- Open access
- Published: 28 March 2022

Experiences of elder abuse: a qualitative study among victims in Sweden
- Mikael Ludvigsson 1 , 2 ,
- Nicolina Wiklund 1 ,
- Katarina Swahnberg 3 &
- Johanna Simmons 1
BMC Geriatrics volume 22 , Article number: 256 ( 2022 ) Cite this article
10k Accesses
12 Citations
7 Altmetric
Metrics details
Elder abuse is underreported and undertreated. Methods for prevention and intervention are being developed, but the knowledge guiding such measures is often insufficiently based on the victims’ own voices due to a paucity of studies. The aim of this study was therefore to explore experiences of elder abuse among the victims themselves.
Consecutive inpatients ≥ 65 years of age at a hospital clinic in Sweden were invited to participate, and 24 victims of elder abuse were identified. Semi-structured qualitative interviews were conducted, and transcripts were analyzed using qualitative content analysis.
The analysis generated four themes that together give a comprehensive picture of elder abuse from the participants’ subjective perspectives. The participants’ experiences of abuse were similar to previous third-party descriptions of elder abuse and to descriptions of abuse among younger adults, but certain aspects were substantially different. Vulnerability due to aging and diseases led to dependance on others and reduced autonomy. Rich descriptions were conveyed of neglect, psychological abuse, and other types of abuse in the contexts of both care services and family relations.
Conclusions
Elder abuse is often associated with an individual vulnerability mix of the aging body, illnesses, and help dependence in connection with dysfunctional surroundings. As individual differences of vulnerability, exposure to violence, and associated consequences were so clear, this implies that components of prevention and intervention should be individually tailored to match the needs and preferences of older victims.
Peer Review reports
Abuse of older adults is recognized as a pervasive and serious problem in society. Prevalence estimates have ranged from 10% upwards in cognitively intact persons from North and South America, with large variations between different countries and subcategories of the population [ 1 , 2 , 3 ]. Elder abuse is defined by the World Health Organization (WHO) as “a single or repeated act or lack of appropriate action, occurring within any relationship where there is an expectation of trust, which causes harm or distress to an older person”. It includes five different types of abuse: physical abuse, psychological abuse, sexual abuse, economic abuse, and neglect [ 4 ]. Elder abuse is associated with various adverse health outcomes including psychosocial distress, morbidity, and mortality [ 1 ]. Exposure to more than one type of abuse or by more than one perpetrator is called poly-victimization, and this common condition is generally associated with even worse health outcomes than single exposure to abuse [ 5 , 6 ]. It is also increasingly acknowledged that elder abuse is associated with previous experiences of violence in childhood and adulthood, motivating a life-course perspective in research on elder abuse [ 7 , 8 ].
The causes and mechanisms of elder abuse are important to understand, to prevent its occurrence more effectively in society. The socio-ecological model (Fig. 1 ) of abuse describes how abuse can be understood as a complex interplay between risk factors on different social levels (individual, relationship, community, or societal level) for the victim [ 5 , 9 ]. By analyzing and handling abuse with help of this model, the circumstances of abuse are concretized which facilitates practical interventions. However, experiences of elder abuse differ between professionals, other surrounding persons, and the older adults themselves [ 10 , 11 ], and the varying conceptions and definitions used have consequences for the types and forms of interventions planned. If supportive resources are not adapted to the victims’ conceptualizations of elder abuse or to their perceived needs, the resources risk being ineffective [ 1 , 12 , 13 ]. Thus, the voices of the victims themselves are important to truly understand their associated needs as well as the causes and mechanisms of elder abuse, in order to develop more effective interventions.
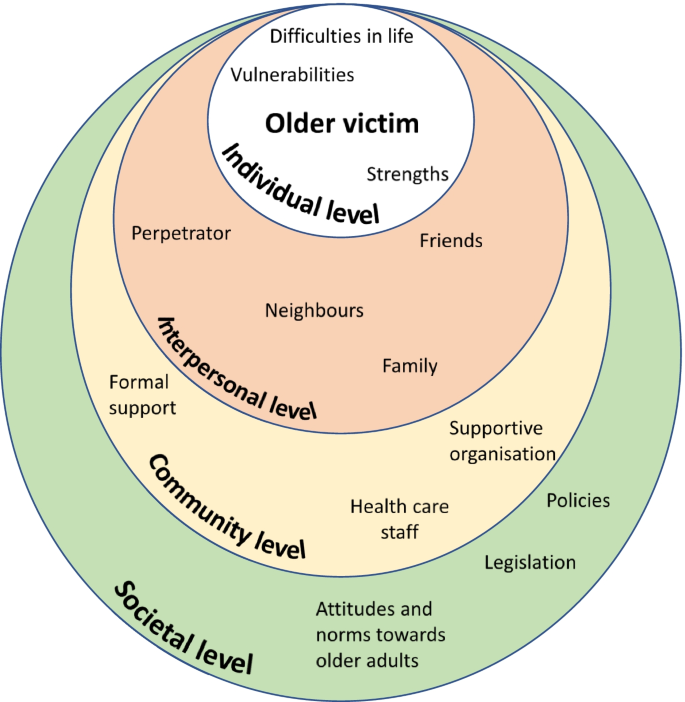
The socioecological model inspired by Bronfenbrenner [ 9 ] and Heise [ 14 ] as a mean to understand the complexity of elder abuse
Furthermore, qualitative studies have been proposed to better understand conceptual and cultural variations of elder abuse [ 1 ]. Some qualitative studies on abuse of older adults have been undertaken within a theoretical framework of intimate partner violence (IPV; [ 15 , 16 ]), but this framework differs from the framework of elder abuse for example by underestimating the categories of abused men, neglect, and abuse by personnel in healthcare or long-term care [ 17 , 18 , 19 ]. Abuse in healthcare and long-term care are particularly relevant for a comprehensive picture of elder abuse as increasing proportions of the population encounter such institutions due to increasing age, frailty, and social dependence [ 2 , 20 ].
Within the framework of elder abuse, several qualitative studies have asked professionals or other third parties about elder abuse [ 11 , 21 , 22 ], but only few have asked the victims themselves [ 21 , 23 , 24 ]. However, these few previous studies do not offer a sufficiently comprehensive picture of the matter which is why we conducted the present study.
The aim of this study was to explore experiences of elder abuse among the victims themselves. By asking the victims directly, our understanding of elder abuse can hopefully deepen and this in turn is essential for adequate prevention and intervention.
Design, setting and sample
Semi structured qualitative interviews were conducted and analyzed using content analysis. The sample was 24 participants from the larger REAGERA (Responding to Elder Abuse in GERiAtric care) project, which included developing and validating the screening instrument REAGERA-S for detecting elder abuse in healthcare [ 25 ]. Consecutive older adults ≥ 65 years of age admitted to a hospital clinic for both acute geriatric and acute medical patients were eligible for inclusion. The consecutive sampling was chosen in the pursuit of naturalistic openness, and this sampling was expected to lead to a wider range of abuse (including mild forms of abuse), compared to alternative purposeful sampling strategies. A parallel goal of gathering information-rich data was reached through a relatively large number of participants. Exclusion criteria were insufficient somatic, cognitive, or linguistic capacity to answer the screening instrument either independently or with the help of healthcare personnel. Patients at the clinic were mostly admitted from the emergency department, and the mean duration of stay for patients over 65 years was 10 days at the acute geriatric ward and 4 days at the acute medical ward during the study period. The setting is described in greater detail elsewhere [ 25 ]. Between January and June 2018, 306 potential participants were asked to participate by nurses on the ward. The screening instrument was completed by 191 participants, of which 135 were interviewed. Of these 135 participants, 24 had been victims of elder abuse and all their 24 recorded interviews were included for this qualitative study. Descriptive data about the 24 included participants are presented in Table 1 . Typically for the setting of the hospital clinic, the mean age was rather high, as were the number of medications and the degree of social dependence for managing activities of daily living—compared to an average patient in health care.
Before the interview, a nurse on the ward distributed a questionnaire to potential participants including the screening instrument REAGERA-S [ 25 ], as well as information about voluntary participation and informed consent. The screening instrument included nine questions about different kinds of abuse (e.g." Has anyone attempted to control you, limit your contact with others, or decide what you may or may not do?”;”Have you been subjected to any form of physical violence, for example being shoved, pinched, held down, hit or kicked?”), and one question about associated suffering. The instrument in total is available elsewhere [ 25 ]. No precise definition of elder abuse was presented for the participants before the interviews. Rather the information preceding the interviews included rather vague descriptions of elder abuse (e.g. “to be subjected to negative actions”) to prevent steering the participants’ thoughts or stories for the data collection. Later that same day or the following day, a qualitative interview was conducted in a private room. The interview was semi-structured using a prepared interview guide (see Supplement 1 ), with four main topics to cover (experiences of abuse, associated thoughts and feelings, effects of the abuse, and support after the abuse). The informants’ experiences of abuse are presented in this study, while their experiences of coping with abuse and their desired support are presented in a separate paper.
For the interviews, we used open-ended questions such as “Can you tell me some more about what you were exposed to?” and “What are your feelings when you think about this today?”. Probing and supplementary questions were also asked. The interviews were audio recorded and transcribed verbatim. The length of the interviews varied between 12 and 97 min. Field notes were written during or after the interviews. Just after each formal interview, the previously completed questionnaire was quickly checked for severe depression or suicidal risk. In two cases, this check – together with the interview – resulted in a referral to an appropriate care unit for support connected to being abused. The individual’s responses from the REAGERA-S were used at a later stage when classifying cases of elder abuse after the interview, described in more detail elsewhere [ 25 ]. All participants received both oral and written information about support services to contact in case of need. In addition to checking the participants’ psychological wellbeing and perceptions of participation in the interviews, additional follow-ups were carried out by phone by the researchers about 1–2 weeks after the interviews. All participants gave written informed consent at the time of participation. A potential ethical problem of the consent process was the principal vulnerability of the participant in the hospital care setting. The interviewers (three of the researchers: JS, NW and ML) usually work as physicians but were not involved in the formal care of the participants, and this was communicated to the patients orally and through a civilian clothing. By signaling thus that the interviewers were separate from the formal health care personnel, elements of vulnerability and potential dependency of the participant was prevented in the participation. Also, security and rapport were built in the meeting through active listening and validation. The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Regional Ethics Review Board in Linköping, Sweden (2017/181–31; 2017/564–32).
Transcripts were analyzed using qualitative content analysis, based on Graneheim and Lundman [ 26 ] and a hermeneutic standpoint with an intermediate level of abstraction and interpretation [ 27 ]. For the purpose of exploring individual experiences, the qualitative content analysis was considered an appropriate method with a focus on subject, context and variation of the data [ 27 ]. The process of analysis involved the following steps: 1) repeated preliminary readings of unique interviews to obtain a sense of the whole; 2) dividing the text into units of meaning; 3) giving codes to condensed meaning units; 4) abstraction within and between interviews by aggregating codes into tentative subcategories/categories (manifest content), and subthemes/themes (latent interpretive content); 5) discussion and revision of tentative codes, subthemes/themes, and subcategories into more definitive ones. The analysis included both a search for convergent patterns and a mirror analytical strategy to investigate divergence (consideration of data that did not fit the dominant patterns) [ 28 ].
Six interviews were coded separately and were then discussed together by all the authors. For the remaining interviews, the coding and development of tentative subcategories and themes were carried out by two of the authors (ML and JS; steps 1–4). The tentative themes/subthemes were then discussed and revised (step 5) by all the authors together. This validation within the research group aimed to strengthen the research design, not by identical statements or consensus but as a form of reflexivity through contesting and supplementing each other’s readings [ 29 ]. The QSR International’s NVivo 12 software program was used as a means for sorting and managing data during the process.
The qualitative analysis generated four themes which are presented in detail below: vulnerability in old age; experiences from earlier in life; perceptions of abuse; consequences and suffering from the abuse. An overview of the themes subthemes and subcategories is depicted in Fig. 2 .
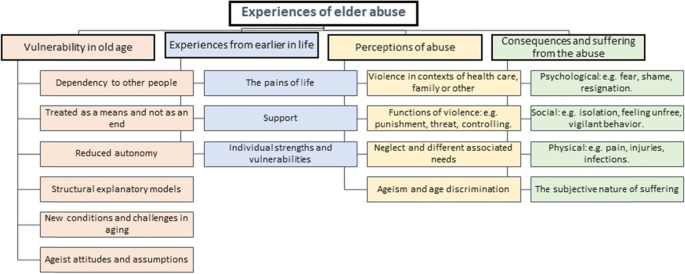
Coding tree as an overview of the themes, subcategories, and subthemes of the qualitative content analysis
Vulnerability in old age
The participants described their life situations as contexts for the adverse events they had been subjected to, and these descriptions expressed a general pattern of vulnerability. This vulnerability largely consisted of different kinds of dependence on other people: social, physical, and medical dependence. Social dependence sometimes reflected efforts to avoid loneliness, conflicts, sorrow, or other adversities for the family members.
Physical dependence could be the need to get a ride to visit friends, or a need for assistance with putting on socks due to reduced mobility, while medical dependence could be a need for assistance with injection treatment. The participants’ vulnerability was due to the natural consequences of normal aging, including a lack of energy or reduced mobility, or the consequences of illness, with reduced capacity for activities and participation. It was also a result of social relationships that had evolved over the course of a long lifetime. When participants asked for help or received help from those around them, they consequently had reduced defense against or increased vulnerability to abuse.
“Well, I’m not a happy person any longer, I’m hardly allowed to laugh, because he doesn’t like that really. […] And I also don’t get outdoors like I did before. Then I could take the bus downtown and go shopping and do whatever I wanted. Now he’s behind my wheelchair, checking me all the time, and that’s not fun.” (Woman, ID 9, 71 years).
The participants often expressed a desire to overcome their dependence, either by managing on their own or by finding alternative helpers. Thus, the dependency was often related to a specific perpetrator, but also in general related to any potential helper. However, a lack of energy or failing capacities during old age often resulted in dependence remaining. As a part of their vulnerability, the participants also expressed that it was hard to defend themselves when exposed to abusive situations:
“… if you have employees who behave a little badly to you, that’s different [that’s one thing]… But if you encounter resistance in healthcare, that’s another story.” (Man, ID 19, 85 years).
How the participants related to their vulnerability or their dependence varied, although a common approach was the desire not to bother their helpers (relatives or personnel).
“[There were] times when they [the care personnel] didn’t come. They have… they had a shortage of staff, and when some of them got sick they skipped [visiting some patients], and I was probably the one they cared about the least, as I was the most alert of us.” (Man, ID 1, 85 years).
Reduced autonomy was also described as an aspect or a consequence of dependence on help, whereby the older adults were not allowed to decide, or could not decide, about their life situation. Their autonomy was sometimes reduced by the limited willingness or ability of those around them to meet their needs. On other occasions, their autonomy was reduced by their physical or social impairments. For example, they were sometimes not allowed to decide where to live, or which activities to engage in.
“And they’re talking about putting me there again [in the nursing home], and I don’t want that, but what the hell can I do [about it]?” (Man, ID 1, 85 years).
The participants also expressed their perceptions of limited autonomy when they were treated like objects rather than individuals, or when the personnel did not show any interest or engagement in their personal needs, desires, or personality. For instance, all residents at the nursing home were invited – or sometimes rather forced – to participate in certain specific activities, due to the mistaken ageist notion that all older adults enjoy the same sort of activities. Thus, the older adults perceived reduced autonomy when grudgingly participating in bingo competitions.
The participants also conveyed their theories about why their dependence became so problematic, and these theories were often about specific members of staff being perceived as unfriendly or incompetent. Other theories related to how structural deficiencies of society – or of healthcare, or of certain organizations – contributed to a general lack of humanity among the older adults’ potential helpers. An example of such a perceived structural deficiency is when financial savings made by an organization are allowed to trump care quality or staff competence in healthcare. Accordingly, a recurrently suggested intervention to prevent elder abuse would be to educate the care staff:
Interviewer: “How would it be possible to … [prevent age-discriminatory care by the assisted living]? Participant: “By educating the care staff, of course…. So to [that they would] understand that an older adult has a background whatever that may be./…/. Perhaps education [for them], to understand the individual, so to say”. (Woman, ID 3, 84 years).
Experiences from earlier in life
In addition to the above descriptions of vulnerability during old age, the participants also spoke about their earlier lives, including time of adversity and joy. Several older participants described that, during old age and beforehand, they could receive strength or support from a friend or a partner, from family members, or by participating in an organization. These surrounding supporting elements helped to create security and meaningfulness, despite the adversities of life.
“She [my wife] was valuable to me… in all kinds of ways. And I have always encountered love through church, and these things have been very valuable to me.” (Man, ID 19, 85 years).
Some participants highlighted their activities or professional experiences that had provided support in life, while others highlighted important insights or mental attitudes that had helped to form their identities, their inner strengths, or their sense of meaning in life.
“When I grew up […] I had to do as I was told. And with this attitude I have managed.” (Man, ID 6, 76 years)
Alongside the participants’ stories about positive experiences and support throughout life, they also conveyed rich stories about difficulties and adversities in life. These stories were often about being a victim of violence during childhood, for example being subjected to school bullying or experiencing different types of violence in the family.
“I was five years old when I saw my father threaten her [my mother] with a loaded rifle, then she was wedged into a corner and he stood in the middle of the floor. […] Then my childhood ended, that day.” (Woman, ID 8, 73 years).
The participants told their stories about being subjected to violence in the past with such passion and emphasis that it became clear during the interviews how violence – even many years ago – could have just as strong an impact on health as recent events of victimization.
Perceptions of abuse
In the interviews, the participants described all five types of abuse. Patterns of neglect and psychological violence were most prominent in their stories, while economic, physical, and sexual violence were generally less prominent.
Neglect occurred in relation to different helpers that the participants were dependent on, and the neglect was related to a variety of needs. Hygiene needs were neglected when the participants had limited access to help with showering, cleaning or washing services, or clothing. Insufficient assistance with buying food or medication was described in association with staff shortages at the care organizations, which could prevent the older adults from initiating treatment prescribed by a doctor.
Neglected medical needs could involve sloppy or incompetent wound dressing, or when staff often forgot to administer medications. Several stories related to how care staff dismissed the older adults’ medical needs or symptoms, on the incorrect ageist assumption that the symptoms were signs of normal aging. The following quotation was interpreted as an example of age discrimination, and at the same time neglect of medical needs when a woman was refused a regular treatment regime. It was unclear whether the neglect was intentional or not.
“I was in France last year. I went down a mountain, skiing, it was slippery. [I] was going down and then got stuck in a fence, and so I twisted my knee. […] [I waited two days to seek healthcare until I came home from the journey.] And then they tell me ‘Well, because of your age you’ll have to wait for six months [to receive care]’, oh my god, and ‘You’ll have to do physiotherapy and attend to the osteoarthritis school’.” (Woman, ID 18, 69 years).
Examples of social needs being neglected varied in nature. This could involve older adults being frequently forgotten, after staff had said “I’ll be right back” in response to a request for help. Alternatively, social needs could be neglected when older residents at a nursing home were forced to attend social activities that were not in line with the individual’s specific preferences or abilities. A lack of staff continuity could mean that the participants were deprived of steady relationships with other people. In such ways, the participants expressed a lack of a meaningful existence, secondary to the social neglect.
“And the nursing home was so… well, it was so boring, damn it! It was as if a lot of… I don’t know what to call it… zombies [demented people] went around. They didn’t talk. That [living situation] wasn’t stimulating, either for me or for them.” (Man, ID 1, 85 years).
Psychological abuse was often connected to neglect and occurred in healthcare as well as in nursing homes and in family environments. The psychological abuse was often perceived as a means by which to control or manipulate the participant’s actions. This control could be about small matters, like the choice of which food to eat, but it could also be about more important matters like whether or not to request home service. Sometimes the abuser used aggressive speech if the participant did not live up to the abuser’s expectations or demands.
“I’ve talked to him about it [getting home service], but he doesn’t want that, because he thinks it’s too expensive. But I just feel I don’t have energy to do anything. And he says [to me]: ‘You’re so damned lazy.’” (Woman, ID 9, 71 years).
Control was sometimes exerted verbally, but often involved more subtle non-verbal expressions, such as constant surveillance in daily activities, or expressing a non-verbal tone of disapproval if the participant met friends. In one case, a woman had even been prevented from seeing her mother on her death bed:
“So when my mother was dying, they called me [from her town] and told me to come as there was not much time left. […] I’ll come right away I said, I’ll get on the first flight. And then my husband told me I couldn’t go as it was the weekend, and that I should wait until Monday. […] I wanted to say goodbye [to her] anyway, I wanted to be with her. But I never got there in time, they called me on Monday morning and said she was gone. […] And I hate this.” (Woman, ID 7, 66 years).
The controlling behavior often turned into direct threats against the participant from a child or a partner. These threats could be related to physical violence or not being allowed to see their grandchildren anymore. Psychological abuse also occurred in care environments, although the expressions were generally less explicit. In healthcare, just as in family environments, the abuse was perceived as an attempt to control the older participant’s behavior. Often the intent of the staff seemed to be well-meaning, but the expression was perceived aggressive or otherwise negative by the participant. One example was the following situation, where the participant had just completed a cardiac exercise test at the hospital:
“… I had cycled very fast, I was in severe pain and I was lying on the bed. […] and then she [the member of staff] would, at the physician’s request, spray nitro medication under my tongue, which she did and said to me: ‘Shut your mouth and swallow’, but I couldn’t because I was just in cramp… so she says again ‘Shut your mouth and swallow!’ but I still couldn’t do it, and then she turns away and says ‘Well then, forget that shit!’.” (Woman, ID 8, 73 years).
The descriptions of economic abuse that emerged during the interviews were many and rich in character. Sometimes the perception of economic abuse was not primarily associated with the lost financial value, but rather with the feeling of deception after a theft within a relationship of trust, or the feeling of sorrow when the lost item had great sentimental value.
“I felt terrible [when the jewelry was stolen by service staff], and after that I have never again… asked [them] for help. […] Yes, I think a lot about the jewelry being gone… it was a necklace that I had inherited from my mother, and a bracelet…” (Woman, ID 23, 73 years).
Stories about physical abuse during aging were few, but there were more examples of this from earlier in life. Examples of physical violence in old age including a robbery necessitating hospital care, being pushed by an official during a home visit, physical violence from a fellow passenger during transportation services, and one participant being hit by hospital staff.
“I’ve been hit on the head with a pillow. Just because I was cranky, she [the nurse] said. And I didn’t like that… And I said: ‘Now you get out of here, because you shouldn’t be working with people.’ […] [I] think it is frightening when you have to go to a care facility to receive care, and then you get hit! I don’t think it is acceptable.” (Man, ID 6, 76 years).
There were several stories about sexual abuse from earlier in life, but only few from old age. In one case the participant had been recurrently raped within the marriage, but the raping had ended some years before the age of 65. In another case, sexual abuse in contact with healthcare staff had obviously occurred during old age.
“Once, there was a physician that made some – it sounds weird now that I’m 84, I think I was ten years younger then – he really made sexual invitations [to me]. Yes, I think it sounds weird, but I felt very awkward.” (Woman, ID 3, 84 years).
The participants’ stories of sexual abuse expressed clearly feelings of shame and disgust.
Consequences and suffering from the abuse
The abuse that the participants had been exposed to led to various consequences. Psychological consequences included uncomfortable or painful feelings or thoughts that tormented the participant long after the abuse. For example, this could include nervousness, depression, disappointment, or guilt on the part of the abuser or the victim. The intensity of these uncomfortable feelings and thoughts varied over time, with a common gradual decrease as time, ordinary life, or support measures had helped to sooth the remaining discomfort. However, even a long time after the abuse had ended, the painful feelings and thoughts could be brought back by events or conversations, so that the intensity became strong again. Even if the interviews themselves evoked such painful feelings, the participants generally perceived the interviews as positive.
“… Because I sense this, how can somebody just do that? It’s [the painful experience]… Yes, it’s inside me. I try to get rid of it when it comes, but it isn’t so easy, sometimes it just comes and yes, it’s just there.” (Woman, ID 10, 67 years).
The participants described feelings of inferiority or uselessness, even though they tried to convince themselves that such feelings or thoughts were not truthful. Feelings of nervousness and fear increased again when experiencing new threats of abuse, for example when facing a new need for hospital care after previous negative experiences of abuse in healthcare.
“I hate being admitted [to hospital] like this, you don’t know which department you will be admitted to or which staff you will meet. […] You’re always prepared for the worst. You never know who you will meet when you’re admitted… Of course, I’m always on my guard… against a punch or such things.” (Man, ID 6, 76 years).
The fear of being robbed again made the participants vigilant and distrustful toward staff, strangers, and authorities. Lasting harm from abuse could include aches due to internal tension. Although the participant conveyed that the physical symptoms were caused by the abuse or medical errors, such causal relationships or physical consequences sometimes seemed uncertain for the researchers.
Social effects of the abuse could include loneliness, avoiding going outdoors due to fear of violence, or social isolation caused by reduced self-confidence or an abuser limiting their personal freedom. Social effects could also include a reluctance to accept care service due to fear, even though the older adult needed such services. Regardless of whether the abuse was ongoing or in the past, the suffering could be so intense that the person had lost the will to live or even planned to take their own life.
“I wouldn’t be alive if I didn’t have them [the children]. Then [without the children] I’d have been gone [dead] a long time ago. Then, I wouldn’t be alive. I don’t like life that much.” (Woman, ID 7, 66 years).
The participants commonly expressed feelings of abandonment and lack of control, in association with the abuse and their situation. By contrast, a few participants instead conveyed how they continued to defend their autonomy and strove to keep control of the situation through different strategies, despite their limited physical condition due to old age.
Discussion and implications
This aim of this study was to explore experiences of elder abuse among the victims themselves, as their own descriptions can help us to better understand how to develop prevention and interventions against elder abuse. The qualitative analysis resulted in four different themes (vulnerability in old age; experiences from earlier in life; perceptions of abuse; and consequences and suffering from the abuse), which describe different aspects of abuse from the participants’ subjective perspectives. In all, many of the participants’ perceptions of abuse were similar to previous descriptions by third party of elder abuse [ 11 , 21 , 22 ]. Some aspects of the descriptions of elder abuse in this study were also similar to previous descriptions of abuse among younger adults, but other aspects were substantially different [ 30 , 31 , 32 ], as discussed below.
Vulnerability in old age and experiences from earlier in life
Vulnerability to abuse during old age was described as different sorts of dependence on other people, and a lack of autonomy. Due to the effects of normal aging or accumulated diseases, the participants had limited mobility and an increasing need for care in everyday life, which meant dependence on care and vulnerability to abuse from others.
When the participants were exposed to abuse, their ability to defend themselves was also low for the same reasons. In general, this contributed to a submissive attitude toward the helper, together with inner reactions of anger, sorrow, and resignation. These descriptions of vulnerability have similarities with descriptions of vulnerability and powerlessness among younger adult victims of abuse in healthcare and other settings [ 32 , 33 ]. At the same time, the context of the aging body is characteristically different for the older adult, with decreasing capabilities and increasing dependence on care. The participants’ vulnerabilities were very varying and unique to each individual in terms of aging, morbidity, and life experiences.
The descriptions of vulnerability in old age were similar to those recounted by Y Mysyuk, RG Westendorp and J Lindenberg [ 23 ]. Dependence was described as a reciprocal process between the abuser and the victim in Mysyuk et al., something that was not spontaneously conveyed from the participants of this study. Nor did we identify the pattern described in Mysyuk et al., whereby increased weakness or dependence would provoke more violence.
The participants’ stories about previous stages of their life contributed to comprehensive individual pictures of how specific abuse in old age had had impact on their health. It was particularly evident that abuse in the past could have a great impact on health in old age, for example when psychological abuse in childhood had additive or synergistic effects on the perception of elder abuse. This is in line with previous literature on poly-victimization, and underlines that understanding elder abuse presupposes considering previous victimization as well as personality and the victims’ experiences of support, attachment styles, and challenges in life [ 5 , 8 , 34 ]. According to the socio-ecological model of abuse (Fig. 1 ), vulnerability can occur on all levels of an individual’s life, although previous experiences of life mainly correspond to the individual and interpersonal levels for the older adult [ 5 , 9 ]. Previous life experiences are important not only for understanding the individual’s unique vulnerability to abuse, but also for considering the victim’s individual strengths and resources when designing interventions and the prevention of elder abuse [ 35 ]. Hence, our results agree well with previous findings that a life-course perspective is essential when trying to understand the causes and consequences of elder abuse [ 6 , 7 , 8 ]. However, our findings also underline that abuse occurs in a context, and factors on all levels of the socioecological model influence the experience of abuse, e.g., ageist attitudes and dysfunctional care organizations described further on. By paying attention to and validating the older adult’s own life story, staff can indirectly contribute to interventions at community level in accordance with the socio-ecological model, as this level includes how the victim is treated by organizations [ 19 ].
Different kinds of elder abuse, ageism, and perceived causes of elder abuse
Neglect was a common kind of abuse in this study, and there were rich descriptions of this from healthcare settings and long-term care institutions. Not only were physical and medical needs neglected – so, too, were social needs, with consequent intense feelings of abandonment and lack of control among the participants. These descriptions were partly similar to those found in previous studies [ 36 ], although the examples of neglect in this study were often modest in character, meaning potentially mild physical adverse effects in the short term. Nevertheless, also modest shortcomings with hygiene or cleaning could have serious or even life-threatening consequences, as they meant an increased risk of serious wound infections. Ageist attitudes were obvious in different types of abuse, and especially in the descriptions of neglect, in which for example all older adults were treated like objects in a routine way without respect for their individual characters, needs, or preferences.
The psychological abuse occurred in both family and care environments and seemed to correspond to the abusers’ attempts to control the participants’ behaviors. In care environments, the abuse could be a way for staff to control behaviors in line with specific care routines or comfortable forms of work for the staff. The descriptions of psychological abuse in this study were similar to previous descriptions of psychological abuse in younger victims in healthcare and in younger persons in other environments [ 30 , 33 , 37 ].
The participants often added their own personal explanations for the abuse. In addition to descriptions of vulnerability and self-blame, common explanations included individual staff members being unfriendly, care organizations being structurally dysfunctional (with a lack of competence and resources), general greed at all levels of society, and discriminatory (ageist) attitudes and actions leading to neglect. Similar explanations have been described in previous studies, with ageism probably corresponding to all levels of the socio-ecological model [ 11 , 23 , 38 , 39 ]. Some people would perhaps think that structural deficiencies are not relevant to abuse, but the very definition of elder abuse by WHO clarifies that also “lack of appropriate action” in a dysfunctional environment can constitute elder abuse [ 4 ].
A general issue from the analysis of the interviews was whether the WHO definition of elder abuse is too narrow since it limits elder abuse to relations of trust. In several examples there was no identified relation of trust in a reported situation, but rather a “situation of trust” in which the abusive action would best be described as an example of elder abuse. For example, when an older adult is exposed to abuse during transportation services, there would be a situation of trust regardless of whether there are any relations of trust. The older adult would typically be vulnerable in this situation due to the physical limitations of ageing. With a narrow interpretation of the WHO definition, this abuse would dysfunctionally not be classified as elder abuse, although the theoretical framework of elder abuse would fit for an adequate understanding and prevention of the same abuse [ 40 ].
Consequences of the abuse
The participants described consequences of abuse in a way that resembled how consequences of trauma have been previously described among both older and younger adults [ 3 , 30 , 41 ]. Whereas patterns of psychological consequences (with negative thoughts and feelings of shame and fear) were rather like descriptions from previous studies among younger adults, the behavioral consequences were different and related to various social and physical preconditions among the older adults compared to younger adults. Social isolation and loneliness were natural consequences of limited mobility in normal aging or disease, and when abuse also contributed to these limitations the sense of isolation grew particularly strong. When participants chose not to receive home-care services because of the fear of recurrent abuse – despite their needs for assistance – the limiting consequences of abuse were particularly evident. There were also examples from the interviews of how neglect could have serious potential physical consequences, as many of the older adults were less physically able to withstand medical mistreatment.
Implications for the prevention of and intervention into elder abuse
Our findings have several implications for the prevention of and intervention into elder abuse. In terms of the socio-ecological model, preventive measures at community (including hospital level) and societal levels could be to ensure a minimum standard (for example by using legislation or economic incentives) for the care of older adults. According to the participants' voices, higher minimum standards of staff competence and resources would be likely to reduce the tendencies toward neglect, psychological abuse, or other kinds of abuse. Vulnerability and abuse could according to the participants also be prevented through education to care staff about different aspects of elder abuse and about aging. Such educational measures were suggested to promote person-centredness and prevent ageist attitudes, as these attitudes seem to contribute to both the vulnerability and elder abuse [ 39 ]. In addition, support units are also needed to offer individual assistance to victims of elder abuse as the negative consequences are substantial. According to a bifocal ecological approach, the assistance should not only be directed to the victim for an effective prevention but also to the perpetrator [ 42 ]. However, an important principle should be to adapt the preventive measures to the individual, as both vulnerability and abuse perceptions vary significantly according to the individual’s unique biopsychosocial conditions and experiences from earlier life. This also underlines the need for a life-course perspective on elder abuse [ 34 , 43 ].
Limitations
In order to minimize bias introduced by the researchers’ preconceptions and instead promote reflexivity, four researchers with different backgrounds have cooperated in the study. Three of the authors work as physicians within geriatrics and psychiatry, while the fourth author works with research, mostly outside hospital environments.
The fact that the sample was selected from inpatient care could be regarded as a disadvantage, as some older adults might have had too little energy to participate actively in interviews while suffering from an acute illness with associated physical exhaustion. On the other hand, the decision to recruit participants from inpatient care meant certain advantages, for example offering the participants a secure context for the interviews while their home or other environments might have been less secure, or more easily controlled by an abuser.
The results are likely to be transferable to older adults in Sweden but should be transferred with caution to countries with other cultures or societal structures.
This is one of few studies to date in which qualitative interviews have been used to explore experiences of elder abuse among the victims themselves. Their stories had similarities with both previous third-party descriptions of elder abuse and previous descriptions of abuse among younger adults. There were also substantial differences, with the consequence that elder abuse needs to be understood and managed by partly different means compared to abuse among younger adults. Vulnerability to elder abuse is often associated with an individual mix of the aging body, illnesses, and a dependence on secondary help. A life-course perspective considering experiences from the individual’s past would be beneficial when designing support for older victims, as such experiences are important to the degree of suffering and disability that the victim develops in relation to elder abuse. Prevention ought to include individually tailored help or support to reduce vulnerability, specific education, and ensuring an acceptable minimum standard of care for older adults in general [ 14 ].
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available and are not available from the corresponding author on request due to reasons concerning participant privacy and confidentiality.
Dong XQ. Elder Abuse: Systematic Review and Implications for Practice. J Am Geriatr Soc. 2015;63(6):1214–38.
Article Google Scholar
Yon Y, Ramiro-Gonzalez M, Mikton CR, Huber M, Sethi D. The prevalence of elder abuse in institutional settings: a systematic review and meta-analysis. Eur J Public Health. 2019;29(1):58–67.
Lachs MS, Pillemer KA. Elder Abuse. N Engl J Med. 2015;373(20):1947–56.
Article CAS Google Scholar
World Health Organisation. Elder Abuse: Fact sheet. Retrieved February 6th, 2021 from https://www.who.int/news-room/fact-sheets/detail/elder-abuse (2020).
Teaster PB. A framework for polyvictimization in later life. J Elder Abuse Negl. 2017;29(5):289–98.
Simmons J, Swahnberg K. Lifetime prevalence of polyvictimization among older adults in Sweden, associations with ill-heath, and the mediating effect of sense of coherence. BMC Geriatr. 2021;21(1):129.
Easton SD, Kong J. Childhood Adversities, Midlife Health, and Elder Abuse Victimization: A Longitudinal Analysis Based on Cumulative Disadvantage Theory. J Gerontol B Psychol Sci Soc Sci. 2021;76(10):2086–97.
Kong J, Easton SD. Re-experiencing Violence Across the Life Course: Histories of Childhood Maltreatment and Elder Abuse Victimization. J Gerontol B Psychol Sci Soc Sci. 2019;74(5):853–7.
Bronfenbrenner U. The ecology of human development : experiments by nature and design. Cambridge, Mass.: Harvard Univ. Press; 1979.
Hempton C, Dow B, Cortes-Simonet EN, Ellis K, Koch S, LoGiudice D, Mastwyk M, Livingston G, Cooper C, Ames D. Contrasting perceptions of health professionals and older people in Australia: what constitutes elder abuse? Int J Geriatr Psychiatry. 2011;26(5):466–72.
Killick C, Taylor BJ, Begley E, Carter Anand J, O’Brien M. Older people’s conceptualization of abuse: a systematic review. J Elder Abuse Negl. 2015;27(2):100–20.
Harbison J, Coughlan S, Beaulieu M, Karabanow J, Vanderplaat M, Wildeman S, Wexler E. Understanding “elder abuse and neglect”: a critique of assumptions underpinning responses to the mistreatment and neglect of older people. J Elder Abuse Negl. 2012;24(2):88–103.
Feltner C, Wallace I, Berkman N, Kistler CE, Middleton JC, Barclay C, Higginbotham L, Green JT, Jonas DE. Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018;320(16):1688–701.
Heise LL. Violence against women: an integrated, ecological framework. Violence Against Women. 1998;4(3):262–90.
Montminy L. Older women’s experiences of psychological violence in their marital relationships. J Gerontol Soc Work. 2005;46(2):3–22.
Eisikovits Z, Band-Winterstein T. Dimensions of Suffering among Old and Young Battered Women. Journal of Family Violence. 2015;30(1):49–62.
Hightower J, Smith MJ, Hightower HC. Hearing the voices of abused older women. J Gerontol Soc Work. 2006;46(3–4):205–27.
Pathak N, Dhairyawan R, Tariq S. The experience of intimate partner violence among older women: A narrative review. Maturitas. 2019;121:63–75.
Weeks LE, Leblanc K. An ecological synthesis of research on older women’s experiences of intimate partner violence. J Women Aging. 2011;23(4):283–304.
Bruggemann AJ, Wijma B, Swahnberg K. Abuse in health care: a concept analysis. Scand J Caring Sci. 2012;26(1):123–32.
Meyer SR, Lasater ME, Garcia-Moreno C. Violence against older women: A systematic review of qualitative literature. PLoS One. 2020;15(9):e0239560.
Erlingsson CL, Carlson SL, Saveman BI. Perceptions of elder abuse: voices of professionals and volunteers in Sweden--an exploratory study. Scand J Caring Sci. 2006;20(2):151–9.
Mysyuk Y, Westendorp RG, Lindenberg J. How older persons explain why they became victims of abuse. Age Ageing. 2016;45(5):696–702.
Yan E. Elder Abuse and Help-Seeking Behavior in Elderly Chinese. J Interpers Violence. 2015;30(15):2683–708.
Simmons J, Wiklund N, Ludvigsson M, Nagga K, Swahnberg K. Validation of REAGERA-S: a new self-administered instrument to identify elder abuse and lifetime experiences of abuse in hospitalized older adults. J Elder Abuse Negl. 2020;32(2):173–95.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Educ Today. 2017;56:29–34.
Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, Calif.: Sage Publications; 2002.
Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358(9280):483–8.
Sleutel MR. Women’s experiences of abuse: a review of qualitative research. Issues Ment Health Nurs. 1998;19(6):525–39.
Lim BH, Valdez CE, Lilly MM. Making Meaning Out of Interpersonal Victimization: The Narratives of IPV Survivors. Violence Against Women. 2015;21(9):1065–86.
Thomas KA, Joshi M, Wittenberg E, McCloskey LA. Intersections of harm and health: a qualitative study of intimate partner violence in women’s lives. Violence Against Women. 2008;14(11):1252–73.
Swahnberg K, Wijma B, Hearn J, Thapar-Bjorkert S, Bertero C. Mentally Pinioned: men’s perceptions of being abused in health care. Int JMen’s Health. 2009;8:60.
Storey J, Perka M. Reaching Out for Help: Recommendations for Practice Based on an In-Depth Analysis of an Elder Abuse Intervention Programme. Br J Soc Work. 2019;49(5):1370–1370.
Ramsey-Klawsnik H, Miller E. Polyvictimization in later life: Trauma-informed best practices. J Elder Abuse Negl. 2017;29(5):339–50.
del Carmen T, LoFaso VM. Elder neglect. Clin Geriatr Med. 2014;30(4):769–77.
Swahnberg K, Thapar-Bjorkert S, Bertero C. Nullified: women’s perceptions of being abused in health care. J Psychosom Obstet Gynaecol. 2007;28(3):161–7.
Walsh CA, Olson JL, Ploeg J, Lohfeld L, MacMillan HL. Elder abuse and oppression: voices of marginalized elders. J Elder Abuse Negl. 2011;23(1):17–42.
Pillemer K, Burnes D, MacNeil A. Investigating the connection between ageism and elder mistreatment. Nature Aging. 2021;1(2):159–64.
Goergen T, Beaulieu M. Critical concepts in elder abuse research. Int Psychogeriatr. 2013;25(8):1217–28.
Pless Kaiser A, Cook JM, Glick DM, Moye J. Posttraumatic Stress Disorder in Older Adults: A Conceptual Review. Clin Gerontol. 2019;42(4):359–76.
Joosten M, Vrantsidis F, Dow B. Understanding Elder Abuse: A scoping study. Melbourne: University of Melbourne and National Ageing Research Institute; 2017.
Google Scholar
Mosqueda L, Burnight K, Gironda MW, Moore AA, Robinson J, Olsen B. The Abuse Intervention Model: A Pragmatic Approach to Intervention for Elder Mistreatment. J Am Geriatr Soc. 2016;64(9):1879–83.
Download references
Acknowledgements
Not applicable.
Open access funding provided by Linköping University. This work was supported by the Swedish Crime Victim Fund, grants no. 3322/2017, 2944/2018, and 03384/2019. The funding source had no involvement in the study design, data collection, analysis, interpretation of the data nor in writing the manuscript.
Author information
Authors and affiliations.
Department of Acute Internal Medicine and Geriatrics and Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden
Mikael Ludvigsson, Nicolina Wiklund & Johanna Simmons
Department of Psychiatry and Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Mikael Ludvigsson
Department of Health and Caring Sciences, Faculty of Health and Life Sciences, Linnaeus University, Kalmar, Sweden
Katarina Swahnberg
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the design of the study. JS, NW and ML performed the interviews and performed proofreading of transcripts. Six interviews were coded separately and were then discussed together by all the authors. For the remaining interviews, the coding and development of tentative subcategories and themes were carried out by ML and JS. Tentative themes/subthemes were then discussed and revised by all the authors together. ML wrote the first draft of the manuscript, and all authors contributed to and approved the final manuscript.
Corresponding author
Correspondence to Mikael Ludvigsson .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Regional Ethics Review Board in Linköping, Sweden (2017/181–31; 2017/564–32) and was conducted in accordance with the principles of the Declaration of Helsinki. All participants gave written informed consent at the time of participation.
Consent for publication
Not applicable .
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1..
Supplement 1. INTERVIEW GUIDE (for two parallel studies).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ludvigsson, M., Wiklund, N., Swahnberg, K. et al. Experiences of elder abuse: a qualitative study among victims in Sweden. BMC Geriatr 22 , 256 (2022). https://doi.org/10.1186/s12877-022-02933-8
Download citation
Received : 12 October 2021
Accepted : 10 March 2022
Published : 28 March 2022
DOI : https://doi.org/10.1186/s12877-022-02933-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mistreatment
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 12 March 2020
Elder abuse and neglect: an overlooked patient safety issue. A focus group study of nursing home leaders’ perceptions of elder abuse and neglect
- Janne Myhre ORCID: orcid.org/0000-0001-8983-7998 1 ,
- Susan Saga 1 ,
- Wenche Malmedal 1 ,
- Joan Ostaszkiewicz 2 &
- Sigrid Nakrem 1
BMC Health Services Research volume 20 , Article number: 199 ( 2020 ) Cite this article
47k Accesses
33 Citations
5 Altmetric
Metrics details
The definition and understanding of elder abuse and neglect in nursing homes can vary in different jurisdictions as well as among health care staff, researchers, family members and residents themselves. Different understandings of what constitutes abuse and its severity make it difficult to compare findings in the literature on elder abuse in nursing homes and complicate identification, reporting, and managing the problem. Knowledge about nursing home leaders’ perceptions of elder abuse and neglect is of particular interest since their understanding of the phenomenon will affect what they signal to staff as important to report and how they investigate adverse events to ensure residents’ safety. The aim of the study was to explore nursing home leaders’ perceptions of elder abuse and neglect.
A qualitative exploratory study with six focus group interviews with 28 nursing home leaders in the role of care managers was conducted. Nursing home leaders’ perceptions of different types of abuse within different situations were explored. The constant comparative method was used to analyse the data.
The results of this study indicate that elder abuse and neglect are an overlooked patient safety issue. Three analytical categories emerged from the analyses: 1) Abuse from co-residents: ‘A normal part of nursing home life’; resident-to-resident aggression appeared to be so commonplace that care leaders perceived it as normal and had no strategy for handling it; 2) Abuse from relatives: ‘A private affair’; relatives with abusive behaviour visiting nursing homes residents was described as difficult and something that should be kept between the resident and the relatives; 3) Abuse from direct-care staff: ‘An unthinkable event’; staff-to-resident abuse was considered to be difficult to talk about and viewed as not being in accordance with the leaders’ trust in their employees.
Conclusions
Findings in the present study show that care managers lack awareness of elder abuse and neglect, and that elder abuse is an overlooked patient safety issue. The consequence is that nursing home residents are at risk of being harmed and distressed. Care managers lack knowledge and strategies to identify and adequately manage abuse and neglect in nursing homes.
Peer Review reports
Little is known about elder abuse in nursing homes, and compared to research on other forms of interpersonal abuse, research about elder abuse in nursing homes is still in its infancy [ 1 , 2 ]. Although no national prevalence data are available in any country internationally, high rates of elder abuse and neglect have been reported in nursing homes, including Norway [ 1 , 3 ]. According to the World Health Organisation (WHO), elder abuse has been identified in almost every country where these institutions exist [ 4 ]. In the Toronto Declaration, WHO defines elder abuse as ‘a single, or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which cause harm or distress to an older person’ [ 5 ] p:3. Prevention of harm is a core principle in health care services and a leadership responsibility [ 6 , 7 , 8 ]. Nursing home leaders are legally and morally responsible for ensuring that required quality and safety standards are met [ 6 , 9 , 10 ]. The National Patient Safety Foundation (United States) defines patient safety as ‘freedom from accidental or preventable injuries or harm produced by medical care’ [ 10 ], p,2. This includes preventing elder abuse and examining the factors that foster an unsafe environment for both residents and staff [ 6 , 7 , 11 ]. Furthermore, elder abuse can be categorized according to type of abuse. The definition from ‘Protecting Our Future: Report from the Working Group on Elder Abuse’ (Ireland) includes physical, psychological, financial and sexual abuse, and neglect (Table 2 ) [ 12 ]. Abuse in nursing homes may also be categorized according to type of relation [ 1 ]; staff-to-resident abuse [ 3 , 13 ], family-to-resident abuse [ 14 , 15 ] and resident-to-resident abuse, also called resident-to-resident aggression [ 16 , 17 ].
A recent meta-analysis of the prevalence of elder abuse in long-term care settings estimated a pooled prevalence of 64.2% of abuse perpetrated by staff in the past year, where psychological abuse and neglect had the highest prevalence [ 1 ]. A survey of 16 nursing homes in the central part of Norway found that 91% of staff had observed a colleague engaging in some form of inadequate care,
and 87% of staff reported that they themselves had perpetrated some form of inadequate care in the past [ 3 ]. Comparably, in a study from Ireland, Drennan et al. found that 57.5% of staff had observed one or more abusive behaviours from a colleague in the previous year [ 13 ]. Neglect and psychological abuse were the most commonly observed or perpetrated acts [ 3 , 13 ]. Living in a nursing home may also mean sharing room and space with co-residents, and in recent literature, resident-to-resident aggression has been identified as a common form of abuse in nursing homes [ 16 , 17 , 18 ]. Lachs and colleagues revealed that 407 of 2011 residents from ten facilities had experienced at least one resident-to-resident event over one month observation, showing a prevalence of 20.2%, and the most common form was verbal abuse [ 16 ]. The literature about elder abuse in domestic settings shows that close family and friends can be perpetrators of abuse [ 15 ], but few studies have investigated the role of family members as perpetrators of abuse in nursing homes. A study from the Czech Republic found that nursing home staff had observed relatives participating in financial exploitation combined with psychological pressure on residents in nursing homes [ 14 ]. However, comparing findings in the literature on elder abuse in nursing homes is challenging because definitions and understandings of abuse can vary in different cultures, jurisdictions, and among health care staff, researchers, family members, and residents themselves [ 1 , 2 , 11 , 19 , 20 , 21 ]. Different understandings of what constitutes abuse and its severity complicate detecting, reporting and managing the problem.
Nursing homes are complex social systems that consist of different participants, including staff, leaders, residents and relatives in constantly shifting interactions [ 22 , 23 ]. The aetiology of abuse in nursing home settings is described as complex, comprising varying associations between personal, social and organisational factors [ 2 , 24 ]. Nursing home residents often have complex care needs, dementia or other forms of cognitive impairment [ 25 ], display challenging behaviour [ 26 ], and depend on assistance in daily activities and care, all factors associated with a high risk of abuse and neglect [ 3 , 13 , 24 , 27 ]. In Norway, 80% of nursing home residents have dementia, and 75% have significant neuropsychiatric symptoms such as agitation, aggression, anxiety, depression, apathy and psychosis [ 25 ]. Residents who display aggressive behaviour toward staff are at greater risk of experiencing abuse [ 13 , 27 , 28 ]. Findings in Drennan et al.’s Irish study revealed that 85% of the nursing home staff had experienced a physical assault from a resident in the previous year [ 13 ]. Aggressive behaviour has also been found to trigger resident-to-resident aggression in nursing homes [ 16 , 17 ]. Related to organisational factors, there is an association between inappropriate environmental conditions for residents, low levels of staffing, and abuse and neglect [ 13 , 14 , 29 ]. As a result of this complexity, elder abuse in nursing homes is difficult to define precisely [ 11 ]. Within the literature, elder abuse in nursing homes is conceptualised as a specific form of institutional abuse [ 30 ] and a setting in which abuse and neglect take place [ 14 ], since rules and regulations in institutions can be abusive themselves, e.g., deciding residents’ sleeping and meal times, the use of restraint, and shared living spaces with other residents.
Good leadership plays a key role in developing staff’s understanding of residents’ needs [ 31 , 32 ] and creating a strong safety culture of respect, dignity, and quality [ 6 , 7 , 9 , 33 ]. The importance of leadership in developing a patient safety culture is highlighted in a report from the National Patient Safety Foundation [ 10 ]. In Norway, governmental strategies to improve leadership and safety culture have been launched, such as the Patient Safety Programme and a system for monitoring health services using quality indicators [ 34 ]. Leadership is defined as a process whereby a person influences a group of individuals to reach a common goal [ 35 ], such as a strong safety culture. The safety culture of an organisation is defined as ‘the product of individual and group values, attitudes, perceptions, competencies, and patterns of behaviour that determine the commitment to, and the style and proficiency of, an organisation’s health and safety management’ [ 10 , 36 ] p:23. This includes detecting situations that can be harmful to residents. However, several studies have shown that underreporting of abuse and neglect is a significant problem [ 1 , 37 , 38 ]. Residents’ own inability to communicate about the abuse or their fear of repercussions and retaliation are important factors of underreporting [ 1 , 2 ]. Therefore, staff should be able to recognise and report situations that can be perceived as harmful or distressful from the perspective of residents. However, a systematic review of staff’s conceptualisation of elder abuse in residential care found that staff were often uncertain about how to identify abuse, especially psychological abuse and caregiver abuse and neglect [ 39 ]. Despite the vast knowledge that exists about the importance of leadership, nursing home research has not yet paid much attention to the role leaders play regarding identifying elder abuse. Consequently, there is a gap in knowledge about elder abuse from the perspective of nursing home leaders. Knowledge about nursing home leaders’ perceptions of elder abuse and neglect are essential because their understanding of the phenomenon will affect what they signal to staff as important to report and what they investigate to create a safe and healthy environment. To our knowledge, this is the first study that seeks to understand the nature of elder abuse from the perspective of nursing home leaders.
Aim of the study
The aim of the study was to explore nursing home leaders’ perceptions of elder abuse and neglect.
The present study is part of a larger study funded by the Research Council of Norway (NFR), project number 262697. A qualitative exploratory design with focus group interviews was conducted to gain greater insight into this important but poorly understood topic. Qualitative methods provide knowledge about people’s experience of their situation and how they interpret, understand and link meaning to events [ 40 , 41 ]. In focus group interviews, group dynamics allow the questions to be discussed from several points of view, and the group’s dynamics can create new perspectives and opinions during the discussion [ 42 ]. This study follows The Consolidated Criteria For Reporting Qualitative Research (COREQ) (Additional file 1 ).
In Norway, approximately 39,600 residents live in nursing homes (12.9% of the population > 80 years), and their mean age is 85 years [ 43 ]. These nursing homes are mainly run by the municipalities and financed by taxes and service user fees. Residents pay an annual fee equal to 75% of the resident’s national age pension. In addition, residents may pay an additional fee if they have income of their assets, but with an upper limit decided by the government. However, the payment cannot exceed the actual expenses of the institutional stay [ 44 ].. Management of care in Norwegian nursing homes is regulated by ‘the regulation of management and quality improvement in health care services’ [ 45 ]. The regulation focusses on the leader’s responsibility to ensure that residents’ basic needs are satisfied. This includes the leader’s responsibility to ensure there is a system in place to monitor residents’ overall quality and safety and to create a safety culture that detects situations and factors that can cause harm to residents and staff [ 45 ].
Each nursing home is required to have an administrative manager, called the nursing home director, and some nursing home directors lead more than one facility. In addition, each nursing home has ward leaders and quality leaders, and in some municipalities, a service leader. Together, individuals in these leader roles form the leadership team in each nursing home [ 46 ]. The ward leader is a registered nurse (RN) who supervises and manages staff. Ward leaders are also responsible for budgets in their own wards and the quality of care for residents. There are often several wards and ward leaders in each nursing home. The quality leader is an RN who monitors the overall quality of care in the nursing home in collaboration with the ward leaders. The service leader supervises and manage service staff members who are in contact with nursing home residents (e.g., activity coordinators, cleaning staff and kitchen staff) and is also responsible for the budget related to his or her staff. Individuals employed in one of these leader positions provide the closest level of leadership to staff and residents but are not part of the daily direct hands-on care of residents. There is no national requirement regarding formal leader education to be employed in these leader positions, but leader education is a high priority in many municipalities. These individuals often have lengthy experience as RNs or have previous leader experience.
The study sample was recruited from 12 nursing homes in six municipalities in Norway. Inclusion criteria were a person who: (a) was employed in a leader position as ward leader, quality leader, or service leader in a nursing home, and (b) was employed full time in the leader position. The inclusion criteria were chosen because these individuals directly affect quality and safety in the nursing home, as they are the closest level of leadership to the staff and residents. Purposive sampling was initially used to ensure that participants recruited could see the phenomenon from the perspective of a leader. During the data collection, each municipality and its nursing home leaders were recruited using a step-wise approach, as we were seeking to get a theoretical sampling until saturation of data was achieved [ 40 , 41 ]. A total of 28 individuals participated in the study, 23 participants were ward leaders, two participants were quality leaders, and three participants were service leaders. However, in this study, all 28 participants are named ‘care managers’. Characteristics of the participants are presented in Table 1 .
Recruitment and data collection
Participants were recruited over a period of six months, from August 2018 through the end of January 2019. A recruitment email was sent to health care managers in 11 municipalities in both urban and rural areas. Health care managers from five municipalities stated that they could not find time to participate in the study, while six health care managers accepted the invitation. Thereafter, a second recruitment email was sent to all nursing home directors in these six municipalities. The email included an invitation letter, which the nursing home director forwarded to all individuals employed in a leader position at their nursing homes. Six focus group interviews were conducted, with three to six participants in each group. The focus groups were composed as follows: one focus group with three participants; two focus groups with four participants; one focus group with five participants; two focus groups with six participants.
All six focus group interviews took place in a meeting room in a nursing home in the participating municipalities. Each focus group interview lasted approximately 90 min. All participants gave informed written consent before the interviews started. Two researchers carried out the interviews. JM was the moderator in all six interviews, SN was co-moderator for two group interviews, and SS was co-moderator in one group interview. In the other three interviews, two researchers from the larger research team were co-moderators. During the introductory information about the focus group interview, we presented a figure (Fig. 1 ), and asked participants about their experience and thoughts on the topic of elder abuse from health care staff, co-residents or relatives. Participants were encouraged to speak freely. However, during the first interview, we experienced that participants were not familiar with the topic. To explore the topic in the ensuing interviews, the moderator gave the participants keywords from the categorization of abuse (e.g., abuse can be described as physical, psychological, sexual, financial, or neglect) (Table 2 ) [ 12 ]. We found that this helped the participants reflect, and they subsequently came up with examples of abusive situations they had heard about or witnessed. During the process of data collection, we further compared our experiences in interview one with interview two, which is in line with the constant comparative method [ 40 ]. This led to including keywords in the interview guide to ensure that all topics were covered (Additional fil 2). To ensure the credibility of an open thematic understanding of participants’ experiences and diminish bias by presenting the keywords, we were conscious about letting the participants speak freely about their experiences and thoughts on this topic. Moreover, they were not given any definition of abuse or examples related to these keywords (Table 2 ) [ 12 ]. The participants freely decided in which order they wanted to talk about different forms and situations of elder abuse. All interviews were recorded and transcribed verbatim, retaining pauses and emotional expressions.
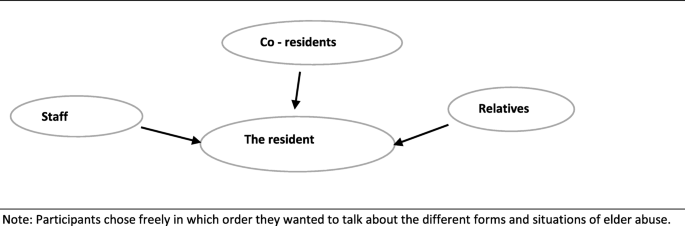
Model of interactions where abuse can occur as used in the interviews
Data analysis
A constant comparative method with a grounded theory approach was used. This allowed us to generate a thematic understanding of elder abuse through an open exploration of the experience described by nursing home leaders [ 40 , 41 ]. The constant comparative method facilitated possible identification of themes and differences between individuals and cases within the data [ 40 ]. Our analysis started right after each interview, where the first author listened to the recorded interview. Memo writing was then used through the whole process of data collection and analysis and served as a record of emerging ideas, questions and categories [ 41 ]. Next, in line with the constant comparative method, open line-by-line coding of the transcribed interviews was performed [ 40 , 41 ], since we wanted to capture the meaning from the participants’ perspectives as they emerged from the interviews. The codes were compared for frequencies and commonalities and then clustered to organise data and develop sub-categories. The sub-categories were examined to construct the final categories and main theme. To add credibility and diminish researcher bias, two researchers (JM and SN) coded the transcribed interviews independently. During the analysis process, the authors held several meetings where codes and their connections were discussed until consensus was reached. To ensure that the emerging categories and themes fit the situations explored, the researchers went back and forth between contextualization, data analysis and memo writing [ 40 ]. An example of the analysis process is shown in Table 3 .
Ethical consideration
Ethical approval for this study was given by the Norwegian Centre for Research Data (NSD), Registration No: 60322. Each participant signed a written consent form after receiving oral and written information about the study. All identifiable characteristics are excluded from the presentation of data to ensure the anonymity of all individuals.
The main theme, ‘Elder abuse in nursing homes, an overlooked patient safety issue’, found in this study indicates an overall lack of awareness of elder abuse and its harm among care managers. Three analytical categories emerged from the analyses: 1) Abuse from co-residents – ‘A normal part of nursing-home life’ , 2) Abuse from relatives – ‘A private affair’ , and 3) Abuse from direct-care staff – ‘An unthinkable event’. Since there were no remarkable differences in care managers’ experiences, we present results without differentiating the participants. Below, we describe each category, together with examples of forms of abuse and neglect. These examples are used to describe the care managers’ perceptions of elder abuse and neglect (Table 4 ).
Abuse from co-residents – ‘A normal part of nursing-home life’
Resident-to-resident aggression was described as the biggest issue related to abuse in nursing homes and a daily challenge for the participants: ‘ That is what I also see, that co-residents are the biggest challenge regarding this topic’ (Group 2). The main cause of resident-to-resident aggression reported by care managers was symptoms of dementia, especially in the initiator, but also in the victim. The care managers expressed that they did not know how to address this problem. As one said, ‘ It happens because of the cognitive failure, so yes. But, at the same time, it is also difficult to do something about it’ (Group 2). Some care managers also stated that the risk of harm caused by resident-to-resident aggression was something residents must accept when living in a nursing home: ‘ There is a predictable risk, when living in nursing homes, [of] such incidents; there is a foreseeable risk that this will happen’ (Group 5) . This demonstrates that resident-to-resident abuse is normalized.
Care managers considered physical abuse to be the most serious form of resident-to-resident aggression, often leading to visible harm and despair. At the same time, all care managers had examples of residents who had been beaten, knocked down, or kicked by co-residents.
‘We have one resident now that is beaten a lot by the other residents. It’s a little extreme, but I think that such things can happen quite often in dementia care because, as in this case, the resident being beaten is not silent for a minute. She speaks and yells all day, and the other residents become annoyed since she disturbs them’ (Group 4).
Care managers described psychological abuse as acts of ‘everyday bullying’ and threats made among residents. They interpreted these situations as a normal consequence of the dementia disease in the individual resident. One care manager noted, ‘ What I think is the challenge is the everyday bullying. It is seen as normal behaviour for that group of residents’ (Group 1). When discussing psychological abuse connected to co-residents, all care managers provided examples of residents trespassing in other residents’ rooms. They interpreted this behaviour as a violation of residents’ privacy. At the same time, it was perceived as normal since it happened quite often. The care managers also reported that when residents trespassed and entered another resident’s room, the risk of other forms of abuse such as financial abuse increased. One care manager remarked , ‘We have some challenges related to residents who enter other residents’ rooms and destroy or take other residents’ possessions. It can be pictures and different things’ (Group 3).
Related to sexual abuse by co-residents, all care managers had examples of residents who had shown sexual interest in another resident. The care managers viewed this sexual interest as an ethical dilemma for them. On the one hand, they want residents to have a healthy sex life in the nursing home, but on the other hand, this is difficult when a resident has dementia and may not be competent to give consent. Several care managers experienced that what seemed to be voluntary sexual interest between residents could not be that, after all:
‘In that situation, she was very interested in him, and he was very interested in her. And it was like, yes, they were in the room together and so on. I remember it as very, very difficult because she often had a lot of pain. I do not know if there was penetration, but it was, in any case, an attempt, yes, it may as well have been that too. I had a lot of trouble because I was unsure whether she understood what happened and who it was happening with because it was often very difficult for her after they had been in the room together. I remember it as a huge ethical dilemma. But I never thought that it was a sexual . . . that it was an assault or something. But, right now, I think it was’ (Group 5).
During the focus group discussion, care managers reflected on the complexity of letting residents express themselves sexually and the risk of sexual assault. From their statements, it was clear that they had not reflected on this topic earlier. A summary of forms of harmful situations related to resident-to-resident aggression reported by participants is presented in Table 4 .
Abuse from relatives – ‘A private affair’
Abuse directed towards residents from their relatives was reported to be a particularly difficult problem. According to the care managers, relative-to-resident abuse was often hidden, occurring behind private closed doors when a relative was visiting the resident. Therefore, participants described it as difficult to discover and associated mainly with the private relationship between the resident and his or her relatives:
‘ It is very difficult. It is a relative who is going to visit her mother in the nursing home, she closes the door to the room and wants to be there alone with her mom, and we have very large rooms, so we thought they were having a nice time inside the rom. But then we discovered that the mom had some bruises, and then we understood that things were happening’ (Group 3).
Not all care managers had knowledge of or experience with relative-to-resident abuse, which highlights the private nature of these forms of abuse. Abuse from relatives was viewed as being linked to past family conflict, which continued inside the nursing home. The care managers deliberated over the extent to which they should interfere in the private relationship when they suspected this form of abuse. They reported that the problem was knowing what to do and when and how to interfere, especially when the resident has dementia or another form of cognitive impairment. One care manager remarked, ‘ It is very difficult. I have a patient who may not be competent to give consent. So, I have a responsibility I must take, but I think it’s challenging to know what to do’ (Group 2). Cases where the resident clearly did not want anyone in the nursing home to know about the abuse or to do anything about it and just wanted to maintain the relationship with his or her family member despite the abuse were reported to be particularly difficult. The care managers expressed that they lacked a strategy or authority in these situations, and harm to the resident being exposed was accepted.
‘ But it is not always that the resident wants us to do something, either. It may have been this way for a long time, and then, maybe it’s okay then. Well, I don’t know’ (Group 5).
Physical and sexual abuse from relatives was regarded as the most hidden form of abuse from relatives. Some care managers provided examples of physical abuse, but none had experienced sexual abuse. However, all care managers commented that when it happened, it took place behind private closed doors. In addition to past family conflict, abuse from relatives was often related to mental problems and/or drug abuse issues. One care manager said, ‘ I have experienced some older people who have children with drug issues and such things. And it is in those cases, I have experienced physical abuse towards residents from relatives’ (Group 4). Related to physical abuse from relatives, care managers also reported situations where a relative forced the resident to, for example, eat, get dressed, wash and groom, or exercise. These situations were linked to unrealistic expectations in relatives, and not trusting the staff is doing a good job.
‘After her husband had been there, we saw that she was so red around the cheek. We then found out that the husband squeezed her mouth open and poured cream into her’ (Group 3).
Care managers viewed psychological abuse from relatives as disrespectful communication with the resident. A participant stated, ‘We experience that relatives can be quite disrespectful to their loved ones. But, at the same time, it may have been this way their whole life’ (Group 6).
Care managers expressed that financial abuse from relatives was a common occurrence. They cited examples of stealing money from residents, threatening residents in order to get money from them, and unauthorized use of a resident’s finances. One participant stated, ‘ What I see most from the relative’s part is financial abuse. It is very common, actually’ (Group 1). Relatives’ economic problems were reported to be a causal factor related to financial abuse. At the same time, care managers indicated that financial problems and financial exploitation by relatives were private issues, and as such, they were reluctant to interfere.
Related to neglect, care managers described that some relatives made decisions on behalf of the resident without considering what the resident wanted and needed or would agree upon. Care managers stated that sometimes the health care staff also disagreed with the relative’s decision. One care manager noted, ‘ We have situations where relatives make decisions on behalf of the resident, which we do not agree upon, and which we might think the resident would not agree upon either’ (Group 3 ). Care managers also described experiences of relatives who refused to allow a resident to buy items the care managers considered necessary and not provided by a nursing home. These could be things such as clothes, hairdressing services, or podiatry, but it could also be related to taking part in activities that cost money. A care manager remarked:
‘ I have a resident who called her son to ask if she could go to a podiatrist because she really needed it, but her son refused and said she has no money for that’ (Group 5).
Thus, because of neglect by their relatives, residents might go without necessities of daily living and may not be able to participate in activities they would like to take part in. A summary of forms of harmful situations related to relative-to-resident abuse reported by participants is presented in Table 4 .
Abuse from direct-care staff – ‘An unthinkable event’
When care managers were prompted to talk about staff-to-resident abuse, they reframed the discussion to focus on the verbal and physical aggression they commonly experienced from nursing home residents. They interpreted aggression directed toward them as a risk to their health and safety. Moreover, they stated this phenomenon was a daily concern. One noted, ‘ We have the opposite focus in our units. We focus on staff being subjected to abuse by residents’ (Group 2). Several care managers also indicated that they understood that staff could become stressed and frustrated in their relationship with an aggressive resident:
‘We have a case that is extremely difficult, where there are many violations against staff by a resident. And then, to be in such a situation where you can quickly retaliate . . . this is difficult’ (Group 6).
Despite this, care managers expressed that elder abuse was not a topic they talked about in their daily work at the nursing home. They indicated that they wanted to trust the employees. Therefore, abuse from staff was difficult to talk about and almost unthinkable to them. One care manager said, ‘I think that no one who works in the nursing home started there just to be able to hurt someone, and that is perhaps why this is such a sensitive and difficult topic’ (Group 5) . The word ‘abuse’ was also reported to be a very strong term and mainly related to intentional physical acts. However, in the discussion, care managers also included unintentional acts in their examples of elder abuse and expressed that, to some degree, it could be difficult to know the full intention of a staff member’s actions. At the same time, they emphasised that staff’s intentions were mainly good, and therefore abuse was unthinkable:
‘Everyone who works in a nursing home is motivated by and has a desire to help someone. So, most of the [incidents] of abuse by staff . . . I think it may be those with a good intention at the heart of it. [For instance, thinking] “I thought he should have a shower, but I forgot to ask” (Group 5).
Care managers discussed examples of the use of physical and chemical forms of restraint and rough handling during care. Utilization of restraints and dilemmas related to their use was discussed in all focus groups, and care managers pointed out that the staff are sometimes compelled to use both physical and chemical restraints to help or protect the resident:
‘I think in relation to, well it is really both physical and psychological abuse. I think of cases, especially at night, where there is low staffing and many residents with aggressive behaviour, where it may be chosen to lock some residents into their rooms to prevent them from being exposed to abuse from co-residents so the staff can deal with the situation, but it is abuse to be locked inside’ (Group 2).
Rough handling was something that all care managers had experienced. This was thought to be mainly unintentional and something that could happen when caring for residents with aggression or those who resist care. Care managers expressed that, to define it as abuse, it had to be significant, or there needed to be visible signs of such handling, such as bruising. At the same time, the care managers also pointed out that residents in nursing homes often bruise easily, and it can be difficult to determine whether such marks are related to abuse:
‘Sometimes, we saw that she was so easy to bruise, and sometimes we clearly noticed hand marks on the bruises around her body. But it can be enough that you handle someone a little hard, and in the old ones, then they get bruises, although it can also indicate that there has been resistance, right. But then this happens all the time’ (Group 4).
Psychological abuse from staff members was linked to verbal abuse. Care managers cited examples of yelling at a resident in anger, speaking to a resident in a disrespectful tone, or being rude, which allegedly occurred in relation to resident-to-staff aggression. When discussing psychological abuse, some care managers also provided examples of violations of residents’ privacy by staff members, such as discussing residents’ health care issues and challenges in public areas in the nursing home:
‘If there has been a resident with a rejection of care responses, for example, that has been difficult to cooperate with, then that frustration can be expressed in public areas with other residents present. Without caution by staff, this is something other residents are going to hear’ (Group 5).
Financial abuse was thought to be related to stealing money or destroying a resident’s property. At the same time, care managers reported that their nursing home policies do not allow residents to keep much money in their rooms in order to protect residents from financial abuse by staff, visitors, or others, and hence, financial abuse from staff rarely happened. One said, ‘Financial abuse only happens if the residents have money laying around’ (Group 1).
When talking about sexual abuse, care managers offered examples of residents who stated that they were sexually assaulted by staff members. These were often female residents who expressed that male staff had sexual intentions towards them during care. At the same time, care managers reported that such statements from residents could be part of the dementia disease, and that resident could have hallucinated the abuse. Care managers indicated that sexual abuse by staff was unthinkable to them:
‘Sometimes, older people with cognitive impairment say things that we can become uncertain about. They say things, but we can’t be sure there has been an assault. Often, we think that it has not happened. It’s about us knowing them; they say a lot of these things and are very sexually oriented’ (Group 4).
Even so, a few care managers mentioned examples of sexual abuse by staff a long time ago that had been reported to the police, and the staff member was convicted.
Related to neglect, care managers reported that staff often did things for residents to save time instead of letting them do it independently. They also reported being aware that, in many situations, staff members do not pay attention to residents’ wishes and thereby neglect to include them in decisions concerning daily life in the nursing home. One care manager noted, ‘ It says on the duty list that you should shower today, so you should shower, even if you might say, “No, I don’t want to.” So, yes, it is your turn today’ (Group 3). Another form of neglect by staff was reported to be linked to health care neglect. Care managers referred to events such as not helping a resident with needed health care, giving a resident an incontinence product instead of helping them use the toilet, not calling for medical help when needed, and not following up on medical conditions:
‘To put on a pad instead of following the patient to the toilet, for those who still manage to use the toilet themselves . . . that can happen’ (Group 6).
The care managers reported that, because of low financial resources, staff must prioritize their work and tasks every day. For this reason, situations not specifically related to medical treatment and physical or health outcomes were given lower priority. This reprioritization was framed as acceptable and was not defined as neglect. One said, ‘ It is about our time. So, no, we don’t have time for you or that need is not important. It is about what we have to prioritize’ (Group 6). A summary of forms of harmful situations related to staff-to-resident abuse reported by participants is presented in Table 4 .
The aim of the study was to explore nursing home leaders’ perceptions of elder abuse and neglect. We found that most of the care managers were not explicitly aware of elder abuse in their daily work. However, when given keywords, they all came up with examples of situations they interpret as harmful or distressful to residents. This shows that care managers need time to reflect on complex aspects of care to become aware of abuse and neglect as a safety issue. At the same time, our findings revealed an ambiguity in the care managers’ examples. The situations, on the one hand, were described as harmful. On the other hand, they were rationalized as care managers attempted to excuse why it was happening. Three main categories are described in the finding: Abuse from co-residents – ‘A normal part of nursing-home life’, Abuse from relatives – ‘A private affair’, Abuse from direct care staff – ‘An unthinkable event’. These findings indicate that this cohort of nursing home care managers lack awareness of the abuse they observe or hear about. Particularly, these findings demonstrate that harm or distress to residents caused by abuse are an overlooked patient safety issue in these nursing homes.
Findings revealed that resident-to-resident aggression is a common form of abuse in nursing homes and a daily challenge. There is a high prevalence of residents with neuropsychiatric symptoms of dementia, including aggression, agitation and psychosis in nursing homes [ 25 , 26 ]. These symptoms impact on co-residents and staff safety, and resident-to-resident aggression is the most common form of abuse in nursing homes [ 16 , 17 ]. However, our findings revealed that harm resulting from resident-to-resident aggression was perceived as normal. This raises the question of whether care managers perceptions place the responsibility on the resident, without accounting for the complexity in the aggressive behaviour and the responsibility of the organization [ 22 ]. It is worth noting that in resident-to-resident aggression, both residents can suffer harm, since the initiator is likely to be confused and usually not responsible for the acts. For the victim, resident-to-resident aggression has both physical and psychological consequences [ 47 ]. However, previous research has also indicated that abusive behaviour can be understood as less abusive when the victim has dementia, and for that reason it is often not reported [ 17 , 48 ]. Recognising that aggressive behaviour has a multifactorial aetiology, best practice recommendations [ 49 ] and research evidence [ 50 , 51 ] call for a comprehensive biopsychosocial approach that investigates the resident’s unmet needs, medical conditions, environmental factors, and interactions between residents and caregivers and a tailored response [ 49 ]. Care managers’ perceptions of resident-to-resident aggression as normal and a foreseeable risk, places residents at risk and is also a failure to deliver much needed care to the initiator.
With respect to relative-to-resident abuse, findings demonstrate that care managers perceive negative events resulting in harm or distress as a private affair between the resident and his or her relatives, and that is difficult to intervene. Similarly, to resident-to-resident abuse, this indicates that the care managers place the responsibility of the observed abuse on the relationship between the resident and his or her relatives, without accounting for the complexity and their own responsibility in these situations. Care managers examples of relatives who force a resident to eat due to unrealistic expectations and distrust in nursing home staff’s care reveals that care managers find it difficult to interact with families. This finding points to potential communication difficulties between staff and resident’s relatives that could adversely affect the resident [ 52 , 53 ]. A Norwegian study that investigated quality of care from the perspective of families in long-term care found that family members saw themselves as an important link between staff and the resident, and an essential voice regarding the resident’s needs and wishes [ 53 ]. However, given the nature of the nursing home and the complexity of its organization and routines [ 22 , 23 ], it can be difficult for someone outside the organization to judge what is and is not adequate clinical practice. Collaboration and communication with the residents and their relatives depend on how the culture in the nursing home view these interactions; the relatives with right to an opinion, or professional as experts and in control [ 6 , 22 , 52 ]. This will in turn affect the quality and safety of the care that is delivered to the residents.
Although some care managers had experience of staff-to-resident abuse within all abuse categories, it was also difficult for them to admit to this form of abuse, and it was viewed as an ‘unthinkable event.’ Instead, care managers were mostly interested in talking about resident-to-staff aggression which they emphasised was a larger problem in their nursing homes. Resident- to-staff aggression can cause physical and psychological harm to staff, reduced job satisfaction, stress and burnout, emotional reactions including sadness, guilt and helplessness [ 28 ]. However, resident-to-staff aggression may also lead to reactive abuse and neglect, due to frustration in staff member being exposed to aggression [ 11 , 13 , 27 , 28 ]. Findings in the present study demonstrate that care managers lack awareness of the staff’s reactive responses to aggression from residents. This might raise the question if they perceive staff as victims in these situations and that abuse from staff is understandable. Unprovoked or intentional abuse towards a resident therefore is unthinkable with justification in their trust to the staff.
Difficulties in defining abuse in nursing home settings have been found in studies that include staff’s perceptions [ 39 , 54 ], where abusive situations are seen as normal in the nursing home culture [ 17 , 33 , 39 , 55 ]. However, these studies did not specifically focus on care managers’ or leaders’ understandings. Our study reveals important information related to detection and management of abuse in nursing homes, since care managers’ perception of abuse affects what they signal to staff as important to report. Care managers have the opportunity to influence the culture and care practice in the nursing home and are responsible for setting policies for the staff, it is therefore essential that they are aware of and able to face situations that constitute potential harm to the residents. But, to be able to define situations that can be experienced as harm and distress, it is essential to see situations from the perspective of the residents. Harm and distress are defined differently from the point of view of the one who causes the harm [ 39 , 54 ], the one observing or hearing about it [ 14 ], or the one who experiences a situation of harm or distress [ 20 , 21 ]. Our findings indicate that the care managers had difficulties in seeing potential harm caused by abuse and neglect from the perspective of the residents. Leaders’ abilities to promote a safety culture for both the resident and staff are linked to their leadership skills, knowledge of the resident’s needs and their capacity to implement effective safety care practices [ 6 , 31 , 32 ]. Care managers’ lack of awareness in identifying and following up on abuse will necessarily affect the safety culture in the organisation and, in the end, clinical outcomes such as quality and safe care for the residents [ 6 , 10 , 56 ].
A recent Norwegian study found that communication, openness and staffing were significant predictors of staff’s overall perception of patient safety in nursing homes, yet the nursing home staff scored low on these dimensions [ 56 ]. This finding aligns with our study, which revealed that care managers find it difficult to distinguish between prioritising and patient neglect. Low financial resources and low staffing can affect the perception of what constitutes harm and safety in the nursing home culture. Low finances, combined with the complexity of residents’ needs, the complex organisation, and demands for improved outcomes, puts great pressure on nursing home leaders [ 22 , 57 ]. The ambiguity in their examples can be understood as an attempt to rationalize abuse and diminish their personal and professional accountability. People in complex social systems will try to make sense of tasks and orders by adapting to internal and external demands [ 22 , 23 ]. Health care policies that mandate efficiency, cost saving, and nursing home care managers’ focus on prioritising contribute to lowering the limit for what is perceived as quality and safety, resulting in low quality and unsafe environment as the norm and accepted in nursing homes.
Strengths and limitations of the study
A strength of this study is that it involves participants who are in leader positions in different nursing homes and municipalities in Norway, which could increase the transferability of these findings. The research team consists of members from two countries, all with broad research experience, which contributed to multiple perspectives and discussions during analyses of the data. This strengthens the trustworthiness of our findings, and the credibility of the research. Three of the authors have worked several years in nursing homes as care managers, but none of those nursing homes participated in this study. The researchers’ backgrounds as care managers has both advantages and disadvantages. A variety of aspects of participants’ experiences was discovered by posing in-depth questions that might not have been possible without the background knowledge. However, the background knowledge can influence the type of follow-up questions that were asked. To counterbalance this possible bias, two researchers were always present during the interview, and the analyses were also independently coded by two researchers (JM and SN). Each focus group consisted of three to six participants, which can be perceived as small groups and a limitation. However, the participants gave a rich description of the phenomenon. Therefore, we decided to include data from the smallest groups.
The examples of abuse and neglect our participants described in the present study could be second-hand information because leaders are not always part of the direct hands-on care residents receive. At the same time, this study has sought to understand the nature of elder abuse from care managers’ perspective, which is of great importance due to their responsibility for creating a safe environment for both residents and staff. Even though the examples are second-hand information, the findings are representative of the care managers’ perceptions of the information and what we thought was important to study.
Many nursing home residents have dementia, neuropsychiatric symptoms, and complex needs, which increases the risk of their being exposed to abuse and neglect. At the same time, little is known about the nature of elder abuse in nursing homes and compared to research on other forms of interpersonal abuse, the study of elder abuse in nursing homes is still in its infancy. Care managers influence the culture and care practice in nursing homes and set policies for staff. Knowledge about their empirical understanding of the phenomenon is important to form more effective intervention and prevention strategies. The present study shows an ambiguity in the nursing home leaders’ examples of abuse and neglect. On the one hand, the situations were described as harmful. On the other hand, they were rationalized with an attempt to excuse their occurrence. Our study revealed that elder abuse and neglect is an overlooked patient safety issue in nursing homes. Care managers lack knowledge and strategies to identify and adequately manage abuse and neglect in nursing homes, and this warrants further research.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to format of the data not allowing for completely anonymizing data but are available from the corresponding author on reasonable request.
Abbreviations
Research Council of Norway
Registered Nurse
World Health Organization
Yon Y, Ramiro-Gonzalez M, Mikton CR, Huber M, Sethi D. The prevalence of elder abuse in institutional settings: a systematic review and meta-analysis. Eur J Pub Health. 2018.
McDonald L, Beaulieu M, Harbison J, Hirst S, Lowenstein A, Podnieks E, et al. Institutional abuse of older adults: what we know, what we need to know. J Elder Abusw Negl. 2012;24(2):138–60.
Article Google Scholar
Malmedal W, Ingebrigtsen O, Saveman BI. Inadequate care in Norwegian nursing homes--as reported by nursing staff. Scand J Caring Sci. 2009;23(2):231–42.
Krug E, Dahlburg L, Mercy J, Zwi A, Lozano RJWH. et al, Abuse of the elderly in World Report on violence and health. 2002.
WHO. The Toronto Declaration on the Global Prevention of Elder Abuse. Geneva: World Health Organization, Availablel at; http://apps.who.int/iris/bitstream/10665/42495/1/9241545615_eng.pdf.; 2002.
American College of Healthcare Executives, The National Patient Safety Foundation, Institute for Healthcare Improvement. Leading a culture of safety. A blueprint for success. 2017.
Sokol-Hessner L, Folcarelli PH, Annas CL, Brown SM, Fernandez L, Roche SD, et al. A road map for advancing the practice of respect in health care: the results of an interdisciplinary modified Delphi consensus study. Jt Comm J Qual Patient Saf. 2018;44:463–76.
PubMed Google Scholar
Pilbeam C, Doherty N, Davidson R, Denyer D. Safety leadership practices for organizational safety compliance: developing a research agenda from a review of the literature. Saf Sci. 2016;86:110–21.
Nakrem S, Vinsnes AG, Harkless GE, Paulsen B, Seim A. Nursing sensitive quality indicators for nursing home care: international review of literature, policy and practice. Int J Nurs Stud. 2009;46(6):848–57.
National Patient Safety Foundation. Free from Harm, Accelrating Patient Safety Improvment Fifteen Year after To Err is Human (NPSF). Boston: Available at; www.npsf.org : National Patient Safety Foundation (NPSF), ; 2015.
Phelan A. Protecting care home residents from mistreatment and abuse: on the need for policy. Risk Manag Healthc Policy. 2015;8:215–23.
Working Group on Elder Abuse. Protecting our future, Report: Dublin, . The Stationery Office. 2002.
Drennan J, Lafferty A, Treacy MP, Fealy G, Phelan A, Lyons I, et al Older people in residential care settings: results of a national survey of staff-resident interactions and conflicts. 2012.
Bužgová R, Ivanová K. Elder abuse and mistreatment in residential settings. Nurs Ethics. 2009;16(1):110–26.
Yon Y, Mikton CR, Gassoumis ZD, Wilber KH. Elder abuse prevalence in community settings: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(2):147–56.
Lachs MS, Teresi JA, Ramirez M, van Haitsma K, Silver S, Eimicke JP, et al. The prevalence of resident-to-resident elder mistreatment in nursing homes. Ann Intern Med. 2016;165(4):229–36.
Rosen T, Pillemer K, Lachs M. Resident-to-resident aggression in long-term care facilities: an understudied problem. NHI Aggression Violent Behav. 2008;13(2):77–87.
Pillemer K, Chen EK, Van Haitsma KS, Teresi J, Ramirez M, Silver S, et al. Resident-to-resident aggression in nursing homes: results from a qualitative event reconstruction study. Gerontologist. 2012;52(1):24–33.
Castle N, Ferguson-Rome JC, Teresi JA. Elder abuse in residential long-term care: an update to the 2003 National Research Council report. J Appl Gerontol. 2015;34(4):407–43.
Lafferty A, Treacy MP, Fealy G, Drennan J, Lyons I. Older people’s experiences of mistreatment and abuse. Dublin: NCPOP, University College, Dublin; 2012.
Google Scholar
World Health Organization (2002). Missing voices; views of Oler persons on elder abuse, Geneva; 2002.
Cilliers P (2002). Complexity and postmodernism: understanding complex systems. London Routledge.
Anderson RA, Issel LM, McDaniel RR Jr. Nursing homes as complex adaptive systems: relationship between management practice and resident outcomes. Nurs Res. 2003;52(1):12–21.
Ostaszkiewicz J. A conceptual model of the risk of elder abuse posed by incontinence and care dependence. Int J Older People Nursing. 2017:1–11.
Helvik A-S, Selbæk G, Benth JŠ, Røen I, Bergh S. The course of neuropsychiatric symptoms in nursing home residents from admission to 30-month follow-u. PLoS One. 2018;13(10):1–18.
Selbaek G, Kirkevold O, Engedal K. The course of psychiatric and behavioral symptoms and the use of psychotropic medication in patients with dementia in Norwegian nursing homes--a 12-month follow-up study. Am J Geriatr Psychiatry. 2008;16(7):528–36.
Malmedal W, Hammervold R, Saveman B-I. The dark side of Norwegian nursing homes: factors influencing inadequate care. J Adult Prot. 2014;16(3):133–51.
Lachs MS, Rosen T, Teresi JA, Eimicke JP, Ramirez M, Silver S, et al. Verbal and physical aggression directed at nursing home staff by residents. J Gen Intern Med. 2013;28(5):660–7.
Goergen T. A multi-method study on elder abuse and neglect in nursing homes. J Adult Prot. 2004;6(3):15–25.
Nerenberg L. Elder abuse prevention: emerging trends and promising strategies. New York: Springer Publishing Company; 2007.
Brady GP, Cummings GG. The influence of nursing leadership on nurse performance: a systematic literature review. J Nurs Manag. 2010;18(4):425–39.
Braithwaite J, Herkes J, Ludlow K, Testa L, GJBO L. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open. 2017;7(11):1–11.
Pickering CEZ, Nurenberg K, Schiamberg L. Recognizing and responding to the "toxic" work environment: worker safety, patient safety, and abuse/neglect in nursing homes. Qual Health Res. 2017;27(12):1870–81.
HOD. (Helse- og omsorgsdepartementet) [Ministry of Health and Care Service] (2013) Kvalitet og pasientsikkerhet 2013 [Quality and patient safety 2013] (St.meld. nr. 11 2014–2015). Oslo: Departementenes servicesenter.2013.
Northouse PG. (2018). Leadership: theory and practice. Los Angeles; Sage publications.
Health and Safety Commission. Third report: organizing for safety. London: HMSO; 1993.
World Health Organization. A global response to elder abuse and Negelct: building primary health care capacity to Deal with the problem worldwide. Geneva: Main Report; 2008.
Cooper C, Selwood A, Livingston G. Knowledge, detection, and reporting of abuse by health and social care professionals: a systematic review. Am J Geriatr Psychiatry. 2009;17(10):826–38.
Radermacher H, Toh YL, Western D, Coles J, Goeman D, Lowthian J. Staff conceptualisations of elder abuse in residential aged care: a rapid review. Aust J Ageing. 2018;37(4):254–67.
Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. J Qual Quantity. 2002;36(4):391–409.
Charmaz K (2006). Constructing grounded theory: a practical guide through qualitative analysis. London; sage publications.
Krueger RA, Casey MA. Focus groups: a practical guide for applied research. Los Angeles: Sage publications; 2014.
SSB. Statistisk Sentralbyrå. [Statistics Norway](2019). Nøkkeltall for helse i Norge [Key number related to health care in Norway]. Available from: https://www.ssb.no/helse/nokkeltall https://www.ssb.no/helse/nokkeltall: Statistisk Sentralbyrå SSB.
HOD. Helse-og omsorgsdepartementet [Ministry of health and care services]. (2014). Egenbetaling for kommunale tjenester i og utenfor instiusjon [User fees for primary care in and outside institution]. [updated 18.12.2014]: https://www.regjeringen.no/no/tema/helse-og-omsorg/helse%2D%2Dog-omsorgstjenester-i-kommunene/innsikt/egenbetaling-i-og-utenfor-institusjon/id434597/ .
HOD. Helse-og omsorgsdepartementet [Ministry of health and care services]. Forskrift om ledelse og kvalitetsforbedring i helse og omsorgstjenesten [Regulation of management and quality improvement in health care services] no. 1036; Amendment 01.01.2017. 2017 https://lovdata.no/dokument/LTI/forskrift/2016-10-28-1250 .
HOD. Helse- og omsorgsdepartementet [Ministry of health and care services]. Forskrift for sykehjem og boform for heldøgns omsorg og pleie [Regulation for nursing homes and residential care] (Updated 01. july 2013) no. 708; Amendment 01.01.1989. 1989. https://lovdata.no/dokument/SF/forskrift/1988-11-14-932 .
Trompetter H, Scholte R, Westerhof G. Resident-to-resident relational aggression and subjective well-being n assisted living facilities. Ageing Mental Health. 2011;15(1):59–67.
Matsuda O. An assessment of the attitudes of potential caregivers toward the abuse of elderly persons with and without dementia. Int Psychogeriatrics. 2007;19(5):892–901.
Kales HC, et al. Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. JAGS. 2014;62(4):762–9.
Lichtwarck B, Selbaek G, Kirkevold O, Rokstad AMM, Benth JS, Lindstrom JC, et al. Targeted interdisciplinary model for evaluation and treatment of neuropsychiatric symptoms: a cluster randomized controlled trial. Am J Geriatr Psychiatry. 2018;26(1):25–38.
Lichtwarck B, Myhre J, Goyal AR, Rokstad AMM, Selbaek G, Kirkevold Ø, et al. Experiences of nursing home staff using the targeted interdisciplinary model for evaluation and treatment of neuropsychiatric symptoms (TIME)–a qualitative study. Aging Ment Health. 2018:1–10.
Utley-Smith Q, Colón-Emeric CS, Lekan-Rutledge D, Ammarell N, Bailey D, Corazzini K, et al. The nature of staff-family interactions in nursing homes: staff perceptions. J Aging Stud. 2009;23(3):168.
Vinsnes AG, Nakrem S, Harkless GE, Seim A. Quality of care in Norwegian nursing homes–typology of family perceptions. J Clin Nurs. 2012;21(1–2):243–54.
Cooper C, Dow B, Hay S, Livingston D, Livingston G. Care workers' abusive behavior to residents in care homes: a qualitative study of types of abuse, barriers, and facilitators to good care and development of an instrument for reporting of abuse anonymously. Int Psychogeriatr. 2013;25(5):733–41.
Jones A, Kelly D. Whistle-blowing and workplace culture in older peoples' care: qualitative insights from the healthcare and social care workforce. Sociol Health Illn. 2014;36(7):986–1002.
Ree E, Wiig S. Employees’ perceptions of patient safety culture in Norwegian nursing homes and home care services. BMC Health Serv Res. 2019;19(1):1–7.
Siegel EO, Young HM, Zysberg L, Santillan V. Securing and managing nursing home resources: director of nursing tactics. Gerontologist. 2015;55(5):748–59.
Download references
Acknowledgements
We would like to express our gratitude to our participants for sharing their experience and thoughts on the topic of elder abuse and neglect in nursing homes. Thanks to Anja Botngård and Stine Borgen Lund for contributing to data collection as co-moderators.
Ethical approval for this study was given by the Norwegian Center for Research Data (NSD), Registration No: 60322. All the participants were provided with written information about the study. They gave written consent to participate in the interviews and for the use of the data from the interviews.
Authors details
JM: RN, MSc, PhD candidate, at Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU, Trondheim, Norway.
SS: RN, MSc, PhD, Associate professor at Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU, Trondheim, Norway.
WM: RN, MSc, PhD, Associate professor at Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU, Trondheim, Norway.
JO: RN, GCert Cont Prom, GCertHE, MNurs-Res, PhD, Research Fellow, Centre for Quality and Patient Safety Research, School of Nursing and Midwifery, Institute for Healthcare Transformation, Deakin University, Geelong, Australia.
SN: RN, MSc, PhD, Professor at Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU, Trondheim, Norway
The study is funded by the Research Council of Norway (NFR) project number: 262697.
Author information
Authors and affiliations.
Department of Public Health and Nursing, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU, Trondheim, Norway
Janne Myhre, Susan Saga, Wenche Malmedal & Sigrid Nakrem
Centre for Quality and Patient Safety Research- Barwon Health Partnership, Institute for Healthcare Transformation, Deakin University, Geelong, Australia
Joan Ostaszkiewicz
You can also search for this author in PubMed Google Scholar
Contributions
JM wrote the manuscript. JM, SS, WM, JO and SN developed the study design. JM transcribed the interviews, and JM and SN performed the analysis of the interviews, with discussion including all authors. SN supervised the project. All authors did critical revisions of the manuscript for important intellectual content and read and approved the final manuscript.
Corresponding author
Correspondence to Janne Myhre .
Ethics declarations
Consent for publication.
The participants consented to the publication of de-identified material from the interviews.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
COREQ checklist.
Additional file 2.
Interview guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Myhre, J., Saga, S., Malmedal, W. et al. Elder abuse and neglect: an overlooked patient safety issue. A focus group study of nursing home leaders’ perceptions of elder abuse and neglect. BMC Health Serv Res 20 , 199 (2020). https://doi.org/10.1186/s12913-020-5047-4
Download citation
Received : 30 September 2019
Accepted : 26 February 2020
Published : 12 March 2020
DOI : https://doi.org/10.1186/s12913-020-5047-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Elder abuse
- Patient safety
- Long-term care
- Nursing homes
- Care managers
- Qualitative
- Focus group
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- News & Views
- Published: 23 September 2022
ELDER ABUSE
Silent suffering: the plague of elder abuse
- Kathleen Wilber ORCID: orcid.org/0000-0001-6211-9726 1 &
- Kelly Marnfeldt 1
Nature Aging volume 2 , pages 771–772 ( 2022 ) Cite this article
201 Accesses
2 Altmetric
Metrics details
- Medical research
- Scientific community
Elder abuse has been recognized as a serious problem for decades. Yet rigorous studies are rare. Burnes and colleagues move the field forward by identifying how pervasive the problem is, the factors that increase and decease vulnerability, and how these factors change over a three-year period.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
111,21 € per year
only 9,27 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Acierno, R. et al. Am. J. Public Health 100 , 292–297 (2010).
Article Google Scholar
Yon, Y., Mikton, C. R., Gassoumis, Z. D. & Wilber, K. H. Lancet Glob. Health 5 , e147–e156 (2017).
Burnes, D., Pillemer, K., Rosen, T., Lachs, M. & Mcdonald, L. Nat. Aging https://doi.org/10.1038/s43587-022-00280-2 (2022).
Centers for Disease Control and Prevention. Elder abuse surveillance: uniform definitions and recommended core data elements. https://www.cdc.gov/violenceprevention/pdf/ea_book_revised_2016.pdf (2016).
McDonald, L. & Thomas, C. Int. Psychogeriatr. 25 , 1235–1243 (2013).
McDonald, L. J. Elder Abuse Negl. 30 , 176–208 (2018).
Beach, S. R., Schulz, R., Castle, N. G. & Rosen, J. Gerontologist 50 , 744–757 (2010).
Yon, Y., Mikton, C., Gassoumis, Z. D. & Wilber, K. H. Trauma Violence Abuse 20 , 245–259 (2019).
Pillemer, K. & Finkelhor, D. Gerontologist 28 , 51–57 (1988).
Article CAS Google Scholar
DeLiema, M., Gassoumis, Z. D., Homeier, D. C. & Wilber, K. H. J. Am. Geriatr. Soc. 60 , 1333–1339 (2012).
Pillemer, K., Burnes, D. & MacNeil, A. Nat. Aging 1 , 159–164 (2021).
Enguidanos, S., DeLiema, M., Aguilar, I., Lambrinos, J. & Wilber, K. Ageing Soc. 34 , 877–903 (2014).
Download references
Acknowledgements
The work of K.W. and K.M. was supported in part by award 2020-75-CX-0001, awarded by the National Institute of Justice, Office of Justice Programs, US Department of Justice. The opinions, findings, and conclusions or recommendations expressed in this publication are those of the authors and do not necessarily reflect those of the Department of Justice.
Author information
Authors and affiliations.
University of Southern California, Los Angeles, CA, USA
Kathleen Wilber & Kelly Marnfeldt
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Kathleen Wilber or Kelly Marnfeldt .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Wilber, K., Marnfeldt, K. Silent suffering: the plague of elder abuse. Nat Aging 2 , 771–772 (2022). https://doi.org/10.1038/s43587-022-00282-0
Download citation
Published : 23 September 2022
Issue Date : September 2022
DOI : https://doi.org/10.1038/s43587-022-00282-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
SYSTEMATIC REVIEW article
The effectiveness of psychosocial interventions for elder abuse in community settings: a systematic review and meta-analysis.

- 1 School of Economic & Management and Law, Hubei Normal University, Huangshi, China
- 2 School of Social Work, Michigan State University, East Lansing, MI, United States
- 3 School of Social Work, University of Michigan, Ann Arbor, MI, United States
- 4 Graduate School of Social Work, University of Denver, Denver, CO, United States
As a global public health concern, elder abuse negatively affects health, psychosocial wellbeing, and mortality among elders. Research and practice efforts made to explore effective prevention and intervention strategies are growing. Despite the growing number of intervention studies on elder abuse, research synthesis on the empirical literature seems lacking. This study aims to identify the pooled effect size of prevention and interventions targeted ultimate and intermediate outcomes for elder abuse that occurred in community settings. Following the Cochrane guideline, our team searched across eight electronic databases and manually searched reference lists of eligible studies and existing systematic reviews for all potentially eligible studies. A random-effects model of 51 effect size estimates reported an overall positive and statistically significant treatment effect of psychosocial interventions for elder abuse, d = 0.63, p < 0.05. The overall treatment effect was approaching statistical significance at 0.1 level for ultimate outcomes, d = 0.32, p = 0.09, and intermediate outcomes, d = 0.75, p = 0.1. An overall significant effect size was found among family-based interventions, d = 0.59, p < 0.05, and interventions targeting older adults and their caregivers, d = 0.45, p < 0.05. Existing evidence supports an overall significant effect for psychosocial interventions for elder abuse. Interventions that used a family-based model, combined education and supportive services, and targeted both caregivers and elders, showed significant effect size, suggesting such features being considered in elder abuse intervention design. Future intervention research is needed to shed light on the link between intervention activities and ultimate change in elder abuse behaviors.
Introduction
Elder abuse refers to intentional or unintentional harmful acts toward an older person where trust is expected. Common types of elder abuse include physical, psychological, sexual abuse, financial exploitation, and neglect ( World Health Organization, 2002 ; Acierno et al., 2010 ). As a global public health concern, about 1 in 6 community-dwelling older adults experienced some form of abuse in the last 12 months as found in a meta-analysis that explored prevalence rates of elder abuse ( Yon et al., 2017 ). The prevalence rate of abuse in elder care facilities is even higher as two-thirds of care staff members reported abusive behaviors ( Yon et al., 2019 ). The profound impact of elder abuse on victim’s health, finances, quality of life, and even mortality ( Acierno et al., 2010 ) deserves attention.
Current elder abuse interventions include public education and advocacy, caregiver support, psychological support for victims, care coordination, and multidisciplinary case management to name a few ( Acierno et al., 2010 ). Based on existing literature, programs that suggest the effectiveness of elder abuse are through providing (1) caregiver supportive services ( Livingston et al., 2013 ), (2) money management coaching ( Sacks et al., 2012 ), (3) telephone helplines ( van Bavel et al., 2010 ), (4) emergency shelters for older victims ( Heck and Gillespie, 2013 ), and (5) access to a multidisciplinary team ( Teaster et al., 2003 ). Educational or training interventions are more accessible than supportive services or case management interventions ( Sacks et al., 2012 ; Livingston et al., 2013 ). Elder abuse preventions and interventions tend to achieve two types of outcomes: reducing the occurrence of abusive behaviors ( Hsieh et al., 2009 ; Khanlary et al., 2016 ), and mitigating elder abuse risk factors, such as psychosocial stress and lack of awareness or competency among nursing staff, family caregivers, and older adults themselves ( Pellfolk et al., 2010 ; Baker et al., 2016 ; Estebsari et al., 2018 ).
Most meta-analysis studies regarding elder abuse focus on the prevalence and risk factors rather than on elder abuse intervention effects ( Yon et al., 2017 , 2019 ). Despite the growing number of intervention studies on elder abuse, research synthesis on the pooled effect for elder abuse interventions remains lacking. From the limited available systematic reviews of elder abuse intervention programs, either found a lack of sufficient evidence to establish the effectiveness of elder abuse ( Ploeg et al., 2009 ; Alt et al., 2011 ; Fearing et al., 2017 ) programs or programs that did not use rigorous evaluations to assess the effectiveness of said programs ( Rosen et al., 2019 ).
Furthermore, the only meta-analysis to our knowledge synthesized 24 studies of elder abuse interventions ( Ayalon et al., 2016 ). This study found an overall small but significant treatment effect for restraint use reduction, d = −0.24, 95% CI (−0.38, −0.09). While highly valuable, this meta-analysis primarily focused on the restraint use as an abuse outcome, which can be questionable as the use of physical restraints with a physician’s order can be medically necessary rather than abusive.
Despite the above evidence that supports the potential effect of intervention programs for elder abuse, the conclusion is far from definitive because of the limited number of studies and a narrowed scope of outcomes reviewed in these systematic reviews ( Ploeg et al., 2009 ; Alt et al., 2011 ; Fearing et al., 2017 ). Elder abuse preventions and interventions typically aim for changes in intermediate or ultimate outcomes. Ultimate outcomes refer to the reduction in the occurrence or reoccurrence of abusive behaviors, while intermediate outcomes include the mitigation of risk factors (e.g., psychosocial stress) and promotion of protective factors (e.g., improving knowledge of abuse and enhancing the competency of addressing abuse) that will lead to the reduction of elder abuse. Both intermediate and ultimate outcomes need to be considered for a competent narrative for the effectiveness of elder abuse interventions.
Therefore, our systematic review and meta-analysis study aims to examine prevention and intervention studies that targeted ultimate and intermediate outcomes for elder abuse that occurred in community settings. Acknowledging that these two outcome types of elder abuse, though interrelated, reflect distinctive features, we hence examined the pooled effect of all outcomes combined and the respective effect for different outcome types.
Materials and Methods
Search strategy.
The identification of relevant studies was performed in two steps. The first step consisted of searching eight academic databases from Jan 1990 to December 2020: Cumulative Index to Nursing and Allied Health (CINAHL), Cochrane Library/Central Register of Controlled Trials, Database of Abstracts of Reviews of Effects (DARE), PsycINFO, PubMed, MEDLINE, BIOSIS, and Science Direct. Key search terms included “older abuse,” “elder abuse,” “elder neglect,” “elder mistreatment/maltreatment,” or “older neglect” and “physical abuse,” or “emotional abuse” or “financial abuse” and “intervention” or “program.” To identify the right design of the intervention, search terms included “control group” or “RCT.” The set of keywords was used for both study title and study abstract search across databases. Second, the reference lists of studies and systematic reviews identified from the database search were reviewed for additional relevant studies.
Inclusion Criteria
The inclusion criteria for studies published in English are those that (1) assessed the effectiveness of a prevention or intervention program designed to address abuse or neglect of elders aged 65 or older living the community settings, (2) targeted at elders or family members, (3) used randomized controlled trials (RCTs) or controlled trials (without random assignment), (4) reported at least one elder abuse intervention outcome, and (5) reported statistical information sufficient to calculate effect size required for meta-analysis. We did not limit the location of the studies. Outcomes consisted of (1) ultimate outcomes: occurrence or reoccurrence of elder abuse behaviors; and (2) intermediate outcomes: reduction of risk factors for elder abuse, such as reduced stress, improved knowledge of abuse, and enhanced competency of addressing abuse.
Data Collection and Extraction
Three researchers conducted data collection and extraction. Two reviewers (YS and FS) screened titles and abstracts for eligible studies independently with decisions blind to one another. If any disagreement existed, two reviewers would discuss first and if unresolvable, a third reviewer (AZ) would intervene and make a final decision. The three-person team adopted the same process in later full article review and quality assessment. Inter-screener reliability was 92% and inter-rater reliability of full articles was 85%.
Measures of ultimate outcomes included occurrence or reoccurrence of elder abuse, here termed as behavioral outcomes, and intermediate outcomes (i.e., risk or protective factors for elder abuse) included psychosocial stress, knowledge of elder abuse, and competency of addressing elder abuse.
Basic information extracted from studies consisted of participant demographic characteristics (i.e., age, gender, and ethnicity), geographic areas of the study (i.e., United States, Asia, and Europe), and study design (i.e., RCT and non-randomized controlled trial). Intervention characteristics consisted of intervention type (i.e., family, individual, and mixed), target population (i.e., elders, family caregivers, or both), intervention approach (i.e., education, supportive services, and mixed), and intervention frequency and duration.
Risk of Biases Assessment
Quality of studies was assessed using the Jadad scale ( Halpern and Douglas, 2005 ), also known as the Oxford quality scoring system. Studies’ risk of bias was assessed using the Cochrane Collaboration’s tool for risk of bias in randomized trials ( Alderson et al., 2008 ). The research team resolved discrepancies and reached a consensus on these ratings. Publication bias was assessed using a funnel plot (visual analysis) and the Vevea and Wood sensitivity weighted function analysis (statistical analysis; Vevea and Woods, 2005 ). For funnel plot, we plotted independent effect sizes only first and then plotted all effect sizes with some of them are dependent of each other.
Meta-Analytic Procedures
We used the R software for data analysis. Treatment effect sizes were estimated for each individual study to determine treatment clinical effects. For continuous outcomes, the standardized mean difference (SMD) was calculated to obtain Hedges’ g statistic ( Cooper et al., 2009 ). For binary outcomes, an odds ratio (OR) was calculated first, followed by taking the log transformation of the odds ratio (i.e., log odds ratio). The log OR statistic was further transformed into the same effect size metric as the Hedges’ g statistic using procedures suggested by Cooper et al. (2009) . The Hedges’ g was further bias corrected using a J function ( Cooper et al., 2009 ) to obtain an unbiased estimation of the treatment effect, noted as d for the rest of the text. When meta-analyzing the effect size estimates, we used the inverse variance weight, which is considered as an optimal weight estimate in meta-analysis ( Marín-Martínez and Sánchez-Meca, 2010 ).
Between-study and between-effect size, heterogeneity was assessed using multilevel modeling with R’s metafor package ( Viechtbauer, 2010 ). A pooled overall treatment effect and potential moderator analyses were achieved through meta-regression with robust variance estimation (RVE) using R’s robumeta package ( Tanner-Smith et al., 2016 ). The intercept only in the meta-regression model offered overall averages of treatment effect sizes across studies; and models with covariates allowed the identification of effects of potential moderators on treatment effect sizes. Meta-regression using the RVE method effectively handles the statistical dependence created by one study reporting multiple effect size estimates on the same outcome ( Hedges et al., 2010 ). For example, a study may use more than one measure to evaluate a provider’s knowledge of elder abuse, resulting in the two knowledge measures within the same study being potentially dependent on each other (see Table 1 , outcome measures). The RVE approach not only effectively addresses the dependent issues but also produces robust estimation regardless of the heterogeneity assumption, meaning results robust across fixed- and random-effects models ( Hedges et al., 2010 ). Given the small number of studies included in this review, we also conducted a small sample size correction to the meta-regression analysis, and for an estimate with degrees of freedom greater than 4, p < 0.05 is considered statistically significant. For an estimate with degrees of freedom lower than 4, p < 0.01 is considered statistically significant. Sensitivity analyses were conducted by averaging dependent effect sizes within each study. Because both methods produced the same statistical inference, we reported the RVE results in this paper ( Tipton, 2015 ).
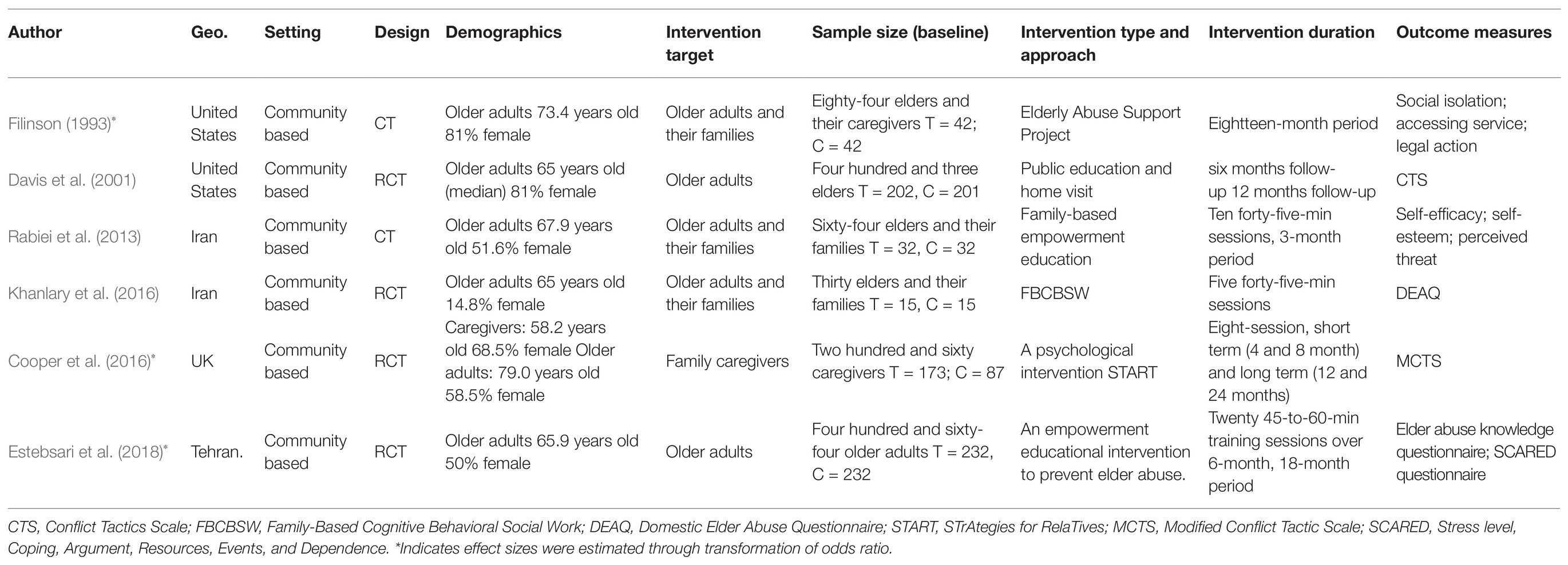
Table 1 . Study characteristics of six included studies.
Search Results
The review process is summarized in Figure 1 . A total of 2,986 studies were identified through a comprehensive search strategy for interventions to prevent or stop elder abuse in the community or an institutional setting. After 1,578 duplicate studies were removed, 1,255 studies were further excluded based on a title and abstract review. Of the remaining 153 studies, 147 studies were excluded for reasons, such as single arm trial without a control group or without statistical data, resulting in an analytical sample of six studies, containing 51 effect size estimates, in the final meta-analysis.
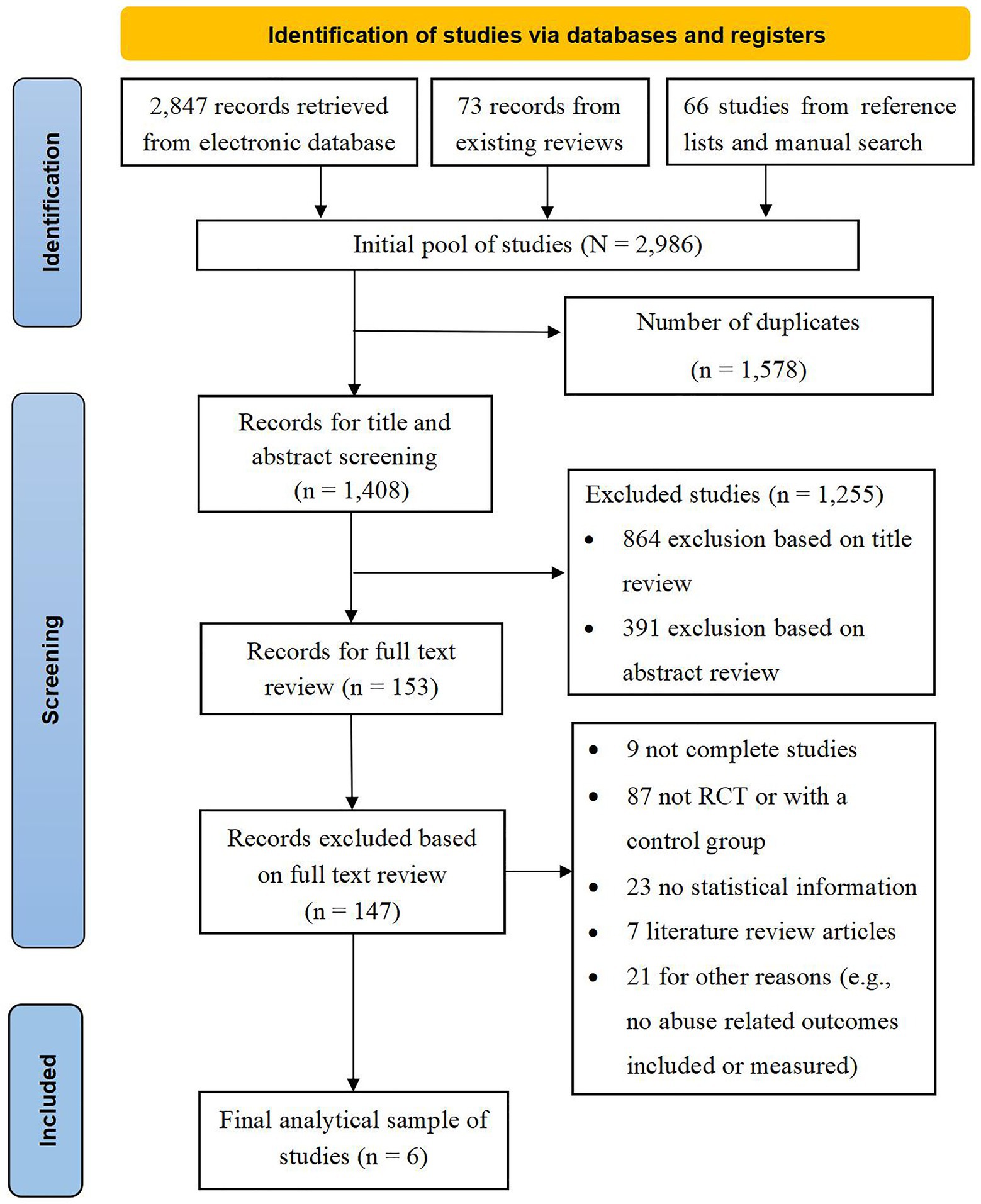
Figure 1 . PRISMA chart of literature search.
Characteristics of Included Studies
Study characteristics are presented in Table 1 . Of the six primary studies, four studies (67%) were published after 2010 and one (17%) was published in the 1990s. The six studies included a total sample of 1,305 participants. Participants’ ages averaged at 64.65 ( SD = 4.15), and 64.52% were female ( SD = 17.13). Four studies (66.7%) included at least one intermediate outcome measure and four studies (66.7%) included at least one ultimate outcome on elder abuse. Specifically, three studies included psychosocial stress outcomes, four studies encompassed outcomes related to knowledge and competency, and four studies addressed ultimate abuse-related behavioral outcomes.
Most interventions in reviewed studies were delivered in a family format ( n = 3, 50%), which lasted on average over 10 months ( SD = 7.55, range = 3–18 months). Two individual-based interventions (33.3%) were on average 21 months in duration ( SD = 4.24, range = 18–24 months) across studies. Three studies directed at both older adults and family members, two studies targeted older adults and one study targeted family members. Two interventions adopted an education approach, three used supportive services, and one incorporated both educational and supportive service interventions. Study sites covered Europe ( n = 2, 33.3%), the United States ( n = 2, 33.3%), and Asia ( n = 2, 33.3%).
Quality Assessment of Included Studies and Risk of Bias
Both RCT studies ( n = 4) and non-randomized controlled trial studies ( n = 2) were rated using the Jadad scale ( Halpern and Douglas, 2005 ) for reporting controlled trials and the Cochrane risk of bias assessment tool. Using the Jadad scale (see Supplementary Table 1), the six trials had an average score of 2.8 ( SD = 1.17) out of 5, indicating acceptable quality. These studies were rated satisfactory in mentioning randomization (5/6), tracking all participants (6/6), and randomization (4/6). However, these studies done were not satisfactory using appropriate blinding, just two studies mentioned blinding. Using the Cochrane Collaboration’s tool for assessing the risk of bias (see Supplementary Table 2), studies were rated most satisfactorily in selective outcome reporting (6/6), random sequence generation (4/6), and handling incomplete outcome data (4/6). Risk of bias was observed in allocation concealment (0/6), blinding of study participants and personnel (0/6), and blinding of outcome data assessment (2/6).
Both visual and statistical examination suggested an absence of publication bias (see Figure 2 ). The funnel plot seemed reasonably symmetric and showed no concerning outliers. The Vevea and Wood sensitivity weighted function analysis further confirmed the absence of publication bias.
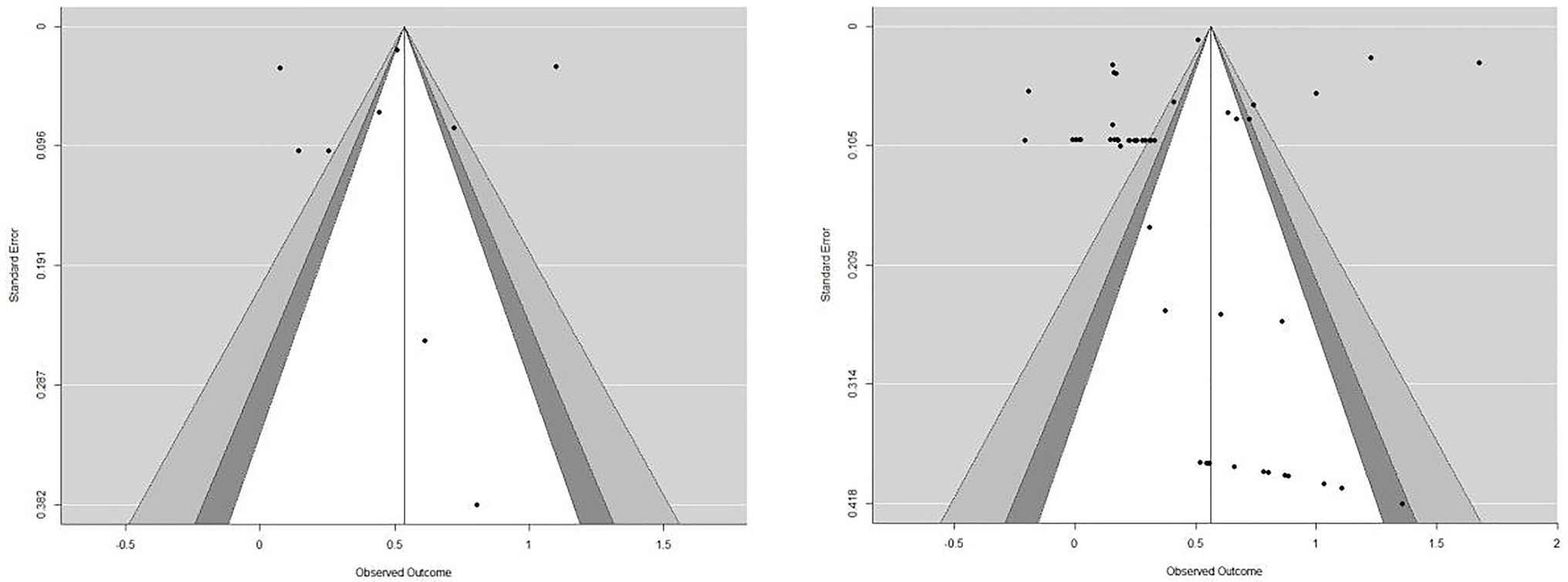
Figure 2 . Funnel plot for publication bias. We plotted independent effect sizes ( n = 9 from 6 studies) in the left plot and plotted all effect sizes (some dependent of each other) in the right plot.

Meta-Analysis Results and Subgroup Analyses
Multilevel modeling and the Q statistic used in heterogeneity assessment indicated a significant amount of heterogeneity across both effect size estimates and studies [ Q (50) = 5914.3, p < 0.01], suggesting a random-effects model is appropriate. We found an overall positive and statistically significant treatment effect ( d = 0.63, 95% CI [0.02, 1.24], p < 0.05).
Effect sizes were found depending on outcomes in subgroup analyses. The overall treatment effect was approaching statistical significance at 0.1 level for ultimate outcomes ( d = 0.32, 95% CI [−0.1, 0.73], p = 0.09) and intermediate outcomes ( d = 0.75, 95% CI [−0.27, 1.77], p = 0.10). More specifically for intermediate outcomes, effect size for psychosocial stress outcomes was 0.57 (95% CI [−0.29, 1.44], p = 0.1), and for knowledge and competency outcomes ( d = 0.66, 95% CI [−0.42, 1.75], p = 0.15).
In terms of intervention characteristics, we found that significant effect sizes across intervention type and target population. An overall significant effect size was found among family-based interventions ( d = 0.59, 95% CI [0.18, 1.01], p < 0.05), but not among individual-based interventions ( d = 0.86, 95% CI [−9.08, 1.8], p = 0.47). In terms of targeted populations, an overall statistically significant treatment effect was observed among interventions targeting both entities (e.g., older adults and their family caregivers; d = 0.45, 95% CI [0.01, 0.89], p < 0.05), but not among those targeting sole older adults or family caregivers.
Subgroup analyses using other study characteristics failed to show significance. Both RCT and non-randomized controlled trial studies reported non statistically significant treatment effect size ( d = 0.67, 95% CI [−0.51, 1.85], p = 0.17) and ( d = 0.54, 95% CI [−0.3, 1.38], p = 0.08) respectively. Subgroup analyses among studies published in the United States, Europe, and Asia did not yield any significance either. Specific results are presented in Table 2 .
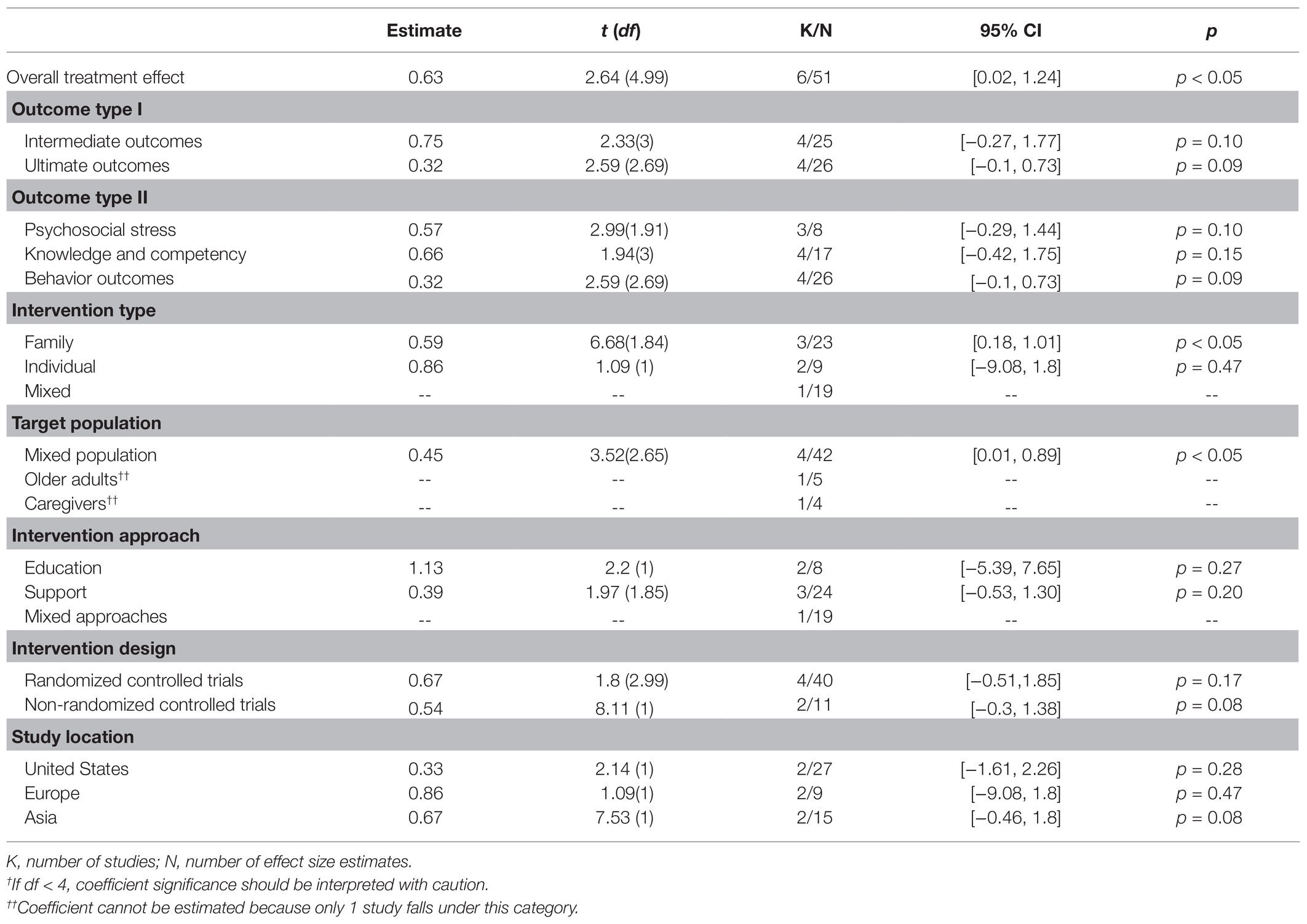
Table 2 . Overall and sub-group meta-analysis.
Moderator Analyses
Results of moderator analyses are presented in Table 3 . Only two univariate meta-regression models revealed a significant moderator that explains the heterogeneity between studies and effect sizes. Interventions targeting older adults reported significantly greater treatment effects than those targeting caregivers, or both. Intervention using a family centered approach had a greater treatment effect than the intervention delivered using a mixed format which included group and individual interventions.
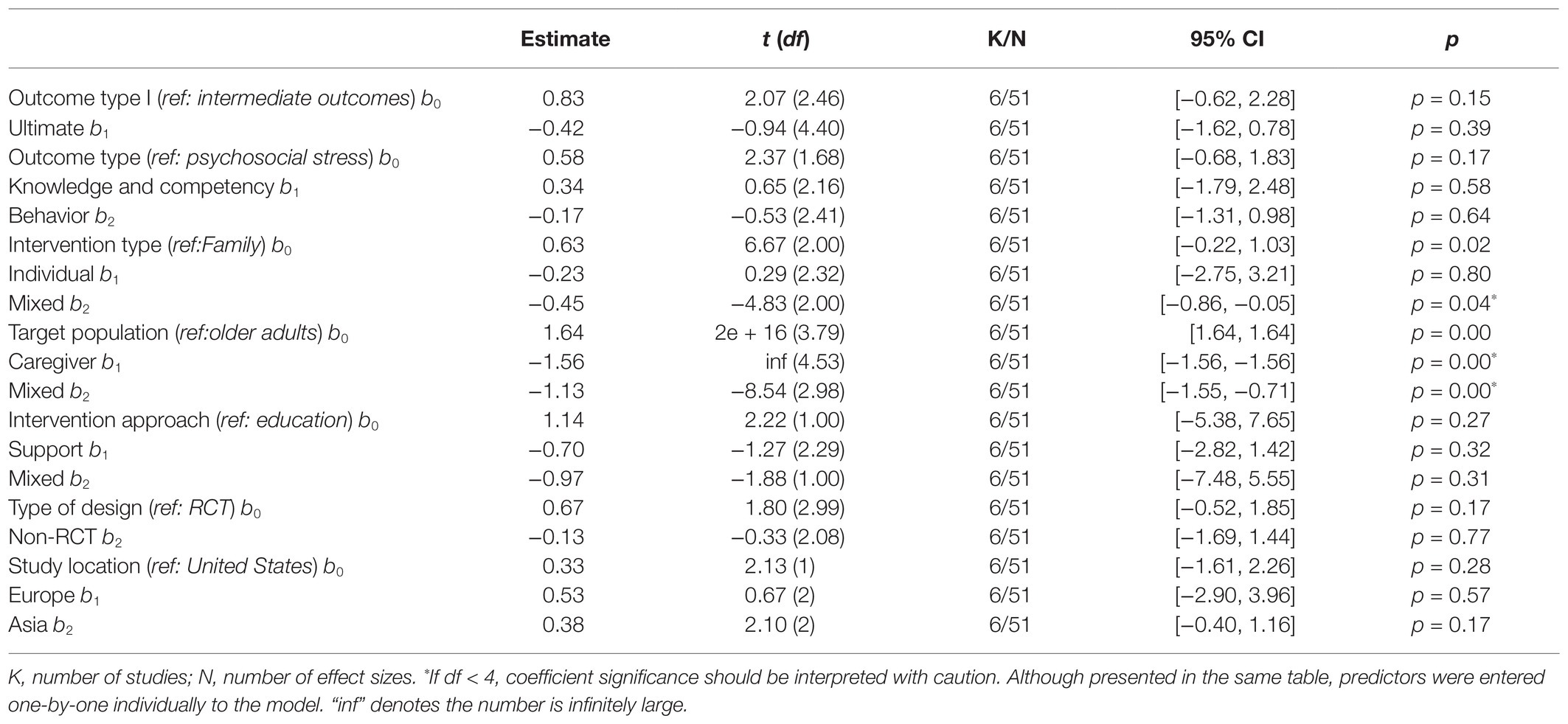
Table 3 . Single-predictor meta-regression analysis.
Our major finding identified a statistically significant effect size ( d = 0.63) of psychosocial interventions for elder abuse, suggesting that the effectiveness of available elder abuse prevention and interventions are moderately supported by evidence. Addressing elder abuse needs a multisystem effort that targets various change agents (e.g., elders, family, and caregivers) and along with multiple domains such as abuse awareness, knowledge, and behaviors ( World Health Organization, 2002 ). Although the overall effect size sounds promising, the findings from the subgroup analyses shed further light on the effectiveness regarding different intervention outcomes and provided specific directions for future research.
The treatment effect for intermediate outcomes ( d = 0.75, p = 0.1) and for the ultimate outcomes ( d = 0.19, p = 0.09) approached significance at 0.1 level. Because of the small power due to a limited number of articles included in the meta-analysis, these findings, though should be interpreted with caution, appear encouraging and promising. Intermediate outcomes can be viewed as mediators which bring about elder abuse reduction. Interventions reviewed in this study leaned toward an effective impact on intermediate outcomes, such as psychosocial stress, knowledge, and competency. This finding corresponds to a conclusion based upon an earlier Cochrane review of interventions for abuse prevention ( Baker et al., 2016 ). As abuse-related knowledge outcomes are often treated as intermediate outcomes, research needs to improve their knowledge-related outcome measures to capture notable changes in abuse awareness and attitude, along with their impact on the occurrence of elder abuse. Moreover, research should not stop arriving at satisfactory intermediate outcomes, but rather continue to disclose the pathway between changes in psychosocial stress and abuse reduction.
Effect size is significant among interventions that were family-based, geared toward elders, and family members, and adopted multiple approaches (e.g., combining education and services). The effectiveness of family-based interventions suggests the change of family dynamics can mitigate abuse. Consistently, an overall statistically significant treatment effect was observed among interventions targeting both elders and family members. As we had a limited number of interventions solely on elders or caregivers, we could not speculate the effect size for each respective group. Elder abuse mostly occurs in family settings, where perpetrators are most family members. Thus, targeting family issues through mitigating risk factors on both sides, potential victims and perpetrators, are likely to yield ideal outcomes ( Dong, 2015 ).
The use of various intervention approaches (e.g., education and supportive services) appeared to be effective, as mixed approach interventions showed an overall significant treatment effect. As there are multiple risks for elder abuse, intervention using mixed approaches can be more effective than interventions using one approach. Future interventions need to incorporate education, support, and services to assist older victims. Enhancing one’s awareness of elder abuse through education is important to the prevention of abuse; however, information itself is far from sufficient to trigger changes in attitude and behavior. Often, elders vulnerable to abuse or have been abused are likely to have other pressing social, health, financial, and legal needs. Similarly, mixed approaches better serve family caregivers who need tangible support to help manage challenging care tasks and emotional support for stress and burden.
Several limitations are inherent to systematic review and meta-analysis studies that should be noted. First, chances could be that one or more studies were missed in our search.
The total number of studies included was small, and a limited sample in subgroup analyses may have failed to show significance due to insufficient power. The small sample size, i.e., a small number of included studies, also prevented us from conducting certain subgroup analyses such as an overall treatment effect for interventions targeting different target population. Future studies should consider these analyses when more studies become available. Second, while two coders independently coded all studies and a team of experienced researchers resolved any disagreements, the results of this study are still subject to human errors. Third, as we used an advanced method to synthesize effect size estimates across outcomes, individual outcome contains distinctiveness in conceptualization. In the subgroup outcome analyses, some outcomes may suffer from a small sample size. As a result, we were unable to identify if the non-significant findings were due to low power. The same issue may exist in the moderator analyses, which prevented us from drawing any definitive conclusions. Fourth, as we focused on our search for psychological interventions, we did not include legal or policy interventions. As this area may play a role in elder abuse, these should be considered in future studies. Furthermore, research with a larger number of studies included will help explain the variations across effect sizes and studies.
This study represents an initial effort to examine the pooled effect of elder abuse preventions and interventions via meta-analyses. Existing evidence is supportive of a modest effect (approaching significance at 0.1 level) of psychosocial interventions for elder abuse. Evidence appears promising for interventions on modifiable intermediate outcomes such as psychosocial stress, knowledge, and competency that are typically theorized to lead to changes in elder abuse occurrence, as well as interventions targeting ultimate outcomes (i.e., abuse reduction). Interventions that used a family-based model, combined education and supportive services, and targeted both caregivers and elders, showed significant effect size, suggesting such features incorporated in elder abuse intervention design. Yet, more research evidence is still needed, in particular, research that will shed further light on the link between intervention activities and changes in elder abuse behaviors.
Community-based approach that draws on the concerted efforts from multiple stakeholders (e.g., elders, families, and service professionals) and tackles multi-domain elder abuse risk factors (e.g., knowledge, competency, and support) is worth pursuing ( Dong, 2015 ). Geriatric health and social care providers as well public health workers in the field of aging should be updated on the status of currently available interventions, adapt evidenced-informed interventions, and account for the heterogeneity of factors at the individual, agency, and cultural levels when promoting a safe and free of abuse environment for older adults.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
YS screened and coded all studies, drafted the entire manuscript. FS screened and coded all studies, drafted the discussion section of the manuscript, and proofread the entire manuscript. AZ designed the search strategy, resolved conflict, conducted preliminary analysis, drafted the entire manuscript, and proofread the entire manuscript. KW conducted all the meta-analysis and led the writing of the method and result section and proofread the entire manuscript. All authors contributed to the article and approved the submitted version.
This project was supported by (1) the China Scholarship Council Visiting Scholar Fellowship Program and (2) the Research Center for the Transformation and Development of Resource-exhausted Cities 2020 Open Fund Project (KF2020Y01) awarded to the first author.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acierno, R., Hernandez, M. A., Amstadter, A. B., Resnick, H. S., Steve, K., Muzzy, W., et al. (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am. J. Public Health 100, 292–297. doi: 10.2105/AJPH.2009.163089
PubMed Abstract | CrossRef Full Text | Google Scholar
Alderson, P., Clarke, M., Mulrow, C. D., and Oxman, A. D. (2008). Cochrane Handbook for Systematic Reviews of Interventions . Chichester, UK: John Wiley & Sons.
Google Scholar
Alt, K. L., Nguyen, A. L., and Meurer, L. N. (2011). The effectiveness of educational programs to improve recognition and reporting of elder abuse and neglect: a systematic review of the literature. J. Elder Abuse Negl. 23, 213–233. doi: 10.1080/08946566.2011.584046
Ayalon, L., Lev, S., Green, O., and Nevo, U. (2016). A systematic review and meta-analysis of interventions designed to prevent or stop elder maltreatment. Age Ageing 45, 216–227. doi: 10.1093/ageing/afv193
Baker, P. R. A., Francis, D. P., Hairi, N. N., Othman, S., and Choo, W. Y. (2016). Interventions for preventing abuse in the elderly. Cochrane Database Syst. Rev. 2016:CD010321. doi: 10.1002/14651858.CD010321.pub2
Cooper, C., Barber, J., Griffin, M., Rapaport, P., and Livingston, G. (2016). Effectiveness of START psychological intervention in reducing abuse by dementia family carers: randomized controlled trial. Int. Psychogeriatr. 28, 881–887. doi: 10.1017/S1041610215002033
Cooper, H., Hedges, L. V., and Valentine, J. C. (2009). The Handbook of Research Synthesis and Meta-Analysis . Russell Sage Foundation.
Davis, R. C., Medina, J., and Avitabile, N. (2001). Reducing Repeat Incidents of Elder Abuse: Results of a Randomized Experiment, Final Report. New York, NY: US Department of Justice.
Dong, X. Q. (2015). Elder abuse: systematic review and implications for practice. J. Am. Geriatr. Soc. 63, 1214–1238. doi: 10.1111/jgs.13454
Estebsari, F., Dastoorpoor, M., Mostafaei, D., Khanjani, N., Khalifehkandi, Z. R., Foroushani, A. R., et al. (2018). Design and implementation of an empowerment model to prevent elder abuse: a randomized controlled trial. Clin. Interv. Aging 13, 669–679. doi: 10.2147/CIA.S158097
CrossRef Full Text | Google Scholar
Fearing, G., Sheppard, C. L., McDonald, L., Beaulieu, M., and Hitzig, S. L. (2017). A systematic review on community-based interventions for elder abuse and neglect. J. Elder Abuse Negl. 29, 102–133. doi: 10.1080/08946566.2017.1308286
Filinson, R. (1993). An evaluation of a program of volunteer advocates for elder abuse victims. J. Elder Abuse Negl. 5, 77–94. doi: 10.1300/J084v05n01_07
Halpern, S. H., and Douglas, M. J. (2005). Appendix: Jadad scale for reporting randomized controlled trials. Evidence-Based Obstetric Anesthesia, Oxford, UK: Blackwell Publishing Ltd., 237–238.
Heck, L., and Gillespie, G. L. (2013). Interprofessional program to provide emergency sheltering to abused elders. Adv. Emerg. Nurs. J. 35, 170–181. doi: 10.1097/TME.0b013e31828ecc06
Hedges, L. V., Tipton, E., and Johnson, M. C. (2010). Robust variance estimation in meta-regression with dependent effect size estimates. Res. Synth. Methods 1, 39–65. doi: 10.1002/jrsm.5
Hsieh, H. F., Wang, J. J., Yen, M. F., and Liu, T. T. (2009). Educational support group in changing caregivers’ psychological elder abuse behavior toward caring for institutionalized elders. Adv. Health Sci. Educ. 14, 377–386. doi: 10.1007/s10459-008-9122-6
Khanlary, Z., Maarefvand, M., Biglarian, A., and Heravi-Karimooi, M. (2016). The effect of a family-based intervention with a cognitive-behavioral approach on elder abuse. J. Elder Abuse Negl. 28, 114–126. doi: 10.1080/08946566.2016.1141738
Livingston, G., Barber, J., Rapaport, P., Knapp, M., Griffin, M., King, D., et al. (2013). Clinical effectiveness of a manual based coping strategy programme (START, STrAtegies for RelaTives) in promoting the mental health of carers of family members with dementia: pragmatic randomised controlled trial. BMJ 347:f6276. doi: 10.1136/bmj.f6276
Marín-Martínez, F., and Sánchez-Meca, J. (2010). Weighting by inverse variance or by sample size in random-effects meta-analysis. Educ. Psychol. Meas. 70, 56–73. doi: 10.1177/0013164409344534
Pellfolk, T. J. E., Gustafson, Y., Bucht, G., and Karlsson, S. (2010). Effects of a restraint minimization program on staff knowledge, attitudes, and practice: a cluster randomized trial. J. Am. Geriatr. Soc. 58, 62–69. doi: 10.1111/j.1532-5415.2009.02629.x
Ploeg, J., Fear, J., Hutchison, B., and Bolan, G. (2009). A systematic review of interventions for elder abuse. J. Elder Abuse Negl. 21, 187–210. doi: 10.1080/08946560902997181
Rabiei, L., Mostafavi, F., Masoudi, R., and Hassanzadeh, A. (2013). The effect of family-based intervention on empowerment of the elders. J. Educ. Health Promot. 2:24. doi: 10.4103/2277-9531.112700
Rosen, T., Elman, A., Dion, S., Delgado, D., Demetres, M., Breckman, R., et al. (2019). Review of programs to combat elder mistreatment: focus on hospitals and level of resources needed. J. Am. Geriatr. Soc. 67, 1286–1294. doi: 10.1111/jgs.15773
Sacks, D., Das, D., Romanick, R., Caron, M., Morano, C., and Fahs, M. C. (2012). The value of daily money management: an analysis of outcomes and costs. J. Evid. Based Soc. Work 9, 498–511. doi: 10.1080/15433714.2011.581530
Tanner-Smith, E. E., Tipton, E., and Polanin, J. R. (2016). Handling complex meta-analytic data structures using robust variance estimates: a tutorial in R. J. Dev. Life-Course Cr. 2, 85–112. doi: 10.1007/s40865-016-0026-5
Teaster, P. B., Nerenberg, L., and Stansbury, K. L. (2003). A national look at elder abuse multidisciplinary teams. J. Elder Abuse Negl. 15, 91–107. doi: 10.1300/J084v15n03_06
Tipton, E. (2015). Small sample adjustments for robust variance estimation with meta-regression. Psychol. Methods 20:375. doi: 10.1037/met0000011
van Bavel, M., Janssens, K., Schakenraad, W., and Thurlings, N. (2010). Elder Abuse in Europe. Background and Position Paper. 14:22.
Vevea, J. L., and Woods, C. M. (2005). Publication bias in research synthesis: sensitivity analysis using a priori weight functions. Psychol. Methods 10, 428–443. doi: 10.1037/1082-989X.10.4.428
Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 36, 1–48. doi: 10.18637/jss.v036.i03
World Health Organization (2002). The Toronto declaration on the global prevention of elder abuse. Geneva: WHO. 3.
Yon, Y., Mikton, C. R., Gassoumis, Z. D., and Wilber, K. H. (2017). Elder abuse prevalence in community settings: a systematic review and meta-analysis. Lancet Glob. Health 5, e147–e156. doi: 10.1016/S2214-109X(17)30006-2
Yon, Y., Ramiro-Gonzalez, M., Mikton, C. R., Huber, M., and Sethi, D. (2019). The prevalence of elder abuse in institutional settings: a systematic review and meta-analysis. Eur. J. Pub. Health 29, 58–67. doi: 10.1093/eurpub/cky093
Keywords: elder abuse, psychosocial intervention, community settings, systematic review, meta-analysis
Citation: Shen Y, Sun F, Zhang A and Wang K (2021) The Effectiveness of Psychosocial Interventions for Elder Abuse in Community Settings: A Systematic Review and Meta-Analysis. Front. Psychol . 12:679541. doi: 10.3389/fpsyg.2021.679541
Received: 15 March 2021; Accepted: 22 April 2021; Published: 26 May 2021.
Reviewed by:
Copyright © 2021 Shen, Sun, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fei Sun, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Interpersonal Violence: a Review of Elder Abuse
- Geriatric Trauma (Bellal Joseph, Section Editor)
- Published: 08 November 2020
- Volume 6 , pages 133–139, ( 2020 )
Cite this article

- Carma Goldstein 1 &
- Nina E. Glass ORCID: orcid.org/0000-0002-6821-4289 1
281 Accesses
Explore all metrics
We review the underappreciated problem of elder abuse with a focus on what trauma surgeons need to know. Because of its prevalence, it is important that clinicians understand types of elder abuse, risk factors in patient and perpetrator, prevention strategies, and the appropriate referral and treatment of potential victims of elder abuse.
Recent Findings
Elder abuse affects at least 10% of older individuals in the USA. Despite much effort to address the problem via legal and societal approaches, data to support particular programs are poor. And even with extensive efforts, the utility of established prevention strategies or existing screening tools to identify victims of elder abuse in the acute care setting has yet to be established.
Elder abuse is a public health problem. As a society, we have only begun to define the extent of the problem. Healthcare systems have failed to effectively prevent or to accurately screen for, diagnose, and report elder abuse. The next steps include broader public awareness, educational initiatives, improved screening tools, and effective intervention strategies. In the meantime, we as trauma surgeons can be more diligent in reporting.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Examining the short and long-term impacts of child sexual abuse: a review study

Intergenerational Trauma and Its Relationship to Mental Health Care: A Qualitative Inquiry
Suggestions to improve outcomes for male victims of domestic abuse: a review of the literature, papers of particular interest, published recently, have been highlighted as: • of importance.
Baker A. Granny battering. Mod Geriatr. 1975;5(8):20–24.
Burston GR. Letter: granny-battering. Br Med J. 1975;3(5983):592. https://doi.org/10.1136/bmj.3.5983.592-a .
Article CAS PubMed PubMed Central Google Scholar
• Mercier E, Nadeau A, Brousseau AA, Emond M, Lowthian J, Berthelot S, et al. Elder abuse in the out-of-hospital and emergency department settings: a scoping review. Ann Emerg Med. 2020;75(2):181–91. https://doi.org/10.1016/j.annemergmed.2019.12.011 A 2020 scoping review which highlights a lot of the available evidence in aspects of elder abuse related specifically to the emergency physician.
Article PubMed Google Scholar
National Adult Protective Services Association. History: about adult protective services from 1960 to 2000. 2020. http://www.napsa-now.org/about-napsa/history/history-of-adult-protective-services/ . Accessed 28 Aug 2020.
National Center on Elder Abuse. Statistics and Data. National Center on Elder Abuse. 2020. https://ncea.acl.gov/About-Us/What-We-Do/Research/Statistics-and-Data.aspx . Accessed 28 Aug 2020.
Colello K. In: Service CR, editor. The elder justice act: background and issues for congress. Washington, DC: Library of Congress; 2014.
Google Scholar
Hall JE, Karch DL, Crosby AE. Elder abuse surveillance: uniform definitions and recommended core data elements for use in elder abuse surveillance, Version 1.0. Atlanta (GA): National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2016.
A profile of older Americans: 2019. U.S. Department of Health and Human Services: Administration on Aging, Administration for Community Living. https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2019ProfileOlderAmericans508.pdf . Accessed 28 Aug 2020.
Lachs MS, Pillemer KA. Elder abuse. N Engl J Med. 2015;373(20):1947–56. https://doi.org/10.1056/NEJMra1404688 .
Article CAS PubMed Google Scholar
Ho CS, Wong SY, Chiu MM, Ho RC. Global prevalence of elder abuse: a meta-analysis and meta-regression. East Asian Arch Psychiatr. 2017;27(2):43–55.
• Yon Y, Mikton CR, Gassoumis ZD, Wilber KH. Elder abuse prevalence in community settings: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(2):e147–e56. https://doi.org/10.1016/S2214-109X(17)30006-2 A 2017, WHO funded, worldwide meta-analysis and systematic review of the known prevalence studies of elder abuse reporting the pooled prevalence as 15.7% and highlighting the global neglect of elder abuse as a public health problem.
World Health Organization. Geneva, Switzerland. World Report on Ageing and Health: World Health Organization; 2015.
Rosen T, Stern ME, Elman A, Mulcare MR. Identifying and initiating intervention for elder abuse and neglect in the emergency department. Clin Geriatr Med. 2018;34(3):435–51. https://doi.org/10.1016/j.cger.2018.04.007 .
Article PubMed PubMed Central Google Scholar
Kojima G, Liljas AEM, Iliffe S. Frailty syndrome: implications and challenges for health care policy. Risk Manag Healthc Policy. 2019;12:23–30. https://doi.org/10.2147/RMHP.S168750 .
Torres-Castro S, Szlejf C, Parra-Rodriguez L, Rosas-Carrasco O. Association between frailty and elder abuse in community-dwelling older adults in Mexico City. J Am Geriatr Soc. 2018;66(9):1773–8. https://doi.org/10.1111/jgs.15489 .
Belisario MS, Dias FA, Pegorari MS, Paiva MM, Ferreira P, Corradini FA, et al. Cross-sectional study on the association between frailty and violence against community-dwelling elderly people in Brazil. Sao Paulo Med J. 2018;136(1):10–9. https://doi.org/10.1590/1516-3180.2017.0203290817 .
Pina-Escudero SD, Garcia-Lara JMA, Avila-Funes JA. Frailty is not associated with mistreatment. J Frailty Aging. 2017;6(4):202–5. https://doi.org/10.14283/jfa.2017.29 .
Gallione C, Dal Molin A, Cristina FVB, Ferns H, Mattioli M, Suardi B. Screening tools for identification of elder abuse: a systematic review. J Clin Nurs. 2017;26(15–16):2154–76. https://doi.org/10.1111/jocn.13721 .
Brijnath B, Gahan L, Gaffy E, Dow B. "Build rapport, otherwise no screening tools in the world are going to help": frontline service providers’ views on current screening tools for elder abuse. Gerontologist. 2020;60(3):472–82. https://doi.org/10.1093/geront/gny166 .
Conrad KJ, Conrad KM. Abuser risk measure: reports by alleged victims to adult protective services. Gerontologist. 2019;59(5):e403–e14. https://doi.org/10.1093/geront/gny091 .
New York State Office of Children and Family Services. Adult Protective Services: Definitions. 2020. https://ocfs.ny.gov/main/psa/adultabuse.asp . Accessed 28 Aug 2020.
Dong X, Simon M, Mendes de Leon C, Fulmer T, Beck T, Hebert L, et al. Elder self-neglect and abuse and mortality risk in a community-dwelling population. JAMA. 2009;302(5):517–26. https://doi.org/10.1001/jama.2009.1109 .
Dong X, Chen R, Chang ES, Simon M. Elder abuse and psychological well-being: a systematic review and implications for research and policy--a mini review. Gerontology. 2013;59(2):132–42. https://doi.org/10.1159/000341652 .
World Health Organization. Geneva, Switzerland. Elder abuse the health sector role in prevention and response: World Health Organization; 2016.
2020 Alzheimer’s disease facts and figures. Alzheimers Dement. 2020. https://doi.org/10.1002/alz.12068 .
Cooper C, Livingston G. Mental health/psychiatric issues in elder abuse and neglect. Clin Geriatr Med. 2014;30(4):839–50. https://doi.org/10.1016/j.cger.2014.08.011 .
Fang B, Yan E. Abuse of older persons with dementia: a review of the literature. Trauma Violence Abuse. 2018;19(2):127–47. https://doi.org/10.1177/1524838016650185 .
Yan E. Abuse of older persons with dementia by family caregivers: results of a 6-month prospective study in Hong Kong. Int J Geriatr Psychiatry. 2014;29(10):1018–27. https://doi.org/10.1002/gps.4092 .
Cooper C, Marston L, Barber J, Livingston D, Rapaport P, Higgs P, et al. Do care homes deliver person-centred care? A cross-sectional survey of staff-reported abusive and positive behaviours towards residents from the MARQUE (managing agitation and raising quality of life) English national care home survey. PLoS One. 2018;13(3):e0193399. https://doi.org/10.1371/journal.pone.0193399 .
• Phelan A. Advances in elder abuse research: practice, legislation, and policy. 1st ed. International Perpectives on Aging, vol 24. Springer International Publishing; 2020. A 2020 book dedicated to examining various aspects of elder abuse including studies where applicable highlighting the current knowledge base and areas to expand.
Yon Y, Ramiro-Gonzalez M, Mikton CR, Huber M, Sethi D. The prevalence of elder abuse in institutional settings: a systematic review and meta-analysis. Eur J Pub Health. 2019;29(1):58–67. https://doi.org/10.1093/eurpub/cky093 .
Article Google Scholar
World Health Organization. World health statistics 2020: monitoring health for the SDGs, sustainable development goals. World Health Organization; 2020. https://apps.who.int/iris/handle/10665/332070 . Accessed 28 Aug 2020.
Powers JS. Common presentations of elder abuse in health care settings. Clin Geriatr Med. 2014;30(4):729–41. https://doi.org/10.1016/j.cger.2014.08.004 .
• USC Department of Family Medicine and Geriatrics, National Center on Elder Abuse. Training resources on elder abuse. https://trea.usc.edu/resources/ . Accessed 8/30/2020. A comprehensive list of resources, some for medical professionals, about different aspects of elder abuse.
National Center on Elder Abuse. NCEA Publications. https://ncea.acl.gov/Resources/Publications.aspx . Accessed 8/30/2020.
Adult protective services. Adult Protective Services Technical Assistance Resource Center: Webinars. https://apstarc.acl.gov/Education/Webinars.aspx . Accessed 8/30/2020.
Schmeidel AN, Daly JM, Rosenbaum ME, Schmuch GA, Jogerst GJ. Health care professionals’ perspectives on barriers to elder abuse detection and reporting in primary care settings. J Elder Abuse Negl. 2012;24(1):17–36. https://doi.org/10.1080/08946566.2011.608044 .
Yaffe MJ, Wolfson C, Lithwick M, Weiss D. Development and validation of a tool to improve physician identification of elder abuse: the elder abuse suspicion index (EASI). J Elder Abuse Negl. 2008;20(3):276–300. https://doi.org/10.1080/08946560801973168 .
Baker PRA, Francis DP, Hairi NN, Othman S, Choo WY. Interventions for preventing abuse in the elderly. Cochrane Database Syst Rev. 2016;8. https://doi.org/10.1002/14651858.CD010321.pub2 .
Rosen T, Elman A, Dion S, Delgado D, Demetres M, Breckman R, et al. Review of programs to combat elder mistreatment: focus on hospitals and level of resources needed. J Am Geriatr Soc. 2019;67(6):1286–94. https://doi.org/10.1111/jgs.15773 .
Cooper C, Barber J, Griffin M, Rapaport P, Livingston G. Effectiveness of START psychological intervention in reducing abuse by dementia family carers: randomized controlled trial. Int Psychogeriatr. 2016;28(6):881–7. https://doi.org/10.1017/s1041610215002033 .
Sirey JA, Halkett A, Chambers S, Salamone A, Bruce ML, Raue PJ, et al. PROTECT: a pilot program to integrate mental health treatment into elder abuse services for older women. J Elder Abuse Negl. 2015;27(4–5):438–53. https://doi.org/10.1080/08946566.2015.1088422 .
Evans CS, Hunold KM, Rosen T, Platts-Mills TF. Diagnosis of elder abuse in U.S. emergency departments. J Am Geriatr Soc. 2017;65(1):91–7. https://doi.org/10.1111/jgs.14480 .
Dudas L, Petrohoy G, Esernio-Jenssen D, Lansenderfer C, Stirparo J, Dunstan M, et al. Every child, every time: hospital-wide child abuse screening increases awareness and state reporting. Pediatr Surg Int. 2019;35(7):773–8. https://doi.org/10.1007/s00383-019-04485-2 .
American Bar Association. Adult protective services reporting laws. American Bar Association Commission on Law and Aging. 2019. https://www.americanbar.org/content/dam/aba/administrative/law_aging/2020-elder-abuse-reporting-chart.pdf . Accessed 28 Aug 2020.
Center for Excellence in Elder Law and the Elder Consumer Protection Program. Guide on U.S. State and Territory Mandatory Reporting Status and Statutes Stetoon University College of Law. 2016. https://www.stetson.edu/law/academics/elder/home/media/Mandatory-reporting-Statutes-for-elder-abuse-2016.pdf . Accessed 28 Aug 2020.
RAINN. Mandatory Reporting Requirements: The Elderly New Jersey. RAINN (Rape, Abuse, & Incest National Network). 2020. https://apps.rainn.org/policy/policy-state-laws-export.cfm?state=New%20Jersey&group=5 . Accessed 28 Aug 2020.
• National Center on Elder Abuse. State Resources. https://ncea.acl.gov/Resources/State.aspx . Accessed 8/30/2020. If you wish to report possible elder abuse in your community, you can find out how via the NCEA State Resources site or the Eldercare Locator at 800–677-1116.
U.S. Administration on Aging. Eldercare Locator. https://eldercare.acl.gov/Public/Index.aspx . Accessed 8/30/2020.
Download references
Author information
Authors and affiliations.
Department of Surgery, Rutgers New Jersey Medical School, Newark, NJ, USA
Carma Goldstein & Nina E. Glass
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nina E. Glass .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Geriatric Trauma
Rights and permissions
Reprints and permissions
About this article
Goldstein, C., Glass, N.E. Interpersonal Violence: a Review of Elder Abuse. Curr Trauma Rep 6 , 133–139 (2020). https://doi.org/10.1007/s40719-020-00205-7
Download citation
Accepted : 23 October 2020
Published : 08 November 2020
Issue Date : December 2020
DOI : https://doi.org/10.1007/s40719-020-00205-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Elder abuse
- Elder mistreatment
- Geriatric trauma
Advertisement
- Find a journal
- Publish with us
- Track your research
- Follow us on Facebook
- Follow us on Twitter
- Criminal Justice
- Environment
- Politics & Government
- Race & Gender
Expert Commentary
Elder abuse: What research says about prevalence, assessment and prevention
We’ve gathered and summarized several relevant studies on elder abuse, including research in the context of the COVID-19 pandemic.

Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
by Sari Boren, The Journalist's Resource July 16, 2020
This <a target="_blank" href="https://journalistsresource.org/politics-and-government/elder-abuse-research-prevalence/">article</a> first appeared on <a target="_blank" href="https://journalistsresource.org">The Journalist's Resource</a> and is republished here under a Creative Commons license.<img src="https://journalistsresource.org/wp-content/uploads/2020/11/cropped-jr-favicon-150x150.png" style="width:1em;height:1em;margin-left:10px;">
Abuse of people age 60 and older is widespread, research shows. According to a 2017 study in The Lancet Global Health , “elder abuse seems to affect 1 in 6 older adults worldwide, which is roughly 141 million people.”
Elder abuse takes many forms. A 2015 review article in The New England Journal of Medicine explains that research on elder abuse generally addresses these five categories: “physical abuse, or acts carried out with the intention to cause physical pain or injury; psychological or verbal abuse, defined as acts carried out with the aim of causing emotional pain or injury; sexual abuse, defined as nonconsensual sexual contact of any kind; financial exploitation, involving the misappropriation of an older person’s money or property; and neglect, or the failure of a designated caregiver to meet the needs of a dependent older person.”
Take for example a 2014 study in the Journal of General Internal Medicine , in which researchers studied nearly 4,000 older residents of New York state. They found that financial abuse afflicted nearly 5% of them during their lifetime, with Black people at higher risk. “If a new disease entity were discovered that afflicted nearly one in 20 adults over their older lifetimes and differentially struck our most vulnerable subpopulations, a public health crisis would likely be declared,” the authors write. “Our data suggest that financial exploitation of older adults is such a phenomenon.”
But as prevalent as elder abuse is, it also goes widely unreported.
A 2018 article in Clinics in Geriatric Medicine , citing research from a 2011 report from the New York City Department for Aging, suggests that about only 1 in 24 cases of elder abuse is identified and reported to social service or legal authorities. The recognition, identification and regulation of elder abuse is complicated by the self-determination granted adults; in other words, while children are mostly seen as a vulnerable population requiring protection, there’s less oversight with vulnerable older adults.
In the past few years federal legislation designed to protect older Americans has passed or been proposed. The Elder Abuse Prevention and Prosecution Act of 2017 , signed into law in October of that year, increased data collection, information sharing, training for federal prosecutors and investigators and penalties for criminal acts for elder abuse. It also established coordinator positions at the Federal Trade Commission and the Department of Justice.
In recent months, the U.S. Senate’s Special Senate Committee on Aging has called attention to increased risk of elder abuse during the COVID-19 pandemic. In May, Sens. Susan Collins, R-Maine; Bob Menendez, D-NJ; and Chuck Grassley, R-Iowa, introduced the “Promoting Alzheimer’s Awareness to Prevent Elder Abuse Act.” That bill builds on the Elder Abuse Prevention and Prosecution Act of 2017 and is paired with companion legislation in the House. When introducing the bill, Sen. Collins said, “During the COVID-19 pandemic, there may be increased risk for elder abuse, including elder financial exploitation. Our bipartisan bill would help to ensure that the frontline professionals who are leading the charge against elder abuse have the training needed to respond to cases where the victim or a witness has Alzheimer’s disease or other forms of dementia.”
Health care providers who work with elderly patients also warn that the pandemic has exacerbated some of the risk factors for elder abuse, for both victims and perpetrators. The COVID-19 stay-at-home orders/recommendations that are meant to keep older people physically safe from the virus may create conditions for abuse. Older adults are now more likely to be isolated and out of sight, for example, making potential abuse harder to detect. Perpetrators, including family members, who experience increased personal or financial stress caused by the pandemic may be more likely to commit abuse.
In addition, there has been increasing ageism rhetoric in the United States during the COVID-19 pandemic, devaluing the lives of older adults, note the authors of a recent letter to the editor in the Journal of the American Geriatrics Society . To combat ageism in our culture, they suggest “increasing representation of older people with decision-making power in public and private sectors.”
To help journalists cover stories of elder abuse, we’ve gathered and summarized several relevant studies, including a recent article on abuse in the context of the COVID-19 pandemic. We also have compiled information on current and pending legislation on the topic, an introduction to a specific type of elder abuse called guardianship abuse, and additional resources for in-depth reporting.
—————————————-
A note on the limitations of data in many studies of elder abuse: Data is often self-reported, depending on the victim to divulge the abuse. Shame of abuse and/or the vulnerable position of older people who may rely on abusers for daily living needs often make older adults less likely to report abuse, leading to underreporting. And most studies exclude participants with dementia or cognitive impairment, even though older people with those issues experience abuse. According to Professor Pamela Teaster , director of the Center for Gerontology at Virginia Tech, these exclusions occur because self-reporting by people with dementia may be unreliable and because of protections for people with dementia regarding research. In an e-mail to Journalist’s Resource she explained, “We have to be very careful because, depending on the degree of the dementia, they may be unable to consent to participate in research.”
Elder Abuse Mark S. Lachs and Karl A. Pillemer. The New England Journal of Medicine , November 2015
The authors of this highly cited paper estimate that across the U.S., approximately 10% of older adults not living in care facilities are victims of abuse. “Thus, a busy physician caring for older adults will encounter a victim of such abuse on a frequent basis, regardless of whether the physician recognizes the abuse,” they write.
People with dementia are at especially high risk, and women are at higher risk than men, the authors note. Those at the younger end of the age group, the so-called “young old,” also have increased risks, as they more often live with the most likely abusers: a partner or adult children.
To help physicians identify elder abuse, the authors create a detailed breakdown of types of elder abuse (physical, verbal/psychological, sexual, financial, neglect) along with ways that abuse manifests itself during physical exams (for example, bone fractures may be a manifestation of physical abuse).
Assessment strategies for physicians include interviewing potential victims separately and alone and recognizing that mental illness resistant to treatment may have its source in emotional abuse. The authors also note that signs of neglect and financial abuse may be more subtle than those of physical abuse (e.g., weight loss and failure to keep appointments or fill prescriptions). Other assessments are specific to the abuse manifestations, such as determining if fractures are from abuse or falls/accidents. Physicians are cautioned that interviews with suspected perpetrators are best conducted by specifically trained professionals.
The authors note that successful treatment usually doesn’t involve just a single intervention of removing the victim from an abusive environment. Instead, successful interventions are typically “interprofessional, ongoing, community-based, and resource-intensive.” They write that the role for physicians is not to lead interventions, but rather to identify abuse, know the local organizations and services that provide resources to victims and refer patients to them, while coordinating care. These services can include Adult Protective Services, police and district attorneys, home health care organizations and appropriate nonprofits, and more.
Elder Abuse in the Time of COVID-19—Increased Risks for Older Adults and Their Caregivers Lena K. Makaroun, Rachel L. Bacrach and Ann-Marie Rosland. The American Journal of Geriatric Psychiatry , May 2020
The stay-at-home orders and recommendations intended to protect people, especially older people, from COVID-19 have created additional risks for elder abuse, note the authors of this perspective article. “Even in the best of times, elder abuse cases are rarely detected, with only 1 in 24 cases identified and reported to the appropriate authorities,” the authors write, citing a 2011 report of elder abuse in New York .
In the pandemic environment, older people and their family caregivers may be especially vulnerable to isolation, anxiety, financial stress and difficulty accessing healthcare and supplies, along with increased co-dependency brought on by the changing living conditions. These stressors increase risk factors for elder abuse.
Health care providers and outside caregivers are now less likely to have in-person contact with their patients, relying instead on technology-based communication; however, many older adults are not adept at technology, may not have the necessary hardware devices, and may not be able to speak privately if living with an abuser. And some elder care must be provided in person. The reduction or loss of this care could lead to neglect.
Existing abusive relationships may become more severe or lethal as mood disorders and substance abuse increase among caregivers. Additionally, during the pandemic, “there was a substantial increase in the purchase of firearms and ammunition.”
The pandemic does offer opportunities for positive change, the authors note. Providers who can contact elder patients via technology can now observe patients in their homes and can provide support for caregivers whom they may not typically see during in-person visits. Institutions and organizations are mobilizing programs and support for elders during the pandemic, including the Veterans Health Administration and local agencies on aging. The authors report that “the new challenges presented by the COVID-19 pandemic present an important opportunity to forge these new partnerships.”
The pandemic also presents opportunities for new research. The authors write, “Perhaps most understudied, and the area where new revelations could have the biggest impact, are caregiver-related risk factors. With many people experiencing caregiving stress and concern about whether loved ones’ needs will be met, caregivers may be more open to participating in research to share their experiences, even uncomfortable ones.”
Elder abuse prevalence in community settings: a systematic review and meta-analysis Yongjie Yon, et al. The Lancet Global Health , February 2017
This meta-analysis of 52 international studies in 28 countries describes how prevention of elder abuse requires a better understanding of the breadth of the problem. The authors report that “elder abuse seems to affect 1 in 6 older adults worldwide, which is roughly 141 million people.” Psychological abuse was reported most often, at a 11.6% pooled prevalence estimate (pooled prevalence is a statistical technique for pooling results of many epidemiological studies), followed by financial abuse, neglect, physical abuse and sexual abuse.
The authors note that reported rates vary widely. “For example, national estimates of past-year abuse prevalence rate ranged between 2.6% in the UK and 4% in Canada to 18.4% in Israel and 29.3% in Spain,” they write. That’s due in part to a lack of consensus on how to define and measure different types of elder abuse, they note, making elder abuse a “neglected global health priority.”
The authors report that if the proportion of elder abuse cases remain constant through the aging global population, they expect elder abuse victims to number 330 million by 2050.
The National Elder Mistreatment Study: An 8-year longitudinal study of outcomes Ron Acierno, et al. Journal of Elder Abuse & Neglect , 2017
This study is the 8-year follow-up to a 2011 study published in the American Journal of Public Health , “ Prevalence and Correlates of Emotional, Physical, Sexual, and Financial Abuse and Potential Neglect in the United States: The National Elder Mistreatment Study. ” The original study analyzed interviews (in English and Spanish) with over 5,500 respondents across the continental U.S., finding that 1 in 10 self-reported some type of elder abuse or neglect. The follow-up study attempted to contact all 752 original participants who reported mistreatment since age 60, of which they reached 183. They also interviewed 591 randomly selected non-mistreated participants from the original study.
The authors of the 2017 paper found that lack of social support increased the likelihood of all forms of abuse, while the presence of social support mitigated negative effects of abuse, particularly anxiety and poor health. Few instances of abuse were reported to authorities.
The authors describe how the 2017 follow-up study “represents the first longitudinal epidemiological study of elder mistreatment to date,” and focuses on how abuse affected victims’ health over time.
In the 2017 study, the authors look at the factors that exacerbated or mitigated the long-term effects of elder abuse. Variables of gender, income, and employment status were not as relevant as levels of social support. Further, beyond the effects on elder mistreatment, the researchers report that “low social support consistently predicted negative outcomes” in mental and physical health, even more consistently than did abuse.
“This is encouraging insofar as these findings speak directly to an actionable intervention to prevent both elder mistreatment and its negative effects,” they write.
They recommend that when family and friends can’t provide sufficient levels of social support, policies should further social support programs “in the form of education, volunteerism, or socialization” with examples including online and in-person classes, and social activities and meal programs through senior centers.
Limitations of both studies were that data was self-reported, respondents were all “community-residing” elders (not living in elder care facilities) who were “cognitively intact,” and the stigma of abuse and mental illness may have led to under-reporting. In the follow-up study a significant proportion of the original respondents were “not available for follow-up, either due to death, relocation, or inability to participate.”
Prevalence of elder abuse in institutional settings: systematic review and meta-analysis Yongjie Yon, et al. The European Journal of Public Health , June 2018
This systematic review and meta-analysis, described by the authors as the “first rigorous quantitative synthesis of prevalence estimates for elder abuse in the institutions” estimates a high global prevalence of elder abuse for those living in elder care facilities during the 12 month period preceding this study.
Based on nine international studies that focused on staff-to-resident abuse in six countries, the authors report more than half of the staff interviewed for these studies admitted to elder abuse, with psychological abuse being most common, followed by physical abuse.
Among self-reporting victims, more than a third had experienced psychological abuse. Next-most common was physical abuse, followed by financial abuse, neglect and sexual abuse. While abuse in elder care facilities also occurs resident-to-resident and visitor-to-resident, the selected papers did not include these categories of data.
The main risk factors in an institutional setting are reported as “being female, presence of a cognitive impairment and disability, and being older than 74 years old,” with a “strong association between increasing dependency and elder abuse occurring” regardless of whether older adults live in an elder care facility or elsewhere.
Staff who self-reported committing abuse described stress from staff shortages and time pressure. The authors also cite staffing data from prior research in which staff who committed abuse described emotional exhaustion. In addition, higher ratios of patients to registered nurses correlated to higher levels of abuse, while “increased presence of qualified nurses” correlated with lower risk.
Comparing older adult and child protection policy in the United States of America Peiyi Lu and Mack Shelley. Ageing & Society , September 2019
This study compares child and adult protection policies in the U.S., noting that by 2050 the U.S. is “expected to have 88.5 million older adults and 79.9 million children.” The authors describe an estimated prevalence of abuse as more than five times higher among older adults than children (10% vs 1.71%); however, they note that the data for elder abuse is not always available or comparable to the detailed data on child abuse.
Overall, U.S. adult protection policies were developed later and more slowly than those for children. The authors include comparisons across multiple factors including response services, post-response services, prevention services and allocation of resources and funding. “Compared to child protection policy, older adult protection policy lacked federal legislative and administrative direction, well-developed diagnosis and evaluation tools, a national data system, sufficient federal funds and a comprehensive response mechanism,” they write.
The autonomy of adults complicates some elements of adult protection. While children are viewed as a vulnerable population requiring protection, “older adults have lived independently for most of their lives and still expect to be independent in most periods of their late life. When abuse happens, especially for the self-neglect and financial exploitation cases, it is difficult to determine whether it is intentional.”
As one example, federal protection policies mandate reporting for both child and adult abuse. Child protection policies are more strictly implemented than those for adults.
“There is a trade-off,” the authors write, “between protecting older adults’ rights to be free from violence and exploitation, and maintaining their individual autonomy.” They cite other researchers who believe that a mandatory system not only interferes with the autonomy of older adults but presents ethical conflicts for physicians.
Financial Exploitation of Older Adults: A Population-Based Prevalence Study Janey C. Peterson, et al. Journal of General Internal Medicine , July 2014
The authors conducted over 4,000 interviews in 2008–2009 with older adults in New York state not living in elder care facilities to identify those who had experienced financial exploitation, defined as: “improper use of funds, property or resources, coerced property transfers, denial of access to assets, fraud, false pretense, embezzlement, conspiracy, or falsifying records.” They found that almost 1 in 20 adults were victims of financial exploitation in their older years.
Older adults who self-reported financial abuse were more likely to already be economically, medically or otherwise demographically vulnerable. Poverty was an indicator for financial exploitation, possibly because individuals in poverty may be sharing homes with others. Family members are most often (57.9 % of the time) the ones financially exploiting victims, with adult children being the primary perpetrators. In addition, living with non-spousal family members put older adults at greater risk. Other perpetrators, in order of occurrence, were friends and neighbors, and home care aides.
Being Black was associated with greater relative risk of being a victim of financial abuse. People who have trouble with the tasks of daily living (e.g. managing finances, shopping, cooking and cleaning, or taking medications) were also at higher risk, as people providing assistance have access to their finances. Other factors associated with financial exploitation were “non-use of social services, need for [assisted daily living] assistance, poor self-rated health, no spouse/partner and lower age.”
The authors conclude, “In addition to robbing older adults of resources, dignity, and quality of life, victims of [financial abuse] likely cost our society dearly in the form of increased entitlement encumbrances, health care, and other costs.”
As with other studies of elder abuse, the limitations are that data was self-reported, did not include participants with dementia, and that elder people are often less likely to report abuse, leading to underreporting.
Risk Factors for Elder abuse and Neglect: A Review of the Literature Jennifer E. Story. Aggression and Violent Behavior , Jan-Feb 2020
To help health care providers identify older adults at risk for abuse, this literature review provides a summary of risk factors that increase the likelihood of becoming either an abuse victim or perpetrator. Many risk factor categories are similar for perpetrators and victims. For example, “dependency” is a risk for a perpetrator, particularly if they are financially dependent on the victim, possibly leading to anger and abuse. For victims, dependency creates a vulnerability because it increases isolation and makes it harder to seek help.
The paper includes a detailed chart with the categories of factors that can increase the likelihood of becoming either a victim or a perpetrator of elder abuse: physical and mental health problems; substance abuse; dependency; problems with stress, coping and attitudes; problems with relationships, and previous experience with or witness to abuse.
Screening for elder mistreatment in emergency departments: current progress and recommendations for next steps Tony Rosen, Timothy F. Platts-Mills & Terry Fulmer. Journal of Elder Abuse & Neglect , June 2020
This paper advocates for universal screening for elder abuse in emergency departments. The authors describe the “dismally low rate at which emergency providers are currently recognizing or reporting abuse” even though, compared with other older adults, victims of elder abuse seek emergency care more frequently and primary care less frequently. They note that “annual rates of ED usage by elder abuse victims are 3 times greater than non-victims.”
Current screening tools, the authors argue, are either likely to miss incidents of elder abuse or are too long and complex for the busy, chaotic emergency department environment. Patients are often screened in the emergency department for safety issues such as domestic abuse with a single vague question: “Do you feel safe at home?”
Instead, the authors propose a two-step screening process: a brief universal screen followed by a comprehensive screen for those positively identified. The initial screen would be designed to more specifically detect elder abuse, with questions such as: “Has anyone close to you harmed you?” or “Has anyone close to you failed to give you the care that you need?” Another option for the initial screen would be to design the electronic health record system to identify at-risk patients. The second-step comprehensive screening would involve a brief cognitive assessment, questions for the patient and a physical exam.
To improve emergency department detection and intervention for elder abuse they also recommend stronger ties between emergency departments and Adult Protection Services, development of multi-disciplinary response teams modeled after similar teams for child protection, and involving emergency medical service providers in initial screenings.
A note on guardianship abuse
There’s a relative dearth of peer-reviewed research on a specific type of abuse called guardianship abuse. This occurs when a court-appointed guardian, who is typically granted control over an elder person’s financial and medical decisions, takes advantage of their position in an abusive way. As described in Rachel Aviv’s 2017 New Yorker article “ How the Elderly Lose Their Rights,” abusive guardians overtly exploit the system to steal from those they’ve been entrusted to protect. Some guardians forge relationships with hospital personnel to help them identify potential vulnerable clients and then convince courts of the need for guardianship, even when family members object. These abusive guardians have convinced physicians to prescribe sedating medications and oftentimes isolate their clients from family or friends.
The scope of the problem and devising remedies has been hindered by lack of data. Testifying before the United States Senate Special Committee on Aging in April, 2018, Dr. Pamela Teaster, professor and director of the Center for Gerontology at Virginia Tech, said that “despite estimates that some 1.5 million adults are under guardianship, in 2018, not one single state in the country can identify its people under guardianship.”
No central national database exists to identify guardians and track potential abuse. Oversight of guardians varies by state. For example, only some states require background checks and few have safeguards to protect against abuse of the system.
In 2018 the U.S. Senate’s Special Senate Committee on Aging published a report on guardianship abuse, Ensuring Trust: Strengthening State Efforts to Overhaul the Guardianship Process and Protect Older Americans . While special committees have no legislative authority, they can study issues and make legislative recommendations. Committee Chairman Sen. Susan Collins and Ranking Member Sen. Bob Casey subsequently sponsored the “ Guardianship Accountability Act of 2019 ,” which, in its most recent action, was sent to the Committee on the Judiciary in February 2019. The bill addresses many of the 2018 report’s recommendations, including the establishment of a National Online Resource Center on Guardianship.
Guardianship may not always be the best way to assist an older adult who needs assistance. As described in the 2018 Senate Ensuring Trust report , “a full guardianship order may remove more rights than necessary and may not be the best means of providing support and protection to an individual.” One relatively new alternative to guardianship is called “supported decision-making. This concept, which first gained traction in the disability rights community, is now proposed as an option to guardianship for some older adults, including those with dementia, and is supported by the American Bar Association. Under supported decision-making the individual relies on support from family, friends, and/or service organizations to help make their own decisions, without having to relinquish legal autonomy. These arrangements can range from informal understandings to written agreements, which are recognized as legally enforceable in nine states.
In a recent issue of Generations , Erica F. Wood, who is the assistant director of the American Bar Association Commission on Law and Aging, provides information for those working with older populations on how to avoid guardianship or how to ensure a proper guardianship. She provides a practical information on how to manage a legal process that will potentially result in the appointment of a guardian.
She suggests obtaining legal representation, and describes possible actions to take before a hearing, including checking applicable laws, assessing for less-restrictive measures than guardianship, and collecting evidence. If the court does appoint a guardian the author describes which aspects of the guardianship to investigate (e.g. who’s the guardian; how will assets be protected), and how to monitor the guardian (e.g. reviewing reports and accounts) and to legally protect the adult under guardianship, by reporting abuse or exploitation or seeking a restoration of rights.
Wood also identifies six common scenarios that can lead to legal guardianship, including a medical crisis, a family feud, discharge from hospital to an elder facility, abuse, eviction and an unpaid care bill.
Additional Resources
Frequently Asked Questions by Guardians about the COVID-19 Pandemic
This COVID-19 resource document for professional and family guardians was jointly created by the American Bar Association, the National Center for State Courts and the National Guardianship Association (a professional association). It includes information on accessing and communicating with older adults living in facilities during the pandemic and protecting the legal, medical and financial rights of older adults under guardianship.
Restoration of Rights in Adult Guardianship: Research & Recommendations American Bar Association Commission on Law and Aging with the Virginia Tech Center for Gerontology, 2017
This report describes that an “unknown number” of adults remain under guardianship longer than necessary or could have benefitted from less-restrictive support from the outset. The report focuses on guardianship for all ages, and includes legal research on restoration of rights by state, as well as court file research to extract data on guardianship.
Guardianship and Supported Decision Making
Among the resources on this American Bar Association page are yearly (2013–2019) summaries of state laws and policies regarding guardianship.
National Center for State Courts: Center for Elders
The National Center for State Courts is an independent, nonprofit “court improvement” organization that provides research, information services, education, and consulting to professionals involved in the workings of state courts. Its Center for Elders includes information on issues likely to concern state courts regarding aging, elder abuse and guardianship.
Government Resources
National Center on Elder Abuse
The National Center on Elder Abuse is a program of the U.S. Administration on Aging , which includes research, statistics and data, risk factors, and the multiple definitions of “How Is Elder Abuse Defined for Research Purposes,” among other resources. They’ve recently added a page on COVID-19 with resources for identifying and reporting abuse during the pandemic.
The Center also published a 2018 guide, “Understanding and Working with Adult Protective Services.”
National Center on Law & Elder Rights
As part of the U.S. Department of Health & Human Services, NCLER has tools and resources for legal assistance regarding elder rights, particularly for those with the “greatest economic and social needs.”
The U.S. Department of Justice Elder Justice Initiative
This site has extensive resources regarding all types categories of elder abuse, focused on the justice system, with information for victim specialists, law enforcement and prosecutors, as well as specific rural and Tribal resources.
Centers for Disease Control and Prevention
The CDC published the report Elder Abuse Surveillance in 2016 , which provides “uniform definitions and recommended core data elements for possible use in standardizing the collection of [elder abuse] data locally and nationally.”
United State Government Accountability Office Elder Abuse , Report to Congressional Requesters, 2016
Focusing on the issue of guardianship for older adults, the report is based on research with federal agencies, relevant state court officials, and nongovernmental organizations with expertise in guardianship-related issues.
Academic Centers that Focus on Elder Abuse
Center of Excellence on Elder Abuse & Neglect, University of California, Irvine, School of Medicine
This center’s website has extensive information across multiple disciplines, including links to national resources and tools for promising practices , along with their own research publications .
Center for Gerontology at Virginia Tech
The center’s Resource page includes resources for preventing abuse, as well as specific information on intimate partner violence and violence against rural older women.
USC Center on Elder Mistreatment
The University of Southern California’s Center on Elder Mistreatment is a multi-disciplinary academic research center specializing on issues of elder mistreatment and includes publications on their research topics. One of their key projects is on the use of multi-disciplinary teams for elder abuse interventions.
For more help with reporting stories related to COVID-19, please visit our archive of resources for covering the coronavirus pandemic.
About The Author
90 Elder Abuse Essay Topic Ideas & Examples
🏆 best elder abuse topic ideas & essay examples, ✅ good essay topics on elder abuse, 📑 interesting topics to write about elder abuse, ❓ questions about elder abuse.
- Child and Elder Abuse: Is It Really Different? The people committing the crime of child abuse are usually people known and trusted by the children as it is in this case.
- Child Abuse Versus Elder Abuse The second distinction is that older people frequently encounter issues that might lead to abuse or neglect, particularly in nursing homes, such as mental disability, loneliness, and physical limitation.
- Elder Abuse Under Sociological Analysis The most prominent kind of elder abuse is abuse by omission, which means that the caretaker fails to provide the elder with necessities.
- The Issue of Elder Abuse and Violence In terms of the public’s perception of elder abuse, it is feasible to state that the opinions and problems among the general society differ from, for example, the specialists within the field of healthcare.
- The Issue of Elder Abuse and Its Management This complex problem has to be addressed on a systemic level, including interventions and solutions to moderate the behavior of both the abusers and the abused, encourage recuperative efforts, and offer mechanisms for reporting abuse.
- Domestic Violence, Child Abuse, or Elder Abuse In every health facility, a nurse who notices the signs of abuse and domestic violence must report them to the relevant authorities.
- Self-Determination of the Elderly Needs and Elder Abuse Thus, the Petrakis family case demonstrates that Magda is an older individual whose needs should have been assessed according to seven domains, and it is necessary to offer additional questions to investigate the situation.
- Dependent Adult and Elderly Neglect and Abuse Dependent elderly are people who need assistance to do daily activities and to protect themselves. They also include sick adults who are in hospitals all the time.
- P-Plan Proposal: Youth, Adult and Elderly Abuse To ensure that equality and sanity is maintained, the government normally has some set rules and regulations that have to be adhered to.
- The Elderly Abuse: Physical and Psychological Aspects It is essential to understand these mistreatments’ similarities and differences and the intervention measures to stop or prevent them. Physical abuse causes bodily harm and can result in impairment, pain, or injury, such as broken […]
- Advocacy in Action: Elderly Abuse and Impact on Society The research suggests that family members and caregivers are the main abusers of the elderly population and, therefore, there should be specific programs that can contribute to enhancing the quality of life of senior members […]
- Elder Abuse Problems: Implementing Health Policies A number of organizations and individuals are already involved in elderly justice, which is the collective action of restoring dignitary to senior citizen care in the country.
- Learning to Detect and Report Elder Abuse The members of the society should be aware of the mechanisms of identifying an elderly individual who is a victim of violence and abuse.
- Elder Abuse and Its Consequences The level of abuse being directed towards elderly people has sort of been under the radar but organizations such as National Centre on Elderly Abuse plus countless others have brought this issue to the forefront […]
- The Issue of Elder Abuse in the US The purpose of this paper is to analyze the problem of elder abuse in America based on the data from the United States.
- Curbing Elder Abuse and Neglect The contemporary evaluation studies of the elderly citizens’ emotional stability prove that there is a consistent percentage of offensive treatment towards the seniors both in the family environments and asylums.
- Financial Abuse of the Elderly When elderly abuse is mentioned, most people think that sexual or physical harassment on the elderly is the only form of mistreatment that qualifies to be abuse.
- Domestic Violence and Elderly Abuse- A Policy Statement Though this figure has been changing with the change in the method of survey that was conducted and the nature of samples that were taken during the research process, it is widely accepted fact that […]
- Community and Domestic Violence: Elder Abuse In addition, the fact the elderly people cannot defend themselves because of the physical frailty that they encounter, they will experience most of the elderly abuse.
- The Elder Abuse in the Russian Culture
- The Harry and Jeanette Weinberg Center for Elder Justice: Elder Abuse Prevention Program
- The Impact of Elder Abuse on a Growing Senior Veteran Population
- Elder Abuse Policy: Considerations in Research and Legislation
- The High Prevalence of Depression and Dementia in Elder Abuse and Neglect
- Prevalence Patterns and Associated Factors of Elder Abuse in an Urban Slum of Eastern India
- Reducing Elder Abuse in Ireland and Germany: Elder Care Programs in Ireland and Germany
- Elder Abuse and Elder Financial Exploitation Statutes
- Legal Help for Different Types of Elder Abuse
- Elderly Abuse, Teenage Pregnancy, and Proposed Solutions to These Two Family Problems
- A Feminist Perspective on Gender and Elder Abuse
- Abuse and Neglect of the Frail Elderly at Home
- Educational Nursing Strategies: Prevention of Elder Abuse and Neglect
- Elder Abuse Issues in Canada: The Most Common Form Is Financial Abuse
- Case of Elderly Abuse: The Alzheimer’s Care of Commerce
- Social Isolation as a Risk Factor for Elder Abuse
- Elder Abuse Is the Main Issue Affecting Around the World
- The Effects of Alcohol Abuse on the Elderly Population
- Social Work Response to Elder Abuse in Uganda
- Enhancing the Justice System’s Response to Elder Abuse.
- Sexual Elder Abuse: Dementia, Alzheimer’s, or Other Cognitive Disabilities
- Elder Abuse Due to Neglect: Trends and Consequences
- The Issue of Elder Abuse and Safeguarding in the UK
- Emotional Elder Abuse: The Most Frequently Reported Type
- Assisted Suicide and Elder Abuse: A Sense of Guilt and Fright Becoming a Burden
- Elder Abuse: Need for Educational Interventions to Create Public
- Elder Abuse and Living Arrangements in Late Adulthood
- California Has the Highest Rate of Elder Abuse
- Barriers to Obtaining Statistics on Elder Abuse
- Abandonment as Elder Abuse: Leaving Without Any Formal Arrangement
- Elder Abuse and Neglect in Latino Families
- Elder Abuse Victimization Patterns: Determining Latent Classes With Victims’ Characteristics
- The Role of the Criminal Justice System in Elder Abuse Cases
- The Seniors’ Rights and Elder Abuse Protection Act
- Using Latent Class Analysis to Identify Profiles of Elder Abuse Perpetrators
- Examination of Explanations for the Occurrence of Elder Abuse
- Elder Abuse in Nursing Homes: Prevention and Resolution Strategies and Barriers
- Helping Prevent Elder Abuse Globally Through the Use of Social Media
- The Most Frequent Perpetrators of Elder Abuse
- Elder Abuse Phenomenon Correlating Relationship to Elder Mortality
- What Are the Most Common Types of Elder Abuse?
- Where Does Elder Abuse Happen the Most?
- Is Gender a Risk Factor for Elder Abuse?
- What Are the Signs of Elder Abuse?
- How Big of a Problem Is Elder Abuse in the US?
- What Are the Major Factors of Elder Abuse?
- Why Are Females More Likely to Be Victims of Elder Abuse?
- How to Prevent Elder Abuse in Nursing Homes?
- What Is the Fastest Form of Elder Abuse?
- Which Type of Elder Abuse Is the Most Unreported?
- Are Statistically Most Victims of Elder Abuse Female?
- What Is the Side Effect of Elder Abuse?
- Who Is the Most Common Perpetrator of Elder Abuse?
- Is Elder Abuse a Crime in the United States?
- What Individuals Are at Higher Risk of Being a Victim of Elder Abuse?
- Why Is It Important to Prevent Elder Abuse?
- What Percent of Elder Abuse Is Caused by Family Members?
- Is There Mandatory Reporting for Elder Abuse in the US?
- Why Is Elder Abuse Becoming More Prevalent in the United States?
- What Is One Reason That Elder Abuse Can Be Difficult to Identify?
- How to Prove Elder Abuse in California?
- What Are the Negative Effects of Elder Abuse?
- How Long Do You Go to Jail for Elder Abuse in California?
- What Can Be Done to End Elder Abuse?
- Is Elder Abuse a Social Issue Worldwide?
- What Increases the Chance of Elder Abuse?
- How Big Is the Problem of Elder Abuse in America?
- What Is the Role Theory of Elder Abuse?
- How Does Culture Affect Elder Abuse?
- What Are the Profiles of the Most Common and Least Common Perpetrators of Elder Abuse?
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 27). 90 Elder Abuse Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/elder-abuse-essay-topics/
"90 Elder Abuse Essay Topic Ideas & Examples." IvyPanda , 27 Feb. 2024, ivypanda.com/essays/topic/elder-abuse-essay-topics/.
IvyPanda . (2024) '90 Elder Abuse Essay Topic Ideas & Examples'. 27 February.
IvyPanda . 2024. "90 Elder Abuse Essay Topic Ideas & Examples." February 27, 2024. https://ivypanda.com/essays/topic/elder-abuse-essay-topics/.
1. IvyPanda . "90 Elder Abuse Essay Topic Ideas & Examples." February 27, 2024. https://ivypanda.com/essays/topic/elder-abuse-essay-topics/.
Bibliography
IvyPanda . "90 Elder Abuse Essay Topic Ideas & Examples." February 27, 2024. https://ivypanda.com/essays/topic/elder-abuse-essay-topics/.
- Caregiver Topics
- Delirium Essay Ideas
- Emergency Department Titles
- Dementia Research Ideas
- Gerontology Titles
- Alcohol Abuse Paper Topics
- Aging Ideas
- Discrimination Essay Titles
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Abuse of Older Persons
- Risk and Protective Factors
- Many older adults require care and are vulnerable to violence perpetrated by a caregiver or someone they trust.
- More research is needed to uncover the causes for, and solutions to, violence against older adults.
What is older person abuse?
Older person abuse is an intentional act or failure to act that causes or creates a risk of harm to an older adult. An older adult is someone aged 60 or older.
The abuse occurs at the hands of a caregiver or other trusted person. Common types of abuse include: 1
- Physical abuse is illness, injury, functional impairment, or death resulting from the intentional use of physical force. Examples include hitting, kicking, or pushing.
- Sexual abuse is forced or unwanted sexual interaction. Examples include unwanted sexual contact or penetration or non-contact acts such as sexual harassment.
- Emotional or psychological abuse refers to verbal or nonverbal behaviors that inflict anguish, fear, or distress. Examples include humiliation, threats, or harassment.
- Neglect is the failure to meet an older adult's basic needs. These needs include food, water, shelter, clothing, hygiene, and essential medical care.
- Financial abuse is the illegal, unauthorized, or improper use of money, benefits, property, or assets for the benefit of someone other than the older adult.
For more information about elder abuse definitions please see Elder Abuse Surveillance: Uniform Definitions and Recommended Core Data Elements .
Quick facts and stats
The older adult population is growing faster in the U.S. than are younger populations. The data underestimate the problem because the number of nonfatal injuries is limited to older adults who are treated in emergency departments. The information doesn’t include those treated by other providers or those that do not need or do not seek treatment. Additionally, many cases are not reported because the older adult is afraid or unable to tell police, friends, or family about the violence.
Abuse, including neglect and exploitation, is experienced by about 1 in 10 older adults who live at home. 2 From 2002 to 2016, more than 643,000 older adults were treated in the emergency department for nonfatal assaults and over 19,000 homicides occurred. 3
Compared with women, men had higher rates of both nonfatal assaults and homicides. 3 4 The rate for nonfatal assaults increased more than 75% among men (2002–2016) and more than 35% among women (2007–2016). The estimated homicide rate for men increased 7% from 2010 to 2016. 3 Compared to non-Hispanic Whites, non-Hispanic Black or African American persons, non-Hispanic American Indian/Alaskan Natives, and Hispanic or Latino persons have higher homicide rates (2002–2016). 3
Overall and firearm-specific older adult homicide rates increased between 2014 and 2017. Of the 6,188 victims, 62% were male. The perpetrator was an intimate partner in 39% of firearm homicides and 12% of non-firearm homicides. Common contexts of firearm homicides were familial or intimate partner problems, robbery or burglary, argument, and illness-related (e.g. the homicide was perpetrated to end the suffering of an ill victim, both victim and perpetrator had an illness, or the perpetrator had a mental illness). 4
Abuse can have several physical and emotional effects on an older adult. Victims are fearful and anxious. They may have problems with trust and be wary of others. 5
Many victims suffer physical injuries. Some are minor, like cuts, scratches, bruises, and welts. Others are more serious and can cause lasting disabilities. These include head injuries, broken bones, constant physical pain, and soreness. Physical injuries can also lead to premature death and make existing health problems worse. 4 5 6 7 8
Violence against older adults can be prevented. Certain factors may increase or decrease the risk of perpetrating or experiencing abuse. Preventing violence requires understanding and addressing the factors that put people at risk for or protect them violence.
We can all help prevent violence against older adults: 9
- Listen to older adults to understand their challenges and provide support.
- Educate yourself and others about how to recognize and report abuse.
- Learn how the signs of abuse differ from the normal aging process.
- Check-in on older adults who may have few friends and family members.
- Encourage or assist persons (caregivers or older adults) who have problems with drugs or alcohol in getting help.
It is also possible to provide over-burdened caregivers with support. This can include help from friends, family, or local relief care groups, adult day care programs, or counseling.
Knowledge about what works to prevent violence against older adults is growing. However, most prevention strategies and practices have not yet been rigorously evaluated to determine their effectiveness. In the absence of proven prevention strategies, program planners may consider the following sources to strengthen their approach: Applying the Principles of Prevention: What do Prevention Practitioners Need to Know About What Works and What Works in Prevention: Principles of Effective Prevention Programs .
Need to report abuse or find services for older adults?
- Hall JE, Karch DL, Crosby AE. Elder Abuse Surveillance: Uniform Definitions and Recommended Core Data Elements For Use In Elder Abuse Surveillance, Version 1.0. Atlanta (GA): National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2016. https://www.cdc.gov/violenceprevention/pdf/ea_book_revised_2016.
- Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, Muzzy W, Kilpatrick DG. (2010).Prevalence and Correlates of Emotional, Physical, Sexual, and Financial Abuse and Potential Neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health; 100:292–7. doi: 10.2105/AJPH.2009.163089 .
- Logan JE, Haileyesus T, Ertl A, Rostad WL, Herbst JH. Nonfatal Assaults and Homicides Among Adults Aged ≥60 Years – United States, 2002-2016. MMWR Morb Mortal Wkly Rep . 2019 Apr 5;68(13):297-302. doi: 10.15585/mmwr.mm6813a1.
- Shawon, R, Adhia, A, DeCou, C et al. (2021). Characteristics and patterns of older adult homicides in the United States. Inj. Epidemiol. 8(5). https://doi.org/10.1186/s40621-021-00299-w.
- Anetzberger, G. The Clinical Management of Elder Abuse. New York: Hawthorne Press, 2004.
- American Medical Association white paper on elderly health. Report of the Council on Scientific Affairs. (1990). Archives of internal medicine , 150 (12), 2459–2472.
- Lachs MS, Williams CS, O'Brien S, et. al. (1998). The Mortality of Elder Mistreatment. Journal of the American Medical Association; 280:428-32. doi: 10.1001/jama.280.5.428.
- Lindbloom EJ, Brandt J, Hough L, Meadows SE. (2007). Elder Mistreatment in the Nursing Home: A Systematic Review. Journal of the American Medical Directors Association ; 8(9):610-16. doi: 10.1016/j.jamda.2007.09.001.
- Fearing G, Sheppard CL, McDonald L, Beaulieu M, Hitzig SL. (2017). A systematic review on community-based interventions for elder abuse and neglect. J Elder Abuse Negl .; 29(2-3): 102-133. doi: 10.1080/08946566.2017.1308286.
Abuse of Older Persons
The abuse of older persons is a serious public health problem in the United States. CDC works to understand the problem of elder abuse and prevent it.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Violence against older women: A systematic review of qualitative literature
Sarah r. meyer.
1 Department of Sexual and Reproductive Health and Research, World Health Organization, Geneva, Switzerland
Molly E. Lasater
2 Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States of America
Claudia García-Moreno
Associated data.
All relevant data are within the manuscript and its Supporting Information files.
The majority of the existing evidence-base on violence against women focuses on women of reproductive age (15–49), and globally there is sparse evidence concerning patterns of and types of violence against women aged 50 and older. Improved understanding of differing patterns and dynamics of violence older women experienced is needed to ensure appropriate policy or programmatic responses. To address these gaps in the evidence, we conducted a systematic review of qualitative literature on violence against older women, including any form of violence against women, rather than adopting a specific theoretical framework on what types of violence or perpetrators should be included from the outset, and focusing specifically on qualitative studies, to explore the nature and dynamics of violence against older women from the perspective of women. Following pre-planned searches of 11 electronic databases, two authors screened all identified titles, abstracts and relevant full texts for inclusion in the review. We extracted data from 52 manuscripts identified for inclusion, and conducted quality assessment and thematic synthesis from the key findings of the included studies. Results indicated that the vast majority of included studies were conducted in high-income contexts, and did not contain adequate information on study setting and context. Thematic synthesis identified several central themes, including the intersection between ageing and perceptions of, experiences of and response to violence; the centrality of social and gender norms in shaping older women’s experiences of violence; the cumulative physical and mental health impact of exposure to lifelong violence, and that specific barriers exist for older women accessing community supports and health services to address violence victimization. Our findings indicated that violence against older women is prevalent and has significant impacts on physical and mental well-being of older women. Implications for policy and programmatic response, as well as future research directions, are highlighted.
Introduction
Violence against women is a major public health problem, a gender inequality issue and a human rights violation. There are significant serious and long-lasting impacts of violence on women’s physical and mental health, including injuries, unintended pregnancy, adverse birth outcomes, abortion (often in unsafe conditions), HIV and sexually transmitted infections, depression, alcohol-use disorders and other mental health problems [ 1 – 5 ]. The 2030 Sustainable Development Goals [SDGs] include as one of their targets (5.2) under Goal 5 on gender equality, the elimination of all forms of violence against women and girls. Indicator 5.2.1, measuring intimate partner violence [IPV]: Proportion of ever-partnered women and girls aged 15 years and older subjected to physical, sexual or psychological violence by a current or former intimate partner in the previous 12 months, is proposed to track the measurement of progress in achieving this goal. The indicator does not include an upper age limit, and data on older women (aged 50 and above), including but not limited to intimate partner violence, are needed to support national and global monitoring of violence against women of all ages, including for monitoring of the SDGs.
The majority of existing violence against women surveys and data have focused on women of reproductive age (15–49), as they suffer the brunt of intimate partner violence and non-partner sexual violence [ 6 ]. A growing number of surveys are now including women older than 49 years, however globally there is sparse evidence concerning patterns of and types of violence against women aged 50 and older, and limited understanding of barriers to reporting and help-seeking amongst older women who are subjected to violence [ 7 ]. Compared to women of reproductive age, women aged 50 and above may experience different relationship dynamics which influence forms of abuse [ 8 , 9 ], and some evidence indicates that older women experience different types of violence, for example, psychological violence and verbal abuse, compared to younger women’s experiences of physical and sexual violence [ 10 ]. For older women, recent exposure to violence may be interlinked with violence victimization at different stages of the life-course [ 11 , 12 ]. Dynamics of ageing may shape experiences of violence, for example, provision of care to a dependent partner may influence decisions to disclose or report abuse [ 10 ]. They are also more likely to experience violence from other family members, including children, and from carers. Currently, the evidence-base of qualitative and quantitative data concerning violence against older women is limited, and a better understanding of these differing patterns and dynamics is needed to ensure appropriate policy or programmatic responses to violence against older women and service development and provision for older women affected by violence [ 10 , 11 ]. To address these gaps in the evidence, we conducted a systematic review of qualitative literature on violence against older women.
Current frameworks on violence against women and existing evidence
Gaps in research and evidence stem in part from conflicting theoretical approaches, definitions and conceptual frameworks concerning violence against older women. The dominant theoretical frameworks are the older adult mistreatment framework and older adult protection framework [ 7 , 13 , 14 ]. The older adult mistreatment framework conceptualizes violence against older women as a form of elder abuse, focusing on age as the primary factor influencing vulnerability to exposure to violence. The older adult protection framework specifically understands violence within the context of care-giving and institutional arrangements, where older adults’ often be gender neutral, and the adult protection framework can result in a framing of older adults as inherently impaired and vulnerable. In addition, the IPV framework primarily understands vulnerability to violence in terms of gender inequality and partnership dynamics, which may neglect analysis of how ageing and partner violence intersect. These differing frameworks inform multiple aspects of research, including study design, data collection and analysis, and reporting, resulting in fragmented data and evidence. For example, some research utilizing the older adult mistreatment framework lacks a focus on the gendered dimensions of violence [ 14 , 15 ], and other studies have solely focused on women in institutional settings, neglecting measurement of violence perpetrated by intimate partners and other family members [ 13 ].
Existing syntheses of evidence on violence against older women often reflect these differing conceptual frameworks. Employing an older adult mistreatment framework, a systematic review of quantitative studies of elder abuse (against men and women aged 60+) found that the global prevalence of elder abuse in community settings is 15.7% in the past year, with psychological abuse and financial abuse as the most prevalent forms of abuse reported [ 16 ]. This review reported prevalence by type of violence, but did not report on perpetrators. Analysis of studies conducted in institutional settings found women, aged 60 and above, to be significantly more vulnerable to abuse, with psychological abuse as the most prevalent form of violence, followed by physical violence, neglect, financial and sexual abuse [ 17 ]; this analysis included data reporting staff-to-resident abuse. Analysis of quantitative data of women aged 60 and above in the systematic review of quantitative studies of elder abuse found a global prevalence of elder abuse against women of 14.1% in the past year, with psychological abuse reported as the most prevalent form of violence, followed by neglect [ 16 ]. The focus of this review was prevalence of different sub-types of violence, and type of perpetrator was not considered. Another systematic review of quantitative data on interpersonal violence (physical and/or sexual violence) against older women (aged 65 and above) in community dwellings primarily employed an IPV framework, finding prevalence of reported interpersonal violence ranged from 6 to 59% over a lifetime, from 6 to 18% since turning 50, and 0.8 to 11% in the past year, however, results indicated that definitions of violence vary widely and affect prevalence estimates [ 18 ]. Syntheses of quantitative literature have identified prevalent forms of violence against older women, highlighting limitations in the evidence-base due to variations in definitions and methodology, and a primary emphasis on populations in high-income, Western countries. These reviews have captured a wide range of types of violence, however, have not considered type of perpetrators or patterns of co-occurring types of violence.
Alongside these systematic reviews of quantitative data, some reviews have included qualitative and mixed methods studies. An empirical review of IPV in later life examined 27 quantitative, 22 qualitative and 7 mixed-methods studies, finding that forms of IPV amongst older women in later life shifted from a higher prevalence of physical and sexual abuse during reproductive years, to a higher prevalence of forms of psychological abuse [ 19 ]. A review of qualitative research on IPV amongst older women identified a number of relevant themes, including patterns of abuse that were continuous and consistent with previous experiences of abuse in families of origin and previous relationships [ 20 ]. A systematic review and meta-synthesis of qualitative studies of IPV and older women focused on how previous exposure to IPV influenced health-seeking behaviours, specifically mental health care [ 21 ]. An empirical review of quantitative and qualitative studies of sexual violence against older people identified widespread variation in prevalence rates across studies, and a range of perpetrators, primarily intimate partners or adult children [ 22 ]. A recent narrative review of quantitative, qualitative and mixed methods studies of IPV against women aged 45 and above concluded that women’s “age and life transitions mean that they may experience abuse differently to younger women. They also face unique barriers to accessing help, such as disability and dependence on their partners” [ 23 ].
However, amongst these existing systematic reviews of qualitative literature, none have focused specifically on older women, while also being inclusive of any form of violence. In order to improve understanding of violence against older women, it is important to explore patterns, dynamics and experiences through examination of the qualitative literature. Qualitative data on violence against older women complements quantitative evidence not only by offering insight into lived experiences of older women subjected to violence, but also by expanding and clarifying types of violence, perpetrators, linkages to particular risk factors, and physical, mental and social impacts of violence against older women.
In the present review, we aimed to build on previous systematic reviews and strengthen the evidence-base by i) including studies and evidence focused specifically on women; ii) including any form of violence against women, rather than adopting a specific theoretical framework on what types of violence or perpetrators should be included from the outset; iii) focusing on women aged 50 and above (as many surveys often specifically focus on women of reproductive age, which is considered to be up to 49 years of age); and iv) focusing specifically on qualitative studies, to explore the nature and dynamics of violence against older women from the perspective of women. We aimed to identify, evaluate and synthesize qualitative studies from all countries, exploring violence against women aged 50 and above, identifying types and patterns of violence, perpetrators of violence, and impacts of violence on various outcomes for older women, including physical and mental health and social support, and women’s responses to experiences of violence. We include the following forms of violence: elder abuse, family violence and intimate partner violence. Elder abuse is defined as “single or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person” [ 24 ]. Intimate partner violence is defined as “behaviour by an intimate partner or ex-partner that causes physical, sexual or psychological harm, including physical aggression, sexual coercion, psychological abuse and controlling behaviours” [ 25 ]. Family violence is often used interchangeable with intimate partner violence, however, also encompasses abuse and violence perpetrated by other family members, for example, adult children or in-laws. While there is no universal agreed-upon definition of older women, for the purposes of this review, we define older women as women aged 50 and above, while recognizing that aging and age are social phenomenon, and definitions vary across organizations, cultures and communities. The protocol was pre-registered with PROSPERO, Registration Number: CRD42019119467, https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019119467 (see also [ 26 ]).
Search strategy
In this systematic review, we searched 11 electronic databases–PubMed, PsycINFO, Embase, CINAHL, PILOTS, ERIC, Social Work Abstracts, International Bibliography of the Social Sciences, Social Services Abstracts, ProQuest Criminal Justice and Dissertations & Theses Global, from 1990. We conducted searches that combined the following domains as part of the research question: 1) age (50 and above); AND 2) women; AND 3) violence; AND 4) qualitative methodology. For each of these domains, we identified the relevant keywords and search terms, which varied by database; the search strategy was appropriately modified for each database, including syntax and specific terms, topics and/ or headings. The search strategy for PubMed is included in S1 File . Searches were conducted in April 2018 and updated in July 2019. We did not limit the search by year of publication or language.
We also hand searched reference lists of relevant existing systematic reviews, which we identified both through background research and through the formal database searches, and reviewed relevant references (44 identified). We consulted with 49 experts on violence against older women or older adults, including researchers, practitioners and policy makers, from all regions globally. All experts were contacted and followed-up with a minimum of 2 contacts. 26 experts responded with 424 articles, 64 of which were duplicates. We reviewed the full text of 43 articles and ultimately included 2 in the full review. Grey literature was not systematically searched; grey literature submitted by experts was initially considered for inclusion, however, conducting comparable data extraction and quality assessment for grey literature alongside the peer-reviewed literature was not possible.
We identified 18 non-English language articles for full-text review. For 17 of these articles, we identified a native speaker external reviewer who was provided with inclusion and exclusion criteria and consulted with authors regarding final inclusion (4 Portuguese, 7 Spanish, 1 Hebrew, 1 Dutch, 1 German, 1 Danish, 2 French). One non-English article (in Farsi) was not reviewed as the research team could not engage a Farsi speaker to review the article. The external reviewers consulted with SRM to decide on inclusion of full texts, and conducted data extraction and quality assessment on 3 articles identified for inclusion (2 Spanish, 1 Portuguese) [ 27 – 29 ].
Study selection and data extraction
After removing duplicates, study selection proceeded in two stages: in the first stage, two authors (SRM and MEL) reviewed titles and abstracts of all identified manuscripts. We included studies that met the following criteria: i) focused on women aged 50 and older, ii) employed qualitative methodology, and iii) focused on women’s experiences of any type of violence perpetrated by any type of perpetrator. Studies including men or also including women aged younger than 50 were included if specific and separate sex and age-specific analyses were included. We included studies employing any type of qualitative methodology, and mixed methods studies were included if qualitative data was presented separately. Studies were excluded if the whole sample was children, adolescents or adults under the age of 50; if the sample only included men; if the methodology was quantitative, or in the case of mixed methods studies, if the qualitative results were not separately presented, and if the data only included the perspectives on violence against women as reported by care providers, health professionals, legal professionals and nursing home managers.
After the first stage of title and abstract review, we reviewed the full text of any manuscript considered relevant by either of the authors. In the second stage, two authors (SRM and MEL) independently reviewed all articles selected for full text review for eligibility, to reach consensus on inclusion. Any discrepancies were resolved with the input of an external reviewer. Fig 1 indicates the full search and study selection process.

From : Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi: 10.1371/journal.pmed1000097 . For more information, visit www.prisma-statement.org .
We designed a data extraction Excel spreadsheet specifically for the purposes of the review, including characteristics of included studies (location of the research, research question), methodology (conceptual framework or theoretical approach, data collection methods, data analysis methods, sampling), characteristics of the sample (inclusion and exclusion criteria, brief description of the sample), types and nature of violence (context of violence, perpetrator and brief description of impacts of violence). We extracted main findings, participant quotations where possible, and study limitations, if reported. Data extraction was conducted by one author (MEL), and checked for accuracy by a second author (SRM), with discrepancies resolved by discussion to reach consensus.
Quality assessment
All included studies were assessed for quality using an adapted version of the Critical Appraisal Skills Programme [CASP] scale. The adapted scale included the following questions [ 30 ]:
- Was there a clear statement of the aims of the research?
- Is a qualitative methodology appropriate?
- Are the setting(s) and context described adequately?
- Was the research design appropriate to address the aims of the research?
- Is the sampling strategy described, and is this appropriate?
- Is the data collection strategy described and justified?
- Is the data analysis described, and is this appropriate?
- Are the claims made/findings supported by sufficient evidence?
- Is there evidence of reflexivity?
- Does the study demonstrate sensitivity to ethical concerns?
Two authors (SRM, MEL) assessed the quality of the studies, assigning a 1 for each affirmative response and 0 for each negative response, for a final score out of 10. Disagreement was resolved by discussion between the two authors. Quality assessment was not used to determine if any studies should be excluded, but rather to assess the strength of each study.
An Excel spreadsheet to compile all relevant findings and quotations from the studies for thematic analysis was developed. Two of the authors (SRM and MEL) coded the main findings extracted from each study. We used line-by-line coding on a sub-set of articles, developing a set of over-arching themes and sub-themes for a draft codebook. The coding proceeded as an iterative process, with the two authors each separately coding the main findings using the draft codebook, discussing coding results, and refining the codebook based on overlap and redundancies identified. After all data were coded, we tallied all occurrences of each code and further explored areas of overlap and merged sub-themes with low numbers of codes, finalizing the broad themes and focused sub-themes. For non-English articles included, the external reviewer translated primary quotations into English and thematic analysis on these articles was conducted alongside the English language articles.
The synthesis and all aspects of the systematic review process are reported following the 21-item checklist provided in the Enhancing Transparency in Reporting the Synthesis of Qualitative Research statement [ 31 ] and the PRISMA checklist [ S2 and S3 Files].
Studies identified and characteristics
Our searches of 11 databases yielded 9318 articles, with an additional 468 articles identified through cross- referencing and expert recommendation. After removing duplicates, 7834 articles remained. We identified 417 articles that were potentially eligible and included in full text screening. Two of these articles had not yet been published. Additionally, 1 Farsi language study was unable to be translated and assessed against the selection criteria. Fifty-two articles met criteria for inclusion in this systematic review ( Fig 1 ). The 52 included articles represent data from 31 studies.
Overview of study characteristics
Study setting ( table 1 ).
Most studies were conducted in high-income countries (HIC), including the United States of America (n = 16), Israel (n = 12), Canada (n = 7), the United Kingdom (n = 4), Hong Kong (n = 2), and Australia (n = 1). Six articles were from upper-middle income countries–Brazil (n = 3), Mexico (n = 2) and Iran (n = 1); and three articles were from low-income countries–Uganda (n = 1) and Ethiopia (n = 2). One article came from India, a lower-middle income country.
Application of the adapted version of CASP scale yielded variable results across the 52 articles assessed [see Table 2 ]. Ratings of research methodology, statement of research aims and selection of appropriate research design were overall high. The majority (46 articles) [ 29 , 32 – 76 ] gave support for research findings with references to primary data (participant quotations, case study vignettes, case file excerpts). Ten articles [ 41 , 46 , 49 , 50 , 59 , 65 , 77 – 80 ] lacked data analysis descriptions.
Only 12 articles [ 29 , 35 , 38 – 40 , 45 , 51 , 58 , 72 – 74 , 79 ] reflected on the relationship between the researchers and the participants (reflexivity). Procedures for ethical research were described in 36 articles [ 27 , 29 , 33 – 37 , 39 – 41 , 45 – 52 , 54 , 55 , 58 , 60 , 61 , 63 , 64 , 66 – 72 , 74 , 76 , 77 , 79 ]. Five articles [ 43 , 44 , 56 , 73 , 75 ] described obtaining consent, but lacked descriptions of ethical approval, and 10 articles [ 32 , 38 , 42 , 53 , 57 , 59 , 62 , 65 , 78 , 80 ] lacked descriptions of both ethical approval and obtaining consent. A significant number of articles [ 32 , 34 – 42 , 45 – 47 , 49 – 51 , 53 , 54 , 56 , 57 , 59 , 61 – 66 , 69 , 70 , 72 – 75 , 77 – 79 ] lacked adequate descriptions of the study setting and context.
Descriptions and patterns of types of violence
Older women described IPV, family violence and elder abuse of various types, perpetrated by a range of perpetrators [ Table 1 ]. Among the specific types of violence reported in the articles in this review, across IPV, elder abuse and family violence, physical violence was most frequently reported [ 27 , 32 – 54 , 57 , 60 – 63 , 66 , 69 – 80 ], followed by emotional/ psychological [ 28 , 32 , 36 – 39 , 41 – 51 , 53 , 54 , 56 , 60 – 62 , 66 – 80 ], economic/ financial [ 34 – 36 , 39 , 41 , 43 – 45 , 48 – 50 , 61 , 62 , 64 , 68 , 71 , 72 , 74 – 78 ], sexual [ 27 , 33 , 34 , 40 , 42 , 49 , 50 , 54 , 57 , 59 , 60 , 67 , 72 , 74 – 76 , 80 ], verbal [ 32 , 40 , 45 , 52 , 62 , 68 – 70 , 73 , 77 ], controlling behaviors [ 45 , 48 , 49 , 51 , 53 , 64 , 67 , 70 , 76 , 77 ], and lastly, neglect [ 28 , 35 , 39 , 61 , 62 , 68 , 71 , 76 ].
Older women’s experience of IPV was the most frequent form of violence reported (42 articles) [ 27 , 29 , 33 , 34 , 36 – 38 , 40 – 42 , 45 – 56 , 59 – 65 , 67 – 80 ]. Older women described on-going instances of neglect, verbal abuse and financial exploitation in a study conducted in India [ 41 ], in other cases, physical violence characterized earlier and on-going experiences of violence within intimate partner relationships [ 37 , 40 , 47 , 54 ]. IPV in particular was described by older women as occurring throughout different stages in the relationship, spanning their youth and into older age. Older women often experienced an escalation of IPV and controlling behaviors despite the age and/ or illness of their partner [ 36 , 40 , 46 , 61 , 69 , 77 ]. Changing relationship dynamics due to ageing–including a husband’s retirement, children leaving the home, women wanting to engage in activities outside of the home, or diagnosis of a chronic or terminal illness–triggered escalating IPV [ 36 , 40 , 46 , 47 , 56 , 69 ]. Shifts in types of violence, from predominantly physical violence to predominant psychological abuse and neglect, were commonly described in studies that encompassed previous and on-going IPV [ 34 , 51 ]. Studies focused on IPV commonly described both previous and on-going violence, and a smaller number described only or primarily violence experienced while aged 50 or above [ 64 , 69 ].
Violence occurring within the family was discussed in 15 articles [ 35 , 39 , 43 , 44 , 46 , 48 , 49 , 55 , 63 , 66 , 68 , 69 , 71 , 76 , 79 ], with perpetrators including family members not including children [ 27 , 43 , 44 , 48 , 49 , 59 , 63 , 68 , 69 , 71 ] and adult children [ 35 , 39 , 48 , 66 , 76 , 79 ]. Studies captured instances of physical and verbal aggression by mentally ill adult children against older women [ 66 ], violence enacted by elderly with dementia against older women who were caregivers [ 46 ], and forms of neglect, financial exploitation and emotional abuse enacted by family members, including children [ 44 ]. The majority of these studies focused on violence experienced in older age, while one study explored dynamics of abuse between children and mothers across the lifespan [ 35 , 39 ].
10 articles reported on experiences of elder abuse [ 28 , 32 , 35 , 43 , 44 , 55 , 57 – 59 , 78 ] with perpetrators including community members [ 43 , 44 ], caregivers [ 57 , 59 ], nursing home residents [ 58 ] and health care providers [ 28 ]. Types of elder abuse included verbal abuse, physical assault and inappropriate sexual advances [ 58 ] and sexual assault [ 59 ].
Financial control spanned instances of elder abuse, family violence and IPV [ 43 , 53 , 62 , 64 , 76 , 78 ], and was described as co-occurring with and resulting in other forms of violence. Financial exploitation could result in emotional and/ or physical violence if older women resisted control [ 62 , 64 ]. An older woman explained that in the context of her relationship with her husband, “If I did not follow his control [over money], he would be verbally abusive” [ 64 ].
Themes and sub-themes identified through coding are displayed in Table 3 .
Intersection of ageing and violence
A number of sub-themes emerged emphasizing the interconnections between the experience of ageing amongst older women, and dynamics, impacts, experiences and perceptions of violence.
Suffering, loneliness, regret and guilt
Older women emphasized suffering, loneliness, regret and guilt in their accounts of living and coping with violence, particularly psychological violence [ 34 , 37 , 38 , 40 , 42 , 44 , 45 , 47 , 50 – 52 , 54 , 56 , 62 , 66 , 75 , 78 , 79 ]. Within the context of IPV, women described experiences of loneliness in terms of detachment from family members, including abusive partners and adult children, who often criticized older women’s responses to violence [ 33 , 34 , 37 , 38 , 40 , 42 , 56 ]. Respondents linked regret with time and age, emphasizing previous decisions, lost opportunities, and wasting time due to living with an abusive partner [ 33 , 34 , 37 , 45 ]. One respondent said, “I was an idiot woman. No woman lives like that, cooking and serving him after the beating… I say that I was an idiot” [ 42 ]. Older women expressed feelings of guilt over the abuse they experienced, and regret and guilt for exposing their children to violence [ 38 , 45 , 50 , 52 , 54 , 66 , 79 ]. Several studies linked suffering, regret and loneliness specifically to psychological violence, which was described as more prominent in older age, pervasive and damaging to social relationships and self-esteem [ 51 , 56 ]. The studies that explored these themes primarily encompassed accounts of violence experienced throughout intimate relationships–while women were younger and through to older age. These experiences were described and conceptualized by older women as interlinked and continuity of victimization by intimate partners was emphasized, rather than viewing women’s experiences of violence in older age as distinct or separate.
Violence, ageing and vulnerabilities
Older women described that ageing diminished their physical and emotional capabilities to cope with experiences of violence [ 33 , 37 , 39 , 47 ]. This sub-theme appeared in 12 manuscripts [ 33 , 37 , 39 , 40 , 43 , 47 , 48 , 53 , 55 , 59 , 62 , 76 ] and was expressed in relation to various forms of violence–IPV [ 33 , 37 , 47 ], including violence perpetrated by a spouse due to dementia [ 40 ], violence in the context of a new relationship or second marriage [ 48 , 53 , 55 , 59 , 62 ], violence perpetrated by a mentally ill child [ 39 ], violence perpetrated by children-in-law [ 76 ], and elder abuse [ 43 ]. These studies primarily focused on current experiences of violence of older women, as changes in physical and emotional capacity to cope was described in relation to present victimization. As a result of diminishing physical and cognitive capacities of ageing, old women experienced vulnerabilities and dependency dynamics–with partners, adult children and caregivers–that exposed them to situations of abuse [ 44 , 47 , 52 , 56 , 57 , 61 , 64 , 66 ]. A mother of an adult son with schizophrenia explained, “When I was younger, I could overcome him faster, save myself, now that I’m old and I have diabetes, now I have to be faster… Now I’m afraid for my life, afraid he will kill me” [ 39 ]. Women reported that lack of financial autonomy, often compounded by years of controlling behaviors perpetrated by a violent spouse, was a central factor in women remaining in abusive spousal, caregiving and family relationships [ 44 , 47 , 52 , 56 , 64 ].
Perpetrator-related factors
Some included studies reported on perpetrator-related factors that initiated or exacerbated forms of violence against older women.
Ageing perpetrators and continuity of abuse
Older women emphasized contexts surrounding IPV in which the perpetrator continues to exercise control, power, and violence, despite their failing health and old age [ 41 , 47 – 49 , 51 , 56 , 59 , 72 , 76 , 77 ]. Women also described shifting forms of violence, predominantly from physical and/ or sexual to psychological violence and controlling behaviours [ 36 , 45 , 50 , 51 , 61 , 72 ]. While sometimes the experience of physical and/ or sexual violence declined, psychological violence persisted and sometimes escalated [ 50 , 51 , 72 ]. While describing the impacts of continual and intense psychological violence, one woman said, “he destroys you; you are not even a person anymore” [ 72 ]. Controlling behaviours were also experienced in the context of cultural norms; for example, in a study of Sri Lankan immigrant women in Canada, older women described forms of control enacted by children and children-in-law. One older women reported, “[h]e [the son-in-law] thinks that I am a widow and why should I have anything on my own name and why can’t I give everything to them and just be a slave to them” [ 76 ].
Perpetrator’s illness as a cause of violence
This sub-theme only emerged in three manuscripts [ 40 , 46 , 69 ], however, it is the only instance among the included studies in which older women described first or new experiences of IPV in older age. Older women who provided care for spouses with dementia reported aggressive behavior, physical violence, and verbal abuse [ 40 , 69 ]. In one study, a woman reported, “I don’t know what’s going on with my husband, he’s never been like that, never hit me before. I’m really worried about him, he’s been changing so much […] We have been married for 47 years…he seems another person [ 46 ].” Another study found that women who had experienced lifelong IPV understood dementia-related violence as a continuation of aggression, dominance and abuse, whereas women who had only been exposed to dementia-related violence took solace in a diagnosis, felt grief over the loss of their spouse as he used to be, and tried to maintain intimacy and affection in a previously caring and loving relationship [ 40 ].
Social and gender norms regarding response to violence
Older women described the ways in which social and gender norms shaped their experiences of and responses to violence.
Silence, stigma and family
Descriptions of social and gender norms that encouraged women to stay in abusive marriages and prioritize children’s needs above their own were common across studies [ 33 – 35 , 38 , 40 – 42 , 46 , 48 , 57 , 65 – 69 , 71 , 73 – 76 , 79 , 80 ]. Older women described several social norms that shaped their past decisions in response to violence including: silence surrounding violence and the reporting of violence [ 41 , 80 ], fears of shame and stigma related to leaving a marriage [ 65 , 69 , 73 ], and ideals of being a good mother by putting up with violence for the sake of her children [ 38 , 42 , 74 ]. One woman explained, “There was violence along with suffering for many years;…but I had a goal behind all this suffering, to have my children grow, get married and get an education…. I don’t know if the suffering was worthwhile for me, I don’t know if it was worthwhile as it was very difficult” [ 42 ]. Remaining in a relationship as a strategy was often employed due to older women feeling obligated to care for an abusive partner who was now sick or unable to live alone [ 33 ]. One respondent explained, “If I leave him, it’s not good. My conscience won’t allow it. At his age, 76, it’s not nice to leave and neglect him. I don’t have feelings for him (because of the violence). I respect him because he’s old and because he’s my husband, I have to care for him” [ 33 ]. These studies primarily focused on previous and current experiences of violence; social norms predominant when women were younger shaped prior and current responses, while one study of Sri Lankan immigrant older women focused on social norms governing current decisions relating to women’s responses to abuse from children and children-in-law [ 76 ].
In several cases, remaining in the relationship was a coping mechanism of last resort, given the multiple barriers present to women leaving the relationship, whether with an intimate partner, other family member or caregiver [ 48 ]. Women also described strong beliefs in social norms that supported staying with a sick or frail abusive partner or abusive child [ 33 , 35 , 40 , 46 , 57 , 66 , 76 ]. Many women viewed seeking help and confiding in others as embarrassing and unacceptable; one woman explained, "I was ashamed. I just didn’t want to admit that’s the situation I was in" [ 80 ].
Perceptions of abuse and violence as normal
In some of the included manuscripts, older women perceived violence as normal, sometimes explaining that they preferred not to term their experiences as abuse or violence [ 32 , 41 , 55 , 70 , 71 , 74 , 75 ]. Older women infrequently perceived verbal and emotional abuse as violence [ 32 ], and some women did not identify as a victim of violence [ 55 , 71 ]. One woman described her process of realizing that her experiences were forms of abuse, “Well, I really didn’t recognize it as abuse. And as soon as I got that message, I felt that I got on a very clear track….Now, I know what I’m dealing with and I can do something about it” [ 74 ]. Moreover, service providers and the legal system, often failed to recognize financial exploitation or verbal abuse as abuse [ 41 , 74 ], or that older women could be affected by IPV [ 75 ]. In rural Kentucky, USA, older women explained that the longer they were in the relationship with their abuser, the more the violence became more normalized and accepted [ 70 ]. Studies also emphasized how ageist attitudes normalizes forms of coercive control, enabling abusers to take advantage of older women’s age, frailty, and illness, for example, appropriating part or all of the victims’ property [ 43 , 44 , 57 ].
Lifelong IPV
Many older women described experiences of IPV throughout their life-course. Several sub-themes were identified related to lifelong patterns of violence, cumulative consequences of IPV, and linkages of violence in older age to earlier experiences of violence.
Continuation of patterns of IPV in old age
Older women described experiences of IPV in older age as a continuation of the patterns of violence experienced throughout the relationship [ 33 , 40 , 49 , 59 , 70 – 72 , 77 ]. Several articles described years to decades long relationships characterized by IPV [ 40 , 70 , 71 , 77 ]. For example, older women living in rural Kentucky, USA explained that the longer they were in the relationship with their abuser, the more the violence became more normalized and accepted [ 70 ].
Earlier experiences of violence
Associations between older women’s earlier experiences with violence, including witnessing of violence as a child, and current experiences of IPV, were discussed in several articles [ 48 , 49 , 61 , 70 , 71 , 80 ]. For example, in a study by Roberto and colleagues, many women who had experienced physical abuse as a child or young woman interpreted controlling behaviors as love, and did not recognize emotional abuse later in life until the abuse became physical or affected their health [ 61 ]. Linkages were also uncovered between experiences of abuse as a child or young woman with current abuse by their adult children [ 57 , 71 ].
Cumulative impacts of violence
Older women described several consequences of experiences of lifelong IPV. In one study, older women related the impacts of lifelong violence to that of a chronic illness, which alters or limits one’s quality of life [ 47 ]. Older women frequently linked experiences of violence with physical health consequences, including bodily pain, reduced mobility, and hearing problems, [ 37 , 47 , 54 , 67 ], as well as mental health and emotional impacts, including depression [ 41 , 50 , 51 , 54 , 67 ], anxiety [ 54 , 67 ], panic attacks [ 54 ], suicidal ideation [ 41 ], loneliness [ 34 , 51 ], and loss of self-esteem [ 34 , 50 , 51 , 54 ].
Needs of older women affected by violence
Older women who reported exposure to violence described various needs in terms of social support, access to services, and issues accessing these services due to their age.
Social and community support
Older women commonly described isolation from family and friends, and a lack of social and community support as a result of violent and controlling behaviors from an intimate partner [ 41 , 45 , 52 , 64 , 65 , 75 – 78 ]. One older woman stated: “I cannot remember, not one time, not having the hell beat out of me. Black and blue, I wasn’t even allowed outside. I couldn’t open my mouth, I couldn’t talk, I couldn’t have friends. I had neighbors, and they didn’t know me …He threatened to kill me if I ever told anyone what was going on” [ 70 ]. Additionally, factors that were reported to impede access to social and community support included being an immigrant with limited language skills [ 67 , 68 , 76 ], and living in rural areas with strong norms against reporting IPV [ 52 ].
Barriers to accessing services
Several articles identified specific barriers for older women to access services and for health care utilization, including lack of awareness of services [ 52 , 54 , 55 , 57 , 74 , 76 ]. Older women reported several concerns when interacting with health care providers, including health care providers’ assumptions that older women could not be experiencing violence due to their age, minimization of forms of abuse common to older women, and lack of confidentiality when using the same provider as their spouse [ 74 ]. One respondent explained, "And when you go to the doctor…they run down the list…and then it’s always, you know, “Well, is it abuse?” “Well, yes emotional.” “Well, what kind of emotional?” “Verbal.” “Oh, OK.” And they mark it, and that’s it” [ 74 ].
Coping mechanisms
Older women reported various approaches to coping with the experience and impacts of different forms of violence, often employing several different coping mechanisms such as leaving relationship with an abuser and emotion-based coping strategies such as alcohol or drug usage, in order to navigate difficult decisions, maintain their health and well-being, and protect other family members in the context of exposure to violence.
Leaving a relationship
In 11 of the included manuscripts older women described remaining in an abusive relationship, family context or caregiver relationship, as a form of coping [ 33 , 34 , 38 , 42 , 45 , 46 , 48 , 57 , 65 , 70 , 73 ], and in six manuscripts, leaving a relationship was employed as a coping mechanism [ 42 , 45 , 61 , 69 , 76 , 77 ]. In one study, older women explained that they had previously not been able to leave a relationship with an intimate partner for the sake of their children, whereas once their children had left the house, they felt freer to reject violent behavior [ 42 ]. Older women’s own health problems were described as a trigger for choosing to leave an abusive relationship [ 61 ].
Isolation, substance use and emotion-based coping strategies
Older women described isolating themselves from family, friends and social support, using alcohol or drugs to cope with experiences of violence, and reframing experiences of violence, often through minimizing experiences [ 33 , 34 , 37 – 39 , 47 , 50 , 51 , 61 , 68 , 69 , 73 , 79 ]. Older women explained that if they were to seek support, family or friends would blame them for their experiences of violence, leading women to choose social isolation as a coping strategy [ 50 , 69 ]. Older women also described using drugs and alcohol as a means to numb themselves to their daily experiences of violence [ 50 ]. One woman explained, “He (my husband) got his medical partner to prescribe Valium for me in the 1970’s and I am still taking it, especially when I feel hopeless and in despair. I know that I am addicted to it and worry that at 68 years I will never be able to survive without them.” [ 50 ]. Older women also reported employing forgiveness of violent and controlling intimate partners as a coping mechanism [ 34 , 38 ]. Older women who remained in a relationship with their abuser often described employing emotional detachment as another coping strategy [ 33 , 37 , 47 , 69 ]. Lastly, older women described how they reframed their experiences of abuse, by excusing abusive spouses for their actions or employing strategies to deliberately diminish the severity of abuse, such as forgetting experiences of abuse [ 34 , 38 , 61 , 68 , 73 ]. While emotional detachment was described as causing isolation and loneliness, older women also perceived it as a form of “inner resistance” [ 37 ], a vital means of opposing intimacy and connection with an abusive partner, and as particularly vital in the case of IPV, where the safety of a woman’s home is threatened by violence [ 47 ].
Behaviors to enhance safety
Older women described taking actions in order to enhance their own safety in the face of violence [ 36 , 67 , 69 , 70 , 75 ]. In some instances, older women first called police or applied for formal legal support, such as a protection order, in the face of violence. In one study, a woman explained, “I called the police because he [my partner] pushed me down on the countertop and poured a cup of tea over me. It was as though he wanted to strangle me. They took him into custody for 24 hours” [ 36 ]. In several instances, legal authorities, including police, provided limited support, leaving women unable to find long-term solutions to the violence they experienced [ 70 ].
This systematic review was motivated by a need to improve understanding of similarities and differences in dynamics, patterns and experiences of violence against older women, in a context whereby the vast majority of research, evidence, policy and service provision is targeted towards women of reproductive age. We reviewed available qualitative studies on violence against older women in order to address existing gaps in evidence and data. We also sought to provide insight into the lived experiences of older women experiencing violence, and an understanding of the types and patterns of violence, perpetrators of violence, and health impacts of violence among older women. The included studies primarily address IPV, with fewer emerging from the older adult mistreatment framework. Most research examined specific types of violence in isolation, for example, IPV or abuse from an adult child, and there were no examples of studies that included polyvictimization or experiences of any type of violence against older women. The strong emphasis on older women’s experiences of IPV gives voice to the experiences of older women subjected to violence and shows how it can persist over time; however, some sites, perpetrators and types of violence against older women may be excluded from view, including that of violence enacted by other family members and non-family caregivers and of women living in institutional care.
The findings in our review confirm results from prior reviews, systematic and otherwise, of similar bodies of literature. For example, Pathak et al.’s review of IPV against older women noted a decline in physical violence against older women, whereas other forms of violence remained stable or increased, a finding that was reflected in our data [ 23 ]. Some of the studies included in the present review also confirm partners’ retirement and children leaving home as precipitating factors for increase of IPV against older women, indicating points for potential intervention and support for older women. In a review of qualitative literature on IPV against older women, Finfgeld-Connett noted that older women actively choose coping strategies that enable them to “make the best of their situations” [ 20 ], a conclusion that is also supported by some of the results of our review. In other cases, staying in a relationship with an abuser appears to be driven by gender norms and feelings of duty towards a partner. In addition [ 34 , 38 ], coping strategies such as use of alcohol and other harmful substances appeared to result in poor health and lack of well-being [ 34 , 37 – 39 , 47 , 50 , 51 , 61 , 68 , 69 , 73 , 79 ]. Recurring themes emphasizing the pervasive impact of violence against older women on physical and mental health, relationships, social networks, hope and sense of well-being, in our systematic review and other previous reviews, indicate the importance of taking violence against older women, in all its manifestations, seriously as a public health and human rights issue. As was identified in previous reviews, there is relatively little evidence concerning the emergence of violence in later life, particularly in the case of IPV. In the case of the majority of studies included in our review, older women described shifting but continuous patterns of violence throughout the life-course, although a small sample of studies identified new relationships and dementia of an intimate partner as factors precipitating the violence [ 40 , 46 , 48 , 53 , 55 , 59 , 62 , 69 ].
Comparing the IPV-specific evidence generated in this review to the existing evidence-base on IPV against women of reproductive age, some notable continuities and differences are evident. Firstly, our findings confirm the extensive impact of IPV exposure on physical and mental health, which has been widely researched amongst women of reproductive age [ 2 , 82 – 85 ]. However, our data indicate that IPV amongst older women is commonly experienced in the context of exposure to lifelong IPV, and that the physical and mental health impacts are cumulative, compounded by ageing processes, and often exacerbated by changes in social situation also triggered by ageing. Ability to employ physical or cognitive coping mechanisms that had been effective earlier in life may diminish for older women [ 33 , 37 , 39 , 47 ]. In addition, alongside depression, anxiety and post-traumatic stress disorder, which are the most commonly measured and reported mental health impacts of IPV amongst women of reproductive age [ 86 – 88 ], older women discussed hopelessness and regret as pervasive and important psychosocial impacts of IPV in older age. There may be some similarities between younger women’s experiences of shame and stigma [ 89 – 93 ] and older women’s feelings of regret, however, regret and hopelessness may be specifically central to older women’s experiences of violence, particularly IPV. Secondly, our results confirm that exposure to IPV is often linked to experiences of violence in childhood; older women in studies included in this review indicated that growing up in families where violence was commonly witnessed and experienced was interlinked with exposure to IPV in adulthood and through to older age, a finding that is evident in data on women of reproductive-age [ 94 – 96 ]. Thirdly, there appear to be common challenges for women of reproductive age and older women in leaving an abusive relationship, including perceptions of the importance of remaining in a relationship for the sake of children, indicating the commonality of the importance of social and gender norms in driving decision-making [ 97 – 101 ]. Implications garnered from research with women of reproductive age experiencing IPV are relevant here; similarly, it should not be assumed that older women want to or can leave an abusive situation, and services provided should recognize and be sensitive to this. Finally, our findings highlight specific issues for consideration in the case of violence against older women, including changes in type and prevalence of controlling behaviours [ 36 , 45 , 50 , 51 , 61 , 72 , 77 ] and forms of financial control that occur alongside IPV [ 43 , 53 , 62 , 64 , 78 ]. These behaviours have the potential to significantly restrict options and limit ability for older women experiencing violence, even more than in younger women. Currently however, these may be under-recognized as specific risk factors for older women.
Global research on violence against women has increasingly explored the significant influence of social and gender norms on prevalence of and risk factors for violence against women of reproductive age [ 102 – 105 ]. Our findings indicate that social and gender norms also continue to strong influence older women’s responses to and experiences of violence. Older women described social and gender norms as shaping their decisions to stay in relationships, to provide care for an abusive spouse, and often as reinforcing shame and social isolation. There is substantial overlap between norms identified in this review with the existing evidence-base on social and gender norms on women of reproductive age, for example, the norm of keeping violence victimization private and overall injunctions concerning silence surrounding IPV. Some evidence indicates positive impacts of violence prevention interventions focused on changing social and gender norms [ 106 ]. However, these programs have not been specifically tested for feasibility and acceptability with older adults, and careful consideration of how and if addressing social and gender norms amongst older adults could result in reduced violence perpetration is needed.
Our review identified significant gaps in the evidence-base concerning older women’s experiences of violence in low and middle-income countries (42 articles in HIC vs. 10 articles LMIC). Within studies conducted in high-income countries, with a few exceptions [ 52 , 61 , 70 , 76 , 80 ], the focus of the included studies was on older women from Western cultural backgrounds. The sparse coverage of several regions globally, and low and middle-income populations overall, indicates that our findings cannot be generalized to older women globally, and that there are likely important influences on and impacts of violence against older women that are currently missing from view. While we can assume that older women in low and middle-income contexts also experience violence, the existing evidence base, for both qualitative and quantitative data, fails to adequately shed light on patterns and prevalence [ 16 , 17 ]. In addition, as found in our quality assessment, included articles contained very little detail on the contexts in which the research was conducted [ 32 , 34 – 42 , 45 – 47 , 49 – 51 , 53 , 54 , 56 , 57 , 59 , 61 – 66 , 69 , 70 , 72 – 75 , 77 – 79 ], which makes it difficult to link the evidence from this review to specific contextual factors. Further exploration of context-specific issues such as living conditions and associated norms, for example, norms governing that older widows live with children and children’s families is needed. In addition, exploration of perceptions of capabilities and appropriate social roles for older women in different socio-cultural contexts is warranted. Perceptions and experiences of ageing processes, and specific issues such as widowhood, differ significantly in different cultural contexts, and existing qualitative and quantitative data do not include these diverse factors or account for their relationship with violence against older women.
Our findings indicate that older women affected by violence need social and community support to help them cope and address the anxiety and stress associated with threats to their safety. Older women affected by violence may be particularly isolated, with social isolation concomitant with ageing compounded by social isolation due to violence victimization. Some of the studies indicated that older women do not understand or define their experiences as abuse or violence, but do seek support regardless. As such, there may be potential for services and interventions designed to address social isolation and targeted for all older women to address violence against older women. Various interventions that have been found to be effective in reducing social isolation and improving social outcomes for older persons, such as group support through discussion groups, individual support through home visiting, and psychosocial education programs, could be effective in improving social support for older women affected by violence [ 107 ]. Currently, services for older persons are overall extremely limited in low and middle-income contexts, and dynamics of social and community support for older persons vary considerably in non-Western cultural contexts. The current qualitative evidence-base does not indicate if older women affected by violence in low and middle-income contexts would benefit from similar interventions or if integrating response to and support for violence against older women into aged-care services are a feasible way to reach older women affected by violence.
In the limited number of included studies that addressed older women’s experiences with and expectations of health-care providers, concerns were raised including lack of confidentiality and health care providers not taking women’s abuse seriously [ 74 ]. Health care providers are in a unique position to provide support and response for women who have been affected by violence. The World Health Organization’s Clinical and Policy Guidelines and Clinical handbook provide guidance for health care providers in providing woman-centred care, compassionate first-line psychosocial support, and linkages to multi-sectoral services [ 108 ]. In the case of older women, women may come in contact with primary, secondary or tertiary health care services for reasons related to chronic disease and ageing-related injuries, for example, or as care-givers for spouses or children. There is a need to explore how and where violence prevention and response for older women in the health system could be feasible and acceptable. For example, gerontologists and other specialists providing elder-care specific services could be provided tools and skills to identify and support women who may be subjected to violence. In addition, as identified in this and other reviews of violence against older women, there are factors that may act as precipitating factors for increase or initiation of violence, including changes in caregiving dynamics or retirement of a spouse, and these could be points of potential intervention and additional support for older women, especially if there is a history of past violence.
Limitations and strengths
Several strengths and limitations should be considered while interpreting the findings of this systematic review. In contrast to previous systematic reviews, we included all qualitative evidence concerning violence against older women, regardless of type of violence and perpetrator, allowing insights into the overall focus of the evidence-base, which revealed limited engagement with elder abuse against women and family violence perpetrated by non-partners, for example, children. Additionally, we followed a rigorous protocol, adhering to a preregistration protocol in line with ENTREQ guidelines [ 31 ]. We carried out an extensive systematic review across 11 databases, supplemented by hand searched references lists and article recommendations from 49 experts on violence against women or older adults, and therefore it is unlikely that published articles would have been overlooked in this review. We reviewed all articles in any language, apart from Farsi.
In order to minimize selection bias or for relevant articles to be missed, two authors screened all titles and abstracts and all articles at the full text review stage. At the data extraction phase, only MEL extracted relevant data, introducing the possibility of transcription errors. Despite this limitation, all extracted data was double checked by SRM to minimize potential of missing descriptive data, and both completed independent quality appraisals to minimize potential for biased assessments. Additionally, during the analysis phase, both authors coded article main findings and key quotes, and developed descriptive and analytical themes to strengthen the interpretation and synthesis of findings.
Another limitation of the findings of this review is the concentration of studies in higher-income contexts, which greatly limits the transferability of findings to low- and middle-income populations. In addition, the small number of studies conducted in low and middle-income countries entailed that comparison of patterns between high-income and low and middle-income contexts was not possible. This review was also limited by the quality of included articles. Many articles did not clearly report on study setting and context, sampling procedures, data analysis, reflexivity, and research ethics. Moreover, many articles included samples of older women across wide age ranges (e.g. 65–85 years old). The available evidence does not disaggregate findings to enable understanding of whether or how women in different age groups experience violence differently, despite significant variation in living conditions, employment and health status of women aged 50–64 vs. 65 and up, for example. This lack of specificity limited our ability to understand the differential causes, experiences and impacts of violence among specific age groups of older women.
Implications for future research
In light of the findings from this review, as noted above, there is an urgent need to address the scarcity of research on violence against older women in low and middle-income contexts, and to expand research in high-income contexts to diverse populations and age groups who may have different risk profiles for violence in older age.
Our results indicate that the focus of the existing qualitative evidence-base is primarily on IPV in older age. It is unclear whether this research focus reflects the actual burden of IPV compared to other forms of violence against older women, and if the evidence-base currently adequately includes accounts of types of violence and perpetrators that are most significant for older women. As noted, assessment of polyvicimization in the evidence-base is lacking. As such, further studies of violence against older women that are inclusive of any type of violence, by any perpetrator, or take an open-ended approach to older women’s accounts of violence, are needed. In the quantitative evidence-base, systematic reviews have focused on elder abuse and on IPV. A review of quantitative evidence on IPV identified 19 studies [ 15 ] and the review of elder abuse against women included 50 studies; as such, the quantitative evidence-base appears to capture more in terms of forms of violence against older women.
Our findings indicate that for older women who had experienced violence throughout the life-course, aspects of ageing, such as frailty, injuries, chronic disease, and cognitive decline, make coping with different forms of violence more difficult than earlier in life. Qualitative and quantitative research does not currently shed light on associations between types of violence, chronicity of violence, and physical and mental health outcomes for older women, and additional research in this area is warranted. Other themes that emerged in our review call for further research. Regret and hopelessness were commonly described as significant issues for older women; these factors appear to significantly influence well-being, psychosocial health and physical and mental health. However, these outcomes are rarely measured, and these may further impact other specific mental health and psychosocial issues for older women subjected to violence. Further research could explore if and how regret and hopelessness amongst older women differs from shame and stigma as currently measured and reported amongst women of reproductive age, and further elucidate its impacts on psychosocial well-being. In addition, economic and financial abuse appeared to be correlated and interlinked with older women’s experiences of violence, and barriers to leaving abusive relationships; terminology and definitions of these forms of abuse are varied and often unclear, and measures often cover several constructs [ 109 ]. While there is some growing consistency in how economic and financial aspects of abuse are conceptualized and measured, there is more work needed on how to assess economic or financial abuse, and understand its linkages with physical and mental health outcomes.
The current qualitative data available on violence against older women has important limitations, including that it is predominantly derived from high-income countries, often does not address context, is focused on IPV to the exclusion of other types of violence and perpetrators, and does not disaggregate by age group. However, our findings highlight some important issues. IPV persists into older age, and shares characteristics and impacts as in younger age groups. In some cases, there may be factors, such as a partner’s retirement or illness such as dementia, which can precipitate or increase violence. As shown in quantitative reviews, physical violence tends to decrease with age while psychological abuse and controlling behaviours increase, and financial and economic abuse are important elements of older women’s experiences of violence and control. Older women described being strongly influenced by social norms that dictate a sense of duty to stay in a relationship with an abusive partner, a desire to protect children, and shame and silence surrounding experiences of violence. More research is needed, particularly from LMICs to fill in the many gaps in the evidence-base. However, it is clear that action to support older women in abusive relationships is needed. Services for older people need to be aware of the prevalence and forms of violence against older women and know when to identify and respond in a sensitive and non-judgmental way, to improve prevention of and response to violence against older women.
Supporting information
Funding statement.
This study is funded by the Department for International Development, UNWomen-World Health Organization Joint Programme on Strengthening Methodologies and Measurement and building national capacities for Violence against Women data. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
- PLoS One. 2020; 15(9): e0239560.
Decision Letter 0
23 Jul 2020
PONE-D-20-10316
Violence against older women: a systematic review of qualitative literature
Dear Dr. Meyer,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
The Reviewers considered the manuscript very positively. They also provided several suggestions to improve the quality of the study and make it suitable for publication.
Please submit your revised manuscript by Sep 06 2020 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
We look forward to receiving your revised manuscript.
Kind regards,
Stefano Federici, Ph.D.
Academic Editor
Additional Editor Comments:
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please cite your published protocol article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6550033/
3. Please include your tables as part of your main manuscript and remove the individual files. Please note that supplementary tables (should remain/ be uploaded) as separate "supporting information" files.
4. PLOS requires an ORCID iD for the corresponding author in Editorial Manager on papers submitted after December 6th, 2016. Please ensure that you have an ORCID iD and that it is validated in Editorial Manager. To do this, go to ‘Update my Information’ (in the upper left-hand corner of the main menu), and click on the Fetch/Validate link next to the ORCID field. This will take you to the ORCID site and allow you to create a new iD or authenticate a pre-existing iD in Editorial Manager. Please see the following video for instructions on linking an ORCID iD to your Editorial Manager account: https://www.youtube.com/watch?v=_xcclfuvtxQ
5. Please include a caption for figure 1.
6. Please include captions for your Supporting Information files at the end of your manuscript, and update any in-text citations to match accordingly. Please see our Supporting Information guidelines for more information: http://journals.plos.org/plosone/s/supporting-information .
<h1> </h1>
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
Reviewer #3: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Recommendation: Publish with minor corrections
1. Summary of Research and Overall Impression
This is an excellent summary of qualitative studies on neglect, abuse, and violence against older women. It makes an important contribution to the literature on this often overlooked population in the domestic violence field. It is well-written and well-researched.
Methodology and selection criteria for studies included in the review are clearly presented. Authors of selected studies are known for their expertise in this area of international domestic violence research on older women. The systematic review presented here complements findings from quantitative including prevalence studies.
This is a particularly appropriate report for UN Women, which has not always been open to considering older women’s experiences with domestic violence as relevant to the field of international domestic violence. The author frames the analysis in a particularly insightful way using a feminist perspective. In doing so, she effectively challenges the ageism inherent in views of older women and domestic violence as “elder abuse” that is disconnected from gender, community, and the life course.
The author chose qualitative research studies that incorporate the words of older women “in their own voices” and use a life course perspective. This very much reflects a feminist perspective. She also makes efforts to include voices of older women from developing countries, which she notes is difficult. Organizations like HelpAge International have done studies on older women and abuse from developing countries, but these studies tend not to reflect the rigor of qualitative studies undertaken by the academy based on her stated selection criteria.
2. Minor issues
101 – Instead of “older adult mistreatment” framework, the author may want to consider substituting “vulnerable older adult” framework and distinguish this from the “intimate partner violence (IPV)” framework and the “active ageing” framework that can incorporate feminist gerontology, although can also reflect a gender neutral perspective. Older adult mistreatment is a generic term, while IPV is more commonly used in domestic violence discussions involving women survivors (and the author makes a point of selecting studies that view older women as women, not elders”). The vulnerable older adult framework reflects a disconnect between women domestic violence survivors and older women, and which this reviewer would argue incorporates an ageist and gender neutral framing of older women survivors. The underlying assumption of this frame is that older victims are frail and dependent by definition: this both narrows the population to be included in the study to a subset of impaired older adults, or alternatively assumes that older women are by definition impaired, care dependent and “vulnerable”. The author has selected studies for the review that quite rightly challenge this assumption.
738 – Under limitations, the author notes that there is a dearth of qualitative studies on older women survivors of domestic violence from developing (low income) countries. This reviewer noted earlier that in fact there may be other studies (for example, those by HelpAge International – Bridget Sleap) but not reflecting the academic rigor sought in this review. However, there are studies conducted in high income countries of older women survivors of domestic violence who are immigrants from low income countries. One example that comes to mind is Guruge et al. (2010), Older women speak about abuse and neglect in the post-immigration context, conducted in Canada with Sri Lankan immigrants.
Polyvictimization is a fairly new concept in older adult abuse, and one that is not prominent in the domestic violence literature to date but is more so in the field of child abuse. Studies by Pamela Teaster and Holly Ramsey-Klawsnik, for example, have found that multiple forms of abuse/multiple abusers experienced by domestic violence victims can lead to increased trauma. If the qualitative studies did not specifically ask about polyvictimization, they may not have captured this.
Overall, these are minor issues. The charts included in the manuscript are very helpful in providing a flavor of the felt experience of older women survivors of domestic violence.
3. Other Points
Overall, an excellent review and one that can serve to educate UN Women staffers, primarily young women, about older women’s lived experience of domestic violence. This will hopefully result in their viewing older women as part of the continuum of “Girls and Women of all Ages” and not “Other”.
Reviewer #2: This is a fascinating study, drawing attention to urgent issues in this field of research and responds to a research gap that it clearly identifies at the outset. It has a well-articulated methodology, discussion and makes powerful conclusions. Further details of the analytical approach would be welcomed, however, as it is currently unclear how themes and sub-themes were reached. There is some overlap between some sub-themes, and in some sub-themes there is a lack of depth where the results could be explored further. Either further details on how the analysis was conducted would address this, or some reorganisation of themes and sub-themes to a smaller number that would allow for exploration of the results in more detail.
Further explanation of why one article in Farsi was not translated and included in the study would also be welcomed.
Reviewer #3: Thank you for giving me the chance to review this important manuscript that addresses a clear gap in the literature. It is very clear that you have done an amazing job in thoroughly going through a vat amount of literature and put a lot of attention in capturing necessary detail. Congratulations on it!
I have some general and specific comments.
General comments:
• The title of the paper is violence against older women and throughout the text you refer to older women. The definition of older women in the text is women aged 50 or older. Is this aligned with existing definition of older or is it a consequence that many other studies have focused on women of reproductive age? Should you not throughout the title and text to simply name them women aged 50 or older or is older women the correct term?
• The review stats that it is “exploring violence against women aged 50 and above, identifying types and patterns of violence, perpetrators of violence, and impacts of violence on various health outcomes for older women”. Reading the review, it seems that much more has been investigated than that, namely associate factors and consequences beyond health outcomes, such as loneliness and social isolation. This could be stated more clearly in the introduction, as I kind of expected it but did not find it reflected in the description of the reviews scope.
• Throughout the results section it was often unclear whether you are summarising violence described actual violence that older women are experiencing now or whether they refer to any violence as it sounds like in the section on loneliness (not only an issue there)? It is important to make that very clear whether women refer to past violence, potentially 20 years ago or current violence. For example, but not only there, in the section “Silence, stigma and family” it is unclear if the women refer to the current violence they experienced or past violence, potentially 20 years ago. The whole paragraph seems to refer to varies time points in which the violence happened and this needs to be clarified, especially since there is a specific sub-section for it
• Have you actually found any differing evidence by different age categories among women aged 50 or above? In the limitation section you mention that the age rages varied widely, but it would be could to situate the results into this as 50 to 64 is quite a different age category than 65 to 99, when women are also more likely to be retired.
• I am a bit surprised by the structuring of the results section and consider reworking it as it jumps from the overview of forms of violence and perpetrators in a summary paragraph to causes, consequences, risk factors to financial abuse- a form of violence experienced, norms, needs, early childhood violence as a risk factor later. While the overall heading make sense, the sub heading sometimes seem to belong somewhere else and do not flow.
• Did you actually find different results by LMIC and HIC?
• The section “Descriptions of types of violence and perpetrators” is actually a quite crucial one, but it is currently very descriptive in terms of numbers. Given that forms of violence and perpetrators are such a key objective, could you expand this section and show what kind of violence was perpetrated by the different perpetrator types or forms of abuse and whether there were any age trends among the older women.
Small, specific comments:
• Abstract p 8, line 31: grammatical mistake
Introduction:
• Page 4, line 77 needs a reference
• Page 6, line 116: Can you state if these systematic reviews said anything about the perpetrators of this violence? Which age ranges did the systematic reviews investigate?
• Page 6, line 128 grammatical error
• Did you use any time limit for the search?
• Did forms/types of violence cluster in certain countries?
• On page 14 under the heading “Descriptions of types of violence and perpetrators” you first describe the terms IPV, family violence and elder abuse, but these terms have not been described before in terms of what they mean and how they are different from each other
• On page 15 when you talk about causes of violence, which types of violence were referred to?
• Is the financial abuse section actually referring to tis as a form of violence or a cause for other violence or a co-occurrence of numerous forms of violence?
• In the discussion section you refer to health care providers response and women’s concerns regarding confidentiality, however, this was not brought up in the results at all and should have been mentioned there too.
• Implication for future research – the scarcity of research only relates to qualitative work or more generally? I understand that your review mainly found studies on IPV, but what did the quantitative reviews find? Would they support your claim?
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: No
Reviewer #2: No
Reviewer #3: Yes: Heidi Stöckl
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Submitted filename: 2020 Plos One review Sarah.docx
Author response to Decision Letter 0
Authors’ response to reviewers
Manuscript title: Violence against older women: a systematic review of qualitative literature
To the Editors, PLoS One
Thank you for the recognition of the contribution of our manuscript, “Violence against older women: a systematic review of qualitative literature.” In response to the reviewers’ comments, some changes have been made to the manuscript. We appreciate the reviewer’s positive comments and feel that our responses to these helpful suggestions helped improve this manuscript. The reviewers’ comments, as well as journal requirements listed, are addressed point-by-point in turn below.
Reviewer 1:
1. 101 – Instead of “older adult mistreatment” framework, the author may want to consider substituting “vulnerable older adult” framework and distinguish this from the “intimate partner violence (IPV)” framework and the “active ageing” framework that can incorporate feminist gerontology, although can also reflect a gender neutral perspective. Older adult mistreatment is a generic term, while IPV is more commonly used in domestic violence discussions involving women survivors (and the author makes a point of selecting studies that view older women as women, not elders”). The vulnerable older adult framework reflects a disconnect between women domestic violence survivors and older women, and which this reviewer would argue incorporates an ageist and gender neutral framing of older women survivors. The underlying assumption of this frame is that older victims are frail and dependent by definition: this both narrows the population to be included in the study to a subset of impaired older adults, or alternatively assumes that older women are by definition impaired, care dependent and “vulnerable”. The author has selected studies for the review that quite rightly challenge this assumption.
We agree with this reviewer that there are other ways to capture and describe the dominant conceptual frameworks in this literature. We feel that the three frameworks that we describe – older adult mistreatment, older adult protection, and IPV – are one way to capture the approaches on the literature. Rather than substituting a different framework, we have added some comments reflecting the problematic aspects of each of these approaches, including the disconnects and underlying assumptions that this reviewer rightly points out. The section now reads:
“The older adult mistreatment framework conceptualizes violence against older women as a form of elder abuse, focusing on age as the primary factor influencing vulnerability to exposure to violence. The older adult protection framework specifically understands violence within the context of care-giving and institutional arrangements, where older adults’ often be gender neutral, and the adult protection framework can result in a framing of older adults as inherently impaired and vulnerable. In addition, the IPV framework primarily understands vulnerability to violence in terms of gender inequality and partnership dynamics, which may neglect analysis of how ageing and partner violence intersect.”
2. 738 – Under limitations, the author notes that there is a dearth of qualitative studies on older women survivors of domestic violence from developing (low income) countries. This reviewer noted earlier that in fact there may be other studies (for example, those by HelpAge International – Bridget Sleap) but not reflecting the academic rigor sought in this review. However, there are studies conducted in high income countries of older women survivors of domestic violence who are immigrants from low income countries. One example that comes to mind is Guruge et al. (2010), Older women speak about abuse and neglect in the post-immigration context, conducted in Canada with Sri Lankan immigrants.
We appreciate the reviewer pointing out this relevant article, and we have included it in our review.
3. Polyvictimization is a fairly new concept in older adult abuse, and one that is not prominent in the domestic violence literature to date but is more so in the field of child abuse. Studies by Pamela Teaster and Holly Ramsey-Klawsnik, for example, have found that multiple forms of abuse/multiple abusers experienced by domestic violence victims can lead to increased trauma. If the qualitative studies did not specifically ask about polyvictimization, they may not have captured this.
We agree with this comment, and have included the following text in the Discussion section to indicate that polyvictimization is not adequately addressed in this literature:
“The included studies primarily address IPV, with fewer emerging from the older adult mistreatment framework. Most research examined specific types of violence in isolation, for example, IPV or abuse from an adult child, and there were no examples of studies that included polyvictimization or experiences of any type of violence against older women. The strong emphasis on older women’s experiences of IPV gives voice to the experiences of older women subjected to violence and shows how it can persist over time; however, some sites, perpetrators and types of violence against older women may be excluded from view, including that of violence enacted by other family members and non-family caregivers and of women living in institutional care.”
“As noted, assessment of polyvicimization in the evidence-base is lacking.”
Reviewer 2:
1. Further details of the analytical approach would be welcomed, however, as it is currently unclear how themes and sub-themes were reached. There is some overlap between some sub-themes, and in some sub-themes there is a lack of depth where the results could be explored further. Either further details on how the analysis was conducted would address this, or some reorganisation of themes and sub-themes to a smaller number that would allow for exploration of the results in more detail.
We agree that further discussion of the analytical approach is warranted, and have added the following description in the Methods section:
“Two of the authors (SRM and MEL) coded the main findings extracted from each study. We used line-by-line coding on a sub-set of articles, developing a set of over-arching themes and sub-themes for a draft codebook. The coding proceeded as an iterative process, with the two authors each separately coding the main findings using the draft codebook, discussing coding results, and refining the codebook based on overlap and redundancies identified. After all data was coded and we tallied all occurrences of codes, we further explored areas of overlap and merged sub-themes with low numbers of codes, finalizing the broad themes and focused sub-themes, displayed in Table 3.”
Further, in response to this comment and Reviewer 3’s comments regarding the Results section, we have reorganized themes and sub-themes to reduce overlap and provide more detail. The themes and sub-themes are now:
• Descriptions and patterns of types of violence
• Intersection of ageing and violence
o Suffering, loneliness, regret and guilt.
o Violence, ageing and vulnerabilities.
• Perpetrator-related factors
o Ageing perpetrators and continuity of abuse.
o Perpetrator’s illness as a cause of violence.
• Social and gender norms regarding response to violence
o Silence, stigma and family.
o Perceptions of abuse and violence as normal.
• Lifelong IPV
o Continuation of patterns of IPV in old age.
o Earlier experiences of violence.
o Cumulative impacts of violence.
• Needs of older women affected by violence
o Social and community support.
o Barriers to accessing services.
• Coping mechanisms
o Leaving a relationship.
o Isolation, substance use and emotion-based coping strategies.
o Behaviors to enhance safety.
2. Further explanation of why one article in Farsi was not translated and included in the study would also be welcomed.
We have added the following sentence to explain this: “One non-English article (in Farsi) was not reviewed as the research team could not engage a Farsi speaker to review the article.”
Reviewer 3:
1. The title of the paper is violence against older women and throughout the text you refer to older women. The definition of older women in the text is women aged 50 or older. Is this aligned with existing definition of older or is it a consequence that many other studies have focused on women of reproductive age? Should you not throughout the title and text to simply name them women aged 50 or older or is older women the correct term?
We have focused this review on women aged 50 and above as a consequence that many other studies have focused on women of reproductive age. Definitions of old and older women vary across organizations and research. However, we found that using the phrase ‘women aged 50 and older’ throughout the manuscript, while more accurate, was difficult to understand and disrupted flow of the narrative. Therefore, we added a sentence in the introduction to explain this:
“While there is no universal agreed-upon definition of older women, for the purposes of this review, we define older women as women aged 50 and above, while recognizing that aging and age are social phenomenon, and definitions vary across organizations, cultures and communities.”
2. The review stats that it is “exploring violence against women aged 50 and above, identifying types and patterns of violence, perpetrators of violence, and impacts of violence on various health outcomes for older women”. Reading the review, it seems that much more has been investigated than that, namely associate factors and consequences beyond health outcomes, such as loneliness and social isolation. This could be stated more clearly in the introduction, as I kind of expected it but did not find it reflected in the description of the reviews scope.
We have altered this statement to include the wider range of outcomes that are considered in this review. The sentence now reads:
“We aimed to identify, evaluate and synthesize qualitative studies from all countries, exploring violence against women aged 50 and above, identifying types and patterns of violence, perpetrators of violence, and impacts of violence on various outcomes for older women, including physical and mental health and social support, and women’s responses to experiences of violence.”
3. Throughout the results section it was often unclear whether you are summarising violence described actual violence that older women are experiencing now or whether they refer to any violence as it sounds like in the section on loneliness (not only an issue there)? It is important to make that very clear whether women refer to past violence, potentially 20 years ago or current violence. For example, but not only there, in the section “Silence, stigma and family” it is unclear if the women refer to the current violence they experienced or past violence, potentially 20 years ago. The whole paragraph seems to refer to varies time points in which the violence happened and this needs to be clarified, especially since there is a specific sub-section for it
We appreciate this important comment, and recognize that throughout the evidence included in this review, there are manuscripts that focus on previous and current violence or current violence only, and that in some cases, given women’s experiences of violence as continuous and interlinked throughout their lifetimes, the distinction is difficult to identify. We have included references to this issue within the Results section where relevant, such as:
“Shifts in types of violence, from predominantly physical violence to predominant psychological abuse and neglect, were commonly described in studies that encompassed previous and on-going IPV. Studies focused on IPV more commonly described both previous and on-going violence, and a small number described only violence experienced while aged 50 or above.”
In the section on Suffering, loneliness, regret and guilt:
“The studies that explored these themes primarily encompassed accounts of violence experienced throughout intimate relationships – while women were younger and through to older age. These experiences were described and conceptualized by older women as interlinked and continuity of victimization by intimate partners was emphasized, rather than viewing women’s experiences of violence in older age as distinct or separate.”
In the section on Violence, ageing and vulnerabilities:
“These studies primarily focused on current experiences of violence of older women, as changes in physical and emotional capacity to cope was described in relation to present victimization.”
In the section on Silence, stigma and family:
These studies primarily focused on previous and current experiences of violence; social norms predominant when women were younger shaped prior and current responses.”
4. Have you actually found any differing evidence by different age categories among women aged 50 or above? In the limitation section you mention that the age rages varied widely, but it would be could to situate the results into this as 50 to 64 is quite a different age category than 65 to 99, when women are also more likely to be retired.
We found this to be one of the major limitations of the available evidence, and have added a sentence to make this limitation clearer based on this comment:
“The available evidence does not disaggregate findings to enable understanding of whether or how women in different age groups experience violence differently, despite significant variation in living conditions, employment and health status of women aged 50-64 vs. 65 and up, for example.”
5. I am a bit surprised by the structuring of the results section and consider reworking it as it jumps from the overview of forms of violence and perpetrators in a summary paragraph to causes, consequences, risk factors to financial abuse- a form of violence experienced, norms, needs, early childhood violence as a risk factor later. While the overall heading make sense, the sub heading sometimes seem to belong somewhere else and do not flow.
We agree with this comment, which is also in line with Reviewer 2’s feedback regarding structure of the Results section. As such, we have refined our coding structure and made the following changes:
• Substantially expanded on the first section of results, renaming if Descriptions and patterns of types of violence, including integrating the sub-theme on increases of violence into this section;
• Removing the section on causes of elder abuse (as we do not have separate sections on causes of other specific types of abuse);
• Creating a theme on issues relating to the perpetrator, and including the sub-themes Ageing Perpetrators and continuity of abuse and
• Removed Ageing and changes in the nature and patterns of IPV theme (sub-themes moved to Descriptions and patterns of types of violence and Perpetrator related factors)
• Removed Control and financial abuse among older women as a sub-theme and incorporated parts of it into Descriptions and patterns of types of violence
6. Did you actually find different results by LMIC and HIC?
Given the very small number of studies conducted in LMIC, this was not possible and we have added a sentence in the Limitations section to indicate this:
“In addition, the small number of studies conducted in low and middle-income countries entailed that comparison of patterns between high-income and low and middle-income contexts was not possible.”
7. The section “Descriptions of types of violence and perpetrators” is actually a quite crucial one, but it is currently very descriptive in terms of numbers. Given that forms of violence and perpetrators are such a key objective, could you expand this section and show what kind of violence was perpetrated by the different perpetrator types or forms of abuse and whether there were any age trends among the older women.
We appreciate this helpful comment, and have substantially expanded this section. We have renamed it Description and patterns of types of violence, and have a separate section focusing more on perpetrators. The section now reads:
Older women described IPV, family violence and elder abuse of various types, perpetrated by a range of perpetrators [Table 1]. Among the specific types of violence reported in the articles in this review, across IPV, elder abuse and family violence, physical violence was most frequently reported [23, 28-50, 53, 56-59, 62, 65-75], followed by emotional/ psychological [24, 28, 32-35, 37-47, 49, 50, 52, 56-58, 62-75], economic/ financial [30-32, 35, 37, 39-41, 44-46, 57, 58, 60, 64, 67, 68, 70-73], sexual [23, 29, 30, 36, 38, 45, 46, 50, 53, 55, 56, 63, 68, 70, 71, 75], verbal [28, 36, 41, 48, 58, 64-66, 69, 72], controlling behaviors [41, 44, 45, 47, 49, 60, 63, 66, 72], and lastly, neglect [24, 31, 35, 57, 58, 64, 67].
Older women’s experience of IPV was the most frequent form of violence reported (41 articles) [23, 25, 29, 30, 32-34, 36-38, 41-52, 55-61, 63-75]. Older women described on-going instances of neglect, verbal abuse and financial exploitation in a study conducted in India; in other cases, physical violence characterized earlier and on-going experiences of violence within intimate partner relationships. IPV in particular was described by older women as occurring throughout different stages in the relationship, spanning their youth and into older age. Older women often experienced an escalation of IPV and controlling behaviors despite the age and/ or illness of their partner [32, 36, 42, 57, 65, 72]. Changing relationship dynamics due to ageing – including a husband’s retirement, children leaving the home, women wanting to engage in activities outside of the home, or diagnosis of a chronic or terminal illness – triggered escalating IPV [32, 36, 42, 43, 52, 65]. Shifts in types of violence, from predominantly physical violence to predominant psychological abuse and neglect, were commonly described in studies that encompassed previous and on-going IPV. Studies focused on IPV commonly described both previous and on-going violence, and a smaller number described only or primarily violence experienced while aged 50 or above.
Violence occurring within the family was discussed in 14 articles [31, 35, 39, 40, 42, 44, 45, 51, 59, 62, 64, 65, 67, 74], with perpetrators including family members not including children [39, 40, 44, 45, 59, 64, 65, 67] and adult children [31, 35, 44, 62, 74]. Studies captured instances of physical and verbal aggression by mentally ill adult children against older women, violence enacted by elderly with dementia against older women who were caregivers and forms of neglect, financial exploitation and emotional abuse enacted by family members, including children. The majority of these studies focused on violence experienced in older age, while one study explored dynamics of abuse between children and mothers across the lifespan.
10 articles reported on experiences of elder abuse [24, 28, 31, 39, 40, 51, 53-55, 73] with perpetrators including community members [39, 40], caregivers [53, 55], nursing home residents [54] and health care providers [24]. Types of elder abuse included verbal abuse, physical assault and inappropriate sexual advances and sexual assault.
Financial control spanned instances of elder abuse, family violence and IPV [39, 49, 58, 60, 73], and was described as co-occurring with and resulting in other forms of violence. Financial exploitation could result in emotional and/ or physical violence if older women resisted control [58, 60]. An older woman explained that in the context of her relationship with her husband, “If I did not follow his control [over money], he would be verbally abusive” [60].
8. Page 4, line 77 needs a reference
We have added a reference.
9. Page 6, line 116: Can you state if these systematic reviews said anything about the perpetrators of this violence? Which age ranges did the systematic reviews investigate?
We have clarified analysis of perpetrators within these systematic reviews and age ranges investigated. This section now reads:
“Employing an older adult mistreatment framework, a systematic review of quantitative studies of elder abuse (against men and women aged 60+) found that the global prevalence of elder abuse in community settings is 15.7% in the past year, with psychological abuse and financial abuse as the most prevalent forms of abuse reported [15]. This review reported prevalence by type of violence, but did not report on perpetrators. Analysis of studies conducted in institutional settings found women, aged 60 and above, to be significantly more vulnerable to abuse, with psychological abuse as the most prevalent form of violence, followed by physical violence, neglect, financial and sexual abuse [16]; this analysis included data reporting staff-to-resident abuse. Analysis of quantitative data of women aged 60 and above in the systematic review of quantitative studies of elder abuse found a global prevalence of elder abuse against women of 14.1% in the past year, with psychological abuse reported as the most prevalent form of violence, followed by neglect. The focus of this review was prevalence of different sub-types of violence, and type of perpetrator was not considered. Another systematic review of quantitative data on interpersonal violence (physical and/or sexual violence) against older women (aged 65 and above) in community dwellings primarily employed an IPV framework, finding prevalence of reported interpersonal violence ranged from 6 to 59% over a lifetime, from 6 to 18% since turning 50, and 0.8 to 11% in the past year, however, results indicated that definitions of violence vary widely and affect prevalence estimates [17]. Syntheses of quantitative literature have identified prevalent forms of violence against older women, highlighting limitations in the evidence-base due to variations in definitions and methodology, and a primary emphasis on populations in high-income, Western countries. These reviews have captured a wide range of types of violence, however, have not considered type of perpetrators or patterns of co-occurring types of violence.”
10. Did you use any time limit for the search?
No, we did not use and time limit for the search. We have clarified this in the methods section.
11. Did forms/types of violence cluster in certain countries?
The studies were primarily conducted in USA and Israel, followed by UK and Canada. While there are some patterns identified within those countries, we concluded that we could not adequately assess whether this reflected true patterns in violence against older women, or the research focus of the research teams in these countries.
12. Results: On page 14 under the heading “Descriptions of types of violence and perpetrators” you first describe the terms IPV, family violence and elder abuse, but these terms have not been described before in terms of what they mean and how they are different from each other
We agree that the manuscript would benefit from definitions of these terms, and have added these definitions into the description of the objectives of the review:
“We include the following forms of violence: elder abuse, family violence and intimate partner violence. Elder abuse is defined as “single or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person” Intimate partner violence is defined as “behaviour by an intimate partner or ex-partner that causes physical, sexual or psychological harm, including physical aggression, sexual coercion, psychological abuse and controlling behaviours.” Family violence is often used interchangeable with intimate partner violence, however, also encompasses abuse and violence perpetrated by other family members, for example, adult children or in-laws.”
13. On page 15 when you talk about causes of violence, which types of violence were referred to?
We have removed the theme Causes of Elder Abuse, given we do not have separate themes for causes of other types of violence analysed. We incorporated the analysis regarding ageist attitudes as a cause of violence into the theme, Social and gender norms regarding response to violence; Sub-theme, Perceptions of abuse and violence as normal.
14. Is the financial abuse section actually referring to tis as a form of violence or a cause for other violence or a co-occurrence of numerous forms of violence?
We agree that in its previous format the inclusion of Financial Abuse as a separate section was not clear enough. As such, we have incorporated aspects of this sub-theme into the Description and patterns of types of violence section, to add further detail there and ensure inclusion of this important type of violence, while improving the structure and flow of the Results.
15. In the discussion section you refer to health care providers response and women’s concerns regarding confidentiality, however, this was not brought up in the results at all and should have been mentioned there too.
We have included the following text in the Results section relating to health car providers’ response:
“Older women reported several concerns when interacting with health care providers, including health care providers’ assumptions that older women could not be experiencing violence due to their age, minimization of forms of abuse common to older women, and lack of confidentiality when using the same provider as their spouse [70].”
16. Implication for future research – the scarcity of research only relates to qualitative work or more generally? I understand that your review mainly found studies on IPV, but what did the quantitative reviews find? Would they support your claim?
The quantitative evidence-base includes a systematic review of elder abuse against older women, and much more literature encompassing different forms of violence against older women. We have added the following text to indicate this:
“In the quantitative evidence-base, systematic reviews have focused on elder abuse and on IPV. A review of quantitative evidence on IPV identified 19 studies and the review of elder abuse against women included 50 studies; as such, the quantitative evidence-base appears to capture more in terms of forms of violence against older women.”
Submitted filename: Response to reviewers.docx
Decision Letter 1
PONE-D-20-10316R1
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
Reviewer #2: All comments have been addressed
Reviewer #3: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
Reviewer #1: (No Response)
Reviewer #2: (No Response)
3. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #3: N/A
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: The author responded to suggestions in my first review of this manuscript and I have nothing further to add. I am comfortable with this manuscript moving to publication.
Reviewer #3: Thank you for addressing all my comments in such a diligent way. The article is a great contribution to the field! Thank you for all your hard work on it
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Acceptance letter
14 Sep 2020
Dear Dr. Meyer:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Prof. Stefano Federici
Research Paper
Elder abuse research paper.

This sample elder abuse research paper is published for educational and informational purposes only. Free research papers, are not written by our writers, they are contributed by users, so we are not responsible for the content of this free sample paper. If you want to buy a high quality research paper on elder abuse at affordable price please use custom research paper writing services.
This sample research paper on elder abuse features: 7400+ words (29 pages), an outline, APA format in-text citations, and a bibliography with 27 sources.
I. Introduction
Ii. defining elder abuse, a. elder abuse as a violation of the criminal law, b. elder abuse as a violation of regulatory law, c. elder abuse as a social construction, d. elder abuse as social harm, 1. physical abuse, 2. financial abuse, 3. sexual abuse, 5. self-neglect, 6. emotional abuse, iii. identifying elder abuse, iv. explaining elder abuse, v. conclusion.
Since the 1970s, elder abuse has been increasingly recognized as a problem across the world. Attention from researchers first surfaced when Baker (1975) discussed the concept of “granny battering” in British medical journals in the mid-1970s. In the United States, interest paralleled a series of political actions, media exposures, and research reports. In 1979, the House Select Committee on Aging held a hearing called “The Hidden Problem.” Around the same time, an episode of Quincy, a late-1970s TV drama series, depicted a case of elder abuse. Katz (1990) argues that the Quincy episode built support for the elder abuse agenda and contributed to public demands for changes in state and federal statutes. Also, The Battered Elder Syndrome was published by Block and Sinnott (1979) around this time, giving increased attention to problems of abuse encountered by older adults.
Since that time, many have accepted that elder abuse is a problem that needs to be addressed by different disciplines and practitioners. Most agree that the best response to elder abuse involves what is called a “multidisciplinary” or “integrated” response. This means that several different agencies are involved in the prevention of and response to elder abuse. To promote a full understanding of the integrated response to elder abuse, this research paper addresses the following areas: defining elder abuse, identifying elder abuse, and explaining elder abuse.
Elder abuse is an underdeveloped area of study. Part of the problem inhibiting the development of research in this area hinges on the lack of uniform definitions of elder about. Generally speaking, elder abuse can be defined in several ways:
- Elder abuse as a violation of the criminal law
- Elder abuse as a violation of regulatory law
- Elder abuse as a social construction
- Elder abuse as social harm
In considering elder abuse as a violation of the criminal law, one can evaluate how elder abuse is criminally defined across the United States. The criminalization of elder abuse is a relatively recent phenomenon. This criminalization involves a surge of criminal justice activity in an effort to apply criminal laws in the area of elder abuse. Criminal laws related to elder abuse can be characterized in three ways. These include (1) laws penalizing offenders for crimes against older individuals, (2) laws specific to the treatment of older persons, and (3) general criminal statutes. First, laws that penalize offenders for crimes against older persons are criminal statutes that call for increased penalties for crimes against persons over a certain age. Known as penalty enhancement laws, they provide for stiffer penalties for individuals who victimize older persons. For example, if an offender robs a 30-year-old victim, the recommended penalty might be 5 years in prison. However, if that offender robs an 80-year-old victim, the penalty might be 8 years.
Second, criminal laws regarding the treatment of older persons include laws that specifically apply to this population. Failure to provide care to an older person is one example. Another example involves states that have specific laws covering crimes occurring in nursing homes or other long-term care settings. For instance, stealing from a vulnerable adult might be classified as “adult abuse” or some other phrase in some states’ statutes.
Third, general criminal statutes apply to elder abuse when states do not have specific laws related to elder abuse. If a grandchild abuses his grandparent, this would be called criminal assault in states where elder abuse laws are not provided. Consider as another example a case where a prosecutor prosecuted a contractor under the burglary criminal statutes when he defrauded an older woman. The prosecutor successfully argued that the contractor entered the woman’s home with the intent to steal from her. Entering a residence with the intention to steal is the basic definition of burglary, and thus the general criminal statute was applied.
There is tremendous variation in the way that states criminally define laws related to elder abuse. According to Lori Stiegel (1995), an elder abuse expert who works for the American Bar Association, the complexity and breadth of the criminal law with regard to elder abuse are evidenced by the fact that the state laws vary in at least six important ways: (1) their definitions of elderly, (2) their definitions of abuse, (3) whether the abuse is classified as criminal or civil, (4) their standards for reporting the abuse, (5) how the abuse should be investigated, and (6) their recommended sanctions for the abuse.
Elder abuse can also be conceptualized as a violation of regulatory law. Indeed, there may be instances when an institution or agency harms an older person. In these cases, it is rare that criminal statutes are used to govern or respond to the harmful behavior; instead, regulations developed by state and federal governments are used to guide the response to the abusive activities. As an illustration, consider that an inordinate number of regulations have been developed to govern the way nursing homes serve their residents. Routinely, licensing investigators visit nursing homes to determine whether the institutions are adhering to regulations. Among the common violations cited against nursing homes are that they fail to adhere to the following regulations:
- Make an adequate comprehensive assessment of resident’s needs.
- Store, prepare, distribute, and serve food under sanitary conditions.
- Develop a comprehensive care plan, with measurable goals and timetables, to meet resident’s medical, nursing, and mental and psychosocial needs.
- Ensure that the resident environment remains as free of accident hazards as possible.
- Promote care for residents in a manner and in an environment that maintains or enhances each resident’s dignity and respect in full recognition of his or her individuality.
Note that when nursing homes commit these actions, they are not criminally prosecuted; instead, because the actions are regulatory violations, the institutions are issued a warning or fined if the actions are not reconciled.
Some have also argued that elder abuse is a socially constructed crime. What this means is that the actions are illegal because society says they are illegal. Consider elder sexual abuse. It is illegal for a caregiver (who is unrelated to the elder) to have sexual relations with the care recipient. However, if the individuals were of the age of consent and under the age determined to be elderly, such relations would not be considered as illegal.
There are other ways to view elder abuse as a social construction. For example, certainly the behaviors that are now labeled elder abuse have occurred throughout time. In fact, some of Shakespeare’s writings have included behaviors that are now cited as elder abuse. During Shakespeare’s time, the phrase “elder abuse” had not yet been socially constructed. Today, the phrase is used to describe a range of behaviors that were defined in different ways in the past.
Some have criticized those who have been instrumental in promoting the study of elder abuse as a separate field. Social scientist Stephen Crystal (1987) argued that the area of study broadly defined the phenomenon of elder abuse so as to increase the number of “elder abuse” victims. This was done, he argued, in order for practitioners to justify their careers and agencies and receive funding and resources for their activities.
Another way to define elder abuse is as social harm. What this means is that whether the crime is defined in statutes as illegal is insignificant; rather, if an older person is harmed, then elder abuse has occurred. Justifying this approach to understanding elder abuse, in his book Crime and Elder Abuse, criminologist Brian Payne (2006) argues the following:
From this perspective, behaviors that harm older persons can be classified as elder abuse. Such a broad conceptualization includes harmful behaviors at the societal, institutional, and individual levels.
Societal abuses include harmful actions, laws, and policies implemented at the societal level that harm older persons. Institutional abuses include the regulatory violations described above. Individual abuses include a range of behaviors. The most commonly cited forms of individual abuse include the following behaviors:
- Physical abuse
- Financial abuse
- Sexual abuse
- Self-neglect
- Emotional abuse
The way that each of these behaviors can be defined as elder abuse within a social harm framework is addressed below.
Physical abuse involves a host of acts that have been committed against elderly persons that range from pinching, slapping, or hitting an older person to committing murder. Five related types of physical abuse have been discussed in the literature: parent abuse, spouse abuse, patient abuse, other violent crimes, and homicides. Parent abuse occurs when an offspring abuses his or her parent. This is among the more commonly reported cases of elder abuse. In these cases, health care professionals or neighbors are the likely reporters, and it is common that the abuser is unemployed and suffering from a drug problem.
Spouse abuse occurs when violence takes place between older persons who are in an intimate relationship. Several patterns have been used to describe elder spouse abuse. Some have noted that it is the result of abuse occurring over the life span. Because abusers do not stop when they become elderly, elder spouse abuse may simply be an indication of a lifetime of violence. Another pattern is that women may become the abusers (after having been victimized by their husbands) once their husbands are physically dependent on them. Also, some experts have noted that elder spouse abuse may occur in second marriages. Difficulty dealing with adult stepchildren, concerns about joint finances, and unfair comparisons to former spouses have been cited as factors contributing to abuse in second marriages. A final pattern is that elder spousal abuse has been attributed to the consequences of dementia.
Patient abuse occurs when a paid care provider physically abuses someone in his or her care. The extent of patient abuse is unknown. Abuse is more commonly attributed to nurse’s aides. Originally, it was believed that such abuse was caused by poor training, difficulties dealing with a stressful work situation, and self-defense against abusive residents. More recently, research by Brian Payne and Randy Gainey (2005) found that a significant proportion of patient abusers were basically predators who had committed prior criminal acts. The need for criminal background checks is being explored by a number of state and federal governments.
Elder physical abuse also includes the range of violent crimes (e.g., robbery, assault, etc.) that can occur at any point during the life course. Robbery is using force or threat of force to steal or attempt to steal another’s property. Assault includes attacks with or without weapons that may or may not result in injury. It seems important to note that the majority of offenders reported in these cases involving older victims were strangers to the victims. The Bureau of Justice Statistics (1994) reports that older violent crime victims “are more likely than younger victims to face assailants who are strangers” and that older robbery victims “are more likely than younger victims to be particularly vulnerable to offenders whom they do not know” (p. 2). Further, findings from the National Crime Victimization Survey (BJS, 1994) show the following results:

- People aged 65 to 74 have a higher victimization rate than those 75 or older.
- Older blacks are more likely to be victimized than older whites.
- Elderly persons with the lowest incomes experience higher rates of violence than elderly with high incomes.
- Separated and divorced elderly persons are more likely to be victims of violent offenses than married elderly persons are.
- Elderly victims of violence are almost twice as likely to be victimized at or near their homes.
Homicides are also committed against the elderly, and it is believed that a high number of elder homicides are misdiagnosed as natural deaths each year. Former homicide investigator Joseph Soos has identified the following five types of homicide committed against elderly persons: (1) murder-for-profit killings, (2) revenge killings, (3) eldercide, (4) gerontophelia, and (5) relief-of-burden killings (cited in Payne, 2006). Murder-for-profit killings occur when individuals kill older persons for their life insurance, inheritance, or other profit. Revenge killings occur when individuals kill older persons out of anger toward the older victim. Eldercide occurs when individuals, typically serial killers, have a fascination with killing older persons. Gerontophelia occurs when individuals kill older persons in order to cover up some other crime. Relief-of-burden killings occur when individuals feel overly stressed about the caregiving experience.
A National Institute of Justice study by Erik Lindbloom and his colleagues (2005) found that four factors in elder deaths often result in referrals to the attorney general’s office for further investigation. These factors included the following:
- Physical condition/quality of care. Specific markers include documented but untreated injuries; undocumented injuries and fractures; multiple, untreated, and/or undocumented pressure sores; medical orders not followed; poor oral care; poor hygiene, and lack of cleanliness of residents; malnourished residents who have no documentation for low weight; bruising on nonambulatory residents; bruising in unusual locations; statements from family concerning adequacy of care; and observations about the level of care for residents with nonattentive family members.
- Facility characteristics. Specific markers include unchanged linens, strong odors (urine, feces), trash cans that have not been emptied, food issues (unclean cafeteria), and documented problems in the past.
- Inconsistencies. Specific markers include inconsistencies between medical records, statements made by staff members, or observations of investigators; inconsistencies in statements among groups interviewed; and inconsistencies between the reported time of death and the condition of the body.
- Staff behaviors. Specific markers include staff members who follow an investigator too closely, lack of knowledge or concern about a resident, unintended or purposeful verbal or nonverbal evasiveness, and a facility’s unwillingness to release medical records (cited in McNamee & Murphy, 2006).
According to criminologist Brian Payne (2006), four general varieties of elder financial abuse include exploitation by primary contacts, nursing home theft by caregivers, fraud by secondary contacts, and other property crimes by strangers. Exploitation by primary contacts refers to those thefts by individuals who supposedly have a close relationship with the victim (e.g., children, caregivers, other relatives, etc.). Exploitation is defined in various ways, depending on one’s orientation. The exploiter is often a relative of the victim and is in many cases financially dependent on the victim.
One scenario that arises in financial abuse cases is that a time may come when an elderly person must rely on someone else to help with his or her financial matters. The assistance may be limited to providing help paying bills or shopping, or it may be that the older adult will grant power of attorney to a trusted primary contact, thus giving the person the authority to make virtually all financial decisions. As already established, many cases of financial exploitation are those where the victim has placed a great deal of trust in a relative, friend, or caregiver.
Nursing home theft by caregivers occurs when nursing home employees steal from residents. Dianne Harris and Michael Benson (1998) have conducted several studies considering various dynamics related to thefts in nursing homes. Based on their estimates from reported victimizations, they claim that up to 2 million thefts possibly occur in nursing homes each year. Items stolen include jewelry, clothing, and cash. New employees and disgruntled employees tend to be implicated as offenders more often than other types of employees. Nursing home administrators use a variety of strategies in an effort to curtail thefts. Harris and Benson argue that the premeditated nature of nursing home thefts potentially makes these thefts “worse” than physical abuse. In effect, thieves plan thefts, whereas some cases of physical abuse may be unplanned and reactive in nature.
Fraud by secondary contacts includes offenses committed by individuals with whom the older victim did not have a long-lasting, trusting relationship. These offenses include home repair fraud, insurance fraud, medical fraud, confidence games, telemarketing fraud, and phony contests. Home repair fraud occurs when offenders steal from the elderly by either overcharging or failing to appropriately provide services for which they were contracted. Insurance fraud occurs when offenders convince older persons to buy useless or unnecessary insurance policies. Medical fraud occurs when health professionals charge older persons for unnecessary services. Confidence games occur when offenders con older persons out of their money, usually through some get-rich-quick scheme. Telemarketing fraud occurs when offenders contact older persons over the phone and steal from them through the offer of some particular service or product. Finally, phony contests fraud entails situations where offenders convince older persons to engage in some contest that they have absolutely no chance of winning. To be sure, each of these offenses could also target younger persons; however, older persons are overrepresented as victims. They are believed to have more money and to be more trusting, so offenders intentionally seek out older persons at church, Bingo halls, or other places that older persons are known to frequent.
Other property crimes by strangers include the range of property offenses that can target all individuals, such as larceny, burglary, arson, and so on. Like the “other violent offenses,” interesting patterns surround these crimes. Of particular interest are the following estimates from the Bureau of Justice Statistics (1994):
- In 1992, the personal theft and household crime rates among the elderly were the lowest since the NCVS started collecting data in 1972.
- Like the rest of the population, older adults are the least susceptible to violent crimes, but most susceptible to household crimes.
- Those 65 and over are about as likely as younger individuals to be victims of purse snatching and pocket picking.
- Older women are more likely than older men to be victims of personal larceny.
- Elderly black women are the least likely to be victims of personal theft.
- Younger victims of personal theft are less likely to tell the police about the act than elderly victims are.
- Separated or divorced elderly persons are more likely to be victims of personal theft than married elderly persons are.
- Elderly renters are less likely than elderly homeowners to be victims of household crimes.
Other patterns also appear from analysis of NCVS data. For example, among elderly persons, white females are most likely to be victimized by personal theft, followed by white males, black males, and black females. These figures are particularly interesting when compared to rates of violence reported in the official crime statistics. In contrast, among elderly persons, elderly black males have the highest rate of violence, followed by black females, white males, and white females. Thus, elderly whites are more likely to be victims of personal theft, and elderly blacks are more likely to be victims of violent crime.
According to the National Center on Elder Abuse (2005), elder sexual abuse is “non-consensual sexual contact of any kind with an elderly person” (National Center on Elder Abuse, 2006, p. 1). Official statistics suggest that older adults are rarely sexually abused (as compared to younger victims). Even so, interviews conducted by elder abuse expert Holly Ramsey-Klawsnik (1991) with Adult Protective Services employees show that most, if not all, individuals working in Adult Protective Services have encountered instances of elder sexual abuse. Ramsey- Klawsnick argues that elderly persons are prime targets of sexual abuse because many are vulnerable and either unwilling or unable to report the abuse. The central premise of her approach to understanding elder sexual abuse is that sexual offenses are more often about power and control, and abusive caregivers find themselves in a position of power. They use sex to maintain the power and subsequently exert even more control over the victim. She further suggests that official statistics underestimate the extent of elder sexual abuse.
Based on this framework, Ramsey-Klawsnick (1999) cites three types of behaviors that are examples of elder sexual abuse. First, hands-off behaviors include activities where the offender does not touch the victim but does things that are sexual in nature that potentially harm the victim. Ramsey-Klawsnick cites “exhibitionism, voyeuristic activity, and forcing an individual to watch pornographic materials” as examples of hands-off behaviors (p. 2). Second, hands-on behaviors involve behaviors where the offender makes contact with the victim. Third, harmful genital practices include “unwarranted, intrusive, and/or painful procedures in caring for the genitals or rectal area” (p. 2).
Neglect is a form of elder abuse that occurs when individuals fail to provide care to a person for whom they are expected to provide care. Some have argued that neglect is the most common form of elder abuse. Experts cite two types of neglect: active and passive. The simplest distinction between the two forms of neglect has to do with intent. In active neglect cases, the offender intends to neglect the care recipient; in passive neglect cases, the caregiver does not intend to commit neglect—the offender often just does not know how to provide care to an older person.
Self-neglect has been described as the most controversial form of elder abuse. It basically refers to instances where individuals fail to provide care to themselves. Technically, it is not criminal in nature. Older persons would never be sent to jail or prison, or placed on probation for that matter, for failing to take their medication, not eating, hoarding goods, or any other self-neglectful behavior. Still, protective services may be called to intervene in situations where self-neglect is believed to be occurring. It is controversial because self-neglect has been regarded, by some, as ageist. That is, if a younger person engages in self-neglectful behaviors, no formal interventions will occur. If an older person engages in these behaviors, however, the individual may be approached by Adult Protective Services for some form of intervention, which in some cases—albeit rarely—may include institutional placement. While it is not criminal behavior, in Family Violence and Criminal Justice: A Life Course Approach, Payne and Gainey (2005) argue that self-neglect is a form of family violence. They suggest that such behavior may be occurring with other forms of abuse. Even if other forms of abuse are not occurring, self-neglect may harm family members who have to witness their loved one not taking care of him- or herself.
The National Center on Elder Abuse defines emotional (or psychological) abuse as the “infliction of anguish, pain, or distress through verbal or nonverbal acts” (http://www.ncea.aoa.gov/). Although this is the least commonly reported form of elder abuse, the harm from such abuse can be devastating. The range of behaviors include using derogatory language, calling people names they don’t want to be called, isolating them, not allowing them to choose how to spend their time, and so on. In some instances, emotional abuse may be subtle. Consider a case in which a caregiver never lets a care recipient choose what to watch on television. In other instances, the behavior may be more blatant. Consider a case in which a caregiver arranges furniture so that the care recipient cannot move around as easily, or the caregiver moves pictures of the care recipient’s loved ones so they are out of the view of the care recipient. Such behavior certainly falls within the framework of a social harm approach to defining elder abuse.
Estimates from the National Center on Elder Abuse show that a number of different groups are involved in identifying elder abuse. The following estimates show how often different representatives reported suspected elder abuse cases to state reporting systems:
- Health care providers reported 22.5% of elder abuse cases to protective services.
- Family members reported 16% of elder abuse cases to authorities.
- Service providers (including paid and volunteer workers) reported 15% of the cases.
- Friends and family members reported 8% of elder abuse cases to protective services.
- Adult protective services workers reported 6% of cases to authorities.
- Law enforcement officials reported 4.7% of cases to protective services.
- An unrelated caregiver reported elder abuse in 3.3% of cases.
- The victim reported the elder abuse in 3.8% of cases.
Given that just 1 in 25 reports is made by the victim him- or herself, it is imperative that those who are in situations where elder abuse might be present are able to identify the cases. Warning signs are related to types of abuse. One set of warning signs demonstrates the possibility of physical abuse, while other sets of warning signs exist for sexual abuse, neglect, financial abuse, and so on.
The California Department of Justice (2002) classifies warning signs into categories of physical, isolation, and behavioral. Physical warning signs of elder abuse include the following:
- Uncombed or matted hair
- Poor skin condition or hygiene
- Unkempt or dirty appearance
- Patches of hair missing or bleeding scalp
- Any untreated medical condition
- Malnourished or dehydrated
- Foul smelling
- Torn or bloody clothing or undergarments
- Scratches, blisters, lacerations, or marks
- Unexplained bruises or welts
- Burns caused by scalding water, cigarettes, or ropes
- Injuries that are incompatible with explanations
- Any injuries that reflect an outline of an object—for example, a belt, cord, or hand (p. 3)
Isolation warning signs refer to instances when older persons are physically separated from others. Experts suggest that abusers use isolation as a strategy to hide the abuse and promote the victim’s dependence on the abuser. Signs of isolation include the following:
- Family members or caregivers have isolated the elder, restricting the elder’s contact with others, including family, visitors, doctors, clergy, or friends.
- Elder is not given the opportunity to speak freely or have contact with others without the caregiver being present. (California Department of Justice, 2002, p. 4)
Behavioral warning signs refer to behaviors of the elder or caregiver that indicate abuse. Consequences of virtually any form of abuse may result in victims acting or behaving differently. Behavioral warning signs for elder physical abuse include instances when the older victim appears to exhibit the following behaviors:
- Helplessness
- Secretiveness
- Fear to communicate
- Fear in general (California Department of Justice, 2002, p. 5)
A different set of warning signs might arise for other forms of elder abuse. For example, discussing ways that health care professionals can identify financial abuse in Crime in the Home Health Care Field, Brian Payne (2003) suggests that the warning signs of financial abuse include the following:
- Sudden changes in banking practice
- Abrupt changes in a will or other documents
- Abrupt and unexplainable disappearance of money or other assets
- Additional names on elder’s bank signature card
- Poor care provided although adequate resources available
- Previously uninvolved relatives become involved and make claims to assets
- Unpaid bills although funds are available
- Sudden withdrawal from accounts
- Extraordinary interest by others in elderly person’s assets
To be sure, when searching for signs of abuse, individuals should focus on all forms and recognize that it is not their job to determine that elder abuse occurred; instead, it is their job to determine if it might have occurred. Investigators are given the task of substantiating the abuse. As an illustration, the American Medical Association suggests that health care practitioners ask the following questions of vulnerable patients who exhibit risk factors for abuse:
- Does anyone hit you?
- Are you afraid of anyone at home?
- Does anyone take things that don’t belong to you without asking?
- Has anyone ever touched you without your consent?
- Are you alone a lot?
- Does anyone yell at you or threaten you?
If a patient answers yes to any of these questions, it does not necessarily mean that abuse occurred. However, it does mean that abuse might have occurred, and health care professionals or other individuals should report their suspicions to social services.
While signs of elder abuse exist and practitioners are given a set of questions to ask to identify the possibility of abuse, the reality is that elder abuse is drastically underreported. Estimates from the National Center on Elder Abuse suggest that anywhere from 1 in 5 to 1 in 14 cases of elder abuse are reported. To address underreporting and other issues related to elder abuse, Attorney General Janet Reno asked a group of 27 experts to participate in a round table in October 2000. The round table was titled Elder Justice: Medical Forensic Issues Relating to Elder Abuse and Neglect. The panel suggested that elder abuse was unreported and undiagnosed for the following reasons:
- No established signs of elder abuse and neglect . There is a paucity of research identifying what types of bruising, fractures, pressure sores, malnutrition, and dehydration are evidence of potential abuse or neglect. This impedes detection and complicates training. Some forensic indicators, however, are known. For example, certain types of fractures or pressure sores almost always require further investigation, whereas others may not require investigation if adequate care was provided and documented.
- No validated screening tool . There is no standardized, validated screening or diagnostic tool for elder abuse and neglect. Such a tool could greatly assist in the detection and diagnosis of elder abuse and neglect and would serve to educate and, where appropriate, to trigger suspicion, additional inquiry, or reporting to Adult Protective Services (APS) or law enforcement. Research is needed to create and validate such a focus.
- Difficulty in distinguishing between abuse and neglect versus other conditions . Older people often suffer from multiple chronic illnesses. Distinguishing conditions caused by abuse or neglect from conditions caused by other factors can be complex. Often the signs of abuse and neglect resemble—or are masked by—those of chronic illnesses. Elder abuse and neglect are very heterogeneous; medical indicators should be viewed in the context of home, family, care providers, decision-making capacity, and institutional environments.
- Ageism and reluctance to report . Ageism results in the devaluation of the worth and capacity of older people. This insidious factor may result in a less vigorous inquiry into the death or suspicious illness of an older person as compared with someone younger. Such ageism may impede and result in inadequate detection and diagnosis, particularly where combined with physicians’ disinclination to report or become involved in the legal process.
- Few experts in forensic geriatrics . In the case of child abuse, doctors who suspect abuse or neglect have the alternative of calling a pediatric forensic expert who will see the child; do the forensic evaluation; do the documentation; and, if necessary, do the reporting and go to court. This eliminates the responsibility of primary care physicians to follow up and relieves them of the burden of becoming involved in the legal process. It increases reporting because the frontline providers feel like they have medical experts backing them up. Training geriatric forensic specialists to serve an analogous role should similarly promote detection, diagnosis, and reporting and increase the expertise in the field.
- Patterns of problems . In the institutional setting, data indicating a pattern of problems may facilitate detection. For example, the minimum data set (MDS) of information for a single facility or for a nursing home chain may include an unacceptably high rate of malnourishment that—absent an explicit formal diagnosis—should trigger additional inquiry. Similarly, a survey may cite a facility for putting its residents in “immediate jeopardy” as a result of providing poor care. Or emergency room staff may identify a pattern of problems from a particular facility. In these examples, the data itself may be a useful tool in facilitating detection of abuse and neglect. This type of information is accessible not only to health care providers but also to others (U.S. Department of Justice, 2002, p. 2).
Mandatory reporting laws and training have been used to improve the ability of professionals to identify suspected cases of elder abuse. Mandatory reporting laws are those that state that certain professionals must report suspected cases of elder abuse to the authorities (which in most cases means social services). In all, 42 states have some form of mandatory reporting law. Mandated reporters include health care professionals, social services professionals, long-term care employees, criminal justice professionals, financial employees, and other professionals who might come into contact with older persons vulnerable to victimization.
Mandatory reporting laws have both strengths and weaknesses. Supporters of the laws contend that they are necessary in order to offer protection to older persons at risk of victimization. They further contend that the laws offer a strategy to educate different groups about elder abuse. In addition, those who support these laws suggest that they send a message to the public that elder abuse will not be tolerated. Finally, supporters note that the laws offer immunity to those who report in good faith. Consequently, the laws protect reporters, thereby removing their concerns about being sued for reporting misconduct.
A number of criticisms have been levied against mandatory reporting laws. Some have pointed out that the laws were developed based on child abuse models and that there was no evidence that elder abuse dynamics were similar to child abuse dynamics. In addition, the lack of research on the need for the laws has been cited as problematic. Critics also note that the laws are ageist because they assume that at a certain point in the life course, individuals are in need of help. A lack of understanding about the laws also has been offered as a criticism. In addition, some have argued that there is no evidence that the laws work; in fact, some have suggested that mandatory reporting laws create more problems then they solve. Also, some have criticized the laws on the grounds that they are not responsive to the actual dynamics of elder abuse. On a similar point, some have noted that the laws were actually unfunded mandates because no funding came along with the passage of the laws. As well, the laws have been criticized for being politically motivated as an ineffective strategy to respond to elder abuse. Finally, some have pointed out that the lack of awareness about how to abide by the law has been problematic.
The development and implementation of different training programs has been one strategy to increase adherence to mandatory reporting laws and promote detection of elder abuse. The United States Department of Justice has provided federal funding to support the development of training curricula on elder abuse. The Office for Victims of Crime has distributed the funding so that the training could actually be carried out. The American Probation and Parole Association recently developed a training curriculum to encourage better responses to elder abuse among probation and parole officers. As well, advocates at the local level have developed training packages and programs.
Despite this increased use of training, a number of concerns have made it difficult to train criminal justice professionals about elder abuse. First, the lack of adequate state laws makes it difficult to train regarding appropriate responses. Second, a lack of specific policies and protocols creates situations where curricula are more emotionally driven, rather than empirically grounded. Third, a lack of concern about elder abuse has made it difficult to get police recruits, law enforcement officers, police executives, court officials, judges, prosecutors, probation and parole officers, and other criminal justice officials willing to participate in the training. Fourth, training is typically given a lower priority when funding decisions are made. Fifth, elder abuse training curricula are not truly based on evidence-based practices simply because no such practices have been developed to guide the criminal justice response to elder abuse. Sixth, it has sometimes been assumed that training will improve the response to elder abuse, yet no evidence has actually made this connection. Finally, curricula are often developed that are devoid of criminological theory. Failing to understand the potential causes of elder abuse results in training packages that are destined for problems.
One of the most basic drives of any field of study involves efforts to explain the behavior being studied. Early elder abuse research tended to focus on the following four explanations:
- Intraindividual explanations
- Dependency explanations
- Caregiver stress explanations
- Cycle-of-violence explanations
More recently, criminologists have demonstrated how different criminological theories can be applied to elder abuse. Criminological explanations that have been applied to elder abuse include the following:
- Deterrence theory
- Strain theory
- Social control theory
- Conflict theory
- Learning theory
- Neutralization theory
- Self-control theory
- Routine activities theory
- Social disorganization theory
In this section, the way that traditional and criminological explanations have been used to explain elder abuse is considered.
Intraindividual explanations suggest that something within either the older person or the offender caused the abuse. For instance, it has been suggested that abusers tend to be unemployed individuals who have drug problems or mental health issues. Among victims, it has been found that dementia and other health-related problems place older individuals at a higher risk for abuse.
Dependency explanations suggest that the care recipient’s dependency on the caregiver places the older individual at risk for abuse. Those citing this explanation often refer to Susan Steinmetz’s (1988) concept of generational inversion to demonstrate how this dependency manifests itself. When individuals are younger, they tend to be dependent on their parents for food, resources, housing, emotional needs, and so on. As the parent ages, and the child does as well, at some point the parent may become unable to care for himself or herself. The parent then may become dependent on the child. While this explanation makes some degree of sense, experts do not all agree that dependency causes elder abuse. Some say that it may cause financial abuse, but it does not necessarily cause physical abuse.
Caregiver stress explanations suggest that abuse occurs because caregivers are unable to cope with the stress that arises from the caregiving situation. From this perspective, it is argued that adult children are not adequately prepared to become caregivers for their parents. When they become caregivers, the burden that comes along with the caregiving creates a situation where individuals may become aggressive in order to cope with the stress. While all agree that caregiving can be stressful, fewer experts agree that stress actually causes abuse. Other factors and dynamics are likely more relevant.
Cycle-of-violence explanations have suggested that elder abuse may be attributed to living in violent families. Initially, it was believed that people who abused older persons were victims of child abuse who were “getting even” with their older parents. Note, however, that no studies have supported this belief. Indeed, it is now believed that child abuse victims, because of the dynamics of their victimization experience, would rarely become the primary caregiver for their aging parents (e.g., an adult offspring will not be likely to become a caregiver for a parent that was abusive).
The above explanations were the early ones for elder abuse. As criminologists have become involved in studying elder abuse, it has become apparent that some criminological explanations can be applied to the phenomenon. For example, using deterrence theory as a guide, it is plausible that cases of elder abuse continue because individuals are able to get away with their offending with minimal, if any, punishment. Criminologist Brian Payne (2006) has argued that strain theory can be used to understand caregiver stress explanations, and self-control theory can be integrated with the intraindividual explanations. In addition, rather than looking at the cycle of violence specifically, criminologists have suggested an examination of how social learning applies to elder abuse. As well, criminologists have noted that routine activities theory easily applies to elder abuse, particularly in nursing homes. The abuser is the motivated offender, the victim is the vulnerable target, and the lack of criminal justice concern about elder abuse equates to the lack of a capable guardian. Criminologists are also now beginning to apply social disorganization theory to elder abuse. In particular, researchers are considering whether elder abuse is distributed equally across communities.
Compared with other forms of abuse, the study of elder abuse is relatively rare among criminologists. With increases in funding from the National Institute of Justice, criminologists are beginning to pay more attention to elder abuse. To better understand the phenomenon, it is imperative that criminologists work with social scientists and hard scientists from other disciplines. Doing so will help to generate increased understanding about this problem, one that is likely to increase as the proportion of older persons in society continues to grow.
Bibliography:
- Anetzberger, G. (1987). The etiology of elder abuse by adult offspring. Springfield, IL: Charles C Thomas.
- Baker,A.A. (1975). Granny-battering. Modern Geriatrics, 5, 20–24.
- Block, M., & Sinnott, J. (1979). The battered elder syndrome. College Park: University of Maryland Center on Aging.
- Bureau of Justice Statistics. (1994). Elderly crime victims: National crime survey. Washington, DC: U.S. Department of Justice.
- California Department of Justice. (2002). A citizen’s guide to preventing and reporting elder abuse. Sacramento: CA: Office of the Attorney General.
- Crystal, S. (1987). Elder abuse: The latest crisis. Public Interest, 88, 56–66.
- Harris, D. K. (1999). Elder abuse in nursing homes: The theft of patients’ possessions. Journal of Elder Abuse & Neglect, 10(3/4), 141–151.
- Harris, D. K., & Benson, M. L. (1998). Nursing home theft: The hidden problem. Journal of Aging Studies, 12(1), 57–67.
- Katz, J. (1990). Seductions of crime. New York: Basic Books.
- Lindbloom, E., Brandt, J., Hawes, C., Phillips, C., Zimmerman, D., Robinson, J., et al. (2005, April). The role of forensic science in identification of mistreatment deaths in long-term care facilities. Final report submitted to the National Institute of Justice, Washington, DC (NCJ 209334). Retrieved August 21, 2013, from https://www.ncjrs.gov/pdffiles1/nij/grants/209334.pdf
- McNamee, C. C., & Murphy, M. B. (2006, November). Elder abuse in the United States. NIJ Journal, 225.
- National Center on Elder Abuse. (2006). Elder abuse: Fact sheet. Rockville, MD: U.S. Department of Health and Human Services.
- Payne, B. K. (2002). An integrated understanding of elder abuse and neglect. Journal of Criminal Justice, 30, 535–547.
- Payne, B. K. (2006). Crime and elder abuse: An integrated perspective (2nd ed.). Springfield, IL: Charles C Thomas.
- Payne, B. K. (2003). Crime in the home health care field: Workplace violence, fraud, and abuse. Springfield, IL: Charles C Thomas.
- Payne, B. K., & Gainey, R. R. (2005). Family violence and criminal justice: A life course approach (2nd ed.). Cincinnati, OH: Anderson.
- Phillips, L. R. (1983). Abuse and neglect of the frail elderly at home: An exploration of theoretical relationships. Journal of Advanced Nursing, 8, 379–392.
- Pillemer, K., & Finkelhor, D. (1988). The prevalence of elder abuse: A random sample survey. Gerontologist, 28, 51–57.
- Pillemer, K., & Suitor, J. J. (1992). Violence and violent feelings: What causes them among family caregivers? Journal of Gerontology, 47, S165–S172.
- Powell, D. E. (1980). The crimes against the elderly. Journal of Gerontological Social Work, 3, 27–39.
- Ramsey-Klawsnick, H. (1991). Elder sexual abuse: Preliminary findings. Journal of Elder Abuse & Neglect, 3(3), 73–90.
- Ramsey-Klawsnick, H. (1995). Investigating suspected elder maltreatment. Journal of Elder Abuse & Neglect, 7(1), 41–67.
- Ramsey-Klawsnick, H. (1999, June 10). Elder sexual abuse: Workshop handouts. Presented at the annual meeting of the Virginia Coalition for the Prevention of Elder Abuse, Richmond.
- Steinmetz, S. K. (1988). Duty bound: Elder abuse and family care. Newbury Park, CA: Sage.
- Stiegel, L. A. (1995). Recommended guidelines for state courts handling cases involving elder abuse. Washington, DC: American Bar Association.
- U.S. Department of Justice. (2002). Elder justice roundtable. National Institute of Justice. Washington, DC: U.S. Government Printing Office.
- Wolf, R. S. (1997). Elder abuse and neglect: Causes and consequences. Journal of Geriatric Psychiatry, 30, 153–174.
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to order a custom research paper on elder abuse and get your high quality paper at affordable price.
ORDER HIGH QUALITY CUSTOM PAPER


IMAGES
VIDEO
COMMENTS
Abuse of older adults is recognized as a pervasive and serious problem in society. Prevalence estimates have ranged from 10% upwards in cognitively intact persons from North and South America, with large variations between different countries and subcategories of the population [1,2,3].Elder abuse is defined by the World Health Organization (WHO) as "a single or repeated act or lack of ...
A systematic review of elder abuse research has not been conducted across disciplines. The purpose of this research was to provide a systematic review of and assign an evidence grade to the research articles on elder abuse. Sixteen healthcare and criminal justice literature databases were searched. The literature review was of English-language ...
Elder abuse is defined as: "(a) intentional actions that cause harm or create a serious risk of harm (whether or not harm is intended) to a vulnerable elder by a caregiver or other person who stands in a trust relationship, or (b) failure by a caregiver to satisfy the elder's basic needs or to protect the elder from harm."
Although elder abuse is a newer field of violence research than domestic violence and child abuse, research indicates that elder abuse is a common, fatal, and costly yet understudied condition. 3-6 An estimated 10% of U.S. older adults have experienced some form of elder abuse, yet only a fraction is reported to Adult Protective Services (APS). 1
In a survey of more than 4000 older people in New York State, the rate of elder abuse was found to be 7.6% 16,17; in a national survey by Laumann et al., the rate was 9%, 12 and in a national ...
Little is known about elder abuse in nursing homes, and compared to research on other forms of interpersonal abuse, research about elder abuse in nursing homes is still in its infancy [1, 2].Although no national prevalence data are available in any country internationally, high rates of elder abuse and neglect have been reported in nursing homes, including Norway [1, 3].
Although research on elder abuse has increased dramatically over several decades, the authors overcome some of the major flaws of past studies (for example, small, convenience samples; cross ...
Introduction. Elder abuse refers to intentional or unintentional harmful acts toward an older person where trust is expected. Common types of elder abuse include physical, psychological, sexual abuse, financial exploitation, and neglect (World Health Organization, 2002; Acierno et al., 2010).As a global public health concern, about 1 in 6 community-dwelling older adults experienced some form ...
Purpose We review the underappreciated problem of elder abuse with a focus on what trauma surgeons need to know. Because of its prevalence, it is important that clinicians understand types of elder abuse, risk factors in patient and perpetrator, prevention strategies, and the appropriate referral and treatment of potential victims of elder abuse. Recent Findings Elder abuse affects at least 10 ...
Elder abuse (EA) (also known as older adult abuse, mistreatment, or maltreatment) can be defined as "a single or repeated act or lack of appropriate action, occurring within a relationship of trust, which causes harm or distress to an older person" (World Health Organization [WHO], 2020, para. 2).EA is a widespread global problem, with a recent study finding a pooled prevalence rate of 15. ...
Abuse of people age 60 and older is widespread, research shows. According to a 2017 study in The Lancet Global Health, "elder abuse seems to affect 1 in 6 older adults worldwide, which is roughly 141 million people.". Elder abuse takes many forms. A 2015 review article in The New England Journal of Medicine explains that research on elder abuse generally addresses these five categories ...
Ethics and Elder Abuse Research Paper. This sample Ethics and Elder Abuse Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write ….
Elder abuse in the COVID-19 era based on calls to the National Center on Elder Abuse resource line: 2022: Cross-sectional V: Souza et al. ... or married (28,35) are information collected from sample characterization in research and listed in the literature as risk factors for EA. Considering the ecological model, such characteristics are ...
The purpose of this research was to provide a systematic review of, and assign an evidence grade to, the research articles on elder abuse. Sixteen health care and criminal justice literature ...
In this paper, I review the epidemiology of elder abuse as well as key practical issues in dealing with the cases of elder abuse. ... (APS). The U.S. National Elder Mistreatment Study, conducted with a representative sample of 5,777 adults aged 60 ... Recent elder abuse research in the Chicago Chinese community has demonstrated success and has ...
An overview of global issues in the field of elder abuse, with a focus on prevention, is provided from an international perspective, highlighting a growing consensus across studies regarding the extent and causes of elder mistreatment. Expand. 469. Highly Influenced.
Introduction. Elder abuse is a growing concern in Canada, as the population ages and the number of seniors in the country continues to increase. Defined as any action or inaction that causes harm or distress to an older person, elder abuse can take many forms, including physical, emotional, financial, or sexual abuse.
Elder Abuse. Abstract Old age is part of the human life cycle. Just as a plant grows from a seed to a full-grown tree, then in its maturity it dies by the hands of a lumberjack, man's fate is just as equal to the tree, humans grow, age, and die. Aging has been a point of discussion for thousands of years, generating ideas like immortality as ...
Elder Abuse: Learn the Signs and Break the Silence. This is an act of emotional abuse and material exploitation by depriving the elderly women of communication, the man tries to get what he wants. We will write. a custom essay specifically for you by our professional experts. 809 writers online.
In this paper, we discuss recent advances in elder abuse research and theory how they can be brought to bear on improved elder abuse intervention program evaluations. To operationalize how these benefits might be achieved, we focus on two popular and rapidly expanding elder abuse interventions as exemplars: Multidisciplinary teams (MDTS) and ...
Anetzberger, G. The Clinical Management of Elder Abuse. New York: Hawthorne Press, 2004. American Medical Association white paper on elderly health. Report of the Council on Scientific Affairs. (1990). Archives of internal medicine, 150(12), 2459-2472. Lachs MS, Williams CS, O'Brien S, et. al. (1998). The Mortality of Elder Mistreatment.
Types of Abuse. Elder abuse occurring either in the home or in an institution can be described as one or more of the following types: physical abuse, neglect, psychological abuse, financial abuse, and sexual abuse. This research-paper focuses on the issues of elder abuse as it occurs in the home. 1.3.1. Physical.
Analysis of quantitative data of women aged 60 and above in the systematic review of quantitative studies of elder abuse found a global prevalence of elder abuse against women of 14.1% in the past year, with psychological abuse reported as the most prevalent form of violence, followed by neglect . The focus of this review was prevalence of ...
This sample elder abuse research paper is published for educational and informational purposes only. Free research papers, are not written by our writers, they are contributed by users, so we are not responsible for the content of this free sample paper. If you want to buy a high quality research paper on elder abuse at affordable price please ...