Combining qualitative and quantitative research within mixed method research designs: a methodological review
Affiliation.
- 1 Division of Nursing, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden. [email protected]
- PMID: 21084086
- PMCID: PMC7094322
- DOI: 10.1016/j.ijnurstu.2010.10.005
Objectives: It has been argued that mixed methods research can be useful in nursing and health science because of the complexity of the phenomena studied. However, the integration of qualitative and quantitative approaches continues to be one of much debate and there is a need for a rigorous framework for designing and interpreting mixed methods research. This paper explores the analytical approaches (i.e. parallel, concurrent or sequential) used in mixed methods studies within healthcare and exemplifies the use of triangulation as a methodological metaphor for drawing inferences from qualitative and quantitative findings originating from such analyses.
Design: This review of the literature used systematic principles in searching CINAHL, Medline and PsycINFO for healthcare research studies which employed a mixed methods approach and were published in the English language between January 1999 and September 2009.
Results: In total, 168 studies were included in the results. Most studies originated in the United States of America (USA), the United Kingdom (UK) and Canada. The analytic approach most widely used was parallel data analysis. A number of studies used sequential data analysis; far fewer studies employed concurrent data analysis. Very few of these studies clearly articulated the purpose for using a mixed methods design. The use of the methodological metaphor of triangulation on convergent, complementary, and divergent results from mixed methods studies is exemplified and an example of developing theory from such data is provided.
Conclusion: A trend for conducting parallel data analysis on quantitative and qualitative data in mixed methods healthcare research has been identified in the studies included in this review. Using triangulation as a methodological metaphor can facilitate the integration of qualitative and quantitative findings, help researchers to clarify their theoretical propositions and the basis of their results. This can offer a better understanding of the links between theory and empirical findings, challenge theoretical assumptions and develop new theory.
Copyright © 2010 Elsevier Ltd. All rights reserved.

Publication types
- Nursing Research*
- Research Design*
Identifiers
Linking ISSN (ISSN-L): 2056-3620
Google https://www.google.com/search?q=ISSN+%222056-3620%22
Bing https://www.bing.com/search?q=ISSN+%222056-3620%22
Yahoo https://search.yahoo.com/search?p=ISSN%20%222056-3620%22
British Library https://explore.bl.uk/primo_library/libweb/action/search.do?fn=search&ct=search&initialSearch=true&mode=Advanced&tab=local_tab&indx=1&tb=t&vl%281UIStartWith0%29=contains&vl%28freeText0%29=2056-3620&SUBMIT
Resource information
Title proper: International journal of quantitative and qualitative research methods.
Country: United Kingdom
Medium: Print
Record information
Last modification date: 23/02/2023
Type of record: Confirmed
ISSN Center responsible of the record: ISSN National Centre for the UK
downloads requested
Discover all the features of the complete ISSN records
Display mode x.
Labelled view
MARC21 view
UNIMARC view
Access, acceptance and adherence to cancer prehabilitation: a mixed-methods systematic review
- Open access
- Published: 06 May 2024
Cite this article
You have full access to this open access article

- Tessa Watts 1 ,
- Nicholas Courtier 1 ,
- Sarah Fry 1 ,
- Nichola Gale 1 ,
- Elizabeth Gillen 1 ,
- Grace McCutchan 1 ,
- Manasi Patil 1 ,
- Tracy Rees 1 ,
- Dominic Roche 1 ,
- Sally Wheelwright 2 &
- Jane Hopkinson 1
542 Accesses
13 Altmetric
Explore all metrics
The purpose of this systematic review is to better understand access to, acceptance of and adherence to cancer prehabilitation.
MEDLINE, CINAHL, PsychINFO, Embase, Physiotherapy Evidence Database, ProQuest Medical Library, Cochrane Library, Web of Science and grey literature were systematically searched for quantitative, qualitative and mixed-methods studies published in English between January 2017 and June 2023. Screening, data extraction and critical appraisal were conducted by two reviewers independently using Covidence™ systematic review software. Data were analysed and synthesised thematically to address the question ‘What do we know about access, acceptance and adherence to cancer prehabilitation, particularly among socially deprived and minority ethnic groups?’
The protocol is published on PROSPERO CRD42023403776
Searches identified 11,715 records, and 56 studies of variable methodological quality were included: 32 quantitative, 15 qualitative and nine mixed-methods. Analysis identified facilitators and barriers at individual and structural levels, and with interpersonal connections important for prehabilitation access, acceptance and adherence. No study reported analysis of facilitators and barriers to prehabilitation specific to people from ethnic minority communities. One study described health literacy as a barrier to access for people from socioeconomically deprived communities.
Conclusions
There is limited empirical research of barriers and facilitators to inform improvement in equity of access to cancer prehabilitation.
Implications for Cancer Survivors
To enhance the inclusivity of cancer prehabilitation, adjustments may be needed to accommodate individual characteristics and attention given to structural factors, such as staff training. Interpersonal connections are proposed as a fundamental ingredient for successful prehabilitation.
Similar content being viewed by others

Reasons for non-participation in cancer rehabilitation: a scoping literature review
Prehabilitation in the lung cancer pathway: a scoping review

Research Priorities in Prehabilitation for Patients Undergoing Cancer Surgery: An International Delphi Study
Avoid common mistakes on your manuscript.
Introduction
Prehabilitation is a core component of supportive care for health and well-being during cancer survivorship. It aims to improve cancer treatment outcomes and long-term health by preparing people awaiting cancer treatments, not only surgery, through support for physical activity, nutrition and emotional well-being either alone or in combination, and from the point of diagnosis [ 1 ]. Growing international evidence indicates that, in specific cancers, engagement with either uni or multimodal prehabilitation interventions can improve individuals’ pre-treatment functional capacity [ 2 , 3 ], reduce treatment-related complications [ 4 , 5 , 6 ], ease anxiety [ 7 ] and enhance post-treatment recovery [ 8 , 9 ]. As the evidence base develops and momentum for prehabilitation grows, the need to embed prehabilitation as the standard of care across different cancers has been recognised [ 10 , 11 , 12 ]. In some regions, multimodal prehabilitation is now offered as the standard of care in certain cancers, particularly lung [ 13 ] and colorectal [ 14 ].
Internationally, there are persistent health disparities following cancer treatment. Treatment and survival outcomes are poor among people from socioeconomically deprived communities and some minority ethnic groups compared to socioeconomically advantaged and majority groups [ 15 , 16 , 17 ]. To ease the overall social and economic impact of cancer on individuals and society, and to reduce the societal and healthcare costs of suboptimal treatment outcomes, it is important to identify the facilitators of and barriers to individuals’ engagement with interventions. People from socioeconomically deprived communities and some minority ethnic groups are known to be underserved in prehabilitation interventions [ 1 , 18 ]. Accordingly, to better understand reasons for informed action, this mixed-methods systematic review aims to identify, critically appraise and synthesise international empirical evidence of the facilitators of and barriers to access, acceptance and adherence of cancer prehabilitation. For this review, prehabilitation is defined as proactive and preventative for all cancer treatments (not only surgery and including neoadjuvant) and includes interventions to support physical activity, nutritional intake or psychological well-being, alone or together, carried out at any time before a course of treatment begins.
Review question
What is known about access, acceptance and adherence to cancer prehabilitation, particularly among socially deprived and minority ethnic groups?
The systematic review was informed by the Joanna Briggs Institute (JBI) mixed-methods systematic reviews (MMSR) methodology [ 19 ]. A convergent, integrated approach to data synthesis and integration was adopted [ 19 , 20 ]. The review was registered in PROSPERO CRD42023403776) on 3 March 2023 and is reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [ 21 ]. Ethical approval was not required.
Database searches
In collaboration with a specialist health service systematic review librarian, the search strategy was developed using medical subject headings (MeSH) and keywords including and relating to cancer, prehabilitation, inequity, inequality, socioeconomic deprivation, ethnic groups and health services accessibility, and then tested and refined. The electronic databases Ovid SP MEDLINE, CINAHL via EBSCO host, PsycINFO, Ovid SP EMBASE, Ovid Emcare, Allied and Complementary Medicine (AMED), Physiotherapy Evidence Database (PEDRo) and Cochrane Central were systematically searched by EG for studies published in English between January 2017 and May 2023. The search strategy was tailored for each database and detailed in online resource (Supplementary information 1 ). Supplementary searches of grey literature using the Overton, Dimensions and Proquest dissertation and theses databases (PQDT), and relevant organisational websites were conducted. Reference lists of papers retrieved for full review were scrutinised for potentially useful papers not identified through the database searches.
Selection criteria
The PICO framework was used to guide inclusion criteria on population (P), Intervention (I), comparators (C) and outcomes (O) and context (Co). It enabled identification of primary qualitative, quantitative and mixed-methods research studies about prehabilitation, published in peer-reviewed journals. Eligibility criteria were used during study selection to screen this body of literature for empirical data about barriers and facilitators of prehabilitation. Non-empirical, opinion pieces, theoretical and methodological articles, reviews and editorials were excluded, as were studies involving children, adolescents and focusing on end-of-life care.
Study selection
All search results were stored in Endnote™. Following deduplication, results were imported into Covidence™ systematic review management software. For study selection, standardised systematic review methods [ 22 ] were used. All project team members were involved in study screening and selection. Firstly, two reviewers independently screened all returned titles and abstracts. Based on eligibility and relevance, these were sifted into ‘yes’, ‘no’ or ‘maybe’ categories. Disagreements were resolved by a third reviewer. Where a definite decision could not be made, full text was retrieved and assessed. Secondly, full text of all potentially relevant abstracts was retrieved and independently assessed for inclusion by two reviewers against the eligibility criteria. Arbitration by an independent reviewer in the event of disagreement was not required at this stage. Reasons for exclusion at full text review were recorded.
Quality assessment
Two reviewers independently assessed the quality of included studies via Covidence ™ using the Mixed Methods Appraisal Tool (MMAT) version 18 [ 23 ]. The MMAT was constructed specifically for quality appraisal in mixed studies reviews and is widely used [ 23 , 24 ]. Within a single tool, Version 18 of the MMAT can be used to appraise the methodological quality of five broad categories of study design, namely qualitative, randomised controlled trials, non-randomised, quantitative descriptive and mixed methods studies. The MMAT comprises two screening questions to establish whether or not the quality appraisal should proceed and 25 core questions: five criteria which mostly relate to the appropriateness of study design and approaches to sampling, data collection and analysis relevant to each of the five study designs [ 23 ]. Each criterion is assessed as being met (Yes) or not (No). There is also scope to indicate uncertainty. A third reviewer independently moderated all quality assessments for accuracy.
Data extraction
Two reviewers independently extracted data systematically via Covidence™ using an adapted, piloted JBI mixed-methods data extraction form. Information extracted included study author, aim, year and country of publication, setting, intervention type, design, sample, data collection, analysis, data relating to prehabilitation facilitators and barriers and, as relevant, data on intervention for support of access, acceptance or adherence to prehabilitation. A third reviewer cross-checked the data extraction tables independently for accuracy and completeness.
Data synthesis and integration
All extracted findings were imported into Microsoft Excel. Quantitative data were ‘qualitised’ into textual descriptions of quantitative results to enable assimilation with qualitative data [ 25 ]. To analyse and synthesise all findings, thematic synthesis [ 26 , 27 ] was used. Thematic analysis is an established process involving the identification and development of patterns and analytic themes in primary research data. Two reviewers coded the findings and then grouped related codes into preliminary descriptive themes which captured patterns across the data describing barriers to and facilitators of cancer prehabilitation [ 26 ]. Preliminary themes were discussed with a third reviewer. Themes were then further combined and synthesised to generate three overarching analytical themes relative to the review question [ 26 ].
Figure 1 shows the PRISMA flow chart of search results. Following the first and second round screening, 56 papers published between 2017 and 2023 were included: 33 quantitative; 14 qualitative and nine mixed methods.
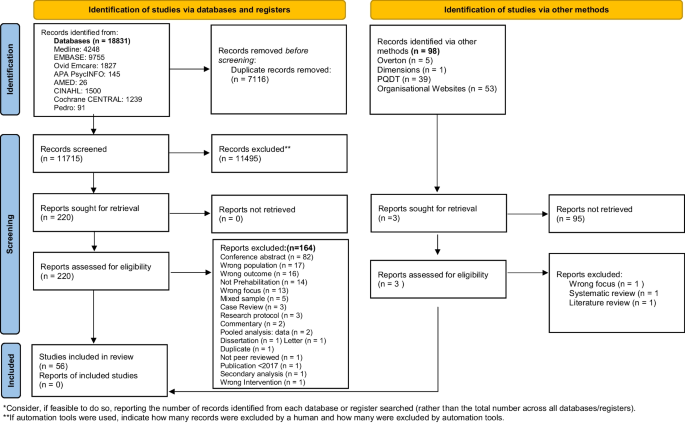
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers and other sources. *Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
A synopsis of study characteristics and the quality appraisal outcomes is found in Table 1 . Brief narrative summaries of the included papers’ findings of relevance to the review question, namely access, acceptance and adherence of prehabilitation interventions, are provided in the online supplementary information (supplementary information 2 ).
Study characteristics
Of the 32 quantitative studies reviewed, there were eight randomised controlled trials, two single-arm multi-centre trials, seven cohort studies and one cross-sectional survey. Others were pilot ( n = 3), feasibility ( n = 7), observational ( n = 1) and prevalence ( n = 1) studies, with one non-randomised trial and one audit. Qualitative studies ( n = 15) mainly used a broad qualitative approach ( n = 12), one used phenomenology, one participatory action research and one used a cross-sectional survey. Nine studies used mixed methods.
Study populations
The majority of included studies were conducted in Europe ( n = 33) (UK ( n = 19), Netherlands ( n = 4), Denmark ( n = 3), Spain ( n = 1), France ( n =1), Portugal ( n = 1), Belgium ( n = 1), Slovenia ( n = 1), Norway ( n = 1) and Sweden ( n = 1)). Eleven were conducted in North America (Canada ( n = 8), United States ( n =3)), and eight were from Australia. The remaining studies were from Japan ( n = 1) and China ( n =1), and two studies were conducted across two countries, Australia and New Zealand and the UK and Norway. Studies focused on prehabilitation in different settings including hospitals ( n = 12), local communities (including universities and local gymnasiums), individuals’ homes ( n = 14) and outdoors ( n = 1). Ten studies reported a hybrid, home and hospital approach to prehabilitation, whilst digital prehabilitation was reported in nine studies. Fifty-three studies were conducted in a range of cancers. Of these, 41 reported data for a single cancer site: colorectal ( n = 11); gastrointestinal ( n = 9); lung ( n = 7); haematology ( n= 4); breast ( n = 3); head and neck ( n =2); bladder ( n = 2) prostate ( n =1) and a range of abdominal surgeries ( n = 3). In 12 studies, cancer sites were pooled. Three studies focused on healthcare professionals ( n = 2) and key stakeholders ( n = 1).
Methodological quality
There was considerable variation in the methodological quality of the 56 studies included. Twelve studies, 10 qualitative and two quantitative, satisfied all the MMAT criteria [ 23 ]. Fourteen studies, nine mixed methods, two qualitative and three quantitative, satisfied just one or two criteria. Thus, data were extracted from a body of literature where one-fifth (21%) of publications were about research of the highest quality, defined as having met 100% of the MMAT criteria [ 23 ]. Detailed results of the MMAT quality assessments are found in supplementary information (supplementary information 3 ).
Thematic synthesis
The thematic synthesis identified three cross-cutting analytic themes. As illustrated in Figure 2 , these themes reflected individual, structural and interpersonal facilitators of and barriers to access, acceptability and adherence of cancer prehabilitation:

Overarching themes
Theme 1 The influence of individual drivers of cancer prehabilitation engagement
Theme 2 Providing acceptable cancer prehabilitation service and interventions
Theme 3 Interpersonal support – the unifying golden thread
Interpersonal support was the unifying golden thread as it facilitated the fit between the individual and the structural for access to, acceptance of and adherence to prehabilitation.
Theme 1. The influence of individual drivers of cancer prehabilitation engagement
Factors at the level of the individual were found to shape prehabilitation access, acceptance and adherence. These included perceived need and benefits, motivations, health status and everyday practicalities.
The perceived need for and potential benefits of prehabilitation
A key stimulus for accessing and adhering to cancer prehabilitation was a belief that engagement might confer benefit. Influences included clinicians’ prehabilitation endorsement and encouragement [ 12 , 13 , 42 , 52 , 55 , 59 , 60 , 65 , 66 , 71 ], positive prior personal experiences of routine physical activities [ 60 , 69 , 70 , 77 ] and weight loss programmes [ 77 ], other patients’ support [ 12 , 71 ] and the perceived need to improve personal fitness [ 60 , 63 ]. Some participants in UK-based studies believed they had a social responsibility to engage in prehabilitation [ 63 , 64 ] as enhanced fitness would benefit healthcare services financially [ 12 , 64 ].
The money, the cost per night in the hospital, goodness knows how much that costs and the follow-up with all the doctors, the dieticians and everyone else behind (….). It’s (prehabilitation) saving the NHS thousands and thousands of pounds of money ([ 64 ] p.4).
Several studies indicated some individuals perceived prehabilitation to be beneficial in that interventions provided a welcome distraction from their illness and situation [ 64 , 72 , 74 ]. Benefit was understood in terms of being psychologically and physically prepared for cancer treatments, potentially enhancing post-treatment recovery and survival [ 12 , 55 , 60 , 63 , 64 , 66 , 67 , 68 , 70 , 71 , 74 ].
I benefited a lot from it because it caught me in that time just after diagnosis when things were pretty scary and pretty awful and I felt like it was one of the key pieces of my plan for positivity during this whole thing, because it was setting a tone for recovery ([ 74 ] p. 8)
Yet, it was also clear that some individuals were disinterested in engaging with prehabilitation [ 56 , 58 , 66 , 74 , 80 ]. Some studies suggested a connection between imminent surgery and patients’ perceptions of little benefit of prehabilitation in the short timescales [ 47 , 54 , 63 , 69 , 77 , 79 ]. Some individuals felt that making additional hospital visits for prehabilitation was onerous [ 54 ]. Others were unaccustomed to or did not want to exercise [ 36 , 70 ] or perceived exercise as demanding [ 41 ], particularly when combined with cancer treatment [ 51 ]. Some considered their existing fitness levels [ 61 , 63 ] and diet [ 61 ] sufficient. A sense of low perceived benefit of or need for prehabilitation meant it was considered a low priority [ 36 ].
Personal motivators
A cancer diagnosis [ 71 , 77 ] conjoined with the desire to improve fitness [ 63 , 64 , 72 ], survive surgery [ 63 , 64 ] and to be present for and enjoy their families [ 64 ] were influential motivators for individuals’ proactively effecting lifestyle change and thus engagement with prehabilitation. Having accessed prehabilitation, exercise logs and diaries [ 64 , 68 , 74 ], personal goal setting [ 61 , 64 , 71 ], progress self-monitoring [ 61 , 64 , 68 , 71 , 77 ], activity tracking and objective feedback [ 56 , 60 ] motivated individuals to maintain participation. They inspired them to remain on track, enabled them to realise their progress, build self-efficacy for prehabilitation adherence [ 60 , 70 , 73 , 76 , 77 ] and, through a process of cognitive reframing, regain a sense of control [ 71 ].
Now I have a feeling of control over my body . . . I don’t want cancer to define me. [ 71 ]
Nonetheless, one study reported that motivation to access prehabilitation may be negatively affected by low levels of health literacy, which is associated with socioeconomic deprivation [ 46 ]. Furthermore, sustaining motivation to continue prehabilitation could be challenging [ 43 , 45 , 58 , 64 , 70 , 74 ], especially when faced with unanticipated setbacks such as delayed surgery [ 57 ] or insufficient peer support [ 64 ].
The enduring problems of health limitations
Individuals’ physical and psychological health status influenced prehabilitation access and adherence, particularly when there was a perception of insufficient on-going professional [ 61 , 72 , 73 ] and family support [ 31 ], and interventions were located away from home. Pancreatic cancer [ 33 ] adversely affected individuals’ access to prehabilitation. Furthermore, physical health problems limited some individuals’ ability to travel and thus access hospital-based prehabilitation [ 54 , 59 , 71 ]. Symptoms experienced and perceived health status influenced individuals’ prehabilitation adherence. Reported adherence barriers included physical symptoms [ 61 , 67 , 70 , 72 , 73 , 81 ] such as fatigue [ 45 , 50 , 57 , 70 , 73 ], pain [ 40 , 45 , 57 , 59 , 70 , 71 , 73 ], digestive problems [ 30 , 35 , 39 , 47 , 55 , 67 ] and feeling unwell [ 40 , 43 , 64 , 79 ]. In addition, functional limitations [ 63 , 70 ] associated with comorbidities [ 31 , 37 , 40 , 49 , 51 , 57 , 64 , 70 , 77 ], disease status [ 37 , 41 ], pre-surgery neoadjuvant treatments [ 37 , 53 , 64 , 70 , 81 ] and mental health problems [ 35 , 39 ] were all reported to negatively affect individuals’ ability to engage with and adhere to prehabilitation, particularly in terms of physical activities.
Several studies reported that psychological distress had a negative effect on prehabilitation access and adherence [ 59 , 61 , 70 , 73 ]. Described by a participant in one study [ 63 ] as ‘dark moments’, as anxiety and stress were often connected with attending hospitals [ 71 ]. In addition, several studies reported that individuals felt overwhelmed, both generally [ 42 , 57 , 74 ] and emotionally [ 12 , 70 ], in advance of their treatments. Information overload [ 62 ] and competing personal matters which required their attention pre-treatment [ 70 , 80 ] contributed to the sense of feeling overwhelmed.
The challenges of everyday life
Across studies, insufficient time for prehabilitation was frequently reported [ 40 , 50 , 51 , 55 , 58 , 66 , 71 , 72 , 74 , 77 , 78 ]. Some individuals described competing priorities in the short space of time between diagnosis and treatment [ 49 , 57 , 59 , 70 , 79 ]. This was partly due to putting affairs in order, prioritising family time [ 61 ] or treatments being scheduled earlier than originally planned [ 35 , 54 , 55 ]. Others were constrained by their employment [ 51 , 70 , 73 , 80 ] and family responsibilities, including caring for other family members [ 55 , 58 , 70 ]. Additional barriers to prehabilitation engagement included geographical distance to hospitals delivering prehabilitation [ 28 , 32 , 41 , 51 , 54 , 57 , 63 , 74 ]; transport difficulties [ 29 , 49 , 51 , 54 , 58 , 60 , 66 , 79 ] and associated financial costs [ 51 , 66 , 71 ]; inclement weather, particularly in relation to prehabilitation with outdoor exercise components [ 45 , 57 , 64 , 70 , 73 , 74 ]; low digital literacy [ 34 , 42 , 76 ]; restricted or limited access to and problems with technology [ 42 , 56 , 76 , 80 ], notably broadband [ 45 , 79 ] and experiencing physical discomfort with exercise equipment [ 60 , 64 ].
Theme 2. Providing acceptable cancer prehabilitation service and interventions
The prehabilitation environment, mode of delivery (which might be technological) and the perceived utility of interventions were important facilitators of access [ 34 , 48 , 57 , 66 , 71 , 75 , 80 ] and adherence [ 36 , 45 , 48 , 61 ] and influenced acceptance [ 36 , 52 , 61 , 64 , 69 , 71 , 77 , 80 , 81 ].
The value of home-based prehabilitation
Home-based prehabilitation interventions with remote professional supervision and support were accepted for their convenience [ 38 , 74 ], capacity to motivate [ 38 , 61 , 64 , 73 ] and build self-efficacy [ 40 , 61 , 64 , 73 ] and perceived benefit [ 40 , 69 , 74 ]. Specifically, individuals reported that home-based prehabilitation enabled them to integrate interventions into their everyday lives [ 61 , 64 ]. Exercising in the safe, private, space of home was enjoyable [ 36 , 66 ], could help with overcoming self-consciousness and engendered a sense of control [ 61 , 64 ].
I couldn’t go to the gym any longer. I can’t very well be running out to the toilet the whole time. So, I had to find something else, so it was that [static bike at home]. ([ 61 ] p. 206) …I don’t want to do it [prehabilitation] in a hospital because I think it then becomes really competitive. And people are, like, if they can’t do it, they feel…. They would feel like, ‘Oh, I’m not strong enough…’ you know what I mean. It might depress them. Whereas if you do it in the house, you can do it at your own pace, there’s nobody watching over you and everything. [ 64 ]
Home-based prehabilitation interventions were important facilitators of access [ 48 , 66 ] and adherence [ 36 , 48 , 61 ]. The provision of portable exercise equipment such as resistance bands enabled sustained adherence, particularly when individuals were temporarily away from home [ 74 ]. Some individuals welcomed the freedom and flexibility of home-based prehabilitation [ 72 ]. Yet despite being provided with resources to monitor [ 34 , 42 , 52 , 64 , 66 , 76 ], supplement and continue physical activity at home [ 48 , 63 , 66 , 74 , 77 ], insufficient in-person healthcare professional engagement and encouragement could mean adherence was often difficult to monitor [ 69 , 81 ] and sustained intervention adherence could be challenging [ 28 , 63 , 64 ] and afforded a low priority by individuals [ 61 , 72 , 73 ].
There had to be real pressure, there really had! And then if suddenly they were not around (the health professionals), then I’m not sure I’d finish it. That’s how I am. You have to keep an eye on me. [ 72 ]
Navigating the technological space of tele-prehabilitation
Sometimes referred to as ‘tele’ or ‘digital’-prehabilitation, technology-based uni and multimodal home-based prehabilitation capitalised on internet and/or telephone communication services and was delivered using smartphones, videos, wearable technology, tablets, mobile applications, video platforms and secure video conferencing [ 34 , 36 , 42 , 45 , 56 , 70 , 71 , 76 , 80 ]. In terms of acceptability, individuals perceived home-based, tele-prehabilitation programmes as accessible, particularly during the SARS-CoV-2 pandemic [ 34 , 71 , 80 ]:
Having prehabilitation outside of the hospital setting made things easier. I wasn’t feeling good with the pain and couldn’t travel too far. Could also do it in my own time ([ 71 ] p. 646)
Home-based tele-rehabilitation was also perceived as motivating [ 36 , 45 , 56 , 76 ], conferred benefit [ 34 , 36 , 45 , 56 , 80 ], particularly when personalised [ 34 , 45 , 56 , 71 ] and reduced transport-associated costs [ 80 ].
Sustained tele-prehabilitation engagement was aided by the provision of smartphones [ 56 , 76 ], tablets with relevant applications and content downloaded [ 34 ], training watches [ 34 , 56 , 76 ], supplementary information and alternate web browser pathways for those without access to or with low digital literacy [ 42 ] and integrated digital training and support during the intervention’s implementation [ 34 , 36 , 42 ].
I would not have been able to endure the treatments and the surgery thereafter had it not been for the continuous support I was receiving through the digital platform. [ 34 ]
Reported barriers were primarily intervention specific. They included technical [ 45 , 80 ] and device connectivity issues [ 34 , 76 ], broadband and website interface problems, particularly for individuals unaccustomed to using technology [ 45 ]. Negative views of mobile mindfulness apps [ 56 ] and equipment aesthetics [ 76 ] were also described.
The perceived utility of prehabilitation interventions
Interventions that were perceived as being accessible in terms of their user-friendliness [ 34 , 56 , 74 , 76 ] and appropriately designed to meet individuals’ needs, preferences and capabilities in terms of their structure [ 40 , 52 , 60 , 68 , 74 , 77 , 78 ], notably coherence [ 36 , 38 , 45 , 75 , 76 ] and components [ 38 , 54 , 55 , 64 , 69 , 74 ], including nutritional supplements [ 44 , 54 , 55 , 67 ], enhanced acceptability. The acceptability of prehabilitation interventions was reflected in the expressions of gratitude [ 12 ] and the positive ways in which interventions were variously described by individuals in some studies [ 12 , 38 , 58 , 64 , 74 ] as ‘excellent’, ‘very good’, ‘great’, ‘brilliant’, ‘hugely beneficial’ and ‘fun’. Some would even recommend home-based prehabilitation to people preparing for cancer treatments [ 52 , 63 , 68 , 74 ]. However, one study [ 42 ] reported that unfamiliarity with the English language had a negative impact on access, whilst in another study [ 56 ], individuals reported adhering to protein targets challenging.
At an individual level, the availability [ 61 ] and extent of integrated healthcare professional supervision and support was perceived to enable intervention access [ 75 ] and adherence [ 42 , 60 , 61 , 64 , 66 , 68 , 69 , 74 , 78 ], particularly when this was personalised [ 34 , 45 , 56 , 65 , 68 , 71 , 78 ]. Unpalatable nutritional interventions had a negative effect on intervention adherence [ 30 , 50 ], and it was reported that inspiratory muscle training devices could be difficult for individuals to use [ 38 ].
Healthcare professionals reported organisational barriers to implementation, and thus individuals’ access to, acceptance of and adherence with prehabilitation. These barriers included workforce capacity limitations [ 12 , 65 , 75 , 79 , 81 ], including insufficient embedded specialist prehabilitation professionals [ 69 , 81 ], delayed or insufficient referral to prehabilitation [ 33 , 44 , 63 ], disconnect in cross-boundary systematic service delivery and communication [ 12 , 28 , 75 , 81 ], inadequate funding [ 12 , 65 , 79 , 81 ] and awareness of local prehabilitation provision, uncertainty regarding what constitutes prehabilitation among some healthcare professionals [ 28 , 79 , 81 ] and space and time constraints [ 69 , 81 ] together with insufficient equipment [ 28 ] in hospital settings to deliver interventions [ 81 ].
Theme 3. Interpersonal support: the unifying golden thread
Across the studies reviewed, the unifying golden thread was interpersonal support, for this was an important, valued enabler of prehabilitation access [ 64 ] acceptance and adherence. It was reported that interpersonal support was derived from family and friends [ 12 , 45 , 60 , 61 , 64 , 70 , 73 ], prehabilitation healthcare professionals [ 42 , 51 , 55 , 60 , 61 , 63 , 64 , 66 , 69 , 71 , 75 , 78 ], prehabilitation peers [ 51 , 59 ], volunteers [ 79 ] and in-person and online peer support groups [ 71 , 79 ]. When embedded within interventions, a network of interpersonal support helped to sustain prehabilitation adherence, particularly in relation to physical activity [ 59 , 60 , 68 , 72 , 79 ]. During what could be challenging times, the interpersonal support experienced during prehabilitation enhanced interventions’ acceptability [ 52 , 60 , 63 , 68 ].
The active involvement of family during physical activities such as walking and exercise routines was reported to generate a sense of companionship, encouragement and motivational and psychological support [ 34 , 60 , 61 , 64 , 70 , 71 , 77 ]. In these ways, prehabilitation interventions with embedded family support enhanced their acceptability [ 52 ].
My wife did the same ones with me so there were two of us doing the same stuff. We did the walks together. Then we would both do the exercises. So that was good company. [ 64 ]
Findings reported in one study [ 31 ] indicated that living alone could have a negative effect on prehabilitation adherence.
The acceptability of prehabilitation interventions was enhanced by relevant healthcare professionals’ supportive dialogue in the shape of information, personalised encouragement, validation and timely, constructive feedback on individuals’ engagement, progress and performance [ 69 , 77 ], signposting to other support services [ 63 ] and broader emotional support [ 77 ]. In addition to sustaining prehabilitation behaviours through collaboration, activation and motivational support [ 60 , 61 , 71 , 72 , 77 , 78 ], healthcare professionals’ presence instilled a sense of trust [ 71 ], comfort [ 51 ] and safety [ 38 , 62 , 63 ] and reduced feelings of social isolation [ 71 ]. The need for and importance of supportive dialogue with healthcare professionals during prehabilitation was identified by participants in one study investigating individuals’ experiences of multimodal prehabilitation delivered via a leaflet and with no embedded healthcare professional support [ 73 ].
I have only been a number. Like I was a garden shovel with a barcode that you scanned at the cash register. There is no one who thinks about what this means for one’s self-understanding–- just to be regarded as a disease [...] There is no one asking about the human being behind it. It is insane [ 73 ]
For some participants, peer support in the shape of information sharing was beneficial and enabled prehabilitation access [ 63 , 71 ]. Integrated group or one to one peer support was reported to enhance an intervention’s acceptability [ 12 , 63 ]. In part, this was because individuals did not always want to engage their families, and peer support reduced their sense of isolation [ 71 ]. Peer support was reported to be beneficial in terms of interaction with others in a similar situation, thereby lending individuals’ social, emotional and motivational support, enabling them to remain on track with their prehabilitation programme [ 51 , 59 , 64 , 66 , 71 ].
Exercising in a group motivates. Let new patients exercise with other patients who are further along and have more experience exercising. They (experienced patients) can then tell them, Yes, you will get muscle aches, but they will subside too. [ 59 ]
It was clear from some studies that the absence of peer support in prehabilitation interventions was lamented [ 64 , 71 ], with some participants exercising agency and accessing online patient forums to derive required support [ 71 ].
This review reports findings from across the globe regarding facilitators of and barriers to access, acceptance and adherence of cancer prehabilitation. The findings draw attention to cross-cutting themes at individual and structural levels and interpersonal factors that connect the levels. As illuminated in Fig. 2 , the multifaceted facilitators and barriers underscore the complexity of cancer prehabilitation access, acceptance and adherence.
This review found interpersonal connections, support either directly obtained from peers, family, healthcare professionals or via digital connectivity, can facilitate a fit between the individual factors and structural factors that affect engagement with prehabilitation. Examples include encouragement from a spouse willing to engage in a recommended physical activity with the patient, practical help with digital technology, peer support during group prehabilitation and health professional supervision. Support through these interpersonal connections may be a core ingredient for successful access, acceptance and adherence. This proposition should now be explored and tested. There may be sub-groups with need or preference for certain sources of interpersonal support. Our review was designed to find out ‘what is known about access, acceptance and adherence to cancer prehabilitation, particularly among socially deprived and minority ethnic groups’ because of the known benefits from prehab for post treatment recovery [ 8 , 9 ]. It found no empirically based analysis of prehabilitation access, acceptance or adherence by people from these groups.
The individual and structural context
This review revealed individual factors enabling or impeding prehabilitation access, acceptance and adherence include personal beliefs and understandings about potential harms or benefits; motivations, for example finding enjoyment in participation; health status and everyday practicalities such as time and transport availability. Structural factors identified included the availability of knowledgeable and supportive health professionals and/or people affected by cancer’ service organisation, such as the availability of a prehabilitation multidisciplinary team and the place and space of service delivery, for example, if it was available in the community.
Individual and structural level factors affecting access to cancer treatment and care are widely reported [ 82 , 83 , 84 , 85 ]. Some are proposed to be modifiable for improved health outcomes in groups at risk of poor health because of poverty and/or discrimination based on age, race, ethnicity or gender [ 84 ]. The findings of the review are consistent with this wider literature on service access, acceptance and adherence. It is notable that although our search was designed to identify all literature about access, acceptance and adherence to cancer prehabilitation from 2017 to 2023, we found no analysis of structural differences. The differential experience of people from structurally vulnerable groups, for example, those who are socioeconomically deprived or from minority communities, had not been considered. Yet, evidence indicates that cancer rehabilitation services are underutilised by people from socioeconomically deprived communities [ 86 , 87 ] and ethnic minorities [ 88 ]. We also know patient engagement with prehabilitation is variable [ 89 ], and third sector organisations claim people from socioeconomically deprived communities, which include people from some ethnic minorities, are underserved by prehabilitation services [ 1 ]. Exploration and understanding of difference in prehabilitation experiences across social groups is needed if support for access, acceptance and adherence is to achieve equity in health outcomes.

Interpersonal connections linking individual experience and structural context
This review identified that it was people, namely peers, family members and friends, who, through their support, influenced the extent to which individual and structural level factors were obstacles or enablers of prehabilitation. In the relational space between individual experience and the infrastructure in place to enable prehabilitation, these people were supportive actors, influencing individuals’ access to, acceptance of and adherence to prehabilitation.
International studies have revealed that interpersonal support is related to mental and physical health. Low perceived social support has been shown to be associated with mental and physical health problems [ 90 ]. In the USA, a high level of perceived social support was found more likely in women and young people and low level of perceived social support more likely for those living in poverty [ 90 ]. Loneliness has been proposed the mediating factor between socioeconomic status and health in a Norwegian population-based study of people aged over 40 years [ 91 ]. Two explanations were suggested. Firstly, people with few social contacts have low levels of physical activity. Secondly, people with poor physical or emotional health are more likely to have low self-esteem and self-efficacy in self-care, which is associated with less successful occupational career and low socioeconomic status and thus fewer social contact resources to manage health [ 91 ].
This review supports an argument that interpersonal connections can be important for prehabilitation access, acceptance and adherence. It found evidence of relationships with family, peers and cancer care staff influencing access to, acceptance of, and adherence to prehabilitation. Perceived social support may have a key role in successful prehabilitation. This proposition should be further explored, paying attention to the known relationship between social support and socioeconomic status in other contexts and the potential for this to be an explanation of any observed difference in access across socioeconomic groups.
Technology as interpersonal connection?
An interesting finding is of data showing some people find web-based resources and/or online help to satisfy their prehabilitation information and support needs. These people experienced interpersonal connection through technology. An online survey among 1037 adults (18+) in the UK found that 80% of those with a long-term condition used technology for managing their health, a majority for seeking information whilst a third used wearable technology or apps. Those most likely to use technologies were younger and/or of high socioeconomic status, leading the authors to caution completely digital approaches because of the potential to exclude some groups from the care they need [ 92 ]. Arguably, technology may provide a partial solution to enabling successful prehabilitation.
What this review adds
Our finding of structural and individual level factors affecting access to, acceptance of and adherence to prehabilitation is consistent with Levesque et al.’s [ 93 ] socioecological model of access to health services. Levesque et al.’s [ 93 ] model sets out access as a process with five dimensions of accessibility (approachability; acceptability; availability and accommodation; affordability; appropriateness) and five corresponding abilities of populations (ability to perceive; ability to seek; ability to reach; ability to pay; ability to engage). The model enables attention to social, service organisation and person-centred factors that influence access. However, the model does not address the relational dimensions derived from our data analysis, i.e. how person-centred and structural factors interrelate for better or poorer service access. Based on our findings, an important ingredient for improving access to prehabilitation may be attention to what happens in the relational space connecting these factors. Voorhees et al. [ 94 ] interpreted findings of participatory research about access to general practice and claimed it is the human abilities of workforce and clients that are an important yet absent consideration in Levesque’s model. They argued that staff training and support for human interaction were needed. We agree. In addition, and based on our analysis, we also consider important the network of interactions between patient and others. Understanding the nature and mechanisms of these interactions may be important for health equity in prehabilitation.
Strengths and limitations
A strength of this review is that established, rigorous systematic review processes were followed to identify and select relevant peer-reviewed literature. Methods and thematic synthesis procedures were reported explicitly, providing an audit trail for dependability. To maximise study identification, the detailed and comprehensive search strategy was developed with the assistance of an expert information specialist, and the review was conducted by a multidisciplinary team with a minimum of two reviewers engaged in the screening and extracting process. Searches were limited from 2017 to 2023 and published in the English language. By limiting the search dates in this way, we have ensured that the evidence assessed has context and relevance to current policy and practices. This systematic review, as a result, provides an overarching picture and holistic understanding of access, acceptance and adherence to cancer prehabilitation. However, this review is not without its limitations. It is possible that some potentially useful studies, notably those not published in the English language have been omitted. Furthermore, we did not take account of study quality in our analysis. To reduce the risk of selection bias, studies were included irrespective of their methodological quality assessment. However, this means that some low quality evidence has been included, and this is a limitation to the credibility of the analysis. Nevertheless, there is some consistency between studies and across international healthcare settings. This does indicate a level of trustworthiness in the review findings. The review was of mixed cancer sites. Cancer site along with its symptoms and treatment-related problems may affect access, acceptance and adherence to prehabilitation. As the body of literature about engagement with prehabilitation grows, further work will be warranted to investigate cancer site–specific factors affecting inclusion in prehabilitation.
ThQueryere is limited empirical study of barriers and facilitators to inform improvement in equity of access to cancer prehabilitation. To enhance the inclusivity of cancer prehabilitation, adjustments may be needed to accommodate individual preferences and characteristics, such as comorbidity, and attention given to structural factors, such as staff training. Based on our findings, we propose interpersonal connections as a fundamental core ingredient for facilitation of prehabilitation access, acceptance and adherence.
Systematic review registration
This systematic review was registered in PROSPERO (CRD42023403776)
Data Availability
All data generated for this review are included in the manuscript and/or the supplementary files.
Macmillan Cancer Support. Prehabilitation for people with cancer: Principles and guidance for prehabilitation within the management and support of people with cancer. Macmillan Cancer Support. 2020. http://www.macmillan.org.uk/healthcare-professionals/news-and-resources/guides/principles-and-guidance-forprehabilitation . Accessed 03 Mar 2023.
Waterland JL, McCourt O, Edbrooke L, Granger CL, Ismail H, Riedel B, Denehy L. Efficacy of prehabilitation including exercise on postoperative outcomes following abdominal cancer surgery: a systematic review and meta-analysis Front Surg. 2021;19(8):628848. https://doi.org/10.3389/fsurg.2021.628848 .
Falz R, Bischoff C, Thieme R, Lässing J, Mehdorn M, Stelzner S, Busse M, Gockel I. Effects and duration of exercise-based prehabilitation in surgical therapy of colon and rectal cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2022;148(9):2187–213. https://doi.org/10.1007/s00432-022-04088-w .
Article PubMed PubMed Central Google Scholar
Moran J, Guinan E, McCormick P, Larkin J, Mockler D, Hussey J, Moriarty J, Wilson F. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery. 2016;160(5):1189–201. https://doi.org/10.1016/j.surg.2016.05.014 .
Article PubMed Google Scholar
Halliday LJ, Doganay E, Wynter-Blyth VA, Hanna GB, Moorthy K. The impact of prehabilitation on post-operative outcomes in oesophageal cancer surgery: a propensity score matched comparison. J Gastrointest Surg. 2021;25(11):2733–41. https://doi.org/10.1007/s11605-020-04881-3 .
Heil TC, Verdaasdonk EGG, Maas HAAM, van Munster BC, Rikkert MGMO, de Wilt JHW, Melis RJF. Improved postoperative outcomes after prehabilitation for colorectal cancer surgery in older patients: an emulated target trial. Ann Surg Oncol. 2023;30(1):244–54. https://doi.org/10.1245/s10434-022-12623-9 .
Scriney A, Russell A, Loughney L, Gallagher P, Boran L. The impact of prehabilitation interventions on affective and functional outcomes for young to midlife adult cancer patients: a systematic review. Psychooncology. 2022;31(12):2050–62. https://doi.org/10.1002/pon.6029 .
Michael CM, Lehrer EJ, Schmitz KH, Zaorsky NG. Prehabilitation exercise therapy for cancer: a systematic review and meta-analysis. Cancer Med. 2021;10(13):4195–205. https://doi.org/10.1002/cam4.4021 .
Minnella EM, Awasthi R, Bousquet-Dion G, Ferreira V, Austin B, Audi C, Tanguay S, Aprikian A, Carli F, Kassouf W. Multimodal prehabilitation to enhance functional capacity following radical cystectomy: a randomized controlled trial. Eur Urol Focus. 2021;7(1):132–8. https://doi.org/10.1016/j.euf.2019.05.016 .
Stout NL, Silver JK, Baima J, Knowlton SE, Hu X. Prehabilitation: an emerging standard in exercise Oncology. In: Schmitz K, editor. Exercise Oncology. Switzerland AG: Springer International Publishing; 2020. p. 111–43.
Chapter Google Scholar
Moore J, Merchant Z, Rowlinson K, McEwan K, Evison M, Faulkner G, Sultan J, McPhee JS, Steele J. Implementing a system-wide cancer prehabilitation programme: the journey of Greater Manchester's Prehab4cancer. Eur J Surg Oncol. 2021; 47(3 Pt A):524-532 https://doi.org/10.1016/j.ejso.2020.04.042
Bingham SL, Small S, Sempl CJ. A qualitative evaluation of a multi-modal cancer prehabilitation programme for colorectal, head and neck and lung cancer patients. PLoS One. 2023;18(10):e0277589. https://doi.org/10.1371/journal.pone.0277589 .
Article CAS PubMed PubMed Central Google Scholar
Bradley P, Marchant Z, Rowlinson-Groves K, Taylor M, Moore J, Evison M. Feasibility and outcomes of a real-world regional lung prehabilitation programme in the UK. Br J Anaesth. 2023;130(1):e47-e55 https://doi.org/10.1016/j.bja.2022.05.034
Sabajo CR, Ten Cate DWG, Heijmans MHM, Koot CTG, van Leeuwen LVL, Slooter GD. Prehabilitation in colorectal cancer surgery improves outcome and reduces hospital costs. Eur J Surg Oncol. 2024;50(1):107302. https://doi.org/10.1016/j.ejso.2023.107302 .
Ammitzbøll G, Levinsen AKG, Kjær TK, Ebbestad FE, Horsbøl TA, Saltbæk L, Badre-Esfahani SK, Joensen A, Kjeldsted E, Halgren Olsen M, Dalton SO. Socioeconomic inequality in cancer in the Nordic countries. A systematic review. Acta Oncol. 2022;61(11):1317–31. https://doi.org/10.1080/0284186X.2022.2143278 .
Boujibar F, Bonnevie T, Debeaumont D, Bubenheim M, Cuvellier A, Peillon C, Gravier FE, Baste JM. Impact of prehabilitation on morbidity and mortality after pulmonary lobectomy by minimally invasive surgery: a cohort study. J Thorac Dis. 2018; 10(4):2240-2248. https://doi.org/10.21037/jtd.2018.03.161
Giaquinto AN, Miller KD, Tossas KY, Winn RA, Jemal A, Siegel RL. Cancer statistics for African American/Black People. CA Cancer J Clin. 2022;72(3):202-229. https://doi.org/10.3322/caac.21718
Lee D, Wang A, Augustin B, Buajitti E, Tahasildar B, Carli F, Gillis C. Socioeconomic status influences participation in cancer prehabilitation and preparation for surgical recovery: a pooled retrospective analysis using a validated area-level socioeconomic status metric. Eur J Surg Oncol. 2023;49(2):512–20. https://doi.org/10.1016/j.ejso.2022.10.023 .
Lizorando L, Stern C, Carrier J, Godfrey C, Rieger K, Salmond S, Apostolo J, Kirkpatrick P, Loveday H (2020) Mixed methods systematic reviews. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. JBI. 2020. https://doi.org/10.46658/JBIMES-20-09
Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. 2017;6(1):61. https://doi.org/10.1186/s13643-017-0454-2 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372):n71. https://doi.org/10.1136/bmj.n71 .
Article Google Scholar
Centre for Reviews & Dissemination. CRD’s guidance on undertaking reviews in health care. York: University of York; 2009.
Google Scholar
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon MP, Griffiths F, Nicolau B, O’Cathain A, Rousseau MC, Vedel I, Pluye P. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Education for Information. 2018;34:285–91. https://doi.org/10.3233/EFI-180221 .
Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53. https://doi.org/10.1016/j.ijnurstu.2011.07.002 .
Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, Apóstolo J, Kirkpatrick P, Loveday H. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. 2020;18(10):2108–18.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. https://doi.org/10.1186/1471-2288-8-45 .
Thomas J, O’Mara-Eves A, Harden A, Newman M. Synthesis methods for combining and configuring textual or mixed methods data. In: Gough D, Oliver S, Thomas J, editors. An introduction to systematic reviews. London: Sage Publishing; 2017. p. 181–209.
PREPARE-ABC Trial Collaborative SupPoRtive Exercise Programmes for Accelerating REcovery after major ABdominal Cancer surgery trial (PREPARE-ABC). Pilot phase of a multicentre randomised controlled trial. Colorectal Dis. 2021;23(11):3008-3022. https://doi.org/10.1111/codi.15856
Argudo N, Rodó-Pin A, Martínez-Llorens J, Marco E, Visa L, Messaggi-Sartor M, Balañá-Corberó A, Ramón JM, Rodríguez-Chiaradía DA, Grande L, Pera M. Feasibility, tolerability, and effects of exercise-based prehabilitation after neoadjuvant therapy in esophagogastric cancer patients undergoing surgery: an interventional pilot study. Dis Esophagus. 2021; 34(4):doaa086. https://doi.org/10.1093/dote/doaa086
Burden ST, Gibson DJ, Lal S, Hill J, Pilling M, Soop M, Ramesh A, Todd C. Pre-operative oral nutritional supplementation with dietary advice versus dietary advice alone in weight-losing patients with colorectal cancer: single-blind randomized controlled trial. J Cachexia Sarcopenia Muscle. 2017;8(3):437–46. https://doi.org/10.1002/jcsm.12170 .
Catho H, Guigard S, Toffart AC, Frey G, Chollier T, Brichon PY, Roux JF, Sakhri L, Bertrand D, Aguirre C, Gorain S, Wuyam B, Arbib F, Borel JC. What are the barriers to the completion of a home-based rehabilitation programme for patients awaiting surgery for lung cancer: a prospective observational study. BMJ Open. 2021;11(2):e041907. https://doi.org/10.1136/bmjopen-2020-041907 .
Crowe J, Francis JJ, Edbrooke L, Loeliger J, Joyce T, Prickett C, Martin A, Khot A, Denehy L; Centre for Prehabilitation Peri-operative Care (CPPOC). Impact of an allied health prehabilitation service for haematologic patients receiving high-dose chemotherapy in a large cancer centre. Support Care Cancer. 2022; 30(2):1841-1852. https://doi.org/10.1007/s00520-021-06607-w
Deftereos I, Yeung JM, Arslan J, Carter VM, Isenring E, Kiss N, On Behalf Of The Nourish Point Prevalence Study Group. Preoperative nutrition intervention in patients undergoing resection for upper gastrointestinal cancer: results from the Multi-Centre NOURISH Point Prevalence Study Nutrients. 2021;13(9):3205. https://doi.org/10.3390/nu13093205
Drummond K, Lambert G, Tahasildar B, Carli F. Successes and challenges of implementing teleprehabilitation for onco-surgical candidates and patients’ experience: a retrospective pilot-cohort study. Sci Rep. 2022;12(1):6775. https://doi.org/10.1038/s41598-022-10810-y .
Ferreira V, Lawson C, Carli F, Scheede-Bergdahl C, Chevalier S. Feasibility of a novel mixed-nutrient supplement in a multimodal prehabilitation intervention for lung cancer patients awaiting surgery: a randomized controlled pilot trial. Int J Surg. 2021;93:106079. https://doi.org/10.1016/j.ijsu.2021.106079 .
Franssen RFW, Bongers BC, Vogelaar FJ, Janssen-Heijnen MLG. Feasibility of a tele-prehabilitation program in high-risk patients with colon or rectal cancer undergoing elective surgery: a feasibility study. Perioper Med (Lond). 2022;11(1):28. https://doi.org/10.1186/s13741-022-00260-5 .
Halliday LJ, Doganay E, Wynter-Blyth V, Osborn H, Buckley J, Moorthy K. Adherence to pre-operative exercise and the response to prehabilitation in oesophageal cancer patients. J Gastrointest Surg. 2021;25(4):890–9. https://doi.org/10.1007/s11605-020-04561-2 .
Karlsson E, Farahnak P, Franzén E, Nygren-Bonnier M, Dronkers J, van Meeteren N, Rydwik E. Feasibility of preoperative supervised home-based exercise in older adults undergoing colorectal cancer surgery - a randomized controlled design. PLoS One. 2019;14(7):e0219158. https://doi.org/10.1371/journal.pone.0219158 .
Lawson C, Ferreira V, Carli F, Chevalier S. Effects of multimodal prehabilitation on muscle size, myosteatosis, and dietary intake of surgical patients with lung cancer - a randomized feasibility study. Appl Physiol Nutr Metab. 2021;46(11):1407–16. https://doi.org/10.1139/apnm-2021-0249 .
Article CAS PubMed Google Scholar
Machado P, Pimenta S, Garcia AL, Nogueira T, Silva S, Oliveiros B, Martins RA, Cruz J. Home-based preoperative exercise training for lung cancer patients undergoing surgery: a feasibility trial. J Clin Med. 2023;12(8):2971. https://doi.org/10.3390/jcm12082971 .
Minnella EM, Baldini G, Quang ATL, Bessissow A, Spicer J, Carli F. Prehabilitation in thoracic cancer surgery: from research to standard of care. J Cardiothorac Vasc Anesth. 2021;35(11):3255–64. https://doi.org/10.1053/j.jvca.2021.02.049 .
Moorthy K, Halliday LJ, Noor N, Peters CJ, Wynter-Blyth V, Urch CE. Feasibility of implementation and the impact of a digital prehabilitation service in patients undergoing treatment for oesophago-gastric cancer. Curr Oncol. 2023;30(2):1673–82. https://doi.org/10.3390/curroncol30020128 .
Naito T, Mitsunaga S, Miura S, Tatematsu N, Inano T, Mouri T, Tsuji T, Higashiguchi T, Inui A, Okayama T, Yamaguchi T, Morikawa A, Mori N, Takahashi T, Strasser F, Omae K, Mori K, Takayama K. Feasibility of early multimodal interventions for elderly patients with advanced pancreatic and non-small-cell lung cancer. J Cachexia Sarcopenia Muscle. 2019;10(1):73–83. https://doi.org/10.1002/jcsm.12351 .
Paynter E, Whelan E, Curnuck C, Dhaliwal S, Sherriff J. Pre-operative immunonutrition therapy in upper gastrointestinal cancer patients: postoperative outcomes and patient acceptance. AMJ. 2017;10(6):466–473. https://doi.org/10.21767/AMJ.2017.2962
Piraux E, Caty G, Reychler G, Forget P, Deswysen Y. Feasibility and preliminary effectiveness of a tele-prehabilitation program in esophagogastric cancer patients. J Clin Med. 2020;9(7):2176. https://doi.org/10.3390/jcm9072176 .
Qin PP, Jin JY, Min S, Wang WJ, Shen YW. Association between health literacy and enhanced recovery after surgery protocol adherence and postoperative outcomes among patients undergoing colorectal cancer surgery: a prospective cohort study. Anesth Analg. 2022;134(2):330–40. https://doi.org/10.1213/ANE.0000000000005829 .
Rupnik E, Skerget M, Sever M, Zupan IP, Ogrinec M, Ursic B, Kos N, Cernelc P, Zver S. Feasibility and safety of exercise training and nutritional support prior to haematopoietic stem cell transplantation in patients with haematologic malignancies. BMC Cancer. 2020;20(1):1142. https://doi.org/10.1186/s12885-020-07637-z .
Santa Mina D, Hilton WJ, Matthew AG, Awasthi R, Bousquet-Dion G, Alibhai SMH, Au D, Fleshner NE, Finelli A, Clarke H, Aprikian A, Tanguay S, Carli F. Prehabilitation for radical prostatectomy: a multicentre randomized controlled trial. Surg Oncol. 2018;27(2):289–98. https://doi.org/10.1016/j.suronc.2018.05.010 .
Shukla A, Granger CL, Wright GM, Edbrooke L, Denehy L. Attitudes and perceptions to prehabilitation in lung cancer. Integr Cancer Ther. 2020;19:1534735420924466. https://doi.org/10.1177/1534735420924466 .
Solheim TS, Laird BJA, Balstad TR, Stene GB, Bye A, Johns N, Pettersen CH, Fallon M, Fayers P, Fearon K, Kaasa S. A randomized phase II feasibility trial of a multimodal intervention for the management of cachexia in lung and pancreatic cancer. J Cachexia Sarcopenia Muscle. 2017;8(5):778–88. https://doi.org/10.1002/jcsm.12201 .
Stalsberg R, Bertheussen GF, Børset H, Thomsen SN, Husøy A, Flote VG, Thune I, Lundgren S. Do breast cancer patients manage to participate in an outdoor, tailored, physical activity program during adjuvant breast cancer treatment, independent of health and socio-demographic characteristics? J Clin Med. 2022;11(3):843. https://doi.org/10.3390/jcm11030843 .
Steffens D, Young J, Beckenkamp PR, Ratcliffe J, Rubie F, Ansari N, Pillinger N, Koh C, Munoz PA, Solomon M. Feasibility and acceptability of a preoperative exercise program for patients undergoing major cancer surgery: results from a pilot randomized controlled trial. Pilot Feasibility Stud. 2021;7(1):27. https://doi.org/10.1186/s40814-021-00765-8 .
Thoft-Jensen B, Jensen JB, Love-Retinger N, Bowker M, Retinger C, Dalbagni G. Implementing a multimodal prehabilitation program to radical cystectomy in a comprehensive cancer center: a pilot study to assess feasibility and outcomes. Urol Nurs. 2019;39(6):303–13. https://doi.org/10.7257/1053-816x.2019.39.6.303 .
Tweed TTT, Sier MAT, Van Bodegraven AA, Van Nie NC, Sipers WMWH, Boerma EG, Stoot JHMB. Feasibility and efficiency of the BEFORE (Better Exercise and Food, Better Recovery) prehabilitation program. Nutrients. 2021;13(10):3493. https://doi.org/10.3390/nu13103493 .
van Rooijen SJ, Molenaar CJL, Schep G, van Lieshout RHMA, Beijer S, Dubbers R, Rademakers N, Papen-Botterhuis NE, van Kempen S, Carli F, Roumen RMH, Slooter GD. Making patients fit for surgery: introducing a four pillar multimodal prehabilitation program in colorectal cancer. Am J Phys Med Rehabil. 2019;98(10):888–96. https://doi.org/10.1097/PHM.0000000000001221 .
Waller E, Sutton P, Rahman S, Allen J, Saxton J, Aziz O. Prehabilitation with wearables versus standard of care before major abdominal cancer surgery: a randomised controlled pilot study (trial registration: NCT04047524). Surg Endosc. 2022;36(2):1008–17. https://doi.org/10.1007/s00464-021-08365-6 .
Waterland JL, Ismail H, Granger CL, Patrick C, Denehy L, Riedel B; Centre for Prehabilitation and Perioperative Care. Prehabilitation in high-risk patients scheduled for major abdominal cancer surgery: a feasibility study. Perioper Med.2022;11(1):32. https://doi.org/10.1186/s13741-022-00263-2
Wu F, Laza-Cagigas R, Pagarkar A, Olaoke A, El Gammal M, Rampal T. The feasibility of prehabilitation as part of the breast cancer treatment pathway. PM R. 2021;13(11):1237–46. https://doi.org/10.1002/pmrj.12543 .
Agasi-Idenburg CS, Zuilen MK, Westerman MJ, Punt CJA, Aaronson NK, Stuiver MM. “I am busy surviving” - views about physical exercise in older adults scheduled for colorectal cancer surgery. J Geriatr Oncol. 2020;11(3):444–50. https://doi.org/10.1016/j.jgo.2019.05.001 .
Banerjee S, Semper K, Skarparis K, Naisby J, Lewis L, Cucato G, Mills R, Rochester M, Saxton J. Patient perspectives of vigorous intensity aerobic interval exercise prehabilitation prior to radical cystectomy: a qualitative focus group study. Disabil Rehabil. 2021;43(8):1084–91. https://doi.org/10.1080/09638288.2019.1651907 .
Beck A, Thaysen HV, Soegaard CH, Blaakaer J, Seibaek L. Investigating the experiences, thoughts, and feelings underlying and influencing prehabilitation among cancer patients: a qualitative perspective on the what, when, where, who, and why. Disabil Rehabil. 2022;44(2):202–9. https://doi.org/10.1080/09638288.2020.1762770 .
Brady GC, Goodrich J, Roe JWG. Using experience-based co-design to improve the pre-treatment care pathway for people diagnosed with head and neck cancer. Support Care Cancer. 2020;28(2):739–45. https://doi.org/10.1007/s00520-019-04877-z .
Collaço N, Henshall C, Belcher E, Canavan J, Merriman C, Mitchell J, Watson E. Patients’ and healthcare professionals’ views on a pre- and post-operative rehabilitation programme (SOLACE) for lung cancer: a qualitative study. J Clin Nurs. 2022;31(1–2):283–93. https://doi.org/10.1111/jocn.15907 .
Cooper M, Chmelo J, Sinclair RCF, Charman S, Hallsworth K, Welford J, Phillips AW, Greystoke A, Avery L. Exploring factors influencing uptake and adherence to a home-based prehabilitation physical activity and exercise intervention for patients undergoing chemotherapy before major surgery (ChemoFit): a qualitative study. BMJ Open. 2022;12(9):e062526. https://doi.org/10.1136/bmjopen-2022-062526 .
Daun JT, Twomey R, Dort JC, Capozzi LC, Crump T, Francis GJ, Matthews TW, Chandarana SP, Hart RD, Schrag C, Matthews J, McKenzie CD, Lau H, Culos-Reed SN. A Qualitative study of patient and healthcare provider perspectives on building multiphasic exercise prehabilitation into the surgical care pathway for head and neck cancer. Curr Oncol. 2022;29(8):5942–54. https://doi.org/10.3390/curroncol29080469 .
Ferreira V, Agnihotram RV, Bergdahl A, van Rooijen SJ, Awasthi R, Carli F, Scheede-Bergdahl C. Maximizing patient adherence to prehabilitation: what do the patients say? Support Care Cancer. 2018;26(8):2717–23. https://doi.org/10.1007/s00520-018-4109-1 .
Hogan SE, Solomon MJ, Carey SK. Exploring reasons behind patient compliance with nutrition supplements before pelvic exenteration surgery. Support Care Cancer. 2019;27(5):1853–60. https://doi.org/10.1007/s00520-018-4445-1 .
McCourt O, Fisher A, Land J, Ramdharry G, Roberts AL, Bekris G, Yong. “What I wanted to do was build myself back up and prepare”: qualitative findings from the PERCEPT trial of prehabilitation during autologous stem cell transplantation in myeloma. BMC Cancer. 2023;23(1):348. https://doi.org/10.1186/s12885-023-10799-1
Murdoch J, Varley A, McCulloch J, Jones M, Thomas LB, Clark A, Stirling S, Turner D, Swart AM, Dresser K, Howard G, Saxton J, Hernon J. Implementing supportive exercise interventions in the colorectal cancer care pathway: a process evaluation of the PREPARE-ABC randomised controlled trial. BMC Cancer. 2021;21(1):1137. https://doi.org/10.1186/s12885-021-08880-8 .
Sun V, Raz DJ, Kim JY, Melstrom L, Hite S, Varatkar G, Fong Y. Barriers and facilitators of adherence to a perioperative physical activity intervention for older adults with cancer and their family caregivers. J Geriatr Oncol. 2020;11(2):256–62. https://doi.org/10.1016/j.jgo.2019.06.003 .
Wu F, Laza-Cagigas R, Rampal T. Understanding patients’ experiences and perspectives of tele-prehabilitation: a qualitative study to inform service design and delivery. Clin Pract. 2022;12(4):640–52. https://doi.org/10.3390/clinpract12040067 .
Beck A, Vind Thaysen H, Hasselholt Soegaard C, Blaakaer J, Seibaek L. What matters to you? An investigation of patients’ perspectives on and acceptability of prehabilitation in major cancer surgery. Eur J Cancer Care. 2021;30(6): e13475. https://doi.org/10.1111/ecc.13475 .
Beck A, Vind Thaysen H, Hasselholt Soegaard C, Blaakaer J, Seibaek L. Prehabilitation in cancer care: patients’ ability to prepare for major abdominal surgery. Scand J Caring Sci. 2021;35(1):143–55. https://doi.org/10.1111/scs .
Brahmbhatt P, Sabiston CM, Lopez C, Chang E, Goodman J, Jones J, McCready D, Randall I, Rotstein S, Santa Mina D. Feasibility of prehabilitation prior to breast cancer surgery: a mixed-methods study. Front Oncol. 2020;10:571091. https://doi.org/10.3389/fonc.2020.571091 .
Deftereos I, Hitch D, Butzkueven S, Carter V, Fetterplace K, Fox K, Ottaway A, Pierce K, Steer B, Varghese J, Kiss N, Yeung JM. Implementing a standardised perioperative nutrition care pathway in upper gastrointestinal cancer surgery: a mixed-methods analysis of implementation using the Consolidated Framework for Implementation Research. BMC Health Serv Res. 2022;22(1):256. https://doi.org/10.1186/s12913-022-07466-9 .
Low CA, Danko M, Durica KC, Kunta AR, Mulukutla R, Ren Y, Bartlett DL, Bovbjerg DH, Dey AK, Jakicic JM. A real-time mobile intervention to reduce sedentary behavior before and after cancer surgery: usability and feasibility study. JMIR Perioper Med. 2020;3(1):e17292. https://doi.org/10.2196/17292 .
Macleod M, Steele RJC, O’Carroll RE, Wells M, Campbell A, Sugden JA, Rodger J, Stead M, McKell J, Anderson AS. Feasibility study to assess the delivery of a lifestyle intervention (TreatWELL) for patients with colorectal cancer undergoing potentially curative treatment. BMJ Open. 2018;8(6):e021117. https://doi.org/10.1136/bmjopen-2017-021117 .
Mawson S, Keen C, Skilbeck J, Ross H, Smith L, Dixey J, Walters SJ, Simpson R, Greenfield DM, Snowden JA. Feasibility and benefits of a structured prehabilitation programme prior to autologous stem cell transplantation (ASCT) in patients with myeloma; a prospective feasibility study. Physiotherapy. 2021;113:88–99. https://doi.org/10.1016/j.physio.2021.08.001 .
Provan D, McLean G, Moug SJ, Phillips I, Anderson AS. Prehabilitation services for people diagnosed with cancer in Scotland-Current practice, barriers and challenges to implementation. Surgeon. 2022;20(5):284–90. https://doi.org/10.1016/j.surge.2021.08.005 .
Waterland JL, Chahal R, Ismail H, Sinton C, Riedel B, Francis JJ, Denehy L. Implementing a telehealth prehabilitation education session for patients preparing for major cancer surgery. BMC Health Serv Res. 2021;21(1):443. https://doi.org/10.1186/s12913-021-06437-w .
Robinson R, Crank H, Humphreys H, Fisher P, Greenfield DM. Time to embed physical activity within usual care in cancer services: a qualitative study of cancer healthcare professionals’ views at a single centre in England. Disabil Rehabil. 2023;45(21):3484–92. https://doi.org/10.1080/09638288.2022.2134468 .
Hewitt M, Simone JC. Ensuring access to cancer care. In: Hewit M, Simone JC, editors. Ensuring Quality Cancer Care. Washingon: National Academy Press; 1999. p. 46–78.
Dunn JG, Garvey PC, Valery D, Ball KM, Fong S, Vinod DL, O’Connell SK, Chambers. Barriers to lung cancer care: health professionals’ perspectives. Support Care Cancer. 2017;25:497–504. https://doi.org/10.1007/s00520-016-3428-3
Bourgeois A, Horrill TC, Mollison A, Lambert LK, Stajduhar KI. Barriers to cancer treatment and care for people experiencing structural vulnerability: a secondary analysis of ethnographic data. Int J Equity in Health. 2023;22:58 https://doi.org/10.1186/s12939-023-01860-3
Pearson SA, Taylor S, Marsden A, Dalton O’Reilly J, Krishan A, Howell S, Yorke J. Geographic and sociodemographic access to systemic anticancer therapies for secondary breast cancer: a systematic review. Systematic Reviews. 2024;13:35 https://doi.org/10.1186/s13643-023-02382-3
Oksbjerg Dalton S, Halgren Olsen M, Moustsen IR, Wedell Andersen C, Vibe-Petersen J, Johansen C. Socioeconomic position, referral and attendance to rehabilitation after a cancer diagnosis: a population-based study in Copenhagen, Denmark 2010-2015. Acta Oncol. 201;58(5):730-736. https://doi.org/10.1080/0284186X.2019.1582800
Ross L, Petersen MA, Johnsen AT, Lundstrøm LH, Groenvold M. Are different groups of cancer patients offered rehabilitation to the same extent? A report from the population-based study “The Cancer Patient’s World.” Support Care Cancer. 2012;20(5):1089–100. https://doi.org/10.1007/s00520-011-1189-6 .
Kristiansen M, Adamsen L, Piil K, Halvorsen I, Nyholm N, Hendriksen C. A three-year national follow-up study on the development of community-level cancer rehabilitation in Denmark. Scand J Public Health. 2019;47(5):511–8. https://doi.org/10.1177/1403494817746535 .
Provan D, McLean G, Moug SJ, Phillips I, Anderson AS. Prehabilitation services for people diagnosed with cancer in Scotland - current practice, barriers and challenges to implementation. Surgeon. 2022;20(5):284–90. https://doi.org/10.1016/j.surge.2021.08.005 .
Moak ZB, Agrawal A. The association between perceived interpersonal social support and physical and mental health: results from the National Epidemiological Survey on Alcohol and Related Conditions. J Public Health (Oxf). 2010;32(2):191–201. https://doi.org/10.1093/pubmed/fdp093 .
Aartsen M, Veenstra M, Hansen T. Social pathways to health: On the mediating role of the social network in the relation between socio-economic position and health. SSM Popul Health. 2017;3:419–26. https://doi.org/10.1016/j.ssmph.2017.05.006 .
NHS Confederation in partnership with Google Health. Patient empowerment: what is the role of technology in transforming care? NHS Confederation. 2023. http://www.nhsconfed.org/publications/patientempowerment-what-role-technology-transforming-care#:~:text=Ensuring%20digital%20access%20and%20inclusion,-There%20are%20disparitiestext=Adopting%20a%20digitalfirst%20approach,and%20centre%20of%20the%20design . Accessed 25 Jan 2024.
Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. https://doi.org/10.1186/1475-9276-12-18 .
Voorhees J, Bailey S, Waterman H, Checkland K. Accessing primary care and the importance of ‘human fit’: a qualitative participatory case study. Br J Gen Pract. 2022;72(718):e342–50. https://doi.org/10.3399/BJGP.2021.0375 .
Download references
Author information
Authors and affiliations.
Cardiff University, Cardiff, UK
Tessa Watts, Nicholas Courtier, Sarah Fry, Nichola Gale, Elizabeth Gillen, Grace McCutchan, Manasi Patil, Tracy Rees, Dominic Roche & Jane Hopkinson
University of Sussex, Brighton, UK
Sally Wheelwright
You can also search for this author in PubMed Google Scholar
Contributions
T.W. and JH wrote the main manuscript. E.G. Designed and tested the search strategy, ran all the searches and prepared supplementary file 1 E.G. and TW prepared figure 1 JH prepared figure 2 All authors contributed to study selection, quality assessment and data extraction TW and MP prepared supplementary file 2 TW prepared supplementary file 3 TW, MP and JH analysed data. All authors reviewed the manuscript.
Corresponding author
Correspondence to Tessa Watts .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 59 KB)
Supplementary file2 (docx 99.3 kb), supplementary file3 (docx 42.6 kb), rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Watts, T., Courtier, N., Fry, S. et al. Access, acceptance and adherence to cancer prehabilitation: a mixed-methods systematic review. J Cancer Surviv (2024). https://doi.org/10.1007/s11764-024-01605-3
Download citation
Received : 29 February 2024
Accepted : 12 April 2024
Published : 06 May 2024
DOI : https://doi.org/10.1007/s11764-024-01605-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Prehabilitation
- Systematic review
- Facilitators
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.9(Suppl); Apr-Jun 2009

Bridging Knowledge in Long Term Care 2009
Qualitative and quantitative methods in health research, m. luisa vázquez navarrete.
Health Policy Research Unit, Consorci Hospitalari de Catalunya, Barcelona, Spain
Introduction
Research in the area of health has been traditionally dominated by quantitative research. However, the complexity of ill-health, which is socially constructed by individuals, health personnel and health authorities have motivated the search for other forms to approach knowledge.
To discuss the complementarities of qualitative and quantitative research methods in the generation of knowledge.
The purpose of quantitative research is to measure the magnitude of an event, to make predictions, develop causal explanations. To achieve this it uses a pre-established design based on hypothesis and theories, conducts extensive data collection to a statistical sample and develops statistical data analysis. Quantitative research objectives can be to establish the incidence or prevalence of a health problem; the health personnel degree of adherence to a new intervention; or, the users’ level of satisfaction with a service. Qualitative research aims at understanding what exists from social actors’ perspectives. Its design is open, flexible and circular, data collection is intensive and based on a purposive sample and results will be achieved through inductive analysis. Qualitative research allows to explore aspects thought as known, understands differences in personnel opinions and practice in front of new interventions or users’ opinion on services utilization.
Quantitative and qualitative methods are different research approaches, that not only provide complementary knowledge that contributes to gaining better understanding of a problem or situation, but that can be used in a combined way, to approach a new research area, to develop instruments and to interpret results.
Presentation slides available from: http://www.bridgingknowledge.net/Presentations/Symp11_Vazquez.pdf
Title: How the green supply chain can transform the economic prosperity
Authors : Muhammad Saeed Shahbaz; Zahoor Ur Rehman; Hassan Raza; Raja Zuraidah Raja Mohd Rasi
Addresses : Shaheed Zulfikar Ali Bhutto Institute of Science and Technology (SZABIST), Pakistan ' Faculty of Technology Management and Business, Universiti Tun Hussein Onn, Malaysia ' Shaheed Zulfikar Ali Bhutto Institute of Science and Technology (SZABIST), Pakistan ' Faculty of Technology Management and Business, Universiti Tun Hussein Onn, Malaysia
Abstract : The green supply chain (GSC) plays a major role in cost reduction and increased supply chain efficiency. The study aim is to determine the impact of GSC on the supply chain of the country, the purpose of which is to assess the impact of value creation on the economic prosperity of the production supply chain. Methodologically, the study used both qualitative and quantitative methods. The data was collected through interviews, and empirical verification was done through a questionnaire. The researcher interviewed the country's employees that belong to either the economic division or supply chain. The collected data was analysed using content analysis and multiple regression through SPSS. The results reveal that creation of value creates increased market share and competitiveness and that there is mutual understanding, close relationships, and contracts between consumers and suppliers to motivate suppliers to improve product quality and reduce inventory costs over the course of time.
Keywords : green supply chain management; economic prosperity; empirical study.
DOI : 10.1504/IJSOM.2024.138594
International Journal of Services and Operations Management, 2024 Vol.48 No.1, pp.99 - 112
Received: 09 Mar 2021 Accepted: 07 Jan 2022 Published online: 14 May 2024 *
Keep up-to-date
- Our Newsletter ( subscribe for free )
- New issue alerts
- Inderscience is a member of publishing organisations including:
- Open access
- Published: 13 May 2024
Sexual and reproductive health implementation research in humanitarian contexts: a scoping review
- Alexandra Norton 1 &
- Hannah Tappis 2
Reproductive Health volume 21 , Article number: 64 ( 2024 ) Cite this article
202 Accesses
6 Altmetric
Metrics details
Meeting the health needs of crisis-affected populations is a growing challenge, with 339 million people globally in need of humanitarian assistance in 2023. Given one in four people living in humanitarian contexts are women and girls of reproductive age, sexual and reproductive health care is considered as essential health service and minimum standard for humanitarian response. Despite growing calls for increased investment in implementation research in humanitarian settings, guidance on appropriate methods and analytical frameworks is limited.
A scoping review was conducted to examine the extent to which implementation research frameworks have been used to evaluate sexual and reproductive health interventions in humanitarian settings. Peer-reviewed papers published from 2013 to 2022 were identified through relevant systematic reviews and a literature search of Pubmed, Embase, PsycInfo, CINAHL and Global Health databases. Papers that presented primary quantitative or qualitative data pertaining to a sexual and reproductive health intervention in a humanitarian setting were included.
Seven thousand thirty-six unique records were screened for inclusion, and 69 papers met inclusion criteria. Of these, six papers explicitly described the use of an implementation research framework, three citing use of the Consolidated Framework for Implementation Research. Three additional papers referenced other types of frameworks used in their evaluation. Factors cited across all included studies as helping the intervention in their presence or hindering in their absence were synthesized into the following Consolidated Framework for Implementation Research domains: Characteristics of Systems, Outer Setting, Inner Setting, Characteristics of Individuals, Intervention Characteristics, and Process.
This review found a wide range of methodologies and only six of 69 studies using an implementation research framework, highlighting an opportunity for standardization to better inform the evidence for and delivery of sexual and reproductive health interventions in humanitarian settings. Increased use of implementation research frameworks such as a modified Consolidated Framework for Implementation Research could work toward both expanding the evidence base and increasing standardization.
Plain English summary
Three hundred thirty-nine million people globally were in need of humanitarian assistance in 2023, and meeting the health needs of crisis-affected populations is a growing challenge. One in four people living in humanitarian contexts are women and girls of reproductive age, and provision of sexual and reproductive health care is considered to be essential within a humanitarian response. Implementation research can help to better understand how real-world contexts affect health improvement efforts. Despite growing calls for increased investment in implementation research in humanitarian settings, guidance on how best to do so is limited. This scoping review was conducted to examine the extent to which implementation research frameworks have been used to evaluate sexual and reproductive health interventions in humanitarian settings. Of 69 papers that met inclusion criteria for the review, six of them explicitly described the use of an implementation research framework. Three used the Consolidated Framework for Implementation Research, a theory-based framework that can guide implementation research. Three additional papers referenced other types of frameworks used in their evaluation. This review summarizes how factors relevant to different aspects of implementation within the included papers could have been organized using the Consolidated Framework for Implementation Research. The findings from this review highlight an opportunity for standardization to better inform the evidence for and delivery of sexual and reproductive health interventions in humanitarian settings. Increased use of implementation research frameworks such as a modified Consolidated Framework for Implementation Research could work toward both expanding the evidence base and increasing standardization.
Peer Review reports
Over the past few decades, the field of public health implementation research (IR) has grown as a means by which the real-world conditions affecting health improvement efforts can be better understood. Peters et al. put forward the following broad definition of IR for health: “IR is the scientific inquiry into questions concerning implementation – the act of carrying an intention into effect, which in health research can be policies, programmes, or individual practices (collectively called interventions)” [ 1 ].
As IR emphasizes real-world circumstances, the context within which a health intervention is delivered is a core consideration. However, much IR implemented to date has focused on higher-resource settings, with many proposed frameworks developed with particular utility for a higher-income setting [ 2 ]. In recognition of IR’s potential to increase evidence across a range of settings, there have been numerous reviews of the use of IR in lower-resource settings as well as calls for broader use [ 3 , 4 ]. There have also been more focused efforts to modify various approaches and frameworks to strengthen the relevance of IR to low- and middle-income country settings (LMICs), such as the work by Means et al. to adapt a specific IR framework for increased utility in LMICs [ 2 ].
Within LMIC settings, the centrality of context to a health intervention’s impact is of particular relevance in humanitarian settings, which present a set of distinct implementation challenges [ 5 ]. Humanitarian responses to crisis situations operate with limited resources, under potential security concerns, and often under pressure to relieve acute suffering and need [ 6 ]. Given these factors, successful implementation of a particular health intervention may require different qualities than those that optimize intervention impact under more stable circumstances [ 7 ]. Despite increasing recognition of the need for expanded evidence of health interventions in humanitarian settings, the evidence base remains limited [ 8 ]. Furthermore, despite its potential utility, there is not standardized guidance on IR in humanitarian settings, nor are there widely endorsed recommendations for the frameworks best suited to analyze implementation in these settings.
Sexual and reproductive health (SRH) is a core aspect of the health sector response in humanitarian settings [ 9 ]. Yet, progress in addressing SRH needs has lagged far behind other services because of challenges related to culture and ideology, financing constraints, lack of data and competing priorities [ 10 ]. The Minimum Initial Service Package (MISP) for SRH in Crisis Situations is the international standard for the minimum set of SRH services that should be implemented in all crisis situations [ 11 ]. However, as in other areas of health, there is need for expanded evidence for planning and implementation of SRH interventions in humanitarian settings. Recent systematic reviews of SRH in humanitarian settings have focused on the effectiveness of interventions and service delivery strategies, as well as factors affecting utilization, but have not detailed whether IR frameworks were used [ 12 , 13 , 14 , 15 ]. There have also been recent reviews examining IR frameworks used in various settings and research areas, but none have explicitly focused on humanitarian settings [ 2 , 16 ].
Given the need for an expanded evidence base for SRH interventions in humanitarian settings and the potential for IR to be used to expand the available evidence, a scoping review was undertaken. This scoping review sought to identify IR approaches that have been used in the last ten years to evaluate SRH interventions in humanitarian settings.
This review also sought to shed light on whether there is a need for a common framework to guide research design, analysis, and reporting for SRH interventions in humanitarian settings and if so, if there are any established frameworks already in use that would be fit-for-purpose or could be tailored to meet this need.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews was utilized to guide the elements of this review [ 17 ]. The review protocol was retrospectively registered with the Open Science Framework ( https://osf.io/b5qtz ).
Search strategy
A two-fold search strategy was undertaken for this review, which covered the last 10 years (2013–2022). First, recent systematic reviews pertaining to research or evaluation of SRH interventions in humanitarian settings were identified through keyword searches on PubMed and Google Scholar. Four relevant systematic reviews were identified [ 12 , 13 , 14 , 15 ] Table 1 .
Second, a literature search mirroring these reviews was conducted to identify relevant papers published since the completion of searches for the most recent review (April 2017). Additional file 1 includes the search terms that were used in the literature search [see Additional file 1 ].
The literature search was conducted for papers published from April 2017 to December 2022 in the databases that were searched in one or more of the systematic reviews: PubMed, Embase, PsycInfo, CINAHL and Global Health. Searches were completed in January 2023 Table 2 .
Two reviewers screened each identified study for alignment with inclusion criteria. Studies in the four systematic reviews identified were considered potentially eligible if published during the last 10 years. These papers then underwent full-text review to confirm satisfaction of all inclusion criteria, as inclusion criteria were similar but not fully aligned across the four reviews.
Literature search results were exported into a citation manager (Covidence), duplicates were removed, and a step-wise screening process for inclusion was applied. First, all papers underwent title and abstract screening. The remaining papers after abstract screening then underwent full-text review to confirm satisfaction of all inclusion criteria. Title and abstract screening as well as full-text review was conducted independently by both authors; disagreements after full-text review were resolved by consensus.
Data extraction and synthesis
The following content areas were summarized in Microsoft Excel for each paper that met inclusion criteria: publication details including author, year, country, setting [rural, urban, camp, settlement], population [refugees, internally displaced persons, general crisis-affected], crisis type [armed conflict, natural disaster], crisis stage [acute, chronic], study design, research methods, SRH intervention, and intervention target population [specific beneficiaries of the intervention within the broader population]; the use of an IR framework; details regarding the IR framework, how it was used, and any rationale given for the framework used; factors cited as impacting SRH interventions, either positively or negatively; and other key findings deemed relevant to this review.
As the focus of this review was on the approach taken for SRH intervention research and evaluation, the quality of the studies themselves was not assessed.
Twenty papers underwent full-text review due to their inclusion in one or more of the four systematic reviews and meeting publication date inclusion criteria. The literature search identified 7,016 unique papers. After full-text screening, 69 met all inclusion criteria and were included in the review. Figure 1 illustrates the search strategy and screening process.
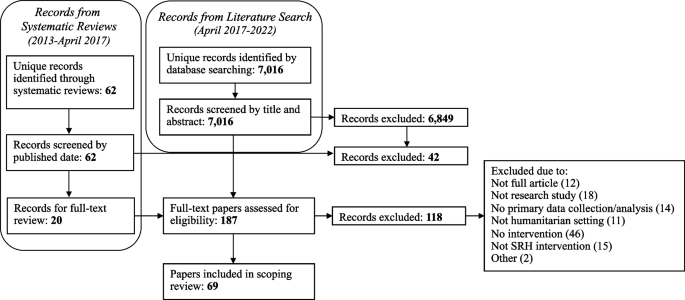
Flow chart of paper identification
Papers published in each of the 10 years of the review timeframe (2013–2022) were included. 29% of the papers originated from the first five years of the time frame considered for this review, with the remaining 71% papers coming from the second half. Characteristics of included publications, including geographic location, type of humanitarian crisis, and type of SRH intervention, are presented in Table 3 .
A wide range of study designs and methods were used across the papers, with both qualitative and quantitative studies well represented. Twenty-six papers were quantitative evaluations [ 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ], 17 were qualitative [ 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ], and 26 used mixed methods [ 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 ]. Within the quantitative evaluations, 15 were observational, while five were quasi-experimental, five were randomized controlled trials, and one was an economic evaluation. Study designs as classified by the authors of this review are summarized in Table 4 .
Six papers (9%) explicitly cited use of an IR framework. Three of these papers utilized the Consolidated Framework for Implementation Research (CFIR) [ 51 , 65 , 70 ]. The CFIR is a commonly used determinant framework that—in its originally proposed form in 2009—is comprised of five domains, each of which has constructs to further categorize factors that impact implementation. The CFIR domains were identified as core content areas influencing the effectiveness of implementation, and the constructs within each domain are intended to provide a range of options for researchers to select from to “guide diagnostic assessments of implementation context, evaluate implementation progress, and help explain findings.” [ 87 ] To allow for consistent terminology throughout this review, the original 2009 CFIR domains and constructs are used.
Guan et al. conducted a mixed methods study to assess the feasibility and effectiveness of a neonatal hepatitis B immunization program in a conflict-affected rural region of Myanmar. Guan et al. report mapping data onto the CFIR as a secondary analysis step. They describe that “CFIR was used as a comprehensive meta-theoretical framework to examine the implementation of the Hepatitis B Virus vaccination program,” and implementation themes from multiple study data sources (interviews, observations, examination of monitoring materials) were mapped onto CFIR constructs. They report their results in two phases – Pre-implementation training and community education, and Implementation – with both anchored in themes that they had mapped onto CFIR domains and constructs. All but six constructs were included in their analysis, with a majority summarized in a table and key themes explored further in the narrative text. They specify that most concerns were identified within the Outer Setting and Process domains, while elements identified within the Inner Setting domain provided strength to the intervention and helped mitigate against barriers [ 70 ].
Sarker et al. conducted a qualitative study to assess provision of maternal, newborn and child health services to Rohingya refugees residing in camps in Cox’s Bazar, Bangladesh. They cite using CFIR as a guide for thematic analysis, applying it after a process of inductive and deductive coding to index these codes into the CFIR domains. They utilized three of the five CFIR domains (Outer Setting, Inner Setting, and Process), stating that the remaining two domains (Intervention Characteristics and Characteristics of Individuals) were not relevant to their analysis. They then proposed two additional CFIR domains, Context and Security, for use in humanitarian contexts. In contrast to Guan et al., CFIR constructs are not used nor mentioned by Sarker et al., with content under each domain instead synthesized as challenges and potential solutions. Regarding the CFIR, Sarker et al. write, “The CFIR guided us for interpretative coding and creating the challenges and possible solutions into groups for further clarification of the issues related to program delivery in a humanitarian crisis setting.” [ 51 ]
Sami et al. conducted a mixed methods case study to assess the implementation of a package of neonatal interventions at health facilities within refugee and internally displaced persons camps in South Sudan. They reference use of the CFIR earlier in the study than Sarker et al., basing their guides for semi-structured focus group discussions on the CFIR framework. They similarly reference a general use of the CFIR framework as they conducted thematic analysis. Constructs are referenced once, but they do not specify whether their application of the CFIR framework included use of domains, constructs, or both. This may be in part because they then applied an additional framework, the World Health Organization (WHO) Health System Framework, to present their findings. They describe a nested approach to their use of these frameworks: “Exploring these [CFIR] constructs within the WHO Health Systems Framework can identify specific entry points to improve the implementation of newborn interventions at critical health system building blocks.” [ 65 ]
Three papers cite use of different IR frameworks. Bolan et al. utilized the Theoretical Domains Framework in their mixed methods feasibility study and pilot cluster randomized trial evaluating pilot use of the Safe Delivery App by maternal and newborn health workers providing basic emergency obstetric and newborn care in facilities in the conflict-affected Maniema province of the Democratic Republic of the Congo (DRC). They used the Theroetical Domains Framework in designing interview questions, and further used it as the coding framework for their analysis. Similar to the CFIR, the Theoretical Domains Framework is a determinant framework that consists of domains, each of which then includes constructs. Bolan et al. utilized the Theoretical Domains Framework at the construct level in interview question development and at the domain level in their analysis, mapping interview responses to eight of the 14 domains [ 83 ]. Berg et al. report using an “exploratory design guided by the principles of an evaluation framework” developed by the Medical Research Council to analyze the implementation process, mechanisms of impact, and outcomes of a three-pillar training intervention to improve maternal and neonatal healthcare in the conflict-affected South Kivu province of the DRC [ 67 , 88 ]. Select components of this evaluation framework were used to guide deductive analysis of focus group discussions and in-depth interviews [ 67 ]. In their study of health workers’ knowledge and attitudes toward newborn health interventions in South Sudan, before and after training and supply provision, Sami et al. report use of the Conceptual Framework of the Role of Attitudes in Evidence-Based Practice Implementation in their analysis process. The framework was used to group codes following initial inductive coding analysis of in-depth interviews [ 72 ].
Three other papers cite use of specific frameworks in their intervention evaluation [ 19 , 44 , 76 ]. As a characteristic of IR is the use of an explicit framework to guide the research, the use of the frameworks in these three papers meets the intention of IR and serves the purpose that an IR framework would have in strengthening the analytical rigor. Castle et al. cite use of their program’s theory of change as a framework for a mixed methods evaluation of the provision of family planning services and more specifically uptake of long-acting reversible contraception use in the DRC. They describe use of the theory of change to “enhance effectiveness of [long-acting reversible contraception] access and uptake.” [ 76 ] Thommesen et al. cite use of the AAAQ (Availability, Accessibility, Acceptability and Quality) framework in their qualitative study assessing midwifery services provided to pregnant women in Afghanistan. This framework is focused on the “underlying elements needed for attainment of optimum standard of health care,” but the authors used it in this paper to evaluate facilitators and barriers to women accessing midwifery services [ 44 ]. Jarrett et al. cite use of the Centers for Disease Control and Prevention’s (CDC) Guidelines for Evaluating Public Health Surveillance Systems to explore the characteristics of a population mobility, mortality and birth surveillance system in South Kivu, DRC. Use of these CDC guidelines is cited as one of four study objectives, and commentary is included in the Results section pertaining to each criteria within these guidelines, although more detail regarding use of these guidelines or the authors’ experience with their use in the study is not provided [ 19 ].
Overall, 22 of the 69 papers either explicitly or implicitly identified IR as relevant to their work. Nineteen papers include a focus on feasibility (seven of which did not otherwise identify the importance of exploring questions concerning implementation), touching on a common outcome of interest in implementation research [ 89 ].
While a majority of papers did not explicitly or implicitly use an IR framework to evaluate their SRH intervention of focus, most identified factors that facilitated implementation when they were present or served as a barrier when absent. Sixty cite factors that served as facilitators and 49 cite factors that served as barriers, with just three not citing either. Fifty-nine distinct factors were identified across the papers.
Three of the six studies that explicitly used an IR framework used the CFIR, and the CFIR is the only IR framework that was used by multiple studies. As previously mentioned, Means et al. put forth an adaptation of the CFIR to increase its relevance in LMIC settings, proposing a sixth domain (Characteristics of Systems) and 11 additional constructs [ 2 ]. Using the expanded domains and constructs as proposed by Means et al., the 59 factors cited by papers in this review were thematically grouped into the six domains: Characteristics of Systems, Outer Setting, Inner Setting, Characteristics of Individuals, Intervention Characteristics, and Process. Within each domain, alignment with CFIR constructs was assessed for, and alignment was found with 29 constructs: eight of Means et al.’s 11 constructs, and 21 of the 39 standard CFIR constructs. Three factors did not align with any construct (all fitting within the Outer Setting domain), and 14 aligned with a construct label but not the associated definition. Table 5 synthesizes the mapping of factors affecting SRH intervention implementation to CFIR domains and constructs, with the construct appearing in italics if it is considered to align with that factor by label but not by definition.
Table 6 lists the CFIR constructs that were not found to have alignment with any factor cited by the papers in this review.
This scoping review sought to assess how IR frameworks have been used to bolster the evidence base for SRH interventions in humanitarian settings, and it revealed that IR frameworks, or an explicit IR approach, are rarely used. All four of the systematic reviews identified with a focus on SRH in humanitarian settings articulate the need for more research examining the effectiveness of SRH interventions in humanitarian settings, with two specifically citing a need for implementation research/science [ 12 , 13 ]. The distribution of papers across the timeframe included in this review does suggest that more research on SRH interventions for crisis-affected populations is taking place, as a majority of relevant papers were published in the second half of the review period. The papers included a wide range of methodologies, which reflect the differing research questions and contexts being evaluated. However, it also invites the question of whether there should be more standardization of outcomes measured or frameworks used to guide analysis and to facilitate increased comparison, synthesis and application across settings.
Three of the six papers that used an IR framework utilized the CFIR. Guan et al. used the CFIR at both a domain and construct level, Sarker et al. used the CFIR at the domain level, and Sami et al. did not specify which CFIR elements were used in informing the focus group discussion guide [ 51 , 65 , 70 ]. It is challenging to draw strong conclusions about the applicability of CFIR in humanitarian settings based on the minimal use of CFIR and IR frameworks within the papers reviewed, although Guan et al. provides a helpful model for how analysis can be structured around CFIR domains and constructs. It is worth considering that the minimal use of IR frameworks, and more specifically CFIR constructs, could be in part because that level of prescriptive categorization does not allow for enough fluidity in humanitarian settings. It also raises questions about the appropriate degree of standardization to pursue for research done in these settings.
The mapping of factors affecting SRH intervention implementation provides an example of how a modified CFIR framework could be used for IR in humanitarian contexts. This mapping exercise found factors that mapped to all five of the original CFIR domains as well as the sixth domain proposed by Means et al. All factors fit well within the definition for the selected domain, indicating an appropriate degree of fit between these existing domains and the factors identified as impacting SRH interventions in humanitarian settings. On a construct level, however, the findings were more variable, with one-quarter of factors not fully aligning with any construct. Furthermore, over 40% of the CFIR constructs (including the additional constructs from Means et al.) were not found to align with any factors cited by the papers in this review, also demonstrating some disconnect between the parameters posed by the CFIR constructs and the factors cited as relevant in a humanitarian context.
It is worth noting that while the CFIR as proposed in 2009 was used in this assessment, as well as in the included papers which used the CFIR, an update was published in 2022. Following a review of CFIR use since its publication, the authors provide updates to construct names and definitions to “make the framework more applicable across a range of innovations and settings.” New constructs and subconstructs were also added, for a total of 48 constructs and 19 subconstructs across the five domains [ 90 ]. A CFIR Outcomes Addendum was also published in 2022, based on recommendations for the CFIR to add outcomes and intended to be used as a complement to the CFIR determinants framework [ 91 ]. These expansions to the CFIR framework may improve applicability of the CFIR in humanitarian settings. Several constructs added to the Outer Setting domain could be of particular utility – critical incidents, local attitudes, and local conditions, each of which could help account for unique challenges faced in contexts of crisis. Sub-constructs added within the Inner Setting domain that seek to clarify structural characteristics and available resources would also be of high utility based on mapping of the factors identified in this review to the original CFIR constructs. As outcomes were not formally included in the CFIR until the 2022 addendum, a separate assessment of implementation outcomes was not undertaken in this review. However, analysis of the factors cited by papers in this review as affecting implementation was derived from the full text of the papers and thus captures content relevant to implementation determinants that is contained within the outcomes.
Given the demonstrated need for additional flexibility within an IR framework for humanitarian contexts, while not a focus of this review, it is worth considering whether a different framework could provide a better fit than the CFIR. Other frameworks have differing points of emphasis that would create different opportunities for flexibility but that do not seem to resolve the challenges experienced in applying the CFIR to a humanitarian context. As one example, the EPIS (Exploration, Preparation, Implementation, Sustainment) Framework considers the impact of inner and outer context on each of four implementation phases; while the constructs within this framework are broader than the CFIR, an emphasis on the intervention characteristics is missing, a domain where stronger alignment within the CFIR is also needed [ 92 ]. Alternatively, the PRISM (Practical, Robust Implementation and Sustainability Model) framework is a determinant and evaluation framework that adds consideration of context factors to the RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) outcomes framework. It has a stronger emphasis on intervention aspects, with sub-domains to account for both organization and patient perspectives within the intervention. While PRISM does include aspects of context, external environment considerations are less robust and intentionally less comprehensive in scope, which would not provide the degree of alignment possible between the Characteristics of Systems and Outer Setting CFIR domains for the considerations unique to humanitarian environments [ 93 ].
Reflecting on their experience with the CFIR, Sarker et al. indicate that it can be a “great asset” in both evaluating current work and developing future interventions. They also encourage future research of humanitarian health interventions to utilize the CFIR [ 51 ]. The other papers that used the CFIR do not specifically reflect on their experience utilizing it, referring more generally to having felt that it was a useful tool [ 65 , 70 ]. On their use of an evaluation framework, Berg et al. reflected that it lent useful structure and helped to identify aspects affecting implementation that otherwise would have gone un-noticed [ 67 ]. The remaining studies that utilized an IR framework did not specifically comment on their experience with its use [ 72 , 83 ]. While a formal IR framework was not engaged by other studies, a number cite a desire for IR to contribute further detail to their findings [ 21 , 37 ].
In their recommendations for strengthening the evidence base for humanitarian health interventions, Ager et al. speak to the need for “methodologic innovation” to develop methodologies with particular applicability in humanitarian settings [ 7 ]. As IR is not yet routinized for SRH interventions, this could be opportune timing for the use of a standardized IR framework to gauge its utility. Using an IR framework to assess factors influencing implementation of the MISP in initial stages of a humanitarian response, and interventions to support more comprehensive SRH service delivery in protracted crises, could lend further rigor and standardization to SRH evaluations, as well as inform strategies to improve MISP implementation over time. Based on categorizing factors identified by these papers as relevant for intervention evaluation, there does seem to be utility to a modified CFIR approach. Given the paucity of formal IR framework use within SRH literature, it would be worth conducting similar scoping exercises to assess for explicit use of IR frameworks within the evidence base for other health service delivery areas in humanitarian settings. In the interim, the recommended approach from this review for future IR on humanitarian health interventions would be a modified CFIR approach with domain-level standardization and flexibility for constructs that may standardize over time with more use. This would enable use of a common analytical framework and vocabulary at the domain level for stakeholders to describe interventions and the factors influencing the effectiveness of implementation, with constructs available to use and customize as most appropriate for specific contexts and interventions.
This review had a number of limitations. As this was a scoping review and a two-part search strategy was used, the papers summarized here may not be comprehensive of those written pertaining to SRH interventions over the past 10 years. Papers from 2013 to 2017 that would have met this scoping review’s inclusion criteria may have been omitted due to being excluded from the systematic reviews. The review was limited to papers available in English. Furthermore, this review did not assess the quality of the papers included or seek to assess the methodology used beyond examination of the use of an IR framework. It does, however, serve as a first step in assessing the extent to which calls for implementation research have been addressed, and identify entry points for strengthening the science and practice of SRH research in humanitarian settings.
With one in 23 people worldwide in need of humanitarian assistance, and financing required for response plans at an all-time high, the need for evidence to guide resource allocation and programming for SRH in humanitarian settings is as important as ever [ 94 ]. Recent research agenda setting initiatives and strategies to advance health in humanitarian settings call for increased investment in implementation research—with priorities ranging from research on effective strategies for expanding access to a full range of contraceptive options to integrating mental health and psychosocial support into SRH programming to capturing accurate and actionable data on maternal and perinatal mortality in a wide range of acute and protracted emergency contexts [ 95 , 96 ]. To truly advance guidance in these areas, implementation research will need to be conducted across diverse humanitarian settings, with clear and consistent documentation of both intervention characteristics and outcomes, as well as contextual and programmatic factors affecting implementation.
Conclusions
Implementation research has potential to increase impact of health interventions particularly in crisis-affected settings where flexibility, adaptability and context-responsive approaches are highlighted as cornerstones of effective programming. There remains significant opportunity for standardization of research in the humanitarian space, with one such opportunity occurring through increased utilization of IR frameworks such as a modified CFIR approach. Investing in more robust sexual and reproductive health research in humanitarian contexts can enrich insights available to guide programming and increase transferability of learning across settings.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Availability, Accessibility, Acceptability and Quality
Centers for Disease Control and Prevention
Consolidated Framework for Implementation Research
Democratic Republic of the Congo
Exploration, Preparation, Implementation, Sustainment
- Implementation research
Low and middle income country
Minimum Initial Service Package
Practical, Robust Implementation and Sustainability Model
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Reach, Effectiveness, Adoption, Implementation, Maintenance
- Sexual and reproductive health
World Health Organization
Peters DH, et al. Implementation research: what it is and how to do it. RESEARCH METHODS. 2013;347:7.
Means AR, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci. 2020;15(1):17.
Article PubMed PubMed Central Google Scholar
Alonge O, et al. How is implementation research applied to advance health in low-income and middle-income countries? BMJ Glob Health. 2019;4(2):e001257.
Ridde V, Pérez D, Robert E. Using implementation science theories and frameworks in global health. BMJ Glob Health. 2020;5(4):e002269.
Gaffey MF, et al. Delivering health and nutrition interventions for women and children in different conflict contexts: a framework for decision making on what, when, and how. Lancet (London, England). 2021;397(10273):543–54.
Article PubMed Google Scholar
Singh NS, et al. Delivering health interventions to women, children, and adolescents in conflict settings: what have we learned from ten country case studies? The Lancet. 2021;397(10273):533–42.
Article Google Scholar
Ager A, et al. Strengthening the evidence base for health programming in humanitarian crises. Science. 2014;345(6202):1290–2.
Article CAS PubMed Google Scholar
Blanchet K, et al. Evidence on public health interventions in humanitarian crises. The Lancet. 2017;390(10109):2287–96.
Sphere A. The Sphere Handbook | Standards for quality humanitarian response. 2018.
Google Scholar
Barot S. In a State of Crisis: Meeting the Sexual and Reproductive Health Needs of Women in Humanitarian Situations. Guttmacher Policy Rev. 2017;20:7.
Crisis, I.-A.W.G.f.R.H.i., Minimum Initial Service Package. 2020: https://www.unfpa.org/resources/minimum-initial-service-package-misp-srh-crisis-situations .
Casey SE. Evaluations of reproductive health programs in humanitarian settings: a systematic review. Confl Heal. 2015;9(1):S1.
Singh NS, et al. A long way to go: a systematic review to assess the utilisation of sexual and reproductive health services during humanitarian crises. BMJ Glob Health. 2018;3(2):e000682.
Singh NS, et al. Evaluating the effectiveness of sexual and reproductive health services during humanitarian crises: A systematic review. PLoS ONE. 2018;13(7):e0199300.
Warren E, et al. Systematic review of the evidence on the effectiveness of sexual and reproductive health interventions in humanitarian crises. BMJ Open. 2015;5(12):e008226.
Dadich A, Piper A, Coates D. Implementation science in maternity care: a scoping review. Implement Sci. 2021;16(1):16.
Tricco AC, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Devine A, et al. Strategies for the prevention of perinatal hepatitis B transmission in a marginalized population on the Thailand-Myanmar border: a cost-effectiveness analysis. BMC Infect Dis. 2017;17(1):552.
Jarrett P, et al. Evaluation of a population mobility, mortality, and birth surveillance system in South Kivu. Democratic Republic of the Congo Disasters. 2020;44(2):390–407.
PubMed Google Scholar
Logie CH, et al. A Psycho-Educational HIV/STI Prevention Intervention for Internally Displaced Women in Leogane, Haiti: Results from a Non-Randomized Cohort Pilot Study. PLoS ONE. 2014;9(2):e89836.
O’Laughlin KN, et al. A cohort study to assess a communication intervention to improve linkage to HIV care in Nakivale Refugee Settlement. Uganda Glob Public Health. 2021;16(12):1848–55.
Adam I. The influence of maternal health education on the place of delivery in conflict settings of Darfur. Sudan Conflict and Health. 2015;9:31.
Adam IF, et al. Relationship between implementing interpersonal communication and mass education campaigns in emergency settings and use of reproductive healthcare services: evidence from Darfur, Sudan. BMJ Open. 2015;5(9):e008285.
Edmond K, et al. Mobile outreach health services for mothers and children in conflict-affected and remote areas: a population-based study from Afghanistan. Arch Dis Child. 2020;105(1):18–25.
Nasir S, et al. Dissemination and implementation of the e-MCHHandbook, UNRWA’s newly released maternal and child health mobile application: a cross-sectional study. BMJ Open. 2020;10(3):e034885.
O’Laughlin KN, et al. Feasibility and acceptability of home-based HIV testing among refugees: a pilot study in Nakivale refugee settlement in southwestern Uganda. BMC Infect Dis. 2018;18(1):332.
Adam I. Evidence from cluster surveys on the association between home-based counseling and use of family planning in conflict-affected Darfur. Int J Gynecol Obstet. 2016;133(2):221–5.
Casey S, et al. Availability of long-acting and permanent family-planning methods leads to increase in use in conflict-affected northern Uganda: Evidence from cross-sectional baseline and endline cluster surveys. Glob Public Health. 2013;8(3):284–97.
Corna F, et al. Supporting maternal mental health of Rohingya refugee women during the perinatal period to promote child health and wellbeing: a field study in Cox’s Bazar. Intervention, the Journal of Mental Health & Psychosocial Support in Conflict Affected Areas. 2019;17(2):160–8.
Glass N, et al. Effectiveness of the Communities Care programme on change in social norms associated with gender-based violence (GBV) with residents in intervention compared with control districts in Mogadishu, Somalia. BMJ Open. 2019;9(3):e023819.
James LE, et al. Development and Testing of a Community-Based Intervention to Address Intimate Partner Violence among Rohingya and Syrian Refugees: A Social Norms-Based Mental Health-Integrated Approach. Int J Environ Res Public Health. 2021;18(21):11674.
Le Roux E, et al. Engaging with faith groups to prevent VAWG in conflict-affected communities: results from two community surveys in the DRC. BMC Int Health Hum Rights. 2020;20(1):27.
Morris CN, et al. When political solutions for acute conflict in Yemen seem distant, demand for reproductive health services is immediate: a programme model for resilient family planning and post-abortion care services. Sex Reprod Health Matters. 2019;27(2):1610279.
Anibueze AU, et al. Impact of counseling visual multimedia on use of family planning methods among displaced Nigerian families. Health Promot Int. 2022;37(3):daac060.
Doocy S, et al. Cash-based assistance and the nutrition status of pregnant and lactating women in the Somalia food crisis: A comparison of two transfer modalities. PLoS ONE. 2020;15(4):e0230989.
Article CAS PubMed PubMed Central Google Scholar
Draiko CV, et al. The effect of umbilical cord cleansing with chlorhexidine gel on neonatal mortality among the community births in South Sudan: a quasi-experimental study. Pan Afr Med J. 2021;38:78.
Edmond KM, et al. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population-based intervention study. BMC Med. 2018;16(1):106.
Edmond KM, et al. Conditional cash transfers to improve use of health facilities by mothers and newborns in conflict affected countries, a prospective population based intervention study from Afghanistan. BMC Pregnancy Childbirth. 2019;19(1):193.
Bakesiima R, et al. Effect of peer counselling on acceptance of modern contraceptives among female refugee adolescents in northern Uganda: A randomised controlled trial. PLoS ONE. 2021;16(9):e0256479.
Greene MC, et al. Evaluation of an integrated intervention to reduce psychological distress and intimate partner violence in refugees: Results from the Nguvu cluster randomized feasibility trial. PLoS ONE. 2021;16(6):e0252982.
Gupta J, et al. Gender norms and economic empowerment intervention to reduce intimate partner violence against women in rural Côte d’Ivoire: a randomized controlled pilot study. BMC Int Health Hum Rights. 2013;13(1):46.
Hossain M, et al. Working with men to prevent intimate partner violence in a conflict-affected setting: a pilot cluster randomized controlled trial in rural Côte d’Ivoire. BMC Public Health. 2014;14(1):339.
Vaillant J, et al. Engaging men to transform inequitable gender attitudes and prevent intimate partner violence: a cluster randomised controlled trial in North and South Kivu, Democratic Republic of Congo. BMJ Glob Health. 2020;5(5):e002223.
Thommesen T, et al. “The midwife helped me … otherwise I could have died”: women’s experience of professional midwifery services in rural Afghanistan - a qualitative study in the provinces Kunar and Laghman. BMC Pregnancy Childbirth. 2020;20(1):140.
Awasom-Fru A, et al. Doctors’ experiences providing sexual and reproductive health care at Catholic Hospitals in the conflict-affected North-West region of Cameroon: a qualitative study. Reprod Health. 2022;19(1):126.
Kabakian-Khasholian T, Makhoul J, Ghusayni A. “A person who does not have money does not enter”: a qualitative study on refugee women’s experiences of respectful maternity care. BMC Pregnancy and Childbirth. 2022;22(1):748.
Lilleston P, et al. Evaluation of a mobile approach to gender-based violence service delivery among Syrian refugees in Lebanon. Health Policy Plan. 2018;33(7):767–76.
Mugo NS, et al. Barriers Faced by the Health Workers to Deliver Maternal Care Services and Their Perceptions of the Factors Preventing Their Clients from Receiving the Services: A Qualitative Study in South Sudan. Matern Child Health J. 2018;22(11):1598–606.
Persson M, et al. A qualitative study on health care providers’ experiences of providing comprehensive abortion care in Cox’s Bazar, Bangladesh. Conflict and Health. 2021;15(1):6.
Phanwichatkul T, et al. The perceptions and practices of Thai health professionals providing maternity care for migrant Burmese women: An ethnographic study. Women Birth. 2022;35(4):e356–68.
Sarker M, et al. Effective maternal, newborn and child health programming among Rohingya refugees in Cox’s Bazar, Bangladesh: Implementation challenges and potential solutions. PLoS ONE. 2020;15(3):e0230732.
Tousaw E, et al. “Without this program, women can lose their lives”: migrant women’s experiences with the Safe Abortion Referral Programme in Chiang Mai. Thailand Reprod Health Matters. 2017;25(51):58–68.
Tousaw E, et al. “It is just like having a period with back pain”: exploring women’s experiences with community-based distribution of misoprostol for early abortion on the Thailand-Burma border. Contraception. 2018;97(2):122–9.
West L, et al. Factors in use of family planning services by Syrian women in a refugee camp in Jordan. Journal of Family Planning and Reproductive Health Care. 2017;43(2):96–102.
O’Connell KA, et al. Meeting the Sexual and Reproductive Health Needs of Internally Displaced Persons in Ethiopia’s Somali Region: A Qualitative Process Evaluation. Glob Health Sci Pract. 2022;10(5):e2100818.
Orya E, et al. Strengthening close to community provision of maternal health services in fragile settings: an exploration of the changing roles of TBAs in Sierra Leone and Somaliland. BMC Health Serv Res. 2017;17(1):460.
Perera SM, et al. Barriers to seeking post-abortion care in Paktika Province, Afghanistan: a qualitative study of clients and community members. BMC Womens Health. 2021;21(1):390.
Tanabe M, et al. Piloting community-based medical care for survivors of sexual assault in conflict-affected Karen State of eastern Burma. Confl Heal. 2013;7(1):12.
Tran NT, et al. Clinical outreach refresher trainings in crisis settings (S-CORT): clinical management of sexual violence survivors and manual vacuum aspiration in Burkina Faso, Nepal, and South Sudan. Reprod Health Matters. 2017;25(51):103–13.
Yankah E, et al. Feasibility and acceptability of mobile phone platforms to deliver interventions to address gender-based violence among Syrian adolescent girls and young women in Izmir. Turkey Vulnerable Children and Youth Studies. 2020;15(2):133–43.
Muuo S, et al. Barriers and facilitators to care-seeking among survivors of gender-based violence in the Dadaab refugee complex. Sex Reprod Health Matters. 2020;28(1):1722404.
Amsalu R, et al. Essential newborn care practice at four primary health facilities in conflict affected areas of Bossaso, Somalia: a cross-sectional study. Conflict and Health. 2019;13(13):27.
Myers A, et al. Facilitators and barriers in implementing the Minimum Initial Services Package (MISP) for reproductive health in Nepal post-earthquake. Conflict and Health. 2018;12:35.
Santo L.C.d, et al. Feasibility and acceptability of a video library tool to support community health worker counseling in rural Afghan districts: a cross-sectional assessment. Conflict and Health. 2020;14:56.
Sami S, et al. Understanding health systems to improve community and facility level newborn care among displaced populations in South Sudan: a mixed methods case study. BMC Pregnancy Childbirth. 2018;18(1):325.
Amsalu R, et al. Effectiveness of clinical training on improving essential newborn care practices in Bossaso, Somalia: a pre and postintervention study. BMC Pediatr. 2020;20(1):215.
Berg M, Mwambali SN, Bogren M. Implementation of a three-pillar training intervention to improve maternal and neonatal healthcare in the Democratic Republic Of Congo: a process evaluation study in an urban health zone. Glob Health Action. 2022;15(1):2019391.
Castillo M, et al. Turning Disaster into an Opportunity for Quality Improvement in Essential Intrapartum and Newborn Care Services in the Philippines: Pre- to Posttraining Assessments. Biomed Res Int. 2016;2016:1–9.
Foster AM, Arnott G, Hobstetter M. Community-based distribution of misoprostol for early abortion: evaluation of a program along the Thailand-Burma border. Contraception. 2017;96(4):242–7.
Guan TH, et al. Implementation of a neonatal hepatitis B immunization program in rural Karenni State, Myanmar: A mixed-methods study. PLoS ONE. 2021;16(12):e0261470.
Logie, C.H., et al., Mixed-methods findings from the Ngutulu Kagwero (agents of change) participatory comic pilot study on post-rape clinical care and sexual violence prevention with refugee youth in a humanitarian setting in Uganda. Global Public Health, 2022((Logie C.H., [email protected]) Factor-Inwentash Faculty of Social Work, University of Toronto, Toronto, Canada(Logie C.H., [email protected]) Women’s College Research Institute, Women’s College Hospital, Toronto, Canada(Logie C.H., carmen.l).
Sami S, et al. “You have to take action”: changing knowledge and attitudes towards newborn care practices during crisis in South Sudan. Reprod Health Matters. 2017;25(51):124–39.
Smith JR, et al. Clinical care for sexual assault survivors multimedia training: a mixed-methods study of effect on healthcare providers’ attitudes, knowledge, confidence, and practice in humanitarian settings. Confl Heal. 2013;7(1):14.
Stevens A, et al. Folate supplementation to prevent birth abnormalities: evaluating a community-based participatory action plan for refugees and migrant workers on the Thailand-Myanmar border. Public Health. 2018;161:83–9.
Nguyen Toan T, et al. Strengthening healthcare providers’ capacity for safe abortion and postabortion care services in humanitarian settings: lessons learned from the clinical outreach refresher training model (S-CORT) in Uganda, Nigeria, and the Democratic Republic of Congo. Conflict and Health. 2021;15(1):20.
Castle S, et al. Successful programmatic approaches to facilitating IUD uptake: CARE’s experience in DRC. BMC Womens Health. 2019;19(1):104.
Deitch J, et al. “They Love Their Patients”: Client Perceptions of Quality of Postabortion Care in North and South Kivu, the Democratic Republic of the Congo. Global health, science and practice. 2019;7(Suppl 2):S285–98.
Ferreyra C, et al. Evaluation of a community-based HIV test and start program in a conflict affected rural area of Yambio County, South Sudan. PLoS ONE. 2021;16(7):e0254331.
Ho LS, Wheeler E. Using Program Data to Improve Access to Family Planning and Enhance the Method Mix in Conflict-Affected Areas of the Democratic Republic of the Congo. Glob Health Sci Pract. 2018;6(1):161–77.
Klabbers RE, et al. Health Worker Perspectives on Barriers and Facilitators of Assisted Partner Notification for HIV for Refugees and Ugandan Nationals: A Mixed Methods Study in West Nile Uganda. AIDS Behav. 2021;25(10):3206–22.
Turner C, et al. Neonatal Intensive Care in a Karen Refugee Camp: A 4 Year Descriptive Study. PLoS ONE. 2013;8(8):e72721.
Vries Id, et al. Key lessons from a mixed-method evaluation of a postnatal home visit programme in the humanitarian setting of Gaza. Eastern Mediterr Health J. 2021;27(6):546–52.
Bolan NE, et al. mLearning in the Democratic Republic of the Congo: A Mixed-Methods Feasibility and Pilot Cluster Randomized Trial Using the Safe Delivery App. Global health, science and practice. 2018;6(4):693–710.
Khan MN, et al. Evaluating feasibility and acceptability of a local psycho-educational intervention for pregnant women with common mental problems affected by armed conflict in Swat, Pakistan: A parallel randomized controlled feasibility trial. Int J Soc Psychiatry. 2017;63(8):724–35.
Hynes M, et al. Using a quality improvement approach to improve maternal and neonatal care in North Kivu, Democratic Republic of Congo. Reprod Health Matters. 2017;25(51):140–50.
Gibbs A, et al. The impacts of combined social and economic empowerment training on intimate partner violence, depression, gender norms and livelihoods among women: an individually randomised controlled trial and qualitative study in Afghanistan. BMJ Glob Health. 2020;5(3):e001946.
Damschroder L, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science: IS; 2009.
Moore GF, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258.
Proctor E, et al. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm Policy Ment Health. 2011;38(2):65–76.
Damschroder LJ, et al. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75.
Damschroder LJ, et al. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): the CFIR Outcomes Addendum. Implement Sci. 2022;17(1):7.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a Conceptual Model of Evidence-Based Practice Implementation in Public Service Sectors. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38(1):4–23.
Feldstein AC, Glasgow RE. A Practical, Robust Implementation and Sustainability Model (PRISM) for Integrating Research Findings into Practice. The Joint Commission Journal on Quality and Patient Safety. 2008;34(4):228–43.
OCHA. Global Humanitarian Overview 2023. 2022 [cited 2023 8/3/2023]; Available from: https://humanitarianaction.info/node/13073/article/glance-0 . Accessed 8 Mar 2023.
Kobeissi L, et al. Setting research priorities for sexual, reproductive, maternal, newborn, child and adolescent health in humanitarian settings. Confl Heal. 2021;15(1):16.
Save the, C., et al. Roadmap to Accelerate Progress for Every Newborn in Humanitarian Settings 2020 – 2024. 2020. p. 52.
Inter-Agency Working Group on Reproductive Health in, C. Inter-Agency Field Manual on Reproductive Health in Humanitarian Settings. 2018.
Download references
Acknowledgements
Not applicable.
The authors received no funding for this study.
Author information
Authors and affiliations.
Duke University School of Medicine, 40 Duke Medicine Circle, Durham, NC, 27710, USA
Alexandra Norton
Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St, Baltimore, MD, 21205, USA
Hannah Tappis
You can also search for this author in PubMed Google Scholar
Contributions
AN and HT designed the scoping review. AN conducted the literature search. AN and HT screened records for inclusion. AN extracted data from included studies. Both authors contributed to synthesis of results. AN drafted the manuscript and both authors contributed to editorial changes.
Corresponding author
Correspondence to Alexandra Norton .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. Literature search terms: Exact search terms used in literature search, with additional detail on the methodology to determine search terms and definitions used for each component of the search
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Norton, A., Tappis, H. Sexual and reproductive health implementation research in humanitarian contexts: a scoping review. Reprod Health 21 , 64 (2024). https://doi.org/10.1186/s12978-024-01793-2
Download citation
Received : 06 November 2023
Accepted : 12 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12978-024-01793-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Humanitarian settings
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
International Journal of Quantitative and Qualitative Research Methods is run by the European Centre for Research, Training and Development, United Kingdom. The journal publishes outstanding academic, theoretical and methodological articles relating to quantitative, qualitative and research in professional and service settings. The journal covers issues addressed by researchers within academic ...
International Journal of Research 8(2):71-87; DOI ... The main aim of this paper is to identify the differences between quantitative and qualitative research methods and to evaluate the bright ...
The International Journal of Qualitative Methods is the peer-reviewed interdisciplinary open access journal of the International Institute for Qualitative Methodology (IIQM) at the University of Alberta, Canada. The journal, established in 2002, is an eclectic international forum for insights, innovations and advances in methods and study designs using qualitative or mixed methods research.
The purpose of this paper is to explain the difference between quantitative research and [qualitative] quantification. The description of the quantification method is based on our own experiences ...
EAJ is an international platform designed for researchers to publish their research. European - American Journals are run by the European Centre for Research, Training and Development (ECRTD), UK.The Centre consists of both researchers in specific fields and multidisciplinary researchers of long-standing and emerging knowledge from around the globe.
International Journal of Quantitative and Qualitative Research Methods, Vol.9, No.3, pp.40-60, 2021 ... survey research, questionnaire survey, sampling ... : Suggested Citation. Bihu, Reuben, Questionnaire Survey Methodology in Educational and Social Science Studies ( 2021). International Journal of Quantitative and Qualitative Research Methods ...
How to combine qualitative with quantitative research? Qualitative methods can be combined with other methods in multi- or mixed methods designs, which "[employ] two or more different methods [ ... Quality of Life Research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2015; 24 (5):1057-1067 ...
Table of contents for International Journal of Qualitative Methods, 20, , Jan 01, ... The COVID-19 pandemic has forced both quantitative and qualitative health researchers to adapt and strategize data collection strategies without causing any harm to the participants or researchers. ... Qualitative research methods have been predominantly used ...
URL http://www.eajournals.org/journals/international-journal-of-quantitative-and-qualitative-research-methods-ijqqrm/. URL http://www.eajournals.org/journals ...
International Journal of Quantitative and Qualitative Research Methods 2021, Vol.9, No.2, pp.1-15 15 Pages Posted: 1 Jun 2021 See all articles by Doreen Said Pace
Significance of Qualitative Research. The qualitative method of inquiry examines the 'how' and 'why' of decision making, rather than the 'when,' 'what,' and 'where.'[] Unlike quantitative methods, the objective of qualitative inquiry is to explore, narrate, and explain the phenomena and make sense of the complex reality.Health interventions, explanatory health models, and medical-social ...
The interaction of quantitative and qualitative methodology in the mixed methods research (MMR) is analysed in a context of distinctions of the meanings between the terms typically used for description, combination, and integration. The interaction in the phases that precede the results, and their interpretation is considered.
International Journal of Quantitative and Qualitative Research Methods, Number of pages: 20 Posted: 31 Mar 2021. Soleman Abu-Bader and Tiffanie Victoria Jones. Howard University - School of Social Work and affiliation not provided to SSRN. Downloads 8,166 (1,494) View PDF. Download. Feedback. Total downloads of all papers by Soleman Abu-Bader.
Generalization, which is an act of reasoning that involves drawing broad inferences from particular observations, is widely-acknowledged as a quality standard in quantitative research, but is more controversial in qualitative research. The goal of most qualitative studies is not to generalize but rather to provide a rich, contextualized ...
Furthermore, the integration of both qualitative and quantitative methods provides new insights to improve and address the complex and multi-faceted issues of primary care ... Authors are thankful to the International Journal of Multiple Research Approaches for providing the permission to reuse from our previous publication Tables 1 and ...
Objectives: It has been argued that mixed methods research can be useful in nursing and health science because of the complexity of the phenomena studied. However, the integration of qualitative and quantitative approaches continues to be one of much debate and there is a need for a rigorous framework for designing and interpreting mixed methods research.
International Journal of Research p-ISSN: 2348-6848 e-ISSN: 2348-795X Volume 08 Issue 02 ... Quantitative and qualitative methods are the engine behind evidence-based outcomes. For decades, one of the
Introduction. Mixed-methods impact evaluation (MMIE) is a route to identifying planned and unplanned outcomes of interventions, causal mechanisms underlying these effects, and the conditions under which these arise to assist both organisational learning and political accountability (Bamberger, Rao, and Woolcock Citation 2010).The general case for combining quantitative and qualitative methods ...
This research holds significance for the fields of social media and communication studies through its comprehensive evaluation of Twitter's quoting encouragement policy enacted during the 2020 U.S. presidential election. In addressing a notable gap in the literature, this study introduces a framework that assesses both the quantitative and qualitative effects of specific platform-wide policy ...
International Journal of Information Management 53: 102118. Google Scholar. Al-Jaradat OM (2021) Research data management (RDM) in Jordanian public university libraries: Present status, challenges and future perspectives. ... (2014), Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 4th edn. Thousand Oaks, CA: SAGE ...
ISSN 2056-3620 (Print) | International journal of quantitative and qualitative research methods Skip to main content. Leave this field blank . Log In; Automatic login IP; PUBLISHERS' AREA DISCOVER ISSN ... International journal of quantitative and qualitative research methods (Print) Identifiers. ISSN : 2056-3620. Linking ISSN (ISSN-L): 2056-3620.
Purpose The purpose of this systematic review is to better understand access to, acceptance of and adherence to cancer prehabilitation. Methods MEDLINE, CINAHL, PsychINFO, Embase, Physiotherapy Evidence Database, ProQuest Medical Library, Cochrane Library, Web of Science and grey literature were systematically searched for quantitative, qualitative and mixed-methods studies published in ...
This research aims to promote diversity and inclusion among higher education students by examining the integration of technology into project-based learning (PBL) for English as a foreign language (EFL) teacher candidates. Based on a mixed-methods approach and convenience sampling (n = 84 participants), this study involved pre-service teachers who collaboratively employed several authoring ...
Quantitative research objectives can be to establish the incidence or prevalence of a health problem; the health personnel degree of adherence to a new intervention; or, the users' level of satisfaction with a service. Qualitative research aims at understanding what exists from social actors' perspectives.
Methodologically, the study used both qualitative and quantitative methods. The data was collected through interviews, and empirical verification was done through a questionnaire. The researcher interviewed the country's employees that belong to either the economic division or supply chain.
International Journal of Quantitative and Qualitative Research Methods Vol.6, No.1, pp.27-38, February 2018 ___Published by European Centre for Research Training and Development UK (www.eajournals.org) 28 ISSN 2056-3620(Print), ISSN 2056-3639(Online) One more important aspect is the population along which it is intended to be measured. This
Abstract. This paper aims to focus on the emerging practical application of mediational analysis in social science research practice. Objectives: The paper introduces simple mediation analysis to social science researchers discusses two statistical methods used to examine the effect of mediating variables on the relationship between the independent and dependent variables. These are the Sobel ...
The main objective of Methodology of Humanities and Social Sciences (MSSH) is to provide an intellectual platform for national and international researchers to discuss their most recent findings related to philosophical foundations and methodology of humanities and social sciences. By doing so, the Journal hopes to improve the status of the field in Iran and in the world and to find solutions ...
Background Meeting the health needs of crisis-affected populations is a growing challenge, with 339 million people globally in need of humanitarian assistance in 2023. Given one in four people living in humanitarian contexts are women and girls of reproductive age, sexual and reproductive health care is considered as essential health service and minimum standard for humanitarian response ...