- Open access
- Published: 29 May 2023

Experiences of water immersion during childbirth: a qualitative thematic synthesis
- E. Reviriego-Rodrigo 1 ,
- N. Ibargoyen-Roteta 1 ,
- S. Carreguí-Vilar 2 ,
- L. Mediavilla-Serrano 3 ,
- S. Uceira-Rey 4 ,
- S. Iglesias-Casás 5 ,
- A. Martín-Casado 6 ,
- A. Toledo-Chávarri 7 ,
- G. Ares-Mateos 8 ,
- S. Montero-Carcaboso 3 ,
- B. Castelló-Zamora 9 ,
- N. Burgos-Alonso 10 ,
- A. Moreno-Rodríguez 11 ,
- N. Hernández-Tejada 12 &
- C. Koetsenruyter 13
BMC Pregnancy and Childbirth volume 23 , Article number: 395 ( 2023 ) Cite this article
4498 Accesses
1 Citations
5 Altmetric
Metrics details
The increasing demand for childbirth care based on physiological principles has led official bodies to encourage health centers to provide evidence-based care aimed at promoting women’s participation in informed decision-making and avoiding excessive medical intervention during childbirth. One of the goals is to reduce pain and find alternative measures to epidural anesthesia to enhance women’s autonomy and well-being during childbirth. Currently, water immersion is used as a non-pharmacological method for pain relief.
This review aimed to identify and synthesize evidence on women’s and midwives’ experiences, values, and preferences regarding water immersion during childbirth.
A systematic review and thematic synthesis of qualitative evidence were conducted. Databases were searched and references were checked according to specific criteria. Studies that used qualitative data collection and analysis methods to examine the opinions of women or midwives in the hospital setting were included. Non-qualitative studies, mixed-methods studies that did not separately report qualitative results, and studies in languages other than English or Spanish were excluded. The Critical Appraisal Skills Program Qualitative Research Checklist was used to assess study quality, and results were synthesized using thematic synthesis.
Thirteen studies met the inclusion criteria and were included in this review. The qualitative studies yielded three key themes: 1) reasons identified by women and midwives for choosing a water birth, 2) benefits experienced in water births, and 3) barriers and facilitators of water immersion during childbirth.
Conclusions
The evidence from qualitative studies indicates that women report benefits associated with water birth. From the perspective of midwives, ensuring safe water births requires adequate resources, midwives training, and rigorous standardized protocols to ensure that all pregnant women can safely opt for water immersion during childbirth with satisfactory results.
Peer Review reports
Childbirth is a significant event in a woman’s life, with short- and long-term consequences that extend beyond her own health. It can also impact the well-being of her child and family, as well as her future reproductive choices and mode of delivery. A long-term follow-up study has found that positive birth experiences can enhance a woman’s self-confidence and self-esteem throughout her life [ 1 ].
In recent years, the demand for care based on the physiology of childbirth has prompted official bodies to encourage evidence-based care in health centers, aimed at empowering women to make informed decisions and minimizing obstetric intervention and medicalization during childbirth. One of the objectives is to reduce pain and explore alternative measures to epidural analgesia that increase women’s autonomy and well-being during childbirth. One such measure is water immersion, which is currently being used as a non-pharmacological method of pain relief [ 2 ].
The Cochrane systematic review “Immersion in water during labor and birth,“ by Cluett et al, defines “water immersion” as the practice of submerging a pregnant woman’s abdomen in water during any stage of labor, including dilation, expulsive, and delivery. On the other hand, “water birth” refers to the delivery of the newborn underwater [ 3 ].
Examining the experiences of mothers and midwives with water immersion is crucial, given the current emphasis on evidence-based care, efficient resource management, and the evaluation of a more humane model that reduces unnecessary interventions during labor. By reducing the need for medical interventions, water immersion may provide a more natural and positive birth experience for both mother and baby.
The objective of this qualitative synthesis of evidence was to investigate the experiences of women and midwives with water immersion during labor.
Systematic review of evidence
We conducted a systematic review of qualitative and mixed-methods studies, utilizing the SPIDER acronym (Sample, Phenomenon of Interest, Design, Evaluation, and Research type) to guide our review [ 4 ].
Our study sample included nulliparous or multiparous women in labor with singleton pregnancies who were healthy and at low risk of complications. In addition, we also included midwives and other professionals who were involved in obstetric care. The focus of our investigation was on the phenomenon of interest, which pertains to the experiences of women and midwives during water birth. Our study was limited to research conducted in hospital settings.
We considered published qualitative studies, studies with mixed methods designs, and surveys with free-text answer options, provided that the qualitative data could be extracted separately and had been formally analyzed using structured approaches such as thematic analysis or content analysis. We assessed the results by analyzing the narrative perspectives, experiences, and viewpoints of both pregnant women and midwives.
Our review included primary research studies and systematic reviews of qualitative studies published in English or Spanish. By synthesizing and analyzing these studies, we aimed to provide a comprehensive understanding of the experiences of women and midwives with water immersion during labor.
Criteria for considering studies for this review
Inclusion criteria.
We included studies that utilized qualitative research methods, such as ethnographic observations, in-depth interviews, focus group discussions, and open-ended survey questions. Studies with appropriate analysis methods, including thematic analysis, narrative analysis, framework analysis, and grounded theory, were also included [ 5 ]. Mixed-methods studies were only considered if they clearly described their qualitative data collection and analysis methods and provided in-depth findings and interpretations. We limited our review to studies published from 2009 to 2022. Including papers from 2009 allowed for a comprehensive review of literature on water immersion in labor and birth, as the first Cochrane review by Cluett et al. in that year was a significant milestone in the development of research in this area.
Exclusion criteria
We have excluded studies conducted outside the hospital setting, such as home births, from our analysis. Additionally, we have excluded studies that were published in languages other than English or Spanish.
By carefully selecting studies that met our inclusion criteria and excluding those that did not, we aimed to ensure that our review provided a comprehensive and high-quality synthesis of the experiences of women and midwives with water immersion during labor.
Search methods for identification of studies
We conducted a comprehensive search to identify all relevant studies, updating it until August 2022. We limited our search to studies published in English or Spanish from 2009 onwards. We searched several databases, including The Cochrane Library (Wiley), Centre for Reviews and Dissemination (CRD) [Database of Abstracts of Reviews of Effects (DARE)], Pubmed/Medline, Embase (OvidWeb), Web of Science (WOS), PsycINFO (OvidWeb), and Cinahl (EBSCOhost), using a combination of controlled and free language terms, such as “Labor”, “Natural Childbirth”, “Waterbirth” or “Water immersion”. The search strategies were adapted to each database, with the use of MESH descriptors and qualifiers to increase specificity when necessary. Alerts were set up in Medline (PubMed) and Embase (OVID) to identify any documents published up to August 2022. We also manually searched the literature cited in the selected studies to locate any relevant information not retrieved in the previous steps.
After completing the searches, we removed any duplicate citations, and the remaining records were uploaded to RefWorks reference manager. To assist with preparing systematic reviews, we used Ryyan, a software designed for this purpose.
Selection of studies
We imported all search results into Rayyan, and removed any duplicates. Subsequently, two review authors independently assessed the retrieved search results against the inclusion criteria. This screening process involved two stages: first, screening titles and abstracts, and then assessing the full-text articles. Employing two reviewers to screen the studies was advantageous as it allowed for an in-depth exploration of the relevance and meaning of the study findings. To arrive at a final selection, we held discussions until a consensus was reached, based on the study eligibility criteria. The entire screening process is summarized in a PRISMA flow diagram (Fig. 1 ), which outlines the number of studies removed and retained at each stage.
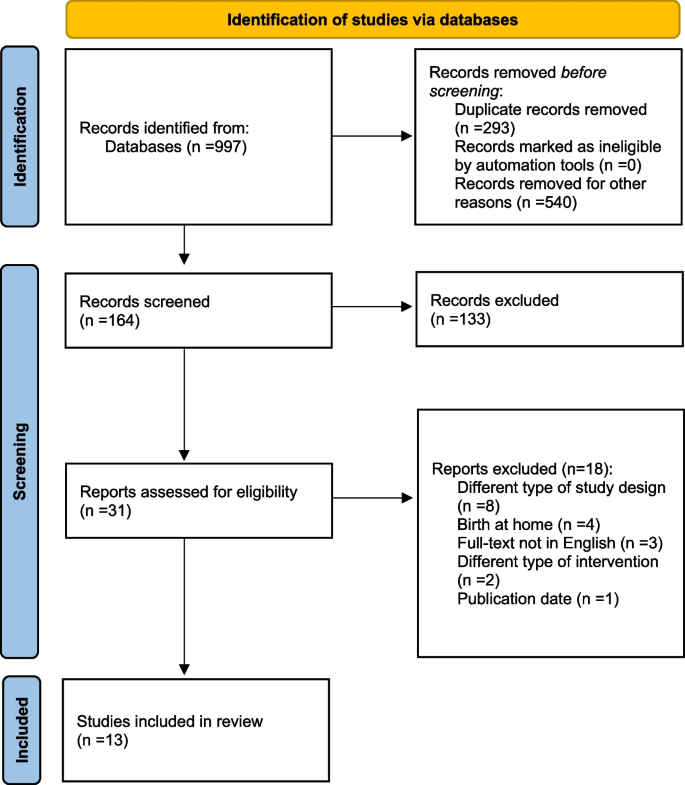
PRISMA flow chart of included studies
Quality appraisal/ assessment of methodological limitations
Prior to comparing findings and reaching a consensus, two reviewers conducted an assessment of methodological limitations for each paper using the Spanish version of the Critical Appraisal Skills Programme tool for qualitative studies (CASPe) [ 6 ]. Any disagreements between the reviewers were addressed and discussed until a consensus was reached. It is important to note that we did not exclude any studies based on our assessment of methodological limitations.
In the case of the systematic review of qualitative studies, the “Enhancing transparency in reporting the synthesis of qualitative research” tool [ 7 ] was applied.
Data extraction and thematic synthesis
We employed a standardized data collection form to extract the relevant data. Thematic synthesis was conducted, following the approach developed by Thomas and Harden [ 5 ]. To ensure a comprehensive analysis, all text in the results or findings sections of the included studies, including participant quotations and interpretations by the authors of the studies, were treated as data.
The lead reviewer (ER) extracted the data into tables and assigned codes to each line of text, based on its meaning and content, in accordance with the method outlined by Thomas and Harden [ 5 ]. These codes were then organized into descriptive themes, some of which corresponded with the original findings of the included studies. Next, the codes were grouped into logical and meaningful clusters in a hierarchical tree structure to form descriptive themes and sub-themes. Finally, the descriptive themes were developed into analytical themes, which enabled us to extend the analysis beyond the original studies.
Internal/external review
The project’s research team conducted an internal review of the work. After completing this stage, the work underwent an external review process, with recognized experts in the field providing feedback to ensure its quality, accuracy, and validity. Before participating in the review, the experts completed a document declaring any potential conflicts of interest.
Included studies and quality assessment
Thirteen studies were identified for the review using PRISMA process (Fig. 1 ).
Characteristics of the included studies
The 13 studies included in this analysis were published between 2013 and 2020, and 9 investigated both the first and second stages of labor, while 4 studies focused solely on the second stage of labor. Eight countries are represented across the studies, Australia ( n = 4), United Kingdom ( n = 2), Sweden ( n = 2), Canada ( n = 1), Portugal ( n = 1), Greece ( n = 1), Scotland ( n = 1), and UU.EE ( n = 1). Methodological approaches varied and qualitative methods used for purposes of data collection from women and midwives, most commonly involved interviews.
Nine studies focussed on women’s experience of water immersion during childbirth (Clews et al., 2019; Poder et al., 2020; Fair et al., 2020; Gonçalves et al., 2019; Lewis et al., 2018; Ulfsdottir et al., 2018; Antonakou et al., 2018; McKenna et al., 2013; Carlsson et al., 2020) [ 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 ], one study (Milosevic et al., 2019) [ 17 ] that explores the factors that determine the use of immersion during childbirth according to the point of view of both women and midwives and medical professionals (obstetricians, neonatologists and pediatricians), and three more studies on midwives’ experience with water immersion during childbirth (Cooper et al., 2019; Lewis et al., 2018; Nicholls et al., 2016 [ 18 , 19 , 20 ].
Tables 1 , 2 and 3 provide a detailed overview of the study characteristics, including information about the author(s)/country, date, study design, participants, method of data collection, method of analysis, recruitment method and setting, study focus, and main findings.
The quality of these studies was evaluated using the CASPe tool, which is widely recognized as a reliable assessment method. For easy reference, the Supplementary Material includes summary tables that provide an overview of the quality of evidence presented in the included studies.
Mothers’ experiences with water immersion during labor and birth
Clews et al. [ 8 ] conducted a metasynthesis of qualitative studies on women’s experiences with water birth. They found four primary themes, which included the mother’s knowledge of water birth, their perception of a physiologic birth, water, autonomy, and control, and water birth easing the transition. The authors concluded that water birth can be an empowering experience for those who choose it and reinforces women’s sense of autonomy and control during the birthing process.
The study conducted by Poder et al. [ 9 ] aimed to identify factors that influence women’s decision to choose water birth or not. They used focus groups to create a validated questionnaire utilizing Discrete Choice Experiments (DCE). The questionnaire considered various attributes that women consider important in making their decision, including type of delivery, duration of labor, pain sensation, risk of severe tearing, risk of newborn death, and general condition (Apgar score at 5 min).
The study by Fair et al. [ 10 ] explored the decision-making process of women who planned to give birth in water. Women sought information from the internet and social networks and desired to limit medical interventions during childbirth. Support from doulas and midwives played a critical role in their decision-making process, while many experienced resistance from family, friends, and colleagues. Although not all women gave birth in water, most reported positive experiences and felt empowered. They encouraged other women to consider water birth and expressed a desire to have a water birth in the future.
In the study conducted by Gonçalves et al. [ 11 ] in Portugal, semi-structured interviews were conducted with mothers who had experienced one or more water births before they were no longer offered by the public health system. The analysis resulted in the identification of seven categories, but the study primarily focuses on two categories: the benefits of water immersion during childbirth, including pain relief and the ability to witness the birth of the child, and the satisfaction of women with the experience.
The study conducted by Lewis et al. in 2018 [ 12 ] aimed to explore the motivations, facilitating and hindering factors, and the birth experiences of women who gave birth in water in a tertiary public hospital in Australia. Telephone interviews were conducted with 296 women 6 weeks after giving birth. Of the participants, only 31% were able to have a water birth, with multiparous women having a higher success rate than primiparous women. Women who planned for a water birth cited pain relief, preference, association with natural childbirth, calming atmosphere, and recommendation as reasons. Support, particularly from midwives, played a crucial role in the success of water birth. The study did not specify which obstetric complications prevented of the women from giving birth in water.
Ulfsdottir et al. [ 13 ] conducted in-depth interviews with primiparous and multiparous mothers three to five months after giving birth. and found that water birth created a comfortable, home-like space that helped women feel relaxed, safe, and in control during childbirth. Three categories emerged: “synergy between body and mind,“ “privacy and discretion,“ and “natural and pleasant.“ The study suggested that water birth could enhance the childbirth experience, but the hospital where the study was conducted provided ongoing support, which may have contributed to positive experiences regardless of whether participants had a water birth or not.
Antonakau et al. [ 14 ] conducted a study on the experiences of women who gave birth using water birth in private facilities in Greece. The study identified three themes: water birth is a natural way of giving birth, healthcare professionals give contradictory messages regarding water births, and the supportive role of partners during the process. All participants reported a positive experience, with water immersion helping them manage pain and feel empowered after birth, resulting in successful breastfeeding for over a year. However, women had difficulty finding healthcare professionals who supported their choices, while they felt very supported by their partners. It is important to note that the participants were a homogenous group, primarily older, more educated, and financially able to afford private maternity care.
McKenna’s study [ 15 ] explored the experiences of women who had a water birth after a previous cesarean section in a Scottish midwifery-led unit. The study found that water birth minimized medical intervention, maximized physical and psychological benefits, and allowed women to have greater control and choice during childbirth. The study also highlighted the women’s management of potential risks associated with water birth and their interactions with healthcare providers, family, and friends.
Carlsson et al. [ 16 ] study included women who gave birth in water. The study identified physical and psychological benefits, including pain relief and improved relaxation, as well as negative experiences such as equipment problems and concerns related to water birth. Participants noted a lack of reliable information on water births and had to seek supplementary information online. The study highlights the need for accessible and reliable information on water births.
Mothers’ and midwives’ experiences with water immersion during labor and birth
Milosevic et al. [ 17 ] conducted a study to investigate factors that influence the use of water immersion during childbirth. The study employed online focus groups with women and midwives, as well as interviews with medical professionals. Eligibility criteria were found to limit access to water births, and obstetrician-led units were described as overly medicalized settings with limited provision of water births. Midwives were found to increase access to water births by proactively offering it as an option during childbirth and providing information to women about water birth during antenatal care.
Midwives’ experiences with water immersion during labor and birth
Cooper, Nicholls, and Lewis have conducted three studies to investigate the experiences of midwives with water immersion during labor or birth [ 18 , 19 , 20 ]. These studies shed light on the benefits and challenges associated with water immersion, as well as the attitudes of midwives towards this birthing option. By examining midwives’ perspectives, these studies provide valuable insights into the implementation and promotion of water immersion.
A study by Cooper et al. [ 18 ] investigated the policies and guidelines for water immersion during labor and birth in Australia, as well as midwives’ experiences and perspectives. The study included a literature search, interviews, and an online questionnaire, and found that midwives must be accredited to facilitate water immersion to promote access to this option. However, midwives faced barriers related to accreditation and inconsistent guidelines across facilities. The study suggests the need for standardized guidelines and improved training opportunities for midwives to ensure the safe and effective use of water immersion during labor and birth. Overall, the study highlights the importance of promoting access to water immersion as a birthing option while ensuring appropriate training and guidelines for healthcare professionals.
Lewis et al. [ 19 ] examined midwives’ perceptions of their education, knowledge, and practice of water immersion during labor and birth in Australia. The study used a two-phase mixed-methods approach, including a questionnaire and focus groups. The results of the questionnaire showed that 93% of midwives felt confident attending water births after attending an average of seven water births, and they enjoyed facilitating water immersion. The focus groups identified several positive aspects of caring for women during water immersion, such as instinctive birth and a woman-centered environment, as well as challenges related to learning through observation and the need for support to enable water births. Overall, the study highlights midwives’ positive experiences and the importance of training and support to ensure safe and effective water immersion during labor and birth.
The study by Nicholls et al. [ 20 ] emphasizes the importance of midwives’ competence and confidence in supporting water births according to local clinical practice guidelines. Interviews with 16 midwives and a focus group with 10 others identified three categories related to confidence acquisition: pre-pathway factors, pathway to confidence, and maintenance of confidence. The study identified three categories that affect midwives’ confidence in supporting water births: 1) factors before entering the profession, 2) factors that contribute to confidence development, and 3) factors that help maintain confidence.
The study’s findings have three significant implications for midwifery practice. Firstly, it is recommended that graduate students and midwives work in maternity wards led by midwives who support normal physiological birth. Secondly, it is suggested that learning directly from experienced midwives who can address their specific needs would benefit maternity wards. Lastly, it is emphasized that midwives have a crucial role as “protectors” of normal physiological birth, and mandatory attendance at sessions highlighting this role and the current evidence supporting normal birth, including water immersion during labor, is necessary.
Thematic synthesis
To summarize the most significant findings from the qualitative studies on water immersion in childbirth, several tables have been created based on the themes that emerged from the studies. Thematic synthesis identified the following three themes:
Theme 1. Reasons for choosing water birth.
This theme investigates the factors that influenced women’s decision to use water immersion during childbirth, such as pain relief, relaxation, and a desire for a more natural birth experience. Some professionals also cited benefits to the baby, such as reducing stress and facilitating a smoother transition to the outside world.
Theme 2. Benefits of water immersion.
This theme includes the positive experiences reported by women who used water immersion during labor and birth, such as reduced pain, increased relaxation, and a greater sense of control. Midwives and other health professionals also noted benefits, including improved maternal-fetal bonding and a decreased need for medical interventions.
Theme 3. Barriers and facilitators of water immersion:
This theme includes factors that can either hinder or promote the use of water immersion during childbirth. For example, midwives’ attitudes and training were identified as critical facilitators, while hospital policies and protocols were seen as significant barriers. Other factors included access to appropriate facilities and equipment, communication and coordination among healthcare providers, and support from partners and family members.
Tables 4 , 5 and 6 provide a comprehensive overview of the themes and subthemes present in the included studies. These tables serve as a visual representation of the key concepts and ideas that emerged from the analysis of the data.
Table 4 presents the reasons for choosing a water birth based on the findings of the included studies.
The table includes 5 identified reasons for choosing water birth and the sources of the evidence supporting each reason. The reasons were identified by four studies: Clews et al. (2019), Poder et al. (2020), Fair et al. (2020), and Lewis et al. (2018) [ 8 , 9 , 10 , 12 ].
The most common reasons for choosing a water birth, as reported the studies, include prior knowledge of water birth [ 8 , 12 ], recommendation by others [ 8 , 12 ], relaxation and decreased anxiety [ 9 , 12 ], sense of comfort and well-being [ 9 ], desire for natural birth [ 10 , 12 ], pain relief during labor [ 9 , 12 ]. Other reported benefits of water birth include reduced likelihood of perineal tearing [ 9 ], shortened active phase of labor [ 9 ], no increased risk of newborn mortality compared to conventional delivery [ 9 ], no adverse effect on newborn’s general condition (Apgar test) [ 9 ], and no increased risk of infection for the newborn [ 9 ].
Overall, the table suggests that women may choose water birth for various reasons, such as personal preference and potential benefits, without increasing the risk of adverse outcomes for the newborn.
Table 5 summarizes the identified benefits of water birth, along with the sources of evidence supporting each benefit.
Table 5 summarizes the reported benefits of water birth as identified by women who had experienced it, as well as midwives who have supported such births. The benefits include a greater feeling of autonomy and control over the childbirth process [ 8 , 11 , 12 , 13 , 16 , 19 ], increased opportunities for experiencing a more natural childbirth [ 8 , 10 , 11 , 12 , 13 , 14 , 16 , 19 ], easing the transition into motherhood [ 8 ], providing pain relief without relying on medical interventions [ 11 , 12 , 16 ], allowing the opportunity to witness the birth of the child [ 11 ], the option of immersion in water [ 11 , 12 ], immersion in water for increased mobility and a sense of lightness [ 11 , 16 ], tranquility, improved breathing, and relaxation leading to synergy between body and mind [ 11 , 12 , 13 , 16 , 19 ], more privacy and discretion during the childbirth process [ 13 ], minimizing the medicalization of childbirth, resulting in less use of analgesia and oxytocin [ 10 , 12 , 15 , 16 , 17 ], a feeling of positive experience [ 8 , 10 , 11 , 12 ], a feeling of success in childbirth [ 11 ], and more physical and psychological benefits [ 15 , 16 ].
Overall, the table highlights the various benefits of water birth as reported by women and midwives, including physical and psychological advantages, which may encourage women to consider water birth as a viable option for childbirth.
Additionally, Table 6 presents a comprehensive overview of the barriers and facilitators that have been identified in the studies analyzed.
Table 6 provides a summary of the barriers and facilitators identified in the studies included in this analysis related to water immersion during childbirth. The references in the table include several studies that investigated water immersion during childbirth, such as Fair et al. 2020 [ 10 ], Lewis et al. 2018 [ 12 ], Antonakou et al. 2018 [ 14 ], McKenna et al. 2013 [ 15 ], Carlsson et al. 2020 [ 16 ], Milosevic et al. 2019 [ 17 ], Cooper et al. 2019 [ 18 ], Lewis et al. 2018 (midwives) [ 19 ], and Nicholls et al. 2016 [ 20 ].
The table lists various factors that could either impede or promote water immersion during childbirth.
The barriers to water immersion during childbirth identified in this study include safety concerns related to potential risks associated with waterbirth after cesarean section [ 15 ] and obstetric complications [ 12 ]. The lack of support from family members and healthcare professionals was also identified as a barrier to water immersion during childbirth [ 10 ].
On the other hand, several facilitators of water immersion in childbirth were identified, including the availability of bathtubs and appropriate usage techniques [ 17 ], clear and consistent eligibility criteria for water immersion during childbirth [ 17 ], and support from health professionals [ 10 , 12 , 14 , 17 , 20 ]. Moreover, training and support for healthcare professionals attending water immersion childbirths, including proper techniques and safety precautions, also facilitate successful water immersion childbirths [ 12 , 17 , 18 , 20 ].
Finally, provision of clear and accurate information to pregnant women about the benefits and risks of water immersion childbirths, promotion of water immersion through education [ 16 , 17 ], and a culture of support for water immersion during childbirth were identified as crucial facilitators for successful water immersion childbirths.
To ensure safe water births, midwives emphasize the importance of having adequate resources, consistent protocols, specialized training, and a supportive culture towards water immersion during childbirth. This support should come from all healthcare professionals involved in the birth process, not just midwives. By ensuring these factors are in place, midwives can confidently attend water births and provide the best care for the mother and baby.
This article examines qualitative studies that explore the experiences of women and healthcare teams caring for mother-newborn pairs.
The results of the qualitative studies suggest that women who choose to use water immersion during labor often have a positive and empowering experience, leading to a more natural childbirth and increased satisfaction [ 8 ]. However, the studies also identified various barriers such as potential obstetric complications, lack of support from family members and healthcare professionals, and inadequate resources and facilities for water births. To offer this service safely and effectively, facilities must have proper equipment, maintenance and cleaning protocols, action protocols, and contingency plans for potential complications. Healthcare professionals must also receive specialized training in water birth practices, and the resource must be readily available upon request [ 10 , 12 ].
One of the studies [ 9 ] examined the factors that can influence a woman’s decision to have a water birth and found that the most significant factors were pain reduction, the risk of neonatal mortality, the risk of severe perineal tears, slightly better general condition of the newborn (as indicated by the Apgar test), and reduction of the duration of the active phase of labor. The study also highlighted the importance of providing accurate and comprehensive information to pregnant women about water immersion during childbirth, as many women reported not receiving enough information on this option.
Two studies conducted by Carlsson et al. (2020) [ 16 ] and Milosevic et al. (2019) [ 17 ] revealed the insufficient provision of information about water births during antepartum classes and midwife consultations. Furthermore, it is essential to incorporate the systematic collection of data obtained from the use of water birth to address the quality-of-care indicators during childbirth. This approach will ensure that pregnant women who choose water births during labor receive the highest level of safe and quality care.
During the final stage of writing this article, the study by Feeley C. et al., 2021 [ 21 ] was retrieved through alerts. This study is a meta-synthesis of qualitative studies and used GRADE-CERQual [ 22 ] to evaluate the results. The meta-synthesis included seven studies to evaluate the impact of water immersion during labor [ 11 , 13 , 14 , 15 , 23 , 24 , 25 ], out of which four were part of the systematic review [ 11 , 13 , 14 , 15 ]. The findings revealed that women who used water immersion during any stage of labor facilitated women’s physical and psychological needs, offering effective analgesia and a versatile tool that women can adapt and influence to best suit their individual needs. Women who used warm water immersion for labor and/or birth described the experience as liberating, transformative, and empowering, resulting in a positive birth experience. Based on these results, the study suggests that maternity professionals and services should improve women’s access to water immersion and offer it as a standard method to of pain relief during labor for low-risk pregnant women.
Qualitative studies have consistently shown that women who have experienced water births associate numerous benefits with the practice. These benefits include reduced pain and discomfort during labor, a greater sense of relaxation and control, increased satisfaction with the birth experience, and improved maternal and fetal outcomes. Additionally, water immersion during labor has been found to reduce the need for pharmacological pain relief, interventions such as episiotomy, and operative deliveries. These findings highlight the potential benefits of water immersion as a safe and effective option for women during labor and delivery.
Midwives emphasize the importance of adequate resources, standardized and rigorous protocols, training for midwives, and a supportive culture for water immersion during childbirth, with input from all professionals involved in attending the birth, including those who care for both mothers and newborns.
It is recommended to improve the information provided to women regarding pain relief options, establish common protocols for water births in NHS hospitals, standardize training for these deliveries, and increase human and material resources to ensure that all pregnant women have the possibility of safely and satisfactorily using hot water immersion during labor, regardless of their location.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Maimburg RD, Væth M, Dahlen H. Women’s experience of childbirth - a five year follow-up of the randomised controlled trial “Ready for Child Trial. Women Birth. 2016;29(5):450–4.
Article PubMed Google Scholar
Mallén Pérez L, Terré Rull C, Palacio Riera M. Inmersión en agua durante el parto: revisión bibliográfica. Matronas Prof. 2015;16(3):108–13.
Google Scholar
Cluett ER, Burns E, Cuthbert A. Immersion in water during labour and birth. Cochrane Database Syst Rev. 2018;5(5):CD000111.
PubMed Google Scholar
Cooke A, Smith D, Booth A, Beyond PICO. The SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8: 45.
Article PubMed PubMed Central Google Scholar
Cano Arana A, González Gil T, Cabello López JB. por CASPe. Plantilla para ayudarte a entender un estudio cualitativo. En: CASPe. Guías CASPe de Lectura Crítica de la Literatura Médica. Alicante: CASPe; 2010. pp. 3–8. Cuaderno III.
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;27(12): 181.
Article Google Scholar
Clews C, Church S, Ekberg M. Women and waterbirth: a systematic meta-synthesis of qualitative studies. Women Birth. 2020;33(6):566–73.
Poder TG, Carrier N, Roy M, Camden C. A discrete choice experiment on women’s preferences for water immersion during labor and birth: identification, refinement and selection of attributes and levels. Int J Environ Res Public Health. 2020;16(6):1936.
Fair CD, Crawford A, Houpt B, Latham V. After having a waterbirth, I feel like it’s the only way people should deliver babies”: the decision making process of women who plan a waterbirth. Midwifery. 2020;82:102622.
Gonçalves M, Coutinho E, Pareira V, Nelas P, Chaves C, Duarte J. Woman’s satisfaction with her water birth experience. Comput Support Qual Res. 2018;861:255.
Lewis L, Hauck YL, Crichton C, Barnes C, Poletti C, Overing H, Keyes L, Thomson B. The perceptions and experiences of women who achieved and did not achieve a waterbirth. BMC Pregnancy Childbirth. 2018;10(1):23.
Ulfsdottir H, Saltvedt S, Ekborn M, Georgsson S. Like an empowering micro-home: a qualitative study of women’s experience of giving birth in water. Midwifery. 2018;67:26–31.
Antonakou A, Kostoglou E, Papoutsis D. Experiences of greek women of water immersion during normal labour and birth. A qualitative study Eur J Midwifery. 2018;12(2):7.
McKenna JA, Symon AG. Water VBAC: exploring a new frontier for women’s autonomy. Midwifery. 2014;30(1):e20-5.
Carlsson T, Ulfsdottir H. Waterbirth in low-risk pregnancy: an exploration of women’s experiences. J Adv Nurs. 2020;76(5):1221–31.
Milosevic S, Channon S, Hughes J, Hunter B, Nolan M, Milton R, Sanders J. Factors influencing water immersion during labour: qualitative case studies of six maternity units in the United Kingdom. BMC Pregnancy Childbirth. 2020;23(1):719.
Cooper M, Warland J, McCutcheon H. Practitioner accreditation for the practice of water immersion during labour and birth: results from a mixed methods study. Women Birth. 2019;32(3):255–62.
Lewis L, Hauck YL, Butt J, Western C, Overing H, Poletti C, Priest J, Hudd D, Thomson B. Midwives’ experience of their education, knowledge and practice around immersion in water for labour or birth. BMC Pregnancy Childbirth. 2018;19(1):249.
Nicholls S, Hauck YL, Bayes S, Butt J. Exploring midwives’ perception of confidence around facilitating water birth in western Australia: a qualitative descriptive study. Midwifery. 2016;33:73–81.
Feeley C, Cooper M, Burns E. A systematic meta-thematic synthesis to examine the views and experiences of women following water immersion during labour and waterbirth. J Adv Nurs. 2021;77(7):2942–56.
Lewin S, Booth A, Glenton C, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13(Suppl 1):2.
Hall SM, Holloway IM. Staying in control: women's experiences of labour in water. Midwifery. 1998;14(1):30–6. https://doi.org/10.1016/s0266-6138(98)90112-7 .
Maude RM, Foureur MJ. It's beyond water: stories of women's experience of using water for labour and birth. Women Birth. 2007;20(1):17–24. https://doi.org/10.1016/j.wombi.2006.10.005 . Epub 2006 Dec 14.
Sprague, Annie G. An investigation into the use of water immersion upon the outcomes and experience of giving birth [Thesis]. Australian Catholic University; 2004. https://doi.org/10.4226/66/5a94ac625e498 .
Download references
Acknowledgements
The authors gratefully acknowledge the contributions of the following individuals and organizations: Arantza Romano Igartua, Mª del Puerto Landa Ortiz de Zárate, Fernando Arizmendi, and Joxe Arizmendi from the Area of Documentation and Specialized Libraries of the Department of Health of the Basque Government, Directorate of Health Research and Innovation. They also thank José Asua Batarrita, who is currently retired from Osteba, Department of Health of the Basque Government; Anaitz Leunda Iñurritegui from Osteba, Health Technology Assessment, Knowledge Management and Evaluation, Basque Foundation for Health Innovation and Research (BIOEF); Rosa María López Rodríguez, Program Director of the Women’s Health Observatory, General Directorate of Public Health, Ministry of Health; José Luis Quintas Díez, Vice-Minister of Health of the Basque Government; and Ignacio Rucandio Alonso, External Technical Support from the Women’s Health Observatory, General Directorate of Public Health, Ministry of Health.
No specific funding has been required to develop this article. The financial support for the activities of the Spanish Network of Agencies for Assessing National Health System Technologies and Performance (RedETS) is provided by the Spanish Ministry of Health.
Author information
Authors and affiliations.
Osteba, Health Technology Assessment, Knowledge Management and Evaluation, Basque Foundation for Health Innovation and Research (BIOEF), Barakaldo-Bizkaia, Spain
E. Reviriego-Rodrigo & N. Ibargoyen-Roteta
La Plana University Hospital, Villarreal-Castellón, Spain
S. Carreguí-Vilar
Osakidetza, OSI Debabarrena, Mendaro Hospital, Mendaro-Gipuzkoa, Spain
L. Mediavilla-Serrano & S. Montero-Carcaboso
Hospital da Barbanza, Ribeira-A Coruña, Spain
S. Uceira-Rey
Hospital do Salnés, Vilagarcía de Arousa-Pontevedra, Spain
S. Iglesias-Casás
Universidad Internacional de La Rioja UNIR, Logroño-La Rioja, Spain
A. Martín-Casado
Canary Islands Health Research Institute Foundation, Network for Research on Chronicity, Primary Care, and Health Promotion (RICAPPS), The Spanish Network of Agencies for Health Technology Assessment and Services of the National Health System (RedETS), Madrid, Spain
A. Toledo-Chávarri
Pediatrics Department, Hospital Universitario Rey Juan Carlos, Madrid, Spain
G. Ares-Mateos
Documentary of the Department of Health of the Basque Government, Territorial Delegation of Health of Bizkaia, Bilbao, Spain
B. Castelló-Zamora
Department of Preventive Medicine and Public Health, Faculty of Medicine and Nursery, UPV/EHU, ES, Leioa, Spain
N. Burgos-Alonso
Osakidetza, OSI Araba, Hospital Txagorritxu, Vitoria-Gasteiz, Spain
A. Moreno-Rodríguez
People with Intellectual Disabilities, Vitoria-Gasteiz, Spain
N. Hernández-Tejada
Mayan Center, Maternity, Yoga and Accompaniment, Bilbao, Spain
C. Koetsenruyter
You can also search for this author in PubMed Google Scholar
Contributions
ER was involved in all aspects of the project, including contributing to the conception and design of the study, as well as coordinating its various stages. ER and NIR both contributed to the interpretation of study results and reviewed relevant documents. SCV, LMS, SUR, SIC, AMC, SMC, and GAM provided a clinical perspective by reviewing the article and sharing their experiences with immersion in water during labor and birth. Their valuable insights have greatly contributed to the quality of this work. ATCh made significant contributions to the development of methods for conducting thematic analysis in qualitative studies. BCZ designed the search strategies, organized the articles in a bibliographic reference manager, retrieved articles, and developed the documentation methodology. NBA has conducted a thorough review of the manuscript with a focus on its public health implications. AMR, NHT, and CK have reviewed the manuscript, analyzed the importance of outcome variables, and provided ideas to improve it. All authors read and approved the final manuscript.
Corresponding author
Correspondence to E. Reviriego-Rodrigo .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was not required in accordance with national legislation and institutional requirements due to fact that the data presented are anonymous, present no potential for identification of specific individuals with the dissemination of the research results, and are not considered to be sensitive or confidential in nature.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Reviriego-Rodrigo, E., Ibargoyen-Roteta, N., Carreguí-Vilar, S. et al. Experiences of water immersion during childbirth: a qualitative thematic synthesis. BMC Pregnancy Childbirth 23 , 395 (2023). https://doi.org/10.1186/s12884-023-05690-7
Download citation
Received : 11 January 2023
Accepted : 08 May 2023
Published : 29 May 2023
DOI : https://doi.org/10.1186/s12884-023-05690-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Natural childbirth
- Water Immersion
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Aug. 15, 2022

Emory University School of Nursing assistant professor Priscilla Hall, PhD, contributed to a recent meta-analysis study on water births that is gaining far-reaching recognition. The study shows that water births provide clear benefits for mothers and their babies, with fewer complications than standard care methods. The new research involving Hall is receiving significant attention from medical professionals and media sources such as “Good Morning America.”
Water birth is when a woman in labor gives birth in a deep bath or birthing pool. The newborn starts breathing as soon as his or her face emerges from the surface of the water. Water birth is relatively uncommon in the United States, and is considered an alternative care modality, despite being an intervention that is safe and valuable to birthing women. The reasons for the lack of availability of this intervention are complex, but one contributing factor is a lack of information about water birth safety in medical education.
“This makes the intervention feel foreign to physicians and facilitates the assumption that water birth is an alternative form of care primarily for midwifery patients in out of hospital settings,” Hall says. “This meta-analysis study was focused mostly on hospital-based care, the setting where physicians provide care and where 98% of U.S. births happen. The study’s focus on the hospital setting made it meaningful to physicians and gave it broader attention.”
The study was done in collaboration with researchers from Oxford Brookes University, with Ethel Burns, PhD, as primary investigator, Jennifer Vanderlaan, PhD, from the University of Nevada Las Vegas, and Claire Feeley, PhD, from King’s College in London. A synthesis of the available evidence led the team to conclude that water births in an obstetric setting have numerous benefits, including lower pain levels and reduced heavy bleeding in labor. The study also showed that waterbirths lead to higher satisfaction levels for mothers and improved odds of avoiding perineal tears or lacerations.
The Royal College of Midwives expressed support for the study , stating, “Research showing the safety and positive benefits for women having a water birth has been welcomed by the Royal College of Midwives. The research showed that women having a water birth in a hospital obstetric unit had fewer medical interventions and complications during and after the birth.”
This meta-analysis research confirms that water births are safe for women, and Hall hopes that medical professionals will consider the intervention as a viable option for all low-risk women, regardless of the birth setting.
“I would like to see water tubs in every hospital. The research shows that water births are safe to offer as a birthing modality. I am hopeful that the attention this study receives will move things in that direction.”
For more information about this study, click here .
About the Nell Hodgson Woodruff School of Nursing
Emory University's Nell Hodgson Woodruff School of Nursing produces nurse leaders who are transforming healthcare through science, education, practice, and policy. Graduates go on to become national and international leaders in patient care, public health, government, research, and education. Others become qualified to seek certification as nurse practitioners and nurse-midwives. The doctor of nurse practice (DNP) program trains nurse anesthetists and advanced leaders in healthcare administration. The school also maintains a PhD program in partnership with Emory's Laney Graduate School. For more information, visit https://www.nursing.emory.edu/ .
About Priscilla Hall, PhD
Hall lectures in the areas of maternal child nursing and midwifery and works in the maternity simulation lab at the Emory University Nell Hodgson Woodruff School of Nursing. She received her PhD from Emory’s Laney Graduate School, where she received the Silver Bowl Award for outstanding work as a PhD candidate. Her dissertation was titled: “Keeping it together and falling apart: women’s experiences of childbirth.” Prior to her academic work, Hall was in clinical practice as a nurse midwife, and she is currently engaged in midwifery practice in the homebirth setting.
- School of Nursing
- Woodruff Health Sciences Center
Recent News
Download emory news photo.
By downloading Emory news media, you agree to the following terms of use:
Creative Commons Attribution-NoDerivatives 4.0 International Public License
By exercising the Licensed Rights (defined below), You accept and agree to be bound by the terms and conditions of this Creative Commons Attribution-NoDerivatives 4.0 International Public License ("Public License"). To the extent this Public License may be interpreted as a contract, You are granted the Licensed Rights in consideration of Your acceptance of these terms and conditions, and the Licensor grants You such rights in consideration of benefits the Licensor receives from making the Licensed Material available under these terms and conditions.
Section 1 – Definitions.
- Adapted Material means material subject to Copyright and Similar Rights that is derived from or based upon the Licensed Material and in which the Licensed Material is translated, altered, arranged, transformed, or otherwise modified in a manner requiring permission under the Copyright and Similar Rights held by the Licensor. For purposes of this Public License, where the Licensed Material is a musical work, performance, or sound recording, Adapted Material is always produced where the Licensed Material is synched in timed relation with a moving image.
- Copyright and Similar Rights means copyright and/or similar rights closely related to copyright including, without limitation, performance, broadcast, sound recording, and Sui Generis Database Rights, without regard to how the rights are labeled or categorized. For purposes of this Public License, the rights specified in Section 2(b)(1)-(2) are not Copyright and Similar Rights.
- Effective Technological Measures means those measures that, in the absence of proper authority, may not be circumvented under laws fulfilling obligations under Article 11 of the WIPO Copyright Treaty adopted on December 20, 1996, and/or similar international agreements.
- Exceptions and Limitations means fair use, fair dealing, and/or any other exception or limitation to Copyright and Similar Rights that applies to Your use of the Licensed Material.
- Licensed Material means the artistic or literary work, database, or other material to which the Licensor applied this Public License.
- Licensed Rights means the rights granted to You subject to the terms and conditions of this Public License, which are limited to all Copyright and Similar Rights that apply to Your use of the Licensed Material and that the Licensor has authority to license.
- Licensor means the individual(s) or entity(ies) granting rights under this Public License.
- Share means to provide material to the public by any means or process that requires permission under the Licensed Rights, such as reproduction, public display, public performance, distribution, dissemination, communication, or importation, and to make material available to the public including in ways that members of the public may access the material from a place and at a time individually chosen by them.
- Sui Generis Database Rights means rights other than copyright resulting from Directive 96/9/EC of the European Parliament and of the Council of 11 March 1996 on the legal protection of databases, as amended and/or succeeded, as well as other essentially equivalent rights anywhere in the world.
- You means the individual or entity exercising the Licensed Rights under this Public License. Your has a corresponding meaning.
Section 2 – Scope.
- reproduce and Share the Licensed Material, in whole or in part; and
- produce and reproduce, but not Share, Adapted Material.
- Exceptions and Limitations . For the avoidance of doubt, where Exceptions and Limitations apply to Your use, this Public License does not apply, and You do not need to comply with its terms and conditions.
- Term . The term of this Public License is specified in Section 6(a) .
- Media and formats; technical modifications allowed . The Licensor authorizes You to exercise the Licensed Rights in all media and formats whether now known or hereafter created, and to make technical modifications necessary to do so. The Licensor waives and/or agrees not to assert any right or authority to forbid You from making technical modifications necessary to exercise the Licensed Rights, including technical modifications necessary to circumvent Effective Technological Measures. For purposes of this Public License, simply making modifications authorized by this Section 2(a)(4) never produces Adapted Material.
- Offer from the Licensor – Licensed Material . Every recipient of the Licensed Material automatically receives an offer from the Licensor to exercise the Licensed Rights under the terms and conditions of this Public License.
- No downstream restrictions . You may not offer or impose any additional or different terms or conditions on, or apply any Effective Technological Measures to, the Licensed Material if doing so restricts exercise of the Licensed Rights by any recipient of the Licensed Material.
- No endorsement . Nothing in this Public License constitutes or may be construed as permission to assert or imply that You are, or that Your use of the Licensed Material is, connected with, or sponsored, endorsed, or granted official status by, the Licensor or others designated to receive attribution as provided in Section 3(a)(1)(A)(i) .
Other rights .
- Moral rights, such as the right of integrity, are not licensed under this Public License, nor are publicity, privacy, and/or other similar personality rights; however, to the extent possible, the Licensor waives and/or agrees not to assert any such rights held by the Licensor to the limited extent necessary to allow You to exercise the Licensed Rights, but not otherwise.
- Patent and trademark rights are not licensed under this Public License.
- To the extent possible, the Licensor waives any right to collect royalties from You for the exercise of the Licensed Rights, whether directly or through a collecting society under any voluntary or waivable statutory or compulsory licensing scheme. In all other cases the Licensor expressly reserves any right to collect such royalties.
Section 3 – License Conditions.
Your exercise of the Licensed Rights is expressly made subject to the following conditions.
Attribution .
If You Share the Licensed Material, You must:
- identification of the creator(s) of the Licensed Material and any others designated to receive attribution, in any reasonable manner requested by the Licensor (including by pseudonym if designated);
- a copyright notice;
- a notice that refers to this Public License;
- a notice that refers to the disclaimer of warranties;
- a URI or hyperlink to the Licensed Material to the extent reasonably practicable;
- indicate if You modified the Licensed Material and retain an indication of any previous modifications; and
- indicate the Licensed Material is licensed under this Public License, and include the text of, or the URI or hyperlink to, this Public License.
- You may satisfy the conditions in Section 3(a)(1) in any reasonable manner based on the medium, means, and context in which You Share the Licensed Material. For example, it may be reasonable to satisfy the conditions by providing a URI or hyperlink to a resource that includes the required information.
- If requested by the Licensor, You must remove any of the information required by Section 3(a)(1)(A) to the extent reasonably practicable.
Section 4 – Sui Generis Database Rights.
Where the Licensed Rights include Sui Generis Database Rights that apply to Your use of the Licensed Material:
- for the avoidance of doubt, Section 2(a)(1) grants You the right to extract, reuse, reproduce, and Share all or a substantial portion of the contents of the database, provided You do not Share Adapted Material;
- if You include all or a substantial portion of the database contents in a database in which You have Sui Generis Database Rights, then the database in which You have Sui Generis Database Rights (but not its individual contents) is Adapted Material; and
- You must comply with the conditions in Section 3(a) if You Share all or a substantial portion of the contents of the database.
Section 5 – Disclaimer of Warranties and Limitation of Liability.
- Unless otherwise separately undertaken by the Licensor, to the extent possible, the Licensor offers the Licensed Material as-is and as-available, and makes no representations or warranties of any kind concerning the Licensed Material, whether express, implied, statutory, or other. This includes, without limitation, warranties of title, merchantability, fitness for a particular purpose, non-infringement, absence of latent or other defects, accuracy, or the presence or absence of errors, whether or not known or discoverable. Where disclaimers of warranties are not allowed in full or in part, this disclaimer may not apply to You.
- To the extent possible, in no event will the Licensor be liable to You on any legal theory (including, without limitation, negligence) or otherwise for any direct, special, indirect, incidental, consequential, punitive, exemplary, or other losses, costs, expenses, or damages arising out of this Public License or use of the Licensed Material, even if the Licensor has been advised of the possibility of such losses, costs, expenses, or damages. Where a limitation of liability is not allowed in full or in part, this limitation may not apply to You.
- The disclaimer of warranties and limitation of liability provided above shall be interpreted in a manner that, to the extent possible, most closely approximates an absolute disclaimer and waiver of all liability.
Section 6 – Term and Termination.
- This Public License applies for the term of the Copyright and Similar Rights licensed here. However, if You fail to comply with this Public License, then Your rights under this Public License terminate automatically.
Where Your right to use the Licensed Material has terminated under Section 6(a) , it reinstates:
- automatically as of the date the violation is cured, provided it is cured within 30 days of Your discovery of the violation; or
- upon express reinstatement by the Licensor.
- For the avoidance of doubt, the Licensor may also offer the Licensed Material under separate terms or conditions or stop distributing the Licensed Material at any time; however, doing so will not terminate this Public License.
- Sections 1 , 5 , 6 , 7 , and 8 survive termination of this Public License.
Section 7 – Other Terms and Conditions.
- The Licensor shall not be bound by any additional or different terms or conditions communicated by You unless expressly agreed.
- Any arrangements, understandings, or agreements regarding the Licensed Material not stated herein are separate from and independent of the terms and conditions of this Public License.
Section 8 – Interpretation.
- For the avoidance of doubt, this Public License does not, and shall not be interpreted to, reduce, limit, restrict, or impose conditions on any use of the Licensed Material that could lawfully be made without permission under this Public License.
- To the extent possible, if any provision of this Public License is deemed unenforceable, it shall be automatically reformed to the minimum extent necessary to make it enforceable. If the provision cannot be reformed, it shall be severed from this Public License without affecting the enforceability of the remaining terms and conditions.
- No term or condition of this Public License will be waived and no failure to comply consented to unless expressly agreed to by the Licensor.
- Nothing in this Public License constitutes or may be interpreted as a limitation upon, or waiver of, any privileges and immunities that apply to the Licensor or You, including from the legal processes of any jurisdiction or authority.
Creative Commons is not a party to its public licenses. Notwithstanding, Creative Commons may elect to apply one of its public licenses to material it publishes and in those instances will be considered the “Licensor.” The text of the Creative Commons public licenses is dedicated to the public domain under the CC0 Public Domain Dedication . Except for the limited purpose of indicating that material is shared under a Creative Commons public license or as otherwise permitted by the Creative Commons policies published at creativecommons.org/policies , Creative Commons does not authorize the use of the trademark “Creative Commons” or any other trademark or logo of Creative Commons without its prior written consent including, without limitation, in connection with any unauthorized modifications to any of its public licenses or any other arrangements, understandings, or agreements concerning use of licensed material. For the avoidance of doubt, this paragraph does not form part of the public licenses.

Rebecca Dekker
The Evidence on: Waterbirth
Originally published on July 8, 2014, and updated on February 14, 2024, by Rebecca Dekker, PhD, RN. Copyright Evidence Based Birth®. All Rights Reserved.
Please read our Disclaimer and Terms of Use . For a printer-friendly PDF, become an EBB Pro Member to access our complete library.
What is Waterbirth, and How is it Different than Water Immersion in Labor?
With water immersion in labor , you get into a tub or pool of warm water during the first stage of labor, before your baby is born. In a waterbirth , you remain in the water during the pushing phase and actual birth of the baby (Nutter et al., 2014a). The baby is then brought to the surface of the water after birth. With a waterbirth, the third stage of labor (when the placenta is born) may take place in or out of the water.
Researchers use the term land birth or conventional birth to refer to a birth in which the baby is born on dry land—not in a tub. And the word hydrotherapy can be used to describe the therapeutic use of water during labor and/or birth.
Waterbirth was first reported in an 1805 medical journal and became more popular in the 1980s and 1990s. The safety of water immersion during labor is well accepted (Cluett and Burns, 2018; Shaw- Battista, 2017). However, doctors and midwives, as well as health care professionals from various countries, often disagree on whether waterbirth is safe.
The purpose of this article is to provide you with the evidence on the safety and health outcomes of waterbirth. Then, we will share an overall summary of the pros and cons of waterbirth.
Before we dive into the evidence on waterbirth, it’s important to understand the impact that laboring in water—regardless of whether you give birth in the water—has on the labor process.
For example, one review of seven randomized trials with 2,615 participants looked at water immersion during labor (before normal land birth) and found that laboring in water posed no extra risks to birthing person or baby (Shaw-Battista, 2017). Water labor helped relieve pain, (leading to less use of pain medication), and led to lower anxiety, better fetal positioning in the pelvis, less use of medications to speed up labor, and higher satisfaction with privacy and the ability to move around.
By the very nature of waterbirth, a birthing person who births in water must also labor in water (for at least a few minutes, but sometimes for hours) prior to the actual waterbirth. Therefore, it is not possible to completely untangle the benefits of water immersion in labor from those of waterbirth. So, with this in mind let us now review what research has demonstrated about waterbirth outcomes.
Overview of Evidence on Waterbirth
In the early 2000s, the American Academy of Pediatrics released their first statement about waterbirth, in which they said: 1) there had not been research on waterbirth, 2) waterbirth posed only dangers for newborns, and 3) there were no benefits for mothers.
But the truth is that researchers from all around the world had been studying waterbirth for decades—and most of the research had found (and continues to find) that with low-risk births, the benefits of waterbirth greatly outweigh the risks.
Waterbirth research includes:
- Randomized, controlled trial s—participants are randomly assigned (like flipping a coin) to give birth in water or give birth on land, and their outcomes are compared.
- Observational studies —researchers enroll people in the study, measure if they have a waterbirth or not, and compare health outcomes. These studies can be prospective (meaning people were enrolled in the study before they gave birth and followed forward in time) or retrospective (meaning researchers look back in time at births that already happened).
- Meta-analyses and systematic reviews —researchers combine data from many randomized trials and/or observational studies to look for overarching trends.
- Qualitative research —researchers use patient interviews or written text to describe what it feels like to have a waterbirth.
- Case studies —each case study contains a report of a single bad outcome (usually a very rare outcome).
Randomized Controlled Trials on Waterbirth
There have been five randomized trials on waterbirth, and so far, they show that waterbirth benefits include:
- Lower pain scores.
- Less use of pain medication during labor.
- Less use of artificial oxytocin (also known as Pitocin®).
- Shorter labors on average.
- Higher rate of normal vaginal birth (birth without the use of forceps, vacuum, or surgery).
- Higher rate of intact perineum (meaning the tissue between the vagina and rectum remains untorn and uncut).
- Less use of episiotomy (a surgical cut to the perineum).
- Greater satisfaction with the birth.
Three trials looked specifically at the effects of giving birth in the water (water immersion was not used earlier in labor) (Nikodem 1999; Woodward & Kelly 1994; Chaichian et al. 2009), and two trials included laboring in water plus waterbirth (Ghasemi et al. 2013; Gayiti et al. 2015).
Table 1: Randomized, controlled trials of waterbirth

Unpublished Student Thesis
One of these trials is an unpublished student thesis from South Africa (Nikodem, 1999). In this study, 60 people were randomly assigned to waterbirth and 60 people to land birth. There was no water labor—participants assigned to waterbirth entered the pool at the start of the pushing phase. The researchers found that the waterbirth group was more satisfied with their birth experience (78% vs. 58%), and that more people who had waterbirths said the pain was less than they expected it to be (57% vs. 28%). They found no difference in overall trauma to the birth canal between groups. The researchers defined trauma to the birth canal as labial tears, perineal tears, or injury to the vaginal wall.
Small Trial with Too Much Crossover
The second trial took place in the United Kingdom (U.K.) (Woodward & Kelly, 2004). In this study, only 10 out of 40 people who were assigned to the waterbirth group actually gave birth in water. Since most people didn’t stay in their assigned groups (this is called crossover), we cannot draw any conclusions from this study.
Small Trial that showed Waterbirth Benefits
The third trial took place in Iran. The researchers assigned 53 people to waterbirth and 53 people to land birth (Chaichian et al. 2009). Everyone in the waterbirth group gave birth in water. The researchers did not find any differences in newborn outcomes, but they found quite a few differences in maternal health outcomes between groups.
Waterbirth led to:
- A higher rate of normal vaginal birth (100% vs. 79.2%)
- A shorter active phase of labor (114 minutes vs. 186 minutes)
- A shorter third stage of labor (6 minutes vs. 7.3 minutes)
- Less use of artificial oxytocin (0% vs. 94.3%)
- Less use of any pain medications (3.8% vs. 100%)
- A 23% lower rate of episiotomy
- A 12% higher rate of perineal tears (reporting that most were mild tears)
There were no differences between groups in the length of the pushing phase of labor or the rate of breastfeeding.
After this trial from Iran was published, two more randomized trials have come out on waterbirth—one from Iran and one from China.
Largest Randomized Trial so far with 200 Participants
A 2013 Iranian trial (Ghasemi et al. 2013) randomly assigned 100 people to waterbirth and 100 people to land birth, making it the largest randomized trial ever done on waterbirth. In the end, 83 people ended up staying in the waterbirth group and 88 people stayed in the land birth group. It’s not clear why people left the study. This study was published in Persian, and we were able to get details thanks to volunteer translators (Personal correspondence, Clausen and Basati, 2017).
The study found that birthing people randomly assigned to the waterbirth group (all of whom labored in water) had a lower chance of needing a Cesarean later in labor compared to the land birth group (5% versus 16%). Participants in the waterbirth group reported less pain than the land birth group, but the researchers did not give any details on how pain was measured.
There was less meconium (baby’s first stool) in the amniotic fluid with waterbirth (2% versus 24%) and fewer low Apgar scores with waterbirth compared to land birth. An Apgar score is a test of how well the baby is doing at birth. A low Apgar score means that the baby may require more medical assistance.
Another Randomized Trial found Benefits to Waterbirth
A study that took place in China (Gayiti et al. 2015) randomly assigned 60 participants to waterbirth and 60 participants to land birth. Everyone who was randomly assigned to the waterbirth group gave birth in the water.
The researchers did not find any differences in newborn health outcomes between groups, but they found several maternal health benefits to waterbirth. Compared to the land birth group, the waterbirth group had a higher rate of intact perineum (25% vs. 8%). The waterbirth group also had a much lower rate of episiotomy (2% vs. 20%), and lower pain scores. The total length of labor was also shorter in the waterbirth group, by an average of 50 minutes. They did not find any difference in the amount of blood loss between groups.
What are the Limitations of these Randomized Trials?
In all these trials, there was no evidence of harm from waterbirth. However, these studies were too small to tell differences in rare health problems. Researchers estimate that there would need to be at least 2,000 people in a waterbirth trial to see at least two rare events occurring (Burns et al. 2012). In one Australian study, only 15% of low-risk research participants said they would be open to being randomly assigned to a waterbirth or land birth (Allen et al. 2022). This means researchers would need to approach 13,000 laboring people to have the 2,000 needed for a waterbirth randomized trial.
Randomized, controlled trials are often considered to be the “gold standard” in research. But when studying an intervention like waterbirth, it can be very hard to carry out a large, randomized, controlled trial. Some birthing people feel very strongly about waterbirth and are not willing to be randomly assigned to waterbirth or land birth. Others may be assigned to have a waterbirth, but then must leave the tub early for some reason.
Because large, randomized trials are unlikely to be published in future due to these constraints, we must turn to other types of evidence about waterbirth. In observational (non-randomized) studies, researchers do not attempt to control who gives birth in the water versus on land, but they record where people choose to give birth and measure their health outcomes.
In the next section, we will look at large analyses where they combined data from randomized trials and observational studies.
Table 2: Meta-Analysis on Randomized Trials and/or Observational Studies on Waterbirth

Systematic Reviews and Meta-Analyses
Since 2009, there have been seven systematic reviews or meta-analyses, where researchers combined research from randomized trials and/or observational studies on waterbirth. For a summary of their findings, see Table 2.
As time has gone on, researchers have been able to include more and more studies in these meta-analyses, giving us lots of information about the safety of waterbirth.
The largest, highest-quality, and most important review on waterbirth was published by Burns et al. in 2022. This review included 36 studies (25 of which examined waterbirths) from hospital and community birth settings from the year 2000 through 2021, resulting in 157,546 participants in the analysis.
The researchers found that laboring and/or giving birth in the water was associated with the following health results compared to no water immersion:
- Less use of Pitocin® to speed up labor.
- Less use of injectable opioids for pain management.
- Less use of epidurals.
- Reduced pain levels.
- Higher rates of intact perineum (positive outcome), but only in obstetric settings; in midwifery settings there were no differences between groups.
- Lower rates of episiotomy.
- Lower risk of postpartum hemorrhage.
- Lower rates of maternal infection.
- Higher rates of maternal satisfaction.
And there were no differences between the laboring and/or giving birth in water group vs. the standard care group with regard to:
- Rates of amniotomy (artificial breaking of the waters).
- Rates of Cesarean (but Cesarean rates were very low overall; average of 3.6%)
- Shoulder dystocia.
- Obstetric anal sphincter injury (3rd or 4th degree tears).
- Need for manual removal of the placenta.
- 5-minute APGAR scores.
- Need for newborn resuscitation.
- Transient fast breathing of the newborn.
- Newborn respiratory distress.
- Newborn death.
- Breastfeeding initiation.
There was a higher risk of the following with waterbirth:
- Cord avulsion (also known as snapping of the umbilical cord after birth, which we will discuss later).
Largest Observational Study on Waterbirth
One of the problems with observational studies is that unlike a randomized trial (when people are randomly assigned to groups), you can’t guarantee that people in the waterbirth group will have similar baseline characteristics to those in the land birth group. For example, it’s expected that people with complications will be asked to “get out of the tub” by the provider, or they might not be offered a water immersion in labor because of risk factors. As a result, waterbirth outcomes are usually better in observational studies—partly because people who end up birthing in water had uncomplicated childbirth experiences.
To address this problem, Bovbjerg et al. (2021) published the largest observational study on waterbirth ever, in which they studied 17,530 waterbirths and 17,530 land births that were matched for more than 80 factors (such as demographics, obstetric history, health conditions, and more). The process they used to match participants, called propensity scoring , resulted in the two groups being as similar as possible at baseline—except that one group was exposed to waterbirth, and the other was not. The researchers only included births that took place at home or in freestanding birth centers, not hospitals.
The Bovbjerg study used a retrospective study design , meaning that researchers looked back in time (“retro”) at medical records to make conclusions. The births they examined came from a data set called the Midwives Alliance of North America Statistics Project (MANA Stats), which collected data on from 2012 to 2018.
Midwives choose to participate in the MANA Stats Project by enrolling clients earlier in pregnancy and collecting data on them all the way through their pregnancy and birth. This is a process called prospective logging , which protects against a type of bias called selection bias. Selection bias happens when the study staff hand pick who they want in each group, based on what they hope the study to show. Selection bias did not occur in this study, because midwives were not allowed to select clients with only good waterbirth outcomes.
To further protect against selection bias, Bovbjerg et al. did not include anyone who was transferred to the hospital during labor. This decision was made because it was unlikely that those transferring to the hospital would be good candidates for waterbirth. Also, if they had included people with transfers during labor, this would have tilted the results in favor of waterbirths at home (because people who transfer and have a hospital land birth typically do so for medical reasons).
The propensity score matching worked—both the waterbirth and land birth groups were quite similar at baseline. About 95% of all participants were married or partnered, 49% had a college degree or higher, 23-24% were eligible for Medicaid, 73-74% had a home birth, 26-27% had a freestanding birth center birth, 72-73% were cared for by a certified professional midwife, 86-87% were white, 26-27% were giving birth to their first baby, and 4% were planning a vaginal birth after Cesarean (VBAC). The average age of participants was 31 years, and the average gestational age at time of birth was 40 weeks 0 days.
The waterbirth group experienced the following positive outcomes (see Table 3):
- Lower rates of postpartum hemorrhage.
- Fewer postpartum transfers to the hospital.
- Fewer postpartum hospitalizations for birthing people.
- Lower rate of severe perineal tears (3rd or 4th degree tears).
- Fewer newborn transfers to the hospital.
- Fewer cases of newborn respiratory distress syndrome.
- Fewer newborn hospitalizations.
There was a lower rate of newborn death in the waterbirth group—0.28 deaths per 1,000 deliveries compared to 0.51 deaths per 1,000 deliveries in the land birth group.
The only negative effects seen with waterbirth were higher rates of umbilical cord avulsion or tearing (sometimes called an umbilical cord snap) (0.57% vs. 0.37%) and higher rates of postpartum uterine infections (0.31% vs. 0.25%). But neither of these resulted in higher hospitalization rates for birthing people or babies, and none of the cases of umbilical cord avulsion resulted in death.
There were no differences between waterbirth and land birth groups in the rate of NICU admissions in the first 6 weeks, or in rates of newborn infections.
Table 3: Benefits and Risks of Waterbirth in the Largest Observational Waterbirth Study to Date by Bovbjerg et al. (2022)

Observational Study on Planned Waterbirths that Become Land Births
Laboring people who are planning a waterbirth may get out of the pool due to personal preference, or because of medical reasons including:
- The midwife or physician may have concerns with the fetal heart rate,
- The birthing person may need pain medication, OR
- Labor may be progressing unusually slow.
In 2016, Bovbjerg et al. published the first study that compared actual waterbirths, intended waterbirths (that ended up being land births), and intended land births.
The study included data from 18,343 midwife-attended births in the U.S. between 2004 and 2009, with 97.6% of births occurring at homes and birth centers. In this study, there were 6,534 waterbirths, 10,290 land births, and 1,573 intended waterbirths that ended up as land births.
Like other researchers, Bovbjerg et al. (2016) found that waterbirth did not appear to increase the risk of bad health outcomes for newborns. In fact, babies born in the water had better health outcomes than babies born on land. The group that fared the worst were those who intended to have waterbirths but left the pool before giving birth. This left the lowest-risk people in the waterbirth group, who had the best outcomes on average.
Since people who birth in water are usually doing well, they (and their newborns) are more likely to have better results. Another way to look at these research results that the U.S. midwives in this study showed good judgment by assessing risk and getting people with complications out of the tub as needed.
Qualitative Research
Qualitative research is a method of research that involves using rich, in-depth data (from interviews or written text) to describe experiences, understand phenomena, and/or look for meaning.
A meta-synthesis is when researchers combine multiple qualitative studies to look for common themes. So far, there have been two meta-syntheses of qualitative studies on waterbirth.
Clews et al. (2020) Meta-Synthesis
In this article, researchers reviewed five qualitative studies that interviewed a total of 30 self-identified birthing women from five different countries. While examining the research, four common themes emerged:
- A knowledge of waterbirth led participants down the path to choosing waterbirth. They learned about waterbirth from books, online articles, and YouTube videos.
- A desire for physiological birth came from feeling that land births did not meet their needs and desires. The participants wanted a more natural or holistic experience. Their decision to get in or out of the water was based on what their body needed. They also felt an instinctive connection with water as soothing and pleasurable.
- Autonomy and control were important. Women reported feeling more in control and increased coping with labor in water. They reported it was easier to avoid interventions they’d had in past births (such as amniotomy, episiotomy, Pitocin®, or the lithotomy birth position with feet in stirrups). They said that the water and tub created a natural barrier that allowed them more privacy and security—nobody could touch them unless they consented to being touched! They also hoped that waterbirth would help them avoid perineal tears.
- An easier transition during the emergence of the baby was meaningful. The mothers felt that their babies were not as shocked when they were birthed from the warmth of the amniotic fluid in the uterus into the warmth of the water of the tub.
The researchers in this study concluded:
“All individuals involved in the care of women during childbirth – from policy makers to midwives – should understand the possibility for waterbirth to offer some women a positive experience and memories of childbirth.”
Large Meta-Synthesis by Reviriego-Rodrigo et al. (2023)
In this study, researchers included 13 qualitative studies from eight countries published between 2013 and 2019. Most of the studies included both water immersion during labor and waterbirth, while some reported only waterbirth findings.
The researchers found four themes across all the qualitative studies:
- Reasons for choosing waterbirth included personal preferences plus knowledge of evidence-based information. Participants were looking for a birth method that would increase relaxation, lower anxiety, decrease pain, increase comfort and well-being, and give them a better chance at a natural birth. They were also interested in a lower chance of perineal tears and a shorter labor. Participants believed that the evidence so far shows no increased risk to babies regarding infection or mortality.
- Perceived benefits of water immersion included more autonomy and control, a higher chance of unmedicated birth, a method of pain relief that doesn’t require interventions, an easier transition into parenthood, mobility and buoyancy in the water, peace/relaxation, improved breathing, privacy, avoiding Pitocin®, and having a positive childbirth experience.
- Perceived barriers of water immersion included safety concerns from vaginal birth after Cesarean (VBAC), pregnancy or labor complications, and a lack of support from family or health care workers.
- Perceived factors that made it possible for them to have a waterbirth included having available tubs and policies that were clear and consistent about who is eligible, support from health care workers trained in waterbirth, clear/accurate information about benefits and risks to aid in decision making, and a culture of respect for waterbirth as a valid option.
Case Reports
The other type of evidence that we have on newborn outcomes after waterbirth comes from case reports. Case reports are published documents about a rare medical event, and they are considered the lowest level of research evidence.
The main advantage of case reports is that they give us information about rare side effects. But the main drawback is that since they only discuss one or two events, we cannot use this evidence to determine how often these events occur. Most case reports are not peer reviewed (some are simply written as letters to the editor), and they often lack enough detail to get a clear picture of what really happened.
In 2020, Vanderlaan and Hall published a systematic review of all the case reports that have ever been published in English about poor newborn outcomes after waterbirth or water immersion during labor. The purpose of their review was to highlight patterns that can be addressed to make waterbirth safer.
The review identified 35 articles with total of 48 cases of poor newborn outcomes (43 events with waterbirth; 11 of which were minor conditions that resolved quickly). Only 14 of the case reports were published in the previous ten years—and so most of the articles did not reflect current waterbirth protocols.
The cases reported difficulty breathing (24 cases), infection (18 cases), and cord avulsion (8 cases). There were seven newborn deaths reported—five due to infection, and two due to unknown causes. Most case reports did not describe the pregnancies, labors, or protocols followed during the water immersion.
The five patterns that the authors reported included:
- Specific bacteria that could be dangerous include Legionella pneumoniae and Pseudomonas aeruginosa .
- These bacteria do not typically cause infection after land births, but 12 cases of infection have been reported after waterbirths.
- Waterbirth providers should ensure a clean water supply and use strict cleaning protocols.
- Eleven case reports described newborn water aspiration, but seven of these cases were misdiagnosed and should have been labeled as transient tachypnea of the newborn.
- Transient tachypnea of the newborn (TTN) is defined as a temporary delay in clearing out the birth fluids from the lungs. This condition occurs in 5.7 out of every 1,000 land births at term.
- Because TTN can happen in any newborn, it makes sense that it would sometimes be seen in newborns after waterbirth.
- Out of the 48 case reports, only a single confirmed case of true water aspiration was reported, and in this case the newborn was dropped in the water, after birth, where it remained for an unreported amount of time.
- There were eight cases of umbilical cord avulsion after waterbirth, and seven were identified and managed quickly (by immediately clamping the cord), leading to no adverse health effects.
- The one case that was not treated quickly did lead to the baby experiencing temporary anemia (a problem of not having enough hemoglobin in red blood cells to carry oxygen to body tissues). This case report was published in 2000 and as a result, protocols were developed and implemented to 1) prevent cord avulsion and 2) identify and clamp the cord quickly if it does happen.
- There were eight case reports that suggest the provider was not trained in safe waterbirth practices.
- Examples of unsafe practices included: 1) permitting a waterbirth even though there were signs of complications such as thick meconium in the amniotic fluid or maternal fever, 2) using hot tubs or home bathtubs (which increase the risk of bacterial growth due to recirculating water in the jets), and 3) keeping the tub filled with warm water for two weeks leading up to the birth (again increasing the risk of infection due water that could be fostering bacterial growth).
- The authors propose that over hydration (drinking too much water) and staying in the tub for many hours could potentially increase the risk of the birthing person having low blood sodium levels.
- The low blood sodium levels in the birthing person could then lower the baby’s sodium levels at birth.
- This is an area that needs more research.
What can we learn from these case reports?
If you read the individual case reports, most of the authors do not recommend a ban on waterbirths. Instead, they make recommendations to improve safety and informed consent. Some of their recommendations are:
- Plastic tubing is the perfect environment for Pseudomonas to grow, especially if the strain of bacteria is resistant to disinfectants (Vochem et al. 2001).
- Providers who offer waterbirth in facilities may want to take frequent cultures from the birthing pool system or after each water birth, shorten the length of filling and exit hoses, and heat disinfect hoses after each use (Rawal et al., 1994).
- Many home birth providers, because of these case study findings, now require their clients to use brand new hoses to fill up a home birthing pool.
- Hospitals should track waterbirth outcomes and have policies in place to prevent infections, such as pool maintenance, decontamination, and universal precautions (Franzin et al. 2004).
- As part of the educational process, inform families who are interested in waterbirth that it is important that they not re-submerge the baby in the water after it has reached the air (Vanderlaan et al. 2020).
- Caution should be used if a birthing person with a recent diarrheal illness is considering a waterbirth (Soileau et al. 2013).
- Spa-like pools with a heater and a re-circulation pump contain complex plumbing that can promote the growth of bacteria and be difficult to disinfect. The environment is especially risky when the tubs are filled in advance of labor and held at a warm temperature. In contrast, a rigid or inflatable tub that is filled at the start of labor poses less risk for bacterial infections (Collins et al. 2016).
Overall Summary of the Pros and Cons
Based on the research studies we’ve reviewed above, here is our summary of the pros and cons of waterbirth.
Pros of Waterbirth
Waterbirth is protective of normal vaginal birth, and can increase the chance of having a faster, less complicated birth. Researchers have found evidence from randomized trials that planning for a birth in water can lead to shorter labors, less need for Pitocin®, and lower rates of giving birth via cesarean or with forceps/vacuum (Caichian et al. 2009; Ghasemi et al. 2013; Gayiti et al. 2015).
Waterbirth can help protect the perineum (the tissue between the vagina and rectum). Both randomized trials and observational studies have found that waterbirth is associated with a higher rate of intact perineum and lower episiotomy rates (Chaichian et al. 2009; Gayiti et al. 2015; Burns et al. 2022). In addition, the largest observational study found that waterbirth is associated with a lower rate of severe perineal tears (3rd or 4th degree lacerations) (Bovbjerg et al 2021).
Waterbirth has been consistently shown to decrease pain in labor . As a result, waterbirth also leads to less use of epidurals and injectable opioids for pain relief during childbirth (Nikodem 1999; Chaichian et al. 2009; Ghasemi et al. 2013; Gayiti et al. 2015; Burns et al. 2022). There is nothing wrong with having an epidural or pain medication during labor—but some birthing people wish to avoid these interventions for personal reasons, or because of potential side effects. Planning a waterbirth can be an effective tool to help families reach their pain management goals . And if water immersion does not provide enough pain relief, then the birthing person can switch to a land birth with pain medications.
Waterbirth is associated with improved health outcomes for birthing people , including lower rates of postpartum hemorrhage and maternal infection (Burns et al. 2022). Observational research has shown that people who have waterbirths at home are less likely to be transferred to the hospital postpartum than their peers who have land births at home (Bovbjerg et al. 2021). In addition, research has consistently shown that waterbirth results in higher birth satisfaction. In qualitative studies, birthing people have described feeling more in control in water, and that water created a natural barrier that helped them feel more safe, private, and secure (Clews et al. 2020; Reviriego-Rodrigo et al. 2023).
Waterbirth is also associated with positive health outcomes for babies . The largest, highest-quality observational study on waterbirth found that babies born via home waterbirth were less likely to be transferred to the hospital, less likely to have newborn respiratory distress syndrome, less likely to be hospitalized, and had a lower mortality rate compared to babies born at home via land birth (Bovbjerg et al. 2021). In addition, one randomized trial found that waterbirth led to a substantially lower risk of meconium in the amniotic fluid, as well as better Apgar scores at birth (Ghasemi et al. 2013). We do not know exactly why these outcomes are better with waterbirth. It’s possible that waterbirth may affect newborn health because of the increased likelihood of a smoother birth with fewer interventions and complications. There may also be better outcomes because only the lowest risk babies are born in water—when there are signs of potential complications, the birthing person is usually asked to get out of the tub.
Cons of Waterbirth
Waterbirth leads to a higher risk of newborn cord avulsion, or snapping . With waterbirths, the baby might be lifted out of the water too quickly, and this might cause the umbilical cord to snap, especially if there is an abnormally short cord. The largest analysis on this subject (Bovbjerg et al. 2021) found a rate of 4.1 cord avulsions per 1,000 waterbirths vs. 1.3 cord avulsions per 1,000 land births. The signs of cord avulsion in a waterbirth can include a dramatic change in the color of the water to deep red, a snapping sound, sudden release of cord tension, seeing the cord snap, and/or signs of the newborn going into shock from losing too much blood. If the cord snaps, someone should immediately clamp the newborn’s end of the umbilical cord and assess the newborn for signs of shock. Researchers do not consider cord avulsion an emergency for a skilled provider, because as long as the cord avulsion is recognized and the cord immediately clamped, then complications can be avoided.
Cord avulsion can be prevented by bringing the baby to the surface gently, assessing cord length/tension at birth, and not excessively pulling on the cord. In a five-year study that took place in eight institutions (Sidebottom et al. 2022), researchers documented three cases of waterbirth-related cord avulsion in the first year. After these cord avulsions occurred, staff were educated on how to prevent cord avulsion, and there were zero cases of cord avulsion during the next four years.
Overall rates of newborn infection do not differ between waterbirth and land birth (Bovbjerg et al. 2021). However, there have been reports of rare cases of newborn infection after waterbirth (Vanderlaan & Hall 2020). Birth attendants and hospital staff should follow evidence-based guidelines for preventing waterborne infection transmission such as using tubs that are easy to disinfect (and avoid tubs with pipes that recirculate water), filling tubs closer to the time of the birth (avoid long-standing water), and regularly testing the hospital water supply, hoses, and birthing pools (Nutter et al. 2014b).
The largest and highest-quality meta-analysis on waterbirth did not find any increase in maternal infection with waterbirth (Burns et al. 2022). However, the largest observational study on waterbirth (Bovbjerg et al. 2021) reported a slightly higher rate of uterine infection in the first six weeks after a waterbirth (0.31% vs. 0.25%) . It is important to note that they reported no increase in the risk of hospitalization, indicating that these uterine infections were successfully treated with antibiotics at home. This is an area that needs further research.
A temporary delay in clearing birth fluids from the lungs (transient tachypnea of the newborn) can occur in babies born on land or in water. There does not seem to be any higher risk of transient tachypnea with waterbirth (Bovbjerg et al. 2021). However, most providers who attend waterbirths recommend that a birth take place on land if there are signs that a fetus may be more likely to experience complications. These signs may include non-reassuring fetal heart tones, maternal fever, meconium-stained amniotic fluid, suspected fetal growth restriction, or other risk factors (Nutter et al. 2014b). If a provider trained in waterbirth asks you to get out of the tub, this is because they believe a waterbirth would not be safe in your case .
Waterbirth cannot be combined with some interventions , including epidurals/spinals and injectable opioids for pain management. If you were hoping for a waterbirth, but these interventions are needed or chosen, then you will need to switch to a land birth (Nutter et al. 2014b). Some hospitals do not permit waterbirth if you need Pitocin® for labor induction or augmentation, while others do (Personal communication, J. Anderson, 2023).
Although most people find water immersion in labor pleasurable, it is possible that you may change your mind and want to get out of the tub . In one survey study from England, a small number of participants said that they got cold, or the baby got cold, that their contractions went away, or that staff were not supportive (Richmond 2003).
It is important that the water temperature is assessed at least every hour, because maintaining the water temperature between 37 to 38 degrees Celsius (98.6 to 100.4 degrees Fahrenheit) helps prevent the baby from experiencing hypothermia or hyperthermia (too low or too high body temperature) (Nutter et al. 2014b).
Sometimes people ask us if waterbirth influences the newborn microbiome. The only study we found on waterbirth and the newborn microbiome did not show any difference in the newborn microbiome between babies born via water vs. land; however, more research is needed (Fehervary et al. 2004).
Healthy babies have a dive reflex that prevents them from taking their first breath until they are exposed to air. A baby being born underwater must be born fully underwater and not exposed to cooler temperatures or air until after their face is brought to the surface. Once the baby’s face is in the air, then their lower body and extremities should rest in the warm water to help keep their body warm. If a birthing person stands up mid-birth, and the baby’s face/skin is exposed to the air, then the birthing person should not squat back down and re-immerse the baby’s head in the water (Nutter et al. 2014b).
The dive reflex can be overridden if a baby is experiencing distress —this may cause a newborn to prematurely gasp underwater before they surface. This is another reason why providers skilled in waterbirth watch to make sure there are no signs of complications before proceeding with a waterbirth (Nutter et al. 2014b).
Professional Guidelines
In the past, the American Academy of Pediatrics (AAP) and American Congress of Obstetricians and Gynecologists (ACOG) have published joint guidelines that denounced and discouraged waterbirth. Their strongly worded 2014 guidelines were not based on research evidence, but mainly on opinion and case reports. In 2016, the AAP and ACOG softened their stance on waterbirth and began to discuss the concept of informed consent. We reviewed the influential 2014 and 2016 AAP/ACOG guidelines on waterbirth here .
In 2022, the AAP released a new statement by Nolt et al. called, “Risk of Infectious Diseases in Newborns Exposed to Alternative Perinatal Practices.” In this latest statement, the authors relied heavily on a meta-analysis by Edwards et al. (2023) that only reviewed six randomized, controlled trials (with a total of 709 participants) and excluded all observational studies (see Table 1 to compare the Edwards et al. meta-analysis to other meta-analyses on waterbirth).
The AAP also mentioned several case reports about Pseudomonas and Legionella infection. In contrast, they never discussed or cited any of the high-quality meta-analyses or large observational studies that we have reviewed in this EBB article. Their opinion was, “Families should be cautioned against water birth during and past the second stage of labor, in the absence of any current evidence to support maternal or neonatal benefit, and with reports of serious and fatal infectious outcomes in infants.” As long as the AAP retains their bias against waterbirth, it is likely that they will continue to ignore the many peer-reviewed studies that have been published on waterbirth. Unfortunately, the AAP’s continued recommendation against waterbirth means that many hospitals will continue to have official or unofficial “bans” on waterbirth. For many families, the only way they can access waterbirth is through home birth or a freestanding birth center.
In contrast to the AAP, the American College of Nurse Midwives (2014) , the American Association of Birth Centers (2014) , the Royal College of Midwives, and the New Zealand College of Midwives (2019) have all released statements endorsing waterbirth as a safe, evidence-based option.
Practical guidelines for clinicians who support waterbirth have been published by the American College of Nurse Midwives (2017), the University Hospital Wishaw (2020) in Scotland, University Hospitals of Leicester (2021) in England, and the National Health Service in Wales (2022).
In 2014, Dr. Nutter, Dr. Shaw-Battista, and Dr. Marowitz of the U.S. published a paper called, “Waterbirth Fundamentals for Clinicians” that includes practical principles for waterbirth, clinical wisdom, and advice for implementing waterbirth in hospitals. The free appendix of their paper includes a waterbirth consent form and clinical guidelines for water immersion in labor and waterbirth.
The bottom line
New research evidence on waterbirth is continuing to emerge! For birthing people, there are benefits associated with waterbirth. There is strong evidence that waterbirth is associated with a lower episiotomy rate, and that planning a waterbirth leads to higher rates of having an intact perineum. People who have waterbirths are less likely to need pain medicine for pain relief compared with people who give birth on land. Waterbirth parents also report higher levels of satisfaction with pain relief and with their experience of childbirth. Some of the benefits of waterbirth (such as decreased pain during the first stage of labor) can also be achieved from using water immersion during labor, before the birth.
Evidence also shows that waterbirth can be safe for babies. The largest and highest-quality meta-analysis on waterbirth found that newborns born via waterbirth had similar health outcomes than babies born on land (Burns et al. 2022). In the single largest study on waterbirth so far, they found that babies in the waterbirth group had better outcomes than those in the land birth group (Burns et al. 2021). This may be partly because waterbirth are associated with faster, easier, less complicated births, and partly because parents experiencing complications are asked to get out of the tub (leaving the healthiest babies in the waterbirth group).
The main waterbirth complication for newborns is umbilical cord avulsion, which occurs in about 4 per 1,000 waterbirths. Simple steps can be taken to prevent cord avulsion, and treat it quickly, if it occurs.
Based on the evidence from many research studies—including randomized trials, large observational studies, and meta-analyses—current evidence suggests that waterbirth is a safe option for families. If you are having a low-risk pregnancy and birth, have a desire for an unmedicated, low-intervention birth, and there are experienced staff who are trained in attending waterbirths, then evidence supports this birth method.
Unfortunately, there are still very few hospitals (outside of the United Kingdom) that provide waterbirth as an option—and in fact, many hospitals “ban” waterbirth. The American Academy of Pediatrics’ negative opinion statements on waterbirth have had a negative influence on the availability of waterbirth in many hospitals. However, it is important to remember that the AAP’s recommendations against waterbirth are not based on the best evidence and should be challenged.
If you are interested in waterbirth, find out which facilities nearby provide waterbirth, and make sure you understand hospital policy. Here at EBB, we have witnessed false advertising—where a hospital advertises that they have waterbirth (to take advantage of the popularity of this option), but in fact do not permit it. If your hospital or hospital-based provider says they provide waterbirth, you can ask the following questions:
- How many birthing rooms have tubs? Are all the tubs functioning? What are the chances that I can get a room with a tub?
- Do you require parents to get out of the tub during the pushing phase? Can the baby be born in the water? [This question helps clarify whether they permit water immersion during labor only and then make you get out for the birth].
- What training do your staff have in caring for parents during waterbirth? What training do they have in managing complications during a waterbirth?
- What are some reasons that I might be asked to get out of the tub? What is your preference for where I birth the placenta?
- Out of the last 10 clients of yours who said they wanted a waterbirth, how many of them gave birth in the water?
- If I need continuous fetal monitoring, do you have wireless, waterproof monitors that can be worn in the tub?
- What infection control measures are in place for waterbirth?
If waterbirth is a high priority for you, and your chosen facility does not support waterbirth, you may want to consider looking at other birth options in your community. Or you could plan to take advantage of water immersion in labor (before the pushing phase), as this also offers many benefits. You are encouraged to print off a copy of the 1-page handout that goes along with this article, to help educate your providers.
Ultimately, as more parents, health care workers, and birth workers request waterbirth and share the evidence, more facilities will begin to provide midwifery-led, evidence-based options—like waterbirth—for families who desire this birth option.
REPLAY – EBB 149: Shifting from Hospital Labor and Delivery Nurse to Home Birth Advocate with Melissa Anne DuBois
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | YouTube For Nurse's Week 2024, we wanted to share a replay of one of our favorite episodes at EBB, and that is an interview with Melissa Anne DuBois about shifting from hospital...

EBB 311 – Creating a Community-Led Birth Center in New York City with Myla Flores of the Womb Bus
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | YouTube Join us in diving deep into Myla Flores' incredible story of becoming a leader and visionary in the birth field! From Myla's early experiences as a birth doula to her...
EBB 310 – Doulas & Nurses Advocating Together for Positive Shifts in Birth Culture with Joyce Dykema, EBB Instructor & Brianna Fields, RN
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | YouTube Dr. Rebecca Dekker is joined by Joyce Dykema, doula and EBB Instructor, and Brianna Fields, a labor and delivery nurse, to discuss advocating for positive shifts in...
Pin It on Pinterest
- https://www.facebook.com/EvidenceBasedBirth/
- https://plus.google.com/106146540771436369846?hl=en
- https://www.pinterest.com/ebbirth/pins/
- https://www.linkedin.com/in/rebecca-dekker-8b3b3b22/
Jump to navigation
- Bahasa Malaysia

Immersion in water in labour and birth
What is the issue?
To assess the effects of water immersion (waterbirth) during labour and/or birth (first, second and third stage of labour) on women and their infants.
Why is this important?
Many women choose to labour and give birth in water (water immersion) and this practice is becoming more popular in many countries, particularly in midwifery-led units. Therefore, it is important to understand more about the benefits of water immersion in labour and birth for women and their newborns, along with any risks.
It is important to examine whether immersion in water during the first and/or the second stage of labour has the potential to maximise women's ability to manage labour pain, and to have a normal birth without increasing the risk of an adverse (harmful) event. Adverse events might be an increased risk of infection for women and/or their newborn; an increased likelihood of a serious tear to the perineum (the area between anus and vagina), and it may make estimating blood loss more difficult in the event of a haemorrhage. In assessing the benefits, we consider well-being to cover both physical and psychological health.
What evidence did we find?
We included 15 trials (3663 women). All the trials compared immersion in water with no immersion in water: eight during the first stage of labour, two during the second stage of labour (waterbirth) only, four during the first and second stages of labour, and one early versus late immersion during the first stage of labour. The evidence was of moderate to very low quality. No trial compared immersion in water with other forms of pain management.
Water immersion during the first stage of labour probably results in fewer women having an epidural, but probably makes little or no difference to the number of women who have a normal vaginal birth, instrumental birth, caesarean section or a serious perineal tear. We are uncertain about the effect on the amount of blood loss after birth because the quality of the evidence was very low. Labouring in water also may make little or no difference to babies being admitted to neonatal intensive care unit (NICU) or developing infections. Stillbirths and baby deaths were not reported.
Two trials compared water immersion during the second stage (birth) with no immersion. We found that immersion may make little or no difference in numbers of women who have a normal vaginal birth. It is uncertain whether immersion makes any difference to instrumental vaginal births, caesarean sections, numbers of babies admitted to NICU, babies' temperatures at birth and fever in babies during the first week, because the quality of the evidence was found to be very low for all of these outcomes. Epidurals were not relevant to this stage of labour. Serious perineal tears and blood loss after birth were not reported in either trial.
Only one trial (200 women) compared women who got into the water early and late in their labour but there was not enough information to show any clear differences between the groups.
What does this mean?
Labouring in water may reduce the number of women having an epidural. Giving birth in water did not appear to affect mode of birth, or the number of women having a serious perineal tear. This review found no evidence that labouring in water increases the risk of an adverse outcome for women or their newborns. The trials varied in quality and further research is needed particularly for waterbirth and its use in birth settings outside hospital labour wards before we can be more certain of these effects. Research is also needed about women’s and caregivers experiences of labour and birth in water.
In healthy women at low risk of complications there is moderate to low-quality evidence that water immersion during the first stage of labour probably has little effect on mode of birth or perineal trauma, but may reduce the use of regional analgesia. The evidence for immersion during the second stage of labour is limited and does not show clear differences on maternal or neonatal outcomes intensive care. There is no evidence of increased adverse effects to the fetus/neonate or woman from labouring or giving birth in water. Available evidence is limited by clinical variability and heterogeneity across trials, and no trial has been conducted in a midwifery-led setting.
Water immersion during labour and birth is increasingly popular and is becoming widely accepted across many countries, and particularly in midwifery-led care settings. However, there are concerns around neonatal water inhalation, increased requirement for admission to neonatal intensive care unit (NICU), maternal and/or neonatal infection, and obstetric anal sphincter injuries (OASIS). This is an update of a review last published in 2011.
To assess the effects of water immersion during labour and/or birth (first, second and third stage of labour) on women and their infants.
We searched Cochrane Pregnancy and Childbirth’s Trials Register, ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform ( ICTRP ) (18 July 2017), and reference lists of retrieved trials.
We included randomised controlled trials (RCTs) comparing water immersion with no immersion, or other non-pharmacological forms of pain management during labour and/or birth in healthy low-risk women at term gestation with a singleton fetus. Quasi-RCTs and cluster-RCTs were eligible for inclusion but none were identified. Cross-over trials were not eligible for inclusion.
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy. Two review authors assessed the quality of the evidence using the GRADE approach.
This review includes 15 trials conducted between 1990 and 2015 (3663 women): eight involved water immersion during the first stage of labour; two during the second stage only; four during the first and second stages of labour, and one comparing early versus late immersion during the first stage of labour. No trials evaluated different baths/pools, or third-stage labour management. All trials were undertaken in a hospital labour ward setting, with a varying degree of medical intervention considered as routine practice. No study was carried out in a midwifery-led care setting. Most trial authors did not specify the parity of women. Trials were subject to varying degrees of bias: the intervention could not be blinded and there was a lack of information about randomisation, and whether analyses were undertaken by intention-to-treat.
Immersion in water versus no immersion (first stage of labour)
There is probably little or no difference in spontaneous vaginal birth between immersion and no immersion (83% versus 82%; risk ratio (RR) 1.01, 95% confidence interval (CI) 0.97 to 1.04; 6 trials; 2559 women; moderate-quality evidence); instrumental vaginal birth (12% versus 14%; RR 0.86, 95% CI 0.70 to 1.05; 6 trials; 2559 women; low-quality evidence); and caesarean section (5% versus 4%; RR 1.27, 95% CI 0.91 to 1.79; 7 trials; 2652 women; low-quality evidence). There is insufficient evidence to determine the effect of immersion on estimated blood loss (mean difference (MD) -14.33 mL, 95% CI -63.03 to 34.37; 2 trials; 153 women; very low-quality evidence) and third- or fourth-degree tears (3% versus 3%; RR 1.36, 95% CI 0.85 to 2.18; 4 trials; 2341 women; moderate-quality evidence). There was a small reduction in the risk of using regional analgesia for women allocated to water immersion from 43% to 39% (RR 0.91, 95% CI 0.83 to 0.99; 5 trials; 2439 women; moderate-quality evidence). Perinatal deaths were not reported, and there is insufficient evidence to determine the impact on neonatal intensive care unit (NICU) admissions (6% versus 6%; average RR 1.30, 95% CI 0.42 to 3.97; 2 trials; 1511 infants; I² = 36%; low-quality evidence), or on neonatal infection rates (1% versus 1%; RR 2.00, 95% CI 0.50 to 7.94; 5 trials; 1295 infants; very low-quality evidence).
Immersion in water versus no immersion (second stage of labour)
There were no clear differences between groups for spontaneous vaginal birth (98% versus 97%; RR 1.02, 95% CI 0.96 to 1.08; 120 women; 1 trial; low-quality evidence); instrumental vaginal birth (2% versus 2%; RR 1.00, 95% CI 0.06 to 15.62; 1 trial; 120 women; very low-quality evidence); caesarean section (0% versus 2%; RR 0.33, 95% CI 0.01 to 8.02; 1 trial; 120 women; very low-quality evidence), and NICU admissions (8% versus 11%; RR 0.78, 95% CI 0.38 to 1.59; 2 trials; 291 women; very low-quality evidence). Use of regional analgesia was not relevant to the second stage of labour. Third- or fourth-degree tears, and estimated blood loss were not reported in either trial. No trial reported neonatal infection but did report neonatal temperature less than 36.2°C at birth (9% versus 9%; RR 0.98, 95% CI 0.30 to 3.20; 1 trial; 109 infants; very low-quality evidence), greater than 37.5°C at birth (15% versus 6%; RR 2.62, 95% CI 0.73 to 9.35; 1 trial; 109 infants; very low-quality evidence), and fever reported in first week (2% versus 5%; RR 0.53, 95% CI 0.10 to 2.82; 1 trial; 171 infants; very low-quality evidence), with no clear effect between groups being observed. One perinatal death occurred in the immersion group in one trial (RR 3.00, 95% CI 0.12 to 72.20; 1 trial; 120 infants; very low-quality evidence). The infant was born to a mother with HIV and the cause of death was deemed to be intrauterine infection.
There is no evidence of increased adverse effects to the baby or woman from either the first or second stage of labour.
Only one trial (200 women) compared early and late entry into the water and there were insufficient data to show any clear differences.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 12, Issue 7
- Systematic review and meta-analysis to examine intrapartum interventions, and maternal and neonatal outcomes following immersion in water during labour and waterbirth
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
This article has a correction. Please see:
- Errata - September 01, 2022
- http://orcid.org/0000-0002-7505-7621 Ethel Burns 1 ,
- Claire Feeley 2 ,
- Priscilla J Hall 3 ,
- Jennifer Vanderlaan 4
- 1 Faculty of Health and Life Sciences , Oxford Brookes University Faculty of Health and Life Sciences , Oxford , UK
- 2 Faculty of Health and Life Sciences , Oxford Brookes University , Oxford , UK
- 3 VA School of Nursing Academic Partnership , Emory University , Atlanta , Georgia , USA
- 4 School of Nursing , University of Nevada Las Vegas , Las Vegas , Nevada , USA
- Correspondence to Dr Ethel Burns; eburns{at}brookes.ac.uk
Objectives Water immersion during labour using a birth pool to achieve relaxation and pain relief during the first and possibly part of the second stage of labour is an increasingly popular care option in several countries. It is used particularly by healthy women who experience a straightforward pregnancy, labour spontaneously at term gestation and plan to give birth in a midwifery led care setting. More women are also choosing to give birth in water. There is debate about the safety of intrapartum water immersion, particularly waterbirth. We synthesised the evidence that compared the effect of water immersion during labour or waterbirth on intrapartum interventions and outcomes to standard care with no water immersion. A secondary objective was to synthesise data relating to clinical care practices and birth settings that women experience who immerse in water and women who do not.
Design Systematic review and meta-analysis.
Data sources A search was conducted using CINAHL, Medline, Embase, BioMed Central and PsycINFO during March 2020 and was replicated in May 2021.
Eligibility criteria for selecting studies Primary quantitative studies published in 2000 or later, examining maternal or neonatal interventions and outcomes using the birthing pool for labour and/or birth.
Data extraction and synthesis Full-text screening was undertaken independently against inclusion/exclusion criteria in two pairs. Risk of bias assessment included review of seven domains based on the Robbins-I Risk of Bias Tool. All outcomes were summarised using an OR and 95% CI. All calculations were conducted in Comprehensive Meta-Analysis V.3, using the inverse variance method. Results of individual studies were converted to log OR and SE for synthesis. Fixed effects models were used when I 2 was less than 50%, otherwise random effects models were used. The fail-safe N estimates were calculated to determine the number of studies necessary to change the estimates. Begg’s test and Egger’s regression risk assessed risk of bias across studies. Trim-and-fill analysis was used to estimate the magnitude of effect of the bias. Meta-regression was completed when at least 10 studies provided data for an outcome.
Results We included 36 studies in the review, (N=157 546 participants). Thirty-one studies were conducted in an obstetric unit setting (n=70 393), four studies were conducted in midwife led settings (n=61 385) and one study was a mixed setting (OU and homebirth) (n=25 768). Midwife led settings included planned home and freestanding midwifery unit (k=1), alongside midwifery units (k=1), planned homebirth (k=1), a freestanding midwifery unit and an alongside midwifery unit (k=1) and an alongside midwifery unit (k=1). For water immersion, 25 studies involved women who planned to have/had a waterbirth (n=151 742), seven involved water immersion for labour only (1901), three studies reported on water immersion during labour and waterbirth (n=3688) and one study was unclear about the timing of water immersion (n=215).
Water immersion significantly reduced use of epidural (k=7, n=10 993; OR 0.17 95% CI 0.05 to 0.56), injected opioids (k=8, n=27 391; OR 0.22 95% CI 0.13 to 0.38), episiotomy (k=15, n=36 558; OR 0.16; 95% CI 0.10 to 0.27), maternal pain (k=8, n=1200; OR 0.24 95% CI 0.12 to 0.51) and postpartum haemorrhage (k=15, n=63 891; OR 0.69 95% CI 0.51 to 0.95). There was an increase in maternal satisfaction (k=6, n=4144; OR 1.95 95% CI 1.28 to 2.96) and odds of an intact perineum (k=17, n=59 070; OR 1.48; 95% CI 1.21 to 1.79) with water immersion. Waterbirth was associated with increased odds of cord avulsion (OR 1.94 95% CI 1.30 to 2.88), although the absolute risk remained low (4.3 per 1000 vs 1.3 per 1000). There were no differences in any other identified neonatal outcomes.
Conclusions This review endorses previous reviews showing clear benefits resulting from intrapartum water immersion for healthy women and their newborns. While most included studies were conducted in obstetric units, to enable the identification of best practice regarding water immersion, future birthing pool research should integrate factors that are known to influence intrapartum interventions and outcomes. These include maternal parity, the care model, care practices and birth setting.
PROSPERO registration number CRD42019147001.
- Pain management
- Maternal medicine
- PRIMARY CARE
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2021-056517
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This study incorporated meta-regression, using covariates identified a priori, to identify sources of heterogeneity in previous studies.
This study included cumulative meta-analysis and fail-safe analysis to provide estimates of the stability of the findings.
Inconsistency of reporting on birth setting, care practices, interventions and outcomes prevented us from achieving our secondary objective to account for intrapartum care variation.
Meta-regression was only possible for three outcomes: intact perineum, episiotomy and postpartum haemorrhage.
Few studies were conducted in midwifery-led settings.
Introduction
Immersion in a birthing pool offers women a non-pharmacological option of pain relief during labour, which also enhances their sense of control. Resting and labouring in water can reduce fear, anxiety and pain perception; it helps optimise the physiology of childbirth through the release of endogenous endorphins and oxytocin. Evidence from randomised controlled trials (RCTs) showed that labouring in water reduces the need for epidural analgesia while identifying no adverse maternal or neonatal effects. 1 In the UK, most birthing pool use occurs in midwifery-led birth settings: these include alongside midwifery units (colocated with a maternity hospital setting) and freestanding midwifery units (in the community setting) and home birth. 2 The outcomes of birthing pool use may be different in midwifery-led settings compared with an obstetric setting because healthy women experience fewer interventions and operative birth when the birth occurs in a midwifery-led setting compared with an obstetric setting. 3
Variations in care between waterbirth services may contribute to the differences in outcomes with water immersion, particularly variations in use of labour augmentation, hands on/off the perineum for the birth, pushing position, use of active management of third stage of labour and placenta birth in the water. 3–9 It is likely that women who use water immersion for labour and birth experience different care practices than women who have standard birth care. Though prior evidence has found no increased risk of adverse events for newborns born in water, heterogeneity in outcomes and limited reporting of the clinical guidance used for water immersion make implementation of evidence-based guidelines difficult. 10–12 There is a need to understand which clinical practices, when performed as part of water immersion care, result in the optimum outcomes for mother and newborn. It has been argued that an international RCT would be desirable. 13 14 However, an RCT proposal is likely to encounter ethical and recruitment challenges due to increasing acknowledgement of the importance of enabling women to take an active part in decision making during labour. Additionally, an unblinded trial and expected uneven crossover carry an inevitable limitation. 15
Water immersion in a birth pool during labour and birth can be divided into two distinct but overlapping categories. Water immersion during labour involves using a birth pool to achieve relaxation and pain relief during the first and possibly part of the second stage of labour but exiting the pool for the birth. With this practice, the infant emerges into air to breathe. With waterbirth, the woman remains in the birth pool for the birth of the baby. The infant emerges into the water and is brought to the surface to initiate breathing.
The primary objective of this systematic review was to compare intrapartum interventions and outcomes for water immersion during labour/waterbirth to standard care with no water immersion. The secondary objective was to analyse data reported for clinical care practices and birth settings experienced by women who use water and women who do not.
Review questions
What interventions do women experience with water immersion for labour and birth?
What are the maternal and newborn outcomes following water immersion during labour and waterbirth compared with similar women who labour and/or give birth on land?
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guideline was followed for conducting this work. 16
Patient and public involvement
Patients were not involved in the development of the research question, study design or selection of outcome measures.
Eligibility criteria included:
Studies using any primary quantitative study design published in peer-reviewed journal or unpublished thesis.
Studies that examined maternal or neonatal interventions and/or outcomes when using the birthing pool for labour and/or birth.
Studies published in 2000 or later.
Studies conducted in any language if it could be translated into English using Google Translate.
A search was conducted using CINAHL, Medline, Embase, BioMed Central (BMC) and PsycINFO during March 2020. The search was replicated in May 2021. A predesigned search strategy was designed using the PICOT/PEOT framework to develop search terms 17 :
Population: women in labour and early post partum.
Intervention/Exposure: water immersion during labour and/or birth.
Comparison: no water immersion during labour or birth.
Outcomes: Maternal: artificial rupture of the membranes, need for labour augmentation, epidural analgesia, opioid injection, planned and actual place of birth, reason for transfer to an obstetric setting, mode of birth, perineal trauma, third-stage management, postpartum haemorrhage (PPH)/blood transfusion, infection, breastfeeding initiation. Newborn: APGAR score, resuscitation, admission to a neonatal intensive care unit (NICU), infection, breastfeeding at 6 weeks.
Time: labour and early puerperium.
A tested, sensitive and reproducible search strategy was developed with the specialist healthcare librarian, VF. 18 The refined search terms and strategy with Boolean operators are provided in online supplemental file 1 . These were adapted for specific database architecture. Additional searches were carried out via referencing, checking all included studies with no further records found. Publication alerts were set up via BMC updates that alerted CF 1 to a new publication that met our inclusion/exclusion criteria. A final search to determine if any additional papers were published after analysis was conducted by VF in May 2021.
Supplemental material
Study selection.
Records were deduplicated in Zotero and collated into Rayyan systematic review software. 19 Initial screening (title/abstract) was carried out blind by HTC, CF 1 , CF 2 against the inclusion/exclusion criteria. Consensus meetings were held to discuss and resolve disagreements. Full-text screening was carried out independently against the inclusion/exclusions criteria and in pairs: JV and CF 1 , EB and PJH. Disagreements were resolved by consensus meeting. In the case of duplication of a sample across multiple papers, the paper which provided the largest sample for each outcome provided the data for synthesis.
Data collection was completed using pilot tested forms created in REDCap data collection software. Researchers worked in teams of two (JV and EB, JV and PJH) to individually abstract data for each study, identify discrepancies and reach consensus when needed. Data collected included the study type; sample characteristics, care practices for water immersion, if it was a midwifery-led setting; rates of interventions including amniotomy, labour induction, augmentation, fetal monitoring, epidural, injected opioid, episiotomy and active management of third stage; and outcome data including mode of birth, level of pain, maternal satisfaction, intact perineum, obstetric anal sphincter injury (OASI), shoulder dystocia, maternal infection defined by symptoms and positive test, primary PPH, manual removal of the placenta, 5 min APGAR, newborn resuscitation, transient tachypnoea of the newborn, respiratory distress of the newborn, neonatal intensive unit admission within the first 24 hours and lasting for 48 hours, death in neonatal period, newborn infection defined by both symptoms and positive test, cord avulsion and breastfeeding initiation.
Risk of bias assessment
Risk of bias assessment included review of seven domains based on the Robbins-I Risk of Bias Tool. 20 The domains included bias due to confounding, bias in selection of participants, bias in measurement of intervention, bias due to departures of intended treatment, bias in measurement of outcomes, bias due to missing data, bias in selection of reported results. Bias due to departure of intended treatment was modified to track studies that did not provide information about water immersion use for the control group. Risk of bias assessment was completed independently by two researchers (JV and EB, JV and PJH). Disagreements were resolved by consensus meeting.
Summary measures and synthesis of results
All outcomes were summarised using an OR and 95% CI. All calculations were conducted in Comprehensive Meta-Analysis V.3, using the inverse variance method. 21 Results of individual studies were converted to log OR and SE for synthesis. Fixed effects models were used when I 2 was less than 50%, otherwise random effects models were used. This decision was made because (1) the population eligible for water immersion is restricted to women at low risk of birth complications and (2) the goal of the analysis was to determine if variations in care practices result in changes in outcomes. Outcomes without adequate heterogeneity in estimates were considered unlikely to be affected by care practices and so a fixed effects model was appropriate for analysis. When possible, subgroup analysis was conducted to determine effect of the birth setting and parity on the estimate. In addition, analysis limited to studies published within the past 10 years was conducted when possible. Per protocol, we intended to conduct subgroup analysis by maternal age, maternal body mass index (BMI), prior caesarean, and pool type, however, the data did not allow for these analyses. Cumulative meta-analysis was used to identify the stability of the estimates over time. 22 The fail-safe N estimates were calculated to determine the number of studies necessary to change the estimates. 23 Forest plots were created in RevMan V.5.4.1. 24
Additional analyses
Begg’s test and Egger’s Regression Risk assessed risk of bias across studies. 25 Trim-and-fill analysis was used to estimate the magnitude of effect of the bias. 26 Meta-regression was completed when at least 10 studies provided data for an outcome when I 2 >50%. 26–28 Tested covariates included the sample characteristics and care practices identified a priori as the structure and process variables likely to be responsible for heterogeneity in the outcomes. Directed acyclic graphs of the covariates and their role are available in online supplemental file 2 . 29 For continuous covariates, the rate of a covariate (eg, the induction rate in the sample) were used for regression. Categorical covariates were coded as dichotomous (eg, described appropriate birth pool or did not describe the immersion receptacle).
Certainty assessment
The fail-safe N estimates were calculated to determine the number of studies necessary to change the estimates. 23 Fail-safe calculates the number of studies needed to change the estimate. Cumulative meta-analysis was used to identify the stability of the estimates over time. 22 Assessment of certainty with GRADE criteria was considered inappropriate for this review because the goal of this study was to identify variations between reports of outcomes with water immersion that contribute to inconsistency, imprecision, variations and confounding—three assessments made when considering certainty of evidence. However, the authors recognise the importance of a standardised GRADE assessment for readers. The individual assessments made in this review were prepared in a table outlining scores per standard Grade criteria as online supplemental file 3 .
The searches generated 2113 hits, reduced to 1667 after duplicates were removed; n=1561 records were discarded at the initial screening stage. Of 106 records that were full-text screened, n=71 records did not meet the criteria. See online supplemental file 4 for the list of excluded studies and the reasons. One additional study was found via BMC updates, therefore, k=36 papers reporting on outcomes for 157 546 women were included into the review. 13 30–64 Figure 1 illustrates the study selection process. 16
- Download figure
- Open in new tab
- Download powerpoint
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers and other sources. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study description
Most studies (k=31) were conducted in an obstetric setting or did not adequately report the setting, while four studies were conducted in midwife-led settings; two included planned home and birth centre births, 33 57 one that involved a birth centre (not explicitly described as freestanding) and an alongside midwifery unit (colocated in an obstetric unit). 32 Studies included RCTs (k=6; n=1862), prospective studies (k=13; n=28 226), retrospective studies (k=16; n=127 477), and one pre–post study (n=11). Studies reported on waterbirth (k=25; n= 151 742), water immersion for labour (k=7; n=1901), both (k=3; n=3688
) and one whose timing of immersion could not be determined (n=215). Full information is available in table 1 .
- View inline
Characteristics of included studies; meta-analysis of water immersion for labour and birth
Few studies provided sample characteristics beyond parity (see table 2 ). Eleven studies reported the sample was restricted to persons in spontaneous labour while seven included the rate of labour induction for each group. Two studies excluded participation based on BMI while six provided weight or BMI distributions in the sample characteristics. Most studies (k=19; n=77 180) excluded multiple pregnancies, the rest did not address this characteristic. Prior caesarean was excluded by seven studies (n=2292) and reported as a sample characteristic for five studies (n=22 439).
Reported characteristics of study samples abstracted from inclusion and exclusion criteria or sample descriptions
Few studies provided descriptions of the care practices used with water immersion and water birth (see table 3 ). The description of the immersion receptacle used was adequate to determine the woman had freedom of movement in seven studies (n=3273). Method of induction was not reported. Sixteen studies reported a fetal heart monitoring method as either intermittent auscultation (k=10; n=50 846), continuous monitoring (k=5; n=967) or a mix of methods (k=1; n=367). Six studies reported using ‘hands-off’ (k=4; n=5595) or ‘hands-on’ (k=2; n=6463) the perineum. Third-stage management was reported by six studies (n=5595), all indicating that active management was used. Three studies indicated whether the placenta and membranes were delivered in the birth pool (k=1; n=513) or out of the birth pool (k=2; n=1396).
Description of care practices reported in included studies
Overall risk of bias is presented in figure 2 . Domain 3, bias due to comparability of the groups, was most often identified in retrospective studies that did not provide adequate sample restriction to ensure comparability. Domain 4, bias due to departure from intended treatment, had the highest potential for bias because studies did not provide information about if or why the comparison group included persons who used water in labour but not during birth. Bias in measurement of outcomes was rare because most outcomes were standard medical record items. However, measurement for pain and maternal satisfaction was not consistently described. Individual study results and risk of bias for each outcome are provided in the forest plots found in figures 3–24 .
Risk of bias assessment.
Forest plot of synthesis of labour induction. IV, inverse variance.
Forest plot of synthesis of amniotomy. IV, inverse variance.
Forest plot of synthesis of augmentation of labour. IV, inverse variance.
Forest plot of synthesis of opioid use. IV, inverse variance.
Forest plot of synthesis of epidural use. IV, inverse variance.
Forest plot of synthesis of pain. IV, inverse variance.
Forest plot of synthesis of caesarean delivery. IV, inverse variance.
Forest plot of synthesis of shoulder dystocia. IV, inverse variance.
Forest plot of synthesis of intact perineum. IV, inverse variance.
Forest plot of synthesis of obstetric anal sphincter injuries. IV, inverse variance.
Forest plot of synthesis of episiotomy. IV, inverse variance.
Forest plot of synthesis of postpartum haemorrhage.
Forest plot of synthesis of manual removal of the placenta. IV, inverse variance.
Forest plot of synthesis for maternal infection. IV, inverse variance.
Forest plot of synthesis of maternal satisfaction measures. IV, inverse variance.
Forest plot of synthesis of 5 min APGAR. IV, inverse variance.
Forest plot of synthesis of neonatal resuscitation. IV, inverse variance.
Forest plot of synthesis of transient tachypnoea of the newborn. IV, inverse variance.
Forest plot of synthesis of respiratory distress. IV, inverse variance.
Forest plot of synthesis of neonatal death. IV, inverse variance.
Forest plot of synthesis of cord avulsion. IV, inverse variance.
Forest plot of synthesis of breastfeeding initiation. IV, inverse variance.
Labour induction
Three studies provided data on labour induction (n=2008), all conducted after 2010. Overall, this analysis found no difference between use of labour induction with water immersion and standard care (OR 0.43; 95% CI 0.16 to 1.16; random effects; Q=20.7 p<0.001; I 2 =90%). Subgroup analysis of studies reporting in an obstetric setting remained no difference. Results of the subgroup analyses are in table 4 . Three studies were too few for cumulative meta-analysis. Two additional studies indicated there was no difference but did not provide data to synthesise. 36 52
Results of subgroup analysis of interventions on outcomes of water immersion for labour and waterbirth compared with standard care
Five studies provided data on amniotomy (n=1627). Overall, this analysis found no difference (OR 0.71; 95% CI 0.37 to 1.39; random effects; Q=23.9 p<0.001; I 2 =83%). Cumulative meta-analysis indicated the available evidence has consistently indicated no difference in the rate of amniotomy. Subgroup analysis of studies reporting in an obstetric setting and the most recent studies remained no difference.
Augmentation
Three studies provided data to compare augmentation of labour (n=1420). This analysis favoured water immersion (OR 0.30; 95% CI 0.10 to 0.92; random effects; Q=19.2 p<0.001; I 2 =90%). Subgroup analysis of studies reporting in an obstetric setting and the most recent studies remained no difference. Fail-safe analysis estimated 34 additional studies finding no difference would be needed to change the estimate to no difference. Three studies were too few for cumulative meta-analysis.
Fetal monitoring
No studies provided data to compare the use of intermittent or continuous fetal monitoring during immersion to standard care.
Eight studies provided data on opioid use (n=27 391), all were conducted in an obstetric setting. Overall, this analysis found reduced use of opioids with water immersion (OR 0.22 95% CI 0.13 to 0.38; random effects; Q=96.1 p<0.001; I 2 =93%). Subgroup analysis of the most recent studies remained no difference. Cumulative meta-analysis indicated the available evidence consistently favoured water immersion. Fail-safe analysis estimated 972 additional studies would be needed to change the estimate to no difference.
Epidural use
Seven studies provided data on epidural use (n=10 993). Overall, this analysis favoured water immersion (OR 0.26 95% CI 0.08 to 0.83; random effects; Q=89.5 p<0.001; I 2 =94%). Cumulative meta-analysis revealed the estimate moved from no difference to favour water immersion in 2007. Fail-safe analysis indicated 100 additional studies would be needed to change the estimate to no difference. Subgroup analysis revealed the use of epidural was reduced with water immersion in an obstetric setting.
Eight studies provided data for analysis of pain (n=1200), all were conducted in an obstetric setting. Because these studies varied in their measurement timing and scale, they were combined with a random effects model for an overall score and the results were stratified by timing of measurement in the forest plot. Overall, the results indicated reduced pain with water immersion (OR 0.24 95% CI 0.12 to 0.51; random effects; Q=76.7 p<0.001; I 2 =91%). One additional study reported in favour of water immersion but did not provide the data in a way that allowed synthesis. 31 Subgroup analysis of the most recent studies indicated reduced reports of pain with water immersion. Cumulative meta-analysis indicated the available evidence moved from no difference to favour water immersion in 2009 and has been stable since. Fail-safe analysis estimated 279 studies finding no difference would be necessary to change the estimate from favouring water to no difference.
Caesarean birth
Eight studies provided data on mode of birth comparing water immersion (n=1190) vs standard care (n=1575), all were conducted in an obstetric setting. All but one study reported on the difference in caesarean with water immersion during labour; the final study was an RCT that analysed using intention to treat. The meta-analysis indicated no difference between water immersion and standard care for caesarean birth (OR 0.92 95% CI 0.58 to 1.48; fixed effects; Q=9.0 p=0.249; I 2 =23%). Subgroup analysis of studies reporting by year of publication remained no difference. Cumulative meta-analysis indicated this result has been stable at no difference since the first time the outcome was reported in 2001.
Shoulder dystocia
Seven studies provided data that could be synthesised for shoulder dystocia (n=53 367). One additional study reported zero events in the sample and could not be included in the synthesis. 16 There was no difference between water immersion and standard care (OR 0.88 95% CI 0.46 to 1.69; random effects; Q=16 p=0.012; I 2 =63%). The subgroup analysis of studies in an obstetric setting and the most recent studies remained no difference. Cumulative meta-analysis indicated there has consistently been no difference.
Intact perineum
Seventeen studies provided data on intact perineum (n=59 070). This analysis favoured water immersion (OR 1.47; 95% CI 1.21 to 1.78; random effects; Q=219.1 p<0.001; I 2 =93%). Note the direction of effect for figure 11 reflects that intact perineum is a positive outcome. Subgroup analysis revealed no difference in odds of intact perineum in midwifery-led settings, in studies that compare waterbirth to no immersion. Subgroup analysis revealed higher odds of intact perineum with water immersion in an obstetric setting and in the most recent studies. Cumulative meta-analysis indicated the available evidence has consistently indicated no difference or favoured water immersion, with evidence stable at favouring water immersion since 2016. Fail-safe analysis estimated 358 additional studies finding no difference would be necessary to change the estimate from favouring water to no difference. Subgroup analysis revealed no difference in odds of intact perineum in midwifery-led settings and in favour of water immersion in an obstetric setting.
Meta-regression identified the episiotomy rate (p<0.001) and the proportion of nulliparas in the sample (p=0.001) accounted for the variation in odds of an intact perineum (R 2 =1.00). Though only six studies provided the necessary data to test this association, the statistically significant result indicated the analysis was adequately powered to find this association. After accounting for these variables, the result was in favour of water immersion (OR 3.03 95% CI 1.52 to 6.04; random effects; Q=2 p=0.504 I 2 =0%).
Obstetric anal sphincter injury
Fifteen studies provided data on OASI (n=93 690). This analysis found no difference (OR 0.84 95% CI 0.59 to 1.18; random effects; Q=52.6 p<0.001; I 2 =73%). Cumulative meta-analysis indicated the estimate has moved between no difference and favouring water, with the most recent change to no difference occurring in 2019. Analysis of subgroups by setting found consistent results of no difference in both settings. Meta-regression of the studies with the a priori selected control variables was not able to reduce the heterogeneity.
Fifteen studies provided data on use of episiotomy (n=36 558). This analysis found reduced use of episiotomy with water immersion (OR 0.16; 95% CI 0.10 to 0.26; random effects; Q=114.3 p<0.001; I 2 =88%). Subgroup analysis revealed a reduction with water immersion in an obstetric setting, for nulliparas, and in the most recent studies. Cumulative meta-analysis indicated the available evidence has consistently favoured water immersion. Fail-safe analysis estimated 1525 additional studies finding no difference would be necessary to change the estimate from favouring water to no difference.
Meta-regression of the studies in an obstetric setting indicated the proportion of nulliparas in the sample accounted for some of the variance (R 2 =0.76; p=0.001; seven studies). Though this analysis was limited to seven studies, the finding of an association indicates the analysis had adequate power to identify the association. After accounting for the variation in proportion of nulliparas, the result remained in favour of water immersion (OR 0.04 95% CI 0.01 to 0.13; random effects; Q=12 p=0.038; I 2 =57%).
Third-stage management
No studies provided comparison data for third-stage management.
Postpartum haemorrhage
Fifteen studies provided data about PPH (n=63 891) using three different measures: count of PPH defined as >500 mL blood loss, mean estimated blood loss, and change in haemoglobin. Overall, this analysis favoured water immersion (OR 0.69 95% CI 0.51 to 0.95; random effects; Q=116.5 p<0.001; I 2 =88%). Subgroup analysis revealed no difference in odds of PPH in midwife-led settings, in studies comparing waterbirth to no water use, and the most recent studies. Subgroup analysis revealed a reduction with water immersion in an obstetric setting. Cumulative meta-analysis of the random effects model found the available evidence has consistently indicated no difference. Fail-safe analysis estimated 198 additional studies finding no difference would be necessary to change the estimate from favouring water to no difference.
Meta-regression of the studies in an obstetric setting identified no association with induction rate (R 2 =0; p=0.777; nine studies). Too few studies provided the data necessary to determine the effect of active management of third stage or the birth of the placenta and membranes into the water.
Manual removal of the placenta
Five studies provided data to assess risk for manual removal of the placenta (n=2893). This analysis indicated no difference (OR 0.73 95% CI 0.38 to 1.42; fixed effects; Q=6.2 p=0.181; I 2 =36%). Cumulative meta-analysis indicated there has consistently been no difference in manual removal of the placenta. Subgroup analysis revealed no difference in an obstetric setting and in the most recent studies.
Maternal infection
Three studies provided data about maternal infection (n=32 653), all were conducted in an obstetric setting. This analysis favoured water immersion (OR 0.64 95% CI 0.52 to 0.80; fixed effects; Q=0.5 p=0.792; I 2 =0%), however, one study carried 97% of the weight for this synthesis. Fail-safe analysis estimated two additional studies finding no difference would be necessary to change the estimate from favouring water to no difference. Three studies were too few for cumulative meta-analysis.

Maternal satisfaction
Six studies provided data on a measure of maternal satisfaction (n=4144). Due to heterogeneity in measurement tool, this analysis used random effects modelling and results were stratified by measurement tool in the forest plot. This analysis indicated increased satisfaction with water immersion (OR 1.95 95% CI 1.28 to 2.96; random effects; Q=24.3 p<0.001; I 2 =33%). Note the direction of effect for figure 17 reflects that maternal satisfaction is a positive outcome. Subgroup analysis revealed increased satisfaction with water immersion in an obstetric setting and in the most recent studies. Cumulative meta-analysis indicated the available evidence moved from no difference to favoured water immersion in 2018. Fail-safe analysis estimated 133 additional studies finding no difference would be necessary to change the estimate from favouring water to no difference.
Five min APGAR
Twenty-one studies provided data for 5 min APGAR (n=98 372). This analysis found no difference (OR 0.63 95% CI 0.38 to 1.05; random effects; Q=146.5 p<0.001; I 2 =87%). Three additional studies reported on 5 min APGAR but did not provide data in a usable format; two found no difference 47 51 and one reported in favour of water immersion. 59 Analysis of subgroups found consistent results of no difference. Cumulative meta-analysis indicated the available evidence has consistently demonstrated no difference.
Meta-regression indicated that study setting accounted for some between-study variance (R 2 =0.85; p=0.001; nine studies). After accounting for setting the analysis favoured water immersion (OR 0.14 95% CI 0.06 to 0.36; random effects; Q=20 p=0.034; I 2 =50%).
Newborn resuscitation
Five studies provided data on newborn resuscitation (n=51 028), all were conducted in an obstetric setting. This analysis found no difference (OR 0.91; 95% CI 0.49 to 1.69; random effects; Q=9.6 p=0.048; I 2 =58%. Cumulative meta-analysis indicated this outcome has been stable at no difference since first reported.
Transient tachypnoea of the newborn
Two studies provided data on transient tachypnoea of the newborn (n=1473), both were conducted in an obstetric setting. This analysis found no difference (OR 0.74; 95% CI 0.33 to 1.65; fixed effects; Q=0.8 p=0.364; I 2 =0%). Too few studies were available to conduct cumulative meta-analysis and subgroup analysis.
Respiratory distress of the newborn
Three studies provided data on respiratory distress of the newborn (n=32 707), all were conducted in an obstetric setting. This analysis indicated no difference (OR 0.34; 95% CI 0.05 to 2.43; random effects; Q=18.1 p<0.001; I 2 =89%). Three studies were too few for cumulative meta-analysis.
NICU admission
No studies met the definition for NICU admission.
Neonatal death
Three studies provided data on neonatal death (n=66 544), all were published after 2010. This analysis indicated no difference (OR 0.94; 95% CI 0.63 to 1.40; fixed effects; Q=1.9 p=0.381; I 2 =0%). Subgroup analysis by setting revealed no difference in midwifery-led settings. Three studies were too few for cumulative meta-analysis.
Infection in newborn period
Only one study met the definition for reporting newborn infection; it reported no difference.
Cord avulsion
Five studies provided data on cord avulsion (n=50 791), all were published after 2010. This analysis favoured standard care (OR 1.94 95% CI 1.30 to 2.88; fixed effects; Q=1.3 p=0.856; I 2 =0%). One study was responsible for 92.7% of the weight of this analysis, when that study was removed the result became no difference (OR 2.92 95% CI 0.67 to 12.77). Subgroup analysis by setting found no difference in an obstetric setting, but increased odds of cord avulsion in midwifery-led settings. Cumulative meta-analysis indicated the estimate moved from no difference to favour standard care in 2019. Fail-safe analysis estimated five additional studies would be needed to change the estimate to no difference.
Breastfeeding initiation
Two studies provided data on breastfeeding initiation (n=692). This analysis found no difference (OR 1.00 95% CI 0.73 to 1.37; fixed effects; Q=1.0 p=0.325; I 2 =0%). Note the direction of effect for figure 24 reflects that breastfeeding initiation is a positive outcome. Two studies were too few for cumulative meta-analysis and subgroup analysis.
Risk of bias across studies
Risk of bias analysis results are available in table 5 . Begg’s test has moderate power with 25 studies, so is underpowered to find publication bias for this review. Egger’s regression identified risk for publication bias in three outcomes: epidural, intact perineum and shoulder dystocia. In each case, trim-and-fill estimates of the magnitude of bias indicate the magnitude was too small to affect the results.
Analysis of risk of bias across studies comparing water immersion for labour and waterbirth to standard care
The main findings of this systematic review and meta-analysis are that labouring and/or giving birth in water has clear benefits to women in the obstetric setting. These findings are interesting because, in general, healthy women are more likely to experience interventions and adverse outcomes in this setting compared with midwifery-led settings and this has been reported for women who labour and/or give birth in water. 3 65–67 Given that globally, most births take place in the obstetric setting, this review shows that water immersion can significantly increase the likelihood of an intact perineum and reduce episiotomy; an intervention which offers no perineal or fetal benefit, can increase postnatal pain, anxiety and impact negatively on a woman’s birth experience. 68 69 Furthermore, labouring and/or giving birth in water does not increase the likelihood of OASI, which corroborates previous waterbirth research. 7 70 71 A significant PPH reduction was another important finding, which is also supported in the literature. 72
In this study, there was no difference in caesarean birth rate between those who used water and those who did not. Interestingly, the caesarean rate in these studies was 3.6%, with all but two studies reporting a caesarean birth rate of less than 10% for the study participants. Given the low caesarean rates reported by most studies, these results should not be generalised to settings with a caesarean rate higher than 10% for women considered low risk. The study with a caesarean rate of 19% is not generalisable to settings with a low-risk caesarean birth rate higher than 10% because it compared the use of water immersion to medical augmentation for women with a stalled labour. 34 One study with a caesarean rate of 26% is generalisable to settings with a higher low-risk caesarean birth rate. 46
Our results for newborns mirror those reported in three substantial newborn specific systematic reviews. 10–12 Additionally, this study improved on prior research, which was limited by variations in definition for reporting newborn infection and NICU admission. The more rigorous definitions used for this study reveals limited reporting of serious complications. Given the lack of association with poor newborn outcomes between this study and prior analyses, it is unlikely that differences in prevalence of serious complications between water immersion and standard care exist.
More cord avulsions were reported for waterbirths and may relate to possible undue traction on the umbilical cord as the newborn is brought up out of the water. 3 73 The incidence of cord avulsion was 4.3 per 1000 births in water compared with 1.3 per 1000 births with standard care. Interestingly, the incidence of cord avulsion varied from 0.2 per 1000 to 11.8 per 1000 in the five studies that reported this outcome, suggesting individual practice characteristics are more relevant to the incidence of cord avulsion than whether the birth occurs in water. A review of case reports of poor newborn outcomes found that when reported, cord avulsion was easily managed by the midwife with no consequences for the newborn. 74
Our results show that water immersion has the potential to make a meaningful contribution to the global agenda towards promoting physiological birth. 75–79 Labouring and/or giving birth in water can reduce maternal pain with no increased risk of an adverse event, and without the risk introduced by epidural and opioids. 80–83 Differences between birth settings in intact perineum and PPH suggest water immersion in an obstetric setting may result in outcomes similar to those achieved in midwifery-led settings. This interpretation is supported by the results of subgroup analysis of studies in an obstetric setting that episiotomy is reduced with water immersion, and maternal satisfaction is increased. Given these results, water immersion for labour and waterbirth is an intervention that can be used to achieve physiological birth and improve the quality of care in the obstetric setting.
One major issue that hindered the potential of this review was that only four studies were conducted in midwifery-led settings. None of the included studies described the care model in operation where the study participants laboured. Healthy women who give birth in a midwifery-led setting are more likely to experience fewer interventions and adverse outcomes compared with those who give birth in an obstetric setting, particularly nullipara. 2 3 There is strong evidence showing that the relational element of care matters to service users, and continuity of carer/care is linked to fewer interventions and adverse outcomes when compared with fragmented care models. 83 This is important because birth pool use is most prevalent in midwifery-led settings. 3 Evidence-based practice of water immersion requires research that reflects the context of care provision.
Few studies provided information generally considered to be relevant to the outcomes reported or controlled for potential confounders. Just over half the studies (k=20, 55%) included some description of the birth pool(s), resulting in uncertainty about whether all participants could move around and adopt different positions with ease. Furthermore, studies did not specify the type of fetal monitoring. Since intermittent auscultation does not inhibit mobility, and continuous electronic fetal monitoring typically does, this could present a confounder. Few studies stratified for parity, even when the outcomes reported occur at higher rates among nullipara. Only six studies (17%) mentioned inclusion of induction of labour while five studies included women with a prior caesarean. Only eight studies (22%) provided birth pool eligibility criteria regarding raised BMI. These studies did not include BMI as a characteristic in their analysis for interventions or outcomes. However, their inclusion in the study populations suggest that water immersion is not considered to be harmful for women who have raised BMI but are otherwise healthy. No studies provided data for the management of the third stage of labour in the studies, to enable examination for any associations between active or physiological management and PPH. Improvements in reporting standards would enable expansion of populations considered appropriate for water immersion and identify best practice for birth pool use.
Strengths and limitations of this work
This was the first substantial systematic review to attempt to include birth setting as an analytic variable. A broad search strategy was developed and all review processes were conducted by at least two reviewers. This study incorporated meta-regression, using covariates identified a priori, to reduce the effect of sources of heterogeneity. The inclusion of analyses of the stability of the results, cumulative meta-analysis and fail-safe, add value to the synthesis by identifying which outcomes may be considered sufficiently researched. The results are further strengthened by use of a trim-and-fill analysis to identify the direction of any potential publication bias.
This review was limited to studies published during or after 2000 or later because earlier studies may not be generalisable to current water immersion practices. This review did not include grey literature, and was limited by language; the search was conducted in English using English-language indices. This analysis was limited to a priori variables for meta-regression. Additional variables, not tested in this study, may contribute to heterogeneity. Inconsistency of reporting on birth setting, care practices, interventions and outcomes prevented us from achieving our secondary objective to account for intrapartum care variation. Meta-regression was only possible for three outcomes: intact perineum, episiotomy and PPH.
Clinical implications
Water immersion provides benefits for the mother and newborn when used in the obstetric setting, making water immersion a low-tech intervention for improving quality and satisfaction with care. In addition, water immersion during labour and waterbirth alter clinical practice resulting in less augmentation, episiotomy and requirements for pharmacological analgesia. Water immersion is an effective method to reduce pain in labour, without increasing risk. Clinicians should be mindful to avoid putting undue traction on the umbilical cord when bringing the newborn to the surface of the water.
Research implications
Water immersion during labour and birth is a low-tech yet complex, nuanced intervention. We suggest that studies incorporate the following fundamentals to advance the evidence: birth pool description, clearly described maternal and obstetric characteristics, the birth setting, the care model and use of standardised definitions. Studies should report potential confounders such as hands-on or hands-off the perineum and third-stage management. When appropriate for the outcome, results should be stratified by maternal parity. The study population should reflect all those now using a birth pool, not just the healthy women who experience an uncomplicated pregnancy. There is a need for additional research conducted in midwifery-led settings to establish best practice.
Water immersion during labour and birth, while low-tech, is a complex, nuanced intervention. Importantly it has clear benefits for healthy women and their newborns when in the obstetric unit setting where the majority of women give birth, and may have benefits for populations previously excluded from water immersion. To enable the identification of best practice regarding water immersion, future birthing pool research should integrate factors that are known to influence intrapartum interventions and outcomes. These include maternal parity, the care model, care practices, birth setting and a clear description of the water immersion receptacle.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
Institutional review board approval was not sought as meta-analyses are not human subjects research.
- Cluett ER ,
- Birthplace in England Collaborative Group ,
- Brocklehurst P ,
- Hardy P , et al
- Boulton MG ,
- Cluett E , et al
- Lucas C , et al
- Edqvist M ,
- Hegaard HK , et al
- Hofmeyr GJ , et al
- Aasheim V ,
- Nilsen ABV ,
- Lukasse M , et al
- Bulchandani S ,
- Sucharitha A , et al
- Begley CM ,
- Pearce M , et al
- Bewley S , et al
- Vanderlaan J ,
- De Rota B ,
- Ferrando A , et al
- Bovbjerg ML
- McKenzie JE ,
- Squires JE ,
- Valentine JC ,
- Grimshaw JM
- Ouzzani M ,
- Hammady H ,
- Fedorowicz Z , et al
- Sterne JA ,
- Hernán MA ,
- Reeves BC , et al
- Biostat Inc
- Koricheva J
- Carson KP ,
- Schriesheim CA ,
- The Nordic Cochrane Center TCC
- Lin L , et al
- Cappelleri JC , et al
- Borenstein M ,
- Hedges LV ,
- Higgins JPT , et al
- Piccininni M ,
- Konigorski S ,
- Rohmann JL , et al
- Bailey JM ,
- Zielinski RE ,
- Emeis CL , et al
- McMahon LE ,
- Banks RA , et al
- Benfield RD ,
- Hortobágyi T ,
- Tanner CJ , et al
- Bovbjerg ML ,
- Cheyney M ,
- Pickering RM ,
- Getliffe K , et al
- da Silva FMB ,
- de Oliveira SMJV ,
- Turnbull D ,
- MacLennan A
- Geissbühler V ,
- Geissbuehler V ,
- Eberhard J ,
- Haslinger C ,
- Burkhardt T ,
- Stoiber B , et al
- Henderson J ,
- Regalia AL , et al
- Hodgson ZG ,
- Comfort LR ,
- Crawford S , et al
- Lathrop A ,
- Bonsack CF ,
- Huang X , et al
- Mallen-Perez L ,
- Roé-Justiniano MT ,
- Colomé Ochoa N , et al
- Menakaya U ,
- Albayati S ,
- Vella E , et al
- Mollamahmutoğlu L ,
- Moraloğlu O ,
- Ozyer S , et al
- Tan A , et al
- Ohlsson G ,
- Buchhave P ,
- Leandersson U , et al
- Otigbah CM ,
- Dhanjal MK ,
- Harmsworth G , et al
- Peacock PJ ,
- Zengeya ST ,
- Cochrane L , et al
- Preston HL ,
- Alfirevic Z ,
- Fowler GE , et al
- Neselioglu S , et al
- Stapleton SR ,
- Wright J , et al
- Moroder L , et al
- Torkamani SA ,
- Kangani F ,
- Ulfsdottir H ,
- Saltvedt S ,
- Georgsson S
- Woodward J ,
- Zanetti-Dällenbach R ,
- Lapaire O ,
- Maertens A , et al
- Zanetti-Daellenbach RA ,
- Tschudin S ,
- Zhong XY , et al
- Ziolkowski R ,
- Czerniawski W , et al
- Alliman J ,
- Meier D , et al
- Rossiter C ,
- Vedam S , et al
- Qian X , et al
- Carroli G , et al
- Carpenter J , et al
- Dahlen HG ,
- Dowling H ,
- Tracy M , et al
- Jardine J ,
- Moitt N , et al
- World Health Organization
- Prosser SJ ,
- Barnett AG ,
- ↵ Supporting healthy and normal physiologic childbirth: a consensus statement by ACNM, manA, and NACPM . J Perinat Educ 2013 ; 22 : 14 – 18 . doi:10.1891/1058-1243.22.1.14 pmid: http://www.ncbi.nlm.nih.gov/pubmed/24381472 OpenUrl PubMed
- National Childbirth Trust
- International Confederation of Midwives
- Thomson G ,
- Cook J , et al
- Fleet J-A ,
- Penuela I ,
- Isasi-Nebreda P ,
- Almeida H , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
- Data supplement 4
- Press release
Twitter @Ethel_Burns_07
Scientific Advisors VF: Methodology, validation & Investigation Vicki Farmilo, Health care librarian, Oxford Brookes University, Oxford, UK RM: Methodology, Review. Dr Reem Malouf, Neurologist, Specialist in Internal Medicine, National Perinatal Epidemiology Units, Oxford UK Cindy Farley (CF2): Methodology, Investigation, Review Associate Professor, Georgetown University, Washington DC, USA HC: Validation, Review Dr Harriet Thorn-Cole, Scientific ColLabourator, University of Health Sciences of Western Switzerland, Lausanne, Switzerland. CR: Methodology, Review Dr Charles Roehr, National Perinatal Epidemiology Unit Clinical Trials Unit, Oxford UK. Academic Consultant Neonatologist, Newborn Services, Southmead Hospital, North Bristol Trust, Bristol.
Contributors EB: conceptualisation, protocol writing, investigation, methodology, writing-original draft, writing-review and editing, project administration, funding acquisition for Open Access publication. EB, Senior Midwifery Lecturer, Midwifery research Lead, Oxford Brookes University, Oxford UKCF1: methodology, protocol writing, validation, writing-original draft, writing- review and editing, visualisation. CF, Midwife Researcher, Associate Lecturer, Oxford Brookes University, Oxford UK. PJH: conceptualisation, investigation, writing - original draft, writing—review and editing. PJH, midwife researcher and senior instructor, Emory University in the Nell Hodgson Woodruff School of Nursing, Atlanta, Georgia USA JV: conceptualisation, methodology, investigation, data curation, formal analysis, writing—original draft, writing—review and editing, visualisation. JV, University of Nevada, Las Vegas School of Nursing, Nevada USA. EB and JV are the guarantors of the article.
Funding This work was supported by Oxford Brookes University.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Linked Articles
- Correction Correction: Systematic review and meta-analysis to examine intrapartum interventions, and maternal and neonatal outcomes following immersion in water during labour and waterbirth British Medical Journal Publishing Group BMJ Open 2022; 12 - Published Online First: 27 Sep 2022. doi: 10.1136/bmjopen-2021-056517corr1
Read the full text or download the PDF:
Center for Women's Health
Water birth.
OHSU was the first hospital in Portland to offer water birth, an option that offers many women relief. You’ll find:
- Certified nurse-midwives with more than 20 years of water birth experience.
- An excellent safety record and high levels of patient satisfaction.
- Access to the resources and expert doctors at OHSU, Oregon’s top hospital, if needed.
What is water birth?
Water birth is the process of laboring and/or giving birth in a tub of warm water. Many women find that sitting or floating in water during labor helps them relax and manage pain. Some women choose to give birth in the water. Others only labor in the tub.
At OHSU, water birth is an option only if you choose delivery with our highly skilled nurse-midwives.
Complete care
- We follow rigorous guidelines to prevent infection.
- We use monitors that work underwater to track your baby’s heart rate.
- We are family-friendly and welcome your partner and doula.
What to expect at OHSU
If you have chosen water birth with a nurse-midwife, a freestanding tub will be set up in your private birthing suite.
The t ubs have a soft floor, high soft sides and a built-in seat. Water is kept warm. The tubs offer plenty of space for your partner. Every birthing suite also has a jetted tub and shower to help you manage labor pain.
Water birth videos
These videos are required viewing if you plan to labor or give birth in the tub. Watch to learn about:
- The benefits of being in water for labor and/or birth
- The guidelines for use of the tub
- Safety issues
Water immersion: Watch this video if you plan to labor in the tub, even if you don’t plan to give birth there.
Water birth: Watch this video if you plan to give birth in the tub.
Water birth benefits
Experts agree that laboring in water is safe and offers benefits. They disagree on whether there’s enough evidence that giving birth in water is safe.
- The American College of Obstetricians and Gynecologists recommends against water birth until there’s more data.
- Other experts, though, say studies already show that water birth with a trained professional is no riskier than a traditional birth.
- You can have the benefits of laboring in water even if you decide not to give birth in the water.
- Many risks of immersion and water birth — such as slips, falls and dehydration — are easy for your nurse-midwife to manage.
At OHSU, we’re committed to helping you understand the research so you can choose the best option for you. We’ve been doing water births with excellent patient outcomes since 1997. Find links to more information in our “Learn more” section below.
Benefits of laboring in water
- A positive birth experience: Women who have labored or given birth in water say they had less pain and a greater sense of control.
- Less pain medication: Some studies show that women who labor in water need less pain medication and may have a shorter first stage of labor.
- Relaxation: Floating in water can be soothing for many women. Your muscles don’t have to work as hard to support you. You can change position more easily. Being relaxed lowers stress hormones. This can give you a sense of reduced pain, and it may help your labor along.
- Improved blood flow: Soaking in warm water up to your shoulders can reduce your blood pressure. Better blood flow may protect your baby against stress during labor.
- Comfortable temperature: Being in water heated to your body temperature can help keep you from becoming chilled or overheated.
Possible benefits of giving birth in water
- Shorter pushing stage: More research is needed, but some women report that being in water shortens the pushing stage of labor.
- Fewer episiotomies: Giving birth in water may mean you’re less likely to need a surgical cut to enlarge the opening of your vagina. More research is needed, though.
Water birth safety concerns
Will the baby try to breathe underwater.
Healthy babies begin to breathe only when they feel air on their mouth and nose. They do not try to breathe underwater.
Our nurse-midwives will make sure that you have your bottom and hips completely underwater when your baby is born. This prevents your baby from trying to take a breath. We lift your baby gently to the surface within seconds of being born. Then the baby starts breathing safely.
How will you know if the baby is stressed?
A change in your baby’s heart rate can be a sign of difficulty coping with labor. All babies are monitored during active labor with a waterproof Doppler.
For water births, we use a Doppler (like the fetal heart tones device used in prenatal care to check the baby’s heart rate) or continuous electronic heart rate monitors. If we see signs that your baby is having a problem, we will have you leave the tub.
What if the umbilical cord tears or tangles?
If the cord tears, the baby could lose blood. Your nurse-midwife will be careful not to tug the cord as she lifts your baby out of the water.
If the umbilical cord is wrapped around the baby’s neck during birth, we may have to unwrap it or move the baby through it. We may ask you to change position or stand up.
How do you prevent infection?
Infection can come from two sources:
- Germs you carry into the pool
- Germs in the tub or water
Our safety precautions include:
- Our tubs contain chlorinated city water. During birth, you may lose fluid from your bag of waters, or pass urine, blood or stool into the tub. Research shows that most germs do not live long in chlorinated water.
- We use a new tub liner and hose for each patient.
- Tubs are cleaned with special products after each use.
- Your nurse-midwife will wear gloves to prevent cross-infection.
Water birth FAQ
Does water birth cost extra.
There is no extra cost to use the water birth tub.
How do I arrange a water birth?
You must be a patient of OHSU’s nurse-midwifery practice to have a water birth with us.
To make an appointment with a nurse-midwife, please call the OHSU Center for Women’s Health at 503-418-4500 .
Can anyone have a water birth?
To be approved for a water birth, you need to have a normal, low-risk pregnancy.
This means:
- You have not had a C-section.
- You are carrying one baby.
- You are at least 37 weeks pregnant when you go into labor.
- You have no sign of high blood pressure or gestational diabetes.
- Your baby is in a head-down position (not breech or transverse).
- You and your baby have no other health problems.
If you qualify for a water birth, you will need to:
- Watch our water immersion and water birth videos. ( See above .)
- Have a hepatitis C test.
- Sign a consent form. This includes agreeing to get out of the tub if your nurse-midwife asks.
How long are babies in the water after birth?
The nurse-midwife will lift the baby out of the water 5 or 10 seconds after birth. She will make sure not to tug on the cord, and she will untangle it if necessary. She may ask you to change position or stand up.
When do babies start to breathe?
As soon as the baby is out of the water, you will hold your baby skin-to-skin to keep the baby warm and to promote breathing.
What happens if there’s a problem?
You will come out of the tub. Any problem for you or the baby will be handled the same way as with a traditional labor. When needed, all labor and delivery patients at OHSU have fast access to:
- Medications
- Anesthesiologists
- Childbirth specialists
- Newborn specialists
- A state-of-the-art NICU (neonatal intensive care unit)
What is the water temperature?
We keep the water temperature close to your body temperature, about 98 degrees. This makes sure that your baby doesn’t get overheated. We encourage you to drink plenty of clear fluids to stay hydrated and comfortable.
When do I get in the tub?
Experts recommend that you get in the tub when your cervix is at least 4 centimeters dilated. Some research suggests that getting in earlier may slow labor.
If your labor slows while you’re in the tub, it’s a good idea to get out and walk around for 30 minutes or so.
Can my partner be in the tub?
Yes. Your partner should bring a swimsuit.
- Certified nurse-midwife Michele Megregian on water birth, water immersion and safety
- Waterbirth International
- How valid are the common concerns raised against water birth? A focused review of the literature , Women and Birth
- Birth, Bath, and Beyond: The Science and Safety of Water Immersion During Labor and Birth , The Journal of Perinatal Education
- Doctors Say Don’t Give Birth to Baby in a Tub, But Midwives Disagree , National Public Radio
- Committee Opinion; Immersion in Water During Labor and Delivery , American College of Obstetricians and Gynecologists
For patients
Call 503-418-4500:
- To schedule an appointment.
- If you’re pregnant, to schedule a free 20-minute “Get to Know You” appointment.
Learn about our midwifery care at Hillsboro Medical Center (formerly Tuality).
Parking is free for patients and their visitors.
Kohler Pavilion, seventh floor 808 S.W. Campus Drive Portland, OR 97239

Promoting midwifery, quality maternity services and professional standards
Professional Practice
- Midwives and Public Health
- Maternity Transformation
- Fetal surveillance
- Safety and Quality Improvement
- Continuity of carer
- Violence against women and girls
Learning & Careers
- How to become a midwife
- Return to midwifery courses
- How to become a maternity support worker
- i-learn and i-folio
- Research Hub
- Apprenticeships
- Access Evidence Based Midwifery Journal
- RCM Library and information services
- Career framework
- Syndeo: a leadership programme for Band 7 midwifery leaders
- Influencing
- Race Matters
Latest news
- Consultation opened on job evaluation matching profiles for midwifery bands
- RCM to ask members in Northern Ireland how many extra hours they’ve worked
- Creating a separate pay spine for nurses is ‘divisive and unfair’ says RCM
- RCM shines light on key member issues at TUC Women’s Conference
Supporting our members, individually and collectively
In this section
- Job evaluation
Getting help
- Pay and Agenda for Change
- NHS Pensions
- Equality and Diversity
- Post supervision across the UK
- Supporting student midwives from day one
- Northern Ireland pay consultation – the background
- Race matters
- Workplace support
- Financial support
- Caring for You
- Media releases
- Midwives in Northern Ireland work thousands of unpaid hours to keep services running safely
- RCM leader calls for a revolution in maternity services
- RCM launch ‘game changing’ set of recommendations to make midwifery education more inclusive
- RCM launches tool to tackle high levels of maternity disadvantage
Influencing on behalf of members and the women and families they care for
- Apply for a fellowship
- Health and Safety Reps webinars
- RCM Networks
- Meet the RCM Fellows
- Honorary Fellows
- Consultations
- RCM Position Statements
- RCM Opinion
- Alliance Partners
- Bereavement Care Network
- Workplace representatives
RCM Activists
- RCM Branches
- Maternity Support Worker Advocates
- Workshops delivered by Learning Reps
- RCM Branch resources
- Professional Advice
- My Membership Benefits
- Media Releases
- RCM Library
- How to become an MSW
- Research and Funding
- RCM Benevolent Fund
- RCM Job Vacancies
RCM welcomes research showing benefits of water birth
Research showing the safety and positive benefits for women having a water birth has been welcomed by the Royal College of Midwives (RCM). The research showed that women having a water birth in a hospital obstetric unit had fewer medical interventions and complications during and after the birth.
Commenting on the research, Clare Livingstone, Professional Policy Advisor at the RCM, said: “This is really good news for women choosing to have a water birth or thinking of having one. There has been previous research outlining the benefits for women and this significant study adds weight to those. It is also positive because it is more information for women when deciding how they want to give birth.
“Water births are becoming more widely available for women across the UK, but this isn’t the case everywhere. The challenge now is to ensure this choice is open to all women wherever they live.”
The study did show a small increase in ‘umbilical cord snaps’ - where the baby’s umbilical cord breaks - though the rates remain very low. This will not hurt the baby and the midwife will respond quickly and clamp the cord to prevent any bleeding. Clare Livingstone added, “What is needed now is to see more research into water births in midwife led settings and in women’s homes. This will give us a broader picture of the impact of water births across all the places in which women give birth.”
The research from Oxford Brookes University will be published in the open access journal BMJ Open tomorrow (6 July).
To contact the RCM Media Office call 020 7312 3456, or email [email protected] .
Notes to Editors
The Oxford Brookes University research can be read at https://bmjopen.bmj.com/content/12/7/e056517.full .
The Royal College of Midwives (RCM) is the only trade union and professional association dedicated to serving midwifery and the whole midwifery team. We provide workplace advice and support, professional and clinical guidance, and information, and learning opportunities with our broad range of events, conferences, and online resources. For more information visit the RCM | A professional organisation and trade union dedicated to serving the whole midwifery team .
Waterbirth: a national retrospective cohort study of factors associated with its use among women in England
Affiliations.
- 1 National Maternity and Perinatal Audit (NMPA), RCOG Centre for Quality Improvement and Clinical Audit, Royal College of Obstetricians and Gynaecologists, 10 -18 Union Street, London, SE1 1SZ, UK. [email protected].
- 2 University Hospitals Bristol NHS Foundation Trust, Bristol, UK. [email protected].
- 3 National Maternity and Perinatal Audit (NMPA), RCOG Centre for Quality Improvement and Clinical Audit, Royal College of Obstetricians and Gynaecologists, 10 -18 Union Street, London, SE1 1SZ, UK.
- 4 Department of Health Service Research and Policy, London School of Hygiene and Tropical Medicine, London, UK.
- 5 Population Health Analytics, Cerner, London, UK.
- 6 Centre for Reproduction Research, De Montfort University, Leicester, UK.
- 7 Royal Free London NHS foundation Trust, London, UK.
- 8 Specialty of Obstetrics, Gynaecology and Neonatology, Westmead Clinical School, University of Sydney, Sydney, Australia.
- 9 Faculty of Health and Life Sciences, De Montfort University, Leicester, UK.
- PMID: 33771115
- PMCID: PMC8004456
- DOI: 10.1186/s12884-021-03724-6
Background: Waterbirth is widely available in English maternity settings for women who are not at increased risk of complications during labour. Immersion in water during labour is associated with a number of maternal benefits. However for birth in water the situation is less clear, with conclusive evidence on safety lacking and little known about the characteristics of women who give birth in water. This retrospective cohort study uses electronic data routinely collected in the course of maternity care in England in 2015-16 to describe the proportion of births recorded as having occurred in water, the characteristics of women who experienced waterbirth and the odds of key maternal and neonatal complications associated with giving birth in water.
Methods: Data were obtained from three population level electronic datasets linked together for the purposes of a national audit of maternity care. The study cohort included women who had no risk factors requiring them to give birth in an obstetric unit according to national guidelines. Multivariate logistic regression models were used to examine maternal (postpartum haemorrhage of 1500mls or more, obstetric anal sphincter injury (OASI)) and neonatal (Apgar score less than 7, neonatal unit admission) outcomes associated with waterbirth.
Results: 46,088 low and intermediate risk singleton term spontaneous vaginal births in 35 NHS Trusts in England were included in the analysis cohort. Of these 6264 (13.6%) were recorded as having occurred in water. Waterbirth was more likely in older women up to the age of 40 (adjusted odds ratio (adjOR) for age group 35-39 1.27, 95% confidence interval (1.15,1.41)) and less common in women under 25 (adjOR 18-24 0.76 (0.70, 0.82)), those of higher parity (parity ≥3 adjOR 0.56 (0.47,0.66)) or who were obese (BMI 30-34.9 adjOR 0.77 (0.70,0.85)). Waterbirth was also less likely in black (adjOR 0.42 (0.36, 0.51)) and Asian (adjOR 0.26 (0.23,0.30)) women and in those from areas of increased socioeconomic deprivation (most affluent versus least affluent areas adjOR 0.47 (0.43, 0.52)). There was no association between delivery in water and low Apgar score (adjOR 0.95 (0.66,1.36)) or incidence of OASI (adjOR 1.00 (0.86,1.16)). There was an association between waterbirth and reduced incidence of postpartum haemorrhage (adjOR 0.68 (0.51,0.90)) and neonatal unit admission (adjOR 0.65 (0.53,0.78)).
Conclusions: In this large observational cohort study, there was no association between waterbirth and specific adverse outcomes for either the mother or the baby. There was evidence that white women from higher socioeconomic backgrounds were more likely to be recorded as giving birth in water. Maternity services should focus on ensuring equitable access to waterbirth.
Keywords: Childbirth; Labour care; Waterbirth.
Publication types
- Observational Study
- Age Factors
- Apgar Score
- Baths / statistics & numerical data*
- Infant, Low Birth Weight
- Infant, Newborn
- Maternal Health Services / statistics & numerical data*
- Natural Childbirth / adverse effects
- Natural Childbirth / methods*
- Natural Childbirth / statistics & numerical data
- Postpartum Hemorrhage / epidemiology*
- Postpartum Hemorrhage / etiology
- Postpartum Hemorrhage / prevention & control
- Retrospective Studies
- Socioeconomic Factors
- Young Adult
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Healthc Eng
- v.2022; 2022

This article has been retracted.
Comparative efficacy of water and conventional delivery during labour: a systematic review and meta-analysis, guanran zhang.
1 Key Laboratory for Experimental Teratology of Ministry of Education, Department of Histology & Embryology, School of Basic Medical Sciences, Shandong University, Jinan, Shandong 250012, China
Qiuhong Yang
2 Department of Obstetrics and Gynecology, Jinan Maternity and Child Care Hospital, Jinan, Shandong 250001, China
3 Department of Gynaecology and Obstetrics, Qilu Hospital Affiliated to Shandong University, Jinan, Shandong 250000, China
Associated Data
All data are already included within the manuscript and supplementary documents.
In many maternal settings, water delivery is widely available for women who do not have an increased risk of complications during childbirth. Soaking in water during labor has been associated with a number of maternal benefits. However, the situation of water birth is not well known, there is lack of hard evidence on safety, and little is known about the characteristics of women who give birth in water. In this paper, we have explored the effects of water delivery compared to the conventional delivery on the health of mothers and babies. For this purpose, clinical trials were conducted including women in labor, in which participants were treated with water labor or conventional labor, respectively, in the experimental and control group. In this analysis, we have selected 17 eligible studies which included 175654 participants. Compared to the conventional birth group, the risk of Apgar score <7 at 5 min of age in the water birth group dropped by 28% (OR = 0.72, 95% CI: 0.52–1.00, I 2 = 25%, P =0.05). Also, the duration of labor was shorter the in water birth group whatever the labor stage was. The patients who underwent water birth showed an obviously lower rate of neonatal intensive care unit (NICU) admission (OR = 0.58, 95% CI: 0.39–0.86, I 2 = 53%, P =0.007). In this meta-analysis, it was seen that water delivery has clinical significance in alleviating the pain of mothers, promoting the safety of mothers and infants, and reducing postpartum complications.
1. Introduction
For most women, childbirth is the most painful experience of their lives [ 1 ]. Warm baths and water delivery have been introduced as a new and natural way to relieve childbirth pain. A relaxing warm bath and water delivery offers an option to satisfy the desire to use a natural method, ideally counterbalancing the anxiety-tension-pain glass cycle. The weightlessness and warmth of the water are relaxing and alleviate pain. Water, in general, is just as integral to the comfort and health of our daily lives as bathing or showering. Relaxing in the water is associated with positive emotions and feelings of life. So it is no surprise that water birth became popular so quickly after it was introduced a decade ago [ 2 – 4 ].
The use of water to treat pain and other ailments, now called hydrotherapy, has been documented as far back as ancient Egyptian, Greek, and Roman civilizations. The immersion in warm water is secure for both the mother and fetus and positive for the mother's birthing experience, including reduced use of epidural anesthesia, improved pain management, shorter labor, and a greater sense of control during labor and delivery [ 5 – 7 ].
The relaxing effects of soaking baths are attributed to the physiological effects of soaking in hot water. Soaking in water during labor and delivery decreases anxiety release, relaxes muscles, and promotes happiness in the water, thereby reducing stress on the limbs and joints and allowing free movement. In addition, water immersion lowers blood pressure definitely through vasodilation and redistribution of blood flow. The technology is considered safe; soak baths were not associated with longer delivery time, increased surgical intervention, or poor neonatal prognosis [ 8 – 10 ].
However, some studies have shown that water delivery can lead to some serious complications [ 11 , 12 ]. So, the pros and cons of water production still need to be further explored. The objective of our study was to explore the effects of water delivery compared to conventional delivery on the health of mothers and babies. The main contributions of this paper are given as follows:
- In the context of increasing water production, we explore the effects of water delivery compared to conventional delivery on the health of mothers and babies
- This article comprehensively compares water and conventional production and can provide guiding suggestions for the future birth of fetuses
- The studies we included were of high quality and included a large number of participants, so they were highly persuasive
The remaining portions of this manuscript are arranged accordingly. In the subsequent section, the proposed methodology which is used to perform meta-analysis is presented in detail along with the detailed discussion on the selection criteria for various research studies. Experimental results and observation, which become visible during the proposed experimental setup, are described in detail both in textual and graphical formats which is followed by a detailed section dedicated to the discussion. Finally, concluding remarks are given at the end of the manuscript.
2. Proposed Method
2.1. search strategy.
We performed the meta-analysis on the basis of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The terms “waterbirth, water birth, labor in water, delivery in water, underwater labor, birth underwater, pregnant, maternal women, and parturient” were used to find all articles that might meet the requirements in PubMed, Cochrane Library, Embase, and Web of Science (last research updated in 2021). The literature is limited to English language, and our study is not intended for inclusion of patients and the public (CRD42021271545).
2.2. Retrieval Strategy
2.2.1. pubmed.
(“natural childbirth” [MeSH Terms] OR (“natural” [All Fields] AND “childbirth” [All Fields]) OR “natural childbirth” [All Fields] OR “waterbirth” [All Fields] OR “waterbirths” [All Fields] OR (“natural childbirth” [MeSH Terms] OR (“natural” [All Fields] AND “childbirth” [All Fields]) OR “natural childbirth” [All Fields] OR (“water” [All Fields] AND “birth” [All Fields]) OR “water birth” [All Fields]) OR ((“labor s” [All Fields] OR “labored” [All Fields] OR “laborer” [All Fields] OR “laborer s” [All Fields] OR “laborers” [All Fields] OR “laboring” [All Fields] OR “labors” [All Fields] OR “labour” [All Fields] OR “work” [MeSH Terms] OR “work” [All Fields] OR “labor” [All Fields] OR “labor, obstetric” [MeSH Terms] OR (“labor” [All Fields] AND “obstetric” [All Fields]) OR “obstetric labor” [All Fields] OR “laboured” [All Fields] OR “labourer” [All Fields] OR “labourers” [All Fields] OR “labouring” [All Fields] OR “labours” [All Fields]) AND (“water” [MeSH Terms] OR “water” [All Fields] OR “drinking water” [MeSH Terms] OR (“drinking” [All Fields] AND “water” [All Fields]) OR “drinking water” [All Fields] OR “watering” [All Fields] OR “waters” [All Fields] OR “water s” [All Fields] OR “watered” [All Fields] OR “waterer” [All Fields] OR “waterers” [All Fields] OR “waterings” [All Fields])) OR ((“deliveries” [All Fields] OR “delivery, obstetric” [MeSH Terms] OR (“delivery” [All Fields] AND “obstetric” [All Fields]) OR “obstetric delivery” [All Fields] OR “delivery” [All Fields]) AND (“water” [MeSH Terms] OR “water” [All Fields] OR “drinking water” [MeSH Terms] OR (“drinking” [All Fields] AND “water” [All Fields]) OR “drinking water” [All Fields] OR “watering” [All Fields] OR “waters” [All Fields] OR “water s” [All Fields] OR “watered” [All Fields] OR “waterer” [All Fields] OR “waterers” [All Fields] OR “waterings” [All Fields])) OR (“underwater” [All Fields] AND (“labor s” [All Fields] OR “labored” [All Fields] OR “laborer” [All Fields] OR “laborer s” [All Fields] OR “laborers” [All Fields] OR “laboring” [All Fields] OR “labors” [All Fields] OR “labour” [All Fields] OR “work” [MeSH Terms] OR “work” [All Fields] OR “labor” [All Fields] OR “labor, obstetric” [MeSH Terms] OR (“labor” [All Fields] AND “obstetric” [All Fields]) OR “obstetric labor” [All Fields] OR “laboured” [All Fields] OR “labourer” [All Fields] OR “labourers” [All Fields] OR “labouring” [All Fields] OR “labours” [All Fields])) OR ((“birth s” [All Fields] OR “birthed” [All Fields] OR “birthing” [All Fields] OR “parturition” [MeSH Terms] OR “parturition” [All Fields] OR “birth” [All Fields] OR “births” [All Fields]) AND “underwater” [All Fields]) OR ((“birth s” [All Fields] OR “birthed” [All Fields] OR “birthing” [All Fields] OR “parturition” [MeSH Terms] OR “parturition” [All Fields] OR “birth” [All Fields] OR “births” [All Fields]) AND “underwater” [All Fields])) AND (“gravidity” [MeSH Terms] OR “gravidity” [All Fields] OR “pregnant” [All Fields] OR “pregnants” [All Fields] OR ((“maternally” [All Fields] OR “maternities” [All Fields] OR “maternity” [All Fields] OR “mothers” [MeSH Terms] OR “mothers” [All Fields] OR “maternal” [All Fields]) AND (“womans” [All Fields] OR “women” [MeSH Terms] OR “women” [All Fields] OR “woman” [All Fields] OR “women s” [All Fields] OR “womens” [All Fields])) OR (“parturient” [All Fields] OR “parturients” [All Fields])).
2.2.2. Embase
(“waterbirth”: ti, ab, kw OR “water birth”: ti, ab, kw OR “labor in water”: ti, ab, kw OR “delivery in water”: ti, ab, kw OR “underwater labor”: ti, ab, kw OR “birth underwater”: ti, ab, kw) AND (“pregnant”: ti, ab, kw OR “maternal women”: ti, ab, kw OR “parturient”: ti, ab, kw).
2.2.3. Web of Science
- #1 TS = (waterbirth OR water birth OR labor in water OR delivery in water OR underwater labor OR birth underwater)
- #2 TS = (pregnant OR maternal women OR parturient)
- #3 #1 AND #2
2.2.4. Cochrane Library
- #1 (waterbirth):ti, ab, kw OR (water birth): ti, ab, kw OR (labor in water): ti, ab, kw OR (delivery in water): ti, ab, kw OR (underwater labor): ti, ab, kw OR (birth underwater): ti, ab, kw
- #2 MeSH descriptor: [waterbirth] explode all trees
- #3 (pregnant): ti, ab, kw OR (maternal women): ti, ab, kw OR (parturient): ti, ab, kw
- #4 MeSH descriptor: [Pregnant Woman] explode all trees
- #5 #1 OR #2
- #6 #3 OR #4
- #7 #5 AND #6
2.3. Study Selection and Data Extraction
We regarded studies as qualified for inclusion as follows: (a) clinical trials in women with ongoing child delivery; (b) participants in the experimental group adopted water delivery, and participants in the control group adopted conventional delivery; (c) Apgar score, blood loss, and labor duration data can be obtained; and (d) articles published in English.
Articles that are not randomized control trials and lack efficacy or validity data will be excluded. For a single clinical trial reported by multiple articles, we selected the article with the most complete clinical trial data as the included literature. When differences arise in the extraction and processing of data, we adopt discussion to resolve them. Extraction of data from included literature was completed by Qiuhong Yang and Guanran Zhang independently. The author, year, median age, and number of participants in the control and experiment group are reported in Table 1 .
Baseline characteristics.
2.4. Quality Assessment
The Cochrane Collaboration risk of bias tool was used to assess the quality of included studies. The domains included sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias. The risk of bias in every study was classified as high, unclear, or low. Any discrepancies were resolved by a consensus discussion (Supplementary Figure 1 ).
2.5. Statistical Analyses
Review Manager 5.3 software (The Cochrane Collaboration; Copenhagen, Denmark) was used to perform statistical analysis. The continuous variable was presented as 95% confidence intervals (95% CIs) of standard mean difference (SMD) or mean difference (MD). The dichotomous variable was expressed by 95% confidence interval (95% CI) of odds ratio (OR). The heterogeneity among studies was calculated by the Q test and I 2 statistic. For data related to time, we uniformly converted it to minutes.
2.6. Patient and Public Involvement
This study did not involve patients and the public.
3. Results and Observations
The baseline characteristics, namely, the author, year, median age, number of participants in the control and experiment group, of the 17 included studies are shown in Table 1 [ 13 – 29 ]. Through keywords search and simply reading abstracts, we found 4417 articles that could be used for further screening. According to inclusion and exclusion criteria, we included 17 clinical trials containing the patients treated with water birth and conventional birth ( Figure 1 ). The present analysis included a total sample of 175654 women.

Study flow diagram.
Data about Apgar score <7 at 5 min of age were acquired from 8 studies. The water birth group had a 28% lower risk of Apgar score <7 at 5 min of age compared to the land birth group (OR = 0.72, 95% CI: 0.52–1.00, I 2 = 25%, P =0.05, Figure 2 ). However, the water birth group had a 115% higher risk of Apgar <7 at 1 min of age compared to the land group (OR = 2.15, 95% CI: 0.97–4.76, I 2 = 66%, P =0.06, Figure 2 ). Forest plots showed that the difference of Apgar score <7 at 5 min of age was statistically significant.

Forest plots of Apgar score <7 at 5 min of age and Apgar score <7 at 1 min of age.
Data about the duration of labor were obtained from 5 studies. According to forest plots, the water birth group had shorter duration of labor whatever the stage was. For the duration of the first stage of labor, the water birth group had a shorter duration compared to the land group (MD = −35.52, 95% CI: [−65.78, −5.27], I 2 = 83%, P =0.02, Figure 3 ). For the duration of the second stage of labor, the water birth group had a shorter duration compared to the conventional birth group (MD = −5.16, 95% CI: [−9.16, −1.15], I 2 = 68%, P =0.01, Figure 3 ), which was statistically significant. The duration of the third stage labor in the water birth group was shorter than in the conventional birth group (MD = −0.28, 95% CI: [−1.71, 1.15], I 2 = 52%, P =0.70, Figure 3 ), which was not statistically significant. The total duration of labor in the water birth group was shorter than in the conventional birth group (MD = −50.41, 95% CI: [−119.88, 19.06], I 2 = 66%, P =0.15, Figure 3 ).

Forest plots of duration of the first, second, and third stage of labor and total duration of labor (min).
Admission to NICU data were obtained from 9 studies. According to the forest plot, the patients who underwent water birth showed an obviously lower risk of NICU admission (OR = 0.58, 95% CI: 0.39–0.86, I 2 = 53%, P =0.007, Figure 4 ).

Forest plots of admission to the NICU.
Data about episiotomy were available from 5 studies. From what has been shown in the forest plots, the risk of episiotomy in the water birth group was lower than that in the conventional birth group (OR = 0.18, 95% CI: 0.05–0.65, I 2 = 91%, P =0.009, Figure 5 ). We obtained the analgesics results from 4 studies. The rate of no analgesics in the water birth group was 243% higher than that in the land birth group (OR = 3.43, 95% CI: 1.62–7.29, I 2 = 98%, P =0.001, Figure 5 ). In the analysis of labor augmentation, we included 4 studies, which showed that OR = 0.17, 95% CI: 0.04–0.67, I 2 = 93%, P =0.01 ( Figure 5 ). Data about dystocia were obtained from 3 studies. The results showed that the water birth group was obviously safe (OR = 0.37, 95% CI: 0.16–0.88, I 2 = 78%, P =0.02, Figure 5 ). All of them were statistically significant.

Forest plots of episiotomy, no analgesics, augmentation, and dystocia.
Data about blood loss >500 ml were available from 3 studies, and the data were not statistically significant (Supplementary Figure 2 ). Data about pelvic floor muscle injury were available from 3 studies, and the data were not statistically significant (Supplementary Figure 2 ). The data of perineum intact or no sutures were obtained from 7 studies, which were not statistically significant. Data about first-degree lacerations and second-degree lacerations with sutures were available from 7 studies. The difference was not statistically significant. Data about third-degree lacerations or fourth-degree lacerations were available from 8 studies, and the data were not statistically significant (Supplementary Figure 2 ).
4. Discussion
Our study is the latest meta-analysis comparing the efficacy and safety of water birth and conventional child birth. We found that water delivery has clinical significance in alleviating the pain of mothers, promoting the safety of mothers and infants, and reducing postpartum complications.
At present, water delivery has been adopted in many areas because it plays a role in alleviating maternal pain and alleviating maternal anxiety. Many clinical studies have confirmed the pain relief effect of water delivery and mentioned that water delivery can enhance the safety of delivery [ 30 ]. But, some case reports suggest that water births are not all good. Water delivery can lead to serious complications in the newborn [ 31 ]. Therefore, the academic community for water delivery is mixed.
We have reviewed all published clinical studies and found that infants born in water had a higher five-minute Apgar score than infants born in conventional birth. That is, infants born in water scored better than infants born in conventional birth at five minutes. But, at the same time, babies born in water had lower one-minute Apgar scores than those born in a conventional way. In this regard, we speculate that water delivery will have a certain chance to lead to different degrees of neonatal asphyxia. The negative effects on newborns were reversed within five minutes of birth, and babies born in water were more active for five minutes after birth than those born in conventional delivery. We speculate that water delivery is just becoming popular, and the methods adopted in many areas are not necessarily appropriate and standardized, thus leading to the poor vitality of newborns in the first minute of birth. Happily, the rate of admission to the Neonatal Intensive Care Unit (NICU) was significantly lower among babies born in water than in conventionally born babies.
Our study found that water has a role in shortening the duration of labor. Water delivery can shorten the first, second, and third stages of labor. This may be related to maternal activity in the water, more relaxed muscles, and psychological factors. Water delivery can reduce the use of analgesics and the number of augmentation, suggesting that water delivery can make labor easier and reduce physical and mental pain. To our surprise, we found that water delivery significantly reduced the rate of dystocia. Although today's advanced technology has reduced the adverse events caused by the use of anesthesia and analgesics during childbirth to a very low level, the risks still exist. Therefore, the use of anesthesia in water delivery will greatly reduce the use of anesthesia and correspondently reduce the harm to the baby caused by anesthesia.
There was no statistically significant difference between water delivery and conventional delivery in terms of pelvic floor muscle injury. In terms of perineal sutures, we found no statistical difference between the two groups involved in most of these outcomes. Even in terms of first-degree lacerations and second-degree lacerations, the incidence of women delivering in water is higher than in women delivering in conventional childbirth. This indicates that water delivery has a weak protective effect on pelvic floor muscles and may even lead to more serious pelvic floor muscle and perineum damage due to the accelerated labor process. Due to the small number of included literature, further studies are needed. If water delivery does cause pelvic floor muscle damage and lacerations, it would be one of the few side effects of water delivery. Considering the benefits of water delivery, if we want to promote water delivery in more hospitals, we should make efforts to protect the pelvic floor muscles and perineum of women in the process of water delivery and take measures to minimize adverse reactions.
Our research has some advantages and limitations. For some outcomes, we included few available studies to make funnel plots to evaluate publication bias. In some funnel plots, we found certain publication bias. However, the studies we included were of high quality and included a large number of participants, so they were highly persuasive. At the same time, compared with the previously published meta-analysis, our study adds new research outcomes, which makes this meta-analysis more comprehensive, and has better clinical guidance significance.
In conclusion, although several limitations existed and further study is required, our study clearly elaborated the advantages and disadvantages of water delivery for mothers and babies and provided a better guiding value for follow-up clinical research.
5. Publication Bias
We tested the outcomes of more than seven included literature for publication bias and made funnel plots. For outcomes such as Apgar score <7 at 5 min of age, we found little publication bias (Supplementary Figure 3 ). For admission to the NICU, the publication bias was not significant (Supplementary Figure 4 ). For perineum intact or no sutures indicated, we found publication bias existed (Supplementary Figure 5 ). For first-degree lacerations or second-degree lacerations with sutures (Supplementary Figure 6 ) and third-degree lacerations or fourth-degree lacerations (Supplementary Figure 7 ), the publication bias was not significant. Thus, the publication bias in included studies of our meta-analysis was little.
6. Conclusions
Compared to the conventional birth group, the water birth group had a 28% lower risk of Apgar score <7 at 5 min of age to the control group. Also, the duration of labor was shorter in the water birth group whatever the labor stage was. The patients who underwent water birth showed an obviously lower risk of NICU admission. Compared with the conventional production group, the rate of episiotomy in the water production group decreased by 82% and the rate of no analgesics increased by 243%, indicating that water birth has alleviated labor pain in most mothers. The water birth group had an 83% lower risk of augmentation to the conventional birth group, and the data show that water birth makes it easier for mothers to deliver their babies. Furthermore, the water birth group had a 63% lower risk of dystocia compared to the conventional birth group, showing that the safety of delivery was improved.
In future, we are eager to extent to the proposed meta-analysis to other disciplines and preferably larger domain.
Data Availability
Conflicts of interest.
The authors declare that they have no conflicts of interest.
Authors' Contributions
Qiuhong Yang planned the study and collected all the suited articles. Guanran Zhang compiled the data and wrote the manuscript. Both of them checked the manuscript.
Supplementary Materials
Funnel plots and part of the forest plots are in the supplementary materials.

Hospital Waterbirth Tied to Less Pain, Increased Patient Satisfaction
S AN FRANCISCO -- People with low-risk pregnancies who opted for an inpatient waterbirth reported reduced pain and higher satisfaction, interim trial results revealed.
In the randomized controlled trial , people who had the option to give birth in an inflatable tub in a hospital room had lower levels of epidural or IV narcotic analgesia use compared to land birth (37.3% vs 82.8%, P <0.0001), reported Emily M. Malloy, PhD, CNM, of Advocate Aurora Health in Milwaukee, in a poster presentation at the American College of Obstetricians and Gynecologists (ACOG) annual meeting.
The waterbirth group also reported significantly higher levels of birth satisfaction, with a median score of 33 compared to land birth at a median of 29 ( P =0.009) on the U.S. Birth Satisfaction Scale Revised, which is a 10-question scale, using a 5-point Likert scale, with answers ranging from "strongly agree" to "strongly disagree."
"A lot of birthing people who don't want to use more traditional medications, like an epidural or an IV, do want some option for pain relief -- and warm water can be a great pain reliever ," Malloy told MedPage Today .
Malloy and colleagues wanted to see if waterbirth was feasible in a hospital setting. Malloy said hospital waterbirth is "something patients have been asking us for" but the hospital does not yet offer, in part because ACOG does not endorse it.
ACOG's current recommendations is that births occur on land, not water, since "there are insufficient data on which to draw conclusions regarding the relative benefits and risks of immersion in water during the second stage of labor and delivery."
Malloy said her group "wanted to do a patient-centered study that could contribute some information," about waterbirth, especially since most research has been retrospective and non-randomized.
Ultimately, the preliminary results "suggest that when offered to low-risk laboring people, hospital water birth reduces pain and increases satisfaction without leading to adverse events [AEs]," the researchers stated.
"People in waterbirth group were very satisfied with having the option, even if they didn't use it, and we had significantly less epidural use and IV narcotic use," Malloy said.
People with low-risk pregnancies between 25 and 34 weeks' gestation were enrolled beginning in January 2022. Of the 182 people enrolled, 157 have given birth and there have been no AEs thus far.
Participants were randomized 2:1 to either waterbirth or land birth. Land birth involved routine care with midwives and obstetricians, and waterbirth involved that same care plus the option to have a give birth in an inflatable tub in a hospital room. About half in the waterbirth group ended up actually giving birth in the water (52.2%).
Patients could opt for different pain relief at any point. If the patient developed risk factors such as hypertension, preterm labor, or non-vertex presentation, they were excluded. This left a total of 96 participants, with 67 in the waterbirth and 29 in the land-birth group.
Participants answered a validated satisfaction questionnaire postpartum. The primary outcome was intrapartum analgesia and anesthesia use and secondary outcomes were maternal and neonatal outcomes as well as maternal satisfaction.
Malloy said the single-study site and non-blind nature of the intervention, as well as only including patients who were open to the idea of waterbirth, were the primary study limitations. The estimated study completion date is December 2025.
Malloy and co-authors disclosed no relationships with industry.

- Follow us on Facebook
- Follow us on Twitter
- Criminal Justice
- Environment
- Politics & Government
- Race & Gender
Expert Commentary
How influencers and content creators discuss birth control on social media: What research shows
TikTok, YouTube and X are full of unsubstantiated claims about the side effects of hormonal contraceptives. Researchers are concerned about the effects of this misinformation.

Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
by Naseem S. Miller, The Journalist's Resource May 15, 2024
This <a target="_blank" href="https://journalistsresource.org/health/how-birth-control-is-discussed-on-social-media/">article</a> first appeared on <a target="_blank" href="https://journalistsresource.org">The Journalist's Resource</a> and is republished here under a Creative Commons license.<img src="https://journalistsresource.org/wp-content/uploads/2020/11/cropped-jr-favicon-150x150.png" style="width:1em;height:1em;margin-left:10px;">
News articles in recent weeks have documented the spread of misinformation about hormonal birth control methods on popular social media platforms like TikTok, YouTube and X, formerly called Twitter. Influencers with large and small followings are sharing unsubstantiated claims about the side effects of contraceptives, while directly or indirectly encouraging others to stop using them.
This trend has not escaped researchers, who for several years have been investigating what people who can get pregnant are posting on social media platforms about hormonal and non-hormonal birth control methods. Understanding the drivers of these trends is important because they have implications for policy and patient care, according to researchers . Some worry that during the post-Dobbs era , when there are continued strikes against reproductive rights in the U.S., misinformation about birth control on social media could have a negative influence on contraceptive preferences — potentially leading to more unwanted pregnancies.
More than 90% of women of reproductive age have used at least one contraceptive method, according to a 2023 report by the U.S. National Center for Health Statistics. However, the report also finds that the use of male condoms and withdrawal methods increased between 2006 and 2019, while the use of the birth control pill decreased. Non-hormonal contraception methods, including condoms, spermicides, withdrawal and menstrual cycle tracking, are 10% or less effective than hormonal contraceptives. The only exceptions are surgical sterilization and the copper intrauterine device.
To be sure, not all birth control-related content posted on social media platforms is negative, studies show. Health care professionals are sharing educational material with a high rate of engagement and non-health care professional users share their positive experiences with the birth control methods they use.
But as you will see in the studies curated below, researchers also find that social media users, including influencers, share inaccurate information about hormonal contraceptives on various social media platforms, discuss their discontinuation of birth control in favor of non-hormonal methods and engage in unsubstantiated fear-mongering of hormonal contraceptives.
Researchers also have learned that the content posted on social media platforms has changed in tone over time, mirroring the shift in the national political discourse.
In a 2021 study published in the American Journal of Obstetrics & Gynecology, researchers analyzed more than 800,000 English-language tweets mentioning at least one contraceptive method between March 2006, when Twitter was founded, and December 2019. They coded the sentiment of tweets as positive, neutral or negative.
“What we found over time was that the number of neutral tweets went down for each and every one of the birth control methods, and people became more polarized with regards to how they talk on these social media platforms over those 13 years,” says study co-author Dr. Deborah Bartz , an OB-GYN at Brigham and Women’s Hospital with expertise in complex family planning and an associate professor at Harvard Medical School.
In a February 2024 commentary in the Journal of Women’s Health, University of Delaware researchers Emily Pfender and Leah Fowler argue that ongoing dialogue about contraception on social media provides “a glimpse into public sentiment about available options” to people who can get pregnant.
The authors also note that misinformation and disinformation about hormonal contraception may have a larger effect on health disparities, especially among historically marginalized groups who may already mistrust the medical establishment.
“This may contribute to unintended pregnancy and delayed care, further widening health disparities and hindering progress toward equitable reproductive health outcomes,” Pfender and Fowler write.
Side effects
There are known side effects to hormonal birth control methods, including headaches, nausea, sore breasts and spotting. Most are mild and disappear with continued use or with switching to another method. Among hormonal contraceptives, only the Depo-Provera injection has been linked with weight gain , studies show .
But some social media influencers have spread false claims about the potential side effects of hormonal birth control methods, ranging from infertility to abortion to unattractiveness. Despite these false claims, physicians and professional organizations such as the American College of Obstetricians and Gynecologists find today’s contraceptive options safe and very effective .
“They’re about the most low-risk prescription that I give,” says Dr. Megana Dwarakanath, an adolescent medicine physician in Pittsburgh. “I always joke that if something goes wrong in someone’s life, they’re within the reproductive years, it always gets blamed on birth control.”
Dwarakanath says her young patients are most worried about two side effects: weight gain and mood. “Those are the things that they will almost always attribute to their birth control at a time that their bodies are also changing very rapidly,” she says. “Things like mental health diagnoses or personality disorders also tend to crop up during the time young people have started or have been on birth control.”
Most research on the link between oral contraceptives and cancer risk comes from observational studies, according to the National Cancer Institute . Overall, the studies have consistently shown that the risks of breast and cervical cancer are slightly increased for women who use oral contraceptives, whereas the risk of endometrial, ovarian and colorectal cancers are reduced.
The use of hormonal birth control has also been associated with an increase in the risk of developing blood clots, studies show . But that risk is not universal for everyone who takes hormonal birth control. This risk is higher for women 35 and older, those who smoke, are very overweight or have a history of cardiovascular disease. Overall, 3 to 9 out of 10,000 women who take the pill are at risk of developing blood clots within a given year. The risk for women who don’t take the pill is 1 to 5 out of 10,000.
There is no association between the pill and mood disorders, according to a large body of research, including a 2021 cohort study of nearly 740,000 young women.
It’s worth noting the dearth of research into women’s reproductive health due to chronic underfunding of women’s health research. An analysis of funding by the U.S. National Institutes of Health finds that in nearly three-quarters of the cases where a disease affects mainly one gender, the institute’s funding pattern favored males. Either the disease affected more women and was underfunded, or the disease affected more men and was overfunded, according to the 2021 study published in the Journal of Women’s Health.
Aside from underfunding, conducting robust research into the long-term effects of birth control is complex.
“Historically, people haven’t felt that it’s ethically OK to randomize people to birth control methods in large part because the outcome of unintended pregnancy is greater,” for people who are given the placebo, Bartz says.
Research on birth control misinformation on social media
Social media use is widespread among young adults. More than 90% of Americans between 18 and 29 reported ever using YouTube, while 78% said they had used Instagram, 62% used TikTok and 42% used Twitter, according to a 2023 survey of 5,733 U.S. adults by Pew Research Center .
These years overlap with the demographic of people who are most likely to use birth control. And because the use of contraceptives is less stigmatized today, people are more likely to talk with one another about their questions and concerns or share that information online.
In addition to investigating the general landscape of social media posts about birth control, researchers are also interested in the type of content influencers, who typically have 20,000 or more followers, post, because of their persuasive power over their audiences.
“When influencers disclose personal experiences and beliefs about various topics, audience members tend to form similar attitudes especially when they feel connected to the influencer,” Pfender and M. Marie Devlin write in a 2023 study published in the journal Health Communication.
Below we have curated several studies published in recent years documenting the spread of birth control misinformation on social media. The roundup is followed by a quick reference guide on female contraceptives and their actual potential side effects.
Contraceptive Content Shared on Social Media: An Analysis of Twitter Melody Huang, et al. Contraception and Reproductive Medicine, February 2024.
The study: The authors explore how contraceptive information is shared on X and understand how those posts affect women’s decisions. They analyze a random 1% of publicly available English-language tweets about reversible prescription contraceptive methods, from January 2014 and December 2019. The 4,434 analyzed tweets included at least 200 tweets per birth control method — IUDs, implants, the pill, patch and ring.
The findings: 26.7% of tweets about contraceptive methods discussed decision-making and 20.5% discussed side effects, especially the side effects of IUDs and the depot medroxyprogesterone acetate (DMPA or Depo-Provera) shot. Discussions about the pill, patch or ring prompted more discussions on logistics and adherence. About 6% of tweets explicitly requested information. Tweets about IUDs were most popular in terms of likes.
More importantly, 50.6% of the tweets were posted by contraceptive users, while only 6% came from official health or news sources. Tweets from news or journalistic sources were more frequent than tweets from a health care professional or organization.
Some tweets contained misinformation represented as facts, such as the unsubstantiated claim that IUDs can cause fertility issues. Others were outwardly misogynistic, shaming women and claiming that they wouldn’t be able to have kids because of using hormonal birth control.
One takeaway: “While Twitter may provide valuable insight, with more tweets being created by personal contraceptive users than official healthcare sources, the available information may vary in reliability. Asking patients about information from social media can help reaffirm to patients the importance of social networks in contraceptive decision-making while also addressing misconceptions to improve contraceptive counseling,” the authors write.
What Do Social Media Influencers Say About Birth Control? A Content Analysis of YouTube Vlogs About Birth Control Emily J. Pfender and M. Marie Devlin. Health Communication, January 2023.
The study : To explore what social media influencers shared on YouTube about their experiences with hormonal and non-hormonal methods of birth control, the researchers analyzed 50 vlogs posted between December 2019 and December 2021. Most of the 50 influencers were categorized on YouTube as Lifestyle (72%) and Fitness (16%). They had between 20,000 and 2.2 million subscribers each.
The findings : In total, 74% of the influencers talked about discontinuing hormonal birth control. About 44% said the main reason they were discontinuing birth control was to be more natural, while 32% said they wanted to improve their mental health and 20% were concerned about weight gain.
Forty percent of influencers mentioned using non-hormonal birth control methods such as menstrual cycle tracking, condoms, non-hormonal IUDs and the pull-out method. Twenty percent reported switching from hormonal to non-hormonal methods.
One takeaway : “Our content analysis revealed that discontinuation of hormonal birth control is commonly discussed among [social media influencers] on YouTube and sexual health information from influencers might not provide accurate educational information and tools… this is especially concerning given that social media is young adults’ primary tool for sexual health information. Future research is needed to understand the effects of SMI birth control content on sexual health behaviors,” the authors write.
Hormonal Contraceptive Side Effects and Nonhormonal Alternatives on TikTok: A Content Analysis Emily J. Pfender, Kate Tsiandoulas, Stephanie R. Morain and Leah R. Fowler. Health Promotion Practice, January 2024.
The study : The authors analyzed the content of 100 TikTok videos that used the hashtags #birthcontrolsideeffects and #nonhormonalcontraception. Their goal was to understand the types of content about side effects of hormonal and non-hormonal contraceptives on TikTok.
The findings : The videos averaged about 1 minute and garnered an average of 27,795 likes, 251 comments and 623 shares. For #birthcontrolsideeffects, 80% of the audience was 18 to 24 years old and videos with that hashtag had 43 million views worldwide as of July 7, 2023.
Thirty-two percent of the videos were by regular users (non-influencers), 26 by clinicians, 13% by health coaches and 2% by companies. Only 3% had a sponsorship disclosure and 6% included a medical disclaimer, that the person was not a doctor or was not providing medical advice.
Most of the 100 videos (71%) mentioned hormonal contraception. Among them 51% discussed unspecific hormonal contraceptives, 31% talked about the pill and 11% about hormonal IUDs. Four of the 71 creators explicitly recommended against using hormonal contraceptives.
Claims about hormonal contraceptives were mostly based on personal experience. About 25% of the creators cited no basis for their claims, 23% included outside evidence, including unspecified studies or information from the FDA insert, and 11% used a combination of personal and outside evidence.
Almost half (49%) mentioned discontinuing their hormonal contraception, with negative side effects cited as the most common reason.
The creators talked about mental health issues, weight gain, headaches, and less common risks of various cancers or chronic illness, change in personality and blood clots. They were less likely to mention the positive aspects of birth control.
About 52% of videos mentioned non-hormonal contraception, including copper IUDs and cycle tracking.
Nine of the 100 creators expressed feeling dismissed, pressured, gaslit or insufficiently informed about contraception by medical providers.
One takeaway : “Our findings support earlier work suggesting social media may fuel ‘hormonophobia,’ or negative framing and scaremongering about hormonal contraception and that this phobia is largely driven by claims of personal experience rather than scientific evidence,” the authors write. “Within these hashtag categories, TikTok creators frame their provider interactions negatively. Many indicate feeling ignored or upset after medical appointments, not sufficiently informed about contraceptive options, and pressured to use hormonal contraceptives. This finding aligns with previous social media research and among the general population, suggesting opportunities for improvements in contraceptive counseling.”
Popular Contraception Videos on TikTok: An Assessment of Content Topics Rachel E. Stoddard, et al. Contraception, January 2024.
The study : Researchers analyzed 700 English-language TikTok videos related to hormonal contraception, with a total of 1.2 billion views and 1.5 million comments, posted between October 2019 and December 2021. Their aim was to explore the types of contraception content on TikTok and to understand how the platform influences the information patients take into birth control counseling visits.
The findings : More than half of the videos (52%) were about patient experiences and how to use contraceptives. Other common topics included side effects (35%) and pregnancy (39%).
Only 19% of the videos were created by health care professionals, including midwives, physician assistants and medical doctors, although those videos garnered 41% of the total views, indicating higher engagement. While 93% of health care providers shared educational content, 23% of non-health care providers shared educational content.
One takeaway : “Our findings show an exceptional opportunity for education around contraception for young reproductive-aged individuals, given the accessibility and popularity of these videos. This may also extend to other topics around sex education and family planning, including sexually transmitted infection prevention and treatment and procuring abortion care,” the authors write.
TikTok, #IUD, and User Experience With Intrauterine Devices Reported on Social Media Jenny Wu, Esmé Trahair, Megan Happ and Jonas Swartz. Obstetrics & Gynecology, January 2023.
The study : Researchers used a web-scraping application to collect the top 100 TikTok videos tagged #IUD on April 6, 2022, based on views, comments, likes and shares. Their aim was to understand the perspectives and experiences of people with IUDs shared on TikTok. The videos had a total of 471 million views, 32 million likes and 1 million shares. Their average length was 33 seconds.
The findings : Some 89% of the creators identified as female and nearly 90% were from the United States; 37% were health care professionals; and 78% were 21 years or older.
Video types included patients’ own experiences with IUD removal (32%), educational (30%) and humorous (25%). More videos (38%) had a negative tone compared with 19% with a positive tone. The videos that portrayed negative user experiences emphasized pain and distrust of health care professionals.
Half of the videos were very accurate, while nearly a quarter were inaccurate (the authors did not use the term misinformation).
One takeaway : “The most liked #IUD videos on TikTok portray negative experiences related to pain and informed consent. Awareness of this content can help health care professionals shape education given the high prevalence of TikTok use among patients,” the authors write. “TikTok differs from other platforms because users primarily engage with an algorithmically curated feed individualized to the user’s interests and demographics.”
Types of female birth control
Most female hormonal contraceptives contain the synthetic version of natural female hormones estrogen and progesterone. They affect women’s hormone levels , preventing mature eggs from being released by the ovaries, a process that’s known as ovulation, hence, preventing a possible pregnancy.
Of the two hormones, progesterone (called progestin in synthetic form) is primarily responsible for preventing pregnancy. In addition to playing a role in preventing ovulation, progesterone inhibits sperm from penetrating through the cervix. Estrogen inhibits the development of follicles in the ovaries.
The information below is sourced from the CDC , the National Library of Medicine , the Cleveland Clinic and the Mayo Clinic .
Intrauterine contraception
Also called Long-Acting Reversible Contraception, or LARC, this method works by thickening the cervical mucus so the sperm can’t reach an egg. There are two types of IUDs: hormonal and non-hormonal.
- Levonorgestrel intrauterine system is a T-shaped device that’s placed inside the uterus by a doctor. It releases a small amount of progestin daily to prevent pregnancy. It can stay in place for 3 to 8 years. Its failure rate is 0.1% to 0.4%.
- Copper T intrauterine device is also T-shaped and is placed inside the uterus by a doctor. It does not contain hormones and can stay in place for up to 10 years. Its failure rate is 0.8%.
- Side effects: Copper IUDs may cause more painful and heavy periods, while progestin IUDs may cause irregular bleeding. In the very rare cases of pregnancy while having an IUD, there’s a greater chance of an ectopic pregnancy, which is when a fertilized egg grows outside of the uterus.
Hormonal methods
- The implant is a single, thin rod that’s inserted under the skin of the upper arm. It releases progestin over 3 years. Its failure rate is 0.1%, making it the most effective form of contraception available.
- Side effects : The most common side effect of an implant is irregular bleeding.
- The injection Depo-Provera or “shot” or “Depo” delivers progestin in the buttocks or arms every three months at the doctor’s office. Its failure rate is 4%.
- Side effects : The shot may cause irregular bleeding. The shot is also the only contraceptive that may cause weight gain. It may also be more difficult to predict when fertility returns once the shot is stopped.
- Combined oral contraceptives or “the pill” contain estrogen and progestin. They’re prescribed by a doctor. The pill has to be taken at the same time daily. The pill is not recommended for people who are older than 35 and smoke, have a history of blood clots or breast cancer. Its failure rate is 7%. Among women aged 15 to 44 who use contraception, about 25% use the pill .
- The skin patch is worn on the lower abdomen, buttocks or upper body, releasing progestin and estrogen. It is prescribed by a doctor. A new patch is used once a week for three weeks. No patch is worn for the fourth week. Its failure rate is 7%.
- Hormonal vaginal contraceptive ring releases progestin and estrogen. It’s placed inside the vagina. It is worn for three weeks and taken out on the fourth week. Its typical failure rate is 7%.
- Side effects : Contraceptives with estrogen, including the pill, the patch and the ring, increase the risk of developing blood clots.
- Progestin-only pill or “mini-pill” only has progestin and is prescribed by a doctor. It has to be taken daily at the same time. It may be a good option for women who can’t take estrogen. Its typical failure rate is 7%.
- Opill is the first over-the-counter daily oral contraceptive in the U.S., approved by the Food and Drug Administration in 2023. Opill only has progestin and like other birth control pills, it has to be taken at the same time every day. It should not be used by those who have or have had breast cancer. Its failure rate is 7%.
- Side effects : The most common side effect of progestin-only pills is irregular bleeding, although the bleeding tends to be light.
Non-hormonal birth control methods include using barriers such as a diaphragm or sponge, condoms and spermicides, withdrawal, and menstrual cycle tracking. Emergency contraception, including emergency contraception pills (the morning-after pill), is not a regular method of birth control.
Additional research studies to consider
Population Attitudes Toward Contraceptive Methods Over Time on a Social Media Platform Allison A. Merz, et al. American Journal of Obstetrics & Gynecology, December 2020.
Social Media and the Intrauterine Device: A YouTube Content Analysis Brian T. Nguyen and Allison J. Allen. BMJ Sexual and Reproductive Health, November 2017.
About The Author
Naseem S. Miller
Pregnant? Researchers want you to know something about fluoride

- Show more sharing options
- Copy Link URL Copied!
Adding fluoride to drinking water is widely considered a triumph of public health. The Centers for Disease Control and Prevention says the cavity-prevention strategy ranks alongside the development of vaccines and the recognition of tobacco’s dangers as signal achievements of the 20th century .
But new evidence from Los Angeles mothers and their preschool-age children suggests community water fluoridation may have a downside.
A study published Monday in JAMA Network Open links prenatal exposure to the mineral with an increased risk of neurobehavioral problems at age 3, including symptoms that characterize autism spectrum disorder. The association was seen among women who consumed fluoride in amounts that are considered typical in Los Angeles and across the country.
The findings do not show that drinking fluoridated water causes autism or any other behavioral conditions. Nor is it clear whether the relationship between fluoride exposure and the problems seen in the L.A.-area children — a cohort that is predominantly low-income and 80% Latino — would extend to other demographic groups.
However, the results are concerning enough that USC epidemiologist Tracy Bastain said she would advise pregnant people to avoid fluoridated water straight from the tap and drink filtered water instead.
“This exposure can impact the developing fetus,” said Bastain, the study’s senior author. “Eliminating that from drinking water is probably a good practice.”

Science & Medicine
A UCLA doctor is on a quest to free modern medicine from a Nazi-tainted anatomy book
Dr. Kalyanam Shivkumar wants to surpass the anatomical atlas created by a fervent supporter of the Nazi regime whose work was fueled by the dead bodies of its victims.
May 20, 2024
About 63% of Americans receive fluoridated water through their taps, including 73% of those served by community water systems, according to the CDC . In Los Angeles County, 62% of residents get fluoridated water, the Department of Public Health says.
The data analyzed by Bastain and her colleagues came from participants in an ongoing USC research project called Maternal and Developmental Risks from Environmental and Social Stressors , or MADRES. Women receiving prenatal care from clinics in Central and South Los Angeles that cater to low-income patients with Medi-Cal insurance were invited to join.
Between 2017 and 2020, 229 mothers took a test to measure the concentration of fluoride in their urine during their third trimester of pregnancy. Then, between 2020 and 2023, they completed a 99-question survey to assess their child’s behavior when their sons and daughters were 3 years old.
Among other things, the survey asked mothers whether their children were restless, hyperactive, impatient, clingy or accident-prone. It also asked about specific behaviors, such as resisting bedtime or sleeping alone, chewing on things that aren’t edible, holding their breath, and being overly concerned with neatness or cleanliness.
Some of the questions the mothers answered addressed health problems with no obvious medical cause, including headaches, cramps, nausea and skin rashes.
Among the 229 children — 116 girls and 113 boys — 35 were found to have a collection of symptoms that put them in the clinical or borderline clinical range for inward-focused problems such as sadness, depression and anxiety. In addition, 23 were in the clinical or borderline clinical range for behaviors directed at others, such as shouting in a classroom or attacking other kids, and 32 were deemed at least borderline clinical for a combination of inward and outward problems.
What interested the researchers was whether there was any correlation between a child’s risk of having clinical or borderline clinical behavioral problems and the amount of fluoride in his or her mother’s urine during pregnancy.
They found that compared to women whose fluoride levels placed them at the 25th percentile — meaning 24% of women in the study had levels lower than theirs — women at the 75th percentile were 83% more likely to have their child score in the “clinical” or “borderline clinical” range for inward and outward problems combined. When the researchers narrowed their focus to children in the clinical range only, that risk increased to 84%, according to the study.
The researchers also found that the same increase in fluoride levels was associated with an 18.5% increase in a child’s symptoms related to autism spectrum disorder, as well as an 11.3% increase in symptoms of anxiety.

What military doctors can teach us about power in the United States
A study of interactions between military doctors and patients of various ranks confirms that people with higher status get resources at other people’s expense.
May 16, 2024
The amount of fluoride needed for mothers to go from the 25th to the 75th percentile was 0.68 milligrams per liter. As it happens, that’s nearly identical to the 0.7 mg per liter standard that federal regulators say is optimal for preventing tooth decay.
Bastain said that allowed the researchers to compare what might happen to children in two parallel universes: a typical one where their mothers consumed fluoridated water during pregnancy, and an alternate one where they didn’t.
“You can use it as a proxy for if they lived in a fluoridated community or not,” she said.
What that thought experiment shows is that children in the fluoridated community face a higher level of risk. That said, it’s not clear when that risk becomes high enough to be worrisome.
“We don’t know what the safe threshold is,” Bastain said. “It’s not like you can say that as long as you’re under the 75th percentile, there are no effects.”
The study authors’ concerns about the effects of fluoride on developing brains didn’t come out of nowhere.
The National Toxicology Program — a joint effort of the CDC, the National Institutes of Health, and the Food and Drug Administration — has been investigating the issue since 2016. In a report last year that reviewed an array of evidence from humans and laboratory animals, a working group concluded “with moderate confidence” that overall fluoride exposure at levels at or above 1.5 mg per liter “is consistently associated with lower IQ in children.”

‘Miracle’ weight-loss drugs could have reduced health disparities. Instead they got worse
Ozempic and other drugs raised the possibility of reversing the country’s obesity crisis. Doctors are frustrated that they’ve made health disparities worse.
April 15, 2024
The working group added that “more studies are needed to fully understand the potential for lower fluoride exposure to affect children’s IQ.”
A 2019 study of hundreds of mothers in Canada — where 39% of residents have fluoridated water — found that a 1-mg increase in daily fluoride intake during pregnancy was associated with a 3.7-point reduction in IQ scores in their 3- and 4-year-old children.
And among hundreds of pregnant women in Mexico, a 0.5-mg-per-liter increase in urinary fluoride went along with a 2.5-point drop in IQ scores for their 6- to 12-year-old children, researchers reported in 2017 .
Bastain and her colleagues write their study is the first they are aware of that examines the link between prenatal fluoride exposure and neurobehavioral outcomes in children in the United States. The results are sure to be controversial, Bastain said, but there’s a straightforward way for pregnant people to reduce the possible risk.
“It’s a pretty easy intervention to get one of those tabletop plastic pitchers ” that filter out metals, she said. “Most of them do a pretty good job of filtering out fluoride.”
More to Read

Drownings rose among young children after decades of decline. It’s ‘highly concerning,’ CDC says
May 14, 2024

Children of Flint water crisis make change as young environmental and health activists
April 22, 2024

Santa Monica school expansion delayed by toxic dry cleaning chemicals in soil

Karen Kaplan covers science and medical research for the Los Angeles Times. She has been a member of the science team since 2005, including 13 years as an editor. Her first decade at The Times was spent covering technology in the Business section as both a reporter and editor. She grew up in San Diego and is a graduate of MIT and Columbia University.
More From the Los Angeles Times

Pro-Palestinian protesters move UC Santa Cruz encampment, join striking workers

Indigenous tribe sues L.A. County, archdiocese over the ‘desecration’ of more than 100 graves

Red Lobster, an icon of casual American dining, files for bankruptcy

Column: In a major rebuke to Exxon Mobil, CalPERS will vote against its entire board

IMAGES
VIDEO
COMMENTS
Of the 20,642 articles identified, 52 were included in the meta-analyses. Based on data from observational studies, water birth was not associated with increased probability of maternal infection compared with land birth (10 articles, 113,395 pregnancies; odds ratio, 0.93; 95% confidence interval, 0.76-1.14).
Water birth vs land birth: a systematic review and meta-analysis. Am J Obstet Gynecol 2024. Download : Download high ... the analysis revealed this finding was stable for many outcomes and is unlikely to change with future research. As such, water immersion during second stage may be considered a safe non-pharmacologic method for managing labor ...
Waterbirth is widely available in English maternity settings for women who are not at increased risk of complications during labour. Immersion in water during labour is associated with a number of maternal benefits. However for birth in water the situation is less clear, with conclusive evidence on safety lacking and little known about the characteristics of women who give birth in water.
Objective: This systematic review and meta-analysis aimed to conduct a thorough and contemporary assessment of maternal and neonatal outcomes associated with water birth in comparison with land-based birth. Data sources: We conducted a comprehensive search of PubMed, EMBASE, CINAHL, and gray literature sources, from inception to February 28, 2023.
The 2014 objection to birth in water voiced by both the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) in ACOG Bulletin #594 on immersion in water during labor and birth is nothing new. The Committee on Fetus and Newborn published the very same opinion in 2005, based on a case report that was published in 2002 in the journal Pediatrics.
The calculated cord avulsion rate is 2.4 per 1000 waterbirths; it is unknown how this compares to conventional birth due to a lack of data that permits direct comparison. Discussion: The majority of waterbirth research to date is observational and descriptive; thus, reported outcomes do not demonstrate causal associations. However, existing ...
The qualitative studies yielded three key themes: 1) reasons identified by women and midwives for choosing a water birth, 2) benefits experienced in water births, and 3) barriers and facilitators of water immersion during childbirth. The evidence from qualitative studies indicates that women report benefits associated with water birth.
The study shows that water births provide clear benefits for mothers and their babies, with fewer complications than standard care methods. The new research involving Hall is receiving significant attention from medical professionals and media sources such as "Good Morning America.". Water birth is when a woman in labor gives birth in a ...
Water immersion in labor and birth is a valuable strategy for pain relief, associated with a significant reduction in the use of epidural anesthesia (Cluett and Burns, 2009). Water immersion has the potential to reduce the cost of care and provide women who want physiologic births with an effective tool for non-pharmacological pain management.
Using meta-ethnography, qualitative research studies were analysed and synthesised using the method of 'reciprocal translational analysis' identifying themes relating to women's experiences of birthing in water. Findings: Four themes were identified: women's knowledge of waterbirth; women's perception of physiological birth; water, autonomy and ...
Water immersion during the second stage of labour including delivery: still undetermined safety levels. The Royal College of Obstetricians and Gynecologists and the Royal College of Midwives, in a Joint Statement issued in 2009, reported that the evidence to support underwater birth is less clear, but complications are apparently rare ().Committee Opinions n°679 from the American College of ...
Researchers use the term land birth or conventional birth to refer to a birth in which the baby is born on dry land—not in a tub.And the word hydrotherapy can be used to describe the therapeutic use of water during labor and/or birth.. Waterbirth was first reported in an 1805 medical journal and became more popular in the 1980s and 1990s.
Introduction Approximately 60 000 (9/100) infants are born into water annually in the UK and this is likely to increase. Case reports identified infants with water inhalation or sepsis following birth in water and there is a concern that women giving birth in water may sustain more complex perineal trauma. There have not been studies large enough to show whether waterbirth increases these poor ...
Giving birth in water did not appear to affect mode of birth, or the number of women having a serious perineal tear. This review found no evidence that labouring in water increases the risk of an adverse outcome for women or their newborns. ... Research is also needed about women's and caregivers experiences of labour and birth in water. If ...
Research implications. Water immersion during labour and birth is a low-tech yet complex, nuanced intervention. We suggest that studies incorporate the following fundamentals to advance the evidence: birth pool description, clearly described maternal and obstetric characteristics, the birth setting, the care model and use of standardised ...
Many women seek alternative birth methods, including water immersion for labor and birth, which several hospitals now offer. Although thousands of water births have occurred with few adverse outcomes documented, research findings on water birth have been sparce and mixed, and further study is necessary. Clinicians should discuss the potential risks and benefits of water birth and utilize ...
Water birth is the process of laboring and/or giving birth in a tub of warm water. Many women find that sitting or floating in water during labor helps them relax and manage pain. Some women choose to give birth in the water. Others only labor in the tub. At OHSU, water birth is an option only if you choose delivery with our highly skilled ...
Although thousands of water births have occurred with few adverse outcomes documented, research findings on water birth have been sparce and mixed, and further study is necessary. Clinicians should discuss the potential risks and benefits of water birth and utilize informed decision-making with women desiring this option. With careful selection ...
The research showed that women having a water birth in a hospital obstetric unit had fewer medical interventions and complications during and after the birth. Commenting on the research, Clare Livingstone, Professional Policy Advisor at the RCM, said: "This is really good news for women choosing to have a water birth or thinking of having one.
September 20, 2023. There are many research studies demonstrating the benefits of water for labour and birth. We have evidence from research involving hundreds of thousands of women and babies that using water for labour and birth is safe and leads to good outcomes. Using water also brings advantages, including less need for other kinds of pain ...
Background: Waterbirth is widely available in English maternity settings for women who are not at increased risk of complications during labour. Immersion in water during labour is associated with a number of maternal benefits. However for birth in water the situation is less clear, with conclusive evidence on safety lacking and little known about the characteristics of women who give birth in ...
The water birth group had an 83% lower risk of augmentation to the conventional birth group, and the data show that water birth makes it easier for mothers to deliver their babies. Furthermore, the water birth group had a 63% lower risk of dystocia compared to the conventional birth group, showing that the safety of delivery was improved.
The waterbirth group also reported significantly higher levels of birth satisfaction, with a median score of 33 compared to land birth at a median of 29 (P=0.009) on the U.S. Birth Satisfaction ...
Water birth is a method of pain relief during labor associated with decreased pain and increased satisfaction. Randomized control trials (RCTs) about water birth and safety outcomes are needed. We conducted an RCT of hospital water birth versus land birth to compare maternal/neonatal outcomes, and differences in analgesia/anesthesia use. ...
The study: To explore what social media influencers shared on YouTube about their experiences with hormonal and non-hormonal methods of birth control, the researchers analyzed 50 vlogs posted between December 2019 and December 2021. Most of the 50 influencers were categorized on YouTube as Lifestyle (72%) and Fitness (16%).
Background: There is a lack of research on the relationship between water fluoridation and pregnancy outcomes. Objectives: We assessed whether hypothetical interventions to reduce fluoride levels would improve birth outcomes in California. Methods: We linked California birth records from 2000 to 2018 to annual average fluoride levels by community water system. Fluoride levels were collected ...
Method . This qualitative study was conducted with 14 mothers who had a vaginal birth with midwives and recommended it to other women. The data were collected using an in-depth interview form and analysed with the thematic analysis technique.
The number of people experiencing poor health and early death caused by metabolism-related risk factors such as high blood pressure, high blood sugar, and high BMI has increased by 50% since 2000, reveals new global study. Last updated. May 16, 2024. News release.
The Night Calver. By Darby Minow Smith & Siri Kaur. May 17, 2024. A prodigal daughter moves from NYC back to Montana to help her family's cattle give birth. At the beginning of March, I began a 32-day shift that started each evening at 7 and ended the next morning at 5. I spent all my waking hours with cattle.
A 2019 study of hundreds of mothers in Canada — where 39% of residents have fluoridated water — found that a 1-mg increase in daily fluoride intake during pregnancy was associated with a 3.7 ...