Advertisement
Supported by

Gearing Up for the ‘New Normal’
In “The New Normal,” Dr. Jennifer Ashton explores the mental health repercussions of the pandemic and ways to rebuild our overall health.
- Share full article

By Anahad O’Connor
As the chief medical correspondent for ABC News, Dr. Jennifer Ashton has spent the past year helping to make sense of the pandemic for the network’s millions of viewers.
But another aspect of the pandemic that she deals with is the toll it has taken on our nation’s mental health, which she sees on a daily basis at her medical practice in New Jersey, where Dr. Ashton is an obstetrician-gynecologist. In the past year, she says, patient after patient has opened up to her about the crippling stress and uncertainty caused by Covid-19 and their struggles with fear, anxiety, loneliness, frustration and depression.
“I have patients ranging in age from teenagers to women in their 70s and 80s, and they all say this to me,” Dr. Ashton said. “They express it to me almost with this tone that they think there’s something wrong with it. The first thing that I do is I help them recognize that it’s appropriate and it’s OK. Everyone is having these feelings.”
Dr. Ashton explores the psychological toll of the pandemic in her new book, “The New Normal,” which shows us how thinking like a doctor may help us to build resilience and strengthen our overall health. We recently caught up with Dr. Ashton to discuss her thoughts on how the pandemic is affecting our mental health, why it’s essential that we practice self-care during these stressful times, and one of the best hacks she found to improve her diet. Here are edited excerpts from our conversation.
Q. How do you define the “new normal”?
This past year has been filled with so much uncertainty and unfamiliarity. Nothing that we are doing today or have lived through in the last year is normal. The approach that I’ve taken to covering this pandemic has been that of viewing the country as one big patient, and the first step in healing or recovery from any illness is accepting the current situation.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplements
- Author Guidelines
- Submission Site
- Open Access
- About Journal of Public Health
- About the Faculty of Public Health of the Royal Colleges of Physicians of the United Kingdom
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- Advertising and Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- < Previous
Adapting to the culture of ‘new normal’: an emerging response to COVID-19
- Article contents
- Figures & tables
- Supplementary Data
Jeff Clyde G Corpuz, Adapting to the culture of ‘new normal’: an emerging response to COVID-19, Journal of Public Health , Volume 43, Issue 2, June 2021, Pages e344–e345, https://doi.org/10.1093/pubmed/fdab057
- Permissions Icon Permissions
A year after COVID-19 pandemic has emerged, we have suddenly been forced to adapt to the ‘new normal’: work-from-home setting, parents home-schooling their children in a new blended learning setting, lockdown and quarantine, and the mandatory wearing of face mask and face shields in public. For many, 2020 has already been earmarked as ‘the worst’ year in the 21st century. Ripples from the current situation have spread into the personal, social, economic and spiritual spheres. Is this new normal really new or is it a reiteration of the old? A recent correspondence published in this journal rightly pointed out the involvement of a ‘supportive’ government, ‘creative’ church and an ‘adaptive’ public in the so-called culture. However, I argue that adapting to the ‘new normal’ can greatly affect the future. I would carefully suggest that we examine the context and the location of culture in which adaptations are needed.
To live in the world is to adapt constantly. A year after COVID-19 pandemic has emerged, we have suddenly been forced to adapt to the ‘new normal’: work-from-home setting, parents home-schooling their children in a new blended learning setting, lockdown and quarantine, and the mandatory wearing of face mask and face shields in public. For many, 2020 has already been earmarked as ‘the worst’ year in the 21st century. 1 Ripples from the current situation have spread into the personal, social, economic and spiritual spheres. Is this new normal really new or is it a reiteration of the old? A recent correspondence published in this journal rightly pointed out the involvement of a ‘supportive’ government, ‘creative’ church and an ‘adaptive’ public in the so-called culture. 2 However, I argue that adapting to the ‘new normal’ can greatly affect the future. I would carefully suggest that we examine the context and the location of culture in which adaptations are needed.
The term ‘new normal’ first appeared during the 2008 financial crisis to refer to the dramatic economic, cultural and social transformations that caused precariousness and social unrest, impacting collective perceptions and individual lifestyles. 3 This term has been used again during the COVID-19 pandemic to point out how it has transformed essential aspects of human life. Cultural theorists argue that there is an interplay between culture and both personal feelings (powerlessness) and information consumption (conspiracy theories) during times of crisis. 4 Nonetheless, it is up to us to adapt to the challenges of current pandemic and similar crises, and whether we respond positively or negatively can greatly affect our personal and social lives. Indeed, there are many lessons we can learn from this crisis that can be used in building a better society. How we open to change will depend our capacity to adapt, to manage resilience in the face of adversity, flexibility and creativity without forcing us to make changes. As long as the world has not found a safe and effective vaccine, we may have to adjust to a new normal as people get back to work, school and a more normal life. As such, ‘we have reached the end of the beginning. New conventions, rituals, images and narratives will no doubt emerge, so there will be more work for cultural sociology before we get to the beginning of the end’. 5
Now, a year after COVID-19, we are starting to see a way to restore health, economies and societies together despite the new coronavirus strain. In the face of global crisis, we need to improvise, adapt and overcome. The new normal is still emerging, so I think that our immediate focus should be to tackle the complex problems that have emerged from the pandemic by highlighting resilience, recovery and restructuring (the new three Rs). The World Health Organization states that ‘recognizing that the virus will be with us for a long time, governments should also use this opportunity to invest in health systems, which can benefit all populations beyond COVID-19, as well as prepare for future public health emergencies’. 6 There may be little to gain from the COVID-19 pandemic, but it is important that the public should keep in mind that no one is being left behind. When the COVID-19 pandemic is over, the best of our new normal will survive to enrich our lives and our work in the future.
No funding was received for this paper.
UNESCO . A year after coronavirus: an inclusive ‘new normal’. https://en.unesco.org/news/year-after-coronavirus-inclusive-new-normal . (12 February 2021, date last accessed) .
Cordero DA . To stop or not to stop ‘culture’: determining the essential behavior of the government, church and public in fighting against COVID-19 . J Public Health (Oxf) 2021 . doi: 10.1093/pubmed/fdab026 .
Google Scholar
El-Erian MA . Navigating the New Normal in Industrial Countries . Washington, D.C. : International Monetary Fund , 2010 .
Google Preview
Alexander JC , Smith P . COVID-19 and symbolic action: global pandemic as code, narrative, and cultural performance . Am J Cult Sociol 2020 ; 8 : 263 – 9 .
Biddlestone M , Green R , Douglas KM . Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19 . Br J Soc Psychol 2020 ; 59 ( 3 ): 663 – 73 .
World Health Organization . From the “new normal” to a “new future”: A sustainable response to COVID-19. 13 October 2020 . https: // www.who.int/westernpacific/news/commentaries/detail-hq/from-the-new-normal-to-a-new-future-a-sustainable-response-to-covid-19 . (12 February 2021, date last accessed) .
| Month: | Total Views: |
|---|---|
| March 2021 | 331 |
| April 2021 | 397 |
| May 2021 | 1,112 |
| June 2021 | 1,714 |
| July 2021 | 1,767 |
| August 2021 | 1,638 |
| September 2021 | 3,977 |
| October 2021 | 8,281 |
| November 2021 | 6,445 |
| December 2021 | 4,287 |
| January 2022 | 6,424 |
| February 2022 | 7,286 |
| March 2022 | 8,709 |
| April 2022 | 7,282 |
| May 2022 | 7,307 |
| June 2022 | 5,175 |
| July 2022 | 2,404 |
| August 2022 | 2,940 |
| September 2022 | 7,021 |
| October 2022 | 7,134 |
| November 2022 | 5,171 |
| December 2022 | 3,236 |
| January 2023 | 3,796 |
| February 2023 | 3,344 |
| March 2023 | 4,316 |
| April 2023 | 2,826 |
| May 2023 | 3,263 |
| June 2023 | 1,742 |
| July 2023 | 988 |
| August 2023 | 1,592 |
| September 2023 | 2,701 |
| October 2023 | 1,847 |
| November 2023 | 1,354 |
| December 2023 | 865 |
| January 2024 | 1,025 |
| February 2024 | 1,232 |
| March 2024 | 1,257 |
| April 2024 | 1,169 |
| May 2024 | 902 |
| June 2024 | 337 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1741-3850
- Print ISSN 1741-3842
- Copyright © 2024 Faculty of Public Health
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- SAGE - PMC COVID-19 Collection

COVID-19 Pandemic and Stress: Coping with the New Normal
Anjana bhattacharjee.
1 Dept. of Psychology, Tripura University, Suryamani Nagar, Tripura, India
Tatini Ghosh
COVID-19 is the new face of pandemic. Since the discovery of COVID-19 in December 2019 in Wuhan, China, it has spread all over the world and the numbers are increasing day by day. Anyone can be susceptible to this infection but children, older adults, pregnant women, and people with comorbidity are more vulnerable. The spread of coronavirus resulted in closures of schools, businesses, and public spaces worldwide and forced many communities to enact stay at home orders, causing stress to all irrespective of their age, gender, or socioeconomic status. The sudden and unexpected changes caused by the outbreak of coronavirus are overwhelming for both adults and children, causing stress and evoking negative emotions like fear, anxiety, and depression, among different populations. The aim of the paper is to ascertain how stress during this pandemic inculcates various psychological health issues like depression anxiety, OCD, panic behavior, and so on. Further, the paper is an attempt to identify different general as well as population specific coping strategies to reduce the stress level among individuals and prevent various stress-induced psychological disorders with reference to different theories and research articles.
COVID-19, also known as coronavirus disease, is a severe respiratory disease first discovered in Wuhan, China, in December 2019. Since then, it has spread globally. The World Health Organization declared it a “Public Health Emergency of International Concern” on the 30 th of January 2020. There were more than 365,000 confirmed cases worldwide by October 2020 ( World Health Organization, 2020 ). According to report by the Ministry of Health and Family Welfare, Government of India (2021), since the inception of COVID-19 in India, there were more than 10,130,000 cases till february 2021. Even though vaccination has started in India and many parts of the world, the COVID-19 cases are still increasing day by day. The common symptoms of coronavirus are fever, cough, shortness of breath, and in some cases no symptoms at all. Anyone can be susceptible to this infection but children, older adults, pregnant women, and people with comorbidity are more vulnerable to this virus ( World Health Organization, 2020 ; National Institute of Mental Health and Neurosciences, 2020 ).
According to the National Institute of Mental Health and Neurosciences ( NIMHANS, 2020 ) the sudden lockdown and restricted mobility, along with isolation and social distancing during the starting of the pandemic, has caused stress, boredom, irritation, adjustment disorder, frustration and aggressive behavior. The sudden drastic change in known usual life acted as a gateway for increasing mental illness. A study shows that any severe epidemic or outbreak in society generally has severe negative effects on the society as well on the lives of humans ( Dodgen et al., 2002 ).
The unexpected outbreak of COVID-19 and its related consequences are causing severe changes in our lifestyle. These sudden changes can be overwhelming for both adults and children causing stress and evoking negative emotions like stress, fear, anxiety, depression among different populations. Several studies stated that the most prevalent mental health issues reported during the pandemic are stress, anxiety, fear, anger, insomnia, and denial. These issues were seen among different population groups ranging from children to older people, frontline workers, and people with pre-existing physical and mental health issues ( Roy et al., 2020 ; Torales et al., 2020 ). Different studies found that stress, anxiety, and depression coincide with the COVID-19 pandemic and due to the ongoing pandemic, there is an increase in the prevalence rate of these mental health issues around the globe ( Mohindra et al., 2020 ; Xiao et al., 2020 ).
A study comprising of 113,285 participants from India, China, Spain, Italy, and Iran revealed that among this surveyed population, the prevalence of depression, anxiety and stress was 20%, 35%, and 53%, respectively, during the pandemic and it seems to be increasing day by day ( Lakhan et al., 2020 ). A similar study found prevalence of post-traumatic stress among the general population has increased from 23.88% to 24.84% during the pandemic ( Cooke et al., 2020 ). A study on racial and ethnic disparity of stress and other mental health conditions during COVID-19 showed that Hispanic adults have four times higher prevalence of psychological stress and mental health issues than any other ethnic groups in the United States, along with increases in substance use and suicidal ideation ( McKnight-Eily et al., 2021 ). Wu et al. (2020) reported in a study that life stress, especially stress associated with uncertainty, has led to mental health disorders. The higher the level of perceived uncertainty stress, the greater the prevalence of mental health disorders. The study further found that the prevalence of mental health disorders due to the COVID-19 pandemic was 22.8%.
Abbott (2021) investigated stress caused by the COVID-19 pandemic and its related consequences and found that there is an increase in prevalence of stress, anxiety, and depression in the U.S. population from 11% to 42% due to this pandemic. The surge in stress among people is also during the rise of new COVID-19 covariant cases. A recent study showed an association between high level of stress, anxiety, and sleep disturbance and the period of social distancing ( Esteves et al., 2021 ).
Currently, several vaccines are being produced and vaccination has started, resulting in the discontinuation of lockdown orders in most countries. Educational institutions and workplaces are reopening and people are returning to the new normal life, maintaining social distancing. Recently Ministry of Health and Family Welfare (2021) reported a sudden surge during December 2020 in COVID-19 cases all over the world, due to a new covariant of COVID-19 virus that was first, testified by the Government of United Kingdom (UK) to World Health Organization (WHO). The new variants are reported to be more infectious and spread more easily among people. This is again aggravating the situation and increasing stress in people even after being vaccinated due to excessive fear and uncertainty.
The objectives of this article are two-fold. First it explores how stress plays a significant role in increasing the number of mental health problems during this pandemic. Second, it tries to identify different general as well as population specific coping mechanisms for dealing with this stressful situation with reference to different theories (both on stress and coping) and research articles.
Methodology
This paper reviews secondary data available through conceptual models, various past journals, research papers, and other useful websites related to coronavirus pandemic and its psychological effect on people. Finally, the paper extensively reviews different articles related to psycho-social coping mechanisms to reduce stress level among individuals.
When conducting this review research, related articles were focused on and keywords like “coronavirus,” “coronavirus and mental health,” “COVID-19,” “stress,” “psychological disorder,” and “coping strategies” were used. In order to identify articles that focused on specific terms like, “stress,” “pandemic and mental health,” “depression,” “anxiety,” “post-traumatic stress disorder,” and other related terms were used. The databases that were used for identifying related articles were Google Scholar, Medline, PubMed, NCBI (National Center for Biotechnology Information), and various other journals. Figure 1

PRISM diagram of systematic literature review process.
The systematic review started with 1137 articles, which were screened and reviewed and some were removed on different grounds. Finally, 106 articles were selected for the review article based on aims and objectives of the paper. The selection process of different articles is shown in the following PRISM flow chart. Finally, conclusions have been made on the basis of findings from different reviewed articles. Figure 2

Table showing discussion.
Theories of Stress
Hans selye’s theory.
In the year of 1930s, 1940s, and 1950s, Han Selye elaborated on the Walter Cannon’s theory of fight-or-flight reaction to stress and named it general adaptation syndrome (GAS). In this theory, Han Selye explained GAS as a physiological reaction to stress consisting of three stage reactions, namely: alarm reaction stage, resistance stage, and exhaustion stage ( Selye, 1956 ). When a person faces a stressful situation, alarm reaction stage is initiated. During this stage the body prepares itself for fight-or-flight reaction and makes the necessary physiological changes in body. If the stressor persists, the body progress to the second stage (the resistance stage), where the body reacts in an opposite way of alarm reaction and tries to repair the body from any damage. If the stressor still continues, in the third stage (exhaustion stage), the body’s energy is depleted and the person succumbs to various mental and physical health issues caused by the extreme stress. Selye (1991) further stated that prolonged exposure to extreme stress can cause mental and physical illness, or even death.
The transactional model of Stress
The transactional model of stress developed by Lazarus and Folkman (1984) explained that the feeling of stress is cumulative in nature. The amount of stress we experience is the result of our thoughts, feelings, emotions, and behaviors attached with our evaluation of our external and internal demands. When the demands of the external and internal environment exceed the resources we possess, it causes stress. If the situational demands are more than that of the available resources, it causes stress in multiple ways: acute, episodic or intermittent, and chronic, which further result in physical and mental dysfunction.
Conservation of resources (COR) theory
This theory ( Hobfoll, 1989 ) proposed a framework of stress and what resources are needed to be conserved for physical and mental well-being, in the face of stressors. According to COR theory, the primary motive of human beings is to conserve resources and tools that would help to maintain their overall well-being. COR states that there are four primary kinds of resources (e.g., objects, conditions, personal characteristics, and energies) that help in fostering and protecting well-being. It proposes that individuals lacking in resources will be more vulnerable to experience stress and those with abundant resources will be resilient to stress ( Hobfoll et al., 1996 ).
Holmes and Rahe’s model of stress
Holmes and Rahe’s (1967) developed a model of stress associated with major life changes, which cause stress and ultimately may result in illness. The model states that there is a positive correlation between stress inducing major life changes and illness. In other words, with an increase in major life events, there is greater likelihood of developing subsequent illness.
Stress-disease model
According to the stress-disease model by Kagan and Levi (1971) , there are several components explain how stress can lead to disease. First, stressors or stressful situations (both social or psychological stressors), second, the individual psychobiological programming (genetic and predisposing factors, learning, and previous experiences), third, how an individual reacts to stress. When the three components work together, it leads to the fourth component, that is, precursors of disease, which ultimately leads to the final outcome which is physical illness. This model explains how different physiological pathways can act as a mediator between stress and physical illness/disease ( Levi & Kagan, 1971 ).
Stress-Induced Mental Health Problems During COVID-19
Humans are social animals and it is a human tendency to establish social interactions with others. Due to COVID-19, our social interactions have been cut down, thus resulting in psychological distress ( Usher et al., 2020 ). Brodeur et al. (2004) revealed that the pandemic is severely affecting our mental health and there is an increase in web searches for loneliness, anxiety, depression, suicide, and divorce. Similarly, other studies also showed that epidemic and post-epidemic situations can cause psychological problems like stress, anxiety, and stigma as well as long lasting effects like post-traumatic stress symptoms and physical conditions like migraines and headaches ( Bhugra, 2004 ; Brooks et al., 2020 ; Cheng et al., 2004 ; Duan & Zhu, 2020 ; Fan et al., 2015 ). Post-traumatic stress disorder is a serious concern in the times of the COVID-19 pandemic, and females were found to be more prone psychological problems ( Alshehri et al., 2020 ; Bridgland et al., 2021 ).
In a recent study, Dubey et al. (2020) revealed that the current pandemic situation has not only affected the health of people but also badly affected the economy of the country. It has caused fear amongst people, which they have termed as “coronaphobia.” Many studies have revealed that stress, anxiety, fear, depression, and other psychological disorders are very commonly experienced during pandemic situations. The pandemic stress has a devastating effect on mental health ( Kumar & Nayar, 2021 ; Montano & Acebes, 2020 ; Van Bortel et al., 2016 ). Many studies over the past few decades proved that the impact of psychological stress is harmful for the immune system and the body’s response to vaccines, and these findings are applicable for COVID-19 vaccine as well ( Madison et al., 2021 ; Xiang et al., 2020 ).
A study by Shrilatha and Durga (2020) revealed that during this pandemic there was a rise in the use of social media and smartphones to is more than four hours a day, and the most used app was found to be WHATSAPP . Along with the increase in social media use, the use of other apps like ZOOM and HOUSE PARTY are also increasing since people are working from home ( Chanchani & Mishra, 2020 ). Even though social media helps in connecting with others from home, still there is a big disadvantage to it. During the coronavirus pandemic, social media is overloaded with misinformation and rumors that create more stress, fear, and panic among all ( Kumar & Nayar, 2021 ). Fear of COVID-19 due to misinformation results in the spread of maladaptive, obsessive-compulsive behaviors. Fear of contamination and regular washing of hands are common symptoms of OCD. Stress during COVID-19 and unavailability of proper treatment and therapy can lead to initiation and maintenance of OCD ( Adams et al., 2018 ).
The study of Kashif et al. (2020) revealed that along with the spike in screen usage, there has been a spike in cyber-crime during the coronavirus period. It has been further reported that personal data have also been stolen and hacked. Similar studies showed that there has been an increase in the number of cyber-crimes and cyber frauds since the first case of coronavirus in China and cyber fraud can lead to fear, panic, and stress ( Gross et al., 2016 ; Lallie et al., 2020 ). At such critical times, when hard earned money is lost, it can cause mental distress that may further develop severe psychological disorders. Hence financial loss and hardships can lead to psychological distress ( Bradshaw & Ellison, 2020 ).
Increased stress also plays a key role in substance abuse and addiction ( Sinha, 2001 ), and the stress, anxiety, and increased isolation lead people to indulge in use of psychoactive substances (like smoking, drugs, and alcohol drinking) and other substance dependent behaviors (like excessive use of social media, online gaming, and pornography). This results in substance abuse disorders during the pandemic ( Clay & Parker, 2020 ; Columb et al., 2020 ).
According to the WHO (2020) , due to the current pandemic and related measures taken to control it like social distancing, lockdown, etc., there has been a rise in the hazardous use of alcohol and drug, as well as suicidal ideation and attempts. Similarly, studies by Cheung et al. (2008) and Gardner et al. (2020) showed that pandemics can increase the rate of suicide among older adults. Not only isolation and loneliness but also death of a near one from COVID-19 are also risk factors for the suicidal ideation of an individual ( Sahoo et al., 2020 ). Figure 3

Summary of review on stress induced mental health problems during COVID-19.
Theories of Coping
Haan’s model of coping, defense, and fragmentation.
Norma Haan (1963) proposed a triarchic model of coping and described how the ego processes different stressors of daily life by using coping, defense, and fragmentation. She proposed in her model that “ego process” is a psychological approach in dealing with the stressors of daily life, which ultimately helps in sustaining a realistic connection with the self and the environment ( Haan, 1969 ). Haan (1993) defined three ways of dealing with stressors: coping, defense, and fragmentation. Coping is an effort to overcome the hardships of life by reaching out and within self for resources. Defense is an unconscious mechanism that greatly helps in reducing anxiety from harmful stimuli. Fragmentation is a method to adapt or accept failure when the stress is too extreme to handle/cope and may result in psychotic behavior. Thus, by controlling belief or behavior (defense), an individual can cope with the stressors, whereas when coping or defense fails, fragmentation occurs ( Haan, 1977 ).
Lazarus and Folkman’s theory of coping
Lazarus and Folkman propounded a theory of coping with stress ( Folkman & Lazarus, 1885 , 1991 ; Lazarus & Folkman, 1984 ), and the theory emphasized how coping transactionally interacts with cognition and emotion. According to the theory ( Lazarus & Folkman, 1987 ), there are two types of coping, namely: problem-focused coping and emotion-focused coping. Problem-focused coping deals with focusing with the problem, planning, and taking action and steps proactively about the problem, which may include gathering resources, seeking social support, or taking action to change or to overcome the problematic situation. On the contrary, emotion-focused coping deals with focusing more on the emotions, while dealing and managing the emotions caused due to the stressors. Emotions can be dealt by meditation, yoga, venting out frustrations, focusing on the positive, etc. Folkman (2013) explained that coping involves resorting to both cognitive and behavioral responses to manage the internal and external stressors.
The Hardiness Theory
Kobasa (1979) had defined hardiness as a personality type that helps in overcoming stress related illness. Hardiness is a general feeling of being satisfied with the environment. Maddi and Kobasa’s (1984) , hardiness theory of coping emphasizes that a hardy person would view stressful or challenging situations as a meaningful and interesting situation and an opportunity for personal growth. Such kind of outlook towards challenges helps people to remain healthy during stress. According to the theory, there are three ways to adhere to hardiness as coping: First, “controlling” the beliefs that can influence their environment; second, “commitment” and deep involvement in their tasks and duties; third, viewing “challenges” as an opportunity for growth and working for it.
The sense of coherence theory
Sense of coherence (SOC) ( Antonovsky, 1987 ) refers to a coping technique to deal with life stressors and emotional distress. It a feeling of confidence that both internal and external environment are predictable. According to the sense of coherence theory, there are three elements that are necessary for coping with daily life stressors: comprehensibility, manageability, and meaningfulness. People with weak SOC have a pessimistic outlook that things will go wrong in the end, whereas people with strong SOC have a good understanding of life and anticipate that all will turn good in the end. By successfully applying the elements of coherency, it is possible to cope with stress without hampering the physical health.
Stress and coping social support theory
The stress and coping social support theory by Cohen and Wills (1985) explained that social support acts as a coping method that protects the people from the stresses of life and the harmful physical effect of stressors. The theory further suggests that social support promotes adaptive appraisal and coping techniques in dealing with stressful events ( Thoits, 2010 ). According to Glanz et al. (2015) there are four types of social support that assist in coping with stress: emotional support comprising love, care, understanding; information support referring to information, guidance, and counseling; appraisal support referring to providing evaluative help; and finally, instrumental support referring to the physical or action-oriented help.
Suggestive Coping Strategies (General and Specific) During Pandemic
General psycho-social coping techniques.
According to various reports by International and National Institutes, like Ministry of Health and Family Welfare, Government of India, 2021 ; National Institute of Mental Health & Neurosciences (NIMHANS), 2020 and World Health Organization, 2020 , different psychological coping strategies have been suggested to reduce stress levels among individuals and to prevent various psychological disorders. COVID-19 has increased people's psychological burden and caused severe stress, which has challenged the resilience and coping ability to overcome hardships ( Polizzi et al., 2020 ). So, it is very requisite of the moment to foster and practice some psycho-social coping strategies to overcome stresses associated with COVID-19.
- 1. Psycho-education refers to educating people about various psychological disorders and their consequences. A study showed that psycho-education has helped people to deal with psychological disorders more successfully than those who were not given psycho-education ( Vieta, 2005 ).
- 2. Acceptance is an important coping mechanism to deal with stressors. If acceptance of the prevailing circumstances is not there, then it can lead to a negative coping strategy known as denial, which is very dangerous. In denial, the person will not follow any guidelines and it may affect others as well. One study shows that acceptance is a good way to cope with stressors and their harmful physical effects ( Lindsay et al., 2018 ).
- 3. Practice Positive Thinking. One negative thought leads to another and it creates a chain reaction of negative thoughts. To break this cycle, positive thinking practice should be adopted. Positive thinking refers to the process of focusing on positive emotions and positive behavioral habits. One study on positive thinking shows that it helps in coping with stress, anxiety, and other psychological disorders as well ( Naseem & Khalid, 2010 ).
- 4. Cognitive redefinition is a psychological coping strategy to redefine or change the way we see, perceive, and feel about any situation or events. Instead of perceiving this current pandemic situation as something very stressful, cognitive redefining can help in perceiving this as time to reconnect with family and to indulge in creative activities and self-care. One study shows that cognitive redefinition or change in mindset is helpful in dealing with stressful situations ( Crum et al., 2013 ).
- 5. Limiting Social Media and News. According to The Centers for Disease Control and Prevention, too much information and news about the COVID-19 pandemic can be overwhelming and upsetting, and it can cause panic among the people. So, it has been suggested to limit social media use and listening/reading news about the current pandemic situation. It has also been suggested by WHO to read about it from trusted sources only, as, factual information can help lessen fear and panic.
- 6. Proper Sleep Hygiene. The current pandemic situation is very crucial for everyone and it is very important to be biologically fit so as to reduce the risk of COVID-19 and its associated issues. Studies proved that having proper sleep hygiene can help in dealing with stress, anxiety, mood disturbances, and other mental health problems associated with the current pandemic ( Jakupcak et al., 2020 ; Thoits, 2010 ).
- 7. Physical Fitness. It has been reported that regular physical exercise not only boosts physical health but also helps in mental health by reducing stress, anxiety, and depression. It would be helpful to do regular physical exercises at home during this pandemic to stay fit both physically and mentally ( Altena et al., 2020 ; Muraki et al., 1993 ; Sunder et al., 2020 ).
- 8. Spending Time on Hobbies. Currently, we are either locked at home or have restricted mobility due to the pandemic situation. So, there is an immense amount of time for us at home now. We can utilize the time by indulging in various activities like cooking, painting, gardening, etc. One study shows that people who indulges in hobbies in their leisure time are less likely to have mental health issues than those who do not have hobbies ( Jeoung et al., 2013 ). Reports by NIMHANS advised people to indulge in various activities so as to distract themselves from the constant worrying about the situation.
- 9. Work life Balance. During the current COVID-19 outbreak when many people are working from home to avoid contamination, it has become very important to maintain work–life balance. Work–life balance is the process of maintaining a proper balance between work and other activities of daily life in a way that one does not hamper the other. Studies also prove that maintaining a proper work life balance boosts positive mental health and reduces anxiety and depression among employees ( LaBrie et al., 2010 ).
- 10. Healthy Daily Routine. Day-to-day routines have been disrupted during the COVID-19 pandemic, and it negatively hampers our both physical and mental health. Various reports show that unhealthy life styles impede our physical and mental health whereas healthy lifestyle like eating healthy, getting enough sleep, focusing on positive thoughts, etc. can boost healthy mind and body ( Haar et al., 2014 ; Takeda et al., 2015 ).
- 11. Mindfulness Practice. Mindfulness refers to the state of physical and mental awareness of a person, without being affected by the surroundings. There are various mindfulness techniques like meditation, physical exercise, yoga, guiding imagery and spiritual practices. Studies also show that mindfulness practices help in dealing with mental and emotional disorders and also boost physical health ( Call et al., 2014 ; Koenig, 2010 ; Mayo Clinic, 2020 ; Melnyk et al., 2006 ).
- 12. Following Government Guidelines. It is being advised all the time to follow the Government guidelines to curb the COVID-19 outbreak. Some of the guidelines by the Ministry of Health and Family Welfare, Government of India suggest to maintain social distancing, wear face coverings whenever outside, wash hands using soap regularly and avoid public gathering.
- 13. Professional Help. Urgent professional help has to be sought if the person is not able to deal with the sudden life changes and if it is severely hampering their physical and mental health. If people are suffering from any kind of physical and emotional disorder, professional help like consulting a psychologist, counselor, or psychiatrist is advisable ( Wang et al., 2020 ).
- 14. Avoid Stigmatization. There has been negative attitudes and stigma about mental health exist. Due to stigma attached to mental health and mental health care providers, people hesitate to express their mental turmoil or stress, which further leads to serious psychological conditions. So, it is suggested to avoid stigmatizing mental health or mental health professionals and seek help whenever needed ( Yang, 2007 ).
- 15. Good Social Support. Studies reveal that people who have good social support are less likely to have any psychological disorders. People with good social networking will have less or no depression, suicidal thoughts, or suicidal risk in the future ( Duan & Zhu, 2020 ). So, it is important to have good social support during this pandemic situation and to stay connected with family or friends through various online mediums.
Specific coping techniques
Besides the above-mentioned general coping strategies, which are suggested for everyone irrespective of any sociodemographic differences to cope up with a stressful life, there are certain coping techniques that are being followed by people belonging to specific age, gender, and community.
- • Age Specific Coping. People of different age groups face different levels of stress, and hence, their coping techniques are different as well ( Paykel, 1983 ). Cognitive behavior therapy seems to help in reducing PTSD, stress, depression, and anxiety among youth during periods of crisis and improves resilience ( Chen et al., 2014 ) whereas, avoidant coping seems to escalate PTSD ( McGregor et al., 2015 ). Youth also seem to apply approach coping and habitual coping styles ( Steiner et al., 2002 ); active coping followed by social coping and avoidant coping style (Brown et al., 2015). Further studies revealed that older adults seem to prefer problem-focused coping in terms of stressful events ( Chen et al., 2017 ); proactive coping ( Pearman et al., 2021 ); adaptive and active strategies of coping ( Kuria, 2012 ).
- • Gender Specific Coping. Several studies have reported gender-differences in terms of coping strategies ( Matud, 2004 ; Ptacek et al., 1994 ). Men seem to resort to approach coping style (Gan et al., 2009), problem-focused approach ( Sinha & Latha, 2018 ; Tolor & Fehon, 1987 ), rational, detachment and rumination coping style ( Matud, 2004) , and cognitive hardiness ( Beasley et al., 2003 ), whereas women are found to use emotion-focused coping style ( Loukzadeh & Mazloom Bafrooi, 2013 ; Manna et al., 2007 ), avoidance coping style followed by approach coping style ( Gan et al., 2009 ), planned-breather leisure coping method ( Tsaur & Tang, 2012 ), active coping strategies ( Lin, 2016 ), and social support ( Linnabery et al., 2014 ).
- • Community Specific Coping. There are variations in the use of coping strategies based on community and racial differences. White Americans are found to use approach behavior coping style, whereas African-Americans are more likely to use avoidance cognitive coping style ( Anshel et al., 2009 ). Similarly, African-American young adults were found to resort to avoidance coping style in comparison to White young adults, who prefer problem-focused coping ( Van Gundy et al., 2015 ). White women seem to use a self-directing coping style, whereas African-American women more often use religious coping ( Ark et al., 2006 ).
COVID-19 is the new face of the pandemic, and it has put the whole world into a pause. It has become a threat to the entire civilization. The COVID-19 pandemic not only affects physical health but also severely affects the mental health of people, whether infected or not. Nationwide lockdowns, social isolation, and restricted mobility have increased the prevalence of mental health problems, and people all over the world are suffering from loneliness, feelings of helplessness, hopelessness, anxiety, stress, and adjustment disorder. Not only these, dependency on social media and alcohol and other psychoactive substances has increased, which further raises the incidents of domestic violence or intimate partner violence. So, healthcare providers should give attention to both physical and psychological well-being of the people. Hence, it is the need of the hour to follow all the physical measures suggested by the healthcare professionals to prevent COVID-19, along with practicing psycho-social coping strategies for better quality of life and overall sound health and well-being of the individual.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Tatini Ghosh https://orcid.org/0000-0002-7221-9381
- Abbott A. (2021). COVID's mental-health toll: how scientists are tracking a surge in depression . Nature , 590 , 194–195. 10.1038/d41586-021-00175-z. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Adams T. G., Kelmendi B., Brake C. A., Gruner P., Badour C. L., Pittenger C. (2018). The role of stress in the pathogenesis and maintenance of obsessive-compulsive disorder . Chronic Stress , 2 , 2470547018758043. 10.1177/2470547018758043. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alshehri F. S., Alatawi Y., Alghamdi B. S., Alhifany A. A., Alharbi A. (2020). Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia . Saudi Pharmaceutical Journal , 28 ( 12 ), 1666–1673. 10.1016/j.jsps.2020.10.013. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Altena E., Baglioni C., Espie C. A., Ellis J., Gavriloff D., Holzinger B., Schlarb A., Frase L., Jernelöv S., Riemann D. (2020). Dealing with sleep problems during home confinementdue to the COVID‐19 outbreak: Practical recommendations from a task force of the European CBT‐I Academy . Journal of Sleep Research , 29 ( 4 ), e13052. 10.1111/jsr.13052. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Anshel M. H., Sutarso T., Jubenville C. (2009). Racial and gender differences on sources of acute stress and coping style among competitive athletes . The Journal of Social Psychology , 149 ( 2 ), 159–178. 10.3200/socp.149.2.159-178. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Antonovsky A. (1987). Unraveling the mystery of health: How people manage stress and stay well : Jossey-Bass. https://psycnet.apa.org/record/1987-97506-000 . [ Google Scholar ]
- Ark P. D., Hull P. C., Husaini B. A., Craun C. (2006). Religiosity, religious coping styles, and health service use: racial differences among elderly women . Journal of Gerontological Nursing , 32 ( 8 ), 20–29. https://pubmed.ncbi.nlm.nih.gov/16915743/ . [ PubMed ] [ Google Scholar ]
- Beasley M., Thompson T., Davidson J. (2003). Resilience in response to life stress: the effects of coping style and cognitive hardiness . Personality and Individual Differences , 34 ( 1 ), 77–95. 10.1016/S0191-8869(02)00027-2. [ CrossRef ] [ Google Scholar ]
- Bhugra D. (2004). Migration and mental health . Acta Psychiatricascandinavica , 109 ( 4 ), 243–258. 10.1046/j.0001-690x.2003.00246.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradshaw M., Ellison C. G. (20201982). Financial hardship and psychological distress: Exploring the buffering effects of religion . Social Science & Medicine , 71 ( 1 ), 196–204. 10.1016/j.socscimed.2010.03.015. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bridgland V. M. E., Moeck E. K., Green D. M., Swain T. L., Nayda D. M., Matson L. A., Hutchison N. P., Takarangi M. K. T. (2021). Why the COVID-19 pandemic is a traumatic stressor . Plos One , 16 ( 1 ), e0240146. 10.1371/journal.pone.0240146. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brodeur A., Clark A. E., Fleche S., Powdthavee N. (2004). Assessing the impact of the coronavirus lockdown on unhappiness, loneliness, and boredom using Google Trends . arXiv preprint arXiv:.12129 https://arxiv.org/abs/2004.12129 .
- Brooks S. K., Webster R. K., Smith L. E., Woodland L., Wessely S., Greenberg N., Rubin G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence . Lancet , 395 ( 10227 ), 912–920. 10.1016/S0140-6736(20)30460-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown S. M., Begun S., Bender K., Ferguson K. M., Thompson S. J. (2015). An exploratory factor analysis of coping styles and relationship to depression among a sample of homeless youth . Community Mental Health Journal , 51 ( 7 ), 818–827. 10.1007/s10597-015-9870-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Call D., Miron L., Orcutt H. (2014). Effectiveness of brief mindfulness techniques in reducing symptoms of anxiety and stress . Mindfulness , 5 ( 6 ), 658–668. 10.1007/s12671-013-0218-6. [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention (2020). U.S. Department of Health & Human Services. Available from: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html .
- Chanchani M., Mishra D. (15th April 2020). “Mobile apps’ usage spikes in lockdown” . Times of India https://timesofindia.indiatimes.com/business/india-business/mobile-apps-usage-spikes-in-lockdown/articleshow/75148768.cms .13
- Cheng S. K. W., Wong C. W., Tsang J., Wong K. C. (2004). Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) . Psychological Medicine , i ( 4 ), 1187–1195. 10.1017/s0033291704002272. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen Y., Peng Y., Xu H., O’Brien W. (2017). Age differences in stress and coping: problem-focused strategies mediate the relationship between age and positive affect . The International Journal of Aging and Human Development , 86 ( 4 ), 347–363. 10.1177/0091415017720890. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen Y., Shen W. W., Gao K., Lam C. S., Chang W. C., Deng H. (2014). Effectiveness RCT of a CBT intervention for youths who lost parents in the Sichuan, China, earthquake . Psychiatric Services , 65 ( 2 ), 259–262. 10.1176/appi.ps.201200470. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cheung Y. T., Chau P. H., Yip P. S. (2008). A revisit on older adults’ suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong . International Journal of Geriatric Psychiatry , 23 ( 12 ), 1231–1238. 10.1002/gps.2056. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clay J. M., Parker M. O. (2020). Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? The Lancet. Public Health , 5 ( 5 ), e259. 10.1016/S2468-2667(20)30088-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen S., Wills T. A. (1985). Stress, social support, and the buffering hypothesis . Psychological Bulletin , 98 ( 2 ), 310–357. 10.1037/0033-2909.98.2.310. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Columb D., Hussain R., O’Gara C. (2020). Addiction psychiatry and COVID-19: Impact on patients and service provision . Irish Journal of Psychological Medicine , 37 ( 3 ), 164–168. 10.1017/ipm.2020.47. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cooke J. E., Eirich R., Racine N., Madigan S. (2020). Prevalence of posttraumatic and general psychological stress during COVID-19: A rapid review and meta-analysis . Psychiatry Research , 292 , 113347. 10.1016/j.psychres.2020.113347. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crum A. J., Salovey P., Achor S. (2013). Rethinking stress: The role of mindsets in determining the stress response . Journal of Personality and Social Psychology , 104 ( 4 ), 716–733. 10.1037/a0031201. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Department of Psychiatry, National Institute of Mental Health & Neurosciences (NIMHANS) (2020). Mental health in the times of COVID-19 Pandemic, guidelines for general medical and specialised mental health care settings (pp. 1–177). National Institute of Mental Health & Neurosciences (NIMHANS). Retrieved from: http://nimhans.ac.in/wp-content/uploads/2020/04/MentalHealthIssuesCOVID-19NIMHANS.pdf . [ Google Scholar ]
- Dodgen D., LaDue L. R., Kaul R. E. (2002). Coordinating a local response to a national tragedy: Community mental health in Washington, DC after the Pentagon attack . Military Medicine , 167 ( 4 ), 87–89. Link: https://pubmed.ncbi.nlm.nih.gov/12363154/ . [ PubMed ] [ Google Scholar ]
- Duan L., Zhu G. (2020). Psychological interventions for people affected by the COVID-19 epidemic . The Lancet Psychiatry , 7 ( 4 ), 300–302. 10.1016/S2215-0366(20)30073-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M. J., Chatterjee S., Lahiri D., Lavie C. J. (2020). Psychosocial impact of COVID-19 . Diabetes & Metabolic Syndrome , 14 ( 5 ), 779–788. 10.1016/j.dsx.2020.05.035. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Esteves C. S., Oliveira C. R. D., Argimon I. I. D. L. (2021). Social distancing: Prevalence of depressive, anxiety, and stress symptoms among Brazilian students during the COVID-19 pandemic . Frontiers in Public Health , 8 , 589966. 10.3389/fpubh.2020.589966. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fan F., Long K., Zhou Y., Zheng Y., Liu X. (2015). Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China . Psychological Medicine , 45 ( 13 ), 2885–2896. 10.1017/S0033291715000884. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Folkman S. (2013). Stress: Appraisal and Coping . In Gellman M.D., Turner J.R. (Eds), Encyclopedia of Behavioral Medicine New York, NY: Springer. 10.1007/978-1-4419-1005-9_215. [ CrossRef ] [ Google Scholar ]
- Folkman S., Lazarus R. S. (1985). If it changes it must be a process: Study of emotion and coping during three stages of a college examination . Journal of Personality and Social Psychology , 48 ( 1 ), 150–170. 10.1037//0022-3514.48.1.150. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Folkman S., Lazarus R. S. (1991). Coping and emotion . In Monat A., Lazarus R. S. (Eds), Stress and Coping: An anthology (pp. 208–227)New York: Columbia University Press. https://www.scirp.org/(S(lz5mqp453edsnp55rrgjct55))/reference/ReferencesPapers.aspx?ReferenceID=1955093 . [ Google Scholar ]
- Gan Q., Anshel M. H., Kim J. K. (2009). Sources and cognitive appraisals of acute stress as predictors of coping style among male and female Chinese athletes . International Journal of Sport and Exercise Psychology , 7 ( 1 ), 68–88. 10.1080/1612197x.2009.9671893. [ CrossRef ] [ Google Scholar ]
- Gardner W., States D., Bagley N. (2020). The Coronavirus and the risks to the elderly in long-term care . Journal of Aging & Social Policy , 32 ( 4-5 ), 310–315. 10.1080/08959420.2020.1750543. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Glanz K., Rimer B. K., Viswanath K. (Eds), (2015). John Wiley & Sons. https://www.wiley.com/en-in/Health+Behavior:+Theory,+Research,+and+Practice,+5th+Edition-p-9781118628980 . Health behavior: Theory, research, and practice [ Google Scholar ]
- Gross M. L., Canetti D., Vashdi D. R. (2016). The psychological effects of cyber terrorism . Bulletin of the Atomic Scientists , 72 ( 5 ), 284–291. 10.1080/00963402.2016.1216502. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haan N. (1963). Proposed model of ego functioning: Coping and defense mechanisms in relationship to IQ change . Psychological Monographs , 77 ( 8 ), 1–23. 10.1037/h0093848. [ CrossRef ] [ Google Scholar ]
- Haan N. (1969). A tripartite model of ego functioning values and clinical and research applications . Journal of Nervous & Mental Disease , 148 ( 1 ), 14–30. 10.1097/00005053-196901000-00003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haan N. (1977). Coping and defending: Processes of self-environment organization : Academic Press. https://www.elsevier.com/books/coping-and-defending/haan/978-0-12-312350-3 . [ Google Scholar ]
- Haan N. (1993). The assessment of coping, defense, and stress . In Goldberger L., Breznitz S. (Eds), Handbook of stress: Theoretical and Clinical Aspects (2nd ed., pp. 258-273)New York: Free Press. https://psycnet.apa.org/record/1993-97397-013 . [ Google Scholar ]
- Haar J. M., Russo M., Suñe A., Ollier-Malaterre A. (2014). Outcomes of work–life balance on job satisfaction, life satisfaction and mental health: A study across seven cultures . Journal of Vocational Behaviour , 85 ( 3 ), 361–373. 10.1016/j.jvb.2014.08.010. [ CrossRef ] [ Google Scholar ]
- Hobfoll S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress . American Psychologist , 44 ( 3 ), 513–524. 10.1037/0003-066X.44.3.513. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hobfoll S. E., Freedy J. R., Green B. L., Solomon S D. (19961996). Coping reactions to extreme stress: The roles of resource loss and resource availability . In Zeidner M, Endler N S. (Eds), Handbook of Coping: Theory, Research, Applications (pp. 322–349)New York: Wiley. https://psycnet.apa.org/record/1996-97004-015 . [ Google Scholar ]
- Holmes T. H., Rahe R. H. (1967). The Social Readjustment Rating Scale . Journal of Psychosomatic Research , 11 ( 2 ), 213–218. 10.1016/0022-3999(67)90010-4. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jakupcak M., Vannoy S., Imel Z., Cook J. W., Fontana A., Rosenheck R., McFall M. (2020). Does PTSD moderate the relationship between social support and suicide risk in Iraq and Afghanistan War Veterans seeking mental health treatment? Depression and Anxiety , 27 ( 11 ), 1001–1005. 10.1002/da.20722. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jeoung B. J., Hong M. S., Lee Y.C. (2013). The relationship between mental health and health-related physical fitness of university students . Journal of Exercise Rehabilitation , 9 ( 6 ), 544–548. 10.12965/jer.130082. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kagan A., Levi L. (1971). Adaptation of the psychosocial environment to man's abilities and needs . Society, Stress and Disease , 1 , 399–404. 10.1002/da.20722. [ CrossRef ] [ Google Scholar ]
- Kashif M., Javed M. K., Pandey D. (2020). A surge in cyber-crime during COVID-19 . Indonesian Journal of Social and Environmental Issues , 1 ( 2 ), 48–52. 10.47540/ijsei.v1i2.22. [ CrossRef ] [ Google Scholar ]
- Kobasa S. C. (1979). Personality and resistance to illness . American Journal of Community Psychology , 7 ( 4 ), 413–423. 10.1007/bf00894383. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koenig H. G. (2010). Spirituality and mental health . International Journal of Applied Psychoanalytic Studies , 7 ( 2 ), 116–122. 10.1002/aps.239. [ CrossRef ] [ Google Scholar ]
- Kumar A., Nayar K. R. (2021). COVID 19 and its mental health consequences . Journal of Mental Health , 30 ( 1 ), 1–2. 10.1080/09638237.2020.1757052. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuria W. (2012). Coping with age related changes in the elderly . Available at: https://www.theseus.fi/handle/10024/42261 .
- LaBrie J. W., Kenney S. R., Lac A. (2010). The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health . Journal of Drug Education , 40 ( 4 ), 361–378. 10.2190/DE.40.4.c. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lakhan R., Agrawal A., Sharma M. (2020). Prevalence of Depression, Anxiety, and Stress during COVID-19 Pandemic . Journal of Neurosciences in Rural Practice , 11 ( 4 ), 519–525. 10.1055/s-0040-1716442. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lallie H. S., Shepherd L. A., Nurse J. R., Erola A., Epiphaniou G., Maple C., Bellekens X. (2020). Cyber security in the age of COVID-19: A timeline and analysis of cyber-crime and cyber-attacks during the Pandemic. Computers & Security . arXiv preprint arXiv:2006.11929, 1–20 10.1016/j.cose.2021.102248. [ PMC free article ] [ PubMed ] [ CrossRef ]
- Lazarus R. S., Folkman S. (1984). Stress, appraisal, and coping New York. Link: Springer Publishing Company. https://books.google.co.in/books?hl=en&lr=&id=i-ySQQuUpr8C&oi=fnd&pg=PR5&ots=DgEPjrjeLa&sig=63fQrxM63vph60T1t7U7oIwhVDw&redir_esc=y#v=onepage&q&f=false . [ Google Scholar ]
- Lazarus R. S., Folkman S. (1987). Transactional theory and research on emotions and coping . European Journal of Personality , 1 ( 3 ), 141–169. 10.1002/per.2410010304. [ CrossRef ] [ Google Scholar ]
- Levi L., Kagan A. (1971). A synopsis of ecology and psychiatry: Some theoretical psychosomatic considerations, review of some studies and discussion of preventive aspects . Excerpta Medica International Congress Series , 274 , 369–379. https://psycnet.apa.org/record/1975-27742-001 . [ Google Scholar ]
- Lin C. C. (2016). The roles of social support and coping style in the relationship between gratitude and well-being . Personality and Individual Differences , 89 , 13–18. 10.1016/j.paid.2015.09.032. [ CrossRef ] [ Google Scholar ]
- Lindsay E. K., Young S., Smyth J. M., Brown K. W., Creswell J. D. (2018). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial . Psychoneuroendocrinology , 87 , 63–73. 10.1016/j.psyneuen.2017.09.015. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Linnabery E., Stuhlmacher A. F., Towler A. (2014). From whence cometh their strength: Social support, coping, and well-being of Black women professionals . Cultural Diversity & Ethnic Minority Psychology , 20 ( 4 ), 541–549. 10.1037/a0037873. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Loukzadeh Z., Mazloom Bafrooi N. (2013). Association of coping style and psychological well-being in hospital nurses . Journal of Caring Sciences , 2 ( 4 ), 313–319. 10.5681/jcs.2013.037. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Maddi S. R., Kobasa S. C. (1984). The hardy executive: Health under stress : Dow Jones-Irwin. [ Google Scholar ]
- Madison A. A., Shrout M. R., Renna M. E., Kiecolt-Glaser J. K. (2021). Psychological and behavioral predictors of vaccine efficacy: Considerations for COVID-19 . Perspectives on Psychological Science , 16 ( 2 ), 191–203. 10.1177/1745691621989243. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Manna G., Foddai E., Di Maggio M., Pace F., Colucci G., Gebbia N., Russo A. (2007). Emotional expression and coping style in female breast cancer . Annals of Oncology , 18 ( 6 ), vi77–vi80. 10.1093/annonc/mdm231. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Matud M. P. (2004). Gender differences in stress and coping styles . Personality and Individual Differences , 37 ( 7 ), 1401–1415. 10.1016/j.paid.2004.01.010. [ CrossRef ] [ Google Scholar ]
- Mayo Clinic (2020). COVID-19 and your mental health : Mayo Clinic. Available from: https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/mental-health-covid-19/art-20482731 . [ Google Scholar ]
- McGregor L. S., Melvin G. A., Newman L. K. (2015). Familial Separations, Coping Styles, and PTSD Symptomatology in Resettled Refugee Youth . The Journal of Nervous and Mental Disease , 203 ( 6 ), 431–438. 10.1097/nmd.0000000000000312. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McKnight-Eily L. R., Okoro C. A., Strine T. W., Verlenden J., Hollis N. D., Njai R., Mitchell E. W., Board A., Puddy R., Thomas C. (2021). Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 Pandemic - United States, April and May 2020 . MMWR. Morbidity and Mortality Weekly Report , 70 ( 5 ), 162–166. 10.15585/mmwr.mm7005a3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Melnyk B. M., Small L., Morrison-Beedy D., Strasser A., Spath L., Kreipe R., Crean H., Jacobson D., Van Blankenstein S. (2006). Mental health correlates of healthy lifestyle attitudes, beliefs, choices, and behaviors in overweight adolescents . Journal of Pediatric Health Care , 20 ( 6 ), 401–406. 10.1016/j.pedhc.2006.03.004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ministry of Health and Family welfare, Government of India (2021). Novel Coronavirus (COVID19) . Available from: https://www.mohfw.gov.in/pdf/ProtectivemeasuresEng.pdf .
- Mohindra R., Ravaki R., Suri V., Bhalla A., Singh S. M. (2020). Issues relevant to mental health promotion in frontline health care providers managing quarantined/isolated COVID19 patients . Asian Journal of Psychiatry , 51 , 102084. 10.1016/j.ajp.2020.102084. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Montano R. L. T., Acebes K. M. L. (2020). Covid stress predicts depression, anxiety and stress symptoms of Filipino respondents . International Journal of Research in Business and Social Science (2147-4478) , 9 ( 4 ), 78–103. 10.20525/ijrbs.v9i4.773. [ CrossRef ] [ Google Scholar ]
- Muraki S., Maehara T., Ishii K., Ajimoto M., Kikuchi K. (1993). Gender difference in the relationship between physical fitness and mental health . The Annals of Physiological Anthropology , 12 ( 6 ), 379–384. 10.2114/ahs1983.12.379. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Naseem Z., Khalid R. (2010). Positive thinking in coping with stress and health outcomes: Literature review . Journal of Research & Reflections in Education (JRRE) , 4 ( 1 ), 42–61. http://www.ue.edu.pk/jrre . [ Google Scholar ]
- Paykel E. S. (1983). Methodological aspects of life events research . Journal of Psychosomatic Research , 27 ( 5 ), 341–352. 10.1016/0022-3999(83)90065-x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pearman A., Hughes M. L., Smith E. L., Neupert S. D. (2021). Age differences in risk and resilience factors in COVID-19-related stress . The Journals of Gerontology: Series B Psychological Sciences and Social Sciences , 76 ( 2 ), e38–e44. 10.1093/geronb/gbaa120. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Polizzi C., Lynn S. J., Perry A. (2020). Stress and coping in the time of COVID-19: pathways to resilience and recovery . Clinical Neuropsychiatry , 17 ( 2 ), 59–62. 10.36131/CN20200204. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ptacek J. T., Smith R. E., Dodge K. L. (1994). Gender differences in coping with stress: When stressor and appraisals do not differ . Personality & Social Psychology Bulletin , 20 ( 4 ), 421–430. 10.1016/0022-3999(83)90065-x. [ CrossRef ] [ Google Scholar ]
- Roy D., Tripathy S., Kar S. K., Sharma N., Verma S. K., Kaushal V. (2020). Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic . Asian Journal of Psychiatry , 51 , 102083. 10.1016/j.ajp.2020.102083. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sahoo S., Rani S., Parveen S., Pal Singh A., Mehra A., Chakrabarti S., Grover S., Tandup C. (2020). Self-harm and COVID-19 Pandemic: An emerging concern - A report of 2 cases from India (Advance online publication) . Asian Journal of Psychiatry , 51 , 102104. 10.1016/j.ajp.2020.102104. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Selye H. (1956). The stress of life . McGraw-Hill Book Company. [ Google Scholar ]
- Selye H. (1991). History and present status of the stress concept In: Stress and coping: An Anthology (pp. 21–35). Columbia University Press. [ Google Scholar ]
- Shrilatha S., Durga M. S. J. (2020). The role of social media apps and its cyber-attacks during Covid-19 lockdown at Vellore City . Purakala with ISSN 0971-2143 is an UGC CARE Journal , 31 ( 17 ), 446–461. 10.4103/IJAM.IJAM_50_20. [ CrossRef ] [ Google Scholar ]
- Sinha R. (2001). How does stress increase risk of drug abuse and relapse? Psychopharmacology , 158 ( 4 ), 343–359. 10.1007/s002130100917. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sinha S., Latha G. S. (2018). Coping response to same stressors varies with gender . National Journal of Physiology, Pharmacy and Pharmacology , 8 ( 7 ), 1053–1057. 10.5455/njppp.2018.8.0206921032018. [ CrossRef ] [ Google Scholar ]
- Steiner H., Erickson S. J., Hernandez N. L., Pavelski R. (2002). Coping styles as correlates of health in high school students . Journal of Adolescent Health , 30 ( 5 ), 326–335. 10.1016/S1054-139X(01)00326-3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sunder P., Prabhu A., Parameswaran U. (2020). Psychosocial interventions for COVID-19-Supporting document . e-Book On Palliative Care Guidelines For Covid-19 Pandemic , 42 , 21–24. https://wp.ufpel.edu.br/francielefrc/files/2020/04/e-book-Palliative-Care-Guidelines-for-COVID19-ver1.pdf . [ Google Scholar ]
- Takeda F., Noguchi H., Monma T., Tamiya N. (2015). How possibly do leisure and social activities impact mental health of middle-aged adults in Japan?: an evidence from a national longitudinal survey . PLoS One , 10 ( 10 ), e0139777. 10.1371/journal.pone.0139777. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thoits P. A. (2010). Perceived social support and the voluntary, mixed, or pressured use of mental health services . Society and Mental Health , 1 ( 1 ), 4–19. 10.1177/2156869310392793. [ CrossRef ] [ Google Scholar ]
- Tolor A., Fehon D. (1987). Coping with stress: A study of male adolescents' coping strategies as related to adjustment . Journal of Adolescent Research , 2 ( 1 ), 33–42. 10.1177/074355488721003. [ CrossRef ] [ Google Scholar ]
- Torales J., O’Higgins M., Castaldelli-Maia J. M., Ventriglio A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health . International Journal of Social Psychiatry , 66 ( 4 ), 317–320. 10.1177/0020764020915212. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tsaur S., Tang Y. (2012). Job stress and well-being of female employees in hospitality: The role of regulatory leisure coping styles . International Journal of Hospitality Management , 31 ( 4 ), 1038–1044. 10.1016/j.ijhm.2011.12.009. [ CrossRef ] [ Google Scholar ]
- Usher K., Durkin J., Bhullar N. (2020). The COVID‐19 pandemic and mental health impacts . International Journal of Mental Health Nursing , 29 ( 3 ), 315–318. 10.1111/inm.12726. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van Bortel T., Basnayake A., Wurie F., Jambai M., Koroma A. S., Muana A. T., Hann K., Eaton J., Martin S., Nellums L. B. (2016). Psychosocial effects of an Ebola outbreak at Individual, Community and International levels . Bulletin of the World Health Organization , 94 ( 3 ), 210–214. 10.2471/BLT.15.158543. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van Gundy K. T., Howerton-Orcutt A., Mills M. L. (2015). Race, coping style, and substance use disorder among non-hispanic African American and white young adults in South Florida . Substance Use & Misuse , 50 ( 11 ), 1459–1469. 10.3109/10826084.2015.1018544. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vieta E. (2005). Improving treatment adherence in bipolar disorder through psychoeducation . The Journal of Clinical Psychiatry , 66 ( 1 ), 24–29. https://pubmed.ncbi.nlm.nih.gov/15693749/ . [ PubMed ] [ Google Scholar ]
- Wang Y., Zhao X., Feng Q., Liu L., Yao Y., Shi J. (2020). Psychological assistance during the coronavirus disease 2019 outbreak in China . Journal of Health Psychology , 25 ( 6 ), 733–737. 10.1177/1359105320919177. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization (2020). Mental health and psychosocial considerations during the COVID-19 outbreak, (No. WHO/2019-nCoV/Mental Health/2020.1) : World Health Organization. Retrieved from https://www.who.int/health-topics/coronavirus . [ Google Scholar ]
- Wu D., Yu L., Yang T., Cottrell R., Peng S., Guo W., Jiang S. (2020). The impacts of uncertainty stress on mental disorders of Chinese college students: Evidence from a nationwide study . Frontiers in Psychology , 11 , 243. 10.3389/fpsyg.2020.00243. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Xiang Y. T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C. H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed . The Lancet Psychiatry , 7 ( 3 ), 228–229. 10.1016/s2215-0366(20)30046-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China . Medical Science Monitor: International Medical Journal of Experimental and Clinical Research , 26 , e923549. 10.12659/MSM.923549. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yang L. H. (2007). Application of mental illness stigma theory to Chinese societies: Synthesis and new direction . Singapore Medical Journal , 48 ( 11 ), 977–985. https://pubmed.ncbi.nlm.nih.gov/17975685/ . [ PubMed ] [ Google Scholar ]
How it works
Transform your enterprise with the scalable mindsets, skills, & behavior change that drive performance.
Explore how BetterUp connects to your core business systems.
We pair AI with the latest in human-centered coaching to drive powerful, lasting learning and behavior change.
Build leaders that accelerate team performance and engagement.
Unlock performance potential at scale with AI-powered curated growth journeys.
Build resilience, well-being and agility to drive performance across your entire enterprise.
Transform your business, starting with your sales leaders.
Unlock business impact from the top with executive coaching.
Foster a culture of inclusion and belonging.
Accelerate the performance and potential of your agencies and employees.
See how innovative organizations use BetterUp to build a thriving workforce.
Discover how BetterUp measurably impacts key business outcomes for organizations like yours.
A demo is the first step to transforming your business. Meet with us to develop a plan for attaining your goals.

- What is coaching?
Learn how 1:1 coaching works, who its for, and if it's right for you.
Accelerate your personal and professional growth with the expert guidance of a BetterUp Coach.
Types of Coaching
Navigate career transitions, accelerate your professional growth, and achieve your career goals with expert coaching.
Enhance your communication skills for better personal and professional relationships, with tailored coaching that focuses on your needs.
Find balance, resilience, and well-being in all areas of your life with holistic coaching designed to empower you.
Discover your perfect match : Take our 5-minute assessment and let us pair you with one of our top Coaches tailored just for you.

Research, expert insights, and resources to develop courageous leaders within your organization.
Best practices, research, and tools to fuel individual and business growth.
View on-demand BetterUp events and learn about upcoming live discussions.
The latest insights and ideas for building a high-performing workplace.
- BetterUp Briefing
The online magazine that helps you understand tomorrow's workforce trends, today.
Innovative research featured in peer-reviewed journals, press, and more.
Founded in 2022 to deepen the understanding of the intersection of well-being, purpose, and performance
We're on a mission to help everyone live with clarity, purpose, and passion.
Join us and create impactful change.
Read the buzz about BetterUp.
Meet the leadership that's passionate about empowering your workforce.

For Business
For Individuals
Adjusting to the new normal: Is COVID-19 ever going to end?

Jump to section
What is the new normal?
What does the new normal look like.
4 impacts of the new normal
How are different generations responding to the new normal?
5 ways to adjust to the new normal
It’s almost two years since the start of the COVID-19 pandemic. Had you told me in March 2020 that COVID-19 would still be around in 2022, I’m not sure I would’ve believed you. But as we all know, living in the age of COVID-19 has become our “new normal.” In a recently released JAMA article, scientists say COVID-19 is here to stay . Much like the flu, it’s anticipated COVID-19 will be endemic.
So, what is the “new normal” as we head into 2022?
While everyone is unique, we all want to live safe, healthy, and fulfilling lives . The truth is we’re remaining flexible and learning as we go. We’re defining (and redefining) what the new normal looks like for our global society, each step of the way.
As you continue your journey to build mental fitness in the face of uncertainty , take these considerations into mind.
A new normal is a state where our global economy and society have settled since the onset of the COVID-19 pandemic. The new normal is evolving as our world adjusts to COVID-19.
We know we’re not going back to life as we know it in 2019. And that’s OK. According to Pew Research, 91% of Americans say coronavirus has changed their lives . As a global society, we’ve suffered grief, loss, and collective trauma . We’ve experienced lockdowns with massive impacts on the economy and jobs. We’re living with the impacts of the coronavirus pandemic on our mental health. We’re navigating uncertainty and the unknown. But we’re resilient. And with change comes opportunity . Together, we’re redefining what “the new normal” looks like for our world.
Every person is unique. There’s not necessarily a one-size-fits-all “new normal” for society. But when we think about our day-to-day lives, there’s a good chance you notice these themes.
Social interactions
If we’re being honest, social interactions could already be awkward pre-pandemic. But with the onset of the coronavirus pandemic, the new normal has brought on a new set of rules with social interactions. Let’s say you run into an old friend in the grocery store. You haven’t seen this friend in a couple of years. Do you go up and give them a hug? Do you pull down your mask so you’re easily recognizable in the store? Do you keep your distance and wave from six feet? One study looked at the impact of COVID-19 and face masks on our social interactions. Scientists found that we’re less likely to be able to read nonverbal body language , like facial expressions. This impedes our ability to evaluate emotions, which has a drastic impact on how we interact. Paired with social distancing, it impedes how we would typically communicate pre-pandemic.
We also know that people reported an increase in symptoms of anxiety since the onset of COVID-19. Anxiety and social interaction often go hand-in-hand. But people are adjusting to social interaction (and anxiety) in the "new normal." One way is through clear communication and boundary setting .
Let’s take the grocery store example. You might overthink whether or not to approach your old friend. You might approach your friend, but perhaps you feel anxious and on edge during the conversation. But what if you simply clearly asked, “What are your COVID boundaries? I’d love to catch up but want to respect your space.” It allows your friend to clearly communicate their boundaries. We’ll likely see an increase in clear communication and boundary setting (if you haven’t already) in our daily social interactions.
Workplace
Before the pandemic, only one in five workers worked remotely . Now, it’s reported that almost 71% of workers are remote. According to our data, workers want a hybrid workforce . They want a place where they have the flexibility to choose where they get their work done.
The new normal in the workplace is ever-evolving. But one thing is for certain: workers aren’t going back to “business as usual” in the physical office space. We see this shift from a binary remote vs. in-office to supporting a hybrid workforce . A workplace where workers are making decisions around how they’d like to spend their days, whether it’s in a home office or a corporate building.
This brings an onslaught of new normal additives to the future work environment . Take virtual meetings, like Zoom or Google Meet. It’s likely that most of your meetings are taking place in virtual rooms. If you’re a new employee, you might onboard to a new job — completely virtually. You might never meet a teammate face-to-face. It's possible you'll experience feelings of social isolation .
At BetterUp, we’ve built a new normal resource kit to help managers and employees transition to the new normal. In it, you’ll find ways to increase empathy and meet the needs of your employees. You’ll also learn how to lean into creativity, turn challenges into opportunities, and stay motivated. If you’re a manager, check out this custom-built new normal checklist specifically built for leaders.
Telehealth
Gone are the days where you had to make a doctor’s appointment in person. The coronavirus pandemic has brought on a new normal in the world of healthcare: telemedicine.
Pre-pandemic, it’s cited that telehealth only reached about 4% of the population . But since COVID-19, it’s seen exponential growth. In the height of 2020, some months reached as high as 4000% growth in telehealth appointments. Right now, more providers are providing patient care completely virtually.
And of all types of virtual appointments, mental health telehealth visits are the highest. Virtual appointments have increased convenience, flexibility , and accessibility for patients. In the world of public health, it seems like a no-brainer to keep telemedicine visits as an available option in the new normal.
4 impacts of the new normal
The new normal is already disrupting the way we live our lives . From always having an extra mask on hand to how we communicate with others, there’s already a lasting impact.
But beyond individual impacts, we’re also experiencing societal and global changes to the new normal as a result of COVID-19.

How (and where) we work
Work — and how we do it — has fundamentally changed since COVID-19. As mentioned, the shift to a hybrid and remote workforce has been a drastic one. We’re seeing more and more companies adjust their work environments to accommodate hybrid workers. Our research says hybrid work arrangements are increasing more rapidly than a return to a physical office .
Candidates aren’t just looking for the option to be remote. It’s now become a necessity. Job searches for remote jobs were reported to be up by 460% . LinkedIn reported a more than 3 50% rise in remote job listings on its platform.
With nearly 10 million open jobs (yet only 6 million people in the job search ), companies are battling for top talent. Employees have deeply examined their purpose in life as a result of the pandemic.
Belonging
Tagging along the shift to a hybrid workforce is something called the belonging tax . It’s the price workers pay for convenience, flexibility, and any semblance of gained work-life balance from remote or hybrid work. It can manifest in a decrease in that sense of innate belonging .
The impact of not having a physical presence in the office could mean employees’ social connections are suffering. Our above-mentioned data says hybrid and remote workers experience increased resilience , optimism, and productivity .
But it can come at a cost. Right now, employees are experiencing their lowest levels of belonging in their organizations since the pandemic began.
We also know social interactions in the workplace have changed since COVID-19. With more remote interactions, COVID-19 has created more isolation . We’ve found the impact on belonging is significant — especially in the workplace.
BetterUp Labs found employees who feel excluded experience a 25% loss in performance. Employees who do not feel they belong are also at a higher risk of turnover .
A renewed focus on the planet
What does COVID-19 have to do with sustainability? In short, a lot more than you might think. In the weeks and months of lockdowns around the globe, many examined their habits and way of life. A 2020 survey by Accenture showed this reflection on sustainability. In fact, 60% of respondents reported that they have been making more sustainable and environmentally friendly purchases since the start of the pandemic.
But beyond consumer habits, the COVID-19 crisis heightened climate crisis concerns globally. In a Boston Consulting Group Survey, the data backs this up. In fact, 70% of respondents said they were more aware now than before COVID-19 that human activity threatens the climate . The pandemic showed our world a sneak peek at what could come with the impacts of climate change. With climate change, we could see the same impacts of COVID-19 — but magnified. Limited resources, panic shopping, and disproportionate impacts on communities of color. Economic impacts — especially on frontline workers — will be a symptom of climate change.
We can also expect economic mobility (or lack thereof) to hinder people from under-resourced communities from re-locating to healthier areas. Because of that, we can expect health and well-being impacts, mostly on communities of color.
It also showed our world how connected we all truly are. This interconnectedness as a global community is rare. It’s not often that crises are experienced on such a grand scale.
But as we’ve learned from COVID-19, no one is immune to global crises. And like COVID-19, climate change is one to continue to battle as a global community.
Education and learning
COVID-19 has changed the education system forever. Much like remote work, remote learning was a quick pivot at the beginning of the pandemic that has since stuck around in this new normal of life.
In March 2021, as much as half of the entire world’s students were still affected by partial or full school closures . As new variants emerge, schools and children aren’t immune to the impact of COVID-19. As such, remote learning has become embedded into the new normal.
Paralleled to the way we work, the way we learn has evolved. Some schools are offering hybrid learning environments. Other schools still consider periods of remote learning and lockdown when cases spike.
There are certainly challenges with online learning. For example, it takes access to tools and resources — like laptops, WiFi, and physical space at home — for learning to take place.
But in the US, the “homework gap” is wide. About 35% of households with school-aged children (and an annual income below $30,000 a year) do not have a high-speed internet connection at home. This leaves a disproportionate impact on students from under-resourced communities, particularly Black and LatinX communities.
But online learning does have its benefits for those who do have access to the right tools and technology. Some research shows that students retain 25-60% more material with online learning . Online learning also requires less time to learn. Students can go at their own pace, accelerate or skip through topics they know well, or revisit topics where they need extra help.
Whether you prefer learning behind a screen or sitting in a physical classroom, online learning is sticking around.
The new normal and mental health
The new normal and mental health are inextricably linked. In August 2020, the Center for Disease Control and Prevention (CDC) reported the impact. About 40% of US adults were struggling with their mental health during the pandemic.

Our data also shows that US employees are sleeping less and worrying more . But if there’s a silver lining here, it’s that mental health has finally been a front-and-center conversation. And slowly, we’re chipping away at associated mental health stigma .
But that doesn’t mean the lasting impacts of mental health are going away. We know that COVID-19 PTSD is real. In fact, 32% of patients who have recovered from COVID-19 displayed symptoms of post-traumatic stress disorder (PTSD).
In July 2021, 40% of adults still reported symptoms of anxiety and depression. Increased loneliness, physical, and financial insecurity make providing access to adequate mental health care more important than ever.
As the impact of the pandemic on mental health continues, mental health professionals are feeling the impact. Psychologists recently reported a large increase in demand for anxiety and depression treatment .
While this demand is exposing cracks in the mental health system, it’s also showing us something else. People are speaking out and seeking help. If you or a loved one are struggling with caring for your mental health, reach out to a trained mental health care worker .
How different generations are responding to the new normal
It’s interesting to examine each generation’s response to the new normal . Let’s break them out.
- Baby boomers. They’re getting comfortable with technology — despite being the generation who is least fearful of COVID-19. Baby boomers are using technology like apps to order groceries. They're Zooming into their grandkids’ birthday parties and FaceTime-ing to stay connected .
- Gen X. As we may already have seen in the lateral moves or job changes , it’s predicted Gen X-ers are coming into this new normal with a renewed look on life. With only a few chapters left in their careers, many might be yearning for that sense of purpose .
- Millennials. Having weathered 2008 financial crisis and now the COVID-19 pandemic, it seems millennials are in search of stability. Similar to Gen X-ers, they are also looking for a purpose in their careers. They’ll continue to make eco-conscious and prosocial decisions that align with their values in their daily lives.
- Gen Z. Let’s start with this stat. Seventy-five percent of Gen Z-ers believe their generation will change the world . Gen Z-ers are in a deep search for purpose and impact. In fact, 70% of Gen Z-ers prefer doing something meaningful as opposed to making a lot of money. Gen Z is arguably going to emerge as the leader of the new normal. Their generation will build what we know to be the new normal.
5 ways to adjust to this new normal
Like any change, the new normal can take some getting used to. But it also takes intention, work, and self-awareness . Here are five ways you can adjust to the new normal.
Build mental fitness
Strong mental fitness and resiliency go hand-in-hand. With personalized coaching support, you can strengthen your mental fitness. At BetterUp, we believe human transformation is the key to thriving. To reach self-actualization , we all need some support along the way.
We took a look at those people who started out in a low state of well-being at the beginning of their personalized coaching journey. Our data shows 77% will significantly improve their well-being state by 3-4 months with personalized support .
When you’re mentally fit, you’re more innovative , productive, and resilient. You are better equipped to handle the peaks and valleys life throws at you.

Practice humility
If we’ve learned anything from the last couple of years, it’s that things change fast. As new data and science emerge about COVID-19 and the new normal, it may rattle what we know to be true. We learn — but it’s almost more important to unlearn .
As cited in the above-mentioned JAMA journal, it’s critical to practice humility. As human beings, we’re lifelong learners. Even the best-laid plans change. It’s important to be flexible, stay humble, and continue to better ourselves as best we can.
Invest in mental health
The impacts of the COVID-19 pandemic have shown our world how critical it is to care for your mental health . Invest in yourself. Seek support if you need it — and lean on your loved ones. Investing in your mental health pays dividends. From dealing with stress to coping with anxiety , it’s important to know you’re not alone.
Stay connected
We might’ve underestimated the value of social connections pre-pandemic. We know that in this new normal, it’s crucial to stay connected with those around you.
We’re human beings. We’re hardwired to connect with others. We crave that aspect of human connection, whether it’s a Friday night Zoom call with friends or a hike with a loved one.
If you’re a heavy social media user, it might be negatively impacting your ability to make meaningful connections. Consider ways you can swap out your time on an app and make connections in other ways.
Do Inner Work®
Looking inward has lasting impacts. In this new normal, it’s important to find ways to continue to do Inner Work® . It looks different for everyone — so personalize Inner Work® so it works for you. Here are some ideas to get started.
- Go on a hike
- Journal
- Volunteer with a local organization
- Practice self-reflection and introspection
- Practice self-care
- Practice meditation or prayer
Start adapting
Any kind of change can be hard. When it comes to the new normal, we know it might take some getting used to.
Take every day with small steps — and celebrate those small wins. Practice the Inner Work® to build strong mental fitness. Stay humble and flexible, two attributes critical to being a lifelong learner .
We can build and shape the new normal together. It starts with intention. It starts with you.
Build resilience for life's challenges
Develop the skills you need to tackle life's ups and downs with confidence. A BetterUp Coach can help you build resilience, set goals, and navigate change.
Madeline Miles
Madeline is a writer, communicator, and storyteller who is passionate about using words to help drive positive change. She holds a bachelor's in English Creative Writing and Communication Studies and lives in Denver, Colorado. In her spare time, she's usually somewhere outside (preferably in the mountains) — and enjoys poetry and fiction.
22 new wellness trends that should be on your radar
Stop feeling so anxious about your new job with these 12 tips, how to stop being jealous by cultivating self-love, radical acceptance—part 1: saying goodbye to the way of life we once knew, feeling lost: signs, causes, and 4 tips for finding your way, believe it or not, not everyone wants to work from home. here’s why., the future of work: how the pandemic changed the picture, what to do in retirement: finding purpose and fulfillment, the work-life balance questions to ask to get yours on the right track, similar articles, what is environmental health and why is it important, post-covid depression: the unknown side effects of the pandemic, supporting frontline employees must be the new normal, millennials and burnout: a guide to finding a way out at any stage, how has belonging changed since covid-19, how remote work will redefine future careers, according to gen z, did covid-19 change us for better or for worse, stay connected with betterup, get our newsletter, event invites, plus product insights and research..
3100 E 5th Street, Suite 350 Austin, TX 78702
- Platform Overview
- Integrations
- Powered by AI
- BetterUp Lead™
- BetterUp Manage™
- BetterUp Care®
- Sales Performance
- Diversity & Inclusion
- Case Studies
- Why BetterUp?
- About Coaching
- Find your Coach
- Career Coaching
- Communication Coaching
- Life Coaching
- News and Press
- Leadership Team
- Become a BetterUp Coach
- BetterUp Labs
- Center for Purpose & Performance
- Leadership Training
- Business Coaching
- Contact Support
- Contact Sales
- Privacy Policy
- Acceptable Use Policy
- Trust & Security
- Cookie Preferences

What Students Are Teaching the Rest of Us about the New Normal
With the COVID-19 pandemic taking a toll on students, personally and academically, many of them are modeling how to respond to the new normal.

So many of us in higher education, and across the world, are exhausted, frustrated, and anxious. Two years ago, everything started to shut down—initially for only two weeks, maybe three—so that we could "bend the curve" to get the COVID-19 pandemic under control and return to normal life.
In those first weeks, which became months, we learned that technology could enable virtual learning in many remarkable ways. But even with all this technology, students still struggled to make real connections with their professors and with each other. And everywhere, all the time, was the risk that the coronavirus was out there, ready to get you if you were not careful or if you were just unlucky. Now, even with vaccines, COVID-19 surges continue as we enter year three.
On another level, however, something interesting is happening in higher education. With the COVID-19 pandemic also taking a toll on students, personally and academically, many of them are modeling, for the rest of us, how to respond to the new normal. In the last week of my class in December 2021, I asked 110 undergraduates:
"How would you say the COVID-19 pandemic has changed you as a student and as a person?"
Mixed Responses
Students stated a variety of ways in which they had matured during the pandemic. Many offered some version of "I've learned how to manage stress and independence." They reported becoming much better at learning independently and developing important life skills. They noted that they are now more aware of the impact of their actions on other people and that they have new appreciation for friends, family, school, and being in nature.
Other students were much less positive. Academically, they reported: "Online learning is really hard—and I am not good at it." They're delighted to be on campus and in person, but they also had to adjust to going back to the classroom. Some students replied more personally: "I'm anxious and sad." "I'm pessimistic and cynical." "I'm burned out." "I'm stressed out." "I have new and worse mental health issues."
Still other students offered a mixed response. Several said something like: "I am a better person but a worse student." Although they considered themselves to be sophisticated social media users, they know that they spend too much time with it. One insightful student reflected that the impact of the pandemic on students was "huge and may not be fully understood for years."
How are students managing all this? Overall, students are coping with their exhaustion, frustration, and anxiety in some healthy ways: through self-care, openness, and empathy.
Students are making a deliberate choice for self-care. For many students, "self-care" may have been considered an indulgent luxury before the pandemic. They heard people telling them: "You should be in school full-time and doing an internship and working at a job and conducting research and volunteering and and and. . . . If you are resting, if you are not interested, don't worry, there is always someone else, ready to work harder, work faster, get ahead. They will win and you will lose—so you better keep going."
But students seem to have made a conscious decision that go-go-go is no longer the only route. Students are saying "no" to things—things that are not essential or not rewarding, things that might advance their careers but not their lives. Students are focusing on healthier relationships, nutrition and exercise, and positive attitudes. Some of my students, for example, began taking—or teaching—Zoom yoga classes. Others incorporated long walks in green spaces into their busy schedules.
Flowing from self-care, students are now being more open with their instructors. They'll say: "I didn't have time to do the assignment"—offering no excuses or apologies (or drama) and willing to accept any consequences. They speak candidly about their own health. "I didn't come to class with my cough. I didn't want to put anyone at risk." Or: "I got tested. It's strep, not Covid." In response, instructors don't need doctors' notes: we are more trusting, with bonds forged from our common threats and from our students' trust in us.
Students are increasingly open about their mental health as well. Sometimes this goes back to self-care: "I just needed a day off." Other times students offer unapologetic candor about specific mental health diagnoses—information that instructors don't need and that students might once have thought carried real stigma. "I am being treated for anxiety"—or depression or ADHD or bipolar disorder. "I'm a recovering alcoholic and drug addict." "My therapist said . . ."
Students are also more open about other parts of their lives: "My dad lost his job." "I came out to my Mom." "My boyfriend dumped me," "I'm failing chemistry." Expecting no judgment or special treatment, they simply think it's now normal to share.
Finally, students are responding to the new normal with empathy. Instead of scrutinizing the decisions of others—especially on social media—they accept each other's decisions more generously and with support. Students know that there is a lot they don't know about each other: lives, backgrounds, struggles. Students may not understand Alex's priorities or Sasha's choices, and that's okay. Let Alex be Alex and let Sasha be Sasha.
We can't know whether these lessons will last beyond the pandemic. The next cadre of college and university students—struggling today through their own middle and high school journeys—will have been through pandemic-era online learning at a much younger age. But for now, all of us working in higher education can learn from how students are responding to the new normal with self-care, openness, and empathy.
Jim Quirk teaches in the School of Public Affairs at American University in Washington, DC.
© 2022 Jim Quirk. The text of this work is licensed under a Creative Commons BY-NC-ND 4.0 International License.
- Find a Doctor
- Our Services
- More at NYP.org

How to Adjust to the ‘New Normal’
As millions face changes brought on by the pandemic and social distancing, an expert offers tips to cope..
Save this to read later.

With most of the country nearing two months of sheltering in place, many of us have suddenly been forced to adjust to a ‘new normal’: parents home-schooling their children, families or roommates suddenly isolating in cramped quarters, donning a mask when leaving the house, and wiping down groceries after a stress-filled visit to the store.
While the changes have been jarring, it’s important to remember the big picture.
“The world is facing a pandemic and in many places across the world, people are following similar lockdowns, shutdowns, or social distancing,” says Dr. Robert Leahy , an attending psychologist at NewYork-Presbyterian/Weill Cornell Medical Center and the author of The Worry Cure . “We have to look at this by putting in perspective that to win the war against COVID-19 we need to make sacrifices and develop a coping mindset.”
Dr. Leahy, a national expert in cognitive therapy, shares his advice on how to cope with the challenges of so much change at once, and how to view the situation through a lens of acceptance.
Give yourself a break
One of the most important things you can do is accept that a new reality should come with a different level of expectations. For example, you’re not going to perfectly juggle remote work with home schooling and child care. “Lower your standards so much that if you fall down, it’s a step up,” says Dr. Leahy. “It’s like if you used to be able to run a 7-minute mile, and now someone tells you to strap a 50-pound bag over your shoulders and do the same thing, it’s going to take you an hour and a half.”
If your children are making noise or interrupting, or you are having trouble staying on top of everything and focusing, normalize that. “You can say to yourself, ‘That is what I would expect right now when I am trying to multitask everything without outside help and during a pandemic,’” says Dr. Leahy. “Anticipate the noise and the interruptions and remind yourself they are not such terrible things, but simply inconveniences.”
For those frustrated by the new limitations on everyday life during quarantine and the ‘new normal’, Dr. Leahy also suggests resetting expectations and identifying what you can do rather than focusing on what you can’t. “A lot of frustration comes from inflexible expectations. We may have an expectation that we should be able to do everything we did before, and as long as we hold on to that expectation, we are going to be frustrated,” says Dr. Leahy.
Consider other things in your life that you expected or hoped for but didn’t pan out, and you survived. “Change the expectation to match reality, realizing it’s not catastrophic,” says Dr. Leahy. “Early Americans from hundreds of years ago wouldn’t even understand the concepts behind some of the luxuries we might miss right now. We are fortunate to even have the things we miss, and maybe we’ll appreciate them even more when they return.”
Be kind and practice acceptance
When hunkered down in close quarters with a lot of stress , Dr. Leahy recommends a “protocol of politeness,” particularly when it comes to your partner or significant other. This is not the time to air every frustration. “Treat your partner like a total stranger you want to please,” he says. “Try to be thoughtful, polite, compassionate, and rewarding. A compliment and a ‘thank you’ can go a long way.”
Being more accepting of family members will help you keep peace in the home, but it’s just as important to accept your situation and the ‘new normal’ as a whole. This doesn’t mean resignation, but rather a realistic observation and a coping mindset, according to Dr. Leahy. “If you’re in northern New England in the middle of winter and it’s 20 degrees outside, you have to accept that. It wouldn’t make sense to say, it shouldn’t be this way, it’s terrible. Accepting the situation is recognizing reality and putting on a warm coat or going back inside.”
People can recognize that it is simply not possible to be on top of everything right now — but they can work to accept the ‘new normal’ as it is and cope as necessary. “Methods of coping can be problem-solving, sharing things, cheering people on, learning from the experience, reevaluating priorities, and reflecting on how people coped with far worse in the past,” says Dr. Leahy. “Resilient people reevaluate their expectations and then focus on new goals.”
Dr. Leahy’s Ingredients for a Coping Mindset
- Adjust your expectations
- Don’t view everything that you had as essential
- Focus on what you can do, not what you cannot do
- Go on a politeness binge
- Think of this as a chapter in the book you are writing
View life as a narrative
Dr. Leahy suggests looking at life as a series of chapters in a book, which can provide a sense of control and agency in what can feel like a helpless situation. “If you look at life as a series of chapters, this chapter is objectively a hard one. But we can adjust our expectations and write a story about how we cope with this chapter to make it as good as it can be,” he says.
Chapters also have an end, which can help you from feeling engulfed in the moment. “This isn’t the chapter we’ll always be in, and not all chapters have to be wonderful,” he says.
We can even view this chapter as a test or philosophy seminar. “Imagine a supreme being we’ll call ‘Chaos and Uncertainty,’ who decided to throw us some really strange stuff right now,” he says with a laugh. “How will we cope? What will we miss and what do we value?”
Each day you can decide to make positive choices, reflect on your values, and cheer on the front-line heroes. “The chapter is up to you,” says Dr. Leahy.
Robert Leahy, Ph.D., is an attending psychologist at NewYork-Presbyterian/Weill Cornell Medical Center and a clinical professor of psychology in psychiatry at Weill Cornell Medicine. He is the director of the American Institute for Cognitive Therapy NYC.
At A Glance
Featured expert.
Psychiatry, Psychology
Consult an Expert
Find a Doctor or call 877-697-9355
Share This Story
Get the latest health and wellness news.
Keep in touch with NewYork-Presbyterian and subscribe to our newsletter.
- Privacy Notice
BRIEF RESEARCH REPORT article
Adjustment to a “new normal:” coping flexibility and mental health issues during the covid-19 pandemic.

- 1 Department of Psychology, The University of Hong Kong, Hong Kong, China
- 2 Department of Psychology, The University of Oslo, Oslo, Norway
- 3 Modum Bad Psychiatric Hospital, Vikersund, Norway
The Coronavirus Disease 2019 (COVID-19) pandemic is an unprecedented health crisis in terms of the scope of its impact on well-being. The sudden need to navigate this “new normal” has compromised the mental health of many people. Coping flexibility, defined as the astute deployment of coping strategies to meet specific situational demands, is proposed as an adaptive quality during this period of upheaval. The present study investigated the associations between coping flexibility and two common mental health problems: COVID-19 anxiety and depression. The respondents were 481 Hong Kong adults (41% men; mean age = 45.09) who took part in a population-based telephone survey conducted from April to May 2020. Self-report data were assessed with the Coping Flexibility Interview Schedule, COVID-19-Related Perception and Anxiety Scale, and Center for Epidemiological Studies Depression Scale. Slightly more than half (52%) of the sample met the criteria for probable depression. Four types of COVID-19 anxiety were identified: anxiety over personal health, others' reactions, societal health, and economic problems. The results consistently revealed coping flexibility to be inversely associated with depression and all four types of COVID-19 anxiety. More importantly, there was a significant interaction between perceived likelihood of COVID-19 infection and coping flexibility on COVID-19 anxiety over personal health. These findings shed light on the beneficial role of coping flexibility in adjusting to the “new normal” amid the COVID-19 pandemic.
Introduction
The emergence of an atypical coronavirus, SARS-CoV-2, instigated a global outbreak of Coronavirus Disease 2019 [COVID-19; e.g., ( 1 )]. Following identification of the earliest cases of COVID-19 in December 2019, the World Health Organization ( 2 ) declared the viral outbreak a health emergency of international concern on January 30, 2020, and then a global pandemic <2 months later. The escalating pandemic has induced anxiety and panic reactions in the general public, and the emotional responses bear some resemblance to those observed amid the severe acute respiratory syndrome (SARS) outbreak in 2003 [e.g., ( 3 , 4 )]. For instance, the panic sell-off of stocks led to a plunge in the global stock market ( 5 ), and long lines for food and the irrational stockpiling of personal protection equipment such as facemasks and hand sanitizers have been widely seen ( 6 , 7 ).
Despite such resemblances, the COVID-19 pandemic is an unprecedented crisis in terms of the scope of its influence on both physical and mental health [e.g., ( 8 , 9 )]. To curb the transmission of this hitherto unknown virus, governments all over the world have enforced strict epidemic-control measures such as nationwide school closures, stay-at-home orders, and physical distancing regulations in public areas ( 10 ). Also, myriad public and private organizations have adopted teleworking policies mandating that their employees work from home ( 11 ). Although employees hold generally favorable attitudes toward home-based teleworking, the sudden drastic change in work mode left many unprepared ( 12 ). Previous research on the office-home transition has revealed major changes in the work environment to induce the most stress and anxiety in employees who feel the least prepared for this alternative work mode ( 13 ). Devastating problems arising from stressful life changes have been documented not only in adults but also in youngsters, with recent studies revealing a significant proportion of children and adolescents to have experienced psychological distress during the school-closure period ( 14 , 15 ). The COVID-19 pandemic has confronted people of all ages with fundamental life changes [e.g., ( 16 , 17 )].
To grapple with the “new normal” and deal with the considerable challenges brought about by the pandemic, individuals need a considerable degree of flexibility. Psychological resilience is a widely recognized mechanism underlying the adjustment process, with coping flexibility a core component [e.g., ( 18 )]. The theory of coping flexibility postulates that effective coping entails (a) sensitivity to the diverse situational demands embedded in an ever-changing environment and (b) variability in deploying coping strategies to meet specific demands ( 19 ). More specifically, psychological adjustment is a function of the extent to which individuals deploy problem-focused coping strategies (e.g., direct action) in controllable stressful situations and emotion-focused coping strategies (e.g., distraction) in uncontrollable ones. Inflexible coping, in contrast, has been linked to psychological symptoms. For example, individuals with heightened anxiety levels are characterized by an illusion of control [e.g., ( 20 , 21 )]. They tend to perceive all events in life as being under their control, and thus predominantly opt for problem-focused coping regardless of the situational characteristics. In contrast, individuals with depression are characterized by a sense of learned helplessness [e.g., ( 22 , 23 )]. They tend to view all events as beyond their control, and thus predominantly deploy emotion-focused coping across stressful events. Coping flexibility has been identified to foster adjustment to stressful life changes, which is indicated by a reduction in symptoms of anxiety and depression commonly experienced in stressful life transitions ( 24 ).
Applying these theories and findings to psychological adjustment during the COVID-19 pandemic, individuals higher in coping flexibility are predicted to experience lower levels of anxiety and depression than those lower in coping flexibility. Clinical trial findings on COVID-19 offer a mixture of promise and disappointment regarding the efficacy of SARS-CoV-2 vaccine candidates [e.g., ( 25 )], and the absence of a thorough understanding of the etiology and treatment of this atypical virus has elicited widespread public panic responses. According to the theory of psychological entropy ( 26 ), uncertainty is a crucial antecedent of anxiety. In accordance with that theory, studies conducted during the pandemic have revealed unusually high prevalence rates of mental health problems such as anxiety and depression, rates ~3-fold higher than both their pre-pandemic prevalence and lifetime prevalence over the past two decades ( 27 , 28 ).
In light of the transactional theory of stress and coping that highlights the importance of primary and secondary appraisals in the coping process ( 29 ), coping flexibility (secondary appraisal) is predicted to explain the association between context-specific health beliefs (primary appraisal) and mental health. Instead of perceiving the COVID-19 pandemic as aversive and uncontrollable, resilient copers tend to espouse a more complex view by recognizing both controllable and uncontrollable aspects of the pandemic. For instance, these individuals tend to take such positive actions as acquiring new information technology and digital skills to meet the demands of home-based teleworking, but engage in meditation to cope with the unpleasant emotions brought about by mandatory stay-at-home orders. Accordingly, coping flexibility is hypothesized to be inversely associated with anxiety and depression during the pandemic.
As individuals high in coping flexibility are characterized by cognitive astuteness in making distinctions in an array of stressful events ( 30 , 31 ), coping flexibility is also predicted to interact with context-specific health beliefs to have a conjoint influence on mental health in the pandemic context. Although COVID-19 shares similar characteristics with other atypical coronaviruses of SARS and Middle East respiratory syndrome (MERS), the case fatality rate of COVID-19 is much lower than the others ( 32 ). Among individuals high in coping flexibility, those who tend to perceive such differences may experience lower COVID-19 anxiety than their counterparts who do not hold this perception. In this respect, mental health experienced during the pandemic is a function of both context-specific health beliefs and coping flexibility.
The present study was conducted during the “second wave” of COVID-19 infections in Hong Kong. Although the first confirmed COVID-19 case was identified on January 23, 2020, with the first death recorded 2 weeks later ( 33 ), Hong Kong remained largely unscathed by the first wave, with only sporadic cases reported and a relatively flat epidemic curve (i.e., fewer than 100 confirmed cases). However, there was a sudden surge in confirmed cases in March, when the viral outbreak swept the globe ( 34 ). The Government of the Hong Kong Special Administrative Region (HKSAR) responded to the health emergency by enacting a travel ban on non-residents, issuing compulsory quarantine orders for residents returning from overseas, and tightening various physical distancing measures in late March and early April [e.g., ( 35 , 36 )]. Special work arrangements for government employees were also implemented, and many organizations followed suit. The psychosocial impact was thus so pervasive that all sectors of society were affected. A population-based survey was therefore deemed the most appropriate method for investigating the psychological reactions to the pandemic among residents of Hong Kong. The method yields heterogeneous community samples, which maximizes representativeness and minimizes sampling errors.
Materials and Methods
Sample size determination and power analysis.
The statistical power analysis showed that the minimum sample size was 276 in order to identify statistically significant associations among the study variables, but a larger sample size was recruited to meet the requirements for conducting principal component analysis (PCA). Considering the general rule of thumb of having at least 50 cases per factor and a maximum number of nine factors to be identified in the PCA, the pre-planned minimum sample size was 450.
Participants and Procedures
The respondents were 481 Hong Kong adults (41% men; mean age = 45.09, SD = 23.42), who were recruited from a population-based telephone survey conducted by a survey research center at the first author's university. Random digit dialing was used for identifying eligible households, and then the most recent birth day method was employed to select a household member. To be eligible for participation, respondents had to be aged 18 or older, a resident of Hong Kong, able to understand Cantonese, and willing to give consent. Participation was voluntary, and all respondents who completed the survey were entered into a lucky draw for a chance to win gift certificates worth 500 Hong Kong dollars (about 65 U.S. dollars).
Trained interviewers conducted the telephone interviews using a structured questionnaire with standard questions. To foster interviewer calibration and minimize measurement bias, the survey was piloted in a small group of respondents from April 2 to 10, 2020. The final set of survey questions was amended to enhance the clarity of a few items, and then the full survey was administered from April 20 to May 19, 2020.
The study was conducted according to the ethical research standards of the American Psychological Association, and the study protocol was reviewed and approved by the human research ethics committee of the first author's university before the survey began (approval number: EA1912046 dated March 4, 2020). All respondents gave verbal consent in accordance with the Declaration of Helsinki.
Instruments
Coping flexibility.
Coping flexibility was assessed by the revised Coping Flexibility Interview Schedule ( 37 ). This interview schedule was originally developed based on clinical samples ( 38 ), and was adjusted for use with heterogeneous non-clinical populations. In the pilot phase, some respondents reported difficulty in understanding the terms of primary and secondary approach coping that was currently used in our interview schedule. The interview questions were revised by combining the terms of primary and secondary approach coping into problem-focused coping and converting the term of avoidant coping style into emotion-focused coping. Problem-focused and emotion-focused coping were originally used in the transactional theory of coping ( 39 ) from which the Coping Flexibility Interview Schedule was derived. The respondents were asked to report their deployment of problem-focused (e.g., information seeking, monitoring) and emotion-focused (e.g., acceptance, relaxation) coping in controllable and uncontrollable stressful situations over the past month.
To obtain a composite score of coping flexibility indicating strategy-situation fit, the individual coping items were subsequently coded by two independent raters according to a coding scheme ( 40 , 41 ) based on coping theories ( 39 , 42 ). One point was given to the deployment of problem-focused coping strategies to handle controllable stressful events and/or the deployment of emotion-focused coping strategies to handle uncontrollable stressful events. Zero points were given otherwise. All of these scores were aggregated, and then averaged to obtain a composite score. Inter-rater agreement was evaluated using Krippendorff alpha coefficients ( 43 ), and the results showed no discrepancies because no subjective codings were required (Krippendorff alpha = 100%).

COVID-19-Related Perceptions
Both perceived likelihood and impact of COVID-19 infection were measured by a modified measure developed and validated during the SARS outbreak ( 44 ). To make this measure relevant to the present pandemic context, the context was altered from “SARS outbreak” to “COVID-19 pandemic.” Respondents gave four-point ratings to indicate their perception of the likelihood of contracting COVID-19 (1 = very unlikely , 4 = very likely ) and the impact of having it (1 = no impact at all , 4 = a large impact ). The measure has been found to display both criterion and predictive validity ( 44 , 45 ).
COVID-19 Anxiety
As the events that have occurred during the COVID-19 pandemic are unprecedented, our team conducted a qualitative study in March 2020 asking participants to list all of the issues that had made them feel anxious during the pandemic. Content analysis of the results revealed 16 distinct themes regarding anxiety-provoking issues experienced amid the pandemic (see Table 1 for details). These items were compiled into a context-specific measure for assessing COVID-19 anxiety. Respondents rated each item on a scale ranging from 1 ( not worried at all ) to 4 ( very worried ).
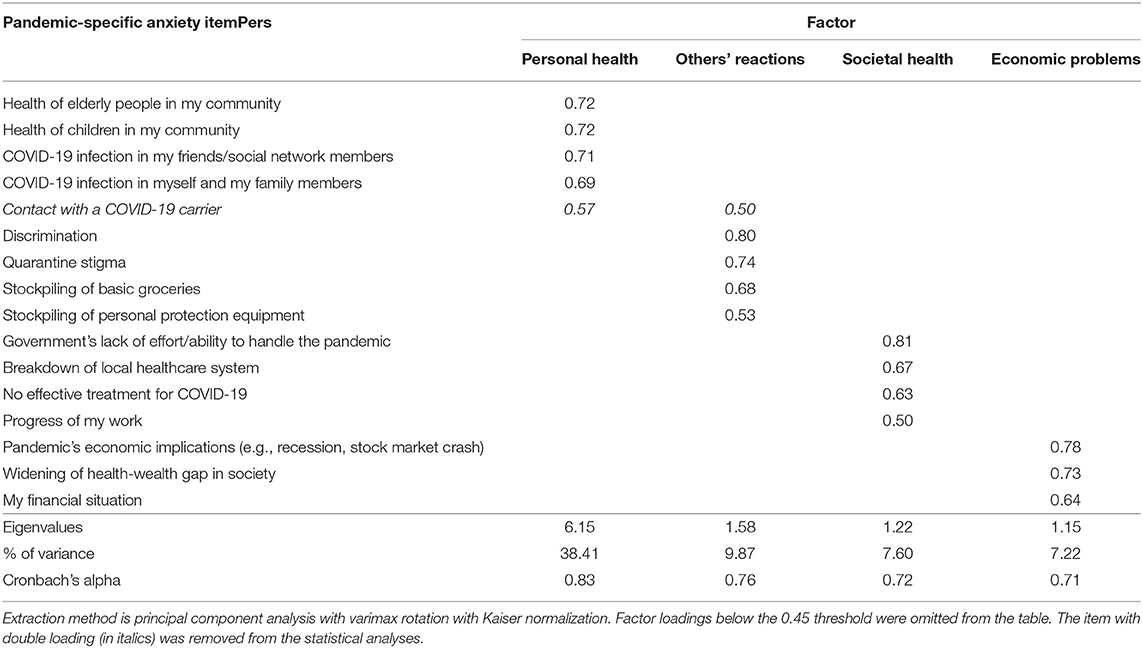
Table 1 . Four-factor promax-rotated factor solution for COVID-19 anxiety ( n = 481).
Depression was measured by the short form of the Center for Epidemiological Studies Depression Scale ( 46 ), which contains 10 items. The translated Chinese version was used in this study ( 47 ). Respondents rated each item on a four-point scale (0 = rarely or none of the time , 3 = most or all of the time ). In this study, we applied the recommended cut-off score of 10 as the classification scheme [e.g., ( 46 , 48 )].
Statistical Analysis
All statistical procedures were conducted using SPSS version 26.0 for Windows (IBM Corporation, 2019, Armonk, NY). Before hypothesis testing, PCA was performed to identify the factorial structure underlying the 16 anxiety-provoking issues. The components were rotated using the varimax method with Kaiser normalization to increase the interpretability of the findings. The number of factors extracted was determined by the Kaiser rule, with factors retained when the eigenvalue exceeded one. The total amount of variance accounted for by the factors needed to exceed 60%, a minimum criterion for factor selection widely adopted in PCA research ( 49 ). Both the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett's test of sphericity were first examined to check the appropriateness for analyzing the dataset, with appropriateness indicated if the KMO index was >0.50 and the test of sphericity was significant. For PCA, items with a factor loading <0.45 or double loading were removed. Cronbach alpha was used to indicate internal consistency for the items within each factor, with an alpha >0.70 considered adequate.
The potential differences among demographic groups were examined. Differences in sex were detected using an independent-samples t -test, and age differences using Pearson zero-order correlation analysis. In addition to testing age as a continuous variable, we also adopted a generational approach proposed by the Pew Research Center that makes comparisons across four age cohorts: (a) Millennials, who were born in 1981 or after; (b) Generation X-ers, who were born between 1965 and 1980; (c) Baby Boomers, who were born between 1946 and 1964; and (d) Silent Gen'ers, who were born before 1946 ( 50 ). A general linear model (GLM) was employed to investigate the differences among the four generations, with post hoc Bonferroni tests conducted if generational differences were found in any of the study variables.
Pearson zero-order correlation analysis was conducted to obtain an overview of the inter-relationships among the study variables. The hypothesized beneficial role of coping flexibility on mental health was then tested using three-step hierarchical regression analysis. First, the two demographic variables (i.e., sex and age) were entered to control for their potential effects on the criterion in question. Second, the variables of perceived likelihood of COVID-19 infection, perceived impact of COVID-19 infection, and coping flexibility were entered simultaneously. Third, the Perceived Likelihood of COVID-19 Infection × Coping Flexibility interaction and the Perceived Impact of COVID-19 Infection × Coping Flexibility interaction were entered. To address the potential multicollinearity problem, all of the variables were centered before conducting these analyses. The procedures were identical for each mental health problem included as the criterion variable. To unpack significant interaction effects, post hoc simple effects analysis was employed to examine the effects of COVID-19-related perception on a criterion at each level of coping flexibility.
PCA was performed because the KMO index was high (.87) and Bartlett's test of sphericity was significant (χ 2 = 3379.31, p < 0.0001). The results with the principal component weights of the 16 anxiety-provoking issues are presented in Table 1 . A four-factor solution was yielded, accounting for 63% of the total variance, with 38% explained by the first factor, personal health issues (e.g., “ COVID-19 infection in myself and my family members ”); 10% by the second factor, other people's undesirable reactions (e.g., “ discrimination ”); 8% by the third factor, societal health issues (e.g., “ government's lack of effort/ability to handle the pandemic ”); and 7% by the fourth factor, economic problems (e.g., “ pandemic's economic implications ”). It is noteworthy that one item (i.e., “ contact with a COVID-19 carrier ”) had a double loading with a difference of <0.10, and was thus discarded. All four factors displayed internal consistency (Cronbach alphas > 0.70), and were thus included in the subsequent analyses as indicators of COVID-19 anxiety.
The GLM results revealed a significant cross-generational difference only for anxiety over societal health, F (3, 477) = 33.92, p < 0.0001, partial eta squared = 0.18. Post hoc Bonferroni tests indicated that Silent Gen'ers aged over 74 ( M = 2.02, SD = 0.62) reported significantly less anxiety over societal health than did Millennials aged 18–39 ( M = 2.87, SD = 0.66) or Generation X-ers aged 40–55 ( M = 2.71, SD = 0.68), p s < 0.0001. However, there were no other differences regarding sex, generation, or the Sex × Generation interaction, p s > 0.05.
The descriptive statistics of and inter-relationships among the study variables are presented in Table 2 . The average depression score was 9.85, which was very close to the cut-off score for probable depression. Adopting the standard cut-off criterion of 10, slightly more than half (52%) of the respondents were categorized as having probable depression. The probable depression group ( M = 2.67, SD = 0.75) generally experienced a higher anxiety level over societal health issues than the no depression group ( M = 2.48, SD = 0.73), t = 2.72, p = 0.007. In addition, the probable depression group ( M = 0.50, SD = 0.21) also reported a generally lower degree of coping flexibility than the no depression group ( M = 0.58, SD = 0.21), t (479) = −3.95, p < 0.0001. However, no other significant differences in depression level were found for sex or generation, p s > 0.21.
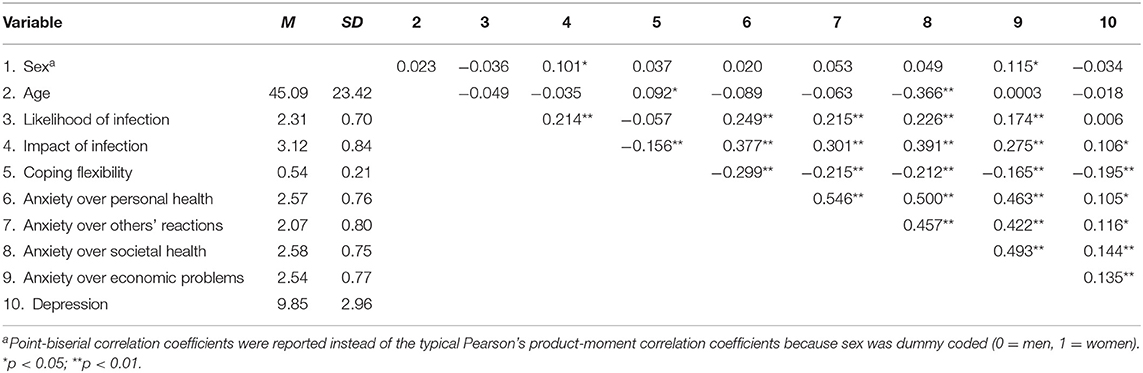
Table 2 . Descriptive statistics of study variables ( n = 481).
Table 3 summarizes the results of hierarchical regression analysis for various mental health problems. As shown in the table, the pattern of results was highly consistent across the four types of COVID-19 anxiety; that is, all four types were positively associated with both the perceived likelihood and impact of COVID-19 infection and inversely associated with coping flexibility. There was also a significant interaction between perceived likelihood of COVID-19 infection and coping flexibility, and the results are presented in Figure 1 . For individuals higher in coping flexibility, those who perceived a lower likelihood of contracting COVID-19 reported less anxiety over their own health than their counterparts who perceived a greater likelihood of such contraction. For individuals lower in coping flexibility, however, such individual differences were absent and they generally reported greater anxiety over their own health than those higher in coping flexibility. In addition, the results revealed depression to also be inversely associated with coping flexibility, although its associations with the two types of COVID-19-related perception were non-significant. In short, these findings provide support for the hypothesized beneficial role of coping flexibility in dealing with mental health issues experienced during the COVID-19 pandemic.
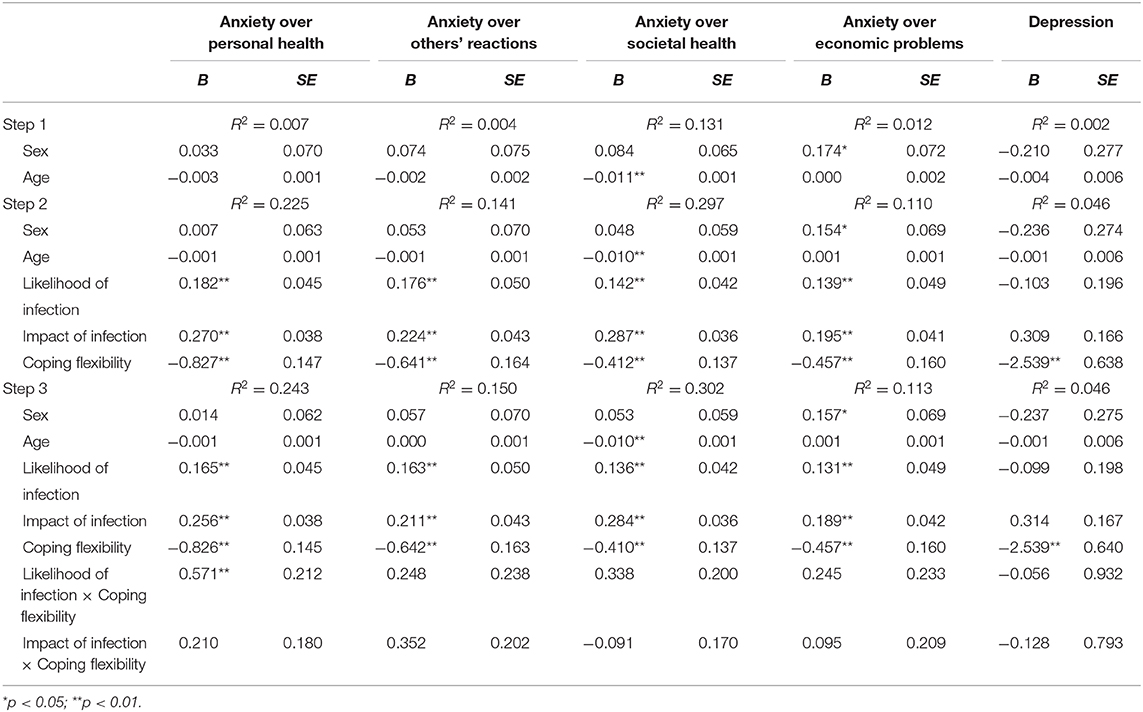
Table 3 . Summary of hierarchical regression analysis by mental health problems ( n = 481).
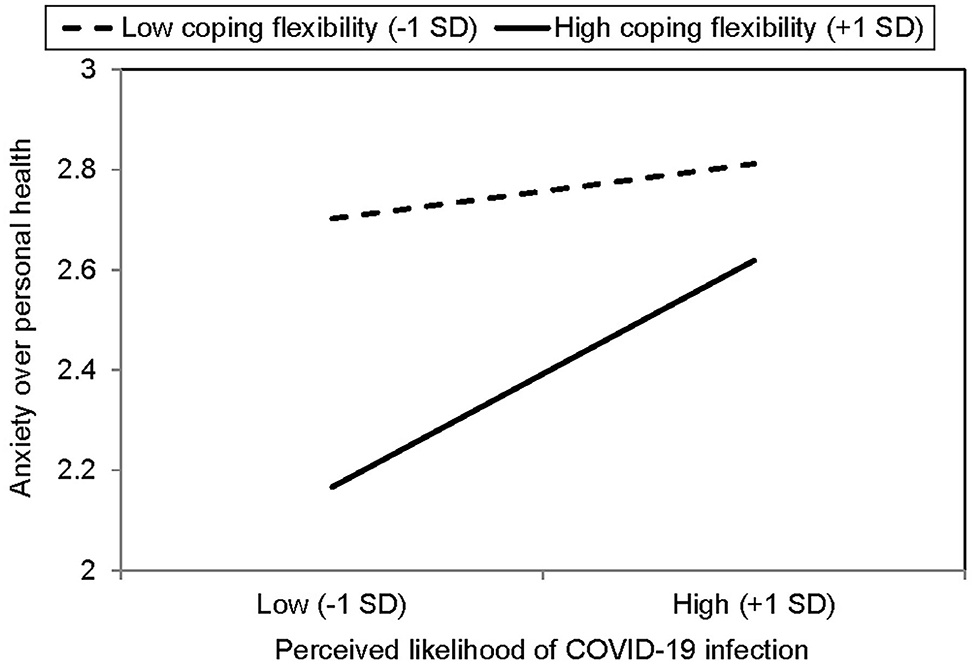
Figure 1 . Simple effects analysis for significant interaction between perceived likelihood of COVID-19 infection and coping flexibility ( n = 481).
In addition to evaluating strategy-situation fit using composite coping flexibility scores, nuanced analysis was conducted to further examine the deployment of individual coping strategies and their associations with mental health problems. Most of the respondents (61%) reported deploying problem-focused coping to handle controllable stressful events during the pandemic, whereas just under half (45%) reported deploying that strategy to deal with uncontrollable stressful events. Fewer respondents said they had used emotion-focused coping to deal with controllable and uncontrollable stressful events (39 and 37%, respectively). Moreover, the deployment of problem-focused coping in controllable stressful events was inversely associated with anxiety over personal health and others' reactions, p s <0.0001, whereas the deployment of emotion-focused coping in controllable stressful events was positively associated with all four types of COVID-19 anxiety and depression, p s < 0.0001. However, neither problem-focused nor emotion-focused coping deployed in uncontrollable stressful events were significantly associated with any of the mental health problems, p s > 0.14.
The present study has investigated coping responses and mental health issues among the general public in Hong Kong amid the second wave of the COVID-19 pandemic. Recent studies have identified high prevalence rates of anxiety and depression among residents of COVID-19-affected regions all over the world [e.g., ( 28 , 51 )]. Our study expands this growing body of research by specifying four major factors of COVID-19 anxiety: personal health, others' reactions, societal health, and economic problems. Although the third factor is characterized primarily by societal health issues, it is interesting to note that a seemingly unrelated item “ progress of my work ” also loaded onto this factor. This perplexing finding may reflect the fact that employees' work progress has been affected more by societal factors (e.g., implementation of prevention and control disease regulations for business and premises, home-based teleworking policy) than personal factors during the pandemic.
A similar phenomenon is found for the fourth factor, economic problems. Most of the items loading onto it involved broad societal issues (e.g., economic recession, widening of health-wealth gap), but an item related to personal financial problems also did so. This finding similarly indicates that individuals' personal financial condition during the pandemic may be influenced to a great extent by the wider economy. Taken together, these interesting findings reflect the intricate interactions between the individual and society in times of crisis, thus attesting to the necessity of identifying anxiety-provoking issues specific to the pandemic in addition to assessing generic mental health issues that are context-free.
In addition to anxiety, our findings also show depression to have been prevalent among Hong Kong adults during the second wave of the pandemic, with slightly more than half the sample identified as having probable depression. Compared with respondents without depression, those with probable depression tended to experience greater anxiety related to societal health issues but not economic problems or personal health issues. These findings indicate that the unusually high prevalence of depression reported during the pandemic is largely related to health-related problems at the societal level (e.g., governmental actions to combat COVID-19, possible breakdown of local healthcare system) rather than personal health issues.
More importantly, the present study is the first to apply the theory of coping flexibility to the context of the COVID-19 pandemic, and the findings provide support for the hypothesized beneficial role of coping flexibility in relieving heightened anxiety and depression when handling the vicissitudes emerged during the pandemic. Astute strategy deployment to meet the specific demands of an ever-changing environment is essential for adjustment to the “new normal,” and a better strategy-situation fit is found to be inversely associated with both COVID-19 anxiety and depression. It is noteworthy that coping flexibility interacts with perceived susceptibility to COVID-19 infection to have a conjoint influence on COVID-19 anxiety. Even within individuals having a higher level of coping flexibility, those tend to experience fewer symptoms of COVID-19 anxiety over personal health if they display cognitive astuteness in assessing their possibility of contracting COVID-19. These novel findings provide support for the notion that the anxiety-buffering role of coping flexibility is highly context-specific ( 24 ), which is confined to infection susceptibility and anxiety over personal health in this stressful encounter. Such context-specificity is not surprising because subjective appraisals of the possibility of contracting a novel virus should be directly linked with concerns over personal health rather than other anxiety-provoking events related to non-health issues or to the society at large. Moreover, these findings further demonstrate that COVID-19 anxiety is not a unidimensional construct and should thus be studied using a multidimensional approach.
We further found the use of problem-focused coping to deal with controllable stressful events to be related to lower levels of anxiety over personal issues (i.e., personal health and others' reactions) rather than broader societal issues (i.e., societal health, economic problems). It is also noteworthy that the use of emotion-focused coping to handle controllable rather than uncontrollable stressful events was related to higher COVID-19 anxiety and depression, a finding consistent with previous studies on clinical samples of depression ( 22 ). Although the unprecedented COVID-19 pandemic is objectively an uncontrollable stressor due to its uncertain nature, the theory of coping flexibility highlights the importance of identifying aspects of life that are controllable and distinguishing these aspects from most other uncontrollable ones in a stressful encounter. For example, when a person high in coping flexibility fails to buy facemasks after visiting many stores, this person still regards the problem as controllable and keeps trying a variety of alternative means (e.g., placing orders in overseas online stores, seeking advice from members of WhatsApp groups). It is the cognitive astuteness in distinguishing between controllable and uncontrollable life aspects that fosters adjustment to stressful life changes.
Such situational differences in coping effectiveness indicate that neither problem-focused nor emotion-focused coping is inherently adaptive or maladaptive. The role of effective coping in mitigating mental health problems depends largely on the extent to which a deployed strategy meets the specific demands of the stressful encounter concerned. For instance, playing online games or browsing social network sites can be stress-relieving during leisure time ( 52 , 53 ), but prolonged gameplay or social media use can impair work or academic performance while working or studying from home ( 54 ). These findings are in line with the theory of coping flexibility, highlighting the beneficial role of flexible coping in soothing mental health problems experienced during the pandemic.
The present findings also have practical implications. Given the beneficial role of coping flexibility, clinicians may work with clients to enhance coping effectiveness with regard to strategy-situation fit. Stress management intervention may involve sharpening clients' skills for (a) distinguishing the key demands stemming from an array of stressful events; (b) assessing whether or not such demands are amendable to a change in effort (i.e., controllable or uncontrollable); (c) applying the meta-cognitive skill of reflection to evaluate strategies that best match the specific demands of diverse stressful situations; and (d) subsequently deploying the most appropriate strategy to handle each stressor. Such flexible coping skills are especially useful for dealing with the psychological distress elicited by a pandemic involving an assortment of stressful events.
Coping flexibility may also be valuable at a broader level because the unpredictable progression of the COVID-19 pandemic across successive waves presents varying challenges for public health authorities worldwide. For instance, the shortage of personal protection equipment aroused immense public anxiety in Hong Kong during the first wave owing to the sudden surge in demand for facemasks and hand sanitizer. After the supply of such equipment had been stabilized, however, new societal problems emerged. For example, during the second wave, public commitment to observing physical distancing measures began to wane owing to “pandemic fatigue” ( 55 ). Public health authorities may need to adopt a certain degree of flexibility in monitoring and identifying emerging issues to allow the timely adjustment of extant disease-control measures or the formulation of new ones to mitigate changing public health threats.
Despite its important findings, several study limitations must be noted. The survey was conducted during the second wave of the pandemic, when the epidemic curve climbed to a high level and then leveled off for a few months before reaching a further peak in the third wave in July and August, 2020 ( 34 ). As the COVID-19 pandemic continues to evolve in an unpredictable manner, some of the anxiety-provoking issues identified in this study may no longer elicit anxiety to the same extent in future waves. The list of issues eliciting COVID-19 anxiety should thus be updated in future research. Given the time sensitivity of these issues, pilot testing is essential to evaluate their relevance in particular phases of the pandemic.
Further, although our findings offer robust support for the hypothesized beneficial role of coping flexibility amid the pandemic, previous meta-analysis indicated that that beneficial role is more prominent in collectivist than individualist regions ( 19 ). A fruitful direction for future research would thus be to replicate the present design in individualist countries, allowing cross-cultural comparisons to be made. In addition to cultural differences, there may also be considerable variations among Chinese adults residing in different regions, as the epidemic trajectory has varied greatly among cities in the Greater Bay Area, such as Guangzhou and Macau ( 56 ). Greater effort can be made to compare the prevalence of psychological disorders and coping processes among Chinese residents of diverse regions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the study protocol was reviewed and approved by the Human Research Ethics Committee of the University of Hong Kong (approval number: EA1912046 dated March 4, 2020). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
CC contributed to project design and administration, coordinated the data collection, performed the statistical analysis, and wrote the first draft of the manuscript. H-yW contributed to project design, survey creation, statistical analysis, and data interpretation. OE contributed to data interpretation and writing parts of the manuscript. All authors contributed to the article and approved the submitted version.
This research project was funded by the Public Policy Research Funding Scheme from the Policy Innovation and Co-ordination Office (Project Number: SR2020.A8.019) and General Research Fund (Project Number: 17400714) of the Government of the Hong Kong Special Administrative Region. The funders had no role in study design and administration, statistical analysis or interpretation, manuscript writing, or the decision to submit the paper for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The author would like to thank Sylvia Lam, Sophie Lau, Janice Leung, Yin-wai Li, Stephanie So, Yvonne Tsui, and Kylie Wong for research and clerical assistance.
1. Lai C, Shih T, Ko W, Tang H, Hsueh P. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. (2020) 55:105924. doi: 10.1016/j.ijantimicag.2020.105924
PubMed Abstract | CrossRef Full Text | Google Scholar
2. World Health Organization. Timeline: WHO's COVID-19 Response . (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed October 8, 2020).
Google Scholar
3. Chen R, Chou K, Huang Y, Wang T, Liu S, Ho L. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. (2006) 43:215–25. doi: 10.1016/j.ijnurstu.2005.03.006
4. Cheng C, Tang CS. The psychology behind the masks: psychological responses to the severe acute respiratory syndrome outbreak in different regions. Asian J Soc Psychol. (2004) 7:3–7. doi: 10.1111/j.1467-839X.2004.00130.x
5. Baker SR, Bloom N, Davis SJ, Kost K, Sammon M, Viratyosin T. The unprecedented stock market reaction to COVID-19. Rev Asset Pricing Studies. (2020) raaa008. doi: 10.3386/w26945
CrossRef Full Text | Google Scholar
6. Arafat SY, Kar SK, Marthoenis M, Sharma P, Apu EH, Kabir R. Psychological underpinning of panic buying during pandemic (COVID-19). Psychiatry Res. (2020) 289:113061. doi: 10.1016/j.psychres.2020.113061
7. Wong JEL, Leo YS, Tan CC. COVID-19 in Singapore—current experience: critical global issues that require attention and action. JAMA. (2020) 323:1243–4. doi: 10.1001/jama.2020.2467
8. Bressington DT, Cheung TCC, Lam SC, Suen LKP, Fong TKH, Ho HSW. Association between depression, health beliefs, and face mask use during the COVID-19 pandemic. Front Psychiatry. (2020) 11:1075. doi: 10.3389/fpsyt.2020.571179
9. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
10. Gostin LO, Wiley LF. Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA. (2020) 323:2137–8. doi: 10.1001/jama.2020.5460
11. Belzunegui-Eraso A, Erro-Garcés A. Teleworking in the context of the Covid-19 crisis. Sustainability. (2020) 12:3662. doi: 10.3390/su12093662
12. Persol Research and Development. Survey of Telework in Japan for COVID-19 . Nagoya: Author (2020).
13. Harris L. Home-based teleworking and the employment relationship: managerial challenges and dilemmas. Pers Rev. (2003) 32:422–37. doi: 10.1108/00483480310477515
14. Tang S, Xiang M, Cheung T, Xiang Y. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J Affect Disord. (2021) 279:353–60. doi: 10.1016/j.jad.2020.10.016
15. Zhang Z, Zhai A, Yang M, Zhang J, Zhou H, Yang C. Prevalence of depression and anxiety symptoms of high school students in shandong province during the COVID-19 epidemic. Front Psychiatry. (2020) 11:1499. doi: 10.3389/fpsyt.2020.570096
16. Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E. Insomnia during the COVID-19 pandemic in a greek population. Psychiatry Res. (2020) 289:113076. doi: 10.1016/j.psychres.2020.113076
17. Cheng C, Ebrahimi OV, Lau Y. Maladaptive coping with the infodemic and sleep disturbance in the COVID-19 pandemic. J Sleep Res. (2020) e13235. doi: 10.1111/jsr.13235
18. Lam CB, McBride-Chang CA. Resilience in young adulthood: the moderating influences of gender-related personality traits and coping flexibility. Sex Roles. (2007) 56:159–72. doi: 10.1007/s11199-006-9159-z
19. Cheng C, Lau HB, Chan MS. Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychol Bull. (2014) 140:1582–607. doi: 10.1037/a0037913
20. Cheng C, Hui W, Lam S. Psychosocial factors and perceived severity of functional dyspeptic symptoms: a psychosocial interactionist model. Psychosom Med. (2004) 66:85–91. doi: 10.1097/01.PSY.0000106885.40753.C1
21. Sanderson WC, Rapee RM, Barlow DH. The influence of an illusion of control on panic attacks induced via inhalation of 5.5% carbon dioxide-enriched air. Arch Gen Psychiatry. (1989) 46:157–162. doi: 10.1001/archpsyc.1989.01810020059010
22. Gan Y, Zhang Y, Wang X, Wang S, Shen X. The coping flexibility of neurasthenia and depressive patients. Pers Individ Differ. (2006) 40:859–71. doi: 10.1016/j.paid.2005.09.006
23. Zong J, Cao XY, Cao Y, Shi YF, Wang YN, Yan C, et al. Coping flexibility in college students with depressive symptoms. Health Quality Life Outcomes. (2010) 8:1–6. doi: 10.1186/1477-7525-8-66
24. Cheng C, Chau C. When to approach and when to avoid? Funct Flex Key Psychol Inquiry. (2019) 30:125–9. doi: 10.1080/1047840X.2019.1646040
25. Jean S, Lee P, Hsueh P. Treatment options for COVID-19: The reality and challenges. J Microbiol Immunol Infect. (2020) 53:436–43. doi: 10.1016/j.jmii.2020.03.034
26. Hirsh JB, Mar RA, Peterson JB. Psychological entropy: a framework for understanding uncertainty-related anxiety. Psychol Rev. (2012) 119:304–20. doi: 10.1037/a0026767
27. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US Adults before and during the COVID-19 pandemic. JAMA Network Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
28. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
29. Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. The dynamics of a stressful encounter. In: Higgins ET, Kruglanski AW, editors. Motivational Science: Social and Personality Perspectives . New York, NY: Psychology Press (2000). p. 111–27.
30. Cheng C. Dialectical thinking and coping flexibility: a multimethod approach. J Pers. (2009) 77:471–94. doi: 10.1111/j.1467-6494.2008.00555.x
31. Cheng C, Chiu C, Hong Y, Cheung JS. Discriminative facility and its role in the perceived quality of interactional experiences. J Pers. (2001) 69:765–86. doi: 10.1111/1467-6494.695163
32. Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. (2020) 26:729–34. doi: 10.1016/j.cmi.2020.03.026
33. Centre for Health Protection. Number of Notifiable Infectious Diseases by Month in 2020 . (2020). Available onlone at: https://www.chp.gov.hk/en/statistics/data/10/26/43/6896.html (accessed October 8, 2020).
34. Statista. Number of Novel Coronavirus COVID-19 Cumulative Confirmed, Recovered and Death Cases in Hong Kong from January 30 to October 25, 2020 . (2020). Available online at: https://www.statista.com/statistics/1105425/hong-kong-novel-coronavirus-covid19-confirmed-death-recovered-trend/ (accessed October 28, 2020).
35. The HKSAR and Government (2020). Government Announces Enhancements to Anti-Epidemic Measures in Four Aspects . Available online at: https://www.info.gov.hk/gia/general/202003/24/P2020032400050.htm (accessed October 8, 2020).
36. news.gov.hk. Restrictions on Bars Gazetted . (2020). Available online at: https://www.news.gov.hk/eng/2020/04/20200402/20200402_195740_071.html (accessed October 8, 2020).
37. Atal S, Cheng C. Socioeconomic health disparities revisited: coping flexibility enhances health-related quality of life for individuals low in socioeconomic status. Health Qual Life Outcomes. (2016) 14:1–7. doi: 10.1186/s12955-016-0410-1
38. Cheng C, Hui W, Lam S. Perceptual style and behavioral pattern of individuals with functional gastrointestinal disorders. Health Psychol. (2000) 19:146–54. doi: 10.1037/0278-6133.19.2.146
39. Lazarus RS, Folkman S. The concept of coping. In: Monat A, Lazarus RS, editors. Stress and Coping: An Anthology . New York, NY: Columbia University (1991). p. 189–206
40. Cheng C, Chan NY, Chio JHM, Chan P, Chan AOO, Hui WM. Being active or flexible? Role of control coping on quality of life among patients with gastrointestinal cancer. Psychooncology. (2012) 21:211–8. doi: 10.1002/pon.1892
41. Cheng C, Cheng F, Atal S, Sarwono S. Testing of a dual process model to resolve the socioeconomic health disparities: a tale of two Asian countries. Int J Environ Res Public Health. (2021) 18:717. doi: 10.3390/ijerph18020717
42. Endler NS. Stress, anxiety and coping: the multidimensional interaction model. Can Psychol. (1997) 38:136–53. doi: 10.1037/0708-5591.38.3.136
43. Hayes AF, Krippendorff K. Answering the call for a standard reliability measure for coding data. Commun Methods Meas. (2007) 1:77–89. doi: 10.1080/19312450709336664
44. Cheng C, Ng A. Psychosocial factors predicting SARS-preventive behaviors in four major SARS-affected regions. J Appl Soc Psychol. (2006) 36:222–47. doi: 10.1111/j.0021-9029.2006.00059.x
45. Cheng C, Cheung MWL. Psychological responses to outbreak of severe acute respiratory syndrome: a prospective, multiple time-point study. J Pers. (2005) 73:261–85. doi: 10.1111/j.1467-6494.2004.00310.x
46. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
47. Yang CF. Measures of Personality and Social Psychological Attitudes , Vol. 1. Taipei: Yuan-Liou (1997).
48. Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. (1999) 14:608–17. doi: 10.1002/(SICI)1099-1166(199908)14:8<608::AID-GPS991>3.0.CO;2-Z
49. Bagozzi RP, Youjae Y. On the evaluation of structural equation models. J Acad Mark Sci. (1988) 16:74–94. doi: 10.1007/BF02723327
50. Wang H, Cheng C. New perspectives on the prevalence and associated factors of gaming disorder in Hong Kong community adults: a generational approach. Comput Hum Behav. (2021) 114:106574. doi: 10.1016/j.chb.2020.106574
51. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. (2020) 16:1–11. doi: 10.1186/s12992-020-00589-w
52. Kardefelt-Winther D. The moderating role of psychosocial well-being on the relationship between escapism and excessive online gaming. Comput Hum Behav. (2014) 38:68–74. doi: 10.1016/j.chb.2014.05.020
53. Young NL, Daria JK, Mark DG, Christina JH. Passive Facebook use, Facebook addiction, and associations with escapism: an experimental vignette study. Comput Hum Behavi. (2017) 71:24–31. doi: 10.1016/j.chb.2017.01.039
54. Cheng C, Lau Y, Luk JW. Social capital–accrual, escape-from-self, and time-displacement effects of internet use during the COVID-19 stay-at-home period: prospective, quantitative survey study. J Med Int Res. (2020) 22:e22740. doi: 10.2196/22740
55. Harvey N. Behavioural fatigue: real phenomenon, naïve construct, or policy contrivance. Front Psychol. (2021) 11:2960. doi: 10.3389/fpsyg.2020.589892
56. Johns Hopkins Coronavirus Resource Center. Coronavirus COVID-19 Global Cases . (2021). Available online at: https://coronavirus.jhu.edu/map.html (accessed January 18, 2021).
Keywords: coronavirus disease, resilience, coping, stress, psychological well-being, adaptation, Chinese, epidemic
Citation: Cheng C, Wang H-y and Ebrahimi OV (2021) Adjustment to a “New Normal:” Coping Flexibility and Mental Health Issues During the COVID-19 Pandemic. Front. Psychiatry 12:626197. doi: 10.3389/fpsyt.2021.626197
Received: 05 November 2020; Accepted: 01 March 2021; Published: 19 March 2021.
Reviewed by:
Copyright © 2021 Cheng, Wang and Ebrahimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cecilia Cheng, ceci-cheng@hku.hk
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Accessibility & Inclusivity
- Breaking News
- International
- Clubs & Orgs
- Humans of SB
- In Memoriam
- Santa Barbara
- Top Features
- Arts & Culture
- Film & TV
- Local Artists
- Local Musicians
- Student Art
- Theater & Dance
- Top A&E
- App Reviews
- Environment
- Nature of UCSB
- Nature of IV
- Top Science & Tech
- Campus Comment
- Letters to the Editor
- Meet Your Neighbor
- Top Opinions
- Illustrations
- Editorial Board
Earth Day Isla Vista – Celebrating Through Music, Nature, and Fun
In photos: men’s basketball: gauchos vs uc davis, art as a weapon against invasion – film reminds us of…, opportunity for all uc office of the president yet to make…, the top boba places in isla vista – a journey into…, getting kozy: isla vista’s newest coffee shop, a call for natural sustainability: the story and mission of the…, tasa night market 2023: fostering community and featuring budding clubs at…, in photos – daedalum luminarium, an art installation, creating characters we love: the screenwriting process in our flag means…, indigo de souza and the best-case anticlimax, a spectrum of songs: ucsb’s college of creative studies set to…, nature in i.v. – black mold, southern california is in super bloom, from love to likes: social media’s role in relationships, the gloom continues: a gray may, the rise of ai girlfriends: connecting with desires and discussing controversy,…, letter to the editor: dining hall laborers have had enough, do…, is studying abroad worth it for a ucsb student, workers at ucsb spotlight: being a writing tutor for clas, the new normal of pandemic life.

Sierra Schumann
Contributing Writer
The introduction of COVID-19 has undoubtedly changed everyone’s lives over the past few years. Living through this event, which will be taught in history classes for years to come, is both terrifying and unique.
While science has made grand improvements and monumental strides in overcoming this earth-shaking virus, it seems that every time we approach “normal” life, a new surge of sickness or a new variant arises, and we are swept back into the tumultuous cycle of mask mandates and online classes. This seemingly never-ending cycle poses a contentious question: will we ever go back to normal life?
Here at UC Santa Barbara (UCSB), students were hopeful, as the fall quarter allowed for the return to in-person instruction. Yet just as school was on its way back to normal, the Omicron variant took over, reintroducing Zoom lectures and asynchronous learning.
COVID-19, despite its unpredictability, has made itself so predictable to the point where the promise of “only two weeks of online classes” is no longer believable. Going online for the full month of January was no surprise to many after the first two-week interval was introduced.
As recent history has proved, and as first-year UCSB undergraduate Annika Hando told The Bottom Line (TBL), “Two weeks is never just two weeks. In 2019, we all were so excited for an extra-long spring break, but those two weeks ended up to be a two-year-and-counting escapade.”
When considering whether we will ever return to normal life again, students hope the answer is yes, but realize that reality disagrees. While we are certainly in a far more advanced and knowledgeable position compared to a year and a half ago, it feels like every time there is a glimpse of hope, something new comes along. It is a never-ending fight, and it is hard to imagine that life will ever be the same as it was before the pandemic.
From the suffering of so many families to drastic changes in mental health, everyone underwent some form of personal change during the months of isolation.
When TBL spoke with Sean Andampour, another freshman at UCSB, he reflected on the pandemic. “It made me feel more sensitive because while being isolated from everyone, there is a certain amount of anxiety that builds up, so I feel like I have become more empathetic and understanding of others,” he said. This illustrates one of the many ways in which COVID-19 has changed people on a level that will remain unaltered, even if life returns to so-called “normal.”
In addition to the personal changes brought on by isolation, there are many logistical areas that have drastically shifted to accommodate social distancing. COVID-19 has shown affluent countries like the United States that we are able to get just about anything done with technology in a much faster, and sometimes simpler way. Time can be used more efficiently as we can multitask Zoom calls and household chores. With this considered, the transition to online schooling and working from home could quite possibly be the new normal.
Furthermore, after seeing how easy and enjoyable it can sometimes be to work or do school from home in one’s pajamas, or order groceries online and forgo the effort of in-person shopping, we got a taste of a new life. For some, they may not be able to or even want to go back to a life where they have to put on a suit and tie and sit in traffic every day.
“The pandemic forced us to become sort of hyper-advanced in using technology for everything. So many things shifted to being online, and I think some of that will stay the same as we move forward,” stated Pavel Tantchev, a first-year undergraduate at UCSB.
While society will most likely, and has already started to, return to many of its old rituals such as the reintroduction of stores, restaurants, parties, concerts, and business as usual, the overall mentality of everyone living through this event will be forever changed.
Pavel captured the sentiments of many students at UCSB when describing how their mindset has changed due to COVID-19. “Since COVID-19, I feel like I am a lot more conscious about germs and overall taking care of my health”, he said. Coming from a world filled with physical touch, large gatherings, and traveling, the new significance of germs has rewired many people’s brains to become hyperaware about the spread of germs and staying healthy and safe. Pavel added, “I think masks will stick around for a while.”
This surge of illnesses brought about by COVID-19 is more widespread than any other in history, and this in itself has the power to change the world’s view of what is “normal.” Changing the way we view disease and intertwining politics with human health in a way we have never seen before, the impact of COVID-19 on the media and polarization of countries like the United States is something that will forever be ingrained in our minds.
Moreover, while this exact moment of online classes, travel bans, and mask-wearing will not always be the new normal, this constant state of change and unpredictability may be.
As said by Sean Andampour, “I think we can try to go back to normal, but it is so hard to say that will happen because I don’t even know what is considered normal anymore. I think eventually we will start to recognize a new normal.”
- Science & Tech
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:

Two Years Into the Pandemic, Americans Inch Closer to a New Normal
Two years after the coronavirus outbreak upended life in the United States, Americans find themselves in an environment that is at once greatly improved and frustratingly familiar.
Around three-quarters of U.S. adults now report being fully vaccinated , a critical safeguard against the worst outcomes of a virus that has claimed the lives of more than 950,000 citizens. Teens and children as young as 5 are now eligible for vaccines . The national unemployment rate has plummeted from nearly 15% in the tumultuous first weeks of the outbreak to around 4% today. A large majority of K-12 parents report that their kids are back to receiving in-person instruction , and other hallmarks of public life, including sporting events and concerts, are again drawing crowds.
This Pew Research Center data essay summarizes key public opinion trends and societal shifts as the United States approaches the second anniversary of the coronavirus outbreak . The essay is based on survey data from the Center, data from government agencies, news reports and other sources. Links to the original sources of data – including the field dates, sample sizes and methodologies of surveys conducted by the Center – are included wherever possible. All references to Republicans and Democrats in this analysis include independents who lean toward each party.
Data essay from March 2021: A Year of U.S. Public Opinion on the Coronavirus Pandemic
The landscape in other ways remains unsettled. The staggering death toll of the virus continues to rise, with nearly as many Americans lost in the pandemic’s second year as in the first, despite the widespread availability of vaccines. The economic recovery has been uneven, with wage gains for many workers offset by the highest inflation rate in four decades and the labor market roiled by the Great Resignation . The nation’s political fractures are reflected in near-daily disputes over mask and vaccine rules. And thorny new societal problems have emerged, including alarming increases in murder and fatal drug overdose rates that may be linked to the upheaval caused by the pandemic.
For the public, the sense of optimism that the country might be turning the corner – evident in surveys shortly after President Joe Biden took office and as vaccines became widely available – has given way to weariness and frustration. A majority of Americans now give Biden negative marks for his handling of the outbreak, and ratings for other government leaders and public health officials have tumbled . Amid these criticisms, a growing share of Americans appear ready to move on to a new normal, even as the exact contours of that new normal are hard to discern.
A year ago, optimism was in the air

Biden won the White House in part because the public saw him as more qualified than former President Donald Trump to address the pandemic. In a January 2021 survey, a majority of registered voters said a major reason why Trump lost the election was that his administration did not do a good enough job handling the coronavirus outbreak.
At least initially, Biden inspired more confidence. In February 2021, 56% of Americans said they expected the new administration’s plans and policies to improve the coronavirus situation . By last March, 65% of U.S. adults said they were very or somewhat confident in Biden to handle the public health impact of the coronavirus.
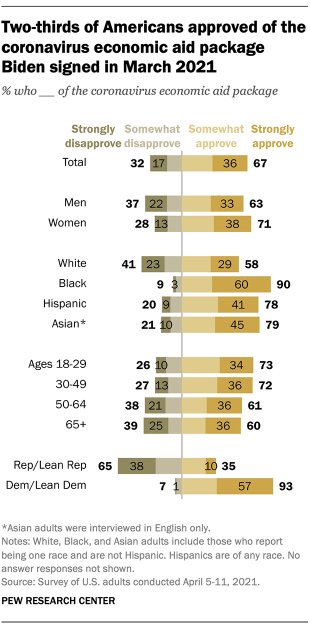
The rapid deployment of vaccines only burnished Biden’s standing. After the new president easily met his goal of distributing 100 million doses in his first 100 days in office, 72% of Americans – including 55% of Republicans – said the administration was doing an excellent or good job overseeing the production and distribution of vaccines. As of this January, majorities in every major demographic group said they had received at least one dose of a vaccine. Most reported being fully vaccinated – defined at the time as having either two Pfizer or Moderna vaccines or one Johnson & Johnson – and most fully vaccinated adults said they had received a booster shot, too.
The Biden administration’s early moves on the economy also drew notable public support. Two-thirds of Americans, including around a third of Republicans, approved of the $1.9 trillion aid package Biden signed into law last March, one of several sprawling economic interventions authorized by administrations of both parties in the outbreak’s first year. Amid the wave of government spending, the U.S. economy grew in 2021 at its fastest annual rate since 1984 .
Globally, people preferred Biden’s approach to the pandemic over Trump’s. Across 12 countries surveyed in both 2020 and 2021, the median share of adults who said the U.S. was doing a good job responding to the outbreak more than doubled after Biden took office. Even so, people in these countries gave the U.S. lower marks than they gave to Germany, the World Health Organization and other countries and multilateral organizations.
Data essay: The Changing Political Geography of COVID-19 Over the Last Two Years

A familiar undercurrent of partisan division
Even if the national mood seemed to be improving last spring, the partisan divides that became so apparent in the first year of the pandemic did not subside. If anything, they intensified and moved into new arenas.
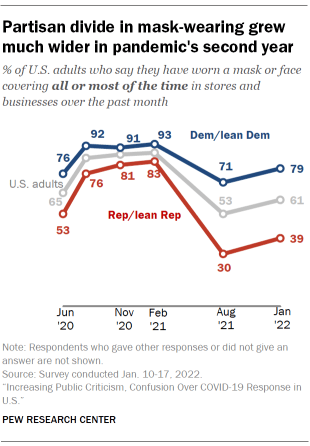
Masks and vaccines remained two of the most high-profile areas of contention. In February 2021, Republicans were only 10 percentage points less likely than Democrats (83% vs. 93%) to say they had worn a face covering in stores or other businesses all or most of the time in the past month. By January of this year, Republicans were 40 points less likely than Democrats to say they had done so (39% vs. 79%), even though new coronavirus cases were at an all-time high .
Republicans were also far less likely than Democrats to be fully vaccinated (60% vs. 85%) and to have received a booster shot (33% vs. 62%) as of January. Not surprisingly, they were much less likely than Democrats to favor vaccination requirements for a variety of activities, including traveling by airplane, attending a sporting event or concert, and eating inside of a restaurant.
Some of the most visible disputes involved policies at K-12 schools, including the factors that administrators should consider when deciding whether to keep classrooms open for in-person instruction. In January, Republican K-12 parents were more likely than Democrats to say a lot of consideration should be given to the possibility that kids will fall behind academically without in-person classes and the possibility that students will have negative emotional consequences if they don’t attend school in person. Democratic parents were far more likely than Republicans to say a lot of consideration should be given to the risks that COVID-19 poses to students and teachers.

The common thread running through these disagreements is that Republicans remain fundamentally less concerned about the virus than Democrats, despite some notable differences in attitudes and behaviors within each party . In January, almost two-thirds of Republicans (64%) said the coronavirus outbreak has been made a bigger deal than it really is . Most Democrats said the outbreak has either been approached about right (50%) or made a smaller deal than it really is (33%). (All references to Republicans and Democrats include independents who lean toward each party.)
New variants and new problems
The decline in new coronavirus cases, hospitalizations and deaths that took place last spring and summer was so encouraging that Biden announced in a July 4 speech that the nation was “closer than ever to declaring our independence from a deadly virus.” But the arrival of two new variants – first delta and then omicron – proved Biden’s assessment premature.
Some 350,000 Americans have died from COVID-19 since July 4, including an average of more than 2,500 a day at some points during the recent omicron wave – a number not seen since the first pandemic winter, when vaccines were not widely available. The huge number of deaths has ensured that even more Americans have a personal connection to the tragedy .

The threat of dangerous new variants had always loomed, of course. In February 2021, around half of Americans (51%) said they expected that new variants would lead to a major setback in efforts to contain the disease. But the ferocity of the delta and omicron surges still seemed to take the public aback, particularly when governments began to reimpose restrictions on daily life.
After announcing in May 2021 that vaccinated people no longer needed to wear masks in public, the Centers for Disease Control and Prevention reversed course during the delta wave and again recommended indoor mask-wearing for those in high-transmission areas. Local governments brought back their own mask mandates . Later, during the omicron wave, some major cities imposed new proof-of-vaccination requirements , while the CDC shortened its recommended isolation period for those who tested positive for the virus but had no symptoms. This latter move was at least partly aimed at addressing widespread worker shortages , including at airlines struggling during the height of the holiday travel season.
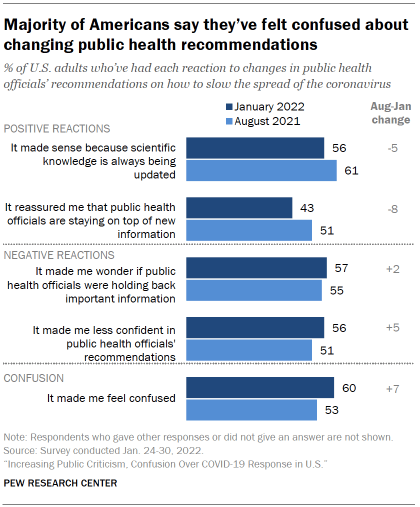
Amid these changes, public frustration was mounting. Six-in-ten adults said in January 2022 that the changing guidance about how to slow the spread of the virus had made them feel confused , up from 53% the previous August. More than half said the shifting guidance had made them wonder if public health officials were withholding important information (57%) and made them less confident in these officials’ recommendations (56%). And only half of Americans said public health officials like those at the CDC were doing an excellent or good job responding to the outbreak, down from 60% last August and 79% in the early stages of the pandemic.
Economic concerns, particularly over rising consumer prices, were also clearly on the rise. Around nine-in-ten adults (89%) said in January that prices for food and consumer goods were worse than a year earlier . Around eight-in-ten said the same thing about gasoline prices (82%) and the cost of housing (79%). These assessments were shared across party lines and backed up by government data showing large cost increases for many consumer goods and services.
Overall, only 28% of adults described national economic conditions as excellent or good in January, and a similarly small share (27%) said they expected economic conditions to be better in a year . Strengthening the economy outranked all other issues when Americans were asked what they wanted Biden and Congress to focus on in the year ahead.
Looking at the bigger picture, nearly eight-in-ten Americans (78%) said in January that they were not satisfied with the way things were going in the country.
Imagining the new normal
As the third year of the U.S. coronavirus outbreak approaches, Americans increasingly appear willing to accept pandemic life as the new reality.
Large majorities of adults now say they are comfortable doing a variety of everyday activities , including visiting friends and family inside their home (85%), going to the grocery store (84%), going to a hair salon or barbershop (73%) and eating out in a restaurant (70%). Among those who have been working from home, a growing share say they would be comfortable returning to their office if it were to reopen soon.
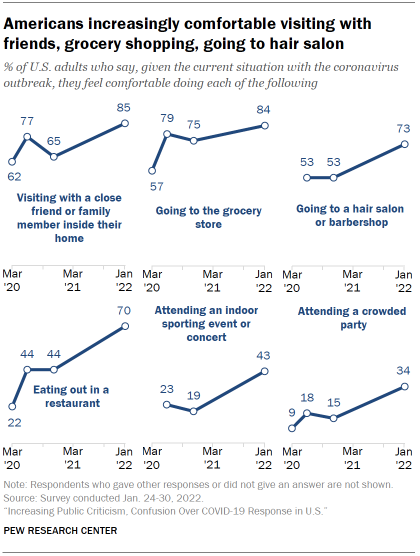
With the delta and omicron variants fresh in mind, the public also seems to accept the possibility that regular booster shots may be necessary. In January, nearly two-thirds of adults who had received at least one vaccine dose (64%) said they would be willing to get a booster shot about every six months. The CDC has since published research showing that the effectiveness of boosters began to wane after four months during the omicron wave.
Despite these and other steps toward normalcy , uncertainty abounds in many other aspects of public life.
The pandemic has changed the way millions of Americans do their jobs, raising questions about the future of work. In January, 59% of employed Americans whose job duties could be performed remotely reported that they were still working from home all or most of the time. But unlike earlier in the pandemic, the majority of these workers said they were doing so by choice , not because their workplace was closed or unavailable.
A long-term shift toward remote work could have far-reaching societal implications, some good, some bad. Most of those who transitioned to remote work during the pandemic said in January that the change had made it easier for them to balance their work and personal lives, but most also said it had made them feel less connected to their co-workers.
The shift away from office spaces also could spell trouble for U.S. downtowns and the economies they sustain. An October 2021 survey found a decline in the share of Americans who said they preferred to live in a city and an increase in the share who preferred to live in a suburb. Earlier in 2021, a growing share of Americans said they preferred to live in a community where the houses are larger and farther apart , even if stores, schools and restaurants are farther away.

When it comes to keeping K-12 schools open, parental concerns about students’ academic progress and their emotional well-being now clearly outweigh concerns about kids and teachers being exposed to COVID-19. But disputes over school mask and vaccine rules have expanded into broader debates about public education , including the role parents should play in their children’s instruction. The Great Resignation has not spared K-12 schools , leaving many districts with shortages of teachers, bus drivers and other employees.
The turmoil in the labor market also could exacerbate long-standing inequities in American society. Among people with lower levels of education, women have left the labor force in greater numbers than men. Personal experiences at work and at home have also varied widely by race , ethnicity and household income level .
Looming over all of this uncertainty is the possibility that new variants of the coronavirus will emerge and undermine any collective sense of progress. Should that occur, will offices, schools and day care providers again close their doors, complicating life for working parents ? Will mask and vaccine mandates snap back into force? Will travel restrictions return? Will the economic recovery be interrupted? Will the pandemic remain a leading fault line in U.S. politics, particularly as the nation approaches a key midterm election?
The public, for its part, appears to recognize that a swift return to life as it was before the pandemic is unlikely. Even before the omicron variant tore through the country, a majority of Americans expected that it would be at least a year before their own lives would return to their pre-pandemic normal. That included one-in-five who predicted that their own lives would never get back to the way they were before COVID-19.
Lead photo: Luis Alvarez/Getty Images.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
© 2024 Pew Research Center
A Year After Coronavirus: An Inclusive ‘New Normal’

Six months into a new decade, 2020 has already been earmarked as ‘the worst’ year in the 21st century. The novel coronavirus has given rise to a global pandemic that has destabilized most institutional settings. While we live in times when humankind possesses the most advanced science and technology, a virus invisible to the naked eye has massively disrupted economies, healthcare, and education systems worldwide. This should serve as a reminder that as we keep making progress in science and research, humanity will continue to face challenges in the future, and it is upon us to prioritize those issues that are most relevant in the 21st century.
Even amidst the pandemic, Space X, an American aerospace manufacturer, managed to become the first private company to send humans to space. While this is a tremendous achievement and prepares humanity for a sustainable future, I feel there is a need to introspect the challenges that we are already facing. On the one hand, we seem to be preparing beyond the 21st century. On the other hand, heightened nationalism, increasing violence against marginalized communities and multidimensional inequalities across all sectors continue to act as barriers to growth for most individuals across the globe. COVID-19 has reinforced these multifaceted economic, social and cultural inequalities wherein those in situations of vulnerability have found it increasingly difficult to get quality medical attention, access to quality education, and have witnessed increased domestic violence while being confined to their homes.
Given the coronavirus’s current situation, some households have also had time to introspect on gender roles and stereotypes. For instance, women are expected to carry out unpaid care work like cooking, cleaning, and looking after the family. There is no valid reason to believe that women ought to carry out these activities, and men have no role in contributing to household chores. With men having shared household chores during the lockdown period, it gives hope that they will realize the burden that women have been bearing for past decades and will continue sharing responsibilities. However, it would be naïve to believe that gender discrimination could be tackled so easily, and men would give up on their decades' old habits within a couple of months. Thus, during and after the pandemic, there is an urgent need to sensitize households on the importance of gender equality and social cohesion.
Moving forward, developing quality healthcare systems that are affordable and accessible to all should be the primary objective for all governments. This can be done by increasing expenditure towards health and education and simultaneously reducing expenditure on defence equipment where the latter mainly gives rise to an idea that countries need to be prepared for violence. There is substantial evidence that increased investment in health and education is beneficial in the long-term and can potentially build the basic foundation of a country.
If it can be established that usage of nuclear weapons, violence and war are not solutions to any problem, governments (like, for example, Costa Rica) could move towards disarmament of weapons and do their part in building a more peaceful planet that is sustainable for the future. This would further promote global citizenship wherein nationality, race, gender, caste, and other categories, are just mere variables and they do not become identities of individuals that restrict their thought process. The aim should be to build responsible citizens who play an active role in their society and work collectively in helping develop a planet that is well-governed, inclusive, and environmentally sustainable.
‘A year after Coronavirus’ is still an unknown, so I think that our immediate focus should be to tackle the complex problems that have emerged from the pandemic so that we make the year after coronavirus one which highlights recovery and acts as a pathway to fresh beginnings. While there is little to gain from such a fatal cause, it is vital that we also use it to make the ‘new normal’ in favour of the environment and ensure that no one is left behind.
Related items
- Country page: India
- UNESCO Office in New Delhi
- SDG: SDG 3 - Ensure healthy lives and promote well-being for all at all ages
This article is related to the United Nation’s Sustainable Development Goals .

Article Terms of Reference for the development of an electronic health database for campus health facilities in Zimbabwe 14 June 2024

Other recent articles

Article PROCUREMENT NOTICE/ADVERTISEMENT: INVITATION TO BID FOR SMALL WORKS – Health Facility Refurbishment 28 May 2024
Article PROCUREMENT NOTICE/ADVERTISEMENT: INVITATION TO BID FOR WORKS – Borehole Drilling & Installation of Water Tanks and Solar Geysers 28 May 2024
- REGISTER TRAVEL
- Engagement Opportunities
- Initiatives
- Travel Resources
Coping with COVID-19: U-M students share their ‘new normal’

Seniors (left to right) Kate Lytchakov, Devin Raymond, Caitlin Shyuu, and Nicole Wozniak take grad photos in the Law Quad while practicing social distancing.
For students, this month with COVID-19 has been framed with uncertainty and stress. Seniors rushed goodbyes, underclassmen quickly vacated dorms, and many found themselves back at home only a few days after spring break. In the middle of this has been the immense university-wide effort to make coursework accessible, engaging and accommodating, a sign of the university’s ability to adapt even in the most turbulent times.
While students say adjusting to coursework online and this “new normal” has been an ongoing challenge, pockets of positivity and optimism have emerged, illuminating now more than ever their support of each other, and faculty commitment to their education.
Here are eight stories from U-M students reflecting on their experiences during this recent transition:
Eric Payerle, junior, Ford School of Public Policy

“While it’s been difficult to spend much of the day at my desk transitioning from video calls and lectures to plugging away at papers and assignments on my laptop — all while my bed sits two feet away — the professors and faculty have brought good humor to this unpredictable experience. One professor noted we’d inevitably see his children running through the background of his lectures at some point; another, while streaming from her children’s closet, proudly displayed her passion for environmental economics by wearing a Severin Borenstein t-shirt, depicting the face of the UC-Berkeley professor of business administration and public policy, one of the authors we had read in the class.
“My family has also found new uses for video conferencing: Euchre. We’ve always played our favorite card game when we’re all home but now, while stuck inside and spread across three different time zones, we’ve moved our game online, and still kept the usual yelling and complaints. Whether it’s new ways of interacting with my family, new ways of relating to our professors, or a host of positive emails from the Ford School dean, this shared experience has given a new perspective to our relationships with our professors and faculty.”
Shannon Habba, biopsychology, cognition, and neuroscience senior, College of Literature, Arts & Sciences
“From football games to spring break, college seniors look forward to celebrating ‘lasts’ surrounded by our best friends, in a community that has become home over the past few years. While this isn’t the end of our college career we imagined, I am determined to focus on the silver lining: I am so thankful to be able to continue my education, to maintain friendships (virtually), and to know that all of these measures taken are for the safety of everyone in our world. On the bright side, I can actually make it to my 9 a.m. class on Blue Jeans, without needing to leave my bed!
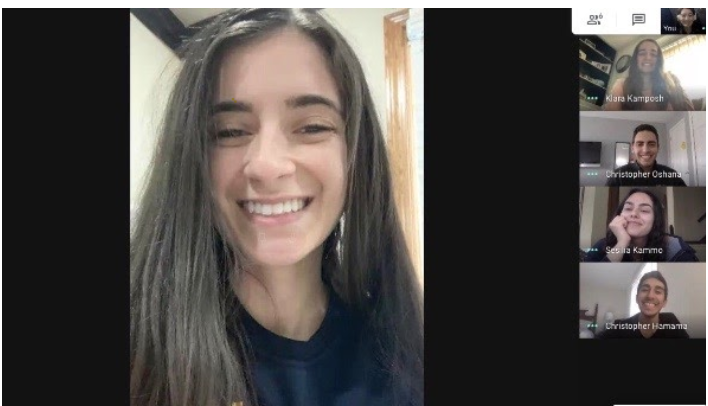
“As much as I miss being with my friends, we’ve been able to keep in touch with constant Facetimes and scheduled Google Hangouts when we want to coordinate with more people in different time zones. We are even able to watch movies together, virtually, thanks to the Netflix watch-party extension. If there is anything that I’ve learned from my time at the University of Michigan, it’s that opportunities are everywhere, whether you need to look for them or create them yourself. I have found comfort in being able to help our health care workers on the front lines against COVID-19, working as a pharmacy technician at CVS and volunteering to make face masks for our doctors and nurses as the need for PPE rises.”
Muriel Steinke, art & design sophomore, Stamps School of Art & Design

“As an art student who is perpetually frustrated when assignments don’t allow me to fully explore my most ambitious ideas, the downtime in light of recent events was something I was actually looking forward to filling with personal projects. In my mind, I pictured myself painting or drawing every day and feeling creatively refreshed. I brought my easel out of hiding and dug out all of my paint. I braced myself for a flood of quarantine-induced inspiration that would surely serve as a catalyst for my greatest work yet.
“This has not happened. I am not painting or drawing. I am, in fact, complaining and eating a lot of chips. I’ve already rewatched all of ‘Fleabag,’ and I call my friends and talk about nothing for two hours every day. My mom and I are trying to watch all of the Bond movies. I’m halfway through the second ‘Harry Potter’ book. But — I honestly feel okay about it. It’s true I’m not creating a magnum opus, but I’m fine, and I keep laughing at myself, which is just about all one could hope for at a time like this.”
Jared Pavlick, biomedical engineering freshman, School of Engineering
“Transitioning to all online classes has been a bit of a struggle. Since coming home, having online classes makes it tempting for me to sleep in, skip class to hang out with my brothers, check my phone when I’m watching a lecture, or forgo a discussion for a Youtube video.
“Yet, there are aspects of the shutdown that have been nice. It has allowed me to be with my family for the longest period of time since I have gone off for college. My brothers and I have found that the best way for us to stay sane is to play basketball. Every day we cycle through every pairing of teams, seeing who can win the most games. After playing basketball every day during this quarantine, I am just waiting to get a call from Juwan Howard asking when I can start playing for the team. Although this transition has not been easy, there are definitely silver linings to the whole situation.”
Alex Mullen, film, TV & media senior, College of Literature, Arts & Sciences
“One of the major disruptions this outbreak has caused is that I was forced to shut down the independent film project that I was working on all semester long. The project, intended to be a sort of senior thesis, required about a month-and-a-half’s worth of pre-production and was only about ¼ of the way finished with principal photography before classes moved online.

“Despite not being able to finish a project I kept close to my heart, this time has given me the opportunity to focus on smaller projects that I never would have thought of creating, like essay films. Spending so much time at home has reminded me of some of the things I love about my childhood house and the things about my house that make it home for me. I’ve decided to create an essay film that focuses on those feelings and all of the memories I’ve made here.
“While the change to remote classes online has been challenging, so far my professors have been very accommodating. Only one of my classes, a seminar of six people, has required synchronous class attendance, and that was a decision made by the students due to the discussion-based nature of the class. A wholesome moment I got out of this experience was the opportunity to get introduced to one of my professor’s one-year-old twin cats (very cute cats, I might add).
“To keep myself motivated, I’ve also started doing fitness challenges with friends — running a mile every day, doing 100 squats and calf raises, and more to make sure we stay in shape and motivate each other throughout our time spent inside. Although the end of my senior year has been more tumultuous than I ever could have expected, I’m excited for the time to try new things and continue to grow as a student and person.”
Anita Michaud, organizational studies & History of Art junior, College of Literature, Arts & Sciences

“Like many other students, my transition to online classes and adjusting to the new normal of working and learning from home has not been without difficulty. Most of my classes this semester are small, and I really enjoyed getting to know my classmates and professor in an intimate setting. Unfortunately, that environment is not easy to replicate virtually, but I think given the circumstances, my professors are doing the best they can. For example, my professor for the history of art class has maintained regular meeting times and has even offered to help students get to the grocery store if they don’t have a car on campus!
“Finding a routine and pockets of normalcy in abnormal times has been instrumental in staying on top of my coursework and extracurricular activities. I’m the business manager of The Michigan Daily, so I’ve been working closely with the student staff to coordinate regular check-in meetings throughout the semester. Now that I’m home all the time and have significantly more free time, I have the opportunity to cook and catch up on other hobbies I enjoy but don’t normally have the time to do! It’s been fun experimenting with new dishes and trying to replicate some of my favorite meals from Ann Arbor restaurants at home. Some of my favorite meals so far have been lentil soups, chili, and stir fry dishes.”
Anna Biberstein, freshman, School of Nursing

“As a freshman nursing student, I understand the importance of staying focused, especially in my nursing classes like Anatomy and Physiology — after all, I wouldn’t trust a nursing student who doesn’t know how the body works or where the femur is.
“This crisis is frightening, but when I look at all of the nurses and other healthcare workers boldly doing their part to care for those impacted by this disease, I am all the more proud of the profession I have chosen. It can be easy to fall into the trap of feeling bad for yourself, but I have been trying to focus on the good that is coming out of this situation instead — finally convincing my parents to get a puppy after 19 years, quality time spent with my family, and doing my best to make sure that my grandma doesn’t feel lonely during this time.

“My professors have been more than helpful and understanding throughout the whole transition; it’s amazing how they have used creativity and technology to adapt. In my Happiness and Health class, for example, my professor asked us to grab some chocolate for a practice in “savoring” — who would have thought that I’d be having a spiritual experience with a Hershey’s bar over Blue Jeans? Not that I’m complaining.”
Caitlin Shyuu, microbiology senior, College of Literature, Arts and Sciences
“When classes switched over to being remote, I had trouble adjusting, not because of the actual switch itself but because of my lack of motivation that followed. Classes being moved online meant my friends slowly started leaving Ann Arbor, and that I would stop seeing the familiar faces that I have been interacting with for four years straight. Graduation being canceled meant that I would not get the opportunity to show my parents, who live in Taiwan and don’t get the chance to visit me on campus, the buildings where my best and worst classes were held, or take them to my go-to restaurants on the weekends.
“But through the ongoing experience, I’m learning to see things from a positive light. Learning that my friends and family are just a call away brings a steady stream of communication, which in turn gives support, encouragement, and motivation. Having to say our goodbyes so suddenly sucks, but it’s important to keep in mind that we are all in this together…and to the class of 2020: I’m proud of all of us.”

- google-plus
Back to In the News
Office of the Provost Alexander G. Ruthven Building Suite 4300 1109 Geddes Avenue Ann Arbor, MI 48109-1079
email: [email protected]
Michigan News 412 Maynard St. Ann Arbor, MI 48109-1399 phone: 734-764-7260

Copyright © 2024 The Regents of the University of Michigan
Website by Michigan Creative Office of the Vice President for Communications
Interested in being featured on the Engaged Michigan twitter account? Fill out the Google Form below for more information. Follow us on Twitter for the latest updates on Engaged Learning throughout U-M.
STUDENTS' STRUGGLES ANG THEIR COPING MECHANISMS IN THE NEW NORMAL

- Department of Education of the Philippines
- This person is not on ResearchGate, or hasn't claimed this research yet.
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Trixie M Lao

- Roselle M. Soriano

- Michelle Gumiran Quijano

- Lalaine E. Ricardo
- Freden S. Delgado

- Eba Christie C. Rivera
- Janet C. Rivera
- Mark Raguindin Limon

- Ruby R Briones
- Mario O Cantanero

- S Valmorida

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
A National Strategy for the “New Normal” of Life With COVID
- 1 Perelman School of Medicine and The Wharton School, University of Pennsylvania, Philadelphia
- 2 Center for Infectious Disease Research and Policy, University of Minnesota, Minneapolis
- 3 Grossman School of Medicine, New York University, New York, New York
- Viewpoint The First 2 Years of COVID-19—Lessons to Improve Preparedness for the Next Pandemic Jennifer B. Nuzzo, DrPH, SM; Lawrence O. Gostin, JD JAMA
- Viewpoint A National Strategy for COVID-19—Testing, Surveillance, and Mitigation Strategies David Michaels, PhD, MPH; Ezekiel J. Emanuel, MD, PhD; Rick A. Bright, PhD JAMA
- Viewpoint A National Strategy for COVID-19 Medical Countermeasures Luciana L. Borio, MD; Rick A. Bright, PhD; Ezekiel J. Emanuel, MD, PhD JAMA
- Viewpoint The Pandemic Preparedness Program Eli Y. Adashi, MD, MS; I. Glenn Cohen, JD JAMA
- Medical News & Perspectives Former Biden-Harris Transition Advisors Propose a New National Strategy for COVID-19 Jennifer Abbasi JAMA
- Comment & Response Strategy for the “New Normal” of Life With COVID—Reply Ezekiel J. Emanuel, MD, PhD; Michael Osterholm, PhD, MPH; Céline R. Gounder, MD, ScM JAMA
- Comment & Response Strategy for the “New Normal” of Life With COVID Afschin Gandjour, MD, PhD, MA JAMA
- Viewpoint COVID-19 Vaccination—Becoming Part of the New Normal Peter Marks, MD, PhD; Janet Woodcock, MD; Robert Califf, MD JAMA
As the Omicron variant of SARS-CoV-2 demonstrates, COVID-19 is here to stay. In January 2021, President Biden issued the “National Strategy for the COVID-19 Response and Pandemic Preparedness.” As the US moves from crisis to control, this national strategy needs to be updated. Policy makers need to specify the goals and strategies for the “new normal” of life with COVID-19 and communicate them clearly to the public.
SARS-CoV-2 continues to persist, evolve, and surprise. In July 2021, with vaccinations apace and infection rates plummeting, Biden proclaimed that “we’ve gained the upper hand against this virus,” and the Centers for Disease Control and Prevention (CDC) relaxed its guidance for mask wearing and socializing. 1 By September 2021, the Delta variant proved these steps to be premature, and by late November, the Omicron variant created concern about a perpetual state of emergency.
In delineating a national strategy, humility is essential. The precise duration of immunity to SARS-CoV-2 from vaccination or prior infection is unknown. Also unknown is whether SARS-CoV-2 will become a seasonal infection; whether antiviral therapies will prevent long COVID; or whether even more transmissible, immune-evading, or virulent variants will arise after Omicron.
Another part of this humility is recognizing that predictions are necessary but educated guesses, not mathematical certainty. The virus, host response, and data will evolve. Biomedical and public health tools will expand, along with better understanding of their limitations. The incidence of SARS-CoV-2, vaccination rates, hospital capacity, tolerance for risk, and willingness to implement different interventions will vary geographically, and national recommendations will need to be adapted locally.
It is imperative for public health, economic, and social functioning that US leaders establish and communicate specific goals for COVID-19 management, benchmarks for the imposition or relaxation of public health restrictions, investments and reforms needed to prepare for future SARS-CoV-2 variants and other novel viruses, and clear strategies to accomplish all of this.
Redefining the Appropriate National Risk Level
The goal for the “new normal” with COVID-19 does not include eradication or elimination, eg, the “zero COVID” strategy. 2 Neither COVID-19 vaccination nor infection appear to confer lifelong immunity. Current vaccines do not offer sterilizing immunity against SARS-CoV-2 infection. Infectious diseases cannot be eradicated when there is limited long-term immunity following infection or vaccination or nonhuman reservoirs of infection. The majority of SARS-CoV-2 infections are asymptomatic or mildly symptomatic, and the SARS-CoV-2 incubation period is short, preventing the use of targeted strategies like “ring vaccination.” Even “fully” vaccinated individuals are at risk for breakthrough SARS-CoV-2 infection. Consequently, a “new normal with COVID” in January 2022 is not living without COVID-19.
The “new normal” requires recognizing that SARS-CoV-2 is but one of several circulating respiratory viruses that include influenza, respiratory syncytial virus (RSV), and more. COVID-19 must now be considered among the risks posed by all respiratory viral illnesses combined. Many of the measures to reduce transmission of SARS-CoV-2 (eg, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.
What should be the peak risk level for cumulative viral respiratory illnesses for a “normal” week? Even though seasonal influenza, RSV, and other respiratory viruses circulating before SARS-CoV-2 were harmful, the US has not considered them a sufficient threat to impose emergency measures in over a century. People have lived normally with the threats of these viruses, even though more could have been done to reduce their risks.
The appropriate risk threshold should reflect peak weekly deaths, hospitalizations, and community prevalence of viral respiratory illnesses during high-severity years, such as 2017-2018. 3 That year had approximately 41 million symptomatic cases of influenza, 710 000 hospitalizations and 52 000 deaths. 4 In addition, the CDC estimates that each year RSV leads to more than 235 000 hospitalizations and 15 000 deaths in the US. 3 This would translate into a risk threshold of approximately 35 000 hospitalizations and 3000 deaths (<1 death/100 000 population) in the worst week.
Today, the US is far from these thresholds. For the week of December 13, 2021, the CDC reported the US experienced more than 900 000 COVID-19 cases, more than 50 000 new hospitalizations for COVID-19, and more than 7000 deaths. 5 , 6 The tolerance for disease, hospitalization, and death varies widely among individuals and communities. What constitutes appropriate thresholds for hospitalizations and death, at what cost, and with what trade-offs remains undetermined.
This peak week risk threshold serves at least 2 fundamental functions. This risk threshold triggers policy recommendations for emergency implementation of mitigation and other measures. In addition, health systems could rely on this threshold for planning on the bed and workforce capacity they need normally, and when to institute surge measures.
Rebuilding Public Health
To cope with pandemic, and eventually, endemic SARS-CoV-2 and to respond to future public health threats requires deploying real-time information systems, a public health implementation workforce, flexible health systems, trust in government and public health institutions, and belief in the value of collective action for public good. 7 , 8
First, the US needs a comprehensive, digital, real-time, integrated data infrastructure for public health. As Omicron has reemphasized, the US is operating with imprecise estimates of disease spread, limited genomic surveillance, projections based on select reporting sites, and data from other countries that may not be generalizable. These shortcomings are threatening lives and societal function.
The US must establish a modern data infrastructure that includes real-time electronic collection of comprehensive information on respiratory viral infections, hospitalizations, deaths, disease-specific outcomes, and immunizations merged with sociodemographic and other relevant variables. The public health data infrastructure should integrate data from local, state, and national public health units, health care systems, public and commercial laboratories, and academic and research institutions. Using modern technology and analytics, it is also essential to merge nontraditional environmental (air, wastewater) surveillance data, including genomic data, with traditional clinical and epidemiological data to track outbreaks and target containment.
Second, the US needs a permanent public health implementation workforce that has the flexibility and surge capacity to manage persistent problems while simultaneously responding to emergencies. Data collection, analysis, and technical support are necessary, but it takes people to respond to crises. This implementation workforce should include a public health agency–based community health worker system and expanded school nurse system.
A system of community public health workers could augment the health care system by testing and vaccinating for SARS-CoV-2 and other respiratory infections; ensuring adherence to ongoing treatment for tuberculosis, HIV, diabetes, and other chronic conditions; providing health screening and support to pregnant individuals and new parents and their newborns; and delivering various other public health services to vulnerable or homebound populations.
School nurses need to be empowered to address the large unmet public health needs of children and adolescents. As polio vaccination campaigns showed, school health programs are an efficient and effective way to care for children, including preventing and treating mild asthma exacerbations (often caused by viral respiratory infections), ensuring vaccination as a condition for attendance, and addressing adolescents’ mental and sexual health needs. School clinics must be adequately staffed and funded as an essential component of the nation’s public health infrastructure.
Third, because respiratory infections ebb and flow, institutionalizing telemedicine waivers, licensure to practice and enable billing across state lines, and other measures that allow the flow of medical services to severely affected regions should be a priority.
Fourth, it is essential to rebuild trust in public health institutions and a belief in collective action in service of public health. 7 Communities with higher levels of trust and reciprocity, such as Denmark, have experienced lower rates of hospitalization and death from COVID-19. 7 Improving public health data systems and delivering a diverse public health workforce that can respond in real time in communities will be important steps toward building that trust more widely.
Conclusions
After previous infectious disease threats, the US quickly forgot and failed to institute necessary reforms. That pattern must change with the COVID-19 pandemic. Without a strategic plan for the “new normal” with endemic COVID-19, more people in the US will unnecessarily experience morbidity and mortality, health inequities will widen, and trillions will be lost from the US economy. This time, the nation must learn and prepare effectively for the future.
The resources necessary to build and sustain an effective public health infrastructure will be substantial. Policy makers should weigh not only the costs but also the benefits, including fewer deaths and lost productivity from COVID-19 and all viral respiratory illnesses. Indeed, after more than 800 000 deaths from COVID-19, and a projected loss of $8 trillion in gross domestic product through 2030, 8 these interventions will be immensely valuable.
Corresponding Author: Ezekiel J. Emanuel, MD, PhD, Medical Ethics and Health Policy, Perelman School of Medicine, University of Pennsylvania, 423 Guardian Dr, Blockley Hall, Philadelphia, PA 19104 ( [email protected] ).
Published Online: January 6, 2022. doi:10.1001/jama.2021.24282
Conflict of Interest Disclosures: Dr Emanuel reported personal fees, nonfinancial support, or both from companies, organizations, and professional health care meetings and being a venture partner at Oak HC/FT; a partner at Embedded Healthcare LLC, ReCovery Partners LLC, and COVID-19 Recovery Consulting; and an unpaid board member of Village MD and Oncology Analytics. Dr Emanuel owns no stock in pharmaceutical, medical device companies, or health insurers. No other disclosures were reported.
Additional Information: Drs Emanuel, Osterholm, and Gounder were members of the Biden-Harris Transition COVID-19 Advisory Board from November 2020 to January 2021.
See More About
Emanuel EJ , Osterholm M , Gounder CR. A National Strategy for the “New Normal” of Life With COVID. JAMA. 2022;327(3):211–212. doi:10.1001/jama.2021.24282
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Adjusting to the New Normal
- Posted August 14, 2020
- By Jacqueline Zeller

As the summer winds down, there are still many unknowns about what school will look like in some communities. Schools and parents are working hard to plan for how to best keep children and educators safe while providing quality education to students.
Below are some ideas parents and other primary caregivers may consider to help children adjust to the circumstances of this school year, with its many uncertainties. Many of these ideas are in line with the National Association of School Psychologists and American School Counselor Association’s Reentry Considerations and guidance regarding talking to children about COVID. This piece is meant to be informational in nature and not to provide medical advice or recommendations. These are general considerations, but parents should contact their own providers for individualized advice for their families and children.
- Talk with your child’s school and/or medical or professional provider to consult on what makes the most sense to support your child and family in the transition back to school. Each child is unique, and parents can adapt ideas to the individual needs of their children and family.
- Provide developmentally appropriate and honest information regarding the beginning of the school year to help students understand what to expect. It is important to leave time for children to ask questions . When adults remain calm in the conversation, while offering information about successfully transitioning back to school, they can help children gain an increased sense of control. It is best not to overly focus on the news or unnecessary details that might cause increased distress to children. In general, with younger children, brief descriptions (with accurate information) are helpful. Children will respond to your emotions. Offer love and reassurance and remind children that adults, including their teachers and parents, are working to keep children safe.
- Listen to children’s questions and concerns . Remember that young children might also communicate through play.
- If children return to in-person school, they will need to be taught new routines regarding physical distancing, hygiene, wearing masks (when required), sharing, etc. It will be important that these new social expectations are taught and reinforced with patience and care. Parents may communicate with the school to understand the new expectations so that they can also have discussions and/or practice at home as needed. For example, parents might practice wearing masks or hand-washing at home. Social stories, books, comic strips, and role-playing that model and educate about the new social routines may also be useful ways to reinforce new school expectations at school and at home.
- Connecting with the school and reading school communications can also help parents reinforce expectations with common words/phrases in both the home and school settings, when appropriate, so that children are better able to connect concepts. For example, if the phrases “social distancing” or “hygiene” are used in the school setting it might be helpful to use the same words at home when reinforcing expectations regarding the new routines.
"When children have predictable routines, feel cared for, and have a sense of safety, they have a stronger foundation to learn. Making sure that there is a balanced approach to the curriculum that acknowledges the importance of supporting children’s well-being during the start of the school year will be important."
- Connect with your child’s school if you have specific questions or concerns regarding fall plans, mental health, and family support needs, including food and/or housing assistance, etc. If parents notice significant behavioral or mood changes, they can also connect with school and/or community agencies to get referrals, if needed. Parents can connect with school counselors, school psychologists, school adjustment counselors and/or school social workers if they feel a child might benefit from additional supports at school and/or in the community. Some families might choose to reach out to their medical providers for referrals and resources for their needs. Even if these needs aren’t apparent at the beginning of the school year, keep lines of communication open with the school and providers should such needs arise at a later point. Every family and child will have their own needs, and connecting with a professional trained to help can offer more tools and resources.
- If children will be returning to school in-person, prior to the start of school, parents may consider walking or driving by the school if it is safe to do so, and if they feel it would support their child’s comfort with the transition back to school or to starting a new school.
- If the school provides a way to do so, connect with the new teacher ahead of time to help increase the child’s comfort level. For example, some schools may have a teacher familiar to the child from a previous year introduce the new teacher or offer back-to-school events to meet teachers (even virtually). This way, students can see the teacher is excited to meet them and work with them.
- Parents of children with special needs may want to communicate any additional questions or concerns to school staff regarding available supports in the upcoming school year and how they can help their children with the beginning of the school year.
- Providing a routine is helpful to children. Knowing that the routine might need to change depending on the ongoing health situation, parents can try to plan and give warnings as much as possible if changes occur. Visual reminders of routines can also be helpful with young children.
Given the current situation, focusing on the well-being of the child will be important — especially during the beginning of the school year. The adjustment back to school is always just that — an “adjustment” — and this year brings unprecedented challenges. When children have predictable routines, feel cared for, and have a sense of safety, they have a stronger foundation to learn. Making sure that there is a balanced approach to the curriculum that acknowledges the importance of supporting children’s well-being during the start of the school year will be important.
Parents are working hard and balancing multiple responsibilities. Parents who remember to be kind and patient with themselves, and to reach out for support when they need it, can more effectively care for their children and model positive coping strategies.

Usable Knowledge
Connecting education research to practice — with timely insights for educators, families, and communities
Related Articles

Hope and Resilience in Childhood

The Art of Talking With Children
Ten ways to jumpstart conversations with kids that will help them bounce back from challenges

The Negative Effects of Remote Learning on Children's Wellbeing

Am I coping well during the pandemic?
Professor of Psychology, The University of Melbourne
Disclosure statement
Nick Haslam receives funding from the Australian Research Council.
University of Melbourne provides funding as a founding partner of The Conversation AU.
View all partners
The pandemic has posed unprecedented challenges. Many of us have lost work, gained carer responsibilities and grappled with social isolation. Experts have warned of a looming wave of mental illness as a result.
Research suggests they’re largely correct. Surveys in Australia , the UK and the USA point to rates of depression, anxiety and suicidal thinking substantially higher than in previous years.
But over time, people have changed how they have responded to the threat of COVID-19. Google searches have shifted from the harm of the pandemic itself to ways of dealing with it, such as exercising and learning new skills.
This pivot points to a new focus on coping with COVID-19.
Many ways of coping
Coping is the process of responding effectively to problems and challenges. To cope well is to respond to the threat in ways that minimise its damaging impact.
Coping can involve many different strategies and it’s likely you have your own preferred ones. These strategies can be classified in many ways, but a key distinction is between problem-focused and emotion-focused strategies.
What’s the difference?
Problem-focused coping involves actively engaging with the outside world. This might mean making action plans, seeking further information about a threat, or confronting an adversary.
Emotion-focused coping, in contrast, is directed inward, attempting to change how we respond emotionally to stressful events and conditions, rather than to change them at their source.
Effective emotion-focused strategies include meditation, humour and reappraising difficulties to find benefits.
Less effective emotion-focused strategies include seeking distractions, denial and substance use. Although these tactics may stave off distress in the short term, they neither address its causes nor prevent its longer term effects.

Which is best?
Neither of these coping strategies is intrinsically more or less effective than the other. Both can be effective for different kinds of challenges.
Problem-focused strategies are said to work best when we can control the problem.
However, when we face an immovable challenge, it can be better to adjust our response to it using emotion-focused strategies, rather than battling fruitlessly against it.
Coping strategies during the pandemic
Physical activity and experiencing nature can offer some protection from depression during the pandemic. One study even points to the benefits of birdwatching .
But there’s more evidence around coping strategies to avoid. Rising levels of substance use during the pandemic are associated with greater distress.
Eating too many snacks and accessing too much COVID-related media have also been linked to higher levels of stress and depression. So these should be consumed in moderation.

How can I tell if I’m not coping well?
We should be able to assess how well we are coping with the pandemic by judging how we’re going compared to our previous normal.
Think of yourself this time last year. Are you drinking more, sleeping poorly or experiencing fewer positive emotions and more negative emotions now?
If the answer to any of these questions is “yes”, then compared to your previous normal, your coping may not been as good as it could be. But before you judge your coping critically, it’s worth considering a few things.
Your coping is relative to your challenge
The pandemic may be shared, but its impacts have been unequal.
If you live alone, are a caregiver or have lost work, the pandemic has been a larger threat for you than for many others. If you’ve suffered more distress than others, or more than you did last year, it doesn’t mean you have coped less well — you may have just had more to cope with.
Read more: Your coping and resilience strategies might need to shift as the COVID-19 crisis continues
Negative emotions can be appropriate
Experiencing some anxiety in the face of a threat like COVID-19 is justified. Experiencing sadness at separation from loved ones under lockdown is also inevitable. Suffering does not mean maladjustment.
In fact, unpleasant emotions draw our attention to problems and motivate us to tackle them, rather than just being signs of mental fragility or not coping.
We should, of course, be vigilant for serious problems, such as thoughts of self-harm, but we should also avoid pathologising ordinary distress. Not all distress is a symptom of a mental health problem.

Read more: 7 mental health coping tips for life in the time of COVID-19
Coping isn’t just about emotions anyway
Coping isn’t all about how we feel. It’s also about action and finding a sense of meaning and purpose in life, despite our distress. Perhaps if we’ve sustained our relationships and done our jobs passably during the pandemic, we have coped well enough, even if we have sometimes been miserable.
Read more: 7 science-based strategies to cope with coronavirus anxiety
Coping with COVID-19 has been an uneven contest
Social distancing and lockdowns have left us with a reduced coping repertoire. Seeking emotional and practical support from others, also known as “social coping”, is made more difficult by pandemic restrictions. Without our usual supports, many of us have had to cope with one arm tied behind our backs.
So remember to cut yourself some slack. For most people, the pandemic has been a unique challenge. When judging how well we’ve coped we should practise self-compassion . Let’s not make things worse by criticising ourselves for failing to cope better.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
- Mental health
- Mental illness
- Social isolation
- Social restrictions

Postdoctoral Research Fellowship

Health Safety and Wellbeing Advisor

Social Media Producer

Dean (Head of School), Indigenous Knowledges

Senior Research Fellow - Curtin Institute for Energy Transition (CIET)

Essay from The New Normal in Asia Series
The “new normal”: thoughts about the shape of things to come in the post-pandemic world.
Nicholas Eberstadt offers insights into the challenges to U.S. leadership in a post-pandemic world. This is the inaugural essay in the series “ The New Normal in Asia ,” which explores ways in which the Covid-19 pandemic might adjust, shape, or reorder the world across multiple dimensions.
Though we are as yet barely weeks into the Covid-19 pandemic, what should already be apparent is that it has precipitated the deepest and most fundamental crisis for Pax Americana that this set of global economic and security arrangements has faced in the past three postwar generations.
We are still very much in the “fog of war” phase of the calamity. The novel coronavirus and its worldwide carnage have come as a strategic surprise to thought leaders and political decision-makers alike. Indeed, it appears to be the intellectual equivalent of an unexpected asteroid strike for almost all who must cope in these unfamiliar new surroundings. Few had seriously considered the contingency that the world economy might be shaken to its foundations by a communicable disease. And even now that this has happened, many remain trapped in the mental coordinates of a world that no longer exists.
Such “prewar” thinking is evident everywhere right now in the earliest phase of what may turn out to be a grave and protracted crisis. Here in the United States, we watch, week by week, as highly regarded financial analysts from Wall Street and economists from the academy misestimate the depths of the damage we can expect—always erring on the side of optimism.
After the March lockdown of the country to “flatten the curve,” the boldest voices dared to venture that the United States might hit 10% unemployment before the worst was over. Four weekly jobless claims reports and 22 million unemployment insurance applications later, U.S. unemployment is already above the 15% mark: north of 1931 levels, in other words. By the end of April, we could well reach or break the 20% threshold, bringing us to 1935 levels, and 1933 levels (25%) no longer sound fantastical. Even so, political and financial leaders talk of a rapid “V-shaped recovery” commencing in the summer, bringing us back to economic normalcy within months. This is prewar thinking, and it is looking increasingly like the economic equivalent of talk in earlier times about how “the boys will be home by Christmas.”
This is moreover a global crisis, and vision has not yet focused on the new realities in other leading powers and major economies. If we try to take an unflinching measure of the impact globally, we can see both good news and bad news—although the two are by no means equally balanced.
The good news is that policymakers the world over have learned from the prewar Great Depression and are unlikely to repeat its exact mistakes. Instead of reducing the money supply and forcing bank collapses, the U.S. Federal Reserve this time is flooding the world with liquidity. Likewise, U.S. fiscal policy, far from attempting to impose further austerity on an already imploding economy through balancing budgets, is embracing Keynesianism with an abandon that might have startled Keynes himself. Given the “stimulus” packages already passed in the last month, this year’s U.S. budget deficit to GDP ratio is already certain to be of World War II scale. And, at least so far, no emanations of Smoot-Hawley-like impulses are on the policy horizon. Last time around, protectionism had devastating reverberations on an already severely stressed international trade and financial system. Confidence in U.S. and international economic management of the current crisis, at least for the time being, is reflected inter alia in the surprisingly sanguine valuations of the stock indices both in the United States and abroad.
The bad news, on the other hand, lies in the nature of the virus itself and in its implications for human life and socioeconomic arrangements. Covid-19 is an extremely contagious virus with high lethality for those exposed to it, and it can be transmitted by asymptomatic “super spreaders.” Further, since this disease is zoonotic (contracted from another species) and novel (our species has no preexisting immunity), the pandemic will roam the world in search of human quarry until an effective vaccine is invented and mass-produced—or until so many people are infected that herd immunity is conferred.
A Darwinian experiment to invite global herd immunity is unthinkable because it could entail untold millions of deaths. New vaccines, for their part, typically take many years to develop. Barring some miracle, even a crash program to perfect a vaccine is currently expected to take at least a year, and it could be a year and a half or longer before a serviceable serum is generally available to the public. Reports now emanating from South Korea, moreover, suggest that survivors might also be susceptible to reinfection. If so, the quest to come up with a lasting inoculation against Covid-19 may be all that much more daunting.
Consequently, societies the world over face the prospect of rolling lockdowns and quarantines until such time as a technological breakthrough rescues them from this condition. This would seem to mean that not just a single national lockdown of a country’s population and economy is in store to fend off mass contagion but rather quite possibly a succession of them—not just one mother-of-all-economic-shocks but an ongoing crisis that presses economic performance severely in countries all around the world simultaneously.
The potential downside of this crisis looks dire enough for affluent societies: even with excellent economic management, they may be in for gruesome recessions, both painful and prolonged. But the situation for the populations of low-income countries—and for least-developed, fragile states—could prove positively catastrophic. Not only are governments in these locales much less capable of responding to pandemics, but malnourished and health-compromised people are much more likely to succumb to them. Even apart from the humanitarian disasters that may result directly from raging outbreaks in poor countries, terrible indirect consequences may also lie in wait for these vulnerable societies. The collapse of economic activity, including demand for commodities, such as minerals and energy, will mean that export earnings and international remittances to poor countries are set to crash in the months ahead and remain low for an indefinite period. Entirely apart from contagion and lockdowns, this can only mean an unavoidable explosion of desperate need—and under governments least equipped to deal with this. While we can hope for the best, the worst could be much, much worse than most observers currently imagine.
Eventually, of course, we will emerge from the current crisis. Envisioning the post-crisis “new normal” is extraordinarily difficult at this early juncture—not that much less demanding, perhaps, than imagining what the postwar world would look like from the vantage point of, say, autumn 1939. Lacking clairvoyance, we can only peer through the glass darkly at what may be the shape of things to come in the post-pandemic order. Yet it is not too soon to offer one safe prediction about that coming order, and to identify three critical but as yet unanswerable questions, the answers to which promise to shape it decisively.
The safe prediction is that the Indo-Pacific, then as now, will be the locus of global economic, political, and military power—and will remain so for at least the coming generation, possibly much longer. Currently, countries belonging to the Asia-Pacific Economic Cooperation (APEC) account for as much as 60% of the world’s estimated GDP and close to half of global trade. If we add India, which is not an APEC member, to that roster, the economic predominance of the region looks even more overwhelming. APEC plus India likewise accounts for much—perhaps most—of the ongoing knowledge production in the world today. By such necessarily imprecise measures as publications in peer-reviewed scientific journals, authors from the APEC-plus-India region are responsible for about three-fifths of current global output. The only state with truly global military capabilities (the United States) is part of this region, as are the only other two governments entertaining global strategic ambitions (China and Russia). In addition to these countries, India and (alas) North Korea are nuclear weapons states. For the moment, the combined nuclear potential of all nuclear powers outside the APEC-plus-India region (France, Britain, Pakistan, and Israel) is dwarfed by the atomic arsenals within it.
Barring a catastrophe of truly biblical proportion (a formulation that may admittedly seem to be tempting fate, given current circumstances) it is impossible to see what configuration of states or regions could displace the Indo-Pacific as the epicenter of world power anytime soon. Someday Africa might in theory become a contender for geopolitical dominance, but that date looks so distant that such scenarios for now are perhaps best narrated by science fiction writers.
“Will the Covid-19 pandemic bring a brutal end to the second age of globalization that began in 1945, just as World War I heralded the cataclysmic death of the first globalization (1870–1914)?”
As for the questions that stand decisively to shape the coming global order, the first concerns the scope and character of what we have been calling “globalization” in the years and decades ahead. Will the Covid-19 pandemic bring a brutal end to the second age of globalization that began in 1945, just as World War I heralded the cataclysmic death of the first globalization (1870–1914)?
At this early point in the crisis, it would take a brave (or foolish) soul to assert confidently that an end to our current far-reaching arrangements for world economic integration simply could not happen. That said, at least for now, it would look as if a lot of things that have not yet gone wrong would have to go wrong, and at the same time sweep away the foundations (and memory plastic) for the networks of trade, finance, communications, technology, culture, and more that have come to deeply connect societies all around the world today. Not much less than a continuing, cascading, and unabated series of worldwide political blunders—not excluding military adventures—would be required to burn this edifice to the ground.
On the other hand, it is also hard to see how a post-pandemic world will pick itself up and carry on with commerce, finance, and global governance as if nothing much happened around the year 2020. Even under the optimistic assumptions—i.e., the assumptions wherein the second age of globalization survives Covid-19’s heavy blow—much will need to be dramatically different. Until the advent of some biometric, post-privacy future, the more or less free movement of peoples across national borders will be a nonstarter. “Davos” stands to become a quaint word, somewhat like “Esperanto,” as national interests and economic nationalism come roaring back. International supply chains will tend to be resourced domestically, notwithstanding the immediate apparent cost in terms of production and profits. At the same time, today’s crisis may explode and wipe out old inefficient business models that had already outlived their usefulness: the “big box” store and retail malls, the unproductive (but sociologically alluring) office, the law firm (with its Soviet-style valuations of its services on the basis of inputs rather than outputs), perhaps the cartelized, price-fixing university as well, and more.
On the positive side, the creative destruction the crisis will unleash will eventually offer immense opportunities for innovation and dynamic improvements in productivity, so long as resources from inefficient or bankrupt undertakings are reallocated to more promising new purposes. To give just one example, the returns on remote communications will likely be high, incentivizing impressive breakthroughs. Post-pandemic economies around the world will need all the productivity surges they can squeeze out of technological and organizational innovation, too—for they will almost certainly be saddled with a far higher burden of public debt than today. Moreover, given current demographic trends and the prospect of significantly less immigration, the shrinking of labor forces and the pronounced aging of national populations may be characteristic of a growing number of economies in the APEC-plus-India region and the rest of the world, and not just in high-income settings. Japan may become a model here, but not in a good way: avoiding “Japanification” could become a preoccupation of policymakers, pundits, and populaces in an epoch of diminished expectations for globalization.
A second huge question for the post-pandemic world concerns China: more specifically, how will the rest of the international community treat this increasingly powerful but intrinsically problematic state?
The world has yet to conduct the authoritative blue-ribbon scientific inquiry into the origins of the coronavirus pandemic that is obviously and urgently needed. However, there is little doubt that heavy responsibility for the global health and economic crisis we are now coping with falls on the Chinese Communist Party (CCP)—and to a lesser but by no means negligible degree, on China’s collaborators within the World Health Organization. Had the CCP placed its population’s health above its own—had it behaved like an open society or followed international transparency norms—there is no question that the global toll from the Covid-19 pandemic would only be a fraction of what has been exacted to date. Epidemiologists from the University of Southampton in the United Kingdom have suggested that the damage might have been contained to just 5% of what we have thus far suffered with an expeditious (and honest) response to the Wuhan outbreak. If that estimate is overly precise, it nonetheless gives a sense of the price the world has paid for the CCP’s priorities and standard operating procedure. We also already know of the complicity of the World Health Organization at its highest levels in buying time for Beijing as the regime figured out how to spin the story of what happened in Hubei Province.
“…the post-pandemic world will have no choice but to contend at last with a problem long in the making: the awful dilemma of global integration without solidarity.”
It would be one thing if this crisis were a one-off—dreadful as the tragedy would be. The problem, unfortunately, is that it is not a one-off, and in fact cannot be. At the heart of the tragedy is an uncomfortable but unavoidable truth: the CCP simply does not share the same interests and norms as the international community into which it has been so momentously and thoroughly integrated. Moreover, there is scant evidence that integration into the world economy and global governance has been “reforming” the Chinese regime, in the sense of bringing its politics and behavior into closer alignment with those acceptable to Western populations. Quite the contrary: in the Xi Jinping era, China’s politics have manifestly been moving away from convergence as the regime has concentrated on perfecting a surveillance state policed by “market totalitarianism” (a social credit system powered by big data, artificial intelligence, and more).
Thus, the post-pandemic world will have no choice but to contend at last with a problem long in the making: the awful dilemma of global integration without solidarity. China is deeply interlinked with every APEC-plus-India economy and with those of the rest of the world as well. Chinese interests are likewise deeply embedded in much of the institutional apparatus that has evolved to facilitate international cooperation. How will the rest of the countries in the international community manage to protect their interests (including health security interests, but by no means limited to this alone) in such a world? Will it be possible to accurately identify and carefully isolate all the areas in which win-win transactions with the CCP are genuinely possible and cordon off everything else? Or will the CCP’s authoritarian influence compromise, corrupt, and degrade these same institutions, and likewise constrain or poison opportunities for truly free international economic cooperation and development after the Covid-19 pandemic?
Last, but by no means least important, there is the question of the United States’ disposition in a post-pandemic world.
Even before the Covid-19 crisis, it was not exactly a secret that the United States—which is to say, Americans—was becoming increasingly reluctant to shoulder responsibility for world leadership in the global order that Washington had been instrumental in creating and that U.S. power was indispensable in supporting. The skepticism and disfavor with which American proponents of internationalism were increasingly greeted at home, however, was not entirely explained by the deep historical roots of isolationism in our country. Nor can it be dismissively described as yet another paroxysm of paranoia and anti-intellectualism on the part of the yahoos, as would-be Hofstadters from today’s chattering classes would like to have it.
Such discontent with our nation’s considerable international obligations skews strongly with socioeconomic status. For those in the bottom half of the country, grievances with the status quo (which not so incidentally includes a strong political commitment to Pax Americana) are by no means delusional. Over the past two generations, the American escalator has broken down for many. Just before the Covid-19 crisis, at the supposed peak of a business cycle, work rates for prime-age American men (the 25–54 age group) were slightly lower than they had been in 1939, near the end of the Great Depression. It is hardly reassuring that this alarming situation has attracted relatively little attention from the talking and deciding classes (many of whom are shielded from personal familiarity with how the other half lives by Charles Murray’s famous bubble).
Scarcely less disconcerting than the work rates for American men are the dismal trends in wealth formation for the less well to do. According to estimates by the Federal Reserve, the mean real net worth for the bottom half of households in the United States was lower in 2019 than it had been in 1989 when the Berlin Wall fell. By these estimates, in fact, the net worth of such households was at least a sixth lower in 2019 than it had been three decades before. Voters from these households might be excused if they were prompted to ask what the fabled “end of the Cold War” had done for them. Recall that these same Americans witnessed a decline in net household worth in a period when overall nominal net worth in the United States soared by almost $80 trillion—an average of almost $250,000 for every man, woman, and child in our country today. Since the arrival of Covid-19 on our shores, the net worth of the bottom half of Americans has dropped still further, as their indebtedness has risen and the value of their assets (mainly homes) declined. It could be quite some time before the balance sheets of those homes look as “favorable” as they did in 2019.
In the United States, the constitutional duty to obtain the consent of the governed obtains for the little people, too, even if they happen to comprise a majority of voters. And in a post-pandemic world, it may be even more difficult to convince a working majority that the globalized economy and other international entanglements actually work in their favor.
If U.S. leaders wanted to generate broad-based domestic support for Pax Americana, they need to devise a formula for generating prosperity for all. Such an agenda, of course, would win on its own merits, with or without an eye toward international security. Absent such a credible agenda, popular support for U.S. international leadership could prove increasingly open to question in the post-pandemic United States. The peril that declining domestic U.S. support poses to the current global order should not be minimized. If or when Pax Americana is destroyed, its demise may be due not to threats from without but rather to pressures from within.
Nicholas Eberstadt holds the Henry Wendt Chair at the American Enterprise Institute in Washington, D.C., and is a Senior Advisor to the National Bureau of Asian Research.
Correction (June 18, 2020): An earlier version of this essay stated that the real net worth for the bottom half of households was a third, rather than a sixth, lower in 2019.

Nicholas Eberstadt
American Enterprise Institute,
- United States
- globlization
- Chinese Communist Party (CCP)


An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
COVID-19: Adjusting to the "new normal" March 27, 2020

The COVID-19 pandemic has rapidly changed how we live, work and learn. First and foremost, I want to assure everyone that the safety of older adults, a population known to be at high risk, is paramount to NIH and NIA leadership.
The "new normal" of this public health emergency coupled with the guidance around physical distancing also makes this a trying time for clinicians, researchers and others who support our crucial science, including trial participants. While no one knows how long our current state will last, for now, I want to let the NIA community know that much-needed help and flexibility is already in motion as you are feeling the impact in your labs and clinical trials.
Grantees with specific questions should reach out directly to their NIA program officers . We are committed to responding as rapidly as possible as we transition to working and meeting online and supporting new research on the effects of this pandemic on older adults.
Resources from NIH OER
The NIH Office of Extramural Research (OER) has an excellent website on Coronavirus Information for NIH Applicants and Recipients , which links to NIH Guide Notices and FAQs, as well as CDC and WHO information. Dr. Mike Lauer, NIH deputy director for extramural research, recently wrote a blog and provided a video update for grantees and applicants on what’s being put into place to help.
Additionally, NIH OER also hosts a helpful FAQs page on COVID-19 flexibilities for applicants and recipients that covers changes regarding late applications , reporting, budgeting, salaries/stipends, travel cancellation fees and more. NIH has also issued guidance for institutions to ensure the safety of human participants and research staff in NIH-funded clinical trials and human subjects studies. Note that NIA peer review will continue during this time but shift from in-person to online meetings.
Time for resilience and perseverance
Above all, this is a time for resilience and perseverance as many studies and trials have put enrollment and follow-up on hold as universities and labs have switched to remote work. But researchers can still do things that don’t involve direct participant contact such as phone visits, data management, and analysis and dissemination activities, or tackle abstracts, presentations and manuscripts. Regardless, please keep in touch with your NIA program officer, your IRB and your institution as plans and policies evolve.
We are all in this together
In the face of realities of the current global crisis, we will need to continue to collaborate and work creatively. Together, we will improvise, adapt and overcome. NIA is here to help while you take actions to keep yourselves, your families, your colleagues and your participants safe and healthy.
We will blog more in the coming weeks about the COVID-19 impact on the NIA community, including about opportunities to contribute to research in this area. Please comment below with any questions or concerns. I wish you safety and wellness.
Subscribe to the NIA blog for weekly updates on funding policies and research priorities
Great information thank you!
Add new comment
A red asterisk ( * ) indicates a required field.
- Allowed HTML tags: <p> <br>
- No HTML tags allowed.
- Lines and paragraphs break automatically.
- Web page addresses and email addresses turn into links automatically.
nia.nih.gov
An official website of the National Institutes of Health

Get Started
PARENTING HUB
A School Psychologist’s Advice For Students On How To Cope During This ‘New Normal’
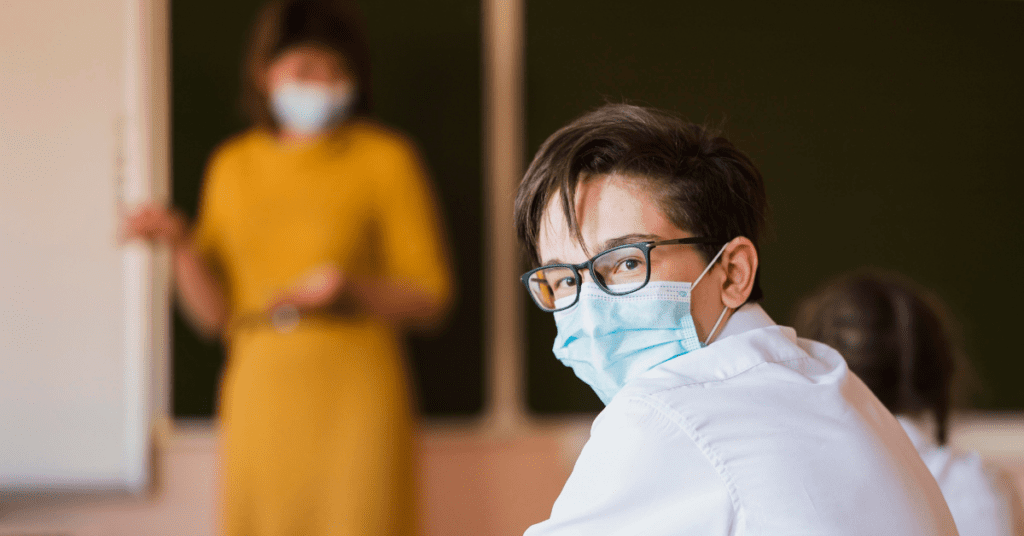
Dr. Roseann Capanna-Hodge
- November 2, 2020
In a recent Article with Broglie Blog titled, “ A School Psychologist’s Advice For Students On How To Cope During This ‘New Normal’ ” Dr. Roseann answers interview questions about Student's mental health during the pandemic. One of the questions she was asked was, “How can students who feel that they have little control over their current situation best combat this thought? What are some helpful ways and methods that could help students feel in control again?” Her response:
“The number one thing a parent can do to help their child feel less overwhelmed by everything that is happening in the world and in their lives, is to empower their child with decision making. Helping them to have more control over the choices they make is a great way to calm anxiety and build a sense of control. Ultimately we all crave control, so why not give your child opportunities to successfully manage things so they can feel better about themselves. ”
Read the Full Article
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:

You can get her books for parents and professionals , including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health , Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Recent Posts

Calm and Confident: How to Reduce Anxiety in an Autistic Child

Empowering Minds: What is Neurotherapy Treatment?

Beyond the Brainwaves: Different Types of Neurofeedback Therapy

Best ADHD Medication for a Child with Anxiety: Holistic Approaches

Sudden Behavioral Changes in Children: Is it PANS/PANDAS?

- Neurofeedback / Biofeedback
- Neurofeedback FAQ
- Terms & Conditions
- Privacy Policy
The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Having Computer issues?
about your child’s behavior that keeps you up at night?
By sending us your question, you give us permission to use your audio clip anonymously in our podcast.

- Siloy is watching

- INQUIRER.net
- RADYO INQUIRER
Coping with challenges in learning under the new normal
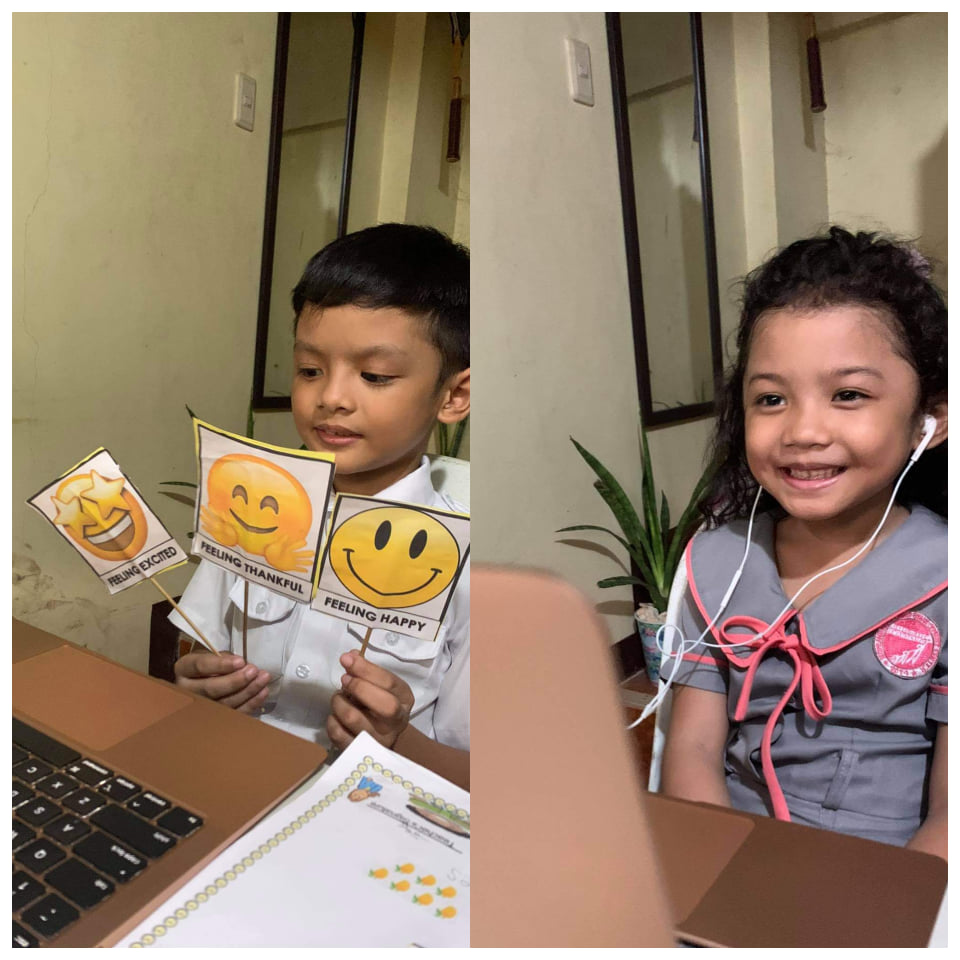
Francis, 8, and Misha, 6, attend their online class at their home in Dumanjug, Cebu.
CEBU CITY, Philippines — Learning in the “new normal” has begun for students and teachers in private institutions.
Although the classes in public schools are set to open on October 5, 2020 yet, some private schools have decided to step into education delivery under the new normal in August, or for some, even earlier.
As classes are mostly carried out online, parents and teachers agree that the challenge in learning under the new normal goes beyond the strength of one’s internet connection.
Eugene Dadol is in his third year in teaching senior high school subjects in a private institution in Cebu City.
But for the 23-year-old, embarking on a journey of teaching under the new normal seems like preparing for his first year in the profession.
Unlike in physical classes, where he can assess how the students comprehend with the materials that he presents, Dadol said virtual classes somehow limits the social cues for him to see if his students have absorbed his lessons.
“There are features I do, like install a plug-in that allows students to ‘notify’ me when they have a question, but it doesn’t capture all the cues that allow a teacher to spontaneously come up with techniques to adapt to the group dynamics,” he explained.
“Classroom management is not much of a risky deal if the routines were incorporated effectively. We limited the maximum students to 15 so it was easier to navigate the virtual class population. Other pedagogical aspects are not of a big problem because there are so many opportunities to transform all conventional learning processes into virtual platforms. However, it requires too much time to prepare for lessons. It feels like I prepared my subject materials all over again when I was first year in teaching,” Dadol added.
Similar to Dadol, Genesis Saquilabon, and Kimberly Mae Moral, who teach junior high school subjects in separate institutions, said both students and teachers are still starting to get the hang of the novel way of holding their classes brought by the precautions against the coronavirus disease (COVID-19).
While faced with the long-standing dilemma of poor internet connection, Saquilabon and Moral said they resort to upgrading connection and having a back-up plan to ensure that they will still be able to deliver their lessons.
“Mas nindot jud if face to face physically but since ma-ask man namo sila to [turn] on their cam, okay ra pod. Better than nothing, I guess,” Moral said.
(It would have been better if it were done face to face physically but since we can ask them to turn their cam on, it’s okay. Better than nothing, I guess.)
Beyond connectivity, Dadol added that technical concerns on the learning management systems used by the school could also pose a challenge in holding classes virtually.
Learning in the new normal
Former CDN Digital General Assignments Reporter Micah Sophia Marcellones, a mother of three, also shared how two of her children engage in school while being safe at home.
Marcellones and her family are living in Dumanjug town, Cebu, where her husband works. Her son, 8, and daughter, 6, are also attending a private school in the southern Cebu town.
“As much as possible I want my kids to keep learning, especially that they are in the initial reading and decoding stage. I want to give them proper education despite this trying time, and I cannot do this alone. Need na ko ang help sa atong mga teachers. Lahi ra man pud if naa interaction with teachers,” Marcellones said as she shared why she chose to enroll her children despite the pandemic.
(I need the help of the teachers. It’s different when there is interaction with the teachers.)
The 28-year-old mother is also “virtually” attending law school herself.
Her children’s school is employing online classes to supplement the modules that they need to accomplish at home.
“[The online classes are held] 2 times a week, 20-30 mins pero depende if tabian ang bata,” she said. (But it depends if the kid talks a lot.)
Aside from the unstable internet connection in their area, Marcellones said keeping her children’s focus on the lesson is another challenge to overcome.
“Knowing that they are just at home, toys ang gihunahuna. Mao na usa sa distraction nila. Another thing pud kung bag-o ang teacher and first time nila magkita online, a bit shy and awkward sa part sa bata. So it requires a lot of adjustment gyud,” she added.
“Knowing that they are just at home, toys are what they think of. That’s one of their distractions. Another thing is that if a teacher is new, and it’s the first time they see each other online, the kids feel a bit shy and awkward. So it really requires a lot of adjustment.)
Despite the challenges and the threats of the pandemic, teachers Dadol, Saquilabon, and Moral, and parents like Marcellones agree that coping with the new normal education is a two-way street.
“As a group, we always try to troubleshoot things immediately and pro-actively patch up some mishaps that might be a result of technological or pedagogical aspects. Best practices are also encouraged. I am not at all [demotivated]. I feel very challenged to come up with innovative and creative ways to implement my plans and troubleshoot challenges. In a way, this is my comfort zone because I get to explore and extract my creative juice,” Dadol said.
Saquilabon adds, “Learning really depends on the effort exerted by the students on their studies. In these trying times, teachers can do their role only that they can not touch their students. So for me, learning could happen anywhere as long as both the teacher and the students are committed. There’s no reason for demotivation.” /bmjo
Read: Councilor to Cebu City gov’t: Study how to help schools gain faster net
Subscribe to our daily newsletter
By providing an email address. I agree to the Terms of Use and acknowledge that I have read the Privacy Policy .
Disclaimer: The comments uploaded on this site do not necessarily represent or reflect the views of management and owner of Cebudailynews. We reserve the right to exclude comments that we deem to be inconsistent with our editorial standards.
Latest News
Filipina on hajj pilgrimage in saudi arabia dies of heatstroke, rescue of injured personnel lasted for 12 hours, featured stories, ora et labora: the guiding principle of cebu’s lone architecture exam topnotcher, palarong pambansa 2024: official billeting quarters revealed, foreigner nabbed for inappropriately touching man in cebu city, why does gov’t repair roads that are still in good condition, ‘misplaced’ street lights in downtown area part of cebu brt project, mactan-cebu airport poised to become next transit hub, coco martin lookalike video was edited, what’s the future of cebu brt phase 1 completion now uncertain.
Subscribe to our regional newsletter
- Environment
© 2024 Cebu Daily News - All Rights Reserved
We use cookies to ensure you get the best experience on our website. By continuing, you are agreeing to our use of cookies. To find out more, please click this link.

IMAGES
VIDEO
COMMENTS
The New Normal: How life has changed due to COVID-19 (and tips to help you cope) By Emilita Cornain. One thing that is certain, we know that adjusting to change can be challenging. Be it planned or unplanned, gradual or sudden, change is inevitable and very much part of being human.
In "The New Normal," Dr. Jennifer Ashton explores the mental health repercussions of the pandemic and ways to rebuild our overall health. As the chief medical correspondent for ABC News, Dr ...
As communities across the world wrangle with a "new normal" amid the coronavirus pandemic, millions are feeling the emotional and mental weight of this unprecedented time. A year ago, most of us had never heard of "social distancing" or "shelter at home.". Now, these are the foundation of our everyday reality.
To live in the world is to adapt constantly. A year after COVID-19 pandemic has emerged, we have suddenly been forced to adapt to the 'new normal': work-from-home setting, parents home-schooling their children in a new blended learning setting, lockdown and quarantine, and the mandatory wearing of face mask and face shields in public.
COVID-19 is the new face of pandemic. Since the discovery of COVID-19 in December 2019 in Wuhan, China, it has spread all over the world and the numbers are increasing day by day. Anyone can be susceptible to this infection but children, older adults, pregnant women, and people with comorbidity are more vulnerable.
Their generation will build what we know to be the new normal. 5 ways to adjust to this new normal. Like any change, the new normal can take some getting used to. But it also takes intention, work, and self-awareness. Here are five ways you can adjust to the new normal. Build mental fitness . Strong mental fitness and resiliency go hand-in-hand.
The next cadre of college and university students—struggling today through their own middle and high school journeys—will have been through pandemic-era online learning at a much younger age. But for now, all of us working in higher education can learn from how students are responding to the new normal with self-care, openness, and empathy.
A compliment and a 'thank you' can go a long way." Being more accepting of family members will help you keep peace in the home, but it's just as important to accept your situation and the 'new normal' as a whole. This doesn't mean resignation, but rather a realistic observation and a coping mindset, according to Dr. Leahy.
To grapple with the "new normal" and deal with the considerable challenges brought about by the pandemic, individuals need a considerable degree of flexibility. ... Adjustment to a "New Normal:" Coping Flexibility and Mental Health Issues During the COVID-19 Pandemic. Front. Psychiatry 12:626197. doi: 10.3389/fpsyt.2021.626197. Received ...
As recent history has proved, and as first-year UCSB undergraduate Annika Hando told The Bottom Line (TBL), "Two weeks is never just two weeks. In 2019, we all were so excited for an extra-long spring break, but those two weeks ended up to be a two-year-and-counting escapade.". When considering whether we will ever return to normal life ...
March 3, 2022. Two years after the coronavirus outbreak upended life in the United States, Americans find themselves in an environment that is at once greatly improved and frustratingly familiar. Around three-quarters of U.S. adults now report being fully vaccinated, a critical safeguard against the worst outcomes of a virus that has claimed ...
Research shows that it takes between 30 and 60 days to establish a new habit or to stop a bad habit, intentionally or coincidentally. That means the things we have been doing, that we didn't do before, will be easy to keep doing, if they are good for us. Similarly, if we started or expanded on unhelpful or unhealthy behaviours while in ...
As a young member of the screening committee for the pan India essay contest on 'A Year After Coronavirus', it has been heartening to realize that regardless of their age, the youth have collectively shared an aspiration to move towards an inclusive future post the global pandemic. Abhinav Kumar. Screening Committee Member.
Coping with COVID-19: U-M students share their 'new normal'. by Stephanie GrauMichigan News. Seniors (left to right) Kate Lytchakov, Devin Raymond, Caitlin Shyuu, and Nicole Wozniak take grad photos in the Law Quad while practicing social distancing. For students, this month with COVID-19 has been framed with uncertainty and stress.
distance learning is the new normal that our students are presently experiencing. In. order to fully understand the experiences of students in m odular distance learning, this. study is conducted ...
To cope with pandemic, and eventually, endemic SARS-CoV-2 and to respond to future public health threats requires deploying real-time information systems, a public health implementation workforce, flexible health systems, trust in government and public health institutions, and belief in the value of collective action for public good. 7,8 First, the US needs a comprehensive, digital, real-time ...
Visual reminders of routines can also be helpful with young children. Given the current situation, focusing on the well-being of the child will be important — especially during the beginning of the school year. The adjustment back to school is always just that — an "adjustment" — and this year brings unprecedented challenges.
Coping strategies during the pandemic. Physical activity and experiencing nature can offer some protection from depression during the pandemic. One study even points to the benefits of ...
Nicholas Eberstadt offers insights into the challenges to U.S. leadership in a post-pandemic world. This is the inaugural essay in the series "The New Normal in Asia," which explores ways in which the Covid-19 pandemic might adjust, shape, or reorder the world across multiple dimensions.
The COVID-19 pandemic has rapidly changed how we live, work and learn. First and foremost, I want to assure everyone that the safety of older adults, a population known to be at high risk, is paramount to NIH and NIA leadership. The "new normal" of this public health emergency coupled with the guidance around physical distancing also makes this ...
Just take it one day at a time and focus on what brings you joy and peace. 4. Limit your exposure to news and social media. To cope well requires being well-informed and updated with the latest. But that doesn't mean you have to be on social media, reading up on everything 24/7. Give yourself a break from social media.
In a recent Article with Broglie Blog titled, "A School Psychologist's Advice For Students On How To Cope During This 'New Normal ... PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS.
But for the 23-year-old, embarking on a journey of teaching under the new normal seems like preparing for his first year in the profession. Unlike in physical classes, where he can assess how the ...