- Login / Register

‘Nearly a week has passed already since International Nurses Day 2024’
STEVE FORD, EDITOR
- You are here: Assessment skills

Communication skills 2: overcoming the barriers to effective communication
18 December, 2017 By NT Contributor
This article, the second in a six-part series on communication skills, a discusses the barriers to effective communication and how to overcome them
Competing demands, lack of privacy, and background noise are all potential barriers to effective communication between nurses and patients. Patients’ ability to communicate effectively may also be affected by their condition, medication, pain and/or anxiety. Nurses’ and patients’ cultural values and beliefs can also lead to misinterpretation or reinterpretation of key messages. This article, the second in a six-part series on communication skills , suggests practical ways of overcoming the most common barriers to communication in healthcare.
Citation: Ali M (2017) Communication skills 2: overcoming barriers to effective communication Nursing Times ; 114: 1, 40-42.
Author: Moi Ali is a communications consultant, a board member of the Scottish Ambulance Service and of the Professional Standards Authority for Health and Care, and a former vice-president of the Nursing and Midwifery Council.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here
- Click here to see other articles in this series
- Read Moi Ali’s comment
Introduction
It is natural for patients to feel apprehensive about their health and wellbeing, yet a survey in 2016 found that only 38% of adult inpatients who had worries or fears could ‘definitely’ find someone in hospital to talk to about them (Care Quality Commission, 2017). There are numerous barriers to effective communication including:
- Time constraints;
- Environmental issues such as noise and privacy;
- Pain and fatigue;
- Embarrassment and anxiety;
- Use of jargon;
- Values and beliefs;
- Information overload.
Time constraints
Time – or lack of it – creates a significant barrier to communication for nurses (Norouzinia et al, 2016). Hurried communication is never as effective as a leisurely interaction, yet in pressured workplaces, nurses faced with competing demands may neglect the quality of communication. It is important to remember that communication does not need to be time-consuming – a smile, hello, or some ‘small talk’ about the weather may suffice. Even when there is no pressing news to tell individual patients, taking the time to get to know them can prepare the ground for difficult conversations that may need to take place in the future.
In a pressured ward or clinic, conversations between patients and nurses may be delayed or interrupted because of the needs of other patients – for example, they may need to respond to an emergency or pain relief. This can be frustrating for patients who may feel neglected. If interruptions occur it is important to explain to patients that you have to leave and why. Arranging to return within a specified time frame may be enough to reassure them that you are aware that their concerns are important (Box 1).
Box 1. Making time for communication
Nurse Amy Green was allocated a bay of four patients and two side wards for her shift. Halfway through the morning one of her patients in a side ward became very ill and Amy realised that she needed to spend a lot of time with him. She quickly visited her other patients to explain what was happening, and reassured them that she had not forgotten about them. She checked that they were comfortable and not in pain, asked them to ring the call bell if they needed her, and explained that she would return as soon as she could. The patients understood the situation and were reassured that their immediate needs had been assessed and they were not being neglected.
Environmental factors
You may be so familiar with your surroundings that you no longer notice the environmental factors that can create communication difficulties. Background noise in a busy clinic can affect patients’ ability to hear, and some may try to disguise this by nodding and ‘appearing’ to hear. If you think your patient has hearing problems, reduce background noise, find a quiet corner or step into a quiet side room or office. Check whether your patient uses physical aids, such as hearing aids or spectacles and that these are in working order.
Noise and other distractions can impede communication with patients with dementia and other cognitive impairments, who find concentration challenging. If you have to communicate an important message to a patient with poor concentration, it is useful to plan ahead and identify the best place and time to talk. It can be helpful to choose a time when you are less busy, without competing activities such as medicine rounds or meal times to interrupt your discussion.
Patients may be reticent to provide sensitive personal information if they are asked about their clinical history within earshot of other people, such as at a busy reception desk or in a cubicle with just a curtain for privacy. It is important to avoid asking sensitive questions where others may hear patients’ replies. Consider alternative ways of gathering pertinent information, such as asking the patient to complete a written form – but remember that some patients struggle with reading and writing or may need the form to be provided in a different language or have someone translate for them.
Pain and fatigue
We often need to gain important information from patients when they are acutely ill and distressed, and symptoms such as pain can reduce concentration. If you urgently need to gather information, it is important to acknowledge pain and discomfort: “I know that it is painful, but it’s important that we discuss.”
Patients may also be tired from a sleepless night, drowsy after an anaesthetic or experiencing the side-effects of medicines. Communicating with someone who is not fully alert is difficult, so it is important to prioritise the information you need, assess whether it is necessary to speak to the patient and ask yourself:
- Is this the best time for this conversation?
- Can my message wait?
- Can I give part of the message now and the rest later?
When patients cannot give their full attention, consider whether your message could be broken down into smaller pieces so there is less to digest in one go: “I will explain your medication now. I’ll return after lunch to tell you about how physiotherapy may help.” Ask if they would like any of the information repeated.
If you have to impart an important piece of information, acknowledge how the patient is feeling: “I know that you’re tired, but …”. Showing empathy can build rapport and make patients more receptive. It may also be useful to stress the need to pay attention: “It’s important that you listen because …”. Consider repeating the message: “It can be difficult to take everything in when you’re tired, so I just wanted to check that you’re clear about …”. If the communication is important, ask the patient to repeat it back to you to check it has been understood.
Embarrassment and anxiety
Would you feel comfortable undressing in front of a complete stranger, or talking about sex, difficult family circumstances, addictions or bowel problems? Patients’ and health professionals’ embarrassment can result in awkward encounters that may hamper effective communication. However, anticipating potential embarrassment, minimising it, and using straightforward, open communication can ease difficult conversations. For example, in a clinic, a patient may need to remove some clothes for an examination. It is important to be direct and specific. Do not say: “Please undress”, as patients may not know what to remove; give specific instructions: “Please remove your trousers and pants, but keep your shirt on”. Clear directions can ease stress and embarrassment when delivered with matter-of-fact confidence.
Patients may worry about embarrassing you or themselves by using inappropriate terms for anatomical parts or bodily functions. You can ease this embarrassment by introducing words such as “bowel movements” or “penis” into your questions, if you think they are unsure what terminology to use. Ambiguous terms such as “stool”, which have a variety of everyday meanings, should be avoided as they may cause confusion.
Many patients worry about undergoing intimate procedures such as bowel and bladder investigations. Explain in plain English what an examination involves, so that patients know what to expect. Explaining any side-effects of procedures – such as flatulence or vomiting – not only warns patients what to expect but reassures them that staff will not be offended if these occur.
Box 2 provides some useful tips on dealing with embarrassment.
Box 2. Managing embarrassment
- Look out for signs of embarrassment – not just obvious ones like blushing, but also laughter, joking, fidgeting and other behaviours aimed at masking it
- Think about your facial expressions when communicating with patients, and use positive, open body language such as appropriate eye contact or nodding
- Avoid disapproving or judgmental statements by phrasing questions carefully: “You don’t drink more than 10 glasses of wine a week, do you?” suggests that the ‘right’ or desired answer is ‘no’. A neutral, open question will elicit a more honest response: “How many glasses of wine do you drink in a typical week?”
Some patients are reluctant to ask questions, seek clarification or request that information be repeated for fear of wasting nurses’ time. It is important to let them know that their health or welfare is an integral part of your job. They also need to know that there is no such thing as a silly question. Encourage questions by using prompts and open questions such as: “You’re bound to have questions – are there any that I can answer for you now?”; “What else can I tell you about the operation?”. It is also possible to anticipate and address likely anxieties such as “Will it be painful?”; “Will I get better?”; or “Will I die?”.
Jargon can be an important communication aid between professionals in the same field, but it is important to avoid using technical jargon and clinical acronyms with patients. Even though they may not understand, they may not ask you for a plain English translation. It is easy to slip into jargon without realising it, so make a conscious effort to avoid it.
A report on health literacy from the Royal College of General Practitioners (2014) cited the example of a patient who took the description of a “positive cancer diagnosis” to be good news, when the reverse was the case. If you have to use jargon, explain what it means. Wherever possible, keep medical terms as simple as possible – for example, kidney, rather than renal and heart, not cardiac. The Plain English website contains examples of healthcare jargon.
Box 3 gives advice on how to avoid jargon when speaking with patients.
Box 3. Avoiding jargon
- Avoid ambiguity: words with one meaning for a nurse may have another in common parlance – for example, ‘acute’ or ‘stool’
- Use appropriate vocabulary for the audience and age-appropriate terms, avoiding childish or over-familiar expressions with older people
- Avoid complex sentence structures, slang or speaking quickly with patients who are not fluent in English
- Use easy-to-relate-to analogies when explaining things: “Your bowel is a bit like a garden hose”
- Avoid statistics such as “There’s an 80% chance that …” as even simple percentages can be confusing. “Eight in every 10 people” humanises the statistic
Values, beliefs and assumptions
Everyone makes assumptions based on their social or cultural beliefs, values, traditions, biases and prejudices. A patient might genuinely believe that female staff must be junior, or that a man cannot be a midwife. Be alert to patients’ assumptions that could lead to misinterpretation, reinterpretation, or even them ignoring what you are telling them. Think about how you can address such situations; for example explain your role at the outset: “Hello, I am [your name], the nurse practitioner who will be examining you today.”
It is important to be aware of your own assumptions, prejudices and values and reflect on whether they could affect your communication with patients. A nurse might assume that a patient in a same-sex relationship will not have children, that an Asian patient will not speak good English, or that someone with a learning disability or an older person will not be in an active sexual relationship. Incorrect assumptions may cause offence. Enquiries such as asking someone’s “Christian name” may be culturally insensitive for non-Christians.
Information overload
We all struggle to absorb lots of facts in one go and when we are bombarded with statistics, information and options, it is easy to blank them out. This is particularly so for patients who are upset, distressed, anxious, tired, in shock or in pain. If you need to provide a lot of information, assess how the patient is feeling and stick to the pertinent issues. You can flag up critical information by saying: “You need to pay particular attention to this because …”.
Box 4 provides tips on avoiding information overload.
Box 4. Avoiding information overload
- Consider suggesting that your patient involves a relative or friend in complex conversations – two pairs of ears are better than one. However, be aware that some patients may not wish others to know about their health
- Suggest patients take notes if they wish
- With patients’ consent, consider making a recording (or asking whether the patient wishes to record part of the consultation on their mobile phone) so they can replay it later or share it with a partner who could not accompany them
- Give written information to supplement or reinforce the spoken word
- Arrange another meeting if necessary to go over details again or to provide further information
It is vital that all nurses are aware of potential barriers to communication, reflect on their own skills and how their workplace environment affects their ability to communicate effectively with patients. You can use this article and the activity in Box 5 to reflect on these barriers and how to improve and refine your communication with patients.
Box 5. Reflective activity
Think about recent encounters with patients:
- What communication barriers did you encounter?
- Why did they occur?
- How can you amend your communication style to take account of these factors so that your message is not missed, diluted or distorted?
- Do you need support to make these changes?
- Who can you ask for help?
- Nurses need to be aware of the potential barriers to communication and adopt strategies to address them
- Environmental factors such as background noise can affect patients’ ability to hear and understand what is being said to them
- Acute illness, distress and pain can reduce patients’ concentration and their ability to absorb new information
- Anticipating potential embarrassment and taking steps to minimise it can facilitate difficult conversations
- It is important to plan ahead and identify the best place and time to have important conversations
Also in this series
- Communication skills 1: benefits of effective communication for patients
- Communication skills 3: non-verbal communication
- Communication 4: the influence of appearance and environment
- Communication 5: effective listening and observation skills
- Communication skills 6: difficult and challenging conversations
Related files
171220 communication skills 2 overcoming barriers to effective communication.
- Add to Bookmarks
Related articles
Have your say.
Sign in or Register a new account to join the discussion.
Dissecting Communication Barriers in Healthcare: A Path to Enhancing Communication Resiliency, Reliability, and Patient Safety
Affiliations.
- 1 Department of Human Factors and Behavioral Neurobiology, Embry-Riddle Aeronautical University, Daytona Beach, Florida.
- 2 Armstrong Institute for Patient Safety and Quality, Johns Hopkins School of Medicine, Department of Surgery, Johns Hopkins Hospital, Baltimore, Maryland.
- PMID: 30418425
- DOI: 10.1097/PTS.0000000000000541
Suboptimal exchange of information can have tragic consequences to patient's safety and survival. To this end, the Joint Commission lists communication error among the most common attributable causes of sentinel events. The risk management literature further supports this finding, ascribing communication error as a major factor (70%) in adverse events. Despite numerous strategies to improve patient safety, which are rooted in other high reliability industries (e.g., commercial aviation and naval aviation), communication remains an adaptive challenge that has proven difficult to overcome in the sociotechnical landscape that defines healthcare. Attributing a breakdown in information exchange to simply a generic "communication error" without further specification is ineffective and a gross oversimplification of a complex phenomenon. Further dissection of the communication error using root cause analysis, a failure modes and effects analysis, or through an event reporting system is needed. Generalizing rather than categorizing is an oversimplification that clouds clear pattern recognition and thereby prevents focused interventions to improve process reliability. We propose that being more precise when describing communication error is a valid mechanism to learn from these errors. We assert that by deconstructing communication in healthcare into its elemental parts, a more effective organizational learning strategy emerges to enable more focused patient safety improvement efforts. After defining the barriers to effective communication, we then map evidence-based recovery strategies and tools specific to each barrier as a tactic to enhance the reliability and validity of information exchange within healthcare.
Copyright © 2018 Wolters Kluwer Health, Inc. All rights reserved.
- Communication Barriers
- Communication*
- Delivery of Health Care
- Medical Errors / prevention & control
- Patient Safety*
- Reproducibility of Results
- Safety Management
- Open access
- Published: 16 May 2024
Comparison of barriers to effective nurse-patient communication in COVID-19 and non-COVID-19 wards
- Hamed Bakhshi ORCID: orcid.org/0009-0008-7865-0149 1 ,
- Mohammad Javad Shariati ORCID: orcid.org/0009-0000-5518-698X 1 ,
- Mohammad Hasan Basirinezhad ORCID: orcid.org/0000-0002-3672-556X 2 &
- Hossein Ebrahimi ORCID: orcid.org/0000-0001-5731-7103 3
BMC Nursing volume 23 , Article number: 328 ( 2024 ) Cite this article
180 Accesses
Metrics details
Communication is a basic need of humans. Identifying factors that prevent effective nurse-patient communication allows for the better implementation of necessary measures to modify barriers. This study aims to compare the barriers to effective nurse-patient communication from the perspectives of nurses and patients in COVID-19 and non-COVID-19 wards.
Materials and methods
This cross-sectional descriptive study was conducted in 2022. The participants included 200 nurses (by stratified sampling method) and 200 patients (by systematic random sampling) referred to two conveniently selected hospitals in Shahroud, Iran. The inclusion criteria for nurses were considered having at least a bachelor’s degree and a minimum literacy level for patients to complete the questionnaires. Data were collected by the demographic information form and questionnaire with 30 and 15 questions for nurses and patients, which contained similar questions to those for nurses, based on a 5-point Likert scale. Data were analysis using descriptive indices and inferential statistics (Linear regression) in SPSS software version 18.
The high workload of nursing, excessive expectations of patients, and the difficulty of nursing work were identified by nurses as the main communication barriers. From the patients’ viewpoints, the aggressiveness of nurses, the lack of facilities (welfare treatment), and the unsanitary conditions of their rooms were the main communication barriers. The regression model revealed that the mean score of barriers to communication among nurses would decrease to 0.48 for each unit of age increase. Additionally, the patient’s residence explained 2.3% of the nurses’ barriers to communication, meaning that native participants obtained a mean score of 2.83 units less than non-native nurses, and there was no statistically significant difference between the COVID and non-COVID wards.
In this study, the domain of job characteristics was identified by nurses as the major barrier, and patients emphasized factors that were in the domain of individual/social factors. There is a pressing need to pay attention to these barriers to eliminate them through necessary measures by nursing administrators.
Peer Review reports
First observed in Wuhan, China, the COVID-19 pandemic is an acute and very severe respiratory syndrome that the World Health Organization has raised as a health problem because of its high spread rate and consequences on an international scale. The number of COVID-19 patients is increasingly on the rise [ 1 , 2 ]. Illness and hospitalization are usually stressful and associated with bad experiences for patients and their family members [ 3 ].
According to Tabandeh Sadeghi et al. (2011) “Communication is a basic need of humans. Any interaction is an opportunity to achieve effective communication and participation in understanding the issue, which leads to the achievement of mutual goals by individuals.” [ 4 ]. The three important aspects of communication that are emphasized the most are the message’s sender, the receiver, and the environment. Communicating is an interaction between the sender and the receiver of the message, and the environment affects them [ 5 , 6 ]. In the context of a hospital, these three aspects of communication can be defined as nurse, patient, and hospital environment, and all three should be considered when examining the obstacles [ 7 ]. “According to Ali Fakhr Movahedi et al. (2012)” Communication is considered a central concept in nursing and an essential part of nursing work [ 8 ]. Patients perceive interaction with nurses as the basis of their treatment [ 9 ]. Nurse-patient communication is an interpersonal process that is created between these two groups during treatment. This process generally includes the start, work, and end stages. Effective communication is an essential aspect of patient care by nurses, and many nursing tasks cannot be performed without this activity [ 10 ]. Effective communication consists of explicit transmission and receipt of message content, in which information is consciously and unconsciously produced by a person and communicated to the recipient through verbal and non-verbal patterns [ 11 ]. The non-verbal aspect of communication plays an essential role and is more important than the verbal aspect of language in emergencies. The mandatory use of face masks during the COVID-19 pandemic negatively influenced nurse-patient communication, notably because this tool significantly reduced the messages arising from non-verbal communication channels [ 12 ]. In this regard, Vitale et al. investigated wearing face masks as a communication barrier between nurses and patients. The results showed no differences in the patients’ opinions before and during the COVID-19 pandemic; patients believed that the mask was not a communication barrier, while nurses thought that wearing masks was a communication barrier [ 12 ]. Unfavorable communication can hamper the patient’s recovery and may even permanently deprive the patient of health or life.
In comparison, good communication affects the patient’s recovery more than medication. In fact, nurses will succeed in their tasks when they can communicate well with their patients [ 13 ]. Effective communication can affect pain control, adherence to a treatment regimen, and the patient’s mental health and play an important role in reducing the patient’s anxiety and fear and faster recovery [ 14 ]. During good communication, patients can disclose and express sensitive and personal information. Consequently, nurses can also transfer necessary information, attitudes, or skills [ 4 ]. Identifying factors that prevent effective nurse-patient communication allows for the better implementation of measures required to adjust obstacles [ 15 ].
The first published reports of the deaths of coronavirus-infected doctors during caring for patients indicate that the virus transmission to healthcare workers in healthcare centers is a hazardous issue [ 16 , 17 ]. Under these stressful conditions, nurses must manage long shift hours and the fear of contagion and overcome communication difficulties through layers of personal protective equipment. These problems may disrupt communication with patients and cause less focus of health workers on the psychosocial well-being of patients [ 18 , 19 ]. Baillie states that the lack of time is a clear barrier to communication between emergency nurses and patients [ 20 ]. Meehan et al. also reported that nurses mentioned the lack of time, fatigue, and workload of personnel to be the factors preventing nurse-patient interaction. In the same research, patients cited the issue of gender as a factor preventing their interaction with nurses. However, male and female patients had difficulty communicating with male nurses [ 21 ].
Identifying factors that prevent effective nurse-patient communication makes it possible to elucidate the direction of necessary measures for the planners and executives of the health sector to eliminate or modify barriers. In particular, when these barriers are identified and expressed with a realistic approach, i.e., from nurses’ and patients’ perspectives [ 22 ]. Before this, no study compared barriers to nurse-patient communication in COVID and non-COVID wards. Therefore, this research aims to compare the barriers to effective nurse-patient communication from nurses’ and patients’ perspectives in COVID-19 and NON-COVID-19 wards. Hopefully, identifying these obstacles and planning to solve them as soon as possible will make us have nurses in the future who can communicate well with patients and improve service delivery.
Study design
This cross-sectional descriptive research was conducted on 200 nurses and 200 patients at hospitals affiliated with the Shahroud University of Medical Sciences. The participants included nurses and patients from different wards of two conveniently selected hospitals in Shahroud. To sample nurses by the stratified method, the sample size was first divided by the total number of nurses in the mentioned hospitals to obtain the sampling fraction. According to Mohammadi et al. study, standard deviations reported for all subscales for barrier’s to effective communication (individual/social factors = 6.22), job characteristics = 6.74, patient’s clinical conditions = 4.22), and environmental factors = 9.09) were utilized to estimate the sample size [ 23 ]. Estimation error was considered 0.15 of standard deviation values. The confidence levels and power were considered at 0.95 and 0.8 respectively with a 15% dropout probability. Also, another sample size was calculated similarly using the standard deviation reported in Norouzinia et al. study for patient’s questionnaire equal to 1.96 [ 24 ]. Finally, among the estimated values; the largest number (200) was considered as the sample size of the present study for nurses and patients.
Considering that the total number of nurses is around 700 and the sample size calculated by the statistics consultant is 200 nurses, our sampling fraction was calculated as \(\frac{2}{7}\) . Therefore, \(\frac{2}{7}\) personnel of each department were included in the study. The patients were sampled by a systematically random method using the hospital list, file number, and dates of admission and discharge. The inclusion criteria for nurses were a bachelor’s degree or higher and a minimum literacy level for patients to complete the questionnaire. Moreover, the questionnaire contained questions about the nurses’ work experience or no experience in COVID-19 wards. The duration of working in COVID-19 wards was included in the questionnaire questions, and the duration was considered in the analysis. Data were collected using a questionnaire provided to the nurses through daily visits to various wards of the mentioned hospitals, including emergency, surgery, special care, internal medicine, gastroenterology, cardiology, urology, orthopedics, ICU, CCU, and other wards. The questionnaire was also provided to the patients hospitalized in surgery, special care, internal medicine, gastroenterology, cardiology, urology, ICU, and CCU wards, among others. Due to the reduced coronavirus spread during that period, the information on COVID-19 patients was accessed using hospital information by obtaining permission, and the questionnaire was completed through phone calls.
Measurements
Demographic information form.
It contained questions about information related to age, gender, marital status, language, and residence.
Communication barrier questionnaire
The barriers to effective nurse-patient communication were investigated using the same questionnaire designed by Anoosheh et al. This questionnaire contains 30 items for nurses and aims to evaluate nurses’ views about the barriers to effective nurse-patient communication. The response of this questionnaire is in the Likert range (completely false = 1, false = 2, I have no opinion = 3, agree = 4, and completely agree = 5). The nurses’ questionnaire contains four dimensions, and the question numbers of each dimension include individual/social factors (1–8), occupational characteristics (9–17), patient’s clinical conditions (18–21), and environmental factors (22–30). The domain of individual/social factors includes questions such as the gender difference between the patient and the nurse, age difference, aggressiveness of nurses, etc. The domain of job characteristics includes questions about the high workload of nursing, the difficulty of nursing work, the low salaries of nurses, etc. The domain of the patient’s clinical condition also includes questions such as the severity of the disease, the presence of the patient’s companion, etc. The domain of environmental factors: where communication occurs is important. The nurse and the patient should feel calm and safe in the treatment environment. This domain also includes questions such as the Lack of facilities (welfare - treatment) for patients, the unsanitary condition of the patient’s room, the High cost of treating patients, etc. A pilot study was carried out to assess the face validity among nurses. In addition, the content validity was assessed by estimation of content validity ratio and content validity index among nursing educators. The internal consistency for the present questionnaire assessed by Cronbach’s alpha coefficient equal to 0.96 [ 25 ].
The patient questionnaire contains 15 questions and aims to evaluate the patients’ views about the barriers to effective nurse-patient communication. The response of this questionnaire is in the Likert range (completely false = 1, false = 2, I have no opinion = 3, agree = 4, and completely agree = 5). No separate dimension was considered for the patient questionnaire. The reliability based on internal consistency was reported using Cronbach’s alpha equal to 0.91 [ 25 ]. The total score of the questionnaire is obtained by summing up the total scores of all questions. The score of each dimension is obtained from the sum of scores for each question of that dimension. Higher scores in each dimension indicate the greater strength of that dimension as a barrier to effective nurse-patient communication and vice versa. After completing the communication barrier questionnaire, a separate question was asked from the patients and nurses about whether or not the face mask was a communication barrier. This question was scored with a Likert scale (completely false = 1, false = 2, I have no opinion = 3, agree = 4, and completely agree = 5). The score of this question was measured separately from the nurse-patient communication barrier questionnaire.
Ethical considerations
Initially, necessary permissions were obtained from the Vice Chancellor of Research and Technology and the Research Ethics Council (code of ethics: IR.SHMU.REC.1401.140) at the Shahroud University of Medical Sciences. Necessary coordination was also made with the administrators of two conveniently selected hospitals in Shahroud. After explaining the purpose of the research and answering the questions of nurses and patients regarding the questionnaire and how to complete them, enough time was given to answer them.
Statistical analysis
Data were analyzed using descriptive statistics (frequency, percentage, mean, and standard deviation) and inferential tests (Linear regression) in SPSS software version 18. All variables with a significance level of less than 0.2 are included in the final regression model. A significance level of 0.05 was considered. Considering that one of the purposes of this study is to determine the barriers to effective nurse-patient communication based on demographic information, three participants were excluded from the data analysis due to a lack of demographic information completion.
The average ages of nurses and patients were respectively 33.28 and 38.57 years, and most nurses (85.3%) and patients (61.5%) were females and males, respectively. Other demographic characteristics are listed in Table 1 .
In this study, the mean score obtained for each domain of the barriers to nurse-patient communication was determined from the nurses’ point of view. According to these results, the highest score with an average of 32.41 ± 6.75 related to the domain of job characteristics, and the lowest score with an average of 11.76 ± 3.17 related to the domain of Patient’s Clinical Conditions. Additional information is presented in Table 2 .
The excessive patients’ expectations in the domain of individual/social factors, the high workload of nursing in the domain of job characteristics, the severity of the disease in the domain of the patient’s clinical conditions, and no appreciation for nurses by authorities in the domain of environmental factors were the major communication barriers. The patient-nurse age difference from the domain of individual/social factors, the patient’s contact with multiple nurses with different attitudes from the domain of job characteristics, previous hospitalization history from the domain of the patient’s clinical conditions, and the high cost of patient treatment from the domain of environmental factors were the least important barriers to communication from the nurses’ viewpoints. From the patients’ views, the aggressiveness of nurses and the patient-nurse age difference were the major and the minor barriers to communication, respectively. Face masks were among the minor barriers to nurse-patient communication from the viewpoints of both groups (Table 3 ); this table is placed at the end of the article.
The relationship between nurses’ age and communication barriers was investigated using a regression model. This model was first run as a univariate type, and variables with a significance of < 0.2 were introduced into a multivariate model using the backward method. Finally, the model showed that the nurses’ age variable explained 3.8% of the score variance. In other words, the regression model revealed that the mean score of nurses would decrease to 0.486 for each year of age increase, and there is no statistically significant difference between the COVID and non-COVID wards (Table 4 ).
Additionally, the patient’s residence variable explained 2.3% of the score variance, meaning that native people obtained a mean score of 2.813 units less than non-native people, and there is no statistically significant difference between the COVID and non-COVID wards (Table 5 ).
The present study aimed to determine the barriers to effective nurse-patient communication from the viewpoints of nurses and patients in COVID-19 and non-COVID-19 wards in hospitals affiliated with the Shahroud University of Medical Sciences. The results of this study showed that in the domains of barriers to effective communication, nurses reported the highest score in job characteristics and the lowest score in the patient’s clinical conditions. In a study on nursing students at Urmia Midwifery School of Nursing, Habibzadeh et al. (2017) reported the highest and the lowest mean scores for questions related to occupational characteristics and the patient’s clinical conditions [ 26 ], which corresponds to our results. Work congestion conditions increase the work pressure of nurses, leading to fatigue, a situation in which nurses lack enough time to discover the patient’s concerns [ 27 ]. Stress and pressure caused by time constraints often result in miscommunication and reduce the satisfaction of nurses and patients [ 28 ].
The results of this study showed that the high workload of nursing and excessive expectations of patients are mentioned as two major obstacles to effective communication with patients from the point of view of nurses. Anoushe et al. (2015) and Baraz Pordanjani et al. (2016) investigated barriers to effective nurse-patient communication. They reported that nurses identify their workload as a major barrier to effective patient communication [ 15 , 22 ]. However, Habibzadeh et al. (2017) claimed that nurses’ lack of information and skills in patient communication was identified as the main communication barrier [ 26 ]. A possible reason for this discrepancy might be that the current study was conducted during the COVID-19 pandemic, concurrent with the increased workload of nurses compared to the pre-pandemic period.
The difficulty of nursing work, the psychophysical fatigue of nurses, the lack of comfort facilities for nurses, and no appreciation for nurses by administrators are in the next ranks of importance. Similarly, Anoushe et al. (2005) reported the difficulty of nursing work, the lack of comfort facilities for nurses, and psychophysical fatigue among the barriers with more emphasis by nurses [ 22 ]. The notable point is that nurses do not have the opportunity to establish effective communication with patients due to their workload. Furthermore, their work type is hard and tiring, and they do not receive proper benefits or appreciation. In such a situation, one cannot expect good nurse-patient communication, and the conditions affect patients’ moods. As expressed by the patients, this issue also negatively affects the quality of their relationships with patients [ 15 ].
The aggressiveness of nurses mentioned as the main obstacle to effective communication with patients from the patients’ point of view. Likewise, Baraz Pordanjani et al. (2009) found a statistically significant difference between the aggressiveness of nurses from the perspectives of nurses and patients [ 15 ].
Regarding the communication barriers from the patient’s perspective, the lack of facilities (welfare treatment) for them and the unsanitary condition of their rooms were among the factors more emphasized by patients than by the nurses. Interestingly, Baraz Pordanjani et al. observed that nurses believed more than patients that the lack of comfort facilities for patients and the unsanitary condition of their rooms would hinder effective communication [ 15 ]. This contradictory result can result from the difference in facilities and health/treatment conditions of the studied hospitals.
The viewpoints of both nurse and patient groups show that age and class differences do not negatively influence their relationships. Since nurses are responsible for initiating and maintaining communication with patients, it can be claimed that they perform their professional tasks, including communication establishment, regardless of the social class and age of patients, who also acknowledge this issue.
The face mask also obtained a low score from the viewpoints of patients and nurses. Vitale et al. investigated the use of face masks as a communication barrier between nurses and patients. The results indicated no difference in the patients’ opinions before and during the COVID-19 pandemic; that is, patients did not consider the mask a communication barrier, which is consistent with the present study. However, nurses thought that using a mask would be a communication barrier [ 12 ].
The present results revealed a significant relationship between the age of nurses and the barriers to effective nurse-patient communication; as such, the total score of nurses decreased for each year of age increase; However, no statistically significant difference was observed in the comparison of COVID and non-COVID wards. In this regard, Gopichandran et al. (2021) aimed to determine communication barriers between doctors and patients during the COVID-19 pandemic in India. They claimed that communication barriers decreased with age [ 29 ]. Nurses gain more experience and skills with rising age. Enough experience is also a characteristic that patients consider necessary for nursing work [ 30 ]. “According to Aram Feizi et al. (2006)” Mark (2001) concluded that the experience of the nursing unit could create satisfaction in both nurses and patients [ 30 ]. The possible reason for obtaining different results could be that the COVID-19 vaccination process was carried out slowly in Iran. For this reason, the nurses, both in the COVID and non-COVID wards, considered all patients with unique viewpoints (all of the patients considered potential cases of COVID-19). For this reason, there was no statistical difference between the communication barriers of the COVID and non-COVID departments.
No statistically significant difference was observed between the scores of male and female nurses and the barriers to effective nurse-patient communication. Unlike this result, Mohammadi et al. (2013) reported a significant difference between job characteristics, patients’ clinical conditions, environmental factors, and the gender of nurses [ 23 ]. The discrepant results might be caused by the heterogeneous distribution of participants in terms of gender, as 56% of the nurses were male in the study of Mohammadi et al. In comparison, less than 20% of the participants were male nurses in the present study.
The present results showed that the patients’ residence was significantly related to the barriers to effective nurse-patient communication, and native people obtained a lower mean score than non-native people: However, there was no any no significant difference between COVID and NON-COVID wards This result might be because nurses are more informed of the accents and dialects of native patients. Caring for patients speaking different languages and accents can lead to problems in the quantity and quality of nurse-patient communication. When patients and caregivers have different cultural values and languages, communication can cause the inability to exchange information [ 27 ]. Tilki and Okoughan presented evidence that differences in spoken language could hinder effective communication [ 31 ]. On the other hand, the results of the study by Vitale et al. showed that there was no difference between the patients before and during the covid-19 pandemic, which is consistent with the results of the present study [ 12 ].
Limitations
Among the limitations of this study, we can mention the low response rate by nurses and patients, which was completed with the continuous presence of the researcher. Since this research is conducted only in public medical centers affiliated to Shahroud University of Medical Sciences, the results may not be generalizable to centers affiliated with other universities of medical sciences in Iran and non-academic centers such as private medical centers. It is recommended that future research be conducted in larger settings.
This study demonstrated that nurses identified the domain of job characteristics as the most critical barrier among the four domains of barriers to effective nurse-patient communication. Patients more emphasized factors that were in the domain of individual/social factors. There is a pressing need to pay attention to these barriers to eliminate them through necessary measures by nursing officials. Hopefully, the elimination of these barriers in the future will lead to nurses who can communicate well with patients and improve service delivery.
Implications
This research helps to identify barriers to effective communication between nurses and patients. In the field of policy and management, the results of this research can help to plan for effective nurse-patient communication. In the field of education, according to the results of this article, necessary training should be given to nurses and patients regarding communication barriers to help improve communication. There will be a basis for further, more comprehensive research in the field of research. Hopefully, these results can help nursing officials and nurses remove communication barriers and improve service delivery.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, et al. Cardiovascular considerations for patients, Health Care Workers, and Health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–71.
Article CAS PubMed PubMed Central Google Scholar
WHO. Coronavirus disease (COVID-19). Situation Report– 161. 2020.[cited 2020 June 29] https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200629-covid-19-sitrep-161.pdf?sfvrsn=74fde64e_2 .
Sheldon LK, Barrett R, Ellington L. Difficult communication in nursing. J Nurs Scholarsh. 2006;38(2):141–7.
Article PubMed Google Scholar
Sadeghi T, Dehghan Nayyeri N, Karimi R. Nursing-patient relationship: a comparison between nurses and adolescents perceptions. Iran J Med Ethics History Med. 2011;4(3):69–78.
Google Scholar
Caris-Verhallen WM, De Gruijter IM, Kerkstra A, Bensing JM. Factors related to nurse communication with elderly people. J Adv Nurs. 1999;30(5):1106–17.
Article CAS PubMed Google Scholar
Kopp P. Better communication with older patients. Professional nurse (London, England). 2001;16(8):1296-9.
Aghamolaei T, Hasani L. Communication barriers among nurses and elderly patients. Hormozgan Med J. 2011;14(4):312–8.
Fakhr-Movahedi A, Negarandeh R, Salsali M. Exploring nurse-patient communication strategies. J Hayat. 2013;18(4):28–46.
Kettunen T, Poskiparta M, Gerlander M. Nurse-patient power relationship: preliminary evidence of patients’ power messages. Patient Educ Couns. 2002;47(2):101–13.
Hagerty BM, Patusky KL. Reconceptualizing the nurse-patient relationship. J Nurs Scholarsh. 2003;35(2):145–50.
Clancy CM, Farquhar MB, Sharp BA. Patient safety in nursing practice. J Nurs Care Qual. 2005;20(3):193–7.
Vitale E, Giammarinaro MP, Lupo R, Archetta V, Fortunato RS, Caldararo C, et al. The quality of patient-nurse communication perceived before and during the COVID-19 pandemic: an Italian pilot study. Acta Biomed. 2021;92(S2):e2021035.
CAS PubMed PubMed Central Google Scholar
Jan Mohamady S, Salami S, Abasi Marei F, Masror D, Nazary Jobrany M. F J. Civilization and Nursing.Tehran: Publication Salemi2002. 107-9 p.
Maskor NA, Krauss SE, Muhamad M, Nik Mahmood NH. Communication competencies of oncology nurses in Malaysia. Asian Pac J Cancer Prev. 2013;14(1):153–8.
Baraz Pordanjani S, Shariati A, Alijani H, Moein Mosavi B. Assessing barriers of nurse-patient’s effective communication in educational hospitals of Ahwaz. Iran J Nurs Res. 2010;5(16):45–52.
Bowdle A, Munoz-Price LS. Preventing infection of patients and Healthcare workers should be the New Normal in the era of Novel Coronavirus Epidemics. Anesthesiology. 2020;132(6):1292–5.
Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67(5):568–76.
Fritzsche K, Scheib P, Ko N, Wirsching M, Kuhnert A, Hick J, et al. Results of a psychosomatic training program in China, Vietnam and Laos: successful cross-cultural transfer of a postgraduate training program for medical doctors. Biopsychosoc Med. 2012;6(1):17.
Article PubMed PubMed Central Google Scholar
Eltaybani S, Igarashi A, Cal A, Lai CK, Carrasco C, Sari DW et al. Long-term care facilities’ response to the COVID‐19 pandemic: An international, cross‐sectional survey. J Adv Nurs. 2023.
Baillie L. An exploration of nurse-patient relationships in accident and emergency. Accid Emerg Nurs. 2005;13(1):9–14.
Cleary M, Edwards C, Meehan T. Factors influencing nurse–patient interaction in the acute psychiatric setting: an exploratory investigation. Aust N Z J Mental Health Nurs. 1999;8(3):109–16.
Article CAS Google Scholar
Anoosheh M, Zarkhah S. Investigating barriers to effective nurse-patient communication. Teb Tazkie. 2006;15(2):49–57.
Mohammadi I, Mozafari M, Beigi EJ, Kaikhavani S. Barriers to effective nurse- patient communication from perspective of nurses employed in Educational hospitals of Ilam. J Neyshabur Univ Med Sci. 2015;2(3):20–7.
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2015;8(6):65–74.
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009;56(2):243–9.
Habibzadeh H, Dehgannejad J, Hoseinzadeghan F, Bafandehzendeh M. Barriers to establishing Effective Communication between Nurse and Patient according to nursing students’ viewpoints Urmia nursing and midwifery Faculty. Nurs Midwifery J. 2019;17(9):696–704.
Mazhariazad F, Taghadosi M, Erami E. Challenges of nurse-patient communication in Iran: a review study. Sci J Nurs Midwifery Paramedical Fac. 2019;4(4):15–29.
Jahromi MK, Ramezanli S. Evaluation of barriers contributing in the demonstration of an effective nurse-patient communication in educational hospitals of Jahrom, 2014. Global J Health Sci. 2014;6(6):54.
Gopichandran V, Sakthivel K. Doctor-patient communication and trust in doctors during COVID 19 times-A cross sectional study in Chennai, India. PLoS ONE. 2021;16(6):e0253497.
Feizi A, Mohammadi R, Nikravesh M. Factors causing patient’s Trust in Nurse from patients’ perspective. Razi J Med Sci. 2006;13(52):177–87.
Okougha M, Tilki M. Experience of overseas nurses: the potential for misunderstanding. Br J Nurs. 2010;19(2):102–6.
Download references
Acknowledgements
The present study is a research project approved under the number 14010048 at Shahroud University of Medical Sciences. The researchers are grateful to the Vice Chancellor of Research and Technology at Shahroud University of Medical Sciences for the necessary financial support of the present study and the participating nurses and patients.
No funding.
Author information
Authors and affiliations.
Student Research Committee, School of Nursing and Midwifery, Shahroud University of Medical Sciences, Shahroud, Iran
Hamed Bakhshi & Mohammad Javad Shariati
Department of Epidemiology and Biostatistics, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Mohammad Hasan Basirinezhad
Center for Health Related Social and Behavioral Sciences Research, Shahroud University of Medical Sciences, Shahroud, Iran
Hossein Ebrahimi
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the writing of the article: design and writing of the article (HB, HE), data collection (HB, MS), analysis and interpretation of data (HB, MB), final approval of the submitted version (HE, HB).
Corresponding author
Correspondence to Hossein Ebrahimi .
Ethics declarations
Ethics approval and consent to participate.
In order to observe ethical considerations, after explaining the study objectives and method to nurses and patients, written informed consent was obtained from them. It should be noted that the principles of the Helsinki Declaration, including the right to enter the research freely, no harm or loss to participants, maintaining the right to withdraw from the study, and confidentiality of information, were observed in this study. Besides, the researchers committed themselves to adhering to the principles of the Committee on Publication Ethics (COPE) set out for the publication of the results. This cross-sectional study was approved by the ethics committee of Shahroud University of Medical Sciences with the registration number: IR.SHMU.REC.1401.140.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bakhshi, H., Shariati, M., Basirinezhad, M. et al. Comparison of barriers to effective nurse-patient communication in COVID-19 and non-COVID-19 wards. BMC Nurs 23 , 328 (2024). https://doi.org/10.1186/s12912-024-01947-4
Download citation
Received : 05 August 2023
Accepted : 18 April 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s12912-024-01947-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Communication barriers
- Communication
- Nurse–patient communication
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Ali M. Communication skills 1: benefits of effective communication for patients. Nursing Times. 2017; 113:(12)18-19
Barber C. Communication, ethics and healthcare assistants. British Journal of Healthcare Assistants. 2016; 10:(7)332-335 https://doi.org/10.12968/bjha.2016.10.7.332
Berlo DK. The process of communication; an introduction to theory and practice.New York (NY): Holt, Rinehart and Winston; 1960
Bramhall E. Effective communication skills in nursing practice. Nurs Stand. 2014; 29:(14)53-59 https://doi.org/10.7748/ns.29.14.53.e9355
Bumb M, Keefe J, Miller L, Overcash J. Breaking bad news: an evidence-based review of communication models for oncology nurses. Clin J Oncol Nurs. 2017; 21:(5)573-580 https://doi.org/10.1188/17.CJON.573-580
Caldwell L, Grobbel CC. The importance of reflective practice in nursing. International Journal of Caring Sciences. 2013; 6:(3)319-326
Communication skills for workplace success employers look for these communication skills. The Balance (online). 2019. http://tinyurl.com/yyx3eeoy (accessed 27 June 2019)
Evans N. Knowledge is power when it comes to coping with a devastating diagnosis. Cancer Nursing Practice. 2017; 16:(10)8-9 https://doi.org/10.7748/cnp.16.10.8.s7
Gibbs G. Learning by doing: a guide to teaching and learning methods.Oxford: Further Education Unit, Oxford Polytechnic; 1988
Gillett A, Hammond A, Martala M. Successful academic writing.Harlow: Pearson Education Limited; 2009
Hanratty B, Lowson E, Holmes L Breaking bad news sensitively: what is important to patients in their last year of life?. BMJ Supportive & Palliative Care. 2012; 2:(1)24-28 https://doi.org/10.1136/bmjspcare-2011-000084
Hemming L. Breaking bad news: a case study on communication in health care. Gastrointestinal Nursing. 2017; 15:(1)43-50 https://doi.org/10.12968/gasn.2017.15.1.43
Macmillan Cancer Support. Cancer clinical nurse specialists (Impact Briefs series). 2014. http://tinyurl.com/yb96z88j (accessed 27 June 2019)
Healthcare professionals: acknowledging emotional reactions in newly-diagnosed patients. 2012. http://www.justgotdiagnosed.com (accessed 27 June 2019)
Oelofsen N. Using reflective practice in frontline nursing. Nurs Times. 2012; 108:(24)22-24
Paterson C, Chapman J. Enhancing skills of critical reflection to evidence learning in professional practice. Phys Ther Sport. 2013; 14:(3)133-138 https://doi.org/10.1016/j.ptsp.2013.03.004
Pincock S. Poor communication lies at heart of NHS complaints, says ombudsman. BMJ. 2004; 328 https://doi.org/10.1136/bmj.328.7430.10-d
Royal College of Nursing. Revalidation requirements: reflection and reflective discussion. 2019. http://tinyurl.com/yy8l68cy (accessed 27 June 2019)
Schildmann J, Cushing A, Doyal L, Vollmann J. Breaking bad news: experiences, views and difficulties of pre-registration house officers. Palliat Med. 2005; 19:(2)93-98 https://doi.org/10.1191/0269216305pm996oa
Shipley SD. Listening: a concept analysis. Nurs Forum. 2010; 45:(2)125-134 https://doi.org/10.1111/j.1744-6198.2010.00174.x
Reflecting on the communication process in health care. Part 1: clinical practice—breaking bad news
Beverley Anderson
Macmillan Uro-oncology Clinical Nurse Specialist, Epsom and St Helier NHS Trust
View articles · Email Beverley
This is the first of a two-part article on the communication process in health care. The interactive process of effective communication is crucial to enabling healthcare organisations to deliver compassionate, high-quality nursing care to patients, in facilitating interactions between the organisation and its employees and between team members. Poor communication can generate negativity; for instance, misperception and misinterpretation of the messages relayed can result in poor understanding, patient dissatisfaction and lead to complaints. Reflection is a highly beneficial tool. In nursing, it enables nurses to examine their practice, identify problems or concerns, and take appropriate action to initiate improvements. This two-part article examines the role of a uro-oncology clinical nurse specialist (UCNS). Ongoing observations and reflections on the UCNS's practice had identified some pertinent issues in the communication process, specifically those relating to clinical practice and the management of practice-related issues and complaints. Part 1 examines the inherent problems in the communication process, with explanation of their pertinence to delivering optimal health care to patients, as demonstrated in four case studies related to breaking bad news to patients and one scenario related to communicating in teams. Part 2 will focus on the management of complaints.
In health care, effective communication is crucial to enabling the delivery of compassionate, high-quality nursing care to patients ( Bramhall, 2014 ) and in facilitating effective interactions between an organisation and its employees ( Barber, 2016 ; Ali, 2017 ). Poor communication can have serious consequences for patients ( Pincock, 2004 ; Barber, 2016 ; Ali, 2017 ). Misperception or misinterpretation of the messages relayed can result in misunderstanding, increased anxiety, patient dissatisfaction and lead to complaints ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ; Evans, 2017 ; Doyle, 2019 ), which, as evidence has shown, necessitates efficient management to ensure positive outcomes for all stakeholders—patients, health professionals and the healthcare organisation ( Barber, 2016 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). Complaints and their management will be discussed in Part 2.
Reflection is a highly beneficial tool ( Oelofsen, 2012 ), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes ( Bramhall, 2014 ). The author, a uro-oncology clinical nurse specialist (UCNS), is required to ensure that appropriate reassurance and support is given to patients following the receipt of a urological cancer diagnosis ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ). Support consists of effective communication, which is vital to ensuring patients are fully informed and understand their condition, prognosis and treatment and, accordingly, can make the appropriate choices and decisions for their relevant needs ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ; Doyle, 2019 ).
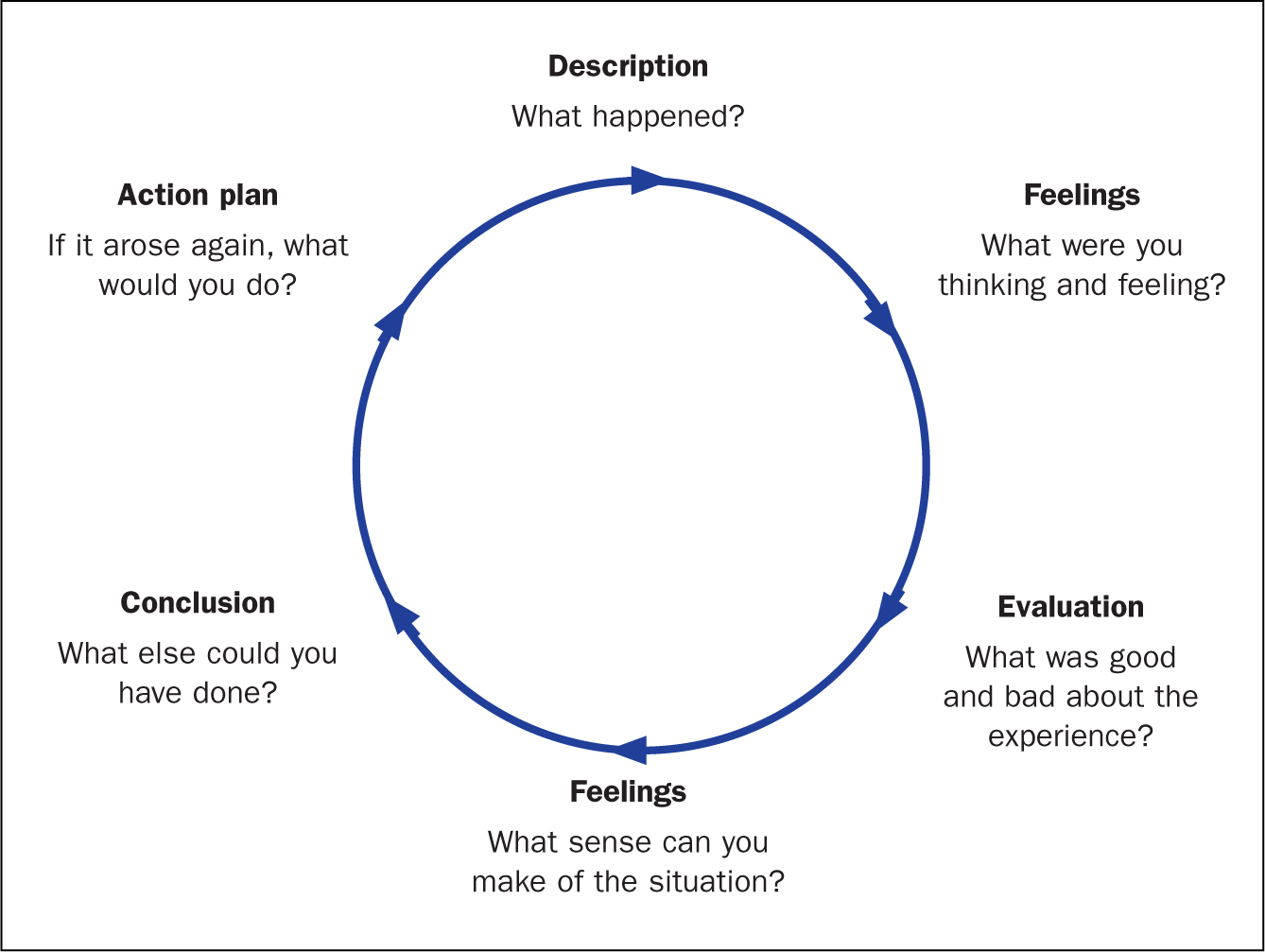
Reflection is a process of exploring and examining ourselves, our perspectives, attributes, experiences, and actions and interactions, which helps us gain insight and see how to move forward ( Gillett et al, 2009:164 ). Reflection is a cycle ( Figure 1 ; Gibbs, 1988 ), which, in nursing, enables the individual to consciously think about an activity or incident, and consider what was positive or challenging and, if appropriate, plan how a similar activity might be enhanced, improved or done differently in the future ( Royal College of Nursing (RCN), 2019 ).
Reflective practice
Reflective practice is the ability to reflect on one's actions and experiences so as to engage in a process of continuous learning ( Oelofsen, 2012 ), while enhancing clinical knowledge and expertise ( Caldwell and Grobbel, 2013 ). A key rationale for reflective practice is that experience alone does not necessarily lead to learning—as depicted by Gibbs' reflective cycle (1988) . Deliberate reflection on experience, emotions, actions and responses is essential to informing the individual's existing knowledge base and in ensuring a higher level of understanding ( Paterson and Chapman, 2013 ). Reflection on practice is a key skill for nurses—it enables them to identify problems and concerns in work situations and in so doing, to make sense of them and to make contextually appropriate changes if they are required ( Oelofsen, 2012 ).
Throughout her nursing career, reflection has been an integral part of the author's ongoing examinations of her practice. The process has enabled numerous opportunities to identify the positive and negative aspects of practice and, accordingly, devise strategies to improve both patient and practice outcomes. Reflection has also been a significant part author's professional development, increasing her nursing knowledge, insight and awareness and, as a result, the author is an intuitive practitioner, who is able to deliver optimal care to her patients.
Communication
Figure 2 provides a visual image of communication—it is both an expressive, message-sending, and a receptive, message-receiving, process ( Berlo, 1960 ; McClain, 2012 ; Evans, 2017 ). This model was originally designed to improve technical communication, but has been widely applied in different fields ( Berlo, 1960 ). Communication is the sharing of information, thoughts and feelings between people through speaking, writing or body language, via phone, email and social media ( Bramhall, 2014 ; Barber, 2016 ; Doyle, 2019 ). Effective communication extends the concept to require that transmitted content is received and understood by someone in the way it was intended.
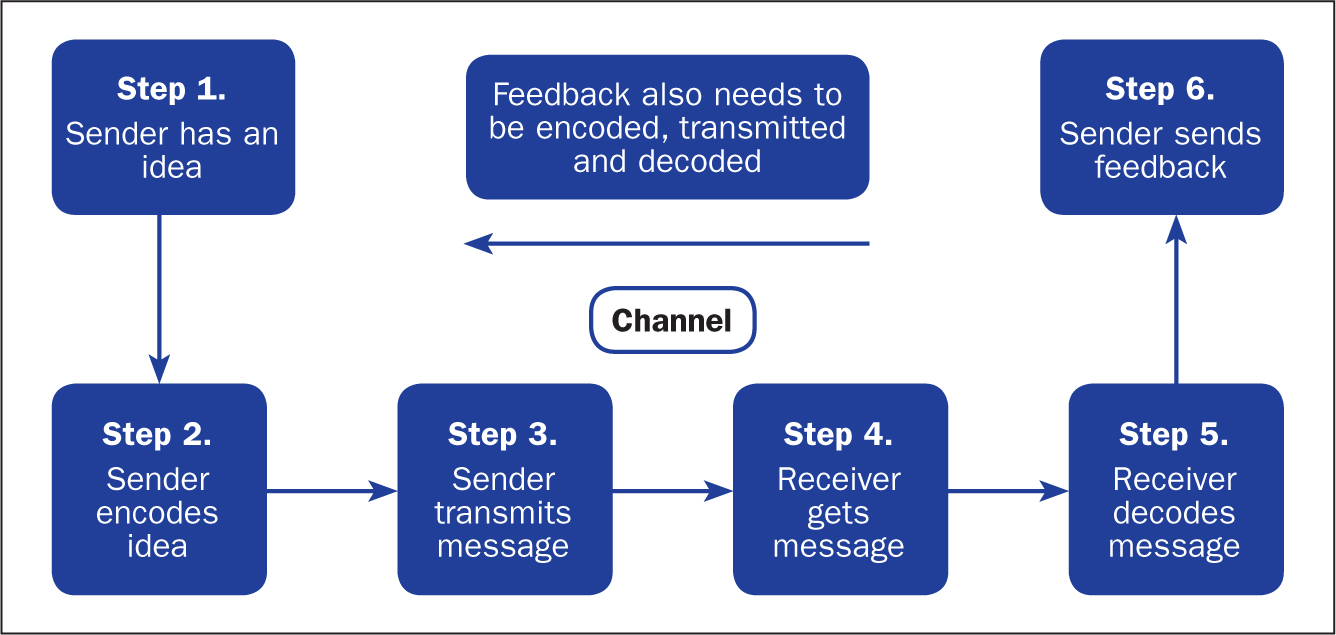
The process is more than just exchanging information. It is about the components/elements of the communication process, ie understanding the emotion and intentions behind the information—the tone of voice, as well as the actual words spoken, hearing, listening, perception, honesty, and ensuring that the messages relayed are correctly interpreted and understood ( Bramhall, 2014 ; Barber, 2016 ; Evans, 2017 ; Doyle, 2019 ). It is about considering emotions, such as shock, anger, fear, anxiety and distress ( Bumb et al, 2017 ; Evans, 2017 ). Language and conceptual barriers may also negatively impact on the efficacy of the communication being relayed.
Challenges of effective communication
The following sections explain the challenges involved in communication—namely, conveying a cancer diagnosis or related bad news.
Tone of voice and words spoken
According to Barber (2016) , when interacting with patients, especially communicating ‘bad news’ to them, both the tone of voice and the actual words spoken are important. The evidence has shown that an empathetic and sensitive tone is conducive to providing appropriate reassurance and in aiding understanding ( McClain, 2012 ; Evans, 2017 ; Hemming, 2017 ). However, an apathetic and insensitive tone will likely evoke fear, anxiety and distress ( Pincock, 2004 ; Ali, 2017 ; Doyle, 2019 ). In terms of the words used, the use of jargon, or highly technical language and words that imply sarcasm and disrespect, can negatively impact on feelings and self-confidence ( Doyle, 2019 ).
Hearing what is being conveyed is an important aspect of effective communication. When interacting with patients it is vital to consider potential barriers such as language (ie, is the subject highly technical or is English not the patient's first language) and emotions (ie shock, anger, fear, anxiety, distress) ( Bumb et al, 2017 ; Evans, 2017 ). A patient may fail to hear crucial information because he or she is distressed during an interaction, or may be unable to fully understand the information being relayed ( Bumb et al, 2017 ). Good communication involves ascertaining what has been heard and understood by the patient, allowing them to express their feelings and concerns, and ensuring these are validated ( Evans, 2017 ).
Listening to the patient
Listening is a deliberate act that requires a conscious commitment from the listener ( Shipley, 2010 ). The key attributes of listening include empathy, silence, attention to both verbal and non-verbal communication, and the ability to be non-judgemental and accepting ( Shipley, 2010 ). Listening is an essential component of effective communication and a crucial element of nursing care ( Shipley, 2010 ; Evans, 2017 ; Doyle, 2019 ). In health care, an inability to fully listen to and appreciate what the patient is saying could result in them feeling that their concerns are not being taken seriously. As observed by the author in practice, effective listening is essential to understanding the patient's concerns.
Perception, interpretation, understanding
Relevant and well-prepared information is key to the patient's perception and interpretation of the messages relayed ( McClain, 2012 ). It is vital to aiding their understanding and to informing their personal choices and decisions. If a patient were to misinterpret the information received, this could likely result in a misunderstanding of the messages being relayed and, consequently, lead to an inability to make clear, informed decisions about their life choices ( McClain, 2012 ; Bramhall, 2014 ).
Fully informing the patient and treating them with honesty, respect and dignity
In making decisions about their life/care, a patient is entitled to all information relevant to their individual situation and needs (including those about the actual and potential risks of treatment and their likely disease trajectory) ( McClain, 2012 ). Information equals empowerment—making a decision based on full information about a prognosis, for example, gives people choices and enables them to put their affairs in order ( Evans, 2017 ). Being honest with a patient not only shows respect for them, their feelings and concerns, it also contributes to preserving the individual's dignity ( Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). However, as observed in practice, a reluctance on the health professional's part to be totally open and honest with a patient can result in confusion and unnecessary emotional distress.
When reflecting on the efficacy of the communication being relayed, it is important for health professionals to acknowledge the challenges and consider how they may actually or potentially impact on the messages being relayed ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Communication and the uro-oncology clinical nurse specialist
It is devastating for a patient to receive the news that they have cancer ( Bumb et al, 2017 ). Providing a patient with a cancer diagnosis—the ‘breaking of bad news’, defined as any information that adversely and seriously affects an individual's view of his or her future ( Schildmann et al 2005 )—is equally devastating for the professional ( Bumb et al, 2017 ; Hemming, 2017 ). It is thus imperative to ensure the appropriate support is forthcoming following receipt of bad news ( Evans, 2017 ).
Integral to the delivery of bad news is the cancer CNS, in this context, the UCNS, who is acknowledged to be in the ideal position to observe the delivery of bad news (usually by a senior doctor in the urology clinic), and its receipt by patients ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ), and to offer appropriate support afterwards ( Evans, 2017 ). Support includes allocating appropriate time with the patient, and their family, after the clinic appointment to ensure they have understood the discussion regarding the diagnosis, prognosis and treatment options ( Evans, 2017 ; Hemming, 2017 ). In this instance, effective communication, as well as the time required, is usually tailored to each individual patient, allowing trust to be built ( Bumb et al, 2017 ; Evans, 2017 ; Hemming, 2017 ).
In the performance of her role, the UCNS is fully aware of the importance placed on delivering bad news well. She has seen first hand how bad news given in a less than optimal manner can impact on the patient's emotions and their subsequent ability to deal with the results. Hence, her role in ensuring that the appropriate support is forthcoming following the delivery of bad news is imperative. It is important to understand that the delivery of bad news is a delicate task—one that necessitates sensitivity and an appreciation of the subsequent impact of the news on the individual concerned. It should also be acknowledged that while the receipt of bad news is, understandably, difficult for the patient, its delivery is also extremely challenging for the health professional ( Bumb et al, 2017 ).
Communicating bad news
The primary functions of effective communication in this instance are to enhance the patient's experience and to motivate them to take control of their situation ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Telling a patient that they have a life-threatening illness such as cancer, or that their prognosis is poor and no further treatment is available to them, is a difficult and uncomfortable task for the health professional ( Bumb et al, 2017 ). It is a task that must be done well nonetheless ( Schildmann, 2005 ). Doing it well is reliant on a number of factors:
- Ensuring communicated information is sensitively delivered ( Hanratty et al 2012 ) to counter the ensuing shock following the patient's receipt of the bad news ( McClain, 2012 )
- Providing information that is clear, concise and tailored to meeting the individual's needs ( Hemming, 2017 )
- Acknowledging and respecting the patient's feelings, concerns and wishes ( Evans 2017 ).
This approach to care is important to empower patients to make the right choices and decisions regarding their life/care, and gives them the chance to ‘put their affairs in order’ ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ).
Choices and decision-making
Case studies 1 and 2 show the importance of honesty, respect, listening and affording dignity to patients by health professionals, in this case senior doctors and the UCNS. The issue of choice and decision-making is highlighted. It is important to note that, while emphasis is placed on patients receiving all the pertinent information regarding their individual diagnosis and needs ( McClain 2012 ), despite receipt of this information, a patient may still be unable to make a definite decision regarding their care. A patient may even elect not to have any proposed treatment, a decision that some health professionals find difficult to accept, but one that must be respected nevertheless ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ).
Case study 1. Giving a poor prognosis and accepting the patient's decision
Jane Green, aged 48, received a devastating cancer diagnosis, with an extremely poor prognosis. It was evident that the news was not what she expected. She had been convinced that she had irritable bowel syndrome and, hence, a cancer diagnosis was quite a shock. Nevertheless, she had, surprisingly, raised a smile with the witty retort: ‘Cancer, you bastard—how dare you get me.’ Mrs Green had been married to her second husband for 3 years. Sadly, her first husband, with whom she had two daughters, aged 17 and 21, had died from a heart attack at the age of 52. His sudden death was hugely upsetting for his daughters; consequently, Mrs Green's relationship with her girls (as she lovingly referred to them) was extremely close. The legacy of having two parents who had died young was not one Mrs Green wished to pass on to her daughters. Her main concern, therefore, was to minimise the inevitable distress that would ensue, following her own imminent death.
In the relatively short time that Mrs Green had to digest the enormity and implications of her diagnosis, she had been adamant that she did not wish to have any life-prolonging interventions, particularly if they could not guarantee a reasonable extension of her life, and whose effects would impact on the time she had left. This decision was driven by previously having observed her mother-in-law's experience of cancer: its management with chemotherapy and the resultant effect on her body and her eventual, painful demise. Mrs Green's memory of this experience was still vivid, and had heightened her fears and anxieties, and reinforced her wish not to undergo similar treatment.
Mrs Green requested a full and honest discussion and explanation from the consultant urologist and the UCNS regarding the diagnosis and its implications. This included the estimated prognosis, treatment interventions and the relevant risks and benefits—specifically, their likely impact on her quality of life. In providing Mrs Green with this information, the consultant and the UCNS had ensured information was clear and concise, empathetic and sensitive to her needs ( Shipley, 2010 ; Hanratty, et al, 2012 ; Evans, 2017 ; Hemming, 2017 ) and, importantly, that her request for honesty was respected. Not disclosing the entire truth can ‘inadvertently create a false sense of hope for a cure and perceptions of a longer life expectancy’ ( Bumb et al, 2017:574 ). Being honest had empowered Mrs Green to come to terms with both the diagnosis and prognosis, to consider the options as well as the risks and benefits. She had a choice between quantity of life and quality of life. Mrs Green elected for quality of life and, accordingly, made decisions that she felt were in her own, and her family's, best interests.
Despite receiving pertinent information and sound advice on why a patient should agree to treatment intervention, they may still elect not to have any treatment ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ). This decision, as observed by the UCNS in practice, is difficult for some health professionals to accept. In Mrs Green's case, accepting her decision not to have any treatment was extremely difficult for both the consultant and the UCNS. In an attempt to try to change Mrs Green's mind, the consultant asked the UCNS to speak to her. The UCNS was aware that the consultant's difficulty to accept the decision was compounded by Mrs Green's age (48) and a desire to give her more time. However, the UCNS had listened closely to Mrs Green's wishes and, in view of her disclosure regarding the experience of her mother-in-law's death, her first husband's untimely death, her fear of upsetting her daughters and her evident determination to keep control of her situation, the UCNS felt compelled to respect her decision.
Following the consultant's request, the UCNS spoke to Mrs Green but, on hearing what she had to say regarding her decision not to have more treatment, concluded that she had to respect Mrs Green's decision. She also clarified whether Mrs Green were willing to continue communication with her GP and ensured that the GP was fully updated regarding current events. Mrs Green had thanked the staff for all their support, but did not wish to continue follow-up with the service. The GP assured the UCNS that she would keep a close eye on Mrs Green and her family.
Case study 2. Giving an honest account of disease progression
The following case study explains how a reluctance by health professionals to be totally honest with a patient had inadvertently hampered the individual's ability to make informed decisions regarding his life choices.
Mr Brown, aged 87, had been previously diagnosed and treated for cancer. On his referral to the urology clinic, his disease had progressed to the metastatic stage, which had limited his management options to palliative care.
Since we have established that delivering bad news to a patient is a difficult task ( Bumb et al, 2017 ), it is not surprising that some health professionals fail to be totally honest with the patient for fear of upsetting them. During the consultation, it transpired that Mr Brown had other serious illnesses and was being managed by other clinicians. Seemingly, previous communications with these clinicians had left Mr Brown and his family unenlightened about his prognosis and his future prospects. In hindsight, the family would have appreciated total honesty sooner, since this would have allowed them to make realistic decisions.
After fully assessing Mr Brown's case (and in light of this disclosure) the doctor decided to be totally honest with Mr Brown and his family regarding his current situation and the choices available to him. Explanations were empathetic and sensitive to Mr Brown's and his family's feelings ( Hanratty et al, 2012 ; Evans, 2017 ). While the news was not entirely unexpected, Mr Brown and his family appreciated the consultant's candour. In this instance, the consultant had respected Mr Brown's entitlement to total honesty. By receiving all the facts, and the appropriate reassurance and support from the UCNS, Mr Brown could now consider his options and, with his family's support, proceed to put his affairs in order.
Management and treatment of cancer
The management and treatment of cancer is determined by several factors. These include: the grade and stage of the individual's disease—whether the disease is low-grade/low-risk, intermediate-grade/intermediate-risk, or high-grade/high-risk. For some low-grade/low-risk disease, the recommended treatment of choice is surgery alone. However, in certain cases, further review of the staging and histology might reveal features of cancer within the sample that are at a high-risk of local recurrence, necessitating additional treatment intervention, ie chemotherapy or radiotherapy, to minimise this threat.
Following the primary treatment intervention (ie surgery), for low-risk/low-grade disease, the risk of local recurrence is usually low, as is the need for additional treatment intervention (chemotherapy or radiotherapy). Nonetheless, local recurrence is still a possibility. A failure to make the patient aware of this possibility creates a lack of trust and a false sense of hope ( Bumb et al, 2017 ), and evokes unnecessary emotional distress for the patient, their families and carers ( McClain, 2012 ).
As previously explained, the term ‘fully informed’ relates to a patient's entitlement to all information relevant to their situation and needs (including those about the actual and potential risks) ( McClain 2012 ). Informed knowledge is power, thus honesty is imperative ( Evans, 2017 ). The following case studies highlight the consequence of failing to fully inform patients about risks and diagnosis.
Case study 3. Consequences of not being fully informed
Mr White, aged 36, had been diagnosed with a low-grade/low-risk cancer. After the initial diagnosis was explained, Mr White was explicitly told by the doctor that after surgery he would not require any additional treatment. However, a subsequent review of his staging and histology revealed features of cancer within the sample that were at a high risk of local recurrence. Therefore the decision was made to offer Mr White additional treatment with radiotherapy to reduce the risk of recurrence down the line. Understandably, this news and the ensuing emotional impact—fear, anxiety and distress—was significant for Mr White. The author contends that, to avoid inciting these emotions, Mr White should have been fully informed, at the initial diagnosis, of the potential risks that further treatment might be necessary, no matter how unlikely these risks were perceived to be. Having observed the emotional impact on Mr White, and other similar cases in local practice, the author proposed that, when delivering a cancer diagnosis, consideration must be given not only to the physical, but also the emotional/psychological impact of the diagnosis on the individuals concerned and all risks, even those deemed small, discussed.
The following case study illustrates how a lack of honesty can lead to misinterpretation and misunderstanding of the messages relayed ( McClain, 2012 ; Bramhall, 2014 ) and, accordingly, raises questions regarding the patient's care.
Case study 4. Consequences of ‘sugar-coating’ a diagnosis
Mrs Black, aged 78, had been diagnosed with a low-grade/low-risk bladder cancer, for which the recommended treatment is a course of six doses of intravesical chemotherapy (mitomycin). In providing Mrs Black with the diagnosis, the doctor had failed to clarify that the term ‘bladder polyp/wort’ in fact meant cancer. It is evident to the UCNS that the doctor's intention was to reduce the impact of the news for Mrs Black. However, if a cancer diagnosis is not clearly explained at the outset ( Evans, 2017 ), then, as the UCNS's personal observations in practice have shown, the offer of subsequent cancer treatments will raise questions. In a follow-up meeting with the UCNS, Mrs Black queried why she was having a cancer treatment, when a cancer diagnosis had not been clearly given ( Bumb et al, 2017 ). In this instance, Mrs Black's query placed the UCNS in an uncomfortable position, but one in which she ultimately had to be honest in her response.
Despite the physician's good intentions, a lack of honesty or in this case ‘sugar-coating’ the truth was an infringement of Mrs Black's right to receive full and honest information regarding her diagnosis and treatments and impacted her ability to make clear decisions regarding her care ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ).
Scenario: communicating in teams
In the UCNS's experience, effective communication is crucial when communicating in teams. The UCNS's observations in practice evoked reflection on past experiences of poor communication and its ensuing impact on her feelings, including hurt and, to some extent, a degree of anger.
Seemingly, poor communication is ingrained in all areas of practice and is highly evident in teams ( Doyle, 2019 ). The ability to communicate effectively is essential to team cohesiveness. One of the chief requirement is to facilitate an environment in which individuals can grow and excel, thus good/effective communication is vital. As previously stated, the tone of voice and actual words spoken are important ( Bramhall, 2014 ; Evans, 2017 ; Doyle, 2019 ). A tone that is respectful and conducive to elevating the individual's self-esteem and morale, ultimately increases self-worth and confidence. Conversely, a patronising attitude—a tone of voice and words spoken that imply sarcasm and disrespect—can, and often does, result in hurt feelings and a significant loss of confidence ( Doyle, 2019 ). Some senior professionals clearly believe in a hierarchy of entitlement to respect in the way that individuals communicate with other team members. A patronising tone of voice and words that imply sarcasm and disrespect impact significantly on individual team members' morale, self-esteem, self-worth, confidence and professional standing. This can lead to disharmony within the clinical environment. This could be communication between a consultant and a junior doctor, or a junior doctor and senior nurse, for example.
As health professionals, admittedly, we could all attest to poor communication at some point in our careers. Nevertheless, we have a responsibility to work and communicate effectively with other team members ( Ali, 2017 ; Doyle, 2019 ). The objective here is in facilitating a happy and functional team, one that demonstrates professionalism and competency in providing the care necessary to improving patients' experiences and outcomes ( Ali, 2017 ; Doyle, 2019 ). Securing improvements necessitates the health professional reflecting on their communication skills, acknowledging their limitations and initiating steps to address these ( Barber, 2016 ).
These case studies and scenario provide an insight into the UCNS's observations and reflections on her area of clinical practice and highlight the importance of effective communication. Acknowledgement of the inherent challenges within the communication process are clearly explained, with consideration given to the actual and potential impact in terms of patient, health professionals and clinical practice outcomes ( Oelofsen, 2012 ; RCN, 2019 ).
Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life, but seemingly few people, including health professionals, have mastered the skill of truly effective communication. There are evident pitfalls that could lead to patient care being compromised as a result of poor communication between health professionals. The UCNS's role in delivering bad news and supporting patients involves ensuring that patients are adequately informed to enable them to take control of their individual situation and, accordingly, that they are able to make the appropriate choices and decisions for their respective needs. Poor communication within teams can affect patient care and staff morale, and learning how to communicate more effectively is beneficial in terms of improving staff interactions with each other. Essentially, communicating effectively is everyone's responsibility; hence, all health professionals should look at the way they interact and communicate with each other and take the necessary steps to improve this extremely important activity.
- The cancer clinical nurse specialist (CNS) role is pivotal when patients receive bad news. It is crucial not only to the individual's understanding of the diagnosis, prognosis and treatment options, but also to the provision of appropriate support following the bad news and countering the ensuing impact of the news on the patient
- Reflection is a powerful tool, one that enables nurses to examine their practice, identifying salient issues and initiate change/improvements
- Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life—few people (in this context health professionals) have mastered the skill of truly effective communication
- Poor communication has implications for the patient, health professional and the health organisation
CPD reflective questions
- Reflection on practice is a key skill for nurses that enables them to identify salient issues and initiate actions to address these. How well do you think you reflect in practice, and does this provide the insight you seek?
- Effective communication is an important interpersonal skill. How well do you communicate with patients and colleagues in your area of practice? Reflect on any situations that you find difficult
- The issue of poor communication within teams and its impact on team members has been highlighted in this article. Have you observed poor communication within your team or within your area of practice? If so, how could this be improved?
- Work Environment
10 Ways to Overcome Communication Barriers in Nursing

Effective communication plays a vital role in nursing, fostering understanding, collaboration, and ultimately improving patient outcomes. However, various barriers can hinder communication within healthcare settings.
In this article, we will explore ten practical ways to overcome these communication barriers and enhance the delivery of care.
Importance of Effective Communication in Nursing
Effective communication lies at the heart of nursing practice. It forms the foundation for building relationships with patients, their families, and the interprofessional healthcare team.
When communication breaks down, patient safety, satisfaction, and overall quality of care are compromised. By understanding and addressing communication barriers, you, as a nurse, can ensure effective and meaningful interactions, leading to improved patient outcomes.
Common Communication Barriers in Nursing
Language and cultural differences.
Language barriers pose significant challenges in nursing, especially in multicultural healthcare settings. Nurses must communicate with patients who have limited English proficiency or speak a different native language. Additionally, cultural differences can influence communication styles and expectations. These barriers can lead to misunderstandings, inadequate information exchange, and reduced patient satisfaction.
Technological Challenges
With the increasing use of technology in healthcare, nurses face communication barriers related to unfamiliarity with electronic health records (EHRs) and other digital systems. Technical difficulties, such as system crashes or slow response times, can impede timely communication and information sharing among healthcare providers.
Hierarchy and Power Dynamics
In healthcare settings, hierarchical structures and power dynamics can hinder effective communication. Nurses may feel hesitant to express their opinions or concerns to physicians or higher-ranking professionals, resulting in vital information being overlooked. Open communication channels and a culture of collaboration are necessary to overcome these barriers.

Emotional and Psychological Factors
Nursing can be emotionally demanding, and stress, fatigue, and burnout can affect communication skills. These factors may lead to misinterpretation of messages, increased conflicts, and decreased empathy. Addressing the emotional well-being of nurses is essential to maintain effective communication in healthcare environments.
1. Active Listening
Active listening is a fundamental skill for effective communication in nursing. By actively engaging with patients, you can demonstrate empathy, gain valuable insights, and establish trust. Here are some techniques to enhance active listening:
- Maintain eye contact : Show your attentiveness and interest in what the patient is saying.
- Provide verbal and non-verbal cues : Nodding or smiling encourages patients to express themselves more openly.
- Practice reflective listening : Summarize and rephrase what the patient has said to ensure mutual understanding.
- Avoid interruptions : Allow patients to fully express their concerns and thoughts without interruption.
2. Clear and Concise Communication
Clear and concise communication is essential to ensure information is accurately conveyed and understood. When communicating with patients, consider the following strategies:
- Use simple language : Avoid complex medical jargon and explain information in a way that patients can easily comprehend.
- Avoid assumptions : Ensure that patients understand by asking open-ended questions and confirming their understanding.
- Confirm understanding through paraphrasing : Summarize the information shared by the patient to validate comprehension.
- Encourage questions and feedback : Create a safe environment for patients to ask questions and provide feedback, ensuring effective communication.
3. Open and Transparent Communication Channels
Creating open and transparent communication channels within healthcare settings is crucial for overcoming barriers. Here’s how you can achieve this:
- Foster a culture of open communication where all team members feel comfortable sharing their thoughts and concerns.
- Encourage feedback from colleagues and actively listen to their perspectives.
- Utilize regular team huddles or meetings to discuss communication challenges and find solutions collaboratively.
- Implement mechanisms such as suggestion boxes or anonymous feedback systems to provide an avenue for open communication.
- Share relevant information and updates with the healthcare team in a timely manner to ensure everyone is well-informed.
4. Empathy and Understanding
Empathy is the ability to understand and share the feelings of another person. In nursing, empathy promotes trust and patient-centered care. Enhance empathy and understanding by:
- Practice active empathy : Put yourself in the patient’s shoes and consider their emotions and experiences.
- Strive for cultural competence : Be mindful of cultural differences and tailor your communication to respect diverse backgrounds.
- Maintain a non-judgmental attitude : Create a supportive environment where patients feel comfortable expressing themselves without fear of judgment.
5. Non-Verbal Communication
Non-verbal cues, such as body language, facial expressions, and gestures, significantly influence communication in nursing. Utilize effective non-verbal communication to enhance your interactions with patients:
- Be aware of your body language and posture : Maintain an open and welcoming stance to convey approachability.
- Use facial expressions : Show empathy, concern, and reassurance through appropriate facial expressions.
- Utilize gestures and touch : Use gentle gestures and appropriate touch to convey comfort and support, when appropriate.
6. Use of Technology
In the modern healthcare landscape, technology plays a significant role in communication. While it offers numerous advantages, it can also present challenges. Embrace technology and leverage its potential for effective communication:
- Utilize electronic health records : Ensure accurate and timely documentation, promoting continuity of care.
- Explore telemedicine and video conferencing : Facilitate remote consultations and improve access to healthcare services.
- Leverage mobile communication devices : Use secure messaging platforms to communicate efficiently with colleagues and share important patient information.
7. Team Collaboration
Collaboration among healthcare professionals is crucial for providing holistic patient care. Effective team communication ensures that everyone involved is well-informed, contributing to seamless coordination. Foster effective collaboration through:
- Interprofessional communication: Maintain open lines of communication with colleagues from different disciplines.
- Participate in regular team meetings : Discuss patient care plans, exchange information, and address any communication challenges.
- Establish clear role expectations : Define each team member’s responsibilities and ensure everyone understands their role in patient care.
8. Patient Education
Patient education empowers individuals to actively participate in their care. As a nurse, you play a vital role in educating patients and breaking down complex medical information. Enhance patient education through:
- Use visual aids : Utilize diagrams, charts, and models to simplify complex concepts and enhance understanding.
- Provide written materials and handouts : Give patients written instructions and resources they can refer to after their interaction with you.
- Ensure patient comprehension : Use teach-back techniques to confirm that patients understand the information you have shared.
9. Language and Cultural Considerations
Language and cultural barriers can significantly impact communication in healthcare. Address these barriers by:
- Utilizing professional interpreters : When language barriers exist, engage the services of interpreters to facilitate effective communication.
- Understanding cultural norms and beliefs : Be culturally sensitive and adapt your communication style to accommodate diverse cultural backgrounds.
- Providing translated materials : Offer translated written materials and resources to assist patients who may have language limitations.
10. Feedback and Continuous Improvement
Feedback is essential for growth and development in nursing communication. Seek feedback from patients and colleagues to identify areas for improvement. Foster a culture of continuous improvement by:
- Seeking feedback from patients : Encourage patients to share their experiences and suggestions for better communication.
- Reflecting on your communication practices : Take time to evaluate your communication techniques and identify areas where you can improve.
- Participating in training and workshops : Attend professional development opportunities to enhance your communication skills and stay up-to-date with best practices.
Benefits of Overcoming Communication Barriers
By overcoming communication barriers, nursing professionals can experience numerous benefits:
- Improved Patient Outcomes: Effective communication leads to better patient understanding of their condition and treatment plans, reducing the risk of medical errors and improving overall healthcare outcomes.
- Enhanced Collaboration and Teamwork: Clear communication fosters collaboration among healthcare professionals, facilitating coordinated care and shared decision-making, ultimately benefiting patient outcomes.
- Increased Patient Satisfaction: When patients feel heard and understood, their satisfaction with the healthcare experience increases, leading to greater patient engagement and adherence to treatment plans.
- Reduced Errors and Misunderstandings: Overcoming communication barriers minimizes the likelihood of misinterpretations, misunderstandings, and errors that can compromise patient safety.
Training and Education for Effective Communication
To equip nurses with effective communication skills, various training and educational opportunities can be provided:
- Communication Skills Workshops: Organizing workshops that focus on active listening, conflict resolution, and effective communication techniques can enhance nurses’ interpersonal skills.
- Cultural Competency Training: Offering training programs that promote cultural awareness, sensitivity, and understanding helps nurses navigate diverse patient populations and communicate effectively across cultures.
- Technology Integration Training: Providing comprehensive training on using digital systems, EHRs, and other communication tools ensures nurses can leverage technology for efficient and secure communication.
In conclusion, effective communication in nursing is vital for providing safe, quality care. By implementing these ten strategies we mentioned above, you can overcome communication barriers, establish meaningful connections, and optimize patient outcomes. Remember, communication is a skill that can always be honed, and fostering open, empathetic, and clear interactions is key to delivering exceptional nursing care.
Q: How can you overcome communication barriers with patients who have limited English proficiency?
A: To overcome language barriers, you can utilize professional interpreters, use visual aids and gestures, and provide translated written materials. It’s important to create a supportive environment and allow extra time for communication with patients who have limited English proficiency.
Q: What are some effective strategies for communicating with patients from diverse cultural backgrounds?
A: When communicating with patients from diverse cultural backgrounds, it is important to be culturally sensitive, respect cultural norms and beliefs, and use culturally appropriate communication styles. Take the time to learn about different cultures, ask open-ended questions, and actively listen to foster effective communication.
Q: How can you promote effective communication during challenging situations, such as delivering difficult news to patients or their families?
A: When delivering difficult news, you can promote effective communication by demonstrating empathy, providing a calm and supportive environment, and using clear and compassionate language. Allow patients and their families to express their emotions, actively listen to their concerns, and offer appropriate support and resources.
Q: What can you do to improve communication within interdisciplinary healthcare teams?
A: To improve communication within interdisciplinary teams, actively participate in regular team meetings, clarify roles and responsibilities, and maintain open and respectful communication channels. Share information, seek input from team members, and foster a collaborative environment to enhance teamwork and patient outcomes.
Q: How can you ensure effective communication during patient handoffs or transitions of care?
A: To ensure effective communication during patient handoffs, use standardized protocols, document important information accurately, and engage in face-to-face or electronic communication with the receiving healthcare team. Provide a comprehensive and concise summary of the patient’s condition, treatment plan, and any ongoing concerns.
Q: How can you incorporate feedback from patients into your communication practices?
A: Actively seek feedback from patients by encouraging them to share their experiences, concerns, and suggestions. Provide patient satisfaction surveys or feedback forms to facilitate the collection of valuable input. By listening to patient feedback and implementing necessary improvements, you can continuously enhance your communication skills.

Sophia Miller
Similar posts.

6 Ways to Overcome Interdisciplinary Challenges in…

10 Ways to Build Positive Workplace Culture…

20 Most Common Ethical Dilemmas in Nursing…

10 Ways to Overcome Leadership Challenges in…

Are Male Nurses Attractive?

Can Nurses Wear Rings?
- Career Advancement 29
- Career Transection 20
- Job Satisfaction 16
- Managing Difficult Situations 6
- Work-Life Balance 14
- NCLEX Guide 50
- New Grad Nurse 21
- Nursing Practice Challenges 35
- Work Environment 23
- Emotional Challenges 3
POPULAR POSTS

What Does Baylor Shift Mean?

Can Male Nurses Have Long Hair?

Can You Take a Picture of Your Nurse?

Do School Nurses Wear Scrubs?

Can Nurses Carry Guns?

How Often Do Travel Nurses Get Audited?
Effective Healthcare Communication Essay
Introduction.
Communication is the transmission of a message, idea, or information between one person and another orally, through signals or gestures, and body language. There should be a sender who conveys the message in such a way that the recipient understands in order for there to be communication. Healthcare communication encompasses the data connections that are; discussion of patient’s condition or tests among the medical team, the interaction between one medical facility and another or one office, and another (Hugman, 2009). However, healthcare communication is mainly relevant in the interaction between a patient, family, and the medical team, and also among the members of the medical team.
It is of utmost importance for effective healthcare communication to ensure proper care and cultural and moral sensitivity to the patient. This paper discusses the basic elements of communication, and how these elements differ from the basic rules of healthcare. It also incorporates the issue of cultural differences and how they influence communication, and how one might encourage a patient to communicate effectively.
Effective Communication
All forms of communication verbal or nonverbal require both the sender of the message and the recipient to understand the message. If the recipient of information acts in accordance with what is expected by the sender, then there is effective communication. However, communication can only be made effective if there are the basic elements of communication which consist of; the sender, the receiver, the message, the channel, and the feedback (Hugman, 2009).
These are the key elements of timely and effective communication since all these five elements are crucial for information to be generated, sent, received, and then understood for the recipient to give feedback. All these aspects are the core attributes for effective communication, and hence the five basic elements of communication are crucial in communicating effectively.
Differences between Basic Elements of Effective Communication and Basic Rules of Health Care Communication
In healthcare communication, more emphasis is put on listening to the patient. Healthcare is more effective when a medical officer listens to the patient, and understands the different modes of care to take. He or she also knows areas that are more sensitive for instance; their cultural and religious beliefs. Ineffective communication, however, the only requirement is for the message to be understood and a course of action taken accordingly.
Healthcare communication also incorporates the nonverbal cues and the facial expressions by both the patient and the attending medical practitioner. Medical facilitators should be highly critical on their facial expressions, and the nonverbal cues they bring forth when attending to patients, because they may make or break the patient. On the other hand, they should also be able to carefully observe the patient’s expressions to be able to communicate effectively. Effective communication does not focus on the nonverbal cues and facial expressions but only focus on sending, receiving the message, and giving positive feedback.
Effective communication does not require both the sender and the recipient of the message to be present in order to communicate effectively. This can be done through mail, telephone, or other means as long as the recipient understands the message and acts accordingly then there is effective communication. Healthcare communication, however, requires both parties to be present at that moment for communication to be effective. The attending medical facilitator should be present together with the patient in order for him or her to assess the patient and give the care needed.
How to Encourage a Reluctant Consumer to Communicate Candidly
A consumer might be reluctant to give information due to different reasons. They may be cultural, religious, gender among others. It is crucial for a medical attendant to spot the reason early, so as to know the approach to take and get all the necessary information he or she may require, to diagnose and treat the patient (McCorry, 2011). One of the methods used is to give the patient guarantee of confidentiality.
Many patients are ashamed of some of their medical conditions and fear other people knowing about their conditions. It is, therefore, important for the medical practitioner to uphold their oath of confidentiality of the patient’s condition, and give their patient assurance that their conversation is confidential (McCorry, 2011).
This will make the patient open up to them. Other patients may be reluctant to give information due to the gender of the attending medical staff. If this is the case, it would be wise for one to get a medical practitioner of the opposite gender and let him or her handle the situation if available. The underlying factor for one to be able to make a patient communicate candidly is listening carefully to the little they say and observing the patient carefully, to assess the barrier in order to be able to look for the best way forward.
Impacts of Cultural Differences in Communication
Different people have different cultures giving rise to different languages and different beliefs. This situation makes it extremely difficult to communicate effectively especially when there is a difference in language. On the other hand, the nonverbal cues are not interpreted the same across all cultures and therefore, making it even more difficult to understand. It is, therefore, necessary for one to take caution while addressing people of a different culture as one may not want to offend them.
It can be concluded that communication is key in healthcare. It is, however, equally important for all members of the medical team to take caution while addressing their patients to ensure proper care. It can also be noted that patients may be reluctant in relaying information and looked at cultural differences impacts on communication. Healthcare communication is, therefore, a wide topic and should be studied comprehensively for proper healthcare.
Hugman, B. (2009). Healthcare communication . London: Pharmaceutical Press.
McCorry, L. K., & Mason, J. (2011). Communication skills for the healthcare professional . Philadelphia: Wolters Williams & Wilkins Health.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, August 29). Effective Healthcare Communication. https://ivypanda.com/essays/effective-healthcare-communication/
"Effective Healthcare Communication." IvyPanda , 29 Aug. 2020, ivypanda.com/essays/effective-healthcare-communication/.
IvyPanda . (2020) 'Effective Healthcare Communication'. 29 August.
IvyPanda . 2020. "Effective Healthcare Communication." August 29, 2020. https://ivypanda.com/essays/effective-healthcare-communication/.
1. IvyPanda . "Effective Healthcare Communication." August 29, 2020. https://ivypanda.com/essays/effective-healthcare-communication/.
Bibliography
IvyPanda . "Effective Healthcare Communication." August 29, 2020. https://ivypanda.com/essays/effective-healthcare-communication/.
- Non-Verbal Cues in Close Relationships
- The Healthcare Communication Strategies
- Nonverbal Communication: The Facial Expression
- How to Get in Shape?
- The Inpatient or Outpatient Setting
- Americans' Health Factors in “Unnatural Causes”
- Prenatal Caffeine Exposure' Effects
- Stem Cell Therapy as a Potential Cure for Diabetes
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Health Serv Res
- PMC10464255

Quality communication can improve patient-centred health outcomes among older patients: a rapid review
Samer h. sharkiya.
Faculty of Graduate Studies, Arab American University, 13 Zababdeh, P.O Box 240, Jenin, Palestine
Associated Data
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Effective communication is a cornerstone of quality healthcare. Communication helps providers bond with patients, forming therapeutic relationships that benefit patient-centred outcomes. The information exchanged between the provider and patient can help in medical decision-making, such as better self-management. This rapid review investigated the effects of quality and effective communication on patient-centred outcomes among older patients.
Google Scholar, PubMed, Scopus, CINAHL, and PsycINFO were searched using keywords like “effective communication,“ “elderly,“ and “well-being.“ Studies published between 2000 and 2023 describing or investigating communication strategies between older patients (65 years and above) and providers in various healthcare settings were considered for selection. The quality of selected studies was assessed using the GRADE Tool.
The search strategy yielded seven studies. Five studies were qualitative (two phenomenological study, one ethnography, and two grounded theory studies), one was a cross-sectional observational study, and one was an experimental study. The studies investigated the effects of verbal and nonverbal communication strategies between patients and providers on various patient-centred outcomes, such as patient satisfaction, quality of care, quality of life, and physical and mental health. All the studies reported that various verbal and non-verbal communication strategies positively impacted all patient-centred outcomes.
Although the selected studies supported the positive impact of effective communication with older adults on patient-centred outcomes, they had various methodological setbacks that need to be bridged in the future. Future studies should utilize experimental approaches, generalizable samples, and specific effect size estimates.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-023-09869-8.
Introduction
Excellent communication is critical for all health professionals [ 1 , 2 ]. It affects the quality of healthcare output, impacts the patient’s health and satisfaction, and benefits both patients and providers [ 3 ]. Communication is a critical clinical competence because it establishes trust between providers and patients, creating a therapeutic relationship [ 4 ]. Physician-patient communication plays several functions, including making decisions, exchanging information, improving the physician-patient relationship, managing the patient’s doubts, addressing emotions, and enhancing self-management [ 5 ]. Features of effective or quality communication include involving patients in decisions, allowing patients to speak without interruptions, encouraging a patient to ask questions and answering the questions, using a language that the patient understands, paying attention to the patient and discussing the next steps [ 5 ]. This communication also includes listening, developing a good interpersonal relationship, and making patient-centred management plans.
The quality of patient-physician communication influences various patient-centred outcomes [ 6 ]. In this review, patient-centred outcomes refer to all the outcomes that contribute to the recovery or indicate the recovery of patients, as well as suggest positive experiences with the care process. For instance, effective communication is associated with enhanced patient satisfaction, regulating emotions, and increasing compliance, leading to improved health and better outcomes [ 7 , 8 ]. According to [ 9 ], quality communication enhances patients’ trust in their providers, making patients more satisfied with the treatment. A trusting provider-patient relationship causes individuals to believe they receive better care [ 10 ]. For instance, [ 11 ] report that effective provider-patient communication improves social, somatic, and psychological health. During communication, the provider may enhance positive motivations and involve the individual in treatment decisions. Communication helps patients to acknowledge their illnesses, the associated risks, and the advantages of consistent treatment [ 5 ]. note that mutual communication between providers and patients stimulates or strengthens patients’ perception of control over their health, the knowledge to discern symptoms and self-care and identify changes in their condition. Effective communication leads to improved perceived quality of health care [ 12 ]. report that physician-patient communication influences the perceived quality of healthcare services. All these outcomes that suggest or contribute to patient’s positive experiences or imply a positive recovery journey, such as shorter hospital stays, are considered patient-centred outcomes.
This rapid review aims to review studies that have previously investigated the influence of quality communication on patient-centred outcomes among older adults, such as psychological well-being, quality of health care, emotional well-being, cognitive well-being, individualised care, health status, patient satisfaction, and quality of life. The specific objectives include (a) exploring the strategies used to ensure quality and effective communication with older patients in various healthcare settings, (b) exploring the patient-centred health outcomes reported by previous studies investigating quality communication between providers and older patients, and (c) to link quality communication strategies with older patients to patient-centred health outcomes among older patients.
The primary rationale for conducting this rapid review is that although many studies have examined the relationship between quality communication and various patient-centred outcomes, few studies have used older patients as their participants. It is a significant research gap because older adults have unique communication needs, which, if not considered, their communication with healthcare providers could be ineffective [ 13 ]. For example, older adults experience age-related changes in cognition, perception, and sensation, which can interfere with the communication process [ 14 ]. As a result, more research is needed to the specific quality communication strategies that could improve patient-centred outcomes among older adults. To my knowledge, no systematic review has focused on this topic. Therefore, this is the first rapid review to explore quality communication and its impact on patient-centred health outcomes among older patients in various healthcare settings.
This rapid review’s findings could inform practitioners of the quality communication strategies they can use to improve patient-reported outcomes. Besides, the rapid review evaluates the quality of studies investigating this matter and makes informed recommendations for future research to advance knowledge on this subject.
This rapid review was conducted in conformity with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [ 15 ]. The main difference between a systematic review and a rapid review is that the former strictly conforms to the PRISMA protocol, whereas the latter can miss a few elements of a typical systematic review. A rapid review was suitable because a single reviewer was involved in the study selection process, whereas at least two independent reviewers are recommended in typical systematic reviews [ 16 ].
Eligibility criteria
Table 1 below summarises the inclusion and exclusion criteria used to guide study selection in this rapid review. Also, justification is provided for each inclusion/exclusion criteria. The inclusion/exclusion criteria were drafted based on the target population, the intervention, the outcomes, year of publication, article language, and geographical location. This approach corresponds with the PICO (P – population, I – intervention, C – comparison, and O – outcomes) framework [ 17 ].
Inclusion and exclusion criteria
Information sources
Four academic databases were searched: PubMed, Scopus, CINAHL, and PsycINFO. These databases were used as sources of information because they publish studies in healthcare sciences on a wide range of topics, including communication and the health outcomes of various interventions. Additionally, Google Scholar was searched to supplement the databases because it indexes academic journal articles in all disciplines, including healthcare. Combining Google Scholar with these databases has been recommended for an optimal search strategy [ 18 ].
Search strategy
Various search terms related to the critical variables of this rapid review, namely quality communication, patient-centred health outcomes, and older patients, were combined using Boolean connectors (AND & OR). Regarding quality communication, some of the keywords that were used include “quality communication,“ “effective communication,“ “doctor-patient communication,“ and “patient-centred communication.“ The keywords that were used for patient-centred outcomes included “well-being,“ “patient satisfaction,“ “quality of care,“ “health status,“ and “quality of life.“ The search terms related to older patients included “nursing home residents,“ “older,“ and “elderly.“ Additionally, since most older patients are institutionalised, search terms like “nursing homes” and “assisted living facilities” were used in the search strategy. Table 2 below presents a sample search strategy executed on PubMed between September 2022 and July 2023. As shown in Table 2 , Mesh terms were used alongside regular keywords. Truncations on the three keywords, namely elderly, nursing homes, and geriatric were used to allow more of their variations to be captured in the search. The use of Mesh terms was only performed on PubMed – Mesh terms are only supported on PubMed and MEDLINE. The rest of the sources of information were searched using the search terms without specifying whether they are Mesh terms or not.
Study selection process
One reviewer (the author) was involved in screening the studies. The reviewer screened each record at least twice for confirmation purposes. Afterwards, an automation tool called ASReview which relies on machine learning to screen textual data was used as a second confirmation [ 19 ]. Research has shown that combining a machine learning tool and a single reviewer can significantly reduce the risk of missing relevant records [ 20 ]. This decision was reached based on previous research that has also demonstrated the good sensitivity of ASReview as a study selection tool in systematic reviews [ 19 ]. The software was trained on the eligibility criteria and the broader context of this study before it was used to screen the studies and confirm the reviewer’s decision. Therefore, if a record were retrieved, the author would screen for its eligibility the first time and confirm it the second time. For the third time confirmation, ASReview was employed. In case of disagreement between the author’s first and second attempts, a third attempt could be made to resolve it. In case of disagreement between the author’s first/second/third attempts and ASReview, a fourth attempt was made to resolve it.
Data collection process
One reviewer (the author) extracted data from the qualifying records. The reviewer could collect data from a given study in the first round, record them, and confirm them in the second round. In case of disagreement between the first and second rounds, the author would extract data from the record for the third time to resolve it. The data points on which data extraction was based include the country where the study was conducted, the study’s research design (if reported), the population and setting of the study, the characteristics of the intervention (communication), and outcomes. Also, the author remained keen to identify ways the studies defined quality or effective communication in the context of older patient care. Regarding the characteristics of the intervention, some of the data sought included the type of communication (e.g., verbal or non-verbal) and the specific communicative strategies, such as touch and active listening.
Regarding outcomes, ‘patient-centred outcomes’ was used as an umbrella term for several variables that relate to the patient’s subjective well-being. Such variables include perceptions of quality of care, quality of life, symptom management, physical health, mental health, health literacy, patient satisfaction, individualised care, and overall well-being, including social processes, self-actualisation, self-esteem, life satisfaction, and psychosocial well-being. If studies reported on the acceptance and usability of communicative strategies, it was also included as a patient-centred outcome because the patient accepts a specific intervention and acknowledges its usability.
Study quality assessment
The study quality assessment in this rapid review entailed the risk of bias and certainty assessments. Risk of bias assessment formed an essential aspect of certainty assessment. The risk of bias in qualitative studies was evaluated using the Critical Appraisal Skills Program (CASP) Qualitative Checklist [ 21 ]; the Cochrane Risk of Bias (RoB) tool was used for randomised studies [ 22 ]; and Risk of Bias in Non-Randomised Studies of Interventions (ROBINS-I) was used for cross-sectional observational studies [ 23 ]. The Grading for Recommendations, Assessment, Development, and Evaluation (GRADE) tool was used to assess the certainty of the evidence for all study designs [ 24 ]. The risk of bias in each study design and its corresponding assessment tool was calculated as a percentage of the total points possible. For example, the CASP Qualitative Checklist has ten items; each awarded one point. If a study scored seven out of 10 possible points, its risk of bias would be rated as 70%. The GRADE Tool has five domains, namely risk of bias, inconsistency, indirectness, imprecision, and publication bias. The first domain, risk of bias, was populated using the findings of risk of bias assessment using the stated tools. The overall quality of a study was based upon all five domains of the GRADE Tool.
Synthesis methods
Both qualitative and quantitative studies were included in this review. The studies were highly heterogeneous in their research designs hence statistical methods like a meta-analysis synthesis were impossible [ 25 ]. Besides, the studies also had substantial heterogeneity in the study settings (some were conducted in primary care settings, but a majority were conducted in long-term care facilities/nursing homes) and outcomes. The studies measured different outcomes under the umbrella variable of patient-centred outcomes. As such, a narrative synthesis approach was considered the most suitable [ 26 ]. The narrative synthesis guidance by [ 27 ] was used. The first step based on the guidelines should be developing a theoretical model of how the interventions work, why, and for whom.
This rapid review’s explanation of how effective or quality communication leads to improved patient-centred outcomes in the introduction section formed the theoretical basis, that is, effective communication facilitates informational exchange between the patient and provider, leading to better decision-making, which positively influences patient outcomes The second step of a narrative synthesis entails organising findings from the included studies to describe patterns across the studies based on the direction of the effect size or effects [ 27 ]. The third step is to explore the relationship in the data by identifying the reasons for the direction of effects or effect size. This rapid review’s reasons were based on the theoretical notions outlined above in this paragraph. The final step is to provide insights into the generalizability of the findings to other populations, which, in the process, further research gaps can be outlined. The results are stated below.
Study selection
After running the search strategy, 40 articles were identified from PubMed, 13 from Google Scholar (records identified from websites (Fig. 1 )), 24 from Scopus, 18 from CINHAL, and 10 from PsycINFO based on the relevance of the titles. It was discovered that 26 were duplicated records between databases and Google Scholar, which reduced the number of identified records to 79. Further, the automation tool (ASReview) marked five records as ineligible based on their title considering the inclusion and exclusion criteria. These articles were excluded because the author confirmed in the fourth round that they were ineligible. After realising they did not focus on older adults, the author excluded three more records. Therefore, 71 records were screened using their abstracts with the help of ASReview (64 records from databases and 7 records from Google Scholar), whereby 44 were excluded (40 records from databases and 4 records from Google Scholar) for various reasons, such as being expert opinions and professional development based on field experiences (e.g., [ 28 ]) and did not have a methodology. The remaining 27 records (24 records from databases and 3 records from Google Scholar) were sought for retrieval, whereby one was excluded because its full text was inaccessible. The remaining 26 articles (23 records from databases and 3 records from Google Scholar) were assessed for eligibility with the help of ASReview, whereby eight records were excluded because they did not report their methodologies (e.g., [ 29 ]), another eight were secondary studies (e.g., [ 30 ]), and three were non-peer-reviewed preprints. Therefore, seven studies met the eligibility criteria for this rapid review.

PRISMA Flowchart summarising the study selection process
Study characteristics
Out of the seven studies, one was an experimental study [ 31 ], one was a cross-sectional observational study [ 32 ], and five were qualitative studies [ 33 – 37 ]. As shown in Table 3 , most of the studies (n = 4) were conducted in the United States. The following countries produced one study each: Australia, Cameroon, the Netherlands, and Hungary. Although all the studies utilised a sample of older patients, the characteristics of the patients differed from one study to another. The studies ranged from primary care settings [ 36 ] and adult medical wards [ 37 ] to long-term care facilities like nursing homes. Apart from [ 36 ], the rest of the studies investigated various non-verbal communication strategies with older adults and their impact on various types of patient-centred outcomes, ranging from health-related outcomes (e.g., smoking cessation) to patient-reported outcomes, such as patient satisfaction, self-esteem, and life satisfaction. These outcomes are within the broader umbrella category of patient-centred m outcomes.
Characteristics of included studies
Further, the studies used different types of communicative strategies that can be used to enhance or promote patient-centred outcomes. In this rapid review, they were categorised into seven, namely (a) touching, (b) smiling, (c) gaze, head nod, and eyebrow movement, (d) active listening, (e) close physical distance, and (f) use of visual aids, and (g) telephone communication. Table 4 summarises the various ways in which each study described its interventions.
Description of interventions used in studies
Quality assessment findings
All seven studies were of high quality based on the GRADE Tool-based Assessment. However, [ 31 ] conducted an experimental study, but they did not provide any details indicating whether there was concealment in participant allocation and blinding of participants and outcome assessors. Therefore, it has a high likelihood of risk of bias. However, they scored excellently in the other domains of the GRADE Tool. All five qualitative studies and the cross-sectional observational study also scored excellently in the domains of the GRADE Tool, apart from the imprecision domain where they could not be scored because none of them reported effect sizes (Table 5 ).
Quality assessment using the GRADE Tool
Results of individual studies
[ 31 ] was the only experimental study used in this rapid review investigating the effect of comfort touch on older patients’ perceptions of well-being, self-esteem, health status, social processes, life satisfaction, self-actualisation, and self-responsibility. The authors did not report the effect sizes but indicated that comforting touch had a statistically significant effect on each of the five variables. In summary, the authors suggested that comfort touch, characterised by a handshake or a pat on the shoulders, forearm, or hand, had a statistically significant positive impact on the various patient-centred outcomes reported in their study. For each variable, the authors used three groups, the first and second control groups and the third experimental group. After delivering the intervention, they investigated whether the scores of these variables changed between three-time points in each of the three groups. The first time point was the baseline data collected before intervention was initiated; the second was two weeks after baseline data; and the third was four weeks after baseline data. The authors found that in each of the five variables, the scores remained almost the same in the three-time points for the two control groups, but there were significant improvements in the experimental group (the one that received the intervention). For example, the self-esteem variable was measured using Rosenberg’s Self-Esteem Scale, with the highest attainable score of 40. In the first control group, the score remained 27.00, 27.27, and 27.13 for Time 1 (baseline), Time 2 (after two weeks), and Time 3 (after four weeks), respectively. The same trend was observed in the second control group. However, in the experimental group, the score improved from 29.17 at baseline to 36.00 at Time 2 and 37.47 at Time 3. These findings suggest that comfort touch was highly effective in improving self-esteem among older patients. The same significant improvements were evident for all the other variables (p.184).
While all the other studies focused on nonverbal communication cues, [ 36 ] focused on telephone communication. They aimed to investigate the effect of a tailored intervention on health behaviour change in older adults delivered through telephone communication. Therefore, the primary rationale for selecting this study for review is that it used a specific communicative strategy (telephone) to deliver the intervention, which is the primary purpose of effective communication in most healthcare settings. The older patients used as participants in this study lived with COPD. The nurses trained to administer the intervention made regular phone calls over 12 months. The intervention was delivered to 90 participants. Of these, 65 were invited for interviews at the end of 12 months. One of the most important outcomes relevant to this rapid review is that the participants reported “being listened to by a caring health professional.“ It means that regular telephone communication improved the patient’s perceptions of the quality of care. Other critical patient-centred outcomes that improved due to this intervention include many participants quitting smoking and increased awareness of COPD effects.
[ 34 ] also conducted a qualitative study but needed to specify the specific research design, which was generally non-experimental. The authors used formative evaluation and a participatory approach to develop a communicative intervention for older adults with limited health literacy. In other words, apart from literature reviews, the authors involved the target population in developing a curated story to improve their health literacy. They developed photo and video-based stories by incorporating narrative and social learning theories. The most important finding of this study was that the authors found the developed communicative strategy appealing and understandable. Such observations imply that the participants’ health literacy also likely improved even though the authors did not evaluate it.
Further, using a sample of 155 older patients, [ 32 ] investigated the relationship between the communication characteristics between nursing practitioners and the older patients and patients’ proximal outcomes, namely patient satisfaction and intention to adhere to the NPs’ recommendations, and patients’ long-term outcomes (presenting problems and physical and mental health). The proximal outcomes (satisfaction and intention to adhere) were measured after visits, whereas the long-term outcomes (presenting problems, mental health, and physical health) were measured at four weeks. The communication and relationship components observed include various non-verbal communication strategies: smile, gaze, touch, eyebrow movement, head nod, and handshakes. The authors recorded videos during patient-provider interactions. These communicative strategies were measured using the Roter Interaction Analysis System (independent variable).
In contrast, the other outcomes (dependent variables) outlined above were each measured separately with a validated tool or single-item instruments [ 32 ]. For example, presenting problems were measured with a single-item instrument, whereas the physical and mental health changes at four weeks were measured using the SF-12 Version 2 Health Survey. The authors found that verbal and nonverbal communication strategies focused on providing patients with biomedical and psychosocial information and positive talk characterised by receptivity and trust were associated with better patient outcomes, such as significant improvements in mental and physical health at four weeks. Although the study did not report effect sizes, the findings agree that effective and quality communication can improve patient-centred outcomes like patient satisfaction.
[ 35 ] conducted a qualitative study with focus groups (eight focus groups with a range of three to nine participants) of 15 older adults in a nursing home. The study used an ethnographic qualitative design. The nonverbal communication strategies observed in this study included active listening (including verbal responses) and touching. The authors found that the characteristics of the communication strategies that make communication quality and effective include mutual respect, equity, and addressing conflict. The patients perceived that their nursing aides gave them better-individualised care if their relationship and communication were characterised by mutual respect. Portraying mutual respect includes showing the patients that they are being listened to and heard, which can include calling them by their names and showing signs of active listening. Some residents (older patients) complained that some nursing aides had favouritism, whereby they liked some patients and not others. When such a perception emerges, the patients could perceive the treatment as unjust, compromising individualised care quality. Also, nursing aides must equip themselves with communicative strategies to address conflict rather than avoid it. For example, knowing about the patient’s history can help nursing aides understand their behaviour in the facility, improving prospects of providing better personalised or individualised care.
[ 33 ] also conducted a qualitative study utilising a sample of 17 older adults in nursing homes and assisted living facilities in the United States. They aimed to identify the types and examples of nurse-aide-initiated communication with long-term care residents during mealtime assistance in the context of the residents’ responses. Using a naturalistic approach, the researchers observed communicative interactions between the nurse aides and the residents during mealtime assistance. Videos were recorded and transcribed and analysed using the grounded theory approach. They found that apart from emotional support, nonverbal communication strategies were used by nurse aides to address the residents, initiate and maintain personal conversations, and check-in. Although the authors did not provide statistical proof that these communication strategies improved well-being, their findings can inform future studies.
Finally, [ 37 ] conducted a qualitative, grounded theory study to develop a model for effective non-verbal communication between nurses and older patients. The authors conducted overt observations of patient-nurse interactions using a sample of eight older patients. They found that the nature of nonverbal communication to be employed depends on the context or environment, and certain external factors influence it. The factors influencing nonverbal communication include the nurses’ intrinsic factors, positive views of older adults, awareness of nonverbal communication, and possession of nonverbal communication skills. Patient factors that can also influence the effectiveness of nonverbal communication include positive moods, financial situations, and non-critical medical conditions. The model developed also emphasised that non-verbal communication, if carried out correctly considering context and environment, can lead to positive outcomes, such as increased adherence to providers’ recommendations, improved quality of care, and shorter hospital stays.
Results of syntheses
Four themes emerged from the narrative synthesis: nonverbal communication, verbal communication, communication strategies, and patient-centred outcomes. Table 6 summarises the subthemes that emerged under each theme. They are discussed below.
Nonverbal communication
Nonverbal communication was a critical theme that emerged in several studies. Five out of the seven studies investigated the effectiveness of touch on various patient-centred outcomes [ 31 ]. found that nonverbal communication strategies such as comfort touch, characterised by a handshake or a pat on the shoulders, forearm, or hand, had a statistically significant positive impact on patient-centred outcomes, such as well-being, self-esteem, health status, social processes, life satisfaction, self-actualisation, and self-responsibility [ 31 ]. implemented comfort touch exclusively without combining it with other nonverbal communication strategies. It means that comfort touch on its own can be effective in improving various patient-centred outcomes. As such, it can be hypothesised that if comfort touch is combined with other nonverbal communication strategies, such as active listening, eye gazing, smiling, maintaining a close distance, eyebrow movement, and nodding/shaking of the head can lead to even better results regarding patient-centred outcomes [ 32 , 33 , 35 , 37 ]. [ 35 ] identified active listening and touching as important nonverbal communication strategies that make communication quality and effective [ 33 ]. found that nurse-aide-initiated communication during mealtime assistance using nonverbal communication strategies, such as emotional support, smiling, laughing, touching, eye gazing, shaking hands, head nodding, leaning forward, and a soft tone were crucial in addressing the residents, initiating (and maintaining) personal conversations, and checking in. Finally, [ 37 ] developed a model that emphasised the importance of effective nonverbal communication in forming effective therapeutic relationships, promoting patient satisfaction, and improving the quality of care. An exhaustive list of the nonverbal communication approaches is shown in Table 6 .
In general, most studies, especially the qualitative ones, supported the utilisation of multiple non-verbal communication strategies in a single communicative episode. The studies also implied that it is the responsibility of healthcare providers to initiate and maintain effective nonverbal communication cues, such as those detailed in Table 6 . Additionally, it is important to note that it is only one study [ 31 ] that investigated the effectiveness of comfort touch on patient-centred outcomes. Therefore, the notion implied in qualitative studies that combining various nonverbal strategies could lead to a better improvement in patient-centred outcomes is subject to further empirical investigation. It was noted that there is a lack of empirical studies investigating how the combination of various non-verbal communication techniques or strategies can influence patient-centred outcomes, such as patient satisfaction and perceptions of quality of care.
Verbal communication
Four out of the seven studies implied that verbal communication improved patient-centred outcomes [ 32 , 34 – 36 ]. Effective and quality verbal communication was found to impact patient satisfaction positively [ 32 ], increased awareness of COPD effects [ 36 ], improved health literacy [ 34 ], presented problems [ 32 ], and mental and physical health [ 32 ]. It is worth noting that [ 32 ] used a cross-sectional survey approach and used regression analyses to investigate the relationship between communication and various patient-centred outcomes, such as patient satisfaction and mental and physical health. Also, it is important noting that the authors combined both verbal (e.g., more positive talk, greater trust, and receptivity) and non-verbal (e.g., smile, gazing, eyebrow movements, and interpersonal touches) in their study. Therefore, it can be a bit challenging to directly conclude that effective verbal communication alone without non-verbal communication is effective on its own in improving patient-centred outcomes. Similarly, [ 34 ] combined both narrative-based and picture-based communication strategies to give patients education about health literacy. Therefore, it can be challenging to know whether narratives comprising of verbal communication (and often non-verbal communication) can improve patient-centred outcomes on their own. The rest of the studies were qualitative [ 35 , 36 ], which means that their findings generally reflected the subjective experiences or opinions of their participants. Therefore, it can be said that although all the four studies supported verbal communication can effectively improve patient-centred outcomes, there is a need for future research to experimentally test its effectiveness without being combined with non-verbal communication strategies.
Moreover, two of the four studies implied that some conditions must be met for verbal communication to be effective [ 32 , 35 ]. some communication strategies, such as higher lifestyle discussion and rapport-building rates, were perceived as patronising and associated with poor outcomes [ 32 ]. Instead, the authors found that communication strategies like seeking and giving biomedical and psychosocial information were more effective in improving patient outcomes [ 32 ]. It implies that healthcare providers should be attentive and intentional of the topics they discuss with patients. Further, in their qualitative study, [ 35 ] found that effective verbal communication also requires mutual respect, equity, and addressing conflict. Indeed, it appears that certain communication strategies like lifestyle discussions can undermine the process of establishing trust, which is why they were associated with adverse patient outcomes. Also, unlike nonverbal communication, the studies that highlighted the effect of verbal communication on patient-centred outcomes did not provide rich descriptions of the specific verbal communication strategies that can be used in a face-to-face healthcare setting. The described strategies like using phone calls to regularly communicate with the patient without having to visit a healthcare facility and things to ensure when communicating with the older patient, such as mutual respect and avoiding too many discussions on lifestyle do not offer rich insights into the specific nature of the verbal communication strategies.
Communication strategies
In 3.5.2 above, it was shown that the sample of participants that [ 32 ] used in their study did not prefer discussions related with healthy lifestyles, which compromised patient-centred outcomes. Therefore, it was also important to determine the best approaches to formulate communication strategies that work. Two out of the seven studies implied how communication strategies can be formulated [ 34 , 36 ] [ 36 ]. found that a tailored intervention delivered through telephone communication improved patient perceptions of the quality of care. In this regard, the authors first identified the needs of the patients to guide the development of the tailored intervention, from which they might have obtained insights into the patients’ communication preferences [ 34 ]. found a participatory approach to developing a curated story that improves health literacy appealing and understandable. The findings emphasised the need for participatory approaches when developing communication interventions for patients with varied health and social needs. Although the studies did not compare or contrast the effectiveness of participatory-based communication strategies and non-participatory-based communication strategies, their findings provide useful insights into the significance of involving patients when developing them. From their findings, it can be anticipated that a participatory approach is more likely to yield better patient-centred outcomes than non-participatory-based communication strategies.
Patient-centred outcomes
All studies reviewed highlighted patient-centred outcomes as the goal of effective communication in older patients. Patient-centred outcomes included well-being, self-esteem, health status, social processes, life satisfaction, self-actualisation, and self-responsibility (Butt, 2001), as well as patient satisfaction [ 32 , 36 ], increased awareness of COPD effects [ 36 ], and improved health literacy [ 34 ]. Others included presenting problems, mental health, and physical health [ 32 ], as well as adherence to providers’ recommendations, improved quality of care, and shorter hospital stays [ 37 ]. All seven studies indicated that the various verbal and nonverbal communication approaches could improve these patient-centred outcomes. The consistency observed between the experimental study by [ 31 ], the qualitative studies, and other quantitative study designs implies the need to pay greater attention to verbal and non-verbal communication strategies used by healthcare professionals as they can directly influence numerous patient-centred outcomes. This consistency further implies that effective communication is the anchor of high-quality care, and its absence will always compromise patient-centred outcomes, such as satisfaction and health outcomes.
Discussion and conclusion
Discussion of findings.
In agreement with various studies and reviews conducted in younger populations [ 1 – 3 ], all the seven studies selected in this rapid review supported that effective communication is a cornerstone of improved patient-centred outcomes. Like [ 5 , 11 , 12 ], the studies reviewed in this rapid review also supported the idea that effective communication with older adults involves the combination of verbal and nonverbal communication cues. However, this rapid review went a step ahead to identify the specific conditions that must be present for effective verbal and nonverbal communication to take place, such as perceptions of equity, mutual respect, and addressing conflict instead of avoiding it. The qualitative studies used in this rapid review also offered rich descriptions of how providers use nonverbal communication strategies.
However, the main shortcoming of the seven studies reviewed is that none aimed to define or describe what constitutes effective communication with older adults, apart from [ 37 ], who described a model of nonverbal communication with older adults. The study was qualitative and only formed a theoretical basis of how effective nonverbal communication with older adults could be shaped. The theory developed needs to be tested in an experimental setting so that its effect size in improving patient-centred outcomes, such as quality of care, quality of life, patient satisfaction, and emotional and cognitive well-being, can be documented unbiasedly and validly. Therefore, as much as the reviewed studies agreed with younger populations regarding the positive effect of effective and quality communication on patient-centred outcomes [ 9 , 10 ], the methodological rigour of studies with older patients needs to be improved.
Although the individual studies reviewed in this rapid review had low risk of bias apart from [ 31 ], the screening was based on the judgment of the individual research designs. Otherwise, if the assessment had been done from the perspective of the focus of this rapid review, the risk of bias in studies could have been high in predicting the influence of effective communication on patient-centred outcomes. First, apart from [ 31 ], none of the studies used a random sample. The qualitative studies used purposively obtained samples, which means the risk of bias from an interventional perspective was high. However, the studies provided in-depth insights into the characteristics and features of verbal and non-verbal communication strategies that can be used to form and maintain provider-patient relationships.
Recommendations for practice and future research
The main recommendation for practice is that nurses and providers serving older patients must be aware of their verbal and non-verbal communication strategies. Besides, they should engage in continuous professional development to enhance their verbal and non-verbal communication skills. Combining a wide range of nonverbal communication, such as touching the patient on the shoulder or arm or even handshaking can help create strong bonds and relationships, which are key in an effective therapeutic relationship. The qualitative studies reviewed showed that nurses and other providers combine a wide range of nonverbal communication in a single interaction instance, such as eye gazing, nodding, touching, and eyebrow movement. Although studies on verbal communication were rare in this rapid review, some lessons learned from the few studies included (e.g., [ 36 ]) is that using telephones to communicate with older patients regularly is potentially effective in improving patient-centred outcomes like better self-management. The information shared by the nurse should be tailored to serve the specific health needs of older patients. For example, for COPD patients, a nurse can make regular calls to old patients to educate them about the importance of quitting smoking and alcohol to improve their health condition and better self-management. However, as [ 32 ] indicated, the nurse should be cautious about how to present the information to the client and be able to detect patronising discussions quickly. For example, the sample of adults used by [ 32 ] found that many lifestyle and rapport-building discussions with the nurse were patronising in ways that may be detrimental to patient-centred outcomes. Some of the strategies providers can employ to ensure that communication is not perceived as patronising by older patients include ensuring mutual respect (e.g., active listening as a sign of mutual respect), creating perceptions of equity rather than favouritism when communicating with multiple patients at a time, and solving conflicts rather than avoiding them, which entails extra efforts, such as understanding the patient’s behaviour in the past and present. Overall, although studies have not provided specific estimates of the effect sizes of effective communication on patient-centred outcomes among older adults, there is a general trend and consensus in studies that effective communication, nonverbal and verbal, is the cornerstone of high-quality healthcare.
Further, future research needs to address various gaps identified in this study. The first gap is that although [ 37 ] tried to develop a model of nonverbal communication with older adults, their study had some drawbacks that limited the comprehensiveness of the model. First, the authors used a sample of only eight older adults in two medical wards in Cameroon. Besides the small sample, the study was conducted in medical wards, which means its findings may not be generalisable to long-term care settings like nursing homes. More older adults who encounter healthcare professionals are admitted in long-term care facilities, calling for developing a more robust communication strategy. Second, [ 37 ] only focused on nonverbal communication, thereby providing limited practical applicability of the model since verbal and nonverbal communication co-exists in a single interactional instance. Therefore, there is a need to develop a model that provides a complete picture into what effective communication is like with older adults.
After developing a valid, reliable, and generalisable model for effective communication with older adults in various healthcare settings, future research should also focus on investigating the impact of such a model on patient-centred outcomes, such as quality of care, quality of life, patient satisfaction, and physical and mental health. More particularly, the developed model can be used to derive communication interventions, which can be applied and tested in various healthcare settings with older adults. That way, research on this subject matter will mature as more and more studies test the effectiveness of such a communication model in various settings and countries. All that is known in the literature is that effective verbal and nonverbal communication can help promote patient-centred outcomes among older adults.
Limitations
Although this rapid review was conducted rigorously by adhering to the PRISMA guidelines, the use of a single reviewer in the study selection process can undermine the quality of the review. When a single reviewer is involved, the probability of missing out relevant studies increases immensely. However, this limitation was mitigated in this review by using an automation tool in the study selection process. In was assumed that combining the automation tool with one independent reviewer could significantly reduce the probability of missing relevant studies.
Another possible limitation is that few studies have been conducted between 2000 and 2023 investigating the effect of effective communication on various patient-centred outcomes. Although the literature recognises the importance of effective communication, and there is a unanimous agreement between studies of various research designs that it is the cornerstone of quality of care, more studies need to be conducted examining how various communication strategies influence patient outcomes, both subjective and objective. For example, [ 31 ] investigated the effect of comfort touch. Other studies using empirical means (e.g., experiments) can also test the other strategies identified, such as eye gazing, head nodding, eyebrow movement, et cetera. In this way, a more specific and structured approach to communication in healthcare settings can be developed using the evidence base.
Moreover, I initially intended to review studies published within the past five years (2018–2023) but later learned there were insufficient studies meeting the eligibility criteria. Consequently, I adjusted the publication date to the past ten years (2013–2023). I also learned insufficient studies published within that period. Consequently, I chose the period of 2000–2023, which yielded seven studies. Thus, some of the studies included may not capture contemporary realities in healthcare settings, raising the need for more empirical studies on this topic.
This rapid review selected seven studies whose narrative synthesis demonstrated that effective verbal and non-verbal communication could improve patient-centred outcomes. However, the studies were mostly qualitative, and hence they only provided rich descriptions of how nurses and older patients communicate in various clinical settings. It is only one study (Butts, 2001) that was experimental. Still, its risk of bias was high since patients were not concealed to allocation, and participants and outcome assessors were not blinded. Future research needs to focus on deriving a valid, reliable, and generalisable communication model with older adults using a larger and more representative sample size of older patients. Such a model should encompass both verbal and nonverbal communication. After developing a robust model, the next phase of future studies is to derive interventions based on the model and then, through experimental research, test their effectiveness. In that way, a standard approach to communicating effectively and in quality will be achieved, which is yet to be achieved in the current studies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
I thank my wife and children for their patience and the great opportunity to devote a lot of time to doing the article in the best possible way.
Authors’ contributions
I am the primary and sole author of this article. My contribution to this article is a full contribution.
Data Availability
Declarations.
The authors declare no competing interests.
‘Not applicable’ for that section. The article is a rapid review type.
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
Internal Noise, Mental/Emotional Distress. Internal noise has an impact on the communication process. Fear and anxiety can affect the person's ability to listen to what the nurse is saying. People with feelings of fear and anger can find it difficult to hear. Illness and distress can alter a person's thought processes.
Hospitalized patients in all ages often experience complex communication needs including mobility, sensory, and cognitive needs as well as language barriers during their stay ( Downey & Happ, 2013 ). Hospitalization is potentially stressful and involves unpleasant experiences for patients and their families. All aspects of care and nursing are ...
Conclusion. The barrier of power and authority can seriously affect the cooperation among healthcare professionals. The discussed example shows how physicians may contribute to ineffective communication by having personal biases, while nurses may do the same by failing to address arising issues.
The first impact of language barriers is miscommunication between medical providers (physicians and nurses) and patients [ Table 2 ]. This miscommunication contributes to a reduction in the satisfaction of both medical providers and patients, the quality of healthcare delivery, and patient safety. The second impact is an increase in indirect ...
Effective communication in health care settings has several components: health literacy, cultural competence, and language barriers (Ratna 2). Any one of these factors causes the organization to deteriorate, and it experiences a phase of stress. Much of the downside of communication barriers in health care has to do with the miscommunication ...
Citation: Ali M (2017) Communication skills 2: overcoming barriers to effective communication Nursing Times; 114: 1, 40-42. Author: Moi Ali is a communications consultant, a board member of the Scottish Ambulance Service and of the Professional Standards Authority for Health and Care, and a former vice-president of the Nursing and Midwifery ...
Communication barriers vary depending on the setting, requiring the nurse to figure out such barriers depending on each patient's individual needs (Sibiya, 2018). One of the most prevalent communication barriers in nursing is the difference in language and culture (Norouzinia et al., 2016).
Dissecting Communication Barriers in Healthcare: A Path to Enhancing Communication Resiliency, Reliability, and Patient Safety J Patient Saf . 2021 Dec 1;17(8):e1465-e1471. doi: 10.1097/PTS.0000000000000541.
1. Introduction. In a medical setting, communication is a core element in the interactions between healthcare providers and patients, and it is with skillful communication that a healthcare provider can earn their patients' trust [].When communication barriers arise, they can compromise the outcome of the care provided [2,3].Effective communication skills of health professionals are vital to ...
Skillful communication is essential to health care. Clear, honest communication between patient and provider paves the way for accurate diagnoses and treatment decisions. Similarly, clear, confidential communication between members of a care team (which often includes patients and multiple providers) results in swiftly and ethically delivered ...
Providing healthcare services that respect and meet patients' and caregivers' needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient ...
The communication barriers in the health sector have been identified in three major domains, namely lack of communication between doctors and nurses, problematic communication between the healthcare team, patients, and their families, and cultural challenges. 4,6,7 Both physician (poor communication skills, no special training during under ...
Background Communication is a basic need of humans. Identifying factors that prevent effective nurse-patient communication allows for the better implementation of necessary measures to modify barriers. This study aims to compare the barriers to effective nurse-patient communication from the perspectives of nurses and patients in COVID-19 and non-COVID-19 wards. Materials and methods This cross ...
Communication is a highly complicated process meant for exchange of ideas or information between two people.1 Although communication is an everyday happening, there is no surety that both sides fully understand each other.1 In fact, the uncertainties of communication are manifold, especially when a group of people or the whole community is ...
To improve the delivery of timely and accurate information and address current barriers in health communication during epidemics and pandemics, there are at least 3 broad areas to consider. These include devising of and investment in accurate, concise, and reliable public health communication frameworks; the improved and advanced use of media ...
Review criteria. A search was carried out on the different databases by means of the (Me SH)terms 'communication', 'primary health care', 'correspondence', 'patient safety', 'patient handoff' and 'continuity of patient care'.Reviewers screened 4609 records and 462 full texts were checked according following inclusion criteria: (1) publication between January 1985 and ...
Introduction. Effective communication is an integral aspect of nursing because nurses constantly interact with patients, families, colleagues, supervisors, and managers in the course of their duties. Rosenblatt and Davis (2009) argue that the nature of communication determines the quality of care that patients receive.
Reflection is a highly beneficial tool (Oelofsen, 2012), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes (Bramhall, 2014).
Confirm understanding through paraphrasing: Summarize the information shared by the patient to validate comprehension. Encourage questions and feedback: Create a safe environment for patients to ask questions and provide feedback, ensuring effective communication. 3. Open and Transparent Communication Channels.
1. For an in-person interpreter, call the interpreter service and specify the language needed and about how much time the interpretation will take. When the interpreter arrives, introduce yourself and provide a brief report on the work needed and a brief patient history. Greet the patient and introduce the interpreter.
One of the biggest challenges that arise the most is language barrier. Language barrier is a major problem in the medical field, this is will lead to patient lack of understanding. Pateron & Taylor (2013), "Language. Free Essay: Health care each day we are faced with new challenges and the decision essentially falls on administrators to ...
Communication is the transmission of a message, idea, or information between one person and another orally, through signals or gestures, and body language. There should be a sender who conveys the message in such a way that the recipient understands in order for there to be communication. Healthcare communication encompasses the data ...
Seamless Communication to Bridge Data Gaps. For hospitals and health systems, eliminating language barriers is essential to providing equitable care for every patient. But simply connecting patients with an interpreter is not enough - health systems need to maintain an accurate report of patient records.
Health is a core element in people's well-being and happiness. Health is an important enabler and a prerequisite for a person's ability to reach his/her goals and aspirations, and for society to reach many of the societal goals (Minister of Social Affairs and Health, Finland, 2013: 3). Health communication has been a part of development communication or communication for development for ...
Effective communication leads to improved perceived quality of health care . report that physician-patient communication influences the perceived quality of healthcare services. All these outcomes that suggest or contribute to patient's positive experiences or imply a positive recovery journey, such as shorter hospital stays, are considered ...