
10 therapy tasks practiced most frequently by survivors of stroke
Stroke can impact all aspects of life—movement, communication, thinking, and autonomic functions such as swallowing and breathing. Research shows that early and specialized stroke rehabilitation can help to optimize an individual’s physical and cognitive recovery and enhance quality of life. Here, we identify the Constant Therapy tasks used most often by those recovering from stroke.
The goal of stroke therapy: help people regain lost skills
According to the Centers for Disease Control , about 87 percent of all strokes are ischemic strokes, in which blood flow to the brain is blocked. According to the American Speech-Language-Hearing Association, individuals with aphasia or other cognitive-communication issues represent up to 20 percent of the adult caseload for speech-language pathologists in the United States.
Typical goals of stroke therapy include:
- Restoring physical function and enhance the skills needed to perform daily activities
- Building strength, improving balance and regaining mobility
- Improving areas such as speech, language, cognition, or swallowing
- Developing new behavioral or compensatory strategies
Analysis: how is Constant Therapy being used with this population?
Constant Therapy uses artificial intelligence and data analytics to provide each user with a personalized brain exercise program targeting areas such as memory, attention, problem-solving, math, language, reading, writing, and many other skills. Research published in the Journal Frontiers in Human Neuroscience showed a significant improvement in standardized tests for survivors of stroke using the iPad-based rehabilitation technology of Constant Therapy.
An analysis of Constant Therapy users identified what tasks are assigned most frequently by clinicians working with survivors of stroke.
- We looked at data on 18,230 users who identified a diagnosis of stroke on the app.
- These 18,230 users completed an average of 572 tasks each
- Total tasks completed numbered 837,700.
The Constant Therapy tasks listed below are the 10 most frequently assigned by clinicians for their clients recovering from stroke.
The top 10 Constant Therapy exercises assigned by clinicians to patients recovering from stroke
1. Follow instructions you hear : Works on auditory memory and auditory comprehension through following directions . Individuals Assigned: 10,207 Percent of Users Identified As Recovering from Stroke 56%
2. Find the same symbols : Cognitive skills such as attention can be affected after a stroke. Find the same symbols targets a variety of skills which includes attention, visuospatial processing, and executive functioning . Individuals Assigned: 9,216 Percent of Users Identified As Recovering from Stroke: 51%
3. Put steps in order : For people recovering from a stroke, executive functioning skills may be affected. In this planning & organizing task , you are presented with steps of daily activities, and must drag these steps into the correct order. This is a great task for people working on sentence level reading comprehension too! Individuals Assigned: 8,814 Percent of Users Identified As Recovering from Stroke: 48%
4. Match pictures : For people with cognitive, speech, or language disorders, this task helps visual memory by matching pictures displayed on a grid. For people recovering from a stroke who are working on word retrieval, they can also practice naming the pairs of pictures that they match . Individuals Assigned: 7,629 Percent of Users Identified As Recovering from Stroke: 42%
5. Remember pictures in order (N-Back) : This memory task specifically targets an aspect of working memory called updating . There are 3 levels of difficulty. In Level 1, you must remember the order of the pictures from 1 picture ago. In level 3 you must recall 3 pictures ago. Want more N-Back Tasks? Do Remember spoken word order (N-Back) and Remember written words in order (N-back) , too! Individuals Assigned: 7,213 Percent of Users Identified As Recovering from Stroke: 40%
6. Do clock math : Stroke can affect number skills, math skills, and word finding. This task helps improve time-based calculation skills by answering math questions associated with clocks . Individuals Assigned: 6,701 Percent of Users Identified As Recovering from Stroke: 37%
7. Name Pictures : Helps improve word retrieval skills by speaking the name of presented images. There are 3 levels to this task, with each level increasing in word difficulty. Different cues include semantic, phonemic, graphemic, and whole word cues . Individuals Assigned: 6,635 Percent of Users Identified As Recovering from Stroke: 36%
8. Repeat a pattern : This task works on attention, visual working memory, and visuospatial skills . Individuals Assigned: 6,433 Percent of Users Identified As Recovering from Stroke: 35%
9. Understand voicemail : This functional task works on comprehension and memory of everyday language by answering questions about voicemails. Looking for a bigger challenge? Check out Infer from voicemail as well . Individuals Assigned: 6,085| Percent of Users Identified As Recovering from Stroke: 33%
10. Remember the right card : This task works on attention, disinhibition, and processing speed. The patient is asked to remember a playing card and tap on that card whenever it is presented in a series of cards . Individuals Assigned: 5,690 Percent of Users Identified As Recovering from Stroke: 31%
- Des Roches, C., Kiran, S. and Balachandran, I. (2015). Frontiers in Human Neuroscience, Effectiveness of an impairment-based individualized rehabilitation program using an iPad-based software platform , 2015 Jan 5. doi: 10.3389/fnhum.2014.01015.
- Centers for Disease Control and Prevention (2018). Stroke Facts .
- ASHA (2017). SLP Healthcare Survey: Caseload Characterisics .
Tackle your speech therapy goals, get top-notch support
Related articles, 11 comments.
Do you get this from the App Store? What is the cost?
Hi Lisa. Yes, check out the app store. Our monthly plan is $25 and an annual plan is $250 with a free tablet. If you want to set up a trial and need support, give us a call or email. 1-888-233-1399 or [email protected]
When I purchased a whole year package in 2023 I never received a free tablet. Is this something new?
Hi Todd, thank you so much for subscribing to Constant Therapy! Apologies for the confusion, this is an older comment and we discontinued this program back in 2019. If you have any questions or concerns about the device you use for Constant Therapy feel free to reach out to our Support Team at [email protected] .
What is the app name please?
- Constant Therapy
Thanks have learnt something. Am struggling with after stroke effects especially speech
Is there a way to have the math word problem questions read to you? My brother is working on math as well as re learning reading. He cannot read the questions yet to do the math problem…
Great question! This is a feature that we are working to add in the near future – keep an eye out for announcements in our weekly emails once we have that feature ready to use!
What exercises are recommended for people with primary progressive apraxia?
Hello Alberta, thank you for your question! We spoke with a Speech Language Pathologist and they said that difficulty levels will depend on the condition’s progression. You may be interested at looking into these exercises: Imitate Words, Imitate Sentences, Form and Say Active Sentences, and Form and Say Passive Sentences . These tasks will allow you practice with articulating speech at various levels of complexity. Hope this is helpful!
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Constant Therapy Health
- Partner with us
- Try for free
- Request a Demo
- Conditions we support
- For clinicians
- For patients
- For veterans
Support + Resources
- Printable Resources
- Testimonials
Join the Conversation
Last updated on June 21, 2024

While games can be enjoyable for individuals of every age, games for stroke patients can actually promote recovery. During rehabilitation, it is critical to stay active, both physically and mentally. While many individuals focus heavily on physical recovery, cognitive recovery can be equally as important.
Because such a wide variety of games have been developed, survivors can often find at least one game that targets the specific cognitive skills they are hoping to improve. Stimulating the brain through games can activate neuroplasticity , the brain’s natural repair mechanism. Therefore, repetitively practicing cognitive skills through games can allow survivors to regain and maintain functions that were impaired or lost after stroke.
This article provides an overview of many fun and challenging games that are ideal for improving cognitive function among stroke patients. These are organized by the types of cognitive skills addressed, with three difficulty levels provided in each category. Use the links below to jump directly to any section.
- Memory and attention games
- Games to improve processing speed
- Developing language skills through games
- Games for improving visual skills
- Further considerations
Memory and Attention Games
The cognitive skills of memory and attention are essential for playing almost any game. Long-term memories may be drawn upon when replaying a game that an individual had played in the past, while working memory is vital to learn and remember how new games are played. The skills of sustained and selective attention are also necessary to focus on game play and tune out any unrelated distractions.
Games that specifically address memory and attention include:
- Beginner: Old Maid or Go Fish . These simple card games can be a great starting point for individuals whose memory and attention skills have been severely affected. Since these games are relatively quick, they require a limited amount of sustained attention. Short-term and working memory can also be challenged when trying to remember which players have which cards.
- Intermediate: Concentration or Guess Who? During the game of Concentration, survivors can challenge their working memory and sustained attention skills by try to pick two matching cards from a set of cards laid out on the table. Guess Who? can also address these skills, while also allowing individuals to work on mental organization and classification skills when grouping characters together by their similarities and differences.
- Advanced: Clue or Azul . These more complex games can be used to fine-tune memory and attention skills, while also exercising reasoning and problem-solving abilities.
Improving Processing Speed through Games
Certain games for stroke patients can also help to increase processing speed. While individuals may require extra time to play these games initially, with practice, their processing speed may improve. Games that can help improve processing speed include:
- Beginner: Dutch Blitz or Spoons . These fast-paced card games require skills such as pattern recognition and sequencing, as well as adequate fine motor skills to quickly grasp and manipulate the cards. Practicing these games independently before playing with more players can be an excellent way to gradually improve processing speed as well.
- Intermediate: Perfection . This game, which involves placing uniquely shaped pieces into their matching holes before a timer goes off, can challenge both fine motor skills and processing speed. To begin with, individuals may choose to practice this game without the timer or use a stopwatch to see how fast they can place all of the pieces into their respective positions.
- Advanced: Pictionary or Charades . Playing games during which individuals draw, act out, or describe a specific item can be a fun yet challenging way to work on improving processing speed. Since the individual depicting the targeted word is constantly adapting their presentation, survivors have to use rapid processing skills in order to provide accurate guesses.
Games that Promote Language Skills
The ability to express and comprehend language is frequently impaired after stroke. The following games may help survivors who experience communication challenges due to aphasia, apraxia of speech, or dysarthria .
- Beginner: Boggle . Played by connecting adjacent letters to create words, Boggle is a great game for individuals targeting word-finding skills. Language expression skills can also be practiced by writing or verbally stating the words found in the game. Some survivors may also benefit from initially playing independently without any time constraints to create a low-pressure and enjoyable atmosphere.
- Intermediate: Catch Phrase or Taboo . These fast-paced word games can challenge both receptive and expressive language skills as players race to guess which word the speaker is describing. Although against the official rules, players may choose to allow gestures to boost communication and even the playing field.
- Advanced: Bananagrams or Scrabble . Both involving small letter tiles to create words, playing Bananagrams or Scrabble can be a great way to promote language skills and word-finding abilities. If trying to use the letters already in play to create words is too challenging, players can simply take 25 tiles and attempt to make as many words as possible.
Games Focused on Visual Skills
A stroke may affect vision , causing challenges such as visual field deficits or problems with visual attention. For example, individuals with hemianopia or hemineglect may be unable to see or perceive anything on one side of their body.
While most games involve at least some visual components, the games below can be particularly helpful for addressing visual skills.
- Beginner: Connect 4 or Sequence . These games, which involve connecting multiple game chips in a row, column or on diagonal, can promote visual scanning skills and cognitive flexibility. Since Sequence is a little more complicated, it may be best to try Connect 4 before playing Sequence. Furthermore, some survivors may benefit from trying the “giant” versions of Connect 4 or Sequence to enhance visual awareness of a larger area and improve gross motor skills.
- Intermediate: Spot It! or Blink . Card games, such as Spot It! or Blink, can exercise skills such as visual memory, visual discrimination, and visual scanning. While these games are designed to be fast-paced, slowing them down can make game play more enjoyable for survivors while they are improving.
- Advanced: Battleship . This game can challenge visuospatial skills while also exercising reasoning and problem-solving abilities. Fine motor precision skills may also be challenged.
Considerations Regarding Games for Stroke Patients
While the list above provides a starting point for stroke survivors hoping to enhance their cognitive skills through games, it is by no means exhaustive. A speech or occupational therapist may be able to provide more personalized recommendations.
Finding a game that is appropriately challenging, yet still enjoyable, can sometimes be difficult. Many games have a junior or kid’s version, which may help survivors who need just a little more practice before trying the standard game. Alternatively, adding more players, time constraints, or external distractions can make games a little more challenging.
Survivors who are looking to fine-tune their cognitive skills may benefit from playing more advanced strategy games. These games often require intense concentration, long periods of sustained attention, and high-level problem-solving skills.
Example strategy games for stroke patients include:
- Carcassonne : a puzzle-based game that can challenge visuospatial skills and problem-solving
- Chess : a traditional game requiring planning, judgement and reasoning
- Catan : a building and trading game requiring constant cognitive flexibility and social skills
Finally, some survivors prefer to use gamified rehabilitation technology, such as the CT Speech and Cognitive Therapy App , FitMi , or the MusicGlove . These devices and programs can address cognitive and/or physical functions while adapting to the survivor’s skill level to provide a just-right challenge. By combining the motivational qualities of gaming with the therapeutic benefits of rehabilitation, survivors can get the best of both worlds.
Finding the Best Games for Stroke Patients
Games can be an engaging option for improving cognitive skills after stroke and can help promote a faster and fuller recovery from stroke. Different games will engage different parts of the brain to target specific cognitive skills.
Therefore, it is important to choose games that will address the survivor’s targeted skills. Games can also be modified to offer an appropriate challenge without becoming overwhelming.
The best games for stroke patients will vary depending on the individual’s needs and skill level. However, games can be an excellent tool to use to boost motivation and brighten a survivor’s recovery journey.
Keep It Going: Download Our Stroke Recovery Ebook for Free
Get our free stroke recovery ebook by signing up below! It contains 15 tips every stroke survivor and caregiver must know. You’ll also receive our weekly Monday newsletter that contains 5 articles on stroke recovery. We will never sell your email address, and we never spam. That we promise.
Related Articles

Top 7 Vitamins for Stroke Recovery Based on the Latest Clinical Evidence

Understanding Chronic Stroke: What It Means & How to Recover

Why "One More Time" Matters in Stroke Rehab
Discover award-winning neurorehab tools.

Do you have these 25 pages of rehab exercises?
Get a free copy of our ebook Full Body Exercises for Stroke Patients. Click here to get instant access.
You're on a Roll: Read More Popular Recovery Articles

“Use It or Lose It:” What This Popular Neurorehab Phrase Means

Shoulder Exercises for Stroke Patients to Improve Stability, Mobility and Strength

10 Swallowing Exercises for Stroke Patients to Recover from Dysphagia
You’re Really on a Roll! See how Jerry is regaining movement with FitMi home therapy

My husband is getting better and better!
“My name is Monica Davis but the person who is using the FitMi is my husband, Jerry. I first came across FitMi on Facebook. I pondered it for nearly a year. In that time, he had PT, OT and Speech therapy, as well as vision therapy.
I got a little more serious about ordering the FitMi when that all ended 7 months after his stroke. I wish I hadn’t waited to order it. He enjoys it and it is quite a workout!
He loves it when he levels up and gets WOO HOOs! It is a wonderful product! His stroke has affected his left side. Quick medical attention, therapy and FitMi have helped him tremendously!”
– Monica & Jerry’s FitMi review

What are these “WOO HOOs” about?
FitMi is like your own personal therapist encouraging you to accomplish the high repetition of exercise needed to improve.
When you beat your high score or unlock a new exercise, FitMi provides a little “woo hoo!” as auditory feedback. It’s oddly satisfying and helps motivate you to keep up the great work.
In Jerry’s photo below, you can see him with the FitMi pucks below his feet for one of the leg exercises:

FitMi is beloved by survivors and used in America’s top rehab clinics
Many therapists recommend using FitMi at home between outpatient therapy visits and they are amazed by how much faster patients improve when using it.
It’s no surprise why over 14,000 OTs voted for FitMi as “Best of Show” at the annual AOTA conference; and why the #1 rehabilitation hospital in America, Shirley Ryan Ability Lab, uses FitMi with their patients.
This award-winning home therapy device is the perfect way to continue recovery from home. Read more stories and reviews by clicking the button below:

Support @ flintrehab.com
1-800-593-5468
Mon-Fri 9am-5pm PST
Get Started
Our Products
Grab a free rehab exercise ebook!
Sign up to receive a free PDF ebook with recovery exercises for stroke, traumatic brain injury, or spinal cord injury below:
Government Contract Vehicles | Terms of Service | Return Policy | Privacy Policy | My Account
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Behav Med

Psychological Stress Management and Stress Reduction Strategies for Stroke Survivors: A Scoping Review
Madeleine hinwood.
School of Medicine and Public Health, The University of Newcastle, Callaghan, NSW, Australia
Hunter Medical Research Institute, New Lambton Heights, NSW, Australia
Marina Ilicic
School of Biomedical Sciences and Pharmacy, The University of Newcastle, Callaghan, NSW, Australia
Priority Research Centre for Stroke and Brain Injury, The University of Newcastle, Callaghan, NSW, Australia
Prajwal Gyawali
School of Health and Wellbeing, Faculty of Health, Engineering and Sciences, University of Southern Queensland, Darling Heights, QLD, Australia
Kirsten Coupland
Murielle g kluge.
Centre for Advanced Training Systems, The University of Newcastle, Callaghan, NSW, Australia
Angela Smith
HNE Health Libraries, Hunter New England Local Health District, New Lambton, NSW, Australia
Consumer Investigator, Moon River Turkey, Bathurst, NSW, Australia
Michael Nilsson
Centre for Rehab Innovations, The University of Newcastle, Callaghan, NSW, Australia
LKC School of Medicine, Nanyang Technological University, Singapore
Frederick Rohan Walker
Associated data.
Stroke can be a life-changing event, with survivors frequently experiencing some level of disability, reduced independence, and an abrupt lifestyle change. Not surprisingly, many stroke survivors report elevated levels of stress during the recovery process, which has been associated with worse outcomes.
Given the multiple roles of stress in the etiology of stroke recovery outcomes, we aimed to scope the existing literature on stress management interventions that have been trialed in stroke survivors.
We performed a database search for intervention studies conducted in stroke survivors which reported the effects on stress, resilience, or coping outcome. Medline (OVID), Embase (OVID), CINAHL (EBSCO), Cochrane Library, and PsycInfo (OVID) were searched from database inception until March 11, 2019, and updated on September 1, 2020.
Twenty-four studies met the inclusion criteria. There was significant variation in the range of trialed interventions, as well as the outcome measures used to assess stress. Overall, just over half (13/24) of the included studies reported a benefit in terms of stress reduction. Acceptability and feasibility were considered in 71% (17/24) and costs were considered in 17% (4/24) of studies. The management of stress was rarely linked to the prevention of symptoms of stress-related disorders. The overall evidence base of included studies is weak. However, an increase in the number of studies over time suggests a growing interest in this subject.
Conclusions
Further research is required to identify optimum stress management interventions in stroke survivors, including whether the management of stress can ameliorate the negative impacts of stress on health.
In this review, we found that interventions to reduce stress in stroke survivors were highly variable, and although more than half reported a positive effect in reducing stress, the feasibility of deploying these interventions in practice was rarely considered.
Introduction
Advances in the treatment of stroke, particularly the introduction of clot-busting drugs and clot retrieval technologies, have significantly reduced stroke mortality [ 1 ]. Improvements in diagnosis and rehabilitation have also improved stroke outcomes; however, many stroke survivors continue to experience poor health outcomes for their remaining lifespan. Stroke is one of the five leading global causes of disability-adjusted life years, and the number of years lost as a result of poor health or disability from cardiovascular disease (CVD), including stroke, is greater than the number of years lost to cardiovascular death globally [ 2 ]. This suggests an urgent need to identify new targets and interventions to improve quality of life (QoL) following stroke.
Psychosocial wellbeing after stroke has been relatively neglected compared with motor and other physical symptoms, which are often the primary focus of rehabilitation efforts. One emerging prognostic factor determining the quality of psychological and emotional recovery from stroke is stress [ 3 , 4 ]. Stroke survivors report experiencing persistently high levels of stress, with greater levels of perceived stress poststroke associated with poorer long-term outcomes [ 5–10 ]. Several observational studies have consistently reported significant correlations between stress and worse stroke outcomes, including functional independence, psychological outcomes such as depression, and cognitive function. Likewise, greater resilience, which is defined as the capacity to withstand adversity and “bounce back” after a stressful event, is associated with better QoL poststroke [ 7 , 11 ]. Further, stress is among the strongest proximal risk factors for depression and anxiety disorders, and the risk of these stress-related mental health disorders is significantly greater in stroke survivors compared with the general population [ 12 ]. In the 2 years immediately following stroke, the risk of depression for stroke survivors was around 25%, compared with 8% in a control group of people the same age [ 12 ]. Stroke survivors are also at increased risk of other stress-related disorders, including post-traumatic stress disorder (PTSD) and anxiety disorders [ 13 , 14 ]. These psychological problems are independently associated with increased morbidity, mortality, and disability [ 15 , 16 ]. In addition to a heightened risk of stress-related disorders, the recovery domains influenced by stress broadly contribute to worse QoL, reduced motivation and lower levels of self-reported wellbeing, which in turn may negatively impact participation in rehabilitation. This is likely to potentiate a positive feedback loop between heightened stress perception and poor participation in rehabilitation.
There is clear evidence that rehabilitation interventions can influence patient outcomes after stroke [ 15 , 17 ]. Therefore, identifying and modifying alternative prognostic factors for recovery outcomes are of vital importance to improve trajectories for stroke survivors. Studies highlighting the association between stress and significant downstream effects such as emotional and cognitive problems and poor functional recovery suggest that managing stress may be beneficial to stroke survivors [ 8–10 ]. There is some evidence that stress management interventions in populations with other chronic illnesses, particularly cancer and CVD, can decrease symptoms of depression, and promote resilience [ 18 , 19 ]. However, it is unclear which interventions to mitigate stress have been trialed for stroke survivors.
Psychological stress is a complex phenomenon, and numerous theoretical models of stress have been proposed. There are also various terminologies in the literature to describe the evaluation of state stress. Variations in terminology connected to stress as a short- or long-term outcome may include stress, distress, depression, anxiety, coping, and QoL. The converse can also be identified; although stress exposure can have lasting negative impacts on psychological health and wellbeing, not all individuals will go on to develop these outcomes, and resilience scores are therefore also frequently examined [ 19 ]. In this study, we conceptualized psychological stress according to the stress, appraisal, and coping framework proposed by Lazarus and Folkman [ 20 ], adapted for the stroke setting in Fig. 1 , where stress is a consequence of an individual’s appraisal of their environment, and their perceived ability to cope with a situation or incident. Therefore, depending on how it is appraised, a stressor may have differential short- and long-term effects upon an individual. Interventions to manage stress may be deployed at any point along a spectrum, with primary interventions primarily concerned with stressor reduction, secondary with stress management, and tertiary with remedial support or treatment of stress-related conditions. Here, we expected to find most interventions at the secondary (stress management) level, with outcomes primarily based on the effectiveness of the intervention in the short term (e.g., reduction in perceived stress or other stress marker; improvement in coping skills; or improvement in resilience), and on the ability of the intervention to prevent other downstream effects of stress, such as symptoms of anxiety and depression. Our framework guided the design of the research questions, literature search, identification of studies, and the collation of results.

Conceptual framework of stress processes after stroke, and spectrum of interventions to manage or reduce stress (adapted from Folkman and Lazarus [ 20 ]).
Given that research into stress management strategies for stroke survivors is an emerging area of research, we collated the results of existing studies under several broad topic areas. In addition to mapping and assessing the reported effectiveness of interventions, we also aimed to collate information on the stress outcome measures used, whether long-term effects of stress were considered, and implementation outcomes (specifically acceptability, feasibility, and economic analyses).
Given the breadth of information to be accumulated, we decided to perform a scoping rather than a systematic review. Scoping reviews are designed to assess the coverage of a body of literature, and to identify gaps and map available evidence. Systematic reviews in health care tend to be more focused on confirming or refuting whether current practice is based on evidence, and to establish the quality of that evidence [ 21 ]. Our overall aim was to broadly map the body of literature concerning stress management interventions in stroke survivors. Further, we aimed to synthesize existing results and approaches around stress interventions in stroke survivors to guide the development and implementation of stress management in future studies, identify knowledge gaps, and clarify key concepts around the measurement of stress in stroke survivors. Therefore, as we were mapping a heterogeneous body of literature rather than synthesizing the best available research to answer a specific question, a scoping review methodology was considered most appropriate.
This scoping review was conducted in accordance with the PRISMA extension for scoping reviews [ 22 ].
A protocol was published prior to conducting this review [ 23 ] based upon the framework proposed by Arksey and O’Malley [ 24 ] and updated by Levac et al. [ 25 ], and the methods outlined in the Joanna Briggs Institute Reviewers’ Manual [ 26 ]. The scoping review process is an iterative one, and the inclusion and exclusion criteria were refined during full-text review for clarity and specificity to the review’s objectives following discussion among the research team. The PRISMA Extension for Scoping Reviews (PRISMA-ScR) checklist was referenced to ensure systematic reporting of this scoping review [ 22 ].
Identification of the Research Question
Overall, we were interested in mapping the existing intervention literature for stress reduction or stress management in stroke survivors. As an emerging and inconsistently defined field, we anticipated enormous heterogeneity in the way stress is defined, operationalized, and measured across studies, and in the way that stress and stress prevention studies are designed. Based on the conceptual framework presented in Fig. 1 , we included any intervention studies which measured stress or a related concept as an outcome; therefore, the included studies encompassed both interventions specifically designed for stress reduction, and interventions that did not explicitly aim to reduce stress, but which reported a reduction in a stress-related outcome, such as self-reported stress. The following broad aims, which attempt to capture this heterogeneity of studies under the Lazarus and Folkman framework [ 20 ], guided this scoping review:
- To map the range of interventions trialed addressing stress management in stroke survivors and to identify which interventions are potentially efficacious for reducing stress, or increasing resilience and coping skills.
- To identify the average duration of study length and follow-up. Stroke is a chronic condition with recovery occurring for months and years after the initial event. Further, it would be of interest to assess the potential impact of interventions on longer-term outcomes that may be affected by acute improvements in stress management. Ideally, stress intervention models would match the natural history of stroke and stress-related problems, and this would be reflected in follow-up times of adequate duration.
- To map the multidimensional range of outcome measures that have been used for stress, resilience, and coping in stroke survivors. We anticipated heterogeneous literature, with no broadly accepted outcome measure for psychological stress. Acute and chronic stress can be quantified using various approaches including self-reported, psychometric assessments, as well as physiological biomarkers.
- To identify whether early intervention for stress translates into a reduction in longer-term stress-related clinical outcomes as shown in Fig. 1 , including depression, anxiety, and PTSD. Although we do not expect psychological stress to be the sole cause of mental disorders poststroke, most cases of depression and anxiety can, to some extent, be traced back to the influence of exogenous or endogenous stressors [ 27 ]. Therefore, although an improvement in stress management or coping, or a reduction in perceived stress will not explain all the variation in poststroke depression or anxiety, we would expect a positive effect on mood disorders due to a preventive effect. However, since stress management does not specifically treat mood symptoms, significant changes in mood, and diagnosis with stress-related disorders, may not be observed.
- The success of any intervention is in part dependent on the successful implementation within its environment and context. Therefore, we collected information on whether studies considered implementation outcomes, including potential barriers and limitations, feasibility and acceptability, and economic considerations. This is particularly relevant for stress management approaches, as they may be time consuming, expensive, and difficult to scale up to larger populations.
Search and Screening Methods
The search strategy was designed around the aims of the review and included two key concepts, stroke and stress. The search was designed to align with the stress, appraisal, and coping framework used to conceptualize stress in this review. Broadly, interventions for stress reduction were operationalized in the following way: any intervention (pharmacological or nonpharmacological) delivered in individual, family, or group settings, incorporating strategies to prevent or delay the development of excessive stress, promote coping strategies or resilience, to improve optimism and wellbeing, or to improve or relieve stress-related outcomes, including symptoms of mood disturbance. We included all types of intervention studies (randomized controlled trials [RCTs] and quasi-experimental designs). The research question and corresponding search strategy are defined using the Population, Intervention, Comparator, Outcome, Study design (PICOS) framework (see Supplementary File 1 ). A complete description of the strategies for database searching, filtering methods, abstract identification, and screening was provided in a previously published protocol [ 23 ]. The search for this scoping review was iterative in nature. It began with a gold standard set of articles that informed the selection of medical subject headings (MeSH), keywords, and keyword phrases. The strategy was further refined through reference checking and forward and backward citation checking. Search strategies from reviews in relevant areas were also searched. The search strategy drew on the work of the Cochrane Stroke Group to operationalize search terms for stroke. The search strategy was developed in Medline before being optimized for Embase, resulting in the need to include some additional Emtree terms to capture additional relevant citations. The strategy was then translated to PsycInfo, CINAHL, and the Cochrane Library. All databases were searched from inception until March 11, 2019, and updated on December 12, 2019. The search was updated again prior to submission on September 1, 2020 ( Supplementary File 2 ). Database searches were restricted to subjects and English language citations only. Primary evidence (empirical research) only was included.
An assessment of study quality is optional in scoping reviews; however, may be conducted to gain an appreciation of the quality of evidence in a field. We did not exclude articles based on quality or design; however, we did conduct an assessment of study quality using the Cochrane Risk of Bias tool or the Mixed Methods Appraisal Tool (MMAT), where appropriate, in order to evaluate the existing quality of evidence in the area.
Identifying Relevant Studies
The search yield was imported into Covidence software and duplicates were removed. Title and abstract, and full-text screening were completed separately by members of the research team (M.H., M.I., P.G., M.K., and KC), with each article independently screened by two team members. Discrepancies during screening and reviewing were resolved by a consensus among all reviewers. Inconsistencies were discussed and resolved, and inclusion criteria were refined to improve the application of inclusion/exclusion criteria.
To be included, studies had to meet the following criteria: (a) include an intervention; (b) involve human adult stroke survivors (age ≥18 years); (c) be written in English; and (d) include at least one outcome measure related to stress or resilience. Outcome measures were consistent with the Lazarus and Folkman [ 20 ] stress–coping–appraisal framework, and incorporated changes in direct measures including perceived stress, resiliency, coping skills, and problem-solving, as well as measures of changes in state stress and aligned constructs, including emotional distress, coping, resilience, QoL, and symptoms of anxiety or depression. Although some of the latter measures do not measure stress directly, they were included as outcomes in several publications consistent with the Lazarus and Folkman framework [ 20 ] which aimed to improve coping or problem-solving skills, were hypothesized to thereby improve QoL, and reduce emotional distress in stroke survivors [ 28–31 ], and were therefore included in this review. This reflects the substantial impact that stress can have on physical and mental health. Exclusion criteria included: (a) nonexperimental (e.g., observational, case–control, cross-sectional, longitudinal) studies (i.e., without implementation of an intervention); and (b) relevant reviews (systematic and meta-analysis), but reference lists were hand-searched to identify additional eligible articles. Studies could be randomized or nonrandomized (quasi-experimental).
Charting the Data
Data extraction was independently completed by five reviewers (M.H., M.I., P.G., M.K., and K.C.). The data extraction spreadsheet was designed to capture all relevant details required to answer the research questions and included: author, year published, country, sample size, and population characteristics were recorded (e.g., age, stroke type, and time since stroke, severity measures, comorbidities), outcome measures associated with stress, length of follow-up, type of intervention, duration of intervention, control group, any measures of acceptability and feasibility, any measures of barriers, study limitations, and any measures of cost or cost-effectiveness. The spreadsheet was refined via an iterative process in collaboration with all reviewers.
Collating, Summarizing, and Reporting the Results
We tabulated key information from included studies descriptively. We categorized interventions by intervention type, study duration, and follow-up (in line with aims 1 and 2), explored how stress and stress-related disorders were measured in these studies (in line with aims 3 and 4), and assessed effectiveness (in line with aim 1) and other measures that may affect implementation, including barriers, acceptability, and cost-effectiveness (in line with aim 5). Records in the PsycInfo database receive a classification code, which is used to categorize the document according to the primary subject matter. We used these classification codes to map interventions to higher-order keywords to categorize them. Findings were presented in a narrative synthesis.
Deviations From the Protocol
We originally stated that we would identify potential findings which may help to inform practice and/or guidelines. Some recent guidelines for CVD identify stress as an important risk factor [ 32 ]; however, there are no best-practice recommendations for the management or reduction of stress in stroke survivors. The included studies were overwhelmingly early phase and/or feasibility trials, and as such no recommendation for an approach to stress management could be determined based on the evidence synthesis included in this review.
Assessment of Study Quality
Quality appraisal was used to broadly assess the quality of the literature, to determine where the field currently lies in terms of evidence development. It was not intended to stratify papers into a hierarchy of evidence, and publications were not excluded from the review based on quality. To assess the quality of the quantitative studies, the Cochrane Risk of Bias 2 (RoB2) quality appraisal tool was used [ 33 ]. For any included qualitative or mixed-method studies, the MMAT was used [ 34 ]. The MMAT does not have an overall rating category, and therefore we used the following guide to assess the overall risk of bias associated with each publication: (a) strong (80% or more of the quality indicators were met), (b) moderate (between 40% and 80% of the quality indicators were met), and (c) weak (less than 40% of the quality indicators were met).
Included and Excluded Articles
The study selection process is summarized in the PRISMA flow diagram ( Fig. 2 ) [ 35 ]. The initial search, which was conducted on March 11, 2019, identified 2,653 references after deduplication. The search was updated on December 12, 2019, and again prior to submission on September 1, 2020, after which there was a total of 3,140 studies imported to Covidence, with 3,048 available for screening following deduplication. Of these, 116 articles were considered potentially relevant after initial exclusions of titles and abstracts. A further 92 were excluded after a two-person review of the full text. A total of 24 articles were included in this review [ 28–31 , 36–55 ].

PRISMA flow diagram [ 35 ].
Study Characteristics
Study characteristics, including country, study design, participants, intervention, comparator, and length of follow-up, are summarized in Supplementary File 3 . Included studies were published between 1992 and 2020, with most ( n = 17; 70%) published in the last 5 years [ 28 , 31 , 36 , 38–42 , 45–48 , 51–55 ].
There was significant variability in study design, including RCTs and non-RCTs, and uncontrolled before and after studies. The type, duration, and frequency of intervention used also varied across studies, with interventions running from five sessions over 1 week (aromatherapy foot bath and massage) [ 46 ], to 6 months (antidepressant treatment with sertraline [ 49 ]; home-based psychoeducational program [ 50 ]). Most interventions ran weekly sessions over approximately 8–12 weeks ( n = 15) [ 29–31 , 40–42 , 44 , 45 , 48–52 , 54 , 55 ]. The duration of follow-up also varied significantly between studies, ranging from 0 (immediate follow-up) to 12 months. Finally, as we placed no restrictions on study type beyond intervention studies, three studies used qualitative thematic analyses (via survey or interview) [ 37 , 40 , 48 ], in which stress emerged as a theme.
Whilst the reported sample sizes varied from 8 to 166 participants, most of the included studies had relatively small sample sizes, with 16 out of 24 studies recruiting fewer than 50 participants [ 28 , 29 , 36 , 37 , 39–42 , 44–48 , 51–54 ].
The populations in the included studies varied in terms of time poststroke, and whether a broad or selected population was recruited. Most studies reported time postonset of stroke; only Nour et al. [ 29 ] and Chouliara and Lincoln [ 40 ] did not explicitly define time poststroke; Nour et al. [ 29 ] stated that participants had finished active rehabilitation. We categorized the populations according to the critical time points of stroke recovery proposed in Bernhardt et al. [ 56 ], including hyperacute (0–24 hr), acute (1–7 days), subacute (7 days to 6 months), and chronic (>6 months) phases. The majority of studies ( n = 15) [ 28 , 30 , 31 , 41 , 43–48 , 50–54 ] involved participants recruited in the chronic phase of recovery. Five studies involved participants recruited during the subacute phase of stroke [ 37 , 38 , 42 , 49 , 55 ]. Two studies recruited participants during the acute period, whilst patients were hospitalized [ 36 , 39 ]. We based our assessments on the mean or median times poststroke reported in the studies; therefore, a small number of studies may have included participants across multiple phases of recovery, primarily subacute to chronic. Studies rarely specified whether included participants were first or recurrent stroke survivors or details of stroke type.
Three of the included studies used a selected population (i.e., those reporting high distress, or those with an existing diagnosis of depression, anxiety, or fatigue [ 41 , 49 , 52 ]), in order to assess the effect of an intervention on these outcomes. Many studies excluded people with a progressive neurological disorder or cognitive dysfunction, reduced life expectancy, subdural hematomas, moderate or severe aphasia, or who partook in excessive drinking or drug abuse [ 31 , 38 , 39 ]. Studies typically justified this approach by stating that collecting and reliably interpreting data from these patients can present significant challenges.
Study Interventions
The types of interventions trialed for stress management across the included studies are summarized in Table 1 .
Characteristics of interventions used to address stress levels in stroke survivors
| Type | Subtype | Theory/hypothesis | Studies |
|---|---|---|---|
| Psychosocial | |||
| Social support networks | Social support | Social support intervention would improve the support experienced by stroke survivors, as such leading to better psychosocial outcome. | Friedland and McColl (1992) [ ] |
| Cognitive processes | MBSR | MBSR will reduce mental fatigue after stroke and TBI. | Johansson et al. (2012) [ ] |
| Problem-solving therapy | Problem-solving therapy will improve coping strategy, QoL, and reduce emotional distress in stroke survivors. | Visser et al. (2016) [ ] Chalmers et al. (2019) [ ] | |
| Meditation | Meditation will cultivate mindfulness to train ttention and awareness, to achieve a mentally clear and emotionally calm and stable state. | Love et al. (2020) [ ] | |
| Rehabilitation/ neuropsychological rehabilitation | Memory rehabilitation | Memory rehabilitation will develop patients’ ability to cope with or compensate for residual memory deficits, as well as promoting participation. | Chouliara and Lincoln (2016) [ ] |
| Leisure rehabilitation | Leisure education will improve QoL and depression in stroke survivors. | Nour et al. (2002) [ ] | |
| Behavioral | Proactive coping intervention | Stroke survivors with better proactive coping skills will experience improved self-efficacy and QoL. | Tielemans et al. (2015) [ ] |
| Motor processes | Physical activity program/exercise | Improving and maintaining physical activity levels will improve the overall health, including psychological functioning, cognitive functioning, and sleep, of adults with acquired brain injury. | Jones et al. (2016) [ ] Colledge et al. (2017) [ ] |
| Aquatic therapy | Aquatic therapy will minimize anxiety, fatigue, and depression, which tend to be barriers to stroke rehabilitation. | Perez-de la Cruz (2020) [ ] | |
| Psychotherapy | Positive psychotherapy | Positive psychotherapy will alleviate psychological distress after acquired brain injury. | Cullen et al. (2018) [ ] Terrill et al. (2018) [ ] |
| SFBT | SFBT will reduce depression and anxiety symptoms, generate a constructive attitude, and increase self-efficacy in patients poststroke. | Wichowicz et al. (2017) [ ] | |
| Creative arts therapy | Person-centered arts program | Participation in an arts program will improve the emotional and mental wellbeing of stroke survivors. | Baumann et al. (2013) [ ] |
| Treatment | cCBT | cCBT will alleviate emotional distress and mental health problems such as anxiety and depression after experiencing a stroke. | Simblett et al. (2017) [ ] |
| PosMT | Training in positivity using the PosMT audio tool could be added to rehabilitation for prevention or management of poststroke psychological problems. | Mavaddat et al. (2017) [ ] | |
| Multicomponent | Psychoeducation (mailed and home visit) | Home-based psychoeducation will improve the perceived health of stroke survivors by decreasing depression, fatigue, and the negative impact of stroke. | Ostwald et al. (2014) [ ] Stubberud et al. (2019) [ ] |
| Promoting psychosocial wellbeing following stroke | Applying a dialog-based intervention drawing on narrative theory, supported conversation for people with aphasia, and guided self-determination will promote a sense of coherence in life and reduce threats to wellbeing after stroke, such as feelings of chaos and lack of control. | Bragstad et al. (2020) [ ] | |
| Training | Skills-based intervention informed by CBT, DBT, and trauma-informed care | Training in areas including cognitive restructuring/reappraisals, adaptive thinking, mindfulness, distress tolerance, impact of the illness/injury, understanding triggers, and role and identity changes will prevent chronic emotional distress in stroke survivors and their caregivers. | Bannon et al. (2020) [ ] |
| Biofeedback training | HRV biofeedback will improve autonomic dysfunction, cognitive impairment, and psychological distress. | Chang et al. (2020) [ ] | |
| Alternative medicine | |||
| Alternative medicine | Aromatherapy (foot bath and massage) | Back massage and foot bath using essential oils will improve stress, body temperature, mood state, and fatigue levels of stroke patients. | Lee et al. (2017) [ ] |
| Pharmacological | |||
| Antidepressant drugs | Sertraline (50–100 mg daily) | Sertraline, a SSRI, will have positive effects on both depressive symptoms and other relevant poststroke domains including emotional distress and QoL. | Murray et al. (2005) [ ] |
cCBT computerized cognitive behavior therapy; DBT dialectical behavior therapy; HRV heart rate variability; MBSR mindfulness-based stress reduction; PosMT positive mental training; QoL quality of life; SFBT solution-focused brief therapy; SSRI selective serotonin reuptake inhibitor; TBI traumatic brain injury.
We used the PsycInfo database to map each intervention to its broader subject heading category and identified the theory or hypothesis associated with each that would lead to an improvement in stress-related outcomes. Although there was wide variability in the types of intervention trialed, most (22; 92%) utilized psychosocial interventions targeted at the individual level. These include social support [ 43 ], cognitive processes including mindfulness-based stress reduction, meditation and problem-solving therapy [ 28 , 31 , 44 , 47 ], rehabilitation or neuropsychological rehabilitation targeted at memory or leisure [ 29 , 40 ], a behavioral proactive coping intervention [ 30 ], physical activity programs [ 41 , 45 , 51 ], psychotherapy including both positive psychotherapy [ 42 , 54 ] and solution-focused brief therapy [ 55 ], creative arts therapy [ 37 ], cognitive behavioral therapy or positive mental training [ 48 , 52 ], multicomponent interventions consisting of home-based visits and mailed information, based on principles of psychoeducation [ 38 , 50 , 53 ] and training modules based on developing skills in either cognitive behavior therapy/cognitive reappraisal or heart rate variability biofeedback [ 36 , 39 ]. The remaining two studies assessed alternative medicine (aromatherapy massage and foot bath [ 46 ]), and pharmacological treatment (the selective serotonin reuptake inhibitor antidepressant sertraline [ 49 ]). There were no organizational-level interventions in the included studies.
Stress Outcome Metrics
Table 2 summarizes how stress or stress-relevant outcomes were measured in the included studies. Not all studies were designed to examine stress or resilience as a primary outcome, and as such the included outcomes were not necessarily primary outcomes. Studies were included into this scoping review only if the stress was specifically discussed in the results section of the study. This may include data from qualitative interviews or surveys, or within a subscale of another measure (e.g., QoL).
Characteristics of outcome measures used to assess interventions for stress measurement
| Outcome type | Outcome measurement scale | Studies |
|---|---|---|
| Stress | 10-item Perceived Stress Scale (PSS-10) | Colledge et al. (2017) [ ] Ostwald et al. (2014) [ ] |
| Depression Anxiety Stress Scales (DASS-21) | Cullen et al. (2018) [ ] | |
| General Health Questionnaire (GHQ) | Friedland and McColl (1992) [ ] | |
| Kessler Psychological Distress Scale (K10) | Jones et al. (2016) [ ] | |
| Mental Fatigue Scale (MFS) | Johansson et al. (2012) [ ] | |
| Social Readjustment Rating Scale (SRRS) | Lee et al. (2017) [ ] | |
| Emotional Distress Scale (EDS) | Murray et al. (2005) [ ] | |
| Coping | Utrecht Proactive Coping Competence scale (UPCC) | Tielemans et al. (2015) [ ] |
| Coping Inventory for Stressful Situations | Visser et al. (2016) [ ] | |
| Problem-solving | Social Problem-Solving Inventory-Revised (SPSIR) | Chalmers et al. (2019) [ ] Visser et al. (2016) [ ] |
| Resilience | 10-item Connor Davidson Resilience Scale (CD-RISC) | Terrill et al. (2018) [ ] Perez-de la Cruz (2020) [ ] |
| Brief Resilience Scale (BRS) | Love et al. (2020) [ ] | |
| Depression/anxiety/mood | Center for Epidemiologic Studies Depression Scale (CES-D) | Chalmers et al. (2019) [ ] Visser et al. (2016) [ ] Love et al. (2020) [ ] |
| Beck Depression Inventory (BDI) | Colledge et al. (2017) [ ] Nour et al. (2002) [ ] Simblett et al. (2017) [ ] | |
| Beck Anxiety Inventory(BAI) | Simblett et al. (2017) [ ] | |
| Hospital Anxiety and Depression Scale (HADS) | Chalmers et al. (2019) [ ] Stubberud et al. (2019) [ ] Tielemans et al. (2015) [ ] Wichowicz et al. (2017) [ ] | |
| Comprehensive Psychopathological Rating Scale (CPRS) | Johansson et al. (2012) [ ] | |
| Multiple Affective Adjective Checklist (MAACL) | Lee et al. (2017) [ ] | |
| Montgomery–Åsberg Depression Rating Scale (MADRS) | Murray et al. (2005) [ ] | |
| Presence of emotionalism (increased tearfulness and pathologic crying was recorded as a dichotomous variable) | Murray et al. (2005) [ ] | |
| Geriatric Depression Scale (GDS) | Ostwald et al. (2014) [ ] | |
| PROMIS-Depression Short Form 8b | Terrill et al. (2018) [ ] | |
| State-Trait Anxiety Inventory (STAI-Y) | Love et al. (2020) [ ] | |
| Quality of life | Stroke Specific Quality of Life Scale (SS-QOL) | Chalmers et al. (2019) [ ] Tielemans et al. (2015) [ ] Visser et al. (2016) [ ] |
| Global subjective rating of change in quality of life (QoL) was measured according to a validated visual analog scale | Murray et al. (2005) [ ] | |
| Sickness Impact Profile | Nour et al. (2002) [ ] Friedland and McColl (1992) [ ] | |
| Older People’s Quality of Life Questionnaire (OPQOL) | Terrill et al. (2018) [ ] | |
| Short From 36 Health Survey (SF-36) | Perez-de la Cruz (2020) [ ] | |
| EuroQol EQ-5D-5L | Visser et al. (2016) [ ] | |
| Life satisfaction | Satisfaction with Life Scale (SWLS) | Colledge et al. (2017) [ ] |
| Authentic Happiness Inventory (AHI) | Cullen et al. (2018) [ ] | |
| Leisure Satisfaction Scale | Nour et al. (2002) [ ] | |
| Likert scales: current life satisfaction, and the difference from prestroke life satisfaction | Cullen et al. (2018) [ ] | |
| Qualitative analysis | Open-ended descriptive survey | Chalmers et al. (2019) [ ] |
| Semi-structured interviews | Chouliara and Lincoln (2016) [ ] Mavaddat et al. (2017) [ ] Baumann et al. (2013) [ ] |
Several different psychometric scales were used to assess stress or related constructs; however, we found no studies assessing stress biomarkers. In our search strategy, we included terms for coping and resilience, resulting in the inclusion of studies that measured stress, and resilience, coping, problem-solving, stress-related disorders (including anxiety, depression, and PTSD), life satisfaction, and QoL measures, where stress was reported as a subcomponent of the measure. Of the 14 studies which included a psychometric measurement of stress, coping, or resilience, 8 reported using a stress-specific outcome measure [ 41–46 , 49 , 50 ], with others recording stress-related constructs via a coping scale [ 30 , 31 ], problem-solving scale [ 28 , 31 ], or resilience scale [ 47 , 51 , 54 ].
Most studies measured stress-related disorders via a scale for symptoms of depression, anxiety, or mood ( n = 16) [ 28–31 , 36 , 39 , 41 , 44 , 46 , 47 , 49 , 50 , 52–55 ]. The Center for Epidemiologic Studies Depression Scale (CES-D) [ 28 , 31 , 47 ], Beck Depression Inventory (BDI) [ 29 , 41 , 52 ], and the Hospital Anxiety and Depression Scale (HADS) [ 28 , 30 , 36 , 39 , 53 , 55 ] were the most commonly used measures.
Ten studies assessed QoL and/or life satisfaction [ 28–31 , 41–43 , 49 , 51 , 54 ]; some studies reported a stress measure as a subscale of this. For example, Friedland and McColl [ 43 ] used the General Health Questionnaire (GHQ) and the Sickness Impact Profile (SIP) to measure “psychosocial adjustment”. As mentioned above three qualitative thematic analysis studies [ 37 , 40 , 48 ] were included which did not measure stress outcomes but which highlighted stress as an emerging theme. For example, Baumann et al. [ 37 ], a descriptive study of an art therapy program aiming to reduce distress during rehabilitation, did not explicitly measure stress but described individual participants’ experiences of distress associated with stroke.
Effectiveness and Implementation Outcomes
For each intervention, we assessed the effectiveness in terms of both reduction in stress or related construct, and reduction in stress-related mental health disorders (anxiety, depression, or PTSD); implementation measures including barriers and limitations, feasibility and acceptability, and any cost analysis or cost-effectiveness, were reported. Collectively, these features are likely to inform the further development of an intervention for eventual use in practice ( Table 3 ).
Measures of effectiveness, acceptability, feasibility, and cost-effectiveness
| Study | Stress reduction | Reduction in anxiety or mood disorder | Barriers and limitations | Feasibility and acceptability | Cost-effectiveness |
|---|---|---|---|---|---|
| Bannon et al. (2020) [ ] | Increased scores on resiliency variables, including self-efficacy, mindfulness, and perceived coping in Recovering Together training dyads, but not control dyads from baseline to post-test. | Participation in Recovering Together was associated with baseline to post-test decrease in symptoms of depression, anxiety, and PTS in stroke survivors and caregivers. | Small feasibility trial Patients discharged before they could be approached Low internal consistency on measures with reversed scored items for patients at baseline | Clinical staff not invested in project Low recruitment Treatment satisfaction was high Adherence and acceptability of procedures was high | NR |
| Baumann et al. (2013) [ ] | Weekly art sessions during rehabilitation. Participants reported that the sessions offered a source of relaxation, tranquility or calmness(qualitative analysis). | NR | No long-term follow-up (1 week after final session) Small sample size ( = 18) | All but one patient indicated a wish to continue arts activities in the future | NR |
| Bragstad et al. (2020) [ ] | No between-group differences in psychosocial wellbeing at 12 months poststroke. | No statistically significant between-group difference in depression, sense of coherence, or health-related QoL at 12 months. | The intervention was designed both to be delivered uniformly and to be individualized. The competing aims may have compromised session delivery Sample may not be representative; informed consent was difficult to obtain in the stroke unit | Composite adherence score showed that 117 (80.1%) of the intervention trajectories satisfied the criteria for high-fidelity intervention adherence Participants reported finding the intervention helpful | NR |
| Chalmers et al. (2019) [ ] | Problem-solving therapy did not produce a significant change in overall problem-solving (SPISR; proxy measure for emotional distress). | Slight reduction after therapy on the CES-D and no reduction on the HADS-A. | No randomization Use of waitlist control group No controlling for confounding Problems with recruitment Small sample size ( = 28) | Participants generally reported that each therapy session was helpful and enjoyable | NR |
| Chang et al. (2020) [ ] | Average HR decreased compared with baseline in the HRVBF, but no significant difference between groups. | HADS score significantly decreased in the HRVBF group at 1 and 3 months but not in the control group. | Small sample size Short follow-up time Did not log self-practice during follow-up | 5/40 patients dropped out after randomization Study reported that the intervention was feasible, but it was not clear on what basis this was reported | NR |
| Chouliara and Lincoln (2016) [ ] | Memory rehabilitation led to perceived benefits in participants’ ability to effectively manage stress (qualitative analysis). | NR | Small sample size ( = 20) Qualitative analysis did not directly assess some aspects Separate results not reported for stroke survivors only | NR | NR |
| Colledge et al. (2017) [ ] | No effect of exercise training on perceived stress. | Descriptive reduction in depressive symptoms at follow-up. | Small sample size ( = 32) Exploratory trial (descriptive analysis only) Selection bias No nonintervention control group | NR | NR |
| Cullen et al. (2018) [ ] | Mean difference of −5.8 points on the DASS-21 Stress scale (intervention vs. controls) at week 20 after positive psychology intervention. | Mean difference of −9.6 points on the DASS-21 Anxiety scale (intervention vs. controls) at week 20 after positive psychology intervention. | Small sample size ( = 37) Exploratory trial Not designed or powered for efficacy | 63% retention (15 completers) Authors considered intervention feasible to deliver and acceptable to participants | NR |
| Friedland and McColl (1992) [ ] | No differences between social support intervention and control groups on psychosocial variables including the GHQ. | NR | Relatively high attrition rate Timing of intervention | NR | NR |
| Johansson et al. (2012) [ ] | Statistically significant reduction in reported mental fatigue, including reduction in sensitivity to stress item, following MBSR compared with baseline and controls. | Significantly decreased scores for depression and anxiety on the CPRS after 8 weeks of MBSR. | Small sample size ( = 29) Some participants who discontinued found the program time consuming, or difficult to travel to attend appointments | NR | NR |
| Jones et al. (2016) [ ] | A statistically significant reduction in psychological distress (K10 scale) of 2.76 points immediately after the myMoves program ( = .001). | NR | Small sample size ( = 24) Contact with study participants occurred outside of the intervention program Mixed population (stroke and TBI) | Participants completed an average of 5.6/6 sessions Participants reported a high level of overall satisfaction with the program (95.7%) The program required little clinician contact time, with an average of 32.8 min per participant over 8 weeks | NR |
| Lee et al. (2017) [ ] | Statistically significant reduction in the social readjustment rating scale (means not reported). | NR | Small sample size ( = 14) Poor reporting of study methodology and results | NR | NR |
| Love et al. (2020) [ ] | Small, but nonsignificant, postmeditation increase in resilience observed. | NR | Small sample size ( = 35) No control group Selection bias Sampling in single stroke clinic Exclusion of participants lost to follow-up | NR | NR |
| Mavaddat et al. (2017) [ ] | In qualitative interviews, stroke survivors reported benefits of the positive mental training program in handling stress, improved mood, and coping ability. | Four stroke survivors had improved scores on PANAS; two stroke survivors had improved scores, and one stroke survivor had a worse score on the HADS. | Small sample size ( = 10) Self-selected sample Not all participants completed the full 12-week program | 7/10 stroke survivors reported positive benefits from listening and would recommend to others Participants with moderate aphasia found it difficult to concentrate and did not persist with the study | £38 for access to the full audio program (in 2013 GBP). |
| Murray et al. (2005) [ ] | No statistically significant effect of sertraline treatment on EDS score, however there was a reduction from baseline in both groups regardless of treatment. Some improvement in QoL and emotionalism. | The MADRS score decreased substantially in both treatment groups, with no significant differences between them at 6 and 26 weeks. | High discontinuation rate (39% in the treatment and 49% in the placebo group) Selection of patients with minor depression only | NR | NR |
| Nour et al. (2002) [ ] | At post-test, the experimental group (leisure rehabilitation) obtained statistically significantly better scores for total, psychological, and physical QoL, although effect sizes were small. | No statistically significant difference between groups for depression (BDI). | Small sample size Extra time (on average 20 min per session) provided to intervention group Some participants did not complete the program | Participants reported satisfaction with leisure activities following the intervention | NR |
| Ostwald et al. (2014) [ ] | No effect of mailed or home-based psychoeducational intervention on stress as measured by the PSS-10. | No effect of mailed or home-based psychoeducational intervention on depression scores (GDS). | Sample size not large enough for subgroup analyses The sample is not representative—included only those over 50 years of age who were being discharged home with a spouse Analysis of multiple outcomes in this study possibly increased the type I error rate. | 84% of the dyads completed the study 12-month follow-up. Dyads that did not complete the study were older, had higher caregiver support scores and spent more days in inpatient rehabilitation than those who finished the study | Number, length, and content of each contact was tracked, allowing for analysis of costs. An average of two home visits a month during the initial 6 months at home postdischarge from inpatient rehabilitation could be delivered at a mean cost of $2,500 per dyad. |
| Perez-de la Cruz (2020) [ ] | In the experimental group, significant differences from baseline were found in the resilience variables ( < .001) and these improvements were maintained 1 month after completing the treatment program. | NR | Small sample size ( = 41) Short follow-up (1 month) | All the participants completed all the sessions and complied with the proposed program | NR |
| Simblett et al. (2017) [ ] | All groups demonstrated a decrease in symptoms of distress, measured via the BDI and BAI, and the NEADL across time associated with computerized CBT and computerized cognitive remediation therapy. | Trend toward reduced depression scores on the BDI for computerized CBT and computerized cognitive remediation therapy. Smaller trend for anxiety symptoms. | Small sample size ( = 28) Feasibility and acceptability were the primary outcomes for this study, not efficacy No blinding to intervention of outcome assessors | Feasibility and acceptability were the primary outcomes for this study. Recruitment rate for the intervention ran below the expected rate Broadly feasible, although some aspects required more flexibility Majority suggested intervention was useful, relevant and easy to use | Not explicitly measured. However, the idea of small groups was primarily introduced as a means of improving the feasibility of delivery by reducing costs associated with providing psychological therapy. |
| Stubberud et al. (2019) [ ] | No change in self-efficacy after training in metacognitive strategies for improving attention, problem-solving, fatigue management, adaptive coping responses, and the use of CBT techniques as measured using the GSE scale. | Decrease in overall score on the HADS, driven by a change in the anxiety subscale. No change in the depression subscale. | Small sample size ( = 8, of which 5 are stroke survivors) Results not presented separately for stroke and TBI survivors Self-reported outcomes only No control group | All subjects completed the interventions | NR |
| Terrill et al. (2018) [ ] | Study not designed to measure effect of intervention—the data collected in this study were used to identify feasibility of a positive psychology app. 8/10 dyads still used positive psychology in their everyday lives at follow-up. Measured CD-RISC, but results not reported. | Measured PROMIS-Depression Short Form 8b, but results not reported. | Small sample size; 11 stroke survivor/carer dyads. One dyad discontinued, final 10 dyads | Participants reported satisfaction with the intervention Stroke survivors were fatigued by training session One of the dyads dropped out of the study Remaining dyads engaged in a mean of 4.08 individual and 3.62 couple activities per week | Not explicitly reported; referenced a Cochrane review stating that use of apps to administer self-management programs was cost-effective. |
| Tielemans et al. (2015) [ ] | No effect of self-management intervention compared with an education intervention in coping skills on the UPCC scale. | Trend favoring the self-management intervention on the HADS. | Study did not include more severely affected stroke survivors Self-assessment used to assess outcomes Outcome measures too generic to detect changes Study too small to detect outcome differences in partners ( = 57 partners) Sample selected by hospital staff Usual care was not controlled | Of 58 patients assigned to the self-management intervention, 56 started the intervention and 46 attended at least three quarters of the intervention sessions | NR |
| Visser et al. (2016) [ ] | Improvement in coping strategy as measured by the Coping Inventory for Stressful Situations between groups (problem-solving therapy vs. control). | Depression score did not differ significantly between the groups over time (CES-D). | No active control groups Intervention was investigated within outpatient rehabilitation and may not be generalizable to other settings Sample reported a relatively high utility score compared with other stroke populations | The low dropout rate and positive feedback suggest that an open group design is feasible and effective in outpatient stroke rehabilitation | NR |
| Wichowicz et al. (2017) [ ] | Increased self-efficacy and constructive attitudes in the SFBT group compared with controls (Mini-Mental Adjustment to Cancer and Self-efficacy Scale). | Reduced anxiety and depression scores in the SFBT group compared with controls (HADS). | 62 completers (100 randomized) Participants relatively fit and may not be representative 35 withdrawals from study Lengthy procedure Lack of complete randomization | Potential SFBT participants who refused to participate may have found the procedure of psychotherapy too lengthy | NR |
BAI Beck Anxiety Inventory; BDI Beck Depression Inventory; CD-RISC 10-item Connor Davidson Resilience Scale; CES-D Center for Epidemiologic Studies Depression Scale; CPRS Comprehensive Psychopathological Rating scale; DASS-21 Depression Anxiety Stress Scales; EDS Emotional Distress Scale; GBP British pounds; GDS Geriatric Depression Scale; GHQ General Health Questionnaire; GSE General Self-Efficacy; HADS Hospital Anxiety and Depression Scale; HR heart rate; HRVBF heart rate variability biofeedback; MADRS Montgomery–Åsberg Depression Rating Scale; MBSR mindfulness-based stress reduction; NEADL Nottingham Extended Activities of Daily Living; NR not reported; PANAS Positive and Negative Affect Schedule; PROMIS Patient-Reported Outcomes Measurement Information System; PSS-10 Perceived Stress Scale; PTS post-traumatic stress; QoL quality of life; SFBT solution-focused brief therapy; SPISR Social Problem-Solving Inventory-revised; TBI traumatic brain injury; UPCC Utrecht Proactive Coping Competence.
In order to address our research question “to identify which interventions are potentially efficacious for reducing stress or increasing resilience and coping” we compiled a descriptive overview of the reported effectiveness of the intervention in each study. Positive effects on stress, resilience, coping, or psychological QoL/life satisfaction were reported in 13 of the 24 included studies [ 29 , 31 , 36 , 37 , 40 , 42 , 44–46 , 48 , 51 , 52 , 55 ]. Baumann et al. [ 37 ] and Chouliara and Lincoln [ 40 ] reported qualitative reductions in stress associated with an inpatient art program and memory rehabilitation, respectively. The other studies reported a quantitative improvement in stress-related outcomes associated with a number of intervention types: skills-based training based on principles of cognitive behavior therapy [ 36 ], positive psychology [ 42 , 48 ], mindfulness-based stress reduction [ 44 ], physical activity program [ 45 ], aromatherapy massage, and footbath [ 46 ], leisure rehabilitation [ 29 ], aquatic therapy [ 51 ], computerized cognitive behavior therapy or cognitive remediation [ 52 ], problem-solving therapy [ 31 ], and solution-focused brief therapy [ 55 ]. Whilst this represents many included studies (54%), most of these had relatively small sample sizes, ranging from 14 to 166, with 10/13 studies recruiting fewer than 30 stroke survivors. Most of these were reported as exploratory, quasi-experimental, or feasibility studies, and reported other methodological concerns including lack of active control group and significant dropout rates. Some of these results were also not numerically reported or reported as a qualitative perceived reduction only.
The impact of the interventions on longer-term stress-related problems, primarily symptoms of depression or anxiety, were considered in 75% (18/24) included studies. Of these, seven reported a quantitative decrease in these symptoms [ 36 , 39 , 42 , 44 , 47 , 53 , 55 ].
In addition to effectiveness results, we also collated implementation outcomes reported across studies, primarily acceptability and feasibility, in order to assess whether the potential long-term sustainability of intervention had been considered in the included studies. Where studies included an explicit measure of feasibility or acceptability from participants, feedback was generally positive [ 28 , 29 , 31 , 36–39 , 42 , 45 , 46 , 48 , 50–52 , 54 ]. Several studies reported low dropout rates and high adherence to the intervention strategy ( n = 8) [ 31 , 36 , 38 , 45 , 50 , 51 , 53 , 54 ]. Broadly, this suggests a willingness to participate in these intervention studies. However, several studies did report problems with recruitment or other barriers to participation, including potential refusal to participate based on the time commitments or participation burden required for some interventions ( n = 8) [ 30 , 36 , 42–44 , 50 , 54 , 55 ]. Further, some interventions reported differential dropout rates for different groups of participants, particularly those with aphasia ( n = 2) [ 30 , 48 ].
We also investigated whether studies reported some measure of cost or cost-effectiveness analysis. This is also an important consideration for upscaling and eventually implementing a novel intervention in practice. Only four of the included studies referred to or measured the costs of the intervention. Mavaddat et al. [ 48 ] and Ostwald et al. [ 50 ] both reported the costs of providing the intervention per participant. In Terrill et al. [ 54 ] and Simblett et al. [ 52 ], although costs were not explicitly measured, both reported that the intervention was expected to be cost-effective based on its features. The cost-effectiveness of any intervention was not reported.
We used the Cochrane Risk of Bias tool to assess intervention studies, and the MMAT to assess mixed-method and qualitative studies ( Supplementary File 4 ). The included quantitative studies ( n = 21) [ 28–31 , 36 , 38 , 39 , 41–47 , 49–55 ] had methodological limitations, including unclear recruitment techniques, small sample sizes, high attrition rates, failure to control for important confounders, use of nonvalidated measures and inconsistent reporting. Studies scored most strongly (low risk of bias) on sequence generation (12/21), allocation concealment (11/21), incomplete outcome data (18/21), and selective outcome reporting (16/21). The categories where studies overall were weaker (associated with a high or unclear risk of bias) included blinding of participants and personnel (16/21), blinding of outcome assessors (14/21), and other sources of bias (20/21). Quality scoring of the qualitative or mixed-methods papers ( n = 3) [ 37 , 40 , 48 ] suggested that these papers had a moderate risk of bias. Studies were not excluded based on quality. The assessment of quality for each of the included studies is presented in Supplementary Appendix .
This scoping review is the first to map the breadth of research that has been conducted around stress interventions for stroke survivors. Here, we have mapped the types and effectiveness of the trialed interventions, as well as the outcome measures used to assess stress or related constructs. We also considered aspects of implementation reported in the studies, including patient acceptability, feasibility, limitations, and cost-effectiveness. We identified a total of 24 studies that recruited mixed populations of stroke survivors in terms of susceptibility to stress-related outcomes and time poststroke and identified a variety of primarily psychosocial interventions delivered to individuals to directly address stress management or promote related constructs such as resilience, problem-solving, or coping. Although all studies reported the effect of the intervention on stress or stress-related outcome measures, a correlation to recovery outcomes was not consistently addressed or investigated across studies. We also identified significant methodological issues associated with most studies, and a tendency for studies to be at an early or feasibility stage. Furthermore, even though the majority of included studies appeared to be feasibility or exploratory trials, our search did not identify any larger subsequent or follow-up studies to this early work. Overall, despite the trend toward positive outcomes, the limitations of the included studies made it difficult to conclusively identify the most effective interventions. Despite these shortcomings, we found that the number of relevant publications increased over time, suggesting that stress and stress management are progressively being considered important for stroke survivors.
Psychological distress is commonly reported following stroke and is associated with a number of significant cognitive and psychological problems, but based on this review, the evidence base for psychotherapeutic interventions is small and equivocal. Any recommendation for an intervention designed to manage excessive stress, with the ultimate aim of preventing stress-related disorders and improving recovery, should be evidence based in order to justify the allocation of resources, and in order to reduce harms from potentially ineffective interventions. Although there is emerging evidence for targeting stress for the prevention of some disorders such as CVD, at present the relevance of intervening on stress in stroke populations remains unclear [ 57 , 58 ]. Broadly, the population with the greatest benefit:risk ratio is not defined, the potential range of interventions remains broad, and there is no agreement on the best outcome measures to use for stress. The studies included here also tended to emphasize treatment rather than prevention of emotional distress. This is in agreement with two recent systematic reviews of dyadic interventions for caregivers and stroke survivors, which focused on interventions to reduce stress in caregivers. The results of these studies highlighted substantial limitations of interventions for carers and stroke survivors including weighting toward treating rather than preventing stress, and a lack of customizable interventions which would allow tailoring to account for the heterogeneity of stroke survivors’ needs [ 59 , 60 ].
Stress Management Interventions and Their Delivery After Stroke
A wide variety of interventions were trialed in the included studies, which were predominantly small in scale and based on very localized or intensive solutions generally run for an 8–12-week period. Often considerations on how such an intervention might scale up to the broader population were not included/made. Several studies reported poor adherence and/or recruitment due to the burden of participation. Stress management interventions that require large amounts of time and travel may lead to adherence problems in stroke survivors and should be an important consideration in the development of any intervention. Unlike pharmaceuticals, funding mechanisms for integrating new psychosocial interventions into health systems are less clear. Further, funding for sufficiently large effectiveness trials and eventual reimbursement should also be considered. These factors were rarely considered in the included studies. Adequate resourcing, and considering the burden of participation for stroke survivors and health systems, are important considerations in the design of any preventive intervention. This is likely to be magnified for an issue such as stress management, which will require significant adherence to achieve its goals.
In order to address issues around implementation, scalability, and cost-effectiveness, it may be worth considering interventions that have been trialed in other populations that may be likely associated with smaller participant burden, lower costs, and high effectiveness. For example, mobile technologies and mHealth interventions might be a low-cost, simple method of delivering modular, customized mental health support to mitigate stress in stroke survivors. Mobile interventions based on cognitive training approaches have been used successfully for stress-related cognitive problems such as memory impairment [ 61 ]. However, to date, there is very little regulation of these interventions and systematic research on the potential benefits of mHealth interventions for stress management is not currently available.
Target Population
The relevant population for targeting stress management to prevent the stress-related sequelae of stroke also remains unclear. Prevention of stress after stroke could be either universal (i.e., offered to all individuals poststroke), or targeted to a higher risk population of stroke survivors identified as having elevated levels of stress prior to the stroke, or those most at risk of developing adverse stress-related outcomes. The studies included in this review were mixed; some included a broader population of stroke survivors (21/24), whilst others included only those at higher risk of stress and related sequelae, such as emotional distress or symptoms of depression (3/24). It is also unclear at which phase of stroke recovery is best to intervene. Although most of the included studies were conducted during the chronic phase of stroke recovery (i.e., >6 months poststroke), at present it remains unknown as to when might be the optimum time to manage stress throughout the recovery trajectory. Whilst the relative risk of negative health outcomes due to stress may be small compared with other risk factors, a recent review highlighted the importance of tackling stress in people with high baseline cardiovascular risk, such as stroke survivors, because this translates into a larger difference in absolute risk [ 62 ]. In order to determine when and in which population stress management might be most clinically and cost-effective, additional studies are required which monitor stress and related sequelae over time.
Additionally, several studies excluded people with a progressive neurological disorder, cognitive dysfunction, or aphasia. Studies typically justified this approach by stating that collecting and reliably interpreting data from these patients can present significant challenges. However, a high proportion of stroke patients have cognitive or speech, and language impairments, and if studies of interventions aiming to reduce psychological distress among stroke patients fail to involve such patients, the findings may not be representative of the wider stroke population [ 37 ]. Therefore, a number of these studies with specific inclusion/exclusion criteria may not be generalizable to the broader population with stroke and have limited external validity.
Measurement of Stress
There was a lack of consistency in measuring stress between studies. Significant uncertainty in the field of stress research more broadly lies in the use of standardized techniques or tools to measure the level of stress. Whilst stress has been linked to an increased risk of secondary stroke, CVD, and psychopathology in stroke survivors, and has a negative impact on the trajectory of recovery from stroke, the best approach to measure stress in research and clinical settings remains unclear [ 63 , 64 ]. Compared with other known behavioral risk factors for chronic diseases, such as smoking, nutrition, and physical activity, psychosocial constructs such as stress are difficult to define objectively [ 65 ]. The response to stress can be measured using self-report, or a physiological measurement. A number of scales have been developed for the measurement of stress. The Perceived Stress Scale (PSS-10) [ 66 ], Symptom Checklist 90 (SCL-90) questionnaire [ 67 ], and the Depression Anxiety Stress Scales (DASS-21) [ 68 ] tend to be the most widely used validated tools found in the literature for the subjective assessment of stress. In this review, we found considerable variation across studies in terms of self-reported approaches for measuring stress. Several studies did not use any stress measurement tool, instead of reporting subscale results of a QoL scale or similar to infer emotional distress, qualitative results, or used an unstandardized tool, making it difficult to compare study results. Related constructs such as resilience also appeared infrequently in our search, with only three studies reporting the results of an intervention on a resilience scale.
Similarly, no studies reported changes in any biomarkers for stress. There are numerous biological pathways linking stress to disease outcomes, and as a result, a number of physiological stress measures or biomarkers are commonly used in stress research, primarily based on stress-related changes in neuroendocrine signaling [ 69 ]. One of the major alternatives to the psychometric assessment of stress is to assess levels of stress hormones, in blood or saliva [ 7 ]. A number of studies have considered a measurement of blood cortisol levels; however, these measures also suffer from serious limitations in terms of their accuracy because stress is not the only factor that evokes changes in the levels of these hormones [ 7 , 63 ]. Stress hormones measured within the saliva and blood can change quickly in their concentration and fluctuate significantly over time [ 70 ]. These issues mean that single-time point analyses using blood or saliva may be noninformative. Of course, it is possible to collect multiple samples across time, but the practical considerations and participant burden mean this is typically not feasible. One recent study has used an objective measure of the stress level in the form of hair cortisol, to associate stroke outcome with stress [ 71 ]. The hair sample for the determination of cortisol level instead of blood, saliva, or urine offers several advantages in stroke–stress research. Firstly, its analysis can provide an accurate assessment of the long-term integrated level of cortisol over the course of the months. Secondly, its measurement is not affected by acute stress variables and is not subject to diurnal variation, and finally, baseline hair samples obtained within the week after stroke provides information about stress and cortisol level prior to the stroke incident. The relatively stable and noninvasive nature of hair cortisol as a stress biomarker may make this an ideal marker in future studies of stress poststroke.
Does Stress Management Prevent Stress-Related Disorders?
Finally, it has not yet been shown that a change on a subjective stress scale is a proxy for patient-relevant outcomes, such as prevention of anxiety or depression. Based on the included studies, there is only limited evidence to suggest that the included interventions to manage stress and related constructs will translate into a reduction in stress-related disorders in stroke survivors. In the included studies, only 7 of the 18 that considered symptoms of stress-related disorders reported a decrease in symptoms associated with the intervention. This may not be unexpected, since these programs were designed to address stress management and not treat existing symptoms of anxiety or depression. Whilst improved stress management is likely to be an important precursor to effective prevention of depression or anxiety, it remains unclear where best to target these efforts. In future studies, it will be important to establish not only consistent and relevant measures of stress, but also the link between an improvement in stress management or stress levels and reductions in the risk of known stress-associated disorders such as depression, anxiety, CVD, and mild cognitive impairment. Further, studies should examine longitudinally the impact of early compared with late stress mitigation, to examine whether stroke survivors who receive these preventive measures at varying time periods in recovery are less likely to develop stress-related problems.
Limitations
There are a number of potential limitations to this review. While we conducted a comprehensive search using key databases and hand searching, it is possible that the review may have missed some relevant studies. We also included only papers in English and did not conduct a search of the gray literature. There may be evidence of program impacts in the evaluation and other technical reports, not available here.
The successful management of chronic stress in stroke survivors is likely to improve psychological and cognitive recovery outcomes and improve rehabilitation contacts. However, most intervention studies we identified were small, primarily consisting of feasibility studies to inform larger trials. There was a trend toward a positive effect of stress management interventions in stroke survivors, in terms of reduction in perceived stress levels, and a smaller trend toward a reduction in symptoms of anxiety and depression associated with improved stress management. It is unclear at this stage which population would benefit most, and which intervention could be recommended based on effectiveness and implementation outcomes. Additionally, it is still unclear how best to measure and monitor stress in stroke survivors. In order for the field to address the gaps and inconsistencies identified here, we must be able to effectively assess stress levels in individuals over time.
Overall, despite the heterogeneity of the studies covered in this review, there was a clear trend toward positive outcomes, and the number of studies conducted is increasing over time. As a field, this area is gaining attention, and future well-designed and properly powered studies will provide important answers to the questions raised in this review. Given that an increasing number of studies have identified that stress represents an unmet need for stroke survivors and is an important contributor to increased risk of poor recovery outcomes, addressing stress provides an opportunity to improve long-term outcomes for stroke survivors.
Supplementary Material
Kaac002_suppl_supplementary_file_1, kaac002_suppl_supplementary_file_2, kaac002_suppl_supplementary_file_3, kaac002_suppl_supplementary_file_4, contributor information.
Madeleine Hinwood, School of Medicine and Public Health, The University of Newcastle, Callaghan, NSW, Australia. Hunter Medical Research Institute, New Lambton Heights, NSW, Australia.
Marina Ilicic, Hunter Medical Research Institute, New Lambton Heights, NSW, Australia. School of Biomedical Sciences and Pharmacy, The University of Newcastle, Callaghan, NSW, Australia. Priority Research Centre for Stroke and Brain Injury, The University of Newcastle, Callaghan, NSW, Australia.
Prajwal Gyawali, School of Health and Wellbeing, Faculty of Health, Engineering and Sciences, University of Southern Queensland, Darling Heights, QLD, Australia.
Kirsten Coupland, Hunter Medical Research Institute, New Lambton Heights, NSW, Australia. School of Biomedical Sciences and Pharmacy, The University of Newcastle, Callaghan, NSW, Australia. Priority Research Centre for Stroke and Brain Injury, The University of Newcastle, Callaghan, NSW, Australia.
Murielle G Kluge, School of Biomedical Sciences and Pharmacy, The University of Newcastle, Callaghan, NSW, Australia. Centre for Advanced Training Systems, The University of Newcastle, Callaghan, NSW, Australia.
Angela Smith, HNE Health Libraries, Hunter New England Local Health District, New Lambton, NSW, Australia.
Sue Bowden, Consumer Investigator, Moon River Turkey, Bathurst, NSW, Australia.
Michael Nilsson, Hunter Medical Research Institute, New Lambton Heights, NSW, Australia. Centre for Rehab Innovations, The University of Newcastle, Callaghan, NSW, Australia. LKC School of Medicine, Nanyang Technological University, Singapore.
Frederick Rohan Walker, Hunter Medical Research Institute, New Lambton Heights, NSW, Australia. School of Biomedical Sciences and Pharmacy, The University of Newcastle, Callaghan, NSW, Australia. Priority Research Centre for Stroke and Brain Injury, The University of Newcastle, Callaghan, NSW, Australia. Centre for Advanced Training Systems, The University of Newcastle, Callaghan, NSW, Australia. Centre for Rehab Innovations, The University of Newcastle, Callaghan, NSW, Australia.
This study was supported by the NHMRC Centre of Research Excellence in stroke rehabilitation and recovery; HMRI MRSP Infrastructure Funding Brain and Mental Health Program; and the University of Newcastle Priority Research Centre for Stroke and Brain Injury.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Madeleine Hinwood, Marina Ilicic, Prajwal Gyawali, Kirsten Coupland, Murielle G. Kluge, Angela Smith, Sue Bowden, Michael Nilsson, and Frederick Rohan Walker declare that they have no conflict of interest.
Authors’ Contributions
M.H. conceived and designed the study, collected and analysed the data, and drafted and revised the paper. M.I. collected and analysed the data, and drafted and revised the paper. P.G., K.C., and M.K. collected and analysed the data and revised the draft paper. A.S. designed and developed the systematic review strategy. S.B. provided consumer advocacy and revised the draft paper. M.N. and F.R.W. conceived the study, initiated the collaborative project, and revised the paper.
Ethical Approval This is a review of published literature, as such ethics approval is not required.
Informed Consent

18 Ways to Improve Cognitive Problems After Stroke
Aug 21, 2019
A Decrease font size. A Reset font size. A Increase font size.
First published on ARNI Institute for Stroke Rehabilitation website
A change in cognitive ability is common after a stroke. Did you know that as many as two-thirds of stroke survivors may experience cognitive impairment as a result of their stroke.? If this is you, or you know someone who seems possibly to be going through such difficulties, here’s 18 steps you can take to try and improve cognition difficulties after stroke:
First, what is cognition?
Put simply, cognition is thinking; it is the processing, organising and storing of information – an umbrella term for all of the mental processes used by your brain to carry you through the day, including perception, knowledge, problem-solving, judgement, language, and memory. The brain’s fantastic complexity means that it can collect vast amounts of information from your senses (sights, sounds, touch, etc) and combine it with stored information from your memory to create thoughts, guide physical actions, complete tasks and understand the world around you.
A stroke can affect the way your brain understands, organises and stores information. This brain injury can result in damage to the areas of the brain that are responsible for perception, memory, association, planning, concentration, etc. The severity and localisation of the stroke will effect the type and level of difficulties experienced by an individual, and will vary from person to person.
It can be difficult to plan and organise daily tasks. The brain is constantly working in the background, allowing us to complete a task based on prior knowledge, experience, and learned behaviour.
You don’t have to consciously think how to boil the kettle, change TV channels or put on your socks before your shoes: you just do it. But damage to the brain can result in problems with these planning and execution mechanisms.
You might not be able to think how to do a simple task, or you may get the sequence wrong (for example, shoes before socks). You might have trouble with orientation, which could include not knowing the date, day of the week, or even who you are with. Problem-solving too can become difficult. Making decisions, solving problems, understanding numbers and managing money can be a challenge.
Good cognitive function also relies on memory. The brain uses 2 types of memory to hold information, the long and short term memory. Short-term memory is the temporary store for small amounts of information. This information is kept readily available and can be recalled quickly. For example, a phone number can be remembered long enough for you to dial it. Long-term memory is where you keep your experiences, thoughts and feelings from the past and things stored here can be stored indefinitely. Memory problems could result in difficulty storing or recalling information. This could include problems remembering appointments, important dates or in the case of short term memory, what you were about to do, or what somebody just said to you.
Problems with concentration are common. Concentration is required for effective cognitive function, as many of your thinking process require concentration. Concentration requires our brain to filter out much of the information coming in from your conscious thinking, so you are not distracted by it.
Stroke can impact on this ability because of damage to the areas of the brain responsible for this, and also because tiredness, pain and emotional problems have an effect of the ability to stay focused and concentrate. This could result in difficulties when trying to follow a television programme, or conduct a conversation with a friend. Multi-tasking too is difficult.
18 Things to try
- Cognitive problems are confusing and frustrating. But, there are some things you can to do help. Most improvements occur in the first 3 months after a stroke, after which they slow down, but the brain will keep creating new neural pathways after this time.
- To help with memory and perception problems, try using a diary, day planner, calendar or notepad. Writing down appointments and creating to-do-lists can help you to remember them.
- Photos and pictures can help to ‘trigger’ your memory.
- Check your calendar, newspaper or diary to help you remember the day and date.
- Make notes of important conversations.
- Use notes, lists and labels around the house and help prompt you to remember. Mobile phones are a great resource. Set alarms, reminders and memos to remind you throughout the day.
- It is important not to overload yourself, finish one task before you start another. Plan your day and prioritise tasks.
- Try slowing the activity down, working through a step at a time.
- Keep instructions clear and short, no more than 5 or 6 words to a sentence, and only 1 or 2 instructions at a time.
Please read the full list here .
Stroke Action Plan for Europe

See our exclusive June offer Click Here

Brain Exercises For Stroke Recovery Patients: Improving Cognitive And Memory Functions

Christopher Ravn
Key takeaways.
1. A stroke is a serious, life-threatening medical condition that happens when the blood supply to part of the brain is cut off. 2. Training and exercising a stroke survivor's brain is known as stroke rehabilitation. 3. Memory exercises are a fundamental part of stroke rehabilitation, helping to retrain the brain and improve cognitive function that may have been affected by the stroke.
Table of Contents
1. What Are The Best Brain Exercises For Stroke Recovery? 2. What Are The Benefits Of Cognitive Exercises For Stroke Patients? 3. How Do You Train And Exercise Your Brain After A Stroke 4. How Effective Are Brain Stroke Recovery Exercises? 5. What Are Cognitive Therapy Activities For Stroke Victims And Survivors? 6. What Cognitive Activities For Adults After Stroke Are Most Effective? 7. How Do Stroke Cognitive Rehabilitation Activities Work? 8. Frequently Asked Questions About Brain Exercises For Stroke Recovery
What Are The Best Brain Exercises For Stroke Recovery?
A stroke is a serious, life-threatening medical condition that happens when the blood supply to part of the brain is cut off. Strokes occur when a blood clot blocks the flow of blood and oxygen to the brain. These blood clots are typically the result of atherosclerosis, or arteries narrowed or blocked over time by fatty deposits. This is the most common type of stroke. Less common are hemorrhagic strokes, where a blood vessel supplying the brain bursts.
People who survive a stroke are often left with long-term problems caused by an injury to their brain . They will face challenges with thinking, reasoning, awareness, and memory. If help is obtained over time, the brain retains some function but needs to reorganize itself. This journey to recovery is arduous and involves relearning skills, improving physical coordination, and maintaining cognitive functions.
The best exercises for stroke recovery focus on cognitive rehabilitation, including problem-solving activities like puzzles and board games, which enhance cognitive flexibility and decision-making skills . These exercises play a crucial role in helping individuals regain cognitive functions affected by stroke, such as memory, problem-solving skills, processing speed, and attention span, ultimately aiding in their recovery journey.

What Does Science Say About Light Therapy?
Find a collection of academic research papers that we, together with top-tier academic research institutions. We are exceedingly proud of our work and incredibly grateful to collaborate with such wonderful research institutions.
What Are The Benefits Of Cognitive Exercises For Stroke Patients?
Cognitive exercises play a crucial role in the rehabilitation of stroke survivors, but they need to be practiced consistently to be most effective. Following a stroke, the brain is busy rewiring new pathways to bypass the affected areas – a process known as neuroplasticity. Functions are being rewired to new, healthy areas of the brain, to compensate for tissue damage sustained in the stroke.
How Do You Train And Exercise Your Brain After A Stroke
Training and exercising a stroke survivor’s brain is known as stroke rehabilitation . These typically are a program of different therapies, designed for the survivor to help them with movement, speech, strength, and daily living skills post-stroke. The aim is to help them regain their independence and quality of life.
What’s involved in stroke rehabilitation is speech and language therapy , focused on improving communication skills affected by the stroke and common post-stroke issues such as swallowing difficulties, otherwise known as dysphagia.
We Believe Prioritizing Brain Health Enhances Your Quality Of Life
Get to know our team, our mission and how our EVY LIGHT® can provide you and your loved ones with a fuller life, letting you breathe a little easier.
How Effective Are Brain Stroke Recovery Exercises?
According to the National Library of Medicine, approximately 40% of patients suffer from functional impairment after stroke onset, and 15–30% experience severe motor, sensory, cognitive, perceptual, and/or language impairments.
Rehabilitation is vital for stroke survivors, and those who undergo consistent and professional rehabilitation tend to recover quickly . Studies have shown that rehabilitation exercise regimens applied soon after a stroke are effective. The programs will need to be tailored to the survivor and how they were affected, so that the correct areas are given the necessary attention.
Cognitive issues are often the most debilitating and difficult-to-address consequences of a stroke. A stroke survivor with memory and attention issues who engages in cognitive therapy, including puzzles and memory games , could experience improvements in their memory and concentration, allowing them to better manage daily tasks and activities.
One may question what the difference is between regular exercises and those intended for stroke patients. The answer lies in their intention. Pre-stroke exercises are typically general and aim to maintain overall health and well-being – cardio, strength training, and muscle toning, for example. In contrast, post-stroke exercises are more targeted, focusing on the rehabilitation and recovery of specific functions affected by the stroke. Post-stroke exercises often involve intensive therapy tailored to individual needs, such as speech therapy, physical therapy, and cognitive exercises.
Studies have shown that brain stroke recovery exercises can be highly effective in improving functional outcomes and quality of life for stroke survivors. Studies published in the Journal of Stroke found that intensive rehabilitation programs significantly improved motor function and activities of daily living in stroke patients. Another study published in the Journal of Neurologic Physical Therapy showed that cognitive rehabilitation can lead to improvements in memory, attention, and executive function in stroke survivors.
What Are Cognitive Therapy Activities For Stroke Victims And Survivors?
Cognitive therapy is designed to improve cognitive functions affected by the stroke, for example, memory, processing speed, problem-solving, language, and executive functions . The aim is to challenge the brain in a supportive way.
Cognitive therapy would include memory exercises, e.g., card games to improve short-term working memory; puzzles, computer games, and reading and summarizing to improve their attention, concentration, and information processing; reading, writing, and conversation practice to help with communication; drawing; navigation tasks to help with visual-spatial orientation, planning, and awareness; and problem-solving tasks to help improve planning and organization skills.
What Cognitive Activities For Adults After Stroke Are Most Effective?
How do stroke cognitive rehabilitation activities work.
A 37-year-old stroke survivor participated in memory-based exercises as part of his rehabilitation program. He regularly played memory games and engaged in storytelling activities with his therapist. Over time, his short-term memory and cognitive function significantly improved . He was able to recall important information, make decisions more confidently, and communicate more effectively with his family and healthcare providers.
Family members can play a crucial role in implementing these activities and supporting stroke rehabilitation. They can be educated on the importance of consistency and patience, as progress may be gradual.
Short-Term Memory Loss Exercises To Train Your Brain After A Stroke
- Repetition: This involves repeating information or tasks multiple times to reinforce memory. For example, repeating a new phone number several times to remember it.
- Association: This technique involves linking new information with existing memories or concepts. For instance, associating a new face with a familiar name or place.
- Visualization: Creating mental images can aid memory recall. For instance, visualizing a grocery list as items in specific locations in your home.
- Chunking: Breaking down information into smaller, manageable chunks can make it easier to remember. For example, remembering a long number by grouping it into smaller sets.
- Memory Games: Playing memory games like matching cards or word recall can be fun and effective. These games challenge the brain and improve memory skills.
Music Stimulation Therapy For Stroke Survivors
Music stimulation therapy can benefit stroke survivors by engaging multiple areas of the brain. Listening to music activates the auditory cortex , which processes sound, while also stimulating areas responsible for memory and emotions. This stimulation can enhance cognitive functions such as memory, attention, and executive function. Additionally, music can evoke emotional responses that may help reduce stress and anxiety, which are common after a stroke.
Some examples of music-based exercises at home include listening to familiar music, such as the stroke survivor’s favorite songs or music from their past. This can evoke memories and emotions, stimulating cognitive function. Caregivers and guardians can sing along to these songs with the patient, to further engage the areas of the brain responsible for these functions.
Enhance your brain performance through the power of light.
Comfortable and easy to use 40Hz light therapy to support and improve your brain function.
Motor Skills Activities For Adults After A Stroke
- Finger Tapping: Tap each finger to your thumb in sequence, then reverse the order. This can improve individual finger movements
- Finger Stretching: Gently stretch your fingers and thumb apart, then bring them back together. Repeat several times to improve flexibility and control.
- Drawing: Encourage drawing simple shapes or patterns, progressing to more complex drawings. This can improve hand-eye coordination and fine motor skills.
- Painting: Use a brush or fingers to paint on paper or canvas. This activity can improve grip strength and coordination.
Practicing Games For Stroke Rehabilitation
- Lumosity: This brain training app offers a variety of games designed to improve memory, attention, and problem-solving skills. Games like “Train of Thought” and “Memory Matrix” are particularly effective for cognitive exercise.
- Nintendo Wii Fit: Games like “Balance Bubble” and “Table Tilt” can improve balance, coordination, and cognitive function through interactive gameplay.

Other Activities That Help Retrain The Brain After A Stroke
An overall change in daily routines is crucial in stroke recovery to promote brain retraining and maximize rehabilitation outcomes.
The most important are physical activity and cognitive stimulation . Incorporating regular physical activity into daily routines can improve blood flow to the brain, promote neuroplasticity, and enhance overall brain health. Activities like walking, yoga, or tai chi can be beneficial.
As for mentally stimulating activities, these include reading, puzzles, or learning new skills, which can help retrain the brain and improve cognitive function . These activities should be challenging but achievable to promote brain plasticity.
Physical Activities In Cognitive Rehabilitation
- Walking: A safe and effective way to improve cardiovascular fitness and mobility. Start with short distances and gradually increase.
- Balance Exercises: Standing on one leg, heel-to-toe walking, and other balance exercises can improve stability and reduce the risk of falls.
Meditation And Relaxation Techniques For Cognitive Stimulation
- Focused Breathing: Sit comfortably and focus on your breath. Inhale deeply through your nose, hold for a moment, and exhale slowly through your mouth. Repeat for several minutes, focusing only on your breath.
- Guided Meditation: Use audio recordings or apps that guide you through a meditation practice, focusing on relaxation, gratitude, or mindfulness.
Social Participation As A Cognitive Exercise
- Support Groups: Joining a stroke support group allows individuals to connect with others who have experienced similar challenges, provide emotional support, and share coping strategies.
- Book Clubs or Discussion Groups: Participating in a book club or discussion group provides opportunities for intellectual stimulation and social interaction.
- You could also recommend light therapy for depression, as most would be negatively impacted by it.
Technology Aid In Stroke Rehabilitation Exercises
Apps and other digital tools can assist in cognitive rehabilitation post-stroke by providing accessible and engaging ways to improve cognitive functions. These tools can offer personalized exercises, real-time feedback, and progress tracking, making rehabilitation more efficient and effective .
View The Video Testimonials Of What Others Have Experienced
See how others have achieved a sharper mind by activating their gamma brainwaves in combination with maintaining a healthy lifestyle.
Frequently Asked Questions About Brain Exercises For Stroke Recovery
The best exercises for stroke recovery focus on cognitive rehabilitation, including problem-solving activities like puzzles and board games, which enhance cognitive flexibility and decision-making skills. These exercises play a crucial role in helping individuals regain cognitive functions affected by stroke, such as memory, problem-solving skills, processing speed, and attention span, ultimately aiding in their recovery journey.
What Are Cognitive Therapy Activities For Stroke Patients?
Receive notification when news, blogs, promotions, or other valuable information drops.

Xanax And Dementia: Potential Risks Between Benzodiazepines And Dementia

What Stage Of Dementia & Alzheimer’s Is Not Sleeping Very Common? Full Insights

What Age Does Dementia Start? Exploring Causes Of Early Onset Dementia

Senile Vs Dementia: Definitions, Differences & How To Deal With Senility

Parkinson’s Vs Alzheimer’s: Learn The Differences, Similarities & Treatment Insights

Mild Cognitive Impairment (MCI) Vs Dementia: In-Depth Exploration Into These Cognitive Issues

Mild Cognitive Impairment Life Expectancy: How It Differs Across Patients

Melatonin For Dementia & Alzheimer’s: Safe Use For Sleep Improvement In Elderly Patients

How To Deal With Dementia Patients Who Are Aggressive: What To Do And Safety Tips

Does Metformin Cause Dementia & Alzheimer’s? Analyzing The Link Between Metformin And Cognitive Issues

Dementia, Alzheimer And Incontinence: Managing Bladder Control & Different Stages
Activities For Dementia Patients: Recreational Good Ideas To Keep People With Dementia Active

Alzheimer’s Hallucinations: Identifying Symptoms And Management Strategies

Why Won’t Dementia Patients Take Showers? Understanding The Refusal & How To Assist Bathing Habits

Why Do Dementia Patients Sleep So Much? Reasons Behind Excessive Sleep & How To Prevent It

What Stage Of Dementia Is Sundowning? How To Manage Changes In Behavior & Treat Early Symptoms

What Sleeping Position Is Linked To Dementia? Different Options To Increase Health & How To Prevent Risks

Subjective Cognitive Impairment: Early Diagnose & How To Prevent Other Types Of Cognitive Decline

Mild Cognitive Impairment & Driving: Safety Issues, Abilities Required & Legal Concerns
Light Therapy Lamp Benefits: How To Use For Physical & Mental Conditions, Safety Considerations

Levels Of Cognitive Impairment: How To Determine Four Levels, Evaluation & Management

How To Talk To Someone With Cognitive Impairment: Creative Ways To Encourage Communication & Active Listening

How Long Do The 7 Stages Of Alzheimer’s Last? Duration, Symptoms & Care Needs For Every Stage

Early Signs Of Alzheimer’s In Your 50s: Risks, Symptoms & Testing Methods

Do Light Therapy Lamps Work: How Useful They Are For Different Disorders & How To Maximize Their Benefits

Signs Death Is Near In Alzheimer’s & Dementia: How To Provide Care & Recognize The Symptoms In The Final Stages

How To Deal With A Spouse With Memory Loss: Caring Tips For Living With Memory Loss & First Steps To Take
Mental Exercises For Mild Cognitive Impairment: Ideas For Improving And Preventing Mild Cognitive Decline

How To Help Someone With Cognitive Impairment: Caring & Communication Techniques To Improve The Quality Of Life Of Persons With MCI

How To Deal With Dementia In A Parent: Techniques To Help & Live With Dementia Parents At Home
How To Deal With Fixation In Dementia: Coping With Dementia Behavior Changes & Ideas To Focus Away From Fixation

How to Help Someone with Dementia Remember: A Comprehensive Guide for Caregivers and Families

Is Mild Cognitive Impairment A Disability? Legal Working Rights And Disability Benefits Advice

Living With A Spouse With Mild Cognitive Impairment: Caring Marital Relations To Adapt And Help A Spouse With MCI

How Long Does It Take For Light Therapy To Work: Duration & Frequency For Optimal Results & Benefits

How Long Can A Person With Dementia Live At Home: Setting Up A Safe Home Care Plan, Living Alone & Memory Care Considerations

How Fast Does Mild Cognitive Impairment (MCI) Progress: Turning Into Other Cognitive Decline, Risks Factors & Timeline

How Do Light Therapy Lamps Work? Best Ways To Maximize The Benefits & Timing Sessions

Brain Exercises For Seniors: Fun Ways Of Cognitive Training & How To Improve Mental Health In Older Adults

Sad Light vs Grow Light: How Different Are They?

Gifts for Dementia Patients: What’s a Good Presents Idea for Someone With Alzheimer’s & Memory Loss

Green Light Therapy Treatment & Its Health Benefits

How to Get Guardianship of an Elderly Parent With Dementia: Legal Steps

Meditation Light Therapy: How to Improve All Relaxation Techniques

Music Therapy for Dementia: Helping Patients Memory Functions

Sensory Activities for Dementia Patients: Improving Abilities & Quality of Life

How To Know When To Call Hospice For Dementia: Qualification Considerations

Which Sense Is Most Affected by Alzheimer’s Disease: Early Signs

What Is the Difference Between Memory Care vs Dementia Care?

Best Gifts for Seasonal Depression & Affective Disorder: Top Ideas

Speech Therapy Memory Activities for Adults: Enhancing Cognitive Skills

Light Therapy Treatment For Depression, SAD And Mood Disorders

How To Talk To Someone With Short-Term Memory Loss: Communication Strategies

Green Light Therapy Treatment For Depression, SAD And Mood Disorders

Brain Exercises To Prevent Alzheimer’s And Dementia: Types & The Best Ones

Transforming Lives: Melissa’s Journey with EVY LIGHT®

5 Warning Signs Of Early Alzheimer’s You Can’t Ignore

Crafting a Brain-Boosting Routine
How Learning Impacts The Brain

Thrive Together: Boosting Brain Health with Group Activities

Proactive Brain Health: Aging Gracefully with Science

Support Memory At All Stages of Life

Harnessing the Power of Dopamine for Keeping Mentally Energized

Strategies for Enhanced Focus: Unleash Your Productivity Potential

Move for Mind: The Link Between Exercise and Mental Health

The Vital Connection Between Your Sleep, Body, and Brain

Unlocking the Sunshine: 6 Tips to Banishing Brain Fog

Unveiling the Astonishing Energy Consumption of the Human Brain
Get exclusive content straight from the scientists who are rooting for you and your brain.
Comfortable Daily Use, Drug Free to Promote Focus, Clarity, and Mental Sharpness.
Privacy Preferences
When you visit our website, it may store information through your browser from specific services, usually in the form of cookies. Here you can change your Privacy preferences. It is worth noting that blocking some types of cookies may impact your experience on our website and the services we are able to offer.
- Study protocol
- Open access
- Published: 27 June 2013
The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled trial
- Marieke M Visser 1 , 2 ,
- Majanka H Heijenbrok-Kal 1 , 2 ,
- Adriaan van ’t Spijker 3 ,
- Gerard M Ribbers 1 , 2 &
- Jan JV Busschbach 3
BMC Neurology volume 13 , Article number: 67 ( 2013 ) Cite this article
6780 Accesses
10 Citations
2 Altmetric
Metrics details
Coping style is one of the determinants of health-related quality of life after stroke. Stroke patients make less use of active problem-oriented coping styles than other brain damaged patients. Coping styles can be influenced by means of intervention. The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients. The secondary aim is to determine the effect of Problem Solving Therapy on depression, social participation, health care consumption, and to determine the cost-effectiveness of the intervention.
Methods/design
We strive to include 200 stroke patients in the outpatient phase of rehabilitation treatment, using a multicenter pragmatic randomized controlled trial with one year follow-up. Patients in the intervention group will receive Problem Solving Therapy in addition to the standard rehabilitation program. The intervention will be provided in an open group design, with a continuous flow of patients. Primary outcome measures are coping style and health-related quality of life. Secondary outcome measures are depression, social participation, health care consumption, and the cost-effectiveness of the intervention.
We designed our study as close to the implementation in practice as possible, using a pragmatic randomized trial and open group design, to represent a realistic estimate of the effectiveness of the intervention. If effective, Problem Solving Therapy is an inexpensive, deliverable and sustainable group intervention for stroke rehabilitation programs.
Trial registration
Nederlands Trial Register, NTR2509
Peer Review reports
Stroke is an increasing public health problem in the Netherlands: every year, 41,000 people suffer from stroke and over 3% of the total health care costs are related to the treatment of stroke and its consequences [ 1 ]. The mortality rate after stroke is 30% and is likely to decrease, which will cause an increase in morbidity [ 2 ]. Almost 50% of stroke survivors experience consequences in daily life that result in a lowered health-related quality of life (HR-QoL) [ 1 ]. The World Health Organization Quality of Life (WHOQOL) Group defines quality of life as “individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns [ 3 ]. HR-QoL refers to the health-related aspects of quality of life. On average, utility scores of HR-QoL after stroke range from 0.47 to 0.68 (a utility score equal to death is 0.0 and full health 1.0), which is substantially lower than the value of a healthy reference population (utility score of 0.93) [ 4 , 5 ]. HR-QoL after stroke is predicted by functional constraints, age, gender, and psychosocial factors, like socioeconomic status, depression, and coping style [ 4 , 6 – 8 ]. Functional constraints, age, gender, and socioeconomic status cannot or are difficult to change, but coping style could be targeted. The question then becomes if HR-QoL after stroke could be improved through a coping style intervention. If this is possible, a secondary question would be how such improvement relates to depression, health care consumption, and costs.
A common definition of coping style is someone’s preferred way of dealing with different situations. Several coping styles can be distinguished, such as active, passive, and avoidant coping. Wolters (2010) shows that in traumatic brain-injured (TBI) patients, higher HR-QoL in the long term is predicted by an increase in active problem-focused coping style and a decrease in passive emotion-focused coping style. Unfortunately, in this population of TBI patients the active coping decreases over time, while passive coping increases [ 9 ]. This suggests that if the decrease of active coping can be stopped, there is room for improvement in HR-QoL. Stroke patients make even less use of active, problem-oriented coping styles compared to other brain damaged patients [ 10 ]. Furthermore, Darlington (2007) shows that in stroke patients, coping becomes more important in determining HR-QoL over time, while the importance of general functioning decreases [ 11 ]. This would mean that long term HR-QoL could benefit from improved coping.
Coping styles can be influenced by several interventions. Backhaus (2010) shows that an intervention aimed at changing maladaptive coping styles positively influenced psychosocial functioning of TBI patients [ 12 ]. However, HR-QoL was not measured in this study. No research is found that investigated an intervention aimed at improving HR-QoL through the change of maladaptive coping styles in stroke patients. We therefore set out to investigate whether Problem Solving Therapy (PST), which aims at active problem-focused coping, might improve HR-QoL in stroke patients. PST has been proved effective in other patient populations [ 13 , 14 ]. In stroke patients, PST has been shown successful for the prevention of post stroke depression [ 15 ]. Effects on coping style and HR-QoL have not been investigated yet.
The primary aim of this study is to investigate whether PST is an effective group intervention for improving active problem-focused coping style and HR-QoL in stroke patients. The secondary aim is to determine the effect of PST on depression, social participation, health care consumption, and the cost-effectiveness of the intervention. The effectiveness of the therapy will be investigated in an open group design, which has not been used in PST research before. PST will be added to the standard care just before the end of the rehabilitation program, as at this moment a relapse in HR-QoL is frequently observed, when patients cannot rely on their therapists anymore [ 16 ]. By teaching patients to actively cope with stressful situations, through adapting and realizing their goals, we expect that patients will use more effective coping styles, which consequently may prevent the relapse in HR-QoL, and possibly increase HR-QoL in the long term. With regard to the secondary aims of this study, we expect the incidence of depression to decrease, social participation to improve, and health care consumption to decrease, resulting in a favorable cost-effectiveness ratio for the intervention.
Study design and procedure
The effectiveness of PST for stroke patients will be evaluated in a multicenter pragmatic randomized controlled trial (RCT) with one year follow-up, with the intervention performed in the daily practice of a sub-acute outpatient stroke rehabilitation program. As such, the potential effects of the intervention have a good external validity, which allows us to calculate the cost-effectiveness of the therapy compared with standard care.
The study will be performed in Rijndam Rehabilitation Center in collaboration with Erasmus MC, both in the Netherlands, and in Ghent University Hospital in Belgium. Patients are invited by their rehabilitation physician to participate in the study. Before the start of the study, patients need to sign the informed consent form. Data will be collected at four time points by one of three research psychologists. T0 is the baseline measurement, performed within three weeks before the start of the intervention phase. T1 will be performed within ten days after the intervention phase, T2 six months and T3 twelve months after the intervention phase (Figure 1 ). The measurements will be performed in the rehabilitation center or at the patients’ home in a face-to-face interview. The study has been approved by the Medical Ethics Committee of Erasmus MC University Medical Center and the Ethics Committee of Ghent University Hospital.
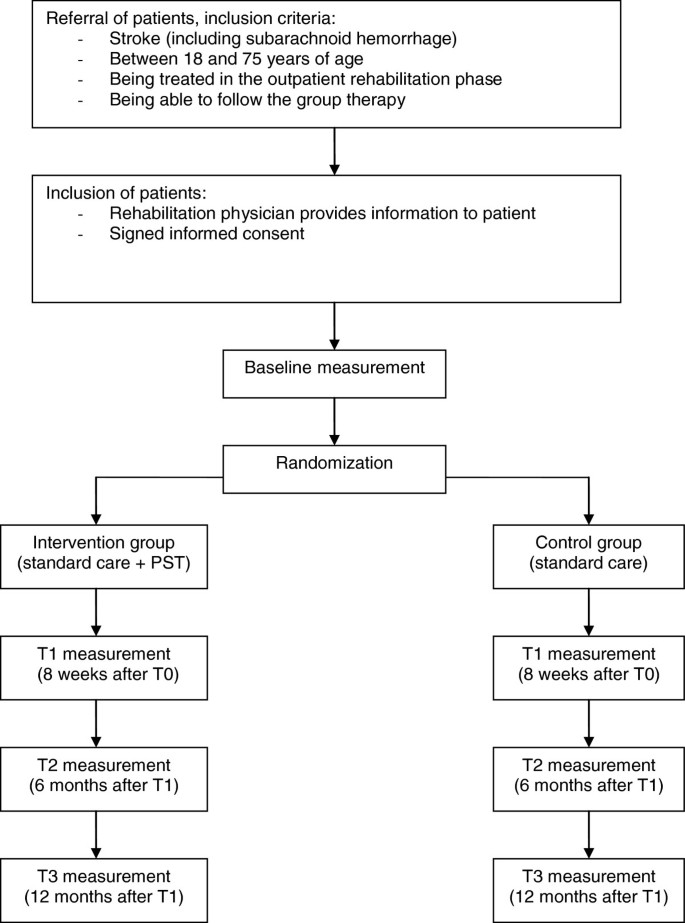
Design of the randomized controlled trial.
Study population
We strive to include 200 stroke patients. Inclusion criteria are: stroke (including subarachnoid hemorrhage), age between 18 and 75 years, being treated in the outpatient rehabilitation phase, and being able to participate in group therapy. Exclusion criteria are: progressive neurological disorders, life expectancy less than one year, insufficient understanding of the Dutch language, excessive drinking or drug abuse, subdural hematomas, moderate and severe aphasia. The same criteria would apply to the implementation of PST in practice, which stresses the pragmatic character of the trial. The inclusion of patients started March 2011 and will end August 2013. The one-year follow-up of all patients will be finished by September 2014.
Randomization
Patients are randomized to the intervention- or control condition using a stratified block randomization procedure with a block size of four. To ensure comparability between the two groups, patients are stratified per rehabilitation center. A member of the research group, who is not involved in the collection of the data, prospectively allocates the patients to the intervention- or control condition in a one-to-one ratio using an online random-number generator. To allow blinded randomization, the allocation information will be put in separate sealed envelopes which are consecutively numbered. At the end of the baseline measurement, the investigator opens the numbered envelop and informs the patient about the condition he or she is assigned to. The research psychologists who perform the baseline and follow-up measurements are blinded for treatment condition. The therapists who provide the intervention are not involved in the collection of the data. The investigator who will analyze the data is not involved in the collection of the follow-up measurements.
Intervention: problem solving therapy
Patients who are assigned to the intervention condition will receive PST in addition to the standard rehabilitation program, which will start during the last eight weeks of outpatient treatment. PST is a widely used and practical intervention method, based on a general model of coping with stress [ 17 , 18 ]. The model states that having a chronic disease causes stressful daily problems, which increase the chance of experiencing psychological stress and depressive feelings. Therefore, the aim of PST is to improve the skills to cope with the stressful daily problems in life after stroke.
The intervention will be provided in an open group design, with a continuous flow of patients, which means that patients can enter the group every week and leave the group after eight sessions (Figure 2 ). The reason for this design is that it studies group therapy in its most feasible form, where patients start and end their programs at different time-points. If we had chosen to study the effect in closed groups, many patients in the similar stage of their programs are necessary. This would only be possible if patients are admitted to large scale rehabilitation centers, which is not the rehabilitation practice in The Netherlands, or patients would have to wait for a long time before entering the group. The open group design has some disadvantages. Patients may feel unsafe when they enter an already existing group. Furthermore, a continuous flow of patients is required to keep a balanced number of patients in the group. Therefore, interventions aimed at rare diseases cannot be studied with an open group design. However, for our population of stroke patients we do expect the design to be suitable and beneficial, because these patients are frequently seen in rehabilitation treatment. An open group design has several benefits as well. Advantages for the patients are that they do not have to wait until they can start with the intervention, they can share their experiences with other ‘experienced’ stroke patients, and there is room for interaction with many fellow patients. Other advantages are that the intervention is relatively easy to organize and implement in the daily practice of the rehabilitation center. This open group design has not been investigated in PST research yet.
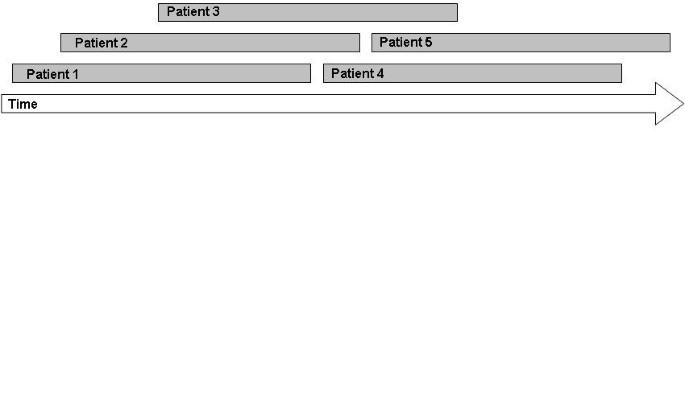
Patient flow in an open group therapy.
The intervention in this study consists of eight group sessions of 1,5 hours a week, with homework exercises after each session. The group consists of a minimum of three and a maximum of six participants. PST is provided by one to three trained neuropsychologists per rehabilitation center. Solving problems will be structured, by dividing the problem solving process in four steps:
Define problem and goal;
Generating multiple solutions;
Considering the possible consequences of the solutions systematically and select the best solution;
Implement the solution and evaluate.
Each session starts with the sharing of experiences from the past week. Then, the model of problem solving will be repeated and explained. If there are some participants who are in the group for a couple of weeks already, they will be asked to explain the model to other new participants. Subsequently, one step of the model will be highlighted every week. With emphasis on this specific step, the model will be applied to one or more examples from the participants. Finally, the participants will be asked to practice the specific step at home by making a homework assignment. During the sessions, inadequate and irrational thoughts will be challenged by common cognitive interventions. A unique aspect of the intervention is the focus on the definition of the problem in the first step of the model. A clear definition of the problem will lead to a better understanding and more solutions to it.
Control condition: standard care
Patients who are assigned to the control condition will receive the standard rehabilitation program, in order to be able to study the additional effect of the intervention to the standard rehabilitation program. This standard rehabilitation program consists of individualized amounts of treatment by a physical therapist, occupational therapist, speech therapist, psychologist, social worker, and rehabilitation physician, depending on the severity of stroke. On average, stroke patients in outpatient rehabilitation receive twelve hours of treatment a week during a nine week rehabilitation program.
Primary outcome measures are changes in task-oriented coping and psychosocial HR-QoL in patients in the intervention group in comparison with the control group. Coping style is measured using the Coping Inventory for Stressful Situations (CISS) and the short version of the Social Problem Solving Inventory-Revised (SPSI-R:SF). The CISS questionnaire consists of 48 questions and contains three subscales; Task-oriented coping, Emotion-oriented coping, and Avoidant coping. The subscale Avoidant coping consists of two subscales; Distraction and Social Diversion [ 18 , 19 ]. Because the PST aims at tasks, ‘Task-oriented coping’ is chosen as a primary endpoint; the other two subscales are used as secondary endpoints. The SPSI-R:SF questionnaire consists of ten questions about problem solving skills regarding daily situations. There are five subscales: Positive Problem Orientation, Rational Problem Solving, Negative Problem Orientation, Impulsivity/Carelessness Style, and Avoidance Style, and all are used as secondary endpoints in this trial [ 20 ].
HR-QoL is measured using the EuroQol (EQ-5D-5L) and the Stroke Specific Quality of Life Scale (SS-QoL-12). The EQ-5D is a generic questionnaire, and consists of five questions regarding mobility, self-care, daily activities, pain/complaints, mood, and a VAS scale. The five dimensions can be combined to one utility scale, representing the societal perspective of the general public [ 21 ]. The SS-QoL-12 is specifically developed for the population of stroke patients [ 22 ]. We will use the abbreviated version containing twelve items, which has been shown valid [ 23 ]. The questionnaire provides a total score and two sub scores: physical and psychosocial, of which the psychosocial sub-score is defined as the primary endpoint. The other HR-QoL scores are used as secondary endpoints.
Other secondary outcome measures are differences in depression, social participation, and health care consumption between patients in the intervention and control group. Additionally, the influence of cognitive functioning, personality characteristics, aphasia, type of stroke, side of stroke, level of functioning, and demographic characteristics on the outcomes will be assessed. Finally, the cost-effectiveness of the intervention will be calculated compared with standard care.
Depression is measured using the Center for Epidemiologic Studies Depression Scale (CES-D). This questionnaire consists of twenty items concerning depression, higher scores indicate more depressive symptoms [ 24 ].
Social participation is measured using the Impact on Participation and Autonomy (IPA). The questionnaire consists of five dimensions; Autonomy indoors, Family role, Autonomy outdoors, Social life and relationships, Work and education [ 25 ].
Health care consumption is measured using the Trimbos Questionnaire for Costs association with Psychiatric Illness (TiC-P). The questionnaire was developed for economic evaluation in mental health care, and measures health care consumption and productivity losses [ 26 ].
Sample size calculation
To determine the sample size for measuring differences between the intervention- and control group in coping style and HR-QoL, we searched for comparable effect sizes in the literature. With regard to coping style, there was no data available for this calculation. With regard to HR-QoL, Studenski (2005) measured an increase in HR-QoL after a physical therapy for stroke patients, with a long term effect size f ranging from 0.06 to 0.18 [ 27 ]. Because of the lack of more comparable data, we used this data and carefully estimated the effect size f to be 0.08. Considering the design of two groups and four repeated measurements, an expected correlation of 0.70, an alpha of 0.05, and a power of 0.80, we calculated a total required sample size of 132 patients based on the F-test. Because potential drop out is estimated at 0.30, we will strive to include 200 patients.
Statistical analyses
Demographic variables will be analyzed with an independent sample T-test for continuous variables, the Mann–Whitney U test for ordinal variables, and the chi-square test for categorical variables. Linear Mixed Models will be used to compare the repeated measurements between treatment groups, taking into account the correlation within and between subjects. We will create models for all the primary and secondary outcome variables, with time, group condition (intervention or control), and the interaction between these variables as predictors. Furthermore, we will control for variables that are accidentally not equally distributed between the two group conditions.
The cost-effectiveness of the intervention will be calculated by counting all the medical and non-medical costs, like productivity losses. The incremental cost-effectiveness ratio will be calculated by dividing the difference in total costs by the difference in quality-adjusted life years (QALYs). These QALYs will be calculated based on the EQ-5D questionnaire. The economic evaluation will be conducted according to the Dutch guidelines [ 28 ] and includes multivariate probabilistic sensitivity analyses. In the base case scenario the time horizon will be one year. If the effect is still present at one year follow up, a Markov model will be made to model a longer time horizon.
This study investigates the effect of PST on coping style and HR-QoL in stroke patients. In addition, the effect on depression, social participation, and health care consumption will be investigated, as well as the cost-effectiveness of the intervention. We will study the effectiveness of PST as close to the implementation in practice as possible, using a pragmatic trial design and an open group therapy. Any pragmatic trial has limitations; MacPherson (2004) argued that a pragmatic trial design cannot be used to determine the specific components of a treatment that caused an effect [ 29 ]. It may be possible that patients in the intervention group show improvement caused by the extra attention they receive and not so much by the assumed effective elements of the therapy; this attention effect may be considered a placebo effect. If we would like to distinguish between this ‘placebo effect’ and the effect of the specific treatment elements, the control group should have received a ‘sham therapy’. Such sham therapy would hinder the estimation of the effect of PST in practice, as in practice such additional effort would not take place. Therefore, one of the advantages of the pragmatic study design is that the external validity is better than using a sham-controlled design; the results will be generalizable to the normal rehabilitation setting [ 30 ]. The study population represents the normal stroke population in the outpatient phase of rehabilitation treatment, and the psychologists will provide the intervention to the patients just as they would do in practice. The results of a pragmatic trial are directly applicable to the usual care setting [ 31 ]. Moreover, if the intervention will prove effective, it will be easy to implement the intervention in the standard rehabilitation program, since it is already in use and the psychologists will already be trained. Other rehabilitation centers can use the therapy manual we developed.
We expect that patients who received PST will use more effective coping styles and experience a higher HR-QoL. Furthermore, we expect that patients after PST will show a decrease in depression score, an increase in social participation, and a decrease in health care consumption, which would lead to a reduction in the health care costs. We expect the intervention to be cost-effective, since the costs of the intervention are relatively low; one psychologist can train three to six patients at the same time. Darlington (2009) estimated the cost-effectiveness of an intervention aimed at coping strategies in stroke patients: the maximum costs for a single patient were 2500 euros, which will be lower if the therapy is provided in a group [ 32 ]. If PST will be proved effective for stroke patients in outpatient rehabilitation, the intervention will be an inexpensive, deliverable and sustainable group intervention that could be added to usual stroke rehabilitation programs.
Abbreviations
Center for Epidemiologic Studies Depression Scale
Coping Inventory for Stressful Situations
- Health-related quality of life
Impact on Participation and Autonomy
- Problem Solving Therapy
Quality-adjusted life years
Randomized controlled trial
Social Problem Solving Inventory-Revised
Stroke Specific Quality of Life Scale
Traumatic brain-injured
Trimbos Questionnaire for Costs association with Psychiatric Illness
World Health Organization Quality of Life.
Evers SM, Engel GL, Ament AJ: Cost of stroke in The Netherlands from a societal perspective. Stroke. 1997, 28 (7): 1375-1381. 10.1161/01.STR.28.7.1375.
Article CAS PubMed Google Scholar
Vaartjes I, van Dis I, Visseren F, Bots M: Hart- en vaatziekten in Nederland 2009, cijfers over leefstijl- en risicofactoren, ziekte en sterfte. 2009, Den Haag: Nederlandse Hartstichting
Google Scholar
Group W, Harper A, Power M: Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998, 28 (3): 551-558.
Article Google Scholar
Sturm JW, Donnan GA, Dewey HM, Macdonell RAL, Gilligan AK, Srikanth V, Thrift AG: Quality of life after stroke - The North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2004, 35 (10): 2340-2345. 10.1161/01.STR.0000141977.18520.3b.
Article PubMed Google Scholar
Mittmann N, Trakas K, Risebrough N, Liu BA: Utility scores for chronic conditions in a community-dwelling population. Pharmaco Economics. 1999, 15 (4): 369-376. 10.2165/00019053-199915040-00004.
Article CAS Google Scholar
Paul SL, Sturm JW, Dewey HM, Donnan GA, Macdonell RAL, Thrift AG: Long-term outcome in the north east Melbourne stroke incidence study - Predictors of quality of life at 5 years after stroke. Stroke. 2005, 36 (10): 2082-2086. 10.1161/01.STR.0000183621.32045.31.
Almborg AH, Ulander K, Thulin A, Berg S: Discharged after stroke - important factors for health-related quality of life. J Clin Nursing. 2010, 19 (15–16): 2196-2206.
Patel MD, Tilling K, Lawrence E, Rudd AG, Wolfe CDA, McKevitt C: Relationships between long-term stroke disability, handicap and health-related quality of life. Age Ageing. 2006, 35 (3): 273-279. 10.1093/ageing/afj074.
Wolters G, Stapert S, Brands I, Van Heugten C: Coping styles in relation to cognitive rehabilitation and quality of life after brain injury. Neuropsychol Rehabil. 2010, 20 (4): 587-600. 10.1080/09602011003683836.
Herrmann M, Curio N, Petz T, Synowitz H, Wagner S, Bartels C, Wallesch CW: Coping with illness after brain diseases - a comparison between patients with malignant brain tumors, stroke, Parkinson's disease and traumatic brain injury. Disabil Rehabil. 2000, 22 (12): 539-546. 10.1080/096382800416788.
Darlington ASE, Dippel DWJ, Ribbers GM, van Balen R, Passchier J, Busschbach JJV: Coping strategies as determinants of quality of life in stroke patients: A longitudinal study. Cerebrovasc Dis. 2007, 23 (5–6): 401-407.
Backhaus SL, Ibarra SL, Klyce D, Trexler LE, Malec JF: Brain Injury Coping Skills Group: A Preventative Intervention for Patients With Brain Injury and Their Caregivers. Archives Physical Med Rehabil. 2010, 91 (6): 840-848. 10.1016/j.apmr.2010.03.015.
Merlijn V, Hunfeld JAM, van der Wouden JC, Hazebroek-Kampschreur A, van Suijlekom-Smit LWA, Koes BW, Passchier J: A cognitive-behavioural program for adolescents with chronic pain - a pilot study. Patient Educ Counseling. 2005, 59 (2): 126-134. 10.1016/j.pec.2004.10.010.
Hopko DR, Armento MEA, Robertson SMC, Ryba MM, Carvalho JP, Colman LK, Mullane C, Gawrysiak M, Bell JL, McNulty JK, et al: Brief Behavioral Activation and Problem-Solving Therapy for Depressed Breast Cancer Patients: Randomized Trial. J Consult Clin Psychol. 2011, 79 (6): 834-849.
Robinson RG, Jorge RE, Moser DJ, Acion L, Solodkin A, Small SL, Fonzetti P, Hegel M, Arndt S: Escitalopram and problem-solving therapy for prevention of poststroke depression - A randomized controlled trial. Jama-Journal The Am Med Assoc. 2008, 299 (20): 2391-2400. 10.1001/jama.299.20.2391.
Ch'ng AM, French D, McLean N: Coping with the Challenges of Recovery from Stroke Long Term Perspectives of Stroke Support Group Members. J Health Psychology. 2008, 13 (8): 1136-1146. 10.1177/1359105308095967.
Nezu AM, Perri MG, Nezu CM, Berking M: Problem-solving therapy for depression: theory, research, and clinical guidelines. 1989, New York: Wiley
Nezu AM, Nezu CM: Problem Solving Therapy. J Psychother Integr. 2001, 11 (2): 187-205. 10.1023/A:1016653407338.
Endler NS, Parker JDA: Coping inventory for stressful situations (CISS) manual. 1990, Toronto: Multi-Health Systems
Hawkins D, Sofronoff K, Sheffield J: Psychometric Properties of the Social Problem Solving Inventory-Revised Short-Form: Is the Short Form a Valid and Reliable Measure for Young Adults?. Cognitive Therapy Res. 2009, 33 (5): 462-470. 10.1007/s10608-008-9209-7.
Lamers LM, McDonnell J, Stalmeier PF, Krabbe PF, Busschbach JJ: The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ. 2006, 15 (10): 1121-1132. 10.1002/hec.1124.
Williams LS, Weinberger M, Harris LE, Clark DO, Biller J: Development of a stroke-specific quality of life scale. Stroke. 1999, 30 (7): 1362-1369. 10.1161/01.STR.30.7.1362.
Post MWM, Boosman H, van Zandvoort MM, Passier P, Rinkel GJE, Visser-Meily JMA: Development and validation of a short version of the Stroke Specific Quality of Life Scale. J Neurol Neurosurg Psychiatry. 2011, 82 (3): 283-286. 10.1136/jnnp.2009.196394.
Radloff LS: The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977, 1: 385-401. 10.1177/014662167700100306.
Cardol M, de Haan RJ, de Jong BA, van den Bos GAM, de Groot IJM: Psychometric properties of the impact on participation and autonomy questionnaire. Arch Physical Med Rehabil. 2001, 82 (2): 210-216. 10.1053/apmr.2001.18218.
Hakkaart-Van Roijen L: Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness (TiC-P). Manual. September 2010, Rotterdam: Erasmus University Rotterdam
Studenski S, Duncan PW, Perera S, Reker D, Lai SM, Richards L: Daily functioning and quality of life in a randomized controlled trial of therapeutic exercise for subacute stroke survivors. Stroke. 2005, 36 (8): 1764-1770. 10.1161/01.STR.0000174192.87887.70.
Oosterbrink JB, Bouwmans CAM, Koopmanschap MA, Rutten FFH: Handleiding voor kostenonderzoek, methoden en standaard kostprijzen voor economische evaluaties in de gezondheidszorg. 2004, Diemen: College voor zorgverzekeringen
Macpherson H: Pragmatic clinical trials. Complement Ther Med. 2004, 12 (2–3): 136-140.
Tunis SR, Stryer DB, Clancy CM: Practical clinical trials - Increasing the value of clinical research for decision making in clinical and health policy. Jama-Journal Am Med Assoc. 2003, 290 (12): 1624-1632. 10.1001/jama.290.12.1624.
Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, Oxman AD, Moher D: Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008, 337: a2390-10.1136/bmj.a2390.
Article PubMed PubMed Central Google Scholar
Darlington ASE, Dippel DWJ, Ribbers GM, van Balen R, Passchier J, Busschbach JJV: A Prospective Study On Coping Strategies And Quality Of Life In Patients After Stroke, Assessing Prognostic Relationships And Estimates Of Cost-Effectiveness. J Rehabil Med. 2009, 41 (4): 237-241. 10.2340/16501977-0313.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2377/13/67/prepub
Download references
Acknowledgements
This study is funded by the National Initiative Brain and Cognition (NIHC 056-11-010), Stichting Coolsingel, and Erasmus MC Cost-Effectiveness Research.
Author information
Authors and affiliations.
Department of Rehabilitation Medicine, Erasmus MC, University Medical Center Rotterdam, PO Box 2040, 3000, CA, Rotterdam, The Netherlands
Marieke M Visser, Majanka H Heijenbrok-Kal & Gerard M Ribbers
Rijndam Rehabilitation Center, PO Box 23181, 3001, KD, Rotterdam, The Netherlands
Department of Psychiatry, Erasmus MC, University Medical Center Rotterdam, Section Medical Psychology and Psychotherapy, PO Box 2040, 3000, CA, Rotterdam, The Netherlands
Adriaan van ’t Spijker & Jan JV Busschbach
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Marieke M Visser .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
All authors contributed to the development of the study protocol. AvtS adapted the PST-manual for the population of stroke patients. MMV implemented the therapy in the rehabilitation program. All authors read and corrected the draft version of this manuscript, and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Visser, M.M., Heijenbrok-Kal, M.H., van ’t Spijker, A. et al. The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled trial. BMC Neurol 13 , 67 (2013). https://doi.org/10.1186/1471-2377-13-67
Download citation
Received : 23 April 2013
Accepted : 20 June 2013
Published : 27 June 2013
DOI : https://doi.org/10.1186/1471-2377-13-67
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rehabilitation
- Coping style
BMC Neurology
ISSN: 1471-2377
- General enquiries: [email protected]
A Neurosurgeon’s Guide to Stroke
Stroke is an abrupt interruption of constant blood flow to the brain that causes loss of neurological function. The interruption of blood flow can be caused by a blockage, leading to the more common ischemic stroke, or by bleeding in the brain, leading to the more deadly hemorrhagic stroke. Ischemic stroke constitutes an estimated 87 percent of all stroke cases. Stroke often occurs with little or no warning, and the results can be devastating.
It is crucial that proper blood flow and oxygen be restored to the brain as soon as possible. Without oxygen and important nutrients, the affected brain cells are either damaged or die within a few minutes. Once brain cells die, they generally do not regenerate and devastating damage may occur, sometimes resulting in physical, cognitive and mental disabilities.
Symptoms + Types
Ischemic stroke.
- Thrombotic (cerebral thrombosis) is the most common type of ischemic stroke. A blood clot forms inside a diseased or damaged artery in the brain resulting from atherosclerosis (cholesterol-containing deposits called plaque), blocking blood flow.
- Embolic (cerebral embolism) is caused when a clot or a small piece of plaque formed in one of the arteries leading to the brain or in the heart, is pushed through the bloodstream and lodges in narrower brain arteries. The blood supply is cut off from the brain due to the clogged vessel.
Transient ischemic attack (TIA)
This is a warning sign of a possible future stroke and is treated as a neurological emergency. Common temporary symptoms include difficulty speaking or understanding others, loss or blurring of vision in one eye and loss of strength or numbness in an arm or leg. Usually these symptoms resolve in less than 10 to 20 minutes and almost always within one hour. Even if all the symptoms resolve, it is very important that anyone experiencing these symptoms call 911 and immediately be evaluated by a qualified physician.
Hemorrhagic Stroke
- Subarachnoid Hemorrhage is bleeding that occurs in the space between the surface of the brain and skull. A common cause of subarachnoid hemorrhagic stroke is a ruptured cerebral aneurysm, an area where a blood vessel in the brain weakens, resulting in a bulging or ballooning out of part of the vessel wall; or the rupture of an arteriovenous malformation (AVM), a tangle of abnormal and poorly formed blood vessels (arteries and veins), with an innate propensity to bleed.
- Intracerebral Hemorrhage is bleeding that occurs within the brain tissue. Many intracerebral hemorrhages are due to changes in the arteries caused by long-term hypertension. Other potential causes may be delineated through testing.
Stroke Statistics
- Stroke is the third leading cause of death in the U.S.
- Statistics indicate that an estimated 135,592 people in the U.S. died from cerebrovascular disease in 2007.
- Of all strokes, 87 percent are ischemic, 10 percent are intracerebral hemorrhage and 3 percent are subarachnoid hemorrhage.
- While the incidence has increased, there has been a steady decline in mortality rates since 2002.
- Of the more than 795,000 people affected every year, about 610,000 of these are first attacks and 185,000 are recurrent.
- About 25 percent of people who recover from their first stroke will have another stroke within five years.
- Stroke is a leading cause of serious long-term disability, with an estimated 5.4 million stroke survivors currently alive today.
- In 2010, stroke cost about $73.7 billion in both direct and indirect costs in the U.S. alone.
Source: American Heart Association (AHA), Heart Disease and Stroke Statistics – 2010 Update.
Risk Factors
Although they are more common in older adults, strokes can occur at any age. Understanding the factors that increase your risk of a stroke and recognizing the symptoms may help you prevent a stroke. Receiving early diagnosis and treatment may improve your chances for complete recovery.
Controllable or treatable risk factors for stroke include:
- Smoking: You can decrease your risk by quitting smoking. Your risk may be increased further if you use some forms of oral contraceptives and are a smoker. There is recent evidence that long-term secondhand smoke exposure may increase your risk of stroke.
- High blood pressure: Blood pressure of 140/90 mm Hg or higher is the most important risk factor for stroke. It usually has no specific symptoms and no early warning signs. That is why it is important to have your blood pressure checked regularly. Controlling your blood pressure is crucial to stroke prevention.
- Carotid or other artery disease: The carotid arteries in your neck supply blood to your brain. A carotid artery narrowed by fatty deposits from atherosclerosis may become blocked by a blood clot. Carotid arteries are treated by neurosurgeons through carotid endarterectomy, a procedure in which an incision is made in the neck and plaque is removed from the artery; or carotid artery angioplasty and stenting, an endovascular procedure that requires no surgical incision in the neck.
- History of TIAs: About 30 percent of strokes are preceded by one or more TIAs that can occur days, weeks or even months before a stroke.
- Diabetes: It is crucial to control your blood sugar levels, blood pressure and cholesterol levels. Diabetes, especially when untreated, puts you at greater risk of stroke and has many other serious health implications.
- High blood cholesterol: A high level of total cholesterol in the blood (240 mg/dL or higher) is a major risk factor for heart disease, which raises your risk of stroke. Recent studies show that high levels of LDL (bad) cholesterol (greater than 100 mg/dL) and triglycerides (blood fats, 150 mg/dL or higher) increase the risk of stroke in people with previous coronary heart disease, ischemic stroke or TIAs. Low levels (less than 40 mg/dL) of HDL (good) cholesterol also may increase stroke risk. You can often improve your cholesterol levels by decreasing the salt and saturated fat in your diet. However, some people inherit genes associated with elevated levels of cholesterol. Although they may eat well and exercise, they still may have high cholesterol and must take medication to control it.
- Physical inactivity and obesity: Being inactive, obese or both can increase your risk of high blood pressure, high blood cholesterol, diabetes, heart disease and stroke. Getting 30 minutes of moderate exercise, five days a week can help reduce your risk of stroke. Check with your doctor first before starting any exercise program if you have any health problems or have been inactive.
- Recent research shows evidence that people receiving hormone replacement therapy (HRT) have an overall 29 percent increased risk of stroke, in particular ischemic stroke.
Uncontrollable risk factors include:
- Age: People of all ages, including children, have strokes. But the older you are, the greater your risk of stroke.
- Gender: Stroke is more common in men than in women. In most age groups, more men than women will have a stroke in a given year. However, women account for more than half of all stroke deaths. Women who are pregnant have a higher stroke risk. Some research has indicated that women may experience and interpret stroke symptoms differently than men, causing them to delay seeking medical care and contributing to their higher stroke mortality rates.
- Heredity and race: You have a greater risk of stroke if a parent, grandparent, sister or brother has had a stroke. African Americans have more than two times the risk of stroke compared to Caucasians, partly related to the prevalence of hypertension. Hispanics also have an elevated stroke risk.
- Prior stroke or heart attack: If you have had a stroke, you are at much higher risk of having another one. If you have had a heart attack, you are also at higher risk of having a stroke.
Stroke Symptoms
The range and severity of early stroke symptoms vary considerably, but they share the common characteristic of being sudden. Warning signs may include some or all of the following symptoms:
- Dizziness, nausea or vomiting
- Unusually severe headache
- Confusion, disorientation or memory loss
- Numbness, weakness in an arm, leg or the face, especially on one side
- Abnormal or slurred speech
- Difficulty with comprehension
- Loss of vision or difficulty seeing
- Loss of balance, coordination or the ability to walk
- It is especially important to note that many strokes may cause an utterly painless loss of neurological function, leading to potential hesitation to call 911 or visit an emergency room.
Stroke Effects
The effects of a stroke depend primarily on the location of the obstruction and the extent of brain tissue affected. One side of the brain controls the opposite side of the body, so a stroke affecting the right side will result in neurological complications on the left side of the body. A stroke on the right side may result in the following:
- Paralysis on the left side of the body
- Vision problems
- Quick, inquisitive or purposeless behavior
- Memory loss
A stroke on the left side may result in the following:
- Paralysis on the right side of the body
- Speech/language problems
- Slow, cautious behavior
Treatment + Care
Rehabilitation following a stroke may involve a number of medical specialists; but the early diagnosis of a stroke, its treatment or its prevention, can be undertaken by a neurosurgeon. Rapid and accurate diagnosis of the kind of stroke and the exact location of its damage is critical to successful treatment. Technical advances such as digital imaging, microcatheters and other neurointerventional technologies, the use of the operating microscope (microsurgery) and the surgical laser have made it possible to treat stroke problems that were inoperable a few years ago.
Ischemic Stroke Treatment
Ischemic stroke is treated by removing obstruction and restoring blood flow to the brain. The only U. S. Food and Drug Administration (FDA)-approved medication for ischemic stroke is tissue plasminogen activator (tPA), which must be administered within a three-hour window from the onset of symptoms to work best. Unfortunately, only 3- 5 percent of those who suffer a stroke reach the hospital in time to be considered for this treatment, and the actual use of tPA is considerably lower. This medication carries a risk for increased intracranial hemorrhage and is not used for hemorrhagic stroke.
Emergency Surgical Stroke Treatment: Neurointerventional Procedures
Microcatheter-based surgical interventions for stroke may include the use of a small microcatheter, delivered through a larger guiding catheter inserted at the groin through a small incision. A microguidewire is used to navigate the microcatheter to the site of obstruction in the brain. Thrombolytic medication, such as tPA, can then be administered directly to the occluding thrombus. This kind of treatment, which delivers thrombolytic medication intraarterially, is more specific than IV (intravenous) tPA and consequently may require significantly lesser dosages of medication. The time limit to implement this type of intervention is also significantly (double) longer than that for IV TPA. Generally, only Comprehensive Stroke Care Centers offer this type of treatment.
Clot Retrieval Devices
The Merci Retriever, approved in 2004 by the FDA, is a corkscrew- shaped device used to help remove blood clots from the arteries of stroke patients. A small incision is made in the patient’s groin, into which a small catheter is fed until it reaches the arteries in the neck. At the neck, a small catheter inside the larger catheter is guided through the arteries into the brain, until it reaches the brain clot. A straight wire inside the small catheter pokes out beyond the clot and automatically coils into a corkscrew shape. It is pulled back into the clot, the corkscrew spinning and grabbing the clot. A balloon inflates in the neck artery, cutting off blood flow, so the device can pull the clot out of the brain safely. The clot is removed through the catheter with a syringe.
Penumbra is also a microcatheter-based system device, which works by an aspiration principle. It was approved by the FDA in 2008.
Stentriever devices are the newest generation of embolectomy devices for stroke. They are still in an investigative phase but work by breaking up the occluding clot, combined with aspiration or withdrawal.
Medical Prevention
Medications used to help prevent stroke in high-risk patients (especially those who have experienced a previous TIA or ischemic stroke) fall into two major categories: anticoagulants and antiplatelet agents.
Anticoagulants thin the blood and prevent clotting. Heparin acts quickly and is given intravenously or subcutaneously (beneath the skin) while a patient is in the hospital. Slower-acting warfarin can be given orally and is used over a longer period. Because these drugs affect the blood’s ability to clot, they require close monitoring by a physician.
Antiplatelet drugs prevent platelet aggregation. Platelets are specialized cells in the blood that initiate a healing process. Large numbers of platelets clump together to form a clot, which can sometimes block an artery or break loose, travel through the bloodstream and block a smaller artery. Antiplatelet drugs make platelets less sticky and less likely to form clots, reducing the risk of ischemic stroke in patients who have had TIA or prior ischemic stroke.
Preventive Surgical Procedures
Carotid endarterectomy surgery (carotid endarterectomy, cea).
Patients will be given either a general or local anesthetic before surgery. In this procedure, the neurosurgeon makes an incision in the carotid artery in the neck and removes the plaque using a dissecting tool. Removing the plaque is accomplished by widening the passageway, which helps to restore normal blood flow. The artery will be repaired with sutures or a graft. The entire procedure usually takes about two hours. One may experience pain near the incision in the neck and some difficulty swallowing during the first few days after surgery. Most patients are able to go home after one or two days and return to work usually within a month. Patients should avoid driving and limit physical activities for a few weeks after surgery.
There are potential complications with carotid endarterectomy surgery, just as there are with any type of surgery. There is a 1-3 percent risk of stroke following surgery. Another fairly rare complication is the reblockage of the carotid artery, called restenosis. This may occur later, especially in cigarette smokers. Numbness in the face or tongue caused by temporary nerve damage is a possibility, but uncommon. This usually clears up in less than one month and most often does not require any treatment.
Carotid Angioplasty and Stenting
An alternative, newer form of treatment, carotid angioplasty and stenting (CAS), shows some promise in patients who may be at too high risk to undergo surgery. Carotid stenting is a neurointerventional procedure in which a tiny, slender metal-mesh tube is fitted inside the carotid artery to increase the flow of blood blocked by plaques. Access is gained through a small (0.5 cm) groin incision, but no incision is made in the neck. The stent is inserted following a procedure called angioplasty, in which the doctor guides a balloon-tipped catheter into the blocked artery. The balloon is inflated and pressed against the plaque, flattening it and reopening the artery. The stent acts as scaffolding to prevent the artery from collapsing or from closing up again after the procedure is completed.
There are several potential complications of endovascular treatment. The most serious risk from carotid stenting is an embolism caused by a disrupted plaque particle breaking free from the site. This can block an artery in the brain, causing a stroke. These risks are minimized using small filters called embolic protection devices in conjunction with angioplasty and stenting. There is also a slight risk of stroke due to a loose piece of plaque or a blood clot blocking an artery during or right after surgery. The risks are balanced against the advantages of a shorter occlusion time (10 seconds, as opposed to 30 minutes for endarterectomy), shorter anesthesia and a small leg incision.
Hyperperfusion, or the sudden increased blood flow through a previously blocked carotid artery and into the arteries of the brain, can cause a hemorrhagic stroke. Other complications include restenosis and short periods of medically treatable reduced blood pressure and heart rate. These risks are similar for CEA and CAS.
Hemorrhagic Stroke Treatment
Hemorrhagic stroke usually requires surgery to relieve intracranial (within the skull) pressure caused by bleeding. Surgical treatment for hemorrhagic stroke caused by an aneurysm or defective blood vessel can prevent additional strokes. Surgery may be performed to seal off the defective blood vessel and redirect blood flow to other vessels that supply blood to the same region of the brain.
For a patient with a ruptured cerebral aneurysm, surgical elimination of the aneurysm is only the beginning. Intensive care recovery for the next 10-14 days is the rule, during which time a multitude of complications related to subarachnoid hemorrhage (SAH) can and do occur. At some time during that period (often immediately upon completion of surgery), cerebral angiography or a substitute study is done to document that the aneurysm has been eliminated. The first two to five days after SAH represent the greatest threat of brain swelling; at which time special measures (both medical and surgical) are used to diminish the effect of swelling on intracranial pressure. Near the end of this initial period, the risk period for delayed cerebral vasospasm begins and lasts the better part of the next 14 days. Intercurrent infections such as pneumonia are common, and hydrocephalus may develop.
Surgery/Clipping
Prior to surgery, the exact location of the subarachnoid hemorrhage or aneursym is identified through cerebral angiography images. An operation to “clip” the aneurysm is performed by doing a craniotomy (opening the skull surgically) and isolating the aneurysm from the normal bloodstream. In addition, a craniectomy, a surgical procedure in which part of the skull is removed and left off temporarily, may be done to help relieve increased intracranial pressure.
One or more tiny titanium clips with spring mechanisms are applied to the base of the aneurysm, allowing it to deflate. The size and shape of the clips is selected based on the size and location of the aneurysm. Clips are permanent, remain in place and generally provide a durable cure for the patient. Angiography is used to confirm exclusion of the aneurysm from the cerebral circulation and the preservation of normal flow of blood in the brain.
Endovascular (Neurointerventional) Treatment
Neurointerventional procedures for cerebral aneurysm share the advantages of no incision made in the skull and an anesthesia time that is often dramatically shorter than for craniotomy and microsurgical clipping.
In endovascular microcoil embolization, a needle is placed into the femoral artery of the leg, and a small catheter is inserted. Utilizing x-ray guidance, the catheter is advanced through the body’s arterial system to one of the four blood vessels that feed the brain. A smaller microcatheter is fed into the aneurysm, and once properly positioned, a thin wire filament or “coil” is advanced into the aneurysm. The flexible, platinum coil is designed to conform to the shape of the aneurysm. Additional coils are advanced into the aneurysm to close the aneurysm from the inside. This prevents flow of blood into the aneurysm by causing a clot to form on the inside.
Balloon-assisted coiling uses a tiny balloon catheter to help hold the coil in place. Although this has been shown in several studies to increase risks, ongoing innovations in this relatively new technology has helped improve its efficacy. Combination stent and coiling utilizes a small flexible cylindrical mesh tube that provides a scaffold for the coiling. Intracranial stenting and other innovations are quite new, and endovascular technology is in a constant state of development. These adjuncts allow coiling to be considered for cerebral aneurysms that may not have an ideal shape for conventional coiling.
Stroke Rehabilitation
Recovery and rehabilitation are among the most important aspects of stroke treatment. As a rule, most strokes are associated with some recovery, the extent of which is variable. In some cases, undamaged areas of the brain may be able to perform functions that were lost when the stroke occurred. Rehabilitation includes physical therapy, speech therapy and occupational therapy. This type of recovery is measured in months to years.
- Physical therapy involves using exercise and other physical means (e.g., massage, heat) and may help patients regain the use of their arms and legs and prevent muscle stiffness in patients with permanent paralysis.
- Speech therapy may help patients regain the ability to speak.
- Occupational therapy may help patients regain independent function and relearn basic skills (e.g., getting dressed, preparing a meal and bathing).
Note from AANS
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon online tool.
We value your privacy
Privacy overview.
| Cookie | Duration | Description |
|---|---|---|
| __cf_bm | 1 hour | This cookie, set by Cloudflare, is used to support Cloudflare Bot Management. |
| ASPSESSIONIDACQATATC | session | ASP Session cookie |
| ASPSESSIONIDACQBSDQD | session | ASP Session cookie |
| ASPSESSIONIDSARBSARA | session | ASP Session cookie |
| ASPSESSIONIDSCDBCDAB | session | ASP Session cookie |
| AWSALBCORS | 7 days | Amazon Web Services set this cookie for load balancing. |
| cookielawinfo-checkbox-advertisement | 1 year | Set by the GDPR Cookie Consent plugin, this cookie records the user consent for the cookies in the "Advertisement" category. |
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| CookieLawInfoConsent | 1 year | CookieYes sets this cookie to record the default button state of the corresponding category and the status of CCPA. It works only in coordination with the primary cookie. |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
| wpEmojiSettingsSupports | session | WordPress sets this cookie when a user interacts with emojis on a WordPress site. It helps determine if the user's browser can display emojis properly. |
| Cookie | Duration | Description |
|---|---|---|
| yt-player-headers-readable | never | The yt-player-headers-readable cookie is used by YouTube to store user preferences related to video playback and interface, enhancing the user's viewing experience. |
| yt-remote-cast-available | session | The yt-remote-cast-available cookie is used to store the user's preferences regarding whether casting is available on their YouTube video player. |
| yt-remote-cast-installed | session | The yt-remote-cast-installed cookie is used to store the user's video player preferences using embedded YouTube video. |
| yt-remote-connected-devices | never | YouTube sets this cookie to store the user's video preferences using embedded YouTube videos. |
| yt-remote-device-id | never | YouTube sets this cookie to store the user's video preferences using embedded YouTube videos. |
| yt-remote-fast-check-period | session | The yt-remote-fast-check-period cookie is used by YouTube to store the user's video player preferences for embedded YouTube videos. |
| yt-remote-session-app | session | The yt-remote-session-app cookie is used by YouTube to store user preferences and information about the interface of the embedded YouTube video player. |
| yt-remote-session-name | session | The yt-remote-session-name cookie is used by YouTube to store the user's video player preferences using embedded YouTube video. |
| ytidb::LAST_RESULT_ENTRY_KEY | never | The cookie ytidb::LAST_RESULT_ENTRY_KEY is used by YouTube to store the last search result entry that was clicked by the user. This information is used to improve the user experience by providing more relevant search results in the future. |
| Cookie | Duration | Description |
|---|---|---|
| AWSALB | 7 days | AWSALB is an application load balancer cookie set by Amazon Web Services to map the session to the target. |
| Cookie | Duration | Description |
|---|---|---|
| _ga | 1 year 1 month 4 days | Google Analytics sets this cookie to calculate visitor, session and campaign data and track site usage for the site's analytics report. The cookie stores information anonymously and assigns a randomly generated number to recognise unique visitors. |
| _ga_* | 1 year 1 month 4 days | Google Analytics sets this cookie to store and count page views. |
| _gcl_au | 3 months | Google Tag Manager sets the cookie to experiment advertisement efficiency of websites using their services. |
| _sp_id.* | 1 year 1 month 4 days | Snowplow sets this cookie to store user information that is created when a user first visits a site and is updated on subsequent visits. |
| _sp_ses.* | 1 hour | Snowplow sets this cookie to store user information that is created when a user first visits a site and is updated on subsequent visits. |
| feathr_session_id | 1 hour | This cookie is set by Feathr. This cookie is used to keep track of user activity. |
| Cookie | Duration | Description |
|---|---|---|
| f_id | 1 year | This cookie is used by feathr to track pages. The cookie establishes a unique identification per browser which helps in advertising. |
| IDE | 1 year 24 days | Google DoubleClick IDE cookies store information about how the user uses the website to present them with relevant ads according to the user profile. |
| test_cookie | 15 minutes | doubleclick.net sets this cookie to determine if the user's browser supports cookies. |
| VISITOR_INFO1_LIVE | 6 months | YouTube sets this cookie to measure bandwidth, determining whether the user gets the new or old player interface. |
| VISITOR_PRIVACY_METADATA | 6 months | YouTube sets this cookie to store the user's cookie consent state for the current domain. |
| YSC | session | Youtube sets this cookie to track the views of embedded videos on Youtube pages. |
| yt.innertube::nextId | never | YouTube sets this cookie to register a unique ID to store data on what videos from YouTube the user has seen. |
| yt.innertube::requests | never | YouTube sets this cookie to register a unique ID to store data on what videos from YouTube the user has seen. |
| Cookie | Duration | Description |
|---|---|---|
| _cfuvid | session | Description is currently not available. |
| ASPSESSIONIDCAQARCSD | session | Description is currently not available. |
| ASPSESSIONIDQCBCDABA | session | Description is currently not available. |
| ASPSESSIONIDQCDCABBB | session | Description is currently not available. |
| AWSALBTG | 7 days | No description available. |
| AWSALBTGCORS | 7 days | No description available. |
| cf_clearance | 1 year | Description is currently not available. |
| OasisLMS | session | Description is currently not available. |

IMAGES
VIDEO
COMMENTS
More than half of all stroke survivors experience a post-stroke cognitive impairment. This may affect many functions, including memory, problem solving skills, and the ability to think clearly, among others. However, survivors can often improve their mental aptitude by practicing cognitive exercises for stroke patients.
Many other thinking processes happen without us being aware of them, known as automatic processes. Together, many of these automatic processes are known as executive function. Executive function is about planning and problem-solving. It includes all the things that allow us to organise, make decisions and know when we need to do something.
same. More than two-thirds of stroke survivors receive rehabilitation services after leaving the hospital. Effective rehabilitation is an essential part of stroke care. Stroke rehabilitation requires a sustainable and coordinated effort from a team with the patient and the patient's goals at the center. In addition to the patient, the team ...
This raises the question whether the intervention should be adapted to increase and prolong the effects found. It may be useful to invite participants for more sessions or a refreshment session 6 months post intervention. ... The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled ...
Decision making is defined as the process of examining possibilities, risks, uncertainties, and options, comparing them, and choosing a course of action. 1, 2 Decisions based on erroneous assessments may result in incorrect patient and family expectations, and potentially inappropriate advice, treatment, or discharge planning (eg, longer length ...
Percent of Users Identified As Recovering from Stroke: 40%. 6. Do clock math: Stroke can affect number skills, math skills, and word finding. This task helps improve time-based calculation skills by answering math questions associated with clocks. Individuals Assigned: 6,701 Percent of Users Identified As Recovering from Stroke: 37%. 7.
problem-solving refers to the "process of finding solutions to specific problems".13 Problem-solving therapy (PST) is an intervention in which patients are taught to increase structure in solving problems and flexibility by using different coping strategies in various situations. In patients with stroke, PST has
Example strategy games for stroke patients include: Carcassonne: a puzzle-based game that can challenge visuospatial skills and problem-solving. Chess: a traditional game requiring planning, judgement and reasoning. Catan: a building and trading game requiring constant cognitive flexibility and social skills.
The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients. The secondary aim is to determine the effect of Problem Solving Therapy on depression, social participation, health care consumption, and to determine the ...
TTES Newsletter: Monthly newsletter provides patients and caregivers information on stroke-related research and resources. Stroke Family Warmline 1-888-478-7653: Connects stroke survivors and their families with specially trained ASA team members — some of whom are stroke family caregivers — for support, information or just a listening ear.
Our framework guided the design of the research questions, literature search, identification of studies, and the collation of results. ... Problem-solving therapy did not produce a significant change in overall problem-solving (SPISR; proxy measure for emotional distress). ... However, a high proportion of stroke patients have cognitive or ...
Making decisions, solving problems, understanding numbers and managing money can be a challenge. Good cognitive function also relies on memory. The brain uses 2 types of memory to hold information, the long and short term memory. Short-term memory is the temporary store for small amounts of information. ... Stroke can impact on this ability ...
ut them. If you're finding it hard, tell someone. Make it clear how they. port you can get.2 Don't be too hard on yourselfHaving cognitive problems after a stroke i. nothing you can control or need to feel bad about. A stroke is a major injury to your br. in, so it's going to take time for it to.
The following are some games that are helpful in stroke recovery cognitive exercises. Lumosity: This brain training app offers a variety of games designed to improve memory, attention, and problem-solving skills. Games like "Train of Thought" and "Memory Matrix" are particularly effective for cognitive exercise.
Coping style is one of the determinants of health-related quality of life after stroke. Stroke patients make less use of active problem-oriented coping styles than other brain damaged patients. Coping styles can be influenced by means of intervention. The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and ...
Stroke Practice Questions. (Asterisks*** indicate correct response) 1. A person presenting with a left lower extremity weakness most likely involves which vascular territory? a. the anterior cerebral artery***. b. the middle cerebral artery. c. the posterior cerebral artery.
The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients.
Nurses provided information, reassurance and problem solving advice using a standardized checklist of topics: Clark 2003, 54 Australia: 62 community stroke patients and spouses: 32 intervention, 30 control. 1) Stroke information package covering stroke consequences, secondary prevention, coping and social support services: A: RCT: 3: S
1) Problem Statement/Research Question and Background. Stroke has been well-known as the most common cause of disability and death worldwide. Every year there are estimated to be 15 million of people who have experienced a stroke [1]. Loss of hand mobility is observed on most stroke patients, which inhibits their activities of daily living (ADL ...
The Health Equity and Actionable Disparities in Stroke: Understanding and Problem-Solving (HEADS-UP) symposium—a collaborative initiative with the American Stroke Association and National Institute of Neurological Disorders and Stroke (NINDS) established in 2020—is the first-ever annual multidisciplinary scientific forum focused on ...
Stroke is a leading cause of serious long-term disability, with an estimated 5.4 million stroke survivors currently alive today. In 2010, stroke cost about $73.7 billion in both direct and indirect costs in the U.S. alone. Source: American Heart Association (AHA), Heart Disease and Stroke Statistics - 2010 Update. Risk Factors
Quinn E, LeLaurin J, Eliazar-Macke N, Orozco T, Montague M, Freytes I and Uphold C (2023) Effect of a telephone and web-based problem-solving intervention for stroke caregivers on stroke patient activities of daily living: A randomized controlled trial, Clinical Rehabilitation, 10.1177/02692155231157301, 37:8, (1062-1073), Online publication ...