- Skip to Nav
- Skip to Main
- Skip to Footer


Why PE matters for student academics and wellness right now
Please try again

This story about PE teachers was produced by The Hechinger Report , a nonprofit, independent news organization focused on inequality and innovation in education. Sign up for Hechinger’s newsletter .
Amanda Amtmanis, an elementary physical education instructor in Middletown, Connecticut, handed out cards with QR codes to a class of third graders, and told them to start running.
The kids sprinted off around the baseball field in a light drizzle, but by the end of the first lap, a fifth of a mile, many were winded and walking. They paused to scan the cards, which track their mileage, on their teacher’s iPad and got some encouragement from an electronic coach — “Way to run your socks off!” or “Leave it all on the track!”
A boy in a red Nike shirt surged ahead, telling Amtmanis his goal was to run 5 miles. “Whoa, look at Dominic!” another boy exclaimed.
“We don’t need to compare ourselves to others,” Amtmanis reminded him.

The third graders finished a third lap, alternating running and walking, and were about to start on a scavenger hunt when the rain picked up, forcing them inside. Amtmanis thanked her students for their willingness to adjust — a skill many of them have practiced far more often than running these past 18 months.
The full impact of the pandemic on kids’ health and fitness won’t be known for some time. But it’s already caused at least a short-term spike in childhood obesity Rates of overweight and obesity in 5- through 11-year-olds rose nearly 10 percentage points in the first few months of 2020.
Amtmanis’ “mileage club,” which tracks students’ running, both in and out of school, and rewards them with Pokémon cards when they hit certain targets, is an example of how PE teachers around the country are trying to get kids back in shape.
But inclement weather isn’t the only thing PE teachers are up against as they confront what might be called “physical learning loss.” Physical education as a discipline has long fought to be taken as seriously as its academic counterparts. Even before the pandemic, fewer than half the states set any minimum amount of time for students to participate in physical education, according to the Society of Health and Physical Educators (SHAPE), which represents PE and health instructors.
Now, as schools scramble to help kids catch up academically, there are signs that PE is taking a back seat to the core subjects yet again. In some California schools, administrators are shifting instructional minutes from PE to academic subjects — or canceling class altogether so PE teachers can sub for classroom teachers; in others, they’re growing class sizes in the gym, so they can shrink them in the classroom.
Meanwhile, innovative instructors like Amtmanis, who has worked in her district for more than 20 years, are struggling to get their ideas off the ground. Over the summer, the principal of Macdonough Elementary, one of two schools where Amtmanis teaches, approved her request to participate in another running program called The Daily Mile, in which kids walk or run 15 minutes a day during school hours.
Daily running breaks “boost attentiveness, which has positive effects on academics,” Amtmanis argued.
But two weeks into the school year, not a single teacher had bought into the idea.
“The issue is their packed schedule,” Amtmanis said.
Last year, many schools conducted gym class remotely, with students joining in from their bedrooms and living rooms.
The online format presented several challenges. Many students lacked the equipment, space, or parental support to participate fully. And many instructors grappled with how to teach and assess motor skills and teamwork online.
Though instructors found creative ways to keep students moving — substituting rolled-up socks for balls, and “disguising fitness” in scavenger hunts and beat-the-teacher challenges — they still fretted that online gym wasn’t giving students the same benefits as in-person classes.
Compounding their concern was the fact that many students were also missing out on recess and extracurricular sports.
In a March 2021 survey conducted by the Cooper Institute, maker of the popular FitnessGram assessments, close to half the PE teachers and school and district administrators responding said their students were “significantly less” physically active during their schools’ closure than before it.
Schools that reopened last year faced their own set of challenges, including bans on shared equipment that made even a simple game of catch impossible. Schools that were open for in-person learning were also much more likely to cut back on PE instructional time, or eliminate it altogether, the survey found.
The consequences of these reductions in physical activity are hard to quantify, especially since many schools suspended fitness testing during the pandemic and have yet to resume it, but some PE teachers say they’re seeing more kids with locomotor delays and weaker stamina than normal.
“The second graders are like first graders, and some are even like kindergarteners,” said Robin Richardson, an elementary PE instructor in Kentucky. They can jump and hop, she said, but they can’t leap. They’re exhausted after 20 seconds of jumping jacks.
An unusually high number of Richardson’s first graders can’t skip or do windmills. Some lack the spatial awareness that’s essential to group games.
“They don’t know how to move without running into each other,” she said.
Other instructors are seeing an increase in cognitive issues, such as difficulty paying attention or following directions, particularly among kids who remained remote for most or all of last year.
Kyle Bragg, an elementary PE instructor in Arizona, has seen kids sitting with their backs to him, staring off into space when he’s talking. “I say ‘Knees, please,’ so they spin around to face me,” he said.
And some PE teachers say their students’ social-emotional skills have suffered more than their gross motor skills. “They forgot how to share; how to be nice to each other; how to relate to each other,” said Donn Tobin, an elementary PE instructor in New York.
PE has a key role to play in boosting those skills, which affect how kids interact in other classes, said Will Potter, an elementary PE teacher in California.
“We’re uniquely situated to handle the social-emotional needs that came out of the pandemic, in a way classroom teachers are not,” Potter said.

Amtmanis, for her part, worries about her students’ mental health. She sees the little signs of strain daily — the kid who got upset because he couldn’t pick his group, for example, and the one who was distressed that his Mileage Club card had gotten mixed up in the front office.
“Their emotional reserves are low,” she said.
Yet not all instructors are reporting drops in their students’ fitness and skill development. Teachers in some middle- and upper-income districts said they haven’t noticed much of a change at all. In some communities, families seemed to spend more time outdoors.
“We saw the skyrocketing sale of bicycles, we saw families going for walks,” said Dianne Wilson-Graham, executive director of the California Physical Education and Health Project.
But in Title I schools like Macdonough, where more than half the students are low-income, some kids didn’t even have access to a safe place to exercise or play during school closures.
“Not only are they not in soccer leagues, but sometimes they don’t even have a park,” Amtmanis said.
Amtmanis came up with the idea of doing the Daily Mile after spring fitness tests revealed drops in her students’ strength, flexibility and endurance.
But many schools still aren’t sure how much physical learning loss their students have experienced as a result of the pandemic. Most schools pressed pause on fitness testing last year, and some elementary-school instructors are reluctant to restart it. They say the tests aren’t valid with young children, even in ordinary times, and argue the time they take could be better spent on Covid catch-up.
Andjelka Pavlovic, director of research and education for the Cooper Institute, said its tests are scientifically proven to be valid for students who are 10 and up, or roughly starting in fourth grade.
Fitness testing requirements vary by state, county or even district. Some states specify how often students must be tested; others leave it largely to the teacher.
Bragg, the Arizona teacher, said he has put testing “on the backburner” because “right now it’s not at the forefront of what’s important.”
Richardson said she is avoiding testing because she doesn’t want to use up precious instructional time or demoralize her students. “I want my kids to enjoy movement,” she said. If they perform poorly on the tests, “they may not feel as strong.”
In Connecticut, where schools are required to test fourth graders’ fitness annually, Amtmanis approached testing cautiously last year. She didn’t want to embarrass her students, so she made it into a series of games.
Instead of Sit-and-Reach, they had a “flexibility contest,” in which kids broke into teams for tag then had to perform stretches if they were tagged. She measured the distances stretched with curling ribbon, tied the ribbons together, and attached a balloon to the end. The team whose balloon soared the highest won fidget putty.
Pushups became a Bingo game, with the center space representing pushups.
“My goal was to get through it without ever using the words ‘fitness” or ‘testing,’” she said.
As the pandemic drags on, some instructors are taking a similar approach to fitness remediation and acceleration.
Bragg likes a warmup called “ Touch Spots ,” in which first graders listen as the instructor reads off the name of a color, then run and touch a corresponding dot on the floor. It works on reaction time, cardiovascular endurance, spatial awareness and sequencing — but the kids don’t know that.
“Students are having so much fun that they don’t realize how much fitness they are doing,” Bragg said.
Differentiation — tailoring instruction to meet individual students’ needs — has become even more essential, with former remote learners often lagging behind their in-person peers, Bragg said.
When playing catch, for example, he offers his students different sized balls — the smaller ones are more challenging.
Potter, the California teacher, spent the first two weeks of school teaching his students how to connect with their partners, stressing the importance of eye contact and body language.
“When you’re on Zoom, you look at the camera to make eye contact,” he said. “It’s a very different environment.”
Bragg reminds his students how to include kids who are standing on the sidelines, modeling excited body language and tone of voice. Lately, he’s noticed that kids who were remote last year are being excluded from groups.
“Social interaction needs to be practiced, just like how to throw a ball,” he said.
Richardson, the Kentucky PE teacher, is trying to build up her students’ stamina gradually, through progressively longer intervals of exercise.
But she works in a school with pods, so she sees each group of kids for five consecutive days, every third week. The two weeks in between, she has to hope that teachers will provide recess and “movement breaks.” She’s trying to get them to give kids breaks “when they get glassy-eyed and frustrated.”
Recently, Richardson was at a staff training session at which depleted teachers were “popping candy in the back.” When she raised her hand and requested a break in the training, her colleagues cheered. She told them to remember how they felt when their students return to the building.
“I always say, ‘If your bum is numb, your brain is the same,’” she said.
Convincing classroom teachers to set aside more time for movement can be challenging, though. As students return from months of online learning, teachers are under enormous pressure to get them caught up academically.
Kate Cox, an elementary and middle-school PE teacher in California, wishes schools would “realize what they’re missing when they cut PE because of learning loss in other areas.” Physical education is “readying their minds and bodies to be more successful in other areas,” Cox said.
Terri Drain, the president of SHAPE, argued that schools fail students when they treat physical learning loss as less serious than its academic counterpart.
“In the primary grades, children develop fundamental motor skills, such as throwing, catching, running, kicking and jumping,” she said. Unless schools commit to helping kids catch up, “the impacts of this ‘missed learning’ will be lifelong.”

In Connecticut, Amtmanis hasn’t given up on convincing teachers to carve out time for the Daily Mile. She recently sent them a list of suggestions on how to fit 15 minutes of running into the day, including by incorporating it as an active transition between academic blocks.
“While it may seem like there aren’t minutes to spare,” she wrote, “the energizing effect of the active transition should result in more on-task behavior and more efficient working.”
In the meantime, Amtmanis plans to keep using the mileage club to motivate her students to run and to monitor their progress.
“I don’t want to call attention to the fact that not everyone is fit,” she said. “This is an unobtrusive way to keep the data.”

35 Fun and Effective PE Exercises for Dynamic Physical Education Classes
Looking for PE exercises that are both enjoyable and effective? Our guide delivers 35 varied activities perfect for energizing students and enriching your physical education classes. Experience an array of PE exercises, from fluid warm-up routines to imaginative obstacle courses, all designed to foster enthusiasm and physical well-being without complicated setups. Ideal for educators seeking practical, inclusive exercises, this guide is your ticket to enlivened gym classes that students will anticipate with excitement.
Table of Contents
Key Takeaways
- Make sure to kick off PE classes with energizing warm-ups like the Jumping Jack PE Game, as they prepare students mentally and physically for the activities ahead, enhance coordination, and build enthusiasm.
- Get creative with obstacle courses and classic games by adding unique tweaks that ensure safety, boost engagement, and teach valuable skills like teamwork, coordination, and strategic thinking.
- Use varying exercises during circuit training and finish with cool-downs and reflection to ensure students of all fitness levels are engaged, prevent post-exercise issues, and discuss what they’ve learned.
PE Exercises! Energizing Warm-Up Routines

Warm-ups are indispensable before any physical education class. But why is that? Well, warming up prepares the students physically and mentally for the PE activities that lie ahead. It’s like revving up the engine before setting off on a journey. Thus, it’s time to get started!
Ever thought of transforming the humble jumping jack into a fun activity? The Jumping Jack PE Game is a brilliant example of how we can turn a simple exercise into a healthy competition. The game not only improves coordination but also sets the tone for the physical education class. It’s no longer about just performing jumping jacks correctly; it’s about the thrill of the game and mastering the technique.
Consider incorporating Stretch & Flex sessions for added flexibility. Guiding students through a variety of stretches prepares their muscles and joints for the day’s activities in PE class. As a physical education teacher, it’s like a gentle wake-up call for the muscles, prepping them for the energetic gym class that awaits.
Beyond enhancing students’ agility, these indoor activities also build their enthusiasm for the class. And the best part is, these exercises don’t require any fancy equipment. A bit of space and a whole lot of enthusiasm are all you need!
Obstacle Course Creations

Want to heighten the excitement? Explore the intriguing sphere of obstacle course creations! While designing an indoor obstacle course, safety comes first. We’re talking cushions, yoga mats, blankets for padding, and keeping sharp corners out of the way. But don’t let that deter you from the fun.
Children can be involved in planning their obstacle course, drawing a few ideas from shows like ‘Ninja Warrior’ or social media for inspiration. Imagine having balance beams made with planks or tape, crepe paper laser mazes, and Shark Zone games to challenge students’ agility and coordination.
However, the excitement doesn’t end here. We can introduce the following elements to enhance the obstacle course experience:
- Tunnels made from items like chairs, play mats, pillowcases, or sleeping bags
- Sack races to add an extra challenge
- Simulated ball pit using laundry baskets
- Timers to enhance hand-eye coordination and motivate children to improve their obstacle course performance
What would an obstacle course be without an accompanying storyline? Let’s turn our students into ninjas or pirates, making the course more captivating and imaginative. An obstacle course that’s not just about physical challenges but also about engaging children’s cognitive skills.
Classic Game Reimagined
Occasionally, traditional games can prove to be enjoyable, particularly when revamped with a novel twist. Classic games like dodgeball and tag can be reimagined to introduce new dynamics, promote teamwork, and boost strategic thinking. Take Blob Ball, for example. It’s a dodgeball variant where players form a ‘Blob’ and can throw dodgeballs while linked, creating a unique team dynamic. Doctor Dodgeball introduces a hidden ‘doctor’ who revives eliminated players, adding a layer of mystery and strategy.
Tag games, like the classic tag game, also offer ample room for creativity. In Blob Tag, students expand the Blob by tagging and linking with others, transforming the game into a collective pursuit. Bridge Tag requires tagged players to form a bridge with their bodies, introducing an element of physical creativity.
By reshaping these classic games, we not only make the learning process enjoyable but also instill valuable skills like teamwork, coordination, and strategic thinking in students. After all, PE classes should be just as mentally stimulating as they are physically!
Circuit Training Stations

Circuit training stations serve as a smorgasbord of PE exercises, catering to a variety of interests and abilities. They offer a variety of exercises targeting different muscle groups and fitness levels, using equipment like cones, hula hoops, and jump ropes to diversify activities.
Circuit training involves sequences of movements such as jumping, agility ladders, or strength exercises, with each station featuring a distinct activity. Students can work individually, with partners, or in small groups, and circuits can serve as a warm-up, cool-down, or main activity.
Using visual aids like exercise cards or videos can guide students through the circuit and indicate when to change stations. And to maintain student engagement, circuits should feature varied and regularly changing activities and exercises.
The beauty of circuit training lies in its flexibility. It caters to various fitness levels and creates an environment where all students can participate and improve their agility and quickness. Plus, it’s a great way to keep the students active and engaged throughout the class!
Rhythmic Activities for All Ages

Why not infuse our PE classes with a touch of rhythm? Rhythmic activities like musical chairs and line dancing not only promote coordination, balance, and cultural appreciation but also engage students in fun, music-based movement.
Musical chairs can be adapted into a dynamic warm-up activity in PE classes, blending the fun of the game with fitness challenges like:
- running backward
- jumping jacks
- side shuffles
And for a little extra zing, we can use hula hoops instead of chairs, encouraging creativity in movement and broadening the game for different ages.
Speaking of age, these rhythmic activities cater to children from age three onwards and become more complex to match the abilities of older children around seven and up. The game enhances:
- physical coordination
- social skills
- emotional regulation
- exposes children to diverse cultural music
And let’s not forget line dancing! The Cupid Shuffle, an easily teachable line dance, promotes coordination and is a familiar favorite at social events, making physical activity appealing.
Therefore, it’s time to get our students moving to the rhythm as they play music during their students walk!
Creative Ball Games
Why not kick things off with some inventive ball games? Games like Balloon Tennis, Basketball Court Quests, and Pac-Man Dribble can enhance hand-eye coordination, teamwork, and strategic thinking in a fun and engaging way.
Balloon Tennis is a safe and child-friendly game where participants use makeshift racquets made from paper plates taped to jumbo popsicle sticks, and a balloon serves as the ball. The game can be diversified with games like Down On One Knee, Smash Down, and Keepy Uppy, each promoting skills such as balance, quick reflexes, and hand-eye coordination.
Basketball Court Quests include shooting and dribbling activities progressing through 9 skill levels to cater to different student abilities, and can be combined with throwing and catching exercises for enhanced skill development.
These games aren’t just about the fun; they’re about teaching students valuable skills while ensuring they’re having a great time playing an enjoyable game. After all, learning is always more effective when it’s enjoyable!
Solo Exercise Endeavors
While group activities effectively encourage teamwork and cooperation, solo exercises have a charm of their own. They allow students to focus on individual progress and self-motivation while honing personal growth and skills.
Take the ‘Whirlwind Challenge,’ for example. It’s a jump rope game that promotes continuous movement and skill enhancement, as eliminated players practice until a timer runs out. And then there’s the ‘Pac-Man Dribble’ exercise that adapts the concept of the video game into a physical activity where players dribble a basketball along gymnasium lines, avoiding being tagged by the ‘Pac-Man’.
These solo exercises encourage students to challenge themselves at their own pace, allowing them to focus on their own progress. After all, every student is unique, and solo exercises provide an opportunity for them to shine in their own light!
Parachute Playtime
Whoever said that parachutes were solely meant for skydiving? Parachute playtime activities like Little Waves, Big Waves, and NASCAR engage students in cooperative play, promoting teamwork, coordination, and quick reaction time.
Activities like ‘Little Waves’ and ‘Big Waves’ teach students coordination by practicing hand movements to create various wave sizes. ‘Travel with the Parachute’ promotes teamwork by requiring all students to move in the same direction and then reverse while holding the parachute.
Dynamic activities like ‘NASCAR’ combine the formation of a parachute tent with movement around the parachute aiming to return to the original spot before it falls. In this game, two teams can compete against each other to make it more exciting. And games like ‘Color Center’ involve students switching places based on the color called out, integrating quick reaction time with fun.
Parachute games not only provide a fun change of pace but also foster vital skills such as teamwork, coordination, and quick reflexes. Plus, they’re a great way to add a touch of adventure and parachute fun to the PE class!
No-Equipment Necessary
At times, a dash of creativity is all it takes to make a PE class enjoyable. No-equipment necessary games like The Floor is Lava, Shadow Tag, and Fitness Charades promote agility, quick decision-making, and physical activity without the need for special equipment.
‘The Floor is Lava’ involves students imagining the gym floor as lava, and they must hop between safe spots like cushions or mats when the music stops, promoting agility and quick decision-making. Shadow Tag, a version of tag played without any equipment, encourages kids to step on each other’s shadows, promoting speed and agility in an engaging way.
Fitness Charades, adapted from Survivor Tag, enables students to act out different sports or exercises and gets them moving without the need for any props or equipment. These games are not only cost-effective but also incredibly fun and engaging. After all, creativity is the best tool we have!
Cool-Down and Reflection
After an exhilarating PE class, a cool-down period and some reflection are in order. Cool-down exercises help prevent lightheadedness or dizziness by allowing blood flow to return to normal and reduce muscle soreness by flushing out lactic acid buildup.
Gentle yoga poses that enhance relaxation and alignment post-exercise include:
- Supine Spinal Twist
- Happy Baby Pose
- Legs Up the Wall Pose
- Corpse Pose
Activities like Pigeon Pose and Supported Bridge Pose can specifically target hip flexors and the spine, increasing mobility after vigorous PE activities.
Additionally, we should never overlook the significance of reflection. A group discussion to reflect on their experiences and learnings from the class can be an excellent way for students to share their thoughts and feedback. It’s a chance for them to express what they enjoyed, what they found challenging, and what they look forward to in future PE classes.
We’ve journeyed through a host of engaging and innovative PE exercises, from energizing warm-up routines to creative ball games, rhythmic activities, parachute playtime, and even no-equipment necessary games. These activities are not only fun but also enhance students’ agility, coordination, teamwork, and strategic thinking. So, let’s keep the spirit of innovation alive in our PE classes, ensuring that every class is a journey of exploration, fun, and learning!
Frequently Asked Questions
What is the best exercise for pe.
The best exercise for premature ejaculation is running, yoga, and pelvic floor workouts. A new study suggests that exercise could be as effective as pharmaceutical treatments.
What do elementary students learn in PE?
In elementary PE, students learn fundamental skills like running, jumping, and throwing, which prepare them for success in middle and high school PE classes. These skills include locomotor, non-locomotor, and manipulative skills.
How to do PE in a classroom?
You can do PE in a classroom by playing games that require minimal equipment, such as a scrunched up piece of paper. Have fun!
Why are warm-up routines important in PE classes?
Warm-up routines are important in PE classes because they prepare students physically and mentally for the activities ahead, enhance agility, and get students excited for the class. So, it’s important to always start with a good warm-up.
How can classic games be reimagined for PE classes?
You can reimagine classic games for PE classes by adding innovative twists that promote teamwork and strategic thinking. For instance, try turning dodgeball into Blob Ball, where players link up and throw dodgeballs as a team.
Share this post: on Twitter on Facebook on Google+
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Physical education for healthier, happier, longer and more productive living

The time children and adults all over the world spend engaging in physical activity is decreasing with dire consequences on their health, life expectancy, and ability to perform in the classroom, in society and at work.
In a new publication, Quality Physical Education, Guidelines for Policy Makers , UNESCO urges governments and educational planners to reverse this trend, described by the World Health Organization (WHO) as a pandemic that contributes to the death of 3.2 million people every year, more than twice as many as die of AIDS.
The Guidelines will be released on the occasion of a meeting of UNESCO’s Intergovernmental Committee for Physical Education and Sport (CIGEPS) in Lausanne, Switzerland, (28-30 January).*
UNESCO calls on governments to reverse the decline in physical education (PE) investment that has been observed in recent years in many parts of the world, including some of the wealthiest countries. According to European sources, for example, funding and time allocation for PE in schools has been declining progressively over more than half of the continent, and conditions are not better in North America.
The new publication on PE, produced in partnership with several international and intergovernmental organizations**, advocates quality physical education and training for PE teachers. It highlights the benefits of investing in PE versus the cost of not investing (cf self-explanatory infographics ).
“The stakes are high,” says UNESCO Director-General Irina Bokova. “Public investment in physical education is far outweighed by high dividends in health savings and educational objectives. Participation in quality physical education has been shown to instil a positive attitude towards physical activity, to decrease the chances of young people engaging in risky behaviour and to impact positively on academic performance, while providing a platform for wider social inclusion.”
The Guidelines seek to address seven areas of particular concern identified last year in UNESCO’s global review of the state of physical education , namely: 1. Persistent gaps between PE policy and implementation; 2. Continuing deficiencies in curriculum time allocation; 3. Relevance and quality of the PE curriculum; 4. Quality of initial teacher training programmes; 5. Inadequacies in the quality and maintenance of facilities; 6. Continued barriers to equal provision and access for all; 7. Inadequate school-community coordination.
The recommendations to policy-makers and education stake-holders are matched by case studies about programmes, often led by community-based nongovernmental organizations. Success stories in Africa, North and Latin America, Asia and Europe illustrate what can be achieved by quality physical education: young people learn how to plan and monitor progress in reaching a goal they set themselves, with a direct impact on their self-confidence, social skills and ability to perform in the classroom.
While schools alone cannot provide the full daily hour of physical activity recommended for all young people, a well-planned policy should promote PE synergies between formal education and the community. Experiences such as Magic Bus (India) which uses physical activity to help bring school drop outs back to the classroom highlight the potential of such school-leisure coordination.
The publication promotes the concept of “physical literacy,” defined by Canada’s Passport for Life organization of physical and health educators as the ability to move “with competence and confidence in a wide variety of physical activities in multiple environments that benefit the healthy development of the whole person. Competent movers tend to be more successful academically and socially. They understand how to be active for life and are able to transfer competence from one area to another. Physically literate individuals have the skills and confidence to move any way they want. They can show their skills and confidence in lots of different physical activities and environments; and use their skills and confidence to be active and healthy.”
For society to reap the benefit of quality physical education, the guidelines argue, planners must ensure that it is made available as readily to girls as it is to boys, to young people in school and to those who are not.
The Guidelines were produced at the request of UNESCO’s Intergovernmental Committee for Physical Education and Sport (CIGEPS) and participants at the Fifth International Conference of Ministers and Senior Officials Responsible for Physical Education and Sport (Berlin 2013). UNESCO and project partners will proceed to work with a number of countries that will engage in a process of policy revision in this area, as part of UNESCO’s work to support national efforts to adapt their educational systems to today’s needs (see Quality physical education contributes to 21st century education ).
Media contact: Roni Amelan, UNESCO Press Service, r.amelan(at)unesco.org , +33 (0)1 45 68 16 50
Photos are available here: http://www.unesco.org/new/en/media-services/multimedia/photos/photo-gallery-quality-physical-education/
* More about the CIGEPS meeting
** The European Commission, the International Council of Sport Science and Physical Education (ICSSPE), the International Olympic Committee (IOC), UNDP, UNICEF, UNOSDP and WHO.
Related items
- Country page: Switzerland

Other recent news


- Annual Meeting

- Generation Public Health
- Public Health Thank You Day
- Who is public health?
- Climate, Health and Equity
- Racial Equity
- Environmental Health
- Gun Violence
- Health Equity
- All Topics and Issues
- Advocacy for Public Health
- Policy Statements
- American Journal of Public Health
- The Nation's Health
- Fact Sheets
- Reports and Issue Briefs
- Advertising
- Public Health Buyers Guide
- Publications Contacts
- Continuing Education
- Public Health CareerMart
- Internships & Fellowships
- Careers at APHA
- Policy Action Institute
- National Public Health Week
- APHA Calendar
- News Releases
- Social Media
- Brand Guidelines
- Member Sections
- Student Assembly
- Member Perks
- Membership Rates
- Agency Membership
- School-Sponsored Student Membership
- Special Member Savings
- Early-Career Professionals
- Gift Membership
- APHA Your Way
- Member Directory
- Policy Statements and Advocacy >
- Policy Statements >
- Policy Statement Database >
Supporting Physical Education in Schools for All Youth
- Policy Statements and Advocacy
- Policy Statement Database
- Development Process
- Archiving Process
- Proposed Policy Statements
- Date: Oct 26 2021
- Policy Number: 20211
Key Words: Physical Activity, Education, School Health, Obesity
Abstract This policy statement provides scientific evidence that schools are unique places where children should be engaged in physical activity. However, most school policies and programs are not supportive of physical activity in the school day, specifically physical education. Considering that 30.4% of youth are overweight or obese and that 76.8% do not meet the daily physical activity recommendations, and considering the benefits of physical activity with respect to increased ability to concentrate and learn, it is of the utmost importance to incorporate policies and programs that facilitate healthy engagement in physical activity in schools. Marginalized youth from low-income families, communities of color, immigrant communities, and others are disproportionately impacted by lack of supportive policies and programming. This policy statement calls for comprehensive and cooperative actions from the public health community, schools, administrators, researchers, and community members to increase physical activity opportunities through physical education in order to engage youth in at least 60 minutes of physical activity daily.
Relationship to Existing Policy Statements
- APHA Policy Statement 20137: Improving Health and Wellness through Access to Nature
- APHA Policy Statement 20172: Supporting the Updated National Physical Activity Plan
- APHA Policy Statement 201515: The Role of Health Education Specialists in a Post-Health Reform Environment
- APHA Policy Statement 20079: Building a Public Health Infrastructure for Physical Activity Promotion
- APHA Policy Statement 9709: Promoting Public Health Through Physical Activity
- APHA Policy Statement 20044: Creating Policies on Land Use and Transportation Systems that Promote Public Health
- APHA Policy Statement 20058: Supporting the WHO Global Strategy on Diet, Physical Activity and Health
- APHA Policy Statement 200619: Urgent Call for a Nationwide Public Health Infrastructure and Action to Reverse the Obesity Epidemic
- APHA Policy Statement 201514: Building Environments and a Public Health Workforce to Support Physical Activity Among Older Adults
- APHA Policy Statement 20121: Supporting the National Physical Activity Plan
- APHA Policy Statement 201415: Support for Social Determinants of Behavioral Health and Pathways for Integrated and Better Public Health
Problem Statement Obesity is an important health issue among children in the United States. According to the 2019 National Health and Nutrition Examination Survey, 16.1% of U.S. youth are overweight and 19.3% are obese.[1] Moreover, racial, socioeconomic, and gender disparities exist in terms of risk factors associated with being overweight or obese. The chronic disease burden is consistent with the disproportionately high percentages of overweight and obese youth in racial minority and socioeconomically disadvantaged populations. According to data from the 2019 Youth Risk Behavior Surveillance System (YRBSS), 37.7% of Black youth and 38.8% of Hispanic youth are overweight or obese, as compared with just 27.7% of White youth.[2]
P hysical inactivity is a significant risk factor for obesity and other chronic conditions.[3] As the proportion of students who are overweight or obese has increased, so has inactivity. Empirical evidence suggests that physical activity may be used as a standalone strategy to decrease adiposity among children.[4] It is recommended that school-aged children and adolescents (6–17 years of age) engage in 60 minutes of physical activity seven days per week.[5] According to data from the 2019 YRBSS, 76.8% of youth do not meet the recommended amounts of physical activity.[2] The same data set indicates that adolescent girls, in particular, are at a higher risk for being inactive as they age; 84.6% of girls do not meet the physical activity guideline of 60 minutes per day seven days a week, as compared with 69.1% of boys.[2] In addition, inactive youth are more likely to be inactive as adults.[6] Starting physical activity early is essential to prevent inactivity in adulthood and older adulthood.
Physical activity provides benefits beyond physical health. For example, it is associated with a reduced risk for depression.[7] Trends for contemplating and making a plan for suicide are increasing among White, Hispanic, and Black youth, and there are racial and ethnic disparities in terms of mental health challenges among youth.[5] In 2019, 40.0% of Hispanic youth reported persistent feelings of sadness or hopelessness, as compared with 36.0% of White youth and 31.5% of Black youth.[5]
In addition to the long-term health benefits of child physical activity, there are numerous academic-related benefits, which the body of evidence continues to expand.[8] Extensive research has demonstrated strong positive correlations between physical activity and higher levels of physical fitness and academic achievement, educational attainment, academic performance, and brain functioning.[8–10] In fact, physical activity participation has both intermediate and long-term benefits with respect to academic performance. Research has shown that, immediately following engagement in physical activity, children have improved concentration on classroom tasks, which may potentially enhance learning.[8]
It is recommended that schools provide 150 minutes of instructional physical education for elementary school children and 225 minutes for middle and high school students per week for the entire school year.[11] However, only Oregon and the District of Columbia have requirements that meet the recommendations for minutes of physical education.[12] Physical education requirements notably decrease after the fifth grade, which aligns with significant decreases in physical activity in youth. Only 8.7% of schools require physical education for 12th grade, as compared with 45.1% of schools for fifth grade.[13]
The lack of universal physical education requirements at all grade levels and the lack of funding dedicated to physical education facilitate inactivity. The median school physical education budget in the United States is just $764 per year,[12] which may further hinder schools from meeting physical education recommendations. Ohinmaa and colleagues suggested that grants, donations, and fundraising account for about half of all funding for school health.[14] Improving physical education policies nationwide has the potential to reduce overall health care costs by $60.5 million within 10 years.[15]
Students who attend physical education in school are two to three times more likely to be physically active outside of school and nearly twice as likely to be active in adulthood.[16] Furthermore, physical education has been shown to be an opportunity for students to gain many of their recommended minutes of physical activity, but many students do not attend or participate in these classes.[13] According to 2019 YRBSS data, about half of high school students attend physical education classes one or more days per week.[2] Therefore, targeting middle and high schools is uniquely important because a significant drop in physical education attendance and physical activity participation occurs between the seventh and 12th grades.[11]
Evidence-Based Strategies to Address the Problem Youth spend a significant portion of their time at school[17]; therefore, schools are one of the most important places for physical activity interventions.[18] According to the Society of Health and Physical Educators, schools should require physical education for students in kindergarten through grade 12.[19] Specifically, all students within secondary school (which includes middle school and high school) should achieve 225 minutes of physical activity per week, while students in primary school (which includes elementary school) should achieve 150 minutes per week.[19]
Current evidence-based strategies to increase physical activity among youth are described below.
Improving school-based physical education: According to the Community Preventive Services Task Force (CPSTF),[20] enhanced school-based physical education involves changing the curriculum and coursework for K–12th-grade students to increase the amount of time students spend engaging in moderate to vigorous physical activity (MVPA) during physical education classes. Enhanced school-based physical education is defined as increasing the amount of time students spend completing MVPA during physical education classes to at least 50% of class time.[20] The CPSTF specifically recommended improving physical education teaching strategies by (1) incorporating modified games and substituting sedentary games with active games and (2) including physical education lesson plans that incorporate fitness and circuit training activities.[20]
Lonsdale and colleagues highlighted effective strategies to increase MVPA, which included teacher professional learning focusing on class organization, management, and instruction and supplementing the usual physical education lessons with high-intensity activity (i.e., fitness infusion).[21] A systematic review of 14 studies showed that students who participated in enhanced school-based physical education classes engaged in 24% more MVPA.[21] Also, groups that received enhanced school-based physical education spent on average 53% of their time engaged in MVPA.[21] In addition, Zhou and Wang found that team games were reported to accumulate the most MVPA time, with movement-based activities (such as gymnastics and dance) having the highest amounts of MVPA and knowledge-based activities (i.e., lesson-based instruction) having the lowest amounts.[22] Implementation of enhanced school-based physical education aligns with the Healthy People 2030 objectives, which aim to increase the proportion of adolescents who meet current federal physical activity guidelines for aerobic physical activity and muscle-strengthening activity.[23]
It is important that physical education classes be taught by state‐licensed or state‐certified teachers who are endorsed to teach physical education. In a meta-analytic review, Hollis and colleagues found that youth were engaged in MVPA for an average of 44.8% of lesson time.[24] Low MVPA levels in physical education lessons could be the result of pedagogical characteristics often observed in typical lessons, such as stopping physical activity to provide instruction, observing demonstrations related to the activity, or organizing equipment or student groups.[25] An examination of time allotment in terms of lesson context revealed that 30% of lesson time was spent in game play, 29% in fitness, 20% in classroom management, 9% in knowledge-related activities, and 5% in skill-related activities.[15] Similar results were found in a study by Powell and colleagues in which the average length of physical education lessons was 35.3 minutes, with only 15 minutes of MVPA during physical education.[26] Results further demonstrated that 34% of the lesson was spent standing and 21.7% was spent sitting, with time sitting being directly linked to knowledge attainment.[26]
In conclusion, a significant proportion of physical education instruction time is spent on classroom management, instruction, and transitional periods. While these periods are necessary, they detract from the overall time youth spend participating in MVPA. It is, therefore, recommended that all physical education courses be taught by qualified individuals who have received formal training in physical education pedagogy. SHAPE America has specifically recommended that physical education be taught by an endorsed state‐licensed or state‐certified teacher.[11] This educational licensure or certification requirement would ensure that the physical education curriculum used in schools is appropriate and maximizes the time students spend engaging in MVPA while also aligning with national and/or state physical education standards for K–12 physical education.[11]
Increasing the frequency of physical education: Scientific evidence has shown that increasing the frequency of physical education can improve overall physical activity among youth. Research indicates that only 25.9% of high school students attend physical education classes five days per week.[5] Findings from the School Health Policies and Practices Study showed that less than 4% of elementary and middle schools require physical education or similar activity every day throughout the school year.[18] Moreover, less than 9% of middle schools require physical education at least three days per week.[18] Physical education instruction for high school students decreased from 29.9% in 2017 to 25.9% in 2019.[5]
The benefits of regular physical activity are well documented and include improvements in bone and muscle development, cardiorespiratory fitness, and weight control; reduced symptoms of depression and anxiety; and reduced risks of heart disease, cancer, type 2 diabetes, and hypertension.[3] Research has demonstrated that physical activity throughout the school day is associated with better school performance.[8] Healthy People 2030 objectives highlight the importance of increased physical activity through improved physical education in both public and private school systems. Specifically, the Educational and Community-Based Programs workgroup aims to increase the proportion of adolescents who participate in daily school-based physical education.[7]
Reduction or removal of waivers, substitutions, and exemptions for physical education: Another important strategy to increase school-based MVPA is the reduction or removal of waivers, substitutions, and exemptions for physical education. According to the Shape of the Nation 2016 report, 30 U.S. states allow student exemptions from physical education classes, and 31 states allow students to substitute activities such as marching band, cheerleading, drill team, or intramural sports for physical education credit.[12] SHAPE America issued a position statement according to which school districts and schools should not allow waivers or exemptions from physical education class time or credit requirements.[11] Specifically, SHAPE firmly asserted that all students should be required to complete physical education courses and that state, district, and school policies should not allow substitutions, waivers, or exemptions for physical education courses, class time, or credit requirements. By allowing waivers, substitutions, and exemptions for physical education, schools and districts eliminate opportunities for students to be active at a time when physical activity levels are at an all-time low among youth.[11] As mentioned, schools offer a unique setting to teach children the value of physical activity as well as a structured, supervised environment in which children can learn the necessary skills to encourage lifelong physical activity.[11]
Culturally tailored physical education: Multiple organizations have reported the need to ensure culturally tailored physical education for all populations, especially marginalized populations such as minority racial, ethnic, and cultural groups; girls and women; refugees; people experiencing homelessness; LGBTQ+ (lesbian, gay, bisexual, transgender, queer or questioning) populations; and others.[27,28] The United Nations Educational, Scientific and Cultural Organization’s Guidelines for Policy-Makers on Quality Physical Education stated the need for and importance of providing physical education for minority groups. According to the guidelines, (1) curricula should be flexible and adaptable for all groups, (2) teachers should be professionally qualified and capable of providing physical education for all students, and (3) school policies and practices should provide appropriate infrastructure, faculties, equipment, and teaching material for all students.[28]
Lastly, it is recommended that teachers have access to resources such as community health workers who can provide culturally specific guidance on physical education. Community health workers are particularly effective because of the cultural and linguistic connections they have with the communities they serve.[29] Providing culturally appropriate physical education may increase physical activity,[30] decrease obesity,[31] and improve the overall health of minority groups by increasing social support, promoting healthy lifestyles, and increasing knowledge of disease prevention.[32]
Adaptive physical education: According to the Physical Activity Guidelines for Americans, children and adolescents with disabilities are more likely to be inactive than those without disabilities.[7] It is recommended that children and adolescents with disabilities still aim to meet the key guideline of 60 minutes of physical activity every day when possible. If youth are unable to participate in the physical activities or durations needed to meet the key guidelines, it is recommended that they be as active as possible and avoid being inactive.[7]
Youth with disabilities should work with health care professionals or physical activity specialists to learn about the types and amounts of physical activity appropriate for them.[7] The Adapted Physical Education National Standards were developed to ensure that physical education for children with disabilities be delivered by a qualified adapted physical educator. According to these standards, physical education teachers should use sound teaching practices to ensure the inclusion and representation of all skill and ability levels.[33] Specifically, master physical educators should be well prepared to provide knowledge acquisition as well as physical activity opportunities for all abilities to create active and healthy lifestyles for all students. In addition, the standards outline high expectations for a physically active lifestyle. Lastly, it is expected that master physical educators will maintain a stimulating, productive learning environment that holds all students to the highest expectations for a physically active lifestyle.[33]
Conclusion: In conclusion, schools are the ideal and recommended setting for the promotion of physical activity among youth, and physical education is the primary vehicle through which to achieve this objective in schools.[34] Improving the quality and quantity of physical education courses will give youth more opportunities to attain the recommended amount of physical activity each day. Reducing physical education waivers would ensure that youth are not exploiting a loophole in the system. Advocating for culturally tailored physical education and adaptive physical education would foster an inclusive environment in which all children are able to be physically active and healthy.
Opposing Arguments/Evidence Few would disagree that physical activity and time spent engaged in physical education are important for youth development and overall health. The primary opposing arguments tend to stem from the poorly designed physical education curriculum and the time taken away from other subjects amid increased pressure to raise standards and scores in subjects such as math, science, and English. As a result, time allocated to physical education and the perceived importance of physical education lessons have been reduced. However, there is a substantial amount of evidence that physical activity can help improve academic achievement, including overall grades and standardized test scores.[34] In a systematic review of 43 articles and 50 studies, the Centers for Disease Control and Prevention (CDC) determined that physical activity has a positive impact on cognitive skills, attitudes, and academic achievement.[34] Specifically, physical activity enhanced concentration and attention and improved classroom behavior.[34] The review also showed that increasing time during the school day for physical activity does not appear to take away from overall academic performance.[34] Therefore, the CDC recommended that schools increase the amount of time students spend in physical education or consider adding components to increase the quality of physical education classes.[34] As highlighted in the evidence-based strategies to improve school-based MVPA, the CPSTF recommended use of enhanced physical education, including improved physical education teaching strategies, by incorporating modified, more active games and physical education lesson plans that involve fitness and circuit training activities.[20]
Alternative Strategies Enhancing, encouraging, and maintaining physical education class duration and quality are vital to the health and well-being of children, particularly in terms of their physical activity behaviors. However, there are several alternative strategies to increase the physical activity of youth that should be considered in conjunction with retaining the importance of physical education.
Before- and after-school physical activity programs: According to the World Health Organization, after-school activities are a key avenue to supplement youth MVPA levels.[35] After-school physical activity could include physical activity clubs, intramural programs, informal play on school grounds, physical activity in school-based before- and after-care programs, and interscholastic sports.[18] Mayorga-Vega and colleagues found that physical activity that took place after school hours achieved 36% of the recommended 60 minutes of MVPA per day.[36] However, adolescents still reported a higher level of MVPA during physical education classes than during school recess and after-school programs.[36]
Only about 26% of the nation’s public and private schools provide access to their physical activity spaces and facilities for all individuals outside of normal school hours. In addition, a steady decline has been observed in provision of access to physical activity facilities during nonschool hours.[37] Therefore, schools can further encourage physical activity by opening up their facilities for community use.[18]
Increasing active transportation to and from school: According to the CPSTF, walking or bicycling to and from school provides children and adolescents with an opportunity to be physically active most days of the week.[38] Interventions such as the Safe Routes to School program could increase active transportation to and from school and reduce pedestrian and bicycle injury rates. However, there is not enough evidence to show that school travel leads to increases in students’ overall daily physical activity.[38]
Recess: Recess is defined as a regularly scheduled period during the school day for physical activity and play that are monitored by trained staff or volunteers.[13] Recess has been directly related to increased physical activity, improved memory, improved attention, improved concentration, decreased classroom disruptive behavior, improved social and emotional development, and academic achievement.[8,39–41] It is recommended that elementary, middle, and high school students have a minimum of 20 minutes of daily recess.[39] The CDC has further recommended that recess and physical education be separate, distinct physical activity opportunities, which creates separate times for skill acquisition (physical education) and active play (recess).[39] Also, the CDC has recommended that schools provide students with adequate, designated, and safe spaces, facilities, equipment, and supplies for both indoor and outdoor recess (e.g., playground markings, physical activity zones, activity cards).[39] Lastly, students should not be excluded from recess for disciplinary reasons or academic performance because such practices promote negative reinforcement.[39]
Classroom-based physical activity: Classroom-based physical activity, including single physical activity sessions, may increase student attention, concentration, and memory; increase motivation and enjoyment of learning; and reduce behavior issues.[8,40] Classroom-based physical activity integration may include physically active lessons, physical activity before a test, physical activity breaks, energizers, brain boosters, and active classrooms (a teaching technique that intentionally blends physical activity into academic lessons to satisfy the learning outcomes of the classroom without sacrificing time spent engaging in physical activity).[8,40,42] Further guidance by the CDC and other national organizations includes providing teachers with ongoing professional development to integrate physical activity into planned academic instruction as a means of reinforcing academic concepts.[40]
Action Steps Increasing physical activity among school-aged children is a vital investment in the health and well-being of youth in the United States. Increasing physical activity at this critical age has the potential to build healthier, happier young adults. Schools should support physical activity through culturally appropriate, high-quality physical education. Schools; local, state, and federal education agencies; public health departments; policymakers; and researchers should address the following objectives relevant to public health priority setting in order to advance school-based physical activity programming and activities:
- Federal agencies should develop national policies on physical education that are consistent with the larger national strategies to increase physical activity among youth.
- Federal and state governments should increase funding for schools to implement high-quality physical education programming
- State and local education departments should improve physical education requirements to provide the opportunity for 60 minutes of MVPA each school day.
- Policymakers at state and local education departments should be made aware of the importance of physical education provided by schools.
- Schools should require that all physical education teachers be appropriately credentialed to deliver culturally appropriate, high-quality physical education.
- Schools should solicit involvement and expertise from state and local public health departments and physical activity researchers on culturally specific, evidence-based strategies to improve school-based physical education.
- Principals and superintendents of schools should develop action plans to improve physical education for all of their students. Youth should have the opportunity to engage in 60 minutes of physical activity during the school day.
- Principals and superintendents should reduce or eliminate policies allowing waivers for physical education. Waivers should be considered on a case-by-case basis.
- Schools and school districts should engage in collaborative efforts to share the results of successfully implemented physical education programs.
- Schools and researchers should collaborate in studying physical activity among diverse youth who have been traditionally understudied and systematically underserved. Furthermore, researchers should be encouraged to develop innovative programs for youth in school settings that promote physical activity for all.
- Greater diversity in programming should be implemented in schools so that youth can be exposed to a variety of activities that those of all abilities and cultures might enjoy.
- Youth, families, community members, and local organizations should advocate to their school districts and legislative bodies for culturally appropriate, high-quality physical education in their local schools.
- Public health departments should partner with and support physical education teachers and programs. This support should include school-based physical activity in community health assessments and community health improvement plans highlighting the importance of physical activity in preventing chronic disease and providing mental and cognitive benefits.
References 1. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. Available at: https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/overweight-obesity-child-H.pdf. Accessed October 20, 2021. 2. Centers for Disease Control and Prevention. 2019 Youth Risk Behavior Survey Questionnaire. Available at: www.cdc.gov/yrbs. Accessed October 20, 2021. 3. Centers for Disease Control and Prevention. Division of Nutrition, Physical Activity, and Obesity at a glance. Available at: https://www.cdc.gov/chronicdisease/resources/publications/aag/dnpao.htm. Accessed October 20, 2021. 4. Laframboise MA, Degraauw C. The effects of aerobic physical activity on adiposity in school-aged children and youth: a systematic review of randomized controlled trials. J Can Chiropractic Assoc. 2011;55(4):256–268. 5. Center for Disease Control and Prevention. High School YRBS 2019. Available at: https://nccd.cdc.gov/youthonline/App/QuestionsOrLocations.aspx?CategoryId=C06. Accessed October 20, 2021. 6. Lounassalo I, Salin K, Kankaanpaa A, et al. Distinct trajectories of physical activity and related factors during the life course in the general population: a systematic review. BMC Public Health. 2019;19:1. 7. U.S. Department of Health and Human Services. Physical activity guidelines for Americans. Available at: https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf. Accessed October 20, 2021. 8. Castelli DM, Glowacki E, Barcelona JM, Calvert HG, Hwang J. Active education: growing evidence on physical activity and academic performance. Available at: https://activelivingresearch.org/sites/activelivingresearch.org/files/ALR_Brief_ActiveEducation_Jan2015.pdf. Accessed October 20, 2021. 9. Kari JT, Pehkonen J, Hutri-Kähönen N, Raitakari OT, Tammelin TH. Longitudinal associations between physical activity and educational outcomes. Med Sci Sports Exerc. 2017;49(11):2158–2166. 10. Kohl HW, Cook HD. Physical activity, fitness, and physical education: effects on academic performance. Available at: https://www.ncbi.nlm.nih.gov/books/NBK201501/. Accessed October 20, 2021. 11. Society of Health and Physical Educators. The essential components of physical education. Available at: https://www.shapeamerica.org/uploads/pdfs/TheEssentialComponentsOfPhysicalEducation.pdf. Accessed October 20, 2021. 12. Society of Health and Physical Educators (2016). 2016 shape of the nation: status of physical education in the U.S. Available at: https://www.shapeamerica.org//advocacy/son/2016/upload/Shape-of-the-Nation-2016_web.pdf. Accessed October 20, 2021. 13. Springboard to Active Schools. Keep recess in schools. Available at: https://www.cdc.gov/healthyschools/physicalactivity/pdf/Recess_Data_Brief_CDC_Logo_FINAL_191106.pdf. Accessed October 20, 2021. 14. Ohinmaa A, Langille JL, Jamieson S, Whitby C, Veugelers PJ. Costs of implementing and maintaining comprehensive school health: the case of the Annapolis Valley Health Promoting Schools program. Can J Public Health. 2011;102(6):451–454. 15. Barrett JL, Gortmaker SL, Long MW, et al. Cost effectiveness of an elementary school active physical education policy. Am J Prev Med. 2015;49(1):148–159. 16. Physical Activity Council. (2017). 2017 participation report. Available at: http://s3.amazonaws.com/ustaassets/assets/822/15/papc_study.pdf. Accessed October 20, 2021. 17. Synder TD, de Brey C, Dillow SA. Digest of education statistics. Available at: https://files.eric.ed.gov/fulltext/ED580954.pdf. Accessed October 20, 2021. 18. Centers for Disease Control and Prevention. School Health Policies and Practices Study, 2014. Available at: https://www.cdc.gov/healthyyouth/data/shpps/pdf/shpps-results_2016.pdf. Accessed October 20, 2021. 19. Society of Health and Physical Educators. A-Z of social justice physical education. Available at: https://www.shapeamerica.org/uploads/pdfs/2020/publications/joperd/The-A%E2%80%93Z-of-Social%20Justice-Physical-Education-P1.pdf. Accessed October 20, 2021. 20. Community Preventive Services Task Force. Annual report to Congress: 2013. Available at: https://www.thecommunityguide.org/content/tffrs-physical-activity-interventions-increase-active-travel-school. Accessed October 20, 2021. 21. Lonsdale C, Rosenkranz R, Peralta L, et al. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical activity lessons. Prev Med. 2013;56:152–161. 22. Zhou Y, Wang L. (2019). Correlates of physical activity of students in secondary school physical education: a systematic review of literature. BioMed Res Int. 2019;2019:4563484. 23. U.S. Department of Health and Human Services. Healthy People 2030 physical activity objectives. Available at: https://health.gov/healthypeople/objectives-and-data/browse-objectives/physical-activity. Accessed October 20, 2021. 24. Hollis JL, Sutherland R, Williams AJ, et al. A systematic review and meta-analysis of moderate-to-vigorous physical activity levels in secondary school physical education lessons. Int J Behav Nutr Phys Act. 2017;14(1):52. 25. Fairclough SJ, Stratton G. A review of physical activity levels during elementary school physical education. J Teach Phys Educ. 2006;25(2):240–258. 26. Powell E, Woodfield LA, Nevill AM, Powell AJ, Myers TD. ‘We have to wait in a queue for our turn quite a bit’: examining children’s physical activity during primary physical education lessons. Euro Phys Educ Rev. 2019;25(4):929–948. 27. Society of Health and Physical Educators. National PE standards. Available at: https://www.shapeamerica.org/standards/pe/. Accessed October 20, 2021. 28. United Nations Educational, Scientific and Cultural Organization. Guidelines for policy makers: quality physical education. Available at: https://en.unesco.org/inclusivepolicylab/sites/default/files/learning/document/2017/1/231101E.pdf. Accessed October 20, 2021. 29. Haughton J, Ayala G, Burke K, Elder J, Montanez J, Arrendondo E. Community health workers promoting physical activity. J Ambul Care Manage. 2015;38(4):309–320. 30. Hovell MF, Mulvihill MM, Buono MJ, et al. Culturally tailored aerobic exercise intervention for low-income Latinas. Am J Health Promotion. 2008;22(3):155–163. 31. Falbe J, Cadiz AA, Tantoco NK, Thompson HR, Madsen KA. Active and healthy families: a randomized controlled trial of a culturally tailored obesity intervention for Latino children. Acad Pediatr. 2015;15(4):386–395. 32. Joo JY, Liu MF. Culturally tailored interventions for ethnic minorities: A scoping review. Nurs Open. 2021;8(5):2078–2090. 33. APENS. Adapted Physical Education National Standards. Available at: https://apens.org/national_standard.html. Accessed October 20, 2021. 34. Centers for Disease Control and Prevention. The association between school based physical activity, including physical education, and academic performance. Available at: https://www.cdc.gov/healthyyouth/health_and_academics/pdf/pa-pe_paper.pdf. Accessed October 20, 2021. 35. World Health Organization. School policy framework: implementation of the WHO global strategy on diet, physical activity and health. Available at: https://www.who.int/dietphysicalactivity/SPF-en-2008.pdf. Accessed October 20, 2021. 36. Mayorga-Vega D, Saldias MP, Viciana J. Comparison of moderate-to-vigorous physical activity levels between physical education, school recess and after-school time in secondary school students: an accelerometer-based study. Kinesiology. 2017;49(2):242–251. 37. U.S. Department of Health and Human Services. Healthy People 2020. Physical activity objectives. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/physical-activity/objectives. Accessed October 20, 2021. 38. Community Guide. Physical activity: interventions to increase active travel to school. Available at: https://www.thecommunityguide.org/content/tffrs-physical-activity-interventions-increase-active-travel-school. Accessed October 20, 2021. 39. Centers for Disease Control and Prevention and Society of Health and Physical Educators. Strategies for recess in schools. Available at: https://www.shapeamerica.org/uploads/pdfs/recess/SchoolRecessStrategies.pdf. Accessed October 20, 2021. 40. Centers for Disease Control and Prevention. Strategies for classroom physical activity in schools. Available at: https://www.cdc.gov/healthyschools/physicalactivity/pdf/classroompastrategies_508.pdf. Accessed October 20, 2021. 41. Zavacky F, Michael SL. Keeping recess in schools. J Phys Educ Recreation Dance. 2017;88(5):46–53. 42. Bedard C, St. John L, Bremer E, Graham JD, Cairney J. A systematic review and meta-analysis on the effects of physically active classrooms on educational and enjoyment outcomes in school age children. PLoS One. 2019;14(6):1–19.

- What is public health
- Topics and Issues
- Policies and Advocacy
- Publications
- Professional Development
- Events and Meetings
- News and Media
- APHA Communities
- Privacy Policy
2024 © American Public Health Association
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Committee on Physical Activity and Physical Education in the School Environment; Food and Nutrition Board; Institute of Medicine; Kohl HW III, Cook HD, editors. Educating the Student Body: Taking Physical Activity and Physical Education to School. Washington (DC): National Academies Press (US); 2013 Oct 30.

Educating the Student Body: Taking Physical Activity and Physical Education to School.
- Hardcopy Version at National Academies Press
3 Physical Activity and Physical Education: Relationship to Growth, Development, and Health
Key messages.
- Regular physical activity promotes growth and development and has multiple benefits for physical, mental, and psychosocial health that undoubtedly contribute to learning.
- Specifically, physical activity reduces the risk for heart disease, diabetes mellitus, osteoporosis, high blood pressure, obesity, and metabolic syndrome; improves various other aspects of health and fitness, including aerobic capacity, muscle and bone strength, flexibility, insulin sensitivity, and lipid profiles; and reduces stress, anxiety, and depression.
- Physical activity can improve mental health by decreasing and preventing conditions such as anxiety and depression, as well as improving mood and other aspects of well-being.
- Physical activity programming specifically designed to do so can improve psychosocial outcomes such as self-concept, social behaviors, goal orientation, and most notably self-efficacy. These attributes in turn are important determinants of current and future participation in physical activity.
- Sedentary behaviors such as sitting and television viewing contribute to health risks both because of and independently of their impact on physical activity.
- Health-related behaviors and disease risk factors track from childhood to adulthood, indicating that early and ongoing opportunities for physical activity are needed for maximum health benefit.
- To be effective, physical activity programming must align with the predictable developmental changes in children's exercise capacity and motor skills, which affect the activities in which they can successfully engage.
- Frequent bouts of physical activity throughout the day yield short-term benefits for mental and cognitive health while also providing opportunities to practice skills and building confidence that promotes ongoing engagement in physical activity.
- Distinct types of physical activity address unique health concerns and contribute in distinct ways to children's health, suggesting that a varied regimen including aerobic and resistance exercise, structured and unstructured opportunities, and both longer sessions and shorter bouts will likely confer the greatest benefit.
The behaviors and traits of today's children, along with their genetics, are determinants of their growth and development; their physical, mental, and psychosocial health; and their physical, cognitive, and academic performance. Technological advances of modern society have contributed to a sedentary lifestyle that has changed the phenotype of children from that of 20 years ago. Children today weigh more and have a higher body mass index (BMI) than their peers of just a generation earlier ( Ogden et al., 2012 ). Behaviorally, most children fail to engage in vigorous- or moderate-intensity physical activity for the recommended 60 minutes or more each day, with as many as one-third reporting no physical activity in the preceding 5 days ( CDC, 2012 ). This lack of participation in physical activity has contributed to a greater prevalence of pediatric obesity, a decrease in fitness (e.g., flexibility, muscular strength, cardiorespiratory capacity), and a greater risk for disease ( Boreham and Riddoch, 2001 ; Eisenmann, 2003 ; Malina, 2007 ; Steele et al., 2008 ). (See Box 3-1 for an overview of the relationship between physical activity and physical fitness.)
Physical Activity and Physical Fitness. As noted in Chapter 1 (see the box titled “Key Terms Used in This Report” on p. 17), physical activity, a behavior, is defined as bodily movement that increases energy expenditure, whereas fitness (more...)
While more can always be learned, the evidence for the health benefits of physical activity is irrefutable ( HHS, 1996 , 2008 ). Adults engaged in regular physical activity have lower rates of chronic disease (e.g., coronary heart disease, cardiovascular disease, type 2 diabetes, hypertension, osteoporosis, and some cancers) and are less likely to die prematurely ( HHS, 1996 , 2008 ; Bauman, 2004 ). And while the ill effects of chronic disease are manifested mainly in adults, it is increasingly better understood that the development of these conditions starts in childhood and adolescence ( Hallal et al., 2006 ; Cook et al., 2009 ; Halfon et al., 2012 ). It appears evident, then, that promotion of health-enhancing behaviors must also start early in life. Indeed, growing evidence points to long-term effects of child and adolescent physical activity on adult morbidity and mortality in addition to its more immediate effects ( Hallal et al., 2006 ) (see Figure 3-1 ).
Conceptual model of how physical activity in childhood and adolescence is beneficial to health. Physical activity has both immediate and long-term health benefits: (a) Physical activity tends to track; early physical activity is associated with physical (more...)
Evidence for both direct and indirect health effects of physical activity has been reported ( Hallal et al., 2006 ), and the need for ongoing participation in physical activity to stimulate and maintain the chronic adaptations that underlie those benefits is well documented. To understand the relationship of physical activity and aerobic fitness to health during childhood, it is important first to recognize the developmental changes that occur throughout maturation. During the early stages of adolescence, for example, participation in physical activity and corresponding physical fitness begin to decline ( Duncan et al., 2007 ). Such differences across stages of development highlight the importance of examining the effects of growth and maturation on physical and cognitive health. Accordingly, this chapter reviews how physical activity may influence developmental processes and other aspects of somatic growth and maturation. A complete review of the effects of physical activity on all tissues and systems is beyond the scope of this report. Rather, the focus is on components of body composition and systems that underlie engagement in physical activity, physical fitness, and chronic disease risk and that in turn influence other aspects of health and academic performance (discussed in Chapter 4 ). Addressed in turn is the relationship between physical activity and physical, psychosocial, and mental health. Structural and functional brain maturation and how physical activity may influence those developmental processes and cognitive health are also reviewed in Chapter 4 .
- PHYSICAL HEALTH
This section reviews what is known about the relationship between physical activity and (1) somatic growth, development, and function and (2) health- and performance-related fitness.
Somatic Growth, Development, and Function
Growth occurs through a complex, organized process characterized by predictable developmental stages and events. Although all individuals follow the same general course, growth and maturation rates vary widely among individuals. Just as it is unrealistic to expect all children at the same age to achieve the same academic level, it is unrealistic to expect children at the same age to have the same physical development, motor skills, and physical capacity. Regular physical activity does not alter the process of growth and development. Rather, developmental stage is a significant determinant of motor skills, physical capacity, and the adaptation to activity that is reasonable to expect (see Box 3-2 ).
Growth, Development, and Maturation. Growth is the normal process of increase in size as a result of accretion of tissues characteristic of the organism; growth is the dominant biological activity for most of the first two decades of life. Changes in (more...)
Developmental Stages
Postnatal growth is commonly divided into three or four age periods. Infancy spans the first year of life. Childhood extends from the end of infancy to the start of adolescence and is often divided into early childhood, which includes the preschool years, and middle childhood, which includes the elementary school years, into the 5th or 6th grade. Adolescence is more difficult to define because of variation in its onset and termination, although it is commonly defined as between 10 and 18 years of age ( WHO, 1986 ). The rapid growth and development of infancy continue during early childhood, although at a decelerating rate, whereas middle childhood is a period of slower, steady growth and maturation. Differences between boys and girls are relatively small until adolescence, which is marked by accelerated growth and attainment of sexual maturity ( Tanner, 1962 ).
Across developmental stages, neurological development and control of movement advance in cephalocaudal and proximodistal directions; that is, they advance “head to toe” (cephalocaudal) and “midline to periphery” (proximodistal), while predictable changes in body proportions also occur. For example, the head accounts for 25 percent of recumbent length in an infant and only 15 percent of adult height, while the legs account for 38 percent of recumbent length at birth and 50 percent of adult height. These changes in body proportions occur because body parts grow at different rates. From birth to adulthood, as the head doubles in size, the trunk triples in length, and arm and leg lengths quadruple.
Coincident with these changes in body proportions, and in part because of them, the capacity to perform various motor tasks develops in a predictable fashion. For example, running speed increases are consistent with the increase in leg length. Neurological development also determines skill progression. Young children, for example, when thrown a ball, catch it within the midline of the body and do not attempt to catch it outside the midline or to either side of the body. As proximodistal development proceeds, children are better able to perform tasks outside their midline, and by adolescence they are able to maneuver their bodies in a coordinated way to catch objects outside the midline with little effort.
Physically active and inactive children progress through identical stages. Providing opportunities for young children to be physically active is important not to affect the stages but to ensure adequate opportunity for skill development. Sound physical education curricula are based on an understanding of growth patterns and developmental stages and are critical to provide appropriate movement experiences that promote motor skill development ( Clark, 2005 ). The mastery of fundamental motor skills is strongly related to physical activity in children and adolescents ( Lubans et al., 2010 ) and in turn may contribute to physical, social, and cognitive development. Mastering fundamental motor skills also is critical to fostering physical activity because these skills serve as the foundation for more advanced and sport-specific movement ( Clark and Metcalfe, 2002 ; Hands et al., 2009 ; Robinson and Goodway, 2009 ; Lubans et al., 2010 ). Physical activity programs, such as physical education, should be based on developmentally appropriate motor activities to foster self-efficacy and enjoyment and encourage ongoing participation in physical activity.
Biological Maturation
Maturation is the process of attaining the fully adult state. In growth studies, maturity is typically assessed as skeletal, somatic, or sexual. The same hormones regulate skeletal, somatic, and sexual maturation during adolescence, so it is reasonable to expect the effect of physical activity on these indicators of maturity to be similar. Skeletal maturity is typically assessed from radiographs of the bones in the hand and wrist; it is not influenced by habitual physical activity. Similarly, age at peak height velocity (the most rapid change in height), an indicator of somatic maturity, is not affected by physical activity, nor is the magnitude of peak height velocity, which is well within the usual range in both active and inactive youth. Discussions of the effects of physical activity on sexual maturation more often focus on females than males and, in particular, on age at menarche (first menses). While some data suggest an association between later menarche and habitual physical activity ( Merzenich et al., 1993 ), most of these data come from retrospective studies of athletes ( Clapp and Little, 1995 ). Whether regular sports training at young ages before menarche “delays” menarche (later average age of menarche) remains unclear. While menarche occurs later in females who participate in some sports, the available data do not support a causal relationship between habitual physical activity and later menarche.
Puberty is the developmental period that represents the beginning of sexual maturation. It is marked by the appearance of secondary sex characteristics and their underlying hormonal changes, with accompanying sex differences in linear growth and body mass and composition. The timing of puberty varies, beginning as early as age 8 in girls and age 9 in boys in the United States and as late as ages 13-15 ( NRC/IOM, 1999 ). Recent research suggests that the onset of puberty is occurring earlier in girls today compared with the previous generation, and there is speculation that increased adiposity may be a cause ( Bau et al., 2009 ; Rosenfield et al., 2009 ). Conversely, some data suggest that excess adiposity in boys contributes to delayed sexual maturation ( Lee et al., 2010 ). Pubescence, the earliest period of adolescence, generally occurs about 2 years in advance of sexual maturity. Typically, individuals are in the secondary school years during this period, which is a time of decline in habitual physical activity, especially in girls. Physical activity trends are influenced by the development of secondary sex characteristics and other physical changes that occur during the adolescent growth spurt, as well as by societal and cultural factors. Research suggests that physical inactivity during adolescence carries over into adulthood ( Malina, 2001a , b ; CDC, 2006 ).
It is critical that adolescents be offered appropriate physical activity programs that take into account the physical and sociocultural changes they are experiencing so they will be inspired to engage in physical activity for a lifetime. As discussed below, adequate physical activity during puberty may be especially important for optimal bone development and prevention of excess adiposity, as puberty is a critical developmental period for both the skeleton and the adipose organ.
Adolescence is the transitional period between childhood and adulthood. The adolescent growth spurt, roughly 3 years of rapid growth, occurs early in this period. An accelerated increase in stature is a hallmark, with about 20 percent of adult stature being attained during this period. Along with the rapid increase in height, other changes in body proportions occur that have important implications for sports and other types of activities offered in physical education and physical activity programs. As boys and girls advance through puberty, for example, biacromial breadth (shoulder width) increases more in boys than in girls, while increases in bicristal breadth (hip width) are quite similar. Consequently, hip-shoulder width ratio, which is similar in boys and girls during childhood, decreases in adolescent boys while remaining relatively constant in girls ( Malina et al., 2004 ). Ratios among leg length, trunk length, and stature also change during this period. Prior to adolescence, boys have longer trunks and shorter legs than girls ( Haubenstricker and Sapp, 1980 ). In contrast, adolescent and adult females have shorter legs for the same height than males of equal stature. Body proportions, particularly skeletal dimensions, are unlikely to be influenced by physical activity; rather, body proportions influence performance success, fitness evaluation, and the types of activities in which a person may wish to engage. For example, there is evidence that leg length influences upright balance and speed ( Haubenstricker and Sapp, 1980 ). Individuals who have shorter legs and broader pelvises are better at balancing tasks than those with longer legs and narrower pelvises, and longer legs are associated with faster running times ( Dintiman et al., 1997 ). Also, longer arms and wider shoulders are advantageous in throwing tasks ( Haubenstricker and Sapp, 1980 ), as well as in other activities in which the arms are used as levers. According to Haubenstricker and Sapp (1980) , approximately 25 percent of engagement in movement-related activities can be attributed to body size and structure.
Motor Development
Motor development depends on the interaction of experience (e.g., practice, instruction, appropriate equipment) with an individual's physical, cognitive, and psychosocial status and proceeds in a predictable fashion across developmental periods. Clark and Metcalfe (2002) provide an eloquent metaphor—“the mountain of motor development”—to aid in understanding the global changes seen in movement across the life span. Early movements, critical for an infant's survival, are reflexive and dominated by biology, although environment contributes and helps shape reflexes. This initial reflexive period is followed quickly by the preadapted period , which begins when an infant's movement behaviors are no longer reflexive and ends when the infant begins to apply basic movement skills (e.g., crawling, rolling, standing, and walking) that generally are accomplished before 12 months of age. The period of fundamental motor patterns occurs approximately between the ages of 1 and 7 years, when children begin to acquire basic fundamental movement skills (e.g., running, hopping, skipping, jumping, leaping, sliding, galloping, throwing, catching, kicking, dribbling, and striking). Practice and instruction are key to learning these skills, and a great deal of time in elementary school physical education is devoted to exploration of movement. Around age 7, during the so-called context-specific period of motor development, children begin to refine basic motor skills and combine them into more specific movement patterns, ultimately reaching what has been called skillfulness . Compensation , the final period of motor development, occurs at varying points across the life span when, as a result of aging, disease, injury, or other changes, it becomes necessary to modify movement.
While all children need not be “expert” in all movement skills, those who do not acquire the fundamental motor skills will likely experience difficulty in transitioning their movement repertoire into specific contexts and engagement in physical activity ( Fisher et al., 2005 ; Barnett et al., 2009 ; Cliff et al., 2009 ; Robinson et al., 2012 ). A full movement repertoire is needed to engage in physical activities within and outside of the school setting. Thus, beyond contributing to levels of physical activity, physical education programs should aim to teach basic fundamental motor skills and their application to games, sports, and other physical activities, especially during the elementary years (i.e., the fundamental motor patterns and context-specific periods). At the same time, it is important to be mindful of the wide interindividual variation in the rate at which children develop motor skills, which is determined by their biological makeup, their rate of physical maturation, the extent and quality of their movement experiences, and their family and community environment.
An increasing amount of evidence suggests that people who feel competent in performing physical skills remain more active throughout their lives ( Lubans et al., 2010 ). Conversely, those who are less skilled may be hesitant to display what they perceive as a shortcoming and so may opt out of activities requiring higher levels of motor competence ( Stodden et al., 2008 ). Children who are less physically skillful tend to be less active than their skillful counterparts ( Wrotniak et al., 2006 ; Williams et al., 2008 ; Robinson et al., 2012 ) and thus have a greater risk of overweight and obesity ( Graf et al., 2004 ). Fundamental skills are the building blocks of more complex actions that are completed in sports, physical activities, and exercise settings. For example, throwing is a fundamental skill that is incorporated into the context-specific throw used in activities such as handball, softball, and water polo. Fundamental skills are of primary interest to both physical education teachers and coaches, and physical education classes should be designed to challenge learners to develop their motor skills.
In 1998 the Centers for Disease Control and Prevention's (CDC's) Division of Nutrition and Physical Activity organized a workshop to determine future directions for research on physical activity. The workshop convened 21 experts from a wide range of academic disciplines. One recommendation resulting from the proceedings was for future research to describe the temporal relationship between motor development and physical activity ( Fulton et al., 2001 ), signifying the importance of better understanding of the nature of the relationship between motor competence and physical activity. The assumption of this relationship is implied in multiple models of motor development ( Seefeldt, 1980 ; Clark and Metcalfe, 2002 ; Stodden et al., 2008 ), which emphasize the importance of motor competence as a prerequisite for engagement in physical activity throughout the life span.
Two models that are commonly used to examine this relationship are Seefeldt's (1980) hierarchical order of motor skills development and the dynamic association model of Stodden and colleagues (2008) . Seefeldt proposed a hierarchical order of motor skills development that includes four levels: reflexes, fundamental motor skills, transitional motor skills (i.e., fundamental motor skills that are performed in various combinations and with variations and that are required to participate in entry-level organized sports, such as throwing for distance, throwing for accuracy, and/or catching a ball while in motion), and specific sports skills and dances. With improved transitional motor skills, children are able to master complex motor skills (e.g., those required for playing more complex sports such as football or basketball). At the end of this developmental period, children's vision is fully mature. The progression through each level occurs through developmental stages as a combined result of growth, maturation, and experience. Seefeldt hypothesized the existence of a “proficiency barrier” between the fundamental and transitional levels of motor skills development. If children are able to achieve a level of competence above the proficiency barrier, they are more likely to continue to engage in physical activity throughout the life span that requires the use of fundamental motor skills. Conversely, less skilled children who do not exceed the proficiency barrier will be less likely to continue to engage in physical activity. Thus, it is assumed that “a confident and competent mover will be an active mover” ( Clark, 2005 , p. 44). For example, to engage successfully in a game of handball, baseball, cricket, or basketball at any age, it is important to reach a minimum level of competence in running, throwing, catching, and striking. The assumption of the existence of a relationship between motor competence and physical activity is at the “heart of our physical education programs” ( Clark, 2005 , p. 44). A thorough understanding of how this relationship changes across developmental stages is crucial for curriculum development and delivery and teaching practices.
Lubans and colleagues (2010) recently examined the relationship between motor competence and health outcomes. They reviewed 21 studies identifying relationships between fundamental motor skills and self-worth, perceived physical competence, muscular and cardiorespiratory fitness, weight status, flexibility, physical activity, and sedentary behavior. Overall, the studies found a positive association between fundamental motor skills and physical activity in children and adolescents, as well as a positive relationship between fundamental motor skills and cardiorespiratory fitness. Other research findings support the hypothesis that the most physically active preschool-age ( Fisher et al., 2005 ; Williams et al., 2008 ; Robinson et al., 2012 ), elementary school–age ( Bouffard et al., 1996 ; Graf et al., 2004 ; Wrotniak et al., 2006 ; Hume et al., 2008 ; Lopes et al., 2011 ), and adolescent ( Okely et al., 2001 ) youth are also the most skilled.
An advantage of the “proficiency barrier” hypothesis proposed by Seefeldt (1980) is its recognition that the relationship between motor competence and physical activity may not be linear. Rather, the hypothesis suggests that physical activity is influenced when a certain level of motor competence is not achieved and acknowledges that below the proficiency barrier, there is bound to be substantial variation in children's motor competence and participation in physical activity. The proficiency barrier is located between the fundamental and transitional motor skills periods. The transition between these two levels of motor competence is expected to occur between the early and middle childhood years. Stodden and colleagues (2008) suggest that the relationship between motor competence and physical activity is dynamic and changes across time. In their model the “development of motor skill competence is a primary underlying mechanism that promotes engagement in physical activity” (p. 290).
The relationship between skills and physical activity is considered reciprocal. It is expected that as motor skills competence increases, physical activity participation also increases and that the increased participation feeds back into motor skills competence. The reciprocal relationship between motor skills competence and physical activity is weak during the early childhood years (ages 2-8) because of a variety of factors, including environmental conditions, parental influences, and previous experience in physical education programs ( Stodden et al., 2008 ). Also, children at this age are less able to distinguish accurately between perceived physical competence and actual motor skills competence ( Harter and Pike, 1984 ; Goodway and Rudisill, 1997 ; Robinson and Goodway, 2009 ; Robinson, 2011 ), and thus motor skills are not expected to strongly influence physical activity. The literature supports this hypothesis, as indicated by low to moderate correlations between motor skills competence and physical activity in preschool ( Sääkslahti et al., 1999 ; Williams et al., 2008 ; Cliff et al., 2009 ; Robinson and Goodway, 2009 ; Robinson, 2011 ) and early elementary school–age ( Raudsepp and Päll, 2006 ; Hume et al., 2008 ; Morgan et al., 2008 ; Houwen et al., 2009 ; Ziviani et al., 2009 ; Lopes et al., 2011 ) children.
In older children, perceived competence is more closely related to actual motor skills competence. Older, low-skilled children are aware of their skills level and are more likely to perceive physical activity as difficult and challenging. Older children who are not equipped with the necessary skills to engage in physical activity that requires high levels of motor skills competence may not want to display their low competence publicly. As children transition into adolescence and early adulthood, the relationship between motor skills competence and physical activity may strengthen ( Stodden et al., 2008 ). Investigators report moderate correlations between motor skills competence and physical activity in middle school–age children ( Reed et al., 2004 ; Jaakkola et al., 2009 ). Okely and colleagues (2001) found that motor skills competence was significantly associated with participation in organized physical activity (i.e., regular and structured experiences related to physical activity) as measured by self-reports. A strength of the model of Stodden and colleagues (2008) is the inclusion of factors related to psychosocial health and development that may influence the relationship between motor skills competence and physical activity, contributing to the development and maintenance of obesity. Other studies have found that perceived competence plays a role in engagement in physical activity ( Ferrer-Caja and Weiss, 2000 ; Sollerhed et al., 2008 ).
Motor skills competence is an important factor; however, it is only one of many factors that contribute to physical activity. For instance, three studies have reported negative correlations between girls' motor competence and physical activity ( Reed et al., 2004 ; Cliff et al., 2009 ; Ziviani et al., 2009 ), suggesting that sex may be another determining factor. A possible explanation for these findings is that since girls tend to be less active than boys, it may be more difficult to detect differences in physical activity levels between high- and low-skilled girls. It is also possible that out-of-school opportunities for physical activity are more likely to meet the interests of boys, which may at least partially explain sex differences in physical activity levels ( Le Masurier et al., 2005 ). Previous research suggests that in general boys are more motor competent than girls ( Graf et al., 2004 ; Barnett et al., 2009 ; Lopes et al., 2011 ) and that this trend, which is less apparent in early childhood, increases through adolescence ( Thomas and French, 1985 ; Thomas and Thomas, 1988 ; Thomas, 1994 ), although one study reports that girls are more motor competent than boys ( Cliff et al., 2009 ).
One component of motor competence is the performance of gross motor skills, which are typically classified into object control and locomotor skills. Consistent evidence suggests that boys are more competent in object control skills, while girls are more competent in locomotor skills ( McKenzie et al., 2004 ; Morgan et al., 2008 ; Barnett et al., 2009 ). In light of these sex differences, it is important to examine the relationships of object control and locomotor skills with physical activity separately for boys and girls. For boys, object control skills are more related to physical activity than are locomotor skills ( Hume et al., 2008 ; Morgan et al., 2008 ; Williams et al., 2008 ; Cliff et al., 2009 ), whereas evidence suggests that the reverse is true for girls ( McKenzie et al., 2002 ; Hume et al., 2008 ; Cliff et al., 2009 ; Jaakkola et al., 2009 ). Three studies report a significant relationship between balance and physical activity for girls but not boys ( Reed et al., 2004 ; Ziviani et al., 2009 ). Cliff and colleagues (2009) suggest that object control and locomotor skills may be more related to boys' and girls' physical activity, respectively, because of the activity type in which each sex typically engages.
The relationship between motor competence and physical activity clearly is complex. It is quite likely that the relationship is dynamic and that motor competence increases the likelihood of participating in physical activity while at the same time engaging in physical activity provides opportunities to develop motor competence ( Stodden et al., 2008 ). Despite some uncertainty, the literature does reinforce the important role of physical education in providing developmentally appropriate movement opportunities in the school environment. These opportunities are the only means of engaging a large population of children and youth and providing them with the tools and opportunities that foster health, development, and future physical activity.
Regular physical activity has no established effect on linear growth rate or ultimate height ( Malina, 1994 ). Although some studies suggest small differences, factors other than physical activity, especially maturity, often are not well controlled. It is important to note that regular physical activity does not have a negative effect on stature, as has sometimes been suggested. Differences in height among children and adolescents participating in various sports are more likely due to the requirements of the sport, selection criteria, and interindividual variation in biological maturity than the effects of participation per se ( Malina et al., 2004 ).
Body Weight
Although physical activity is inversely related to weight, correlations are generally low (~r–0.15), and differences in body weight between active and inactive boys and girls tend to be small ( Mirwald and Bailey, 1986 ; Saris et al., 1986 ; Beunen et al., 1992 ; Lohman et al., 2006 ;), except in very obese children and adolescents. Similarly, physique, as represented in somatotypes, does not appear to be significantly affected by physical activity during growth ( Malina et al., 2004 ). In contrast, components of weight can be influenced by regular physical activity, especially when the mode and intensity of the activity are tailored to the desired outcome. Much of the available data in children and adolescents is based on BMI, a surrogate for composition, and indirect methods based on the two-compartment model of body composition in which body weight is divided into its fat-free and fat components ( Going et al., 2012 ). While studies generally support that physical activity is associated with greater fat-free mass and lower body fat, distinguishing the effects of physical activity on fat-free mass from expected changes associated with growth and maturation is difficult, especially during adolescence, when both sexes have significant growth in fat-free mass. The application of methods based on the two-compartment model is fraught with errors, especially when the goal is to detect changes in fat-free mass, and no information is available from these methods regarding changes in the major tissue components of fat-free mass—muscle and skeletal tissue.
Skeletal muscle is the largest tissue mass in the body. It is the main energy-consuming tissue and provides the propulsive force for movement. Muscle represents about 23-25 percent of body weight at birth and about 40 percent in adults, although there is a wide range of “normal” ( Malina, 1986 , 1996 ). Postnatal muscle growth is explained largely by increases in cell size (hypertrophy) driving an increase in overall muscle mass. The increase in muscle mass with age is fairly linear from young childhood until puberty, with boys having a small but consistent advantage ( Malina, 1969 , 1986 ). The sex difference becomes magnified during and after puberty, driven primarily by gender-related differences in sex steroids. Muscle, as a percentage of body mass, increases from about 42 percent to 54 percent in boys between ages 5 and 11, whereas in girls it increases from about 40 percent to 45 percent between ages 5 and 13 and thereafter declines ( Malina et al., 2004 ). It should be noted that absolute mass does not decline; rather, the relative decline reflects the increase in the percentage of weight that is fat in girls. At least part of the sex difference is due to differences in muscle development for different body regions ( Tanner et al., 1981 ). The growth rate of arm muscle tissue during adolescence in males is approximately twice that in females, whereas the sex difference in the growth of muscle tissue in the leg is much smaller. The sex difference that develops during puberty persists into adulthood and is more apparent for the musculature of the upper extremities.
Sex-related differences in muscular development contribute to differences in physical performance. Muscle strength develops in proportion to the cross-sectional area of muscle, and growth curves for strength are essentially the same as those for muscle ( Malina and Roche, 1983 ). Thus the sex difference in muscle strength is explained largely by differences in skeletal muscle mass rather than muscle quality or composition. Aerobic (endurance) exercise has little effect on enhancing muscle mass but does result in significant improvement in oxygen extraction and aerobic metabolism ( Fournier et al., 1982 ). In contrast, numerous studies have shown that high-intensity resistance exercise induces muscle hypertrophy, with associated increases in muscle strength. In children and adolescents, strength training can increase muscle strength, power, and endurance. Multiple types of resistance training modalities have proven effective and safe ( Bernhardt et al., 2001 ), and resistance exercise is now recommended for enhancing physical health and function ( Behringer et al., 2010 ). These adaptations are due to muscle fiber hypertrophy and neural adaptations, with muscle hypertrophy playing a more important role in adolescents, especially in males. Prior to puberty, before the increase in anabolic sex steroid concentrations, neural adaptations explain much of the improvement in muscle function with exercise in both boys and girls.
The skeleton is the permanent supportive framework of the body. It provides protection for vital organs and is the main mineral reservoir. Bone tissue constitutes most of the skeleton, accounting for 14-17 percent of body weight across the life span ( Trotter and Peterson, 1970 ; Trotter and Hixon, 1974 ). Skeletal strength, which dictates fracture risk, is determined by both the material and structural properties of bone, both of which are dependent on mineral accrual. The relative mineral content of bone does not differ much among infants, children, adolescents, and adults, making up 63-65 percent of the dry, fat-free weight of the skeleton ( Malina, 1996 ). As a fraction of weight, bone mineral (the ash weight of bone) represents about 2 percent of body weight in infants and about 4-5 percent of body weight in adults ( Malina, 1996 ). Bone mineral content increases fairly linearly with age, with no sex difference during childhood. Girls have, on average, a slightly greater bone mineral content than boys in early adolescence, reflecting their earlier adolescent growth spurt. Boys have their growth spurt later than girls, and their bone mineral content continues to increase through late adolescence, ending with greater skeletal dimensions and bone mineral content ( Mølgaard et al., 1997 ). The increase in total body bone mineral is explained by both increases in skeletal length and width and a small increase in bone mineral density ( Malina et al., 2004 ).
Many studies have shown a positive effect of physical activity on intermediate markers of bone health, such as bone mineral content and density. Active children and adolescents have greater bone mineral content and density than their less active peers, even after controlling for differences in height and muscle mass ( Wang et al., 2004 ; Hind and Burrows, 2007 ; Tobias et al., 2007 ). Exercise interventions support the findings from observational studies showing beneficial effects on bone mineral content and density in exercise participants versus controls ( Petit et al., 2002 ; Specker and Binkley, 2003 ), although the benefit is less than is suggested by cross-sectional studies comparing active versus inactive individuals ( Bloomfield et al., 2004 ). The relationship between greater bone mineral density and bone strength is unclear, as bone strength cannot be measured directly in humans. Thus, whether the effects of physical activity on bone mineral density translate into similar benefits for fracture risk is uncertain ( Karlsson, 2007 ). Animal studies have shown that loading causes small changes in bone mineral content and bone mineral density that result in large increases in bone strength, supporting the notion that physical activity probably affects the skeleton in a way that results in important gains in bone strength ( Umemura et al., 1997 ). The relatively recent application of peripheral quantitative computed tomography for estimating bone strength in youth has also provided some results suggesting an increase in bone strength with greater than usual physical activity ( Sardinha et al., 2008 ; Farr et al., 2011 ).
The intensity of exercise appears to be a key determinant of the osteogenic response ( Turner and Robling, 2003 ). Bone tissue, like other tissues, accommodates to usual daily activities. Thus, activities such as walking have a modest effect at best, since even relatively inactive individuals take many steps (>1,000) per day. Activities generating greater muscle force on bone, such as resistance exercise, and “impact” activities with greater than ordinary ground reaction forces (e.g., hopping, skipping, jumping, gymnastics) promote increased mineralization and modeling ( Bloomfield et al., 2004 ; Farr et al., 2011 ). Far fewer randomized controlled trials (RCTs) examining this relationship have been conducted in children than in adults, and there is little evidence on dose response to show how the type of exercise interacts with frequency, intensity, and duration. Taken together, however, the available evidence supports beneficial effects of physical activity in promoting bone development ( Bailey et al., 1996 ; Modlesky and Lewis, 2002 ).
Physical activity may reduce osteoporosis-related fracture risk by increasing bone mineral accrual during development; by enhancing bone strength; and by reducing the risk of falls by improving muscle strength, flexibility, coordination, and balance ( Bloomfield et al., 2004 ). Early puberty is a key developmental period. Approximately 26 percent of the mineral content in the adult skeleton is accrued during the 2 years around the time of peak height velocity ( Bailey et al., 2000 ). This amount of mineral accrual represents approximately the same amount of bone mineral that most people will lose in their entire adult lives ( Arlot et al., 1997 ). The increase in mineral contributes to increased bone strength. Mineral is accrued on the periosteal surface of bone, such that the bone grows wider. Increased bone width, independent of the increased mineral mass, also contributes to greater bone strength. Indeed, an increase of as little as 1 mm in the outer surface of bone increases strength substantially. Adding bone to the endosteal surface also increases strength ( Parfitt, 1994 ; Wang et al., 2009 ). Increases in testosterone may be a greater stimulus of periosteal expansion than estrogen since testosterone contributes to wider and stronger bones in males compared with females. Retrospective studies in tennis players and gymnasts suggest structural adaptations may persist many years later in adulthood and are greatest when “impact” activity is initiated in childhood ( Kannus et al., 1995 ; Bass et al., 1998 ). RCTs on this issue are few, although the available data are promising ( McKay et al., 2000 ; Fuchs et al., 2001 ; MacKelvie et al., 2001 , 2003 ; Lindén et al., 2006 ). Thus, impact exercise begun in childhood may result in lasting structural changes that may contribute to increased bone strength and decreased fracture risk later in life ( Turner and Robling, 2003 ; Ferrari et al., 2006 ).
Adipose tissue
The adipose “organ” is composed of fat cells known as adipocytes ( Ailhaud and Hauner, 1998 ). Adipocytes are distributed throughout the body in various organs and tissues, although they are largely clustered anatomically in structures called fat depots, which include a large number of adipocytes held together by a scaffold-like structure of collagen and other structural molecules. In the traditional view of the adipocyte, the cell provides a storage structure for fatty acids in the form of triacylglycerol molecules, with fatty acids being released when metabolic fuel is needed ( Arner and Eckel, 1998 ). While adipocytes play this critical role, they are also involved in a number of endocrine, autocrine, and paracrine actions and play a key role in regulating other tissues and biological functions, for example, immunity and blood pressure, energy balance, glucose and lipid metabolism, and energy demands of exercise ( Ailhaud and Hauner, 1998 ; Frühbeck et al., 2001 ). The role of adipocytes in regulation of energy balance and in carbohydrate and lipid metabolism and the potential effects of physical activity on adipocyte function are of particular interest here, given growing concerns related to pediatric and adult obesity ( Ogden et al., 2012 ) and the associated risk of cardiometabolic disease ( Weiss et al., 2004 ; Eisenmann, 2007 a,b; Steele et al., 2008 ). Metabolic differences among various fat depots are now well known ( Frühbeck et al., 2001 ), and there is significant interest in the distribution of adipose tissue, the changes that occur during childhood and adolescence, and their clinical significance.
Adipocytes increase in size (hypertrophy) and number (hyperplasia) from birth through childhood and adolescence and into young adulthood to accommodate energy storage needs. The number of adipocytes has been estimated to increase from about 5 billion at birth to 30 billion to 50 billion in the nonobese adult, with an increase in average diameter from about 30-40 μm at birth to about 80-100 μm in the young adult ( Knittle et al., 1979 ; Bonnet and Rocour-Brumioul, 1981 ; Chumlea et al., 1982 ). In total the adipose organ contains about 0.5 kg of adipocytes at birth in both males and females, increasing to approximately 10 kg in average-weight-for-height males and 14 kg in females ( Malina et al., 2004 ). There is wide interindividual variation, however, and the difficulty of investigating changes in the number and size of adipocytes is obvious given the invasiveness of the required biopsy procedures; understandably, then, data on these topics are scarce in children and adolescents. Also, since only subcutaneous depots are accessible, results must be extrapolated from a few sites.
Based on such information, the average size of adipocytes has been reported to increase two- to threefold in the first year of life, with little increase in nonobese boys and girls until puberty ( Malina et al., 2004 ). A small increase in average adipocyte size at puberty is more obvious in girls than in boys. There is considerable variation in size across various subcutaneous sites and between subcutaneous and internal depots. The number of adipocytes is difficult to estimate. Available data suggest that the cellularity of adipose tissue does not increase significantly in early postnatal life ( Malina et al., 2004 ). Thus, gain in fat mass is the result of an increase in the size of existing adipocytes. From about 1-2 years of age and continuing through early and middle childhood, the number of adipocytes increases gradually two- to threefold. With puberty the number practically doubles, followed by a plateau in late adolescence and early adulthood. The number of adipocytes is similar in boys and girls until puberty, when girls experience a greater increase than boys.
The increases in the number of adipocytes during infancy and puberty are considered critical for enlargement of the adipose tissue organ and for the risk of obesity. Since size and number are linked, the number of adipocytes can potentially increase at any age if fat storage mechanisms are stimulated by chronic energy surfeit ( Hager, 1981 ; Chumlea et al., 1982 ). Energy expenditure through regular physical activity is a critical element in preventing energy surfeit and excess adiposity. While cellularity undoubtedly is strongly genetically determined, regular physical activity, through its contribution to energy expenditure, can contribute to less adipocyte hyperplasia by limiting hypertrophy.
Fat distribution
Fat distribution refers to the location of fat depots on the body. The metabolic activities of fat depots differ, and small variation can have a long-term impact on fat distribution. Differences in metabolic properties across depots also have clinical implications. Visceral adipose tissue in the abdominal cavity is more metabolically active (reflected by free fatty acid flux) than adipose tissue in other areas ( Arner and Eckel, 1998 ), and higher amounts of visceral adipose tissue are associated with greater risk of metabolic complications, such as type 2 diabetes and cardiovascular disease ( Daniels et al., 1999 ; He et al., 2007 ; Dencker et al., 2012 ). In contrast, subcutaneous fat, particularly in the gluteofemoral region, is generally associated with a lower risk of cardiometabolic disease. Age- and sex-associated variations in fat distribution contribute to age- and sex-associated differences in cardiometabolic disease prevalence. Girls have more subcutaneous fat than boys at all ages, although relative fat distribution is similar. After a rapid rise in subcutaneous fat in the first few months of life, both sexes experience a reduction through age 6 or 7 ( Malina and Roche, 1983 ; Malina and Bouchard, 1988 ; Malina, 1996 ). Girls then show a linear increase in subcutaneous fat, whereas boys show a small increase between ages 7 and 12 or 13 and then an overall reduction during puberty. The thickness of subcutaneous fat on the trunk is approximately one-half that of subcutaneous fat on the extremities in both boys and girls during childhood. The ratio increases with age in males during adolescence but changes only slightly in girls. In males the increasing ratio of trunk to extremity subcutaneous fat is a consequence of slowly increasing trunk subcutaneous fat and a decrease in subcutaneous fat on the extremities. In girls, trunk and extremity subcutaneous fat increase at a similar rate; thus the ratio is stable ( Malina and Bouchard, 1988 ). As a consequence, the sex difference in the distribution of body fat develops during adolescence. It is important to note that changes in subcutaneous fat pattern do not necessarily represent changes in abdominal visceral adipose tissue.
Tracking of subcutaneous fat has been investigated based on skinfold thicknesses and radiographs of fat widths in males and females across a broad age range ( Katzmarzyk et al., 1999 ; Campbell et al., 2012 ). Results indicate that subcutaneous fat is labile during early childhood. After age 7 to 8, correlations between subcutaneous fat in later childhood and adolescence and adult subcutaneous fat are significant and moderate. Longitudinal data on tracking of visceral adipose tissue are not available, but percent body fat does appear to track. Thus children and especially adolescents with higher levels of body fat have a higher risk of being overfat at subsequent examinations and in adulthood, although variation is considerable, with some individuals moving away from high fatness categories, while some lean children move into higher fatness categories.
In cross-sectional studies, active children and adolescents tend to have lower skinfold thicknesses and less overall body fat than their less active peers ( Loftin et al., 1998 ; Rowlands et al., 2000 ; Stevens et al., 2004 ; Lohman et al., 2006 ), although the correlations are modest, reflecting variation in body composition at different levels of physical activity, as well as the difficulty of measuring physical activity. Longitudinal studies indicate small differences in fatness between active and inactive boys and girls. Although some school-based studies of the effects of physical activity on body composition have reported changes in BMI or skinfolds in the desired direction ( Gortmaker et al., 1999 ; McMurray et al., 2002 ), most have not shown significant effects. High levels of physical activity are most likely needed to modify skinfold thicknesses and percent body fat. In adults, visceral adipose tissue declines with weight loss with exercise. In contrast, in a study of obese children aged 7-11, a 4-month physical activity program resulted in minimal change in abdominal visceral adipose tissue but a significant loss in abdominal subcutaneous adipose tissue ( Gutin and Owens, 1999 ). In adults, decreases in fatness with exercise are due to a reduction in fat cell size, not number ( You et al., 2006 ); whether this is true in children is not certain but appears likely. Given that adipocyte hypertrophy may trigger adipocyte hyperplasia ( Ballor et al., 1998 ), energy expenditure through regular physical activity may be important in preventing excess adipose tissue cellularity. Regular physical activity also affects adipose tissue metabolism so that trained individuals have an increased ability to mobilize and oxidize fat, which is associated with increased levels of lipolysis, an increased respiratory quotient, and a lower risk of obesity ( Depres and Lamarche, 2000 ).
Cardiorespiratory System
The ability to perform sustained activity under predominantly aerobic conditions depends on the capacity of the cardiovascular and pulmonary systems to deliver oxygenated blood to tissues and on the ability of tissues (primarily skeletal muscle) to extract oxygen and oxidize substrate. By age 2 the systems are fully functional, although young children lack the cardiorespiratory capacity of older children and adults because of their small size ( Malina et al., 2004 ). Children's aerobic capacity and consequently their ability to exercise for longer periods of time increase as they grow. Maximal aerobic power (liters per minute) increases fairly linearly in boys until about age 16, whereas it increases in girls until about age 13 and then plateaus during adolescence ( Malina et al., 2004 ; Eisenmann et al., 2011 ). Differences between boys and girls are small (~10 percent) during childhood and greater after the adolescent growth spurt, when girls have only about 70 percent of the mean value of boys. Changes with age and sex differences are explained largely by differences in the size of the relevant tissues. Dimensions of the heart and lungs enlarge with age in a manner consistent with the increase in body mass and stature ( Malina et al., 2004 ). The increase in the size of the heart is associated with increases in stroke volume (blood pumped per beat) and cardiac output (product of stroke volume and heart rate, liters per minute), despite a decline in heart rate during growth. Similarly, increase in lung size (proportional to growth in height) results in greater lung volume and ventilation despite an age-associated decline in breathing frequency. From about age 6 to adulthood, maximal voluntary ventilation approximately doubles (50–100 L/min) ( Malina et al., 2004 ). The general pattern of increase as a function of height is similar in boys and girls. In both, lung function tends to lag behind the increase in height during the adolescent growth spurt. As a result, peak gains in lung function occur about 2 years earlier in girls than in boys.
Blood volume is highly related to body mass and heart size in children and adolescents, and it is also well correlated with maximal oxygen uptake during childhood and adolescence ( Malina et al., 2004 ). Blood volume increases from birth through adolescence, following the general pattern for changes in body mass. Both red blood cells and hemoglobin have a central role in transport of oxygen to tissues. Hematocrit, the percentage of blood volume explained by blood cells, increases progressively throughout childhood and adolescence in boys, but only through childhood in girls. Hemoglobin content, which is related to maximal oxygen uptake, heart volume, and body mass, increases progressively with age into late adolescence. Males have greater hemoglobin concentrations than females, especially relative to blood volume, which has functional implications for oxygen transport during intense exercise.
Growth in maximal aerobic power is influenced by growth in body size, so controlling for changes in body size during growth is essential. Although absolute (liters per minute) aerobic power increases into adolescence relative to body weight, there is a slight decline in both boys and girls, suggesting that body weight increases at a faster rate than maximal oxygen consumption, particularly during and after the adolescent growth spurt ( Malina et al., 2004 ). Changes in maximal oxygen consumption during growth tend to be related more closely to fat-free mass than to body mass. Nevertheless, sex differences in maximal oxygen consumption per unit fat-free mass persist, and maximal oxygen consumption per unit fat-free mass declines with age.
Improvements in cardiorespiratory function—involving structural and functional adaptations in the lungs, heart, blood, and vascular system, as well as the oxidative capacity of skeletal muscle—occur with regular vigorous- and moderate-intensity physical activity ( Malina et al., 2004 ). Concern about the application of invasive techniques limits the available data on adaptations in the oxygen transport system in children. Nevertheless, it is clear that aerobic capacity in youth increases with activity of sufficient intensity and that maximal stroke volume, blood volume, and oxidative enzymes improve after exercise training ( Rowland, 1996 ). Training-induced changes in other components of the oxygen transport system remain to be determined.
Health- and Performance-Related Fitness
Physical fitness is a state of being that reflects a person's ability to perform specific exercises or functions and is related to present and future health outcomes. Historically, efforts to assess the physical fitness of youth focused on measures designed to evaluate the ability to carry out certain physical tasks or activities, often related to athletic performance. In more recent years, the focus has shifted to greater emphasis on evaluating health-related fitness ( IOM, 2012a ) and assessing concurrent or future health status. Health- and performance-related fitness, while overlapping, are different constructs. Age- and sex-related changes in the components of both are strongly linked to the developmental changes in tissues and systems that occur during childhood and adolescence. Although genetic factors ultimately limit capacity, environmental and behavioral factors, including physical activity, interact with genes to determine the degree to which an individual's full capacity is achieved.
Health-Related Fitness
Cardiorespiratory endurance, muscular strength and endurance, flexibility, and body composition are components of health-related fitness historically assessed in school-based fitness assessment programs ( IOM, 2012a ). These components of health-related fitness are considered important since they can be linked to the risk of cardiometabolic disease and musculoskeletal disability, chronic hypokinetic-related diseases.
Cardiorespiratory endurance
Cardiorespiratory (aerobic) endurance reflects the functioning of the pulmonary and cardiovascular systems to deliver oxygen and the ability of tissues (primarily skeletal muscle) to extract oxygen from the blood. Defined clinically as the maximum oxygen consumption during a maximal graded exercise test, in practice it is usually measured indirectly as performance on a field test of endurance, such as 1- or 2-mile run time ( IOM, 2012a ). During childhood, aerobic capacity approximately doubles in both boys and girls, although girls on average possess a lower capacity. Males continue to improve during adolescence, up to ages 17-18, while aerobic capacity plateaus around age 14 in females ( Malina et al., 2004 ), resulting in an approximately 20 percent difference between males and females ( Rowland, 2005 ).
Favorable associations have been found between aerobic endurance and high-density lipoproteins, systolic blood pressure, diastolic blood pressure, BMI, measures of fatness, arterial stiffness, and measures of insulin sensitivity ( Boreham et al., 2004 ; Imperatore et al., 2006 ; Hussey et al., 2007 ; Ondrak et al., 2007 ). Some evidence suggests a decline in aerobic endurance among U.S. youth in recent decades ( Eisenmann, 2003 ; Carnethon et al., 2005 ; Pate et al., 2006 ), coincident with increased sedentariness and obesity and a greater prevalence of metabolic syndrome in youth. Aerobic exercise has been shown to increase cardiorespiratory endurance by about 5-15 percent in youth ( Malina et al., 2004 ; HHS, 2008 ). The programs that produce this benefit involve continuous vigorous- or moderate-intensity aerobic activity of various types for 30-45 minutes per session at least 3 days per week over a period of at least 1-3 months ( Baquet et al., 2002 ); improvements are greater with more frequent exercise ( Baquet et al., 2003 ).
Muscle strength and endurance
Muscle strength is defined as the highest force generated during a single maximum voluntary contraction, whereas muscle endurance is the ability to perform repeated muscular contraction and force development over a period of time. Muscle strength and endurance are correlated, especially at higher levels of force production. Muscle strength is proportional to the cross-sectional area of skeletal muscle; consequently, strength growth curves parallel growth curves for body weight and skeletal muscle mass ( Malina et al., 2004 ).
Both males and females show impressive increases in muscle strength from childhood to adolescence. Strength in children increases linearly, with boys having a slight advantage over girls. However, these sex differences are magnified during the adolescent years as a result of maturation ( Malina and Roche, 1983 ). Differences in muscle strength between boys and girls become more apparent after puberty, primarily as a result of the production of sex steroid hormones. In boys the increase in strength during adolescence lags behind the growth spurt by at least a year (peak height velocity), which may explain why some boys experience a brief period of clumsiness or awkwardness during puberty, as they have not yet acquired the muscle strength necessary to handle the changes associated with their larger bodies. Muscle strength increases at its greatest rate approximately 1 year after peak height velocity in boys, whereas for girls the strength spurt generally occurs during the same year as peak height velocity ( Bar-Or, 1983 ).
A compelling body of evidence indicates that with resistance training children and adolescents can significantly increase their strength above that expected as a result of normal growth and maturation, provided that the training program is of sufficient intensity, volume, and duration ( Committee on Sports Medicine Fitness, 2001 ). Both boys and girls can benefit, and strength gains in children as young as 5-6 have been reported ( Faigenbaum et al., 2009 ), although most studies are of older children and adolescents. Gains in muscle strength of about 30 percent are typical, although considerably larger gains have been reported. Adolescents make greater gains than preadolescents in absolute strength, whereas reported relative (percent above initial strength) gains in strength during preadolescence and adolescence are similar. A variety of programs and modalities have proved efficacious ( Council on Sports Medicine Fitness, 2008 ), as long as load (~10-15 repetitions maximum) and duration (~8-20 weeks) are adequate. As in adults, training adaptations in youth are specific to the muscle action or muscle groups that are trained, and gains are transient if training is not maintained ( Faigenbaum et al., 2009 ).
Youth resistance training, as with most physical activities, does carry some degree of risk of musculoskeletal injury, yet the risk is no greater than that associated with other sports and activities in which children and adolescents participate ( Council on Sports Medicine Fitness, 2008 ; Faigenbaum et al., 2009 ) as long as age-appropriate training guidelines are followed. A traditional area of concern has been the potential for training-induced damage to growth cartilage, which could result in growth disturbances. However, a recent review found no reports of injury to growth cartilage in any prospective study of resistance training in youth and no evidence to suggest that resistance training negatively impacts growth and maturation during childhood and adolescence ( Faigenbaum et al., 2009 ). Injuries typically occur in unsupervised settings and when inappropriate loads and progressions are imposed.
In addition to the obvious goal of gaining strength, resistance training may be undertaken to improve sports performance and prevent injuries, rehabilitate injuries, and enhance health. Appropriately supervised programs emphasizing strengthening of trunk muscles in children theoretically benefit sport-specific skill acquisition and postural control, although these benefits are difficult to study and thus are supported by little empirical evidence ( Council on Sports Medicine Fitness, 2008 ). Similarly, results are inconsistent regarding the translation of increased strength to enhanced athletic performance in youth. Limited evidence suggests that strength-training programs that address common overuse injuries may help reduce injuries in adolescents, but whether the same is true in preadolescents is unclear ( Council on Sports Medicine Fitness, 2008 ). Increasing evidence suggests that strength training, like other forms of physical activity, has a beneficial effect on measurable health indices in youth, such as cardiovascular fitness, body composition, blood lipid profiles and insulin sensitivity ( Faigenbaum, 2007 ; Benson et al., 2008 ), bone mineral density and bone geometry ( Morris et al., 1997 ; MacKelvie et al., 2004 ), and mental health ( Holloway et al., 1988 ; Faigenbaum et al., 1997 ; Annesi et al., 2005 ; Faigenbaum, 2007 ). Some work has shown that muscle fitness, reflected in a composite index combining measures of muscle strength and endurance, and cardiorespiratory fitness are independently and negatively associated with clustered metabolic risk ( Steene-Johannessen et al., 2009 ). Moreover, children with low muscle strength may be at increased risk of fracture with exercise ( Clark et al., 2011 ). Finally, muscle hypertrophy, which adds to fat-free mass, contributes to resting metabolic rate and therefore total daily energy expenditure. Resistance training may be particularly useful for raising metabolic rate in overweight and obese children without the risk associated with higher-impact activities ( Watts et al., 2005 ; Benson et al., 2007 ).
Flexibility
Flexibility has been operationally defined as “the intrinsic property of body tissues, including muscle and connective tissues, that determines the range of motion achievable without injury at a joint or group of joints” ( IOM, 2012b , p. 190). At all ages, girls demonstrate greater flexibility than boys, and the difference is greatest during the adolescent growth spurt and sexual maturation. Perhaps the most common field measure of flexibility in children and youth is the sit-and-reach test ( IOM, 2012b ) of low-back flexibility. Low-back flexibility as measured by this test is stable in girls from age 5 to 11 and increases until late adolescence. In boys, low-back flexibility declines linearly starting at age 5, reaching its nadir at about age 12, and then increases into late adolescence. The unique pattern of age- and sex-associated variation is related to the growth of the lower extremities and the trunk during adolescence. In boys the nadir in low-back flexibility coincides with the adolescent growth spurt in leg length. In both boys and girls, the increase during adolescence coincides with the growth spurt in trunk length and arm length, which influences reach. Flexibility in both males and females tends to decline after age 17, in part as a result of a decline in physical activity and normal aging.
The principal health outcomes hypothesized to be associated with flexibility are prevention of and relief from low-back pain, prevention of musculoskeletal injury, and improved posture. These associations have been studied in adults, with equivocal results ( Plowman, 1992 ). Although flexibility has long been included in national youth fitness tests, it has proven difficult to establish a link between flexibility and health ( IOM, 2012a ). In contrast to other fitness components that are general or systemic in nature, flexibility is highly specific to each joint of the body. Although appropriate stretching may increase flexibility, establishing a link to improved functional capacity and fitness is difficult. A few studies suggest that improvements in flexibility as measured by the sit-and-reach test may be related to less low-back pain ( Jones et al., 2007 ; Ahlqwist et al., 2008 ), but the evidence is weak. Consequently, the Institute of Medicine (IOM) Committee on Fitness Measures and Health Outcomes in its recent report elected to forego recommending a flexibility test for a national youth fitness test battery pending further research to confirm the relationship between flexibility and health and to develop national normative data ( IOM, 2012a ).
Body composition
Body composition is the component of health-related fitness that relates to the relative amount of adipose tissue, muscle, bone, and other vital components (e.g., organs, connective tissues, fluid compartments) that make up body weight. Most feasible methods for assessing body composition are based on models that divide the body into fat and fat-free (all nonfat constituents) components ( Going et al., 2012 ). Although fat mass and adipose tissue are not equivalent components, fat mass is easier to estimate than adipose tissue, and it is correlated with performance and disease risk. In settings in which estimation of body fat is difficult, weight-for-height ratios often are used as surrogates for body composition. Indeed, definitions of pediatric overweight and obesity have been based on BMI, calculated as weight in kilograms divided by height squared. Child and adolescent obesity defined by BMI remains at all-time highs. Population surveys indicate that approximately 33 percent of all boys and girls are overweight, and nearly one in five are obese ( Ogden and Flegal, 2011 ). The tendency for excess fatness to persist from childhood and adolescence into adulthood ( Daniels et al., 2005 ), coupled with the strong association between obesity and chronic disease ( Weiss and Caprio, 2005 ; Barlow, 2007 ), has caused great concern for future obesity levels and the health of youth and adults alike ( IOM, 2005 , 2012b ).
The increase in prevalence of obesity is undoubtedly due to a mismatch between energy intake and expenditure. Population surveys have shown that few children and youth meet recommended levels of daily physical activity (see Chapter 2 ). Prospective studies have shown a significant and inverse relationship between habitual physical activity and weight gain ( Berkey et al., 2003 ), and in some studies physical activity is a better predictor of weight gain than estimates of calorie or fat intake ( Berkey et al., 2000 ; Janssen et al., 2005 ). These relationships are better established in adults than in children and youth, although even in preschool children, low levels of physical activity, estimated from doubly labeled water, were found to be indicative of higher body fat content ( Davies et al., 1995 ). While studies of exercise without caloric restriction generally show only small effects on body weight, significant albeit moderate reductions of body fat are generally reported ( Eisenmann, 2003 ). Moreover, even in the absence of significant weight loss, exercise has beneficial effects on risk factors for cardiometabolic disease ( Ross and Bradshaw, 2009 ; Gutin and Owens, 2011 ).
Body mass index
Changes in weight for height with growth and maturation for U.S. boys and girls are described in CDC growth curves ( Kuczmarski et al., 2000 ). Current growth curves were derived from U.S. population surveys conducted before the increase in weight for height that defines today's pediatric obesity epidemic. In boys and girls, BMI declines during early childhood, reaching its nadir at about ages 5-6, and then increases through adolescence. A gender difference emerges during puberty, with males gaining greater fat-free mass than females. Both the period of “adiposity rebound” (the increase in BMI in midchildhood following the decline in early childhood) and puberty are times of risk for excess fat gain that correlates with future adiposity ( Rolland-Cachera et al., 1984 ). Physical activity and BMI are inversely correlated in children and adolescents, although the correlations are modest ( Lohman et al., 2006 ), reflecting the difficulty of measuring physical activity, as well as variation in body composition and physical activity at a given weight ( Rowlands et al., 2000 ). Indeed, when studied separately, fat mass index (FMI, or fat mass divided by height squared) and fat-free mass index (FFMI, or fat-free mass divided by height squared) are both inversely related to physical activity. With FMI controlled, however, FFMI is positively related to physical activity, indicating that, for a given level of body fat, individuals with more fat-free mass are more active ( Lohman et al., 2006 ). BMI cut-points for defining overweight and obesity have historically been based on age- and gender-specific population distributions of BMI. Recent work has shown good correspondence between BMI standards and percent fat standards that are referenced to health criteria ( Laurson et al., 2011 ). These new standards should prove useful for identifying children and adolescents at risk for higher levels of cardiometabolic risk factors.

Percent body fat
Direct measures of body fat as a percent of weight provide a better index of adiposity and health risk than BMI ( Zeng et al., 2012 ), which is confounded by variation in lean tissue mass relative to height. Recently, percent fat growth curves were established for representative samples of U.S. boys and girls using National Health and Nutrition Examination Survey (NHANES) data ( Laurson et al., 2011 ; Ogden and Flegal, 2011 ). Median percent fat for boys aged 5-18 ranged from 14 to 19 percent and for girls across the same ages 15 to 28 percent. In both boys and girls, percent fat increases slowly during early childhood, with girls having a consistently greater relative fatness than boys after ages 5-6. In girls, percent fat increases gradually throughout adolescence in the same manner as fat mass. In boys, percent fat increases gradually until the adolescent growth spurt and thereafter gradually declines until about age 16-17, reflecting the rapid growth in fat-free mass relative to fat mass. After age 17, percent fat in males gradually increases again into adulthood.
The increased prevalence of child and adolescent obesity as defined by BMI presumably also reflects increased adiposity, although the degree is not certain as population-based estimates of percent fat have only recently been developed ( Laurson et al., 2011 ). Health-related percent fat standards recently were developed by determining levels of body fat associated with greater occurrence of chronic disease risk factors defined by metabolic syndrome ( Going et al., 2011 ). In boys and girls aged 12-18, body fat above 20-24 percent and above 27-31 percent, respectively, was predictive of metabolic syndrome.
Physical activity is inversely correlated with percent body fat ( Rowlands et al., 2000 ; Lohman et al., 2006 ), although the correlations are modest, and changes in overall fatness as well as subcutaneous adipose tissue with habitual physical activity are reasonably well documented in children and adolescents ( Gutin and Humphries, 1998 ; Gutin and Owens, 1999 ; Dionne et al., 2000 ). In youth, as in adults, the effects of exercise without caloric restriction are modest and are influenced by the initial level of body fat and the duration and regimen of exercise ( Going, 1999 ). Experimental studies have documented reductions in percent body fat with aerobic exercise, especially in children and adolescents who are overweight or obese at the initiation of an exercise program ( Davis et al., 2012 ). Regular physical activity also affects adipose tissue metabolism ( Gutin and Owens, 1999 ). Individuals who engage in aerobic endurance exercise training have an increased ability to mobilize and oxidize fat, which is associated with increased levels of lipolysis ( Depres and Lamarche, 2000 ). Similar information on adipose tissue metabolism in children and youth is lacking, although one can reasonably expect similar adaptations in older adolescents.
Metabolic syndrome
The tendency for risk factors for cardiometabolic disease to cluster, now called metabolic syndrome, is well recognized in adults ( Alberti and Zimmet, 1998 ). Similar clustering occurs in older children and especially adolescents ( Cook et al., 2003 ), and interest in metabolic syndrome has increased, driven by the increased prevalence of pediatric obesity and the increasing incidence and earlier onset of type 2 diabetes in youth. There is as yet no accepted definition of metabolic syndrome for use in pediatric populations ( Jolliffe and Janssen, 2007 ). Typically, adult definitions are extrapolated to children and adolescents, with appropriate adjustments of the thresholds for the defining variables. Perhaps the most common approach is to emulate the National Cholesterol Education Program (NCEP), which defines metabolic syndrome as exceeding thresholds on three of five components: waist circumference, blood pressure (systolic or diastolic), blood lipids (high-density lipoprotein [HDL] and triglycerides), and blood glucose levels ( NIH, 2001 ).
The concept of metabolic syndrome is useful as it provides an integrated index of risk, and it recently was used to derive health-related percent-body-fat standards ( Laurson et al., 2011 ). Based on NHANES data, the prevalence of metabolic syndrome varies with the degree of obesity, and it is estimated at 4-6 percent of children and adolescents ( Cook et al., 2003 ; Dubose et al., 2007 ); among obese youth it may be as high as 30-50 percent ( Weiss et al., 2004 ). Youth with metabolic syndrome have an increased risk of type 2 diabetes and cardiovascular disease. In adults a loss of 5-10 percent of body weight through calorie restriction and exercise has been shown to reduce the risk of cardiometabolic disease by improving risk factors ( Diabetes Prevention Program Research Group, 2002 ; Ross and Janiszewski, 2008 ). In particular, weight loss results in reduced visceral adipose tissue, a strong correlate of risk ( Knowler et al., 2002 ), as well as lower blood pressure and blood glucose levels due to improved insulin sensitivity. Even without significant weight loss, exercise can have significant effects in adults by improving glucose metabolism, improving lipid and lipoprotein profiles, and lowering blood pressure, particularly for those who are significantly overweight ( Ross and Bradshaw, 2009 ). Similar benefits have been observed in adolescents.
A growing body of literature addresses the associations of physical activity, physical fitness, and body fatness with the risk of metabolic syndrome and its components in children and especially adolescents ( Platat et al., 2006 ; McMurray et al., 2008 ; Rubin et al., 2008 ; Thomas and Williams, 2008 ; Christodoulos et al., 2012 ). Studies in adults have shown that higher levels of physical activity predict slower progression toward metabolic syndrome in apparently healthy men and women ( Laaksonen et al., 2002 ; Ekelund et al., 2005 ), an association that is independent of changes in body fatness and cardiorespiratory fitness ( Ekelund et al., 2007 ). Few population studies have focused on these relationships in children and adolescents, and the use of self-reported activity, which is imprecise in these populations, tends to obscure associations. In a large sample of U.S. adolescents aged 12-19 in the 1999–2002 NHANES, for example, there was a trend for metabolic syndrome to be more common in adolescents with low activity levels than in those with moderate or high activity levels, although the differences among groups were not statistically significant ( Pan and Pratt, 2008 ). Moreover, for each component of metabolic syndrome, prevalence was generally lower with higher physical activity levels, and adolescents with low physical activity levels had the highest rates of all metabolic syndrome components.
The association between cardiorespiratory fitness and metabolic syndrome also was examined in the 1999–2002 NHANES ( Lobelo et al., 2010 ). Cardiorespiratory fitness was measured as estimated peak oxygen consumption using a submaximal treadmill exercise protocol, and metabolic syndrome was represented as a “clustered score” derived from five established risk factors for cardiovascular disease, an adiposity index, insulin resistance, systolic blood pressure, triglycerides, and the ratio of total to HDL cholesterol. Mean clustered risk score decreased across increasing fifths (quintiles) of cardiorespiratory fitness in both males and females. The most significant decline in risk score was observed from the first (lowest) to the second quintile (53.6 percent and 37.5 percent in males and females, respectively), and the association remained significant in both overweight and normal-weight males and in normal-weight females. Other studies, using the approach of cross-tabulating subjects into distinct fitness and fatness categories, have examined associations of fitness and fatness with metabolic syndrome risk ( Eisenmann et al., 2005 , 2007a , b ; Dubose et al., 2007 ). Although different measures of fitness, fatness, and metabolic syndrome risk were used, the results taken together across a wide age range (7–18) show that fitness modifies the influence of fatness on metabolic syndrome risk. In both males and females, high-fit/low-fatness subjects have less metabolic syndrome risk than low-fit/high-fatness subjects ( Eisenmann, 2007 ).
That many adult chronic health conditions have their origins in childhood and adolescence is well supported ( Kannel and Dawber, 1972 ; Lauer et al., 1975 ; Berenson et al., 1998 ; IOM, 2004 ). Both biological (e.g., adiposity, lipids) and behavioral (e.g., physical activity) risk factors tend to track from childhood and especially adolescence into adulthood. Childhood BMI is related to adult BMI and adiposity ( Guo et al., 1994 , 2000 ; Freedman et al., 2005 ), and as many as 80 percent of obese adolescents become obese adults ( Daniels et al., 2005 ). Coexistence of cardiometabolic risk factors, even at young ages ( Dubose et al., 2007 ; Ramírez-Vélez et al., 2012 ), has been noted, and these components of metabolic syndrome also have been shown to track to adulthood ( Bao et al., 1994 ; Katzmarzyk et al., 2001 ; Huang et al., 2008 ). Landmark studies from the Bogalusa Heart Study ( Berenson et al., 1998 ; Li et al., 2003 ) and others ( Mahoney et al., 1996 ; Davis et al., 2001 ; Morrison et al., 2007 , 2008 ) have demonstrated that cardiometabolic risk factors present in childhood are predictive of adult disease.
The benefits of exercise for prevention and treatment of cardiometabolic disease in adults are well described ( Ross et al., 2000 ; Duncan et al., 2003 ; Gan et al., 2003 ; Irwin et al., 2003 ; Lee et al., 2005 ; Sigal et al., 2007 ; Ross et al., 2012 ). Prospective studies examining the effects of exercise on metabolic syndrome in children and adolescents remain limited, and it is important to refrain from extrapolating intervention effects observed in adults to youth, although one might reasonably assume the benefits in older adolescents to be similar to those in young adults. Indeed, based on the inverse associations of physical activity and physical fitness with metabolic syndrome ( Kim and Lee, 2009 ) and on the available intervention studies, some experts have recommended physical activity as the main therapeutic tool for prevention and treatment of metabolic syndrome in childhood ( Brambilla et al., 2010 ). Comparative studies in adults have shown that the effect of exercise on weight is limited and generally less than that of calorie restriction ( Brambilla et al., 2010 ). Moreover, the relative effectiveness of diet and exercise depends on the degree of excess fatness ( Brambilla et al., 2010 ). Comparative studies in children and youth are few, as behavioral interventions in overweight children and adolescents commonly combine exercise and dietary restriction, making it difficult to disentangle their independent effects. Nonetheless, diet and exercise have different effects on body composition: While both contribute to fat loss, only exercise increases muscle mass and thus has a direct effect on metabolic health. In children and youth, as in adults, the effect of exercise on cardiometabolic risk factors is greater in overweight/obese youth than in their normal-weight peers ( Kang et al., 2002 ; Lazaar et al., 2007 ).
Exercise also may have important benefits even without significant modification of body composition ( Bell et al., 2007 ). Experimental studies in overweight and obese youth have shown that exercise leads to reductions in visceral fat ( Owens et al., 1999 ; Gutin et al., 2002 ; Lee at al., 2005 ; Barbeau et al., 2007 ; Kim and Lee, 2009 ) without a significant change in BMI, as well as improvement in markers of metabolic syndrome, primarily fasting insulin and insulin resistance ( Treuth et al., 1998 ; Ferguson et al., 1999 ; Carrel et al., 2005 ; Nassis et al., 2005 ; Meyer et al., 2006 ; Shaibi et al., 2006 ; Bell et al., 2007 ). Results from experimental studies of the effects of exercise on lipids and lipoproteins ( Stoedefalke et al., 2000 ; Kelley and Kelley, 2008 ; Janssen and LeBlanc, 2010 ) are mixed. Although some studies have shown improved lipid and lipoprotein profiles, primarily a decrease in low-density lipoprotein (LDL) cholesterol and triglyceride concentrations and an increase in HDL cholesterol ( Ferguson et al., 1999 ), other studies have shown no improvement in these outcomes ( Kelley and Kelley, 2008 ). In part, such conflicting results are likely due to initial differences in body composition and severity of hyperlipidemia. Well-controlled exercise training studies in obese children ( Escalante et al., 2012 ) and children with adverse blood lipid and lipoprotein profiles have shown positive alterations in their profiles ( Stoedefalke et al., 2000 ), whereas results in normolipid-emic children and adolescents are equivocal. Similarly, exercise has little effect on resting blood pressure in normotensive children and adolescents ( Kelley and Kelley, 2008 ), whereas reductions in resting systolic and sometimes diastolic pressures have been reported in youth with high blood pressure ( Hagberg et al., 1983 , 1984 ; Danforth et al., 1990 ; Ewart et al., 1998 ; Farpour-Lambert et al., 2009 ; Janssen and LeBlanc, 2010 ).
In adults, physical activity is inversely associated with low-grade inflammation ( Wärnberg et al., 2010 ; Ertek and Cicero, 2012 ), which is now recognized as a significant feature of metabolic syndrome and an independent predictor of cardiometabolic disease ( Malina, 2002 ). In obese children and adolescents, as in their adult counterparts, elevation of inflammatory markers is evident, and observational studies have shown significant relationships among physical activity, physical fitness, and inflammation ( Isasi et al., 2003 ; Platat et al., 2006 ; Ruiz et al., 2007 ; Wärnberg et al., 2007 ; Wärnberg and Marcos, 2008 ). These relationships are better studied and stronger in adolescents than in children. In one study of boys and girls aged 10-15, those who were obese and unfit had the highest levels of systemic inflammation, whereas those who were obese yet fit had levels as low as those who were lean and fit ( Halle et al., 2004 ). In another study, low-grade inflammation was negatively associated with muscle strength in overweight adolescents after controlling for cardiorespiratory fitness, suggesting that high levels of muscle strength may counteract some of the negative consequences of higher levels of body fat ( Ruiz et al., 2008 ). Experimental studies of the effects of exercise and markers of low-grade inflammation in children and adolescents are lacking. Improved cardiorespiratory fitness in adults ( Church et al., 2002 ), however, has been shown to be inversely related to concentration of C-reactive protein (CRP), a marker of low-grade inflammation. In a small study of a lifestyle intervention entailing 45 minutes of physical activity 3 times per week for 3 months, a small reduction in body fat and an overall decrease in inflammatory factors (CRP, interleukin [IL]-6) were seen in obese adolescents ( Balagopal et al., 2005 ).
Performance-Related Fitness
Speed, muscle power, agility, and balance (static and dynamic) are aspects of performance-related fitness that change during body development in predictable ways associated with the development of tissues and systems discussed above ( Malina et al., 2004 ). Running speed and muscle power are related, and both depend on full development of the neuromuscular system. Running speed and muscle power are similar for boys and girls during childhood ( Haubenstricker and Seefeldt, 1986 ). After puberty, largely because of differences in muscle mass and muscle strength, males continue to make significant annual gains, while females tend to plateau during the adolescent years. Sociocultural factors and increasing inactivity among girls relative to boys, along with changes in body proportion and a lowering of the center of gravity, may also contribute to gender differences ( Malina et al., 2004 ).
Balance—the ability to maintain equilibrium—generally improves from ages 3 to 18 ( Williams, 1983 ). Research suggests that females outperform males on tests of static and dynamic balance during childhood and that this advantage persists through puberty ( Malina et al., 2004 ).
Motor performance is related in part to muscle strength. Increases in muscle strength as a result of resistance exercise were described above. A question of interest is whether gains in strength transfer to other performance tasks. Available results are variable, giving some indication that gains in strength are associated with improvement in some performance tasks, such as sprinting and vertical jump, although the improvements are generally small, highlighting the difficulty of distinguishing the effects of training from changes expected with normal growth. Changes in body size, physique, and body composition associated with growth and maturation are important factors that affect strength and motor performance. The relationships vary among performance measures and with age, and these factors often are inadequately controlled in studies of components of performance-related fitness and performance tasks.
- PSYCHOSOCIAL HEALTH
Research supports the positive impact of physical activity on the overall psychological health and social engagement of every student. A well-designed physical education curriculum provides students with social and emotional benefits ( NASPE, 2001 ). Simultaneously, exposure to failure experiences, emphasis on competitive sports, and elitism for naturally inclined athletes, along with bullying and teasing of unfit, uncoordinated, and overweight youth, may be important factors discouraging participation in current and future physical activity ( Kohl and Hobbs, 1998 ; Sallis et al., 2000 ; Allender et al., 2006 ). School-based physical activity, including physical education and sports, is designed to increase physical activity while also improving motor skills and development, self-efficacy, and general feelings of competency and engaging children socially ( Bailey, 2006 ). The hoped-for psychosocial outcomes of physical education and other physical activity programs in the school setting have been found to be critical for continued physical activity across the life span and are themselves powerful long-term determinants of physical activity ( Bauman et al., 2012 ). Unfortunately, significant gaps exist between the intent and reality of school-based physical education and other activity programs ( HHS, 2013 ).
A large number of psychological and social outcomes have been examined. Specific aspects of psychosocial health showing a beneficial relationship to physical activity include, among others, self-efficacy, self-concept, self-worth ( Haugen et al., 2011 ), social behaviors ( Cradock et al., 2009 ), pro-school attitudes, motivation and goal orientation ( Digelidis et al., 2003 ), relatedness, friendships ( de la Haye et al., 2011 ; Macdonald-Wallis et al., 2011 ), task orientation, team building, bullying, and racial prejudice ( Byrd and Ross, 1991 ). Most studies are descriptive, finding bidirectional associations between psychosocial outcomes and physical activity. Reviews and meta-analyses confirm a positive association between physical activity and self-esteem, especially for aerobic activities ( McAuley, 1994 ).
Among psychosocial factors, self-efficacy (confidence in one's ability to be physically active in specific situations) has emerged as an important correlate of physical activity from a large body of work based on the durable and practically useful social learning theory ( Bandura and McClelland, 1977 ; Bandura, 1995 ). Bandura's theory compels consideration of the psychosocial and physical environments, the individual, and in this case the behavior of physical activity. Using this framework, physical activity itself has been shown to be a consistent positive correlate as well as a determinant of physical activity in children and adolescents. A large amount of reviewed research has found that physical education and physical activity experiences can increase children's confidence in being active and lead to continued participation in physical activity ( Bauman et al., 2012 ). RCTs have shown that both self-efficacy and social interactions leading to perceived social support influence changes in physical activity ( Dishman et al., 2009 ). Skill mastery, confidence building, and group support are well-known strategies for advancing student learning and well-being in many educational domains in the school setting and apply equally to school physical education and other physical activity. Early observational studies of physical, social, and environmental determinants of physical activity at home, school, and recess indicated that prompts to be active (or not) from peers and adults accounted for a significant amount of the variance in directly observed physical activity ( Elder et al., 1998 ). One longitudinal study following the variability and tracking of physical activity in young children showed that most of the variability in both home and recess activity was accounted for by short-term social and physical environmental factors, such as prompts from others and being outdoors ( Sallis et al., 1995 ). Another study, examining activity among preschool children, found that, contrary to common belief, most of the time spent in preschool was sedentary, and correlates of activity were different for preschool boys and girls ( Byun et al., 2011 ). In addition, significant variation in activity by preschool site was noted, indicating that local environmental conditions, including physical environment and equipment, policies, and teacher and administrative quality characteristics, play an important role in promoting physical activity ( Brown et al., 2009 ).
Studies in middle and high school populations have strengthened the evidence base on relationships among self-efficacy, physical activity, and social support (from adults and peers). This research has highlighted the central contribution of self-efficacy and social support in protecting against a decline in activity levels among adolescent girls ( Dishman et al., 2009 , 2010 ). Evidence indicates further that these impacts spread to activities outside the school setting ( Lytle et al., 2009 ). Findings of a related study suggest that leisure-time physical activity among middle school students was linked to motivation-related experiences in physical education ( Cox et al., 2008 ).
A recent review of reviews ( Bauman et al., 2012 ) found that population levels of physical activity are low and that consistent individual-level correlates of physical activity are age, sex, health status, self-efficacy, and previous physical activity. Physical activity declines dramatically as children progress from elementary through high school ( Nader et al., 2008 ). Boys are consistently found to be more active than girls from ages 4 to 9. For other age groups of children and adolescents, sex is correlated with but not a determinant of activity ( Bauman et al., 2012 ). These findings suggest the need to tailor physical education and physical activity programs for youth specifically to increase self-efficacy and enjoyment of physical activity among girls ( Dishman et al., 2005 ; Barr-Anderson et al., 2008 ; Butt et al., 2011 ).
In summary, a broad range of beneficial psychosocial health outcomes have been associated with physical activity. The promotion of more physical activity and quality physical education in the school setting is likely to result in psychosocially healthier children who are more likely to engage in physical activity as adults. Schools can play an important role in ensuring opportunities for physical activity for a segment of the youth population that otherwise may not have the resources to engage in such activity. It makes sense to assume that, if physical activity experiences and environments were once again structured into the daily school environment of children and adolescents, individuals' feelings of self-efficacy regarding physical activity would increase in the U.S. population.
- MENTAL HEALTH
Mental illness is a serious public health issue. It has been estimated that by 2010 mental illness will account for 15 percent of the global burden of disease ( Biddle and Mutrie, 2008 ; Biddle and Asare, 2011 ). Young people are disproportionately affected by depression, anxiety, and other mental health disorders ( Viner and Booy, 2005 ; Biddle and Asare, 2011 ). Approximately 20 percent of school-age children have a diagnosable mental health disorder ( U.S. Public Health Service, 2000 ), and overweight children are at particular risk ( Ahn and Fedewa, 2011 ). Mental health naturally affects academic performance on many levels ( Charvat, 2012 ). Students suffering from depression, anxiety, mood disorders, and emotional disturbances perform more poorly in school, exhibit more behavioral and disciplinary problems, and have poorer attendance relative to mentally healthy children. Thus it is in schools' interest to take measures to support mental health among the student population. In addition to other benefits, providing adequate amounts of physical activity in a way that is inviting and safe for children of all ability levels is one simple way in which schools can contribute to students' mental health.
Impact of Physical Activity on Mental Health
Several recent reviews have concluded that physical activity has a positive effect on mental health and emotional well-being for both adults and children ( Peluso and Guerra de Andrade, 2005 ; Penedo and Dahn, 2005 ; Strong et al., 2005 ; Hallal et al., 2006 ; Ahn and Fedewa, 2011 ; Biddle and Asare, 2011 ). Numerous observational studies have established the association between physical activity and mental health but are inadequate to clarify the direction of that association ( Strong et al., 2005 ). It may be that physical activity improves mental health, or it may be that people are more physically active when they are mentally healthy. Most likely the relationship is bidirectional.
Several longitudinal and intervention studies have clarified that physical activity positively impacts mental health ( Penedo and Dahn, 2005 ; Strong et al., 2005 ). Physical activity has most often been shown to reduce symptoms of depression and anxiety and improve mood ( Penedo and Dahn, 2005 ; Dishman et al., 2006 ; Biddle and Asare, 2011 ). In addition to reducing symptoms of depression and anxiety, studies indicate that regular physical activity may help prevent the onset of these conditions ( Penedo and Dahn, 2005 ). Reductions in depression and anxiety are the commonly measured outcomes ( Strong et al., 2005 ; Ahn and Fedewa, 2011 ). However, reductions in states of confusion, anger, tension, stress, anxiety sensitivity (a precursor to panic attacks and panic disorders), posttraumatic stress disorder/psychological distress, emotional disturbance, and negative affect have been observed, as well as increases in positive expectations; fewer emotional barriers; general well-being; satisfaction with personal appearance; and improved life satisfaction, self-worth, and quality of life ( Heller et al., 2004 ; Peluso and Guerra de Andrade, 2005 ; Penedo and Dahn, 2005 ; Dishman et al., 2006 ; Hallal et al., 2006 ; Ahn and Fedewa, 2011 ; Biddle and Asare, 2011 ). Among adolescents and young adult females, exercise has been found to be more effective than cognitive-behavioral therapy in reducing the pursuit of thinness and the frequency of bingeing, purging, and laxative abuse ( Sundgot-Borgen et al., 2002 ; Hallal et al., 2006 ). The favorable effects of physical activity on sleep may also contribute to mental health ( Dishman et al., 2006 ).
The impact of physical activity on these measures of mental health is moderate, with effect sizes generally ranging from 0.4 to 0.7 ( Biddle and Asare, 2011 ). In one meta-analysis of intervention trials, the RCTs had an effect size of 0.3, whereas other trials had an effect size of 0.57.
Ideal Type, Length, and Duration of Physical Activity
Intervention trials that examine the relationship between physical activity and mental health often fail to specify the exact nature of the intervention, making it difficult to determine the ideal frequency, intensity, duration, and type of physical activity involved ( Penedo and Dahn, 2005 ; Ahn and Fedewa, 2011 ; Biddle and Asare, 2011 ).
Many different types of physical activity—including aerobic activity, resistance training, yoga, dance, flexibility training, walking programs, and body building—have been shown to improve mood and other mental health indicators. The evidence is strongest for aerobic physical activity, particularly for reduction of anxiety symptoms and stress ( Peluso and Guerra de Andrade, 2005 ; Dishman et al., 2006 ; Martikainen et al., 2013 ), because more of these studies have been conducted ( Peluso and Guerra de Andrade, 2005 ). One meta-analysis of RCTs concluded that physical activity interventions focused exclusively on circuit training had the greatest effect on mental health indicators, followed closely by interventions that included various types of physical activity ( Ahn and Fedewa, 2011 ). Among studies other than RCTs, only participation in sports had a significant impact on mental health ( Ahn and Fedewa, 2011 ). The few studies that investigated the impact of vigorous- versus lower-intensity physical activity ( Larun et al., 2006 ; Biddle and Asare, 2011 ) found no difference, suggesting that perhaps all levels of physical activity may be helpful. Among adults, studies have consistently shown beneficial effects of both aerobic exercise and resistance training. Ahn and Fedewa (2011) concluded that both moderate and intense physical activity have a significant impact on mental health, although when just RCTs were considered, only intense physical activity was significant ( Ahn and Fedewa, 2011 ). While physical activity carries few risks for mental health, it is important to note that excessive physical activity or specialization too early in certain types of competitive physical activity has been associated with negative mental health outcomes and therefore should be avoided ( Peluso and Guerra de Andrade, 2005 ; Hallal et al., 2006 ). Furthermore, to reach all children, including those that may be at highest risk for inactivity, obesity, and mental health problems, physical activity programming needs to be nonthreatening and geared toward creating a positive experience for children of all skill and fitness levels ( Amis et al., 2012 ).
Various types of physical activity programming have been shown to have a positive influence on mental health outcomes. Higher levels of attendance and participation in physical education are inversely associated with feelings of sadness and risk of considering suicide ( Brosnahan et al., 2004 ). Classroom physical activity is associated with reduced use of medication for attention deficit hyperactivity disorder ( Katz et al., 2010 ). And participation in recess is associated with better student classroom behavior, better focus, and less fidgeting ( Pellegrini et al., 1995 ; Jarrett et al., 1998 ; Barros et al., 2009 ).
Strong evidence supports the short-term benefits of physical activity for mental health. Acute effects can be observed after just one episode and can last from a few hours to up to 1 day after. Body building may have a similar effect, which begins a few hours after the end of the exercise. The ideal length and duration of physical activity for improving mental health remain unclear, however. Regular exercise is associated with improved mood, but results are inconsistent for the association between mood and medium- or long-term exercise ( Dua and Hargreaves, 1992 ; Slaven and Lee, 1997 ; Dimeo et al., 2001 ; Dunn et al., 2001 ; Kritz-Silverstein et al., 2001 ; Sexton et al., 2001 ; Leppamaki et al., 2002 ; Peluso and Guerra de Andrade, 2005 ). Studies often do not specify the frequency and duration of physical activity episodes; among those that do, interventions ranged from 6 weeks to 2 years in duration. In their meta-analysis, Ahn and Fedewa (2011) found that, comparing interventions entailing a total of more than 33 hours, 20-33 hours, and less than 20 hours, the longer programs were more effective. Overall, the lack of reporting and the variable length and duration of reported interventions make it difficult to draw conclusions regarding dose ( Ahn and Fedewa, 2011 ).
In addition to more structured opportunities, naturally occurring physical activity outside of school time is associated with fewer depressive symptoms among adolescents ( Penedo and Dahn, 2005 ). RCTs have demonstrated that physical activity involving entire classrooms of students is effective in alleviating negative mental health outcomes ( Ahn and Fedewa, 2011 ). Non-RCT studies have shown individualized approaches to be most effective and small-group approaches to be effective to a more limited extent ( Ahn and Fedewa, 2011 ). Interventions have been shown to be effective in improving mental health when delivered by classroom teachers, physical education specialists, or researchers but may be most effective when conducted with a physical education specialist ( Ahn and Fedewa, 2011 ). Many physical activity interventions include elements of social interaction and support; however, studies to date have been unable to distinguish whether the physical activity itself or these other factors account for the observed effects on mental health ( Hasselstrom et al., 2002 ; Hallal et al., 2006 ). Finally, a few trials ( Larun et al., 2006 ; Biddle and Asare, 2011 ) have compared the effects of physical activity and psychosocial interventions, finding that physical activity may be equally effective but may not provide any added benefit.
Subgroup Effects
Although studies frequently fail to report the age of participants, data on the effects of physical activity on mental health are strongest for adults participating in high-intensity physical activity ( Ahn and Fedewa, 2011 ). However, evidence relating physical activity to various measures of mental health has shown consistent, significant effects on individuals aged 11-20. A large prospective study found that physical activity was inversely associated with depression in early adolescence ( Hasselstrom et al., 2002 ; Hallal et al., 2006 ); fewer studies have been conducted among younger children. Correlation studies have shown that the association of physical activity with depression is not affected by age ( Ahn and Fedewa, 2011 ).
Few studies have examined the influence of other sociodemographic characteristics of participants on the relationship between physical activity and mental health ( Ahn and Fedewa, 2011 ), but studies have been conducted in populations with diverse characteristics. One study of low-income Hispanic children randomized to an aerobic intensity program found that the intervention group was less likely to present with depression but did not report reduced anxiety ( Crews et al., 2004 ; Hallal et al., 2006 ). A study that included black and white children (aged 7-11) found that a 40-minute daily dose of aerobic exercise significantly reduced depressive symptoms and increased physical appearance self-worth in both black and white children and increased global self-worth in white children compared with controls ( Petty et al., 2009 ). Physical activity also has been positively associated with mental health regardless of weight status (normal versus overweight) or gender (male versus female) ( Petty et al., 2009 ; Ahn and Fedewa, 2011 ); however, results are stronger for males ( Ahn and Fedewa, 2011 ).
Improvements in mental health as a result of physical activity may be more pronounced among clinically diagnosed populations, especially those with cognitive impairment or posttraumatic stress disorder ( Craft and Landers, 1998 ; Ahn and Fedewa, 2011 ; Biddle and Asare, 2011 ). Evidence is less clear for youth with clinical depression ( Craft and Landers, 1998 ; Larun et al., 2006 ; Biddle and Asare, 2011 ). Individuals diagnosed with major depression undergoing an intervention entailing aerobic exercise have shown significant improvement in depression and lower relapse rates, comparable to results seen in participants receiving psychotropic treatment ( Babyak et al., 2000 ; Penedo and Dahn, 2005 ). One program for adults with Down syndrome providing three sessions of exercise and health education per week for 12 weeks resulted in more positive expectations, fewer emotional barriers, and improved life satisfaction ( Heller et al., 2004 ; Penedo and Dahn, 2005 ). Ahn and Fedewa (2011) found that, compared with nondiagnosed individuals, physical activity had a fivefold greater impact on those diagnosed with cognitive impairment and a twofold greater effect on those diagnosed with emotional disturbance, suggesting that physical activity has the potential to improve the mental health of those most in need.
In sum, although more studies are needed, and there may be some differences in the magnitude and nature of the mental health benefits derived, it appears that physical activity is effective in improving mental health regardless of age, ethnicity, gender, or mental health status.
Sedentary Behavior
Sedentary behavior also influences mental health. Screen viewing in particular and sitting in general are consistently associated with poorer mental health ( Biddle and Asare, 2011 ). Children who watch more television have higher rates of anxiety, depression, and posttraumatic stress and are at higher risk for sleep disturbances and attention problems ( Kappos, 2007 ). Given the cross-sectional nature of these studies, however, the direction of these associations cannot be determined. A single longitudinal study found that television viewing, but not playing computer games, increased the odds of depression after 7-year follow-up ( Primack et al., 2009 ; Biddle and Asare, 2011 ), suggesting that television viewing may contribute to depression. Because of design limitations of the available studies, it is unclear whether this effect is mediated by physical activity.
Television viewing also is associated with violence, aggressive behaviors, early sexual activity, and substance abuse ( Kappos, 2007 ). These relationships are likely due to the content of the programming and advertising as opposed to the sedentary nature of the activity. Television viewing may affect creativity and involvement in community activities as well; however, the evidence here is very limited ( Kappos, 2007 ). Studies with experimental designs are needed to establish a causal relationship between sedentary behavior and mental health outcomes ( Kappos, 2007 ).
Although the available evidence is not definitive, it does suggest that sedentary activity and television viewing in particular can increase the risk for depression, anxiety, aggression, and other risky behaviors and may also affect cognition and creativity ( Kappos, 2007 ), all of which can affect academic performance. It would therefore appear prudent for schools to reduce these sedentary behaviors during school hours and provide programming that has been shown to be effective in reducing television viewing outside of school ( Robinson, 1999 ; Robinson and Borzekowski, 2006 ).
It is not surprising that physical activity improves mental health. Both physiological and psychological mechanisms explain the observed associations. Physiologically, physical activity is known to increase the synaptic transmission of monoamines, an effect similar to that of anti-depressive drugs. Physical activity also stimulates the release of endorphins (endogenous opoids) ( Peluso and Guerra de Andrade, 2005 ), which have an inhibitory effect on the central nervous system, creating a sense of calm and improved mood ( Peluso and Guerra de Andrade, 2005 ; Ahn and Fedewa, 2011 ). Withdrawal of physical activity may result in irritability, restlessness, nervousness, and frustration as a result of a drop in endorphin levels. Although more studies are needed to specify the exact neurological pathways that mediate this relationship, it appears that the favorable impact of physical activity on the prevention and treatment of depression may be the result of adaptations in the central nervous system mediated in part by neurotropic factors that facilitate neurogenerative, neuroadaptive, and neuroprotective processes ( Dishman et al., 2006 ). It has been observed, for example, that chronic wheel running in rats results in immunological, neural, and cellular responses that mitigate several harmful consequences of acute exposure to stress ( Dishman et al., 2006 ). A recent study found that children who were more physically active produced less cortisol in response to stress, suggesting that physical activity promotes mental health by regulating the hormonal responses to stress ( Martikainen et al., 2013 ).
Psychological mechanisms that may explain why physical activity improves mental health include (1) distraction from unfavorable stimuli, (2) increase in self-efficacy, and (3) positive social interactions that can result from quality physical activity programming ( Peluso and de Andrade, 2005 ) (see also the discussion of psychosocial health above). The relative contribution of physiological and psychological mechanisms is unknown, but they likely interact. Poor physical health also can impair mood and mental function. Health-related quality of life improves with physical activity that increases physical functioning, thereby enhancing the sense of well-being ( McAuley and Rudolph, 1995 ; HHS, 2008 ).
Physical activity during childhood and adolescence may not only be important for its immediate benefits for mental health but also have implications for long-term mental health. Studies have shown a consistent effect of physical activity during adolescence on adult physical activity ( Hallal et al., 2006 ). Physical activity habits established in children may persist into adulthood, thereby continuing to confer mental health benefits throughout the life cycle. Furthermore, physical activity in childhood may impact adult mental health regardless of the activity's persistence ( Hallal et al., 2006 ).
Physical activity can improve mental health by decreasing and preventing conditions such as anxiety and depression, as well as improving mood and other aspects of well-being. Evidence suggests that the mental health benefits of physical activity can be experienced by all age groups, genders, and ethnicities. Moderate effect sizes have been observed among both youth and adults. Youth with the highest risk of mental illness may experience the most benefit. Although evidence is not adequate to determine the ideal regimen, aerobic and high-intensity physical activity are likely to confer the most benefit. It appears, moreover, that a variety of types of physical activity are effective in improving different aspects of mental health; therefore, a varied regimen including both aerobic activities and strength training may be the most effective. Frequent episodes of physical activity are optimal given the well-substantiated short-term effects of physical activity on mental health status. Although there are well-substantiated physiological bases for the impact of physical activity on mental health, physical activity programming that effectively enhances social interactions and self-efficacy also may improve mental health through these mechanisms. Quality physical activity programming also is critical to attract and engage youth of all skills level and to effectively reach those at highest risk.
Sedentary activity may increase the risk of poor mental health status independently of, or in addition to, its effect on physical activity. Television viewing in particular may lead to a higher risk of such conditions as depression and anxiety and may also increase violence, aggression, and other high-risk behaviors. These impacts are likely the result of programming and advertising content in addition to the physiological effects of inactivity and electronic stimuli.
In conclusion, frequently scheduled and well-designed opportunities for varied physical activity during the school day and a reduction in sedentary activity have the potential to improve students' mental health in ways that could improve their academic performance and behaviors in school.
Good health is the foundation of learning and academic performance (see Chapter 4 ). In children and youth, health is akin to growth. An extensive literature demonstrates that regular physical activity promotes growth and development and has multiple benefits for physical, mental, cognitive, and psychosocial health that undoubtedly contribute to learning. Although much of the evidence comes from cross-sectional studies showing associations between physical activity and various aspects of health, available prospective data support this cross-sectional evidence. Experimental evidence, although more limited for younger children, is sufficient among older children and adolescents to support the notion that children and young adults derive much the same health benefits from physical activity.
Moreover, many adult diseases have their origins in childhood. This finding, together with the finding that health-related behaviors and disease risk factors may track from childhood into adulthood, underscores the need for early and ongoing opportunities for physical activity.
Children's exercise capacity and the activities in which they can successfully engage change in a predictable way across developmental periods. For example, young children are active in short bursts, and their capacity for continuous activity increases as they grow and mature (see Figure 3-2 ). In adults and likely also adolescents, intermittent exercise has much the same benefit as continuous exercise when mode and energy expenditure are held constant. The health benefits of sporadic physical activity at younger ages are not well established. However, the well-documented short-term benefits of physical activity for some aspects of mental and cognitive health suggest that maximum benefit may be attained through frequent bouts of exercise throughout the day.
Changes in physical activity needs with increasing age of children and adolescents. SOURCE: Adapted from Malina, 1991. Reprinted with permission from Human Kinetics Publishers.
Children require frequent opportunities for practice to develop the skills and confidence that promote ongoing engagement in physical activity. Physical education curricula are structured to provide developmentally appropriate experiences that build the motor skills and self-efficacy that underlie lifelong participation in health-enhancing physical activity, and trained physical education specialists are uniquely qualified to deliver them (see Chapter 5 ). However, physical education usually is offered during a single session. Therefore, other opportunities for physical activity can supplement physical education by addressing the need for more frequent exercise during the day (see Chapter 6 ). In addition to the immediate benefits of short bouts of physical activity for learning and for mental health, developmentally appropriate physical activity during those times, along with the recommended time in physical education, can contribute to daily energy expenditure and help lessen the risk of excess weight gain and its comorbidities. Specific types of activities address specific health concerns. For example, vertical jumping activities contribute to energy expenditure for obesity prevention and also promote bone development (via the resulting ground reaction forces), potentially contributing to lower fracture risk. Other activities contribute to prevention of chronic disease. Since different types of physical activity contribute to distinct aspects of physical, mental, and psychosocial health, a varied regimen is likely to be most beneficial overall.
The quality of physical activity programming also is critical; psychosocial outcomes and improvements in specific motor skills, for example, are likely the result of programming designed specifically to target these outcomes rather than just a result of increases in physical activity per se. These psychosocial outcomes also are likely to lead to increased levels of physical activity in both the short and long terms, thereby conferring greater health benefits. Unstructured physical activity or free play also confers unique benefits and is an important supplement to more structured opportunities. Quality physical activity programming that makes these activities attractive, accessible, and safe for children and youth of all skill and fitness levels is critical to ensure that all youth participate in these activities and can therefore derive the health benefits.
Sedentary activities, such as screen viewing and excessive time spent sitting, may contribute to health risks both because of and independent of their impact on physical activity. Thus specific efforts in school to reduce sedentary behaviors, such as through classroom and playground design and reduction of television viewing, are warranted.
In sum, a comprehensive physical activity plan with physical education at the core, supplemented by other varied opportunities for and an environment supportive of physical activity throughout the day, would make an important contribution to children's health and development, thereby enhancing their readiness to learn.
- Ahlqwist A, Hagman M, Kjellby-Wendt G, Beckung E. Physical therapy treatment of back complaints on children and adolescents. Spine. 2008; 33 (20):E721–E727. [ PubMed : 18794746 ]
- Ahn S, Fedewa AL. A meta-analysis of the relationship between children's physical activity and mental health. Journal of Pediatric Psychology. 2011; 36 (4):385–397. [ PubMed : 21227908 ]
- Ailhaud G, Hauner H. Development of white adipose tissue. In: Bray GA, James WPT, editors. In Handbook of Obesity. New York: Marcel Dekker; 1998. pp. 359–378.
- Alberti K, Zimmet P. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabetic Medicine. 1998; 15 (7):539–553. [ PubMed : 9686693 ]
- Allender S, Cowburn GG, Foster C. Understanding participation in sport and physical activity among children and adults: A review of qualitative studies. Health Education Research. 2006; 21 (6):826–835. [ PubMed : 16857780 ]
- Amis JM, Wright PM, Dyson B, Vardaman JM, Ferry H. Implementing Childhood Obesity Policy in a New Educational Environment: The Cases of Mississippi and Tennessee. American Journal of Public Health. 2012; 102 (7):1406–1413. [ PMC free article : PMC3478004 ] [ PubMed : 22420819 ]
- Annesi JJ, Westcott WL, Faigenbaum AD, Unruh JL. Effects of a 12-week physical activity protocol delivered by YMCA after-school counselors (Youth Fit for Life) on fitness and self-efficacy changes in 5-12-year-old boys and girls. Research Quarterly for Exercise and Sport. 2005; 76 (4):468–476. [ PubMed : 16739685 ]
- Arlot ME, Sornay-Rendu E, Garnero P, Vey-Marty B, Delmas PD. Apparent pre- and postmenopausal bone loss evaluated by DXA at different skeletal sites in women: The OFELY cohort. Journal of Bone and Mineral Research. 1997; 12 (4):683–690. [ PubMed : 9101381 ]
- Arner P, Eckel RH. Adipose tissue as a storage organ. In: Bray GA, James WPT, editors. In Handbook of obesity. New York: Marcel Dekker; 1998. pp. 379–396.
- Babyak M, Blumenthal JA, Herman S, Khatri P, Doraiswamy M, Moore K, Craighead WE, Baldewicz TT, Krishnan KR. Exercise treatment for major depression: Maintenance of therapeutic benefit at 10 months. Psychosomatic Medicine. 2000; 62 (5):633–638. [ PubMed : 11020092 ]
- Bailey DA, Faulkner RA, McKay HA. Growth, physical activity, and bone mineral acquisition. Exercise and Sport Science Reviews. 1996; 24 (1):233–266. [ PubMed : 8744252 ]
- Bailey DA, Martin AD, McKay HA, Whiting S, Mirwald R. Calcium accretion in girls and boys during puberty: A longitudinal analysis. Journal of Bone and Mineral Research. 2000; 15 (11):2245–2250. [ PubMed : 11092406 ]
- Bailey R. Physical education and sport in schools: A review of benefits and outcomes. Journal of School Health. 2006; 76 (8):397–401. [ PubMed : 16978162 ]
- Balagopal P, George D, Patton N, Yarandi H, Roberts WL, Bayne E, Gidding S. Lifestyle-only intervention attenuates the inflammatory state associated with obesity: A randomized controlled study in adolescents. Journal of Pediatrics. 2005; 146 (3):342–348. [ PubMed : 15756217 ]
- Ballor D, Poehlman E, Toth M. Exercise as a treatment for obesity. In: Bray GA, Bouchard C, James WPT, editors. Handbook of obesity. New York: Marcel Dekker; 1998. pp. 891–910.
- Bandura A. Self-efficacy in changing societies. New York: Cambridge University Press; 1995.
- Bandura A, McClelland DC. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1977.
- Bao W, Srinivasan SR, Wattigney WA, Berenson GS. Persistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood: The Bogalusa Heart Study. Archives of Internal Medicine. 1994; 154 (16):1842. [ PubMed : 8053753 ]
- Baquet G, Berthoin S, Dupont G, Blondel N, Fabre C, Van Praagh E. Effects of high intensity intermittent training on peak VO(2) in prepubertal children. International Journal of Sports Medicine. 2002; 23 (6):439. [ PubMed : 12215964 ]
- Baquet G, Van Praagh E, Berthoin S. Endurance training and aerobic fitness in young people. Sports Medicine. 2003; 33 (15):1127–1143. [ PubMed : 14719981 ]
- Barbeau P, Johnson MH, Howe CA, Allison J, Davis CL, Gutin B, Lemmon CR. Ten months of exercise improves general and visceral adiposity, bone, and fitness in black girls. Obesity. 2007; 15 (8):2077–2085. [ PubMed : 17712126 ]
- Barlow S. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007; 120 (S4):S164–S192. [ PubMed : 18055651 ]
- Barnett LM, Van Beurden E, Morgan PJ, Brooks LO, Beard JR. Childhood motor skill proficiency as a predictor of adolescent physical activity. Journal of Adolescent Health. 2009; 44 (3):252–259. [ PubMed : 19237111 ]
- Bar-Or O. Pediatric sports medicine for the practitioner. New York: Springer-Verlag; 1983.
- Barr-Anderson DJ, Neumark-Sztainer D, Schmitz KH, Ward DS, Conway TL, Pratt C, Baggett CD, Lytle L, Pate RR. But I like PE: Factors associated with enjoyment of physical education class in middle school girls. Research Quarterly for Exercise and Sport. 2008; 79 (1):18–27. [ PMC free article : PMC2430627 ] [ PubMed : 18431947 ]
- Barros RM, Silver EJ, Stein REK. School recess and group classroom behavior. Pediatrics. 2009; 123 (2):431–436. [ PubMed : 19171606 ]
- Bass S, Pearce G, Bradney M, Hendrich E, Delmas PD, Harding A, Seeman E. Exercise before puberty may confer residual benefits in bone density in adulthood: Studies in active prepubertal and retired female gymnasts. Journal of Bone and Mineral Research. 1998; 13 (3):500–507. [ PubMed : 9525351 ]
- Bau AM, Ernert A, Schenk L, Wiegand S, Martus P, Grüters A, Krude H. Is there a further acceleration in the age at onset of menarche? A cross-sectional study in 1840 school children focusing on age and bodyweight at the onset of menarche. European Journal of Endocrinology. 2009; 160 (1):107–113. [ PubMed : 18974233 ]
- Bauman AE. Updating the evidence that physical activity is good for health: An epidemiological review 2000–2003. Journal of Science and Medicine in Sport. 2004; 7 (1):6–19. [ PubMed : 15214597 ]
- Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW. Lancet Physical Activity Series Working Group. Correlates of physical activity: Why are some people physically active and others not. Lancet. 2012; 380 (9838):258–271. [ PubMed : 22818938 ]
- Behringer M, vom Heede A, Yue Z, Mester J. Effects of resistance training in children and adolescents: A meta-analysis. Pediatrics. 2010; 126 (5):e1199–e1210. [ PubMed : 20974785 ]
- Bell LM, Watts K, Siafarikas A, Thompson A, Ratnam N, Bulsara M, Finn J, O'Driscoll G, Green DJ, Jones TW. Exercise alone reduces insulin resistance in obese children independently of changes in body composition. Journal of Clinical Endocrinology & Metabolism. 2007; 92 (11):4230–4235. [ PubMed : 17698905 ]
- Benson AC, Torode ME, Fiatarone Singh MA. A rationale and method for high-intensity progressive resistance training with children and adolescents. Contemporary Clinical Trials. 2007; 28 (4):442–450. [ PubMed : 17185043 ]
- Benson A, Torode M, Fiatarone Singh M. Effects of resistance training on metabolic fitness in children and adolescents: A systematic review. Obesity Reviews. 2008; 9 (1):43–66. [ PubMed : 18154602 ]
- Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. New England Journal of Medicine. 1998; 338 (23):1650–1656. [ PubMed : 9614255 ]
- Berkey CS, Rockett HR, Field AE, Gillman MW, Frazier AL, Camargo CA, Colditz GA. Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics. 2000; 105 (4):e56. [ PubMed : 10742377 ]
- Berkey CS, Rockett HR, Gillman MW, Colditz GA. One-year changes in activity and in inactivity among 10- to 15-year-old boys and girls: Relationship to change in body mass index. Pediatrics. 2003; 111 (4):836–843. [ PubMed : 12671121 ]
- Bernhardt D, Gomez J, Johnson M, Martin T, Rowland T, Small E, LeBlanc C, Malina R, Krein C, Young J. Strength training by children and adolescents. Pediatrics. 2001; 107 (6):1470. [ PubMed : 11389279 ]
- Beunen GP, Malina RM, Renson R, Simons J, Ostyn M, Lefevre J. Physical activity and growth, maturation and performance: A longitudinal study. Medicine and Science in Sports and Exercise. 1992; 24 (5):576. [ PubMed : 1569854 ]
- Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: A review of reviews. British Journal of Sports Medicine. 2011; 45 (11):886–895. [ PubMed : 21807669 ]
- Biddle S, Mutrie N. Psychology of physical activity: Determinants, well-being and interventions, 2nd ed. London: Routledge; 2008.
- Bloomfield SA, Little KD, Nelson ME, Yingling VR. American College of Sports Medicine ® position stand. Medicine & Science in Sports & Exercise. 2004; 195 (9131/04):1985. [ PubMed : 15514517 ]
- Bonnet FP, Rocour-Brumioul D. Normal growth of human adipose tissue. In: Bonnet F, editor. In Adipose tissue in childhood. Boca Raton, FL: CRC Press; 1981. pp. 81–107.
- Boreham C, Riddoch C. The physical activity, fitness and health of children. Journal of Sports Sciences. 2001; 19 (12):915–929. [ PubMed : 11820686 ]
- Boreham CA, Ferreira I, Twisk JW, Gallagher AM, Savage MJ, Murray LJ. Cardiorespiratory fitness, physical activity, and arterial stiffness: The Northern Ireland Young Hearts Project. Hypertension. 2004; 44 (5):721–726. [ PubMed : 15452034 ]
- Bouchard C. Genomic predictors of trainability. Experimental Physiology. 2012; 97 (3):347–352. [ PubMed : 21967902 ]
- Bouffard ME, Watkinson EJ, Thompson LP, Dunn JLC, Romanow SKE. A test of the activity deficit hypothesis with children with movement difficulties. Adapted Physical Activity Quarterly. 1996; 13 :61–73.
- Brambilla P, Pozzobon G, Pietrobelli A. Physical activity as the main therapeutic tool for metabolic syndrome in childhood. International Journal of Obesity. 2010; 35 (1):16–28. [ PubMed : 21139560 ]
- Brosnahan J, Steffen LM, Lytle L, Patterson J, Boostrom A. The relation between physical activity and mental health among Hispanic and non-Hispanic white adolescents. Archives of Pediatrics and Adolescent Medicine. 2004; 158 (8):818–823. [ PubMed : 15289257 ]
- Brown WH, Pfeiffer KA, McIver KL, Dowda M, Addy CL, Pate RR. Social and environmental factors associated with preschoolers' nonsedentary physical activity. Child Development. 2009; 80 (1):45–58. [ PMC free article : PMC2648129 ] [ PubMed : 19236392 ]
- Butt J, Weinberg RS, Breckon JD, Claytor RP. Adolescent physical activity participation and motivational determinants across gender, age, and race. Journal of Physical Activity and Health. 2011; 8 (8):1074–1083. [ PubMed : 22039125 ]
- Byrd CE, Ross SM. The influence of participation in junior high athletics on students' attitudes and grades. Physical Educator. 1991; 48 (4):170–176.
- Byun W, Dowda M, Pate RR. Correlates of objectively measured sedentary behavior in US preschool children. Pediatrics. 2011; 128 (5):937–945. [ PMC free article : PMC3208960 ] [ PubMed : 22007010 ]
- Campbell PT, Katzmarzyk PT, Malina RM, Rao D, Pérusse L, Bouchard C. Stability of adiposity phenotypes from childhood and adolescence into young adulthood with contribution of parental measures. Obesity Research. 2012; 9 (7):394–400. [ PubMed : 11445661 ]
- Carnethon MR, Gulati M, Greenland P. Prevalence and cardiovascular disease correlates of low cardiorespiratory fitness in adolescents and adults. Journal of the American Medical Association. 2005; 294 (23):2981–2988. [ PubMed : 16414945 ]
- Carrel AL, Clark RR, Peterson SE, Nemeth BA, Sullivan J, Allen DB. Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: A randomized, controlled study. Archives of Pediatrics and Adolescent Medicine. 2005; 159 (10):963. [ PubMed : 16203942 ]
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Reports. 1985; 100 (2):126. [ PMC free article : PMC1424733 ] [ PubMed : 3920711 ]
- CDC (Centers for Disease Control and Prevention). Overweight and obesity: Frequently asked questions. 2006. [November 27, 2012]. http://www .cdc.gov/obesity/index.html .
- CDC. Youth risk behavior surveillance: United States, 2011. Morbidity and Mortality Weekly Report. 2012; 61 (4):1–162. [ PubMed : 22673000 ]
- Charvat J. Research on the relationship between mental health and academic achievement. Bethesda, MD: National Association of School Psychologists; 2012.
- Christodoulos AD, Douda HT, Tokmakidis SP. International Journal of Pediatrics. 2012. Cardiorespiratory fitness, metabolic risk, and inflammation in children. epub ahead of print. [ PMC free article : PMC3270402 ] [ PubMed : 22315623 ]
- Chumlea W, Siervogel R, Roche A, Mukherjee D, Webb P. Changes in adipocyte cellularity in children ten to 18 years of age. International Journal of Obesity. 1982; 6 (4):383–389. [ PubMed : 7129750 ]
- Church T, Barlow C, Earnest CP, Kampert J, Priest E, Blair S. Associations between cardiorespiratory fitness and C-reactive protein in men. Arteriosclerosis, Thrombosis, and Vascular Biology. 2002; 22 (11):1869–1876. [ PubMed : 12426218 ]
- Clapp J III, Little KD. Effect of recreational exercise on pregnancy weight gain and subcutaneous fat deposition. Medicine and Science in Sports and Exercise. 1995; 27 (2):170. [ PubMed : 7723638 ]
- Clark ME, Tobias JH, Murray L, Boreham C. Children with low muscle strength are at an increased risk of fracture with exposure to exercise. Journal of Musculoskeletal and Neuronal Interactions. 2011; 11 (2):196–202. [ PubMed : 21625056 ]
- Clark JE. From the beginning: A developmental perspective on movement and mobility. Quest. 2005; 57 :37–45.
- Clark JE, Metcalfe JS. The mountain of motor development: A metaphor. Clark E, Humphrey JH, editors. Reston, VA: National Association for Sport and Physical Education; 2002. pp. 62–95. (In Motor development: Research and review, vol. 2).
- Cliff D, Okely A, Smith L, McKeen K. Relationships between fundamental movement skills and objectively measured physical activity in preschool children. Pediatric Exercise Science. 2009; 21 (4):436. [ PubMed : 20128363 ]
- Committee on Sports Medicine Fitness. Strength training by children and adolescents. Pediatrics. 2001; 107 (6):1470–1472. [ PubMed : 11389279 ]
- Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the Third National Health and Nutrition Examination Survey, 1988–1994. Archives of Pediatrics and Adolescent Medicine. 2003; 157 (8):821. [ PubMed : 12912790 ]
- Cook S, Auinger P, Huang TTK. Growth curves for cardio-metabolic risk factors in children and adolescents. Journal of Pediatrics. 2009; 155 (3):S6. [ PMC free article : PMC2789447 ] [ PubMed : 19732566 ]
- Council on Sports Medicine Fitness. Strength training by children and adolescents. Pediatrics. 2008; 121 (4):835–840. [ PubMed : 18381549 ]
- Cox AE, Smith AL, Williams L. Change in physical education motivation and physical activity behavior during middle school. Journal of Adolescent Health. 2008; 43 (5):506–513. [ PubMed : 18848680 ]
- Cradock AL, Kawachi I, Colditz GA, Gortmaker SL, Buka SL. Neighborhood social cohesion and youth participation in physical activity in Chicago. Social Science and Medicine. 2009; 68 (3):427–435. [ PubMed : 19036490 ]
- Craft LL, Landers DM. The effect of exercise on clinical depression and depression resulting from mental illness: A meta-analysis. Journal of Sport and Exercise Psychology. 1998; 20 :339–357.
- Crews DJ, Lochbaum MR, Landers DM. Aerobic physical activity effects on psychological well-being in low-income Hispanic children. Perceptual and Motor Skills. 2004; 98 (1):319–324. [ PubMed : 15058892 ]
- Danforth JS, Allen KD, Fitterling JM, Danforth JA, Farrar D, Brown M, Drabman RS. Exercise as a treatment for hypertension in low-socioeconomic-status black children. Journal of Consulting and Clinical Psychology. 1990; 58 (2):237. [ PubMed : 2335640 ]
- Daniels SR, Morrison JA, Sprecher DL, Khoury P, Kimball TR. Association of body fat distribution and cardiovascular risk factors in children and adolescents. Circulation. 1999; 99 (4):541–545. [ PubMed : 9927401 ]
- Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, Robinson TN, Scott BJ, Jeor SS, Williams CL. Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation. 2005; 111 (15):1999–2012. [ PubMed : 15837955 ]
- Davies PS, Gregory J, White A. Physical activity and body fatness in preschool children. International Journal of Obesity and Related Metabolic Disorders. 1995; 19 (1):6. [ PubMed : 7719393 ]
- Davis CL, Pollock NK, Waller JL, Allison JD, Dennis BA, Bassali R, Meléndez A, Boyle CA, Gower BA. Exercise dose and diabetes risk in overweight and obese children: A randomized controlled trial. Journal of the American Medical Association. 2012; 308 (11):1103–1112. [ PMC free article : PMC3487697 ] [ PubMed : 22990269 ]
- Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine study. Circulation. 2001; 104 (23):2815–2819. [ PubMed : 11733400 ]
- de la Haye K, Robins G, Mohr P, Wilson C. How physical activity shapes, and is shaped by, adolescent friendships. Social Science and Medicine. 2011; 73 (5):719–728. [ PubMed : 21802807 ]
- Dencker M, Wollmer P, Karlsson MK, Lindén C, Andersen LB, Thorsson O. Body fat, abdominal fat and body fat distribution related to cardiovascular risk factors in prepubertal children. Acta Paediatrica. 2012; 101 (8):852–857. [ PubMed : 22452521 ]
- Depres JP, Lamarche B. Physical activity and the metabolic complications of obesity. Bouchard C, editor. Champaign, IL: Human Kinetics; 2000. pp. 331–354. (In Physical activity and obesity).
- Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002; 25 (12):2165–2171. [ PMC free article : PMC1282458 ] [ PubMed : 12453955 ]
- Digelidis N, Papaioannou A, Laparidis K, Christodoulidis T. A one-year intervention in 7th grade physical education classes aiming to change motivational climate and attitudes towards exercise. Psychology of Sport and Exercise. 2003; 4 (3):195–210.
- Dimeo F, Bauer M, Varahram I, Proest G, Halter U. Benefits from aerobic exercise in patients with major depression: A pilot study. British Journal of Sports Medicine. 2001; 35 (2):114–117. [ PMC free article : PMC1724301 ] [ PubMed : 11273973 ]
- Dintiman G, Ward B, Telez T. Sports speed. Champaign, IL: Human Kinetics; 1997.
- Dionne I, Almeras N, Bouchard C, Tremblay A. The association between vigorous physical activities and fat deposition in male adolescents. Medicine and Science in Sports and Exercise. 2000; 32 :392–395. [ PubMed : 10694122 ]
- Dishman RK, Motl RW, Saunders R, Felton G, Ward DS, Dowda M, Pate RR. Enjoyment mediates effects of a school-based physical-activity intervention. Medicine and Science in Sports and Exercise. 2005; 37 (3):478–487. [ PubMed : 15741848 ]
- Dishman RK, Hales DP, Pfeiffer KA, Felton GA, Saunders R, Ward DS, Dowda M, Pate RR. Physical self-concept and self-esteem mediate crosssectional relations of physical activity and sport participation with depression symptoms among adolescent girls. Health Psychology. 2006; 25 (3):396–407. [ PubMed : 16719612 ]
- Dishman RK, Saunders RP, Motl RW, Dowda M, Pate RR. Self-efficacy moderates the relation between declines in physical activity and perceived social support in high school girls. Journal of Pediatric Psychology. 2009; 34 (4):441–451. [ PMC free article : PMC2671981 ] [ PubMed : 18812410 ]
- Dishman RK, Dunn AL, Sallis JF, Vandenberg RJ, Pratt CA. Social-cognitive correlates of physical activity in a multi-ethnic cohort of middle-school girls: Two-year prospective study. Journal of Pediatric Psychology. 2010; 35 (2):188–198. [ PMC free article : PMC2902830 ] [ PubMed : 19468040 ]
- Dua J, Hargreaves L. Effect of aerobic exercise on negative affect, positive affect, stress, and depression. Perceptual and Motor Skills. 1992; 75 (2):355–361. [ PubMed : 1408588 ]
- Dubose KD, Eisenmann JC, Donnelly JE. Aerobic fitness attenuates the metabolic syndrome score in normal-weight, at-risk-for-overweight, and overweight children. Pediatrics. 2007; 120 (5):e1262–e1268. [ PubMed : 17974719 ]
- Duncan GE, Perri MG, Theriaque DW, Hutson AD, Eckel RH, Stacpoole PW. Exercise training, without weight loss, increases insulin sensitivity and postheparin plasma lipase activity in previously sedentary adults. Diabetes Care. 2003; 26 (3):557–562. [ PubMed : 12610001 ]
- Duncan SC, Duncan TE, Strycker LA, Chaumeton NR. A cohort-sequential latent growth model of physical activity from ages 12 to 17 years. Annals of Behavioral Medicine. 2007; 33 (1):80–89. [ PMC free article : PMC2729662 ] [ PubMed : 17291173 ]
- Dunn AL, Trivedi MH, O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Medicine and Science in Sports and Exercise. 2001; 33 (6 Suppl):S587–S597. [ PubMed : 11427783 ]
- Eisenmann JC. Secular trends in variables associated with the metabolic syndrome of North American children and adolescents: A review and synthesis. American Journal of Human Biology. 2003; 15 (6):786–794. [ PubMed : 14595870 ]
- Eisenmann JC. Aerobic fitness, fatness and the metabolic syndrome in children and adolescents. Acta Paediatrica. 2007; 96 (12):1723–1729. [ PubMed : 17971189 ]
- Eisenmann J, Katzmarzyk P, Perusse L, Tremblay A, Despres J, Bouchard C. Aerobic fitness, body mass index, and CVD risk factors among adolescents: The Quebec Family Study. International Journal of Obesity. 2005; 29 (9):1077–1083. [ PubMed : 15917844 ]
- Eisenmann JC, Welk GJ, Wickel EE, Blair SN. Combined influence of cardiorespiratory fitness and body mass index on cardiovascular disease risk factors among 8-18 year old youth: The Aerobics Center Longitudinal Study. International Journal of Pediatric Obesity. 2007a; 2 (2):66–72. [ PubMed : 17763013 ]
- Eisenmann JC, Welk GJ, Ihmels M, Dollman J. Fatness, fitness, and cardiovascular disease risk factors in children and adolescents. Medicine and Science in Sports and Exercise. 2007b; 39 (8):1251. [ PubMed : 17762357 ]
- Eisenmann JC, Laurson KR, Welk GJ. Aerobic fitness percentiles for US adolescents. American Journal of Preventive Medicine. 2011; 41 (4):S106–S110. [ PubMed : 21961609 ]
- Ekelund U, Brage S, Franks PW, Hennings S, Emms S, Wareham NJ. Physical activity energy expenditure predicts progression toward the metabolic syndrome independently of aerobic fitness in middle-aged healthy Caucasians the Medical Research Council Ely Study. Diabetes Care. 2005; 28 (5):1195–1200. [ PubMed : 15855588 ]
- Ekelund U, Franks PW, Sharp S, Brage S, Wareham NJ. Increase in physical activity energy expenditure is associated with reduced metabolic risk independent of change in fatness and fitness. Diabetes Care. 2007; 30 (8):2101–2106. [ PubMed : 17536069 ]
- Elder JP, Broyles SL, McKenzie TL, Sallis JF, Berry CC, Davis TB, Hoy PL, Nader PR. Direct home observations of the prompting of physical activity in sedentary and active Mexican- and Anglo-American children. Journal of Developmental and Behavioral Pediatrics. 1998; 19 (1):26–30. [ PubMed : 9524302 ]
- Ertek S, Cicero A. Impact of physical activity on inflammation: Effects on cardiovascular disease risk and other inflammatory conditions. Archives of Medical Science. 2012; 8 (5):794. [ PMC free article : PMC3506236 ] [ PubMed : 23185187 ]
- Escalante Y, Saavedra JM, García-Hermoso A, Domínguez AM. Improvement of the lipid profile with exercise in obese children: A systematic review. Preventive Medicine. 2012; 54 (5):293–301. [ PubMed : 22387009 ]
- Ewart CK, Young DR, Hagberg JM. Effects of school-based aerobic exercise on blood pressure in adolescent girls at risk for hypertension. American Journal of Public Health. 1998; 88 (6):949–951. [ PMC free article : PMC1508242 ] [ PubMed : 9618627 ]
- Faigenbaum AD. State of the art reviews: Resistance training for children and adolescents: Are there health outcomes. American Journal of Lifestyle Medicine. 2007; 1 (3):190–200.
- Faigenbaum A, Zaichkowsky L, Westcott W, Long C, LaRosa-Loud R, Micheli L, Outerbridge A. Psychological effects of strength training on children. Journal of Sport Behavior. 1997; 20 (2):164–175.
- Faigenbaum AD, Kraemer WJ, Blimkie CJ, Jeffreys I, Micheli LJ, Nitka M, Rowland TW. Youth resistance training: Updated position statement paper from the National Strength and Conditioning Association. Journal of Strength and Conditioning Research. 2009; 23 (5 Suppl):S60–S79. [ PubMed : 19620931 ]
- Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. Journal of the American College of Cardiology. 2009; 54 (25):2396–2406. [ PubMed : 20082930 ]
- Farr JN, Lee VR, Blew RM, Lohman TG, Going SB. Quantifying bone-relevant activity and its relation to bone strength in girls. Medicine and Science in Sports and Exercise. 2011; 43 (3):476. [ PMC free article : PMC3152309 ] [ PubMed : 20631644 ]
- Ferguson M, Gutin B, Le N, Karp W, Litaker M, Humphries M, Okuyama T, Riggs S, Owens S. Effects of exercise training and its cessation on components of the insulin resistance syndrome in obese children. International Journal of Obesity and Related Metabolic Disorders. 1999; 23 (8):889. [ PubMed : 10490792 ]
- Ferrari SL, Chevalley T, Bonjour JP, Rizzoli R. Childhood fractures are associated with decreased bone mass gain during puberty: An early marker of persistent bone fragility. Journal of Bone and Mineral Research. 2006; 21 (4):501–507. [ PubMed : 16598368 ]
- Ferrer-Caja E, Weiss MR. Predictors of intrinsic motivation among adolescent students in physical education. Research Quarterly for Exercise and Sport. 2000; 71 (3):267–279. [ PubMed : 10999264 ]
- Fisher A, Reilly JJ, Kelly LA, Montgomery C, Williamson A, Paton JY, Grant S. Fundamental movement skills and habitual physical activity in young children. Medicine and Science in Sports and Exercise. 2005; 37 (4):684. [ PubMed : 15809570 ]
- Fournier M, Ricci J, Taylor AW, Ferguson RJ, Montpetit RR, Chaitman BR. Skeletal muscle adaptation in adolescent boys: Sprint and endurance training and detraining. Medicine and Science in Sports and Exercise. 1982; 14 (6):453. [ PubMed : 6219266 ]
- Freedman DS, Kettel Khan L, Serdula M, Dietz W, Srinivasan S, Berenson G. The relation of childhood BMI to adult adiposity: The Bogalusa Heart Study. Pediatrics. 2005; 115 (1):22–27. [ PubMed : 15629977 ]
- Frühbeck G, Gómez-Ambrosi J, Muruzábal FJ, Burrell MA. The adipocyte: A model for integration of endocrine and metabolic signaling in energy metabolism regulation. American Journal of Physiology-Endocrinology and Metabolism. 2001; 280 (6):E827–E847. [ PubMed : 11350765 ]
- Fuchs RK, Bauer JJ, Snow CM. Jumping improves hip and lumbar spine bone mass in prepubescent children: A randomized controlled trial. Journal of Bone and Mineral Research. 2001; 16 (1):148–156. [ PubMed : 11149479 ]
- Fulton JE, Burgeson CR, Perry GR, Sherry B, Galuska DA, Alexander MP, Caspersen CJ. Assessment of physical activity and sedentary behavior in preschool-age children: Priorities for research. Pediatric Exercise Science. 2001; 13 :113–126.
- Gan SK, Kriketos AD, Ellis BA, Thompson CH, Kraegen EW, Chisholm DJ. Changes in aerobic capacity and visceral fat but not myocyte lipid levels predict increased insulin action after exercise in overweight and obese men. Diabetes Care. 2003; 26 (6):1706–1713. [ PubMed : 12766098 ]
- Going S. Body composition alterations with exercise. Rippe JM, editor. Blackwell Science; 1999. pp. 1089–1097. (In Lifestyle medicine).
- Going SB, Lohman TG, Cussler EC, Williams DP, Morrison JA, Horn PS. Percent body fat and chronic disease risk factors in US children and youth. American Journal of Preventive Medicine. 2011; 41 (4):S77–S86. [ PubMed : 21961616 ]
- Going S, Hingle M, Farr J. Body composition. 11th. Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, editors. Baltimore, MD: Lippincott, Williams & Wilkins; 2012. p. 1648. (In Modern nutrition in health and disease).
- Goodway JD, Rudisill ME. Perceived physical competence and actual motor skill competence of African American preschool children. Adapted Physical Activity Quarterly. 1997; 14 :314–326.
- Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, Laird N. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet health. Archives of Pediatrics and Adolescent Medicine. 1999; 153 (4):409–418. [ PubMed : 10201726 ]
- Graf C, Koch B, Dordel S, Schindler-Marlow S, Icks A, Schüller A, Bjarnason-Wehrens B, Tokarski W, Predel HG. Physical activity, leisure habits and obesity in first-grade children. European Journal of Cardiovascular Prevention and Rehabilitation. 2004; 11 (4):284–290. [ PubMed : 15292761 ]
- Guo SS, Roche AF, Chumlea WC, Gardner JD, Siervogel RM. The predictive value of childhood body mass index values for overweight at age 35 y. American Journal of Clinical Nutrition. 1994; 59 (4):810–819. [ PubMed : 8147324 ]
- Guo S, Huang C, Maynard L, Demerath E, Towne B, Chumlea WC, Siervogel R. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: The Fels Longitudinal Study. International Journal of Obesity and Related Metabolic Disorders. 2000; 24 (12):1628. [ PubMed : 11126216 ]
- Gutin B, Humphries M. Exercise, body composition, and health in children. In: Lamb DR, Murray R, editors. In Perspectives in exercise science and sports medicine. Vol. 11. Carmel, IN: Cooper Publishing Group; 1998. pp. 295–347.
- Gutin B, Owens S. Role of exercise intervention in improving body fat distribution and risk profile in children. American Journal of Human Biology. 1999; 11 (2):237–247. [ PubMed : 11533947 ]
- Gutin B, Owens S. The influence of physical activity on cardiometabolic biomarkers in youths: A review. Pediatric Exercise Science. 2011; 23 (2):169. [ PubMed : 21633131 ]
- Gutin B, Barbeau P, Owens S, Lemmon CR, Bauman M, Allison J, Kang HS, Litaker MS. Effects of exercise intensity on cardiovascular fitness, total body composition, and visceral adiposity of obese adolescents. American Journal of Clinical Nutrition. 2002; 75 (5):818–826. [ PubMed : 11976154 ]
- Hagberg JM, Goldring D, Ehsani AA, Heath GW, Hernandez A, Schechtman K, Holloszy JO. Effect of exercise training on the blood pressure and hemodynamic features of hypertensive adolescents. American Journal of Cardiology. 1983; 52 (7):763–768. [ PubMed : 6624669 ]
- Hagberg JM, Ehsani AA, Goldring D, Hernandez A, Sinacore DR, Holloszy JO. Effect of weight training on blood pressure and hemodynamics in hypertensive adolescents. Journal of Pediatrics. 1984; 104 (1):147–151. [ PubMed : 6690660 ]
- Hager A. Adipose tissue cellularity in childhood in relation to the development of obesity. British Medical Bulletin. 1981; 37 (3):287–290. [ PubMed : 7034854 ]
- Halfon N, Verhoef PA, Kuo AA. Childhood antecedents to adult cardiovascular disease. Pediatrics in Review. 2012; 33 (2):51–61. [ PubMed : 22301031 ]
- Hallal PC, Victora CG, Azevedo MR, Wells JC. Adolescent physical activity and health: A systematic review. Sports Medicine. 2006; 36 (12):1019–1030. [ PubMed : 17123326 ]
- Halle M, Korsten-Reck U, Wolfarth B, Berg A. Low-grade systemic inflammation in overweight children: Impact of physical fitness. Exercise Immunology Review. 2004; 10 :66–74. [ PubMed : 15633587 ]
- Hands B, Larkin D, Parker H, Straker L, Perry M. The relationship among physical activity, motor competence and health related fitness in 14-year-old adolescents. Scandinavian Journal of Medicine and Science in Sports. 2009; 19 (5):655–663. [ PubMed : 18694431 ]
- Harter S, Pike R. The pictorial scale of perceived competence and social acceptance for young children. Child Development. 1984; 55 (6):1969–1982. [ PubMed : 6525886 ]
- Hasselstrom H, Hansen S, Froberg K, Andersen LB. Physical fitness and physical activity during adolescence as predictors of cardiovascular disease risk in young adulthood. Danish Youth and Sports Study. An eight-year follow-up study. International Journal of Sports Medicine. 2002; 23 (1):27. [ PubMed : 12012259 ]
- Haubenstricker J, Sapp M. A brief review of the Bruininks-Oseretsky test of motor proficiency. Reston, VA: National Association for Sport and Physical Education; 1980.
- Haubenstricker J, Seefeldt V. Acquisition of motor skills during childhood. In: Seefeldt V, editor. In Physical activity and well-being. Reston, VA: American Alliance for Health, Physical Education, Recreation and Dance; 1986. pp. 41–92.
- Haugen T, Säfvenbom R, Ommundsen Y. Physical activity and global self-worth: The role of physical self-esteem indices and gender. Mental Health and Physical Activity. 2011; 4 (2):49–56.
- He Q, Zhang X, He S, Gong L, Sun Y, Heshka S, Deckelbaum RJ, Gallagher D. Higher insulin, triglycerides, and blood pressure with greater trunk fat in Tanner 1 Chinese. Obesity. 2007; 15 (4):1004–1011. [ PMC free article : PMC2726721 ] [ PubMed : 17426336 ]
- Heller T, Hsieh K, Rimmer JH. Attitudinal and psychosocial outcomes of a fitness and health education program on adults with Down syndrome. American Journal on Mental Retardation. 2004; 109 (2):175–185. [ PubMed : 15000672 ]
- HHS (U.S. Department of Health and Human Services). Physical activity and health: A report of the Surgeon General. Atlanta, GA: HHS, CDC, National Center for Chronic Disease Prevention and Health Promotion; 1996.
- HHS. Physical activity guidelines for Americans. Washington, DC: HHS; 2008.
- HHS. Physical activity guidelines for Americans midcourse report: Strategies to increase physical activity among youth. Washington, DC: HHS; 2013.
- Hind K, Burrows M. Weight-bearing exercise and bone mineral accrual in children and adolescents: A review of controlled trials. Bone. 2007; 40 (1):14–27. [ PubMed : 16956802 ]
- Holloway JB, Beuter A, Duda JL. Self-efficacy and training for strength in adolescent girls. Journal of Applied Social Psychology. 1988; 18 (8):699–719.
- Houwen S, Hartman E, Visscher C. Physical activity and motor skills in children with and without visual impairments. Medicine and Science in Sports and Exercise. 2009; 41 (1):103. [ PubMed : 19092701 ]
- Huang TTK, Nansel TR, Belsheim AR, Morrison JA. Sensitivity, specificity, and predictive values of pediatric metabolic syndrome components in relation to adult metabolic syndrome: The Princeton LRC follow-up study. Journal of Pediatrics. 2008; 152 (2):185–190. [ PMC free article : PMC2414260 ] [ PubMed : 18206687 ]
- Hume C, Okely A, Bagley S, Telford A, Booth M, Crawford D, Salmon J. Does weight status influence associations between children's fundamental movement skills and physical activity. Research Quarterly for Exercise and Sport. 2008; 79 (2):158–166. [ PubMed : 18664040 ]
- Hussey J, Bell C, Bennett K, O'Dwyer J, Gormley J. Relationship between the intensity of physical activity, inactivity, cardiorespiratory fitness and body composition in 7-10-year-old Dublin children. British Journal of Sports Medicine. 2007; 41 (5):311–316. [ PMC free article : PMC2659066 ] [ PubMed : 17395610 ]
- Imperatore G, Cheng YJ, Williams DE, Fulton J, Gregg EW. Physical activity, cardiovascular fitness, and insulin sensitivity among US adolescents: The National Health and Nutrition Examination Survey, 1999–2002. Diabetes Care. 2006; 29 (7):1567–1572. [ PubMed : 16801580 ]
- IOM (Institute of Medicine). Children's health, the nation's wealth. Washington, DC: The National Academies Press; 2004.
- IOM. Preventing childhood obesity: Health in the balance. Washington, DC: The National Academies Press; 2005. [ PubMed : 22379642 ]
- IOM. Accelerating progress in obesity prevention: Solving the weight of the nation. Washington, DC: The National Academies Press; 2012a. [ PMC free article : PMC3648752 ] [ PubMed : 22983849 ]
- IOM. Fitness measures and health outcomes in youth. Washington, DC: The National Academies Press; 2012b. [ PubMed : 25187939 ]
- Irwin ML, Yasui Y, Ulrich CM, Bowen D, Rudolph RE, Schwartz RS, Yukawa M, Aiello E, Potter JD, McTiernan A. Effect of exercise on total and intra-abdominal body fat in postmenopausal women. Journal of the American Medical Association. 2003; 289 (3):323–330. [ PubMed : 12525233 ]
- Isasi CR, Deckelbaum RJ, Tracy RP, Starc TJ, Berglund L, Shea S. Physical fitness and C-reactive protein level in children and young adults: The Columbia University Biomarkers Study. Pediatrics. 2003; 111 (2):332–338. [ PubMed : 12563060 ]
- Jaakkola T, Kalaja S, Liukkonen J, Jutila A, Virtanen P, Watt A. Relations among physical activity patterns, lifestyle activities, and fundamental movement skills for Finnish students in grade 7. Perceptual and Motor Skills. 2009; 108 (1):97–111. [ PubMed : 19425451 ]
- Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. International Journal of Behavioral Nutrition and Physical Activity. 2010; 7 (40):1–16. [ PMC free article : PMC2885312 ] [ PubMed : 20459784 ]
- Janssen I, Katzmarzyk P, Boyce W, Vereecken C, Mulvihill C, Roberts C, Currie C, Pickett W. Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obesity Reviews. 2005; 6 (2):123–132. [ PubMed : 15836463 ]
- Jarrett OS, Maxwell DM, Dickerson C, Hoge P, Davies G, Yetley A. Impact of recess on classroom behavior: Group effects and individual differences. Journal of Educational Research. 1998; 92 (2):121–126.
- Jolliffe CJ, Janssen I. Development of age-specific adolescent metabolic syndrome criteria that are linked to the Adult Treatment Panel III and International Diabetes Federation criteria. Journal of the American College of Cardiology. 2007; 49 (8):891–898. [ PubMed : 17320748 ]
- Jones M, Stratton G, Reilly T, Unnithan V. The efficacy of exercise as an intervention to treat recurrent nonspecific low back pain in adolescents. Pediatric Exercise Science. 2007; 19 (3):349–359. [ PubMed : 18019593 ]
- Kang HS, Gutin B, Barbeau P, Owens S, Lemmon CR, Allison J, Litaker MS, Le NA. Physical training improves insulin resistance syndrome markers in obese adolescents. Medicine and Science in Sports and Exercise. 2002; 34 (12):1920. [ PubMed : 12471297 ]
- Kannel WB, Dawber TR. Atherosclerosis as a pediatric problem. Journal of Pediatrics. 1972; 80 (4):544–554. [ PubMed : 4552435 ]
- Kannus P, Haapasalo H, Sankelo M, Sievänen H, Pasanen M, Heinonen A, Oja P, Vuori I. Effect of starting age of physical activity on bone mass in the dominant arm of tennis and squash players. Annals of Internal Medicine. 1995; 123 (1):27. [ PubMed : 7762910 ]
- Kappos AD. The impact of electronic media on mental and somatic children's health. International Journal of Hygiene and Environmental Health. 2007; 210 (5):555–562. [ PubMed : 17869577 ]
- Karlsson M. Does exercise during growth prevent fractures in later life. Medicine and Sport Science. 2007; 51 :121–136. [ PubMed : 17505123 ]
- Katz DL, Cushman D, Reynolds J, Njike V, Treu JA, Walker J, Smith E, Katz C. Putting physical activity where it fits in the school day: Preliminary results of the ABC (Activity Bursts in the Classroom) for fitness program. Preventing Chronic Disease. 2010; 7 (4):A82. [ PMC free article : PMC2901580 ] [ PubMed : 20550840 ]
- Katzmarzyk PT, Pérusse L, Malina RM, Bouchard C. Seven-year stability of indicators of obesity and adipose tissue distribution in the Canadian population. American Journal of Clinical Nutrition. 1999; 69 (6):1123–1129. [ PubMed : 10357729 ]
- Katzmarzyk PT, Pérusse L, Malina RM, Bergeron J, Després JP, Bouchard C. Stability of indicators of the metabolic syndrome from childhood and adolescence to young adulthood: The Quebec Family Study. Journal of Clinical Epidemiology. 2001; 54 (2):190–195. [ PubMed : 11166535 ]
- Kelley GA, Kelley KS. Effects of aerobic exercise on non-high-density lipoprotein cholesterol in children and adolescents: A meta-analysis of randomized controlled trials. Progress in Cardiovascular Nursing. 2008; 23 (3):128–132. [ PMC free article : PMC2596632 ] [ PubMed : 19039893 ]
- Kim YKY, Lee SLS. Physical activity and abdominal obesity in youth. Applied Physiology, Nutrition, and Metabolism. 2009; 34 (4):571–581. [ PubMed : 19767790 ]
- Knittle J, Timmers K, Ginsberg-Fellner F, Brown R, Katz D. The growth of adipose tissue in children and adolescents. Cross-sectional and longitudinal studies of adipose cell number and size. Journal of Clinical Investigation. 1979; 63 (2):239. [ PMC free article : PMC371945 ] [ PubMed : 429551 ]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine. 2002; 346 (6):393–403. [ PMC free article : PMC1370926 ] [ PubMed : 11832527 ]
- Kohl HW, Hobbs KE. Development of physical activity behaviors among children and adolescents. Pediatrics. 1998; 101 (Suppl 2):549–554. [ PubMed : 12224661 ]
- Kritz-Silverstein D, Barrett-Connor E, Corbeau C. Cross-sectional and prospective study of exercise and depressed mood in the elderly: The Rancho Bernardo Study. American Journal of Epidemiology. 2001; 153 (6):596–603. [ PubMed : 11257068 ]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC growth charts: United States. Advance Data. 2000; 314 :1. [ PubMed : 11183293 ]
- Laaksonen DE, Lakka HM, Salonen JT, Niskanen LK, Rauramaa R, Lakka TA. Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care. 2002; 25 (9):1612–1618. [ PubMed : 12196436 ]
- Larun L, Nordheim L, Ekeland E, Hagen K, Heian F. Cochrane Database of Systematic Reviews. 3. 2006. Exercise in prevention and treatment of anxiety and depression among children and young people; p. CD004691. [ PubMed : 16856055 ]
- Lauer RM, Connor WE, Leaverton PE, Reiter MA, Clarke WR. Coronary heart disease risk factors in school children: The Muscatine Study. Journal of Pediatrics. 1975; 86 (5):697–706. [ PubMed : 1133650 ]
- Laurson KR, Eisenmann JC, Welk GJ. Body fat percentile curves for US children and adolescents. American Journal of Preventive Medicine. 2011; 41 (4):S87–S92. [ PubMed : 21961617 ]
- Lazaar N, Aucouturier J, Ratel S, Rance M, Meyer M, Duché P. Effect of physical activity intervention on body composition in young children: Influence of body mass index status and gender. Acta Paediatrica. 2007; 96 (9):1321–1325. [ PMC free article : PMC2040215 ] [ PubMed : 17718785 ]
- Le Masurier G, Beighle A, Corbin C, Darst P, Morgan C, Pangrazi R, Wilde B, Vincent S. Pedometer-determined physical activity levels of youth. Journal of Physical Activity and Health. 2005; 2 (2):159–168.
- Lee JM, Kaciroti N, Appugliese D, Corwyn RF, Bradley RH, Lumeng JC. Body mass index and timing of pubertal initiation in boys. Archives of Pediatrics and Adolescent Medicine. 2010; 164 (2):139. [ PMC free article : PMC4172573 ] [ PubMed : 20124142 ]
- Lee S, Kuk JL, Davidson LE, Hudson R, Kilpatrick K, Graham TE, Ross R. Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without type 2 diabetes. Journal of Applied Physiology. 2005; 99 (3):1220–1225. [ PubMed : 15860689 ]
- Leppamaki S, Partonen TT, Hurme J, Haukka JK, Lonnqvist J. Randomized trial of the efficacy of bright-light exposure and aerobic exercise on depressive symptoms and serum lipids. Journal of Clinical Psychiatry. 2002; 63 (4):316–321. [ PubMed : 12000205 ]
- Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, Berenson GS. Childhood cardiovascular risk factors and carotid vascular changes in adulthood. Journal of the American Medical Association. 2003; 290 (17):2271–2276. [ PubMed : 14600185 ]
- Lindén C, Stenevi-Lundgren S, Gardsell P, Karlsson M. A five-year school curriculum-based exercise program in girls during early adolescence is associated with a large bone size and a thick cortical shell—pQCT data from the prospective pediatric osteoporosis prevention study (POP study). Journal of Bone and Mineral Research. 2006; 21 :S38.
- Lobelo F, Pate RR, Dowda M, Liese AD, Daniels SR. Cardiorespiratory fitness and clustered cardiovascular disease risk in US adolescents. Journal of Adolescent Health. 2010; 47 (4):352–359. [ PubMed : 20864004 ]
- Loftin M, Strikmiller PK, Warren B, Myers L, Schroth L, Pittman J, Harsha D, Sothern M. Original research comparison and relationship of vo2 peak and physical activity patterns in elementary and high school females. Pediatric Exercise Science. 1998; 10 :153–163.
- Lohman TG, Ring K, Schmitz KH, Treuth MS, Loftin M, Yang S, Sothern M, Going S. Associations of body size and composition with physical activity in adolescent girls. Medicine and Science in Sports and Exercise. 2006; 38 (6):1175. [ PMC free article : PMC2441868 ] [ PubMed : 16775560 ]
- Lopes VP, Rodrigues LP, Maia JA, Malina RM. Motor coordination as predictor of physical activity in childhood. Scandinavian Journal of Medicine and Science in Sports. 2011; 21 (5):663–669. [ PubMed : 21917017 ]
- Lubans DR, Morgan PJ, Cliff DP, Barnett LM, Oakley AD. Fundamental movement skills in children and adolescents: Review of associated health benefits. Sports Medicine. 2010; 40 (12):1019–1035. [ PubMed : 21058749 ]
- Lytle LA, Murray DM, Evenson KR, Moody J, Pratt CA, Metcalfe L, Parra-Medina D. Mediators affecting girls' levels of physical activity outside of school: Findings from the trial of activity in adolescent girls. Annals of Behavioral Medicine. 2009; 38 (2):124–136. [ PMC free article : PMC2819204 ] [ PubMed : 20012810 ]
- Macdonald-Wallis K, Jago R, Page AS, Brockman R, Thompson JL. School-based friendship networks and children's physical activity: A spatial analytical approach. Social Science and Medicine. 2011; 73 (1):6–12. [ PMC free article : PMC3133642 ] [ PubMed : 21680072 ]
- MacKelvie KJ, Khan KM, Petit MA, Janssen PA, McKay HA. A school-based exercise intervention elicits substantial bone health benefits: A 2-year randomized controlled trial in girls. Pediatrics. 2003; 112 (6 Pt 1):e447–e452. [ PubMed : 14654643 ]
- MacKelvie KJ, Petit MA, Khan KM, Beck TJ, McKay HA. Bone mass and structure are enhanced following a 2-year randomized controlled trial of exercise in prepubertal boys. Bone. 2004; 34 (4):755–764. [ PubMed : 15050908 ]
- MacKelvie KJ, McKay HA, Khan KM, Crocker PRE. A school-based exercise intervention augments bone mineral accrual in early pubertal girls. Journal of Pediatrics. 2001; 139 (4):501–508. [ PubMed : 11598595 ]
- Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, Lauer RM. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: The Muscatine Study. Journal of the American College of Cardiology. 1996; 27 (2):277–284. [ PubMed : 8557894 ]
- Malina RM. Quantification of fat, muscle and bone in man. Clinical Orthopaedics and Related Research. 1969; 65 :9–38. [ PubMed : 4895801 ]
- Malina RM. Growth of muscle tissue and muscle mass. In: Falkner F, Tanner JM, editors. In Human growth. Vol. 2. New York: Plenum; 1986. pp. 77–99.
- Malina RM. Fitness and performance: Adult health and the culture of youth. In: Park RJ, Eckert HM, editors. In New possibilities, new paradigms? American Academy of Physical Education, No. 24. Champaign, IL: Human Kinetics Publishers; 1991. pp. 30–38.
- Malina RM. Physical growth and biology maturation of young athletes. Exercise and Sports Sciences Review. 1994; 22 :389–433. [ PubMed : 7925550 ]
- Malina RM. Regional body composition: Age, sex, and ethnic variation. In: Roche AF, Heymsfield S, Lohman TG, editors. In Human body composition. Champaign, IL: Human Kinetics Publishers; 1996. pp. 217–255.
- Malina RM. Adherence to physical activity from childhood to adulthood: A perspective from tracking studies. Quest. 2001a; 53 (3):346–355.
- Malina RM. Tracking of physical activity across the lifespan. President's Council on Physical Fitness and Sports Research Digest. 2001b; 3 (14)
- Malina RM. In Human growth and development. San Diego: Academic Press; 2002. 15—exercise and growth: Physical activity as a factor in growth and maturation; pp. 321–348.
- Malina R. Physical fitness of children and adolescents in the United States: Status and secular change. Medicine and Sports Science. 2007; 50 :67–90. [ PubMed : 17387252 ]
- Malina RM, Bouchard C. Subcutaneous fat distribution during growth. In: Bouchard C, Johnston FE, editors. In Fat distribution during growth and later health outcomes. New York: Alan R. Liss; 1988. pp. 63–84.
- Malina RM, Roche AF. Manual of physical status and performance in childhood, Vol. 2. New York: Plenum; 1983.
- Malina RM, Bouchard C, Bar-Or O. Growth, maturation, and physical activity. 2nd. Champaign, IL: Human Kinetics Publishers; 2004.
- Martikainen S, Pesonen AK, Lahti J, Heinonen K, Feldt K, Pyhälä R, Tammelin T. Journal of Clinical Endocrinology & Metabolism. 2013. Higher levels of physical activity are associated with lower hypothalamic-pituitary-adrenocortical axis reactivity to psychosocial stress in children. epub ahead of print. [ PubMed : 23471978 ]
- McAuley E. Physical activity and psychosocial outcomes. In: Bouchard C, Shepard RJ, Stephens T, editors. In Physical activity, fitness and health. Champaign IL: Human Kinetics Publishers; 1994. pp. 551–568.
- McAuley E, Rudolph D. Physical activity, aging, and psychological well-being. Journal of Aging and Physical Activity. 1995; 3 (1):67–98.
- McKay HA, Petit MA, Schutz RW, Prior JC, Barr SI, Khan KM. Augmented trochanteric bone mineral density after modified physical education classes: A randomized school-based exercise intervention study in prepubescent and early pubescent children. Journal of Pediatrics. 2000; 136 (2):156–162. [ PubMed : 10657819 ]
- McKenzie TL, Sallis JF, Broyles SL, Zive MM, Nader PR, Berry CC, Brennan JJ. Childhood movement skills: Predictors of physical activity in Anglo American and Mexican American adolescents. Research Quarterly for Exercise and Sport. 2002; 73 (3):238–244. [ PubMed : 12230330 ]
- McKenzie TL, Prochaska JJ, Sallis JF, Lamaster KJ. Coeducational and single-sex physical education in middle schools: Impact on physical activity. Research Quarterly for Exercise and Sport. 2004; 75 (4):446–449. [ PubMed : 15673045 ]
- McMurray RG, Harrell JS, Bangdiwala SI, Bradley CB, Deng S, Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. Journal of Adolescent Health. 2002; 31 (2):125–132. [ PubMed : 12127382 ]
- McMurray R, Bangdiwala S, Harrell J, Amorim L. Adolescents with metabolic syndrome have a history of low aerobic fitness and physical activity levels. Dynamic Medicine. 2008; 7 (1):5. [ PMC free article : PMC2358885 ] [ PubMed : 18394155 ]
- Merzenich H, Boeing H, Wahrendorf J. Dietary fat and sports activity as determinants for age at menarche. American Journal of Epidemiology. 1993; 138 (4):217–224. [ PubMed : 8356963 ]
- Meyer AA, Kundt G, Lenschow U, Schuff-Werner P, Kienast W. Improvement of early vascular changes and cardiovascular risk factors in obese children after a six-month exercise program. Journal of the American College of Cardiology. 2006; 48 (9):1865–1870. [ PubMed : 17084264 ]
- Mirwald R, Bailey D. Maximal aerobic power. London, Ontario: Sports Dynamics; 1986.
- Modlesky CM, Lewis RD. Does exercise during growth have a long-term effect on bone health. Exercise and Sport Sciences Reviews. 2002; 30 (4):171–176. [ PubMed : 12398114 ]
- Mølgaard C, Thomsen BL, Prentice A, Cole TJ, Michaelsen KF. Whole body bone mineral content in healthy children and adolescents. Archives of Disease in Childhood. 1997; 76 (1):9–15. [ PMC free article : PMC1717036 ] [ PubMed : 9059153 ]
- Morgan PJ, Okely AD, Cliff DP, Jones RA, Baur LA. Correlates of objectively measured physical activity in obese children. Obesity. 2008; 16 (12):2634–2641. [ PubMed : 18927553 ]
- Morris FL, Naughton GA, Gibbs JL, Carlson JS, Wark JD. Prospective ten-month exercise intervention in premenarcheal girls: Positive effects on bone and lean mass. Journal of Bone and Mineral Research. 1997; 12 (9):1453–1462. [ PubMed : 9286762 ]
- Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: The Princeton Lipid Research Clinics Follow-up Study. Pediatrics. 2007; 120 (2):340–345. [ PubMed : 17671060 ]
- Morrison JA, Friedman LA, Wang P, Glueck CJ. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. Journal of Pediatrics. 2008; 152 (2):201–206. [ PubMed : 18206689 ]
- Nader PR, Bradley RH, Houts RM, McRitchie SL, O'Brien M. Moderate-to-vigorous physical activity from ages 9 to 15 years. Journal of the American Medical Association. 2008; 300 (3):295–305. [ PubMed : 18632544 ]
- NASPE (National Association for Sport and Physical Education). Physical education is critical to a complete education—position statement. Reston, VA: NASPE; 2001.
- Nassis GP, Papantakou K, Skenderi K, Triandafillopoulou M, Kavouras SA, Yannakoulia M, Chrousos GP, Sidossis LS. Aerobic exercise training improves insulin sensitivity without changes in body weight, body fat, adiponectin, and inflammatory markers in overweight and obese girls. Metabolism: Clinical and Experimental. 2005; 54 (11):1472. [ PubMed : 16253636 ]
- NIH (National Institutes of Health). Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Bethesda, MD: NIH; 2001.
- NRC (National Research Council)/IOM. Adolescent development and the biology of puberty: Summary of a workshop on new research. Washington, DC: National Academy Press; 1999. [ PubMed : 25077230 ]
- Ogden CL, Flegal KM. Smoothed percentage body fat percentiles for US children and adolescents, 1999–2004. National Health Statistics Report. 2011; 43 :1–7. [ PubMed : 22164513 ]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among U.S. children and adolescents, 1999–2010. Journal of the American Medical Association. 2012; 307 (5):483–490. [ PMC free article : PMC6362452 ] [ PubMed : 22253364 ]
- Okely AD, Booth ML, Patterson JW. Relationship between physical activity to fundamental movement skills among adolescents. Medicine and Science in Sports and Exercise. 2001; 33 (11):1899–1904. [ PubMed : 11689741 ]
- Ondrak KS, McMurray RG, Bangdiwala SI, Harrell JS. Influence of aerobic power and percent body fat on cardiovascular disease risk in youth. Journal of Adolescent Health. 2007; 41 (2):146–152. [ PubMed : 17659218 ]
- Owens S, Gutin B, Allison J, Riggs S, Ferguson M, Litaker M, Thompson W. Effect of physical training on total and visceral fat in obese children. Medicine and Science in Sports and Exercise. 1999; 31 (1):143. [ PubMed : 9927022 ]
- Pan Y, Pratt CA. Metabolic syndrome and its association with diet and physical activity in US adolescents. Journal of the American Dietetic Association. 2008; 108 (2):276. [ PubMed : 18237576 ]
- Parfitt A. The two faces of growth: Benefits and risks to bone integrity. Osteoporosis International. 1994; 4 (6):382–398. [ PubMed : 7696836 ]
- Pate RR, Wang CY, Dowda M, Farrell SW, O'Neill JR. Cardiorespiratory fitness levels among US youth 12 to 19 years of age: Findings from the 1999–2002 National Health and Nutrition Examination Survey. Archives of Pediatrics & Adolescent Medicine. 2006; 160 (10):1005. [ PubMed : 17018458 ]
- Pellegrini AD, Huberty PD, Jones I. The effects of recess timing on children's playground and classroom behaviors. American Educational Research Journal. 1995; 32 (4):845–864.
- Peluso MA, Guerra de Andrade LH. Physical activity and mental health: The association between exercise and mood. Clinics (São Paulo, Brazil). 2005; 60 (1):61–70. [ PubMed : 15838583 ]
- Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005; 18 (2):189–193. [ PubMed : 16639173 ]
- Petit M, McKay H, MacKelvie K, Heinonen A, Khan K, Beck T. A randomized school-based jumping intervention confers site and maturity-specific benefits on bone structural properties in girls: A hip structural analysis study. Journal of Bone and Mineral Research. 2002; 17 (3):363–372. [ PubMed : 11874228 ]
- Petty KH, Davis CL, Tkacz J, Young-Hyman D, Waller JL. Exercise effects on depressive symptoms and self-worth in overweight children: A randomized controlled trial. Journal of Pediatric Psychology. 2009; 34 (9):929–939. [ PMC free article : PMC2744328 ] [ PubMed : 19223278 ]
- Platat C, Wagner A, Klumpp T, Schweitzer B, Simon C. Relationships of physical activity with metabolic syndrome features and low-grade inflammation in adolescents. Diabetologia. 2006; 49 (9):2078–2085. [ PubMed : 16791618 ]
- Plowman SA. Physical activity, physical fitness, and low back pain. Exercise and Sport Sciences Review. 1992; 20 (1):221–242. [ PubMed : 1385572 ]
- Primack BA, Swanier B, Georgiopoulos AM, Land SR, Fine MJ. Association between media use in adolescence and depression in young adulthood: A longitudinal study. Archives of General Psychiatry. 2009; 66 (2):181–188. [ PMC free article : PMC3004674 ] [ PubMed : 19188540 ]
- Ramírez-Vélez R, Suaréz-Ortegón MF, Aguilar de Plata AC. Association between adiposity and cardiovascular risk factors in prepubertal children. Endocrinología y Nutrición (English Edition). 2012; 58 (9):457–463. [ PubMed : 21962397 ]
- Raudsepp L, Päll P. The relationship between fundamental motor skills and outside-school physical activity of elementary school children. Pediatric Exercise Science. 2006; 18 (4):426–435.
- Reed J, Metzker A, Phillips D. Relationships between physical activity and motor skills in middle school children. Perceptual and Motor Skills. 2004; 99 (2):483. [ PubMed : 15560336 ]
- Robinson LE. Effect of a mastery climate motor program on object control skills and perceived physical competence in preschoolers. Research Quarterly for Exercise and Sport. 2011; 82 (2):355–359. [ PubMed : 21699116 ]
- Robinson LE, Goodway JD. Instructional climates in preschool children who are at risk. Part I: Object-control skill development. Research Quarterly for Exercise and Sport. 2009; 80 (3):533–542. [ PubMed : 19791639 ]
- Robinson LE, Wadsworth DD, Peoples CM. Correlates of school-day physical activity in preschoolers: A preliminary study. Research Quarterly for Exercise and Sport. 2012; 83 (1):20–26. [ PubMed : 22428408 ]
- Robinson TN. Reducing children's television viewing to prevent obesity. Journal of the American Medical Association. 1999; 282 (16):1561–1567. [ PubMed : 10546696 ]
- Robinson TN, Borzekowski DLG. Effects of the smart classroom curriculum to reduce child and family screen time. Journal of Communication. 2006; 56 (1):1–26.
- Rolland-Cachera M, Deheeger M, Bellisle F, Sempe M, Guilloud-Bataille M, Patois E. Adiposity rebound in children: A simple indicator for predicting obesity. American Journal of Clinical Nutrition. 1984; 39 (1):129–135. [ PubMed : 6691287 ]
- Rosenfield RL, Lipton RB, Drum ML. Thelarche, pubarche, and menarche attainment in children with normal and elevated body mass index. Pediatrics. 2009; 123 (1):84–88. [ PubMed : 19117864 ]
- Ross R, Bradshaw AJ. The future of obesity reduction: Beyond weight loss. Nature Reviews Endocrinology. 2009; 5 (6):319–325. [ PubMed : 19421242 ]
- Ross R, Janiszewski PM. Is weight loss the optimal target for obesity-related cardiovascular disease risk reduction. Canadian Journal of Cardiology. 2008; 24 (Suppl D):25D. [ PMC free article : PMC2794451 ] [ PubMed : 18787733 ]
- Ross R, Dagnone D, Jones PJ, Smith H, Paddags A, Hudson R, Janssen I. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. Annals of Internal Medicine. 2000; 133 (2):92–103. [ PubMed : 10896648 ]
- Ross R, Janssen I, Dawson J, Kungl AM, Kuk JL, Wong SL, Nguyen-Duy TB, Lee S, Kilpatrick K, Hudson R. Exercise-induced reduction in obesity and insulin resistance in women: A randomized controlled trial. Obesity Research. 2012; 12 (5):789–798. [ PubMed : 15166299 ]
- Rowland TW. Developmental exercise physiology. Champaign, IL: Human Kinetics Publishers; 1996.
- Rowland TW. Children's exercise physiology. Champaign, IL: Human Kinetics Publishers; 2005.
- Rowlands A, Ingledew D, Eston R. The effect of type of physical activity measure on the relationship between body fatness and habitual physical activity in children: A meta-analysis. Annals of Human Biology. 2000; 27 (5):479–497. [ PubMed : 11023118 ]
- Rubin DA, McMurray RG, Harrell JS, Hackney AC, Thorpe DE, Haqq AM. The association between insulin resistance and cytokines in adolescents: The role of weight status and exercise. Metabolism: Clinical and Experimental. 2008; 57 (5):683. [ PMC free article : PMC2678573 ] [ PubMed : 18442634 ]
- Ruiz J, Ortega F, Wärnberg J, Sjöström M. Associations of low-grade inflammation with physical activity, fitness and fatness in prepubertal children: The European Youth Heart Study. International Journal of Obesity. 2007; 31 (10):1545–1551. [ PubMed : 17653064 ]
- Ruiz JR, Ortega FB, Wärnberg J, Moreno LA, Carrero JJ, Gonzalez-Gross M, Marcos A, Gutierrez A, Sjöström M. Inflammatory proteins and muscle strength in adolescents: The Avena Study. Archives of Pediatrics & Adolescent Medicine. 2008; 162 (5):462–468. [ PubMed : 18458193 ]
- Sääkslahti A, Numminen P, Niinikoski H, Rask-Nissilä L, Viikari J, Tuominen J, Välimäki I. Is physical activity related to body size, fundamental motor skills, and CHD risk factors in early childhood. Pediatric Exercise Science. 1999; 11 :327–340.
- Sallis JF, Berry CC, Broyles SL, McKenzie TL. Variability and tracking of physical activity over 2 yrs in young children. Medicine and Science in Sports and Exercise. 1995; 27 (7):1042–1049. [ PubMed : 7564971 ]
- Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Medicine and Science in Sports and Exercise. 2000; 32 (5):963–975. [ PubMed : 10795788 ]
- Sardinha LB, Andersen LB, Anderssen SA, Quitério AL, Ornelas R, Froberg K, Riddoch CJ, Ekelund U. Objectively measures time spent sedentary is associated with insulin resistance independent of overall and central body fat in 9- to 10-year-old Portuguese children. Diabetes Care. 2008; 31 (3):569–575. [ PubMed : 18070991 ]
- Saris WHM, Elvers JWH, van't Hof MA, Binkhorst RA. Changes in physical activity of children aged 6 to 12 years. In: Rutenfranz J, Mocellin R, Klimt F, editors. In Children and exercise XII. Champaign, IL: Human Kinetics; 1986. pp. 121–130.
- Seefeldt V. Developmental motor patterns: Implications for elementary school physical education. In: Nadeau WHC, Newell K, Roberts G, editors. In Psychology of motor behavior and sport. Champaign, IL: Human Kinetics; 1980. pp. 314–323.
- Sexton H, Søgaard A, Olstad R. How are mood and exercise related? Results from the Finnmark study. Social Psychiatry and Psychiatric Epidemiology. 2001; 36 (7):348–353. [ PubMed : 11606004 ]
- Shaibi GQ, Cruz ML, Ball GDC, Weigensberg MJ, Salem GJ, Crespo NC, Goran MI. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Medicine and Science in Sports and Exercise. 2006; 38 (7):1208. [ PubMed : 16826016 ]
- Sigal RJ, Kenny GP, Boulé NG, Wells GA, Prud'homme D, Fortier M, Reid RD, Tulloch H, Coyle D, Phillips P. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes. Annals of Internal Medicine. 2007; 147 (6):357–369. [ PubMed : 17876019 ]
- Slaven L, Lee C. Mood and symptom reporting among middle-aged women: The relationship between menopausal status, hormone replacement therapy, and exercise participation. Health Psychology. 1997; 16 (3):203. [ PubMed : 9152697 ]
- Sollerhed AC, Apitzsch E, Råstam L, Ejlertsson G. Factors associated with young children's self-perceived physical competence and self-reported physical activity. Health Education Research. 2008; 23 (1):125–136. [ PubMed : 17347524 ]
- Specker B, Binkley T. Randomized trial of physical activity and calcium supplementation on bone mineral content in 3- to 5-year-old children. Journal of Bone and Mineral Research. 2003; 18 (5):885–892. [ PubMed : 12733728 ]
- Steele RM, Brage S, Corder K, Wareham NJ, Ekelund U. Physical activity, cardiorespiratory fitness, and the metabolic syndrome in youth. Journal of Applied Physiology. 2008; 105 (1):342–351. [ PMC free article : PMC2494842 ] [ PubMed : 18369096 ]
- Steene-Johannessen J, Anderssen SA, Kolle E, Andersen LB. Low muscle fitness is associated with metabolic risk in youth. Medicine and Science in Sports and Exercise. 2009; 41 (7):1361–1367. [ PubMed : 19516166 ]
- Stevens J, Suchindran C, Ring K, Baggett CD, Jobe JB, Story M, Thompson J, Going SB, Caballero B. Physical activity as a predictor of body composition in American Indian children. Obesity Research. 2004; 12 (12):1974–1980. [ PubMed : 15687399 ]
- Stodden DF, Goodway JD, Langendorfer SJ, Roberton MA, Rudisill ME, Garcia C, Garcia LE. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest. 2008; 60 (2):290–306.
- Stoedefalke K, Armstrong N, Kirby B, Welsman J. Effect of training on peak oxygen uptake and blood lipids in 13- to 14-year-old girls. Acta Paediatrica. 2000; 89 (11):1290–1294. [ PubMed : 11106038 ]
- Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, Hergenroeder AC, Must A, Nixon PA, Pivarnik JM, Rowland T, Trost S, Trudeau F. Evidence based physical activity for school-age youth. Journal of Pediatrics. 2005; 146 (6):732–737. [ PubMed : 15973308 ]
- Sundgot-Borgen J, Rosenvinge J, Bahr R, Schneider L. The effect of exercise, cognitive therapy, and nutritional counseling in treating bulimia nervosa. Medicine and Science in Sports and Exercise. 2002; 34 (2):190. [ PubMed : 11828224 ]
- Tanner JM. Growth at adolescence, 2nd ed. Oxford, England: Blackwell Scientific Publications; 1962.
- Tanner J, Hughes P, Whitehouse R. Radiographically determined widths of bone muscle and fat in the upper arm and calf from age 3-18 years. Annals of Human Biology. 1981; 8 (6):495–517. [ PubMed : 7337414 ]
- Thomas JR. Effects of training on gender differences in overhand throwing: A brief quantitative literature analysis. Research Quarterly for Exercise and Sport. 1994; 65 (1):67–71. [ PubMed : 8184213 ]
- Thomas JR, French KE. Gender differences across age in motor performance: A meta-analysis. Psychological Bulletin. 1985; 98 (2):260. [ PubMed : 3901062 ]
- Thomas JR, Thomas KT. Development of gender differences in physical activity. Quest. 1988; 40 (3):219–229.
- Thomas N, Williams D. Inflammatory factors, physical activity, and physical fitness in young people. Scandinavian Journal of Medicine & Science in Sports. 2008; 18 (5):543–556. [ PubMed : 18627553 ]
- Tobias JH, Steer CD, Mattocks CG, Riddoch C, Ness AR. Habitual levels of physical activity influence bone mass in 11-year-old children from the United Kingdom: Findings from a large population-based cohort. Journal of Bone and Mineral Research. 2007; 22 (1):101–109. [ PMC free article : PMC2742715 ] [ PubMed : 17014381 ]
- Treuth MS, Hunter GR, Figueroa-Colon R, Goran MI. Effects of strength training on intra-abdominal adipose tissue in obese prepubertal girls. Medicine and Science in Sports and Exercise. 1998; 30 (12):1738. [ PubMed : 9861608 ]
- Trotter M, Hixon BB. Sequential changes in weight, density, and percentage ash weight of human skeletons from an early fetal period through old age. Anatomical Record. 1974; 179 (1):1–18. [ PubMed : 4821360 ]
- Trotter M, Peterson RR. Weight of the skeleton during postnatal development. American Journal of Physical Anthropology. 1970; 33 (3):313–323. [ PubMed : 5490179 ]
- Turner CH, Robling AG. Designing exercise regimens to increase bone strength. Exercise and Sport Science Reviews. 2003; 31 (1):45–50. [ PubMed : 12562170 ]
- Umemura Y, Ishiko T, Yamauchi T, Kurono M, Mashiko S. Five jumps per day increase bone mass and breaking force in rats. Journal of Bone and Mineral Research. 1997; 12 (9):1480–1485. [ PubMed : 9286765 ]
- U.S. Public Health Service. Report of the Surgeon General's conference on children's mental health: A national action agenda. Washington, DC: HHS; 2000. [ PubMed : 20669515 ]
- Viner R, Booy R. Epidemiology of health and illness. British Medical Journal. 2005; 330 (7488):411–414. [ PMC free article : PMC549118 ] [ PubMed : 15718543 ]
- Wang Q, Suominen H, Nicholson P, Zou L, Alen M, Koistinen A, Cheng S. Influence of physical activity and maturation status on bone mass and geometry in early pubertal girls. Scandinavian Journal of Medicine & Science in Sports. 2004; 15 (2):100–106. [ PubMed : 15773864 ]
- Wang Q, Cheng S, Alén M, Seeman E. Bone's structural diversity in adult females is established before puberty. Journal of Clinical Endocrinology and Metabolism. 2009; 94 (5):1555–1561. [ PubMed : 19223517 ]
- Wärnberg J, Marcos A. Low-grade inflammation and the metabolic syndrome in children and adolescents. Current Opinion in Lipidology. 2008; 19 (1):11–15. [ PubMed : 18196981 ]
- Wärnberg J, Nova E, Romeo J, Moreno LA, Sjöström M, Marcos A. Lifestyle-related determinants of inflammation in adolescence. British Journal of Nutrition. 2007; 98 (Suppl 1):S116–S120. [ PubMed : 17922948 ]
- Wärnberg J, Cunningham K, Romeo J, Marcos A. Session 6: Role of physical activity on immune function physical activity, exercise and low-grade systemic inflammation. Proceedings of the Nutrition Society. 2010; 69 (3):400–406. [ PubMed : 20598198 ]
- Watts K, Jones TW, Davis EA, Green D. Exercise training in obese children and adolescents: Current concepts. Sports Medicine. 2005; 35 (5):375–392. [ PubMed : 15896088 ]
- Weiss R, Caprio S. The metabolic consequences of childhood obesity. Best Practice and Research Clinical Endocrinology and Metabolism. 2005; 19 (3):405–419. [ PubMed : 16150383 ]
- Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, Allen K, Lopes M, Savoye M, Morrison J. Obesity and the metabolic syndrome in children and adolescents. New England Journal of Medicine. 2004; 350 (23):2362–2374. [ PubMed : 15175438 ]
- WHO (World Health Organization). Young people's health—a challenge for society. Report of a study group on young people and health for all by the year 2000. 1986. [March 1, 2013]. http://whqlibdoc .who .int/trs/WHO_TRS_731.pdf . [ PubMed : 3085358 ]
- Williams HG. Perceptual and motor development. Englewood Cliffs, NJ: Prentice Hall; 1983.
- Williams HG, Pfeiffer KA, O'Neill JR, Dowda M, McIver KL, Brown WH, Pate RR. Motor skill performance and physical activity in preschool children. Obesity. 2008; 16 (6):1421–1426. [ PubMed : 18388895 ]
- Wrotniak BH, Epstein LH, Dorn JM, Jones KE, Kondilis VA. The relationship between motor proficiency and physical activity in children. Pediatrics. 2006; 118 (6):e1758–e1765. [ PubMed : 17142498 ]
- You T, Murphy K, Lyles M, Demons J, Lenchik L, Nicklas B. Addition of aerobic exercise to dietary weight loss preferentially reduces abdominal adipocyte size. International Journal of Obesity. 2006; 30 (8):1211–1216. [ PubMed : 16446745 ]
- Zeng Q, Dong SY, Sun XN, Xie J, Cui Y. Percent body fat is a better predictor of cardiovascular risk factors than body mass index. Brazilian Journal of Medical and Biological Research. 2012; 45 (7):591–600. [ PMC free article : PMC3854278 ] [ PubMed : 22510779 ]
- Ziviani J, Poulsen A, Hansen C. Movement skills proficiency and physical activity: A case for Engaging and Coaching for Health (EACH)-child. Australian Occupational Therapy Journal. 2009; 56 (4):259–265. [ PubMed : 20854526 ]
- Cite this Page Committee on Physical Activity and Physical Education in the School Environment; Food and Nutrition Board; Institute of Medicine; Kohl HW III, Cook HD, editors. Educating the Student Body: Taking Physical Activity and Physical Education to School. Washington (DC): National Academies Press (US); 2013 Oct 30. 3, Physical Activity and Physical Education: Relationship to Growth, Development, and Health.
- PDF version of this title (4.4M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Physical Activity and Physical Education: Relationship to Growth, Development, a... Physical Activity and Physical Education: Relationship to Growth, Development, and Health - Educating the Student Body
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
New Research Examines Physical Education in America
By Morgan Clennin, PhD, MPH, Kaiser Permanente of Colorado, University of South Carolina, and National Physical Activity Plan
School-based physical education (PE) is recommended by the Community Guide as an effective strategy to promote physical activity among youth. Unfortunately, many have speculated that PE exposure has declined precipitously among U.S. students in the past decade. Limited resources and budgets, prioritization of core academic subjects, and several other barriers have been cited as potential drivers of these claims. However, few large-scale studies have explored the merit of these claims – leaving the answers following questions unknown:
Has PE attendance decreased among U.S. students in the past decades?
What policies and practices are in place to support quality PE?
To answer these questions, the President’s Council on Sports, Fitness & Nutrition tasked the National Physical Activity Plan Alliance (NPAPA) to review the available evidence and summarize their findings. The primary objective of this effort was to better understand PE exposure over time to inform national recommendations and strategies for PE.
The NPAPA began by establishing a collaborative partnership with experts in the federal government, industry, and academia. The group analyzed existing national data sources that could be used to examine changes in PE attendance and current implementation of PE policies and practices. These efforts culminated in a final report and two peer-reviewed manuscripts. A summary of the group’s findings are outlined below.
Key Findings:
- 1/2 of U.S. high school students did not attend PE classes—which is consistent over the 24-year period studied (1991-2015).
- The percentage of U.S. high school students reporting PE attendance did not change significantly between 1991 and 2015 for the overall sample or across sex and race/ethnicity subgroup.
- Daily PE attendance did decrease 16% from 1991 to 1995 then attendance rates remained stable through 2015.
- > 65% of schools implemented 2-4 of the 7 essential PE policies
- Implementation of PE policies varied by region, metropolitan status, and school level.
- Data indicates minority students have been disproportionately affected by cuts to school PE programs during the past two decades.
Recommendations Based on Key Findings:
- Prioritize efforts to expand collection of surveillance data examining trends in PE attendance among elementary and middle school students.
- Develop policies to improve PE access for all students in order for PE to contribute to increased physical activity among youth.
- Adopt policies and programs that prioritize PE to maximize the benefits of PE.
- Utilize the findings of these efforts to target professional development and technical assistance for PE practitioners.
The Education sector of the NPAP provides evidence-based strategies and tactics that can guide efforts to support the provision of quality PE to all students. More information, and links to the respective manuscripts, can be found on the NPAPA website: http://physicalactivityplan.org/projects/physicaleducation.html
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.

- Pete Charrette
Why Is Physical Education Important? 10 Powerful Reasons We Need PE In Our Schools Today
According to the CDC, children 6 to 17 years old should do 60 minutes or more of moderate-to-vigorous physical activity every day. The tragic reality is that less than 25% of kids follow those guidelines. Many children are extremely inactive and do not participate in any extracurricular activities. What would happen if our students were no longer granted access to quality physical education?

Participating in a high-quality PE program may provide numerous benefits for students, perhaps more than any other subject. Physical education is critical to our health, well-being, and overall development. Unfortunately, it is not always understood by everyone. The fact is that we, as educators, must be our students' and others' own strongest advocates. We must identify and promote the unique benefits of physical education to all members of our community. Here are ten of the many reasons why physical education is so important:
Physical Education...
1. encourages physical activity for life.

Regular exercise and movement are required for optimum health in our lives. A physical education class is the ideal setting for instilling healthy habits and acquiring an understanding of one's own fitness and mobility abilities. Daily physical education is an essential component of a complete educational program. It encourages children to be physically active and develop the abilities and confidence they need to be active throughout their lives, which is beneficial for them both physically and emotionally.
Keeping active for life as a result of a quality PE program directly correlates with Shape America's Standard 4 : Develops personal skills, identifies personal benefits of movement, and chooses to engage in physical activity.
Rationale : Through learning experiences in physical education, the student develops an understanding of how movement is personally beneficial and subsequently chooses to participate in physical activities that are personally meaningful (e.g., activities that offer social interaction, cultural connection, exploration, choice, self-expression, appropriate levels of challenge, and added health benefits). A student's personal development can be acquired early and maintained for a lifetime.
National Physical Education Standards are used under license from SHAPE America. © 2024, SHAPE America, https://www.shapeamerica.org/ . All rights reserved.

For in-depth exploration of the physiological changes that occur during exercise, check out my article:
What Happens to My Body When I Exercise? A Physical Educator's Guide .
2. Helps prevent sickness and disease

Regular exercise can not only improve your physical health, but it may also help you avoid illness and disease. Physical activity has been linked to a strengthened immune system, which makes us less likely to get sick. It also aids in the reduction of stress, improvement of mental health, weight management, and overall energy levels. And since PE classes are a great way to get people moving, they can play a big role in keeping our students healthy.
Additionally, regular physical education helps manage chronic conditions like diabetes and heart disease. By incorporating cardiovascular activities, PE classes improve students' physical stamina and promote a higher quality of life. These healthy habits, formed during formative years, often extend into adulthood, offering lifelong health benefits and aiding in disease prevention. Thus, maintaining physical education in school is crucial for cultivating a healthier future generation.
Check out the following article on my blog to see 8 health habits students can develop now that will instill lifetime benefits: Healthy Habits for Students: Teaching SELF CARE for Lifelong Wellness .
3. Provides an outlet for creativity and self-expression

PE gives young people the opportunity to express themselves in a different way than they do in the classroom. They can let loose, have fun, and be creative without having to worry about grades or competition. PE is a great outlet for kids who may not be as academically inclined as their peers. It allows them to still feel like they're part of the class and gives them a chance to show their personality.
Physical education also provides an outlet for kids who are shy or introverted. It's a great way for them to get out of their shell and interact with other kids in a non-threatening environment. It may be a wonderful opportunity for kids to have some fun, discover their talents, and just be themselves.
Do you need some great ideas for engaging students with physical education stations? Check out this article: PE Stations: 15 Fun Ideas for Active Engagement in Elementary Physical Education Classes .
4. Develops cooperation and teamwork
Physical education helps students develop social skills and the ability to work cooperatively and effectively with others. In PE, students learn how to share, take turns, and cooperate with classmates to accomplish a common goal. These skills are essential for success in school and later on, in the workplace. It can also help a student develop teamwork skills by teaching them how to communicate effectively, set goals, and problem-solve as a team. These skills are essential for success in any endeavor.
Developing a cooperative, collaborative attitude is crucial for meeting Shape America's Standard 3 : Develops social skills through movement.
Rationale: Through learning experiences in physical education, students develop the social skills necessary to exhibit empathy and respect for others and foster and maintain relationships. In addition, students develop skills for communication, leadership, cultural awareness, and conflict resolution in a variety of physical activity settings. The capacity to respect oneself and others may be extended to all aspects of a child's or adolescent's life.

Great character makes cooperative and team-oriented students. Check out this article that delves into the world of character education within the physical education setting :
Cultivating Positive Character Traits for Students in Physical Education: Shaping Tomorrow's Leaders .
5. Builds self-confidence
Physical education classes help to develop self-assurance and determination in children. It can help to boost confidence, as they see themselves achieving their goals and improving their abilities. A student's confidence can be greatly enhanced if they improve their fitness level or acquire new movement skills. They also learn how to cooperate with others and handle winning and losing gracefully. These are all vital abilities for youngsters who compete in outside individual and team sports.

Self-confidence is highlighted when a young person learns a new skill or movement in a PE class. They can then apply that knowledge to be more self-assured in a game or performance-based sports setting. Moreover, this newfound confidence can spill over into other areas of their lives, enhancing their willingness to take on new challenges and participate in activities that were previously outside their comfort zones. By fostering a positive self-image and an attitude of resilience, physical education helps mold students into empowered individuals who feel capable of navigating various aspects of their lives.
Students love challenges which help boost their self-confidence! Check out this blog post that examines valuable insights on creating, implementing, and assessing skill-based challenge activities:
Skill-Based Activity Challenges in PE: Practical, Self-Guided Activities for Elevated PE
6. Provides opportunities for personal goal-setting

One of the most outstanding features of PE is the opportunity it provides students to create individual goals and self-discipline. This could be anything from improving their fitness levels to learning a new sport or perfecting a particular skill set. Having something to aim for gives children a real sense of purpose and motivation in PE, which can carry over into other areas of their lives.
Setting goals also helps children to track their progress and see how far they've come. This can be a great source of pride and satisfaction. Teachers can help students establish goals for themselves, which is an excellent approach to motivate them to reach Shape America's Standard 2 which highlights this PE concept: Applies knowledge related to movement and fitness concepts.
Rationale : Through learning experiences in physical education, the student uses their knowledge of movement concepts, tactics, and strategies across a variety of environments. This knowledge helps the student become a more versatile and efficient mover. Additionally, the student applies knowledge of health-related and skill-related fitness to enhance their overall well-being.

A well-constructed Physical Education Exit Checklist can play a crucial role in helping students assess their PE performance .The following article delves into the different components of such a checklist, how it promotes self-assessment, self-improvement, and why it's an essential tool in the modern PE environment: Enhancing Self-Reflection in Physical Education: The PE Exit Checklist Approach.
7. Helps reduce stress and anxiety
PE can be the perfect outlet to reduce stress and anxiety for young people. When kids are allowed to be active and move their bodies at school, it becomes a natural body and mind energizer that makes the rest of the day far more enjoyable. According to recent research, physical education may play an important role in lowering cortisol levels, which is linked to stress. Physical activity may help to improve mood and emotional stability. Regular physical exercise can also aid in the prevention of anxiety disorders. These anti-stress benefits, in the end, assist children and adolescents to become better students.

Furthermore, engaging in physical activities can serve as a constructive distraction, allowing students to break away from the daily pressures of academics and social interactions. This mental break is crucial for emotional rejuvenation, as it provides an opportunity to clear the mind, leading to increased concentration and improved overall mental health. The supportive environment of PE classes also promotes social interaction and teamwork, which are essential for developing coping mechanisms and a sense of belonging, further helping to alleviate feelings of stress and anxiety.
Are you ever stuck in a classroom for the day or know teachers that could use some GREAT Brain Breaks and Brain Boosts to recharge their students minds and bodies? Check out this blog :
Energizing Education: The Power of Brain Breaks in the Classroom; Includes 12 Practical Activities
8. Increases personal fitness and motor skill development
Physical education is a prime outlet for kids and adolescents to intentionally develop both their health and skill-related components of fitness. Students who participate in regular physical activity can get a lot out of their PE lessons. This is accomplished through repetition, practice, and creative movement situations. They may learn more about their bodies and how to use them appropriately in a variety of settings.

PE is a broad discipline that includes numerous options for students to participate in team and individual sports, dance, and gymnastics. A skill acquired early in life may be transferred to other similar skills or activities and put to use for the remainder of one's life, resulting in better health as an adult.
The physical benefits of developing personal fitness and motor skills are directly linked to Shape America's Standard 1: Develops a variety of motor skills.
Rationale : Through learning experiences in physical education, the student develops motor skills across a variety of environments. Motor skills are a foundational part of child development and support the movements of everyday life. The development of motor skills contributes to an individual’s physical literacy journey. Physical education class may be the only opportunity for younger individuals to learn a variety of motor skills and move their bodies in a meaningful way.

Learn how school physical education can combat childhood obesity in the following article. It offers strategies, insights, and personal experiences to guide you in creating a PE program that truly impacts student health and well-being :
Physical Education and Childhood Obesity: Empowering a Healthier Generation
9. Strengthens relationships with others
Physical education is not only about enhancing one's physical capabilities and motor skills. It's also about teaching individuals to collaborate and develop leadership skills. Students are frequently forced to work together as part of their PE lessons to complete assigned activities or objectives. This allows them to strengthen relationships with their classmates. In some cases, these relationships can last a lifetime. PE can also help to build communication skills and teach students how to better manage conflict. All of these factors contribute to the development of strong, healthy relationships with others.

Moreover, through group activities and team sports, PE classes provide an excellent platform for students to interact in a structured yet relaxed environment. This setting encourages them to understand and appreciate diverse perspectives, fostering empathy and mutual respect among peers. Such interactions not only enhance teamwork skills but also help in building a supportive community within the school. These social connections are vital for personal growth and contribute significantly to a student's emotional and social development.
Conflict resolution in physical education is an essential part of a PE teacher's role. Learn how to help students work through issues using the RESOLVE method. Click below for the article : Conflict Resolution in PE: A Teacher's Guide to Problem-Solving Using the RESOLVE Method .
10. Boosts academic learning
Numerous studies have demonstrated a strong correlation between physical activity and academic performance. Physical education plays a crucial role in enhancing concentration, attention, and memory, while also alleviating stress and fatigue. These benefits collectively contribute to better grades and higher test scores for students. Moreover, engaging in physical activity increases blood flow and oxygen supply to the brain, which in turn improves cognitive functions. PE also fosters the development of executive functioning skills, including planning, organizing, and multitasking, which are essential for academic success.

Additionally, physical education significantly enhances students' energy levels and mood, which are critical for effective learning. The increased production of endorphins triggered by physical activity not only uplifts mood but also boosts energy, making students more alert and receptive in the classroom. This positive shift in mood and energy facilitates easier focus and absorption of new information, thereby enhancing overall academic learning.
Discover the transformative power of word walls in physical education as the following blog post explores practical tips and strategies for their effective use. Unlock new avenues for engagement and learning with innovative approaches tailored to enhance your PE curriculum.
PE Word Walls: Engaging Strategies for Active Learning in Physical Education
Final Thoughts
Physical education is an important part of a student's overall education. It provides opportunities for students to improve their physical fitness and motor skills, while also developing teamwork skills and relationships with others. PE can also boost their academic performance by improving focus, concentration, and energy levels.
All of these benefits make PE an essential part of the educational experience for students of all ages. Physical education is an important part of a well-rounded education and should be required in all schools. So let's do our part to promote physical education in schools and keep our students strong in body and mind!
Do you think PE should be a mandatory part of the educational curriculum? Why or why not? Share your thoughts in the comments below!
Video- Why Physical Education?
Check out Pete's video entitled Why Physical Education? 10 Reasons for and 6 Steps to Advocate.

FREE advocacy bundle
Need some graphics to advocate for your physical education program? Download this FREE visual packet to create wall posters or post them on your gym or school bulletin board!!

Need More Visual Resources for Your Learning Area?
Teaching physical education can be difficult. There are so many different things to cover, and it's hard to know what is the most important. I can help you make teaching PE simpler with engaging, student-friendly graphics that you may utilize on your gym wall or via a monitor. Visual aids can assist make physical education instruction much more simple. They break down complex topics into easy-to-understand visuals that will engage your students and help them learn.
If you're looking for high-quality visuals to help you teach PE and health, go with the Cap'n Pete's Top Physical Education Posters - 25 Set Super Bundle.

You can download the bundle (or individual resources) from either of the following platforms: Cap'n Pete's Power PE Website or Teachers Pay Teachers- Cap'n Pete's TPT Store

- PE Advocacy
- Inspirational Articles
- The PE Community
Related Posts
Understanding the New SHAPE America Physical Education Standards for 2024
Physical Education Advocacy Amplified: Elevating Your Voice
PE is a good thing for kids. and im a kid so i will explan the joys of PE. when ever i walk in =to the gym i wonder what are we doing to day. these are my favs: doge ball and kick ball.
When was this powere pe thing made
my pronouns are before/after and was
Recent Posts

18 Top PE Activities for Dynamic Physical Education Classes

Mastering the Dynamics of PE Classroom Management: A Comprehensive Guide

PE Games for Elementary Students: 6 Dynamic Physical Education Games to Transform Your Classes

Run, Walk, Thrive: How to Implement a Mileage Club at Your School

Engaging At-Home PE Activities for Effective Distance Learning in Physical Education

Adopt-a-Gym: Enhancing Physical Education for Underfunded Schools

Best Physical Education Equipment Providers 2024: Your Complete Resource

PE Stations: 15 Fun Ideas for Active Engagement in Elementary Physical Education Classes

Exploring the Role of AI in Physical Education: Enhancing Efficiency and Effectiveness in Teaching PE

Cultivating Positive Character Traits for Students in Physical Education: Shaping Tomorrow's Leaders

What is Physical Education? A Comprehensive Overview for Physical Educators

Educating the Student Body: Taking Physical Activity and Physical Education to School (2013)
Chapter: 6 approaches to physical activity in schools.
Approaches to Physical Activity in Schools
Key Messages
• Data are insufficient to permit assessment of opportunities for and participation in sedentary activities in schools.
• Schools need to strive to reduce unnecessary opportunities for sedentary behavior.
• When embracing the advantages of technology for learning, schools need to be aware of its negative impact on students’ physical activity behavior.
• Recess has been shown to be beneficial for academic achievement. It is counterproductive to withhold recess or replace it with classroom activities as a punishment.
• Several models and examples demonstrate that scheduling multiple daily recess periods during the school day is feasible.
• School-based sports and active transport provide opportunities for physical activity but may not be accessible or attractive for all youth.
These opportunities need to be reexamined to address disparities based on socioeconomic status, school location and resources, students’ disabilities, or cultural/religious barriers.
• Participation in intra- and extramural sports has flourished over the past 40 years; however, school systems need to ensure that equitable sports opportunities are available for youth in all types of school settings and at all levels of socioeconomic status.
• Nonsport after-school programs should include physical activity.
• Active transport to and from school can be a safe and effective way to increase students’ daily physical activity, especially where a large proportion of students live close to their school.
• Each community needs to examine systematically opportunities for community-based promotion of physical activity.
• Inviting students’ families and other community members to participate in developing before- and after-school programs, including sports and active transport, will increase program sustainability.
I t has been argued that, while reversing the obesity epidemic is not solely the responsibility of schools, the trend is unlikely to change without schools’ assistance (Siedentop, 2009). Schools are an ideal venue for the implementation of healthy behaviors because they serve more than 56 million youth in the United States; because youth spend such a large amount of time in school; and because schools already have the access, personnel, equipment, and space to implement physical activity programming.
Physical activity opportunities in schools take the form primarily of formal instruction in physical education for all students and sport-based athletics for the talented and interested. Although physical education is a required school subject, the classes may occur infrequently, and children taking them often accrue only low levels of physical activity (Simons-Morton et al., 1994). According to Tudor-Locke and colleagues (2006), physical education programs typically provide only 8-11 percent of a student’s daily recommended physical activity. However, a meta-analysis of the literature revealed that physical education can help children achieve up to 40 percent of the recommended 60 or more minutes of daily vigorous- or
moderate-intensity physical activity per day (Bassett et al., 2013; see also Chapter 5 ).
Mahar (2011) states that children’s physical activity levels are directly related to the opportunities they have to be active. Schools have the potential to influence the physical activity behaviors of their students through various opportunities in addition to physical education (e.g., recess periods, classroom physical activity breaks, active transport to and from school; van Landeghem, 2003). Furthermore, children are sedentary for much of the school day, and emerging evidence suggests that long periods of inactivity should be avoided. Thus it is essential for the school setting to provide opportunities outside of physical education for school-age children to be physically activity throughout the school day.
This chapter reviews the status and trends of sedentary behavior in schools and describes opportunities for physical activity in the school environment other than physical education, including classroom activity Breaks, recess, intra- and extramural sports, active transport, and after-school programs. Also reviewed are policies that may affect these opportunities, as well as barriers to and enablers of the opportunities. Chapter 7 examines the evidence on the effectiveness of these physical activity opportunities.
SEDENTARISM IN SCHOOLS
The committee did not identify a widely recognized definition of sedentarism, a new word in the English language, but one that exists in other languages to describe sedentary behaviors, sedentary activities, a sedentary lifestyle, or physical inactivity. Bernstein and colleagues (1999) describe sedentarism in terms of energy expenditure, while Ricciardi (2005) defines it in terms of what it is not, that is, not engaging in physical activity. Probably the most commonly accepted definition is time spent other than in sleep, or time spent in vigorous-, moderate-, or light-intensity physical activity. The word also is used to describe the status of a person or a population with high levels of sedentary behaviors or a sedentary lifestyle.
Sedentarism can be categorized as (1) recreational sedentarism, which refers mainly to media use or “screen time” but can also include more traditional sedentary activities such as recreational reading or having a conversation while sitting, and (2) nonrecreational sedentarism, which refers to schoolwork or other types of work that occur while sitting and also to other sedentary activities that are necessary to perform daily tasks, such as motorized transportation or eating a meal. Most of the public health interest in sedentarism has focused on decreasing recreational sedentarism, especially screen time, but there is increasing interest in ways to alter sedentary work so it can be performed while engaging in light physical activity or even while standing. Standing desks and treadmill desks are becoming popular
for adults in the workplace, for example, and many schools are seeking creative ways to integrate light physical activity into traditionally sedentary schoolwork. Such efforts are important given the amount of sedentary time entailed in schoolwork. In Australia, for example, 42 percent of nonscreen sedentary time is school related (Olds et al., 2010).
Such efforts to address nonrecreational sedentarism are just emerging, and much research and innovation are needed to move these efforts forward. On the other hand, significant research already exists on decreasing recreational sedentarism, especially among children, to treat or prevent obesity. Today, 46 percent of U.S. children aged 6-11 fail to meet the recommendation of less than 2 hours of recreational sedentarism (screen time) per day (Fakhouri et al., 2013). In addition to the nonrecreational sedentarism that occurs while children sit to perform schoolwork, significant recreational sedentarism takes place on the way to school and in school during breaks, recess, lunch, and after-school programs. Data are not available on the extent to which recreational sedentarism occurs on school grounds and on whether recreational sedentarism in school should be an important public health target as it already is outside of school. What is known, however, is that “eight- to eighteen-year-olds spend more time with media than in any other activity besides (maybe) sleeping—an average of more than 7½ hours a day, seven days a week” (Rideout et al., 2010, p. 1).
One of the lessons of pediatric obesity research is that behavioral approaches designed to increase physical activity are different from those designed to decrease recreational sedentarism and have different effects on behavior and health. Using behavioral economic theory, Epstein and colleagues (1995) demonstrated that monitoring children and encouraging them to decrease recreational sedentarism was more successful in treating obesity than either promoting physical activity or targeting both physical activity and sedentarism at the same time. Furthermore, the children randomized to the intervention targeting only sedentarism increased their enjoyment of vigorous- or moderate-intensity physical activity, while enjoyment of moderate-intensity physical activity decreased among those randomized to physical activity promotion; changes in enjoyment among those in the combined intervention group were between those in the other two groups. The importance of targeting a decrease in sedentarism was further highlighted when Robinson (1999) published the first successful school-based obesity prevention intervention that targeted only sedentarism, with no behavioral intervention focused on physical activity promotion or dietary changes. Since then, several randomized trials have confirmed the causal link between recreational sedentarism and childhood obesity (Tremblay et al., 2011). Despite this evidence, however, the approach of specifically targeting sedentarism has received only limited attention. While academic research has focused on using school as a setting in which to teach
students how to decrease sedentarism outside of school, this approach has not translated into widespread policies or curricula. Such efforts may be particularly important as sedentarism appears to track among individuals from childhood to adulthood (Gordon-Larsen et al., 2004; Nelson et al., 2006).
Of interest, a large nationally representative survey found that, “contrary to the public perception that media use displaces physical activity, those young people who are the heaviest media users report spending similar amounts of time exercising or being physically active as other young people their age who are not heavy media users” (Rideout et al., 2010, p. 12). The question was, “Thinking just about yesterday, how much time did you spend being physically active or exercising, such as playing sports, working out, dancing, running, or another activity?” This finding suggests that media use does not displace vigorous- or moderate-intensity physical activity but more likely displaces light-intensity physical activity, schoolwork, and sleep. Light-intensity physical activity, including playing or even just standing, is more difficult to measure than vigorous-or moderate-intensity physical activity, but its positive health impact is increasingly being recognized (see Box 2-4 in Chapter 2 ). The finding of this survey also suggests that promotion of vigorous- or moderate-intensity physical activity may not decrease sedentarism but rather might replace light-intensity physical activity. Therefore, the optimal way to promote an overall increase in physical activity (including light-intensity physical activity) may be to use behavioral approaches to decrease sedentarism, as has been shown in behavioral research (Epstein et al., 1995; Robinson, 1999).
One of the challenges to monitoring sedentarism is the fact that children and adolescents frequently multitask. As noted earlier, Rideout and colleagues (2010) found that U.S. youth aged 8-18 spent more than 7.5 hours per day using recreational media; 29 percent of this time was spent multitasking, resulting in a total media exposure of almost 10.5 hours per day. This figure represents an overall increase in sedentarism since 1999, when the corresponding figures were 6.2 hours and 7.3 hours per day, respectively. Television content still dominated sedentary time, accounting for 4.3 hours per day. Computer use for schoolwork (not included in these totals) averaged 16 minutes, while computer use for recreational purposes totaled 1.3 hours per day. On a typical day, 70 percent of youth went online for any purpose, including 57 percent at home, 20 percent at school, and 14 percent elsewhere. It is unknown whether all online activities at school were related to schoolwork.
In addition to displacing physical activity and schoolwork, recreational media use exposes youth to “a constant stream of messages” that shape their perception of what is normative, including food choices, physical appearance, physical activity, and even sedentarism itself (Rideout et al.,
2010). Usually, these perceived norms are not in line with healthy or academically productive behaviors, and cannot be countered by the best efforts of parents and teachers. As a consequence, compared with those who used recreational media the least, “heavy users” tended to have lower school grades and to report that they were getting in trouble “a lot,” unhappy, sad, or bored (Rideout et al., 2010). Furthermore, in the face of rapidly advancing technology, parents and teachers are not always fully aware of the many ways in which media and marketing are part of youth’s lives. In addition to television and desktop computers, laptops, tablets, and cell phones often follow children and adolescents into the school bus, class, recess, and after-school activities unless such access is limited by policy, providing increasing opportunities to be sedentary on school grounds. In 2009 an average of 20 percent of media consumption, more than 2 hours per day, occurred with mobile devices, some of this media use likely occurring on school grounds. This figure probably has increased since then. Rideout and colleagues also note that children whose parents make an effort to limit media use spend less time consuming media, but whether this holds true for limits on recreational sedentarism in the school setting is unknown.
Both recreational and nonrecreational sedentarism in schools need to be monitored separately from physical activity. Specific school policies, based on updated knowledge of media use, need to focus on decreasing recreational sedentarism in school and integrating prevention of recreational sedentarism outside of school into the education curriculum. Because media use among youth already is significantly higher than recommended, schools should not provide students with increased opportunities for sedentarism, such as television sets in classrooms, the cafeteria, or after-school programs; access to social networks and recreational media on school computers; or the ability to use cell phones anywhere and at any time on school grounds or school transportation.
Research is needed to explore sedentarism and media use in schools more systematically so that evidence-based school policies to decrease these behaviors can be implemented to increase overall, including light-intensity, physical activity. In particular, surveys of media use are needed to document the amount of recreational sedentarism taking place in the school setting, where, in contrast with the home setting, public health policy can potentially be implemented.
OPPORTUNITIES TO INCREASE PHYSICAL ACTIVITY IN THE SCHOOL ENVIRONMENT
School physical activity programs are needed so that schools can ensure they are providing students with 60 minutes or more of vigorous-
or moderate-intensity physical activity per day. Physical activity programs are neither equivalent to nor a substitute for physical education, and both can contribute meaningfully to the development of healthy, active children (NASPE and AHA, 2012). The former are behavioral programs, whereas the latter are instructional programs. Box 6-1 presents the Healthy People 2020 objectives for non–physical education physical activity opportunities in school settings.
The following sections describe various non–physical education opportunities for physical activity in the school environment. The discussion includes relevant policies, barriers, and enablers.
Healthy People 2020 Objectives for Non– Physical Education Physical Activity Opportunities in School Settings
• Increase the number of States that require regularly scheduled elementary school recess.
• Increase the proportion of school districts that require regularly scheduled elementary school recess.
• Increase the proportion of school districts that require or recommend elementary school recess for an appropriate period of time.
• Increase the proportion of the Nation’s public and private schools that provide access to their physical activity spaces and facilities for all persons outside of normal school hours (that is, before and after the school day, on weekends, and during summer and other vacations).
• Increase the proportion of trips of 1 mile or less made to school by walking by children and adolescents aged 5 to 15 years.
• Increase the proportion of trips of 2 miles or less made to school by bicycling by children and adolescents aged 5 to 15 years.
SOURCE: HHS, 2012.
Classroom Activity breaks
An emerging strategy for increasing daily participation in physical activity in schools is the implementation of structured, classroom-based physical activity breaks. Classroom physical activity includes all activity regardless of intensity performed in the classroom during normal classroom time. It includes activity during academic classroom instruction as well as breaks from instruction specifically designed for physical activity. It also includes time spent learning special topics (e.g., art, music) even if not taught by the usual classroom teacher. It excludes physical education and recess even if conducted in the classroom by the usual classroom teacher. It also excludes physical activity breaks during lunchtime. Although some discussions of schooltime activity breaks include such breaks during lunchtime (Turner and Chaloupka, 2012), the committee views lunchtime physical activity as more akin to activity during recess and before and after school than to physical activity during normal academic classroom time. While a number of programs specifically designed to increase the volume of students’ physical activity during usual classroom time exist, the committee found no information about changes in such programs over time at the population level.
A typical break consists of 10-15 minutes focused on vigorous- or moderate-intensity physical activity. This strategy has been found to be effective in significantly increasing physical activity levels of school-age children (Ernst and Pangrazi, 1999; Scruggs et al., 2003; Mahar et al., 2006). Bassett and colleagues (2013) found that classroom activity breaks provide school-age children with up to 19 minutes of vigorous- or moderate-intensity physical activity, and the sustained use of such breaks was shown to decrease body mass index (BMI) in students over a period of 2 years (Donnelly et al., 2009). The effectiveness of classroom physical activity breaks is discussed further in Chapter 7 .
An example of an effective school-based physical activity program is Take 10! Kibbe and colleagues (2011) provide consistent evidence that the Take 10! program has been effective in increasing physical activity levels among a variety of samples of children enrolled in kindergarten through 5th grade in various countries. Likewise, Mahar and colleagues (2006) found that, with the implementation of 10-minute physical activity breaks called “Energizers,” students increased their time on task while averaging approximately 782 more steps in a day. Another example, supported by the Robert Wood Johnson Foundation Center to Prevent Childhood Obesity (2012), is Jammin’ Minute, a realistic and effective “bridge” tool for increasing children’s physical activity until schools have sufficient resources to develop more comprehensive physical education programs. Jammin’ Minute has important implications for advocates and policy makers, as well
as administrators and teachers, seeking ways to make school environments healthier for children. At the same time, it should be emphasized that, while the benefits of small increases in physical activity during the school day need to be recognized, the ultimate goal of policy makers and advocates should be to ensure that all schools have comprehensive physical education programs (see Chapter 5 ).
Another program, Texas I-CAN!, helped teachers incorporate physical activity by modifying lesson plans to include more active activities, thereby increasing vigorous- or moderate-intensity physical activity by 1,000 steps per day (Bartholomew and Jowers, 2011). It was found that these curriculum-based activities improved time on task immediately following the breaks, especially in children who were overweight; these students went from being on task 58 percent of the time on typical instruction days to 93 percent of the time after the breaks (Grieco et al., 2009).
These findings emphasize the effectiveness and feasibility of providing classroom-based structured opportunities for physical activity. Breaks in the classroom provide an additional opportunity for physical activity throughout the school day with minimal planning, no equipment, and a short amount of time required; they can also incorporate learning opportunities for students. It should be noted that the literature tends to focus on the effect of classroom physical activity breaks on elementary school rather than secondary school students.
For classroom-based physical activity breaks to become a priority, it will be important to provide evidence that such breaks do not detract from academic achievement. Chapter 4 provides an extensive review of the evidence showing that physical activity in general has positive effects on academic performance. With respect to classroom-based physical activity, the Centers for Disease Control and Prevention (CDC) (2010) reviewed studies examining the association between such activity and academic performance in elementary school–age children. Eight of nine published studies found positive effects on such outcomes as academic achievement and classroom behavior; only one study found no relationship (Ahamed et al., 2007), but that study also found that the breaks did increase physical activity levels and did not adversely affect academic achievement. Donnelly and Lambourne (2011) provide further support for the link between physical activity and positive cognitive and academic outcomes in elementary school–age children. In addition, studies in elementary school–age children have found an increase in on-task behavior in the classroom after participation in a physical activity break (Jarrett et al., 1998; Mahar et al., 2006; Mahar, 2011; see also Chapter 4 ). For example, Mahar and colleagues (2006) found that time on task increased by 8 percent ( p < .017) with the implementation of a 10-minute break. They also found that the 20 percent of students who were off task improved the most in time on task. Similar
results were found in Georgia, where 4th graders exhibited significantly less fidgeting behaviors and significantly better on-task behaviors on days when activity breaks were conducted (Jarrett et al., 1998). Finally, a meta-analysis by Erwin and colleagues (2012) found that breaks increase the frequency of physical activity behaviors and have positive learning outcomes. It should be noted that the effect and benefits of classroom-based physical activity breaks in preschool populations have not been thoroughly investigated.
Policies That Affect Classroom Physical Activity Breaks
Classroom physical activity breaks are a relatively new approach to promoting physical activity during the school day. Consequently, research on policies that support or hinder the use of this approach is sparse. For this approach to become more prevalent, supportive policies will be necessary, an observation supported by the fact that just one in four U.S. public elementary schools offered children and youth physical activity breaks apart from physical education and recess during the 2009-2011 school years (Turner and Chaloupka, 2012). Research clearly demonstrates the important role of state laws and school district policies in promoting physical activity opportunities in schools. For example, schools are more likely to meet physical education recommendations when state laws and school district policies mandate a specific amount of time for physical education classes (Slater et al., 2012; see also Chapter 5 ). Currently, few if any school districts require that physical activity opportunities be provided throughout the school day or within the classroom (Chriqui et al., 2010). Therefore, research is needed to identify strategies for implementing classroom-based physical activity breaks and providing teachers with the skills and confidence necessary to engage students in these activities. In addition, questions remain about the optimal duration, timing, and programming (e.g., types of activities) for physical activity breaks (Turner and Chaloupka, 2012).
Barriers to Classroom Physical Activity Breaks
One factor that influences classroom physical activity breaks is competition for time during the school day, arising from the need for schools to meet the academic requirements of the No Child Left Behind Act (see Chapter 5 ). As discussed above and in Chapter 4 , however, the literature clearly supports that classroom physical activity breaks are not only beneficial in promoting physical activity in children and youth but also can occur in the classroom without compromising learning and in fact improve academic performance and related classroom behaviors. In addition, research has shown that using innovative curriculum change, such as Physical Activity Across the Curriculum (Donnelly et al., 2009), can increase daily
physical activity and improve academic performance. Additionally, schools often have a scarcity of resources related to staffing, teacher training, funding, champions, and/or facilities for physical activity. Dwyer and colleagues (2003), for example, document the lack of facilities and equipment for physical activity breaks. As a result of these barriers, it has been found that, although teachers see the importance of physical activity breaks for children’s health and development, they infrequently integrate movement into the classroom (Parks et al., 2007).
From the literature, classroom physical activity breaks appear to be heavily implemented in early childhood and elementary classrooms (CDC, 2010). Few if any classroom physical activity breaks appear to occur in middle and high school settings. The lack of physical activity breaks for this age group may be due to the increased academic demands of testing, along with difficulty of implementing breaks that target these older students. However, classroom-based physical activity curricula are emerging at a rapid rate. Programs available for purchase include Active and Healthy Schools activity break cards, Promoting Physical Activity and Health in the Classroom activity cards, Energizers, and TAKE 10! Other resources for classroom physical activity breaks are available at no cost to schools, such as Jammin’ Minute, ABS for Fitness, Activity Bursts in the Classroom, Game On! The Ultimate Wellness Challenge, and approximately 50 others. These resources can be found through the Alliance for a Healthier Generation at www.healthiergeneration.org . They provide an excellent starting point for teachers and are flexible enough to be modified to meet the needs of specific classrooms.
Space is another concern for classroom teachers, who must consider the safety of students. The classroom (e.g., desks and tables) needs to be arranged to provide adequate open space for students to move during physical activity breaks. Figure 6-1 shows the activity area/space available in a traditionally organized classroom. Figures 6-2 and 6-3 show how the classroom can be arranged to optimize the space for movement and physical activity.
One of the most common forms of physical activity break during the school day is recess. Children can accumulate up to 40 percent of their daily physical activity time during recess (Ridgers et al., 2006). Recess, according to Pellegrini and colleagues (1995), is the time of day set aside for students to take a break from their class work; engage in play with their peers; and take part in independent, unstructured activities. Recess is most common in elementary schools and is rare during the secondary years.
While separate and distinct from physical education, recess is an essential component of the total educational experience for elementary-age chil-

FIGURE 6-1 Traditional layout of a classroom with limited space for physical activity breaks. SOURCE: Personal communication from Heather Erwin. Reprinted with permission from Heather Erwin.

FIGURE 6-2 One classroom layout designed to accommodate physical activity breaks. SOURCE: Personal communication from Hearther Erwin. Rseprinted with permission from Heather Erwin.

FIGURE 6-3 Another classroom layout designed to accommodate physical activity breaks. SOURCE: Personal communication from Heather Erwin. Reprinted with permission from Heather Erwin.
dren (Ramstetter et al., 2010). In addition to providing children the opportunity to engage in physical activity, develop healthy bodies, and develop an enjoyment of movement, it provides them with a forum in which they are able to practice life skills, including conflict resolution, problem solving, communicating with language, cooperation, respect for rules, taking turns, and sharing. Moreover, it serves as a developmentally appropriate outlet for reducing stress in children (National Association for the Education of Young Children, 1998). Furthermore, recess facilitates attention and focus on learning in the classroom (NASPE, 2001). This dedicated period of time further allows children the opportunity to make choices, plan, and expand their creativity (National Association for the Education of Young Children, 1998). Indeed, the American Academy of Pediatrics (AAP) recently released a policy statement in support of recess and free play as “fundamental component[s] of a child’s normal growth and development” (Council on School Health, 2013, p. 188).
The AAP further asserts that cognitive processing and academic performance depend on regular breaks from concentrated class work. The AAP believes that
• Recess is a complement to but not a replacement for physical education. Physical education is an academic discipline.
• Recess can serve as a counterbalance to sedentary time and contribute to the recommended 60 minutes or more of vigorous- or moderate-intensity physical activity per day.
• Peer interactions during recess are a unique complement to the classroom. The lifelong skills acquired for communication, negotiation, cooperation, sharing, problem solving, and coping are not only foundations for healthy development but also fundamental measures of the school experience.
The Decline of Recess
Since passage of the No Child Left Behind Act in 2001, several studies and reports across the literature have pointed to a decline in recess to make more time for academic subjects. Approximately 40 percent of schools in the United States have either eliminated or reduced recess in order to free up more time for academics (RWJF, 2010). See Table 6-1 for a summary of changes in recess time between 2001 and 2007; see also the detailed discussion of time shifting in Chapter 5 .
The Recess Gap
In addition to the general decline in recess time, the Center for Public Education (2008) has identified a “recess gap” across school settings. This finding is supported by the results of a survey sponsored by the U.S. Department of Education and the National Center for Education Statistics (Parsad and Lewis, 2006), which collected information from a representative sample of 1,198 U.S. elementary schools on whether they scheduled any recess for each grade, typically grades 1 through 5 or 6. Respondents reported the number of days per week of scheduled recess, the number of times per day, and the total minutes per day for each elementary grade in
TABLE 6-1 Change in Recess Time, 2001-2007
SOURCE: Center on Education Policy, 2007.

FIGURE 6-4 Percent of schools that do not provide recess to 1st graders. NOTE: Poverty rate is based on the proportion of students eligible for free or reduced-price lunches. SOURCE: Parsad and Lewis, 2006. Reprinted with permission.
2005. The survey found that while most children, regardless of location, continue to get recess on a regular basis, children who attend high-minority, high-poverty, or urban schools are far more likely than other children to get no recess at all (see Figure 6-4 ). Also:
- The proportion of public elementary schools with any scheduled recess ranged from 87 to 93 percent across elementary grades.
- The proportion of public elementary schools with no scheduled recess ranged from 7 to 13 percent across elementary grades.
- Fourteen percent of elementary schools with a minority enrollment of at least 50 percent scheduled no recess for 1st graders, compared with 4 percent of schools with 21-49 percent minority enrollment, 5 percent of those with 6-20 percent minority enrollment, and 2 percent of those with less than 6 percent minority enrollment.
- Eighteen percent of elementary schools with a poverty rate over 75 percent (based on the proportion of students eligible for free or reduced-price lunches) provided 1st graders with no recess, compared with 3 percent of schools with a 50-74 percent poverty rate, 4 percent with a 35-49 percent poverty rate, and 4 percent with a less than 35 percent poverty rate.
- Fourteen percent of urban elementary schools did not offer recess to 1st graders, compared with 6 percent of schools on the urban fringe, 6 percent of those in towns, and 3 percent of rural schools.
The above patterns for 1st graders persisted through 6th grade: 24 percent of 6th graders in high-minority schools, 28 percent in high-poverty schools, and 24 percent in urban schools did not get recess, compared with 13 percent of 6th graders overall.
The National Association of State Boards of Education’s (NASBE’s) Center for Safe and Healthy Schools (2013) State School Healthy Policy Database supports the above survey findings. It shows that most public elementary schools (83-88 percent) offer daily recess across elementary grades, while 47 percent offer it 1-4 days per week:
- Large schools generally are less likely than small- and medium-sized schools to have daily recess for 1st through 3rd grades.
- City schools are less likely than schools in other locales to offer daily recess for 1st graders. City schools also are less likely than schools in urban fringes and rural areas to schedule daily recess for 2nd through 5th grades.
- Schools with the highest poverty concentrations are less likely than those with lower poverty concentrations to offer daily recess for elementary grades.
- Differences also exist by minority enrollment, with schools with the highest minority enrollment being less likely than those with lower minority enrollment to provide daily recess.
The percentage of public elementary schools offering more than 30 minutes per day of recess ranges from 19 to 27 percent across elementary grades. The average number of minutes per day of scheduled recess for elementary grades differs by school characteristics. Large schools on average offer fewer average minutes per day of recess than small- and medium-sized schools; the same is true for schools with the highest and lowest poverty concentrations, respectively. For further detail, a state-by-state list of policies from the NASBE State School Health Policy Database can be found in Appendix C .
Since physical activity, such as recess, has been shown to improve academic achievement, this recess gap may contribute to, not decrease, disparities in academic achievement.
Support for Recess
Both international and U.S. organizations support the importance of recess.
International organizations Aside from the historical literature on the need for children to play (dating back to the 1600s), the most prominent and widespread support for recess is rooted in the International Play Association and its work through the United Nations (UN). The International Play Association, founded in 1961 in Denmark, is a global nongovernmental organization that protects, preserves, and promotes children’s fundamental human right to play. The UN’s Declaration of the Rights of the Child (1959), Article 7, Paragraph 3, states:
The child shall have full opportunity for play and recreation which should be directed to the same purposes as education; society and the public authorities shall endeavor to promote the enjoyment of this right.
The declaration asserts that spontaneous play fulfills a basic childhood developmental need. It further defines play as “a combination of thought and action that is instinctive and historical and that teaches children how to live” (IPA, 2013). At the 1989 UN General Assembly, the International Play Association played a key role in the inclusion of “play” in Article 31 of the UN Convention on the Rights of the Child. It reads:
That every child has the right to rest and leisure, to engage in play and recreational activities appropriate to the age of the child and to participate freely in cultural life and the arts. That member governments shall respect and promote the right of the child to participate fully in cultural and artistic life and shall encourage the provision of appropriate and equal opportunities for cultural, artistic, recreational and leisure activity. (IPA, 2013)
The U.S. affiliate of the International Play Association has as its primary goal to protect, preserve, and promote play as a fundamental right for all children.
U.S. organizations In a 2013 policy statement, the AAP asserts that recess is a crucial and necessary component of a child’s development and as such should not be withheld for punitive or academic reasons. The AAP stresses that minimizing or eliminating recess may be counterproductive to academic
achievement, as mounting evidence suggests that recess promotes physical health, social development, and cognitive performance (AAP, 2013).
Through three sponsored research studies, the Robert Wood Johnson Foundation (RWJF) further supports the need for recess in schools. Recess Rules: Why the Undervalued Playtime May Be America’s Best Investment for Healthy Kids in Healthy Schools (RWJF, 2007) states that recess represents an unparalleled chance to increase physical activity among a large number of children in the United States, as well as an underutilized opportunity to improve the overall learning environment in the nation’s schools. For a second study conducted by RWJF (2010), The State of Play , 1,951 elementary school principals participated in a Gallup survey devoted to the subject of recess. The survey sample was provided by the National Association of Elementary School Principals, and it reflects a balance of urban, suburban, and rural schools and schools of different income levels, as defined by the percentage of students receiving free or reduced-price lunches. The results show that principals overwhelmingly believe that recess has a positive impact not only on the development of students’ social skills but also on achievement and learning in the classroom. When asked what would improve recess at their schools, they highlighted an increase in the number of staff to monitor recess, better equipment, and playground management training, in that order.
According to a third RWJF and Active Living Research study, School Policies on Physical Education and Physical Activity (Ward, 2011):
- “Whole-school programs that provide opportunities for physical activity across the school day—through recess, in-class breaks, and after-school events—increase children’s physical activity levels.”
- “Schools that provide ample time for supervised recess and access to equipment, as well as those that make low-cost modifications to improve play spaces, have more physically active students.”
- “Activity breaks during classes not only increase physical activity but also help children focus better on academic tasks and enhance academic achievement.”
Other national organizations and studies further support the need for recess in elementary schools:
- The National Association of Early Childhood Specialists in State Departments of Education takes the position that “recess is an essential component of education and that preschool and elementary school children must have the opportunity to participate in regular periods of active play with peers” (National Association of Early Childhood Specialists in State Departments of Education, 2001, p. 1).
- The National Association for the Education of Young Children (2001) believes that unstructured play is a developmentally appropriate outlet for reducing stress in children, improves children’s attentiveness, and decreases restlessness.
- Through a position statement, Recess in Elementary Schools , the National Association for Sport and Physical Education, Council on Physical Education for Children, asserts:
Recess also provides the opportunity for students to develop and improve social skills. During recess, students learn to resolve conflicts, solve problems, negotiate, and work with others without adult intervention. Cognitive abilities may also be enhanced by recess. Studies have found that students who do not participate in recess may have difficulty concentrating on specific tasks in the classroom, are restless and may be easily distracted. In addition, recess serves as a developmentally appropriate strategy for reducing stress. Contemporary society introduces significant pressure and stress for many students because of academic demands, family issues, and peer pressures. (NASPE, 2001)
- The National Parent Teacher Association (PTA) and the Cartoon Network launched “Rescuing Recess” in 2006 to help sustain and revitalize the importance of recess in schools across the country. The goal of the campaign is to recognize unstructured break time as an essential element of the school day and to connect educators, parents, and children as advocates for bringing back or retaining recess. A 2006 nationwide survey of PTA leaders found that parents and teachers also think taking a break is a vital part of a child’s school day (National Parent Teacher Association, 2006).
Barriers to Recess
The evidence supporting the cognitive, health, and social benefits of recess could become a thesis on its own merits. Despite these benefits, however, few states have specific policies requiring recess, and those that do have such policies often defer to local school districts to allow individual schools to determine whether students will have a recess period.
Policies requiring increased activity at school each day have the potential to affect large numbers of children and are an effective strategy for promoting regular physical activity. However, external and internal barriers to policy implementation need to be considered (Amis et al., 2012). Competing time demands, shorter school days, lack of teacher participation, and lack of adequate facilities have all been cited as barriers to providing recess (Evenson et al., 2009). Further, weak policies suggesting or recommending changes have shown little or no effect on changing behavior
(Ward, 2011; Slater et al., 2012). Additional barriers to enacting effective policies include a lack of earmarked resources devoted to policy implementation, principals’ lack of knowledge of the policy, and no accountability mechanisms to ensure policy implementation (Belansky et al., 2009).
In addition, the National Association of Early Childhood Specialists in State Departments of Education (2002) identifies issues of student safety, lack of adult supervision, potential lawsuits for injured students, and potential for children to come into contact with strangers entering school grounds as barriers to recess. Elementary school principals responding to the above-referenced RWJF (2010) Gallup survey also cited liability and safety issues, as well as access to space and weather.
Strategies for Reviving Recess
Several strategies can be used to promote recess in schools, along with engagement in physical activity among youth participating in these programs. First, it is necessary to provide a safe environment with ample recreational equipment to encourage physical activity. Additionally, regulations should be in place to ensure that schools offer at least 20 minutes of recess per day. It is imperative as well that training be provided to recess supervisors and staff, with a focus on both safety issues and ways to interact with students to better promote physical activity. Recess is not a common occurrence for secondary students; however, they could participate in a civic- or service-oriented program whereby they would oversee and engage in recess for local elementary schools.
Intra- and Extramural Sports
Sports programs have long been an integral part of the school setting. Sport is one of the four human activities, along with play, games, and work. According to Woods (2011, pp. 5-6), play is a “free activity that involves exploration, self-expression, dreaming, and pretending. Play has no firm rules and can take place anywhere.” Children’s play often involves physical movement. Games are forms of play “that have greater structure and are competitive. Games have clear participation goals … [and] are governed by informal or formal rules” (p. 5). Games can be sedentary or physical; involve competition, planning, and strategizing; and result in “prestige or status.” Sport is a specialized or higher order of play or games with special characteristics. It must involve physical movement and skill. It must be “competitive with outcomes that are important to those involved,” and “winning and losing are a critical part of competition.” Thus, an important aspect of sport is institutionalized competition under formal rules. Lastly, work is “purposeful activity that may include physical and mental effort
to perform a task, overcome an obstacle, or achieve a desired outcome.” Sport can be work.
It is important to note that children in schools can participate in sports as either players or spectators. Kretchmar (2005) suggests that playing sports at a young age tracks to becoming a loyal spectator in later years; however, being a spectator at a young age may not necessarily lead to active participation as a player. Chen and Zhu (2005) analyzed intuitive interest in physical activity among 5-year-olds using the nationally representative sample from the U.S. Department of Education’s Early Childhood Longitudinal Study. The results of a logistic regression analysis showed that early exposure to watching a sport may have a negative effect on developing interest in actually playing the sport.
The discussion here focuses on institutionalized in-school sports and on children’s participation as players. In-school sports programs typically fall into two categories: intramural , or within a school, and extramural or interscholastic , or competition between schools (AAHPERD, 2011). The type and scope of each of these categories of sports vary by school size (Landis et al., 2007), location, and the socioeconomic status of students (Edwards et al., 2013).
In the past 40 years, participation in sports has flourished both within and outside of schools. Although young children are not eligible for formal interscholastic competition until they reach secondary school, children (or their parents) with athletic aspirations start preparation for competition at a very young age. Results of the National Survey of Children’s Health (2007) showed that approximately 58.3 percent of 6- to 17-year-olds participated in sports teams or lessons over a 12-month period. The Centers for Disease Control and Prevention (CDC) (2012) reports that in 2011, 58 percent of high school students played on at least one sports team. Intramural sports clubs in middle and high schools also involve large numbers of students.
Participation in sports inside and outside school has increased in the past 20 years. According to the latest report of the National Federation of State High School Associations (NFSHSA) (2012), participation in high school sports nearly doubled in 2011-2012 relative to 1971-1972. While boys’ participation increased by about 22 percent during these years, girls’ participation increased about 10-fold. Table 6-2 documents the change by decade.
Figure 6-5 shows the ratio of growth in boys’ and girls’ participation in sports relative to the total enrollment in U.S. high schools during the five decades. The data show that while the ratio for boys has remained steady at about 40-50 percent, the ratio for girls has increased from 4 percent in 1971-1972 to 40 percent in 2011-2012.
Nationwide, 77 percent of middle schools and 91 percent of high schools offer at least one interscholastic sport (Lee et al., 2007), and 48 per-
TABLE 6-2 Change in Participation in High School Sports in the Past Five Decades
NOTE: Rounded to the nearest 1,000. Participants total is the sum of participants in school sports; if a student participated in more than one sport, he or she would be counted for each of those sports. SOURCE: Adapted from NFSHSA, 2012.

FIGURE 6-5 Change in the ratio of males’ and females’ participation in sports relative to enrollment, 1971-2011. NOTE: Ratio is number of participants divided by estimated number of males or females enrolled in high school in October of the enrollment year. Enrollment data were adapted from the U.S. Census Bureau’s October Current Population Survey. For 1971 and 1981, only the total number of students was available, and the proportion of male students was assumed to be 0.515. SOURCE: U.S. Census Bureau, 1971-2011.
cent of middle and high schools offer intramural sports or physical activity clubs (NASPE and AHA, 2010). Based on data from a nationally representative sample of middle schools, Young and colleagues (2007) found that 83 percent of schools offered interscholastic sports, and 69 percent offered intramural sports and clubs. No reports indicate that interscholastic or intramural sports were offered in elementary schools.
Many students who do not play on school teams may participate in sports programs outside of school. CDC (2012) data indicate that 58 percent of high school–age youth played on at least one sports team in 2011, which suggests that an estimated 31 million of the 55 million youth in this age group participated in sports outside of school. The committee was unable to find a national estimate of the number of students who participated in school intramural sports or physical activity clubs. However, one study of four middle schools with similar demographic populations based on race/ethnicity, income, and geographic location suggests that the intramural sports environment may be more conducive to increased physical activity levels than the environment of varsity sports, at least for middle school boys (Bocarro et al., 2012). This may be due in part to the fact that all children can participate in intramural activities without having the high skill levels required for interscholastic sports.
Students have many choices of interscholastic sports. Lee and colleagues (2007) cite 23 popular sports, grouped in Table 6-3 as team or individual sports. Lee and colleagues (2007) believe that most individual sports may be more likely than team sports to become lifelong activities for individual students.
Policies That Affect Participation in Sports
As with physical education and recess policies, data from both the Shape of the Nation Report (NASPE and AHA, 2010) and the NASBE State School Health Policy Database (see Appendix C ) show variations in amounts, accountability, and regulations for high school sports. Twenty-one states (41 percent) had state requirements regarding sports, most relating to gender equity, concussion management, and local requirements. Although NFSHSA remains the governing body for individual state athletic associations, the governance of district sports opportunities is determined largely by local athletic associations in accordance with individual state association requirements. However, decisions on what sports to offer, the frequency of sport competitions, and other factors are made at the local level. In its report on the Comprehensive School Physical Activity Program (CSPAP), the American Alliance for Health, Physical Education, Recreation and Dance (AAHPERD) (2011) notes that 65 percent of high
TABLE 6-3 Interscholastic Sports Choices and Percentage of Middle and High Schools Offering Them
schools implemented various forms of team-cut policies for participation in interscholastic sports. The practice requires students to meet minimum performance qualifications before joining a school-sponsored sports team. Such policies include maintaining a designated grade point average, meeting daily attendance requirements, and adhering to individual school district code-of-conduct policies. One might speculate that such policies may prohibit interscholastic sports from becoming a viable means of promoting maximum student participation in sports and other physical activity.
In summary, trends in participation in sports are encouraging. Compared with physical education, however, it is difficult to expect every child to participate in sports. Although the available data indicate a nearly 60 percent participation rate, the data do not provide specific information
about the participants. In addition, studies and national surveys have not provided useful information about those children who do not participate in sports, who may be in the greatest need of physical activity. Although the opportunity for physical activity through participation in interscholastic and/or intramural sports does exist in most secondary schools, the extent to which participation in sports contributes to children’s health and positive behavior change for active living is unclear.
Barriers to Participation in Sports
Although the literature documents the benefits of participating in high school sports in such areas as academic achievement, attendance, and self-esteem, opportunities for participation in sports have not escaped the effects of the budget cuts that have plagued education over the past several years (Colabianchi et al., 2012).
In addition, interscholastic sports have been dominated by a competitive sports model (Lee et al., 2007), which may fail to engage and support all students. Policies encouraging and funding intramural sports, which are usually more inclusive and less competitive, can increase student participation in sports. The CDC recommends inclusive policies and programs as a strategy for enabling students to meet the 2008 Physical Activity Guidelines (HHS, 2008).
According to the Government Accountability Office (GAO) (2012) report K-12 Physical Education: School-Based Physical Education and Sports Programs , school district officials assert that budget cuts have impacted predominantly transportation and facilities, both critical to after-school sports programs (GAO, 2012). According to data from the School Health Policies and Practices Study (SHPPS) (2006) (Lee et al., 2007), an estimated 29 percent of schools that offered interscholastic sports in 2006 also provided transportation home for participating students, up from 21 percent in 2000. Transportation costs, a large part of overall school athletic budgets, are impacted not only by the need to transport students to practice facilities and competition venues and then home but also by increases in fuel prices and maintenance costs.
Facilities and equipment are another recognized barrier to participation. Budget cuts have hindered school districts from building new facilities or upgrading existing ones. Where facility and land limitations prevail, school districts have resorted to developing partnerships and contractual agreements with local community recreation centers or universities to use their facilities for various sports program. A lack of funding for sports equipment has further reduced the number of participating students, as the number of uniforms available per sport has caused the selection process to become more stringent. Colabianchi and colleagues (2012) also conclude
that the percentage of students participating in interscholastic sports is contingent on the type and number of facilities (see Figure 6-6 ).
Another challenge to implementing quality sports programs is the availability of quality coaches. Fewer school personnel are coaching in the face of a decline in coaching supplements and increased time commitments. Funding for staffing or staff training is an important aspect of successful sports or after-school physical activity programs. According to the 2006 SHPPS data, more than half of schools surveyed paid staff for involvement in intramural sports programs (Lee et al., 2007). Policies to support supervisory staff can facilitate increased opportunities for physical activity for students.
Constrained budgets also have reduced the number of sports offerings, with the primary sports being retained and the second-tier sports, such as golf and tennis, either being eliminated or requiring that students pay 100 percent of the cost of participation. Indeed, many school districts across the United States have implemented a pay-to-play policy. According to the 2006 SHPPS data, 33 percent of schools require students to pay to participate in interscholastic sports. A study released by the University of Michigan, C.S. Mott Children’s Hospital (2012), reports that pay-to-play fees are preventing lower-income children from participating in both middle and high school sports. The study found that the average fee was $93 per sport, while some respondents to the survey reported paying $150 or more.

FIGURE 6-6 Participation in interscholastic sports among boys and girls by availability of sports facilities, 2009-2011. SOURCE: Colabianchi et al., 2012. Figure 6-6 .eps
When combined with the cost of equipment, uniforms, and additional team fees, the average total cost for a child’s participation in sports was $381. Nineteen percent of families making under $60,000 reported that costs had led to at least one of their children being unable to participate in sports. Figure 6-7 shows the study results regarding participation in school sports among youth aged 12-17 by household income. The study found further that
- More than 60 percent of children who played school sports were subject to a pay-to-play fee; only 6 percent received waivers for the fee.
- Only one-third of lower-income parents reported that their child participated in school sports, compared with more than half of higher-income parents.
- In lower-income households, nearly one in five parents reported a decrease in their child’s participation in school sports because of cost.
Colabianchi and colleagues (2012) further determined that the percentage of students participating in sports varied with the students’ socioeconomic status. Participation was higher at schools of mid-socioeconomic status than at those of low socioeconomic status, and even higher at schools of high socioeconomic status compared with those of mid-socioeconomic status (see Figure 6-8 ).
Interscholastic sports have been criticized for perpetuating racial and gender segregation (Lee et al., 2007). Further study by Kelly and colleagues (2010) and Bocarro and colleagues (2012) confirmed the relationship

FIGURE 6-7 Participation in school sports for youth aged 12-17 by household income. SOURCE: C.S. Mott Children’s Hospital, 2012.

FIGURE 6-8 Participation in interscholastic sports by school socioeconomic status among boys and girls, 2009-2011. NOTE: SES = socioeconomic status. SOURCE: Colabianchi et al., 2012.
between socioeconomic status and sports participation, finding that fewer children and adolescents in schools of low socioeconomic status or with a relatively high proportion of racial and ethnic minority groups participated in sports programs.
To provide the physical activity and psychosocial benefits of engaging in sports at school, education systems need to reevaluate their budgets to ensure that equitable sports opportunities are available for youth in all types of school settings and at all levels of socioeconomic status. The same holds true with respect to ensuring that school-based intramural sports opportunities are available before or after school hours to increase participation in physical activity among all students.
Programs for Students with Disabilities
The 2010 GAO report Students with Disabilities: More Information and Guidance Could Improve Opportunities in Physical Education and Athletics notes that students with and without disabilities were provided similar opportunities to participate in physical education in schools but identifies several challenges to serving students with disabilities. Likewise, for sports, opportunities were provided for students to participate, but students with disabilities participated at lower rates than those without disabilities. Yet sports programs for students without disabilities have shown
similar benefits for students with disabilities, including not only obesity reduction but also higher self-esteem, better body image, and greater academic success; more confidence and a greater likelihood of graduating from high school and matriculating in college; and greater career success and more career options (GAO, 2010; Active Policy Solutions, 2013; U.S. Department of Education, 2013).
To ensure that students with disabilities have opportunities to participate in extracurricular athletics equal to those of other students, the GAO report recommends that the U.S. Department of Education clarify and communicate schools’ responsibilities under Section 504 of the Rehabilitation Act of 1973 regarding the provision of extracurricular athletics. Most important, the report recommends improving physical education and athletic opportunities for students with disabilities and recommends that (1) the Secretary of Education facilitate information sharing among agencies, including schools, on ways to provide opportunities, and (2) clarify schools’ responsibilities under federal law, namely Section 504 of the Rehabilitation Act of 1973, through the Office for Civil Rights, which is responsible for enforcing Section 504. In January 2013, in a landmark response to the release of the 2010 GAO report, the U.S. Department of Education, Office for Civil Rights (2013), clarified a school’s role in providing extracurricular athletic opportunities for students with disabilities.
Active Transport
Active transport or active commuting refers to the use of walking, biking, or other human-powered methods (e.g., skateboarding). It includes using public transportation or “walking school buses,” or being driven to a point closer to but not at school from which students walk the remainder of the way. Active transport equates to moderate-intensity physical activity, which, as discussed in earlier chapters, provides crucial health benefits. In light of these benefits, the CDC has launched programs to encourage parents to walk their children to school.
Active commuting has been proposed as an ideal low-cost strategy to increase physical activity within the general population and can account for one-quarter of an individual’s recommended total daily steps (Whitt et al., 2004). Studies have found that active transport provides children with physical activity (Tudor-Locke et al., 2002) and increased energy expenditure (Tudor-Locke et al., 2003). Bassett and colleagues (2013) suggest that active transport to and from school contributes on average 16 minutes of vigorous- or moderate-intensity physical activity for youth. These benefits, together with concern about increased traffic congestion and air pollution, have led to growing interest in the use of active transport by youth to get to and from school (Kahlmeier et al., 2010). In addition, it has been suggested
that active transport enhances social interaction among children and promotes independent mobility (Collins and Kearns, 2001; Kearns et al., 2003).
Five decades ago, children actively commuting to school were a common sight. Nearly 90 percent of children who lived within a 1-mile radius of school either walked or biked to school (USDOT, 1972). Since 1969 the prevalence of youth walking or biking to school has steadily declined (McDonald, 2007), paralleling a decline in active commuting among American adults (Pucher et al., 2011). Data from the U.S. Department of Transportation show the decline in active transportation to and from school between 1969 and 2001 (see Figure 6-9 ).
From an international perspective, active transport among children and adolescents is more prevalent in European countries such as the Netherlands and Germany, which have a culture of active transport, than in other regions. These countries tend to have a lower risk of obesity, diabetes, and hypertension in youth compared with the United States. Indeed, the data support an inverse relationship between the percentage of active transport and obesity rates among residents of the United States, Canada, Australia, and 14 European countries (Bassett et al., 2008). In this study

FIGURE 6-9 Decline in active transportation to and from school among youth from 1969 to 2001 in the United States. SOURCE: CDC, 2008; 1969 Nationwide Personal Transportation Survey (USDOT, 1972); and 2001 National Household Travel Survey.
the United States ranked the lowest on active transport and the highest on obesity prevalence.
Policies That Affect Active Transport
Various environmental and policy factors support or hinder active transport to and from school. For example, school siting policies that encourage the construction of schools on large campuses far from residential areas and not integrated with housing development are a hindrance (Council of Educational Facility Planners International, 1991). Accordingly, efforts are being made to stop “school sprawl,” including eliminating minimum acreage guidelines so that schools can be located closer to where school-age children live (Salvesen and Hervey, 2003).
At the national level, the U.S. Secretary of Transportation has called for a “sea change” in transportation planning in the United States. He has expressed the need to put cyclists and walkers on even ground with motorists and issued a policy statement on accommodations for active transport (USDOT, 2010). His statement calls for the redesign of existing neighborhoods with bicycle lanes, sidewalks, and shared paths. Additionally, the reauthorization of federal transport legislation charged the Federal Highway Administration with providing funds for states to create and implement Safe Routes to School programs (National Safe Routes to School Task Force, 2008). Provision of this funding may increase the percentage of children who walk or bike to school through a variety of initiatives, including engineering (e.g., building sidewalks), enforcement (e.g., ticketing drivers who speed in school zones), education (e.g., teaching pedestrian skills in the classroom), and encouragement (e.g., having students participate in walk-to-school days) (CDC, 2005).
Eyler and colleagues (2008) examined policies related to active transport in schools. In 2005, six states (California, Colorado, Massachusetts, North Carolina, South Carolina, and Washington) had statewide safe routes to school or active transport programs. California, Colorado, and South Carolina had regulations regarding the required distance students must live from a school to be eligible for bus transportation (more than 1.5 miles in South Carolina). A review of the NASBE (2012) State School Health Policy Database revealed that only 11 states (21 percent) had legislation requiring walk/bike programs, most in partnership with the state departments of transportation (see Appendix C ).
Barriers to Active Transport
Several factors contribute to the lack of active transport of youth to and from school. The first is accessibility (Frank et al., 2003), which refers to the proximity (i.e., within a 1-mile radius) of a child’s home to school
(Bassett, 2012). Nearly half of the decline in youth walking to and from school from 1969 to 2001 is attributable to the increased distance between home and school (McDonald, 2007). Proximity to school is influenced by families moving farther away from school; schools are being built farther away from homes compared with the small neighborhood schools of the past (see Figures 6-10 and 6-11 ). Proximity also is influenced by the decrease in the number of schools since 1960 even as the number of students enrolled in schools has increased (Wirt et al., 2003).
Proximity to school is not the only factor accounting for the decline in active transport among youth, as a significant decline also has been seen among youth living within a 1- to 2-mile radius of school. A second key determinant is infrastructure (Frank et al., 2003). The built environment is key to facilitating active transport. For active transport to be effective, not only must schools be in close proximity to the neighborhoods of students, but sidewalks, pedestrian crossings, and traffic lights must be adequate (Boarnet et al., 2005; Fulton et al., 2005). Boarnet and colleagues (2005) found that children’s walking and cycling to and from school greatly increased in urban areas with improvements in sidewalks, traffic lights, pedestrian crossings, and bike paths. In a national study of 4th to 12th graders, the presence of sidewalks was the main modifiable characteristic associated with active transport to and from school (Fulton et al., 2005). Other parental concerns include street connectivity, busy streets on

FIGURE 6-10 Distance to school for youth aged 5-18, 1969. SOURCE: CDC, 2008.

FIGURE 6-11 Distance to school for youth aged 5-18, 2001. SOURCE: CDC, 2008.
routes, and mixed land uses (Ewing and Greene, 2003; Fulton et al., 2005; Schlossberg et al., 2006; Timperio et al., 2006).
All nine schools interviewed for one study by active transport programs reported that the environmental factors that most affected these programs were sidewalks, crossing guards/crosswalks, funding, personal safety concerns, and advocacy group involvement. All schools also reported that a school speed zone was the greatest concern (Eyler et al., 2008). Other environmental factors include weather (heat, humidity, precipitation) and geographic location (Pucher and Buehler, 2011), with the South having a built environment less conducive to active transport compared with the Northeast, Midwest, and West (Bassett, 2012).
Related to infrastructure issues are parental concerns about safety (Loprinzi and Trost, 2010). These concerns include traffic dangers (Dellinger and Staunton, 2002). For example, 50 percent of children hit by cars near schools are hit by cars driven by parents of students (CDC, 2008), and drivers often exceed the posted speed limit and/or violate traffic signage in school zones (CDC, 2008). Safe routes to school initiatives that have linked engineers and educators to make school trips safer have seen a 64 percent increase in the percentage of students walking to school (Boarnet et al., 2005). In urban areas, infrastructure is conducive to active commuting to and from school, but these areas may be characterized by high crime rates. Dellinger and Staunton (2002) propose that safety is of particular concern for primary school children, which may account for their finding
that parents rated their child’s age as the most important factor in their decision to allow the child to walk to school. Other studies confirm that many 5- to 6-year-olds lack the skills to cope with traffic issues (Whitebread and Neilson, 2000), although other studies have found that neighborhood safety is unrelated to commuting practices in children (Humpel et al., 2004; Wilson et al., 2004). The “walking school bus” (i.e., when an adult escorts a group of children to school) has been shown to be an effective means of safely transporting children to and from school (Collins and Kearns, 2005). It may be noted that pedestrian and bicycling injury/death rates among youth have declined by 51 percent and 60 percent, respectively. However, the decrease in walking or biking among youth may have contributed to this downward trend (CDC, 2008).
Finally, parents identify the perceived fitness level of their children as a determinant of the children’s participation in active transport. Specifically, parents who perceive their children as being unfit prefer passive transportation (Yeung, 2008).
“Walking School Bus” Programs
School-endorsed “walking school buses” may address several of the barriers identified above—in particular, traffic and crime dangers (White House Task Force on Childhood Obesity, 2010). “Walking school buses” are popular means for walking young children to school securely in Europe and Australia but are just starting to emerge in the United States. A “walking school buses” often entails one or two adult volunteers escorting a group of children from pickup points or their homes to school along a fixed route, starting with the pickup point or home that is farthest from the school and stopping at other pickup points or homes along the way. For increased security for the youngest children, a rope that surrounds the group can be used. On the way back from school, the same system is used in the opposite direction.
The White House Task Force on Childhood Obesity’s (2010) Report to the President identifies “walking school buses” as a low-cost initiative that communities can undertake to increase physical activity among elementary school children. The prevalence of “walking school buses” remains low in the United States but is growing; in 2008-2009, about 4.2 percent of a representative sample of public elementary schools organized “walking school buses”, with an increase to 6.2 percent in 2009-2010 (Turner et al., 2012). Examples of “walking school buse” programs are described in Box 6-2 .
Parents’ engagement in school-based health promotion activities is another significant benefit of “walking school buses”. In some communities, “walking school buses” have provided opportunities for parents and
other volunteers to remain engaged in the life of the community while increasing their own physical activity.
Differences in Opportunities for Active Transport
The literature demonstrates that active transport varies among socioeconomic and ethnic groups and with the type of area (suburban, urban, or rural) (Davis and Jones, 1996; Dovey, 1999). Data from Bridging the Gap (Turner et al., 2010) demonstrate that one in four middle school students and one in eight high school students commute actively to and from school. Students of low socioeconomic status and those who attend schools where the majority of students are nonwhite (i.e., black and Latino) are more likely to walk or bike to and from school than those of high socioeconomic status and those who attend schools with a predominantly white student body.
Facilitators of Active Transport to School
Four common themes have been identified among schools with successful active transport to school programs (Eyler et al., 2008):
- collaboration among many organizations and individuals, including school personnel, public safety officials, city officials, parents, and school district representatives;
- funding for personnel, program materials, and improvements to the built environment;
- concerns about both traffic and crime being addressed; and
- efforts to make the built environment more conducive to active transport by students.
The same study identified a number of important and specific factors and policies to be considered (see Table 6-4 ).
A useful five-component framework for planning programs to enhance active transport to school has been suggested (Fesperman et al., 2008). This framework begins with the development of a plan and the enlistment of key individuals and organizations for input and support. The planning phase is crucial and may take a full year. The implementation of programmatic activities (e.g., training in pedestrian and bicycle safety, walk-to-school days), policy changes (e.g., school speed zones, modification of school start and dismissal times), and physical changes (e.g., sidewalk improvement, installment of traffic calming devices) follow in a sequence appropriate for the specific school and plan. For all activities, promotional materials to ensure understanding and continued support should be disseminated.
Examples of “Walking School Bus” Programs
The Safe Passage program in Chicago, a comprehensive initiative designed to help keep children safe on their way to and from school, includes a “walking school bus” program (see http://www.cps.edu/Programs/Wellness_and_transportation/SafetyandSecurity/SafePassage/Documents/SafePassageGuide.pdf [accessed February 1, 2013]). To further improve children’s safety, military veterans have been enlisted to escort the children, on the assumption that their training enables early detection of any crime-related problems along the way to school ( http://www.npr.org/2013/02/15/172130142/checking-in-on-chicago-schools-safe-passage-program [accessed February 1, 2013]). “Walking school bus” programs also have been undertaken in Columbia, Missouri ( http://activelivingbydesign.org/communities/featured-community/albd-sustainability-columbias-walking-school-bus [accessed February 1, 2013]), and in Cleveland, Ohio ( http://activelivingbydesign.org/communities/featured-community/clevelands-schools-are-taking-walking-school-bus [accessed February 1, 2013]).
Many resources are available to schools and communities that are interested in starting a “walking school bus” program. See the following websites:
In summary, active transport to and from school can be a safe and effective way to increase students’ daily physical activity, especially where a large proportion of students live close to their school. Increasing the proportion of children who walk or bike to school commonly requires collaboration among school personnel, public safety officials, city officials, parents, and school district representatives, as well as the funding necessary to address the factors and policies listed in Table 6-4 .
After-School Programs
After-school programs are emerging as another potential means of promoting physical activity in the context of the school environment. After-school programs are organized school or community-based extracurricular activities that take place outside of the school day, typically between 3:00
• The CDC’s Nutrition and Physical Activity Program has developed KidsWalk-to-School, a community-based program that encourages children to walk and bicycle to school. It provides resources and training models for creating walk-to-school programs. The program increases awareness of the importance of physical activity for children and mobilizes communities to advocate for the creation of safe routes to school ( http://www.cdc.gov/nccdphp/dnpa/kidswalk [accessed February 1, 2013]).
• The Santa Clarita, California, 2010 Walking School Bus Training Guidebook provides suggestions on how to create “walking school bus” programs, identify route leaders, plan routes, manage logistics, and raise funds ( http://www.altaprojects.net/files/1712/6662/3993/SC%20WSB%20Training%20Guidebook%20WEB.pdf [accessed February 1, 2013]).
• The Walking School Bus model encourages children to walk or bicycle together in groups, supervised by one or two adults ( http://www.walkingschoolbus.org [accessed February 1, 2013]).
• Fire Up Your Feet provides additional perspectives on community methods for creating walking school buses ( http://fireupyourfeet.org/resources/walking-school-bus [accessed February 1, 2013]).
and 6:00 PM (Granger et al., 2007) and are characterized by opportunities to build competencies in a wide range of areas (Mahoney et al., 2005). They are conducted on most afternoons during the school week for school-age children. Common areas of focus are nutrition and health education, physical activity and recreation, art, and music. After-school programs also provide academic assistance (i.e., tutoring and assistance with homework) and opportunities to develop leadership. Personal and social skills are a common theme.
The past two decades have seen a rapid increase in after-school programs in the United States, and these programs have become an integral part of the community for many families. In 1988, just 22 percent of K-8 school principals reported offering an after-school program, whereas two-thirds reported offering such a program in 2001 (National Association of Elementary School Principals, 2001). This increase in after-school programs is associated with a growing number of parents working beyond the regu-
TABLE 6-4 Factors and Policies That Influence Promotion of Walking or Biking to School
lar school hours and a rise in maternal employment, which have created a need to provide children with a safe and adult-supervised environment (U.S. Department of Labor, 2005; Afterschool Alliance, 2009). Emerging data indicate that more than 8.4 million youth attend after-school programs for an average of 8.1 hours per week (Afterschool Alliance, 2009). The After-School Programs and Activities Survey, a nationally representative survey of the 2005 National Household Education Surveys Program (Carver and Iruka, 2006), revealed that 40 percent of students in grades K-8 were in at least one weekly nonparental after-school care program, 20 percent of which were school- or center-based programs. Overall, after-school programs have the opportunity to reach large numbers of school-age children. A wealth of research and emerging findings demonstrate the benefits of after-school programs with respect to academic performance; social and emotional development; and health and wellness, including prevention of risky behaviors.
Public opinion supports the need for after-school programs. In 1999 the Mott Foundation reported that 94 percent of people believed “there should be some type of organized activity or place for children and teens to go after school every day” (Afterschool Alliance, 1999, p. 1). The federal government also supports after-school programs, especially in low-income communities. Funding for the 21st Century Community Learning Centers, an after-school program established by the Clinton administration, has increased dramatically over the years, from $40 million in fiscal year 1998 to $1 billion in fiscal year 2002. This grant program supports after-school programs in about 7,500 rural and inner-city public schools in more than 1,400 communities (U.S. Department of Education, 2003).
Policies That Affect After-School Programs
Despite their popularity, there is an absence of nationally recognized standards or policies for promoting physical activity in after-school pro-
grams. Moreover, while some states have taken the initiative to create benchmarks, standards and policies are rare, existing in only 70 percent of states (Beets et al., 2010). Table 6-5 provides an overview of state-level policies, standards, recommendations, and guidelines for physical activity in after-school programs. The table shows wide variation. For example, policies in North Carolina state that 20 percent of the time in an after-school program must be spent in vigorous- or moderate-intensity physical activity, while in California all children must be engaged in a minimum of 30 minutes of vigorous- or moderate-intensity physical activity (Beets et al., 2010). Some standards suggest 30-60 minutes of vigorous- or moderate-intensity physical activity, while others suggest ‘‘frequent opportunities’’ for physical activity or 30 minutes out of a 3-hour block. By comparison, one recommendation is to allocate at least 50 percent of program time to physical activity (Beighle et al., 2010).
After-school programs can be used to combat physicalinactivity and obesity while promoting physical activity on school grounds outside of the normal school-day hours (Lee et al., 2007; Levi et al., 2009). However, national organizations and state entities need to develop appropriate policies and standards for the implementation of after-school programs whose goal is to promote health and physical activity in school-age children. Doing so would help promote physical activity among school-age children in these settings, aiding them in achieving the recommended levels of daily physical activity. However, it is important not only to have such policies in place but also to ensure that the policies are being implemented (i.e., accountability).
Facilitators of and Barriers to After-School Programs
Various factors serve as barriers and facilitators for after-school programs. The school environment is a facilitator for after-school programs because the setting provides for a wide range of activities (Grossman et al., 2001). Schools are equipped with gymnasiums, libraries, auditoriums, and computer labs that provide unique equipment and space. Second, schools have immediate access to participants, and their after-school programs offer legitimacy for parents who may be hesitant to allow their children to participate in a program elsewhere.
Using schools as a venue for after-school programs is not as easy as it may seem, however. First, their facilities may not always be available for use. Safety, lack of staffing, insufficient funding, risk of vandalism, and insurance liability concerns are often cited as barriers to making school grounds available outside of school hours (Filardo et al., 2010; Cox et al., 2011; Spengler et al., 2011; Evenson et al., 2012). For instance, teachers use classrooms to prepare for the next day’s lesson or to provide extra academic assistance to students, students use the library and computer lab to
TABLE 6-5 State Policies, Standards, Recommendations, and Guidelines for Physical Activity in After-School Programs
NOTE: PA = physical activity. SOURCE: Beets et al., 2010. Reprinted with permission.
complete classroom assignments, and sports teams need the gymnasium for practice. Thus, after-school programs often compete for space, particularly in the gymnasium. The availability of school space is critical to the effectiveness and quality of after-school programs, most of which require open multipurpose space to accommodate a range of activities.
In addition to competing for space, after-school programs entail costs to schools, after-school community partners, and families. In addition to personnel to run the program, there are costs for upkeep and maintenance of school facilities. After-school programs also entail custodial costs for
room cleaning. For parents the average cost for after-school programs is $67.00 per week, a $20.00 increase over the past 5 years (Afterschool Alliance, 2009). Thus, public funds are needed to defray some of these costs to schools and families.
In addition, the inability of an after-school program to provide transportation home is a major barrier to participation for a large number of students. Programs have an advantage in recruiting participants when operating in schools where a majority of the students live within safe walking distance (in particular, urban city schools) (Grossman et al., 2001). For children not living within walking distance of school, busing is an alternative, but the limited supply of buses and drivers, as well as their cost, is a major barrier. There are substantial negative consequences of inadequate transportation. Youth who live beyond walking distance from their school and who cannot be picked up by a parent or adult at the designated time are unable to participate in programs. For schools that can provide busing for after-school programs, the number of seats available on those buses limits the number of children who can participate. Even when children live within walking distance of their school, many parents feel uncomfortable about their child walking home alone in the dark at 5:00 or 6:00 PM. School districts have struggled with easing this transportation problem. Money has been unavailable in schools’ budgets, or there have been restrictions on how transit money can be spent. For example, some school districts give transportation funding only to academic programs, and after-school programs are considered nonacademic.
Staff training is another concern for after-school programs. If training does occur, it is often in house. Existing training programs tend to focus on games and to use prepackaged materials, and they fail to address promotion of physical activity (Ajja et al., 2012; Weaver et al., 2012).
Differences in Opportunities in After-School Programs
In addition to providing children with enrichment opportunities, a key factor behind the policy interest in after-school programs is the increasing need for child care. Almost all adults agree that elementary school children need adult supervision. Young people aged 10-14 are often seen as old enough to stay on their own for short periods of time, but they are also old enough to get into serious trouble. Unfortunately, these older children are much less likely to participate in supervised after-school programs, whether the programs take place at youth-serving organizations or at school. It is easier to recruit elementary school children to these programs than middle and high school students, who tend to have busier schedules, increased responsibilities, and greater freedom (Grossman et al., 2001). Grossman and colleagues also found that 30 percent of enrollees in after-
school programs were in 3rd grade or lower, 45 percent were in 4th through 6th grades, 23 percent were in 7th and 8th grades, and only 2 percent were in 9th grade or higher. Additionally, elementary-age children who enrolled attended more frequently than older youth.
In addition to physical education, schools can offer students non-instructional opportunities to engage in beneficial physical activity before, during, or after the school day. These opportunities take various forms, such as interscholastic sports teams, intramural sport clubs, recess, and in-class physical activity breaks. Interscholastic sports provide opportunities for students with athletic talent. But budgetary constraints, team-cut policies, transportation, lack of facilities, and pay-to-play policies and practices in many high schools may limit participation. Intramural sports clubs in middle and high schools are a viable way for the majority of children to engage in in-school or after-school physical activities. Research data consistently show, however, that although these programs can serve a large number of children, not every child will opt to participate or be able to find transportation home after an activity. Recess and classroom physical activity breaks have become valuable opportunities for elementary school students to be active during the school day. Their value in middle and high schools is questionable when they are combined with lunch, and at the secondary level classroom activity breaks are lost to valuable and limited academic time. Evidence supporting the integration of physical activity into academic lessons does exist but only for elementary schools. Given the nature of institutionalized education and its emphasis on academic achievement, it is unclear that the approach will be embraced by school officials and most classroom teachers.
One consensus from the literature is that, to take advantage of and enhance the many opportunities for physical activity outside of physical education, policy makers and practitioners must acknowledge the anchor function of physical education (National Physical Activity Plan, 2010). Curriculum time is insufficient for all of the recommended 60 minutes or more of vigorous- or moderate-intensity physical activity to take place during physical education, so the activity in which children engage throughout the school day is important. Therefore, a holistic, comprehensive approach is increasingly being advocated to promote physical activity in schools. School environments encourage more physical activity, both before and after school, if they include well-designed playgrounds; open spaces; and facilities and equipment that are available, accessible, and inviting to children. AAHPERD’s CSPAP program can serve as an example. It provides opportunities anchored in the knowledge and skills learned in physical
education and uses a flexible programming method that allows local decision makers and teachers to integrate physical activity opportunities into relevant school activities before, during, and after the school day. It must be emphasized that, while school-based physical activity should be used to support physical activity in the school environment, it should not be used as a replacement for physical education, whose importance is explained in Chapter 5 .
AAP (American Academy of Pediatrics). 2013. The crucial role of recess in school. Pediatrics 131(1):183-188.
AAHPERD (American Alliance for Health, Physical Education, Recreation and Dance). 2011. 2011 Comprehensive School Physical Activity Program (CSPAP) survey report. Reston, VA: AAHPERD.
Active Policy Solutions. 2013. Active policy solutions: Analysis and history of the Department of Education’s January 2013 guidance. Washington, DC: Active Policy Solutions.
Afterschool Alliance. 1999. A report of findings from the December 1999 Mott foundation/JCPenney nationwide survey on afterschool programs. Washington, DC: Afterschool Alliance.
Afterschool Alliance. 2009. America after 3pm: The most in-depth study of how America’s children spend their afternoons. Washington, DC: Afterschool Alliance.
Ahamed, Y., H. Macdonald, K. Reed, P. J. Naylor, T. Liu-Ambrose, and H. McKay. 2007. School-based physical activity does not compromise children’s academic performance. Medicine and Science in Sports and Exercise 39(2):371-376.
Ajja, R., M. W. Beets, J. Huberty, A. T. Kaczynski, and D. S. Ward. 2012. The healthy afterschool activity and nutrition documentation instrument. American Journal of Preventive Medicine 43(3):263-271.
Amis, J. M., P. M. Wright, B. Dyson, J. M. Vardaman, and H. Ferry. 2012. Implementing childhood obesity policy in a new educational environment: The cases of Mississippi and Tennessee. American Journal of Public Health 102(7):1406-1413.
Bartholomew, J. B., and E. M. Jowers. 2011. Physically active academic lessons in elementary children. Preventive Medicine 52(Suppl):S51-S54.
Bassett, D. R. 2012. Encouraging physical activity and health through active transportation. Kinesiology Reviews 1(1):91-99.
Bassett, D. R., Jr., J. Pucher, R. Buehler, D. L. Thompson, and S. E. Crouter. 2008. Walking, cycling, and obesity rates in Europe, North America, and Australia. Journal of Physical Activity and Health 5(6):795-814.
Bassett, D. R., E. C. Fitzhugh, G. W. Heath, P. C. Erwin, G. M. Frederick, D. L. Wolff, W. A. Welch, and A. B. Stout. 2013. Estimated energy expenditures for school-based policies and active living. American Journal of Preventive Medicine 44(2):108-113.
Beets, M. W., M. Wallner, and A. Beighle. 2010. Defining standards and policies for promoting physical activity in afterschool programs. Journal of School Health 80(8):411-417.
Beighle, A., M. W. Beets, H. Erwin, J. L. Huberty, J. B. Moore, and M. B. Stellino. 2010. Physical activity promotion in after-school programs. After-School Matters 11:24-32.
Belansky, E. S., N. Cutforth, E. Delong, C. Ross, S. Scarbro, L. Gilbert, B. Beatty, and J. A. Marshall. 2009. Early impact of the federally mandated local wellness policy
on physical activity in rural, low-income elementary schools in Colorado. Journal of Public Health Policy 30(Suppl 1):S141-S160.
Bernstein, M. S., A. Morabia, and D. Sloutskis. 1999. Definition and prevalence of sedentarism in an urban population. American Journal of Public Health 89(6):862-867.
Boarnet, M. G., C. L. Anderson, K. Day, T. McMillan, and M. Alfonzo. 2005. Evaluation of the California Safe Routes to School legislation: Urban form changes and children’s active transportation to school. American Journal of Preventive Medicine 28(2 Suppl 2):134-140.
Bocarro, J. N., M. A. Kanters, E. Cerin, M. F. Floyd, J. M. Casper, L. J. Suau, and T. L. McKenzie. 2012. School sport policy and school-based physical activity environments and their association with observed physical activity in middle school children. Health and Place 18(1):31-38.
Carver, P. R., and I. U. Iruka. 2006. After school programs and activities: 2005 . Washington, DC: U.S. Department of Education.
CDC (U.S. Centers for Disease Control and Prevention). 2005. Barriers to children walking to and from school—United States, 2004. Morbidity and Mortality Weekly Report 54:949-952.
CDC. 2008. Kids walk to school: Then and now—barriers and solutions . http://www.cdc.gov/nccdphp/DNPA/kidswalk/then_and_now.htm (accessed April 15, 2013).
CDC. 2010. The association between school based physical activity, including physical education, and academic performance. Atlanta, GA: U.S. Department of Health and Human Services, CDC.
CDC. 2012. Trends in the prevalence of physical activity and sedentary behaviors; YRBS 1991-2011. Atlanta, GA: U.S. Department of Health and Human Services, CDC, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of Adolescent and School Health.
Center for Public Education. 2008. Time out: Is recess in danger? http://www.centerforpubliceducation.org/Main-Menu/Organizing-a-school/Time-out-Is-recess-in-danger (accessed March 5, 2013).
Center on Education Policy. 2007. Choices, changes, and challenges: Curriculum and instruction in the NCLB era. Washington, DC: Center on Education Policy.
Chen, A., and W. Zhu. 2005. Young children’s intuitive interest in physical activity: Personal, school, and home factors. Journal of Physical Activity and Health 2(1):1-15.
Chriqui, J. F., L. Schneider, F. J. Chaloupka, C. Gourdet, A. Bruursema, K. Ide, and O. Pugach. 2010. School district wellness policies: Evaluating progress and potential for improving children’s health three years after the federal mandate: School years 2006-07, 2007-08 and 2008-09, volume 2. Chicago, IL: Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois.
Colabianchi, N., L. Johnston, and P. M. O’Malley. 2012. Sports participation in secondary schools: Resources available and inequalities in participation—a BTG research brief. Ann Arbor, MI: Bridging the Gap Program, Survey Research Center, Institute for Social Research, University of Michigan.
Collins, D. C. A., and R. A. Kearns. 2001. The safe journeys of an enterprising school: Negotiating landscapes of opportunity and risk. Health and Place 7(4):293-306.
Collins, D. C., and R. A. Kearns. 2005. Geographies of inequality: Child pedestrian injury and walking school buses in Auckland, New Zealand. Social Science and Medicine 60(1):61-69.
Council of Educational Facility Planners International. 1991. Guide for planning educational facilities. Scottsdale, AZ: Council of Educational Facility Planners International.
Council on School Health. 2013. The crucial role of recess in school. Pediatrics 131(1):183-188.
Cox, L., V. Berends, J. F. Sallis, J. M. St. John, B. McNeil, M. Gonzalez, and P. Agron. 2011. Engaging school governance leaders to influence physical activity policies. Journal of Physical Activity and Health 8(Suppl 1):S40-S48.
C.S. Mott Children’s Hospital. 2012. Pay-to-play sports keeping lower-income kids out of the game. Ann Arbor: University of Michigan Health System.
Davis, A., and L. J. Jones. 1996. Children in the urban environment: An issue for the new public health agenda. Health and Place 2(2):107-113.
Dellinger, A. M., and C. E. Staunton. 2002. Barriers to children walking and biking to school—United States, 1999. Morbidity and Mortality Weekly Report 51(32):701-704.
Donnelly, J. E., and K. Lambourne. 2011. Classroom-based physical activity, cognition, and academic achievement. Preventive Medicine 52(Suppl):S36-S42.
Donnelly, J. E., J. L. Greene, C. A. Gibson, B. K. Smith, R. A. Washburn, D. K. Sullivan, K. DuBose, M. S. Mayo, K. H. Schmelzle, J. J. Ryan, D. J. Jacobsen, and S. L. Williams. 2009. Physical Activity Across the Curriculum (PAAC): A randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Preventive Medicine 49(4):336-341.
Dovey, K. 1999. Framing places: Mediating power in built form . London, UK: Routledge.
Dwyer, J. J., K. R. Allison, M. Barrera, B. Hansen, E. Goldenberg, and M. A. Boutilier. 2003. Teachers’ perspective on barriers to implementing physical activity curriculum guidelines for school children in Toronto. Canadian Journal of Public Health 94(6):448-452.
Edwards, M. B., J. N. Bocarro, and M. A. Kanters. 2013. Place disparities in supportive environments for extracurricular physical activity in North Carolina middle schools. Youth and Society 45(2):265-285.
Epstein, L. H., A. M. Valoski, L. S. Vara, J. McCurley, L. Wisniewski, M. A. Kalarchian, K. R. Klein, and L. R. Shrager. 1995. Effects of decreasing sedentary behavior and increasing activity on weight change in obese children. Health Psychology 14(2):109-115.
Ernst, M. P., and R. P. Pangrazi. 1999. Effects of a physical activity program on children’s activity levels and attraction to physical activity. Pediatric Exercise Science 11(4):393-405.
Erwin, H. E., A. Beighle, C. F. Morgan, and M. Noland. 2011. Effect of a low-cost, teacher-directed classroom intervention on elementary students’ physical activity. Journal of School Health 81(8):455-461.
Erwin, H., A. Fedewa, A. Beighle, and S. Ahn. 2012. A quantitative review of physical activity, health, and learning outcomes associated with classroom-based physical activity interventions. Journal of Applied School Psychology 28(1):14-36.
Evenson, K. R., K. Ballard, G. Lee, and A. Ammerman. 2009. Implementation of a school-based state policy to increase physical activity. Journal of School Health 79(5):231-238.
Evenson, K. R., J. F. Sallis, S. L. Handy, R. Bell, and L. K. Brennan. 2012. Evaluation of physical projects and policies from the active living by design partnerships. American Journal of Preventive Medicine 43(5):S309-S319.
Ewing, R., and W. Greene. 2003. Travel and environmental implications of school siting . http://www.epa.gov/smartgrowth/pdf/school_travel.pdf (accessed April 1, 2013).
Eyler, A. A., R. C. Brownson, M. P. Doescher, K. R. Evenson, C. E. Fesperman, J. S. Litt, D. Pluto, L. E. Steinman, J. L. Terpstra, P. J. Troped, and T. L. Schmid. 2008. Policies related to active transport to and from school: A multisite case study. Health Education Research 23(6):963-975.
Fakhouri, T. H., J. P. Hughes, D. J. Brody, B. K. Kit, and C. L. Ogden. 2013. Physical activity and screen-time viewing among elementary school-aged children in the United States from 2009 to 2010. Journal of the American Medical Association Pediatrics 167(3):223-229.
Fesperman, C. E., K. R. Evenson, D. A. Rodríguez, and D. Salvesen. 2008. A comparative case study on active transport to and from school. Preventing Chronic Disease 5(2):A40.
Filardo, M., J. M. Vincent, M. Allen, and J. Franklin. 2010. Joint use of public schools: A framework for a new social contract . Berkeley: University of California, Berkeley, Center for Cities & Schools.
Frank, L., P. Engelke, and T. Schmid. 2003. Health and community design: The impact of the built environment on physical activity : Washington, DC: Island Press.
Fulton, J. E., J. L. Shisler, M. M. Yore, and C. J. Caspersen. 2005. Active transportation to school: Findings from a national survey. Research Quarterly for Exercise and Sport 76(3):352-357.
GAO (U.S. Government Accountability Office). 2010. Students with disabilities: More information and guidance could improve opportunities in physical education and athletics . Washington, DC: GAO.
GAO. 2012. K-12: School-based physical education and sports programs. Washington, DC: GAO.
Gordon-Larsen, P., M. C. Nelson, and B. M. Popkin. 2004. Longitudinal physical activity and sedentary behavior trends: Adolescence to adulthood. American Journal of Preventive Medicine 27(4):277-283.
Granger, R., J. A. Durlak, N. Yohalem, and E. Reisner. 2007. Improving afterschool program quality. New York: William T. Grant Foundation.
Grieco, L. A., E. M. Jowers, and J. B. Bartholomew. 2009. Physically active academic lessons and time on task: The moderating effect of body mass index. Medicine and Science in Sports and Exercise 41(10):1921-1926.
Grossman, J. B., K. Walker, and R. Raley. 2001. Challenges and opportunities in after-school programs: Lessons for policymakers and funders. Philadelphia, PA: Public/Private Ventures.
HHS (U.S. Department of Health and Human Services). 2008. Physical activity guidelines for Americans. Washington, DC: HHS.
HHS. 2012. Healthy people 2020: Physical activity objectives . http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=33 (accessed December 3, 2012).
Humpel, N., N. Owen, D. Iverson, E. Leslie, and A. Bauman. 2004. Perceived environment attributes, residential location, and walking for particular purposes. American Journal of Preventive Medicine 26(2):119-125.
IPA (International Play Association). 2013. International Play Association: Promoting the child’s right to play . http://ipaworld.org (accessed March 4, 2013).
Jarrett, O. S., D. M. Maxwell, C. Dickerson, P. Hoge, G. Davies, and A. Yetley. 1998. Impact of recess on classroom behavior: Group effects and individual differences. Journal of Educational Research 92(2):121-126.
Kahlmeier, S., F. Racioppi, N. Cavill, H. Rutter, and P. Oja. 2010. “Health in all policies” in practice: Guidance and tools to quantifying the health effects of cycling and walking. Journal of Physical Activity and Health 7(Suppl 1):S120-S125.
Kearns, R. A., D. C. A. Collins, and P. M. Neuwelt. 2003. The walking school bus: Extending children’s geographies? Area 35(3):285-292.
Kelly, I. R., M. A. Phillips, M. Revels, and D. Ujamaa. 2010. Contribution of the school environment to physical fitness in children and youth. Journal of Physical Activity and Health 7(3):333-342.
Kibbe, D. L., J. Hackett, M. Hurley, A. McFarland, K. G. Schubert, A. Schultz, and S. Harris. 2011. Ten years of TAKE 10! ® : Integrating physical activity with academic concepts in elementary school classrooms. Preventive Medicine 52(Suppl):S43-S50.
Kretchmar, S. 2005. Teaching games for understanding and the delights of human activity. In Teaching games for understanding: Theory, research, and practice , edited by L. Griffin and J. Butler. Champaign, IL: Human Kinetics. Pp. 199-212.
Landis, M. J., P. P. Peppard, and P. L. Remington. 2007. Characteristics of school-sanctioned sports: Participation and attrition in Wisconsin public high schools. Wisconsin Medical Journal 106(6):312-318.
Lee, S. M., C. R. Burgeson, J. E. Fulton, and C. G. Spain. 2007. Physical education and physical activity: Results from the school health policies and programs study 2006. Journal of School Health 77(8):435-463.
Levi, J., S. Vinter, L. Richardson, R. St. Laurent, and L. M. Segal. 2009. F as in fat: How obesity policies are failing in America. Washington, DC: Trust for America’s Health.
Loprinzi, P. D., and S. G. Trost. 2010. Parental influences on physical activity behavior in preschool children. Preventive Medicine 50(3):129.
Mahar, M. T. 2011. Impact of short bouts of physical activity on attention-to-task in elementary school children. Preventive Medicine 52(Suppl):S60-S64.
Mahar, M. T., S. K. Murphy, D. A. Rowe, J. Golden, A. T. Shields, and T. D. Raedeke. 2006. Effects of a classroom-based program on physical activity and on-task behavior. Medicine and Science in Sports and Exercise 38(12):2086-2094.
Mahoney, J. L., H. Lord, and E. Carryl. 2005. Afterschool program participation and the development of child obesity and peer acceptance. Applied Developmental Science 9(4):202-215.
McDonald, N. C. 2007. Active transportation to school. Trends among U.S. school-children, 1969-2001. American Journal of Preventive Medicine 32(6):509-516.
NASBE (National Association of State Boards of Education). 2012. State School Health Policy Database. Reston, VA: AAHPERD.
NASBE Center for Safe and Healthy Schools. 2013. State School Health Policy Database. Reston, VA: AAHPERD.
NASPE. 2001. Integrating physical activity into the complete school day. Reston, VA: AAHPERD.
NASPE (National Association for Sport and Physical Education) and AHA (American Heart Association). 2010. Shape of the nation report: Status of physical education in the USA. Reston, VA: AAHPERD.
NASPE and AHA. 2012. Shape of the nation report: Status of physical education in the USA. Reston, VA: AAHPERD.
National Association for the Education of Young Children. 1998. The value of school recess and outdoor play. Washington, DC: National Association for the Education of Young Children.
National Association of Early Childhood Specialists in State Departments of Education. 2001. Recess and the importance of play: A position statement on young children and recess. Denver, CO: National Association of Early Childhood Specialists in State Departments of Education.
National Association of Early Childhood Specialists in State Departments of Education. 2002. Recess and the importance of play: A position statement on young children and recess. Washington, DC: National Association of Early Childhood Specialists in State Departments of Education.
National Association of Elementary School Principals. 2001. Principals and after-school programs: A survey of pre-K-8 principals. http://www.naesp.org/after-school-programs-archives-0 (accessed April 20, 2013).
National Parent Teacher Association. 2006. Recess is at risk, new campaign comes to the rescue . http://www.peacefulplaygrounds.com/pdf/right-to-recess/national-pta-recess-at-risk.pdf (accessed April 24, 2013).
National Physical Activity Plan. 2010. U.S. National Physical Activity Plan. Columbia, SC National Physical Activity Plan. http://www.physicalactivityplan.org/theplan.php (accessed August 12, 2013).
National Safe Routes to School Task Force. 2008. Safe routes to school: A transportation legacy—a national strategy to increase safety and physical activity among American youth. Washington, DC: U.S. Department of Transportation.
National Survey of Children’s Health. 2007. The child and adolescent health measurement initiative . www.childhealthdata.org/browse/survey/results?q=928&r=1 (accessed February 1, 2013).
Nelson, M. C., D. Neumark-Stzainer, P. J. Hannan, J. R. Sirard, and M. Story. 2006. Longitudinal and secular trends in physical activity and sedentary behavior during adolescence. Pediatrics 118(6):e1627-e1634.
NFSHSA (National Federation of State High School Associations). 2012. 2011-2012 high school athletics participation survey results. Indianapolis, IN: NFSHSA.
Olds, T. S., C. A. Maher, K. Ridley, and D. M. Kittel. 2010. Descriptive epidemiology of screen and non-screen sedentary time in adolescents: A cross sectional study. International Journal of Behavioral Nutrition and Physical Activity 7:92.
Parks, M., M. Solmon, and A. Lee. 2007. Understanding classroom teachers’ perceptions of integrating physical activity: A collective efficacy perspective. Journal of Research in Childhood Education 21(3):316-328.
Parsad, B., and L. Lewis. 2006. Calories in, calories out: Food and exercise in public elementary schools, 2005. Washington, DC: National Center for Education Statistics.
Pellegrini, A. D., P. D. Huberty, and I. Jones. 1995. The effects of recess timing on children’s playground and classroom behaviors. American Educational Research Journal 32(4):845-864.
Pucher, J., R. Buehler, D. Merom, and A. Bauman. 2011. Walking and cycling in the United States, 2001-2009: Evidence from the National Household Travel Surveys. American Journal of Public Health 101(Suppl 1):S310-S317.
Ramstetter, C. L., R. Murray, and A. S. Garner. 2010. The crucial role of recess in schools. Journal of School Health 80(11):517-526.
Ricciardi, R. 2005. Sedentarism: A concept analysis. Nursing Forum 40(3):79-87.
Rideout, V., U. G. Foehr, and D. F. Roberts. 2010. Generation M2: Media in the lives of 8- to 18-year-olds. Washington, DC: Kaiser Family Foundation.
Ridgers, N. D., G. Stratton, and S. J. Fairclough. 2006. Physical activity levels of children during school playtime. Sports Medicine 36(4):359-371.
RWJF (Robert Wood Johnson Foundation). 2007. Recess rules: Why the undervalued playtime may be America’s best investment for healthy kids and healthy schools. Princeton, NJ: RWJF.
RWJF. 2010. The state of play: Gallup survey of principals on school recess. Princeton, NJ: RWJF.
RWJF Center to Prevent Childhood Obesity. 2012. Jammin’ Minute. Princeton, NJ: RWJF.
Robinson, T. N. 1999. Reducing children’s television viewing to prevent obesity: A randomized controlled trial. Journal of the American Medical Association 282(16):1561-1567.
Salvesen, D., and P. Hervey. 2003. Good schools—good neighborhoods. Chapel Hill, NC: Center for Urban and Regional Studies, University of North Carolina at Chapel Hill.
Schlossberg, M., J. Greene, P. P. Phillips, B. Johnson, and B. Parker. 2006. School trips: Effects of urban form and distance on travel mode. Journal of the American Planning Association 72(3):337-346.
Scruggs, P. W., S. K. Beveridge, and D. L. Watson. 2003. Increasing children’s school time physical activity using structured fitness breaks. Pediatric Exercise Science 15(2):156-169.
Siedentop, D. L. 2009. National plan for physical activity: Education sector. Journal of Physical Activity and Health 6(Suppl 2):S168-S180.
Simons-Morton, B. G., W. C. Taylor, S. A. Snider, I. W. Huang, and J. E. Fulton. 1994. Observed levels of elementary and middle school children’s physical activity during physical education classes. Preventive Medicine 23(4):437-441.
Slater, S. J., L. Nicholson, J. Chriqui, L. Turner, and F. Chaloupka. 2012. The impact of state laws and district policies on physical education and recess practices in a nationally representative sample of U.S. public elementary schools. Archives of Pediatrics & Adolescent Medicine 166(4):311-316.
Spengler, J. O. 2012. Promoting physical activity through the shared use of school and community recreational resources. Princeton, NJ: RWF.
Timperio, A., K. Ball, J. Salmon, R. Roberts, B. Giles-Corti, D. Simmons, L. A. Baur, and D. Crawford. 2006. Personal, family, social, and environmental correlates of active commuting to school. American Journal of Preventive Medicine 30(1):45-51.
Tremblay, M. S., A. G. LeBlanc, M. E. Kho, T. J. Saunders, R. Larouche, R. C. Colley, G. Goldfield, and S. C. Gorber. 2011. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. International Journal of Behavioral Nutrition and Physical Activity 8:98.
Tudor-Locke, C., L. Neff, B. E. Ainsworth, C. Addy, and B. M. Popkin. 2002. Omission of active commuting to school and the prevalence of children’s health-related physical activity levels: The Russian Longitudinal Monitoring Study. Child Care Health and Development 28(6):507-512.
Tudor-Locke, C., B. E. Ainsworth, L. S. Adair, and B. M. Popkin. 2003. Objective physical activity of Filipino youth stratified for commuting mode to school. Medicine and Science in Sports and Exercise 35(3):465-471.
Tudor-Locke, C., S. M. Lee, C. F. Morgan, A. Beighle, and R. P. Pangrazi. 2006. Children’s pedometer-determined physical activity during the segmented school day. Medicine and Science in Sports and Exercise 38(10):1732-1738.
Turner, L., J. Chriqui, and F. Chaloupka. 2012. Walking school bus programs in US public elementary schools. Journal of Physical Activity and Health [epub ahead of print].
Turner, L., and F. J. Chaloupka. 2012. Activity breaks: A promising strategy for keeping children physically active at school. Chicago, IL: Bridging the Gap Program, University of Illinois at Chicago Health Policy Center, Institute for Health Research and Policy.
Turner, L., F. Chaloupka, J. Chiriqui, and A. Sandoval. 2010. School policies and practices to improve health and prevent obesity: National Elementary School Survey Results: School years 2006-07 and 2007-08. Chicago, IL: Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago.
U.S. Census Bureau. 1971-2011. Current Population Survey data on school enrollment. Washington, DC: U.S. Census Bureau.
U.S. Department of Education. 2003. When schools stay open late: The national evaluation of the 21st century community learning centers program, first year findings. Washington, DC: U.S. Department of Education.
U.S. Department of Education. 2013. Dear colleague (clarifying guidance) . Washington, DC: U.S. Department of Education, Office for Civil Rights.
U.S. Department of Labor. 2005. Women in the labor force: A databook . www.bls.gov/cps/wlf-databook2005.htm (accessed November 27, 2012).
USDOT (U.S. Department of Transportation). 1972. 1969 National Personal Transit Survey: Travel to school, June 1972. Washington, DC: USDOT.
USDOT. 2010. United States Department of Transportation policy statement on bicycle and pedestrian accommodation regulations and recommendations . Washington, DC: USDOT.
van Landeghem, K. 2003. Preventing obesity in youth through school-based efforts . Washington, DC: National Governors Association Center for Best Practices, Health Policy Studies Division.
Wallis, A., B. Cody, and A. Mickalide. 2003. Report to the nation: Trends in unintentional childhood injury mortality, 1987-2000 . Washington, DC: National SAFE KIDS Campaign.
Ward, D. 2011. School policies on physical education and physical activity: Research synthesis . San Diego, CA: Active Living Research, A Program of the Robert Wood Johnson Foundation.
Weaver, R. G., M. W. Beets, C. Webster, A. Beighle, and J. Huberty. 2012. A conceptual model for training after-school program staffers to promote physical activity and nutrition. Journal of School Health 82(4):186-195.
White House Task Force on Childhood Obesity. 2010. Solving the problem of childhood obesity within a generation: Report to the President . Washington, DC: Executive Office of the President of the United States.
Whitebread, D., and K. Neilson. 2000. The contribution of visual search strategies to the development of pedestrian skills by 4-11 year old children. British Journal of Educational Psychology 70(4):539-557.
Whitt, M. C., K. D. DuBose, B. E. Ainsworth, and C. Tudor-Locke. 2004. Walking patterns in a sample of African American, Native American, and Caucasian women: The cross-cultural activity participation study. Health Education and Behavior 31(4 Suppl):45S-56S.
Wilson, D. K., K. A. Kirtland, B. E. Ainsworth, and C. L. Addy. 2004. Socioeconomic status and perceptions of access and safety for physical activity. Annals of Behavioral Medicine 28(1):20-28.
Wirt, J., S. Choy, S. Provasnik, P. Rooney, A. Sen, and R. Tobin. 2003. The condition of education 2003 . Washington, DC: U.S. Department of Education.
Woods, R. 2011. Social issues in sport . Chicago, IL: Human Kinetics.
Yeung, J. 2008. Child transport practices and perceived barriers in active commuting to school. Transportation Research Part A 42:895-900.
Young, D. R., G. M. Felton, M. Grieser, J. P. Elder, C. Johnson, J. S. Lee, and M. Y. Kubik. 2007. Policies and opportunities for physical activity in middle school environments. Journal of School Health 77(1):41-47.
This page intentionally left blank.
Physical inactivity is a key determinant of health across the lifespan. A lack of activity increases the risk of heart disease, colon and breast cancer, diabetes mellitus, hypertension, osteoporosis, anxiety and depression and others diseases. Emerging literature has suggested that in terms of mortality, the global population health burden of physical inactivity approaches that of cigarette smoking. The prevalence and substantial disease risk associated with physical inactivity has been described as a pandemic.
The prevalence, health impact, and evidence of changeability all have resulted in calls for action to increase physical activity across the lifespan. In response to the need to find ways to make physical activity a health priority for youth, the Institute of Medicine's Committee on Physical Activity and Physical Education in the School Environment was formed. Its purpose was to review the current status of physical activity and physical education in the school environment, including before, during, and after school, and examine the influences of physical activity and physical education on the short and long term physical, cognitive and brain, and psychosocial health and development of children and adolescents.
Educating the Student Body makes recommendations about approaches for strengthening and improving programs and policies for physical activity and physical education in the school environment. This report lays out a set of guiding principles to guide its work on these tasks. These included: recognizing the benefits of instilling life-long physical activity habits in children; the value of using systems thinking in improving physical activity and physical education in the school environment; the recognition of current disparities in opportunities and the need to achieve equity in physical activity and physical education; the importance of considering all types of school environments; the need to take into consideration the diversity of students as recommendations are developed.
This report will be of interest to local and national policymakers, school officials, teachers, and the education community, researchers, professional organizations, and parents interested in physical activity, physical education, and health for school-aged children and adolescents.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.

How to Stay Safe During Physical Activity
Young people will learn how to stay safe during physical activity. This includes wearing the right equipment, warming up before play, when not to play, and rules of the game.
3-8 Years Old
What You Need
- Staying Safe Coloring Sheet
Healthy Families Newsletter
English (pdf)
Spanish (pdf)
To find out how this health safety lesson fits Physical Education and Health Education standards click here .
Newsletter sign-up
Be the first to know when new lessons come out.
Lesson Overview
This health safety lesson helps young people understand the equipment they need to stay safe during different sports and activities. They will color images of athletes and then label the different gear that keeps them safe.
Introduction
Explain to the youth that using the wrong or improperly fitted equipment is a major cause for injuries in playing games and sports. For example, playing tennis with a badly strung racquet while wearing worn-out shoes can be just as dangerous as playing football without shoulder pads!
Ask young people if they can think of any equipment they have used or have seen others wear while playing sports or doing other physical activities.
Remind young people during this health safety lesson , that before wearing protective equipment or playing, they should always check equipment for proper fit and replace worn -o ut equipment. For example, replace a child’s bike helmet if it:
- has been in a bike accident
- is damaged from being used (such as cracked or dented).
Activity: Staying Safe Coloring Sheet
Distribute the Staying Safe Coloring Sheet. As you walk through the different kinds of equipment below, have the youth color the athletes and label the different gear that keeps them safe.
Here are the “Most Valuable Pieces” of equipment that you s hould mention when teaching kids how to stay safe during physical activities .
- Always wear a helmet made for the sport you are playing.
- Bike helmets should have a CPSC sticker. The U.S. Consumer Product Safety Commission (CPSC) set up the federal safety standard that all bike helmets must meet. Helmets that meet this standard will have this sticker attached.
- Helmets should fit snugly but comfortably on your head and shouldn’t tilt backward or forward.
Eye Protection:
- Eye gear for sports is made from a plastic called polycarbonate.
- Facemasks, either a guard or shield, attached to helmets should also be made of polycarbonate.
- Goggles should be worn to cover prescription eyeglasses. You can also purchase prescription polycarbonate goggles.
Mouth Guards:
- Mouth guards can protect your mouth, teeth, and tongue.
- Mouth guards should be worn in contact sports.
- If you wear a retainer, always take it out before you start to exercise, practice or play.
Wrist, Knee, and Elbow Guards or Pads:
- You should wear guards or pads when doing any activity that requires moving on wheels, such as skateboarding.
- Guards or pads can prevent breaks, cuts, and absorb shock from falls.
- Guards or pads should fit snugly and comfortably.
Protective Cup
- Boys who play contact sports should wear a protective cup.
- Boys should wear an athletic supporter when playing non-contact sports that involve running.
- If you are unsure, ask your coach if you need a protective cup for your sport.
- Football, baseball, softball and soccer are some sports that require cleats.
- Skateboarding and biking have special types of shoes that are best for performing well.
- Replace cleat and shoes that have worn out or are no longer supportive.
Activity: Safety Tips
Here are a few other tips on how to stay safe during physical activities .
Warm Up for Injury-Free Play: Muscles that have not been warmed up the right way tend to be injured more easily.
- Start out with some light cardiovascular activities, such as easy jogging, jumping jacks, or brisk walking, to get your muscles moving and blood circulating.
- Follow your warm-up with some stretches. Stretching works best after a warm-up because your ligaments and tendons are more elastic (flexible) due to the increase in heat and blood flow to the muscle.
- Do not overdo your play, game, or sport. If you increase how often, how long or how hard you play too fast, you might see better performance at first, but this can lead to injuries later.
Stay Off the Court When You Are Hurt: If you have been injured and you try to come back too soon, you run the risk of re-injuring yourself – maybe even more seriously than before.
- Concussion: A concussion is a blow to the head that affects how the brain works. A concussion can also happen after a hit to the body that causes the head to move quickly back and forth. Because you cannot see this type of injury, it is easy to come back too soon from a concussion. Always listen to your doctor and get the OK from him or her to play again.
- Pain relief: Some athletes use pain relievers to avoid pain. Pain is your body’s way of signaling it is not happy with what you are doing. If you have pain, get treatment so you can fix what’s causing it.
The Rules of the Game: Rules are made to keep you and your teammates in the game and to avoid injuries. Follow all the rules to have a safe season.
- Rules are made to promote safety so that everyone can enjoy the game.
- You need to follow other rules even if they don’t relate to the sport. For example, if you are inline skating on a public street, pay strict attention to all traffic laws.
- You need to use the right techniques when playing a sport. This will help you or your opponent not get injured. For example, when playing football, always keep your head up when tackling, neck injuries are common when players tackle with head down. In hockey, high sticking is a violation because it can be dangerous to other players. The right technique would be to keep the stick below waist level. It is also important to use the right technique when lifting weights. This will keep you from holding your breath and possibly fainting.
Whether you are following rules, regulations, or proper techniques, remember that they are not there to restrict you, they are there to keep you safe and injury free.
At the end of this health safety lesson , a sk the young people to think of one way they will keep themselves safe during sports or other activities this week. If time permits, allow the youth to share their reflections. Conclude this lesson on health safety by reminding young people that rules and protective equipment are not there to restrict you, they are there to keep you safe and injury-free! Depend on Health Powered Kids for safe and simple exercises for children .
Continuing the Conversation
Hand out the Healthy Families Newsletter in English or Spanish , so that families can continue discussing ways they will stay safe during sports and other activities.
Additional Instructor Resources
Concussions in Sports: What You Should Know

Power Chargers
A set of quick activities to ignite bursts of energy. See all >
Q and A Stretching

Food and Fitness Freeze Frames

Heart Pumping Activity

Race in Place
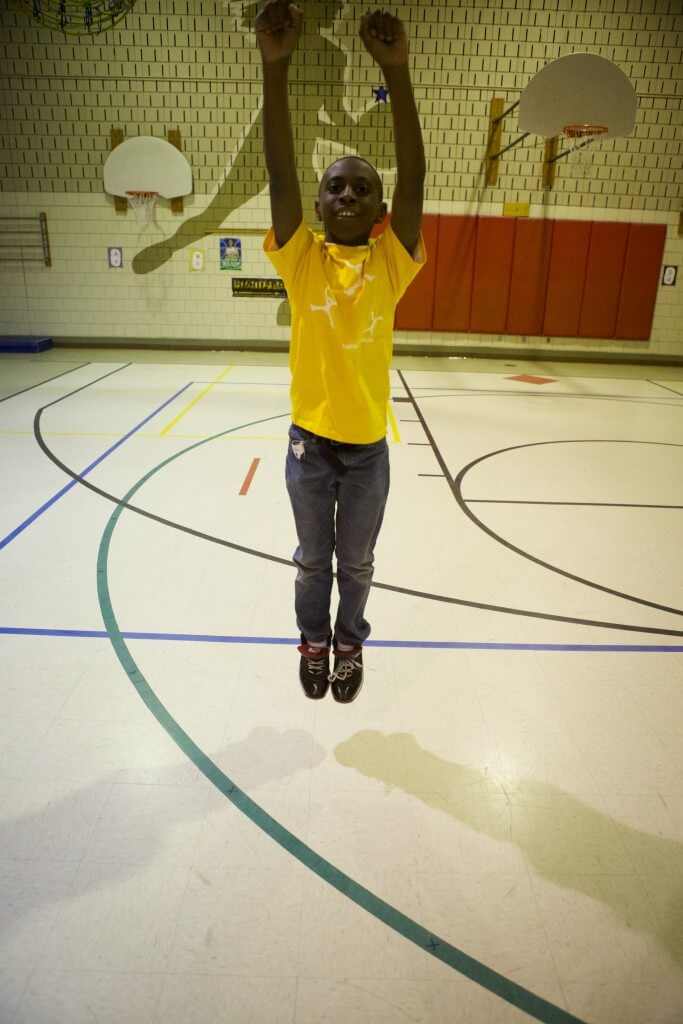
Sports Charades

Tricep Dips
This site is presented for information only and is not intended to substitute for professional medical advice. Health Powered Kids is a trademark of Allina Health System. Presentation and Design © 2015 Allina Health. All Rights Reserved.

Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
High Quality Physical Education
Appropriate actions must be taken in four main areas to ensure a high quality physical education program:
- Curriculum.
- Policies and environment.
- Instruction.
- Student assessment.
Policy and environmental actions that support high quality physical education require the following:
- Adequate instructional time (at least 150 minutes per week for elementary school students and 225 minutes per week for middle and high school students).
- All classes be taught by qualified physical education specialists.
- Reasonable class sizes.
- Proper equipment and facilities.
Instructional strategies that support high quality physical education emphasize the following:
- The need for inclusion of all students.
- Adaptations for students with disabilities.
- Opportunities to be physically active most of class time.
- Well-designed lessons.
- Out-of-school assignments to support learning.
- Not using physical activity as punishment.
Regular student assessment within a high quality physical education program features the following:
- The appropriate use of physical activity and fitness assessment tools.
- Ongoing opportunities for students to conduct self-assessments and practice self-monitoring of physical activity.
- Communication with students and parents about assessment results.
- Clarity concerning the elements used for determining a grading or student proficiency system.
A curriculum is a sequential system for delivering learning experiences to students. A physical education curriculum is the framework that provides guidance for teaching skills and providing physical activity instruction.
A high quality physical education curriculum will be based on the national standards in the document Moving Into the Future: National Standards for Physical Education ,1 which describes what a physically educated student should know and be able to do. It emphasizes meaningful content, which includes the following:
- Instruction in a variety of motor skills designed to enhance child and adolescent development.
- Fitness education and assessment that allows for understanding and improvement of physical well-being.
- Development of cognitive concepts related to motor skills and fitness.
- Opportunities to improve social and cooperative skills.
- Opportunities to increase the value placed on physical activity for health, enjoyment, self expression, and confidence.
Appropriate sequencing of learning activities is critical to developing a high quality physical education curriculum. Appropriate sequencing involves the following:
- Ensuring that motor skills, physical activity, and fitness assessments are age and developmentally appropriate.
- Methods of teaching motor and movement skills that ensure that basic skills lead to more advanced skills.
- Plans to appropriately monitor, reinforce, and prepare for student learning.
The effectiveness of school physical education is enhanced when it is implemented as an integral part of Whole School, Whole Community, Whole Child (WSCC) and when physical education outcomes are reinforced by other components of a school health program.
- National Association of Sport and Physical Education. Moving into the Future: National Standards for Physical Education . 2nd ed. Reston, VA: National Association for Sport and Physical Education; 2004.

Healthy Youth
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

IMAGES
VIDEO
COMMENTS
Physical education is the foundation of a Comprehensive School Physical Activity Program. 1, 2 It is an academic subject characterized by a planned, sequential K-12 curriculum (course of study) that is based on the national standards for physical education. 2-4 Physical education provides cognitive content and instruction designed to develop motor skills, knowledge, and behaviors for ...
Physical education as a discipline has long fought to be taken as seriously as its academic counterparts. Even before the pandemic, fewer than half the states set any minimum amount of time for students to participate in physical education, according to the Society of Health and Physical Educators (SHAPE), which represents PE and health ...
is defined as any physical activity done in the classroom. Classroom physical activity can take place at any time and occur in one or several brief periods of time during the school day. Classroom physical activity should be offered in addition to physical education and recess and at all school levels (elementary, middle, and high school).
Our guide delivers 35 varied activities perfect for energizing students and enriching your physical education classes. Experience an array of PE exercises, from fluid warm-up routines to imaginative obstacle courses, all designed to foster enthusiasm and physical well-being without complicated setups. Ideal for educators seeking practical ...
Physical education for healthier, happier, longer and more productive living. The time children and adults all over the world spend engaging in physical activity is decreasing with dire consequences on their health, life expectancy, and ability to perform in the classroom, in society and at work. In a new publication, Quality Physical Education ...
Although academic performance stems from a complex interaction between intellect and contextual variables, health is a vital moderating factor in a child's ability to learn.The idea that healthy children learn better is empirically supported and well accepted (Basch, 2010), and multiple studies have confirmed that health benefits are associated with physical activity, including ...
Physical education should be a cornerstone for a total of 60 minutes of physical activity before, during and after the school day. Physical education is the only physical activity-related policy or program that can reach and benefit all students - including students with disabilities.
8. Recommendations. This chapter presents the committee's recommendations for strengthening and improving programs and policies for physical activity and physical education in the school environment, including before, during, and after school.These recommendations were developed in accordance with the guiding principles outlined in Chapter 1, which included recognizing the benefits of ...
Physical education is a formal content area of study in schools that is standards based and encompasses assessment based on standards and benchmarks.It is defined in Chapter 1 as "a planned sequential K-12 standards-based program of curricula and instruction designed to develop motor skills, knowledge, and behaviors of healthy active living, physical fitness, sportsmanship, self-efficacy ...
Supporting Physical Education in Schools for All Youth. Date: Oct 26 2021. Policy Number: 20211. Key Words: Physical Activity, Education, School Health, Obesity. Abstract. This policy statement provides scientific evidence that schools are unique places where children should be engaged in physical activity.
Source: Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion. Children and adolescents should do 60 minutes (1 hour) or more of physical activity each day. Physical education benefits students by increasing their level of physical activity, improving their grades and test scores, and helping them ...
Move Your Way® Toolkit for Schools. This toolkit is for anyone working to encourage physical activity in a school setting — like physical education and health education teachers, classroom teachers, coaches, after-school program leaders, and school administrators. Others promoting student health and well-being — like school nurses and ...
Students that attend physical education are: Approximately 2-3 times more likely to be active outside of school.5. Almost twice as likely to continue to be active to a healthy level in adulthood.5. *Doing any kind of physical activity that increased their heart rate and made them breathe hard some of the time during the 7 days before the survey ...
While more can always be learned, the evidence for the health benefits of physical activity is irrefutable (HHS, 1996, 2008).Adults engaged in regular physical activity have lower rates of chronic disease (e.g., coronary heart disease, cardiovascular disease, type 2 diabetes, hypertension, osteoporosis, and some cancers) and are less likely to die prematurely (HHS, 1996, 2008; Bauman, 2004).
1/2 of U.S. high school students did not attend PE classes—which is consistent over the 24-year period studied (1991-2015). The percentage of U.S. high school students reporting PE attendance did not change significantly between 1991 and 2015 for the overall sample or across sex and race/ethnicity subgroup. Daily PE attendance did decrease 16 ...
Energizing Education: The Power of Brain Breaks in the Classroom; Includes 12 Practical Activities. 8. Increases personal fitness and motor skill development. Physical education is a prime outlet for kids and adolescents to intentionally develop both their health and skill-related components of fitness.
ALT-PE is the time in physical education class during which children are exposed to motor skill development, understanding of movement principles, attainment of health-enhancing levels of fitness, regular engagement in physical activity, socially responsible behaviors in physical activity settings, and an appreciation of the importance of ...
in the classroom. Classroom physical activity can take place at any time and occur in one or several brief periods of time during the school day. Classroom physical activity should be offered in addition to physical education and recess and at all school levels (elementary, middle, and high school). The two primary approaches for
taught in school is it give kids: regular fitness activity, builds self-confidence, develops motor. skills, health and nutrition, relieves stress, and considerations. Physical fitness is not only an. important component to living a healthy lifestyle; the teaching of physical education helps students maintain fitness.
2 Physical Activity Should Not Be Used as Punishment and/or Behavior Management Educators who use appropriate practices: 1. Promote a physically active lifestyle; 2. Provide a safe and inclusive learning environment, allowing students to experience positive, challenging, and enjoyable physical activity while learning about the benefits
It must be emphasized that, while school-based physical activity should be used to support physical activity in the school environment, it should not be used as a replacement for physical education, whose importance is explained in Chapter 5. REFERENCES. AAP (American Academy of Pediatrics). 2013. The crucial role of recess in school.
Activity: Safety Tips. Here are a few other tips on how to stay safe during physical activities. Warm Up for Injury-Free Play: Muscles that have not been warmed up the right way tend to be injured more easily. Start out with some light cardiovascular activities, such as easy jogging, jumping jacks, or brisk walking, to get your muscles moving ...
Appropriate actions must be taken in four main areas to ensure a high quality physical education program: Curriculum. Policies and environment. Instruction. Student assessment. Policy and environmental actions that support high quality physical education require the following: Adequate instructional time (at least 150 minutes per week for ...