- Search Menu
- Sign in through your institution
- Browse content in Disability assessment
- Assessment for capacity to work
- Assessment of functional capability
- Browse content in Fitness for work
- Civil service, central government, and education establishments
- Construction industry
- Emergency Medical Services
- Fire and rescue service
- Healthcare workers
- Hyperbaric medicine
- Military - Other
- Military - Fitness for Work
- Military - Mental Health
- Oil and gas industry
- Police service
- Rail and Roads
- Remote medicine
- Telecommunications industry
- The disabled worker
- The older worker
- The young worker
- Travel medicine
- Women at work
- Browse content in Framework for practice
- Health and Safety at Work etc. Act 1974 and associated regulations
- Health information and reporting
- Ill health retirement
- Questionnaire Reviews
- Browse content in Occupational Medicine
- Blood borne viruses and other immune disorders
- Dermatological disorders
- Endocrine disorders
- Gastrointestinal and liver disorders
- Gynaecology
- Haematological disorders
- Mental health
- Neurological disorders
- Occupational cancers
- Opthalmology
- Renal and urological disorders
- Respiratory Disorders
- Rheumatological disorders
- Browse content in Rehabilitation
- Chronic disease
- Mental health rehabilitation
- Motivation for work
- Physical health rehabilitation
- Browse content in Workplace hazard and risk
- Biological/occupational infections
- Dusts and particles
- Occupational stress
- Post-traumatic stress
- Advance articles
- Editor's Choice
- Themed and Special Issues
- Author Guidelines
- Submission Site
- Open Access
- Books for Review
- Become a Reviewer
- About Occupational Medicine
- About the Society of Occupational Medicine
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Permissions
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Introduction, acknowledgements, competing interests, data availability.
- < Previous
Healthcare worker burnout during a persistent crisis: a case–control study
- Article contents
- Figures & tables
- Supplementary Data
S Appelbom, A Nordström, A Finnes, R K Wicksell, A Bujacz, Healthcare worker burnout during a persistent crisis: a case–control study, Occupational Medicine , Volume 74, Issue 4, May 2024, Pages 297–303, https://doi.org/10.1093/occmed/kqae032
- Permissions Icon Permissions
During the immediate outbreak of the COVID-19 pandemic, burnout symptoms increased among healthcare workers. Knowledge is needed on how early symptoms developed during the persistent crisis that followed the first pandemic wave.
To investigate if high levels of burnout symptoms during the first pandemic wave led to high burnout and depressive symptoms up to a year later, and if participation in psychological support was related to lower levels of symptoms.
A longitudinal case–control study followed 581 healthcare workers from two Swedish hospitals. Survey data were collected with a baseline in May 2020 and three follow-up assessments until September 2021. The case group was participants reporting high burnout symptoms at baseline. Logistic regression analyses were performed separately at three follow-ups with case–control group assignment as the main predictor and burnout and depression symptoms as outcomes, controlling for frontline work, changes in work tasks and psychological support participation.
One out of five healthcare workers reported high burnout symptoms at baseline. The case group was more likely to have high burnout and depressive symptoms at all follow-ups. Participation in psychological support was unrelated to decreased burnout and depressive symptoms at any of the follow-ups.
During a persistent crisis, healthcare organizations should be mindful of psychological reactions among staff and who they place in frontline work early in the crisis. To better prepare for future healthcare crises, preventive measures on burnout are needed, both at workplaces and as part of the curricula in medical and nursing education.
Increased prevalence of burnout symptoms has been reported among healthcare workers during the COVID-19 pandemic.
For a sub-group of healthcare workers with higher symptoms, burnout rates were elevated also later in the crisis.
It is not known whether burnout and depressive symptoms later in the pandemic were predicted mainly by the early burnout symptoms or the recurring periods of frontline work for this group of healthcare workers.
High burnout symptoms in response to the work environment during the first pandemic wave were the main predictor of both high burnout and depressive symptoms during later periods of the crisis, regardless of the intensity of frontline work or participation in psychological support.
When forming policies on how to respond to future crises in healthcare, healthcare workers’ psychological reactions to the work environment during the initial stages of the crisis should be a key focus.
If the crisis persists over a longer period, healthcare organizations may benefit from being extra mindful of the work environment of staff members who showed signs of burnout right before, or early in the crisis.
During the immediate outbreak of the COVID-19 pandemic, healthcare workers faced high emotional and physical demands at the same time as resources to cope with them were limited [ 1 , 2 ]. The prevalence of burnout symptoms also increased among healthcare workers during this period with pooled prevalence between 34% and 52% [ 3 , 4 ]. In the ICD-11, the World Health Organization defines burnout as ‘a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed’ [ 5 ]. More specifically, burnout refers to the combination of high job demands and insufficient job resources that implicates the workers’ ability to cope with those demands [ 6 , 7 ]. When faced with this imbalance, the worker experiences symptoms of emotional exhaustion and depersonalization from work [ 8 ]. Although burnout is an occupational phenomenon [ 5 ], conflicting demands in personal life can also lead to burnout symptoms [ 9 ].
Even before the COVID-19 pandemic, healthcare workers had increased risks of burnout. In 2020, pre-pandemic burnout prevalence of 12% among early-career nurses in Sweden [ 10 ], and 10% among nurses in Europe and Central Asia [ 11 ] was reported.
Although burnout is not a clinical condition, a long-term imbalance between demands and resources is related to higher risk of sickness absence [ 12 ]. Still, experiencing high burnout symptoms during a shorter period of a demanding work environment does not necessarily mean that the worker will face symptoms long term [ 13 ]. Several studies on burnout trajectories among healthcare workers during the COVID-19 pandemic reported elevated burnout symptoms during the first outbreak of the COVID-19 pandemic, which would later decrease [ 14–17 ].
However, for a sub-group of healthcare workers with strong stress reactions during the first pandemic wave, the high symptom levels were persistent also during later periods of the COVID-19 pandemic [ 14 , 18–20 ]. A possible reason for this may be that their strong reaction to the immediate crisis during the pandemic outbreak led to an elevated risk of later psychological strain in terms of both depressive and burnout-related symptoms [ 10 , 13 , 21 , 22 ]. This group of healthcare workers may, therefore, have been more vulnerable to changes in the work environment during the recurring periods of increased patient intake later in the pandemic [ 15 ].
To the best of our knowledge, only one study has explicitly studied the relationship between early onset of burnout symptoms and the risk of later strain among healthcare workers during the COVID-19 pandemic. The results showed that burnout symptoms during the first pandemic wave predicted about 37% of burnout symptoms among US frontline healthcare workers during the second wave. However, it was not clear how job demands related to the treatment of COVID-19 patients impacted the burnout rates [ 20 ]. More knowledge is needed on the persistence of burnout and depressive symptoms during different stages of a long-term crisis in relation to early onset of burnout rates and changes in the work environment, both between and during consecutive pandemic waves [ 23 ].
Occupational health services can support workplaces in the implementation of organizational changes that prevent burnout by fostering a healthy work environment [ 24 ]. However, during a crisis, demands are high, and the resources limited, so health-promoting interventions should rather focus on secondary interventions that help healthcare workers cope with the crisis [ 24 ]. During the COVID-19 pandemic, many healthcare organizations implemented psychological support with the aim to limit psychological stress reactions, such as burnout and depressive symptoms, caused by the demanding work environment [ 25–27 ].
The aim of the present study was to (i) describe the prevalence of burnout and depressive symptoms among healthcare workers up to a year after the onset of the COVID-19 pandemic, (ii) examine if high levels of burnout symptoms early in the pandemic led to high burnout and depressive symptoms up to a year later, and (iii) additionally examine if those who participated in psychological support initiatives displayed lower levels of burnout or depressive symptoms across the first year of the COVID-19 pandemic.
Healthcare workers from two hospitals in the Stockholm Region, Sweden, were invited to participate in a longitudinal survey during the COVID-19 pandemic. Data were collected at four timepoints with baseline in May and June 2020, and follow-ups in September 2020, February 2021 and June 2021. Compared to the timeline of the COVID-19 pandemic in Sweden, the surveys coincided with the first pandemic wave (baseline), between the first and second waves (follow-up 1), the overlap between the second and third waves (follow-up2), and after the third wave (follow-up 3) [ 28 ]. The study was reviewed and approved by the Swedish Ethical Review authority (reference numbers 2020-01795, 2020-03495, 2020-04959, 2020-06602, 2022-01546-02). The participants involved provided written informed consent before answering the baseline survey.
A case–control design was applied to investigate the association between high burnout symptoms during the early stages of the COVID-19 pandemic and high symptoms throughout the first year of the pandemic. Out of 2262 invited, 681 healthcare workers were enrolled in the study (see Figure 1 , available as Supplementary data at Occupational Medicine Online). Participants ( n = 581) who answered the burnout questionnaire at baseline were included in the analytic sample and assigned to the case and control groups based on high or low burnout symptoms at baseline.
Case and control groups were created based on the level of work-related burnout symptoms measured using the seven-item version of the Oldenburg Burnout Inventory (OLBI). Items were rated on a 4-point scale, ranging from 1 = ‘Not accurate at all’ to 4 = ‘Totally accurate’. A cut-off mean score of 3 or higher was considered a high level of burnout symptoms. The version used in the present study was validated in a Swedish healthcare context, and the cut-off values were established for nurses as the norm group [ 7 ]. To limit missing data, mean values were calculated for all participants who answered at least six out of seven items. Scale means were 2.39, 2.20, 2.35 and 2.41 for baseline and each follow-up, respectively. The scale reliability was high at all timepoints (see Table 4 , available as Supplementary data at Occupational Medicine Online).
At follow-ups, burnout symptoms were measured with the Shirom-Melamed Burnout Questionnaire (SMBQ). SMBQ is a validated screening tool for detecting clinical symptom levels of burnout within a general population in Sweden [ 29 ]. For this study, a six-item version was used, measuring emotional and physical exhaustion, as well as cognitive weariness [ 30 ]. Items were rated on a 7-point scale, ranging from 1 = ‘Almost never’ to 7 = ‘Almost always’. Cut-off values were chosen based on pre-pandemic data from the general population in Sweden, where the 75% percentile corresponded to an average of 4 for women and 3.5 for men on a 7-point scale [ 30 ]. A mean value of 4 was chosen as a cut-off for high burnout symptoms in the present study. A mean value was calculated for all participants who answered at least five out of six items. Scale means were 2.68, 2.97 and 3.02 for each follow-up, respectively. The scale reliability was high for all time points (see Table 4 , available as Supplementary data at Occupational Medicine Online).
Depressive symptoms were measured using the two-item screening version of the Patient Health Questionnaire (PHQ-2). PHQ-2 measures symptoms of anhedonia and low mood within a 2-week period [ 31 ]. Items were rated on a 4-point scale ranging from 0 = ‘Not at all’ to 3 = ‘Nearly every day’. A cut-off value of 1.5 or higher on the mean scale was considered an indicator of high levels of depressive symptoms [ 31 , 32 ]. Due to high correlations between the two items, a mean value was calculated for all participants who answered at least one out of the two items. Scale means were 0.60, 0.58, 0.76 and 0.69 from baseline and each follow-up, respectively (see Table 5 , available as Supplementary data at Occupational Medicine Online).
Frontline work was recoded based on whether participants were frequently exposed to COVID-19 due to their work at frontline with COVID-19 patients. Participants indicating that they had treated COVID-19 patients within the last 2 weeks on several occasions or daily were coded as 1 = Frontline workers. Participants who had not treated COVID-19 patients or had treated them on one occasion were coded as 0 = non-frontline workers.
Participants stated whether their work tasks had changed due to the COVID-19 pandemic with a single item coded as 1 = Yes, and 0 = No. In the baseline survey, changed tasks since the beginning of the COVID-19 pandemic were noted while follow-ups measured changes since the previous survey.
Participants rated their level of participation in seven different psychological support types, using a single item: ‘Have you been offered any of the following types of support during the current pandemic?’, with 1 = ‘No’, 2 = ‘Yes, I have been offered but not used or participated in them’, 3 = ‘Yes, I have occasionally used or participated in them’, and 4 = ‘Yes, I have used them or participated in them on several occasions’ as response options. The response options were dichotomized, with options 1 and 2 coded as having not participated, and options 3 and 4 coded as having participated. The support types were categorized into two variables: passive and active psychological support, presented in Table 1 . Participation in each category (active/passive) was noted if participants had indicated participation in at least one support type belonging to that category.
Description of types of psychological support measured in the surveys
| Support variable . | Type of support . |
|---|---|
| Passive support | Access to a quiet space, for example, a staff room to rest or recover |
| Access to information on stress management or mental health | |
| Education or other training regarding the COVID-19 disease or personal protective equipment | |
| Education or other training in potentially traumatic situations at work | |
| Active support | Scheduled appointments to meet with colleagues to check in on or discuss how they feel |
| Collegial support interventions, for example, peer support or mentorships | |
| Scheduled group sessions lead by psychologists, counsellors, priests, HR or others | |
| Individual conversations led by psychologists, counsellors, priests, HR or others |
| Support variable . | Type of support . |
|---|---|
| Passive support | Access to a quiet space, for example, a staff room to rest or recover |
| Access to information on stress management or mental health | |
| Education or other training regarding the COVID-19 disease or personal protective equipment | |
| Education or other training in potentially traumatic situations at work | |
| Active support | Scheduled appointments to meet with colleagues to check in on or discuss how they feel |
| Collegial support interventions, for example, peer support or mentorships | |
| Scheduled group sessions lead by psychologists, counsellors, priests, HR or others | |
| Individual conversations led by psychologists, counsellors, priests, HR or others |
Prevalence of burnout at baseline and at each of the three follow-ups was estimated for the entire sample. The association between high burnout levels at baseline and symptoms at each follow-up was analysed using logistic regression, with case and control group membership as the main predictor and cut-off scores for high levels of burnout and depressive symptoms as outcome measures (Model 1). Second, the model was extended by controlling for frontline work and change of work tasks (Model 2), and psychological support participation (Model 3). Analyses were conducted for each outcome separately. All statistical analyses were conducted using Jamovi version 2.2 [ 33 ].
Baseline sample characteristics and differences between the case ( n = 119) and control ( n = 462) groups are presented in Table 2 . Of the 581 participants enrolled at baseline, 436 (75%) completed the first follow-up, 385 (66%) the second and 329 (57%) the third. See Supplementary Materials for more details on dropouts. The overall number of responses on burnout (SMBQ) at follow-ups 1, 2 and 3 were 414, 352 and 300, respectively. For depressive symptoms, the number of responses were 405, 339 and 294 for follow-up 1, 2 and 3, respectively. Proportions of participants engaged in frontline work, with changed work tasks, and psychological support participation at follow-ups are outlined in Table 6 (available as Supplementary data at Occupational Medicine Online).
Characteristics of the analytic sample
| Characteristics . | Analytic sample . | Case group . | Control group . | (193) . | χ . | ( ) . | -value . | |||
|---|---|---|---|---|---|---|---|---|---|---|
| . | (SD) . | (%) . | (SD) . | (%) . | (SD) . | (%) . | . | . | . | . |
| Age | 45 (11.3) | 41 (10.4) | 46 (11.3) | 3.98 | <0.001 | |||||
| Women | 455 (79) | 88 (76) | 367 (80) | 0.781 | 1 (577) | >0.05 | ||||
| Occupation | 30.3 | 3 (577) | <0.001 | |||||||
| Nurse | 218 (38) | 68 (58) | 150 (33) | |||||||
| Assistant nurse | 126 (22) | 24 (20) | 102 (22) | |||||||
| Physician | 102 (18) | 16 (14) | 86 (19) | |||||||
| Non-medical | 131 (23) | 10 (9) | 121 (26) | |||||||
| Previous treatment mental illness | 14.7 | 2 (576) | <0.001 | |||||||
| No treatment | 449 (78) | 77 (65) | 372 (81) | |||||||
| More than 3 months prior | 104 (18) | 32 (27) | 72 (16) | |||||||
| Within 3 months | 23 (4) | 9 (8) | 14 (3) | |||||||
| Frontline work | 313 (62) | 98 (85) | 215 (55) | 33.5 | 1 (509) | <0.001 | ||||
| Changed tasks | 309 (54) | 77 (65) | 232 (51) | 7.26 | 1 (575) | <0.01 | ||||
| Passive support | 442 (78) | 94 (81) | 348 (78) | 0.612 | 1 (564) | >0.05 | ||||
| Active support | 316 (56) | 84 (74) | 232 (52) | 17.7 | 1 (562) | <0.001 | ||||
| Characteristics . | Analytic sample . | Case group . | Control group . | (193) . | χ . | ( ) . | -value . | |||
|---|---|---|---|---|---|---|---|---|---|---|
| . | (SD) . | (%) . | (SD) . | (%) . | (SD) . | (%) . | . | . | . | . |
| Age | 45 (11.3) | 41 (10.4) | 46 (11.3) | 3.98 | <0.001 | |||||
| Women | 455 (79) | 88 (76) | 367 (80) | 0.781 | 1 (577) | >0.05 | ||||
| Occupation | 30.3 | 3 (577) | <0.001 | |||||||
| Nurse | 218 (38) | 68 (58) | 150 (33) | |||||||
| Assistant nurse | 126 (22) | 24 (20) | 102 (22) | |||||||
| Physician | 102 (18) | 16 (14) | 86 (19) | |||||||
| Non-medical | 131 (23) | 10 (9) | 121 (26) | |||||||
| Previous treatment mental illness | 14.7 | 2 (576) | <0.001 | |||||||
| No treatment | 449 (78) | 77 (65) | 372 (81) | |||||||
| More than 3 months prior | 104 (18) | 32 (27) | 72 (16) | |||||||
| Within 3 months | 23 (4) | 9 (8) | 14 (3) | |||||||
| Frontline work | 313 (62) | 98 (85) | 215 (55) | 33.5 | 1 (509) | <0.001 | ||||
| Changed tasks | 309 (54) | 77 (65) | 232 (51) | 7.26 | 1 (575) | <0.01 | ||||
| Passive support | 442 (78) | 94 (81) | 348 (78) | 0.612 | 1 (564) | >0.05 | ||||
| Active support | 316 (56) | 84 (74) | 232 (52) | 17.7 | 1 (562) | <0.001 | ||||
Notes : Comparison groups were men, non-frontline workers, unchanged work tasks, and not having participated in passive/active support.
At baseline, 119 (21%) participants reported high burnout symptoms (i.e. the case group). The burnout prevalence during each follow-up was then estimated using SMBQ scores, presented in Figure 1 .

Prevalence of burnout (SMBQ) and depressive symptoms (PHQ) at follow-ups.
Figure 2 displays the logistic regression results for each outcome separately. At follow-up 1, cases were more likely to have high burnout symptoms compared to the controls (odds ratio [OR] = 3.061, 95% confidence interval [CI]: 1.798–5.211, P < 0.001, Model 1). The effect remained both at follow-up 2 (OR = 5.018, 95% CI: 2.868–8.780, P < 0.001, Model 1) and follow-up 3 (OR = 4.874, 95% CI: 2.699–8.802, P < 0.001, Model 1).

Odds ratios and 95% CI for each predictor in Model 3 and for each follow-up, respectively (T2 to T4).
Across all follow-ups, the association was unchanged also after controlling for frontline work and change of work tasks in Model 2 (follow-up 1 OR = 3.120, 95% CI: 1.774–5.489, P < 0.001; follow-up 2 OR = 4.594, 95% CI: 2.593–8.140, P < 0.001; follow-up 3 OR = 4.434, 95% CI: 2.383–8.250, P < 0.001), as well as psychological support participation in Model 3 (follow-up 1 OR = 2.979, 95% CI: 1.687–5.260, P < 0.001; follow-up 2 OR = 4.496, 95% CI: 2.451–8.249; follow-up 3 OR = 4.622, 95% CI: 2.443–8.746, P < 0.001).
At the third follow-up, participants categorized as frontline workers were also more likely to report high burnout symptoms. This was the case in both Model 2 (OR = 3.357, 95% CI: 1.741–6.473, P < 0.001), and after adding the psychological support in Model 3 (OR = 3.511, 95% CI: 1.765–6.983, P < 0.001). No other predictor had a statistically significant association with burnout symptoms (see Figure 2 ). A more detailed presentation of all model results is presented in Tables 7–9 (available as Supplementary data at Occupational Medicine Online).
Cases were also more likely to have high depressive symptoms later in the pandemic. The effect was similar at follow-up 1 (Model 1 OR = 3.175, 95% CI: 1.795–5.615, P < 0.001), follow-up 2 (Model 1 OR = 3.415, 95% CI: 1.917–6.083, P < 0.01), and follow-up 3 (Model 1 OR = 2.808, 95% CI: 1.502–5.250, P < 0.01).
This effect remained unchanged also after controlling for frontline work and change of work tasks in Model 2 (follow-up 1 OR = 3.051, 95% CI: 1.669–5.578, P < 0.001; follow-up 2 OR = 3.086, 95% CI: 1.710–5.570, P < 0.001; follow-up 3 OR = 2.657, 95% CI: 1.388–5.088, P < 0.01), and after adding psychological support in Model 3 (follow-up 1 OR = 2.927, 95% CI: 1.591–5.384, P < 0.001; follow-up 2 OR = 2.794, 95% CI: 1.478–5.280, P < 0.01; follow-up 3 OR = 2.872, 95% CI: 1.481–5.569, P < 0.01). No other predictor had a statistically significant association with depressive symptoms (see Figure 2 ). See Tables 10 – 12 for details of all model results (available as Supplementary data at Occupational Medicine Online).
The results of this study showed that one out of five healthcare workers experienced high burnout symptoms during the first wave of the COVID-19 pandemic. Affected healthcare workers were also more likely to experience both high burnout and depressive symptoms during follow-ups, compared to those with low burnout symptoms at baseline. Participation in psychological support was unrelated to the level of reported symptoms at follow-ups.
One strength of this study is the longitudinal design which allowed us to measure burnout symptoms over the course of a persistent crisis. We were also able to capture changes in the work environment over the course of the COVID-19 pandemic. By using burnout instruments validated within a Swedish healthcare context, we were able to compare the burnout prevalence with pre-pandemic levels and generalize our findings to Swedish healthcare workers.
The main limitation of our study is that we lack pre-pandemic data for our sample. It was more common among cases to have a previous history of mental illness and we do not know to what extent previous health problems overshadow the COVID-19-related effects on burnout. Another limitation was the use of self-reported data, which introduces the risk of biases (e.g. social desirability or inaccurate recollections). The low inclusion rate (26%) also introduces the risk of selection bias. Regarding our statistical analysis, the use of a single model might have led to a more straightforward conclusion, but our analytical approach enables a closer perspective on the specific issue of the persistence of high symptoms at different stages of a prolonged crisis.
At baseline, the prevalence of high burnout symptoms was 21%. Which is a considerable increase compared to the reported pre-pandemic prevalence of 10% among nurses in Sweden [ 10 ], and 12% among nurses in Europe and Central Asia [ 11 ]. This indicates that, like other countries [ 34 ], the COVID-19 pandemic negatively impacted the psychological well-being among healthcare workers in Sweden.
Experiencing high burnout symptoms during the first wave was the main predictor of high symptoms of both burnout and depression later in the pandemic. Building on the already existing literature on the long-term consequences of burnout [ 10 , 22 , 35 ], this finding implies that the early onset of symptoms is the main risk factor for continuing symptoms also during a persistent crisis.
When comparing the case to control group at baseline, we found important differences. Known risk factors related to burnout such as being a nurse, work in the frontline and have changed work tasks were more common in the case group [ 16 , 17 , 36–38 ]. It was also more common in the case group to have sought help for mental health issues. This group was therefore likely more vulnerable to the increased demands in the early pandemic [ 21 ].
Interestingly, at the last time point, over a year after the pandemic outbreak, frontline work increased the risk of burnout. This suggests that, over the course of a persistent crisis, there may be an added burden from being re-exposed to high job demands that increase the risk of both burnout and depressive symptoms [ 15 ].
Across all follow-ups, psychological support participation was not related to the likelihood of experiencing high symptoms. However, it was more common among the case group to use the active psychological support at baseline. Because of the strong relationship between case group membership and symptoms, the association between psychological support and stress symptoms may have been difficult to capture within the context of this study. Also, due to lack of pre-pandemic data, the effect of the interventions was not possible to assess.
An effect of psychological support on stress reactions during healthcare crises has been difficult to establish in many studies [ 23 , 27 ]. Future research should use more objective measurements such as participation logs and, if possible, pre-crisis data for comparison. Rather than measuring the changes in symptoms, it might be beneficial to investigate changes in resources that help healthcare workers cope better [ 39 ]. Such a resource could be perceived social support, a resource known to mitigate burnout symptoms when the demands are high [ 40 ].
During a persistent crisis, healthcare workers’ responses to the strained work environment in the immediate outbreak is a major risk factor for developing high burnout and depressive symptoms later in the crisis. A strained work environment may be difficult to avoid, but, if possible, healthcare organizations should be mindful of who they place in the frontline. Especially among those healthcare workers with a strong initial burnout reaction. Future research should address how and when changes in the work environment translate into burnout and depressive symptoms over time during a persistent crisis. Occupational health researchers should focus on identifying individual-centred interventions [ 24 ] that in a feasible way support healthcare workers experiencing strong stress reactions during an ongoing crisis.
The research was funded by a grant from AFA Insurance (AFA Försäkring) reference number 200136.
We thank all participants for answering multiple surveys during the ongoing COVID-19 pandemic. We would also like to thank managers and collaborators at the study sites who helped make the data collection possible.
The authors have no Competing Interests to declare.
Raw data will not be shared due to the constraints in the information included in the written consent.
Cai H , Tu B , Ma J et al. . Psychological impact and coping strategies of frontline medical staff in Hunan Between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China . Med Sci Monit 2020 ; 26 : e924171 .
Google Scholar
Newman KL , Jeve Y , Majumder P. Experiences, and emotional strain of NHS frontline workers during the peak of the COVID19 pandemic . Int J Soc Psychiatr 2021 ; 68 : 783 – 790 .
Salazar de Pablo G , Vaquerizo-Serrano J , Catalan A et al. . Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis . J Affect Disord 2020 ; 275 : 48 – 57 .
Ghahramani S , Lankarani KB , Yousefi M , Heydari K , Shahabi S , Azmand S. A systematic review and meta-analysis of burnout among healthcare workers during COVID-19 . Front Psychiatry 2021 ; 12 : 758849 .
WHO. World Health Organization . [cited 2022 Nov 13]. Burn-out an ‘occupational phenomenon’: International Classification of Diseases . Available from: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
Aronsson G , Theorell T , Grape T et al. . A systematic review including meta-analysis of work environment and burnout symptoms . BMC Public Health. 2017 ; 17 : 264 .
Gustavsson P , Hallsten L , Rudman A. Early career burnout among nurses: modelling a hypothesized process using an item response approach . Int J Nurs Stud 2010 ; 47 : 864 – 875 .
Demerouti E , Bakker AB , Nachreiner F , Schaufeli WB. The job demands-resources model of burnout . J Appl Psychol 2001 ; 86 : 499 – 512 .
Amoafo E , Hanbali N , Patel A , Singh P. What are the significant factors associated with burnout in doctors ? Occup Med (Lond) 2015 ; 65 : 117 – 121 .
Rudman A , Arborelius L , Dahlgren A , Finnes A , Gustavsson P. Consequences of early career nurse burnout: a prospective long-term follow-up on cognitive functions, depressive symptoms, and insomnia . EClinicalMedicine 2020 ; 27 : 100565 .
Woo T , Ho R , Tang A , Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis . J Psychiatr Res 2020 ; 123 : 9 – 20 .
Glise K , Wiegner L , Jonsdottir IH. Long-term follow-up of residual symptoms in patients treated for stress-related exhaustion . BMC Psychol 2020 ; 8 : 26 .
Williams R , Kemp V. Principles for designing and delivering psychosocial and mental healthcare . BMJ Mil Health. 2020 ; 166 : 105 – 110 .
Dionisi T , Sestito L , Tarli C et al. .; Gemelli Against COVID-19 Group . Risk of burnout and stress in physicians working in a COVID team: a longitudinal survey . Int J Clin Pract 2021 ; 75 : e14755 .
Goss CW , Duncan JG , Lou SS , Holzer KJ , Evanoff BA , Kannampallil T. Effects of persistent exposure to COVID-19 on mental health outcomes among trainees: a longitudinal survey study . J Gen Intern Med 2022 ; 37 : 1204 – 1210 .
Ju TR , Mikrut EE , Spinelli A et al. . Factors associated with burnout among resident physicians responding to the COVID-19 pandemic: a 2-month longitudinal observation study . Int J Environ Res Public Health 2022 ; 19 : 9714 .
Maunder RG , Heeney ND , Hunter JJ et al. . Trends in burnout and psychological distress in hospital staff over 12 months of the COVID-19 pandemic: a prospective longitudinal survey . J Occup Med Toxicol 2022 ; 17 : 11 .
Melnikow J , Padovani A , Miller M. Frontline physician burnout during the COVID-19 pandemic: national survey findings . BMC Health Serv Res 2022 ; 22 : 365 .
Sasaki N , Asaoka H , Kuroda R , Tsuno K , Imamura K , Kawakami N. Sustained poor mental health among healthcare workers in COVID‐19 pandemic: a longitudinal analysis of the four‐wave panel survey over 8 months in Japan . J Occup Health 2021 ; 63 : e12227 .
Kachadourian L , Murrough J , Kaplan C et al. . A prospective study of transdiagnostic psychiatric symptoms associated with burnout and functional difficulties in COVID-19 frontline healthcare workers . J Psychiatr Res 2022 ; 152 : 219 – 224 .
Oosterholt BG , Maes JHR , Van der Linden D , Verbraak MJPM , Kompier MAJ. Getting better, but not well: a 1.5 year follow-up of cognitive performance and cortisol levels in clinical and non-clinical burnout . Biol Psychol 2016 ; 117 : 89 – 99 .
Bianchi R , Schonfeld IS , Laurent E. Burnout—depression overlap: a review . Clin Psychol Rev 2015 ; 36 : 28 – 41 .
Pappa S , Sakkas N , Sakka E. A year in review: sleep dysfunction and psychological distress in healthcare workers during the COVID-19 pandemic . Sleep Med 2022 ; 91 : 237 – 245 .
Kinman G , Dovey A , Teoh K. Burnout in Healthcare: Risk Factors and Solutions [Internet] . London, UK : The Society of Occupational Medicine , 2023 [cited 2024 Feb 4]. Available from: https://www.som.org.uk/sites/som.org.uk/files/Burnout_in_healthcare_risk_factors_and_solutions_July2023_0.pdf
Google Preview
Albott CS , Wozniak JR , McGlinch BP , Wall MH , Gold BS , Vinogradov S. Battle Buddies: rapid deployment of a psychological resilience intervention for healthcare workers during the Covid-19 pandemic . Anesthesia Analgesia 2020 ; 131 : 43 – 54 .
Galanis P , Vraka I , Fragkou D , Bilali A , Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis . J Adv Nurs 2021 ; 77 : 3286 – 3302 .
Pollock A , Campbell P , Cheyne J et al. . Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review . Cochrane Database Syst Rev 2020 ; 11 : CD013779 .
Bartelink V , Lager A (redaktörer). Folkhälsorapport 2023 . Stockholm : Centrum för Epidemiologi och Samhällsmedicin , 2023 .
Lundgren-Nilsson A , Jonsdottir IH , Pallant J , Ahlborg G. Internal construct validity of the Shirom-Melamed Burnout Questionnaire (SMBQ) . BMC Public Health 2012 ; 12 : 1 .
Almén N , Jansson B. The reliability and factorial validity of different versions of the Shirom-Melamed Burnout Measure/Questionnaire and normative data for a general Swedish sample . Int J Stress Manag. 2021 ; 28 : 314 – 325 .
Gilbody S , Richards D , Brealey S , Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis . J Gen Intern Med 2007 ; 22 : 1596 – 1602 .
Kroenke K , Spitzer RL , Williams JBW. The Patient Health Questionnaire-2: validity of a Two-Item Depression Screener . Med Care 2003 ; 41 : 1284 – 1292 .
The jamovi project . Jamovi [Internet] . 2021 . Available from: https://www.jamovi.org/
van den Broek A , van Hoorn L , Tooten Y , de Vroege L. The moderating effect of the COVID-19 pandemic on the mental wellbeing of health care workers on sustainable employability: a scoping review . Front Psychiatry 2023 ; 13 : 1067228 .
Fagerlind Ståhl AC , Ståhl C , Smith P. Longitudinal association between psychological demands and burnout for employees experiencing a high versus a low degree of job resources . BMC Public Health 2018 ; 18 : 915 .
Guastello AD , Brunson JC , Sambuco N et al. . Predictors of professional burnout and fulfilment in a longitudinal analysis on nurses and healthcare workers in the COVID-19 pandemic . J Clin Nurs 2023 ; 33 : 1 – 16 .
Kok N , van Gurp J , Teerenstra S et al. . Coronavirus disease 2019 immediately increases burnout symptoms in ICU professionals: a longitudinal cohort study . Crit Care Med 2021 ; 49 : 419 – 427 .
Nishimura Y , Miyoshi T , Sato A et al. . Burnout of healthcare workers amid the COVID-19 pandemic: a follow-up study . Int J Environ Res Public Health 2021 ; 18 : 11581 .
de Jonge J , Dormann C. Stressors, resources, and strain at work: a longitudinal test of the triple-match principle . J Appl Psychol 2006 ; 91 : 1359 – 1374 .
Velando‐Soriano A , Ortega‐Campos E , Gómez‐Urquiza JL , Ramírez‐Baena L , De La Fuente EI , Cañadas‐De La Fuente GA. Impact of social support in preventing burnout syndrome in nurses: a systematic review . Jpn J Nurs Sci. 2020 ; 17 : e12269 .
Supplementary data
| Month: | Total Views: |
|---|---|
| May 2024 | 357 |
| June 2024 | 217 |
Email alerts
Citing articles via.
- Contact SOM
- Recommend to your Library
Affiliations
- Online ISSN 1471-8405
- Print ISSN 0962-7480
- Copyright © 2024 Society of Occupational Medicine
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Stroke risk higher for the chronically lonely
Testing fitness of aging brain

DNR orders for Down syndrome patients far exceeded pandemic norm

Doctors not the only ones feeling burned out
BWH Communications
COVID survey finds more than half of healthcare workers stressed, overworked, and ready to leave
Although much focus has been placed on physician and nurse burnout, a new study finds the COVID-19 pandemic increased stress across the entire healthcare workforce.
Led by Brigham and Women’s Hospital investigators, the survey included over 15,000 physicians and 11,000 nurses as well as more than 5,000 other clinical staff such as pharmacists, nursing assistants, therapists, medical assistants, or social workers and over 11,000 non-clinical staff including housekeeping, administrative staff, lab technicians, or food service staff. The results are published in the Journal of General Internal Medicine.
“Teams are crucial for good healthcare delivery and our study emphasizes a need to improve the well-being of the many role types that comprise our healthcare teams,” said corresponding author Lisa S. Rotenstein, a primary care physician at the Brigham and assistant professor at Harvard Medical School.
Rotenstein’s team analyzed burnout, intent to leave the profession, and feelings of work overload reported in the American Medical Association’s Coping with COVID Survey from April to December 2020. Through the survey, 43,026 responses were collected from 206 healthcare organizations.
“There’s an opportunity here to both identify and address workload across all role types.” Lisa S. Rotenstein
“Individuals in other clinical roles or non-clinical roles such as technicians, food service workers or nursing assistants may be more likely to be from underrepresented minority groups or hold multiple jobs,” Rotenstein said. “They may be less likely to be in a position to speak up about their own working conditions.”
Approximately 50 percent of all respondents reported burnout, with the highest levels among nurses (56 percent) and other clinical staff (54.1 percent) reporting burnout. Intent to leave the job was reported by 28.7 percent of healthcare workers, with 41 percent of nurses, 32.6 percent of non-clinical staff and 31.1 percent of clinical staff reporting the sentiment. The intent to leave was higher for both physicians and nurses in an in-patient setting compared to out-patient settings.
The prevalence of perceived work overload ranged from 37.1 percent among physicians to 47.4 percent in other clinical staff. And this work overload was significantly associated with both burnout and intent to leave the job.
“That is something potentially actionable. There isn’t a standard way to quantify work overload in the healthcare setting,” said Rotenstein. “There’s an opportunity here to both identify and address workload across all role types.”
Rotenstein advocates for more innovative approaches that do not simply shift responsibilities from some members of the healthcare workforce to others, but to automate or reimagine some of these responsibilities.
Survey completion was voluntary, so the population is not necessarily representative of the healthcare workforce. Additionally, the data were collected at the height of the pandemic, and levels of burnout could have changed. Still, the survey responses underscore the importance of looking at the experience of all healthcare workers.
“We are acutely seeing the effects of burnout across the workforce,” Rotenstein said. “There are staffing shortages in healthcare facilities across the country and it’s not just physicians. It is nurses, medical assistants, and more. We need to take care of all types of healthcare workers.”
Disclosures: Co-author Mark Linzer was supported through his employer Hennepin Healthcare, and by the AMA. His other scholarly work is supported by NIH and AHRQ. Rotenstein has received research support from the American Medical Association, FeelBetter Inc., and AHRQ. Linzer is also supported through his employer for work on burnout reduction projects for IHI, ABIM, ACP, Optum Office for Provider Advancement, Essentia Health Systems, Gillette Children’s Hospital, and the California AHEC System, and consults for Harvard University on a grant assessing relationships between work conditions and diagnostic accuracy (consultation funds donated to Hennepin Healthcare Foundation).
Share this article
You might like.
Study of adults over 50 examines how feelings boost threat over time

Most voters back cognitive exams for older politicians. What do they measure?

Co-author sees need for additional research and earlier, deeper conversations around care
When should Harvard speak out?
Institutional Voice Working Group provides a roadmap in new report
Had a bad experience meditating? You're not alone.
Altered states of consciousness through yoga, mindfulness more common than thought and mostly beneficial, study finds — though clinicians ill-equipped to help those who struggle
College sees strong yield for students accepted to Class of 2028
Financial aid was a critical factor, dean says
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Burnout in healthcare:...
Burnout in healthcare: the case for organisational change
- Related content
- Peer review
- A Montgomery , professor in work and organizational psychology 1 ,
- E Panagopoulou , associate professor 2 ,
- A Esmail , professor of general practice 3 ,
- T Richards , senior editor, BMJ patient partnership initiative 4 ,
- C Maslach , professor 5
- 1 University of Macedonia, Thessaloniki, Greece
- 2 Hygiene Laboratory, Aristotle Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 3 Division of Population Health, Health Services Research and Primary Care, University of Manchester, Manchester, UK
- 4 BMJ, London, UK
- 5 University of California, Berkeley, CA, USA
- Correspondence to: A Montgomery monty5429{at}hotmail.com
Burnout is an occupational phenomenon and we need to look beyond the individual to find effective solutions, argue A Montgomery and colleagues
Burnout has become a big concern within healthcare. It is a response to prolonged exposure to occupational stressors, and it has serious consequences for healthcare professionals and the organisations in which they work. 1 Burnout is associated with sleep deprivation, 2 medical errors, 3 4 5 poor quality of care, 6 7 and low ratings of patient satisfaction. 8 Yet often initiatives to tackle burnout are focused on individuals rather than taking a systems approach to the problem.
Evidence on the association of burnout with objective indicators of performance (as opposed to self report) is scarce in all occupations, including healthcare. 9 But the few examples of studies using objective indicators of patient safety at a system level confirm the association between burnout and suboptimal care. For example, in a recent study, intensive care units in which staff had high emotional exhaustion had higher patient standardised mortality ratios, even after objective unit characteristics such as workload had been controlled for. 10
The link between burnout and performance in healthcare is probably underestimated: job performance can still be maintained even when burnt out staff lack mental or physical energy 11 as they adopt “performance protection” strategies to maintain high priority clinical tasks and neglect low priority secondary tasks (such as reassuring patients). 12 Thus, evidence that the system is broken is masked until critical points are reached. Measuring and assessing burnout within a system could act as a signal to stimulate intervention before it erodes quality of care and results in harm to patients.
Burnout does not just affect patient safety. Failing to deal with burnout results in higher staff turnover, lost revenue associated with decreased productivity, financial risk, …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £33 / $40 / €36 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
Preventing Nurse Burnout With Workplace Interventions Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Project proposal topic, capstone proposal, literature review.
This capstone project’s goal is to explore the issue of nurse burnout in the healthcare industry. Burnout is a widespread problem that affects not only the health and well-being of nurses but also the quality of patient care (Fitzpatrick et al., 2019). According to Bogue and Bogue (2020), burnout emerges as an epidemic in healthcare. This research will look at the origins and consequences of nurse burnout and identify strategies for preventing and managing burnout in the workplace. The research is conducted through a review of relevant literature and a survey of healthcare facilities and nurses.
The project proposal focuses on the exploration of nurse burnout in the healthcare industry. The aim is to understand the causes, consequences, and strategies for preventing and managing nurse burnout in the workplace. According to Buckley et al. (2020), peer-reviewed literature ensures the quality of the data reviewed. Therefore, the research will include a literature review and a survey of healthcare facilities and nurses. This project aims to contribute to developing practical solutions for reducing nurse burnout and improving the quality of patient care.
Project Question (PICOT): What is the impact of workplace interventions on reducing nurse burnout in the healthcare industry? Title of the Project: Preventing Nurse Burnout: An Examination of Workplace Interventions. Proposal: Nurse burnout is a serious issue that affects not only the health and well-being of nurses but also the quality of patient care (Fitzpatrick et al., 2019). This capstone project examines workplace interventions’ impact on reducing nurse burnout in the healthcare industry. It sheds light on the effectiveness of workplace interventions in reducing nurse burnout.
One of the interventions that will be explored is the implementation of workplace wellness programs. These programs can include activities such as exercise classes, stress management workshops, and counseling services. Another intervention that will be studied is flexible scheduling, allowing nurses more control over their work-life balance (Mlambo et al., 2021). Generally, the role of nurse managers in promoting a healthy work environment and addressing nurse burnout will also be examined. This project aims to explore the effectiveness of workplace wellness programs.
The findings provide valuable insight into the effectiveness of workplace interventions in reducing nurse burnout. It informs the development of strategies to promote a healthier work environment for nurses. The work environment is the conditions in which nurses work (Buckley et al., 2020). Ultimately, this project aims to improve the quality of patient care by reducing nurse burnout. It also promotes a sustainable work environment for nurses and other healthcare practitioners.
The issue of nurse burnout is a pressing concern in the healthcare industry, affecting the standard of patient care and the nurses’ health and well-being. The signs of burnout entail emotional exhaustion, depersonalization, and decreased personal accomplishment (Bogue & Bogue, 2020). It can lead to reduced job satisfaction and increased healthcare costs. This capstone project aims to address nurse burnout by exploring the impact of workplace interventions on reducing burnout levels. The project addresses nurse burnout by examining the effect of workplace interventions.
A literature study and a survey of hospitals and nurses will be used to conduct the research. It will focus on identifying effective strategies for preventing and managing nurse burnout in the workplace. This project was selected because nurse burnout is a critical issue in the healthcare industry and significantly impacts nurses’ and patients’ care quality (Johnson et al., 2017). Nurses have witnessed the toll that burnout can take on their colleagues. Finding ways to address this issue is crucial for nurses’ well-being and the healthcare industry’s sustainability.
Nurse burnout has multiple causes, including extended hours and high stress. It results in burnout symptoms like exhaustion and feeling overwhelmed. It can also result in excessive workload and increased pressure on nurses to perform their duties efficiently. The study will explore ways to enhance the work environment for nurses and reduce burnout through practical solutions. It aims to contribute to a healthier and more sustainable workplace for nursing professionals.
The literature review plays a crucial role in this capstone project. It provides a comprehensive understanding of the current research on nurse burnout and workplace interventions to reduce burnout levels (Bogue & Bogue, 2020). It will examine peer-reviewed articles and other academic sources to identify the key themes and findings related to the problem of nurse burnout and effective strategies for reducing it (Buckley et al., 2020). This information will inform the design of the survey component and the development of recommendations for improving the work environment for nurses. It serves as a foundation for the project, ensuring that the methodology is well-informed and based on the latest scientific evidence.
Methods of Searching
A literature review was conducted using both electronic and manual resources. Relevant databases such as PubMed, CINAHL, and ProQuest were searched using keywords related to nursing burnout and workplace interventions (Norful et al., 2018). The manual search involved reviewing reference lists of relevant articles and books. The investigation was limited to English language sources published in the last five years. The sources were then evaluated for relevance, quality, and credibility before being included in the literature review. This comprehensive and systematic approach ensured that the information gathered was up-to-date and relevant to the current state of the research.
Review of the Literature
The literature review examined the growing issue of nurse burnout and the potential solutions to address this problem. The study used electronic and manual resources, including PubMed, CINAHL, and ProQuest databases, to compile the most recent information. It was restricted to sources published within the last five years. The restriction ensured that the information gathered was up-to-date and relevant to the current state of the research. Filtering occurred in the database used to produce peer-reviewed articles.
The literature found that nurse burnout is a growing concern in nursing. High levels of burnout impact the quality of care and contribute to high turnover rates. Contributing factors to nurse burnout include heavy workloads, lack of support from colleagues and supervisors, and poor working conditions (Dall’Ora et al., 2020). The nurse will ultimately reduce their work performance, and some will desire to quit. Eventually, the healthcare system faces challenges whenever there are scarce nurses.
The literature review identified several workplace interventions that have shown promise in reducing burnout. These include programs to improve work-life balance and provide nurses with support and resources. Another intervention is to improve the working conditions of the nurses. One study found that a workplace wellness program, which provided education and resources for stress management and self-care, significantly reduced nurse burnout (Johnson et al., 2017). It highlights the significance of nurse burnout and the need for effective interventions to address this issue.
Further research shows more interventions that could reduce nurse burnout. According to another study, offering opportunities for professional development and growth, such as continuing education and leadership training, reduced burnout and improved job satisfaction among nurses (Fitzpatrick et al., 2019). Regular skill renewal and upgrading are necessary for healthcare workers. The literature review also highlighted the importance of addressing burnout at the organizational level. It includes creating a supportive work environment, promoting work-life balance, and providing resources and support for nurses.
Nurse burnout is a significant problem in the healthcare industry. It affects both the well-being of nurses and the quality of patient care. Workplace interventions, such as wellness programs and professional development opportunities, have shown promise in reducing burnout and improving nurses’ job satisfaction (Johnson et al., 2017). However, the most practical methods for reducing nurse burnout and enhancing the working conditions for nurses require more investigation. This capstone project aims to contribute to the ongoing effort to reduce nurse burnout and improve the work environment for nurses.
The literature has shown that nurse burnout is a growing concern in nursing. Burnout harms the quality of care nurses provide. Heavy workloads, a lack of support from peers and managers, and unfavorable working circumstances are all factors that contribute to nursing burnout (Dall’Ora et al., 2020). The literature review identified several workplace interventions that have shown promise in reducing burnout. These include programs to improve work-life balance, provide nurses with support and resources, and improve working conditions.
Additionally, addressing nurse burnout at the organizational level through supportive work environments and involving nurses in decision-making can help reduce burnout. It is found that continued professional development in nursing is an effective strategy for reducing nurse burnout and enhancing the nursing workforce (Mlambo et al., 2021). A nurse practitioner is an example of a registered nurse holding a doctoral degree. The findings intend to lessen nurse burnout and enhance the working conditions for nurses. These findings provide valuable insight into the most successful strategies for promoting a healthy and sustainable work environment for nurses.
The project targets nurse burnout with three objectives. Objective 1: Evaluate the workplace wellness program’s impact on nurse burnout (Ernawati et al., 2022). Objective 2: Boost nurse engagement by involving them in decision-making (Fitzpatrick et al., 2019). Objective 3: Improve nurse work-life balance with flexible arrangements and resources for stress management. These objectives ensure that the project is focused and aligned to reduce nurse burnout.
Two strategies will be employed to achieve the first objective: to identify the extent of nurse burnout in healthcare facilities. Firstly, a survey will be administered to a sample of nurses to assess their level of burnout (Ernawati et al., 2022). The survey will include questions about the frequency and intensity of symptoms associated with burnout. These may entail emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. Secondly, a focus group will be organized to allow nurses to share their experiences and perspectives on nurse burnout.
The second objective is to understand the contributing factors to nurse burnout. Two strategies will be used in order to achieve this. Firstly, the survey and focus group results will be analyzed to identify patterns or trends. Secondly, a review of the relevant literature will be conducted to identify gaps in the current understanding of nurse burnout (Buckley et al., 2020). All this will ensure that all relevant factors are considered when developing strategies to reduce nurse burnout.
The third objective is to develop and implement an intervention to reduce nurse burnout. A customized program will be designed that addresses the contributing factors identified in the analysis of the survey and focus group results. It may include training sessions on stress management for nurses and healthcare administrators (Ernawati et al., 2022). Secondly, workplace practices will be implemented to support work-life balance for nurses. It includes flexible schedules and opportunities for professional development for nurses.
Evaluation of the project will be crucial to determine its success in achieving the objectives and improving patient outcomes/safety. Several methods will be used to evaluate the capstone project. These include data analysis, surveys, random interviews, and focus groups. The data collected from these methods will be used to determine the effectiveness of the strategies implemented in addressing the objectives (Dall’Ora et al., 2020). One of the required evaluation methods will be data analysis.
The patient data is analyzed to determine any improved outcomes and safety. It includes patient satisfaction levels, patient outcomes, and the number of adverse events. The collection of data is before and after the implementation of the strategies. A comparison of the two data sets will be used to determine if there has been any improvement. In addition to data analysis, surveys and focus groups will gather feedback from patients and healthcare providers.
The evaluations will provide insight into the perceived effectiveness of the strategies and any potential areas for improvement. This feedback will refine the plan and make any necessary changes to improve patient safety (Fitzpatrick et al., 2019). The project evaluation will be ongoing and will provide valuable information on its effectiveness. The assessment results will be used to make necessary changes to the project and ensure that it continues improving patient outcomes and safety. Upon thorough evaluation, the project is ready to be actualized.
The budget for this project will include various items necessary for its successful implementation. These items include resources for conducting workshops and training sessions for the nursing staff, materials for disseminating information and awareness, and software and tools required for data collection and analysis. The funding for these budget items will come from various sources, such as grants, sponsorships, and in-kind contributions from the healthcare organization where the project will be implemented. The total budget required for the successful completion of the project will be determined after carefully considering all the necessary expenses. It will be subject to change as per the needs of the project.
Nurse burnout is a pressing issue affecting the quality of patient care and nursing professionals’ overall health and well-being. The capstone project aims to combat nurse burnout, which affects patient care and health (Ernawati et al., 2022). Evidence supports the need for stress-reducing interventions to enhance work-life balance. The project targets the issue of nurse burnout and its negative impact on patients and healthcare workers. The study aims to offer a solution to improve outcomes for both patients and healthcare professionals.
The objectives and strategies outlined in this proposal are well-defined and achievable. The evaluation plan will help determine the effectiveness of the interventions. The initiative has the potential to significantly influence many people’s lives and the healthcare system as a whole, with sufficient financing and support. It is a valuable contribution to the field of nursing and healthcare. The project will help advance the understanding of mitigating nurse burnout and promoting better patient care outcomes.
The project aims to address the issue of nurse burnout through research and interventions. It, therefore, offers solutions to promote healthy work environments for nurses. New nurses face challenges and often lack resilience, but this project can guide the healthcare industry in supporting these professionals (Buckley et al., 2020). The insights gained will benefit nurses and patients, creating a brighter future in the healthcare field. This project serves as a blueprint for governments and institutions to follow in preventing nurse burnout.
Bogue, T. L., & Bogue, R. L. (2020). Extinguish Burnout in Critical Care Nursing . Critical Care Nursing Clinics of North America , 32 (3), 451–463. Web.
Buckley, L., Berta, W., Cleverley, K., Medeiros, C., & Widger, K. (2020). What is known about paediatric nurse burnout: a scoping review . Human Resources for Health , 18 (1). Web.
Dall’Ora, C., Ball, J., Reinius, M., & Griffiths, P. (2020). Burnout in nursing: a theoretical review . Human Resources for Health , 18 (1). Web.
Ernawati, E., Mawardi, F., Roswiyani, R., Melissa, M., Wiwaha, G., Tiatri, S., & Hilmanto, D. (2022). Workplace wellness programs for working mothers: A systematic review . Journal of Occupational Health , 64 (1). Web.
Fitzpatrick, B., Bloore, K., & Blake, N. (2019). Joy in Work and Reducing Nurse Burnout: From Triple Aim to Quadruple Aim . AACN Advanced Critical Care , 30 (2), 185–188. Web.
Johnson, J., Hall, L. H., Berzins, K., Baker, J., Melling, K., & Thompson, C. (2017). Mental healthcare staff well-being and burnout: A narrative review of trends, causes, implications, and recommendations for future interventions . International Journal of Mental Health Nursing , 27 (1), 20–32. Web.
Mlambo, M., Silén, C., & McGrath, C. (2021). Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature . BMC Nursing , 20 (1). Web.
Norful, A. A., De Jacq, K., Carlino, R., & Poghosyan, L. (2018). Nurse Practitioner–Physician Comanagement: A Theoretical Model to Alleviate Primary Care Strain . The Annals of Family Medicine , 16 (3), 250–256. Web.
- The Capstone Project: The Analysis of Uipath
- Capstone Change Project Resources in Acute Care
- The Effects of Child Abuse: Capstone Project Time Line
- The H.R. 198 Bill's Impact on Nursing Practice
- Nurse-to-Patient Ratios' Effect on Nurse Retention
- Nurses' Role in National Patient Safety Goals
- Narrative and Bearing Witness in Nursing
- Cultural and Social Considerations in Health Assessment
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, January 30). Preventing Nurse Burnout With Workplace Interventions. https://ivypanda.com/essays/preventing-nurse-burnout-with-workplace-interventions/
"Preventing Nurse Burnout With Workplace Interventions." IvyPanda , 30 Jan. 2024, ivypanda.com/essays/preventing-nurse-burnout-with-workplace-interventions/.
IvyPanda . (2024) 'Preventing Nurse Burnout With Workplace Interventions'. 30 January.
IvyPanda . 2024. "Preventing Nurse Burnout With Workplace Interventions." January 30, 2024. https://ivypanda.com/essays/preventing-nurse-burnout-with-workplace-interventions/.
1. IvyPanda . "Preventing Nurse Burnout With Workplace Interventions." January 30, 2024. https://ivypanda.com/essays/preventing-nurse-burnout-with-workplace-interventions/.
Bibliography
IvyPanda . "Preventing Nurse Burnout With Workplace Interventions." January 30, 2024. https://ivypanda.com/essays/preventing-nurse-burnout-with-workplace-interventions/.
Understanding and prioritizing nurses’ mental health and well-being
Healthcare organizations continue to feel the effects of the COVID-19 pandemic, including prolonged workforce shortages, rising labor costs, and increased staff burnout. 1 The World Health Organization defines burnout as “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed,” with symptoms including “feelings of energy depletion or exhaustion; increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; and reduced professional efficacy.” For more, see “Burn-out an ‘occupational phenomenon’: International Classification of Diseases,” World Health Organization, May 28, 2019; and “Doctors not the only ones feeling burned out,” Harvard Gazette , March 31, 2023. Although nurses routinely experience job-related stress and symptoms of burnout, the COVID-19 pandemic exacerbated the challenges of this high-intensity role.
About the research collaboration between the American Nurses Foundation and McKinsey
The American Nurses Foundation is a national research, educational, and philanthropic affiliate of the American Nurses Association committed to advancing the nursing profession by serving as a thought leader, catalyst for action, convener, and funding conduit. The American Nurses Foundation and McKinsey are partnering to assess and report on trends related to the nursing profession. A foundational part of this effort is jointly publishing novel insights related to supporting nurses throughout their careers.
In April and May 2023, the American Nurses Foundation and McKinsey surveyed 7,419 nurses in the United States to better understand their experiences, needs, preferences, and career intentions. All survey questions were based on the experiences of the individual professional. All questions were also optional for survey respondents; therefore, the number of responses may vary by question. Additionally, publicly shared examples, tools, and healthcare systems referenced in this article are representative of actions that stakeholders are taking to address workforce challenges.
As part of an ongoing, collaborative research effort, the American Nurses Foundation (the Foundation) and McKinsey surveyed more than 7,000 nurses in April and May 2023 to better understand mental health and well-being in the nursing workforce (see sidebar “About the research collaboration between the American Nurses Foundation and McKinsey”). The survey results revealed that symptoms of burnout and mental-health challenges among nurses remain high; the potential long-term workforce and health implications of these persistent pressures are not yet fully understood.
In this report, we share the highlights of our most recent survey and trends over the past few years. As healthcare organizations and other stakeholders continue to evolve their approaches to these important issues, this research provides additional insight into the challenges nurses face today and highlights opportunities to ensure adequate support to sustain the profession and ensure access to care for patients.
Current state of the nursing workforce
Although many organizations have taken steps to address the challenges facing the nursing workforce, findings from the joint American Nurses Foundation and McKinsey survey from May 2023 indicate that continued action is required. Nursing turnover is beginning to decline from its 2021 high but remains above prepandemic levels. 2 2023 NSI national health care retention & RN staffing report , NSI Nursing Solutions, 2023. Intent to leave also remains high: about 20 percent of surveyed nurses indicated they had changed positions in the past six months, and about 39 percent indicated they were likely to leave their current position in the next six months. 3 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4. Intent to leave was roughly 41 percent among nurses who provide direct care to patients, compared with 30 percent for nurses not in direct-patient-care roles. 4 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4.
Surveyed nurses who indicated they were likely to leave cited not feeling valued by their organizations, insufficient staffing, and inadequate compensation as the top three factors influencing their decisions. 5 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4. Insufficient staffing was especially important to respondents with less than ten years of experience 6 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4. —a population that will be critical to retain to ensure future workforce stability.
Key survey insights on mental health and well-being
Our joint research highlighted the magnitude of the health and well-being challenges, both physical and mental, facing the nursing workforce. More than 57 percent of surveyed nurses indicated they had been diagnosed with COVID-19, and 11 percent of those indicated they had been diagnosed with post-COVID-19 conditions (PCC or “long COVID”). Additional research may be needed to fully understand the impact of PCC on nurses, but in the meantime, employers could consider augmenting their PCC services for clinicians.
Research conducted by both the Foundation and McKinsey over the past three years has identified sustained feelings of burnout among surveyed nurses—a trend that continued this year. 7 For more, see the following articles: “Mental health and wellness survey 1,” American Nurses Foundation, August 2020; “Mental health and wellness survey 2,” American Nurses Foundation, December 2020; “Mental health and wellness survey 3,” American Nurses Foundation, September 2021; Gretchen Berlin, Meredith Lapointe, Mhoire Murphy, and Molly Viscardi, “ Nursing in 2021: Retaining the healthcare workforce when we need it most ,” McKinsey, May 11, 2021; Gretchen Berlin, Meredith Lapointe, Mhoire Murphy, and Joanna Wexler, “ Assessing the lingering impact of COVID-19 on the nursing workforce ,” McKinsey, May 11, 2022; “ Nursing in 2023: How hospitals are confronting shortages ,” McKinsey, May 5, 2023. Reported contributors to burnout include insufficient staffing, high patient loads, poor and difficult leadership, and too much time spent on administrative tasks. In our joint survey, 56 percent of nurses reported experiencing symptoms of burnout, such as emotional exhaustion (Exhibit 1). Well more than half (64 percent) indicated they feel “a great deal of stress” because of their jobs. Additionally, although there have been slight improvements year over year in respondents’ reports of stress, anxiety, and feeling overwhelmed, reports of positive emotions such as feeling empowered, grateful, and confident have declined. 8 “Pulse on the Nation’s Nurses Survey Series results,” American Nurses Foundation, accessed October 20, 2023.
Our results indicate that mental health and well-being vary by nurse experience levels (Exhibit 2). Less-tenured nurse respondents were more likely to report less satisfaction with their role, had a higher likelihood of leaving their role, and were more likely to be experiencing burnout.
Despite these sustained and high levels of burnout, approximately two-thirds of surveyed nurses indicated they were not currently receiving mental-health support (a figure that remained relatively consistent in Foundation surveys over the past two years), and 56 percent of surveyed nurses believe there is stigma attached to mental-health challenges. 9 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4; “Pulse on the Nation’s Nurses,” accessed October 20, 2023.
Reasons cited by nurse respondents for not seeking professional mental-health support have remained consistent over the past two years, 10 “Mental health and wellness survey 3,” September 2021. with 29 percent indicating a lack of time, 23 percent indicating they feel they should be able to handle their own mental health, and 10 percent citing cost or a lack of financial resources (Exhibit 3). For nurses with ten or fewer years of experience, lack of time ranked as the top reason for not seeking professional mental help.
Despite slight improvements to the most severe symptoms over the past six to 12 months, reported levels of sustained burnout and well-being challenges have remained consistently high since we began assessing this population in 2021. Moreover, research indicates that burnout has several adverse, long-term health effects; for example, it is a predictor of a wide range of illnesses. 11 Denise Albieri Jodas Salvagioni et al., “Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies,” PLoS One , October 2017, Volume 12, Number 10; D. Smith Bailey, “Burnout harms workers’ physical health through many pathways,” Monitor on Psychology , June 2006, Volume 37, Number 7. These health conditions incur not only personal costs but also societal and organizational costs because they influence productivity, employee retention, presence at work, and career longevity. 12 Prioritise people: Unlock the value of a thriving workforce , Business in the Community and the McKinsey Health Institute, April 2023.
Actions stakeholders can take to address mental health and well-being
To address these sustained levels of burnout, stakeholders will need to take steps to support nurses’ mental health and well-being. They will also need to address the underlying structural issues—for example, workload and administrative burden—that affect the nursing profession and that have been consistently acknowledged as root causes of burnout. Simultaneously reducing workload demands and increasing resources available to meet those demands will be critical.
A variety of interventions could address the drivers and effects of adverse nursing mental health and well-being, bolstering support for individuals, organizations, and the healthcare system at large. Various stakeholders are deploying a number of initiatives.
Applying process and operating-model interventions
Addressing the underlying drivers of burnout could help to prevent it in the first place. Research from the McKinsey Health Institute shows that the day-to-day work environment has a substantial impact on the mental health and well-being of employees. 13 “ Addressing employee burnout: Are you solving the right problem? ,” McKinsey Health Institute, May 27, 2022. Process and operating-model shifts—in the context of ongoing broader shifts in care models—could enable organizations and care teams to evolve working practices to better support job satisfaction and sustainability.
In our most recent collaborative research, almost a quarter of surveyed nurses believed their teams were not working efficiently; more than 40 percent reported that they had poor control over their workloads and that their day-to-day work was hectic and intense. 14 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4. Evaluating and addressing structural aspects of the job that contribute to workload—for example, by identifying opportunities to delegate activities and enable nurses to use technology—could help support these themes. 15 Gretchen Berlin, Ani Bilazarian, Joyce Chang, and Stephanie Hammer, “ Reimagining the nursing workload: Finding time to close the workforce gap ,” McKinsey, May 26, 2023. However, providing these resources without also addressing the underlying structural drivers contributing to mental-health and well-being challenges is insufficient and can unintentionally appear to place the burden for solving problems on employees themselves. Both individual-level supports and collaborative efforts to drive structural change are required.
In addition to addressing workload challenges, employers could provide flexible work options—for example, in shift length, start time, shift commitments, and virtual activities 16 Erica Carbajal, “‘Resilience isn’t a pillar by itself’: CommonSpirit’s plan to support 44,000 nurses in 2023,” Becker’s Clinical Leadership, December 9, 2022. —to better enable employees to recharge from high levels of demands and to reduce conflicts with demands outside of work.
Finally, employers could take steps to reduce the administrative burden on nurses. More than a third of nursing respondents in our joint survey felt they spent excessive time working on electronic health records on breaks or after shifts, and 45 percent reported this activity adds frustration to their day. 17 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4. Employers can look for opportunities to delegate some documentation to nursing scribes, reduce documentation requirements, or use AI to aid with documentation to help reduce this burden.
Increasing availability, awareness, and accessibility of evidence-based resources
When nurses experience symptoms of burnout or other mental-health and well-being challenges, evidence-based resources need to be available. In addition, employees need to know these resources are available, and they need to feel comfortable accessing them within the organization’s cultural context.
Investments in resources for mental health and well-being span the continuum—from mental healthcare for those experiencing clinical symptoms to well-being support tools and programs to promote healthy behaviors and mitigate sources of stress. On the higher-acuity end of the continuum, providing employees with free or subsidized access to professionally provided therapy or counseling services could help reduce the barriers employees face in getting the care they need. On the lower-acuity end, providing access to resources and training on mental-health literacy, self-monitoring, and adaptability skills could help nurses identify and mitigate sources of stress.
Investments in awareness and accessibility are important to ensure available resources are used. Roughly 19 percent of surveyed nurses who indicated they had not sought mental-health support in the past 12 months cited lack of knowledge, lack of resources, fear of losing their job, or concern about colleagues finding out as reasons for not seeking support. 18 Based on data from Pulse on the Nation’s Nurses Survey Series: Mental Health and Wellness Survey 4. To reinforce their support, employers can take steps such as establishing support networks for communities and allies, providing forums to share stories of mental health, and introducing avenues for peer-to-peer support. Additionally, resources such as a behavioral-health concierge can help all employees (including nurses) navigate, find, and access care and support.
Resources available through the Foundation
The American Nurses Foundation (the Foundation) and the American Nurses Association (ANA) provide numerous free support resources, including the following:
Well-Being Initiative. The Foundation launched the Well-Being Initiative to offer resources that focus on caring for nurses as they tirelessly care for others. 1 “Well-Being Initiative,” American Nurses Foundation, accessed October 20, 2023. These free, multimodal resources are accessible to all US nurses at any time and are completely anonymous.
Stress and Burnout Prevention Pilot Program. The Foundation launched the Stress and Burnout Prevention Pilot Program with support from the United Health Foundation to address nurse burnout and manage stress, among other goals. 2 “Stress & Burnout Prevention Program,” American Nurses Foundation, accessed October 20, 2023. The program uses the “Stress First Aid” model to facilitate discussions about stress and burnout and reduce stigma for nurses in need of support. The program goes beyond identification of burnout to intervention by helping nurses speak about stress and burnout using a common language, normalizing talking about and understanding support resources for them and their peers.
Healthy Nurse, Healthy Nation (HNHN). This ANA Enterprise program is designed to improve the nation’s health, “one nurse at a time.” 3 “Healthy Nurse, Healthy Nation,” American Nurses Foundation, accessed October 20, 2023. HNHN supports nurses in six areas: physical activity, rest, nutrition, quality of life, safety, and mental health. An online platform offers nurses inspiration, friendly competition, content and resources, and connections with other nurses, employers, and organizations.
Nurse suicide prevention. Nurses are at higher risk of suicide than the general population. 4 Christopher R. Friese and Kathryn A. Lee, “Deaths by suicide among nurses: A rapid response call,” Journal of Psychosocial Nursing and Mental Health Services , August 2021, Volume 59, Number 8. The multiple stressors they face in their profession may lead to emotional turmoil, moral distress or injury, and cognitive overload. ANA offers resources to educate nurses about suicide prevention and strategies to help them support themselves and one another. 5 “Nurse suicide prevention/resilience,” American Nurses Association, accessed October 20, 2023; “Suicide among nurses: What we don’t know might hurt us,” American Nurses Association, accessed October 20, 2023.
Accessibility of resources within the organization’s cultural context is also important, given that stigmatization of beliefs, behaviors, and policies can prevent people from feeling able to seek help when they need it. Because mental-illness stigma includes self-stigma, public stigma, and structural stigma, companies can take a holistic approach to root it out, 19 Erica Coe, Jenny Cordina, Kana Enomoto, and Nikhil Seshan, “ Overcoming stigma: Three strategies toward better mental health in the workplace ,” McKinsey Quarterly , July 23, 2021. including with education, leadership role modeling, and policies addressing discriminatory behaviors. 20 Allison Nordberg and Marla J. Weston, “Stigma: A barrier in supporting nurse well-being during the pandemic,” Nurse Leader , April 2022, Volume 20, Number 2. They can also provide information about free support resources, such as those provided by the American Nurses Foundation and the American Nurses Association (see sidebar “Resources available through the Foundation”).
Bolstering skills and capabilities
Efforts to address structural issues can be advanced by investing in training opportunities to help individuals and teams proactively support their own mental health and that of their colleagues. Training areas could include workplace mental-health intervention; critical skills for leaders and managers, such as conflict resolution and bystander intervention; and resilience and adaptability training to inculcate mindsets and behaviors across the organization that ultimately support employee mental health and well-being.
Toward a healthier future for nurses
Tackling these sustained challenges for mental health and well-being will be critical for addressing near-term workforce shortages and ensuring the health and well-being of the nursing profession in the long term. In our joint survey, many surveyed nurses indicated they chose the profession because they wanted to make a difference—by helping improve patients’ lives and care for patients in their most vulnerable moments. They value their colleagues and the care and trust of their teams. However, with less than half of surveyed nurses feeling satisfied with their jobs, they clearly need more in return to sustain them in the profession. There isn’t a one-size-fits-all approach to tackling some of the sustained well-being challenges that face nurses, but now is the time to bring additional energy and commitment to tackle the multifaceted drivers of symptoms of burnout and to support the profession in improving sustainability and fulfillment for years to come.
Gretchen Berlin, RN , is a senior partner in McKinsey’s Washington, DC, office, where Faith Burns is an associate partner; Brad Herbig is an associate partner in the Philadelphia office; and Mhoire Murphy is a partner in the Boston office. Amy Hanley is a program manager at the American Nurses Foundation, and Kate Judge is the executive director of the American Nurses Foundation.
The authors wish to thank the nurses, physicians, and staff on the front lines who are caring for patients and communities. They also wish to thank Nitzy Bustamante, Stephanie Hammer, and Brooke Tobin for their contributions to this article.
Explore a career with us
Related articles.

Nursing in 2023: How hospitals are confronting shortages

Nurses are still under pressure—here’s what healthcare organizations can do about it
Reimagining the nursing workload: finding time to close the workforce gap.
- INNOVATION FESTIVAL
- Capital One
06-25-2024 WORKPLACE EVOLUTION
The burnout epidemic is hitting healthcare workers hard
According to research, high levels of microstress may be behind the rise of burnout in industries like healthcare.

[Photo: Karolina Kaboompics /Pexels]
BY Karen Dillon and Rob Cross 7 minute read
Many experts are calling attention to a so-called burnout epidemic among workers . Unfortunately, healthcare workers are being especially impacted. Both of us have seen that impact firsthand through our work with healthcare groups.
We interviewed workers to better understand why the burnout epidemic is hitting healthcare workers so hard. Here’s what we found:
“I end up feeling exhausted”
“I have the best job in the world,” says Carlos, who asked that his last name be withheld. His job as chief diagnostic medical physicist for a major health system requires him to ensure that the sophisticated medical equipment for the 700-bed hospital is always working properly. It’s a hectic job that keeps him on his toes most days. But some days the incoming requests are so fast and furious that Carlos silently declares them “laughing days”—because if he didn’t do that, he says, he “would just shut down.”
Like many of us, Carlos tries to be easily accessible to his colleagues, via landline, mobile phone, email, text, pager, or in person in his office. “But there are times I will get a call on my office phone, then someone else will call my cellphone, and I’ll be in the middle of two different conversations, and I’ll get a page about the same issue from someone else,” he explains. “Then as I’m on the phone, I’ll see so many emails popping into my inbox that it almost looks like my inbox is scrolling. And I’ll look up and someone else is standing in my door with something they need me to sign, and so on.”
ABOUT THE AUTHORS
Karen Dillon is a former editor of Harvard Business Review and coauthor of The Microstress Effect: How Little Things Pile Up and Create Big Problems — and What to Do About It (Harvard Business Review Press, 2023). She is also coauthor of three books with Clayton Christensen, including the New York Times best-seller How Will You Measure Your Life? More
Rob Cross is the Edward A. Madden Professor of Global Leadership at Babson College and a Senior Vice President of Research for the Institute for Corporate Productivity. He is also coauthor of The Microstress Effect: How Little Things Pile Up and Create Big Problems — and What to Do About It and the author of Beyond Collaboration Overload. More
Explore Topics
- Workplace Evolution
- Tech Video assistant referees to smart rings: Here’s the soccer tech at Euro 2024
- Tech What is a passkey? Why Apple is betting on password-free tech
- Tech How to find and search YouTube video transcripts on your phone
- News 32 of the nation’s 200 largest housing markets are back to pre-pandemic inventory levels
- News Tour de France 2024: How to watch coverage of the cycling event live without cable
- News White House to expand its influencer engagement efforts with its first-ever Creator Economy Conference
- Design Verizon’s new CMO Leslie Berland wants to make sure you can hear the brand now
- Design Fujifilm can’t keep up with TikTok’s retro-camera craze for the X100
- Design The Stonewall Inn Monument gets a slick new visitor center
- Work Life 6 tips to stay on track with your investing goals after losing a job
- Work Life Employers believe this is the age you’re too old to hire. This is why they’re wrong
- Work Life Does having more women in VC circles lead to more funding for woman-led businesses? No, says new study
MINI REVIEW article
Burnout among healthcare workers in the covid 19 era: a review of the existing literature.

- 1 Institute of Clinical Physiology, National Research Council, Lecce, Italy
- 2 Institute for Research on Population and Social Policies, National Research Council, Brindisi, Italy
- 3 Institute for Applied Mathematics and Information Technologies “E. Magenes,” National Research Council, Milan, Italy
- 4 Respiratory Diseases Unit, “A. Perrino” P.O., Brindisi, Italy
In the current period of global public health crisis due to the COVID-19, healthcare workers are more exposed to physical and mental exhaustion – burnout – for the torment of difficult decisions, the pain of losing patients and colleagues, and the risk of infection, for themselves and their families. The very high number of cases and deaths, and the probable future “waves” raise awareness of these challenging working conditions and the need to address burnout by identifying possible solutions. Measures have been suggested to prevent or reduce burnout at individual level (physical activity, balanced diet, good sleep hygiene, family support, meaningful relationships, reflective practices and small group discussions), organizational level (blame-free environments for sharing experiences and advices, broad involvement in management decisions, multi-disciplinary psychosocial support teams, safe areas to withdraw quickly from stressful situations, adequate time planning, social support), and cultural level (involvement of healthcare workers in the development, implementation, testing, and evaluation of measures against burnout). Although some progress has been made in removing the barrier to psychological support to cope with work-related stress, a cultural change is still needed for the stigma associated with mental illness. The key recommendation is to address the challenges that the emergency poses and to aggregate health, well-being and behavioral science expertise through long term researches with rigorous planning and reporting to drive the necessary cultural change and the improvement of public health systems.
Introduction
Burnout is a psychological syndrome described as a self-reported state of care- or work- related physical and mental stress ( 1 ) that induces emotional exhaustion (EE), depersonalization (DP), and a sense of reduced personal accomplishment (PA) ( 2 ). It is an unexpected consequence of an organizational culture unable to balance the personal identity of the worker with that of the work organization and the social context, and of the consequent continuous mental effort to cope with the perceived friction ( 3 ). Burnout was first applied to healthcare workers (HCWs) by Freudenberger in 1974 ( 4 ). Due to substantial disagreement in the health literature on what exactly constitutes burnout and therefore on how to measure it ( 5 ), there is a great heterogeneity in the prevalence of this phenomenon: Rodrigues and colleagues, in their meta-analysis on different medical resident specialties ( 2 ), reported that the overall prevalence of burnout for all specialties was 35.1%; Rotenstein and colleagues, in their meta-analysis on practicing physicians ( 5 ), estimate an overall burnout ranging from 0 to 80.5% with pooled prevalence of 21.3% on overall burnout; they also calculate a pooled prevalence of 34.4% on EE, 25.8% on DP, and of 23.5% on PA.
In the recent period due to the coronavirus disease 2019 (COVID-19) pandemic ( 6 ) the world is experiencing an unprecedented global public health crisis with a significant strain on the healthcare system. In fact, the very high number of globally confirmed cases (195,266,156) and deaths (4,180,161) ( 7 ) and the probable additional “waves” to come as new variants emerge despite increased vaccination coverage ( 8 ) are having a serious impact on health systems: rationing or cessation of routine services, repurposing of clinical areas, redeployment of staff to unfamiliar clinical environments, shortage of personal protective equipment, extensive responsibilities, constant risk of complaints for negligence ( 9 , 10 ) with medical resources and services placed at their maximum capacity due to unprecedented demands, especially for emergency departments ( 11 ). Frontline HCWs involved in the management and diagnosis of COVID-19 are more exposed to overwhelming pressure with consequent psychological stress. As referred in recent publications, medical staff report physical and mental exhaustion – due to the ethical dilemmas and moral injuries for the torment of life-or-death decisions required to be made fast and without the support of optimal care protocols, the pain of losing patients and colleagues, and the risk of infection for themselves and their families ( 12 , 13 ). All these issues are especially true for residents and young HCWs who, as discussed in Zoorob et al. ( 14 ), received ever-changing information on protective measures, and are asked to work in services other than their specialty, particularly in frontline situations ( 15 ).
With this narrative review, we aim to discuss the magnitude of burnout among HCWs in the COVID-19 era analyzing emerging concepts to grasp the complexity of the problem. In particular we wanted to identify the health professionals exposed to a greater risk, the effects of burn-out on an individual and organization level and how it has been recommended to address this issue. We also wanted to highlight current research gaps that need to be filled so that health systems can be prepared for future challenges.
With this broad perspective in mind, to grasp the complexity of the problem, we performed, as also suggested by Greenhalgh and colleagues ( 16 ), a narrative review. The of review of literature has been done without date restrictions; it was conducted on MEDLINE/Pubmed, ISI Web of Knowledge, Scopus, and Google Scholar by a multi-disciplinary team of socio-economists, methodologists, healthcare workers. We limited our search to works published in English or Italian and used the following search terms: “healthcare workers,” “physicians,” “residents,” “nurses,” “burnout,” “chronic pain,” “pain syndrome,” “painful disorders,” “stress,” “workloads,” “suicide,” “Covid19,” “coronavirus disease,” “pandemic”. Study inclusion was assessed through visual inspection of abstracts. Forward citation of relevant papers was also adopted to increase the sensitivity of the search process.
Who Is Affected
Before COVID-19, Rodrigues and colleagues ( 2 ) reported an high variability of the prevalence of burnout across specialties: high prevalence (42.5%), when grouping general surgery, anesthesiology, obstetrics and gynecology, and orthopedics; moderate prevalence (29.4%), for internal medicine, plastic surgery and pediatrics; low prevalence (23.5%), for otolaryngology and neurology. Emergency routine results a key determinant of heterogeneity: prevalence is higher among residents from medical specialty schools who deal directly with life-threatening situations and shift overload. Age emerges as a protective factor: burnout levels in physicians tend to decrease with increasing age, possibly due to the more “idealistic” and empathic approach in younger physicians ( 17 ).
In the COVID-19 pandemic, more HCWs are facing life-threatening situations, pathogen exposure, and shift overload and other major changes in work organization ( 9 ). Moreover, increased supervision and regulation reduced autonomy of HCWs and their time with patients ( 18 ). Prevalence of burnout was higher in intensive care units and sub-intensive care wards, and for residents and nurses. In an Italian survey, higher levels of burnout were found in females, in young (aged <30 years) HCWs, in those who frequently change job duties and family habits, and in residents ( 19 ).
In a recent systematic review, Prasad and colleagues ( 20 ) found higher stress scores in US health organizations among women, black and Latino individuals, hospital workers and nursing assistants, medical assistants, and social workers. Stress and burnout were associated with fear of exposure or transmission, self-reported anxiety/depression, and work overload. The high exposure to risk for female workers may be linked to their predominance in patient-facing roles, gender discrimination, gender expectations in care, and inattention at “double shift” work with high workloads at home. The high exposure to risk for black and Latino HCWs was linked to a greater fear of exposure to COVID-19 due to racial concordance between workers and patients (black and Latino were overrepresented among patients hospitalized with COVID-19) and entry-level positions to their employment that expose them to a direct contact with patients and with few opportunities for advancement. The risk of infection may be higher in low- or middle-income countries due to a very limited access to personal protective equipment ( 21 ).
The above energy drain factors are summarized in Figure 1 along with the consequences of burnout which are discussed in the next section.
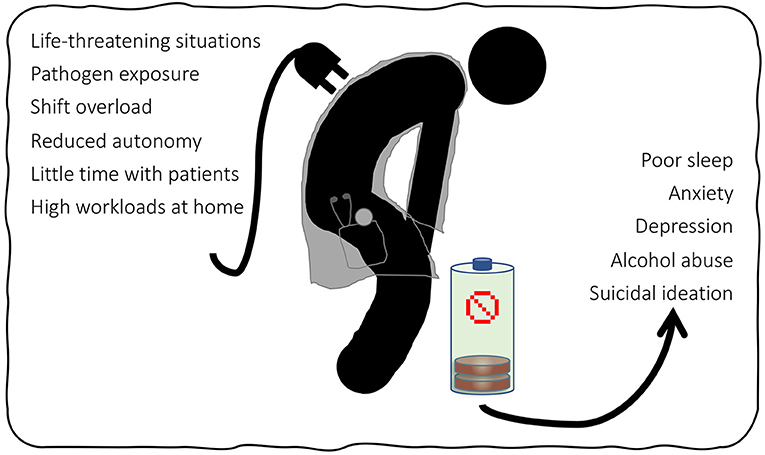
Figure 1 . Summary of energy drain factors and consequences of burnout on HCWs.
Effects on Healthcare Workers and on Healthcare Systems
A first direct effect of burnout is, of course, on HCWs' own care and safety. The rate of depressive disorder among HCWs is alarming when compared with that of the general population and is closely related to high levels of occupational stress ( 22 ). During the COVID-19 outbreak, a relatively high prevalence of anxiety (24.94%), depression (24.83%) and sleep disorders (44.03%) was reported in meta-analyses investigating the mental health of HCWs ( 23 , 24 ). Healthcare workers tend to hide their difficulties due to the perceived stigma associated with mental illness as well as to the fear of an impact on their careers ( 25 ).
In turn, these mental conditions are associated with further criticalities, including a 25% increased odds of alcohol abuse or dependence and a doubled risk of suicidal ideation ( 18 ). When considering the extreme act, it is well known that the rates are higher among physicians than in the general populations ( 26 ). Dutheil and colleagues ( 27 ) recently reported an overall standardized mortality rate for suicide in physicians of 1.44 with an higher level in females of 1.99. They also found a higher risk for anesthesiologists, psychiatrists, general practitioners and general surgeons. Although, at present, no data sets regarding the impact of COVID-19 on physician mental health and suicide are available, the many news published in the newspapers of various countries about the suicide of doctors active in the pandemic leave no doubt that the situation is getting worse ( 28 ).
An indirect effect of burnout could be the lowering of the quality of healthcare systems in terms of adherence to guidelines, poor communication, medical errors, and patient outcomes and safety ( 29 ). However, as clearly stated by Tawfik and colleagues ( 30 ), the relationship between the two phenomena may be bi-directional: HCWs suffering from burnout may not be able to provide high-quality healthcare services, take more unnecessary risks, pay less attention to details, and, conversely, exposure to adverse events or recognition of poor quality of care may lead to psychological distress. The authors conclude that the real strength of the relationship may be less than that reported and that more randomized trials with adequate power and design are needed to understand how exactly burnout and quality of care influence each other.
Burnout is a critical issue that generate inefficiency in healthcare organizations. Shanafelt and colleagues ( 31 ) reported that the economic cost of physicians' reduced wellbeing can be mainly assessed in terms of the organizational cost of replacing them, decreased productivity and other “blind” issues. They estimated these costs to be between $ 500,000 and $ 1,000,000 for replacing a single physician with the invaluable training and experience consequently lost. Moreover, they reported a 30% reduction in work effort for each 1-point increase in burnout (on a 7-point scale), and highlighted other costs arising from losing mentors for junior faculty and grants, or from managing medical errors and complaints of negligence.
How to Address It
Defining strategies to cope with HWC burnout is a relevant research topic regardless of the outbreak of COVID-19 (in the Table 1 we have summarized the measures found that prevent and reduce physician burnout). In 2016, West and colleagues ( 32 ) performed a meta-analysis on interventions to prevent and reduce physician burnout. These were focused on both individuals and organizations: facilitating small group curricula, stress management, and training in self-care and communication skills, as interventions on individuals, and shortening the duration of attending rotation and resident shifts, and improvements in clinical work processes, as organizational strategies.
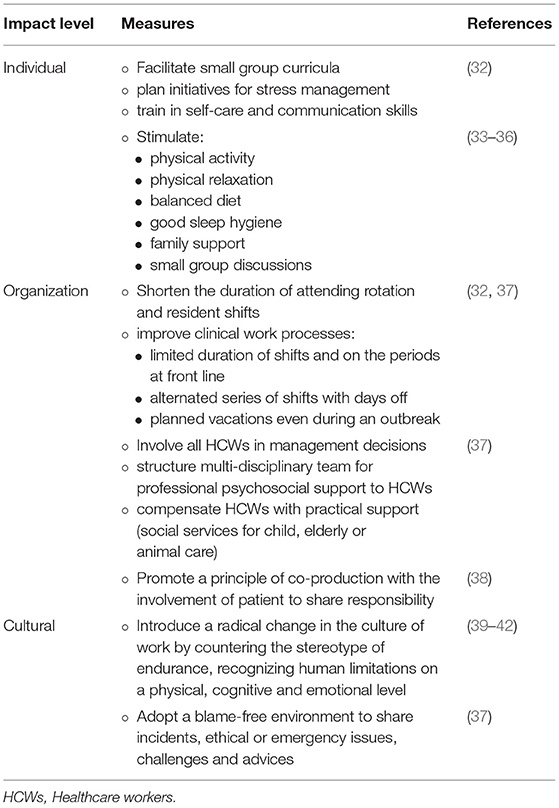
Table 1 . Measures to prevent and reduce physician burnout.
In addition, Epstein and Privitera ( 39 ), called for a radical change in the culture of work by countering the stereotype of endurance which “overvalues stoicism and dismisses complaints as signs of weakness” and recognizing human limitations on a physical, cognitive and emotional level.
Since the COVID-19 outbreak, a great deal of evidence has been generated on burnout in HCWs, leading to extensive discussions on how to address it in this specific context.
Regarding individual measures, self-care is suggested as a line of defense for HCWs to manage requests for assistance of COVID-19 patients, especially when recovery times are short and long-terms efforts are required. Physical activity, physical relaxation, balanced diet, good sleep hygiene, family support, meaningful relationships (also maintained through digital channels), job satisfaction, self-awareness though reflective practices and small group discussions are the reported interventions with evidence of efficacy ( 33 – 36 ).
Based on a scoping review and expert interviews, several recommendations focused on organizations have been proposed to build and maintain the resilience of frontline HCWs exposed to COVID-19 ( 37 ). Authors invite to support communication, even during busy periods, by: (a) adopting a blame-free environment to share incidents, ethical or emergency issues, and challenges and advices; (b) involving nurses in management decisions (to promote a sense of togetherness and positivity where every voice has the opportunity to be heard); (c) allowing someone to talk before, during and after a shift. In addition, they recommend structuring a multi-disciplinary team with psychologists, spiritual counselors, social professionals, occupational health and safety physicians for professional psychosocial support to HCWs based on natural coping strategies (acceptance, active coping, positive framing). They also suggest creating a safe area to provide HCWs with the opportunity to quickly withdraw from an emotionally stressful situation and get peer support. Authors propose planning time limitations on the duration of the shifts (distinguishing between day and night, and between light and intense tasks) and on the periods at front line, alternating series of shifts with days off, and planning vacations even during an outbreak. Finally, they report the importance of compensating HCWs with practical support such as social services for child, elderly or animal care.
Regarding the cultural dimension, it was noted that the widely adopted short-term mood boosters that contributed to depict HCWs as “healthcare heroes”, while offering recognitions in the short, can obscure the human needs for support, especially in contexts where mental health is still perceived as a stigma across society ( 43 ). Even if some progress has been made in removing the barrier to seeking psychological support in coping with work-related stress ( 40 , 41 ), a cultural change is still needed for the stigma ( 42 ). In our opinion, it is important to promote a principle of co-production ( 38 ) which also includes the involvement of patients in the effort to improve healthcare services through their feed-back on the quality and organization of services. Sharing responsibilities allows to reduce the work-related pressures that may lead to burnout.
Current Research Gap
Research plays a key role in transforming the challenges that the COVID-19 era poses to society, especially healthcare systems, into an opportunity for improvement. Although a large volume of studies since the COVID-19 outbreak have examined the impact of the pandemic on the mental health of HCWs ( 44 ), solid evidence on the effectiveness of interventions to support mental well-being during stressful situations is available only from previous healthcare crises and general contexts ( 45 ). To adequately address the burnout issue in times of crisis, both large-sized quantitative longitudinal studies and qualitative studies based on first-person reports are needed. These would allow to better understand the impact on mental health of HCWs during and after the pandemic and to identify the best solutions ( 46 ). Practice guidelines are needed ( 47 ) which also integrate organizational, social, personal, and psychological factors ( 45 ). Acceptability, resources, feasibility, long-term sustainability, the impact on patients, and potential harm are reported as additional key themes to be investigated. Due to the difficulty of conducting research during a pandemic, a great heterogeneity and suboptimal designs characterize the current body of evidence. It is advisable, for future researches, to realize rigorous, standardized and transparent protocols for replicability in other settings [better if using reporting standards such as the Template for Intervention Description and Replication, TIDieR ( 48 )], to develop shared definitions of burnout, to use standardized and validated measurement tools and more representative sample sizes, to include follow-up for long-term mental health implications and comparisons with other time periods ( 5 , 44 , 45 , 49 – 51 ). However, one must be aware of the risks of considering only metrics, and health care organizations must focus on process rather than outcome alone, on goals that demonstrate effective improvement of working conditions and not just on achieving a specific threshold score or ranking ( 52 ).
Burnout was a major concern for HCWs since before the COVID-19 pandemic. The current emergency context has added new social and job-related factors that increase the risk of burnout with associated effects on quality of care and efficiency of the system. Based on our knowledge, this is the first work that discusses recently emerging concepts with a comprehensive view. Several measures have been suggested to prevent or reduce this parallel epidemic that calls for action at individual, organizational or cultural level. The key recommendation is to take up the challenges that the emergency imposes and to aggregate competences in health, well-being and behavioral science through rigorously planned and reported long term researches to guide the necessary cultural change and the improvement of public health systems.
Author Contributions
CL, SS, and PM conceived the work. All authors performed the search and analysis of the literature. CL, SS, and PM wrote the original draft of the manuscript. MT, AB, GP, and ES critically reviewed the manuscript. All authors have read and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. (2016) 15:103–11. doi: 10.1002/wps.20311
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS ONE. (2018) 13:e0206840. doi: 10.1371/journal.pone.0206840
3. Kunda G. Engineering Culture . Control and Commitment in a High-Tech Corporation Revised and Expanded Edition Temple University Press. (2006).
Google Scholar
4. Freudenberger HJ. Staff Burn-Out. J Soc Issues. (1974) 30:159–65. doi: 10.1111/j.1540-4560.1974.tb00706.x
CrossRef Full Text | Google Scholar
5. Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. (2018) 320:1131–50. doi: 10.1001/jama.2018.12777
6. Organization WH. Coronavirus disease 2019 (COVID-19): situation report, 51. Geneva PP - Geneva: World Health Organization Available online at: https://apps.who.int/iris/handle/10665/331475
7. World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online at: https://covid19.who.int . (accessed July 29, 2021)
8. Planas D, Veyer D, Baidaliuk A, Staropoli I, Guivel-Benhassine F, Rajah MM, et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature . (2021) 596:276–80 doi: 10.1038/s41586-021-03777-9
9. Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: a multinational cross-sectional study. PLoS ONE. (2021) 16:e0238666. doi: 10.1371/journal.pone.0238666
10. Elghazally SA, Alkarn AF, Elkhayat H, Ibrahim AK, Elkhayat MR. Burnout impact of COVID-19 pandemic on health-care professionals at assiut university hospitals, 2020. Int J Environ Res Public Health . (2021) 18:5368. doi: 10.3390/ijerph18105368
11. Tuan NQ, Phuong ND, Co DX, Son DN, Chinh LQ, Dung NH, et al. Prevalence and factors associated with psychological problems of healthcare workforce in vietnam: findings from COVID-19 hotspots in the national second wave. Healthc . (2021) 9:718. doi: 10.3390/healthcare9060718
12. The Lancet. COVID-19: protecting health-care workers. Lancet. (2020) 395:922. doi: 10.1016/S0140-6736(20)30644-9
13. Søvold LE, Naslund JA, Kousoulis AA, Saxena S, Qoronfleh MW, Grobler C, et al. Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front Public Heal. (2021) 9:514. doi: 10.3389/fpubh.2021.679397
14. Zoorob D, Shah S, La Saevig D, Murphy C, Aouthmany S, Brickman K. Insight into resident burnout, mental wellness, and coping mechanisms early in the COVID-19 pandemic. PLoS ONE. (2021) 16:e0250104. doi: 10.1371/journal.pone.0250104
15. Lasalvia A, Amaddeo F, Porru S, Carta A, Tardivo S, Bovo C, et al. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. (2021) 11:e045127. doi: 10.1136/bmjopen-2020-045127
16. Greenhalgh T, Thorne S, Malterud K. Time to challenge the spurious hierarchy of systematic over narrative reviews? Eur J Clin Invest. (2018) 48:e12931. doi: 10.1111/eci.12931
17. Wiederhold BK, Cipresso P, Pizzioli D, Wiederhold M, Riva G. Intervention for physician burnout: a systematic review. Open Med. (2018) 13:253–63. doi: 10.1515/med-2018-0039
18. Kalmoe MC, Chapman MB, Gold JA, Giedinghagen AM. Physician suicide: a call to action. Mo Med. (2019) 116:211–6.
19. Gramaglia C, Marangon D, Azzolina D, Guerriero C, Lorenzini L, Probo M, et al. The mental health impact of 2019-nCOVID on healthcare workers from north-eastern piedmont, Italy. Focus on burnout front public. Heal. (2021) 9:667379. doi: 10.3389/fpubh.2021.667379
20. Prasad K, McLoughlin C, Stillman M, Poplau S, Goelz E, Taylor S, et al. Prevalence and correlates of stress and burnout among US healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. E Clin Med. (2021) 35:100879. doi: 10.1016/j.eclinm.2021.100879
21. Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. (2021) 8:535–50. doi: 10.1016/S2215-0366(21)00025-0
22. Lancet T. Suicide among health-care workers: time to act. Lancet. (2017) 389:2. doi: 10.1016/S0140-6736(17)30005-3
23. Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 107:110247. doi: 10.1016/j.pnpbp.2021.110247
24. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
25. Brower KJ. Professional stigma of mental health issues: physicians are both the cause and solution. Acad Med. (2021) 96:635–40. doi: 10.1097/ACM.0000000000003998
26. Schernhammer E. Taking their own lives — the high rate of physician suicide. N Engl J Med. (2005) 352:2473–6. doi: 10.1056/NEJMp058014
27. Dutheil F, Aubert C, Pereira B, Dambrun M, Moustafa F, Mermillod M, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0226361. doi: 10.1371/journal.pone.0226361
28. Jahan I, Ullah I, Griffiths MD, Mamun MA. COVID-19 suicide and its causative factors among the healthcare professionals: case study evidence from press reports. Perspect Psychiatr Care. (2021) 57:1707–11. doi: 10.1111/ppc.12739
29. Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. (2017) 32:475–82. doi: 10.1007/s11606-016-3886-9
30. Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. (2019) 171:555–67. doi: 10.7326/M19-1152
31. Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. (2017) 177:1826–32. doi: 10.1001/jamainternmed.2017.4340
32. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272–81. doi: 10.1016/S0140-6736(16)31279-X
33. Heath C, Sommerfield A, von Ungern-Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. (2020) 75:1364–71. doi: 10.1111/anae.15180
34. Organization WH. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. World Health Organization. (2020).
35. Treluyer L, Tourneux P. Burnout among paediatric residents during the COVID-19 outbreak in France. Eur J Pediatr. (2021) 180:627–33. doi: 10.1007/s00431-020-03907-x
36. Zhang M, Murphy B, Cabanilla A, Yidi C. Physical relaxation for occupational stress in healthcare workers: A systematic review and network meta-analysis of randomized controlled trials. J Occup Health. (2021) 63:e12243. doi: 10.1002/1348-9585.12243
37. Rieckert A, Schuit E, Bleijenberg N, Ten Cate D, de Lange W, de Man-van Ginkel JM, et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. (2021) 11:e043718. doi: 10.1136/bmjopen-2020-043718
38. Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf. (2016) 25:509–17. doi: 10.1136/bmjqs-2015-004315
39. Epstein RM, Privitera MR. Doing something about physician burnout. Lancet. (2016) 388:2216–7. doi: 10.1016/S0140-6736(16)31332-0
40. Moutier C. Physician mental health: an evidence-based approach to change. J Med Regul. (2018) 104:7–13. doi: 10.30770/2572-1852-104.2.7
41. Hengerer AS, Staz ML, Chaudhry HJ. FSMB efforts on physician wellness and burnout. J Med Regul. (2018) 104:14–6. doi: 10.30770/2572-1852-104.2.14
42. Feist J, Feist C, Cipriano P. Stigma Compounds the Consequences of Clinician Burnout During COVID-19: A Call to Action to Break the Culture of Silence. NAM Perspectives . Washington, DC: Commentary, National Academy of Medicine (2020). doi: 10.31478/202008b
43. Wei EK, Long T, Katz MH. Nine lessons learned from the COVID-19 pandemic for improving hospital care and health care delivery. JAMA Intern Med. (2021) 181:1161–3. doi: 10.1001/jamainternmed.2021.4237
44. Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. (2020) 277:347–57. doi: 10.1016/j.jad.2020.08.034
45. Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane database. Syst Rev. (2020) 11:CD013779. doi: 10.1002/14651858.CD013779
46. Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthc . (2020) 8:421. doi: 10.3390/healthcare8040421
47. Babamiri M, Alipour N, Heidarimoghadam R. Research on reducing burnout in health care workers in critical situations such as the COVID-19 outbreak. Work. (2020) 66:379–80. doi: 10.3233/WOR-203189
48. Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. (2014) 348:g1687. doi: 10.1136/bmj.g1687
49. Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J Affect Disord. (2020) 275:48–57. doi: 10.1016/j.jad.2020.06.022
50. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
51. Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Kazeminia M, Mohammadi M, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. (2020) 18:100. doi: 10.1186/s12960-020-00544-1
52. Marchalik D, Shanafelt T. Addressing Burnout Among Health Care Professionals by Focusing on Process Rather Than Metrics. JAMA Heal Forum. (2020) 1:e201161. doi: 10.1001/jamahealthforum.2020.1161
Keywords: COVID-19, burnout, healthcare workers, mental health, public health
Citation: Leo CG, Sabina S, Tumolo MR, Bodini A, Ponzini G, Sabato E and Mincarone P (2021) Burnout Among Healthcare Workers in the COVID 19 Era: A Review of the Existing Literature. Front. Public Health 9:750529. doi: 10.3389/fpubh.2021.750529
Received: 02 August 2021; Accepted: 07 October 2021; Published: 29 October 2021.
Reviewed by:
Copyright © 2021 Leo, Sabina, Tumolo, Bodini, Ponzini, Sabato and Mincarone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Rosaria Tumolo, mariarosaria.tumolo@irpps.cnr.it
† These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Empathy - Advanced Research and Applications
From Empathy to Compassion Fatigue: A Narrative Review of Implications in Healthcare
Submitted: 20 July 2022 Reviewed: 25 August 2022 Published: 18 October 2022
DOI: 10.5772/intechopen.107399
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Empathy - Advanced Research and Applications
Edited by Sara Ventura
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
332 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Overall attention for this chapters
Evidence is clear regarding the importance of empathy in the development of effective relationships between healthcare professionals (HCPs) and patients in the delivery of successful healthcare. HCPs have pledged to relieve patient suffering, and they value the satisfaction felt from caring for their patients. However, empathy may lead to negative consequences for the empathiser. If there is a personal identification with the emotions of the distressed person, empathic concern may evolve into personal distress leading to compassion fatigue over time. A narrative review was used to explore the connection between empathy and compassion fatigue. A search of MEDLINE, PsychINFO and CINAHL resulted in 141 articles meeting the inclusion criteria. The results included in this chapter explore the practical implications of empathy in relation to compassion fatigue, examining the impact on HCPs as well as the potential risk factors and effective strategies to reduce compassion fatigue. The negative impact of compassion fatigue can have a severe impact on HCP well-being and can in turn impact the care received by the patient. Nevertheless, and despite existing effective strategies to support and manage those experiencing compassion fatigue, more needs to be done to prevent its development in HCPs.
- compassion fatigue
- healthcare profession
secondary traumatic stress
- vicarious trauma
Author Information
Jane graves.
- Western Sydney University, Sydney, Australia
Caroline Joyce
Iman hegazi *.
*Address all correspondence to: [email protected]
1. Introduction
1.1 empathy and compassion in the healthcare profession.
Compassion and respect for human dignity is enshrined in the codes of conduct for healthcare professionals (HCPs). Providing high-quality compassionate care is a fundamental aim of the helping professions and provides them with job satisfaction and a sense of value [ 1 ]. Being treated with compassion also has many patient benefits including increasing compliance with professional advice, improving satisfaction with services and enhancing health and quality of life [ 2 ]. Providing compassionate care requires kindness, empathy, and sensitivity [ 3 ].
Empathy refers to the capacity to understand and share the feelings of others such as pain, joy, fear, and other emotions [ 4 , 5 ]. Historically, emotional responses to patients were seen as threats to objectivity and doctors strived for detachment to be able to care, reliably, for all patients regardless of their personal feelings. Blumgart [ 6 ] recalls Sir William Osler’s “Aequanimitas” in his definition of ‘neutral empathy’ which states that a physician will do what needs to be done without feeling grief, regret, or other difficult emotions. Osler argues that by neutralising their emotions to the point that they feel nothing in response to patient suffering, physicians can ‘see into’ and, thereby, be able to ‘study’ the patient’s ‘inner life’ [ 7 ].
To avoid this conceived conflict between emotions and objectivity, ‘professional empathy’ was defined, on purely ‘cognitive’ basis, as “the act of correctly acknowledging the emotional state of another without experiencing that state oneself” [ 8 ]. This model of ‘detached concern’ assumes that knowing how the patient feels is no different from knowing that the patient is in a certain emotional state. However, the function of empathy is to recognise what it feels like to experience something, not merely to label emotional states [ 9 ]. Halpern [ 9 ] emphasises that patients sense when physicians are ‘emotionally attuned’ and that patients trust ‘emotionally attuned’ physicians and adhere better to their treatment.
In the clinical context, Stepien and Baernstein [ 10 ] combined the different definitions within the literature to put forward an expanded definition of empathy. This proposed definition includes four distinct dimensions: ‘ moral, emotive, cognitive, and behavioural’, all working in harmony to benefit the patient.
1.2 From empathy to compassion fatigue
Empathic perspective-taking is the level of empathy which most psychologists refer to when they speak of ‘empathy’. In this view, empathy is a cognitive state—dependent on imagination and mental attribution—combined with emotional engagement. A major manifestation of empathic perspective-taking is ‘targeted helping’ i.e., help and care based on a cognitive appreciation of the other’s specific need or situation [ 11 ]. The emotional component in providing care and support to people in distress can, over time, deplete the caregiver’s emotional resources engendering ‘compassion fatigue’; which is characterised by feelings of indifference to the suffering of others [ 12 ]. Joinson [ 13 ] in 1992 described compassion fatigue as a form of ‘occupational burnout’ experienced by those in the caring professions. Figley [ 14 ] then described compassion fatigue as ‘caregiver burnout’ and his 2002 model of compassion fatigue emphasised “the costs of caring, empathy, and emotional investment in helping the suffering” [ 15 ]. These ‘costs’ include the increased risk of mental and physical health problems in helping professionals [ 16 , 17 ]. Radey and Figley [ 12 ] suggest, “as our hearts go out to our clients through our sustained compassion, our hearts can give out from fatigue” (p. 207).
Compassion fatigue exists across a diverse range of healthcare professional groups, disciplines, and specialties [ 18 , 19 , 20 ]. Close to 7% of professionals who work with traumatised individuals exhibit emotional reactions that are similar to symptoms of post-traumatic stress disorder (PTSD). This is not only seen in the healthcare sector, where it has been demonstrated in physicians, psychotherapists, and nurses—especially those working with critically ill children, in oncology and in trauma care [ 21 , 22 , 23 , 24 ]—but also, beyond the hospital setting in first responders, emergency teams, social workers, police officers, migration workers, and those working with the homeless [ 25 , 26 , 27 , 28 , 29 ].
Levels of compassion fatigue have increased over the last decade [ 30 ]. More recently, compassion fatigue has become a significant concern during the COVID-19 crisis which has intensified the feelings of burnout, and compassion fatigue in healthcare workers, especially those working in specific COVID-19 units and in emergency departments, leaving no mental space for clinicians to experience authentic clinical empathy [ 31 , 32 , 33 , 34 ]. Recent pooled subscale scores indicate average to high levels compassion fatigue across a diverse healthcare practitioner groups [ 18 ]. For nurses, compassion fatigue rates are currently reported as just above 50% [ 35 ].
2. Aim of this chapter
The aim of this narrative review is to describe and synthesise the literature to explore the associations between empathy and compassion fatigue, and the impact of the latter in the healthcare profession. Also, to examine screening and management strategies of compassion fatigue in HCPs and deduce a conclusion from the evidence.
3. Methodology
We conducted a narrative review using the process described by Green et al. [ 36 ] to present objective conclusions based upon previously published literature that we have comprehensively reviewed. We opted for a narrative overview as narrative reviews can often serve to provoke thought and controversy and may be an excellent venue for presenting philosophical perspectives in a balanced manner [ 36 ].
3.1 Identifying relevant studies
We determined the search strategy through team discussions and pilot explorations of the different databases. We searched MEDLINE (Ovid), APA PsycINFO (EBSCOhost), and CINAHL Plus using the Boolean/Phrase (Empathy AND (‘Compassion Fatigue’ OR ‘Vicarious Trauma’) AND Health). We conducted the search during May and June of 2022 and included literature published between 2003 and 2022, including articles published online ahead of print. Initial search recovered 290 results from MEDLINE, 112 from CINAHL Plus, and 215 from PsycINFO.

3.2 Study selection
EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA) was used to download the bibliographic details of studies yielded from the database searches and duplicates were deleted. Researchers screened article titles and abstracts to determine eligibility for full-text review based on relevance to the research topic. After this initial screening, all researchers read full texts of articles to determine eligibility for inclusion.
Inclusion criteria: The literature review included full text empirical research, which described empathy and compassion fatigue in healthcare workers, published in the English language in academic peer-reviewed journals over the last 20 years.
Exclusion criteria: Studies which covered other forms of vicarious trauma and post-traumatic stress, and studies which explored compassion fatigue in other professions, e.g., police officers, chaplaincy, caregivers, and migration agents, were excluded from this review.
Figure 1 shows a flowchart indicating the search and selection process. Following screening and full-text review, 92 articles were included in this literature review. Subsequent to the full text review, additional related references reported in the 92 examined articles were inspected, and those satisfying the inclusion criteria (n = 49) were also included in this literature review as secondary sources, leading to a total of 141 studies included in this review.

Flow diagram showing records identified from databases and the screening and selection process.
3.3 Collating, summarising, and reporting results
Authors read and objectively evaluated each of the 141 articles. They recorded how each article relates to the objectives of this narrative review. The authors are all HCPs, a chiropractor, psychologist, and a physician. This expertise in the area was useful in interpreting the literature but the authors were careful not to incorporate predispositions or biases by having multiple discussions throughout the review process.
The connection between empathy and compassion fatigue
The impact of compassion fatigue in healthcare
The detection and assessment of compassion fatigue
Management of compassion fatigue in healthcare professionals
HCPs are continually exposed to stressful events in their day-to-day work including frequent encounters with: (a) death and dying, (b) grieving families, (c) personal grief, (d) traumatic stories, (e) observing extreme physical pain in patients, (f) strong emotional states such as anger and depression, and (g) emotional and physical exhaustion [ 37 , 38 , 39 ]. Over time, high levels of stress can lead to burnout [ 39 , 40 ]. Burnout, a much-researched topic in the helping professions, has been defined as “a syndrome composed of emotional exhaustion, depersonalization, and reduction of personal accomplishments” [ 41 ]. Burnout may also lead to negative self-concept, negative attitudes about work, and a loss of caring about work-related issues [ 38 ].
Compassion fatigue, a construct similar to burnout, is a topic that has emerged in the literature in recent years [ 42 , 43 , 44 ]. Radley and Figley [ 12 ] define compassion as a “deep sense or quality of knowing or an awareness [among helping professionals] of the suffering of another coupled with the wish to relieve it” (p. 207). Compassion fatigue, a possible effect of long-term demonstrations of compassion, is defined as “a deep physical, emotional, and spiritual exhaustion accompanied by acute emotional pain” [ 45 ]. Compassion fatigue is thought to be a result of long exposure to the suffering of others, listening to descriptions of traumatic events experienced by others, little to no emotional support in the workplace, and poor self-care [ 12 ].
4.1 The connection between empathy and compassion fatigue
Compassion is an essential component of patient care provided by health professionals [ 46 ]. The care-giving relationship is founded on empathy and a critical characteristic of compassion fatigue is a loss or lack of empathy [ 47 , 48 ].
4.1.1 Temporary lapses in empathy
Temporary lapses in empathy are not uncommon in professional intervention and can have a variety of causes, ranging from experiences in the professional’s own life to reactions to clients’ situation [ 49 , 50 ]. Most clinicians experience them from time to time, and they rarely arouse major distress. There are reports of self-perceived lapses of empathy among emergency workers who provide services in the acute phase of the disaster and psychotherapists engaged in long-term psychotherapeutic relationships that started before and continued during and after the disaster. Many experience the conflict of ‘attention-to-self versus attention-to-client’ as temporary and normal for the situation. Reports by these professionals suggest that their lapses in availability and empathy cause them distress by impairing their self-esteem and fostering feelings of guilt, shame, and inadequacy [ 51 , 52 ].
Baum [ 53 ] suggests that the source of much of the widely reported distress among clinicians is an intra-psychic conflict between two conflicting psychological needs: the need to distance themselves from their clients and their need to raise their self-esteem, especially in experienced professionals whose anxiety is doubly intensified by their prior experiences. Much of the identity and self-esteem of helping professionals is anchored in their ability to be empathic, present, and containing towards those they help. The conflict from the fact that distancing helps the professionals to cope but reduces their ability to empathise with their clients, can lead to feelings of guilt, shame, and self-reproach.
Empathy is seen as comprising affective and cognitive components, whereas compassion is defined in terms of affective and behavioural elements. More specifically, compassion is perceived as comprising both of ‘feelings for’ the person who is suffering and a desire to act to relieve the suffering. The desire to act is distinct from the act itself [ 54 , 55 ].
Compassion fatigue involves a decline in one’s energy, desire, and/or ability to love, nurture, care for, or empathise with another’s suffering [ 56 , 57 , 58 ]. These critical defining attributes were used to develop a theoretical definition: “Compassion fatigue is the physical, emotional, and spiritual result of chronic self-sacrifice and/or prolonged exposure to difficult situations that renders a person unable to love, nurture, care for, or empathize with another’s suffering” [ 59 ].
4.1.2 Compassion fatigue and burnout
Compassion fatigue is strongly correlated with burnout [ 21 , 60 , 61 , 62 ]. Whilst stress and exhaustion are critical attributes of both concepts [ 21 , 60 ] the experience is of being in a ‘tired’ state in burnout and being in a ‘drained’ state in compassion fatigue [ 60 ] and thus devoid of ones resources [ 14 , 60 ].
Wynn [ 60 ] performed a comparative concept analysis examining the terms ‘burnout’ and ‘compassion fatigue’ using Walker and Avant methodology. The ability to recognise both concepts is pivotal in helping to establish strategies that support healthcare workers cope and achieve optimal occupational health. Wynn noted that burnout can be an antecedent of compassion fatigue. The important difference is that burnout as a precursor may be more readily responsive than compassion fatigue to restorative strategies such as time away from the work environment and behaviour modification [ 14 , 60 ]. If not addressed in its early stages compassion fatigue can permanently alter the compassionate ability of the individual [ 63 ]. Thus compassion fatigue may be considered to be a consequence of ongoing burnout in healthcare and indicate a further decline in the wellbeing of the healthcare professional.
The development of compassion fatigue is understood to be a cumulative and progressive process [ 64 ] Whist the development is cumulative, the onset of the experience compassion fatigue for the healthcare worker is a rapid one [ 35 , 65 ]. Comparatively burnout, a larger overarching construct, is experienced as a slowly progressing disorder and is associated with working in burdensome organisational environments [ 65 ]. Thus, in burnout conflict associated with the employer-employee relationship, and in compassion fatigue the conflict is primarily an internal one which is associated with the relationship between the healthcare professional and their patient [ 60 , 66 ].
4.1.3 Vicarious trauma and secondary traumatic stress
Meadors et al. [ 67 ] investigated the relationships between the terms associated with secondary traumatization using a correlational design. They established that there is a significant overlap between compassion fatigue, secondary traumatic stress (STS), and burnout, but that each of the concepts also had significant unexplained variance which suggests that there were differences between the concepts ( Table 1 ).
| Term | Definition |
|---|---|
| Primary traumatization | Primary traumatization is the process that can occur from having direct contact with a traumatic event [ ] |
| Secondary traumatization (ST) | Secondary traumatization (ST), via an indirect exposure, may develop from hearing about a traumatic event or caring for someone who has experienced such an event [ ] |
| Compassion fatigue (CF) | The consequence of working with a significant number of traumatised individuals in combination with a strong empathic orientation [ ] or a formal caregiver’s reduced capacity and interest in being empathetic for a suffering individual [ ] |
| Secondary traumatic stress (STS) | The distress and emotional disruption connected to an encounter with an individual who has experienced a primary traumatization [ ] |
| Burnout | Burnout is a “defensive response to prolonged occupational exposure to demanding interpersonal situations that produce psychological strain and provide inadequate support” [ ]. (p. 424) |
Definition of compassion fatigue and related terms.
Adapted from [ 67 ].
Secondary traumatization (ST) occurs as a natural consequence of caring between two people: one who has been traumatised and the other who is affected by the first’s traumatic experience [ 70 , 71 ]. Empathy and exposure are central in the development of ST [ 72 ] and can alter the way in which the healthcare worker experiences self, others, and the world [ 73 ].
The potential for ST begins with exposure to a client’s experience that is sufficient to evoke an arousal or emotional response [ 71 , 74 ]. Vulnerability to the client’s experience may be heightened by pre-existing conditions (risk factors) that produce greater sensitivity to the elements in the client’s situation leading to one’s absorption of the suffering itself [ 70 ]. The vicarious experiencing of the feelings, thoughts, or attitudes of another may result in the development of empathy, or the emotional connection that occurs through listening and bearing witness to graphic depictions of traumatic events. While bearing witness to the client’s suffering, the healthcare worker is susceptible to responses or reactions that may be physiological, behavioural, emotional, and/or cognitive in nature. Figley describes this as the “cost of caring” for those in emotional pain [ 71 ]. Alternate discussions such as those by Ledoux contest the notion of a ‘ cost to caring’ and propose that compassion fatigue occurs when ‘ care is obstructed’ [ 54 ].
Osland [ 75 ] reported that dietitians in high-risk workloads reported higher levels of STS than those with low-risk workloads, those in smaller facilities reported higher STS than larger facilities, and that working for >5 years as a dietitian was associated with higher rates of STS and burnout than in those working for <5 years. Those who perceived greater levels of support reported lower rates of burnout and higher rates of compassion satisfaction.
Zeidner et al. [ 47 ] examined the role of some personal and professional factors in compassion fatigue among health-care professionals. Research participants included 182 healthcare professionals who completed an assessment battery measuring compassion fatigue, emotion management, trait emotional intelligence, situation-specific coping strategies, and negative affect. Major findings indicate that self-reported traits ‘emotional intelligence’ and ‘ability-based emotion management’ are inversely associated with compassion fatigue; ‘adaptive coping’ is inversely related to compassion fatigue. Furthermore, problem-focused coping appeared to mediate the association between trait emotional intelligence and compassion fatigue. These findings highlighted the role of emotional factors in compassion fatigue among health-care professionals [ 47 ].
Rayner et al. [ 76 ] examined STS and related factors of empathetic behaviour and trauma caseload among 190 social workers and psychologists. Approximately 30 percent of participants met the criteria for a diagnosis of STS. Results indicated that there was a significant interaction between caseload trauma and personal trauma history on STS. Similarly, empathy alone was not directly related to changes in STS, yet the trauma in caseload effect on STS was moderated by empathy. A personal history of trauma was found to be related to increased levels of STS. However, contrary to expectation of prior research, empathy contributed to a reduction in STS, meaning that lower empathy levels were associated with a higher risk of developing STS.
Hubbard et al. [ 77 ] demonstrated consistency between the five key concepts of ST discussed in the literature, i.e., exposure, vulnerability, empathic engagement, reaction, and transformation. The analysis revealed a dynamic, fluid process in which the energy of the nurse, client, and environment were integrated and part of a diverse whole [ 78 ]. The dynamic nature of the nurses’ experiences created a “kaleidoscope of potentialities” [ 78 ], the outcome of which was either a positive or a negative trajectory. This revealed a new aspect of the dimension of alteration/transformation, which was the identification of a positive outcome during the ST process. These results suggest the importance of further research to assess the role and value of reflective supervision for HCPs and how this may enhance their personal and professional resilience.
4.2 Risk factors for compassion fatigue
Risk factors for the development of compassion fatigue include the intensity of the patient setting as healthcare professionals who care for traumatised individuals in critical care environments are at greater risk of acquiring compassion fatigue [ 20 ]. Engaging with the patients loved ones also places the healthcare professional at risk, particularly if the interactions involve conflict [ 20 ]. Other factors that place the professional at risk including undertaking difficult discussion with patients and families such as breaking bad or uncertain news to patients and their families. A lack of perceived managerial support compounds the risk [ 20 , 65 ] and working more hours perpetuates emotional exhaustion in providers [ 79 ].
Personal factors also appear to play a role in the risk of the development of compassion fatigue. Those who have less experience working as a healthcare professional are at greater risk [ 20 , 80 ] as are those with less maturity [ 80 ] or those who have not acquired a higher level of education or qualification in their profession [ 35 , 46 ].
Poor coping strategies and difficulty with emotional regulation also place providers at greater risk. These include being unable to process feelings in relation to trauma and caring for those who are impacted by suffering [ 20 , 47 ]. Being unable to identify effective coping mechanisms, adapt, manage emotion and develop one’s emotional intelligence [ 20 , 47 ]
There is some indication that one’s personality may also play a role and people with high sensitivity may be more vulnerable to compassion fatigue. People with an increased ability to perceive others feelings may have stronger emotional and physiological reactivity [ 81 ] and thus be more prone to compassion fatigue [ 82 ]. This may be compounded by the contract between the quality of care the healthcare professional may want to provide with what they are actually able to achieve [ 80 ].
Negative life events and pre-existing mental illnesses such as anxiety or depression have been found to increases a person’s susceptibility for compassion fatigue [ 18 ]. Similarly coexisting physical and emotional stress increases levels of existing compassion fatigue [ 80 ].
Certain workplace conditions and events are more likely to trigger the onset of compassion fatigue [ 60 ]. These include continuous and intense contact with patients, exposure to high levels of stress, exposure to suffering and work which requires a high use of self [ 83 ].
4.3 The impact of compassion fatigue
Compassion fatigue negatively impacts the healthcare professional, the patient, the organisation, and the healthcare system [ 19 ].
4.3.1 Impact on the healthcare professional
In order to support patient autonomy healthcare providers practice patient centred care. This care requires genuine engagement and an empathetic approach making exposure to patient trauma and suffering unavoidable for the health care professional [ 79 ].
4.3.1.1 Signs of compassion fatigue
Indicators of compassion fatigue frequently cited in the literature include exhaustion [ 14 , 60 ], reduced capacity for self-care [ 13 , 60 ], ineffective coping, poor judgement [ 83 ], inability to function [ 63 , 83 ], loss of empathy [ 60 , 83 ] and depersonalisation of patients [ 83 ].
4.3.1.1.1 Exhaustion
The experience of the depth of exhaustion has a number of descriptors in the literature. These include a include feelings of weariness [ 63 , 64 ] emptiness, of being drained [ 14 , 60 ] and a ‘profound fatigue of mind and body’ [ 80 ]. People with compassion fatigue feel completely depleted of one’s “biological, psychological, and social resources” [ 14 ] such that they have nothing more to give [ 14 , 60 ]. The individual wants to rest although concerningly rest does not result in increased energy levels or a sense of rejuvenation [ 14 , 60 ]. Individuals may try various attempts to replenish and yet the feeling of exhaustion remains [ 14 , 60 ].
4.3.1.1.2 Reduced capacity for self-care
In 1992 Joinson described compassion fatigue as the reduced capacity to self-care as a result of the sustained fatigue acquired by caring for others [ 13 ]. Recent synthesised descriptions of the experience of compassion fatigue include being left so physically and mentally exhausted and drained by patient care that the provider lacks empathy and is unable to cope [ 60 ].
4.3.1.1.3 Ineffective coping
Ineffective coping is a critical indicator of the occurrence of compassion fatigue [ 13 , 60 ]. When healthcare professionals are no longer able to recover from a depleted state despite using coping strategies the result is ineffective coping [ 60 ]. Coping strategies that may have worked successfully in the past become no longer effective [ 60 ]. Recovery from the stress and exhaustion of providing patient care [ 60 ], is no longer possible. Emotional responses may include feeling emotionally overwhelmed [ 63 , 84 , 85 ] and potentially experiencing an emotional breakdown [ 15 , 20 , 63 ].
4.3.1.1.4 Inability to function
Inability to function may be experienced as a diminished ability [ 15 ] or reduced endurance and output [ 63 , 83 ], leading to a diminished or ineffective work performance [ 13 , 63 , 83 ]. The experience of trauma-based symptoms, in addition to significant exhaustion results in a deterioration of function [ 63 ]. The compassionate energy required to care for patients has been consumed over time is distinguished beyond the point of possible replenishment. An inability to compassionately care for patients moves beyond the work environment and leads to an inability to function which impacts all aspects of the professionals life [ 63 ].
4.3.1.1.5 Loss of empathy
Whilst attempting to employ coping strategies to manage the stress of caregiving a loss of empathy occurs. In response to the relentless overwhelming stress and resultant exhaustion of care-giving a deep psychological shift occurs [ 60 , 86 ]. Health professionals lose their sensitivity to and understanding of the patient’s needs. The professional is no longer able to comprehend the patient’s perspectives or recognise their thoughts and feelings [ 60 , 86 ]. Thus patient experiences are no longer relatable and the health professional experiences compassion fatigue [ 60 , 86 ]. Factors that inhibit sustained energy and perpetuate compassion fatigue include time constraints, burnout [ 87 ] and caring for high-stakes patients [ 60 ]. Health professionals with their own personal history of trauma are also at greater risk of acquiring compassion fatigue [ 88 ] due to their sensitivity to secondary traumatic stress [ 76 ]. As a consequence of their empathy loss, the healthcare professional appears indifferent [ 14 , 15 ], unresponsive [ 63 ], callous [ 15 , 84 , 89 ] and unable to share in or alleviate the patients suffering [ 15 ].
4.3.1.1.6 Depersonalisation
Depersonalisation is a sense of detachment from oneself in which individuals perform tasks in a robotic fashion without emotion. It presents as a coping mechanism used to manage exhaustion [ 90 ] and to avoid the feelings of distress that may arise when a person is experiencing compassion fatigue. Whilst the response does not arise from a lack of empathy for the patient [ 60 ] the depersonalisation coping mechanism once triggered in the professional results in a lack human feelings or emotions in the work place. Consequently, this translates to a lack of human feelings in how the professional provides care, which results in substandard care [ 83 ]. The serious implications of depersonalisation in healthcare professionals arises when the lack of emotion in self, results in the professional viewing the patient as also inert or an ‘object’ and approaches the patient with an attitude of indifference [ 90 ].
Depersonalisation is a maladaptive coping mechanism seen in both burnout and compassion fatigue and occurs when individuals detach from their feelings and emotions in order to be able to function and complete work-related tasks [ 60 ]. Yet the severity of depersonalisation experienced in compassion fatigue leads the provider to view the patient as an ‘object’ [ 90 ] and the provider is no longer able to respond to the humanity within the patient. This emotionally dissociated approach sharply contrasts with anticipated patient expectations.
4.3.1.2 Symptoms of compassion fatigue
Compassion fatigue is a significant risk factor for well-being [ 20 , 25 ]. Compassion fatigue impacts ones physical and mental health [ 63 , 64 ] and leading to an array of potentiation indicators including psychological, physical, spiritual, and social symptoms [ 86 ]. As the condition progresses the professional experiences an increase in the scope and severity of symptoms [ 63 ]. For example the individual may experience physical symptoms of burnout, reduced work performance and physical complaints, the intellectual effects of impaired concentration, emotional effects of breakdown, the social symptoms of indifference towards patients and desire to quit, the spiritual effects of disinterest in introspection and dysfunctional coping behaviours [ 63 ].
4.3.1.2.1 Physical symptoms
Physical symptoms may include health complaints, intellectual effects and fatigue [ 15 , 63 ]. Health complaints may include gastrointestinal conditions and stomach pain, and headaches, including migraine [ 20 , 83 , 91 ]. Sleep disturbance is frequently cited [ 20 , 65 , 91 , 92 ] and people may be at greater risk of accidents [ 15 , 83 ]. Intellectual effects include impaired ability to concentrate [ 13 , 14 , 15 , 63 ], poor judgement [ 20 ] and disorganisation [ 63 , 89 ]. Fatigue may manifest as weariness [ 63 , 85 ] lack of energy [ 13 , 15 , 63 , 85 , 89 ] loss of strength [ 63 , 85 ] loss of endurance [ 63 , 85 ] and power of physical recovery [ 63 ] Complications of fatigue include weight gain or weight loss [ 83 ].
4.3.1.2.2 Psychological impact
The psychological impact of compassion fatigue is well established in the literature and manifests as stress, burnout [ 13 ], intrusive and pervasive thoughts [ 65 , 91 ] anxiety [ 13 , 63 , 64 ], and depression [ 13 , 20 , 60 , 63 , 64 , 65 ]. Compassion fatigue has been found to have a moderate correlation with anxiety and depression [ 93 ].
4.3.1.2.3 Emotional impact
The emotional impact of a loss of compassion is typically one of devastation for those in healthcare professions [ 13 ]. Compassion for others drives workplace motivation to serve and alleviate suffering [ 54 ]. People in nurturing roles are rewarded for putting others needs ahead of their own [ 13 ], and ethically a drive to nurture others connects with the ideal archetype of those in caring professions and a societal sense of social justice [ 54 ].
Emotional exhaustion and its consequential impact on one’s personal life are the most frequently reported emotional effects of compassion fatigue [ 20 , 94 ]. A person’s capacity to communicate with others is impaired and this extended into personal relationships. Individuals feel emotionally distressed or bereft and may well experience an emotional breakdown [ 15 , 60 , 63 , 65 , 80 , 83 ].
Indicators of compassion fatigue may include fluctuations in emotional states [ 91 , 92 ] or mood swings [ 20 ]. Impacted healthcare professionals may feel emotionally overwhelmed [ 63 , 84 , 85 ], irritable [ 14 , 20 , 63 , 64 ] angry, fearful, out of control [ 13 ]. or apathetic [ 13 , 63 , 84 ]. Ones outlook is likely to become negative [ 60 ] and people experience ‘work related dreads’. [ 91 ] Healthcare professionals are no longer able to feel empathy for those in their care or respond compassionately. They have an inability to share in, or alleviate suffering [ 15 ] and may respond with indifference [ 14 , 15 ], callousness [ 15 , 84 , 89 ] or be unresponsiveness [ 63 ] to patients at times when they previously would have been empathetic.
Spiritual effects include a lack of spiritual awareness and disinterest in introspection [ 15 , 63 , 85 ] which has the potential to result in poor judgement [ 15 , 63 ] cynical humour and dysfunctional coping behaviours such an increased consumption of alcohol, unhealthy food or pornography [ 91 ]. The impact is a loss of self-worth [ 95 ] which may be compounded by weight gain or loss [ 83 ] and its emotional impact.
4.3.2 The impact of compassion fatigue on patients
Patient care is negatively impacted by compassion fatigue and this impact is recognisable to patients. Health professionals effected by compassion fatigue experience a decreased ability to feel empathy and hence lack meaning in their work [ 20 , 96 ]. which results in substandard care [ 20 , 83 , 96 ]. The stress of the working environment is palpable to patients and is identifiable as a consequence of poor-quality care [ 60 , 97 ]. Patients depend on health professionals to alleviate the stress, anxiety and fear associated with their illness [ 90 ]. When patients sense the impact of compassion fatigue they question the quality and appropriateness of care which in turn escalates patient stress [ 60 ].
The relationship between the healthcare professional and the patient becomes compromised. The trauma response associated with compassion fatigue results in reduced or decreased workplace engagement [ 21 ] and avoidance of particular situations or patients [ 96 ]. The ultimate consequence of compassion fatigue and burnout is poor patient outcomes [ 60 ]. Indeed significant concerns arise regarding the potential for increased medical errors and patient safety [ 21 , 64 , 83 ].
4.3.3 The impact of compassion fatigue on organisations and the healthcare system
Staff who are experiencing compassion fatigue have reduced job satisfaction [ 21 ] and reduced efficiency levels resulting in reduced service quality [ 98 ]. Patient satisfaction levels are lower in institutions where job satisfaction and burnout levels are reduced [ 97 ]. Poor patient satisfaction levels result in reduced patient recommendation rates of same facility to family and friends [ 60 , 97 ].
Relationships with co-workers become negatively impacted [ 20 , 96 ] when a person is impacted by compassion fatigue. If working with colleagues who are equally exhausted and apathic [ 13 ] productivity and workplace morale decline [ 95 ]. The result is a poor work environment with lower levels of productivity, patient satisfaction and patient care outcomes [ 21 ]. Compassion fatigue is triggered by the ongoing use of empathy while caring for those who are suffering and the effect of a poor work environment [ 18 , 99 ]. Thus, the cycle of compassion fatigue perpetuates.
As staff fatigue, the rates of sick leave increase [ 83 ]. More staff members experience an intensifying desire to leave their workplace, profession [ 15 , 24 , 60 ] and specialty [ 80 ]. Compassion fatigue and burnout result in workplace imbalances [ 24 , 60 ] with higher rates of staff turnover [ 95 ], and attrition and eventually, workforce dropout [ 98 ]. Staff turnover rates are particularly volatile in in high-stakes environments [ 100 ] such as oncology and emergency medicine. Staff seek alternate employment opportunities in an attempt to combat excessive workplace stress. As turnover rates increase, the stress in the workplace intensifies as remaining staff attempt to continue short staffed [ 60 ].
Compounding the impact of compassion fatigue is the perception that indicators of a poor working environment, such as increased rates of absenteeism, reduced service quality, low levels of efficiency are being ignored by the organisation and healthcare system [ 18 , 98 ]. Concerns include the conclusion by staff that administrators do not consider caregiver stress when allocating tasks [ 13 ]. The impact of compassion fatigue is intensified when management fail to provide workplace acknowledgement, fail to provide opportunities for peer support and appear not to value work-life balance [ 80 ]. When the workplace culture is not addressed with opportunity for employee training, and a shift towards a compassionate organisational culture [ 65 ] staff in healthcare will continue to experience moderate to high levels of compassion fatigue.
As a consequence of the negative impact on productivity, job satisfaction and staff turnover, compassion fatigue also impedes workplace focus on patient safety [ 21 ] and thus has the potential to lead to an increase in medical errors and diminished patient outcomes [ 21 ]. Healthcare professionals experiencing burnout and compassion fatigue are more prone to medical error [ 83 ] as a result of compassion fatigue symptoms including exhaustion [ 14 , 60 ] and a diminished work performance [ 13 , 63 , 83 ].
In addition to the potential harm to patients and families, compassion fatigue related medical error has the potential to result in legal, reputational and economic loss, for individual healthcare providers [ 101 ]. The economic impact of an institution impacted by compassion fatigue staff turnover, patient dissatisfaction and concerns regarding medical error and patient safety is institutional financial loss [ 64 , 102 , 103 , 104 ]. Compassion is valued by patients and healthcare professionals alike and both patients and professionals raise concerns regarding a widespread and escalating lack of compassion in healthcare systems [ 30 , 101 ].
4.4 Detection and assessment of compassion fatigue
Compassion fatigue is commonly measured using the Professional Quality of Life Scale (ProQOL) [ 105 , 106 ]. The self-score scale is a freely available to measure the negative and positive effects of caring and helping others who have experiences significant trauma or suffering.
The Compassion Fatigue Self-Test (CFST) was originally developed to measure compassion fatigue [ 107 ]. The CFST measures the level of risk of an individual to developing compassion fatigue. The scale included 40 items, divided into two subscales, compassion fatigue and job burnout; 23 items measure compassion fatigue and 17 items burnout. Using a five-point scale, respondents are asked to indicate how frequently a situation or particular characteristic is true of themselves (1 = rarely/never, 2 = at times, 3 = not sure, 4 = often, 5 = very often). On the subscale compassion fatigue, scores of 26 or below, indicate being at an extremely low risk, a score between 27 and 30, low risk, between 31 and 35 moderate risk, scores between 36 and 40 high risk and scores between 41 and above, indicate an extreme high risk of compassion fatigue. Scores on the subscale for burnout below 36 indicated an extremely low risk, between 37 and 50 moderate risk, 51–75 indicates high risk, and scores between 76 and 85 indicated an extremely high risk of burnout. The reported internal consistency alphas are reported to be between .86 to .94 [ 108 ]. The scale has been widely used in a variety of settings and has adequate reliability and validity [ 69 ]. The measure was specifically developed to measure both direct and indirect trauma making it a widely applied measure [ 108 ].
The CFST scale was revised and re-developed [ 106 ] into the Professional Quality of Life (ProQOL). The revised scale included an additional subscale to measure compassion satisfaction. The three subscales total 30 items, using a six-point scale (0 = never, 1 = rarely, 2 = a few times, 3 = somewhat, 4 = often, 5 = very often). Respondents are asked about their thoughts, feelings and behaviour at work. The first of the three sub-scales measures compassion satisfaction, a higher score on this scale represents a greater satisfaction as a caregiver and helping others. The second subscale, measures burnout and feelings of hopelessness at not being able to do a good job, and the third subscale measures compassion fatigue/secondary traumatic stress. A higher score on this subscale represents high levels of compassion fatigue/secondary traumatic stress. Each subscale includes 10 items, and the subscale scores cannot be combined to calculate a total score. The ProQOL scale improved on the psychometric properties of the CFST scale [ 105 , 106 ]. The scale with the additional subscale measuring compassion satisfaction incorporates the more positive and psychologically protective aspect of caring, capturing the rewarding and gratifying aspects of caring [ 105 , 106 ]. The Cronbach’s α values reported by Stamm for these scales were .82 for compassion satisfaction, .71 for burnout, and .78 for compassion fatigue [ 105 ]. The ProQOL is free to use and is readily available, as are guidelines for interpreting the results from the scale.
4.5 Management of compassion fatigue in healthcare professionals
Figley [ 70 ] believed to manage compassion fatigue in health professional a multifaceted approach is required that includes prevention, assessment and minimising the consequences. The impacts of compassion fatigue are far reaching for both the individual health professional and organisations. Helping protect healthcare professionals from developing compassion fatigue and managing those experiencing high levels of job burnout and secondary traumatic stress can be done through self-care, evidence-based interventions and creating organisations that are better able to support and protect their workers. By protecting health professionals ensures high quality patient care. Over the past few decades’ interventions have been developed to help reduce symptoms of compassion fatigue. Self-care techniques that can be used to help reduce the risk of developing compassion fatigues and managing the risks of providing compassionate care to patients and clients have been developed and promoted among health care professionals. Organisations also play a role in helping reduce the risk to their workers through better training, ongoing support and creating a support environment that recognises the risks to their staff.
4.5.1 Interventions for compassion fatigue
Interventions have been developed to both prevent and manage compassion fatigue in healthcare professionals. The strategies have included education interventions and developing skills such as resilience [ 109 ]. The Accelerated Recovery Program (ARP) is a program developed to reduce compassion fatigue, including secondary traumatic stress and burnout in healthcare professionals. The ARP was originally developed in 1997 [ 110 ], based on Figley’s work on compassion fatigue (1995). The main aim of the program is to build resilience skills to prevent compassion fatigue. The program duration is 5 weeks, consisting of a weekly 90–120-minute training sessions. A full assessment is undertaken in the first session, along with a discussion exploring the symptoms participants are experiencing. In the second session treatment goals and a timeline is discussed using self-visualisation techniques. The third session focuses on reframing and reprocessing the trauma experienced using eye movement desensitisation and reprocessing therapy and reviewing self-regulation strategies for managing situations. The fourth session incorporates video-dialogue techniques to enable the individuals to supervise themselves through the development of externalisation techniques. In the final session, closure and aftercare are addressed with the use of Pathways to recovery that include skill acquisition; self-care; connection with others; and internal conflict resolution. The program works by developing a person’s self-awareness of compassion fatigue and practicing regular self-care activities [ 110 ]. The ARP primarily focused on mental health and trauma workers [ 110 ] but its potential to be effective in reducing compassion fatigue among nurses and other healthcare profession is growing [ 24 ]. Evidence supports the use of the ARP to reduce compassion fatigue among health care professionals [ 24 , 111 , 112 ]. An adaptation of the ARP that reduced the training into a single four-hour session reported a similar significant reduction in compassion fatigue [ 113 ].
The Compassion Fatigue Resiliency program (CFRP) was based on the concepts of the ACP [ 110 ]. The program is a five-week formalised program to educate participants about compassion fatigue, the factors that contribute to it and the effects of chronic stress. The program interventions aim to reduce the effects of compassion fatigue with participants taking part in small group activities that allow them to build resilience through self-regulation, intentionality, self-validation, connection and self-care.
Evidence supports the effectiveness of the CRRP to reduce secondary traumatic stress by providing nurses with the ability to manage intrusive thoughts [ 24 ]. The program aids greater relaxation enabling individuals to better manage perceive threats, enabling them to manage chronic stress through self-regulation [ 114 ]. The benefits of the CFRP have been reported for healthcare providers in reducing the symptoms of compassion fatigue [ 115 , 116 , 117 ].
To improve the resilience of military healthcare professionals and reduce compassion fatigue the Army’s Care Provider Support Program (CPSP) was developed. During one-hour sessions, healthcare providers are educated to be able to assess themselves for compassion fatigue and identify when they need to take action. The program activities focus on developing self-awareness through group discussion and interactive participation, along with providing education on stress and resilience. Support for the intervention significantly reducing burnout was demonstrated by Weidleich et al. [ 118 ]. However, although a decrease in secondary trauma was reported this was not significant [ 118 ].
Overall, the usefulness of formal intervention programs developed to target reducing compassion fatigue have been reported in a number of healthcare professionals. Although, there is only limited evidence to support the effectiveness of the CPSP. Despite the evidence to support the use of these intervention programs provided in this section, due to the nature of health care settings it is not always practical or cost effective to run these programs for staff. Staff would be expected to attend these programs in their own time and the financial impact to organisations with other competing costs make these types of interventions unfeasible.
4.5.2 Self-care
Organisational resources may not be available or sufficient to address compassion fatigue in employees, therefore promoting self-care can be an effective way to support staff. Self-care interventions are commonly prescribed for health professions experiencing compassion fatigue. Successfully managing compassion fatigue can be done by developing strategies that enhance awareness and provide thoughtful self-care [ 119 ]. There are numerous self-care strategies that can be adopted and utilised by healthcare professionals.
Strategies and techniques that can be used to reduce the risk of compassion fatigue involve looking after general wellbeing, including diet, exercise and sleep. Evidence supports maintaining a healthy diet and getting the recommended amount of physical exercise help regulates mood [ 120 ] and reduce the risk of compassion fatigue [ 121 ]. Regular sleep also plays an important role in regulating mood. Sleep deprivation is associated with decrease cognitive performance and increases the risk of low mood such as anxiety and anger [ 122 ].
Nurturing the self can be done using a number of different techniques. Developing and practicing self-compassion can increase a person psychological wellbeing and assist professionals to better respond to the difficulties experienced in their jobs [ 123 , 124 ]. Self-care interventions developed aim to help healthcare professionals achieve work-life balance by developing coping skills to maintain both emotional and physical health [ 125 ], along with maintaining healthy social networks and participating in activities to promote relaxation such as meditation and mindfulness [ 126 , 127 ]. Other self-care activities that can be adopted to help to support emotional wellbeing involve creative writing [ 128 ]. Strategies have included the use of writing poems to explore difficulties with emotional connection [ 129 ], or the use of creative cafes to reaffirm the core values involved in nursing [ 130 ].
4.5.3 Peer support programs
Peer support programs can be effective strategies to support healthcare professionals to help mitigate compassion fatigue. Encouraging individuals to utilise their social support networks has a protective quality, by providing opportunities to process traumatic experiences at work [ 131 ]. Chambers [ 132 ] developed the Care for Caregivers program for physicians, nurses and other frontline staff. The staff were trained in peer support techniques that covered active listening, normalising emotions, reframing situations, sharing stories and offering ideas of coping mechanisms. The program was reported as being well utilised by staff members, especially those dealing with patients experiencing trauma or patient death. Within 2 years of the program running staff surveys reported an increase in feeling adequately supported by the hospital from 16% to 86%, helping change the workplace culture to being more emphatic [ 132 ].
4.5.4 Protection through training
Preventing healthcare from the risks of developing compassion fatigue can be included in training programs. There are ways in training healthcare professionals to equipped them with strategies to help protect them from developing compassion fatigue. For example, trauma therapists utilising evidence-base practices when treating their clients had significantly decreased amounts of compassion fatigue and burnout compared to specialists not using evidence-based practices [ 133 ]. This demonstrates the use of evidence-based practices to prevent the negative outcomes of compassion fatigue therefore improving both the therapists and clients experience of therapy [ 133 , 134 ]. A study by Deighton [ 135 ] reported the exposure to the clients traumatic event was not as important in therapists developing compassion fatigue as the therapist’s t ability to help the client work through their trauma [ 135 ]. Being able to identify possible strategies to be better equipped to deal with exposure to clients’ traumas can reduce the impact on healthcare professionals.
4.5.5 Culture change in healthcare facilities
Organisations can help mitigate the effects of compassion fatigue experienced by their employees. Organisations need to assess whether and to what extent compassion fatigue is a concern of their workers to be able to start to address the problem [ 136 ]. Prevention is recommended as the first line of defence against compassion fatigue [ 137 ]. Organisations should provide regular education and training around the importance of building employees self-care routines [ 138 ]. The Hospital, University Pennsylvania, is an example of an organisation that has provided their own wellness programs to support their staff. A Centre for Nursing Renewal was developed to minimise the ill effects of compassion fatigue and promote wellness among its staff [ 139 ]. The centre offered relaxation, meditation, yoga, group exercise classes, along with other classes and spaces to support nurses emotional and physical wellbeing. The centre assisted in creating a culture where nurse leaders were increasing awareness of nurses experiencing compassion fatigue and burnout and could therefore encourage staff to engage in discussion and renewal practices such as exercise, talking, reflection and getting adequate rest [ 139 ].
Staff wellness programs and initiatives have been implemented and trialled in other health care providers organisations. These programs range in the types of resources provided, include from professional counselling, employee health screening, role modelling, mentor program, o providing healthy snacks and relaxation. These types of programs offered by organisations and led by trained professional can help reduce compassion fatigue [ 119 , 128 ]. These include employee health screening, role modelling, mentor program and staff retreats.
Staff wellness programs and initiatives have been implemented and trialled in other organisations. These programs range in the types of resources provided and included professional counselling, employee health screening, role modelling, mentor program, staff retreats, providing healthy snacks and relaxation. These types of programs were offered by organisations and led by trained professional can help reduce compassion fatigue [ 116 , 125 ].
More practical strategies that could be provided from an organisational level include providing adequate staffing levels, having good leadership support and experienced staff [ 140 ]. By creating workplaces where it is encouraged to acknowledge that providing emphatic care to patients in difficult situations can cause compassion fatigue is a response of caring, can help to address the phenomenon [ 66 ]. At an organisational level demonstrating compassion is genuinely appreciated through celebrating staff acts of compassion [ 136 ] can help make staff feel valued and supported. Providing staff with personal development opportunities promoting psychological wellbeing [ 141 ], along with debriefing after stressful events could promote healing [ 140 ]. Organisations can play a major role in supporting staff provide the best patients care in a safe and nurturing environment.
5. Limitations of this review
While every attempt was made to search the appropriate databases for articles systematically, it is important to note that this is not a systematic review. The search was limited to three major databases: MEDLINE (Ovid), APA PsycINFO (EBSCOhost), and CINAHL Plus using the Boolean/Phrase (Empathy AND (“Compassion Fatigue” OR “Vicarious Trauma”) AND Health). Two main limitations influenced the studies identified by the database search; the first was not including the term “Secondary Traumatic Stress” as an alternative to “Vicarious Trauma” in the search terms, and the second was limiting the search to literature published between 2003 and 2022 and missing essential articles published in the 90s. These dates were initially selected due to the escalation in volume of relevant publications during that timeframe. Fortunately, these limitations were identified by the authors during the review process and were corrected by including all relevant secondary sources which retrieved the essential articles before 2003 in addition to studies examining Secondary Traumatic Stress.
6. Conclusion
Empathy and compassion are fundamental aspirations for HCPs as they provide them with job satisfaction, a sense of value, as well as greatly benefiting their patients. However, caring and supporting people in distress can, over time, lead to compassion fatigue which negatively impacts the healthcare professional, the patient, the organisation, and the healthcare system. Although there are clear risk factors, identifying tools and effective strategies to support and manage those experiencing compassion fatigue, compassion fatigue in HCPs continues to grow reaching alarming levels over the last decade. Further research is needed to quantify the escalation and impact of compassion fatigue, and in a broader array of healthcare professionals. Exploration of the unique impact of loss of compassion beyond the experience of burnout is also an area requiring an enhanced understanding.
We propose that organisations implement regular screening and targeted support for at-risk individuals. More practical strategies could be provided from an organisational level to prevent the development of compassion fatigue in HCPs and support staff to provide the best patient care in a safe and nurturing environment. Ensuring a positive work culture, which includes peer support programs, is a managerial responsibility. Evidence supports the use of formal intervention programs such as CFRP and the ARP to be effective in reducing compassion fatigue, yet these programs required the HCP to commit a substantial amount of time, usually outside of their working day. For the benefits of these programs to reach HCP, shorter programs preferably accessible during work hours could be incorporated. Future research should focus on identifying components of these programs that could be adapted into modified shorter training sessions that could become part of ongoing professional development.
Crucially, we propose that ensuring adequate staffing levels be a key responsibility of management and, therefore, we advise the meticulous implementation of quality assurance, evaluation, and formal reporting of staffing ratios.
Acknowledgments
This study was supported by the School of Medicine at University of Western Sydney University, Australia.
Conflict of interest
The authors declare no conflict of interest.
A special thank you to the medical librarians at Western Sydney University for their literature search and Endnote support.
Nomenclature and abbreviations
healthcare professionals or providers
post-traumatic stress disorder
secondary traumatization
- 1. Roney LN, Acri MC. The cost of caring: An exploration of compassion fatigue, compassion satisfaction, and job satisfaction in pediatric nurses. Journal of Pediatric Nursing. 2018; 40 :74-80
- 2. Kinman G, Grant L. Enhancing empathy in the helping professions. In: Psychology and neurobiology of empathy. Nova Biomedical Books; 2016. pp. 297-319
- 3. Cole-King A, Gilbert P. Compassionate care: The theory and the reality. Journal of Holistic Healthcare. 2011; 8 (3):30
- 4. Hein G, Singer T. I feel how you feel but not always: The empathic brain and its modulation. Current Opinion in Neurobiology. 2008; 18 (2):153-158
- 5. Hoffman ML. Chapter 4—Varieties of empathy-based guilt. In: Bybee J, editor. Guilt and Children. San Diego: Academic Press; 1998. pp. 91-112
- 6. Blumgart HL. Caring for the patient. The New England Journal of Medicine. 1964; 270 :449-456
- 7. Osler W. Aequanimitas: With Other Addresses to Medical Students, Nurses and Practitioners of Medicine. Philadelphia: P. Blakiston's Son & Co.; 1920. p. 475
- 8. Markakis K, Frankel R, Beckman H, Suchman A. Teaching empathy: It can be done. Annual Meeting of the Society of General Internal Medicine; April 29–May 1; San Francisco, California. 1999
- 9. Halpern J. What is clinical empathy? Journal of General Internal Medicine. 2003; 18 (8):670-674
- 10. Stepien KA, Baernstein A. Educating for empathy. A review. Journal of General Internal Medicine. 2006; 21 (5):524-530
- 11. de Waal FB. The antiquity of empathy. Science. 2012; 336 (6083):874-876
- 12. Radey M, Figley CR. The social psychology of compassion. Clinical Social Work Journal. 2007; 35 (3):207-214
- 13. Joinson C. Coping with compassion fatigue. Nursing (Jenkintown, Pa). 1992; 22 (4):116-121
- 14. Figley CR. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those Who Treat the Traumatized. New York: Brunner/Mazel; 1995
- 15. Figley CR. Compassion fatigue: Psychotherapists' chronic lack of self care. Journal of Clinical Psychology. 2002; 4 (11):1433-1441
- 16. Adams RE, Boscarino JA, Figley CR. Compassion fatigue and psychological distress among social workers: A validation study. American Journal of Orthopsychiatry. 2006; 76 (1):103-108
- 17. Bourassa DB. Compassion fatigue and the adult protective services social worker. Journal of Gerontological Social Work. 2009; 52 (3):215-229
- 18. Cavanagh N, Cockett G, Heinrich C, Doig L, Fiest K, Guichon JR, et al. Compassion fatigue in healthcare providers: A systematic review and meta-analysis. Nursing Ethics. 2020; 27 (3):639-665
- 19. Peters E. Compassion fatigue in nursing: A concept analysis. Nursing Forum (Hillsdale). 2018; 53 (4):466-480
- 20. Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: A review of current literature. Journal of Nursing Scholarship. 2016; 48 (5):456-465
- 21. Bleazard M. Compassion fatigue in nurses caring for medically complex children. Journal of Hospice and Palliative Nursing: JHPN: The Official Journal of the Hospice and Palliative Nurses Association. 2020; 22 (6):473-478
- 22. Osofsky JD. Perspectives on helping traumatized infants, young children, and their families. Infant Mental Health Journal. 2009; 30 (6):673-677
- 23. Katz A. Compassion in practice: Difficult conversations in oncology nursing. Canadian Oncology Nursing Journal. 2019; 29 (4):255-257
- 24. Potter P, Deshields T, Berger JA, Clarke M, Olsen S, Chen L. Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncology Nursing Forum. 2013; 40 (2):180-187
- 25. Kinman G, Grant L. Emotional demands, compassion and mental health in social workers. Occupational Medicine. 2020; 70 (2):89-94
- 26. Lemieux-Cumberlege A, Taylor EP. An exploratory study on the factors affecting the mental health and well-being of frontline workers in homeless services. Health & Social Care in the Community. 2019; 27 (4):e367-ee78
- 27. Pietrantoni L, Prati G. Resilience among first responders. African Health Sciences. 2008; 8 (Suppl. 1):S14-S20
- 28. Tehrani N. Compassion fatigue: Experiences in occupational health, human resources, counselling and police. Occupational Medicine. 2010; 60 (2):133-138
- 29. Turgoose D, Glover N, Barker C, Maddox L. Empathy, compassion fatigue, and burnout in police officers working with rape victims. Traumatology. 2017; 23 (2):205-213
- 30. Xie W, Chen L, Feng F, Okoli CTC, Tang P, Zeng L, et al. The prevalence of compassion satisfaction and compassion fatigue among nurses: A systematic review and meta-analysis. International Journal of Nursing Studies. 2021; 120 :103973
- 31. Anzaldua A, Halpern J. Can clinical empathy survive? Distress, burnout, and malignant duty in the age of Covid-19. Hastings Center Report. 2021; 51 (1):22-27
- 32. Becker J, Dickerman M. Impact of narrative medicine curriculum on burnout in pediatric critical care trainees. Critical Care Medicine. 2021; 49 (1 Suppl. 1):473
- 33. Carver ML. Another look at compassion fatigue. Journal of Christian Nursing: A Quarterly Publication of Nurses Christian Fellowship. 2021; 38 (3):E25-EE7
- 34. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. Journal of Clinical Nursing. 2020; 29 (21-22):4321-4330
- 35. Zhang YY, Han WL, Qin W, Yin HX, Zhang CF, Kong C, et al. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: A meta-analysis. Journal of Nursing Management. 2018; 26 (7):810-819
- 36. Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. Journal of Chiropractic Medicine. 2006; 5 (3):101-117
- 37. DiTullio M, MacDonald D. The struggle for the soul of hospice: Stress, coping, and change among hospice workers. American Journal of Hospice and Palliative Medicine®. 1999; 16 (5):641-655
- 38. Keidel GC. Burnout and compassion fatigue among hospice caregivers. American Journal of Hospice and Palliative Medicine®. 2002; 19 (3):200-205
- 39. Payne N. Occupational stressors and coping as determinants of burnout in female hospice nurses. Journal of Advanced Nursing. 2001; 33 (3):396-405
- 40. O'Halloran TM, Linton JM. Stress on the job: Self-care resources for counselors. Journal of Mental Health Counseling. 2000; 22 (4):354
- 41. Jenaro C, Flores N, Arias B. Burnout and coping in human service practitioners. Professional Psychology: Research and Practice. 2007; 38 (1):80
- 42. Bride BE, Figley CR. The fatigue of compassionate social workers: An introduction to the special issue on compassion fatigue. Clinical Social Work Journal. 2007; 35 (3):151-153
- 43. Figley CR. Compassion Fatigue: Toward a New Understanding of the Costs of Caring. Philadelphia, PA, US: Brunner/Mazel; 1995
- 44. Rourke MT. Compassion Fatigue in Pediatric Palliative Care Providers. Pediatric Clinics of North America. 2007; 54 (5):631-644
- 45. Pfifferling J-H, Gilley K. Overcoming compassion fatigue. Family Practice Management. 2000; 7 (4):39
- 46. Arkan B, Yılmaz D, Düzgün F. Determination of compassion levels of nurses working at a university hospital. Journal of Religion and Health. 2020; 59 (1):29-39
- 47. Zeidner M, Hadar D, Matthews G, Roberts RD. Personal factors related to compassion fatigue in health professionals. Anxiety, Stress & Coping: An International Journal. 2013; 26 (6):595-609
- 48. Lynch SH, Shuster G, Lobo ML. The family caregiver experience – Examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes. Aging & Mental Health. 2018; 22 (11):1424-1431
- 49. Goldblatt H, Buchbinder E. Challenging Gender Roles. Journal of Social Work Education. 2003; 39 (2):255-275
- 50. Gerson JI. The Development of Empathy in the Male Psychotherapist: A Researched Essay. Ohio, United States of America: The Union Institute; 1996
- 51. Kogan I. The role of the analyst in the analytic cure during times of chronic crises. Journal of the American Psychoanalytic Association. 2004; 52 (3):735-757
- 52. Batten SV, Orsillo SM. Therapist reactions in the context of collective trauma. The Behavior Therapist. 2002; 25 (2):36-40
- 53. Baum N. Trap of conflicting needs: Helping professionals in the wake of a shared traumatic reality. Clinical Social Work Journal. 2012; 40 (1):37-45
- 54. Ledoux K. Understanding compassion fatigue: Understanding compassion. Journal of Advanced Nursing. 2015; 71 (9):2041-2050
- 55. Tanner D. 'The love that dare not speak its Name': The role of compassion in social work practice. British Journal of Social Work. 2020; 50 (6):1688-1705
- 56. Coetzee SK, Klopper HC. Compassion fatigue within nursing practice: A concept analysis. Nursing & Health Sciences. 2010; 12 (2):235-243
- 57. Gilmore C. Compassion fatigue-what it is and how to avoid it. Kai Tiaki: Nursing New Zealand. 2012; 18 (5):32
- 58. Stewart DW. Casualties of war: Compassion fatigue and health care providers. Medsurg Nursing. 2009; 18 (2):91-94
- 59. Walker LO, Avant KC. Strategies for Theory Construction in Nursing. Prentice Hall Upper Saddle River, NJ: Pearson; 2005
- 60. Wynn F. Burnout or compassion fatigue? A comparative concept analysis for nurses caring for patients in high-stakes environments. International Journal for Human Caring. 2020; 24 (1):59-71
- 61. Zhang Y-Y, Zhang C, Han X-R, Li W, Wang Y-L. Determinants of compassion satisfaction, compassion fatigue and burn out in nursing: A correlative meta-analysis. Medicine (Baltimore). 2018; 97 (26):e11086
- 62. Sukut O, Sahin-Bayindir G, Ayhan-Balik CH, Albal E. Professional quality of life and psychological resilience among psychiatric nurses. Perspectives in Psychiatric Care. 2022; 58 (1):330-338
- 63. Coetzee SK, Klopper HC. Compassion fatigue within nursing practice: A concept analysis: Concept analysis of compassion fatigue. Nursing & Health Sciences. 2010; 12 (2):235-243
- 64. Stamm R, Lambert J, Garritano N, Miller J, Donnellan A. Advanced practice registered nurse subspecialty compassion satisfaction and compassion fatigue. The Journal for Nurse Practitioners. 2022; 18 (3):310-315
- 65. Slatten LA, Carson KD, Carson PP. Compassion fatigue and burnout: What managers should know. The Health Care Manager. 2020; 39 (4):181-189
- 66. Harris C, Griffin MTQ. Nursing on empty: Compassion fatigue signs, symptoms, and system interventions. Journal of Christian Nursing : A Quarterly Publication of Nurses Christian Fellowship. 2015; 32 (2):80-87
- 67. Meadors P, Lamson A, Swanson M, White M, Sira N. Secondary traumatization in pediatric healthcare providers: Compassion fatigue, burnout, and secondary traumatic stress. Omega: Journal of Death and Dying. 2009; 60 (2):103-128
- 68. Peebles-Kleiger MJ. Pediatric and neonatal intensive care hospitalization as traumatic stressor: Implications for intervention. Bulletin of the Menninger Clinic. 2000; 64 (2):257-280
- 69. Jenkins SR, Baird S. Secondary traumatic stress and vicarious trauma: A validational study. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2002; 15 (5):423-432
- 70. Figley CR. Treating Compassion Fatigue. Routledge; 2002
- 71. Figley CR. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those Who Treat the Traumatized. Routledge; 2013
- 72. Sinclair HA, Hamill C. Does vicarious traumatisation affect oncology nurses? A literature review. European Journal of Oncology Nursing. 2007; 11 (4):348-356
- 73. Simon CE, Pryce JG, Roff LL, Klemmack D. Secondary traumatic stress and oncology social work: Protecting compassion from fatigue and compromising the worker's worldview. Journal of Psychosocial Oncology. 2005; 23 (4):1-14
- 74. Beck CT. Secondary traumatic stress in nurses: A systematic review. Archives of Psychiatric Nursing. 2011; 25 (1):1-10
- 75. Osland EJ. An investigation into the professional quality of life of dietitians working in acute care caseloads: Are we doing enough to look after our own? Journal of Human Nutrition and Dietetics: The Official Journal of the British Dietetic Association. 2015; 28 (5):493-501
- 76. Rayner S, Davis C, Moore M, Cadet T. Secondary traumatic stress and related factors in Australian social workers and psychologists. Health & Social Work. 2020; 45 (2):122-130
- 77. Hubbard GB, Beeber L, Eves E. Secondary traumatization in psychiatric mental health nurses: Validation of five key concepts. Perspectives in Psychiatric Care. 2017; 53 (2):119-126
- 78. Rogers ME. Nursing science and the space age. Nursing Science Quarterly. 1992; 5 (1):27-34
- 79. Huang Y-H, Kim H, Le M, Martinez J, Martin J, Maghen E, et al. Predictors and risk factors of compassion satisfaction, burnout, and compassion fatigue among OTs. The American Journal of Occupational Therapy. 2019; 73 (4_Supplement_1):7311505161-p1
- 80. Perry B, Toffner G, Merrick T, Dalton J. An exploration of the experience of compassion fatigue in clinical oncology nurses. Canadian Oncology Nursing Journal. 2011; 21 (2):91-97
- 81. Aron EN, Aron A, Jagiellowicz J. Sensory processing sensitivity: A review in the light of the evolution of biological responsivity. Personality and Social Psychology Review. 2012; 16 (3):262-282
- 82. Pérez-Chacón M, Chacón A, Borda-Mas M, Avargues-Navarro ML. Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. International Journal of Environmental Research and Public Health. 2021; 18 (2):611
- 83. Jenkins B, Warren NA. Concept analysis: Compassion fatigue and effects upon critical care nurses. Critical Care Nursing Quarterly. 2012; 35 (4):388-395
- 84. Benoit LG, Veach PM, LeRoy BS. When you care enough to do your very best: Genetic counselor experiences of compassion fatigue. Journal of Genetic Counseling. 2007; 16 (3):299-312
- 85. Thomas RB, Wilson JP. Issues and controversies in the understanding and diagnosis of compassion fatigue, vicarious traumatization, and secondary traumatic stress disorder. International Journal of Emergency Mental Health. 2004; 6 (2):81-92
- 86. Lynch SH, Lobo ML. Compassion fatigue in family caregivers: A Wilsonian concept analysis. Journal of Advanced Nursing. 2012; 68 (9):2125-2134
- 87. Rawal S, Strahlendorf C, Nimmon L. Challenging the myth of the attrition of empathy in paediatrics residents. Medical Education. 2020; 54 (1):82-87
- 88. Turgoose D, Maddox L. Predictors of compassion fatigue in mental health professionals: A narrative review. Traumatology. 2017; 23 (2):172-185
- 89. Mendenhall TJ. Trauma-response teams: Inherent challenges and practical strategies in interdisciplinary fieldwork. Families, Systems & Health. 2006; 24 (3):357-362
- 90. Lee H-F, Kuo C-C, Chien T-W, Wang Y-R. A meta-analysis of the effects of coping strategies on reducing nurse burnout. Applied Nursing Research. 2016; 31 :100-110
- 91. Howard H, Navega N. Pivotal events: 'I’m not a normal person anymore'—Understanding the impact of stress among helping professionals. Best Practices in Mental Health: An International Journal. 2018; 14 (2):32-47
- 92. Sansbury BS, Graves K, Scott W. Managing traumatic stress responses among clinicians: Individual and organizational tools for self-care. Trauma (London, England). 2015; 17 (2):114-122
- 93. Jo M, Na H, Jung Y-E. Mediation effects of compassion satisfaction and compassion fatigue in the relationships between resilience and anxiety or depression among hospice volunteers. Journal of Hospice and Palliative Nursing: JHPN: The Official Journal of the Hospice and Palliative Nurses Association. 2020; 22 (3):246-253
- 94. Mason VM, Leslie G, Clark K, Lyons P, Walke E, Butler C, et al. Compassion fatigue, moral distress, and work engagement in surgical intensive care unit trauma nurses: A pilot study. Dimensions of Critical Care Nursing. 2014; 33 (4):215-225
- 95. Showalter SE. Compassion fatigue: What is it? Why does it matter? Recognizing the symptoms, acknowledging the impact, developing the tools to prevent compassion fatigue, and strengthen the professional already suffering from the effects. American Journal of Hospice & Palliative Medicine. 2010; 27 (4):239-242
- 96. Lombardo B, Eyre C. Compassion fatigue: A nurse's primer. Online Journal of Issues in Nursing. 2011; 16 (1):3
- 97. McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs. 2011; 30 (2):202-210
- 98. Nimmo A, Huggard P. A systematic review of the measurement of compassion fatigue, vicarious trauma, and secondary traumatic stress in physicians. Australasian Journal of Disaster and Trauma Studies. 2013; 2013 (1):37
- 99. Circenis K, Millere I. Compassion fatigue, burnout and contributory factors among nurses in Latvia. Procedia, Social and Behavioral Sciences. 2011; 30 :2042-2046
- 100. Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. American Journal of Critical Care. 2015; 24 (5):412-420
- 101. Brito-Pons G, Librada-Flores S. Compassion in palliative care: A review. Current Opinion in Supportive and Palliative Care. 2018; 12 (4):472-479
- 102. Pereira-Lima K, Mata DA, Loureiro SR, Crippa JA, Bolsoni LM, Sen S. Association between physician depressive symptoms and medical errors: A systematic review and meta-analysis. JAMA Network Open. 2019; 2 (11):e1916097-e
- 103. Willard-Grace RMPH, Knox MMPH, Huang BBA, Hammer HMD, Kivlahan CMDM, Grumbach KMD. Burnout and health care workforce turnover. Annals of Family Medicine. 2019; 17 (1):36-41
- 104. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. An official critical care societies collaborative statement: Burnout syndrome in critical care health care professionals: A call for action. American Journal of Critical Care. 2016; 25 (4):368-376
- 105. Stamm BH. The ProQOL Manual: The Professional Quality of Life Scale: Compassion Satisfaction, Burnout & Compassion Fatigue/Secondary Trauma Scales. Baltimore, MD: Sidran; 2005
- 106. Stamm BH. Measuring Compassion Satisfaction as Well as Fatigue: Developmental History of the Compassion Satisfaction and Fatigue Test. Treating Compassion Fatigue. Psychosocial Stress Series, no. 24. New York, NY, US: Brunner-Routledge; 2002. pp. 107-119
- 107. Figley CR. In: Figley CR, editor. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized. Vol. xxii. Philadelphia, PA, US: Brunner/Mazel; 1995. 268-xxii p
- 108. Bride BE, Radey M, Figley CR. Measuring compassion fatigue. Clinical Social Work Journal. 2007; 35 (3):155-163
- 109. Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: A meta-narrative review of the healthcare literature. International Journal of Nursing Studies. 2017; 69 :9-24
- 110. Gentry JE, Baranowsky AB. Treatment Manual for Accelerated Recovery from Compassion Fatigue. Toronto, Ontario, Canada: Psych Ink Resources; 1998
- 111. Robinson LK, Sterling L, Jackson J, Gentry E, Araujo F, LaFond C, et al. A secondary traumatic stress reduction program in emergency room nurses. SAGE Open Nursing. 2022; 8 :23779608221094530
- 112. Rajeswari H, Sreelekha BK, Nappinai S, Subrahmanyam U, Rajeswari V. Impact of accelerated recovery program on compassion fatigue among nurses in South India. Iranian Journal of Nursing and Midwifery Research. 2020; 25 (3):249
- 113. Flarity K, Gentry JE, Mesnikoff N. The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Advanced Emergency Nursing Journal. 2013; 35 (3):247-258
- 114. Cohen-Katz J, Wiley SD, Capuano T, Baker DM, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout, part II: A quantitative and qualitative study. Holistic Nursing Practice. 2005; 19 (1):26-35
- 115. Pfaff KA, Freeman-Gibb L, Patrick LJ, DiBiase R, Moretti O. Reducing the 'cost of caring' in cancer care: Evaluation of a pilot interprofessional compassion fatigue resiliency programme. Journal of Interprofessional Care. 2017; 31 (4):512-519
- 116. Aycock N, Boyle D. Interventions to manage compassion fatigue in oncology nursing. Clinical Journal of Oncology Nursing. 2009; 13 (2):183-191
- 117. Meadors P, Lamson A. Compassion fatigue and secondary traumatization: Provider self care on intensive care units for children. Journal of Pediatric Health Care. 2008; 22 (1):24-34
- 118. Weidlich CP, Ugarriza DN. A pilot study examining the impact of care provider support program on resiliency, coping, and compassion fatigue in military health care providers. Military Medicine. 2015; 180 (3):290-295
- 119. Nolte AG, Downing C, Temane A, Hastings-Tolsma M. Compassion fatigue in nurses: A metasynthesis. Journal of Clinical Nursing. 2017; 26 (23-24):4364-4378
- 120. Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005; 18 (2):189-193
- 121. Neville K, Cole DA. The relationships among health promotion behaviors, compassion fatigue, burnout, and compassion satisfaction in nurses practicing in a community medical center. The Journal of Nursing Administration. 2013; 43 (6):348-354
- 122. National Sleep Foundation. Sleep-Wake Cycle: Its Physiology and Impact on Health. 2006
- 123. Neff KD, Kirkpatrick KL, Rude SS. Self-compassion and adaptive psychological functioning. Journal of Research in Personality. 2007; 41 (1):139-154
- 124. Hall CW, Row KA, Wuensch KL, Godley KR. The role of self-compassion in physical and psychological well-being. The Journal of Psychology. 2013; 147 (4):311-323
- 125. Houck D. Helping nurses cope with grief and compassion fatigue: An educational intervention. Clinical Journal of Oncology Nursing. 2014; 18 (4):454-458
- 126. Hevezi JA. Evaluation of a meditation intervention to reduce the effects of stressors associated with compassion fatigue among nurses. Journal of Holistic Nursing. 2016; 34 (4):343-350
- 127. Owens RA, Alfes C, Evans S, Wyka K, Fitzpatrick JJ. An exploratory study of a 3-minute mindfulness intervention on compassion fatigue in nurses. Holistic Nursing Practice. 2020; 34 (5):274-281
- 128. Warren J, Morgan MM, Morris LB, Morris TM. Breathing words slowly: Creative writing and counselor self-care—The writing workout. Journal of Creativity in Mental Health. 2010; 5 (2):109-124
- 129. Groninger H. Palliative medicine fellows attend to compassion fatigue using John Stone’s ‘talking to the family’. Perspectives on Medical Education. 2015; 4 (2):83-85
- 130. Winch S, Henderson AJ, Kay M, Burridge LH, Livesay GJ, Sinnott MJ. Understanding compassion literacy in nursing through a clinical compassion café. The Journal of Continuing Education in Nursing. 2014; 45 (11):484-486
- 131. Killian KD. Helping till it hurts? A multimethod study of compassion fatigue, burnout, and self-care in clinicians working with trauma survivors. Traumatology. 2008; 14 (2):32-44
- 132. Chambers RS. Developing a peer support program to mitigate compassion fatigue in health care: A quality improvement project. Iowa Nurse Reporter. 2021; 4 (4):19
- 133. Craig CD, Sprang G. Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress & Coping: An International Journal. 2010; 23 (3):319-339
- 134. Kadambi MA, Ennis L. Reconsidering vicarious trauma: A review of the literature and its' limitations. Journal of Trauma Practice. 2004; 3 (2):1-21
- 135. Deighton RM, Gurris N, Traue H. Factors affecting burnout and compassion fatigue in psychotherapists treating torture survivors: Is the therapist's attitude to working through trauma relevant? Journal of Traumatic Stress. 2007; 20 (1):63-75
- 136. Hofmann PB. Addressing compassion fatigue. The problem is not new, but it requires more urgent attention. Healthcare Executive. 2009; 24 (5):40-42
- 137. Tjeltveit AC, Gottlieb MC. Avoiding the road to ethical disaster: Overcoming vulnerabilities and developing resilience. Psychotherapy: Theory, Research, Practice, Training. 2010; 47 (1):98
- 138. Paiva-Salisbury ML, Schwanz KA. Building compassion fatigue resilience: Awareness, prevention, and intervention for pre-professionals and current practitioners. Journal of Health Service Psychology. 2022; 48 (1):39-46
- 139. Romano J, Trotta R, Rich VL. Combating compassion fatigue: An exemplar of an approach to nursing renewal. Nursing Administration Quarterly. 2013; 37 (4):333-336
- 140. Al-Majid S, Carlson N, Kiyohara M, Faith M, Rakovski C. Assessing the degree of compassion satisfaction and compassion fatigue among critical care, oncology, and charge nurses. The Journal of Nursing Administration. 2018; 48 (6):310-315
- 141. Why emergency nurses are said to succumb to “burnout” while other nurse specialties are said to succumb to “compassion fatigue”; is there a difference? Journal of Emergency Nursing. 2019; 45 (1):4-5
© 2022 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Published: 22 March 2023
By Bruce W. Newton
138 downloads
By Sara Ventura and Alison Jane Martingano
194 downloads
By Neil E. Grunberg and Erin S. Barry
347 downloads
- Corpus ID: 245950995
Understanding the Occupational Burnout Experience of Medical Specialists at the Time of Education and Career Launch: A Case Study of the Sechenov First Moscow State Medical University Students and Residents of the Alekseev Psychiatric Hospital N1
- Anzhela Avagimyan , N. Kasimovskaya , +3 authors N. Nikishina
- Published 2022
- Medicine, Psychology
Figures and Tables from this paper

42 References
Burnout among psychiatry residents, the relationship between burnout syndrome and emotional intelligence in healthcare professionals, the evolution of representations about the syndrome of emotional burnout, medical student and physician burnout in the gulf region: a systematic review, the role of emotional intelligence in health care professionals burnout, burnout in medical students before residency: a systematic review and meta-analysis, display rule "regulators": the relationship between supervisors and worker emotional exhaustion., resources, coping strategies, and emotional exhaustion: a conservation of resources perspective, professional burnout: recent developments in theory and research: w b schaufeli, c maslach, t marek (eds) taylor & francis, 1995. isbn 156032 262 4, £36, research companion to organizational health psychology, related papers.
Showing 1 through 3 of 0 Related Papers
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Stress, anxiety, depression and burnout in frontline healthcare workers during two peaks of COVID-19 pandemic in Russia
Affiliations.
- 1 Faculty of Basic Medicine, Lomonosov Moscow State University, Moscow, Russian Federation.
- 2 Department of Psychiatry, Russian Medical Academy of Continuous Professional Education, Ministry of Public Health of Russian Federation, Moscow, Russian Federation.
- 3 Department of Psychiatry, Russian Medical Academy of Continuous Professional Education, Ministry of Public Health of Russian Federation, Moscow, Russian Federation; Moscow Research Institute of Psychiatry, Moscow, Russian Federation. Electronic address: [email protected].
- PMID: 34619519
- PMCID: PMC8480133
- DOI: 10.1016/j.psychres.2021.114226
Purpose: In this study we aimed to assess the range of psychopathological symptoms (anxiety, stress, depression, burnout) and risk factors in frontline HCWs during spring and autumn outbreaks of the new coronavirus infection in Russian Federation.
Methods: We conducted two independent, cross-sectional hospital-based online surveys. Data of 2195 HCWs were collected between May 19th and May 26th 2020 and between October 10th and October 17th 2020. Stress, anxiety, depression, burnout and perceived stress were assessed using the Russian versions of SAVE-9 and GAD-7, PHQ-9, MBI and PSS-10 scales. Logistic regression analysis was performed to determine the influence of different variables.
Results: The study revealed the rates of anxiety, stress, depression, emotional exhaustion and depersonalization and perceived stress as 32.3%, 31.1%, 45.5%, 74.2%, 37.7%,67.8%, respectively. Moreover, 2.4% of HCWs reported suicidal thoughts. The rate of anxiety was higher in October 2020 compared with May 2020. Revealed risk factors included: female gender, younger age, being a physician, working for over a week, living outside of Moscow or Saint Petersburg, being vaccinated against COVID-19.
Conclusion: These results demonstrate the need for urgent supportive programs for HCWs fighting COVID-19 that fall into higher risk factors groups and its increasing importance over time.
Keywords: Anxiety; Burnout; COVID-19; Depression; Healthcare workers; Stress; Suicide.
Copyright © 2021 Elsevier B.V. All rights reserved.
PubMed Disclaimer
Conflict of interest statement
We declare no competing interests.
Similar articles
- Development, validation, and accuracy of ORCHESTRA emotional exhaustion screening questionnaire among healthcare workers during COVID-19 Pandemic. Gan RK, Arcos González P, Fernandez-Tardon G, Zerbo A, Calota VC, Klöslová Z, Otelea MR, Fabiánová E, Rodriguez-Suarez MM, Tardon A. Gan RK, et al. Br J Health Psychol. 2024 May;29(2):430-453. doi: 10.1111/bjhp.12706. Epub 2023 Nov 13. Br J Health Psychol. 2024. PMID: 37957891 Review.
- [Stress, anxiety, depression and burnout in healthcare workers during the first two outbreaks of COVID-19 in Russia]. Mosolova ES, Sosin DN. Mosolova ES, et al. Zh Nevrol Psikhiatr Im S S Korsakova. 2022;122(6):128-133. doi: 10.17116/jnevro2022122061128. Zh Nevrol Psikhiatr Im S S Korsakova. 2022. PMID: 35758958 Russian.
- Prevalence of Burnout, Depression, Anxiety, Stress, and Hopelessness Among Healthcare Workers in COVID-19 Pandemic in Turkey. Akova İ, Kiliç E, Özdemir ME. Akova İ, et al. Inquiry. 2022 Jan-Dec;59:469580221079684. doi: 10.1177/00469580221079684. Inquiry. 2022. PMID: 35232291 Free PMC article.
- The Sustained Psychological Impact of the COVID-19 Pandemic on Health Care Workers One Year after the Outbreak-A Repeated Cross-Sectional Survey in a Tertiary Hospital of North-East Italy. Lasalvia A, Bodini L, Amaddeo F, Porru S, Carta A, Poli R, Bonetto C. Lasalvia A, et al. Int J Environ Res Public Health. 2021 Dec 19;18(24):13374. doi: 10.3390/ijerph182413374. Int J Environ Res Public Health. 2021. PMID: 34948981 Free PMC article.
- Reported effects of the COVID-19 pandemic on the psychological status of emergency healthcare workers: A scoping review. Alanazi TNM, McKenna L, Buck M, Alharbi RJ. Alanazi TNM, et al. Australas Emerg Care. 2022 Sep;25(3):197-212. doi: 10.1016/j.auec.2021.10.002. Epub 2021 Nov 12. Australas Emerg Care. 2022. PMID: 34802977 Free PMC article. Review.
- COVID-19, new challenges to human safety: a global review. Aikebaier S. Aikebaier S. Front Public Health. 2024 Mar 14;12:1371238. doi: 10.3389/fpubh.2024.1371238. eCollection 2024. Front Public Health. 2024. PMID: 38550317 Free PMC article. Review.
- Perceived stress and psychological disorders in healthcare professionals: a multiple chain mediating model of effort-reward imbalance and resilience. Tao Y, Cheng Z, Wang C, Liu T, Yan M, Huang X, Jian S, Sun L, Chen Z. Tao Y, et al. Front Public Health. 2023 Dec 14;11:1320411. doi: 10.3389/fpubh.2023.1320411. eCollection 2023. Front Public Health. 2023. PMID: 38155891 Free PMC article.
- Family support, anger and aggression in health workers during the first wave of the pandemic. Pachi A, Anagnostopoulou M, Antoniou A, Papageorgiou SM, Tsomaka E, Sikaras C, Ilias I, Tselebis A. Pachi A, et al. AIMS Public Health. 2023 Jun 15;10(3):524-537. doi: 10.3934/publichealth.2023037. eCollection 2023. AIMS Public Health. 2023. PMID: 37842274 Free PMC article.
- Factors Associated with Burnout in Medical Staff: A Look Back at the Role of the COVID-19 Pandemic. Țăranu SM, Ștefăniu R, Rotaru TȘ, Turcu AM, Pîslaru AI, Sandu IA, Herghelegiu AM, Prada GI, Alexa ID, Ilie AC. Țăranu SM, et al. Healthcare (Basel). 2023 Sep 13;11(18):2533. doi: 10.3390/healthcare11182533. Healthcare (Basel). 2023. PMID: 37761730 Free PMC article.
- Differential impact of COVID-19 on mental health and burnout. Maniero C, Ng SM, Collett G, Godec T, Siddiqui I, Antoniou S, Kumar A, Janmohamed A, Nair S, Kotecha A, Khan R, Khanji MY, Kapil V, Gupta J, Gupta AK. Maniero C, et al. Occup Med (Lond). 2024 Feb 19;74(1):45-52. doi: 10.1093/occmed/kqad011. Occup Med (Lond). 2024. PMID: 37040624 Free PMC article.
- Albert P. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015;40:219–221. doi: 10.1503/jpn.150205. - DOI - PMC - PubMed
- Alenazi T.H., BinDhim N.F., Alenazi M.H., Tamim H., Almagrabi R.S., Aljohani S.M., H Basyouni M., Almubark R.A., Althumiri N.A., Alqahtani S.A. Prevalence and predictors of anxiety among healthcare workers in Saudi Arabia during the COVID-19 pandemic. J. Infect. Public Health. 2020;13:1645–1651. doi: 10.1016/j.jiph.2020.09.001. - DOI - PMC - PubMed
- Alonso J., Vilagut G., Mortier P., Ferrer M., Alayo I., Aragón-Peña A., Aragonès E., Campos M., Cura-González I.D., Emparanza J.I., Espuga M., Forjaz M.J., González-Pinto A., Haro J.M., López-Fresneña N., Salázar, A.D.M de, Molina J.D., Ortí-Lucas R.M., Parellada M., Pelayo-Terán J.M., Pérez-Zapata A., Pijoan J.I., Plana N., Puig M.T., Rius C., Rodríguez-Blázquez C., Sanz F., Serra C., Kessler R.C., Bruffaerts R., Vieta E., Pérez-Solà V. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: a large cross-sectional survey. Rev. Psiquiatr. Salud Ment. 2020 doi: 10.1016/j.rpsm.2020.12.001. - DOI - PMC - PubMed
- Alshekaili M., Hassan W., Al Said N., Al Sulaimani F., Jayapal S.K., Al-Mawali A., Chan M.F., Mahadevan S., Al-Adawi S. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042030. - DOI - PMC - PubMed
- An Y., Yang Y., Wang A., Li Y., Zhang Q., Cheung T., Ungvari G.S., Qin M.-.Z., An F.-.R., Xiang .Y..-T. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. - DOI - PMC - PubMed
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Europe PubMed Central
- PubMed Central
- Genetic Alliance
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Artificial intelligence in healthcare

traffic_analyzer/DigitalVision V
What Are the Top Challenges of Clinical Decision Support Tools?
Clinical decision support tools can provide actionable information, but issues like alarm fatigue can increase clinician burnout..
- Editorial Staff
Clinical decision support tools can help organizations manage large volumes of data while enabling them to deliver quality, value-based care.
Designed to sort through large amounts of data and provide clinicians with actionable insights, these tools can suggest next steps for treatment, catch potential problems, and alert providers to information they may have missed.
However, if poorly designed or implemented, clinical decision support systems can cause more problems than they solve. Alarm fatigue, physician burnout, and medication errors are all detrimental side effects of unintuitive clinical decision support technology, with these events harming patient outcomes and organizations’ bottom lines.
What are the major challenges with clinical decision support implementation and use, and how can developers and provider organizations overcome these barriers?
CLINICAL DECISION SUPPORT SYSTEMS AND BURNOUT
Clinical decision support systems embedded into the electronic health record (EHR) have the potential to reduce care errors and improve medication adherence rates .
But these tools can also contribute to clinician frustration and burnout. According to a national survey co-authored by the American Medical Association (AMA), physician burnout rates spiked to 63 percent at the end of 2021.
In a 2020 study conducted by researchers at Stanford University School of Medicine, the group stated that an estimated 35 to 60 percent of clinicians experienced symptoms of burnout and called for increased efforts to address it.
The team recommended that healthcare stakeholders consider several factors when designing and implementing clinical decision support to minimize clinician burnout.
“End-users should be involved in all aspects of design, pre-testing, and implementation. [Clinical decision support] requires ongoing maintenance based on feedback and outcomes, as well as updates to clinical practice standards,” the group said.
Previous research has highlighted the importance of user feedback and involvement in clinical decision support tool development. A 2018 study published in JAMIA showed that using natural language processing (NLP) techniques to analyze user feedback and override comments in clinical decision support systems could help organizations identify malfunctioning or broken alerts.
This could help eliminate unnecessary notifications, reducing clinician burnout and fatigue.
The research team emphasized that user feedback provided via override comments is an underutilized but valuable data source for improving clinical decision support tools. They recommended that healthcare organizations with the resources to do so should evaluate all override comments and use these to guide system improvement efforts.
However, increased integration of advanced analytics technologies like NLP in clinical decision support tools comes with additional challenges that healthcare organizations must navigate.
THE GROWING INFLUENCE – AND POTENTIAL RISK – OF AI
With the rise of artificial intelligence (AI) and machine learning (ML) in healthcare, researchers and provider organizations have begun to apply these technologies to clinical decision support tools.
However, combining these systems with advanced analytics often introduces its own set of challenges.
Experts from Mass General Brigham and Brigham and Women’s Hospital have cautioned that physicians may blindly accept the outputs generated by AI and ML systems, which could lead to unintended harms stemming from racial bias in algorithms and impaired clinical decision-making .
Healthcare leaders are familiar with concerns around automation bias and clinician dependency on AI , but these anxieties are growing as health systems increasingly pursue AI deployment.
However, many agree that the risk of clinicians becoming over-reliant on AI and ML is low as long as care teams understand how these tools make their recommendations and view the technologies as assistants, instead of replacements for clinical expertise.
Further, healthcare already has some strategies that have worked in the past to help prevent and address potential over-reliance, as the implementation of EHRs and other tools also created concerns about automation bias.
Creating transparency around how these tools work and how they should be used is a key part of addressing these concerns, and involving clinicians in that process can help build trust and ensure the responsible use of AI and ML.
Building accountability into the AI-driven decision-making process by establishing governance infrastructure and ensuring that a human being is involved at every step of a tool’s use can provide additional safeguards.
In doing so, monitoring and flagging an AI-driven clinical decision support system if issues arise becomes easier.
Clinician involvement can also improve the on-site development of clinical decision support tools in health systems with the resources to do so. Clinical knowledge is useful for troubleshooting why a model may not be successful for a particular use case or helping guide modifications to enhance an algorithm’s performance.
Some healthcare systems have already been utilizing this ‘human in the loop’ approach to improve clinical decision making and care delivery.
For example, AI and ML tools can act as “ real-time listeners ,” that utilize clinician dictations to generate reports. This streamlines workflows for creating reports and can provide clinical decision support by making recommendations for next steps based on relevant report details.
However, before clinicians use these tools, they should undergo educational training to understand best practices for leveraging the technologies in different use cases.
Some organizations have also found success pulling patient cases and running them through the tools in order to test their performance against a provider’s actual recommendations. In doing so, healthcare organizations can ensure suggestions are aligned with clinical practice standards.
Organizations should also have multiple real-time feedback mechanisms for clinicians to report any false negatives or false positives generated by the tools, or any other issues that may arise. Feedback should be sent to the organization’s data science team for troubleshooting and model retraining in the event of a tool providing incorrect outputs.
Having a framework to monitor and address potential issues with the clinical decision support tools ensures that the tools can make the workflow more efficient for clinicians, while the educational and feedback components help avoid automation bias.
But if a clinical decision support tool is missing critical information, its utility will be severely limited.
ADDRESSING MISSED INFORMATION, DIAGNOSTIC ERRORS
Diagnostic errors are a massive patient safety hazard, resulting in care gaps, unnecessary procedures, and patient harm.
Sometimes, these errors can be attributed to missing information or interoperability issues present in clinical decision support systems. While the use of AI has the potential to reduce some of these errors, these technologies cannot currently solve the problem.
Diagnostic errors are common in the United States, with the Agency for Healthcare Research and Quality (AHRQ) estimating that one in 20 adults experiences such an error in outpatient settings and 250,000 Americans experience them in hospitals each year.
These errors – which result from a diagnosis being delayed, poorly communicated, or incorrect – can have serious consequences for patients. The Society to Improve Diagnosis in Medicine indicates that evidence of a major diagnostic error is found in anywhere from 10 to 20 percent of US autopsies, suggesting that these errors contribute to 40,000 to 80,000 deaths annually.
Clinical decision support tools can help prevent diagnostic errors by flagging incidental findings in a patient’s record that may warrant follow-up or by identifying ordered tests that haven’t yet been completed.
Clinical decision support tools that incorporate ‘hard stops’ – in which a response is required before a user can move forward with a task – can help improve patient outcomes when used appropriately.
Hard stops are one of three alert categories common in clinical decision support systems, alongside ‘soft stops’ and passive alerts, according to a 2018 JAMIA study .
The researchers defined soft stop alerts as “those in which the user is allowed to proceed against the recommendations presented in the alert as long as an active acknowledgement reason is entered.” Passive alerts are those “in which information is presented but does not interrupt the user workflow and does not require any interaction on the part of the user.”
In a 2023 article , the Institute for Safe Medication Practices (ISMP) demonstrated that alert fatigue – a phenomenon that occurs when clinicians become desensitized to alerts due to the sheer number and frequency of such alerts – can lead providers disregarding valuable information that could prevent patient harm.
Passive alerts are easiest to ignore as they require no user action, but soft stops may only require clinicians to acknowledge the alert with minimal or no action, making them relatively easy to ignore.
Hard stops, however, completely halt the progression of a process like medication prescription or administration that could harm a patient. In certain cases, a hard stop can help identify and prevent a potential adverse event before it occurs, improving patient outcomes.
But hard stops are not without their pitfalls.
ISMP further indicated that clinicians must sometimes work around barriers like hard stops in order to provide patient care, leading them to circumvent these alerts. Often, this occurs because they do not recognize the issue the alert is trying to prevent or that the rationale for the hard stop is unclear.
While alerts in clinical decision support tools play a key role in preventing diagnostic errors, the presence of alert fatigue and inappropriate alerts – like a hard stop that clinicians must work around – can undermine patient safety by increasing cognitive load for clinicians .
To combat this, the ISMP recommends certain best practices for hard stop implementation, including establishing oversight, evaluating EHR systems, assessing if and where hard stops are necessary, using hard stops judiciously, developing an escalation process to tackle hard stop workarounds, using objective measures to evaluate alert appropriateness and utility, performing functional testing, gathering feedback, and collaborating with clinical decision support technology vendors.
Across the board, user testing and feedback are critical to ensure that clinical decision support systems are pulling and flagging all the information needed to guide decision-making in a way that positively impacts diagnostic error rates and patient safety.
- How Machine Learning is Transforming Clinical Decision Support Tools
- Understanding the Basics of Clinical Decision Support Systems
- FDA Releases Guidance on AI-Driven Clinical Decision Support Tools
Related Resources
- Enabling High-Quality Healthcare And Outcomes With Better Analytics –Teradata
Dig Deeper on Artificial intelligence in healthcare

clinical decision support system (CDSS)

Clinical Decision Support Associated with Improved Patient Outcomes

Potential Risks, Benefits of Patient Access to EHR Clinical Notes

Mayo Clinic Announces Partnership, Clinical Decision Support EHR Integration
UW Health nurses are piloting a generative AI tool that drafts responses to patient messages to improve clinical efficiency ...
Industry stakeholders are working with DirectTrust to create a data standard for secure cloud fax to address health data exchange...
A new HHS final rule outlines information blocking disincentives for healthcare providers across several CMS programs, including ...

Make a gift to PBS News Hour and your donation will be doubled !
Support Intelligent, In-Depth, Trustworthy Journalism.

Devna Bose, Associated Press Devna Bose, Associated Press
Leave your feedback
- Copy URL https://www.pbs.org/newshour/health/health-care-must-diversify-workforce-to-get-rid-of-racial-inequalities-according-to-new-report
Health care must diversify workforce to get rid of racial inequalities, according to new report
Racial and ethnic inequities in health care are found in every state in the U.S. despite the passage of legislation intended to improve health outcomes for minorities and increased awareness of health care disparities over the past two decades, according to a new national report released Wednesday.
The 300-plus-page document from the National Academies of Sciences, Engineering, and Medicine detailed how structural racism and people’s surroundings have contributed to worse health outcomes for minorities. It also offers recommendations and solutions to health care organizations and the federal government, like a more diverse workforce and adjusting payment systems to make health care more affordable.
WATCH: President Joe Biden and Bernie Sanders join forces to promote lower health care costs
Dr. Georges Benjamin, executive director of the American Public Health Association and co-chair of the committee that wrote the report, said people of color in the U.S. are more likely to experience maternal and infant mortality, lower life expectancy and many chronic diseases.
“Inequities are baked into our health care system, and if we address them, everyone benefits,” Benjamin said.
Racism and bias from health care providers have also contributed to worse health outcomes, according to the report, which comes 21 years after the first from the organization.
The committee behind the report suggested that more practicing physicians who are from diverse backgrounds and from the communities they serve would improve several problem areas; studies show that people of color generally receive better care when treated by those who look like them.
The research also showed language barriers persist in health care and that trainings on bias management and ways to become more familiar with cultural issues don’t create long-term improvements in health outcomes for minorities.
WATCH: Research reveals depths of racial and ethnic bias in health care
Health care systems should work to strengthen the ties between patients and providers — so the patient has a voice in their treatment — and bring in important community voices, the report recommended.
“Health systems should work with the community to understand what their needs are, and engage them early and often,” Benjamin said.
The policies that have been put into place to bridge racial and ethnic gaps haven’t been widely implemented, the report said, and there’s little oversight to ensure their enforcement. It points out the 10 holdout states that have yet to expand Medicaid under the Affordable Care Act, as well as legal challenges that have halted broad implementation of several provisions.
The report’s authors urged Congress, the U.S. Department of Health and Human Services, National Institutes of Health and Centers for Medicare & Medicaid Services to better coordinate their health care equity plans — which the report said are siloed — and to establish a federal oversight body for the implementation of these plans.
Other suggested steps involve collecting better health care data at the federal level and providing more money for research and programs proven to reduce racial and ethnic inequities.
The quality of health care in the U.S. is not what it should be compared to other high-income countries largely “because we haven’t addressed health inequities,” said Dr. Lisa Cooper, director of the Johns Hopkins Center for Health Equity and one of the report’s reviewers. She said that became even more apparent during the COVID-19 pandemic.
“The only way we will make progress is if we really pay close attention to this issue,” she said. “We’re failing everybody in our health care system. It’s just that some groups of people are suffering even more.”
Even if it takes years, the recommendations should be implemented, Benjamin said. If not, he said, people will continue to “die unnecessarily, in an unjust way.”
The Associated Press Health and Science Department receives support from the Robert Wood Johnson Foundation. The AP is solely responsible for all content.
Support Provided By: Learn more
Support PBS News:

Educate your inbox
Subscribe to Here’s the Deal, our politics newsletter for analysis you won’t find anywhere else.
Thank you. Please check your inbox to confirm.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.10(12); 2018 Dec

Burnout in United States Healthcare Professionals: A Narrative Review
Thomas p reith.
1 Internal Medicine, Medical College of Wisconsin, Milwaukee, USA
Burnout has reached rampant levels among United States (US) healthcare professionals, with over one-half of physicians and one-third of nurses experiencing symptoms. The burnout epidemic is detrimental to patient care and may exacerbate the impending physician shortage. This review gives a brief history of burnout and summarizes its main causes, effects, and prevalence among US healthcare workers. It also lists some strategies that physicians, organizations, and medical schools can employ to counter the epidemic.
Introduction and background
What is burnout?
Broadly speaking, burnout is a combination of exhaustion, cynicism, and perceived inefficacy resulting from long-term job stress. It was first described in 1974 by the clinical psychologist Herbert Freudenberger, who often volunteered at a free clinic in the then drug-ridden East Village of New York City. Over time, Freudenberger observed emotional depletion and accompanying psychosomatic symptoms among the clinic’s volunteer staff. He called the phenomenon “burnout,” borrowing the term from drug-addict slang. Freudenberger defined burnout as exhaustion resulting from “excessive demands on energy, strength, or resources” in the workplace, characterizing it by a set of symptoms including malaise, fatigue, frustration, cynicism, and inefficacy:
There is a feeling of exhaustion, being unable to shake a lingering cold, suffering from frequent headaches and gastrointestinal disturbances, sleeplessness and shortness of breath. … The burn-out candidate finds it just too difficult to hold in feelings. He cries too easily, the slightest pressure makes him feel overburdened and he yells and screams. With the ease of anger may come a suspicious attitude, a kind of suspicion and paranoia. The victim begins to feel that just about everyone is out to screw him. … He becomes the ‘house cynic.’ Anything that is suggested is bad rapped or bad mouthed. … A sign that is difficult to spot until a closer look is taken is the amount of time a person is now spending in the free clinic. A greater and greater number of physical hours are spent there, but less and less is being accomplished. He just seems to hang around and act as if he has nowhere else to go. Often, sadly, he really does not have anywhere else to go, because in his heavy involvement in the clinic, he has just about lost most of his friends [ 1 ].
In addition, Freudenberger noted that burnout often occurred in contexts requiring large amounts of personal involvement and empathy, primarily among “the dedicated and the committed.”
Over the next decade, the social psychologist Christina Maslach built upon Freudenberger’s work. At the University of California, Berkeley, Maslach developed a model of burnout consisting of three dimensions: emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment [ 2 ]. In 1981, she proposed the Maslach Burnout Inventory (MBI), which consists of three subscales to measure the extent of an individual’s symptoms along each dimension [ 2 ]. The MBI remains the most commonly used instrument to assess burnout to this day [ 3 ].
Why should we care about burnout?
The consequences of burnout are not limited to the personal well-being of healthcare workers; many studies have demonstrated that provider burnout is detrimental to patient care. For example, the number of major medical errors committed by a surgeon is correlated with the surgeon's degree of burnout [ 4 ] and likelihood of being involved in a malpractice suit [ 5 ]. Among nurses, higher levels of burnout are associated with higher rates of both patient mortality [ 6 ] and dissemination of hospital-transmitted infections [ 7 ]. In medical students, burnout has been linked to dishonest clinical behaviors, a decreased sense of altruism [ 8 ], and alcohol abuse [ 9 ]. High rates of physician burnout also correlate with lower patient satisfaction ratings [ 10 ].
At an institutional level, burnout results in greater job turnover and increased thoughts of quitting among physicians [ 11 ] and nurses [ 12 ]. It also results in decreased workforce efficiency: a recent Mayo Clinic study estimated the loss of productivity due to physician burnout as the equivalent of eliminating seven entire medical school graduating classes [ 13 ]. Consequently, burnout may contribute to an already impending physician and nursing shortage.
How prevalent is burnout?
Attending Physicians
Over half of physicians in the United States (US) experience symptoms of burnout, a rate nearly double that of workers in other professions after controlling for hours worked, age, sex, and other factors [ 14 ]. Furthermore, burnout among physicians has shown signs of increasing. The 2013 Medscape Lifestyle Report – based on the surveyed responses of over 20,000 physicians – reported a nationwide burnout rate of 40% [ 15 ], yet the 2017 Report found a rate of 51% [ 16 ], representing a 25% increase in four years. Another recent study supports the Medscape findings, reporting a 9% increase in burnout between 2011 and 2014 [ 17 ]. Physicians working the front lines of care (emergency medicine, family medicine, internal medicine and obstetrics/gynecology (OB/GYN)) are at especially high risk for burnout, and female physicians are more likely to experience burnout than their male colleagues [ 16 ].
Nurses & Physician Assistants
Burnout is not limited to physicians. A 2001 study found that 43% of nurses working at US hospitals experience symptoms of emotional exhaustion [ 18 ], and a 2011 study reported burnout prevalences of 37% among nurses providing direct patient care in nursing homes, and 33% among hospital nurses [ 19 ]. While burnout in physician assistants is less studied, initial reports suggest it may be similarly high [ 20 ].
Residents & Medical Students
Burnout is especially prevalent among physicians in training. A 2016 study of residents of all specialties at a tertiary academic center reported an overall burnout rate of 69%, with a 78% rate among surgical residents and a 66% rate among non-surgical residents [ 21 ]. A 2009 review supports these findings, reporting overall rates of resident burnout up to 75% [ 22 ]. In medical students, burnout levels are not much better. A 2013 review estimated that at least half of students at US medical schools experience symptoms [ 23 ], and a 2018 meta-analysis of over 16,000 students worldwide found that 44% suffered from burnout [ 24 ].
What causes burnout?
Although burnout is caused by a myriad of factors, surveys of physicians have helped to identify common themes. As part of its annual Physician Lifestyle Report, Medscape gives physicians a list of possible burnout causes and asks them to rank their significance. Over the last five years, “too many bureaucratic tasks (e.g., charting, paperwork),” “spending too many hours at work,” and “increasing computerization of practice (electronic health records (EHRs)),” have consistently been ranked as three of the top four factors [ 15 , 16 ].
Too Many Bureaucratic Tasks
Today’s physicians spend a large amount of time on documentation required for a growing number of quality programs initiated by Medicare, Medicaid, and private insurance companies. Such programs cause burnout by impeding physicians from spending time with their patients [ 17 ]. On average, US physicians spend 2.6 hours per week complying with external quality measures; in an outpatient setting, this is enough time to see approximately nine additional patients [ 25 ]. Moreover, for each hour of clinical face time that physicians spend with patients, an additional two are consumed by administrative and clerical work [ 26 ]. The former president of the American Medical Association (AMA), Robert M. Wah, attempted to summarize the collective feelings of US physicians in the following statement:
Physicians want to provide our patients with the best care possible, but today there are confusing, misaligned and burdensome regulatory programs that take away critical time physicians could be spending to provide high-quality care for their patients [ 27 ].
Too Much Time at Work
The average US physician works 51 hours per week, with one quarter of US physicians working more than 60 hours per week [ 28 ]. When surveyed by the AMA, one half of physicians responded that they would prefer to work fewer hours [ 29 ]. Inverse correlations have been found between hours worked and job satisfaction. Physicians working in specialties requiring more hours report lower job satisfaction, and physicians working in specialties requiring fewer hours report higher job satisfaction [ 30 ].
Increasing Computerization of Practice
When EHRs were first introduced, they were touted as a way to streamline workflows and reduce the clerical burden on physicians. In this respect, however, EHRs have had the opposite effect of creating more work. In one recent study, primary care physicians spent nearly six hours out of an 11.4-hour workday on EHR tasks, including around 1.5 hours at night after the clinic was closed [ 31 ]. Such tasks included documentation, order entry, billing and coding, and inbox management. Put another way, physicians spent more time in the EHR than they did treating patients. In a recent interview, Steven Strongwater, CEO of Massachusetts-based Atrius Health, summarized the impact of EHRs on Atrius’s physicians as follows:
The electronic medical record has clearly added work to a physician’s day, and people who are so dedicated and committed are working late into the evenings in what we would call ‘pajama time.’ In general, what seems to happen is that our docs will work during the day — they’ll work a full day, sometimes 8 or 10 hours or longer — they’ll go home for a brief period of time, and then they’ll get back on their record in order to finish the work of the day that evening [ 32 ].
Is burnout a distinct disorder?
The validity of burnout as an independent diagnosis remains controversial. While the majority of studies use the MBI for measurement, the scales and cutoff values employed are often arbitrary. Indeed, one recent review concludes that the measurement of burnout in the literature is so heterogenous that it is impossible to conclude anything about its prevalence [ 3 ]. Another criticizes the MBI as being “neither grounded in firm clinical observation nor based on sound theorizing” [ 33 ]. A third calls it “unrealistic”:
The three-dimensional structure of the burnout syndrome is unrealistic [and] the mere fact of defining burnout as job-related is not nosologically discriminant. … The arbitrariness surrounding the elaboration of the MBI constitutes a fundamental problem, especially given the central role of the instrument in the definition of the burnout phenomenon [ 34 ].
Furthermore, the symptoms of burnout seem to overlap with those of depressive disorders. In one study, over 90% of participants assessed as “burned out” by the MBI also met diagnostic criteria for depression and scored 15 or greater on the Patient Health Questionnaire-9 (PHQ-9) [ 35 ]. In another study, depressed and “burned out” participants displayed similar attentional and behavioral alterations [ 36 ].
Burnout is also not recognized in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) , the official classification of psychiatric disorders in the United States [ 37 ].
How can we combat burnout?
Regardless of burnout’s nosological classification, an epidemic of unhappy and demoralized physicians seems worthy of acknowledgement. Unfortunately, there remains a relative paucity of evidence on how to address the problem. Still, recent research indicates that efforts at both the individual and organizational levels can prove effective; indeed, the best way forward likely involves a combination of the two [ 38 ]. To that end, major health organizations have begun developing guidelines aimed at decreasing burnout and increasing well-being. Last year, the Mayo Clinic described nine strategies that, when implemented, resulted in a 7% decrease in burnout over a two-year period [ 39 ]. In April 2018, a number of physician educators and wellness experts published a Charter on Physician Well-being [ 40 ], which presents guiding principles that individuals and groups should use when addressing burnout. Some suggestions for addressing burnout are listed below.
Involve Leadership
There is an ancient saying that the fish begins to stink at the head. In other words, problems within any organization often stem from its executive leadership. Evidence suggests that greater leadership qualities in physician supervisors decreases burnout and increases job satisfaction among the physicians they oversee [ 41 ]. Consequently, healthcare administrators must acknowledge burnout as a systemic problem and promote a culture of self-care among their employees, starting from the top down. To help accomplish this, some hospitals, such as Stanford and Mount Sinai, have created the administrative position of chief wellness officer [ 42 ]. If leadership is inadequate, however, organizations must be willing to make changes. In most companies, the board of directors has no problem ousting a CEO who is not delivering profits. Similarly, a healthcare executive overseeing a majority of unhappy physicians may need to be replaced.
Choose Incentives Wisely
Many healthcare systems motivate physicians with financial rewards, either adjusting physicians’ salaries based on productivity (i.e., revenue generation) or handing out performance-based bonuses [ 43 ]. Yet productivity-based compensation often leads to overwork and/or shortening the time spent per patient, which in turn leads to increased burnout. Such consequences are by no means a modern phenomenon. In The Wealth of Nations , the 18 th century economist Adam Smith offered the following warning:
Workmen, … when they are liberally paid by the piece, are very apt to overwork themselves, and to ruin their health and constitution in a few years [ 44 ].
To avoid these problems, organizations may want to consider performance-independent salary models or offer alternative rewards such as greater schedule flexibility or time off [ 39 ]. They may also want to incorporate measures of well-being into performance assessments [ 40 ].
Encourage a Work-Life Balance
Physicians often find it difficult to balance long hours at work with their personal lives. Organizations can help mitigate this problem by allowing physicians to work fewer hours in exchange for reduced compensation, or by granting them greater flexibility. For example, physicians could choose to start the work day earlier or later, or work longer hours on certain days and shorter hours on others. Organizations can also let physicians devote more time to their favorite aspect of work (e.g., patient care, education, administration, or research). Physicians who spend at least 20% of their time on the part of work they find most fulfilling significantly lower their chances of burning out [ 45 ]. On an individual level, physicians can work to improve their time management skills. Eliminating time used inefficiently at work allows more time to be spent at home.
Encourage Peer Support
Recent years have seen diminished personal interaction between physicians. Increased documentation requirements and the rise of EHRs have caused physicians to spend increasing amounts of time on computer systems. Moreover, doctors’ lounges – where physicians historically relaxed and discussed cases – have disappeared from many hospitals, resulting in a loss of camaraderie and an increased sense of isolation [ 42 ]. Yet evidence suggests that encouraging physician solidarity reduces burnout: when Mayo physicians engaged in one hour of small group discussions every other week, they experienced significant reductions in depersonalization and emotional exhaustion [ 46 ]. One small way for hospitals to promote physician interaction might be providing coffee and snacks at gathering spots analogous to the office “water cooler.” Recently, Stanford has taken a more creative approach, paying for small groups of doctors to dine together at local restaurants [ 42 ].
Furnish Resources for Self-care and Mental Health
Mental health remains a taboo subject among physicians, and many are reluctant to pursue treatment due to potential shame, income loss, or licensure actions [ 47 ]. Organizations can counter this stigma by helping physicians seek treatment in ways that minimize repercussions. Examples include extending the hours of confidential mental health services to include times that physicians are not at work, and/or providing coverage to allow physicians to attend appointments [ 40 ]. Organizations can also furnish resources encouraging individual physicians to practice self-care; examples include offering healthy food in cafeterias, providing mindfulness or exercise programs at the hospital or clinic, and facilitating memberships to local gyms. Furthermore, physicians can be equipped with protected time to devote to these practices.
Target Burnout from Day One of Medical School
Finally, burnout must be addressed from the onset of medical training. This problem cannot be addressed at the resident and attending levels if students are already burned out by the time they get there. Recent efforts addressing burnout at select schools have been met with success. Vanderbilt University's School of Medicine has implemented a wellness program where students promote healthy habits by holding each other accountable [ 48 ]. At Northwestern University's Feinberg School of Medicine, second-year medical students are tasked with improving their self-care by choosing a personal health behavior to change and tracking their progress towards it [ 49 ]. Perhaps the most drastic changes, however, have been made at the Saint Louis University (SLU) School of Medicine, where the curriculum has been redesigned over the past decade to reduce student stressors and “produce a less toxic educational environment.” Changes included the implementation of a pass/fail grading system, reducing unnecessary detail in coursework, and introducing electives throughout the preclinical years. As a result, SLU students experienced reductions in depression, stress, and anxiety while maintaining similar levels of academic performance [ 50 ].
Conclusions
Burnout has emerged as a major problem plaguing 21 st century American medicine. If not addressed, the burnout epidemic may continue to worsen, to the detriment of patients and physicians alike. Experts have identified good starting points to confront this problem, and it is time for healthcare institutions nationwide to put their suggestions into practice.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.

IMAGES
COMMENTS
Overall, the current paper discussed the problem of burnout among healthcare workers. Firstly, it was established that the symptoms of burnout include exhaustion, depersonalization, and reduced performance. Secondly, it was shown that this issue could have a negative impact on all the stakeholders involved in the healthcare process.
Burnout in Physicians. Burnout has been shown to occur in all kinds of jobs. However, the incidence seems to be higher in physicians. In a study comparing incidences of burnout between US physicians and a population control sample, Shanafelt et al observed an incidence of symptoms of burnout of 37.9% in physicians compared to 27.8% in the control population (p < 0.001). 23 Physicians in ...
Health worker burnout is a serious threat to the nation's health and economic security. The time for incremental change has passed. We need bold, fundamental change that gets at the roots of the ...
In the current period of global public health crisis due to the COVID-19, healthcare workers are more exposed to physical and mental exhaustion - burnout - for the torment of difficult decisions, the pain of losing patients and colleagues, and the risk of infection, for themselves and their families. The very high number of cases and deaths ...
During the COVID-19 pandemic, this systematic review and meta-analysis aims to provide a complete assessment of the prevalence of burnout across various healthcare personnel. Until January 2021, systematic searches for English language papers were conducted using PubMed, Scopus, EMBASE, Web of Science, Cochrane Library, and ProQuest.
The prevalence of burnout symptoms also increased among healthcare workers during this period with pooled prevalence between 34% and 52% [3, 4]. In the ICD-11, the World Health Organization defines burnout as 'a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed' .
COVID survey finds more than half of healthcare workers stressed, overworked, and ready to leave. Although much focus has been placed on physician and nurse burnout, a new study finds the COVID-19 pandemic increased stress across the entire healthcare workforce. Led by Brigham and Women's Hospital investigators, the survey included over ...
Burnout is an occupational phenomenon and we need to look beyond the individual to find effective solutions, argue A Montgomery and colleagues Burnout has become a big concern within healthcare. It is a response to prolonged exposure to occupational stressors, and it has serious consequences for healthcare professionals and the organisations in which they work.1 Burnout is associated with ...
DOI: 10.7759/cureus.3681. Work-related stress can lead to burnout for anyone. Even before the COVID-19 pandemic, it was especially prevalent among healthcare workers (HCWs) [i]. Based on initial responses to MHA's Healthcare Worker Survey, many frontline employees have experienced increases in sleep trouble, physical exhaustion, emotional ...
Burnout among healthcare professionals is thought to affect the standard of treatment, but little is known about how consistently and significantly it affects patient outcomes. The performance (quality, patient experience) and safety of the treatment are often connected to provider burnout (emotional weariness, depersonalization, and lower ...
Jean Watson. ABSTRACT. Work-related stress (of which burnout might be an example) is one of the most common work-related health problems. Currently, psychiatric illness (particularly depression, anxiety disorders, and stress related conditions) is the most common cause for long-term sick-leave in Sweden for women, and the second largest for men.
Nurse burnout is a significant problem in the healthcare industry. It affects both the well-being of nurses and the quality of patient care. Workplace interventions, such as wellness programs and professional development opportunities, have shown promise in reducing burnout and improving nurses' job satisfaction (Johnson et al., 2017).
Healthcare organizations continue to feel the effects of the COVID-19 pandemic, including prolonged workforce shortages, rising labor costs, and increased staff burnout. 1 The World Health Organization defines burnout as "a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed," with symptoms including "feelings of energy depletion or ...
Implementing strategies to mitigate burnout in healthcare involves fostering a supportive work environment, promoting teamwork, and providing resources for emotional support and resilience training. Overall, optimizing workload, reducing excesive working hours and sharing tasks are important for improving job performance, yet it is also ...
Healthcare professionals are in the midst of one of the most challenging and traumatic periods in the history of healthcare in America. Dealing with the COVID-19 pandemic has taken its toll, exacerbating burnout and mental health issues to extreme levels. We've worked with our friends at Headspace to look at the impacts of burnout on mental ...
Jerry L. Halverson, MD, FACPsych, DFAPA, is a board-certified adult psychiatrist with a subspecialty in Consult Liaison Psychiatry. He serves as senior physician executive for Rogers Behavioral Health supporting strategic planning for future growth, external partnerships, and physician recruitment. He has been honored by his colleagues for clinical and leadership excellence, receiving numerous ...
Many experts are calling attention to a so-called burnout epidemic among workers. Unfortunately, healthcare workers are being especially impacted. Both of us have seen that impact firsthand ...
The COVID-19 pandemic exacerbated already rising rates of burnout among American health care workers. A new Northwestern University study found learning and practicing skills that increase positive emotion like gratitude, mindful awareness and self-compassion helped improve health care workers' well-being and reduce stress and anxiety.
Guest Essay. Doctors Aren't Burned Out From Overwork. ... burnout. Nearly two-thirds of ... It's revealing to look at the crisis among health care workers as at least in part a crisis of ...
Effects on Healthcare Workers and on Healthcare Systems. A first direct effect of burnout is, of course, on HCWs' own care and safety. The rate of depressive disorder among HCWs is alarming when compared with that of the general population and is closely related to high levels of occupational stress ().During the COVID-19 outbreak, a relatively high prevalence of anxiety (24.94%), depression ...
Investigating links between stress, burnout, mental state, and well-being among healthcare workers in the Czech Republic revealed that emotional exhaustion, a core component of burnout, was associated with increased feelings of anxiety and depression. Stress and burnout can negatively affect performance, mental health, and the overall well-being of healthcare workers. The study aims to examine ...
Introduction. Clinician burnout is a threat to US health and health care. 1 At more than 6 million in 2019, 2 nurses are the largest segment of our health care workforce, making up nearly 30% of hospital employment nationwide. 3 Nurses are a critical group of clinicians with diverse skills, such as health promotion, disease prevention, and direct treatment.
The Accelerated Recovery Program (ARP) is a program developed to reduce compassion fatigue, including secondary traumatic stress and burnout in healthcare professionals. The ARP was originally developed in 1997 [ 110 ], based on Figley's work on compassion fatigue (1995).
The score of the Integrative Burnout Index ranges from 48.99 in students of the [BLINDED] University to 23.52 in psychiatrists of the Alekseev Psychiatric Hospital N1. Occupational burnout syndrome is spread in medical students worldwide, with its level higher than in the overall population, in students of other specialties.
Purpose: In this study we aimed to assess the range of psychopathological symptoms (anxiety, stress, depression, burnout) and risk factors in frontline HCWs during spring and autumn outbreaks of the new coronavirus infection in Russian Federation. Methods: We conducted two independent, cross-sectional hospital-based online surveys. . Data of 2195 HCWs were collected between May 19th and May ...
The team recommended that healthcare stakeholders consider several factors when designing and implementing clinical decision support to minimize clinician burnout. "End-users should be involved in all aspects of design, pre-testing, and implementation.
The 300-plus-page document from the National Academies of Sciences, Engineering, and Medicine detailed how structural racism and people's surroundings have contributed to worse health outcomes for ...
A covert campaign to target a writer critical of the country's Communist Party has extended to sexually suggestive threats against his 16-year-old daughter. Deng Yuwen, a Chinese dissident ...
The European Union will impose economic penalties aimed at some shipments of Russian natural gas, hoping to deprive Moscow of income. By Melissa Eddy The European Union has agreed to a new raft of ...
Burnout has reached rampant levels among United States (US) healthcare professionals, with over one-half of physicians and one-third of nurses experiencing symptoms. The burnout epidemic is detrimental to patient care and may exacerbate the impending physician shortage. This review gives a brief history of burnout and summarizes its main causes ...