- What Is Back Pain?
- Tests & Diagnosis
- Living With
- View Full Guide

An Overview of Spondylolisthesis

What Is Spondylolisthesis?
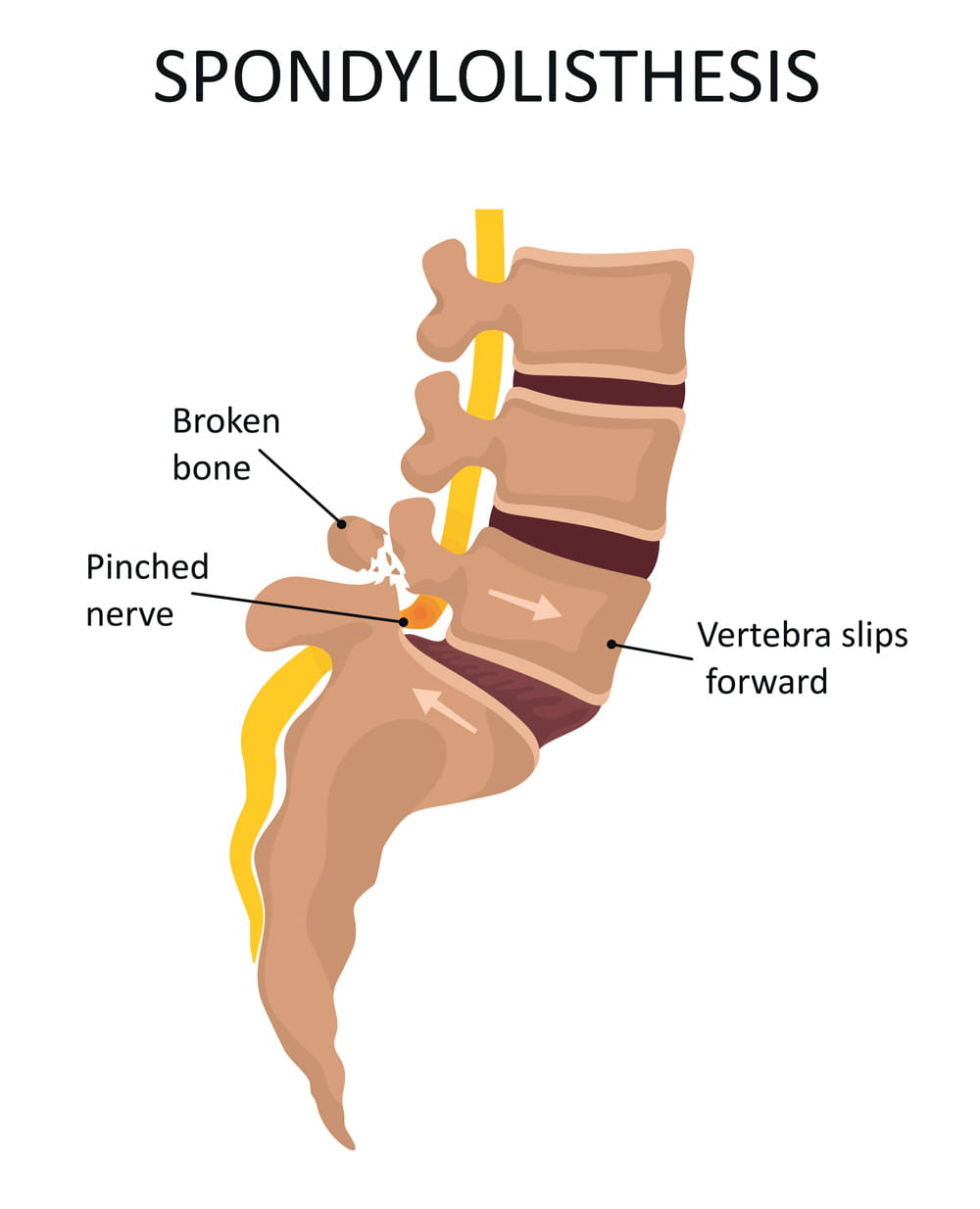
Spondylolisthesis (pronounced spahn-duh-low-liss-thee-sus) is a condition in which one of the bones in your spine (the vertebrae) slips out of place and moves on top of the vertebra next to it.
It usually happens at the base of your spine (lumbar spondylolisthesis). When the slipped vertebra puts pressure on a nerve, it can cause pain in your lower back or legs.
Spondylolisthesis Symptoms
Sometimes, people with this condition don't notice anything is wrong. But you can have symptoms that include:
- Lower back pain
- Muscle tightness and stiffness
- Pain in your buttocks
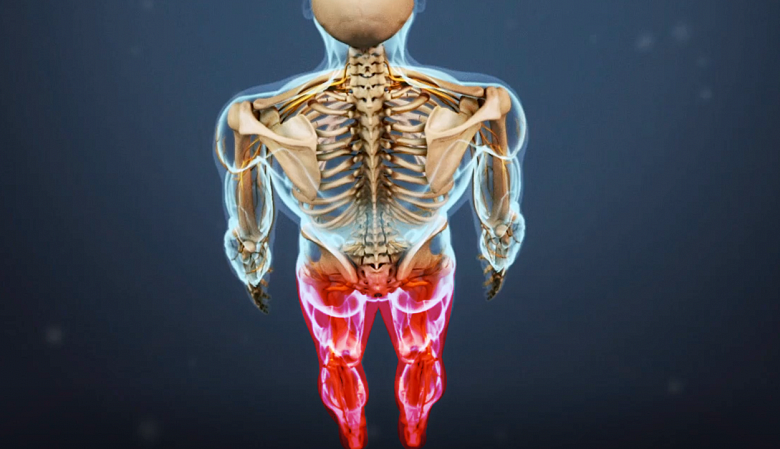
- Pain that spreads down your legs (due to pressure on nerve roots)
- Pain that gets worse when you move around
- Tight hamstrings (muscles in the back of your thighs)
- Trouble standing or walking
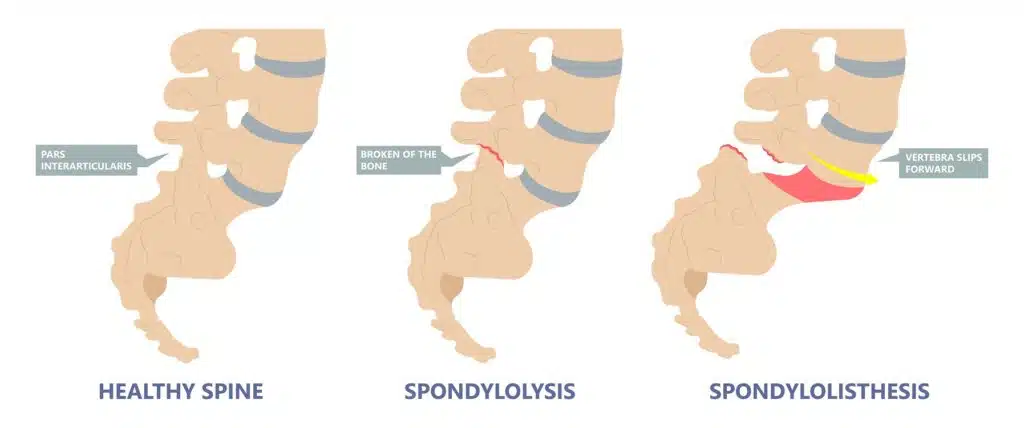
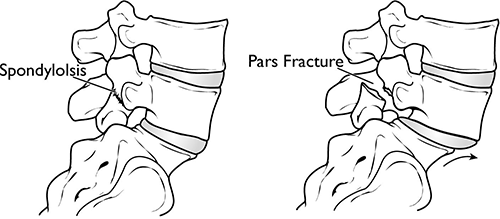
Spondylolisthesis vs. Spondylolysis
Spondylolysis (pronounced spahn-duh-loll-iss-us) and spondylolisthesis are different conditions of the spine, though they're sometimes related. Both conditions cause pain in your lower back .
Spondylolysis is a weakness or small fracture (crack) in one of your vertebrae. This usually affects your lower back, but it can also happen in the middle of your back or your neck. It's most often found in kids and teens, especially those involved in sports that repeatedly overstretch the lower spine, like football or gymnastics.
It's not uncommon for people with spondylolysis to also have spondylolisthesis. That's because the weakness or fracture in your vertebra may cause it to move out of place.
Types of Spondylolisthesis
Doctors divide this condition into six main types, determined by cause.
Degenerative spondylolisthesis: This is the most common type. As people age, the disks that cushion vertebrae can become worn, dry out, and get thinner. This makes it easier for the vertebra to slip out of place.
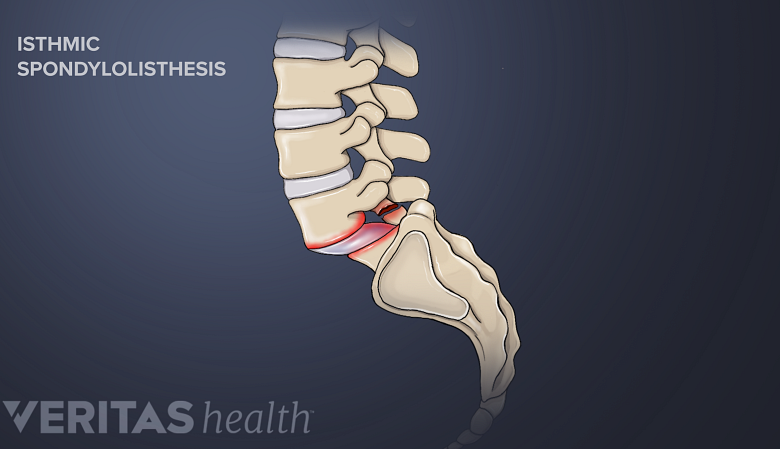
Isthmic spondylolisthesis: This type is caused by spondylosis. A crack in the vertebra can lead it to slip backward, forward, or over a bone below. It may affect kids and teens who do gymnastics, do weightlifting, or play football because they repeatedly overextend their lower backs. But it also sometimes happens when you're born with vertebrae whose bone is thinner than usual.
Congenital spondylolisthesis: Also known as dysplastic spondylolisthesis, this happens when your vertebrae are aligned incorrectly due to a birth defect.
Traumatic spondylolisthesis: In this type, an injury (trauma) to the spine causes the vertebra to move out of place.
Pathological spondylolisthesis: This type is caused by another spine condition, such as osteoporosis or a spinal tumor.
Postsurgical spondylolisthesis: Also called iatrogenic spondylolisthesis, this happens when a vertebra slips out of place after spinal surgery.
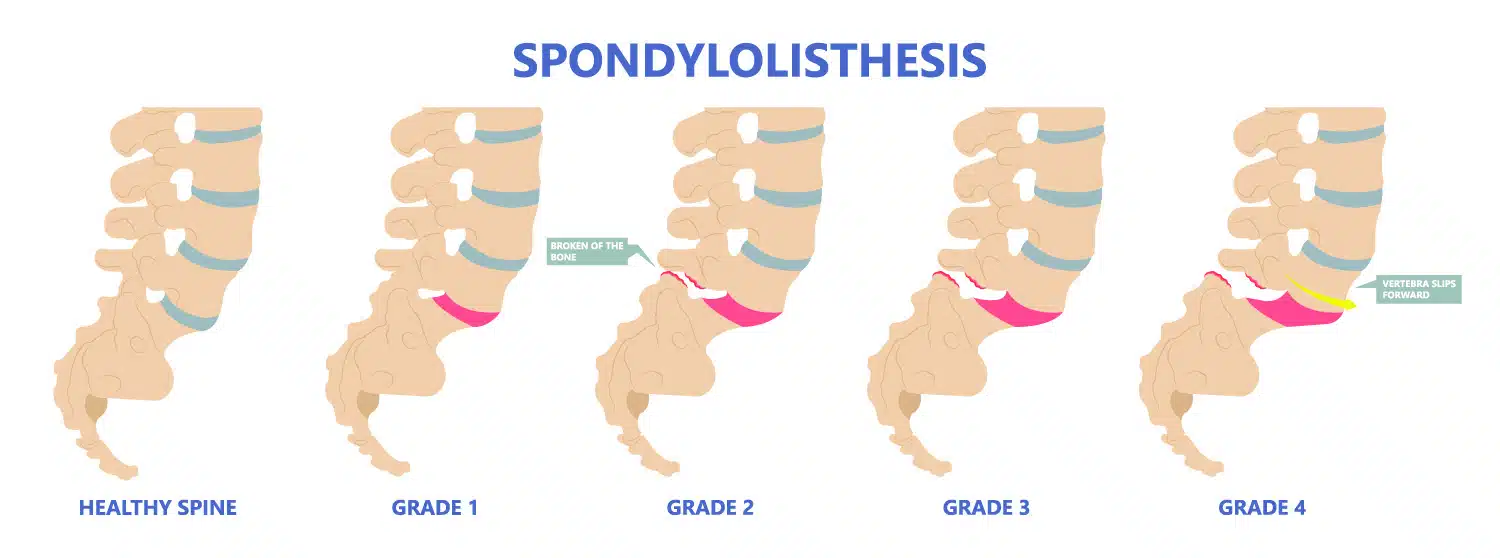
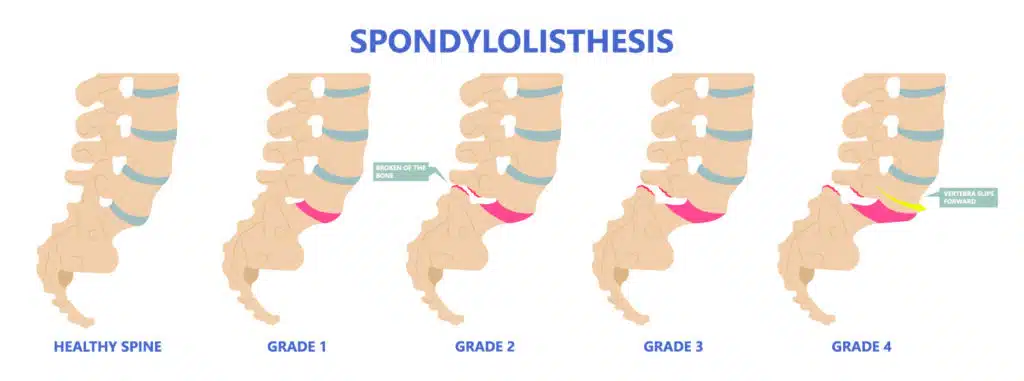
Grades of Spondylolisthesis
Your doctor may give your spondylolisthesis a grade based on how serious it is. The most common grading system is called Meyerding's classification and includes:
- Grade I : The most common grade, this is defined as 1%-25% slippage of the vertebra
- Grade II : Up to 50% slippage of the vertebra
- Grade III : Up to 75% slippage
- Grade IV : 76%-100% slippage
- Grade V : More than 100% slippage, also known as spondyloptosis
Grades I and II are considered low grade. Grades III and up are considered high grade.
Spondylolisthesis Causes and Risk Factors
Causes of spondylolisthesis include:
- Wear and tear with age
- Birth defects
- Spondylolysis
- Injury to the spine
- Another condition such as a spinal tumor or osteoporosis
- Spinal surgery
You're more likely to get this condition if you:
- Take part in sports that put stress on your spine
- Were born with thinner areas of vertebrae that are prone to breaking and slipping
- Are 50 or older
- Have a degenerative spinal condition
Spondylolisthesis Diagnosis
If your doctor thinks you might have this condition, they'll ask about your symptoms and run imaging tests to see if a vertebra is out of place. These tests may include:
These tests can also help your doctor determine a grade for your spondylolisthesis.
Spondylolisthesis Treatments
The treatment you'll need depends on what grade of spondylolisthesis you have, as well as your age, symptoms, and your medical history. Low grade can usually be treated with physical therapy or medications. With high grade, you may need surgery, especially if you're in a lot of pain.
Nonsurgical treatment options include:
- Rest : You may need to take some time off from sports and other vigorous activities.
- Medications : Your doctor may recommend over-the-counter anti-inflammatory medicines to relieve your pain, such as ibuprofen or naproxen.
- Injections : Steroid shots in the area where you have pain can bring relief.
- Physical therapy : Daily exercises that stretch and strengthen your supportive abdominal and lower back muscles can lower your pain.
- Braces : For children with fractures in the vertebrae (spondylolysis), a back brace can restrict movement so the fractures can heal.
Spondylolisthesis Surgery
If you have high-grade spondylolisthesis or if you still have serious pain and disability after nonsurgical treatments, you may need surgery. This usually means spinal decompression, often along with spinal fusion.
Spinal surgery is always done under general anesthesia , which means you're asleep during the operation.
Spinal decompression: Decompression lessens the pressure on the nerves in your spine to relieve pain. There are several techniques your surgeon can use to give your nerves more room. They may remove bone from your spine, take out part or all of a disk, or make the opening in your spinal canal larger. Your surgeon might need to use all these methods during your surgery.
Spinal fusion: In spinal fusion, the doctor joins, or fuses, the affected vertebrae together to prevent them from slipping again. After this surgery, you may have a bit less flexibility in your spine.
Pars repair: This surgery repairs fractures in the vertebrae using small wires or screws. Sometimes, a bone graft is used to reinforce the fracture so it can heal better.
After spinal surgery, you'll likely need to stay in the hospital for at least a day. Most people can go home within a week. You may be able to stand or even walk the day after the operation. You may go home with pain medication to ensure that your recovery is as easy as possible.
You'll need to limit physical activity for 8-10 weeks after your surgery so your spine can heal. But you should still move around and even walk every day. This can make your recovery go faster and help keep complications at bay.
Around 10-12 weeks after your surgery, you'll start physical therapy to stretch and strengthen your muscles and help you move more easily. Ideally, you should have physical therapy for a year.
For the first year after your surgery, you'll need to see your surgeon about every 3 months. You'll likely have X-rays taken at these follow-ups to make sure your spine is healing well.
Spondylolisthesis Complications
Serious spondylolisthesis sometimes leads to another condition called cauda equina syndrome . This is a serious condition in which nerve roots in part of your lower back called the cauda equina get compressed. It can cause you to lose feeling in your legs. It also can affect your bladder.
This is a medical emergency. If left untreated, cauda equina syndrome can lead to a loss of bladder control and paralysis.
See your doctor if you:
- Have trouble controlling your bladder or bowels
- Notice numbness or a strange sensation between your legs or on your buttocks, inner thighs, backs of your legs, feet, or heels
- Have pain or weakness in a leg or both legs that may cause stumbling
The symptoms may come on slowly and vary in how serious they are.
Spondylolisthesis Outlook
For most people, rest and nonsurgical treatments bring long-term relief within several weeks. But sometimes, spondylolisthesis comes back again after treatment. This happens more often when it was a higher grade.
If you've had surgery, you'll most likely do well afterward. Most people get back to normal activities within a few months. But your spine may not be as flexible as it was before.
Spondylolisthesis is when one of your vertebrae moves out of place. This sometimes leads to back pain and other symptoms. It can be usually treated with rest, medication, and/or physical therapy. But serious cases may require surgery.
Spondylolisthesis FAQs
What is the main cause of spondylolisthesis?
In adults, it most often happens when cartilage and bones in the spine become worn from conditions such as arthritis. It's more common in people age 50 and older. In kids and teens, the most common causes are either a spinal birth defect or injury to the spine.
Is spondylolisthesis a serious condition?
For most people, it's not serious. Many people have few symptoms or no symptoms at all. It's only a problem when it causes pain or limits your ability to move. If that happens, you'll need to see a doctor for treatment.

Top doctors in ,
Find more top doctors on, related links.
- Back Pain News
- Back Pain Reference
- Back Pain Slideshows
- Back Pain Quizzes
- Back Pain Videos
- Back Pain Medications
- Find a Neurologist
- Find a Pain Medicine Specialist
- WebMDRx Savings Card
- Ankylosing Spondylitis
- Drug Interaction Checker
- Osteoporosis
- Pain Management
- Pill Identifier
- Second Opinions
- SI Joint Pain
- More Related Topics
Spondylolisthesis: Definition, Causes, Symptoms, and Treatment
by Dave Harrison, MD • Last updated November 26, 2022
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
What is Spondylolisthesis?
The spine is comprised of 33 bones, called vertebra , stacked on top of each other interspaced by discs . Spondylolisthesis is a condition where one vertebra slips forward or backwards relative to the vertebra below. More specifically, retrolisthesis is when the vertebra slips posteriorly or backwards, and anterolisthesis is when the vertebra slips anteriorly or forward.
Spondylosis vs Spondylolisthesis
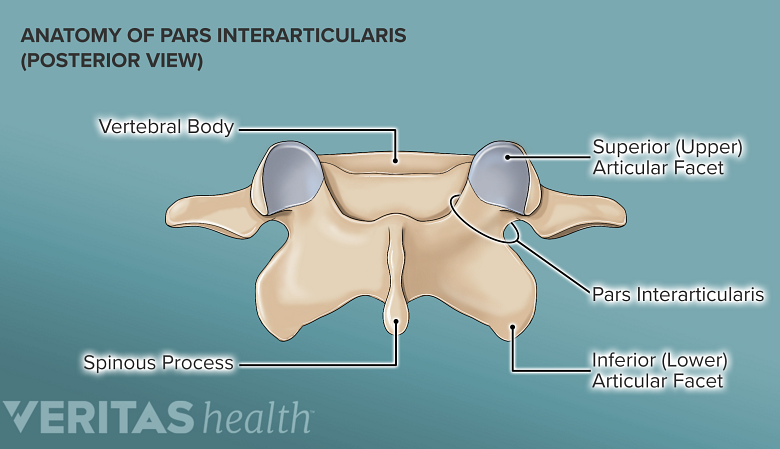
Spondylosis and Spondylolisthesis are different conditions. They can be related but are not the same. Spondylosis refers to a fracture of a small bone, called the pars interarticularis, which connects the facet joint of the vertebra to the one below. This may lead to instability and ultimately slippage of the vertebra. Spondylolisthesis, on the other hand, refers to slippage of the vertebra in relation to the one below.
Types and Causes of Spondylolisthesis
There are several types of spondylolisthesis, often classified by their underlying cause:
Degenerative Spondylolisthesis
Degenerative spondylolisthesis is the most common cause, and is due to general wear and tear on the spine. Overtime, the bones and ligaments which hold the spine together may become weak and unstable.
Isthmic Spondylolisthesis
Isthmic spondylolisthesis is the result of another condition, called “ spondylosis “. Spondylosis refers to a fracture of a small bone, called the pars interarticularis, which connects the facet joint of the vertebra to the one below. If this interconnecting bone is broken, it can lead to slippage of the vertebra. This can sometimes occur during childhood or adolsence but go unnoticed until adulthood when degenerative changes cause worsening slippage.
Congenital Spondylolisthesis
Congenital spondylolisthesis occurs when the bones do not form correctly during fetal development
Traumatic Spondylolisthesis
Traumatic spondylolisthesis is the result of an injury such as a motor vehicle crash
Pathologic Spondyloslisthesis
Pathologic spondylolisthesis is when other disorders weaken the points of attachment in the spine. This includes osteoporosis, tumors, or infection that affect the bones and ligaments causing them to slip.
Iatrogenic Spondylolisthesis
Iatrogenic spondylolisthesis is the result of a prior surgery. Some operations of the spine, such as a laminectomy, may lead to instability. This can cause the vertebra to slip post operatively.
Spondylolisthesis Grades
Spondylolisthesis is classified based on the degree of slippage relative to the vertebra below
- Grade 1 : 1 – 25 % forward slip. This degree of slippage is usually asymptomatic.
- Grade 2: 26 – 50 % forward slip. May cause mild symptoms such as stiffness and pain in your lower back after physical activity, but it’s not severe enough to affect your everyday activities.
- Grade 3 : 51 – 75 % forward slip. May cause moderate symptoms such as pain after physical activity or sitting for long periods.
- Grade 4: 76 – 99% forward slip. May cause moderate to severe symptoms.
- Grade 5: Is when the vertebra has slipped completely of the spinal column. This is a severe condition known as “spondyloptysis”.
Symptoms of Spondylolisthesis
Spondylolisthesis can cause compression of spinal nerves and in severe cases, the spinal cord. The symptoms will depend on which vertebra is affected.
Cervical Spondylolisthesis (neck)
- Arm numbness or tingling
- Arm weakness
Lumbar Spondylolisthesis (low back)
- Buttock pain
- Leg numbness or tingling
- Leg weakness
Diagnosing Spondylolisthesis
Your doctor may order imaging tests to confirm the diagnosis and determine the severity of your spondylolisthesis. The most common imaging tests used include:
- X-rays : X-rays can show the alignment of the vertebrae and any signs of slippage.
- CT scan: A CT scan can provide detailed images of the bones and soft tissues in your back, allowing your doctor to see any damage or abnormalities.
- MRI: An MRI can show the spinal cord and nerves, as well as any herniated discs or other soft tissue abnormalities.
Treatments for Spondylolisthesis
Medications.
For those experiencing pain, oral medications are first line treatments. This includes non-steroidal anti-inflammatory medications (NSAIDs) such as ibuprofen, acetaminophen, or in severe cases opioids or muscle relaxants (with extreme caution). Topical medications such as lidocaine patches are also sometimes used.
Physical Therapy
Physical therapy can help improve mobility and strengthen muscles around your spine to stabilize your neck and lower back. You may also receive stretching exercises to improve flexibility and balance exercises to improve coordination.
Surgery is reserved for severe cases of spondylolisthesis in which there is a high degree of instability and symptoms of nerve compression.
In these cases a spinal fusion may be necessary. This surgery joins two or more vertebra together using rods and screws, in order to improve stability.
Reference s
- Alfieri A, Gazzeri R, Prell J, Röllinghoff M. The current management of lumbar spondylolisthesis. J Neurosurg Sci. 2013 Jun;57(2):103-13. PMID: 23676859.
- Stillerman CB, Schneider JH, Gruen JP. Evaluation and management of spondylolysis and spondylolisthesis. Clin Neurosurg. 1993;40:384-415. PMID: 8111991.
About the Author
Dave Harrison, MD
Dr. Harrison is a board certified Emergency Physician with a part time appointment at San Francisco General Medical Center and is an Assistant Clinical Professor-Volunteer at the UCSF School of Medicine. Dr. Harrison attended medical school at Tufts University and completed his Emergency Medicine residency at the University of Southern California. Dr. Harrison manages the editorial process for SpineInfo.com.
- skip to Cookie Notice
- skip to Main Navigation
- skip to Main Content
- skip to Footer
- Find a Doctor
- Find a Location
- Appointments & Referrals
- Patient Gateway
- Español
- Leadership Team
- Quality & Safety
- Equity & Inclusion
- Community Health
- Education & Training
- Centers & Departments
- Browse Treatments
- Browse Conditions A-Z
- View All Centers & Departments
- Clinical Trials
- Cancer Clinical Trials
- Cancer Center
- Digestive Healthcare Center
- Heart Center
- Mass General for Children
- Neuroscience
Orthopaedic Surgery
- Information for Visitors
- Maps & Directions
- Parking & Shuttles
- Services & Amenities
- Accessibility
- Visiting Boston
- International Patients
- Medical Records
- Billing, Insurance & Financial Assistance
- Privacy & Security
- Patient Experience
- Explore Our Laboratories
- Industry Collaborations
- Research & Innovation News
- About the Research Institute
- Innovation Programs
- Education & Community Outreach
- Support Our Research
- Find a Researcher
- News & Events
- Ways to Give
- Patient Rights & Advocacy
- Website Terms of Use
- Apollo (Intranet)
- Like us on Facebook
- Follow us on Twitter
- See us on LinkedIn
- Print this page
Spondylolysis & Spondylolisthesis
Orthopaedic spine center.
- 617-724-8636
Contact Information
Phone: 617-724-8636 Fax: 617-726-7587
Our spine team sees patients at these locations:
Mass General - Boston 55 Fruit Street Yawkey Center for Outpatient Care, Suite 3A Boston, MA 02114
Orthopaedics at Mass General Brigham Healthcare Center (Waltham) 52 Second Avenue Building 52, 1st Floor, Suite 1150 Waltham, MA 02451
Newton-Wellesley Spine Center 159 Wells Avenue Newton, MA 02459
Mass General Brigham Healthcare Center (Danvers) 102-104 Endicott Street Danvers, MA 01923
Mass General Brigham Healthcare Center (20 Patriot Place, Foxborough) 20 Patriot Place Foxborough, MA 01923
Explore Spondylolysis & Spondylolisthesis
What is spondylolysis.
Spondylolysis is a condition when the fifth (last) vertebra of the lumbar (lower) spine is fractured.
What is Spondylolisthesis?
Spondylolisthesis is a condition when the spondylolysis (fracture of the fifth lumbar vertebra) weakens the bone so much that it cannot maintain proper position and vertebrae start to shift out of place.
Who is affected by Spondylolysis and Spondylolisthesis?
Adolescent athletes, especially football players, gymnasts and weight lifters, are prone to spondylolysis. Sports that require athletes to put a great deal of stress on their lower backs, and athletes that are required to constantly overextend their back are more prone to spondylolysis.
Symptoms of spondylolysis and spondylolisthesis often do not present right away, and when they do present, it can feel like muscle strain across the lower back. Spondylolisthesis can also cause muscle spasms.
After taking a medical history and performing a thorough physical exam, your doctor probably will request that you have an x-ray, CT scan or an MRI scan, which will be able to show the spondylolysis or spondylolisthesis.
Nonsurgical treatment
For most people with spondylolysis or spondylolisthesis, your doctor will try nonsurgical treatments first. Resting and taking a break from any sports or other physical activities is a good idea to give the fracture time to heal. Your doctor also might recommend physical therapy and exercise to strengthen muscles in your back and abdomen, which can help stabilize your spine. Anti-inflammatory medications (like ibuprofen) may be recommended to reduce pain, discomfort and inflammation.
In more severe cases, a back brace or back support might be used to stabilize the spine. And epidural steroid injections can help reduce inflammation and pain. The steroid is injected into the space surrounding the spine.
Surgical treatment
Surgery may be recommended if none of the nonsurgical treatment options help keep the pain at a tolerable level. Surgery for spondylolisthesis typically is a spinal fusion and sometimes involves screws and rods to hold everything together as the fusion heals. Another type of surgery that is used sometimes is called a vertebral body replacement.
Meet our Spine Team
Contact the orthopaedic spine center..
Have questions about spondylolysis & spondylolisthesis? Get in touch.
Spondylolisthesis
Spondylolisthesis is slippage of a lumbar vertebra in relation to the vertebra below it. Anterior slippage (anterolisthesis) is more common than posterior slippage (retrolisthesis). Spondylolisthesis has multiple causes. It can occur anywhere in the spine and is most common in the lumbar and cervical regions. Lumbar spondylolisthesis may be asymptomatic or cause pain when walking or standing for a long time. Treatment is symptomatic and includes physical therapy with lumbar stabilization.
There are five types of spondylolisthesis, categorized based on the etiology:
Type I, congenital: caused by agenesis of superior articular facet
Type II, isthmic: caused by a defect in the pars interarticularis (spondylolysis)
Type III, degenerative: caused by articular degeneration as occurs in conjunction with osteoarthritis
Type IV, traumatic: caused by fracture, dislocation, or other injury
Type V, pathologic: caused by infection, cancer, or other bony abnormalities
Spondylolisthesis usually involves the L3-L4, L4-L5, or most commonly the L5-S1 vertebrae.
Types II (isthmic) and III (degenerative) are the most common.
Type II often occurs in adolescents or young adults who are athletes and who have had only minimal trauma; the cause is a weakening of lumbar posterior elements by a defect in the pars interarticularis (spondylolysis). In most younger patients, the defect results from an overuse injury or stress fracture with the L5 pars being the most common level.
Type III (degenerative) can occur in patients who are > 60 and have osteoarthritis ; this form is six times more common in women than men.
Anterolisthesis requires bilateral defects for type II spondylolisthesis. For type III (degenerative) there is no defect in the bone.

ZEPHYR/SCIENCE PHOTO LIBRARY
Spondylolisthesis is graded according to the percentage of vertebral body length that one vertebra subluxes over the adjacent vertebra:
Grade I: 0 to 25%
Grade II: 25 to 50%
Grade III: 50 to 75%
Grade IV: 75 to 100%
Spondylolisthesis is evident on plain lumbar x-rays. The lateral view is usually used for grading. Flexion and extension views may be done to check for increased angulation or forward movement.
Mild to moderate spondylolisthesis (anterolisthesis of ≤ 50%), particularly in the young, may cause little or no pain. Spondylolisthesis can predispose to later development of foraminal stenosis . Spondylolisthesis is generally stable over time (ie, permanent and limited in degree).
Treatment of spondylolisthesis is usually symptomatic. Physical therapy with lumbar stabilization exercises may be helpful.

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Cookie Preferences

Neurology and Neurosurgery
- Spondylolisthesis: Individualized approach for optimal outcomes
March 27, 2021

High-grade spondylolisthesis has diverse etiologies and presentations, as well as multiple treatment options. Mayo Clinic spinal surgeons tailor treatment to the individual patient to maximize outcomes and avoid future revision surgery.
"We treat many patients who had surgery elsewhere that used inadequate sacral and pelvic fixation. Inadequate fixation leads to higher rates of failed fusion, which requires more-complex surgery to repair," says Jeremy L. Fogelson, M.D. , a neurosurgeon specializing in spine care at Mayo Clinic in Rochester, Minnesota. "When we perform an initial surgery for spondylolisthesis, we take a safe but aggressive approach to fixation if needed."

Treating complex curvature
Preoperative X-ray shows severe spinal curvature in a 30-year-old woman with high-grade congenital spondylolisthesis. She presented at Mayo Clinic with intractable back pain and leg pain, which did not resolve with nonoperative treatments.

Successful fusion
Postoperative X-ray shows treatment with a fusion from L4 to S1, including pelvic fixation with S2 alar-iliac screws, and fixation into L5 with S1 to L5 transdiscal screws. Her pain was resolved and the fusion successfully healed, with eventual removal of the iliac screws.
As a high-volume center, Mayo Clinic regularly sees children and adults with congenital or degenerative spondylolisthesis. Full-body electro-optical system (EOS) imaging, a low-radiation X-ray technology, is routinely used for diagnosis. Mayo Clinic, which has a long history of imaging expertise, was among the first centers in the United States to offer EOS .
" EOS allows us to evaluate the entire spine as well as whole-body and leg alignment," Dr. Fogelson says. "We can factor in all features — cervical spine misalignment, bent knees or hips, leg-length discrepancy — into our treatment plan."
If surgery is needed, Mayo Clinic bases the approach not on a surgeon's preference but on the patient's condition. "We are able to perform the fusion posteriorly, anteriorly or laterally, or in some combination, depending on the individual patient's needs," Dr. Fogelson says. Less invasive surgical techniques also can be used.
In addition to neurosurgeons, Mayo Clinic's spondylolisthesis care team includes specialists in neurology, physical medicine and rehabilitation, and pain medicine. "We work from the beginning of each case with our colleagues in those specialties, to make sure we've maximized any nonoperative treatment possibilities," Dr. Fogelson says.
If surgery is needed, Mayo Clinic's neurosurgeons and orthopedic surgeons routinely collaborate on complex spinal procedures. 3D spinal navigation can be used to guide the placement of spinal hardware, and intraoperative CT checks screw placement. All members of the care team have spinal deformity expertise, including nurses and anesthesiologists dedicated to caring for patients during complex spinal procedures.
Mayo Clinic also works to learn more about optimal surgical approaches to spondylolisthesis. Within the field of spinal surgery, iliac fixation has sometimes been avoided, due to concerns about screws loosening over time and eventually requiring surgical removal related to pain. To investigate one aspect of this issue, Mayo Clinic is participating in a multicenter clinical trial comparing the outcomes of patients having multilevel lumbar fusion with or without simultaneous sacroiliac joint fusion.
Postoperative rehabilitation is an important aspect of treatment. At Mayo Clinic, rehabilitation care is provided by specialists in pain medicine and in physical medicine and rehabilitation, as well as physical and occupational therapists who routinely work with people who have had spinal deformity surgery.
A commitment to rehabilitation, combined with skilled surgical techniques, allows for positive results from spondylolisthesis surgery. "People facing lumbar fixation surgery often worry about loss of motion in the spine and further disability," Dr. Fogelson says. "But once the pain generator is fixed, most patients gain function. Spinal fusion can have very good outcomes when performed well and for the right reasons."
For more information
SI-BONE Inc. SI Joint Stabilization in Long Fusion to the Pelvis (SILVIA). ClinicalTrials.gov.
Receive Mayo Clinic news in your inbox.
- Medical Professionals
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.

- See All Locations
- Primary Care
- Urgent Care Facilities
- Emergency Rooms
- Surgery Centers
- Medical Offices
- Imaging Facilities
- Browse All Specialties
- Diabetes & Endocrinology
- Digestive & Liver Diseases
- Ear, Nose & Throat
- General Surgery
- Neurology & Neurosurgery
- Obstetrics & Gynecology
- Orthopaedics
- Pain Medicine
- Pediatrics at Guerin Children’s
- Urgent Care
- Medical Records Request
- Insurance & Billing
- Pay Your Bill
- Advanced Healthcare Directive
- Initiate a Request
- Help Paying Your Bill
Spondylolisthesis
Spondylolisthesis is a displacement of a vertebra in which the bone slides out of its proper position onto the bone below it. Most often, this displacement occurs following a break or fracture.
Surgery may be necessary to correct the condition if too much movement occurs and the bones begin to press on nerves.
Other complications may include:
- Chronic back pain
- Sensation changes
- Weakness of the legs
- Temporary or permanent damage of spinal nerve roots
- Loss of bladder control
When a vertebra slips out of proper alignment, discs can be damaged. To surgically correct this condition, a spinal surgeon removes the damaged disc. The slipped vertebra is then brought back into line, relieving pressure on the spinal nerve.
Types of spondylolisthesis include:
- Dysplastic spondylolisthesis , caused by a defect in part of the vertebra
- Isthmic spondylolisthesis , may be caused by repetitive trauma and is more common in athletes exposed to hyperextension motions
- Degenerative spondylolisthesis , occurs with cartilage degeneration because of arthritic changes in the joints
- Traumatic spondylolisthesis , caused by a fracture of the pedicle, lamina or facet joints as a result of direct trauma or injury to the vertebrae
- Pathologic spondylolisthesis , caused by a bone defect or abnormality, such as a tumor
Symptoms may vary from mild to severe. In some cases, there may be no symptoms at all.
Spondylolisthesis can lead to increased lordosis (also called swayback), and in later stages may result in kyphosis, or round back, as the upper spine falls off the lower.
Symptoms may include:
- Lower back pain
- Muscle tightness (tight hamstring muscle)
- Pain, numbness or tingling in the thighs and buttocks
- Tenderness in the area of the vertebra that is out of place
- Weakness in the legs
- Stiffness, causing changes in posture and gait
- A semi-kyphotic posture (leaning forward)
- A waddling gate in advanced cases
- Lower-back pain along the sciatic nerve
- Changes in bladder function
Spondylolisthesis may also produce a slipping sensation when moving into an upright position and pain when sitting and trying to stand.
Spondylolisthesis may appear in children as the result of a birth defect or sudden injury, typically occurring between the fifth bone in the lower back (lumbar vertebra) and the first bone in the sacrum (pelvis).
In adults, spondylolisthesis is the result of abnormal wear on the cartilage and bones from conditions such as arthritis , trauma from an accident or injury, or the result of a fracture, tumor or bone abnormality.
Sports that place a great deal of stress on bones may cause additional deterioration, fractures and bone disease, which may cause the bones of the spine to become weak and shift out of place.
A simple X-ray of the back will show any cracks, fractures or vertebrae slippage that are the signs of spondylolisthesis.
A CT scan or an MRI may be used to further diagnose the extent of the damage and possible treatments.
Treatment for spondylolisthesis will depend on the severity of the vertebra shift. Stretching and exercise may improve some cases as back muscles strengthen.
Non-invasive treatments include:
- Heat/Ice application
- Pain medicine (Tylenol and/or NSAIDS)
- Physical therapy
- Epidural injections
Surgery may be needed to fuse the shifted vertebrae if the patient has:
- Severe pain that does not get better with treatment
- A severe shift of a spine bone
- Weakness of muscles in a leg or both legs
Surgical process realigns the vertebrae, fixing them in place with a small rod that is attached with a pedicle screw, adding stability to the spine with or without the addition to an interbody (bone graft or cage) placed between the vertebra from the side or front.
Choose a doctor and schedule an appointment.
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.
(1-800-233-2771)
Available 7 days a week, 6 am - 9 pm PT
Expert Care for Life™ Starts Here
Looking for a physician.
- Spondylolysis and Spondylolisthesis
By: Adaku Nwachuku, DO, Physiatrist
Peer-Reviewed
Spondylolysis refers to a defect in the short, flat strip of bone called pars interarticularis (or pars). The pars is located at the back of the spine and forms a bridge (or isthmus) between the upper and lower joint surfaces of each facet of a vertebra (spinal bone).

Show Transcript
Lumbar spondylolysis is a condition in the lower back where there is a defect or fracture in the part of the vertebra known as the pars interarticularis. The pars interarticularis, also known as the isthmus, is a segment of bone that connects the facet joints at the back of the spine. It is a small, thin part of the lamina that has a poor blood supply, which makes it susceptible to stress fractures.
Fractures of the pars interarticularis, known as spondylolysis, usually occur at the L5-S1 level,and rarely at L4-L5 or higher. They can occur on one side of the vertebra or on both.
Spondylolysis usually occurs in children between the ages of 5 and 7. It is sometimes called the “gymnastics fracture” because it is associated with sports that require a lot of bending backward. It is thought that repetitive stress on the spine has a cumulative effect that causes the pars interarticularis to break.
Spondylolysis sometimes causes spondylolisthesis, which is when one vertebra slips forward on the vertebra below it.
Symptoms include a deep ache in the lower back, pain that is worse with movement, and tightness in the hamstrings. If the vertebral slippage is severe, nerve roots can be compressed.
However, most people do not experience symptoms from lumbar spondylolysis at all, and those who do tend to develop problems in adulthood or in adolescence.
Spondylolisthesis is a condition where a vertebra slips forward over the vertebra below it. When spondylolisthesis occurs due to spondylolysis, the condition is called isthmic spondylolisthesis .
Spondylolysis and isthmic spondylolisthesis rarely cause pain, but when symptoms do occur, they typically affect children and adolescents. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/ , 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/ , 3 Mikhael MM, Shapiro GS, Wang JC. High-grade adult isthmic L5-s1 spondylolisthesis: a report of intraoperative slip progression treated with surgical reduction and posterior instrumented fusion. Global Spine J. 2012;2(2):119-124. doi:10.1055/s-0032-1307257 Spondylolysis occurs in the lumbar spine (low back) and primarily affects the L5 vertebra. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
In This Article:
- Symptoms and Diagnosis of Spondylolysis
- Spondylolysis Treatment
Lumbar Spondylolysis Video
Understanding spondylolysis.
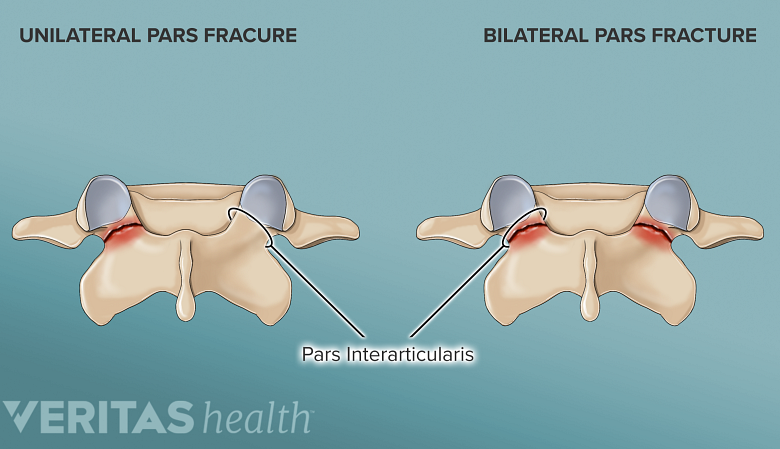
A stress fracture of the pars can occur on one side or both sides.
Spondylolysis occurs when a stress fracture in the pars does not fuse or heal completely as a part of the bone’s natural healing process, leaving the bone permanently split into two pieces. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Research shows that the pars is subjected to the greatest force compared to any other structure in the lumbar spine, making it vulnerable to stress fractures. In susceptible individuals, the pars may fracture, heal, and fracture again—repeatedly. 4 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
The fracture can involve the right pars, left pars, or both. Pars fractures involving both sides (also called bilateral fractures) are more common than one-sided (or unilateral) fractures. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
A stress fracture of the pars can occur as a result of 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/ , 4 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/ :
- Hereditary causes that make the pars more likely to fracture
- Weak bone tissue in the pars that is present at birth (congenital)
- Abnormally long pars bone
- Sudden trauma to the spine
The condition is more common in genetically susceptible children and adolescents who frequently participate in activities or sports that involve repeated forward bending and rotation of the spine. These actions, coupled with the genetic defect or weak bone tissue, cause excessive microtrauma to the growing, immature pars interarticularis, leading to a fracture. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Classic Symptoms and Signs of Spondylolysis
A dull ache in the lower back and buttock area is a common symptom of spondylolysis.
Spondylolysis pain feels like a dull ache that spans across the low back area. The buttocks and the back of the thigh may also feel sore, and the muscles in these areas tend to feel stiff or tight. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Bending backward or performing twisting movements increases spondylolysis pain in the low back. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
If there is associated isthmic spondylolisthesis, the symptoms may differ and include nerve pain, tingling, and leg weakness based on the severity of the vertebral slippage and spinal nerve compression. 4 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
See Isthmic Spondylolisthesis Symptoms
Spondylolysis Causes and Risk Factors
Activities and sports that have a high impact on the spine may cause pars fractures.
In addition to those with high genetic susceptibility, the following individuals are also likely to be affected by spondylolysis 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/ :
- Males (spondylolysis is twice as likely to occur in males than females)
- Children who are diagnosed with abnormal bone and nerve conditions such as spina bifida occulta, Marfan syndrome, or osteogenesis imperfecta
- Adolescents who are actively involved in high-impact sports
- Adults diagnosed with spinal osteopetrosis (weak, brittle bone)
Spondylolysis is usually identified during adolescence, around the age of 15, when symptoms start to manifest. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Specific sports that increase the likelihood of a pars fracture are 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/ :
- Gymnastics and weightlifting
- Football, soccer, and rugby
- Basketball and volleyball
- Swimming (butterfly and breaststroke)
Approximately 4% of 6-year-old children and 6% of teenagers aged 14 have this condition. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Progression of Spondylolysis to Isthmic Spondylolisthesis
When spondylolysis causes the vertebra to slip forward, it results in spondylolisthesis.
When a bilateral stress fracture of the pars interarticularis does not heal, the affected vertebra becomes incapable of bearing the heavy loads of the spine, causing the upper and lower surfaces of the facet joints to disconnect and separate. This separation makes the vertebra lose connection with the rest of the spine, resulting in isthmic spondylolisthesis – a forward slippage of the vertebral body, typically in a horizontal pattern. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Spondylolysis typically impacts the L5 vertebra in approximately 90% of cases, and if the condition progresses, L5 slips over S1. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
If only one of the pars interarticularis bone gets fractured (unilateral spondylolysis), the condition does not progress to isthmic spondylolisthesis. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
While spondylolysis is more common in adolescent males, the progression to isthmic spondylolisthesis is more common in adolescent females. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Spondylolisthesis can also occur due to degenerative changes in the spine ( degenerative spondylolisthesis ), trauma (traumatic spondylolisthesis), or bone diseases, such as spinal cancer (pathologic spondylolisthesis).
Why Spondylolysis Is More Common in Adolescents
The bone along the outer side of the upper joint surface of the facets has a small, rounded projection called the mammillary process. This bony projection serves as an attachment point for the thin strips of deep spinal multifidi muscles, which stabilize the facet joints and provide stability to the spine. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
The mammillary process is not completely formed until the age of 25, making the facet joint complex (which includes the pars) vulnerable to injury. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
A similar structure called the neural arch (an arch of bone at the back of a vertebra) also does not develop until the age of 25, contributing to the risk of spondylolysis and subsequent spondylolisthesis. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Progression to spondylolisthesis is less likely to occur in adults compared to adolescents. 5 Gagnet P, Kern K, Andrews K, Elgafy H, Ebraheim N. Spondylolysis and spondylolisthesis: A review of the literature. J Orthop. 2018 Mar 17;15(2):404-407. doi: 10.1016/j.jor.2018.03.008. PMID: 29881164; PMCID: PMC5990218.
The Course of Spondylolysis
Spondylolysis is not considered a serious condition and typically has an excellent long-term outlook when treated appropriately. For individuals with no symptoms, treatment, activity restriction, or other precautions are not needed. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
How long spondylolysis takes to heal
For symptomatic patients, complete healing generally occurs within 6 to 12 weeks of nonsurgical treatments. One-sided pars fractures heal sooner than bilateral fractures. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
In cases that have progressed to spondylolisthesis, the bone may not heal completely but the symptoms usually subside with treatment. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Return to work or play after spondylolysis
Over 75% of patients achieve complete relief from their symptoms with nonsurgical treatments. 1 , In adolescents, the healing process is more favorable, with approximately 92% of adolescent athletes returning to competitions after conservative treatment. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Surgery for spondylolysis is rare and when considered, about 90% of young athletes have a successful return to sports activities. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Potential complications of spondylolysis
While rare, if left untreated, spondylolysis may progress to spondylolisthesis and subsequent nerve or spinal cord damage if the vertebral slippage is severe. 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
Spondylolysis may also accelerate the progression of co-occurring degenerative spinal conditions, such as degenerative disc disease and spondylosis, potentially leading to severe spinal stenosis and lumbar radiculopathy . 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
When to See a Doctor for Spondylolysis
Progressive weakness and numbness in the legs may require immediate medical attention.
Certain red flags suggest potential complications or severe underlying issues associated with spondylolysis and must be evaluated immediately by a medical professional. These signs and symptoms include but are not limited to:
- Progressive neurological symptoms. Progressive weakness, numbness, or tingling in the legs, or feet may indicate severe nerve compression due to spondylolysis-related spinal instability.
- Unrelenting pain. Experiencing intense and unrelenting back pain, especially after a traumatic event or fall, indicates a more serious injury or fracture.
- Bowel or bladder dysfunction. Difficulty controlling bowel or bladder movements, or experiencing urinary or fecal incontinence, may indicate cauda equina syndrome , a rare but severe complication of spondylolysis that requires urgent medical attention.
- Sudden worsening of symptoms. If the existing symptoms suddenly intensify, it could indicate a significant progression of the condition or a related complication.
- Pain at rest or night pain. Pain that persists when resting or worsens at night might indicate a more severe underlying problem, such as a spinal tumor .
- Fever or signs of infection. Fever, chills, and signs of infection (redness, swelling, or a discharge) around the back area may suggest an infection in the spine , which requires urgent medical assessment and treatment.
Recognizing these red flag signs and symptoms is vital to ensure timely intervention and prevent potential complications associated with spondylolysis.
See When Back Pain May Be a Medical Emergency
Medical Professionals Who Treat Spondylolysis
If spondylolysis is suspected, it is advisable to consult with a qualified healthcare professional for a thorough evaluation and personalized treatment plan. Physiatrists (PM&R specialists), sports management specialists, orthopedic surgeons, physical therapists, and chiropractors have specialized training in managing musculoskeletal disorders and can effectively treat spondylolysis and spondylolisthesis.
- 1 McDonald BT, Hanna A, Lucas JA. Spondylolysis. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513333/
- 2 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
- 3 Mikhael MM, Shapiro GS, Wang JC. High-grade adult isthmic L5-s1 spondylolisthesis: a report of intraoperative slip progression treated with surgical reduction and posterior instrumented fusion. Global Spine J. 2012;2(2):119-124. doi:10.1055/s-0032-1307257
- 4 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
- 5 Gagnet P, Kern K, Andrews K, Elgafy H, Ebraheim N. Spondylolysis and spondylolisthesis: A review of the literature. J Orthop. 2018 Mar 17;15(2):404-407. doi: 10.1016/j.jor.2018.03.008. PMID: 29881164; PMCID: PMC5990218.
Dr. Adaku Nwachuku is a physiatrist with Privium Consultants, where she specializes in treating musculoskeletal and spine pain. Dr. Nwachuku has been published in the Oxford Handbook of Physical Medicine & Rehabilitation as well as in several medical journals. She also coordinates and participates in medical missions to Nigeria.
- Spondylolysis and Spondylolisthesis "> Share on Facebook
- Spondylolysis and Spondylolisthesis "> Share on Pinterest
- Spondylolysis and Spondylolisthesis "> Share on X
- Subscribe to our newsletter
- Print this article
- Spondylolysis and Spondylolisthesis &body=https://www.spine-health.com/conditions/spondylolisthesis/spondylolysis-and-spondylolisthesis&subject= Spondylolysis and Spondylolisthesis "> Email this article
Editor’s Top Picks
Isthmic spondylolisthesis symptoms, spinal fusion surgery for isthmic spondylolisthesis, isthmic spondylolisthesis video, answers to common spondylosis questions, degenerative spondylolisthesis video.
Popular Videos

Sciatica Causes and Symptoms Video

Cervical Disc Replacement Surgery Video

Lower Back Strain Video

3 Gentle Stretches to Prevent Neck Pain Video
Undergoing a Spinal Fusion?
Learn how bone growth stimulation therapy can help your healing process
Sponsored by Orthofix
Health Information (Sponsored)
- Learn How Bone Growth Therapy Can Help You
- Don't Push Through the Pain: Contact the Experts at Cedars-Sinai
- Suffering from Lumbar Spinal Stenosis? Obtain Long Term Pain Relief
- Take the Chronic Pain Quiz
Utility Menu
- Request an Appointment
Popular Searches
- Adult Primary Care
Orthopedic Surgery
Spondylolisthesis.
Select your language:
In spondylolisthesis, one of the bones in your spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar spine). In some people, this causes no symptoms at all. Others may have back and leg pain that ranges from mild to severe.
(Left) In spondylolysis, a fracture often occurs at the pars interarticularis. (Right) Because of the pars fracture, only the front part of the bone slips forward.
What are the different types of spondylolisthesis?
Many types of spondylolisthesis can affect adults. The two most common types are degenerative and spondylolytic. There are other less common types of spondylolisthesis, such as slippage caused by a recent, severe fracture or a tumor.
What is degenerative spondylolisthesis?
As we age, general wear and tear causes changes in the spine. Intervertebral discs begin to dry out and weaken. They lose height, become stiff, and begin to bulge. This disc degeneration is the start to both arthritis and degenerative spondylolisthesis (DS).
As arthritis develops, it weakens the joints and ligaments that hold your vertebrae in the proper position. The ligament along the back of your spine (ligamentum flavum) may begin to buckle. One of the vertebrae on either side of a worn, flattened disc can loosen and move forward over the vertebra below it. This can narrow the spinal canal and put pressure on the spinal cord. This narrowing of the spinal canal is called spinal stenosis and is a common problem in patients with DS.
Women are more likely than men to have DS, and it is more common in patients who are older than 50. A higher incidence has been noted in the African-American population.
What is spondylolytic spondylolisthesis?
One of the bones in your lower back can break and this can cause a vertebra to slip forward. The break most often occurs in the area of your lumbar spine called the pars interarticularis.
In most cases of spondylolytic spondylolisthesis, the pars fracture occurs during adolescence and goes unnoticed until adulthood. The normal disc degeneration that occurs in adulthood can then stress the pars fracture and cause the vertebra to slip forward. This type of spondylolisthesis is most often seen in middle-aged men.
Because a pars fracture causes the front (vertebra) and back (lamina) parts of the spinal bone to disconnect, only the front part slips forward. This means that narrowing of the spinal canal is less likely than in other kinds of spondylolisthesis, such as DS in which the entire spinal bone slips forward.
What are the symptoms of degenerative spondylolisthesis?
Patients with DS often visit the doctor's office once the slippage has begun to put pressure on the spinal nerves. Although the doctor may find arthritis in the spine, the symptoms of DS are typically the same as symptoms of spinal stenosis. For example, DS patients often develop leg and/or lower back pain. The most common symptoms in the legs include a feeling of vague weakness associated with prolonged standing or walking.
Leg symptoms may be accompanied by numbness, tingling, and/or pain that is often affected by posture. Forward bending or sitting often relieves the symptoms because it opens up space in the spinal canal. Standing or walking often increases symptoms.
What are the symptoms of spondylolytic spondylolisthesis?
Most patients with spondylolytic spondylolisthesis do not have pain and are often surprised to find they have the slippage when they see it in x-rays. They typically visit a doctor with low back pain related to activities. The back pain is sometimes accompanied by leg pain.
How is a spondylolisthesis diagnosed?
Doctors diagnose both DS and spondylolytic spondylolisthesis using the same examination tools.
After discussing your symptoms and medical history, your doctor will examine your back. This will include looking at your back and pushing on different areas to see if it hurts. Your doctor may have you bend forward, backward, and side- to-side to look for limitations or pain.
Other tests which may help your doctor confirm your diagnosis include:
X-rays. These tests visualize bones and will show whether a lumbar vertebra has slipped forward. X-rays will show aging changes, like loss of disc height or bone spurs. X-rays taken while you lean forward and backward are called flexion-extension images. They can show instability or too much movement in your spine.
Magnetic resonance imaging (MRI). This study can create better images of soft tissues, such as muscles, discs, nerves, and the spinal cord. It can show more detail of the slippage and whether any of the nerves are pinched.
Computed tomography (CT). These scans are more detailed than x-rays and can create cross-section images of your spine.
How is spondylolisthesis treated without surgery?
Although nonsurgical treatments will not repair the slippage, many patients report that these methods do help relieve symptoms.
Physical therapy and exercise . Specific exercises can strengthen and stretch your lower back and abdominal muscles.
Medication . Pain killers and non-steroidal anti-inflammatory medicines may relieve pain.
Steroid injections . Cortisone is a powerful anti-inflammatory. Cortisone injections around the nerves or in the "epidural space" can decrease swelling, as well as pain. It is not recommended to receive these, however, more than three times per year. These injections are more likely to decrease pain and numbness, but will not relieve weakness of the legs.
When should someone with degenerative spondylolisthesis be treated with surgery?
Patients should consider surgery for degenerative spondylolisthesis if they have tried the nonsurgical treatments for 3 to 6 months with no improvement.
Before committing to surgery, your provider will take a close look at the extent of the arthritis in your spine and whether your spine has excessive movement.
DS patients who are candidates for surgery are usually not able to walk or stand, and have a poor quality of life due to the pain and weakness.
When should someone with spondylolytic spondylolisthesis be treated with surgery?
Patients should consider surgery for spondylolytic spondylolisthesis if they have tried the nonsurgical treatments for at least 6 to 12 months with no improvement.
If the slippage is getting worse or the patient has progressive neurologic symptoms, such as weakness, numbness, or falling, and/or symptoms of cauda equina syndrome, surgery may help.
How is spondylolisthesis treated with surgery?
Surgery for both DS and spondylolytic spondylolisthesis includes removing the pressure from the nerves and spinal fusion.
Removing the pressure involves opening up the spinal canal. This procedure is called a laminectomy. Spinal fusion is essentially a "welding" process. The basic idea is to fuse together the painful vertebrae so that they heal into a single, solid bone.
Departments and Programs Who Treat This Condition
Spine surgery.

Popular Services
- Patient & Visitor Guide

Committed to improving health and wellness in our Ohio communities.
Health equity, healthy community, classes and events, the world is changing. medicine is changing. we're leading the way., featured initiatives, helpful resources.
- Refer a Patient
Spondylolisthesis
We design a unique treatment plan for your condition of spondylolisthesis and take into account your life goals., what is spondylolisthesis.
Low back pain, leg pain and weakness in the legs can happen if the bone that’s out of position significantly narrows the spinal column and begins to press on nerves.
Causes of spondylolisthesis
- Birth defect of the vertebral joint – This usually occurs in the lower spine where the lumbar spine and sacrum come together
- Stress “micro-fracture” in the bone due to overstretching and overuse – This can occur with sports activities such as gymnastics, weight lifting, ice skating and football
- Aging or overuse-related wear on the spinal joints
Rest and anti-inflammatory medication resolve most cases.
If it’s more severe, you may need physical therapy or surgery.
Spondylolisthesis grades
Doctors commonly describe spondylolisthesis as either high-grade or low-grade, depending on how severe your condition is. Grades are from 1 to 4.
- Low-grade (grade 1 and grade 2) usually occurs in adolescents and is considered less severe. Low-grade doesn’t typically require surgery.
- High-grade (grade 3 and grade 4) may require surgery if you’re experiencing severe pain.
The grade of your condition is based on how far away from proper alignment your spine has become.
Spondylolisthesis symptoms
In many cases, people who have spondylolisthesis don’t have any symptoms. You may not be aware you have the condition until an X-ray is taken for an unrelated reason. If you do have symptoms, the most common are:
- Lower back pain that feels like a muscle strain
- Muscle spasms or tightness in your hamstring
- Lower back pain that worsens with activity and improves with rest
- Difficulty walking or standing
- Pain when bending over
- Stiffness in your back
- Pain extending down from your lower back to your thighs
If you have high-grade spondylolisthesis, you may experience tingling, numbness or weakness in one or both legs.
Diagnosing spondylolisthesis
Following a thorough medical history, physical and neurological exams, our spine surgeons may recommend any of the following tests to confirm whether a bone in your spine is out of alignment. All tests are available at Ohio State Spine Care :
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI) scan
- Electromyography (EMG) to test your muscles and nerves
Spondylolisthesis treatment
Ohio State’s Spine Care team has the benefit of extra expertise from treating many people with spondylolisthesis. Because of this, the Spine Care team, composed of orthopedic and neurological specialists, is uniquely qualified to determine whether you’re likely to benefit from nonsurgical treatment. We also recommend lifestyle changes to prevent future problems with your spine.
We offer treatments ranging from physical therapy to the most complex spine surgeries. Physicians, therapists and other care providers work together to provide you with options that increase mobility and reduce pain.
Most people who come to Ohio State Spine Care don’t require surgery.
Lifestyle changes
- Exercise, such as Pilates or yoga, to strengthen muscles in your back
- Quitting smoking
- Guidance on weight loss to reduce pressure on your spine
Nonsurgical treatments
- Physical therapy – We’ll work with you one-on-one to customize a treatment plan for your needs and goals
- Spine orthobiologics use substances in your body to activate the healing process naturally
- Wearing a back brace to limit spine movement
- Medication for pain management
Most people return slowly to full function, including athletic activity.
Spondylolisthesis surgery
You may need surgery if a spinal bone that has slipped is likely to cause damage to nerves and the surrounding spinal structure, or if it’s causing severe pain or muscle weakness in one or both legs.
Our surgeons can perform minimally invasive surgery to correct the symptoms of spondylolisthesis. The surgeon makes tiny incisions in the back and works through a tube to minimize skin and muscle damage, reduce blood loss and reduce postsurgical pain.
At Ohio State, we can use both minimally invasive surgery and conventional surgical techniques for these procedures:
- Decompression surgery (laminectomy) to remove part of the vertebra and relieve pressure on your spinal cord or nerves
- Spinal fusion surgery to fuse a severely slipped bone with the vertebra below it and restore stability to the spinal column
Most people who have decompression or fusion surgery can return to full function, including athletic activities.
Ohio State conducts innovative research in the laboratory, as well as through clinical trials.
Those who have a pinched nerve may be eligible to participate in one of the following areas of research at The Ohio State University Wexner Medical Center.
Biomechanical testing: We’re doing biomechanical testing to assess the spine before and after surgery. A specialized vest helps us assess your spinal movement and measure the effectiveness of surgery. It ultimately may provide valuable information about which treatment methods will best increase mobility and function of the spine.
Back pain consortium: We’re members of the International Consortium for Health Outcomes Measurement (ICHOM). Membership in this elite organization allows us to engage with other top U.S. medical centers in global research studies on back pain. As we measure our results against established international standards, we share best practices and elevate our standard of care.
Enroll in a clinical trial
- Learn more about spine care at Ohio State Download our guide
Patient Education Animation Library
How would you like to schedule.
Don’t have MyChart? Create an account
Subscribe. Get just the right amount of health and wellness in your inbox.
Spondylolisthesis
Spondylolisthesis is where one of the bones in your spine, called a vertebra, slips forward. It can be painful, but there are treatments that can help.
It may happen anywhere along the spine, but is most common in the lower back.
Check if you have spondylolisthesis
The main symptoms of spondylolisthesis include:
- pain in your lower back, often worse when standing or walking and relieved when sitting or bending forward
- pain spreading to your bottom or thighs
- tight hamstrings (the muscles in the back of your thighs)
- pain, numbness or tingling spreading from your lower back down 1 leg ( sciatica )
Spondylolisthesis does not always cause symptoms.
Spondylolisthesis is not the same as a slipped disc . This is when the tissue between the bones in your spine pushes out.
Non-urgent advice: See a GP if:
- you have lower back pain that does not go away after 3 to 4 weeks
- you have pain in your thighs or bottom that does not go away after 3 to 4 weeks
- you're finding it difficult to walk or stand up straight
- you're worried about the pain or you're struggling to cope
- you have pain, numbness and tingling down 1 leg for more than 3 or 4 weeks
What happens at your GP appointment
If you have symptoms of spondylolisthesis, the GP may examine your back.
They may also ask you to lie down and raise 1 leg straight up in the air. This is painful if you have tight hamstrings or sciatica caused by spondylolisthesis.
The GP may arrange an X-ray to see if a bone in your spine has slipped forward.
You may have other scans, such as an MRI scan , if you have pain, numbness or weakness in your legs.
Treatments for spondylolisthesis
Treatments for spondylolisthesis depend on the symptoms you have and how severe they are.
Common treatments include:
- avoiding activities that make symptoms worse, such as bending, lifting, athletics and gymnastics
- taking anti-inflammatory painkillers such as ibuprofen or stronger painkillers on prescription
- steroid injections in your back to relieve pain, numbness and tingling in your leg
- physiotherapy to strengthen and stretch the muscles in your lower back, tummy and legs
The GP may refer you to a physiotherapist, or you can refer yourself in some areas.
Waiting times for physiotherapy on the NHS can be long. You can also get it privately.
Surgery for spondylolisthesis
The GP may refer you to a specialist for back surgery if other treatments do not work.
Types of surgery include:
- spinal fusion – the slipped bone (vertebra) is joined to the bone below with metal rods, screws and a bone graft
- lumbar decompression – a procedure to relieve pressure on the compressed spinal nerves
The operation is done under general anaesthetic , which means you will not be awake.
Recovery from surgery can take several weeks, but if often improves many of the symptoms of spondylolisthesis.
Talk to your surgeon about the risks and benefits of spinal surgery.
Causes of spondylolisthesis
Spondylolisthesis can:
- happen as you get older – the bones of the spine can weaken with age
- run in families
- be caused by a tiny crack in a bone (stress fracture) – this is more common in athletes and gymnasts
Page last reviewed: 01 June 2022 Next review due: 01 June 2025
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Lumbar spondylolysis and spondylolisthesis.
Alan G. Shamrock ; Chester J. Donnally III ; Matthew Varacallo .
Affiliations
Last Update: August 7, 2023 .
- Continuing Education Activity
Spondylolysis refers to a posterior defect in the vertebral body at the pars interarticularis. Usually, this defect is due to trauma or from a chronic repetitive loading and hyperextension. If this instability results in translation of the vertebral body, spondylolisthesis has occurred. This process requires a fracture or deformation of the posterior spine elements creating an elongation of the pars. This condition occurs in all ages with the underlying cause varying based on the age group. This activity describes the pathophysiology, evaluation, and management of lumbar spondylolysis/spondylolisthesis and highlights the role of the interprofessional team in improving care for affected patients.
- Identify the different types of spondylolisthesis, differentiating the patholological features that distinguish each variety.
- Outline the components of a proper evaluation and assessment of a patient presenting with lumbar spondylolysis/spondylolisthesis, including any indicated imaging studies.
- Describe management strategies for spondylolisthesis, based on which variant of the condition with which the patient presents.
- Review the interprofessional team strategies for improving care coordination and communication regarding the management of patients with lumbar spondylolysis/spondylolisthesis.
- Introduction
Spondylolysis refers to a posterior defect of the vertebral body occurring at the pars interarticularis. [1] Typically, this defect results from trauma or chronic repetitive loading and hyperextension. If this instability leads to translation of the vertebral body, this is spondylolisthesis. [1] [2] This process requires either a fracture or deformation of the posterior spinal elements resulting in elongation of the pars interarticularis. This condition can potentially occur in all age groups, with the underlying cause varying based on age. If the slip progresses to the point of neurologic compromise, then surgical intervention may be necessary to decompress and stabilize affected segments. [3] Absent any motor deficits, a nonoperative course of analgesia, activity modification, and injections should be the initial therapeutic approach for several months. [4]
Isthmic spondylolisthesis refers to a defect within the pars interarticularis usually from repetitive microtrauma and accounts for the vast majority of cases in children and adolescents. [1] [5]
Degenerative spondylolisthesis is the most common form of spondylolisthesis seen in adults. [6] It is due to chronic degenerative changes at the posterior elements resulting in the incompetence of the surrounding ligamentous structures, leading to elongation and slippage. [6]
Acutely, a traumatic spondylolisthesis can occur following a high-energy injury flexion/extension that causes a fracture-dislocation at the posterior elements. [7]
Another type is dysplastic spondylolisthesis which is a result of an abnormal formation of the posterior elements resulting in this subsequent instability. [8]
- Epidemiology
The rates of spondylosis and spondylolisthesis vary widely by age group. In the pediatric population, spondylosis is present in about 5% of the population, most commonly (90%) at the L5 to S1 motion segment, although pathology at L4 is more likely to be symptomatic. [1] [9] Long-term studies estimate that about 15% of those with a defect (spondylosis) will develop a slip (spondylolisthesis). [10] [11] Regarding adults, lumbar spondylolisthesis without a defect in the pars is present in 5% of men, 10% of women. [12] It is not always symptomatic. This degenerative type usually occurs at the L4 to L5 levels (versus isthmic noted at L5 to S1). [6] Degenerative spondylolisthesis is an acquired type of spondylolisthesis occurring much more frequently and gradually in the adult population. [6] Cohorts with degenerative spondylolisthesis will rarely develop a high-grade spondylolisthesis. [13] Furthermore, the chronic natural history of this disease process is such that with further degenerative changes, the vertebral segments may eventually stabilize, and the patients can have subsequent clinical improvements. [13]
- Pathophysiology
Repetitive micro-traumas from hyperextension lead to elongated or absent pars interarticularis. This force applies additional stress to the facet joints and subsequent hypermobility leading to advanced degeneration of the disc space. [14] The reduced disc and facet stability results in the translation of the vertebral body, creating a stenotic effect on the exiting nerve roots and/or the spinal canal. In the traumatic setting, flexion-distraction energy may cause a localized vertebral body failure at this segment, predisposing the patient to chronic issues if instability develops.
- History and Physical
Initial evaluation of lower back pain initiates by obtaining a history from the patient. This history should pertain to the timeline of pain, radiation of pain, and inciting events. The clinician should pay careful attention to prior episodes of trauma. Low-grade slips and stenotic spinal canals may decompress and relieve pain with leaning forward or sitting. It is crucial to note patient comments such as decreased pain with pushing a grocery cart or walking upstairs as both common actions have the spinal column in forwarding flexion. [15] It is also important in any evaluation of extremity issues to inspect circulation as vascular claudication may mirror or mimic the neurogenic problems.
Classically patients may complain of pain radiating down both buttocks and lower extremities. An evaluation of the patient's walking is also critical to better assess the daily impact that pain or neurological deficits cause. All physical examinations will include assessing the neurologic function of the arms, legs, bladder, and bowels. The keys to a thorough exam are organization and patience. One should evaluate not only strength but also sensation and reflexes. It is also essential to inspect the skin along the back and document the presence of tenderness to compression or palpable step-off.
Performing a straight leg test in a patient positioned supine may also reveal a stenotic canal. [16] This test may also cause local sites of pain as hamstring contractures are often associated with spondylolisthesis. [17] As mentioned above, a thorough neurologic examination is required. Commonly a patient will have L5 radiculopathy resulting in weakness of ankle dorsiflexion and extension of the great toe. This deficit may also diminish the Achilles tendon reflex. L4 radiculopathy may present with weakness at the quadriceps and a decreased patellar tendon reflex.
Documentation is paramount as these initial findings will likely serve as a baseline for all future evaluations.
Evaluation of patients with low-back pain typically includes anterior-posterior (AP) and lateral radiographs of the impacted area. Some physicians will obtain radiographs of the entire spine. A key component to radiographic evaluation is obtaining flexion/extension films, which illustrates vertebral segment stability. [18] Serial standing lateral radiographs obtained in the clinic will help track any potential progression of the slip.
One of the crucial measurements to note regarding slips is the amount of translation between vertebral bodies. The amount of “uncovering” of one endplate from the other determines the grade. There are four grades of spondylolisthesis: Grade 1: 0% to 25%, Grade 2: 26% to 50%, Grade 3: 51% to 75% and Grade 4: 76% to 99%. [12] [19] At 100% displacement, patients have developed spondyloptosis. [20] Grades 1 and 2 are considered low-grade slips. [21] Grades 3 and 4 are considered high-grade spondylolisthesis. [19]
An MRI is critical when evaluating patients with suspected spondylosis and spondylolisthesis. Frequently these patients will initially trail a six-week course of physical therapy. Upon follow-up, if the symptomology is still present, the clinician can obtain an MRI at that time. [1] The focus should be on the T2 weighted sagittal and axial images, as these will illustrate any compression of neurologic elements.
- Treatment / Management
Non-surgical intervention includes modification of the activity that may have exacerbated the pain, non-steroidal anti-inflammatory medications (NSAIDs), physical therapy, stretching, and occasionally using a lumbosacral orthosis. A 2009 meta-analysis evaluating spondylolysis and grade 1 spondylolisthesis showed almost 84% of adolescent patients treated nonoperatively had a successful clinical outcome at one year. [22] This study also showed no difference in those who did and did not use a brace. [22] Likely it is the activity restriction and not bracing, which determines the overall outcome. Additionally, a course of at least six weeks of physical therapy with an emphasis on core exercise strengthening and stretching should be attempted. Additionally, temporary pain relief is possible with epidural injections, but the potential for subsequent infection risk, while low, is possible. [23] [24]
While most patients improve with nonoperative treatment alone, those failing a conservative treatment course have three options- continued pain, complete avoidance of activities that elicit pain, or surgical intervention. Again, the surgical options for spondylolysis (as well as low-grade spondylolisthesis) should be reserved for those with either neurologic deficits, the progression of a slip, or pain limiting daily functions. [3] The literature regarding the optimal surgical procedure, approach, and roles for decompression and instrumentation remains controversial. While there is still controversy regarding the need for posterior decompression for patients who have just radicular symptoms, what is agreed upon is the need for decompression when a true motor deficit is present. [3] [11] [25] Additionally, in the setting of retrolisthesis and disc herniation at L5-S1, recent long-term follow-up from the SPORT database has shown non-inferior outcomes in patients with surgically treated disc herniations in the setting of retrolisthesis. [26] The patient needs to understand that while surgical intervention has favorable outcomes for relieving radicular pains, the results are less predictable for non-radiating lower back pain.
- Differential Diagnosis
- Lumbosacral disc injuries
- Lumbosacral discogenic pain syndrome
- Lumbosacral facet syndrome
- Lumbosacral spine acute bony injuries
- Lumbosacral spine sprain/strain injuries
- Lumbosacral spondylolisthesis
- Lumbosacral spondylosis
- Myofascial pain in athletes
- Sacroiliac joint injury
The prognosis for patients with spondylolisthesis is generally good. Most patients will respond to conservative treatment. For those with ongoing, severe symptoms not relieved by conservative approaches, surgery can potentially relieve radicular leg symptoms by decompressing nerve roots. Localized lumbar pain may require lumbar fusion in more extreme cases. [27] [28]
- Complications
Complications of spondylolisthesis tend to be neurological. These can include chronic pain in the lower back or legs, and numbness, tingling, or weakness in the lower extremities. Severe nerve compression can lead to problems with bowel or bladder control; however, this is quite uncommon. [27]
- Deterrence and Patient Education
Patients will need to understand their condition and its imposed limitations based on the severity of their particular case. The clinician should review the relevant anatomy and explain the disruption, using spinal models if necessary. A review of the patient's activities and physical demands is prudent (e.g., heavy lifting, prolonged sitting, etc.). Based on the severity of the condition, the clinician may impose physical limitations.
- Pearls and Other Issues
Many patients will improve with a nonoperative treatment course directed at activity modification. [22] Patients should understand that surgery frequently will not relieve all pain as irreversible damage to the nerves may have already occurred. The future of minimally invasive treatment options will continue to perfect outcomes for spinal stenosis. Advancements in pain control and endoscopic technologies now allow for select patients and facilities to perform endoscopic disc debridement followed by percutaneous instrumentation on an outpatient basis. Additional research will focus on optimizing treatment outcomes and predicting which patients will develop symptomatic progression of a slip.
- Enhancing Healthcare Team Outcomes
Patients with low back pain are best managed by an interprofessional team that includes the emergency department physician, therapist, orthopedic nurse, primary care physician, an orthopedic surgeon. The initial treatment for low back pain is non-surgical and involves a change in lifestyle. Most patients can benefit from exercise, weight loss, and leading an active lifestyle. Surgery is only a recommendation when there is nerve compression, or the patient has failed conservative treatment. The patient must understand that surgery is not always effective, and many patients still experience residual pain and limited range of motion of the lumbar spine. The patient needs to understand that while surgical intervention has favorable outcomes for relieving radicular pains, the results are less predictable for non-radiating lower back pain.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Isthmic Spondylolisthesis intervention Contributed by Chester J Donnally III, MD
Spondylolysis with Spondylolisthesis, showing spino pelvic parameters, slip, dysplasia of upper endplate of S1, Slip angle (SA = angle between inferior endplate of L5 and line perpendicular to the S1 posterior wall) and lumbo sacral angle (LSA = angle (more...)
Disclosure: Alan Shamrock declares no relevant financial relationships with ineligible companies.
Disclosure: Chester Donnally III declares no relevant financial relationships with ineligible companies.
Disclosure: Matthew Varacallo declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Shamrock AG, Donnally III CJ, Varacallo M. Lumbar Spondylolysis and Spondylolisthesis. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Pars Interarticularis Injury. [StatPearls. 2024] Pars Interarticularis Injury. Pereira Duarte M, Camino Willhuber GO. StatPearls. 2024 Jan
- Review Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. [J Am Acad Orthop Surg. 2006] Review Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. Cavalier R, Herman MJ, Cheung EV, Pizzutillo PD. J Am Acad Orthop Surg. 2006 Jul; 14(7):417-24.
- Review Lumbosacral Spondylolysis and Spondylolisthesis. [Clin Sports Med. 2021] Review Lumbosacral Spondylolysis and Spondylolisthesis. Chung CC, Shimer AL. Clin Sports Med. 2021 Jul; 40(3):471-490.
- Pars Interarticularis Defect. [StatPearls. 2024] Pars Interarticularis Defect. Mansfield JT, Wroten M. StatPearls. 2024 Jan
- Spondylolisthesis with spondylolysis in a 17-month-old: a case report. [J Spine Surg. 2017] Spondylolisthesis with spondylolysis in a 17-month-old: a case report. O'Donnell M, Lavelle WF, Sun MH. J Spine Surg. 2017 Dec; 3(4):689-692.
Recent Activity
- Lumbar Spondylolysis and Spondylolisthesis - StatPearls Lumbar Spondylolysis and Spondylolisthesis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- GP practice services
- Health advice
- Health research
- Medical professionals
Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
- Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Spondylolisthesis and spondylolysis
Peer reviewed by Dr Laurence Knott Last updated by Dr Colin Tidy, MRCGP Last updated 20 Nov 2021
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Cervical spondylosis article more useful, or one of our other health articles .
In this article :
What is spondylolisthesis, spondylolisthesis vs spondylolysis.
- Who gets spondylolisthesis and spondylolysis? (Epidemiology)
Spondylolisthesis causes (aetiology)
- Types of spondylolisthesis
- Presentation
Differential diagnosis
Investigations.
- Spondylolisthesis treatment and management
Complications of surgical repair
Spondylolisthesis prognosis.
Continue reading below
Spondylolisthesis is the movement of one vertebra relative to the others in either the anterior or posterior direction due to instability. Degenerative spondylolisthesis is a common pathology, often causing lumbar canal stenosis 1 .
Anatomy of the vertebrae
The vertebrae can be divided into three portions:
Centrum - involved in weight bearing. This is the body of the vertebra and is formed of cancellous bone.
Dorsal arch - surrounds and protects the spinal cord. It carries the upper and lower facet joints of each vertebra which articulate with the facet joints of the vertebra above and below, respectively. The part of the vertebral arch between them is the thinnest part and is called the pars interarticularis, or the isthmus.
Posterior aspect - protrudes and can be palpated on the lower back.
Lumbar vertebra 1 inferior surface
Lumbar vertebra 1 anterior surface
Images by Anatomography, via Wikimedia Commons . Click here to see a lumbar vertebra 1 close-up superior surface animation.
Spondylolysis and spondylolisthesis are separate conditions, although spondylolysis often precedes spondylolisthesis.
Spondylolysis is a bony defect (commonly due to a stress fracture but it may be a congenital defect) in the pars interarticularis of the vertebral arch, separating the dorsum of the vertebra from the centrum. It may occur unilaterally or bilaterally. It most commonly affects the fifth lumbar vertebra and may cause back pain.
Spondylolisthesis refers to the anterior slippage of one vertebra over another (or the fifth vertebra over the sacrum). There are five forms:
Isthmic : the most common form, usually acquired in adolescence as a consequence of spondylolysis but often unnoticed until adulthood.
Degenerative : developing in older adults as a result of facet joint osteoarthritis and bone remodelling.
Traumatic (rare): resulting from fractures of the neural arch.
Pathologic : from metastases or metabolic bone disease.
Dysplastic : (rare): congenital, resulting from malformation of the pars.
Spondylosis is a general term for degenerative osteoarthritic changes in the spine. It involves dehydration of the intervertebral discs with consequent narrowing of the intervertebral spaces. There may be changes in the facet joints with osteophyte formation and this may put pressure on the nerve roots, causing motor and sensory disturbance.
Who gets spondylolisthesis and spondylolysis? (Epidemiology) 2
Spondylolysis is a common diagnosis with a high prevalence in children and adolescents complaining of low back pain.
There is an increased risk of spondylolysis in young athletes like gymnasts, presumably due to impact-related stress fractures . However most cases are low-grade. At-risk activities include gymnastics, diving, tennis, cricket, weightlifting, football and rugby.
Isthmic spondylolisthesis affects around 5% of the population but is more common in young athletes. 60-80% of people with spondylolysis have associated spondylolisthesis 3 4 .
The majority of cases of spondylolysis and spondylolisthesis affect L5 and most of the remainder affect L4.
Degenerative spondylolisthesis is more common in older people, particularly women.
Traumatic, metastatic and dysplastic spondylolistheses are relatively rare.
Many cases of spondylolisthesis are asymptomatic.
Spondylolisthesis commonly occurs due to a fracture or defect in the pars interarticularis, the narrowest part of the posterior vertebral arch between the upper and lower facet joints. When this is breached, the upper facet joint may no longer be able to hold the vertebra in place against the downward force of body weight and forward/downward slippage occurs.
Risk factors that increase the risk of spondylolysis developing into spondylolisthesis include 5 :
Female gender.
Presence of spina bifida or spina bifida occulta .
Vertebral wedging.
Hyperlordosis.
Positive family history.
Certain high-impact sports, as evidenced by increased rates in athletes and gymnasts 3 .
Types of spondylolisthesis 2
Stable or unstable.
Asymptomatic or symptomatic.
Graded according to degree of slippage; the Meyerding classification is based on the ratio of the overhanging part of the superior vertical body to the anterio-posterior length of the inferior vertebral body:
Grade I: 0-25%.
Grade II: 26-50%.
Grade III: 51-75%.
Grade IV: 76-100%.
Grade V (spondyloptosis): >100%.
Graded according to type; the Wiltse classification (1976):
Type I: dysplastic (congenital).
Type II: isthmic: secondary to a lesion involving the pars interarticularis:
Subtype A: secondary to stress fracture.
Subtype B: result of multiple healed stress fractures resulting in an elongated pars.
Subtype C: acute pars fracture (rare).
Type III: degenerative.
Type IV: post-traumatic: fracture in a region other than the pars.
Type V: pathological: diffuse or local disease.
Type VI: iatrogenic.
Presentation 4
Spondylolysis symptoms.
Most cases of spondylolysis are asymptomatic and identified incidentally.
It may present with low back pain provoked by lumbar extension, paraspinal spasm and tight hamstrings.
It frequently does not show on X-ray. It is important to consider it in the differential diagnosis of back pain, as its identification can prevent progression and avoid the potential need for aggressive intervention.
Spondylolisthesis symptoms
Presentation varies slightly by type although common spondylolisthesis symptoms include exercise-related back pain, radiating to the lower thighs, which tends to be eased by rest, particularly in positions of spinal flexion.
Isthmic spondylolisthesis
Most patients are asymptomatic, even with progressing slippage.
Symptoms often begin around the adolescent growth spurt.
Back pain - worse with activity (particularly back extension) - this may come on acutely or insidiously.
Pain may flare with sudden or trivial activities and is relieved by resting.
Pain is worse with higher grades of disease.
Pain may radiate to buttocks or thighs
There are usually no neurological features with lower grades of slippage but radicular pain becomes common with larger slips. Pain below the knee due to nerve root compression or disc herniation would suggest more severe slippage. High degrees of spondylolisthesis may present with neurogenic claudication or even cauda equina impingement.
Tightened hamstrings are very common
There may be enhanced lordosis and a waddling gait with shortened step length.
There may be gluteal muscular wasting.
Degenerative spondylolisthesis
Pain is aching in nature and insidious in onset.
Pain is in the low back and posterior thighs.
Neurogenic claudication may be present with lower-extremity symptoms worsening with exercise.
Symptoms are often chronic and progressive, sometimes with periods of remission.
If lumbar stenosis is also present, reflexes may be diminished.
Dysplastic spondylolisthesis
Presentation and physical findings are similar to isthmic spondylolisthesis but with a greater likelihood of neurological compromise.
Traumatic spondylolisthesis
Patients will have experienced acute trauma and are likely to have significant pain.
Severe slips may cause cauda equina compression with bladder and bowel dysfunction, radicular symptoms or neurogenic claudication.
Physical findings are as for the other types.
Pathological spondylolisthesis
Symptoms may be insidious in onset and associated with radicular pain.
Other causes of back pain need to be ruled out - eg:
Osteoarthritis .
Ankylosing spondylitis .
Mechanical lower back pain .
Spinal cord lesion.
Multiple myeloma .
Vertebral compression fracture .
Lumbar disc prolapse.
Discitis/other spinal disc problems .
Blood tests - looking for infection, myeloma, hypercalcaemia/hypocalcaemia.
Lateral spinal X-rays - will show spondylolisthesis. These are best performed in the position of maximal pain.
Oblique spinal X-rays - may (but will often not) detect spondylolysis.
Radionuclide scintigraphy and CT may help in cases of spondylolysis in distinguishing progressing lesions of the pars from stable lesions.
MRI is often performed perioperatively to look at relationships between the bony and neurological structures in the compromised area.
Spondylolisthesis treatment and management 1 2 4
The goal of treatment is to relieve pain, stabilise the spinal segment and stop or reverse the slippage. Patients need to be evaluated for the presence of instability, as if there is an unstable segment early surgery will be needed.
Depending on the severity of the spondylolysis and symptoms associated it may be treated either conservatively or surgically, both of which have shown significant success.
Conservative treatments such as bracing and decreased activity have been shown to be most effective with patients who have early diagnosis and treatment. Low-intensity pulsed ultrasound in addition to conservative treatment appears to achieve a higher rate of bony union. Surgery may be required if conservative treatment, for at least six months, failed to give sustained pain relief for the activities of daily living.
For degenerative spondylolisthesis, surgery is indicated mainly for perceived functional impairment. Improvement in neurological symptoms is one of the main treatment objectives. For this, it is useful to perform radicular decompression. The most frequent technique is direct posterior decompression.
Conservative treatment
Complete bed rest for 2-3 days can be helpful in relieving pain, particularly in spondylolysis, although longer periods are likely to be counterproductive. Patients should try to sleep on their side as much as possible, with a pillow between the knees.
Activity modification to prevent further injury. This may mean avoidance of activities if there is >25% slippage.
Analgesia - eg, paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), codeine phosphate.
Steroid and local anaesthetic injections are sometimes used around compressed nerve roots or even into the fracture area of the pars for diagnostic purposes.
Bracing: a brace or corset may be recommended for a pars interarticularis fracture which is likely to heal. Bracing with exercise may be beneficial for patients with mild or even more severe degrees of slippage.
Physiotherapy: this includes massage, ultrasound, bracing, mobilisation, biomechanical correction, hydrotherapy, exercises for flexibility, strength and core stability and a gradual return to activity programme.
More than 80% of children treated non-surgically will have full resolution of symptoms.
A meta-analysis of observation studies suggested that around 80% of all patients treated non-operatively would have a successful clinical outcome after one year. Lesions diagnosed at the acute stage and unilateral lesions were the best subgroups 6 .
Surgical treatment
If there is evidence of progression or if conservative measures are ineffective then surgical therapy may be offered. This depends also on degree and aetiology.
Surgical intervention involves a prolonged rehabilitation period so it is generally not considered until conservative treatments have failed. An exception would be in the case of significant instability or neurological compromise and in high-grade slips.
Surgical therapy involves fusing the affected vertebra with a neighbouring normally aligned vertebra (both anteriorly and posteriorly). The intervertebral disc is usually also removed, as it is inevitably damaged. The slipped vertebra may be realigned.
Whilst most surgeons agree that decompression of the nerves is of benefit to patients, the benefit of realigning slipped vertebrae is uncertain. For example, when the spondylolisthesis is very gradual in onset, or in cases of congenital spondylolisthesis, compensatory changes in the spine and musculature occur so that realignment may increase the possibility of further injury.
There is good evidence that surgical treatment of symptomatic spondylolisthesis is significantly superior to non-surgical management in the presence of 7 :
Significant neurological deficit.
Failed response to conservative therapy.
Instability with neurological symptoms.
Degree of subluxation of III or more.
Unremitting pain affecting quality of life.
A large systematic review concluded that reduction of displacement carried benefits over fusion alone, although a large retrospective review showed high complication rates, particularly for older patients with more severe disease 8 9 10 11 .
Fusion techniques can be associated with neurological complications in older patients with degenerative spondylolisthesis, but in adolescent patients outcomes are good 9 .
Surgery is commonly complicated by pseudoarthrosis (non-union) which may result in chronic pain years down the line.
In the case of spondylolysis, if surgery is offered it would involve pinning the defect. However, most cases are managed conservatively.
Implant failure.
Pseudoarthrosis (failure of bone healing leading to a 'false joint').
Poor alignment of the fusion.
Neurological damage: foot drop, spinal cord compression . Chronic nerve injury/inflammation: neuropathic pain can persist in the face of apparent surgical success, possibly due to permanent changes in the nerves or a deregulation of pain control mechanisms.
Spondylolisthesis is generally a benign condition; however, it runs a chronic course and is therefore a cause of much morbidity and disability. In degenerative spondylolisthesis this will relate in part to the progress and prognosis of the underlying changes.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Guigui P, Ferrero E ; Surgical treatment of degenerative spondylolisthesis. Orthop Traumatol Surg Res. 2017 Feb;103(1S):S11-S20. doi: 10.1016/j.otsr.2016.06.022. Epub 2016 Dec 30.
- Gagnet P, Kern K, Andrews K, et al ; Spondylolysis and spondylolisthesis: A review of the literature. J Orthop. 2018 Mar 17;15(2):404-407. doi: 10.1016/j.jor.2018.03.008. eCollection 2018 Jun.
- Toueg CW, Mac-Thiong JM, Grimard G, et al ; Prevalence of spondylolisthesis in a population of gymnasts. Stud Health Technol Inform. 2010;158:132-7.
- Syrmou E, Tsitsopoulos PP, Marinopoulos D, et al ; Spondylolysis: a review and reappraisal. Hippokratia. 2010 Jan;14(1):17-21.
- Sadiq S, Meir A, Hughes SP ; Surgical management of spondylolisthesis overview of literature. Neurol India. 2005 Dec;53(4):506-11.
- Klein G, Mehlman CT, McCarty M ; Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Orthop. 2009 Mar;29(2):146-56. doi: 10.1097/BPO.0b013e3181977fc5.
- Alfieri A, Gazzeri R, Prell J, et al ; The current management of lumbar spondylolisthesis. J Neurosurg Sci. 2013 Jun;57(2):103-13.
- Weinstein JN, Lurie JD, Tosteson TD, et al ; Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009 Jun;91(6):1295-304. doi: 10.2106/JBJS.H.00913.
- Sansur CA, Reames DL, Smith JS, et al ; Morbidity and mortality in the surgical treatment of 10,242 adults with spondylolisthesis. J Neurosurg Spine. 2010 Nov;13(5):589-93. doi: 10.3171/2010.5.SPINE09529.
- Kasliwal MK, Smith JS, Kanter A, et al ; Management of high-grade spondylolisthesis. Neurosurg Clin N Am. 2013 Apr;24(2):275-91. doi: 10.1016/j.nec.2012.12.002. Epub 2013 Feb 21.
- Longo UG, Loppini M, Romeo G, et al ; Evidence-based surgical management of spondylolisthesis: reduction or arthrodesis in situ. J Bone Joint Surg Am. 2014 Jan 1;96(1):53-8. doi: 10.2106/JBJS.L.01012.
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 19 Nov 2026
20 nov 2021 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Influence of slippage reduction and correction of lumbosacral kyphosis by single-level posterior lumbar interbody fusion on spinal alignment in patients with dysplastic spondylolisthesis
Affiliations.
- 1 Department of Orthopaedic Surgery, Keio University School of Medicine, 35 Shinanomachi Shinjuku-Ku, Tokyo, 1608582, Japan.
- 2 Department of Orthopedic Surgery, International University of Health and Welfare School of Medicine, Tokyo, Japan.
- 3 Department of Orthopaedic Surgery, Keio University School of Medicine, 35 Shinanomachi Shinjuku-Ku, Tokyo, 1608582, Japan. [email protected].
- PMID: 38926256
- DOI: 10.1007/s43390-024-00917-9
Purpose: To investigate the influence of slippage reduction and correction of lumbosacral kyphosis by L5-S1 single-level posterior lumbar interbody fusion (PLIF) on spinal alignment and clinical outcomes including postoperative complications in patients with dysplastic spondylolisthesis (DS).
Methods: Twenty consecutive patients with symptomatic and severe DS who underwent L5-S1 single-level PLIF with a minimum of 2 years of follow-up after surgery were included. Clinical outcomes were evaluated using the Japanese Orthopaedic Association (JOA) and visual analog scale (VAS) scores for low back and leg pain obtained on preoperative and postoperative examinations. Postoperative instrumentation failure and L5 radiculopathy were also evaluated. The preoperative and postoperative spinopelvic parameters were measured.
Results: The JOA score significantly improved from 21.5 ± 4.8 (preoperative) to 27.0 ± 2.5 (postoperative), with a mean recovery rate of 75.0% ± 30.4%. The VAS score for low back pain significantly improved from 44.5 ± 30.1 (preoperative) to 11.5 ± 15.9 (postoperative), and that for leg pain significantly improved from 31.0 ± 33.2 (preoperative) to 5.0 ± 10.2 (postoperative). The slip percentage (% slip) significantly improved from 59.6% ± 13.5% (preoperative) to 25.2% ± 15.0% (postoperative). The lumbosacral angle (LSA) significantly improved from 12.3° ± 9.5° (preoperative) to 1.0° ± 4.9° (postoperative). L5-S1 PLIF led to significant improvement of lumbar lordosis (from 52.0° ± 15.9° to 59.7° ± 8.0°) and pelvic incidence - lumbar lordosis mismatch (from 23.9° ± 20.6° to 13.3° ± 10.0°). Correction of lumbosacral kyphosis had a significant positive correlation with postoperative pelvic tilt (PT) (r = 0.50, P = 0.02), while postoperative % slip did not have a significant correlation with postoperative PT.
Conclusions: L5-S1 PLIF for DS provided good clinical outcomes. Correction of lumbosacral kyphosis had a positive impact on regaining ideal spinopelvic balance and may be beneficial in the setting of treating DS.
Keywords: Correction of lumbosacral kyphosis; Dysplastic spondylolisthesis; Lumbosacral kyphosis; Retroverted pelvis; Single-level posterior lumbar interbody fusion; Slippage reduction.
© 2024. The Author(s), under exclusive licence to Scoliosis Research Society.
PubMed Disclaimer
Similar articles
- Risk factors for early-onset radiographical adjacent segment disease in patients with spondylolytic spondylolisthesis after single-level posterior lumbar interbody fusion. Takeda K, Okada E, Shinozaki Y, Ozaki M, Kono H, Yasuda A, Suzuki S, Tsuji O, Nagoshi N, Yagi M, Fujita N, Ogawa J, Nakamura M, Matsumoto M, Watanabe K. Takeda K, et al. Spine J. 2022 Jul;22(7):1112-1118. doi: 10.1016/j.spinee.2022.02.001. Epub 2022 Feb 11. Spine J. 2022. PMID: 35158045
- Double-level lumbar spondylolysis and spondylolisthesis: A retrospective study. Zhang S, Ye C, Lai Q, Yu X, Liu X, Nie T, Zhan H, Dai M, Zhang B. Zhang S, et al. J Orthop Surg Res. 2018 Mar 16;13(1):55. doi: 10.1186/s13018-018-0723-3. J Orthop Surg Res. 2018. PMID: 29548343 Free PMC article. Review.
- Utility of multilevel lateral interbody fusion of the thoracolumbar coronal curve apex in adult deformity surgery in combination with open posterior instrumentation and L5-S1 interbody fusion: a case-matched evaluation of 32 patients. Theologis AA, Mundis GM Jr, Nguyen S, Okonkwo DO, Mummaneni PV, Smith JS, Shaffrey CI, Fessler R, Bess S, Schwab F, Diebo BG, Burton D, Hart R, Deviren V, Ames C; for the International Spine Study Group. Theologis AA, et al. J Neurosurg Spine. 2017 Feb;26(2):208-219. doi: 10.3171/2016.8.SPINE151543. Epub 2016 Oct 21. J Neurosurg Spine. 2017. PMID: 27767682
- [Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis]. Zencica P, Chaloupka R, Hladíková J, Krbec M. Zencica P, et al. Acta Chir Orthop Traumatol Cech. 2010 Apr;77(2):124-30. Acta Chir Orthop Traumatol Cech. 2010. PMID: 20447355 Czech.
- Posterior lumbar interbody fusion for lytic spondylolisthesis: restoration of sagittal balance using insert-and-rotate interbody spacers. Sears W. Sears W. Spine J. 2005 Mar-Apr;5(2):161-9. doi: 10.1016/j.spinee.2004.05.256. Spine J. 2005. PMID: 15749616 Clinical Trial.
- Cai T, Yang L, Cai W et al (2015) Dysplastic spondylolysis is caused by mutations in the diastrophic dysplasia sulfate transporter gene. Proc Natl Acad Sci U S A 12(26):8064–8069. https://doi.org/10.1073/pnas.1502454112 - DOI
- Moke L, Debeer P, Moens P (2011) Spondylolisthesis in twins: multifactorial etiology: a case report and review of the literature. Spine (Phila Pa 1976) 36(11):E741–746. https://doi.org/10.1097/BRS.0b013e3181f9f575
- Al-Khawashki H, Wasef Al-Sebai M (2001) Combined dysplastic and isthmic spondylolisthesis: possible etiology. Spine (Phila Pa 1976) 26(23):E542–546. https://doi.org/10.1097/00007632-200112010-00021
- Cavalier R, Herman MJ, Cheung EV, Pizzutillo PD (2006) Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg 14(7):417–424. https://doi.org/10.5435/00124635-200607000-00004
- Bourassa-Moreau E, Mac-Thiong JM, Joncas J, Parent S, Labelle H (2013) Quality of life of patients with high-grade spondylolisthesis: minimum 2-year follow-up after surgical and nonsurgical treatments. Spine J 13(7):770–774. https://doi.org/10.1016/j.spinee.2013.01.048 - DOI - PubMed
Related information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 27 June 2024
Ancient Egyptian scribes and specific skeletal occupational risk markers (Abusir, Old Kingdom)
- Petra Brukner Havelková 1 , 2 ,
- Veronika Dulíková 2 ,
- Šárka Bejdová 3 ,
- Jana Vacková 2 , 4 ,
- Petr Velemínský 1 &
- Miroslav Bárta 2
Scientific Reports volume 14 , Article number: 13317 ( 2024 ) Cite this article
692 Accesses
690 Altmetric
Metrics details
- Archaeology
- Biological anthropology
Men with writing proficiency enjoyed a privileged position in ancient Egyptian society in the third millennium BC. Research focusing on these officials of elevated social status (“scribes”) usually concentrates on their titles, scribal statues, iconography, etc., but the individuals themselves, and their skeletal remains, have been neglected. The aim of this study is to reveal whether repetitive tasks and maintained postures related to scribal activity can manifest in skeletal changes and identify possible occupational risk factors. A total of 1767 items including entheseal changes, non-metric traits, and degenerative changes were recorded from the human remains of 69 adult males of well-defined social status categories from the necropolis at Abusir (2700–2180 BC). Statistically significant differences between the scribes and the reference group attested a higher incidence of changes in scribes and manifested themselves especially in the occurrence of osteoarthritis of the joints. Our research reveals that remaining in a cross-legged sitting or kneeling position for extended periods, and the repetitive tasks related to writing and the adjusting of the rush pens during scribal activity, caused the extreme overloading of the jaw, neck and shoulder regions.
Similar content being viewed by others

The influence of occupation on the longevity of Japanese traditional artists
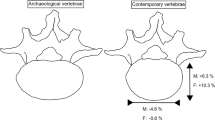
Temporal Trends in Vertebral Dimensions – a case study from Finland
Association between changes in working status and hand-grip strength among Korean middle-aged and older adults: a longitudinal panel study
Introduction.
The term “scribes” in relation to ancient Egypt in the third millennium BC covers men who held a wide range of administrative posts or functions. These individuals enjoyed a privileged position in society at that time, since only 1% of the population would have been literate 1 . A whole range of scribal titles associated with various departments or specific tasks is attested in the Old Kingdom 2 , but literacy and writing skills/scribal ability were an integral part of the employment of all administrative officials. Depending upon their hierarchical grade within a given office, it is supposed that the working activity of such officials in large part encompassed activities related to the writing of administrative documents. Those who headed a department (overseers) also managed its relevant agenda.
In recent years, scholars have directed their research towards various aspects associated with scribes, e.g., with their titles, scribal statues, iconography in wall decoration, writing materials, writing systems and analyses of single documents 2 , 3 . However, thorough research into the skeletal remains of these ancient Egyptian scribes, focusing on scribal activities and their possible influence on the development of activity-related skeletal changes, has been missing or limited to single case studies 4 .
Various skeletal markers manifesting on the human skeleton are supposed to be activity-induced in nature, and reflect a mechanical loading and repetitive tasks throughout life; and vice versa specific occupational physical activities may represent risk factors for the development of various changes to the skeleton. These include in particular the presence and character of entheseal changes (EC) at the insertion sites of tendons and ligaments 5 , 6 or the size of muscle attachment sites 7 ; selected non-metric traits (NMT) as accessory facets, notches, etc., on the infra-cranial skeleton 8 , 9 , 10 , 11 , 12 ; degenerative changes, specifically osteoarthritis (OA) of joints of appendicular skeleton and vertebral column and intervertebral disc disease (IDD) at vertebral bodies 13 , 14 , 15 , 16 , 17 ; and analysis of the cross-sectional geometric properties 18 , 19 .
In addition to the presumed effects of physical stress on the development of changes, more factors such as age, sex, metabolic disorders, or hormonal and genetic influences contribute to their aetiology. The link between physical activity and skeletal changes is still not entirely clear and is widely discussed 16 , 20 , 21 , 22 , 23 also applies to osteoarthritic changes 16 , 24 . A clear association between degenerative changes and activity thus cannot easily be demonstrated 25 , 26 . Although the multifactorial aetiology of the aforementioned skeletal markers complicates the interpretations of the results, it seems that physical stress still remains among important factors influencing the development and character of change, but non-mechanical factors should also be controlled or discussed 20 , 22 , 23 .
When attempting to reconstruct a possible pattern of habitual activities in individuals from past populations, the archaeological and/or historical context is crucial. For the scribes in ancient Egypt, there is evidence (textual, wall relief decoration in tombs and statues) that provides insights into the way working activities were carried out. Ancient Egyptian officials used a thin brush-like pen made of rush during the Pharaonic era, until it was substituted by the Greek-origin reed pen around 100 BC. They regularly wrote on papyrus, ostraca or wooden boards 27 , 28 . We also have a fairly accurate knowledge of the postures in which they performed their profession, and in which they spent relatively long periods. Simplistically, it may be assumed that they mainly adopted three typical poses: (a) the cross-legged position (sartorial), where the stretched skirt served as a table (Fig. 1 A); (b) the kneeling-squatting position, one leg squatting with the second knee on the floor (usually seen in two-dimensional depictions; Fig. 1 B 29 ); (c) the standing position (Fig. 1 C 29 ). It is very likely that while specific positions varied (Fig. 1 D 30 ), there could have been a general tendency for an individual to revert to a preferred position 31 . It may also have depended on the circumstances and the environment in which the scribal activity was carried out. Although, these positions and movements were by no means physically demanding, it can be assumed that daily repetition and maintaining them could affect specific areas of the skeleton.

Working positions of scribes. ( A ) cross-legged (sartorial) position (the scribal statue of the high-ranking dignitary Nefer, Abusir; photo Martin Frouz); ( B ) kneeling-squatting position (wall decoration from the mastaba of the dwarf Seneb 29 ); ( C ) standing position (wall decoration from the mastaba of the dwarf Seneb 29 ); ( D ) based on tomb relief decoration, different position of the legs when sitting 30 . Drawing Jolana Malátková.
In this paper we seek to reveal whether the repetitive tasks and positions related to scribal activity in Old Kingdom Egypt can manifest themselves in recorded changes in the skeleton, as well as which areas of the skeleton, i.e. attachment sites or joint articular surfaces, are significantly affected in comparison to the reference group. The identification of these areas, and especially their combinations, could then be useful in the identification of the “scribal profession” in the skeletons of those individuals whose titles have not been preserved—a practical outcome and the main aim of this and future research. We would also like to focus on identifying the most likely preferred position for scribes to perform their duties, and compare it with the archaeological evidence. To date, no analogous study has been published that comprehensively evaluates the occupational risk factors on the entire skeleton, while at the same time being based on a homogenous and relatively large sample of individuals whose employment was related to scribal activity.
Of the 1767 evaluated items in total, a statistically significant difference at the level of significance alpha 0.05 between the scribes and the reference group based on Mann–Whitney U test and/or Chi-square test was found in only 68 (3.85%); 34 significant differences were recorded on the skull and appendicular skeleton and 34 on the vertebrae. The results of the statistical analyses for these 68 traits are shown in Tables 1 and 2 , separately for the skull and appendicular skeleton, and vertebrae (the complete results for all 1767 items are given in Supplementary Data S1 and Data S2 ). After adjustment using the Holm-Bonferroni correction, the number of statistically significant traits was reduced to 40. The traits that appeared non-significant after this correction were mainly scored on the lower limb and vertebrae. Although we recognize that the explanatory value of the differences between the scribes and the reference group is lower for those traits that were found to be significant using only the Mann–Whitney or chi-squared tests, we address them in the results and discussion.
The observed statistically significant differences indicate a higher incidence of changes in scribes compared to the reference sample (61/68; 90%; respective 37/40; 92.5% after Holm-Bonferroni correction) and manifested themselves especially in the occurrence of degenerative changes to the joints (OA and/or minor criteria) for both the appendicular skeleton and vertebrae.
In terms of the OA changes on the skull and appendicular skeleton in scribes, a higher incidence was observed at the areas of both temporomandibular joints (Figs. 2 , 3 ), the right clavicle, the right humeral caput, proximal articular surface of the right first metacarpal bone (CMC1) and the medial condyle of the right femur (Fig. 4 ). Differences in minor changes (SC, MC, JC, NB) were also recorded on other joints of the appendicular skeleton (see Table 1 ), almost exclusively more frequently in scribes. Only two minor osteoarthritic changes showed a higher incidence in the reference sample: marginal changes (MC) on the right lateral surface of the patella and the trochlea of the humerus.

Osteoarthritis of the temporomandibular joint of a supposed family member (174/AS79/2015) of Khemetnu, the presumed owner of family tomb AS 79. Khemetnu’s working activity was associated with the household management and the arranging of the funerary cult of the judge Inti (AS 22). ( A ) Base of the skull with both mandibular fossae exhibiting OA; ( B ) Eburnation in the left mandibular fossa; ( C ) Subchondral lesions in the right mandibular fossa; ( D ) Joint contour deformation and marginal changes of the left condylar process. Photo Šárka Bejdová.

Comparison of the incidence of osteoarthritis (OA) in the temporomandibular joint (TMJ) and the apophyseal joints of the vertebrae (C1-S1) between scribes and the reference group (OA for the whole joint/vertebra was scored as present if OA occurred in at least one articular surface of an apophyseal joint). The number of individuals with OA (presence of OA/total number of individuals evaluated) is shown in the table below the graph.
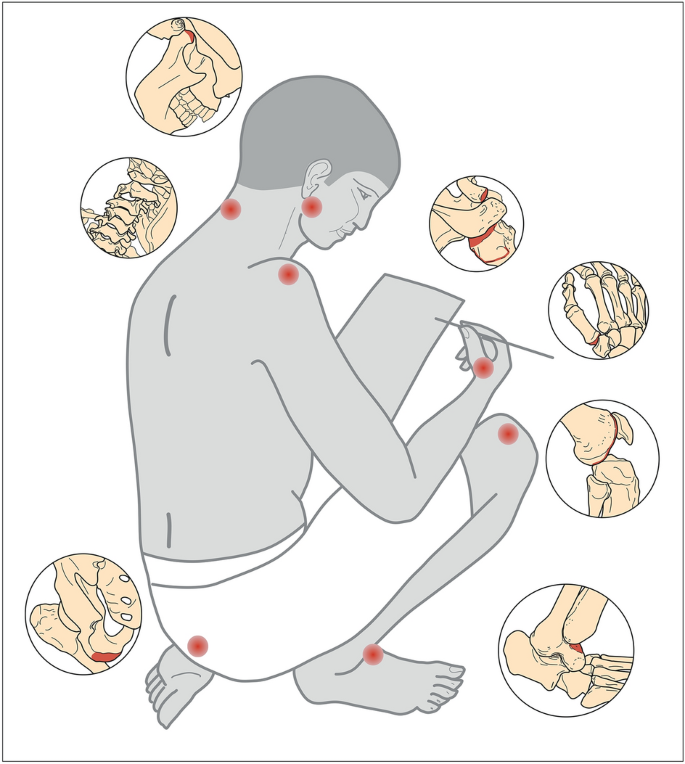
Drawing indicating the most affected regions of the skeletons of scribes with higher prevalence of evaluated changes compared to reference group: both temporomandibular joints (OA); cervical spine (OA, spondylosis); right shoulder (OA of the acromial facet of the clavicle and humeral head, EC on the greater tubercle of the humerus); right first metacarpal bone (OA); left ischial tuberosity (EC); right femoral medial condyle (OA) and the medial squatting facet on the right talus. Drawing Jolana Malátková.
As for the vertebral column, statistically significant differences of OA changes of apophyseal joints were more common than the alterations of vertebral bodies, i.e., intervertebral disc disease (IDD; Table 2 ). All significant OA changes including the minor criteria occurred more often in scribes, except for the left upper facet of the T2 vertebra. A higher prevalence of OA in scribes was observed especially on the cervical vertebrae (C1, C2, C3, C7) and the T7 and L5 vertebra (Fig. 3 ). Minor OA changes were also noted on other vertebrae (Table 2 ). Differences in the incidence of IDD were recorded only on the lower surface of the C3 vertebra and the upper surface of the T3 vertebra, with a higher prevalence in scribes, and surface changes of the L2 upper surface in the reference sample.
A statistically significantly higher incidence of EC in the scribes was noted at two attachment sites on the humerus (the margin of the left entheses of the subscapularis; HSC Out, and the right infra-/supraspinatus; HSI Out) and on the left hip bone (ischial tuberosity), while in the reference sample only on the right femur (gluteus maximus). In the case of vertebral bodies, EC on the inferior part of the T4 body were significantly higher in the reference sample, while on the superior part of the L4 in scribes.
Regarding NMT, vastus fossa on the both patellae and medial squatting facet on the right talus, were recorded more often in scribes, while a rounded edge pit on the right acetabulum was more typical for the reference sample.
The results of the statistical tests did not indicate significant differences in the age-at-death distribution between all the scribes and the reference group when all individuals evaluated were included (χ 2 = 0.208 < χ 2 α=0.05 = 5.991; Mann–Whitney: Z = − 0.242, p-level = 0.809). However, due to differences in the preservation of the traits assessed, the representation of scribes and reference individuals in each age category varies for each trait. The consistency of the distribution of individuals in the age categories was therefore monitored separately for each trait using the Mann–Whitney U test (see last two columns of the Tables 1 and 2 for selected traits; Supplementary Data S1 and Data S2 for complete results). These results reveal a different age distribution between scribes and the reference group for 35% of the traits evaluated (Supplementary Data S1 and Data S2 ). Traits for which we found a statistically significant difference between scribes and the reference group show a different age distribution in half of the cases (see Table 1 and Table 2 ). Typically, there is a higher number of older individuals among the scribes. The possible influence of age on the observed differences should thus be taken into account for these traits.
All evaluated markers were tested for side asymmetry by Wilcoxon Matched Pairs Test, separately for scribes and the reference sample. Statistically significant differences between the right and left sides were noted only for three traits in the scribes—EC: biceps brachii insertion on the radius (N = 12; T = 0.000; Z = 2.023; p-level = 0.043), OA: mandibular fossa on the mandible (N = 22; T = 0.000; Z = 2.023; p-level = 0.043), NB: trochlea of humerus (N = 20; T = 0.000; Z = 2.023; p-level = 0.043) and three traits in the reference group – EC: ischial tuberosity on the pelvis (N = 18; T = 0.000; Z = 2.201; p-level = 0.028); NMT: lateral extension of the trochlear surface on the talus (N = 24; T = 0.000; Z = 2.023; p-level = 0.043), SC: glenoid cavity on the scapula (N = 31; T = 0.000; Z = 2.201; p-level = 0.028).
Professions involving scribal agenda was certainly not physically demanding, but neither can it be assumed that individuals of lower status buried at Abusir performed physically demanding activities on a daily basis. These were not labourers, but usually members of the household or relatives, performing activities related to the running of the household 32 , 33 . The similar lifestyle of the two studied samples was manifested in the low number of evaluated traits showing statistically significant differences (3.85%), most of them showing a higher incidence among scribes (90%).
These statistically significant differences are in most cases reflected in the occurrence of degenerative joint changes. The intensity of these traits is usually attributed to increasing age 14 , 16 , 34 , 35 . Although the statistical tests did not reveal any significant differences in the age-at-death distribution between the compared groups, the possible influence of advanced age in the scribesʼ group on the higher incidence of degenerative changes cannot be completely ruled out, because for half of the traits for which statistically significant differences were found, the distribution across age categories is not the same—scribes tend to be older. Simplistically, we can conclude that these differences do not apply to the temporomandibular joint region, the acromial facet of the clavicle, the wrist and metacarpus, the pelvic and talar traits, and the upper cervical and mid-thoracic spine, where the distribution of individuals in the age categories is similar. Conversely, the observed differences in the prevalence of changes assessed in the humerus, femur, and patella, as well as the lower cervical and lumbar spine, may be influenced by this unequal age distribution. However, in the study presented it would be highly likely that statistically significant differences in the incidence of degenerative changes between scribes and the reference group would occur in a much larger number, or even the majority, of the articular surfaces assessed, rather than in a minority of them, localised to a few regions of the skeleton. This permits the assumption that the observed differences could to some extent be related to the scribal activity associated with well-defined repetitive tasks and stationary posture.
One of the areas significantly more affected in the group of scribes was the spine, especially in the cervical region . Two separate areas of vertebrae were examined: (zyg)apophyseal joints with osteoarthritic changes (OA/minor criteria) and intervertebral joints (bodies) with marginal spondylosis (SP) and surface changes (IDD). The prevalence of changes in a particular vertebra is different for each marker; they are basically uncorrelated, which is due to the different function of the apophyseal and intervertebral joints of the spine. The intervertebral joints allow a minimum of movement and provide support, while the apophyseal joints provide less support with varying degrees of movement.
Compared to previous studies 15 , 36 , 37 , 38 , the curves characterizing the degree of loading of individual vertebrae in the present study approximately correspond for both scribes and the reference sample, but some atypical manifestations are worth mentioning. All cervical vertebrae show more degenerative changes in the scribes compared to the reference group, but the statistically significant differences concern mainly OA at the apophyseal joints. The C7 vertebra exhibited the highest incidence of OA changes at apophyseal joints among the cervical vertebrae, and significantly exceeded the frequency in the reference sample and frequencies recorded in previous studies. The location of the C7 vertebra at a point where the lordotic curvature of the cervical spine ends and the thoracic kyphosis begins implies that the lower facets are under continuous tension, partially due to the action of the nuchal ligament that ends at the spinous process of the C7 37 . The C7 vertebra is thus usually one of the most affected vertebrae in OA 25 . This explains the frequent occurrence of OA at the C7 vertebra, but not the enormous increase in OA in scribes compared to the reference group. It cannot be ruled out that this could be related to the constant overloading of the cervical spine.
In a typical scribe’s working position, the head had to be forward, and the spine flexed, changing the centre of gravity of the head and putting stress on the spine. An exaggerated dorsal kyphosis (round back) places the head ahead of the centre of gravity, increasing the cervical lordosis. The weight of the head in this position is borne by the apophyseal joints 38 . The forward head posture with a flexed neck is a position characteristic of many of modern occupations. In a sitting work position characterized by flexion of the whole spine to accommodate the eye-object distance to a horizontal working surface (as with scribes), the load moment for the C7-T1 motion segment induced by the weight of the head and neck increases 3.6 times in comparison to the neutral position 39 . Prolonged cross-legged sitting could result in a significant increase of degenerative changes to the cervical spine among scribes.
Atypical and excessive loading of the cervical spine in the group of scribes is also accompanied by the extreme prevalence of OA in the temporomandibular joint (TMJ). The prevalence of TMJ OA ranges from 16% to 38% in living populations and from 2.4% to 40% in archaeological samples 40 , 41 , 42 . The prevalence of TMJ OA in individuals in the reference sample (30%) falls exactly within this range. However, the temporomandibular joints of the scribes were affected far beyond the reported incidence of TMJ OA in previous studies (64%). The development of TMJ OA is most commonly associated with dental pathologies, dental attrition or antemortem tooth loss of the posterior dentition 40 or with dietary habits 43 . The significant loading of the TMJ could also be closely related directly to scribal activity. The tools that scribes used to write were made from rush ( Juncus ), which was cut at a slant and chewed at the end to form a brush-like head 28 . When the pen became ragged or clogged with ink, the scribe cut off the end again and chewed the next section. Frequent or long-term chewing may be a risk factor for TMJ disorders with a high percentages of osteoarthritis 44 . This scribal habit of retting by chewing the rush brush used to write hieroglyphs might also have led to the asymmetrical dental wear evidenced in the mandible of the scribe Horemkenesi (21st Dynasty, Thebes), where it resulted in mesio-distal depressions along the molar teeth 45 .
However, the existing relationship between the load on the cervical spine and the temporomandibular joint cannot be ignored. The correlation between temporomandibular disorders and cervical spine dysfunction or neck/shoulder area symptoms is well documented or reviewed by clinical studies 46 , 47 , 48 , 49 . The TMJ and cervical spine are anatomically and functionally interrelated, and the malposition of one can affect the position and function of the other 50 . Postural maintenance of the head is achieved through a muscle chain which is formed, among others, by the large posterior neck muscles and anterior muscle attachments to the mandible and hyoid bones, as they link the cranium to the shoulder girdle. Any alteration of this functional chain anywhere along its course will be reflected elsewhere along its length 48 . Therefore, we cannot exclude that the high incidence of TMJ OA among scribes compared to the reference sample may to some extent be related to extreme overloading of the cervical spine. While scribes probably alternated the position of the arms and leg, the head and cervical spine remained in a forward position, resulting in excessive strain. It should be noted that in the case of the temporomandibular joint and upper cervical vertebrae, no statistically significant differences in age distribution were found between the scribes and the reference group. Therefore, in this case, the differences observed between the groups of individuals evaluated are not due to differences in age distribution.
As in the case of the cervical spine and TMJ, statistically significant differences in the shoulder and the whole upper limb were higher in the group of scribes for most of the studied traits. Nevertheless, statistically significant differences were observed for only a few traits, linked mainly to OA or its minor criteria. The scribes’ group manifested a significant increase in OA changes at the right shoulder (humeral head, acromial facet of clavicle) and the right first metacarpal bone. The pattern of right shoulder loading is complemented by an increased occurrence of entheseal changes at the margin of the supra- and infraspinatus muscle attachment on the humeral greater tubercle (HSI), which belongs to the rotator cuff group. The prevalence of shoulder osteoarthritis is usually low comparison to other large joints 34 , 51 , 52 . The shoulder and hip are usually less severely involved than the knee or elbow 15 . By contrast, among scribes the shoulder is the most affected joint compared to the hip and knee (unlike the reference group, where it was the elbow area; Fig. 5 ). However, apart from the acromial facet of the clavicle and the first metacarpal, the age distribution of the scribes differs from that of the reference group for the traits evaluated, with the scribes having a greater number of older individuals. The influence of age cannot be excluded in this case.
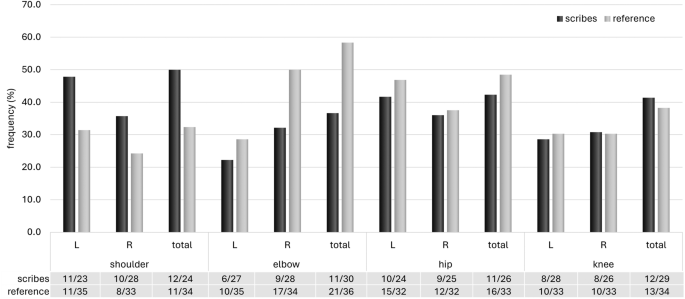
Comparison of the incidence of osteoarthritis (OA) in large joints (shoulder, elbow, hip, knee) between scribes and the reference group (OA for the whole joint was scored as present if OA.
In conjunction with the involvement of the supra- and infraspinatus muscle tendons, this could indicate an overall overloading of the shoulder region. Stress to the rotator cuff, specifically the supraspinatus muscle, usually occurs when the arm is in an elevated position, such as among painters 53 . However, it could also be related to a static sitting position with arms unsupported, such as during typing 54 , 55 . Last but not least, the shoulder area is connected to the cervical spine, both functionally and by innervation. Especially in the C7/T1 joint area, where an enormous load was recorded among scribes, the upper girdle and vertebral column are linked 25 . Studies focused on the impact of disorders in the ‘upper quarter’ of the body on posture and pain experienced in different parts of the body have found a relationship between the presence of signs and symptoms in the jaw and neck/shoulder areas 46 , 49 .
Based on the iconography and statues, it can be assumed that scribes wrote with their right hands and rolled the papyrus scroll left-handed. A papyrus 6 m length, when tightly rolled, yielded a cylinder 5–6 cm thick, which could easily be spanned by the fingers of a hand 28 . Writing with a rush pen required dexterity that allowed the creation of clearly written ligatured as well as non-ligatured signs of l cm or less 28 . These repetitive movements and positions can lead to excessive strain on the wrists and hands, which could be reflected in changes to the bones. Occupational risk factors of the hand and wrist are however usually closely related to tendon-related disorders (tendinitis, carpal tunnel syndrome, etc.) caused by the chronic performance of forceful exertions or highly repetitive hand-intensive tasks 56 . These work-related musculoskeletal disorders are difficult to identify on the skeleton and to interpret appropriately. As for the wrist area of the studied skeletons, only minor osteoarthritic changes (MC, SC) exhibited a significantly higher incidence in the group of scribes, on both hands localized to the scaphoid and lunate area. Unlike tendon-related disorders, OA of the wrist is usually traceable to a secondary to posttraumatic sequel, such as fracture, dislocation, ligament injury or metabolic disease 57 , 58 . Although there are several studies referencing an association between wrist/hand OA and specific movements (pinch grip, power grip, impact loading), occupations or kinds of activity 35 , 59 , 60 , 61 , it is still very difficult to define how a scribal activity would affect such a complex joint as the wrist and hand.
In addition to the minor changes on the aforementioned articular surfaces, a significantly higher occurrence of OA on the proximal articular surface of the right first metacarpal bone (CMC1) was detected among scribes. This could be related to specific thumb motions, their frequency and duration, and specific thumb positions, which may constitute long-term low-level mechanical stresses, resulting in degenerative changes in the articular cartilage and initiating OA 62 . The development of OA of the CMC1 has been shown to be closely associated with pinch grip work especially 61 , 63 , which corresponds well to the repetitive use of the right hand during scribal activity. However, further research focusing on other musculoskeletal markers (e.g., entheseal changes) in the wrist and hand will be needed, following some of the current methods 64 , 65 .
One of the initial hypotheses was that differences among groups would manifest themselves in the lower part of the body , especially in the area of the knees due to the kneeling working position. However, this assumption was not confirmed. After adjusting the data by Holm-Bonferroni correction, the only significant trait was the vastus fossa on the patella, the presence of which is problematic in terms of interpretation due to unclear aetiology and the lack of literature. Its higher incidence in scribes may also be associated with heredity 66 , given the familial nature of the tombs.
Focusing only on the significant results of the Mann–Whitney test, individuals from both groups also exhibited similar degrees of OA changes at the knee and the hip region (Fig. 5 ). However, OA on the medial condyle of the right femur manifested significantly more among scribes. During knee flexion there is a load imbalance between medial and lateral tibiofemoral contact forces, created by an adduction moment in the knees 67 . Contact stresses increase significantly during deep knee flexion and medial peak pressures are greater than pressures in the lateral tibiofemoral compartment 68 . Occupational kneeling (e.g., for floor layers) also increases the risk of degenerative tears in the medial, but not the lateral, menisci 69 . Therefore, it cannot be excluded that the OA on the right medial condyle of the femur is related to repetitive deep knee flexion in the kneeling posture of scribes. Given the right-sided loading of the joint in question, it is possible that they preferred kneeling/squatting on the right knee, which would correspond with a higher incidence of the medial squatting facet on the right talus among scribes. The other probable preferred position, cross-legged sitting, could put more pressure on the buttock, especially the ischial tuberosity where the common origin of the biceps femoris, semitendinosus and semimembranosus is located. This enthesis on the left side manifested a significantly higher occurrence of ECs in the scribes’ group compared to the reference sample. The aforementioned muscles are mainly involved in thigh extension at the hip joint, in flexion of the leg at the knee joint, and rotation of the leg with flexed knee 70 , which corresponds to the cross-legged siting position. Bioarchaeological studies focusing on the relationship between the intensity of physical loading and the occurrence of EC on the ischial tuberosity rate this correlation as very weak and they cite age as a major factor in their occurrence 70 , 71 . However, in the present study there was no difference in age distribution for this trait between the scribes and the reference group. Clinical studies, particularly from Asia where cross-legged sitting position is still frequently used, have highlighted the health risks associated with this position when the lower legs are folded and crossed at the ankles or calves 72 . Gluteal/buttock pressure varies depending on the position of the lumbar spine (lordosis, flat, slump); anterior and posterior tilts of the upper body in the slump and lordosis postures may result in more pressure concentration in the feet or buttocks, respectively 72 , 73 . Increasing gluteal pressure could thus be one of the factors related to the changes found in the ischial tuberosity among scribes. Cross-legged sitting positions also significantly alter all of the spinopelvic alignment—the lumbar lordotic angle, sacral slope, pelvic tilt, and pelvic incidence 74 —which may lead to a reduction in lumbar lordosis (becoming more kyphotic) and an increased compression load, especially at the L4-5 vertebrae 72 , 75 . This may explain the higher minor OA changes on the lumbar vertebrae (and OA in L4) in the group of scribes, but the effect of greater age cannot be ruled out, as in the case of the medial condyle of the right femur.
Nevertheless, if we accept that the changes observed in the lower limbs of scribes (EC on the left ischial tuberosity, OA on the right femoral medial condyle, the medial squatting facet on the right talus) are related to their activity, then this would indicate a preferred position where the left leg is in a kneeling or cross-legged sitting position and the right leg in a squatting position as visible in Fig. 1 B and D (a, d) and Fig. 4 .
The overall non-significant differences between the scribes and the reference group in the lower limb region may also indicate that kneeling or a cross-legged sitting position was a common posture in the Old Kingdom, unrelated to any specific occupation, as reflected in various tomb scenes where family members and dependents are sitting on the floor and in so-called “servant statues” depicting people performing everyday tasks 33 .
The present research provides a first insight into possible occupational risk factors related to scribal activity and the most affected areas of the scribes’ skeletons. Further research will focus on the examination of selected skeletal regions where significant differences have been recorded and on evaluation of a similar population (e.g., Giza).
Conclusions
The scribes and reference group significantly differ in only 3.85% of all the evaluated skeletal traits, which might reflect an overall likeness (male sex, identical age distribution) and similarity in their lifestyle, including the absence of physically demanding activities in both groups.
Most of these statistically significant differences, show a higher prevalence of the observed changes among the scribes (90%), which allows us to deduce that they might be related to scribal activity, but the significant effect of age cannot be ruled out for some traits, for which an unequal age distribution between scribes and the reference group was recorded.
The different kinds of changes (OA, EC, NMT) recorded at a significantly higher frequency among scribes were clustered in a few well-defined regions or structures of the skeleton: the temporomandibular joint, the cervical spine, the right shoulder, the right first metacarpal bone, the femoral medial condyle of the right knee, the left ischial tuberosity and the right talus (Fig. 4 ).
Upper body region: the occurrence of TMJ OA is probably related to the excessive and frequent chewing of rush pens by scribes, but in addition TMJ disorders are often related to extreme loading of the cervical spine and vice versa. The latter is also significantly loaded in the scribes’ group, probably in relation to prolonged forward head positioning in a sitting or kneeling posture during scribal activity. The loading of the shoulder area may also be connected to the cervical spine, but the observed changes could also be related to a static sitting position with arms unsupported, such as during scribing. The development of OA of the right first metacarpal bone probably reflects pinch grip work, such as frequent gripping of the pen.
Lower body region: the higher incidence of changes in the aforementioned traits (right knee, left ischial tuberosity, right talus) among scribes compared to the reference group, and their combination, could indicate a preferential position for scribes where the left leg is in a kneeling or cross-legged sitting position and the right leg in a squatting position, which could also cause overloading of the lumbar spine.
Risk factors for the occupation of scribe very likely did not include kneeling or squatting, which were probably also common in the rest of the population and could be alternated with standing, but extreme overloading of the neck and shoulder region.
Materials and methods
Sample of study.
At its height in the age of the pyramid builders (the third millennium BC), kings and royal family members (5th Dynasty) and non-royal elite (5th and 6th Dynasties) built their tombs in the necropolis at Abusir where archaeological research is carried out by the Czech Institute of Egyptology (Faculty of Arts, Charles University, Prague) since 1960. To date, almost two hundred tombs dating back to the Old Kingdom (2700–2180 BC) have been discovered. Although Abusir is perceived primarily as a burial ground of the Old Kingdom elite population, the arrangement of tombs within the necropolis reflects differences in the social status of their owners 76 . Although the first skeletal remains of Old Kingdom individuals were unearthed in the Abusir region in 1976, the process of collecting sufficient material for a “population” study took several decades 77 . Research focusing on the health status and activity related markers on the scribes’ skeletons began in 2009, but it took another 10 years to uncover enough skeletons for a comprehensive study. Currently, the Abusir skeletal collection contains 221 Old Kingdom individuals, of which 102 are estimated to be male; 26 male skeletons from previous research have been reburied and therefore could not be evaluated for this study.
Unambiguous dating to the Old Kingdom period, precise social status determination and successful sex and age-at-death estimation were the basic criteria for the inclusion of an individual in the assemblage. Our study includes the human remains of 69 adult males of different age-at-death and social status categories (Supplementary Data S3 ). The complete numbers and frequencies of individuals according to age-at-death for both groups (scribes and reference group) are summarized in Table 3 .
Social status definition
An essential prerequisite for successful assessment of occupational risk factors impacting the skeletons of Old Kingdom officials who carried out scribal activity is a precise social status definition. The titles held by ancient Egyptians are often indicators of their social status. However, when a title is lacking, the status enjoyed by individuals in society can be identified quite precisely from an archaeological point of view. Based on tomb appearance and architecture, 11 criteria were used for social status assessment of the evaluated individuals: tomb ownership, tomb dimensions, tomb type, chapel dimensions, chapel decoration, the form and execution of false doors, burial shaft depth, the appearance and dimensions of the burial place, the burial manner and the body position (Supplementary Data S3 ). An overview of the statistical assessment of single criteria decisive for the determination of social status categories is summarized in Supplementary Table S1 ).
The identities of the high-ranking and higher individuals (their personal names and titles) are known with one exception, while every individual of lower status remains anonymous with no title, and thus evidence of their exact professions is lacking. However, scribal ability was an integral part of the performance of all administrative roles, and not only for those who held the title sesh (scribe); the skeletal remains of all individuals of elevated social status have therefore been included in the group of “scribes” for the purposes of this study.
Concerning titles, at least one is attested for 24 (16.6%) of the 69 individuals under study. This set comprises manifold occupations ranging from a vizier, the heads of important administrative departments, priests of the royal mortuary cult and two physicians, to rank-and-file members of institutions or working phyles. A large proportion (10 of 24) worked in the department of legal matters. Six individuals held an actual scribal title: “scribe of treasury” Sekhemka; “scribe of the crews” and “scribe of the archives” Nyankhseshat; “overseer of the scribes of the crew” Nefershepes; “overseer of the scribes of the crew” and “overseer of the royal document scribes” Nefer; “scribe of the royal children” and “scribe of the king” Idu Faaf; and “inspector of the scribes of royal documents in the presence” Inti Pepyankh, who was even buried with scribal tools.
The high-ranking officials were interred in large stone-built mastabas or rock-cut tombs incorporating a decorated funerary chapel equipped with a false door. The deceased, in outstretched position, lay in a spacious burial chamber inside a stone sarcophagus. They were the tomb owners. As a general rule, they headed a crucial administrative department or held an important position in the king’s household.
The individuals categorized as the higher held hierarchically inferior positions to the high-ranking officials. Their burial customs were very similar, but the dimensions of their tombs, chapels and burial chambers could be smaller than those of top-level dignitaries.
The middle-ranking officials might be family members of the tomb owner. They were buried in a roughly dressed sarcophagus, burial pit or a wooden coffin. They usually worked in the area of legal matters and/or as a priest of the royal mortuary cult.
The individuals categorized as being of low-middle are somewhere on the dividing line between the low- and middle-ranking men. Their burials were usually part of that of highly positioned men. The depth of the burial shaft was shallower. They were usually buried in a contracted position in a small burial chamber or in a burial niche. Their identity is known in 4 of 12 cases, and working position in 3 cases (members of the priesthood or working groups providing mortuary cults).
Low-ranking individuals were placed in humble mud-brick tombs with a simple niche instead of a false door. Their body, in a contracted position, was put into a confined niche or simply at the bottom of the shaft. Their identities are unknown. Although the occupation of low-ranking men is not recorded in textual sources, it is very likely that they were involved in the running of their masters’ households, or were members of the priesthood or working groups providing mortuary cults as shown by the depictions on the walls of the tombs 78 , 79 .
Distinctive differences between both groups under study
Distinctive differences between the group of scribes and the reference set are: First group (scribes)—the individuals (whose identities are largely known) were mainly buried in large stone-built mastabas or rock-cut tombs, usually placed in a spacious burial chamber in an outstretched position, their bodies protected by a stone sarcophagus or at least a wooden coffin; they were of statuses defined as high-ranking, higher or middle-ranking. Their employment was mainly connected with important administrative offices of the country, which largely involved and required activities related to writing records and creating documents of an administrative nature.
Second group (reference set)—these predominantly anonymous individuals were usually buried in smaller mudbrick tombs or single burial shafts and their bodies of were often put in a contracted position in a confined niche or simply at the bottom of the shaft; they were of statuses defined as low-middle or low. These were usually members of the household or relatives, performing activities related to the running of the household. At the same time, they could also have been members of the priesthood or working groups providing mortuary cults. Thus, scribal activity was not a significant part of their work agenda. From this it can be inferred that low-middle and low status individuals very likely performed different physical activities on a daily basis from officials with a scribal agenda.
Anthropological methods
Methods used for sex and age-at-death estimation are described in detail in previously published work 77 . The metrical approach 80 , 81 was used for primary sex diagnosis where possible, together with morphological evaluation of pelvic structures 82 , 83 , 84 . Where the pelvic bones were missing, the descriptive morphological features 83 , 84 and discriminant function analysis of the visually assessed traits 85 of the skull were used. Metric standards for estimating sex using a discriminant function based on selected measurements of other bones 86 , 87 , 88 were used as auxiliary methods. The estimation of age-at-death was based on morphoscopic evaluation of morphological changes of pelvic structures: the auricular surface 89 , 90 , the pubic symphysis 91 , 92 , 93 , and the acetabulum 94 . In addition, changes to the sternal end of the clavicle 95 , the inner architecture of the proximal femur and humerus 96 and the degree of dental wear 97 , 98 , 99 were evaluated where possible.
Four groups of changes that might have been related to physical activity were evaluated: entheseal changes, infra-cranial non-metric traits, osteoarthritis of joints of the appendicular skeleton, and degenerative changes of the vertebral column. An overview, including the range of assessed stages and the number of evaluated traits in each category, is presented in Table 4 . A total of 1767 items were recorded on each skeleton where preservation allowed. Although some of the evaluated traits show a correlation with age (e.g., entheseal changes, degenerative changes), individuals over 50 years of age were not excluded for the purposes of our study. However, the distribution of individuals in age-at-death categories was statistically tested for scribes and the reference sample.
All joints of the appendicular skeleton (except for hand and foot phalanges), including the temporomandibular joint, were evaluated for OA according to the recommendations of Waldron 14 . A total of 72 articular surfaces on each side were included in the analysis (Supplementary Table S2 and Table S3 ). Not only the final presence or absence of OA, but also the occurrence of single changes (minor criteria) such as marginal changes (MC), surface changes (SC), new bone (NB), joint contour (JC) and eburnation (Eb) were compared between the two study samples.
Degenerative changes of the vertebral column (C1-S1) were analysed for both apophyseal joints and vertebral bodies (Supplementary Table S4 ). OA of apophyseal joints were evaluated according to the same method as joints of the appendicular skeleton 14 . Several markers were observed on the vertebral bodies: intervertebral disc disease IDD 14 , inclusive of evaluation of the marginal osteophytes/spondylosis (SP), pitting/porosity and new bone production (SC). Degrees of spondylosis were stated according to Stloukal and Vyhnánek 17 and were included in the final analysis. Occurrences of Schmorl’s nodes were also recorded 25 . In addition to the methods mentioned above, degenerative changes of the cervical vertebrae were evaluated using a complex method designed only for the cervical spinal section. 13 .
Entheseal changes were recorded on 18 attachment sites of the appendicular skeleton and on 46 vertebral bodies (Supplementary Table S4 and Table S5 ) according to the method of Villotte 5 , which was current in 2009 when research began. Since most of the skeletons included in this study had already been evaluated at the time of publication of the more recent Coimbra method 100 , and a subsequent study suggest that recording entheseal changes using the revised Coimbra method does not reflect activity more effectively than earlier methods 101 , Villotte’s method was considered appropriate.
NMTs cannot be considered as a homogenous group of markers of uniform origin and/or methodological approach; 28 selected non-metric traits of the infra-cranial skeleton were evaluated and are listed in Supplementary Table S6 , including a description of NMT and references to relevant publications based on which evaluated the trait. The presence or absence of NMT was recorded, except for traits at the anterior aspect of the proximal femur (Poirier’s facet, plaque and the cribra/fossa of Allen), where the methodology of Radi et al. 102 was applied.
Statistical analysis
Age-at-death distribution in the group of scribes and the reference sample was tested using the Mann–Whitney U test (Python, scipy.stats) and Chi-square test (Python, scipy.stats).
The same tests were used to reveal differences in the incidence of the evaluated changes between scribes and the reference sample. In the case of entheseal changes, all stages (A, B, C respectively 0, 1, 2) were included in the analysis by Mann–Whitney U test, while stages were reduced to presence and absence (0, 1) for testing using the Chi-square test. The Chi-square test was used in the classic form, unless a low sample size or zero frequencies appeared in the contingency table; in such cases, Yates’s correction for continuity was applied. Also, the correction for tied data in the Mann–Whitney U test was applied, since the examined data are categorical.
Considering the discussed issue of using p values and null hypothesis significance tests 103 , odds ratios (Python: scipy.stats) and their 95% and 97.5% confidence intervals were calculated to find other ways to interpret the findings.
Since the independence of two variables in a contingency table is equivalent to an odds ratio equal to 1, only the Mann–Whitney U test (null hypothesis: the scribes and reference group distribution functions are equal; alternative hypothesis: the scribes and reference group distribution functions are not equal) and the Chi-square test (null hypothesis: the presence of the trait is independent of the scribes and reference group; alternative hypothesis: the presence of the trait depends on the scribes and reference group) are assumed for each trait to establish a family of hypotheses. In other words, both tests are performed for each trait separately, first with their p-values. Then, the intersection of the two constituent null hypotheses (the joint null hypothesis) is evaluated against the union of their constituent alternative hypotheses , while the family-wise error rate is fixed as the significance level alpha 0.05 in accordance with the Holm-Bonferroni correction. The Holm-Bonferroni correction for the intersection of two constituent null hypotheses (as in this case) works as follows: the minimum p-value of their constituent p-values is compared to alpha/2 (0.025), and the maximum p-value is compared to alpha (0.05). If at least one of the two constituent null hypotheses is rejected (while the significance level alpha 0.05 for each constituted test is adjusted by applying the Holm-Bonferroni correction), the union of their constituent alternative hypotheses is statistically significant, which means that the examined trait is statistically significant for the difference between the scribes and the reference group (where the family-wise error rate did not exceed the predefined significance level alpha). The establishment of the family of hypotheses follows Rubin’s paper 104 and the desired outcome of the analysis, which is the individual statistical significance of each trait. For these reasons, any other alpha adjustment would be redundant.
Side asymmetry was assessed for all bilaterally occurring traits and was tested using the Sign test and Wilcoxon test (STATISTICA software).
Data availability
All data and complete results of statistical tests for all traits evaluated are available in the main text or the Supplementary Information. Raw data are available on request from the corresponding author.
Baines, J. & Eyre, C. Four notes on literacy. In Visual and Written Culture in Ancient Egypt (ed. Baines, J.) 63–94 (Oxford University Press, 2007).
Chapter Google Scholar
Piacentini, P. Les Scribes dans la Société Égyptienne de l’Ancien Empire I (Cybele, 2002).
Google Scholar
Yuen-Collingridge, R. Observing the scribe at work. In Observing the Scribe at Work: Scribal Practice in the Ancient World (eds Ast, R. et al. ) 1–8 (Peeters Publishers, 2021).
Kennedy, K. A. R., Plummer, J. & Chiment, J. Identification of the eminent dead: Penpi, a scribe of ancient Egypt. In Forensic Osteology: The Recovery and Analysis of Unknown Skeletal Remains (ed. Reichs, K.) (Charles C Thomas, 1986).
Villotte, S. Enthésopathies et activités des hommes préhistoriques - recherche méthodologique et application aux fossiles européens du Paléolithique supérieur et du Mésolithique. (Archaeopress, 2009).
Henderson, C. Y. & Alvez Cardoso, F. Special issue entheseal changes and occupation: Technical and theoretical advances and their applications. Int. J. Osteoarchaeol. 23 , 127–134. https://doi.org/10.1002/oa.2298 (2013).
Article Google Scholar
Karakostis, F. A. & Harvati, K. New horizons in reconstructing past human behavior: Introducing the “Tübingen University Validated Entheses-Based Reconstruction of Activity” method. Evol. Anthropol. 30 , 185–198. https://doi.org/10.1002/evan.21892 (2021).
Article PubMed Google Scholar
Mafart, B. Description, significance and frequency of the acetabular crease of the hip bone. Int. J. Osteoarchaeol. 15 , 208–215. https://doi.org/10.1002/oa.770 (2005).
Dlamini, N. & Morris, A. G. An investigation of the frequency of squatting facets in later stone age foragers from South Africa. Int. J. Osteoarchaeol. 15 , 371–376. https://doi.org/10.1002/Oa.791 (2005).
Capasso, L., Kennedy, K. A. R. & Wilczak, C. A. Atlas of occupational markers on human remains (Edigrafital, 1998).
Finnegan, M. Non-metric variation of the infracranial skeleton. J. Anat. 125 , 23–37 (1978).
CAS PubMed PubMed Central Google Scholar
Radi, N. Diversity of the proximal femur in humans: morphological variations of the head-neck junction Dissertation thesis, Università di Bologna, (2014).
Sager, P. Spondylosis cervicalis. A pathological and osteoarchaeological study of osteochondrosis intervertebralis cervicalis, arthrosis uncovertebralis, and spondylarthrosis cervicalis (Munksgaard, 1986).
Waldron, T. Palaeopathology (Cambridge University Press, 2009).
Jurmain, R. D. & Kilgore, L. Skeletal evidence of osteoarthritis: A palaeopathological perspective. Ann. Rheum. Dis. 54 , 443–450. https://doi.org/10.1136/ard.54.6.443 (1995).
Article CAS PubMed PubMed Central Google Scholar
Weiss, E. & Jurmain, R. D. Osteoarthritis revisited: A contemporary review of aetiology. Int. J. Osteoarchaeol. 17 , 437–450. https://doi.org/10.1002/oa.889 (2007).
Stloukal, M. & Vyhnánek, L. Slované z velkomoravských Mikulčic . (Academia, 1976).
Ruff, C. B. Biomechanical analyses of archaeological human skeletons. In Biological Anthropology of the Human Skeleton (eds Katzenberg, M. A. & Grauer, A. L.) (Wiley Online Library, 2018).
Stock, J. T. et al. Body Size, Skeletal Biomechanics, Mobility and Habitual Activity from the Late Palaeolithic to the Mid-Dynastic Nile Valley. In Human Bioarchaeology of the Transition to Agriculture (eds Pinhasi, R. & Stock, J. T.) (John Wiley, 2011).
Meyer, C., Nicklisch, N., Held, P., Fritsch, B. & Alt, K. W. Tracing patterns of activity in the human skeleton: An overview of methods, problems, and limits of interpretation. HOMO J. Comp. Hum. Biol. 62 , 202–217. https://doi.org/10.1016/j.jchb.2011.03.003 (2011).
Alves-Cardoso, F. & Assis, S. Exploring, “wear and tear” of joints and “muscle function” assumptions in skeletons with known occupation at death. Am. J. Phys. Anthropol. 175 , 689–700. https://doi.org/10.1002/ajpa.24334 (2021).
Jurmain, R. D., Alves Cardoso, F., Henderson, C. Y. & Villotte, S. Bioarchaeology’s holy grail: the reconstruction of activity. In A companion to Palaeopathology (ed. Grauer, A. L.) 531–552 (Wiley-Blackwell, 2012).
Tihanyi, B. et al. “Brothers in arms”: Activity-related skeletal changes observed on the humerus of individuals buried with and without weapons from the 10th-century CE Carpathian Basin. Int. J. Osteoarchaeol. 30 , 798–810. https://doi.org/10.1002/oa.2910 (2020).
Brandt, K. D., Dieppe, P. & Radin, E. L. Commentary: Is it useful to subset “primary” osteoarthritis? A critique based on evidence regarding the etiopathogenesis of osteoarthritis. Semin. Arthritis. Rheum. 39 , 81–95. https://doi.org/10.1016/j.semarthrit.2009.06.001 (2009).
Knüsel, C. J., Goggel, S. & Lucy, D. Comparative degenerative joint disease of the vertebral column in the medieval monastic cemetery of the Gilbertine priory of St. Andrew, Fishergate, York. England. Am. J. Phys. Anthropol. 103 , 481–495. https://doi.org/10.1002/(SICI)1096-8644(199708)103:4<481::AID-AJPA6>3.0.CO;2-Q (1997).
Jurmain, R. D. Degenerative changes in peripheral joints as indicators of mechanical stress: Opportunities and limitations. Int. J. Osteoarchaeol. 1 , 247–252. https://doi.org/10.1002/oa.1390010319 (1991).
Polis, S. Methods, tools, and perspectives of hieratic palaeography. In The Oxford Handbook of Egyptian Epigraphy and Palaeography (eds Laboury, D. & Davies, V.) 550–565 (Oxford University Press, 2020).
Allon, N. & Navrátilová, H. Ancient Egyptian scribes: a cultural exploration (Bloomsbury Publishing, 2017).
Junker, H. Gîza V. Die Mastaba des Snb (Seneb) und die umliegenden Gräber. Bericht über die von der Akademie der Wissenschaften in Wien auf gemeinsame Kosten mit Dr. Wilhelm Pelizaeus unternommenen Grabungen auf dem Friedhof des Alten Reiches bei den Pyramiden von Giza. Akademie der Wissenschaften in Wien Philosophisch-historische Klasse Denkschriften 71, Abhandlung 2 . (Hölder-Pichler-Tempsky 1941).
Schäfer, H. Von ägyptischer Kunst. Eine Grundlage. 3. neugestaltete und stark vermehrte Auflage . (Hinrichs, 1930).
Molleson, T. Bones of work at the origins of labour. In Archaeology and women: Ancient and modern issues (eds Hamilton, S. et al. ) 185–198 (Routledge, 2007).
Havelková, P. & Dulíková, V. What skeletal remains reveal about ancient Egypt’s inhabitants. In Kings of the Sun Studies (ed. Bárta, M.) 347–352 (National Museum and Charles University, 2020).
Roth, A. M. The meaning of menial labor: “Servant Statues” in Old Kingdom Serdabs. JARCE 39 , 103–121. https://doi.org/10.2307/40001151 (2002).
Domett, K., Evans, C., Chang, N., Tayles, N. & Newton, J. Interpreting osteoarthritis in bioarchaeology: Highlighting the importance of a clinical approach through case studies from prehistoric Thailand. J. Archaeol. Sci. Rep. 11 , 762–773. https://doi.org/10.1016/j.jasrep.2016.12.030 (2017).
Felson, D. T. et al. Osteoarthritis: New insights. Part 1: The disease and its risk factors. Ann. Intern. Med. 133 , 635–646. https://doi.org/10.7326/0003-4819-133-8-200010170-00016 (2000).
Article CAS PubMed Google Scholar
Knüsel, C. J. On the biomechanical and osteoarthritic differences between hunter-gatherers and agriculturalists. Am. J. Phys. Anthropol. 91 , 523–525. https://doi.org/10.1002/ajpa.1330910409 (1993).
Ezra, D., Kedar, E., Salame, K., Alperovitch-Najenson, D. & Hershkovitz, I. Osteophytes on the zygapophyseal (facet) joints of the cervical spine (C3–C7): A skeletal study. Anat. Rec. 305 , 1065–1072. https://doi.org/10.1002/ar.24751 (2022).
Al-Bustany, D. A. & Aziz, Z. A. Cervical spondylosis among group of computer users in Erbil City. Zanco J. Med. Sci. 13 , 28–36. https://doi.org/10.15218/zjms.2009.016 (2009).
Harms-Ringdahl, K., Ekholm, J., Schüldt, K., Németh, G. & Arborelius, U. P. Load moments and myoelectric activity when the cervical spine is held in full flexion and extension. Ergonomics 29 , 1539–1552. https://doi.org/10.1080/00140138608967267 (1986).
Suby, J. A. & Giberto, D. A. Temporomandibular joint osteoarthritis in human ancient skeletal remains from late holocene in Southern Patagonia. Int. J. Osteoarchaeol. 29 , 14–25. https://doi.org/10.1002/oa.2709 (2019).
Stone, J. H., Nelson, G. C. & Fitzpatrick, S. M. Temporomandibular joint osteoarthritis at Chelechol ra Orrak Palau. Int. J. Paleopathol. 28 , 20–31. https://doi.org/10.1016/j.ijpp.2019.12.001 (2020).
Rando, C. & Waldron, T. TMJ osteoarthritis: A new approach to diagnosis. Am. J. Phys. Anthropol. 148 , 45–53. https://doi.org/10.1002/ajpa.22039 (2012).
Akmal, N. L. H. B. I., Kumar, S. & Duraisamy, R. Evaluation of association between dietary habits and temporomandibular joint disorders. JRMDS 8 , 291–297 (2020).
Almashraqi, A. A., Ahmed, E. A., Mohamed, N. S. & Halboub, E. S. An MRI evaluation of the effects of qat chewing habit on the temporomandibular joint. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 126 , 272-282.e272. https://doi.org/10.1016/j.oooo.2018.05.005 (2018).
Molleson, T. A method for the study of activity related skeletal morphologies. Bioarchaeol. Near East 1 , 5–33. https://doi.org/10.31826/9781463222505-002 (2007).
Wiesinger, B., Malker, H., Englund, E. & Wänman, A. Does a dose-response relation exist between spinal pain and temporomandibular disorders?. BMC Musculoskelet. Disord. 10 , 28. https://doi.org/10.1186/1471-2474-10-28 (2009).
Article PubMed PubMed Central Google Scholar
Babalola, K., Potluri, A., Rengasamy, K. & Tadinada, A. Correlation between arthritic changes in cervical vertebrae and TMJ. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 127 , 33–34. https://doi.org/10.1016/j.oooo.2018.07.018 (2019).
Reggars, J. W. The relationship between primary temporomandibular joint disorders and cervical spine dysfunction: A summary and review. COMSIG Rev. 3 , 35–39 (1994).
PubMed Central Google Scholar
Aloosi, S. N., Mohammad, S. M., Qaradakhy, T. A. & Hasa, S. O. Contribution of cervical spine in temporomandibular joint disorders: A cross-sectional study. JBR J. Interdiscip. Med. Dental Sci. 4 , 204. https://doi.org/10.4172/2376-032X.1000204 (2016).
Friedman, M. H. & Weisberg, J. Temporomandibular Joint Disorders: Diagnosis and Treatment (Quintessence Books, 1985).
Lieverse, A. R., Weber, A. W., Bazaliiskiy, V. I., Goriunova, O. I. & Savel’ev, N. A. Osteoarthritis in Siberia’s Cis-Baikal: Skeletal indicators of hunter-gatherer adaptation and cultural change. Am. J. Phys. Anthropol. 132 , 1–16. https://doi.org/10.1002/ajpa.20479 (2007).
Kaczmarek, M. & Kozieradzka-Ogunmakin, I. Anthropology. Demographic, metric and palaeopathological study of human remains recovered from the Lower necropolis at Saqqara in Saqqara V. Old Kingdom Structures Between the Step Pyramid Complex and the Dry Moat. Part 2: Geology, Anthropology, Finds, Conservation (ed. Mysliwiec, K.) 345–422 (Editions Neriton, 2013).
Loew, M. et al. Could long-term overhead load in painters be associated with rotator cuff lesions? A pilot study. PLoS One 14 , e0213824. https://doi.org/10.1371/journal.pone.0213824 (2019).
Sommerich, C. M., McGlothlin, J. D. & Marras, W. S. Occupational risk factors associated with soft tissue disorders of the shoulder: A review of recent investigations in the literature. Ergonomics 36 , 697–717. https://doi.org/10.1080/00140139308967931 (1993).
Keyserling, W. M. Workplace risk factors and occupational musculoskeletal disorders, part 2: A review of biomechanical and psychophysical research on risk factors associated with upper extremity disorders. Am. Ind. Hyg. Assoc. J. 61 , 231–243. https://doi.org/10.1080/15298660008984532 (2000).
Article CAS Google Scholar
Keir, P. J., Farias Zuniga, A., Mulla, D. M. & Somasundram, K. G. Relationships and mechanisms between occupational risk factors and distal upper extremity disorders. Hum. Factors 63 , 5–31. https://doi.org/10.1177/0018720819860683 (2021).
Laulan, J., Marteau, E. & Bacle, G. Wrist osteoarthritis. Orthop. Traumatol. Surg. Res. 101 , S1–S9. https://doi.org/10.1016/j.otsr.2014.06.025 (2015).
Cayci, C. & Carlsen, B. T. Osteoarthritis of the Wrist. Plast. Reconst. Surg. 133 , 605–615. https://doi.org/10.1097/01.prs.0000438463.90968.d6 (2014).
Dillon, C., Petersen, M. & Tanaka, S. Self-reported hand and wrist arthritis and occupation: Data from the U.S. National Health Interview survey-occupational health supplement. Am. J. Ind. Med. 42 , 318–327. https://doi.org/10.1002/ajim.10117 (2002).
Williams, W. V. et al. Metacarpophalangeal arthropathy associated with manual labor (missouri metacarpal syndrome). clinical, radiographic, and pathologic characteristics of an unusual degenerative process. Arthritis Rheum. 30 , 1362–1371. https://doi.org/10.1002/art.1780301207 (1987).
Hammer, P. E. C., Shiri, R., Kryger, A. I., Kirkeskov, L. & Bonde, J. P. Associations of work activities requiring pinch or hand grip or exposure to hand-arm vibration with finger and wrist osteoarthritis: A meta-analysis. Scand. J. Work Environ. Health 40 , 133–145. https://doi.org/10.5271/sjweh.3409 (2014).
Fontana, L., Neel, S., Claise, J.-M., Ughetto, S. & Catilina, P. Osteoarthritis of the thumb carpometacarpal joint in women and occupational risk factors: A case-control study. J. Hand. Surg. Am. 32 , 459–465. https://doi.org/10.1016/j.jhsa.2007.01.014 (2007).
Wolf, J. M., Turkiewicz, A., Atroshi, I. & Englund, M. Occupational load as a risk factor for clinically relevant base of thumb osteoarthritis. Occup. Environ. Med. 77 , 168. https://doi.org/10.1136/oemed-2019-106184 (2020).
Cashmore, L. A. & Zakrzewski, S. R. Assessment of musculoskeletal stress marker development in the hand. Int. J. Osteoarchaeol. 23 , 334–347. https://doi.org/10.1002/oa.1254 (2013).
Karakostis, F. A., Hotz, G., Scherf, H., Wahl, J. & Harvati, K. A repeatable geometric morphometric approach to the analysis of hand entheseal three-dimensional form. Am. J. Phys. Anthropol. 166 , 246–260. https://doi.org/10.1002/ajpa.23421 (2018).
Voisin, J.-L. & Condemi, S. Non-metric traits in the Spy remains. Anthropologica et praehistorica 124 (2013), 1–16 (2014).
Andriacchi, T. P. Dynamics of knee malalignment. Orthop. Clin. North Am. 25 , 395–403. https://doi.org/10.1016/S0030-5898(20)31924-6 (1994).
Thambyah, A., Goh, J. C. H. & De, S. D. Contact stresses in the knee joint in deep flexion. Med. Eng. Phys. 27 , 329–335. https://doi.org/10.1016/j.medengphy.2004.09.002 (2005).
Rytter, S., Jensen, L. K., Bonde, J. P., Jurik, A. G. & Egund, N. Occupational kneeling and meniscal tears: A magnetic resonance imaging study in floor layers. J. Rheumatol. 36 , 1512–1519. https://doi.org/10.3899/jrheum.081150 (2009).
Niinimaki, S. & Sotos, L. B. The relationship between intensity of physical activity and entheseal changes on the lower limb. Int. J. Osteoarchaeol. 23 , 221–228. https://doi.org/10.1002/oa.2295 (2013).
Listi, G. A. The use of entheseal changes in the femur and os coxa for age assessment. J. Forensic. Sci. 61 , 12–18. https://doi.org/10.1111/1556-4029.12905 (2016).
Kwon, Y. et al. Classification of spinal postures during cross-legged sitting on the floor. J. Mech. Med. Biol. 19 , 1940056. https://doi.org/10.1142/s0219519419400566 (2019).
Woo, Y., Jun, I. & Je, W. Effects of a good posture belt on buttock pressure during cross-legged sitting. J. Phys. Ther. Sci. 28 , 976–978. https://doi.org/10.1589/jpts.28.976 (2016).
Moon, M.-S. et al. Spinopelvic orientation on radiographs in various body postures: upright standing, chair sitting, japanese style kneel sitting, and korean style cross-legged sitting. Clin. Orthop. Surg. 10 , 322–327. https://doi.org/10.4055/cios.2018.10.3.322 (2018).
Bae, J. S., Jang, J.-S., Lee, S.-H. & Kim, J. U. A comparison study on the change in lumbar lordosis when standing, sitting on a chair, and sitting on the floor in normal individuals. J. Korean Neurosurg. Soc. 51 , 20–23. https://doi.org/10.3340/jkns.2012.51.1.20 (2012).
Bárta, M. Kings of the Sun. Studies (National Museum and Charles University, 2020).
Brukner Havelková, P., Dulíková, V., Bejdová, Š., Velemínský, P. & Bárta, M. Anthropological evaluation of Old Kingdom human burials from the pyramid field of Abusir. PES XXVIII/2022 , 28–81 (2022).
Baines, J. Modelling the integration of elite and other social groups in Old Kingdom Egypt. In Élites et pouvoir en Égypte ancienne (ed. Moreno García, J. C.) 117–144 (Université Charles-de-Gaulle/Lille, 2010).
Seyfried, K. J. Dienstpflicht mit Selbstversorgung: die Diener des Verstorbenen im Alten Reich in Grab und Totenkult im Alten Ägypten (eds. Guksch, H., Hofmann, E., & Bommas, M.) 41–59 (C.H.Beck, 2003).
Brůžek, J., Santos, F., Dutailly, B., Murail, P. & Cunha, E. Validation and reliability of the sex estimation of the human os coxae using freely available DSP2 software for bioarchaeology and forensic anthropology. Am. J. Phys. Anthropol. 164 , 440–449. https://doi.org/10.1002/ajpa.23282 (2017).
Murail, P., Brůžek, J., Houët, F. & Cunha, E. DSP: A tool for probabilistic sex diagnosis using worldwide variability in hip-bone measurements. Bull. Mém. Soc. Anthropol. Paris 17 , 167–176 (2005).
Brůžek, J. A method for visual determination of sex, using the human hip bone. Am. J. Phys. Anthropol. 117 , 157–168. https://doi.org/10.1002/ajpa.10012 (2002).
Buikstra, J. E. & Ubelaker, D. H. Standards for data collection from human skeletal remains (Arkansas Archeological Survey, 1994).
Ferembach, D., Schwidetzky, I. & Stloukal, M. Recommendations for age and sex diagnoses of skeletons. J. Hum. Evol. 9 , 517–549 (1980).
Walker, P. L. Sexing skulls using discriminant function analysis of visually assessed traits. Am. J. Phys. Anthropol. 136 , 39–50. https://doi.org/10.1002/ajpa.20776 (2008).
Raxter, M. H. Metric sex estimation in an ancient Egyptian skeletal sample. SAS Bull. Newsl. Soc. Archaeol. Sci. 30 , 9–12 (2007).
Dabbs, G. Sex determination using the scapula in new kingdom skeletons from Tell El-amarna. HOMO 61 , 413–420. https://doi.org/10.1016/j.jchb.2010.09.001 (2010).
Marlow, E. J. & Kozieradzka-Ogunmakin, I. Metric sex estimation of ancient Egyptian skeletal remains.: Part II: Testing of new population-specific methods. Bioarchaeol. Near East 10 , 27–46 (2016).
Lovejoy, C. O., Meindl, R. S., Pryzbeck, T. R. & Mensforth, R. P. Chronological metamorphosis of the auricular surface of the ilium: A new method for the determination of adult skeletal age at death. Am. J. Phys. Anthropol. 68 , 15–28. https://doi.org/10.1002/ajpa.1330680103 (1985).
Schmitt, A. Une nouvelle méthode pour estimer l’âge au décès des adultes à partir de la surface sacro-pelvienne iliaque. Bull. Mém. Soc. Anthropol. Paris 17 , 89–101. https://doi.org/10.4000/bmsap.943 (2005).
McKern, T. W. & Stewart, T. D. Skeletal Age Changes in Young American Males . (U.S. Army, 1957).
Brooks, S. T. & Suchey, J. M. Skeletal age determination based on the os pubis: A comparison of the Acsádi-Nemeskéri and Suchey-Brooks methods. Hum. Evol. 5 , 227–238. https://doi.org/10.1007/BF02437238 (1990).
Schmitt, A. Age-at-death assessment using the os pubis and the auricular surface of the ilium: A test on an identified Asian sample. Int. J. Osteoarchaeol. 14 , 1–6. https://doi.org/10.1002/oa.693 (2004).
Calce, S. E. A new method to estimate adult age-at-death using the acetabulum. Am. J. Phys. Anthropol. 148 , 11–23. https://doi.org/10.1002/ajpa.22026 (2012).
Szilvássy, J. Age determination on the sternal articular faces of the clavicula. J. Hum. Evol. 9 , 906–910. https://doi.org/10.1016/0047-2484(80)90090-1 (1980).
Szilvássy, J. & Kritscher, H. Estimation of chronological age in man based on the spongy structure of long bones. Anthropol. Anz. 48 , 289–298 (1990).
Lovejoy, C. O. Dental wear in the Libben population: Its functional pattern and role in the determination of adult skeletal age at death. Am. J. Phys. Anthropol. 68 , 47–56. https://doi.org/10.1002/ajpa.1330680105 (1985).
Miles, A. E. W. The dentition in the assessment of individual age in skeletal material. In Dental Anthropology (ed. Brothwell, D. R.) 191–209 (Pergamon, 1963).
Brothwell, D. R. Digging Up Bones: The Excavation, Treatment, and Study of Human Skeletal Remains (Cornell University Press, 1981).
Henderson, C. Y., Mariotti, V., Pany-Kucera, D., Villotte, S. & Wilczak, C. A. The new “Coimbra Method’: A biologically appropriate method for recording specific features of fibrocartilaginous entheseal changes. Int. J. Osteoarchaeol. 26 , 925–932. https://doi.org/10.1002/oa.2477 (2016).
Michopoulou, E., Nikita, E. & Henderson, C. Y. A test of the effectiveness of the coimbra method in capturing activity-induced entheseal changes. Int. J. Osteoarchaeol. 27 , 409–417. https://doi.org/10.1002/oa.2564 (2017).
Radi, N. et al. Variation of the anterior aspect of the femoral head-neck junction in a modern human identified skeletal collection. Am. J. Phys. Anthropol. 152 , 261–272. https://doi.org/10.1002/ajpa.22354 (2013).
Smith, R. J. The continuing misuse of null hypothesis significance testing in biological anthropology. Am. J. Phys. Anthropol. 166 , 236–245. https://doi.org/10.1002/ajpa.23399 (2018).
Rubin, M. Inconsistent multiple testing corrections: The fallacy of using family-based error rates to make inferences about individual hypotheses. Methods Psychol. 10 , 100140. https://doi.org/10.1016/j.metip.2024.100140 (2024).
Download references
Acknowledgements
We would to thank Sébastien Villotte for his helpful comments, which improved the quality of the present paper, and Marek Bukáček for consultation on statistical analysis. Alastair Millar provided a linguistic review. This study was funded by the Ministry of Culture of the Czech Republic (DKRVO 2024-2028/7.I.a., National Museum, 00023272); by the Cooperatio Program provided by Charles University implemented at the Faculty of Arts of Charles University (research area: Archaeology); a non-investment subsidy from the Ministry of Education, Youth and Sports (1-VEG 2024, MSMT 1232/2024-8) and by the Czech Science Foundation through the research project “Titles and bones of ancient Egyptian officials: New mathematical approach to analysing Old Kingdom data” (GACR 24-10275M).
Author information
Authors and affiliations.
Department of Anthropology, National Museum in Prague, Cirkusová 1740, 193 00, Prague 9, Czech Republic
Petra Brukner Havelková & Petr Velemínský
Czech Institute of Egyptology, Faculty of Arts, Charles University, 110 00, Prague, Czech Republic
Petra Brukner Havelková, Veronika Dulíková, Jana Vacková & Miroslav Bárta
Department of Anthropology and Human Genetics, Faculty of Science, Charles University, 128 00, Prague, Czech Republic
Šárka Bejdová
Department of Applied Mathematics, Faculty of Information Technology, Czech Technical University in Prague, 160 00, Prague, Czech Republic
Jana Vacková
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: P.B.H., V.D., M.B. Methodology: P.B.H., V.D., J.V., P.V. Investigation: P.B.H., V.D., Š.B., J.V., P.V. Supervision: P.B.H., V.D., M.B. Writing—original draft: P.B.H., V.D. Writing—review & editing: P.B.H., V.D., J.V., Š.B., P.V., M.B.
Corresponding author
Correspondence to Petra Brukner Havelková .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information 1., supplementary information 2., supplementary information 3., supplementary information 4., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Brukner Havelková, P., Dulíková, V., Bejdová, Š. et al. Ancient Egyptian scribes and specific skeletal occupational risk markers (Abusir, Old Kingdom). Sci Rep 14 , 13317 (2024). https://doi.org/10.1038/s41598-024-63549-z
Download citation
Received : 01 December 2023
Accepted : 30 May 2024
Published : 27 June 2024
DOI : https://doi.org/10.1038/s41598-024-63549-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
VIDEO
COMMENTS
Spondylolisthesis (pronounced spahn-duh-low-liss-thee-sus) is a condition in which one of the bones in your spine (the vertebrae) slips out of place and moves on top of the vertebra next to it. It ...
Spondylolisthesis is a condition involving spine instability, which means the vertebrae move more than they should. A vertebra slips out of place onto the vertebra below. It may put pressure on a nerve, which could cause lower back pain or leg pain. The word spondylolisthesis (pronounced spohn-di-low-less-THEE-sis) comes from the Greek words ...
Spondylolysis (spon-dee-low-lye-sis) and spondylolisthesis (spon-dee-low-lis-thee-sis) are common causes of low back pain in children and adolescents. Spondylolysis is a weakness or stress fracture in one of the vertebrae, the small bones that make up the spinal column. This condition or weakness can occur in up to 5% of children as young as ...
Spondylolisthesis is a spinal condition that affects the lower vertebrae (spinal bones). This disease causes one of the lower vertebrae to slip forward onto the bone directly beneath it.
Symptoms of Spondylolisthesis. Spondylolisthesis can cause compression of spinal nerves and in severe cases, the spinal cord. The symptoms will depend on which vertebra is affected. Cervical Spondylolisthesis (neck) Neck pain. Arm pain. Arm numbness or tingling. Arm weakness.
Spondylolisthesis may present with symptoms of a radiculopathy due to compression of the nerve roots. When spondylolisthesis occurs in the lumbar vertebrae, pain, numbness, tingling, or weakness will be present in the lower. Patients may also complain of sharp shooting pains down their legs with certain activities that involve extension of the ...
Spondylolisthesis is the slippage of one vertebral body with respect to the adjacent vertebral body causing mechanical or radicular symptoms or pain. It can be due to congenital, acquired, or idiopathic causes. Spondylolisthesis is graded based on the degree of slippage of one vertebral body on the adjacent vertebral body.[1]
Spondylolysis is a condition when last vertebra of the lower spine is fractured. Spondylolisthesis is a condition when the spondylolysis weakens the bone so much that it cannot maintain proper position and vertebrae start to shift. Orthopaedic Spine Center. 617-724-8636.
In lumbar spondylolisthesis, a vertebrae in the lower back slips forward. This disorder usually occurs during adolescence or young adulthood (often in athletes). It is usually caused by a birth defect or an injury that causes fractures (breaks) in a part of the vertebra. If both sides of the vertebra are involved, the vertebra can then slip ...
Spondylolisthesis is slippage of a lumbar vertebra in relation to the vertebra below it. Anterior slippage (anterolisthesis) is more common than posterior slippage (retrolisthesis). Spondylolisthesis has multiple causes. It can occur anywhere in the spine and is most common in the lumbar and cervical regions.
Spondylolisthesis is the displacement of one spinal vertebra compared to another. While some medical dictionaries define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it (or the sacrum ), [1] [2] it is often defined in medical textbooks as displacement in any direction.
Spondylolisthesis is a common complication of spondylolysis. Spondylolisthesis progression is typically small and most likely in young individuals. Significant progression in adults is rare. The finding of spondylolysis and spondylolisthesis in an adult patient is usually incidental and not likely to be a direct source of pain unless there is ...
March 27, 2021. High-grade spondylolisthesis has diverse etiologies and presentations, as well as multiple treatment options. Mayo Clinic spinal surgeons tailor treatment to the individual patient to maximize outcomes and avoid future revision surgery. "We treat many patients who had surgery elsewhere that used inadequate sacral and pelvic ...
Spondylolisthesis is a displacement of a vertebra in which the bone slides out of its proper position onto the bone below it. Most often, this displacement occurs following a break or fracture. Surgery may be necessary to correct the condition if too much movement occurs and the bones begin to press on nerves.
Spondylolysis and Spondylolisthesis. Spondylolysis refers to a defect in the short, flat strip of bone called pars interarticularis (or pars). The pars is located at the back of the spine and forms a bridge (or isthmus) between the upper and lower joint surfaces of each facet of a vertebra (spinal bone).
In spondylolisthesis, one of the bones in your spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar spine). In some people, this causes no symptoms at all. Others may have back and leg pain that ranges from mild to severe.
In spondylolisthesis, one of the bones in your spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar spine). In some people, this causes no symptoms at all. Others may have back and leg pain that ranges from mild to severe.
Spondylolisthesis is a condition in which a bone in the spine (a vertebra) slips forward or backward in relation to the bone below it. It occurs most frequently in the lower back, but any vertebra in the spine can be affected. Low back pain, leg pain and weakness in the legs can happen if the bone that's out of position significantly narrows ...
The main symptoms of spondylolisthesis include: pain in your lower back, often worse when standing or walking and relieved when sitting or bending forward. pain spreading to your bottom or thighs. tight hamstrings (the muscles in the back of your thighs) pain, numbness or tingling spreading from your lower back down 1 leg ( sciatica)
Spondylolysis and spondylolisthesis are related conditions that affect your spine. Spondylolisthesis is when one vertebra slips out of place over the vertebra below it in your spine. Spondylolysis is a common cause of spondylolisthesis, because the crack (called a pars fracture) in a vertebra can cause it to slip out of place and become ...
Acutely, a traumatic spondylolisthesis can occur following a high-energy injury flexion/extension that causes a fracture-dislocation at the posterior elements. Another type is dysplastic spondylolisthesis which is a result of an abnormal formation of the posterior elements resulting in this subsequent instability.
Degenerative spondylolisthesis. Pain is aching in nature and insidious in onset. Pain is in the low back and posterior thighs. Neurogenic claudication may be present with lower-extremity symptoms worsening with exercise. Symptoms are often chronic and progressive, sometimes with periods of remission.
Purpose: To investigate the influence of slippage reduction and correction of lumbosacral kyphosis by L5-S1 single-level posterior lumbar interbody fusion (PLIF) on spinal alignment and clinical outcomes including postoperative complications in patients with dysplastic spondylolisthesis (DS). Methods: Twenty consecutive patients with symptomatic and severe DS who underwent L5-S1 single-level ...
Men with writing proficiency enjoyed a privileged position in ancient Egyptian society in the third millennium BC. Research focusing on these officials of elevated social status ("scribes ...