Obesity Research - Science topic

- asked a question related to Obesity Research
- Oct 1, 2019
- 2015 - COMPARISON OF HEPATIC PROFILE IN PRE AND POSTOPERATIVE OF BARIATRIC SURGERY - PRIVATE VS PUBLIC NETWO RK.pdf 328.17 KB

- Oct 15, 2019
- 48 Recommendations

- Jul 9, 2016

- May 18, 2019
- 9 Recommendations

- Jun 16, 2016
- Feb 8, 2019
- 0 Recommendations

- Oct 25, 2016

- Oct 28, 2016
- 4 Recommendations

- Jun 22, 2016
- 3 Recommendations

- Jun 8, 2016

- Jun 9, 2016
- 5 Recommendations

- Jan 27, 2016

- Jan 29, 2016
- 8 Recommendations

- Nov 8, 2015

- Jan 28, 2016
- 11 Recommendations

- Dec 17, 2015

- Dec 28, 2015
- asthma&obesity&childhood_ RS.pdf 1.13 MB
- 2 Recommendations

- Nov 20, 2015

- Nov 21, 2015
- 18 Recommendations

- Aug 6, 2015

- Oct 13, 2015
- AMY1 gene on obesity risk in Mexican childr en.pdf 148.50 KB
- art-3A10.1007-2Fs0012501006 49.pdf 65.42 KB
- Diurnal Salivary Cortisol Is Associated20 13.pdf 417.16 KB
- Low copy number of the salivary amylase ge ne.pdf 774.65 KB
- Serum Leptin, Salivary Cortisol, and Obesity in Swedish Men 20 02.pdf 69.36 KB
- Sustained Exendin-4 Secretion through Gene Thera py.pdf 1.87 MB
- 6 Recommendations
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Effectiveness of...
Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials
- Related content
- Peer review
- Claire D Madigan , senior research associate 1 ,
- Henrietta E Graham , doctoral candidate 1 ,
- Elizabeth Sturgiss , NHMRC investigator 2 ,
- Victoria E Kettle , research associate 1 ,
- Kajal Gokal , senior research associate 1 ,
- Greg Biddle , research associate 1 ,
- Gemma M J Taylor , reader 3 ,
- Amanda J Daley , professor of behavioural medicine 1
- 1 Centre for Lifestyle Medicine and Behaviour (CLiMB), The School of Sport, Exercise and Health Sciences, Loughborough University, Loughborough LE11 3TU, UK
- 2 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
- 3 Department of Psychology, Addiction and Mental Health Group, University of Bath, Bath, UK
- Correspondence to: C D Madigan c.madigan{at}lboro.ac.uk (or @claire_wm and @lboroclimb on Twitter)
- Accepted 26 April 2022
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care.
Design Systematic review and meta-analysis of randomised controlled trials.
Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary care compared with no treatment, attention control, or minimal intervention and weight change at ≥12 months follow-up.
Data sources Trials from a previous systematic review were extracted and the search completed using the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021.
Data extraction and synthesis Two reviewers independently identified eligible studies, extracted data, and assessed risk of bias using the Cochrane risk of bias tool. Meta-analyses were conducted with random effects models, and a pooled mean difference for both weight (kg) and waist circumference (cm) were calculated.
Main outcome measures Primary outcome was weight change from baseline to 12 months. Secondary outcome was weight change from baseline to ≥24 months. Change in waist circumference was assessed at 12 months.
Results 34 trials were included: 14 were additional, from a previous review. 27 trials (n=8000) were included in the primary outcome of weight change at 12 month follow-up. The mean difference between the intervention and comparator groups at 12 months was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, P<0.001), favouring the intervention group. At ≥24 months (13 trials, n=5011) the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, P<0.001) favouring the intervention. The mean difference in waist circumference (18 trials, n=5288) was −2.5 cm (−3.2 to −1.8 cm, I 2 =69%, P<0.001) in favour of the intervention at 12 months.
Conclusions Behavioural weight management interventions for adults with obesity delivered in primary care are effective for weight loss and could be offered to members of the public.
Systematic review registration PROSPERO CRD42021275529.
Introduction
Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality. 1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19. 4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight. 6
Primary care is an ideal setting for delivering weight management services, and international guidelines recommend that doctors should opportunistically screen and encourage patients to lose weight. 7 8 On average, most people consult a primary care doctor four times yearly, providing opportunities for weight management interventions. 9 10 A systematic review of randomised controlled trials by LeBlanc et al identified behavioural interventions that could potentially be delivered in primary care, or involved referral of patients by primary care professionals, were effective for weight loss at 12-18 months follow-up (−2.4 kg, 95% confidence interval −2.9 to−1.9 kg). 11 However, this review included trials with interventions that the review authors considered directly transferrable to primary care, but not all interventions involved primary care practitioners. The review included interventions that were entirely delivered by university research employees, meaning implementation of these interventions might differ if offered in primary care, as has been the case in other implementation research of weight management interventions, where effects were smaller. 12 As many similar trials have been published after this review, an updated review would be useful to guide health policy.
We examined the effectiveness of weight loss interventions delivered in primary care on measures of body composition (weight and waist circumference). We also identified characteristics of effective weight management programmes for policy makers to consider.
This systematic review was registered on PROSPERO and is reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. 13 14
Eligibility criteria
We considered studies to be eligible for inclusion if they were randomised controlled trials, comprised adult participants (≥18 years), and evaluated behavioural weight management interventions delivered in primary care that focused on weight loss. A primary care setting was broadly defined as the first point of contact with the healthcare system, providing accessible, continued, comprehensive, and coordinated care, focused on long term health. 15 Delivery in primary care was defined as the majority of the intervention being delivered by medical and non-medical clinicians within the primary care setting. Table 1 lists the inclusion and exclusion criteria.
Study inclusion and exclusion criteria
- View inline
We extracted studies from the systematic review by LeBlanc et al that met our inclusion criteria. 11 We also searched the exclusions in this review because the researchers excluded interventions specifically for diabetes management, low quality trials, and only included studies from an Organisation for Economic Co-operation and Development country, limiting the scope of the findings.
We searched for studies in the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021 (see supplementary file 1). Reference lists of previous reviews 16 17 18 19 20 21 and included trials were hand searched.
Data extraction
Results were uploaded to Covidence, 22 a software platform used for screening, and duplicates removed. Two independent reviewers screened study titles, abstracts, and full texts. Disagreements were discussed and resolved by a third reviewer. All decisions were recorded in Covidence, and reviewers were blinded to each other’s decisions. Covidence calculates proportionate agreement as a measure of inter-rater reliability, and data are reported separately by title or abstract screening and full text screening. One reviewer extracted data on study characteristics (see supplementary table 1) and two authors independently extracted data on weight outcomes. We contacted the authors of four included trials (from the updated search) for further information. 23 24 25 26
Outcomes, summary measures, and synthesis of results
The primary outcome was weight change from baseline to 12 months. Secondary outcomes were weight change from baseline to ≥24 months and from baseline to last follow-up (to include as many trials as possible), and waist circumference from baseline to 12 months. Supplementary file 2 details the prespecified subgroup analysis that we were unable to complete. The prespecified subgroup analyses that could be completed were type of healthcare professional who delivered the intervention, country, intensity of the intervention, and risk of bias rating.
Healthcare professional delivering intervention —From the data we were able to compare subgroups by type of healthcare professional: nurses, 24 26 27 28 general practitioners, 23 29 30 31 and non-medical practitioners (eg, health coaches). 32 33 34 35 36 37 38 39 Some of the interventions delivered by non-medical practitioners were supported, but not predominantly delivered, by GPs. Other interventions were delivered by a combination of several different practitioners—for example, it was not possible to determine whether a nurse or dietitian delivered the intervention. In the subgroup analysis of practitioner delivery, we refer to this group as “other.”
Country —We explored the effectiveness of interventions by country. Only countries with three or more trials were included in subgroup analyses (United Kingdom, United States, and Spain).
Intensity of interventions —As the median number of contacts was 12, we categorised intervention groups according to whether ≤11 or ≥12 contacts were required.
Risk of bias rating —Studies were classified as being at low, unclear, and high risk of bias. Risk of bias was explored as a potential influence on the results.
Meta-analyses
Meta-analyses were conducted using Review Manager 5.4. 40 As we expected the treatment effects to differ because of the diversity of intervention components and comparator conditions, we used random effects models. A pooled mean difference was calculated for each analysis, and variance in heterogeneity between studies was compared using the I 2 and τ 2 statistics. We generated funnel plots to evaluate small study effects. If more than two intervention groups existed, we divided the number of participants in the comparator group by the number of intervention groups and analysed each individually. Nine trials were cluster randomised controlled trials. The trials had adjusted their results for clustering, or adjustment had been made in the previous systematic review by LeBlanc et al. 11 One trial did not report change in weight by group. 26 We calculated the mean weight change and standard deviation using a standard formula, which imputes a correlation for the baseline and follow-up weights. 41 42 In a non-prespecified analysis, we conducted univariate and multivariable metaregression (in Stata) using a random effects model to examine the association between number of sessions and type of interventionalist on study effect estimates.
Risk of bias
Two authors independently assessed the risk of bias using the Cochrane risk of bias tool v2. 43 For incomplete outcome data we defined a high risk of bias as ≥20% attrition. Disagreements were resolved by discussion or consultation with a third author.
Patient and public involvement
The study idea was discussed with patients and members of the public. They were not, however, included in discussions about the design or conduct of the study.
The search identified 11 609 unique study titles or abstracts after duplicates were removed ( fig 1 ). After screening, 97 full text articles were assessed for eligibility. The proportionate agreement ranged from 0.94 to 1.0 for screening of titles or abstracts and was 0.84 for full text screening. Fourteen new trials met the inclusion criteria. Twenty one studies from the review by LeBlanc et al met our eligibility criteria and one study from another systematic review was considered eligible and included. 44 Some studies had follow-up studies (ie, two publications) that were found in both the second and the first search; hence the total number of trials was 34 and not 36. Of the 34 trials, 27 (n=8000 participants) were included in the primary outcome meta-analysis of weight change from baseline to 12 months, 13 (n=5011) in the secondary outcome from baseline to ≥24 months, and 30 (n=8938) in the secondary outcome for weight change from baseline to last follow-up. Baseline weight was accounted for in 18 of these trials, but in 14 24 26 29 30 31 32 44 45 46 47 48 49 50 51 it was unclear or the trials did not consider baseline weight. Eighteen trials (n=5288) were included in the analysis of change in waist circumference at 12 months.

Studies included in systematic review of effectiveness of behavioural weight management interventions in primary care. *Studies were merged in Covidence if they were from same trial
- Download figure
- Open in new tab
- Download powerpoint
Study characteristics
Included trials (see supplementary table 1) were individual randomised controlled trials (n=25) 24 25 26 27 28 29 32 33 34 35 38 39 41 44 45 46 47 50 51 52 53 54 55 56 59 or cluster randomised controlled trials (n=9). 23 30 31 36 37 48 49 57 58 Most were conducted in the US (n=14), 29 30 31 32 33 34 35 36 37 45 48 51 54 55 UK (n=7), 27 28 38 41 47 57 58 and Spain (n=4). 25 44 46 49 The median number of participants was 276 (range 50-864).
Four trials included only women (average 65.9% of women). 31 48 51 59 The mean BMI at baseline was 35.2 (SD 4.2) and mean age was 48 (SD 9.7) years. The interventions lasted between one session (with participants subsequently following the programme unassisted for three months) and several sessions over three years (median 12 months). The follow-up period ranged from 12 months to three years (median 12 months). Most trials excluded participants who had lost weight in the past six months and were taking drugs that affected weight.
Meta-analysis
Overall, 27 trials were included in the primary meta-analysis of weight change from baseline to 12 months. Three trials could not be included in the primary analysis as data on weight were only available at two and three years and not 12 months follow-up, but we included these trials in the secondary analyses of last follow-up and ≥24 months follow-up. 26 44 50 Four trials could not be included in the meta-analysis as they did not present data in a way that could be synthesised (ie, measures of dispersion). 25 52 53 58 The mean difference was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, τ 2 =3.38; P<0.001) in favour of the intervention group ( fig 2 ). We found no evidence of publication bias (see supplementary fig 1). Absolute weight change was −3.7 (SD 6.1) kg in the intervention group and −1.4 (SD 5.5) kg in the comparator group.

Mean difference in weight at 12 months by weight management programme in primary care (intervention) or no treatment, different content, or minimal intervention (control). SD=standard deviation
Supplementary file 2 provides a summary of the main subgroup analyses.
Weight change
The mean difference in weight change at the last follow-up was −1.9 kg (95% confidence interval −2.5 to −1.3 kg, I 2 =81%, τ 2 =2.15; P<0.001). Absolute weight change was −3.2 (SD 6.4) kg in the intervention group and −1.2 (SD 6.0) kg in the comparator group (see supplementary figs 2 and 3).
At the 24 month follow-up the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, τ 2 =3.13; P<0.001) (see supplementary fig 4). As the weight change data did not differ between the last follow-up and ≥24 months, we used the weight data from the last follow-up in subgroup analyses.
In subgroup analyses of type of interventionalist, differences were significant (P=0.005) between non-medical practitioners, GPs, nurses, and other people who delivered interventions (see supplementary fig 2).
Participants who had ≥12 contacts during interventions lost significantly more weight than those with fewer contacts (see supplementary fig 6). The association remained after adjustment for type of interventionalist.
Waist circumference
The mean difference in waist circumference was −2.5 cm (95% confidence interval −3.2 to −1.8 cm, I 2 =69%, τ 2 =1.73; P<0.001) in favour of the intervention at 12 months ( fig 3 ). Absolute changes were −3.7 cm (SD 7.8 cm) in the intervention group and −1.3 cm (SD 7.3) in the comparator group.

Mean difference in waist circumference at 12 months. SD=standard deviation
Risk of bias was considered to be low in nine trials, 24 33 34 35 39 41 47 55 56 unclear in 12 trials, 25 27 28 29 32 45 46 50 51 52 54 59 and high in 13 trials 23 26 30 31 36 37 38 44 48 49 53 57 58 ( fig 4 ). No significant (P=0.65) differences were found in subgroup analyses according to level of risk of bias from baseline to 12 months (see supplementary fig 7).

Risk of bias in included studies
Worldwide, governments are trying to find the most effective services to help people lose weight to improve the health of populations. We found weight management interventions delivered by primary care practitioners result in effective weight loss and reduction in waist circumference and these interventions should be considered part of the services offered to help people manage their weight. A greater number of contacts between patients and healthcare professionals led to more weight loss, and interventions should be designed to include at least 12 contacts (face-to-face or by telephone, or both). Evidence suggests that interventions delivered by non-medical practitioners were as effective as those delivered by GPs (both showed statistically significant weight loss). It is also possible that more contacts were made with non-medical interventionalists, which might partially explain this result, although the metaregression analysis suggested the effect remained after adjustment for type of interventionalist. Because most comparator groups had fewer contacts than intervention groups, it is not known whether the effects of the interventions are related to contact with interventionalists or to the content of the intervention itself.
Although we did not determine the costs of the programme, it is likely that interventions delivered by non-medical practitioners would be cheaper than GP and nurse led programmes. 41 Most of the interventions delivered by non-medical practitioners involved endorsement and supervision from GPs (ie, a recommendation or checking in to see how patients were progressing), and these should be considered when implementing these types of weight management interventions in primary care settings. Our findings suggest that a combination of practitioners would be most effective because GPs might not have the time for 12 consultations to support weight management.
Although the 2.3 kg greater weight loss in the intervention group may seem modest, just 2-5% in weight loss is associated with improvements in systolic blood pressure and glucose and triglyceride levels. 60 The confidence intervals suggest a potential range of weight loss and that these interventions might not provide as much benefit to those with a higher BMI. Patients might not find an average weight loss of 3.7 kg attractive, as many would prefer to lose more weight; explaining to patients the benefits of small weight losses to health would be important.
Strengths and limitations of this review
Our conclusions are based on a large sample of about 8000 participants, and 12 of these trials were published since 2018. It was occasionally difficult to distinguish who delivered the interventions and how they were implemented. We therefore made some assumptions at the screening stage about whether the interventionalists were primary care practitioners or if most of the interventions were delivered in primary care. These discussions were resolved by consensus. All included trials measured weight, and we excluded those that used self-reported data. Dropout rates are important in weight management interventions as those who do less well are less likely to be followed-up. We found that participants in trials with an attrition rate of 20% or more lost less weight and we are confident that those with high attrition rates have not inflated the results. Trials were mainly conducted in socially economic developed countries, so our findings might not be applicable to all countries. The meta-analyses showed statistically significant heterogeneity, and our prespecified subgroups analysis explained some, but not all, of the variance.
Comparison with other studies
The mean difference of −2.3 kg in favour of the intervention group at 12 months is similar to the findings in the review by LeBlanc et al, who reported a reduction of −2.4 kg in participants who received a weight management intervention in a range of settings, including primary care, universities, and the community. 11 61 This is important because the review by LeBlanc et al included interventions that were not exclusively conducted in primary care or by primary care practitioners. Trials conducted in university or hospital settings are not typically representative of primary care populations and are often more intensive than trials conducted in primary care as a result of less constraints on time. Thus, our review provides encouraging findings for the implementation of weight management interventions delivered in primary care. The findings are of a similar magnitude to those found in a trial by Ahern et al that tested primary care referral to a commercial programme, with a difference of −2.7 kg (95% confidence interval −3.9 to −1.5 kg) reported at 12 month follow-up. 62 The trial by Ahern et al also found a difference in waist circumference of −4.1 cm (95% confidence interval −5.5 to −2.3 cm) in favour of the intervention group at 12 months. Our finding was smaller at −2.5 cm (95% confidence interval −3.2 to −1.8 cm). Some evidence suggests clinical benefits from a reduction of 3 cm in waist circumference, particularly in decreased glucose levels, and the intervention groups showed a 3.7 cm absolute change in waist circumference. 63
Policy implications and conclusions
Weight management interventions delivered in primary care are effective and should be part of services offered to members of the public to help them manage weight. As about 39% of the world’s population is living with obesity, helping people to manage their weight is an enormous task. 64 Primary care offers good reach into the community as the first point of contact in the healthcare system and the remit to provide whole person care across the life course. 65 When developing weight management interventions, it is important to reflect on resource availability within primary care settings to ensure patients’ needs can be met within existing healthcare systems. 66
We did not examine the equity of interventions, but primary care interventions may offer an additional service and potentially help those who would not attend a programme delivered outside of primary care. Interventions should consist of 12 or more contacts, and these findings are based on a mixture of telephone and face-to-face sessions. Previous evidence suggests that GPs find it difficult to raise the issue of weight with patients and are pessimistic about the success of weight loss interventions. 67 Therefore, interventions should be implemented with appropriate training for primary care practitioners so that they feel confident about helping patients to manage their weight. 68
Unanswered questions and future research
A range of effective interventions are available in primary care settings to help people manage their weight, but we found substantial heterogeneity. It was beyond the scope of this systematic review to examine the specific components of the interventions that may be associated with greater weight loss, but this could be investigated by future research. We do not know whether these interventions are universally suitable and will decrease or increase health inequalities. As the data are most likely collected in trials, an individual patient meta-analysis is now needed to explore characteristics or factors that might explain the variance. Most of the interventions excluded people prescribed drugs that affect weight gain, such as antipsychotics, glucocorticoids, and some antidepressants. This population might benefit from help with managing their weight owing to the side effects of these drug classes on weight gain, although we do not know whether the weight management interventions we investigated would be effective in this population. 69
What is already known on this topic
Referral by primary care to behavioural weight management programmes is effective, but the effectiveness of weight management interventions delivered by primary care is not known
Systematic reviews have provided evidence for weight management interventions, but the latest review of primary care delivered interventions was published in 2014
Factors such as intensity and delivery mechanisms have not been investigated and could influence the effectiveness of weight management interventions delivered by primary care
What this study adds
Weight management interventions delivered by primary care are effective and can help patients to better manage their weight
At least 12 contacts (telephone or face to face) are needed to deliver weight management programmes in primary care
Some evidence suggests that weight loss after weight management interventions delivered by non-medical practitioners in primary care (often endorsed and supervised by doctors) is similar to that delivered by clinician led programmes
Ethics statements
Ethical approval.
Not required.
Data availability statement
Additional data are available in the supplementary files.
Contributors: CDM and AJD conceived the study, with support from ES. CDM conducted the search with support from HEG. CDM, AJD, ES, HEG, KG, GB, and VEK completed the screening and full text identification. CDM and VEK completed the risk of bias assessment. CDM extracted data for the primary outcome and study characteristics. HEJ, GB, and KG extracted primary outcome data. CDM completed the analysis in RevMan, and GMJT completed the metaregression analysis in Stata. CDM drafted the paper with AJD. All authors provided comments on the paper. CDM acts as guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: AJD is supported by a National Institute for Health and Care Research (NIHR) research professorship award. This research was supported by the NIHR Leicester Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. ES’s salary is supported by an investigator grant (National Health and Medical Research Council, Australia). GT is supported by a Cancer Research UK fellowship. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: This research was supported by the National Institute for Health and Care Research Leicester Biomedical Research Centre; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
The lead author (CDM) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported, and that no important aspects of the study have been omitted.
Dissemination to participants and related patient and public communities: We plan to disseminate these research findings to a wider community through press releases, featuring on the Centre for Lifestyle Medicine and Behaviour website ( www.lboro.ac.uk/research/climb/ ) via our policy networks, through social media platforms, and presentation at conferences.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- Renehan AG ,
- Heller RF ,
- Bansback N ,
- Birmingham CL ,
- Abdullah A ,
- Peeters A ,
- de Courten M ,
- Stoelwinder J
- Aghili SMM ,
- Ebrahimpur M ,
- Arjmand B ,
- KETLAK Study Group
- ↵ Department of Health and Social Care. New specialised support to help those living with obesity to lose weight UK2021. www.gov.uk/government/news/new-specialised-support-to-help-those-living-with-obesity-to-lose-weight [accessed 08/02/2021].
- U.S. Preventive Services Task Force
- ↵ National Institute for Health and Care Excellence. Maintaining a Healthy Weight and Preventing Excess Weight Gain in Children and Adults. Cost Effectiveness Considerations from a Population Modelling Viewpoint. 2014, NICE. www.nice.org.uk/guidance/ng7/evidence/evidence-review-2-qualitative-evidence-review-of-the-most-acceptable-ways-to-communicate-information-about-individually-modifiable-behaviours-to-help-maintain-a-healthy-weight-or-prevent-excess-weigh-8733713.
- ↵ The Health Foundation. Use of primary care during the COVID-19 pandemic. 17/09/2020: The Health Foundation, 2020.
- ↵ Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings, 2017-18. 2019 ed. Canberra, Australia, 2018. www.abs.gov.au/AUSSTATS/[email protected]/Lookup/4839.0Main+Features12017-18?OpenDocument.
- LeBlanc ES ,
- Patnode CD ,
- Webber EM ,
- Redmond N ,
- Rushkin M ,
- O’Connor EA
- Damschroder LJ ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- McKenzie JE ,
- Bossuyt PM ,
- ↵ WHO. Main terminology: World Health Organization; 2004. www.euro.who.int/en/health-topics/Health-systems/primary-health-care/main-terminology [accessed 09.12.21].
- Aceves-Martins M ,
- Robertson C ,
- REBALANCE team
- Glasziou P ,
- Isenring E ,
- Chisholm A ,
- Wakayama LN ,
- Kettle VE ,
- Madigan CD ,
- ↵ Covidence [program]. Melbourne, 2021.
- Welzel FD ,
- Carrington MJ ,
- Fernández-Ruiz VE ,
- Ramos-Morcillo AJ ,
- Solé-Agustí M ,
- Paniagua-Urbano JA ,
- Armero-Barranco D
- Bräutigam-Ewe M ,
- Hildingh C ,
- Yardley L ,
- Christian JG ,
- Bessesen DH ,
- Christian KK ,
- Goldstein MG ,
- Martin PD ,
- Dutton GR ,
- Horswell RL ,
- Brantley PJ
- Wadden TA ,
- Rogers MA ,
- Berkowitz RI ,
- Kumanyika SK ,
- Morales KH ,
- Allison KC ,
- Rozenblum R ,
- De La Cruz BA ,
- Katzmarzyk PT ,
- Martin CK ,
- Newton RL Jr . ,
- Nanchahal K ,
- Holdsworth E ,
- ↵ RevMan [program]. 5.4 version: Copenhagen, 2014.
- Sterne JAC ,
- Savović J ,
- Gomez-Huelgas R ,
- Jansen-Chaparro S ,
- Baca-Osorio AJ ,
- Mancera-Romero J ,
- Tinahones FJ ,
- Bernal-López MR
- Delahanty LM ,
- Tárraga Marcos ML ,
- Panisello Royo JM ,
- Carbayo Herencia JA ,
- Beeken RJ ,
- Leurent B ,
- Vickerstaff V ,
- Hagobian T ,
- Brannen A ,
- Rodriguez-Cristobal JJ ,
- Alonso-Villaverde C ,
- Panisello JM ,
- Conroy MB ,
- Spadaro KC ,
- Takasawa N ,
- Mashiyama Y ,
- Pritchard DA ,
- Hyndman J ,
- Jarjoura D ,
- Smucker W ,
- Baughman K ,
- Bennett GG ,
- Steinberg D ,
- Zaghloul H ,
- Chagoury O ,
- Leslie WS ,
- Barnes AC ,
- Summerbell CD ,
- Greenwood DC ,
- Huseinovic E ,
- Leu Agelii M ,
- Hellebö Johansson E ,
- Winkvist A ,
- Look AHEAD Research Group
- LeBlanc EL ,
- Wheeler GM ,
- Aveyard P ,
- de Koning L ,
- Chiuve SE ,
- Willett WC ,
- ↵ World Health Organization. Obesity and Overweight, 2021, www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Starfield B ,
- Sturgiss E ,
- Dewhurst A ,
- Devereux-Fitzgerald A ,
- Haesler E ,
- van Weel C ,
- Gulliford MC
- Fassbender JE ,
- Sarwer DB ,
- Brekke HK ,
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NEWS FEATURE
- 11 October 2023
Why BMI is flawed — and how to redefine obesity
- McKenzie Prillaman 0
McKenzie Prillaman is a freelance science journalist in Washington DC.
You can also search for this author in PubMed Google Scholar
Players in an ‘overweight football league’ warm up before a match in Germany. To join, members must have a BMI of at least 31. Credit: Ina Fassbender/AFP via Getty
As an obesity physician, Fatima Cody Stanford has treated many people whose weight was causing them health problems. She has plenty of success stories: one woman, for instance, returned “stunning” cholesterol, blood-pressure and blood-sugar readings after working with Stanford for about ten years.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 622 , 232-233 (2023)
doi: https://doi.org/10.1038/d41586-023-03143-x
Visaria, A. & Setoguchi, S. PLoS ONE 18 , e0287218 (2023).
Article PubMed Google Scholar
Flegal, K. M., Kit, B. K., Orpana, H. & Graubard, B. I. JAMA 309 , 71–82 (2013).
Li, J. et al. PLoS ONE 16 , e0253696 (2021).
Eknoyan G. Nephrol . Dial. Transplant. 23 , 47–51 (2008).
Keys, A., Fidanza, F., Karvonen, M. J., Kimura, N. & Taylor, H. L. J. Chron. Dis. 25 , 329–343 (1972).
Tomiyama, A. J., Hunger, J. M., Nguyen-Chu, J. & Wells, C. Int. J. Obes. 40 , 883–886 (2016).
Article Google Scholar
Sharma, A. M. & Kushner, R. F. Int. J. Obes. 33 , 289–295 (2009).
Download references
Reprints and permissions
Related Articles

- Health care
- Public health

Father’s diet influences son’s metabolic health through sperm RNA
News & Views 05 JUN 24

A dad’s diet affects his sperm — and his sons’ health
News 05 JUN 24

Ozempic keeps wowing: trial data show benefits for kidney disease
News 24 MAY 24

Huge amounts of bird-flu virus found in raw milk of infected cows
Underfunding cannabis research hampers sensible policymaking and boosts the black market
Correspondence 04 JUN 24

Negotiating a pandemic treaty is just the first step — how will countries comply?
World View 04 JUN 24
Postdoctoral fellow at USC (Dr. Jian-Fu Chen lab), Los Angeles
Two post-doc positions for studying neuroscience and craniofacial biology, crosstalk, and disease using mouse and iPSC models.
Los Angeles, California
USC - Center for Craniofacial Molecular Biology
Associate Editor, Physics of Living Systems
The Associate Editor will decide on publishing the most exciting and consequential results in the physics of living systems.
United States (US) - Remote
American Physical Society
Senior Project Manager
The Senior Project Manager will play a key role in enabling Springer Nature’s OA transformation, and optimising and expanding our OA business.
London – Hybrid Working Model
Springer Nature Ltd
Senior Commercial Manager (Open Access)
This position offers a unique opportunity to influence the future of open access publishing.
Postdoctoral Fellow in Immunology at Northwestern University
Our T cell biology lab is looking for fellows interested in improving immunotherapies for cancer and autoimmune disease through immune engineering.
Chicago, Illinois
Choi Laboratory at Northwestern
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 12, Issue 7
- Setting the top 10 priorities for obesity and weight-related research (POWeR): a stakeholder priority setting process
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-8577-6574 Ailsa R Butler 1 ,
- http://orcid.org/0000-0001-9301-7458 Nerys M Astbury 1 ,
- Lucy Goddard 1 ,
- Anisa Hajizadeh 1 ,
- Philippa Seeber 2 ,
- Bruce Crawley 2 ,
- http://orcid.org/0000-0002-1802-4217 Paul Aveyard 1 ,
- Susan A Jebb 1
- 1 Nuffield Department of Primary Care Health Sciences , University of Oxford , Oxford , UK
- 2 Patient and Public contributor , N/A , UK
- Correspondence to Nerys M Astbury; nerys.astbury{at}phc.ox.ac.uk
Objectives To identify and prioritise the most impactful, unanswered questions for obesity and weight-related research.
Design Prioritisation exercise of research questions using online surveys and an independently facilitated workshop.
Setting Online/virtual.
Participants We involved members of the public including people living with obesity, researchers, healthcare professionals and policy-makers in all stages of this study.
Primary outcome measures Top 10 research questions to be prioritised in future obesity and weight-related research.
Results Survey 1 produced 941 questions, from 278 respondents. Of these, 49 questions held satisfactory evidence in the scientific literature and 149 were out of scope. The remaining 743 questions were, where necessary, amalgamated and rephrased, into a list of 149 unique and unanswered questions. In the second survey, 405 respondents ranked the questions in order of importance. During the workshop, a subset of 38 survey respondents and stakeholders, agreed a final list of 10 priority research questions through small and large group consultation and consensus. The top 10 priority research questions covered: the role of the obesogenic environment; effective weight loss and maintenance strategies; prevention in children; effective prevention and treatment policies; the role of the food industry; access to and affordability of a healthy diet; sociocultural factors associated with weight; the biology of appetite and food intake; and long-term health modelling for obesity.
Conclusions This systematic and transparent process identified 149 unique and unanswered questions in the field of obesity and weight-related research culminating in a consensus among relevant stakeholders on 10 research priorities. Targeted research funding in these areas of top priority would lead to needed and impactful knowledge generation for the field of obesity and weight regulation and thereby improve population health.
- GENERAL MEDICINE (see Internal Medicine)
- NUTRITION & DIETETICS
- PREVENTIVE MEDICINE
- PUBLIC HEALTH
Data availability statement
Data are available on reasonable request. Requests can be made for the deidentified participant level data collected during this study from the Nuffield Department of Primary Care hosted Datasets Independent Scientific Committee (PrimDISC): [email protected] on approval of a protocol, statistical analysis plan and the signing of a suitable data sharing agreement.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/bmjopen-2021-058177
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This is the first research priority setting specific to the field of obesity and weight-related research.
This exercise involved input from a large number of participants from a broad range of relevant stakeholder groups including patients, members of the pubic, researchers, policy-makers and charities.
The final list of priorities was reached through consultation and consensus in a workshop guided by independent facilitators to minimise bias towards certain questions or areas.
Obesity is a major preventable cause of ill health and is affecting an increasing number of children and adults globally. 1 2 Obesity is defined as a body mass index (BMI) of ≥27.5 kg/m 2 (or ≥30 kg/m 2 if of white ethnic groups). No country has managed to achieve a sustained decrease in the prevalence of obesity, despite evidence-based clinical and public health guidelines and polices aimed at tackling obesity. 3 4 Obesity increases the risk of developing several conditions including type 2 diabetes, cardiovascular disease, osteoarthritis and some cancers. 4 The cost attributable to overweight and obesity are substantial. For example, in the UK’s National Health Service the cost is projected to reach £9.7 billion per annum, with wider costs to society projected to reach £49.9 billion by 2050 per year. 5 6 The detrimental effects of excess weight are not restricted to those who meet the BMI threshold of obesity as the increased morbidity is seen in people with any degree of excess adiposity. 7 Accordingly, strategies to prevent obesity or excess weight or adiposity are needed, defined here as obesity and weight-related research.
Presently, the research agenda is mainly driven by the interests and concerns of researchers, or research commissioners. A more transparent, systematic and collaborative approach involving multiple stakeholders to identify research priorities could accelerate progress. The James Lind Alliance (JLA) priority setting process brings patients, carers and clinicians together on an equal basis to define uncertainties, consider their importance and thereby set research priorities. 7 8 The output should, and typically has, informed researchers and research funders about the key questions to address in research because it is based on what matters most to people with lived experience of having a condition and those treating it. 9 Policies to prevent obesity typically affect the whole of society, for example fiscal policies or policies restricting the promotion or selling of some goods. Likewise, providing treatment for obesity as part of publicly funded healthcare is contested, and thus questions about research in this area seem to call for a much wider group of stakeholders than patients, carers, and clinicians. As in a previous tobacco control priority setting partnership (PSP), 10 we adapted the JLA approach to incorporate the perspectives of this wider range of stakeholders including people without experience of obesity, policy-makers, charities and, as for JLA, patients and members of the public with a lived experience of obesity (or related disease) and clinicians. 10 The objective of this work, as the first prioritisation project in obesity and weight-related research, was to identify unanswered questions across the whole of the field, from basic science through to health policy.
Patient and public involvement
We involved two members of the public (BC and PS) with lived experience of overweight in all stages of the project, from conception and design of the study, to its conduct, data collection and analysis. Our wider public involvement (surveys and workshop) incorporated members of the public with and without lived experience of being overweight and patients, defined as people with lived experience of being overweight and experience of receiving clinical treatment for overweight, obesity or an associated condition. Members of the public were involved in all stages of the work alongside and as equal partners with other stakeholders.
Subjects and methods
The priorities for obesity and weight-related research (POWeR) project took place between December 2019 and December 2020. The process was guided by Viergever et al, 11 which outlines principles of priority setting in health research and by the priority setting process carried out by Lindson et al. 11 We were guided by the general principles of the JLA PSP, however, we involved a wider range of stakeholders. We engaged a diverse and representative group of stakeholders comprising members of the public, people with lived experience of overweight and/or obesity, and people who work for organisations and charities, funders, policy-makers, clinicians and academic researchers all involved in the field of overweight and obesity. The prioritisation process had three stages: first an online survey to collect research questions stakeholders deemed to be priorities; a second online survey to rank the priority questions amalgamated from survey 1; and finally, an online workshop to reduce the ranked questions from survey 2 to produce a final list of top 10 priorities. The scope was limited to research questions on the aetiology, consequences, prevention or treatment of overweight and obesity in both adults and children, and did not include questions about whether currently evidenced interventions or polices should be implemented. For example, research questions relating to the prevention or treatment of eating disorders were not within the scope of this prioritisation project, however, eating disorders and related psychological adverse events related to weight management programmes were within scope. There was a study management group of investigators and patient and public involvement representatives that met regularly. Survey respondents provided consent to survey 1 and survey 2. Participants in the online workshop gave explicit consent prior to participation.
Survey 1: gathering questions and identifying those unanswered
Gathering questions:
The first survey in the process asked respondents to submit up to four questions that they felt should be prioritised in the field of obesity and weight-related research. The survey was administered online using JISC Online Survey and was piloted with our public coauthors and colleagues in the research team, prior to being launched. The survey asked respondents to identify research questions that they felt were the most important unanswered questions on the topic and to say why they felt each question was important. The latter information was used by the team to interpret, contextualise, group and sort questions.
We publicised the survey passively via a web link on our POWeR project website ( https://www.phc.ox.ac.uk/research/participate/power ), and actively via email to relevant stakeholders and Facebook adverts targeted to men. We invited our stakeholders to circulate the link, resulting in the distribution of the survey by more than 40 organisations to their members, visitors to their webpages and readers of their newsletters ( online supplemental table S1 ). We targeted organisations relevant to the field which included but was not limited to, obesity charities, community groups, funding bodies, hospital trusts, general practices and city councils. Participation in survey 1 was incentivised through a prize draw. We made physical copies of the survey, and versions with a large font size readily available on request. The survey was only available in English, and open for responses for 37 days between 15 January 2020 and 21 February 2020.
Supplemental material
Identifying unanswered questions:
Survey 1 questions were grouped by topic area and rephrased to form answerable research questions ( online supplemental tables S2 and S3 ). We used a multilevel coding system to categorise questions into overarching categories that were iteratively deduced throughout the grouping. For example, the submitted question ‘which diets work’ fell into a macro category, ‘treatment’ and was then further filtered into the sub-category ‘behavioural’ over ‘pharmaceutical’. Questions organised into groups were then rephrased as research questions in collaboration with our public coauthors who ensured that the groupings and rephrasing retained the intent of the original questions, and that they were understandable to a lay audience while making them tractable to empirical research. For example, a question such as ‘Are there medications to treat obesity?’ would have been combined with others to become a tractable research question such as ‘What is the effectiveness, safety, tolerability and cost-effectiveness of medications to treat obesity?’
We then searched the literature using keywords and MeSH terms informed by the questions, to determine if these were areas that were already adequately addressed in the scientific literature. Questions were deemed ‘answered’ if there was satisfactory evidence. We accepted satisfactory evidence primarily in the form of preprocessed literature in: (1) systematic reviews published within the last 10 years, with little to no uncertainty; (2) proof of evidence in national clinical guidelines (eg, National Institute for Health and Care Excellence, and Scottish Intercollegiate Guidelines Network). We also accepted primary literature by way of high certainty if there was evidence in randomised controlled trials (RCTs). Such an approach would indicate that the question on currently available pharmacotherapy for obesity, for example, was at least partially answered by current reviews and trials.
We noted how many questions fed into each research question.
Survey 2: prioritising unanswered research questions
The second online survey was piloted with members of the public and colleagues in the research team. The survey was administered via REDCap, and sent to the 256 survey 1 respondents who had provided us with their email addresses, as well as to the organisations approached to share survey 1 (see online supplemental table S1 ).
The second survey remained open for 30 days between 6 August 2020 and 14 September 2020. Survey 2 asked respondents to prioritise the unanswered questions gleaned from survey 1, which were sent in batches of about 50 questions to lower the response burden. The questions in each batch covered the whole range of submitted research questions. Respondents were asked to rate each question on a scale of 1–10 with 10 representing ‘very important’ and 1 representing ‘not important’. The mean priority score was calculated for the resulting rated questions and ranked ( online supplemental table S3 ) to create a list of the top 30 priority research questions.
Workshop: determining the top 10 research priorities
We invited a subset of survey respondents and other stakeholders including NGO representatives, healthcare professionals, public members including people with lived experience of overweight to take part in a 3-hour online workshop in the winter of 2020 to determine the top 10 questions. This was a real-time, facilitator-led consultation, replacing a full-day in person event that was not possible due to local COVID-19 restrictions. The group was representative of the multidisciplinary stakeholders involved in the project; patients and members of the public, researchers, policy-makers, clinicians and relevant research funders. The workshop was held via a videoconferencing platform (Zoom), and led by external facilitators from Hopkins van Mil, a service that specialises in guiding impartial discussions to elucidate views and opinions of a diverse group of people in a safe, productive space. 12 Prior to the workshop, participants were given the resulting top 30 questions from survey 2, in addition to a list of 10 other questions from survey 1 that had been asked by more than 10 people ( online supplemental table S4 ). The difference between the mean ranked scores in survey 2 was subtle. Workshop participants were offered the opportunity to advocate to include any of these extra 10 that they felt should be considered in the workshop to be as inclusive as possible. The workshop was divided into small groups of 4–6 people representing the range of stakeholders involved, to balance expertise and experience. Each small group was guided by a Hopkins van Mil facilitator.
The 3-hour workshop was divided into three parts with a final plenary session. Throughout the workshop participants were asked to justify their choices, and reveal the values and reasoning behind their prioritisation. Important questions were defined as those that would have the most impact if answered by research. In the first session, each group was asked to debate what they considered to be the four most and least important research questions from the 30 questions. In session 1, the highest and lowest questions were determined.
In session 2, facilitators shared a list of questions that were of medium importance, that is, not the highest or lowest priority questions determined in session 1. Facilitators asked participants to categorise these as either: (1) a priority, (2) low priority, (3) not a priority. This was determined by debate, discussion and justification of the participants’ reasoning. The facilitator moved the questions around on the shared slide. The highest ranking questions from session 1 and session 2 were brought together. By the end of the second session each group had a list of top 14 questions ranked in order of importance.
The facilitators then met to combine the top 14 questions from all the small groups, this led to one list of 16 questions. In the third session of the workshop, this combined list of 16 questions was shared with the individual groups for debate. Here the groups were asked to determine and rank their final list of 10 research questions. Facilitators guided this final prioritisation stage by asking groups to focus on questions that would have the highest impact if taken forward as a research question. The groups then came together in a final plenary session and the top two questions from each group were shared with the larger group. After an amalgamation of the top two questions from each group and invariable overlap, the third and fourth questions from each group were added to produce a final list of the top 10 questions.
This three-stage prioritisation project involved a diverse group of stakeholders in prioritising a list of top 10 unanswered research questions for obesity and weight-related research, which are presented here and at: https://www.phc.ox.ac.uk/research/participate/power
Demographics of respondents and questions gathered:
Survey 1 received 278 responses ( table 1 ), yielding 941 original questions ( figure 1 online supplemental table S2 ). Demographic information collected during the survey indicated a diverse range of ages, ethnicities and stakeholder groups among survey respondents. Thirty-seven per cent of respondents had lived experience of obesity, and 80% were educated to degree level or above ( table 1 ).
- View inline
Demographic characteristics for respondents to survey 1 and survey 2
- Download figure
- Open in new tab
- Download powerpoint
Flow diagram for the priority research questions. RQ, Research questions.
Final top 10 priority research questions*
What are the most effective methods for weight maintenance following weight loss? What are the effective components of treatments/programmes incorporating a behavioural element? How many and in what combination are most effective? What is the optimal duration of these programmes?
What are the most effective methods for weight loss? What are the effective components of treatments/programmes incorporating a behavioural element? How many and in what combination are most effective? What is the optimal duration of these programmes?
What is the most effective and cost-effective mix of population/public health and individual interventions to tackle obesity?
Do interventions that target the ‘obesogenic environment’, such as community interventions, urban planning, placement of fast-food outlets or workplace polices, affect population mean weight and do these effects differ by baseline weight status (underweight, healthy weight, overweight, obesity)? Which interventions are most effective at reaching low socioeconomic groups?
Do interventions (eg, nutrition education and physical activity) in preschool, primary school and secondary school reduce children’s risk of unhealthy weight gain and, if so, how do they act? Does the effect of such interventions differ by social and cultural groups?
What changes in supermarkets or the wider food industry are effective in promoting healthier diets? Does changing labelling and/or packaging on foods affect purchasing, consumption and body weight?
What is the cost and affordability of a healthy balanced diet? How can we make healthier foods more affordable? How can we improve access to healthy diets for social and cultural groups, such as people in poverty, people in inner cities, or young and older people?
How do demographic, social and cultural factors (eg, age, socioeconomic status, lifestyle, environment, psychosocial functioning) affect weight status, weight gain and regional fat distribution? What are the mechanisms involved? Does the effectiveness of weight loss methods depend on social and cultural background and, if so, can the effects be made more equitable? Are weight loss methods tailored to people’s background more effective for weight loss and weight maintenance than general methods?
How accurate are existing models of health consequences of excess weight and the impact of weight loss? Which assumptions are critical in determining the long-term effectiveness and cost effectiveness of weight loss interventions? What do these models predict is the impact of weight loss interventions on health and disease incidence and the cost-effectiveness of such interventions? What is the impact of weight regain on the incidence of disease and cost-effectiveness of weight loss interventions?
What are the drivers of food choice, appetite and intake and do variations in these drives explain who develops obesity and who does not? How does the brain control food intake and can we use these mechanism to aid weight loss? What are the brain responses (neural correlates) in response to food during weight loss and following weight regain?
The 941 questions were grouped by topic. We excluded 49 (5.2%) questions as already answered, and 149, (15.8%) as out of scope ( figure 1 , online supplemental table S2 ). The remaining 743 questions were rephrased following the process above to yield 149 individual research questions ( online supplemental table S3 ). These questions covered a range of topics ( figure 2 ). Of the 941 submitted questions most questions concerned: prevention and intervention; mental health; illness, disease and health; and food industry, policy and environment ( figure 2A ). Of the 149 grouped research questions taken forward ‘illness, disease and health’ and ‘metabolism, physiology and appetite’, were the most popular categories and fewer questions concerned age of onset and duration of obesity ( figure 2B ).
(A) 941 submitted questions by topic; (B) 149 research questions grouped by topic. BMI, body mass index; NHS, National Health Service.
Survey 2 received 405 responses; 61% of respondents reported lived experience with obesity and 74% held an education to degree level or above ( table 1 ). A total of 149 questions to be taken forward from survey 1 were divided into three batches of up to 50 questions, and randomly assigned to respondent’s survey 2. Each question was rated in order of importance, by a mean of 115 people (SD 9.7) ( online supplemental table S3 ).
We invited 64 stakeholders, 39 people confirmed their acceptance and one person dropped out on the day. Thirty-eight attendees (20 female, 18 male) were made up of 4 public members, 8 participants from related organisations, 13 researchers, 7 policy makers and 6 healthcare professionals. One person asked for the question on the role of the gut microbiome to be included from the list of 10 extra questions. At the workshop 31 questions were debated in small groups. In the first session the groups sorted questions into highest and lowest priority. In the second session, the top 14 questions were determined by all groups except one that determined their top 10 and another that grouped questions as high medium and low priority. The facilitators combined the lists from all the groups into a list of 16 as many of the top 14 from each group overlapped. In the third session participants ranked the 16 questions into a top 10 list. The top two from all these lists was shared at a final plenary session. Consolidation of the top two questions and the questions ranked third and fourth resulted in 11 unique research questions by the end of the workshop. On analysis of recordings of each group’s discussion, multiple participants noted that two questions in the 11 that were similar in meaning. We, therefore, combined these two questions (concerning food choice, appetite and the brain’s control of food intake) post hoc to produce a final list of the top 10 research questions ( box 1 ). There was consistency between the top questions in this final list produced from the workshop, and popular questions submitted in the surveys as indicated by number of people asking each question ( online supplemental table S3 ). Five of the final top 10 questions were among the 10 most frequently submitted questions in survey 1. Seven of the final questions were in the top 10 from survey 2, ranked by mean score. The final list of the top 10 priorities are not listed in order of priority ( box 1 ).
Summary of findings
Our priority setting exercise identified the top 10 research questions that stakeholders in the field, and those with an interest overweight and obesity, believe to be the key priorities to advance obesity and weight-related research. In two online surveys and a workshop, we collated nearly 1000 questions, and guided participants in a structured and systematic prioritisation process to reach the final list of 10 ( box 1 ). These questions cover a wide spectrum of areas, and if answered by research, would generate knowledge applicable for individuals, healthcare, public health and policy.
Strengths and limitations
The main strength of this project was the successful collaboration between a diverse range of stakeholder groups, though it was not without its challenges. Our stakeholders included patients, members of the public, clinicians, charities, researchers and policy-makers connected to the field. Identifying the most appropriate group for a condition where a third of the adult population are clinically obese and more than 60% are overweight, while at the same time, considering how to prevent the condition developing which is relevant to the whole population, resulted in the inclusion of both patients and members of the public. Members of the public naturally included some people without lived experience of overweight or obesity, though it seems unlikely that they would not be aware of family members, and friends who are affected, and they may become affected themselves, justifying their inclusion in this prioritisation process. To have found consistency in the questions being posed throughout the entire process by a variety of individuals bringing different experience and expertise to a common area of focus, supports the validity of the resulting top 10 questions. The majority of survey respondents and workshop participants appear to be highly educated. Nonetheless there was evidence of an awareness of the need for interventions to help reduce inequalities and the top 10 priorities include questions on social determinants of health like low-socioeconomic status and cultural factors. We commissioned third-party, impartial facilitators to guide the workshop without input from the research team, so as to not inadvertently sway the prioritisation of questions being considered in each session. Additionally, the number of questions submitted and finally categorised is in line with similar priority setting exercises in health research, using an analogous process set out by the JLA, with a comparable number of stakeholders involved. 13 14
There are limitations that we identified and strived to address throughout the stages of the process. To begin with survey 1, we deemed that 5.2% of all questions submitted were already answered by empirical evidence. We assessed this through a thorough search of the literature to identify systematic reviews, clinical and public health guidelines and high-quality primary studies in the form of RCTs. Although this necessitated some subjective judgement, we ensured that all decisions were made in duplicate, and discrepancies were resolved by a third researcher. Our confidence in the categorisation of answered versus unanswered questions is strengthened by consensus among stakeholders involved, some of whom were researchers with expertise in the question areas being considered. That 5.2% of the submitted questions were considered answered indicates that research may not being adequately communicated in these areas. This could be addressed by improved or targeted communication.
In survey 2, we asked participants to rate questions on a scale of 1–10, but found that participants were disinclined to use the full range. Many questions had means between 6 and 8 meaning that differences in the scoring were subtle. Future work could consider using a condensed scale to perhaps mirror ratings that people are more familiar with (eg, 5-point ratings seen in 5-star reviews or 4-point grading of evidence 15 however unless people used the top and the bottom of the scale a condensed scale could lead to questions being rated as even more similar. In regards to the workshop, while facilitators had standardised methods for the structure of the small group discussion, one group did not rank their questions during the workshop, and instead batched them as high, medium and low priority. This made no difference to the outcome, as the group’s top three high-priority questions were included in the final priority list across all groups.
An additional limitation of the workshop was the shift to a virtual vs in-person meeting due to local COVID-19 restrictions, which limited the length of the discussions. On analysis of the recordings from each group’s consultations, it was clear that the virtual setting maintained a clean discussion where moderators were clearly able to garner input from each participant without anyone talking over-another, as may have been the case in an in-person discussion. It was possible to rank the top 10 in the small groups in the workshop, however, it was harder to achieve this with 38 participants in the plenary sessions so we did not seek to order the final 10 priorities. Lastly, obesity is a worldwide problem calling for a global research response, but we only involved UK-based stakeholders. It is likely that the process identified questions that are generalisable outside of the UK, but it is unlikely that this process fully captured priorities that may be relevant to low-income countries or countries with a low prevalence of overweight and obesity.
Implications for research and policy
The main implication of this work is for the top 10 POWeR to be considered by funding bodies concerned with advancing the field. Similar priority setting work in other areas of health research have resulted in research calls that reflect priorities identified by stakeholders. 16 Along with the top 10 questions, this project identified a further 139 unanswered questions that may also serve as a resource for researchers trying to match gaps in the evidence with perceived needs.
We make two recommendations for future priority setting exercises in this area based on what we learnt from the process. The first would be to limit the focus to a prespecified area in the field. The breadth of topic areas produced by the large number of stakeholders engaged was onerous to process, and resulted in high level areas for research. Future exercises may wish to restrict their scope to a certain area of research, such as treatment for people living with obesity, or population-wide prevention strategies to allow more granular questions to emerge. The second would be to incorporate work to boost awareness of the existing research evidence for common questions that were submitted, but deemed to be answered. Questions that were commonly submitted, but already answered and therefore excluded from progressing through the prioritisation process are telling of a discrepancy between published research and knowledge dissemination.
We have identified 10 priorities that cover: the role of the obesogenic environment; effective weight loss and maintenance; prevention in children; effective prevention and treatment policies; the role of the food industry; access to and affordability of healthy diets; the sociocultural factors associated with weight; the biology of appetite and food intake and long-term health modelling. Research funders may want to prioritise these questions when considering research proposals, or commissioning programmes of research to answer these key questions.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
The study was approved by the University of Oxford Medical Sciences Inter Divisional Research Ethics Committee (Ref: R6721/RE003). Participants gave informed consent to participate in the study before taking part.
Acknowledgments
We would like to thank Nicola Lindson and Jamie Hartmann Boyce for help and guidance and David Dyson, Gavin Hubbard, Alice Crouch and Dan Richard-Doran for support with the surveys and webpages, Michaela Noriek for help with public engagement, Goher Ayman for helpful advice We also want to thank everyone who worked on the POWER project including all the members of the health behaviours team who helped us with questions from survey 1. Elizabeth Morris, Carmen Piernas-Sanchez, Dimitrios Koutoukidis, Tanisha Spratt, Anne Ferrey, and Jenny Brooks. We would like to thank all the people who took the surveys and provided us with their original questions, everyone who ranked the questions and to all the workshop participants and the many organisations that distributed the surveys on our behalf. We are grateful to the workshop participants for giving us their time. We would like to thank Hopkins Van Mil for conducting the workshop.
- NHS DIgital
- World Health Organization
- Caballero B
- Jaacks LM ,
- Vandevijvere S ,
- Pan A , et al
- Alliance JL
- Chalmers I ,
- Atkinson P ,
- Fenton M , et al
- Nygaard A ,
- Halvorsrud L ,
- Linnerud S , et al
- Lindson N ,
- Richards-Doran D ,
- Heath L , et al
- Viergever RF ,
- Olifson S ,
- Ghaffar A , et al
- Hopkins Van Mil
- Goodridge D ,
- Cowan K , et al
- Strachan JA ,
- McLennan N , et al
- Schünemann HJ ,
- Vist G , et al
- Nasser MC S
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors NMA, PA and SAJ conceived the concept. ARB, LG and NMA were responsible for collecting and collating data with guidance from PS and BC. ARB, LG, AH and NMA produced an initial draft of the manuscript, PA, SAJ, PS and BC provided comments and edited the original draft. All authors reviewed and approved the final submitted version of the manuscript. NMA is responsible for the overall content as the guarantor and accepts full responsibility for the work and/or the conduct of the study, had access to the data and controlled the decision to publish.
Funding The study was funded by the National Institute for Health Research (NIHR) Oxford and Thames Valley Applied Research Collaboration. NMA, PA and SAJ are supported by the NIHR Oxford Biomedical Research Centre. PA and SAJ are NIHR senior investigators.
Disclaimer The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The views are those expressed by the authors and not necessarily those of the NHS, NIHR, or Department of Health.
Competing interests NA, PA, and SAJ led an investigator-initiated study funded by Cambridge Weight Plan. PA has spoken at two symposia organised by the Royal College of General Practitioners that were funded by Novo Nordisk. None of these activities led to personal payment. ARB, LG, AH, PS and BC have no interests to declare.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- For Authors
- Collaboration
- Privacy Policy

- Conferences & Symposiums
Tools & Methods
The ‘fundamental questions of obesity’: asked and answered.
Scientific progress requires the ability to discover which questions are essential and which are trivial. Yet until recently, there were three fundamental questions that were ignored in nutrition & obesity research:
- What is the defining characteristic of obesity?
- Why would humans or non-human animals habitually consume more calories than they ‘burn’?
- Why would the excess calories be stored more as ‘fat’ than as muscle or bone?
Answer #1: The Defining Characteristic of Obesity Animals are comprised of cells. Smaller animals have fewer cells than larger animals. So, it is not surprising that elephants have more cells than mice. This relation is also true within species. For example, ceteris paribus, larger humans have more cells than smaller humans. Thus, because obese individuals have more fat-cells than lean individuals, the defining characteristic of obesity is not ‘diet’, ‘genes’, ‘exercise’, or bodyweight and fat-mass, but a greater number of fat-cells relative to other cell types.
Answer #2: Overconsumption There are two reasons for the chronic overconsumption of calories. First, the more fat-cells an individual has, the more calories s/he will store as fat after each meal. Yet if more calories are stored as fat, less calories are available to keep other cells alive. Therefore, excess calories must be consumed to replace the calories lost to fat storage.
The second reason is physical inactivity. As physical activity (PA) levels drop below an individual’s “metabolic tipping point”, appetite and fat storage increase (Fig. 1A). Thus, as fewer calories are burned, more calories are stored as fat. With extreme inactivity, you can eat very little and still gain fat.

Fig. 1 A. Relations between physical activity (PA), body mass, and energy intake. As physical activity declines below the “Metabolic Tipping Point” (i.e., into the “Sedentary” range), energy intake and energy expenditure become dissociated due to insufficient metabolic-flux; as a result, body mass increases as energy balance becomes positive. B. Body and fat mass trajectories of individuals varying in adipocyte cellularity (i.e., relative # of fat-cells). Body and fat mass trajectories return to the initial slope (i.e., rate of gain) after diet-induced weight loss. The initial slope was determined by fat-cell number.
Answer #3: Why Gain ‘Fat’ and not Muscle or Bone? A fat-cell’s ‘job’ is not to ‘burn’ calories but to store them. Therefore, the more fat-cells a person or animal is born with, the more calories they store as fat. Conversely, a person born with more muscle-cells will ‘burn’ or store more calories in muscle-cells.
Importantly, the number of calories reaching the fetus during gestation is the major determinant of the number of muscle- and fat-cells present at birth. If too few calories reach the fetus, s/he will be born with too few muscle- and bone-cells and a stunted, unhealthy body. If too many calories reach the fetus, s/he will be born with too many fat-cells and prone to obesity and metabolic disease. Interestingly, the individual’s genes and those of his/her parents have little influence on the number of cells present at birth. In fact, a mother’s prenatal metabolism is the main determinant of obesity and health. This is known as a “maternal effect” .
Summary & Conclusion The defining characteristic of obesity is not ‘genes’ nor ‘diet’, but the number of fat-cells relative to other cell-types. Obesity can be ‘inherited’ via non-genetic prenatal processes (i.e., “maternal effects” ) or ‘acquired’ after puberty via physical inactivity and concomitant appetite dysregulation and overconsumption.
Our work suggests that ‘inherited’ obesity is irreversible because losing weight merely changes the size, but not the number of fat-cells in the body (Fig. 1B). Thus, no amount of ‘diet & exercise’ can overcome the metabolic effects of having too many fat-cells. This explains why no matter how much weight you lose, you will quickly gain it back. Conversely, ‘acquired’ obesity may be susceptible to ‘diet & exercise’, but only if no new fat cells were created.
In summary, people born with a large number of fat-cells will almost always be obese — and more importantly, their ‘diet’, ‘genes’, and physical activity levels are not the cause.
Edward Archer EvolvingFX, Jupiter FL, USA
Publication
The Contributions of ‘Diet’, ‘Genes’, and Physical Activity to the Etiology of Obesity: Contrary Evidence and Consilience. Archer E, Lavie CJ, Hill JO Prog Cardiovasc Dis. 2018 Jul – Aug

Related Articles:
| Muscle and nerve communicate at the level of a specialized region, namely the neuromuscular junction (NMJ), a synaptic connection where the peripheral nervous system contacts skeletal muscle fibers, governing crucial… | |
| Obesity typically occurs when a person eats more calories than they need for their daily activity. It results in a build-up of fatty tissue around all organs. In lean people,… | |
| Pain comes in all shapes and sizes. Ranging from acute to chronic, from nociceptive and myofascial to neuropathic, pain is a part of life. Myofascial or muscle pain, is among… | |
| Diet is important to fuel growth and cellular machinery and thus, plays an important role in the survival of a living organism. One of the important components of our diet… | |
| People choose vegetarian/vegan diets and for many reasons, however, these diets require careful dietary planning. The essential polyunsaturated n-6 (omega-6) and n-3 (omega-3) fatty acids are required for synthesis of… | |
| Campylobacteriosis has been the most frequently reported zoonotic disease in humans in Europe since 2005, and the annual number of notified campylobacteriosis cases has increased in many European countries in… |
Leave a Reply Cancel reply
You must be logged in to post a comment.
Top Keywords
Diabetes | Alzheimer’s disease Cancer | Breast cancer | Tumor Blood pressure | Heart Brain | Kidney | Liver | Lung Stress | Pain | Therapy Infection | Inflammation | Injury DNA | RNA | Receptor | Nanoparticles Bacteria | Virus | Plant
See more …

Proofread or Perish: Editing your scientific writing for successful publication

Lab Leader makes software applications for experiment design in life science

Cyagen Biosciences – Helping you choose the right animal model for your research
Labcollector lims and eln for improving productivity in the lab.

Image Cytometer – NucleoCounter® NC-3000™
Recent posts.
- The Manikin Challenge: manikin-based simulation in the psychiatry clerkship
- Does UV-B radiation modify gene expression?
- Ferrate technology: an innovative solution for sustainable sewer and wastewater management
- Sleep abnormalities in different clinical stages of psychosis
- A compact high yield isotope enrichment system
| M | T | W | T | F | S | S |
|---|---|---|---|---|---|---|
| 1 | 2 | |||||
| 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| 10 | 11 | 12 | 13 | 14 | 15 | 16 |
| 17 | 18 | 19 | 20 | 21 | 22 | 23 |
| 24 | 25 | 26 | 27 | 28 | 29 | 30 |
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Setting the top 10 priorities for obesity and weight-related research (POWeR): a stakeholder priority setting process
Affiliations.
- 1 Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, UK.
- 2 Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, UK [email protected].
- 3 Patient and Public contributor, N/A, UK.
- PMID: 35858732
- PMCID: PMC9305808
- DOI: 10.1136/bmjopen-2021-058177
Objectives: To identify and prioritise the most impactful, unanswered questions for obesity and weight-related research.
Design: Prioritisation exercise of research questions using online surveys and an independently facilitated workshop.
Setting: Online/virtual.
Participants: We involved members of the public including people living with obesity, researchers, healthcare professionals and policy-makers in all stages of this study.
Primary outcome measures: Top 10 research questions to be prioritised in future obesity and weight-related research.
Results: Survey 1 produced 941 questions, from 278 respondents. Of these, 49 questions held satisfactory evidence in the scientific literature and 149 were out of scope. The remaining 743 questions were, where necessary, amalgamated and rephrased, into a list of 149 unique and unanswered questions. In the second survey, 405 respondents ranked the questions in order of importance. During the workshop, a subset of 38 survey respondents and stakeholders, agreed a final list of 10 priority research questions through small and large group consultation and consensus. The top 10 priority research questions covered: the role of the obesogenic environment; effective weight loss and maintenance strategies; prevention in children; effective prevention and treatment policies; the role of the food industry; access to and affordability of a healthy diet; sociocultural factors associated with weight; the biology of appetite and food intake; and long-term health modelling for obesity.
Conclusions: This systematic and transparent process identified 149 unique and unanswered questions in the field of obesity and weight-related research culminating in a consensus among relevant stakeholders on 10 research priorities. Targeted research funding in these areas of top priority would lead to needed and impactful knowledge generation for the field of obesity and weight regulation and thereby improve population health.
Keywords: GENERAL MEDICINE (see Internal Medicine); NUTRITION & DIETETICS; PREVENTIVE MEDICINE; PUBLIC HEALTH.
© Author(s) (or their employer(s)) 2022. Re-use permitted under CC BY. Published by BMJ.
PubMed Disclaimer
Conflict of interest statement
Competing interests: NA, PA, and SAJ led an investigator-initiated study funded by Cambridge Weight Plan. PA has spoken at two symposia organised by the Royal College of General Practitioners that were funded by Novo Nordisk. None of these activities led to personal payment. ARB, LG, AH, PS and BC have no interests to declare.
Flow diagram for the priority…
Flow diagram for the priority research questions. RQ, Research questions.
(A) 941 submitted questions by…
(A) 941 submitted questions by topic; (B) 149 research questions grouped by topic.…
Similar articles
- Identifying and prioritising unanswered research questions for people with hyperacusis: James Lind Alliance Hyperacusis Priority Setting Partnership. Fackrell K, Stratmann L, Kennedy V, MacDonald C, Hodgson H, Wray N, Farrell C, Meadows M, Sheldrake J, Byrom P, Baguley DM, Kentish R, Chapman S, Marriage J, Phillips J, Pollard T, Henshaw H, Gronlund TA, Hoare DJ. Fackrell K, et al. BMJ Open. 2019 Nov 21;9(11):e032178. doi: 10.1136/bmjopen-2019-032178. BMJ Open. 2019. PMID: 31753886 Free PMC article.
- Identifying trial recruitment uncertainties using a James Lind Alliance Priority Setting Partnership - the PRioRiTy (Prioritising Recruitment in Randomised Trials) study. Healy P, Galvin S, Williamson PR, Treweek S, Whiting C, Maeso B, Bray C, Brocklehurst P, Moloney MC, Douiri A, Gamble C, Gardner HR, Mitchell D, Stewart D, Jordan J, O'Donnell M, Clarke M, Pavitt SH, Guegan EW, Blatch-Jones A, Smith V, Reay H, Devane D. Healy P, et al. Trials. 2018 Mar 1;19(1):147. doi: 10.1186/s13063-018-2544-4. Trials. 2018. PMID: 29490702 Free PMC article.
- Research priorities in foot and ankle conditions: results of a UK priority setting partnership with the James Lind Alliance. Mangwani J, Hau M, Thomson L. Mangwani J, et al. BMJ Open. 2023 May 16;13(5):e070641. doi: 10.1136/bmjopen-2022-070641. BMJ Open. 2023. PMID: 37192795 Free PMC article.
- Top research priorities for preterm birth: results of a prioritisation partnership between people affected by preterm birth and healthcare professionals. Oliver S, Uhm S, Duley L, Crowe S, David AL, James CP, Chivers Z, Gyte G, Gale C, Turner M, Chambers B, Dowling I, McNeill J, Alderdice F, Shennan A, Deshpande S. Oliver S, et al. BMC Pregnancy Childbirth. 2019 Dec 30;19(1):528. doi: 10.1186/s12884-019-2654-3. BMC Pregnancy Childbirth. 2019. PMID: 31888523 Free PMC article.
- What are the most important unanswered research questions in trial retention? A James Lind Alliance Priority Setting Partnership: the PRioRiTy II (Prioritising Retention in Randomised Trials) study. Brunsdon D, Biesty L, Brocklehurst P, Brueton V, Devane D, Elliott J, Galvin S, Gamble C, Gardner H, Healy P, Hood K, Jordan J, Lanz D, Maeso B, Roberts A, Skene I, Soulsby I, Stewart D, Torgerson D, Treweek S, Whiting C, Wren S, Worrall A, Gillies K. Brunsdon D, et al. Trials. 2019 Oct 15;20(1):593. doi: 10.1186/s13063-019-3687-7. Trials. 2019. PMID: 31615577 Free PMC article.
- Identifying the top 10 research priorities for the school food system in the UK: a priority setting exercise. Schliemann D, Spence S, O'Kane N, Chiang CC, Olgacher D, McKinley MC, Woodside JV; GENIUS network. Schliemann D, et al. BMJ Open. 2024 Mar 14;14(3):e081400. doi: 10.1136/bmjopen-2023-081400. BMJ Open. 2024. PMID: 38485482 Free PMC article.
- Self-management interventions for adults living with obesity to improve patient-relevant outcomes: An evidence map. Sunol R, González-González AI, Valli C, Ballester M, Seils L, Heijmans M, Poortvliet R, van der Gaag M, Rocha C, León-García M, Salas-Gama K, de Guzman EN, Kaloteraki C, Santero M, Spoiala C, Gurung P, Moaddine S, Wilemen F, Cools I, Bleeker J, Kancheva A, Ertl J, Laure T, Kancheva I, Veroniki AA, Zevgiti S, Beltrán J, Canelo-Aybar C, Zafra-Tanaka JH, Seitidis G, Mavridis D, Groene O, Alonso-Coello P, Orrego C; COMPAR-EU consortium. Sunol R, et al. Patient Educ Couns. 2023 May;110:107647. doi: 10.1016/j.pec.2023.107647. Epub 2023 Jan 24. Patient Educ Couns. 2023. PMID: 36739705 Free PMC article.
- NHS DIgital . Health Survey for Engalnd 2019 2020 [updated 15 December 2020. Available: https://digital.nhs.uk/data-and-information/publications/statistical/hea...
- World Health Organization . Obesity and overweight 2020 [updated 1 April 2020. Available: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Caballero B. The global epidemic of obesity: an overview. Epidemiol Rev 2007;29:1–5. 10.1093/epirev/mxm012 - DOI - PubMed
- Jaacks LM, Vandevijvere S, Pan A, et al. . The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol 2019;7:231–40. 10.1016/S2213-8587(19)30026-9 - DOI - PMC - PubMed
- PHE . Health matters: obesity and the food environment 2017. Available: https://www.gov.uk/government/publications/health-matters-obesity-and-th...
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Europe PubMed Central
- PubMed Central
- Genetic Alliance
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Strategic Plan
Strategic Plan for NIH Obesity Research
The Purpose of the Strategic Plan
The Strategic Plan for NIH Obesity Research serves as a guide to accelerate a broad spectrum of research toward developing new and more effective approaches to address the tremendous burden of obesity, so that people can look forward to healthier lives.
The Plan was originally published in 2011. In 2018-2019, the Obesity Research Task Force confirmed that the challenges and opportunities identified in the Plan reflect the current research landscape and should continue to guide obesity research.
- Full Report for the scientific community (PDF, 716.76 KB)
- Summary Report non-technical (PDF, 627.47 KB)
- View a video of former NIH Director Dr. Francis Collins discussing the Strategic Plan
Development of the Strategic Plan
The Strategic Plan was developed by the NIH Obesity Research Task Force with crucial input from researchers external to the NIH, professional and other health-focused organizations, and others through a public comment period. Research challenges and opportunities identified at meetings and workshops also helped shape the Strategic Plan, and will continue to inform NIH research planning.
Major Themes for Research Highlighted in the Strategic Plan
Research Opportunities:
- Discover fundamental biological processes that regulate body weight and influence behavior
- Understand the factors that contribute to obesity and its consequences
- Design and test new interventions for achieving and maintaining a healthy weight
- Evaluate promising strategies for obesity prevention and treatment in real-world settings and diverse populations
- Harness technology and tools to advance obesity research and improve healthcare delivery
Application of Research Findings:
- Facilitate integration of research results into community programs and medical practice
Questions and Answers
What are the goals of the plan.
The efforts of many individuals and institutions are essential to reducing the prevalence of obesity – including government, businesses, community organizations, healthcare professionals, schools, and families. Research can provide the foundation for these efforts. As the country's medical research agency, the NIH funds a spectrum of research to reduce the prevalence and burden of obesity. Research can lead to a better understanding of the causes and consequences of obesity and will give us the evidence for what works to prevent and treat obesity. In addition, research will help us reduce health disparities and inform policies.
Researchers seek to answer many questions, for example:
- How can we increase and use our knowledge of human biology and behavior to develop new and more effective prevention and treatment approaches?
- What aspects of our community environments and daily lives contribute to unhealthy eating and insufficient physical activity–and what can we change to make it easier for people to achieve a healthy weight?
- How can we rigorously evaluate interventions–whether based on individual lifestyle changes, pharmacological or surgical approaches, community-based programs, policy changes, or other environmental changes–to determine which really work?
- How do we scale up the approaches that show promise and expand those proven effective, in order to reach more people?
- Given that no single intervention will solve this complex problem, how can we continue to develop new and innovative approaches?
We hope that the plan will serve as a guide to accelerate progress in obesity research, and that this research will ultimately help extend healthy life and reduce the burdens of illness and disability.
Why create a strategic plan for obesity research?
Obesity is highly prevalent in the United States. Obesity increases a person’s chance of developing many health problems, including type 2 diabetes, heart disease, high blood pressure, fatty liver disease, respiratory problems (e.g., asthma and sleep apnea), and some cancers. Obesity adversely affects people's quality of life and exacts a substantial economic toll on the nation.
Obesity arises from a complex interplay of forces and affects some populations disproportionately. We need to take a multifaceted approach to combat it. Simply telling people to "eat less and exercise more" is not enough.
Research is the foundation for finding viable solutions. Research allows us to explore the roles that genetics and biology, our environment, and our lifestyles play in obesity – and to transform that knowledge into better prevention and treatment strategies. Through research, we rigorously evaluate interventions to see which ones really work and who can benefit most.
How can scientists apply to the NIH for funding for obesity-related research?
Information on funding opportunities , including lists of NIH obesity-related research solicitations, is available.
The strategic plan identifies and encourages a broad range of research opportunities and priorities to accelerate obesity research.
Researchers can obtain information about applying for NIH funding, and about the peer review system through which applications are evaluated, on the NIH Grants and Funding website . NIH publishes Notices of Funding Opportunities to solicit research on topics specific to many diseases and conditions, including obesity. Additionally, researchers are invited to submit applications independent of these topic-specific solicitations. View complete listings of all NIH research solicitations .
Grant applications that fall within the areas covered in the strategic plan are considered under the same review processes as other NIH research applications.
Who can be involved in implementing the strategic plan?
Advancing the progress of obesity research requires a strong pool of researchers with diverse areas of expertise who are dedicated to understanding and ameliorating obesity and its many adverse outcomes.
But researchers alone can't solve the obesity problem. We need the commitment of policymakers, healthcare practitioners, businesses, communities, families, and individuals to partner in research and implement what we learn. The NIH works with groups across the country and around the world—including universities, medical centers, businesses, schools, and communities—to study obesity, develop and evaluate strategies for prevention and treatment, train researchers, and teach people about science-based interventions to improve their health.
How can people act on the plan?
Everyone can play a role in enhancing obesity research and moving research results to longer and healthier lives. For example:
- Researchers can submit obesity-related grant applications that align with the areas of opportunity highlighted in the plan.
- When taking actions to reduce obesity—such as adding sidewalks or playgrounds to increase opportunities for physical activity or improving access to fresh, healthy foods—policymakers, community organizations, and others can participate in research to evaluate these efforts, to determine what is working, and how successful approaches could be expanded.
- The public can participate in clinical research studies to help inform the science of obesity – helping scientists to identify contributing factors and evaluate new prevention and treatment strategies.

- MJC Library & Learning Center
- Research Guides
- Obesity in America
Research Obesity
Obesity in america: research obesity, start learning about your topic.
It's important to begin your research learning something about your subject; in fact, you won't be able to create a focused, manageable thesis unless you already know something about your topic.
Use the words below to search for useful information in books including eBooks and articles at the MJC Library.
- overweight persons
- morbid obesity
Top Picks for Background Reading:
All of these resources are free for MJC students, faculty, & staff.
- CQ Researcher Online This link opens in a new window This is the resource for finding original, comprehensive reporting and analysis to get background information on issues in the news. It provides overviews of topics related to health, social trends, criminal justice, international affairs, education, the environment, technology, and the economy in America.
- Gale eBooks This link opens in a new window Use this database for preliminary reading as you start your research. You'll learn about your topic by reading authoritative topic overviews on a wide variety of subjects.
- Issues & Controversies This link opens in a new window This is a great database to use when you want to explore different viewpoints on controversial or hot-button issues. It includes reports on more than 800 hot topics in business, politics, government, education, and popular culture. Use the search or browse topics by subject or A to Z.
Create Research Questions to Focus Your Topic
Obesity is a complex issue with many causes and consequences. You could concentrate on one set of issues and do in-depth research on that or use several of the questions below to focus on the topic of obesity more generally.
- Is obesity a serious problem?
- What factors cause obesity?
- Is obesity hereditary?
- Is obesity harmful to your health?
- Is obesity a physical or mental health issue?
- What are the economic consequences to society of obesity?
- Who should take responsibility for obesity?
- What steps should be taken to fight obesity?
- Should sodas and junk food be banned in school cafeterias?
- Based on what I have learned from my research what do I think about the issue of obesity in America?
Find Articles in Library Databases
All of these resources are free for MJC students, faculty, & staff.
If you're working from off campus, you'll need to sign in just like you do for your MJC email and Canvas classes.
- Gale Databases This link opens in a new window Search over 35 databases simultaneously that cover almost any topic you need to research at MJC. Gale databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- EBSCOhost Databases This link opens in a new window Search 22 databases simultaneously that cover almost any topic you need to research at MJC. EBSCO databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Nursing & Health Databases @ MJC Select a database from our list of nursing & health databases
- Facts on File Databases This link opens in a new window Facts on File databases include: Issues & Controversies , Issues & Controversies in History , Today's Science , and World News Digest .
- Access World News This link opens in a new window Search the full-text of editions of record for local, regional, and national U.S. newspapers as well as full-text content of key international sources. This is your source for The Modesto Bee from January 1989 to the present. Also includes in-depth special reports and hot topics from around the country. To access The Modesto Bee , limit your search to that publication. more... less... Watch this short video to learn how to find The Modesto Bee .
Search the Web
Use the Web to explore cutting-edge topics and to read current information.
Google Scholar is a great way to use Google to find scholarly information on the Web. Search Google Scholar below:

You may also be interested in these two relevant and reliable Website below:
- Overweight and Obesity From the Centers for Disease Control and Prevention, this site provides data and statistics on obesity.
- Obesity: MedlinePlus Produced by the National Library of Medicine, MedlinePlus brings you information about diseases, conditions, and wellness issues in language you can understand. MedlinePlus offers reliable, up-to-date health information, anytime, anywhere, for free.
Selected Library eBooks
Cite Your Sources
Your teacher should have told you what style you should use.
Click on a citation style below to learn how to cite your sources and format your paper using that style.
- Chicago Style
- Other Styles
Email: [email protected]
Drop-In research help
Meet with a librarian
- 209-575-6230 (East Campus) or
- 209-575-6949 (West Campus)
Text: (209) 710-5270

- Last Updated: Apr 25, 2024 1:28 PM
- URL: https://libguides.mjc.edu/obesity
Except where otherwise noted, this work is licensed under CC BY-SA 4.0 and CC BY-NC 4.0 Licenses .
Advertisement
Research priority setting in obesity: a systematic review
- Review Article
- Open access
- Published: 03 December 2021
- Volume 31 , pages 1285–1301, ( 2023 )
Cite this article
You have full access to this open access article

- Halima Iqbal ORCID: orcid.org/0000-0003-0895-1479 1 , 2 ,
- Rosemary R. C. McEachan 2 ,
- Jane West 2 &
- Melanie Haith-Cooper 1
2552 Accesses
7 Citations
3 Altmetric
Explore all metrics
Obesity research priority setting, if conducted to a high standard, can help promote policy-relevant and efficient research. Therefore, there is a need to identify existing research priority setting studies conducted in the topic area of obesity and to determine the extent to which they followed good practice principles for research priority setting.
Studies examining research priority setting in obesity were identified through searching the MEDLINE, PBSC, CINAHL, PsycINFO databases and the grey literature. The nine common themes of good practice in research priority setting were used as a methodological framework to evaluate the processes of the included studies. These were context, use of a comprehensive approach, inclusiveness, information gathering, planning for implementation, criteria, methods for deciding on priorities, evaluation and transparency.
Thirteen articles reporting research prioritisation exercises conducted in different areas of obesity research were included. All studies reported engaging with various stakeholders such as policy makers, researchers and healthcare professionals. Public involvement was included in six studies. Methods of research prioritisation commonly included both Delphi and nominal group techniques and surveys. None of the 13 studies fulfilled all nine of the good practice criteria for research priority setting, with the most common limitations including not using a comprehensive approach and lack of inclusivity and evaluating on their processes.
There is a need for research priority setting studies in obesity to involve the public and to evaluate their exercises to ensure they are of high quality.
Similar content being viewed by others

Health research priority setting in selected high income countries: a narrative review of methods used and recommendations for future practice

What do we know about evidence-informed priority setting processes to set population-level health-research agendas: an overview of reviews
Information sources for obesity prevention policy research: a review of systematic reviews.
Avoid common mistakes on your manuscript.
Introduction
Setting priorities for research helps to direct the most effective use of resources, such as research capacity, time and funds, to ensure an optimal health impact (Terry et al. 2018 ). Research priority setting in health, informed by stakeholders, can assist in the identification of topical and relevant issues, and unresolved questions regarding prevention, diagnosis and treatment of health conditions using a process that is explicit, iterative and inclusive (Rudan et al. 2010 ). There is currently no consensus on the definition of research priority setting, but there is agreement on a range of activities that centre on identifying, prioritising and reaching agreement on the research areas or questions deemed important to stakeholders (Tong et al. 2019 ). In the past, research-funding organisations and researchers developed their own research agendas without consulting key stakeholders (Graham et al. 2020 ). In recent times, however, there has been a focus on research needing to address questions that have relevance to those very people it intends to help (Dawson et al. 2017 ). It has been advocated that priority setting processes must also be fair, informed by credible evidence, of high quality and involve a broad range of stakeholders (Nasser et al. 2013 ; Sibbald et al. 2009 ; Viergever et al. 2010 ). Adopting a systematic and transparent approach to the identification of health research priorities can help to ensure that funded research has a public health benefit and make efficient and equitable use of limited resources (Bryant et al. 2014 ). Developing research agendas with target populations increases the potential for success and is more likely to be well received and relevant to their needs.
Nine common themes of good practice in research priority setting
There are currently no published guidelines for reporting priority setting for health research (Tong et al. 2019 ). In the absence of a gold standard approach, a checklist of nine common themes for good practice in health research prioritisation was developed by Viergever et al. ( 2010 ). In developing the checklist, expert consultation was initiated, and a literature review identified several methodological approaches which were combined to draw together a comprehensive outline of common views on what constituted good practice in health research priority setting (Viergever and Roderik 2010 ). The aim was to facilitate a transparent and comprehensive priority setting via this checklist and accommodate the flexibility required by different contexts.
The nine themes contained within the checklist broadly fall into three different categories: preparatory work, deciding on priorities and after priorities have been set. Each category contains corresponding practices that further identify the goals in each step. There are five related practices within preparatory work , namely context, use of a comprehensive approach (established frameworks providing structured guidance for research prioritisation), inclusiveness, information gathering and planning for implementation. There are two related practices within deciding on priorities, namely criteria and methods for deciding on priorities, and two within after priorities have been set, namely evaluation and transparency. See Table 1 for a detailed description of each theme.
The worldwide prevalence of obesity has significantly increased over the past few decades, leading the trend to be termed a ‘global epidemic’ by the World Health Organization and a serious threat to public health (World Health Organization 2017 ). Moreover, obesity is a global issue because it concerns both developed and developing countries (Cassi et al. 2017 ). The most recent available statistics from 2018/19 show that in England, a significant proportion of adults were overweight or obese, namely 67% of men and 60% of women (NHS Digital 2020 ). Of these, 26% of men and 29% of women were obese, and morbid obesity has also increased, from under 1% in 1993, to 3% in 2018 (NHS Digital 2020 ). Excess levels of fat in the body increase the risk of disease (Pollack et al. 2020 ) and obesity is a major risk factor for developing a range of conditions including cardiovascular disease, type 2 diabetes, muscular disorders, respiratory conditions and a host of psychological problems (Fruh 2017 ). A recent report by Public Health England highlights that the COVID-19 pandemic has brought to the fore the health crisis caused by overweight and obesity (Public Health England 2020 ). Both international and national research has consistently identified obesity as one of the key factors linked with severe outcomes from COVID-19 (Dietz and Santos-Burgoa 2020 ; Halvatsiotis et al. 2020 ). The direct annual costs resulting from obesity to the UK National Health Service (NHS) are reportedly estimated to reach £9.7 billion ($13.2 billion) by 2050, with wider costs to society predicted to reach just under £50 billion ($67.8 billion) per year by 2050 (Bradford Metropolitan District Council 2019 ).
Research is critical to inform prevention and treatment strategies to tackle obesity. Although there is a plethora of research examining the multitude of factors influencing obesity, research budgets are finite. Research priority setting can assist in making the most effective use of budgets by identifying the most relevant research areas according to different stakeholders. There is an emphasis on the need for research priority setting exercises to be explicit in their processes (Tong et al. 2019 ). Research priority setting guidelines and/or frameworks can help improve future research prioritisation in obesity, thus increasing the value and contribution of research aimed at reducing the obesity levels of populations.
The aim of this systematic review was to identify research priority setting exercises that have been conducted in obesity and to examine whether they had applied good practice principles in health research priority setting.
The systematic review followed the standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Shamseer et al. 2015 ).
Search strategy and process of study selection
The search was undertaken between 14–15 November 2020, using four electronic health databases, namely MEDLINE, PBSC, CINAHL and PsychINFO. The following Boolean search term combinations were used:
‘research priority setting’ [all fields] OR ‘research prioritization’ [all fields] OR ‘research prioritisation’ [all fields] OR ‘research priorities’ [all fields] OR ‘research agenda’ [all fields]
‘obesity’ OR ‘child obesity’ [all fields] OR ‘childhood obesity’ [all fields] OR ‘pediatric obesity’ [all fields] OR ‘obesity prevention’ [all fields] OR ‘obesity treatment’ [all fields]
We searched databases from their inception to November 2020. Only titles and abstracts published in English were included. The principal researcher (HI) independently conducted the article search. Searches in the grey literature included Google Scholar, Cochrane methods priority setting, the James Lind Alliance (a well-established priority-setting partnership method) and reference lists of selected articles to identify eligible papers. The search string ‘research priority setting and obesity’ was applied to Google Scholar. The first ten pages of Google Scholar were examined for additional articles. All authors contributed and refined the review’s search strategy.
Inclusion and exclusion criteria
The review included any study describing a process of conducting a research prioritisation exercise in obesity. To be included in the review, studies must have outlined participants’ characteristics, stated the methods used to obtain research and identified well-established outcomes. International studies were included provided they were written in the English language. Studies were excluded if they did not mention health research, had not described the research prioritisation process or had assessed priorities for practice and policy rather than research (quality indicators). Also excluded were studies that did not focus on obesity research prioritisation.
Across all databases, the search yielded 249 citations, of which 203 remained after duplicates were removed. After the titles and abstracts had been screened, 26 articles underwent full-text screening. Of these publications, 13 studies met our inclusion criteria and were finally included in the analysis. Of the 13 excluded studies, four did not focus mainly on research prioritisation, one was a study protocol, two did not focus on obesity, four were non-research articles and two failed to include the methods and processes. All authors discussed and agreed on the selected papers. References were managed with EndNote X9 for ease. The PRISMA flowchart is displayed in Fig. 1 .
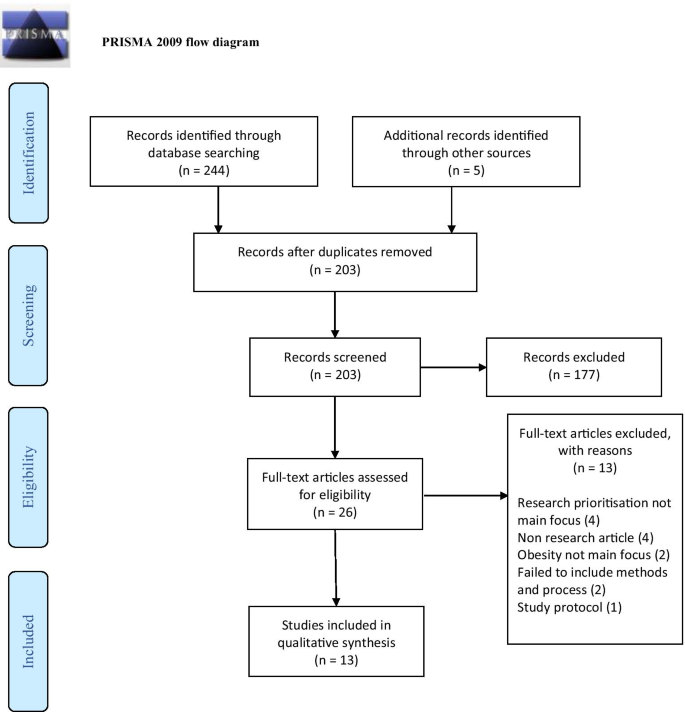
PRISMA 2009 flow diagram
Quality assessment tool
In the absence of a gold standard approach to research priority setting, the checklist of nine common themes for good practice in health research priority setting by Viergever et al. ( 2010 ) was used to ascertain whether the research prioritisation exercises in each included study complied with good practice principles in their processes. This checklist has been previously used to evaluate or guide research prioritisation exercises (Doolan-Noble et al. 2019 ; Iqbal et al. 2021 ; Mador et al. 2016 ; Reveiz et al. 2013 ; Tong et al. 2015 ;) and has identified weaknesses prevalent in their processes. The checklist was specifically designed for health research priority setting and, as such, can identify issues that may have been otherwise overlooked by traditional quality appraisal tools.
Data synthesis and extraction
A descriptive synthesis was conducted to outline study characteristics and outcomes, and to determine how many good practice principles each study followed. Studies could score between 0 (demonstrated none of the good practice principles) to 20 (demonstrated all of the good practice principles). One researcher (HI) independently extracted study characteristics, methods and outcomes. The relevant data were inserted into comprehensive data extraction checklist forms developed specifically for the quality synthesis. The quality appraisal criteria were applied by two researchers and resolved through discussion (HI and MC).
Studies were conducted in research priority setting in the area of obesity for childhood obesity (Botchwey et al. 2018 ; Byrne et al. 2008 ; Curtin et al. 2017 ; Gallagher et al. 2010 ; Hennessy et al. 2018 ; McPherson et al. 2016 ; Ramirez et al. 2011 ; Taylor et al. 2013 ; Ward et al. 2013 ), adult obesity (Hill et al. 2019 ; Hill et al. 2020 ; Mama et al. 2014 ), and obesity more generally (McKinnon et al. 2009 ). Studies were conducted in the areas of childhood obesity prevention or treatment (Byrne et al. 2008 ; Gallagher et al. 2010 ; Hennessy et al. 2018 ; Taylor et al. 2013 ), youth physical activity and healthy weight (Botchwey et al. 2018 ), healthy weight among youth with autism spectrum disorder and other developmental disabilities (Curtin et al. 2017 ), preconception priorities for maternal obesity prevention (Hill et al. 2019 ), pregnancy priorities for maternal obesity prevention (Hill et al. 2020 ), obesity reduction (Mama et al. 2014 ), obesity in children with physical disabilities (McPherson et al. 2016 ), obesity in Latino children (Ramirez et al. 2011 ), obesity policy (McKinnon et al. 2009 ) and obesity prevention in early care and education settings (Ward et al. 2013 ). The prioritisation exercises were all conducted in high income countries, namely Australia (4), the UK (1) and the US (8).
Seven studies did not include any patient or public involvement in their establishment of research priorities, yet involved a wide range of other stakeholders such as researchers, policy makers/leaders and healthcare professionals (Botchwey et al. 2018 ; Byrne et al. 2008 ; Gallagher et al. 2010 ; Hennessy et al. 2018 ; McKinnon et al. 2009 ; Taylor et al. 2013 ; Ward et al. 2013 ). One study solely involved the public in identifying priorities (Mama et al. 2014 ) and the remaining five studies involved the public alongside other stakeholders (Curtin et al. 2017 ; Hill et al. 2019 ; Hill et al. 2020 ; McPherson et al. 2016 ; Ramirez et al. 2011 ). Frequently cited methods used to identify priorities were surveys, Delphi techniques and the nominal group technique.
The main outcome of the studies was the generation of research priorities relevant to the topic and scope of each study. The priorities were described as prioritised research ideas/gaps/areas, prioritised lists, research priorities and prioritised themes. All 13 studies are displayed in Table 2 below.
When matched against the checklist of good practice principles in research priority setting as defined by Viergever et al. ( 2010 ), none of the studies adhered to all the principles outlined in the checklist (see Table 3 ).
Summary of the comprehensiveness of studies in reporting good practice principles
Theme 1: context.
The focus of the exercise was made clear in all studies, as were the underlying values and principles of each study. These included the need to engage the community in identifying obesity research priorities (Mama et al. 2014 ), or to foster collaboration amongst interdisciplinary research experts in the field of healthy weight, prevention of weight gain and maintenance of healthy weight (Gallagher et al. 2010 ; Hennessy et al. 2018 ; Taylor et al. 2013 ), or to develop a research agenda leveraging the collective expertise of a range of stakeholders (McPherson et al. 2016 ). However, the resources used for the exercises were made explicit in very few studies. Where information was provided, these included the use of materials used during the exercise such as cards to write knowledge gaps on (McPherson et al. 2016 ), flipcharts and numbered stickers for ranking (Hennessy et al. 2018 ), the use of audio-recorders (Mama et al. 2014 ) and the use of facilitators (Gallagher et al. 2010 ; Hennessy et al. 2018 ; Hill et al. 2020 ; Hill et al. 2019 ; McKinnon et al. 2009 ; McPherson et al. 2016 ) and project staff members to take notes and capture details around the issues raised (Ward et al. 2013 ), as well as the use of a statistician, data analyst and administrative support staff (Curtin et al. 2017 ). In one study, the use of a transcription service was disclosed (Mama et al. 2014 ). The economic/financial and political environment in which the prioritisation exercise took place was not disclosed in any of the studies.
Theme 2: Use of a comprehensive approach
None of the studies reported the use of established, structured, step-by-step frameworks specifically designed for research priority setting to guide their prioritisation processes, such as the James Lind Alliance (JLA) methodology (JLA 2020 ), the Essential National Health Research (ENHR) strategy (COHRED 2009 ), the Combined Approach Matrix (CAM) (Ghaffar 2009 ) and the Child Health and Nutrition Research Initiative (CHNRI) (Rudan 2016 ). None of the studies developed their own frameworks to guide their exercises.
Theme 3: Inclusiveness
Across prioritisation exercises, participants comprised a diverse range of stakeholders. Samples were inclusive of health service managers, medical practitioners, healthcare practitioners, academics, interdisciplinary researchers, dietitians, scientists, government agencies, policy leaders and experts in the field of child obesity more generally. Two studies solely involved researchers in the process (Gallagher et al. 2010 ; Taylor et al. 2013 ). Public involvement in the exercise was made explicit in six studies only (Curtin et al. 2017 ; Hill et al. 2020 ; Hill et al. 2019 ; Mama et al. 2014 ; McPherson et al. 2016 ; Ramirez et al. 2011 ). Although all studies discussed participant characteristics, some were more detailed in their descriptions by disclosing the sex of participants (Hennessy et al. 2018 ; Mama et al. 2014 ; Ramirez et al. 2011 ), with women overwhelmingly outnumbering men in two studies (Hennessy et al. 2018 ; Ramirez et al. 2011 ). An appropriate representation of regional participation was included in most studies that did not involve the public, as well as the incorporation of relevant sectors.
Theme 4: Information gathering
In some studies, a core planning group or committee suggested initial priorities to direct the process (Gallagher et al. 2010 ; Ramirez et al. 2011 ; Ward et al. 2013 ), or researchers identified the initial areas and other stakeholders prioritised the selected areas (Botchwey et al. 2018 ; Byrne et al. 2008 ). The use of technical data was reported in most studies. These included reviews of guidelines and recommendations (Hill et al. 2020 ; Hill et al. 2019 ), as well as literature searches, reports and systematic reviews (Botchwey et al. 2018 ; Hill et al. 2020 ; Ramirez et al. 2011 ). Surveys were conducted to obtain broad input on the selected topic areas (Botchwey et al. 2018 ; Byrne et al. 2008 ; Curtin et al. 2017 ), as were questionnaires (Ramirez et al. 2011 ; Taylor et al. 2013 ). Workshops (Gallagher et al. 2010 ; Hennessy et al. 2018 ; Hill et al. 2019 ; Hill et al. 2020 ; McPherson et al. 2016 ), group meetings (Curtin et al. 2017 ; McPherson et al. 2016 ; Ward et al. 2013 ) and brainstorming sessions were also reported as a means of generating information (Curtin et al. 2017 ), as well as presentations (McPherson et al. 2016 ; Ward et al. 2013 ).
Theme 5: Planning for implementation
Most of the studies did not report their plans for implementing identified priorities. Several community projects were established from two research priority setting studies (Gallagher et al. 2010 ; Ramirez et al. 2011 ). Plans for implementing pilot studies were established from a research agenda (Ramirez et al. 2011 ). Ongoing activities influenced by the identified priorities were reported in two studies (Hill et al. 2019 ; Hill et al. 2020 ). The research agenda shaped four initial projects in another study (Botchwey et al. 2018 ) and finally, one study secured a large team grant to address some items on their research agenda (McPherson et al. 2016 ).

Theme 6: Criteria
Criteria to focus discussion on research priorities were mentioned in six studies (Botchwey et al. 2018 ; Hill et al. 2020 ; Hill et al. 2019 ; McKinnon et al. 2009 ; McPherson et al. 2016 ; Ramirez et al. 2011 ). Cited criterion included research priorities that had the greatest long-term impact, and what would have the most immediate impact (Botchwey et al. 2018 ), prevalence or burden attributable to the proposed problem (Hill et al. 2019 ), provision, potential and proposed transformation attributable to the problem (Hill et al. 2020 ), preventative effect with respect to obesity development, and implementation feasibility (Hill et al. 2020 ), and the most appropriate and feasible methods for initiating research efforts (McPherson et al. 2016 ).
Theme 7: Methods for deciding on priorities
Studies either adopted a metrics approach (Botchwey et al. 2018 ; Byrne et al. 2008 ; Curtin et al. 2017 ; Gallagher et al. 2010 ; Taylor et al. 2013 ; Ward et al. 2013 ), a consensus approach (McPherson et al. 2016 ; Ramirez et al. 2011 ) or a combination of both (Hennessy et al. 2018 ; Hill et al. 2019 ; Hill et al. 2020 ). Likert scales were utilised in one study for ranking priorities (Ramirez et al. 2011 ), as were numbered stickers (Hennessy et al. 2018 ). The Delphi method was the most used method for deciding on priorities, both in its original form (Byrne et al. 2008 ; Ramirez et al. 2011 ; Taylor et al. 2013 ) and adapted versions, followed by the nominal group technique (Hennessy et al. 2018 ). In two studies, the Delphi technique was combined with the nominal group technique (Hill et al. 2019 ; Hill et al. 2020 ). One study used a modified nominal group technique to determine priorities (McKinnon et al. 2009 ). Another study did not use ranking and/or consensus to determine priorities, and instead searched for themes in the data and described these as the priorities (Mama et al. 2014 ).
Theme 8: Evaluation
There were no reported plans to update the priorities. One study mentioned that the research agenda would be reviewed, re-evaluated and refined (Curtin et al. 2017 ).
Theme 9: Transparency
Most of the studies were explicit in their priority setting processes, despite not using a well-established framework, although some were more transparent than others (Gallagher et al. 2010 ; Hennessy et al. 2018 ; Hill et al. 2020 ; Hill et al. 2019 ; Ramirez et al. 2011 ). The majority of studies outlined how the priorities were set. In most cases, it was clear which stakeholders identified initial topics, which stakeholders added generated additional input and who exactly prioritised.
Some studies also highlighted the limitations of their prioritisation exercise, such as acknowledging the lack of public involvement altogether (Hennessy et al. 2018 ), the possibility of unequal representation of disciplines (Hill et al. 2019 ; Hill et al. 2020 ), the lack of participation in person by children or youth (McPherson et al. 2016 ) and the lack of men that participated (Hennessy et al. 2018 ). Further highlighted limitations were around the issue of generalisability. This included the small sample size (Taylor et al. 2013 ), method of sample recruiting (Mama et al. 2014 ) and the possibility of selection bias due to the participants not being randomly selected (Ramirez et al. 2011 ). Other challenges were also highlighted, such as issues encountered in achieving consensus during the prioritisation phases (Hennessy et al. 2018 ), and the steps taken to reduce potential limitations when using the nominal group technique (Hennessy et al. 2018 ; Hill et al. 2019 ). One study reported pilot testing the questionnaire used to elicit priorities utilising a survey instrument, and subsequently revising it for improvement (Ramirez et al. 2011 ).
This review provides an assessment of research priority setting initiatives in the area of obesity. Most of the prioritisation exercises focussed on obesity topics including causes, prevention and management. Of the 13 identified studies, ten concentrated on child obesity, three on adult obesity and one focussed on obesity more generally. The application of a checklist of good practice principles in research priority setting identified the strengths and weaknesses inherent in each study. None of the studies fulfilled all the good practice principles as outlined by the checklist. It is clear that more effort needs to be made in studies examining obesity research priority setting to ensure that their processes are of a high quality. It is important to note however, that two studies (Byrne et al. 2008 ; McKinnon et al. 2009 ) were conducted before the checklist of nine common themes of good practice was published in 2010. In addition, literature advocating the need for research priority setting to be fair, legitimate, informed by credible evidence, include a wide range of stakeholders and be transparent, has only more recently been strongly advocated (Bhaumik et al. 2015 ; Nasser et al. 2013 ; Tong et al. 2019 ; Viergever et al. 2010 ) which may be as a result of the increase in research prioritisation exercises in the past two decades. Our findings suggest that the greatest limitations of studies when applied to the checklist of good practice concerned the criteria use of comprehensive approach, inclusiveness and evaluation.
None of the studies used comprehensive well-established research priority setting frameworks such as the JLA methodology, the ENHR strategy, the CAM and the CHNRI initiative. These established schemata were all developed before the studies were undertaken and provide step-by-step guidance for the entire process, while covering many of the points on the checklist (Viergever et al. 2010 ). It is argued by Viergever et al. ( 2010 ) that the use of these structurally well-defined tools and methods should at least be considered, and that they will gradually replace commonly used methods such as the Delphi method (Yoshida 2016 ), which was a frequently used method used to establish obesity priorities in the identified studies.
It is concerning that only six of the 13 studies in this review involved the public as stakeholders and even then, the public were significantly underrepresented in the sample (Hill et al. 2020 ; Hill et al. 2019 ; McPherson et al. 2016 ; Ramirez et al. 2011 ), with another study not making clear how many public stakeholders were involved in the process (Curtin et al. 2017 ). Interestingly, of the seven studies that scored the highest in this review, six of them involved the public in the generation of priorities. It is well established in the literature that community engagement in research priority setting is crucial for establishing research questions that are relevant to them. Previous studies have demonstrated that the research priorities of other stakeholders do not align with those of the public (Brady et al. 2020 ; Manikam et al. 2017 ; Owens et al. 2008 ; Tallon et al. 2000 ; Voigt et al. 2010 ). A 2014 report systematically reviewed research priority setting studies from the period 1966 to 2014 and found that in the 91 studies, researcher and government involvement was strong, yet involvement of other key stakeholders was limited (McGregor et al. 2014 ). To ensure the incorporation of public and patients in the process, guidelines are available such as the Guidance for Reporting Involvement of Patients and the Public (GRIPP) checklist (Staniszewska et al. 2017 ), which was developed to aid in improving the quality, consistency and transparency of reporting the inclusion of patients and the public in research. The checklist offers a comprehensive list of issues that require consideration when reporting activities in relation to public and patient involvement. It must be noted, however, that it fails to offer information on how the public and patient contributors are to be recruited (Dawson et al. 2017 ). Additionally, it does not offer explicit consideration for representing the diversity of the population relevant to the topic area (Dawson et al. 2017 ). It is unclear in the current review whether public stakeholders were representative of the community at large, i.e. whether there was inclusion of Black and minority ethnic stakeholders in the samples. In addition to ensuring the inclusion of the public in research priority setting exercises, it is recommended that key characteristics of the sample are recorded and reported so that issues in relation to inclusion and diversity can be understood.
With regard to evaluation, a small number of studies in this review described strategies for the implementation of identified priorities, yet none measured the impact of the prioritisation. This can be done, for example, by performing an impact assessment reviewing the research performed (Viergever and Roderik 2010 ). The authors of a 2014 report (McGregor et al. 2014 ) argued that many of the exercises failed to translate the result of the prioritisation process into implementation of projects. It was further highlighted that the exercises were rarely repeated due to the lack of follow-up. The authors of the current review would strongly endorse the use of good practice guidelines, such as the one used to critically appraise the studies in this review, or the Reporting Guideline for Priority Setting of Health Research (REPRISE) by Tong et al. ( 2019 ).
In summary, one can say that while research priority setting studies in the topic area of obesity do exist, they vary in scope and in quality. Although a wide range of stakeholders were involved in the prioritisation processes, public involvement was either non-existent or limited. The use of a comprehensive approach in research priority setting and/or adherence to good practice guidelines could enrich obesity priority setting processes to ensure the identified obesity priorities are relevant, transparent and can assist in implementation efforts. It is imperative that the public be involved in the obesity research priority setting process, resulting in research agendas that have incorporated their unmet needs. This can improve the relevance and legitimacy of research and ultimately achieve better health outcomes in obesity.
Availability of data and material
DOI’s are cited in the reference list
Bradford District Metropolitan Council) (BDMC) (2019) Living well: overweight and obesity. Available online at: https://jsna.bradford.gov.uk/documents/People%20are%20living%20their%20lives%20well%20and%20ageing%20well/4.2%20LIfestyle%20Factors/Overweight%20and%20Obesity.pdf . Accessed 16 Nov 2020
Bhaumik S, Rana S, Karimkhani C, Welch V, Armstrong R, Pottie K, Dellavalle R, Dhakal P, Oliver S, Francis DK, Nasser M, Crowe S, Aksut B, Amico RD (2015) Ethics and equity in research priority-setting: stakeholder engagement and the needs of disadvantaged groups. Indian J Med Ethics 12:110-3. https://doi.org/10.20529/IJME.2015.030
Botchwey N, Floyd MF, Pollack Porter K, Cutter CL, Spoon C, Schmidt TL, Conway TL, Hipp JA, Kim AJ, Umstattd Meyer MR, Walker AL, Kauth TJ, Sallis JF (2018) Policy and Practice-Relevant Youth Physical Activity Research Center Agenda. J Phys Act Health 15:626–634. https://doi.org/10.1123/jpah.2017-0327
Article PubMed Google Scholar
Brady PC, Horne AW, Saunders PTK, Thomas AM, Missmer SA, Farland LV (2020) Research priorities for endometriosis differ among patients, clinicians, and researchers. Am J Obstet Gynecol 222:630–632. https://doi.org/10.1016/j.ajog.2020.02.047
Bryant J, Sanson-Fisher R, Walsh J, Stewart J (2014) Health research priority setting in selected high income countries: a narrative review of methods used and recommendations for future practice. Cost Eff Resour 12:23
Article Google Scholar
Byrne S, Wake M, Blumberg D, Dibley M (2008) Identifying priority areas for longitudinal research in childhood obesity: Delphi technique survey. Int J Pediatr Obes 3:120-122. https://doi.org/10.1080/17477160701830796
Cassi L, Lahattel A, Rafols I, Sauther P, De Turckheim É (2017) Improving fitness: Mapping research priorities against societal needs on obesity. J Informetr 11:1095–1113. https://doi.org/10.1016/j.joi.2017.09.010
COHRED (2009) A manual for research priority setting using the ENHR strategy. Available online at: http://www.cohred.org/downloads/578.pdf . Accessed 16 Nov 2020
Curtin C, Must A, Phillips S, Bandini L (2017) The healthy weight research network: a research agenda to promote healthy weight among youth with autism spectrum disorder and other developmental disabilities. Pediatr Obes 12:e6–e9. https://doi.org/10.1111/ijpo.12109
Article CAS PubMed Google Scholar
Dawson S, Campbell SM, Giles SJ, Morris RL, Cheraghi-sohi S (2017) Black and minority ethnic group involvement in health and social care research: a systematic review. Health Expect 21:3–22. https://doi.org/10.1111/hex.12597
Article PubMed PubMed Central Google Scholar
Dietz W, Santos-burgoa C (2020) Obesity and its implications for COVID-19 mortality. Obesity 28:1005. https://doi.org/10.1002/oby.22818
Doolan-Noble F, Mehta P, Waters D, Baxter GD (2019) Supporting ageing well research: Findings from a research priority setting exercise. Australas J Ageing 38:136–143. https://doi.org/10.1111/ajag.12615
Fruh SM (2017) Obesity: risk factors, complications, and strategies for sustainable long-term weight management. J Am Ass Nurse Pract 29:S3-S14. https://doi.org/10.1002/2327-6924.12510
Gallagher D, Larson EL, Wang YHC, Richards B, Weng C, Hametz P, Begg MD, Chung WK, Boden-Albala B, Akabas SR (2010) Identifying interdisciplinary research priorities to prevent and treat pediatric obesity in New York City. Clin Transl Sci 3:172–177. https://doi.org/10.1111/j.1752-8062.2010.00210.x
Ghaffar A (2009) Setting research priorities by applying the combined approach matrix. The Indian Journal Of Medical Research 129:368–375
PubMed Google Scholar
Graham L, Illingworth BJG, Showell M, Vercoe M, Crosbie EJ, Gingel LJ, Farguhar CM, Horne AW, Prior M, Stephenson JM, Magee LA, Duffy JMN, Crosbie (2020) Research priority setting in women's health: a systematic review. BJOG 127:694-700. https://doi.org/10.1111/1471-0528.16150
Halvatsiotis P, Kotanidou A, Tzannis K, Jahaj E, Magira E, Theodorakopoulou M, Konstandopoulou G, Gkeka E, Pourzitaki C, Kapravelos N, Papoti S, Sileli M, Gogos C, Velissaris D, Markou N, Stefanatou E, Vlachogianni G, Aimoniotou E, Komnos A, Zafeiridis T, Koulouvaris P, Armaganidis A, Bamias A, Dimopoulos G (2020) Demographic and clinical features of critically ill patients with COVID-19 in Greece: The burden of diabetes and obesity. Diabetes Res Clin Pract 166:108331. https://doi.org/10.1016/j.diabres.2020.108331
Hennessy M, Byrne M, Laws R, Mc Sharry J, O'malley G, Heary C (2018) Childhood obesity prevention: priority areas for future research and barriers and facilitators to knowledge translation, coproduced using the nominal group technique. Transl Behav Med 9(4):759–767. https://doi.org/10.1093/tbm/iby074
Hill B, Skouteris H, Boyle JA, Bailey C, Walker R, Thangaratinam S, Sundseth H, Stephenson J, Steegers E, Redman LM, Montanaro C, Lim S, Jorgensen L, Jack B, Borges ALV, Bergmeier HJ, Baxter JAB, Harrison CL, Teede HJ (2020) Health in preconception, pregnancy and postpartum global alliance: international network pregnancy priorities for the prevention of maternal obesity and related pregnancy and long-term complications. J Clin Med 9(3):822. https://doi.org/10.3390/jcm9030822
Hill B, Skouteris H, Teede HJ, Bailey C, Baxter JAB, BergmeierHJ BALV, Harrison CL, Jack B, Jorgensen L, Lim S, Montanaro C, Redman L, Steegers E, Stephenson J, Sundseth H, Thangaratinam S, Walker R, Boyle JA (2019) Health in preconception, pregnancy and postpartum global alliance: international network preconception research priorities for the prevention of maternal obesity and related pregnancy and long-term complications. J Clin Med 8(12):2119. https://doi.org/10.3390/jcm8122119
Iqbal H, West J, Haith-Cooper M, Mceachan RRC (2021) A systematic review to identify research priority setting in Black and minority ethnic health and evaluate their processes. Plos One 16:e0251685. https://doi.org/10.1371/journal.pone.0251685
Article CAS PubMed PubMed Central Google Scholar
James Lind Alliance (JLA) (2020) JLA guidebook. Available online at: https://www.jla.nihr.ac.uk/jla-guidebook/chapter-7/collating-and-scoring-interim-priorities.html Accessed 23 Nov 2020
Mador RL, Kornas K, Simard A, Haroun V (2016) Using the Nine Common Themes of Good Practice checklist as a tool for evaluating the research priority setting process of a provincial research and program evaluation program. Health Res Policy Syst 14:1–9. https://doi.org/10.1186/s12961-016-0092-5
Mama SK, Soltero EG, Ledoux TA, Gallagher MR, Lee RE (2014) Solving the obesity epidemic: voices from the community. Nurs Inq 21:192–201. https://doi.org/10.1111/nin.12054
Manikam L, Shah R, Reed K, Santini G, Lakhanpaul M (2017) Using a co-production prioritization exercise involving South Asian children, young people and their families to identify health priorities requiring further research and public awareness. Health Expect 20:852–861. https://doi.org/10.1111/hex.12524
McGregor S, Henderson KJ, Kaldor JM (2014) How are health research priorities set in low and middle income countries? A systematic review of published reports. Plos One 9:e108787. https://doi.org/10.1371/journal.pone.0108787
McKinnon RA, Orleans CT, Kumanyika SK, Haire-Joshu D, Krebs-Smith SM, Finkelstein EA, Brownell KD, Thompson JW, Ballard-Barbash R, Mckinnon RA, Orleans CT, Kumanyika SK, Haire-Joshu D, Krebs-Smith SM, Finkelstein EA, Brownell KD, Thompson JW, Ballard-Barbash R (2009) Considerations for an obesity policy research agenda. Am J Prev Med 36:351–357. https://doi.org/10.1016/j.amepre.2008.11.017
McPherson AC, Ball GDC, Maltais DB, Swift JA, Cairney J, Knibbe TJ, Krog K (2016) A call to action: Setting the research agenda for addressing obesity and weight-related topics in children with physical disabilities. Child Obes 12:59–69. https://doi.org/10.1089/chi.2015.0119
Nasser M, Welch V, Tugwell P, Ueffing E, Doyle J, Waters E (2013) Ensuring relevance for Cochrane reviews: evaluating processes and methods for prioritizing topics for Cochrane reviews. J Clin Epidemiol 66:474–482. https://doi.org/10.1016/j.jclinepi.2012.01.001
NHS Digital (2020) Statistics on obesity, physcial activity and diet, England. Available online at: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020 . Accessed 16 Nov 2020
Owens C, Ley A, Aitken P (2008) Do different stakeholder groups share mental health research priorities? A four-arm Delphi study. Health Expect 11:418–431. https://doi.org/10.1111/j.1369-7625.2008.00492.x
Public Health England (2020) Excess weight and COVID-19: insights from new evidence . Public Health England. Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/907966/PHE_insight_Excess_weight_and_COVID-19__FINAL.pdf . Accessed 17 Nov 2020
Pollack LM, Wang M, Leung MYM, Colditz G, Herrick C, Chang SH (2020) Obesity-related multimorbidity and risk of cardiovascular disease in the middle-aged population in the United States. Prev Med 139:106225. https://doi.org/10.1016/j.ypmed.2020.106225
Ramirez AG, Chalela P, Gallion KJ, Green LW, Ottoson J (2011) Salud America! Developing a national Latino childhood obesity research agenda. Health Educ Behav 38:251–260. https://doi.org/10.1177/1090198110372333
Reveiz L, Elias V, Terry RF, Alger J, Becerra-Posada F (2013) Comparison of national health research priority-setting methods and characteristics in Latin America and the Caribbean, 2002-2012. Revista Panamericana de Salud Publica 34:1–13
Rudan I (2016) Setting health research priorities using the CHNRI method: IV. Key conceptual advances. J Global Health 6:010501–010501
Rudan I, Kapiriri L, Tomlinson M, Balliet M, Cohen B, Chopra M (2010) Evidence-based priority setting for health care and research: tools to support policy in maternal, neonatal, and child health in Africa. Plos Med 7:e1000308. https://doi.org/10.1371/journal.pmed.1000308
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) elaboration and explanation. BMJ (Clinical research ed.) 350:g7647. https://doi.org/10.1136/bmj.g7647
Sibbald SL, Singer PA, Upshur R, Martin DK (2009) Priority setting: what constitutes success? A conceptual framework for successful priority setting. BMC Health Serv Res 9:43
Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, Altman DG, Moher D, Barber R, Denegri S, Entwistle A, Littlejohns P, Morris C, Suleman R, Thomas V, Tysall C (2017) GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 358:j3453. https://doi.org/10.1136/bmj.j3453
Tallon D, Chard J, Dieppe P (2000) Relation between agendas of the research community and the research consumer. Lancet 355:2037–2040. https://doi.org/10.1016/S0140-6736(00)02351-5
Taylor RW, Robinson A, Espinel PT, Baur LA, Wake M, Sabin MA (2013) Research priorities in 2012 for the effective management of childhood obesity. Clin Obes 3:3–6. https://doi.org/10.1111/cob.12014
Terry RF, Charles E, Purdy B, Sanford A (2018) An analysis of research priority-setting at the World Health Organization - how mapping to a standard template allows for comparison between research priority-setting approaches. Health Res Policy Syst 16:116. https://doi.org/10.1111/cob.12014
Tong A, Chando S, Crowe S, Manns B, Winkelmayer WC, Hemmelgarn B, Craig JC (2015) Research priority setting in kidney disease: a systematic review. Am J Kidney Dis 65:674–683
Tong A, Synnot A, Crowe S, Hill S, Matus A, Scholes-Robertson N, Oliver S, Cowan K, Nasser M, Bhaumik S, Gutman T, Baumgart A, Craig JC (2019) Reporting guideline for priority setting of health research (REPRISE). BMC Med Res Methodol 19:1–11. https://doi.org/10.1186/s12874-019-0889-3
Article CAS Google Scholar
Viergever and Roderik (2010) Health research prioritization at WHO - an overview of methodology and high level analysis of WHO led health research priority setting exercises pp 2-30. https://www.ip-watch.org
Viergever RF, Olifson S, Ghaffar A, Terry RF (2010) A checklist for health research priority setting: nine common themes of good practice. Health Res Policy Syst 8:36
Voigt I, Wrede J, Diederichs-Egidi H, Dierks ML, Junius-Walker U (2010) Priority setting in general practice: Do health priorities of older patients differ from treatment priorities of their physicians. Croatian Med J 51:483–492. https://doi.org/10.3325/cmj.2010.51.483
Ward DS, Vaughn A, Story M (2013) Expert and stakeholder consensus on priorities for obesity prevention research in early care and education settings. Child Obes 9:116–124. https://doi.org/10.1089/chi.2013.9204
World Health Organization (WHO) (2017) Obesity and overweight. Available online at: http://www.who.int/mediacentre/factsheets/fs311/en . Accessed 20 Nov 2020
Yoshida S (2016) Approaches, tools and methods used for setting priorities in health research in the 21st century. J Global Health 6:010507–010507
Download references
This work was supported by the National Institute for Health Research (NIHR) under its Applied Research Collaboration (ARC) Yorkshire and Humber in the form of Ph.D. funding to HI [NIHR200166], the UK Prevention Research Partnership (UKPRP) in the form of funding to JW and RM [MR/S037527/1], the NIHR Clinical Research Network in the form of funding to JW, and the NIHR ARC Yorkshire and Humber in the form of funding to RM
Author information
Authors and affiliations.
Faculty of Health Studies, University of Bradford, Richmond Road, Bradford, BD7 1DP, UK
Halima Iqbal & Melanie Haith-Cooper
Bradford Institute for Health Research, Bradford Teaching Hospital NHS Foundation Trust, Bradford, UK
Halima Iqbal, Rosemary R. C. McEachan & Jane West
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation: Halima Iqbal, Melanie Haith-Cooper, Rosie McEachan, Jane West; Methodology: Halima Iqbal; Formal analysis and investigation: Halima Iqbal, Melanie Haith-Cooper; Writing – original draft preparation: Halima Iqbal; Writing – review and editing: Halima Iqbal, Melanie Haith-Cooper, Rosie McEachan, Jane West; Resources: Halima Iqbal; Supervision: Halima Iqbal
Corresponding author
Correspondence to Halima Iqbal .
Ethics declarations
Conflicts of interest.
The authors declare they have no financial or non-financial interests to disclose.
Ethics approval
This is a systematic review. The University of Bradford Ethics Committee has confirmed that no ethical approval is required
Consent to participate
Not applicable
Consent for publication
Code availability, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Iqbal, H., McEachan, R.R.C., West, J. et al. Research priority setting in obesity: a systematic review. J Public Health (Berl.) 31 , 1285–1301 (2023). https://doi.org/10.1007/s10389-021-01679-8
Download citation
Received : 23 July 2021
Accepted : 11 November 2021
Published : 03 December 2021
Issue Date : August 2023
DOI : https://doi.org/10.1007/s10389-021-01679-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- research priority setting
- obesity research agenda
- Find a journal
- Publish with us
- Track your research

- June 9, 2024 | Mayo Clinic Study Reveals Startling Connection Between Energy Drinks and Sudden Cardiac Arrest
- June 9, 2024 | Quantum Theory Unveils Surprising Black Hole Shortage
- June 9, 2024 | Cracking the Code: Scientists Solve Reynolds’ Century-Old Fluid Flow Mystery
- June 9, 2024 | A Sustainable Solution to Fighting Global Warming – New Catalyst Efficiently Converts CO2 to Natural Gas
- June 9, 2024 | Beware the Rise of Superweeds: Mowing’s Unintended Consequences
New Research Finds That With Obesity, the Problem Isn’t an Excess of Fat but Its Loss of Function
By Cell Press February 3, 2022
Obesity’s detrimental health effects, such as hypertension and diabetes, stem not merely from an excess of fat, but rather from the loss of fat’s plasticity — its ability to respond to changes — according to a review published in the Cell journal. The researchers explain that fat, besides storing energy, plays crucial roles in immune response, insulin sensitivity regulation, and body temperature maintenance. As fat loses its plasticity due to aging and obesity, it can’t respond to bodily cues, leading to insulin resistance, inflammation, and cell death due to the fast growth of adipose tissue that outstrips its blood supply.
A review in the Cell journal reveals that the negative health impacts of obesity are not merely due to excess fat, but rather a loss of fat’s plasticity, its ability to respond to changes. This decline leads to health issues such as insulin resistance and inflammation. The researchers highlight the potential of altering fat tissue phenotypes for therapeutic benefits, pointing to an exciting avenue for future medical advancements.
Obesity is known to cause cardiometabolic diseases like hypertension and diabetes but attributing these diseases to merely an overabundance of fat is a simplification. On a basic level, fat acts as a receptacle to store energy, but upon a closer look it is an essential actor in vital bodily processes like the immune response, the regulation of insulin sensitivity, and maintenance of body temperature. In a review published in the journal Cell on February 3rd, 2022, researchers argue that the negative health effects of obesity stem not simply from an excess of fat but from the decline in its ability to respond to changes, or in other words, its plasticity.
The makeup and functioning of this tissue changes in response to weight fluctuations and aging. As fat declines in plasticity due to aging and obesity, it loses its ability to respond to bodily cues. In the current model of this phenomenon, the rapid growth of adipose tissue outpaces its blood supply, depriving the fat cells of oxygen and causing the accumulation of cells that no longer divide. This leads to insulin resistance, inflammation, and cell death accompanied by the uncontrolled spill of lipids from these cells.
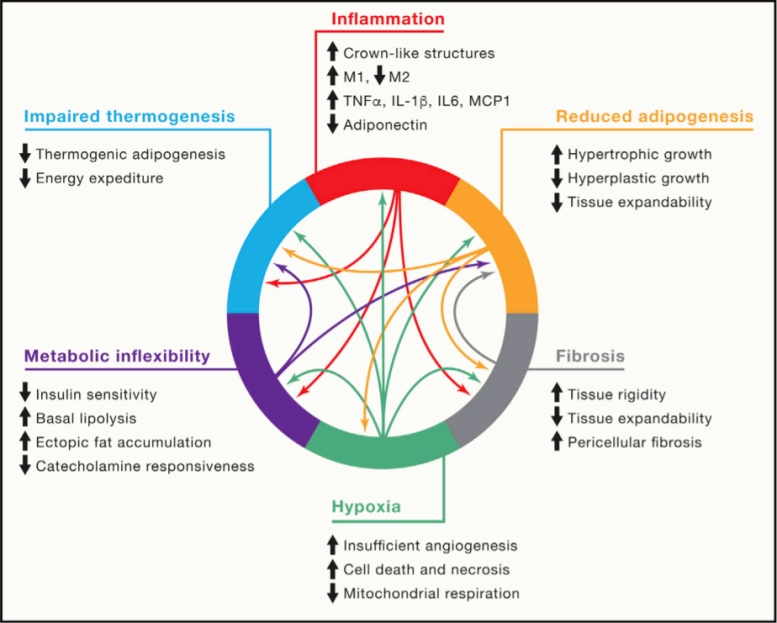
The hallmarks of adipose tissue dysfunction. Credit: Sakers et al./Cel
“The central role of adipose tissue dysfunction in disease and the incredible plasticity of fat tissue supports the promise of modulating fat tissue phenotypes for therapeutic purposes,” write the authors, led by Claudio J. Villanueva from the College of Life Sciences/David Geffen School of Medicine and Patrick Seale from Perelman School of Medicine at the University of Pennsylvania. “Many questions and opportunities for future discovery remain, which will yield new insights into adipose tissue biology and hopefully lead to improved therapies for human disease.”
Reference: “Adipose tissue plasticity in health and disease” by Alexander Sakers, Mirian Krystel De Siqueira, Patrick Seale and Claudio J. Villanueva, 3 February 2022, Cell . DOI: 10.1016/j.cell.2021.12.016
Research reported in this publication was supported by NIDDK at the National Institutes of Health , the UCLA Life Sciences Fund, and UCLA Graduate Council Diversity Fellowship. The authors declare no competing interests.
More on SciTechDaily
Columbia University Obesity Treatment: Nanotechnology Reduces Fat at Targeted Locations

Neuroscientists Discover Beige Fat “Indispensable” in Protecting Brain From Dementia

Scientists Discover How To “Flavor” Your Food To Burn Excess Fat
Healthy Obesity: Blood Vessels Can Make You Fat, and yet Fit

Beige Fat May Have Therapeutic Potential for Treating Obesity

The Obesity Society Issues New Position Statement on COVID-19 Vaccines

Insulin in a Pill? New Research Answers a Question That Has Puzzled Diabetes Researchers for 100 Years
Researchers Develop a New Ultrafast Insulin for Management of Blood Sugar in Diabetes
314 comments on "new research finds that with obesity, the problem isn’t an excess of fat but its loss of function".
a sensitive society will tell itself anything to make fat people feel well about themselves, while neglecting that their bodies might shut down at any moment
Spoken like a typical body shaming bigot. Mounting scientific evidence clearly points to obesity having genetic origin as well as pathogenic causes. An exhaustive study by the World Health Organization concluded obesity isn’t as simple as poor habits. No indigenous animals on the Earth deliberately over except for survival. Even those animals resume their normal eating habits when hyperphagia (gorging)is no longer necessary. I suggest it’s you with the problem and it’s called superiority complex. It’s a psychological disorder where someone is compelled to demean others in order to feel good about themselves and you have it in spades. Seek help.
We shame criminals so that they shape up. We shame presidents so that they shape up. We shame other countries so that they shape up.
Shame gets sh*t done. If you really care about human life, you need to speak up. Give them the truth or you are complicit in the silent murder.
We shame criminals so that they shape up. And most reoffend. We shame presidents so that they shape up. And they never do. We shame other countries so that they shape up. And it caused WWII among other problems. We shame mental illnesses. And they commit suicide.
Shame gets sh*t done is a bad excuse for poor behavior not a solution.
Actually, no. That’s extremely ignorant and misinformed. Shame is PROVEN to be ineffective at “getting sh*t” done. There’s an enormous body of research showing that it’s actually counterproductive to change. I can actually prove it. Easily. You are currently being shamed in the comments for being a a**hole. Do you feel motivated to change your veiwpoint and behavior? Because if shaming bad behavior is effective at producing change, right now you should be rethinking your stance on this. So tell me, how effective is shame?
“we” shame people because we are self righteous and passive aggressive, not to to get them to shape up. People shame themselves with their own actions, and society punishes criminals. Twitter bullies and morality enforcers weaponize shame.
Nah… shaming me is just your immature response to seeing something you find offensive. Thing is… I don’t give two craps what you think.
Dan here finished off a whole bag of Chips and a liter of soda while whining about intelligent fit people.
Dan has a point, all you bigots out their need to get off your high horses and stop shaming people for their bad health practices like smoking, heavy drinking, and eating too many calories.
Also some percent, maybe 40%, might be a disposition towards obesity, which means people can’t help it that they eat too much pizza and don’t exercise, and if they can’t help it, why try? True, obesity rates have increased 27-47% worldwide over the past 30 years, and while our genetics don’t mutate that quickly, those people 30+ years ago who were genetically predisposed just didn’t realize it. Now that we are informed, we know it’s not our fault and we can choose our own unhealthy lifestyles. Enough already with medical professionals and society trying to get us healthy, it’s obviously not going to work, we’re also genetically predisposed to resisting critiques, even if it can make us healthier. “Healthy” is probably a made up word without any scientific basis. Mental health is also important, and eating potato chips while binging shows on my couch makes me happy, so leave me alone!!!
Dan, Reality is correct. Anyone can lose weight. Literally anyone. I assume, Dan, you are fat and want to justify it by shaming Reality for speaking the truth? There is a lot of that going around these days. Truth shaming. A lot. But truth is thruth, and you’re not speaking truth. You are enabling…fat behavior. And it has its foundation in marxism (everyone is the SAME-fat people are thin too….whine). No Dan we are NOT like you. We don’t OVEREAT junk food. We don’t overeat. No matter how hard you try to justify your own lack of good eating hygiene, it won’t get you normo-weight. Put down the ho-hos Dan!
Overeat, that is.
While I agree that society is not only turning a blind eye to obesity (ostensibly trying to fight it), it seems in many ways certain powers that be want obesity worse.
However, this article does say that greater fat quantity is bad. The article also claims that greater fat quantity contributes, with age, to a loss of fat plasticity, which compounds the negative effects of having too much fat.
From what I can tell, the article isn’t diminishing the negative effects of fat quantity, it illuminates how fat becomes more dangerous the faster one is.
That same sensitive society probably told you that your reading comprehension is great and that you’re a smart boy while handing you your participation trophy.
Quit body shaming others that isn’t skinny. It is ALSO HEREDITARY! I have a 13yr old daughter, who has had medical problems since birth. She is also boarder line diabetic and takes Metformin. She is over weight ever since she was a toddler and yes she had seen a dietitian for a Cple of years. On her father’s side of the family, every single one of her father’s immediate family is obese and has been for generations,that is including her father. She also has fatty liver disease (found out in an ultrasound they ran on her back during the summer). Her father has heart failure and really high blood pressure (also runs in his family). My 18yr old daughter isn’t as big as her younger sister, she also has medical problems. High Blood pressure, high cholesterol, she doesn’t get periods very often (2-3 times a yr but lasts only 1 day), she has OCD and has been in and out of therapy since she was 8. She was also been verbally abused by her father until she was 14, when I got the courage to leave their dad and move back home. I also went thru the same thing on getting verbally abused by her father also off and on from not long after I gotten married in 2001 and got worse in Feb 2017, when his mom had a major heart attack and passed. He became a heavy drinker and bar hop every weekend and not come home til next morning. He was also cheating on me by a so called “lesbian”(his excuse hanging out with his lesbian friend on Friday and Saturdays). Well… Maybe there are others that is obese and CAN NOT help it. Maybe they went thru a similar situation like mine and my kids. Depression can cause obesity, being hereditary can cause obesity, stress can also cause it. Heart problems runs in BOTH my family’s and my kids dad’s family. So does becoming diabetic (type 2, kids dad, my dad, my oldest brother, kids dad’s mom and grandmother and biological father, 2 of my uncle’s. Type 1 runs in my family also, my mom’s cousin was type 1). NOT everyone that is obese can NOT help it! Some can yes, but some can not. The same with super skinny ppl.. My late step father in law was type 1 diabetic and he could NOT gain weight at all. He was under 130lbs. I have a friend in MI who can not help being really skinny, she eats all of the time and alot of ppl body shames her cause you can see her ribcage. She can NOT help it(she’s also type 1)… Quit being a male version of a Karen and stop that body shaming nonsense. As long as the person is happy about their body and tries to take care of their body is all that matters. Your nonsense crap is the reason why ppl ends up having medical issues and mental issues from constantly having others body shame them… ESPECIALLY when a 38yr old ADULT starts body shaming a 13yr old and she’s big herself. Body shaming = BULLYING
An anecdotal account of “my daughter is obese” or “all the immediate family members are obese” by itself proves nothing. It must be hard with your situation and your daughter, lots of challenges to be sure. But as a whole, the “They can’t help it” examples are very rare and don’t inform the whole.
With personal examples, please also provide their exact daily activity, amount of calories eaten, when they eat, what kind of food, how much sleep they get, and how much water they drink. This is important to make an informed conclusion, and most of the time this is the reason people are overweight, and even in rare cases where there’s an underlying genetic issue, that and their weight can still be managed if these other things are addressed properly with that in mind.
If we begin with, “I can’t help it,” or, “I’ve been to a dietician and I’m still overweight,” then we will quit trying. Will you quit, or will you take what you know and strive to make it better?
I speak from experience also, I too have underlying genetic issues, I too have been to a dietician, but for me, if I’m overweight it’s mostly a combination of these other things, NOT my generltics, only I can’t eat the same things others can … but it’s about what I can do to be healthy based on my body & genetics, not someone else’s
Arrogant prick. Shut it
Good luck getting doxxed.
This is so dumb, can’t believe people still spout this nonsense. Even if obesity is not exacerbated by genes which it in many cases is. The fact that society is set up to make people fat is always completely neglected. There is a reason people weren’t as fat decades ago and it’s not because people nowadays lack willpower or don’t practise self control.
If you REALLY want to stop people from becoming obese, tackle the CAUSE. Want to guess what it is? It’s corporations designing foods that are addictive and bad for our health. Not only that but using smart strategies to advertise said “food” so that people become influenced into buying more of it. It’s all so clearly obvious that that is at heart of the issue but people just don’t see it. Because muh choice and muh freedom. Get the f*ck out of here and fight against the real problem and stop shaming the victims.
So, according to you someone who’s fat because of a pinhead sized tumor on their pituitary gland has only themselves to blame? (The name for such a tumor is called Cushing’s disease)
Is telling a bipolar person they are unfixable helpful? Is telling a slow person they’ll never get faster helpful? >Muh genetics tho
A perfect example of when very rare medical problems are given as the reason for, “I can’t help being overweight.”
Let’s not forget that having Cushing’s does not guarantee obesity, it only makes it more of a challenge, AND it can be cured in most.
What’s harder to cure? Unhealthy habits like not eating well and insufficient exercise.
We live in a world where the habits of those with anorexia are given as weight loss tips for those fighting obesity. Science is starting to catch up to the reality that losing weight is a whole lot more than willpower, starvation, and working out until you drop while being ridiculed for “allowing yourself to look like that.” The world is moving on. Maybe you should update your programming before you get left behind.
Fiber. Turn off AC and heater. Toss any pills with side effects. Limit calorie and sucrolose intake. Eat fish daily.
Worry and thinking hard have been shown to be able to burn off a whole Whopper daily, too. The brain uses calories, too.
You’re a bully and you’re embarrassingly wrong and playing doctor all at the same time. Congratulations.
What a s****y comment,”Reality”. I don’t even think you read the article.
Okay, but what causes obesity? It’s simply an excess of fructose from ingesting an over abundance of addictive sugars and carbs. While food scientists have taken full advantage of this in engineering highly processed and hybridized foods. Though unfortunately, dieting and fitness is way more psychological than anything else.
This is the most uneducated comment on here. Your ignorance is astonishing!
>what is fiber
I get the gist of your remark and agree that rationalizing a problem away for someone to save face is common. That said, however, this is a really interesting article that I will be reading more into. I bet there’s a lot of truth to this and probably, hopefully, this research will lead to good, new strategies to help people with real obesity problems. Please don’t dismiss it as just another excuse people with weight problems use, to do nothing at all about their situation.
More like weak people enabling weak people. It’s the liberal way. Like what they do with drug addicts and how they raise weak dysfunctional children.
Gopher Cakes are for everyone, fren. Open wide; stuff your face. There’s always room for moar Gopher Cakes. https://youtu.be/AHmVcYOqGe0
Rather than talk about the nutrition fed to Americans the previous comment or states an obvious fact. We need to spend more of medicines attention on factory, processed and fast foods as the source of much of obesity.
We put corn subsidies in our soda as a sweetener. This is a problem at the federal level.
The article just tells you the why that having too much fat tissue is bad. Adipose tissue loses its ideal function in the body. It is not an excuse to stay that way. As a matter of fact it gives encouragement to lose weight to be healthy. Thank You.
I had a ruptured brain aneurysm and subarachnoid hemorrhage stroke. I was in ICU and rehab for 6 weeks. While I was in ICU they determined I had sleep apnea and they had to add supplemental oxygen. Not only did my brain blow a gasket, my entire body went to a place of its own. I had a seizure, fell off the porch and crushed my wrist. I have developed cysts on my thyroid gland and while they were doing a CT to find the blockage for my PAD, they found another cyst on my kidney. My veins have collapsed. I can’t walk and breath at the same time. I can’t lay down without my BiPap and oxygen concentrator on. I also can’t talk and breath at the same time. I have a PCP, a neurologist, neurosurgeon, vascular surgeon, pulmonologist and eye, nose and throat specialist. I’ve had 3 rounds of rehab and will be having my 6th brain angioplasty. With all this medical assistance why and how did I get 100 pounds overweight and how do I exercise to lose it when I can’t breath? And how can I walk with a large blockage in my femoral artery? They don’t have an answer… diet pills cause fluctuation of the arteries and the last thing they want to mess with are my arteries. And so I eat eggs and I eat salad. I have an occasional piece of baked fish.. about once every 3 months. So far none of the “experts” have any answers.
My grandmother had similar. I suggest getting off any unnecessary medications, intake fiber (metafucil even), and to walk every day. It will not be easy but it will be worth it.
Wrong again “Fren”.
Look into the Gerson Clinic and Gerson therapy. God bless you. You can reclaim your health. Believe.
Fatness still has little/nothing to do with personal choice and please cite articles about “causal” relationships of obesity to disease as the science typically indicates correlation, not the same. This would be a percentage of populations just as many fat people may have risk so do thin people (hint: everyone based on many factors of health like genetics- not just 1 factor of weight.)
Well I see you don’t belong to the sensitive society…..so what are your suggestions for us FAT people?
Fiber, fiber, fiber No AC and limited home heating Daily fish intake Limit calories and even sucralose Brain exercise Daily movement, even driving
And absolutely no antidepressants or birth control of any kind! These do all sorts of damage.
I am so wildly sick the reading medical advice from someone who probably barely graduated high school
Many people can NOT choose not to take birth control or antidepressants. Steroids both inhaled and oral (IM/IV etc as well) also cause weight gain as do antipsychotics. Shall they not take meds either.
Stop sticking your nose where it does not belong.
Reality, did you even read the article?
The bottom line is: lose the fat and gain your life back.
>insert fight club soap joke
No society on earth tracks nutrition and goes to the gym the way this nation does, yet we’re fatter than ever and dying of it. If the adipose tissue is lose its plasticity and function, isn’t it time we look at the chemicals, including vitamin “fortification” that we load into our food? Nobody has the obesity issue we have here.
Nobody else adds HFCS to bread, has free soda refills, waxy Hershey’s chocolate, AC running all day, and doctors getting kickbacks for prescribing all this medication with obesity as a side effect. America is too spoiled and Wall-E was a prophecy.
Gee, where are all the kickbacks? Where do I apply for these kickbacks of which you speak? Because, yeah, no.
But hey, you just keep telling everyone all your outlandish ideas about medicine. Did you get your degree from Trump University or Google U? How embarrassing for you.
What can we do about it?
Turn down the d*mn heater, for one. Activate some of our brown fat in our sleep.
OMG! What are the thin “normal” people gonna do when their perfect bodies give out??!!🤔🤷
Hopefully, by then, we’ll be dead; what will it matter. Until then, we’ll continue to be coveted and feeling great in our clothes. And, why not? We’ve worked hard for it (usually).
So basically the type of fats that are in the food you eat still have an effect on their ability to be useful ?
“Reality” you’re an @sshole.
I hope you continue to study this and figure something out. The article is very interesting. I have dieted much and do much work outs and I never lose much. Thanks
Dump all meds and consume more fiber. It really is that simple.
Superficial article st bedt that totally ignores very complex metabolic processes other than adipose deposition and retention. Loss of function.
Replying to myself. Article ststes that plasticity decreases eith she and therefore does not respond to bidy changes. This totally totally ignores the function of the liver. If you cut caloric intake by 50% for 14 days your liver starts turning fat back into energy for use by your body. Done it.
If reading comprehension is a problem then you should just say so. The article is giving additional reasons why fat is bad 🙄🙄
This was in reply to Reality
I can’t seem to loss weight it won’t come off
To Dan, most people who are fat do not have those kinds of tumors, they are overweight, inactive, and eat terrible food that makes them feel terrible and have no energy. If you really want a narrative that will tell you it’s OK you’re fat, you can’t help it, then no one can convince you otherwise. Why are there not more obese lions and obese woves? Because they eat a species appropriate diet that gives them energy and they burn the calories being active. Obesity has so little to do with genetics it’s ridiculous.
I say try walking in my shoes for 54 years of battling obesity. I was put on a diet at 6 years of age and I will be 60 this year. I have weighed over 650 lbs. I weighed 185 lbs at 13. My thyroid and my metabolism are both messed up dying my whole life and I plateaued at 450 lbs. A year ago I started my current weight journey and I now weigh 176 lbs. I don’t remember weighing this little in my lifetime. I feel like there’s always a monkey on my back trying to get me to 650 again. I have a goal to be 150 and would do anything to get there and stay there. I would be willing to take part in medical trials and or experimental pills. I would try anything to get that monkey off my back. It has never been a lack of willpower but a lifetime of trying not to be fat. Any advice or help would be appreciated. Please help me!
Stop all unnecessary medication. Consume more fiber. Get outside daily.
Dietary fat and carbohydrate (glucose) turned into stored body fat by insulin are two different things.
The jews have been poisoning the goyim for centuries. We put poison in your Wells, threw plague infected bodies into your cities, and now we just feed you processed food filled with industrial waste and artificial estrogen.
We used your worship of “science” to convince you to stop eating meat and eggs and that hydrogenated soy oil was healthier for you than natural butter.
Our word for you means “livestock” for a reason.
Imagine using the comments of a site reporting on advances in science to spew anti-Semitic garbage (and that’s describing your comment EXTREMELY generously). Scientists, engineers, etc. are trying to improve the world, and you just want to regress it to the 40s.
At the end of your life, how will you feel knowing that your only influence in this world was making it worse and that people will remember you around as much as used gum on a sidewalk (and think of you just as negatively)?
How about you do everyone here a favor and preach your lunacy on a street corner instead? Maybe ask some of the gum how it feels while you’re at it.
Soy made me a very sexy femboy. I freaking love science. Between xenoestrogens, soy, and neoteny… the world is becoming a very beautiful place for us femboys.
A willfully ignorant society is judgemental and tends not to look at what science can tell us. Instead they look at correlation and confuse that with causation which allows for victim blaming rather than working on reasonable solutions which are effective at treating the issue.
Eat fiber alongside quick carbs. Turn off the heater and AC. Watch you calorie intake. Stop all medications with obesity as a side effect. Obesity solved.
That seems like a non sequitur considering the evidence from this study would imply you can do something by about it.
>sleeping in the cold doesnt burn calories and activate brown fat simultaneously
who cares either way if people are fat? if they die from it, they’re the ones dying, not me. i can’t understand interfering with someone else’s life like that. maybe people who care this much need to feel a sense of control over others because they have no sense of control over themselves.
>t. based libertarian.
What does the overall well-being of the society I live in even matter bro? Ho-lee, give your head a shake bud.
Nice! Now if we can figure out the best method to get adipose tissue to *regain* function we’ll be able to help people. So many people struggle with maintaining their weight dispute diet and exercise, while others don’t seem able to gain any at all.
Brown fat activates when you turn off your heater. It helps save energy, too. Win-win.
This is common sense, not a scientific discovery.
People did not want to be Fat.
Yeah because fat people feel SO good about themselves already 🙄
There’s always someone to turn a scientific finding into an excuse for a political speech, in the foregoing example to condemn a “sensitive society.” Yes, those with unhealthy overweight should know of consequences, but much of the concern with minor deviations from that “ideal” weight is itself unhealthy.
America has men chasing other men the women have become so obese. This is hardly a minor deviation.
Im deveely detaerted
I look forward to my body finally shutting down.
Told my Dr this 25 years ago ! He says you need to loose weight you might feel better if you do ! I have arthritis in everything, all my joints swell up ! and ive got spores sticking out of and into my spine my vertebrate are splintered ive got bad spondolosis that feels like somebodys stabbing me in the spine 24/7 and when i exercise if i move the wrong way it knocks the air out of me ! Ive got shadows on my lungs and it looks like i might have half to 3/4 of a good lung left ! You want me to exercise so i might feel better ! Now 25 years later i dieted and exercised down to the weight he wanted me at ! Im in even worse pain cause im older !im In pain 24/7 cause i might get addicted to pain meds ! News flash im gonna die no matter what ! Most of my friends are dead cause they bought fetanyl pain pills cause they were also in pain 24/7 you would rather they buy fake pain meds that ended up killing them so it makes more sense to force me to go get fetanyl on the streets cause thats what most fake pain pills are now days than to allow me to live a pain free managable life ! Somebody checked their brains at the desk when they got accepted into college and it wasn’t me ! You are all fueling the cartels illegal drug trade and shipping pallets of money to China the world’s 1 producer of fetanyl because your government masters would rather you kill off your patients with fetanyl pills than prescribe them pills of known value and known origins ! That is exactly what you are doing ! You are killing americans to make mexican cartels and chineese labs billions ! You doctors are killing americans by refusing to prescribe opioids and the fda and dea are killing even more by waging war they will never win ! Legalize it all or face 90% of the USA dying from fetanyl ! That is in fact what will happen because at some point in a person’s life if they work a job which entails any real work they will at one point get injured its inevitable you cannot stop it ! My wife worked in the medical field she got flesh eating virus during a surgery she was doing ! It destroyed her kidneys so now she needs a transplant nobody cares shes in pain 24/7 we both gave our lives to saving others now we are trash because we are no longer tax payers ! With obesity the problem isn’t excess fat ! It’s immobility because we move for more than 10 minutes we are in pain and cannot do anymore fools ! I take illegal pain meds wham I loose all that weight like a bodybuilder going from 18 to 22inch biceps in 8 months cause hes spot injecting steroids ! Drugs exist for a reason ! Because they work ! Stop killing people by forcing them to buy fetanyl off the street !
Definitely based.
As my belly gets bigger and bigger, I just tell people, “Like the mighty camel, I’m just storing up fat for that LONG walk across the desert.”
It’s fun to watch all the anorexics come out of the woodwork and flex.
I have fought weight gain for over 40 years. I have been on every diet trend, worked 60+ hours a week at a physical demanding job (not a desk job) I was an industrial machine mechanic and spent 10-12 hours a day walking and on my feet. During this time I was on a low fat, low carb, high protein and sugar free meal plan. I also had a home gym (bowflex) that I used every night 7 nights a week. I lost 15 pounds over a 5 year period. I have been in construction and manual labor 95% of my life and regardless of the activity I could never keep my weight down. I have been told I have thyroid issues but medication would be unsafe due to the fact my thyroid enzymes fluctuate to severe highs and lows. I hate people who think it is about over eating and have no idea. I was on dietician recommend meal plans and activity recommendations on top of working 2 jobs and still retained weight. Stop assuming all people are gluttonous pigs and understand some seriously just have to starve and literally put their lives at risk just to lose weight. I pray they can find a medical reason and reverse it for the sake of those who have issues losing weight (not talking about the creepy people who call themselves FEEDERS for perverted sexual pleasure which is disturbing and disgusting).
Brown fat is why children don’t gain weight. Fiber in soda and banning air conditioning would solve the obesity epidemic instantly.
A lot of people use food to feel good because eating is an activity after all, but what you choose to eat is critical. Either we eat simple sugars that may appeal to us for a minute or we eat something more healthy that will actually make us feel better for hours. As far as exercise goes we need to do things but it can be so many different things. Life is short so we should enjoy whatever it is. I don’t like grinding at the gym. A walk in the park seems much more appealing to me nowadays!
Overall reality is that people who are overweight – especially obese that by simply eating properly & exercise regularly will in the VAST MAJORITY OF CASES will loose weight – quickly – there are rare exceptions & should NOT be considered unless a person has been supervised in diet & activity for at least 30 days with no loss of weight – otherwise in over 98.99% of the cases weight loss always occured with proper diet & activity.
There’s some people on here that don’t like the hard truth. And that its not healthy and a major risk to be fat. Yes genetics play a role in it. Im much more easily addicted to substances than my paternal cousin. So in our lives I had to grapple with and finally fight and win against addiction. While he and I did the same amount of experimentation, nothing seemed to grab him. These people need to understand that the fattest person in the world 100 years ago weighed like 400 lbs. We have like five 400+ pounders at my work alone. Yes our modern society doesn’t play to genetic weakness like substance abuse and weight gain susceptibility. But yelling at people telling you the hard truth that “in this specific battle you are gonna have to try harder than some others or else you will fail” will not help you. I witnessed my uncle die from a life of lethargy, bad eating and major weight issues. And it was the longest most brutal 3 months of blood clots and comas that I ever have seen a family member go through. He was 63
Kris E, you are my hero!! Rock on! I am so proud of you. I have never been at a constant weight my entire life. I am a diet professional – which means, I can take it off, but can’t keep it off. The news flash for everyone here is that, we are all going to die. Tall, short, young, old, black and white. I have known healthy people that drink plenty of water and are physically active, yet die from cancer. Your body is in control – NOT you. You can not prevent or stop cancer, dementia, strokes, and a host of other disease. The Dr’s will tell you – just like with Covid 19 – “we do not have all the answers” Anyone can find themselves havibg to take steroids for a medical condition and start blowing up like a ballon. Take care that you show compassion, as weight, may have never beem your battle. No matter what state you are in enjoy life – you are going to die – that is a fact.
A bigot for being real? Dan, let me help you get your head out of your ass.. Bleeding hearts like you encourage an unnatural way of life and you justify your “logic” by scrutinizing those of us who point you out. You say it’s “fat shaming”, I say it’s reality. Fat people need to make healthier choices and stop making excuses.
I think this info. may help someone someday. Research is good. Keep up the good work!
Getting molested and eating/drinking one’s feelings away is also a good way to get fat. Find a good listener. And your own conception of a God.
Before ‘discussing’ this article, or any other, some of you may want to think about why you are so hostile. Articulating your opinion while demeaning others demonstrates a lack of emotional intelligence and maturity. Are you this unpleasant face to face, or are you simply feeling powerful in your anonymity? In other words, see if you can converse with other humans without being such an @sshole.
So Dan is a whiny fat bastard himself huh? Don’t blame your genetics bro, get off your ass or put down the potato chips. Not that hard.
Don’t diet change your diet
https://youtu.be/LWcsT1RDpSY
Obesity is a result of a lack of willpower.
Here is an easy road map:
1. 25-50% calorie deficit indefinitely 2. Enable thermogenesis (caffeine-no sugar, green tea, certain peppers, etc) 3. Walk (elevation is a plus) for 30-60 mins daily 4.Drink WATER, no more sugar, if you must drink juice, dilute with water 3. Eat lean meat (chicken, turkey, fish) 5. Boost your metabolism: eat fiber, coffee, flaxseeds, lentils, GINGER
No Larry your path is ridiculous you are asking people to suddenly be able to deprive themselves it never last.
Instead just encourage people to add avocados and spinach or Kale to their diet and increase their protein and fiber intake. Adding these things will eventually crowd out their urges.
There are now protein chips, protein donuts, and fiber based oatmeal raisin cookies. Eat as much as you want and eventually the fiber intake, protein, and healthy fat in take just shuts down your other urges
Reality is a arrogant prick. God complex.
Seems like people claim calories like they claim tips. They say they haven’t eaten all day. Didn’t count the 44oz soda twice, the candy bar. You have to burn more than you consume.
First and foremost aging is a process where our body is incapable of burning the amount of energy we use as we were younger. We have different metabolism rate as we grow older. Hormonal changes in our body have a lot to do with weight gain and weight loss. Don’t forget about the stress of life changing in health and disease. I went through chemo treatment for two years and gained 40 lb from the steroids they have put my body through. The destruction of chemotherapy destroyed my entire body, physically,mentally and emotionally.
I have known people who were overweight, I have seen them eat large quantities of food, two, maybe three times what”normal” people eat. I know why they are fat. I eat normally, same meal for breakfast everyone else eats, salads as a meal, avoid sodas for the most part, skip the fries most of the time. I eat fruit often, nothing to axcess, semi low carb. I don’t eat sweets and dessert often. I am still overweight and nothing seems to affect it. I have no mobility issues and am fully functional. I excercise some, need to do more, but nothing seems to work. In many People’s cases, there is more going on then we understand yet
Americans will come up with any excuse to avoid responsibility for their actions. Obesity is caused by over consumption of food that is why bariatric surgery works.
I don’t see why the cause matters; doing your best to management weight is key. We’re all born into some undesirable trait, but that doesn’t preclude us (or someone else, in instances where one is incompetent) from seeking help and USING it. The word “shame” should be banned. …unless it’s only used to describe capable folks who fail to help themselves.
Actually all the people claiming this is body shaming or that if you are obese it’s just generic and there is nothing you can do about it is so ridiculous.
Anybody on the planet who decides to do the following:
#1 Everday eat more avocados, spinach or kale even if it’s a smoothie
#2 Increase protein intake
#3 5,000-10,000 steps a day
#4 Walk 5,000-10,000 steps
#5 Lower white carb intake
Will lose weight. The spinach and avocado combination causes your brain to fill fuller and it changes your urges over the long term.
Try this and tell me you don’t lose weight and this is even if you continue to eat cheeseburgers and sugar.
Because over time your sugar urges will reduce.
You don’t always have to try to starve yourself you can just add healthier foods. So when it actually is this simple and someone declines to do it then there shouldn’t be such a high level of acceptance.
If you haven’t tried these things then don’t lecture me. Instead try it for 30 days and then tell me it doesn’t work. Except that wont be possible
Lol Dan. What a clown you are. My guess is your wife and daughter are disgusting fat bodies.
Let’s face it, we allow companies to put every chemical known to man in our food. It’s dangerous and often poisonous to some degree yet we still consume it. Coke is a prime example it will eat the paint off of a car but we’re more than happy to drink it by the truck loads and you think that that’s not going to do something to you? Don’t get me wrong I’m as guilty as the next guy of eating all the things with all these chemicals but it does stand to reason that that is going to change how your body functions and destroy a good piece of the mechanisms that make it work properly. So logically anyone with half a brain can see this is the real cause for obesity. Everything is a chain reaction and your body is no different.
Body shaming is wrong. Obesity is usually a medical problem. No history in my family of obesity. My daughter is obese first gastroenterologist told me to starve her. I didn’t agree so brought her to Boston Children’s. She has an auto immune disease (celiac), took her off gluten she lost weight. She was malnourished cause her body couldn’t absorb nutrients. Wasn’t an over eating problem. Maybe educate yourself before judging. A little kindness goes a long way.
Hello… If you all are still taking the advice of a conventional doctor, AMA, and the FDA. You all are suffering because of greed.
I guarantee you ALL are suffering from LEAKY GUT. FOOD INTOLERANCES. MOLD, HEAVY METAL TOXICITY, YEAST are possibilities.
MTHFR…serious
EPIGENETICS… you can not change your DNA. YOU can change your genetic path.
I wish I could speak with all of you. I have experiences that would help.
Research. Feel better🌻
Everyone needs a “Fren”! Fren’s delivery is brutal AF, but who’d not get off their arse and make changes with Fren as a Life Coach? …and, nothing Fren said is wrong. Who was born obese? I’ll wait.
Wow this comment section is a dumpster fire. All they did was report on an interesting study and y’all be making it so personal and political. We all have better things to do.
I have pcwest polycystic ovarian syndrome and it’s hard for person like me to lose weight but unfortunately I had thyroid surgery 10 years ago and I went from 235 lb woman down to under a hundred my diabetes is under control but I still have high cholesterol hypertension and all that other stuff even though I followed the books and rules and I can’t digest food anymore because missing my thyroid glands they proved that with many tests so it doesn’t matter if you’re fat you appreciate that person for who they are they might not can help being fat there is nothing wrong with that as long as they’re healthy and even you skinny b****** that are healthy can’t have underlying conditions so just don’t blame fat people for all we’re lazy where this word at because we’re not we’re wonderful people so stop judging us until you know what’s wrong with us stop putting labels on our asses thank you
It doesn’t matter if you’re skinny or overweight. What matters is if you’re healthy. There are skinny people that are unhealthy and there are obese people that are very healthy and vice versa. We need to quit having this perfect mold of what “normal” is.
And to the prior poster, FYI some babies are born obese. Babies that are more than 8 lb 13 Oz are considered large or obese. That is about 10% of the babies that are born today.
Obesity is a choice, most you people just need to stop being whiny p*ssies I went from 160 lb to 260, because I stopped exercising and increased what I was eating, now that I’m 40 years old I have to fast all day long and only eat once a day so that I can stay around 200 lb otherwise I will blow up to 300 obesity is a choice I do not starve myself billions of people have done day fasting for thousands of years and this is actually a proven practice to defeat obesity so if you don’t even want to try there’s a plenty ways out there to try so just shove it up your butt
PSR suggests pesticides and plastics and other poisons especially when in the womb and first few years life. I like their fact sheets that mention things like dryer sheets, “cleaning” products, popcorn bags, shampoos, HF corn syrup, and tobacco.
Fren, Are you saying shame is a motivator? Prisons are full of repeat offenders. Presidents? Seriously? Other countries? Again, seriously? Shame just makes someone feel bad or get defensive. Doesn’t change behavior.
And I also have to say that as of 150 years ago there was no such thing as obesity obesity is a brand new thing in society so therefore is completely controllable you never heard of it in ancient times you don’t hear of it in the Bible going Jesus walk by a fat guy and made him skinny because there was no fat people you need to get this straight it is a new age problem it is a problem and it is completely controllable these are facts
In Chinese medicine, this s nothing new and was well documented thousands years ago.
A decline in general health leads to improper weight. Especially digestive and respiratory health.
Modern diet and lifestyles just help exacerbate this phenomenon.
Living in a society where money is the only thing that matters is shameful. The reason for belly fat is processed foods and throwing sugar in our face. We are a busy society and the media knows it stuffing junk in all our foods causing us to have health problems later. Where’s the healthy food? Media doesn’t care. They just want your money honey. That’s it!
Dear fren The the only advice you did not give is grow your own food and raise your own meat so you know how it was processed .
This article is very informative. Fat shaming to me is putting someone down that is obese, by calling the fatso, big, etc. Explaining what causes obesity is not. Explaining how bad it gets when we get older is not. We live in the most sensitive era of human beings that I’ve seen in my 46 years here on earth. Stop acting like yal don’t know that politicians get kickbacks for allowing these chemicals in our food. They do it to make food last longer on the shelves so they make more money. Then we get sick so big Pharma now gets paid. It’s all about money! The greed levels are at an all time high. If people stop buying foods with 40 ingredients their health will get better. In families with lower income they buy the crap that is full of junk because the price is right for their budget. Go to Walmart, then go to Jewel, Marianos, or Whole Foods. Totally different products. Walmart carries the crap at a low price while the other stores sell high quality food. I am overweight myself and have learned this info through experience. Now that I read labels and don’t eat at McDonald’s and other fast food restaurants my health is better. My fatty tissue in my liver isn’t increasing. I hope scientists continue to enlighten me and others on the dangers of obesity. As society will have you canceling everybody that speaks truth.
The article and many others is merely to share and show research and discoveries related to obesity. Body weight/size is not a measure of beauty or worth. It is a matter of health. As a person who was 320, now 150, I can attest to the damage it does to the body, both mechanically and physiologically ….until we approach people about health, eliminating all statements referring to any other aspects we will not help others to change. Learning food is fuel, bodies need certain nutrients and in certain balance, is the 1st step. Remember change is hard, will be and should be gradually or you burn out and say screw it
Recognizing and addressing health concerns is not shaming.
People who fixate on anti-shaming narratives tend to frequently disparage those with whom they disagree while failing to define the contours of the shame they allege they or someone else suffered.
People hold preferences to establish direction in life. Parents who prefer their children to enjoy the most physical potential from their young bodies avoid dietary approaches that contribute to obesity. That is not shaming, nor is it shaming to hold that aspiration for one’s progeny.
Thank you for this information. I want to learn the science of how my body works. If there is information that I don’t understand or question, I don’t look at it as shaming
Always a reason… Calories in vs out It’s that simple Stop stuffing the pie hole
The facts: At least 2.8 million people each year die as a result of being overweight or obese.
Obesity is definitely a concern. It is not like most obese people want to be obese. What is needed is a solution not gimics that don’t work and fad diets that get little to no results. I see so many different diet plans out there and tons “miracle pills”. All they do is rip people off. So many have been tried by people who spent their hard earned money only to be scammed. Those need to be stopped. We all know moderation eating and exercise are important but for some that just isn’t enough. We all know that one person who can eat and eat and never gain. There needs to be a real solution with real results that is affordable for everyone. This country allows big pharma to control who can get the help they need and who can’t. I know people who have struggled with their weight all their lives and were never able to lose enough to be considered non obese. Only narrow minded people believe it is due to a lack of self control.
Being fat or obese is extremely unhealthy. Now please tell me how I shamed someone by stating obvious fact you prick.
It’s about common sense , eat a balanced healthy meals and exercise. If you get way overweight that’s on you. You are in control of your body !!!
Since when did shaming help anything? Do you think our criminal shaming has worked? How’s the churches doing with their attendance? Bringing people to the alters in masses because shaming is so succesful? Ludicrous!
Obesity has a myriad of causes and complications…not the least of which is a dopamine deficiency that is rampant. More science, less BS…
I like this article. Some of these comments I could do without.
I believe more people started becoming obese with the over processed fake foods in the ’80s. High fructose corn syrup. It’s in everything. You put the wrong kind of fuel in a car and it will break down. The lack of exercise is another and lastly the lack of sleep. I’m not well versed but I think it is a simple fix but would be a costly one. Just think how empty a grocery store would be if you took all the non nutrient foods off the shelves.
Thank you. To all the nasty posts…I am someone who eats right, exercises everyday and can’t lost weight no matter what I do. I also now have severe inflammatory diseases that have impacted me even more so I can’t exercise as much as I would like..so this makes sense. Science will show the truth. Our society is the way it is because of closed minded bitter people.
Based on most of the comments, a lot of people must think the laws of thermodynamics are nonsense
What you all neglected to mention: American people have been poisoned by Elites who GMO our food(not allowed in other Countries) and our water has poison in it,waste items like floride😳and we’re given vaccines practically from birth which contain poison (flu shots alone contain horrific heavy metals)Every other commercial is on drug brought to U.S. by big PHARMA.. They’re killing us..pay better ATTENTION 🎉
I’m sure some will call this fat shaming. I mean an extra couple hundred pounds can’t really be unhealthy can it??
Hey “The Truth”, you’re wearing a MAGA aren’t you? I can tell by the judging you do to people you know nothing about. typical redneck, ignorant republican bulls****. If you and Trump are so smart, why has it taken more than a year to realize you lost the election in 2020. Go back to your hole in the woods and reflect on why you’ll believe that Fox News is an actual news outlet.
Reality, You need to look up fecal transplants. When a slender persons stool transplanted into an obese person’s colon, they lose weight. And when a slender person has the same transplant from an obese person they gain weight. This is about the microbiome.
News flash- Skinny people die too. May wanna eat a few donuts. The sugar may make you happy and less of a nosey, it’s none of your business what strangers do- whole. Enjoy your inevitable death. I’m so glad I’m fat so I can annoy you with my disgusting ways!
Fat is nothing new. Fat people, again, nothing new. If the scientific community would spend as much time and energy on solutions for ending cancer as they do on obesity and erectile dysfunction, maybe – just MAYBE – cancer could be eradicated. Seems reasonable to me.
I saw no shaming in this article only facts telling you too much fat on your body amplifies and causes a cascade of other unwanted ailments. I have been there and it took effort and will to change it but I feel so much better physically now.
Thank you Dan
To all the people that say treating obese people critically is fat-shaming because some people “can’t help it”, I say total bullsh@$. It is a math problem, consume more calories than you burn and you gain weight. Every body uses fuel in the same order… glucose then fat then protein and finally itself. It’s like a campfire. I can put nice dry logs in the fire ring, douse them with gasoline and light it. I’ll get a huge blaze and when the gasoline is consumed the fire goes out with the logs almost untouched. The gasoline is glucose and the logs are protein in that example. If I put dry logs, kindling, paper and gasoline, the gas will catch the kindling and paper which will then catch the logs. Kindling and paper joining this example as fats. So if you have sufficient glucose from eating the wrong foods to meet the fuel needs of your body, you’ll never burn fat and the proteins will also be untouched… and you get fat
Hey Fren What is brown fat?
Shop in produce and meat department at grocery store and get off of medication that only mask the problem.Also excercise and get off of social media
Thanks reality. I Lol’ed at the fat guy who called you a “body shaming bigot.”
Stop eating so much. It’s disgusting
Damn, anything about health really brings out the nutty people. Why do they let people comment under these things? Nothing of value is ever said.
None of these comments have much to do with the article. If what it said is true, carrying excess weight in middle age and beyond wouldn’t necessarily mean a death sentence if the fat cells can, be means of medicine, be returned to the way they were. I hope I’m understanding this correctly. It could be a game changer. Weightloss is great too but no one deserves to die from obesity.
Hey Fren, there are 3 basic body types. All of which are predicted by genetics. GENETICS!!! Can shame change someone genetics make up? I can eat 500 calories a day and stay the exact same weight. My grandmother’s brothers were 6’5 and up. Close to 300 lbs of solid muscle. My genetics come from their mother mostly. She was 5’10 200 lb. Not a fat woman and not a slim woman. I am 5’9 and have always struggled with my weight. My mother’s side of the family have very very plump short women. I got the best of both I guess. I have two sons and my oldest has always been 99th percentile for height and weight his whole life. He was over 10 lb as a baby. Straight out the hospital and a size 2. Not even 14 yet and 6 ft 1 and 215.lb. His father is 175 and 5’9. Can you tell who’s genetics have played a major role in his body type? Both he and I have 22 inch calves. All muscle. We both also have horrible knee problems and vericose veins along with circulatory problems. Neither one of us can run to save our lives. All from dad’s mom’s mom side of the family. Since childhood. It’s predetermined from the day you’re born and if you think any different you’re just clueless to human geneology. I of course got bullied and so does my kid for something neither one of us can control. The worst thing is watching my son have to go through the same thing that I did with family and friends who don’t understand scientific facts either. Please do yourself and society a favor and educate yourself. It’s ignorant bullies like you who never bother to look at the facts. Ignoring facts causes 99% of the problems in this world. Change. Be a better person.
When in doubt blame genetics. Check.
Know 2 fat people who blame it on insulin resistant but been around these folks THEY EAT too much and too often. And do not exercise.
Ok,so with all that explained. How does a person that has these issues fix them with fixing the gut first? We are in 2022 I think we need to figure what foods can help fixing these diseases instead of putting a blanket over the real issue by pumping one with pills after pills after pills, many many years ago what one could plant that’s what they ate and the animals were not eating food with chemicals and people and animals lived much longer, why? Because the ate the foods God intended for us too eat. Our bodies are not designed for us to only fix our bodies with pills alone the biggest factor is nutrition. What we are eating is killing us little by little …Our bodies are a machine that needs to keep feeding our stem cells,our vessels, and our organs then all things along with meds if need be, our bodies work properly……Nutrition needs to be taught way more in medical school then 4 months. You know thr old saying you are what you eat.
Have you ever met a fat person that runs marathons? Don’t think so. Genetics. Lol.
For 99 percent of people who follow a healthy lifestyle and exercise this isn’t a problem. Our American lifestyle is. We eat to many processed foods and spend to much time behind the computer or TV.
Fern is a bit. Eat more fiber indeed machine, god speed.
Here’s my unbiased opinion…kiss my entire fat ass! I am 50 you skinny hungry bastards need to eat real food and stop smoking that CBD OIL. At no point in my FAT LIFE did you ever consider my weight to be a necessary evil? Hell no…you compare pencil thin people to fat people and then have the audacity to say we’re the ones with a problem? You’re a jealous dumbass! Now wake up and go eat.
I would like to see regulations on some of the garbage that is added to foods that we buy. Why to we need tons of sugars added to foods. Why, so we become addicted and buy more of the same. There is just not one answer to this problem, it is multi level. To much screen time on phones, computers,TV, fast foods etc. Internet as great as it is has been our downfall. Greed has been our downfall. This has all contributed to weight gain. And so much more. And yes there are some genetics involved and diseases. Unless people are willing to cook meals with little processed food this issue is not going away. Remember decades ago it was homecooked meals of meat, vegetables and potatoes or what ever filler was served. Soda was a treat once in awhile. I could go on and on.
I was always fit & active, till I settled down and got married. My wife is an excellent cook, and I got lazy… 250 lbs lazy. I had never dieted before, so I read lots about it. I’m not smart, but it occurred to me that if our ancestors from the distant past stayed trim, I should only eat what they ate. So, I stopped eating white foods (potatoes, pasta, rice, sugar, breads) and just ate fatty meats, cheese, butter, nuts, seeds, salad greens, eggs, coffee, coconut oil & fat, MCT oil, avocados, Brussels sprouts, and all berries (straw’, blue’, ras’.) I stopped shopping in “the aisles” and only shopped “the outside edges” of the grocery store. Turns out, without knowing it I was on a peculiar diet they call, “low carb,” or “Atkinson,” or “keto,” or something else (that I can’t remember.)
Anyway, I lost 75 lbs in a year. My friend says it’s because I’ve been eating like a big ape, lol. Maybe he’s right, I don’t know. When asked casually about looking trim again, I just answer, “I cut out white foods, mainly sugars in anything, pasta & bread.)
YER FAT !!!🤣
Time restrictive eating and intermittent fasting every other day helps restore the functionality because people who do this have increased insensitivity and better functioning fat cells
Supertoilet, Have your daughters been checked for Polycystic Ovary Syndrome? You may want to read about it, or ask your daughters doctor This may give you some answers. I see where your daughter is taking Metformin, and that’s what is often prescribed for PCOS. I hope you will you will find this helpful.
Would you goofs stop complaining in the comments about things entirely irrelevant to the article? None of this shame stuff (pro or con) is pertinent to the studies mentioned or the article about them.
I have been up and down the scale due to medical issues and this article pin points the fact that fat can make your body weak ,it is very True for myself when your muscles or lack of muscles are weak you can not move as well or as safe it allows for movement in joints that shouldn’t happen ,so ending up on high end of the scale im weaker and tired more Have more scrapes , when im lower on the scale it is easier to move about but I still have to exercise to build back muscle that helps tendons to keep things in place and moving well this adding the flexibility we need to move well. To those who have trouble due to medical conditions and want to improve ,my approach is one step at a time each day one more step Then add on and on and soon who knows where you’ll be .set your own goals wish all the best
Dan, doth protest too much. Eat better and get some exercise. This is the new progressive ideaology: fat is good, fit is bad, cops are bad, and people are born victims or aggressors purely based off biology. Pretty weak and ignorant.
This is a great conversation with many good points. Is it possible to carry on while loving the person who opposes your opinion?
As a fat person, let me say that every doctor i see tell me im fat first thing when talking to me. I ask every one of them to help me with my weight BUT NONE of them will.
But society shames smokers, drinkers, etc in the name of health. Being overweight is very unhealthy, so eat less move more. Maybe try intermittent fasting or keto, worked for me.
There’s a difference between having no solution and just not liking/choosing to implement the solution. Noone is meant to be overweight, it’s a direct result of our diet/ eating patterns
Reality…no one hates my fat as much as I do. It has made my life miserable. I assume you have no excess pounds & I’m happy for you. In today’s judgmental society you fit in! But don’t forget you may drop dead at any moment or you may have a stroke or heart attack & be damaged for the rest of your life.
Can’t we all love one another and have a friendly debate? I can tell some of you are on social media 22 hours a day.
My dad use to say, “All you have to do is watch the History Channel.” to learn how to get skinny. Whenever a POW camp was liberated by Allied Forces in WWll, every prisoner was super thin. That was because they worked them hard, and feed them little. A lot of fat people will argue but it’s true.
Obesity is a societal problem. Fast food on every corner. TONS OF COMMERCIALS advertising unhealthy food,limited exercise opportunities, poor health care. NO emphasis on healthy food and drink.
Can we all agree that any food sold on any shelve is ran through the FDA system? Yeah , most of it is. Y’all need to snap out of it, IT’S CALLED SUGAR! SUGAR IS THE PARASITE THAT THRIVES ON OUR IMMUNE SYSTEM. IT MULTIPLIES THE MOMENT IT REACHES THE BACTERIA.,
So why don’t you all mind your own business. Leave people be! Who even cares what your opinions are, I don’t Cheers
To those with a transgenerational obesity problem.. fats kids are 100% your fault no matter which way you look at it. Knowing you have a higher genetic component to put on and store fat but never decided to eat real food, shame. Diets don’t work, healthy lifestyles do. Learn the difference.
It’s an allergic reaction to whatever additives they put in food nowadays. I’m a decent weight female but I have to work nonstop at it. I’m literally eating nothing but triscuits that taste like hay and drinking nothing but water through the week. I don’t lose weight but don’t gain any either. Maintaining a decent weight is expensive,time consuming and just plain hard. Some times after a bad day I just want a twinkie but that’s an extra ten minutes to my workout routine. I ate the damn frosting off a cupcake once and gained three pounds overnight from it!! If it not food allergy that caused it then I sure want to know what it was!!
🙋♀️ I have been overweight since I was born I lost weight was on yo-yo diets took diet pills anything to try to keep my weight down. 21 I had a set of twins I got back on the diet pills I lost the weight I stayed thin until 10 years later when I had my last child. I had C-sections and I have had other surgeries but I have noticed but then the last 10 years of my life I do not move as much, I do not go as much, this fat does not move at all it stays right in the front and Lord I pray for all of us because it’s hard give us the courage Amen ❤️🙏🙋♀️💯
Stop ! Obese people do not want to be obese from my experience. There are underlying legitimate reasons why people gain weight – medical, emotional, mental, environmental etc. What I do know is that gaining weight has had detrimental effects on my physical, emotional, and mental wellbeing. I did not cause all that led to my weight gain but Im responsible for my weight loss and how I treat people in my life. Stop the hate , people all have to deal with life problems. I plan to get strong to help myself and others.
Cant we all just agree that its the gov and SUGAR manufacturers that is to blame for all of this everybody is so caught up in my side is right and your side is wrong nobody is looking at who put us as people on the mutha f×^kin board wake up
So instead of telling facts as that obesity kills in many ways such as diabetes, heart problems, ect.ect. We say or do nothing because it’s shaming ? I have watched a dear friend for 30 yes Kill herself by eating and drinking tons of soda, oh but it’s diet soda. Ya ok. I’ve watched her be sick her entire life and reject help from all of us whom love her . When you care about your friends, family, society, you tell the truth . Your heart cannot take that kind of abuse , fluid forms , always. And carrying that weight is devastating. It kills many people everyday. So we just sit silent Because we are accused of FAT SHAMING ? Think of the children and how it’s a fact The younger you are The easier it is to lose weight and be in shape . Get these kids off the computers and get outside and run and play as we use to do .sports helps kids and exercising is the best for anyone . So no one is shaming They are concerned about people’s health And this growing concern we see . Be there and help people or at least try .Instead of enabling them due to Hurt feelings .. What happens when the Dr tells you the truth ? My friend changed drs as she was mad .. How sad …
Not everyone who opens this is a brainiac…Speak English
People who make fun of some one for their appearance are scandalous but it is importtto keep your weight good health is important always inform or be truthful with friends or family members about their weight. And people who lie about that are evil.
Judge not lest you be judged….You don’t have to agree,you have a right to your own opinion,just don’t expect others to agree,but be respectful.I know first hand what it’s like to feel like your body has been highjacked, and no matter what you do to get that termer body back you hit a brick wall. In 2007 I came down with Lyme disease and did not catch it in time and through the years it took control of my whole body and has moved from one organ to another and has effected my whole being, I’ve tried everything I can search to get me back,My metabolism is shot,but I’m working to get it built back up, I’ve watched my fat in take and cooked on the healthy side, yet my insulin just increases its at the point now that I have insulin resistant, and with that push my cholesterol up in to the 300s putting me 80 lbs. Over weight, So it’s not coming from over eating, it’s a condition that I need help with because all I’ve done to help myself just it’s working, If someone can, I’m so in please contact me at [email protected]
1 pound of fat = about 3500 calories ingested and not burned off. Count calories, make adjustments, and monitor results. It is much easier to watch what you eat than try to burn off the calories or make excuses.
Well i went from 290 to 210 by walking an i stop sugar hit my a1c frist year out i dont drink pop only water an a little milk in cearal you give up the sh*t food you can loss it its in you to do it just do it you will see everything eles is bull sh*t do what it take just will power stop eating crap
Those who believe in fat shaming, are the same ones that personally don’t like only skinny people. They are the ones that say “fat people have no right to be seen at the beach”. And similar insults. They don’t really care about the health of those they enjoy shaming. It’s just an excuse. They used to shame women for having sex outside of wedlock and for having abortions. Now they promote it, saying “shout your abortion”. They used to shame people for not getting a job. Now “the great resignation” is promoted as virtuous. Whatever is politically correct is what is promoted. Whatever isn’t is what is shamed. It’s about politics, not health
If you don’t want to be shamed don’t be grossly overweight. And you know what I mean as there are plenty of fat people not getting shamed. I’m talking wearing big athletic shorts in 20 degree temps because you’re too big for pants or your behind hadn’t seen denim or a no stretch material since your youth.
Wow your religion teaches you better you should be ashamed!Judgment will come to you remember one day! Body shaming is no different than racism. You should know that being your culture. I feel sorry for you!
Seems to me comments in reference to this article should be encouraging and helpful. Not a battle ground for opinions on fat people skinny people etc. Adult discussion about the article and helpful ideas would be great.
So I have eaten actually the same thing my BF ate for a whole 2 months and he lost weight and I did not. So you can’t say to eat fiber and cut out sugar. People are made differently. Female and Man are not equal women are scientific proven to carry more fat (aka to carry a baby ect). So don’t you think that Genes also play a part. Those people that say eat less and body shame I bet are white 20-30 year old men/women that Daddy paid for everything for them because they can’t take a sh*t by himself….if they had to survive by by themselves they would just die because Daddy did everything for them got them a job and everything…karma is a b*tch remember that
Obesity is caused by eating more calories than you burn for a prolonged period of time. Yes we can cherry pick infrequent cases where someone has awful genetics but the majority of overweight and obese people just eat too much among other bad habits. It’s not body shaming to call a fat person fat.
Are people really arguing over fat people? Some people can’t help their mass x gravity = bulldozer. Science has proven that chicken + flour + grease = bulldozerass. There is nothing genetic about poor diet decisions or lack of exercise which is the main cause of fat bodies in the US.
If you notice, the same overweight person is in the comments on every thread justifying the over-intake of calories on a daily basis. Don’t blame corporations or anyone else, the fact is we choose what we eat.
If you choose better you’ll feel better, making excuses will keep you in your current belt size.
Just quit being a fat f**k!!!….try a salad for God sakes!!….its not that hard!!
lol so in other words being fat is still bad. All this article is doing is dancing around this established fact while drawing the same conclusion. Fatties are unhealthy.
Maybe if you stopped eating like a pig and exercised (not walked for 30 mins once every 2 days) you would actually lose some weight? The only “genetic” factor in an obese family is the passed down stupidity from parent to child and lack of self respect to allow one’s self to live past 50 and be able to tie their own shoelaces.
And surprise its a loss of function due to fat
I think your write up here left out one very important role that fat cells also play in our physiology. That being their role in cell division which is something I think that people should have some consideration of when they think about what it is to provide yourself with a well balanced diet. And is likely to have a significant part in why you will sometimes hear the phrase “healthy fats”??
When your born into a family who are already overweight, have Thyroid,diabetes, and heart disease, the battles and genetics are real! Now I’m not saying this is an excuse for being fat but when you’ve tried everything under the sun, including several dieticians that say eat this, not that, you get so many mixed emotions when it’s all different information. Everything from pills to powders, exercise and gyms feed off this! It drives a person stir crazy. I wish instead of logistics, genetical info, and money hungry lions taking advantage, someone would say they specialize in caring about making “you” healthy and loosing weight along the way would be a better approach. So do you see counselors, trainers, dr”s, dieticians and Endocrinologists? Yup, done it all! Guess what, I’m a overweight, happy. Fat cat!! And still engage and be and engage into society. I have 2 degrees, substitute teach and a caregiver to many! Good luck to all on your journey.
After reading through these comments , one thing occurred to me there is alot we need to learn about this subject yet from further scientific research which is not the same necessarily as my opinion. One thing that comes from the statistical world and demography. Correlations are not cause but they begin to help direct science research.
Great article. The people leaving comments need to see a shrink.
People MUST be honest about caloric intake. The three meal day plus snacks & dessert is a Western antiquated paradigm. Genetics by themselves will NOT make you FAT. The term “Fat Shaming” is ploy by the Food & Pharma industries b/c over indulging is very profitable
It’s the food and what’s being put into our foods we need to go back to the natural way
If the answer is old fat please explain the phenomenon of the 450 pound 12 year old.
I don’t have time to read through ALL the nasty comments, but what studies have been done about other contributing factors to obesity, such as plastics, chemicals or environmental triggers? It’s true that humans were very rarely fat in previous generations, making genetics the unlikely universal cause. I also know plenty of people (including myself) who follow strict diet and exercise guidelines and keep gaining anyway, so it’s not just about willpower. Something is definitely makes us sick, and fighting with each other over cheeseburgers will not get us any closer to answers!
At the end of the day eating healthy food matters the most whether you are obese or not.
Very interested in this article. Where can I find this study. Everything I read makes perfect good sense. Please disregard the turkeys and ignorants leaving absurd and sad comments.
Expert find that asphyxiation death isn’t cause by lack of oxygen but by the heart not beating…
Really Is stupid
On my, that’s the problem in our world, all the judgement on one another, the separation, the lack of support, lack of love and empathy. Any addiction is accepted more than being over weight, there is sex, drug, shopping, porn, video, internet, tv, addiction and the list goes on and on. Most of them are to cope or avoid feelings. I have met a lot of so called healthy people who feed their children fast food, sit at Applebees order a salad, down three beers, put their children in the car and drive home. Yes, being overweight has complications that CAN come with it, but unless you are GOD no matter how you have lived your life it’s all in his hands when and how that life ends. We all have a right to our opinions, but we don’t have a right to think we are better than others. Oh and yes I am overweight with health issues, but I am also a human being just like YOU.
Articles that are about the medical and overall well being of being overweight is not fat shaming. Fat shaming is making a fun of those by how they look. Society has gotten to the point that they’re offended by anything.
I think people have been interchangeably using the terms “overweight”, “fat”, and obese, which all have different meanings. those who are concerned about being “overweight”…. are you happy? if not then keep trying. those whom are arguing about “fat” …. this is subjective, I can call a 105lb 5ft woman fat because it is my opinion. Obese has medical implications. so most of you sham fools full of shaming shamers should consider much more than attacking opinionated statements as the ones that know won’t help you to know which often perpetuates your idiosyncratic self serving ego boost for the day. obvious unfortunate stories, are just that…unfortunate, genetics should be used in moderation as what evernody considers to be normal within one family may be completely normal in another, thus causing “hereditary” features, this can easily be as simple as not washing your bed sheets weekly . all baby’s are born fat…that’s just how they look lol
What are you people talking about? Did you even read the article? Do you see the pictures and you think you understand the article, Geez..please read before you write a pointless opinion and start a controversy that is isn’t there.
What are you people talking about? Did you even read the article? Do you see the pictures and you think you understand the article, Geez..please read before you write a pointless opinion and start a controversy that isn’t there.
The one thing that I’ve taken from this article for sure is that Dan, is an @sshole…
Still; which one of us isn’t adversly affected by the weekly loss of the art Linkletter and petticoat junction show’s.
Great answer Fran, eat less, drink a lot of water, fast, walk or do Tai chi, stop making excuses, do a little everyday and you will loose weight
If body shaming worked everyone would be skinny. Overweight people know they are overweight. If dieting worked we would not have an obesity issue. Obesity is a complex issue which has lots of causes physical, economic, ethnic, genetic, emotional and social. Bodies developed to hold on to and store fat. Cutting calories and increasing exercise are no guarantee for weight loss. It is a chronic problem which needs to be addressed with gradual changes of life style. And the American “ideal” of the skinny body is not healthy, realistic or attainable. Bodies can be healthy by making gradual changes. And kind support from others.
Don’t eat and lose weight. Simple. Takes discipline which is what fat people lack.
My cousin was living with his girlfriend who weighed 615 lbs. One day, he came home and found her dead on the living room sofa. She was 59. They had to take the front door off the hinges to remove her body from the home. She wouldn’t fit into the hearse, so the funeral home had to send out for a box truck. Ask yourself if this is how you want to go out
@Stormy Look into the Gerson clinic.
The leading cause of most diseases are grains and sugars. Vegetables are extremely important and they actually cure most diseases because of their vitamin content and the fact that they contain living cells which replace dying cells, and and their alkaline forming and hydrating cleansing effects. Yes fiber is important, but its even more important what kind of fiber we consume. If its grain fiber, it causes lots of issues where as veggy fibers heal. And yes anything that is chemical based is a bad idea. All natural diets provide tons of energy, and keep us more naturally active and bustling around. Natural fats and lipids like avocados and olives lubricate our systems and are good for us just like oil for the tin man, while refined sugars and simple carbs are what cause weight gain. Most people over exhert them selves in exercise, which makes them actually keep their weight cuz they insight their stress response. Mixing bursts of muscle building cardio 15 min a day is better then running for an hour.
For those of you who say that shaming people get results obviously have no idea what kind of damage that can do to a person. It isn’t always over eating. There are health problems that can prevent people from losing weight especially if it is a hormone imbalance or even a tumor. There is a long list of reasons as to why a person is obese. Unless if you have walked in their shoes and lived in their body then you should probably keep your negative opinions to yourself. Maybe the best way to handle it is to be supportive and not negative. Shaming someone for their weight is cruel.
A hormone imbalance!? Orrrr a tumor???! Haaaah that is so funny. Like they all have one of those. A hormone Imbalance or tumor! Lol. Ummmm, NO
Plain English please?
For the lady on here saying that her daughter has been fat since she was a toddler because her father’s family members are fat you decided to have kids with this man knowing the risks but now you want to blame his family.
You can’t talk about the problem of obesity without being accused of fat shaming. My state has one of the highest obesity rates in the country which makes it also one of the fattest places in the world. The US in general has extremely high obesity rates making us one of the heaviest countries in the world. It was not always like that but people are less active and eat too much junk, consume too much sugar and other empty calories. I have a gut myself, not as big as it was before I was diagnosed with diabetes but I’m still a little overweight. I’m not tryouts g to far shame people but we must acknowledge that we have a problem and try to correct it even if it hurts some peoples tender feelings. Covid has torn my state up in large part because we are so overweight and because conditions like diabetes and heart problems an so on that go hand in hand with obesity are so common here. But you can’t bring it up or you’re fat shaming, now pour me another glass of sweet tea and it better be thick like syrup with all the sugar in it. Then we’ll go get McDonalds and maybe stop at Starbucks for a 900 calorie coffee drink.
Despite how other people are interpreting this particular article, the information I received from it is important to me.
I understand that body fat is not the best thing for anybody. I understand that body fat does play an important role in the human body – when the body is healthy. Comprehending how body fat functions is essential to understanding its role.
When obesity occurs, it definitely does contribute to certain types of disease, which in turn make obesity even more of a problem. The flip side of this coin is that when fats are consumed in the diet, these lipids are NOT the same thing as body fat. This is where people get the wrong idea.
While a small amount of dietary lipids are essential to healthy bodily function – an unhealthy body requires even fewer dietary lipids. So, when a person is obese, they require fewer dietary lipids along with muscle use in the form of exercise, which could be as simple as going for a daily walk.
This article provides some basic information that has garnered interest in my brain and this has resulted in my desire to research this subject even further. This is the primary reason articles of this type are written.
Also, from the comments, I have developed a strong repulsion to anyone who believes that shame is a good idea in any situation. Why do something that has proven itself to be counterproductive? It amazes me that people are comfortable spewing shame. Just. Why?
Wow. Has anyone studied the effects of reading the comments sections of ANY ARTICLE on the prevalence of stress and its pals, raised blood pressure and stress eating? It would be so nice to see a thoughtful conversation. I will now go thank my book club, and try to resist eating a handful of Wilbur Buds (the best chocolate) by going for a walk. Sign me “Not skinny, not obese, a little fat, over 65, out of estrogen and low on thyroid hormone”. We all have our problems. Be happy nobody in this thread is starving to death. Geez.
Reality, only posted a premise which could be true in many cases. As far genes go, yes that might be true but the mind should be more powerful; keeping a good diet will drop the weight, feeling happy about eating the right things is something that takes practice and patience…again Molding the Brain.
Okay, I read some of these. And please guys! We have always known what causes people to be fat. Overweight. Obese. I do appreciate the conversation. It does expose the underline narratives the Marxists are trying to put forth in every aspect of our lives. There are no differences, we are all the same. No, we are all only all the same in the sense that we are all human beings. And there’s a large variety of us. And we all know that. Some are fat. Not because of a hormone imbalance, or because they have a tumor, those CAN happen but are rarities. People are fat because they eat too much for their activity level. And if someone gets so heavy they look like a ball, It is pretty odd. And yes we will stare. Because it’s such an extreme neglect and abuse of the human body. We truly can’t imagine how they can let themselves go like that. Just eat nonstop? Maybe they do have a real illness. But come on people, that is rare indeed. And NOT the reason for most of the obesity we see. Most of those extremely, disgustingly fat people are just over-indulging. And it is as simple as that. Gluttony used to be a sin. One of the 7 deadly sins. For a good reason. Gluttony destroys people. Kills them. It’s about time the time we take it seriously again.
When I was growing up in the 60s I rarely saw people as fat as the ones I see in profusion today. Moreover,what was consudered “fat” at that time would now be considered average. What has changed over this oeriod other than diet, lack of discipline and acceptance? Why is it that I see normal- (yes normal) size children with hugely obese parents? I have to assume their parents started out normal and and year after year of first 10, then 20, then 30 poubd weight gains led them to be immensely fat. Why is it that I go to any European or Asian city and find that the people I pass on the street are not fat the way their American counterparts are?
If obesity was only due to eating unhealthy or eating to much then this wouldn’t be possible. I am very skinny. I always have been very skinny. However my son has been big since the day he was born. We basically ate the same foods for 16 years until he started working so he didnt eat at home all the time. But im still skinny and he is overweight with us both eating the same foods. His brother has some extra weight now that he doesn’t live at home but he didnt have any extra weight when he lived at home. So thats 2 skinny people and 1 overweight person all eating the same food and amounts of food. Infact I probably ate more than they did. But im still skinny and he still struggles with his weight constantly. This proves it isn’t what we eat or even how much. Uts something else in our genetics or something that causes it. Thats the ONLY WAY to explain this situation. Oh just to let yall know my sons thyroid has been check many times and its fine. Also my thyroid has also been checked and its fine.
Is there anything that can help one lose some degree of weight, even if it’s a slow process? The problem I have with psoriatic arthritis is the incredible pain that never stops. Tylenol does nothing for it and I really need to walk. I love to walk, but my body dorsn’t allow for mich of it without paying me back. My doctor doesn’t have any answers…just do the best you can. Unfortunayely, any weight-bearing exercize is excruciating.
Not everyone can afford a gym membership or getting exercise equipment.
Survival of the fittest . Only the strong survive . Call it what you want . If your obese, get some medical help, push the chair back from the buffet. Take a walk . Proven fact , slim people live longer . If you have no self esteem, just keep pounding the donuts.
My comment is that why is that people tend to attack the obesity person because of high blood pressure or diabetes why it can’t be because they are kidney failure or any other symptoms because it is hard when you are in these people shoes trying to lose weight and maintain a positive impact and weight loss
Change is required rather than shame. Obesity is a health issue and can be prevented with better food choices and moderate exercise. We should never accept or encourage what we know to be bad for us. We need better choices when it comes to food and encouragement to be healther. We don’t need name calling.
Why be so quick on you hateful comments on this report? Keep your negativity to yourself. How can you be so critical of as study that was done to prevent and restore health for people that have a problem? Would you have told Dr. Salk and Dr. Sabinthe same when he was finding his vaccine?
I was looking at a group photo of my 110 classmates from 1965. Maybe one or two students were overweight. Not a lot. Different story now.
In the August 2019 of Good Housekeeping, it states 1) fat cells serve as hormone command centers. 2) They can suffocate if they get too big and oxygen can’t get in and causes them that something is very wrong and starts releasing cytokines. and 3) Once you’re an adult, you almost always have a fixed number of fat cells. Childhood obesity tees you up for weight struggles as an adult.
Mmm…I love seeing all the comments that led to my mother putting an extremely active and happy 13 year old me on a strict 700 calorie a day starvation diet for over a year desperately trying to turn 250lb me into a 130lb me so that my bullies would stop bullying (news flash: they didn’t) and my mom’s side of the family would stop calling her a bad mother and saying “she would be so pretty if she just lost the weight..” despite the fact that I hit all the same landmarks every single woman in my dad’s side hit. Like a sudden intense weight gain at the onset of puberty with no changes to diet or activity level.
Did so much damage to my mind and body that I am now nearly 400, severely depressed, suffering over whelming anxiety, and unable to work. I love having had my whole life obliterated by shamers.
I love having doctors actively harming me by attributing everything to my weight and pushing severe body deformity onto me every time I seek medical attention…because obviously I should allow them to permanantly mutilate me for a CHANCE to lose weight.
I love having a broken tailbone and a lifetime of pain and misery because when I complained of severe pain in my ass they x-ray’d my lower back and said “It is because you are fat and sitting too long.” No doc it is because my tail bone snapped and got shoved the wrong way and healed that way because when I said “I don’t remember falling.” You took it as “I didn’t fall” and x-ray’d the wrong damn area.
I also love being tuned out and told my sudden leg weakness and worsening condition was not being used to exercise after my physical therapist STOPPED TREATMENT because my legs were doing things they should not be doing and she wanted it looked into before she continued so I was not permanently injured. I loved demanding he have blood work done so I could prove that my back is potentially Psoriatic Arthritis. I loved watching him roll his eyes and order it, only to come back next appointment like EVERY DOCTOR I have ever been to going “You’re right, I am sending you to a Rhumatologist because it is most likely Psoraisis related.
Screw shamers. If I wasn’t treated worse then a dog my entire life I would probably be fine now doing the job I wanted to do since childhood instead of trying desperately to think of things I can do to support myself without it leading to panic, terror, and suicidal mental breaks.
I don’t care that this is ‘just anecdotal evidence’ either. I really don’t because it is MY reality and that should be good enough to make people think about their own actions and how it affects others!
Oh and yes, every single doctor I have ever had has PRAISED my mother’s actions. “Good! Anything to get the weight off!” And every mental health professional and Dietician has been horrified and emotional distraught because what my mom did was beyond cruel and I defend my mother because she was doing what she thought was best at the time and was desperate to protect me from all the garbage spewing from the mouth of shamers.
I came from a fat mother. I became a fat mother. I have a fat daughter. Until someone lives in this cycle I am sorry but you really don’t get it. Our society loves to help you and has plenty to say about it. Example I went to a doctor for an ear infection and before leaving I had to endure the help of how I was wrong and not handling my tragic weight problem. My ear?
My grandfather was fat(RIP), my dad was fat and lost over 80 pounds(all in his 40s) when the doctor told him he was gonna get diabetes. I was fat and lost 40 pounds when I wasn’t as fit as I wanted to. Calories in, calories out: exercise more and eat less calorie dense food. Notice I didn’t say less food, me and my dad still eat a ton of food but we eat healthy and workout to burn extra calories. I went from a 10:30 mile 2 years ago to a 6:05 now, I plan to run for track and get a sub 5 by senior year. Its doable, you can lose weight, but not if u pretend it’s impossible.
Chubby people give the best hugs! I’ve dated those labeled “overweight”, and I think they wear their weight very well. Fat can be beautiful. Some people are just made bigger, and I’m happy for it! I was made slim, and I’ve never put much effort into staying this way. I have watched loved ones put loads of effort into losing pounds, and when that amount of time & effort became unmanageable the pounds came right back. I didn’t mind… The things that we hate in others are just reminding us of what we subconsciously hate about ourselves. I say don’t hate; Ask a chubby person on a date!🤗
Fren…you are an ignorant, pompous, supercilious, self absorbed, self righteous, arrogant ass. You sense of intellectual superiority is only exceeded by the size of the anal sphincter you have your cranium pushed pass and inserted into your fiber filled alimentary canal
“Being fat is beautiful, name a thing you can’t do? Jumping Jack’s, run a mile, Live past 42?”
Good to see new research showing up on this topic.
Calories in, calories out. I used to be pretty fat and could barely run a 10 minute mile. I lost around 40 pounds in 6 months because I knew it was better my health. For a lot of people the problem isn’t they have to big of an appetite, it’s that they chose the wrong foods to satisfy themselves or don’t exercise. for me all I needed was to be more active, I did a lot of running, but other activities can work too, you just have to find what is best for you. We are not presisposed to obesity, it’s just that nowadays foods are wayyy more calorie dense and people are wayyy less active.
Why is this picture Black??
It’s genetics y’all. Everyone in my family is tall and athletic. I’m 6’5″ 185lbs. And have been this size since high school. I’m 52 now and couldn’t gain weight even if I ate at Golden Corral three times a day. Americans waste billions on diets to lose weight and they rarely work. Control what you can to keep healthy. Exercise is beneficial even if you’re fat. Quit drinking, smoking and doing drugs. And most importantly focus on your spiritual and mental well-being.
NO NO NO! You idiots! How many times do we have to tell you that fat IS HEALTHY AND BEAUTIFUL!? 😑😑
Stop telling us bad things about being fat. WE. ARE. HEALTHY. AND. BEAUTIFUL.
My 3XL grandfather suffered from bad knees, constipation, diabetes, senility from obesity (lived to 98). His wive had a heart attack which is how she found out she was diabetic. She would ask me the same question 4 times within an hour. She had her knees replaced. Their daughters and son all overweight as well affecting cognition.
Myself had afib, congestive heart failure, diabetes, chronic kidney disease, high blood pressure (149/90 mmHg) memory decline, and grumpiness. November 2020 I switched to Whole Food, Plant Based, no salt, no oil, no sugar (WFPB-SOS)lost 50 pounds, reversed my type diabetes, my blood pressure is now 110/70 mmHg. My memory, mood and cognition is as good as 20 years ago. I am 66 now and went back to work last year designing bumper, fascias and grilles.
2/3 of obese people suffer major medical issues from the condition. BMI of 35 and higher were 7 times more likely to be hospitalized from COVID-19. Uncontrolled diabetes with a1c of 8.0 or higher were 14 times more likely to end up in the hospital. My advice is to get your BMI in the 18 to 25 range and definitely under 30. Sumo wrestlers do fairly well with their weight until they retire with lower activity.
Question is are you fat on the inside (fatty liver, interstitial abdominal fat) which is the most dangerous. Table sugar, fruit juice, fructose and alcohol all raise triglyercides abd cause fatty liver (so stop soft drinks including diet, use of sugars and sugar subsitutes, alcohol and enjoy your senior years as well as the early years.
Six million people of every physical and genetic makeup occupied concentration camps in WWII, all on calorie-restricted diets. Not one case of obesity.
According to Cyrus Khambatta and Robbie Barbaro of Mastering Diabetes the insulin resistance is due to intramyocellular lipids blocking insulin from entering into cell. I followed advice from their book and removed meat and processed foods from my diet (including oils) and dropped 50 pounds in 10 months and got off metformin and blood pressure medicine. Many Whole Food, Plant Based doctors, dieticians and nutritionist follow this advice of getting rid of saturated fats from the diet.
Our country is in death spiral. We either change or our country could be just like Rome. All empires must end.
Fren you are an idiot. Throw away meds and AC? Hell, don’t stop there. Get rid of anything discovered since the 18th Century and return the actuarial tables back to about a 40 year life expectancy.Everyone will be skinny b/c they are either sick or starving. What a fool…
Wow..I seen more drug addicts the so called skinny cocaine,meth,pilly people drop dead nobody escapes it stop living your skinny lies ..😂🤣😂🌍
Obesity is as simple as poor habits. Which leads to poor health. If you don’t want to be a fat f*ck put down the fork. Absolutely that simple
Well,well,well!! I see after reading through a ton of these comments that 1)quite a few of you must be terribly miserable with your own lives. 2)others really are fat just because they spend all day watching “soaps” and gobbling down ho hos and bon bons.3)there are actually a few level headed comments here. with those 3 realizations in mind I will now add my two cents. Regardless of what you try to say to defend yourself period bottom line unavoidable, unequivocally truthful,and absolute fact is if your here defending fat shaming or any “shaming” whatsoever you are in fact a ignorant turd Regardless if it’s because your miserable in your own life or you just get your (sick/demented) kicks from hurting another human. If your excuse for being obese is “its impossible to lose weight” no matter your reasoning you are a liar because whether it’s lying to yourself therefore lying to others or lying as a defense mechanism it’s still a lie. Anyone can lose weight although it may be extremely difficult for some and to the point that it’s just not worth the trade off to do what it takes to lose the weight.Shaming someone for being illiterate is looked down upon by society as a whole and will get you the “pos” lable instantly although there isn’t any acceptable excuse for being illiterate just like being fat. You can always seek help with literacy. There is literally numbers to call and help on the web(not sure how effective since you can’t read smh) and family members etc. So bottom line the only way a person can remain illiterate through their lives is because they actively “choose” to remain that way. I’ll only use this one example for the sake of time and space. So while you are being scolded by society you are also told what? Your unsolicited negative commentary against this illiterate person is a big part of the reason the person is still illiterate because shaming them makes them scared to reach out because they don’t want to be ridiculed. So with this line of thought think about this, your fat/obese every where you go you get “looks and negative comments” you actually want to go to the gymn but just stepping out of your vehicle at the gymn and walking toward the entrance with your bag you get chuckles,laughs,sneers and looks of disgust before even entering the establishment and can only imagine how bad it would be inside so you get back in your car defeated,sad and guess what “hungry” for food or is it for feeling something other than rejection? You go to the nearest McDonald’s and drown your misery with a big Mac and fries. You go to the grocery store and get the same negative experience with people looking in your cart and you knowing they are searching for the pizza pockets and snack cakes but only finding healthy foods so mumble something about it being the only salad you eat all year.Are you starting to get it yet? When you are openly ridiculed both for being obese and trying to do something about it then you are way less likely to be successful at losing the weight or more often than not you actually get worse because it becomes a mental issue.For all you “tough guys/gals who would retaliate to me with the well they should suck it up let’s be honest you would fold like a chair in the same situation. This is the most ignorant assanine meat crob I’ve heard in my entire life.All you punks are looking for is an excuse to bully. Would any of you walk up to random people and tell them their hair cut looks like complete sh*t? Would any of you walk up to someone built like a MMA fighter just to tell them they are ugly as a horses ass? Let me answer hell no! Do you honestly think their haircut or looks require you to go out of your way to tell them how sh*t they look? Again let me answer hell no! So when you walk up to an obese individual and call them fat ass or sneer and/or laugh what is it that your trying to achieve? Once again let me answer but in parts 1) most often you think because they are fat that they are automatically weak and at the very least slower than you at running and a easy mark to try and bolster your self esteem by ridiculing them like your mother when she accurately screamed that you are worthless and will never amount to anything. 2)You suffer from a mental issue like low self esteem and somehow feel better after (again) insulting a person who a) you think is too weak to pose a threat b)too slow to catch a coward on the run. Then there is 3) You are trying to impress someone i.e. girlfriend/boyfriend or friend and or family. The bottom line is no matter the reason it all comes down to the same shameful cowardly reasons and has absolutely nothing to do with wanting the “best” for anyone and everything to do with your (sick/depraved) needs to feel dominant or better about yourself by bringing down another person
Just like any doctors office that wants ti weight you! It’s degrading and depressing! So this year I’m telling my doctors, if they can’t give me a valid reason for why they need to know my weight,then I’m not getting on the scales! And if they want to put me on BP meds, I’m asking for blood work to check my adrenal gland! People don’t realize some meds cause high BP.
We have to weigh you because that is an important vital sign. Jesus folks. Stop playing doctor. You aren’t good at it.
I’ve made major discoveries checking people’s weight, like heart failure, when I’ve found massive weight gain with no reason for it. If you have high blood pressure or diabetes or just about any medication, we need to know your weight. We may also need to know for dosing medications (not always, but some medications).
If you don’t want to know the number, ask your doctor’s office to weigh you backwards, as we do with our patients with disordered eating. We CAN’T just not weigh you because it’s depressing anymore than we can stop taking someone’s blood pressure because that’s depressing for some.
Regarding adrenal testing…we can’t just do that because you want it. It has to be medically indicated for it to be covered and for the results to be medically significant (due to the potential for any test t have false negatives and false positives).
I know it’s depressing. Most of us are overweight or obese too.
I see a lot of comments, none which point to the more obvious explanations. Obesity is the result of food loaded with sugar and animal protein. Americans eat way more protein than needed, and if not used will be stored as fat. About 45 grams of protein a day is more than enough for a body builder and 1 grand slam from Dennys tops that.. Sugar is unatural, and I’m not talking about fruit, I’m talking about processed sugars. To your liver, alcohol and processed sugar are no different. So you might as well drink instead of eating a sleeve of orios because either way we are doing liver damage, gaining weight, and becoming addicted.. One soda a day will add 17 unuseable very hard to get rid of pounds per year. Don’t expect your main stream health professionals and poloticians to tell you America’s largest cash generators such as sugar, beef, and dairy, are making you sick and now need Surgeon General warning labels too.. Ag laws and anti terrorism laws prevent them legally from doing so. Also don’t wait for your doctor to tell you because it’s practically illegal and not beneficial to the industry to do so until you are sick or diabetic, it’s just not something Doctors are trained to teach you in preventing. Everything legally on this topic is on the consumer as of now until everyone is aware and sick of being sick. It benefits the peddlers of these poisons to keep us dumb and addicted, and yes, animal protein and sugar are more addictive than cocaine. Yet harder to quit because we know about cocaine, its expensive, it’s illegal,, and it’s not in our face every place we go.. Anyone working in health care would be putting themselves out of business if they spoke the truth about how dangerous the American diet of meat and sugar really is because that is what is fueling a very large majority of their revenue and almost all our illness. Our diseases are caused by food that we pay for. Then that disease is treated by the health care we pay for. America makes twice the revenue off of unhealthy food vs healthy food. Every one wins except for the purposely uneducated victims like us who then unwittingly pass this cycle of life to our children. That’s why holidays like Halloween and Easter make me sick anymore because to the kids it’s all about the candy and I don’t want to tell them no when the whole world around them is doing it.. Knowing isn’t easy and many will read this and get angry, deny the facts that are out there and published. That’s how I felt at one time too, however, I should have known then that the only one I could count on to be honest with me is my instincts and they were trying to tell me all along. Now I’m skinny again. Also if you want to loose weight a little quicker, stop eating meat as much as possible or never. Yes, it’s delicious, yes it takes a lot of effort to avoid and work around, but if your overweight you don’t need all that protein. Plants are all you need, they won’t give you diabetes and heart disease, only animal protein will do that. Also anyone who eats daily will not die of a protein deficiency. Have you ever heard of such a thing? It’s actually quite opposite in America.
Fat is an organ just like skin or a kidney. This article addresses its function and disfunction. I see no “fat shaming” here.
You guys have some serious emotional problems. Just want to hear yourself cry. I’m over overweight its good not to just bandaid everything stop being so sensitive 🙃 little pu##ies thats whats wrong with this country. Take responsibility fix your health balance your hormones stop being little snowflakes….. the end
Oh yeah….you sound REALLY healthy. 🙄
If cutting weight is impossible for someone through diet they can always try amputation. I dropped 25lbs instantly and it’s stayed off. And I no longer eat processed garbage food and lie to myself about everything being not my false. Personal responsibility concerning your health is so last century
Fat placicity, well that says it all there. People need to question what isn’t being said, such as how have the processed foods affected our cells, fat and otherwise. Not just the foods but the packaging. Pretty sure it has much to do with our illnesses and the stubbornness of losing fat. Corporations pay good money to squash studies that show any rhetoric involving lawsuit possibilities.
You dip-sh*t know-nothings. This is a SCIENCE article. It’s not written to make anyone feel better or to negate personal responsibility. It’s meant to inform and educate. There has been growing research over the years indicating that there are a number of reasons why an individual is overweight and has problems losing it. Hormonal imbalances, insulin resistance, genetics. Even someone eating all of the “right” foods might still be missing a key component.
I hope anyone who needs this information is able to ignore the self-righteous d**kheads and use it to their benefit.
Some people on here need to stop playing doctor.
Do NOT stop taking meds without medical approval. If you have a serious medical condition (like myself and many of my own patients), you cannot go off meds.
Science has proven no statistically significant improvement in metabolism with “turning off the heat and AC”. 😂 Wow. Just wow. Likewise, there no consistent data to breaking up meals and eating more frequently. In fact, many overeat doing so and do better with regular meal times.
Many people gain considerable weight on medications.edications which can’t be stopped without serious medical consequences. Many people DO overeat and many Americans in particular overeat due to stress and UNDER sleeping due to being overextended with family and work.
Obesity is multifactorial. There is no one cause and even one obese individual typically has more than one reason they are overweight. Shaming doesn’t help and studies show it is counterproductive.
In medicine, we look for peer reviewed randomized control study data to drive medical decision making. Which is in fact why we have not solved the issue of obesity and overweight in the US. It is a combination of eating too many calories, the wrong kind of calories, public science and health policies that favor subsidy of all the wrong foods and corn sugar, lack of public education in health and diet, decreasing physical activity, increasing rates of disability and poor health both related and unrelated to obesity and overweight, pollution and obesogens… And not even taking into consideration that countries with better public safety nets, paid vacation for workers, public transportation and universal health care have lower rates of obesity.
A certain segment of the population likes to cry about everyone else’s feelings while exhibiting the most embarrassing displays of emotions and feelfeels. If we addressed obesity as the public health crisis it is instead of using it as an opportunity to bully others, we’d all be better off for it.
Go back and read the first comment. I don’t think this is shaming. Regardless of the reasons, overweight people are more prone to serious physical ailments. Not all overweight people are unhealthy, but the propensity is there.If you can’t agree with that, then you very likely believe the Earth is flat, vaccines are for population control, and Trump won the election. Why do so many statements need to attacked as an attack on others. Full disclaimer, I’m 6 ft 3 and 230 lb. I don’t like my weight that high. My knees, my lungs, and my digestion were much happier when I weighed less. One thing worsens the other and it becomes a negative spiral. I believe I can get myself back into shape, but this is an ongoing battle for me as it is for many other people.
Everyone wants to tell everybody else what to do & think. It’s been like that since the origin of Homo sapiens. In fact, it may predate that to pre-humans since chimpanzees can also be pretty nasty animals. We can’t seem to mind our own business. It’s all about who has power & influence since most of us are basically so insecure that we must lord it over others to feel secure & superior. We just can’t “let it be.” Our downfall as a species. Unfortunately,other more noble animals will be dragged down with us when we annihilate each other.
Reality hasn’t ever heard of thyroid disorders or weight gain caused from medicines. Reality has never stayed on a diet for one day. I’ll not be taking weight loss advice from reality. Reality won’t be reading the comments because it’s his choice to remain incredibly ignorant.
Obesity itself is a symptom of underlying disease at times.
To all those folks who struggle with obesity – I feel your pain. To those who have never been obese, count your blessings. The bottom line: If you don’t have anything helpful or nice to say about a very serious health issue, consider saying nothing – especially if you lack perspective and experience regarding the same.
Shame and Blame. Truly American. Speaking of getting fat, anyone remember the Crazy 20’s when they sent us to our room for 2 years? A we get older it’s more difficult to get around, certain injuries from the past crop up and it’s harder to keep weight off. Let alone lose weight.in my 20-50’s I said “I’ll never let myself go!!”. I never anticipated stenosis or spondylitis. Nor bein sent to my room, out of work, for 2 years either. Nor RA. You fat shamers can take a breather. There’s nothing you can say or write that’s half as cruel as what we say to ourselves about ourselves. But bc you’re head is up yourself-righteous arse you won’t hear a word of this. Get over yourself and do something nice for someone today, how about a lift to my PT ? My car died after my Dad died after my 18 y/o best friend, my dog SnoopDogg died. Depression is fattening,too. Judge that. 1 finger pointing out leaves your other 3 pointing back.
By the by, I’m not critiquing the Article, which is 💯 on target. The Arrival did not blame shame or judge. It spoke about additional, scientific information meant to help and guide. I’m critiquing the idiot critics deciding what’s fact and what’s not. If your friend wants to eat herself to death, you can’t change her,foo. Move on, find new friends to mend that broken(seriously?) heart. If it’s a good addiction, go to an OA Meeting and listen to reality. If you are so good at looking good, get away from your toy, hit a club and bore someone else who can look at you with you. Foo don’t know what they don’t know but in this forum,finally an audience! Let out your outrage. Yawn.
It all boils down to the many use the true medical problems of the few as cover for a problem that has no medical bearing laziness and indulgence
“Reality” he says lmao. braindead. the only way a fat persons body is shutting down is if they have a bmi of 50+. maybe stop pretending like you’re some genius and read the article and realize its not anything about giving unhealthy people an exscuse. its about how the fat itself in overweight individuals is not the killer. its what the excess fat causes. uneducated skinny guy pretending hes superman bc he was born with a fast metabolism. how about you get off your ass and get some muscle on your body and thn talk. ive been fat, skinny, and now fit. you’ve probably been an unfit lazy mf ur whole life acting like you’re greater thn those that arent as fortunate to be able to get good food to eat that isnt hotpockets and ramen. open your eyes.
As well as some intentions may be on this comment trace instead of fixing everyone else how about we fix ourselves. You do you I’ll do mean and when our time on this rock is done whether we were thin or fat, tall or short, race creed or color what will matter how those we interacted with that are left behind remember us. Will we kind compassionate loving forgiving or we self-centered self-loathing projecting ourselves on other people to make ourselves feel better. there’s all kinds of science behind weight loss and genetics The biggest picture of all is how we treat each other. every culture and faith has its own basis in you reap what you sow, yin and yang, do you want to others as you would want them to do unto you. basically you do you I’ll do me and when I’m gone I hope my children in my friends remember me kindly in loving. I don’t believe if there is a next life it’s not judged on our waistline or bank accounts rather how we treated each other.
It’s hilarious how many lazy fat people here are using every psychologically warped angle that they can muster, to stave off those commenting truth. If they spent half the energy they are using to do this, on exercise, they’d lose weight and feel free, and better about themselves. Groupthink and Marxism keeps them fat and in denial.
Your diet can turn on or off genetic markers resulting in your health outcome. Exercise also has a profound effect on turning these markers off for obesity through epigenetics. I come from both obese parents and grandparents. My siblings are all obese. I am Vegan and I workout 5 days a week with both weightlifting and cardio. I have 20 percent body fat (considered athlete for woman). I do believe genetically we are predisposed to many things but we also have control over what we can do about it.
I have done some research and it is true that obesity from one or both parents is passed to the born child. Something in the genetics becomes deformed and mutated and it causes a child to have an obesity problem from the day they are born to the rest of their life. The other driver of course is lack of exercise and our poor eating diets. In 1998 my car broke down and so the only thing I can do because I didn’t have the funds to buy now the car was to ride my bike for 6 months in Seattle here to Seattle has several Hills and I had the bike up those Hills I tell you what that was really hard. But within a few months all my body fat had literally disappeared and turned into lean muscle. I felt really really healthy that felt like a spring word it was amazing. Now I’m over 50 and I’m alway obese cuz I don’t exercise. Part of the reason why I’m obese has cuz my age every year the metabolic burn rate drops a little bit. There’s a true story that I heard. A sixteen-year-old kid that is sitting in a chair burns more calories per hour did a four year old that is jogging down a track
Sounds to me like a wana be know it all. Listen, much of the food we eat are meant to make us fat. Rather, made for shelf life or look pretty & the result is harmful to some more than others. Sadly, no one wants to lobby for a Better quality of food ie; gmo, pesticides hormones you name it. Quit screwing w/the food & the food fed to the cattle & animal meats. If food was not so full of toxins that harm fat cells & metabolism & glucose etc etc those with weight issues would be able to live a healthier life, in turn a thinner less body fat, life.
Enough Already. Everyone is different, situations are different. I wonder why people are concerned about people who have drug and alcohol addiction. Smoking sessation programs are available that are covered by insurance, and there is no help for the overweight or obese people. Other than very expensive programs that insurance companies don’t cover. Financial situations need to be looked at, families have difficulties buying inexpensive healthy food. Unless you have been there in the poverty level with several children don’t even comment about it. If you think eating canned food from a food bank is healthy. There are so many legitament reasons. I guess why nearly everyone on here uses a fake name so they can hide behind hurtful, shameful or ignorant comments.
@Reality you should be ashamed of yourself for breathing the air other people can use to be healthier. Go take your participation trophy for not being able to spell empathy and hold it over your face till you stop moving. It’s a fun way for you to stay in shape.
Nothing ever justifies shaming or bullying. Science has proven that people are so much more likely to meet their goals in a supportive environment. e.g. a child will just grow to hate reading if laughed at every time they make a mistake.
So just stop being a jerky jerk hater who wants others to fail.
Having said that, do not let our blame focused society give you an excuse not to get better. Whether you truly have special circumstances or not let me ask you this: who holds the power to make a change?
1. Interesting article. I would love to see what more research and practical applications of the research can do. 2. A lot of people commenting here are full of themselves. Wouldnt have commented, but damn…There are a number of reasons people are fat that have nothing to do with inactivity r over eating. Nor does it have anything to do with fiber, ac or heaters. If people turn off ac or heat they can die or become quite ill in many places Fren. Oh, and Fren, some medications cause weight gain but keep people from dying. So stop offering that little nugget too. Shaming heavy people doesn’t help either. But it tells a lot about fat headed egos and who to avoid. Rather a heavy good person than a fit egotistical idiot. When Dr’s can figure out hormone imbalances, genetic tendencies, and healthy food becomes more affordable and more available to all, then maybe we will see some more progress. In the meantime, until you walk in others shoes, don’t be mean. And maybe all you smarty pants should go back to preschool and learn some more social skills.
People are unhealthy. The fat is a byproduct. It’s not shame. People are literally wearing there health on their body
Since I had an early hysterectomy, at fifty two i.had a great healthy figure I’m sixty one and am fifty pounds over weight I eat healthy I excersize even more and I still can’t lose weight oh I also took lithium for bipolar so some times the body just doesn’t metabolize food fast enough I also walk my dog every day ride my bike everywhere don’t own a car live in a town house so I walk up and down stairs several times a day I don’t eat junk food never have don’t eat sweets don’t drink pop koolaid I drink one cup of coffee water and two percent milk oj I squeeze but I’m still fifty pounds overweight of course I’m swiss and nezperce five eight I was ran over last April and broke my femur had to have surgery was unable to get around for about three months gained twenty three pounds because I couldn’t do my daily excersize the fat went to my boobs belly and butt it won’t come off I even eat very small meals with low calories it’s my age the meds I took but shame me all you want I’m happy and can kick a guy twenty years younger ass I’m strong healthy have great immune system. Don’t take pills but I smoke pot to help me sleep nights i.havent been to a resteraunt or fast food resteraunt in years I grow my veggies in my garden every year and home can them don’t eat prossessed food so why am I still fifty pounds over weight it doesn’t bother me to much but why does it bother you. I’m still a good person I’m still healthy and funny and happy to bad you all are not by the comments I read you can try to shame me but I have no shame to my game. SINCERLY Laughing Dove.
The real question is…If its not YOUR body, YOUR health, why do you care so much? Ah, not care..As Americans we are incapable of minding our own damn business..
I remember participating in after work activities, not understanding why my body was aching so bad, and HEART kept racing B4 I even got started and remained on fast all night, so much that I couldn’t sleep, yet everyone wanted my life…jus show-up at a physical activity, hardly do anything and continue to loose weight, despite having both height & weight, within portion at the time of my 30yrs of age. In the meantime, I felt so fatigued & alwayz hungry. I was also feeling Anxious, Confused and out of Sorts. My new normal appearance went from well kept to unkept & lack lusted, behind extremely dry skin & hair that both shedded on command, like a snake. Pretty soon the almentioned and thinner frame, became the source of drug rumors, yet I barely ever took a pill to relieve my monthly cramps. Fast forward, I began going the other way, gaining 25lbs in one month, while all the other symptoms remained unchanged. Nobody was envying me now, so new rumors of over eating began, jus as my doctor was telling me to halt exercising, because test results showed that my heart could only function for three months at it’s current rythmn. Topped off with Iodine treatment, I easily put on 100lbs with this thing call Hashimotos… although I got hospitalized, behind the whole ordeal, fat shaming is what it came down to, no matter how much I tried to explain.
We live in a sedentary lifestyle. Processed food is cheaper and faster to make and does have a short term filling sensation. People in general don’t want to be bothered in preparing healthy options. Healthy options that are pre-prepared are more costly. It’s the excuses I’ve heard of. Convenience=unhealthy. Just don’t have the drive to actually get up and move anymore.
So since I became handicapped 3 years ago and as a result, I gained weight since I’m not a active as I once was, now I’m supposed to be shamed for it? Well since this has become a country that’s ‘o so sensitive , do I get to cry and whine too with the rest of the candy asses? Can I cry that I’m being discrimated against? ? Sounds great. Where do I start since I finally have a legitimate bitch? Can I punch out the idiots that hurt my feelings? Will Rev. Jesse Jackson or Rev. AL Sharpton come to my rescue? I think that if people have that much time in their hands that they have to find a new way to make a person or persons miserable then they are neglecting their own imperfections. And why am I handicapped now- because an illegal citizen with no drivers license or insurance was driving drunk and I got hit by their illegal vehicle. They made bond and hauled ass to parts unknown. I not only ended up like Iam now, but the best part of an the money I lost from drs, having to replace my car, and loss of employment. Priorities are definitely screwed up in this county now. Let’s kick a person down and destroy anything positive they had to offer.
I totally agree with a couple of you guys.WE NEED TO REINSTATE SHAME!! IT WAS LOVINGLY GIVEN TO US BY OUR CREATOR.it helps us to get back on track. America has tried to cancel SHAME, and we are just now seeing the obvious results. When I was a child there were very few FatFkrs. Why. SHAME.
Go to YouTube and look up a few who can bring you out of the calorie in/out dark ages. Dr. pradip Jamnadas “Amazing Fasting Benefits” & “Insane Fasting Benefits”, Dr Jason Fung, Sten Elbert, David Sinclair and others intermittent fasting and insulin reality, a hormone that once triggered often turns body into a fat saving haven and then our bodies just don’t get the chance to use the fat. They’ve know for over a 100 years calorie in/out is BS in the long run. Look around the 70’s and at the food pyramid and the statistics show the truth. Stop your insulin spikes then you’ll see change for those of us Insulin Sensitive folks and finally we can see light at the end of the tunnel. Everybody is unique and it’s insanity to think most of the world wants to be fat We evolved through feast and famine and now there’s no famine and those who tell us to follow a flawed system such as the food pyramid that was constructed under false theories of the heart not body composition realities.
I am a 48 year old female with PCOS/stein leventhal disease. I was diagnosed at age 17. I suffered from lack of periods which we thought was from my extreme workout routine. I was a semi professional athlete moving towards being a professional athlete. 5’5” and very muscular. As it turns out my lack of periods was caused by PCOS. String of pearls cysts on both ovaries, high androgen and other markers. As a professional athlete over the years I have had access to Olympic team nutritionists and trainers and each decade despite eating healthy and training up to 7 hours a day I have GAINED WEIGHT. BMI is a terrible marker for muscular people but now at age 48 I am considered clinically obese…and yet I still exercise and lift weights for hours each day and make extremely educated food choices both in glycemic index, fodmap, and portions. I cannot begin to tell you the resentment and I’ll say it, utter hatred, I have for people who make comments like those in this thread about lack of self control, sedentary lifestyle and gluttony or poor diet choices.
Peer pressure, societal pressure and norms a proven methods of behavior modification that governments use successfully all the time without people even noticing it.it is not shaming and it is effective across the board, including in most obese people. The answer is not to simply celebrate obesity and shame those people who care about others enough to not ignore it.
Lose fucion
People keep making poor choices and they end up being fat. I am still the same weight that I was when I left high school and that was over 30 years ago. Stop eating crappy food and start getting active.
I will share my experience. My mom had 6 children. By the time I was 2 she had 5 of us. She started to ask the doctor why I was so fat. All my siblings were normal but I was getting fatter and fatter
The doctor poo-pooed and said it’s babyfat. A 5 year old is not feeding themselves. I was eating same food, same portions but my body was processing it differently.
I grew up in the 70s when Twiggy was the thing. Believe me I know shame intimately. It does NOTHING other than reinforce a horrible self-loathing.
I don’t blame others anymore for being jerks. We are so ignorant about science and biology but pretend like we know. And jerks have been told fat people are just lazy and have no discipline. They believe that.
I hope one day they can figure out to help those like me where it isn’t psychological but until then it will continue to cause psychological harm because of jerks and well intentioned shaming.
so I remember my parents both of them weighed over 300 pounds.They decided to do keto, and yes at first it was hard but it was worth it.my mom I’m so proud of her she dropped over 150 pounds and is in the best shape of her life.my dad is at 230 right now and is still dropping.they do not exercise they just ate healthier nutrient dense foods.now what works for my mom and dad may not work for others that’s the thing,I know countless people that are obese that eat healthy,but don’t work out.some people need to diet some need to exercise,it’s what your body needs.God created this glorious body it is formidable it will tell you what you need that’s how it was designed.now it’s up to you to decide to listen to your body or neglect it. Now on the other hand there are people that are either born or diagnosed with obesity or other weight disorders that is what’s not there fault.If I get skin cancer because I don’t put sunscreen on that’s my fault.If I get skin cancer genetically,well there’s nothing I can really do about it other than hope that someone figures out how to help
Leave a comment Cancel reply
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
- Dissertation
- PowerPoint Presentation
- Book Report/Review
- Research Proposal
- Math Problems
- Proofreading
- Movie Review
- Cover Letter Writing
- Personal Statement
- Nursing Paper
- Argumentative Essay
- Research Paper
- Discussion Board Post
How To Write A Strong Obesity Research Paper?

Table of Contents

Obesity is such a disease when the percent of body fat has negative effects on a person’s health. The topic is very serious as obesity poisons the lives of many teens, adults and even children around the whole world.
Can you imagine that according to WHO (World Health Organization) there were 650 million obese adults and 13% of all 18-year-olds were also obese in 2016? And scientists claim that the number of them is continually growing.
There are many reasons behind the problem, but no matter what they are, lots of people suffer from the wide spectrum of consequences of obesity.
Basic guidelines on obesity research paper
Writing any research paper requires sticking to an open-and-shut structure. It has three basic parts: Introduction, Main Body, and Conclusion.
According to the general rules, you start with the introduction where you provide your reader with some background information and give brief definitions of terms used in the text. Next goes the thesis of your paper.
The thesis is the main idea of all the research you’ve done written in a precise and simple manner, usually in one sentence.
The main body is where you present the statements and ideas which disclose the topic of your research.
In conclusion, you sum up all the text and make a derivation.
How to write an obesity thesis statement?
As I’ve already noted, the thesis is the main idea of your work. What is your position? What do you think about the issue? What is that you want to prove in your essay?
Answer one of those questions briefly and precisely.
Here are some examples of how to write a thesis statement for an obesity research paper:
- The main cause of obesity is determined to be surfeit and unhealthy diet.
- Obesity can be prevented no matter what genetic penchants are.
- Except for being a problem itself, obesity may result in diabetes, cancers, cardiovascular diseases, and many others.
- Obesity is a result of fast-growing civilization development.
- Not only do obese people have health issues but also they have troubles when it comes to socialization.

20 top-notch obesity research paper topics
Since the problem of obesity is very multifaceted and has a lot of aspects to discover, you have to define a topic you want to cover in your essay.
How about writing a fast food and obesity research paper or composing a topic in a sphere of fast food? Those issues gain more and more popularity nowadays.
A couple of other decent ideas at your service.
- The consequences of obesity.
- Obesity as a mental problem.
- Obesity and social standards: the problem of proper self-fulfilment.
- Overweight vs obesity: the use of BMI (Body Mass Index).
- The problem of obesity in your country.
- Methods of prevention the obesity.
- Is lack of self-control a principal factor of becoming obese?
- The least obvious reasons for obesity.
- Obesity: the history of the disease.
- The effect of mass media in augmentation of the obesity level.
- The connection between depression and obesity.
- The societal stigma of obese people.
- The role of legislation in reducing the level of obesity.
- Obesity and cultural aspect.
- Who has the biggest part of the responsibility for obesity: persons themselves, local authorities, government, mass media or somebody else?
- Why are obesity rates constantly growing?
- Who is more prone to obesity, men or women? Why?
- Correlation between obesity and life expectancy.
- The problem of discrimination of the obese people at the workplace.
- Could it be claimed that such movements as body-positive and feminism encourage obesity to a certain extent?
Best sample of obesity research paper outline
An outline is a table of contents which is made at the very beginning of your writing. It helps structurize your thoughts and create a plan for the whole piece in advance.
…Need a sample?
Here is one! It fits the paper on obesity in the U.S.
Introduction
- Hook sentence.
- Thesis statement.
- Transition to Main Body.
- America’s modern plague: obesity.
- Statistics and obesity rates in America.
- Main reasons of obesity in America.
- Social, cultural and other aspects involved in the problem of obesity.
- Methods of preventing and treating obesity in America.
- Transition to Conclusion.
- Unexpected twist or a final argument.
- Food for thought.
Specifics of childhood obesity research paper

A separate question in the problem of obesity is overweight children.
It is singled out since there are quite a lot of differences in clinical pictures, reasons and ways of treatment of an obese adult and an obese child.
Writing a child obesity research paper requires a more attentive approach to the analysis of its causes and examination of family issues. There’s a need to consider issues like eating habits, daily routine, predispositions and other.
Top 20 childhood obesity research paper topics
We’ve gathered the best ideas for your paper on childhood obesity. Take one of those to complete your best research!
- What are the main causes of childhood obesity in your country?
- Does obesity in childhood increase the chance of obesity in adulthood?
- Examine whether a child’s obesity affects academic performance.
- Are parents always guilty if their child is obese?
- What methods of preventing childhood obesity are used in your school?
- What measures the government can take to prevent children’s obesity?
- Examine how childhood obesity can result in premature development of chronic diseases.
- Are obese or overweight parents more prone to have an obese child?
- Why childhood obesity rates are constantly growing around the whole world?
- How to encourage children to lead a healthy style of life?
- Are there more junk and fast food options for children nowadays? How is that related to childhood obesity rates?
- What is medical treatment for obese children?
- Should fast food chains have age limits for their visitors?
- How should parents bring up their child in order to prevent obesity?
- The problem of socializing in obese children.
- Examine the importance of a proper healthy menu in schools’ cafeterias.
- Should the compulsory treatment of obese children be started up?
- Excess of care as the reason for childhood obesity.
- How can parents understand that their child is obese?
- How can the level of wealth impact the chance of a child’s obesity?
Childhood obesity outline example
As the question of childhood obesity is a specific one, it would differ from the outline on obesity we presented previously.
Here is a sample you might need. The topic covers general research on child obesity.
- The problem of childhood obesity.
- World’s childhood obesity rates.
- How to diagnose the disease.
- Predisposition and other causes of child obesity.
- Methods of treatment for obese children.
- Preventive measures to avoid a child’s obesity.
On balance…
The topic of obesity is a long-standing one. It has numerous aspects to discuss, sides to examine, and data to analyze.
Any topic you choose might result in brilliant work.
How can you achieve that?
Follow the basic requirements, plan the content beforehand, and be genuinely interested in the topic.
Option 2. Choose free time over struggle on the paper. We’ve got dozens of professional writers ready to help you out. Order your best paper within several seconds and enjoy your free time. We’ll cover you up!

What Makes A Good Leader: Essay Hints

10 College Tips for Sophomore Students
Essay writing checklist.
394 Obesity Essay Topics & Research Questions + Examples
Are you looking for the best obesity essay topics? You are at the right place! We’ve compiled a list of obesity research questions and catchy titles about various aspects of this problem. Read on to discover the most controversial topics about obesity for your research paper, project, argumentative essay, persuasive speech, and other assignments.
🧃 TOP 10 Obesity Essay Topics
🏆 best essay topics on obesity, 👍 good obesity research topics & essay examples, 🍔 obesity argumentative essay topics, 🌶️ hot obesity essay titles, 🥤 obesity topics for presentation, 🎓 most interesting obesity research titles, 💡 simple research topics on obesity, 📝 obesity essay examples, 📌 easy obesity essay topics, 🔎 obesity topics for research paper, ❓ research questions about obesity.
- The Causes and Effects of Obesity
- Childhood Obesity: The Parents’ Responsibility
- Causes and Consequences of Childhood Obesity
- Childhood Obesity: Causes and Solutions
- Parents Are Not to Blame for Obesity in Children
- Obesity: A Personal Problem and a Social Issue
- Obesity as a Disease: Arguments For and Against
- Link Between Watching Television and Obesity
- Health Promotion Proposal Obesity Prevention
- Children Obesity Prevention Proposals
- Health Promotion Strategies for Obesity The paper outlines and critically analyses the population based strategy as a method of managing and preventing obesity used in United Kingdom.
- Health Promotion for Obesity in Adults This is a health promotion proposal for preventing obesity among adults in the US. People get obesity when they acquire a given body mass index.
- Obesity From Sociological Perspectives The social problem under focus is obesity originating from Latino food norms. The problem of obesity is the direct result of adherence to social norms.
- Unhealthy Food Culture and Obesity Unhealthy food culture plays a significant role in developing health-related diseases, including its contribution to obesity.
- Junk Food and Children’s Obesity Eating junk foods on a regular basis causes weight gain and for one in five Americans, obesity, is a major health concern though no one seems to be sounding the alarm.
- Obesity Issue: Application of Nursing Theory This analysis will show that well-established theories are valuable to nursing problem-solving as frameworks for analyzing issues and planning solutions.
- Depression as It Relates to Obesity This paper will argue that there is a positive correlation between depression and obesity. The paper will make use of authoritative sources to reinforce this assertion.
- Link Between Obesity and Genetics Obesity affects the lives through limitations implemented on the physical activity, associated disorders, and even emotional pressure.
- Childhood Obesity and Health Promotion Today, childhood obesity is one of the critical health concerns. Being an important factor impacting the future of the nation, children`s health should be cultivated.
- Nature vs. Nurture: Child Obesity On the basis of the given assessment, it is evident that a child’s environment is a stronger influencer than his or her genetic makeup
- Obesity: Background and Preventative Measures Obesity is an epidemic. It tends to have more negative than positive effects on the economy and can greatly reduce one’s life expectancy.
- Obesity Prevention and Weight Management Theory The issue of obesity prevention will be guided by a nursing theory. One of the theories applicable in the case of childhood overweight is a theory of weight management.
- Obesity as a Global Health Issue The purpose of this research is to identify obesity as a global health issue, evaluate the methods and findings conducted on obesity, and find solutions to reduce obesity globally.
- Childhood Obesity: Causes and Effects Childhood obesity has many causes and effects, which denotes that parents and teachers should make children with obesity engage in regular physical exercise in school and at home.
- Obesity Management and Intervention Many patients within the age brackets of 5-9 admitted in hospital with obesity cases have a secondary diagnosis of cardiovascular disease exceptionally high blood pressure.
- Obesity in Children and Adolescents: Quantitative Methods Obesity in children and adolescents has increasingly become prevalent in the recent past and is now a major problem in most developed countries.
- Childhood Obesity: Methods and Data Collection The first instrument that will be used in data collection is body mass index (BMI). The BMI is measured by dividing a patient’s weight in kilograms by height in meters squared.
- Childhood Obesity Study and Health Belief Model A field experiment will be used in the research to identify the impact of a healthy lifestyle intervention on children diagnosed with obesity.
- Childhood Obesity in the US From an Economic Perspective Looking at the problem of childhood obesity from an economic point of view offers an understanding of a wider range of causes and the definition of government intervention.
- Childhood Obesity and Nutrition The prevalence of childhood obesity in schools can be compared to an epidemic of a virulent disease on a global scale.
- Childhood Obesity Prevention: Physical Education and Nutrition The paper examines how physical education in schools can prevent child obesity and how to educate parents about the importance of proper nutrition.
- Eating Fast Food and Obesity Correlation Analysis The proposed study will attempt to answer the question of what is the relationship between eating fast food and obesity, using correlation analysis.
- Obesity Rates and Global Economy The process of obesity in modern society is undoubtedly a severe obstacle to the development of the global economy, as well as to the achievement of its sustainability.
- Food Ads Ban for Childhood Obesity Prevention In order to prevent childhood obesity, it is necessary to ban food ads because they have adverse effects on children’s food preferences, consumption, and purchasing behaviors.
- Addressing Teenage Obesity in America The paper states that adolescence is one of the most crucial developmental phases of human life during which the issue of obesity must be solved.
- Obesity in the World: the Prevalence, Its Effects to Human Health, and Causes There are various causes of obesity ranging from the quantity of food ingested to the last of physical exercises that utilize the accumulated energy.
- Childhood Obesity: Problem Analysis The introduced project addresses childhood obesity problem and highlights the inconsistency between the existing programs and their implementation in real life.
- Prevention of Obesity in Teenagers This paper aims to create an education plan for teenage patients and their parents to effectively inform them and help them avoid obesity.
- Obesity Prevention: Social Media Campaign A variety of programs aimed at reducing the risk of obesity has been suggested by healthcare practitioners and scholars. Among them, diet interventions are highly popular.
- Childhood Obesity and Public Policies in England The study identifies the preventive measures of the English government to deal with childhood obesity and compares the trends in England with the rest of the UK.
- The Role of Nurses in the Problem of Obesity Nurses cannot control people’s daily activities, but they can educate people regarding the principles of a healthy lifestyle to avoid risks of developing cardiovascular diseases.
- Childhood Obesity and Socio-Ecological Model Childhood obesity can be significantly reduced through a public health intervention grounded in the socio-ecological model.
- Technological Progress as the Cause of Obesity Obesity is the increase of the body’s weight over the natural limit because of accumulated fats. Technology is a cost to the lost creativity and control over the required healthy lifestyle.
- The Science Behind Obesity and Its Impact on Cancer The paper addresses the connection between cancer and physical activity, diet, and obesity in Latin America and the USA. The transitions in dietary practices may be observed.
- Impact of Obesity on Healthcare System Patients suffering from obesity suffer immensely from stigma during the process of care due to avoidance which ultimately affects the quality of care.
- Childhood Obesity: Medical Complications and Social Problems The children have also suffered from the adverse effects that have been instilled into our society. Obesity has become a common problem in children of American and European countries.
- Depression and Other Antecedents of Obesity Defeating the inertia about taking up a regular programme of sports and exercise can be a challenging goal. Hence, more advocacy campaigns focus on doing something about obesity with a more prudent diet.
- Adolescent Obesity: Theories and Interventions This paper explores the issue of adolescent obesity and provides a cohesive action plan to propose how to remedy barriers to the success of implemented interventions.
- Physical Exercises as Obesity Treatment Exercise cannot be considered an effective tool for weight loss, but it does help individuals to maintain their normal and healthy weight.
- The Role of Family in Childhood Obesity Families and healthcare providers develop numerous interventions in order to provide their children with a chance to avoid obesity complications.
- Obesity Interventions and Nursing Contributions Detecting health problems that may affect children later in their adulthood is worthwhile. This paper reviews roles of nurses’ actions in replacing obesity with wellness.
- Childhood Obesity: Prevention and Mitigation Over the past three decades, childhood obesity has developed into an epidemic and is considered as one of the major health issues in the world.
- Obesity in Miami-Dade Children and Adults The problem of childhood obesity is rather dangerous and may produce a short-term and long-term effect on young patients’ social, emotional, and physical health.
- Humanistic Theory in Childhood Obesity Research The humanistic theory will assist in research investigating how the use of dieting and parental supervision can help to resolve the issue of obesity.
- Childhood Obesity During the COVID-19 Pandemic While the COVID-19 pandemic elicited one of the worst prevalences of childhood obesity, determining its extent was a problem due to the lockdown.
- Trending Diets to Curb Obesity There are many trending diets that have significant effects on shedding pounds; however, the discourse will focus on the Mediterranean diet.
- Dealing with Obesity as a Societal Concern This essay shall discuss the health issue of obesity, a social health problem that is, unfortunately, growing at a rapid rate.
- Health Psychology and Activists’ Views on Obesity This paper examines obesity from the psychological and activists’ perspectives while highlighting some of the steps to be taken in the prevention and curbing of the disease.
- Care Plan: Quincy Town, Massachusetts With Childhood Obesity This study will develop a community assessment program based on the city with the aim of creating a care plan for tackling the issue of child obesity in the town.
- Obesity in Hispanic American Citizens The issue of obesity anong Hispanic Americans occurs as a result of poor dieting choices caused by misinformed perceptions of proper eating.
- Obesity: Cause and Treatment The sphere of contemporary medicine faces the problem of obesity as a troublesome trend that proceeds to embrace the global citizens.
- Screen Time and Pediatric Obesity Obese and overweight children have a high likelihood of proceeding with the problem into adulthood, in addition to the threat of chronic illnesses.
- Technology as the Cause of Obesity Today, humanity witnesses the third industrial revolution, or the broad implementation of innovative solutions into various spheres of activity.
- How to Reduce Obesity and Maintain Health? Health is becoming a matter of grave concern, especially the health of teenagers and adolescents, who are becoming increasingly overweight and obese.
- Approaches to Childhood Obesity Treatment As parents have a decisive influence on children as well as their dietary and activity patterns, it is only logical that education interventions must be aimed at them and not just the child.
- Motivational Interviewing in Obesity Reduction: Statistical Analysis The research determines the effect the methods like motivational interviews and specific web tools will have on people suffering from different degrees of obesity.
- Obesity in Miami as a Policy-Priority Issue Obesity is a health condition associated with unhealthy eating practices. Many states in the US have outlined obesity as one of the health issues affecting their citizens.
- Childhood Obesity Causes: Junk Food and Video Games The problem of “competitive foods and beverages” that are sold in schools outside the existing breakfast and lunch programs has been discussed for a while now.
- Diet and Lifestyle vs Surgery in Obesity Treatment The research would assess the effectiveness of dietary interventions and lifestyle changes in comparison with the bariatric surgery to determine the methods’ advantages.
- Childhood Obesity Risks, Reasons, Prevention In the modern world, obesity is the most widely spread health problem among children. That is why it should be the primary concern of the public.
- Fast Food as a Cause of Obesity in the US and World In the contemporary rapidly developing world people are always on the move. They want to save time whenever it is possible.
- Betty Neuman’s System Model for Adult Obesity Betty Neuman’s system model can beneficially influence a physical and emotional state of the person who is experiencing difficulties with being overweight.
- Obesity Education Plan for Older Adults The given paper presents an obesity education plan targeted at adults and older adults who are overweight or obese and, therefore, are at risk of developing various diseases.
- Childhood Obesity, Social Actions and Intervention This literature review presents the major social actions and family-based interventions that have been in use to address the problem of obesity in children.
- Childhood Obesity and Overweight Issues The paper discusses childhood obesity. It has been shown to have a negative influence on both physical health and mental well-being.
- Childhood Obesity: Quantitative Annotated Bibliography Childhood obesity is a problem that stands especially acute today, in the era of consumerism. Children now have immense access to the Internet.
- Behavioral Modifications for Patients With Obesity This paper aims to find out in obese patients, do lifestyle and behavioral changes, compared to weight loss surgery, improve patients’ health and reduce complications.
- Obesity, Diabetes and Self-Care The paper discusses being overweight or obese is a high-risk factor for diabetes mellitus and self-care among middle-aged diabetics is a function of education and income.
- The Effects of Gender on Child Obesity The high percentage of women’s obesity prevalence is a result of poor nutrition in childhood and access to greater resources in adulthood.
- Obesity Problem in the United States Obesity is not just people going fat; it is a disease that causes maladies like type-2 diabetes, heart disease, cancer and strokes.
- Should fast-food restaurants be liable for increasing obesity rates?
- Does public education on healthy eating reduce obesity prevalence?
- Is obesity a result of personal choices or socioeconomic circumstances?
- Should the government impose taxes on soda and junk food?
- Weight loss surgery for obesity: pros and cons.
- Should restaurants be required to display the caloric content of every menu item?
- Genetics and the environment: which is a more significant contributor to obesity?
- Should parents be held accountable for their children’s obesity?
- Does weight stigmatization affect obesity treatment outcomes?
- Does the fashion industry contribute to obesity among women?
- Eating Healthy and Its Link to Obesity A careful analysis will reveal that obesity is a silent killer, and that it has created an unnecessary pressure in the U.S.
- Childhood Obesity: Research Methodology Based on their body mass index measurement or diagnosis by a qualified physician, all children in the sample should be qualified as having obesity.
- Obesity Prevention in Community: Strategic Plan This paper is a plan of how to change the way the community should treat obesity and improve people’s health through the required number of interventions.
- Childhood Obesity Prevention: The Role of Nursing Education Nurse practitioners have to deal with childhood obesity challenges and identity healthy physical and environmental factors to help pediatric patients and their parents.
- Pediatric Obesity and Self-Care Nursing Theory The presence of excess body fat in children has to be given special consideration since healthy childhood is a prerequisite to normal physical and psychological maturation.
- Childhood Obesity Interventions: Data Analysis The described analysis of research variables will make it possible to test the research and null hypotheses and contribute to the treatment of obesity in children.
- Obesity in School-Aged Children as a Social Burden In addition to personal concerns, overweight and obese children are at risk for long-term health consequences, including cardiovascular problems and additional comorbidities.
- Childhood Obesity and Public Health Intervention Childhood obesity can be significantly reduced through a public health intervention grounded in the socio-ecological model, in particular, parents’ active participation.
- Treat and Reduce Obesity Act and Its Potential The paper discusses the background, processing, and potential consequences of a Congress bill presented as H.R.1953: Treat and Reduce Obesity Act of 2017.
- Advocacy Campaign: Childhood Obesity This paper will review two articles studying different advocacy campaigns: a community-based approach and a youth-led intervention for childhood obesity.
- Ways of Treating Obesity in Older Patients The researching obesity management and treatment in older adults is important, as it could help to raise the quality of life of the elderly.
- Evidence Based Practice Related to Patient Obesity An effective weight management plan should be designed to tackle the health problem. The plan should also be implemented using desirable processes.
- Obesity, Its Contributing Factors and Consequences Obesity is one of the issues that are often discussed by medical workers and researchers. This topic has been chosen for several reasons.
- Children Obesity Research Method and Sampling This paper presents a research method and sampling on the investigation of the issue of childhood obesity and the impact parents` education might have on reducing excess weight.
- Childhood Obesity: A Global Public Health Crisis Karnik and Kanekar try to show the threatening tendency towards the deterioration of children`s health and the actions that should be performed to change the situation.
- Obesity in African Americans: Prevention and Therapy According to the official statistics, African American people present the group of American citizens which is the most susceptible to obesity.
- Food Allergies and Obesity This short research paper will examine how food allergies can lead to food addiction that can cause obesity in individuals suffering from these allergies.
- Obesity: High Accumulation of Adipose Tissue It is important to point out that obesity is a complex and intricate disease that is associated with a host of different metabolic illnesses.
- Obesity and Iron Deficiency Among College Students The study seeks to establish the relationship between obesity and iron deficiency by analyzing the serum hepcidin concentration among individuals aged between 19 to 29 years.
- Overweight and Obesity Prevalence in the US Obesity is a significant public health problem recognized as one of the leading causes of mortality in the United States. Obesity and overweight are two common disorders.
- Obesity Screening Training Using the 5AS Framework The paper aims to decrease obesity levels at the community level. It provides the PCPs with the tools that would allow them to identify patients.
- Prevalence and Control of Obesity in Texas Obesity has been a severe health issue in the United States and globally. A person is obese if their size is more significant than the average weight.
- Nutrition: Obesity Pandemic and Genetic Code The environment in which we access the food we consume has changed. Unhealthy foods are cheaper, and there is no motivation to eat healthily.
- Preventing Obesity Health Issues From Childhood The selected problem is childhood obesity, the rates of which increase nationwide yearly and require the attention of the government, society, and parents.
- Describing the Problem of Childhood Obesity Childhood obesity is a problem that affects many children. If individuals experience a health issue in their childhood, it is going to lead to negative consequences.
- Researching of Obesity in Florida It is important to note that Florida does not elicit the only state with an obesity problem, as the nation’s obesity prevalence stood at 42.4% in 2018.
- Preventing Obesity Health Issues From the Childhood The paper is valuable for parents of children who are subject to gaining excess weight because the report offers how to solve the issue.
- The Role of Social Workers in Addressing Teenage Obesity The social worker should be the bridge uniting obese individuals and society advertising social changes, and ending injustice and discrimination.
- Obesity and Health Outcomes in COVID-19 Patients The COVID-19 pandemic has posed many challenges over the last three years, and significant research has been done regarding its health effects and factors.
- Childhood Obesity in the US from Economic Perspective The economic explanation for the problem of childhood obesity refers to the inability of a part of the population to provide themselves and their children with healthy food.
- Obesity in the United States of America The article discusses the causes of the obesity pandemic in the United States of America, which has been recognized as a pandemic due to its scope, and high prevalence.
- The Problem of Childhood Obesity Obesity in childhood is a great concern of current medicine as the habits of healthy eating and lifestyle are taught by parents at an early age.
- Oral Health and Obesity Among Adolescents This research paper developed the idea of using dental offices as the primary gateway to detect potential obesity among Texas adolescents.
- Obesity, Weight Loss Programs and Nutrition The article addresses issues that can help increase access to information related to the provision of weight loss programs and nutrition.
- Obesity From Sociological Imagination Viewpoint Most obese individuals understand that the modern market is not ready to accept them due to negative sociological imagination.
- The Current Problem of Obesity in the United States The paper raises the current problem of obesity in the United States and informs people about the issue, as well as what effect obesity can have on health.
- Childhood and Adolescent Obesity and Its Reasons Various socio-economic, health-related, biological, and behavioral factors may cause childhood obesity. They include an unhealthy diet and insufficient physical activity and sleep.
- Pediatric Obesity and Its Treatment Pediatric obesity is often the result of unhealthy nutrition and the lack of control from parents but not of health issues or hormonal imbalance.
- Issues of Obesity and Food Addiction Obesity and food addiction have become widespread and significant problems in modern society, both health-related and social.
- Diet, Physical Activity, Obesity, and Related Cancer Risk One’s health is affected by their lifestyle, which should be well managed since childhood to set a basis for a healthier adulthood.
- The link between excess weight and chronic diseases.
- The role of genetics in obesity.
- The impact on income and education on obesity risks.
- The influence of food advertising on consumer choices.
- Debunking the myths related to weight loss.
- Obesity during pregnancy: risks and complications.
- Cultural influences on eating patterns and obesity prevalence.
- Community initiatives for obesity prevention.
- The healthcare and societal costs of obesity.
- The bidirectional relationship between sleep disorders and obesity.
- Articles About Childhood Obesity The most straightforward technique to diagnose childhood obesity is to measure the child’s weight and height and compare them to conventional height and weight charts.
- Obesity: Causes, Consequences, and Care Nowadays, an increasing number of people suffer from having excess weight. This paper analyzes the relationship between obesity and other diseases.
- Discussion of Freedman’s Article “How Junk Food Can End Obesity” David Freedman, in article “How Junk Food Can End Obesity”, talks about various misconceptions regarding healthy food that are common in society.
- Obesity Prevention Policy Making in Texas Obesity is a national health problem, especially in Texas; therefore, the state immediately needed to launch a policy to combat and prevent obesity in the population.
- Obesity and How It Can Cause Chronic Diseases Obesity is associated with increased cardiovascular diseases, and cancer risks. The modifications in nutrition patterns and physical activity are effective methods to manage them.
- Physical Wellness to Prevent Obesity Heart Diseases Heart disease remains to be one of the most severe health concerns around the world. One of the leading causes of the condition is obesity.
- Obesity and General State of Public Health Obesity is a condition caused by an abnormal or excessive buildup of fat that poses a health concern. It raises the risk of developing various diseases and health issues.
- Ways of Obesity Interventions The paper discusses ways of obesity interventions. It includes diet and exercise, patient education, adherence to medication, and social justice.
- Obesity, Cardiovascular and Inflammatory Condition Under Hormones The essay discusses heart-related diseases and obesity conditions in the human body. The essay also explains the ghrelin hormone and how it affects the cardiovascular system.
- Aspects of Obesity Risk Factors Obesity is one of the most pressing concerns in recent years. Most studies attribute the rising cases of obesity to economic development.
- Obesity in Adolescence in the Hispanic Community The health risks linked to Hispanic community adolescent obesity range from diabetes, heart problems, sleep disorders, asthma, and joint pain.
- Obesity as a Wellness Concern in the Nursing Field A critical analysis of wellness can provide an understanding of why people make specific health-related choices.
- Physio- and Psychological Causes of Obesity The paper states that obesity is a complex problem in the formation of which many physiological and psychological factors are involved.
- How Junk Diets Can Reduce Obesity To control obesity there is a need to ensure that the junk foods produced are safe for consumption before being released into the foods market.
- The Problem of Obesity: Weight Management Obesity is now a significant public health issue around the world. The type 2 diabetes, cardiac conditions, stroke, and metabolism are the main risk factors.
- Sleep Deprivation Effects on Adolescents Who Suffer From Obesity The academic literature on sleep deprivation argues that it has a number of adverse health effects on children and adolescents, with obesity being one of them.
- Hypertensive Patients Will Maintain Healthy Blood Pressure and Prevent Obesity Despite hypertension and obesity are being major life threats, there are safer lifeways that one can use to combat the problem.
- The Consequences of Obesity: An Annotated Bibliography To review the literature data, the authors searched for corresponding articles on the PubMed database using specific keywords.
- Evolving Societal Norms of Obesity The primary individual factors that lead to overeating include limited self-control, peer pressure, and automatic functioning.
- Obesity: Racial and Ethnicity Disparities in West Virginia Numerous social, economic, and environmental factors contribute to racial disparities in obesity. The rates of obesity vary depending on race and ethnicity in West Virginia.
- The Worldwide Health Problem: Obesity in Children The paper touch upon the main causes of obesity, its spread throughout the world, the major effects of the condition and ways of prevention.
- Mental Stability and Obesity Interrelation The study aims to conduct an integrative review synthesizing and interpreting existing research results on the interrelation between mental stability and obesity.
- Crutcho Public School: Obesity in School Children Numerous school children at Crutcho Public elementary school, Oklahoma City, are obese revealing how obesity is a threat to that community.
- Obesity in Low-Income Community: Diet and Physical Activity The research evaluates the relationship between family earnings and physical activity and overweight rates of children in 8 different communities divided by race or ethnicity.
- Adolescent Obesity in the United States The article reflects the problem of overweight in the use, a consideration which the authors blame on influential factors such as age and body mass index.
- Obesity Problem Solved by Proper Nutrition and Exercise Most people who suffer from obesity are often discouraged to pursue nutrition and exercise because their bodies cannot achieve a particular look.
- Girls with Obesity: Hospital-Based Intervention This paper includes a brief description of a hospital-based intervention targeting middle-school girls with obesity.
- Hispanic Obesity in the Context of Cultural Empowerment This paper identifies negative factors directly causing obesity within the Hispanic people while distinguishing positive effects upon which potential interventions should be based.
- Childhood Obesity Teaching Experience and Observations The proposed teaching plan aimed at introducing the importance of healthy eating habits to children between the ages of 6 and 11.
- Exercise for Obesity Description There are numerous methods by which obesity can be controlled and one of the most effective ways is through exercising.
- Obesity and Disparity in African American Women Several studies indicate that the rate of developing obesity is the highest in African American populations in the US.
- Factors Increasing the Risk of Obesity The consumption of fast food or processed products is one of the major factors increasing the risk of obesity and associated health outcomes.
- Childhood Obesity in Modern Schools Most schools have poor canteens with untrained staff and poor equipment for workers. That’s why they can’t cook quality food and offer better services to students.
- Effectiveness of a Diet and Physical Activity on the Prevention of Obesity Research indicates that obesity is the global epidemic of the 21st century, especially due to its prevalent growth and health implications.
- Community Obesity and Diabetes: Mississippi Focus Study The paper provides a detailed discussion of the correct method to be used in the state of Mississippi to control and avoid obesity and diabetes issues.
- Multicausality: Reserpine, Breast Cancer, and Obesity All the factors are not significant in the context of the liability to breast cancer development, though their minor influence is undeniable.
- The Home Food Environment and Obesity-Promoting Eating Behaviours Campbell, Crawford, Salmon, Carver, Garnett, and Baur conducted a study to determine the associations between the home food environment and obesity.
- The Problem of Childhood Obesity in the United States Childhood obesity is one of the reasons for the development of chronic diseases. In the US the problem is quite burning as the percentage of obese children increased significantly.
- Children Obesity in the United States Together with other problems and illnesses, obesity stands as one of the main difficulties in modern societies.
- The Situation of Obesity in Children in the U.S. The paper will discuss the situation of obesity in Children in the U.S. while giving the associated outcomes and consequences.
- Childhood Obesity and Healthy Lifestyles
- Screen Time and Pediatric Obesity Among School-Aged Children
- Policymaker Visit About the Childhood Obesity Problem
- Public Health Interventions and Economics: Obesity
- Obesity Overview and Ways to Improve Health
- Nursing: Issue of Obesity, Impact of Food
- Childhood Overweight and Obesity
- Childhood Obesity as an International Problem
- Obesity Negative Influence on Public Health
- Problematic of Obesity in Mexican Americans
- Child Obesity Problem in the United States
- Screen Time and Pediatric Obesity in School-Aged Children
- Obesity Treatment – More Than Food
- Effects of Exercise on Obesity Reduction in Adults
- The Problem of Obesity in the Latin Community
- Obesity Prevention in Ramsey County, Minnesota
- Childhood Obesity and Its Potential Prevention
- Non-Surgical Reduction of Obesity and Overweight in Young Adults
- Obesity Prevention Due to Education
- Physical Activity and Obesity in Children by Hills et al.
- The Best Way to Address Obesity in the United States
- Nursing Diabetes and Obesity Patients
- Obesity Problem Description and Analysis
- The Issues with Obesity of Children and Adolescents
- Obesity in People with Intellectual Disabilities’: The Article Review
- Non-Surgical Reduction of Obesity in Young Adults
- Obesity in Children in the United States
- Childhood Obesity in Ocean Springs Mississippi
- The Problem of Children Obesity
- “Physical Activity and Obesity in Children” by A. P. Hills
- “Physical Activity and Obesity in Children” by Hills
- The Current State of Obesity in Children Issue
- Effects of Obesity on Human Lifespan Development
- Obesity and High Blood Pressure as Health Issues
- Adult Obesity: Treatment Program
- The Prevention of Childhood Obesity in Children of 1 to 10 Years of Age
- Obesity as a Major Health Concern in the United States
- Janet Tomiyama’s “Stress and Obesity” Summary
- A Dissemination Plan on Adolescent Obesity and Falls in Elderly Population
- The Issue of Obesity: Reasons and Consequences
- “Obesity and the Growing Brain” by Stacy Lu
- Obesity Disease: Symptoms and Causes
- Obesity Among Mexican-American School-Age Children in the US
- Obesity as a One of the Major Health Concerns
- Obesity: Diet Management in Adult Patients
- Children’s Obesity in the Hispanic Population
- Prevention of Childhood Obesity
- Assessing Inputs and Outputs of a Summer Obesity Prevention Program
- Designing a Program to Address Obesity in Florida
- Widespread Obesity in Low-Income Societies
- Health Policy: Obesity in Children
- Youth Obesity In Clark County in Vancouver Washington
- Obesity in Clark County and Health Policy Proposal
- Obesity: Is It a Disease?
- Clark County Obesity Problem
- Obesity Action Coalition Website Promoting Health
- How to Address Obesity in the United States
- The Epidemic of Obesity: Issue Analysis
- Child Obesity in North America
- Personal Issues: Marriage, Obesity, and Alcohol Abuse
- Obesity in Children: Relevance of School-Based BMI Reporting Policy
- Obesity in the United States: Defining the Problem
- Obesity in Children in the US
- Childhood Obesity: Issue Analysis
- Data Mining Techniques for African American Childhood Obesity Factors
- Researching Childhood Obesity Issues
- Infant Feeding Practices and Early Childhood Obesity
- Prevalence of Obesity and Severe Obesity in U.S. Children
- Problem of Obesity: Analytic Method
- Obesity as National Practice Problem
- Obesity Management: Hypothesis Test Study
- Practice Problem of the Obesity in United States
- Exercise for Obesity Management: Evidence-Based Project
- Obesity in African-American Women: Methodology
- The Epidemiology of Obesity
- Pediatric Obesity Study Methodology
- Adult Obesity Causes & Consequences
- Community Health: Obesity Prevention
- Obesity Treatment in Primary Care: Evidence-Based Guide
- Childhood Obesity and Mothers’ Education Project
- Childhood Obesity Research Critiques
- Childhood Obesity: Medication and Parent Education
- Obesity Caused by Fast-Food as a Nursing Practice Issue
- Cardiometabolic Response to Obesity Treatment
- Childhood Obesity Study: Literature Review
- Obesity Among the Adult Population: Research Planning
- Research and Global Health: Obesity and Overweight
- Childhood Obesity as a Topic for Academic Studies
- Adolescent Obesity Treatment in Primary Care
- The Issues of Childhood Obesity: Overweight and Parent Education
- Childhood Obesity and Parent Education: Ethical Issues
- Obesity Reduction and Effectiveness of Interventions
- Obesity Counteractions in Clark County, Washington
- Childhood and Adult Obesity in the US in 2011-12
- Anti-Obesity Project’s Sponsors in the USA
- Obesity Prevention Advocacy Campaigns
- Childhood Obesity Study, Ethics, and Human Rights
- Childhood Obesity, Demographics and Environment
- Childhood Obesity and Self-Care Deficit Theory
- Overweight and Obesity in 195 Countries Since 1980
- Childhood Obesity and American Policy Intervention
- Efficient Ways to Manage Obesity
- Childhood Obesity and Healtcare Spending in the US
- Childhood Obesity, Medical and Parental Education
- Nursing Role in Tackling Youth Obesity
- Childhood Obesity: Problem Issues
- Adolescent Obesity and Parental Education Study
- Childhood Obesity: Data Management
- Obesity Prevention and Patient Teaching Plan
- “Management of Obesity” by Dietz et al.
- Nutrition and Obesity: Management and Prevention
- Obesity, Diet Modification and Physical Exercises
- Obesity, Its Definition, Treatment and Prevention
- Childhood Obesity and Eating Habits in Low-Income Families
- Obesity: Society’s Attitude and Media Profiling
- Childhood Obesity and Family’s Responsibility
- Childhood Obesity: Parental Education vs. Medicaments
- Childhood Obesity and Healthy Lifestyle Education
- Childhood Obesity and Health Promoting Schools Program
- Obesity Prevention and Education in Young Children
- Childhood Obesity: The Relationships Between Overweight and Parental Education
- Obesity, Its Demographics and Health Effects
- Obesity Treatment: Surgery vs. Diet and Exercises
- Child Obesity as London’s Urban Health Issue
- Childhood Obesity Problem Solution
- Obesity Prevention in Young Children: Evidence-Based Project
- Obesity as American Social Health Issue
- Prevalence of Childhood and Adult Obesity in the US
- The Role of Nurses in the Obesity Problem
- The Issue of Obesity in Youth in the U.S.
- Obesity Among Children of London Borough of Southwark
- Childhood Obesity Risks and Preventive Measures
- Life Expectancy and Obesity Health Indicators
- The Overuse of Antibiotics and Its Role in Child Obesity
- Children and Adolescents With Obesity: Physical Examination
- Obesity in the United States: Learning Process
- Pharmacotherapy for Childhood Obesity
- “Let’s Move” Intervention for Childhood Obesity
- Obesity Prevention in Childhood
- Patient Education for Obesity Treatment
- Childhood Obesity Prevention Trends
- Obesity Prevention in Young Children in US
- Wellness, Academics & You: Obesity Intervention
- Childhood Obesity, Health and Psychological State
- Parents’ Education in Childhood Obesity Prevention
- Childhood Obesity in the US
- Childhood Obesity and Its Solutions
- Obesity Problem among the Adult Population
- Obesity Education in Social Media for Children
- Childhood Obesity and Governmental Measures
- Childhood Obesity Research and Ethical Concerns
- Obesity among the Adult Population
- Multimodal-Lifestyle Intervention for Obesity
- Technological Education Programs and Obesity Prevention
- Childhood Obesity and Independent Variable in Parents
- Childhood Obesity, Its Definition and Causes
- Public Health Initiative for Childhood Obesity
- Childhood Obesity in the US: Factors and Challenges
- Obesity: Genetic, Hormonal and Environmental Influences
- The Problem of Obesity in the USA
- Childhood Obesity in the USA
- Prevention of Obesity in Children
- Racial and Ethnic Trends in Childhood Obesity in the US
- Diabetic Patients with Obesity or Overweight
- Age and Gender in Childhood Obesity Prevention
- Childhood Obesity and Public Health Interventions
- Obesity in Florida and Prevention Programs
- Obesity in Afro-Americans: Ethics of Intervention
- Helping Children with Obesity and Health Risks
- Healthy Nutrition: Obesity Prevention in Young Children
- Myocardial Infarction, Obesity and Hypertension
- Childhood Obesity and Parent Education
- Obesity’s Effect on Children and Elderly People
- Childhood Obesity and Community Nursing Intervention
- Obesity Trends Among Non-Hispanic Whites and Blacks
- Family-Based Childhood Obesity and Parental Weight
- Childhood Obesity and Depression Intervention
- Problem of the Childhood Obesity
- Advocacy Campaign: the Problem of Childhood Obesity
- Childhood Obesity and Control Measures in the US
- Decreasing Obesity in Jewish Children
- Nutrition: Obesity Epidemics in America
- Fast Food and Obesity Link – Nutrition
- Dairy Products Consumption and Obesity – Nutrition
- Nutrition Issues: Obesity and Breastfeeding
- The Evidence of Association between Iron Deficiency and Childhood Obesity
- Childhood Obesity: a Population Health Issue
- Nutrition: Fighting the Childhood Obesity Epidemic
- What Factors Causes Obesity?
- What Are Five Problems With Obesity?
- Can the Government Help the Obesity Issue?
- What Are the Three Dangers of Obesity?
- What Are Ten Health Problems Associated With Obesity?
- Are the Parents to Blame for Childhood Obesity?
- What Are the Social Effects of Obesity?
- Does Adolescent Media Use Cause Obesity and Eating Disorders?
- How Is Obesity Affecting the World?
- How Does Obesity Impact Quality of Life?
- Does Society Affect America’s Obesity Crisis?
- How Does Obesity Affect You Mentally?
- How Does Obesity Impact Children?
- How Does Obesity Affect Self-Esteem?
- How Does Obesity Cause Depression?
- Are First Generation Mexican Children More Prone to Obesity Than Their Second Generation Counterparts?
- Should Fast Food Companies Be Held Responsibility for Children’s Obesity?
- Does Obesity Cause Mood Swings?
- What Are the Causes and Effects of Childhood Obesity?
- Is Obesity a Mental or Physical Illness?
- What Comes First: Depression or Obesity?
- What Makes Obesity Dangerous?
- Which European Country Has the Highest Rate of Obesity?
- What Is the Obesity Rate in Africa?
Cite this post
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2021, September 9). 394 Obesity Essay Topics & Research Questions + Examples. https://studycorgi.com/ideas/obesity-essay-topics/
"394 Obesity Essay Topics & Research Questions + Examples." StudyCorgi , 9 Sept. 2021, studycorgi.com/ideas/obesity-essay-topics/.
StudyCorgi . (2021) '394 Obesity Essay Topics & Research Questions + Examples'. 9 September.
1. StudyCorgi . "394 Obesity Essay Topics & Research Questions + Examples." September 9, 2021. https://studycorgi.com/ideas/obesity-essay-topics/.
Bibliography
StudyCorgi . "394 Obesity Essay Topics & Research Questions + Examples." September 9, 2021. https://studycorgi.com/ideas/obesity-essay-topics/.
StudyCorgi . 2021. "394 Obesity Essay Topics & Research Questions + Examples." September 9, 2021. https://studycorgi.com/ideas/obesity-essay-topics/.
These essay examples and topics on Obesity were carefully selected by the StudyCorgi editorial team. They meet our highest standards in terms of grammar, punctuation, style, and fact accuracy. Please ensure you properly reference the materials if you’re using them to write your assignment.
This essay topic collection was updated on January 21, 2024 .

Responsibility
Unravelling the Link Between Socioeconomic Status and Obesity

- Share on LinkedIn
- Share on Facebook
- Share on Twitter
- Share via Email
- Download PDF
The world is getting bigger, quite literally. By 2035, just over half of humankind will be overweight or obese , with associated costs on the global economy.
As complex and multifaceted a disease as obesity is, its link with socioeconomic status is clear: Obesity is more common among people of lower socioeconomic standing. In the United Kingdom , for example, obesity is nearly twice as common in the country’s most deprived regions than its least deprived (36 percent vs. 20 percent).
The question is why.
Research has identified five factors as possible links between modern-day obesity and socioeconomic status: stress, temporal focus or whether one is focused on the past or the future, well-being expectations, time spent outdoors and food scarcity. However, studies typically examine only one or two factors at a time and not the relative importance of all five. In addition, past research has typically been cross-sectional, meaning it examined data in a single point in time, which limits the ability to infer causality.
The Covid-19 pandemic threw up the rare opportunity to probe these mechanisms and their impact on weight gain over time. In a study published in the Journal of the Association for Consumer Research, we found that people of lower socioeconomic status gained more weight than the higher-status ones during the pandemic, further exacerbating the existing association between socioeconomic status and obesity.
Significantly, we found that this was driven by a higher level of stress among people with a lower socioeconomic status, and not by any of the other four factors. Our research also indicates that stress drives weight gain because it leads people to eat more, eat less healthily and exercise less .
Lower status, higher stress
We launched the study shortly after the outbreak of the coronavirus pandemic. We surveyed a total of 892 Americans three times between March and May 2020 (see graphic below), and a final time 18 months later, in November 2021.

Notably, we asked participants to indicate their socioeconomic status – in terms of financial wealth, education and job – on a 10-point ladder, with 10 being the highest. As it happens, past research shows that self-assessed social standing and perceived inequality may be stronger determinants of health outcomes than objective measures such as income .
We assessed respondents’ stress levels by asking them to indicate how often each of eight statements, such as “I find myself getting agitated”, described them. Temporal focus was measured by items such as “I replay memories of the past in my mind” and “I focus on my future”. Well-being expectations were measured by respondents indicating where they thought they would stand on a 10-point ladder scale, with 10 representing their best possible life, in a year’s time.
Analyses of the responses revealed that, in the early, chaotic months of the pandemic, lower-status respondents gained more weight than higher-status ones. This was brought on by a higher level of stress and not by respondents being less focused on the future, having worse expectations about the future, spending less time outdoors or being deprived of food.
Sadly, lower-status respondents continued to display elevated stress 20 months into the crisis. Meanwhile those of higher status, who suffered less strain to begin with, experienced significantly less stress. People who initially reacted to the pandemic by eating more, eating less healthily and exercising less were likely to still be doing so 20 months later, while those who ate less and better and exercised more also persisted with their new habits. As a result, those who gained weight retained most of the extra pounds whereas those who lost weight kept it off.

Healthy nudges for the less privileged
A similar association between stress and weight gain during Covid-19 has been observed in a separate study involving British participants. Taken together, that study and ours suggest that although Covid-19 is no longer a global health emergency, it is likely to cast a long shadow in the form of worsened health inequalities by fuelling elevated, chronic stress among lower-status members of society. For not only does stress lead to weight gain and possibly obesity over time, it is also associated with inflammations that can cause diseases such as cancer and diabetes, and impact general health.
Our study offers takeaways for the ongoing, long-term war on obesity. The first is that governments and responsible corporations should design interventions with socioeconomic differences in mind. These might include measures that directly target higher and persistent levels of stress among the less-privileged, as well as behavioural nudges or programmes that offer financial rewards for engaging in healthy behaviours, since monetary incentives appear to be particularly effective among this demographic. Think discount coupons, rather than cognitive nudges like nutritional labelling .
Health authorities might also look into tightening regulations around marketing tactics designed to frame nutritionally poor food as healthy , in light of Pierre's recent research that shows that people with obesity are more responsive to these tactics than those of normal weight.
Our findings hopefully shed light on the strong albeit complex link between socioeconomic status and obesity. The sobering fact is that the less advantaged among us are also more vulnerable to stress, weight gain and a whole host of adverse health outcomes, including being sickened by the coronavirus. These factors in turn trigger more stress and eventually a vicious spiral. More research on the underlying causes of the stress and measures to tackle them will go a long way towards alleviating health inequalities.
About the author(s)
Pierre Chandon
is the L’Oréal Chaired Professor of Marketing - Innovation and Creativity at INSEAD and the Director of the INSEAD-Sorbonne Université Behavioural Lab .
Maria Langlois
is an Assistant Professor in Marketing at the Cox School of Business, Southern Methodist University, in the United States. She obtained her PhD at INSEAD.
About the research
"Inequality, Stress, and Obesity: Socioeconomic Disparities in the Short- and Long-Term Effects of the COVID-19 Pandemic" is published in Journal of the Association for Consumer Research.
Related Tags
About the series, healthcare management, share this post, view comments.
18/08/2023, 07.38 pm
I found this article to be incredibly enlightening. It's crucial to understand the complex relationship between socioeconomic status and obesity. Well-researched and thought-provoking!
- Log in or register to post comments
Leave a Comment
Please log in or sign up to comment., related reads.

Weight Loss Surgery Reduces Susceptibility to Food Marketing
H. Plassman, P. Chandon

How Focusing on the Pleasure of Eating Can Reduce Obesity

Overcoming Obesity: Can Big Food Help?

Our website has a lot of features which will not display correctly without Javascript.
Please enable Javascript in your browser
Here how you can do it: http://enable-javascript.com
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Weight Management
- Choosing a Safe & Successful Weight-loss Program
Choosing a Safe & Successful Weight-loss Program
On this page:
What is a weight-loss program?
Is a weight-loss program a good option for me, what should i look for in a weight-loss program, what if the program is offered online, which weight-loss programs should i avoid, what questions should i ask about a weight-loss program, clinical trials for weight-loss programs.
If you’ve been thinking about trying a weight-loss program, you’re not alone. Nearly 3 in 4 U.S. adults (73%) have overweight or obesity , and many would like to lose excess weight. 1
A number of these programs are advertised on social media, the internet, magazines, and other media. But are they safe? And will they work for you?
Here are some tips on how to choose a weight-loss program that may help you lose weight safely. You’ll also learn how to talk with a health care professional about your weight and what questions to ask program staff before you decide to join a weight-loss program.
A weight-loss program is more than a book or app that promises to help you lose weight. It is a formal program that gives you ongoing guidance and support to build healthy lifestyle habits that may promote weight loss. 2 The program should include
- a healthy, reduced-calorie eating and drinking plan
- a plan for increasing physical activity if appropriate
- guidance and support for adopting these lifestyle habits
- a plan for keeping the weight off
If you have overweight or obesity, losing weight may prevent or reduce weight-related problems , such as high blood pressure , heart disease , and diabetes . Losing weight may also improve your quality of life. Ask your health care professional about safe and effective ways to lose weight.
Talk with your health care professional about your weight

Talking with a health care professional about your weight is an important first step. Sometimes, health care professionals may not address issues such as the benefits of choosing healthy food and drinks , physical activity, and weight during a general office visit. You may need to bring up these issues yourself.
If you feel uneasy talking about your weight, practice talking about your concerns before your office visit and bring your questions with you. Sample questions can include
- “Am I at a healthy weight?”
- “How is my weight affecting my health?”
- “Will losing weight improve my general health, as well as specific health problems I have?”
During your visit, your health care professional may
- ask you about your eating, drinking, and physical activity habits
- measure your body mass index (BMI) and other health factors to find out if you are at a healthy weight
- review any medical problems you have and medicines or dietary supplements you take to see whether they may be affecting your weight or your ability to lose weight
Ask about safe and effective ways to lose weight
If your health care professional advises you to lose weight, ask about safe and effective ways to do so. For many adults, treating overweight and obesity starts with lifestyle changes. Your health care professional may work with you to develop a weight-loss program tailored to your needs and preferences. They may also refer you to a registered dietitian or a specific program. If you already have a weight-loss program in mind, ask your health care professional if the program may be a good fit for you.
Overweight and obesity may also be treated with weight-loss medicines and weight-loss surgery , also called metabolic and bariatric surgery. Health care professionals most often recommend lifestyle changes along with medicines or surgery. Ask your health care professional whether you should consider these options.
Successful weight-loss programs promote healthy behaviors that may help you lose weight safely and keep the weight off.
Check for these features in any weight-loss program you are thinking about trying.
Realistic weight-loss goals
Successful weight-loss programs help you set realistic goals for weight loss. Experts recommend an initial weight-loss goal of 5% to 10% of your starting weight within 6 months. 2 For example, if you weigh 200 pounds, your goal may be to lose about 10 pounds in the first 6 months.
A healthy eating plan that is low in calories
Successful weight-loss programs provide guidance and support for adopting a healthy eating plan that is low in calories. Although studies suggest that different eating and drinking plans may promote weight loss, some plans may be better suited for you than others. 3 The best plan is one that is backed by science and is tailored to your health, cultural needs and preferences, and values—so you can stick with it over the long term.
Physical activity plan

The weight-loss program should include a plan for getting regular physical activity . The amount and type of activity will depend on your personal health and ability. Over time, some people may work up to 150 minutes or more per week of aerobic activities—activities that make you breathe harder and make your heart beat faster. 2 Although increased physical activity may not have a big impact on your weight loss, it has important health benefits that are independent of weight loss itself. Physical activity may also help you keep off any weight you lose.
Guidance and support for adopting healthy habits
Successful weight-loss programs help you set specific goals for adopting healthy lifestyle habits and tracking your progress. 2
The program should provide 3,4,5
- counseling on how to develop and stick with healthier lifestyle habits, including how to set goals, address barriers, and overcome setbacks
- support for monitoring your eating, drinking, sleep, and physical activity every day and for checking your weight every week
- regular feedback, monitoring, and support throughout the program—either in person, by phone, online, or using a combination of these approaches
- the option of social support from a group
A plan for keeping the weight off
Maintaining weight loss can be hard. Sticking with your new lifestyle habits is key to long-term success. Strategies that may help prevent weight regain include 3
- following an eating plan appropriate for your new weight
- getting 150 to 300 minutes or more of physical activity per week 6
- monitoring your weight at least once a week
Look for a program that will give ongoing support, such as counseling sessions, for keeping the weight off.
Most weight-loss programs use the internet, smartphones, or other digital devices in some way. But some programs may be delivered fully online or using these devices, with no in-person contact.
Digital weight-loss programs, also called virtual weight-loss programs, are still being researched. Studies suggest that some virtual programs may work if they include the key features described above. 3,7 But researchers are still studying whether virtual weight-loss programs are effective, especially in the long term.
If you’re thinking about joining a virtual weight-loss program, make sure it includes
- weekly sessions, offered online, that are tailored to your personal goals
- support from a trained professional , such as a registered dietitian, health counselor, or lifestyle coach to meet your goals
- a plan to track your progress on changing your lifestyle habits—such as healthy eating and physical activity—using tools such as cellphones, activity counters, and online journals
- regular feedback on your goals, progress, and results provided by a counselor through email, phone, or text messages
- the option of social support from a group through online meetings or chat groups

Whether a program is virtual or in person, you should get as much background as you can before you decide to join. Here are some warning signs to consider.
Too many promises
Stay away from weight-loss programs that make these types of promises
- Lose weight without diet or exercise!
- Lose weight while eating as much as you want of all your favorite foods!
- Lose 30 pounds in 30 days!
- Lose weight in a specific part of your body!
Other warning signs
Other warning signs to look out for include
- very small print, asterisks, and footnotes, which may make it easy to miss important information
- before-and-after photos or personal endorsements that seem too good to be true
Talk with your health care professional about these types of claims. You can report false claims or scams by weight-loss programs to the Federal Trade Commission .
Weight-loss program staff should be able to answer questions about a program’s features, safety, costs, and results.
Do studies show that your program works?
Find out if there is evidence that the program works. If not, you may want to consider a different program.
- Has your program been formally studied to find out if it is safe and effective?
- Have study results been published in a scientific journal?
- Can I get a copy or a link to the study findings?
If you have questions about a study’s findings, discuss the findings with your health care professional.
How does your program work?
- How can your program help me lose weight?
- How long does your program last?
- How is the program delivered? In person? Online? By smartphone?
- Can I change the program to meet my lifestyle, work schedule, and cultural needs and preferences?
How much does your program cost?
- What is the total cost of the program, from beginning to end?
- weekly visits
- food, meal replacements, supplements, or other products
- medical tests
- counseling sessions
- follow-up to maintain the weight I’ve lost
- online chat access
What does your program include?
Healthy eating guidance.
- Do I need to follow a specific meal plan?
- Do I need to track what I eat each day?
- Do I have to buy special meals or supplements? If so, what are the daily or weekly costs?
- Does your program offer healthy meal plan suggestions that are easy for me to follow?
- If your program requires special foods, can I make changes based on my likes, dislikes, cultural preferences, and any food allergies I may have?
Physical activity guidance
- Does your program include a physical activity plan?
- How does your program address different ability levels and intensity of physical activity?
- Do I need to join a gym or structured exercise program?
- Does your program include physical activities that can be done in short periods of time and in different locations—for example, at home, work, or during travel?
- How can your program help me be more physically active and stay motivated?
- Does your program offer one-on-one or group counseling to help me develop and stick with my healthier habits?
- Does your program include a trained coach or counselor who can help me overcome roadblocks and stay on track?
- Will the program help me cope with issues such as stress or social eating, getting enough sleep, changes in work schedules, lack of motivation, and injury or illness?
- Does your program include a plan to help me keep off the weight I’ve lost?
- How long is the weight-loss maintenance program?
- What does the weight-loss maintenance program include?
What kind of education or training do staff members have?
- Does a doctor or other certified health professional run or oversee the program? Can I speak with a doctor or certified health professional if I need to?
- Does the program include certain experts, such as a registered dietitian, mental health counselor, or exercise physiologist?
- What type of certifications, education, experience, and training do staff members have? How long, on average, have most of the staff been working with the program?
- Are your staff members trained in cultural competence?
What results do people in your program typically achieve?
- How much weight does the average person lose?
- How long does the average person keep the weight off?
What are the risks of your program?
- Could the program cause health problems or be harmful to me in any way?
- Is there ongoing input and follow-up to ensure my safety while I’m in the program?
- Will the program’s doctor or staff work with my health care professional if needed—for example, to address how the program may affect an ongoing medical issue?
NIDDK conducts and supports clinical trials in many diseases and conditions, including overweight and obesity. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for weight-loss programs?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of weight-loss programs, such as
- strategies to promote weight loss and help prevent type 2 diabetes
- family-based programs to encourage healthy habits and weight management for parents and children
- new ways to use digital technology to enhance weight-loss programs
- how lifestyle programs can support patients taking weight-loss medications
Find out if clinical studies are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies on weight-loss programs are looking for participants?
You can view a filtered list of federally funded, open, and recruiting clinical studies that focus on weight-loss programs at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your health care provider before you participate in a clinical study.
What have we learned about weight-loss programs from NIDDK-funded research?
NIDDK has supported many research projects to learn more about weight-loss programs, including the Look AHEAD (Action for Health in Diabetes) study. The Look AHEAD study showed that people who had type 2 diabetes as well as overweight or obesity can lose weight and maintain some of that weight loss through a program of intense lifestyle changes, such as healthy eating and increased physical activity. The study also showed that weight loss provides other health benefits, such as better physical mobility and improved blood glucose, blood pressure, and cholesterol levels.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Samuel Klein, M.D., Washington University School of Medicine
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.6(11); 2016

‘Now I care’: a qualitative study of how overweight adolescents managed their weight in the transition to adulthood
Helen sweeting.
1 MRC/CSO Social and Public Health Sciences Unit, Institute of Health and Wellbeing, University of Glasgow,, Glasgow, UK
Emily Smith
2 University Hospital Southampton NHS Foundation Trust, Southampton, UK
Joanne Neary
3 Department of Public Health, Institute of Health and Wellbeing, University of Glasgow, Glasgow, UK
Charlotte Wright
4 School of Medicine, University of Glasgow,, Glasgow, UK
Associated Data
bmjopen-2015-010774supp1.pdf
bmjopen-2015-010774supp2.pdf
bmjopen-2015-010774supp_tables.pdf
A qualitative study of recalled experiences of early adolescent overweight/obesity revealed low levels of weight-related concern. This further analysis aimed to explore weight-related concern and weight-loss efforts as participants transitioned into adulthood.
Design, participants and methods
Participants were 35 young adults from a population-based cohort study who had body mass index (BMI) >95th centile between ages 11 and 15 and participated in semistructured interviews aged 24. At age 24, they were categorised as: ‘ slimmers ’ (N=13) who had lower BMI Z-scores at 24 than their adolescent peak and were not obese (BMI<30 kg/m 2 ); ‘ relapsers ’ (N=8, of whom 2 were morbidly obese (BMI>35 kg/m 2 ) at age 24); ‘ stable ’ (N=3, of whom 1 morbidly obese); and ‘ gainers ’ (N=11, of whom 5 morbidly obese). Themes were identified and coded using NVivo qualitative data analysis software, blind to participants’ current weight status.
Contrasting with the lack of concern recalled in respect of earlier adolescence, weight-related concerns and/or desire to lose weight generally increased around the time of school leaving and almost all participants described some form of exercise (formal/informal) and dietary weight-control strategies. Among ‘slimmers’, there was some (subtle) evidence of more consistent use of exercise, self-monitoring of diet and exercise and of lifestyle changes becoming habitual and/or part of identity. Few participants had accessed professional support. Diet clubs seemed to have been used most by ‘gainers’, some only recently. Labour-market and housing transitions were strong influences, described as facilitating weight losses by some, but increases by others. For some participants, it appeared that weight loss was simply a by-product of these transitions.
Conclusions
In contrast to earlier adolescence, even the heaviest participants tended to show actual weight loss action or preparation for action. The transition to adulthood could thus be a key life stage for interventions.
Strengths and limitations of this study
- This is one of very few qualitative studies, and the first in the UK, to explore reasons why overweight community-based adolescents do or do not lose weight, in the transition to adulthood.
- It subsampled from a longitudinal study with measured body mass index (BMI) at several points in adolescence, enabling objective categorisation of BMI changes over time.
- Our findings resulted from secondary analysis of qualitative data from a study which did not specifically set out to identify some of the highlighted themes.
- Not all adolescent weight changes described by participants were detected by our measurement schedule (eg, some described losing then regaining weight in the years between) and some categorised as ‘slimmers’ had experienced BMI increases since their very lowest point.
Introduction
Adolescent overweight is associated with greatly increased likelihood of adult obesity, 1 but up to a third of obese adolescents do not go on to be obese adults. 2 What is not clear is why and how some overweight/obese adolescents (defined broadly, by the WHO, as those aged 10–19 3 ) lose weight and others do not, 4 and why some adolescents maintain weight loss while others regain weight. The few population-based studies that have examined this question have generally found very limited or inconsistent behavioural differences between adolescent weight losers, gainers and/or maintainers. A national US survey of adolescents found differences in physical activity, but none in reported diet. 5 Two smaller US and New Zealand studies found ‘healthful’ dietary and PA behaviours, and self-monitoring were associated with loss, but specific dietary plans were not 6 7 and a study of female Swedish adolescents found no clear behavioural differences. 8 Analysis of the Scottish cohort from which participants in the present study were drawn found no differences in reported dieting at either 11 or 15 between the continually obese and those who had slimmed. 9
Active initiation of weight loss behaviours requires that overweight/obesity is recognised and perceived as a problem. 10–13 Community-based quantitative studies have shown obese children and adolescents tend to have more negative body image than non-obese peers. 14 15 However, a qualitative UK study found high acceptance of body size among disadvantaged overweight/obese Scottish 13–14 years, 16 while qualitative US and Australian studies have found that adolescents recognise obesity as a societal issue, but not in themselves, and thus have low motivation to implement behavioural changes. 17–19
One reason why so little is known about how young adults view overweight/obesity or approach weight loss is that while it is relatively easy to study adolescents ‘captive’ in school or treatment programmes, they become largely invisible to researchers once they leave school. We have previously reported findings from a qualitative study of young adults nested within a large Scottish cohort study, where participants were well documented as having been overweight/obese in adolescence. This revealed widespread recalled recognition of, but lack of major recalled concern about their overweight/obesity during adolescence, 20 consistent with other studies. 16–19 This data set also included reflections by participants on their lives since adolescence which have not so far been reported. Thus, this new qualitative analysis aimed to explore their transition to adulthood, by examining postschool weight-related concerns, behaviours and experiences related to young adult transitions among 24 year-olds categorised in terms of measured adolescent body mass index (BMI) trajectories and current BMI. Specifically, we considered whether they described more concern about their overweight/obesity in the postschool transition to adulthood and how other aspects of their late adolescent/young adult lives impacted on their weight-related behaviours.
Participants and recruitment
In 2008, 35 young adults (age 24; 17 males; 33 White Scottish and 2 mixed/Asian ethnicity) participated in a study of recalled adolescent experiences of obesity conducted by ES. 21 They were purposively subsampled from the longitudinal West of Scotland 11–16/16+ Study, which obtained data from school pupils at age 11 (N=2586; 93% of issued sample), 13, 15 9 and 19 (N=1256). Height and weight measurements were taken at each stage, allowing calculation of BMI and BMI z-scores 22 and identification of participants with BMI z-scores >95th centile compared with British 1990 growth references 22 between ages 11 and 15, as described previously. 20 21
University of Glasgow ethical approval was obtained for the qualitative substudy and participants completed consent forms, including permission to publish anonymised extracts from their interviews.
Semistructured interviews were conducted by ES and audio-recorded with consent. They began with a picture task designed for this study (paired images of young people with a range of BMIs and diet/exercise behaviours) to stimulate discussion around perceptions of bodies and health. Next, participants were asked to describe themselves and their lives as a teenager and changes as they became young adults. These generally prompted discussion of postschool labour market transitions, health, concerns (including in relation to health/weight), interests and activities, eating patterns and relationships/support (see online supplementary file 1 —interview topic guide and example picture task items).
supplementary file
The interviews were transcribed verbatim and pseudonyms applied. For this paper, a secondary analysis approach was taken. Previous analyses 20 21 meant ES, HS and CW were already familiar with the data set. A researcher with no prior knowledge of the study (JN) familiarised herself with the transcripts, then, with HS and CW, identified themes relating to postschool late adolescent/young adult experiences. Themes, identified deductively (based on previous literature) and inductively (from the data), were coded by JN using NVivo qualitative data analysis software, blind to participant BMI. These were then reviewed with HS and CW and checked against transcripts by HS during write-up of the paper. Separately, CW converted all adolescent BMIs into age-specific and gender-specific Z-scores compared with the UK 1990 reference. 23 24 Age 24 BMIs were converted to Z-scores for age 19.99, the highest age of the reference. She then categorised participants into one of four relatively homogenous BMI trajectory groups on the basis of adolescent (age 11–15) and young adult BMI: ‘ slimmers ’ had lower BMI Z-scores at age 24 than their adolescent peak and were not obese (BMI<30 kg/m 2 ); ‘ relapsers ’ had shown a decrease from their peak adolescent BMI Z-score, followed by regain and were currently obese; the BMI Z-scores of ‘ stable ’ participants had remained largely unchanged throughout; finally, the BMI Z-scores of ‘ gainers ’ had steadily increased since adolescence.
This paper describes the most common themes raised by participants in relation to late adolescence/young adulthood (weight-related concerns; exercise; diet; professional support; young adult transitions) and relates these to their adolescent/young adult BMI categories.
Table 1 shows 13 participants were ‘slimmers’, of whom 3 were of normal weight (BMI<25 kg/m 2 ) and 10 were overweight at age 24. Eight were ‘relapsers’ (6 obese, 2 morbidly obese—BMI>35 kg/m 2 ), 3 were ‘stable’ (1 overweight, 1 obese, 1 morbidly obese) and 11 were ‘gainers’ (6 obese, 5 morbidly obese). Individual graphs show considerable variations in BMI trajectory (see online supplementary file 2 —individual BMI Z-score trajectories). Some participants also described weight changes not apparent in these study measurements and discussed the circumstances in which they had occurred.
Table 1
Participants categorised according to current body mass index (BMI), change since highest BMI in adolescence and whether had slimmed and relapsed previously
| As adolescent (ages 11–15) | As young adult (age 24) | ||||
|---|---|---|---|---|---|
| Pseudonym | Peak adolescent BMI Z-score | Age of max adolescent BMI | BMI | BMI Z-score | BMI category |
| ‘ 6 7 | |||||
| Lower BMI than in adolescence and not obese as young adult | |||||
| Catherine | 2.37 | 15 | 24.0 | 0.55 | Normal |
| Nina | 1.82 | 13 | 23.8 | 0.49 | Normal |
| Noel* | 2.46 | 15 | 20.7 | −1.04 | Normal |
| Alan | 2.06 | 13 | 27.4 | 1.33 | Overweight |
| Charlie | 2.90 | 15 | 28.7 | 1.64 | Overweight |
| Clare | 1.94 | 11 | 27.1 | 1.39 | Overweight |
| Eilidh | 3.08 | 13 | 29.3 | 1.88 | Overweight |
| Emma | 2.37 | 11 | 28.4 | 1.68 | Overweight |
| Janine | 2.37 | 15 | 25.4 | 0.95 | Overweight |
| Mark | 2.18 | 15 | 29.5 | 1.83 | Overweight |
| Pete | 2.17 | 15 | 28.0 | 1.47 | Overweight |
| Rachel | 1.71 | 15 | 26.1 | 1.14 | Overweight |
| Scott | 2.38 | 11 | 26.5 | 1.07 | Overweight |
| 5 3 | |||||
| Obese, slimmed previously | |||||
| Colin | 2.68 | 15 | 30.2 | 1.98 | Obese |
| Laura | 1.66 | 15 | 30.2 | 2.06 | Obese |
| Malcolm | 2.02 | 15 | 30.8 | 2.09 | Obese |
| Patricia | 2.82 | 13 | 33.1 | 2.55 | Obese |
| Patrick | 1.66 | 15 | 30.5 | 2.04 | Obese |
| Philip | 1.88 | 11 | 30.4 | 2.01 | Obese |
| Donna | 3.24 | 15 | 37.8 | 3.20 | Morbidly obese |
| Geoff | 3.14 | 13 | 44.3 | 3.87 | Morbidly obese |
| ‘ 1 2 | |||||
| No change since adolescence | |||||
| Chris | 1.90 | 13 | 29.6 | 1.84 | Overweight |
| Christina | 2.55 | 15 | 32.4 | 2.44 | Obese |
| Jenny | 3.24 | 15 | 38.3 | 3.25 | Morbidly obese |
| 5 6 | |||||
| Increased obesity since adolescence | |||||
| Jamie | 2.37 | 15 | † | 2.57† | Obese |
| Matthew | 1.91 | 15 | 32.9 | 2.49 | Obese |
| Michael | 1.88 | 13 | 31.9 | 2.31 | Obese |
| Natasha | 2.03 | 15 | 32.0 | 2.37 | Obese |
| Neil | 2.06 | 13 | 34.9 | 2.75 | Obese |
| Sarah | 2.28 | 15 | 32.7 | 2.49 | Obese |
| Anne | 3.64 | 15 | 43.1 | 3.74 | Morbidly obese |
| Elizabeth | 3.21 | 15 | 41.2 | 3.56 | Morbidly obese |
| Kirsty | 2.65 | 15 | 43.5 | 3.78 | Morbidly obese |
| Lisa | 3.19 | 15 | ‡ | 3.79‡ | Morbidly obese |
| Richard | 2.84 | 15 | 42.7 | 3.71 | Morbidly obese |
*Weight loss attributed by participant to severe postviral illness at age 17.
†Did not consent to be weighed at age 24 but observed to be obese; age 19 BMI Z-score provided.
‡Did not consent to be weighed at age 24 but observed to be extremely obese; age 19 BMI Z-score provided.
Weight-related concerns
Most participants, regardless of BMI trajectory group, described increasing weight-related concerns and/or desire to lose weight as they progressed into later adolescence ( table 2 ; see online supplementary table S1 for extensive illustrative quotes). Several related their increasing concerns to a wish for a new identity as part of the postschool transition; Eilidh ‘ realised that I was going to uni, I didn't want to be big, it was like a new kinda fresh start ’. However, most described their attitudinal change in terms of more general maturity and acknowledgement of weight as personal responsibility. Examples among ‘slimmers’ included Janine, who became ‘ conscious ’ of her weight around age 15–16 and Mark who noted ‘ it was only in my late teens that I started to be aware of this concept of healthy living, yeah, it wasn't something that ever kinda touched me as a, as a fifteen year-old boy ’. Malcolm (‘relapser’) ‘ left school thinking “nah, I don't care about dieting” … and then that kinda stopped and I was like that, “oh wait a minute, need to try and do something ”’. Such accounts were also evident among ‘gainers’: Anne said that ‘ as I got older I realised that I had to do something ’, Elizabeth had ‘ changed since I've been a teenager, because I watch what I'm eating ’ and Sarah, who was ‘ finally on a diet for the first time properly in my life ’ described herself as ‘ far more mature than I used to be ’. There was no evidence that increasing concern was limited to those who had at some stage lost weight, apart from hints that perhaps non-‘slimmers’ expressed concerns in slightly vaguer terms and, for a small number, they appeared to have occurred more recently.
Table 2
Illustrative quotes according to participant ‘slimmer’, ‘relapser’, ‘stable’ and ‘gainer’ categorisation—weight-related concerns
| Slimmer | |
| Eilidh | Yeah I don't know I think when I started coming to the end of high school and realised that I was going to Uni, I didn't want to be big, it was like a new kinda fresh start Once I got to a size 16 I just got kinda lazy and went ‘well, I'm fine now’, do you know. I'd, I would like to lose a wee bit more but I'm quite content the way I am do you know |
| Relapser | |
| Malcolm | I still left school thinking, ‘nah I don't care about dieting’, again ‘if I eat I'm just gonna burn it off, quicker than anyone else’ and then that kinda stopped and I was like that ‘oh wait a minute, need to try and do something’ |
| Stable | |
| Christina | But I'm quite vain, even though I'm big, I think I'm shit hot, do you know what I mean? … I am quite vain, even though there's things that I would like tae change, but I'm no gonna bust a gut tae change them, do you know what I mean? |
| Gainer | |
| Sarah | I am now finally on a diet for the first time properly in my life, so I've joined Weight Watchers a couple of months ago so I've now lost just over a stone … so I'm finally trying to do something about it cos it bothers me |
supplementary tables
However, some participants expressed current acceptance of their size. For example, Geoff (‘relapser’) was not ‘ overly concerned ’, having decided ‘ this is what I'm are ’ [sic], Christina (‘stable’) described herself as ‘ quite vain, even though I'm big, I think I'm shit hot’ and Jenny (‘stable’) did not want to ‘ go to all these classes to get healthy. As long as I don't feel like crap I'm not too bothered like ’. Two ‘slimmers’ expressed acceptance only once they felt more comfortable with their clothes size. Eilidh described herself as becoming ‘ lazy’ and ‘ content ’ on reaching size 16, and Rachel ‘ realised as I got older that I was never supposed to be a size six or a size eight, that's just not the way I'm built ’.
In response to these concerns, almost all participants described behavioural changes, including diet (next section) and exercise, particularly in gyms, but also team sports, swimming, use of home exercise DVDs/gym equipment, running and walking ( table 3 ; see online supplementary table S2).
Table 3
Illustrative quotes according to participant ‘slimmer’, ‘relapser’, ‘stable’ and ‘gainer’ categorisation—exercise and diet
| Slimmers | |
| Mark | I don't remember the moment of making the decision, but I do remember coming home from school and getting changed and going to the gym and that was, that was very… it was a bit of a departure from the way life was for me before then … it became part of my life and it has remained so to this day |
| Catherine | So aye, it was losing the weight, it was, it was hard at the start, but see once you get into a routine of knowing what you do, what you can eat, what you can't eat, what you need to keep yourself away fae, it is quite easy |
| Relapsers | |
| Geoff | When I left school I went to I done, I done boxing, fitba, I went to the gym. … I wis I say I wis playing aw the sports. So if I could eat that but I, I wisny putting on any weight cos I wis going to the gym, playing fitba and that. I don't play a lot o’ fitba noo right enough. I'd like tae but it's getting the time and the people tae play it |
| Laura | Maybe in the last couple of years or so, in the sense that, yeah, you go out and do lunches with your friends and this and that, and you think that I could really do with cutting some of that out. You know, weekend fry-ups and stuff like that. Trying to be healthier and, you know, the healthy option … |
| Stable | |
| Chris | I never did anything particularly excessive. I never did anything too… you know, tried… sort of stuck to anything very long I don't think when I was, when I was younger, so I guess that's probably why nothing ever worked |
| Jenny | I can just eat really good foods and be really good but it never makes that much of a difference |
| Gainers | |
| Anne | I used to go to the gym on a Monday but it's shut now, the gym that I go to, it's not opened anymore. Em, for refurbishment. But like, I've got like exercise DVDs now that I'll do in the house |
| Jamie | Just cut out junk, I cut out a lot of carbs I remember… Yeah it was that what I did I remember doing, I remember saying ‘no junk’… You really do need a disciplined and healthy eating plan. You know says the man who had a bag of crisps and a Mars Bar last night … |
Most ‘slimmers’ mentioned the gym. Pete and Mark started attending while still at school, which for Mark was ‘ a bit of a departure from the way life was for me before ’. Scott's, Charlie's, Claire's and Rachel's gym attendance began at university. Charlie found it ‘ wasn't even difficult ’ and this ‘ total change in lifestyle ’ resulted in weight loss. Claire used the gym ‘ throughout my uni life ’, and Rachel managed gym attendance, university classes and bar work. Exercise had been sustained by all this group. For Mark, the gym environment ‘ became part of my life and has remained so to this day ’, Scott continued to ‘ train hard ’ and Charlie described how ‘ now I jist sorta sustain ’ exercise. Claire's exercise had become ‘ kind of habit … I don't think I have to go to the gym or do this, to exercise I would just do, walking, jogging, whatever ’ and Rachel went ‘ to the gym a lot ’. Among the other ‘slimmers’, Emma's police training involved time at the gym, circuits and swimming and was ‘ the most active I think I have ever been in my life ’; she also continued to attend. Eilidh and Catherine had tried a gym, but preferred other activities; Eilidh ‘ loved’ cycling and Catherine walked with her baby buggy. While acknowledging impact on weight, Nina and Noel were vaguer about their exercise.
Some ‘relapsers’ linked weight loss to exercise. At around 17–18, Patricia ‘ lost a drastic amount of weight … and I was exercising an awful lot ’, Colin had a ‘ fitness freak stage ’ and Geoff found he could maintain his weight by balancing eating with exercise. However, only Patricia's gym attendance continued. Exercise featured less in the accounts of other ‘relapsers’, including Malcolm, for whom ‘ there's not been any exercise really, not much ’, Laura, who occasionally used a home trampoline, although ‘ there's just those weeks when you can't be bothered ’, and Donna who had recently tried to increase her exercise via walking. Similarly, Chris (‘stable’) thought not sticking with anything was ‘ probably why nothing ever worked ’ while Christina who regularly walked her dog ‘ wouldnae go tae a gym ’.
In exactly the same way, several male ‘gainers’ described earlier periods of significant exercise which had ceased for reasons, including the need to focus on academic work, injuries, lack of time or motivation. Some female ‘gainers’ described exercising: Anne had attended a gym which was now closed, but used home exercise DVDs, Elizabeth had discovered aqua-aerobics and Kirsty had recently joined a gym.
Participants tended to discuss diet in two ways. First, the importance of having a balanced diet that used home cooking rather than relying on frozen/take-away meals, with healthy choices such as less cheese or cream-based sauces and more fruit. Second, they described their experiences of participating in calorie-controlled diets, either as promoted by commercial slimming clubs or unsustainable ‘fad’ diets (eg, liquid diets, drinking vinegar, avoiding dairy/gluten/carbohydrates or foods of a particular colour) ( table 3 ; see online supplementary table S3 ).
Several female ‘slimmers’ related their weight loss to reduced food intake and meal-skipping: Rachel ‘ just changed the way I ate ’. Many ‘slimmers’ described the need to be constantly mindful of food choices: Mark had not bought certain foods in order to control his intake; Scott self-monitored, ‘ there's times whereby I'll pick up a biscuit and I'll go “no, I don't want it”’ ; Nina noted ‘ the [weight-related] worrying's definitely stayed there ’; and Eilidh described herself as ‘ very, very always watching about not getting bigger ’. However, some appeared slightly more relaxed, including Catherine who described ‘ a routine of knowing what you do, what you can eat, what you can't eat, what you need to keep yourself away fae. It is quite easy ’.
A similar range of strategies was described by participants in the other groups, but with perhaps less emphasis on real and sustainable reductions in intake or continued vigilance. Among the ‘relapsers’, Patricia had lost weight by meal skipping, Donna had achieved weight loss via severe dieting but now ate ‘healthy’ food, while one of Colin's adolescent weight-loss strategies had been to make himself sick; this had stopped and he was trying to ‘ eat something a bit more healthier ’. Malcolm believed controlling food intake was more important than exercise for weight loss, but did so by skipping breakfast. He and Philip talked about home-cooked meals while Laura mentioned ‘ you know, the healthy option ’. Christina (‘stable’) noted that ‘ I dae eat quite healthily but it's my amounts ’; she had unsuccessfully tried a range of ‘fad’ diets. However, Jenny (stable) believed ‘ I can just eat really good foods and be really good but it never makes that much of a difference ’.
Two ‘gainers’, Sarah and Kirsty, had recently started seriously dieting, using commercial slimming club regimes. Elizabeth reported losing weight when on a commercial club diet, and was currently focusing on ‘ watch[ing] what I'm eating ’, but Anne believed dieting had caused stomach problems so ‘ I'd had to eat things to suit my stomach, rather than suit my diet ’. Lisa also reported losing weight via a commercial club, but it increased once she ‘ stopped recording things and checkin g’. Although more often described by females, a small number of male ‘gainers’ also described dieting: Michael had reduced his calorie intake on the advice of his GP, and Richard ‘ didn't have a takeaway for six mon ths’, but then, to use Jamie's description, his diet went ‘ a bit awry again ’.
Professional support
Contrasting with self-initiated and/or unsupported behavioural changes, professional support (eg, slimming clubs, fitness classes, GP advice) was mentioned by very few participants ( table 4 ; see online supplementary table S4 ). Only one ‘slimmer’, Pete, mentioned that at around age 19–20, he had asked his GP and been helped by simple advice on portion control, exercise and social support. Patricia (‘relapser’) reported her GP had told her ‘ och it's OK you don't need to lose weight ’. She had also attended a council-run weight-management service, Weight-Watchers and used a personal trainer.
Table 4
Illustrative quotes according to participant ‘slimmer’, ‘relapser’, ‘stable’ and ‘gainer’ categorisation—professional support
| Slimmer | |
| Pete | I went to you know like my GP a couple of times to try and get advice on how to, you know what I should do. … [was advised] just to try and control portions and try to, to count, you know not count calories but be mindful of what the intake was and perhaps to, to exercise regularly you know with, either with friends or you know try and get support you know. So that did help a lot. That did help |
| Relapser | |
| Patricia | I was referred to the Council's weight-management service by my doctor, and I went and never lost any weight there, and because I never lost any weight, they just never got back in contact. And my doctor I feel because she's so big, when I go and I say ‘I would really, really like to lose weight and I'll, I can show you a food diary of what I've been eating, I can show you my exercise, I can show you how much water I've been drinking’, my doctor will go, ‘och it's ok you don't need to lose weight’ |
| Gainers | |
| Lisa | I went to Weight Watchers classes and lost a good bit of weight … the reason I left was a lot of it was getting me down because, em, there was too much emphasis on figures, like you've lost or you've gained or you're this or you're that |
| Richard | My cousin dragged me tae Weight Watchers. … It's actually alright. I liked it. I went for aboot four months … I've got a family doctor … She's always geeing me an earful to get oan at me, and every time I go up that's the first thing she does. If I go up for a sore throat she weighs me, so she's always on my back to get me to lose weight. … So I've no been up for aboot eight month noo, coz I'm terrified of going up again in case she shouts at me again |
Similar, if not more, professional input was mentioned by ‘gainers’, some describing this as helpful. Anne spoke vaguely about ‘slimming clubs’, but Lisa lost ‘ a good bit of weight ’ via 2 years' Weight-Watchers attendance. Richard reported losing around 15 kg, having been ‘ dragged ’ to Weight-Watchers. However, he subsequently regained the weight and stopped attending his GP because ‘ She's always geeing me an earful to get oan at me, and every time I go up that's the first thing she does. If I go up for a sore throat she weighs me, so she's always on my back to get me to lose weight ’. Similarly, Michael reported his GP said ‘ if I keep cerry on the way I was, I was gonna have a heart attack by the time I was thirty-five, and that put the shitters right up me ’. However, he found her simple dietary and exercise advice useful. Two ‘gainers’ had started attending slimming clubs only very recently, with Kirsty reporting that ‘ I'm ready to take that step to lose weight ’.
Young adult transitions
Participants had experienced a range of young adult transitions: 23 had attended tertiary education in the past (university and college, including college-based apprenticeships) and 4 were doing so at the time of the interview; 29 were working and 5 had performed so in the past; 19 were living in their own homes and 3 had left the parental home in the past but were living back there at the time of the interview; 1 was a parent. These young adult transitions (which were broadly similar across BMI trajectory groups) appeared key to weight changes for many participants, regardless of BMI trajectory group ( table 5 ; see online supplementary table S5 ). Thus, across the groups, some described college/university as a fresh start and/or facilitator to exercise which then meant they met active peers. A few learnt about nutrition or PA, enabling reflection on personal choices. However, others felt college/university was connected with weight-gain, mainly via poor diet and alcohol. Employment was also described as both facilitating and impeding weight loss. Several described loss resulting from active jobs and a few used their earnings to join a gym. However, others worked in sedentary jobs, felt too exhausted by work to bother with home cooking or exercise, or spent their earnings on ‘junk’ food and alcohol. Leaving home was also linked to increased dietary control and so healthier options for some but less balanced meals for others; the small number living with a partner described this as increasing the likelihood of home-cooking.
Table 5
Illustrative quotes according to participant ‘slimmer’, ‘relapser’, ‘stable’ and ‘gainer’ categorisation—young adult transitions
| Slimmers | |
| Catherine | WORK: I changed my jobs in August last year, and since then, the amount of weight I have lost is unbelievable. I think I've lost about a stone and a half since August … it's just through daen more, being more active, than compared to what I was doing |
| Scott | EDUCATION: The lifestyle wasn't so much a big thing about until I turned maybe eighteen, nineteen and started doing my degree then I started learning how to use a gym properly and what sort of exercise that I can do and just I'm now very aware of cos I'm working in nutrition what it is I actually take in and what it is I actually expend |
| Relapsers | |
| Donna | EDUCATION/LEAVING HOME: That wasn't actually so much of a help because I was living on my own. At student houses and everything else and takeaways was a much more tempting option than cooking for yourself more often than not. Again throughout my Uni career, first to fourth year, I gradually, I definitely improved. I got a grip of that and decided that eating healthy was, was the best option so I started cooking for myself |
| Stable | |
| Chris | EDUCATION/LEAVING HOME: When I was at uni and I joined the gym and pretty much spent all the money I had on cigarettes and alcohol and didn't eat as much as probably I should have, but not in a you, know, not in a deliberate way, just like I used to never have any money for food and so I lost quite a lot of weight then |
| Gainers | |
| Jamie | EDUCATION: There was first, first and second year at Uni when I just, you know I discovered you know booze. And then that really was us off to the races in terms of overweight |
| Neil | WORK: I was labouring for a wee while. I must have laboured for about six months. … I didn't try to lose weight, when I started the job, I didn't try to lose weight, initially, at all—it didn't enter my mind. … then it became, for me, at my work, at my workplace, where I could be getting paid for losing weight, basically |
Among the ‘slimmers’, Charlie, Clare, Mark and Scott all described weight loss associated with attending university. Charlie's close friends also went to the gym, while Mark was encouraged by a coach; for him ‘ coming to uni was the sort of the biggest change ever ’. When Eilidh started university, she ‘ just started really healthy eating ’ and took up swimming. Catherine and Scott's courses involved nutrition, with Catherine noting ‘ it kinda opens your eyes to things that you're eating and what it is doing to you ’. Weight loss was a requirement for Alan's admission to the RAF and Emma's police job, and their subsequent training involved PA. Both had maintained weights well below the adult obesity level, but Emma described consciously relaxing her regime since achieving her goal of becoming a police officer. Janine had worked as a show dancer, which required physical fitness, but also encouraged high levels of social drinking, ‘ so it was a bit of both—bad and good ’. Catherine had recently left a job at a fast food counter and ‘ the amount of weight I have lost is unbelievable ’.
‘Relapsers’ and those for whom our measurements showed ‘stable’ BMIs provided largely similar accounts. Patricia and Chris described losing weight at university, Patricia by meal-skipping attributed to a busy routine and Chris because he ‘ pretty much spent all the money I had on cigarettes and alcohol and didn't eat as much as probably I should have ’. Donna dealt with university workload stress by eating, and in student accommodation ‘ takeaways was a much more tempting option than cooking for yourself ’. Although several ‘relapsers’ mentioned gym attendance, Chris was the only one who linked this with university. Philip lost weight after leaving school without conscious effort because ‘ I was working full-time. … I wasn't able to go to like Gregg's [bakers] twice a day and stuff like that ’. Christina thought she had lost weight ‘ by accident ’ due to stress and other changes involved in moving into her own home, while living with a friend/partner had forced Malcolm and Philip to begin home cooking.
Weight loss facilitated by young adult transitions was also mentioned by some ‘gainers’: Jamie attended the gym and dieted during his third university year and that was ‘ probably the best shape I was in ’ and Richard attributed weight loss at college to football and gym attendance. Neil found he ‘ could be getting paid for losing weight ’ while working as a building labourer for 6 months. He also ascribed weight fluctuations to his relationship status: ‘ whenever I meet a lassie I'll be in tip top condition and then, within a year I've put on like a stone and a half’. Sarah thought her current nursing job meant ‘ I can't really preach healthy living to people if I'm not actually doing it myself ’. However, accounts in this group also tended to describe transition-related barriers to weight loss. Jamie ‘ discovered booze ’ at university ‘ and then that really was us off to the races in terms of overweight ’. Other ‘gainers’ described the impact of shift-work, on diet (‘ no eating breakfast again, and grabbing a bar of chocolate ’—Kirsty) and motivation to exercise (‘ after a day's work I'm absolutely knackered and I don't want to go out for a run ’—Matthew).
Studies that track from adolescence into adulthood are relatively rare. In our sample of previously overweight or obese adolescents, over a third had not gone on to become obese adults, but almost a quarter were already morbidly obese. The interviews revealed clearly that, contrasting with the recalled lack of concern in mid-adolescence, 20 weight-related concerns and/or desire to lose weight generally increased around the time of school-leaving and most participants described some form of both exercise (formal/informal) and dietary weight-control strategies. These changes may have partly resulted from increasing autonomy (independent/voluntary functioning), 25 self-determination 26 or self-esteem 27 with age: many participants described perceiving postschool transitions as a fresh start and acknowledgement of weight as personal responsibility; most had left the parental home and controlled their own diet and leisure activities.
Differences between ‘slimmers’ and those who had become or remained obese were subtle and hard to detect, even using qualitative methods. A qualitative study of 22 US overweight adolescents, identified via health centre records, found those whose BMI decreased over a 2-year period were more likely to describe ‘transformative experiences’ and family support as well as intense daily exercise. 4 Other qualitative studies have identified successful weight loss maintenance strategies including dietary change, ‘overwhelmingly increased’ exercise and rigorous self-correction after going ‘off course’ among US 14–20 years with sustained weight loss, 28 and a ‘healthy obsession’ with monitoring food, activity and weight among eight formerly obese US adolescents who had attended an immersion treatment. 29 A qualitative study of 20 overweight Taiwanese nursing students highlighted ‘the struggle’, of continuing to practise a new lifestyle and so reducing/maintaining bodyweight. 30 These findings are consistent with suggestions in our data of lifestyle changes becoming habitual and/or part of identity among ‘slimmers’, and of their appearing more likely to self-monitor diet and PA.
Few participants described receiving professional support and, although numbers are small, diet clubs seemed to have been used most by ‘gainers’. In contrast, ‘slimmers’ had achieved weight loss, without support, sometimes fairly easily. A previous qualitative study of obese Australian adults similarly found that few received long-term professional guidance or support as adolescents. 31 Although important for adolescent weight loss, 4 28 it has been suggested that exercise is less acceptable as a weight-loss solution because it is perceived as harder, 31 yet in this study, slimmers commonly used and sustained exercise as a method of weight-control and did not generally describe it as hard.
Our analysis highlights complex relationships between postschool transitions and weight-control behaviours. University/college, work and independent living were each described as facilitating weight losses by some and increases by others. Analysis of US longitudinal youth survey data has identified subgroups with distinctive patterns of weight-gain risk at different periods from middle-school to work/family formation. 32 Other studies have found evidence of declines in PA, increases in alcohol consumption and poor nutrition at University 33–35 36 and in young adulthood, 37 38 but these life-stages have not previously been described before as promoting weight loss. Relationships have also been found between obesity and work conditions including long hours, but again not weight loss. 39
The main strength of this paper is its objective categorisation of participants as ‘slimmer’, ‘gainer’, etc, based on (measured) BMI at several points throughout adolescence. The threshold used in childhood (95th centile) is not a stringent definition of childhood obesity, though widely used for public health analyses. 40 When compared with the more stringent clinical definition of obesity, 40 the 98th centile (Z score 2, equivalent to BMI of about 30 at age 20), nine of the participants were only overweight as adolescents, but it is of note that five of these went on to be obese as adults. Several not categorised as ‘slimmers’ or ‘relapsers’ also mentioned weight loss, not detected by our measurement schedule. Gaps and possible weight changes between measurements, and the sometimes vague nature of participants' recollections mean that precise chronological mapping of these against weight changes is impossible. As the original study did not set out to specifically identify some of the themes highlighted here, particularly professional support, identity and vigilance, we cannot know if other participants might have discussed these issues had the interview included them. The fact they emerged spontaneously is a strength, but because they were not a consistent focus of the study, conclusions on differences between the BMI trajectory groups must remain tentative. However, future research on late adolescent/young adult weight-related concerns, behaviours and experiences could explore these issues more explicitly. Another limitation of all interview data is that participants might have been providing acceptable ‘public’ accounts to a public health researcher 41 about a stigmatised issue. 42 43
In conclusion, this exploratory paper adds insights on experiences of obesity and weight loss during a rarely studied life-stage when research participants are hard to access. In contrast to their recollections of adolescence, as young adults even the heaviest participants tended to show contemplation or preparation for weight-loss action. 12 13 Although there were few really distinctive differences between those who successfully lost weight and those who became ever more obese, their accounts suggest the importance of social context and highlight potential health-change opportunities during the transition to adulthood. This could be a key life-stage for interventions, which should include workplace and educational 44 settings.
Acknowledgments
The authors would like to thank the young people, nurse interviewers, schools and all those involved in the West of Scotland 11-16/16+Study.
Contributors: HS and CW conceived the research questions and analysis, ES gathered the data as part of a wider study. JN identified relevant themes, CW categorised participants on the basis of their adolescent and age 24 BMIs, HS identified relevant literature and first-drafted the paper. All authors contributed to subsequent redrafts.
Funding: HS is funded by the MRC at the MRC/CSO Social and Public Health Sciences Unit, University of Glasgow (MC_UU_12017/12 and SPHSU12). These data were gathered by ES while funded by a UK Medical Research Council (MRC) PhD studentship. JN was funded by a small grant from a Feeding Research Fund held by CW. CW is funded by Glasgow University and NHS Greater Glasgow and Clyde.
Competing interests: None declared.
Ethics approval: Approval to conduct each stage of the 11-16/16+ Study was given by the University of Glasgow Ethics Committee for Non-Clinical Research Involving Human Subjects; approval for the qualitative substudy was obtained from the University of Glasgow Law, Business, and Social Science Faculty Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The current MRC/CSO Social and Public Health Sciences Unit Data Sharing Policy does not cover data collected by research students. Anyone with a particular interest in this qualitative data set should contact HS.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- Health Topics
- < Back To High Blood Pressure
- Causes and Risk Factors
- What Is High Blood Pressure?
- Living With High Blood Pressure
- Pregnancy and High Blood Pressure
MORE INFORMATION
High Blood Pressure Causes and Risk Factors
Language switcher, what are the risk factors.
Many factors raise your risk of high blood pressure. You can change some risk factors, such as unhealthy lifestyle habits. A healthy lifestyle can lower your risk for developing high blood pressure.
Other risk factors, such as age, family history and genetics, race and ethnicity, and sex, cannot be changed. But, you can still take steps to reduce your risk of high blood pressure and its complications .
Blood pressure tends to rise with age. Blood vessels naturally thicken and stiffen over time. These changes increase the risk for high blood pressure.
However, the risk of high blood pressure is rising for children and teens, possibly because more children and teens have overweight or obesity .
Family history and genetics
High blood pressure often runs in families. Much of what we know about high blood pressure has come from genetic studies. Many genes are linked to small increases in high blood pressure risk. Research suggests that as an unborn baby grows in the womb, some DNA changes may also raise the risk for high blood pressure later in life.
Some people have a high sensitivity to salt in their diet, which can play a role in high blood pressure. This can also run in families.
Lifestyle habits
Lifestyle habits can increase the risk of high blood pressure, including if you:
- Eat unhealthy foods often, especially foods that are high in salt and low in potassium. Some people, including Black people, older adults, and people who have chronic kidney disease, diabetes, or metabolic syndrome, are more sensitive to salt in their diet.
- Drink too much alcohol or caffeine
- Don’t get enough physical activity
- Don’t get enough good-quality sleep
- Experience high-stress situations
- Use substances such as cocaine, methamphetamine, “bath salts,” or other stimulants
Some medicines can make it harder for your body to control your blood pressure. Antidepressants, decongestants (medicines to relieve a stuffy nose), hormonal birth control pills, and non-steroidal anti-inflammatory drugs such as aspirin or ibuprofen can all raise your blood pressure.
Other medical conditions
Other medical conditions change the way your body controls fluids, sodium, and hormones in your blood. Other conditions that can cause high blood pressure include:
- Some tumors
- Chronic kidney disease
- Metabolic syndrome
- Overweight and obesity
- Sleep apnea
- Thyroid problems
Race or ethnicity
High blood pressure is more common in Black adults than in White, Hispanic, or Asian adults. Compared with other racial or ethnic groups, Black people tend to have higher average blood pressure numbers and get high blood pressure earlier in life. Also , some high blood pressure medicines may not work as well for Black people.
During pregnancy , Black women are more likely than White women to develop preeclampsia . Preeclampsia is a pregnancy disorder that causes sudden high blood pressure and problems with the kidneys and liver.
Men are more likely than women to develop high blood pressure throughout middle age. But in older adults, women are more likely than men to develop high blood pressure.
Women who have high blood pressure during pregnancy are more likely to have high blood pressure later in life. Research shows that medicines used to control high blood pressure during pregnancy lower the chance of pregnancy complications and won’t harm the developing baby.
Social and economic factors
Research shows that factors such as income, education level, where you live, and the type of job you have, as well as stressors on the job may raise your risk of high blood pressure. Working early or late shifts is one example of a social factor that can raise your risk.
Experiencing discrimination and poverty has been linked to high blood pressure. Also , some research has shown that experiencing stress, danger, harm, or trauma as a child may raise the risk of high blood pressure.
Can High Blood Pressure be prevented?
How to prevent high blood pressure.
A heart-healthy lifestyle can help prevent high blood pressure and its complications.
- Choose heart-healthy foods that are lower in salt (sodium) and are rich in potassium. Fruits and vegetables are high in potassium. For more ways to limit your sodium, visit the DASH Eating Plan page or print out the Tips to Reduce Salt and Sodium handout.
- Avoid or limit alcohol.
- Get regular physical activity . Even modest amounts can make a difference. Reducing the amount of time you sit each day can help lower your blood pressure.
- Aim for a healthy weight .
- Quit smoking .
- Control your cholesterol and blood sugar levels. To learn some tips to help manage your cholesterol level, read our booklet Therapeutic Lifestyle Changes to Lower Cholesterol .
- Manage stress .
- Get enough good-quality sleep .

IMAGES
VIDEO
COMMENTS
Answer. Kent, It depends on the question you are asking. Our lab studies the effects of maternal high fat diet on DOHaD in offspring. Others use a Western diet (high fat and carbohydrates). There ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the prevalence of 30.5% during 1999 to 2002. 2 Among those afflicted with ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
In spite of an increasing recognition of the integral role of patient experience in health research [25, 26], the voices of patients remain largely underrepresented in obesity research [27, 28]. Systematic reviews and syntheses of qualitative studies are recognised as a useful contribution to evidence and policy development . To the best of the ...
Abstract. This review has examined the scientific basis for our current understanding of obesity that has developed over the past 100 plus years. Obesity was defined as an excess of body fat ...
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health, increases the risk of long-term medical complications and reduces lifespan. 1 Epidemiologic studies define obesity using the body mass index (BMI; weight/height 2), which can stratify obesity-related health risks at the population level.Obesity is operationally defined as a BMI exceeding 30 kg ...
Introduction. Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality.1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19.4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight.6
Current research on obesity and sleep. An NHLBI-funded study is looking at whether energy balance and obesity affect sleep in the same way that a lack of good-quality sleep affects obesity. The researchers are recruiting equal numbers of men and women to include sex differences in their study of how obesity affects sleep quality and circadian ...
The main diagnostic test for obesity — the body mass index — accounts for only height and weight, leaving out a slew of factors that influence body fat and health. Players in an 'overweight ...
Objectives To identify and prioritise the most impactful, unanswered questions for obesity and weight-related research. Design Prioritisation exercise of research questions using online surveys and an independently facilitated workshop. Setting Online/virtual. Participants We involved members of the public including people living with obesity, researchers, healthcare professionals and policy ...
Answer #2: Overconsumption. There are two reasons for the chronic overconsumption of calories. First, the more fat-cells an individual has, the more calories s/he will store as fat after each meal. Yet if more calories are stored as fat, less calories are available to keep other cells alive. Therefore, excess calories must be consumed to ...
Currently, there are 13.7 (around 17% of US population) million children and adolescents with obesity. Children with obesity face a lifetime of physical and psychological complications, yet this condition is often ignored and under addressed at most office visits. 1,2 Many reasons have been proposed for this gap in care services, including lack of effectiveness of any currently available ...
Objectives: To identify and prioritise the most impactful, unanswered questions for obesity and weight-related research. Design: Prioritisation exercise of research questions using online surveys and an independently facilitated workshop. Setting: Online/virtual. Participants: We involved members of the public including people living with obesity, researchers, healthcare professionals and ...
The Strategic Plan for NIH Obesity Research serves as a guide to accelerate a broad spectrum of research toward developing new and more effective approaches to address the tremendous burden of obesity, so that people can look forward to healthier lives. The Plan was originally published in 2011. In 2018-2019, the Obesity Research Task Force ...
This is the resource for finding original, comprehensive reporting and analysis to get background information on issues in the news. It provides overviews of topics related to health, social trends, criminal justice, international affairs, education, the environment, technology, and the economy in America. Gale eBooks.
Aim. Obesity research priority setting, if conducted to a high standard, can help promote policy-relevant and efficient research. Therefore, there is a need to identify existing research priority setting studies conducted in the topic area of obesity and to determine the extent to which they followed good practice principles for research priority setting.
Obesity represents a significant public health concern, with one-third of adults classified as living with obesity in the United States. Obesity correlates with cardiometabolic comorbidities that can decrease the quality of life.[1][2] Researchers have proposed that exercise is an important lifestyle measure to maintain a healthy weight. This review will cover the role of exercise in obesity ...
By Cell Press February 3, 2022. Obesity's detrimental health effects, such as hypertension and diabetes, stem not merely from an excess of fat, but rather from the loss of fat's plasticity — its ability to respond to changes — according to a review published in the Cell journal. The researchers explain that fat, besides storing energy ...
Childhood obesity outline example. As the question of childhood obesity is a specific one, it would differ from the outline on obesity we presented previously. Here is a sample you might need. The topic covers general research on child obesity. Introduction. Hook sentence. Thesis statement. Transition to Main Body. Main Body. The problem of ...
The high percentage of women's obesity prevalence is a result of poor nutrition in childhood and access to greater resources in adulthood. Obesity Problem in the United States. Obesity is not just people going fat; it is a disease that causes maladies like type-2 diabetes, heart disease, cancer and strokes.
Published: 17 August 2018. Updated: 20 January 2022. The donations that can be done through this webpage are exclusively for the benefit of Hospital Clínic of Barcelona through Fundació Clínic per a la Recerca Biomèdica and not for BBVA Foundation, entity that collaborates with the project of PortalClínic.
The question is why. Research has identified five factors as possible links between modern-day obesity and socioeconomic status: stress, temporal focus or whether one is focused on the past or the future, well-being expectations, time spent outdoors and food scarcity. However, studies typically examine only one or two factors at a time and not ...
Abstract. Obesity is a complex condition that interweaves biological, developmental, environmental, behavioral, and genetic factors; it is a significant public health problem. The most common cause of obesity throughout childhood and adolescence is an inequity in energy balance; that is, excess caloric intake without appropriate caloric ...
This study analyzed data from 6,138 American adults aged 20 and older from the National Health and Nutrition Examination Survey (NHANES) years 2003 to 2006.. The researchers excluded pregnant ...
It is a formal program that gives you ongoing guidance and support to build healthy lifestyle habits that may promote weight loss. 2 The program should include. a healthy, reduced-calorie eating and drinking plan. a plan for increasing physical activity if appropriate. guidance and support for adopting these lifestyle habits.
The UX designer role is to make a product or service usable, enjoyable, and accessible. While many companies design user experiences, the term is most often associated with digital design for websites and apps. While the exact process varies from product to product and company to company, the general phases of design tend to stay the same.
Introduction. Adolescent overweight is associated with greatly increased likelihood of adult obesity, 1 but up to a third of obese adolescents do not go on to be obese adults. 2 What is not clear is why and how some overweight/obese adolescents (defined broadly, by the WHO, as those aged 10-19 3) lose weight and others do not, 4 and why some adolescents maintain weight loss while others ...
Research shows that factors such as income, education level, where you live, and the type of job you have, as well as stressors on the job may raise your risk of high blood pressure. Working early or late shifts is one example of a social factor that can raise your risk. Experiencing discrimination and poverty has been linked to high blood ...