University Library, University of Illinois at Urbana-Champaign


Research Posters
- Elements of a poster
CREATING YOUR POSTER
Color scheme choices.
- WHAT TO INCLUDE IN YOUR POSTER
- More helpful tips
- Visualizations & images
- Illinois logo
- Archiving - Grad Students
- More Resources
- Oral Presentations
- 2024 Undergraduate Research Symposium This link opens in a new window
You have two choices when creating a research poster:
- You can create your poster from scratch by using PowerPoint, Adobe InDesign, or a similar design program.
- You can use one of the University of Illinois Research Poster Templates .
Sizing your Poster
- If you are presenting for the Undergraduate Research Symposium , resize your slide to width 48 inches by height 36 inches.
- If you are presenting at a professional conference , your instructions should indicate the size limits of your poster. Standard U.S. conference poster size is 48" by 36".
IMPORTANT: You must change the size of your slide before you start working on your poster. This will ensure that your images and text do not become pixilated when the poster is printed. See below for specific instructions.
How to correctly size your poster in PowerPoint:
- Select the "Design" tab
- Click "Slide Size"
- Select "Page Setup"
- Under the "Slides sized for:" dropdown menu, select "Custom"
- Set the "Width" and "Height" to what is needed for your poster
- Click "OK"

How to correctly size your poster in Adobe InDesign:
When a new document is created in Adobe InDesign, a dialogue box prompts you to enter dimensions:

- Change the dimension metric to inches from the drop down box.
- Margins are intentional space from an object to the edge of the poster, intended not to be trimmed. You can set this to 0 inches on all sides unless you have a specific plan to use margins in your design.
- Bleed shows the printer where to trim white space that occurs when printing color onto white poster paper. If you are printing your poster, include at least a 0.25 inch bleed on each side; remember not to place any content in the bleed as it will be trimmed by the printer.
- Slug is a space for the creator to leave any notes for the printer. You can set this to 0 inches unless you have notes.
If you ever want to change your poster dimensions after starting the poster, you can do so through the Document Setup Menu .
Using multiple font styles can really make your poster stand out and look professional. Consult this graphic to understand different font styles, what fonts work best together, and what fonts to avoid.
Sticking to a color scheme can help your poster look professional. Consistent use of color can help your viewer understand how information is organized on your poster. Not sure where to start with color?
- Pick colors from an image (including a custom one you're planning to use on your poster)
- Use Illinois branding colors
Not sure what to do with the hex code from a brand guide or color palette generator?
- Adobe InDesign
Always check that your text is accessible on background colors using WebAIM's free contrast checker.
If printing your poster, it's a good idea to do a small-scale test print of your poster before getting it printed. Colors often appear brighter and more vibrant on a screen than when printed. There still might be some variation in color depending on the color scale the printer uses, but it will be a closer match on paper than what you see on screen.
- << Previous: Examples
- Next: Visualizations & images >>
- Last Updated: May 13, 2024 2:05 PM
- URL: https://guides.library.illinois.edu/poster
How to Create a Research Poster
- Poster Basics
- Design Tips
- Logos & Images
What is a Research Poster?
Posters are widely used in the academic community, and most conferences include poster presentations in their program. Research posters summarize information or research concisely and attractively to help publicize it and generate discussion.
The poster is usually a mixture of a brief text mixed with tables, graphs, pictures, and other presentation formats. At a conference, the researcher stands by the poster display while other participants can come and view the presentation and interact with the author.
What Makes a Good Poster?
- Important information should be readable from about 10 feet away
- Title is short and draws interest
- Word count of about 300 to 800 words
- Text is clear and to the point
- Use of bullets, numbering, and headlines make it easy to read
- Effective use of graphics, color and fonts
- Consistent and clean layout
- Includes acknowledgments, your name and institutional affiliation
A Sample of a Well Designed Poster
View this poster example in a web browser .
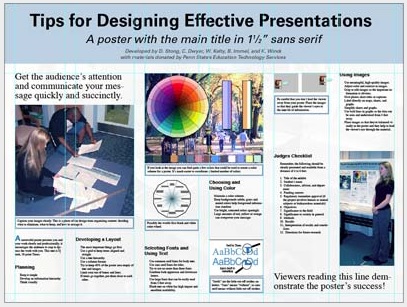
Image credit: Poster Session Tips by [email protected], via Penn State
Where do I begin?
Answer these three questions:.
- What is the most important/interesting/astounding finding from my research project?
- How can I visually share my research with conference attendees? Should I use charts, graphs, photos, images?
- What kind of information can I convey during my talk that will complement my poster?
What software can I use to make a poster?
A popular, easy-to-use option. It is part of Microsoft Office package and is available on the library computers in rooms LC337 and LC336. ( Advice for creating a poster with PowerPoint ).
Adobe Illustrator, Photoshop, and InDesign
Feature-rich professional software that is good for posters including lots of high-resolution images, but they are more complex and expensive. NYU Faculty, Staff, and Students can access and download the Adobe Creative Suite .
Open Source Alternatives
- OpenOffice is the free alternative to MS Office (Impress is its PowerPoint alternative).
- Inkscape and Gimp are alternatives to Adobe products.
- For charts and diagrams try Gliffy or Lovely Charts .
- A complete list of free graphics software .
A Sample of a Poorly Designed Poster
View this bad poster example in a browser.
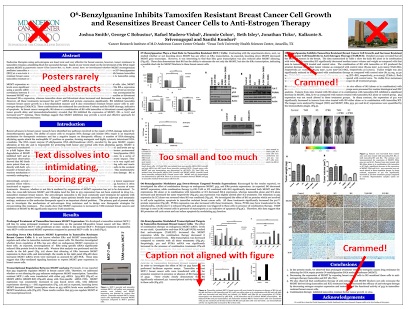
Image Credit: Critique by Better Posters
- Next: Design Tips >>
- Last Updated: Jul 11, 2023 5:09 PM
- URL: https://guides.nyu.edu/posters
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Serv Res
- v.42(1 Pt 1); 2007 Feb
Preparing and Presenting Effective Research Posters
Associated data.
APPENDIX A.2. Comparison of Research Papers, Presentations, and Posters—Contents.
Posters are a common way to present results of a statistical analysis, program evaluation, or other project at professional conferences. Often, researchers fail to recognize the unique nature of the format, which is a hybrid of a published paper and an oral presentation. This methods note demonstrates how to design research posters to convey study objectives, methods, findings, and implications effectively to varied professional audiences.
A review of existing literature on research communication and poster design is used to identify and demonstrate important considerations for poster content and layout. Guidelines on how to write about statistical methods, results, and statistical significance are illustrated with samples of ineffective writing annotated to point out weaknesses, accompanied by concrete examples and explanations of improved presentation. A comparison of the content and format of papers, speeches, and posters is also provided.
Each component of a research poster about a quantitative analysis should be adapted to the audience and format, with complex statistical results translated into simplified charts, tables, and bulleted text to convey findings as part of a clear, focused story line.
Conclusions
Effective research posters should be designed around two or three key findings with accompanying handouts and narrative description to supply additional technical detail and encourage dialog with poster viewers.
An assortment of posters is a common way to present research results to viewers at a professional conference. Too often, however, researchers treat posters as poor cousins to oral presentations or published papers, failing to recognize the opportunity to convey their findings while interacting with individual viewers. By neglecting to adapt detailed paragraphs and statistical tables into text bullets and charts, they make it harder for their audience to quickly grasp the key points of the poster. By simply posting pages from the paper, they risk having people merely skim their work while standing in the conference hall. By failing to devise narrative descriptions of their poster, they overlook the chance to learn from conversations with their audience.
Even researchers who adapt their paper into a well-designed poster often forget to address the range of substantive and statistical training of their viewers. This step is essential for those presenting to nonresearchers but also pertains when addressing interdisciplinary research audiences. Studies of policymakers ( DiFranza and the Staff of the Advocacy Institute 1996 ; Sorian and Baugh 2002 ) have demonstrated the importance of making it readily apparent how research findings apply to real-world issues rather than imposing on readers to translate statistical findings themselves.
This methods note is intended to help researchers avoid such pitfalls as they create posters for professional conferences. The first section describes objectives of research posters. The second shows how to describe statistical results to viewers with varied levels of statistical training, and the third provides guidelines on the contents and organization of the poster. Later sections address how to prepare a narrative and handouts to accompany a research poster. Because researchers often present the same results as published research papers, spoken conference presentations, and posters, Appendix A compares similarities and differences in the content, format, and audience interaction of these three modes of presenting research results. Although the focus of this note is on presentation of quantitative research results, many of the guidelines about how to prepare and present posters apply equally well to qualitative studies.
WHAT IS A RESEARCH POSTER?
Preparing a poster involves not only creating pages to be mounted in a conference hall, but also writing an associated narrative and handouts, and anticipating the questions you are likely to encounter during the session. Each of these elements should be adapted to the audience, which may include people with different levels of familiarity with your topic and methods ( Nelson et al. 2002 ; Beilenson 2004 ). For example, the annual meeting of the American Public Health Association draws academics who conduct complex statistical analyses along with practitioners, program planners, policymakers, and journalists who typically do not.
Posters are a hybrid form—more detailed than a speech but less than a paper, more interactive than either ( Appendix A ). In a speech, you (the presenter) determine the focus of the presentation, but in a poster session, the viewers drive that focus. Different people will ask about different facets of your research. Some might do policy work or research on a similar topic or with related data or methods. Others will have ideas about how to apply or extend your work, raising new questions or suggesting different contrasts, ways of classifying data, or presenting results. Beilenson (2004) describes the experience of giving a poster as a dialogue between you and your viewers.
By the end of an active poster session, you may have learned as much from your viewers as they have from you, especially if the topic, methods, or audience are new to you. For instance, at David Snowdon's first poster presentation on educational attainment and longevity using data from The Nun Study, another researcher returned several times to talk with Snowdon, eventually suggesting that he extend his research to focus on Alzheimer's disease, which led to an important new direction in his research ( Snowdon 2001 ). In addition, presenting a poster provides excellent practice in explaining quickly and clearly why your project is important and what your findings mean—a useful skill to apply when revising a speech or paper on the same topic.
WRITING FOR A VARIED PROFESSIONAL AUDIENCE
Audiences at professional conferences vary considerably in their substantive and methodological backgrounds. Some will be experts on your topic but not your methods, some will be experts on your methods but not your topic, and most will fall somewhere in between. In addition, advances in research methods imply that even researchers who received cutting-edge methodological training 10 or 20 years ago might not be conversant with the latest approaches. As you design your poster, provide enough background on both the topic and the methods to convey the purpose, findings, and implications of your research to the expected range of readers.
Telling a Simple, Clear Story
Write so your audience can understand why your work is of interest to them, providing them with a clear take-home message that they can grasp in the few minutes they will spend at your poster. Experts in communications and poster design recommend planning your poster around two to three key points that you want your audience to walk away with, then designing the title, charts, and text to emphasize those points ( Briscoe 1996 ; Nelson et al. 2002 ; Beilenson 2004 ). Start by introducing the two or three key questions you have decided will be the focus of your poster, and then provide a brief overview of data and methods before presenting the evidence to answer those questions. Close with a summary of your findings and their implications for research and policy.
A 2001 survey of government policymakers showed that they prefer summaries of research to be written so they can immediately see how the findings relate to issues currently facing their constituencies, without wading through a formal research paper ( Sorian and Baugh 2002 ). Complaints that surfaced about many research reports included that they were “too long, dense, or detailed,” or “too theoretical, technical, or jargony.” On average, respondents said they read only about a quarter of the research material they receive for detail, skim about half of it, and never get to the rest.
To ensure that your poster is one viewers will read, understand, and remember, present your analyses to match the issues and questions of concern to them, rather than making readers translate your statistical results to fit their interests ( DiFranza and the Staff of the Advocacy Institute 1996 ; Nelson et al. 2002 ). Often, their questions will affect how you code your data, specify your model, or design your intervention and evaluation, so plan ahead by familiarizing yourself with your audience's interests and likely applications of your study findings. In an academic journal article, you might report parameter estimates and standard errors for each independent variable in your regression model. In the poster version, emphasize findings for specific program design features, demographic, or geographic groups, using straightforward means of presenting effect size and statistical significance; see “Describing Numeric Patterns and Contrasts” and “Presenting Statistical Test Results” below.
The following sections offer guidelines on how to present statistical findings on posters, accompanied by examples of “poor” and “better” descriptions—samples of ineffective writing annotated to point out weaknesses, accompanied by concrete examples and explanations of improved presentation. These ideas are illustrated with results from a multilevel analysis of disenrollment from the State Children's Health Insurance Program (SCHIP; Phillips et al. 2004 ). I chose that paper to show how to prepare a poster about a sophisticated quantitative analysis of a topic of interest to HSR readers, and because I was a collaborator in that study, which was presented in the three formats compared here—as a paper, a speech, and a poster.
Explaining Statistical Methods
Beilenson (2004) and Briscoe (1996) suggest keeping your description of data and methods brief, providing enough information for viewers to follow the story line and evaluate your approach. Avoid cluttering the poster with too much technical detail or obscuring key findings with excessive jargon. For readers interested in additional methodological information, provide a handout and a citation to the pertinent research paper.
As you write about statistical methods or other technical issues, relate them to the specific concepts you study. Provide synonyms for technical and statistical terminology, remembering that many conferences of interest to policy researchers draw people from a range of disciplines. Even with a quantitatively sophisticated audience, don't assume that people will know the equivalent vocabulary used in other fields. A few years ago, the journal Medical Care published an article whose sole purpose was to compare statistical terminology across various disciplines involved in health services research so that people could understand one another ( Maciejewski et al. 2002 ). After you define the term you plan to use, mention the synonyms from the various fields represented in your audience.
Consider whether acronyms are necessary on your poster. Avoid them if they are not familiar to the field or would be used only once or twice on your poster. If you use acronyms, spell them out at first usage, even those that are common in health services research such as “HEDIS®”(Health Plan Employer Data and Information Set) or “HLM”(hierarchical linear model).
Poor: “We use logistic regression and a discrete-time hazards specification to assess relative hazards of SCHIP disenrollment, with plan level as our key independent variable.” Comment: Terms like “discrete-time hazards specification” may be confusing to readers without training in those methods, which are relatively new on the scene. Also the meaning of “SCHIP” or “plan level” may be unfamiliar to some readers unless defined earlier on the poster.
Better: “Chances of disenrollment from the State Children's Health Insurance Program (SCHIP) vary by amount of time enrolled, so we used hazards models (also known as event history analysis or survival analysis) to correct for those differences when estimating disenrollment patterns for SCHIP plans for different income levels.” Comment: This version clarifies the terms and concepts, naming the statistical method and its synonyms, and providing a sense of why this type of analysis is needed.
To explain a statistical method or assumption, paraphrase technical terms and illustrate how the analytic approach applies to your particular research question and data:
Poor : “The data structure can be formulated as a two-level hierarchical linear model, with families (the level-1 unit of analysis) nested within counties (the level-2 unit of analysis).” Comment: Although this description would be fine for readers used to working with this type of statistical model, those who aren't conversant with those methods may be confused by terminology such as “level-1” and “unit of analysis.”
Better: “The data have a hierarchical (or multilevel) structure, with families clustered within counties.” Comment: By replacing “nested” with the more familiar “clustered,” identifying the specific concepts for the two levels of analysis, and mentioning that “hierarchical” and “multilevel” refer to the same type of analytic structure, this description relates the generic class of statistical model to this particular study.
Presenting Results with Charts
Charts are often the preferred way to convey numeric patterns, quickly revealing the relative sizes of groups, comparative levels of some outcome, or directions of trends ( Briscoe 1996 ; Tufte 2001 ; Nelson et al. 2002 ). As Beilenson puts it, “let your figures do the talking,” reducing the need for long text descriptions or complex tables with lots of tiny numbers. For example, create a pie chart to present sample composition, use a simple bar chart to show how the dependent variable varies across subgroups, or use line charts or clustered bar charts to illustrate the net effects of nonlinear specifications or interactions among independent variables ( Miller 2005 ). Charts that include confidence intervals around point estimates are a quick and effective way to present effect size, direction, and statistical significance. For multivariate analyses, consider presenting only the results for the main variables of interest, listing the other variables in the model in a footnote and including complex statistical tables in a handout.
Provide each chart with a title (in large type) that explains the topic of that chart. A rhetorical question or summary of the main finding can be very effective. Accompany each chart with a few annotations that succinctly describe the patterns in that chart. Although each chart page should be self-explanatory, be judicious: Tufte (2001) cautions against encumbering your charts with too much “nondata ink”—excessive labeling or superfluous features such as arrows and labels on individual data points. Strive for a balance between guiding your readers through the findings and maintaining a clean, uncluttered poster. Use chart types that are familiar to your expected audience. Finally, remember that you can flesh out descriptions of charts and tables in your script rather than including all the details on the poster itself; see “Narrative to Accompany a Poster.”
Describing Numeric Patterns and Contrasts
As you describe patterns or numeric contrasts, whether from simple calculations or complex statistical models, explain both the direction and magnitude of the association. Incorporate the concepts under study and the units of measurement rather than simply reporting coefficients (β's) ( Friedman 1990 ; Miller 2005 ).
Poor: “Number of enrolled children in the family is correlated with disenrollment.” Comment: Neither the direction nor the size of the association is apparent.
Poor [version #2]: “The log-hazard of disenrollment for one-child families was 0.316.” Comment: Most readers find it easier to assess the size and direction from hazards ratios (a form of relative risk) instead of log-hazards (log-relative risks, the β's from a hazards model).
Better: “Families with only one child enrolled in the program were about 1.4 times as likely as larger families to disenroll.” Comment: This version explains the association between number of children and disenrollment without requiring viewers to exponentiate the log-hazard in their heads to assess the size and direction of that association. It also explicitly identifies the group against which one-child families are compared in the model.
Presenting Statistical Test Results
On your poster, use an approach to presenting statistical significance that keeps the focus on your results, not on the arithmetic needed to conduct inferential statistical tests. Replace standard errors or test statistics with confidence intervals, p- values, or symbols, or use formatting such as boldface, italics, or a contrasting color to denote statistically significant findings ( Davis 1997 ; Miller 2005 ). Include the detailed statistical results in handouts for later perusal.
To illustrate these recommendations, Figures 1 and and2 2 demonstrate how to divide results from a complex, multilevel model across several poster pages, using charts and bullets in lieu of the detailed statistical table from the scientific paper ( Table 1 ; Phillips et al. 2004 ). Following experts' advice to focus on one or two key points, these charts emphasize the findings from the final model (Model 5) rather than also discussing each of the fixed- and random-effects specifications from the paper.

Presenting Complex Statistical Results Graphically

Text Summary of Additional Statistical Results
Multilevel Discrete-Time Hazards Models of Disenrollment from SCHIP, New Jersey, January 1998–April 2000
Source : Phillips et al. (2004) .
SCHIP, State Children's Health Insurance Program; LRH, log relative-hazard; SE, standard error.
Figure 1 uses a chart (also from the paper) to present the net effects of a complicated set of interactions between two family-level traits (race and SCHIP plan) and a cross-level interaction between race of the family and county physician racial composition. The title is a rhetorical question that identifies the issue addressed in the chart, and the annotations explain the pattern. The chart version substantially reduces the amount of time viewers need to understand the main take-home point, averting the need to mentally sum and exponentiate several coefficients from the table.
Figure 2 uses bulleted text to summarize other key results from the model, translating log-relative hazards into hazards ratios and interpreting them with minimal reliance on jargon. The results for family race, SCHIP plan, and county physician racial composition are not repeated in Figure 2 , averting the common problem of interpreting main effect coefficients and interaction coefficients without reference to one another.
Alternatively, replace the text summary shown in Figure 2 with Table 2 —a simplified version of Table 1 which presents only the results for Model 5, replaces log-relative hazards with hazards ratios, reports associated confidence intervals in lieu of standard errors, and uses boldface to denote statistical significance. (On a color slide, use a contrasting color in lieu of bold.)
Relative Risks of SCHIP Disenrollment for Other * Family and County Characteristics, New Jersey, January 1998–April 2000
Statistically significant associations are shown in bold.
Based on hierarchical linear model controlling for months enrolled, months-squared, race, SCHIP plan, county physician racial composition, and all variables shown here. Scaled deviance =30,895. Random effects estimate for between-county variance =0.005 (standard error =0.006). SCHIP, State Children's Health Insurance Program; 95% CI, 95% confidence interval.
CONTENTS AND ORGANIZATION OF A POSTER
Research posters are organized like scientific papers, with separate pages devoted to the objectives and background, data and methods, results, and conclusions ( Briscoe 1996 ). Readers view the posters at their own pace and at close range; thus you can include more detail than in slides for a speech (see Appendix A for a detailed comparison of content and format of papers, speeches, and posters). Don't simply post pages from the scientific paper, which are far too text-heavy for a poster. Adapt them, replacing long paragraphs and complex tables with bulleted text, charts, and simple tables ( Briscoe 1996 ; Beilenson 2004 ). Fink (1995) provides useful guidelines for writing text bullets to convey research results. Use presentation software such as PowerPoint to create your pages or adapt them from related slides, facilitating good page layout with generous type size, bullets, and page titles. Such software also makes it easy to create matching handouts (see “Handouts”).
The “W's” (who, what, when, where, why) are an effective way to organize the elements of a poster.
- In the introductory section, describe what you are studying, why it is important, and how your analysis will add to the existing literature in the field.
- In the data and methods section of a statistical analysis, list when, where, who, and how the data were collected, how many cases were involved, and how the data were analyzed. For other types of interventions or program evaluations, list who, when, where, and how many, along with how the project was implemented and assessed.
- In the results section, present what you found.
- In the conclusion, return to what you found and how it can be used to inform programs or policies related to the issue.
Number and Layout of Pages
To determine how many pages you have to work with, find out the dimensions of your assigned space. A 4′ × 8′ bulletin board accommodates the equivalent of about twenty 8.5″ × 11″ pages, but be selective—no poster can capture the full detail of a large series of multivariate models. A trifold presentation board (3′ high by 4′ wide) will hold roughly a dozen pages, organized into three panels ( Appendix B ). Breaking the arrangement into vertical sections allows viewers to read each section standing in one place while following the conventions of reading left-to-right and top-to-bottom ( Briscoe 1996 ).
- At the top of the poster, put an informative title in a large, readable type size. On a 4′ × 8′ bulletin board, there should also be room for an institutional logo.

Suggested Layout for a 4′ × 8′ poster.
- In the left-hand panel, set the stage for the research question, conveying why the topic is of policy interest, summarizing major empirical or theoretical work on related topics, and stating your hypotheses or project aims, and explaining how your work fills in gaps in previous analyses.
- In the middle panel, briefly describe your data source, variables, and methods, then present results in tables or charts accompanied by text annotations. Diagrams, maps, and photographs are very effective for conveying issues difficult to capture succinctly in words ( Miller 2005 ), and to help readers envision the context. A schematic diagram of relationships among variables can be useful for illustrating causal order. Likewise, a diagram can be a succinct way to convey timing of different components of a longitudinal study or the nested structure of a multilevel dataset.
- In the right-hand panel, summarize your findings and relate them back to the research question or project aims, discuss strengths and limitations of your approach, identify research, practice, or policy implications, and suggest directions for future research.
Figure 3 (adapted from Beilenson 2004 ) shows a suggested layout for a 4′ × 8′ bulletin board, designed to be created using software such as Pagemaker that generates a single-sheet presentation; Appendix C shows a complete poster version of the Phillips et al. (2004) multilevel analysis of SCHIP disenrollment. If hardware or budget constraints preclude making a single-sheet poster, a similar configuration can be created using standard 8.5″ × 11″ pages in place of the individual tables, charts, or blocks of text shown in Figure 3 .
Find out well in advance how the posters are to be mounted so you can bring the appropriate supplies. If the room is set up for table-top presentations, tri-fold poster boards are essential because you won't have anything to attach a flat poster board or pages to. If you have been assigned a bulletin board, bring push-pins or a staple gun.
Regardless of whether you will be mounting your poster at the conference or ahead of time, plan how the pages are to be arranged. Experiment with different page arrangements on a table marked with the dimensions of your overall poster. Once you have a final layout, number the backs of the pages or draw a rough sketch to work from as you arrange the pages on the board. If you must pin pages to a bulletin board at the conference venue, allow ample time to make them level and evenly spaced.
Other Design Considerations
A few other issues to keep in mind as you design your poster. Write a short, specific title that fits in large type size on the title banner of your poster. The title will be potential readers' first glimpse of your poster, so make it inviting and easy to read from a distance—at least 40-point type, ideally larger. Beilenson (2004) advises embedding your key finding in the title so viewers don't have to dig through the abstract or concluding page to understand the purpose and conclusions of your work. A caution: If you report a numeric finding in your title, keep in mind that readers may latch onto it as a “factoid” to summarize your conclusions, so select and phrase it carefully ( McDonough 2000 ).
Use at least 14-point type for the body of the poster text. As Briscoe (1996) points out, “many in your audience have reached the bifocal age” and all of them will read your poster while standing, hence long paragraphs in small type will not be appreciated! Make judicious use of color. Use a clear, white, or pastel for the background, with black or another dark color for most text, and a bright, contrasting shade to emphasize key points or to identify statistically significant results ( Davis 1997 ).
NARRATIVE TO ACCOMPANY A POSTER
Prepare a brief oral synopsis of the purpose, findings, and implications of your work to say to interested parties as they pause to read your poster. Keep it short—a few sentences that highlight what you are studying, a couple of key findings, and why they are important. Design your overview as a “sound byte” that captures your main points in a succinct and compelling fashion ( Beilenson 2004 ). After hearing your introduction, listeners will either nod and move along or comment on some aspect of your work that intrigues them. You can then tailor additional discussion to individual listeners, adjusting the focus and amount of detail to suit their interests. Gesture at the relevant pages as you make each point, stating the purpose of each chart or table and explaining its layout before describing the numeric findings; see Miller (2005) for guidelines on how to explain tables and charts to a live audience. Briscoe (1996) points out that these mini-scripts are opportunities for you to fill in details of your story line, allowing you to keep the pages themselves simple and uncluttered.
Prepare short answers to likely questions about various aspects of your work, such as why it is important from a policy or research perspective, or descriptions of data, methods, and specific results. Think of these as little modules from an overall speech—concise descriptions of particular elements of your study that you can choose among in response to questions that arise. Beilenson (2004) also recommends developing a few questions to ask your viewers, inquiring about their reactions to your findings, ideas for additional questions, or names of others working on the topic.
Practice your poster presentation in front of a test audience acquainted with the interests and statistical proficiency of your expected viewers. Ideally, your critic should not be too familiar with your work: A fresh set of eyes and ears is more likely to identify potential points of confusion than someone who is jaded from working closely with the material while writing the paper or drafting the poster ( Beilenson 2004 ). Ask your reviewer to identify elements that are unclear, flag jargon to be paraphrased or defined, and recommend changes to improve clarity ( Miller 2005 ). Have them critique your oral presentation as well as the contents and layout of the poster.
Prepare handouts to distribute to interested viewers. These can be produced from slides created in presentation software, printed several to a page along with a cover page containing the abstract and your contact information. Or package an executive summary or abstract with a few key tables or charts. Handouts provide access to the more detailed literature review, data and methods, full set of results, and citations without requiring viewers to read all of that information from the poster ( Beilenson 2004 ; Miller 2005 ). Although you also can bring copies of the complete paper, it is easier on both you and your viewers if you collect business cards or addresses and mail the paper later.
The quality and effectiveness of research posters at professional conferences is often compromised by authors' failure to take into account the unique nature of such presentations. One common error is posting numerous statistical tables and long paragraphs from a research paper—an approach that overwhelms viewers with too much detail for this type of format and presumes familiarity with advanced statistical techniques. Following recommendations from the literature on research communication and poster design, this paper shows how to focus each poster on a few key points, using charts and text bullets to convey results as part of a clear, straightforward story line, and supplementing with handouts and an oral overview.
Another frequent mistake is treating posters as a one-way means of communication. Unlike published papers, poster sessions are live presentations; unlike speeches, they allow for extended conversation with viewers. This note explains how to create an oral synopsis of the project, short modular descriptions of poster elements, and questions to encourage dialog. By following these guidelines, researchers can substantially improve their conference posters as vehicles to disseminate findings to varied research and policy audiences.
CHECKLIST FOR PREPARING AND PRESENTING AN EFFECTIVE RESEARCH POSTERS
- Design poster to focus on two or three key points.
- Adapt materials to suit expected viewers' knowledge of your topic and methods.
- Design questions to meet their interests and expected applications of your work.
- Paraphrase descriptions of complex statistical methods.
- Spell out acronyms if used.
- Replace large detailed tables with charts or small, simplified tables.
- Accompany tables or charts with bulleted annotations of major findings.
- Describe direction and magnitude of associations.
- Use confidence intervals, p -values, symbols, or formatting to denote statistical significance.
Layout and Format
- Organize the poster into background, data and methods, results, and study implications.
- Divide the material into vertical sections on the poster.
- Use at least 14-point type in the body of your poster, at least 40-point for the title.
Narrative Description
- Rehearse a three to four sentence overview of your research objectives and main findings.
- Summary of key studies and gaps in existing literature
- Data and methods
- Each table, chart, or set of bulleted results
- Research, policy, and practice implications
- Solicit their input on your findings
- Develop additional questions for later analysis
- Identify other researchers in the field
- Prepare handouts to distribute to interested viewers.
- Print slides from presentation software, several to a page.
- Or package an executive summary or abstract with a few key tables or charts.
- Include an abstract and contact information.
Acknowledgments
I would like to thank Ellen Idler, Julie Phillips, Deborah Carr, Diane (Deedee) Davis, and two anonymous reviewers for helpful comments on earlier drafts of this work.
Supplementary Material
The following supplementary material for this article is available online:
APPENDIX A.1. Comparison of Research Papers, Presentations, and Posters—Materials and Audience Interaction.
Suggested Layout for a Tri-Fold Presentation Board.
Example Research Poster of Phillips et al. 2004 Study.
- Beilenson J. Developing Effective Poster Presentations. Gerontology News. 2004; 32 (9):6–9. [ Google Scholar ]
- Briscoe MH. Preparing Scientific Illustrations: A Guide to Better Posters, Presentations, and Publications. 2. New York: Springer-Verlag; 1996. [ Google Scholar ]
- Davis M. Scientific Papers and Presentations. New York: Academic Press; 1997. [ Google Scholar ]
- DiFranza JR. A Researcher's Guide to Effective Dissemination of Policy-Related Research. Princeton, NJ: The Robert Wood Johnson Foundation; 1996. the Staff of the Advocacy Institute, with Assistance from the Center for Strategic Communications. [ Google Scholar ]
- Fink A. How to Report on Surveys. Thousand Oaks, CA: Sage Publications; 1995. [ Google Scholar ]
- Friedman GD. Be Kind to Your Reader. American Journal of Epidemiology. 1990; 132 (4):591–3. [ PubMed ] [ Google Scholar ]
- Maciejewski ML, Diehr P, Smith MA, Hebert P. Common Methodological Terms in Health Services Research and Their Symptoms. Medical Care. 2002; 40 :477–84. [ PubMed ] [ Google Scholar ]
- McDonough J. Experiencing Politics: A Legislator's Stories of Government and Health Care. Berkeley: University of California Press; 2000. [ Google Scholar ]
- Miller JE. The Chicago Guide to Writing about Multivariate Analysis. Chicago Guides to Writing, Editing and Publishing. Chicago: University of Chicago Press; 2005. [ Google Scholar ]
- Nelson DE, Brownson RC, Remington PL, Parvanta C, editors. Communicating Public Health Information Effectively: A Guide for Practitioners. Washington, DC: American Public Health Association; 2002. [ Google Scholar ]
- Phillips JA, Miller JE, Cantor JC, Gaboda D. Context or Composition. What Explains Variation in SCHIP Disenrollment? Health Services Research. 2004; 39 (4, part I):865–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Snowdon D. Aging with Grace: What the Nun Study Teaches Us about Leading Longer, Healthier, and More Meaningful Lives. New York: Bantam Books; 2001. [ Google Scholar ]
- Sorian R, Baugh T. Power of Information Closing the Gap between Research and Policy. Health Affairs. 2002; 21 (2):264–73. [ PubMed ] [ Google Scholar ]
- Tufte ER. The Visual Display of Quantitative Information. 2. Cheshire, CT: Graphics Press; 2001. [ Google Scholar ]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to prepare an...
How to prepare an effective research poster
- Related content
- Peer review
- Lucia Hartigan , registrar 1 ,
- Fionnuala Mone , fellow in maternal fetal medicine 1 ,
- Mary Higgins , consultant obstetrician 1 2
- 1 National Maternity Hospital, Dublin
- 2 Obstetrics and Gynaecology, Medicine and Medical Sciences, University College Dublin
- mhiggins{at}nmh.ie
Being asked to give a poster presentation can be exciting, and you need not be daunted by the prospect of working out how to prepare one. As Lucia Hartigan and colleagues explain, many options are available
The long nights are over, the statistics have been run, the abstract has been written, and the email pops into your inbox: “Congratulations! You have been accepted for a poster presentation.”
All that work has been worthwhile. Your consultant congratulates you and your colleagues are envious of your having a legitimate excuse to go away for a couple of days, but now you have to work out how to prepare a poster. Do not despair, for you have many options.
Firstly, take this seriously. A poster is not a consolation prize for not being given an oral presentation. This is your chance to show your work, talk to others in the field, and, if you are lucky, to pick up pointers from experts. Given that just 45% of published abstracts end in a full paper, 1 this may be your only chance to get your work out there, so put some effort into it. If you don’t have access to the services of a graphic designer, then some work will be entailed as it normally takes us a full day to prepare the layout of a poster. If you are lucky enough to have help from a graphic designer, then you will need to check that the data are correct before it is sent to the printer. After all, it will be your name on the poster, not the graphic designer’s.
Secondly, check the details of the requirements. What size poster should you have? If it is too big, it may look arrogant. If it is too small, then it may seem too modest and self effacing. Should it be portrait or landscape? Different meetings have different requirements. Some may stay with traditional paper posters, so you need to factor in printing. Others present them electronically, but may have a deadline by which you need to have uploaded the poster. When planning a meeting the organisers work out how many poster boards there will be and then the numbers, so follow their requirements and read the small print.
Then make a template. It can be tempting to “borrow” a poster template from someone else, and this may buy you some time, but it is important to check what page set-up and size have been selected for the template. If it’s meant for an A2 size and you wish to print your poster on A0 paper, then the stretching may lead to pixillation, which would not look good.
Next, think about your layout. Use text boxes to cover the following areas: title (with authors, institution, and logo), background, methods, results, and conclusions. Check that the text boxes are aligned by using gridlines, and justify your text. Use different colours for titles, and make sure you can read the title from 3 metres away. Some people will put their abstract in a separate box in the top right hand corner underneath the title, and then expand a little in the other areas. That is fine, so long as you follow the golden rule of writing a poster: do not include too much text. One study showed that less than 5% of conference attendees visit posters at meetings and that few ask useful questions. 2 The same research found that, in addition to the scientific content of a poster, the factors that increase visual appeal include pictures, graphs, and a limited use of words. 2 The ideal number of words seems to be between 300 and 400 per square metre.
Now make it look pretty and eye catching, and use lots of graphics. Outline text boxes or fill them with a different colour. If you can present the data using a graph, image, or figures rather than text, then do so, as this will add visual appeal. If you want to put a picture in the background, and it is appropriate to do so, fade the image so that it does not distract from the content.
Fonts are important. Check whether the meeting has set criteria for fonts; if they have, then follow them. You do not want to stand out for the wrong reason. If there are no specified criteria, then the title should be in point size 72-84, depending on the size of the poster. The authors’ names should be either the same size, but in italics, or else a couple of sizes smaller.
If you are including the hospital logo, don’t take a picture that will not size up properly when enlarged. Instead, obtain a proper copy from the hospital administrators.
References can be in small writing. No one is likely to read them, and you are including them only to remind yourself what you learnt in the literature review. One intriguing possibility is the use of a trigger image to link the poster to online content. 3
Finally, there are also things you should not do. Don’t leave your figures unlabelled, include spelling errors, use abbreviations without an explanation, or go outside the boundaries of the poster. Don’t be ashamed that you “only” have a poster. At a good meeting you may find that the comments from passers by are an amazing peer review. We have presented at meetings where world experts have given feedback, and with that feedback we have written the paper on the flight home.
Competing interests: We have read and understood the BMJ Group policy on declaration of interests and have no relevant interests to declare.
- ↵ Scherer RW, Langenberg P, von Elm E. Full publication of results initially presented in abstracts. Cochrane Database Syst Rev 2007 ; 2 : MR000005 . OpenUrl PubMed
- ↵ Goodhand JR, Giles CL, Wahed M, Irving PM, Langmead L, Rampton DS. Poster presentations at medical conferences: an effective way of disseminating research? Clin Med 2011 ; 1 : 138 -41. OpenUrl
- ↵ Atherton S, Javed M, Webster S, Hemington-Gorse S. Use of a mobile device app: a potential new tool for poster presentations and surgical education. J Visual Comm Med 2013 ; 36 (1-2): 6 -10. OpenUrl
Gerstein Science Information Centre
Posters and presentations.
- Planning it out
General Poster Design Guides
Video: making an academic research poster using powerpoint, scientific research poster design guides and templates, design inspiration, handout tips.
- Presentation Tips
- Using Images and Data
- Citing Sources
- Printing Posters
- Campus Resources
- U of T poster session opportunities
- Your Comments

Pro tip: Not using a template and starting from scratch?
Remember to resize your canvas to the right size in PowerPoint (often 36x 48 inches or 36x 56 inches , instead of the default 8.5x11 inches).
Photo Credit: widdowquinn via Compfight cc
- Poster Buzz Resource created by design firm SCP; content created in consultation with science faculty from various universities. - Contains Microsoft PowerPoint templates for scientific research - various sizes and content/format types available (e.g. Quantitative, Qualitative, Mixed Methods, etc). - Also contains other resources for academic poster design and printing.
- Faculty of 1000 posters An open access repository of biology and medicine posters from 180+ international conferences
- Couldn't fit everything into your poster? Include extra key information , in an concise 1-page handout.
- Include your Works Cited list and any supplementary readings your audience might find of interest.
- Don't have time to make a handout from scratch? Print out colour mini copies of your poster to distribute, so that attendees won't have to rely on their grainy photos of your poster.
- << Previous: Planning it out
- Next: Presentation Tips >>
- Last Updated: May 1, 2024 12:49 AM
- URL: https://guides.library.utoronto.ca/posters_presentations
Library links
- Gerstein Home
- U of T Libraries Home
- Renew items and pay fines
- Library hours
- Contact Gerstein
- University of Toronto Libraries
- UT Mississauga Library
- UT Scarborough Library
- Information Commons
- All libraries
© University of Toronto . All rights reserved.
Connect with us
Learn more about how the Cal Poly Humboldt Library can help support your research and learning needs.
Stay updated at Campus Ready .

- Cal Poly Humboldt Library
- Research Guides
Creating a Research Poster
- Creating your poster step by step
- Getting Started
- Citing Images
- Creative Commons Images
- Printing options
- More Resources
Preparing your poster
There are three components to your poster session:
- Your poster
All three components should complement one another, not repeat each other.
Poster: Your poster should be an outline of your research with interesting commentary about what you learned along the way.
You: You should prepare a 10-30 second elevator pitch and a 1-2 minute lightning talk about your research. This should be a unique experience or insight you had about your research that adds depth of understanding to what the attendee can read on your poster.
Handout: Best practices for handouts - Your handout should be double-sided. The first side of the paper should include a picture of your poster (this can be in black and white or color). The second side of the handout should include your literature review, cited references, further information about your topic and your contact information.
Creating your poster by answering 3 questions:
- What is the most important and/or interesting finding from my research project?
- How can I visually share my research with conference attendees? Should I use charts, graphs, images, or a wordcloud?
- What kind of information do I need to share during my lightning talk that will complement my poster?
- *Title (at least 72 pt font).
- Research question or hypothesis (all text should be at least 24 pt font).
- Methodology. What is the research process that you used? Explain how you did your research.
- Your interview questions.
- Observations. What did you see? Why is this important?
- *Findings. What did you learn? Summarize your conclusions.
- Pull out themes in the literature and list in bullet points.
- Consider a brief narrative of what you learned - what was the most interesting/surprising part of your project?
- Interesting quotes from your research.
- Turn your data into charts or tables.
- Use images (visit the "Images" tab in the guide for more information). Take your own or legally use others.
- Recommendations and/or next steps for future research.
- You can include your list of citations on your poster or in your handout.
- *Make sure your name, and Cal Poly Humboldt University is on your poster.
*Required. Everything else is optional - you decide what is important to put on your poster. These are just suggestions. Use the tabs in this guide for more tips on how to create your poster.
Poster Sizes
You can create your poster from scratch by using PowerPoint or a similar design program.
Resize the slide to fit your needs before you begin adding any content. Standard poster sizes range from 40" by 30" and 48" by 36" but you should check with the conference organizers. If you don't resize your design at the beginning, when it is printed the image quality will be poor and pixelated if it is sized up to poster dimensions.
The standard poster sizes for ideaFest are 36" x 48" and 24" by 36".
To resize in PowerPoint, go to "File" then "Page Setup..." and enter your dimensions in the boxes for "width" and "height". Make sure to select "OK" to save your changes.
To resize in Google Slides, go to "File" then "Page setup" and select the "Custom" option in the drop down menu. Enter the dimensions for your poster size and then select "Apply" to save your changes.
Step Four: Final checklist
Final checklist for submitting your poster for printing:.
- Proofread your poster for spelling and grammar mistakes. Ask a peer to read your poster, they will catch the mistakes that you miss. Print your poster on an 8 1/2" by 11" sheet of paper - it is easier to read for mistakes and to judge your design.
- Make sure you followed Step 3 and resized your PPT slide correctly.
- Does your poster have flow? Did you "chunk" information into easily read pieces of information?
- Do your visualizations (e.g. charts, graphs, tag clouds, etc.) tell a story? Are they properly labeled and readable?
- Make sure that your images we not resized in PPT. You should use the original size of the image or try an image editor (e.g. Photoshop). Did you cite your image?
- Is your name, department, and affiliation on your poster?
- Did you want to include acknowlegments on your poster? This may be appropriate if your advisor and a graduate student provided leadership during the research process.
- Most importantly- Save your PPT slide to PDF before you send to the printer in order to avoid any printing mishaps. You should also double-check the properties to make sure it is still sized correctly in PDF.
- << Previous: Getting Started
- Next: Images >>
Undergraduate Research: Posters
- Topics & Search Tools
- Search Strategies
- Literature Reviews
- Annotated Bibliographies
- Office of Undergraduate Research
- Tips for Designing Better Research Posters
Online Tutorials
- UT at Austin: Guide to Creating Research Posters This sources contains samples and examples of posters alongside tips for messaging, reviewing, printing, and presenting your poster.
- UNC: Poster and Presentation Resources The academic poster design portion of this guide contains useful links to support creating a research poster. Other portions of this site will help with presenting your research and poster.
- NCSU: Creating Effective Poster Presentations Designed and organized like a research poster, this source contains an introduction to research posters along with other tools to support poster creation.
Blogs and Sites
- Better Posters: A Resource for Improving Poster Presentations Blog
- Colin Purrington: Designing Conference Posters This page gives a summary of what research posters are and how to get started. The subpages detail what you should put in different sections, provide free templates, and give tips on avoiding common mistakes.
Free Fonts and Palettes
- Fontsquirrel
- 1001 Free Fonts
- Coolors Palette Generator
- COLOURlovers
Undergraduate Research Services Librarian

Print on Campus
- Biological Sciences Department
- Newman Library Posting printing information is available under the dropdown "Plotter Printer."
- << Previous: Annotated Bibliographies
- Next: Citation >>
- Last Updated: Jul 11, 2020 3:06 PM
- URL: https://guides.lib.vt.edu/ur

How to create a research poster
- Getting Started
- Planning your Poster
- Designing a Poster
- Poster Templates & Examples
- Printing your Poster
- Additional Guides
What is a research poster?
A research poster is a visual way to summarize and communicate the results of a research project to a general audience. A good poster should include the goal of the research, its methodology, results, and discussion/conclusion, in clear and concise language.
Research posters will often include photos, maps, graphs and other images to present information in an attractive way.
Why a poster?
Research posters are a common form of research presentation in conferences, seminars, and symposiums. Some of the main advantages of presenting a poster rather than a conference paper are:
- Knowledge sharing with a wider audience: with poster presentations, researchers usually stand beside their posters and can interact directly with the public.
- Opportunity to explore different ways to present information: posters are ideal for highly visual topics.
- Networking: presenting posters can help researchers identify potential collaborators, spark further discussion, make contacts, etc.
- Opportunity to improve verbal presentation skills: researchers can talk about their research without having to observe the stricter guidelines of other types of conference presentations.
- Opportunity to showcase research to potential employers.
Branding requirements
Yukon University's branding guidelines may be applicable when presenting research results. This can vary depending on course/assignment requirements, whether the research is directly sponsored/funded by the institution, and how and where the poster will be presented.
For YukonU students: check with your instructor if branding is required for your situation.
YukonU faculty/staff: YukonU's branding guidelines can be found on https://yukoncollege.sharepoint.com/sites/yc/offices/relations (Sharepoint login required).
- Next: Planning your Poster >>
- Last Updated: Apr 12, 2023 2:45 PM
- URL: https://yukonu.libguides.com/research_poster
- Skip to main content
- Skip to primary sidebar
- Skip to footer
Additional menu
FreshSpectrum - Data Visualization Made Easy
Learn how you can use simple methods and tools, like Canva, Flourish, and Datawrapper, to improve your data communication skills.

How to design a research poster using Canva
Today’s post is about designing research poster presentations using Canva. Even if you’ve never created a research poster in your life, I think this post can really help you get a solid jump on your next design.
Because ready or not, it’s happening. After a long COVID-19 break, a bunch of evaluation conferences are going to be live again. And with live conferences you also get actual live presentations. And you also get those big poster presentation nights.
In this post:
- I’ll show you how to create a research poster, including a new approach I really appreciate.
- Grid based design and why planning your poster in content blocks is a good idea.
- A bunch of alternative poster styles that use the same underlying grid.
- Free research poster Canva templates, and some tools to help you design your next poster.

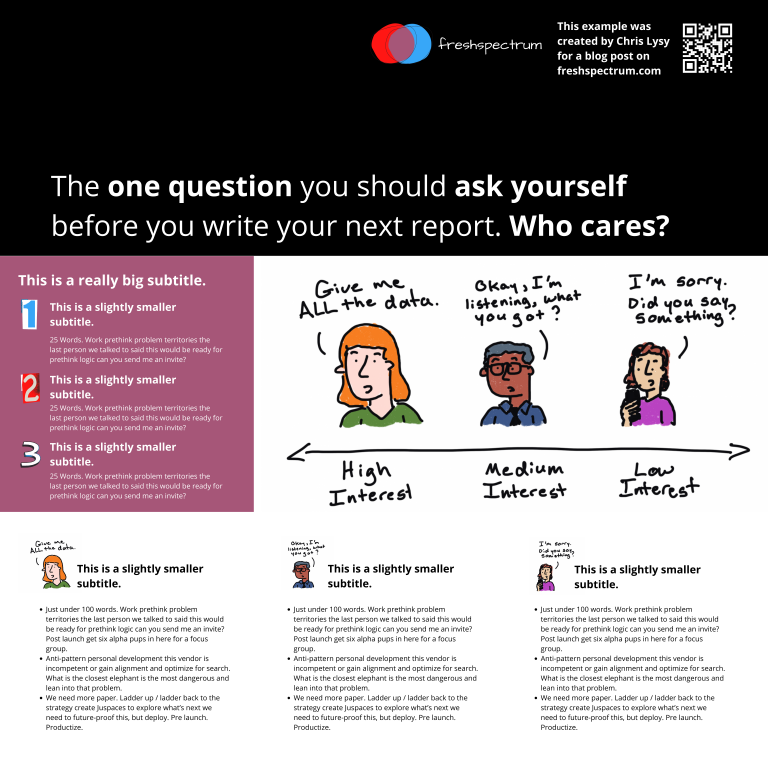
The research poster presentation mindset.
So imagine yourself in a room standing in front of a research poster surrounded by people just like you. The attendees at the session might be holding drinks and are continuously running into old friends. Some glance at your work and keep right on walking. Others might ask you a question or two as they peruse your poster.
And there you are, standing in front of your poster that you’ve agonized over. The one you had to carry in a big tube through a crowded airport and then inside a crowded airport shuttle.
A research poster isn’t some stand alone document or social media infographic. It’s your wingman. Your partner in crime. It stays by your side, supporting the communication of your work. A better poster design won’t just help you communicate, it can also make your time in that room feel a little less awkward.
The usual approach to research poster design.
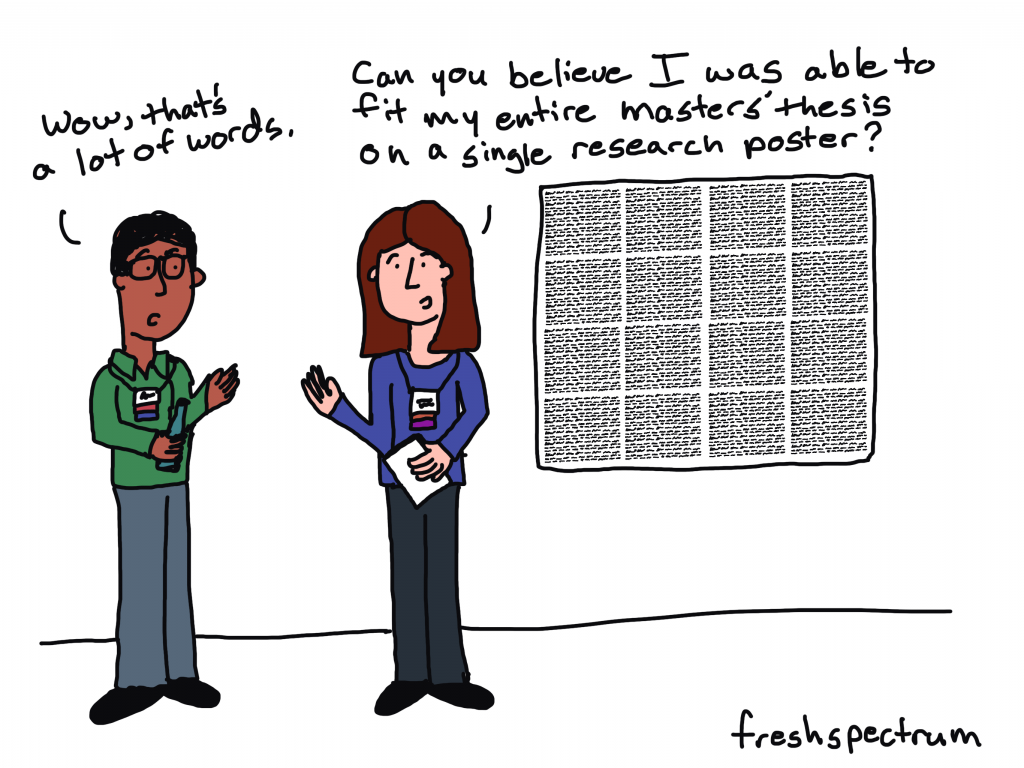
Most research posters tend to just be adaptations of a research paper. As such, a lot of academics will simply take their paper title and put it at the top of the research poster. They will then create sections on the poster that mirror the sections in their paper.
Ultimately they end up with a research poster outline that looks just like a research paper outline. This is definitely not my preferred approach to research poster design. But if this is the way that you decide to create your poster, at least take some basic steps to ensure it’s readable.
Years ago, Stephanie Evergreen and Chris Metzner created a quick little guide on how to design a research poster for the American Evaluation Association’s Potent Presentations Initiative. Definitely check it out . Especially if you just want to polish a poster you’ve already created.
How to create a better research poster in less time.
I really like the poster approach outlined by Mike Morrison .
The gist, if you don’t feel like watching the video, is that research posters should be designed more like billboards than infographics.
Because during a poster session there is a lot of competing information. So instead of trying to capture and retain the attention of just a few attendees, focus on sharing a very specific point to a lot of attendees. And then use a QR code to link to the full paper and other more in-depth information.
What is the standard size for a research poster?
Okay this is kind of a trick question. There are standardish sizes, but the people who decide on the size are almost always the ones putting on the conference.
In the past at least, the American Evaluation Association has required a square 44 inch by 44 inch design. Other common sizes include 36 inch tall by 48 inch wide and 42 inch tall by 56 inch wide.
But before you start designing, always check the specific conference’s website and follow their design guidelines.
A research poster design process using Canva.
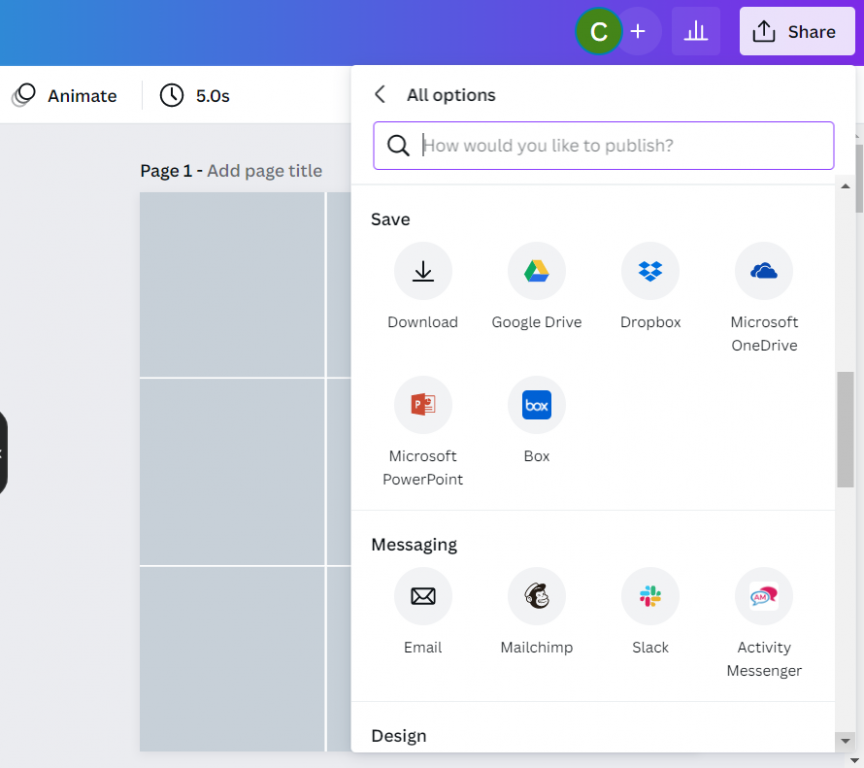
So for my research poster designs I’m going to use Canva.com .

Instead of starting with a base template, we’ll just click on the “Create a design” and click custom size. I’ll be creating a square 48 inch by 48 inch poster.

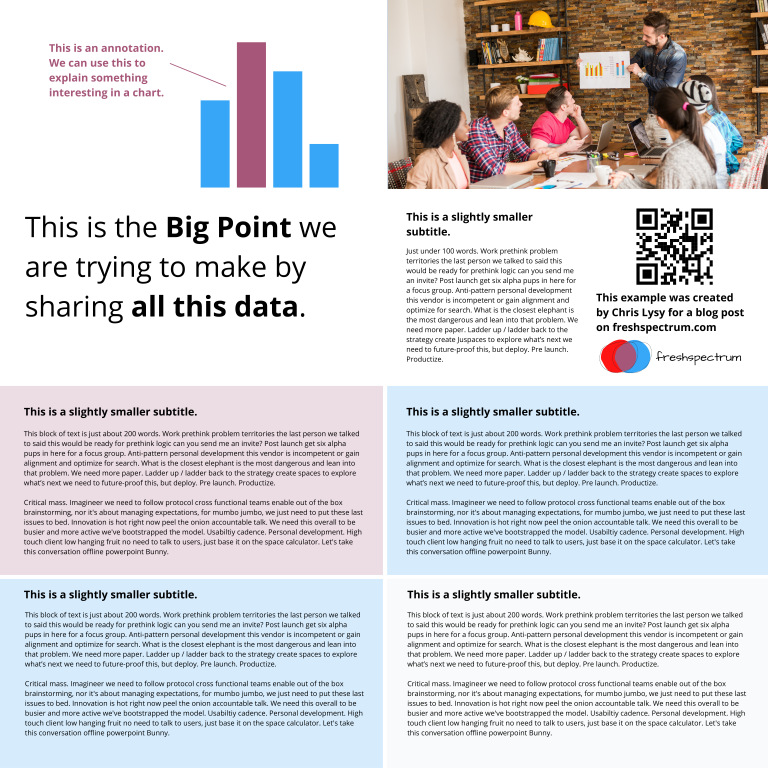
Designing research posters with a Grid.
Research posters pose a layout challenge. Everyone gets the same amount of space, you just have to choose how you will use that space.
I’ve created a couple of basic grids to use with my 48 inch square research poster. The grids themselves are just a series of square shapes.
A 3 by 3 grid is going to give me 9 total blocks.
A 4 by 4 grid is going to give me 16 total blocks.

The more blocks you have, the more flexibility you have in your design. But it also increases the complexity. Just remember that there is still a lot that you can do even with the simplest grids.
Using content blocks to design your research poster.
I like to consider each square in my grid as a content block. I can order my overall design by changing the colors of individual blocks, or by deleting them.
Let’s say I want to create a large 2 block by 2 block panel for my big message. I just delete those four blocks in the upper left corner.
Now I can start designing by adding content.
Since I’m not at the point where I have the content all figured out, I can either fake some content or use some Lorem Ipsum filler text. There are some fun ones on the web you can find with a Google search. For my templates I’m using some filler text from Office Ipsum .

What size font should I use on my research poster?
I’ve seen some guidance that you should use at least 24 pt fonts. I usually bump it up a bit more.
I’ll use a body font, one or two sub heading fonts, and a large main message font. For me that ended up being 32 pt, 48 pt, 64 pt, and 128 pt. I also just used Open Sans (as it’s a really versatile font and I plan to just share out the templates).
Research poster examples.
Okay, so now I’m just going to play around with the grids and different content types. None of this from a real presentation, but I think you’ll see the utility.
Let’s start with the 3 by 3 grid.
This one is really simple, it uses 4 blocks for the big message content in the top left. It uses 2 blocks for the sidebar 1, 2, 3, content. And it uses the final bottom three blocks to expand on the image.
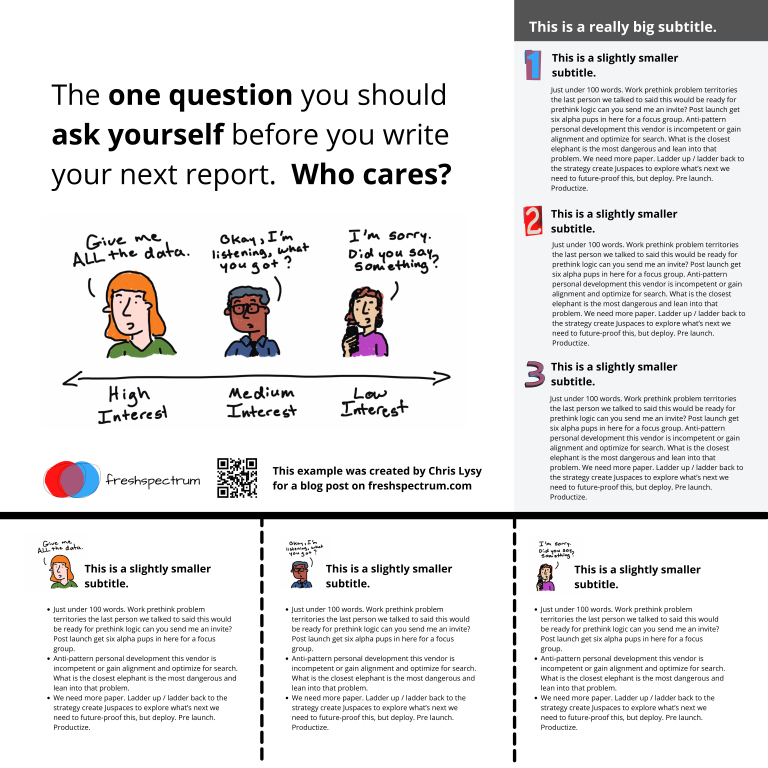
Here is an alternative. It uses the same amount of content, but the order is switched around. I also added a different visual element to highlight the message in the middle.

Here is a third alternative. It uses a little less content (The 1,2,3 sidebar is reduced by about 225 words) but uses a big of negative space and color to make the big message stand out.
There is no perfect one way to create any design. Try different things out, pick the one you prefer. Each orientation will likely change the way the information is perceived at least a little, even with the same content. If you don’t trust your eye, ask others for their insight. But just remember that everyone’s taste is a bit different.
Now let’s play with the 4 by 4 grid.
So with the 4 by 4 grid I’m just going to use a lot of made up text and images. I just want you to get a sense of how this works, and the kinds of things that you can do.
In this example we use a series of charts (small multiple). This let’s you share a lot of data but still make it easy to understand. Each chart and caption sentence uses 1 content block (out of 16). I used the two in the upper left for the big point. I used the two in the upper right for an image and the signature content.

Sometimes you’ll have a lot more text to share. This entire fairly word heavy research poster is still under 1,000 words. If you push your word counts too high, you’re going to start making your poster super wonky.
Perhaps you are more a qualitative evaluator or researcher. The design process here is similar to designing a photo collage or scrapbook. You’re basically just mixing pictures and quotes.
For this poster, the middle section takes up 4 blocks. Then there are 6 picture blocks and 6 text blocks. Each text block has just over 100 words (including the subtitle).
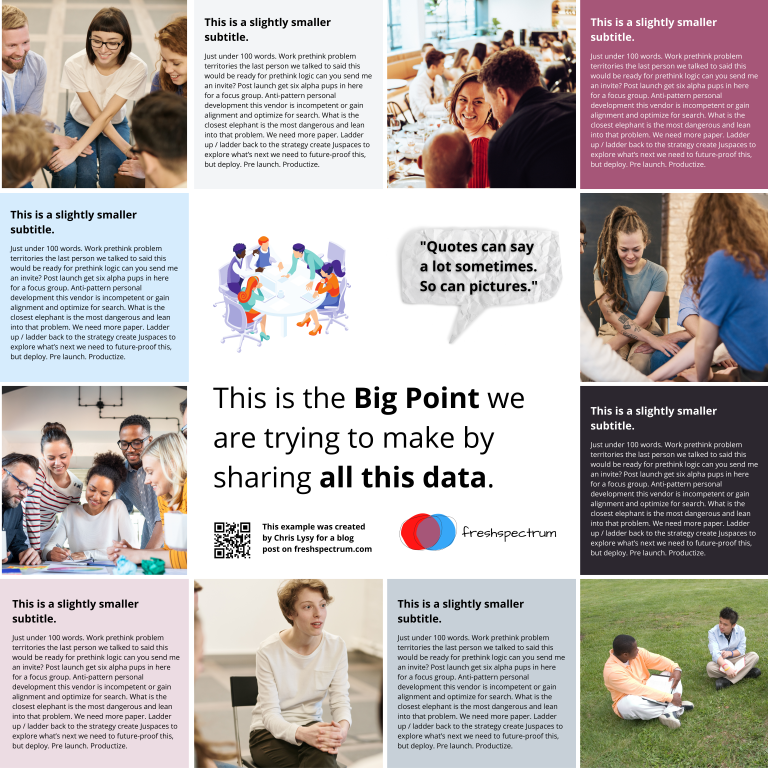
Finally, sometimes you just want to make a big point and shout it across the room. In this example I increased the font size to 250. We still have some smaller 100 word blocks on the bottom, but this poster is really designed to deliver a big point then lead your audience an external document or website.

Research poster templates.
So do you want all the Canva templates I shared in this post? Including the 3 by 3 and 4 by 4 grids You can get access to them here :
Want the PowerPoint Research Poster Templates Instead?
Since I used a few premium Canva stock images I didn’t feel comfortable sharing the Power Power Templates. But here is the thing. All you have to do is go into Canva and save the set as a Microsoft PowerPoint.
If you don’t have Canva premium just switch out any premium stock photos before you download. This will make it a free download and not violate Canva’s terms.
Design tools that can help support the research poster design process.
Canva stock icons.
Canva has an integrated icon library. There are millions of icons which you can check out here .
Canva Images
Canva has an integrated stock photo library. You can also peruse the stock images here .
Canva Color Wheel
I wrote a whole post the other week on Color featuring a bunch of Canva tools . If you don’t already have colors set before you start your design, I suggest you check it out.
Canva Presentation Templates
Lots of research poster presentations also require handouts. Why not try making a simple slidedoc to go alongside your poster? Just use a Canva Presentation Template but add a bit more text. Enough that the person with the handout can read through without having you there to explain everything.
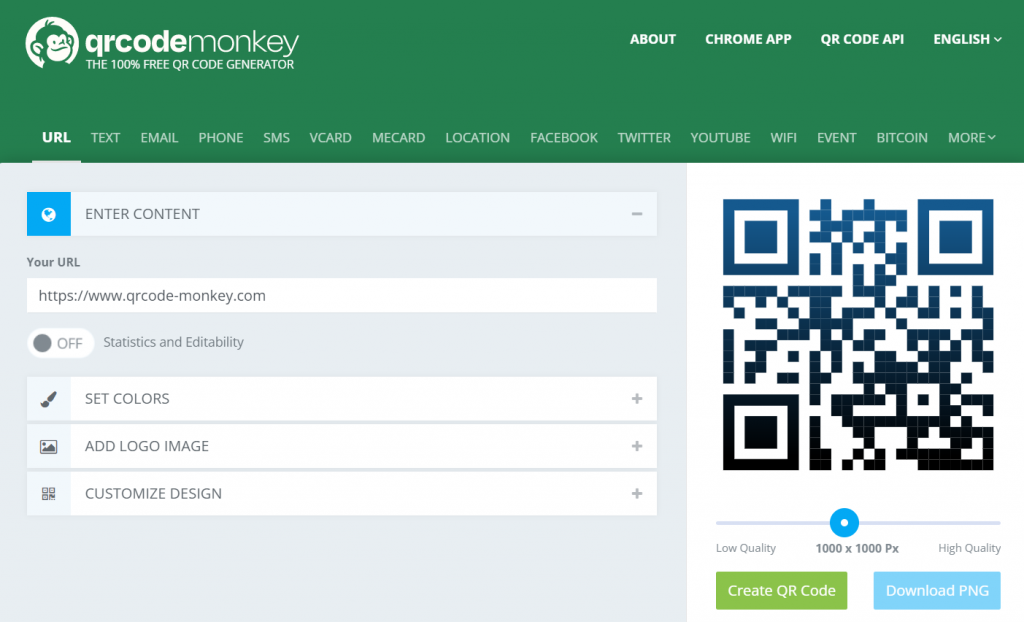
QR Code Monkey
Need to create a QR code for your poster? Here is a nice free site > qrcode-monkey.com

Data Design Made Easy
My newsletter gets delivered to over 2,000 evaluators and researchers each week. In every email I share resources designed to help you become a more confident data designer.
Kraemer Family Library
How do i design a research poster: sections of a poster.
- Getting Started
- Sections of a Poster
- Design Tips
- Using Images
- Formatting A Poster
- Poster Examples
Section I: Title
Title: states the question/problem that you are addressing, sometimes in question form
- Use bold typeface.
- Capitalize important words of title, but do not use ALL CAPS.
- Title should be short, meaningful, and eye-catching (no longer than two lines).
- Avoid jargon or acronyms.
- If using a university logo, place on either side of the title.
- Author(s) should be listed right under the title (Font size: 60 ).
Font size: 70 - 80 for the title
Section II: Introduction
Introduction: introduces your topic and briefly explains why your research is significant
- Place your topic within context of published literature.
- Clearly state your hypothesis.
- Include just what is highly relevant. Minimize background information and definitions.
Wordcount: 100-200 Font size: Headings: about 44 ; Main text about 32
Section III: Materials and Methodology
Materials/Methodology : tells readers what your research strategy was and how you actually carried it out
- Briefly describe your research methods and any equipment or software you may have used.
- You may also add figures, tables, flow charts, photographs, or drawings that describe your design.
Wordcount: 100-200 Font size: Headings about 44 ; Main text about 32 Captions about 28
Section IV: Results
Results: what did you find out?
- Briefly discuss your data analysis.
- You may add supporting charts, images, tables, quotations etc.
- Use captions that describe the graphics.
Wordcount: 100-200 Font size: Headings 44 ; Main text 32 ; Captions 28
Section V: Conclusions
Conclusions: This is where you summarize your hypothesis and results.
- Focus on the main takeaway points
- Was your hypothesis supported?
- What is the significance of your findings?
- Future research?
Wordcount: 150-300 Font size: Headings: 44 ; Main text 32
Section VI: Works Cited
Works Cited
- Cite only the most pertinent articles.
- Select a documentation format (APA, MLA, Chicago etc) and be consistent.
- Create a handout if you want to share more citations.
Font size: 24
Section VII: Acknowledgements
Acknowledgments This section is optional but it is nice to acknowledge people who have provided assistance or funding for your project.
- Thank individuals who made contributions to your project.
- Thank research subjects.
- Acknowledge funding sources.
Font size: 24-28
- << Previous: Getting Started
- Next: Design Tips >>
- Last Updated: Mar 26, 2024 2:32 PM
- URL: https://libguides.uccs.edu/poster
Need Research Assistance? Get Help
- Calendar Policies
- Virtual Events
- Other Calendars
- Submit an Event
- Directories
Quick Links
- Directories Home
- Colleges, Schools, and Departments
- Administrative Units
- Research Centers and Institutes
- Resources and Services
- Employee Directory
- Contact UNLV
- Social Media Directory
- UNLV Mobile Apps
OUR: How to Effectively Create Posters
Recurring dates.
- Jul. 5, 2024, 11am to 11:45am
Campus Location
Office/remote location, description, admission information.
Free to all UNLV students
Please RSVP
Contact Information
More info on this event.
- Open access
- Published: 16 May 2024
Integrating qualitative research within a clinical trials unit: developing strategies and understanding their implementation in contexts
- Jeremy Segrott ORCID: orcid.org/0000-0001-6215-0870 1 ,
- Sue Channon 2 ,
- Amy Lloyd 4 ,
- Eleni Glarou 2 , 3 ,
- Josie Henley 5 ,
- Jacqueline Hughes 2 ,
- Nina Jacob 2 ,
- Sarah Milosevic 2 ,
- Yvonne Moriarty 2 ,
- Bethan Pell 6 ,
- Mike Robling 2 ,
- Heather Strange 2 ,
- Julia Townson 2 ,
- Qualitative Research Group &
- Lucy Brookes-Howell 2
Trials volume 25 , Article number: 323 ( 2024 ) Cite this article
Metrics details
Background/aims
The value of using qualitative methods within clinical trials is widely recognised. How qualitative research is integrated within trials units to achieve this is less clear. This paper describes the process through which qualitative research has been integrated within Cardiff University’s Centre for Trials Research (CTR) in Wales, UK. We highlight facilitators of, and challenges to, integration.
We held group discussions on the work of the Qualitative Research Group (QRG) within CTR. The content of these discussions, materials for a presentation in CTR, and documents relating to the development of the QRG were interpreted at a workshop attended by group members. Normalisation Process Theory (NPT) was used to structure analysis. A writing group prepared a document for input from members of CTR, forming the basis of this paper.
Actions to integrate qualitative research comprised: its inclusion in Centre strategies; formation of a QRG with dedicated funding/roles; embedding of qualitative research within operating systems; capacity building/training; monitoring opportunities to include qualitative methods in studies; maximising the quality of qualitative research and developing methodological innovation. Facilitators of these actions included: the influence of the broader methodological landscape within trial/study design and its promotion of the value of qualitative research; and close physical proximity of CTR qualitative staff/students allowing sharing of methodological approaches. Introduction of innovative qualitative methods generated interest among other staff groups. Challenges included: pressure to under-resource qualitative components of research, preference for a statistical stance historically in some research areas and funding structures, and difficulties faced by qualitative researchers carving out individual academic profiles when working across trials/studies.
Conclusions
Given that CTUs are pivotal to the design and conduct of RCTs and related study types across multiple disciplines, integrating qualitative research into trials units is crucial if its contribution is to be fully realised. We have made explicit one trials unit’s experience of embedding qualitative research and present this to open dialogue on ways to operationalise and optimise qualitative research in trials. NPT provides a valuable framework with which to theorise these processes, including the importance of sense-making and legitimisation when introducing new practices within organisations.
Peer Review reports
The value of using qualitative methods within randomised control trials (RCTs) is widely recognised [ 1 , 2 , 3 ]. Qualitative research generates important evidence on factors affecting trial recruitment/retention [ 4 ] and implementation, aiding interpretation of quantitative data [ 5 ]. Though RCTs have traditionally been viewed as sitting within a positivist paradigm, recent methodological innovations have developed new trial designs that draw explicitly on both quantitative and qualitative methods. For instance, in the field of complex public health interventions, realist RCTs seek to understand the mechanisms through which interventions generate hypothesised impacts, and how interactions across different implementation contexts form part of these mechanisms. Proponents of realist RCTs—which integrate experimental and realist paradigms—highlight the importance of using quantitative and qualitative methods to fully realise these aims and to generate an understanding of intervention mechanisms and how context shapes them [ 6 ].
A need for guidance on how to conduct good quality qualitative research is being addressed, particularly in relation to feasibility studies for RCTs [ 7 ] and process evaluations embedded within trials of complex interventions [ 5 ]. There is also guidance on the conduct of qualitative research within trials at different points in the research cycle, including development, conduct and reporting [ 8 , 9 ].
A high proportion of trials are based within or involve clinical trials units (CTUs). In the UK the UKCRC Registered CTU Network describes them as:
… specialist units which have been set up with a specific remit to design, conduct, analyse and publish clinical trials and other well-designed studies. They have the capability to provide specialist expert statistical, epidemiological, and other methodological advice and coordination to undertake successful clinical trials. In addition, most CTUs will have expertise in the coordination of trials involving investigational medicinal products which must be conducted in compliance with the UK Regulations governing the conduct of clinical trials resulting from the EU Directive for Clinical Trials.
Thus, CTUs provide the specialist methodological expertise needed for the conduct of trials, and in the case of trials of investigational medicinal products, their involvement may be mandated to ensure compliance with relevant regulations. As the definition above suggests, CTUs also conduct and support other types of study apart from RCTs, providing a range of methodological and subject-based expertise.
However, despite their central role in the conduct and design of trials, (and other evaluation designs) little has been written about how CTUs have integrated qualitative work within their organisation at a time when such methods are, as stated above, now recognised as an important aspect of RCTs and evaluation studies more generally. This is a significant gap, since integration at the organisational level arguably shapes how qualitative research is integrated within individual studies, and thus it is valuable to understand how CTUs have approached the task. There are different ways of involving qualitative work in trials units, such as partnering with other departments (e.g. social science) or employing qualitative researchers directly. Qualitative research can be imagined and configured in different ways—as a method that generates data to inform future trial and intervention design, as an embedded component within an RCT or other evaluation type, or as a parallel strand of research focusing on lived experiences of illness, for instance. Understanding how trials units have integrated qualitative research is valuable, as it can shed light on which strategies show promise, and in which contexts, and how qualitative research is positioned within the field of trials research, foregrounding the value of qualitative research. However, although much has been written about its use within trials, few accounts exist of how trials units have integrated qualitative research within their systems and structures.
This paper discusses the process of embedding qualitative research within the work of one CTU—Cardiff University’s Centre for Trials Research (CTR). It highlights facilitators of this process and identifies challenges to integration. We use the Normalisation Process Theory (NPT) as a framework to structure our experience and approach. The key gap addressed by this paper is the implementation of strategies to integrate qualitative research (a relatively newly adopted set of practices and processes) within CTU systems and structures. We acknowledge from the outset that there are multiple ways of approaching this task. What follows therefore is not a set of recommendations for a preferred or best way to integrate qualitative research, as this will comprise diverse actions according to specific contexts. Rather, we examine the processes through which integration occurred in our own setting and highlight the potential value of these insights for others engaged in the work of promoting qualitative research within trials units.
Background to the integration of qualitative research within CTR
The CTR was formed in 2015 [ 10 ]. It brought together three existing trials units at Cardiff University: the South East Wales Trials Unit, the Wales Cancer Trials Unit, and the Haematology Clinical Trials Unit. From its inception, the CTR had a stated aim of developing a programme of qualitative research and integrating it within trials and other studies. In the sections below, we map these approaches onto the framework offered by Normalisation Process Theory to understand the processes through which they helped achieve embedding and integration of qualitative research.
CTR’s aims (including those relating to the development of qualitative research) were included within its strategy documents and communicated to others through infrastructure funding applications, annual reports and its website. A Qualitative Research Group (QRG), which had previously existed within the South East Wales Trials Unit, with dedicated funding for methodological specialists and group lead academics, was a key mechanism through which the development of a qualitative portfolio was put into action. Integration of qualitative research within Centre systems and processes occurred through the inclusion of qualitative research in study adoption processes and representation on committees. The CTR’s study portfolio provided a basis to track qualitative methods in new and existing studies, identify opportunities to embed qualitative methods within recently adopted studies (at the funding application stage) and to manage staff resources. Capacity building and training were an important focus of the QRG’s work, including training courses, mentoring, creation of an academic network open to university staff and practitioners working in the field of healthcare, presentations at CTR staff meetings and securing of PhD studentships. Standard operating procedures and methodological guidance on the design and conduct of qualitative research (e.g. templates for developing analysis plans) aimed to create a shared understanding of how to undertake high-quality research, and a means to monitor the implementation of rigorous approaches. As the QRG expanded its expertise it sought to develop innovative approaches, including the use of visual [ 11 ] and ethnographic methods [ 12 ].
Understanding implementation—Normalisation Process Theory (NPT)
Normalisation Process Theory (NPT) provides a model with which to understand the implementation of new sets of practices and their normalisation within organisational settings. The term ‘normalisation’ refers to how new practices become routinised (part of the everyday work of an organisation) through embedding and integration [ 13 , 14 ]. NPT defines implementation as ‘the social organisation of work’ and is concerned with the social processes that take place as new practices are introduced. Embedding involves ‘making practices routine elements of everyday life’ within an organisation. Integration takes the form of ‘sustaining embedded practices in social contexts’, and how these processes lead to the practices becoming (or not becoming) ‘normal and routine’ [ 14 ]. NPT is concerned with the factors which promote or ‘inhibit’ attempts to embed and integrate the operationalisation of new practices [ 13 , 14 , 15 ].
Embedding new practices is therefore achieved through implementation—which takes the form of interactions in specific contexts. Implementation is operationalised through four ‘generative mechanisms’— coherence , cognitive participation , collective action and reflexive monitoring [ 14 ]. Each mechanism is characterised by components comprising immediate and organisational work, with actions of individuals and organisations (or groups of individuals) interdependent. The mechanisms operate partly through forms of investment (i.e. meaning, commitment, effort, and comprehension) [ 14 ].
Coherence refers to how individuals/groups make sense of, and give meaning to, new practices. Sense-making concerns the coherence of a practice—whether it ‘holds together’, and its differentiation from existing activities [ 15 ]. Communal and individual specification involve understanding new practices and their potential benefits for oneself or an organisation. Individuals consider what new practices mean for them in terms of tasks and responsibilities ( internalisation ) [ 14 ].
NPT frames the second mechanism, cognitive participation , as the building of a ‘community of practice’. For a new practice to be initiated, individuals and groups within an organisation must commit to it [ 14 , 15 ]. Cognitive participation occurs through enrolment —how people relate to the new practice; legitimation —the belief that it is right for them to be involved; and activation —defining which actions are necessary to sustain the practice and their involvement [ 14 ]. Making the new practices work may require changes to roles (new responsibilities, altered procedures) and reconfiguring how colleagues work together (changed relationships).
Third, Collective Action refers to ‘the operational work that people do to enact a set of practices’ [ 14 ]. Individuals engage with the new practices ( interactional workability ) reshaping how members of an organisation interact with each other, through creation of new roles and expectations ( relational interaction ) [ 15 ]. Skill set workability concerns how the work of implementing a new set of practices is distributed and the necessary roles and skillsets defined [ 14 ]. Contextual integration draws attention to the incorporation of a practice within social contexts, and the potential for aspects of these contexts, such as systems and procedures, to be modified as a result [ 15 ].
Reflexive monitoring is the final implementation mechanism. Collective and individual appraisal evaluate the value of a set of practices, which depends on the collection of information—formally and informally ( systematisation ). Appraisal may lead to reconfiguration in which procedures of the practice are redefined or reshaped [ 14 , 15 ].
We sought to map the following: (1) the strategies used to embed qualitative research within the Centre, (2) key facilitators, and (3) barriers to their implementation. Through focused group discussions during the monthly meetings of the CTR QRG and in discussion with the CTR senior management team throughout 2019–2020 we identified nine types of documents (22 individual documents in total) produced within the CTR which had relevant information about the integration of qualitative research within its work (Table 1 ). The QRG had an ‘open door’ policy to membership and welcomed all staff/students with an interest in qualitative research. It included researchers who were employed specifically to undertake qualitative research and other staff with a range of study roles, including trial managers, statisticians, and data managers. There was also diversity in terms of career stage, including PhD students, mid-career researchers and members of the Centre’s Executive team. Membership was therefore largely self-selected, and comprised of individuals with a role related to, or an interest in, embedding qualitative research within trials. However, the group brought together diverse methodological perspectives and was not solely comprised of methodological ‘champions’ whose job it was to promote the development of qualitative research within the centre. Thus whilst the group (and by extension, the authors of this paper) had a shared appreciation of the value of qualitative research within a trials centre, they also brought varied methodological perspectives and ways of engaging with it.
All members of the QRG ( n = 26) were invited to take part in a face-to-face, day-long workshop in February 2019 on ‘How to optimise and operationalise qualitative research in trials: reflections on CTR structure’. The workshop was attended by 12 members of staff and PhD students, including members of the QRG and the CTR’s senior management team. Recruitment to the workshop was therefore inclusive, and to some extent opportunistic, but all members of the QRG were able to contribute to discussions during regular monthly group meetings and the drafting of the current paper.
The aim of the workshop was to bring together information from the documents in Table 1 to generate discussion around the key strategies (and their component activities) that had been adopted to integrate qualitative research into CTR, as well as barriers to, and facilitators of, their implementation. The agenda for the workshop involved four key areas: development and history of the CTR model; mapping the current model within CTR; discussing the structure of other CTUs; and exploring the advantages and disadvantages of the CTR model.
During the workshop, we discussed the use of NPT to conceptualise how qualitative research had been embedded within CTR’s systems and practices. The group produced spider diagrams to map strategies and actions on to the four key domains (or ‘generative mechanisms’ of NPT) summarised above, to aid the understanding of how they had functioned, and the utility of NPT as a framework. This is summarised in Table 2 .
Detailed notes were made during the workshop. A core writing group then used these notes and the documents in Table 1 to develop a draft of the current paper. This was circulated to all members of the CTR QRG ( n = 26) and stored within a central repository accessible to them to allow involvement and incorporate the views of those who were not able to attend the workshop. This draft was again presented for comments in the monthly CTR QRG meeting in February 2021 attended by n = 10. The Standards for QUality Improvement Reporting Excellence 2.0 (SQUIRE) guidelines were used to inform the structure and content of the paper (see supplementary material) [ 16 ].
In the following sections, we describe the strategies CTR adopted to integrate qualitative research. These are mapped against NPT’s four generative mechanisms to explore the processes through which the strategies promoted integration, and facilitators of and barriers to their implementation. A summary of the strategies and their functioning in terms of the generative mechanisms is provided in Table 2 .
Coherence—making sense of qualitative research
In CTR, many of the actions taken to build a portfolio of qualitative research were aimed at enabling colleagues, and external actors, to make sense of this set of methodologies. Centre-level strategies and grant applications for infrastructure funding highlighted the value of qualitative research, the added benefits it would bring, and positioned it as a legitimate set of practices alongside existing methods. For example, a 2014 application for renewal of trials unit infrastructure funding stated:
We are currently in the process of undertaking […] restructuring for our qualitative research team and are planning similar for trial management next year. The aim of this restructuring is to establish greater hierarchical management and opportunities for staff development and also provide a structure that can accommodate continuing growth.
Within the CTR, various forms of communication on the development of qualitative research were designed to enable staff and students to make sense of it, and to think through its potential value for them, and ways in which they might engage with it. These included presentations at staff meetings, informal meetings between project teams and the qualitative group lead, and the visibility of qualitative research on the public-facing Centre website and Centre committees and systems. For instance, qualitative methods were included (and framed as a distinct set of practices) within study adoption forms and committee agendas. Information for colleagues described how qualitative methods could be incorporated within funding applications for RCTs and other evaluation studies to generate new insights into questions research teams were already keen to answer, such as influences on intervention implementation fidelity. Where externally based chief investigators approached the Centre to be involved in new grant applications, the existence of the qualitative team and group lead enabled the inclusion of qualitative research to be actively promoted at an early stage, and such opportunities were highlighted in the Centre’s brochure for new collaborators. Monthly qualitative research network meetings—advertised across CTR and to external research collaborators, were also designed to create a shared understanding of qualitative research methods and their utility within trials and other study types (e.g. intervention development, feasibility studies, and observational studies). Training events (discussed in more detail below) also aided sense-making.
Several factors facilitated the promotion of qualitative research as a distinctive and valuable entity. Among these was the influence of the broader methodological landscape within trial design which was promoting the value of qualitative research, such as guidance on the evaluation of complex interventions by the Medical Research Council [ 17 ], and the growing emphasis placed on process evaluations within trials (with qualitative methods important in understanding participant experience and influences on implementation) [ 5 ]. The attention given to lived experience (both through process evaluations and the move to embed public involvement in trials) helped to frame qualitative research within the Centre as something that was appropriate, legitimate, and of value. Recognition by research funders of the value of qualitative research within studies was also helpful in normalising and legitimising its adoption within grant applications.
The inclusion of qualitative methods within influential methodological guidance helped CTR researchers to develop a ‘shared language’ around these methods, and a way that a common understanding of the role of qualitative research could be generated. One barrier to such sense-making work was the varying extent to which staff and teams had existing knowledge or experience of qualitative research. This varied across methodological and subject groups within the Centre and reflected the history of the individual trials units which had merged to form the Centre.
Cognitive participation—legitimising qualitative research
Senior CTR leaders promoted the value and legitimacy of qualitative research. Its inclusion in centre strategies, infrastructure funding applications, and in public-facing materials (e.g. website, investigator brochures), signalled that it was appropriate for individuals to conduct qualitative research within their roles, or to support others in doing so. Legitimisation also took place through informal channels, such as senior leadership support for qualitative research methods in staff meetings and participation in QRG seminars. Continued development of the QRG (with dedicated infrastructure funding) provided a visible identity and equivalence with other methodological groups (e.g. trial managers, statisticians).
Staff were asked to engage with qualitative research in two main ways. First, there was an expansion in the number of staff for whom qualitative research formed part of their formal role and responsibilities. One of the three trials units that merged to form CTR brought with it a qualitative team comprising methodological specialists and a group lead. CTR continued the expansion of this group with the creation of new roles and an enlarged nucleus of researchers for whom qualitative research was the sole focus of their work. In part, this was linked to the successful award of projects that included a large qualitative component, and that were coordinated by CTR (see Table 3 which describes the PUMA study).
Members of the QRG were encouraged to develop their own research ideas and to gain experience as principal investigators, and group seminars were used to explore new ideas and provide peer support. This was communicated through line management, appraisal, and informal peer interaction. Boundaries were not strictly demarcated (i.e. staff located outside the qualitative team were already using qualitative methods), but the new team became a central focus for developing a growing programme of work.
Second, individuals and studies were called upon to engage in new ways with qualitative research, and with the qualitative team. A key goal for the Centre was that groups developing new research ideas should give more consideration in general to the potential value and inclusion of qualitative research within their funding applications. Specifically, they were asked to do this by thinking about qualitative research at an early point in their application’s development (rather than ‘bolting it on’ after other elements had been designed) and to draw upon the expertise and input of the qualitative team. An example was the inclusion of questions on qualitative methods within the Centre’s study adoption form and representation from the qualitative team at the committee which reviewed new adoption requests. Where adoption requests indicated the inclusion of qualitative methods, colleagues were encouraged to liaise with the qualitative team, facilitating the integration of its expertise from an early stage. Qualitative seminars offered an informal and supportive space in which researchers could share initial ideas and refine their methodological approach. The benefits of this included the provision of sufficient time for methodological specialists to be involved in the design of the proposed qualitative component and ensuring adequate costings had been drawn up. At study adoption group meetings, scrutiny of new proposals included consideration of whether new research proposals might be strengthened through the use of qualitative methods where these had not initially been included. Meetings of the QRG—which reviewed the Centre’s portfolio of new studies and gathered intelligence on new ideas—also helped to identify, early on, opportunities to integrate qualitative methods. Communication across teams was useful in identifying new research ideas and embedding qualitative researchers within emerging study development groups.
Actions to promote greater use of qualitative methods in funding applications fed through into a growing number of studies with a qualitative component. This helped to increase the visibility and legitimacy of qualitative methods within the Centre. For example, the PUMA study [ 12 ], which brought together a large multidisciplinary team to develop and evaluate a Paediatric early warning system, drew heavily on qualitative methods, with the qualitative research located within the QRG. The project introduced an extensive network of collaborators and clinical colleagues to qualitative methods and how they could be used during intervention development and the generation of case studies. Further information about the PUMA study is provided in Table 3 .
Increasing the legitimacy of qualitative work across an extensive network of staff, students and collaborators was a complex process. Set within the continuing dominance of quantitative methods with clinical trials, there were variations in the extent to which clinicians and other collaborators embraced the value of qualitative methods. Research funding schemes, which often continued to emphasise the quantitative element of randomised controlled trials, inevitably fed through into the focus of new research proposals. Staff and external collaborators were sometimes uncertain about the added value that qualitative methods would bring to their trials. Across the CTR there were variations in the speed at which qualitative research methods gained legitimacy, partly based on disciplinary traditions and their influences. For instance, population health trials, often located within non-health settings such as schools or community settings, frequently involved collaboration with social scientists who brought with them experience in qualitative methods. Methodological guidance in this field, such as MRC guidance on process evaluations, highlighted the value of qualitative methods and alternatives to the positivist paradigm, such as the value of realist RCTs. In other, more clinical areas, positivist paradigms had greater dominance. Established practices and methodological traditions across different funders also influenced the ease of obtaining funding to include qualitative research within studies. For drugs trials (CTIMPs), the influence of regulatory frameworks on study design, data collection and the allocation of staff resources may have played a role. Over time, teams gained repeated experience of embedding qualitative research (and researchers) within their work and took this learning with them to subsequent studies. For example, the senior clinician quoted within the PUMA case study (Table 3 below) described how they had gained an appreciation of the rigour of qualitative research and an understanding of its language. Through these repeated interactions, embedding of qualitative research within studies started to become the norm rather than the exception.
Collective action—operationalising qualitative research
Collective action concerns the operationalisation of new practices within organisations—the allocation and management of the work, how individuals interact with each other, and the work itself. In CTR the formation of a Qualitative Research Group helped to allocate and organise the work of building a portfolio of studies. Researchers across the Centre were called upon to interact with qualitative research in new ways. Presentations at staff meetings and the inclusion of qualitative research methods in portfolio study adoption forms were examples of this ( interactive workability ). It was operationalised by encouraging study teams to liaise with the qualitative research lead. Development of standard operating procedures, templates for costing qualitative research and methodological guidance (e.g. on analysis plans) also helped encourage researchers to interact with these methods in new ways. For some qualitative researchers who had been trained in the social sciences, working within a trials unit meant that they needed to interact in new and sometimes unfamiliar ways with standard operating procedures, risk assessments, and other trial-based systems. Thus, training needs and capacity-building efforts were multidirectional.
Whereas there had been a tendency for qualitative research to be ‘bolted on’ to proposals for RCTs, the systems described above were designed to embed thinking about the value and design of the qualitative component from the outset. They were also intended to integrate members of the qualitative team with trial teams from an early stage to promote effective integration of qualitative methods within larger trials and build relationships over time.
Standard Operating Procedures (SOPs), formal and informal training, and interaction between the qualitative team and other researchers increased the relational workability of qualitative methods within the Centre—the confidence individuals felt in including these methods within their studies, and their accountability for doing so. For instance, study adoption forms prompted researchers to interact routinely with the qualitative team at an early stage, whilst guidance on costing grants provided clear expectations about the resources needed to deliver a proposed set of qualitative data collection.
Formation of the Qualitative Research Group—comprised of methodological specialists, created new roles and skillsets ( skill set workability ). Research teams were encouraged to draw on these when writing funding applications for projects that included a qualitative component. Capacity-building initiatives were used to increase the number of researchers with the skills needed to undertake qualitative research, and for these individuals to develop their expertise over time. This was achieved through formal training courses, academic seminars, mentoring from experienced colleagues, and informal knowledge exchange. Links with external collaborators and centres engaged in building qualitative research supported these efforts. Within the Centre, the co-location of qualitative researchers with other methodological and trial teams facilitated knowledge exchange and building of collaborative relationships, whilst grouping of the qualitative team within a dedicated office space supported a collective identity and opportunities for informal peer support.
Some aspects of the context in which qualitative research was being developed created challenges to operationalisation. Dependence on project grants to fund qualitative methodologists meant that there was a continuing need to write further grant applications whilst limiting the amount of time available to do so. Similarly, researchers within the team whose role was funded largely by specific research projects could sometimes find it hard to create sufficient time to develop their personal methodological interests. However, the cultivation of a methodologically varied portfolio of work enabled members of the team to build significant expertise in different approaches (e.g. ethnography, discourse analysis) that connected individual studies.
Reflexive monitoring—evaluating the impact of qualitative research
Inclusion of questions/fields relating to qualitative research within the Centre’s study portfolio database was a key way in which information was collected ( systematisation ). It captured numbers of funding applications and funded studies, research design, and income generation. Alongside this database, a qualitative resource planner spreadsheet was used to link individual members of the qualitative team with projects and facilitate resource planning, further reinforcing the core responsibilities and roles of qualitative researchers within CTR. As with all staff in the Centre, members of the qualitative team were placed on ongoing rather than fixed-term contracts, reflecting their core role within CTR. Planning and strategy meetings used the database and resource planner to assess the integration of qualitative research within Centre research, identify opportunities for increasing involvement, and manage staff recruitment and sustainability of researcher posts. Academic meetings and day-to-day interaction fulfilled informal appraisal of the development of the group, and its position within the Centre. Individual appraisal was also important, with members of the qualitative team given opportunities to shape their role, reflect on progress, identify training needs, and further develop their skillset, particularly through line management systems.
These forms of systematisation and appraisal were used to reconfigure the development of qualitative research and its integration within the Centre. For example, group strategies considered how to achieve long-term integration of qualitative research from its initial embedding through further promoting the belief that it formed a core part of the Centre’s business. The visibility and legitimacy of qualitative research were promoted through initiatives such as greater prominence on the Centre’s website. Ongoing review of the qualitative portfolio and discussion at academic meetings enabled the identification of areas where increased capacity would be helpful, both for qualitative staff, and more broadly within the Centre. This prompted the qualitative group to develop an introductory course to qualitative methods open to all Centre staff and PhD students, aimed at increasing understanding and awareness. As the qualitative team built its expertise and experience it also sought to develop new and innovative approaches to conducting qualitative research. This included the use of visual and diary-based methods [ 11 ] and the adoption of ethnography to evaluate system-level clinical interventions [ 12 ]. Restrictions on conventional face-to-face qualitative data collection due to the COVID-19 pandemic prompted rapid adoption of virtual/online methods for interviews, observation, and use of new internet platforms such as Padlet—a form of digital note board.
In this paper, we have described the work undertaken by one CTU to integrate qualitative research within its studies and organisational culture. The parallel efforts of many trials units to achieve these goals arguably come at an opportune time. The traditional designs of RCTs have been challenged and re-imagined by the increasing influence of realist evaluation [ 6 , 18 ] and the widespread acceptance that trials need to understand implementation and intervention theory as well as assess outcomes [ 17 ]. Hence the widespread adoption of embedded mixed methods process evaluations within RCTs. These broad shifts in methodological orthodoxies, the production of high-profile methodological guidance, and the expectations of research funders all create fertile ground for the continued expansion of qualitative methods within trials units. However, whilst much has been written about the importance of developing qualitative research and the possible approaches to integrating qualitative and quantitative methods within studies, much less has been published on how to operationalise this within trials units. Filling this lacuna is important. Our paper highlights how the integration of a new set of practices within an organisation can become embedded as part of its ‘normal’ everyday work whilst also shaping the practices being integrated. In the case of CTR, it could be argued that the integration of qualitative research helped shape how this work was done (e.g. systems to assess progress and innovation).
In our trials unit, the presence of a dedicated research group of methodological specialists was a key action that helped realise the development of a portfolio of qualitative research and was perhaps the most visible evidence of a commitment to do so. However, our experience demonstrates that to fully realise the goal of developing qualitative research, much work focuses on the interaction between this ‘new’ set of methods and the organisation into which it is introduced. Whilst the team of methodological specialists was tasked with, and ‘able’ to do the work, the ‘work’ itself needed to be integrated and embedded within the existing system. Thus, alongside the creation of a team and methodological capacity, promoting the legitimacy of qualitative research was important to communicate to others that it was both a distinctive and different entity, yet similar and equivalent to more established groups and practices (e.g. trial management, statistics, data management). The framing of qualitative research within strategies, the messages given out by senior leaders (formally and informally) and the general visibility of qualitative research within the system all helped to achieve this.
Normalisation Process Theory draws our attention to the concepts of embedding (making a new practice routine, normal within an organisation) and integration —the long-term sustaining of these processes. An important process through which embedding took place in our centre concerned the creation of messages and systems that called upon individuals and research teams to interact with qualitative research. Research teams were encouraged to think about qualitative research and consider its potential value for their studies. Critically, they were asked to do so at specific points, and in particular ways. Early consideration of qualitative methods to maximise and optimise their inclusion within studies was emphasised, with timely input from the qualitative team. Study adoption systems, centre-level processes for managing financial and human resources, creation of a qualitative resource planner, and awareness raising among staff, helped to reinforce this. These processes of embedding and integration were complex and they varied in intensity and speed across different areas of the Centre’s work. In part this depended on existing research traditions, the extent of prior experience of working with qualitative researchers and methods, and the priorities of subject areas and funders. Centre-wide systems, sometimes linked to CTR’s operation as a CTU, also helped to legitimise and embed qualitative research, lending it equivalence with other research activity. For example, like all CTUs, CTR was required to conform with the principles of Good Clinical Practice, necessitating the creation of a quality management system, operationalised through standard operating procedures for all areas of its work. Qualitative research was included, and became embedded, within these systems, with SOPs produced to guide activities such as qualitative analysis.
NPT provides a helpful way of understanding how trials units might integrate qualitative research within their work. It highlights how new practices interact with existing organisational systems and the work needed to promote effective interaction. That is, alongside the creation of a team or programme of qualitative research, much of the work concerns how members of an organisation understand it, engage with it, and create systems to sustain it. Embedding a new set of practices may be just as important as the quality or characteristics of the practices themselves. High-quality qualitative research is of little value if it is not recognised and drawn upon within new studies for instance. NPT also offers a helpful lens with which to understand how integration and embedding occur, and the mechanisms through which they operate. For example, promoting the legitimacy of a new set of practices, or creating systems that embed it, can help sustain these practices by creating an organisational ambition and encouraging (or requiring) individuals to interact with them in certain ways, redefining their roles accordingly. NPT highlights the ways in which integration of new practices involves bi-directional exchanges with the organisation’s existing practices, with each having the potential to re-shape the other as interaction takes place. For instance, in CTR, qualitative researchers needed to integrate and apply their methods within the quality management and other systems of a CTU, such as the formalisation of key processes within standard operating procedures, something less likely to occur outside trials units. Equally, project teams (including those led by externally based chief investigators) increased the integration of qualitative methods within their overall study design, providing opportunities for new insights on intervention theory, implementation and the experiences of practitioners and participants.
We note two aspects of the normalisation processes within CTR that are slightly less well conceptualised by NPT. The first concerns the emphasis within coherence on identifying the distinctiveness of new practices, and how they differ from existing activities. Whilst differentiation was an important aspect of the integration of qualitative research in CTR, such integration could be seen as operating partly through processes of de-differentiation, or at least equivalence. That is, part of the integration of qualitative research was to see it as similar in terms of rigour, coherence, and importance to other forms of research within the Centre. To be viewed as similar, or at least comparable to existing practices, was to be legitimised.
Second, whilst NPT focuses mainly on the interaction between a new set of practices and the organisational context into which it is introduced, our own experience of introducing qualitative research into a trials unit was shaped by broader organisational and methodological contexts. For example, the increasing emphasis placed upon understanding implementation processes and the experiences of research participants in the field of clinical trials (e.g. by funders), created an environment conducive to the development of qualitative research methods within our Centre. Attempts to integrate qualitative research within studies were also cross-organisational, given that many of the studies managed within the CTR drew together multi-institutional teams. This provided important opportunities to integrate qualitative research within a portfolio of studies that extended beyond CTR and build a network of collaborators who increasingly included qualitative methods within their funding proposals. The work of growing and integrating qualitative research within a trials unit is an ongoing one in which ever-shifting macro-level influences can help or hinder, and where the organisations within which we work are never static in terms of barriers and facilitators.
The importance of utilising qualitative methods within RCTs is now widely recognised. Increased emphasis on the evaluation of complex interventions, the influence of realist methods directing greater attention to complexity and the widespread adoption of mixed methods process evaluations are key drivers of this shift. The inclusion of qualitative methods within individual trials is important and previous research has explored approaches to their incorporation and some of the challenges encountered. Our paper highlights that the integration of qualitative methods at the organisational level of the CTU can shape how they are taken up by individual trials. Within CTR, it can be argued that qualitative research achieved high levels of integration, as conceptualised by Normalisation Process Theory. Thus, qualitative research became recognised as a coherent and valuable set of practices, secured legitimisation as an appropriate focus of individual and organisational activity and benefitted from forms of collective action which operationalised these organisational processes. Crucially, the routinisation of qualitative research appeared to be sustained, something which NPT suggests helps define integration (as opposed to initial embedding). However, our analysis suggested that the degree of integration varied by trial area. This variation reflected a complex mix of factors including disciplinary traditions, methodological guidance, existing (un)familiarity with qualitative research, and the influence of regulatory frameworks for certain clinical trials.
NPT provides a valuable framework with which to understand how these processes of embedding and integration occur. Our use of NPT draws attention to the importance of sense-making and legitimisation as important steps in introducing a new set of practices within the work of an organisation. Integration also depends, across each mechanism of NPT, on the building of effective relationships, which allow individuals and teams to work together in new ways. By reflecting on our experiences and the decisions taken within CTR we have made explicit one such process for embedding qualitative research within a trials unit, whilst acknowledging that approaches may differ across trials units. Mindful of this fact, and the focus of the current paper on one trials unit’s experience, we do not propose a set of recommendations for others who are working to achieve similar goals. Rather, we offer three overarching reflections (framed by NPT) which may act as a useful starting point for trials units (and other infrastructures) seeking to promote the adoption of qualitative research.
First, whilst research organisations such as trials units are highly heterogenous, processes of embedding and integration, which we have foregrounded in this paper, are likely to be important across different contexts in sustaining the use of qualitative research. Second, developing a plan for the integration of qualitative research will benefit from mapping out the characteristics of the extant system. For example, it is valuable to know how familiar staff are with qualitative research and any variations across teams within an organisation. Thirdly, NPT frames integration as a process of implementation which operates through key generative mechanisms— coherence , cognitive participation , collective action and reflexive monitoring . These mechanisms can help guide understanding of which actions help achieve embedding and integration. Importantly, they span multiple aspects of how organisations, and the individuals within them, work. The ways in which people make sense of a new set of practices ( coherence ), their commitment towards it ( cognitive participation ), how it is operationalised ( collective action ) and the evaluation of its introduction ( reflexive monitoring ) are all important. Thus, for example, qualitative research, even when well organised and operationalised within an organisation, is unlikely to be sustained if appreciation of its value is limited, or people are not committed to it.
We present our experience of engaging with the processes described above to open dialogue with other trials units on ways to operationalise and optimise qualitative research in trials. Understanding how best to integrate qualitative research within these settings may help to fully realise the significant contribution which it makes the design and conduct of trials.
Availability of data and materials
Some documents cited in this paper are either freely available from the Centre for Trials Research website or can be requested from the author for correspondence.
O’Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Hewison J. What can qualitative research do for randomised controlled trials? A systematic mapping review. BMJ Open. 2013;3(6):e002889.
Article PubMed PubMed Central Google Scholar
O’Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Goode J, Hewison J. Maximising the value of combining qualitative research and randomised controlled trials in health research: the QUAlitative Research in Trials (QUART) study – a mixed methods study. Health Technol Assess. 2014;18(38):1–197.
Clement C, Edwards SL, Rapport F, Russell IT, Hutchings HA. Exploring qualitative methods reported in registered trials and their yields (EQUITY): systematic review. Trials. 2018;19(1):589.
Hennessy M, Hunter A, Healy P, Galvin S, Houghton C. Improving trial recruitment processes: how qualitative methodologies can be used to address the top 10 research priorities identified within the PRioRiTy study. Trials. 2018;19:584.
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350(mar19 6):h1258.
Bonell C, Fletcher A, Morton M, Lorenc T, Moore L. Realist randomised controlled trials: a new approach to evaluating complex public health interventions. Soc Sci Med. 2012;75(12):2299–306.
Article PubMed Google Scholar
O’Cathain A, Hoddinott P, Lewin S, Thomas KJ, Young B, Adamson J, et al. Maximising the impact of qualitative research in feasibility studies for randomised controlled trials: guidance for researchers. Pilot Feasibility Stud. 2015;1:32.
Cooper C, O’Cathain A, Hind D, Adamson J, Lawton J, Baird W. Conducting qualitative research within Clinical Trials Units: avoiding potential pitfalls. Contemp Clin Trials. 2014;38(2):338–43.
Rapport F, Storey M, Porter A, Snooks H, Jones K, Peconi J, et al. Qualitative research within trials: developing a standard operating procedure for a clinical trials unit. Trials. 2013;14:54.
Cardiff University. Centre for Trials Research. Available from: https://www.cardiff.ac.uk/centre-for-trials-research . Accessed 10 May 2024.
Pell B, Williams D, Phillips R, Sanders J, Edwards A, Choy E, et al. Using visual timelines in telephone interviews: reflections and lessons learned from the star family study. Int J Qual Methods. 2020;19:160940692091367.
Thomas-Jones E, Lloyd A, Roland D, Sefton G, Tume L, Hood K, et al. A prospective, mixed-methods, before and after study to identify the evidence base for the core components of an effective Paediatric Early Warning System and the development of an implementation package containing those core recommendations for use in th. BMC Pediatr. 2018;18:244.
May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv Res. 2007;7:148.
May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology. 2009;43(3):535–54.
Article Google Scholar
May CR, Mair F, Finch T, Macfarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci. 2009;4:29.
Ogrinc G, Davies L, Goodman D, Batalden PB, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Quality and Safety. 2016;25:986-92.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655.
Jamal F, Fletcher A, Shackleton N, Elbourne D, Viner R, Bonell C. The three stages of building and testing mid-level theories in a realist RCT: a theoretical and methodological case-example. Trials. 2015;16(1):466.
Download references
Acknowledgements
Members of the Centre for Trials Research (CTR) Qualitative Research Group were collaborating authors: C Drew (Senior Research Fellow—Senior Trial Manager, Brain Health and Mental Wellbeing Division), D Gillespie (Director, Infection, Inflammation and Immunity Trials, Principal Research Fellow), R Hale (now Research Associate, School of Social Sciences, Cardiff University), J Latchem-Hastings (now Lecturer and Postdoctoral Fellow, School of Healthcare Sciences, Cardiff University), R Milton (Research Associate—Trial Manager), B Pell (now PhD student, DECIPHer Centre, Cardiff University), H Prout (Research Associate—Qualitative), V Shepherd (Senior Research Fellow), K Smallman (Research Associate), H Stanton (Research Associate—Senior Data Manager). Thanks are due to Kerry Hood and Aimee Grant for their involvement in developing processes and systems for qualitative research within CTR.
No specific grant was received to support the writing of this paper.
Author information
Authors and affiliations.
Centre for Trials Research, DECIPHer Centre, Cardiff University, Neuadd Meirionnydd, Heath Park, Cardiff, CF14 4YS, UK
Jeremy Segrott
Centre for Trials Research, Cardiff University, Neuadd Meirionnydd, Heath Park, Cardiff, CF14 4YS, UK
Sue Channon, Eleni Glarou, Jacqueline Hughes, Nina Jacob, Sarah Milosevic, Yvonne Moriarty, Mike Robling, Heather Strange, Julia Townson & Lucy Brookes-Howell
Division of Population Medicine, School of Medicine, Cardiff University, Neuadd Meirionnydd, Heath Park, Cardiff, CF14 4YS, UK
Eleni Glarou
Wales Centre for Public Policy, Cardiff University, Sbarc I Spark, Maindy Road, Cardiff, CF24 4HQ, UK
School of Social Sciences, Cardiff University, King Edward VII Avenue, Cardiff, CF10 3WA, UK
Josie Henley
DECIPHer Centre, School of Social Sciences, Cardiff University, Sbarc I Spark, Maindy Road, Cardiff, CF24 4HQ, UK
Bethan Pell
You can also search for this author in PubMed Google Scholar
Qualitative Research Group
- , D. Gillespie
- , J. Latchem-Hastings
- , R. Milton
- , V. Shepherd
- , K. Smallman
- & H. Stanton
Contributions
JS contributed to the design of the work and interpretation of data and was responsible for leading the drafting and revision of the paper. SC contributed to the design of the work, the acquisition of data and the drafting and revision of the paper. AL contributed to the design of the work, the acquisition of data and the drafting and revision of the paper. EG contributed to a critical review of the manuscript and provided additional relevant references. JH provided feedback on initial drafts of the paper and contributed to subsequent revisions. JHu provided feedback on initial drafts of the paper and contributed to subsequent revisions. NG provided feedback on initial drafts of the paper and contributed to subsequent revisions. SM was involved in the acquisition and analysis of data and provided a critical review of the manuscript. YM was involved in the acquisition and analysis of data and provided a critical review of the manuscript. MR was involved in the interpretation of data and critical review and revision of the paper. HS contributed to the conception and design of the work, the acquisition and analysis of data, and the revision of the manuscript. JT provided feedback on initial drafts of the paper and contributed to subsequent revisions. LB-H made a substantial contribution to the design and conception of the work, led the acquisition and analysis of data, and contributed to the drafting and revision of the paper.
Corresponding author
Correspondence to Jeremy Segrott .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not sought as no personal or identifiable data was collected.
Consent for publication
Competing interests.
All authors are or were members of staff or students in the Centre for Trials Research. JS is an associate editor of Trials .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Segrott, J., Channon, S., Lloyd, A. et al. Integrating qualitative research within a clinical trials unit: developing strategies and understanding their implementation in contexts. Trials 25 , 323 (2024). https://doi.org/10.1186/s13063-024-08124-7
Download citation
Received : 20 October 2023
Accepted : 17 April 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s13063-024-08124-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Qualitative methods
- Trials units
- Normalisation Process Theory
- Randomised controlled trials
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 15 May 2024
“I do not know the advantages of having a general practitioner” - a qualitative study exploring the views of low-acuity emergency patients without a regular general practitioner toward primary care
- Lisa Kümpel ORCID: orcid.org/0000-0003-3214-6189 1 ,
- Sarah Oslislo 1 ,
- Rebecca Resendiz Cantu 2 ,
- Martin Möckel ORCID: orcid.org/0000-0002-7691-3709 2 ,
- Christoph Heintze ORCID: orcid.org/0000-0002-2179-8192 1 &
- Felix Holzinger ORCID: orcid.org/0000-0002-8400-7757 1
BMC Health Services Research volume 24 , Article number: 629 ( 2024 ) Cite this article
Metrics details
Emergency departments (ED) worldwide have to cope with rising patient numbers. Low-acuity consulters who could receive a more suitable treatment in primary care (PC) increase caseloads, and lack of PC attachment has been discussed as a determinant. This qualitative study explores factors that contribute to non-utilization of general practitioner (GP) care among patients with no current attachment to a GP.
Qualitative semi-structured telephone interviews were conducted with 32 low-acuity ED consulters with no self-reported attachment to a GP. Participants were recruited from three EDs in the city center of Berlin, Germany. Data were analyzed by qualitative content analysis.
Interviewed patients reported heterogeneous factors contributing to their PC utilization behavior and underlying views and experiences. Participants most prominently voiced a rare need for medical services, a distinct mobility behavior, and a lack of knowledge about the role of a GP and health care options. Views about and experiences with GP care that contribute to non-utilization were predominantly related to little confidence in GP care, preference for directly consulting medical specialists, and negative experiences with GP care in the past. Contrasting their reported utilization behavior, many interviewees still recognized the advantages of GP care continuity.
Understanding reasons of low-acuity ED patients for GP non-utilization can play an important role in the design and implementation of patient-centered care interventions for PC integration. Increasing GP utilization, continuity of care and health literacy might have positive effects on patient decision-making in acute situations and in turn decrease ED burden.
Trial registration
German Clinical Trials Register: DRKS00023480; date: 2020/11/27.
Peer Review reports
Many countries record rising numbers of patients in emergency departments (ED) [ 1 , 2 ]. A substantial share of these ED consulters present with low-acuity care needs and could potentially receive a more suitable treatment in primary care (PC) [ 3 , 4 ]. Concerning these cases, achieving a shift toward a more appropriate use of general practitioner (GP) care could benefit not only the patients concerned but also the entire ED care system, as crowded EDs are associated with poorer quality of care [ 5 ].
The use of ED care for low-acuity complaints is influenced by multiple factors. Among others, a lack of knowledge about alternative acute care options was identified [ 6 , 7 ] and attributed to a lack of health literacy [ 8 , 9 ]. There is evidence that lower levels of heath literacy are associated with higher subjectively perceived treatment urgency [ 9 ]. In this context, GP care has been advocated not only as an adequate alternative treatment option for low-acuity health issues but also as an important source of health information and facilitator for care coordination, helping patients navigate in the sometimes complex structures of the health care system [ 10 , 11 ]. Consequently, it is assumed that patients with no continuous GP attachment are more likely to visit the ED for low-acuity care needs [ 12 ]. Integrating GP care by reducing access barriers could reduce demand for ED services by both providing a fixed first point of contact and promoting continuity of care, which in turn facilitates the management of long-term health care needs [ 13 , 14 , 15 , 16 ].
With regard to these findings, it is problematic that every tenth person in Germany has no GP [ 17 ]. In our health care system, there is no obligation to register for GP care at a practice and attachment is completely voluntary. Patients are free to choose or change providers anytime, and anyone can likewise visit the ED at own discretion without following any gatekeeping procedure [ 18 ]. Having the current absence of regulations and patient steering in mind, it is important to explore the roots of lacking PC integration. This is a prerequisite for the development of concepts to promote attachment and thus to potentially influence future ED utilization behavior [ 19 ]. Accordingly, our research questions for this qualitative interview study of ED patients without current attachment to a GP were as follows: What factors are associated with their health care utilization behavior and non-utilization of GP care? Which views and previous experiences of GP care could contribute to GP non-utilization and lack of attachment?
EMAPREPARE study
This qualitative evaluation was conducted as part of the multicenter mixed-methods study EMAPREPARE (Emergency and Acute Medicine– Primary Care Demands in Patients Resorting to Emergency Departments), which is a subproject of the research network EMANet (Emergency and Acute Medicine Network for Health Care Research Berlin). EMAPREPARE explores the redirection potential of low-acuity ED patients without a GP. The project includes a pilot intervention and complementary qualitative interviews. The results and implications of the intervention have been reported in a previous publication [ 20 ]. Our paper presents findings on participants’ views and experiences of GP care from the qualitative interview study accompanying the intervention. The core team of researchers for this project consisted of L.K. and S.O. (female health scientists), F.H. and C.H. (male general practitioners and senior researchers), and R.R.C. (female ED physician). The EMAPREPARE study was registered a priori in the German Clinical Trials Register (trial registration number: DRKS00023480, registration date 27/11/2020) [ 21 ]. Qualitative data are reported in this article according to the COREQ guidelines (Additional file 2 ) [ 22 ].
Participants
Interviewees were selected as a subsample of the EMAPREPARE cohort. Recruitment was conducted in three inner city EDs in Berlin, including two university medical centers. Patients were recruited in the ED waiting room, informed about the project’s aims, and asked for written informed consent to participate in the study and an optional qualitative interview. Consent included audio recording, storage and pseudonymized analysis of the interview material. The EMAPREPARE inclusion criteria needed participants to be of age (≥ 18 years) and fluent in German. Patients also had to be self-referred walk-in outpatient cases, triaged in the Manchester Triage System (MTS) lower priority categories 3–5 [ 23 ]. A further eligibility prerequisite was that patients did not have a regular GP, meaning no current self-reported attachment to a particular practice, or regular recent visits. Patients were excluded if they were not able to formally give informed consent. Researchers had no relationship with the participants prior to the study. The patients’ reasons for refusing to participate in the study were not recorded.
Recruitment for the interviews was based on the principle of purposive sampling [ 24 ]. We tried to balance gender and intentionally over-represented participants willing to make use of the GP appointment service, which was part of the pilot intervention. Further information on sampling details can be found in a previous paper [ 20 ]. Patients who consented to a qualitative interview were called after ED discharge to schedule an interview appointment within two weeks after ED presentation to facilitate recall.
Data collection
A semi-structured interview guide based on the literature was compiled with the intention to capture and understand patients’ views and experiences [ 25 ]. The questions were thoroughly discussed within the study team and in an interdisciplinary methods working group at the institute, and pilot tested in two interviews. After the first two interviews, the guide was revised further. The final interview guide consisted of three parts (see Additional file 1 for complete interview guide). The results presented here correspond to the first part of the interview guide, which addressed patients’ experiences and views about GP care (see Table 1 ), while parts two and three covered participants’ views on the EMAPREPARE intervention, with results reported elsewhere [ 20 ]. During the interviews, questions were individually adapted to the conversation flow.
Interviews were carried out between March 2021 and January 2022 by L.K. and S.O. by telephone (to avoid COVID-19 infection risk) and were concluded after thirty-two interviews once no more new themes emerged, indicating content saturation [ 26 ]. The interviewees did not receive any questions in advance, and interviews were conducted only once with each patient. Interviews were audio-recorded, and field notes were taken to document additional impressions or specifics of interview circumstances. Recordings were then transcribed verbatim and pseudonymized by L.K. and S.O., the transcripts were not returned to the patients for corrections and/or comments.
Data analysis
The transcripts of the interviews were analyzed by qualitative content analysis according to Mayring using a combined deductive and inductive approach for coding text segments. This interpretative but rule-guided process is based on coding guidelines. The method allows focusing on essential interview topics and facilitates thematic structuring and summarizing of the content [ 27 ]. Due to the exploratory nature of the study, no pre-existing framework was used to guide analysis. The first draft of the coding tree was based on the themes of the interview guide, and additional themes were then inductively derived from the material during coding. This allowed for consideration of both theoretical aspects and interview content. All derived codes had defined coding rules and anchor examples. Transcription, coding, and data analysis were performed in MAXQDA 2020. The majority of interviews were independently coded by two scientists (L.K. and S.O., experienced in qualitative research) to enable comparison and discussion of discrepancies. As interviews were conducted in German, quotes were translated to English by the authors for presentation in this paper.
Sample characteristics
Thirty-two interviews were conducted. An overview of the participants’ characteristics is given in Table 2 . The interviews had a mean duration of 20 min.
After categorizing the interview data, diverse factors contributing to the non-utilization of GP care emerged. These factors were in turn associated with thematic categories related to patient characteristics and underlying views and experiences with past GP care (see Table 3 ). In the following, these thematic categories are presented in detail with exemplary interview quotes.
Patient characteristics related to non-utilization of GP care
Rare need for medical care.
With regard to the reasons for the low relevance of GP care for their individual care context, interviewees most prominently described a rare need for regular medical care in the past due to their good state of health.
“There is no doctor I have consulted more than five times, except for my gynecologist.” (P23). “So, I have not really been ill until now and therefore I do not have a GP I regularly visit.” (P20).
Distinct mobility behavior
Apart from the rare need for regular medical care, many patients attributed the lack of continuity in their GP utilization patterns to attachment difficulties rooted in their individual mobility patterns.
“Before I came to Germany, I had a GP, but since I moved, I no longer have a GP.” (P28). “I have simply moved too often. Quite often within Berlin, in different cities, abroad.” (P1). “My parents still have the same GP that I had as a child. That has changed in modern times because people are much more mobile and move around more often. You no longer stay in one place for twenty to thirty years and have all your doctors in the neighborhood for your whole life.” (P18).
Due to circumstances such as the aforementioned infrequent need for medical care and distinct mobility behavior, many participants depicted a rather situational consultation pattern with sporadic visits to various physicians based on short-term needs. In this context, a personal relationship and continuous attachment to a specific GP practice were frequently described as less relevant than solving acute health problems by consulting a doctor selected on an as-needed basis.
“There is a GP practice where I go when something comes up. However, I do not consider this my GP of choice.” (P26). “Otherwise, I just do not have any relationship [to a GP] at all because I always just sat down in the acute consultation of some doctor. I described the problem and was treated once-off.” (P25). “As I said, I do not really have a GP in the true sense. I have been to GPs here and there, depending on which district I was living in at the time, and whether it was an urgent matter or not” (P18).
Lack of knowledge about the role of a GP and health care options
Many of the interviewed patients reported a self-perceived lack of knowledge about the responsibility of a GP.
“I do not truly understand [what a GP does], I am of course familiar with the word though.” (P1). “I do not know the advantages of having a GP. That is why I never truly thought about it.” (P26). “It is probably good to have an overview of the types of occasions for which people go to the GP. […] because it is not at all clear to me, actually.” (P11).
Some interviewees explicitly mentioned this lack of knowledge about GP care as a factor that made it difficult for them to navigate the care system and find the right doctor for their specific health problems.
“Then it is difficult for me to say, if I have an issue with my ears, whether I should go straight to an ear, nose and throat specialist, or whether I should go to the GP first.” (P13). “And it is not so clear to me now to what extent the tasks of the GP overlap or differ from the tasks of the respective specialists to whom I have turned thus far. If I were aware of what a GP actually does differently and how this could be of use to me, then I naturally would be open to it.” (P2).
In this context, one patient with a migration history depicted his limited understanding of German health care structures and the role of the GP within the system.
“Because I cannot understand the health system in Germany. It is very different from my country and completely ineffective. In my country you automatically have a GP. Everyone has.” (P28).
Views about and experiences with previous GP care
Little confidence in gp care.
Several interviewees also attributed their low utilization of GP care to a lack of confidence in the skills and knowledge of GPs compared to other specialists.
“I always have such a bad feeling about GPs, so sorry about that.” (P4). “From my experience, it is always the case that the normal doctors [GPs] are a little less experienced and can help a little less with acute cases. They can give great check-ups, they can give great recommendations […], little things like that. Unfortunately, this is not the case for acute cases. They have no experience.” (P4). “I also understand that the GPs are often not extremely qualified here […], the specialists are usually much more qualified and I do not expect anything.” (P16).
Some patients also considered consulting a GP time-consuming, complicated, and a pointless additional step in the care process. In this regard, patients portrayed the GP as a mere intermediary to medical specialists.
“My general experience is that going through GPs just delays everything even more. However, that is probably a perspective you have as a young person.” (P11). “I […] find it cumbersome to be sent from a GP to a specialist. It is an outdated concept for me.” (P25).
Preference of consulting specialists
Consequently, direct consultation with medical specialists was a pattern of utilization frequently depicted in the interviews.
“When I look back, whenever I went to the doctor, it was usually directly to specialists.” (P12). “If I am concerned about a specific problem anyway, then I can also sit down in the emergency consultation hour of the specialist.” (P2).
In addition to the aforementioned view that GP care is an intermediary step to be bypassed, some patients explicitly expressed a belief in the professional superiority of medical specialists over GPs.
“Because I often have the feeling that when I go to the GP, he does not really know what to do either, and that I always end up with a specialist.” (P7).
Negative experiences with GP care
Regarding past contacts with GP care and their potential role in explaining current individual consultation decisions, some respondents described negative experiences. An important theme in this context was frustration about long waiting times for appointments and in practice.
“ […] I have also always experienced GP surgeries as very crowded.” (P3). “You cannot always get to an acute consultation right away. You also have to wait.” (P25).
In addition, many participants described previous access problems, such as not being able to obtain a timely GP appointment, or futile attempts to find a practice that would accept new patients.
“I felt very rejected. I called different doctors’ offices and they said, “Do not come!” (P15). “For three or four months I was looking for a GP, but the answer is always that they do not take new patients.” (P29).
Participants also reported that they had not been satisfied with the treatment they received in the past from the GP.
“When I think about my GP experience, they were less able to help me there.” (P21).
“Thus far, my experience has not been so good, which is why I went straight to the ED. When I had truly severe pain, they [GPs] only ever prescribed me painkillers.” (P27).
Some interviewees described experiencing GP care as impersonal, including the impression that the respective GP was overworked and did not take enough time for consultations.
“[…] because the GPs are so overburdened.” (P16). “That is always so sobering, you ask yourself, has he [GP] truly listened to what you have to say? You tell him and he types on the computer and you get a prescription and that is it. This personal factor is also missing. It does not exist like that anymore.” (P19).
Views on the concept of having a regular GP
Participants interviewed were also asked what the concept of ‘having a regular GP’ implied for them. While most patients had a general idea of this, for some it seemed to be a completely foreign concept.
“So probably, it [having a regular GP] just means that someone has a regular doctor that they always go to.” (P1). “I do not know [what it means to “have a regular GP”].” (P23). “I do not truly understand it, the term is familiar to me, of course, and I have observed with my grandmother, for example, that she had something like a GP who actually also came to her home. In addition, she knew him for decades.” (P1).
Although some patients did not understand the concept or need for a GP, most interviewees indicated that they could see clear benefits from the continuity of GP-based care. Having a fixed contact person in case of illness who knows the individual medical history was frequently mentioned as the main advantage.
“To have a doctor where you can go if something is wrong and who also knows you and already has the data.” (P30). “I would say someone who actually knows me. Someone I do not just go to when I have cut off my finger, but who actually knows my history and accompanies me like that. Maybe not through life, but at least for a period of life. Who can then perhaps also assess what the better treatment options are, because I have certain previous illnesses, or because they know that I take certain other medicines or have taken certain other medicines until recently?” (P6).
Summary of findings
In the interviewed sample of low-acuity ED patients without a regular GP, a number of central contributing factors for GP non-utilization and an associated lack of continuity of care were identified. Patients’ characteristics and lifestyles are linked to underlying views about PC and individual past experiences. In particular, a rare need for medical care due to good general health, mobility, and a lack of knowledge about the role and responsibilities of GPs and health care options were identified as important factors for GP non-utilization. Little confidence in PC providers emerged as a widespread view, possibly contributing to a preference for specialist care. Interviews suggested that this constellation is often due to negative experiences with GP care in the past.
Results in context
Implications of sample composition and study setting.
Our study investigated factors that contribute to GP non-utilization in low-acuity ED patients. With regard to our interview sample, it is important to note that it consisted of relatively young patients, corresponding to the overall mean age of 30.6 years in the EMAPREPARE cohort. Regarding the prevalence of a first-generation migration history ( ∼ 30%), the qualitative sample likewise reflects the composition of the larger cohort from which it was recruited. The two mentioned sample characteristics have been identified in previous studies as factors that increase the odds of not having a GP [ 17 ]. Furthermore, previous work has described young age and not having a GP as factors contributing to low-acuity ED usage, which is also consistent with our findings [ 28 , 29 ]. However, other population groups have also been identified as contributive to rising ED utilization, particularly older people and people living in nursing homes, which is not reflected by our results as to the selection criteria of the study [ 30 ].
The results might also reflect specifics of the urban study setting with a high availability of specialists and care choices, where patients are less tied to one provider and have many options, which may play a role in GP care utilization and attachment motives. Other studies also found that low-acuity ED patients in urban settings, compared to rural settings, are less connected to GP care [ 31 ] and show lower commitment to their PC provider [ 11 ].
Understanding utilization motives and potential implications
Need to adapt gp care to individual life situations and to diminish access barriers.
Many of the comparably young patients from our cohort reported being rarely ill and having no regular need for medical care. Concerning age, findings by Tillmann et al. show that young people are often attached to a pediatrician during their childhood and might miss the transition to GP care as young adults. The authors stress the importance of improving this transition to support GP attachment [ 17 ].
Even though utilization of GP care was depicted as rare and sporadic in many interviews, some of the participants notably consulted a GP in the past 6 months (see Table 2 ). This utilization was prevailingly described as situational, with no attachment or long-term continuity. Accordingly, a qualitative study on the attachment of patients to GP practices by Frederiksen et al. highlighted that patients with higher morbidity and vulnerability have a greater need to have a regular GP [ 32 ]. This is consistent with our findings.
Against the backdrop of patient characteristics associated with non-utilization, such as young age, good health and related situational contacts with GP care, it is worth taking a closer look at negative experiences with PC depicted by the participants. Access problems (waiting times, appointment scheduling problems) play an important role in this context. Difficulties in obtaining a timely appointment at a GP practice were also described in a qualitative study from France by Durand et al. and identified as a reason for seeking low-acuity ED care [ 33 ]. Access problems may also be related to the problem of patient mobility, which in turn is a feature associated with younger age groups. For people who move between neighborhoods or cities, it might be quite burdensome to connect to a GP and to schedule appointments. The interviews describe experiences of rejection by practices, even for acute complaints. In a recent qualitative study, Korczak et al. investigated determinants of low-acuity ED presentations and found three main factors specifically associated with GP care: having no GP, failure to attend an appointment, and negative previous experiences with a GP practice. In turn, the main reason for not having a GP identified by this study was that patients move around or do not understand the health care system and the most appropriate care paths. The authors suggested that there should be services to enable patients to find a GP who meets their individual needs, arguing that this would increase GP attachment and continuity of care in the long term [ 34 ]. A targeted GP attachment program, as piloted in the interventional module of EMAPREPARE, could help to connect patients with GPs [ 20 ].
Another aspect underlying the deliberate non-utilization of GP care, which came up repeatedly in our interviews, was little confidence in GP care, which was related to negative experiences with PC in the past. In an Australian study, Wong and Hall examined how ED patients’ experiences with GP care affected their ED attendance and found that patients who had negative experiences with GP care in the past were more likely to visit the ED [ 35 ]. A general lack of trust in GP treatment can also play a role in ED utilization decisions [ 31 ]. Previous research by our study group has also stressed the potentially negative influence of GP-aversive views and negative PC experiences on utilization behavior [ 36 ].
Need for patient education
Patients often do not know where to access appropriate care for their needs, or struggle to obtain suitable medical attention. A surprising finding in our data was that many interviewed patients were not familiar with the role and tasks of a GP and the concept of having a regular GP practice. Even if these statements cannot be generalized – especially regarding other settings and populations – they could indicate a lack of health literacy in this patient group. While we did not survey health literacy in our study population, other works however have shown lower health literacy in low-acuity ED patients than in the general population [ 37 , 38 ]. On that score, Strauß et al. found that health literacy in low-acuity ED patients was positively related to GP attachment. Therefore, they assumed that improving GP attachment among these patients would help them to receive personalized information from their GP about different health care options and therefore make more adequate ED utilization decisions [ 10 ]. Likewise, Oedekoven et al. stressed the importance of GPs as a source of health-related information [ 39 ].
In line with the theme that non-utilization of GP care is associated with knowledge deficits about the functions and potential of PC, our interviews indicated that beliefs about the professional superiority of specialists frequently seem to play a role in not having a regular GP. Promoting information about the role of GPs and their care capabilities seems crucial in this context. However, it is certainly a challenge to reach people who have no contact with PC. Himmel et al. suggested that– especially for younger patients who are frequently not attached to a GP– health insurance personnel could educate patients about the benefits of having a GP and continuity of care [ 40 ]. Other authors have likewise stressed that specific information on the importance of having a regular GP could help to increase patients’ commitment to PC [ 11 ]. For patients with utilization patterns that are detached from PC, the ED may appear to be a particularly attractive care pathway or may be perceived as without alternatives. A patient-oriented approach to promoting and improving health literacy is therefore important to support informed decision-making processes [ 9 ]. Altogether, we must stress that our results highlight the need to improve the public perception of GPs’ important coordinating role in the healthcare system as well as their medical expertise.
Attachment to a GP and continuity of care
Interestingly, our interviews revealed that many patients embrace the theoretical concept of having a regular GP and the associated advantages of having a health care provider who knows their medical history and is available as a point of contact for any medical problems that arise. However, translating this agreement in principle into actual utilization reality is not achieved, with barriers mentioned in our interviews likely playing a central role.
Numerous works have emphasized the link between continuity of care and potentially inadequate ED utilization, and promoting PC attachment appears to be a promising leverage point for streamlining utilization [ 41 , 42 , 43 ]. A study by van den Berg et al. showed that patients with regular GP attachment are more likely to consider PC as a primary care option in an acute situation [ 12 ]. Other works have stressed that in addition to continuity of care, the doctor-patient relationship plays a central role in the decision to either consult a GP or turn to the ED for a problem that is perceived as urgent [ 41 , 42 ]. In line with this, Strauß et al. reported that both the quality of a GP-patient relationship and the experienced continuity of care are crucial factors in reducing ED utilization beyond mere attachment to a GP [ 10 ]. Our own research points in a similar direction [ 20 ]. Notably, the importance of continuity of care extends well beyond the acute care context, and some studies even suggest potential benefits in terms of mortality [ 42 , 44 , 45 ].
Our findings of a fundamental openness to attach to primary care in this patient group however raise the question of how this can best be promoted. The study’s approach is based on voluntary participation in an appointment scheduling service, but this is by no means the only conceivable measure. Internationally, many health care systems (e.g. Denmark) are based on mandatory registration with a particular practice, frequently associated with gatekeeping regulations [ 46 ]. Respective policy changes toward a primary care-based healthcare system could alleviate many of the issues raised in our study, with our findings suggesting that this could potentially be well accepted. However, as this was not part of our research question, further investigation is required.
Strengths and limitations
This qualitative study provides new insights into the views and experiences of low-acuity ED patients without PC integration toward GP care, and their complex reasons for non-utilization. While conducting our study, measures such as independent coding and reflection of results with independent researchers were taken to reduce interviewer bias, but such cannot be completely eliminated [ 47 , 48 ]. Other caveats include possible bias due to social desirability among interview respondents [ 49 ] and selection effects related to patients who may have felt offended when approached by a project about redirection to a GP and the appropriateness of their visit, and therefore refused to participate in the study. A member check with interviewed patients was not performed. Furthermore, qualitative research is inherently subjective, and characteristics of the sample must be considered when reflecting on the results [ 50 ]. Due to the inclusion criteria of the pilot study, our qualitative results only reflect the views of a selected population of patients without GP attachment. However, for context and potential contrast with a less selective patient sample, we can refer to a previous qualitative study by our research group [ 36 ]. The fact that only patients who had sufficient German language skills were able to take part in the study may also limit transferability to unselected ED users. Moreover, it must be stressed that GP attachment is not formalized (and therefore not associated with e.g. a registration process) in Germany, and ‘having a GP’ or not is a personal subjective definition for the individual patient. As described, part of our sample had made use of GP care in the recent past, but nevertheless participants described themselves as ‘unattached’ to a GP. Apart from the fact that our results reflect peculiarities of the German health care system with its absence of gatekeeping regulations, the urban study setting, as mentioned above, might also have distinctly impacted the results and limits the conclusions derived from it. This requires further research to correspondingly explore the issue in rural settings, for example.
Conclusions
Factors that contribute to non-utilization of GP care in low-acuity ED patients are multifaceted. Patients’ personal life situations, health literacy, and experiences with GPs, play an important role in their behavior when seeking medical care and choosing acute care options. As the themes identified were found to be interrelated, this study highlights individual non-utilization as a complex configuration, for which the insights derived from our data provide a framework useful for understanding and better description. This can be very helpful in targeting future intervention approaches to promote PC attachment and continuity of care and in turn strengthen GP-mediated health literacy. Our EMAPREPARE pilot intervention is a first step in this direction, providing both information material about alternative care paths and an optional GP appointment scheduling service [ 20 ].
Data Availability
The datasets used and analyzed in this study are available from the corresponding author upon reasonable request.
Abbreviations
emergency department
primary care
general practitioner
Emergency and Acute Medicine Network for Health Care Research Berlin
Emergency and Acute Medicine– Primary Care Demands in Patients Resorting to Emergency Departments
Manchester Triage System
Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Al Shabanah H, Anderson PD, et al. International perspectives on Emergency Department Crowding. Acad Emerg Med. 2011;18(12):1358–70.
Article PubMed Google Scholar
Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS ONE. 2018;13(8):e0203316.
Article PubMed PubMed Central Google Scholar
Scherer M, Lühmann D, Kazek A, Hansen H, Schäfer I. Patients attending emergency departments. Dtsch Arzteblatt Int. 2017;114(39):645–52.
Google Scholar
Parkinson B, Meacock R, Checkland K, Sutton M. Clarifying the concept of avoidable emergency department attendance. J Health Serv Res Policy. 2021;26(1):68–73.
Carter EJ, Pouch SM, Larson EL. The relationship between Emergency Department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014;46(2):106–15.
Minderhout RN, Venema P, Vos HMM, Kant J, Bruijnzeels MA, Numans ME. Understanding people who self-referred in an emergency department with primary care problems during office hours: a qualitative interview study at a Daytime General Practice Cooperative in two hospitals in the Hague, the Netherlands. BMJ Open. 2019;9(6):e029853.
Oslislo S, Kümpel L, Cantu RR, Möckel M, Heintze C, Holzinger F. Bin Ich ein Notfall? Notfallempfinden und Entscheidungskompetenz in akuten Situationen: eine qualitative Erhebung bei Notaufnahmepatient*innen. Z Evid Fortbild Qual Gesundhwes. 2021;165:43–50.
Balakrishnan MP, Herndon JB, Zhang J, Payton T, Shuster J, Carden DL. The Association of Health Literacy With Preventable Emergency Department Visits: A Cross-sectional Study. Acad Emerg Med. 2017;24(9):1042–50.
Wehler M, Kalch A, Bilandzic H, Händl T. Gesundheitskompetenz und Notfallverhalten. Notf Rettungsmedizin. 2022;25(6):427–33.
Article Google Scholar
Strauß A, Zimmermann T, Schäfer I, Scherer M. Gesundheitskompetenz und Hausarztbindung nicht dringlicher Patientinnen und Patienten in Notaufnahmen: Ergebnisse Der PiNo-Studie in Hamburg Und Schleswig-Holstein. Z Evid Fortbild Qual Gesundhwes. 2022;175:50–8.
Hansen H, Schäfer I, Porzelt S, Kazek A, Lühmann D, Scherer M. Regional and patient-related factors influencing the willingness to use general practitioners as coordinators of the treatment in northern Germany - results of a cross-sectional observational study. BMC Fam Pract. 2020;21(1):110.
van den Berg MJ, van Loenen T, Westert GP. Accessible and continuous primary care may help reduce rates of emergency department use. An international survey in 34 countries. Fam Pract. 2016;33(1):42–50.
Willson KA, Lim D, Toloo G, FitzGerald G, Kinnear FB, Morel DG. Potential role of general practice in reducing emergency department demand: a qualitative study. Emerg Med Australas. 2022;34(5):717–24.
Pak A, Gannon B. Do access, quality and cost of general practice affect emergency department use? Health Policy. 2021;125(4):504–11.
Wensing M, Szecsenyi J, Laux G. Continuity in general practice and hospitalization patterns: an observational study. BMC Fam Pract. 2021;22(1):21.
Adamczyk C, Huber M, Engelbrecht C, Kowalski L, Sanftenberg L, Schelling J, et al. Der Hausarzt als Koordinator Im Notfallsystem / the Family Physician: a coordinator in the Emergency System. Z Allg Med. 2019;5/2019:203–7.
Tillmann J, Puth MT, Frank L, Weckbecker K, Klaschik M, Münster E. Determinants of having no general practitioner in Germany and the influence of a migration background: results of the German health interview and examination survey for adults (DEGS1). BMC Health Serv Res. 2018;18(1):755.
Busse R, Blümel M, Knieps F, Bärnighausen T. Statutory health insurance in Germany: a health system shaped by 135 years of solidarity, self-governance, and competition. Lancet. 2017;390(10097):882–97.
Afilalo J. Nonurgent Emergency Department Patient Characteristics and barriers to primary care. Acad Emerg Med. 2004;11(12):1302–10.
Kümpel L, Oslislo S, Resendiz Cantu R, Möckel M, Heintze C, Holzinger F. Exploring the views of low-acuity emergency department consulters on an educational intervention and general practitioner appointment service: a qualitative study in Berlin, Germany. BMJ Open. 2023;13(4):e070054.
German Clinical Trials Register. Emergency and Acute Medicine - Primary Care demands in patients resorting to emergency departments [Internet]. DRKS00023480; https://drks.de/search/en/trial/DRKS00023480
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51.
Gräff I, Goldschmidt B, Glien P, Bogdanow M, Fimmers R, Hoeft A, et al. The German version of the Manchester Triage System and its Quality Criteria– First Assessment of Validity and Reliability. PLoS ONE. 2014;9(2):e88995.
Robinson OC. Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol. 2014;11(1):25–41.
Merriam SB, Tisdell EJ. Qualitative research: a guide to design and implementation. Fourth edition. San Francisco, CA: John Wiley & Sons; 2015. 1 p.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Mayring P. Qualitative content analysis: theoretical foundation, basic procedures and software solution. Klagenfurt: Beltz; 2014.
Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Deciding to visit the Emergency Department for non-urgent conditions: a systematic review of the literature. Am J Manag Care. 2013;19(1):47–59.
PubMed PubMed Central Google Scholar
Dinh MM, Berendsen Russell S, Bein KJ, Chalkley DR, Muscatello D, Paoloni R, et al. Statewide retrospective study of low acuity emergency presentations in New South Wales, Australia: who, what, where and why? BMJ Open. 2016;6(5):e010964.
Hoffmann F, Habbinga K. Notaufnahmebesuche Von Pflegeheimbewohnern: Analyse von Routinedaten einer städtischen Klinik der Schwerpunktversorgung. Med Klin Intensivmed Notfmed. 2023;118(7):549–55.
Schmiedhofer M, Möckel M, Slagman A, Frick J, Ruhla S, Searle J. Patient motives behind low-acuity visits to the emergency department in Germany: a qualitative study comparing urban and rural sites. BMJ Open. 2016;6(11):e013323.
Frederiksen HB, Kragstrup J, Dehlholm-Lambertsen B. Attachment in the doctor-patient relationship in general practice: a qualitative study. Scand J Prim Health Care. 2010;28(3):185–90.
Durand AC, Palazzolo S, Tanti-Hardouin N, Gerbeaux P, Sambuc R, Gentile S. Nonurgent patients in emergency departments: rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res Notes. 2012;5(1):525.
Korczak V, Yakubu K, Angell B, Middleton P, Dinh M, Lung T, et al. Understanding patient preferences for emergency care for lower triage acuity presentations during GP hours: a qualitative study in Australia. BMC Health Serv Res. 2022;22(1):1442.
Wong CY, Hall J. Does patients’ experience of general practice affect the use of emergency departments? Evidence from Australia. Health Policy. 2018;122(2):126–33.
Oslislo S, Heintze C, Möckel M, Schenk L, Holzinger F. What role does the GP play for emergency department utilizers? A qualitative exploration of respiratory patients’ perspectives in Berlin, Germany. BMC Fam Pract. 2020;21(1):154.
Wehler M, Kalch A, Bilandzic H, Händl T. Gesundheitskompetenz und Notfallverhalten. Notf Rettungsmedizin. 2022;25:427-33.
Herndon JB, Chaney M, Carden D. Health Literacy and Emergency Department Outcomes: a systematic review. Ann Emerg Med. 2011;57(4):334–45.
Oedekoven M, Herrmann WJ, Ernsting C, Schnitzer S, Kanzler M, Kuhlmey A, et al. Patients’ health literacy in relation to the preference for a general practitioner as the source of health information. BMC Fam Pract. 2019;20(1):94.
Himmel W, Dieterich A, Kochen MM. Will German patients accept their family physician as a gatekeeper? J Gen Intern Med. 2000;15(7):496–502.
Article CAS PubMed PubMed Central Google Scholar
Henninger S, Spencer B, Pasche O. Deciding whether to consult the GP or an emergency department: a qualitative study of patient reasoning in Switzerland. Eur J Gen Pract. 2019;25(3):136–42.
Sandvik H, Hetlevik Ø, Blinkenberg J, Hunskaar S. Continuity in general practice as predictor of mortality, acute hospitalisation, and use of out-of-hours care: a registry-based observational study in Norway. Br J Gen Pract. 2022;72(715):e84–90.
Wong AH, Ray JM, Eixenberger C, Crispino LJ, Parker JB, Rosenberg A, et al. Qualitative study of patient experiences and care observations during agitation events in the emergency department: implications for systems-based practice. BMJ Open. 2022;12(5):e059876.
Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. 2018;8(6):e021161.
Wolinsky FD, Bentler SE, Liu L, Geweke JF, Cook EA, Obrizan M, et al. Continuity of care with a primary care physician and mortality in older adults. J Gerontol Biol Sci Med Sci. 2010;65A(4):421–8.
OECD. Primary Care in Denmark [Internet]. OECD. 2017. (OECD Reviews of Health Systems). https://www.oecd-ilibrary.org/social-issues-migration-health/primary-care-in-denmark_9789264269453-en .
Erlingsson C, Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med. 2017;7(3):93–9.
Mruck K, Breuer F. Subjectivity and reflexivity in qualitative research—the FQS issues. Forum Qual Soc Res. 2003;4(2).
Paulhus DL. Socially desirable responding on Self-Reports. In: Zeigler-Hill V, Shackelford TK, editors. Encyclopedia of personality and individual differences. Springer International Publishing; 2017.
Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol. 2018;18(1):148.
Download references
Acknowledgements
We would like to thank all patients who participated in our study and the study team for their persistent recruitment efforts at the ED.
This study is funded by the Federal Ministry of Education and Research (BMBF), grant number 01GY1914. The funding body had no role in the design and conduct of the study, data collection, analysis, and interpretation of the data, or in the preparation, review and approval of the manuscript. We acknowledge financial support from the Open Access Publication Fund of Charité– Universitätsmedizin Berlin.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Charité– Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Institute of General Practice, Charitéplatz 1, 10117, Berlin, Germany
Lisa Kümpel, Sarah Oslislo, Christoph Heintze & Felix Holzinger
Charité– Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Division of Emergency Medicine, Campus Virchow Klinikum and Campus Charité Mitte, Berlin, Germany
Rebecca Resendiz Cantu & Martin Möckel
You can also search for this author in PubMed Google Scholar
Contributions
M.M. initiated the network EMANet and is the principal investigator and speaker of the network. S.O. (health scientist), F.H. (GP and senior researcher), R.R.C. (ED physician) and C.H. (GP and senior researcher) designed the subproject EMAPREPARE. S.O., F.H. and R.R.C. developed the study protocol and research questions for the qualitative study module. S.O and L.K. (health scientists) developed the interview guide. L.K. and S.O. carried out the interviews and transcribed audio files. L.K. and S.O. analyzed and interpreted the data. L.K. drafted the manuscript for this paper. S.O., F.H., R.R.C., C.H. and M.M. critically revised the manuscript. All the authors have read and approved the final version of this manuscript. All authors qualify as authors according to ICMJE guidelines.
Corresponding author
Correspondence to Lisa Kümpel .
Ethics declarations
Ethics approval and consent to participate.
The ethics committee of Charité– Universitätsmedizin Berlin approved the EMAPREPARE study (EA1/120/20). Written informed consent was obtained from all study participants, and methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kümpel, L., Oslislo, S., Resendiz Cantu, R. et al. “I do not know the advantages of having a general practitioner” - a qualitative study exploring the views of low-acuity emergency patients without a regular general practitioner toward primary care. BMC Health Serv Res 24 , 629 (2024). https://doi.org/10.1186/s12913-024-10977-2
Download citation
Received : 20 October 2023
Accepted : 10 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12913-024-10977-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency department
- GP attachment
- GP non-utilization
- Continuity of care
- Qualitative research
- General practitioners
- Primary care
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Get 7 Days Free
Gate Neurosciences to Share New Data and Research Insights on its Synaptic Function Molecules with Multiple Posters at 2024 ASCP Annual Meeting
- Two poster presentations will feature novel findings of preclinical metaplasticity research and updated data from the recent apimostinel Phase 1 qEEG biomarker study
- Company will host its 3 rd annual R&D Day with investigators and key opinion leaders to share new insights ahead of an upcoming Phase 2 MDD study with zelquistinel
Gate Neurosciences , a clinical-stage biotechnology company using precision medicine to develop next-generation neuroscience therapies, today announced upcoming activities at the 2024 annual meeting of the American Society of Clinical Psychopharmacology (ASCP), being held in Miami Beach, FL, from May 28-31, 2024.
The company will present new preclinical and clinical data supporting its NMDAR PAM portfolio and will share novel insights from internal research on the biological mechanisms of neuroplasticity and synaptic function.
Specifically, Gate Neurosciences will highlight its cutting-edge research on how a single dose of neuroplasticity-enhancing drugs can trigger both rapid-onset (i.e. hours) and long-lasting therapeutic effects (i.e. weeks), a phenomenon termed ‘event-driven pharmacology’. Gate’s new preclinical and clinical insights have yielded critical findings on CNS-specific ‘event-driven pharmacology’ and the importance of dosing intervals to optimize plasticity treatments.
The company plans to share these new insights at its 3 rd annual R&D Day at the conference with leading members of the scientific community in attendance. The session will also include updates on an upcoming Phase 2 study with a once-weekly oral program, zelquistinel (GATE-251), for Major Depressive Disorder.
Gate Neurosciences 3 rd Annual R&D Day at ASCP 2024: Location: Loews Hotel Miami Beach, Florida Date: Tuesday, May 28, 2024 Time: 12:15 p.m. to 1:45 p.m.
“Over the past few years, the Gate team has made considerable progress in understanding mechanisms that rapidly and durably enhance synaptic function for treating CNS diseases. Dosing these compounds the right way is critical to success,” stated Mike McCully, CEO of Gate Neurosciences. “We look forward to sharing our new data and insights with the psychiatry community at the ASCP conference and discussing updated plans for our Phase 2 study of once-weekly oral zelquistinel in depression.”
Poster Presentation Details: Poster #T14 Title: Apimostinel, a Novel NMDAR Modulator with Rapid-Acting, Sustained Effects and Favorable Drug-Like properties: Preclinical Studies Abstract Number: T14 Presentation Session: Poster Session II, Salon 4 Presentation Date and Time: 12:30pm – 2:25pm, Thursday May 30 th 2024 Lead Author: Jeffrey Burgdorf, PhD
Poster #T14 details new preclinical data supporting apimostinel as an acute psychiatry drug candidate with lasting metaplasticity effects. Key takeaways include:
- Single dose of apimostinel acutely enhanced LTP with metaplasticity lasting 7 days, and produced robust antidepressant-like effects without ketamine-like side effects
- Apimostinel dose-dependently enhanced qEEG alpha in correlation with CSF exposure, as a biomarker of NMDA receptor target activation
- Repeat doses of apimostinel led to larger and longer-lasting metaplastic effects
At the Society of Biological Psychiatry (SOBP) Annual Meeting earlier this month, Gate presented additional data on the specific NMDAR PAM mechanism of action of apimostinel.
Poster #T21 Title: A Phase 1 Safety, Pharmacokinetics (PK) and Quantitative Electroencephalography (qEEG) Pharmacodynamics Study of Single and Multiple Ascending Doses of Intravenous Apimostinel Compared with Placebo in Healthy Volunteers Abstract Number: T21 Presentation Session: Poster Session II, Salon 4 Presentation Date and Time: 12:30pm – 2:25pm, Thursday May 30 th 2024 Lead Author: Ronald M. Burch, MD PhD
Poster #T21 is the first scientific presentation of findings from the apimostinel Phase 1 clinical trial assessing safety and qEEG biomarkers. Key takeaways include:
- Apimostinel was generally safe and well-tolerated following multiple doses from 1-25mg
- Apimostinel dose-dependently stimulated qEEG alpha power
- qEEG alpha power stimulation with apimostinel was consistent with CSF Cmax drug concentrations that maximally stimulate NMDA receptors in vitro
- qEEG alpha power stimulation with apimostinel was consistent with efficacious doses in a previous Phase 2a clinical MDD study
Full abstracts will be published by ASCP following the conclusion of the 2024 Annual Meeting.
About Gate Neurosciences
Gate Neurosciences, headquartered in Indianapolis, is a precision medicine biotechnology company focused on advancing next-generation central nervous system (CNS) treatments that address the growing needs in mental health. The company is developing a portfolio of novel mechanisms of action that enhance synaptic function to address neuropsychiatric and neurocognitive diseases, including major depressive disorder. Using learnings from extensive clinical, preclinical and translational data, along with a better understanding of CNS development challenges, the company is advancing its clinical pipeline using evidence-driven, precision psychiatry approaches.
Media Contact: Azeem Zeekrya HDMZ [email protected] 312-506-5244
Corporate Contact: Rob Houghtaling - Sr. Director, Corporate Development Gate Neurosciences, Inc. [email protected]
View source version on businesswire.com: https://www.businesswire.com/news/home/20240515180606/en/
Market Updates
How anti-obesity drugs are innovating the healthcare market, why immigration has boosted job gains and the economy, what to invest in during high inflation, never mind market efficiency: are the markets sensible, starbucks stock could use a pick-me-up after big selloff; is it a buy, 5 cheap stocks to buy from an attractive part of the market, markets brief: all eyes on inflation, 5 things we learned from the q1 earnings season, stock picks, baidu earnings: weakness in advertising offset by continued double-digit growth in cloud business, going into earnings, is target stock a buy, a sell, or fairly valued, walmart earnings: low prices and strong digital presence drive market share gains, after earnings and a big selloff, is shopify stock a buy, a sell, or fairly valued, cisco earnings: positive guidance and splunk inclusion align with our long-term thesis, 3 warren buffett stocks to buy after berkshire hathaway’s just-released 13f filing, going into earnings, is nvidia stock a buy, a sell, or fairly valued, after earnings, is arista stock a buy, a sell, or fairly valued, sponsor center.

IMAGES
VIDEO
COMMENTS
Find sources of qualitative training & support at UNC. How to search for and evaluate qualitative research, integrate qualitative research into systematic reviews, report/publish qualitative research. Includes some Mixed Methods resources. Some examples and thoughts on presenting qualitative research, with a focus on posters
How to correctly size your poster in PowerPoint: Select the "Design" tab. Click "Slide Size". Select "Page Setup". Under the "Slides sized for:" dropdown menu, select "Custom". Set the "Width" and "Height" to what is needed for your poster. Click "OK". How to correctly size your poster in Adobe InDesign:
The title should be clear, succinct, and by far the largest text on the poster. I make my research question and conclusion stand out, and I lay out the rest of the content in a way that is visually intuitive to follow in the correct order. I also spend a lot of time on typography. The right typesetting can turn a dense-looking wall of text into ...
Insights to Make Your Poster Better. To fully realize the potential of both the poster genre and the opportunity that presenting posters provide, we recommend: 1. Don't Copy Most Other Posters. Most academic posters are ineffective. This trend makes it harder for good posters to be created.
Research posters summarize information or research concisely and attractively to help publicize it and generate discussion. The poster is usually a mixture of a brief text mixed with tables, graphs, pictures, and other presentation formats. At a conference, the researcher stands by the poster display while other participants can come and view ...
Please find attached a presentation that includes the presentation of qualitative quotes for Study 2 and Study 3. I try and trim quotes down as much as possible. Leave lots of white space on the ...
Research Poster Template. Title: Keep it short, 10 words or less. Abstract: Should be concise and to the point, including the essential components of research. (not required for URC Conference - use an introduction) Introduction: Introduce your topic or issue, what is the purpose of your work, and provide any critical information needed for ...
Conclusions. Effective research posters should be designed around two or three key findings with accompanying handouts and narrative description to supply additional technical detail and encourage dialog with poster viewers. Keywords: Communication, poster, conference presentation. An assortment of posters is a common way to present research ...
Firstly, take this seriously. A poster is not a consolation prize for not being given an oral presentation. This is your chance to show your work, talk to others in the field, and, if you are lucky, to pick up pointers from experts. Given that just 45% of published abstracts end in a full paper, 1 this may be your only chance to get your work ...
Video: Making an academic research poster using PowerPoint. Scientific Research Poster Design Guides and Templates. Design of Scientific Posters. ... (e.g. Quantitative, Qualitative, Mixed Methods, etc). - Also contains other resources for academic poster design and printing. Design Inspiration. Faculty of 1000 posters.
2. What are the characteristics of a good poster session? a. One part billboard, one part research paper. i. Good posters, like billboards, should capture the interest of the potential audiencefrom a distance. ii. Make sure your poster is memorable. b. A poster should be self-sustaining i. The poster should be able to stand alone.
Poster: Your poster should be an outline of your research with interesting commentary about what you learned along the way. ... You can create your poster from scratch by using PowerPoint or a similar design program. Resize the slide to fit your needs before you begin adding any content. Standard poster sizes range from 40" by 30" and 48" by 36 ...
The first section describes objectives of research posters. The second shows how to describe statistical results to viewers with varied levels of statistical training, and the third provides guidelines on the contents and organization of the poster. Later sections address how to prepare a narrative and handouts to accompany a research poster.
Online Tutorials. This sources contains samples and examples of posters alongside tips for messaging, reviewing, printing, and presenting your poster. The academic poster design portion of this guide contains useful links to support creating a research poster. Other portions of this site will help with presenting your research and poster.
Welcome! Welcome to the Social Sciences and Humanities Research Poster Design library guide! This guide will introduce you to the content, formatting, and presention best practices needed to make an effective and engaging research poster. You will also be able to view sample posters to help guide your design.
A research poster is a visual way to summarize and communicate the results of a research project to a general audience. A good poster should include the goal of the research, its methodology, results, and discussion/conclusion, in clear and concise language. Research posters will often include photos, maps, graphs and other images to present ...
A research poster design process using Canva. So for my research poster designs I'm going to use Canva.com. Instead of starting with a base template, we'll just click on the "Create a design" and click custom size. I'll be creating a square 48 inch by 48 inch poster.
Once you've picked a research poster layout to personalize, utilize our intuitive design dashboard and easy-to-use editing tools to make it your own. Drag and drop graphic elements from our extensive library into your creative research poster template. Feel free to include the ones you need according to your purpose.
How do I Design a Research Poster?: Poster Examples. Getting Started; Sections of a Poster; Design Tips; Using Images; Formatting A Poster
1) The core message. Often, a study will have a single-sentence, clear takeaway. In traditional poster designs, this is commonly lost in the conclusions, and is easily missed by a conference attendee just strolling past your poster. The #BetterPoster 's biggest design change is to place your key message right in the middle of your poster, in ...
Determine the elements in a poster to show, not tell, your research story in graphical terms. Display the essential content to deliver the message, by being bold, explicit and concise. Review the ethical and professional behavior when presenting a poster. Use it as a means to deliver your research story and generate active discussion.
Introduction: introduces your topic and briefly explains why your research is significant Place your topic within context of published literature. Clearly state your hypothesis. Include just what is highly relevant. Minimize background information and definitions.
Have contrast between text and background. Have an icon or image at the top showing what the general topic is (i.e. hands for hand therapy) Add a QR code for people to access your handouts. Poster presentation designs were the first thing I started with at OT Graphically and I was excited to share them at the American Occupational Therapy ...
Description. The art of crafting a research poster is important for the successful illustration of your research. In this interactive workshop, students will learn about the design basics of research posters. Students will also learn how to strategically craft the poster content and execute the delivery. Learning objectives: By participating in ...
The value of using qualitative methods within clinical trials is widely recognised. How qualitative research is integrated within trials units to achieve this is less clear. This paper describes the process through which qualitative research has been integrated within Cardiff University's Centre for Trials Research (CTR) in Wales, UK. We highlight facilitators of, and challenges to, integration.
Follow this poster making tutorial in order or jump ahead to a section of your interest. Step #1: Identify the Purpose of Your Poster. Step #2: Choose a Poster Template. Step #3: Add in Your Text Content. Step #4: Add Photos and Graphics. Step #5: Customize Colors and Fonts. Step #6: Include a Call-to-Action.
Background Emergency departments (ED) worldwide have to cope with rising patient numbers. Low-acuity consulters who could receive a more suitable treatment in primary care (PC) increase caseloads, and lack of PC attachment has been discussed as a determinant. This qualitative study explores factors that contribute to non-utilization of general practitioner (GP) care among patients with no ...
Background and aim: Research on international students conducted during the COVID-19 pandemic has persistently highlighted the vulnerabilities and challenges that they experienced when staying in the host country to continue with their studies. The findings from such research can inevitably create a negative image of international students and their ability to respond to challenges during ...
How we use your information depends on the product and service that you use and your relationship with us. We may use it to: Verify your identity, personalize the content you receive, or create ...