- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences

Barriers and Gateways to Communication
- Carl R. Rogers
- F. J. Roethlisberger
This article originally appeared in HBR July–August 1952. Part I: Carl R. Rogers It may seem curious that someone like me, a psychotherapist, should be interested in problems of communication. But, in fact, the whole task of psychotherapy is to deal with a failure in communication. In emotionally maladjusted people, communication within themselves has broken […]
Part I: Carl R. Rogers
It may seem curious that someone like me, a psychotherapist, should be interested in problems of communication. But, in fact, the whole task of psychotherapy is to deal with a failure in communication. In emotionally maladjusted people, communication within themselves has broken down, and as a result, their communication with others has been damaged. To put it another way, their unconscious, repressed, or denied desires have created distortions in the way they communicate with others. Thus they suffer both within themselves and in their interpersonal relationships.
- CR The late Carl R. Rogers was a professor of psychology at the University of Chicago when he wrote this article. His many books include the groundbreaking Client-Centered Therapy (Houghton Mifflin, 1951).
- FR The late F.J. Roethlisberger was the Wallace Brett Donham Professor of Human Relations at the Harvard Business School. He is the author of Man-in-Organization (Harvard University Press, 1968) and other books and articles.
Partner Center
- Research article
- Open access
- Published: 11 February 2019
A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients
- Vida Maame Kissiwaa Amoah 2 ,
- Reindolf Anokye ORCID: orcid.org/0000-0002-7669-7057 1 ,
- Dorothy Serwaa Boakye 2 ,
- Enoch Acheampong 1 ,
- Amy Budu-Ainooson 3 ,
- Emelia Okyere 2 ,
- Gifty Kumi-Boateng 2 ,
- Cynthia Yeboah 2 &
- Jennifer Owusu Afriyie 2
BMC Nursing volume 18 , Article number: 4 ( 2019 ) Cite this article
133k Accesses
39 Citations
Metrics details
Therapeutic communication is essential in the provision of quality healthcare to patients. The purpose of this study was to explore the perceived barriers to effective therapeutic communication among patients and nurses at Komfo Anokye Teaching Hospital,Kumasi.
An exploratory study design was employed using a qualitative approach. A purposive sampling technique was used to select 13 nurses and patients who were interviewed using an unstructured interview guide. Interviews were audio-taped, transcribed verbatim and analyzed using thematic content analysis.
Patient-related characteristics that were identified as barriers to effective therapeutic communication included socio-demographic characteristics, patient-nurse relationship, language, misconception, as well as pain. Nurse-related characteristics such as lack of knowledge, all-knowing attitude, work overload and dissatisfaction were also identified as barriers to effective therapeutic and environmental-related issues such as noisy environment, new to the hospital environment as well as unconducive environment were identified as barriers to effective therapeutic communication among patients and nurses at Komfo Anokye Teaching Hospital,Kumasi.
Nurse-patient communication is an inseparable part of the patients’ care in every health setting; it is one of the factors that determine the quality of care. Several patient-related characteristics, nurse- related characteristics and environmental-related issues pose as barriers to effective therapeutic communication at Komfo Anokye Teaching Hospital,Kumasi and have ultimately; resulted in reducing effective communication at the wards. Therefore, all the barriers must be eradicated to promote effective therapeutic communication.
Peer Review reports
Therapeutic communication is essential in the provision of quality healthcare to patients. According to the American Nurses Association [ 1 ], nurses serve the role as patient advocates and must, therefore, preserve a therapeutic and professional nurse-patient relationship in their professional role with specific boundaries to their role. This makes it necessary that nurses adopt techniques in interacting with patients within the clinical setting which is an important part of their work in the provision of healthcare to patients.
Therapeutic communication involves a direct face to face contact with patients that focus on enhancing the physical and emotional well-being of patients [ 2 ]. A variety of techniques are used by nurses in communicating with patients. In therapeutic communication, there is a verbal and non-verbal flow of information between nurses and patients [ 3 ]. The verbal aspect of communication employs the use of words whilst non-verbal communication makes use of non-verbal cues such as eye contact, body language, and facial expression [ 3 ].
Bournes and Mitchell [ 4 ] state, “Health is the way people go on and live what is important to them, moment to moment and day to day”. The recognition of effective therapeutic communication as a critical part of healthcare provision has been highlighted in several studies [ 5 ]. Therapeutic communication has the potency of increasing patients’ knowledge and understanding, enhancing trust and self-health skills, increase adherence, providing comfort and facilitating the management of emotions key to patients’ health and well-being [ 2 ]. Again, it has been well documented in several studies that medical practice is affected with the quality of communication between patients and clinicians as more medical errors occur with less effective communication within the clinical setting [ 6 , 7 ].
Nevertheless, several factors such as the environment/surroundings, circumstances and timing affect the restorative and soothing facets of patients that give significance to therapeutic communication [ 8 ]. For instance, in emergency cases where there will be little time for verbal interaction, the use of non-verbal cues such as the holding of hand could carry much more words to patients [ 8 ]. Even in cases where nurses are much experienced in therapeutic communication, there can still be a gap in communication as sometimes it becomes difficult to understand patients from their own viewpoints [ 8 ].
Therefore, this study sought to investigate the barriers to effective therapeutic communication among patients and nurses at the Komfo Anokye Teaching Hospital in Kumasi.
Komfo Anokye Teaching Hospital (KATH) is a tertiary health facility premise in the environs of Kumasi within the Ashanti Region and ranked as the second largest hospital in Ghana. Komfo Anokye Teaching Hospital (KATH) has a bed capacity of about 1000 with twelve (12) clinical directorates providing healthcare services to the people within the region as well as handling referrals from other closer regions.
Study design
The study employed an exploratory based design which followed a qualitative approach to investigate Nurses’ and Patients’ experiences and views on the barriers to effective therapeutic communication to serve as a springboard for further studies.
Study population
The study population included patients and nurses at Komfo Anokye Teaching Hospital.
Inclusion criteria
Participants included in the study were individuals who had been admitted for a minimum of 3 to 4 days. This meant that participants would have communicated regularly with the nurses during their stay. Registered nurses employed full-time and having worked for four months or more at KATH were also included.
Exclusion criteria
Unconscious and patients who had not been on admission for up to a minimum of 3 days were excluded from the study. Nurses who were not full time and had not worked for more than 4 months were also excluded.
Techniques, instruments for data collection and analysis
An in-depth interview guide was used as the data collection instrument to gather in-depth information from participants. The interview guide allowed the researcher to probe further in order to understand and explore participant contributions in as much depth as possible. An unstructured interview guide which followed an open-ended approach permitted the in-depth investigation of experiences and views regarding nurse-patient communication. The interview guide contained interview questions on the demographic profile of nurses and patients as well as interview questions on Nurse-related barriers; Patient-related barriers and Environmental-related barriers to Therapeutic Communication.
The interview days and time were discussed with participants and each interview was scheduled at their convenience. Interviews were then audio-taped so that participants’ responses could later be transcribed verbatim. The researcher used two weeks for data collection (3rd March to 17th March 2016) with each interview lasting approximately 45 to 60 min. The collection of data was done by two of the authors (sixth and seventh authors) and assisted by two (2) research assistants. Participants were informed about the time before commencement. The data collected was then transcribed verbatim and analyzed through thematic content analysis. This was done by listening to tape recordings and transcribing the content. The transcript was coded by going through the transcript line by line and paragraph by paragraph, to find significant statements and codes according to the topics addressed. The similarities and contrast within the data were compared by the investigators and data that seemed to cluster together were sorted into categories.
Sampling and sampling techniques
The participants were purposively selected to participate in the study based on the characteristics they exhibited which were of interest to the researchers and were able to provide the needed information. According to Patton [ 9 ], the logic and power of purposeful sampling lie in selecting information-rich cases for in-depth study. A sample of 13 participants was used for the study which was made up of 6 nurses and 7 patients. The interviews were conducted till a saturation point was reached after interviewing the 13th participant. Saturation refers to the point at which new data collected and analyzed does not provide further meaning to the research question [ 10 ].
Validity and reliability
To ensure rigour, or the integrity in which the study was conducted, and ensure the credibility of findings in relation to qualitative research, several steps were taken to enhance the validity and reliability of the study [ 11 ].
Firstly, comparisons were done to find out similarities and differences across accounts to ensure that all different perspectives were represented.
Also, active and continuous reflection was done by the researcher during the interpretation of data to ensure the quality of the data and to mirror participants’ experiences to add credibility to the study. The context of the research and assumptions central to the study were thoroughly described to achieve transferability. The criteria applied were made explicit, according to the purpose and orientation of the study [ 12 ].
Furthermore, other researchers were engaged to reduce research bias and the researchers and supervisor again ensured that the findings, conclusions, and recommendations were braced by the data collected and that the interpretation of the data was meaningful and relevant to the study.
Limitations of the study
The study was conducted at Komfo Anokye Teaching Hospital which is a single facility and therefore the findings cannot be generalized. Some of the participants were not willing to respond to some of the interview questions due to its sensitive nature. However, these limitations did not influence the findings of this study in any negative way.
Thematic content analysis was used to analyze data collected based on the aims of the study. The results included background characteristics of study participants as well as the main and sub-themes of the study. Three main themes were derived from the data collected. The themes included; patient-related barriers with sub-themes personal/ social characteristics; patient-nurse relationship; language barriers as well as misconception and pain. The nurse related barriers came with sub-themes such as availability of nurses; inadequate knowledge; all-knowing attitude; dissatisfaction as well as the disease state and family interference. The environmental barriers included sub-themes such as noisy environment; new to the hospital environment and unconducive environment.
Background characteristics of study participants
Table 1 shows the background characteristics of the study participants.From the table,five (5) of the study participants were females whiles eight (8) were males. The participants were between the ages of 20 and 50 years and most of them were between the ages of 20 and 30 years. Moreover, six of the participants were married and seven were single. Most of the patient participants have attained their tertiary education while most of the nurses have attained their degree in nursing.
Main findings
Patient-related barriers.
Patient-related barriers are those obstacles directly from patients that inhibit effective therapeutic communication. Sub-themes that emerged are personal/social characteristics, patient-nurse relationship, language barriers, misconception, and pain.
Personal / social characteristics
These included characteristics such as age, religion, ethnicity among others that have the tendency of influencing communication .
One Participant revealed that;
Once they age, conditions such as dementia sets in and this causes their level of interpretation and understanding to go down and it becomes difficult communicating with them. Those at the extremes of age will have difficulty as compared to those who are in their middle ages. Sometimes the younger ones act like they understand what we tell them and they are okay but in actual sense, they do not understand (Participant 2).
One nurse also reported that religious beliefs and culture play a key role;
Some patients are Muslims and would not want females to attend to them but they prefer males. People from different parts of Ghana have different cultures thus, culture and religion, patient status, all do count to add up to the personal barriers. There are also patients who would say no to blood but as a nurse, you have to use your discretion and this can alter effective communication between you and the patient (Participant 13).
A greater number of the nurses admitted that the cultural background of patients affected their communications. One echoed;
Sometimes the culture of some people will require you to bow whenever you attend to or meet them but as a nurse, you work with limited time and therefore cannot be bowing to everyone you meet and this may portray you the nurse as been insolent thus, affecting the level of communication (Participant 11).
Patient-nurse relationship
Patient-Nurse Relationship is essential for effective healthcare delivery. In this study, patients complained about their relationship with the nurses and the way the nurses attend to them when they are in need. The nurses also admitted that the kind of relationship between the client and them also influences the level of effective communication.
One patient admitted that;
Our relationship is okay but I think their swiftness is a little questionable, they sit always but I think maybe it’s because they are busy but for me, their swiftness is not too good just not too good (Participant 1).
Misconception
Misconceptions can distort effective communication. One individual may perceive another to be of a certain trait, character or of a certain attitude.
Patient revealed that;
I think we come with preconceived ideas because of what we hear about the nurses (Participant 2).
Some of us have misconceptions about nurses that they are rude and disrespectful so we already have something in mind before coming to the ward (Participant 3).
Pain is one thing that can change one’s mood and influence his/her behaviour. Participants verbalized how pain act as a barrier to effective therapeutic communication;
Sometimes I don’t blame the patients, because the pain is too much for them to bear, they wouldn’t want to engage themselves in the conversation going on. In fact, whiles you are in pains and someone tries to even communicate with you, you sometimes get angry (Participant 2).
Another participant had this to say:
Because of the fact that the person is suffering and going through a lot when they call the nurses for one or two times and we don’t attend to them they lose their temper and begin to alter insults (Participant 5).
Language can act as a barrier to any form of communication and effective therapeutic communication is not an exception. Some of the patients complained that nurses mostly resorted to the Twi language when most of the patients have difficulties in understanding Twi.
I am a Voltarian and would like the nurses to speak English because I do not understand Twi but they always speak Twi. They should speak in languages that we will understand and I know every nurse can speak English so I do not know why they normally prefer to speak Twi whiles they know some of us cannot speak Twi well (Participant 3).
There was a patient here who was a northerner and could not communicate so whenever he needed something he had to wait for his relatives to come so that he will communicate his needs through them to the nurses (Participant 7).
Ghana is an Anglophone speaking country and most residents don’t speak French. Therefore, if a patient cannot speak English, it will be difficult communicating. Occasionally, foreigners who speak French and other languages and are living in Ghana visit the Hospital. Majority of the nurses commented on how language was a problem to effective therapeutic communication. Nurses complained of having patients from different tribes and countries which makes it difficult for them to communicate effectively.
There are people admitted here who speak French and as for me, I have never spoken French before so it makes it difficult for me to communicate with them. Also, because KATH is a referral point for many hospitals and clinics we admit people from mostly Nigeria and China and its quite difficult talking to those who cannot speak English, sometimes we have to resort to sign language and even that we are not good in it. There was an occassion when we had a patient from Upper West who couldn’t speak Twi so we had to resort to sign language (Participant 12).
Nurse-related barriers
This category includes barriers related to attributes of the nurse. These attributes can be barriers in establishing a therapeutic nurse-patient relationship in the hospital. Six sub-themes emerged from it and they are inadequate knowledge, disease state, availability of nurses, all-knowing attitude, family interference, and dissatisfaction.
Availability of nurses
The Nurses complained that due to the small number of nurses and the workload it becomes difficult attending to all patients as and when they call.
One Nurse revealed;
Workload has been a factor, when nurses have a lot of work to do they will not have time to explain things to patients they will tell the patient ‘don’t you know I am very busy, don’t you know I am overburden’ especially with women whose threshold of managing stress is low as compared to men so that is a point (Participant 11). Ooh! because there are few nurses at the ward sometimes you would want a nurse to attend to you but he or she might be working on another patient so in such case the nurse cannot divide him or herself into two to attend to you both. So you have to wait for quite some time and at times due to stress they end up forgetting that you called them (Participant10).
A patient stressed that;
One thing is that the nurses that are taking care of us are very few. So most at times the nurses here, lets say patients are 31 and only 4 nurses are taking care of us. Anytime you call the nurse, she will be busy doing something else and will tell you that she will be back soon. And as a human being, you can forget about things so easily. So as the nurse is attending to a sick patient, she may also come to your direction and another sick person will also call the nurse so hardly do we communicate with them as often. They are always busy (Participant 6).
Another Nurse commented;
Because there are few nurses at the ward, sometimes you would like a nurse to attend to you but he/she might be working on another patient (Participant 13).
Inadequate knowledge
Most nurses admitted and verbalized that, some nurses had little knowledge on how to communicate with others. Lack of knowledge on therapeutic communication on the part of some nurses also contributed to ineffective therapeutic communication. If there is a close relationship between the patient and the nurse, a patient can speak out all their problems to the nurse.
One of the Nurses echoed;
I will say ignorance or nurse is not well abreast of what effective therapeutic communication is. A nurse who knows what effective therapeutic communication is will use it, especially if the nurse knows what it does to the healing process (Participant 10).
All-knowing attitude
Attitude refers to the predisposition to behave in a certain manner. Majority of the nurses verbalized that because some of the patients have stayed at the ward for a long time and in an era where most patients are educated, they think they know more about the nursing procedures and thus, do not adhere to whatever their health care provider says.
The nurses revealed;
Patients who are learned tend to give a lot of instructions when performing any procedures on them. For example, when they are allergic to pethidine injection they assume every injection you give them is pethidine and will start complaining, this makes communication difficult (Participant 12).
You see when the patients stay on the ward for a very long time, they begin to act that they know everything you do for them. So for instance, when you are dressing their wounds, they go like do this do that trying to dictate or tell you what to do and if you resist they will claim you are all-knowing (Participant 11).
Dissatisfaction
When one is not pleased with a service provider or a process, it may distort effective communication between the individual and another person. Most of the nurses identified dissatisfaction with services provided by nurses as the predominant barrier to effective communication.
I would not say so; I wouldn’t say they are satisfied. Even when you get the time to talk to them the duration of the conversation is usually minimal okay, because of the work overload and the number of nurses to attend to patients you won’t get the time to communicate with our patients. But sometimes we do try but I will say that it is not the best (Participant 10).
Another echoed;
In terms of the level of satisfaction of patients, it may vary from one patient to another. Generally, I will give them 40% because I think they are not satisfied since we don’t explain things thoroughly to them. We don’t normally explain the condition and even the adverse effect of their drugs to them. All these things must be done by us and are not effectively done (Participant 11).
Disease state
All nurses verbalized that, the disease state and mental status of patients also affect the level of communication between nurses and patients.
One of the Nurses’ commented;
When the patient is unconscious or just returned from surgery, it becomes difficult communicating with them and this can also reduce the quality of care provided to them (Participant 1) .
Another Nurse also added;
Currently we have a mental disoriented patient on the ward and in this case, communicating with such a patient is a problem which also leads to ineffective therapeutic communication (Participant 9).
Family interference
A family may interfere in a service process in order to influence outcomes. Another problem that the nurses admitted to facing is family interference in most of the procedures at the ward. Also, the kind of behaviour exhibited by clients’ families also affects how they communicate with them.
A Nurse said;
Sometimes the patient may be very sick and may not need any relatives to be there, they need some rest and when you want to restrict them (relatives) there is trouble. Some want to even dictate to you. They want to plan with you how to care for their relatives. In fact, some of the family members are troublesome (Participant 8).
Another added:
There are some instances where nurses or doctors will give them (relatives) an order; the relatives will rather give the patient drugs from a spiritualist or a herbalist which may lead to contradiction of information which resulting to ineffective therapeutic communication (Participant 13).
Environmental barriers
Environmental barriers are obstacles within the environment that inhibit effective therapeutic communication. Almost all nurses and some of the patients asserted that environmental barriers influence therapeutic communication at the ward. Most of the patients expressed how they felt when things they didn’t expect emerged.
Sub-themes that emerged were a noisy environment, new to the hospital environment smell, work overload, mosquitoes, and unconducive environment.
New to the hospital environment
Adapting to a new environment can be problematic for some people at times, therefore, influencing their ability to communicate effectively.
One Nurse stated;
You see some of the patients are new to the hospital environment and the mere fact that he or she is in the hospital makes them feel that they are really sick and can’t even communicate with the nurses. They are also already anxious the moment they get to the hospital. This alone can delay therapeutic communication (Participant 11).
Noisy environment
Noise can affect any form of communication and in this case therapeutic communication.
The issue of noise is reflected in the following;
Yeah, some patients put on their radio, some talk on top of their voices and even the nurses chat too much especially, when you call them and they are chatting they do not attend to or mind you because they are concentrating on their talking (Participant 9).
Unconducive environment
Communication can be effective only in an environment that is conducive enough for everyone. Participants shared their views on how unconducive the hospital environment is for effective communication. One participant had this to say;
The mosquitoes disturb us because there are no mosquito nets etc. here at night so when you manage to sleep through your own ways and means and the nurses wake us up because time is due for our medications, it becomes a challenge and we need to exercise patience so not to fight or get angry with the nurses that are at the ward (Participant 5).
The hospital settings itself is also a barrier. The fact that sometimes the environment is not conducive enough, it may be too warm or cold. Sometimes the patient will tell you that they don’t like the fan whiles others will say that they don’t like the light (Participant 13).
Discussions
The study explored the barriers to effective therapeutic communication among patients and nurses in Kumasi. The barriers that were explored include nurses related, patient-related, and environment-related barriers. A key demographic characteristic of patients that were identified as a barrier was age. Similarly, Payne et al., [ 13 ], reported that age can serve as a barrier to effective communication. This implies that conditions such as dementia that may set in once you age and causes the level of interpretation and understanding to go down makes it difficult to communicate effectively. Religion was also identified as a barrier as patients who were Muslims would not want females to attend to them but preferred males. People from different parts of Ghana have different cultures and thus patient status, culture, and religion are key barriers to effective therapeutic communication. This implies that religion, age as well as culture has a tendency to influence therapeutic communication. There may be cases where both may belong to the same ethnic group, however, different social orientations and circumstances may affect their communication. Payne et al., [ 13 ], also found generational gaps between the elderly and young nurses as key barriers to effective communication. However, culture and ethnic group were not mentioned by Payne et al., [ 13 ], but reported by Anderson et al., [ 14 ] who emphasized that nurses in interacting with patients from different backgrounds should be sensitive, effective and attach professional attitude.
Language was also identified as a barrier to effective therapeutic communication in this study. Similarly, Quesada [ 15 ] reported that in general, the majority of the nurses and patients report that language barrier is an impediment to quality care. The findings corroborate with this study results where patients complained that nurses mostly resort to the Twi language when some of the patients had difficulties in communicating in Twi. Nurses also complained of having patients from different tribes and countries which also makes it difficult for them to communicate effectively.
This study reports that patients complained that they feel like they have been neglected by nurses because they do not promptly attend to them while nurses also complained that, due to the small number of nurses and the workload it becomes difficult attending to all patients as and at when they call. This gives credence to the findings that heavy work schedules of nurses, tough and intensive nursing tasks and the absence of welfare facilities for nurses obstruct communication as reported by Anoosheh et al., [ 16 ].
This study reported that several patients complain about their relationship with the nurses and lack of attention. Teutsch [ 17 ], reported that nurses undivided attention for patients as they listen to them and observe them gives patients a high level of satisfaction. Interactions with patients therefore eliminate scary thoughts, doubts, and misinterpretations. The researchers do believe that if there is a close relationship between the patient and the nurse, the patient can voice out all their problems to the nurse.
Loghmani, Borhani, and Abbaszadeh [ 18 ] in their studies came to the conclusion that nurse-patient communication is declining due to family interference. This gives credence to this current study reporting that family interference is a barrier to effective therapeutic communication. Most of the patients were dissatisfied due to inattention on the part of the nurses and this was a predominant barrier to effective communication in this study. In a similar study, the majority of patients that recounted their experiences on nursing care felt dissatisfied due to neglect [ 19 ]. According to McQueen [ 20 ], patients in a healthcare facility require information,education, encouragement and support, and nurses are in an ideal position to meet this need.
Conclusions
Nurse-patient communication is an inseparable part of the patients’ care in every health setting; it is one of the factors that determine the quality of care. However, the results of this study have shown that several factors, which are patient-related, nurse- related and environmental-related pose as barriers to effective therapeutic communication and has ultimately, resulted in reducing effective communication which could affect the quality and comprehensive care delivery at the hospital wards. Authorities at the hospital must ensure that all barriers are eradicated to promote effective therapeutic communication.
Abbreviations
Komfo Anokye Teaching Hospital
American Nurses Association. Correctional nursing scope and standards of practice. Silver Sping: MD: American Nurses Association; 2013.
Google Scholar
Richard L.S, Gregory M., Neeraj K.A., Ronald M.E. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns Elsevier, 2009: 74(295–301).
Sherko E, Sotiri E, Lika E. Therapeutic communication. JAHR. 2013;4(7):457–66.
Bournes DA, Mitchell GJ. Waiting: the experience of persons in a critical care waiting room. Research in nursing & health. 2002;25(1):58–67.
Article Google Scholar
McGilton K, Robinson HI, Boscart V, Spanjevic L. Communication enhancement: nurse and patient satisfaction outcomes in a complex continuing care facility. J Adv Nurs. 2006;54(1):35–44.
Swasey, M. L. Physician, and Patient Communication: A Grounded Theory Analysis of Physician and Patient Web-Logs (doctoral dissertation, southern Utah University. Department of Communication 2013.
Alvarez G, Coiera E. Interdisciplinary communication: an uncharted source of medical error? J Crit Care. 2006;21(3):236–42.
Montgomery CL. Healing through communication: the practice of caring: Sage; 1993.
Patton, M. Q. Qual Res & evaluation methods: Integrating theory and practice (4th ed.). Thousand oaks, CA: Sage, 2015.
Mack N, Woodsong C, MacQueen KM, Guest G, Namey E. Qualitative research methods: a data collector’s field guide; 2005.
Noble H, Smith J. Issues of validity and reliability in qualitative research. Evidence-Based Nursing 2015:ebnurs-2015.
Patton, M. Q. Qualitative research John Wiley & Sons, Ltd, 2005.
Payne S, Kerr C, Hawker S, Hardey M, Powell J. The communication of information about older people between health and social care practitioners. Age and aging. 2002;31(2):107–17.
Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Culturally competent healthcare systems: a systematic review. Am J Prev Med. 2003;24(3):68–79.
Quesada GM. Language and communication barriers for health delivery to a minority group. Soc Sci Med. 1967;10(6):323–7.
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009;56(2):243–9.
Article CAS Google Scholar
Teutsch C. Patient-doctor communication. Med Clin N Am. 2003;87(5):1115–45.
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patient' family communication in intensive care unit of Kerman: a qualitative study. J Caring Sci. 2014;3(1):67.
PubMed PubMed Central Google Scholar
Rauseo MM. Effective communication in nursing: is it necessary to know your own sociological Bias? 2016.
McQueen A. Nurse-patient relationships, and partnership in hospital care. J Clin Nurs. 2000;9(5):723–31.
Download references
Acknowledgements
Our gratitude goes out to the management and staff of Komfo Anokye Teaching Hospital, Kumasi as well as all patients and nurses who took part in this study. Further thanks to all whose works on therapeutic communication helped in putting this work together.
There were no external grants received for the conduction of this study. Researchers of this study bear all expenses related to the study.
Availability of data and materials
The whole document, data, materials, and results of this work are available at the Library of the Garden City University College, Kumasi. If someone wants to request the data the corresponding author should be contacted.
Author information
Authors and affiliations.
Centre for Disability and Rehabilitation Studies, Department of Community Health, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Reindolf Anokye & Enoch Acheampong
Department of Nursing, Garden City University College, Kumasi, Ghana
Vida Maame Kissiwaa Amoah, Dorothy Serwaa Boakye, Emelia Okyere, Gifty Kumi-Boateng, Cynthia Yeboah & Jennifer Owusu Afriyie
School of Public Health, Department of Health Education and Promotion, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Amy Budu-Ainooson
You can also search for this author in PubMed Google Scholar
Contributions
The collection of data was done by sixth and seventh authors (EO and GKB). The secondary data compilation, data analysis, and interpretation were done by the second author (RA). The first and third authors (VMKA and EA) in their individual capacities reviewed the manuscript thoroughly. Authors DSB, ABA, CY and JOA played a significant role during data collection, data analysis, and interpretation. All authors contributed to the designing, preparation of manuscripts, the analysis of the data, proofreading and the final approval process of the manuscript. The authors all approved the submission of this manuscript for publication.
Corresponding author
Correspondence to Reindolf Anokye .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Committee on Human Research, Publication and Ethics (CHRPE) at Komfo Anokye Teaching Hospital (KATH) and Kwame Nkrumah University of Science and Technology (KNUST). The participants were reassured that information taking will be confidential. Participation was voluntary and participants were informed of their right to pull out of the study at any point of the research which was not going to affect the care they were receiving. Written consent was obtained from participants before they participated in the study. The study was well explained to the participants and also the recording tape was locked to prevent other people from getting access to it. All the participants were given pseudonyms to protect their anonymity. All authors have agreed to the submission of this manuscript for publication.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Amoah, V.M.K., Anokye, R., Boakye, D.S. et al. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs 18 , 4 (2019). https://doi.org/10.1186/s12912-019-0328-0
Download citation
Received : 25 April 2018
Accepted : 28 January 2019
Published : 11 February 2019
DOI : https://doi.org/10.1186/s12912-019-0328-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Therapeutic communication
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Browse All Articles
- Newsletter Sign-Up
Communication →
- 22 May 2024
Banned or Not, TikTok Is a Force Companies Can’t Afford to Ignore
It may be tempting to write off TikTok, the highly scrutinized social media app whose cat clips and dance videos propelled it to the mainstream. However, business leaders could learn valuable lessons about engaging consumers from the world's most-used platform, says Shikhar Ghosh in a case study.

- 15 May 2024
- Research & Ideas
A Major Roadblock for Autonomous Cars: Motorists Believe They Drive Better
With all the advances in autonomous vehicle technology, why aren't self-driving cars chauffeuring more people around? Research by Julian De Freitas, Stuti Agarwal, and colleagues reveals a simple psychological barrier: Drivers are overconfident about their own abilities, so they resist handing over the wheel.
- 09 May 2024
Called Back to the Office? How You Benefit from Ideas You Didn't Know You Were Missing
As companies continue to weigh the benefits and drawbacks of remote work, a study of how knowledge flows among academic researchers by Karim Lakhani, Eamon Duede, and colleagues offers lessons for hybrid workplaces. Does in-person work provide more opportunities for innovation than people realize?
- 06 May 2024
The Critical Minutes After a Virtual Meeting That Can Build Up or Tear Down Teams
Weak communication and misunderstandings during virtual meetings can give way to resentment and rifts when the cameras turn off. Research by Leslie Perlow probes the nuances of digital communication. She offers advice for improving remote teamwork.

- 16 Feb 2024
Is Your Workplace Biased Against Introverts?
Extroverts are more likely to express their passion outwardly, giving them a leg up when it comes to raises and promotions, according to research by Jon Jachimowicz. Introverts are just as motivated and excited about their work, but show it differently. How can managers challenge their assumptions?

- 06 Nov 2023
Did You Hear What I Said? How to Listen Better
People who seem like they're paying attention often aren't—even when they're smiling and nodding toward the speaker. Research by Alison Wood Brooks, Hanne Collins, and colleagues reveals just how prone the mind is to wandering, and sheds light on ways to stay tuned in to the conversation.
.jpg)
- 31 Oct 2023
Checking Your Ethics: Would You Speak Up in These 3 Sticky Situations?
Would you complain about a client who verbally abuses their staff? Would you admit to cutting corners on your work? The answers aren't always clear, says David Fubini, who tackles tricky scenarios in a series of case studies and offers his advice from the field.

- 24 Jul 2023
Part-Time Employees Want More Hours. Can Companies Tap This ‘Hidden’ Talent Pool?
Businesses need more staff and employees need more work, so what's standing in the way? A report by Joseph Fuller and colleagues shows how algorithms and inflexibility prevent companies from accessing valuable talent in a long-term shortage.

- 23 Jun 2023
This Company Lets Employees Take Charge—Even with Life and Death Decisions
Dutch home health care organization Buurtzorg avoids middle management positions and instead empowers its nurses to care for patients as they see fit. Tatiana Sandino and Ethan Bernstein explore how removing organizational layers and allowing employees to make decisions can boost performance.

- 24 Jan 2023
Passion at Work Is a Good Thing—But Only If Bosses Know How to Manage It
Does showing passion mean doing whatever it takes to get the job done? Employees and managers often disagree, says research by Jon Jachimowicz. He offers four pieces of advice for leaders who yearn for more spirit and intensity at their companies.

- 10 Jan 2023
How to Live Happier in 2023: Diversify Your Social Circle
People need all kinds of relationships to thrive: partners, acquaintances, colleagues, and family. Research by Michael Norton and Alison Wood Brooks offers new reasons to pick up the phone and reconnect with that old friend from home.

- 15 Nov 2022
Why TikTok Is Beating YouTube for Eyeball Time (It’s Not Just the Dance Videos)
Quirky amateur video clips might draw people to TikTok, but its algorithm keeps them watching. John Deighton and Leora Kornfeld explore the factors that helped propel TikTok ahead of established social platforms, and where it might go next.

- 03 Nov 2022
Feeling Separation Anxiety at Your Startup? 5 Tips to Soothe These Growing Pains
As startups mature and introduce more managers, early employees may lose the easy closeness they once had with founders. However, with transparency and healthy boundaries, entrepreneurs can help employees weather this transition and build trust, says Julia Austin.

- 15 Sep 2022
Looking For a Job? Some LinkedIn Connections Matter More Than Others
Debating whether to connect on LinkedIn with that more senior executive you met at that conference? You should, says new research about professional networks by Iavor Bojinov and colleagues. That person just might help you land your next job.

- 08 Sep 2022
Gen Xers and Millennials, It’s Time To Lead. Are You Ready?
Generation X and Millennials—eagerly waiting to succeed Baby Boom leaders—have the opportunity to bring more collaboration and purpose to business. In the book True North: Emerging Leader Edition, Bill George offers advice for the next wave of CEOs.

- 05 Aug 2022
Why People Crave Feedback—and Why We’re Afraid to Give It
How am I doing? Research by Francesca Gino and colleagues shows just how badly employees want to know. Is it time for managers to get over their discomfort and get the conversation going at work?

- 23 Jun 2022
All Those Zoom Meetings May Boost Connection and Curb Loneliness
Zoom fatigue became a thing during the height of the pandemic, but research by Amit Goldenberg shows how virtual interactions can provide a salve for isolation. What does this mean for remote and hybrid workplaces?

- 13 Jun 2022
Extroverts, Your Colleagues Wish You Would Just Shut Up and Listen
Extroverts may be the life of the party, but at work, they're often viewed as phony and self-centered, says research by Julian Zlatev and colleagues. Here's how extroverts can show others that they're listening, without muting themselves.

- 24 May 2022
Career Advice for Minorities and Women: Sharing Your Identity Can Open Doors
Women and people of color tend to minimize their identities in professional situations, but highlighting who they are often forces others to check their own biases. Research by Edward Chang and colleagues.
- 12 May 2022
Why Digital Is a State of Mind, Not Just a Skill Set
You don't have to be a machine learning expert to manage a successful digital transformation. In fact, you only need 30 percent fluency in a handful of technical topics, say Tsedal Neeley and Paul Leonardi in their book, The Digital Mindset.
- Research article
- Open access
- Published: 24 March 2021
Exploring the barriers and facilitators of psychological safety in primary care teams: a qualitative study
- Ridhaa Remtulla ORCID: orcid.org/0000-0003-4037-8959 1 na1 ,
- Arwa Hagana 2 na1 ,
- Nour Houbby 2 na1 ,
- Kajal Ruparell 2 na1 ,
- Nivaran Aojula 2 ,
- Anannya Menon 2 ,
- Santhosh G. Thavarajasingam 2 &
- Edgar Meyer 3
BMC Health Services Research volume 21 , Article number: 269 ( 2021 ) Cite this article
17k Accesses
21 Citations
5 Altmetric
Metrics details
Psychological safety is the concept by which individuals feel comfortable expressing themselves in a work environment, without fear of embarrassment or criticism from others. Psychological safety in healthcare is associated with improved patient safety outcomes, enhanced physician engagement and fostering a creative learning environment. Therefore, it is important to establish the key levers which can act as facilitators or barriers to establishing psychological safety. Existing literature on psychological safety in healthcare teams has focused on secondary care, primarily from an individual profession perspective. In light of the increased focus on multidisciplinary work in primary care and the need for team-based studies, given that psychological safety is a team-based construct, this study sought to investigate the facilitators and barriers to psychological safety in primary care multidisciplinary teams.
A mono-method qualitative research design was chosen for this study. Healthcare professionals from four primary care teams ( n = 20) were recruited using snowball sampling. Data collection was through semi-structured interviews. Thematic analysis was used to generate findings.
Three meta themes surfaced: shared beliefs, facilitators and barriers to psychological safety. The shared beliefs offered insights into the teams’ background functioning, providing important context to the facilitators and barriers of psychological safety specific to each team. Four barriers to psychological safety were identified: hierarchy, perceived lack of knowledge, personality and authoritarian leadership. Eight facilitators surfaced: leader and leader inclusiveness, open culture, vocal personality, support in silos, boundary spanner, chairing meetings, strong interpersonal relationships and small groups.
This study emphasises that factors influencing psychological safety can be individualistic, team-based or organisational. Although previous literature has largely focused on the role of leaders in promoting psychological safety, safe environments can be created by all team members. Members can facilitate psychological safety in instances where positive leadership behaviours are lacking - for example, strengthening interpersonal relationships, finding support in silos or rotating the chairperson in team meetings. It is anticipated that these findings will encourage practices to reflect on their team dynamics and adopt strategies to ensure every member’s voice is heard.
Peer Review reports
Psychological safety is the notion where individuals feel empowered to ask questions, admit mistakes or voice concerns without fear of negative repercussions from their team [ 1 ]. This concept has been explored in varying contexts, including healthcare teams as psychological safety can have an impact on patient safety and quality of care. For healthcare professionals, psychological safety creates an environment of trust and openness to discuss concerns and raise errors [ 2 , 3 ]. This enables focus on providing high quality care, as opposed to managing the expectations around voicing dissent and disagreement. It has also been shown that psychological safety increases physician engagement [ 4 ], reduces burnout [ 5 ] and promotes creativity [ 6 ].
Appelbaum et al. surveyed 106 physicians in the United States in order to investigate the perceptions of psychological safety and various other parameters including the intention to report adverse events. Psychological safety was found to be a direct predictor of the intention to report adverse events by physicians, highlighting the importance of psychological safety in creating safer care for patients [ 7 ]. Yanchus et al. investigated 11,726 healthcare workers including psychiatrists and mental health nurses and determined that psychological safety was a direct predictor of turnover intent, emphasising the value of psychological safety in employee retention [ 8 ].
Indeed, the positive effects of psychological safety are not limited to the individual or team level - rather, they permeate throughout the entire organisational infrastructure. This draws on the concept of organisational resilience, which can be described as how well supported workers within an organisation are by across three specific levels: the individual level, team level, and organisational level [ 9 ]. Organisations which are resilient will facilitate workers to predict when a problem will arise (foresight), help individuals cope with problems which do occur (coping), and finally, find suitable ways to recover from problems and prevent them in the future (recovery) [ 9 ]. In turn, organisational resilience allows for problem management, which in a healthcare setting translates to improved patient safety measures – a typical example of organisational resilience in healthcare is the clinical handover which aims to facilitate foresight, coping and recovery across the three levels of an organisation [ 9 ]. Psychological safety is integral to maintaining organisational resilience. For example, an individual healthcare worker should feel able to raise a concern regarding a patient showing clinical signs of deteriorating (foresight) without fear of repercussions from seniors [ 9 ].
In light of the well-evidenced benefits of psychological safety on healthcare teams, it is imperative to understand the key drivers which either facilitate or act as a barrier to establishing psychological safety. Specific facilitators which have already been identified in the literature include those pertaining to the actions of leaders. For example, inclusive behaviours displayed by a leader such as active invitation and appreciation of opinions from fellow team members regardless of factors such as hierarchical differences between a leader and team member have been shown to facilitate psychological safety, exemplified by Hirak et al’s [ 10 ] study which investigated the correlation between leader inclusiveness and psychological safety within a hospital [ 3 , 11 ]. 224 team members and 55 team leaders consisting of various hospital employees including doctors and nurses were surveyed, and a positive relationship was found to exist within teams with more inclusive leaders [ 10 ].
The literature also links psychological safety with change-oriented leadership. Change-oriented leadership as described by Yuki et al [ 12 ] refer to a set of behaviours which promote innovation and change amongst teams. For example, leaders who monitor the external environment to identify opportunities or potential threats to a team, envision change, encourage innovation from their subordinates and take on personal risk to enact change are seen to be change-oriented leaders. Ortega et al [ 2 ] surveyed 107 nursing teams from various healthcare settings including primary care, intensive care and surgical settings to investigate the relationship between psychological safety and change-oriented leadership. Ortega et al. reported that teams with change-oriented leaders also reported higher psychological safety within teams [ 2 ]. This has great implications for healthcare considering innovation and non-traditional problem-solving strategies have historically proved beneficial for the industry.
Ethical leaders i.e. individuals who demonstrate appropriate conduct themselves and by doing so encourage and model exemplary conduct in their subordinates have also been cited in the literature as encouraging psychological safety [ 13 ]. Gong et al [ 14 ] surveyed the opinions of feedback-seeking behaviour amongst subordinate nurses and nurse leaders – in total, 60 leaders and 458 subordinates were investigated. Teams, where leaders were deemed to be more ethical, were found to have higher levels of psychological safety and feedback-seeking behaviour, particularly in teams with a high-power distance [ 14 ].
Barriers to psychological safety include workplace bullying and hierarchy. Arnetz et al [ 15 ] investigated the experience of workplace bullying amongst 331 registered nurses from a specific American regional healthcare system. 36.9% of responders reported being bullied in the preceding 6 months [ 14 ]. An inverse relationship was found between personal experiences of disengagement with work following personal bullying and psychological safety. Psychological safety was also associated with less personal bullying as well as witnessing others being bullied [ 15 ]. Hierarchy has also been cited in the literature, with Appelbaum et al [ 7 ] investigating the influences of power distance and leader inclusiveness on psychological safety amongst 106 medical residents. A higher perceived power distance predicted lower levels of psychological safety, whilst leader inclusiveness was positively correlated with psychological safety [ 7 ]. Higher levels of psychological safety by consequence were positively correlated with intentions to report adverse medical events, further highlighting the importance of mitigating barriers to psychological safety in order to maintain and improve patient safety.
Whilst the literature makes clear that leaders are crucial in facilitating psychological safety in healthcare teams, there is less focus on how other team members may help to improve the psychological safety of their environment. Circumstances where individuals speak up regardless of the leadership style they work under, suggests that other factors external to the leader are at play in facilitating psychological safety. Given that the literature has a strong focus on the role of the leader, attempts should be made to determine if general team behaviours, environmental factors, team culture or innate personality traits contribute to the psychological safety of a team environment and if so, what these factors may be. Likewise, are there alternative intrinsic or extrinsic factors that individuals may possess which can facilitate or impede the establishment of a psychologically safe environment.
Most of these findings on psychological safety in healthcare teams however, focuses on secondary care, with limited studies examining the application of this construct within primary care teams [ 3 , 11 ]. Arguably, the dynamics of teamwork can vary greatly between primary and secondary care multidisciplinary teams, thus a focused exploration into psychological safety in these teams is warranted.
This qualitative study aimed to identify the specific barriers and facilitators of psychological safety in primary care teams. In the context of this study, barriers and facilitators refer to the various psychological, environmental, interpersonal and organisational aspects of the multidisciplinary teams investigated. This was with a view to establish behaviours that practices can implement to harbour psychologically safe environments.
Given that the aim of this study is to identify barriers and facilitators of psychological safety within primary care teams, an inductive study approach was deemed to be a more suitable study design as opposed to a traditional hypothetico-deductive approach [ 16 ]. The lack of specific premises to prove or disprove in the context of psychological safety further supports the use of an inductive methodology [ 17 ].
Research philosophy and approach
This study utilised a mono-method qualitative research design which uses semi-structured interviews as the only mode of data collection. The present study seeks to investigate multi-disciplinary team members’ perceptions of the facilitators and barriers of PS in primary care teams. Such perspectives and insights can only be explored using a qualitative inquiry which, crucially, uses methods such as open-ended interviewing to surface opinions unconducive to quantification [ 18 ].
This study employed an interpretivist approach which leverages qualitative methods to elicit narratives, capture stories and probe perceptions to articulate and conceptualise aspects of social phenomena which cannot be quantified [ 19 ]. Interpretivism champions subjectivity, and calls on the researcher to engage their own values and beliefs, making their empathetic viewpoint a central part of the research process [ 20 ]. Critical to the interpretivist philosophy is its acknowledgement of multiple realities and therefore, this approach facilitates a deep understanding of participants’ lived experiences [ 21 ].
The very notion that within the same context there exist multiple realities experienced by different people makes an interpretivist approach appropriate for the present study exploring MDT members’ views on PS in primary care teams. By exploring PS through the lens of different MDT members, this research acknowledges the complexity of the social world and seeks to develop a deep understanding of the phenomenon under investigation.
This study applies an inductive approach to theory development, which recognises the existence of a gap between observed data and derived conclusions [ 22 ]; a gap filled with underlying complexities which cannot always be distilled to ‘cause and effect’ mechanisms [ 20 ]. Inductive reasoning therefore traverses the rigid structural boundaries which govern deductive approaches and does not seek to mechanistically verify or oppose existing theory. Rather, an inductive approach is limitless. It utilises a ‘bottom up approach’ beginning with primary data collection followed by the identification of patterns and themes in an effort to construct theory [ 23 ]. Consistent with an inductive approach, this study uses qualitative methods focussed on meaning-making, allowing for a detailed exploration of participants’ lived experiences [ 24 ].
Methodology is reported in accordance with the Consolidated Criteria for Reporting Qualitative Research Checklist [ 25 ].
Snowball sampling enabled the recruitment of a team-focused study population, thus facilitating comparison between the perceptions of different MDT members. This was vital given that psychological safety is a team construct. Utilising snowball sampling methodology, a sample of 20 individuals from four different primary care teams ( n = 5, n = 6, n = 6, n = 3) were obtained. The sampling approach was employed in two stages. First-line participants were recruited through LinkedIn and the Royal Colleges, subject to specified inclusion and exclusion criteria (Table 1 ). These participants then recruited colleagues from their multidisciplinary team. For example, to recruit the participants in team 1, the head partner GP was contacted through LinkedIn. They then initiated contact with the head nurse from the team which resulted in a sample of five participants in team 1. Their employment information was verified at the time of the interview by asking their role in the practice. The response rate through LinkedIn was approximately 70% and recruitment was completed in one month. The inclusion/exclusion criteria were checked prior to the interview by asking preliminary questions to obtain their professional role. The roles included were general practitioners, practice managers, partners, healthcare assistants and nurses. The demographic information has been anonymised due to the inclusion of direct quotes being used in this report. All recruitment was in line with the approved ethics protocol. A brief synopsis outlining the study purpose and objectives were sent to the participants. Once interest was confirmed, they were provided with a participant information sheet detailing the purpose of the study and information regarding data confidentiality alongside an informed consent form to obtain consent prior to interview conduction. Participants were informed that they could withdraw from the study at any time. This was repeated until no further recruitment occurred [ 26 ] and data saturation was reached. Data saturation was deemed the point at which similar responses were being surfaced in the interviews with repeating rather than novel ideas, referred to by Sandelowski [ 27 ] as ‘informational redundancy’. In qualitative research, significant ambiguity exists around what is deemed an appropriate sample size [ 20 ] with limited guidance on this. Guest et al. 2006 suggest that 12 interviews are sufficient [ 28 ], while Creswell [ 29 ] recommends between 5 and 30 interviews for qualitative research. An accepted sample size of between 5 and 25 participants has been cited for studies utilising semi-structured or in-depth interviews [ 30 ]. Therefore, given the fact that data saturation was achieved at 20 interviews, this was deemed an appropriate sample size for the study.
Data collection
Data was collected using semi-structured interviews (SSIs), as they are adaptable in nature and allow stakeholders to share answers openly and independently [ 31 ]. Interviews with all 20 participants were conducted via video-conferencing (due to Covid-19 restrictions). Video conferencing platforms utilised included Zoom and Skype. Conducting the interviews in this manner offered numerous advantages including; convenience for both the interviewer and the interviewee as well as deducting travel time, thus increasing efficiency of data collection. Furthermore, this facilitates visual interaction with the added advantage that it allows the interviewer and interviewee to remain in their own comfortable locations [ 32 ]. However, video-conferencing limited our non-verbal communication which could have helped contextualise the responses. Overall, utilising video-conferencing proved advantageous in our data collection process. Interviews were audio-recorded, anonymised and stored on a secure drive before being destroyed post-transcription.
The interview schedule was designed to be open-ended to encourage participants to speak freely to allow detailed accounts to be elicited [ 33 ]. This was recommended by the five-step framework by Kallio et al [ 34 ] to create a qualitative interview guide. Kallio et al. recommended first to evaluate if a semi-structured interview is necessary. The conclusion of conducting interviews was reached as this study needed the perceptions and opinions of our participants in order to contextualise their answers. Next, a literature review was conducted to establish existing knowledge and identify the gap the interview needs to fill. This helped us with the third step of devising the questions, which included the main themes and follow up questions.
As per Kallio et al’s fourth step [ 34 ], two pilot interviews with GPs were conducted to verify the initial interview guide developed. The pilot interviews demonstrated significant overlap in the interview guide questions within the subsection “Roles and Responsibilities”, hence this subsection was summarised into three questions. Secondly, the question ‘How do you view your relationship with other team members? was removed since it required extensive clarification in both pilots. Finally, one question was added to the interview protocol, ‘Which member of the team is most influential in ensuring a psychologically safe environment?’, due to both interviewees referring frequently to the influential role of team leaders in facilitating PS within their teams. Yin [ 35 ] advocates the conduction of pilot studies as an effective method for developing ‘relevant lines of informed questioning’, enabling the refinement of data collection methods. The conduction of pilot interviews further informed the modification of the interview guide to ensure data gauged from the questions was sufficient for answering our research question.
The semi-structured interview format allowed for probing questions to be used to encourage participants to develop and elaborate on their responses, facilitating a more detailed inquiry [ 36 ]. All SSIs ranged from 20 to 45 min in duration due to differences in individual availability and commitment of the respondents. This is in line with accepted practice in the literature [ 37 ]. Three researchers (KR, NA and NH) conducted the interviews which introduced different perspectives who were able to individually interpret the participants’ non-verbal cues and the emotional aspects which often do not surface in the transcripts and are only picked up in the interview. The triangulation of researchers [ 38 ] in this manner minimised individual biases and contributed to the validity of our research. An interview schedule ( Supplementary file A ) was devised with open-ended questions to encourage participants to speak freely, facilitating a detailed inquiry [ 33 ].
Data analysis
Braun and Clarke’s six-phase methodology [ 39 ] of thematic analysis was utilised for the interview data. Phase 1 involved three researchers (RR, NH and AH) transcribing the interviews ad verbatim and developing transcript summaries. In line with an inductive approach, within phase 2, ‘in-vivo’ codes were derived from the data. Codes were reviewed and compared at the team level in phase 3 and were subsequently categorised into themes, beginning the process of theory inception. In the fourth phase, candidate themes and subthemes were reviewed against the coded data to ensure intra-theme coherence and against the entire data to ensure representability. Further refinement of themes was undertaken in phase 5 before being used to construct a coherent analytic narrative in phase six.
Reflexive statement
Reflexivity serves as a conscious acknowledgement of the researcher’s assumptions and experiences which influence the research process [ 40 ]. This study was conducted by a team of seven medical students alongside our supervisor, each with varying experiences which have shaped our perceptions of primary care. We are aware of our biases towards hierarchy in healthcare teams. However, to reduce the influence of preconceived biases we used open questions to allow free expression and had three researchers conduct the interviews to ensure triangulation.
This study explored the facilitators and barriers of psychological safety in the four primary care teams. The data analysis yielded three meta-themes: Barriers to psychological safety, facilitators of psychological safety, and shared beliefs.
Facilitators and barriers of psychological safety are the main focus of this study, however, the additional meta-theme of shared beliefs was found to be significantly distinct from barriers and facilitators. Notably, the meta-theme shared beliefs refers to the characteristics of the team, including team dynamics and relationships, and hence provides a common basis for the interpretation of how the facilitators and barriers of psychological safety influence the respective primary care team. Figure 1 summarises the shared beliefs across the four primary care teams, as well as their relation to barriers and facilitators of psychological safety.
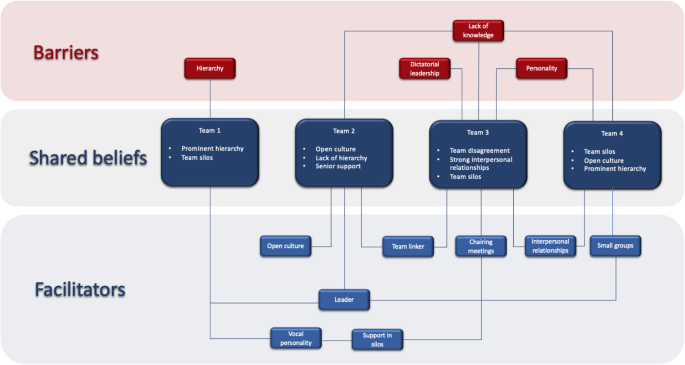
Illustration of primary care teams with their respective shared beliefs, alongside the barriers and facilitators to psychological safety. Lines connecting barriers and facilitators to shared beliefs indicate contextual relation
The four barriers (hierarchy, lack of knowledge, authoritarian leadership, personality) identified in this study were categorised as either organisational, team-based or individual-level barriers. An overview of the barriers and supporting quotes are shown in Table 2 .
Hierarchy was identified as an organisational level barrier to psychological safety within team 1. This fostered feelings of inferiority and a perception that other members valued their opinions less, increasing hesitancy to voice opinions. Team-based barriers included a lack of knowledge (team 2, 3 and 4) and authoritarian leadership (team 3). The perceived lack of knowledge was attributed to a lack of awareness around the respective discussion topic. This subsequently increased anxiety related to saying something incorrect or appearing as the lone member lacking in knowledge. Furthermore, authoritarian leadership hindered psychological safety with individuals feeling that decisions were enforced rather than discussed. This fostered a lack of ownership and members feeling powerless. Frustrations were two-fold: some participants were discouraged at the domineering approach to decision making, while others expressed concerns over the decisions made.
On an individual level, personality was cited as a barrier to psychological safety. Dominating personalities, particularly of those in leadership roles, acted as a barrier to psychological safety in Teams 3 and 4, by causing unequal dynamics and participation within conversations. Members also expressed that their opinions had to be repeated multiple times to be heard. Furthermore, one team member discussed intrinsic barriers such as shy personality or a fear of public speaking.
Facilitators
The eight key facilitators (leaders and leader inclusiveness, open culture, support in silos, boundary spanner, interpersonal relationships, small groups, vocal personality, chairing meetings) identified in this study were categorised as either team-based or individual-level barriers. An overview of the facilitators and supporting quotes are shown in Table 3 .
Leaders (teams 1,2 and 4) were cited as a prominent facilitator of psychological safety. Within team 1 and 2, leaders exhibiting a friendly attitude, acting in a supportive manner and inviting participation of members made them influential in facilitating psychological safety. An interesting facilitator of psychological safety which surfaced was that of groups of similar individuals in the same profession; silos (teams 1 and 3). Here, psychological safety was facilitated via two mechanisms: identifying within the silo which strengthened voice and empowerment via a silo leader, an individual with reduced power distance who acted as a spokesperson for the group. For example, several members felt more comfortable approaching their nursing team leader or a GP colleague rather than practice leadership directly.
The presence of a boundary spanner, an individual responsible for linking sub-groups within the wider MDT, was cited by participants in teams 2 and 3 as an influential facilitator of psychological safety. Fostering strong interpersonal relationships was an important facilitator of psychological safety in team 3 and 4. One member contrasted their ability to speak up as a longstanding team member compared to being a newcomer, highlighting that knowing the team enabled them to speak up. The presence of a smaller group made participants of Team 4 more comfortable and confident in voicing their opinions.
Individual level facilitators were having a vocal personality and chairing meetings. Vocal personality was a prominent facilitator in teams 1 and 3, with members in team 1 acknowledging their inherent confidence allowed them to voice opinions confidently. An interesting facilitator reported in team 3 was chairing meetings. Some participants referred to the dual perspective of the chairing role, describing that it facilitated them to speak up but they, in turn, acted as a facilitator for others.
To the authors’ knowledge, this is the first qualitative team-based study investigating barriers and facilitators of psychological safety in primary care teams. Obtaining the viewpoints of different healthcare professionals across four primary care teams enabled intra- and inter-group analysis, on the background of shared beliefs, which provided a contextual representation of the team dynamic. The themes that surfaced from this study can be considered at three levels; organisation, team and individual levels.
Barriers and facilitators of psychological safety emerged at an individual level, with personality influencing team dynamics significantly. Whilst the literature reporting on healthcare teams highlights how the behaviour and personality of a leader specifically can be a barrier to psychological safety [ 4 , 41 , 42 , 43 ], the impacts of dominating personalities amongst other team members is less explored. A shy personality was reported as a barrier, and whilst this may be viewed as an innate characteristic, the influence of the team in negating this should be considered. In contrast, a vocal personality emerged as a facilitator of psychological safety in this study. A relationship between personal control and voicing behaviours has been documented in healthcare literature, whereby individuals with greater autonomy feel empowered to speak up [ 44 ], however there is less exploration of the impacts of personality on speaking up behaviours in the context of psychological safety. These findings indicate that psychological safety relies on exploring the personality of both oneself and others in a team in order to establish how individuals can be best supported in the work environment.
Furthermore, our results identified barriers and facilitators at the team level. Our findings revealed that leadership roles are influential as facilitators or barriers to psychological safety. Teams 1,2 and 4 highlighted leaders who displayed support and inclusiveness as facilitators of psychological safety. Where leadership was not cited as a facilitator, it surfaced as a barrier in the form of authoritarian leadership. Literature corroborates this, highlighting a correlation between effective or inclusive leadership and psychological safety in healthcare teams [ 2 , 7 , 12 , 18 , 21 , 45 , 46 , 47 ]. In contrast, leader unreceptiveness has been reported as a barrier to raising patient concerns [ 18 , 19 ]. A key differentiator between the teams is their leadership structure in the GP practice. Members of a mono-leadership referred to their leader centralising control; this phenomenon may not have emerged in teams with multiple GP partners in the leadership structure. Although this authoritarian leadership style presents benefits in certain situations, such as emergencies occurring commonly in secondary care which require fast decision making by a single leader [ 48 ],, this is arguably less applicable and useful in primary care. Crucially, high-performing healthcare organisations are associated with broad leadership distributions [ 49 ]; our findings suggest that this should be reflected in primary care.
Through this study, various leadership traits emerged as facilitators to psychological safety, offering practical actions that can be adopted going forwards. This includes showing support, actively listening to team members and inclusive behaviours, such as encouraging contributions or introducing new members of the team to their colleagues. Developing these positive leadership traits is an important step for the NHS, with action already demonstrated by the General Practice Forward View (GPFV), which states that a larger proportion of the primary care budget is being allocated towards the leadership development of more senior GPs [ 50 ]. These findings are further supported by the literature, which has highlighted the correlation between effective leadership behaviours and psychological safety in healthcare teams [ 46 , 47 , 51 ] Additional traits that should be adopted by healthcare leaders highlighted by literature include transformational leadership behaviours [ 52 ], encouraging innovative change [ 2 ] and displaying role-modelling behaviours [ 15 , 43 , 53 , 54 ].
Associating within a silo enabled members in teams 2 and 3 to speak up. It appears counterintuitive that profession-based silos, often considered destructive to team cohesiveness [ 55 ], could facilitate psychological safety. Perhaps individuals find ‘strength in numbers [ 56 ] and subsequently leverage their silos to be heard. This appeared to be particularly noted in teams who reported poor leadership and a prominent hierarchy, both of which emerged as barriers to psychological safety. Although we have identified support in silos as a potential facilitator of psychological safety, caution is needed regarding its practical use. It is possible that this emerges within teams lacking psychological safety, resulting in a reliance rather than support within the silos. This is a novel finding, and further research is required to investigate the underlying role of silos in ensuring psychological safety.
As shown by Jain et al [ 57 ], our results also demonstrated the importance of a boundary spanner as a facilitator of psychological safety. However, our study builds on existing literature by suggesting that the practice manager, a non-clinical member of a primary care team, is most appropriate for this role. This likely stems from their knowledge of both clinical and non-clinical activities occurring within a GP practice [ 58 ]. This was a facilitator common to two highly contrasting teams (teams 2 and 3), built on different underlying shared beliefs. As primary care teams become increasingly diverse [ 59 ], our findings therefore call for the designation of a boundary spanner, given their inextricable value for unifying any team regardless of underlying dynamics. Furthermore, given this increasing diversity in healthcare teams, the traditional hierarchical view whereby doctors are seen as ‘automatic leaders’ [ 60 ] is outdated. Our findings show that providing individuals with the opportunity to chair meetings can facilitate voicing behaviour amongst members who are typically reluctant to speak up.
Of particular note is the obstructive effects of hierarchy on psychological safety. The hindering nature of hierarchy is supported by literature, and both our study alongside other research highlight that open cultures can help to negate the impact of hierarchy [ 61 ]. However, adopting a team view on hierarchy and open cultures is perhaps too restrictive; rather, a broader view which encompasses the entire healthcare organisation is warranted. Hierarchy is a deep-rooted cultural aspect of healthcare, and while some literature suggests that it can improve role clarity and coordination within teams [ 62 ], it is becoming apparent that the resulting detriment to teams should be further acknowledged in healthcare [ 63 ]. Our study has shed light on the numerous methods by which teams can help to foster psychological safety. However, if the underlying problems surrounding hierarchies are not addressed at the organisational level, it will still be difficult to foster psychological safety. We propose larger organisations such as professional bodies work towards informing key stakeholders - both clinicians and management teams, of the benefits of psychological safety as well as the role of hierarchy as a barrier to implementing this.
An element of hierarchy may also be responsible for perceived lack of knowledge acting as a barrier, where those ‘lower’ in hierarchy status incorrectly assume others in the team possess more important information and consider their own knowledge to be irrelevant to the discussion [ 64 ]. These cognitive biases can have detrimental effects to patient safety, where individuals do not raise crucial information resulting in patient harm [ 65 ]. Many junior HCPs also struggle to speak up against senior, more experienced colleagues when errors are occurring, due to an assumption of superior knowledge possessed by their supervisors [ 66 ]. These findings where a perceived lack of knowledge acts as a barrier to psychological safety are widely supported by existing literature on healthcare teams [ 43 , 51 , 67 ]. This indicates that building the confidence of each individual team member is a fundamental step to increasing psychological safety, with the leader’s role being to validate input and encourage contribution from every individual, regardless of position.
Limitations
The findings of this study should be considered in the context of several limitations. Firstly, we were unable to recruit every team member from the four primary care teams, and therefore may have missed key viewpoints. Secondly, despite the effectiveness of snowball sampling for recruitment, this method can incur selection biases as participants are recruited upon referral [ 68 ]. Finally, this study was conducted during the COVID-19 pandemic where primary care was overstretched resulting in heightened workplace stress and altered team dynamics. These unique circumstances may have altered participants’ opinions of psychological safety within their team, which may have impacted our data.
Implications for practice
This study offers a unique insight to the specific barriers and facilitators of psychological safety in primary care, identifying tangible changes that can be adopted at the individual, team and organisation level. The importance of psychological safety in healthcare is well established, underpinning the patient care that is provided and holding potential to benefit both healthcare workers and patients alike [ 7 , 69 ].
Implications for future research
During this study, common themes arose regarding perceptions of psychological safety in primary care. Profession based differences are reported in literature, however, are often generalised across healthcare [ 70 , 71 , 72 ]. A direct focus on profession analysis would provide an important insight to the field of psychological safety. By identifying profession specific attitudes, barriers and facilitators, personalised support can be offered to increase the psychological safety within general practice.
Importantly, many of the underlying barriers to psychological safety appear to be ingrained into the culture of the healthcare system. This would require multifaceted changes to deep-rooted beliefs and systems, with scope for future research to identify the most effective methods to achieve this. Alongside these efforts, the focus should be directed on the new generation of healthcare professionals and students. Psychological safety remains a relatively unknown concept to both healthcare students and educators alike [ 73 ]. Further research should explore their experience and perceptions of psychological safety, particularly whilst exposed on clinical placements, and identify methods to equip students with the ability to ensure psychological safety is prominent within their future multidisciplinary teams.
This qualitative study aimed to identify facilitators and barriers of psychological safety in primary care, considered at the individual, team and organisation levels. Leaders are influential within a team since their behaviours can directly facilitate or act as a barrier to psychological safety. However, our study highlights that the responsibility and influence does not solely lie with the leader. Rather, there are several behaviours the team can engage in to directly facilitate or impede psychological safety. By strengthening interpersonal relationships, encouraging a rotating chairperson for meetings and finding support in silos to reduce power distances, a team can create a positive team culture that ultimately supports psychological safety. It is anticipated that these findings will encourage primary care teams to reflect on their team dynamics and adopt the aforementioned strategies to ensure every member’s voice is heard.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Edmondson A. Psychological safety and learning behavior in work teams. Adm Sci Q. 1999;44(2):350–83.
Article Google Scholar
Ortega A, Van den Bossche P, Sánchez-Manzanares M, Rico R, Gil F. The influence of change-oriented leadership and psychological safety on team learning in healthcare teams. J Bus Psychol. 2014;29(2):311–21.
Google Scholar
Edmondson AC. Learning from mistakes is easier said than done: group and organizational influences on the detection and correction of human error. J Appl Behav Sci. 2004;40(1):66–90.
Yanchus NJ, Carameli KA, Ramsel D, Osatuke K. How to make a job more than just a paycheck: understanding physician disengagement. Health Care Manag Rev. 2020;45(3):245–54.
LeNoble CA, Pegram R, Shuffler ML, Fuqua T, Wiper DW III. To address burnout in oncology, we must look to teams: reflections on an organizational science approach. JCO Oncol Pract. 2020;16(4):e377–83.
Article PubMed Google Scholar
Kessel M, Kratzer J, Schultz C. Psychological safety, knowledge sharing, and creative performance in healthcare teams. Creat Innov Manag. 2012;21(2):147–57.
Appelbaum NP, Dow A, Mazmanian PE, Jundt DK, Appelbaum EN. The effects of power, leadership and psychological safety on resident event reporting. Med Educ. 2016;50(3):343–50.
Yanchus NJ, Periard D, Moore SC, Carle AC, Osatuke K. Predictors of job satisfaction and turnover intention in VHA mental health employees: a comparison between psychiatrists, psychologists, social workers, and mental health nurses. Hum Serv Organ Manage Leadership Governance. 2015;39(3):219–44.
Rangachari P, Woods JL. Preserving organizational resilience, patient safety, and staff retention during COVID-19 requires a holistic consideration of the psychological safety of healthcare workers. Int J Environ Res Public Health. 2020;17(12):4267.
Article PubMed Central Google Scholar
Hirak R, Peng AC, Carmeli A, Schaubroeck JM. Linking leader inclusiveness to work unit performance: the importance of psychological safety and learning from failures. Leadersh Q. 2012;23(1):107–17.
Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27(7):941–66.
Yukl G, Gordon A, Taber T. A hierarchical taxonomy of leadership behavior: integrating a half century of behavior research. J Leadership Organ Stud. 2002;9(1):15–32.
Brown ME, Treviño LK, Harrison DA. Ethical leadership: a social learning perspective for construct development and testing. Organ Behav Hum Decis Process. 2005;97(2):117–34.
Gong Z, Van Swol L, Xu Z, Yin K, Zhang N, Gilal FG, Li X. High-power distance is not always bad: ethical leadership results in feedback seeking. Front Psychol. 2019;10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6781884/ .
Arnetz JE, Sudan S, Fitzpatrick L, Cotten SR, Jodoin C, Chang CH, Arnetz BB. Organizational determinants of bullying and work disengagement among hospital nurses. J Adv Nurs. 2019;75(6):1229–38.
Hammond, M., 2016. Inductive or deductive approaches. [online] Warwick.ac.uk. Available at: https://warwick.ac.uk/fac/soc/ces/research/current/socialtheory/maps/when/ . [Accessed 6 December 2020].
Wilson, R., 2016. Deductive and inductive reasoning. [online] mscc.Edu. Available at: https://www.mscc.edu/documents/writingcenter/Deductive-and-Inductive-Reasoning.pdf . [Accessed 6 December 2020].
Saunders M, Lewis P, Thornhill A. Research methods for business. London: Pitman; 2007. p. 124–6.
Wellington J, Szczerbinski M. Research methods for the social sciences. London: A&C Black; 2007.
Saunders M, Lewis P, Thornhill A. Research methods for business students. 8th ed. Harlow: Pearson; 2019.
Creswell JW, Poth CN. Qualitative inquiry and research design: choosing among five approaches. California: Sage publications; 2016
Ketokivi M, Mantere S. Two strategies for inductive reasoning in organizational research. Acad Manag Rev. 2010;35(2):315–33.
Lodico MG, Spaulding DT, Voegtle KH. Methods in educational research: from theory to practice. San Francisco: Wiley; 2010.
Merriam SB, Tisdell ET. Qualitative research: a guide to design and implementation. San Francisco: Wiley.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Johnson TP. Snowball sampling. Encyclopedia Biostatistics. 2005;15:7.
Sandelowski M. Theoretical saturation. In: Given LM, editor. The SAGE encyclopedia of qualitative research methods. Thousand Oaks: Sage; 2008. p. 875–6.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field methods. 2006;18(1):59–82.
Creswell J, Creswell J. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 5th ed. SAGE Publications; 2017.
Saunders MN, Lewis P. Doing research in business & management: an essential guide to planning your project. Harlow: Pearson; 2012.
Cohen D, Crabtree B. Semi-structured interviews. In: Qualitative research guidelines project; 2006. p. 2.
Hanna P. Using internet technologies (such as Skype) as a research medium: a research note. Qual Res. 2012;12(2):239–42.
Patton MQ. Qualitative research. In: Encyclopedia of statistics in behavioral science; 2005. p. 15.
Kallio H, Pietilä AM, Johnson M, Kangasniemi M. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72(12):2954–65.
Yin RK. Case study research: design and methods. Thousand oaks: Sage publications; 2009.
Rubin HJ, Rubin IS. Qualitative interviewing: The art of hearing data. California: Sage; 2011.
Jamshed S. Qualitative research method-interviewing and observation. J Basic Clin Pharm. 2014;5(4):87.
Article PubMed PubMed Central Google Scholar
Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum. 2014;41(5):545–7.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101 Available from: https://www.tandfonline.com/doi/abs/10.1191/1478088706qp063oa . [cited 15 July 2020].
Hammond M. reflexivity [Internet]. Warwick.ac.uk . 2017 [cited 23 July 2020]. Available from: https://warwick.ac.uk/fac/soc/ces/research/current/socialtheory/maps/reflexivity/
Yanchus NJ, Derickson R, Moore SC, Bologna D, Osatuke K. Communication and psychological safety in veterans health administration work environments. J Health Organ Manage. 2014;28:754–76.
Etchegaray JM, Ottosen MJ, Dancsak T, Thomas EJ. Barriers to speaking up about patient safety concerns. J Patient Saf. 2017;1 (Published Online First: 4 November 2017). https://doi.org/10.1097/PTS.0000000000000334 .
Omura M, Stone TE, Maguire J, Levett-Jones T. Exploring Japanese nurses' perceptions of the relevance and use of assertive communication in healthcare: a qualitative study informed by the theory of planned behaviour. Nurse Educ Today. 2018;67:100–7.
Tangirala S, Ramanujam R. Exploring nonlinearity in employee voice: The effects of personal control and organizational identification. Acad Manage J. 2008;51(6):1189–203.
Munn L. Team dynamics and learning behavior in hospitals: a study of error reporting by nurses. https://doi.org/10.17615/tab9-xg64 .
Edmondson AC, Higgins M, Singer S, Weiner J. Understanding psychological safety in health care and education organizations: a comparative perspective. Res Hum Dev. 2016;13(1):65–83.
Wholey DR, Disch J, White KM, Powell A, Rector TS, Sahay A, Heidenreich PA. Differential effects of professional leaders on health care teams in chronic disease management groups. Health Care Manag Rev. 2014;39(3):186–97.
Sfantou DF, Laliotis A, Patelarou AE, Sifaki-Pistolla D, Matalliotakis M, Patelarou E. Importance of leadership style towards quality of care measures in healthcare settings: a systematic review. Healthcare. 2017;5(4):73 Multidisciplinary Digital Publishing Institute.
McKee L, West M, Flin R, Grant A, Johnston D, Jones M, et al. Understanding the dynamics of organisational culture change: creating safe places for patients and staff. Southampton, United Kingdom: NIHR Service Delivery and Organisation programme; 2010. p. 423.
General Practice Forward View [Internet]. England.nhs.uk . 2016 [cited 7 December 2020]. Available from: https://www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf
Schwappach DL, Gehring K. Trade-offs between voice and silence: a qualitative exploration of oncology staff’s decisions to speak up about safety concerns. BMC Health Serv Res. 2014;14(1):303.
Raes E, Decuyper S, Lismont B, Van den Bossche P, Kyndt E, Demeyere S, Dochy F. Facilitating team learning through transformational leadership. Instr Sci. 2013;41(2):287–305.
Leroy H, Dierynck B, Anseel F, Simons T, Halbesleben JR, McCaughey D, Savage GT, Sels L. Behavioral integrity for safety, priority of safety, psychological safety, and patient safety: a team-level study. J Appl Psychol. 2012;97(6):1273.
Alingh CW, van Wijngaarden JD, van de Voorde K, Paauwe J, Huijsman R. Speaking up about patient safety concerns: the influence of safety management approaches and climate on nurses’ willingness to speak up. BMJ Qual Saf. 2019;28(1):39–48.
Braithwaite J, Clay-Williams R, Vecellio E, Marks D, Hooper T, Westbrook M, Westbrook J, Blakely B, Ludlow K. The basis of clinical tribalism, hierarchy and stereotyping: a laboratory-controlled teamwork experiment. BMJ Open. 2016;1:6(7).
Kreindler SA, Dowd DA, Dana Star NO, Gottschalk T. Silos and social identity: the social identity approach as a framework for understanding and overcoming divisions in health care. Milbank Q. 2012;90(2):347–74.
Jain AK, Fennell ML, Chagpar AB, Connolly HK, Nembhard IM. Moving toward improved teamwork in cancer care: the role of psychological safety in team communication. J Oncol Pract. 2016;12(11):1000–11.
McLaren S, Woods L, Boudioni M, Lemma F, Rees S, Broadbent J. Developing the general practice manager role: managers’ experiences of engagement in continuing professional development. Qual Prim Care. 2007;15(2):85–91.
General Practice: Forward View [Internet]. England.nhs.uk . 2016 [cited 23 July 2020]. Available from: https://www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf
van Schaik SM, O'Brien BC, Almeida SA, Adler SR. Perceptions of interprofessional teamwork in low-acuity settings: a qualitative analysis. Med Educ. 2014;48(6):583–92.
Padmore JS, Jaeger J, Riesenberg LA, Karpovich KP, Rosenfeld JC, Patow CA. “Renters” or “owners”? Residents' perceptions and behaviors regarding error reduction in teaching hospitals: a literature review. Acad Med. 2009;84(12):1765–74.
Cantimur Y, Rink F, van der Vegt GS. When and why hierarchy steepness is related to team performance. Eur J Work Organ Psychol. 2016;25(5):658–73.
Bould MD, Sutherland S, Sydor DT, Naik V, Friedman Z. Residents’ reluctance to challenge negative hierarchy in the operating room: a qualitative study. Can J Anesthesia. 2015;62(6):576–86.
Moneypenny MJ, Guha A, Mercer SJ, O'Sullivan H, McKimm J. Don't follow your leader: challenging erroneous decisions. Br J Hosp Med. 2013;74(12):687–90.
Salazar MJ, Minkoff H, Bayya J, Gillett B, Onoriode H, Weedon J, Altshuler L, Fisher N. Influence of surgeon behavior on trainee willingness to speak up: a randomized controlled trial. J Am Coll Surg. 2014;219(5):1001–7.
Beament T, Mercer SJ. Speak up! Barriers to challenging erroneous decisions of seniors in anaesthesia. Anaesthesia. 2016;71(11):1332–40.
Article CAS PubMed Google Scholar
Reese J, Simmons R, Barnard J. Assertion practices and beliefs among nurses and physicians on an inpatient pediatric medical unit. Hosp Pediatrics. 2016;6(5):275–81.
Sedgwick P. Snowball sampling. Bmj. 2013;20:347.
Edmondson A. Learning from mistakes is easier said than done: group and organizational influences on the detection and correction of human error. J Appl Behav Sci. 1996;32(1):5–28.
Rahmati A, Poormirzaei M. Predicting nurses' psychological safety based on the forgiveness skill. Iran J Nurs Midwifery Res. 2018;23(1):40.
Pfeifer LE, Vessey JA. Psychological safety on the healthcare team. Nurs Manag. 2019;50(8):32–8.
Moore L, McAuliffe E. To report or not to report? Why some nurses are reluctant to whistleblow. In: Clinical Governance: An International Journal; 2012.
Torralba KD, Jose D, Byrne J. Psychological safety, the hidden curriculum, and ambiguity in medicine. Clin Rheumatol. 2020;4:1–5.
Download references
Acknowledgements
Not applicable.
Funding was not required for this study.
Author information
Ridhaa Remtulla, Arwa Hagana, Nour Houbby and Kajal Ruparell are joint co-first authors.
Authors and Affiliations
College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK
Ridhaa Remtulla
Imperial College London, School of Medicine, London, UK
Arwa Hagana, Nour Houbby, Kajal Ruparell, Nivaran Aojula, Anannya Menon & Santhosh G. Thavarajasingam
Leeds University Business School, University of Leeds, Leeds, UK
Edgar Meyer
You can also search for this author in PubMed Google Scholar
Contributions
RR, AH, NH and KR are co-first authors and have contributed substantially to the conduct of this study and the writing of the manuscript. KR, NA and NH were responsible for data collection. RR, NH and AH were responsible for transcribing, coding, data analysis and interpretation. NA, AM and SGT substantially contributed to the study design, recruitment, interview schedule and preliminary drafts of the work. EM substantially contributed to the conception and design of the study, forming the basis of the thematic analysis used, and made substantial revisions to the manuscript, alongside overseeing the overall study conduct. The authors read and approved the final manuscript.
Authors information
RR is a female 6th year medical student but was a 5th year medical student at the time of the study.
AH, NH, KR and AM are female 5th year medical students, but were 4th year medical students at the time of the study.
NA and SGT are male 5th year medical students but were 4th year medical students at the time of the study.
EM (PhD) is a male professor at Leeds Business school. At the time of the study, EM was an associate Dean at Imperial College London business school.
Corresponding author
Correspondence to Ridhaa Remtulla .
Ethics declarations
Ethics approval and consent to participate.
This study was granted Ethical Approval by Imperial College Research Ethics Committee (ICREC). Informed, written consent was obtained from all participants.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: supplementary file a.
- Interview Schedule.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions

About this article
Cite this article.
Remtulla, R., Hagana, A., Houbby, N. et al. Exploring the barriers and facilitators of psychological safety in primary care teams: a qualitative study. BMC Health Serv Res 21 , 269 (2021). https://doi.org/10.1186/s12913-021-06232-7
Download citation
Received : 12 August 2020
Accepted : 02 March 2021
Published : 24 March 2021
DOI : https://doi.org/10.1186/s12913-021-06232-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological safety
- Primary care
- General practice
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Language: English | Danish
Barriers to and facilitators for supporting patient communication in the adult ICU during the COVID ‐19 pandemic: A qualitative study
Laura istanboulian.
1 Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto Ontario, Canada
2 Michael Garron Hospital, Toronto Ontario, Canada
Louise Rose
3 Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, King's College London, James Clerk Maxwell Building, London UK
4 Lane Fox Clinical Respiratory Physiology Research Centre, St Thomas' Hospital, Guy's and St. Thomas' NHS Foundation Trust, London UK
Yana Yunusova
5 Department of Speech Language Pathology, University of Toronto, Toronto Ontario, Canada
6 Toronto Rehabilitation Institute, University Health Network, Toronto Ontario, Canada
7 Harvitz Brain Sciences Program, Sunnybrook Research Institute Wellness Way, Toronto Ontario, Canada
8 Tory Trauma Program, Sunnybrook Health Sciences Centre, Toronto Ontario, Canada
Associated Data
The data that support the findings of this study are available from the corresponding author upon reasonable request.
To explore barriers to and facilitators for supporting communication with and for patients treated with invasive mechanical ventilation in the intensive care unit during the COVID‐19 pandemic.
A qualitative descriptive study reported according to the Consolidated Criteria for Reporting Qualitative Research.
Adult intensive care unit patients treated with an advanced airway for mechanical ventilation, their family members and healthcare providers (nurses, intensivists and allied health) were recruited for interviews between January and April 2021. Interviews were audio‐recorded, transcribed verbatim and analysed using content analysis methods. Reported communication barriers and facilitators were mapped to the theoretical framework of acceptability to identify potentially modifiable clinical and institutional practices.
We recruited 29 participants (20 healthcare providers, four patients and five family member). Provider communication barriers included isolation procedures, lack of personal protective equipment and inadequate communication tools/training, which reduced perceived communication frequency and effectiveness. Patients and families reported infrequent proactive provision of communication tools, which contributed to a crisis of unmet needs. Reported facilitators included adequate access to personal protective equipment to mitigate the risk of patient proximity and communication tools/training to improve communication effectiveness. Authentic unit leadership helped to assuage pandemic work stressors and encourage humanistic care. Our analysis indicates low acceptability of existing communication practices during the COVID‐19 pandemic and the importance of leadership to reduce the burden of communication through provision of key necessary resources.
COVID‐19 conditions have precipitated a communication crisis in the ICU. The results of this study have practice and policy implications and will be used to co‐design a communication intervention for use during and beyond the COVID‐19 pandemic.
The study contributes a better understanding of resources necessary to support patient communication. Results apply beyond the pandemic to routine use of infection prevention and control precautions in the intensive care unit.
1. INTRODUCTION
Intensive care unit (ICU) patients and their healthcare providers (HCPs) have persistently reported communication difficulty due to impaired vocalization associated with placement of advanced airways (e.g. endotracheal or tracheostomy tubes) for mechanical ventilation. Globally, ICU survivors have described communication impairment during mechanical ventilation as one of the most stressful and dehumanizing events of hospital admission (Baumgarten & Poulsen, 2015 ; Karlsen et al., 2019 ). Communication difficulty can result in the inability to self‐report major physical (e.g. pain, dyspnea, thirst) and psychological symptoms (e.g. sadness, fear, confusion) of critical illness and its treatment (Choi et al., 2017 ; Radtke et al., 2011 ). Unrelieved symptoms contribute to long‐term patient morbidity including depression, anxiety and post‐traumatic stress disorder, rendering communication an important target for practice improvement (Ijssennagger et al., 2018 ; Inoue et al., 2019 ; Khalaila et al., 2011 ).
ICU nurses most frequently interact with critically ill patients and require pragmatic strategies to address communication impairment. ICU nurses may also be required to guide other HCPs including allied health team members and intensivists about communication strategies and tools that match patient abilities and preferences (Istanboulian et al., 2020 ). Current recommendations include but are not limited to the use of augmentative and alternative communication (AAC). Defined as alternatives to speech, AAC consists of ‘unaided’ strategies (e.g. mouthing words and gesturing) or ‘aided’ strategies such as low‐tech (e.g. picture or word boards) and high‐tech (e.g. computer interface) devices (Augmentative and Alternative Communication, 2019 ). Prospective use of AAC is demonstrated to be effective in reducing patient communication difficulty and improving HCP satisfaction with care (Carruthers et al., 2017 ; Karlsen et al., 2019 ; Ten Hoorn et al., 2016 ; Zaga et al., 2019 ). In support of this evidence, recent research has identified the importance of all ICU HCPs having access to communication tools and training in their use (Happ et al., 2014 ; Istanboulian et al., 2020 ; Trotta et al., 2019 ) to avoid patient and HCP emotional distress (i.e. frustration, anger) over failed communication attempts (Istanboulian et al., 2020 ). The burden associated with failed communication may lead to emotional disengagement and reduced communication frequency by both patients and HCPs (Ijssennagger et al., 2018 ; Istanboulian et al., 2020 ).
In Canada and the US, to date approximately 18–28% of people with confirmed COVID‐19 infection have been reported to require ICU admission (Canada Go, 2022 ; Nguyen et al., 2021 ). Those treated with mechanical ventilation often experience a prolonged ICU admission, thereby increasing the need for consistent and effective communication support (Attaway et al., 2021 ). However to date, infection control conditions, such as those enacted during the COVID‐19 pandemic, have not been the primary context for research informing ICU communication guidance (Istanboulian et al., 2020 ). COVID‐19 infection prevention and control measures including the use of personal protective equipment (PPE) and visiting restrictions may complicate utilization of current guidance to support communication with patients (i.e. AAC) and support of communication for patients (i.e. family education in AAC) in the adult ICU (Freeman‐Sanderson et al., 2020 ; Ontario PH, 2021 ). As the pandemic presents a significant change in the global healthcare landscape, exploratory research is needed to understand barriers to and facilitators for communication among nurses, patients, family and other ICU professional stakeholders to inform practice recommendations (Akgun et al., 2020 ; Barreras‐Espinoza et al., 2021 ; Freeman‐Sanderson et al., 2020 ; Richards et al., 2021 ; Rose et al., 2021 ).
Theoretical frameworks are recommended to explore practice barriers and facilitators, and inform the design and implementation of complex interventions, such as patient communication (O'Cathain et al., 2019 ). The theoretical framework of acceptability (TFA) defines acceptability as a multifaced construct that reflects the cognitive and emotional responses of people delivering or receiving a healthcare intervention (Sekhon et al., 2017 ). The TFA includes seven constructs, namely: affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness and self‐efficacy (Sekhon et al., 2017 ). The TFA posits that patients, families and HCPs form judgements about the acceptability of an intervention, based on anticipated or actual experience, that will impact their engagement with or commitment to the intervention. Because aspects of an intervention can be modified to increase acceptability, an important element of the present study was to identify dimensions of communication that may be amenable to improvement.
2. THE STUDY
Our aim was to explore barriers to and facilitators for supporting communication with and for mechanically ventilated adult patients admitted to ICU during the COVID‐19 pandemic according to TFA constructs.
2.1.1. Design and setting
We conducted a prospective qualitative descriptive study, which is an approach for exploring participants' perceptions of clinical processes and how they might be improved (Doyle et al., 2020 ). We recruited participants from a 17‐bed medical‐surgical ICU in a community teaching hospital in Toronto, Canada (January–April 2021) admitting COVID‐19 patients experiencing hypoxemic respiratory failure. The unit is managed under a closed intensivist model and nurses are assigned to mechanically ventilated patients in a 1:1 or 1:2 ratio. Respiratory therapists (RTs) are also present in the unit to manage ventilator support and weaning. The study unit followed COVID‐19 infection prevention and control standards set by the Government of Ontario, including the use of PPE, isolation of patients with suspected or confirmed infection and restricting family visitors except in the case of imminent death (Ontario PH, 2021 ). The Consolidated Criteria for Reporting Qualitative Research (COREQ) was used as a guide for reporting this research (Tong et al., 2007 ).
2.2. Participants
Eligible participants were: (1) patients (≥18 years of age, discharged from ICU and able to speak English) admitted to the study unit and treated with an advanced airway during the COVID‐19 pandemic; (2) family members (≥18 years of age, discharged from ICU and able to speak English) of patients admitted to the study unit; (3) HCPs including registered nurses, intensivists and allied health team members (i.e. RTs, speech and language therapists [SLP], occupational and physical therapists, registered dietitians, pharmacists, social workers, spiritual care providers) employed in the study unit during the COVID‐19 pandemic. We used convenience sampling in the study setting to recruit participants. This comprised the use of paper and electronic posters advertising the study. Patients and family were identified by HCPs on discharge from ICU and all participants were approached and consented by the principal investigator (LI).
2.2.1. Data collection
Following informed consent, participants took part in one interview exploring their communication experiences using a semi‐structured interview guide ( Material S1 ) previously piloted with an external sample. All interviews were conducted by LI who identifies as a woman and has graduate training in the conduct of semi‐structured interviews. LI works professionally as a nurse practitioner with prior clinical experience caring for mechanically ventilated patients and their families in adult ICUs and a long‐term ventilation and weaning centre in the study site.
Interviews were conducted privately either face to face (in an office), by telephone or video call. Data collection and analysis occurred concurrently and data collection was discontinued when no new information was being identified during interviews (Cope, 2014 ). No one refused participation, no participant dropped out and no repeat interviews were carried out. Interviews were digitally audio‐recorded and transcribed verbatim. Prior to the interview, LI ensured participants understood the rationale for the study and that participation was voluntary and confidential.
2.2.2. Ethical considerations
Ethics approval for the study was given by the Michael Garron Hospital (820‐2010‐Mis‐347) and the University of Toronto Research Ethics Boards (40495). Written informed consent was obtained from all participants prior to interview.
2.2.3. Data analysis and rigour
We completed a team‐based deductive content analysis with author coders working in pairs together, multiple rounds of group discussions and NVIVO 12 software to identify, code and categorize barriers and facilitators to supporting patient communication (Bengtsson, 2016 ). The four stages of content analysis (i.e. decontextualization, recontextualization, categorization and compilation) were used (Bengtsson, 2016 ). In the categorization phase, barriers and facilitators were mapped to the TFA's seven constructs. Definitions for the TFA constructs were adapted to communication with adult ICU patients (Table 1 ). To enhance credibility of the analysis a code book was constructed and modified using an audit trail through the multiple rounds of coding and discussions among the research team (Cope, 2014 ; De Cuir‐Gunby et al., 2011 ). Further meanings in and across the acceptability constructs and participant groups were elaborated during the compilation stage.
Context‐specific definitions for theoretical framework of acceptability (TFA)
| Constructs | Definition |
|---|---|
| Affective attitude | How the individual (HCP or patient/family) describes feeling about communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Burden | The perceived physical, psychological and cognitive effort required of the individual (HCP or patient/family) to engage in communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Ethicality | The extent to which supporting patient communication has a good fit with the individual's (HCP or patient/family) personal or professional values in the context of infection control practices for COVID‐19 in the adult ICU |
| Intervention coherence | The extent to which the individual (HCP or patient/family) understands how to support communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Opportunity costs | The extent to which benefits (e.g. time, money, personal safety) must be given up by the individual (HCP or patient/family) to engage in communication in the context of infection control practices for COVID‐19 in the adult ICU |
| Perceived effectiveness | The extent to which communication is perceived by the individual (HCP or patient/family) to be effective. Strategies that support selecting what is thought to be the most effective intervention in the context of infection control practices for COVID‐19 in the adult ICU |
| Self‐efficacy | The individual's (HCP or patient/family) confidence that they can support communication in the context of infection control practices for COVID‐19 in the adult ICU |
Abbreviations: HCP, healthcare provider; ICU, intensive care unit.
3. FINDINGS
We conducted 29 semi‐structured telephone (15, 52%), face to face (9, 31%) and video call (5, 17%) interviews. Most interviews (23, 79%) were between 30 and 60 min (average 35 min) and six (21%) lasted between 15 and 30 min. Data were collected from nurses and other HCPs (20, 69%) and patients/family (9, 31%). HCPs were primarily women (17, 85%); patient participants were mostly men (3, 75%). Family members largely identified as women (4, 80%) and spouses (2, 40%) and included both members of surviving and deceased ICU patients (Table 2 ). Patient and family interviews occurred from 11 to 305 days post discharge from ICU, and all participants were able to recall communication experiences in ICU during COVID‐19 pandemic conditions. Patient and family interviews were conducted in dyads (4, 44%) or stand alone when only a patient or family member was available (5, 56%).
Participant demographics ( N = 29)
| Demographics | (%) |
|---|---|
| Healthcare providers | 20 (69) |
| Women | 17 (85) |
| Education level | |
| Diploma | 3 (15) |
| Bachelor | 7 (35) |
| Graduate | 10 (50) |
| Profession | |
| Registered Nurse | 9 (45) |
| Allied | 10 (50) |
| Intensivist | 1 (5) |
| Intensive care unit experience | |
| <1 year | 5 (25) |
| 1–10 years | 12 (60) |
| 11–20 years | 2 (10) |
| >20 years | 1 (5) |
| Employment | |
| Full‐time | 11 (55) |
| Patients | 4 (44) |
| Age (range) | 55–71 |
| Gender | |
| Women | 1 (25) |
| Family | 5 (56) |
| Gender | |
| Woman | 4 (80) |
| Relation to patient | |
| Spouse | 2 (40) |
| Sibling | 2 (40) |
| Child | 1 (20) |
| Patient deceased | |
| Yes | 1 (20) |
Though a variety of interview modes were used, each in accordance with participant preference, the quality of data collected afforded by video and face to face methods offered better access to non‐verbal communication for all participants, and in the case of HCPs time constraints in the form of interruptions were observed. Participant checking did not occur after data collection was complete, however, clarification with participants was sought throughout each interview. Participants largely expressed gratitude for the opportunity to share their experiences.
HCPs described using a range of communication strategies with patients individualized to each person's level of consciousness and functional capacities. The primary method described was lip reading/gesture interpretation. Examples of AAC use for awake patients included alphabet boards found online and printed locally or a clipboard and paper if available. For patients who were not awake, some HCP participants described explaining procedures, that is, step‐by‐step guidance. Patient participants recalled more extensive communication efforts by individual providers as the exception rather than the norm. Communication strategies for patients in the context of visitor restrictions included facilitating telephone and video calls between patients and family members (Figure 1 ).

Summary of HCP reported communication strategies. Abbreviations: HCP, health care provider; SLP, speech and language pathologist
Overall participants described communication with and for mechanically ventilated patients in the context of the COVID‐19 pandemic as being significantly constrained, inconsistent, frequently ineffective and unacceptable, thereby contributing to a crisis of communication. Reported barriers and facilitators associated with communication interventions spanned all TFA constructs. The following results are organized by barrier (Table 3 ) and facilitator (Table 4 ) categories and described with theoretical concepts from the TFA (identified by italics). In the barrier and facilitator categories, HCP results are separated from patient and family results, permitting comparison across these groups. The source of HCP quotes from members of the allied team were not separated by profession to protect the privacy of participants for whom there were one or few from each class in the study setting. Additional quotes are included as Table S1A–D ).
Summary of HCP and patient/family reported barriers to supporting communication with and for patients according to the TFA (Rose et al., 2021 )
| Construct | HCP | Patient/family |
|---|---|---|
| Affective attitude | Negative feelings about distal or insufficient communication | Anger and frustration with failed communication |
| Burden | Shortage of PPE Physical discomfort of PPE Fear of spreading infection Insufficient time Perceived futility Emotional and cognitive load | Fear to see patient sick Physical weakness Confusion about situation Loss of family presence |
| Ethicality | Lack of proximity and time | Strategies not supportive of patient humanity and autonomy |
| Intervention coherence | Insufficient tools and training | Inconsistent availability of tools Inconsistent HCP skill |
| Opportunity costs | Risk of infection Other priorities in ICU | |
| Perceived effectiveness | Patient decreased level of consciousness and weakness PPE impedes verbal and non‐verbal messages | Decreased level of consciousness PPE blocks verbal and non‐verbal messages |
| Self‐efficacy | HCP lack of skill | HCP and family lack of skill |
Abbreviations: HCP, healthcare provider; PPE, Personal protective equipment; TFA, theoretical framework of acceptability.
Summary of HCP and patient/family reported facilitators for supporting communication with and for patients according to the TFA (Rose et al., 2021 )
| Construct | HCP | Patient/family |
|---|---|---|
| Affective attitude | Feeling good with successful communication | |
| Burden | PPE availability Voice modulation Exaggerate gestures Mental health support Spiritual support Leadership support | Trust in HCP Connecting patients and family |
| Ethicality | Empathy Professional values | Strategies that support patient humanity and autonomy |
| Intervention coherence | Access to tools and training | Access to tools Coaching from HCP |
| Opportunity costs | Flexibility with timing of video calls | |
| Perceived effectiveness | Communication assessment and treatment algorithm | Increased level of consciousness |
| Self‐efficacy |
Abbreviations: HCP, Healthcare provider; PPE, personal protective equipment; TFA, Theoretical framework of acceptability.
3.1. Communication barriers
3.1.1. hcp barriers.
Participants described patient proximity as a prerequisite for assessing mechanically ventilated patient communication needs and executing collaborative strategies such as lip reading, symbol/word boards or reading handwritten messages. Impaired patient proximity under isolation procedures led several HCPs to reported negative affective attitudes concerning patient communication. For example, one participant described having to communicate from outside the glass door of the patient's room using a telephone as ‘awful’ (Allied). This HCP explained that communication at a distance was required to reduce excess consumption of PPE, due to shortages at the onset of the pandemic. Conservation of PPE added to the burden of communication, whereby essential communication opportunities were constrained or ineffective at a distance, resulting in concerns about the ethicality of care.
Masks and visors also negatively impacted perceived effectiveness of communication through reduced transmission of verbal and non‐verbal messages. This warranted additional time spent communicating in discomforting conditions:
Also, sometimes you're wearing an N95 mask and you're wearing a shield on top of that, and you know, and you're wearing a gown and hairnet and everything, you have to speak really loudly. And, and your words don't come out as clear. Nurse
HCPs described communication with mechanically ventilated patients as a time‐intensive endeavour under normal or non‐pandemic circumstances. This is because a process of trial and error is required to identify modes of communication best suited to each patient's level of consciousness and functional capacities. The opportunity costs of supporting patient communication in a pandemic context included having to balance patient care needs, infection risk for themselves, as well as physical discomfort and a time‐compressed work environment. One participant explained:
I mean, it's not just a coincidence that we leave the room without saying ‘Do you need anything else.’ We're trying to get out so that we can get to the next person. Allied
HCPs described volatile emotions such as sadness as a significant communication burden in this context. Some participants speculated that strong emotions might negatively impact the willingness of HCPs to participate in patient communication interventions. For example, the increased proportion of patient deaths due to COVID‐19 led to what some described as an overriding feeling of futility:
…And no matter what you do, sometimes it just doesn't work. They die …. And then, here comes another one, you know, like, and again, the same presentation. Allied.
The emotional, physical and psychological demands of this work were well exemplified by accounts of facilitated communication for patients and families via video call at the time of death. Some family members asked HCPs to perform extended acts of patient intimacy such as ‘holding their hand’ (Nurse). These encounters placed HCPs in sustained contact with dying patients and grieving family members adding to the emotional burden of communication.
Many HCP reported a lack of ready access to communication tools contributing to the burden of communication with mechanically ventilated patients. Lack of access to communication tools, particularly in isolation rooms was frequently reported. One participant stated:
So, I usually have to open the door and be like, “Can I please have a clipboard? paper? Anything? A pen? pencil?” Allied
Others described low intervention coherence and self‐efficacy leading to frequent communication failures. Resolution of such difficulty required time‐consuming workarounds, such as ‘calling a colleague for help’, which increased the opportunity costs of communication (Nurse). Furthermore, while SLPs were available for communication consultation at the study site, there was variable awareness of their services among staff.
In summary, HCP barriers for communicating with mechanically ventilated patients emerged from isolation requirements and PPE shortage, which impeded the proximity required for communication support. PPE impediments to message transmission and limited access to communication tools further complicated this work. The opportunity costs of supporting patient communication in a pandemic context included having to balance patient needs, infection risk, physical discomfort and a time‐compressed work environment. The cumulative physical, emotional and psychological barriers contributed to negative affective attitudes , low intervention coherence and self‐efficacy, reduced ethicality and high burden of communication with and for patients.
3.1.2. Patient and family barriers
Like HCP, patients and families described barriers to communication with respect to visiting restrictions and the deployment of telephone and video calls, which did not uniformly meet their needs. For example, some families did not characterize facilitated telephone or video calls with the patient as ‘real communication’:
Well, I couldn't communicate with xxx because I couldn't be there. Family
In this instance, proximity to the mechanically ventilated patient was considered essential for meaningful expression of verbal (i.e. comforting words) and non‐verbal messages (i.e. physical touch). The limitations of video call methods were made particularly clear in instances where the patient was sedated or comatose:
He was unconscious … the first while so there was no real communicating with him. Family
The non‐responsive nature of sedated or comatose mechanically ventilated patients during some video calls aroused discomfort for some participants and added to the emotional burden of communication and reduced intervention coherence . Some participants felt ill prepared for these encounters:
She's gonna be scarred forever from that first view of the ICU and seeing her dad like that. Family
When reflecting back on their inability to communicate verbally during mechanical ventilation, most patients described negative affective attitudes including frustration with their non‐verbal status and clinicians who they perceived as unable to understand them when they mouthed words:
I couldn't [speak], nothing would come out. It was frustrating for me. I'm trying to talk and then I would get very upset because why isn't she listening to me? Why isn't she understanding me? Patient
Family members confirmed how few HCPs were able to lip read, leading to frequent communication failures:
Because there was one, I remember who was really good at lip reading, but the rest of them weren't. Family
In rare instances, family members reported HCPs introducing low‐tech strategies such as communication boards when lip reading was unsuccessful. However, barriers to their use included patient functional deficits, which negatively impacting perceived effectiveness of this strategy:
He'd play with the [word] boards, and those would get frustrating … Family
Patients confirmed infrequent provision of tools such as communication boards and writing instruments, despite their interest in using them. For most, this culminated in a lack of ethicality related to expectations for communication support:
Did anyone ever bring you an alphabet board? Interviewer No. Never. Patient
Patients emphasized how unresolved communicate barriers during mechanical ventilation left them vulnerable and afraid in isolation rooms, compromising their feelings of autonomy and humanity ( ethicality ). For example, one patient repeatedly struggled to capture the attention of HCPs, who often appeared distracted or rushed during their encounters. In addition to the negative impact on their feelings of humanity, these events left patients in a state of crisis:
Well, when you have absolutely no voice [it] is little things that just can bring a little control. They turn around, they walk out. So, I'm waving at a back. […] I have no idea whether they even saw me. Patient
Like HCP, patient and family participants reported impaired verbal and non‐verbal message transmission with PPE, but also described difficulty in identifying which HCP they were communicating with and understanding general information about the treatment plan. On PPE and perceived effectiveness of communication, one family member who was able to visit the ICU stated:
So much of our communication is nonverbal, as you know … And if you've got that taken away, it's very, very, very difficult to really absorb what's going on. Family
In summary, patient and family participants reported communication barriers during mechanical ventilation such as isolation procedures, functional deficits, HCP skill and PPE use as contributing to low intervention coherence and negative affective attitude s. Patients and family also reported a high emotional burden of communication via video calls without adequate preparation as well as confusion about HCP identity. An overall gap in the provision of proactive and effective communication support compromised the ethicality of care and left some participants in a state of crisis.
3.2. Communication facilitators
3.2.1. hcp facilitators.
Several strategies were reported to manage the challenges of working with PPE and mechanically ventilated patients managed in isolation. Reduced verbal and non‐verbal message transmission while wearing masks and visors was mitigated through exaggerated gestures and voice modulation.
You have to talk in short sentences loudly and we have to be very clear and concise because … the mask and the shields. Nurse
Adequate availability of PPE was a reported facilitator that increased the acceptability of supporting patient communication during the COVID‐19 pandemic. As the PPE supply increased and rationing was lessened, clinicians were able to spend more time at the patient bedside:
And we feel a little bit more liberal with our PPE than we did previously. So, I think the actual hands on with the patients enhance the communication with the patient; [it] is a little bit better. Intensivist
Greater time spent in ‘hands on’ care at the bedside enabled more frequent communication opportunities and aligned with ethical tenets of professional practice. For example, one participant explained how PPE enabled them to better fulfil their role in emotionally and psychologically safeguarding patients:
But that's what you're there for. You're there to keep them alive. But you want to reassure them; too, it's just part of the job. Allied
Balancing opportunity costs of patient care needs, infection risk and the physical discomfort of PPE was facilitated through supportive acknowledgement of care stressors by unit leaders (e.g. daily staff‐leadership huddles) and access to the spiritual care team who helped to process feelings of burden for HCPs. Intervention coherence for facilitating communication with and for patients was advanced by communication tool availability and training of staff to assist in appropriate tool selection and implementation:
I think there's room for a structured process in terms of “if this doesn't work, try this. If it doesn't work, try this, this doesn't work try this”. Allied
Choosing the appropriate strategy for mechanically ventilated patients based on communication assessments was a suggestion to reduce frustration associated with communication failure. Recommendations included a decisional algorithm to improve perceived effectiveness of communication interactions.
In summary, HCPs acknowledged the importance of adequate PPE and communication tools/training to support the intervention coherence and sustained proximity required for communication work with mechanically ventilated patients. They also described examples of unit leadership mitigating some of the emotional burden and opportunity costs of supporting patient communication in the pandemic context. Improvements in perceived effectiveness through individual workarounds such as accentuating gestures and speaking louder were described, as was the suggestion to use an assessment‐based communication algorithm.
3.2.2. Patient and family facilitators
Some patients described positive affective attitudes in response to the proactive facilitation of communication needs during mechanical ventilation. For example, a few patients recalled proactive provision of writing instruments. The time HCPs invested in facilitating and reviewing written communication was described as reducing the burden of voicelessness during mechanical ventilation:
Yeah. I said why I have no voice. Thank God there's a pen and paper. Patient
Like I have to be able to write something and then have the person actually take the time to read it […]. And ask you about it. Do you mean this? Yes or no? Patient
Similarly, a patient aligned the proactive application of a speaking valve to their tracheostomy tube with positive affective attitudes about their treatment and recovery:
Yeah, I remember the day I got [the speaking valve]. And I just said a few words. And I just felt so good. Patient
Patients also described the provision of technology for telephone and video calls as reducing the emotional burden of isolation and advancing the ethicality of care, as it facilitated a connection with family members, who offered emotional support and reassurance.
… if it wasn't for the actual iPad that was provided from the hospital, yeah, they would literally have no means of communication whatsoever. Zero. Patient
With respect to preparation for communication with a non‐verbal mechanically ventilated patient, one family member shared how coaching from a speech language pathologist in the ICU improved the coherence and perceived effectiveness of video call communication:
And she [SLP] actually spent some time with xxx coaching him on different things to do. She also coached me in terms of, you know, I'm used to asking open ended questions. Family
In summary, patients and family participants reported proactive provision of communication tools/training and associated use of technology as therapeutic during mechanical ventilation. Such support improved perceived effectiveness in communication and advanced perceptions of role self‐efficacy , care ethicality and reducing the burden of communication barriers.
4. DISCUSSION
The aim of this qualitative study was to explore barriers to and facilitators for supporting communication with and for mechanically ventilated adult patients admitted to ICU during the COVID‐19 pandemic according to TFA constructs. To our knowledge, this is the first study to explore ICU patient communication needs in ICU during pandemic conditions. Study results revealed substantial gaps in support for patients and a practice context fraught with unanticipated challenges, often culminating in a crisis of communication. Stakeholder reported communication barriers and facilitators spanned all constructs of the TFA and comprised potentially modifiable clinical and institutional practices including proactive and systematic provision of communication tools, training, emotional/spiritual support, as well as leadership practices that may encourage effective and timely communication with and for mechanically ventilated patients.
4.1. Communication barriers
Patients, family members and HCPs reported how isolation precautions contributed to negative affective attitudes and burden , as they counteracted the proximity and time required for successful communication support during mechanical ventilation. Negative affective attitudes were described by patients who were frustrated by abbreviated or non‐existent communication encounters and family members who experienced distress in their attempts to communicate with non‐responsive patients. HCPs also reported feeling badly about insufficient or ineffective communication interventions, such as those conducted from a distance or under time‐compressed circumstances. Sustained proximity, for example when using a communication board, tablet for video calls, or lip reading was described, but HCPs explained they often did so with fear of contracting COVID‐19 from patients and infecting their own family members at home. These pandemic‐related reported risks add to known moral difficulties associated with the patient proximal nature of nursing work (Peter & Liaschenko, 2004 ). The high opportunity costs of patient care were similarly reported in a prospective cross‐sectional survey from an Australian ICU, where 90% of responding nurses shared the fear of contracting and transmitting COVID‐19 (Lord et al., 2021 ). Furthermore, prior research suggests HCPs exposed to high patient acuity, advanced technology, families in crisis and morally distressing situations are at high risk of burnout and depersonalization (Epp, 2012 ). These issues may impede the proximity need to identity patient communication needs and provide effective support.
Described shortages of essential resources (e.g. PPE, time, communication tools) and the physical challenges of wearing PPE contributed to perceived ineffective communication , and ethical‐moral conflict for HCPs balancing professional accountability and personal safety. While the lack of available PPE reduced bedside communication encounters, its use often negatively influenced perceived communication effectiveness . Other authors have described impaired verbal and non‐verbal message transmission due to PPE and shortages in supply as major communication barriers in care settings outside of ICU (Knollman‐Porter & Burshnic, 2020 ; Richards et al., 2021 ). Masks and visors inhibit what SLPs call the ‘speech chain’; the listener's ability to simultaneously hear, lip read and interpret facial expressions (Reidy et al., 2020 ). In addition to muffling voices, masks and visors render recognition of clinicians, and therefore their purpose at the bedside, difficult for patients. These challenges may contribute to communication breakdown, increased frustration and decreased quality of care.
As in previous studies, a lack of uniform awareness of local communication experts, such as SLPs, lack of easily accessible communication tools and limited family presence negatively impacted communication encounters and perceived empathic care by mechanically ventilated patients (Istanboulian et al., 2020 ). Insufficient training and ready access to communication tools, such as video call tablets, were reported as barriers to supporting patient communication with family members. A UK multicentre survey of how communication between families, patients and the ICU team was enabled during the pandemic similarly reported insufficient staff time, rapid implementation of and unequal availability of video call technology as well as some centres restricting their use at end‐of‐life (Rose et al., 2021 ). Our study describes the immense emotional nature of end‐of‐life video supported communication on HCPs. The negative psychological effects of remote‐only communication for family of ICU patients during the COVID‐19 pandemic have been recently described (Cattelan et al., 2021 ). Family participants in our study, though appreciative of video calls, suggested the need for better preparation and emotional support for technology‐mediated patient encounters.
4.2. Communication facilitators
Authentic leadership, with its attributes of transparency, honesty and mutual respect, may play an important role in creating work environments that promote humanistic care, including communication support through reducing staff moral distress (Spence Laschinger & Fida, 2015 ). Key facilitators reported in this study included the role leadership played in reducing the burden of communication with mechanically ventilated patients through ensuring adequate provision of PPE and transparent policy information. Tabah and colleagues previously identified an association between shortage of PPE and low HCP confidence in the adequacy of protection from COVID infection (Tabah et al., 2020 ). Likewise, a recent US study reported a reduction in moral distress among nurses during COVID‐19 when leadership provided clear communication and adequate PPE supplies (Lake et al., 2021 ). Adequacy of PPE and clear communication from unit leadership may increase confidence in personal safety, thereby enabling more time spent in direct patient care supporting communication interventions.
While provision of PPE was an institutional responsibility, strategies to overcome other communication resource gaps were most often left to the individual HCP to resolve. Clinicians frequently employed time‐intensive workarounds, such as trial and error, to manage patient communication impairment during mechanical ventilation. Resource gaps are known to contribute to HCPs feeling time compressed, which is a predictor of patient communication omission (Ausserhofer et al., 2014 ). Systemic efforts to place communication tools for staff to use in or near patient rooms (i.e. communication cart), and provide just‐in‐time training, may potentially reduce the burden of communication (Happ et al., 2014 ; Trotta et al., 2019 ). Access to evidence‐based tools and training may improve intervention coherence, perceived effectiveness and self‐efficacy in communication efforts and decrease long‐term negative outcomes of communication impairment (Happ et al., 2014 , 2015 ; Radtke et al., 2011 ; Simeone et al., 2021 ; Vento‐Wilson et al., 2015 ).
While evidence‐based communication treatment algorithms exist for use in the adult ICU, none consider telephone and video calls as optional supports for mechanically ventilated patients treated under infection control precautions (Happ, 2013 ; Ten Hoorn et al., 2016 ). Facilitating communication for patients and family through telephone and video calls was reported by HCPs, patients and family members in this study. The endorsement of these communication adjuncts (e.g. telephones and tablets) in communication guidance may be important in expanding communication opportunities for mechanically ventilated patients in pandemic and other infection control contexts. The use of tablet and video call technology in this and other ICUs has become an emerging practice to connect patients and family members when in‐person visiting is restricted (Negro et al., 2020 ; Rose et al., 2021 ). Standardized access to institution tablets, sufficient wireless technology, secure video call programs and accessories such as charging cables and mounting structures may facilitate intervention coherence and the acceptability of these communication practices in the ICU.
4.3. Acceptability
Our analysis indicates low acceptability of existing communication practices for mechanically ventilated patients in the adult ICU during COVID‐19 restrictions from the perspective of diverse ICU stakeholders. Barriers aligned with the TFA constructs burden, affective attitudes, effectiveness, ethicality and intervention coherence suggest a need to address the physical safety and emotional needs of ICU nurses and other HCPs to allow them to maintain proximity to and time with patients to support their communication needs. Many facilitators were also reported and were aligned with the TFA constructs burden, intervention coherence, self‐efficacy, opportunity costs, ethicality and effectiveness suggesting a need for consistent availability of communication tools, staff training and awareness of support roles such as SLP, spiritual care and unit leadership to improve cognitive and emotional responses to communication in pandemic and other infection control conditions.
Looking beyond the COVID‐19 pandemic, critically ill patients will continue to require treatment with advanced airways for mechanical ventilation, ICU nurses and other HCPs will need to wear PPE for infection control purposes, and family members may not be available to attend the patient's bedside. Accurate patient‐HCP communication is essential to providing safe and effective care. The communication challenges experienced during the COVID‐19 pandemic identify the need to expand current guidance to address communication challenges during infection control and prevention precautions. Future research should explore implementation of communication interventions under infection prevention and control precautions and evaluate outcomes using TFA domains.
4.4. Strengths and limitations
Strengths of this study include the use of a theoretical framework and the inclusion of patient, family and professionally diverse stakeholders. The TFA provided a systematic and multilevel approach to exploring acceptability that may inform the design and implementation of communication interventions. In addition, we employed an interprofessional team approach to analysis to expand interpretive insights and implications. Limitations include a single study site and limited numbers of patients, which may impact transferability of the results. Time constraints in the pandemic context contributed to some shorter interviews for some HCPs. The researcher conducing the interviews is an NP working in the same institution, which may have influenced stakeholder reporting during interviews.
5. CONCLUSION
COVID‐19 conditions have precipitated a communication crisis in the ICU. The TFA was a useful framework to analyse reported barriers to and facilitators for supporting communication with and for patients treated with invasive mechanical ventilation in the intensive care unit during the COVID‐19 pandemic. Aligning reported barriers and facilitators to the TFA constructs unveiled multiple dimensions of unacceptability of current communication practices in the COVID‐19 ICU context. The results of this study can be used to inform ICU practice as well as communication and visiting policies that can be used during and beyond the COVID‐19 pandemic. The results will be used to co‐develop with patient, family and clinician stakeholders, an intervention for this context that will undergo further acceptability evaluation.
AUTHOR CONTRIBUTIONS
LI, LR, YY, CD: made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15212 .
Supporting information
Acknowledgement.
The authors thank the patients, families and healthcare provider participants of this study for their generous participation.
Istanboulian, L. , Rose, L. , Yunusova, Y. & Dale, C. (2022). Barriers to and facilitators for supporting patient communication in the adult ICU during the COVID‐19 pandemic: A qualitative study . Journal of Advanced Nursing , 78 , 2548–2560. 10.1111/jan.15212 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Funding informationThis study is supported by the Canadian Nurses Foundation, the Bertha Rosenstadt Health Research Fund, the Bluma Appel and Jeannie Butler Graduate Award in Nursing, the Mary Kathleen King Graduate Awards, the Staples Family Graduate Student Award in Nursing and the Michael Garron Hospital TD Community Health Fund Solutions for COVID‐19 Research Grant.
Contributor Information
Laura Istanboulian, Email: [email protected] , @Laura_lista .
Craig Dale, @Craig_dale1 .
DATA AVAILABILITY STATEMENT
- Akgun, K. M. , Shamas, T. L. , Feder, S. L. , & Schulman‐Green, D. (2020). Communication strategies to mitigate fear and suffering among COVID‐19 patients isolated in the ICU and their families . Heart & Lung , 49 ( 4 ), 344–345. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Attaway, A. H. , Scheraga, R. G. , Bhimraj, A. , Biehl, M. , & Hatipoglu, U. (2021). Severe covid‐19 pneumonia: Pathogenesis and clinical management . BMJ , 372 , n436. [ PubMed ] [ Google Scholar ]
- Augmentative and Alternative Communication . Augmentative and Alternative Communication [June 21, 2019]. Available from: http://www.asha.org/public/
- Ausserhofer, D. , Zander, B. , Busse, R. , Schubert, M. , De Geest, S. , Rafferty, A. M. , et al. (2014). Prevalence, patterns and predictors of nursing care left undone in European hospitals: Results from the multicountry cross‐sectional RN4CAST study . BMJ Quality and Safety , 23 ( 2 ), 126–135. [ PubMed ] [ Google Scholar ]
- Barreras‐Espinoza, J. A. , Leyva‐Moraga, F. A. , Leyva‐Moraga, E. , Leyva‐Moraga, F. , Soualhi, A. , Juanz‐Gonzalez, A. , et al. (2021). Communication in the ICU during the COVID‐19 pandemic . European Journal of Anaesthesiology , 38 ( 10 ), 1009–1011. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Baumgarten, M. , & Poulsen, I. (2015). Patients' experiences of being mechanically ventilated in an ICU: A qualitative metasynthesis . Scandinavian Journal of Caring Sciences , 29 ( 2 ), 205–214. [ PubMed ] [ Google Scholar ]
- Bengtsson, M. (2016). How to plan and perform a qualitative study using content analysis . NursingPlus Open , 2 , 8–14. [ Google Scholar ]
- Canada Go . COVID‐19 daily epidemiology update 2022. [Available from: https://health‐infobase.canada.ca/src/data/covidLive/Epidemiological‐summary‐of‐COVID‐19‐cases‐in‐Canada‐Canada.ca.pdf .
- Carruthers, H. , Astin, F. , & Munro, W. (2017). Which alternative communication methods are effective for voiceless patients in intensive care units? A systematic review . Intensive & Critical Care Nursing , 42 , 88–96. [ PubMed ] [ Google Scholar ]
- Cattelan, J. , Castellano, S. , Merdji, H. , Audusseau, J. , Claude, B. , Feuillassier, L. , Cunat, S. , Astrié, M. , Aquin, C. , Buis, G. , Gehant, E. , Granier, A. , Kercha, H. , Le Guillou, C. , Martin, G. , Roulot, K. , Meziani, F. , Putois, O. , & Helms, J. (2021). Psychological effects of remote‐only communication among reference persons of ICU patients during COVID‐19 pandemic . Journal of Intensive Care , 9 ( 1 ), 5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Choi, J. , Campbell, M. L. , Gelinas, C. , Happ, M. B. , Tate, J. , & Chlan, L. (2017). Symptom assessment in non‐vocal or cognitively impaired ICU patients: Implications for practice and future research . Heart & Lung , 46 ( 4 ), 239–245. [ PubMed ] [ Google Scholar ]
- Cope, D. G. (2014). Methods and meanings: Credibility and trustworthiness of qualitative research . Oncology Nursing Forum , 41 ( 1 ), 89–91. [ PubMed ] [ Google Scholar ]
- De Cuir‐Gunby, J. T. , Marshall, P. L. , & McCulloch, A. W. (2011). Developing and using a codebook for the analysis of interview data: An example from a professional development research project . Field Methods , 23 ( 2 ), 136–155. [ Google Scholar ]
- Doyle, L. , McCabe, C. , Keogh, B. , Brady, A. , & McCann, M. (2020). An overview of the qualitative descriptive design within nursing research . Journal of Research in Nursing , 25 ( 5 ), 443–455. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Epp, K. (2012). Burnout in critical care nurses: A literature review . Dynamics (Pembroke, Ont.) , 23 ( 4 ), 25–31. [ PubMed ] [ Google Scholar ]
- Freeman‐Sanderson, A. , Rose, L. , & Brodsky, M. B. (2020). Coronavirus disease 2019 (COVID‐19) cuts ties with patients' outside world . Australian Critical Care , 33 ( 5 ), 397–398. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Happ MB. 2013. SPEACS – 2 Communication Training Program 2013 . Available from: https://nucleus.con.ohio‐state.edu/media/speacs2/speacs.htm .
- Happ, M. B. , Garrett, K. L. , Tate, J. A. , DiVirgilio, D. , Houze, M. P. , Demirci, J. R. , George, E. , & Sereika, S. M. (2014). Effect of a multi‐level intervention on nurse‐patient communication in the intensive care unit: Results of the SPEACS trial . Heart & Lung , 43 ( 2 ), 89–98. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Happ, M. B. , Seaman, J. B. , Nilsen, M. L. , Sciulli, A. , Tate, J. A. , Saul, M. , & Barnato, A. E. (2015). The number of mechanically ventilated ICU patients meeting communication criteria . Heart & Lung , 44 ( 1 ), 45–49. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ijssennagger, C. , Ten Hoorn, S. , Van Wijk, A. , Van den Broek, J. M. , Girbes, A. R. , & Tuinman, P. R. (2018). Caregivers' perceptions towards communication with mechanically ventilated patients: The results of a multicenter survey . Journal of Critical Care , 48 , 263–268. [ PubMed ] [ Google Scholar ]
- Inoue, S. , Hatakeyama, J. , Kondo, Y. , Hifumi, T. , Sakuramoto, H. , Kawasaki, T. , Taito, S. , Nakamura, K. , Unoki, T. , Kawai, Y. , Kenmotsu, Y. , Saito, M. , Yamakawa, K. , & Nishida, O. (2019). Post‐intensive care syndrome: Its pathophysiology, prevention, and future directions . Acute Medicine and Surgery , 6 ( 3 ), 233–246. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Istanboulian, L. , Rose, L. , Gorospe, F. , Yunusova, Y. , & Dale, C. M. (2020). Barriers to and facilitators for the use of augmentative and alternative communication and voice restorative strategies for adults with an advanced airway in the intensive care unit: A scoping review . Journal of Critical Care , 57 , 168–176. [ PubMed ] [ Google Scholar ]
- Karlsen, M. W. , Olnes, M. A. , & Heyn, L. G. (2019). Communication with patients in intensive care units: A scoping review . Nursing in Critical Care , 24 ( 3 ), 115–131. [ PubMed ] [ Google Scholar ]
- Khalaila, R. , Zbidat, W. , Anwar, K. , Bayya, A. , Linton, D. M. , & Sviri, S. (2011). Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation . American Journal of Critical Care , 20 ( 6 ), 470–479. [ PubMed ] [ Google Scholar ]
- Knollman‐Porter, K. , & Burshnic, V. L. (2020). Optimizing effective communication while wearing a mask during the COVID‐19 pandemic . Journal of Gerontological Nursing , 46 ( 11 ), 7–11. [ PubMed ] [ Google Scholar ]
- Lake, E. T. , Narva, A. M. , Holland, S. , Smith, J. G. , Cramer, E. , Rosenbaum, K. E. F. , French, R. , Clark, R. R. S. , & Rogowski, J. A. (2021). Hospital nurses' moral distress and mental health during COVID‐19 . Journal of Advanced Nursing , 78 , 799–809. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lord, H. , Loveday, C. , Moxham, L. , & Fernandez, R. (2021). Effective communication is key to intensive care nurses' willingness to provide nursing care amidst the COVID‐19 pandemic . Intensive & Critical Care Nursing , 62 , 102946. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Negro, A. , Mucci, M. , Beccaria, P. , Borghi, G. , Capocasa, T. , Cardinali, M. , Pasculli, N. , Ranzani, R. , Villa, G. , & Zangrillo, A. (2020). Introducing the video call to facilitate the communication between health care providers and families of patients in the intensive care unit during COVID‐19 pandemia . Intensive & Critical Care Nursing , 60 , 102893. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nguyen, N. , Chinn, J. , Nahmias, J. , Yuen, S. , Kirby, K. , Hohmann, S. , et al. (2021). Outcomes and mortality among adults hospitalized with COVID‐19 at US medical centres . JAMA Network Open , 4 ( 3 ), e210417. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- O'Cathain, A. , Croot, L. , Duncan, E. , Rousseau, N. , Sworn, K. , Turner, K. M. , Yardley, L. , & Hoddinott, P. (2019). Guidance on how to develop complex interventions to improve health and healthcare . BMJ Open , 9 ( 8 ), e029954. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ontario PH . 2021. IPAC Recommendations for Use of Personal Protective Equipment for Care of Individuals with Suspect or Confirmed COVID‐19 2021 [Available from: https://www.publichealthontario.ca/‐/media/documents/ncov/updated‐ipac‐measures‐covid‐19.pdf?la=en .
- Peter, E. , & Liaschenko, J. (2004). Perils of proximity: A spatiotemporal analysis of moral distress and moral ambiguity . Nursing Inquiry , 11 ( 4 ), 218–225. [ PubMed ] [ Google Scholar ]
- Radtke, J. V. , Baumann, B. M. , Garrett, K. L. , & Happ, M. B. (2011). Listening to the voiceless patient: Case reports in assisted communication in the intensive care unit . Journal of Palliative Medicine , 14 ( 6 ), 791–795. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Reidy, J. , Brown‐Johnson, C. , McCool, N. , Steadman, S. , Heffernan, M. B. , & Nagpal, V. (2020). Provider perceptions of a humanizing intervention for health care workers‐a survey study of PPE portraits . Journal of Pain and Symptom Management , 60 ( 5 ), e7–e10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Richards, D. A. , Sugg, H. V. , Cockcroft, E. , Cooper, J. , Cruickshank, S. , Doris, F. , et al. (2021). COVID‐NURSE: Evaluation of a fundamental nursing care protocol compared with care as usual on experience of care for noninvasively ventilated patients in hospital with the SARS‐CoV‐2 virus‐protocol for a cluster randomised controlled trial . BMJ Open , 11 ( 5 ), e046436. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rose, L. , Yu, L. , Casey, J. , Cook, A. , Metaxa, V. , Pattison, N. , Rafferty, A. M. , Ramsay, P. , Saha, S. , Xyrichis, A. , & Meyer, J. (2021). Communication and virtual visiting for families of patients in intensive care during COVID‐19: A UKNational Survey . Annals of the American Thoracic Society , 18 , 1685–1692. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sekhon, M. , Cartwright, M. , & Francis, J. J. (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework . BMC Health Services Research , 17 ( 1 ), 88. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Simeone, I. M. , Berning, J. N. , Hua, M. , Happ, M. B. , & Baldwin, M. R. (2021). Training chaplains to provide communication‐board‐guided spiritual care for intensive care unit patients . Journal of Palliative Medicine , 24 ( 2 ), 218–225. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spence Laschinger, H. K. , & Fida, R. (2015). Linking nurses' perceptions of patient care quality to job satisfaction: The role of authentic leadership and empowering professional practice environments . The Journal of Nursing Administration , 45 ( 5 ), 276–283. [ PubMed ] [ Google Scholar ]
- Tabah, A. , Ramanan, M. , Laupland, K. B. , Buetti, N. , Cortegiani, A. , Mellinghoff, J. , Conway Morris, A. , Camporota, L. , Zappella, N. , Elhadi, M. , Povoa, P. , Amrein, K. , Vidal, G. , Derde, L. , Bassetti, M. , Francois, G. , Ssi Yan Kai, N. , de Waele, J. J. , & PPE‐SAFE contributors . (2020). Personal protective equipment and intensive care unit healthcare worker safety in the COVID‐19 era (PPE‐SAFE): An international survey . Journal of Critical Care , 59 , 70–75. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ten Hoorn, S. , Elbers, P. W. , Girbes, A. R. , & Tuinman, P. R. (2016). Communicating with conscious and mechanically ventilated critically ill patients: A systematic review . Critical Care , 20 ( 1 ), 333. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups . International Journal for Quality in Health Care , 19 ( 6 ), 349–357. [ PubMed ] [ Google Scholar ]
- Trotta, R. L. , Hermann, R. M. , Polomano, R. C. , & Happ, M. B. (2019). Improving nonvocal critical care patients' ease of communication using a modified SPEACS‐2 program . Journal for Healthcare Quality , 42 , e1–e9. [ PubMed ] [ Google Scholar ]
- Vento‐Wilson, M. T. , McGuire, A. , & Ostergren, J. A. (2015). Role of the speech‐language pathologist: Augmentative and alternative communication for acute care patients with severe communication impairments . Dimensions of Critical Care Nursing , 34 ( 2 ), 112–119. [ PubMed ] [ Google Scholar ]
- Zaga, C. , Berney, S. , & Vogel, A. (2019). The feasibility, utility, and safety of communication interventions with mechanically ventilated intensive care unit patients: A systematic review . American Journal of Speech‐Language Pathology , 28 , 1335–1255. [ PubMed ] [ Google Scholar ]
Psychological Barriers to Communication: Examples & How to Overcome
Table of Contents
Definition of psychological barriers
Psychological barriers are defined as “mental and emotional obstacles that interfere with the smooth flow of communication, such as individual differences in perception, interpretation, and emotional states.” In the book “Communication in Everyday Life” by Steve Duck and David T. McMahan.
What are Psychological barriers?
Psychological barriers to communication are internal factors that can create obstacles in the effective exchange of information and emotions between individuals. These barriers arise from our thoughts, emotions, beliefs, and perspectives, influencing how we interpret and respond to messages.
They impact the clarity, understanding, and connection in communication. For instance, our subjective perception can shape how we interpret information, leading to misunderstandings. Emotions play a significant role as well, as negative emotions can cloud our judgment and limit our ability to accurately process and express information.
Cultural and language differences can also create barriers , as differing norms and communication styles can lead to misinterpretations. Additionally, trust and self-confidence affect communication, with a lack of trust restricting open dialogue and low self-confidence affecting self-expression.
By understanding and addressing these psychological barriers, we can enhance our communication skills, establish stronger connections, and avoid misunderstandings.
What are socio-psychological barriers to effective communication?
Socio-psychological barriers to effective communication refer to the combined impact of social and psychological factors that prevent the smooth and meaningful exchange of ideas and emotions between individuals or groups. These barriers emerge from the complex interplay between social dynamics and individual psychological processes, impacting how people communicate and connect.
What are the examples of psychological barriers?
The following illustration list the five common psychological barriers to effective communication with their causes.
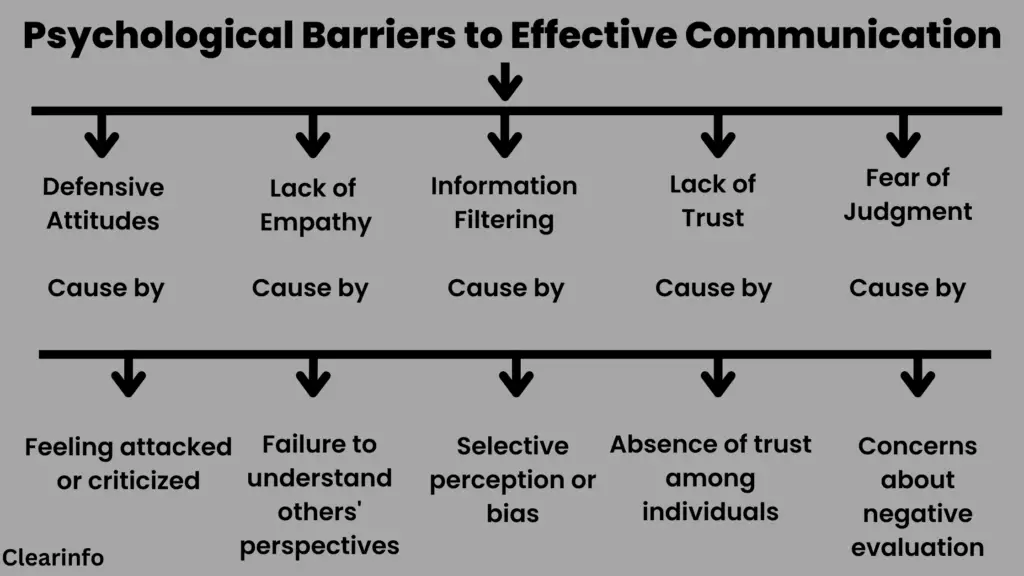
Example of psychological barriers in a sentence
“Due to his strongly held prejudice, John struggled to engage in open and inclusive communication with individuals from different cultural backgrounds.” “The defensive attitudes of both parties prevented constructive communication, as they were more focused on proving themselves right rather than understanding each other’s perspectives.”
Different kinds of Psychological barriers to communication
1/ perception and interpretation: .
Perception and interpretation refer to how individuals perceive and make sense of the information they receive during the communication process . This psychological barrier arises from the fact that people have unique perspectives, experiences, and filters through which they interpret messages.
Perception is the process by which individuals select, organize, and interpret sensory information from their environment. It involves filtering information through personal filters, biases, and prior knowledge. This filtering process can lead to differences in how individuals perceive and prioritize information, resulting in potential communication barriers.
Interpretation involves assigning meaning to the perceived information. It is influenced by an individual’s cognitive frameworks, cultural context, and personal beliefs. Two individuals can interpret the same message differently based on their distinct perspectives, leading to misunderstandings or conflicting interpretations.
Psychological barriers arising from perception and interpretation can include:
- Selective Attention
- Stereotyping
- Halo or Horns Effect
- Confirmation Bias
- Perceptual Constrain
2/ Emotional Barriers
Emotional barriers are psychological factors that can affect the process of communication. Our emotions significantly influence how we process and express information, as well as how we interpret the messages received from others. When individuals experience strong or negative emotions, it can create barriers that block the smooth exchange of ideas and feelings.
Emotional barriers can originate in several ways:
- Anger and Hostility : When individuals feel angry or hostile, their ability to communicate calmly and rationally can be compromised. They may engage in aggressive or confrontational communication, making it difficult to have a constructive dialogue or find common ground.
- Fear and Anxiety : Feelings of fear or anxiety can create barriers to effective communication . When individuals are afraid of judgment, criticism, or negative outcomes, they may hesitate to express themselves honestly or openly. This fear can limit the depth of communication and prevent the establishment of trust and mutual understanding.
- Stress and Overwhelm : High levels of stress or feeling overwhelmed can impact communication effectiveness. When individuals are preoccupied with stress or mentally overloaded, their ability to focus and engage fully in communication may be compromised.
Must Read : Emotional Barriers to Communication: Examples & Solutions
3/ Stereotyping and Prejudice
Stereotyping and prejudice refer to the cognitive biases and preconceived opinions that individuals hold about others based on characteristics such as race, gender, age, religion, or social status. These biases can create barriers to communication by influencing how individuals perceive, interpret, and interact with others.
Stereotyping and prejudice can prevent effective communication in the following ways:
- Misinterpretation : Stereotyping and prejudice can lead to misinterpretation of messages. When individuals hold preconceived views about someone based on stereotypes or biases, they may interpret their words or actions in a manner consistent with those stereotypes, rather than understanding their intended meaning.
- Lack of Understanding : Stereotyping and prejudice can lead to a lack of understanding and awareness of diverse perspectives. When individuals hold to inflexible beliefs about others, they may become less receptive to exploring alternative perspectives or practicing empathetic listening .
Bias and Discrimination: Prejudice involves the presence of biased attitudes or discriminatory behaviors towards individuals or groups. These biases can impact communication by affecting how individuals perceive and treat others.
4/ Filtering and Selective Listening
Filtering and selective listening are psychological barriers to communication that can impact the transmission and reception of messages. These barriers involve the conscious or unconscious process of screening information based on personal interests, or preferences.
Filtering refers to the act of intentionally withholding or manipulating information before communicating it to others. Individuals may filter information based on their own desire to control the narrative or fear of negative reactions. This can result in incomplete communication, as certain details or perspectives are intentionally altered.
Similarly, selective listening occurs when individuals choose to pay attention to only certain aspects of a message while ignoring or disregarding others. This can be influenced by preconceived beliefs or a lack of interest. Selective listening can lead to a failure to fully understand the intended message.
5/ Communication Apprehension
Communication apprehension refers to the anxiety or fear that individuals experience when faced with the prospect of engaging in communication. It is characterized by a sense of discomfort, nervousness, or self-consciousness that can impact effective communication.
Communication apprehension often comes from a fear of being judged, criticized, or negatively evaluated by others. Individuals might experience concerns about making errors, being seen as inadequate, or facing embarrassment. This fear can hold back their willingness to communicate openly and confidently.
In addition, communication apprehension can also be associated with performance anxiety. When individuals feel pressure to perform well or meet certain expectations in their communication, they may experience increased anxiety. This anxiety can affect their ability to articulate their thoughts clearly and coherently.
Therefore Individuals with communication apprehension may avoid or minimize their participation in conversations, group discussions, or public speaking engagements.
6/ Status Consciousness
Status consciousness refers to the awareness and concern individuals have regarding their social standing, rank, or perceived importance in relation to others. It involves the tendency to perceive communication through the lens of hierarchy and power dynamics, which can impact effective communication.
Status consciousness often arises from power variations within social or professional contexts. Individuals who are more status-conscious may be overly concerned with maintaining a sense of superiority. This can create barriers in communication by preventing open and equal participation in discussions and decision-making processes.
People may also attribute greater credibility or value to the ideas or perspectives of individuals with higher status while overlooking the contributions of those with lower status. This perception bias can limit the exchange of diverse viewpoints.
In a workplace environment when individuals are overly concerned about maintaining or improving their status, they may prioritize personal achievements over collective goals. This can lead to competition, a lack of cooperation, and limited information sharing, discouraging effective communication within teams or groups.
7/ Defensiveness
Defensiveness is a psychological barrier that affects communication interactions. It arises when individuals feel the need to protect themselves from perceived threats, criticism, or attacks. It involves reacting with a guarded or resistant attitude, which can prevent open and constructive communication.
Defensiveness often leads to a closed-minded attitude, where individuals resist considering alternative perspectives, ideas, or feedback. They become rigid in their thinking, rejecting information that challenges their existing beliefs or self-perception. Consequently, communication breakdowns occur, as individuals prioritize self-preservation over active listening and understanding.
Moreover, defensiveness creates a negative communication climate characterized by tension, mistrust, and conflict. Others may hesitate to express their thoughts or concerns openly due to the defensive responses they anticipate.
8/ Self-Centered Attitude
A self-centered attitude is a psychological barrier that refers to an excessive focus on oneself, where individuals prioritize their own needs, interests, and opinions above those of others. A self-centered attitude restrains genuine listening, understanding, and empathy in communication interactions.
When individuals possess a self-centered attitude, they tend to dominate conversations, steer discussions toward their own concerns, and disregard the perspectives and experiences of others. This can lead to communication breakdowns and interrupt the establishment of meaningful connections.
When individuals possess a self-centered attitude, they tend to:
- Lack of Empathy : A self-centered attitude often results in a diminished capacity for empathy . Individuals may struggle to understand or relate to the feelings, thoughts, and experiences of others.
- Monopolizing Conversations : People with a self-centered attitude tend to monopolize conversations by constantly bringing the focus back to themselves. They may interrupt others, shift attention to their own experiences, or dismiss the contributions of others.
- Disregard Others’ Perspectives : Individuals with a self-centered attitude may dismiss or downplay the perspectives, ideas, or opinions of others. They may prioritize their own viewpoints or ignore alternative viewpoints.
9/ Attitudes and Values
Attitudes and values play a significant role in shaping communication dynamics. They influence how individuals perceive, interpret, and respond to information, ideas, and interactions. Attitudes refer to individuals’ general feelings towards certain topics, while values represent deeply held beliefs and principles that guide behavior.
Attitudes and values can act as potential barriers to good communication when they are inflexible or divergent between individuals. Here are some key considerations:
- Communication Style : Attitudes and values shape communication styles, including assertiveness, directness, or indirectness. Individuals with differing attitudes and values may have contrasting preferences in how they express themselves, leading to misunderstandings or conflicts in communication.
- Preconceived Notions : Attitudes and values can lead to preconceived beliefs that affect how individuals interpret and respond to information. These preconceptions may cause individuals to make assumptions or judgments, limiting their openness to different perspectives.
10/ Distrust
Distrust is a psychological barrier that poses challenges to effective communication. It refers to a lack of confidence or suspicion towards others, their intentions, or the information they provide. Distrust can arise due to past negative experiences, perceived dishonesty, or a lack of credibility. This barrier undermines open and transparent communication, making it difficult to establish rapport and build collaborative relationships.
Simultaneously distrust can color the interpretation of messages, leading to a tendency to doubt or question the motives behind what others say. Individuals may read negative intentions into neutral or positive messages, further boosting suspicion and preventing effective communication.
In addition, when individuals distrust one another, they are less likely to share ideas, offer support, or engage in cooperative efforts. This can limit the exchange of diverse perspectives and hamper problem-solving processes.
How to overcome psychological barriers in communication
Overcoming psychological barriers in communication requires a proactive and mindful approach. Here are some strategies to help overcome various barriers:
1/ Overcoming Perception and Interpretation Barriers
Overcoming perception and interpretation barriers requires developing self-awareness and understanding that others may have different perspectives. Effective communication involves actively listening, seeking clarification, and being open to different interpretations.
Employing clear and precise language, using examples or visuals, and encouraging dialogue can help bridge the gap in perception and interpretation, fostering better understanding and reducing miscommunications.
2/ Overcoming Emotional Barriers
To overcome emotional barriers, it is essential to cultivate emotional intelligence and create a supportive communication environment. This involves recognizing and managing one’s own emotions, as well as being empathetic and understanding toward the emotions of others.
Validating emotions, and creating a safe space for open expression can help individuals navigate emotional barriers and foster more effective communication. Furthermore, discovering constructive methods to cope with stress , such as engaging in mindfulness practices or seeking assistance, can positively impact emotional well-being and enhance communication.
3/ Overcoming Stereotyping and Prejudice Barriers
Overcoming the barrier of stereotyping and prejudice requires promoting awareness, empathy, and inclusivity. By actively seeking diverse perspectives, engaging in meaningful dialogues with individuals from various backgrounds, and consistently questioning their own assumptions, individuals can effectively confront and challenge their own stereotypes and prejudices.
Education, cultural sensitivity training, and fostering a culture of respect and acceptance can help break down these barriers and promote more inclusive and effective communication.
4/ Overcoming Filtering and Selective Listening Barriers
To overcome the barriers of filtering and selective listening, individuals can cultivate active listening skills and practice open-mindedness. This includes being fully present in the communication interaction, actively seeking to understand the speaker’s perspective, and setting aside personal biases or preconceived perspectives.
By actively listening to the complete message, considering non-verbal cues , and being open to diverse viewpoints, individuals can enhance their understanding, minimize misinterpretation, and foster more effective communication.
5/ Overcoming Communication Apprehension Barriers
To address communication apprehension, individuals can employ various strategies:
- Building Self-Confidence : Enhancing self-confidence through practice, preparation, and positive self-talk can help individuals overcome communication apprehension.
- Seeking Support : Seeking support from mentors, or communication coaches, or participating in supportive communication groups can provide guidance and encouragement to overcome communication apprehension.
- Relaxation Techniques : Utilizing relaxation techniques like deep breathing, visualization, or mindfulness can assist in effectively managing anxiety and fostering a state of calmness during communication scenarios.
6/ Overcoming Status Consciousness Barriers
To mitigate the impact of status consciousness on communication, it is essential to promote a culture of equality, respect, and inclusivity. Strategies to address this barrier include:
- Encouraging Open Dialogue: Fostering an environment that encourages open dialogue and active participation, regardless of status, can help mitigate the effects of status consciousness.
- Developing Empathy and Perspective-Taking : Encouraging individuals to develop empathy and practice perspective-taking can help break down status barriers.
- Promoting Effective Feedback : Establishing a feedback culture that values constructive criticism and learning can help reduce status-related concerns.
Related Reading : What is the purpose of feedback in communication
7/ Overcoming Defensiveness Barriers
To overcome defensiveness and promote constructive communication, individuals can be open to feedback, engage in self-reflection and awareness, and develop conflict-resolution skills. These strategies help individuals overcome defensiveness, foster a more positive communication climate, and promote open and meaningful interactions.
8/ Overcoming Barriers Due to Resistance to Change
To address barriers due to resistance to change and facilitate effective communication, several strategies can be employed:
- Open Dialogue : Encourage open dialogue about the proposed changes, allowing individuals to express their concerns, questions, and opinions.
- Transparent Communication : Provide clear and transparent communication about the reasons behind the change, its potential benefits, and the expected outcomes.
- Collaboration and Involvement : Involve individuals in the change process, seeking their input and participation.
- Providing Support : Offer support and resources to help individuals navigate through the change.
9/ Overcoming Attitudes and Values Barriers
To address the impact of attitudes and values on communication, several strategies can be employed. First, developing self-awareness regarding one’s own attitudes and values is crucial. This involves reflecting on how these factors influence communication, enabling individuals to recognize potential biases and be more open to alternative perspectives.
Cultivating an open-minded attitude is also essential, as it helps individuals approach communication with curiosity and a willingness to consider different viewpoints. This requires challenging one’s own assumptions, suspending judgment, and actively seeking diverse perspectives.
10/ Overcoming Distrust Barriers
To overcome the barrier of distrust and foster effective communication, consider the following strategies:
- Establishing trust is crucial for effective communication. This involves consistent and reliable behavior, keeping promises, and demonstrating honesty and integrity. Trust can be built gradually through open and transparent communication over time.
- Practicing transparency in communication helps to clear doubts and suspicions. Being clear, honest, and open about intentions, decisions, and information fosters trust and encourages more two-way communication exchanges .
- Effectively resolving conflicts is crucial for rebuilding trust. Employing constructive conflict resolution techniques, such as active listening, mutual respect, and finding common ground, can help restore trust in communication.
Ways to overcome psychological barriers in a working environment
Overcoming psychological barriers in a working environment requires specific approaches tailored to the workplace context. Here are some additional strategies to address psychological barriers in a professional setting:
- Encourage Psychological Safety : Foster an environment of psychological safety where employees feel comfortable expressing their thoughts and opinions without fear of negative consequences.
- Provide Communication Training : Offer communication skills training to employees at all levels of the organization. Equip them with the necessary tools and techniques to communicate effectively, such as active listening, conflict resolution, and assertiveness.
- Establish Clear Communication Channels : Ensure that communication channels are clear, accessible, and well-defined within the organization. This includes both formal and informal channels .
- Regularly Assess Communication Climate : Conduct regular assessments or surveys to measure the communication climate within the organization. Collect feedback from employees to understand their experiences and identify potential areas for improvement.
How to overcome socio-psychological barriers in communication
- Foster empathy and understanding for diverse socio-psychological backgrounds.
- Establish an inclusive environment that appreciates and values a wide range of perspectives.
- Practice active listening to truly understand others’ viewpoints.
- Build trust through transparent and consistent communication.
- Adapt your communication style to accommodate different socio-psychological contexts.
- Encourage open dialogue and honest expression of thoughts and ideas.
- Develop cultural competence to appreciate and respect diverse customs.
- Seek clarification to ensure mutual understanding across socio-psychological differences.
How psychological barriers affect communication
Psychological barriers have a profound impact on communication, affecting various aspects of the process. One aspect is how we encode and decode messages. Our thoughts, beliefs, and perceptions shape how we interpret information, and when influenced by biases or preconceived viewpoints, they can affect our understanding of the message, leading to misunderstandings.
Another critical aspect affected by psychological barriers is emotional interference. Emotions play a vital role in communication, but barriers such as fear, anxiety, anger, or stress can prevent our ability to express ourselves clearly and listen attentively.
When strong emotions are present, they can cloud our judgment and trigger defensive responses. As a result, effective communication becomes challenging as emotions block our capacity to communicate and understand messages accurately.
What are the causes of psychological interference in a communication process?
Psychological interference in the communication process can be caused by several factors that impact our ability to communicate effectively. These causes include
- Past Experiences
- Cultural and Social Conditioning
- Emotional States
- Limited Self-Awareness
- Cognitive Biases
- Lack of Empathy
- Communication Apprehension
How does psychological noise create barriers to effective communication?
Psychological noise refers to internal distractions and interferences that occur within an individual’s mind. These internal factors impact the encoding and decoding of messages, leading to barriers in communication. Here’s how psychological noise creates barriers to effective communication:
- Psychological noise can distort how individuals perceive and interpret messages.
- Psychological noise includes emotional factors such as anxiety, stress, anger, or fear, which can interfere with communication.
- Psychological noise contributes to cognitive biases, such as confirmation bias or stereotyping.
- Psychological noise can limit empathetic understanding.
Examples of psychological noise Self-consciousness Personal Beliefs Negative Self-talk Closed-mindedness Emotional Distractions Mental Fatigue Defensive Attitudes
Difference between physical barriers and psychological barriers
A comparison table highlighting the key differences between physical barriers and psychological barriers to communication:
Frequently Asked Questions
Q1) what are psychological barriers and examples .
Ans: Psychological barriers are internal obstacles that prevent effective communication by influencing individuals’ thoughts, emotions, beliefs, and perceptions. Some examples of psychological barriers include differences in perception and interpretation, emotional interference, cognitive biases, low self-confidence, defensive attitudes, lack of empathy, and cultural differences.
Q2) What are physiological barriers in communication examples?
Ans: Physiological barriers in communication are related to physical conditions or limitations that block effective communication. Examples of physiological barriers include Hearing Impairment, Speech Disorder, Visual Impairment, Neurological Conditions, and Physical Disabilities.
Q3) What is the definition of a psychological firewall?
Share your read share this content.
- Opens in a new window
Aditya Soni
You might also like.

Ethics in Business Communication: Examples, Types & Importance

Interpersonal Barriers to Communication: Examples & Solutions

Top 10 Business Communication Skills With Examples & Importance
Leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.

Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

COMMUNICATION BARRIERS AT THE WORKPLACE A CASE STUDY 3299 13072 2 PB

2020, European Journal of Education Studies
The success of an organization does not only rely on the rapid growth of their profits. Behind each success of the projects, there is a good relationship and cooperation between all members of the company. To ensure the work goes smoothly, communication is the vital key in achieving it. Without proper communication between the members of the company, the agreement while working cannot be accomplished. Therefore, this study aims to seek the various types of communications at the workplace. At the same time, this study investigates how the communication barriers affect the flow of communication and information at the workplace. A set of questionnaires was developed and distributed to employees in different companies. The questionnaire comprises different sections; demographic profile, the types of communications and the communication barriers. The participants contributed to this survey were in total of 31 respondents. The respondents involved had assessed the survey based on their personal experiences in their respective organizations. The results of the study showed that both verbal and non-verbal communications at the workplace played big roles in ensuring the smooth flow of the company. Other than that, the communication barriers at the workplace existed in which it could affect the growth of the company. Therefore, the findings of this study can help employers to be aware of the challenges and plan on how to overcome it. Recommendations for future research in this area are concluded at the end of this study.
Related Papers
International Journal of Asian Social Science
Noor Hanim Rahmat, (Associate Professor, Dr) , SITI KHADIJAH OMAR
Effective communication creates a positive working environment and thus increases the job performance of the staff. However, the absence of proper communication between the members of an organisation or a company would result in failure to achieve the agreement while working. Therefore, this study aims to investigate how perceptual factors, verbal, and non-verbal communication can be barriers to effective communication in the workplace. A set of questionnaires is used and distributed to workers of various industries in different companies. It consists of five parts: the demographic profile, verbal communication, non-verbal communication, work environment, and organisational values. A total of ninety-four (94) responses are received and recorded. Findings reveal how perceptual, verbal, and non-verbal factors influence the flow of communication in the workplace. Consequently, the findings of this study can help employers and employees to improve communication at all levels for the betterment of the work performance of all workers. Contribution/ Originality: This paper contributes to the existing literature by offering clear explanations of how perceptual, verbal, and non-verbal barriers affect the communication flow in the workplace. By analysing the highlighted barriers, employers can be mindful of the challenges in communication at work and strategise systematic ways on how to ensure effective communication among workers for a smooth flow of the company.
Oghenethoja Umuteme
Research evidence shows that managers spend 70-90% of their time in communication, in order to keep reinforcing the organisation's goals and bottom line.The 21st century workplace with its hi-tech communication process is becoming more of a social structured and complex technological workplace; coupled with global issues of terrorism, climate change, and changing demographics. Ineffective communication can affect employees’ output overtime, as they begin to experience both physiological and psychosocial withdrawals, which gradually leads to job stress.Communication barriers are impediments that distort the intended meaning and intention conveyed in a message. Channels of communication arises from where communication is needed – such as among employees within the business, customers and clients, vendors and distributors, and engagement with government regulatory bodies. This work shows that effective communication is an important factor that can enhance productivity in the workplace.
European Journal of Social Science Studies, Vol 4(5)
Noor Hanim Rahmat, (Associate Professor, Dr)
Among the many types of interaction at the workplace are communication at the organisation level and communication among employees. Effective communication at the operational level provides good foundation for interaction within and outside the organisation. effective communication at individual levels among the employers' help create positive work environment and therefore enhance productivity of each employee in the long run. This quantitative pilot study was carried out in a government organisation. 68 respondents answered a 34-item survey on 5-likert scales. Findings showed that employees felt that besides effective communication at top-down level, there should also be good communication within the organisation and among the employees themselves. Positive interaction would lead to positive communication and thus improve motivation at work as well as productivity.
abhilasha ram
Excellent employee communication is must for any thriving organization. Effective internal communication is key to success of any organization. The need for communicating information to an organization's internal public — its employees — has become of utmost importance in the recent years. This research article studied internal / employee communication in terms of openness of communication and adequacy of information. The openness should be followed across the organization – between the employer and employee as well as amongst employees. Giving too little information as well as too much information to the concerned employee makes him/her confused; so, the importance of adequate information. The effectiveness of information studied on the basis of communication tools and practices used in the organization for the proper dissemination of communication.
Chia Shun Kit
As a manager, we need to know the different aspects of communication in order to communicate effectively and efficiently. And at this moment, barriers of communication will occur. Barriers of communication are obstacles that affects in the workplace from exchanging ideas and thoughts. By eliminating those barriers, it helps us to prevent misunderstanding. Put it in a simple way, barriers are equivalent to “Noise” (Danny, 2009). The objective of this report aims to achieve the following targets: 1. To scrutinize five types of communication barriers that will distort the message delivery process. 2. To elicit three ways how managers can improve their communication skills.
NHRD Network Journal
Prasenjit Bhattacharya
e-Academia Journal
zamri miskam
Communication effectiveness has been one of important factors in daily life covering workplaces, relationships, and all sorts of human interaction. As a workplace or even learning centres, any organisation shall need to practise good and effective communication, from within and outside organisation, to achieve its goals. Many researchers have developed and shared various theories, models and frameworks with regards to this topic of interest due to its cruciality to be achieved and practised. However, communication is a very broad subject and is affected by many internal and external factors. The internal and external factors may both refer to communication barriers, which could be a stimulus, a situation or even an object that may hinder or prohibit any part of a communication process making it harder for messages to be encoded and decoded precisely by parties involved. The purpose of this research is to investigate the factors influencing effective communication in an organisation....
Sureyya ECE
Individuals, as a social being, need to communicate with their external environment. When a baby is born, he/she trying to communicate with the outside environment by crying, it begins to communicate verbally after learning to speak. An individual who does not have the ability to speak or loses this ability tries to communicate with those around him with the sign language. Therefore, it can be said that the communication process starts with the birth of human being and continues until the end of life. The importance of communication has led researchers to work on communication in firms. But before that, it is useful to examine the history of communication….
Karlene Roberts
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Amadosi Mosugu
misbah memon
Review of European Studies
Saul Rick Fernandez Hurtado
Hamdan Said
Communication Management Review
Jana Chrenková
Clement OKHAKHU, Ph.D.
Constantin Stoican
Journal of Humanities and Education Development (JHED)
Bayad Jamal Ali
Academic Voices: A Multidisciplinary Journal
ganesh niraula
Kenan Spaho
George Bakkur
Organisational Behaviour
Iim Rohimah
Kelebogile Ngwenya
Ana Lucia Magalhaes
Asian Journal of Management
Dasarathi Sahu
Economics and Culture
sllavka kurti
Marek Makowiec
Anna Rogala
International Virtual Symposium: Research, Industry & Community Engagement (RICE)
Hajime Okano
Dr. Sharon Campbell-Phillips
Worldwide Hospitality and Tourism Themes
Juan Fernando Villadiego Madera
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

- Free Case Studies
- Business Essays
Write My Case Study
Buy Case Study
Case Study Help
- Case Study For Sale
- Case Study Services
- Hire Writer
Case Study on Psychological Barriers to Communication
Psychological barriers to communication case study:.
Psychological barriers to communication are the obstacles which occur in the process of communication because of the personal emotional condition of both sides of the conversation.Psychological barriers occur quite frequently during conversation because of numerous reasons, which most often depend on the current human psychological condition and the human temperament. Sometimes it happens that the human being is an introvert, so it is often difficult to persuade such a person to communicate a lot, because she simply does not need it.Of course, there are more distinct barriers which are characterized with the human experience, for example, the individual has inner barriers which depend on his bringing up, education, stereotypes and prejudices. When the person has had experience in communication with the definite type of people, he will treat this type according to his first impression.Then, if the individual has serious problems at work, family or other close people and he is always stressed or even depressed, he will not be a positive communicant, because he will not be able to catch the information and concentrate on it.
This type of barrier is called filtering.Finally, there is an obstacle which is connected with the social status of the participants of the conversation. This psychosocial barrier exists between the boss and the employee, between the teacher and his student, between the mature and young people. This sort of barriers is associated with the fact that the communicant of the “lower” level can not present the information in the way he wants. He will try to behave better and use more formal and sophisticated language.Psychological barriers to communication are the barriers which occur because of the human psychological condition and her personal experience.
We Will Write a Custom Case Study Specifically For You For Only $13.90/page!
The student who is interested in the research of the problem about the psychological barriers to communication should focus on the explanation of these barriers, enumerating their types, etc. Then, one is expected to collect information about the case under analysis and define its problem. It is important to think about the cause and effect of the psychological barriers to communication and then to take efforts to solve the problem efficiently.Sometimes students do not have the slightest idea about the appropriate organization of the paper and the Internet becomes the single reliable helper in this occasion. The young professional who requires a piece of the friendly advice on writing is able to find the assistance in the form of a free sample case study on psychological barriers to communication designed by the well-educated author.
It is reasonable to improve one’s knowledge and writing skills with the help of the free example case study on psychological barriers to communication and succeed in writing your own paper.
Related posts:
- Case Study on Barriers of Communication
- Case Study on Barriers to Effective Communication
- Case Study on Physical Barriers to Communication
- Barriers to Effective Communication
- Case Study on Psychological Abuse
- Cross Cultural Barriers in Nonverbal Communication
- Case Study on Barriers to Learning
Quick Links
Privacy Policy
Terms and Conditions
Testimonials
Our Services
Case Study Writing Services
Case Studies For Sale
Our Company
Welcome to the world of case studies that can bring you high grades! Here, at ACaseStudy.com, we deliver professionally written papers, and the best grades for you from your professors are guaranteed!
[email protected] 804-506-0782 350 5th Ave, New York, NY 10118, USA
Acasestudy.com © 2007-2019 All rights reserved.

Hi! I'm Anna
Would you like to get a custom case study? How about receiving a customized one?
Haven't Found The Case Study You Want?
For Only $13.90/page
- DOI: 10.29333/OJCMT/2541
- Corpus ID: 151152194
Study on Communication Barriers in the Classroom: A Teacher’s Perspective
- Nilanjana Pal , Santoshi Halder , Abhijit Guha
- Published 15 January 2016
Ask This Paper
By using this feature, you agree to AI2's terms and conditions and that you will not submit any sensitive or confidential info.
AI2 may include your prompts and inputs in a public dataset for future AI research and development. Please check the box to opt-out.
Ask a question about " "
Supporting statements, 15 citations, communication barriers in english language classroom: a study of teachers' perceptions in pakistan, student effective communication, communication barriers faced by english language learners at a university level: factors and solutions, perception of classroom communication barriers of the undergraduate students of general degree colleges : its relationship with and prediction from their attitude towards communication skills, effective communication in indonesian high school: the ombuds office criteria, the investigation of classroom communication strategies used by english department lecturers, an investigation of perceptual, verbal, and non-verbal barriers in the workplace, factors contributing low english language literacy in rural primary schools of karachi, pakistan, identifying the factors contributing to students’ difficulties in the english language learning, student communication skills from internalizing religious values to energy modules in life systems.
- Highly Influenced
24 References
Analysis of communication barriers to distance education: a review study, overcoming transactional distance as a barrier to effective communication over the internet, communication barriers: a study of eastern mediterranean university students' and teachers' of online program and courses, overcoming social and psychological barriers to effective on-line collaboration, major linguistic barriers of oral communication in english as perceived by the tertiary level esl students.
- Highly Influential
The Methodology of Educational Research
Pygmalion teaching style, is there a need for it, role of non-verbal communication in education, evaluating teaching methods: is it worth doing right, related papers.
Showing 1 through 3 of 0 Related Papers
Case Study Hub | Samples, Examples and Writing Tips
Case study on psychological barriers to communication, psychological barriers to communication case study:.
Psychological barriers to communication are the obstacles which occur in the process of communication because of the personal emotional condition of both sides of the conversation.
Psychological barriers occur quite frequently during conversation because of numerous reasons, which most often depend on the current human psychological condition and the human temperament. Sometimes it happens that the human being is an introvert, so it is often difficult to persuade such a person to communicate a lot, because she simply does not need it.
Of course, there are more distinct barriers which are characterized with the human experience, for example, the individual has inner barriers which depend on his bringing up, education, stereotypes and prejudices. When the person has had experience in communication with the definite type of people, he will treat this type according to his first impression.
We can write a Custom Case Study on Barriers to Communication for you!
Then, if the individual has serious problems at work, family or other close people and he is always stressed or even depressed, he will not be a positive communicant, because he will not be able to catch the information and concentrate on it. This type of barrier is called filtering.
Finally, there is an obstacle which is connected with the social status of the participants of the conversation. This psychosocial barrier exists between the boss and the employee, between the teacher and his student, between the mature and young people. This sort of barriers is associated with the fact that the communicant of the “lower” level can not present the information in the way he wants. He will try to behave better and use more formal and sophisticated language.
Psychological barriers to communication are the barriers which occur because of the human psychological condition and her personal experience. The student who is interested in the research of the problem about the psychological barriers to communication should focus on the explanation of these barriers, enumerating their types, etc. Then, one is expected to collect information about the case under analysis and define its problem. It is important to think about the cause and effect of the psychological barriers to communication and then to take efforts to solve the problem efficiently.
Sometimes students do not have the slightest idea about the appropriate organization of the paper and the Internet becomes the single reliable helper in this occasion. The young professional who requires a piece of the friendly advice on writing is able to find the assistance in the form of a free sample case study on psychological barriers to communication designed by the well-educated author. It is reasonable to improve one’s knowledge and writing skills with the help of the free example case study on psychological barriers to communication and succeed in writing your own paper.
At EssayLib.com writing service you can get a custom case study on Family Conflict topics. Your case study will be written from scratch. We hire top-rated Ph.D. and Master’s writers only to provide students with professional case study help at affordable rates. Each customer will get a non-plagiarized paper with timely delivery. Just visit our website and fill in the order form with all paper details:

Related Posts:
- Case Study on Zappos – How They Did It
- Apple Inc Case Study Sample
- Case Study – Zara International: Fashion at…
- Health Management: Business Case Study
- Case Study – Amazon: One E-Store to Rule Them All
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

IMAGES
VIDEO
COMMENTS
Abstract: The success of an organization does not only rely on the rapid growth of their profits. Behind each success of the projects, there is a good relationship and cooperation between. all ...
In emotionally maladjusted people, communication within themselves has broken down, and as a result, their communication with others has been damaged. To put it another way, their unconscious ...
The common. barriers that take place within the course of effective communication are, noise, physical. environment, mental attitude, inappropriate feedback, poor listening skills, selection of ...
Results. Exploratory factor analysis of the items relating to barriers to communication resulted in three latent factors ('stigma, diagnosis and risk'; 'service structure'; and 'individual circumstances' such as the person receiving the diagnosis being young, having a culturally and linguistically diverse background or being unwell at the time of conversation).
The most impactful psychosocial barriers were English learning experiences in the previous class. Teachers' teaching styles are the riskiest barriers that cause the negative impacts of students ...
this study investigates how the communication barriers affect the flow of communication and information at the workplace. A set of questionnaires was developed and distributed to employees in different companies. The questionnaire comprises different sections; demographic profile, the types of communications and the communication barriers. The
Therapeutic communication is essential in the provision of quality healthcare to patients. The purpose of this study was to explore the perceived barriers to effective therapeutic communication among patients and nurses at Komfo Anokye Teaching Hospital,Kumasi. An exploratory study design was employed using a qualitative approach. A purposive sampling technique was used to select 13 ...
People who seem like they're paying attention often aren't—even when they're smiling and nodding toward the speaker. Research by Alison Wood Brooks, Hanne Collins, and colleagues reveals just how prone the mind is to wandering, and sheds light on ways to stay tuned in to the conversation. 31 Oct 2023. HBS Case.
Background Psychological safety is the concept by which individuals feel comfortable expressing themselves in a work environment, without fear of embarrassment or criticism from others. Psychological safety in healthcare is associated with improved patient safety outcomes, enhanced physician engagement and fostering a creative learning environment. Therefore, it is important to establish the ...
Psychological Barriers to Communication. AA CCURATE munication and between adequate groups com- and sible the greatest distortions of reality. condition for almost all forms of social ence. The semantic movement is the. progress. Physical barriers to com- current effort to cope with the woeful. munication are rapidly disappearing, inadequacies ...
Communication-Related Barriers. Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [7, 16, 27, 28].
Earlier it was stated that their use of English is poor. Second, Physical barriers leads to communication disconnect, because of the hierarchy structure - hence decision from top management does not get to the bottom objectively. Third, Psychological barriers are evident as the workforce feel discriminated against.
Stakeholder reported communication barriers and facilitators spanned all constructs of the TFA and comprised potentially modifiable clinical and institutional practices including proactive and systematic provision of communication tools, training, emotional/spiritual support, as well as leadership practices that may encourage effective and ...
b. Generational (age) barriers: Currently there are 4 generations in the workforce and each potentially has a different preferred method of communication. While the younger generation might prefer to receive text messages as their preferred way of communication, older employees may not find this method of communication acceptable.
10/ Distrust. Distrust is a psychological barrier that poses challenges to effective communication. It refers to a lack of confidence or suspicion towards others, their intentions, or the information they provide. Distrust can arise due to past negative experiences, perceived dishonesty, or a lack of credibility.
An analysis of the problems of interpersonal communication, as viewed from a human behavior standpoint. Real communication occurs when one listens to another person's viewpoint with empathic understanding. It is possible to facilitate achievement of this communication breakthrough by summarizing the speaker's thoughts and feelings to his or her satisfaction before presenting a rebuttal. This ...
European Journal of Education Studies - Volume 7 │ Issue 10 │ 2020 234 Ain Nur Amilia Md Yusof, Noor Hanim Rahmat COMMUNICATION BARRIERS AT THE WORKPLACE: A CASE STUDY 4.6 Findings for Environmental Barrier 4.5 4 3.5 3 2.5 2 1.5 1 0.5 0 4 3.4 3.1 2.7 not enough time to do not given suitable feel that inharmonious fear the power of the ...
He will try to behave better and use more formal and sophisticated language.Psychological barriers to communication are the barriers which occur because of the human psychological condition and her personal experience. We Will Write a Custom Case Study Specifically. For You For Only $13.90/page! order now.
part of the manuscript, steps have been identified to overcome the communication. barriers, these are, eliminating differences in perception, use of simple language, reduction and elimination of ...
The present study is undertaken with the objective to analyse the opinion of secondary school teachers regarding barriers in classroom communication. It is evident from the result of the analysis that barriers existmore, or less, though there is significant difference in opinion among the teachers regarding various dimensions of communication. The majority of the teachers opined that barriers ...
to focus on physiological barriers in communication. Additionally, a critical analysis of past case studies will also be looked at. The research method that is going to be used is looking at the past case study. The study is vital as it will help us find the root cause for physiological barriers in communication in an organization and ways of
The psychological barrier of communication is the influence of psychological state of the communicators (sender and receiver) which creates an obstacle for effective communication. Causes of Psychological Barriers. Lack of Attention: When a person's mind is distracted or preoccupied with other things, the person is not able to form proper ...
Psychological Barriers to Communication Case Study: Psychological barriers to communication are the obstacles which occur in the process of communication because of the personal emotional condition of both sides of the conversation. Psychological barriers occur quite frequently during conversation because of numerous reasons, which most often ...
Since communication is a unique and important process, it becomes an object of study from the point of view of many fields, such as linguistics, psychology, pedagogy, social sciences, political ...