giombini, L., Leppanen, J. & Kinnaird, E. Evidence for cognitive remediation therapy in young people with anorexia nervosa: systematic review and meta‐analysis of the literature. Eur. Eat. Disord. Rev. 25 , 227–236 (2017).
Witt, K. G. et al. Interventions for self-harm in children and adolescents. Cochrane Database Syst. Rev. 3 , CD013667 (2021).
Zang, Y. Impact of physical exercise on children with attention deficit hyperactivity disorders: evidence through a meta-analysis. Medicine 98 , e17980 (2019).
Zhou, X. et al. Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: a systematic review and network meta-analysis. Lancet Psychiatry 7 , 581–601 (2020).
Abboud, M. Vitamin D supplementation and blood pressure in children and adolescents: a systematic review and meta-analysis. Nutrients 12 , 1163 (2020).
Anagnostis, P. et al. Efficacy and safety of statin use in children and adolescents with familial hypercholesterolaemia: a systematic review and meta-analysis of randomized-controlled trials. Endocrine 69 , 249–261 (2020).
Bricarello, L. P. et al. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: a systematic review. Clin. Nutr. ESPEN 28 , 1–11 (2018).
Burrello, J. et al. Pharmacological treatment of arterial hypertension in children and adolescents: a network meta-analysis. Hypertension 72 , 306–313 (2018).
Cilliers, A., Adler, A.J. & Saloojee, H. Anti-inflammatory treatment for carditis in acute rheumatic fever. Cochrane Database Syst. Rev. 5 , CD003176 (2015).
Gartlehner, G. et al. Screening for hypertension in children and adolescents: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 324 , 1884–1895 (2020).
Gomes-Neto, M. et al. Impact of exercise training in aerobic capacity and pulmonary function in children and adolescents after congenital heart disease surgery: a systematic review with meta-analysis. Pediatr. Cardiol. 37 , 217–224 (2016).
Guillem, C. M., Loaiza-Betancur, A. F., Rebullido, T. R., Faigenbaum, A. D. & Chulvi-Medrano, I. The effects of resistance training on blood pressure in preadolescents and adolescents: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 17 , 7900 (2020).
Hauger, H. et al. Effects of vitamin D supplementation on cardiometabolic outcomes in children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Eur. J. Nutr. 59 , 873–884 (2020).
Leyvraz, M. et al. Sodium intake and blood pressure in children and adolescents: a systematic review and meta-analysis of experimental and observational studies. Int. J. Epidemiol. 47 , 1796–1810 (2018).
Mantovani, L. M. & Pugliese, C. Phytosterol supplementation in the treatment of dyslipidemia in children and adolescents: a systematic review. Rev. Paul. Pediatr. 39 , e2019389 (2020).
Meyer, M. et al. Current state of home-based exercise interventions in patients with congenital heart disease: a systematic review. Heart 106 , 333–341 (2020).
Mirkowski, M. et al. Nonpharmacological rehabilitation interventions for motor and cognitive outcomes following pediatric stroke: a systematic review. Eur. J. Pediatr. 178 , 433–454 (2019).
Oosterhoff, M., Joore, M. & Ferreira, I. The effects of school‐based lifestyle interventions on body mass index and blood pressure: a multivariate multilevel meta‐analysis of randomized controlled trials. Obes. Rev. 17 , 1131–1153 (2016).
Pacheco, J. T. et al. Safety and efficacy of recanalization therapy in pediatric stroke: a systematic review and meta-analysis. Eur. J. Paediatr. Neurol. 22 , 1035–1041 (2018).
Pozuelo-Carrascosa, D. P. et al. School-based exercise programs and cardiometabolic risk factors: a meta-analysis. Pediatrics 142 , e20181033 (2018).
Vuorio, A. et al. Statins for children with familial hypercholesterolemia. Cochrane Database Syst. Rev . 11 , CD006401 (2017).
Williams, C. A. et al. Physical activity interventions for people with congenital heart disease. Cochrane Database Syst. Rev. 10 , CD013400 (2020).
Xu, C. et al. Effects of exercise training in postoperative patients with congenital heart disease: a systematic review and meta‐analysis of randomized controlled trials. J. Am. Heart Assoc. 9 , e013516 (2020).
Al-Hosni, K., Chan, M. F. & Al-Azri, M. The effectiveness of interventional cancer education programs for school students aged 8–19 years: a systematic review. J. Cancer Educ. 36 , 229–239 (2021).
Bhardwaj, T. & Koffman, J. Non-pharmacological interventions for management of fatigue among children with cancer: systematic review of existing practices and their effectiveness. BMJ Support. Palliat. Care 7 , 404–414 (2017).
Bukola, I. M. & Paula, D. The effectiveness of distraction as procedural pain management technique in pediatric oncology patients: a meta-analysis and systematic review. J. Pain Symptom Manage. 54 , 589–600 (2017).
Burns, M. A. et al. School and educational support programmes for paediatric oncology patients and survivors: a systematic review of evidence and recommendations for future research and practice. Psychooncology 30 , 431–443 (2021).
Cheng, L. et al. The effect of digital health technologies on managing symptoms across pediatric cancer continuum: a systematic review. Int. J. Nurs. Sci. 8 , 22–29 (2021).
Cheuk, D. K. L., Chiang, A. K. S., Chan, G. C. F. & Ha, S. Y. Urate oxidase for the prevention and treatment of tumour lysis syndrome in children with cancer. Cochrane Database Syst. Rev . 3 , CD006945 (2017).
Cheuk, D. K. L., Sieswerda, E., van Dalen, E. C., Postma, A. & Kremer, L. C. M. Medical interventions for treating anthracycline-induced symptomatic and asymptomatic cardiotoxicity during and after treatment for childhood cancer. Cochrane Database Syst. Rev. 8 , CD008011 (2016).
Cheung, A. T. et al. Physical activity for pediatric cancer survivors: a systematic review of randomized controlled trials. J. Cancer Surviv. 15 , 876−889 (2021).
Cohen, J. E., Wakefield, C. E. & Cohn, R. J. Nutritional interventions for survivors of childhood cancer. Cochrane Database Syst. Rev. 8 , CD009678 (2016).
da Silva Santa, I. N., Schveitzer, M. C., Dos Santos, M. L., Ghelman, R. & Odone Filho, V. Music interventions in pediatric oncology: systematic review and meta-analysis. Complement. Ther. Med. 59 , 102725 (2021).
Daneshdoost, S. M. et al. Bisphosphonate therapy for treating osteonecrosis in pediatric leukemia patients: a systematic review. J. Pediatr. Hematol. Oncol. 43 , e365 (2021).
Hu, X., Fang, Y., Hui, X., Jv, Y. & You, C. Radiotherapy for diffuse brainstem glioma in children and young adults. Cochrane Database Syst. Rev. 6 , CD010439 (2016).
Kelada, L., Wakefield, C. E., Silva, M. C. & Signorelli, C. Camps for children with cancer and their families: a systematic review of psychosocial and physical impacts. J. Dev. Behav. Pediatr. 41 , 145–56 (2020).
Loefen, E. A. H., te Poele, E. M., Tissing, W. J. E., Boezen, H. M. & de Bont, E. S. J. M. Very early discharge versus early discharge versus non-early discharge in children with cancer and febrile neutropenia. Cochrane Database Syst. Rev. 2 , CD008382 (2016).
Lopes-Júnior, L. C. et al. Effectiveness of complementary therapies for the management of symptom clusters in palliative care in pediatric oncology: a systematic review. Rev. Esc. Enferm. USP 55 , 03709 (2021).
Lopez-Rodriguez, M. M., Fernández-Millan, A., Ruiz-Fernández, M. D., Dobarrio-Sanz, I. & Fernández-Medina, I. M. New technologies to improve pain, anxiety and depression in children and adolescents with cancer: a systematic review. Int. J. Environ. Res. Public Health 17 , 3563 (2020).
Michiels, E. M. C., Schouten-Van Meeteren, A. Y. N., Doz, F., Janssens, G. O. & van Dalen, E. C. Chemotherapy for children with medulloblastoma. Cochrane Database Syst. Rev. 1 , CD006678 (2015).
Nunns, M. et al. Effectiveness of nonpharmacological interventions to reduce procedural anxiety in children and adolescents undergoing treatment for cancer: a systematic review and meta‐analysis. Psychooncology 27 , 1889–1899 (2018).
O’Connor, M. & Halkett, G. K. A systematic review of interventions to reduce psychological distress in pediatric patients receiving radiation therapy. Patient Educ. Couns. 102 , 275–283 (2019).
Pelland-Marcotte, M. C., Tole, S., Pechlivanoglou, P. & Brandão, L. R. Effectiveness and safety of primary thromboprophylaxis in children with cancer: a systematic review of the literature and network meta-analysis. Thromb. Haemost. 119 , 2034–2042 (2019).
Phillips, R. S. et al. Antiemetic medication for prevention and treatment of chemotherapy-induced nausea and vomiting in childhood. Cochrane Database Syst. Rev. 2, CD007786 (2016).
Ranmal, R., Prictor, M. & Scott, J. T. Interventions for improving communication with children and adolescents about their cancer. Cochrane Database Syst. Rev. 4 , CD002969 (2008).
Rensen, N. et al. Hypothalamic-pituitary-adrenal (HPA) axis suppression after treatment with glucocorticoid therapy for childhood acute lymphoblastic leukaemia. Cochrane Database Syst. Rev. 11 , CD008727 (2017).
Ryan, D. et al. Interventions to improve the aftercare of survivors of childhood cancer: a systematic review. Pediatr. Hematol. Oncol. J. 3 , 90–98 (2018).
Strzebonska, K. et al. Risk and benefit for targeted therapy agents in pediatric phase II trials in oncology: a systematic review with a meta-analysis. Target. Oncol. 16 , 415–424 (2021).
van As, J. W., van den Berg, H. & van Dalen, E. C. Medical interventions for the prevention of platinum-induced hearing loss in children with cancer. Cochrane Database Syst. Rev. 5 , CD009219 (2019).
van Atteveld, J. E. et al. Vitamin D supplementation for children with cancer: a systematic review and consensus recommendations. Cancer Med. 10 , 4177–4194 (2021).
Ward, E. J., Henry, L. M., Friend, A. J., Wilkins, S. & Phillips, R. S. Nutritional support in children and young people with cancer undergoing chemotherapy. Cochrane Database Syst. Rev. 8 , CD003298 (2015).
Yalçin, B., Kremer, L. C. M., Caron, H. N. & van Dalen, E. C. High-dose chemotherapy and autologous haematopoietic stem cell rescue for children with high-risk neuroblastoma. Cochrane Database Syst. Rev. 8 , CD006301 (2013).
Alquran, A. et al. Smartphone applications for encouraging asthma self-management in adolescents: a systematic review. Int. J. Environ. Res. Public Health 15 , 2403 (2018).
Axelsson, I., Naumburg, E., Prietsch, S. O. M. & Zhang, L. Inhaled corticosteroids in children with persistent asthma: effects of different drugs and delivery devices on growth. Cochrane Database Syst. Rev. 6 , CD010126 (2019).
Berger, W. E. & Meltzer, E. O. Intranasal spray medications for maintenance therapy of allergic rhinitis. Am. J. Rhinol. Allergy 29 , 273–282 (2015).
Cai, K. J., Su, S. Q., Wang, Y. G. & Zeng, Y. M. Dexamethasone versus prednisone or prednisolone for acute pediatric asthma exacerbations in the emergency department: a meta-analysis. Pediatr. Emerg. Care 37 , e1139–e1144 (2021).
Chan, M. et al. Community-based interventions for childhood asthma using comprehensive approaches: a systematic review and meta-analysis. Allergy Asthma Clin. Immunol. 17 , 19. 1–6 (2021).
Chauhan, B. F., Chartrand, C., Chroinin, M. N., Milan, S. J. & Ducharme, F.M. Addition of long‐acting beta 2‐agonists to inhaled corticosteroids for chronic asthma in children. Cochrane Database of Systematic Reviews 11, CD007949 (2015).
Chen, X. et al. Addition to inhaled corticosteroids of leukotriene receptor antagonists versus theophylline for symptomatic asthma: a meta-analysis. J. Thorac. Dis. 7 , 644−652 (2015).
Culmer, N. et al. Telemedical asthma education and health care outcomes for school-age children: a systematic review. J. Allergy Clin. Immunol. Pract. 8 , 1908–1918 (2020).
Das, R. R., Sankar, J. & Kabra, S. K. Role of breathing exercises and yoga/pranayama in childhood asthma: a systematic review. Curr. Pediatr. Rev. 15 , 175–183 (2019).
Day, M., Clarke, S. A., Castillo-Eito, L. & Rowe, R. Psychoeducation for children with chronic conditions: a systematic review and meta-analysis. J. Pediatr. Psychol. 45 , 386–398 (2020).
de Boer, G. M. et al. Bacterial lysate therapy for the prevention of wheezing episodes and asthma exacerbations: a systematic review and meta-analysis. Eur. Respir. Rev. 29 , 190175 (2020).
Drummond, D., Monnier, D., Tesnière, A. & Hadchouel, A. A systematic review of serious games in asthma education. Pediatr. Allergy Immunol. 28 , 257–265 (2017).
Fares, M. M., Alkhaled, L. H., Mroueh, S. M. & Akl, E. A. Vitamin D supplementation in children with asthma: a systematic review and meta-analysis. BMC Res. Notes 8 , 23 (2015).
Feng, B. et al. Efficacy and safety of sublingual immunotherapy for allergic rhinitis in pediatric patients: a meta-analysis of randomized controlled trials. Am. J. Rhinol. Allergy 31 , 27–35 (2017).
Fortescue, R., Kew, K. M., Leung, M. & Leung, M. S. T. Sublingual immunotherapy for asthma. Cochrane Database Syst. Rev. 9 , CD011293 (2020).
Fu, Z., Xu, Y. & Cai, C. Efficacy and safety of omalizumab in children with moderate-to-severe asthma: a meta-analysis. J. Asthma 58 , 1350–1358 (2021).
Hall, K. K., Petsky, H. L., Chang, A. B. & O’Grady, K. F. Caseworker-assigned discharge plans to prevent hospital readmission for acute exacerbations in children with chronic respiratory illness. Cochrane Database Syst. Rev. 11 , CD012315 (2018).
Harris, K. et al. School-based self-management interventions for asthma in children and adolescents: a mixed methods systematic review. Cochrane Database Syst. Rev. 1 , CD011651 (2019).
Isik, E., Fredland, N. M. & Freysteinson, W. M. School and community-based nurse-led asthma interventions for school-aged children and their parents: a systematic literature review. J. Pediatr. Nurs. 44 , 107–114 (2019).
Janjua, S., Schmidt, S., Ferrer, M. & Cates, C. J. Inhaled steroids with and without regular formoterol for asthma: serious adverse events. Cochrane Database Syst. Rev. 9 , CD006924 (2019).
Kelly, C. et al. Macrolide antibiotics for bronchiectasis. Cochrane Database Syst. Rev. 3 , CD012406 (2018).
Kew, K. M., Carr, R. & Crossingham, I. Lay-led and peer support interventions for adolescents with asthma. Cochrane Database Syst. Rev. 4 , CD012331 (2017).
Kew, K. M. & Cates, C. J. Home telemonitoring and remote feedback between clinic visits for asthma. Cochrane Database Syst. Rev. 8 , CD011714 (2016).
Kew, K. M., Malik, P., Aniruddhan, K. & Normansell, R. Shared decision-making for people with asthma. Cochrane Database Syst. Rev. 10 , CD012330 (2017).
Kew, K. M., Quinn, M., Quon, B. S., & Ducharme, F. M. Increased versus stable doses of inhaled corticosteroids for exacerbations of chronic asthma in adults and children. Cochrane Database Syst. Rev. 6 , CD007524 (2016).
Khattiyawittayakun, L., Seresirikachorn, K., Chitsuthipakorn, W., Kanjanawasee, D. & Snidvongs, K. Effects of double‐dose intranasal corticosteroid for allergic rhinitis: a systematic review and meta‐analysis. Int. Forum Allergy Rhinol. 9 , 72–78 (2019).
Leung, J. S. et al. A systematic review of adverse drug events associated with administration of common asthma medications in children. PLoS ONE 12 , e0182738 (2017).
Li, C. Y. & Liu, Z. Effect of budesonide on hospitalization rates among children with acute asthma attending paediatric emergency department: a systematic review and meta-analysis. World J. Pediatr. 17 , 152–163 (2021).
Lin, J., Zhang, Y., He, C. & Dai, J. Probiotics supplementation in children with asthma: a systematic review and meta‐analysis. J. Paediatr. Child Health 54 , 953–961 (2018).
McCallum, G. B., Morris, P. S., Brown, N. & Chang, A. B. Culture-specific programs for children and adults from minority groups who have asthma. Cochrane Database Syst. Rev . 8 , CD006580 (2017).
Murphy, K. R. & Chipps, B. E. Tiotropium in children and adolescents with asthma. Ann. Allergy Asthma Immunol. 124 , 267–276 (2020).
Payares‐Salamanca, L. et al. Metered‐dose inhalers versus nebulization for the delivery of albuterol for acute exacerbations of wheezing or asthma in children: a systematic review with meta‐analysis. Pediatr. Pulmonol. 55 , 3268–3278 (2020).
Pike, K. C., Akhbari, M., Kneale, D. & Harris, K. M. Interventions for autumn exacerbations of asthma in children. Cochrane Database Syst. Rev . 3 , CD012393 (2018).
Pincheira, M. A., Bacharier, L. B. & Castro-Rodriguez, J. A. Efficacy of macrolides on acute asthma or wheezing exacerbations in children with recurrent wheezing: a systematic review and meta-analysis. Pediatr. Drugs 22 , 217–228 (2020).
Ramachandran, H. J., Jiang, Y., Shan, C. H., San Tam, W. W. & Wang, W. A systematic review and meta-analysis on the effectiveness of swimming on lung function and asthma control in children with asthma. Int. J. Nurs. Stud. 120 , 103953 (2021).
Sauni, R. et al. Remediating buildings damaged by dampness and mould for preventing or reducing respiratory tract symptoms, infections and asthma. Evid. Based Child Health. Cochrane Rev. J. 8 , 944–1000 (2013).
Su, Z., Li, R. & Gai, Z. Intravenous and nebulized magnesium sulfate for treating acute asthma in children: a systematic review and meta-analysis. Pediatr. Emerg. Care 34 , 390–395 (2018).
Velentza, L., Maridaki, Z., Blana, E. & Miligkos, M. Antihistamines in the management of pediatric allergic rhinitis: a systematic review. Pediatr. Drugs 22 , 673–683 (2020).
Wang, Y. et al. Role of nasal saline irrigation in the treatment of allergic rhinitis in children and adults: a systematic analysis. Allergol. Immunopathol. 48 , 360–367 (2020).
Article CAS Google Scholar
Zhang, W., Wang, Q., Liu, L., Yang, W. & Liu, H. Effects of physical therapy on lung function in children with asthma: a systematic review and meta-analysis. Pediatr. Res. 89 , 1343–1351 (2021).
Daniels, S. R. Complications of obesity in children and adolescents. Int. J. Obes. 33 , S60–S65 (2009).
Han, J. C., Lawlor, D. A. & Kimm, S. Y. Childhood obesity. Lancet 375 , 1737–1748 (2010).
Weiss, R. & Lustig, R. H. in Pediatric Endocrinology (ed M. Sperling) 956–1014.e1011 (Elsevier, 2014).
Bukhman, G. et al. The Lancet NCDI Poverty Commission: bridging a gap in universal health coverage for the poorest billion. Lancet 396 , 991–1044 (2020).
Sheffler, J. L., Stanley, I. & Sachs-Ericsson, N. in: Adverse Childhood Experiences (eds Asmundson, G. J. G. & Afifi, T. O.) Ch. 4, 47–69 (Academic Press, 2020).
Ramaswamy, S., Seshadri, S. & Bunders-Aelen, J. Shifting landscapes of global child mental health: imperatives for transdisciplinary approaches. Asian J. Psychiatry 69 , 103002 (2022).
Mosca, S. et al. Dyslipidemia diagnosis and treatment: risk stratification in children and adolescents. J. Nutr. Metab. 2022 , 4782344 (2022).
Asadi-Lari, M., Ahmadi Teymourlouy, A., Maleki, M. & Afshari, M. Opportunities and challenges of global health diplomacy for prevention and control of noncommunicable diseases: a systematic review. BMC Health Serv. Res. 21 , 1193 (2021).
Jailobaeva, K. et al. An analysis of policy and funding priorities of global actors regarding noncommunicable disease in low- and middle-income countries. Global. Health 17 , 68 (2021).
The WHO–UNICEF–Lancet Commissioners After COVID-19, a future for the world’s children? Lancet 396 , 298–300 (2020).
One Year Into Covid: Prioritizing Education Recovery to Avoid a Generational Catastrophe (UNESCO, 2021); https://en.unesco.org/news/one-year-covid-prioritizing-education-recovery-avoid-generationalcatastrophe
Whitehead, M., Taylor-Robinson, D. & Barr, B. Poverty, health, and Covid-19. BMJ 372 , n376 (2021).
Browne, N. T. et al. When pandemics collide: the impact of COVID-19 on childhood obesity. J. Pediatr. Nurs. 56 , 90 (2021).
Mak, I. L. et al. The spill-over impact of the novel coronavirus-19 pandemic on medical care and disease outcomes in non-communicable diseases: a narrative review. Public Health Rev. 43 , 1604121 (2022).
Luijten, M. A. et al. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. Qual. Life Res. 30 , 2795–2804 (2021).
Scull, T. M., Kupersmidt, J. B. & Weatherholt, T. N. The effectiveness of online, family‐based media literacy education for substance abuse prevention in elementary school children: Study of the Media Detective Family program. J. Community Psychol. 45 , 796–809 (2017).
Khatib, M. N. et al. A systematic review on effect of electronic media among children and adolescents on substance abuse. Indian J. Community Med. 43 , S66-S72 (2018).
Bala, M. M., Strzeszynski, L., & Topor-Madry, R. Mass media interventions for smoking cessation in adults. Cochrane Database Syst. Rev. 11, CD004704 (2017).
Weissberg-Benchell, J., Wolpert, H. & Anderson, B. J. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care 30 , 2441–2446 (2007).
Laing, S. P., Jones, M. E., Swerdlow, A. J., Burden, A. C. & Gatling, W. Psychosocial and socioeconomic risk factors for premature death in young people with type 1 diabetes. Diabetes Care 28 , 1618–1623 (2005).
Lotstein, D. S. et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics 131 , e1062–e10670 (2013).
Chater, N. & Loewenstein, G. The i-frame and the s-frame: how focusing on individual-level solutions has led behavioral public policy astray. Behav. Brain Sci. 46, e147 1–84 (2022).
Lamptey, P., Dirks, R., Torpey, K. & Mastro, T. Discussion Paper on How to Promote the Inclusion of the Prevention and Control of Noncommunicable Diseases within Other Programmatic Areas WHO GCM/NCD Working Group (WHO, 2016).
Covidence Systematic Review Software (Veritas Health Innovation); (2023). www.covidence.org
Thomas, J., Brunton, J. & Graziosi, S. (2010) EPPI Reviewer 4.0: software for research synthesis. EPPI Centre Software (Social Science Research Unit, Institute of Education, Univ. London) (2010).
Download references
Acknowledgements
This paper represents independent research funded by the NCD Child Secretariat. NCD Child is supported through grants to the Hospital for Sick Children, Toronto, from the AstraZeneca Young Health Programme and Friends of Cancer Patients (Z.A.B., L.L.-W.). The Hospital for Sick Children, Toronto, also provides in-kind contributions to support the NCD Child Secretariat. We would also like to acknowledge A. R. Rahman from the Institute for Global Health and Development, Aga Khan University Hospital, for his assistance with the graphs and maps for the paper.
Author information
Authors and affiliations.
The Daffodil Centre, The University of Sydney, a joint venture with Cancer Council NSW, Sydney, New South Wales, Australia
Rehana A. Salam
Institute for Global Health and Development, Aga Khan University Hospital, Karachi, Pakistan
Maryam Hameed Khan, Syed Saqlain Ali Meerza & Jai K. Das
Centre for Global Child Health, The Hospital for Sick Children (SickKids), Toronto, Ontario, Canada
Laura Lewis-Watts & Zulfiqar A. Bhutta
You can also search for this author in PubMed Google Scholar
Contributions
Z.A.B. conceptualized the study, assembled the writing team and assigned tasks. R.A.S. and J.K.D. oversaw the methods and training for study identification and data extraction. Screening and coding of studies were carried out by M.H.K., S.S.A. and R.A.S. L.L.-W. gave technical support and conceptual advice. All the authors contributed to the drafting of the paper, maps and figures. The paper was reviewed by all authors, with further editing and revision support.
Corresponding author
Correspondence to Zulfiqar A. Bhutta .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Medicine thanks Christian Loret de Mola and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Jennifer Sargent, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended data fig. 1 publications over time..
Graph depicting number of publications overtime showing that the majority of included studies were published from 2010 to 2020 with a noticeable increase in publications overtime.
Extended Data Fig. 2 Delivery platforms.
Graph depicting various delivery platforms utilized in the included studies to deliver interventions for risk factors and non-communicable diseases.
Extended Data Fig. 3 Outcomes evaluated.
Graph showing distribution of the included studies across broad categories of outcomes reported.
Extended Data Fig. 4 Evidence summary for obesity.
Figure summarizing the existing evidence on interventions for obesity.
Extended Data Fig. 5 Evidence summary for substance abuse.
Figure summarizing the existing evidence on interventions for substance abuse.
Extended Data Fig. 6 Evidence summary for diabetes.
Figure summarizing the existing evidence on interventions for diabetes.
Extended Data Fig. 7 Evidence summary for mental health conditions.
Figure summarizing the existing evidence on interventions for mental health conditions.
Extended Data Fig. 8 Evidence summary for cardiovascular diseases.
Figure summarizing the existing evidence on interventions for cardiovascular diseases.
Extended Data Fig. 9 Evidence summary for cancers.
Figure summarizing the existing evidence on interventions for cancers.
Extended Data Fig. 10 Evidence summary for chronic respiratory diseases.
Figure summarizing the existing evidence on interventions for chronic respiratory diseases.
Supplementary information
Supplementary information.
Supplementary Tables 1–9 and Supplementary Appendix.
Reporting Summary
Source data, source data fig. 2.
Statistical source data for the global map depicting the distribution of primary studies.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Salam, R.A., Khan, M.H., Meerza, S.S.A. et al. An evidence gap map of interventions for noncommunicable diseases and risk factors among children and adolescents. Nat Med 30 , 290–301 (2024). https://doi.org/10.1038/s41591-023-02737-2
Download citation
Received : 03 February 2023
Accepted : 27 November 2023
Published : 09 January 2024
Issue Date : January 2024
DOI : https://doi.org/10.1038/s41591-023-02737-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Loading metrics
Open Access
Peer-reviewed
Research Article
Implementation research on noncommunicable disease prevention and control interventions in low- and middle-income countries: A systematic review
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Global Health and Population, Harvard TH Chan School of Public Health, Boston, Massachusetts, United States of America
Roles Data curation, Writing – review & editing
Affiliation School of Population and Public Health, University of British Columbia, Vancouver, British Columbia, Canada
Affiliation School of Public Health, University of Illinois Chicago, Chicago, Illinois, United States of America
Roles Conceptualization, Investigation, Methodology, Writing – review & editing
Affiliation Alliance for Health Policy and Systems Research, WHO, Geneva, Switzerland
Roles Conceptualization, Investigation, Methodology
Affiliation Department of NCD, WHO, Geneva, Switzerland
Affiliations The George Institute for Global Health, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia, School of Public Health, Harbin Medical University, Harbin, China
Affiliation The George Institute for Global Health, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Roles Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing
- Celestin Hategeka,
- Prince Adu,
- Allissa Desloge,
- Robert Marten,
- Ruitai Shao,
- Maoyi Tian,
- Ting Wei,
- Margaret E. Kruk

- Published: July 25, 2022
- https://doi.org/10.1371/journal.pmed.1004055
- Peer Review
- Reader Comments
While the evidence for the clinical effectiveness of most noncommunicable disease (NCD) prevention and treatment interventions is well established, care delivery models and means of scaling these up in a variety of resource-constrained health systems are not. The objective of this review was to synthesize evidence on the current state of implementation research on priority NCD prevention and control interventions provided by health systems in low- and middle-income countries (LMICs).
Methods and findings
On January 20, 2021, we searched MEDLINE and EMBASE databases from 1990 through 2020 to identify implementation research studies that focused on the World Health Organization (WHO) priority NCD prevention and control interventions targeting cardiovascular disease, cancer, diabetes, and chronic respiratory disease and provided within health systems in LMICs. Any empirical and peer-reviewed studies that focused on these interventions and reported implementation outcomes were eligible for inclusion. Given the focus on this review and the heterogeneity in aims and methodologies of included studies, risk of bias assessment to understand how effect size may have been compromised by bias is not applicable. We instead commented on the distribution of research designs and discussed about stronger/weaker designs. We synthesized extracted data using descriptive statistics and following the review protocol registered in PROSPERO (CRD42021252969). Of 9,683 potential studies and 7,419 unique records screened for inclusion, 222 eligible studies evaluated 265 priority NCD prevention and control interventions implemented in 62 countries (6% in low-income countries and 90% in middle-income countries). The number of studies published has been increasing over time. Nearly 40% of all the studies were on cervical cancer. With regards to intervention type, screening accounted for 49%, treatment for 39%, while prevention for 12% (with 80% of the latter focusing on prevention of the NCD behavior risk factors). Feasibility (38%) was the most studied implementation outcome followed by adoption (23%); few studies addressed sustainability. The implementation strategies were not specified well enough. Most studies used quantitative methods (86%). The weakest study design, preexperimental, and the strongest study design, experimental, were respectively employed in 25% and 24% of included studies. Approximately 72% of studies reported funding, with international funding being the predominant source. The majority of studies were proof of concept or pilot (88%) and targeted the micro level of health system (79%). Less than 5% of studies report using implementation research framework.
Conclusions
Despite growth in implementation research on NCDs in LMICs, we found major gaps in the science. Future studies should prioritize implementation at scale, target higher levels health systems (meso and macro levels), and test sustainability of NCD programs. They should employ designs with stronger internal validity, be more conceptually driven, and use mixed methods to understand mechanisms. To maximize impact of the research under limited resources, adding implementation science outcomes to effectiveness research and regional collaborations are promising.
Author summary
Why was the study done.
- While the evidence for the clinical effectiveness of most noncommunicable disease (NCD) prevention and treatment interventions is well established, care delivery models and means of scaling these up to entire populations in need in heterogeneous and resource-constrained health systems are not.
- Implementation research on NCD program delivery can illuminate what does and does not work in preventing NCDs or achieving NCD control. This can promote faster, more efficient, and more effective scale-up of life-saving and health-preserving health system strategies.
- Evidence needed on the current state of implementation research on World Health Organization (WHO) priority NCD prevention and control interventions to help inform research priority.
What did the researchers do and find?
- We performed a systematic review search in MEDLINE and EMBASE databases from 1990 through 2020 to identify implementation research studies that focused on the WHO priority NCD prevention and control interventions targeting cardiovascular disease, cancer, diabetes, and chronic respiratory disease and provided within health systems in low- and middle-income countries (LMICs).
- We identified 222 eligible studies that evaluated 265 priority NCD prevention and control interventions implemented in 62 countries (6% in low-income countries and 90% in middle-income countries). The number of studies published has been increasing over time. The majority of interventions were focused on either screening (49%) or treatment (39%), while prevention accounted for only 12%.
- Reviewed studies emphasized a few health areas, such as cervical cancer, with many other high-burden conditions little researched. The majority of studies were proof of concept or pilot, quantitative using weaker study designs and targeted the micro level of health system.
What do these findings mean?
- While implementation research on priority NCDs has grown substantially, from under 10 studies per year in early 2000s to 51 studies in 2020, this is still vastly incommensurate with the health burden of NCDs.
- Future studies should prioritize implementation at scale, target higher levels health systems (meso and macro levels), and test sustainability of NCD programs. They should employ designs with stronger internal validity, be more conceptually driven, and use mixed methods to understand mechanisms.
- To maximize impact of the research under limited resources, adding implementation science outcomes to effectiveness research and regional collaborations are promising.
Citation: Hategeka C, Adu P, Desloge A, Marten R, Shao R, Tian M, et al. (2022) Implementation research on noncommunicable disease prevention and control interventions in low- and middle-income countries: A systematic review. PLoS Med 19(7): e1004055. https://doi.org/10.1371/journal.pmed.1004055
Academic Editor: Elvin Hsing Geng, Washington University in St Louis School of Medicine, UNITED STATES
Received: December 8, 2021; Accepted: June 21, 2022; Published: July 25, 2022
Copyright: © 2022 Hategeka et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its supporting information files.
Funding: The Alliance for Policy and Health Systems Research and The World Health Organization funded the study. CH received support through a Banting Postdoctoral Fellowship from the Canadian Institutes of Health Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: I have read the journal’s policy and the authors of this manuscript have the following competing interests: CH, PA and MEK report personal fees from the funders, during the conduct of the study. MEK is an Academic Editor on PLOS Medicine’s editorial board. RM and RS are employed by the study funders.
Abbreviation: COVID-19, Coronavirus Disease 2019; LIC, low-income country; LMIC, low- and middle-income country; NCD, noncommunicable disease; SDG, Sustainable Development Goal; UMIC, upper middle-income country
Introduction
Noncommunicable diseases (NCDs) have become the leading contributors to morbidity and mortality worldwide. They are now responsible for 74% of all global deaths, 77% of which occur in low- and middle-income countries (LMICs) [ 1 , 2 ]. Approximately 85% of NCD deaths among people aged 30 and 69 years occur in LMICs [ 1 ]. Cardiovascular diseases are the leading causes of NCD mortality, followed by cancers, respiratory diseases, and diabetes [ 1 ]. Together, these 4 NCDs are responsible of over 80% of all premature NCD deaths [ 1 ]. Risk factors such as tobacco and alcohol use, physical inactivity, and unhealthy diets result in significantly greater risk of dying from NCDs. Primary, secondary, and tertiary prevention strategies are vital in addressing NCD burden [ 1 ]. Sustainable Development Goal (SDG) target 3.4 commits countries to reduce premature mortality from NCDs by a third by 2030 relative to 2015 levels. Recent analysis shows that no LMIC is on track to meet this target for both men and women if they maintain their 2010 to 2016 average rates of decline [ 3 ].
NCD prevention and control should not be regarded as a vertical issue separated from other health conditions. The ongoing Coronavirus Disease 2019 (COVID-19) pandemic has put a spotlight on NCDs, as these increased the risk of death for people with COVID infection. Similarly, NCDs increase mortality risk among people with other infectious diseases such as tuberculosis and HIV. It further highlighted the economic and social inequities in who is afflicted with NCDs, in both high-income countries and LMICs. While primary prevention relies on public health, taxation, and other public policy measures, mitigating the health consequences of NCDs also requires strong health systems. Health systems that recognize this challenge and address modifiable risk factors and prioritize the management of NCDs will be better positioned to promote and maintain health. Data from the 2019 World Health Organization (WHO) NCD Country Capacity surveys reveal that only half of 160 countries have national guidelines for NCDs, half have the 6 essential technologies for early detection, diagnosis, and monitoring of NCDs available in primary care facilities of the public health sector, and 20% of countries have 6 (or fewer) of the 11 essential medicines available [ 4 ]. Greater prioritization of NCDs within health systems and high-quality care are essential to achieving SDG 3.4 [ 3 ]. Beyond this lies an important agenda for tackling the cumulatively large group of rarer NCDs that afflict the world’s poorest people [ 5 ].
To support countries in crafting effective NCD strategies, the WHO Assembly endorsed the Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020 (GAP-NCD) in May 2013 together with a set of evidence-based interventions (best-buys) and policy options in its appendix 3 that was updated in 2016 and provides 84 interventions or policy options [ 6 , 7 ]. Furthermore, WHO has developed a compendium including all available health interventions. The list and compendium aim to assist Member States, as appropriate in specific national contexts, in implementing measures to achieve the 9 global voluntary targets for NCDs and Target 3.4 of the SDGs. Despite recent calls for a new commitment to implementation research for NCDs, a mid-point evaluation of the WHO NCD Global Action Plan 2013–2030 (NCD-GAP) found that “research has been the weakest NCD-GAP objective in terms of implementation and that progress in implementing research linked to the NCD-GAP has been slow and incremental” [ 8 , 9 ].
While the evidence for the clinical effectiveness of most NCD prevention and treatment interventions is well established, care delivery models and means of scaling these up to entire populations in need in heterogeneous and resource-constrained health systems are not. Implementation research on NCD program delivery, including cost effectiveness in various regions, can illuminate what does and does not work in achieving NCD control [ 8 , 10 – 12 ]. This can promote faster, more efficient, and more effective scale-up of life-saving and health-preserving health system strategies [ 13 , 14 ]. In this systematic review, we aim to synthesize evidence on the current state of implementation research on WHO priority NCD prevention and control interventions provided within health systems in LMICs [ 6 , 7 , 15 – 17 ].
This systematic review was conducted according to a study protocol registered in PROSPERO (#CRD42021252969) [ 18 ].
Search strategy
Following the Systematic Reviews and Meta-Analyses (PRISMA) checklist [ 19 ], we searched for implementation research studies that focused on relevant NCD prevention and control interventions (Table A in S1 Appendix ) provided within health systems in LMICs and were published in peer-reviewed journals indexed in MEDLINE and EMBASE databases from 1990 to 2020. The databases were last searched on January 20, 2021. Our search terms included medical subject heading (MeSH) terms and/or key words for 4 key themes (implementation research; NCDs; NCD interventions; LMICs) that were adjusted for each database:
- Implementation research (e.g., implementation research, implementation science, diffusion of innovations, implementation strategies, dissemination science, implementation outcomes).
- NCDs (e.g., cardiovascular disease, cancer, diabetes, chronic respiratory disease).
- Interventions (e.g., smoking cessation, management of hypertension, treatment of acute myocardial infarction, cervical and colorectal cancer screening).
- LMICs as defined by the World Bank in 2019 (Table C in S1 Appendix ).
Language restrictions were not applied. Full details of the search strategy are provided in Table B in S1 Appendix .
Inclusion and exclusion criteria
Table 1 summarizes our review’s specific eligibility criteria. This review includes peer-reviewed, empirical quantitative, qualitative, and mixed method study designs conducted in LMICs that described the implementation of relevant NCD preventive and/or control interventions provided within health systems. Using the updated Appendix 3 of the WHO Global NCD Action Plan 2013–2020, we identified the WHO priority NCD prevention and control interventions [ 6 ]. Of these interventions, we selected those that are specifically provided by health systems. This was achieved through discussions and consensus. Table 2 summarizes the intervention categories across eligible NCD risk factors (i.e., tobacco and alcohol use, physical inactivity, and unhealthy diets) and NCDs (i.e., cardiovascular disease, diabetes, cancer, and chronic respiratory disease), and full details are provided in Table A in S1 Appendix . While our search in databases was not restricted to any language, during study screening/review processes, we only retained eligible studies that were in 6 official languages of the United Nations (i.e., Arabic, Chinese, English, French, Russian, and Spanish). We drew on Proctor and colleagues and Glasgow and colleagues to define implementation outcomes eligible for inclusion [ 20 , 21 ]. Nonempirical/primary research studies are not eligible for inclusion ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1004055.t001
https://doi.org/10.1371/journal.pmed.1004055.t002
Data extraction and analysis
The titles and abstracts of unique results from the databases were reviewed independently by 2 researchers for potential inclusion using COVIDENCE review software [ 22 ]. The full texts of studies retained at the title and abstract screening stage were retrieved and independently assessed for inclusion. Any discrepancies were resolved through discussion and consensus. Data extraction on each included study was conducted by a single researcher using a data extraction tool, developed and piloted a priori (Table D in S1 Appendix ). Data elements included study characteristics (e.g., publication year, country of implementation, study funding), NCD conditions (risk factors and disease), intervention details (e.g., type of intervention, level of health system), methods (e.g., research approach, study design), implementation outcomes (e.g., fidelity, feasibility), and equity lens (e.g., disaggregated by key SES stratifiers, targeted vulnerable population). We also extracted data on implementation strategies including actor (i.e., who delivered the intervention), action target, and recipients; details of other implementation strategies were not sufficiently described to permit extraction [ 23 ]. The recipients of the action/strategy were further aggregated by demographic subgroup (e.g., people eligible for cancer screening including cervical and colorectal), disease risk subgroup (e.g., patients with myocardial infarction, patients with diabetes or hypertension, people who smoke), general population, healthcare workers (e.g., physicians, nurses, pharmacists, and midwives), and community health workers. We synthesize extracted data using descriptive statistics and following the review protocol registered in PROSPERO. Specifically, we provide an overview of NCD priority intervention implementation study characteristics across NCD conditions to shed light on the current state of implementation research of priority NCD prevention and control interventions in LMICs. Given this review does not focus on effect size of NCD interventions, we did not perform a meta-analysis.
Risk of bias assessment
This review focuses on implementation of multiple interventions across various NCDs, rather than effectiveness of any single set of interventions. Further, studies with heterogenous aims and methodologies (including qualitative methodology) were included. Therefore, risk of bias assessment to understand how effect size may have been compromised by bias is not applicable in this review. We instead commented on the distribution of research designs and discussed about stronger/weaker designs.
Our search strategy implemented in MEDLINE and EMBASE identified 9,683 publications, of which 7,419 unique records were screened for inclusion. Abstract and full-text screening identified 222 studies that met our inclusion criteria (Tables 1 and 2 ) [ 24 – 245 ]. A summary of this process is presented in the PRISMA flow diagram in Fig 1 .
Intervention refers to studies excluded because they studied the implementation of interventions that did not meet the eligible criteria. Study design refers to studies excluded because they used study designs that did not meet eligibility criteria (e.g., nonempirical studies including reviews and commentaries). Outcomes refer to studies excluded based on not having focused on relevant implementation outcomes. Settings refer to studies excluded because they were not conducted in LMICs. Full text means that studies were excluded because full text was not available. Time refers to studies that were excluded because they were published before/conducted before 1990.
https://doi.org/10.1371/journal.pmed.1004055.g001
The 222 studies included in this review evaluated 265 priority NCD prevention and control interventions implemented in 62 countries, of which 6% were in low-income countries (LICs), 45% in LMICs, and 46% in upper middle-income countries (UMICs) ( Table 3 and Figs 2 , 3 , and 4A and Table E in S1 Appendix ). The NCD conditions targeted varied by income groups of countries (Fig A in S1 Appendix ). Eight of the included studies were multicountry studies. The number of studies published has been increasing over time ( Fig 5A ). Overall, the majority of interventions were focused on either screening (49%) or treatment (39%), while prevention accounted for only 12%, with nearly 80% of these tackling prevention of the shared NCD behavioral risk factors—tobacco use, unhealthy diet, physical inactivity, and harmful use of alcohol. The NCD interventions varied by conditions and type (prevention, screening, and treatment) (Figs 2, B, and C in S1 Appendix ). Notably, over one-third of the interventions studied (37%) were for cervical cancer ( Fig 2 ), which accounts for 0.35% of DALYs lost and 0.5% of deaths globally, with similar figures for LMICs ( https://vizhub.healthdata.org/gbd-compare/ ). Diabetes was the focus of nearly one-quarter of the research with hypertension the topic of another 9% ( Fig 2 ). Each of the other recommended interventions represented 5% or less of the implementation research output. Chronic respiratory disease was understudied relative to its prevalence: less than 1% of the studies examined chronic respiratory disease treatment and only 3% smoking cessation programs. The intervention focus appears to vary by income groups of countries (Fig D in S1 Appendix ). Feasibility was the most studied implementation outcome followed by adoption ( Fig 6 ). Most of the actors were researchers, which accounted for 58%; whereas government/ministry of health, providers, and NGOs accounted for 18%, 10%, and 6%, respectively. The majority of intervention targeted improvement in health outcomes (45%) followed by change in behavior (34%).
https://doi.org/10.1371/journal.pmed.1004055.g002
We used country population size in 2020 ( https://data.worldbank.org/indicator/SP.POP.TOTL ) to standardized estimates expressed as number of studies per 1 million population. We used “rworldmap” package ( https://cran.r-project.org/web/packages/rworldmap/rworldmap.pdf ) available in R software to present these standardized estimates across countries where interventions were implemented. Country borders in this package are derived from Natural Earth data. Table E in S1 Appendix shows number of included studies per country.
https://doi.org/10.1371/journal.pmed.1004055.g003
https://doi.org/10.1371/journal.pmed.1004055.g004
Growth of research over time (A) and distributions of NCD interventions by type (B). Fig 5A shows number of studies published each year ( N = 222 studies); Fig 5B shows distributions by type of interventions ( N = 265 NCD interventions evaluated in studied included in the review).
https://doi.org/10.1371/journal.pmed.1004055.g005
https://doi.org/10.1371/journal.pmed.1004055.g006
https://doi.org/10.1371/journal.pmed.1004055.t003
Most studies used quantitative methods, which accounted for 86%, whereas mixed methods and qualitative methods accounted for 9% and 5%, respectively ( Table 2 ). The majority of studies used observational designs, with cross-sectional designs used in 45 studies. Among evaluations, preexperimental studies (such as pre-post without a comparison group or post-only) was the most frequently employed ( n = 56 or 25% of all studies); experimental designs were used in a quarter of studies ( n = 53 or 24% of all studies); quasi-experimental evaluation designs (such as pre-post comparison group or time series) were used in 15 papers (7% of all studies) ( Fig 7 ). Study designs also appear to vary by NCD conditions targeted (Fig E in S1 Appendix ). The sample size among included studies varied, ranging from 11 to 350,581, with median of 658. Most studies were standalone implementation studies (85%), with some variations by NCD conditions (Fig F in S1 Appendix ). Hybrid implementation and effectiveness studies accounted only for 15%. Less than 5% of studies reported they were guided by widely known implementation science framework. Majority of studies were proof of concept or pilot versus scale-up studies (88% versus 12%), with variations by NCD conditions (Fig G in S1 Appendix ). The level of health system targeted most often was micro level, accounting for 79% of studies, with variations by NCD conditions. The meso and macro levels of health systems were targeted by 14% and 7% of studies, respectively (Fig H in S1 Appendix ). Approximately 42% of studies employed an equity lens—i.e., studies disaggregated by SES stratifiers (e.g., age, sex, education, income, and rural versus urban) and/or targeted vulnerable population.
https://doi.org/10.1371/journal.pmed.1004055.g007
A majority of studies (72%) reported funding, with international funding being the predominant source ( Fig 4B ). There seems to be some variations by NCD conditions (Figs I–K in S1 Appendix ). For example, while 78% of studies focused on cervical cancer reported funding, of which 77% were from international sources, those focused on colorectal cancer and treatment of acute myocardial infarction received most of their funding from the countries where implementation research was conducted (Fig K in S1 Appendix ). Majority of reported funding was provided by government/universities (43.6%), 35% reported multiple funders, 16% were foundations/NGOs, and 6% were private funders (e.g., pharmaceutical companies, professional associations) (Fig L in S1 Appendix ). Approximately 62% of corresponding authors were from the country of implementation ( Fig 4C ); however, this varied by funding sources, with studies funded by international funders having the highest number of international corresponding authors.
We conducted a systematic review of implementation research studies on NCD prevention and control strategies in LMICs published between 1990 and 2020. We focused our analysis on WHO-recommended NCD interventions carried out by the health system rather than through policy, legislation, or public health approaches [ 6 , 7 ]. These studies therefore represent the state of the implementation science in prevention and control of NCDs by health systems in the countries bearing the bulk of disease burden from noncommunicable conditions.
Of the 222 implementation science studies included in this review, 94% were conducted in middle-income countries (evenly split between lower- and upper-middle) and 6% in LICs. UMICs were slightly overrepresented compared to their share of the LMIC population (approximately 40%). Only 8 of the studies were multicountry studies, suggesting that cross-national generalizability is not the primary motivation for this type of research. India and China, with 43% of the population of LMICs, comprised one-third of the studies. South Africa, Brazil, Iran, Kenya, and Nigeria, were well represented, each contributing more than 3% of the research.
The studies described 265 different NCD interventions, ranging from screening to prevention to treatment and palliation. Conditions studied varied substantially by region. All 13 of the interventions studied in LICs were for cervical cancer screening. In low-middle income countries, cervical cancer accounted for 37%, diabetes for 29%, and hypertension for 8% of interventions. There was a larger variety of conditions studied in UMICs: while cervical cancer and diabetes comprised half the studies, hypertension, myocardial infarction, colorectal cancer, other cardiovascular diseases, and unhealthy diet each comprised more than 5% of studies. The 2 countries with the largest research output and populations, China and India, differed substantially in focus. In India over 70% of studies were on 2 conditions: diabetes (51%) and cervical cancer (19%), whereas the research was more evenly distributed across the NCDs in China.
Half of all studied interventions in this review evaluated screening for disease, nearly 40% treatment and 12% prevention. Over 70% of all screening studies were for cervical cancer, with less research on other conditions for which screening can be cost effective, such as diabetes, colorectal cancer, and breast cancer. Primary and secondary prevention can reduce incidence of disease and forestall disease progression and disability. We found that only 31 (12%) of the studied interventions addressed prevention with nearly 80% of these tackling prevention of the NCD behavior risk factors (e.g., tobacco use, inactivity, unhealthy diet). Less than 10% of the interventions evaluated in this review focused on management of hypertension (the leading metabolic risk factor worldwide, accounting for approximately 19% of global deaths) [ 246 ]. This suggests a substantial implementation research gap in secondary prevention, a critical function of primary care and other levels of health systems. Primary care services such as hypertension management and glucose control play a major role in reducing mortality, thus insufficient research on their optimal implementation is a major missed opportunity. Recent work shows that treatment and control rates for hypertension were below 25% and 10%, respectively, in many countries in South Asia and sub-Saharan Africa. These countries also showed the slowest rates of improvement from 1990 [ 247 ].
The preponderance of interventions studied was in pilot phase, with fewer than 15% studying large-scale implementation. Along the same lines, feasibility and adoption were the most studied implementation outcomes, suggesting the research is focused on introduction of new approaches. While proof of concept studies is vital with new implementation strategies, arguably WHO-proposed interventions are well established and evidence on (clinical) effectiveness abound. To provide useful guidance to health system planners and realize population health gains, there needs to be a greater investment in large-scale NCD implementation research to promote sustainability of evidence-based interventions. To best scale scarce research resources and accelerate impact, countries could join regional consortia to study interventions and undertake factorial designs that compare locally adapted implementation approaches.
Over three-quarters of the studies were situated at the micro level of the health system—targeting patient, provider, or clinic levels. Nearly 1 in 5 tested a new technology, despite evidence that technology adoption without substantial integration into policies, data, and workflows is typically ineffective in transforming care [ 248 , 249 ]. Education was another common target featuring in 3 of 10 studies; researchers accounted for the majority of the actors. While micro-level approaches are the most “researchable,” as they are easiest to implement and analyze; positive results are difficult to scale and sustain in the absence of systemic health system change. The Lancet Commission on High Quality Health Systems notes that high-quality care results from structures that align system aims and policies with strong governance, management, and appropriately trained workforce [ 250 ]. In this context, micro-level innovation cannot raise quality system wide and is only effective if undertaken as part of a learning health system that can determine whether it offers sufficient benefit over current practice in complexity, cost, and health benefit, and if so, how to best integrate into the health system [ 251 ].
Nearly 9 in 10 studies were stand-alone implementation research. This also points to an opportunity to add implementation research to ongoing effectiveness trials. Integrated or hybrid effectiveness-implementation studies are increasingly being used in high-income countries to shed light on both the outcome and extent and quality of service/program delivery [ 252 ]. Notably, fewer than 5% of studies cited use of an implementation science framework consistent with prior research showing that the use of implementation science framework is substantially lower in LMICs compared with high-income countries [ 253 ]. The use of a tested conceptual framework can improve the rigor of the research and promote comparability of results. Of the studies that reported a funding source, 60% was from international sources, 33% from the country of the research, and the remaining from both local and international sources. This reflects the low spending for health research and especially for health systems and implementation research in LMICs. The lack of domestic support is unlikely to be offset by global funding going forward; a recent analysis showed that NCDs were under prioritized in bilateral agency portfolios relative to their health impacts [ 254 ]. Over 40% of development assistance for health in LICs for NCDs came from NGOs and philanthropies, which are less inclined to support research than operations [ 254 ]. Indeed, we found that only 16% of studies with funding information reviewed were supported by philanthropies or NGOs, while the other remaining studies reported funding sources from government, private, and/or multiple sources.
Scarcity of funding for research is a key constraint to needed implementation research for NCDs. While there are proposals for coordinating and increasing global support, it is unrealistic to expect this to meet the scale of needed research without a substantial increase in countries’ investment in research [ 255 ]. Such an investment is likely to pay off in better health and higher quality, more efficient service delivery [ 256 ]. To make best use of research funds, implementation science should strive to be as generalizable as possible—at minimum at a regional level where health systems share similarities. International and regional institutions can play an important role in supporting research consortia and partnerships to promote efficiency of and accelerate the pace of research and, ultimately its uptake into routine care at scale.
Over 50 of the 222 included studies used an experimental research design. While this is the strongest design to yield causal inference, it is not always feasible to implement. Quasi-experimental designs, such as pretest, posttest comparison group designs, and interrupted time series, which can offer robust information were used in only 15 studies. Preexperimental designs that do not include a comparison group or tracking over time, comprised nearly a quarter of the studies. These designs have very low internal validity and should generally be avoided. The remainder of the studies used cross-sectional descriptions, cohort studies, and qualitative research or multiple study types. Given the disproportionate health harms of NCDs among the poor and other vulnerable groups within countries, disaggregated or stratified analysis is crucial. Forty percent of the assessed studies included stratification by age, sex, education, or urbanicity. Going forward, greater use of quasi-experimental designs, hybrid implementation studies and mixed methods approaches, would benefit the field. An expanded focus on equity of implementation outcomes is also needed.
Strengths and limitations
Our study had several strengths, notably the extensive scope for the search that covered LMICs, a wide range of outcomes and study types, and a large contingent of conditions and health services. We had no language restrictions permitting a comprehensive assessment of the published literature. The review also had several limitations. We focused on WHO-recommended interventions, which at present do not include guidance for some prevalent conditions such as mental health problems and kidney disease [ 6 , 12 ]. Mental health is a major contributor to the global burden of disease and future work should assess the implementation science for the growing range of mental health interventions that appear to be effective in lower-income settings [ 257 , 258 ]. The studies we assessed used differing definitions of implementation outcomes (e.g., acceptability was measured in some studies by self-report and in others by behavior change). This limits direct comparison of study outcomes. Greater use of implementation science frameworks can promote coherence in the research approaches and terminology used to the benefit of end users. Similarly, given the implementation strategies were not specified well enough in the included studies, we elected to focus on actors, action target, and recipients in our description of implementation strategies. Clearly, reporting empirical implementation studies using existing framework to describe implementation strategies would help bolster uptake of implementation research in NCDs.
We also did not search the gray literature and as such, some relevant studies may have been missed. However, studies in gray literature that were not peer reviewed would have not have been eligible for inclusion in this review. Despite using rigorous search strategies without language restrictions, studies published in journals not indexed in MEDLINE and EMBASE were not captured [ 259 – 263 ]. Given the focus on this review and the heterogeneity in aims and methodologies of included studies, risk of bias assessment to understand how effect size may have been compromised by bias is not applicable. As such, we only commented on the distribution of research designs and discussed about stronger/weaker designs. Lastly, we reported year of publication and not time of when study/implementation was conducted.
High-quality implementation science can play a key role in informing effective delivery of health system interventions to mitigate the burden of NCDs and avoiding expensive mistakes. While implementation research on priority NCDs has grown substantially, from under 10 studies per year in early 2000s to 51 studies in 2020, this is still vastly incommensurate with the health importance of the topic. Further, the concentration of studies in a few geographies and a few health areas, such as cervical cancer, highlights the dearth of research for other key conditions. We found a major gap in research on secondary prevention, i.e., management of risk factors or early disease to prevent disease progression and premature death. Research on ways in which health systems can be strengthened, including primary care levels, to provide optimal care for NCDs is critically needed. Future studies should use implementation science frameworks, and, when testing interventions, strong research designs with strong internal validity, including well-designed quasi-experimental studies. Opportunities exist for adding implementation science studies to planned effectiveness research.
Supporting information
S1 prisma checklist. prisma 2020 checklist..
https://doi.org/10.1371/journal.pmed.1004055.s001
S1 Appendix. Appendix tables and figures.
Table A in S1 Appendix. Interventions provided within health systems. Table B in S1 Appendix. Sample of the search strategy used in the MEDLINE database. Table C in S1 Appendix. List of low- and middle-income countries. Table D in S1 Appendix. Data extraction tool. Table E in S1 Appendix. Distribution of studies by countries where they were implemented. Fig A in S1 Appendix. Variation of conditions evaluated by income group. Fig B in S1 Appendix. Priority NCD interventions ( n = 265) identified in 222 studies included in the review. Fig C in S1 Appendix. Distribution of included studies by NCD. Fig D in S1 Appendix. Distribution of intervention type by income group. Fig E in S1 Appendix. Distributions by research designs. Fig F in S1 Appendix. Distributions by standalone implementation studies vs. embedded or hybrid effectiveness-implementation studies. Fig G in S1 Appendix. Distributions by pilot vs. scale-up project. Fig H in S1 Appendix. Variation by level of health system. Fig I in S1 Appendix. Studies that reported funding (vs. those that did not) by NCD conditions. Fig J in S1 Appendix. Distributions by funding type. Fig K in S1 Appendix. Distribution of funding sources by NCDs and their risk factors. Fig L in S1 Appendix. Types of reported funding sources ( N = 222 included studies).
https://doi.org/10.1371/journal.pmed.1004055.s002
- View Article
- Google Scholar
- PubMed/NCBI
- 18. Systematic Review of NCD Implementation Research in Low- and Middle-Income Countries. [Internet]. PROSPERO 2021. [cited 2021 Oct 2]. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021252969 .
- 22. Veritas Health Innovation. Covidence systematic review software. 2020 [cited 2021 Nov 5]. Available from: https://get.covidence.org/systematic-review?campaignid=11343712044&adgroupid=114130876511&gclid=Cj0KCQjwtrSLBhCLARIsACh6RmjH6RwcJalTVCaL76kpSCeqErC2sP8uX4Vj8wZYdEQWQxdXWVwD0eMaAsz1EALw_wcB .
- 264. Beard P, Greenall J, Hoffman C, Nettleton S, Popescu I, Ste-Marie M. Incident Analysis Collaborating Parties. Canadian Incident Analysis Framework. Edmonton, AB: Canadian Patient Safety Institute; 2012.
- Utility Menu
- Join Our Team
- Mailing List
Non Communicable Diseases
Sylvia Kehlenbrink, James Smith, Eimhin Ansbro, Daniela C Fuhr, Anson Cheung, and Ruwan Ratnayake . 8/1/2019. “ The burden of diabetes and use of diabetes care in humanitarian crises in low-income and middle-income countries .” The Lancet, 7, 8, Pp. 638-647. Abstract Human suffering as a result of natural disasters or conflict includes death and disability from non-communicable diseases, including diabetes, which have largely been neglected in humanitarian crises. The objectives of this Series paper were to examine the evidence on the burden of diabetes, use of health services, and access to care for people with diabetes among populations affected by humanitarian crises in low-income and middle-income countries, and to identify research gaps for future studies. We reviewed the scientific literature on this topic published between 1992 and 2018. The results emphasise that the burden of diabetes in humanitarian settings is not being captured, clinical guidance is insufficient, and diabetes is not being adequately addressed. Crisis-affected populations with diabetes face enormous constraints accessing care, mainly because of high medical costs. Further research is needed to characterise the epidemiology of diabetes in humanitarian settings and to develop simplified, cost-effective models of care to improve the delivery of diabetes care during humanitarian crises.
Philippa Boulle, Sylvia Kehlenbrink, James Smith, David Beran, and Kiran Jobanputra . 3/13/2019. “ Challenges associated with providing diabetes care in humanitarian settings .” The Lancet, 7, 8, Pp. 648-656. Publisher's Version Abstract The humanitarian health landscape is gradually changing, partly as a result of the shift in global epidemiological trends and the rise of non-communicable diseases, including diabetes. Humanitarian actors are progressively incorporating care for diabetes into emergency medical response, but challenges abound. This Series paper discusses contemporary practical challenges associated with diabetes care in humanitarian contexts in low-income and middle-income countries, using the six building blocks of health systems described by WHO (information and research, service delivery, health workforce, medical products and technologies, governance, and financing) as a framework. Challenges include the scarcity of evidence on the management of diabetes and clinical guidelines adapted to humanitarian contexts; unavailability of core indicators for surveillance and monitoring systems; and restricted access to the medicines and diagnostics necessary for adequate clinical care. Policy and system frameworks do not routinely include diabetes and little funding is allocated for diabetes care in humanitarian crises. Humanitarian organisations are increasingly gaining experience delivering diabetes care, and interagency collaboration to coordinate, improve data collection, and analyse available programmes is in progress. However, the needs around all six WHO health system building blocks are immense, and much work needs to be done to improve diabetes care for crisis-affected populations.
Sylvia Kehlenbrink and Lindsay M Jaacks . 6/6/2019. “ Diabetes in humanitarian crises: the Boston Declaration .” The Lancet, 7, 8. Publisher's Version Abstract Nearly three out of every four deaths worldwide in 2017 were caused by non-communicable diseases (NCDs). Many countries have made progress reducing risk factors for NCDs such as tobacco use, hyperlipidaemia, and hypertension, but no countries have successfully reversed the increasing trends in diabetes prevalence and mortality from diabetes. This situation represents a massive global health failure, since type 2 diabetes is largely preventable with lifestyle modification and cost-effective treatments exist for both type 2 and type 1 diabetes. Type 1 diabetes is of particular concern, since it is fatal in the absence of insulin treatment.

Sylvia Kehlenbrink, MD
Sylvia Kehlenbrink is an Endocrinologist and Director of Global Endocrinology at Brigham and Women’s Hospital, Part-time Instructor at Harvard Medical...
- Humanitarian Negotiation Strategies (23)
- Evaluation and Implementation Science (24)
- Transitional Justice (12)
- Education in Crisis (1)
- Children in Crisis (2)
- Infectious Diseases and Epidemics Program (2)
- Peace and Human Rights Data (25)
- Program on Resilient Communities (37)
- Gender, Rights and Resilience (30)
- Emergency Health Systems (10)
- Humanitarian Action and the Environment (3)
- Non Communicable Diseases (4)
- Urbanization and Resilience (20)
- Global Childhood Cancer (1)
- Front Line Indigenous Partnership (1)
- Ohiyesa Premedical Program (1)
- DataPop (2)
- KoBoToolbox (2)
- Humanitarian Geoanalytics (8)
- Signal Program (27)
- HHI Scholars at Risk (2)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Unmet Medical Needs in Chronic, Non-communicable Inflammatory Skin Diseases
Affiliations.
- 1 Department of Dermatology, Faculty of Medicine and Graduate School of Medicine, Hokkaido University, Sapporo, Japan.
- 2 Department of Dermatology, Tufts Medical Center, Boston, MA, United States.
- 3 Department of Dermatology, Venereology and Allergology, University Medical Center Göttingen, Göttingen, Germany.
- 4 Lower Saxony Institute of Occupational Dermatology, University Medical Center Göttingen, Göttingen, Germany.
- 5 Center for Chronic Pruritus, Department of Dermatology, University Hospital Muenster, Muenster, Germany.
- 6 Department of Dermatology, University of Lübeck, Lübeck, Germany.
- 7 Institute for Allergology, Charité-Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany.
- 8 Fraunhofer Institute for Translational Medicine and Pharmacology (ITMP), Allergology and Immunology, Berlin, Germany.
- 9 Institute and Comprehensive Center for Inflammation Medicine, University of Lübeck, Lübeck, Germany.
- 10 Lübeck Institute of Experimental Dermatology and Center for Research on Inflammation of the Skin, University of Lübeck, Lübeck, Germany.
- 11 Division of Dermatology, Rush University Medical Center, Chicago, IL, United States.
- 12 Department of Internal Medicine, Rush University Medical Center, Chicago, IL, United States.
- 13 Department of Dermatology and Allergology, Philipps-Universität, Marburg, Germany.
- 14 Department of Rheumatology and Clinical Immunology, University of Lübeck, Lübeck, Germany.
- 15 Department of Dermatology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States.
- 16 Corporal Michael J. Crescenz Veterans Affairs Medical Center, Philadelphia, PA, United States.
- 17 Department of Dermatology, Columbia University Medical Center, New York, NY, United States.
- 18 Psoriasis Research and Treatment Centre, Charité-Universitätsmedizin Berlin, Berlin, Germany.
- 19 Interdisciplinary Group Molecular Immunopathology, Dermatology/Medical Immunology, Charité-Universitätsmedizin Berlin, Berlin, Germany.
- 20 Azrieli Faculty of Medicine, Bar-Ilan University, Safed, Israel.
- PMID: 35755063
- PMCID: PMC9218547
- DOI: 10.3389/fmed.2022.875492
An estimated 20-25% of the population is affected by chronic, non-communicable inflammatory skin diseases. Chronic skin inflammation has many causes. Among the most frequent chronic inflammatory skin diseases are atopic dermatitis, psoriasis, urticaria, lichen planus, and hidradenitis suppurativa, driven by a complex interplay of genetics and environmental factors. Autoimmunity is another important cause of chronic skin inflammation. The autoimmune response may be mainly T cell driven, such as in alopecia areata or vitiligo, or B cell driven in chronic spontaneous urticaria, pemphigus and pemphigoid diseases. Rare causes of chronic skin inflammation are autoinflammatory diseases, or rheumatic diseases, such as cutaneous lupus erythematosus or dermatomyositis. Whilst we have seen a significant improvement in diagnosis and treatment, several challenges remain. Especially for rarer causes of chronic skin inflammation, early diagnosis is often missed because of low awareness and lack of diagnostics. Systemic immunosuppression is the treatment of choice for almost all of these diseases. Adverse events due to immunosuppression, insufficient therapeutic responses and relapses remain a challenge. For atopic dermatitis and psoriasis, a broad spectrum of innovative treatments has been developed. However, treatment responses cannot be predicted so far. Hence, development of (bio)markers allowing selection of specific medications for individual patients is needed. Given the encouraging developments during the past years, we envision that many of these challenges in the diagnosis and treatment of chronic inflammatory skin diseases will be thoroughly addressed in the future.
Keywords: alopecia areata; atopic dermatitis; chronic spontaneous urticaria; hidradenitis suppurativa; inflammation; medical need; psoriasis; skin.
Copyright © 2022 Ujiie, Rosmarin, Schön, Ständer, Boch, Metz, Maurer, Thaci, Schmidt, Cole, Amber, Didona, Hertl, Recke, Graßhoff, Hackel, Schumann, Riemekasten, Bieber, Sprow, Dan, Zillikens, Sezin, Christiano, Wolk, Sabat, Kridin, Werth and Ludwig.
PubMed Disclaimer
Conflict of interest statement
HU has received research grants from JB, Otsuka, Taiho, Boehringer Ingelheim, Kyowa Kirin, Kaken, Sun Pharma, Shionogi, Teijin, Mitsubishi Tanabe, Nihon Zoki, Eisai, Torii and Tokiwa, consultant fees from Ono, Nihon-Pharmaceutical, Sun Pharma, argenx and Ishin Pharma, and speaker's fees from Nihon-Pharmaceutical, Maruho, Eli Lilly, Abbie, Eisai, Sanofi, Janssen, Kyowa Kirin, Ono, UCB, Novartis, Sun Pharma, Torii, Taiho, Mitsubishi Tanabe, and Boehringer Ingelheim during the last 3 years, DR has received honoraria or research support from AbbVie, Abcuro, AltruBio, Amgen, Boehringer-Ingelheim, Bristol Meyers Squibb, Celgene, Concert, CSL Behring, Dermavant, Dermira, Galdrema, Incyte, Janssen, Kyowa Kirin, Lilly, Merck, Novartis, Pfizer, Regeneron, Sanofi, Sun Pharmaceuticals, UCB, and VielaBio during the last 3 years, MS has received consulting/speakers' fees, or grant support from AbbVie, Almirall, Amgen, Biogen, BMS, Janssen, Novartis, and UCB during the last 3 years, SS has received funding and personal fees from Celldex, Clexio, Dermasence, Galderma, GSK, Kiniksa, Menlo, Trevi, Novartis, Sanofi (investigator all), Abbvie, Almirall, Beiersdorf, Bellus Health, Benevolent, Bionorica, Cara, Celgene, CelloHealth, Clexio, DS Biopharma, Eli Lilly, Escient, Galderma, Grünenthal, Kiniksa, Klinge Pharma, Menlo, Sanofi, Sienna, Trevi, P.G. Unna Academy, Perrigo, Pfizer, Vanda, Vifor, WebMD (Consultancy/Advisory board) and Almirall, Eli Lilly, Sanofi, Galderma, Menlo, Omnicuris, Beiersdorf, Leo Pharma, Novartis, P. G. Unna Academy, Pfizer, Pierre Fabre (speaker) during the last 3 years, MMe has received honoraria as a speaker and/or consultant for Amgen, Aralez, argenx, Bayer, Beiersdorf, Celgene, Escient, Galderma, GSK, Menlo, Moxie, Novartis, Pharvaris, Pfizer, Roche, Sanofi, Siennabio, and Uriach, MMa was a speaker and/or advisor for and/or has received research funding from Allakos, Amgen, Aralez, ArgenX, AstraZeneca, Celldex, Centogene, CSL Behring, FAES, Genentech, GIInnovation, Innate Pharma, Kyowa Kirin, Leo Pharma, Lilly, Menarini, Moxie, Novartis, Roche, Sanofi/Regeneron, Third HarmonicBio, UCB, and Uriach during the last 3 years, is a consultant, advisory board member, and/or investigator for AbbVie, Almirall, Amgen, Beiersdorf, BMS, Boehringer Ingelheim, Eli Lilly, Galapagos, Janssen-Cilag, LEO Pharma, MorphoSys, Novartis, Pfizer, Regeneron Pharmaceuticals, Inc., Samsung, Sandoz, Sanofi, Sun Pharma, and UCB, ES has received research grants from UCB, Incyte, Biotest, ArgenX, Dompe, Fresenius Medical Care, Bayer, AstraZenca, and Euroimmun and honoraria from Biotest, Thermo Fisher, ArgenX, Fresenius Medical care, Topas, Leo, Chugai, AstraZenca, and Almirall during the last 3 years, MH has received honoraria from Novartis, Sanofi, Celgene, and unrestricted grants from Biotest, Janssen Cilag and Topas durimg the last 3 years, KBi has received research funds from ArgenX during the last 3 years, DZ has received support for research and development work, lecturing and consulting from Euroimmun AG, UCB Pharma, ArgenX, Biotest, Abbvie, Janssen, Sanofi in the last 3 years, KW has received research grants, travel grants, consulting honoraria or lecturer's honoraria from Amgen, Bristol Myers Squibb, Celgene, Charité Research Organization, Flexopharm, Janssen-Cilag, Novartis Pharma, Sanofi-Aventis, and Trial Form Support during the last 3 years, RS has received research grants or honoraria for participation in advisory boards, clinical trials, or as speaker for one or more of the following: AbbVie, Amgen, Bayer, Boehringer Ingelheim Pharma, Bristol Myers Squibb, Celgene, Charité Research Organization, CSL Behring, Dr. Willmar Schwabe, Flexopharm, Incyte, Janssen-Cilag, La Roche-Posay Laboratoire Dermatologique, Novartis Pharma, Parexel International, Sanofi–Aventis, TFS, and UCB Biopharma during the last 3 years, VW has received grants from Celgene, Amgen, Janssen, Biogen, Gilead, Viela; Horizon therapeutics, Pfizer, Corbus, CSL Behring, consulted Astra-Zeneca, Pfizer, Biogen, Celgene, Resolve, Janssen, Gilead, Lilly, BMS, Nektar, Abbvie, Viela, GSK, EMD Serona, Sanofi, Anaptysbio, Amgen, Merck, Pfizer, Janssen, Neovacs, Idera, Octapharma, CSL Behring, Corbus, Novartis, Romefor during the last 3 years, RL has received honoraria for speaking or consulting or has obtained research grants from Novartis, Lilly, Bayer, Dompe, Synthon, Argen-X, and Incyte during the last 3 years. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Clinical images of patients with…
Clinical images of patients with chronic skin inflammatory diseases. (A) Blurry erythema and…
Similar articles
- Aberrant inflammasome activation as a driving force of human autoimmune skin disease. Fetter T, de Graaf DM, Claus I, Wenzel J. Fetter T, et al. Front Immunol. 2023 May 30;14:1190388. doi: 10.3389/fimmu.2023.1190388. eCollection 2023. Front Immunol. 2023. PMID: 37325658 Free PMC article. Review.
- Epigenetic Dysregulation in Autoimmune and Inflammatory Skin Diseases. Gibson F, Hanly A, Grbic N, Grunberg N, Wu M, Collard M, Alani RM. Gibson F, et al. Clin Rev Allergy Immunol. 2022 Dec;63(3):447-471. doi: 10.1007/s12016-022-08956-8. Epub 2022 Nov 8. Clin Rev Allergy Immunol. 2022. PMID: 36346551 Review.
- Multimorbidity and mortality risk in hospitalized adults with chronic inflammatory skin disease in the United States. Narla S, Silverberg JI. Narla S, et al. Arch Dermatol Res. 2020 Sep;312(7):507-512. doi: 10.1007/s00403-020-02043-8. Epub 2020 Feb 11. Arch Dermatol Res. 2020. PMID: 32047999
- Comorbidities in Dermatology: What's Real and What's Not. Qureshi A, Friedman A. Qureshi A, et al. Dermatol Clin. 2019 Jan;37(1):65-71. doi: 10.1016/j.det.2018.07.007. Epub 2018 Nov 1. Dermatol Clin. 2019. PMID: 30466689 Review.
- Dissecting susceptibility from exogenous triggers: the model of alopecia areata and associated inflammatory skin diseases. Garzorz N, Alsisi M, Todorova A, Atenhan A, Thomas J, Lauffer F, Ring J, Schmidt-Weber C, Biedermann T, Eyerich S, Eyerich K. Garzorz N, et al. J Eur Acad Dermatol Venereol. 2015 Dec;29(12):2429-35. doi: 10.1111/jdv.13325. Epub 2015 Sep 28. J Eur Acad Dermatol Venereol. 2015. PMID: 26416203
- Inhibition of interferon gamma impairs induction of experimental epidermolysis bullosa acquisita. Gross N, Marketon J, Mousavi S, Kalies K, Ludwig RJ, Bieber K. Gross N, et al. Front Immunol. 2024 May 10;15:1343299. doi: 10.3389/fimmu.2024.1343299. eCollection 2024. Front Immunol. 2024. PMID: 38799441 Free PMC article.
- Improving systemic therapy selection for inflammatory skin diseases: A clinical need survey. Brownstone ND, Farberg AS, Litchman GH, Quick AP, Siegel JJ, Hurton LV, Goldberg MS, Lio PA. Brownstone ND, et al. JAAD Int. 2024 Apr 6;16:49-56. doi: 10.1016/j.jdin.2024.03.019. eCollection 2024 Sep. JAAD Int. 2024. PMID: 38774343 Free PMC article.
- Incorporating Dermatologic Clinical Research Into Private Practice: A Review. Slater KN, Fivenson D. Slater KN, et al. Cureus. 2024 Apr 6;16(4):e57733. doi: 10.7759/cureus.57733. eCollection 2024 Apr. Cureus. 2024. PMID: 38711732 Free PMC article. Review.
- Patient-reported assessment of medical care for chronic inflammatory skin diseases: an enterprise-based survey. Wolk K, Schielein M, Maul JT, Widmayer F, Wanke K, Fischmann W, Nathan P, Sabat R. Wolk K, et al. Front Med (Lausanne). 2024 Apr 18;11:1384055. doi: 10.3389/fmed.2024.1384055. eCollection 2024. Front Med (Lausanne). 2024. PMID: 38698787 Free PMC article.
- Blood MALT1 expression could help predict treatment outcomes in psoriasis patients, especially in those receiving biologics. Liu Q, Zhang Y, Xu B, Jin X, Yang T, Fan L. Liu Q, et al. Immun Inflamm Dis. 2024 Apr;12(4):e1235. doi: 10.1002/iid3.1235. Immun Inflamm Dis. 2024. PMID: 38578002 Free PMC article.
- Schmidt T, Solimani F, Pollmann R, Stein R, Schmidt A, Stulberg I, et al. . TH1/TH17 cell recognition of desmoglein 3 and bullous pemphigoid antigen 180 in patients with lichen planus. J Allergy Clin Immunol. (2018) 142:669–72.e7. 10.1016/j.jaci.2018.02.044 - DOI - PubMed
- Arakawa A, Siewert K, Stöhr J, Besgen P, Kim SM, Rühl G, et al. . Melanocyte antigen triggers autoimmunity in human psoriasis. J Exp Med. (2015) 212:2203–12. 10.1084/jem.20151093 - DOI - PMC - PubMed
- Christophers E, van de Kerkhof PCM. Severity, heterogeneity and systemic inflammation in psoriasis. J Eur Acad Dermatol Venereol. (2019) 33:643–7. 10.1111/jdv.15339 - DOI - PubMed
- Meijer JM, Lamberts A, Luijendijk HJ, Diercks GFH, Pas HH, Zuidema SU, et al. . Prevalence of pemphigoid as a potentially unrecognized cause of pruritus in nursing home residents. JAMA Dermatol. (2019) 155:1423–4. 10.1001/jamadermatol.2019.3308 - DOI - PMC - PubMed
- Eyerich K, Eyerich S. Immune response patterns in non-communicable inflammatory skin diseases. J Eur Acad Dermatol Venereol. (2018) 32:692–703. 10.1111/jdv.14673 - DOI - PMC - PubMed

Publication types
- Search in MeSH
Related information
Grants and funding.
- P30 AR069632/AR/NIAMS NIH HHS/United States
- P50 AR070588/AR/NIAMS NIH HHS/United States
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Frontiers Media SA
- PubMed Central
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
REVIEW article
Management and prevention strategies for non-communicable diseases (ncds) and their risk factors.

- 1 Panevezys Faculty of Technology and Business, Kaunas Technology University (KTU), Panevezys, Lithuania
- 2 Department of Biochemistry, Faculty of Science, King Abdulaziz University (KAU), Jeddah, Saudi Arabia
- 3 Division of Protein Science, Kungliga Tekniska Högskolan Royal Institute of Technology, Stockholm, Sweden
- 4 Department of Medical Laboratory Science, Charmo University, Chamchamal, Iraq
- 5 Procomcure Biotech, GmbH, Thalgau, Austria
- 6 Prosthetics, Biomechanics and Biomaterial Research, Paracelsus Medical University Salzburg, Salzburg, Austria
- 7 Bioprospecting Departament, Baltic Institute of Advanced Technology, Vilnius, Lithuania
- 8 Faculty of Medicine, Ludwig Maximilian University of Munich (LMU), Munich, Germany
Non-communicable diseases (NCDs) are of increasing concern for society and national governments, as well as globally due to their high mortality rate. The main risk factors of NCDs can be classified into the categories of self-management, genetic factors, environmental factors, factors of medical conditions, and socio-demographic factors. The main focus is on the elements of self-management and to reach a consensus about the influence of food on risk management and actions toward the prevention of NCDs at all stages of life. Nutrition interventions are essential in managing the risk of NCDs. As they are of the utmost importance, this review highlights NCDs and their risk factors and outlines several common prevention strategies. We foresee that the best prevention management strategy will include individual (lifestyle management), societal (awareness management), national (health policy decisions), and global (health strategy) elements, with target actions, such as multi-sectoral partnership, knowledge and information management, and innovations. The most effective preventative strategy is the one that leads to changes in lifestyle with respect to diet, physical activities, cessation of smoking, and the control of metabolic disorders.
Introduction
Non-communicable diseases (NCDs), also known as chronic diseases, are medical conditions that are associated with long durations and slow progress ( Figure 1 ). Most NCDs are non-infectious and are the result of several factors, including genetic, physiological, behavioral, and environmental factors ( 1 ). According to the World Health Organization (WHO), NCDs are the leading cause of death worldwide, responsible for 71% of the total number of deaths each year. The top four killers among NCDs with the highest number of deaths are cardiovascular diseases (17.9 million deaths annually), cancers (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million) ( Figure 1 ) ( 1 ). However, the term of NCDs has been extended to cover a wide range of health problems, such as hepatic, renal, and gastroenterological diseases, endocrine, hematological, and neurological disorders, dermatological conditions, genetic disorders, trauma, mental disorders, and disabilities (e.g., blindness and deafness) ( 2 ). The main risk factors contributing to NCDs involve unhealthy diets, physical inactivity, tobacco use, and alcohol misuse. Hence, most of these diseases are preventable as they eventually progress in early life due to lifestyle aspects ( 3 ). There is an increasing concern that poor diet has increased the potential risk, causing chronic diseases, and nutrition problems in the public health sector ( 4 ). Historically, many NCDs have been directly linked to economic growth and were called “diseases of the rich.” Now, the burden of NCDs in developing countries has increased. Further, mortality in low and middle-income countries has doubled the burden of NCDs. The growing interest in population well-being and economic growth, based on Gross National Happiness (GNH), has recently attracted more attention. The epidemic of NCDs hinders the progress of GNH because good health is necessary in order to achieve happiness ( 5 ). Bhutan's experience suggests that strategic opportunities to minimize NCDs and to promote population well-being can be taken advantage of by joining the health sector with other sectors at the individual and organizational levels ( 5 ).
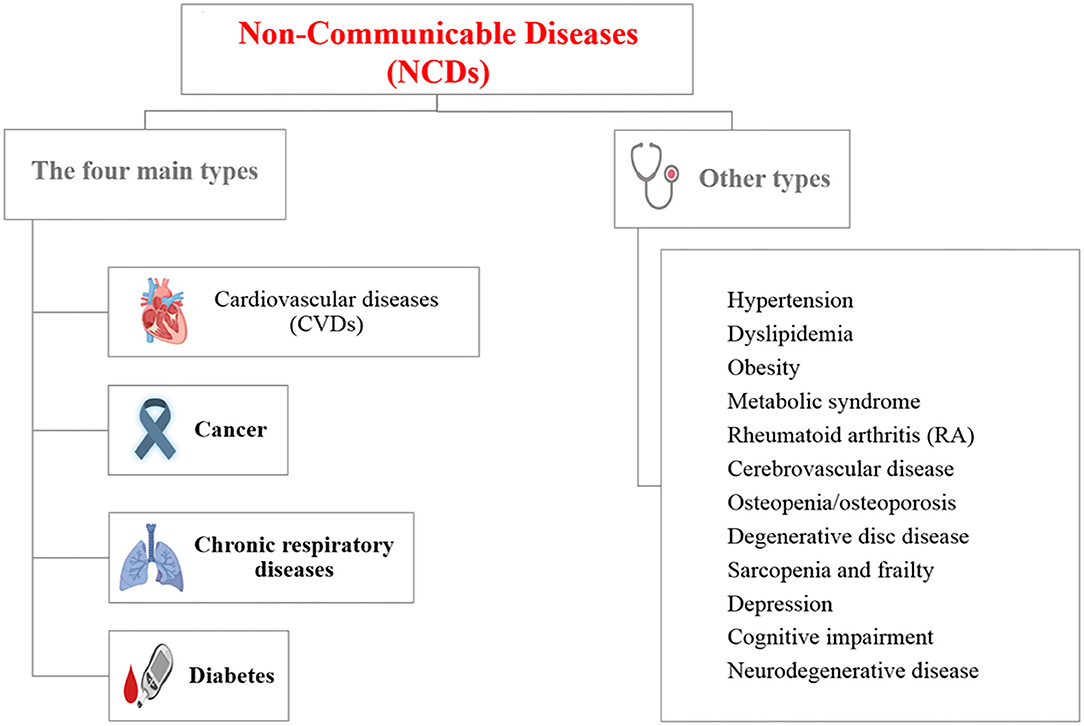
Figure 1 . List of non-communicable diseases (NCDs) [Created with BioRender].
Health and well-being are the primary goals of society in regards to food choice ( 6 ). Researchers have pointed out that the core of the health-conscious lifestyle is directed toward a wellness-oriented lifestyle ( 5 ) and the behavior of people determines their health status ( 7 ). Nutritionists have been reported to be associated with many chronic diseases, but designed studies exploring the association between diet, nutrition, and NCDs are rare ( 8 ). Thus, lifestyle modifications and interventions to reduce the risk of NCDs is the priority in the primary prevention of diseases. Hence, finding answers to the following questions can significantly contribute to a better and healthier society:
• What are NCDs and their risk factors?
• What are the most used interventions in managing the risk of NCDs?
• What are the contemporary prevention strategies for NCDs?
The current review focuses on the answers to the previous questions and highlights several strategic models in the contemporary management of NCDs.
Key Risk Factors of NCDs
Several factors can increase the amount of opportunities to develop NCDs and can be classified in different ways. In one approach, risk factors are classified as modifiable or non-modifiable factors that can have changeable or non-changeable conditions, respectively. The modifiable risk factors involve high blood pressure, smoking, diabetes mellitus, physical inactivity, obesity, and high blood cholesterol, while the non-modifiable risk factors involve age, gender, genetic factors, race, and ethnicity ( 9 – 12 ). Interestingly, although age and gender are non-modifiable factors, most of their associated factors are modifiable. Figure 2 represents a model to classify the risk factors of NCDs. The non-modifiable factors can also be classified into three classes: (i) biological factors, such as being overweight, dyslipidemia, hyper-insulinaemia, and hypertension; (ii) behavioral factors, such as diet, lack physical activity, tobacco smoking, and alcohol consumption; and (iii) societal factors, which involve complex combinations of interacting socioeconomic, cultural and environmental parameters ( 13 ). In the next section, examples of the identified risk factors for NCDs, including age, diet, and economic context, are highlighted.
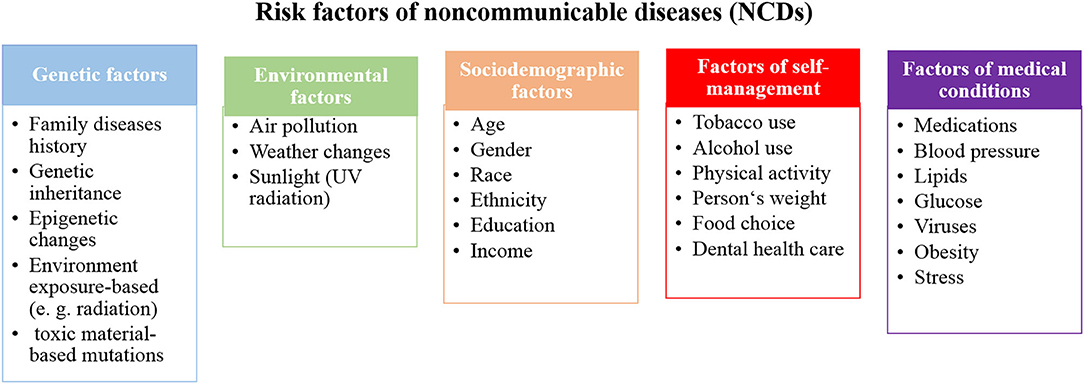
Figure 2 . A proposed model to classify the risk factors of NCDs.
While NCDs are usually associated with elderly people, all ages are at risk, even before birth. These diseases may start in the earliest years of life and keep progressing during childhood, adolescence, and old age ( 14 ). However, 15 million deaths due to NCDs were recorded from people aged between 30 and 69 years of age and more than 82% of these “premature” deaths were from low and middle-income countries ( 15 ). The life-course perspective is evidence of the origin of adult NCDs, which are determined in uterus. Barker ( 16 ) showed that maternal nutrition plays a significant role in adult diseases. He found that adapting human fetuses to a limited supply of nutrients resulted in permanent structure and metabolism changes. Subsequently, such programmed changes may have attributed to several diseases, such as heart disease, diabetes and hypertension in later life ( 16 , 17 ). Moreover, unborn babies are not only negatively influenced by maternal habits, such as diet, drug, stress, alcohol and tobacco consumption during pregnancy, but environmental factors, such as air pollution, also have an effect. These factors influence the fetal and early brain development, for example, a low birth weight is attributable to poor long-term health and poor cognition ( 14 , 18 ).
In the period of childhood, new risks of NCDs may appear due to the easy access to unhealthy food and drinks in kindergartens and schools. Thus, this leads to a high number of overweight and obese children ( 19 ). After that stage of life, young people in the adolescence stage can acquire new and harmful habits, such as smoking and drinking alcohol, which can significantly contribute to NCD risk ( 20 , 21 ). These bad habits may continue during adulthood with additional aspects facing adults in workplaces, including financial stressors, unemployment, unsatisfying careers, and low social engagement, which influence the progress of NCDs ( 20 , 22 ). Retirement and leaving a workplace can provide new challenges among elderly people and influence the development of NCDs. Poor nutrition, lack of physical activity, alcohol and tobacco use, social isolation, and financial stress directly affect older people and strongly promotes NCDs ( 20 ).
The prevention and control of NCDs can be achieved at all ages. The health status of women before and during pregnancy influences the susceptibility of children to NCDs in later life ( 20 , 23 ). This is the most important strategy to control NCDs because it targets the root of the problem. Applying high standards for food and drinks, increased physical activity in schools and workplaces, in addition to monitoring air quality and offering smoke-free zones can largely prevent NCDs at all stages of life. However, taxation and creating restricted policy for the marketing of unhealthy food, sugary drinks, tobacco, and alcohol can largely improve health statistics. Further, as obese children and elderly people are at a high risk of social isolation, it is important, for their mental and physical health, to be involved in social activities ( 20 , 24 ).
Diets and Lifestyle
In the past, infectious and parasitic diseases were the main causes of death, but in the recent decades, NCDs have replaced them and have become the main cause of deaths ( 25 ). This may be attributed to the change of diet habits and lifestyle over the years, which can be classified as a shift of disease patterns in humans. Various dietary factors, such as meat, whole grain products, healthy dietary patterns, sugar-sweetened beverage consumption, and iron-based diets have an obvious relationship with NCDs ( 11 , 12 ). Additionally, the high consumption of processed meat and sugar-sweetened beverages, combined with other unhealthy lifestyle factors, such as a high body mass index (BMI), physical inactivity, and smoking have a marked association with NCDs ( 26 , 27 ). Whole-grain products are independent of the BMI and have protective effects, due to their high fiber contents and ability to slowly release glucose into circulation; subsequently, this reduces the postprandial insulin response and may improve insulin sensitivity ( 26 , 28 – 31 ).
Dietary transition describes the changes in production, processing, availability, dietary consumption, and energy expenditure. Further, the concept becomes wider and involves body composition, anthropometrical parameters, and physical activity ( 32 , 33 ). The use of dietary transition terms arises due to the shift to western diets in developing countries in particular. Traditional food in most countries is healthier, natural, and richer in fiber, and cereal has been replaced by unhealthy processed food that is rich in sugars and fats, animal-source foods, and refined carbohydrates. Hence, low and middle-income countries have seen rapid changes in nutrition transition and rapid increases in NCDs ( 34 ). High food consumption and declining physical activity rates occur simultaneously, resulting in NCDs. The main factor, attributable to physical inactivity, is the rapid and continuous development in technology. The easy access to modern technology and manufacturing in houses and workplaces, including machines, vehicles and labor-saving technology, make life easier but unhealthier from the perspective of reducing the risk of NCDs ( 34 ).
The Economic Context
NCDs are already common in developed countries and rapidly propagate. Spreading western lifestyle in low and middle-income countries, due to global population aging and commercial pressures for unhealthy diets and cigarettes, contributes to the increasing rate of NCDs in these countries ( 35 ). There is a direct relationship between poor health and low-income, which contributes to food poverty, purchasing of cheaper and unhealthy dietary products, and expensive treatments, in addition to psychosocial factors. People with low-incomes have the feeling that they occupy a lower status in society, which prevents them from participating in social life ( 36 ). However, food poverty, poor mobility and lack of physical activity are also serious problems in high-income countries ( 37 ).
There is a growing trend to consider social, political, and economic systems as critical factors that impact NCDs besides individual behavior/lifestyle ( 38 , 39 ). Krieger's Ecosocial theory highlights ecosocial disease distribution which describes how diversity between historical, societal, and ecological conditions significantly contributes to changes in the health outcomes of various social groups ( 39 ). For example, the bad side of economic and health inequality that already exists for many years becomes obvious with the current coronavirus COVID-19 pandemic. According to Krieger's research, the higher number of COVID-19 deaths in African American than whites in the US is attributed to several factors involve living in crowded places, using public transportation to commute to work, working in service jobs in close contact with others, and shortage of protective equipment at workplaces. Furthermore, the lack of access to health care and health insurance, and pre-existing health conditions may be increased the risk from COVID-19 in the African American population ( 40 ).
Key Diseases
Cardiovascular diseases (cvds).
CVDs are the leading contributors to the global burden of disease among the NCDs and account for the most deaths worldwide each year—even more than the number of deaths from cancer and chronic respiratory diseases combined ( 41 , 42 ). CVDs are a group of disorders that are not only related to heart conditions, such as ischaemic heart disease (IHD), stroke, congenital heart disease, coronary heart disease, cerebrovascular disease, peripheral arterial disease, and rheumatic heart disease, but also to blood vessels that involve hypertension, and conditions associated with cerebral, carotid, and peripheral circulation ( 43 ). While CVDs equally affect both sexes, men suffer from higher incidences than women. Still, CVDs are the leading cause of death of women in developed countries ( 44 ). Moreover, many epidemiological studies show the relationship between periodontal disease (PD) and cardiovascular disease. Mild forms of PD affect 75% of adults in the US, and more severe forms affect 20 to 30% of adults. Since PD is common, it is responsible for a significant proportion of proposed infection-associated risks of cardiovascular diseases ( 45 , 46 ).
According to the American Heart Association, there are seven key health factors and behaviors that contribute to the increasing risks of heart disease and stroke: nutrition, smoking, overweight/obesity, physical inactivity, uncontrolled blood pressure, elevated levels of cholesterol, and blood sugar ( 42 ).
Most CVDs can be prevented by addressing the seven risk factors, which involves healthy diets, regular physical activity, avoiding smoking and second-hand smoking, reaching and maintaining a healthy weight, and keeping blood pressure, cholesterol, and blood sugar levels under control ( 42 ).
Cancer is the main public health problem and the second main cause of death globally [who]. It shares the common risk factors with other key diseases of NCDs and several identified and unidentified factors can be attributed to cancer. The causes of cancer can be classified into three categories, including: (i) biological carcinogens (e.g., viral, bacterial, or parasites infections, hormonal and genetics factors); (ii) chemical carcinogens (such as food and water contamination, and tobacco smoking); and (iii) physical carcinogens (such as ultraviolet and ionizing radiation). However, tobacco smoking is considered to be the main cause of cancer, followed by poor diets ( 47 – 49 ). Moreover, together, body weight and lack physical activity are also associated with the most common cancers, including breast (postmenopausal), colon, endometrium, kidney, and esophagus cancers ( 50 ). According to WHO report in 2018, the most common cancers are lung, breast, colorectal, prostate, skin, and stomach, while the most cancer deaths are from cancer of the lung, colorectal, stomach, liver, and breast ( 48 ). A noticeable decrease in the cancer death rates of lung, breast, colon/rectum, and prostate is achieved in high-income countries, but are still high in low and middle-income countries ( 51 ). Further, the incidence of several cancers, including lung, breast, prostate, colon, and rectum, is commonly elevated concurrently with economic development. In contrast, the incidence of stomach cancer declines with economic development ( 48 ). The guidelines for oncological disease prevention and early detection are based on cancer risk assessment, including past medical history, lifestyle factors, family diseases history, and genetic testing ( 10 ).
Lung cancer, which is the most common cancer in the world, is mainly the result of smoking and the risk increases in heavy smokers ( 52 ). Further, several studies reported low intakes of fruits, vegetables and related nutrients in lung cancer patients ( 53 , 54 ). Hence, it is possible to prevent lung cancer by stopping the prevalence of smoking and by increasing fruit and vegetable consumption. Furthermore, dietary habits and physical activity contribute to breast cancer, which is the second most common cancer in the world and the most common cancer among women. Excess adiposity and hormonal mechanisms appeared to play key roles in breast cancer progress, and are effected by dietary intake during childhood and adolescence ( 51 , 55 , 56 ). Hence, maintaining a healthy weight throughout life can minimize the chances of breast cancer. Another type of cancer that is strongly associated with diet is colorectal cancer. High intakes of meat and fat, and low intakes of fruits and vegetables, dietary fiber, vitamins and minerals are related to an increased risk of colorectal cancer ( 57 ). Hence, minimizing or stopping the consumption of meat, especially preserved meats, can reduces the risk of this cancer. Stomach cancer was the main cause of mortality globally, but is currently decreasing in industrialized countries. It is associated with dietary habits and vitamin C intake ( 48 ). Helicobacter pylori infection is considered to be a type I carcinogen and as the strongest known risk factor of gastric cancer ( 58 ). Cancers caused by infections are three times lower in developed countries than in developing ones. It is important to avoid the infection in order to prevent cancer, and that can be achieved by eating food that is properly prepared, drinking water from clean sources, taking vitamins according to the recommended dietary allowance, and avoiding the extensive use of antibiotics in order to reduce antibiotic resistant strains ( 51 ).
Chronic Respiratory Diseases (CRDs)
CRDs cover a wide range of diseases in the airways and the other structures of the lungs. Most of the morbidity and mortality of CRDs is increased with age. CRDs include chronic obstructive pulmonary disease (COPD), occupational lung diseases, asthma and respiratory allergies, sleep apnoea syndrome, and pulmonary hypertension. Asthma and COPD account for most of the deaths among CRDs in low and middle-income countries ( 59 – 61 ). Genetic and environmental factors are the risk factors of CRDs; environmental factors are more dominant. These factors include air pollution exposure, including tobacco smoke and second-hand tobacco smoke, indoor and outdoor air pollution, occupational exposures, and socioeconomic factors ( 62 , 63 ).
CRDs are not fully reversible and are partially preventable ( 64 ). During pregnancy, maternal smoking contributes to lung dysfunction in children at birth. Further, in early life, a child's health affects their subsequent respiratory health. Thus, following a healthy lifestyle in the early ages of life, avoiding respiratory infections, and avoiding environmental and occupational agents can effectively prevent CRDs. Preventing exposure to indoor and outdoor pollutants can be achieved by filtration and ventilation, in addition to the use of natural gas ( 27 ).
Diabetes Mellitus
Diabetes has attracted global attention due to its elevating prevalence and incidence. It is not only a chronic disease, but also an acutely life-threatening condition. Further, it may cause other serious diseases such as heart diseases, kidney failure, and eye damage, which may subsequently lead to blindness, and foot ulcers, which may require limb amputation. The main two types of diabetes are both lead to hyperglycemia. In type 1, the pancreatic β-cells cannot produce a sufficient amount of insulin, while in type 2, the body cells cannot respond properly to insulin ( 64 ). Other types of diabetes involve gestational diabetes mellitus, which occurs in pregnant women with glucose intolerance ( 65 ), and type 3 diabetes, which is associated with Alzheimer's disease, where neurons in the brain cannot respond to insulin ( 66 ). While diabetes can be partially inherited, several lifestyle factors, such as obesity, high sugar consumption, and lack of physical activity can significantly contribute to the progress diabetes. However, lifestyle changes can prevent diabetes and the long-term complications of diabetes. Patients with type 2 diabetes can control or even reverse the diabetes by changing their lifestyle and eating habits. The term “healthy dietary pattern” includes a variety of diets and nutritional factors, for example, reducing the consumption of red and processed meat, sugar-sweetened beverages and alcohol, while increasing the consumption of whole-grain products ( 67 ).
Management of Risk Factors and NCDs
The following sections outline the developed and proposed strategies to manage NCDs and their risk factors from several perspectives.
Management of Risk Factors
The most common causes of NCDs are metabolic and behavioral risk factors and can be largely preventable by several available means. Most global discussions concern the risk factors of self–management (tobacco and alcohol consumption, physical activity, weight, food, and dental health care) and focus on the role of individual responsibility to manage the risk factors of NCDs. Health care specialists should educate patients about their nutrition value and raise the profile of didactics, practicums, and workshops in daily practice ( 68 ). Further, the management of NCDs is the priority of the public health sector in most countries, because management in society is the main direction of NCD prevention strategies. Interventions are used in public health management in an effort to promote good health behavior. For example, India, with its wide sociocultural, economic, and geographical diversity, is implementing multi-sectoral (partnership between different sectors) actions to prevent NCDs, including school health programs, initiatives of National Cancer Control Programme, National Trauma Control program, National Program for Control of Blindness, National Mental Health Programme, the National Tobacco Control Program, and the National Program for Control of Diabetes, Stroke, and Cardiovascular Diseases initiatives ( 69 ). From another approach, researchers also highlight the environmental factors (air pollution, climate changes, sunlight) and their impact on NCD development. Air pollution will be an important challenge in the future and new technologies, such as microchips, will have more of an impact in air monitoring ( 27 ).
Since diet is a common risk factor among most NCDs, it attracts more attention in an effort to find effective strategies to provide healthy food to the community and at all stages of life. Evidence-based nutrition interventions should be a global health priority and the role of the dietary fat studied should be a modifiable variable in the prevention of NCDs ( 29 ). Recent evidence suggests that a diet that is high in healthy fat and rich in unsaturated fatty acids prevents the development of metabolic diseases and reduces cardiovascular events ( 29 ). Many interventions addressing poverty and development have an impact on NCD prevalence and risk ( 69 ). The current evidence is limited to diets, and a positive effect of agricultural-based food security programs on diet indicators has been suggested ( 7 ). A suboptimal diet is the leading risk factor for NCDs and consumption of specific foods, rather than macronutrients or micronutrients; it may be the most significant risk factor for NCDs ( 70 ). Strategic health communication in the population-wide intervention includes engaging the food industry in order to reduce the salt content in foods ( 71 ). The concept of a sustainable diet combines health and environmental concerns and includes the abovementioned risk factors as part of the recommendations to reduce processed meat consumption and to increase whole-grain consumption ( 72 ). Lifestyle activities include healthy diets and focus on limiting the use of salt, sugar, and saturated fats ( 73 ). While our body can synthesize many of the molecules required to function properly, essential nutrients are obtained from food. Carbohydrates, proteins, and fats are the primary components of food. Minerals are inorganic essential nutrients that must be obtained from food. The omega−3 alpha-linolenic and the omega−6 linoleic acids are essential fatty acids that are needed to make some membrane phospholipids. Vitamins (B, C, A, D, E, and K) are the classes of essential organic molecules (such as cofactors) that are required in small quantities for most enzymes to function properly. The absence or low levels of vitamins can have a dramatic effect on health. A focus on the need to meet adequate dietary intakes of essential nutrients ( 74 ) through a healthy diet is considered to be very significant for the aging society ( 74 ). Food supplements are concentrated sources of nutrients (minerals and vitamins) or other substances with a nutritional or physiological effect, which are marketed in the form of pills, capsules, and/or liquids ( Table 1 ). These dietary supplements offer many benefits, including the maintaining of an adequate intake of certain nutrients, to correct nutritional deficiencies, or to support specific physiological functions. Recently, researchers have been looking for new solutions to implement an efficient food production process and to discover the benefits of starch waste on human health.
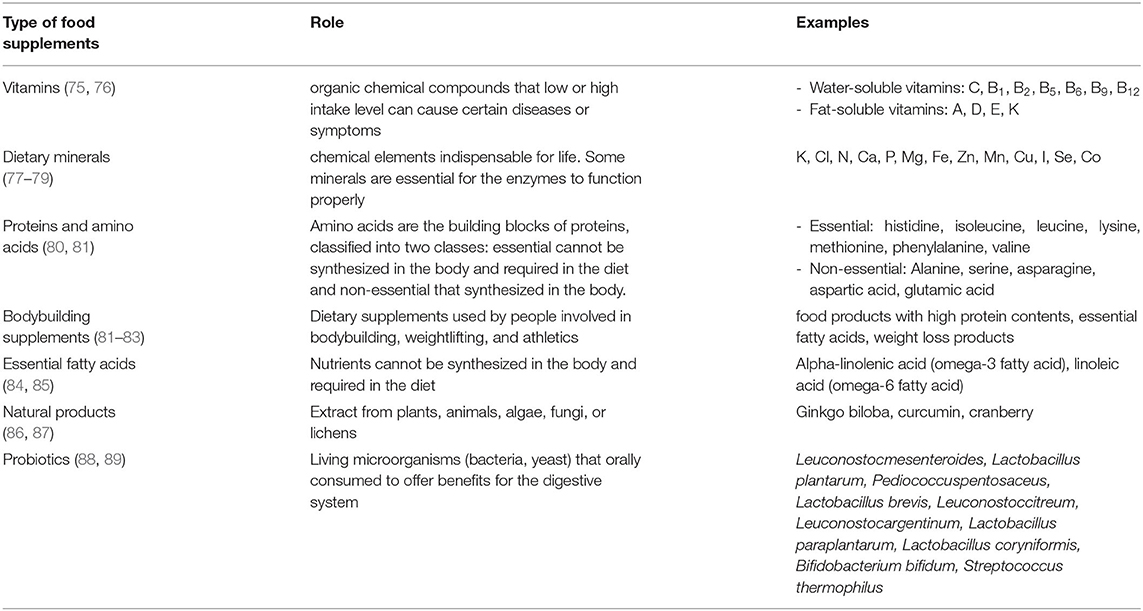
Table 1 . Types of food supplements.
Management of NCDs
NCDs are the silent killers threatening health without showing any symptoms until the problem progresses to an advanced stage. Patients with NCDs, or people with a susceptibility to develop one, need long-term care that is personalized, proactive, and sustainable. Primary health care can organize and deliver healthcare strategies to manage NCDs in each community and to detect diseases at early stages. Thus, they can significantly overcome the challenges linked to a high cost in the health sector. For example, several studies have proved that lifestyle factors have direct links to cancer risk and changing lifestyles, in a positive approach, can considerably minimize the cancer burden. The main risk factors of cancer are age, gender, alcohol, smoking, family disease history, and food ( 90 – 92 ). Cancer can be prevented by changing behavior: dietary improvements, physical activity, weight control, obesity management, tobacco prevention, safe sex and control of oncogenic viruses, sun protection, medications, and lower alcohol consumption ( 26 ).
A dramatic decrease in all cardiovascular disease-related deaths has been recorded in high-income countries, whereas a significant increase was registered in low and middle-income countries ( 93 , 94 ). Checkley et al. reported on NCDs' management in low and middle-income countries ( 95 ). While some people in these countries can access the same treatments that are available in high-income countries, the majority of the population lacks access. The main obstacle causes an increase in the number of patients with NCDs in low and middle-income communities is the absence of a well-designed plan to stop disease occurrence and spreading. Each country needs to prepare its management plan, not just with coping models from high-income countries. Several successful models have been verified, taking into consideration the low-cost strategies to prevent, diagnose and treat NCDs. For example, a cost-effective strategy has been developed in Kenya to diagnose diabetes and hypertension in the early stages of life. While health workers are visiting homes to examine human immunodeficiency virus (HIV) infection, they also measure blood glucose levels and blood pressure. Further, type 2 diabetes is a global pandemic that highly affects human health and global economic development ( 96 ). The International Diabetes Federation reported that there were 415 million people living with type 2 diabetes in 2015, and estimated that the number by 2040 might increase to 642 million, which is attributable to genetic and environmental factors ( 96 ). The genetic–environmental interaction induces insulin resistance and β-cell dysfunction ( 96 ). The epidemic of type 2 diabetes in recent decades has not only attributed to the alteration of the gene pool, but environmental changes also play significant roles in the rapid increase in the prevalence of type 2 diabetes ( 96 ). However, global diabetes mellitus epidemics require the looking for innovative approaches to prevention ( 7 ).
Contemporary Prevention Strategy of NCDs
The prevention strategies of NCDs can include small and large-scale human cooperation ( Figure 3 ). The importance of preventing NCDs arises from the direct impact of NCDs on the decreasing rate of national income. Loss productivity on a large-scale is the result of the inability to work and the frequent absence threats to the national economy. The management strategy to prevent NCDs is based on risk factor management that addresses individual, society, country, and global levels, with actions, such as resource allocation, multi-sectoral partnership, knowledge and information management and innovations. The most critical dimension of the prevention strategy is lifestyle management at the individual level and with a focus on actions, such innovations, which can help the society to increase the awareness of risk factors management, to take health policy decisions at a country level and to develop a health strategy at the global level. The importance of leadership for the change management process is underscored and requires the creation of new approaches to the prevention of NCDs ( 96 , 97 ).
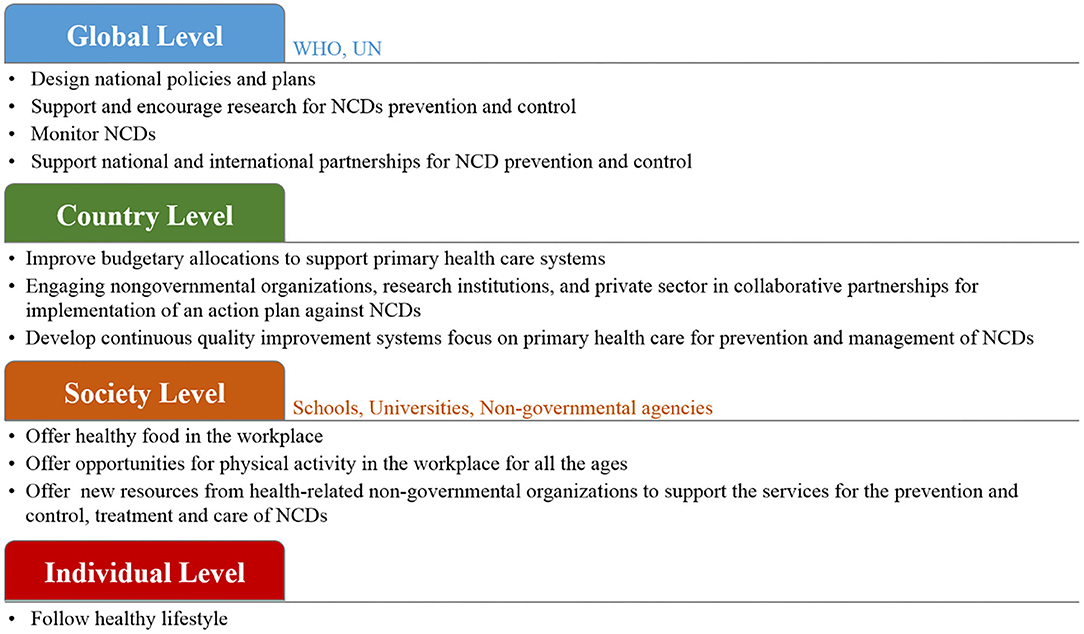
Figure 3 . The proposed prevention management of NCDs with small and large-scale human cooperation.
At the global level, WHO and UN agencies can work together to design policies and strategies to reduce the risk of NCDs ( 98 , 99 ). It is important to monitor NCDs and to assess their progress at the national, regional and global levels. These organization can support research and encourage collaborations among national and international health agencies and academic institutions. Further, tobacco smoke, as a common factor of the four main types of NCDs, must be put under control. The WHO offers help to smokers who have the desire to stop using tobacco products and to implement rules to propose a smoke-free environment. Further, WHO can, by law, protect tobacco control policies from the commercial interests of the tobacco industry. At the country level, each government needs to design its plan based on its economy. Several low-cost and highly effective strategies are available to prevent and manage NCDs ( 100 – 103 ). For example, encouraging people to play sports for physical activity is the most effective factor that can easily influence the prevention of NCDs, and at the same it is time and cost-effective. Moreover, improved budgetary allocations to support primary health care systems should be put in place in order to provide health services to all community members. To achieve large-scale progress, collaboration between governments and various non-governmental organizations, schools, and universities, to provide advice on lifestyle modifications and to warn people about the risks of NCDs, is in high demand. At the society level, research centers and institutes can significantly contribute to the prevention of NCDs by conducting research projects and programs. Focusing research on food biotechnology and agriculture has a direct influence on NCDs risk ( 7 , 104 ). The development of diagnostic tools allows for the rapid detection of NCDs biomarkers with high sensitivity to help detect diseases at their early stages, which subsequently contributes to easier treatment and fast cures ( 105 – 107 ). However, in order to reach the highest attainable standard of health, it is important to encourage individuals and families to follow a healthy lifestyle in order to get an effective response for prevention and the control of NCDs and to improve health outcomes ( 100 , 108 ).
Conclusions
In modern society, NCDs are the main challenge in health systems. Risk factor management is essential in NCDs' management. The management of NCDs requires many strategies from several perspectives and on different levels, including the individual and country levels. Based on the hypotheses that were raised during the above scientific discussion, it can be concluded that modern strategies for the management of NCDs should be oriented toward the individual level, where the individual is responsible for their health by simply following a healthy lifestyle. It is important to combine modern scientific achievements and innovative decisions, with regard to the rationality of nutrition and positive effects on human health. Governments and international organizations should make people aware of their health and their environment to make the world a safe and healthy place. From another perspective, support research to find new techniques to improve food biotechnology is in high demand. Further, finding rapid and sensitive diagnostic platforms to detect NCDs at the point-of-care offers huge benefits to personnel and the healthcare system. The innovations are vital to address the growing crisis of NCDs successfully, and most often use lifestyle projects, the promotion of healthy eating behaviors and smoking cessation. We believe that there is a need to look for further innovations to build better lives in society.
Author Contributions
The manuscript was prepared by AB, SD, and RK. Writing review and editing was done by AB, SD, DS, KO, PS-G, GP, AK, SK, and RK. Final revision and approval was done by RK. All authors contributed to the article and approved the submitted version.
This research was funded by the European Regional Development Fund according to the supported activity Attracting scientists from abroad to carry out research (RK) under Measure No. 01.2.2-LMT-K-718 (project No. 01.2.2-LMT-K-718-02-0012).
Conflict of Interest
KO was employed by the company Procomcure Biotech, GmbH.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. World Health Organization. Noncommunicable Diseases (NCD) . (2019). Available online at: https://www.who.int/gho/ncd/mortality_morbidity/en/ (accessed January 03, 2020).
2. World Health Organization. Global Action Plan: For the Prevention and Control of Non-communicable Diseases . (2013–2020). Available online at: https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf (accessed January 13,2020).
3. Noor NAM, Yap SF, Liew KH, Rajah E. Consumer attitudes toward dietary supplements consumption: implications for pharmaceutical marketing. Int J Pharm Healthc Mark. (2014) 8:6–26. doi: 10.1108/IJPHM-04-2013-0019
CrossRef Full Text | Google Scholar
4. Sithey G, Li M, Thow MA. Strengthening non–communicable disease policy with lessons from Bhutan: linking gross national hapiness and health policy action. J Public Health Policy. (2018) 39:327–42. doi: 10.1057/s41271-018-0135-y
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Goetzke BI, Spiller A. Health-improving lifestyles of organic and functional food consumers. Brit Food J. (2014) 116:510–26. doi: 10.1108/BFJ-03-2012-0073
6. Yang ZY, Yang Z, Zhu L, Qiu C. Human behaviors determine health: strategic thoughts on the prevention of chronic non-communicable diseases in China. Int J Behav Med. (2011) 18:295–301. doi: 10.1007/s12529-011-9187-0
7. Pullar J, Allen L, Townsend N, Williams J, Foster C, Roberts N, et al. The impact of poverty reduction and development interventions on non-communicable diseases and their behavioural risk factors in low and lower-middle income countries. a systematic review. PLoS ONE. (2018) 13:e0193378. doi: 10.1371/journal.pone.0193378
8. Na L, Wu X, Feng R, Li J, Han T, Lin L, et al. The harbin cohort study on diet, nutrition and chronic non communicable diseases: study design and baseline characteristics. PLoS ONE. (2015) 10:e0122598. doi: 10.1371/journal.pone.0122598
9. International Diabetes Federation. IDF Diabetes Atlas . 7th Edn. Brussels: International Diabetes Federation (2015).
Google Scholar
10. Kahn SE, Cooper ME, Del PS. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. (2014) 383:1068–83. doi: 10.1016/S0140-6736(13)62154-6
11. Aune D, Ursin G, Veierød MB. Meat consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Diabetologia . (2009) 52:2277–87. doi: 10.1007/s00125-009-1481-x
12. Imamura F, O'Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ . (2015) 351:h3576. doi: 10.1136/bmj.h3576
13. World Health Organization Technical Report Series. Diet, Nutrition and the Prevention of Chronic Diseases . Geneva: WHO (2003). p. 1–149.
14. Fair Society. Healthy Lives: Strategic Review of Health Inequalities in England Post 2010. London, UK: Marmo Review (2010).
15. World Health Organization. Noncommunicable Diseases: Key Facts . (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
16. Barker DJP. In utero programming of chronic disease. Clin Sci. (1998) 95:115–28. doi: 10.1042/cs0950115
17. Gluckman PD, Hanson MA. Adult disease: echoes of the past. Euro J Endocrin. (2006) 155 (Suppl. 1):S47–50. doi: 10.1530/eje.1.02233
18. Jefferis BJMH, Power C, Hertzman C. Birth weight, childhood socioeconomic environment, and cognitive development in the 1958 British birth cohort study. BMJ . (2002) 325:305. doi: 10.1136/bmj.325.7359.305
19. Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics . (1998) 101 (Suppl. 2):518–25.
PubMed Abstract | Google Scholar
20. Mikkelsen B, Williams J, Rakovac I, Wickramasinghe K, Hennis A, Shin HR, et al. Life course approach to prevention and control of non-communicable diseases. BMJ . (2019). 364:l257. doi: 10.1136/bmj.l257
21. Pechmann C, Levine L, Loughlin S, Leslie F. Impulsive and self-conscious: adolescents' vulnerability to advertising and promotion. J Public Policy Mark . (2005) 24:202–21. doi: 10.1509/jppm.2005.24.2.202
22. World Health Organization (EURO). The Health and Well-Being of Men in the WHO European Region: Better Health Through a Gender Approach . (2018). Available online at: http://www.euro.who.int/en/health-topics/health-determinants/gender/publications/2018/the-health-and-well-being-of-men-in-the-who-european-region-better-health-through-a-gender-approach-2018 (accessed January 13, 2020).
23. World Health Organization. (2016). Good Maternal Nutrition the Best Start in Life . WHO. Available online at: http://www.euro.who.int/__data/assets/pdf_file/0008/313667/Good-maternal-nutrition-The-best-start-in-life.pdf?ua=1 (accessed January 13, 2020).
24. Billingsley M. New advice on physical activity aims to prevent chronic disease from early years. BMJ . (2016) 343:d4457. doi: 10.1136/bmj.d4457
25. Martorell R, Kettel Khan L, Hughes ML, Grummer-Strawn LM. Overweight and obesity in preschool children from developing countries. Int J Obesity . (2000) 24:959–67. doi: 10.1038/sj.ijo.0801264
26. Stein CJ, Colditz GA. Modifiable risk factors of cancer. Br J Cancer . (2004) 90:299–303. doi: 10.1038/sj.bjc.6601509
27. Schultze F, Gao X, Virzonis D, Damiati S, Schneider MR, Kodzius R. Air quality effects on human health and approaches for its assessment through microfluidic chips. Genes . (2017) 8:244. doi: 10.3390/genes8100244
28. Kumar A. The impact of obesity on cardiovascular disease risk factor. Asian J Med Sci . (2019) 10:21294. doi: 10.3126/ajms.v10i1.21294
29. Billingsley HE, Carbone S, Lavie CJ. Dietary fats and chronic noncommunicable diseases. Nutrients . (2018) 10:1385. doi: 10.3390/nu10101385
30. Katileviciute A, Plakys G, Budreviciute A, Onder K, Damiati S, Kodzius RA. Sight to wheat bran: high value-added products. Biomolecules . (2019) 9:887. doi: 10.3390/biom9120887
31. WHO/FAO. Diet, Nutrition and the Prevention of Chronic Diseases. Draft Joint WHO/FAO Consultation on Diet Nutrition and the Prevention of Chronic Disease . (2003). Available online at: https://www.who.int/dietphysicalactivity/publications/trs916/en/ (accessed January 13, 2020).
32. WHO. (2002). The World Health Report 2002 . Geneva: WHO.
33. Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nut Rev . (1997) 55:31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x
34. Popkin BM. Nutrition transition and the global diabetes epidemic. Curr Diab Rep . (2015) 15:64. doi: 10.1007/s11892-015-0631-4
35. The Lancet Global Health. Getting to the heart of non-communicable diseases. (2018) 6:e933. doi: 10.1016/S2214-109X(18)30362-0
36. Marmot M. Social causes of social inequalities in health. In: Anand S, Fabienne P, Sen A, editors. Public Health, Ethics, and Equity . Oxford: Oxford University Press (2004). p. 37–46.
37. Lundberg O, Åberg YM, Stjärne M, Björk L, Fritzell J. The Nordic Experience: Welfare States and Public Health . Stockholm. Centre for Health Equity Studies (2008). Available online at: https://www.chess.su.se/polopoly_fs/1.54170.1321266667!/menu/standard/file/NEWS_Rapport_080819.pdf
38. Yang JS, Mamudu HM, John R. Incorporating a structural approach to reducing the burden of non-communicable diseases. Global Health . (2018) 14:66. doi: 10.1186/s12992-018-0380-7
39. Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol . (2001) 30:668–77. doi: 10.1093/ije/30.4.668
40. Krieger N. COVID-19 Pandemic Highlights Longstanding Health Inequities in U.S . Harvard T.H. Chan School of Public Health (2020). Available online at: https://www.hsph.harvard.edu/news/hsph-in-the-news/covid-19-pandemic-highlights-longstanding-health-inequities-in-u-s/ (accessed August 11, 2020).
41. Blundell HJ, Hine P. Non-communicable diseases: ditch the label and recapture public awareness. Int Health . (2019) 11:5–6. doi: 10.1093/inthealth/ihy063
42. World Health Organization. Noncommunicable Diseases: Key Facts . (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed January 22, 2020).
43. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics−2018 update: a report from the american heart association. Circulation . (2018) 137:e67–492. doi: 10.1161/CIR.0000000000000573
44. Popkin BM, Horton SH, Kim S. The Nutrition Transition and Prevention of Diet-Related Diseases in Asia and the Pacific . Washington, DC: International Food Policy Research Institute (IFPRI) (2001).
45. Brands A, Yach D. NMH Reader. Women and the Rapid Rise of Noncommunicable Diseases . World Health Organization (2002). Available online at: https://apps.who.int/iris/bitstream/handle/10665/67256/WHO_NMH_02.01.pdf;jsessionid=92EE99BB43827D58A0DFDCD7A7E5F5AE?sequence=1 (accessed January 22, 2020).
46. Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidem. (2013) 28:845–58. doi: 10.1007/s10654-013-9852-5
47. Fung TT, Hu FB, Pereira MA, Liu S, Stampfer MJ, Colditz GA, et al. Whole-grain intake and the risk of type 2 diabetes: a prospective study in men. Amer J Clin Nutr . (2002) 76:535–40. doi: 10.1093/ajcn/76.3.535
48. Centers for Disease Control and Prevention(US) National Center for Chronic Disease Prevention and Health Promotion(US) Office on Smoking and Health(US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General . Atlanta, GA: Centers for Disease Control and Prevention (2010).
49. Joint WHO/FAO. Expert Consultation on Diet, Nutrition and the Prevention of Chronic Diseases . Geneva, Switzerland (2002). Available online at: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed January 22,2020).
50. Willet MC. Diet, nutrition, and avoidable cancer. Environ Health Perspect . (1995) 103:S165–70. doi: 10.1289/ehp.95103s8165
51. Vainio H, Bianchini F. Weight control and physical activity. In: IARC Handbooks of Cancer Prevention . Vol. 6. Lyon: IARC Press (2002).
52. International Agency for Research on Cancer. Cancer: causes, occurrence and control. In: Thomas L, Aitio O, Day NE, Heseltine E, Kadlor J, Miller AB, Parkin DM, Riboli, editors. Lyon, International Agency for Research on Cancer . Lyon: IARC Scientific Publications (1990).
53. Ferlay J. Globocan 2000: Cancer Incidence, Mortality and Prevalence Worldwide. Version 1.0 . Lyon: International Agency for Research on Cancer (2001).
54. Potter J. Food, Nutrition and the Prevention of Cancer: A Global Perspective . Washington, DC: World Cancer Research Fund/American Institute for Cancer Research (1997).
55. Nutritional Aspects of the Development of Cancer. Report of the working group on diet and cancer of the committee on medical aspects of food and nutrition policy. Rep Health Soc Subj . (1998) 48:i–xiv:1–274.
56. Key TJ, Verkasalo PK, Banks E. Epidemiology of breast cancer. Lancet Oncol . (2001) 2:133–40. doi: 10.1016/S1470-2045(00)00254-0
57. Norat T, Lukanova A, Ferrari P, Riboli E. Meat consumption and colorectal cancer risk: a dose–response meta-analysis of epidemiological studies. Int J Cancer . (2002) 98:241–56. doi: 10.1002/ijc.10126
58. Wroblewski LE, Peek RM J, Wilson KT. Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbio Rev. (2010) 23:713–39. doi: 10.1128/CMR.00011-10
59. Navarro-Torné A, Vidal M, Trzaska DK, Passante L, Crisafulli A, Laang H, et al. Chronic respiratory diseases and lung cancer research: a perspective from the European Union. Eur Resp J . (2015) 46:1270–80. doi: 10.1183/13993003.00395-2015
60. Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global burden of disease study 2015. Lancet . (2016) 388:1459–544. doi: 10.1016/S0140-6736(16)31012-1
61. de-Graft Aikins A, Unwin N, Agyemang C, Allotey P, Campbell C, Arhinful D. Tackling Africa's chronic disease burden: from the local to the global. Global Health. (2010) 6:5. doi: 10.1186/1744-8603-6-5
62. Bousquet J, Dahl R, Khaltaev N. Global alliance against chronic respiratory diseases. Eur Respir J . (2007) 29:233–9. doi: 10.1183/09031936.00138606
63. Leynaert B, Sunyer J, Garcia-Esteban R, Svanes C, Jarvis D, Cerveri I, et al. Gender differences in prevalence, diagnosis and incidence of allergic and non-allergic asthma: a population-based cohort. Thorax . (2012) 67:625–31. doi: 10.1136/thoraxjnl-2011-201249
64. Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS ONE . (2018) 13:e0194127. doi: 10.1371/journal.pone.0194127
65. Gilmartin AB, Ural SH, Repke JT. Gestational diabetes mellitus. Rev Obstet Gynecol . (2008) 1:129–34.
66. De la Monte SM, Wands JR. Alzheimer's disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol . (2008) 2:1101–13. doi: 10.1177/193229680800200619
67. Esposito K, Chiodini P, Maiorino MI, Bellastella G, Panagiotakos D, Giugliano D. Which diet for prevention of type 2 diabetes? a meta-analysis of prospective studies. Endocrine . (2014) 47:107–16. doi: 10.1007/s12020-014-0264-4
68. Johnston E, Mathews T, Aspry K, Aggarwal M, Gianos E. Strategies to fill the gaps in nutrition education for health professionals through continuing medical education. Curr Atheroscler Rep . (2019) 21:13. doi: 10.1007/s11883-019-0775-9
69. Arora M, Chauhan K, John S, Mukhopadhyay A. Multi-sectoral action for addressing social determinants of noncommunicable diseases and mainstreaming health promotion in national health programmes in India. Indian J Commun Med . (2011) 36:S43–9. doi: 10.4103/0970-0218.94708
70. Mutie PM, Giordano GN, Franks PW. Lifestyle precision medicine: the next generation in type 2 diabetes prevention? BMC Med . (2017) 15:171. doi: 10.1186/s12916-017-0938-x
71. Micha R, Khatibzadeh S, Shi P, Andrews KG, Engell RE, Mozaffarian D. Global, regional and national consumption of major food groups in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open . (2015) 5:e008705. doi: 10.1136/bmjopen-2015-008705
72. Webster J, Pillay A, Suku A, Gohil P, Santos JA, Schultz J, et al. Process evaluation and costing of a multifaceted population-wide intervention to reduce salt consumption in fiji. Nutrients . (2018) 10:155. doi: 10.3390/nu10020155
73. Springmann M, Wiebe K, Mason-D'Croz D, Sulser TB, Rayner M, Scarborough P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: a global modelling analysis with country-level detail. Lancet Planet Health . (2018) 2:e451–61. doi: 10.1016/S2542-5196(18)30206-7
74. Bruins MJ, van Dael P, Eggersdorfer M. The role of nutrients in reducing the risk for noncommunicable diseases during aging. Nutrients . (2019) 11:85. doi: 10.3390/nu11010085
75. USDA. (2020). U.S.D.o.A. Dietary Guidelines and MyPlate . Available online at: https://www.choosemyplate.gov/dietary-guidelines (accessed Feburary 16, 2020).
76. Fletcher RH, Fairfield KM. Vitamins for chronic disease prevention in adults. JAMA . (2002) 287:3127–9. doi: 10.1001/jama.287.23.3127
77. Castiglione D, Platania A, Conti A, Falla M, D'Urso M, Marranzano M. Dietary micronutrient and mineral intake in the mediterranean healthy eating, ageing, and lifestyle (MEAL) study. Antioxidants . (2018) 7:79. doi: 10.3390/antiox7070079
78. Higdon J. An evidence-based approach to vitamins and minerals: health benefits and intake recommendations. United States: Thieme Medical Publishers (2003). 253p.
79. Huskisson E, Maggini S, Ruf M. The role of vitamins and minerals in energy metabolism and well-being. J Int Med Res . (2007) 5:277–89. doi: 10.1177/147323000703500301
80. Damodaran S Parkin KL Fenema OR. Fennema‘s Food Chemistry . Boca Raton, FL: Taylor and Francis Group (2007). 1144p.
81. Wu G. Amino acids: metabolism, functions, and nutrition. Amino Acids . (2009) 37:1–17. doi: 10.1007/s00726-009-0269-0
82. Applegate EA, Grivetti LE. Search for the competitive edge: a history of dietary fads and supplements. J Nutr . (1997) 127:869–73. doi: 10.1093/jn/127.5.869S
83. Helms ER, Aragon AA, Fitschen PJ. Evidence-based recommendations for natural bodybuilding contest preparation: nutrition and supplementation. J Int Soc Sports Nutr . (2014) 11:20. doi: 10.1186/1550-2783-11-20
84. Simopoulos AP. Essential fatty acids in health and chronic disease. Am Clin Nutr . (1999) 70:560–9. doi: 10.1093/ajcn/70.3.560s
85. Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation . (2002) 106:2747–57. doi: 10.1161/01.CIR.0000038493.65177.94
86. Harvey AL. Natural products in drug discovery. Drug Discov Today . (2008) 13:894–901. doi: 10.1016/j.drudis.2008.07.004
87. Dias DA, Urban S, Roessner U. A historical overview of natural products in drug discovery. Metabolites . (2012) 2:303–36. doi: 10.3390/metabo2020303
88. Kaur IP, Chopra K, Saini A. Probiotics: potential pharmaceutical applications. Eur J Pharm Sci . (2002) 15:1–9. doi: 10.1016/S0928-0987(01)00209-3
89. Parvez S, Malik KA, Kang SA, Kim HY. Probiotics and their fermented food products are beneficial for health. J App Microbiol. (2006) 100:1171–85. doi: 10.1111/j.1365-2672.2006.02963.x
90. Curry S, Byers T, Hewitt M. Fulfilling the Potential of Cancer Prevention and Early Detection . Washington DC: National Academy Press (2003).
91. Jhajharia S, Verma S, Kumar R. Risk factors, susceptibility, and machine learning techniques for cancer prediction. Drug Intervent Today . (2018) 10:580–92.
92. Thun MJ, DeLancey JO, Center MM, Jemal A, Ward EM. The global burden of cancer: priorities for prevention. Carcinogenesis . (2010) 31:100–10. doi: 10.1093/carcin/bgp263
93. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol . (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
94. Rarau P, Pulford J, Gouda H, Phuanukoonon S, Bullen C, Scragg R, et al. Socio-economic status and behavioural and cardiovascular risk factors in Papua New Guinea: a cross-sectional survey. PLoS ONE . (2019) 14:e0211068. doi: 10.1371/journal.pone.0211068
95. Checkley W, Ghannem H, Irazola V, Kimaiyo S, Levitt NS, Miranda JJ, et al. Management of NCD in low- and middle-income countries. Glob Heart . (2014) 9:431–43. doi: 10.1016/j.gheart.2014.11.003
96. International Diabetes Federation. IDF Diabetes Atlas . 7th ed. Brussels: International Diabetes Federation (2015).
97. World Health Organization (WHO). Global Action Plan for the Prevention and Control of NCDs 2013-2020 . (2013). Available online at: https://www.who.int/nmh/events/ncd_action_plan/en/ (accessed January 22, 2020).
98. Lim J, Chan MM, Alsagoff FZ, Ha D. Innovations in non-communicable diseases management in ASEAN: a case series. Glob Health Action . (2014) 7:25110. doi: 10.3402/gha.v7.25110
99. World Health Organization (WHO). Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-resource Settings . (2010). Available online at: https://www.who.int/nmh/publications/essential_ncd_interventions_lr_settings.pdf (accessed January 22,2020).
100. Rogge J. Statement by Dr Jacques Rogge. In: Proceedings of High-level meeting of the UN General Assembly on the Prevention and Control of Non-communicable Diseases, New York, NY: New York (2018).
101. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet . (2012) 380:219–29. doi: 10.1016/S0140-6736(12)61031-9
102. Phillips CM, Chen LW, Heude B, Bernard JY, Harvey NC, Duijts L, et al. Dietary inflammatory index and non-communicable disease risk: a narrative review. Nutrients . (2019) 11:1873. doi: 10.3390/nu11081873
103. Zarocostas J. Need to increase focus on non-communicable diseases in global health, says WHO. BMJ . (2010) 341:c7065. doi: 10.1136/bmj.c7065
104. Francesco R, Anna L, Stineke O, Victor A, Gunhild S, Ruth R, et al. Transforming the food system to fight non-communicable diseases. BMJ . (2019) 364:l296. doi: 10.1136/bmj.l296
105. Damiati S, Küpcü S, Peacock M, Eilenberger C, Zamzami M, Qadri I, et al. Acoustic and hybrid 3D-Printed electrochemical biosensors for the real-time immunodetection of liver cancer cells (HepG2). Biosens Bioelectron . (2017) 94:500–6. doi: 10.1016/j.bios.2017.03.045
106. Damiati S, Peacock M, Leonhardt S, Baghdadi MA, Damiati L, Becker H, et al. Embedded disposable functionalized electrochemical biosensor with a 3D-printed flow-cell for detection of hepatic oval cells. Genes . (2018) 9:89. doi: 10.3390/genes9020089
107. Damiati S, Hersman C, Søpstad S, Peacock M, Whitley T, Davey P, et al. Sensitivity comparison of macro- and micro-electrochemical biosensors for human chorionic gonadotropin (hCG) biomarker detection. IEEE Access. (2019) 7:94048–58. doi: 10.1109/ACCESS.2019.2928132
108. Matheson GO, Klugl M, Engebretsen L, Bendiksen F, Blair SN, Borjesson M, et al. Prevention and management of noncommunicable disease: the IOC consensus statement, Lausanne 2013. Clin J Sport Med . (2013) 23:419–29. doi: 10.1097/JSM.0000000000000038
Keywords: risk factors, non-communicable diseases, health policy, prevention strategies, healthcare-management
Citation: Budreviciute A, Damiati S, Sabir DK, Onder K, Schuller-Goetzburg P, Plakys G, Katileviciute A, Khoja S and Kodzius R (2020) Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front. Public Health 8:574111. doi: 10.3389/fpubh.2020.574111
Received: 18 June 2020; Accepted: 26 October 2020; Published: 26 November 2020.
Reviewed by:
Copyright © 2020 Budreviciute, Damiati, Sabir, Onder, Schuller-Goetzburg, Plakys, Katileviciute, Khoja and Kodzius. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rimantas Kodzius, kodzius@envirola.com
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
How micro- and nanoplastics may worsen non-communicable diseases
- Download PDF Copy

In a recent study published in Cell Reports Medicine , researchers review and assess the potential exacerbation of non-communicable diseases (NCDs) by micro- and nanoplastics (MnPs) through their impact on inflammation and disease mechanisms.

What causes NCDs?
The global incidence of NCDs, such as cardiovascular diseases, cancers, diabetes, and chronic lung diseases, is rising. Current estimates indicate that NCDs are responsible for about 71% of annual deaths and will be responsible for an economic burden exceeding $30 trillion USD over the next two decades.
Environmental pollution exacerbates NCD burden, with MnPs now ubiquitous throughout nature. Despite their prevalence in lungs, blood, breast milk, placenta, and stool samples, the health risks of MnP exposure remain unclear due to the lack of standardized protocols and mechanistic understanding. Thus, further research is needed to accurately assess the health risks of MnP exposure and their potential role in exacerbating NCDs.
Human exposure to MnPs
Environmental prevalence of mnps.
Since the 1950s, many studies have indicated a significant rise in MnP concentrations in the environment, reflecting the increase in the production, use, and disposal of plastics worldwide. Plastics are integral to daily life, thus leading to widespread exposure and potential health risks. MnP toxicity, like other pollutants such as soot and lead, is linked to exposure and dosage.
Routes of MnP exposure
Humans encounter MnPs through various pathways, including outdoor air, indoor environments, food, water, and even cosmetics. Direct sources include MnPs in food and beverages, inhalation of particles from local emissions, and household items like plastic clothing and furniture. Indirect sources include contamination from fertilizers, soil, and atmospheric deposition, which can lead to MnP uptake in food crops.
Inhalation of MnPs
MnP inhalation has been confirmed by several studies identifying the presence of MnPs in human lungs, with polypropylene and polyethylene terephthalate fibers being the most common. These particles can induce cytotoxicity, inflammation, and oxidative stress in the lungs.
Related Stories
- Ketogenic diet a potential therapy for autism by reshaping gut bacteria and brain inflammation
- Cinnamon, curcumin, and resveratrol show promise in diabetes inflammation fight
- Non-viral gene therapy offers hope for chronic low back pain sufferers
Human exposure to airborne MnPs varies by location, with higher concentrations present in urban areas. Indoor air often contains higher MnP levels than outdoor air, primarily from household sources like carpets and furnishings.
Ingestion of MnPs
MnPs have been found in human feces, indicating ingestion and entry into the gastrointestinal (GI) tract. Infants exhibit higher MnP concentrations due to exposure to plastics in food preparation and storage. Furthermore, MnPs have been found in breast milk and formula, highlighting exposure from early life.
MnPs are also present in various foods and beverages, including seafood, salad, salt, and bottled water. Previous studies suggest that food preparation and packaging also contribute to MnP exposure.
MnP material properties and health risks
MnP properties such as size, shape, and surface conditions influence human health risks. While larger particles are less likely to penetrate biological barriers, smaller particles can enter the bloodstream and other tissues, potentially causing inflammation and oxidative stress.
MnPs have been detected in human blood, stool, placenta, and breast milk, thus indicating systemic circulation. However, understanding of retention and egestion rates in the human body remains limited.
Potential impacts of MnPs on NCDs
MnP exposure can exacerbate symptoms of NCDs like inflammation, oxidative stress, and cell damage. Initial evidence links MnPs to inflammation in the GI tract and respiratory system, which can potentially worsen conditions like Crohn's disease and chronic obstructive pulmonary disease (COPD), respectively.
MnPs may also disrupt tight junctions in epithelial membranes, thereby increasing permeability and facilitating further MnP uptake. This cycle can aggravate pre-existing NCDs and contribute to new health issues.
Pre-existing NCDs can increase MnP uptake due to inflammation and dysregulation of epithelial barriers. This can lead to further translocation of MnPs throughout the body, thereby exacerbating health impacts. For example, colon and liver inflammation from MnP exposure has been linked to insulin resistance in mice, which suggests similar risks in humans.
Health risks from MnP leachates
In addition to their physical effects, MnPs exposure is also associated with chemical risks through their leachates, which include harmful substances like bisphenols and phthalates. These chemicals can cause endocrine disruption, reproductive issues, and cancer. MnPs can also act as carriers for environmental contaminants and subsequently introduce additional health risks upon entering the body.
Future directions
A transdisciplinary one-health approach that integrates ecology, chemistry, biology, and other fields is essential to study MnP transport, fate, dose-response effects, as well as particle and leachate mechanisms. Improved analytical methods, such as micro Raman (μRaman) spectroscopy and mass spectrometry, are also needed to detect smaller MnPs in the environment and human tissues.
Additionally, the utilization of advanced models like organ-on-a-chip and three-dimensional (3D) cell culture can elucidate MnP interactions with human tissues. The insights provided by these studies have the potential to guide risk assessments and interventions to understand MnP impacts on NCDs.
Conclusions
There remains an urgent need for the systematic investigation of MnP impacts on NCD prevalence and severity. Understanding the links between MnP exposure and NCDs is crucial, especially in low-income countries, to designing effective risk reduction strategies and mitigating global health burdens. Taken together, these efforts will align with the United Nations (UN) Sustainable Development Goal Target 3.4 to reduce premature mortality from NCDs.
- Krause, S., Ouellet, V., Allen, D., et al. (2024). The potential of micro- and nanoplastics to exacerbate the health impacts and global burden of non-communicable diseases. Cell Reports Medicine. doi:10.1016/j.xcrm.2024.101581
Posted in: Medical Science News | Medical Research News | Medical Condition News | Disease/Infection News | Healthcare News
Tags: Blood , Breast Milk , Cancer , Cell , Cell Culture , Chemicals , CHIP , Chronic , Chronic Obstructive Pulmonary Disease , Colon , Contamination , Cosmetics , Crohn's Disease , Cytotoxicity , Diabetes , Endocrine , Food , Global Health , Inflammation , Insulin , Insulin Resistance , Liver , Lungs , Mass Spectrometry , Medicine , micro , Mortality , Oxidative Stress , Phthalates , Placenta , Pollution , Research , Respiratory , Salad , Spectrometry , Spectroscopy , Stress
Vijay Kumar Malesu
Vijay holds a Ph.D. in Biotechnology and possesses a deep passion for microbiology. His academic journey has allowed him to delve deeper into understanding the intricate world of microorganisms. Through his research and studies, he has gained expertise in various aspects of microbiology, which includes microbial genetics, microbial physiology, and microbial ecology. Vijay has six years of scientific research experience at renowned research institutes such as the Indian Council for Agricultural Research and KIIT University. He has worked on diverse projects in microbiology, biopolymers, and drug delivery. His contributions to these areas have provided him with a comprehensive understanding of the subject matter and the ability to tackle complex research challenges.
Please use one of the following formats to cite this article in your essay, paper or report:
Kumar Malesu, Vijay. (2024, June 21). How micro- and nanoplastics may worsen non-communicable diseases. News-Medical. Retrieved on June 29, 2024 from https://www.news-medical.net/news/20240621/How-micro-and-nanoplastics-may-worsen-non-communicable-diseases.aspx.
Kumar Malesu, Vijay. "How micro- and nanoplastics may worsen non-communicable diseases". News-Medical . 29 June 2024. <https://www.news-medical.net/news/20240621/How-micro-and-nanoplastics-may-worsen-non-communicable-diseases.aspx>.
Kumar Malesu, Vijay. "How micro- and nanoplastics may worsen non-communicable diseases". News-Medical. https://www.news-medical.net/news/20240621/How-micro-and-nanoplastics-may-worsen-non-communicable-diseases.aspx. (accessed June 29, 2024).
Kumar Malesu, Vijay. 2024. How micro- and nanoplastics may worsen non-communicable diseases . News-Medical, viewed 29 June 2024, https://www.news-medical.net/news/20240621/How-micro-and-nanoplastics-may-worsen-non-communicable-diseases.aspx.
Suggested Reading

Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

Revolutionizing Life Science: An Interview with SCIEX on ASMS, the SCIEX 7500+ System, and AI-Driven Quantitation
Jose Castro-Perez and Chris Lock, SCIEX
In our latest interview, News Medical speaks with SCIEX, a global leader in life science analytical technologies, about their exciting announcements at ASMS, the SCIEX 7500+ System, and how they utilize AI quantitation software to streamline solutions.

From Discovery Biology to ELRIG Chair
Melanie Leveridge
In this interview, we speak with Melanie Leveridge, Vice President of Discovery Biology at AstraZeneca and Chair of the Board for ELRIG UK, to discuss her extensive career in the pharmaceutical industry, her role in fostering scientific innovation, and her vision for ELRIG's future.

Breathing New Life into Diagnostics: Plasmion's SICRIT Technology
Revolutionizing Non-Invasive Diagnostics with Plasmion’s SICRIT Breath Analysis.

Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback

- Open access
- Published: 28 June 2024
Burden and trends of infectious disease mortality attributed to air pollution, unsafe water, sanitation, and hygiene, and non-optimal temperature globally and in different socio-demographic index regions
- Qiao Liu 1 ,
- Jie Deng 1 ,
- Wenxin Yan 1 ,
- Chenyuan Qin 1 ,
- Yaping Wang 1 ,
- Shimo Zhang 1 ,
- Min Liu 1 , 2 &
- Jue Liu ORCID: orcid.org/0000-0002-1938-9365 1 , 2 , 3 , 4 , 5
Global Health Research and Policy volume 9 , Article number: 23 ( 2024 ) Cite this article
Metrics details
Environmental factors greatly impact infectious disease-related mortality, yet there's a lack of comprehensive global studies on the contemporary burden and trends. This study aims to evaluate the global burden and trends of infectious disease mortality caused by air pollution, unsafe water, poor sanitation, and non-optimal temperature across Socio-Demographic Index (SDI) regions from 1990 to 2019.
This observational study utilized data from the Global Burden of Diseases Study to examine mortality rates from infectious diseases attributed to environmental risk factors between 1990 and 2019, including air pollution, unsafe water, sanitation, handwashing facilities (UWSH), and non-optimal temperatures. Age-standardized mortality rates (ASMRs) and estimated annual percentage change (EAPC) were utilized to present infectious disease mortality, and its trajectory influenced by environmental risk factors over the years. Nonlinear regression was conducted to explore the association between the SDI and ASMRs across regions from 1990 to 2019.
In 2019, global infectious disease deaths linked to air pollution, UWSH, and non-optimal temperature reached a startling 2,556,992. Disease mortality varied widely across SDI regions, with the highest number of deaths due to air pollution and UWSH in Low SDI regions, and deaths from non-optimal temperature primarily in High SDI regions. Age disparities emerged, with children under five and the elderly most affected. However, an increasing mortality trend was observed among seniors (65–69, 75–79, and over 80) in High SDI regions due to enteric infections linked to UWSH. Globally, a consistent decrease in ASMR was seen from 1990 to 2019 for all diseases connected to these factors, except for respiratory infections linked to non-optimal temperature.
Conclusions
Our study underscores the significant impact of air pollution, UWSH, and non-optimal temperatures on global infectious disease mortality, particularly among vulnerable groups such as children and the elderly. It's important to tackle these challenges with targeted interventions aiming to enhance environmental quality, improve water and sanitation systems, and control extreme temperatures. In addition, international cooperation is essential for bridging regional disparities and driving global public health initiatives forward, thereby helping achieve Sustainable Development Goals more effectively.
Introduction
Human well-being is significantly impacted by various environmental factors. According to the World Health Organization (WHO), in 2016, 13.7 million deaths, constituting 24% of global mortality, were attributed to modifiable environmental risks, underscoring that nearly one in four global deaths was linked to environmental conditions [ 1 ]. Specifically, air pollution, a contributor to both communicable and noncommunicable diseases, was responsible for approximately one in eight deaths [ 2 ]. Furthermore, cholera, primarily transmitted through faecally contaminated water or food, has affected 47 countries, with an annual report of about 2.9 million cases [ 2 ]. Additionally, inadequate water, sanitation, and hygiene lead to 829 thousand preventable deaths from diarrheal diseases each year, including 297 thousand deaths of children aged 5 and under [ 2 ]. It was also estimated that 1.69 million deaths were attributable to non-optimal temperature globally in 2019 [ 3 ]. These compelling statistics underscore the imperative to recognize and address the pervasive impact of environmental factors on health. The emphasis on the profound influence of environmental factors on global mortality rates necessitates increased awareness and concerted efforts to foster healthier living environments worldwide.
The impact of environmental factors on health is prominently demonstrated in the domain of infectious diseases. Environmental conditions play crucial roles in disease transmission and prevalence, shaping patterns that significantly contribute to global morbidity and mortality. Recent reports have highlighted the close association between emerging infectious diseases and environmental factors, particularly the rise in diseases originating from wildlife [ 4 ]. Previous studies have validated a correlation between common air pollutants and death from lower respiratory infections, revealing that nitrogen dioxide (per 10 μg/m 3 ) and black carbon (per 0.5 10 −5 m −1 ) are linked to a 10% to 12% increase in combined mortality from pneumonia and influenza [ 5 ]. In contrast to air pollution, which primarily leads to noncommunicable disease-related deaths, illnesses resulting from unsafe drinking water predominantly manifest as infectious diseases, including diarrhea and parasitic infections. Prior research has demonstrated that interventions to improve drinking water, sanitation, and hygiene can effectively reduce the incidence of childhood diarrhea in low- and middle-income countries [ 6 , 7 , 8 , 9 ]. However, despite these findings, as of 2020, 2.0 billion people lacked access to safely managed drinking water services, 3.6 billion lacked access to safely managed sanitation services, and 2.3 billion lacked access to handwashing facilities with soap and water at home [ 10 ]. Moreover, climate and weather significantly influence the duration, timing, and intensity of disease outbreaks, reshaping the global landscape of infectious diseases [ 11 ]. For example, a study in China has revealed that each 5 °C increase in average temperature above 10 °C was associated with a 22% (95% CI, 17% to 28%) increase in malaria cases [ 12 ]. Furthermore, the potential expansion of pathogen or vector ranges due to climate change, coupled with increased global connectivity, can potentially facilitate a faster dissemination of pathogens into new areas [ 13 ].
Considering the paramount significance of environmental factors and their profound influence on global welfare, they emerge as vital touchstones within the framework set by the Sustainable Development Goals (SDGs). Notably, they feature prominently in Goal 3 – “Ensure healthy lives and promote well-being for all at all ages”, Goal 6 – “Ensure availability and sustainable management of water and sanitation for all”, and Goal 13 – “Take urgent action to combat climate change and its impacts” [ 14 ]. In this context, the intersection of environmental factors and infectious diseases becomes a critical focus of inquiry. However, a noticeable dearth exists in global-scale studies examining the contemporary burden and trends of infectious diseases attributed to environmental factors, representing a significant gap hindering the realization of SDGs.
This study, acknowledging the existing research void, aims to shed light on the global burden and trends in infectious disease mortality linked to certain environmental factors, focusing on different Socio-Demographic Index (SDI) regions from 1990 to 2019. Through a meticulous exploration of this inquiry, our findings have the potential to offer valuable insights into the evolving landscape of infectious diseases influenced by certain environmental factors and the regional variations therein. This contribution seeks to enhance our nuanced understanding of the intricate interplay between global health and environmental conditions, ultimately contributing to the fulfillment of SDGs.
Study design
This was an observational study using data obtained from the 2019 Global Burden of Disease study (GBD 2019) result tools. The GBD results, a comprehensive regional and global research program encompassing hundreds of diseases, injuries, and risk factors, allows researchers access to a wealth of global health data [ 15 ]. This observational study capitalized on this extensive dataset to analyze and draw conclusions about particular health concerns.
The number of deaths with its 95% uncertainty interval (UI) per year, and their mortality rates with 95% UIs of infectious diseases attributed to environmental risk factors were extracted. Infectious diseases included enteric infections (diarrheal diseases, specifically referring to infectious diarrheal diseases), respiratory infections (lower respiratory infections, upper respiratory infections, and otitis media), and other infectious diseases (encephalitis and meningitis). Environmental risk factors in this study included air pollution (ambient particulate matter pollution and household air pollution from solid fuels), non-optimal temperature (high temperature and low temperature), and unsafe water, sanitation, and handwashing (UWSH) (unsafe water source, unsafe sanitation, and no access to handwashing facility). The Socio-demographic Index (SDI) of 21 GBD regions from 1990 to 2019 was also extracted from the GBD 2019 result tools. The SDI is a composite indicator of development status strongly correlated with health outcomes. It is the geometric mean of 0 to 1 indices of total fertility rate under the age of 25, mean education for those ages 15 and older, and lag distributed income per capita. As a composite, a country with an SDI of 0 would have a theoretical minimum level of development relevant to health, while a country with an SDI of 1 would have a theoretical maximum level. Low SDI was between 0 and 0.455, Low-middle SDI was between 0.455 and 0.608, Middle SDI was between 0.608 and 0.690, High-middle SDI was between 0.690 and 0.805, and High SDI was between 0.805 and 1 [ 16 ].
Data collection and processing
Data was gathered from the GBD 2019 result tools, established by the GBD group [ 15 ]. The general methodological approaches to estimate the mortality were described elsewhere [ 17 ]. Briefly, all available data on causes of death and exposure of risk factors were standardized and pooled into a single database used to generate cause-specific estimates by age, sex, year, and geography; then multiple models, such as cause of death ensemble modelling, disease model-Bayesian meta-regression, comorbidity correction and so on were used to estimate comparable data of different diseases across the world [ 17 ]. Furthermore, GBD study used a model to link the death rates of infectious diseases to environmental risk factors. The GBD measured how people are exposed to these risks, how these exposures are related to health outcomes, and the percentage of deaths that would be prevented by reducing exposure to these risks. This approach, however, may vary, and captures uncertainty regarding the quality of data and the certitude of the used models [ 18 ].
We reported the death results of infectious diseases attributed to air pollution, UWSH, and non-optimal temperature, in five SDI regions (High, High-middle, Middle, Low-middle, and Low SDI regions) and the global total data from 1990 to 2019, and arranged incidence and death data into successive 5-year age intervals from < 5 years to 75–79 years, plus the 80 + years group.
Statistical analysis
The absolute number of deaths represented the actual impact of infectious disease mortality attributed to environmental risk factors in each SDI region and at global level, and its relative change was defined as \(\frac{{Number}_{2019}-{Number}_{1990}}{{Number}_{1990}}\times 100\%\) , which showed the overall change between 1990 and 2019. Age-standardized mortality rate (ASMR), which were directly extracted from the GBD result tool, [ 15 ] were calculated by applying the age-specific rates to a GBD World Standard Population, and were used to compare populations with different age structures or for the same population over time in which the age profiles changed accordingly.
The Estimated Annual Percentage Change (EAPC) is a commonly used tool to quantified the rate trend over a specific interval [ 19 , 20 ]. A regression line was fitted to the natural logarithm of the rates ( y = α + βx + ε , where y = ln(rate) and x = calendar year). EAPC was calculated as \(({e}^{\beta }-1)\times 100\%\) , with 95% confidence intervals (CIs) obtained from the linear regression model. In this study, overall EAPC was calculated by the annual ASMR of each category of infectious diseases attributed to environmental risk factors in five SDI regions and at global level, and EAPC in different age groups was calculated by the age-specific mortality rate. The term “increase” was used to describe trends when the EAPC and its lower boundary of 95% CI were both > 0. In contrast, “decrease” was used when the EAPC and its upper boundary of 95% CI, were both < 0. Otherwise, the term “stable” was used.
The population attributable fraction (PAF), which represents the proportion of risk that would be reduced in a given year if the exposure to a risk factor in the past were reduced to an ideal exposure scenario [ 17 ]. In this study, we extracted mortality data for all causes of infectious diseases and calculated the PAF of certain risk factors for certain infectious diseases in each year by the formula: \(\frac{death\;number\;attributed\;to\;certain\;risk\;factors}{death\;number\;by\;all\;causes}\times100\%\) .
Finally, we conducted a non-linear regression (second order polynomial) to explore the association between SDI and ASMRs in 21 GBD regions throughout 1990 to 2019. A regression curve was fitted to the ASMR ( y = α + βx + γx 2 , where y = the value of ASMRs and x = SDI).
All the statistical analyses were conducted using the R program (version 4.4.1).
Burden and trends of infectious disease mortality attributed to air pollution, UWSH, and non-optimal temperature from 1990 to 2019
In 2019, global infectious disease deaths attributed to environmental risk factors reached a staggering 2,556,992, with contributions from air pollution, UWSH, and non-optimal temperature of 763,291, 1,656,887, and 245,814 deaths, respectively. The predominant cause of infectious disease deaths associated with air pollution was respiratory infections, contributing to 749,254 fatalities globally in 2019 (95% UI, 573,848 to 959,290). UWSH primarily resulted in deaths from enteric infections, while non-optimal temperature mainly caused respiratory infections, with 1,386,769 (95% UI, 978,063 to 2,009,500) and 245,814 (95% UI, 174,760 to 342,302) deaths, respectively, in 2019.
Examining different SDI regions in 2019, the highest number of infectious disease deaths attributed to air pollution and UWSH occurred in the Low SDI region, with 330,074 (95% UI, 250,942 to 423,208) respiratory infections attributed to air pollution, 6,546 (95% UI, 5,096 to 8,419) enteric infections attributed to air pollution, 2,529 (95% UI, 1,962 to 3,317) deaths from other infectious diseases attributed to air pollution, 640,329 (95% UI, 480,412 to 858,264) enteric infections attributed to UWSH, and 130,090 (95% UI, 58,429 to 200,590) respiratory infections attributed to UWSH. However, in the case of respiratory infections attributed to non-optimal temperatures, the highest death toll was observed in High SDI regions, with 69,216 (95% UI, 51,479 to 88,585) deaths in 2019 (Table 1 ).
On a global scale, enteric infections, attributed to UWSH, were responsible for the highest number of deaths from 1990 to 2019, ranging from 52.01% to 54.67%. This trend persisted in Middle, Low-middle, and Low SDI regions, where enteric infections attributed to UWSH constituted 44.88% to 49.03%, 59.35% to 61.57%, and 55.10% to 56.89% of all deaths, respectively, from 1990 to 2019. Conversely, in the High-middle SDI region, respiratory infections attributed to air pollution dominated deaths from 1990 to 2015 (34.65% to 38.30%). Subsequently, respiratory infections attributed to non-optimal temperature became the primary cause of deaths from 2016 to 2019, accounting for over 37%. Moreover, in the High SDI region, respiratory infections attributed to non-optimal temperature constituted more than 60% of deaths from 1990 to 2019 (Fig. 1 ).

Proportions of deaths of infectious diseases attributed to air pollution, UWSH, and non-optimal temperature from 1990 to 2019, globally and by SDI regions. SDI, Socio-Demographic Index; UWSH, unsafe water, sanitation, and handwashing
Among the three categories of infectious diseases tied to air pollution, respiratory infections had the highest ASMR both in 1990 (27.71 per 100,000 population, 95% UI, 21.66 to 34.76) and 2019 (10.38 per 100,000 population, 95% UI, 7.89 to 13.28). UWSH and non-optimal temperature primarily resulted in enteric infections and respiratory infections, with ASMRs of 18.94 (95% UI, 13.59 to 26.96) and 3.41 (95% UI, 2.42 to 4.77) per 100,000 population in 2019 (Table 1 ).
All infectious diseases attributed to air pollution, UWSH, and non-optimal temperature exhibited declining trends in ASMR globally from 1990 to 2019, with the most rapid decrease observed in enteric infections attributed to air pollution (EAPC = -5.20%, 95% CI, -5.52% to -4.78%). This category decreased from 0.74 (95% CI, 0.52 to 0.93) per 100,000 population in 1990 to 0.16 (95% CI, 0.13 to 0.20) per 100,000 population in 2019. Following closely were enteric infections attributed to UWSH, exhibiting an average annual decrease of 3.73% (95% CI, 3.60% to 3.85%), declining from 8.44 (95% UI, 3.63 to 12.97) per 100,000 in 1990 to 3.74 (95% UI, 1.66 to 5.83) per 100,000 in 2019.
Analyzing within different SDI regions, the highest ASMRs of infectious diseases associated with air pollution, UWSH, and non-optimal temperature were consistently observed in Low SDI regions, in both 1990 and 2019. Across all SDI regions, the ASMRs of infectious diseases attributed to air pollution, UWSH, and non-optimal temperature demonstrated declining patterns from 1990 to 2019 (all p < 0.05) (Fig. 2 ).

Trends of ASMRs of infectious diseases attributed to air pollution, UWSH, and non-optimal temperature from 1990 to 2019, globally and by SDI regions. ASMR, Age-standardized mortality rate; SDI, Socio-Demographic Index; UWSH, unsafe water, sanitation, and handwashing
Age disparities of infectious disease mortality attributed to air pollution, UWSH, and non-optimal temperature
Figure 3 illustrated the global mortality rates of infectious diseases that are attributable to air pollution, UWSH, and non-optimal temperature, in various SDI regions, and across different age groups for the years 1990 and 2019. Notably, air pollution was exclusively linked with deaths from enteric infections and other infectious diseases only in children under the age of 5, with this correlation not being observed in other age groups. The highest mortality rates were observed in the Low SDI region in 2019: 3.83 (95% UI, 2.98 to 4.93) per 100,000 for enteric infections and 1.48 (95% UI, 1.15 to 1.94) per 100,000 for other infectious diseases.

Mortality of infectious diseases attributed to air pollution, UWSH, and non-optimal temperature in different age groups, in 1990 and 2019, globally and by SDI regions. SDI, Socio-Demographic Index; UWSH, unsafe water, sanitation, and handwashing
In cases of respiratory infections attributed to air pollution, non-optimal temperature, UWSH, and enteric infections due to UWSH, both children under five years old and the elderly were significantly impacted. In 2019, the global mortality rates for these conditions in children under 5 were 45.90 (95% UI, 33.50 to 60.41), 8.69 (95% UI, 4.90 to 16.17), 17.24 (95% UI, 7.78 to 27.39), and 71.02 (95% UI, 54.77 to 92.29) per 100,000 population, respectively. In individuals aged over 80, the rates were 101.96 (95% UI, 74.03 to 135.37), 66.46 (95% UI, 49.13 to 87.47), 33.08 (95% UI, 14.11 to 52.85), and 202.05 (95% UI, 116.59 to 330.79) per 100,000 population, respectively. Low SDI regions consistently reported the highest mortality rates across all age groups.
From 1990 to 2019, most age brackets showed a downward trend in mortality rates for respiratory infections resulting from air pollution, non-optimal temperature, UWSH, along with enteric infections attributed to UWSH. Children under the age of 5 exhibited the most significant decline in all diseases and SDI regions. However, in High SDI region, there were increasing trends in mortality rates for enteric infections attributed to UWSH among individuals aged 65–69 (EAPC = 0.38%, 95% CI, 0.02% to 0.75%), 75–79 (EAPC = 0.61%, 95% CI, 0.02% to 1.20%), and over 80 years (EAPC = 1.81%, 95% CI, 1.20% to 2.42%) (Fig. 4 ).

EAPC of mortality of infectious diseases attributed to air pollution, UWSH, and non-optimal temperature in different age groups, from 1990 to 2019, globally and by SDI regions. EAPC, Estimated Annual Percentage Change; SDI, Socio-Demographic Index; UWSH, unsafe water, sanitation, and handwashing
PAF of environmental risk factors for infectious disease mortality
On a global scale, diarrheal diseases emerged as the predominant cause of death among infectious diseases linked to environmental risk factors, with lower respiratory infections following closely. The primary contributors to diarrheal disease deaths were unsafe sanitation, an insecure water source, and lack of access to handwashing facilities. Ambient particulate matter pollution and household air pollution from solid fuel played subsidiary roles in a minority of diarrheal disease deaths. Lower respiratory infections were attributed to factors such as the absence of handwashing facilities, ambient particulate matter pollution, household air pollution from solid fuel, high temperature, and low temperature. These conditions persisted across Middle, Low-middle, and Low SDI regions. However, in High and High-middle SDI regions, lower respiratory infections accounted for the majority of infectious disease deaths (Fig. 5 ).

Contribution Proportion of air pollution, UWSH, and non-optimal temperature to Infectious Disease Mortality, in 1990 and 2019, globally and by SDI regions. SDI, Socio-Demographic Index
Examining the global scenario, for deaths related to diarrheal diseases, the highest PAF in 2019 was associated with an unsafe water source (PAF = 80.17%), followed by unsafe sanitation (49.31%), and lack of access to handwashing facilities (23.32%). Concerning lower respiratory infections, household air pollution stemming from solid fuels had the highest PAF (16.96% in 2019), followed by ambient particulate matter pollution (13.09%), and the absence of handwashing facilities (10.83%). Moreover, the PAF of household air pollution played a central role in lower respiratory infections across Middle, Low-middle, and Low SDI regions. In contrast, High and High-middle SDI regions were primarily impacted by low temperature (17.43% in High SDI region and 11.77% in High-middle SDI region, in 2019). Notably, the PAF of ambient particulate matter pollution for lower respiratory infections exhibited an upward trend from 1990 to 2019. This trend was consistent in Middle (from 13.10% to 16.77%), Low-middle (from 7.62% to 18.16%), and Low (from 4.79% to 10.33%) SDI regions. Similarly, the PAF of high temperature for lower respiratory infections also exhibited an upward trajectory in these three SDI regions, rising from 2.50% to 2.61%, 5.12% to 5.58%, and 5.09% to 5.41%, from 1990 to 2019 respectively (Table 2 ).
Association between SDI and infectious disease mortality attributed to air pollution, UWSH, and non-optimal temperature in 21 GBD regions
For enteric infections attributed to air pollution and UWSH, as well as other infectious diseases attributed to air pollution, and respiratory infections attributed to air pollution and UWSH, there was a consistent decrease in the ASMR of infectious diseases with the rise in SDI. The second order polynomial regression revealed a strong correlation (R-squared ranging from 0.78 to 0.91). Nonetheless, for respiratory infections triggered by non-optimal temperatures, the association between ASMR and SDI lacked statistical significance (R-squared of the second order polynomial regression was lower than 0.1).
On analyzing particular diseases, the Caribbean displayed the highest ASMR for enteric infections and other infectious diseases resulting from air pollution, surpassing other regions with similar SDIs. In contrast, Central, Western, and Southern Sub-Saharan Africa reported the highest ASMR for respiratory infections attributed to air pollution and UWSH compared to other regions with comparable SDIs. Additionally, South Asia recorded the highest ASMR for enteric infections attributed to UWSH when compared to regions with similar SDIs (Fig. 6 ).

The correlation between ASMR of infectious diseases attributed to air pollution, UWSH, and non-optimal temperature and SDI in 21 GBD regions. ASMR, Age-standardized mortality rate; SDI, Socio-Demographic Index; GBD, Global Burden of Disease Study; UWSH, unsafe water, sanitation, and handwashing
To the best of our knowledge, this study represented the first comprehensive effort to outline the current burden of infectious disease mortality attributed to air pollution, UWSH, and non-optimal temperature, both globally and within various SDI regions, encompassing the estimation of its longitudinal trends over the past three decades. In summary, the analysis highlights the significant impact of certain environmental risk factors on global infectious disease mortality. Respiratory infections attributed to air pollution and enteric infections attributed to UWSH were particularly noteworthy, causing a substantial number of deaths globally, with the Low SDI region recording the highest infectious disease deaths. Both children under five years old and the elderly bore the greatest impact from air pollution, UWSH, and non-optimal temperature. While overall mortality rates showed a declining trend from 1990 to 2019, an increasing trend was observed in the High SDI region in mortality rates for enteric infections attributed to UWSH among individuals aged 65–69, 75–79, and over 80 years. Interestingly, non-optimal temperatures served as the main causes for respiratory infection deaths in High and High-middle SDI regions, while household air pollution was a fundamental contributor in lower respiratory infections across Middle, Low-middle, and Low SDI regions. Furthermore, specific infectious diseases exhibited higher mortality rates in the Caribbean, Sub-Saharan Africa (especially Central, Western, and Southern regions), and South Asia. A thorough understanding of these intricate trends and geographical variations is essential in crafting targeted interventions and policies to mitigate the impact of environmental risk factors on infectious disease mortality.
In our study, we found that respiratory infections attributed to air pollution was particularly noteworthy, contributing to 749,254 fatalities globally in 2019. This finding underscores the previously acknowledged contribution of air pollution to one in eight deaths from all diseases, emphasizing the substantial impact on infectious disease mortality [ 2 ]. Inhalation of combustion-derived material has been shown to heighten vulnerability to airway infections, as evidenced by Logan's seminal Lancet paper reporting a threefold increase in pneumonia-related deaths during the 1952 London smog, particularly affecting the very young and elderly [ 21 ]. Pneumonia notifications surged 1.4-fold during the smog and 2.4- to 2.7-fold in the following two weeks compared to the 1947–1951 weekly average. Bell et al. estimated pneumonia as a significant cause of the 12,000 excess deaths from the 1952 London smog [ 22 ]. Additionally, various combustion sources, such as environmental tobacco smoke in Vietnam, have been associated with a 1.5-fold increased risk for childhood pneumonia, with 28% of cases attributable to environmental tobacco smoke [ 23 ]. Mechanistic evidence was also emerging for bacterial pneumonia, with urban PM found to enhance pneumococcal adhesion by boosting platelet-activating factor receptor expression on airway epithelial cells, and NO 2 exposure increasing the expression of the rhinovirus entry receptor in nasal epithelial cells [ 24 , 25 ]. However, the precise impact of PM and NO 2 on RSV infection remains uncertain [ 26 ]. Moving forward, policies aimed at reducing air pollution and mitigating its adverse health effects, particularly targeting vulnerable populations, are imperative to combating the burden of infectious diseases associated with air pollution.
In addition to air pollution, our study highlights the impact of non-optimal temperature on mortality from lower respiratory infections, particularly in High and High-middle SDI regions. Previous research has demonstrated that low temperatures were the second leading risk factor for respiratory infection deaths in America in 2019, accounting for 15.3% of fatalities, with smoking as the first leading risk factor [ 27 ]. Moreover, studies have shown that a 1 °C increase in maximum temperature was associated with a 4.2% and 3.4% increase in hospital admissions for acute lower respiratory infections among children aged 3–5 years during the dry and rainy seasons, respectively [ 28 ]. While cold effects predominate in most regions, areas with high prevailing temperatures can experience substantial heat-related effects that far exceed the burden attributable to cold temperatures [ 3 ]. Non-optimal temperatures can significantly impact respiratory infections by influencing the formation and development of microbial biofilms, a major factor in respiratory tract infection pathologies, whereby the growth and virulence of pathogenic microorganisms such as Streptococcus pneumoniae and nontypeable Haemophilus influenzae can be enhanced under such stressed conditions, further promoting the recurrence and chronicity of diseases [ 29 , 30 ]. Given these findings, it is imperative to implement strategies aimed at mitigating the adverse health impacts of temperature extremes. This may include initiatives to improve urban planning and infrastructure to mitigate the urban heat island effect and enhance resilience to extreme temperatures. Additionally, targeted public health interventions and awareness campaigns could help vulnerable populations better adapt to temperature extremes and reduce their susceptibility to respiratory infections.
Moreover, we found that the PAF of ambient particulate matter pollution and high temperature for lower respiratory infections exhibited an upward trend from 1990 to 2019, in Middle, Low-middle, and Low SDI regions. In areas with lower SDI, potential issues such as inadequate public health facilities, malnutrition, and low awareness of preventive measures among residents make these populations more susceptible to the impacts of environmental particulate matter pollution and high temperatures. This might be a contributing factor to the observed phenomenon. In one study, Zhao and his team found a clear association between particulate matter pollution and respiratory diseases in Dongguan, China [ 31 ]. High temperatures are another major factor causing an increase in the rate of respiratory infections. A research study by Horne et al. stated that a rise in the concentration of particulate pollution exacerbateed the effects of weather on acute lower respiratory infections [ 32 ]. From these studies, it can be inferred that in low SDI areas, the PAF of lower respiratory infections caused by environmental particulate matter pollution and high temperatures shows an upward trend, reflecting the effects of these factors and regional characteristics on population health.
Enteric infection deaths, primarily stemming from diarrheal diseases and attributed to UWSH, were observed to be of concern across all SDI regions in our study. Even in the High SDI region, there were discernible increasing trends in mortality rates for enteric infections attributed to UWSH among individuals aged 65–69, 75–79, and over 80 years. Diarrhea could have a devastating effect on quality of life in the elderly, and the impact of diarrhea might be more pronounced in the elderly due to various causes, such as age-related structural and functional intestinal changes, consume of preventive and therapeutic drugs, compromised nutrition and hydration to withstand the effect of diarrhea, more frequent hospital admissions and courses of antibiotics, and more subtle clinical presentation than in younger patients [ 33 ]. Moreover, in nations with higher SDIs, robust health surveillance systems enable more accurate detection and documentation of diarrheal cases. However, the reliance on centralized water supply systems in these countries may also be a contributing factor. Despite being more prevalent and reliable in developed societies, these systems may still face water quality challenges, impacting diarrheal incidence [ 34 ]. Conversely, in countries with lower SDIs, the risk of diarrheal transmission may escalate due to insufficient sanitation facilities and limited hygiene education. Water quality issues, even with access to basic water supply, could contribute to diarrheal outbreaks if the water becomes contaminated. For instance, in many African cities, anthropogenic contamination of groundwater often arises from industrial discharge and untreated sewage [ 35 ]. Ensuring safe and readily available water is crucial for public health, whether for drinking, domestic use, and food production, or recreational activities. Improving water supply and sanitation, alongside enhanced management of water resources, can not only enhance economic growth but also significantly contribute to poverty reduction [ 36 ]. The multifaceted benefits of prioritizing safe water management underscore the interconnectedness of water-related initiatives with broader socio-economic goals, highlighting the pivotal role of water resources in advancing overall community well-being.
Children under 5 and the elderly, were disproportionately affected. Globally, acute lower respiratory infection remains one of the leading causes of morbidity and mortality in children younger than 5 years [ 37 ]. Antenatal exposure to air pollution may increase infants' vulnerability to respiratory infections [ 38 ]. This vulnerability could be due to underdeveloped lungs in infants with lower birth weight [ 39 ]. Postnatal lung development is crucial, with early insults potentially having lasting impacts [ 40 ]. In a Czech Republic study monitoring 1,130 children for 4.5 years, a 30% higher risk of bronchitis was found in children under 2 for every 25 mg/m 3 increase in 30-day average PM2.5 [ 41 ]. A recent meta-analysis of 10 European birth cohorts associated PM10 and traffic exposure with increased pneumonia risk in 16,059 children across six countries [ 42 ]. While the specific timing of pollution exposure wasn't pinpointed, chronic exposure to traffic-derived air pollution was strongly linked to heightened childhood respiratory infection risk. Unsafe water, sanitation, and hygiene cause over 1 million infectious disease deaths annually, with children under 5 bearing a disproportionate burden [ 18 , 43 ]. Diarrhea profoundly affects the elderly's quality of life, possibly exacerbated by age-related intestinal changes, medication use, nutritional challenges, frequent hospitalizations, antibiotic courses, and subtle clinical presentations [ 33 ]. To mitigate the impact of environmental factors on vulnerable populations such as children and the elderly, comprehensive protective measures should be implemented. This includes enhancing environmental protection measures for pregnant women to safeguard fetal health and improving the quality of drinking water to prevent contamination-related illnesses in both age groups. Additionally, efforts to monitor and improve air quality are essential to minimize the respiratory health risks posed by air pollution to both children and the elderly. Regular health check-ups for these vulnerable populations, along with prompt identification and management of potential infection symptoms, are crucial steps in safeguarding their overall health and well-being.
In our findings, Low SDI region recording the highest infectious disease deaths attributed to air pollution, UWSH, and non-optimal temperature. Moreover, the Caribbean, Sub-Saharan Africa (especially Central, Western, and Southern regions), and South Asia displayed higher mortality rates for enteric infections attributed to air pollution, respiratory infections attributed to air pollution and UWSH, and enteric infections attributed to UWSH. Given the significant disparities in infectious disease mortality attributed to environmental factors across different regions, strengthening international cooperation and health assistance is imperative. This could involve collaborative efforts in sharing knowledge, expertise, and resources to address the specific challenges faced by each region. Additionally, international aid programs focused on improving healthcare infrastructure, sanitation facilities, and access to clean water can play a crucial role in reducing the burden of infectious diseases attributed to environmental factors in regions with higher mortality rates. By fostering global partnerships and solidarity, we can work towards achieving better health outcomes for all populations, regardless of geographical location.
This study had some limitations. First, the use of yearly data from the GBD database may have led to misestimation of the disease burden in instances where original data were sparse or missing, as estimates were derived from models. Secondly, due to statistical constraints of the GBD results, only six individual diseases and seven individual risk factors were reported. Thirdly, our analysis was limited to regional-level findings, overlooking potential variations at the national level within each region. Fourth, our analysis is based on the GBD 2019 dataset, which does not cover the extensive changes in environmental factors and health outcomes that have potentially been influenced by the global COVID-19 pandemic. Therefore, the findings of this study may not reflect the situation after the COVID-19 onset. As such, a follow-up study with the GBD 2021 dataset is warranted to provide valuable insights into post-COVID-19 changes. However, despite these limitations, our findings underscore the critical need for regional cooperation in addressing infectious disease mortality attributable to environmental factors, serving as a vital call to action for global health initiatives.
Our findings emphasize the significant role that air pollution, UWSH, and non-optimal temperature play in global infectious disease mortality. Respiratory and enteric infections attributed to air pollution and UWSH present considerable challenges, particularly for vulnerable populations such as children under five and the elderly. Addressing these challenges calls for targeted interventions and policies that focus on improving environmental quality, bolstering water and sanitation infrastructure, and controlling temperature extremes. Prioritizing the health and well-being of these vulnerable populations is crucial in reducing the burden of infectious diseases and further advancing global public health. Moreover, fortifying international cooperation is key to bridging the disparities across regions, propelling global public health endeavors, and achieving the SDGs.
Availability of data and materials
Data are available from the corresponding author by request.
World Health Organization. Environmental health: Impact. 2024. https://www.who.int/health-topics/environmental-health#tab=tab_2 . Accessed 5 Feb 2024.
Google Scholar
World Health Organization. Healthy environments for healthier populations: Why do they matter, and what can we do? 2019–9–13. https://iris.who.int/bitstream/handle/10665/325877/WHO-CED-PHE-DO-19.01-eng.pdf?sequence=1 . Accessed 5 Feb 2024.
Burkart KG, Brauer M, Aravkin AY, et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet. 2021;398(10301):685–97. https://doi.org/10.1016/s0140-6736(21)01700-1 .
Article PubMed PubMed Central Google Scholar
Jones KE, Patel NG, Levy MA, et al. Global trends in emerging infectious diseases. Nature. 2008;451(7181):990–3. https://doi.org/10.1038/nature06536 .
Article CAS PubMed PubMed Central Google Scholar
Liu S, Lim YH, Chen J, et al. Long-term Air Pollution Exposure and Pneumonia-related Mortality in a Large Pooled European Cohort. Am J Respir Crit Care Med. 2022;205(12):1429–39. https://doi.org/10.1164/rccm.202106-1484oc .
Article CAS PubMed Google Scholar
Freeman MC, Garn JV, Sclar GD, et al. The impact of sanitation on infectious disease and nutritional status: A systematic review and meta-analysis. Int J Hyg Environ Health. 2017;220(6):928–49. https://doi.org/10.1016/j.ijheh.2017.05.007 .
Article PubMed Google Scholar
Clasen TF, Alexander KT, Sinclair D, et al. Interventions to improve water quality for preventing diarrhoea. Cochrane Database Syst Rev. 2015;2015(10):Cd004794. https://doi.org/10.1002/14651858.cd004794.pub3 .
Norman G, Pedley S, Takkouche B. Effects of sewerage on diarrhoea and enteric infections: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10(8):536–44. https://doi.org/10.1016/s1473-3099(10)70123-7 .
Wolf J, Hubbard S, Brauer M, et al. Effectiveness of interventions to improve drinking water, sanitation, and handwashing with soap on risk of diarrhoeal disease in children in low-income and middle-income settings: a systematic review and meta-analysis. Lancet. 2022;400(10345):48–59. https://doi.org/10.1016/s0140-6736(22)00937-0 .
World Health Organization, UNICEF, World Health Organization, United Nations Children’s Fund. Progress on household drinking water, sanitation and hygiene 2000–2020: five years into the SDGs. 2021. https://www.who.int/publications-detail-redirect/9789240030848 . Accessed 5 Feb 2024.
Bezirtzoglou C, Dekas K, Charvalos E. Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Anaerobe. 2011;17(6):337–40. https://doi.org/10.1016/j.anaerobe.2011.05.016 .
Liu Z, Wang S, Zhang Y, et al. Effect of temperature and its interactions with relative humidity and rainfall on malaria in a temperate city Suzhou. China Environ Sci Pollut Res Int. 2021;28(13):16830–42. https://doi.org/10.1007/s11356-020-12138-4 .
Baker RE, Mahmud AS, Miller IF, et al. Infectious disease in an era of global change. Nat Rev Microbiol. 2022;20(4):193–205. https://doi.org/10.1038/s41579-021-00639-z .
United Nations. Sustainable Development Goals. 2024. https://sdgs.un.org/goals . Accessed 5 February 2024.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. 2019. https://vizhub.healthdata.org/gbd-results/ . Accessed 5 Feb 2024.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. 2020. http://ghdx.healthdata.org/record/ihme-data/gbd-2019-socio-demographic-index-sdi-1950-2019 . Accessed 5 Feb 2024.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. https://doi.org/10.1016/s0140-6736(20)30925-9 .
Article Google Scholar
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49. https://doi.org/10.1016/s0140-6736(20)30752-2 .
Article CAS Google Scholar
Li XY, Hou MJ, Kong XM, et al. The congenital birth defects burden in children younger than 14 years of age, 1990–2019: An age-period-cohort analysis of the global burden of disease study. J Glob Health. 2024;14:04012. https://doi.org/10.7189/jogh.14.04012 .
Liu Q, Jing W, Liu M, Liu J. Health disparity and mortality trends of infectious diseases in BRICS from 1990 to 2019. J Glob Health. 2022;12:04028. https://doi.org/10.7189/jogh.12.04028 .
Logan WP. Mortality in the London fog incident, 1952. Lancet. 1953;1(6755):336–8. https://doi.org/10.1016/s0140-6736(53)91012-5 .
Bell ML, Davis DL. Reassessment of the lethal London fog of 1952: novel indicators of acute and chronic consequences of acute exposure to air pollution. Environ Health Perspect. 2001;109 Suppl 3(Suppl 3):389–94. https://doi.org/10.1289/ehp.01109s3389 .
Suzuki M, Thiem VD, Yanai H, et al. Association of environmental tobacco smoking exposure with an increased risk of hospital admissions for pneumonia in children under 5 years of age in Vietnam. Thorax. 2009;64(6):484–9. https://doi.org/10.1136/thx.2008.106385 .
Mushtaq N, Ezzati M, Hall L, et al. Adhesion of Streptococcus pneumoniae to human airway epithelial cells exposed to urban particulate matter. J Allergy Clin Immunol. 2011;127(5):1236-42.e2. https://doi.org/10.1016/j.jaci.2010.11.039 .
Spannhake EW, Reddy SP, Jacoby DB, et al. Synergism between rhinovirus infection and oxidant pollutant exposure enhances airway epithelial cell cytokine production. Environ Health Perspect. 2002;110(7):665–70. https://doi.org/10.1289/ehp.02110665 .
Grigg J. Air Pollution and Respiratory Infection: An Emerging and Troubling Association. Am J Respir Crit Care Med. 2018;198(6):700–1. https://doi.org/10.1164/rccm.201804-0614ed .
Zhong W, Bragazzi NL, Kong JD, et al. Burden of Respiratory Infection and Tuberculosis Among US States from 1990 to 2019. Clin Epidemiol. 2021;13:503–14. https://doi.org/10.2147/clep.s314802 .
Ngo HKT, Luong LMT, Le H, et al. Impact of temperature on hospital admission for acute lower respiratory infection (ALRI) among pre-school children in Ho Chi Minh City. Vietnam Int J Biometeorol. 2021;65(7):1205–14. https://doi.org/10.1007/s00484-021-02104-1 .
Kyd JM, Krishnamurthy A, Kidd S. Interactions and mechanisms of respiratory tract biofilms involving Streptococcus pneumoniae and nontypeable Haemophilus influenzae. In: Dharumadurai D, Nooruddin T, editors. Microbial Biofilms-Importance and Applications. InTech; 2016. Available from: https://doi.org/10.5772/61499 .
Alotaibi GF, Bukhari MA. Factors influencing bacterial biofilm formation and development. Am J Biomed Sci Res. 2021;12(6):617–26. https://doi.org/10.34297/AJBSR.2021.12.001820 .
Zhao Y, Wang S, Lang L, et al. Ambient fine and coarse particulate matter pollution and respiratory morbidity in Dongguan. China Environ Pollut. 2017;222:126–31. https://doi.org/10.1016/j.envpol.2016.12.070 .
Horne BD, Joy EA, Hofmann MG, et al. Short-Term Elevation of Fine Particulate Matter Air Pollution and Acute Lower Respiratory Infection. Am J Respir Crit Care Med. 2018;198(6):759–66. https://doi.org/10.1164/rccm.201709-1883oc .
Truninger K. Diarrhea in the elderly. Ther Umsch. 2014;71(9):545–50. https://doi.org/10.1024/0040-5930/a000550 .
Mac Kenzie WR, Hoxie NJ, Proctor ME, et al. A massive outbreak in Milwaukee of cryptosporidium infection transmitted through the public water supply. N Engl J Med. 1994;331(3):161–7. https://doi.org/10.1056/nejm199407213310304 .
Reaver KM, Levy J, Nyambe I, et al. Drinking Water Quality and Provision in Six Low-Income, Peri-Urban Communities of Lusaka, Zambia. Geohealth. 2021;5(1):e2020GH000283. https://doi.org/10.1029/2020gh000283 .
World Health Organization. Drinking-water: overview. 2023. https://www.who.int/news-room/fact-sheets/detail/drinking-water#:~:text=Safe%20and%20readily%20available%20water%20is%20important%20for,growth%20and%20can%20contribute%20greatly%20to%20poverty%20reduction . Accessed 5 February 2024.
Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027–35. https://doi.org/10.1016/s0140-6736(16)31593-8 .
Jedrychowski WA, Perera FP, Spengler JD, et al. Intrauterine exposure to fine particulate matter as a risk factor for increased susceptibility to acute broncho-pulmonary infections in early childhood. Int J Hyg Environ Health. 2013;216(4):395–401. https://doi.org/10.1016/j.ijheh.2012.12.014 .
Brugha R, Grigg J. Urban air pollution and respiratory infections. Paediatr Respir Rev. 2014;15(2):194–9. https://doi.org/10.1016/j.prrv.2014.03.001 .
Shaheen SO, Barker DJ, Shiell AW, et al. The relationship between pneumonia in early childhood and impaired lung function in late adult life. Am J Respir Crit Care Med. 1994;149(3 Pt 1):616–9. https://doi.org/10.1164/ajrccm.149.3.8118627 .
Hertz-Picciotto I, Baker RJ, Yap PS, et al. Early childhood lower respiratory illness and air pollution. Environ Health Perspect. 2007;115(10):1510–8. https://doi.org/10.1289/ehp.9617 .
MacIntyre EA, Gehring U, Mölter A, et al. Air pollution and respiratory infections during early childhood: an analysis of 10 European birth cohorts within the ESCAPE Project. Environ Health Perspect. 2014;122(1):107–13. https://doi.org/10.1289/ehp.1306755 .
Prüss-Ustün A, Wolf J, Bartram J, et al. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: An updated analysis with a focus on low- and middle-income countries. Int J Hyg Environ Health. 2019;222(5):765–77. https://doi.org/10.1016/j.ijheh.2019.05.004 .
Download references
Acknowledgements
We appreciate the works by the GBD collaborators.
This work was supported by the National Key Research and Development Project of China (grant numbers 2021ZD0114101). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the paper.
Author information
Authors and affiliations.
Department of Epidemiology and Biostatistics, School of Public Health, Peking University, No. 38, Xueyuan Road, Haidian District, Beijing, 100191, China
Qiao Liu, Jie Deng, Wenxin Yan, Chenyuan Qin, Min Du, Yaping Wang, Shimo Zhang, Min Liu & Jue Liu
Key Laboratory of Epidemiology of Major Diseases, Ministry of Education, Peking University, Haidian District, Beijing, China
Min Liu & Jue Liu
Institute for Global Health and Development, Peking University, Haidian District, Beijing, China
Global Center for Infectious Disease and Policy Research & Global Health and Infectious Diseases Group, Peking University, Beijing, China
Institute of Environmental Medicine, Peking University, Beijing, China
You can also search for this author in PubMed Google Scholar
Contributions
QL, JD and WY searched the literature and collected the data. QL, CQ and MD analyzed the data and interpreted the results. QL drafted the paper. ML and JL conceived of the study, designed the study, supervised the study, and interpreted the results. QL, JD, MD, YW, SZ, WY, ML and JL revised the paper. All authors contributed to the writing of the paper.
Corresponding author
Correspondence to Jue Liu .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
We declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Liu, Q., Deng, J., Yan, W. et al. Burden and trends of infectious disease mortality attributed to air pollution, unsafe water, sanitation, and hygiene, and non-optimal temperature globally and in different socio-demographic index regions. glob health res policy 9 , 23 (2024). https://doi.org/10.1186/s41256-024-00366-x
Download citation
Received : 21 February 2024
Accepted : 20 June 2024
Published : 28 June 2024
DOI : https://doi.org/10.1186/s41256-024-00366-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Global Health Research and Policy
ISSN: 2397-0642
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Public ranks long-term challenges and health determinants as top priorities for new EU
To enhance public health, the post-election European Union (EU) should prioritise long-term challenges such as climate change and the ageing population, as well as factors that influence our health, according to a new report . The findings, derived from a seven-month public debate led by the European Observatory on Health Systems and Policies, highlight a collective call for the EU to play a more significant role in health.
The report, which is based on the public debate commissioned by the European Commission’s Directorate General for Health and Food Safety ( DG SANTE ), outlines the key priorities and actions desired by citizens and stakeholders from a wide range of sectors and mostly from Europe. The analysis included more than 800 responses in conference polls and a survey, plus comprehensive inputs across three webinars .
The large and participatory initiative allowed to collect public opinion on nine critical health topics: health security; determinants of health; health system transformation; the health workforce; universal health coverage; digital solutions and AI; performance and resilience; long-term challenges like climate change and ageing; and the EU’s global role in health.
The public’s calls for action – including across sectors
Participants called for the European Commission to coordinate across its different policy branches. Collaborating across sectors is considered key to deliver health priorities, making the concepts of ‘ Health in All Policies’ and ‘Health for All Policies ’ important tools for addressing the determinants of health. Interestingly, the topics which garnered the highest consensus in the discussion framework were those least controlled by the health sector alone.
Significant measures should be taken to mitigate the health impacts of environmental risks, including promoting environmental health and supporting health equity through integrated policies. Participants also considered addressing the needs of an ageing population essential, by improving health services and ensuring that health systems are prepared to meet the demands of older adults.
The public opinion suggested several actions to achieve universal health coverage (UHC) across the EU, such as ensuring equal access to comprehensive health care services for all EU citizens and financial protection for all. Other recommendations ranged from establishing a common minimum coverage package and a European health insurance scheme to focusing on underserved groups, improving health literacy, and including mental health in UHC policies.
What role for the EU?
Participants highlighted the importance of EU legal frameworks and instruments in promoting and safeguarding health, such as funding and technical support. They advocated both for new tools and for better implementation and coordination of existing mechanisms.
Aligning educational standards was raised as a key topic in the context of addressing shortages of health workers , regional disparities and managing the demands for new skills. Better addressing health workforce needs and improving their working conditions to mitigate existing gaps was also discussed. There was consensus on the need for EU approaches to health workforce issues, including better coordination of initiatives and pursuit of EU wide policies.
Digital solutions , health security and strengthening the EU’s global voice and leadership were widely discussed but ranked slightly lower. Possible explanations outlined in the report include the “transversal nature of digital solutions, which voters may have perceived as a means to achieving other priorities”. The COVID-19 pandemic and sustained EU action on health security may have elicited some voters to opt for other topics that have received less policy attention in recent years.
Survey, webinars, and conference polls
Media Contacts
Débora Miranda
Communications and Dissemination Officer
Subscribe to our newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Asian Pac J Cancer Prev
- v.18(7); 2017

Non Communicable Disease Risk Factors and their Trends in India
Suzanne nethan.
1 Division of Clinical Oncology, ICMR - National Institute of Cancer Prevention and Research (NICPR), Noida, India
Dhirendra Sinha
2 ICMR - National Institute of Cancer prevention and Research (NICPR), Noida, India
Ravi Mehrotra
Background:.
India is a populous country of about 1.3 billion. Non communicable diseases (NCDs) contribute to around 5.87 million (60%) of all deaths in India. Hence, the objectives of this paper are to find baseline information on different NCD risk factors coverage and to determine their trends in India.
For this systematic review, PubMed, Google and different surveillance systems were searched. Of the search results, 41 papers/survey reports were eventually assessed for eligibility. National and state representative data on NCD risk factors (for the major NCDs like cardiovascular diseases, chronic respiratory disease, cancer and diabetes) having World Health Organization(WHO) indicator definitions, covering rural and urban population, were included in the study. Thereafter, state-wise population proportion was added and divided by the total Indian population to determine the percentage of population coverage for each risk factor by the surveys. Also, the old and current data of the periodic surveys were compared to assess prevalence trends.
Various national/state level surveys in India include single or multiple risk factors. Nationwide coverage is available for tobacco use, alcohol drinking, raised blood pressure and overweight and obesity. Periodic National Family Health Surveys provide information on selected risk factors during 2005-16 among adults aged 15-49 years. An overall significant increase was noted in overweight and obesity while decline was noted in tobacco and alcohol use during the same period. From GATS 1 (2009-10) to 2 (2016-17) also, the prevalence of tobacco consumption decreased in India.
Conclusion:
India has a much delayed response on NCD risk factors surveillance and information of the same are sporadic and incomplete. In order to increase information comprehensiveness, standard WHO NCD risk factors questions must be incorporated in the ongoing surveys. India should also plan for cost and time effective NCD surveillance system.
Introduction
Non-communicable diseases (NCDs) encompass a vast group of diseases such as cardiovascular diseases, cancer, diabetes and chronic respiratory diseases. NCDs contribute to around 38 million (68%) of all the deaths globally and to about 5.87 million (60%) of all deaths in India. Four NCDs mainly responsible for the total NCD mortality and morbidity are cardiovascular diseases, chronic respiratory disease, cancers and diabetes, contributing to about 82% of all NCD deaths (World Health Organization - WHO, 2014).
The majority of NCD deaths occur in low and middle-income countries such as India, which is undergoing an epidemiological health transition owing to rapid urbanization, which in turn has led to an overall economic rise, but with certain associated flipsides (risk factors) (Chakma and Gupta, 2014). A risk factor is defined as “An aspect of personal behavior or lifestyle, an environmental exposure, or a hereditary characteristic that is associated with an increase in the occurrence of a particular disease, injury, or other health condition” (Centers for Disease Control and Prevention, 2006). These behavioral and biological risk factors, with a predisposition to the development of NCDs, are use of tobacco and alcohol, physical inactivity, overweight and obesity, increased fat and sodium intake, low fruit and vegetable intake, raised blood pressure (BP), blood glucose and cholesterol levels (WHO, 2013).
India being a populous country of about 1.3 billion, contributes to more than 2/3rd of the total deaths due to NCDs in the South-East Asia Region (SEAR) of WHO (WHO, 2014; United Nations Statistics Division). As per the 2011 report on NCD status in SEAR, raised BP, raised blood glucose and tobacco use were the three major risk factors responsible for majority of deaths annually in this region. The prevalence of raised BP was greater in Myanmar (highest – 42%), Indonesia, Sri Lanka, Bhutan and Thailand as compared to that in India (about 35%); however, Nepal, Maldives, Bangladesh and Democratic Republic of Korea (lowest -19%) showed a relatively lesser prevalence of the same. For raised blood glucose (diabetes), Bhutan showed the highest prevalence i.e. 12-13% and India, second highest i.e. 11%, among the SEAR countries. The prevalence of smoked tobacco products use was slightly lesser in Sri Lanka (14.1%) while it was much higher in Thailand (24%), Bangladesh (24%), Myanmar (24%), Maldives (27%), Nepal (32%) and Indonesia (highest - 33%), as compared to in India (15%). The prevalence of smokeless tobacco (SLT) products usagewas higher in India (25.9%) as compared to that in Thailand (1.3%), Sri Lanka (15.8%), Nepal (18.6%) and Bhutan (19.4%); however, Bangladesh (27.2%) and Myanmar (51.4%) showed relatively higher SLT consumption than in India (WHO, 2011).
WHO in its World Health Assembly in May 2008 put forth an Action Plan of Global Strategy for the Prevention and Control of NCDs. India also, as a WHO member state, is committed to implementing the same and taking the required steps and initiative to meet the objectives . As part of this plan, India has developed and is gradually developing a wide number of national public health programs. It has also performed various periodic surveys, both at the national and subnational/state levels, which directly or indirectly target NCDs (Chakma and Gupta, 2014). Few examples of these surveys are the National Family Health Survey (NFHS), Global Adult Tobacco Survey (GATS) etc. However, these are associated with a number of shortcomings, which need to be addressed in order to improvise NCD control in India. A similar study demonstrating the availability of data regarding NCD risk factors in India was published in 2012 by Raban et al, however without the representation and/or analysis of the same. Various authors have also published systematic reviews demonstrating trends in these surveys (which have been discussed subsequently) however only for one or few more risk factors, thereby rendering them non-comprehensive and incomplete. Also, these details regarding trends of NCD risk factors prevalence are available only upto 2012 (example: trend analysis of National Sample Survey Organization - NSSO surveys held between 1999-2012, for tobacco use prevalence by Bhan et al., 2016). For NFHS, previously, prevalence trends for tobacco consumption and overweight and obesity have been determined through data from 1998 to 2006; however, here this information has been updated till 2016. Thus, this paper examines the epidemiology and data availability of all the NCD risk factors.
Materials and Methods
For this systematic review on the NCD risk factors in India, national or state-level (subnational) surveys, which collected information on at least one NCD risk factor (for the major NCDs such as like cardiovascular diseases, chronic respiratory disease, cancer and diabetes), irrespective of the period of data collection or reporting or the sample size, were searched for and evaluated, between October 2016 to January 2017.
The online literature search strategy performed is shown in Figure 1 :

Search Strategy to Identify Surveys Documenting Non Communicable Disease Risk Factors in India
- Extensive PubMed literature search was performed using a combination of keywords such as noncommunicable diseases, NCD, risk factors, India, prevalence, tobacco, alcohol, fruit intake, vegetable intake, salt intake, physical activity, BMI, overweight, obesity, blood pressure, hypertension, blood glucose, diabetes, saturated fat, cholesterol. This search produced 332 results, the titles and abstracts of which were assessed and those clearly not relevant were excluded. Abstracts of the remaining publications and full papers were reviewed to identify those that fulfilled the inclusion criteria. Among these, 2 articles were found to be of potential interest and were thereby included.
- Also, Google and some of the known surveillance systems, known to conduct routine household surveys across various States and Union Territories (UTs) of India, were searched, like the NFHS, GATS, District Level Household and Facility Survey (DLHS), Integrated Disease Surveillance Program (IDSP) and Indian Council of Medical Research (ICMR), which revealed 5 eligible survey systems with 8 reports, performed between 1998-2016.
- The criteria for data selection, obtained from the search above, was as follows:
» Inclusion Criteria – studies/surveys which are national (representative of states or nationally representative), multiple-state representative or single state representative; surveys following the WHO indicator definitions for each risk factor; surveys covering both rural and urban population; manuscripts in English language:
1. Tobacco use - of any tobacco form in last 30 days (WHO, 2008).
2. Alcohol use - at least once previously in 30 days (WHO, 2008).
3. Physical inactivity - adults aged 18+ years not meeting any of these criteria: 150 minutes of moderate-or 75 minutes of vigorous or an equivalent combination of both types of physical activity accumulating atleast 600 MET (Metabolic Equivalent - ratio of a person’s working metabolic rate relative to the resting metabolic rate) minutes per week (WHO, 2013)
4. Salt Intake – >5 gm (2 gm sodium) (WHO, 2012).
5. Low fruit and/or vegetables consumption - <5 servings (400 grams) per day (WHO, 2013).
6. Raised blood pressure - Systolic blood pressure ≥140 and/or diastolic blood pressure ≥90 among persons aged 18+ years (WHO, 2013).
7. Raised blood glucose - an adult aged 18+ years with fasting plasma glucose value ≥7.0 mmol/L (126 mg/dl) or on medication for it (WHO, 2013).
8. Overweight and Obesity- Body mass index (BMI) ≥25 kg/m2 denotes overweight and ≥ 30 kg/m2 denotes obesity in adults aged 18+ years (WHO, 2013).
9. Increased saturated fat consumption - intake >150 mg/dL (WHO, 2013).
10. Raised cholesterol - if >5.0 mmol/L (190 mg/dl) (WHO, 2013).
» Exclusion Criteria – studies not set in India; surveys which are multiple or single state non-representative; surveys not following the WHO indicator definitions; surveys not covering both the rural and urban population; documents in languages other than English.
In total, 10 eligible surveys were identified through the aforementioned literature search.
Thereafter, state-wise population proportion was added and divided by the total Indian population to determine the percentage of population coverage for each risk factor by the surveys. The population count for all the Indian states and UTs are available in the Population Projection Report 2006 by the Office of the Registrar Generaland Census Commissioner, India – RGI (RGI, 2006). Also, the old and current data of the periodic surveys were compared to assess prevalence trends.
The details of the various surveys have been summarized in Table 1 . Of all the NCD risk factors, assessment by surveys for the prevalence of tobacco use, alcohol use, raised blood pressure and overweight and obesity, has been done almost nationwide. Specific details for each risk factor have been mentioned henceforth.
Survey Systems Representing Data on Non Communicable Disease Risk Factors in India that Met the Inclusion Criteria
| Name Of Survey | Period Of Survey | Total No. Of States/Union Territories Covered | Age Group (In Years) | Rural/Urban/Both | Number Of Risk Factors Covered | N | Periodic Survey |
|---|---|---|---|---|---|---|---|
| National, Representative Of States/Regions | |||||||
| National Family Health Survey | 1998-2016 | 36 | Women = 15-49, Men = 15-54 | Both | Tobacco Use, Alcohol Use, Raised Blood Pressure, Overweight and Obesity | 803,211 | Yes |
| Global Adult Tobacco Survey | 2009-2016 | 31 | 15 and Above | Both | Tobacco Use | 69,296 | Yes |
| District Level Household And Facility Survey | 2012-13 | 21 | 15-49 | Both | Raised Blood Pressure | Yes | |
| Multi State Representative | |||||||
| Integrated Disease Surveillance Program | 2007-08 | 7 | 15 – 64 | Both | Tobacco Use, Alcohol Use, Physical Inactivity, Raised Blood Pressure, Overweight and Obesity, Low Fruits and Vegetables Intake | 38,054 | No |
| Indian Council Of Medical Research India Diabetes Study | 2008-11 | 4 | 20 And Above | Both | Physical Inactivity, Raised Blood Pressure, Overweight & Obesity, Raised Blood Glucose | 14,277 | No |
| Single State Representative | |||||||
| Punjab Survey | 2014-15 | 1 | 18 – 69 | Both | Tobacco use, Salt use, Physical Inactivity, Raised Blood Pressure, Overweight and Obesity, Low Fruits & Vegetables Intake, Saturated Fat intake, Total Cholestrol | 5,127 | No |
| Kerala Survey | 2003-04 | 1 | 30-74 | Both | Tobacco use, Overweight and Obesity | 6,579 | No |
Behavioral Risk Factors for NCDs
1. tobacco use.
Tobacco consumption has been recorded extensively for 100% (12,62,940,000)of the population in all Indian states and UTs, by NFHS (International Institute for Population Sciences- IIPS, 2007, 2015-16) and GATS (IIPS, 2009; Tata Institute of Social Sciences- TISS, 2017). Other surveys which have also recorded the prevalence of tobacco use among adults are IDSP (National Institute of Medical Statistics - NIMS, ICMR, 2009), the Punjab (Thakur et al., 2016) and Kerala (Sugathan et al., 2008) state surveys ( Figure 2 ).

Percentage of Population Coverage for Each Non Communicable Disease Risk Factor by the Various Surveys. 1, National Family Health Survey; 2, District Level Household and Facility Survey; 3, Integrated Disease Surveillance Program; 4, Global Adult Tobacco Survey; 5, Indian Council of Medical Research India Diabetes Study; 6, Punjab State Survey; 7, Kerala State Survey
In NFHS, between 2005-16, a significant decline in tobacco use was noted among both males and females in India ( Figure 3 )(IIPS, 2007; 2015-16).

Pan-India Prevalence Trends Observed Among Males and Females During the National Family Health Surveys 3 (2005-06) and 4 (2015-16)
From GATS 1 (2009-10) (IIPS, 2009) to GATS 2 (2016-17) (TISS, 2017), the prevalence of tobacco consumption has decreased from 34.6 to 28.6% in India.
2. Alcohol Use
Alcohol usage has also been recorded by NFHS for 100% (12,62,940,000)of the Indian states and UTs (IIPS, 2007; 2015-16). Other survey which has recorded the prevalence of alcohol consumption is the IDSP (NIMS, ICMR, 2009) ( Figure 2 ).
In NFHS, between 2005-16, an overall decline was seen in alcohol consumption among both males and females ( Figure 3 )(IIPS 2007; 2015-16).
3. Physical Inactivity
Physical inactivity has been recorded for a maximum of 36.9% of the total Indian population i.e. in 7 states by IDSP (NIMS, ICMR, 2009), followed by the ICMR India Diabetes (INDIAB) study (4 states/UTs) (ICMR, 2016) and the Punjab survey (single state) (Thakur et al., 2016) ( Figure 2 ).
4. Salt Intake
The Punjab state survey documented salt intake by the residents of the state, constituting about 2.3% (290,10,000) of the Indian population ( Figure 2 ) (Thakur et al., 2016).
5. Low Fruit and Vegetable Consumption
The IDSP (NIMS, ICMR, 2009) and Punjab state survey (Thakur et al., 2016) together recorded information for about 34.1% (4,30,501,000) of the Indian population, in a total of 8 states ( Figure 2 ).
6. Saturated Fat Intake
Prevalence of increased saturated fat intake has been documented by the Punjab state survey for about 2.2% (290,10,000) of the Indian population ( Figure 2 ) (Thakur et al., 2016).
Biological Risk Factors for NCDs
1. raised blood pressure.
Data regarding this NCD risk factor is available for population residing in 100% (12,62,940,000)of the Indian statesand UTs, through surveys like NFHS 4 (IIPS, 2015-16), DLHS (IIPS, 2012-13), IDSP (NIMS, ICMR, 2009), ICMR INDIAB (ICMR, 2016) and Punjab state survey (Thakur et al., 2016) ( Figure 2 ). Although NFHS 4 follows the WHO indicator definition for raised blood pressure levels, it categorized the same as slightly above normal, moderately high and very high (IIPS, 2015-16).
2. Raised Blood Glucose
Raised blood glucose levels have been documented for about 17.7% (223,986,000) of the Indian population by the ICMR INDIAB (ICMR, 2016) survey ( Figure 2 ).
3. Overweight and Obesity
Information regarding raised BMI has been documented for 100% (12,62,940,000) of the Indian population, mainly by NFHS (IIPS, 1998-99; 2007; 2015-16), along with IDSP (NIMS, ICMR, 2009), ICMR INDIAB (ICMR, 2016), Punjab (Thakur et al., 2016) and Kerala (Sugathan et al., 2008) state surveys ( Figure 2 ).
In NFHS 2 and 3 (1998-2006), 6% increase in prevalence was seen in all states except Delhi (Sengupta et al., 2015); Garg et al. (2010) and Balarajan and Villamor (2009) also showed increased prevalence of obesity among Indian women from 10.6% to 12.6% and 10.6 to 14.8% respectively. In NFHS 3 and 4 (2005-16), an overall significant increase was noted both among males and females ( Figure 3 ) (IIPS, 2007; 2015-16).
4. Raised Total Cholestrol
The Punjab state survey (2014-15) documented information regarding raised cholesterol levels from 2.2% (290,10,000) of the Indian population residing there ( Figure 2 ) (Thakur et al., 2016).
NCDs are a leading global public health problem, as established by the United Nations Summit on NCDs in September 2011 (Samuels et al., 2014). Regulating the increasing burden of NCDs in low and middle-income countries involves establishing adequate systems for monitoring the same and using the data obtained to upgrade or implement control strategies. In this paper we examined the availability of data measuring the NCD risk factor indicators as collected by household based surveys in India since 1998 till 2016. Based on the aforementioned observations among the various national and subnational surveys, the involved pitfalls have been elicited and discussed below:
1. Inadequate Coverage of the NCD Risk Factors –
Most surveys, national or sub-national, do not report data pertaining to every NCD risk factor. Only the survey performed in Punjab between 2014-15 has covered all of them (Thakur et al., 2016). Other surveys such as IDSP (NIMS, ICMR, 2009), NFHS 4 (2015-16) (IIPS, 2015-16), NFHS 3 (2005-06) (IIPS, 2007) etc. have recorded fewer number of risk factors, in the descending order.
2. Incomplete Geographical Coverage –
Inspite of being national level surveys, some have reported data only for a limited number of Indian states; the IDSP (NIMS, ICMR, 2009) and the ICMR INDIAB study (ICMR, 2016) have covered 7 and 4 Indian states respectively. NFHS (IIPS, 1998-99; 2007; 2015-16) and GATS (IIPS, 2009; TISS, 2017) covered most of the Indian states, along with the UTs but have information on limited risk factors.
Also, very few states have performed similar independent surveys till now, for example Punjab (Thakur et al., 2016) and Kerala (Sugathan et al., 2008).
3. Periodicity of Surveying –
The NFHS and GATS surveys have been held periodically till date i.e. NFHS from 1998 -2016 (IIPS, 1998-99; 2007; 2015-16), GATS in 2009 (IIPS, 2009) and 2016 (TISS, 2017). However, examples of other surveys which haven’t followed the same continuum are the IDSP performed only once in 2007-08 (NIMS, ICMR, 2009), the ICMR INDIAB study in 2008-11 (ICMR, 2016), the Punjab state survey in 2014-15 (Thakur et al., 2016) and the Kerala state survey in 2003-04 (Sugathan et al., 2008).
4. Lack of a Standardised Methodology –
Many surveys measured the WHO recommended core indicators incompletely or were missed because of the use of different indicator definitions, which have been elaborated upon below. Also, the variables covered differed amongst most surveys, i.e. some surveys accounted for data coverage based on gender, some based on the type of residence of the population while few surveys represented data with regard to both. Thus, a standardized approach should be employed while NCD risk factor data collection. Considering that large scale collection of blood samples is not an easy task, some of the biological risk factors requiring the same (example: blood cholesterol) were covered mostly by surveys of smaller geographic representativeness. However, as has been seen in NFHS (IIPS, 1998-99; 2007; 2015-16) and DLHS (IIPS, 2012-13), wherein blood samples were collected for testing for anaemia and Human Immunodeficiency Virus infection, the task does not seem impossible. Other easier or feasible alternatives for sample collection can be tried, for example, blood spots on filter paper instead of venous blood for measuring blood cholesterol in large surveys (Raban et al., 2015).
In addition to enumerating the various lacunae in the surveys, the current trends in the prevalence of the NCD risk factors have been demonstrated in this paper. The disparities or additional observations in other published data have been discussed below.
Bhan et al., (2016), in their analysis of the NSSO surveys (1999-2012) showed decline in bidi (from 24.9% to 14.9%) and increase in cigarette use (from 3.4% to 3.8%), especially among lower socioeconomic status (SES) groups; increased use of SLT (from 18.5% to 24%) across all SES groups was also noted. Mishra et al., (2016) compared the Special Fertility and Mortality Survey (1998), Sample Registration System Baseline Survey (2004) and GATS, wherein, despite decrease in the smoking prevalence, an increased number of male smokers, aged 15–69 years, was noted between 1998-2015. Sinha et al., (2015) showed a significantly increasing trend of SLT consumption among men (27.1% to 33.4%) and women (10.1% to 15.7%) in NFHS 2, 3 and GATS.
An increase in the prevalence of overweight and obese individuals from 7 % in 1975-79 to 24% in 2011-12 in National Nutrition Monitoring Board Surveys was noted by Meshram et al., (2016) and from 10.6% and 1.6% in 1998–99 to 12.6% and 1.5% in 2005-06, in women and pre-school children respectively, in NFHS by Wang et al., (2009).
In terms of alcohol intake, the Organization for Economic Co-operation and Development report, 2015 (Sassi, 2015) showed a major rise between 1992 and 2002. The WHO Global status report on Alcohol and Health, 2014 (WHO, 2014) also showed the same from 2003-05 to 2008-10.
Anjana et al., (2014) showed, that of the total sample in the ICMR INDIAB study (2008-11), 54.4% individuals were inactive, inactivity was more prevalent in the urban than rural areas and among females than males.
Bhansali et al., (2014) showed a higher prevalence of hypertension among the urban (31.5, 28.9, 30.7 and 28.1%) than the rural (26.2, 21.7, 19.8 and 24.0%) residents of Tamil Nadu, Jharkhand, Chandigarh and Maharashtra respectively, in the ICMR INDIAB study (2008-11).
In conclusion, surveillance and procurement of details regarding NCD risk factors is essential for health programs/policy planning and implementation, particularly in a country like India with a rapidly increasing burden of NCDs. Currently, a relative lack of adequate risk factor data in its entirety, inadequate coverage (geographically and demographically) and absence of a standardized methodology are the major deficiencies which need to be overcome for a superior and more effective NCD control in the country, which in turn would facilitate reduction of the overall NCD burden by 2025.
- Anjana RM, Pradeepa R, Das AK, et al. Physical activity and inactivity patterns in India –results from the ICMR-INDIAB study (Phase-1) [ICMR-INDIAB-5] Int J Behav Nutr Phys Act. 2014; 11 :1–11. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Balarajan Y, Villamor E. Nationally representative surveys show recent increases in the prevalence of overweight and obesity among women of reproductive age in Bangladesh, Nepal, and India. J Nutr. 2009; 139 :2139–44. [ PubMed ] [ Google Scholar ]
- Bhan N, Karan A, Srivastava S, et al. Have socioeconomic inequalities in Tobacco use in India increased over time?Trends from the national sample surveys (2000–2012) Nicotine Tob Res. 2016; 18 :1711–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bhansali A, Dhandania VK, Deepa M, et al. Prevalence of and risk factors for hypertension in urban and rural India: the ICMR–INDIAB study. J Hum Hypertens. 2015; 29 :204–9. [ PubMed ] [ Google Scholar ]
- Centers for disease control and prevention. In ‘Glossary’. U.S. department of health and human services. Atlanta: Centers for disease control and prevention (CDC); 2006. Principles of epidemiology in public health practice third edition, An introduction to applied epidemiology and biostatistics. [ Google Scholar ]
- Chakma JK, Gupta S. Lifestyle and non-communicable diseases: A double edged sword for future India. Indian J Comm Health. 2014; 26 :325–32. [ Google Scholar ]
- Garg C, Khan SA, Ansari SH, Garg M. Prevalence of obesity in Indian women. Obes Rev. 2010; 11 :105–8. [ PubMed ] [ Google Scholar ]
- Indian council of medical research (ICMR) India diabetes (INDIAB) Study phase I, 2008-11. New Delhi, India: ICMR; 2016. [ Google Scholar ]
- International institute for population sciences (IIPS) and Macro international. National family health survey (NFHS-2), 1998-99. Mumbai, India: IIPS; 1998-99. [ Google Scholar ]
- International institute for population sciences (IIPS) and Macro international. National family health survey (NFHS-3), 2005–06: India: volume I. Mumbai, India: IIPS; 2007. [ Google Scholar ]
- International institute for population sciences (IIPS) Global adult Tobacco survey GATS India report 2009-10. Mumbai, India: IIPS; 2009. [ Google Scholar ]
- International institute for population sciences (IIPS) District level household and facility survey-4, 2012-13. Mumbai, India: IIPS; 2012-13. [ Google Scholar ]
- International institute for population sciences (IIPS) and Macro international. National family health survey (NFHS-4), State data fact sheets. Mumbai, India: IIPS; 2015-16. [ Google Scholar ]
- Meshram II, Balakrishna N, Sreeramakrishna N, et al. Trends in nutritional status and nutrient intakes and correlates of overweight/obesity among rural adult women (≥18–60 years) in India: National nutrition monitoring Bureau (NNMB) national surveys. Public Health Nutr. 2015; 19 :767–76. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mishra S, Joseph RA, Gupta PC, et al. Trends in bidi and cigarette smoking in India from 1998 to 2015, by age, gender and education. BMJ Glob Health. 2016; 1 :e000005. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- National institute of medical statistics, Indian council of medical research (ICMR) IDSP non-communicable disease risk factors survey, Phase-I states of India, 2007-08. New Delhi, India: National institute of medical statistics and division of non-communicable diseases, Indian council of medical research; 2009. [ Google Scholar ]
- Office of the registrar generaland census commissioner, India (RGI) Population projections for India and states 2001-2026. New Delhi, India: RGI; 2006. [ Google Scholar ]
- Raban MZ, Dandona R, Dandona L. Availability of data for monitoring noncommunicable disease risk factors in India. Bull World Health Organ. 2012; 90 :20–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rai RK. Factors associated with nutritional status among adult women in urban India, 1998-2006. Asia Pac J Public Health. 2015; 27 :NP1241–52. [ PubMed ] [ Google Scholar ]
- Samuels TA, Kirton J, Guebert J. Monitoring compliance with high-level commitments in health: the case of the CARICOM Summit on chronic non-communicable diseases. Bull World Health Organ. 2014; 92 :270–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sassi F. Tackling harmful alcohol use: Economics and public health policy. Paris: OECD Publishing; 2015. [ Google Scholar ]
- Sengupta A, Angeli F, Syamala TS, et al. Overweight and obesity prevalence among Indian women by place of residence and socio-economic status: Contrasting patterns from 'underweight states'and 'overweight states'of India. Soc Sci Med. 2015; 138 :161–9. [ PubMed ] [ Google Scholar ]
- Sinha DN, Rizwan SA, Aryal KK, et al. Trends of smokeless tobacco use among adults (aged 15-49 years) in Bangladesh, India and Nepal. Asian Pac J Cancer Prev. 2015; 16 :6561–8. [ PubMed ] [ Google Scholar ]
- Sugathan TN, Soman CR, Sankaranarayan K. Behavioural risk factors for noncommunicable diseases among adults in Kerala, India. Indian J Med Res. 2008; 127 :555–63. [ PubMed ] [ Google Scholar ]
- Tata institute of social sciences (TISS) Global adult tobacco survey GATS-2 India 2016-17. Mumbai, India: TISS; 2017. [ Google Scholar ]
- Thakur JS, Jeet G, Pal A, et al. Profile of risk factors for non-communicable diseases in Punjab, Northern India: Results of a state-wide STEPS survey. PLoS One. 2016; 11 :e0157705. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- United nations statistics division. World statistics pocket book. 2017. [[Accessed 12 January 2017]]. Available at: http://data.un.org/CountryProfile.aspx?crName=INDIA .
- Wang Y, Chen HJ, Shaikh S, Mathur P. Is obesity becoming a public health problem in India?Examine the shift from under- to overnutrition problems over time. Obes Rev. 2009; 10 :456–74. [ PubMed ] [ Google Scholar ]
- World health organization. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance. Geneva, Switzerland: WHO; 2008. [ Google Scholar ]
- World health organization. Noncommunicable diseases in the South-East Asia region: Situation and response 2011. New Delhi, India: World health organization regional office for South-East Asia; 2011. [ Google Scholar ]
- World health organization. Guideline: Sodium intake for adults and children. Geneva, Switzerland: World health organization; 2012. [ PubMed ] [ Google Scholar ]
- World health organization. Noncommunicable diseases global monitoring framework: Indicator definitions and specifications. Geneva, Switzerland: World health organization; 2013. [ Google Scholar ]
- World health organization. Global status report on alcohol and health 2014. Geneva, Switzerland: World health organization; 2014. [ Google Scholar ]
- World health organization. Global status report on noncommunicable diseases 2014. Geneva, Switzerland: World health organization; 2014. [ Google Scholar ]
- Posted on: 26 June 2024
Tenure-track Assistant Research Professor in Non-Communicable Disease Epidemiology
Job Information
Offer description.
The Barcelona Institute for Global Health (ISGlobal) is a cutting-edge institute addressing global public health challenges through research, translation into policy and education. ISGlobal has a broad portfolio in communicable and non-communicable diseases, including environmental, lifestyle and climate determinants, and applies a multidisciplinary scientific approach ranging from the molecular to the population level. Research is organized in five programmes: Climate, Air Pollution, Nature and Urban Health; Environment and Health over the Lifecourse; Global Viral and Bacterial Infections; Malaria and Neglected Parasitic Diseases and Maternal, Child and Reproductive Health. The Environment and Health over the Lifecourse research programme aims to conduct high-quality integrative research to expand knowledge on the causes and mechanisms of non-communicable diseases (NCDs). Work in the programme ranges from local to national and global efforts in high and low-and-middle income countries, with international leadership in areas such as exposome, radiation, child health, cancer, and respiratory health research. ISGlobal is accredited with the Severo Ochoa distinction, a seal of excellence of the Spanish Science Ministry.
What We Are Looking for We are seeking applicants for two full-time tenure-track assistant research professor positions in the field of non-communicable disease (NCD) epidemiology . Applications are invited from dynamic researchers with experience in NCD epidemiology and demonstrated excellence and intellectual leadership. The researcher is expected to develop a research group within the Environment and Health over the Lifecourse Programme. The researcher should develop high quality research to expand knowledge on the causes and mechanisms of NCDs development or progression, in populations in high and low-medium income countries, with the ultimate goal to inform, improve and promote interventions and policies for prevention of NCDs. Experience in the following areas will be an asset: respiratory health, cancer, circadian disruption, cognition and aging-related diseases, in relation to environmental risk factors.
Training and Experience/Qualifications
- Candidates must have a PhD
- At least 5 years of accredited postdoctoral experience
- A record of peer review publications
- Demonstrate potential for obtaining external research funding
- Experience in training early career researchers will be an asset
Key Responsibilities
- Develop a research group within the Environment and Health over the Lifecourse Programme at ISGlobal
- Collaborate across ISGlobal research programs
- Publish scholarly work
- Obtain grant funding to support research
- Teach at the masters and doctorate level and
- Participate in advancing the strategic goals of ISGlobal in policy translation and innovation.
- Problem resolution
- Ability to apply for competitive grants at EU (Horizon Europe, ERC…) and NIH level
Language level:
- English proficiency
Conditions:
- Assistant Research Professor Tenure Track full time, open-ended contract
- Starting date: January 2025 (negotiable)
- Gross Annual Salary Range: ̴37.500 – 47.500 €
- Broad training offer adapted to the different profiles
Measures to reconcile work and family life: flexible schedule working hours, teleworking possibilities, 23 working days of paid holidays, 13 leave days for personal matters, among other. The successful candidate will be periodically evaluated (at least every 5 years) by external international experts, according to ISGlobal’s Tenure track researcher’s evaluation and promotion policy. Technical support for grant application and management will be provided, as well as limited administrative support.
How to apply: Applicants must complete the request form including the following reference: AssistantResearchProfessorNCDs_June24 . Applications must include to be considered: A cover letter describing research interests and plans in ISGlobal
- Curriculum Vitae
- Copies of 3 key publications
- The names and contact information for three references.
Please contact [email protected] for questions about this position. Each attached document must be named with the candidate name and surname. The receipt of applications will be open until 12th September 2023 Applications will be accepted until 17.00 CET of the closing date. Only the applications submitted through the request form will be considered. Only shortlisted candidates will be contacted. In ISGlobal we are committed to maintaining and developing a work environment in which the values and principles of our organization are respected and equal opportunities between women and men be promoted in each of the areas in which we operate, not tolerating discrimination based on criteria such as age, gender, marital status, race, ethnicity, functional diversity, political leanings, religion, sexual orientation, gender identity or gender expression. In order to promote gender balance, if no female candidate is selected for interview, the position will be re-advertised.
Selection criteria and procedure The evaluation of candidates will be based on criteria of excellence in research, leadership and service in a two-step evaluation process: 1. Scoring of each candidate according to the documents presented and their fit in the position by the selection panel 2. Seminar and interview for the top scored 2-3 candidates
In ISGlobal we are committed to maintaining and developing a work environment in which the values and principles of our organization are respected and equal opportunities between women and men be promoted in each of the areas in which we operate, not tolerating discrimination based on criteria such as age, gender, marital status, race, ethnicity, functional diversity, political leanings, religion, sexual orientation, gender identity or gender expression. ISGlobal supports the initiative #ScienceforUkraine. Therefore, to sustain Ukraine’s presence in the European Research Area and international scholarly community, candidates from Ukraine on all levels of scholarly career are welcome: students, PhD candidates, early career researchers and senior scholars. We confirm our commitment towards the value of the diversity of our staff and student population and seek to promote peace, equity, diversity and inclusion as essential elements in contribution to improving health worldwide.
Where to apply
Requirements, additional information, work location(s), share this page.

IMAGES
VIDEO
COMMENTS
Introduction. Non-communicable diseases (NCDs), also known as chronic diseases, are medical conditions that are associated with long durations and slow progress (Figure 1).Most NCDs are non-infectious and are the result of several factors, including genetic, physiological, behavioral, and environmental factors ().According to the World Health Organization (WHO), NCDs are the leading cause of ...
Noncommunicable diseases (NCDs), also known as chronic diseases, are not passed from person to person. They are of long duration and generally slow progression. The four main types of noncommunicable diseases are cardiovascular diseases (like heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma) and diabetes.
Historically, communicable diseases, such as HIV/AIDS, viral hepatitis, malaria, poliomyelitis, tuberculosis, influenza and, more recently, the coronavirus disease 2019, have been at the center of global health concerns and initiatives, as they are transmitted from one person to another with a variety of ways, easily spread across national borders, and threaten the lives of millions of people ...
Non-communicable diseases (NCDs) are a huge group of illnesses that comprise chronic respiratory illnesses (asthma, COPD), malignant growth, diabetes, and cardiovascular ailments (including stroke and respiratory failures). The mortality rate of NCDs is considerably higher in low-income and middle-income countries (LICs and MICs), which makes ...
Addressing non-communicable disease (NCDs) is a global priority in the Sustainable Development Goals, especially for adolescents. However, existing literature on NCD burden, risk factors and determinants, and effective interventions and policies for targeting these diseases in adolescents, is limited. This study develops an evidence-based conceptual framework, and highlights pathways between ...
Collins, T., Akselrod, S., Berlina, D., et al. Unleashing implementation research to accelerate national noncommunicable disease responses. Global Health 18, 6 (2022) Marten, Robert et al. Committing to implementation research for health systems to manage and control non-communicable diseases. The Lancet Global Health, Volume 9, Issue 2, e108-e109.
A recent report from the World Health Organization 1 identified six risk factors associated with noncommunicable diseases as the leading global risk factors for death: high blood pressure, tobacco ...
Noncommunicable diseases (NCDs), including heart disease, stroke, cancer, diabetes and chronic lung disease, are collectively responsible for 74% of all deaths worldwide. More than three-quarters of all NCD deaths, and 86% of the 17 million people who died prematurely, or before reaching 70 years of age, occur in low- and middle-income ...
Non-communicable diseases in low- and middle-income countries can be tackled with integrated health systems interventions that consider multimorbidity, supported by patient involvement and new ...
In The Lancet, David Watkins and colleagues explore how countries can get back on track to reach the Sustainable Development Goal (SDG) 3.4 target of reducing premature mortality from cancers, cardiovascular diseases, chronic respiratory diseases, and diabetes by a third by 2030. Drawing on the Disease Control Priorities Project and what WHO considers the "best buys", they synthesise the ...
In recent years, pronounced shifts have occurred in patterns of communicable to non-communicable diseases (NCDs). Globally, NCDs account for around 40 million deaths per annum, having increased by seven million since 2008 [ Citation 1 ]. 87% of premature mortality and morbidity is borne in low- and middle-income countries (LMICs) and 40% is ...
Haregu, T. N. et al. A scoping review of non-communicable disease research capacity strengthening initiatives in low and middle-income countries. Glob. Health Res. Policy 4, 31 (2019).
Non-communicable diseases (NCDs) represent the leading cause of death worldwide, killing 41 million people each year—equivalent to 71% of all deaths globally. Among NCDs, the four top killers that together account for more than 80% of all premature NCD deaths include cardiovascular diseases (17·9 million deaths annually), cancers (9·0 million), respiratory diseases (3·9 million), and ...
Celestin Hategeka and colleagues evaluate the current state of implementation research on Non-Communicable Disease prevention and control interventions in low-and middle ... Holmer H. Implementation of non-communicable disease policies from 2015 to 2020: a geopolitical analysis of 194 countries. Lancet Glob Health. 2021;9(11):e1528-e1538. ...
Non Communicable Disease. Noncommunicable disease surveillance is the ongoing systematic collection and analysis of data to provide appropriate information regarding noncommunicable disease burden, the population groups at risk, mortality, morbidity, risk factors, and determinants, coupled with the ability to track health outcomes and risk factor trends over time [28].
Summary. 1. This paper is for policy makers that are involved in making investments to tackle the main. non-communicable diseases (NCDs), namely cardiova scular disease, cancers, diabetes and ...
Non-communicable diseases (NCDs) remain the largest global public health threat. The emerging field of precision public health (PPH) offers a transformative opportunity to capitalize on digital health data to create an agile, responsive and data-driven public health system to actively prevent NCDs. ... From 2015, research accelerated in the use ...
Further research is needed to characterise the epidemiology of diabetes in humanitarian settings and to develop simplified, cost-effective models of care to improve the delivery of diabetes care during humanitarian crises. ... Nearly three out of every four deaths worldwide in 2017 were caused by non-communicable diseases (NCDs). Many countries ...
5 Conceptual Framework 1.9 Genetics for prevention and control of noncommunicable diseases. Paper 9. Geneva, World Health Organization, 2011. 1.10 Promoting use of research findings to policies and practice for prevention and control of noncommunicable diseases in low- and middle-income
Non-Communicable Diseases. NCDs such as Diabetes mellites, cardiac disorders, cardiac failure, obesity, renal diseases, lung disease, dyslipidemia and. stroke are among the few. NSDs hav e become ...
Non-communicable diseases are the number one cause of mortality in women worldwide. Gestational diabetes refers to hyperglycaemia first diagnosed during pregnancy that does not fulfil the criteria of overt type 2 diabetes (ie, glycated haemoglobin >6·5%, fasting glucose concentration >7 mmol/L, or 2-h glucose >11·1 mmol/L on a 75 g oral ...
An estimated 20-25% of the population is affected by chronic, non-communicable inflammatory skin diseases. Chronic skin inflammation has many causes. Among the most frequent chronic inflammatory skin diseases are atopic dermatitis, psoriasis, urticaria, lichen planus, and hidradenitis suppurativa, d …
Introduction. Non-communicable diseases (NCDs), also known as chronic diseases, are medical conditions that are associated with long durations and slow progress ().Most NCDs are non-infectious and are the result of several factors, including genetic, physiological, behavioral, and environmental factors ().According to the World Health Organization (WHO), NCDs are the leading cause of death ...
In a recent study published in Cell Reports Medicine, researchers review and assess the potential exacerbation of non-communicable diseases (NCDs) by micro- and nanoplastics (MnPs) through their ...
The research agenda aligns with the fourth objective of the Sixty-first World Health Assembly, which endorsed the Global Strategy Action Plan for the Prevention and Control of Non-communicable Diseases. Its aim is to "promote research for the prevention and control of non-communicable diseases." [28,29].
Environmental factors greatly impact infectious disease-related mortality, yet there's a lack of comprehensive global studies on the contemporary burden and trends. This study aims to evaluate the global burden and trends of infectious disease mortality caused by air pollution, unsafe water, poor sanitation, and non-optimal temperature across Socio-Demographic Index (SDI) regions from 1990 to ...
Most respondents worked in the public sector, with significant representation from academia, research organizations, government, multilateral organizations, civil society, and the private sector.Topics beyond the framework were raised with a set of common concerns emerging, namely: non-communicable and chronic diseases, including cancer and ...
Background: India carries the greatest burden of non-communicable diseases (NCDs) amongst nations. It is estimated that by the year 2030 there will be 101 million diabetics, 218 million ...
Non-communicable diseases (NCDs) encompass a vast group of diseases such as cardiovascular diseases, cancer, diabetes and chronic respiratory diseases. NCDs contribute to around 38 million (68%) of all the deaths globally and to about 5.87 million (60%) of all deaths in India. Four NCDs mainly responsible for the total NCD mortality and ...
We are seeking applicants for two full-time tenure-track assistant research professor positions in the field of non-communicable disease (NCD) epidemiology. Applications are invited from dynamic researchers with experience in NCD epidemiology and demonstrated excellence and intellectual leadership.