2.1 Why is Research Important
Learning objectives.
By the end of this section, you will be able to:
- Explain how scientific research addresses questions about behavior
- Discuss how scientific research guides public policy
- Appreciate how scientific research can be important in making personal decisions
Scientific research is a critical tool for successfully navigating our complex world. Without it, we would be forced to rely solely on intuition, other people’s authority, and blind luck. While many of us feel confident in our abilities to decipher and interact with the world around us, history is filled with examples of how very wrong we can be when we fail to recognize the need for evidence in supporting claims. At various times in history, we would have been certain that the sun revolved around a flat earth, that the earth’s continents did not move, and that mental illness was caused by possession (figure below). It is through systematic scientific research that we divest ourselves of our preconceived notions and superstitions and gain an objective understanding of ourselves and our world.

Some of our ancestors, across the work and over the centuries, believed that trephination – the practice of making a hole in the skull, as shown here – allowed evil spirits to leave the body, thus curing mental illness and other diseases (credit” “taiproject/Flickr)
The goal of all scientists is to better understand the world around them. Psychologists focus their attention on understanding behavior, as well as the cognitive (mental) and physiological (body) processes that underlie behavior. In contrast to other methods that people use to understand the behavior of others, such as intuition and personal experience, the hallmark of scientific research is that there is evidence to support a claim. Scientific knowledge is empirical : It is grounded in objective, tangible evidence that can be observed time and time again, regardless of who is observing.
We can easily observe the behavior of others around us. For example, if someone is crying, we can observe that behavior. However, the reason for the behavior is more difficult to determine. Is the person crying due to being sad, in pain, or happy? Sometimes, asking about the underlying cognitions is as easy as asking the subject directly: “Why are you crying?” However, there are situations in which an individual is either uncomfortable or unwilling to answer the question honestly, or is incapable of answering. For example, infants would not be able to explain why they are crying. In other situations, it may be hard to identify exactly why you feel the way you do. Think about times when you suddenly feel annoyed after a long day. There may be a specific trigger for your annoyance (a loud noise), or you may be tired, hungry, stressed, or all of the above. Human behavior is often a complicated mix of a variety of factors. In such circumstances, the psychologist must be creative in finding ways to better understand behavior. This chapter explores how scientific knowledge is generated, and how important that knowledge is in forming decisions in our personal lives and in the public domain.

USE OF RESEARCH INFORMATION
Trying to determine which theories are and are not accepted by the scientific community can be difficult, especially in an area of research as broad as psychology. More than ever before, we have an incredible amount of information at our fingertips, and a simple internet search on any given research topic might result in a number of contradictory studies. In these cases, we are witnessing the scientific community going through the process of coming to an agreement, and it could be quite some time before a consensus emerges. In other cases, rapidly developing technology is improving our ability to measure things, and changing our earlier understanding of how the mind works.
In the meantime, we should strive to think critically about the information we encounter by exercising a degree of healthy skepticism. When someone makes a claim, we should examine the claim from a number of different perspectives: what is the expertise of the person making the claim, what might they gain if the claim is valid, does the claim seem justified given the evidence, and what do other researchers think of the claim? Science is always changing and new evidence is alwaus coming to light, thus this dash of skepticism should be applied to all research you interact with from now on. Yes, that includes the research presented in this textbook.
Evaluation of research findings can have widespread impact. Imagine that you have been elected as the governor of your state. One of your responsibilities is to manage the state budget and determine how to best spend your constituents’ tax dollars. As the new governor, you need to decide whether to continue funding the D.A.R.E. (Drug Abuse Resistance Education) program in public schools (figure below). This program typically involves police officers coming into the classroom to educate students about the dangers of becoming involved with alcohol and other drugs. According to the D.A.R.E. website (www.dare.org), this program has been very popular since its inception in 1983, and it is currently operating in 75% of school districts in the United States and in more than 40 countries worldwide. Sounds like an easy decision, right? However, on closer review, you discover that the vast majority of research into this program consistently suggests that participation has little, if any, effect on whether or not someone uses alcohol or other drugs (Clayton, Cattarello, & Johnstone, 1996; Ennett, Tobler, Ringwalt, & Flewelling, 1994; Lynam et al., 1999; Ringwalt, Ennett, & Holt, 1991). If you are committed to being a good steward of taxpayer money, will you fund this particular program, or will you try to find other programs that research has consistently demonstrated to be effective?

The D.A.R.E. program continues to be popular in schools around the world despite research suggesting that it is ineffective.
It is not just politicians who can benefit from using research in guiding their decisions. We all might look to research from time to time when making decisions in our lives. Imagine you just found out that a close friend has breast cancer or that one of your young relatives has recently been diagnosed with autism. In either case, you want to know which treatment options are most successful with the fewest side effects. How would you find that out? You would probably talk with a doctor or psychologist and personally review the research that has been done on various treatment options—always with a critical eye to ensure that you are as informed as possible.
In the end, research is what makes the difference between facts and opinions. Facts are observable realities, and opinions are personal judgments, conclusions, or attitudes that may or may not be accurate. In the scientific community, facts can be established only using evidence collected through empirical research.
THE PROCESS OF SCIENTIFIC RESEARCH
Scientific knowledge is advanced through a process known as the scientific method . Basically, ideas (in the form of theories and hypotheses) are tested against the real world (in the form of empirical observations), and those observations lead to more ideas that are tested against the real world, and so on. In this sense, the scientific process is circular. We continually test and revise theories based on new evidence.
Two types of reasoning are used to make decisions within this model: Deductive and inductive. In deductive reasoning, ideas are tested against the empirical world. Think about a detective looking for clues and evidence to test their “hunch” about whodunit. In contrast, in inductive reasoning, empirical observations lead to new ideas. In other words, inductive reasoning involves gathering facts to create or refine a theory, rather than testing the theory by gathering facts (figure below). These processes are inseparable, like inhaling and exhaling, but different research approaches place different emphasis on the deductive and inductive aspects.

Psychological research relies on both inductive and deductive reasoning.
In the scientific context, deductive reasoning begins with a generalization—one hypothesis—that is then used to reach logical conclusions about the real world. If the hypothesis is correct, then the logical conclusions reached through deductive reasoning should also be correct. A deductive reasoning argument might go something like this: All living things require energy to survive (this would be your hypothesis). Ducks are living things. Therefore, ducks require energy to survive (logical conclusion). In this example, the hypothesis is correct; therefore, the conclusion is correct as well. Sometimes, however, an incorrect hypothesis may lead to a logical but incorrect conclusion. Consider the famous example from Greek philosophy. A philosopher decided that human beings were “featherless bipeds”. Using deductive reasoning, all two-legged creatures without feathers must be human, right? Diogenes the Cynic (named because he was, well, a cynic) burst into the room with a freshly plucked chicken from the market and held it up exclaiming “Behold! I have brought you a man!”
Deductive reasoning starts with a generalization that is tested against real-world observations; however, inductive reasoning moves in the opposite direction. Inductive reasoning uses empirical observations to construct broad generalizations. Unlike deductive reasoning, conclusions drawn from inductive reasoning may or may not be correct, regardless of the observations on which they are based. For example, you might be a biologist attempting to classify animals into groups. You notice that quite a large portion of animals are furry and produce milk for their young (cats, dogs, squirrels, horses, hippos, etc). Therefore, you might conclude that all mammals (the name you have chosen for this grouping) have hair and produce milk. This seems like a pretty great hypothesis that you could test with deductive reasoning. You go out an look at a whole bunch of things and stumble on an exception: The coconut. Coconuts have hair and produce milk, but they don’t “fit” your idea of what a mammal is. So, using inductive reasoning given the new evidence, you adjust your theory again for an other round of data collection. Inductive and deductive reasoning work in tandem to help build and improve scientific theories over time.
We’ve stated that theories and hypotheses are ideas, but what sort of ideas are they, exactly? A theory is a well-developed set of ideas that propose an explanation for observed phenomena. Theories are repeatedly checked against the world, but they tend to be too complex to be tested all at once. Instead, researchers create hypotheses to test specific aspects of a theory.
A hypothesis is a testable prediction about how the world will behave if our theory is correct, and it is often worded as an if-then statement (e.g., if I study all night, I will get a passing grade on the test). The hypothesis is extremely important because it bridges the gap between the realm of ideas and the real world. As specific hypotheses are tested, theories are modified and refined to reflect and incorporate the result of these tests (figure below).

The scientific method of research includes proposing hypotheses, conducting research, and creating or modifying theories based on results.
To see how this process works, let’s consider a specific theory and a hypothesis that might be generated from that theory. As you’ll learn in a later chapter, the James-Lange theory of emotion asserts that emotional experience relies on the physiological arousal associated with the emotional state. If you walked out of your home and discovered a very aggressive snake waiting on your doorstep, your heart would begin to race and your stomach churn. According to the James-Lange theory, these physiological changes would result in your feeling of fear. A hypothesis that could be derived from this theory might be that a person who is unaware of the physiological arousal that the sight of the snake elicits will not feel fear.
A scientific hypothesis is also falsifiable, or capable of being shown to be incorrect. Recall from the introductory chapter that Sigmund Freud had lots of interesting ideas to explain various human behaviors (figure below). However, a major criticism of Freud’s theories is that many of his ideas are not falsifiable. The essential characteristic of Freud’s building blocks of personality, the id, ego, and superego, is that they are unconscious, and therefore people can’t observe them. Because they cannot be observed or tested in any way, it is impossible to say that they don’t exist, so they cannot be considered scientific theories. Despite this, Freud’s theories are widely taught in introductory psychology texts because of their historical significance for personality psychology and psychotherapy, and these remain the root of all modern forms of therapy.

Many of the specifics of (a) Freud’s theories, such ad (b) his division on the mind into the id, ego, and superego, have fallen out of favor in recent decades because they are not falsifiable (i.e., cannot be verified through scientific investigation). In broader strokes, his views set the stage for much psychological thinking today, such as the idea that some psychological process occur at the level of the unconscious.
In contrast, the James-Lange theory does generate falsifiable hypotheses, such as the one described above. Some individuals who suffer significant injuries to their spinal columns are unable to feel the bodily changes that often accompany emotional experiences. Therefore, we could test the hypothesis by determining how emotional experiences differ between individuals who have the ability to detect these changes in their physiological arousal and those who do not. In fact, this research has been conducted and while the emotional experiences of people deprived of an awareness of their physiological arousal may be less intense, they still experience emotion (Chwalisz, Diener, & Gallagher, 1988).
Scientific research’s dependence on falsifiability allows for great confidence in the information that it produces. Typically, by the time information is accepted by the scientific community, it has been tested repeatedly.
Scientists are engaged in explaining and understanding how the world around them works, and they are able to do so by coming up with theories that generate hypotheses that are testable and falsifiable. Theories that stand up to their tests are retained and refined, while those that do not are discarded or modified. IHaving good information generated from research aids in making wise decisions both in public policy and in our personal lives.
Review Questions:
1. Scientific hypotheses are ________ and falsifiable.
a. observable
b. original
c. provable
d. testable
2. ________ are defined as observable realities.
a. behaviors
c. opinions
d. theories
3. Scientific knowledge is ________.
a. intuitive
b. empirical
c. permanent
d. subjective
4. A major criticism of Freud’s early theories involves the fact that his theories ________.
a. were too limited in scope
b. were too outrageous
c. were too broad
d. were not testable
Critical Thinking Questions:
1. In this section, the D.A.R.E. program was described as an incredibly popular program in schools across the United States despite the fact that research consistently suggests that this program is largely ineffective. How might one explain this discrepancy?
2. The scientific method is often described as self-correcting and cyclical. Briefly describe your understanding of the scientific method with regard to these concepts.
Personal Application Questions:
1. Healthcare professionals cite an enormous number of health problems related to obesity, and many people have an understandable desire to attain a healthy weight. There are many diet programs, services, and products on the market to aid those who wish to lose weight. If a close friend was considering purchasing or participating in one of these products, programs, or services, how would you make sure your friend was fully aware of the potential consequences of this decision? What sort of information would you want to review before making such an investment or lifestyle change yourself?
deductive reasoning
falsifiable
hypothesis: (plural
inductive reasoning
Answers to Exercises
Review Questions:
1. There is probably tremendous political pressure to appear to be hard on drugs. Therefore, even though D.A.R.E. might be ineffective, it is a well-known program with which voters are familiar.
2. This cyclical, self-correcting process is primarily a function of the empirical nature of science. Theories are generated as explanations of real-world phenomena. From theories, specific hypotheses are developed and tested. As a function of this testing, theories will be revisited and modified or refined to generate new hypotheses that are again tested. This cyclical process ultimately allows for more and more precise (and presumably accurate) information to be collected.
deductive reasoning: results are predicted based on a general premise
empirical: grounded in objective, tangible evidence that can be observed time and time again, regardless of who is observing
fact: objective and verifiable observation, established using evidence collected through empirical research
falsifiable: able to be disproven by experimental results
hypothesis: (plural: hypotheses) tentative and testable statement about the relationship between two or more variables
inductive reasoning: conclusions are drawn from observations
opinion: personal judgments, conclusions, or attitudes that may or may not be accurate
theory: well-developed set of ideas that propose an explanation for observed phenomena

Share This Book
- Increase Font Size

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Chapter 1: The Science of Psychology
Science and Clinical Practice
Learning Objectives
- Define the clinical practice of psychology and distinguish it from the science of psychology.
- Explain how science is relevant to clinical practice.
- Define the concept of an empirically supported treatment and give some examples.
Psychology is the scientific study of behaviour and mental processes. But it is also the application of scientific research to “help people, organizations, and communities function better” (American Psychological Association, 2011) [1] . By far the most common and widely known application is the clinical practice of psychology —the diagnosis and treatment of psychological disorders and related problems. Let us use the term clinical practice broadly to refer to the activities of clinical and counseling psychologists, school psychologists, marriage and family therapists, licensed clinical social workers, and others who work with people individually or in small groups to identify and help address their psychological problems. It is important to consider the relationship between scientific research and clinical practice because many students are especially interested in clinical practice, perhaps even as a career.
The main point is that psychological disorders and other behavioural problems are part of the natural world. This means that questions about their nature, causes, and consequences are empirically testable and therefore subject to scientific study. As with other questions about human behaviour, we cannot rely on our intuition or common sense for detailed and accurate answers. Consider, for example, that dozens of popular books and thousands of websites claim that adult children of alcoholics have a distinct personality profile, including low self-esteem, feelings of powerlessness, and difficulties with intimacy. Although this sounds plausible, scientific research has demonstrated that adult children of alcoholics are no more likely to have these problems than anybody else (Lilienfeld et al., 2010) [2] . Similarly, questions about whether a particular psychotherapy is effective are empirically testable questions that can be answered by scientific research. If a new psychotherapy is an effective treatment for depression, then systematic observation should reveal that depressed people who receive this psychotherapy improve more than a similar group of depressed people who do not receive this psychotherapy (or who receive some alternative treatment). Treatments that have been shown to work in this way are called empirically supported treatments .
Empirically Supported Treatments
An empirically supported treatment is one that has been studied scientifically and shown to result in greater improvement than no treatment, a placebo, or some alternative treatment. These include many forms of psychotherapy, which can be as effective as standard drug therapies. Among the forms of psychotherapy with strong empirical support are the following:
- Cognitive behavioural therapy. For depression, panic disorder, bulimia nervosa, and post-traumatic stress disorder.
- Exposure therapy. For post-traumatic stress disorder.
- Behavioural therapy. For depression.
- Behavioural couples therapy. For alcoholism and substance abuse.
- Exposure therapy with response prevention. For obsessive-compulsive disorder.
- Family therapy. For schizophrenia.
For a more complete list, see the following website, which is maintained by Division 12 of the American Psychological Association, the Society for Clinical Psychology: Evidence-based practice in psychology .
Many in the clinical psychology community have argued that their field has not paid enough attention to scientific research—for example, by failing to use empirically supported treatments—and have suggested a variety of changes in the way clinicians are trained and treatments are evaluated and put into practice. Others believe that these claims are exaggerated and the suggested changes are unnecessary (Norcross, Beutler, & Levant, 2005) [3] . On both sides of the debate, however, there is agreement that a scientific approach to clinical psychology is essential if the goal is to diagnose and treat psychological problems based on detailed and accurate knowledge about those problems and the most effective treatments for them. So not only is it important for scientific research in clinical psychology to continue, but it is also important for clinicians who never conduct a scientific study themselves to be scientifically literate so that they can read and evaluate new research and make treatment decisions based on the best available evidence.
Key Takeaways
- The clinical practice of psychology—the diagnosis and treatment of psychological problems—is one important application of the scientific discipline of psychology.
- Scientific research is relevant to clinical practice because it provides detailed and accurate knowledge about psychological problems and establishes whether treatments are effective.
- a potential client of the clinician
- a judge who must decide whether to allow the clinician to testify as an expert witness in a child abuse case
- an insurance company representative who must decide whether to reimburse the clinician for his or her services
- Practice: Create a short list of questions that a client could ask a clinician to determine whether he or she pays sufficient attention to scientific research.
- American Psychological Association. (2011). About APA . Retrieved from http://www.apa.org/about ↵
- Lilienfeld, S. O., Lynn, S. J., Ruscio, J., & Beyerstein, B. L. (2010). 50 great myths of popular psychology . Malden, MA: Wiley-Blackwell. ↵
- Norcross, J. C., Beutler, L. E., & Levant, R. F. (Eds.). (2005). Evidence-based practices in mental health: Debate and dialogue on the fundamental questions . Washington, DC: American Psychological Association. ↵
The diagnosis and treatment of psychological disorders and related problems.
Treatments that have been shown to work through systematic observation.
Research Methods in Psychology - 2nd Canadian Edition Copyright © 2015 by Paul C. Price, Rajiv Jhangiani, & I-Chant A. Chiang is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
Clinical Psychology Research
Clinical psychology research is as important to the nation’s health and well being as medical research. In the same way that medical scientists work to understand the prevention, genesis, and spread of various genetic and infectious diseases, scientists conduct rigorous psychological research studies to understand, prevent, and treat the human condition as it applies psychologically to individuals, couples, families, cultures, and diverse communities.
Empirical results gathered from psychological research studies guide practitioners in developing effective interventions and techniques that clinical psychologists employ – proven, reliable results that improve lives, mend troubled relationships, manage addictions, and help manage and treat a variety of other mental health issues. Clinical psychology by definition marries science with practical knowledge, integrates the two, and produces a field that encourages a robust, ongoing process of scientific discovery and clinical application.
Trained at how to evaluate this large body of research, clinical psychology students continue to make significant professional contributions to the field even after graduation, staying current and up-to-date with psychological research taking place at universities and research labs across the world. Some decide to stay in research, investigating new ways to understand the human mind, and developing solutions to enrich the lives of all others.
Research in the area of clinical psychology is vast, containing hundreds if not thousands of topics. However, most of these research studies generally fall within one of three main areas integral to clinical psychology:
A large part of a clinical psychologist’s job, and therefore clinical psychology research, involves assessment – or developing valid and reliable tests. Assessments take the form of written tests, such as intelligence and achievement tests, vocational tests, and other tests designed to measure aptitude and skill levels for specific jobs, careers, interests, and personality types.
Clinical psychologists also interview individuals, review their medical records, and conduct clinical observations as part of the assessment process. A comprehensive assessment approach ensures that psychologists apply the most effective and appropriate psychological treatments and interventions.
In addition, assessment research in clinical psychology also involves developing valid and reliable ways to measure the outcome of specific treatments and interventions. Michael C. Roberts and Stephen S. Hardi state in their article, “Research Methodology and Clinical Psychology: An Overview,” that improvements in therapy and psychotherapeutic effects rest on targeted research informed by scientific methodologies.
“Measurement of treatment procedures, treatment integrity, behavioral changes, functional performance, objective measurements, perceptions of change, and satisfaction from a variety of sources, follow-up assessment, etc., are needed to establish the ‘scientific credentials’ of each therapeutic approach,” Roberts and Hardi state.
They also stress the importance of robust research assessments to measure the costs and benefits associated with psychotherapeutic outcomes and prevention interventions.
After gathering assessment data, psychologists consult the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-R), which lists criteria and standardized definitions for mental illnesses and conditions. Categories of symptoms differentiate one mental illness from another, and the usual course of each illness.
Beyond the DSM-IV-R, however, research in the area of diagnosing mental health problems remains one of the most exciting research areas in the field today – thanks to rapid advances in technology. Numerous brain imaging techniques that map brain structure and function now give researchers “images” of both normal and abnormal brain functioning. Scientists are using computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) to come up with greater precision and accuracy in diagnosing various mental illnesses.
Psychotherapies
The number of psychotherapies – a set of procedures or techniques that evaluate psychological problems, and come up with alternative ways of thinking, behaving, or feeling – has exploded in popularity since the middle of the last century. Most psychotherapies fall within one of the four main psychotherapeutic frameworks:
What is Psychodynamic Therapy?
Psychodynamic therapy explores an individual’s unconscious, seeking reasons or explanations for the individual’s current behavior. This therapy, also called insight-oriented therapy, attempts to bring underlying factors grounded in early life to the individual’s attention, increasing self-awareness and self-understanding.
Psychodynamic therapy stems from Sigmund Freud’s focus on psychoanalysis, making it the oldest form of psychotherapy. As a result, a large body of research exists to either support or refute the effectiveness of this approach.
Because the results of psychoanalysis research are harder to measure than behavioral-oriented therapies, research methodologies and outcomes of treatment have been questioned – especially those of the earliest studies. Psychodynamic therapy requires long-term treatment, sometimes a year or more, also complicating the research process. However, researchers today apply the most rigorous scientific processes, including meta-analysis studies completed over a number of years, to study of efficacy of psychodynamic practice and techniques, and many studies report significant positive outcomes.
In 2008, the Journal of the American Medical Association (JAMA) used a meta-analysis process to examine studies published between January 1, 1960, and May 31, 2008, identifying the possible effects of long-term psychodynamic psychotherapy. JAMA reported positive outcomes – especially for those with complex mental disorders, such as patients with personality disorders, chronic mental disorders, multiple mental disorders, and complex depressive and anxiety disorders .
Current Sample Topics in Research Psychodynamic Therapy Include:
- Psychodynamic therapy with addicted individuals.
- Childhood neurosis and adult mental health.
- Dreams and emotions in situations of childhood abuse.
- Psychodynamic psychology and sexuality.
- Structure and function of the psyche.
- Psychoanalytic play therapy.
- Psychic suffering.
- The practice and art of psychotherapeutic dialogue.
- Treating schizophrenia with psychodynamic therapies.
- Individuation and wholeness.
- Psychodynamic psychology and human development.
- Transference and psychodynamic psychology.
What is Humanistic Therapy?
According to the Association of Humanistic Psychology (AHP) , humanistic psychology today emphasizes “the independent dignity and worth of human beings and their conscious capacity to develop personal competence and self respect. This value orientation has led to the development of therapies to facilitate personal and interpersonal skills, and to enhance the quality of life.”
Humanistic therapy, founded by psychologist Carl Rogers, grew out of a reaction to psychoanalysis and behaviorism, two schools of thought that Rogers considered too “pessimistic.” Through psychoanalysis, Freud dwelled on unconscious motivators for behavior, while behaviorism, which followed developments in psychoanalysis, attributed behaviors to learned conditioning processes.
Instead, Rogers believed in downplays the pathological dimensions to an individual’s life, and alternatively, focusing on healthy aspects or behaviors. Rogers emphasized human potential, inherent goodness, the ability to self-direct by making choices; his form of psychotherapy came to be known as client-centered therapy. Self-actualization and developing a strong “sense of self” became the groundwork for this psychological framework and area of research.
AHP also acknowledges that negative and destructive forces in society can affect the mind, causing harm and dysfunction. Therefore, many humanistic psychologists also stress the importance of social change, modifying institutions and organizations to support human development, and acknowledging and building connectedness throughout a globally interdependent world.
Research, therefore, in humanistic psychology focuses not only on finding appropriate interventions toward helping individuals find their purpose and meaning in life, but also on peace and social justice issues within communities, nations, and the world. Transpersonal and quantum psychology, metaphysics, politics, economics, neuroconsciousness, and the environment are examples of topics explored in humanistic psychology research.
Some of the Current Research Topics in Humanistic Therapy and Theory:
- Feminism and psychology.
- Issues of Identity.
- The self and authenticity.
- The connection between people, the environment and spirituality.
- The psychology of climate change.
- Diet: physiological, psychological, and spiritual growth.
- Creative, empathetic, and critical thinking with self-reflection.
- Finding meaning in one’s work and career.
- Finding meaning in suffering.
- The psychology of creativity.
- Community-building.
- Evolving consciousness.
- Spirituality and personal growth.
- Existential psychotherapy.
What is Cognitive Behavioral Therapy (CBT)?
As the name implies, this therapy addresses both cognition – thoughts, feelings, emotions – and behaviors, attempting to change dysfunctional ways of thinking or misguided thought patterns that often lead to dysfunctional and sometimes harmful behaviors.
The therapy focuses on the present, current thought patterns, identifying distortions, and applying interventions that specifically target those errant thoughts. These interventions and techniques are problem-solving solutions, first guiding individuals in how to evaluate and modify beliefs, and then, how to change correspondingly unhealthy behaviors and interactions. Metaphorically, CBT interventions resemble a step-by-step “how-to” manual, giving instructions, and then empowering the individual to follow the steps, observe how they feel, and report back to the therapist the successes or challenges encountered. Typically, this type of therapy is short-term and goal-oriented, with occasional “checkups” to gauge progress and help in correcting any missteps.
CBT is “evidence-based” therapy, meaning that psychologists seek interventions that have been proven empirically through rigorously controlled experiments. The National Association of Cognitive-Behavioral Therapists bases its definition of evidence-based therapy on the following explanation by Aldo R. Pucci, MA, DCBT:
- an approach to therapy that emphasizes the pursuit of evidence on which to base its theory and techniques, as well as encourages its patients or clients to consider evidence before taking action; or
- an approach to therapy is supported by research findings, and those findings provide evidence that it is effective.
Because cognitive behavioral therapists base their applications on evidence-based research, the amount of CBT research surpasses the amount of psychotherapeutic research in nearly all other areas.
Some of the Popular Research Topics that CBT Addresses:
- Controlling chronic pain
- Treating anxiety and panic disorders
- CBT techniques for criminal offenders
- Using CBT for substance abuse and addiction disorders
- Eating disorders
- Post traumatic stress disorder
- Trauma from abusive relationships and situations
- Seasonal Affect Disorder
- Agoraphobia
**In addition, CBT research often addresses the management and treatment of a number of medical conditions through cognitive behavioral therapies and interventions, including: side effects of cancer; sickle cell; disease pain; irritable-bowel syndrome; obesity; asthma; rheumatic disease pain; temporomandibular disorder; erectile dysfunction; infertility; chronic fatigue syndrome; pre-menstrual syndrome.
What is Family Systems Therapy or Family Therapy?
Family systems therapy is psychotherapy that treats families, couples, and close-knit groups of people or extended families, as a system. This means that the psychologist treats the family, couple, or group as a unit, which scientists believe function as one organism or system, operating with a distinct set of communication and interaction patterns, and internal rules – all directly affecting behaviors. Rather than focus on the dysfunction or problems of one individual, the entire system receives therapy.
Over the past 20 years, this form of psychotherapy that began with a focus on the traditional family unit has expanded to include therapy for all types of familial relationships, including gay and lesbian couples and families, extended families related through divorce and re-marriage, and other groups that resemble family systems, such as church or religious groups.
For this reason, researchers of family systems theory and therapy have experienced an exponential growth in the number of topics and issues for study and investigation.
Family systems research projects fall within the following categories:
- School and learning difficulties
- Adjustments to bereavement
- Adjustments to geographical location
- Adjustment to physical or mental illness or disability
- Marital or relationship problems
- Divorce issues
- Substance abuse and behavioral disorders
- Nutritional, physiological and health issues
Within each research category, researchers study specific issues, issues that often cross into other categories as well. Below are some additional research topics studied today in family systems therapy
Eating Disorders Research:
- Is family therapy or individual therapy most effective for treating adolescent anorexia nervosa?
- Does dysfunctional family communication and relationship patterns cause eating disorders? Or does the stress associated with raising a child with an eating disorder cause dysfunctional family problems?
- What is the impact of eating disorders on families?
- How do family dynamics affect individuals with eating disorders?
- How does the mother-infant relationship affect future eating disorders?
- How does the Maudsley Method of treating eating disorders work compared to other more traditional forms of family systems therapy? (Maudsley takes a behavioral approach of giving all family members responsibility of ensuring that the suffering individual eats, finishes each meal, and receives incentives and rewards for eating.)
School and Learning Research:
- How do learning disabilities of one family member affect the entire family? Parents? Other siblings? And how the family functions?
- Should the assessment and treatment of a person with ADHD ( Attention Deficit Hyperactivity Disorder ) occur in the context of an individual’s family system?
- What are effective family therapies for childhood behavioral disorders?
- What are the psychological effects on parents and families of autistic children?
Adjustments to Bereavement Research:
- What are the needs of bereaved families?
- What are the long-term effects of a child’s death on a family?
- How do social/cultural influences affect how families cope with the loss of a family member?
- How does disenfranchised grief affect families? (Disenfranchised grief is grief not acknowledged by society, such as loss of a pet, an aborted or miscarried pregnancy, the loss of a child to adoption, the death of a celebrity, or a fictional character.)
Adjustments to Geographical Location Research:
- Re-location effects on military children and spouses.
- Re-location effects on civilian children: social, behavioral and cognitive development.
- Immigration and family emotional process.
Marital or Relationship Research:
- Does emotion-focused couples therapy work and facilitate forgiveness?
- Does a couple-based approach work to reduce the effects of post traumatic stress disorder (ptsd)?
- How can couples restore emotional intimacy and passion?
- What are the most effective interventions for aiding better communication between couples?
- The interplay between healthy relationships and reproduction.
- Genetics, physiology and relationships
Substance Abuse and Behavioral Disorders Research:
- How does family structure and functioning affect drug abusers?
- How does drug abuse by a family member affect siblings/parents/family functioning?
- What is the importance of parent-child relationships on preventing drug use and abuse?
Adjustment to Physical and Mental Illness or Disability Research:
- Family involvement in the treatment of mentally ill relatives.
- Multimedia interventions for families where one or more members suffer with a genetic disease.
- What are the effects of family network support and mental health recovery?
- Family functioning and depression in low-income Latino families and couples.
- Implications of violence and abuse on the family.
- The effect of AIDS on the family.
Nutritional, Physiological and Health Research:
- Cancer prevention for families.
- Family functioning and the effects of obesity.
Divorce Research:
- Does therapeutic divorce mediation work? (Divorce mediation is a therapeutic intervention for helping highly conflicted parents resolve disputes about their children.)
- What are the effects of divorce on young children, adolescents, and young adults?
- Reconciliation issues after divorce.
- Inter-parental conflict and its effects on children of divorce.
- How to establish healthy co-parenting roles.
Related Links Browse Links Browse Links Media Psychologist Career Profiles Childhood Developmental Psychology Existential Psychology Gender Identity Obesity Psychological Assessments Health Psychology Community Psychology Peer Pressure Entrepreneurship and Innovation
- Privacy Policy
- Terms of Use
- Do Not Sell My Personal Information (CA and NV)
- Psychologist
- Social Worker
- Military Psychology
- Psychology Schools
- Counseling Schools
- Psychology Degree Programs
- Counseling Degree Programs
- Associate’s in Psychology
- Bachelor’s in Psychology
- Master’s in Psychology
- PHd in Psychology
- Psychologist License
- Counseling License
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Conducting research in clinical psychology practice: Barriers, facilitators, and recommendations
Affiliation.
- 1 Oxford Centre for Anxiety Disorders and Trauma, Department of Experimental Psychology, University of Oxford, UK.
- PMID: 28569400
- PMCID: PMC5575503
- DOI: 10.1111/bjc.12142
Objectives: The combination of clinical psychologists' therapeutic expertise and research training means that they are in an ideal position to be conducting high-quality research projects. However, despite these skills and the documented benefits of research to services and service users, research activity in practice remains low. This article aims to give an overview of the advantages of, and difficulties in conducting research in clinical practice.
Method: We reviewed the relevant literature on barriers to research and reflected on our clinical and research experiences in a range of contexts to offer practical recommendations.
Results: We considered factors involved in the planning, sourcing support, implementation, and dissemination phases of research, and outline suggestions to improve the feasibility of research projects in post-qualification roles.
Conclusions: We suggest that research leadership is particularly important within clinical psychology to ensure the profession's continued visibility and influence within health settings.
Practitioner points: Clinical implications Emerging evidence suggests that clinical settings that foster research are associated with better patient outcomes. Suggestions to increase the feasibility of research projects in clinical settings are detailed. Limitations The present recommendations are drawn from the authors' practical experience and may need adaptation to individual practitioners' settings. This study does not attempt to assess the efficacy of the strategies suggested.
Keywords: barriers to research; clinical psychology; clinical psychology training; professional issues; research; research in practice.
© 2017 The Authors. British Journal of Clinical Psychology published by John Wiley & Sons Ltd on behalf of British Psychological Society.
PubMed Disclaimer
Similar articles
- The Experience and Effectiveness of Nurse Practitioners in Orthopaedic Settings: A Comprehensive Systematic Review. Taylor A, Staruchowicz L. Taylor A, et al. JBI Libr Syst Rev. 2012;10(42 Suppl):1-22. doi: 10.11124/jbisrir-2012-249. JBI Libr Syst Rev. 2012. PMID: 27820153
- Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. Eddy K, Jordan Z, Stephenson M. Eddy K, et al. JBI Database System Rev Implement Rep. 2016 Apr;14(4):96-137. doi: 10.11124/JBISRIR-2016-1843. JBI Database System Rev Implement Rep. 2016. PMID: 27532314 Review.
- New ways of working in mental health services: a qualitative, comparative case study assessing and informing the emergence of new peer worker roles in mental health services in England. Gillard S, Edwards C, Gibson S, Holley J, Owen K. Gillard S, et al. Southampton (UK): NIHR Journals Library; 2014 Jul. Southampton (UK): NIHR Journals Library; 2014 Jul. PMID: 27466663 Free Books & Documents. Review.
- Clinical psychologists' experiences of reflective staff groups in inpatient psychiatric settings: a mixed methods study. Heneghan C, Wright J, Watson G. Heneghan C, et al. Clin Psychol Psychother. 2014 Jul-Aug;21(4):324-40. doi: 10.1002/cpp.1834. Epub 2013 Jan 28. Clin Psychol Psychother. 2014. PMID: 23355325
- [A proposal for reforming psychologists' training in France and in the European Union]. Bouchard JP. Bouchard JP. Encephale. 2009 Feb;35(1):18-24. doi: 10.1016/j.encep.2007.11.008. Epub 2008 Apr 2. Encephale. 2009. PMID: 19250989 French.
- Healthcare Quality Improvement Competency: A Clinical and Training Imperative for Geropsychology. Jacobs ML, Mlinac ME. Jacobs ML, et al. J Clin Psychol Med Settings. 2021 Dec;28(4):897-908. doi: 10.1007/s10880-021-09824-x. Epub 2021 Oct 1. J Clin Psychol Med Settings. 2021. PMID: 34596823 Free PMC article.
- Barrom, C. P. , Shadish, W. R. , & Montgomery, L. M. (1988). PhDs, PsyDs, and real‐world constraints on scholarly activity: Another look at the Boulder Model. Professional Psychology: Research and Practice, 19(1), 93 https://doi.org/10.1037/0735-7028.19.1.93 - DOI
- British Psychological Society . (2006). Code of ethics and conduct. Leicester, UK: Author.
- British Psychological Society . (2014). Code of human research ethics. Leicester, UK: Author.
- Cooper, M. , & Graham, C. (2009). Research and evaluation. In Beinart H., Kennedy P. & Llewellyn S. (Eds.), Clinical psychology in practice (pp. 46–58). Leicester, UK: British Psychology Society and Blackwell.
- Cooper, M. , & Turpin, G. (2007). Clinical psychology trainees’ research productivity and publications: An initial survey and contributing factors. Clinical Psychology & Psychotherapy, 14(1), 54–62. https://doi.org/10.1002/cpp.513 - DOI
- Search in MeSH
Grants and funding
- WT_/Wellcome Trust/United Kingdom
- 102176/WT_/Wellcome Trust/United Kingdom
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central
Other Literature Sources
- scite Smart Citations

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Science of Psychology

The Go-To Science
Curiosity is part of human nature. One of the first questions children learn to ask is “why?” As adults, we continue to wonder. Using empirical methods, psychologists apply that universal curiosity to collect and interpret research data to better understand and solve some of society’s most challenging problems.
It’s difficult, if not impossible, to think of a facet of life where psychology is not involved. Psychologists employ the scientific method — stating the question, offering a theory and then constructing rigorous laboratory or field experiments to test the hypothesis. Psychologists apply the understanding gleaned through research to create evidence-based strategies that solve problems and improve lives.
The result is that psychological science unveils new and better ways for people to exist and thrive in a complex world.
Psychologists in Action

Helping Businesses
Dr. Jack Stark uses psychological science to help NASCAR drivers achieve optimal performance and keep their team in the winner’s circle.

Improving Lives
Dr. David Strayer uses psychological science to study distracted driving by putting people through rigorous concentration tests during driving simulations.

Promoting Health
Dr. Deborah Tate uses psychological science to identify strategies for improving weight loss . Her research brings the proven benefits of face-to-face weight loss programs to more people through technology.

Helping Organizations
As an organizational psychologist, Dr. Eduardo Salas studies people where they work — examining what they do and how they make decisions.

Working in Schools
Dr. Kathleen Kremer knows a thing or two about fun. Using psychological science, she studies user attitudes, behaviors and emotions to learn what makes a child love a toy.
Science in Action
Psychology is a varied field. Psychologists conduct basic and applied research, serve as consultants to communities and organizations, diagnose and treat people, and teach future psychologists and those who will pursue other disciplines. They test intelligence and personality.
Many psychologists work as health care providers. They assess behavioral and mental function and well-being. Other psychologists study how human beings relate to each other and to machines, and work to improve these relationships.
The application of psychological research can decrease the economic burden of disease on government and society as people learn how to make choices that improve their health and well-being. The strides made in educational assessments are helping students with learning disabilities. Psychological science helps educators understand how children think, process and remember — helping to design effective teaching methods. Psychological science contributes to justice by helping the courts understand the minds of criminals, evidence and the limits of certain types of evidence or testimony.
The science of psychology is pervasive. Psychologists work in some of the nation’s most prominent companies and organizations. From Google, Boeing and NASA to the federal government, national health care organizations and research groups to Cirque du Soleil, Disney and NASCAR — psychologists are there, playing important roles.

Brain science and cognitive psychology

Climate and environmental psychology

Clinical psychology

Counseling psychology

Developmental psychology

Experimental psychology

Forensic and public service psychology

Health psychology

Human factors and engineering psychology

Industrial and organizational psychology

Psychology of teaching and learning

Quantitative psychology

Rehabilitation psychology

Social psychology

Sport and performance psychology
Psychology Careers: What to Know
CALL TO BOOK

- Why Choose Us
- About The Artwork
- Vision and Mission Statement
- Referral Pathways
- Fees, Rebates & Services
- Your Rights
- Carer Rights
- Mental Health Adelaide Help
- SA Intensive Gambling Help Service
- Trauma Services
- Suicide Prevention
- The Matrix Program
- The RPG Program
- Disability (NDIS)
- Rural and Remote Help
- Psychological Assessments and Reports
- Employee Assistance Programs
- Therapy for Internet Gaming Disorder (IGD)
- Remedial Massage
- Game Therapy (Lego® / Minecraft)
- Trauma-Informed Care
- Adelaide Clinic (City)
- Gilles Plains Clinic
- Seaview Downs Clinic
- Sunshine Coast
The role of research in the practice of psychology

‘I’ve done my research,’ is a phrase that seems to be spoken more and more often. As information continues to become easier to produce and access, doing research is likely to become more relevant for everybody. In psychology, research plays an essential part in understanding human behaviour, and in the assessment, diagnosis and treatment of psychological disorders.
As a science, the body of knowledge under the heading ‘psychology’ concerns our knowledge of human behaviour that has been acquired through scientific research. Behaviour can be researched through an array of techniques and study designs, which gives individual studies unique qualities that affect the conclusions that can be drawn from them. This means a single piece of research will rarely provide a comprehensive understanding of a particular problem, and that research needs to be ongoing.
In Australia, registration as a psychologist requires university study involving both training in research and conducting research itself. This enables psychologists to do their own research, and also to understand, critique and apply others’ research to reach their own conclusions. Conducting high-quality research requires critical thinking, rigour, logic, and objectivity, which can be applied to assessing the quality of studies they use to inform their practice.
A key area of application for research in psychology is in developing, administering and interpreting psychological assessments. To provide real world meaning of the results, development of psychological assessments requires research in actual populations. The research that is used to develop an assessment has a substantial effect on determining if it is appropriate to use, how the test should be administered, and how the results should be interpreted. Because of this, understanding the research behind an assessment is important in psychological practice. It enables psychologists to better explain what results ‘mean’.
Research is also conducted in psychology to develop treatments for psychological disorders, determine whether they are effective, and use them in clinical practice. As psychologists are required to follow evidence-based practice, treatments used by psychologists have been demonstrated under scientific conditions to produce results. Research into the efficacy of treatments enables psychologists to better understand the variables involved and ensures treatments are applied in the most effective way. As an example, a study conducted by PsychMed on rates of remission for methamphetamine addiction showing that people who gave up tobacco and methamphetamine had higher rates of remission than those who quit methamphetamine alone, has helped us to advise on issues around co-substance use.
Finally, research plays a role in measurement-based treatment/care. Measurement-based treatment is a systematic approach to mental health care that involves using standardised assessments to track a patient’s progress and adjust their treatment plan as needed. This approach is based on the idea that regular monitoring and assessment can help identify changes in a patient’s symptoms or functioning, and allow for timely adjustments to their treatment plan to address any changes that may be occurring in different aspects of a patient’s mental health, including their symptoms, functioning, and overall well-being.
One of the main advantages of measurement-based treatment is that it provides a systematic and objective way to monitor a patient’s progress over time. This can be particularly helpful for patients with chronic mental health conditions, as it can allow for more precise tracking of their symptoms and functioning and can help ensure that their treatment plan is appropriate and effective. In addition to tracking a patient’s progress, measurement-based treatment may also involve setting specific treatment goals and working with the patient to develop strategies to achieve those goals.
In summary, research is crucial in understanding human behaviour, as well as in the assessment, diagnosis, and treatment of psychological disorders. Psychological assessments and interventions are developed through rigorous research, and psychologists being trained in research enables them to understand, critique, and apply this research in their own practice. Measurement-based treatment, which involves using standardised assessments to track a patient’s progress and adjust their treatment plan as needed, can be seen as research on the smallest, but also most relevant scale. Understanding the research behind these tools and approaches is vital for psychologists to provide the most effective care for their patients.

Engaging with research as a clinician
The following two articles consider the challenges and opportunities of engaging with research as an early career practitioner psychologist.
03 January 2023
How to become more research active
Dr Eleanor Chatburn's brief guide for Early Career Practitioner Psychologists
Are you an early career practitioner psychologist with a keen interest in research? Want to know how to become more research active but unsure where to start? Then this article is for you!
In this short guide, I share some top tips and resources that you can use to make your next steps into research. I have drawn on my own experiences of starting out on a clinical academic career pathway since I qualified as a clinical psychologist one year ago as well as the reflections of several research active practitioner psychologists who kindly shared their advice with me.
Why become more research active?
Becoming more research active in your role as a practitioner psychologist can have multiple benefits. For the individual practitioner, "being research active helps you to be the most effective therapist you can, and it also helps retain curiosity and enthusiasm in the work", Professor Barney Dunn, a research clinical psychologist at the University of Exeter, told me. "But equally importantly, practitioners bring a fresh, clinically grounded perspective", he added", "which helps ensure that the research that is being done in the field genuinely reflects the needs of the clients we serve and the services that are delivering care, closing the research practice gap."
Did you know that the value of clinical research is actually written into The NHS Constitution? It emphasises that one aspect of providing high quality care is "through the promotion, conduct and use of research to improve the current and future health and care of the population" (Department of Health, 2015). So far, so good. A big problem until fairly recently has been a scarcity of funding opportunities for allied health professionals or psychological practitioners to engage in research activity; many funding schemes prioritised medics which effectively shut out other practitioners from research (Newington et al., 2021).
But there is good news for practitioner psychologists. "There has been a real shift in the last few years", one research active Cognitive Behaviour Therapy (CBT) therapist* told me. "Both the academic side and the clinical lead side now recognise that there is a pool of talented, willing and interested clinicians in the field who could make a meaningful and patient-focussed contribution to research."
We now have a greater range of resources and funding streams available to practitioners who want to become research active such as the National Institute for Health and Care Research (NIHR) Integrated Clinical and Practitioner Academic (ICA) scheme. I have collated a list of useful resources and weblinks where you can explore these opportunities further (see Box).
What are the challenges?
Although we have made some great progress in supporting practitioners to become more research active, there is still space for improvement. The literature documents that the common barriers to becoming more research active include funding issues, interference with work/life balance, a lack of clarity for the career path, and insufficient support for clinical academics (Deane & Clunie, 2021; Newington et al., 2021).
I decided to ask a small group of practitioner psychologists with a passion for research to tell me more about the barriers they had experienced to see what we could learn from their experience. Back in 2019, a group of us wrote an article for CBT Today about some of these challenges after we participated in a research workshop led by Professors Barney Dunn and Shirley Reynolds at the BABCP annual conference. At the time, many workshop participants reported a lack of knowledge about how to get started and limited time, money, or support for research activity (Dunn et al., 2019).
I followed up with some of my co-authors to check in on their progress three years later. One person had been awarded an NIHR fellowship, another had worked as a therapist on two research trials, and a third person was running their own small-scale research projects, but others told me they had struggled to make much progress. All the practitioners I spoke to were very clear how tough it can be to get involved in research. As one CBT therapist put it, "I must admit [the progress I have made] has predominantly been through perseverance".
Some specific barriers to research activity that practitioners described include:
- Lack of protected time or resources for research activity within a clinical role. Newly qualified practitioners in particular can be under considerable pressure to focus on clinical appointments, leaving no time (or headspace) within the working day to shift gear and work on any kind of research.
- Research not prioritised by senior leaders or service managers. One CBT therapist* told me that "the service just want me to get through the waiting list". Another therapist described a "lack of support by management structures with some research topics being discouraged".
- Limited specific clinical-academic roles and career structures within the NHS. Once a fixed-term research fellowship or trial therapist job ends, it can be a real challenge to maintain both your research and your practice unless you can get more funding.
- Isolation and difficulty making contacts. It can feel lonely trying to pursue research on your own in a service that is not supportive of this activity. Practitioners are also unlikely to have an extensive network of research contacts and may not know of a suitable supervisor within their chosen topic. "I had difficulties making links with academic research departments who did not respond to emails", one CBT therapist explained, and another told me that the researchers they contacted "were not willing to engage" with practitioners.
- Personal impact. Several practitioners reported they ended up having to work on their research passions in their evenings/weekends as realistically they were otherwise unable to make any progress. Some people even chose to drop some of their contracted hours to collaborate on research projects in an unpaid capacity which they described as not financially sustainable.
It seems clear that there are some structural barriers to research activity for practitioner psychologists that are outside the control of individual practitioners, which require more action from our senior leaders and funders. I am keen to emphasise though that if you are passionate about research, there are some great resources and like-minded people out there who want to help you to navigate this challenging but hopefully rewarding journey. In the next sections, I have collated all the best advice that I could find for practical, doable ways that you can take that next step into research.
Write up a case study. Prof. Dunn's top tip is to start by writing up some routine clinical work. "Add a little more methodological rigour to the routine outcome monitoring we typically do in therapy for example, by using a single case experimental design that tracks symptom change over time from a baseline to a treatment phase. This kind of paper can make a useful contribution to the literature in helping us to "characterise the individuals who present to routine services and how well their needs are met". You could submit your case study to a publication like The Cognitive Behaviour Therapist which also runs an excellent mentoring scheme for new authors.
Create opportunities within your current role. Looking for some "quick wins" can be a great starting point, advises Dr Tim Clarke, Principal Research Clinical Psychologist at Norfolk and Suffolk Foundation Trust. You could take a lead on an audit or service development project and disseminate the results for example, as a poster at a professional conference, or in a professional magazine or peer-reviewed publication.
Publish any existing work. If you completed a Masters or Professional Doctorate thesis, then now is a great time to revisit your previous work and turn it into a publishable paper or present your findings as a poster or short talk at a conference. Your previous supervisor should be able to help you. Demonstrating output from prior research is important for some fellowship applications.
Work with a trainee. Supervise or co-supervise a trainee's case study, service development or main research project. This can be a great way to learn new research methods and to link with staff at the trainee's academic institution. You could then collaborate with the trainee on any dissemination activities and outputs.
Get a mentor. Clinical psychologist Dr Maria Loades is an NIHR Development & Skills Enhancement Award Holder at the University of Bath. Her best advice? "Get mentorship from and link into a university department who are interested in a similar topic and/or method to you". In my experience, getting the right mentor makes all the difference and it is worth spending time speaking to a range of people to get the right 'fit' for you. If you end up working with an academic/research supervisor from a different professional background to you, I highly recommend also finding a research active practitioner mentor (even if they work on a different topic or population) who can help you to negotiate the dual role of researcher and practitioner.
Contact your R&D team. Most NHS Trusts have an internal Research and Development team who are a great source of information about current research projects that the Trust is supporting such as opportunities to get involved in recruitment for large multi-site studies.
Train as a P.I. The NIHR runs an Associate Principal Investigator (PI) Scheme where you can shadow a PI to learn about the role. You may want to then become a site PI on a study, which is a great way to develop skills with clinical recruitment and research governance. Some regional NIHR Clinical Research Networks (CRNs) also run a "Greenshoots" scheme that offers extra funding for clinicians who are involved in recruitment for a study. Ask your R&D team for more information.
Network. "Linking with colleagues and like-minded individuals" is essential, as one CBT therapist told me. Dr Loades also advised, "look out for special interest groups of relevance to your topic area and conferences that will help you link up with others with similar interests." Clinical research is not done in isolation, and in my experience you need a team of collaborators and supervisors around you to make progress. Do reach out to others to learn about their research, explain why you are passionate about their topic, and explore any opportunities to collaborate.
Collaborate on an existing project. Getting your own new project idea off the ground can be challenging without buy-in from more established researchers. You may choose to build your research skills and ideas first by joining an existing project and research team. You could ask the lead researcher if they have any existing projects where you could make a defined contribution (e.g., screening studies for a systematic review). Working as part of a team on a larger project can be a great way to learn different research methods. Once you have these links, you may decide you want to apply for a fellowship to develop your own spin-off project (perhaps using the same data set or drawing on their methodology) so you can continue working with your new collaborators.
Work on a trial. One newly qualified clinical psychologist* told me about their experience of working as a trial therapist. "As an early career psychologist this was a brilliant opportunity to continue to build on my developing therapeutic skills after training", they explained, and added "and it also gave me an insight into some of the 'behind the scenes' work on a trial". You may be able to take on some additional sessions within your current role or to apply for full-time trial therapist jobs when you see these advertised.
Join a higher education institution (HEI). If you are passionate about teaching and supervising trainees, there are Teaching Fellow or teaching-track Lectureship roles on practitioner training programmes at many HEIs which often do not require much evidence of prior research activity. Once in post, you could then look for opportunities to supervise trainee research or to run small-scale projects. A good and supportive HEI should offer you career development support to apply for fellowships or to move across to a research-track position.
Apply for your own funding. There are dedicated funding streams for clinicians and practitioners who want dedicated time for research (see Box). Be aware that completing an application for a fellowship is a time-consuming process! A full NIHR doctoral research fellowship could take up to one year to develop. Many fellowships schemes are also highly competitive, and you should be prepared to receive rejections or requests for extensive revisions. Funders have recognised some of these difficulties, and there are now predoctoral schemes that will give you funding to spend time with a supervisor to work up your initial project idea into a fully costed, detailed fellowship application.
I hope that this article has given you some ideas for practical ways in which you can take your interest in research to the next level. Good luck with your research endeavours!
Further reading
- The NIHR Incubator for Mental Health Research. A great resource for mental health professionals who want to explore opportunities in research. It includes career case studies and provides information on training, funding, and finding a mentor, plus it has a whole section with specific advice for practitioner psychologists. https://mentalhealthresearch.org.uk/advice-for-psychologists/
- NIHR Integrated Clinical Academic programme: https://www.nihr.ac.uk/explore-nihr/academy-programmes/hee-nihr-integrated-clinical-and-practitioner-academic-programme.htm
- NIHR Local Authority Academic Fellowship programme: https://www.nihr.ac.uk/explore-nihr/funding-programmes/nihr-local-authority-academic-fellowship-programme-and-associated-opportunities.htm
- Wellcome Trust PhD Fellowship for Health Professionals: https://wellcome.org/grant-funding/schemes/phd-fellowships-health-professionals
- Your regional NIHR Research Design Service (RDS). These services run useful careers and training events and offer one-to-one appointments with a research advisor to help practitioners who are drafting fellowship or grant applications. https://www.nihr.ac.uk/explore-nihr/support/research-design-service.htm
- Your regional NIHR Applied Research Collaboration (ARC). There are 15 ARCs across England which support applied health and care research. ARCs can be a great way of linking up with other researchers in your region, and some of them run an annual research fellowship programme for practitioners: https://www.nihr.ac.uk/explore-nihr/support/collaborating-in-applied-health-research.htm
- There are some Health Education England (HEE) regionally funded predoctoral and postdoctoral bridging schemes. These tend to be advertised locally, for example, see Clinical Academic Careers East of England: https://www.claceast.net/
- The Healthcare Professionals in Research Facebook group: a peer-run group for early to mid-stage allied health professionals and practitioner psychologists interested in clinical academic careers. You will need to apply to the group's administrators to join:. https://www.facebook.com/groups/351873385356662/
- The Council for Allied Health Professions Research (CAHPR) is a national organisation with regional hubs, it runs events and shares useful information: https://cahpr.csp.org.uk
- The Cognitive Behaviour Therapist, a peer-reviewed journal run by the British Association for Behavioural and Cognitive Psychotherapies (BABCP), offers a mentoring scheme for practitioners who are interested in publishing a paper but are unsure where to start. The journal is also recruiting experienced researchers to become volunteer mentors: https://www.cambridge.org/core/journals/the-cognitive-behaviour-therapist/tcbt-mentorship-scheme
About the author
Dr Eleanor Chatburn qualified as a Clinical Psychologist in 2021 from the University of Bath. She is a Lecturer at the Department of Clinical Psychology and Psychological Therapies, University of East Anglia and a Visiting Researcher at the Department of Psychiatry, University of Cambridge. Twitter: @eleanorchats
Key sources
Deane, J.A. & Clunie, G. (2021). Healthcare professionals in research (HPiR) Facebook community: a survey of UK doctoral and postdoctoral healthcare professionals outside of medicine. BMC medical Education, 21(1), 1-9.
Department of Health. (2015). NHS Constitution. https://www.gov.uk/government/publications/the-nhs-constitution-for-england/the-nhs-constitution-for-england
Dunn B., Reynolds, S., Blacklock, J., et al. (2019). Turning research ideas into reality: How can we better support 'on the ground' clinicians to become research active?. CBT Today, 47(4), 18-20.
Newington, L., Wells, M., Adonis, A., et al. (2021). A qualitative systematic review and thematic synthesis exploring the impacts of clinical academic activity by healthcare professionals outside medicine. BMC Health Services Research, 21(1), 1-20.
Assistant Psychologists in clinical research delivery
Danae Palate with challenges and opportunities
Clinical research is essential for innovation in healthcare. The NHS is committed to promoting and conducting clinical research to provide the best patient care. Recent policy (The Future of UK Clinical Research Delivery: 2021 to 2022) has highlighted the need for more joined-up clinical research delivery across the NHS, including greater funding for academic institutions and third sector services, with the shared goal of better health outcomes for patients. This policy also details steps for more innovative clinical research, enabled by new digital data and tools.
One of the themes for the vision of UK clinical research implementation moving forward is a change in the culture of research within the NHS. Unfortunately, as pressures on the NHS have continued to increase, staff have needed to prioritise clinical contact over engagement with clinical research. Whilst this has been essential to make a dent in lengthy patient waiting lists, it means that research engagement has been neglected, even though clinical contact and research are both key to providing a good service and improving long term health outcomes.
Improving engagement with research
Assistant Psychologist roles are often undertaken by ECRs and include some level of clinical contact with patients as well as a research component. The job plan and experiences of Assistant Psychologists can vary enormously, and are dependent on both service pressures and the managing Clinical Psychologist.
Assistant Psychologists with primarily clinical roles can engage with the plan for clinical research delivery by being informed about the research relevant to the population(s) they are supporting. A searchable database of ongoing research has been developed by the National Institute for Health and Care Research (NIHR) (Be Part of Research) which ensures that staff can remain informed about current research in their area. Clinical staff can then signpost eligible people they are working with to get involved with ongoing research projects.
Disseminating research
The processes for gaining permission to disseminate clinical research are often confusing and can deter staff from disseminating research findings outside of their specific team or NHS Trust. This means that by the time research is disseminated, it might be less current, relevant and meaningful for both patients and staff.
Ensuring research has a meaningful impact means working to identify the target audience for dissemination in the early stages of research planning. Assistant Psychologist posts are often limited by fixed-term contracts. Therefore, planning dissemination early makes it more likely that Assistant Psychologists will have the time and resources to appropriately disseminate their work, so that their research can create maximum impact. Research and development teams are being transformed under new policy plans, and the hope is that Assistant Psychologists will be able to draw on increased resources to support and plan their research.
Increasing diversity in clinical research
New policy outlines the development of data and digital services to improve the diversity of study participants to include those groups that are often under-represented in research. There are also ongoing investigations to better understand how to reach under-represented communities.
Patient, Public and service user Involvement (PPI) is needed to better understand the challenges preventing under-represented populations from engaging with research. The value of service-user insight has been recognised as making research more effective and relevant, although the process for reimbursing service users for their time and expertise has been challenging to implement.
Successful PPI engagement requires shared expectations to be established between service users and professionals. Assistant Psychologists might support this process by informing service users of opportunities for research engagement, and by seeking to establish a shared understanding between service users and professionals about what research collaboration involves.
In conclusion, the plans for improving clinical research in the UK and the steps taken so far are exciting from the point of view of Assistant Psychologists wishing to increase their engagement with research. As policy documents often focus on long term changes, Assistant Psychologists may feel like proposed changes are less relevant to them, due to their fixed-term contracts. However, as I have demonstrated in this article, there are ways in which Assistant Psychologists can meaningfully engage with plans for research delivery in the context of the barriers and opportunities they face.
Danae Palate moved to the UK to study her undergraduate in psychology, now holds Graduate Basis for Chartered Membership with the BPS, and works as an Assistant Psychologist in the NHS alongside training as a psychological therapist at the Centre for Psychological Therapies at the University of Edinburgh.
Related articles

- Careers and professional development
- Teaching and learning
- Work and occupational

- Trainees and training

30 March 2020
- History and philosophy
This dialog contains the full navigation menu for this site.
- School of Humanities and Social Sciences
- Academic Programs
- Master of Arts in Clinical Psychology
Program Requirements for Clinical Psychology
Academic eligibility requirements.
For admission to the Graduate School at Penn State , an applicant must hold either: (1) a baccalaureate degree from a regionally accredited U.S. institution or (2) a tertiary (postsecondary) degree that is deemed comparable to a four-year bachelor's degree from a regionally accredited U.S. institution. This degree must be from an officially recognized degree-granting institution in the country in which it operates.
Admission decisions are based on the complete application portfolio. Admission to the Clinical Psychology program is granted jointly by The Graduate School of Penn State University and Penn State Behrend's School of Humanities and Social Sciences .
In addition to the general requirements for admission to the Graduate School , the following is required by the Clinical Psychology program:
Students must have a cumulative grade-point average of 3.0 or above (on a 4.0 scale) in the last 60 credits of course work. The undergraduate work must include a statistics course and a psychology research methods course with grades of B or higher.
The applicant must have completed at least 18 credits in psychology as part of their four-year bachelor’s degree from an accredited institution.
Supporting Materials
- Before you apply, be sure to have official transcripts from all institutions attended. In the application, skip any questions that don’t apply, such as junior/senior GPA, GMAT/GRE scores, etc.
- A copy of an official transcript from each institution attended except Penn State
- Three professional letters of recommendation, at least two of which should be academic
- Include any and all job experience, research experience, and/or clinical or clinically-related experience
- Include any and all skills that would assist you in completing a rigorous graduate program
- The writing sample should demonstrate your ability to write in a scientific manner (i.e., command of APA style, reference to and synthesis of scholarly sources) and your overall writing ability.
- Why have you chosen to pursue a Clinical Psychology degree at Penn State Behrend?
- How will these studies help you achieve your personal and professional goals?
- How will your participation contribute to Penn State Behrend's Clinical Psychology program?
- Indicate your current or most recent work, internship, and/or clinical experiences.
- You also can address any concerns that you have regarding GRE scores, undergraduate GPA, or the like.
- GRE scores are not required for admission, but students who do not submit GRE scores will not be eligible for most graduate assistantships and/or scholarships.
- A personal interview is required.
Clinical Psychology Application Deadlines
The deadline to apply for admission to the fall semester is April 30.
- The Admissions Review Committee will begin reviewing completed applications in mid-February. A second round of applications will be reviewed beyond April 30, if space is available in the program.
- Domestic applicants can apply now for Fall 2025. A complete application should be ready for review by April 30.
- International applicants should have a complete application ready for review by mid-February.
- All application requirements, including references, are due by the deadline.
- Once your application is accessible, Graduate Admissions will begin assembling your application portfolio and will send a confirmation email.
- View semester dates and student action guidelines on Penn State's academic calendar .
- Early application is encouraged, especially for anyone who is hoping to be considered for merit-based awards. Decisions are made on a rolling basis beginning in February. Only completed applications received by April 30 will be considered for the subsequent fall semester.
Admissions Timeline
- Submit completed application and application fee, including all components listed below, through the application portal. Please note: Your application will not be reviewed by the program faculty until it is complete, including your letters of recommendation.
- The Program Coordinator will review your application to verify you have met the minimum application requirements. They will then determine, based on the strength of your application, whether you will be interviewed.
- A core faculty member will interview selected applicants via Zoom. Interviews typically last 20-30 minutes; applicants should come prepared with any questions they might have. If the interviewing faculty member feels more information is needed after an interview, or believes a specific faculty may want to discuss the program further with an applicant (e.g., an applicant with an addictions focus may benefit from a second interview with a faculty member in that research area), a second interview may be required. Request for a second interview does not automatically indicate that the first interview was subpar.
- Interviewing faculty member(s) will share their impressions with the Program Coordinator, who will make a final decision in admittance.
- Given the rolling admissions nature of our application process, applicants who have been offered acceptance must decide about their standing in the program within two weeks of their offer. The Program Coordinator may allow extensions on a case-by-case basis.
- University Bulletin
- Trauma-Informed Psychotherapy Graduate Credit Certificate Program
- Graduate Programs
- Graduate Financial Aid
- RSVP for Graduate Events or Request Information
Exploring the role of dysfunctional attitudes and unhelpful thoughts in the relationship between personality traits and psychological distress in Australian University students
- Open access
- Published: 28 June 2024
Cite this article
You have full access to this open access article

- Ronan J. Galloghly 1 ,
- Pragalathan Apputhurai 2 &
- Simon R. Knowles ORCID: orcid.org/0000-0001-8000-1000 1
The impact of dysfunctional attitudes and unhelpful thinking upon clients presenting with personality-related psychological distress is an important clinical area of investigation as it informs psychological interventions. Despite this, there is limited research in this area. Thus, this study had two main aims: (1) examine the interrelationships between maladaptive personality traits, dysfunctional attitudes, unhelpful thinking, and psychological distress; and (2) explore the potential mediating roles of dysfunctional attitudes and unhelpful thinking on the relationship between maladaptive personality traits and psychological distress. A convenience sample of 728 undergraduate psychology students (mean age: 31.57 years; 76% female) completed an online questionnaire for course credit. The results supported the first hypothesis that after controlling for gender and age, there would be significant positive correlations among maladaptive personality traits, dysfunctional attitudes, and psychological distress. A structural equation model with an excellent fit (CMIN/df = 2.23, p = .063, TLI = 0.98, CFI = 0.99, SRMR, = 0.01, and RMSEA = 0.04) provided partial support for the second hypothesis in that dysfunctional attitudes and unhelpful thoughts mediated the relationship between maladaptive personality traits and psychological distress. Specifically, negative affectivity and detachment’s relationship with psychological distress were partially mediated via dysfunction attitudes and unhelpful thoughts, and dysfunctional attitudes respectively. These findings suggest that while dysfunctional attitudes and unhelpful thinking contribute to the relationship between personality traits and psychological distress, identification of other factors are required to improve theoretical understanding and subsequently psychological interventions.
Avoid common mistakes on your manuscript.
Introduction
Psychological distress is transdiagnostic, in that it features in all psychiatric disorders, and is defined as a combination of stress, anxiety and depressive symptoms in response to daily or chronic stressors (Lovibond & Lovibond, 1995 ; Barry et al., 2020 ). Gender and age represent the main biological predictors of psychological distress, with literature suggesting females experience significantly more psychological distress than males (Bracken & Reintjes, 2010 ; Mirowsky & Ross, 2017 ; Watkins & Johnson, 2018 ). Further, the Australian Institute of Health and Welfare (AIHW; 2018 ) found that - irrespective of gender - psychological distress increased throughout adulthood peaking at middle age (~ 50 years), before gradually decreasing. In addition to the biological contributors, two important psychological factors found to influence psychological distress are dysfunctional attitudes and personality (Buschmann et al., 2018 ; Jourdy & Petot, 2017 ).
Dysfunctional attitudes/beliefs reflect the attention, encoding, and interpreting of information in a negatively based format (Beck, 1976 ). Examples of these include rigid ‘must’ statements (e.g., “Everyone must love me’) and extreme “if-then” rules such as “If I do not pass this exam, then this confirms I am stupid”. A meta-analysis by Vîslă et al. ( 2016 ) found that across 83 primary studies including both clinical and community samples, dysfunctional attitudes predicted 20% of psychological distress variance independent of age, gender, income, educational, occupational, and marital status. Dysfunctional attitudes have also been identified to precede and perpetuate unhelpful thoughts (also known as thinking errors, negative automatic thoughts, or cognitive distortions) such as filtering, polarized thinking, overgeneralizing, and catastrophising (McKay et al., 2011 ). Understandably, like dysfunctional attitudes, unhelpful thoughts have been found to be related to, or associated with, changes in depression and anxiety (DeRubeis et al., 2008 ; Ross et al., 1986 ). Due to their significant role in underpinning and perpetuating psychological distress, dysfunctional attitudes and/or unhelpful thoughts are often primary targets for clinicians using psychological interventions such as cognitive behaviour therapy (Beck & Clark, 1997 ; Bowler et al., 2012 ; DeRubeis et al., 2008 ).
Along with dysfunctional attitudes and unhelpful thinking patterns, another primary contributor linked to psychological distress is personality traits (i.e., enduring patterns of perception, relation and thinking of the environment and oneself that are expressed in a wide variety of social and personal contexts; American Psychiatric Association [APA], 2013 ). Although the current approach for classifying personality disorders is based on the much-criticised categorial approach (e.g., Bach & Sellbom, 2016 ; Widiger & Gore, 2014 ), the fifth edition of the Diagnostic and Statistical Manual (DSM-5; APA, 2013 ) took tentative steps to move towards a dimensional approach to personality-based psychopathology (referred to as the alternative model of personality disorders; AMPD). According to the AMPD, personality disorders are dichotomous, and thus evaluated by both the level of personality dysfunction, and the specific personality traits (i.e., negative affectivity, detachment, antagonism, disinhibition, and psychoticism) which mirror the dysfunction. Recent literature supports the AMPD’s validity and usability across multiple mental health disorders including psychological distress (Chauhan et al., 2023 ; Clark & Watson, 2022 ; Nysaeter et al., 2023 ; Uliaszek et al., 2023 ; Vittengl et al., 2023 ).
Research to date provides evidence that personality traits, such as those based on the Big Five personality model (i.e., openness, conscientiousness, extraversion, agreeableness, and neuroticism) account for approximately one third of variance in depression symptoms, with the trait neuroticism (the tendency to experience negative emotions) being the most frequent and strongest contributor (Strickhouser et al., 2017 ; Kotov et al., 2010 ). More broadly, neuroticism has been identified to both predict and perpetuate psychological distress (Pollak et al., 2020 ; Widiger & Oltmanns, 2017 ).
Given personality traits, unhelpful thoughts, and dysfunctional attitudes independently predict psychological distress, it may be unsurprising the three variables are strongly interrelated. Research indicates that neuroticism is particularly correlated with dysfunctional attitudes and unhelpful thoughts (Blau et al., 2006 ; Hopwood et al., 2013 ; Samar et al., 2013 ). However, less is known about the role dysfunction attitudes and unhelpful thoughts play in the relationship between personality traits and psychological distress. Specifically, there is a lack of research examining whether dysfunctional attitudes and/or unhelpful thoughts mediate the relationship between personality traits and psychological distress.
Using a sample comprised of undergraduate psychology students, McDermut et al. ( 2019 ) found dysfunctional attitudes significantly and partially mediated the relationship between personality traits and psychological distress, and concluded that personality traits predicted psychological distress via the mechanism of dysfunctional attitudes. However, findings from McDermut et al. ( 2019 ) were limited by a relatively small sample size ( n = 167), using just one personality trait (neuroticism) in the mediation model, and not investigating potential mediating role of unhelpful thoughts in personality-related psychological distress.
Given the limited research to date, this study aimed to examine the role of dysfunctional attitudes and/or unhelpful thoughts in personality traits and psychological distress. The study will also seek to address the limited research using Personality Inventory for DSM-5 brief form (PID-5-BF) which assesses the five personality traits (i.e., negative affectivity, detachment, antagonism, disinhibition, and psychoticism) underpinning the AMPD. It was hypothesised that after controlling for gender and age, there would be significant positive correlations among personality traits, unhelpful thoughts, dysfunctional attitudes, and psychological distress. It was also hypothesised that dysfunctional attitudes and unhelpful thoughts would mediate the relationship between personality traits and psychological distress.
Participants and design
This study was based on an observational cross-design design using a convenience sampling method. Seven hundred and twenty-eight first year undergraduate psychology students enrolled at a medium-sized Australian university completed an online survey. The sample was predominantly female (76%), married/defacto (48.8%), and aged ranged between 18 and 74 years ( M = 31.57, SD = 20.84).
Depression anxiety and stress scale (DASS-21; Lovibond & Lovibond, 1995 )
The DASS-21 is a 21-item self-report questionnaire which assesses psychological distress via three subscales each containing seven items: depression, anxiety, and stress. Participants were requested to report the degree to which each item (e.g., ‘I felt I had nothing to look forward to’) applied to them during the preceding week. Each item is measured on a four-point Likert-type scale ranging from 0 (‘never’) to 3 (‘almost always’). As the DASS-21 is a short-form version of the original 42-item DASS, the final score was multiplied by two. Thus, total scores range from 0 to 126, with higher scores reflecting higher levels of psychological distress. The DASS-21 is reliable and valid amongst undergraduate student populations (Lemma et al., 2012 ; Osman et al., 2012 ), whilst demonstrating excellent internal consistency in this sample (Cronbach’s α = 0.94).
Dysfunctional attitude scale-short-form 1 (DAS-SF1: Beevers et al., 2007 )
The DAS-SF1 assesses dysfunctional attitudes across multiple domains including the need for approval from others (e.g., “My value as a person depends greatly on what others think of me”). Each item is scored on a four-point Likert-type scale ranging from 1 (‘totally disagree’) to 4 (‘totally agree). Total scores range from 9–36 with higher scores indicating more severe dysfunctional attitudes. In this study, the short-form version of the DAS (i.e., DAS-SF1) was used to decrease participant burden. The DAS-SF1 has displayed sound psychometrics amongst undergraduate student populations (McDermut et al., 2019 ) and good internal consistency in this sample (Cronbach’s α = 0.87).
The brief unhelpful thinking scale (BUTS; Knowles et al., 2017 )
The BUTS is an 11-item questionnaire examines unhelpful thoughts across several domains such as polarised thinking (e.g., “Things are either black or white, good or bad”). Each item is scored on a six-point Likert-type scale ranging from 0 (‘strongly disagree’) to 5 (‘strongly agree). Total scores range from 0–55 with higher scores indicating greater tendency toward unhelpful thinking. The BUTS demonstrated good internal consistency in this sample (Cronbach’s α = 0.82).
The PID-5 – Brief Form (PID-5-BF; Krueger et al., 2013 )
The PID-5-BF comprises 25 items with five items for five personality traits: Negative affectivity, Detachment, Disinhibition, Antagonism, and Psychoticism. Each item asked respondents whether they felt a statement accurately described them (e.g., ‘I often have to deal with people who are less important than me’). Items were measured on a Likert-type scale ranging from 0 (‘Very False or Often False’) to 3 (‘Very True or Often True’). Each trait domain score ranged from 0 to 15, with higher scores indicating greater personality trait dysfunction. The PID-5-BF is a reliable and valid instrument among university students which its brevity was designed to reduce participant burden (Anderson et al., 2018 ). The PID-5-BF demonstrated excellent internal consistency in this study (Cronbach’s α = 0.90).
Participants were provided a link to the study via course research experience program. Prior to commencing, students were informed that their survey was intended for respondents aged 18 years old and above, their participation was voluntary, they had a right to withdraw any time without reasons, and their responses were anonymous. Agreeing to begin the survey implied informed consent. Following completion of the questionnaire, information was provided explaining the study’s purpose, and contact information for support was provided in the unlikely event that completing the survey caused psychological distress. Course credit was given in compensation for completing the study survey. Ethical approval for the study was obtained by the university human research ethics committee. Pre-testing of the online (Qualtrics) questionnaire was tested by the members of the research team. The questionnaire took approximately 30 min to complete with all questions requiring a response to minimise missing data.
Data analysis strategy
All analyses were performed with SPSS (version 27) and AMOS (version 27) Data were screened, and all assumptions were tested prior to analyses. Bivariate correlations and Multivariate Analysis of Variance (MANOVA) were performed to examine the relationships of the demographic variables age and gender with study variables, evaluating the first hypothesis. The mediation model employing structural equation modeling was developed to evaluate the second hypothesis and the model fit being evaluated using the following criteria recommended by Hu and Bentler ( 1999 ): CMIN/Chi-square goodness of fit test [χ²] p > .05; Normed Chi-square [χ2/df] = 1–3, Tucker–Lewis index [TLI] > 0.95, Steiger-Lind Root Mean Square Error of Approximation [RMSEA] < 0.08, and Standardized Root Mean Square Residual [SRMR] < 0.06. The final model was derived by a stepwise approach of adding or removing paths based on theoretical and AMOS reported modification indices.
There were significant positive correlations among psychological distress, dysfunctional attitudes, unhelpful thoughts, and all five PID-5 personality traits (See Table 1 ). Psychological distress, dysfunctional attitudes, and the PID-5 personality traits were negatively correlated with unhelpful thinking. Negative affectivity produced the strongest correlations with psychological distress ( r = .59), unhelpful thinking ( r = .59), and dysfunctional attitudes ( r = .54). Detachment produced moderate correlations with psychological distress ( r = .45), unhelpful thinking ( r = .42), and dysfunctional attitudes ( r = .43). Unhelpful thoughts were also strongly correlated with dysfunctional attitudes ( r = .59) and psychological distress ( r = .52). Age was found to be a significantly related to negative affectivity ( r = −.29, p < .001), detachment ( r = − .10, p = .01), disinhibition ( r = − .22, p < .001), psychoticism ( r = − .26, p < .001), antagonism ( r = − .27, p < .001), Unhelpful thinking ( r = .27, p < .001), Dysfunctional attitudes ( r = - .21, p < .001), and psychological distress ( r = − .21, p < .001), and therefore age was controlled for in the subsequent analysis. A MANOVA (IV: gender; DVs: study variables) identified result was significant for gender, Pillai’s Trace = 0.01, F (14,1428) = 5.42, p < .001. A subsequent, univariate F test indicated that females had a significantly higher mean psychoticism compared to males ( F (2,719) = 3.35, p = .036). No other gender-based difference across the study variables was found.
In relation to the second hypothesis, a final model was developed based on an iterative approach where nonsignificant paths were removed from a saturated mediation model. Initially the model controlled for age and gender, however its inclusion produced a poorer fit and was therefore removed from the model. Similarly, psychoticism found to be a poor predictor and was also removed from the model. Overall, the final model (see Fig. 1 ) had an excellent fit (CMIN/df = 2.23, p = .063, TLI = 0.98, CFI = 0.99, SRMR, = 0.01, and RMSEA = 0.04). The total amount of variance accounted for in each of the variables was 33% of dysfunctional attitudes, 40% of unhelpful thinking, and 44% of psychological distress. As shown in Fig. 1 , Disinhibition had a significant direct influence on psychological distress and the relationship between Antagonism and psychological distress is fully mediated via BUTS and DAS-SF. The relationship between Negative affectivity and psychological distress is partially mediated via BUTS and DAS-SF while the relationship between Detachment and psychological distress is partially mediated via DAS-SF. The configural model fit indices indicated an adequate fit (χ2(36) = 1.65, p = .009, TLI = 0.98, CFI = 0.99, SRMR = 0.05, RMSEA = 0.02, Akaike information criterion (AIC) = 155.28), and the measurement weights model, with equal factor loadings on males and female groups, fit indices were also acceptable (χ2(46) = 1.42, p = .031, TLI = 0.99, CFI = 0.99, SRMR = 0.05, RMSEA = 0.02, AIC = 144.47). Comparisons across models showed that the increase in chi-squared values (Δχ2(10) = 6.19, p = .799) was not statistically significant and changes in other model fit indices were small, indicating robust measurement consistency across gender.
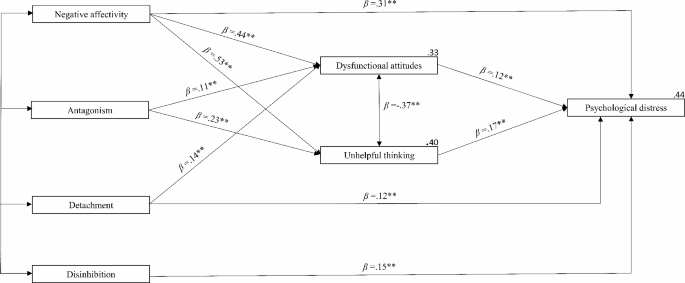
Final mediation model (** = p < .001)
The results supported the first hypothesis in that after controlling for gender and age, there would be significant positive correlations among PID-5 personality traits, dysfunctional attitudes, and psychological distress. These findings were consistent with the cognitive theory model linking these variables (Góngora & Castro Solano, 2017 ; Hopwood et al., 2013 ; Kotov et al., 2010 ; Pretzer & Beck, 2005 ). Also consistent with past research were the findings that Negative affectivity and Detachment produced the strongest correlations with psychological distress, dysfunctional attitudes, and the significant positive correlations between all five PID-5 personality traits and dysfunctional attitudes (Hakulinen et al., 2015 ; Hopwood et al., 2013 ; McDermut et al., 2019 ; Thimm et al., 2016 ). Additionally, there were no significant differences between male and female for individuals concerning dysfunctional attitudes, unhelpful thoughts, psychological distress, and personality traits, except for psychoticism.
The results also partially supported the second hypothesis in that dysfunctional attitudes and unhelpful thoughts would mediate the relationship between PID-5 personality traits and psychological distress. Specifically, Negative affectivity and Detachment’s relationship with psychological distress were partially mediated via dysfunction attitudes and unhelpful thoughts, and dysfunctional attitudes respectively. Further, supporting the second hypothesis was the finding that Antagonism’s effect on psychological distress was fully mediated by both dysfunctional attitudes and unhelpful thoughts. Not supporting the second hypothesis were the findings that neither dysfunctional attitudes nor unhelpful thoughts had any impact on Disinhibition’s effect on psychological distress.
The partial mediation of dysfunctional attitudes and unhelpful thoughts upon Negative affectivity’s relationship with psychological distress was consistent with McDermut and colleagues’ ( 2019 ) findings, and subsequently indicates that Negative affectivity predicts psychological distress, at least partially, by operating through these two cognitive mediators. Moreover, the novel findings that dysfunctional attitudes and unhelpful thoughts fully explained the relationship between Antagonism and psychological distress suggests they are the primary cognitive processes inherent within this relationship. Conversely, neither dysfunctional attitudes nor unhelpful thoughts had any impact upon Disinhibition’s relationship with psychological distress which indicates that this relationship exists outside of these cognitive models linking personality and psychological distress (Beck et al., 2015 ).
Clinical implications
The findings suggest that dysfunctional attitudes and unhelpful thoughts play a role in explaining the relationship between psychological distress and the AMPD PID-5 personality traits Negative affectivity, Detachment, and Antagonism. Subsequently, clients who present with psychological distress and score highly on these three scales may benefit from therapeutic interventions which focus on clients’ attitudes and unhelpful thinking patterns via well-established approaches such as cognitive behavioural therapy. Antagonism specifically, may be efficaciously treated by interpersonal therapy (IPT) given that it’s key feature interpersonal problems (Vize et al., 2022 ; Wright, 2019 ). Conversely, this approach may not be as efficacious for clients scoring high on Disinhibition, as this trait’s characteristics include irresponsibility, impulsivity, and risk taking; all of which infer potential treatment-interfering behaviours including missed appointments, difficulty focusing in-session, and nonadherence to homework tasks (APA, 2013 ). The utilisation of an intervention to such specific personality traits may be more efficacious, rather than focusing on attitudes and thoughts which may be symptoms of the trait. For instance, Conrod et al. ( 2013 ) created personality-specific interventions which included psychoeducation of personality traits and goalsetting to enhance motivation to change. The authors found that the intervention significantly reduce disinhibition-related behaviours (i.e., substance use) among adolescents. However, more research is required to determine the efficacy of this approach across wider community and clinical populations.
Limitations and future studies
This study has several limitations. The cross-section design lacks the robustness of a longitudinal approach from which casual inferences (true mediation) could be attained. The study also utilised a largely homogeneous non-clinical convenience sample of university students thus limiting the generalisability of findings, including age, cultural, socioeconomic, and educational diversity. It is also important to recognise the potential impact and limitations associated with social desirability and selection and response bias given the student-based convenience sample. Future research should investigate if these results can be replicated using community and clinical populations. Additionally, this paper utilised dysfunctional attitudes and unhelpful thoughts broadly. A more judicious approach might be to explore which specific dysfunctional attitudes and unhelpful thoughts are associated with specific personality traits. This could improve theory and potentially offer a more targeted approach to treating personality-related psychological distress.
In addition to addressing the above limitations, future studies should also look to explore and address other potential processes or confounders which may influence the identified relationships. These include coping strategies, comorbid psychological and/or physical conditions, and psychosocial stressors (e.g., relationship, employment, educational, financial). For instance, Huang et al. ( 2021 ) found that other psychological processes such as self-efficacy, coping styles, and psychological resilience mediated this relationship between personality traits and psychological distress among Chinese nurses. Similarly, a recent paper by Kestler-Peleg and colleagues ( 2023 ) found intolerance to uncertainty mediated the relationship between personality traits and a form on adjustment disorder-associated psychological distress.
In conclusion, this study’s findings indicate that three AMPD PID-5 personality traits (i.e., Negative affectivity, Detachment, and Antagonism) predicted psychological distress via the dysfunctional attitudes and unhelpful thoughts. This study is the first to extend the limited research to date by exploring the potential mediating role of dysfunctional attitudes and unhelpful thoughts on the relationship between personality and psychological distress. The findings provide evidence for the mediating role of dysfunctional attitudes and unhelpful thoughts. While limited by the cross-sectional design and evidence for true causal mediation, the findings highlight the relevance and importance of targeting dysfunctional attitudes and unhelpful thoughts in therapy.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request and after relevant ethical approval.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Anderson, J. L., Sellbom, M., & Salekin, R. T. (2018). Utility of the personality inventory for DSM-5-Brief form (PID-5-BF) in the measurement of maladaptive personality and psychopathology. Assessment , 25 (5), 596–607. https://doi.org/10.1177/1073191116676889
Article PubMed Google Scholar
Australian Institute of Health and Welfare (2018). Australia’s Health 2018. (Cat. No. AUS 221; Australia’s Health Series No. 16) , 570. https://doi.org/10.25816/5ec1e56f25480
Bach, B., & Sellbom, M. (2016). Continuity between DSM-5 categorical criteria and traits criteria for borderline personality disorder. The Canadian Journal of Psychiatry, 61 (8), 489–494. https://doi.org/10.1177/0706743716640756
Barry, V., Stout, M. E., Lynch, M. E., Mattis, S., Tran, D. Q., Antun, A., Ribeiro, M. J., Stein, S. F., & Kempton, C. L. (2020). The effect of psychological distress on health outcomes: A systematic review and meta-analysis of prospective studies. Journal of Health Psychology , 25 (2), 227–239. https://doi.org/10.1177/1359105319842931
Beck, A. T. (1976). Cognitive Therapy and the Emotional Disorders New York, New American Library.
Beck, A. T., & Clark, D. A. (1997). An information processing model of anxiety: Automatic and strategic processes. Behaviour Research and Therapy , 35 (1), 49–58. https://doi.org/10.1016/S0005-7967(96)00069-1
Beck, A. T., Freeman, A., & Davis, D. D. (2015). Cognitive therapy of personality disorders 3rd edition / New York, The Guilford Press.
Beevers, C. G., Strong, D. R., Meyer, B., Pilkonis, P. A., & Miller, I. R. (2007). Efficiently assessing negative cognition in depression: An item response theory analysis of the dysfunctional attitude scale. Psychological Assessment , 19 (2), 199–209. https://doi.org/10.1037/1040-3590.19.2.199
Blau, S., Fuller, J. R., & Vaccaro, T. P. (2006). Rational-emotive disputing and the five-factor model: Personality dimensions of the Ellis emotional efficiency inventory. Journal of Rational-Emotive and Cognitive-Behavior Therapy , 24 (2), 87–100. https://doi.org/10.1007/s10942-005-0020-z
Article Google Scholar
Bowler, J. O., Mackintosh, B., Dunn, B. D., Mathews, A., Dalgleish, T., & Hoppitt, L. (2012). A comparison of cognitive bias modification for interpretation and computerized cognitive behavior therapy: Effects on anxiety, depression, attentional control, and interpretive bias. Journal of Consulting and Clinical Psychology , 80 (6), 1021–1033. https://doi.org/10.1037/a0029932
Article PubMed PubMed Central Google Scholar
Bracken, B. A., & Reintjes, C. (2010). Age, race, and gender differences in depressive symptoms: A lifespan developmental investigation. Journal of Psychoeducational Assessment , 28 (1), 40–53. https://doi.org/10.1177/0734282909336081
Buschmann, T., Horn, R. A., Blankenship, V. R., Garcia, Y. E., & Bohan, K. B. (2018). The relationship between automatic thoughts and irrational beliefs predicting anxiety and depression. Journal of Rational-Emotive & Cognitive-Behavior Therapy , 36 (2), 137–162. https://doi.org/10.1007/s10942-017-0278-y
Chauhan, K., Donahue, J., & Thompson, R. (2023). The predictive validity of the DSM-5 alternative model for borderline personality disorder: Associations with coping strategies, general distress, rumination, and suicidal ideation across one year. Personality and Mental Health , 17 (3), 272–281. https://doi.org/10.1002/pmh.1580
Clark, L. A., & Watson, D. (2022). The trait model of the DSM-5 alternative model of personality disorder (AMPD): A structural review. Personality Disorders , 13 (4), 328–336. https://doi.org/10.1037/per0000568
Conrod, P. J., O’Leary-Barrett, M., Newton, N., Topper, L., Castellanos-Ryan, N., Mackie, C., et al. (2013). Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA Psychiatry , 70 (3), 334–342. https://doi.org/10.1001/jamapsychiatry.2013.651
DeRubeis, R. J., Siegle, G. J., & Hollon, S. D. (2008). Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nature Reviews Neuroscience , 9 (10), 788–796. https://doi.org/10.1038/nrn2345
Góngora, V. C., & Castro Solano, A. (2017). Pathological personality traits (DSM-5), risk factors, and Mental Health. SAGE Open , 7 (3), 2158244017725129. https://doi.org/10.1177/2158244017725129
Hakulinen, C., Elovainio, M., Pulkki-Råback, L., Virtanen, M., Kivimäki, M., & Jokela, M. (2015). Depression and Anxiety , 32(7), 461–470. https://doi.org/10.1002/da.22376
Hopwood, C. J., Schade, N., Krueger, R. F., Wright, A. G., & Markon, K. E. (2013). Connecting DSM-5personality traits and pathological beliefs: Toward a unifying model. Journal of Psychopathology and Behavioral Assessment , 35 (2), 162–172. https://doi.org/10.1007/s10862-012-9332-3
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal , 6 (1), 1–55. https://doi.org/10.1080/10705519909540118
Huang, W., Cai, S., Zhou, Y., Huang, J., Sun, X., Su, Y., Dai, M., & Lan, Y. (2021). Personality profiles and personal factors Associated with psychological distress in Chinese nurses. Psychology Research and Behavior Management , 14 , 1567–1579. https://doi.org/10.2147/PRBM.S329036
Jourdy, R., & Petot, J. M. (2017). Relationships between personality traits and depression in the light of the big five and their different facets. L’Évolution Psychiatrique , 82 (4), e27–e37. https://doi.org/10.1016/j.evopsy.2017.08.002
Kestler-Peleg, M., Mahat-Shamir, M., Pitcho-Prelorentzos, S., & Kagan, M. (2023). Intolerance to uncertainty and self-efficacy as mediators between personality traits and adjustment disorder in the face of the COVID-19 pandemic. Current Psychology (New Brunswick N J) , 42 (10), 8504–8514. https://doi.org/10.1007/s12144-023-04465-9
Knowles, S. R., Apputhurai, P., & Bates, G. (2017). Development and validation of the brief unhelpful thoughts scale (BUTs). Journal of Psychology & Psychotherapy , 4 , 61–70. https://savvysciencepublisher.com/index.php/jppr
Kotov, R., Gamez, W., Schmidt, F., & Watson, D. (2010). Linking big personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin , 136 (5), 768–821. https://doi.org/10.1037/a0020327
Krueger, R., Derringer, J., Markon, K., Watson, D., & Skodol, A. (2013). The personality inventory for DSM-5—brief form (PID-5-BF)—adult . American Psychiatric Association.
Google Scholar
Lemma, S., Gelaye, B., Berhane, Y., Worku, A., & Williams, M. A. (2012). Sleep quality and its psychological correlates among university students in Ethiopia: A cross-sectional study. Bmc Psychiatry , 12 (1), 1–7. https://doi.org/10.1186/1471-244X-12-237
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression anxiety stress scales (DASS) with the Beck Depression and anxiety inventories. Behaviour Research and Therapy , 33 (3), 335–343. https://doi.org/10.1016/0005-7967(94)00075-u
McDermut, W., Pantoja, G., & Amrami, Y. (2019). Dysfunctional beliefs and personality traits. Journal of Rational-Emotive & Cognitive-Behavior Therapy , 37 (4), 338–357. https://doi.org/10.1007/s10942-019-00315-5
McKay, M., Davis, M., & Fanning, P. (2011). Thoughts and feelings: Taking control of your moods and your life . New Harbinger.
Mirowsky, J., & Ross, C. E. (2017). Social causes of psychological distress (2nd ed.). Routledge.
Book Google Scholar
Nysaeter, T. E., Hummelen, B., Christensen, T. B., Eikenaes, I. U., Selvik, S. G., Pedersen, G., Bender, D. S., Skodol, A. E., & Paap, M. C. S. (2023). The Incremental Utility of Criteria A and B of the DSM-5 Alternative Model for Personality disorders for Predicting DSM-IV/DSM-5 section II personality disorders. Journal of Personality Assessment , 105 (1), 111–120. https://doi.org/10.1080/00223891.2022.2039166
Osman, A., Wong, J. L., Bagge, C. L., Freedenthal, S., Gutierrez, P. M., & Lozano, G. (2012). The Depression anxiety stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. Journal of Clinical Psychology , 68 (12), 1322–1338. https://doi.org/10.1002/jclp.21908
Pollak, A. J., Dobrowolska, M., Timofiejczuk, A., & Paliga, M. M. (2020). The Effects of the Big Five Personality Traits on Stress among Robot Programming Students. Sustainability, 12 , 1–11. https://doi.org/10.3390/su12125196
Pretzer, J. L., & Beck, A. T. (2005). A cognitive theory of personality disorders. In M. F. Lenzen- weger & J. F. Clarkin (Eds.), Major Theories of Personality Disorder (2nd ed., pp. 43–113). New York, The Guilford Press.
Ross, S. M., Gottfredson, D. K., Christensen, P., & Weaver, R. (1986). Cognitive self-statements in depression: Findings across clinical populations. Cognitive Therapy and Research , 10 (2), 159–165. https://doi.org/10.1007/BF01173722
Samar, S. M., Walton, K. E., & McDermut, W. (2013). Personality traits predict irrational beliefs. Journal of Rational-Emotive & Cognitive-Behavior Therapy , 31 (4), 231–242. https://doi.org/10.1007/s10942-013-0172-1
Strickhouser, J. E., Zell, E., & Krizan, Z. (2017). Does personality predict health and well-being? A metasynthesis. Health Psychology , 36 (8), 797–810. https://doi.org/10.1037/hea0000475
Thimm, J. C., Jordan, S., & Bach, B. (2016). The personality inventory for DSM-5 short form (PID-5-SF): Psychometric properties and association with big five traits and pathological beliefs in a Norwegian population. BMC Psychol , 4 (1), 61. https://doi.org/10.1186/s40359-016-0169-5
Uliaszek, A. A., Amestoy, M. E., Fournier, M. A., & Al-Dajani, N. (2023). Criterion a of the alternative model of personality disorders: Structure and validity in a community sample. Psychological Assessment, 35(5), 453–461. https://doi.org/10.1037/pas0001225
Vittengl, J. R., Jarrett, R. B., Ro, E., & Clark, L. A. (2023). How can the DSM-5 alternative model of personality disorders advance understanding of depression?. Journal of Affective Disorders, 320, 254–262. https://doi.org/10.1016/j.jad.2022.09.146
Vîslă, A., Flückiger, C., Holtforth, G., M., & David, D. (2016). Irrational beliefs and psychological distress: A meta-analysis. Psychotherapy and Psychosomatics , 85 (1), 8–15. https://doi.org/10.1159/000441231
Vize, C. E., Ringwald, W. R., Edershile, E. A., & Wright, A. G. C. (2022). Antagonism in Daily Life: An exploratory ecological momentary Assessment Study. Clinical Psychological Science , 10 (1), 90–108. https://doi.org/10.1177/21677026211013507
Watkins, D. C., & Johnson, N. C. (2018). Age and gender differences in psychological distress among African americans and whites: Findings from the 2016 National Health interview survey. Healthcare (Basel Switzerland) , 6 (1), 6. https://doi.org/10.3390/healthcare6010006
Widiger, T. A., & Gore, W. L. (2014). Dimensional versus categorical models of psychopathology. The Encyclopedia of Clinical Psychology , 1–12. https://doi.org/10.1002/9781118625392.wbecp108
Widiger, T. A., & Oltmanns, J. R. (2017). Neuroticism is a fundamental domain of personality with enormous public health implications. World Psychiatry , 16 (2), 144–145. https://doi.org/10.1002/wps.20411
Wright, A. G. C. (2019). Antagonism from the perspective of interpersonal theory. In J. D. Miller, & D. R. Lynam (Eds.), The handbook of antagonism: Conceptualizations, assessment, consequences, and treatment of the low end of agreeableness (pp. 155–170). Elsevier Academic. https://doi.org/10.1016/B978-0-12-814627-9.00011-6
Chapter Google Scholar
Download references
Acknowledgements
The authors would like to thank all the individuals who participated in this research.
Provenance and peer review
Not commissioned, externally peer reviewed.
Open Access funding enabled and organized by CAUL and its Member Institutions. None.
Author information
Authors and affiliations.
Department of Psychological Sciences, Swinburne University of Technology, John St, Hawthorn, Melbourne, VIC, 3122, Australia
Ronan J. Galloghly & Simon R. Knowles
Department of Health Science and Biostatistics, School of Health Sciences, Swinburne University of Technology, Melbourne, Australia
Pragalathan Apputhurai
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Simon R. Knowles .
Ethics declarations
Ethical approval.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Informed consent to publish the study findings was obtained from all individual participants included in the study.
Conflict of interest
The authors have no conflict of interests in relation to this study.

Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Galloghly, R.J., Apputhurai, P. & Knowles, S.R. Exploring the role of dysfunctional attitudes and unhelpful thoughts in the relationship between personality traits and psychological distress in Australian University students. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06239-3
Download citation
Accepted : 05 June 2024
Published : 28 June 2024
DOI : https://doi.org/10.1007/s12144-024-06239-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Australian university students
- Dysfunctional attitudes
- Personality traits
- Psychological distress
- Unhelpful thinking
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 24 June 2024
Effects of memory and attention on the association between video game addiction and cognitive/learning skills in children: mediational analysis
- Amani Ali Kappi 1 ,
- Rania Rabie El-Etreby 2 ,
- Ghada Gamal Badawy 3 ,
- Gawhara Ebrahem 3 &
- Warda El Shahat Hamed 2
BMC Psychology volume 12 , Article number: 364 ( 2024 ) Cite this article
212 Accesses
Metrics details
Video games have become a prevalent source of entertainment, especially among children. Furthermore, the amount of time spent playing video games has grown dramatically. The purpose of this research was to examine the mediation effects of attention and child memory on the relationship between video games addiction and cognitive and learning abilities in Egyptian children.
A cross-sectional research design was used in the current study in two schools affiliated with Dakahlia District, Egypt. The study included 169 children aged 9 to 13 who met the inclusion criteria, and their mothers provided the questionnaire responses. The data collection methods were performed over approximately four months from February to May. Data were collected using different tools: Socio-demographic Interview, Game Addiction Scale for Children (GASC), Children’s Memory Questionnaire (CMQ), Clinical Attention Problems Scale, Learning, Executive, and Attention Functioning (LEAF) Scale.
There was a significant indirect effect of video game addiction on cognitive and learning skills through attention, but not child memory. Video game addiction has a significant impact on children’s attention and memory. Both attention and memory have a significant impact on a child’s cognitive and learning skills.
Conclusions
These results revealed the significant effect of video game addiction on cognitive and learning abilities in the presence of mediators. It also suggested that attention-focused therapies might play an important role in minimizing the harmful effects of video game addiction on cognitive and learning abilities.
Peer Review reports
Introduction
The use of video games has increased significantly in recent years. Historically, such games are used more often by children. Despite the positive impacts of video games on socialization and enjoyment, empirical and clinical research has consistently demonstrated that many children can become addicted due to excessive use. Among Arab children and adolescents, the prevalence of video game addiction is 62% of 393 adolescents in Saudi Arabia, 5% in Jordan, 6% in Syria, and 7.8% in Kuwait [ 1 , 2 ]. The varying incidence rates can be attributable to variations in the research population, cultural determinants, and evaluation or diagnostic standards.
In addition, video games, the internet, and other new technologies have become children’s top leisure pursuits. Today, they comprise a virtual environment in which thousands of gamers simultaneously participate worldwide; rather than being a personal or lonely leisure activity, they are often a group activity that establishes new social networks [ 3 ]. Although playing video games in moderation can have many positive effects, their exploitation may lead to addictions and societal issues [ 4 ]. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), identifies repetitive and persistent behavior related to online video games as the core element of addiction. This behavior should persist for at least 12 months and result in significant impairment. Additionally, addiction should be accompanied by psychological and social symptoms, as well as tolerance and withdrawal symptoms [ 5 ].
Different studies have examined the impact of video games on children’s cognitive abilities and school performance [ 6 , 7 ]. The recent literature has shown how video games affect the brain and alter its functioning while being played. It demonstrates how specific cortical and subcortical structures are involved [ 8 , 9 , 10 ]. Research indicates that excessive play of the same typees of games might negatively impact school-age children’s cognitive and academic skills as well as their capacity to maintain and enhance memories [ 7 ]. Possible consequences of video game addiction may include memory and attention-related difficulties [ 4 , 6 , 11 ]. For instance, children’s memory scores negatively correlated with greater levels of video game addiction in Lebanon [ 6 ]. Furthermore, studies show that action-game players are more likely to succeed at short-term concentration tests while they perform below average in long-term, less exciting activities. At the point of game addiction, difficulties with focus are likely to become much more apparent [ 12 ]. Studies show a substantial association between gaming addiction and inattention, even after controlling other variables such as personality factors, anxiety and depression symptoms, and attention deficit hyperactivity disorder [ 13 , 14 ].
Prior studies have illustrated the association between video game addiction and psychiatric disorders, social phobia, mental well-being, and risky health behaviors [ 15 , 16 , 17 ]. Another study shows an association between video game addiction and memory, attention, cognitive, and learning abilities among Lebanese children [ 18 ]. However, all of these studies explain the association without controlling for any history of mental or behavioral disorders such as ADHD, anxiety, or depression. However, to the best of our knowledge, a few studies have specifically investigated the effect of attention and child memory on the relationship between video game addiction and cognitive and learning abilities in Egyptian children. Therefore, this study aimed to explore the mediation effect of attention and child memory on the association between addiction to video game and cognitive and learning abilities among Egyptian children. Our hypotheses were: (1) child attention mediates the relationship between video game addiction and cognitive and learning abilities among Egyptian children; and (2) child memory mediates the relationship between video game addiction and cognitive and learning abilities among Egyptian children.
Literature review
Video games have transformed into complex experiences that embody principles recognized by psychologists, neuroscientists, and educators as crucial for behavior, learning, and cognitive functions. While video games offer social and entertainment benefits, extensive research indicates that their excessive use can lead to adverse psychological consequences and even addiction in a minority of players. Symptoms like impaired control over gaming and prioritizing games over daily responsibilities may signify gaming addiction [ 19 ].
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) acknowledged video game addiction as an internet gaming disorder in its fifth edition, highlighting the need for further research [ 20 ]. Similarly, the 11th edition of the International Classification of Diseases (ICD-11) classified gaming disorder as a recurrent pattern of gaming behavior that encompasses both online and offline gaming [ 21 ]. Scientific evidence indicates that addictions can develop due to a combination of genetic susceptibility and repeated exposure to specific stimuli [ 22 ].
Growing public concerns have emerged regarding the potential negative impacts of video games, notably on children’s memory [ 23 ]. Individuals with various behavioral disorders and those with addictive tendencies often find their memory, crucial for comprehension and cognitive abilities like memory updating and working memory, compromised [ 24 ]. Although some research delves into video games’ effects on cognitive functions and academic achievement in children [ 25 , 26 ], the impact on memory remains a contentious topic.
Despite being a leisure activity, video gaming can pose issues for certain children, impacting their ability to focus. Meta-analysis and systematic reviews by Ho et al. and Carli et al. indicated a link between inattention and addiction to the internet and gaming [ 27 ]. Additionally, numerous studies corroborated this connection, demonstrating a robust correlation between the severity of inattention in ADHD and addiction to the internet or gaming. This correlation persisted even after controlling for factors such as depression and anxiety symptoms, as well as personality traits [ 27 ].
Study design and sample
This study has a cross-sectional descriptive design. It was conducted in two convienient selected preparatory schools, Emam Mohamed Abdo Preparatory and Omar Ibn Elkhatab Preparatory School. The two schools are affiliated with xxx. The participants were selected at random from the list of school principals. The research was open to all students between the ages of 9 and 13 with no history of physical, mental, or cognitive disorders. Each student’s parents provided the questionnaire responses. Using the G-power software 3.1.9.2, the study’s sample size was determined. Based on an average effect size of f = 0.15, a 2-sides test at alpha = 0.05, a statistical power (1-β) of 0.95, and eight predictors (age, gender, educational level of the child and mother, video game addiction, memory, attention, and learning abilities), power analysis was performed. A minimum of 166 participants were required based on these criteria.
Ethical consideration
The study approved by the Research Ethics Committee (REC) of Mansoura University’s Faculty of Nursing (IRB P0506/9/8/2023). The study’s purpose, methodology, duration, and benefits were also explained to the directors of the two selected institutions. Mothers’ consents obtained after explaining the study’s objective and the data kept confidential. The participants were informed that they had their right to withdraw from the study at any time.
Data Collection
The following tools were utilized in the study:
Socio-demographic questionnaire
Child and mother’s information was collected, such as age, sex, number of children, and level of education.
- Video game addiction
We used the Game Addiction Scale for Children (GASC) to measure children’s video game addiction. The GASC developed by Yılmaz, Griffiths [ 28 ] according to DSM criteria to evaluate gaming addiction. It includes 21 self-reported items rated on five-point Likert scale (from 1 = never to 5 = very frequently), where higher score shows more hazardous online gaming usage. An individual’s total score can range from a minimum of 21 to a maximum of 105; a score above 90 may be a sign of a video game addiction. It is also emphasized that this is not a diagnostic tool, however, but merely an indicator that a child may have a gaming addiction. Such a diagnosis could only be made by a comprehensive clinical evaluation. Seven criteria for video game addiction are determined by the scale: salience, tolerance, mood modification, withdrawal, relapse, conflict, and issues. The scale shows an acceptable internal consistency reliability ( r = 0.89, p < 0.001) [ 19 ].
Children’s memory
We used the Children’s Memory questionnaire (CMQ) to assess children’s memory rated by their parents. The CMQ developed by Drysdale, Shores [ 29 ]. It included 34 items that rated on a five-point Likert scale ranging from 1 = never or almost never, to 5 = more than once a day. Higher scores indicate a more significant reduction in the cognitive domain. The scale is divided into three subscales: working memory and attention, visual memory, and episodic memory. The Cronbach alpha value for the episodic memory subscale was 0.88, the visual memory is 0.77, and the working memory is 0.84 [ 29 ].
Attention of children
The Clinical Attention Problems Scale was used to measure children’s attention level in the morning and afternoon. This scale was developed by Edelbrock and Rancurello [ 30 ] and includes 12 items. The possible responses are 0 = not true, 1 = somewhat or sometimes true, and 2 = very often or often true. The higher the scores, the more attention there is. The Cronbach alpha values for the clinical attention problem in the morning is 0.84 and for the afternoon is 0.83.
Cognitive and learning skills
We used the Learning, Executive, and Attention Functioning (LEAF) scale to measure children’s cognitive and learning skills. The LEAF scale is a self-reported 55 items scale developed by Castellanos, Kronenberger [ 31 ]. The scale assesses core cognitive abilities and related academic and learning abilities. The LEAF assesses cognitive skills such as attention, processing speed, working memory, sustained sequential processing to accomplish goals (such as planning and carrying out goal-directed tasks), and new problem-solving. Moreover, the LEAF approach takes into account academic functioning, declarative/factual memory, and understanding and concept formulation.
The LEAF includes 55 items, with 11 academic subscales that rate a person’s reading, writing, and mathematics proficiency. The LEAF is divided into subscales that measure comprehension and conceptual learning, factual memory, attention, processing speed, visual-spatial organization, sustained sequential processing, working memory, new problem-solving, mathematics, basic reading, and written expression skills. Each subscale has the same number of items. The responses were rated on a three-point scale ranging from 0 to 3. Higher scores indicate more significant issues with cognition. The five component items are added to provide the subscale score for each of the 11 subject areas. Three criterion-referenced ranges are established for the interpretation of LEAF subscale raw scores. Out of nine, a score of five to nine is classified as the “borderline problem range,” a score of less than five as the “no problem range,” and a score of nine or above as the “problem range.” The Cronbach alpha value for the LEAF scale is 0.96.
Validity and reliability
Study tools were translated into Arabic by the researchers. Five pediatric nursing and psychiatric and mental health nursing experts tested them for content validity. At first, the scales were translated into Arabic using a forward and backward translation method. The translated questionnaires were then adapted to fit Arabic cultural norms. Two highly proficient native Arabic speakers who are accomplished academics in the fields of psychiatry and mental health nursing, and hold the academic status of Full Professor translated the questionnaire from English to Arabic. An English-language expert who is fluent in Arabic back translated the Arabic version. Native Arabic speakers who were not involved in the translation process verified the final translation. The forward-to-back translation process was repeated until the comparative findings matched exactly. The questionnaires were then given to three Arabic psychiatric nursing professionals, who provided their opinions on its importance, relevance, and simplicity. The tools’ reliability was tested using Cronbach’s alpha test (tool I α = 0.86, tool II α = 0.81, tool III α = 0.95, and tool IV α = 0.95, respectively). Additionally, a confirmatory factor analysis were carried out to validate the content of the four scales after translation. The data collection methods were performed over approximately four months from February to May. Also, a pilot study was conducted to assess the study tools’ feasibility and determine the time required to complete the tools. 10% of the initial participants were randomly selected from the same schools. Minimal modifications were then made to the tools. Mothers of students who participated in the pilot study were excluded from the primary study. The data was collected for four months (February to May). An online Google form was created to collect data. The link was then shared with selected student parents through WhatsApp groups. The link outlined the study’s purpose and methods, and participants signed a consent form.
Data collection procedure
We obtained permission to translate the study scales into Arabic. We collected data from February to May using an online Google Form for four months. The Google Form included full details regarding the study’s aims and processes to ensure transparency and establish participants’ trust. An extensive description of the response process additionally supports the Attention Problems Scale. For instance, mothers are required to respond to the items and their relevance to their children in the morning and afternoon. We distributed the survey link to the selected students’ mothers through WhatsApp groups as it was convenient and widespread among the target demographic. Before proceeding to the survey questions, participants were required to read and sign this consent form to ensure that participants received information about the study and voluntarily consented.
Statistical analysis
We employed the Statistical Package for Social Science version 26 [ 23 ] to analyze the data. We analyzed the demographic data using descriptive statistics such as means, standard deviations, frequency, and percentages. In order to evaluate the mediator effects of memory and attention on the relationship between cognitive, academic, and learning skills and video gaming addiction, we ran the multiple regression PROCESS macro with 5,000 bootstraps in SPSS version 3.4 [ 24 ]. We also included confounding variables, such as the age of the child, gender, the age of the mother, education, and job status, as covariates in the mediation model.
Sample characteristics
There were 169 children their mothers responded to the study surveys. The children’s mean age was 13 (SD = 3.9), while the mothers’ mean age was 41 (SD = 7.1). According to mothers, the children were ranked third in their household. Most mothers (72%) said they lived in rural areas. About 61% of the families had at least three children. Half of the mothers had high school or less education, and more than half were unemployed. Most children were in middle school (72%), see Table 1 .
Study variables description
The mean scores for all scales are presented in Table 2 . The mean score of the video gaming addiction total scale was 61 ± 19.3, indicating a moderate level of addiction. The attention total scale mean was 9 ± 6.50, indicating moderate attention problems. The mean score on the total scale for child memory was 80 ± 31,4, indicating moderate memory issues. Eight subscales of the LEAF had mean scores of 5: factual memory, processing speed, visual-spatial organization, sustained sequential processing, working memory, novel problem-solving, mathematics skills, and written expression skills. These mean scores indicate that a borderline problem exists. However, the mean scores for the comprehension and conceptual learning subscale, attention subscale, and basic reading skills subscale were below five, indicating that there was no problem.
Mediating effect of memory, attention problem on the association between video gaming addiction and cognitive, learning, and academic skills
Video game addiction had a significant impact on attention problems (b = 0.34, p < 0.001; a1), and child memory (b = 0.18, p < 0.001; a2). In turn, both attention problems (b = 0.48, p < 0.001; b1) and child memory (b = 0.38, p < 0.001; b2) had significant impact on cognitive and learning skills. The results reveal a significant indirect effect of video game addiction on cognitive and learning skills through attention problems (b = 0.17, CI: 0.82, 0.25; c ’ 1). However, there was no significant indirect effect of video game addiction on cognitive and learning skills through child memory (b = 0.07, CI: -0.01, 0.16; c ’ 2). The analysis revealed that confounding variables had no significant effect on the direct or indirect pathways linking video game addiction to cognitive and learning skills. The direct effect of video game addiction on cognitive and learning skills in the presence of the mediators was also found to be significant (b = 0.11, CI: 0.008, 0.401; c ’ -c). Figure 1 displays the mediation analysis findings.
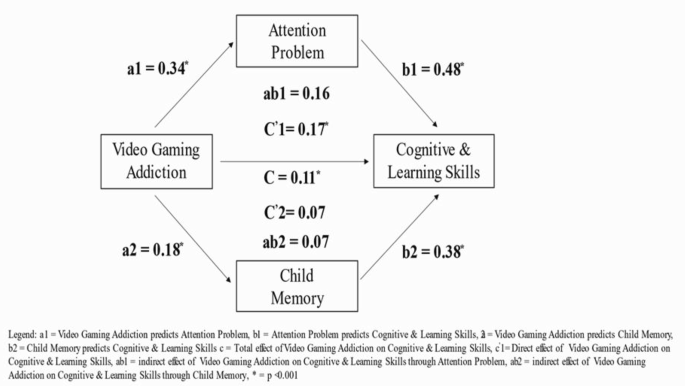
Mediation effect of attention problem and child memory on the association between video gaming addiction and cognitive and learning skills
Previous research has explored the relationship between video game addiction, attention, and memory. Some studies have focused on the relationship between video game addiction and cognitive and learning skills. Others have examined the association between video gaming addiction and all other variables (attention, memory, learning, and cognitive skills). However, no study has explicitly examined the direct and indirect effect of video gaming addiction on learning and cognitive skills through the mediation effect of attention and memory.
This study was done on a sample of Egyptian school children to evaluate the mediation effect of attention and memory on the relationship between video game addiction and cognitive and learning abilities in children. The present study reveals that a gaming addiction can significantly impact attention and memory. This result agrees with Farchakh, Haddad [ 6 ], who conducted a study on a group of Lebanese school children aged 9 to 13 to investigate the association between gaming addiction, attention, memory, cognitive, and learning skills. They found that a greater degree of addiction to video gaming was significantly associated with worse attention scores and worse memory scores. An earlier study suggests that the link between inattention and video game addiction could be described by game genres’ immediate response and reward system. Alrahili, Alreefi [ 2 ] suggest that this may alleviate the boredom typically reported by inattentive users while simultaneously introducing a lack of responsiveness to real-world rewards. Another study on Turkish schoolchildren aged 10 to 16 years old revealed that the total recall scores of the subject group (children who regularly play video games) are significantly lower than those of the control group (children who do not regularly play video games; [ 7 ]).
The current study demonstrates that attention and child memory significantly impacted cognitive and learning skills. This agrees with the opinion of, Gallen, Anguera [ 32 ], who argues that children and young people process information differently, affecting the performance of various cognitive tasks. Additionally, this result disagrees with the findings of Ellah, Achor, and Enemarie [ 26 ], who have stated that students’ working memory has no statistically significant correlation with learning and problem-solving skills. Moreover, their same study showed that different measures of working memory can be attributed to a small variation in low-ability students’ problem-solving skills.
The results revealed a significant indirect effect of video game addiction on cognitive and learning skills through attention. This could be related to the relationship between attention and learning skills. Attention is an essential factor in the learning process because it helps a person make efficient use of data by directing their learning to relevant components and relationships in the input material. If a student can pay attention, they may be able to better retain and understand this material; if not, a lack of attention may lead to difficulties in learning and academic performance. As video gaming addiction affects students’ attention, it may directly affect learning skills [ 33 ]. Another study agrees with the current result, revealing that video game addiction negatively affects adolescents’ learning skills and grade point average [ 34 ].
A child’s memory has an effect on their cognitive and learning skills. Encoding, consolidating, and retrieving experiences and information are the foundation for learning new skills and knowledge [ 35 ]. Video game addiction affects children’s memory. Hence, the expectation is that video game addiction directly affects cognitive and learning skills. However, the present study reveals no significant indirect effect of video game addiction on cognitive and learning skills through child memory. For example, perceptual attention to the exterior world and reflective attention to interior memories need modification of shared representational components in the occipitotemporal cortex. This is shown in episodic memory by recovering an experience from memory, which includes reactivating some of the same sensory areas used during encoding. Furthermore, the prefrontal cortex involves continuous and reflecting attention [ 36 ]. The prefrontal cortex controls memory recall by choosing target memories and filtering or suppressing competing memories [ 36 ].
Another aspect that may be responsible for the absence of a mediating effect of memory on the association between video game addiction and cognitive and learning skills is the presence of the many factors that affect learning and cognitive skills besides memory alone. Life circumstances can affect learning skills rather than memory itself, for example. Problem solving (one of the learning skills) requires a brain that works effectively. Therefore, it is critical to address needs such as physical health, which is influenced by self-care needs such as diet, sleep, and relaxation, as well as children’s social and emotional needs. Furthermore, learning experiences that use all the senses, rather than only hearing or seeing information, result in effective and straightforward information retrieval from memory during problem-solving processes. Such abilities are supposed to be acquired by active participation in learning activities by children [ 37 ]. Finally, long-term focus on online gaming may eventually lead to neglect in learning, leading to a deterioration in learning performance [ 38 ].
Limitations
Our study has some limitations. First, we administered the Clinical Attention Problems Scale only once per student rather than conducting repeated measurements in the morning and afternoon. This approach overlooks potential daytime variations in attention levels, limiting our understanding of each child’s attentional profile. This choice was driven by practical considerations such as reducing the testing burden and participant fatigue. Future research could address this limitation by implementing repeated assessments to comprehend better daytime patterns in children’s attention levels and their implications for learning and behavior. Causality analysis was not possible due to the use of a cross-sectional sample. In addition, some results may be attributable to the small sample size. To fully understand the complex interplay between video game addiction and cognitive outcomes, longitudinal studies and controlled experiments are necessary to provide more conclusive insights into the relationship. It was difficult to include both parents in the study, as most of the fathers said they were too busy to participate. Hence, mothers were the subjects of the study. Certain differences (or lack thereof) are probably artifacts of the sample size. As a result, our findings must be validated by analyzing larger samples. Despite these limitations, this work has the potential to provide insights and open new research avenues.
Implications
Healthcare professionals should be aware of how much children participate in these games and be willing to engage in in-depth conversations with parents about the impact these games may have on children’s health. Therefore, periodical workshops should be held by pediatric and community mental health nurses to enhance student awareness of the effects of video games on their memory, attention, and academic performance. In addition, teaching programs should be held at schools to improve students’ attention, memory, learning, and cognitive skills.
Video game addiction has a significant impact on children’s attention and memory. Both attention and memory have a significant impact on a child’s cognitive and learning skills. These results reveal a significant indirect effect of video game addiction on cognitive and learning skills through attention. However, video game addiction had no significant indirect effect on cognitive and learning skills through child memory. In the presence of the mediators, the direct impact of video game addiction on cognitive and learning skills was also significant.
Data availability
No datasets were generated or analysed during the current study.
Almutairi TA et al. Prevalence of internet gaming disorder and its association with psychiatric comorbidities among a sample of adults in three arab countries. Middle East Curr Psychiatry. 2023;30(1).
Alrahili N, et al. The prevalence of video game addiction and its relation to anxiety, depression, and attention deficit hyperactivity disorder (ADHD) in children and adolescents in Saudi Arabia: a cross-sectional study. Cureus. 2023;15(8):e42957–42957.
PubMed PubMed Central Google Scholar
Johannes N, Vuorre M, Przybylski AK. Video game play is positively correlated with well-being. Royal Soc open Sci. 2021;8(2):202049–202049.
Article Google Scholar
Esposito MR, et al. An investigation into video game addiction in pre-adolescents and adolescents: a cross-sectional study. Med (Kaunas Lithuania). 2020;56(5):221.
Google Scholar
American Psychiatric Association, D., &, Association AP. Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5). American psychiatric association Washington. DC; 2013.
Farchakh Y, et al. Video gaming addiction and its association with memory, attention and learning skills in Lebanese children. Child Adolesc Psychiatry Mental Health. 2020;14(1):46–46.
Özçetin M, et al. The relationships between video game experience and cognitive abilities in adolescents. Neuropsychiatr Dis Treat. 2019;15:1171–80.
Article PubMed PubMed Central Google Scholar
Kwak KH, et al. Comparison of behavioral changes and brain activity between adolescents with internet gaming disorder and student pro-gamers. Int J Environ Res Public Health. 2020;17(2):441.
Lee D, et al. Gray Matter differences in the anterior cingulate and orbitofrontal cortex of young adults with internet gaming disorder: surface-based morphometry. J Behav Addictions. 2018;7(1):21–30.
Mondéjar T, et al. Analyzing EEG waves to support the design of serious games for cognitive training. J Ambient Intell Humaniz Comput. 2019;10:2161–74.
Bediou B, et al. Meta-analysis of action video game impact on perceptual, attentional, and cognitive skills. Psychol Bull. 2018;144(1):77–110.
Article PubMed Google Scholar
García-Redondo P, et al. Serious games and their effect improving attention in students with Learning Disabilities. Int J Environ Res Public Health. 2019;16(14):2480.
Evren C, et al. Relationships of Internet addiction and internet gaming disorder symptom severities with probable attention deficit/hyperactivity disorder, aggression and negative affect among university students. ADHD Atten Deficit Hyperactivity Disorders. 2019;11(4):413–21.
Stavropoulos V, et al. Associations between attention deficit hyperactivity and internet gaming disorder symptoms: is there consistency across types of symptoms, gender and countries? Addict Behav Rep. 2019;9:100158–100158.
Ahmed GK, et al. Relation between internet gaming addiction and comorbid psychiatric disorders and emotion avoidance among adolescents: a cross-sectional study. Psychiatry Res. 2022;312:114584.
Raouf SYA, et al. Video game disorder and mental wellbeing among university students: a cross-sectional study. Pan Afr Med J. 2022;41:89–89.
Purwaningsih E, Nurmala I. The impact of online game addiction on adolescent mental health: a systematic review and meta-analysis. Open Access Macedonian J Med Sci (OAMJMS). 2021;9(F):260–74.
Farchakh Y, et al. Video gaming addiction and its association with memory, attention and learning skills in Lebanese children. Child Adolesc Psychiatry Mental Health. 2020;14(1):1–11.
Nogueira M, et al. Addictive video game use: an emerging pediatric problem? Acta Med Port. 2019;32(3):183–8.
Christakis DA. The challenges of defining and studying digital addiction in children. JAMA. 2019;321(23):2277–8.
Kök Eren H, Örsal Ö. Computer game addiction and loneliness in children. Iran J Public Health. 2018;47(10):1504–10.
Choi BY, et al. Transitions in problematic internet use: a one-year longitudinal study of boys. Psychiatry Investig. 2019;16(6):433–42.
Du X, et al. Compensatory increase of functional connectivity density in adolescents with internet gaming disorder. Brain Imaging Behav. 2017;11(6):1901–9.
Lim JA, et al. Changes of quality of life and cognitive function in individuals with internet gaming disorder: a 6-month follow-up. Med (Baltim). 2016;95(50):e5695.
Teng Z, et al. A longitudinal study of link between exposure to violent video games and aggression in Chinese adolescents: the mediating role of moral disengagement. Dev Psychol. 2019;55(1):184–95.
van den Eijnden R, et al. The impact of heavy and disordered use of games and social media on adolescents’ psychological, social, and school functioning. J Behav Addict. 2018;7(3):697–706.
Evren C, et al. Relationships of Internet addiction and internet gaming disorder symptom severities with probable attention deficit/hyperactivity disorder, aggression and negative affect among university students. Atten Defic Hyperact Disord. 2019;11(4):413–21.
Yılmaz E, Griffiths MD, Kan A. Development and validation of videogame addiction scale for children (VASC). Int J Mental Health Addict. 2017;15(4):869–82.
Drysdale K, Shores A, Levick W. Use of the everyday memory questionnaire with children. Child Neuropsychol. 2004;10(2):67–75.
Edelbrock C, Rancurello MD. Childhood hyperactivity: an overview of rating scales and their applications. Clin Psychol Rev. 1985;5(5):429–45.
Castellanos I, Kronenberger WG, Pisoni DB. Questionnaire-based assessment of executive functioning: psychometrics applied neuropsychology. Child. 2018;7(2):93–109.
Gallen CL, et al. Enhancing neural markers of attention in children with ADHD using a digital therapeutic. PLoS ONE. 2021;16(12):e0261981–0261981.
Lindsay GW. Attention in psychology, neuroscience, and machine learning. Front Comput Neurosci. 2020;14:29–29.
van den Eijnden R, et al. The impact of heavy and disordered use of games and social media on adolescents’ psychological, social, and school functioning. J Behav Addictions. 2018;7(3):697–706.
Scerif G, et al. Making the executive ‘function’for the foundations of mathematics: the need for explicit theories of change for early interventions. Educational Psychol Rev. 2023;35(4):110.
Miller EK, Lundqvist M, Bastos AM. Working memory 2.0. Neuron. 2018;100(2):463–75.
Aydoğan Y, Özyürek A. The relationship between problem-solving skills and memory development in preschool children. J History Cult Art Res. 2020;9(3):43.
Jin Y, et al. Social Factors Associated with Video Game Addiction among teenagers: School, Family and Peers, in advances in Social Science, Education and Humanities Research. Atlantis; 2021.
Download references
Acknowledgements
The authors extend their heartfelt appreciation and gratitude to all parents who willingly participated in the study.
The authors gratefully acknowledge the funding of the Deanship of Graduate Studies and Scientific Research, Jazan University, Saudi Arabia, through Project Number: GSSRD-24.
Author information
Authors and affiliations.
Department of Nursing, College of Nursing, Jazan University, Jazan, Kingdom of Saudi Arabia
Amani Ali Kappi
Psychiatric and Mental Health Nursing Department, College of Nursing, Mansoura University, Mansoura, Egypt
Rania Rabie El-Etreby & Warda El Shahat Hamed
Pediatric Nursing Department, College of Nursing, Mansoura University, Mansoura, Egypt
Ghada Gamal Badawy & Gawhara Ebrahem
You can also search for this author in PubMed Google Scholar
Contributions
Amany Ali Kappi contributed to the project by designing the methodology, performing formal analysis, analyzing the data, and writing both the original draft and the manuscript. Rania Rabie El-Etreby contributed to conceptualizing, methodology, conducting, drafting, reviewing, and editing the manuscript. Ghada Gamal Badawy, was responsible for designing, executing, and documenting the investigation, including methodology, and manuscript preparation. Gawhara Ebrahem was responsible for designing, executing, and documenting the investigation, including methodology, and manuscript preparation Warda El Shahat Hamed conceptualized and prepared the methodology and investigation and contributed to writing the original draft. She also reviewed and edited the document. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Warda El Shahat Hamed .
Ethics declarations
Ethics approval and consent to participate.
The researchers obtained approval for this study and data collection in this study from the Research Ethical Committee (REC) of Mansoura University’s Faculty of Nursing (IRB P0506/9/8/2023). All procedures were conducted in accordance with ethical standards outlined by the responsible committee on human experimentation and the Helsinki Declaration of 2008. Consent forms were obtained from all participants. Informed consent was obtained from all the participants in this study (from the mothers of the participant children).
Consent for publication
Not applicable.
Patient or public contributions
No patient or public contributions.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kappi, A.A., El-Etreby, R.R., Badawy, G.G. et al. Effects of memory and attention on the association between video game addiction and cognitive/learning skills in children: mediational analysis. BMC Psychol 12 , 364 (2024). https://doi.org/10.1186/s40359-024-01849-9
Download citation
Received : 16 April 2024
Accepted : 10 June 2024
Published : 24 June 2024
DOI : https://doi.org/10.1186/s40359-024-01849-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Child memory
- Learning skills
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Pandemics and Clinical Psychology
Pandemics are complex events involving a range of stressors affecting mental health. The recent COVID-19 pandemic served as a catalyst, accelerating preexisting trends in clinical care such as the rise of e-health for rapidly and broadly disseminating psychological services. The process of adapting face-to-face clinical services to online formats occurred rapidly during COVID-19, underscoring the adaptability of clinicians to meet new challenges. However, COVID-19 also highlighted important shortcomings in clinical care, including planning deficiencies and shortages of clinicians with specialized training for treating various psychological problems (e.g., prolonged grief disorder). These problems and potential solutions are discussed.
11.11.1. Introduction
Pandemics are outbreaks of infectious diseases that spread globally, affecting millions of people. Epidemics, in comparison, are lesser, more localized outbreaks, limited to a few countries. Pandemics and some epidemics arise from emerging infectious diseases; that is, diseases for which most people have no pre-existing immunity. Pandemics are an inevitable part of human existence and likely to become more prevalent in the coming years, given the rapidly growing global population, increasing population mobility due to mass transportation (e.g., air travel), and the likely change in disease dynamics that will come with climate change (e.g., increasing prevalence of tropical diseases in formerly temperate regions).
The psychological footprint of pandemics, particularly the more severe outbreaks, tends to be larger than the medical footprint, in that psychological effects are more pronounced, widespread, and longer-lasting than the purely somatic effects of infection ( Taylor, 2019 , 2021d ). To illustrate, for every COVID-19 fatality, there is an average of five bereaved immediate family members ( Verdery et al., 2020 ). This underscores the fact that pandemics can have wide-reaching effects even on people who may not have been infected.
Historically, the importance of psychological factors in pandemics has been neglected by scientists and health authorities despite evidence that pandemics are, to a large extent, psychological phenomena in which beliefs and behaviors influence the spreading versus containment of infection ( Taylor, 2019 ). Psychological factors are important in determining (a) adherence to pandemic-mitigation methods (e.g., social distancing protocols, mask-wearing, vaccine uptake), (b) pandemic-related socially disruptive events (e.g., panic-buying, protest rallies against social restrictions), and (c) pandemic-related psychopathology such as anxiety or mood disorders, contamination-related obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and prolonged grief disorder ( Taylor, 2019 , 2021b ).
Although each pandemic had its characteristic features, such as its sociocultural context and disease characteristics, many of the basic psychological phenomena observed in the COVID-19 pandemic were apparent in past pandemics and other major outbreaks, particularly the more lethal outbreaks, such as the 1889 Russian flu pandemic, the 1918 Spanish flu pandemic, and the 2003 outbreak of Severe Acute Respiratory Syndrome (SARS). Notable similarities include the following: (a) the role of the news media in both calming and alarming the populace; (b) the initial efforts of political leaders to downplay the seriousness of the outbreak so as to calm people and keep the economy running; (c) the rise of anticipatory anxiety ahead of the arrival of infection in one's community; (d) the rise of xenophobia, rumors, and conspiracy theories; panic buying; (e) the new onset of mental disorders and worsening of preexisting ones; (f) protests over social distancing restrictions and related mandates; (g) the rise of quack cures and profiteering; and, (h) the occasional rioting and violent protests but, more commonly, a rise of altruism as people come together to help one another ( Taylor, 2019 , 2021b ).
Important differences between COVID-19 and past pandemics include, for COVID-19, the effects of the 24/7 news cycle and social media, and differences in medical management (e.g., availability of treatments for secondary pneumonia). Not all past pandemics or outbreaks had significant impacts on mental health. Although the Russian flu, Spanish flu, and SARS outbreaks had deleterious effects on mental health ( Taylor, 2019 ), other pandemics such as the 1957 and 1968 influenza pandemics had apparently little impact ( Honigsbaum, 2020 ). Differences can be attributed to a range of factors including disease lethality and contagiousness, whether the disease killed in gruesome or excruciating ways, and the extent to which health authorities and the news media reacted with alarm about the outbreak.
Pandemics are dynamic events, often occurring in waves. These are caused, in part, by fluctuations in patterns of human aggregation. This occurs, for example, as part of seasonal movements of people away from and then into contact with one another, as occurs when schools are closed for the summer and then reopen ( Herrera-Valdez et al., 2011 ). Pandemics are also dynamic in terms of psychological reactions, with anxiety levels rising, for example, as infection rates rise in communities, and anxiety abating as social restrictions are lifted ( Asmundson and Taylor, 2020 ). Psychological reactions may also change as the pandemic progresses, especially if government-mandated restrictions such as social distancing are implemented. With the prolonged stress of rolling lockdowns (i.e., recurrent stay-at-home orders), and other restrictions on social gatherings, a phenomenon known as pandemic fatigue can occur, characterized by progressively worsening adherence to social distancing guidelines accompanied by negative emotions such as depression, irritability, and apathy ( World Health Organization, 2020 ).
In summary, pandemics are not simply about some microbe “going viral.” Behaviors, emotions, and attitudes play a key role in the spreading versus containment of disease, distress, and societal disruption. Psychology plays a vital role in every aspect of pandemic management, including the development of effective public messaging to encourage adherence to pandemic mitigation measures, and methods for managing pandemic-related mental health problems. Strategies for improving public health messaging have been discussed at length in various publications (e.g., World Health Organization, 2020 ). The purpose of this chapter is to focus specifically on the role of clinical psychology in pandemics and pandemic management. That is, to (a) review the types of psychopathology arising during pandemics such as COVID-19, (b) discuss the state-of-the-art of clinical services for pandemics, and (c) consider the clinical psychological needs and services for future pandemics. In the following sections, discussion is put in context with a brief review of pandemic-related stressors and how they are linked to psychopathology, along with a summary of contemporary methods of pandemic management.
11.11.2. Pandemic-Related Stressors
Uncertainty is a pervasive, abstract stressor during pandemics ( Taylor, 2021b ). Examples include uncertainties about whether a disease outbreak will become a pandemic, how dangerous it will be, whether there are effective prophylactic measures, how long the pandemic will last, who is infected (e.g., who is an asymptomatic carrier), and whether the pandemic is over or whether there will be another wave of infection. The voluminous amount of pandemic-related news and social media information—the so-called infodemic —adds to the uncertainties, including uncertainties about which news stories or rumors are accurate and which are misinformed or even fake. Uncertainties can lead to high levels of worry (as in generalized anxiety disorder; GAD), particularly for people who have high levels of intolerance of uncertainty, as discussed later in this chapter.
In addition to uncertainty-related stressors, there are several other pandemic-related stressors, which are potentially associated with various forms of psychopathology. Examples include (a) the loss of loved ones, potentially leading to prolonged grief disorder, (b) threats to, or loss of, occupation and income (e.g., due to lockdown or economic recession), leading to potential problems including anxiety and mood disorders, substance use disorders, and suicide (c) trauma exposure (e.g., exposure to death, child or spousal abuse during lockdown, life-threatening infection), and trauma-related disorders, (d) exposure to infection and the development of contamination-related OCD, especially in people with preexisting risk factors for these disorders (e.g., preexisting obsessive-compulsive tendencies), and (e) persistent direct effects of the infection itself such as chronic dyspnea or fatigue (i.e., the stress of chronic disease) ( Taylor, 2019 , 2021b ).
11.11.3. Goals of Pandemic Management
There are two broad goals in managing pandemics, of which psychology is central to both: (a) to encourage people to take the pandemic seriously and to adopt the recommended pandemic mitigation practices such as social distancing, and (b) to encourage these practices without precipitating mass panic. Governments and health authorities have long expressed concerns about pandemic-precipitated mass panic or mass hysteria, reflecting the tendency for government leaders to regard crowds as sources of irrational thinking and dangerous behavior ( Tomes, 2010 ). While many people might become highly anxious or engage in panic buying during a pandemic, mass panic tends to be rare ( Taylor, 2019 ). Nevertheless, such episodes have occurred (see Taylor, 2019 , for examples). Accordingly, the World Health Organization (WHO) (2005) raised concerns about mass panic during pandemics.
Pandemic mitigation involves risk communication in which health authorities and other community leaders inform the public about the degree of risk posed by the pandemic, and make recommendations or mandates about pandemic mitigation strategies. These involve hygiene practices (e.g., handwashing, covering coughs), social distancing strategies (e.g., remaining six feet apart from strangers when out in public), stay-at-home recommendations or mandates, adherence to mask-wearing and vaccination, and strategic closures of places of congregation such as bars, restaurants, places of amusement (e.g., cinemas), schools, and churches. Clearly, people in the community need to agree to adhere to these behaviors, restrictions, or closures in order for these methods to be effective.
Sometimes, pandemic mitigation methods are more important for calming the public than for reducing the risk of infection. In the early months of 2020 during the COVID-19 pandemic, for example, health authorities emphasized the importance of cleaning and disinfecting surfaces and objects that might be contaminated with the SARS-CoV-2 virus. In later months, as research on the transmission of the virus accumulated, it became apparent that contaminated surfaces or objects were not as important as previously thought, and that infection was spread primarily through droplets and erosols (e.g., coughing, sneezing) ( Goldman, 2020 ). In fact, the WHO acknowledged that there is limited evidence of SARS-COV-2 being transmitted via contaminated surfaces ( Lewis, 2021 ). Yet, vigorous cleaning and disinfecting persisted; trains, buses, and public spaces were vigorously washed, restaurant tables were scrubbed, and objects touched by people were assiduously sanitized. This excessive cleaning was dubbed hygiene theater ( Thompson, 2020 ), which served more to reassure the public than to reduce the spread of infection. Hygiene theater fostered a sense of control during the pandemic, albeit a largely illusory one. Note that the notion of hygiene theater is not new; a very similar idea was raised in 1918 during in the Spanish flu in which some medical authorities believed that facemasks provided a false sense of security, which could nonetheless be useful in alleviating public anxiety ( Price, 1919 ). In other words, donning a mask gave the wearer a false sense of control, which was useful in allaying public anxiety about infection.
11.11.4. Pandemic-Related Psychopathology: an Overview
11.11.4.1. covid-19.
Pandemic-related stressors can amplify or exacerbate various types of mental health problems, including anxiety and related disorders, mood disorders, and substance-use disorders. Accordingly, it is not surprising that the severity of these disorders tended to be exacerbated during COVID-19 ( Asmundson et al., 2020 ). During COVID-19, clinically significant anxiety or depression also occurred in some people who had no prior history of anxiety or mood disorders. During the early stages of the pandemic in 2020, for example, there was widespread distress in communities, with about 20% of people having elevated levels of anxiety or depression ( Taylor et al., 2020a ). Meta-analytic research indicates that the mental health consequences of COVID-19 during the short-term (i.e., during the pandemic) were equally high among countries in which COVID-19 was widespread and equally prevalent across genders ( Cénat et al., 2021 ).
Longitudinal surveys conducted over the course of COVID-19 in 2020 indicated that, on average, there was a progressive deterioration in mental health as pandemic mitigation restrictions were drawn out. This occurred for people of all walks of life including older adults, young adults, and youth ( Prati and Mancini, 2021 ). Although people tend to be resilient, a substantial minority were emotionally affected by COVID-19. Deterioration in mental health mainly involved increases in depression, but also increases in anxiety, insomnia, and substance abuse ( Prati and Mancini, 2021 ). Longitudinal studies during 2020 further found that depressed mood tended to persist or progressively worsen whereas anxiety levels tended to fluctuate; for example, anxiety rose as cases of infection increased and anxiety diminished as infection rates abated and social distancing restrictions were eased ( Yarrington et al., 2021 ).
Deterioration of mental health during 2020 was linked to a range of factors, particularly the restrictions placed by lockdown and associated effects such as reductions in both income and physical activity ( Prati and Mancini, 2021 ). Lockdown required many people to work from home. Working from home can be stressful if the home environment is not conducive to this arrangement, such as when one is working from home while also caring for young children.
After communities were released from lockdown, mental health tended to improve on average, even when other pandemic restrictions (e.g., restrictions on social gatherings) were still in place and vaccines had not yet become available ( Richter et al., 2021 ). However, not all people are likely to recover unaided from pandemic-related stress. Forecasting modeling from England in 2020 suggested that about 20% of the UK population would need either new or additional mental health support as a direct consequence of the COVID-19 pandemic ( O'Shea, 2020 ). The long-term mental health effects of COVID-19 may not become fully apparent until many years after the pandemic is over. This could include the long-term effects of disrupted education and restricted socialization opportunities for children, and job loss for adults. For both children and adults, long-term effects could also include persistent bereavement and lingering health effects of SARS-COV-2 infection.
11.11.4.2. Past Outbreaks
Many past pandemics and outbreaks, such as the Russian flu, Spanish flu, 2009 Swine flu pandemic, and SARS, were associated with community-wide increases in emotional distress ( Honigsbaum, 2013 ; Taylor, 2019 ). In the years following both the Russian and the Spanish flu pandemics there were increases in first-time admissions to psychiatric hospitals ( Mamelund, 2010 ). In the years following the 2003 SARS outbreak there was a rise in mental disorders in people who had acquired the disease, as compared to those who were not infected ( Tzeng et al., 2020 ). In contrast to these pandemics and outbreaks, other pandemics, such as the 1957 and 1968 influenza pandemics, were apparently associated with very little distress or lingering effects. Compared to the Russian flu, Spanish flu, and COVID-19, the pandemics of 1957 and 1968 were milder. That, along with the lack of government restrictions and the lack of media attention, may account for the relative lack of public anxiety. The pandemics of 1957 and 1968 are instructive because they show that widespread anxiety is not an inevitable reaction to pandemics.
11.11.5. Specific Clinical Conditions Associated with Pandemics
11.11.5.1. fear of infection.
During pandemics, it is expected and reasonable for people to experience some degree of fear or anxiety, especially when infection is serious and widespread. These emotional reactions can be adaptive if they motivate the person to take necessary precautions (e.g., wear a mask, get vaccinated). In comparison, our focus here is on extreme, impairing, and disproportionate levels of fear or anxiety in response to infection. Historical descriptions of pandemic-related excessive fears have, in many ways, resembled contemporary definitions of specific phobias, in which fear, avoidance, and anticipatory anxiety were cardinal features ( Taylor, 2019 , 2021a ). Examples include “flu-phobia” during the Spanish flu pandemic, descriptions of phobic responses during the Zika virus and Swine flu pandemics, and references to “coronaphobia” during COVID-19 ( Taylor, 2021a ).
During COVID-19, some clinical investigators began questioning the assumption that pandemic-related fears are simple mono-phobias. There were strong hints from previous outbreaks that fear of infection was part of a broader syndrome or set of syndromes. Research on past pandemics (e.g., Zika, Swine flu) and SARS showed that fear of infection was correlated with obsessive-compulsive contamination symptoms (i.e., health-related checking and reassurance seeking) and with traumatic stress symptoms (i.e., pandemic-related nightmares or intrusive thoughts) ( Taylor et al., 2020a ). The question remained, however, as to whether some combination of these symptoms co-occurred to form a psychopathologic syndrome.
To investigate the issue further, my colleagues and I developed a battery of scales to assess COVID-19-related anxiety reactions, called the COVID Stress Scales ( Taylor et al., 2020b ). Through a process of multivariate statistical analyses, involving factor analyses and other methods, we identified a stable, replicable factor structure consisting of five inter-correlated elements that we termed the COVID Stress Syndrome ( Taylor et al., 2020a , 2020b ). The COVID Stress Syndrome comprises (a) fear of becoming infected with SARS-COV-2 and fear of coming into contact with potentially infected objects or surfaces, (b) COVID-19-related xenophobia (i.e., fear of coming into contact with foreigners for fear that they might be infected), (c) fear of the personal socio-economic consequences of the pandemic (e.g., job loss, financial hardships), (d) compulsive checking and reassurance-seeking about pandemic-related threats (e.g., repetitively checking the news and social media for pandemic-related information), and (e) traumatic stress symptoms about the pandemic (e.g., nightmares, intrusive thoughts pertaining to the pandemic).
The five scales were strongly intercorrelated ( rs ranging from 0.41 to 0.73) and essentially defined a dimensional (rather than present/absent) syndrome ( Taylor et al., 2020a ). Network analyses indicated that fear of becoming infected was at the core of the syndrome. The severity of the syndrome was correlated with a range of preexisting (pre-COVID-19) emotional vulnerability factors, including intolerance of uncertainty, negative emotionality, obsessive-compulsive symptoms, general anxiety about one's health, and heightened perceived vulnerability to disease ( Taylor et al., 2020a , 2020b ).
Severe scores on the scales, combined with evidence of functional impairment due to COVID-19-related distress, are indicative of a COVID Stress Disorder ( Asmundson and Taylor, 2020 ). This disorder represents a combination of symptoms that don't neatly fit into diagnostic categories of major anxiety-related disorders because it combines elements of various disorders (e.g., OCD, PTSD, specific phobia). Instead, severe, impairing forms of the COVID Stress Syndrome are best conceptualized as representing an adjustment disorder, where symptoms wax and wane over time in relation to the perceived degree of threat posed by COVID-19. That is, the severity fluctuated in concert with the prevalence of COVID-19 in the community ( Asmundson and Taylor, 2020 ). Adjustment disorders are not trivial conditions and merit serious attention from clinicians, especially because not all adjustment disorders are transient; some evolve into chronic, progressively intensifying psychopathology ( Bachem and Casey, 2018 ). Further research is needed to investigate the extent to which this occurs for the COVID Stress Syndrome, and whether future pandemics will be associated with similar syndromes. Nevertheless, the findings support the view that pandemic-related fear is more than simply a mono-phobia; instead, fear of infection is an important element of a broader constellation of psychopathology. Accordingly, when assessing patients with pandemic-related anxiety, it is important to conduct a broad assessment of the sources of anxiety or distress in order to identify important targets for treatment.
11.11.5.2. Obsessive-Compulsive Disorder
Research indicates that OCD arises, in part, from gene-environment interactions, where vulnerability genes interact with particular environmental stressors ( Taylor, 2011 ). The specific genes have yet to be delineated, although there are several promising candidate polymorphisms. Pandemics are stressful, protracted environmental events involving uncertainty and the threat of infection and other (e.g., socioeconomic) threats. Pandemic-related stressors are likely to interact with genetic factors for OCD, such as the genetic factors associated with contamination-related obsessions and compulsions ( Taylor, 2011 ). Some forms of contamination-related OCD are associated with fears of becoming infected with pathogens. Such people may have unwanted intrusive thoughts (i.e., obsessions) about becoming infected and may engage in extensive washing or cleaning rituals, and seek out reassurance about their health from loved ones or from medical professionals. These types of OCD symptoms, along with OCD in general, have been exacerbated during the COVID-19 pandemic, leading to heightened anxiety, checking, cleaning, and avoidance of germ-related places or situations (e.g., Taylor et al., 2020a ). Contamination-related OCD, in addition to related disorders such as the COVID Stress Syndrome, may also arise de novo for people with a genetic predisposition that interacts with pandemic-related stressors.
In addition to giving rise to, or worsening, OCD, pandemics can also interfere with the treatment of the disorder. The effects of cognitive-behavior therapy (CBT) for OCD, involving exposure and response prevention, were attenuated during the COVID-19 pandemic ( Storch et al., 2021 ), likely due to a range of factors, including disruptions in access to treatment and reluctance to engage in exposure therapy (e.g., touching contaminated surfaces) because of fears of becoming infected with SARS-COV-2. Research suggests that the COVID-19 pandemic has not interfered with the effects of pharmacotherapy for OCD ( Sharma et al., 2021 ). Given the problems in administering exposure-based therapies during COVID-19, it has been argued that pharmacotherapy should be the first-line treatment for OCD during the pandemic ( Fineberg et al., 2020 ). This recommendation, based on limited research, requires further evaluation. If CBT involving exposure and response prevention is used, it should take into account guidance from health authorities (e.g., hand-washing and cleaning guidelines from the WHO or the Centers for Disease Control and Prevention) rather than ceasing handwashing altogether. Patients also should be discouraged from exceeding the health guidelines, such as the unnecessary use of disinfectants.
11.11.5.3. Posttraumatic Stress Disorder
PTSD can be triggered by traumatic pandemic-related stressors such as the death of a loved one, exposure to widespread death, or personal life-threatening experiences linked to severe infection ( Taylor, 2019 ). PTSD and posttraumatic stress symptoms have been documented in many studies during outbreaks of SARS, Middle East Respiratory Syndrome (MERS), and COVID-19 ( Asmundson and Taylor, 2021 ). A problem in interpreting the findings is that many of the studies were based on flawed methodology; for example, failing to assess whether the person experienced a traumatic stressor, failing to assess whether the putative PTSD symptoms were linked to a traumatic stressor, and failing to determine whether symptoms had been present for at least a month, as required to diagnose PTSD ( Asmundson and Taylor, 2021 ). Some studies have treated the mere experience of living during COVID-19 as a “traumatic stressor.” This excessively broad definition confuses traumatic stressors with milder stressors and does not meet DSM-5 or ICD-11 criteria for a traumatic stressor.
Some of these problematic studies have been included in PTSD meta-analyses, thereby casting doubt on the validity of the meta-analytic findings ( Asmundson and Taylor, 2021 ). A meta-analysis of survivors of MERS and SARS estimated the rate of infection-related PTSD to be 32% ( Rogers et al., 2020 ). Meta-analytic estimates of PTSD prevalence during COVID-19 have ranged widely from 5% to 50% ( Asmundson and Taylor, 2021 ), with findings suggesting that PTSD during COVID-19 was more prevalent among healthcare workers (HCWs) and COVID-19 patients, as compared to the general population. In light of the aforementioned methodological problems, the validity of these findings remains in question.
Very few studies of COVID-19, SARS, or MERS assessed PTSD using a structured clinical interview, which is the diagnostic gold standard. An exception is an Italian study of patients presenting to a hospital emergency department with COVID-19, most of whom were severely ill and hospitalized ( Janiri et al., 2021 ). During their convalescence from COVID-19, patients were assessed with a diagnostic psychiatric interview. The prevalence of PTSD was 30%. Risk factors for COVID-19-related PTSD were female gender, past history of psychiatric disorders, delirium or agitation during the acute phase of COVID-19 infection, and persistent COVID-19 symptoms (i.e., Long COVID). For the latter, the symptoms were most commonly fatigue and dyspnea. Female gender, delirium, and a past history of psychopathology are all previously established risk factors for PTSD in general ( Taylor, 2017 ).
11.11.5.4. Prolonged Grief Disorder
A likely consequence of the COVID-19 pandemic, and probably other severe pandemics, is an increase in the prevalence of prolonged grief disorder, as diagnosed in ICD-11, also known as persistent complex bereavement disorder in DSM-5. This is a severe, chronic grief reaction characterized by persistent yearning and preoccupation with the deceased, combined with intense emotional distress about the loss (e.g., sadness, guilt, anger, blame) ( Shear and Gribbin, 2016 ). Research conducted prior to COVID-19 suggested that prolonged grief disorder occurs in about 10% of bereaved people ( Lundorff et al., 2017 ). The percentage might be higher for COVID-19 because the social restrictions of the pandemic curtailed normal expressions of grief and culturally prescribed mourning, with some people dying in hospitals or long-term care facilities, isolated from friends and family, and even funerals were held virtually. Prolonged grief disorder is likely to afflict a large number of people during COVID-19 because of the prevalence of the disorder among the bereaved (10%) and the large number of people bereaved as a result of COVID-19. As mentioned above, for every COVID-19 death there is an average of five bereaved immediate family members ( Verdery et al., 2020 ). Cognitive-behavioral interventions show promise in treating prolonged grief disorder ( Iglewicz et al., 2020 ).
11.11.5.5. Addictive Behaviors
Substance use and abuse increased substantially during the COVID-19 pandemic. This included increases in alcohol, cannabis, and other drugs such as opiates ( Taylor et al., 2020d ). To illustrate, in a population-representative sample of over 3000 adults from the US and Canada, for people who reported consuming alcohol prior to COVID-19%, 23% reported that their consumption had increased during the pandemic ( Taylor et al., 2020d ). For people who consumed recreational drugs prior to the pandemic, 31% reported that their consumption had increased ( Taylor et al., 2020d ). Substance use and abuse were associated with various pandemic-related stressors, including the stress of social restrictions, such as the extremes of crowding or isolation, child care challenges, and pandemic-related socioeconomic stressors. Substance use and abuse were associated with the COVID Stress Syndrome ( Taylor et al., 2020d ).
Paralleling the pandemic-related increase in substance use and abuse in adults, there was an increase in video gaming disorder and internet gaming disorder among youth, particularly adolescents, likely reflecting an attempt to cope with the stress and boredom of stay-at-home restrictions ( Teng et al., 2021 ). For some people with gambling disorder, their gambling migrated to online gambling when in-person gambling was thwarted due to the pandemic-related closure of casinos ( Xuereb et al., 2021 ). Other problem gamblers reported a shift in addiction from gambling to substance abuse when casinos were closed ( Xuereb et al., 2021 ).
11.11.6. Burnout and Moral Injury Among Frontline Workers
11.11.6.1. burnout.
Workplace-related burnout, as defined in ICD-11, is a syndrome arising from chronic workplace stress that has not been successfully managed. Burnout is characterized by three features, including (a) feeling depleted of energy and exhausted, (b) diminishing commitment to, or involvement with one's job, or negative or cynical attitudes toward one's job, and (c) a sense of ineffectiveness and lack of accomplishment ( WHO, 2019 ). Workplace-related burnout among HCWs is a longstanding problem that worsens during health crizes such as pandemics, especially for frontline HCWs involved in the care of infected patients ( Chor et al., 2020 ). Work-related factors linked to high levels of burnout among HCWs include heavy workload and high job demands, working in unsafe settings (e.g., lack of personal protective equipment), lack of training and experience, limited opportunities for downtime (i.e., limited time for sleep, recreation, or time with friends or family), and lack of support from peers and management ( Morgantini et al., 2020 ).
11.11.6.2. Moral Injury
A phenomenon related to burnout is moral injury, also known as moral stress. Moral injury involves exposure to events or actions that violate one's moral code or values ( Litz et al., 2009 ). That is, moral injury refers to the psychological, social, and spiritual impact of events involving betrayal or transgression of one's own deeply held moral beliefs and values occurring in high stakes situations ( Phoenix Australia, 2020 ). Moral stressors are an unavoidable part of clinical practice where patients are numerous and resources may be comparatively scarce. Moral transgression events can involve people doing or failing to do something, or witnessing such transgressions unfold without being able to remedy the situation. Severe moral stress can involve, for example, a HCW having to decide which patients receive life-saving resources in limited supply, such as ventilators. Moral injury can involve reactions such as shame, guilt, anger, disgust, sadness, anxiety, self-condemnation, and demoralization ( Phoenix Australia, 2020 ). People experiencing moral injury may lose faith in their profession, workplace, or leaders, and often experience existential or spiritual crizes (e.g., loss of previously held religious beliefs, or loss of belief in a just world) ( Phoenix Australia, 2020 ). Moral injury can occur with or without burnout, although the two often co-occur. Moral injury is part of a broader constellation of work-related stressors encountered by HCWs during pandemics, including stigma against HCWs for fear that they are sources of infection ( Taylor et al., 2020 ).
11.11.6.3. Managing Burnout and Moral Injury
Both burnout and moral injury are risk factors for job turnover and absenteeism, and risk factors for various mental health problems including PTSD, anxiety disorders, mood disorders, and substance-use disorders ( Phoenix Australia, 2020 ). Burnout has also been implicated in HCW suicide. Burnout is also a safety issue for patients in that burnout may undermine the ability of HCWs to provide optimal treatment. Burnout and moral injury involve more than simply a failure to cope with chronic workplace stressors; they involve HCWs being unable to provide the level of care needed by patients ( Phoenix Australia, 2020 ). Treatment of burnout and moral injury requires both structural resources (e.g., a safe, adequately supplied work environment), along with organizational support, social support (including peer support) and individual-focused interventions. Promising forms of the latter involve forms of CBT, self-care interventions, and stress management (e.g., Mollica et al., 2020 ). Organizational changes can help protect HCWs from burnout, such as changes that alleviate various workload burdens; for example, changes that lessen the administrative burdens.
11.11.7. Suicide
11.11.7.1. does suicide increase during pandemics.
Wasserman (1992) argued that pandemics involving social restrictions should lead to an increase in suicide because the restrictions decrease social integration, interaction, and support. Accordingly, there has been a great deal of research on whether pandemics and related outbreaks are associated with an increase in attempted or completed suicides. Determining the cause of suicide can be difficult. During COVID-19, for example, there has been an increase in drug overdose deaths ( Centers for Disease Control and Prevention, 2020 ) and in such cases it can be difficult to determine whether the overdose was deliberate or accidental. In other cases, the intent is clearer, such as when a suicide note is left or when the manner of death clearly involved deliberate self-harm (e.g., use of firearms). The determination of whether a death is suicide is made by coroners and, inevitably, research into pandemic-related suicide largely depends on the accuracy of coroners' reports. Accordingly, the following findings need to be interpreted with caution.
The Russian flu coincided with a reportedly marked rise in suicide rate ( Honigsbaum, 2013 ). With regard to the Spanish flu, an analysis of US Census data from 1910 to 1920 revealed that suicide rates increased during the Spanish flu, even after controlling for the effects of the coincident World War I ( Wasserman, 1992 ). An analysis of US Spanish flu data found that social distancing (e.g., school and business closures) predicted suicide rates ( Stack and Rockett, 2021 ), presumably through lowering social interaction and social support in the context of rising financial hardship. During the SARS outbreak in 2003 in Hong Kong there was an increase in suicides among seniors aged over 65 years ( Yip et al., 2010 ). Here, the suicide rate of seniors tripled from previous years to 38 suicides per 100,000 people. A spike in suicides coincided with the peak of SARS infection. SARS was also associated with an increase in suicide in Taiwan ( Tzeng et al., 2020 ). During the 2009 Swine flu pandemic in South Korea, a time series investigation found that the development of influenza-like illness was predictive of suicide mortality ( Jung et al., 2021 ). Collectively, these findings suggest an increase in suicide during pandemics and related outbreaks.
The relationship between COVID-19 and suicide is less clear because, at the time of writing this article (August 2021) the pandemic was ongoing and most of the relevant research on suicide had been conducted during the early phases (first year) of the pandemic. The research has so far failed to resolve into a clear picture about the relationship between COVID-19 and suicide, with studies reporting either increases, no changes or decreases, or a fluctuating pattern during the first year of the pandemic. Numerous studies reported that suicidal ideation increased in the US and Canada during the first year of COVID-19 (e.g., Czeisler et al., 2021 ). Ethnic minorities, younger adults (18–24 years), unpaid caregivers for adults, and essential workers were more likely to report suicidal ideation in these studies. In Nepal, during lockdown early in COVID-19, the rate of suicide increased, as compared to pre-lockdown ( Pokhrel et al., 2021 ). In Germany, suicide rates in early 2020, as compared to previous years, were unusually high ( Radeloff et al., 2021 ). In Japan, the suicide rate initially declined early in the COVID-19 pandemic and then rose later in 2020 ( Tanaka and Okamoto, 2021 ). Many other studies, however, conducted during the first year of COVID-19, found that suicidal ideation or attempted or completed suicide had not increased from previous years (e.g., Radeloff et al., 2021 ).
The impact of pandemics on attempted and completed suicides likely depends on a variety of factors, including the suicide prevention measures and other barriers to self-harm that might be put in place. Accordingly, suicide rates may vary across pandemics, across time periods during a given pandemic (e.g., early vs. late), across economic impacts (e.g., suicide increases when there is massive unemployment), and the availability of self-harm mitigation resources (e.g., clinics, helplines). Given these considerations, it is not surprising that inconsistent findings have emerged during COVID-19. A coherent picture of the relationship between COVID-19 and suicide might not be available until some years after the pandemic ends particularly because some of the effects of COVID-19 (e.g., economic effects) might not be fully apparent for some years.
11.11.7.2. Healthcare Worker Suicide
Even during non-pandemic times, physicians tend to have higher suicide rates than the general population ( Dutheil et al., 2019 ). Physicians are often reluctant to seek mental health services out of career concerns, work culture, or a predisposition toward self-reliance ( Duarte et al., 2020 ). During both COVID-19 and the Spanish flu pandemics there were many cases in which physicians, nurses, paramedics, and other HCWs committed or attempted suicide ( Mortier et al., 2021 ). Risk factors for suicidal ideation or attempts included (a) being a frontline worker coming in contact with pandemic patients, (b) having suspected or confirmed pandemic infection and fear of transmitting this infection to others, including loved ones, (c) having a preexisting mental disorder, (d) having relationship or career difficulties, and (e) work-related stress, burnout, and moral injury ( Duarte et al., 2020 ; Mortier et al., 2021 ). It is unclear whether the suicide rate of HCWs increased during COVID-19, as compared to pre-pandemic periods. Nevertheless, there have been numerous reports of physicians and other HCWs taking their lives because they felt unable to provide adequate care for COVID-19 patients ( Moutier et al., 2021 ).
11.11.7.3. Suicide Mitigation
Suicide mitigation during COVID-19 has involved a variety of methods, including public education, government assistance to offset economic stressors, e-health resources (e.g., internet-based stress management advice, as described below), telephone hotlines, and preemptive approaches targeting at-risk populations, such as resiliency training for HCWs and outreach programs for socially isolated seniors ( Moutier et al., 2021 ). The methods for reducing burnout and moral injury may also reduce HCW suicide.
11.11.8. Vulnerability Factors for Pandemic-Related Emotional Disorders
11.11.8.1. biopsychosocial factors.
A range of factors can contribute to pandemic-related worsening or new-onset of psychological problems. Vulnerability factors for pandemic-related psychopathology include the biopsychosocial factors for psychopathology in general ( Taylor, 2019 ). Traumatic stressors during the pandemic (e.g., exposure to death on a wide scale, or personal life-threatening infection) are examples ( Taylor, 2017 , 2019 ). In other cases, gene-environment interactions may be at play, as discussed earlier with regard to OCD. Cognitive factors such as dysfunctional beliefs and misinterpretations about health-related stimuli can also play a role in exacerbating pandemic-related negative emotions, including health anxiety. Cognitive-behavioral factors in pandemic-related anxiety are discussed elsewhere ( Taylor, 2019 , 2021a , 2021c ). Personality traits can also pandemic-related emotional disorders, as described below.
11.11.8.2. Personality Traits
In the following sections, we focus on pre-pandemic vulnerability traits that may predispose people to experience pandemic-related psychopathology. The list of traits is not exhaustive but focuses rather on the most promising traits for understanding pandemic-related emotional disorders, as suggested by studies before and during COVID-19.
11.11.8.2.1. Negative Emotionality
Negative emotionality (i.e., neuroticism) is the tendency to experience negative emotions in response to all kinds of stressors, large and small. This broad trait is thought to confer vulnerability for many kinds of psychopathology ( Brandes et al., 2019 ). Negative emotionality predicted fears of infection in past pandemics and outbreaks ( Taylor, 2019 ) and was associated with heightened distress levels in the community during COVID-19 ( Taylor et al., 2021 ). Although negative emotionality is composed of narrow traits, research supports of bifactor model of negative emotionality, consisting of a general factor (negative emotionality) in addition to distinct, but correlated, narrow traits ( Brandes et al., 2019 ). Narrow traits include the intolerance of uncertainty.
11.11.8.2.2. Intolerance of Uncertainty
Intolerance of uncertainty is a personality trait characterized by the extent to which a person is anxious about uncertainties in daily life ( Birrell et al., 2011 ). People with high levels of intolerance of uncertainty have a strong desire for predictability and tend to worry about uncertainties ( Birrell et al., 2011 ). Research conducted before COVID-19 shows that a high degree of intolerance of uncertainty is associated with a range of disorders, including GAD, OCD, and other clinical conditions such as severe health anxiety ( Rosser, 2018 ). People with high levels of intolerance of uncertainty try to reduce uncertainty by behaviors such as checking and reassurance-seeking ( Dugas and Robichaud, 2007 ). In the case of health-related uncertainty, this can involve repeatedly checking the Internet for medical information, or persistently seeking reassurance from doctors. The intolerance of uncertainty is likely to be a particularly important contributor to pandemic-related anxiety. This is because pandemics are associated with all kinds of uncertainties, as discussed earlier. People with a high degree of intolerance of uncertainty tend to become highly anxious about the threat of infectious disease, especially if they perceive themselves as having limited control over the threat. The news media can fuel uncertainties with speculative reports about what “might” happen during an outbreak of infectious disease ( Taylor, 2019 ). During COVID-19, high levels of intolerance of uncertainty were associated with the COVID Stress Syndrome, panic buying, maladaptive coping, and high levels of distress during lockdown ( Taylor, 2021c ; Taylor et al., 2020a ). CBT for GAD ( Dugas and Robichaud, 2007 ) can be beneficial because one of the targets of treatment involves improving one's tolerance for uncertainty.
11.11.8.2.3. Boredom Proneness
Lockdown, quarantine, and other social distancing restrictions in which people are required to remain home for long periods are conducive to boredom. Boredom is an unpleasant state of being weary and restless, where time drags and nothing maintains one's interest or focus of attention. Boredom motivates people to seek out new experiences, even if those experiences have negative consequences ( Bench and Lench, 2019 ). Boredom proneness is a trait characterized by the tendency to experience boredom in a wide range of situations ( Farmer and Sundberg, 1986 ). Boredom proneness is correlated with (a) the tendency to experience negative emotions such as depression, anxiety, and irritability, (b) substance-use disorders and related conditions such as problem gambling, mobile phone addiction, and internet addiction, (c) low adherence to home-schooling during pandemic-related school closures, and (d) the tendency to disregard social distancing guidelines (e.g., Boylan et al., 2021 ; Yang et al., 2020 ). Little is known about the best way to reduce boredom proneness. It is negatively correlated with mindfulness ( Regan et al., 2020 ), which raises questions of whether the two are causally related and whether training in mindfulness might reduce boredom proneness.
11.11.8.2.4. Stress Buffering Traits
Some personality traits are protective, stress-buffering factors that enable the person to cope with life stressors without developing emotional disorders. Trait optimism and trait resilience are buffering factors against stressors in general. Research conducted during COVID-19 suggests that trait optimism and trait resilience modulate (inhibit) the effects of negative emotionality on COVID-19-related distress such as the COVID Stress Syndrome ( Taylor et al., 2021 ).
It could be argued that introversion is a protective factor during lockdown because introverted people, compared to extraverts, may be better able to endure the social isolation of lockdown because introverts do not require or desire high levels of social interaction. However, COVID-19 research conducted during lockdown suggests that introversion/extraversion is not a strong predictor of distress; instead, other personality traits, particularly negative emotionality and intolerance of uncertainty, are more important predictors ( Taylor et al., 2021 ).
11.11.8.2.5. Other Personality Traits
Several other traits have been examined in relation to pandemics and other outbreaks. These include various anxiety-related traits such as trait anxiety, harm avoidance, the overestimation of threat, perfectionism, and anxiety sensitivity ( Taylor, 2019 ). Further research is needed to better understand how these traits are related to pandemic-related distress.
11.11.8.3. The Behavioral Immune System
Pathogens such as viruses are too small to directly observe and so a person's biological immune system is insufficient for avoiding exposure to these threats. It is necessary to use perceptible cues to detect and avoid pathogens. Such cues include noxious smells, visual stimuli, and auditory cues, like the sights and sounds of people coughing. The behavioral immune system (BIS) is conceptualized as a system for detecting such cues ( Schaller and Park, 2011 ). When cues are detected, this triggers an emotional response (e.g., fear, disgust), which motivates the person to avoid or escape the aversive cues. The BIS is biased toward false positives (i.e., false alarms) in detecting pathogens, which is adaptive to the extent that it minimizes exposure to potentially fatal pathogens ( Schaller and Park, 2011 ). Thus, the BIS can be sensitive to cues that only superficially resemble environmental signs of infection; for example, the sight of someone sneezing is a superficial disease cue that could be due to any of a number of things (e.g., allergies, dust exposure, or the common cold).
There are individual differences in BIS sensitivity, known as the perceived vulnerability to disease ( Duncan et al., 2009 ). People who have a high degree of perceived vulnerability to disease tend to be excessively worried about becoming infected during a pandemic such as COVID-19 ( Taylor et al., 2020a ), and also tend to generally worry about their health ( Taylor, 2019 ). Perceived vulnerability to disease is also tied to racism. A common way of acquiring an infectious disease is from other people, especially when foreign groups intermingle, in which one group introduces a disease that the other group has never encountered and has no immunity against. Given that many infections are transmitted through interpersonal interactions, the BIS is said to have evolved to influence social attitudes and interactions, including ethnocentrism and negative attitudes toward immigrants and other foreigners ( Schaller and Park, 2011 ). Consistent with this, research shows that when people feel threatened about becoming infected with some pathogen, they tend to avoid or stigmatize out-groups (i.e., a group which a person does not belong to, or identify with) ( Taylor, 2019 ). Thus, out-groups are blamed for causing or spreading diseases, such as being blamed for lack of hygiene, education, self-control, or other factors such as cultural practices. Moreover, people who are most frightened of infection are most likely to avoid foreigners and have negative attitudes toward such people ( Taylor, 2019 ; Taylor et al., 2020a ).
If a population is threatened with severe infection, the BIS will be activated in almost everyone, with some people having particularly intense levels of activation. This suggests that during times of pandemic there will be a general increase in stigmatization and xenophobia, where foreigners and other out-groups are blamed for being sources of infection. Indeed, racism was a common feature of past pandemics and other outbreaks ( Taylor, 2019 ). Racism and other forms of xenophobia were widely documented during COVID-19, including a number of racist attacks against Asians in the US ( Man, 2020 ). Xenophobic fears that foreigners are spreading SARS-CoV-2 is also a feature of the COVID Stress Syndrome ( Taylor et al., 2020a ).
11.11.9. Long-Term Effects of Infection
11.11.9.1. long covid.
Long COVID was a term coined by people who suffered from persistent COVID-19 symptoms; that is, symptoms persisting even after the person had recovered from the acute phase of infection. The term was created in an effort to raise awareness among members of the medical community and government leaders about persistent COVID-19-related symptoms ( Callard and Perego, 2021 ). The diagnostic criteria for Long COVID are imprecize in terms of the nature and duration of symptoms. There have been efforts at developing specific criteria ( National Institute for Clinical Excellence, 2020 ), but further research is needed. Despite this limitation, the available research provides an approximate indication of the prevalence of various symptoms.
A prospective study of over 4000 cases of COVID-19 found that symptoms persisted for at least 2 months in 5% of patients, and for at least 3 months in 2% ( Sudre et al., 2021 ). Here, Long COVID was characterized by fatigue, headache, dyspnea, and anosmia. The odds of having persistent symptoms were higher with greater age and body mass index, and female gender ( Sudre et al., 2021 ). Other studies reported that a quarter or more of COVID-19 survivors described having at least one persistent symptom for at least 2 months after disease onset (e.g., Carfì et al., 2020 ). Patients who were hospitalized for COVID-19 were most likely to have persistent symptoms. More than 75% of hospitalized patients reported symptoms 6 months after getting ill despite having no detectable virus load, and even patients who initially experienced mild symptoms may develop Long COVID ( Ludvigsson, 2021 ). Cases of Long COVID are not restricted to adults. Pediatric cases (ages 9–15 years) have been described, where symptoms persisted for at least 6–8 months after an initial diagnosis of COVID-19 ( Ludvigsson, 2021 ). Common persistent symptoms included fatigue, dyspnea, palpitations, headaches, and concentration difficulties, which were similar to those reported in adults.
Clinical accounts of Long COVID suggest that there may be periods of remission and relapse, along with the emergence of new symptoms ( Altmann and Boyton, 2021 ). In such cases, it can be challenging to determine which symptoms are due to COVID-19 and which are coincidental, perhaps due to some pathophysiology other than that associated with COVID-19. A further issue for investigation is whether there are different pathophysiological types of Long COVID. Long COVID in which fatigue is a central feature has been compared to Chronic Fatigue Syndrome (CFS), also known as myalgic encephalomyelitis. Although Long COVID could be a post-viral form of CFS, it is hazardous to label Long COVID as simply “chronic fatigue”, because such a label could dissuade medical practitioners from adequately investigating the cause of the symptoms. With regard to treatment, aside from medical management, CBT for chronic fatigue has been suggested, although its efficacy in reducing COVID-related fatigue has been questioned ( Vink and Vink-Niese, 2020 ).
11.11.9.2. Comparison with Other Outbreaks
Similar to Long COVID, there is evidence of long-term effects of SARS and MERS. For example, there were descriptions of patients assessed 3 months or longer after recovering from acute SARS or MERS who reported persistent fatigue, breathlessness, and other symptoms such as concentration difficulties ( Ahmed et al., 2020 ). Similarly, historical records suggest that there were long forms of the Russian and Spanish flu. Post-infection chronic fatigue was observed in both pandemics. Commenting on patients seen during the Russian flu pandemic, one physician observed that “many patients recovering from a case of influenza which had run a normal unchecked course frequently suffered for six or nine months, or even a year, from pronounced symptoms such as depression, neurasthenia, neuritis, and other ills which we could only describe as ‘nervous’” ( Turner, 1919 , p. 77).
11.11.10. Managing and Treating Pandemic-Related Psychopathology
11.11.10.1. understanding coping in order to enhance resilience.
Resilience is the ability to successfully adapt to stress and adversity. It involves, among other things, the ability to implement adaptive coping skills. Understanding naturally occurring patterns of coping during pandemics is important for understanding how to improve the resilience of communities. Human beings are social creatures and so lockdown and related social distancing interventions can lead to loneliness, depression, and other forms of distress. Not surprisingly, higher levels of social support are associated with lower levels of lockdown-related distress ( Taylor et al., 2020a ). With regard to coping during COVID-19, several salient findings have emerged. Adaptive coping behaviors, including problem-solving (e.g., trying new activities), adopting a healthy lifestyle, and emotion regulation skills (e.g., limiting exposure to distressing news media), tend to be associated with lower levels of COVID-19-related distress ( Fullana et al., 2020 ). CBT can improve resilience in various ways, such as training people in coping skills ( Joyce et al., 2018 ), including the coping skills associated with lower pandemic-related distress.
11.11.10.2. Enhancing the Resilience of Healthcare Workers
During COVID-19, increases in physical activity and exercise were among the most commonly used coping behaviors of HCWs, although many also expressed interest in resiliency training programs ( Shechter et al., 2020 ). Military organizations, such as the US Department of Defense, have developed training programs for enhancing the resiliency of soldiers and medical staff working in theaters of combat. Recently, there have been efforts to adapt these procedures for improving the resiliency of HCWs during COVID-19 ( Albott et al., 2020 ). This involved a combination of educational webinars, skills training, and structural changes to workplace operations. HCWs received education about the nature and risk factors for workplace-related burnout and PTSD. Skills training involved education about simple, practical, readily implemented coping strategies (e.g., reaching out to colleagues, positive self-talk, limiting exposure to disturbing news media, maintaining a healthy lifestyle, and other stress-reducing activities such as yoga or meditation) ( Albott et al., 2020 ). Stress reactions were framed as normal reactions that one should expect and plan to address. In addition, self-assessment tools can be used to improve awareness among HCWs of whether they are developing problems such as burnout and whether they should seek help ( Wei et al., 2020 ).
Structural changes to the workplace can reduce the demands placed on HCWs, thereby reducing workplace stress. Changes to the workplace environment may involve, among other things, the use of peer support groups and other forms of social support, including an on-site mental health consultant, who could facilitate training in stress management, provide additional support, and coordinate referrals for external professional consultation ( Albott et al., 2020 ).
The Battle Buddies component of the HCW resiliency training ( Albott et al., 2020 ) is particularly promising because it is simple to implement and likely to be very useful in dealing with workplace stress. It involves HCWs pairing up, such that pairs are similar in demographics, occupational roles, and seniority. Buddies are matched as far as possible on these variables because the nature of occupational stressors can differ considerably across demographics, roles, and seniority (e.g., people in managerial positions face different stressors than people in junior positions). Members of each pair are able to debrief with one another each day, brainstorming potential solutions to problems and providing mutual support. During daily check-ins, buddies share their reactions to stressors (e.g., “I'm afraid I'm going to bring the virus home”), validate each other's experiences (rather than debating or arguing), offer their perspectives and discuss possible solutions, and encourage the seeking of additional help if stressors or anxieties escalate ( Albott et al., 2020 ). Battle Buddies are selected specifically not to be close friends or confidantes (or spouses) because sometimes difficult conversations or observations must be made without the fear of jeopardizing close friendships. Further research is needed to evaluate the efficacy of resiliency training programs for reducing burnout and other psychological problems in HCWs.
11.11.10.3. Community-wide Interventions: the Rise of E-Health
Pandemics, especially those in which social restrictions are imposed, impact the delivery of mental health services and increase the number of people requiring such services ( O'Shea, 2020 ). Accordingly, there is a need for free, widely available, and remotely accessible mental health services during a pandemic and likely afterward. Face-to-face psychological consultations may not be possible due to social distancing restrictions, and the sheer magnitude of people requiring such services makes one-to-one consultations untenable.
During pandemics, methods are needed for rapidly providing services widely, for a range of psychological problems. For the most part, the development of these during COVID-19 was reactive rather than proactive; that is, programs were not developed in anticipation of the rise of pandemic-related mental health needs but rather arose once it became apparent that there was widespread distress in the community. Such services tended to be piecemeal in nature; that is, the development of a single type of service or intervention (e.g., a phone app for stress management) instead of developing a comprehensive approach to mental health.
Although piecemeal approaches are unlikely to be sufficient in addressing community-wide pandemic-related distress, studies of specific interventions have identified promising interventions for inclusion in broader programs. Research has demonstrated the value of online cognitive-behavioral reappraisal exercises for reducing distress during COVID-19 ( Wang et al., 2021 ). Reappraisal exercises are simple, adaptable, efficient, and among the most effective cognitive interventions for changing emotional responses ( Webb et al., 2012 ). Two types of reappraisal were found to be effective in reducing distress during COVID-19, including reconstrual and repurposing ( Wang et al., 2021 ). Reconstrual involves changing how the situation is construed or mentally represented. For example, instead of saying to oneself, “We will never get through this pandemic”, one could say “I know from world history that keeping calm and carrying on gets us through tough times.” Repurposing involves focusing on potentially positive outcomes of a situation. For example, instead of saying to oneself, “Lockdown is horrible,” one could say, “Lockdown helps me realize the importance of social connections and helps me identify the most important people in my life.”
Simple cognitive restructuring methods, while useful, are not new in their application to pandemic-related distress. During the Spanish flu, simple cognitive strategies were also recommended for anxious people, involving distraction (“Think of something else”) and positive thinking, and reappraisal strategies (e.g., warning people about misinterpreting cold symptoms as indications of a far more serious infection) ( Literary Digest, 1918 ).
Regarding other interventions, research shows that a brief online self-guided cognitive-behavioral intervention is useful in reducing excessive worry about COVID-19 ( Wahlund et al., 2020 ). Mindfulness training, which can be delivered digitally, also shows promise in improving resilience during COVID-19 ( Yuan, 2021 ). Empathy-focused telephone calls delivered by lay counselors reduced loneliness, depression, and anxiety in housebound adults during COVID-19 ( Kahlon et al., 2021 ). Brief CBT, delivered online or as a phone application can improve sleep quality for people suffering from insomnia ( Cheng et al., 2020 ).
Various types of online stress management interventions, as used in non-pandemic times, have been shown to be useful in reducing distress ( Amanvermez et al., 2020 ), and can be adapted for managing distress during COVID-19 lockdown ( Jasti et al., 2020 ). Innovative interventions using online-administered virtual reality are also under development, providing interventions such as imagery-augmented relaxation exercises ( Riva and Riva, 2020 ). Videoconferencing methods can also be used to deliver, for suitable patients, cognitive restructuring and exposure therapies for PTSD ( Fina et al., 2020 ). For people hospitalized for COVID-19 but not on a ventilator, preliminary evidence suggests that either in-person or online CBT can reduce distress ( Shaygan et al., 2021 ).
In summary, there are a number of promising treatment resources that can be accessed by large numbers of people, including those living in remote settings, far from the consulting rooms of major metropolitan areas. Clearly, however, there are limits to e-health and some patients will require inpatient hospitalization, such as for suicidal ideation, severe depression, psychosis, or substance dependence.
11.11.10.4. Comprehensive Mental Health Management
During COVID-19, arguably the most comprehensive multicomponent program for pandemic-related mental health problems was developed in Chengdu, China, by He and colleagues ( He et al., 2020 ). This program was rapidly deployed in the early months of COVID-19. Administered by a multidisciplinary team of mental health professionals, the program was designed to reach members of the community as well as at-risk groups. The program had four main components:
- • TV and radio programs, broadcast nightly, discussing COVID-19-related psychological problems and offering information and advice. These were supplemented and promoted through Chinese social media platforms (i.e., WeChat, Weibo, and TikTok), drawing the attention of millions of viewers.
- • 24-h hotline consultations were provided free through six dedicated hotlines. Complex or urgent cases were referred on for consultation sessions.
- • Online video consultation sessions involved the use of psychological interventions and pharmacotherapy. Cases were referred from the hotline or from COVID-19 hospitals.
- • On-site (hospital or clinic) crisis intervention for two groups of people: (a) COVID-19 confirmed, suspected, or quarantined cases who showed signs of psychological distress, and (b) frontline HCWs, who were provided with training in stress management.
Preliminary data showed that this rapidly deployed, comprehensive program was feasible, well-received by the community, and attracted large numbers of calls and consultations, sometimes numbering hundreds of hotline calls per day ( He et al., 2020 ). The merits of the program require further evaluation. The program will likely be insufficient for treating all types of pandemic-related psychopathology, particularly for patients requiring inpatient admission and patients requiring specialized psychological services. To illustrate the latter, specialty clinics have emerged, offering CBT for chronic fatigue associated with Long COVID ( Vink and Vink-Niese, 2020 ; and see below). Accordingly, the comprehensive program developed in Chengdu could be augmented in various ways, such as by adding, as needed, specialized treatment services and in-patient psychiatric services.
11.11.11. Future Directions for Research and Clinical Practice
11.11.11.1. covid-19 as catalyst.
COVID-19 has served as a catalyst, altering the delivery and scope of clinical psychological services. Regarding delivery, treatment approaches during the COVID-19 pandemic have involved an increasing use of e-health (e.g., cognitive-behavioral programs via phone or internet) as well as interventions to boost the resilience of frontline workers. Psychologists and other healthcare professionals rapidly adapted to the restrictions imposed by COVID-19 by moving their clinical practices to online or telephone formats when face-to-face consultations became impractical during stay-at-home and related restrictions. This enhanced a trend already in place prior to COVID-19 for practitioners to increasingly rely on e-health forms of delivery. The treatment program developed by He and colleagues (2020) , as described earlier, serves as an exemplary model of how mental health needs in the community can be rapidly and widely addressed with the aid of e-health. This program highlighted the importance of planning for forthcoming problems, such as planning to deal with a surge in mental health problems; that is, being proactive in order to anticipate and prepare for problems, rather than taking a reactive approach in which problems are not addressed until they become too great to be ignored. Research is needed to evaluate the potential merits of proactive versus reactive approaches to developing clinics and other clinical services.
COVID-19 shifted the scope of clinical practice, with a growing number of patients requiring help for pandemic-related anxiety and for symptoms associated with PTSD, OCD, Long COVID, and prolonged grief disorder. Treatments for these disorders require specialized clinical training. To the extent that there is a shortage of suitably qualified clinicians, there will be a shortfall in meeting the mental health needs of communities. Based on COVID-19 research so far accumulated, there will likely be a strong demand for mental health services during the post-pandemic period. To meet these needs, clinical training programs may need to alter their focus by giving greater emphasis to pandemic-related disorders such as PTSD and prolonged grief disorder.
To better meet the clinical psychological needs of communities, the scope of clinical practice needs to change in other ways, such as in the type and mode of delivery of psychoeducation. Psychoeducation is a key ingredient of clinical practice, in which patients gain, among other things, a better understanding of the nature and treatment of their problems. During pandemics, patients may ask for advice from their treating clinicians about a range of pandemic-related issues, such as issues related to personal safety (e.g., mask-wearing, vaccine uptake), advice on coping (e.g., what to do if there is an outbreak of panic buying in one's community), issues about managing anxieties about returning to work or resuming social recreational activities, and issues about how patients might communicate with friends or family members who subscribe to conspiracy theories or other extreme beliefs. Ideally, clinicians would be informed and able to provide evidence-based advice on these issues, tailored to the specifics of the patient's circumstances. Patients may also benefit from advice about how to manage the infodemic; that is, advice about how to locate and evaluate authoritative, reliable health-related information (see Taylor, 2021b ).
With the rise of e-health, the question arises about the best way of delivering psychoeducation in order to address the needs of communities. For issues relevant to many people (e.g., stress management), psychoeducation could be delivered via the news or social media (as per He et al., 2020 ). During the COVID-19 pandemic, community-wide psychoeducation was implemented on an ad hoc, unsystematic basis, with some psychological organizations producing psychoeducational fact sheets for consumers, and psychologists and other mental health practitioners offering advice to the public via news stories, social media, and other formats. This approach could be refined for future pandemics and other disasters. For example, leading psychological associations could set up an expert panel to provide advice to the public about important psychological matters, with an emphasis on providing practical, evidence-based guidance. That is, moving away from glib, pop psychological pronouncements seen in midday talk shows toward evidence-based advice that is presented in a way that engages the audience without sensationalizing the subject matter.
As part of psychoeducation, communities need to be made aware of online and other mental health resources. Many distressed people during COVID-19 did not make use of mental health resources (e.g., online programs) ( Taylor et al., 2020a ), possibly because of a lack of awareness of such programs, or difficulty deciding which programs would be useful. Clinical psychologists can address this problem by offering authoritative advice, both in their consultations with patients and in broader community work (e.g., public service announcements, media interviews).
11.11.11.2. Psychological Field Clinics
Pandemics, just like natural disasters, require clinicians to be flexible and creative, adapting established treatments in non-traditional ways in order to meet the mental health needs of communities. The rise of e-health is one example. During pandemics such as COVID-19, there is also a need for psychological field clinics, just like the temporary, “pop-up” testing and vaccination clinics during COVID-19. These clinics were placed throughout communities in order to make them readily available to the public. In a similar way, temporary psychological field clinics could be established to address the mental health needs of any particular widespread emergency, whether it be a pandemic or some other stressor. Such clinics could serve as drop-in resources for people wanting information or advice about psychological issues, including advice about referral resources. To enhance their utilization, psychological field clinics could be integrated into medical clinics; for example, a pandemic testing clinic could have an on-site psychological clinic, offering brief consultations and advice about referrals and other useful resources for people. Research on health anxiety shows that such psychological clinics are more likely to be utilized by people if the clinics are integrated into general medical clinics ( Taylor, 2019 ).
11.11.11.3. Psychological Triage
The concept of triage is well-developed in general medicine. Here, the degree of severity and urgency of cases are evaluated in order to determine the course of treatment in circumstances in which the demand for medical resources exceeds their availability. Regarding the triage of psychological services, there are screen-and-treat protocols in which the degree and type of intervention increase with the severity and complexity of the patient's problems. An example of a pandemic-related screen-and-treat protocol appears in Fig. 1 ( Taylor, 2019 ). Here, interventions may involve some combination of educational online materials, self-help phone apps or internet self-guided cognitive-behavioral programs, and telehealth (e.g., videoconferencing) sessions with a mental health professional. This protocol, which was developed prior to the onset of COVID-19, has many similarities to the protocol independently developed and implemented in Chengdu by He et al. (2020) . Details of screen-and-treat approaches, along with a discussion of screening methods and patient handouts, are discussed elsewhere ( He et al., 2020 ; Taylor, 2019 ). Such protocols can be readily adapted to the specifics of a particular community-wide stressor (e.g., a pandemic), although the protocols may need to be fine-tuned and evaluated to ensure they meet the mental health needs associated with a given stressor.

Screen-and-treat flowchart for targeting mental health problems.
11.11.12. Conclusion
Pandemics are complex, dynamic events involving a range of stressors that can seriously affect mental health. Pandemics tend to be particularly stressful when it becomes necessary for governments to impose social restrictions, such as stay-at-home orders. Those restrictions are necessary to stem the spread of infection, but impact the mental health of many people. Although most people are resilient to stress, a substantial minority are likely to have psychological disorders that may persist if untreated. This includes worsening or new onset of various disorders, including mood and anxiety disorders, substance use disorders, PTSD, OCD, and prolonged grief disorder. Frontline HCWs, compared to the community at large, are especially vulnerable to developing symptoms of these disorders. Additionally, people diagnosed with COVID-19 are at risk for both PTSD and Long COVID. To treat pandemic-related clinical problems, it was necessary for clinicians to adapt existing practices (e.g., face-to-face psychotherapy) to meet the challenges of pandemics; for example, by moving to e-health. COVID-19 served as a catalyst for such developments. Further research is needed to refine and evaluate these methods. Research is needed to evaluate and refine specific interventions and the comprehensive treatment programs that contain these interventions. It is also necessary to identify and overcome potential barriers to mental healthcare, including financial barriers to accessing mental health services. Widespread, freely available e-health services may help offset this problem. Further research is also needed to refine and evaluate mental health services for various vulnerable populations, including the elderly, children, indigent and incarcerated individuals, and ethnic minorities.
- Ahmed H., Patel K., Greenwood D.C., Halpin S., Lewthwaite P., Salawu A., et al.Sivan M. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J. Rehabil. Med. 2020; 52 (5):jrm00063. doi: 10.2340/16501977-2694. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Albott C.S., Wozniak J.R., McGlinch B.P., Wall M.H., Gold B.S., Vinogradov S. Battle Buddies: rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. Anesth. Analg. 2020; 131 (1):43–54. doi: 10.1213/ANE.0000000000004912. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Altmann D.M., Boyton R.J. Decoding the unknowns in long COVID. BMJ. 2021; 372 :n132. doi: 10.1136/bmj.n132. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Amanvermez Y., Rahmadiana M., Karyotaki E., de Wit L., Ebert D.D., Kessler R.C., Cuijpers P. Stress management interventions for college students: a systematic review and meta-analysis. Clin. Psychol. Sci. Pract. 2020:e12342. doi: 10.1111/cpsp.12342. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Asmundson G.J.G., Paluszek M.M., Landry C.A., Rachor G.S., McKay D., Taylor S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J. Anxiety Disord. 2020; 74 :102271. doi: 10.1016/j.janxdis.2020.102271. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Asmundson G.J.G., Taylor S. Coronaphobia revisited: a state-of-the-art on pandemic-related fear, anxiety, and stress. J. Anxiety Disord. 2020; 76 :102326. doi: 10.1016/j.janxdis.2020.102326. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Asmundson G.J.G., Taylor S. Garbage in, garbage out: the tenuous state of research on PTSD in the context of the COVID-19 pandemic and infodemic. J. Anxiety Disord. 2021; 78 :102368. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bachem R., Casey P. Adjustment disorder: a diagnosis whose time has come. J. Affect. Disord. 2018; 227 :243–253. doi: 10.1016/j.jad.2017.10.034. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bench S.W., Lench H.C. Boredom as a seeking state: boredom prompts the pursuit of novel (even negative) experiences. Emotion. 2019; 19 :242–254. doi: 10.1037/emo0000433. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birrell J., Meares K., Wilkinson A., Freeston M. Toward a definition of intolerance of uncertainty: a review of factor analytical studies of the intolerance of uncertainty scale. Clin. Psychol. Rev. 2011; 31 :1198–1208. doi: 10.1016/j.cpr.2011.07.009. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boylan J., Seli P., Scholer A.A., Danckert J. Boredom in the COVID-19 pandemic: trait boredom proneness, the desire to act, and rule-breaking. Pers. Indiv. Differ. 2021; 171 :110387. doi: 10.1016/j.paid.2020.110387. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brandes C.M., Herzhoff K., Smack A.J., Tackett J.L. The p factor and the n factor: associations between the general factors of psychopathology and neuroticism in children. Clin. Psychol. Sci. 2019; 7 :1266–1284. doi: 10.1177/2167702619859332. [ CrossRef ] [ Google Scholar ]
- Callard F., Perego E. How and why patients made Long Covid. Soc. Sci. Med. 2021; 268 :113426. doi: 10.1016/j.socscimed.2020.113426. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carfì A., Bernabei R., Landi F. Persistent symptoms in patients after acute COVID-19. J. Am. Med. Assoc. 2020; 324 (6):603–605. doi: 10.1001/jama.2020.12603. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.-G., Mukunzi J.N., McIntee S.-E., et al.Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatr. Res. 2021; 295 :113599. doi: 10.1016/j.psychres.2020.113599. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention . 2020. Overdose Deaths Accelerating during COVID-19. https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html [ Google Scholar ]
- Cheng P., Casement M.D., Kalmbach D.A., Castelan A.C., Drake C.L. Digital cognitive behavioral therapy for insomnia promotes later health resilience during the coronavirus disease 19 (COVID-19) pandemic. Sleep. 2020; 44 (4):zsaa258. doi: 10.1093/sleep/zsaa258. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chor W.P.D., Ng W.M., Cheng L., Situ W., Chong J.W., Ng L.Y.A., et al.Lin Z. Burnout amongst emergency healthcare workers during the COVID-19 pandemic: a multi-center study. AJEM (Am. J. Emerg. Med.) 2020; 46 :700–702. doi: 10.1016/j.ajem.2020.10.040. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Czeisler M.É., Lane R.I., Wiley J.F., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, September 2020. JAMA Net. Open. 2021; 4 (2):e2037665. doi: 10.1001/jamanetworkopen.2020.37665. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duarte D., El-Hagrassy M.M., Couto T.C.E., Gurgel W., Fregni F., Correa H. Male and female physician suicidality: a systematic review and meta-analysis. JAMA Psychiatr. 2020; 77 (6):587–597. doi: 10.1001/jamapsychiatry.2020.0011. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dugas M.J., Robichaud M. Routledge; New York: 2007. Cognitive-behavioral Treatment for Generalized Anxiety Disorder: From Science to Practice. [ Google Scholar ]
- Duncan L.A., Schaller M., Park J.H. Perceived vulnerability to disease: development and validation of a 15-item self-report instrument. Pers. Indiv. Differ. 2009; 47 :541–546. doi: 10.1016/j.paid.2009.05.001. [ CrossRef ] [ Google Scholar ]
- Dutheil F., Aubert C., Pereira B., Dambrun M., Moustafa F., Mermillod M., et al.Navel V. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One. 2019; 14 (12):e0226361. doi: 10.1371/journal.pone.0226361. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Farmer R., Sundberg N.D. Boredom proneness—the development and correlates of a new scale. J. Pers. Assess. 1986; 50 :4–17. doi: 10.1207/s15327752jpa5001_2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fina B.A., Wright E.C., Rauch S.A.M., Norman S.B., Acierno R., Cuccurullo L.-A.J.…Foa E.B. Conducting prolonged exposure for PTSD during the COVID-19 pandemic: considerations for treatment. Cognit. Behav. Pract. 2020 doi: 10.1016/j.cbpra.2020.09.003. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fineberg N.A., Van Ameringen M., Drummond L., Hollander E., Stein D.J., Geller D., et al.Dell'Osso B. How to manage obsessive-compulsive disorder (OCD) under COVID-19: a clinician's guide from the international college of obsessive compulsive spectrum disorders (ICOCS) and the obsessive-compulsive and related disorders research network (OCRN) of the European college of neuropsychopharmacology. Compr. Psychiatr. 2020; 100 :152174. doi: 10.1016/j.comppsych.2020.152174. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fullana M.A., Hidalgo-Mazzei D., Vieta E., Radua J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020; 275 :80–81. doi: 10.1016/j.jad.2020.06.027. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goldman E. Exaggerated risk of transmission of COVID-19 by fomites. Lancet Infect. Dis. 2020; 20 :892–893. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- He Z., Chen J., Pan K., Yue Y., Cheung T., Yuan Y., et al.Xiang Y.-T. The development of the “COVID-19 Psychological Resilience Model” and its efficacy during the COVID-19 pandemic in China. Int. J. Biol. Sci. 2020; 16 :2828–2834. doi: 10.7150/ijbs.50127. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Herrera-Valdez M.A., Cruz-Aponte M., Castillo-Chavez C. Multiple outbreaks for the same pandemic: local transportation and social distancing explain the different “waves” of A-H1N1pdm cases observed in México during 2009. Math. Biosci. Eng. 2011; 8 :21–48. doi: 10.3934/mbe.2011.8.21. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Honigsbaum M. “An inexpressible dread”: psychoses of influenza at fin-de-siècle. Lancet. 2013; 381 :988–989. doi: 10.1016/S0140-6736(13)60701-1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Honigsbaum M. Revisiting the 1957 and 1968 influenza pandemics. Lancet. 2020; 395 :1824–1826. doi: 10.1016/S0140-6736(20)31201-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Iglewicz A., Shear M.K., Reynolds C.F., 3rd, Simon N., Lebowitz B., Zisook S. Complicated grief therapy for clinicians: an evidence-based protocol for mental health practice. Depress. Anxiety. 2020; 37 (1):90–98. doi: 10.1002/da.22965. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Janiri D., Carfì A., Kotzalidis G.D., Bernabei R., Landi F., Sani G. Posttraumatic stress disorder in patients after severe COVID-19 infection. JAMA Psychiatr. 2021; 78 :567–569. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jasti N., Bhargav H., George S., Varambally S., Gangadhar B.N. Tele-yoga for stress management: need of the hour during the COVID-19 pandemic and beyond? Asian J. Psychiatr. 2020; 54 :102334. doi: 10.1016/j.ajp.2020.102334. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Joyce S., Shand F., Tighe J., Laurent S.J., Bryant R.A., Harvey S.B. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. 2018; 8 (6):e017858. doi: 10.1136/bmjopen-2017-017858. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jung S.J., Lim S.-S., Yoon J.-H. Fluctuations in influenza-like illness epidemics and suicide mortality: a time-series regression of 13-year mortality data in South Korea. PLoS One. 2021; 16 (2):e0244596. doi: 10.1371/journal.pone.0244596. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kahlon M.K., Aksan N., Aubrey R., Clark N., Cowley-Morillo M., Jacobs E.A., et al.Tomlinson S. Effect of layperson-delivered, empathy-focused program of telephone calls on loneliness, depression, and anxiety among adults during the COVID-19 pandemic: a randomized clinical trial. JAMA Psychiatr. 2021; 78 (6):616–622. doi: 10.1001/jamapsychiatry.2021.0113. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lewis D. COVID-19 rarely spreads through surfaces. Nature. 2021 https://www.nature.com/articles/d41586-021-00251-4 [ PubMed ] [ Google Scholar ]
- Literary Digest How to fight Spanish influenza. Literary Digest. 1918:13. October 12. [ Google Scholar ]
- Litz B.T., Stein N., Delaney E., Lebowitz L., Nash W.P., Silva C., Maguen S. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin. Psychol. Rev. 2009; 29 :695–706. doi: 10.1016/j.cpr.2009.07.003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ludvigsson J.F. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr. 2021; 110 (3):914–921. doi: 10.1111/apa.15673. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lundorff M., Holmgren H., Zachariae R., Farver-Vestergaard I., O'Connor M. Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J. Affect. Disord. 2017; 212 :138–149. doi: 10.1016/j.jad.2017.01.030. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mamelund S.-E. Paper Presented at the Historical Influenza Pandemics: Lessons Learned Meeting and Workshop, Copenhagen, Denmark. 2010. The impact of influenza on mental health in Norway 1972–1929. [ Google Scholar ]
- Man S. Anti-Asian violence and US imperialism. Race Class. 2020; 62 (2):24–33. doi: 10.1177/0306396820949779. [ CrossRef ] [ Google Scholar ]
- Mollica R.F., Augusterfer E.F., Fricchione G.L., Graziano S. 2020. New Self-Care Protocol: Practice Guide for Healthcare Practitioners and Staff. https://hprtselfcare.org/ [ Google Scholar ]
- Morgantini L.A., Naha U., Wang H., Francavilla S., Acar Ö., Flores J.M., et al.Weine S.M. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey. PLoS One. 2020; 15 :e0238217. doi: 10.1371/journal.pone.0238217. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mortier P., Vilagut G., Ferrer M., Serra C., Dios Molina J., López-Fresneña N., et al.Alonso J. Thirty-day suicidal thoughts and behaviors among hospital workers during the first wave of the Spain Covid-19 outbreak. Depress. Anxiety. 2021; 38 :528–544. doi: 10.1002/da.23129. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moutier C.Y., Myers M.F., Feist J.B., Feist J.C., Zisook S. Preventing clinician suicide: a call to action during the COVID-19 pandemic and beyond. Acad. Med. 2021; 96 :624–628. doi: 10.1097/ACM.0000000000003972. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Institute for Clinical Excellence . Author; London: 2020. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19. [ PubMed ] [ Google Scholar ]
- O'Shea N. Centre for Mental Health; 2020. Covid-19 and the Nation's Mental Health. https://www.centreformentalhealth.org.uk/sites/default/files/publication/download/CentreforMentalHealth_COVID_MH_Forecasting3_Oct20_0.pdf [ Google Scholar ]
- Phoenix Australia . Author; Melbourne, Australia: 2020. Moral Stress Amongst Heathcare Workers during COVID-19: A Guide to Moral Injury. [ Google Scholar ]
- Pokhrel S., Sedhai Y.R., Atreya A. An increase in suicides amidst the coronavirus disease 2019 pandemic in Nepal. Med. Sci. Law. 2021; 61 (2):161–162. doi: 10.1177/0025802420966501. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021; 51 :201–211. doi: 10.1017/S0033291721000015. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Price G.M. Influenza—destroyer and teacher. The Survey. 1919; 41 :367–369. [ Google Scholar ]
- Radeloff D., Papsdorf R., Uhlig K., Vasilache A., Putnam K., von Klitzing K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol. Psychiatr. Sci. 2021; 30 :e16. doi: 10.1017/S2045796021000019. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Regan T., Harris B., Van Loon M., Nanavaty N., Schueler J., Engler S., Fields S.A. Does mindfulness reduce the effects of risk factors for problematic smartphone use? Comparing frequency of use versus self-reported addiction. Addict. Behav. 2020; 108 :106435. doi: 10.1016/j.addbeh.2020.106435. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Richter D., Riedel-Heller S., Zuercher S. Mental health problems in the general population during and after the first lockdown phase due to the SARS-CoV-2 pandemic: rapid review of multi-wave studies. Epidemiol. Psychiatr. Sci. 2021; 30 :e27. doi: 10.1017/S2045796021000160. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Riva G., Riva E. COVID Feel Good: a free VR self-help solution for providing stress management and social support during the COVID-19 pandemic. Cyberpsychol., Behav. Soc. Netw. 2020; 23 (9):652–653. doi: 10.1089/cyber.2020.29195.ceu. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., et al.David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatr. 2020; 7 (7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rosser B.A. Intolerance of uncertainty as a transdiagnostic mechanism of psychological difficulties: a systematic review of evidence pertaining to causality and temporal precedence. Cognit. Ther. Res. 2018; 43 :438–463. doi: 10.1007/s10608-018-9964-z. [ CrossRef ] [ Google Scholar ]
- Schaller M., Park J.H. The behavioral immune system (and why it matters) Curr. Dir. Psychol. Sci. 2011; 20 :99–103. doi: 10.1177/0963721411402596. [ CrossRef ] [ Google Scholar ]
- Sharma L.P., Balachander S., Thamby A., Bhattacharya M., Kishore C., Shanbhag V.…Reddy J.Y.C. Impact of the COVID-19 pandemic on the short-term course of obsessive-compulsive disorder. J. Nerv. Ment. Dis. 2021; 209 :256–264. doi: 10.1097/NMD.0000000000001318. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shaygan M., Yazdani Z., Valibeygi A. The effect of online multimedia psychoeducational interventions on the resilience and perceived stress of hospitalized patients with COVID-19: a pilot cluster randomized parallel-controlled trial. BMC Psychiatr. 2021; 21 (1):93. doi: 10.1186/s12888-021-03085-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shear M.K., Gribbin C.E. In: Trauma- and Stressor-Related Disorders: A Handbook for Clinicians. Casey P.R., Strain J.J., editors. American Psychiatric Publishing; Arlington, VA: 2016. Persistent complex bereavement disorder and its treatment; pp. 133–154. [ Google Scholar ]
- Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., et al.Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatr. 2020; 66 :1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stack S., Rockett I.R.H. Social distancing predicts suicide rates: analysis of the 1918 flu pandemic in 43 large cities. Suicide Life-Threatening Behav. 2021 doi: 10.1111/sltb.12729. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Storch E.A., Sheu J.C., Guzick A.G., Schneider S.C., Cepeda S.L., Rombado B.R.…Goodman W.K. Impact of the COVID-19 pandemic on exposure and response prevention outcomes in adults and youth with obsessive-compulsive disorder. Psychiatr. Res. 2021; 295 :113597. doi: 10.1016/j.psychres.2020.113597. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sudre C.H., Murray B., Varsavsky T., Graham M.S., Penfold R.S., Bowyer R.C., et al.Steves C.J. Attributes and predictors of long COVID. Nat. Med. 2021 doi: 10.1038/s41591-021-01292-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Human Behav. 2021; 5 (2):229–238. doi: 10.1038/s41562-020-01042-z. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor S. Etiology of obsessions and compulsions: a meta-analysis and narrative review of twin studies. Clin. Psychol. Rev. 2011; 31 (8):1361–1372. doi: 10.1016/j.cpr.2011.09.008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor S. second ed. Guildford; New York: 2017. Clinician's Guide to PTSD. [ Google Scholar ]
- Taylor S. Cambridge Scholars Publishing; Newcastle upon Tyne: 2019. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease. [ Google Scholar ]
- Taylor S. COVID stress syndrome: clinical and nosological considerations. Curr. Psychiatr. Rep. 2021; 23 :19. doi: 10.1007/s11920-021-01226-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor S. The psychology of pandemics: lessons learned for the future. Can. Psychol. 2021 [ Google Scholar ]
- Taylor S. Understanding and managing pandemic-related panic buying. J. Anxiety Disord. 2021; 78 :102364. [ PubMed ] [ Google Scholar ]
- Taylor S. The psychology of pandemics. Ann. Rev. Clinical Psychol. 2021 [ PubMed ] [ Google Scholar ]
- Taylor S., Fong A., Asmundson G.J.G. Predicting the severity of symptoms of the COVID stress syndrome from personality traits: a prospective network analysis. Front. Psychol. 2021; 12 :632227. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Covid stress syndrome: concept, structure, and correlates. Depress. Anxiety. 2020; 37 :706–714. doi: 10.1002/da.23071. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J.G. Development and initial validation of the COVID stress scales. J. Anxiety Disord. 2020; 72 :102232. doi: 10.1016/j.janxdis.2020.102232. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor S., Landry C.A., Rachor G.S., Paluszek M.M., Asmundson G.J.G. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J. Anxiety Disord. 2020; 75 :102289. doi: 10.1016/j.janxdis.2020.102289. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor S., Paluszek M., Landry C., Rachor G.S., Asmundson G.J.G. Predictors of distress and coping during pandemic-related self isolation: the relative importance of personality traits and beliefs about personal threat. Pers. Indiv. Differ. 2021; 176 :110779. [ Google Scholar ]
- Taylor S., Paluszek M., Rachor G.S., McKay D., Asmundson G.J.G. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: a network analysis. Addict. Behav. 2020; 114 :106754. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Teng Z., Pontes H.M., Nie Q., Griffiths M.D., Guo C. Depression and anxiety symptoms associated with internet gaming disorder before and during the COVID-19 pandemic: a longitudinal study. J. Behav. Addict. 2021; 10 :169–180. doi: 10.1556/2006.2021.00016. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thompson D. Hygiene theater is a huge waste of time. Atlantic. 2020 https://www.theatlantic.com/ideas/archive/2020/07/scourge-hygiene-theater/614599/ [ Google Scholar ]
- Tomes N. “Destroyer and teacher”: managing the masses during the 1918–1919 influenza pandemic. Publ. Health Rep. 2010; 125 (Suppl. 3):48–62. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Turner E.B. Discussion on influenza. Proc. Roy. Soc. Med. 1919; 12 :76–90. https://pubmed.ncbi.nlm.nih.gov/19980438 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tzeng N.-S., Chung C.-H., Chang C.-C., Chang H.-A., Kao Y.-C., Chang S.-Y., Chien W.-C. What could we learn from SARS when facing the mental health issues related to the COVID-19 outbreak? A nationwide cohort study in Taiwan. Transl. Psychiatr. 2020; 10 (1):339. doi: 10.1038/s41398-020-01021-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Verdery A.M., Smith-Greenaway E., Margolis R., Daw J. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc. Natl. Acad. Sci. USA. 2020; 117 :17695. doi: 10.1073/pnas.2007476117. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vink M., Vink-Niese A. Could cognitive behavioural therapy be an effective treatment for long COVID and post COVID-19 fatigue syndrome? Lessons from the qure study for Q-fever fatigue syndrome. Healthcare. 2020; 8 :552. doi: 10.3390/healthcare8040552. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wahlund T., Mataix-Cols D., Olofsdotter Lauri K., de Schipper E., Ljótsson B., Aspvall K., Andersson E. Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 Pandemic: a randomised controlled trial. Psychother. Psychosom. 2020; 90 :191–199. doi: 10.1159/000512843. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang K., Goldenberg A., Dorison C.A., Miller J.K., Uusberg A., Lerner J.S.…Moshontz H. A multi-country test of brief reappraisal interventions on emotions during the COVID-19 pandemic. Nat. Human Behav. 2021 doi: 10.1038/s41562-021-01173-x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wasserman I.M. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life-Threatening Behav. 1992; 22 (2):240–254. [ PubMed ] [ Google Scholar ]
- Webb T.L., Miles E., Sheeran P. Dealing with feeling: a meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychol. Bull. 2012; 138 (4):775–808. doi: 10.1037/a0027600. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wei E.K., Segall J., Linn-Walton R., Eros-Sarnyai M., Fattal O., Toukolehto O., et al.Cho H.J. Combat stress management and resilience: adapting department of defense combat lessons learned to civilian healthcare during the COVID-19 pandemic. Health Security. 2020 doi: 10.1089/hs.2020.0091. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization . Author; Geneva: 2005. WHO Checklist for Influenza Pandemic Preparedness Planning. [ Google Scholar ]
- World Health Organization . 2019. ICD-11: Burnout. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281 [ Google Scholar ]
- World Health Organization . 2020. Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19. https://apps.who.int/iris/bitstream/handle/10665/335820/WHO-EURO-2020-1160-40906-55390-eng.pdf [ Google Scholar ]
- Xuereb S., Kim H.S., Clark L., Wohl M.J.A. Substitution behaviors among people who gamble during COVID-19 precipitated casino closures. Int. Gambl. Stud. 2021 doi: 10.1080/14459795.2021.1903062. [ CrossRef ] [ Google Scholar ]
- Yang X.-J., Liu Q.-Q., Lian S.-L., Zhou Z.-K. Are bored minds more likely to be addicted? The relationship between boredom proneness and problematic mobile phone use. Addict. Behav. 2020; 108 :106426. doi: 10.1016/j.addbeh.2020.106426. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yarrington J.S., Lasser J., Garcia D., Vargas J.H., Couto D.D., Marafon T., et al.Niles A.N. Impact of the COVID-19 pandemic on mental health among 157,213 Americans. J. Affect. Disord. 2021; 286 :64–70. doi: 10.1016/j.jad.2021.02.056. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yip P.S.F., Cheung Y.T., Chau P.H., Law Y.W. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. 2010; 31 :86–92. [ PubMed ] [ Google Scholar ]
- Yuan Y. Mindfulness training on the resilience of adolescents under the COVID-19 epidemic: a latent growth curve analysis. Pers. Indiv. Differ. 2021; 172 :110560. doi: 10.1016/j.paid.2020.110560. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Accountancy and Control (master)
- Accountancy and Control (premaster)
- Actuarial Science (bachelor)
- Actuarial Science and Mathematical Finance (master)
- American Studies (master)
- Ancient Studies (bachelor)
- Arabische taal en cultuur (bachelor)
- Arbeidsrecht (master)
- Archaeology (master)
- Archaeology (premaster)
- Archaeology (bachelor), EN
- Archaeology and Heritage (research master)
- Archeologie (bachelor), NL
- Archival and Information Studies (duale master)
- Art and Performance Research Studies (research master)
- Artificial Intelligence (master)
- Bèta-gamma (bachelor)
- Bioinformatics and Systems Biology (master, joint degree)
- Biological Sciences (master)
- Biologie (bachelor)
- Biomedical Sciences (master)
- Biomedische wetenschappen (bachelor)
- BMS: Cell Biology and Advanced Microscopy (master)
- BMS: Cognitive Neurobiology and Clinical Neurophysiology (master)
- BMS: Developmental and Therapeutic Biology (master)
- BMS: Experimental Internal Medicine (master)
- BMS: Infection and Immunity (master)
- BMS: Medical Biochemistry and Biotechnology (master)
- BMS: Molecular Neurosciences (master)
- BMS: Oncology (master)
- BMS: Physiology of Synapses and Networks (master)
- BMS: Psychopharmacology and Pathophysiology (master)
- Boekwetenschap (master)
- Boekwetenschap (schakelprogramma)
- Brain and Cognitive Sciences (research master)
- BS: Ecology and Evolution (master)
- BS: Freshwater and Marine Biology (master)
- BS: General Biology (master)
- BS: Green Life Sciences (master)
- Business Administration (bachelor)
- Business Administration (master)
- Business Administration (premaster)
- Business Analytics (bachelor)
- Business Economics (master)
- Business Economics (premaster)
- Chemistry (master, joint degree)
- Chemistry (premaster)
- Chemistry: Analytical Sciences (master, joint degree)
- Chemistry: Molecular Sciences (master, joint degree)
- Chemistry: Science for Energy and Sustainability (master, joint degree)
- Child Development and Education (research master)
- Classics and Ancient Civilizations (master)
- Cognition, Language and Communication (bachelor)
- Commerciële rechtspraktijk (master)
- Communicatiewetenschap (bachelor)
- Communication and Information (duale master)
- Communication Science (bachelor)
- Communication Science (master)
- Communication Science (premaster)
- Communication Science (research master)
- Comparative Cultural Analysis (master)
- Comparative Literature (master)
- Computational Science (master, joint degree)
- Computational Social Science (bachelor)
- Computer Science (master, joint degree)
- Conflict Resolution and Governance (master)
- Conservation and Restoration of Cultural Heritage (master)
- Cultural Analysis (research master)
- Cultural and Social Anthropology (master)
- Cultural and Social Anthropology (premaster)
- Cultural Anthropology and Development Sociology (bachelor)
- Cultural Data & AI (master)
- Culturele antropologie en ontwikkelingssociologie (bachelor)
- Cultuurwetenschappen (bachelor)
- Curating Art and Cultures (duale master)
- Data Science (master)
- Data Science and Business Analytics (master)
- Documentaire en fictie (duale master)
- Duits, Educatie en communicatie (master)
- Duits, Educatie en communicatie (schakelprogramma)
- Duitslandstudies (bachelor)
- Duitslandstudies (master)
- Earth Sciences (master)
- East European Studies (master)
- Econometrics (master)
- Econometrics (premaster)
- Econometrics and Data Science (bachelor)
- Economics (master)
- Economics (premaster)
- Economics and Business Economics (bachelor)
- Engels, Educatie en communicatie (master)
- Engels, Educatie en communicatie (schakelprogramma)
- English Language and Culture (bachelor)
- English Literature and Culture (master)
- Entrepreneurship (master)
- ES: Environmental Management (master)
- ES: Future Planet Ecosystem Science (master)
- ES: Geo-Ecological Dynamics (master)
- European Competition Law and Regulation (master)
- European Policy (master)
- European Private Law (master)
- European Studies (bachelor)
- European Studies (premaster)
- European Union Law (master)
- Europese studies (bachelor)
- Exchange programme Economics and Business
- Exchange programme Humanities
- Exchange programme Law - Amsterdam Law School
- Exchange programme PPLE - Politics, Psychology, Law and Economics
- Exchange programme Science
- Exchange programme Social and Behavioural Sciences
- Film Studies (master)
- Filosofie (bachelor)
- Filosofie (master)
- Finance (master)
- Fiscaal Recht (bachelor)
- Fiscaal Recht (master)
- Fiscale Economie (bachelor)
- Fiscale Economie (master)
- Fiscale Economie (premaster)
- Forensic Science (master)
- Frans, Educatie en communicatie (master)
- Frans, Educatie en communicatie (schakelprogramma)
- Franse taal en cultuur (bachelor)
- Future Planet Studies (bachelor)
- Geneeskunde (bachelor)
- Geneeskunde (master)
- Geneeskunde (schakelprogramma)
- General Linguistics (master)
- Geschiedenis (bachelor)
- Geschiedenis (master)
- Geschiedenis (research master)
- Geschiedenis (schakelprogramma)
- Geschiedenis van de internationale betrekkingen (master)
- Geschiedenis, Educatie en communicatie (master)
- Gezondheidsrecht (master)
- Gezondheidszorgpsychologie (master)
- Global Arts, Culture and Politics (bachelor)
- Griekse en Latijnse taal en cultuur (bachelor)
- Hebreeuwse taal en cultuur (bachelor)
- Heritage and Memory Studies (duale master)
- Holocaust and Genocide Studies (master)
- Human Geography (master)
- Human Geography (premaster)
- Human Geography and Planning (bachelor)
- Identity and Integration (master)
- Informatica (bachelor)
- Informatiekunde (bachelor)
- Informatierecht (master)
- Information Studies (master)
- Information Systems (master)
- Interdisciplinaire sociale wetenschap (bachelor)
- Internationaal en Europees belastingrecht (master)
- International and Transnational Criminal Law (master)
- International Criminal Law - Joint programme with Columbia Law School (master)
- International Development Studies (master)
- International Development Studies (premaster)
- International Development Studies (research master)
- International Dramaturgy (duale master)
- International Dramaturgy and Theatre Studies (premaster)
- International Tax Law (advanced master)
- International Trade and Investment Law (master)
- Italië Studies (bachelor)
- Jewish Studies (master)
- Journalism, Media and Globalisation (Erasmus Mundus Master's - joint degree)
- Journalistiek en media (duale master)
- Kunst, cultuur en politiek (master)
- Kunst, cultuur en politiek (schakelprogramma)
- Kunstgeschiedenis (bachelor)
- Kunstgeschiedenis (master)
- Kunstgeschiedenis (schakelprogramma)
- Kunstmatige intelligentie (bachelor)
- Language and Society (master)
- Language, Literature and Education (master)
- Language, Literature and Education (premaster)
- Latin American Studies (master)
- Latin American Studies (premaster)
- Law & Finance (master)
- Lerarenopleidingen
- Linguistics (bachelor)
- Linguistics (premaster)
- Linguistics and Communication (research master)
- Literary and Cultural Analysis (bachelor)
- Literary Studies (premaster)
- Literary Studies (research master)
- Literature, Culture and Society (master)
- Logic (master)
- Mathematics (master)
- Media and Culture (bachelor)
- Media and Information (bachelor)
- Media en cultuur (bachelor)
- Media Studies (premaster)
- Media Studies (research master)
- Medical Anthropology and Sociology (master)
- Medical Anthropology and Sociology (premaster)
- Medical informatics (master)
- Medische informatiekunde (bachelor)
- Midden-Oostenstudies (master)
- Midden-Oostenstudies (schakelprogramma)
- Militaire geschiedenis (master)
- Museum Studies (duale master)
- Music Studies (master)
- Music Studies (premaster)
- Muziekwetenschap (bachelor)
- Natuurkunde en sterrenkunde (bachelor, joint degree)
- Nederlands als tweede taal en meertaligheid (duale master)
- Nederlands als tweede taal en meertaligheid (schakelprogramma)
- Nederlands, Educatie en communicatie (master)
- Nederlands, Educatie en communicatie (schakelprogramma)
- Nederlandse taal en cultuur (bachelor)
- Nederlandse taal en cultuur (master)
- New Media and Digital Culture (master)
- Nieuwgriekse taal en cultuur (bachelor)
- Onderwijswetenschappen (bachelor)
- Onderwijswetenschappen (master)
- Onderwijswetenschappen (schakelprogramma)
- (Forensische) Orthopedagogiek (schakelprogramma)
- Oudheidwetenschappen (bachelor)
- P&A: Advanced Matter and Energy Physics (master, joint degree)
- P&A: Astronomy and Astrophysics (master, joint degree)
- P&A: Biophysics and Biophotonics (master, joint degree)
- P&A: General Physics and Astronomy (master, joint degree)
- P&A: GRAPPA - Gravitation, Astro-, and Particle Physics (master, joint degree)
- P&A: Science for Energy and Sustainability (master, joint degree)
- P&A: Theoretical Physics (master, joint degree)
- Pedagogical Sciences (master)
- Pedagogische wetenschappen (bachelor)
- Pedagogische wetenschappen (master)
- Philosophy (master)
- Philosophy (research master)
- Philosophy of the Humanities and the Social Sciences (master)
- Philosophy of the Humanities and the Social Sciences (schakelprogramma)
- Physics and Astronomy (master, joint degree)
- Political Science (bachelor)
- Political Science (master)
- Political Science (premaster)
- Politicologie (bachelor)
- PPLE - Politics, Psychology, Law and Economics (bachelor)
- Preservation and Presentation of the Moving Image (duale master)
- Preventieve jeugdhulp en opvoeding (schakelprogramma)
- Privaatrechtelijke rechtspraktijk (master)
- Psychobiologie (bachelor)
- Psychologie (schakelprogramma)
- Psychologie (bachelor), NL
- Psychologie (master), NL
- Psychology (premaster)
- Psychology (bachelor), EN
- Psychology (master), EN
- Psychology (research master), EN
- Public International Law (master)
- Publieksgeschiedenis (master)
- Rechtsgeleerdheid (bachelor)
- Rechtsgeleerdheid met HBO-vooropleiding (schakelprogramma)
- Rechtsgeleerdheid met WO-vooropleiding (schakelprogramma)
- Redacteur/editor (duale master)
- Religiewetenschappen (bachelor)
- Religious Studies (research master)
- Russische en Slavische studies (bachelor)
- Scandinavië studies (bachelor)
- Scheikunde (bachelor, joint degree)
- Science, Technology & Innovation (bachelor)
- Security and Network Engineering (master)
- Sign Language Linguistics (bachelor)
- Social Sciences (research master)
- Sociale geografie en Planologie (bachelor)
- Sociologie (bachelor)
- Sociology (bachelor)
- Sociology (master)
- Sociology (premaster)
- Software Engineering (master)
- Spaanse en Latijns-Amerikaanse studies (bachelor)
- Spirituality and Religion (master)
- Spirituality and Religion (schakelprogramma)
- Staats- en bestuursrecht (master)
- Stads- en architectuurgeschiedenis (master)
- Stochastics and Financial Mathematics (master)
- Strafrecht (master)
- Taalwetenschappen (bachelor)
- Technology Governance (advanced master)
- Television and Cross-Media Culture (master)
- Theaterwetenschap (bachelor)
- Theatre Studies (master)
- Universitaire Pabo van Amsterdam (bachelor)
- Urban and Regional Planning (master)
- Urban and Regional Planning (premaster)
- Urban Studies (research master)
- Vertalen (master)
- Vertalen (schakelprogramma)
- Wiskunde (bachelor)

Presentation Master's thesis - Levi Legdeur - Clinical Psychology
Roeterseilandcampus, Building: G, Street: Nieuwe Achtergracht 129-b, Room: GS.05
Collaboration between the security- (SCD) and mental health domain (MHD) towards radicalization paves the way towards more effective service of the general public with regards to individual (mental) healthcare and societal safety and stability. Intersectional collaboration shows efficacious towards clinical and safety outcomes, making radicalization a suitable problem to be targeted by such efforts. The current study investigates how perceptions of these domains towards radicalization and collaboration on the matter differ, providing insights for collaboration. Earlier, focus groups on the same subject were conducted. The focus groups presented controversial points of domains on radicalization, reduced to five themes. The 81-item quantitative survey used in the current study corresponding to each theme. Themes were all hypothesized differ by domains. Furthermore, reference frames were explicitly modelled with an exploratory cluster analysis. Validation of internal consistency indicated two out of five themes to be insufficient, leading to the hypotheses of Radicalization and Content of Work being dropped. Results do however indicate several significant differences on these themes, as well as Roles and Responsibilities and Relationship; which had their hypotheses supported. Only the Contact theme did not. Subsequent greatest differences were visualized in figures. The clustering model fitted best into a 2-cluster solution and converged to an interpretable structure separating between domains. Both analyses suggest there are many different perceptions between domains on radicalization. The final cluster solution furthermore supports the idea of domains holding distinct reference frames towards radicalization. Specific results mostly support similar notions, visualized by figures and discussed.

IMAGES
VIDEO
COMMENTS
Discuss how scientific research guides public policy. Appreciate how scientific research can be important in making personal decisions. Scientific research is a critical tool for successfully navigating our complex world. Without it, we would be forced to rely solely on intuition, other people's authority, and blind luck.
Introduction. Psychology is an ever-growing and popular field (Gough and Lyons, 2016; Clay, 2017).Due to this growth and the need for science-based research to base health decisions on (Perestelo-Pérez, 2013), the use of research methods in the broad field of psychology is an essential point of investigation (Stangor, 2011; Aanstoos, 2014).Research methods are therefore viewed as important ...
We suggest that research leadership is particularly important within clinical psychology to ensure the profession's continued visibility and influence within health settings. ... Clinical psychology trainees' research productivity and publications: An initial survey and contributing factors. Clinical Psychology & Psychotherapy, 14 (1), 54-62.
The application of their research and the science behind their work make clinical psychologists invaluable in mental health and health care settings alike and in hospitals, schools, courts, the government, the military — almost anywhere you can imagine. 1 Compas, Bruce & Gotlib, Ian. (2002). Introduction to Clinical Psychology.
An important aim of basic research in Clinical Psychology is to improve clinical practice (e.g., by developing novel interventions or improving the efficacy of existing ones) based on an improved understanding of key mechanisms involved in psychopathology. In the first part of this article, we examine how frequently this translation has happened in the past by reviewing all 40 evidence-based ...
However, research studies focusing on professional issues pertinent to the field of clinical psychology (e.g., survey of clinical psychologists regarding the importance of training in ethical standards) may, on occasion, be considered.
Why research is important 3 concepts or constructs. A piece of research is embedded in a frame-work or way of seeing the world. Second, research involves the application of a method, which has been designed to achieve knowledge that is as valid and truthful as possible. 4 The products of research are propositions or statements. There is a
Clinical psychology—a field anchored on the deep integration of basic science and clinical practice—is uniquely positioned to serve as a transdisciplinary hub for this research (Baker et al 2008, McFall et al 2015). But rising to this challenge requires an honest reckoning with the strengths and weaknesses of current training practices.
Psychology is the scientific study of behaviour and mental processes. But it is also the application of scientific research to "help people, organizations, and communities function better" (American Psychological Association, 2011) [1]. By far the most common and widely known application is the clinical practice of psychology —the ...
second edition, entitled Research Methods in Clinical Psychology, focused on clinical psychologists as a primary readership, with counseling, health, educational, and ... bullet‐point summaries of the important points in boxes, and a chapter summary and suggested reading at the end of each chapter. In this edition, we have added ques- ...
Clinical psychological research is a rapidly evolving field using a diverse set of methodologies to answer critical questions about etiology and treatment of psychological disorders in various populations. Every day researchers in this field make numerous decisions on how and when to apply specific methods, and these decisions are frequently made within a specific research laboratory and not ...
An important aim of basic research in Clinical Psychology is to improve clinical practice (e.g., by developing novel interventions or improving the efficacy of existing ones) based on an improved understanding of key mechanisms involved in psychopathology. In the first part of this article, we exami …
Evidence-based practice designates a process of clinical decision-making that integrates research evidence, clinical expertise, and patient preferences and characteristics. Evidence-based practice is a transdisciplinary, idiographic approach that promotes lifelong learning. Empirically supported treatments (ESTs) are an important component of ...
Clinical psychology research is as important to the nation's health and well being as medical research. In the same way that medical scientists work to understand the prevention, genesis, and spread of various genetic and infectious diseases, scientists conduct rigorous psychological research studies to understand, prevent, and treat the human condition as it applies psychologically to ...
Central to research in clinical psychology is the evaluation of treatment outcomes. Research evaluations of the efficacy and effectiveness of therapeutic interventions have evolved from single-subject case histories to complex multimethod experimental investigations of carefully defined treatments applied to genuine clinical samples.
This article aims to give an overview of the advantages of, and difficulties in conducting research in clinical practice. Method: We reviewed the relevant literature on barriers to research and reflected on our clinical and research experiences in a range of contexts to offer practical recommendations. Results: We considered factors involved in ...
An important aim of basic research in Clinical Psychology is to improve clinical practice (e.g., by developing novel interventions or improving the efficacy of existing ones) based on an improved understanding of key mechanisms involved in psychopathology.
The science of psychology is pervasive. Psychologists work in some of the nation's most prominent companies and organizations. From Google, Boeing and NASA to the federal government, national health care organizations and research groups to Cirque du Soleil, Disney and NASCAR — psychologists are there, playing important roles.
Because of this, understanding the research behind an assessment is important in psychological practice. It enables psychologists to better explain what results 'mean'. Research is also conducted in psychology to develop treatments for psychological disorders, determine whether they are effective, and use them in clinical practice.
For the individual practitioner, "being research active helps you to be the most effective therapist you can, and it also helps retain curiosity and enthusiasm in the work", Professor Barney Dunn, a research clinical psychologist at the University of Exeter, told me. "But equally importantly, practitioners bring a fresh, clinically grounded ...
Abstract. The goal of this review was to present the essential steps in the entire process of clinical research. Research should begin with an educated idea arising from a clinical practice issue. A research topic rooted in a clinical problem provides the motivation for the completion of the research and relevancy for affecting medical practice ...
A systematic review of empirical research into ethical decision-making in clinical psychology and related fields was therefore indicated, with the aim of summarising the literature available. Although there are some important differences between professions in terms of the training backgrounds and regulatory frameworks, the search was extended ...
Selective outcome reporting in clinical trials involves reporting only some of the prespecified outcomes examined, including outcomes that were not prespecified, and/or changing the importance of outcomes in terms of primary and secondary importance (Kirkham et al., Citation 2010; Thomas & Heneghan, Citation 2022).Outcome reporting bias (ORB) arises from selective outcome reporting and ...
The undergraduate work must include a statistics course and a psychology research methods course with grades of B or higher. Education The applicant must have completed at least 18 credits in psychology as part of their four-year bachelor's degree from an accredited institution.
The impact of dysfunctional attitudes and unhelpful thinking upon clients presenting with personality-related psychological distress is an important clinical area of investigation as it informs psychological interventions. Despite this, there is limited research in this area. Thus, this study had two main aims: (1) examine the interrelationships between maladaptive personality traits ...
Background Video games have become a prevalent source of entertainment, especially among children. Furthermore, the amount of time spent playing video games has grown dramatically. The purpose of this research was to examine the mediation effects of attention and child memory on the relationship between video games addiction and cognitive and learning abilities in Egyptian children. Methods A ...
However, COVID-19 also highlighted important shortcomings in clinical care, including planning deficiencies and shortages of clinicians with specialized training for treating various psychological problems (e.g., prolonged grief disorder). These problems and potential solutions are discussed. Keywords: Clinical psychology ... as research on the ...
Intersectional collaboration shows efficacious towards clinical and safety outcomes, making radicalization a suitable problem to be targeted by such efforts. The current study investigates how perceptions of these domains towards radicalization and collaboration on the matter differ, providing insights for collaboration.