An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob J Health Sci
- v.8(6); 2016 Jun

Communication Barriers Perceived by Nurses and Patients
Roohangiz norouzinia.
1 School of Paramedical, Alborz University of Medical Sciences, Karaj, Iran
Maryam Aghabarari
2 Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
3 School of Nursing and Midwifery, Alborz University of Medical Sciences, Karaj, Iran
Maryam Shiri
Mehrdad karimi.
4 School of Public Health, Department of Epidemiology and Biostatistics, Tehran University of Medical Sciences, Tehran, Iran
Elham Samami
Communication, as a key element in providing high-quality health care services, leads to patient satisfaction and health. The present Cross sectional, descriptive analytic study was conducted on 70 nurses and 50 patients in two hospitals affiliated to Alborz University of Medical Sciences, in 2012. Two separate questionnaires were used for nurses and patients, and the reliability and validity of the questionnaires were assessed. In both groups of nurses and patients, nurse-related factors (mean scores of 2.45 and 2.15, respectively) and common factors between nurses and patients (mean scores of 1.85 and 1.96, respectively) were considered the most and least significant factors, respectively. Also, a significant difference was observed between the mean scores of nurses and patients regarding patient-related (p=0.001), nurse-related (p=0.012), and environmental factors (p=0.019). Despite the attention of nurses and patients to communication, there are some barriers, which can be removed through raising the awareness of nurses and patients along with creating a desirable environment. We recommend that nurses be effectively trained in communication skills and be encouraged by constant monitoring of the obtained skills.
1. Introduction
Communication is a multi-dimensional, multi-factorial phenomenon and a dynamic, complex process, closely related to the environment in which an individual’s experiences are shared. Since the time of Florence Nightingale in 19 th century until today, specialists and nurses have paid a great deal of attention to communication and interaction in nursing ( Fleischer, Berg, Zimmermann, Wüste, & Behrens, 2009 ). Effective communication is an important aspect of patient care, which improves nurse-patient relationship and has a profound effect on the patient’s perceptions of health care quality and treatment outcomes ( Li, Ang, & Hegney, 2012 ). Effective communication is the key element in providing high-quality nursing care, and leads to patient satisfaction and health ( Cossette, Cara, Ricard, & Pepin, 2005 ). Effective communication skills of health professionals are vital to effective health care provision, and can have positive outcomes including decreased anxiety, guilt, pain, and disease symptoms. Moreover, they can increase patient satisfaction, acceptance, compliance, and cooperation with the medical team, and improve physiological and functional status of the patient; it also has a great impact on the training provided for the patient ( Aghabarari, Mohammadi, & Varvani, 2009 ).
However, most studies have reported poor nurse-patient relationships ( McCabe, 2004 ; Jangland, Gunningberg, & Carlsson, 2009 ; Gilmartin, & Wright 2008 ). Therefore, overall, nurse-patient communication has not led to personal satisfaction ( Jangland, Gunningberg, & Carlsson, 2009 ). This is due to the fact that health care quality is strongly affected by nurse-patient relationship, and lack of communication skills (or not using them) has a negative impact on services provided for the patients. The results of previous studies have shown that nurses have been trained to establish an effective communication; however, they do not use these skills to interact with their patients in clinical environments ( Heaven, Clegg, & Maguire, 2006 ). Similarly, the results of other studies show that nurses and nursing professionals in general, have not made a lot of effort for establishing positive interactions with the patients. Many reported problems are related to the decreased sense of altruism among hospital staff including nurses ( Bridges et al., 2013 ).
Communication pitfalls are 5-10% in general population and more than 15% in hospital admissions ( Bartlett, Blais, Tamblyn, Clermont, & MacGibbon, 2008 ). Hospitalized patients in all ages often experience complex communication needs including mobility, sensory, and cognitive needs as well as language barriers during their stay ( Downey & Happ, 2013 ). Hospitalization is potentially stressful and involves unpleasant experiences for patients and their families. All aspects of care and nursing are of high importance in communication with patients, as the patients consider interaction with the nurses as a key to their treatment. Also, through communication, nurses become familiar with the needs of their patients, and therefore, they can deliver high-quality health care services ( Cossette et al., 2005 ; Sheldon, Barrett, & Ellington, 2006 ; Thorsteinsson, 2002 ). Patients with communication disability were three times more likely to experience medical or clinical complications compared to other patients ( Bartlett et al., 2008 ).
Iran is a multicultural country with recognized cultural pluralism. In Iranian religious context, nurses are not allowed to gaze or touch patients of the opposite-sex, except in emergency cases. In addition, although Iranian formal language is Farsi, there are many dialects such as Lurish, Kurdish, and Baluchi, which might act as communication barriers between nurses and patients ( Anoosheh, Zarkhah, Faghihzadeh, & Vaismoradi, 2009 ). In Iran, some communication facilitators and barriers have been reported including low educational preparation, governmental policies, and inappropriate environment as barriers, and religious and cultural norms, role modeling, and previous exposure of patients as facilitators ( Rejeh, Heravi-Karimooi, & Vaismoradi, 2011 ).
The first step in eradicating the problems related to nurse-patient communication is two-sided (nurse and patient) awareness of communication barriers. It is of no doubt that building an effective relationship is dependent on the understanding of both sides of the interaction ( Park & Song, 2005 ). In this study, we aimed to determine the barriers to nurse-patient relationship from the perspective of nurses and patients. Through this evaluation, we can improve the quality of nursing services and increase the satisfaction of patients and their families. We also assessed the barriers to using communication skills by the nurses in nurse-patient interactions.
2.1 Study Design
Cross sectional, descriptive analytic study.
2.2 Participants
This study was conducted on nurses and patients of two public hospitals affiliated to Alborz University of Medical Sciences, Karaj, Iran. Simple random sampling method was applied.
2.3 Questionnaires
Data were collected via two separate questionnaires for nurses and patients. The reliability and validity of the questionnaires were assessed. Content validity was approved by eight professors of Tehran University of Medical Sciences and Tarbiat Modares University, and reliability was assessed using the split-half method. Pearson’s correlation coefficient between the two halves was calculated, and reliability of patient (correlation coefficient of 0.76) and nurse (correlation coefficient of 0.82) questionnaires were approved.
The questionnaires consisted of two sections. The first part included demographic questions and the second part was concerned with the present barriers to nurses’ use of communication skills. The nurse questionnaire contained 44 items and patient questionnaire consisted of 29 items; each item included 5 options: none, little, average, high, and not included. The participants chose one of the options with regard to the importance of each barrier; “not included” was selected if the subjects had not dealt with such a barrier before.
The barriers were divided to four categories: common barriers between patient and nurse, nurse-related barriers, patient-related barriers, and environmental barriers. To determine the importance of each barrier, the qualitative data were converted to quantitative data and the options were scored as follows: none: 1 score, low: 2 scores, average: 3 scores, and high: 4 scores. The difference in the number of items between patient and nurse questionnaires was related to the number of nurse-related factors. Some items were designed with regard to nurses’ working conditions, and there was a possibility that patients were unaware of these conditions; therefore, these cases were removed from the patient questionnaire, and the remainders were included in both questionnaires.
2.4 Data Collection
After obtaining the required approval, nurses and patients in the two hospitals were asked to participate in the study. In order to collect the data, the researchers visited the wards on a daily basis during different shifts. After explaining the study objectives to the nurses and taking informed consents, the questionnaires were given to the participants; after completion, the questionnaires were collected by the researchers.
The nurse sample included nurses of medical, surgical, intensive care unit, and emergency wards. They were working in morning, evening, night, evening and night, and circulating shifts. The sample size was calculated according to the number of nurses in the ward.
The inclusion criteria for the nurse group were as follows: 1) bachelor’s degree (minimum education level), 2) minimum of 6-month working experience, and 3) willingness to participate in the study.
The participants in the patient group were selected based on the inclusion criteria of the patient sample: 1) willingness to participate in the study, 2) ability to establish communication, 3) literacy, and 4) older than 15 years of age. The exclusion criteria for the patients were poor speech ability, hearing difficulty, language impairment following a stroke, and intubation.
The subjects were selected from hospitalized patients. After explaining the objectives of the study, an informed consent was obtained and the patient was given a questionnaire, which was collected after 1 hour. The patient sample was randomly selected from medical, surgical, and emergency wards.
2.5 Statistical Analysis
For data analysis, descriptive and inferential statistics (Binomial, Mann-Whitney, and Friedman tests) were used and SPSS version 14 was utilized. P-value less than or equal to 0.05 was considered statistically significant.
3.1 Demographic Characteristics
According to the results, the mean age of the nurses was 30.95 yrs, and the mean working experience was 7.02 yrs. The mean age of the patients was 29.30 yrs and the mean of hospitalization days was 2.3 days. Tables Tables1 1 and and2 2 show the demographic characteristics of the subjects.
Demographic characteristics of nurses
Demographic characteristics of patients
3.2 The Most and Least Important Barriers
The findings suggest that among four categories of communication barriers in nurse and patient groups, nurse-related factors (mean scores of 2.45 and 2.15, respectively) and common factors between nurses and patients (mean scores of 1.85 and 1.96, respectively) were the most and least important factors, respectively.
3.3 Compare the Nurses and Patients’ Viewpoint
Regarding patient-related factors (P=0.001), nurse-related factors (P=0.012) and environmental factors (P=0.019), there was a significant difference between the mean scores of nurses and patients ( Table 3 ).
Comparison of four groups of barriers in two groups of nurses and patients
The most frequent communication barriers from the nurses’ viewpoint were as follows: differences in colloquial languages of nurses and patients, nurses’ being overworked, family interference, and presence of emergency patients in the ward. According to the patients, gender differences between nurse and patient, nurse’s reluctance for communication, hectic environment of the ward, and patient’s anxiety, pain, and physical discomfort were the most important barriers to communication ( Table 4 ).
The most important barriers from the viewpoint of nurses and, based on the type of barrier
According to the data obtained from Man Whitney Test, comparison of patients’ and nurses’ mean scores of barriers (to using communication skills by nurses) indicated that of 29 items common between nurse and patient questionnaires, the mean scores of 13 items were significantly different ( Table 5 ).
Comparison of the mean scores of barriers to communication skills by nurses in interacting with patients from the viewpoint of nurses and patients
4. Discussion
The results of this study showed that in both groups of nurses and patients, the most and the least important barriers were nurse-related factors and common factors between nurses and patients, respectively. These results were consistent with the findings of Aghabarari et al., who performed a study to determine the barriers to applying communication skills by nurses, from the viewpoint of nurses and patients ( Aghabarari et al., 2009 ). Also, in the study of Aghamolaei et al., nurse- and patient-related barriers were more important than environmental barriers ( Aghamolaei & Hasani, 2011 ). In terms of common factors between nurses and patients, colloquial language, and cultural and gender differences were of high importance; however, priorities were not quite similar between nurses and patients. Through establishing an appropriate verbal communication, the nurse could thoroughly understand the patient’s problems; hence, in many studies, the nurse’s unfamiliarity with the patient’s colloquial language has been mentioned as a communication barrier ( Anoosheh et al., 2009 ; Baraz, Shariati, Alijani, & Moein, 2010 ; del Pino, Soriano, & Higginbottom, 2013 ; Li et al., 2012 ). If there is a difference in spoken language, effective communication cannot be established; even non-verbal communication in different cultures may have different interpretations. Patients are also less acceptant of nurses with different languages and cultures (culture has an impact on individuals’ attitudes and behaviors). Based on previous studies, communicative needs and ways of expressing emotions vary in different cultures and religions. Sufficient knowledge of nurses regarding patients’ culture, language, customs, and beliefs can help them communicate with the patients without having any pre-judgments or prejudice. Indeed, culture can act as both a facilitator and a barrier to communication ( Okougha & Tilki, 2010 ).
Alborz province is also called “little Iran”, meaning that all ethnicities and cultures are present in this region; therefore, the variety of cultures should not be neglected. Considering the population concentration of specific ethnic groups in particular regions of this province, it is recommended that the patient’s language and ethnicity be considered for the allocation of medical staff.
In this study, another factor affecting communication, particularly from the viewpoint of patients, was gender differences; the results were consistent with those of previous studies ( Anoosheh et al., 2009 ; Baraz et al., 2010 ). The impact of gender differences on communication is mostly emphasized by the patients; in fact, nurses are less affected by patients’ gender while performing their professional duties. According to cultural and religious beliefs in Iran, touching and gazing are inconsistent with the principles of the society ( Anoosheh et al., 2009 ). Similar to many Asian cultures, speaking about sexual problems is also considered impolite ( Im et al., 2008 ). Given the aforementioned principles, the number of male nursing students should increase considering the shortage of male nurses in hospital wards.
As to the patients’ viewpoint, another influential factor was age differences. Similarly, Sung and Park considered generation gap as a communication barrier ( Park & Song, 2005 ). In another study, differences in age and social class were included as communication barriers ( Anoosheh et al., 2009 ). However, according to a study by Baraz, age differences had no negative impact on nurse-patient relationship ( Baraz et al., 2010 ). Generally, communicating with different age groups has its own challenges and complexities. Nurses can have good interactions with patients through developing awareness of each age group’s attitudes to health, disease, and body function ( Bridges et al., 2013 ).
Evaluation of the viewpoints of nurses and patients showed that among nurse-related barriers, being overworked, shortage of nurses, and lack of time were the most important barriers for the nurse group. Also, the nurses’ unwillingness to communicate, and lack of understanding of patients’ needs were the most important barriers from the patients’ perspective. Shortage of nurses increases the work load, and therefore, there is not enough time to establish a good therapeutic relationship ( Park & Song, 2005 ); also, nurses’ low income has been mentioned as a barrier to nurse-patient interaction ( Aghamolaei & Hasani, 2011 ; Baraz et al., 2010 ; Mendes, Trevizan, Nogueira, & Sawada, 1999 ). Stress, being overworked, and lack of welfare facilities could decrease nurses’ satisfaction and quality of health care provision ( Nayeri, Nazari, Salsali, & Ahmadi, 2005 ). Based on the results of the study by Park and Song, being overworked is a nurse-related communication barrier, which affects the quality and quantity of the relationship between nurses and patients ( Park & Song, 2005 ).
In the present study, comparison of the viewpoints of nurses and patients regarding patient-related barriers showed that interference by family, patients’ unawareness of the status and duties of the nurses, patients’ physical pain, discomfort, and anxiety, lack of attention, and the presence of patients’ companions were the most important factors; these results were considerably consistent with previous studies ( Aghabarari et al., 2009 ).
Definitely, the patient’s disease and dependence after hospitalization result in anxiety, tension, and fear in the patient; moreover, the patient’s family also experiences a difficult time and has different needs and demands. Negligence of the patient and the family of the status and duties of nurses leads to misconceptions about the nurses’ role in the improvement or deterioration of the patient’s health and may even result in the patient’s death. If nurses are not successful in establishing an effective communication with the patients, they can apply communication facilitators; if they still do not succeed, they can explain the problems to the patients so that they can obtain positive treatment results without having a good communication ( Ammentorp, Sabroe, Kofoed, & Mainz, 2007 ).
Nurse is considered the direct care provider and the smallest delay in care provision will be considered as medical negligence. However, it is quite obvious that a medical team consisting of physicians, nurses, clinical departments, and even medical center crew are all responsible for the patient’s health care. Thus, given the direct relationship between nurses and patients, the image created by nurses affects their being accepted as professional staff, and their role will be highlighted in establishing an effective communication ( Aghabarari et al., 2009 ).
In terms of environmental barriers, the presence of critically ill patients in the ward, the hectic environment of the hospital, and unsuitable environmental conditions are considered the main barriers in both groups. The findings of previous studies confirm the aforementioned results. The shortage of nurses and the presence of critically ill patients in the ward cause a lot of stress for the patient and lead to decreased ability and motivation to communicate with other patients; on the other hand, medical environment conditions have great effects on the quantity and quality of communication ( Bartlett et al., 2008 ). Factors disturbing the communication process can be improper temperature, excessive noise, poor ventilation, and lack of respect for the privacy of the two sides of the relationship ( Mendes et al., 1999 ). Thus, providing a safe and comfortable environment leads to psychological and physical comfort of the nurse and patient, and facilitates using communication skills and establishing an effective communication.
One of the limitations of this study was the low number of male nurses. Another limitation was lack of evaluation of cultural forces operating between patients and nurses, regardless of the country of origin or background in the hospitals (active, passive, or power relationships). It is recommended that future studies pay more attention to communication facilitators and divide the participants to male and female groups. It is also suggested that religious and cultural beliefs as well as language barriers be more thoroughly evaluated in patients and nurses.
5. Conclusion
The purpose of any system is to provide services with optimal quality and quantity, and health care systems are no exception. One of the best ways to gain the patients’ satisfaction, as major clients of health care systems, is through establishing effective and appropriate communication. Thus, according to the results of this study and previous studies, the following measures will be considerably helpful in establishing an effective nurse-patient communication: allocation of medical staff with regard to the language and culture of the region, motivating nurses to provide high-quality health care services, upgrading medical clinics and facilities, holding periodic workshops of communication skills, holding nursing quality assurance committees, and most importantly, changing attitudes of nursing managers and administrators from offering task-based services toward following a holistic approach.
Acknowledgments
This study is financially supported by Research Affairs, Alborz University of Medical Sciences, Karaj, Iran. The authors wish to express their sincere gratitude to the study participants without whom this study could not have been conducted.
Conflict of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
- Aghabarari M, Mohammadi I, Varvani-Farahani A. Barriers to Application of Communication Skills by Nurses in Nurse-Patient Interaction. Nurses and Patients’ Perspective. Iranian Journal of Nursing. 2009; 22 (16):19–31. [ Google Scholar ]
- Aghamolaei T, Hasani L. Communication barriers among nurses and elderly patients. Bimonthly Journal of Hormozgan University of Medical Sciences. 2011; 14 (4):312–318. [ Google Scholar ]
- Ammentorp J, Sabroe S, Kofoed P.-E, Mainz J. The effect of training in communication skills on medical doctors’ and nurses’ self-efficacy: A randomized controlled trial. Patient Education and Counseling. 2007; 66 (3):270–277. http://dx.doi.org/10.1016/j.pec.2006.12.012 . [ PubMed ] [ Google Scholar ]
- Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. International Nursing Review. 2009; 56 (2):243–249. http://dx.doi.org/10.1111/j.1466-7657.2008.00697.x . [ PubMed ] [ Google Scholar ]
- Baraz P. S, Shariati A. A, Alijani R. H, Moein M. S. Assessing barriers of nurse-patient’s effective communication in educational hospitals of Ahwaz. Iranian Journal of Nursing Research. 2010; 5 (16):45–52. [ Google Scholar ]
- Bartlett G, Blais R, Tamblyn R, Clermont R. J, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. Canadian Medical Association Journal. 2008; 178 (12):1555–1562. http://dx.doi.org/10.1503/cmaj.070690 . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bridges J, Nicholson C, Maben J, Pope C, Flatley M, Wilkinson C, Tziggili M. Capacity for care: Meta-ethnography of acute care nurses’ experiences of the nurse-patient relationship. Journal of Advanced Nursing. 2013; 69 (4):760–772. http://dx.doi.org/10.1111/jan.12050 . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cossette S, Cara C, Ricard N, Pepin J. Assessing nurse-patient interactions from a caring perspective: Report of the development and preliminary psychometric testing of the Caring Nurse-Patient Interactions Scale. International Journal of Nursing Studies. 2005; 42 (6):673–686. http://dx.doi.org/10.1016/j.ijnurstu.2004.10.004 . [ PubMed ] [ Google Scholar ]
- Del Pino F. J. P, Soriano E, Higginbottom G. M. Sociocultural and linguistic boundaries influencing intercultural communication between nurses and Moroccan patients in southern Spain: A focused ethnography. BMC Nursing. 2013; 12 (1):14. http://dx.doi.org/10.1186/1472-6955-12-14 . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Downey D, Happ M. B. The Need for Nurse Training to Promote Improved Patient-Provider Communication for Patients with Complex Communication Needs. Perspectives on Augmentative and Alternative Communication. 2013; 22 (2):112–119. http://dx.doi.org/10.1044/aac22.2.112 . [ Google Scholar ]
- Fleischer S, Berg A, Zimmermann M, Wüste K, Behrens J. Nurse-patient interaction and communication: A systematic literature review. Journal of Public Health. 2009; 17 (5):339–353. http://dx.doi.org/10.1007/s10389-008-0238-1 . [ Google Scholar ]
- Gilmartin J, Wright K. Day surgery: Patients’ felt abandoned during the preoperative wait. Journal of Clinical Nursing. 2008; 17 (18):2418–2425. http://dx.doi.org/10.1111/j.1365-2702.2008.02374.x . [ PubMed ] [ Google Scholar ]
- Heaven C, Clegg J, Maguire P. Transfer of communication skills training from workshop to workplace: The impact of clinical supervision. Patient Education and Counseling. 2006; 60 (3):313–325. http://dx.doi.org/10.1016/j.pec.2005.08.008 . [ PubMed ] [ Google Scholar ]
- Im E.-O, Chee W, Guevara E, Lim H.-J, Liu Y, Shin H. Gender and ethnic differences in cancer patients’ needs for help: An Internet survey. International Journal of Nursing Studies. 2008; 45 (8):1192–1204. http://dx.doi.org/10.1016/j.ijnurstu.2007.09.006 . [ PubMed ] [ Google Scholar ]
- Jangland E, Gunningberg L, Carlsson M. Patients’ and relatives’ complaints about encounters and communication in health care: Evidence for quality improvement. Patient Education and Counseling. 2009; 75 (2):199–204. http://dx.doi.org/10.1016/j.pec.2008.10.007 . [ PubMed ] [ Google Scholar ]
- Li H, Ang E, Hegney D. Nurses’ perceptions of the barriers in effective communicaton with impatient cancer adults in Singapore. Journal of Clinical Nursing. 2012; 21 (17-18):2647–2658. http://dx.doi.org/10.1111/j.1365-2702.2011.03977.x . [ PubMed ] [ Google Scholar ]
- McCabe C. Nurse-patient communication: An exploration of patients’ experiences. Journal of Clinical Nursing. 2004; 13 (1):41–49. http://dx.doi.org/10.1111/j.1365-2702.2004.00817.x . [ PubMed ] [ Google Scholar ]
- Mendes I. A. C, Trevizan M, Nogueira M, Sawada N. Humanizing nurse-patient communication: A challenge and a commitment. Medicine and Law. 1999; 18 (1):639–644. [ PubMed ] [ Google Scholar ]
- Nayeri N. D, Nazari A. A, Salsali M, Ahmadi F. Iranian staff nurses’ views of their productivity and human resource factors improving and impeding it: A qualitative study. Human Resources for Health. 2005; 3 (1):9. http://dx.doi.org/10.1186/1478-4491-3-9 . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Okougha M, Tilki M. Experience of overseas nurses: The potential for misunderstanding. British Journal of Nursing. 2010; 19 (2):102–106. http://dx.doi.org/10.12968/bjon.2010.19.2.46293 . [ PubMed ] [ Google Scholar ]
- Park E.-k, Song M. Communication barriers perceived by older patients and nurses. International Journal of Nursing Studies. 2005; 42 (2):159–166. http://dx.doi.org/10.1016/j.ijnurstu.2004.06.006 . [ PubMed ] [ Google Scholar ]
- Rejeh N, Heravi-Karimooi M, Vaismoradi M. Iranian nursing students’ perspectives regarding caring for elderly patients. Nursing & Health Sciences. 2011; 13 (2):118–125. http://dx.doi.org/10.1111/j.1442-2018.2011.00588.x . [ PubMed ] [ Google Scholar ]
- Sheldon L. K, Barrett R, Ellington L. Difficult communication in nursing. Journal of Nursing Scholarship. 2006; 38 (2):141–147. http://dx.doi.org/10.1111/j.1547-5069.2006.00091.x . [ PubMed ] [ Google Scholar ]
- Thorsteinsson L. S. The quality of nursing care as perceived by individuals with chronic illnesses: The magical touch of nursing. Journal of Clinical Nursing. 2002; 11 (1):32–40. http://dx.doi.org/10.1046/j.1365-2702.2002.00575.x . [ PubMed ] [ Google Scholar ]
- Work Environment
10 Ways to Overcome Communication Barriers in Nursing

Effective communication plays a vital role in nursing, fostering understanding, collaboration, and ultimately improving patient outcomes. However, various barriers can hinder communication within healthcare settings.
In this article, we will explore ten practical ways to overcome these communication barriers and enhance the delivery of care.
Importance of Effective Communication in Nursing
Effective communication lies at the heart of nursing practice. It forms the foundation for building relationships with patients, their families, and the interprofessional healthcare team.
When communication breaks down, patient safety, satisfaction, and overall quality of care are compromised. By understanding and addressing communication barriers, you, as a nurse, can ensure effective and meaningful interactions, leading to improved patient outcomes.
Common Communication Barriers in Nursing
Language and cultural differences.
Language barriers pose significant challenges in nursing, especially in multicultural healthcare settings. Nurses must communicate with patients who have limited English proficiency or speak a different native language. Additionally, cultural differences can influence communication styles and expectations. These barriers can lead to misunderstandings, inadequate information exchange, and reduced patient satisfaction.
Technological Challenges
With the increasing use of technology in healthcare, nurses face communication barriers related to unfamiliarity with electronic health records (EHRs) and other digital systems. Technical difficulties, such as system crashes or slow response times, can impede timely communication and information sharing among healthcare providers.
Hierarchy and Power Dynamics
In healthcare settings, hierarchical structures and power dynamics can hinder effective communication. Nurses may feel hesitant to express their opinions or concerns to physicians or higher-ranking professionals, resulting in vital information being overlooked. Open communication channels and a culture of collaboration are necessary to overcome these barriers.
Emotional and Psychological Factors
Nursing can be emotionally demanding, and stress, fatigue, and burnout can affect communication skills. These factors may lead to misinterpretation of messages, increased conflicts, and decreased empathy. Addressing the emotional well-being of nurses is essential to maintain effective communication in healthcare environments.
1. Active Listening
Active listening is a fundamental skill for effective communication in nursing. By actively engaging with patients, you can demonstrate empathy, gain valuable insights, and establish trust. Here are some techniques to enhance active listening:
- Maintain eye contact : Show your attentiveness and interest in what the patient is saying.
- Provide verbal and non-verbal cues : Nodding or smiling encourages patients to express themselves more openly.
- Practice reflective listening : Summarize and rephrase what the patient has said to ensure mutual understanding.
- Avoid interruptions : Allow patients to fully express their concerns and thoughts without interruption.
2. Clear and Concise Communication
Clear and concise communication is essential to ensure information is accurately conveyed and understood. When communicating with patients, consider the following strategies:
- Use simple language : Avoid complex medical jargon and explain information in a way that patients can easily comprehend.
- Avoid assumptions : Ensure that patients understand by asking open-ended questions and confirming their understanding.
- Confirm understanding through paraphrasing : Summarize the information shared by the patient to validate comprehension.
- Encourage questions and feedback : Create a safe environment for patients to ask questions and provide feedback, ensuring effective communication.
3. Open and Transparent Communication Channels
Creating open and transparent communication channels within healthcare settings is crucial for overcoming barriers. Here’s how you can achieve this:
- Foster a culture of open communication where all team members feel comfortable sharing their thoughts and concerns.
- Encourage feedback from colleagues and actively listen to their perspectives.
- Utilize regular team huddles or meetings to discuss communication challenges and find solutions collaboratively.
- Implement mechanisms such as suggestion boxes or anonymous feedback systems to provide an avenue for open communication.
- Share relevant information and updates with the healthcare team in a timely manner to ensure everyone is well-informed.
4. Empathy and Understanding
Empathy is the ability to understand and share the feelings of another person. In nursing, empathy promotes trust and patient-centered care. Enhance empathy and understanding by:
- Practice active empathy : Put yourself in the patient’s shoes and consider their emotions and experiences.
- Strive for cultural competence : Be mindful of cultural differences and tailor your communication to respect diverse backgrounds.
- Maintain a non-judgmental attitude : Create a supportive environment where patients feel comfortable expressing themselves without fear of judgment.
5. Non-Verbal Communication
Non-verbal cues, such as body language, facial expressions, and gestures, significantly influence communication in nursing. Utilize effective non-verbal communication to enhance your interactions with patients:
- Be aware of your body language and posture : Maintain an open and welcoming stance to convey approachability.
- Use facial expressions : Show empathy, concern, and reassurance through appropriate facial expressions.
- Utilize gestures and touch : Use gentle gestures and appropriate touch to convey comfort and support, when appropriate.
6. Use of Technology
In the modern healthcare landscape, technology plays a significant role in communication. While it offers numerous advantages, it can also present challenges. Embrace technology and leverage its potential for effective communication:
- Utilize electronic health records : Ensure accurate and timely documentation, promoting continuity of care.
- Explore telemedicine and video conferencing : Facilitate remote consultations and improve access to healthcare services.
- Leverage mobile communication devices : Use secure messaging platforms to communicate efficiently with colleagues and share important patient information.
7. Team Collaboration
Collaboration among healthcare professionals is crucial for providing holistic patient care. Effective team communication ensures that everyone involved is well-informed, contributing to seamless coordination. Foster effective collaboration through:
- Interprofessional communication: Maintain open lines of communication with colleagues from different disciplines.
- Participate in regular team meetings : Discuss patient care plans, exchange information, and address any communication challenges.
- Establish clear role expectations : Define each team member’s responsibilities and ensure everyone understands their role in patient care.
8. Patient Education
Patient education empowers individuals to actively participate in their care. As a nurse, you play a vital role in educating patients and breaking down complex medical information. Enhance patient education through:
- Use visual aids : Utilize diagrams, charts, and models to simplify complex concepts and enhance understanding.
- Provide written materials and handouts : Give patients written instructions and resources they can refer to after their interaction with you.
- Ensure patient comprehension : Use teach-back techniques to confirm that patients understand the information you have shared.
9. Language and Cultural Considerations
Language and cultural barriers can significantly impact communication in healthcare. Address these barriers by:
- Utilizing professional interpreters : When language barriers exist, engage the services of interpreters to facilitate effective communication.
- Understanding cultural norms and beliefs : Be culturally sensitive and adapt your communication style to accommodate diverse cultural backgrounds.
- Providing translated materials : Offer translated written materials and resources to assist patients who may have language limitations.
10. Feedback and Continuous Improvement
Feedback is essential for growth and development in nursing communication. Seek feedback from patients and colleagues to identify areas for improvement. Foster a culture of continuous improvement by:
- Seeking feedback from patients : Encourage patients to share their experiences and suggestions for better communication.
- Reflecting on your communication practices : Take time to evaluate your communication techniques and identify areas where you can improve.
- Participating in training and workshops : Attend professional development opportunities to enhance your communication skills and stay up-to-date with best practices.
Benefits of Overcoming Communication Barriers
By overcoming communication barriers, nursing professionals can experience numerous benefits:
- Improved Patient Outcomes: Effective communication leads to better patient understanding of their condition and treatment plans, reducing the risk of medical errors and improving overall healthcare outcomes.
- Enhanced Collaboration and Teamwork: Clear communication fosters collaboration among healthcare professionals, facilitating coordinated care and shared decision-making, ultimately benefiting patient outcomes.
- Increased Patient Satisfaction: When patients feel heard and understood, their satisfaction with the healthcare experience increases, leading to greater patient engagement and adherence to treatment plans.
- Reduced Errors and Misunderstandings: Overcoming communication barriers minimizes the likelihood of misinterpretations, misunderstandings, and errors that can compromise patient safety.
Training and Education for Effective Communication
To equip nurses with effective communication skills, various training and educational opportunities can be provided:
- Communication Skills Workshops: Organizing workshops that focus on active listening, conflict resolution, and effective communication techniques can enhance nurses’ interpersonal skills.
- Cultural Competency Training: Offering training programs that promote cultural awareness, sensitivity, and understanding helps nurses navigate diverse patient populations and communicate effectively across cultures.
- Technology Integration Training: Providing comprehensive training on using digital systems, EHRs, and other communication tools ensures nurses can leverage technology for efficient and secure communication.
In conclusion, effective communication in nursing is vital for providing safe, quality care. By implementing these ten strategies we mentioned above, you can overcome communication barriers, establish meaningful connections, and optimize patient outcomes. Remember, communication is a skill that can always be honed, and fostering open, empathetic, and clear interactions is key to delivering exceptional nursing care.
Q: How can you overcome communication barriers with patients who have limited English proficiency?
A: To overcome language barriers, you can utilize professional interpreters, use visual aids and gestures, and provide translated written materials. It’s important to create a supportive environment and allow extra time for communication with patients who have limited English proficiency.
Q: What are some effective strategies for communicating with patients from diverse cultural backgrounds?
A: When communicating with patients from diverse cultural backgrounds, it is important to be culturally sensitive, respect cultural norms and beliefs, and use culturally appropriate communication styles. Take the time to learn about different cultures, ask open-ended questions, and actively listen to foster effective communication.
Q: How can you promote effective communication during challenging situations, such as delivering difficult news to patients or their families?
A: When delivering difficult news, you can promote effective communication by demonstrating empathy, providing a calm and supportive environment, and using clear and compassionate language. Allow patients and their families to express their emotions, actively listen to their concerns, and offer appropriate support and resources.
Q: What can you do to improve communication within interdisciplinary healthcare teams?
A: To improve communication within interdisciplinary teams, actively participate in regular team meetings, clarify roles and responsibilities, and maintain open and respectful communication channels. Share information, seek input from team members, and foster a collaborative environment to enhance teamwork and patient outcomes.
Q: How can you ensure effective communication during patient handoffs or transitions of care?
A: To ensure effective communication during patient handoffs, use standardized protocols, document important information accurately, and engage in face-to-face or electronic communication with the receiving healthcare team. Provide a comprehensive and concise summary of the patient’s condition, treatment plan, and any ongoing concerns.
Q: How can you incorporate feedback from patients into your communication practices?
A: Actively seek feedback from patients by encouraging them to share their experiences, concerns, and suggestions. Provide patient satisfaction surveys or feedback forms to facilitate the collection of valuable input. By listening to patient feedback and implementing necessary improvements, you can continuously enhance your communication skills.

Sophia Miller
Similar posts.

6 Ways to Overcome Interdisciplinary Challenges in…

10 Ways to Build Positive Workplace Culture…

20 Most Common Ethical Dilemmas in Nursing…

10 Ways to Overcome Leadership Challenges in…

Are Male Nurses Attractive?

Can Nurses Wear Rings?
- Career Advancement 29
- Career Transection 20
- Job Satisfaction 16
- Managing Difficult Situations 6
- Work-Life Balance 14
- NCLEX Guide 50
- New Grad Nurse 21
- Nursing Practice Challenges 35
- Work Environment 23
- Emotional Challenges 3
POPULAR POSTS

What Does Baylor Shift Mean?

Can Male Nurses Have Long Hair?

Can You Take a Picture of Your Nurse?

Do School Nurses Wear Scrubs?

Can Nurses Carry Guns?

How Often Do Travel Nurses Get Audited?

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

3.7: Barriers to Effective Communication
- Last updated
- Save as PDF
- Page ID 49264

- Maureen Nokuthula Sibiya
- Gümüşhane University via IntechOpen
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Effective communication skills and strategies are important for nurses. Clear communication means that information is conveyed effectively between the nurse, patients, family members and colleagues. However, it is recognized that such skills are not always evident and nurses do not always communicate well with patients, family members and colleagues. The message sent may not be the message received. The meaning of a message depends on its literal meaning, the non-verbal indicators accompanying it and the context in which it is delivered. It is therefore, easy to misinterpret the message, or to interpret it correctly, but to decide not to pursue its hidden meaning this leads to obstruction to communication. Continuous barriers to effective communication brings about a gradual breakdown in relationships. The barriers to effective communication outlined below will help nurses to understand the challenges [ 8 ].
Language Barrier
Language differences between the patient and the nurse are another preventive factor in effective communication. When the nurse and the patient do not share a common language, interaction between them is strained and very limited [ 9 , 10 , 11 ]. Consequently, a patient may fail to understand the instructions from a nurse regarding the frequency of taking medication at home.
Cultural Differences
Culture is another hindrance. The patient’s culture may block effective nurse–patient interactions because perceptions on health and death are different between patients [ 12 , 13 , 14 ]. The nurse needs to be sensitive when dealing with a patient from a different culture [ 9 , 15 , 16 ]. What is acceptable for one patient may not be acceptable for another. Given the complexity of culture, no one can possibly know the health beliefs and practices of every culture. The nurse needs check with the patient whether he/she prefers to be addressed by first name or surname. The use of eye contact, touching and personal space is different in various cultures and rules about eye contact are usually complex, varying according to race, social status and gender. Physical contact between sexes is strictly forbidden in some cultures and can include handshakes, hugging or placing a hand on the arm or shoulder. A ‘yes’ does not always mean ‘yes’. A smile does not indicate happiness, recognition or agreement. Whenever people communicate, there is a tendency to make value judgements regarding those perceived as being different. Past experiences can change the meaning of the message. Culture, background and bias can be good if they allow one to use past experiences to understand something new; it is when they change meaning of the message that they interfere with the communication process [ 12 ]. It is important for nurses to think about their own experiences when considering cultural differences in communication and how these can challenge health professionals and service users.
Conflict is a common effect of two or more parties not sharing common ground. Conflict can be healthy in that it offers alternative views and values. However, it becomes a barrier to communication when the emotional ‘noise’ detracts from the task or purpose. Nurses aim for collaborative relationships with patients, families and colleagues.
Setting in Which Care is Provided
The factors in care setting may lead to reduction in quality of nurse–patient communication. Increased workload and time constraints restrict nurses from discussing their patients concerns effectively [ 16 ]. Nurses work in busy environments where they are expected to complete a specific amount of work in a day and work with a variety of other professionals, patients and their families. The roles are hard, challenging and tiring. There is a culture to get the work done. Some nurses may consider colleagues who spend time talking with patients to be avowing the ‘real’ work and lazy. Nurses who might have been confident in spending time with patients in an area where this was valued, when faced with a task-orientated culture have the dilemma of fitting into the group or being outside the group and spending time engaging with patients. Lack of collaboration between the nurses and the doctors in information sharing also hinder effective communication. This leads to inconsistencies in the information given to patients making comprehension difficult for the patient and their families.
Internal Noise, Mental/Emotional Distress
Internal noise has an impact on the communication process. Fear and anxiety can affect the person’s ability to listen to what the nurse is saying. People with feelings of fear and anger can find it difficult to hear. Illness and distress can alter a person’s thought processes. Reducing the cause of anxiety, distress, and anger would be the first step to improving communication.
If a healthcare professional feels that the person is talking too fast, not fluently, or does not articulate clearly etc., he/she may dismiss the person. Our preconceived attitudes affect our ability to listen. People tend to listen uncritically to people of high status and dismiss those of low status.
Difficulty With Speech and Hearing
People can experience difficulty in speech and hearing following conditions like stroke or brain injury. Stroke or trauma may affect brain areas that normally enable the individual to comprehend and produce speech, or the physiology that produces sound. These will present barriers to effective communication.
Medication can have a significant effect on communication for example it may cause dry mouth or excess salivation, nausea and indigestion, all of which influence the person’s ability and motivation to engage in conversation. If patients are embarrassed or concerned that they will not be able to speak properly or control their mouth, they could be reluctant to speak.
Equipment or environmental noise impedes clear communication. The sender and the receiver must both be able to concentrate on the messages they send to each other without any distraction.
- Login / Register

‘Let’s hear it for the midwives and everything they do’
STEVE FORD, EDITOR
- You are here: Assessment skills
Communication skills 2: overcoming the barriers to effective communication
18 December, 2017 By NT Contributor
This article, the second in a six-part series on communication skills, a discusses the barriers to effective communication and how to overcome them
Competing demands, lack of privacy, and background noise are all potential barriers to effective communication between nurses and patients. Patients’ ability to communicate effectively may also be affected by their condition, medication, pain and/or anxiety. Nurses’ and patients’ cultural values and beliefs can also lead to misinterpretation or reinterpretation of key messages. This article, the second in a six-part series on communication skills , suggests practical ways of overcoming the most common barriers to communication in healthcare.
Citation: Ali M (2017) Communication skills 2: overcoming barriers to effective communication Nursing Times ; 114: 1, 40-42.
Author: Moi Ali is a communications consultant, a board member of the Scottish Ambulance Service and of the Professional Standards Authority for Health and Care, and a former vice-president of the Nursing and Midwifery Council.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here
- Click here to see other articles in this series
- Read Moi Ali’s comment
Introduction
It is natural for patients to feel apprehensive about their health and wellbeing, yet a survey in 2016 found that only 38% of adult inpatients who had worries or fears could ‘definitely’ find someone in hospital to talk to about them (Care Quality Commission, 2017). There are numerous barriers to effective communication including:
- Time constraints;
- Environmental issues such as noise and privacy;
- Pain and fatigue;
- Embarrassment and anxiety;
- Use of jargon;
- Values and beliefs;
- Information overload.
Time constraints
Time – or lack of it – creates a significant barrier to communication for nurses (Norouzinia et al, 2016). Hurried communication is never as effective as a leisurely interaction, yet in pressured workplaces, nurses faced with competing demands may neglect the quality of communication. It is important to remember that communication does not need to be time-consuming – a smile, hello, or some ‘small talk’ about the weather may suffice. Even when there is no pressing news to tell individual patients, taking the time to get to know them can prepare the ground for difficult conversations that may need to take place in the future.
In a pressured ward or clinic, conversations between patients and nurses may be delayed or interrupted because of the needs of other patients – for example, they may need to respond to an emergency or pain relief. This can be frustrating for patients who may feel neglected. If interruptions occur it is important to explain to patients that you have to leave and why. Arranging to return within a specified time frame may be enough to reassure them that you are aware that their concerns are important (Box 1).
Box 1. Making time for communication
Nurse Amy Green was allocated a bay of four patients and two side wards for her shift. Halfway through the morning one of her patients in a side ward became very ill and Amy realised that she needed to spend a lot of time with him. She quickly visited her other patients to explain what was happening, and reassured them that she had not forgotten about them. She checked that they were comfortable and not in pain, asked them to ring the call bell if they needed her, and explained that she would return as soon as she could. The patients understood the situation and were reassured that their immediate needs had been assessed and they were not being neglected.
Environmental factors
You may be so familiar with your surroundings that you no longer notice the environmental factors that can create communication difficulties. Background noise in a busy clinic can affect patients’ ability to hear, and some may try to disguise this by nodding and ‘appearing’ to hear. If you think your patient has hearing problems, reduce background noise, find a quiet corner or step into a quiet side room or office. Check whether your patient uses physical aids, such as hearing aids or spectacles and that these are in working order.
Noise and other distractions can impede communication with patients with dementia and other cognitive impairments, who find concentration challenging. If you have to communicate an important message to a patient with poor concentration, it is useful to plan ahead and identify the best place and time to talk. It can be helpful to choose a time when you are less busy, without competing activities such as medicine rounds or meal times to interrupt your discussion.
Patients may be reticent to provide sensitive personal information if they are asked about their clinical history within earshot of other people, such as at a busy reception desk or in a cubicle with just a curtain for privacy. It is important to avoid asking sensitive questions where others may hear patients’ replies. Consider alternative ways of gathering pertinent information, such as asking the patient to complete a written form – but remember that some patients struggle with reading and writing or may need the form to be provided in a different language or have someone translate for them.
Pain and fatigue
We often need to gain important information from patients when they are acutely ill and distressed, and symptoms such as pain can reduce concentration. If you urgently need to gather information, it is important to acknowledge pain and discomfort: “I know that it is painful, but it’s important that we discuss.”
Patients may also be tired from a sleepless night, drowsy after an anaesthetic or experiencing the side-effects of medicines. Communicating with someone who is not fully alert is difficult, so it is important to prioritise the information you need, assess whether it is necessary to speak to the patient and ask yourself:
- Is this the best time for this conversation?
- Can my message wait?
- Can I give part of the message now and the rest later?
When patients cannot give their full attention, consider whether your message could be broken down into smaller pieces so there is less to digest in one go: “I will explain your medication now. I’ll return after lunch to tell you about how physiotherapy may help.” Ask if they would like any of the information repeated.
If you have to impart an important piece of information, acknowledge how the patient is feeling: “I know that you’re tired, but …”. Showing empathy can build rapport and make patients more receptive. It may also be useful to stress the need to pay attention: “It’s important that you listen because …”. Consider repeating the message: “It can be difficult to take everything in when you’re tired, so I just wanted to check that you’re clear about …”. If the communication is important, ask the patient to repeat it back to you to check it has been understood.
Embarrassment and anxiety
Would you feel comfortable undressing in front of a complete stranger, or talking about sex, difficult family circumstances, addictions or bowel problems? Patients’ and health professionals’ embarrassment can result in awkward encounters that may hamper effective communication. However, anticipating potential embarrassment, minimising it, and using straightforward, open communication can ease difficult conversations. For example, in a clinic, a patient may need to remove some clothes for an examination. It is important to be direct and specific. Do not say: “Please undress”, as patients may not know what to remove; give specific instructions: “Please remove your trousers and pants, but keep your shirt on”. Clear directions can ease stress and embarrassment when delivered with matter-of-fact confidence.
Patients may worry about embarrassing you or themselves by using inappropriate terms for anatomical parts or bodily functions. You can ease this embarrassment by introducing words such as “bowel movements” or “penis” into your questions, if you think they are unsure what terminology to use. Ambiguous terms such as “stool”, which have a variety of everyday meanings, should be avoided as they may cause confusion.
Many patients worry about undergoing intimate procedures such as bowel and bladder investigations. Explain in plain English what an examination involves, so that patients know what to expect. Explaining any side-effects of procedures – such as flatulence or vomiting – not only warns patients what to expect but reassures them that staff will not be offended if these occur.
Box 2 provides some useful tips on dealing with embarrassment.
Box 2. Managing embarrassment
- Look out for signs of embarrassment – not just obvious ones like blushing, but also laughter, joking, fidgeting and other behaviours aimed at masking it
- Think about your facial expressions when communicating with patients, and use positive, open body language such as appropriate eye contact or nodding
- Avoid disapproving or judgmental statements by phrasing questions carefully: “You don’t drink more than 10 glasses of wine a week, do you?” suggests that the ‘right’ or desired answer is ‘no’. A neutral, open question will elicit a more honest response: “How many glasses of wine do you drink in a typical week?”
Some patients are reluctant to ask questions, seek clarification or request that information be repeated for fear of wasting nurses’ time. It is important to let them know that their health or welfare is an integral part of your job. They also need to know that there is no such thing as a silly question. Encourage questions by using prompts and open questions such as: “You’re bound to have questions – are there any that I can answer for you now?”; “What else can I tell you about the operation?”. It is also possible to anticipate and address likely anxieties such as “Will it be painful?”; “Will I get better?”; or “Will I die?”.
Jargon can be an important communication aid between professionals in the same field, but it is important to avoid using technical jargon and clinical acronyms with patients. Even though they may not understand, they may not ask you for a plain English translation. It is easy to slip into jargon without realising it, so make a conscious effort to avoid it.
A report on health literacy from the Royal College of General Practitioners (2014) cited the example of a patient who took the description of a “positive cancer diagnosis” to be good news, when the reverse was the case. If you have to use jargon, explain what it means. Wherever possible, keep medical terms as simple as possible – for example, kidney, rather than renal and heart, not cardiac. The Plain English website contains examples of healthcare jargon.
Box 3 gives advice on how to avoid jargon when speaking with patients.
Box 3. Avoiding jargon
- Avoid ambiguity: words with one meaning for a nurse may have another in common parlance – for example, ‘acute’ or ‘stool’
- Use appropriate vocabulary for the audience and age-appropriate terms, avoiding childish or over-familiar expressions with older people
- Avoid complex sentence structures, slang or speaking quickly with patients who are not fluent in English
- Use easy-to-relate-to analogies when explaining things: “Your bowel is a bit like a garden hose”
- Avoid statistics such as “There’s an 80% chance that …” as even simple percentages can be confusing. “Eight in every 10 people” humanises the statistic
Values, beliefs and assumptions
Everyone makes assumptions based on their social or cultural beliefs, values, traditions, biases and prejudices. A patient might genuinely believe that female staff must be junior, or that a man cannot be a midwife. Be alert to patients’ assumptions that could lead to misinterpretation, reinterpretation, or even them ignoring what you are telling them. Think about how you can address such situations; for example explain your role at the outset: “Hello, I am [your name], the nurse practitioner who will be examining you today.”
It is important to be aware of your own assumptions, prejudices and values and reflect on whether they could affect your communication with patients. A nurse might assume that a patient in a same-sex relationship will not have children, that an Asian patient will not speak good English, or that someone with a learning disability or an older person will not be in an active sexual relationship. Incorrect assumptions may cause offence. Enquiries such as asking someone’s “Christian name” may be culturally insensitive for non-Christians.
Information overload
We all struggle to absorb lots of facts in one go and when we are bombarded with statistics, information and options, it is easy to blank them out. This is particularly so for patients who are upset, distressed, anxious, tired, in shock or in pain. If you need to provide a lot of information, assess how the patient is feeling and stick to the pertinent issues. You can flag up critical information by saying: “You need to pay particular attention to this because …”.
Box 4 provides tips on avoiding information overload.
Box 4. Avoiding information overload
- Consider suggesting that your patient involves a relative or friend in complex conversations – two pairs of ears are better than one. However, be aware that some patients may not wish others to know about their health
- Suggest patients take notes if they wish
- With patients’ consent, consider making a recording (or asking whether the patient wishes to record part of the consultation on their mobile phone) so they can replay it later or share it with a partner who could not accompany them
- Give written information to supplement or reinforce the spoken word
- Arrange another meeting if necessary to go over details again or to provide further information
It is vital that all nurses are aware of potential barriers to communication, reflect on their own skills and how their workplace environment affects their ability to communicate effectively with patients. You can use this article and the activity in Box 5 to reflect on these barriers and how to improve and refine your communication with patients.
Box 5. Reflective activity
Think about recent encounters with patients:
- What communication barriers did you encounter?
- Why did they occur?
- How can you amend your communication style to take account of these factors so that your message is not missed, diluted or distorted?
- Do you need support to make these changes?
- Who can you ask for help?
- Nurses need to be aware of the potential barriers to communication and adopt strategies to address them
- Environmental factors such as background noise can affect patients’ ability to hear and understand what is being said to them
- Acute illness, distress and pain can reduce patients’ concentration and their ability to absorb new information
- Anticipating potential embarrassment and taking steps to minimise it can facilitate difficult conversations
- It is important to plan ahead and identify the best place and time to have important conversations
Also in this series
- Communication skills 1: benefits of effective communication for patients
- Communication skills 3: non-verbal communication
- Communication 4: the influence of appearance and environment
- Communication 5: effective listening and observation skills
- Communication skills 6: difficult and challenging conversations
Related files
171220 communication skills 2 overcoming barriers to effective communication.
- Add to Bookmarks

Related articles
Have your say.
Sign in or Register a new account to join the discussion.
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Abdolrahimi M, Ghiyasvandian S, Zakerimoghadam M, Ebadi A. Therapeutic communication in nursing student: a Walker and Avant concept analysis. Electron Physician.. 2017; 9:(8)4968-4977 https://doi.org/10.19082/4968
Communication skills 1: benefits of effective communication for patients. 2017. https://tinyurl.com/y3nzu222 (accessed 10 August 2020)
Communication skills 3: non-verbal communication. 2018. https://tinyurl.com/y5ay4uhd (accessed 10 August 2020)
Bandura A. Self-efficacy: toward a unifying theory of behavior change. Psychol Rev.. 1977; 84:191-215 https://doi.org/10.1016/0146-6402(78)90002-4
Barratt J. Developing clinical reasoning and effective communication skills in advanced practice. Nurs Stand.. 2019; 34:(2)37-44 https://doi.org/10.7748/ns.2018.e11109
Bergdahl E, Berterö CM. Concept analysis and the building blocks of theory: misconceptions regarding theory development. J Adv Nurs.. 2016; 72:(10)2558-2566 https://doi.org/10.1111/jan.13002
Bloomfield J, Pegram A. Care, compassion and communication. Nurs Stand.. 2015; 29:(25)45-50 https://doi.org/10.7748/ns.29.25.45.e7653
Bramhall E. Effective communication skills in nursing practice. Nurs Stand.. 2014; 29:(14)53-59 https://doi.org/10.7748/ns.29.14.53.e9355
Brown R. An analysis of loneliness as a concept of importance for dying persons. In: McKenna H, Cutcliffe J (eds). Philadelphia (PA): Elsevier Churchill Livingstone; 2005
Burley D. Better communication in the emergency department. Emerg Nurse.. 2011; 19:(2)32-36 https://doi.org/10.7748/en2011.05.19.2.32.c8509
Cambridge University Press. Effective. 2018. https://tinyurl.com/y7dqcypc (accessed 10 August 2020)
Campbell JD, Lavallee LF. Who am I? The role of self-concept confusion in understanding the behavior of people with low self-esteem. In: Baumeister RF (ed). New York (NY): Plenum Press; 1993
Carment DW, Miles CG, Cervin VB. Persuasiveness and persuasibility as related to intelligence and extraversion. Br J Soc Clin Psychol.. 1965; 4:(1)1-7 https://doi.org/10.1111/j.2044-8260.1965.tb00433.x
Casey A, Wallis A. Effective communication: principle of nursing practice E. Nurs Stand.. 2011; 25:(32)35-37 https://doi.org/10.7748/ns2011.04.25.32.35.c8450
Daly L. Effective communication with older adults. Nurs Stand.. 2017; 31:(41)55-62 https://doi.org/10.7748/ns.2017.e10832
Department of Health and Social Care. Essence of care 2010: benchmarks for the fundamental aspects of care. 2010. https://tinyurl.com/y3z8grqe (accessed 10 August 2020)
Dithole KS, Thupayagale-Tshweneagae G, Akpor AO, Moleki MM. Communication skills intervention: promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs.. 2017; 16:(74)1-6 https://doi.org/10.1186/s12912-017-0268-5
Draper P. A critique of concept analysis. J Adv Nurs.. 2014; 70:(6)1207-1208 https://doi.org/10.1111/jan.12280
Duldt BW, Giffin K, Patton BR. Interpersonal communication in nursing: a humanistic approach.Philadelphia (PA): FA Davis; 1983
Fakhr-Movahedi A, Salsali M, Negharandeh R, Rahnavard Z. Exploring contextual factors of the nurse-patient relationship: a qualitative study. Koomesh.. 2011; 13:(1)23-34
Fleischer S, Berg A, Zimmermann M, Wuste K, Behrens J. Nurse-patient interaction and communication: a systematic literature review. J Public Health.. 2009; 17:339-353 https://doi.org/10.1007/s10389-008-0238-1
Foley A, Davis A. A guide to concept analysis. Clin Nurse Spec.. 2017; 31:(2)70-73 https://doi.org/10.1097/NUR.0000000000000277
Gadamer HG. Philosophical hermeneutics. Translated by DE Linge.Berkeley (CA): University of California Press; 1976
Gallagher L. Continuing education in nursing: a concept analysis. Nurse Educ Today.. 2007; 27:(5)466-473 https://doi.org/10.1016/j.nedt.2006.08.007
Ghafouri R, Rafii F, Oskouie F, Parvizy S, Mohammadi N. Nursing professional regulation: Rodgers' evolutionary concept analysis. Int J Med Res Health Sci. 2016; 5:(9S)436-442
Griffiths J. Person-centred communication for emotional support in district nursing: SAGE and THYME model. Br J Community Nurs.. 2017; 22:(12)593-597 https://doi.org/10.12968/bjcn.2017.22.12.593
Hazzard A, Harris W, Howell D. Taking care: practice and philosophy of communication in a critical care follow-up clinic. Intensive Crit Care Nurs.. 2013; 29:(3)158-165 https://doi.org/10.1016/j.iccn.2013.01.003
Jevon P. Clinical examination skills.Chichester: Wiley-Blackwell Publications; 2009
Jones A. The foundation of good nursing practice: effective communication. J Renal Nurs.. 2012; 4:(1)37-41 https://doi.org/10.12968/jorn.2012.4.1.37
Kelton D, Davis C. The art of effective communication. Nurs Made Incred Easy.. 2013; 11:(1)55-56 https://doi.org/10.1097/01.NME.0000423378.98763.96
Kourkouta L, Papathanasiou IV. Communication in nursing practice. Mater Sociomed.. 2014; 26:(1)65-67 https://doi.org/10.5455/msm.2014.26.65-67
McCabe C. Nurse patient communication: an exploration of patients' experiences. J Clin Nurs.. 2004; 13:41-49 https://doi.org/10.1111/j.1365-2702.2004.00817.x
McCabe C, Timmins F. Communication skills for nursing practice, 2nd edn. Basingstoke: Palgrave; 2013
McCarthy DM, Buckley BA, Engel KG, Forth VE, Adams JG, Cameron KA. Understanding patient-provider conversations: what are we talking about?. Acad Emerg Med.. 2013; 20:(5)441-448 https://doi.org/10.1111/acem.12138
McCroskey JC, Richmond VP. Willingness to communicate: differing cultural perspectives. South Commun J.. 1990; 56:(1)72-77 https://doi.org/10.1080/10417949009372817
McCuster M. Apathy: who cares? A concept analysis. Ment Health Nurs.. 2015; 36:693-697 https://doi.org/10.3109/01612840.2015.1022844
McKenna HP. Nursing theories and models.London: Routledge; 1997
McKinnon J. The case for concordance: value and application in nursing practice. Br J Nurs.. 2013; 22:(13)16-21 https://doi.org/10.12968/bjon.2013.22.13.766
Miller L. Effective communication with older people. Nurs Stand.. 2002; 17:(9)45-50 https://doi.org/10.7748/ns2002.11.17.9.45.c3298
Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital settings: a qualitative systematic review protocol. JBI Database System Rev Implement Rep.. 2015; 13:(1)76-87 https://doi.org/10.11124/jbisrir-2015-1072
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci.. 2016; 8:(6)65-74 https://doi.org/10.5539/gjhs.v8n6p65
Nuopponen A. Methods of concept analysis: a comparative study. LSP.. 2010; 1:(1)4-12
Nursing and Midwifery Council. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. 2018. https://tinyurl.com/zy7syuo (accessed 10 August 2020)
O'Hagan S, Manias E, Elder C What counts as effective communication in nursing? Evidence from nurse educators' and clinicians' feedback on nurse interactions with simulated patients. J Adv Nurs.. 2013; 70:(6)1344-1355 https://doi.org/10.1111/jan.12296
Orem DE. Nursing: concepts of practice, 4th edn. St. Louis (MO): Mosby-Year Book; 1991
Oxford University Press. Communication. 2018. https://tinyurl.com/y7k22yxb (accessed 10 August 2020)
Communication barriers. 2016. https://tinyurl.com/y3sn342h (accessed 10 August 2020)
Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf.. 2014; 23:(8)678-689 https://doi.org/10.1136/bmjqs-2013-002437
Rodgers BL. Concepts, analysis and the development of nursing knowledge: the evolutionary cycle. J Adv Nurs.. 1989; 14:(4)330-335 https://doi.org/10.1111/j.1365-2648.1989.tb03420.x
Rodgers BL, Knafi KA. Concept development in nursing: foundations, techniques and applications, 2nd edn. Philadelphia (PA): WB Saunders; 2000
Royal College of Nursing. Communication-end of life care. 2015. https://tinyurl.com/go28vsm (accessed 10 August 2020)
Schirmer JM, Mauksch L, Lang F Assessing communication competence: a review of current tools. Fam Med.. 2005; 37:(3)184-192
Skär L, Söderberg S. Patients' complaints regarding healthcare encounters and communication. Nurs Open.. 2018; 5:(2)224-232 https://doi.org/10.1002/nop2.132
Snowden A, Martin C, Mathers B, Donnell A. Concordance: a concept analysis. J Adv Nurs.. 2014; 70:(1)46-59 https://doi.org/10.1111/jan.12147
Tay LH, Ang E, Hegney D. Nurses' perceptions of the barriers in effective communication with inpatient cancer adults in Singapore. J Clin Nurs. 2011; 21:(17-18)2647-2658 https://doi.org/10.1111/j.1365-2702.2011.03977.x
Thompson CJ. Nursing theory and philosophy terms: a guide.South Fork (CO): CJT Consulting and Education; 2017
Tofthagen R, Fagerstrøm LM. Rodgers' evolutionary concept analysis – a valid method for developing knowledge in nursing science. Scand J Caring Sci. 2010; 24:21-31 https://doi.org/10.1111/j.1471-6712.2010.00845.x
Nursing, admission assessment and examination. 2018. https://tinyurl.com/y4ykv2uo (accessed 10 August 2020)
Walker LO, Avant KC. Strategies for theory construction in nursing, 5th edn. Norwalk (CT): Appleton and Lange; 2011
Webb L. Exploring the characteristics of effective communicators in healthcare. Nurs Stand.. 2018; 33:(9)47-51 https://doi.org/10.7748/ns.2018.e11157
Wikström B, Svidén G. Exploring communication skills training in undergraduate nurse education by means of a curriculum. Nurs Rep.. 2011; 1:(1) https://doi.org/10.4081/nursrep.2011.e7
Effective communication between nurses and patients: an evolutionary concept analysis
Dorothy Afriyie
Student Nurse, University of West London, Brentford
View articles · Email Dorothy

Communication can be considered as the basis of the nurse-patient relationship and is an essential element in building trust and comfort in nursing care. Effective communication is a fundamental but complex concept in nursing practice. This concept analysis aims to clarify effective communication and its impact on patient care using Rodgers's (1989) evolutionary framework of concept analysis. Effective communication between nurses and patients is presented along with surrogate terms, attributes, antecedents, consequences, related concepts and a model case. Effective communication was identified to be a multifactorial concept and defines as a mutual agreement between nurses and patients. This influences the nursing process, clinical reasoning and decision-making. Consequently, promotes high-quality nursing care, positive patient outcome and patient's and nurse's satisfaction of care.
Communication is an essential element of building trust and comfort in nursing, and it is the basis of the nurse–patient relationship ( Dithole et al, 2017 ). Communication is a complex phenomenon in nursing and is influenced by multiple factors, such as relationship, mood, time, space, culture, facial expression, gestures, personal understanding and perception ( McCarthy et al, 2013 ; Kourkouta and Papathanasiou, 2014 ). Effective communication has been linked to improved quality of care, patient satisfaction and adherence to care, leading to positive health outcomes ( Burley, 2011 ; Kelton and Davis, 2013 ; Ali, 2017 ; Skär and Söderberg, 2018 ). It is an important part of nursing practice and is associated with health promotion and prevention, health education, therapy and treatment as well as rehabilitation ( Fakhr-Movahedi et al, 2011 ). The Nursing and Midwifery Council (NMC) (2018) emphasised effective communication as one of the most important professional and ethical nursing traits. Nonetheless, communication remains a complicated phenomenon in nursing, and most patient-reported complaints in healthcare are around failed communication ( Reader et al, 2014 ). The aim of the present concept analysis is to explore and clarify the complexity of establishing effective communication between nurses and patients in practice.
Concept analysis
Concept analysis is the foundation and preparatory phase of nursing research ( Walker and Avant, 2011 ). Concept analysis aids in clarifying concepts in nursing by using simpler elements to reduce ambiguity and identify all aspects of a concept ( Nuopponen, 2010 ; Foley and Davis, 2017 ). Draper (2014) criticised concept analysis as being methodologically weak and philosophically dubious, further arguing that there is no evidence of its contribution to patient care. However, concept analysis facilitates the review of literature on a concept of interest, thereby enabling a thorough examination of the concept ( Bergdahl and Berterö, 2016 ). This helps in understanding the concept and, therefore, applying it appropriately. Correspondingly, understanding key concepts in nursing practice enables the nurse to identify strategic interventions that could benefit patients. Although McKenna (1997) argued that there is no definite meaning of a concept because they are experienced and perceived differently by people, Walker and Avant (2011) highlighted that the ability of the nurse to describe concepts in an exploratory way is an important means to demonstrate evidence base in practice. Nursing is an evidence-based practice; hence it is the responsibility of the nurse to keep up-to-date with quality evidence and demonstrate it in practice ( Thompson, 2017 ). Therefore, it is paramount for nurses to understand concept analysis and be able to analyse key concepts in nursing.
This concept analysis aims to clarify the concept of effective communication and address the gap in knowledge using Rodgers's (1989) theoretical framework. The evolutionary method of concept analysis was chosen because it adopts a systematic approach with focused phases ( Tofthagen and Fagerstrøm, 2010 ). Rodgers's (1989) method is perceived as a simultaneous task approach, which does not seek boundaries to restrict a concept and considers its application within multiple contexts ( Gallagher, 2007 ). However, the framework will be used because it facilitates an exploration and deep comprehension of a concept ( McCuster, 2015 ). Additionally, the framework offers an alternative to a positivist approach to concepts, allowing different findings depending on the situation ( Ghafouri et al, 2016 ). Moreover, the framework provides an opportunity to identify attributes and related features in a manner that minimises bias ( McCuster, 2015 ). Effective communication between patients and nurses was analysed using the seven phases of Rodgers's (1989) evolutionary method ( Box 1A ). Further, the following four questions were addressed ( Box 1B ).
Box 1A.Rodgers's method of analysis (1989)
Box 1B.Rationale for the four focused questionsThe focus questions were driven by the Rodgers's (1989) framework of concept analysis; the four questions are aimed at analysing the concept of effective communication using the seven stages of the framework in a systematic manner to engender an understanding of effective communication
- What is effective communication?
- What are the surrogate terms and related use of the concept of effective communication?
- What attributes, antecedents and consequences apply to the concept of effective communication?
- Who benefits from effective communication between nurses and patients?
Identifying the appropriate realm for data collection
As endorsed by Brown (2005) , a comprehensive review of the literature was conducted for this analysis. Explicit inclusion and exclusion criteria were used to select relevant articles, as recommended by Tofthagen and Fagerstrøm (2010) . Two electronic databases-Cumulative Index for Nursing and Allied Health (CINAHL) and MEDLINE (Ovid)-were searched using the keywords ‘effective communication’ and ‘nurses’ and ‘patients’. The inclusion criteria allowed selection of only peer-reviewed academic journals written in the English language. Studies exploring or analysing effective communication among nurses and patients with underlying communication difficulties and cognitive disabilities were excluded, because it is likely that such patients or nurses represent a special challenge in communicating. Only articles exploring effective communication and factors that influence communication between nurses and patients were considered. A total of 2086 articles were retrieved from the databases, and these articles were screened for relevance by reading the abstract. Finally, 30 articles were determined to meet the inclusion criteria for the analysis ( Figure 1 ). The articles selected were published between 1965 and 2019.
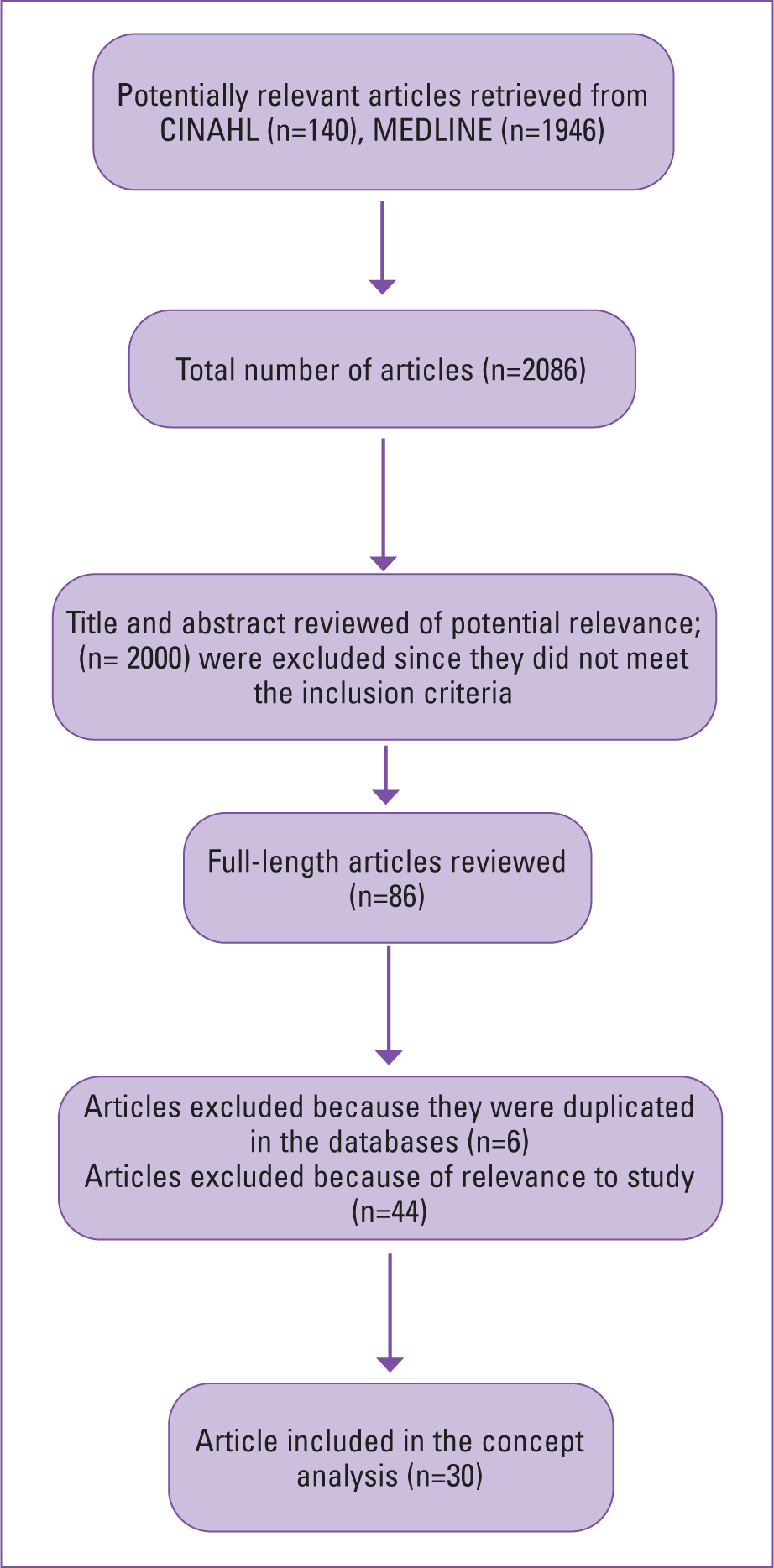
Defining effective communication
The Cambridge English dictionary defines ‘effective’ as ‘successful or achieving the results that you want’ ( Cambridge University Press, 2018 ). According to the Oxford English Dictionary, communication is ‘imparting or exchanging information by speaking, writing or using some other medium’ ( Oxford University Press, 2018 ). The Department of Health and Social Care (2010) described communication as the meaningful exchange of facts, needs, opinions, thoughts, feelings or other information between two or more people. Further, communication can be face-to-face, over the phone or by written words. McCabe and Timmins (2013) also described communication as a cyclical and dynamic process, involving transmission, receiving and interpretation of information between people using verbal or non-verbal means. Rani (2016) simply described communication as ‘sharing meaning’.
Interestingly, Hazzard et al (2013) described communication as a primary condition of human consciousness. They further explained that people always identify themselves in a communicative state. This would imply that people are always exchanging information. The authors, however, described communication as the actions taken after speaking to someone; this highlights communication as responsive. This may be the action and reaction people adopt after a communicated request or statement. Nonetheless, Gadamer (1976) , a twentieth-century philosopher, highlighted communication as what we are and not just what we do. Kourkouta and Papathanasiou (2014) defined communication as the use of speech or other means to exchange information, thoughts and feelings among people. Therefore, effective communication may be classified as exchanging information, thoughts and feelings using either verbal or non-verbal expressions to successfully produce a desired or intended result.
Effective communication between nurses and patients may be analysed from both the nurse's and the patient's perspective. McCabe (2004) identified that the patients' perspective of effective communication entails patient-centred interaction. On the other hand, O'Hagan et al (2013) found that nurses' perspective of effective communication revolves around time, task, rapport and patients' agreement on what has been communicated. Although both perspectives appear to differ, they are both driven by the expectations of the patient and nurse. A nurse may ultimately identify effective communication as the ability to engage with patients and to achieve clinical goals. Similarly, patients may be influenced by their expectation regarding their management outcome ( Schirmer et al, 2005 ). Therefore, effective communication between nurses and patients may be defined as mutual agreement and satisfaction with care (provided and received).
Surrogate terms and relevant uses
The terms most commonly serving a manifestation of effective communication include: therapeutic communication, interpersonal relationship, intercommunication, interpersonal communication and concordance. From a literature search, these terms appear frequently, highlighting their close usage with the concept of effective communication ( Fleischer et al, 2009 ; Casey and Wallis, 2011 ; Jones, 2012 ; Bloomfield and Pegram, 2015 ; Daly, 2017 ). For example, through intercommunication or interpersonal communication, a nurse can encourage a patient to participate in their care decision-making. However, a patient's acceptance to engage in shared decision-making regarding care and agree with a negotiated care plan could reflect effective communication. This act of mutual agreement through negotiation and shared decision-making suggests concordance ( Mckinnon, 2013 ; Snowden et al, 2014 ). Abdolrahimi et al (2017) pointed out that therapeutic communication is the basis for effective communication. They highlighted therapeutic communication as an important means for establishing interpersonal relationships. These concepts are different from effective communication; however, these notions express an idea of the concept of effective communication and highlight an understanding of effective communication as emphasised by Rodgers (1989) .
Daly (2017) described communication as dynamic and cyclical, because it involves a process of transmission, receiving and interpretation through verbal or non-verbal means. This reflects the complexity of communication, which involves speaking, being heard, listening, understanding or being accepted, as well as being seen and acknowledged. Hence, assessing factors that could affect communication, such as noise or interference, is always crucial for effective communication ( McCabe and Timmins, 2013 ; Webb, 2018 ). Daly (2017) explained that other skills for effective communication, which are consciousness, compassion, competence, professionalism and person-centredness, are all important concepts in nursing studies and practice. This indicates that communication is intentional in nature, so the purpose and perspective of individuals involved should be valued and respected ( Jones, 2012 ). In the case of the nurse–patient relationship, a nurse must consider a patient's perspective, background and concerns when communicating. It is important for a nurse to be competent, ethical and professional and exhibit an individualised approach in communicating with patients ( Bramhall, 2014 ; Bloomfield and Pegram, 2015 ). For example, when communicating with a patient with no medical background, medical terms should be explained further or avoided. This promotes person-centredness, which is a determinant for effective communication for patients.
A nurse must respect human rights and be professional ( NMC, 2018 ). However, it can be challenging when communicating with a patient who does not want to communicate about their health, which reflects their right to autonomy. Nonetheless, it is paramount for a nurse to identify the purpose of communication and the difficulties, so that they can mitigate them as part of their professional and ethical duties ( Royal College of Nursing, 2015 ; NMC, 2018 ). This can be done by reassuring and encouraging patients. Correspondingly, this act of communication features in Duldt et al's (1983) theory of humanistic nursing communication. This theory is reflected in Bramhall (2014) and Kourkouta and Papathanasiou's (2014) exploration on communication in nursing. The theory explains the need for comprehensive and exclusive communication among nurses and clients as well as colleagues. The focus of the theory is on interpersonal communication and emphasises the need for humanistic approaches to help improve professional communication. These approaches include empathy, deeper respect, encouragement and interpersonal relationship. For example, listening to people, providing privacy when communicating, giving patients ample time, using kind and courteous words such as ‘please’ and ‘thank you’, as well as being frank and honest when communicating. All these approaches may promote effective communication between nurses and patients ( Jevon, 2009 ; Bramhall, 2014 ; Bloomfield and Pegram, 2015 ).
Further, Miller (2002) , Burley (2011) , Casey and Wallis (2011) , Jones (2012) Bloomfield and Pegram (2015) and Daly (2017) demonstrated how effective communication is key in the assessment, planning and implementation of personalised nursing care. Holistic assessment in nursing includes history-taking, general appearance, physical examination, vital signs and documentation ( Toney-Butler and Unison-Pace, 2018 ). Patient assessment aids in identifying the communication needs of a patient in order to promote person-centred care ( Toney-Butler and Unison-Pace, 2018 ). Moreover, non-verbal cues such as general appearance or posture are vital in communication, and understanding them could help in the assessment process. General appearance such as facial expressions, dressing, hair or skin integrity may convey information that may be helpful in the nursing assessment process. Although not ideal, however, appearance can be a powerful transmitter of intentional or unintentional messages ( Ali, 2018 ). For instance, a nurse may sense neglect or abuse when a patient appears physically unkempt, with bruises or sores. This may inform the nurse on appropriate questions to ask during history-taking in order to ascertain the patient's situation and safeguard, signpost or refer them for support if necessary. Nurses' ability to identify these concerns may aid in providing the best necessary care for their patients. This promotes person-centredness, which is perceived as a means of effective communication by patients ( McCabe, 2004 ).
Effective communication promotes comprehensive history-taking. History-taking involves communicating with patients to collect subjective data and using this information to determine management plans ( Jevon, 2009 ). In history-taking, inaccurate information may be collected when communication is not effective ( Burley, 2011 ; Jones, 2012 ; Daly, 2017 ). However, it is important for nurses to establish good personal relationships with patients, so the latter can feel comfortable in sharing their complaints ( Casey and Wallis, 2011 ). It needs to be noted that, since patients are experts in their own lives, the nurse's ability to make patients feel comfortable may encourage patients to share valuable information, as well as their expectations, concerns and fears. Effective communication is important if nurses are to implement their roles effectively with regard to holistic assessment, considering the subjective experience and characteristics of their patient. Further, a well-informed collaborative assessment through effective communication may contribute to positive patient management outcomes ( Kourkouta and Papathanasiou, 2014 ). For instance, a patient may convey all necessary information to a nurse during assessment, and this may inform the nurse and patient of the necessary examination and investigations to aid in evidence-based nursing diagnosis and a collaborative management plan. The ability to establish a mutual agreement for the nursing process suggests effective communication for both parties.
Effective communication aids in planning and implementing personalised care. It helps patients to set realistic goals and choose preferred management for better outcomes. Communication is a bidirectional process in which a sender becomes a receiver and vice versa ( Kourkouta and Papathanasiou, 2014 ). Therefore, there is a need for both patients and nurses to realise that they are partners in communicating care planning and implementation ( Bloomfield and Pegram, 2015 ). This realisation may promote the patient's dignity and may also influence patients' desire to adhere to their plan when they feel involved in decision-making ( Casey and Wallis, 2011 ). Conversely, patients may be reluctant and unhappy if they feel dictated to or patronised. Most importantly, involving patients through effective communication can empower them to have full control over their health and wellbeing. This is reflected in the self-care theory proposed by Orem (1991) and the theory of self-efficacy proposed by Bandura (1977) . These theories focus on the role of the individual in initiating and sustaining change and healthy behaviours. Orem (1991) reinforced the importance of communication, as self-care is learned through communication and interpersonal relationships.
Attributes of effective communication
Certain attributes can be used to develop a definition of effective communication that is more realistically reflective of how patients and nurses use the term in healthcare settings ( Rodgers and Knafi, 2000 ). The most common attributes identified in the literature include: effective communication as ‘a building foundation for interpersonal-relationship’, ‘a determinant of promoting respect and dignity’, ‘a precedent of achieving concordance’, ‘an important tool in empowering self-care in patient’, ‘a significant tool in planning and implementing person-centred care’ and ‘a determinant of clinical reasoning and the nursing process’ ( Casey and Wallis, 2011 ; Jones, 2012 ; McCabe and Timmins, 2013 ; Bramhall, 2014 ; Bloomfield and Pegram, 2015 ; Daly, 2017 ; Webb, 2018 ; Barratt, 2019 ). These attributes make it possible to identify situations that can be categorised under the concept of effective communication.
Antecedents of effective communication
According to the literature, antecedents to effective communication include: personality trait, perceived communication competence and level of education on communication. Personality traits were linked with communication in early research. Carment et al (1965) demonstrated that people who are introverts are less likely to communicate well compared with extroverts. McCroskey and Richmond (1990) also indicated that people with low self-esteem are less willing to communicate. This is because they are more sensitive to environmental cues ( Campbell and Lavallee, 1993 ). Additionally, McCroskey and Richmond (1990) asserted that people who perceived themselves as poor communicators may be less willing to communicate. Nonetheless, people who may be very capable of communicating may not be willing to, due to low self-esteem, anxiety or fear. As a result, such people may have low communication efficacy despite having high actual competence ( McCroskey and Richmond, 1990 ). Therefore, it is important for nurses to consider these factors when communicating with patients in order to identify their communication needs and manage them accordingly ( Daly, 2017 ). Furthermore, Dithole et al (2017) and Norouzinia et al (2016) highlighted that the nurse's level of education on communication may influence the ability to communicate effectively. Thus, incorporation of targeted communication skills education in the training curriculum and on-the-job training will empower nurses to communicate effectively with their patients.
Consequences of effective communication
The consequences of effective communication can be classified into patient–nurse-related and healthcare system-related outcomes. Skär and Söderberg (2018) mentioned that effective communication ensures a good healthcare encounter for patients. In the community settings, effective communication empowers patients to talk about their concerns and expectations ( Griffiths, 2017 ). Further, effective communication promotes a pleasant and comfortable hospital experience for patients as well as their families; this can also be reflected in the community settings, where patients may report pleasant and comfortable nursing care ( Newell and Jordan, 2015 ; Barratt, 2019 ). Kourkouta and Papathanasiou (2014) and Wikström and Svidén (2011) pointed out that the success of a nurse mostly depends on how effectively they can communicate with their patient. Conversely, ineffective communication may lead to unsuccessful outcomes. For example, a patient may convey their fears, signs and symptoms to a nurse and how the nurse decodes and applies the information may influence the intervention given ( Kourkouta and Papathanasiou, 2014 ). Likewise, a nurse may convey a piece of information to a patient, but the patient's understanding of the information will determine their action. Therefore, how the message is understood determines the action taken ( Kourkouta and Papathanasiou, 2014 ). Additionally, through effective communication, a patient may be empowered to have full control over their health and wellbeing ( Newell and Jordan, 2015 ) and may not require extended care. Clearly, effective communication can lead to positive and cost-saving consequences for patients, nurses and the healthcare system.
The final phase of Rodgers's (1989) method of analysis highlights an application of the concept in an exploratory case scenario. A model case for effective communication between a nurse and a patient is given in Box 2 . This case portrays effective communication between a nurse and a patient, revealing some surrogate terms, defining attributes, antecedents and consequences of the concept. The case model highlighted Audrey's positive engagement in her care decision-making when the nurse Dani communicated effectively. Dani visited Audrey in her home, where Audrey had spatial and environmental control, but she was reluctant to engage in her own care. Audrey perceived that other nurses did not involve her in her care decision-making. This indicates ineffective communication and may be attributed to factors such as age difference, generational gap, gender and culture and ethnic differences between Audrey and the other nurses ( Tay et al, 2011 ; Norouzinia et al, 2016 ).
Box 2.Model caseAudrey, a 90-year-old housebound patient with bilateral leg ulcers was visited by Dani, a 45-year-old community staff nurse working in a diverse multicultural district nursing team. On arrival, Dani introduced herself in a suitable tone, maintaining eye contact. Audrey responded in a low tone, without maintaining eye contact. Audrey appeared to be quiet and in a low mood; Dani identified this nonverbal cue and was determined to engage Audrey in conversation. Dani knew from her experience that leg ulcer treatment can affect a person's mental health, causing low self-esteem, fear and anxiety. Dani asked how Audrey felt and if there was something she could help her with. Audrey mentioned she was fine; her carers had visited and supported her with personal care, breakfast and medication, she had been waiting for the nurse's visit. Dani asked Audrey about her ulcers and how she felt about her dressings; Audrey mentioned she was fine, but expressed concerns about the ulcers not healing. Dani reassured Audrey, explained leg ulcers to her and advised Audrey about some effective practice to promote the healing process.Dani asked Audrey ‘How best can I help you, and how do you want your care to be delivered?’. Audrey responded, ‘You are the nurse, you know better’. Dani took ample time to explain to Audrey how she understands her own body better than any other person. Dani also reassured and encouraged Audrey that her opinions mattered, as this helped empower her, promoted her dignity and informed the nurse on how to care for her. Audrey then expressed to Dani that her other nurses, who are much younger than Dani, never ask her opinion regarding the ulcer management; hence, she was not willing to speak. Audrey mentioned that those nurses came in to re-dress her ulcers and they spoke to her about the care plan, but she did not feel involved in decision-making about her care. Audrey then mentioned that she did not mean to create problems or report anyone. Dani reassured Audrey that there would be no trouble, so she should not be afraid to speak up. Audrey thought that having an honest communication about her needs and views could create problems for her or for the nurses if it seemed that she had reported them.Dani then reassured and encouraged Audrey that the situation will be addressed in a professional manner, and none of the other nurses would feel they had been reported; however, they would involve her in her care and decision-making, which is the expectation. Audrey was then comfortable, communicated in a suitable tone and maintained eye contact with Dani. She asked Dani if she could bandage her right leg first, as she tends to be in pain for a long time when the left one is dressed first. Dani gained consent from Audrey, explained the procedure and advised Audrey to stop her whenever she experienced pain. Dani also asked Audrey a bit more about her pain and her analgesia. Dani identified that Audrey's analgesia had not been reviewed for over 3 years. Dani explained to Audrey that she would be making a referral to her GP about this matter. Audrey was very pleased and indicated she was happy with how Dani had communicated with her; she felt she could trust her. Dani was also pleased, because she could provide the best care for Audrey.
Another important factor that can affect effective communication is the environmental factor. Norouzinia et al (2016) revealed that the hospital environment is a barrier to effective communication for patients. Additionally, Tay et al. (2011) indicated the possibility of unilateral communication due to the hierarchical structure of the hospital environment. Conversely, although nurses may feel quite comfortable in the hospital or inpatient setting, they might feel relatively intimidated when visiting a patient's home. Therefore, an awareness of the contextual discomfort and how it may affect communication is important and should be considered when planning for effective two-way communication between the nurse and patient during home visits. Although all these factors are important in communication, a full discussion of these is beyond the scope of this paper and should be the focus of another complete work.
In the model case described in Box 2 , the nurse acknowledged that she was privileged to be a guest in Audrey's home, and she tailored her strategy to gain Audrey's perspective. The nurse's aim was to get Audrey involved in her care decision-making since Audrey knows herself best. Additionally, Audrey's participation in the decision-making made it possible for her to receive her preferred care. This shows that effective communication is bidirectional, and both partners (nurse and patient) must work together to achieve their desired outcomes, in this case, the patient's satisfaction with care and the nurse's ability to provide the best care.
Effective communication in nursing is clearly a complex, multidimensional and multifactorial concept. Factors such as emotions, general appearance, personality trait, mood and level of education on communication may influence the practice and outcome of effective communication. However, effective communication is an ultimate determinant of success for a nurse. Effective communication was defined as a mutual agreement and satisfaction of care for both patients and nurses. It has been linked to precede the achievement of concordance in patients, and in nurses, it influences clinical reasoning and the nursing process. This aids in implementing compassionate person-centred care and, when successful, it promotes positive patient outcomes and satisfaction with nursing care. Thus, effective communication is an important concept to prioritise in nursing education and practice. For this reason, engaging nurses in communication skills and on-the-job training will empower them to communicate effectively with their patients. As endorsed by Rodgers's (1989) , the outcome of this analysis is not the endpoint of the concept but should direct the future exploration of effective communication. Therefore, a systematic study of effective communication between nurses and patients as well as a systematic review considering effective communication among nurses and patients with underlying communication difficulties, cognitive disabilities and intercultural perspectives can ultimately enhance nursing science.
- Effective communication is a key component of nursing practice
- Effective communication is intentional in nature and can be improved through direct actions taken by the nurse
- Communication is a complex phenomenon and is an essential element of building trust and comfort in nursing
- Concept analysis is the basic way of understanding complex concepts and developing different meanings and perceptions
CPD REFLECTIVE QUESTIONS
- How might concept analysis be relevant in nursing studies or practice?
- What does effective communication mean to you?
- What are some challenges nurses face in communicating effectively?
- How can an interpersonal relationship between nurses and patients influence effective communication?
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Ali M. Communication skills 1: benefits of effective communication for patients. Nursing Times. 2017; 113:(12)18-19
Barber C. Communication, ethics and healthcare assistants. British Journal of Healthcare Assistants. 2016; 10:(7)332-335 https://doi.org/10.12968/bjha.2016.10.7.332
Berlo DK. The process of communication; an introduction to theory and practice.New York (NY): Holt, Rinehart and Winston; 1960
Bramhall E. Effective communication skills in nursing practice. Nurs Stand. 2014; 29:(14)53-59 https://doi.org/10.7748/ns.29.14.53.e9355
Bumb M, Keefe J, Miller L, Overcash J. Breaking bad news: an evidence-based review of communication models for oncology nurses. Clin J Oncol Nurs. 2017; 21:(5)573-580 https://doi.org/10.1188/17.CJON.573-580
Caldwell L, Grobbel CC. The importance of reflective practice in nursing. International Journal of Caring Sciences. 2013; 6:(3)319-326
Communication skills for workplace success employers look for these communication skills. The Balance (online). 2019. http://tinyurl.com/yyx3eeoy (accessed 27 June 2019)
Evans N. Knowledge is power when it comes to coping with a devastating diagnosis. Cancer Nursing Practice. 2017; 16:(10)8-9 https://doi.org/10.7748/cnp.16.10.8.s7
Gibbs G. Learning by doing: a guide to teaching and learning methods.Oxford: Further Education Unit, Oxford Polytechnic; 1988
Gillett A, Hammond A, Martala M. Successful academic writing.Harlow: Pearson Education Limited; 2009
Hanratty B, Lowson E, Holmes L Breaking bad news sensitively: what is important to patients in their last year of life?. BMJ Supportive & Palliative Care. 2012; 2:(1)24-28 https://doi.org/10.1136/bmjspcare-2011-000084
Hemming L. Breaking bad news: a case study on communication in health care. Gastrointestinal Nursing. 2017; 15:(1)43-50 https://doi.org/10.12968/gasn.2017.15.1.43
Macmillan Cancer Support. Cancer clinical nurse specialists (Impact Briefs series). 2014. http://tinyurl.com/yb96z88j (accessed 27 June 2019)
Healthcare professionals: acknowledging emotional reactions in newly-diagnosed patients. 2012. http://www.justgotdiagnosed.com (accessed 27 June 2019)
Oelofsen N. Using reflective practice in frontline nursing. Nurs Times. 2012; 108:(24)22-24
Paterson C, Chapman J. Enhancing skills of critical reflection to evidence learning in professional practice. Phys Ther Sport. 2013; 14:(3)133-138 https://doi.org/10.1016/j.ptsp.2013.03.004
Pincock S. Poor communication lies at heart of NHS complaints, says ombudsman. BMJ. 2004; 328 https://doi.org/10.1136/bmj.328.7430.10-d
Royal College of Nursing. Revalidation requirements: reflection and reflective discussion. 2019. http://tinyurl.com/yy8l68cy (accessed 27 June 2019)
Schildmann J, Cushing A, Doyal L, Vollmann J. Breaking bad news: experiences, views and difficulties of pre-registration house officers. Palliat Med. 2005; 19:(2)93-98 https://doi.org/10.1191/0269216305pm996oa
Shipley SD. Listening: a concept analysis. Nurs Forum. 2010; 45:(2)125-134 https://doi.org/10.1111/j.1744-6198.2010.00174.x
Reflecting on the communication process in health care. Part 1: clinical practice—breaking bad news
Beverley Anderson
Macmillan Uro-oncology Clinical Nurse Specialist, Epsom and St Helier NHS Trust
View articles · Email Beverley
This is the first of a two-part article on the communication process in health care. The interactive process of effective communication is crucial to enabling healthcare organisations to deliver compassionate, high-quality nursing care to patients, in facilitating interactions between the organisation and its employees and between team members. Poor communication can generate negativity; for instance, misperception and misinterpretation of the messages relayed can result in poor understanding, patient dissatisfaction and lead to complaints. Reflection is a highly beneficial tool. In nursing, it enables nurses to examine their practice, identify problems or concerns, and take appropriate action to initiate improvements. This two-part article examines the role of a uro-oncology clinical nurse specialist (UCNS). Ongoing observations and reflections on the UCNS's practice had identified some pertinent issues in the communication process, specifically those relating to clinical practice and the management of practice-related issues and complaints. Part 1 examines the inherent problems in the communication process, with explanation of their pertinence to delivering optimal health care to patients, as demonstrated in four case studies related to breaking bad news to patients and one scenario related to communicating in teams. Part 2 will focus on the management of complaints.
In health care, effective communication is crucial to enabling the delivery of compassionate, high-quality nursing care to patients ( Bramhall, 2014 ) and in facilitating effective interactions between an organisation and its employees ( Barber, 2016 ; Ali, 2017 ). Poor communication can have serious consequences for patients ( Pincock, 2004 ; Barber, 2016 ; Ali, 2017 ). Misperception or misinterpretation of the messages relayed can result in misunderstanding, increased anxiety, patient dissatisfaction and lead to complaints ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ; Evans, 2017 ; Doyle, 2019 ), which, as evidence has shown, necessitates efficient management to ensure positive outcomes for all stakeholders—patients, health professionals and the healthcare organisation ( Barber, 2016 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). Complaints and their management will be discussed in Part 2.
Reflection is a highly beneficial tool ( Oelofsen, 2012 ), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes ( Bramhall, 2014 ). The author, a uro-oncology clinical nurse specialist (UCNS), is required to ensure that appropriate reassurance and support is given to patients following the receipt of a urological cancer diagnosis ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ). Support consists of effective communication, which is vital to ensuring patients are fully informed and understand their condition, prognosis and treatment and, accordingly, can make the appropriate choices and decisions for their relevant needs ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ; Doyle, 2019 ).
Reflection is a process of exploring and examining ourselves, our perspectives, attributes, experiences, and actions and interactions, which helps us gain insight and see how to move forward ( Gillett et al, 2009:164 ). Reflection is a cycle ( Figure 1 ; Gibbs, 1988 ), which, in nursing, enables the individual to consciously think about an activity or incident, and consider what was positive or challenging and, if appropriate, plan how a similar activity might be enhanced, improved or done differently in the future ( Royal College of Nursing (RCN), 2019 ).
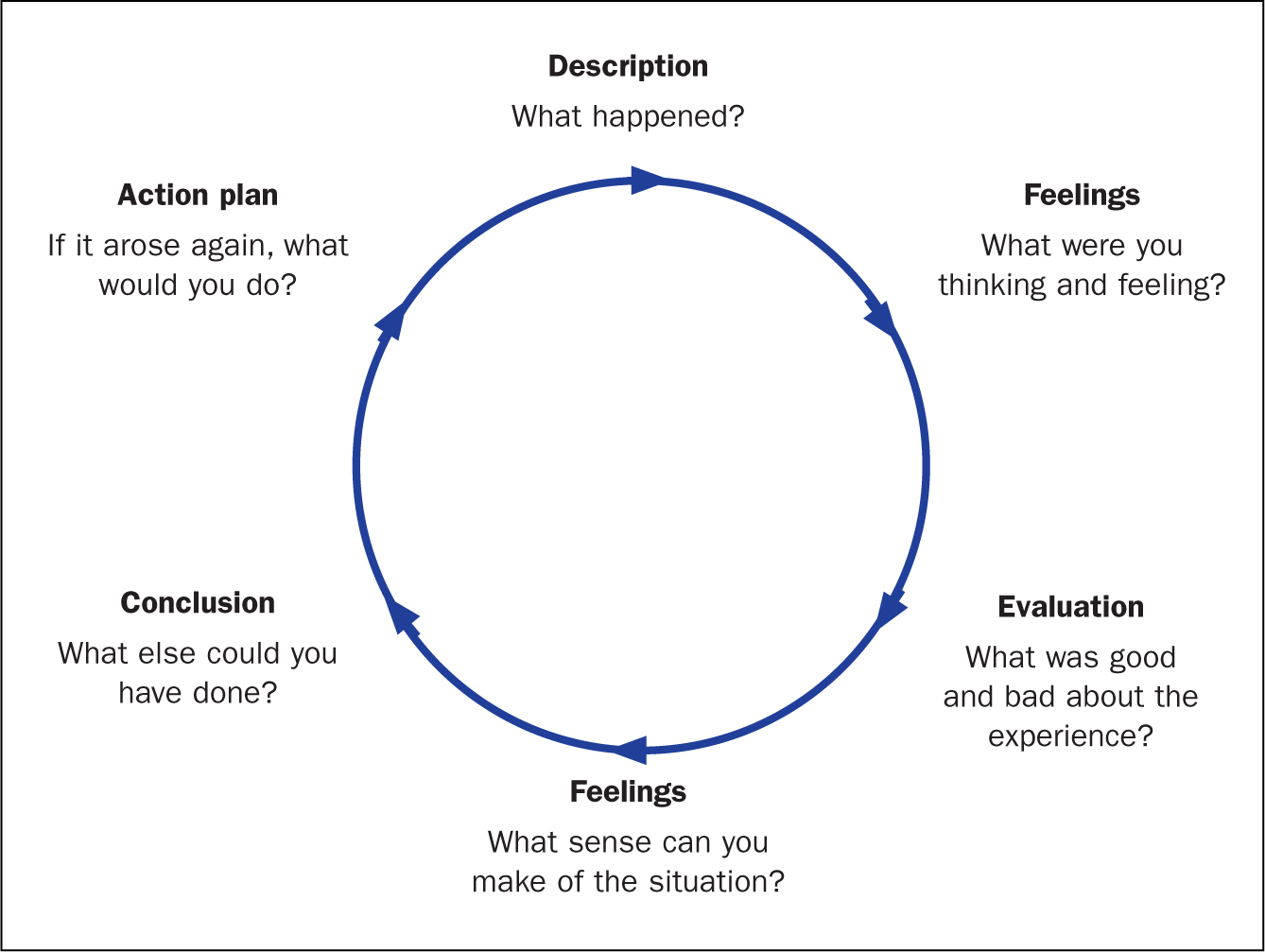
Reflective practice
Reflective practice is the ability to reflect on one's actions and experiences so as to engage in a process of continuous learning ( Oelofsen, 2012 ), while enhancing clinical knowledge and expertise ( Caldwell and Grobbel, 2013 ). A key rationale for reflective practice is that experience alone does not necessarily lead to learning—as depicted by Gibbs' reflective cycle (1988) . Deliberate reflection on experience, emotions, actions and responses is essential to informing the individual's existing knowledge base and in ensuring a higher level of understanding ( Paterson and Chapman, 2013 ). Reflection on practice is a key skill for nurses—it enables them to identify problems and concerns in work situations and in so doing, to make sense of them and to make contextually appropriate changes if they are required ( Oelofsen, 2012 ).
Throughout her nursing career, reflection has been an integral part of the author's ongoing examinations of her practice. The process has enabled numerous opportunities to identify the positive and negative aspects of practice and, accordingly, devise strategies to improve both patient and practice outcomes. Reflection has also been a significant part author's professional development, increasing her nursing knowledge, insight and awareness and, as a result, the author is an intuitive practitioner, who is able to deliver optimal care to her patients.
Communication
Figure 2 provides a visual image of communication—it is both an expressive, message-sending, and a receptive, message-receiving, process ( Berlo, 1960 ; McClain, 2012 ; Evans, 2017 ). This model was originally designed to improve technical communication, but has been widely applied in different fields ( Berlo, 1960 ). Communication is the sharing of information, thoughts and feelings between people through speaking, writing or body language, via phone, email and social media ( Bramhall, 2014 ; Barber, 2016 ; Doyle, 2019 ). Effective communication extends the concept to require that transmitted content is received and understood by someone in the way it was intended.
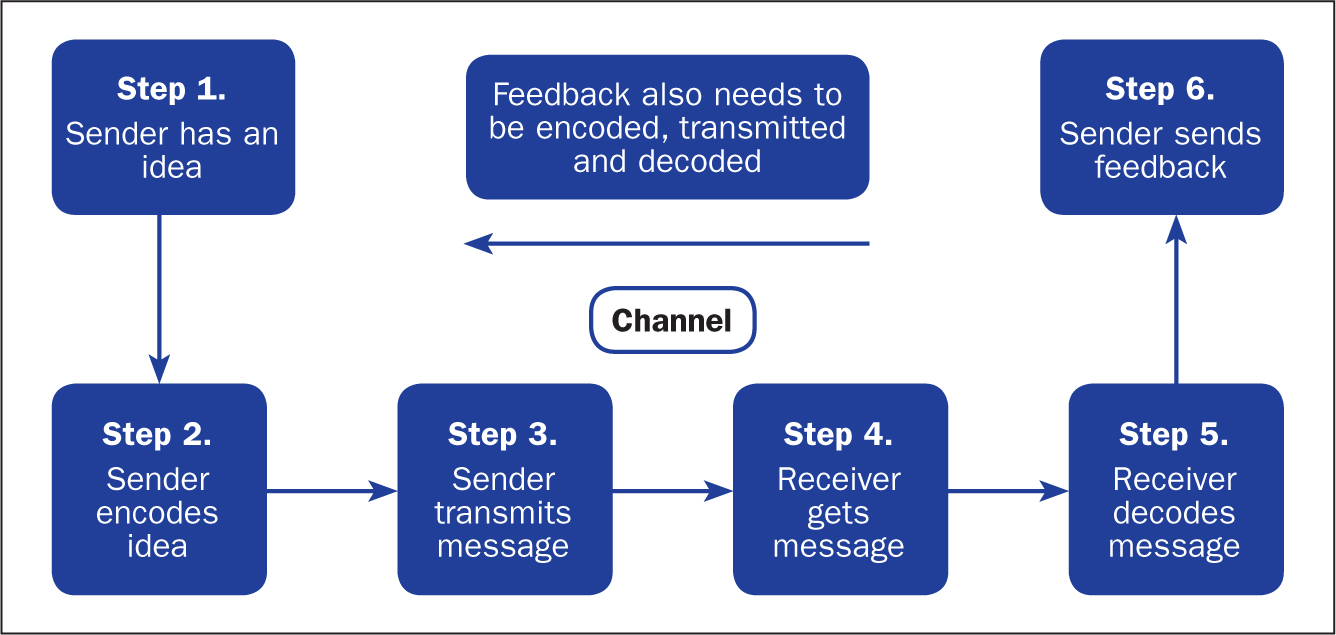
The process is more than just exchanging information. It is about the components/elements of the communication process, ie understanding the emotion and intentions behind the information—the tone of voice, as well as the actual words spoken, hearing, listening, perception, honesty, and ensuring that the messages relayed are correctly interpreted and understood ( Bramhall, 2014 ; Barber, 2016 ; Evans, 2017 ; Doyle, 2019 ). It is about considering emotions, such as shock, anger, fear, anxiety and distress ( Bumb et al, 2017 ; Evans, 2017 ). Language and conceptual barriers may also negatively impact on the efficacy of the communication being relayed.
Challenges of effective communication
The following sections explain the challenges involved in communication—namely, conveying a cancer diagnosis or related bad news.
Tone of voice and words spoken
According to Barber (2016) , when interacting with patients, especially communicating ‘bad news’ to them, both the tone of voice and the actual words spoken are important. The evidence has shown that an empathetic and sensitive tone is conducive to providing appropriate reassurance and in aiding understanding ( McClain, 2012 ; Evans, 2017 ; Hemming, 2017 ). However, an apathetic and insensitive tone will likely evoke fear, anxiety and distress ( Pincock, 2004 ; Ali, 2017 ; Doyle, 2019 ). In terms of the words used, the use of jargon, or highly technical language and words that imply sarcasm and disrespect, can negatively impact on feelings and self-confidence ( Doyle, 2019 ).
Hearing what is being conveyed is an important aspect of effective communication. When interacting with patients it is vital to consider potential barriers such as language (ie, is the subject highly technical or is English not the patient's first language) and emotions (ie shock, anger, fear, anxiety, distress) ( Bumb et al, 2017 ; Evans, 2017 ). A patient may fail to hear crucial information because he or she is distressed during an interaction, or may be unable to fully understand the information being relayed ( Bumb et al, 2017 ). Good communication involves ascertaining what has been heard and understood by the patient, allowing them to express their feelings and concerns, and ensuring these are validated ( Evans, 2017 ).
Listening to the patient
Listening is a deliberate act that requires a conscious commitment from the listener ( Shipley, 2010 ). The key attributes of listening include empathy, silence, attention to both verbal and non-verbal communication, and the ability to be non-judgemental and accepting ( Shipley, 2010 ). Listening is an essential component of effective communication and a crucial element of nursing care ( Shipley, 2010 ; Evans, 2017 ; Doyle, 2019 ). In health care, an inability to fully listen to and appreciate what the patient is saying could result in them feeling that their concerns are not being taken seriously. As observed by the author in practice, effective listening is essential to understanding the patient's concerns.
Perception, interpretation, understanding
Relevant and well-prepared information is key to the patient's perception and interpretation of the messages relayed ( McClain, 2012 ). It is vital to aiding their understanding and to informing their personal choices and decisions. If a patient were to misinterpret the information received, this could likely result in a misunderstanding of the messages being relayed and, consequently, lead to an inability to make clear, informed decisions about their life choices ( McClain, 2012 ; Bramhall, 2014 ).
Fully informing the patient and treating them with honesty, respect and dignity
In making decisions about their life/care, a patient is entitled to all information relevant to their individual situation and needs (including those about the actual and potential risks of treatment and their likely disease trajectory) ( McClain, 2012 ). Information equals empowerment—making a decision based on full information about a prognosis, for example, gives people choices and enables them to put their affairs in order ( Evans, 2017 ). Being honest with a patient not only shows respect for them, their feelings and concerns, it also contributes to preserving the individual's dignity ( Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). However, as observed in practice, a reluctance on the health professional's part to be totally open and honest with a patient can result in confusion and unnecessary emotional distress.
When reflecting on the efficacy of the communication being relayed, it is important for health professionals to acknowledge the challenges and consider how they may actually or potentially impact on the messages being relayed ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Communication and the uro-oncology clinical nurse specialist
It is devastating for a patient to receive the news that they have cancer ( Bumb et al, 2017 ). Providing a patient with a cancer diagnosis—the ‘breaking of bad news’, defined as any information that adversely and seriously affects an individual's view of his or her future ( Schildmann et al 2005 )—is equally devastating for the professional ( Bumb et al, 2017 ; Hemming, 2017 ). It is thus imperative to ensure the appropriate support is forthcoming following receipt of bad news ( Evans, 2017 ).
Integral to the delivery of bad news is the cancer CNS, in this context, the UCNS, who is acknowledged to be in the ideal position to observe the delivery of bad news (usually by a senior doctor in the urology clinic), and its receipt by patients ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ), and to offer appropriate support afterwards ( Evans, 2017 ). Support includes allocating appropriate time with the patient, and their family, after the clinic appointment to ensure they have understood the discussion regarding the diagnosis, prognosis and treatment options ( Evans, 2017 ; Hemming, 2017 ). In this instance, effective communication, as well as the time required, is usually tailored to each individual patient, allowing trust to be built ( Bumb et al, 2017 ; Evans, 2017 ; Hemming, 2017 ).
In the performance of her role, the UCNS is fully aware of the importance placed on delivering bad news well. She has seen first hand how bad news given in a less than optimal manner can impact on the patient's emotions and their subsequent ability to deal with the results. Hence, her role in ensuring that the appropriate support is forthcoming following the delivery of bad news is imperative. It is important to understand that the delivery of bad news is a delicate task—one that necessitates sensitivity and an appreciation of the subsequent impact of the news on the individual concerned. It should also be acknowledged that while the receipt of bad news is, understandably, difficult for the patient, its delivery is also extremely challenging for the health professional ( Bumb et al, 2017 ).
Communicating bad news
The primary functions of effective communication in this instance are to enhance the patient's experience and to motivate them to take control of their situation ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Telling a patient that they have a life-threatening illness such as cancer, or that their prognosis is poor and no further treatment is available to them, is a difficult and uncomfortable task for the health professional ( Bumb et al, 2017 ). It is a task that must be done well nonetheless ( Schildmann, 2005 ). Doing it well is reliant on a number of factors:
- Ensuring communicated information is sensitively delivered ( Hanratty et al 2012 ) to counter the ensuing shock following the patient's receipt of the bad news ( McClain, 2012 )
- Providing information that is clear, concise and tailored to meeting the individual's needs ( Hemming, 2017 )
- Acknowledging and respecting the patient's feelings, concerns and wishes ( Evans 2017 ).
This approach to care is important to empower patients to make the right choices and decisions regarding their life/care, and gives them the chance to ‘put their affairs in order’ ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ).
Choices and decision-making
Case studies 1 and 2 show the importance of honesty, respect, listening and affording dignity to patients by health professionals, in this case senior doctors and the UCNS. The issue of choice and decision-making is highlighted. It is important to note that, while emphasis is placed on patients receiving all the pertinent information regarding their individual diagnosis and needs ( McClain 2012 ), despite receipt of this information, a patient may still be unable to make a definite decision regarding their care. A patient may even elect not to have any proposed treatment, a decision that some health professionals find difficult to accept, but one that must be respected nevertheless ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ).
Case study 1. Giving a poor prognosis and accepting the patient's decision
Jane Green, aged 48, received a devastating cancer diagnosis, with an extremely poor prognosis. It was evident that the news was not what she expected. She had been convinced that she had irritable bowel syndrome and, hence, a cancer diagnosis was quite a shock. Nevertheless, she had, surprisingly, raised a smile with the witty retort: ‘Cancer, you bastard—how dare you get me.’ Mrs Green had been married to her second husband for 3 years. Sadly, her first husband, with whom she had two daughters, aged 17 and 21, had died from a heart attack at the age of 52. His sudden death was hugely upsetting for his daughters; consequently, Mrs Green's relationship with her girls (as she lovingly referred to them) was extremely close. The legacy of having two parents who had died young was not one Mrs Green wished to pass on to her daughters. Her main concern, therefore, was to minimise the inevitable distress that would ensue, following her own imminent death.
In the relatively short time that Mrs Green had to digest the enormity and implications of her diagnosis, she had been adamant that she did not wish to have any life-prolonging interventions, particularly if they could not guarantee a reasonable extension of her life, and whose effects would impact on the time she had left. This decision was driven by previously having observed her mother-in-law's experience of cancer: its management with chemotherapy and the resultant effect on her body and her eventual, painful demise. Mrs Green's memory of this experience was still vivid, and had heightened her fears and anxieties, and reinforced her wish not to undergo similar treatment.
Mrs Green requested a full and honest discussion and explanation from the consultant urologist and the UCNS regarding the diagnosis and its implications. This included the estimated prognosis, treatment interventions and the relevant risks and benefits—specifically, their likely impact on her quality of life. In providing Mrs Green with this information, the consultant and the UCNS had ensured information was clear and concise, empathetic and sensitive to her needs ( Shipley, 2010 ; Hanratty, et al, 2012 ; Evans, 2017 ; Hemming, 2017 ) and, importantly, that her request for honesty was respected. Not disclosing the entire truth can ‘inadvertently create a false sense of hope for a cure and perceptions of a longer life expectancy’ ( Bumb et al, 2017:574 ). Being honest had empowered Mrs Green to come to terms with both the diagnosis and prognosis, to consider the options as well as the risks and benefits. She had a choice between quantity of life and quality of life. Mrs Green elected for quality of life and, accordingly, made decisions that she felt were in her own, and her family's, best interests.
Despite receiving pertinent information and sound advice on why a patient should agree to treatment intervention, they may still elect not to have any treatment ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ). This decision, as observed by the UCNS in practice, is difficult for some health professionals to accept. In Mrs Green's case, accepting her decision not to have any treatment was extremely difficult for both the consultant and the UCNS. In an attempt to try to change Mrs Green's mind, the consultant asked the UCNS to speak to her. The UCNS was aware that the consultant's difficulty to accept the decision was compounded by Mrs Green's age (48) and a desire to give her more time. However, the UCNS had listened closely to Mrs Green's wishes and, in view of her disclosure regarding the experience of her mother-in-law's death, her first husband's untimely death, her fear of upsetting her daughters and her evident determination to keep control of her situation, the UCNS felt compelled to respect her decision.
Following the consultant's request, the UCNS spoke to Mrs Green but, on hearing what she had to say regarding her decision not to have more treatment, concluded that she had to respect Mrs Green's decision. She also clarified whether Mrs Green were willing to continue communication with her GP and ensured that the GP was fully updated regarding current events. Mrs Green had thanked the staff for all their support, but did not wish to continue follow-up with the service. The GP assured the UCNS that she would keep a close eye on Mrs Green and her family.
Case study 2. Giving an honest account of disease progression
The following case study explains how a reluctance by health professionals to be totally honest with a patient had inadvertently hampered the individual's ability to make informed decisions regarding his life choices.
Mr Brown, aged 87, had been previously diagnosed and treated for cancer. On his referral to the urology clinic, his disease had progressed to the metastatic stage, which had limited his management options to palliative care.
Since we have established that delivering bad news to a patient is a difficult task ( Bumb et al, 2017 ), it is not surprising that some health professionals fail to be totally honest with the patient for fear of upsetting them. During the consultation, it transpired that Mr Brown had other serious illnesses and was being managed by other clinicians. Seemingly, previous communications with these clinicians had left Mr Brown and his family unenlightened about his prognosis and his future prospects. In hindsight, the family would have appreciated total honesty sooner, since this would have allowed them to make realistic decisions.
After fully assessing Mr Brown's case (and in light of this disclosure) the doctor decided to be totally honest with Mr Brown and his family regarding his current situation and the choices available to him. Explanations were empathetic and sensitive to Mr Brown's and his family's feelings ( Hanratty et al, 2012 ; Evans, 2017 ). While the news was not entirely unexpected, Mr Brown and his family appreciated the consultant's candour. In this instance, the consultant had respected Mr Brown's entitlement to total honesty. By receiving all the facts, and the appropriate reassurance and support from the UCNS, Mr Brown could now consider his options and, with his family's support, proceed to put his affairs in order.
Management and treatment of cancer
The management and treatment of cancer is determined by several factors. These include: the grade and stage of the individual's disease—whether the disease is low-grade/low-risk, intermediate-grade/intermediate-risk, or high-grade/high-risk. For some low-grade/low-risk disease, the recommended treatment of choice is surgery alone. However, in certain cases, further review of the staging and histology might reveal features of cancer within the sample that are at a high-risk of local recurrence, necessitating additional treatment intervention, ie chemotherapy or radiotherapy, to minimise this threat.
Following the primary treatment intervention (ie surgery), for low-risk/low-grade disease, the risk of local recurrence is usually low, as is the need for additional treatment intervention (chemotherapy or radiotherapy). Nonetheless, local recurrence is still a possibility. A failure to make the patient aware of this possibility creates a lack of trust and a false sense of hope ( Bumb et al, 2017 ), and evokes unnecessary emotional distress for the patient, their families and carers ( McClain, 2012 ).
As previously explained, the term ‘fully informed’ relates to a patient's entitlement to all information relevant to their situation and needs (including those about the actual and potential risks) ( McClain 2012 ). Informed knowledge is power, thus honesty is imperative ( Evans, 2017 ). The following case studies highlight the consequence of failing to fully inform patients about risks and diagnosis.
Case study 3. Consequences of not being fully informed
Mr White, aged 36, had been diagnosed with a low-grade/low-risk cancer. After the initial diagnosis was explained, Mr White was explicitly told by the doctor that after surgery he would not require any additional treatment. However, a subsequent review of his staging and histology revealed features of cancer within the sample that were at a high risk of local recurrence. Therefore the decision was made to offer Mr White additional treatment with radiotherapy to reduce the risk of recurrence down the line. Understandably, this news and the ensuing emotional impact—fear, anxiety and distress—was significant for Mr White. The author contends that, to avoid inciting these emotions, Mr White should have been fully informed, at the initial diagnosis, of the potential risks that further treatment might be necessary, no matter how unlikely these risks were perceived to be. Having observed the emotional impact on Mr White, and other similar cases in local practice, the author proposed that, when delivering a cancer diagnosis, consideration must be given not only to the physical, but also the emotional/psychological impact of the diagnosis on the individuals concerned and all risks, even those deemed small, discussed.
The following case study illustrates how a lack of honesty can lead to misinterpretation and misunderstanding of the messages relayed ( McClain, 2012 ; Bramhall, 2014 ) and, accordingly, raises questions regarding the patient's care.
Case study 4. Consequences of ‘sugar-coating’ a diagnosis
Mrs Black, aged 78, had been diagnosed with a low-grade/low-risk bladder cancer, for which the recommended treatment is a course of six doses of intravesical chemotherapy (mitomycin). In providing Mrs Black with the diagnosis, the doctor had failed to clarify that the term ‘bladder polyp/wort’ in fact meant cancer. It is evident to the UCNS that the doctor's intention was to reduce the impact of the news for Mrs Black. However, if a cancer diagnosis is not clearly explained at the outset ( Evans, 2017 ), then, as the UCNS's personal observations in practice have shown, the offer of subsequent cancer treatments will raise questions. In a follow-up meeting with the UCNS, Mrs Black queried why she was having a cancer treatment, when a cancer diagnosis had not been clearly given ( Bumb et al, 2017 ). In this instance, Mrs Black's query placed the UCNS in an uncomfortable position, but one in which she ultimately had to be honest in her response.
Despite the physician's good intentions, a lack of honesty or in this case ‘sugar-coating’ the truth was an infringement of Mrs Black's right to receive full and honest information regarding her diagnosis and treatments and impacted her ability to make clear decisions regarding her care ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ).
Scenario: communicating in teams
In the UCNS's experience, effective communication is crucial when communicating in teams. The UCNS's observations in practice evoked reflection on past experiences of poor communication and its ensuing impact on her feelings, including hurt and, to some extent, a degree of anger.
Seemingly, poor communication is ingrained in all areas of practice and is highly evident in teams ( Doyle, 2019 ). The ability to communicate effectively is essential to team cohesiveness. One of the chief requirement is to facilitate an environment in which individuals can grow and excel, thus good/effective communication is vital. As previously stated, the tone of voice and actual words spoken are important ( Bramhall, 2014 ; Evans, 2017 ; Doyle, 2019 ). A tone that is respectful and conducive to elevating the individual's self-esteem and morale, ultimately increases self-worth and confidence. Conversely, a patronising attitude—a tone of voice and words spoken that imply sarcasm and disrespect—can, and often does, result in hurt feelings and a significant loss of confidence ( Doyle, 2019 ). Some senior professionals clearly believe in a hierarchy of entitlement to respect in the way that individuals communicate with other team members. A patronising tone of voice and words that imply sarcasm and disrespect impact significantly on individual team members' morale, self-esteem, self-worth, confidence and professional standing. This can lead to disharmony within the clinical environment. This could be communication between a consultant and a junior doctor, or a junior doctor and senior nurse, for example.
As health professionals, admittedly, we could all attest to poor communication at some point in our careers. Nevertheless, we have a responsibility to work and communicate effectively with other team members ( Ali, 2017 ; Doyle, 2019 ). The objective here is in facilitating a happy and functional team, one that demonstrates professionalism and competency in providing the care necessary to improving patients' experiences and outcomes ( Ali, 2017 ; Doyle, 2019 ). Securing improvements necessitates the health professional reflecting on their communication skills, acknowledging their limitations and initiating steps to address these ( Barber, 2016 ).
These case studies and scenario provide an insight into the UCNS's observations and reflections on her area of clinical practice and highlight the importance of effective communication. Acknowledgement of the inherent challenges within the communication process are clearly explained, with consideration given to the actual and potential impact in terms of patient, health professionals and clinical practice outcomes ( Oelofsen, 2012 ; RCN, 2019 ).
Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life, but seemingly few people, including health professionals, have mastered the skill of truly effective communication. There are evident pitfalls that could lead to patient care being compromised as a result of poor communication between health professionals. The UCNS's role in delivering bad news and supporting patients involves ensuring that patients are adequately informed to enable them to take control of their individual situation and, accordingly, that they are able to make the appropriate choices and decisions for their respective needs. Poor communication within teams can affect patient care and staff morale, and learning how to communicate more effectively is beneficial in terms of improving staff interactions with each other. Essentially, communicating effectively is everyone's responsibility; hence, all health professionals should look at the way they interact and communicate with each other and take the necessary steps to improve this extremely important activity.
- The cancer clinical nurse specialist (CNS) role is pivotal when patients receive bad news. It is crucial not only to the individual's understanding of the diagnosis, prognosis and treatment options, but also to the provision of appropriate support following the bad news and countering the ensuing impact of the news on the patient
- Reflection is a powerful tool, one that enables nurses to examine their practice, identifying salient issues and initiate change/improvements
- Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life—few people (in this context health professionals) have mastered the skill of truly effective communication
- Poor communication has implications for the patient, health professional and the health organisation
CPD reflective questions
- Reflection on practice is a key skill for nurses that enables them to identify salient issues and initiate actions to address these. How well do you think you reflect in practice, and does this provide the insight you seek?
- Effective communication is an important interpersonal skill. How well do you communicate with patients and colleagues in your area of practice? Reflect on any situations that you find difficult
- The issue of poor communication within teams and its impact on team members has been highlighted in this article. Have you observed poor communication within your team or within your area of practice? If so, how could this be improved?
- Open access
- Published: 03 September 2021
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
- Abukari Kwame 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 20 , Article number: 158 ( 2021 ) Cite this article
369k Accesses
160 Citations
97 Altmetric
Metrics details
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Peer Review reports
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 , 6 , 7 , 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.
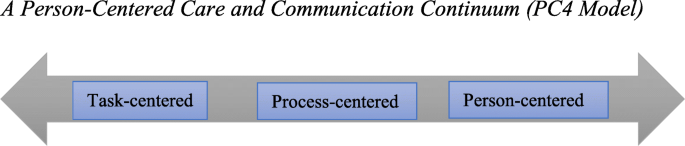
A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.
Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Availability of data and materials
Not applicable.
Abbreviations
Intensive Care Unit
Institution of Medicine
Person-Centered Care and Communication Continuum
Etheredge HR. “Hey sister! Where’s my kidney?“ Exploring ethics and communication in organ transplantation in Gauteng, South Africa, Ph.D. dissertation, Johannesburg. University of the Witwatersrand; 2015.
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clin Nurs. 2018 Apr;27(7–9):e1651-9. doi: https://doi.org/10.1111/jocn.14315 .
Long KA. The Institute of Medicine report on health professions education: A bridge to quality. Policy Polit Nurs Pract. 2003 Nov;4(4):259–62. doi: https://doi.org/10.1177/1527154403258304 .
Crawford T, Candlin S, Roger P. (2017). New perspectives on understanding cultural diversity in nurse-patient communication. Collegian, 2017 Feb 1;24(1):63 – 9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Madula P, Kalembo WF, Yu H, Kaminga CA. Healthcare provider-patient communication: A qualitative study of women’s perceptions during childbirth. Reprod Health. 2018 Dec;15(135):1–10. https://doi.org/10.1186/s12978-018-0580-x .
McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004 Jan;13(1):41–9.
Schöpf AC, Martin GS, Keating MA. Humor as a communication strategy in provider-patient communication in a chronic care setting. Qual Health Res. 2017 Feb;27(3):374–90. doi: https://doi.org/10.1177/1049732315620773 .
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: the core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Google Scholar
Boykins AD. Core communication competences in patient-centered care. The ABNF J. 2014 Apr 1;25(2):40 – 5.
Henly SJ. Health communication research for nursing science and practice. Nurs Res [Editorial] 2016:257–8. doi: https://doi.org/10.1097/NNR.0000000000000171 .
Ruben BD. Communication theory and health communication practice: The more things change, the more they stay the same. Health Commun. 2016 Jan 2;31(1):1–11. doi: https://doi.org/10.1080/10410236.2014.923086 .
Bello P. Effective communication in nursing practice: A literature review. BSc Nursing Thesis. Arcada; 2017. Available at https://core.ac.uk/download/pdf/84798372.pdf Accessed 20 Jan 2021.
McLean A. The person in dementia: A study of nursing home care in the US. Toronto, University of Toronto Press; 2007.
Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. Doi: https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article Google Scholar
Amoah KMV, Anokye R, Boakye SD, Acheampong E, Budu-Ainooson A, Okyere E, Kumi-Boateng G, Yeboah C, Afriyie OJ. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs. 2019 Dec;18(4)1–8. https://doi.org/10.1186/s12912-019-0328-0 .
Ddumba-Nyanzia I, Kaawa-Mafigiria D, Johannessen H. Barriers to communication between HIV care providers (HCPs) and women living with HIV about childbearing: A qualitative study. Patient Educ Couns. 2016 May 1:99(5):754–9. https://doi.org/10.1016/j.pec.2015.11.023 .
Al-Kalaldeh M, Amro N, Qtait M. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2021 Mar 2;29(2). doi: https://doi.org/10.7748/en.2020.e1969 .
Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017 Oct. 2016;9(4):30. doi: https://doi.org/10.5958/j.2320-8651.2.1.001 .
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of Kerman: A qualitative study. J Caring Sci. 2014 Mar;3(1):67–2. doi: https://doi.org/10.5681/jcs.2014.008 .
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2016 Jun;8(6):65–4. https://doi.org/10.5539/gjhs.v8n6p65 .
Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694 .
Murira N, Lützen K, Lindmark G, Christensson K. Communication patterns between healthcare providers and their clients at an antenatal clinic in Zimbabwe. Health Care Women Int. 2003 Feb 1;24(2):83 – 2. https://doi.org/10.1080/07399330390170060 .
Papadopoulos I, Lazzarino R, Koulouglioti C, Aagard M, Akman O, Alpers L-M, Apostolara P, Araneda Bernal J, Biglete-Pangilinan S, Eldar-Regev O, Gonzalez-Gil MT, Kouta C, Zorba A. Obstacles to compassion-giving among nursing and midwifery managers: An international study. Int Nurs Rev. 2020 Aug;11:1–13.
Camara BS, Belaid L, Manet H, Kolie D, Guilard E, Bigirimana T, Delamou A. What do we know about patient-provider interactions in sub-Saharan Africa? A scoping review. Pan Afr Med J. 2020;88(88):1–13. doi: https://doi.org/10.11604/pamj.2020.37.88.24009 .
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. Int J Afr Nurs Sci. 2020 Jan 1;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009 Jun;56(2):243–9.
Vuković M, Gvozdenović BS, Stamatović-Gajić B, Ilić M, Gajić T. Development and evaluation of the nurse quality of communication with patient questionnaire. Srp Arh Celok Lek. 2010;138(1–2):79–4. doi: https://doi.org/10.2298/SARH1002079V .
Article PubMed Google Scholar
Mastors P. (2018). What do patients want, need, and have the right to expect? Nurs Adm Q. 2018 Jul 1;42(3):192-8. doi: https://doi.org/10.1097/NAQ.0000000000000297 .
Harvard Medical School. The Eight Principles of Patient Centered Care; 2015 Nov 18. Available from OneView: https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ Accessed 28 Dec 2020.
White J, Phakoe M, Rispel LC. ‘Practice what you preach’: Nurses’ perspectives on the Code of Ethics and Service Pledge in five South African hospitals. Glob Health Action. 2015 Dec 1;8(1):26341. https://doi.org/10.3402/gha.v8.26341 .
Kruger L-M, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol. 2010 Feb 1;28(1):84–101. doi: https://doi.org/10.1080/02646830903294979 .
International Council of Nurses. ICN Code of Ethics for Nurses; 2012. Available from www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 20 Dec 2020.
Stievano A, Tschudin V. The ICN code of ethics for nurses: A time for revision. Nurs Health Policy Perspect. 2019 Jun;66(2):154–6.
Liu W, Manias E, Gerdtz M. Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health 2012 Mar. 2012;17(2):113–34. doi: https://doi.org/10.1177/1363459312447257 .
Hoglind TA. Healthcare language barriers affect deaf people, too. 2018 Oct 11. Retrieved from Boston University [BU] School of Public Health: Available from https://www.bu.edu/sph/news/articles/2018/healthcare-language-barriers-affect-deaf-people-too/ Accessed 15 Jan 2021.
Cuellar NG. Humility. A concept in cultural sensitivity. JTranscult Nurs [Editorial]. 2018 Apr 26; 29(4):317. https://doi.org/10.1177/1043659618772384 .
Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int J Nurs Stud. 2019 Nov 1;99(103386):1–8. https://doi.org/10.1016/j.ijnurstu.2019.103386 .
Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018 Jul;26(4):590–603. doi: https://doi.org/10.1111/hsc.12556 .
Download references
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwame, A., Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs 20 , 158 (2021). https://doi.org/10.1186/s12912-021-00684-2
Download citation
Received : 05 May 2021
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12912-021-00684-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered care
- Therapeutic communication
- Nurse-patient interactions
- Clinical discourse space
- Patient-centered care and communication continuum
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

- Teacher Education
Nursing Education
- Behavioral Sciences
- Sign & Foreign Languages
- Performing Arts
- Communication
- Any Skill You Teach
WATCH FOR FREE
ReAction On-Demand!
Dive into our on-demand library from the skills based conference.

SEE GOREACT IN ACTION
Try for Free
See how GoReact can help empower confident skills
CONTENT TYPE
- Case Studies
- Product Demos

ReAction On-Demand
Dive into our on-demand library from ReAction, the skills based conference. Whether you missed a session or want to rewatch, it's all here (and free)!
- CONTACT SALES EXPLORE GOREACT TRY FOR FREE CONTACT SALES
3 Barriers to Effective Communication in Nursing (And How to Overcome Them)

Nursing is built on communication skills. To provide the highest level of care, it’s crucial for nurses to master the soft skills that allow them to excel in healthcare.
But nursing is also a high-workload profession. As duties pile up throughout a shift, nurses can find themselves rushing to complete their tasks. A nurse may not spend adequate time talking with patients, listening to concerns, or perceiving needs.
To make sure vital communication doesn’t fall between the cracks, it’s important for educators to set the foundation for soft skills early on in a nurse’s career. When a nurse understands the skills required for good communication—as well as the barriers that exist—patient care improves.
In “ Communication and Language Needs ,” Dawn Weaver identifies three types of barriers to effective communication in nursing : physical, psychological, and social. Let’s take a deeper look at where these barriers come from and how we can avoid them.
1. Physical Barriers
Physical environment can make a huge difference in successful communication. Have you ever tried to talk with someone from a different level of the house? Shouting down a flight of stairs doesn’t exactly make for great correspondence. Similarly, according to Weaver, insufficient lighting, room size, ambient noise, and lack of privacy can prevent effective communication in nursing.
But are nurses really in control of their physical environment? Not entirely, but a few measures can be taken to improve surroundings.
For example, busy, distracting environments can increase patient stress. If it’s extra hectic on a particular day, a nurse may explain this to a patient. Closing doors, keeping outside noises to a minimal level, and opening blinds are additional small practices to increase patient comfort. A safe and comfortable environment facilitates constructive communication.
2. Psychological Barriers
Obesity, sexuality, disease, and death aren’t exactly pleasant conversation starters. And the anxiety and stress that comes from addressing sensitive topics can block effective communication in nursing .
Along with delicate conversations, nurses face a variety of emotionally exhausting situations. A study in the Journal of Advanced Nursing found that many nurses experience anxiety due to a patient’s medical needs.
Patients may also be in a vulnerable state. For many, a simple visit to the doctor is enough to get their heart pounding. Stress, anxiety, and weakness are common emotions experienced by patients, and it’s understandable why. But there are ways to help.
One answer is for nurses to develop a strong bedside manner . Bedside manner encompasses sensitivity, dedication, and empathy. It also fosters good communication and builds trust and confidence.
3. Social Barriers
Gender, education, religion, and age all drive human behavior. We can’t change others’ behavior, let alone the way they see the world. So how do we overcome cultural barriers?
Awareness is key. According to “ Nurse Perceived Barriers to Effective Nurse-Client Communication ,” sufficient knowledge of a patient’s culture, language, and customs can help nurses communicate clearly and avoid prejudice.
What if you don’t know about a patient’s particular culture or religion? If you are unsure about something, ask polite questions. This may help the patient feel valued. It’s much easier to communicate and sympathize with someone else when you understand where they’re coming from.
Nurses can effectively practice verbal and nonverbal communication skills using video. Use this quick start guide to see how easy it is to create video assignments for role-playing tasks like educating new patients and taking health history.
You can also learn more about the correlation between age and health. A 14-year-old and a 60-year-old may have different ideas of what it means to take care of their body. That’s why nurses should learn more about each age group’s attitudes toward health, disease, and body function.
It’s possible to overcome barriers to communication, and small changes can make a big difference. A comfortable environment, strong bedside manner skills, and awareness of needs foster the nurse-patient relationship. Knowing how to successfully communicate and interact with patients allows nurses to improve overall care. Effective communication in nursing can promote health and patient well-being nationwide.
Personalize Your GoReact Experience
Importance of the Communication in Nursing Essay
Introduction, types of communication, communication models, barriers to productive communication, ways to improve communication.
In the nursing field, productive communication is an important aspect of successful activities and the key to effective patient care. In case the management of a particular medical institution promotes creating conditions for such interaction, performance increases due to the minimization of errors and the exchange of experience among colleagues. Based on the modern principles of professional communication, one can distinguish several basic strategies of building relationships in nursing teams.
In addition, there are special models that characterize the features of information transfer among the parties involved and determine the possibilities of interaction. At the stage of building such relationships, some barriers may arise, which are essential to overcome timely. Respecting colleagues’ personal dignity and following the principles of professional ethics can help maintain productive communication in the nursing environment, thereby increasing the potential success of activities.
While examining the types of nursing communication in the context of the importance of specific approaches, classic concepts may be cited. In particular, Sibiya (2018) notes that there are two key types of interaction – verbal and non-verbal, and each of them has its unique goals and purposes. Verbal communication is carried out through speaking directly and exchanging words among the parties involved. Sibiya (2018) argues that this style of interaction is an important aspect of the nursing field and healthcare sector in general. Also, in addition to interpersonal professional contacts, employees can communicate with other stakeholders, for instance, patients and their relatives. Therefore, this form of interaction is significant in the considered environment.
The non-verbal mechanism is based not on speech but on body language. As Sibiya (2018) remarks, looks, gestures, emotional movements of hands, and other elements of non-verbal communication are involved in nursing, and about 60% of all interaction is carried out in this format (p. 21). In some situations, for instance, emergency cases, this type of contact is more effective than speech due to the natural ability of a person to perceive visual information more quickly.
While taking into account the specifics of the work of junior medical employees, additional communication methods may be identified based on the profile of their activities. However, the two styles considered are the most common principles of transmitting relevant information.
The analysis of nursing communication at a deeper level can make it possible to single out specific models that form the principles of transmission and perception of information. Sibiya (2018) cites three key interaction concepts – linear, interactive, and transactional. All these strategies are subordinate to the basic principles of communication, in particular, conveying data from one party to the other one, but the features of this transfer are distinctive.
The linear model is a classic strategy when speakers direct their messages to listeners and intend to convey certain information in the most understandable form. This principle is basic and does not have any unique features and associated conditions. The interactive model is a more complex form of interaction and involves a communication mode in which recipients of information can interpret certain data individually.
An example of communication among senior and junior nurses may be given in order to convey the meaning of such relationships in the context of advice and recommendations. Finally, the transactional model is the most complex form of interaction because, for its implementation, additional factors should be taken into account, for instance, time, place, environment, and other criteria that can affect the communication process. All the three models may be utilized in nursing and help healthcare providers understand one another successfully.
Despite clear instructions that medical employees should follow during their work, the communication process can be complicated by barriers caused by concomitant circumstances and affecting relationships. Norouzinia, Aghabarari, Shiri, Karimi, and Samami (2016) consider these aspects that make it difficult to maintain effective interaction and note several key obstacles – language, cultural, and educational. In addition, in some cases, more global factors may arise, for instance, political ones, when legal conventions affect nurses’ work (Norouzinia et al., 2016). These obstacles may occur both in verbal and non-verbal communication forms, which complicates the work to eliminate them.
These obstacles can be interconnected and create increased discomfort for employees. For instance, language barriers are characteristic of a diverse cultural environment, and accusations based on personal bias may cause conflicts in the workplace. Also, Norouzinia et al. (2016) mention the religious context and note that in some countries, nurses cannot touch colleagues or patients of the opposite sex, which creates challenges for non-verbal communication. As a result, performance indicators are reduced due to the inability to maintain a productive work environment in which each employee can count on effective interaction and support. Therefore, searching for methods to improve communication in the nursing area is one of the priority tasks in case one or more of the aforementioned barriers are identified.
In order to minimize potential barriers to productive communication in nursing, it is essential for all employees to be aware of the importance of appropriate behavioral patterns. For this purpose, MacLean, Kelly, Geddes, and Della (2017) offer to use special training materials at the early stages of education so that future employees could have an idea of the basics of ethical interaction. The manifestation of bias based on individual prejudices is unacceptable since any conflicts can lower patient outcomes, which is unacceptable. The dignity of each employee is to be respected in order to avoid interpersonal contradictions.
To enhance unique communication skills, for instance, non-verbal ones, the management of medical institutions should promote the exchange of experience among subordinates and encourage teamwork. In the context of intense activities that many nurses face, Sibiya (2018) recommends avoiding unclear messages in order to prevent misunderstandings and make the exchange of information more productive.
In addition, the ability to be convincing is a valuable quality that may allow earning authority among colleagues and become an example for them. To train this skill, it is necessary to follow all the aforementioned aspects of work and take into account ethical forms of interaction in a professional nursing environment. These measures can improve the quality of communication and, therefore, expand opportunities for successful collaboration.
Compliance with the principles of ethical interaction can help improve nursing communication in all its manifestations and increase patient outcomes, which is the ultimate goal of all interventions. Both verbal and non-verbal contacts are common in the medical environment in question, and appropriate models may be applied. In nursing practice, some communication barriers arise periodically due to various factors. In order to exclude them and minimize the likelihood of conflicts, rejecting bias should be a mandatory attribute of junior medical employees’ activities, and the exchange of experience may help maintain productive interaction.
MacLean, S., Kelly, M., Geddes, F., & Della, P. (2017). Use of simulated patients to develop communication skills in nursing education: An integrative review. Nurse Education Today , 48 , 90-98.
Norouzinia, R., Aghabarari, M., Shiri, M., Karimi, M., & Samami, E. (2016). Communication barriers perceived by nurses and patients. Global Journal of Health Science , 8 (6), 65-74.
Sibiya, M. N. (2018). Effective communication in nursing. In N. Ulutasdemir (Ed.), Nursing (pp. 19-36). London, UK: IntechOpen.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, June 21). Importance of the Communication in Nursing. https://ivypanda.com/essays/importance-of-the-communication-in-nursing/
"Importance of the Communication in Nursing." IvyPanda , 21 June 2021, ivypanda.com/essays/importance-of-the-communication-in-nursing/.
IvyPanda . (2021) 'Importance of the Communication in Nursing'. 21 June.
IvyPanda . 2021. "Importance of the Communication in Nursing." June 21, 2021. https://ivypanda.com/essays/importance-of-the-communication-in-nursing/.
1. IvyPanda . "Importance of the Communication in Nursing." June 21, 2021. https://ivypanda.com/essays/importance-of-the-communication-in-nursing/.
Bibliography
IvyPanda . "Importance of the Communication in Nursing." June 21, 2021. https://ivypanda.com/essays/importance-of-the-communication-in-nursing/.
- Verbal and Nonverbal Communication: Principles and Cues
- Non-Verbal Communication in "When They See Us" TV Show
- Nonverbal Communication in Nursing
- APN Professional Development Plan in Missouri
- Nurses and Virtual Learning Environments: Understanding Limits in Nursing Education
- The Role of the Nurse in Rehabilitation
- Nursing: Advanced Technology and New Opportunities
- The Intravenous Tubing Changes Policy Review

IMAGES
VIDEO
COMMENTS
Hospitalized patients in all ages often experience complex communication needs including mobility, sensory, and cognitive needs as well as language barriers during their stay ( Downey & Happ, 2013 ). Hospitalization is potentially stressful and involves unpleasant experiences for patients and their families. All aspects of care and nursing are ...
Confirm understanding through paraphrasing: Summarize the information shared by the patient to validate comprehension. Encourage questions and feedback: Create a safe environment for patients to ask questions and provide feedback, ensuring effective communication. 3. Open and Transparent Communication Channels.
Language Barrier. Language differences between the patient and the nurse are another preventive factor in effective communication. When the nurse and the patient do not share a common language, interaction between them is strained and very limited [9, 10, 11].Consequently, a patient may fail to understand the instructions from a nurse regarding the frequency of taking medication at home.
Communication barriers vary depending on the setting, requiring the nurse to figure out such barriers depending on each patient's individual needs (Sibiya, 2018). One of the most prevalent communication barriers in nursing is the difference in language and culture (Norouzinia et al., 2016).
18 December, 2017By NT Contributor. This article, the second in a six-part series on communication skills, a discusses the barriers to effective communication and how to overcome them. Abstract. Competing demands, lack of privacy, and background noise are all potential barriers to effective communication between nurses and patients.
Other studies have also reported that, nurse's work load was perceived as barrier to effective communication which supports the finding of the current study (Kourkouta, 2014), and (Norouzinia et al., 2016, OC, ot, 2014, S. A.-H. 2013) which reported, increased work load, limited or inadequate time to establish a good relationship, presence of ...
Abstract. Effective nurse-patient communication, also described as therapeutic communication, is essential for providing high quality nursing care. It increases patient satisfaction and health, decreases patient anxiety and disease symptoms, and increases patient cooperation and compliance to treatment.
Background Communication is a basic need of humans. Identifying factors that prevent effective nurse-patient communication allows for the better implementation of necessary measures to modify barriers. This study aims to compare the barriers to effective nurse-patient communication from the perspectives of nurses and patients in COVID-19 and non-COVID-19 wards. Materials and methods This cross ...
6.1 Barriers to effective communication in nursing practice. 28 6.2 How effective communication relates with patients and nurses. 30 6.3 Means to improve effective communication in nursing settings 32 7. DISCUSSION 34 7.1 Discussion of results 34 7.1.1 Discussion of Results as related to theoretical concept 35
Emaliyawati et al. (2020) reported communication barriers in the ICU between patient families and healthcare workers related to high workload, educational background of the family, cultural ...
Communication is an essential element of building trust and comfort in nursing, and it is the basis of the nurse-patient relationship (Dithole et al, 2017).Communication is a complex phenomenon in nursing and is influenced by multiple factors, such as relationship, mood, time, space, culture, facial expression, gestures, personal understanding and perception (McCarthy et al, 2013; Kourkouta ...
Barriers To Effective Communication In Nursing Nursing Essay. A nurse with good communication skill is someone who really listens to the patients, understands their problems and queries and answers in a way the patients will understand. Communication in nursing profession can be a complicated process, and the possibility of sending or receiving ...
Reflection is a highly beneficial tool (Oelofsen, 2012), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes (Bramhall, 2014).
In " Communication and Language Needs ," Dawn Weaver identifies three types of barriers to effective communication in nursing: physical, psychological, and social. Let's take a deeper look ...
Effective communication is crucial aspect of nursing yet too often is placed low on the priority list, especially at shift change. Information related to the care of patients is frequently disseminated at a crowded, noisy nurse station with several nurses rushing to leave and others attempting to get the information necessary to plan care and limit the constant distractions.
Providing healthcare services that respect and meet patients' and caregivers' needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient ...
In " Communication and Language Needs," Dawn Weaver identifies three types of barriers to effective communication in nursing: physical, psychological, and social. Let's take a deeper look at where these barriers come from and how we can avoid them. 1. Physical Barriers. Physical environment can make a huge difference in successful ...
Effective communication is an integral aspect of nursing because nurses constantly interact with patients, families, colleagues, supervisors, and managers in the course of their duties. Rosenblatt and Davis (2009) argue that the nature of communication determines the quality of care that patients receive. In essence, effective communication ...
In order to minimize potential barriers to productive communication in nursing, it is essential for all employees to be aware of the importance of appropriate behavioral patterns. For this purpose, MacLean, Kelly, Geddes, and Della (2017) offer to use special training materials at the early stages of education so that future employees could ...
Barriers To Effective Communication In Nursing Nursing Essay. A nurse with good communication skill is someone who really listens to the patients, understands their problems and queries and answers in a way the patients will understand. Communication in nursing profession can be a complicated process, and the possibility of sending or receiving ...