

How to Write an Evidence-Based Practice Paper in Nursing
Some call it an EBP paper while some evidence-based research paper, and it comes in many other forms as well, including EBP case reports, EBP capstone projects, EBP coursework, or EBP thesis. Regardless of the name, without explicit knowledge on how to write an evidence-based practice paper, you cannot wrap your mind around it. Evidence-based papers are written by students so that they can develop confidence, research interests, critical thinking, creativity, and decision-making skills that are applicable in real-world clinical settings.
Any nursing school student must write an evidence-based practice paper. In most cases, EBP papers can come in the form of change management papers where quality improvement processes are recommended. To avoid making blunders when writing, it is vital to grasp the entire writing process.
Unlike other nursing papers and essays, evidence-based practice papers require in-depth reasoning, research, and reading. We acknowledge that writing a great evidence-based paper that is gradable takes sweat and is very challenging.
We have compiled this guideline for writing an evidence-based nursing paper to ease the burden on your side. If you quite can't find it easy even after reading this article, we have experienced nursing paper writers who can always help you.
We are the best nursing paper writing service; we do this to help you take care of your wellbeing, achieve freedom, and extend your time caring for others in your clinical. Let us dig right into it, won't we?
What is Evidence-Based Practice?
Evidence-Based Practice in the field of nursing focuses on the premise that medical practice should focus on adapted and developed principles through a cycle of evidence, research, and analysis of theory. Evidence-based practice intends to address the changes in practice based on the nursing and non-nursing theories developed through proper research.
In nursing, the implementation of EBP comes in the form of a systematic review, where research is reviewed based on a particular guideline to determine its suitability for being used as a gold standard in practice.
The systematic review helps in sense-making from the mammoth of information available for effective change management, implementation, and institutionalization.
The EBP process involves six significant steps:
- Assessment of the need for change : This entails the formulation of a research question or hypothesis based on the gaps in current practice.
- Location of the best evidence : Depending on the levels of nursing resources or evidence, the next step entails assessing the credibility, reliability, and relevance of the evidence or peer-reviewed articles.
- Synthesis of evidence : This step involves the comparison and contrast of available sources of evidence to establish similarities and differences to determine the best course of approach.
- Designing change : through the results of the synthesis of the available evidence, the next step is to create an effective change based on the evidence collected. It also involves drafting the change implementation plan within the clinical setting.
- Implementing and Evaluating Change : After the design comes to the process of initiating the change through change advocates such as nurse leaders and nurses themselves, it is the phase where the new process is established into practice. Various change management theories can be followed to ensure the fruition of the change management plan.
- Integration and Sustaining Change : Once the new evidence has been used to implement change, it is adopted through policy or guidelines within the clinical settings. It also entails the process of continuous improvement to achieve the best.
Steps of Writing an EBP Research Paper in Nursing
Once you have been assigned to write an evidence-based paper, you need to follow the steps below to write the best essay.
1. Choose a Topic for your Paper
There are many methods you can use when choosing an EBP topic. You can get ideas from your coursework, peer-reviewed sources, class assignments, and past evidence-based projects done. Thanks to the Internet, there are various evidence-based practice topic ideas. However, choose a topic that resonates well with your passion and interest in nursing practice. For instance, if you are looking forward to improving patient flow in the ED using technology, be sure that you are cognizant of such technology as EHR or HIT. Begin by exploring the assignment and make some notes; you should then settle for a tentative topic.
2. Consult with your Professor/Instructor
Nursing education, just like nursing practice, calls for collaboration and getting feedback. Therefore, once you have selected a creative, evidence-based practice topic , you must make an appointment with either the writing center or the professor/instructor for confirmation. In some instances, your professor/instructor will request for an evidence-based practice proposal. In the EBP proposal, you must state the nursing issue you intend to solve, the change management process, and the rationale for the change. If it is convincing enough, you will get a go-ahead. Otherwise, you will need to revise the EBP nursing proposal.
Tip: SELECT a good health indicator (disease, health conditions, working/living conditions) , DESCRIBE the population or sub-population of the target, find EVIDENCE of around 7-10 peer-reviewed sources that support your proposal, and DESCRIBE the intended outcomes and rationale of the change proposed in the clinical setting.
Some of the health indicators you can use for your EBP paper include socio-economic status; gender, education, environment, employment, genetic endowment, culture, child development, healthcare services, access, quality, cost of care, social support, coping skills, etc.
The EBP papers can include a change model, population health model, nursing theory, and nursing interventions and each must be justified using credible evidence.
3. Gathering Supporting Evidence - Research
The backbone of an evidence-based paper is evidence. Therefore, you need to extensively research both online and print sources to get facts to support your EBP paper thesis statement. Once you have developed the problem statement and outlined the thesis statement, you should critically evaluate the sources to determine those that support the thesis.
In some instances, the instructor might request you to write an annotated bibliography or critically analyze each of the articles or the main article that supports your evidence-based practice paper. A common approach is through using an evidence evaluation table. When selecting the sources, remember that there are both primary and secondary sources.
You can get primary and secondary sources from databases such as PubMed, EBSCO, UpToDate, TRIP Database, OVID, The Cochrane Collaboration, and CINAHL. Besides, you can depend on .gov, .org, and .edu websites to get information. Professional and government organizations, as well as NGOs, can be a starting point of research. They are an excellent resource for statistics, epidemiology data, and further information. Excellent research means that the research question, hypothesis, and thesis statement will be supported and answered.
Related: How to write a great thesis statement for any paper.
Deciding on the Best Resources for EBP Papers
There are primary and secondary data sources when it comes to scientific writing. Instead of collecting and analyzing real data as students do for qualitative and quantitative or mixed methods thesis, dissertation, and research papers, an EBP paper is purely based on the published findings from primary research. It is imperative, therefore, that a nursing student only uses credible, valid, and reliable sources. Here are three criteria to select a good source for your EBP paper:
- A research journal article is only reliable if published in a reliable database/journal and is peer-reviewed. It depends on the level of the evidence as well. Will the same test yield similar results if replicated?
- A valid research study has followed the strict research protocols, is up to date, and is relevant to the chosen EBP paper topic selected. Does the study measure what it says it intends to measure?
- Credible research that can be incorporated into an EBP paper must have verifiable findings, published in a reputable journal, and is scholarly. Is the research study from a reputable journal?
- Is the research report, article, or journal primary research such as qualitative research, quantitative research, randomized controlled trial, controlled case studies, or quasi-experimental study?
It is only natural that you can dislike the entire process of writing an EBP paper, not because you don't know how to, but probably because of the strict and laborious process. If this is the case, our nursing writing service is all you need for your peace of mind. We have experienced nursing assignment help experts who can craft the best papers for you. Stop, think about it, and let us know if you need some help.
Related reading: How to title an article in an academic paper.
Outline of an Evidence-Based Practice Paper
A good evidence-based paper in nursing must have several parts, each of which are completed with precision, care, and wit. If you have researched online for evidence-based practice paper examples , you will agree with us that the format or structure is more or less as broken down below. It is the same structure you will see on an evidence-based practice paper template that you will likely receive from class. Here is a critical breakdown of what to include in your nursing evidence-based practice paper:
1. Title of the EBP Paper
A good title will either attract and keep or turn off your audience, instructor/professor. Therefore, having an excellent title for your evidence-based practice case study, report, write-up, or research paper is paramount. The title aims to set the scope of the EBP paper and provide a hint about the hypothesis or thesis statement. It is, therefore, imperative that it is concise, clear, and fine-tuned. If you decide to write the title as a question, you could paraphrase the PICOT statement, for example. Otherwise, it can also take forms such as statements or facts opposing the status quo. Whichever direction you choose to align to, the aim remains constant to give more insight to the reader from the onset.
2. Thesis Statement
While the PICOT statement can already tell what your entire EBP paper is all about, you need to develop a great thesis statement. A thesis statement, usually the last sentence or two, is like a blueprint of the entire paper. It is the foundation upon which the whole paper is built. Take note that a thesis is not a hypothesis, which is an idea that you either want to prove or refute based on a set of available evidence. An evidence-based practice paper with a thesis ultimately earns the best grade without leaving the reader to look for it the entire paper.
The thesis statement must be specific, manageable, and enjoyable. A sample EBP thesis statement can be: According to new developments in genomics and biotechnology, stem cells have reportedly been used in breast cancer treatment with higher chances of remission in the patients. Novel approaches to pain management dictate that a nurse must obtain three kinds of knowledge to respond effectively to patients' pain: knowledge of self, knowledge of standards of care, and knowledge of pain.
A thesis can also be an implied argument, which makes it descriptive. However, not so many professors like such. This paper discusses
3. Introduction
The introduction of evidence-based practice must reflect certain elements. First, you must present a background to the research question or nursing issue. It would help if you also painted a clear picture of the problem through a thorough and brief problem statement and at the same time, provide the rationale. You can organize your intro into a PICO:
Patient/Problem : What problems does the patient group have? What needs to be solved?
Intervention : What intervention is being considered or evaluated? Cite appropriate literature.
Comparison : What other interventions are possible? Cite appropriate literature.
Outcome : What is the intended outcome of the research question?
The thesis statement we have discussed above then comes in as either a sentence or two in the last part of the introduction. The research problem should help generate the research question or hypothesis for the entire EBP paper.
4. Methodology
As indicated before, an EBP research paper does not focus on research; instead, it focuses on a body of knowledge or evidence. For that matter, when writing an EBP paper, you only collect data from literature produced on your chosen topic. A confusing bit when researching evidence to use is deciding on what level of evidence to use. There are systematic reviews, literature reviews, white papers, opinion papers, practice papers, peer-reviewed journals, critically appraised topics, RCTs, Case-controlled studies, or cohort studies, you name it. You must decide which level of evidence is appropriate. It trickles down to the scholarly source's validity, reliability, and credibility. Your methodology should include:
- The databases you searched, the search terms, the total articles yielded per search, the inclusion and selection criteria, the exclusion criteria.
- You should indicate the inclusion and exclusion criteria for the articles and the number of articles you finally end up with.
You can further choose to use knowledge as evidence based on authority, a priori, theory, and tenacity, as advised by Fawcett and Garity in their book Evaluating research for evidence-based nursing practice.
5. EBP Literature Review
In the literature review section, you aim to explore the associations of the evidence chosen given your topic. It aims at either finding the gap in those studies or using the knowledge to build on the topic. For instance, if you are to come up with a new management approach for pressure ulcers in palliative care, choose credible evidence on the topic. Find the effectiveness of your proposed approach in other environments, what works well, and what precautions should be taken. It is more of comparing and contrasting the sources. You also ought to be critical as it is the only way you can develop the best EBP paper. It is here that you report your findings from the literature. You can do it in the form of a table outlining the aspects of each study including demographics, samples, methodology, and level of evidence, results, and limitations.
6. Discussion
Like any other professional research setting, the discussion section often discusses the changed practice, implementation approach, and evaluation strategies. This can be your approach as well in your EBP paper. However, go further to explore how the findings led to a given change in practice, the efficiency after that, and suggest the best strategy for implementing the change in your chosen organization. Make comparisons if necessary.
7. Conclusion
In your conclusion, you should wind up the paper, summarize the EBP paper, and leave the readers satisfied. Your revamped thesis statement can feature in the conclusion. Make your conclusion count.
Finally, your EBP paper must have references, works cited, or a bibliography section. You realize that most EBP papers are written in either APA formatting or Harvard formatting .
Furthermore, it would be best if you wrote your abstract section last, which is about 150-250 words. It aims to offer a highlight of the entire evidence-based paper.
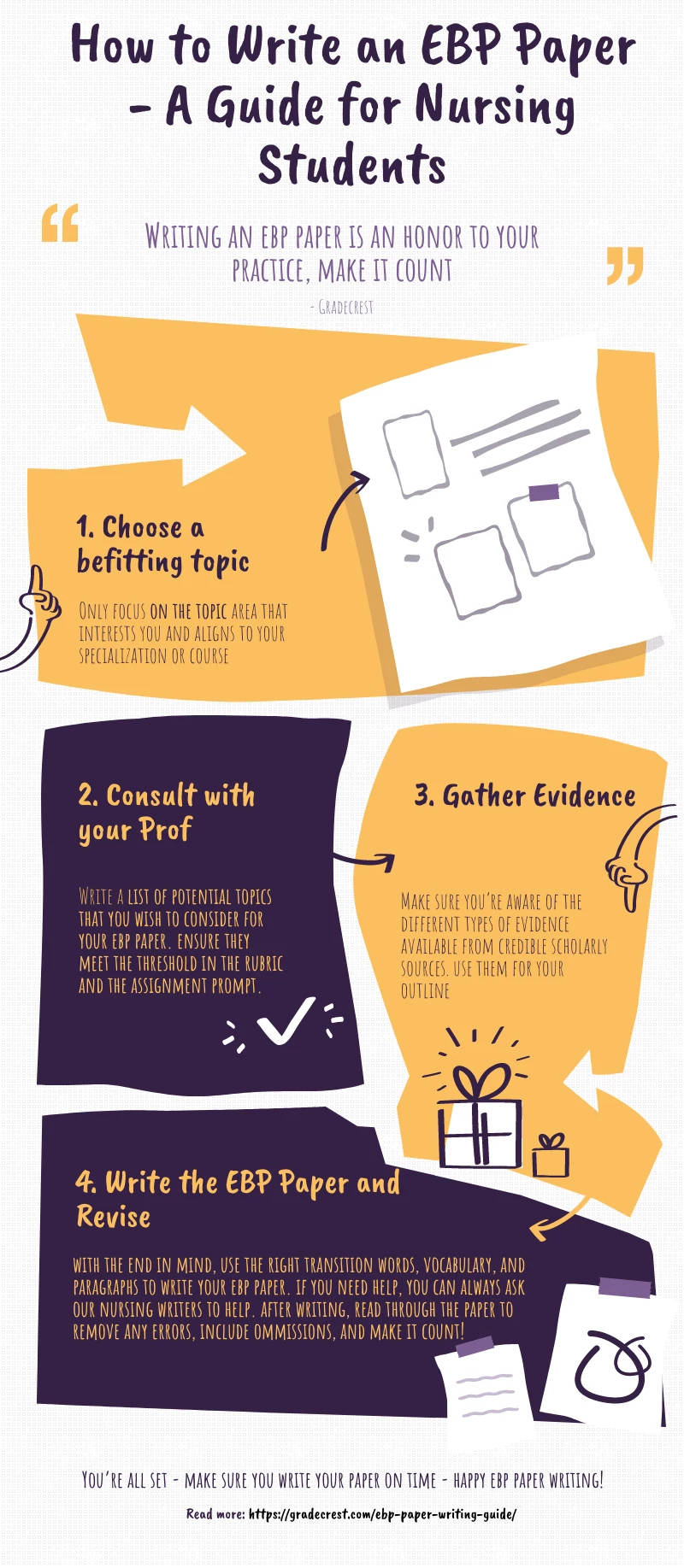
Here is a graphic/visual representation of the entire EBP writing process for students.
You can Buy Evidence-Based Papers in Nursing Here!
If your worry was how to write an evidence-based practice paper in nursing at the beginning, it is possible that you feel like a pro to this end. It is a super feeling that every reader who interacted with our article on how to write nursing care plans had, and they suggested we do this article as well.
As the best nursing assignment help service , we gave in to the pressure and put our best feet forward. We intend to create a resource for nursing students and learners. We also have expert writers to help in various academic fields. If you feel stuck with anything, do not hesitate to ask for help.
You can get a sample EBP research paper to benchmark on as you complete your nursing evidence-based research paper. Apart from the EBP research paper examples online, we offer you the chance to have a custom sample that matches your instructions.
In this article, we have answered the question: what is EBP? What is an EBP research paper? and how to write an APA evidence-based research paper in nursing.
If you are far ahead in your nursing level, our article on nursing capstone ideas can also be an excellent place to sojourn and drink from the fountain of wisdom. The students who have sourced examples of evidence-based practice assignments from us have ended up mastering concepts. Do not just wait, be part of the excelling team!

Gradecrest is a professional writing service that provides original model papers. We offer personalized services along with research materials for assistance purposes only. All the materials from our website should be used with proper references. See our Terms of Use Page for proper details.

1.2 Evidence-Based Practice
Learning objectives.
By the end of this section, you will be able to:
- Analyze how different theories influence nursing knowledge
- Describe how nursing research has evolved
- Identify the steps for translating evidence-based research into evidence-based practice
This section will explore the world of nursing theory and how it has shaped evidence-based practice (EBP) and the nursing profession as a whole. As nursing evolved from reliance on complete medical direction into independent professional practice, nursing theories were developed by leaders in the field to shape nursing practice into what it is today. This section will guide you through these important aspects, helping you grasp the connections between theory, research, and practice.
Interdisciplinary Theories Used in Nursing
A theory that integrates knowledge and concepts from one or more disciplines to enhance nursing practice, research, and education is known as an interdisciplinary theory . These are an essential part of nursing as they provide a broader perspective and more comprehensive understanding of healthcare issues.
In nursing, interdisciplinary theories are used in various ways. They assist in the development of nursing models and frameworks that guide the delivery of patient care. By incorporating theories from disciplines such as psychology, sociology, and biology, nurses can better understand the complex factors influencing health and apply holistic approaches to patient care.
Interdisciplinary theories also facilitate collaboration among healthcare professionals from various disciplines. Nurses frequently work as part of interdisciplinary teams, including physicians, therapists, social workers, and others. By understanding and integrating theories from different fields, nurses can effectively communicate and collaborate with team members, promoting coordinated and holistic patient care.
General Systems Theory
The general systems theory is a conceptual framework that describes how systems function and interact with their environment (American Psychological Association, 2023). General systems theory views the world not as a collection of individual elements operating independently, but as a network of interconnected systems. A system is defined as a set of elements that are interrelated and work together to achieve a common goal. An element can be an object, person, process, or concept. General systems theory emphasizes the interdependence, relationships, and dynamics within and between systems.
General systems theory is highly beneficial in healthcare settings as it provides a holistic perspective and promotes a comprehensive understanding of complex healthcare systems. It encourages healthcare professionals to view the entire system, including patients, healthcare providers, and community resources, as interconnected components. By adopting a systems thinking approach, healthcare teams can analyze the relationships and interdependencies within the system, identify patterns, and address underlying causes of problems.
Adaptation Theory
Roy’s adaptation model , developed by nursing theorist Sister Callista Roy, is a conceptual framework based on the belief that individuals strive to maintain balance and achieve a state of equilibrium in response to changes in their internal and external environments, and aims to promote adaptation for optimal health and well-being (Marudhar & Josefina, 2019).
According to Roy’s adaptation model, adaptation is influenced by both internal and external stimuli. An internal stimulus includes physiological, psychological, and cognitive factors, while an external stimulus encompasses the physical, social, and cultural aspects of the environment.
Roy’s model proposes four major adaptive modes: physiological, self-concept, role function, and interdependence. These adaptive modes represent different aspects of an individual’s life and are interconnected ( Figure 1.4 ). The model also highlights the importance of coping strategy mechanisms and the role of the nursing profession in facilitating adaptive responses.
Nurses using Roy’s adaptation model assess individuals’ adaptive responses, identify stimuli that may disrupt adaptation, and intervene to promote adaptation. Interventions may include modifying the environment, providing education and support, or assisting individuals in developing effective coping strategies. See 1.1 Principles of Nursing Practice for a more detailed description of strategies that nurses can give to their patients to help promote adaptation and adapt effective coping strategies.
Developmental Theory
A developmental theory is a framework that aims to explain and understand how individuals grow, change, and develop across various stages of life, emphasizing the interaction between biological, cognitive, social, and emotional factors in shaping human development. Erik Erikson’s psychosocial development theory and Abraham Maslow’s hierarchy of needs theory are two of the most important developmental theories that have influenced nursing theory .
Erikson’s psychosocial development theory outlines eight stages of human development, each characterized by a unique psychosocial crisis or challenge (Orenstein & Lewis, 2022). These stages span from infancy to old age and emphasize the importance of successfully resolving these crises for healthy psychosocial development ( Figure 1.5 ). Nursing theories influenced by Erikson’s model recognize the significance of addressing psychosocial aspects of patient care, such as identity, intimacy, and generativity. These theories focus on promoting patients’ psychological well-being, fostering positive relationships, and supporting patients in their developmental journeys. Examples include Jean Watson’s caring science and human caring theory, Imogene King’s theory of goal attainment, and Betty Neuman’s systems model.
On the other hand, Maslow’s hierarchy of needs theory posits that individuals have a hierarchical structure of needs, ranging from basic physiological needs to self-actualization (Toney-Butler & Thayer, 2023). This theory suggests that individuals must fulfill their basic physiological and safety needs before progressing to higher-level needs such as belonging, self-esteem, and self-actualization. Nursing theories inspired by Maslow’s model prioritize providing holistic care that addresses patients’ physiological, psychological, and social needs. Examples include Hildegard Peplau’s theory of interpersonal relations, Virginia Henderson’s nursing theory, Madeleine Leininger’s culture care theory, and Sister Callista Roy’s adaptation model.
These theories emphasize the importance of creating a supportive and nurturing environment that promotes patients’ well-being and enables them to reach their full potential. Figure 1.6 depicts Maslow’s hierarchy and illustrates the various human needs encompassed by holistic care.
Both Erikson’s and Maslow’s theories have influenced nursing theorists in recognizing the importance of addressing the multidimensional needs of patients. They have contributed to the development of nursing theories that embrace a holistic perspective, acknowledging the influence of psychological, social, and developmental factors on patients’ health and well-being.
Nursing Theory
The nursing theory refers to a set of organized concepts, principles, and relationships that guide and inform nursing practice. It is a systematic and evidence-based framework developed by nursing theorists to describe, explain, predict, and prescribe nursing care. Ultimately, nursing theories shape how nurses interact with their patients.
Framework of Nursing Theory
The framework of nursing theory provides a structured and organized approach to understanding and applying nursing concepts and principles. It serves as the foundation ( Table 1.1 ) upon which nursing theories are built and helps to organize and categorize nursing knowledge.
| Key Components of Nursing Theory Framework | Definition |
|---|---|
| Concepts | Concepts are the building blocks of nursing theory. They are abstract ideas or phenomena that represent various aspects of nursing practice and patient care. Examples of nursing concepts include health, environment, nursing process, adaptation, and caring. |
| Propositions | Propositions are statements that describe the relationships between concepts within a nursing theory. They articulate the connections and interactions between different elements of the theory and provide a basis for understanding and explaining nursing situations. |
| Assumptions | Assumptions are underlying beliefs or values that guide the development and application of nursing theory. They are the foundation upon which theories are built and shape the perspective and approach of the theory. Assumptions may relate to the nature of health, the role of the nurse, or the influence of the environment, among others. |
| Models or frameworks | Some nursing theories are presented in the form of models or frameworks that provide a visual representation of the theory’s key concepts, relationships, and processes. These models or frameworks offer a visual guide for understanding and applying the theory in practice. |
The framework of nursing theory is dynamic and evolves as new knowledge and evidence emerge. Nursing theories and their frameworks contribute to the development of EBP, improve patient outcomes, and enhance the professional identity and autonomy of the nursing profession. There are two main types of nursing theories: descriptive and prescriptive.
Descriptive Theories
A descriptive theory in nursing, also known as phenomenological theories, focuses on describing and understanding the lived experiences of individuals in the context of health care (Watkins, 2020). These theories aim to provide a deeper understanding of the meaning and significance of various phenomena related to health, illness, and nursing care.
Descriptive nursing theories often employ qualitative research methods to explore and analyze the subjective experiences, perspectives, and perceptions of patients, families, and healthcare providers. They seek to uncover the essence of these experiences and the underlying meanings attributed to them. These theories may explore topics such as the experience of chronic illness, the process of decision-making in health care, the impact of cultural beliefs on health behaviors, or the challenges faced by nurses in providing end-of-life care. They delve into the lived experiences of individuals to gain insights into the complexity and nuances of healthcare phenomena.
Leininger’s theory of culture care diversity and universality is an example of a descriptive nursing theory . This theory focuses on describing the impact of cultural beliefs, values, and practices on health and nursing care (McFarland & Wehbe-Alamah, 2019). It explores how individuals from different cultural backgrounds experience and perceive health, illness, and health care, highlighting the importance of cultural competence in nursing practice.
Prescriptive Theories
A prescriptive theory in nursing provides guidance and direction for nursing practice by offering recommendations, interventions, or guidelines to achieve desired outcomes (Watkins, 2020). These theories focus on prescribing actions or strategies that nurses can implement to promote health, prevent illness, and facilitate healing. One example of a prescriptive nursing theory is Watson’s theory of human caring . Watson’s theory emphasizes the significance of caring in nursing practice (Watson Caring Science Institute, 2023). It prescribes that nurses should demonstrate genuine caring attitudes, compassion, and empathy toward patients. Nurses then integrate caring behaviors into their interactions, creating a healing environment that nurtures the physical, emotional, and spiritual well-being of patients.
Concepts of Nursing Theories
The nursing metaparadigm refers to the four foundational concepts that are central to the discipline of nursing (Deliktas et. al, 2019). These concepts are person, environment, health, and nursing. They form the overarching framework that guides nursing theory, research, and practice ( Figure 1.7 ). The nursing metaparadigm guides nurses in understanding the interconnectedness of the person, environment, health, and nursing, and serves as a foundation for delivering patient-centered and evidence-based care.
The person refers to the individual, family, group, or community receiving nursing care. It recognizes that each person is unique, with physical, emotional, social, and spiritual dimensions. Nurses support the concept of person by considering the patient’s beliefs, values, and preferences when developing a plan of care.
Environment
The environment encompasses the physical, social, cultural, and economic settings in which the person exists. It includes both the immediate healthcare setting and the broader societal and environmental factors that can influence health outcomes. Nurses support the concept of environment by recognizing the impact of the environment on the patient’s well-being and working to create a supportive, safe, and healing environment.
Health encompasses the physical, mental, and social well-being of the person. It goes beyond the absence of illness and emphasizes optimal functioning and quality of life. Nurses support the concept of health by providing education and preventive care, managing symptoms, and facilitating the person’s overall well-being.
Nursing is the art and science of providing care to individuals, families, communities, and populations. It involves the application of knowledge, skills, and compassion in promoting and maintaining health, preventing illness, and supporting individuals in their healing processes. Nursing is characterized by utilizing a unique body of knowledge, ethical principle s, and commitment to provide holistic care.
Evolution of Nursing Research
Nursing research has undergone significant evolution over time, transitioning from a tradition-based practice to a scientifically rigorous discipline. Initially, nursing relied on personal experience and tradition, but beginning in the nineteenth century, the need for evidence-based practice became evident (U.S. Department of Health and Human Services, n.d.). The term evidence-based practice (EBP) refers to the integration of the best available research information, clinical expertise, and patient preferences or values to guide healthcare decision-making and improve patient outcomes ( American Nurses Association (ANA) , 2023). With the establishment of research organizations and journals, nursing research gained recognition and contributed to the improvement of patient care. The adoption of different kinds of research methodologies allowed for more robust investigations into nursing education, practice improvement, and patient outcomes. The emergence of EBP ( Table 1.2 ) further integrated research findings into nursing practice, ensuring that decisions are based on the best available evidence. Nursing research has expanded its focus to encompass diverse topics such as chronic illness management, mental health, and healthcare disparities. Technological advancements and interdisciplinary collaborations continue to shape the evolution of nursing research, further advancing the field and its impact on patient care.
| ANA Standard 13, Evidence-Based Practice and Research |
|---|
| The ANA’s Standards of Professional Performance are a set of guidelines that outline the behaviors and competencies expected of nurses in their professional roles. These standards encompass various domains, including quality of care, professional practice evaluation, education, collaboration, ethics, research, resource utilization, leadership, and advocacy. |
| Standard 13, Evidence-Based Practice and Research, states “the registered nurse integrates evidence and research findings into practice” (American Nurses Association, 2021). |
| The ANA Standard 13 on Evidence-Based Practice and Research is an indispensable cornerstone of nursing practice. This standard is paramount because it emphasizes the integration of the best available evidence into clinical decision-making. By adhering to Standard 13, nurses are equipped with the tools to critically appraise research, identify relevant findings, and translate them into evidence-based interventions. This elevates nursing practice by ensuring that patient care is grounded in scientifically sound principles. Moreover, embracing evidence-based practice fosters a culture of lifelong learning and professional growth. By implementing this standard, nurses become steadfast advocates for quality and safety, driving the delivery of patient-centered care. |
Protection of Human Rights in Nursing Research
The protection of human rights is of utmost importance in nursing research to ensure the ethical treatment of participants and uphold their dignity, privacy, and well-being (Burke, 2023c). Several principles and guidelines are in place to safeguard human rights during the research process:
- Informed consent: Obtaining informed consent is a fundamental requirement in nursing research. Participants must be provided with comprehensive information about the study, including its purpose, procedures, risks, benefits, and their right to withdraw at any time. Informed consent ensures that individuals can make voluntary and autonomous decisions about their participation.
- Confidentiality and privacy: The ethical and legal duty to safeguard and protect sensitive and private information from unauthorized disclosure or access, ensuring it remains secure from others is known as confidentiality . Respecting the confidentiality and privacy of research participants is crucial. Nurses must take measures to protect participants’ identities and ensure that data are handled securely. Confidentiality allows individuals to share sensitive information without fear of it being disclosed to unauthorized individuals.
- Beneficence and nonmaleficence: Nursing researchers have an ethical obligation to promote the well-being of participants (beneficence) and minimize any potential harm (nonmaleficence). This includes carefully designing research protocols, minimizing risks, and monitoring participants’ welfare throughout the study.
- Research ethics committees: Institutional review boards or research ethics committees play a vital role in safeguarding human rights in nursing research. These committees review research protocols to ensure that ethical principles are upheld, participants’ rights are protected, and potential risks are minimized.
- At-risk populations: Special considerations must be given when conducting research involving at-risk populations. The term at-risk population refers to a group of individuals who are at higher risk of experiencing adverse health, social, or economic outcomes due to various factors such as limited access to resources, socioeconomic disparities, or health conditions. This includes children, older adults, individuals with cognitive impairments, or those with limited decision-making capacity. Extra safeguards are necessary to protect the rights and welfare of these individuals.
- Ethical guidelines and standards : Nursing research adheres to ethical guidelines and standards and national regulatory bodies’ guidelines. These documents provide ethical frameworks and principles that guide researchers in conducting ethical and responsible research.
By upholding the protection of human rights in nursing research, nurses contribute to the integrity, validity, and ethical conduct of research. Ensuring participants’ autonomy, privacy, confidentiality, and overall well-being enhances the trustworthiness of research findings and upholds the ethical principles central to the nursing profession.
Link to Learning
The U.S. Department of Health and Human Services offers free, comprehensive training on human research protections on their website. This training is mandatory for researchers who wish to participate in studies involving human subjects that are funded by the National Institutes of Health (NIH) . Certificates can be printed for each lesson to demonstrate completion of the course.
Methodology of Nursing Research
Nursing research methodology uses both quantitative and qualitative research methods ( Figure 1.8 ). The quantitative research refers to a systematic and empirical approach that involves the collection, analysis, and interpretation of numerical data to answer research questions and explore phenomena related to health care. Quantitative research provides numerical data and statistical analysis, allowing for objective measurements, generalizations, and statistical significance. It helps identify trends, assess treatment effectiveness, and inform evidence-based practice.
On the other hand, qualitative research in nursing refers to a systematic and subjective approach that focuses on understanding and interpreting human experiences, meanings, and social phenomena in the context of health care. Qualitative research explores the subjective experiences, perspectives, and meanings behind healthcare phenomena through in-depth interviews, observations, and narratives. It provides rich, contextual insights into patients’ lived experiences, healthcare provider interactions, and social determinants of health. By combining both approaches, nurses can obtain a holistic view of patient care, integrating objective data with the humanistic aspects of health care (Curtis et al., 2016).
Quantitative Research
Quantitative research is a methodical investigation that utilizes statistical analysis and objective measurements to generate numerical findings. Statistical analysis techniques are used to summarize the data, draw conclusions, and test hypotheses. Quantitative research aims to identify patterns, relationships, and associations between variables ( Table 1.3 ). The results of quantitative research are presented using statistical tables, charts, and statistical measures such as means, percentages, correlations, or regression analyses.
| Type | Description |
|---|---|
| Correlational | The researcher aims to identify a relationship between two variables, without any outside influence (extraneous variables). A positive correlation means both variables change in the same direction, a negative correlation means the variables change in opposite directions, and a zero correlation means there is no relationship observed. |
| Descriptive | The researcher observes and measures variables in order to identify trends, or to understand a population, phenomenon, or situation. |
| Experimental | The researcher aims to identify the relationship between two or more variables using the scientific method. The researcher has control over the extraneous variable, and can recreate and verify the outcomes. |
| Quasi-experimental | The researcher aims to identify a relationship between two variables, but participants are placed in random groups (extraneous variables) to compare results. |
| Survey | The researcher uses surveys to collect information. Cross-sectional surveys are given at any point in time; Longitudinal surveys are given for various durations of time. |
In quantitative nursing research, researchers use data collection instruments, such as surveys, questionnaires, or structured observations, to gather data from a sample or population. The collected data are typically in the form of numerical values or categorical responses. An example of quantitative research would be a hospital giving surveys to patients upon discharge, asking them to rate their experience on a numerical scale of 0 to 10, and then evaluating the responses to see which areas most need improvement.
Qualitative Research
Qualitative research is a methodological approach that emphasizes exploring the depth, complexity, and richness of individuals’ perspectives and the social context in which they occur.
In qualitative nursing research, researchers use various data collection methods, such as interviews, focus groups, observations, or document analysis, to gather non-numerical data. The data collected often consist of words, narratives, descriptions, and images that provide a detailed understanding of the participants’ experiences, beliefs, and perceptions ( Table 1.4 ).
| Type | Description |
|---|---|
| Ethnography | The researcher is directly involved/immersed in the participant’s environment; different data techniques are used to document the behaviors, actions, and events of the research population. |
| Grounded theory | The researcher observes or studies a population, and then develops a comparative analysis based on studied social interactions and experiences. |
| Phenomenology | The researcher looks into “lived experiences” of the participants, and focuses on examining why the participant behaved a certain way from the perspective of the participant who experienced it. |
| Narrative | The researcher strings together a sequence of events, usually from just one or two participants, to create a narrative, or cohesive story. |
The results of qualitative research are typically presented through rich descriptions, quotes, and narratives that capture the essence of the participants’ experiences. An example of a simple qualitative research study may be “the effect of having a designated nursing preceptor on the perceived satisfaction of new nurses.” Qualitative research in nursing enables a deeper understanding of the subjective aspects of health care, such as patients’ lived experiences, cultural beliefs, and social interactions. It explores the complexities and context in which healthcare phenomena occur, allowing for the exploration of multiple perspectives and uncovering novel insights. It also helps generate hypotheses and inform the development of quantitative research studies.
Understanding the Parts of a Research Article
Understanding the parts of an article is crucial for interpreting and extracting valuable information from scholarly literature. Each section of the article serves a specific purpose and provides essential insights for critical appraisal (Carey et al., 2020). Here’s a step-by-step look at how to interpret and analyze each component:
- Abstract: The abstract serves as a concise summary of the entire article. Pay attention to the research question, key findings, and implications. It provides a quick overview of the study’s relevance and helps determine if the article aligns with your information needs.
- Introduction: The introduction sets the stage for the research. Evaluate the background information provided and the clarity of the research question. Consider how well the authors justify the need for the study and their ability to connect it with existing literature.
- Methods: Scrutinize the methods section to understand how the study was conducted. Assess the appropriateness of the study design, sample size, data collection methods, and statistical analyses. This section should provide sufficient details to allow for replication and assess the validity of the findings.
- Results: Thoroughly analyze the results section to grasp the main findings. Examine any statistical analyses, figures, or qualitative descriptions presented. Consider the clarity of the results and the extent to which they support the research question. Assess whether the data analysis methods are appropriate and the results are accurately reported.
- Discussion: The discussion section is where authors interpret the findings and relate them to existing knowledge. Evaluate the authors’ ability to critically analyze the results, address any limitations, and consider alternative explanations. Look for implications for nursing practice, education, or future research that are supported by the findings.
- Conclusion: The conclusion summarizes the main points of the study. Assess whether the conclusions align with the results and discussion. Consider the authors’ ability to synthesize the findings and provide a concise summary of the study’s contributions.
- References: Review the reference list to identify the sources cited in the article. Assess the credibility and relevance of the references to determine if the authors have relied on reputable sources to support their claims.
Translating Research into Practice
Translating research findings to clinical nursing practice is a crucial process that involves applying evidence-based knowledge to improve patient care and outcomes It begins with critically appraising the research to assess its quality and validity (Titler, 2018). Nurses then consider the relevance and generalizability of the findings to their specific patient population and clinical setting. By integrating research findings with their clinical expertise, nurses can develop strategies for implementation , such as creating guidelines or protocols. Ongoing evaluation and monitoring of the implemented practices help nurses assess their impact on patient outcomes. Lifelong learning and staying up to date with current research ensure nurses remain informed and continue to enhance the quality of care they provide.
Steps of Evidence-Based Practice
Evidence-based practice (EBP) refers to the integration of the best available research evidence, clinical expertise, and patient preferences or values to guide healthcare decision-making and improve patient outcomes (ANA, 2023). According to the ANA, there are five key steps in implementing EBP: ask a clinical question, acquire the evidence, appraise the evidence, apply the evidence, and assess outcomes.
Ask a Clinical Question
The first step in implementing EBP is to formulate clear and focused clinical questions that address specific patient care issues. By framing questions in this format, nurses can identify the specific information needed to guide their practice.
Acquire the Evidence
Once the clinical questions are defined, nurses conduct a thorough search for the best available evidence to answer those questions. This involves accessing reputable databases, journals, and other reliable sources to find relevant research studies, systematic reviews, or clinical guidelines that address the identified clinical issues.
Appraise the Evidence
In this step, nurses critically appraise the quality and validity of the evidence gathered. They assess the methodology, study design, sample size, data analysis, and overall strength of the research. They decide if the information is applicable to the patient. This critical appraisal helps determine the credibility and applicability of the evidence to the clinical context.
When you have gathered all of the necessary evidence, the next step is to evaluate it for quality and validity. But how do you know what evidence is strongest and most applicable to your clinical question?
In the steps of EBP, the hierarchy of evidence refers to a ranking system that classifies different types of research studies based on their reliability and validity. The hierarchy helps healthcare professionals determine the strength and quality of evidence when making clinical decisions. The commonly recognized hierarchy includes systematic reviews and meta-analyses at the top, followed by randomized controlled trials (RCTs), cohort studies, case-control studies, cross-sectional studies, case series, and expert opinions at the bottom. The hierarchy of evidence serves as a guide, with studies higher up being considered more rigorous and providing stronger evidence to inform healthcare practices ( Figure 1.9 ).
Nursing and other healthcare professions also frequently use Melnyk and Fineout-Overholt’s levels of evidence ( Figure 1.10 ). Instead of a hierarchy, Melnyk and Fineout-Overholt list seven levels of evidence based on their methodological quality (2023).
Apply the Evidence
The next step involves implementing evidence-based interventions or changes in practice based on nursing knowledge and new expertise. Nurses integrate the findings from the new evidence with their clinical expertise and knowledge of individual patient values and preferences. They consider factors such as patient preferences, available resources, and feasibility of implementation when making decisions about patient care.
Assess Outcomes
The final stage of implementing evidence-based practices involves evaluating their impact on patient outcomes. Nurses collect data, monitor outcomes, and assess the effectiveness of the implemented interventions. This can help determine if the treatment will be effective for other patients as well. This ongoing evaluation helps identify areas for improvement and supports the continuous cycle of EBP implementation.
Clinical Safety and Procedures (QSEN)
Qsen competency: evidence-based practice (ebp).
Definition : Provide optimal patient care while integrating best current evidence and expertise with patient/family values and preference.
Knowledge : The nurse will describe reliable sources for locating clinical practice guidelines and evidence, and describe how the strength of evidence influences patient care.
Skill : Provide patient-centered care utilizing current evidence. The nurse will:
- Create individualized care plans based on EBP and patient values.
- Examine evidence reports and research relative to area of expertise.
- Locate evidence related to clinical practice guidelines and topics.
- Engage in the integration of new EBP in the work environment.
- Consult with experts before deviating from EBP.
Attitude : The nurse will recognize the importance of reading professional journals and improving patient care based on new evidence.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/clinical-nursing-skills/pages/1-introduction
- Authors: Christy Bowen
- Publisher/website: OpenStax
- Book title: Clinical Nursing Skills
- Publication date: Jun 26, 2024
- Location: Houston, Texas
- Book URL: https://openstax.org/books/clinical-nursing-skills/pages/1-introduction
- Section URL: https://openstax.org/books/clinical-nursing-skills/pages/1-2-evidence-based-practice
© Jun 12, 2024 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.
What is Evidence-Based Practice in Nursing? (With Examples, Benefits, & Challenges)

Are you a nurse looking for ways to increase patient satisfaction, improve patient outcomes, and impact the profession? Have you found yourself caught between traditional nursing approaches and new patient care practices? Although evidence-based practices have been used for years, this concept is the focus of patient care today more than ever. Perhaps you are wondering, “What is evidence-based practice in nursing?” In this article, I will share information to help you begin understanding evidence-based practice in nursing + 10 examples about how to implement EBP.
What is Evidence-Based Practice in Nursing?
When was evidence-based practice first introduced in nursing, who introduced evidence-based practice in nursing, what is the difference between evidence-based practice in nursing and research in nursing, what are the benefits of evidence-based practice in nursing, top 5 benefits to the patient, top 5 benefits to the nurse, top 5 benefits to the healthcare organization, 10 strategies nursing schools employ to teach evidence-based practices, 1. assigning case studies:, 2. journal clubs:, 3. clinical presentations:, 4. quizzes:, 5. on-campus laboratory intensives:, 6. creating small work groups:, 7. interactive lectures:, 8. teaching research methods:, 9. requiring collaboration with a clinical preceptor:, 10. research papers:, what are the 5 main skills required for evidence-based practice in nursing, 1. critical thinking:, 2. scientific mindset:, 3. effective written and verbal communication:, 4. ability to identify knowledge gaps:, 5. ability to integrate findings into practice relevant to the patient’s problem:, what are 5 main components of evidence-based practice in nursing, 1. clinical expertise:, 2. management of patient values, circumstances, and wants when deciding to utilize evidence for patient care:, 3. practice management:, 4. decision-making:, 5. integration of best available evidence:, what are some examples of evidence-based practice in nursing, 1. elevating the head of a patient’s bed between 30 and 45 degrees, 2. implementing measures to reduce impaired skin integrity, 3. implementing techniques to improve infection control practices, 4. administering oxygen to a client with chronic obstructive pulmonary disease (copd), 5. avoiding frequently scheduled ventilator circuit changes, 6. updating methods for bathing inpatient bedbound clients, 7. performing appropriate patient assessments before and after administering medication, 8. restricting the use of urinary catheterizations, when possible, 9. encouraging well-balanced diets as soon as possible for children with gastrointestinal symptoms, 10. implementing and educating patients about safety measures at home and in healthcare facilities, how to use evidence-based knowledge in nursing practice, step #1: assessing the patient and developing clinical questions:, step #2: finding relevant evidence to answer the clinical question:, step #3: acquire evidence and validate its relevance to the patient’s specific situation:, step #4: appraise the quality of evidence and decide whether to apply the evidence:, step #5: apply the evidence to patient care:, step #6: evaluating effectiveness of the plan:, 10 major challenges nurses face in the implementation of evidence-based practice, 1. not understanding the importance of the impact of evidence-based practice in nursing:, 2. fear of not being accepted:, 3. negative attitudes about research and evidence-based practice in nursing and its impact on patient outcomes:, 4. lack of knowledge on how to carry out research:, 5. resource constraints within a healthcare organization:, 6. work overload:, 7. inaccurate or incomplete research findings:, 8. patient demands do not align with evidence-based practices in nursing:, 9. lack of internet access while in the clinical setting:, 10. some nursing supervisors/managers may not support the concept of evidence-based nursing practices:, 12 ways nurse leaders can promote evidence-based practice in nursing, 1. be open-minded when nurses on your teams make suggestions., 2. mentor other nurses., 3. support and promote opportunities for educational growth., 4. ask for increased resources., 5. be research-oriented., 6. think of ways to make your work environment research-friendly., 7. promote ebp competency by offering strategy sessions with staff., 8. stay up-to-date about healthcare issues and research., 9. actively use information to demonstrate ebp within your team., 10. create opportunities to reinforce skills., 11. develop templates or other written tools that support evidence-based decision-making., 12. review evidence for its relevance to your organization., bonus 8 top suggestions from a nurse to improve your evidence-based practices in nursing, 1. subscribe to nursing journals., 2. offer to be involved with research studies., 3. be intentional about learning., 4. find a mentor., 5. ask questions, 6. attend nursing workshops and conferences., 7. join professional nursing organizations., 8. be honest with yourself about your ability to independently implement evidence-based practice in nursing., useful resources to stay up to date with evidence-based practices in nursing, professional organizations & associations, blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. what did nurses do before evidence-based practice, 2. how did florence nightingale use evidence-based practice, 3. what is the main limitation of evidence-based practice in nursing, 4. what are the common misconceptions about evidence-based practice in nursing, 5. are all types of nurses required to use evidence-based knowledge in their nursing practice, 6. will lack of evidence-based knowledge impact my nursing career, 7. i do not have access to research databases, how do i improve my evidence-based practice in nursing, 7. are there different levels of evidence-based practices in nursing.
• Level One: Meta-analysis of random clinical trials and experimental studies • Level Two: Quasi-experimental studies- These are focused studies used to evaluate interventions. • Level Three: Non-experimental or qualitative studies. • Level Four: Opinions of nationally recognized experts based on research. • Level Five: Opinions of individual experts based on non-research evidence such as literature reviews, case studies, organizational experiences, and personal experiences.
8. How Can I Assess My Evidence-Based Knowledge In Nursing Practice?


Evidence-Based Practice Nursing Research Paper Guide

The world now has more health researchers than ever before in history. Because of this, many quality health studies are being published virtually every week. These studies provide new ideas, systems, and theories that are helping to improve patient care. Evidence-Based Practice (EBP) nursing research papers are academic writings that help to document how the new studies are helping or can help to improve patient care.
In this post, you will discover everything you need to know about EBP papers, including how to write one from start to finish.
But before proceeding further, let's get solid on what Evidence-Based Practice means in nursing.
What is Evidence-Based Practice in Nursing?
Evidence-Based Practice (EBP) in nursing is a field of nursing focusing on helping nurses to learn how to find and adopt patient care strategies, theories, and systems that are based on scientific evidence. It has significantly improved patient care over the last two decades. In evidence-based practice, nurses ask, acquire, appraise, apply, and assess. The five steps of EBP are integral in nursing and medical practice.
Nursing degree programs that include this field in their curriculum produce nurses who know that patient care should almost always be based on evidence from research.
EBP is implemented methodically in actual nursing practice, beginning with assessing the need for change. It is then followed by locating the best evidence from credible, reliable, reputable, and authoritative sources.
The next step entails a systematic review of the evidence using a specific guideline, enabling the synthesis of the gathered evidence. The evaluation aims to ensure that the evidence being considered for adoption or implementation is suitable for use.
Since so many health studies are published weekly, adopting evidence from random studies is insufficient. The evidence must first be reviewed before adoption.
The review results help design change, which leads to implementation and evaluation and, finally, integration and maintenance of the EBP change.
The methodical review of the evidence for adoption in EBP is done through an EBP nursing research paper , aka EBP research paper .
Learn what exactly makes up the structure of a typical EBP research paper in the section below and then how to write a brilliant EBP research paper in the section after the section below.
The standard structure of a nursing EBP research paper
A good nursing EBP research paper has several vital parts. All the parts must be included for it to be considered complete.
If you have seen or read many EBP research papers, you must have noticed that a typical EBP research paper includes an introduction, methodology, literature review, discussion, and conclusion. These are perhaps the most crucial parts of an EBP paper. Nevertheless, they are not the only ones. Below is a breakdown of the critical parts of a nursing EBP research paper:
1. Title page
The first part of an EBP paper is the title page. Like every other academic paper, an EBP research paper must have a title page, and the title page must be formatted appropriately. Ensuring your title page is formatted correctly is vital so you do not get penalized during grading. Probably the most critical element of your title page is the title itself. The title should be an attention-grabber to make your professor highly interested in your research paper.
When developing a title for your research paper, you should ensure it sets the scope of your EBP research paper. It should also provide a hint at what your thesis statement will be. Moreover, it should also be concise and fine-tuned. A clear, concise title that provides the scope of the paper is more than sufficient for any academic paper.
2. Introduction
The introduction of your EBP paper is one of its most critical parts. This is because it introduces the reader to the rest of your paper. Therefore, a good EBP research paper introduction presents background information on the research topic or question.
The best way to provide background information on the research topic or nursing issue is to use the PICO approach. PICO is an acronym for Problem, Intervention, Comparison, and Outcome. You can use the PICO approach to organize your introduction as follows:
- Problem: Present the problem that needs to be solved.
- Intervention: Present the intervention or solution being evaluated. (Reference relevant literature)
- Comparison: Present other possible interventions. (Reference relevant literature)
- Outcome: Present the expected outcome of the intention on the problem.
In addition to organizing your introduction using the PICO approach, as shown above, you must ensure it ends with your thesis statement.
Related Reading:
- Steps for writing a nursing diagnosis.
- Writing a nursing case study.
- Nursing Research topics
3. Thesis statement
The second part of your EBP paper is your thesis statement. Every adequately written EBP paper must have a thesis statement. A thesis statement in an EBP paper is its central argument. It is usually the last sentence or statement in the introduction paragraph, and the entire paper is based on it. Only an EBP paper with a good thesis statement can get a top grade. This is because it does not force the reader to read the entire paper to get what it is all about.
A proper thesis statement is specific, argumentative, and manageable. If your thesis statement is not specific, your EBP research paper will be too broad and lose significance. If your thesis is not argumentative, your EBP paper will be too descriptive and not analytic enough to be considered a good research paper. Lastly, completing your EBP paper will be challenging if your thesis statement is not manageable.
4. Methodology
At the core of every EBP research paper is the systematic review of recent literature on a particular topic to find information that can help improve a nursing or patient care issue. Because the literature review is a vital element of every nursing EBP paper, it is essential to ensure the literature chosen for review is of the highest quality.
You cannot just go on Google and find random papers or sources to use for your EBP research paper literature review. You must use credible evidence from cohort studies, case-controlled studies, RCTs, peer-reviewed journals, practice papers, white papers, literature reviews, and systematic reviews. And you must get them orderly and systematically in trustworthy databases. How you get them is what is referred to as methodology. Your professor expects to see details about your methodology immediately after your EBP paper introduction.
The most crucial methodology details your professor expects to see include the names of the databases you searched for evidence (sources), the search terms you used, and the inclusion and exclusion criteria. One can use different methodologies to choose evidence for their literature review.
Under methodology, explain the databases you used, including the search terms, total articles yielded, and your inclusion and exclusion criteria. You should consider the credibility, validity, and reliability of each study. You can use qualitative or quantitative studies. Qualitative studies focus on subjective analysis, interviews, and description, while quantitative studies use objective figures that can be measured, calculated, and counted.
5. EBP Literature Review
The most crucial part of every nursing EBP paper is the literature review. Because it is in the literature review section, you are supposed to analyze and compare the links between the evidence (sources) you have settled on in your methodology.
What is essential in the literature review section is not the evidence used but the associations or analysis of the evidence. As long as the evidence (sources) are gotten using the proper methodology, what matters is how you show the links between the different pieces of evidence you include in your literature review. The best way to show the links between the sources is to show how the sources compare and contrast. Doing this will help you to develop an excellent EBP paper.
After reviewing the evidence you collected, you should create a table to show how different aspects of your pieces of evidence associate in terms of year of publication, sample size, demographics, methodology, limitations, results, and confidence level.
6. Discussion
After your EBP literature review section, you will want to discuss your findings or what you've noted in the evidence. A typical discussion will discuss the critical aspects of the different sources used as evidence, including the interventions, the approaches used for implementation, the evaluation strategies, and so on. You should start the discussion by discussing the findings first, followed by a discussion of the change in practice and then a discussion of the efficiency of the change. This should be followed by a discussion of the most appropriate implementation strategy.
7. Conclusion
The last written part of every EBP research paper is the conclusion. You must professionally conclude your EBP paper. For your conclusion to be professional, it must have a summary of your EBP paper and nicely wrap the whole thing.
8. References
After writing your conclusion, you must add a references page that correctly references all the sources you have used in your paper. Without a references page, your EBP research paper will be considered incomplete. Make sure you add the references following the formatting style advised by your professor.
Most EBP research papers usually have an abstract. An abstract is a short (less than 250 words) summary of a scientific paper. It is used to highlight what is contained in the paper.
Steps to writing an EBP nursing paper
When given an EBP paper assignment, there are specific steps you need to follow to ensure that the paper you develop is quality and 100 percent complete. Below we will highlight these steps.
1. Select a good topic for your EBP paper
The first thing you need to do when given an EBP paper assignment is to pick a topic. Ensure the topic is viable (not too hard to write about). There are different ways to pick a topic for your nursing EBP paper. You can get inspiration from your class notes, assignments, coursework, peer-reviewed sources, etc. You can also search on Google for nursing EBP paper topics to get inspiration for your own paper topic.
As you look at different things for inspiration for your own topic, you should ensure that the topic you come up with is one in which you have great interest. If you do this, it will be evident in your paper that the topic you are writing about is one you are interested in. If you don't, your EBP paper will probably sound dull or flat and won't even excite your reader.
Sometimes, your professor/instructor will give you a topic to focus on. If that is true in your EBP paper assignment, jump to the next step below.
2. Ask your professor for confirmation
You should ask your professor for confirmation after choosing a nursing topic for your EBP paper. Ask them if your chosen topic is good enough to help you develop a good EBP paper. If they say it is good enough, start collecting evidence for your paper. If they suggest you edit the topic in any way, do it immediately. By asking your professor for confirmation before you start writing your EBP paper, you will write it will so much confidence when they agree it is good enough. Even if they ask you to refine it, you will have a lot of confidence writing it because you will know the refined topic is on the right track.
Sometimes professors ask students to write a research proposal before starting the EBP research paper. If you have been asked to write a research proposal, you will need to write it before you begin researching the paper. To accept your research proposal, you must ensure it clearly highlights the issue you want to solve, the change process, and the basis for change. If your proposal is not good enough, your professor will most likely recommend changes you can implement to improve it.
3. Gather evidence to support your topic
Once you choose a topic (a problem you want to solve) and your professor confirms it, you should start gathering evidence to support your topic. Good evidence is probably the most essential part of an essay. If your EBP paper does not have good evidence, it is improbable that you will get a top grade when graded. Therefore, it is crucial to do good research to ensure you get credible and trustworthy sources for your EBP paper. Sources should be all the papers that can help you to provide a solution to the problem you want to solve.
Once you have many sources, read through them to find out how to solve the problem. When you have a good idea of how to do this, you should create a proper problem statement and a strong thesis statement. A problem statement describes the problem you want to solve unambiguously, while a thesis statement defines how you will do it. With a thesis statement written, you should evaluate the sources you collected and choose only those that are very credible for your literature review.
The right way to choose sources or find evidence for your EBP nursing paper is to search for your chosen topic in a credible or reliable science database. Examples of credible nursing article databases include The Cochrane Collaboration, CINAHL, OVID, TRIP Database, PubMed, and EBSCO. You can also search for sources in your university's online database. Mark all the sources you believe have information that could help you answer your research question and/or support your thesis statement.
Related reading: Important nursing theories and nursing theorists.
4. Choose sources for your nursing EBP paper
It is crucial to choose sources carefully to ensure you do not mess up. The best sources to use in the literature review section of your EBP paper are those that are credible and verifiable. Do not choose or use any source that is not credible and verifiable to use in your paper.
It is crucial to note that most nursing EBP papers focus on the research and its credibility. This is the reason why they have a methodology section. In the section, you are supposed to explain your inclusion and exclusion criteria. You are supposed to write down the conditions the sources you want to use should meet and the conditions that will disqualify a source.
So make sure you create inclusion and exclusion criteria for your EBP paper at this stage. Then, use these two criteria to identify the most relevant and credible sources for the literature review section of your paper.
5. Create an outline
You should create an outline after choosing a nursing topic, gathering evidence, and selecting sources. There are many outline templates available online for writing nursing EBP research papers. Download a good template and print it. After printing it, fill it in with all the crucial points you intend to write your paper in the order you intend to write them.
Once you have written them down, make sure they make sense to you from an organizational point of view. If they do, your outline is good to go. Creating an outline is an important thing to do when writing an EBP paper. This is because once you create it, you have to follow it, and you will have all the forward momentum you need to write your paper from the first paragraph to the last. In addition, you won't get stuck because whenever you feel like you are getting stuck, you can refer back to your outline for direction, and just like that, you will know what to write next.
6. Write a good title for your EBP paper
You need to ensure your EBP paper has an interesting title if you want your reader/professor to read it with high interest. If your paper's title is dull or flat, the reader will read it with the same mood from start to finish. In addition to your title being interesting, it should set the scope for your entire paper.
The best EBP paper title is clear, precise, relevant, and fine-tuned. The title of your paper can be a statement, a PICOT statement, a question, or a fact against the status quo. Whatever approach you take, you must ensure it provides good insight into your paper.
7. Write your introduction
The introduction of an EBP paper is one of its most essential elements. This is because it presents background information on the problem plus the solution blueprint. In other words, it tells the reader what the paper is about. The best way to write an EBP paper introduction is to provide background information on the paper's topic. And best way to provide background information on the topic is to use the PICO approach. PICO is an acronym for Problem, Intervention, Comparison, and Outcome. You can use the PICO approach to organize your introduction as follows:
In addition to organizing your introduction using the PICO approach shown above, the last statement in your introduction needs to be your thesis statement.
Related Reading : Does a picot question or statement have to be in order ?
8. Write the methodology section
You can't just go on Google and find random papers or sources to use for your EBP research paper literature review. You must use credible evidence from cohort studies, case-controlled studies, RCTs, peer-reviewed journals, practice papers, white papers, literature reviews, and systematic reviews. And you must get them orderly and systematically in trustworthy databases. How you find credible sources is what is referred to as methodology. Your professor expects to see details about your methodology immediately after your EBP paper introduction.
The most crucial methodology details your professor expects to see include the names of the databases you searched for evidence (sources), the search terms you used, and the inclusion and exclusion criteria. In addition, highlight the methodology you used earlier in step 4.
9. Develop the EBP Literature Review
The analysis of the evidence is essential in the literature review section. As long as the evidence (sources) are gotten using a sound methodology, what matters is how you show the links between the different pieces of evidence you include in your literature review. The best way to show the links between the sources is to show how the sources compare and contrast. Doing this will help you to develop an excellent EBP paper literature review section.
After reviewing the evidence you collected, you should create a table to show how different aspects of your pieces of evidence link in terms of year of publication, sample size, demographics, methodology, limitations, results, and confidence level.
10. Write the discussion section
After writing your EBP literature review section, you should discuss your findings. You should start the discussion by examining the findings first, followed by a discussion of the change in practice and then a discussion of the efficiency of the change. This should be followed by a discussion of the most appropriate implementation strategy.
11. Write the conclusion
You must professionally conclude your EBP paper. For your conclusion to be professional, it must have a summary of your EBP paper. The right way to write this summary is to start with a restatement of the thesis, followed by a restatement of the main points. The main points should be followed by an overview of the proposed change, its implementation strategy, and the intended benefits.
12. Develop the references page
After writing your conclusion, you must add a references page that correctly references all the sources you have used in your paper. Without a references page, your EBP research paper will be considered incomplete. The references on your references page must be formatted appropriately.
13. Edit and proofread
After completing your references page, you should begin editing and proofreading your paper. Your paper will most likely contain typing errors, grammar errors, and so on. You can only make it perfect by proofreading it. The best way to proofread is first to do it using an AI-powered proofreader like Grammarly.com. It will help you to quickly catch and eliminate most of the obvious or basic mistakes in your work.
After proofreading and editing using an AI proofreader, you should do it with your own two eyes and brain. This will help you to catch the errors the computer software might have missed. It will also help you to find and correct sentences and paragraphs in your work that are not clear.
Once you are done editing and proofreading, your paper will be ready for submission.
Also Read: How to formulate an excellent nursing care plan for a nursing school assignment.
Evidence-based Practice Topics in Nursing Research
Check out the sample EBP topics below for inspiration to develop your own topic.
- How to reduce the likelihood of child injury during birth
- How to improve the diagnosis of childhood respiratory illnesses
- How to improve child malnutrition programs
- How to enhance neonatal care
- Ethics of pediatric care
- Effective methods to enhance nurse emotional health
- How to improve ADHD treatment
- How to reduce child mortality
- How to improve nonchemical bipolar disorder treatments
- How to minimize the spread of infectious illnesses by nurses
- Improvement of treatment of restless leg syndrome
- How to better identify chronic anxiety disorders
- How to enhance midwifery practices in rural areas
- How to improve nonchemical pain management during labor
- Enhanced care strategies for the elderly
- How to improve the treatment of Alzheimer's disease
- How to improve breast cancer diagnosis in women
- The enhancement of acne treatments for women
- How to improve ADHD stimulant treatments
- How to enhance remote care in nursing
You can also consider the list of nursing informatics research topics we have developed to help you select the best.
Types of studies to use when writing an EBP nursing paper
You can include several types of studies in the literature review section of your EBP paper. They include case reports, control studies, and so on. Discover all the important ones below:
- Meta-analysis. A meta-analysis is a research paper that utilizes a qualitative method to compare study results and combine their conclusions. Meta-analyses are considered to have the best quality for EBP research papers.
- Systematic review. A systematic review uses various methods to compare and synthesize information from credible sources.
- Case report. A case report is a story written on a hypothetical patient or group of patients to analyze treatment plans.
- Cohort study. This study looks at a population subset over an extended period to examine the effects of a particular experiment.
- Randomized control study. This is a clinical trial that looks at the effects of a treatment plan on a specific population. This paper is known as a gold standard research paper or source because it is randomized.
Levels of Evidence to consider when writing EBP nursing paper
There are seven levels of evidence you can use in your literature review. They include:
- Level I: Evidence from the systematic review of related RCTs.
- Level II: Evidence is from a minimum of one RCT.
- Level III: Evidence from controlled trials but without randomization.
- Level IV: Evidence from cohort studies and case-control studies.
- Level V: Evidence from qualitative and descriptive studies.
- Level VI: Evidence from a single qualitative or descriptive study.
- Level VII: Evidence from reports by expert committees or the opinion pieces authored by government or medical agencies.
Tips for writing an excellent research paper
- Make sure your thesis statement is strong and clear. This will ensure your resulting paper is similarly solid and well-structured.
- Create an outline before you start writing. This will help you to have a paper that is well-organized and structured from start to finish.
- Reference your paper correctly . Proper references will help to make your paper stronger. It will also help to ensure your paper is not penalized for poor referencing during grading.
- Revise your paper before submitting it. Never submit your research paper before you revise it thoroughly. Thoroughly revising your paper will help you to identify and eliminate errors to ensure your paper is perfect before submission.
- Never forget to follow all your paper instructions. This seems like something small, but it isn't. Following your paper's instructions will ensure it is what your professor expects. This will put you in an excellent position to get a good grade.
Before you Close this Guide, ...
Using the knowledge, tips, and insights we shared in this article, you should be able to write a nursing EBP research paper effortlessly.
If you can't because of time or other reasons, you should order your nursing EBP paper from NurseMyGrade. We assure you a brilliant nursing EBP research paper that is 100% original, 100% error-free, and formatted correctly in either APA, AMA, or Harvard formatting styles.
In other words, you will get a research paper that will guarantee you a good grade. Try our nursing assignment help service today; you will not be disappointed.
- Ideas and topics for nursing research papers.
Struggling with
Related Articles
Tips to Write a Plagiarism-Free Nursing Research Paper or Assignmen

List of 500 Plus Nursing Capstone Project Ideas to Consider as a nursing Student

Top Guide and Hints for Writing Great Nursing Competency Statements
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Evidence-Based Practice: Step by Step: The Seven Steps of Evidence-Based Practice
Melnyk, Bernadette Mazurek PhD, RN, CPNP/PMHNP, FNAP, FAAN; Fineout-Overholt, Ellen PhD, RN, FNAP, FAAN; Stillwell, Susan B. DNP, RN, CNE; Williamson, Kathleen M. PhD, RN
Bernadette Mazurek Melnyk is dean and distinguished foundation professor of nursing at Arizona State University in Phoenix, where Ellen Fineout-Overholt is clinical professor and director of the Center for the Advancement of Evidence-Based Practice, Susan B. Stillwell is clinical associate professor and program coordinator of the Nurse Educator Evidence-Based Practice Mentorship Program, and Kathleen M. Williamson is associate director of the Center for the Advancement of Evidence-Based Practice.
Contact author: Bernadette Mazurek Melnyk, [email protected] .

This is the second article in a new series from the Arizona State University College of Nursing and Health Innovation's Center for the Advancement of Evidence-Based Practice. Evidence-based practice (EBP) is a problem-solving approach to the delivery of health care that integrates the best evidence from studies and patient care data with clinician expertise and patient preferences and values. When delivered in a context of caring and in a supportive organizational culture, the highest quality of care and best patient outcomes can be achieved.
The purpose of this series is to give nurses the knowledge and skills they need to implement EBP consistently, one step at a time. Articles will appear every two months to allow you time to incorporate information as you work toward implementing EBP at your institution. Also, we've scheduled "Ask the Authors" calls every few months to provide a direct line to the experts to help you resolve questions. See details below.
In this second article on implementing evidence-based practice, the authors offer an overview of the multistep process.
Research studies show that evidence-based practice (EBP) leads to higher quality care, improved patient outcomes, reduced costs, and greater nurse satisfaction than traditional approaches to care. 1-5 Despite these favorable findings, many nurses remain inconsistent in their implementation of evidence-based care. Moreover, some nurses, whose education predates the inclusion of EBP in the nursing curriculum, still lack the computer and Internet search skills necessary to implement these practices. As a result, misconceptions about EBP—that it's too difficult or too time-consuming—continue to flourish.
In the first article in this series ("Igniting a Spirit of Inquiry: An Essential Foundation for Evidence-Based Practice," November 2009), we described EBP as a problem-solving approach to the delivery of health care that integrates the best evidence from well-designed studies and patient care data, and combines it with patient preferences and values and nurse expertise. We also addressed the contribution of EBP to improved care and patient outcomes, described barriers to EBP as well as factors facilitating its implementation, and discussed strategies for igniting a spirit of inquiry in clinical practice, which is the foundation of EBP, referred to as Step Zero. ( Editor's note : although EBP has seven steps, they are numbered zero to six.) In this article, we offer a brief overview of the multistep EBP process. Future articles will elaborate on each of the EBP steps, using the context provided by the Case Scenario for EBP: Rapid Response Teams .
Step Zero: Cultivate a spirit of inquiry. If you've been following this series, you may have already started asking the kinds of questions that lay the groundwork for EBP, for example: in patients with head injuries, how does supine positioning compared with elevating the head of the bed 30 degrees affect intracranial pressure? Or, in patients with supraventricular tachycardia, how does administering the β-blocker metoprolol (Lopressor, Toprol-XL) compared with administering no medicine affect the frequency of tachycardic episodes? Without this spirit of inquiry, the next steps in the EBP process are not likely to happen.
Step 1: Ask clinical questions in PICOT format. Inquiries in this format take into account patient population of interest (P), intervention or area of interest (I), comparison intervention or group (C), outcome (O), and time (T). The PICOT format provides an efficient framework for searching electronic databases, one designed to retrieve only those articles relevant to the clinical question. Using the case scenario on rapid response teams as an example, the way to frame a question about whether use of such teams would result in positive outcomes would be: "In acute care hospitals (patient population), how does having a rapid response team (intervention) compared with not having a response team (comparison) affect the number of cardiac arrests (outcome) during a three-month period (time)?"
Step 2: Search for the best evidence. The search for evidence to inform clinical practice is tremendously streamlined when questions are asked in PICOT format. If the nurse in the rapid response scenario had simply typed "What is the impact of having a rapid response team?" into the search field of the database, the result would have been hundreds of abstracts, most of them irrelevant. Using the PICOT format helps to identify key words or phrases that, when entered successively and then combined, expedite the location of relevant articles in massive research databases such as MEDLINE or CINAHL. For the PICOT question on rapid response teams, the first key phrase to be entered into the database would be acute care hospitals , a common subject that will most likely result in thousands of citations and abstracts. The second term to be searched would be rapid response team , followed by cardiac arrests and the remaining terms in the PICOT question. The last step of the search is to combine the results of the searches for each of the terms. This method narrows the results to articles pertinent to the clinical question, often resulting in fewer than 20. It also helps to set limits on the final search, such as "human subjects" or "English," to eliminate animal studies or articles in foreign languages.
Step 3: Critically appraise the evidence. Once articles are selected for review, they must be rapidly appraised to determine which are most relevant, valid, reliable, and applicable to the clinical question. These studies are the "keeper studies." One reason clinicians worry that they don't have time to implement EBP is that many have been taught a laborious critiquing process, including the use of numerous questions designed to reveal every element of a study. Rapid critical appraisal uses three important questions to evaluate a study's worth. 6-8
- Are the results of the study valid? This question of study validity centers on whether the research methods are rigorous enough to render findings as close to the truth as possible. For example, did the researchers randomly assign subjects to treatment or control groups and ensure that they shared key characteristics prior to treatment? Were valid and reliable instruments used to measure key outcomes?
- What are the results and are they important? For intervention studies, this question of study reliability addresses whether the intervention worked, its impact on outcomes, and the likelihood of obtaining similar results in the clinicians' own practice settings. For qualitative studies, this includes assessing whether the research approach fits the purpose of the study, along with evaluating other aspects of the research such as whether the results can be confirmed.
- Will the results help me care for my patients? This question of study applicability covers clinical considerations such as whether subjects in the study are similar to one's own patients, whether benefits outweigh risks, feasibility and cost-effectiveness, and patient values and preferences.
After appraising each study, the next step is to synthesize the studies to determine if they come to similar conclusions, thus supporting an EBP decision or change.
Step 4: Integrate the evidence with clinical expertise and patient preferences and values. Research evidence alone is not sufficient to justify a change in practice. Clinical expertise, based on patient assessments, laboratory data, and data from outcomes management programs, as well as patients' preferences and values are important components of EBP. There is no magic formula for how to weigh each of these elements; implementation of EBP is highly influenced by institutional and clinical variables. For example, say there's a strong body of evidence showing reduced incidence of depression in burn patients if they receive eight sessions of cognitive-behavioral therapy prior to hospital discharge. You want your patients to have this therapy and so do they. But budget constraints at your hospital prevent hiring a therapist to offer the treatment. This resource deficit hinders implementation of EBP.
Step 5: Evaluate the outcomes of the practice decisions or changes based on evidence. After implementing EBP, it's important to monitor and evaluate any changes in outcomes so that positive effects can be supported and negative ones remedied. Just because an intervention was effective in a rigorously controlled trial doesn't mean it will work exactly the same way in the clinical setting. Monitoring the effect of an EBP change on health care quality and outcomes can help clinicians spot flaws in implementation and identify more precisely which patients are most likely to benefit. When results differ from those reported in the research literature, monitoring can help determine why.
Step 6: Disseminate EBP results. Clinicians can achieve wonderful outcomes for their patients through EBP, but they often fail to share their experiences with colleagues and their own or other health care organizations. This leads to needless duplication of effort, and perpetuates clinical approaches that are not evidence based. Among ways to disseminate successful initiatives are EBP rounds in your institution, presentations at local, regional, and national conferences, and reports in peer-reviewed journals, professional newsletters, and publications for general audiences.
When health care organizations adopt EBP as the standard for clinical decision making, the steps outlined in this article naturally fall into place. The next article in our series will feature a staff nurse on a medical–surgical unit who approached her hospital's EBP mentor to learn how to formulate a clinical question about rapid response teams in PICOT format.
Ask the Authors on January 22!
On January 22 at 3:30 PM EST, join the "Ask the Authors" call. It's your chance to get personal consultation from the experts! And it's limited to the first 50 callers, so dial-in early! U.S. and Canada, dial 1-800-947-5134 (International, dial 001-574-941-6964). When prompted, enter code 121028#.
Go to www.ajnonline.com and click on "Podcasts" and then on "Conversations" to listen to our interview with the authors.
Case Scenario for EBP: Rapid Response Teams
You're a staff nurse on a busy medical–surgical unit. Over the past three months, you've noticed that the patients on your unit seem to have a higher acuity level than usual, with at least three cardiac arrests per month, and of those patients who arrested, four died. Today, you saw a report about a recently published study in Critical Care Medicine on the use of rapid response teams to decrease rates of in-hospital cardiac arrests and unplanned ICU admissions. The study found a significant decrease in both outcomes after implementation of a rapid response team led by physician assistants with specialized skills. 9 You're so impressed with these findings that you bring the report to your nurse manager, believing that a rapid response team would be a great idea for your hospital. The nurse manager is excited that you have come to her with these findings and encourages you to search for more evidence to support this practice and for research on whether rapid response teams are valid and reliable.
- Cited Here |
- Google Scholar
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Evidence-based practice, step by step: asking the clinical question: a key step ..., evidence-based practice: step by step: igniting a spirit of inquiry, evidence-based practice, step by step: searching for the evidence, evidence-based practice step by step: critical appraisal of the evidence: part i, evidence-based practice, step by step: implementing an evidence-based practice....

- MJC Library & Learning Center
- Research Guides
Evidence-Based Practice
- APA Style, 7th Edition
- Defining Evidence
- Getting Started With EBP
- EBP @ the Library
What is APA Style?
APA style was created by social and behavioral scientists to standardize scientific writing. APA style is most often used in:
- psychology,
- social sciences (sociology, business), and
If you're taking courses in any of these areas, be prepared to use APA style.
For in-depth guidance on using this citation style, refer to Publication Manual of the American Psychological Association , 7th ed. We have several copies available at the MJC Library at the call number BF 76.7 .P83 2020 .
APA Style, 7th ed.
Apa tutorial.
In October 2019, the American Psychological Association made radical changes its style, especially with regard to the format and citation rules for students writing academic papers. Use this guide to learn how to format and cite your papers using APA Style, 7th edition.
You can start by viewing the video tutorial .
Formatting Your Paper
For help on all aspects of formatting your paper in APA Style, see The Essentials page on the APA Style website.
- sans serif fonts such as 11-point Calibri, 11-point Arial, or 10-point Lucida Sans Unicode, or
- serif fonts such as 12-point Times New Roman, 11-point Georgia, or normal (10-point) Computer Modern (the default font for LaTeX)
- There are exceptions for the title page , tables , figures , footnotes , and displayed equations .
- Margins : Use 1-in. margins on every side of the page.
- Align the text of an APA Style paper to the left margin . Leave the right margin uneven, or “ragged.”
- Do not use full justification for student papers.
- Do not insert hyphens (manual breaks) in words at the end of line. However, it is acceptable if your word-processing program automatically inserts breaks in long hyperlinks (such as in a DOI or URL in a reference list entry).
- Indent the first line of each paragraph of text 0.5 in . from the left margin. Use the tab key or the automatic paragraph-formatting function of your word-processing program to achieve the indentation (the default setting is likely already 0.5 in.). Do not use the space bar to create indentation.
- There are exceptions for the title page , section labels , abstract , block quotations , headings , tables and figures , reference list , and appendices .
Paper Elements
Student papers generally include, at a minimum:
- Title Page (2.3)
- Text (2.11)
- References (2.12)
Student papers may include additional elements such as tables and figures depending on the assignment. So, please check with your teacher!
Student papers generally DO NOT include the following unless your teacher specifically requests it:
- Running head
- Author note
For complete information on the order of pages , see the APA Style website.
Number your pages consecutively starting with page 1. Each section begins on a new page. Put the pages in the following order:
- Page 1: Title page
- Page 2: Abstract (if your teacher requires an abstract)
- Page 3: Text
- References begin on a new page after the last page of text
- Footnotes begin on a new page after the references (if your teacher requires footnotes)
- Tables begin each on a new page after the footnotes (if your teacher requires tables)
- Figures begin on a new page after the tables (if your teacher requires figures)
- Appendices begin on a new page after the tables and/or figures (if your teacher requires appendices)
Sample Papers With Built-In Instructions
To see what your paper should look like, check out these sample papers with built-in instructions.
Headings Organize Your Paper (2.27)
APA Style uses five (5) levels of headings to help you organize your paper and allow your audience to identify its key points easily. Levels of headings establish the hierarchy of your sections just like you did in your paper outline.
APA tells us to use "only the number of headings necessary to differentiate distinct section in your paper." Therefore, the number of heading levels you create depends on the length and complexity of your paper.
See the chart below for instructions on formatting your headings:

Video Tutorials
Use word to format your paper:.
Use Google Docs to Format Your Paper:
Reference List Format (9.43)
Placement: The reference list appears at the end of the paper, on its own page(s). If your research paper ends on page 8, your References begin on page 9.
Heading: Place the section label References in bold at the top of the page, centered.
Arrangement: Alphabetize entries by author's last name. If source has no named author, alphabetize by the title, ignoring A, An, or The. (9.44-9.48)
Spacing: Like the rest of the APA paper, the reference list is double-spaced throughout. Be sure NOT to add extra spaces between citations.
Indentation: To make citations easier to scan, add a hanging indent of 0.5 in. to any citation that runs more than one line. Use the paragraph-formatting function of your word processing program to create your hanging indent.
See Sample References Page (from APA Sample Student Paper):

Elements of Reference List Entries: (Chapter 9)

References generally have four elements, each of which has a corresponding question for you to answer:
- Author: Who is responsible for this work? (9.7-9.12)
- Date: When was this work published? (9.13-9.17)
- Title: What is this work called? (9.18-9.22)
- Source: Where can I retrieve this work? (9.23-9.37)
By using these four elements and answering these four questions, you should be able to create a citation for any type of source.
For complete information on all of these elements, checkout the APA Style website.
This infographic shows the first page of a journal article. The locations of the reference elements are highlighted with different colors and callouts, and the same colors are used in the reference list entry to show how the entry corresponds to the source.
To create your references, you'll simple look for these elements in your source and put them together in your reference list entry.
American Psychological Association. Example of where to find reference information for a journal article [Infographic]. APA Style Center. https://apastyle.apa.org/style-grammar-guidelines/references/basic-principles
Reference Examples (Chapter 10)
Below you'll find two printable handouts showing APA citation examples. The first is an abbreviated list created by MJC Librarians. The second, which is more comprehensive, is from the APA Style website. Feel free to print these for your convenience or use the links to reference examples below:
- APA Citation Examples Created by MJC Librarians for you.
- Common References Examples (APA Handout) Printable handout from the American Psychological Association.
- Journal Article
- Magazine Article
- Newspaper Article
- Edited Book Chapter
- Webpage on a Website
Classroom or Intranet Sources
- Classroom Course Pack Materials
- How to Cite ChatGPT
- Dictionary Entry
- Government Report
- Legal References (Laws & Cases)
- TED Talk References
- Religious Works
- Open Educational Resources (OER)
- Archival Documents and Collections
You can view the entire Reference Examples website below and view a helpful guide to finding useful APA style topics easily:
- APA Style: Reference Examples
- Navigating the not-so-hidden treasures of the APA Style website
- Missing Reference Information
Sometimes you won't be able to find all the elements required for your reference. In that case, see the instructions in Table 9.1 of the APA style manual in section 9.4 or the APA Style website below:
- Direct Quotation of Material Without Page Numbers
DOIs and URLs (9.34-9.36)
The DOI or URL is the final component of a reference list entry. Because so much scholarship is available and/or retrieved online, most reference list entries end with either a DOI or a URL.
- A DOI is a unique alphanumeric string that identifies content and provides a persistent link to its location on the internet. DOIs can be found in database records and the reference lists of published works.
- A URL specifies the location of digital information on the internet and can be found in the address bar of your internet browser. URLs in references should link directly to the cited work when possible.
When to Include DOIs and URLs:
- Include a DOI for all works that have a DOI, regardless of whether you used the online version or the print version.
- If an online work has both a DOI and a URL, include only the DOI.
- For works without DOIs from websites (not including academic research databases), provide a URL in the reference (as long as the URL will work for readers).
- For works without DOIs from most academic research databases, do not include a URL or database information in the reference because these works are widely available. The reference should be the same as the reference for a print version of the work.
- For works from databases that publish original, proprietary material available only in that database (such as the UpToDate database) or for works of limited circulation in databases (such as monographs in the ERIC database), include the name of the database or archive and the URL of the work. If the URL requires a login or is session-specific (meaning it will not resolve for readers), provide the URL of the database or archive home page or login page instead of the URL for the work. (See APA Section 9.30 for more information).
- If the URL is no longer working or no longer provides readers access to the content you intend to cite, try to find an archived version using the Internet Archive , then use the archived URL. If there is no archived URL, do not use that resource.
Format of DOIs and URLs:
Your DOI should look like this:
https://doi.org/10.1037/a0040251
Follow these guidelines from the APA Style website.
In-Text Citations
APA Style uses the author–date citation system , in which a brief in-text citation points your reader to the full reference list entry at the end of your paper. The in-text citation appears within the body of the paper and briefly identifies the cited work by its author and date of publication. This method enables your reader to locate the corresponding entry in the alphabetical reference list at the end of your paper.
Each work you cite must appear in the reference list, and each work in the reference list must be cited in the text (or in a table, figure, footnote, or appendix) except for the following (See APA, 8.4):
- Personal communications (8.9)
- General mentions of entire websites, whole periodicals (8.22), and common software and apps (10.10) in the text do not require a citation or reference list entry.
- The source of an epigraph does not usually appear in the reference list (8.35)
- Quotations from your research participants do not need citations or reference list entries (8.36)
- References included in a statistical meta-analysis, which are marked with an asterisk in the reference list, may be cited in the text (or not) at the author’s discretion. This exception is relevant only to authors who are conducting a meta-analysis (9.52).
Formatting Your In-Text Citations
Parenthetical and Narrative Citations: ( See APA Section 8.11)
In APA style you use the author-date citation system for citing references within your paper. You incorporate these references using either a parenthetical or a narrative style.
Parenthetical Citations
- In parenthetical citations, the author name and publication date appear in parentheses, separated by a comma. (Jones, 2018)
- A parenthetical citation can appear within or at the end of a sentence.
- When the parenthetical citation is at the end of the sentence, put the period or other end punctuation after the closing parenthesis.
- If there is no author, use the first few words of the reference list entry, usually the "Title" of the source: ("Autism," 2008) See APA 8.14
- When quoting, always provide the author, year, and specific page citation or paragraph number for nonpaginated materials in the text (Santa Barbara, 2010, p. 243). See APA 8.13
- For most citations, the parenthetical reference is placed BEFORE the punctuation: Magnesium can be effective in treating PMS (Haggerty, 2012).

Narrative Citations
In narrative citations, the author name or title of your source appears within your text and the publication date appears in parentheses immediately after the author name.
- Santa Barbara (2010) noted a decline in the approval of disciplinary spanking of 26 percentage points from 1968 to 1994.
In-Text Citation Checklist
- In-Text Citation Checklist Use this useful checklist from the American Psychological Association to ensure that you've created your in-text citations correctly.
In-Text Citations for Specific Types of Sources
Quotations from Research Participants
Personal Communications
Secondary Sources
NoodleTools
Use noodletools to cite your sources .
NoodleTools can help you create your references and your in-text citations.
- NoodleTools Express No sign in required . When you need one or two quick citations in MLA, APA, or Chicago style, simply generate them in NoodleTools Express then copy and paste what you need into your document. Note: Citations are not saved and cannot be exported to a word processor using NoodleTools Express.
- NoodleTools (Login Full Database) This link opens in a new window Create and organize your research notes, share and collaborate on research projects, compose and error check citations, and complete your list of works cited in MLA, APA, or Chicago style using the full version of NoodleTools. You'll need to Create a Personal ID and password the first time you use NoodleTools.
See How to Use NoodleTools Express to Create a Citation in APA Format
Additional NoodleTools Help
- NoodleTools Help Desk Look up questions and answers on the NoodleTools Web site
- << Previous: EBP @ .GOV
- Last Updated: May 1, 2024 2:04 PM
- URL: https://libguides.mjc.edu/ebp
Except where otherwise noted, this work is licensed under CC BY-SA 4.0 and CC BY-NC 4.0 Licenses .
Evidence Based Practice Essays
Smoking and the risk of developing lung cancer, disseminating effective and widely cited ebp, implementing evidence-based practice for improved patient care: a comprehensive approach in a psychiatric hospital setting, thoughts on the dnp degree, nursing journey reflection, healthcare crisis: young people’s mental health, nursing: evidence-based practice in clinical settings, qualitative research and evidence-based practice, exploring nursing practice through a patient-centered lens: a critical reflection, using a pico(t) framework and evidence to develop care practices, critical factors in evidence-based practice, enhancing patient safety through evidence-based practice, exploring evidence-based practice in nursing, locating credible databases and research, ebp and quadruple aim, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail

How to Write an EBP Nursing Research Paper – Helpful Guide for APA Nursing Research Papers [+ 6 Examples & Outline]
Rachel andel rn, bsn.
- August 12, 2022
- Nursing Writing Guides
Writing an evidence-based practice nursing research paper is a structured process that requires extensive research and the help of the right tools and guidance. An EBP nursing research paper has different components requiring systematic research, writing, and editing.
In this guide, we provide a structured approach on how to write an effective EBP Nursing Research Paper .
How to Write an Evidence-Based Paper – Step By Step Guide for APA Nursing Research Papers
EBP Nursing Research Paper Writing
Get EBP Paper Writing Help
- Experienced and Qualified Writers
- 100% Plagiarism Free
- Timely Delivery
- 🎓 MSN & DNP – LeveL Writing
- Confidentiality and Privacy
When writing an EBP nursing research paper, it is important to consider the components of an effective nursing research paper. Here are the different elements of an EBP paper and how to write each.
Introduction to the EBP Nursing Research Papers
In an introduction, you should briefly overview the topic you will discuss. This will help your instructor understand the main points of your paper.
How do you write an introduction for an EBP Nursing Research Paper?
The introduction should be brief but provide enough information to orient readers to the topic and guide them through the rest of the paper. It should also introduce key concepts and explain what will come.
When writing your introduction, make sure it;
- Defines the problem; it answers the question
- Patient/Problem: What problems does the patient group have? What needs to be solved?
- Intervention: What intervention is being considered or evaluated? Cite appropriate literature.
- Comparison: What other interventions are possible? Cite appropriate literature.
- Outcome: What is the intended outcome of the research question?
- Introduces the key concept, thus providing a transition to the next section, which reveals that the target population
- Clearly states the purpose of the report
- Identifies the target population.
- Relates to the significance of the problem
- also relates to the significance of the problem
You should include a clear statement of the research problem at the beginning or end of the introduction. This research problem can also generate the research question used to conduct the research itself.
Here’s an EBP Nursing Research Paper example ;
(1) Root caries is a disease of humans, which manifests as lesions on the root surfaces of teeth producing loss of the natural tooth structure. (2) The lesions progress to deeper and deeper levels of the root as well as spreading laterally to enwrap it. (3) Ultimately a lesion can progress to involve the pulp, threatening the viability of the tooth resulting in pain and eventual tooth loss. (4) When located between the teeth, the lesions are difficult to acess and therefore difficult to excise and restore. (5) In otherwise healthy, North American populations, root caries lesions increase with age. (6) This report sets out to provide evidence-based guidelines on the prevention of root caries for Toronto Public Helath staff on the best available evidence. https://www.una.edu/writingcenter/docs/Writing-Resource
Working on an EBP Nursing Research Paper?
Get nursing writing help for EBP nursing research papers, capstone papers, DNP projects, and Nursing Capstone Presentations. ZERO AI, ZERO Plagiarism and 💯 Timely Delivery.
EBP Nursing Literature Review
The literature review is one of the most important sections of an EBP paper. It should provide a detailed overview of the studies conducted on your topic. You should also include any relevant quotes from these studies.
When writing an effective EBP literature review, it is important to keep in mind the following tips:
- Take the time to read all the articles you cite in your review. This will help you understand the literature better and contextualize it.
- Be sure to cite your sources correctly. If you use a journal article, for example, include the author’s last name and publication year in your citations.
- Be concise in your writing. A literature review should not exceed 10 pages in length. Try to focus on key points and highlight why they are important.
- Use analytical techniques to help you evaluate the literature. For example, consider using qualitative or quantitative methods to analyze data.
- Make sure that your writing is accessible to a broad audience. If your research is technical, explain clearly how it was conducted and what it suggests.
EBP Nursing Research Paper Methodology
The methods section should describe how you researched the topic you are writing about. You should include details about the study you chose to utilize and any statistical analysis you performed.
How to write a methodology in an EBP Nursing Research Paper
Instead of collecting data through surveys, interviews, or clinical records, as in a quantitative or qualitative study, the data you collect is the literature produced on your topic.
Remember, the research you obtain is evidence like quantitative or qualitative data. But what evidence do you select to analyze?
It can be difficult to select evidence. Don’t just go with sources that work well for you, as this will only discredit your ideas. Consider assessing the dependability of the source, ensuring you have different viewpoints when considering a change in practice.
- What database did you search?
- Which search terms did you use, and how many total articles came up with those searches?
- If the search yielded few or fewer results, that may be because the search was too narrow.
The author considers many factors when evaluating sources. Here’s how to evaluate sources for your nursing research Papers
- Assess how trustworthy the source is, how accurate it is, and whether the source has a bias.
- The credibility of study material—is the study/journal credible and original? Research can be found in scholarly journals rather than general reading material.
- Validity: Does the study measure what it says it measures? What demographic sample did the study use? A study may be invalid or inaccurate if it does not produce an accurate margin of error.
- The same test needs to be done to get a true sense of reliability and yield the same results. The test needs to end when the results have been favorable. The results of the study are valid. The report suggests high levels of consistency and validity.
Here’s How to write a Critical Analysis in Nursing
Findings – How to present findings in the EBP Nursing Research Paper
The results and discussion section should provide a detailed analysis of your findings. Discuss the implications of findings and how policymakers can use them.
Your findings will be an analysis, possibly including a chart or table. You should present the studies you selected as the most appropriate sources for studying your problem and instituting your proposed change.
Be sure to compare the following aspects of each study:
- Demographics, pools, and samples
- Methods of discovery and analysis
- Results and limitations
Remember that these studies are supposed to be the most reliable and valid ones for answering the problem you found or the practice you wish to change. Your findings should lay the groundwork for making this argument in your discussion section.
Discussion: Conclusion and Recommendations for the EBP Nursing Research Paper
The conclusion section should summarize everything that has been discussed in the paper. It should provide a summary of your findings, and make any recommendations that you have for policymakers. Be Sure to:
- Argue that the findings lead to the specific change in practice you identified in your introduction.
- Suggest a strategy for implementation. Will the change you recommend (which these studies probably also recommend) work in your situation? Why? What changes might be needed?
Here’s a video guide
Here are a few key points to remember when writing your conclusion for an EBP Research Paper. First, combine all the information and data you’ve gathered throughout your paper.
Second, summarize your study’s findings and what they mean for nursing practice. Finally, provide recommendations for future research in this area.
History of Evidence-based Practice
The history of evidence-based practice (EBP) can be traced back to the early 1990s, when the Institute of Medicine published “To Err Is Human: Building a Safer Health System” which called for more use of evidence in health care decision making.
In 1992, the National Academies Press published “Principles of Evidence-Based Practice” which was a synthesis of work from multiple organizations and aimed to provide guidance on how to use evidence to improve patient care.
Since then, EBP has evolved into an increasingly popular approach to nursing practice. Today, EBP is used by nurses at all levels of education and experience, and it is becoming more integral to the way nurses deliver care. There are many reasons why EBP has become such an important tool in nursing practice, and this article will discuss some of them.
First, EBP helps nurses make informed decisions about patient care. Nurses need reliable information to provide quality care for their patients, and EBP provides that information by providing systematic reviews of research studies. Systematic reviews are a type of scientific literature review that systematically assess the quality and applicability of research studies in order to provide recommendations for clinical practice.
Steps of the EBP process
There are six steps in the Evidence-based Practice process:
Evidence-based practice involves the following six steps:
- Assess the need for change: Formulate the research question based on the inadequacies of current practice.- Identification of a problem or issue. Nurses should identify problems they see in their clinical practice and believe could benefit from intervention. For example, nurses may want to investigate whether patients who experience poor patient-centred outcomes after surgery have different factors, such as pain medication use or depression, that need to be addressed.
- Locate the best evidence: Obtain sources and assess their credibility and relevancy to the research question. Locate the best evidence & Synthesize evidence: Assessment of the current state of knowledge. To determine which interventions are likely to be effective, nurses should review the evidence on the effectiveness of interventions. This evidence can come from studies that have been conducted on interventions, from reviews of existing studies, or from clinical guidelines .
- 1) the target population for the intervention,
- 2) the severity of the problem or issue,
- 3) the feasibility of implementing the intervention
- 4) the cost of the intervention.
- Design the change: Apply the synthesized evidence to create a change in practice that reflects the new understanding. Selection and implementation of interventions. Nurses should select interventions that are likely effective for their target population, based on the factors listed in Step 3. They should then implement the interventions in a feasible and affordable way.
- Implement and evaluate: Apply the necessary changes and assess the changes to acquire new evidence. Evaluation of outcomes. After implementing interventions, nurses should evaluate their outcomes to determine their effectiveness. This evaluation can be done in several ways, such as through surveys or focus groups.
- Integrate and maintain changes: Reassess based on new evidence to continue improvement.
Nurses can use these steps to guide their EBP research in a number of ways. For example, they may want to investigate which interventions are most likely to be effective for a particular target population or problem, or they may want to determine which interventions are the most feasible and affordable to implement.
As you continue, nursingstudy.org/ has the top and most qualified writers to help with any of your assignments. All you need to do is place an order with us.
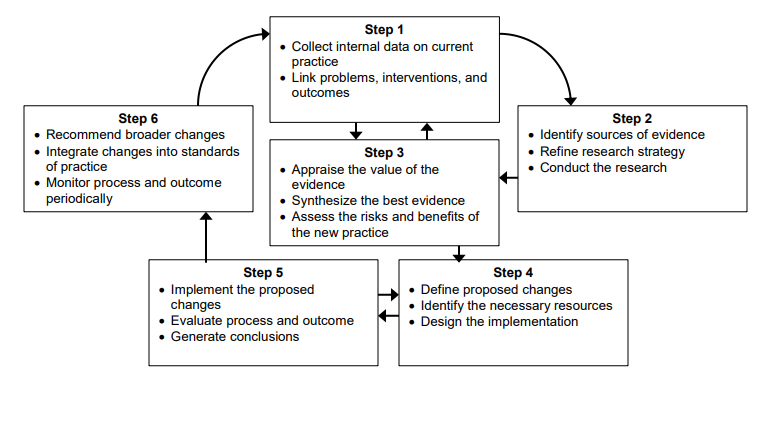
Find out more on
- How to write DNP capstone project Methodology Chapter
- How to write a DNP Capstone Project Literature Review
- How to write a DNP capstone project chapter 1 – Introduction
- DNP Capstone project Abstract Examples [Outline & How-to]
Evidence-Based Research Paper topics in Nursing
List of twenty EBP Nursing Research Paper ideas in nursing to write about
- Effectiveness of interventions for preventing falls in the elderly
- A pilot study of the efficacy of a home-based intervention to reduce falls in older adults
- Evaluating the effectiveness of a community-wide fall prevention intervention for older adults
- The impact of diabetes on balance and falls in older adults
- The effect of social isolation on falls in older adults
- The influence of ethnicity on falls in older adults
- Assessment and management of postural instability in the elderly
- Trends in hip fracture rates among older adults in the United States over time
- Reducing the risk factors for institutionalization among elders with Alzheimer’s disease
- Promoting healthy sleep habits among elders with dementia
- Assessing and managing sleep disturbances in elders with dementia
- Effects of exercise interventions on balance, mobility, and safety in seniors
- Rehabilitation after stroke: Targeting fall prevention
- The Effect of Nurse-Family Partnership on maternal and child health outcomes
- The Relationship of Depression to Nursing Home Use and Mortality
- Factors Influencing Patient Compliance with Diabetes Management Guidelines
- Contributions of Breastfeeding to Infant and Young Child Nutrition
- Role of the nurse in community-acquired pneumonia prevention
- Effectiveness of home health aide services on elder quality of life
- Impact of Acute Care Hospitals on the Nation’s Health
Plan of the EBP Nursing Research Paper
Writing an EBP Nursing research paper can be daunting, but it can be much easier with a plan. This guide will provide you with the essential steps you need to take to produce high-quality research papers. First, you will need to identify the problem you are researching. Next, identify the population most likely to experience the problem and/or share its consequences.
Finally, using evidence-based practices as your guide, develop a plan of action that will address the problem.
Read more on How to Format a CV for a Nursing Position Examples
Identify the Problem
The first step in writing an EBP nursing research paper is to identify the problem you are researching. This can be difficult, as the problem may be subtle or complex. However, you can use rigorous research methods to identify the problem and its consequences.
Once you have identified the problem, you must identify the population most likely to experience it and/or share its consequences. This can be a difficult task, as it may be difficult to differentiate between those affected by the problem and those not. However, by using reliable sources of information, you can develop a profile of the population that will help you identify which groups are most at risk.
Once you have identified the population most likely to experience the problem, you to develop a plan of action to address it. This action plan should be based on evidence-based practices, ensuring that your proposal is effective and efficient.
Find out more on Nursing Essay Thesis Statement [+How to & Examples]
Develop a Plan of Action
The next step in writing an EBP nursing research paper is to develop a plan of action. This action plan should be based on the evidence you have gathered and the population you have identified as most at risk.
Your action plan should include specific objectives, targets, timelines, and budgetary constraints. It should also include measures to resolve the problem, including benchmarks and measurements.
Finally, your action plan should be evaluated and revised based on stakeholder feedback. This feedback will help you ensure that your proposal is effective and efficient.
Writing an EBP nursing research paper can be daunting, but it can be much easier with a plan. This guide will provide you with the essential steps you need to take to produce high-quality research papers. First, you will need to identify the problem you are researching. Next, identify the population most likely to experience the problem and/or share its consequences. Finally, using evidence-based practices as your guide, develop a plan of action that will address the issue.
Steps of Writing an EBP Research Paper in Nursing
1. Determine the purpose of your EBP study. 2. Choose a relevant population or setting. 3. Identify the specific question you wish to answer. 4. Collect and analyze data. 5. Construct a hypothesis or theory based on your findings. 6. Write a conclusion that supports your thesis statement. 7. Offer suggestions for future research on evidence-based practice in nursing.
EBP Research Paper Literature Review Writing- Evidence-Based Practice (EBP)
Evidence-based practice (EBP) is an approach to nursing that focuses on using evidence to guide clinical decisions. EBP is effective in improving patient outcomes and reducing healthcare costs. To write an effective EBP literature review, it is important to understand the concepts of evidence and research.
The following section will provide a brief overview of the concept of evidence and its role in EBP. After this, the section will outline the different types of research used in EBP and discuss how to select appropriate research for your paper. Finally, the section will provide tips for writing an effective literature review.
You might be interested in Nursing Case Study Analysis [10 Examples & How-To Guides]
What is Evidence?
Evidence is information that supports a belief or theory. It can come from either personal experience or empirical research. Personal experience includes things like doctor’s orders or patient statements. Empirical research includes studies that use scientific methods to collect data about a particular topic.
Why Use Evidence in Nursing?
There are many reasons why using evidence in nursing is important. First, it can help improve patient outcomes. For example, using evidence-based practices when caring for patients with diabetes can help control their blood sugar levels and reduce the risk of complications.
Second, using evidence can reduce healthcare costs. For example, using evidence-based interventions when caring for patients with heart disease can help reduce the risk of death and hospitalization.
Finally, using evidence can help nurses make better decisions. For example, when caring for a patient with cancer, it is important to use evidence-based treatments that are effective in reducing the risk of cancer recurrence.
What Types of Research is Used in EBP?
There are many different types of research used in EBP. The following section will outline the different types of research and discuss how to select appropriate research for your paper.
- Clinical trials: Clinical trials are experiments that are designed to test the effectiveness of a new treatment or intervention. Clinical trials can be conducted in hospitals or clinics.
- Evaluation studies: Evaluation studies compare the outcomes of two or more treatments or interventions. Evaluation studies can be conducted in hospitals or clinics.
- Observational studies: Observational studies collect data about how people behave without Intervention. Observational studies can be conducted at home, work, or anywhere people gather data.
How to Select Appropriate Research for Your Paper
When selecting research for your EBP nursing research paper, it is important to consider the topic you are writing about and the audience you are writing for. The following tips can help you select appropriate research for your paper.
- First, consider the topic you are writing about. If you are writing about a new treatment or intervention, it is important to use clinical trials. Clinical trials are experiments that are designed to test the effectiveness of a new treatment or intervention.
- If you are writing about an existing treatment or intervention, it is important to use observational studies. Observational studies are studies that collect data about how people behave without Intervention. These studies can be conducted at home, work, or anywhere else people gather data.
- Second, consider the audience you are writing for. If you are writing for a healthcare provider, using evidence-based practices that effectively improve patient outcomes and reduce healthcare costs is essential. If you are writing for a patient or their family, using understandable and relatable information is essential.
- Finally, always check the credibility of any sources used in your paper. Credible sources will typically have references that can be verified.
Using credible sources for Evidence-based practice paper
Evidence-based practice (EBP) is a nursing research methodology that draws on published, peer-reviewed scientific studies to develop rationales for and recommendations for patient care.
- It is important to use credible sources to write an EBP paper that is both credible and useful. Credible sources have been examined by experts in the field and found to be reliable. To identify credible sources, it is helpful first to understand what constitutes evidence-based practice.
- The five types of evidence considered most important in EBP are randomized clinical trials (RCTs), systematic reviews, meta-analyses, case reports, and expert opinion.
- When using any of these types of evidence, it is important to ensure the study was conducted according to strict methodological standards.
- For example, RCTs must be blinded (i.e., the participants and investigators should not know which group is receiving the treatment being studied). Furthermore, all data collected during an RCT must be reported accurately and completely.
- Once you have identified a study as credible, the next step is to determine whether the study’s findings are relevant to your topic. It is important to note that not all studies that qualify as evidence-based practice apply to every topic.
- For example, a study that explores the use of acupuncture as a treatment for chronic neck pain would not apply to writing an EBP paper on the use of epidural analgesia in childbirth.
- Finally, it is important to consider the implications of the study’s findings when writing an EBP paper.
- For example, if a study found that a particular treatment was ineffective, it is important to discuss why this might be the case and what can be done to address the issue.
What are the 5 A’s in evidence-based practice?
Evidence-based practice is a healthcare approach that is based on the use of evidence from research studies to make decisions about care. Here are the A’s in evidence-based practice:
- Anchor: The anchor for your paper should be a specific and meaningful study that provides the basis for your argument.
- Background: State the purpose of your paper, including why you are studying the issue.
- Methods: Describe how you conducted your study and collected the data.
- Results: Discuss the findings of your study in detail, including any relevant conclusions.
- Discussion: Explain how this information can be used to improve patient care.
How do nurses write evidence based practice papers?
There are a few key steps that nurses should take when writing evidence based practice papers, including conducting research, analyzing data, and writing effective conclusions.
Here are more specific tips on how to go about each of these steps:
1. Conduct Research: The first step in writing an evidence-based practice paper is to conduct research. This means gathering information from reliable sources to support your arguments. You can find information on different types of research in the library, online databases, and journals. When selecting sources, be sure to select studies that are relevant to your topic and that you can trust.
2. Analyze Data: After you have gathered your data, it is important to analyze it carefully. This means looking at the data from different perspectives and using logic and reasoning to arrive at a conclusion. Be sure to state your findings clearly and concisely so that others can understand them.
3. Write Effective Conclusions: The final step in writing an evidence-based practice paper is to write effective conclusions. This section should summarize your findings and include any recommendations that you have for improving patient care. Remember to support your recommendations with credible evidence.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Careers
- Nursing Paper Solutions
- Nursing Theories
- Nursing Topics and Ideas
Related Posts
- Types of Analysis in a DNP Project: A Guide for Doctor of Nursing Practice Students
- How to Write a DNP Project Executive Summary: Comprehensive Guide for Nursing Students
- DNP Project Gantt Chart Guide for Nursing Students
Important Links
Knowledge base.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Center for Nursing Inquiry
Evidence-based practice, what is ebp.
As nurses, we often hear the term evidence-based practice (EBP). But, what does it actually mean? EBP is a process used to review, analyze, and translate the latest scientific evidence. The goal is to quickly incorporate the best available research, along with clinical experience and patient preference, into clinical practice, so nurses can make informed patient-care decisions ( Dang et al., 2022 ). EBP is the cornerstone of clinical practice. Integrating EBP into your nursing practice improves quality of care and patient outcomes.
How do I get involved in EBP?
As a nurse, you will have plenty of opportunities to get involved in EBP. Take that “AHA” moment. Do you think there’s a better way to do something? Let’s turn to the evidence and find out!
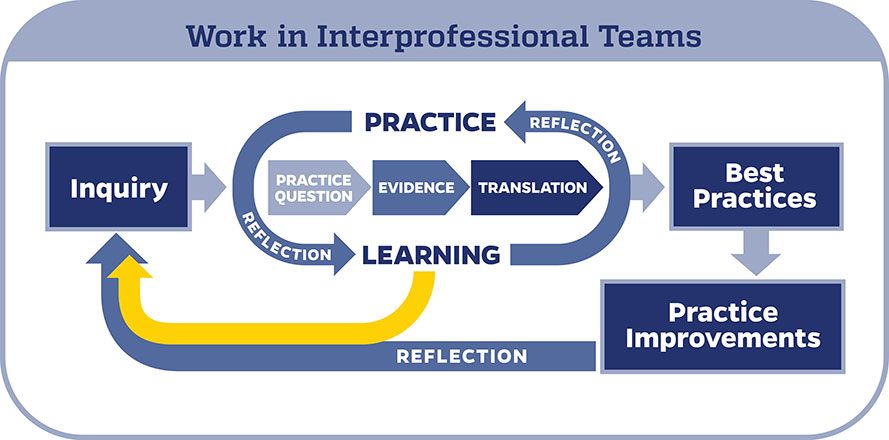
When conducting an EBP project, it is important to use a model to help guide your work. In the Johns Hopkins Health System, we use the Johns Hopkins Evidence-Based Practice (JHEBP) model. It is a three-phase approach referred to as the PET process: practice question, evidence, and translation. In the first phase, the team develops a practice question by identifying the patient population, interventions, and outcomes (PICO). In the second phase, a literature search is performed, and the evidence is appraised for strength and quality. In the third phase, the findings are synthesized to develop recommendations for practice.
The JHEBP model is accompanied by user-friendly tools. The tools walk you through each phase of the project. Johns Hopkins nurses can access the tools via our Inquiry Toolkit . The tools are available to individuals from other institutions via the Institute for Johns Hopkins Nursing (IJHN) .
If you’re interested in learning more about the JHEBP model and tools, Johns Hopkins nurses have access to a free online course entitled JHH Nursing | Central | Evidence-Based Practice Series in MyLearning. The course follows the JHEBP process from beginning to end and provides guidance to the learner on how to use the JHEBP tools. The course is available to individuals from other institutions for a fee via the Institute for Johns Hopkins Nursing (IJHN) .
Where should I start?
All EBP projects need to be submitted to the Center for Nursing Inquiry for review. The CNI ensures all nurse-led EBP projects are high-quality and value added. We also offer expert guidance and support, if needed.
Who can help me?
The Center for Nursing Inquiry can answer any questions you may have about the JHEBP tools. All 10 JHEBP tools can be found in our Inquiry Toolkit : project management guide, question development tool, stakeholder analysis tool, evidence level and quality guide, research evidence appraisal tool, non-research evidence appraisal tool, individual evidence summary tool, synthesis process and recommendations tool, action planning tool, and dissemination tool. The tools walk you through each phase of an EBP project.
The Welch Medical Library serves the information needs of the faculty, staff, and students of Johns Hopkins Medicine, Nursing and Public Health. Often, one of the toughest parts of conducting an EBP project is finding the evidence. The informationist assigned to your department can assist you with your literature search and citation management.
When do I share my work?
Your project is complete. Now what? It’s time to share your project with the scholarly community.
To prepare your EBP project for publication, use the JHEBP Dissemination Tool . The JHEBP Dissemination Tool (Appendix J) details what to include in each section of your manuscript, from the introduction to the discussion, and shows you which EBP appendices correspond to each part of a scientific paper. You can find the JHEBP Dissemination Tool in our Inquiry Toolkit .
You can also present your project at a local, regional, or national conference. Poster and podium presentation templates are available in our Inquiry Toolkit .
To learn more about sharing your project, check out our Abstract & Manuscript Writing webinar and our Poster & Podium Presentations webinar !
Submit Your Project
Do you have an idea for an EBP project?
Evidence Based Practice’ Impact on Nursing Essay (Article)
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Article: APA Format
Brief discussion, ebp discussions.
Reid, J., Briggs, J., Carlisle, S., Scott, D., & Lewis, C. (2017). Enhancing utility and understanding of the evidence-based practice through undergraduate nurse education. BMC Nursing, 16 (58), 1-8. Web.
The selected article offers meaningful insights that can empower nursing educationists and practitioners to embrace the power of evidence-based practice (EBP). The authors describe a new course (Evidence-Based Nursing 1) that was implemented as part of an undergraduate nursing program. The researchers observed that the targeted learners were willing to make evidence-based practices part of their nursing philosophies after completing the course. The practice can encourage practitioners to integrate EBP into their respective care delivery models (Reid, Briggs, Carlisle, Scott, & Lewis, 2017). The judicious use of emerging or current evidence in care delivery and health decision-making processes can result in improved patient outcomes and support advanced practice nursing. This article describes the meaning of EBP and how it can be implemented in nursing institutions to ensure that advanced practice nurses (APNs) are prepared to meet their patients’ health needs. The use of emerging evidence and concepts from research studies can guide nurses to offer advanced care. When APNs embrace the power of EBP, they will achieve their potential and offer quality and equitable health services.
The concept of EBP revolves around the use of best evidence to improve patient outcomes. Mackey and Bassendowski (2016) indicate that external clinical findings, results from systematic studies, and personal nursing expertise constitutes “best evidence” for EBP. Nurses should combine such concepts to develop appropriate care delivery models and make desirable decisions to support their patients. EBP is a powerful approach that can be used at the point of care. Proficient nurses can diagnose and educate patients depending on their conditions. Such practitioners will identify signs and symptoms, offer timely patient education, and empower individuals to engage in disease management practices. These tasks at the point of care will be informed by every nurse’s current evidence and information backed by the latest research findings.
Informatics can bring the best available evidence to support AGPC practice. Modern technologies empower nurses to use standardized terminologies that can result in desirable health outcomes. Digital sources of timely or latest evidence can also be used to meet patients’ needs. Practitioners can use informatics processes to acquire and apply evidence to different clinical situations (Reid et al., 2017). Informatics competencies empower nurses to minimize sentinel events and meet patients’ needs.
I am planning to embrace the future by using EBP in my practice. I will incorporate the concept using a powerful strategy. The approach will be implemented using the notion of lifelong learning. I will also undertake numerous researches and use modern informatics to improve my nursing philosophy. Unfortunately, some barriers can affect the implementation and development of an EBP culture. The first one is the existing gap in education and practice. This limitation affects nurses’ ability to use evidence accurately and efficiently. The lack of appropriate policies to support the use of EBP is the second challenge (Mackey & Bassendowski, 2016). The third obstacle is that many institutions and practitioners have failed to embrace the power of informatics. These gaps affect patients’ health outcomes negatively.
EBP is expected to impact advanced nursing practice positively. The concept can sanction practitioners to make informed decisions and offer desirable care depending on their patients’ expectations. The approach results in improved care delivery systems. It also encourages practitioners to improve their nursing philosophies using emerging ideas (or concepts) and their competencies (Reid et al., 2017). EBP empowers nurses to make informed decisions, develop superior care delivery models, and update their skills. APNs using the concept will, therefore, offer safe, affordable, and sustainable care to their patients.
Mackey, A., & Bassendowski, S. (2016). The history of evidence-based practice in nursing education and practice. Journal of Professional Nursing, 33 (1), 51-55. Web.
Reid, J., Briggs, J., Carlisle, S., Scott, D., & Lewis, C. (2017). Enhancing utility and understanding of evidence based practice through undergraduate nurse education. BMC Nursing, 16 (58), 1-8. Web.
- Reflection of Professional Experience: EBP
- Evidence-Based Practice in Informatics
- Evidence-Based Practice Changes in a Clinical Setting
- The Future of Nursing
- Interdisciplinary Cooperation in Nursing
- Teaching Beliefs in Nursing Education
- Nursing Theory: Evidence-Based Practice
- Nursing Research: Clinical Performance
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, December 17). Evidence Based Practice' Impact on Nursing. https://ivypanda.com/essays/evidence-based-practice-impact-on-nursing/
"Evidence Based Practice' Impact on Nursing." IvyPanda , 17 Dec. 2020, ivypanda.com/essays/evidence-based-practice-impact-on-nursing/.
IvyPanda . (2020) 'Evidence Based Practice' Impact on Nursing'. 17 December.
IvyPanda . 2020. "Evidence Based Practice' Impact on Nursing." December 17, 2020. https://ivypanda.com/essays/evidence-based-practice-impact-on-nursing/.
1. IvyPanda . "Evidence Based Practice' Impact on Nursing." December 17, 2020. https://ivypanda.com/essays/evidence-based-practice-impact-on-nursing/.
Bibliography
IvyPanda . "Evidence Based Practice' Impact on Nursing." December 17, 2020. https://ivypanda.com/essays/evidence-based-practice-impact-on-nursing/.

Evidence-Based Practice (EBP)
- The EBP Process
- Forming a Clinical Question
- Inclusion & Exclusion Criteria
- Acquiring Evidence
- Appraising the Quality of the Evidence
- Writing a Literature Review
- Finding Psychological Tests & Assessment Instruments
What Is a Literature Review?
A literature review is an integrated analysis of scholarly writings that are related directly to your research question. Put simply, it's a critical evaluation of what's already been written on a particular topic . It represents the literature that provides background information on your topic and shows a connection between those writings and your research question.
A literature review may be a stand-alone work or the introduction to a larger research paper, depending on the assignment. Rely heavily on the guidelines your instructor has given you.
What a Literature Review Is Not:
- A list or summary of sources
- An annotated bibliography
- A grouping of broad, unrelated sources
- A compilation of everything that has been written on a particular topic
- Literary criticism (think English) or a book review
Why Literature Reviews Are Important
- They explain the background of research on a topic
- They demonstrate why a topic is significant to a subject area
- They discover relationships between research studies/ideas
- They identify major themes, concepts, and researchers on a topic
- They identify critical gaps and points of disagreement
- They discuss further research questions that logically come out of the previous studies
To Learn More about Conducting and Writing a Lit Review . . .
Monash University (in Australia) has created several extremely helpful, interactive tutorials.
- The Stand-Alone Literature Review, https://www.monash.edu/rlo/assignment-samples/science/stand-alone-literature-review
- Researching for Your Literature Review, https://guides.lib.monash.edu/researching-for-your-literature-review/home
- Writing a Literature Review, https://www.monash.edu/rlo/graduate-research-writing/write-the-thesis/writing-a-literature-review
Keep Track of Your Sources!
A citation manager can be helpful way to work with large numbers of citations. See UMSL Libraries' Citing Sources guide for more information. Personally, I highly recommend Zotero —it's free, easy to use, and versatile. If you need help getting started with Zotero or one of the other citation managers, please contact a librarian.
- << Previous: Appraising the Quality of the Evidence
- Next: Finding Psychological Tests & Assessment Instruments >>
- Last Updated: May 16, 2024 2:44 PM
- URL: https://libguides.umsl.edu/ebp
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 7 the evidence for evidence-based practice implementation.
Marita G. Titler .
Affiliations
Overview of evidence-based practice.
Evidence-based health care practices are available for a number of conditions such as asthma, heart failure, and diabetes. However, these practices are not always implemented in care delivery, and variation in practices abound. 1–4 Traditionally, patient safety research has focused on data analyses to identify patient safety issues and to demonstrate that a new practice will lead to improved quality and patient safety. 5 Much less research attention has been paid to how to implement practices. Yet, only by putting into practice what is learned from research will care be made safer. 5 Implementing evidence-based safety practices are difficult and need strategies that address the complexity of systems of care, individual practitioners, senior leadership, and—ultimately—changing health care cultures to be evidence-based safety practice environments. 5
Nursing has a rich history of using research in practice, pioneered by Florence Nightingale. 6–9 Although during the early and mid-1900s, few nurses contributed to this foundation initiated by Nightingale, 10 the nursing profession has more recently provided major leadership for improving care through application of research findings in practice. 11
Evidence-based practice (EBP) is the conscientious and judicious use of current best evidence in conjunction with clinical expertise and patient values to guide health care decisions. 12–15 Best evidence includes empirical evidence from randomized controlled trials; evidence from other scientific methods such as descriptive and qualitative research; as well as use of information from case reports, scientific principles, and expert opinion. When enough research evidence is available, the practice should be guided by research evidence in conjunction with clinical expertise and patient values. In some cases, however, a sufficient research base may not be available, and health care decision making is derived principally from nonresearch evidence sources such as expert opinion and scientific principles. 16 As more research is done in a specific area, the research evidence must be incorporated into the EBP. 15
Models of Evidence-Based Practice
Multiple models of EBP are available and have been used in a variety of clinical settings. 16–36 Although review of these models is beyond the scope of this chapter, common elements of these models are selecting a practice topic (e.g., discharge instructions for individuals with heart failure), critique and syntheses of evidence, implementation, evaluation of the impact on patient care and provider performance, and consideration of the context/setting in which the practice is implemented. 15 , 17 The learning that occurs during the process of translating research into practice is valuable information to capture and feed back into the process, so that others can adapt the evidence-based guideline and/or the implementation strategies.
A recent conceptual framework for maximizing and accelerating the transfer of research results from the Agency for Healthcare Research and Quality (AHRQ) patient safety research portfolio to health care delivery was developed by the dissemination subcommittee of the AHRQ Patient Safety Research Coordinating Committee. 37 This model is a synthesis of concepts from scientific information on knowledge transfer, social marketing, social and organizational innovation, and behavior change (see Figure 1 ). 37 Although the framework is portrayed as a series of stages, the authors of this framework do not believe that the knowledge transfer process is linear; rather, activities occur simultaneously or in different sequences, with implementation of EBPs being a multifaceted process with many actors and systems.
AHRQ Model of Knowledge Transfer Adapted from Nieva, V., Murphy, R., Ridley, N., et al. Used with permission. http://www.ahrq.gov/qual/advances/
Steps of Evidence-Based Practice
Steps of promoting adoption of EBPs can be viewed from the perspective of those who conduct research or generate knowledge, 23 , 37 those who use the evidence-based information in practice, 16 , 31 and those who serve as boundary spanners to link knowledge generators with knowledge users. 19
Steps of knowledge transfer in the AHRQ model 37 represent three major stages: (1) knowledge creation and distillation, (2) diffusion and dissemination, and (3) organizational adoption and implementation. These stages of knowledge transfer are viewed through the lens of researchers/creators of new knowledge and begin with determining what findings from the patient safety portfolio or individual research projects ought to be disseminated.
Knowledge creation and distillation is conducting research (with expected variation in readiness for use in health care delivery systems) and then packaging relevant research findings into products that can be put into action—such as specific practice recommendations—thereby increasing the likelihood that research evidence will find its way into practice. 37 It is essential that the knowledge distillation process be informed and guided by end users for research findings to be implemented in care delivery. The criteria used in knowledge distillation should include perspectives of the end users (e.g., transportability to the real-world health care setting, feasibility, volume of evidence needed by health care organizations and clinicians), as well as traditional knowledge generation considerations (e.g., strength of the evidence, generalizability).
Diffusion and dissemination involves partnering with professional opinion leaders and health care organizations to disseminate knowledge that can form the basis of action (e.g., essential elements for discharge teaching for hospitalized patient with heart failure) to potential users. Dissemination partnerships link researchers with intermediaries that can function as knowledge brokers and connectors to the practitioners and health care delivery organizations. Intermediaries can be professional organizations such as the National Patient Safety Foundation or multidisciplinary knowledge transfer teams such as those that are effective in disseminating research-based cancer prevention programs. In this model, dissemination partnerships provide an authoritative seal of approval for new knowledge and help identify influential groups and communities that can create a demand for application of the evidence in practice. Both mass communication and targeted dissemination are used to reach audiences with the anticipation that early users will influence the latter adopters of the new usable, evidence-based research findings. Targeted dissemination efforts must use multifaceted dissemination strategies, with an emphasis on channels and media that are most effective for particular user segments (e.g., nurses, physicians, pharmacists).
End user adoption, implementation, and institutionalization is the final stage of the knowledge transfer process. 37 This stage focuses on getting organizations, teams, and individuals to adopt and consistently use evidence-based research findings and innovations in everyday practice. Implementing and sustaining EBPs in health care settings involves complex interrelationships among the EBP topic (e.g., reduction of medication errors), the organizational social system characteristics (such as operational structures and values, the external health care environment), and the individual clinicians. 35 , 37–39 A variety of strategies for implementation include using a change champion in the organization who can address potential implementation challenges, piloting/trying the change in a particular patient care area of the organization, and using multidisciplinary implementation teams to assist in the practical aspects of embedding innovations into ongoing organizational processes. 35 , 37 Changing practice takes considerable effort at both the individual and organizational level to apply evidence-based information and products in a particular context. 22 When improvements in care are demonstrated in the pilot studies and communicated to other relevant units in the organization, key personnel may then agree to fully adopt and sustain the change in practice. Once the EBP change is incorporated into the structure of the organization, the change is no longer considered an innovation but a standard of care. 22 , 37
In comparison, other models of EBP (e.g., Iowa Model of Evidence-based Practice to Promote Quality of Care 16 ) view the steps of the EBP process from the perspective of clinicians and/or organizational/clinical contexts of care delivery. When viewing steps of the EBP process through the lens of an end user, the process begins with selecting an area for improving care based on evidence (rather than asking what findings ought to be disseminated); determining the priority of the potential topic for the organization; formulating an EBP team composed of key stakeholders; finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations, with the type and strength of evidence used to support each clearly documented; determining if the evidence findings are appropriate for use in practice; writing an EBP standard specific to the organization; piloting the change in practice; implementing changes in practice in other relevant practice areas (depending on the outcome of the pilot); evaluating the EBP changes; and transitioning ongoing quality improvement (QI) monitoring, staff education, and competency review of the EBP topic to appropriate organizational groups as defined by the organizational structure. 15 , 40 The work of EBP implementation from the perspective of the end user is greatly facilitated by efforts of AHRQ, professional nursing organizations (e.g., Oncology Nursing Society), and others that distill and package research findings into useful products and tools for use at the point of care delivery.
When the clinical questions of end users can be addressed through use of existing evidence that is packaged with end users in mind, steps of the EBP process take less time and more effort can be directed toward the implementation, evaluation, and sustainability components of the process. For example, finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations with documentation of the type and strength of evidence for each recommendation; and determining appropriateness of the evidence for use in practice are accelerated when the knowledge-based information is readily available. Some distilled research findings also include quick reference guides that can be used at the point of care and/or integrated into health care information systems, which also helps with implementation. 41 , 42
Translation Science: An Overview
Translation science is the investigation of methods, interventions, and variables that influence adoption by individuals and organizations of EBPs to improve clinical and operational decisionmaking in health care. 35 , 43–46 This includes testing the effect of interventions on promoting and sustaining adoption of EBPs. Examples of translation studies include describing facilitators and barriers to knowledge uptake and use, organizational predictors of adherence to EBP guidelines, attitudes toward EBPs, and defining the structure of the scientific field. 11 , 47–49
Translation science must be guided by a conceptual model that organizes the strategies being tested, elucidates the extraneous variables (e.g., behaviors and facilitators) that may influence adoption of EBPs (e.g., organizational size, characteristics of users), and builds a scientific knowledge base for this field of inquiry. 15 , 50 Conceptual models used in the translating-research-into-practice studies funded by AHRQ were adult learning, health education, social influence, marketing, and organizational and behavior theories. 51 Investigators have used Rogers’s Diffusion of Innovation model, 35 , 39 , 52–55 the Promoting Action on Research Implementation in Health Services (PARIHS) model, 29 the push/pull framework, 23 , 56 , 57 the decisionmaking framework, 58 and the Institute for Healthcare Improvement (IHI) model 59 in translation science.
Study findings regarding evidence-based practices in a diversity of health care settings are building an empirical foundation of translation science. 19 , 43 , 51 , 60–83 These investigations and others 18 , 84–86 provide initial scientific knowledge to guide us in how to best promote use of evidence in practice. To advance knowledge about promoting and sustaining adoption of EBPs in health care, translation science needs more studies that test translating research into practice (TRIP) interventions: studies that investigate what TRIP interventions work, for whom, in what circumstances, in what types of settings; and studies that explain the underlying mechanisms of effective TRIP interventions. 35 , 49 , 79 , 87 Partnership models, which encourage ongoing interaction between researchers and practitioners, may be the way forward to carry out such studies. 56 Challenges, issues, methods, and instruments used in translation research are described elsewhere. 11 , 19 , 49 , 78 , 88–97
- Research Evidence
What Is Known About Implementing Evidence-Based Practices?
Multifaceted implementation strategies are needed to promote use of research evidence in clinical and administrative health care decisionmaking. 15 , 22 , 37 , 45 , 64 , 72 , 77 , 79 , 98 , 99 Although Grimshaw and colleagues 65 suggest that multifaceted interventions are no more effective than single interventions, context (site of care delivery) was not incorporated in the synthesis methodology. As noted by others, the same TRIP intervention may meet with varying degrees of effectiveness when applied in different contexts. 35 , 49 , 79 , 80 , 87 , 100 , 101 Implementation strategies also need to address both the individual practitioner and organizational perspective. 15 , 22 , 37 , 64 , 72 , 77 , 79 , 98 When practitioners decide individually what evidence to use in practice, considerable variability in practice patterns result, 71 potentially resulting in adverse patient outcomes.
For example, an “individual” perspective of EBP would leave the decision about use of evidence-based endotracheal suctioning techniques to each nurse and respiratory therapist. Some individuals may be familiar with the research findings for endotracheal suctioning while others may not. This is likely to result in different and conflicting practices being used as people change shifts every 8 to 12 hours. From an organizational perspective, endotracheal suctioning policies and procedures based on research are written, the evidence-based information is integrated into the clinical information systems, and adoption of these practices by nurses and other practitioners is systematically promoted in the organization. This includes assuring that practitioners have the necessary knowledge, skills, and equipment to carry out the evidence-based endotracheal suctioning practice. The organizational governance supports use of these practices through various councils and committees such as the Practice Committee, Staff Education Committee, and interdisciplinary EBP work groups.
The Translation Research Model, 35 built on Rogers’s seminal work on diffusion of innovations, 39 provides a guiding framework for testing and selecting strategies to promote adoption of EBPs. According to the Translation Research Model, adoption of innovations such as EBPs are influenced by the nature of the innovation (e.g., the type and strength of evidence, the clinical topic) and the manner in which it is communicated (disseminated) to members (nurses) of a social system (organization, nursing profession). 35 Strategies for promoting adoption of EBPs must address these four areas (nature of the EBP topic; users of the evidence; communication; social system) within a context of participative change (see Figure 2 ). This model provided the framework for a multisite study that tested the effectiveness of a multifaceted TRIP intervention designed to promote adoption of evidence-based acute pain management practices for hospitalized older adults. The intervention improved the quality of acute pain management practices and reduced costs. 81 The model is currently being used to test the effectiveness of a multifaceted TRIP intervention to promote evidence-based cancer pain management of older adults in home hospice settings. * This guiding framework is used herein to overview what is known about implementation interventions to promote use of EBPs in health care systems (see Evidence Table ).
*Implementation Model Redrawn from Rogers EM. Diffusion of innovations. 5th ed. New York: The Free Press; 2003; Titler MG, Everett LQ. Translating research into practice: considerations for critical care investigators. Crit Care Nurs Clin North Am 2001a;13(4):587-604. (more...)
Evidence Table
Evidence-Based Practice in Nursing
Nature of the Innovation or Evidence-Based Practice
Characteristics of an innovation or EBP topic that affect adoption include the relative advantage of the EBP (e.g., effectiveness, relevance to the task, social prestige); the compatibility with values, norms, work, and perceived needs of users; and complexity of the EBP topic. 39 For example, EBP topics that are perceived by users as relatively simple (e.g., influenza vaccines for older adults) are more easily adopted in less time than those that are more complex (acute pain management for hospitalized older adults). Strategies to promote adoption of EBPs related to characteristics of the topic include practitioner review and “reinvention” of the EBP guideline to fit the local context, use of quick reference guides and decision aids, and use of clinical reminders. 53 , 59 , 60 , 65 , 74 , 82 , 102–107 An important principle to remember when planning implementation of an EBP is that the attributes of the EBP topic as perceived by users and stakeholders (e.g., ease of use, valued part of practice) are neither stable features nor sure determinants of their adoption. Rather it is the interaction among the characteristics of the EBP topic, the intended users, and a particular context of practice that determines the rate and extent of adoption. 22 , 35 , 39
Studies suggest that clinical systems, computerized decision support, and prompts that support practice (e.g., decisionmaking algorithms, paper reminders) have a positive effect on aligning practices with the evidence base. 15 , 51 , 65 , 74 , 80 , 82 , 102 , 104 , 107–110 Computerized knowledge management has consistently demonstrated significant improvements in provider performance and patient outcomes. 82 Feldman and colleagues, using a just-in-time e-mail reminder in home health care, have demonstrated (1) improvements in evidence-based care and outcomes for patients with heart failure, 64 , 77 and (2) reduced pain intensity for cancer patients. 75 Clinical information systems should deploy the evidence base to the point of care and incorporate computer decision-support software that integrates evidence for use in clinical decisionmaking about individual patients. 40 , 104 , 111–114 There is still much to learn about the “best” manner of deploying evidence-based information through electronic clinical information systems to support evidence-based care. 115
Methods of Communication
Interpersonal communication channels, methods of communication, and influence among social networks of users affect adoption of EBPs. 39 Use of mass media, opinion leaders, change champions, and consultation by experts along with education are among strategies tested to promote use of EBPs. Education is necessary but not sufficient to change practice, and didactic continuing education alone does little to change practice behavior. 61 , 116 There is little evidence that interprofessional education as compared to discipline-specific education improves EBP. 117 Interactive education, used in combination with other practice-reinforcing strategies, has more positive effects on improving EBP than didactic education alone. 66 , 68 , 71 , 74 , 118 , 119 There is evidence that mass media messages (e.g., television, radio, newspapers, leaflets, posters and pamphlets), targeted at the health care consumer population, have some effect on use of health services for the targeted behavior (e.g., colorectal cancer screening). However, little empirical evidence is available to guide framing of messages communicated through planned mass media campaigns to achieve the intended change. 120
Several studies have demonstrated that opinion leaders are effective in changing behaviors of health care practitioners, 22 , 68 , 79 , 100 , 116 , 121–123 especially in combination with educational outreach or performance feedback. Opinion leaders are from the local peer group, viewed as a respected source of influence, considered by associates as technically competent, and trusted to judge the fit between the innovation and the local situation. 39 , 116 , 121 , 124–127 With their wide sphere of influence across several microsystems/units, opinion leaders’ use of the innovation influences peers and alters group norms. 39 , 128 The key characteristic of an opinion leader is that he or she is trusted to evaluate new information in the context of group norms. Opinion leadership is multifaceted and complex, with role functions varying by the circumstances, but few successful projects to implement innovations in organizations have managed without the input of identifiable opinion leaders. 22 , 35 , 39 , 81 , 96 Social interactions such as “hallway chats,” one-on-one discussions, and addressing questions are important, yet often overlooked components of translation. 39 , 59 Thus, having local opinion leaders discuss the EBPs with members of their peer group is necessary to translate research into practice. If the EBP that is being implemented is interdisciplinary in nature, discipline-specific opinion leaders should be used to promote the change in practice. 39
Change champions are also helpful for implementing innovations. 39 , 49 , 81 , 129–131 They are practitioners within the local group setting (e.g., clinic, patient care unit) who are expert clinicians, passionate about the innovation, committed to improving quality of care, and have a positive working relationship with other health care professionals. 39 , 125 , 131 , 132 They circulate information, encourage peers to adopt the innovation, arrange demonstrations, and orient staff to the innovation. 49 , 130 The change champion believes in an idea; will not take “no” for an answer; is undaunted by insults and rebuffs; and, above all, persists. 133 Because nurses prefer interpersonal contact and communication with colleagues rather than Internet or traditional sources of practice knowledge, 134–137 it is imperative that one or two change champions be identified for each patient care unit or clinic where the change is being made for EBPs to be enacted by direct care providers. 81 , 138 Conferencing with opinion leaders and change champions periodically during implementation is helpful to address questions and provide guidance as needed. 35 , 66 , 81 , 106
Because nurses’ preferred information source is through peers and social interactions, 134–137 , 139 , 140 using a core group in conjunction with change champions is also helpful for implementing the practice change. 16 , 110 , 141 A core group is a select group of practitioners with the mutual goal of disseminating information regarding a practice change and facilitating the change by other staff in their unit/microsystem. 142 Core group members represent various shifts and days of the week and become knowledgeable about the scientific basis for the practice; the change champion educates and assists them in using practices that are aligned with the evidence. Each member of the core group, in turn, takes the responsibility for imparting evidence-based information and effecting practice change with two or three of their peers. Members assist the change champion and opinion leader with disseminating the EBP information to other staff, reinforce the practice change on a daily basis, and provide positive feedback to those who align their practice with the evidence base. 15 Using a core-group approach in conjunction with a change champion results in a critical mass of practitioners promoting adoption of the EBP. 39
Educational outreach, also known as academic detailing, promotes positive changes in practice behaviors of nurses and physicians. 22 , 64 , 66 , 71 , 74 , 75 , 77 , 81 , 119 , 143 Academic detailing is done by a topic expert, knowledgeable of the research base (e.g., cancer pain management), who may be external to the practice setting; he or she meets one-on-one with practitioners in their setting to provide information about the EBP topic. These individuals are able to explain the research base for the EBPs to others and are able to respond convincingly to challenges and debates. 22 This strategy may include providing feedback on provider or team performance with respect to selected EBP indicators (e.g., frequency of pain assessment). 66 , 81 , 119
Users of the Innovation or Evidence-Based Practice
Members of a social system (e.g., nurses, physicians, clerical staff) influence how quickly and widely EBPs are adopted. 39 Audit and feedback, performance gap assessment (PGA), and trying the EBP are strategies that have been tested. 15 , 22 , 65 , 66 , 70–72 , 81 , 98 , 124 , 144 PGA and audit and feedback have consistently shown a positive effect on changing practice behavior of providers. 65 , 66 , 70 , 72 , 81 , 98 , 124 , 144 , 145 PGA (baseline practice performance) informs members, at the beginning of change, about a practice performance and opportunities for improvement. Specific practice indicators selected for PGA are related to the practices that are the focus of evidence-based practice change, such as every-4-hour pain assessment for acute pain management. 15 , 66 , 81
Auditing and feedback are ongoing processes of using and assessing performance indicators (e.g., every-4-hour pain assessment), aggregating data into reports, and discussing the findings with practitioners during the practice change. 22 , 49 , 66 , 70 , 72 , 81 , 98 , 145 This strategy helps staff know and see how their efforts to improve care and patient outcomes are progressing throughout the implementation process. Although there is no clear empirical evidence for how to provide audit and feedback, 70 , 146 effects may be larger when clinicians are active participants in implementing change and discuss the data rather than being passive recipients of feedback reports. 67 , 70 Qualitative studies provide some insight into use of audit and feedback. 60 , 67 One study on use of data feedback for improving treatment of acute myocardial infarction found that (1) feedback data must be perceived by physicians as important and valid, (2) the data source and timeliness of data feedback are critical to perceived validity, (3) time is required to establish credibility of data within a hospital, (4) benchmarking improves the validity of the data feedback, and (5) physician leaders can enhance the effectiveness of data feedback. Data feedback that profiles an individual physician’s practices can be effective but may be perceived as punitive; data feedback must persist to sustain improved performance; and effectiveness of data feedback is intertwined with the organizational context, including physician leadership and organizational culture. 60 Hysong and colleagues 67 found that high-performing institutions provided timely, individualized, nonpunitive feedback to providers, whereas low performers were more variable in their timeliness and nonpunitiveness and relied more on standardized, facility-level reports. The concept of useful feedback emerged as the core concept around which timeliness, individualization, nonpunitiveness, and customizability are important.
Users of an innovation usually try it for a period of time before adopting it in their practice. 22 , 39 , 147 When “trying an EBP” (piloting the change) is incorporated as part of the implementation process, users have an opportunity to use it for a period of time, provide feedback to those in charge of implementation, and modify the practice if necessary. 148 Piloting the EBP as part of implementation has a positive influence on the extent of adoption of the new practice. 22 , 39 , 148
Characteristics of users such as educational preparation, practice specialty, and views on innovativeness may influence adoption of an EBP, although findings are equivocal. 27 , 39 , 130 , 149–153 Nurses’ disposition to critical thinking is, however, positively correlated with research use, 154 and those in clinical educator roles are more likely to use research than staff nurses or nurse managers. 155
Social System
Clearly, the social system or context of care delivery matters when implementing EBPs. 2 , 30 , 33 , 39 , 60 , 84 , 85 , 91 , 92 , 101 , 156–163 For example, investigators demonstrated the effectiveness of a prompted voiding intervention for urinary incontinence in nursing homes, but sustaining the intervention in day-to-day practice was limited when the responsibility of carrying out the intervention was shifted to nursing home staff (rather than the investigative team) and required staffing levels in excess of a majority of nursing home settings. 164 This illustrates the importance of embedding interventions into ongoing processes of care.
Several organizational factors affect adoption of EBPs. 22 , 39 , 79 , 134 , 165–167 Vaughn and colleagues 101 demonstrated that organizational resources, physician full-time employees (FTEs) per 1,000 patient visits, organizational size, and whether the facility was located in or near a city affected use of evidence in the health care system of the Department of Veterans Affairs (VA). Large, mature, functionally differentiated organizations (e.g., divided into semiautonomous departments and units) that are specialized, with a focus of professional knowledge, slack resources to channel into new projects, decentralized decisionmaking, and low levels of formalization will more readily adopt innovations such as new practices based on evidence. Larger organizations are generally more innovative because size increases the likelihood that other predictors of innovation adoption—such as slack financial and human resources and differentiation—will be present. However, these organizational determinants account for only about 15 percent of the variation in innovation adoption between comparable organizations. 22 Adler and colleagues 168 hypothesize that while more structurally complex organizations may be more innovative and hence adopt EBPs relatively early, less structurally complex organizations may be able to diffuse EBPs more effectively. Establishing semiautonomous teams is associated with successful implementation of EBPs, and thus should be considered in managing organizational units. 168–170
As part of the work of implementing EBPs, it is important that the social system—unit, service line, or clinic—ensures that policies, procedures, standards, clinical pathways, and documentation systems support the use of the EBPs. 49 , 68 , 72 , 73 , 103 , 140 , 171 Documentation forms or clinical information systems may need revision to support changes in practice; documentation systems that fail to readily support the new practice thwart change. 82
Absorptive capacity for new knowledge is another social system factor that affects adoption of EBPs. Absorptive capacity is the knowledge and skills to enact the EBPs; the strength of evidence alone will not promote adoption. An organization that is able to systematically identify, capture, interpret, share, reframe, and recodify new knowledge, and put it to appropriate use, will be better able to assimilate EBPs. 82 , 103 , 172 , 173 A learning organizational culture and proactive leadership that promotes knowledge sharing are important components of building absorptive capacity for new knowledge. 66 , 139 , 142 , 174 Components of a receptive context for EBP include strong leadership, clear strategic vision, good managerial relations, visionary staff in key positions, a climate conducive to experimentation and risk taking, and effective data capture systems. Leadership is critical in encouraging organizational members to break out of the convergent thinking and routines that are the norm in large, well-established organizations. 4 , 22 , 39 , 122 , 148 , 163 , 175
An organization may be generally amenable to innovations but not ready or willing to assimilate a particular EBP. Elements of system readiness include tension for change, EBP-system fit, assessment of implications, support and advocacy for the EBP, dedicated time and resources, and capacity to evaluate the impact of the EBP during and following implementation. If there is tension around specific work or clinical issues and staff perceive that the situation is intolerable, a potential EBP is likely to be assimilated if it can successfully address the issues, and thereby reduce the tension. 22 , 175
Assessing and structuring workflow to fit with a potential EBP is an important component of fostering adoption. If implications of the EBP are fully assessed, anticipated, and planned for, the practice is more likely to be adopted. 148 , 162 , 176 If supporters for a specific EBP outnumber and are more strategically placed within the organizational power base than opponents, the EBP is more likely to be adopted by the organization. 60 , 175 Organizations that have the capacity to evaluate the impact of the EBP change are more likely to assimilate it. Effective implementation needs both a receptive climate and a good fit between the EBP and intended adopters’ needs and values. 22 , 60 , 140 , 175 , 177
Leadership support is critical for promoting use of EBPs. 33 , 59 , 72 , 85 , 98 , 122 , 178–181 This support, which is expressed verbally, provides necessary resources, materials, and time to fulfill assigned responsibilities. 148 , 171 , 182 , 183 Senior leaders need to create an organizational mission, vision, and strategic plan that incorporate EBP; implement performance expectations for staff that include EBP work; integrate the work of EBP into the governance structure of the health care system; demonstrate the value of EBPs through administrative behaviors; and establish explicit expectations that nurse leaders will create microsystems that value and support clinical inquiry. 122 , 183 , 184
A recent review of organizational interventions to implement EBPs for improving patient care examined five major aspects of patient care. The review suggests that revision of professional roles (changing responsibilities and work of health professionals such as expanding roles of nurses and pharmacists) improved processes of care, but it was less clear about the effect on improvement of patient outcomes. Multidisciplinary teams (collaborative practice teams of physicians, nurses, and allied health professionals) treating mostly patients with prevalent chronic diseases resulted in improved patient outcomes. Integrated care services (e.g., disease management and case management) resulted in improved patient outcomes and cost savings. Interventions aimed at knowledge management (principally via use of technology to support patient care) resulted in improved adherence to EBPs and patient outcomes. The last aspect, quality management, had the fewest reviews available, with the results uncertain. A number of organizational interventions were not included in this review (e.g., leadership, process redesign, organizational learning), and the authors note that the lack of a widely accepted taxonomy of organizational interventions is a problem in examining effectiveness across studies. 82
An organizational intervention that is receiving increasing attention is tailored interventions to overcome barriers to change. 162 , 175 , 185 This type of intervention focuses on first assessing needs in terms of what is causing the gap between current practice and EBP for a specified topic, what behaviors and/or mechanism need to change, what organizational units and persons should be involved, and identification of ways to facilitate the changes. This information is then used in tailoring an intervention for the setting that will promote use of the specified EBP. Based on a recent systematic review, effectiveness of tailored implementation interventions remains uncertain. 185
In summary, making an evidence-based change in practice involves a series of action steps and a complex, nonlinear process. Implementing the change will take several weeks to months, depending on the nature of the practice change. Increasing staff knowledge about a specific EBP and passive dissemination strategies are not likely to work, particularly in complex health care settings. Strategies that seem to have a positive effect on promoting use of EBPs include audit and feedback, use of clinical reminders and practice prompts, opinion leaders, change champions, interactive education, mass media, educational outreach/academic detailing, and characteristics of the context of care delivery (e.g., leadership, learning, questioning). It is important that senior leadership and those leading EBP improvements are aware of change as a process and continue to encourage and teach peers about the change in practice. The new practice must be continually reinforced and sustained or the practice change will be intermittent and soon fade, allowing more traditional methods of care to return. 15
- Practice Implications From Translation Science
Principles of Evidence-Based Practice for Patient Safety
Several translation science principles are informative for implementing patient safety initiatives:
- First, consider the context and engage health care personnel who are at the point of care in selecting and prioritizing patient safety initiatives, clearly communicating the evidence base (strength and type) for the patient safety practice topic(s) and the conditions or setting to which it applies. These communication messages need to be carefully designed and targeted to each stakeholder user group.
- Second, illustrate, through qualitative or quantitative data (e.g., near misses, sentinel events, adverse events, injuries from adverse events), the reason the organization and individuals within the organization should commit to an evidence-based safety practice topic. Clinicians tend to be more engaged in adopting patient safety initiatives when they understand the evidence base of the practice, in contrast to administrators saying, “We must do this because it is an external regulatory requirement.” For example, it is critical to converse with busy clinicians about the evidence-based rationale for doing fall-risk assessment, and to help them understand that fall-risk assessment is an external regulatory agency expectation because the strength of the evidence supports this patient safety practice.
- Third, didactic education alone is never enough to change practice; one-time education on a specific safety initiative is not enough. Simply improving knowledge does not necessarily improve practice. Rather, organizations must invest in the tools and skills needed to create a culture of evidence-based patient safety practices where questions are encouraged and systems are created to make it easy to do the right thing.
- Fourth, the context of EBP improvements in patient safety need to be addressed at each step of the implementation process; piloting the change in practice is essential to determine the fit between the EBP patient safety information/innovation and the setting of care delivery. There is no one way to implement, and what works in one agency may need modification to fit the organizational culture of another context.
- Finally, it is important to evaluate the processes and outcomes of implementation. Users and stakeholders need to know that the efforts to improve patient safety have a positive impact on quality of care. For example, if a new barcoding system is being used to administer blood products, it is imperative to know that the steps in the process are being followed (process indicators) and that the change in practice is resulting in fewer blood product transfusion errors (outcome indicators).
Research Implications
Translation science is young, and although there is a growing body of knowledge in this area, we have, to date, many unanswered questions. These include the type of audit and feedback (e.g., frequency, content, format) strategies that are most effective, the characteristics of opinion leaders that are critical for success, the role of specific context variables, and the combination of strategies that are most effective. We also know very little about use of tailored implementation interventions, or the key context attributes to assess and use in developing and testing tailored interventions. The types of clinical reminders that are most effective for making EBP knowledge available at the point of care require further empirical explanation. We also know very little about the intensity and intervention dose of single and multifaceted strategies that are effective for promoting and sustaining use of EBPs or how the effectiveness differs by type of topic (e.g., simple versus complex). Only recently has the context of care delivery been acknowledged as affecting use of evidence, and further empirical work is needed in this area to understand how complex adaptive systems of practice incorporate knowledge acquisition and use. Lastly, we do not know what strategies or combination of strategies work for whom, in what context, why they work in some settings or cases and not others, and what is the mechanism by which these strategies or combination of strategies work.
This is an exciting area of investigation that has a direct impact on implementing patient safety practices. In planning investigations, researchers must use a conceptual model to guide the research and add to the empirical and theoretical understanding of this field of inquiry. Additionally, funding is needed for implementation studies that focus on evidence-based patient safety practices as the topic of concern. To generalize empirical findings from patient safety implementation studies, we must have a better understanding of what implementation strategies work, with whom, and in what types of settings, and we must investigate the underlying mechanisms of these strategies. This is likely to require mixed methods, a better understanding of complexity science, and greater appreciation for nontraditional methods and realistic inquiry. 87
Although the science of translating research into practice is fairly new, there is some guiding evidence of what implementation interventions to use in promoting patient safety practices. However, there is no magic bullet for translating what is known from research into practice. To move evidence-based interventions into practice, several strategies may be needed. Additionally, what works in one context of care may or may not work in another setting, thereby suggesting that context variables matter in implementation. 80
- Search Strategy
Several electronic databases were searched (MEDLINE ® , CINAHL ® , PubMed ® ) using terms of evidence-based practice research, implementation research, and patient safety. (The terms “quality improvement” or “quality improvement intervention research” were not used.) The Cochrane Collaboration–Cochrane Reviews was also searched to look for systematic reviews of specific implementation strategies, and the Journal of Implementation Science was also reviewed. I also requested the final reports of the TRIP I and TRIP II studies funded by AHRQ. Classic articles known to the author were also included in this chapter (e.g.,Locock et al. 123 ).
*Principal Investigator: Keela Herr (R01 grant no. CA115363-01; National Cancer Institute (NCI))Background
- Cite this Page Titler MG. The Evidence for Evidence-Based Practice Implementation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 7.
- PDF version of this page (470K)
In this Page
Other titles in this collection.
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". [Int J Health Policy Manag. 2015] It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". Bucknall T, Fossum M. Int J Health Policy Manag. 2015 Jul 28; 4(11):787-8. Epub 2015 Jul 28.
- Nursing implementation science: how evidence-based nursing requires evidence-based implementation. [J Nurs Scholarsh. 2008] Nursing implementation science: how evidence-based nursing requires evidence-based implementation. van Achterberg T, Schoonhoven L, Grol R. J Nurs Scholarsh. 2008; 40(4):302-10.
- Review The science of implementation: changing the practice of critical care. [Curr Opin Crit Care. 2008] Review The science of implementation: changing the practice of critical care. Weinert CR, Mann HJ. Curr Opin Crit Care. 2008 Aug; 14(4):460-5.
- Review Integrative review of implementation strategies for translation of research-based evidence by nurses. [Clin Nurse Spec. 2014] Review Integrative review of implementation strategies for translation of research-based evidence by nurses. Wuchner SS. Clin Nurse Spec. 2014 Jul-Aug; 28(4):214-23.
- Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study [ 2015] Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study Herepath A, Kitchener M, Waring J. 2015 Sep
Recent Activity
- The Evidence for Evidence-Based Practice Implementation - Patient Safety and Qua... The Evidence for Evidence-Based Practice Implementation - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- How we work
No Idea How to Write an Evidence Based Paper?
Why rely on our help with your ebp paper, how to write an evidence based paper: from explanation to outline.
An evidence based practice paper can take a lot of forms, from a standard essay or case report to coursework or even a thesis. Regardless of the name, mastering the art of writing such a paper is crucial for any nursing school student. The reason is simple: these papers serve to foster confidence, cultivate research interests, nurture critical thinking, stimulate creativity, and hone decision-making — skills indispensable in real-world clinical settings. However, crafting high-quality evidence-based papers is not easy and presents significant challenges, especially for beginners.
To ease your burden, we’ve put together this comprehensive guide on how to write an evidence based practice research paper.
What Is Evidence-Based Practice and Its Components
Evidence-based practice (EBP) is a process for reviewing, analyzing, and integrating the most recent research discoveries in everyday patient care routines and clinical decision-making. It also entails merging the most reliable evidence with clinical expertise, all while taking into account individuals’ needs and preferences. When employed consistently, EBP enhances the likelihood of achieving optimal outcomes.
Below are the three components of EBP:
- Best available evidence
While EBP extends beyond solely relying on the best available evidence, much of the challenges and obstacles in implementing it revolve around sourcing and applying research. Our nursing writing services assist students in discovering and utilizing evidence based resources.
- Preferences and needs of patients
Incorporating the preferences and needs of patients is a fundamental aspect of nursing evidence based care. It requires the ability to integrate their cultural considerations, requirements, and values, ensuring the delivery of optimal services, and we can help with that, too.
- Knowledge and skills of clinicians
The expertise of physical therapists and therapist assistants like the ones we have on our platform plays a crucial role in the EBP process. This encompasses activities undertaken by each practitioner within their unique body of knowledge, education, training, and competency.
Now that you know what is evidence-based practice and its key components, let’s take a quick look at some examples of EBP you can implement in your work.
Guarantees provided with our evidence based paper assistance
Get your evidence based practice paper written in 3 steps, 12 examples of good topics to consider.
There are a lot of examples of evidence-based practice in nursing , including the following that you can use:
- Enforcing safety measures at home and educating individuals about their importance.
- Raising the head of a patient’s bed to an angle from 30 to 45 degrees.
- Following medication reconciliation, barcode scanning, and double-check procedures to prevent drug events and medication errors.
- Providing oxygen therapy to patients diagnosed with Chronic Obstructive Pulmonary Disease (COPD).
- Implementing care coordination models, such as transitional care programs and interprofessional collaboration, to improve patient outcomes and reduce healthcare costs.
- Minimizing the frequency of scheduled changes to ventilator circuits.
- Providing patient education materials to promote self-management of chronic conditions, medication adherence, and lifestyle modifications.
- Promoting the adoption of balanced diets for children experiencing gastrointestinal symptoms.
- Using standardized nursing terminology and electronic health record systems to improve the accuracy, completeness, and efficiency of nursing documentation.
- Revising approaches for bathing bedbound patients.
- Implementing palliative care interventions, advance care planning discussions, and symptom management strategies to improve the quality of end-of-life care for individuals and their families.
- Advocating for proper nurse staffing ratios based on research demonstrating the impact of nurse staffing levels on patient outcomes, including mortality rates, infection rates, and satisfaction scores.
Moving forward, let’s find out how to write an evidence based paper from A to Z.
Steps to Writing Nursing Evidence Based Practice Papers
When assigned to create an evidence based paper, follow these nine key steps to produce high-quality work.
- Select a good topic
There are numerous methods for choosing a topic. You can derive ideas from class assignments and past nursing evidence based practice papers. With the abundance of resources available online, you have access to various topic ideas. However, it is essential to choose one that aligns with your passion and interest in nursing practice.
- Conduct a literature review
Look for peer-reviewed articles, systematic reviews, and meta-analyses related to the chosen subject area. Evaluate the evidence to determine its quality and relevance to your clinical question.
- Formulate a clinical question
Develop a clear and focused question that addresses the identified problem or issue. Use the PICO framework (Population, Intervention, Comparison, Outcome) to structure your question.
- Gather and evaluate evidence
The foundation of evidence-based practice papers lies in the evidence. Therefore, thorough research of both online and print sources is essential to obtain facts supporting your thesis statement. Once you’ve formulated the problem statement and outlined the thesis statement, critically evaluate sources to identify those that support your thesis.
In case your instructor requests an annotated bibliography or critical analysis of each source or the main article supporting your work, consider using an evidence evaluation table. When selecting sources, remember there are both primary and secondary sources.
Pro tip: Primary and secondary sources can be found in databases such as EBSCO, PubMed, TRIP Database, UpToDate, OVID, The Cochrane Collaboration, and CINAHL. Additionally, reliable information can be sourced from .org, .gov, and .edu websites, government agencies, professional organizations, and NGOs. These sources provide valuable statistics, epidemiological data, and other evidence based information. Thorough research ensures that the clinical question, hypothesis, and thesis statement are adequately supported and addressed.
- Develop an intervention
Based on your analysis, propose an intervention that addresses the clinical question you formulated. Ensure that it’s evidence-based and feasible within the context of nursing.
- Implement the intervention
Describe how you would implement the intervention in a real-world clinical setting. Consider factors such as staffing, resources, and potential barriers to implementation.
- Evaluate outcomes
Determine how you’ll measure the effectiveness of your intervention. Identify specific outcomes or indicators that will indicate whether the intervention has achieved its intended goals.
- Write your paper
Organize your writing according to standard academic conventions, including a well-structured introduction, body, and conclusion. Make sure to cite all sources of evidence properly using a citation style specified in your nursing assignment brief.
- Revise your paper carefully
Review your paper for clarity, coherence, and accuracy. Check for grammatical errors, typos, and inconsistencies in formatting. Consider seeking feedback from mentors or nursing evidence based practice writing services to improve the quality of your paper.
Detailed Outline of an Evidence Based Practice Paper
A good project in nursing should include the following components:
II. Introduction
Background Information:
- Overview of the subject matter.
- Importance of the issue in nursing.
- Brief history/context of the problem.
Problem Statement:
- A clear statement of the problem or PICO question.
- Identification of the gap in knowledge.
- Relevance of the problem to nursing practice.
Purpose/Objectives:
- Specific aims or objectives of the evidence based paper.
- What the nursing paper seeks to achieve or address.
Significance:
- Why is the topic important or relevant to nursing practice?
- Potential impact of addressing the problem.
Review of Literature:
- Summary of existing research on the topic.
- Analysis of key studies, theories, and evidence.
- Identification of gaps or limitations in current knowledge.
Methodology:
- Description of research design (e.g., systematic review, randomized controlled trial).
- Details of data collection methods (e.g., search strategy, inclusion criteria).
- Explanation of data analysis procedures (e.g., statistical analysis, thematic analysis).
- Presentation of findings from the literature review.
- Summary of key outcomes, trends, or patterns identified.
Discussion:
- Interpretation and analysis of the results.
- Comparison of findings with existing literature.
- Implications of the results for nursing practice.
- Strengths and limitations of the study.
IV. Conclusion
Summary of Findings:
- Recap of the main findings or conclusions from the nursing paper.
Implications for Practice:
- Practical implications of the findings for nursing practice.
- Recommendations for healthcare providers or policymakers.
Future Directions:
- Suggestions for future study or initiatives.
- Areas that warrant further investigation or exploration.
Closing Remarks:
- Final thoughts on the significance of the study.
- Call to action or reflection on the importance of evidence based practice in nursing.
V. References
Pro tip: Always take the time to choose a relevant health indicator (e.g., disease, health conditions, working/living conditions), describe the target population or sub-population, and settle for around 7-10 peer-reviewed sources supporting your proposal.
Still Struggling? Opt for Nursing Evidence Based Practice Writing Services
We are available to assist you 24/7. Our team comprises highly qualified experts with RN, MSN, and DNP degrees and 4+ years of hands-on expertise in writing evidence-based papers on diverse nursing-related topics. Let them take over your paper so you can focus on other priorities or just relax and enjoy your free time. 100% satisfaction, compliance with your instructions, and on-time delivery are guaranteed!
Key EBP Nursing Topics: Enhancing Patient Results through Evidence-Based Practice
This article was written in collaboration with Christine T. and ChatGPT, our little helper developed by OpenAI.

Evidence-based practice (EBP) is the use of the best available evidence to inform clinical decision-making in nursing. EBP has become increasingly popular in nursing practice because it ensures that patient care is based on the most current and relevant research. In this article, we will discuss the latest evidence-based practice nursing research topics, how to choose them, and where to find EBP project ideas.
What is Evidence-Based Practice Nursing?
EBP nursing involves a cyclical process of asking clinical questions, seeking the best available evidence, critically evaluating that evidence, and then integrating it with the patient’s clinical experience and values to make informed decisions. By following this process, nurses can provide the best care for their patients and ensure that their practice is informed by the latest research.
One of the key components of EBP nursing is the critical appraisal of research evidence. Nurses must be able to evaluate the quality of studies, including study design, sample size, and statistical analysis. This requires an understanding of research methodology and the ability to apply critical thinking skills to evaluate research evidence.
EBP nursing also involves the use of clinical practice guidelines and protocols, which are evidence-based guidelines for clinical practice. These guidelines have been developed by expert groups and are based on the best available evidence. By following these guidelines, nurses can ensure that their practice is in line with the latest research and can provide the best possible care for their patients.
Finally, EBP nursing involves continuous professional development and a commitment to lifelong learning. Nurses must keep abreast of the latest research and clinical practice guidelines to ensure that their practice is informed by the latest research. This requires a commitment to ongoing learning and professional development, including attending conferences, reading scholarly articles, and participating in continuing education programs.
You can also learn more about evidence-based practice in nursing to gain a deeper understanding of the definition, stages, benefits, and challenges of implementing it.
Medical Studies Overwhelming?
Delegate Your Nursing Papers to the Pros!
Get 15% Discount
+ Plagiarism Report for FREE
How to Choose Evidence-Based Practice Nursing Research Topics
Choosing a science-based topic for nursing practice can be a daunting task, especially if you are new to the field. Here are some tips to help you choose a relevant and interesting EBP topic:
- Look for controversial or debated issues
Look for areas of nursing practice that are controversial or have conflicting evidence. These topics often have the potential to generate innovative and effective research.
- Consider ethical issues
Consider topics related to ethical issues in nursing practice. For example, bereavement care, informed consent , and patient privacy are all ethical issues that can be explored in an EBP project.
- Explore interdisciplinary topics
Nursing practice often involves collaboration with other health professionals such as physicians, social workers, and occupational therapists. Consider interdisciplinary topics that may be useful from a nursing perspective.
- Consider local or regional issues
Consider topics that are relevant to your local or regional healthcare facility. These topics may be relevant to your practice and have a greater impact on patient outcomes in your community.
- Check out the latest research
Review recent research in your area of interest to identify gaps in the literature or areas where further research is needed. This can help you develop a research question that is relevant and innovative.
With these tips in mind, you can expand your options for EBP nursing research topics and find a topic that fits your interests and goals. Remember that patient outcomes should be at the forefront of your research and choose a topic that has the potential to improve treatment and patient outcomes.
Where to Get EBP Project Ideas
There are several sources that nurses can use to get EBP project ideas. These sources are diverse and can provide valuable inspiration for research topics. By exploring these sources, nurses can find research questions that align with their interests and that address gaps in the literature. These include:
- Clinical Practice Guidelines
Look for clinical practice guidelines developed by professional organizations or healthcare institutions. These guidelines provide evidence-based guidelines for clinical practice and can help identify areas where further research is needed.
- Research databases
Explore research databases such as PubMed, CINAHL, and the Cochrane Library to find the latest studies and systematic reviews. These databases can help you identify gaps in the literature and areas where further research is needed.
- Clinical Experts
Consult with clinical experts in your practice area. These experts may have insights into areas where further research is needed or may provide guidance on areas of practice that may benefit from an EBP project.
- Quality Improvement Projects
Review quality improvement projects that have been implemented in your healthcare facility. These projects may identify areas where further research is needed or identify gaps in the literature that could be addressed in an EBP project.
- Patient and family feedback
Consider patient and family feedback to identify areas where further research is needed. Patients and families can provide valuable information about areas of nursing practice that can be improved or that could benefit from further research.
Remember, when searching for ideas for EBP nursing research projects, it is important to consider the potential impact on patient care and outcomes. Select a topic that has the potential to improve patient outcomes and consider the feasibility of the project in terms of time, resources, and access to data. By choosing a topic that matches your interests and goals and is feasible at your institution, you can conduct a meaningful and productive EBP research project in nursing.
Nursing EBP Topics You Can Use in Your Essay
Here are some of the latest evidence-based practice nursing research topics that you can use in your essay or explore further in your own research:
- The impact of telehealth on patient outcomes in primary care
- The use of music therapy to manage pain in post-operative patients
- The effectiveness of mindfulness-based stress reduction in reducing stress and anxiety in healthcare workers
- Combating health care-associated infections: a community-based approach
- The impact of nurse-led discharge education on readmission rates for heart failure patients
- The use of simulation in nursing education to improve patient safety
- The effectiveness of early mobilization in preventing post-operative complications
- The use of aromatherapy to manage agitation in patients with dementia
- The impact of nurse-patient communication on patient satisfaction and outcomes
- The effectiveness of peer support in improving diabetes self-management
- The impact of cultural competence training on patient outcomes in diverse healthcare settings
- The use of animal-assisted therapy in managing anxiety and depression in patients with chronic illnesses
- The effectiveness of nurse-led smoking cessation interventions in promoting smoking cessation among hospitalized patients
- Importance of literature review in evidence-based research
- The impact of nurse-led care transitions on hospital readmission rates for older adults
- The effectiveness of nurse-led weight management interventions in reducing obesity rates among children and adolescents
- The impact of medication reconciliation on medication errors and adverse drug events
- The use of mindfulness-based interventions to manage chronic pain in older adults
- The effectiveness of nurse-led interventions in reducing hospital-acquired infections
- The impact of patient-centered care on patient satisfaction and outcomes
- The use of art therapy to manage anxiety in pediatric patients undergoing medical procedures
- Pediatric oncology: working towards better treatment through evidence-based research
- The effectiveness of nurse-led interventions in improving medication adherence among patients with chronic illnesses
- The impact of team-based care on patient outcomes in primary care settings
- The use of music therapy to improve sleep quality in hospitalized patients
- The effectiveness of nurse-led interventions in reducing falls in older adults
- The impact of nurse-led care on maternal and infant outcomes in low-resource settings
- The use of acupressure to manage chemotherapy-induced nausea and vomiting
- The effectiveness of nurse-led interventions in promoting breastfeeding initiation and duration
- The impact of nurse-led palliative care interventions on end-of-life care in hospice settings
- The use of hypnotherapy to manage pain in labor and delivery
- The effectiveness of nurse-led interventions in reducing hospital length of stay for surgical patients
- The impact of nurse-led transitional care interventions on readmission rates for heart failure patients
- The use of massage therapy to manage pain in hospitalized patients
- The effectiveness of nurse-led interventions in promoting physical activity among adults with chronic illnesses
- The impact of technology-based interventions on patient outcomes in mental health settings
- The use of mind-body interventions to manage chronic pain in patients with fibromyalgia
- Optimizing the clarifying diagnosis of stomach cancer
- The effectiveness of nurse-led interventions in reducing medication errors in pediatric patients
- The impact of nurse-led interventions on patient outcomes in long-term care settings
- The use of aromatherapy to manage anxiety in patients undergoing cardiac catheterization
- The effectiveness of nurse-led interventions in improving glycemic control in patients with diabetes
- The impact of nurse-led interventions on patient outcomes in emergency department settings
- The use of relaxation techniques to manage anxiety in patients with cancer
- The effectiveness of nurse-led interventions in improving self-management skills among patients with heart failure
- The impact of nurse-led interventions on patient outcomes in critical care settings
- The use of yoga to manage symptoms in patients with multiple sclerosis
- The effectiveness of nurse-led interventions in promoting medication safety in community settings
- The impact of nurse-led interventions on patient outcomes in home healthcare settings
- The role of family involvement in the rehabilitation of stroke patients
- Assessing the effectiveness of virtual reality in pain management
- The impact of pet therapy on mental well-being in elderly patients
- Exploring the benefits of intermittent fasting on diabetic patients
- The efficacy of acupuncture in managing chronic pain in cancer patients
- Effect of laughter therapy on stress levels among healthcare professionals
- The influence of a plant-based diet on cardiovascular health
- Analyzing the outcomes of nurse-led cognitive behavioral therapy sessions for insomnia patients
- The role of yoga and meditation in managing hypertension
- Exploring the benefits of hydrotherapy in post-operative orthopedic patients
- The impact of digital health applications on patient adherence to medications
- Assessing the outcomes of art therapy in pediatric patients with chronic illnesses
- The role of nutrition education in managing obesity in pediatric patients
- Exploring the effects of nature walks on mental well-being in patients with depression
- The impact of continuous glucose monitoring systems on glycemic control in diabetic patients
The Importance of Incorporating EBP in Nursing Education
Evidence-based practice is not just a tool for seasoned nurses; it’s a foundational skill that should be integrated early into nursing education. By doing so, students learn the mechanics of nursing and the rationale behind various interventions grounded in scientific research.
- Bridging Theory and Practice:
Introducing EBP in the curriculum helps students bridge the gap between theoretical knowledge and clinical practice. They learn how to perform a task and why it’s done a particular way.
- Critical Thinking:
EBP promotes critical thinking. By regularly reviewing and appraising research, students develop the ability to discern the quality and applicability of studies. This skill is invaluable in a rapidly evolving field like healthcare.
- Lifelong Learning:
EBP instills a culture of continuous learning. It encourages nurses to regularly seek out the most recent research findings and adapt their practices accordingly.
- Improved Patient Outcomes:
At the heart of EBP is the goal of enhanced patient care. We ensure patients receive the most effective, up-to-date care by teaching students to base their practices on evidence.
- Professional Development:
Familiarity with EBP makes it easier for nurses to contribute to professional discussions, attend conferences, and conduct research. It elevates their professional stature and opens doors to new opportunities.
To truly prepare nursing students for the challenges of modern healthcare, it’s essential to make EBP a core part of their education.
In summary, evidence-based practice nursing is an essential component of providing quality patient care. As a nurse, it is important to stay up to date on the latest research in the field and incorporate evidence-based practices into your daily work. Choosing a research topic that aligns with your interests and addresses a gap in the literature can lead to valuable contributions to the field of nursing.
When it comes to finding EBP project ideas, there are many sources available, including professional organizations, academic journals, and healthcare conferences. By collaborating with colleagues and seeking feedback from mentors, you can refine your research question and design a study that is rigorous and relevant.
The nursing evidence-based practice topics listed above provide a starting point for further exploration and investigation. By studying the effectiveness of various nursing interventions and techniques, we can continue to improve patient outcomes and deliver better care. Ultimately, evidence-based practice nursing is about using the best available research to inform our decisions and provide the highest quality care possible to our patients.
📎 Related Articles
1. Top Nursing Research Topics for Students and Professionals 2. Nursing Debate Topics: The Importance of Discussing and Debating Nursing Issues 3. Mental Health Nursing Research Topics: Inspiring Ideas for Students 4. Top Nursing Argumentative Essay Topics: Engage in Thought-Provoking Debates 5. Top Nursing Topics for Discussion: Engaging Conversations for Healthcare Professionals 6. Exploring Controversial Issues in Nursing: Key Topics and Examples 7. Pediatric Nursing Research Topics for Students: A Comprehensive Guide
Table of content
Crafted with Care:
Nursing Essays!
Precision, Passion, & Professionalism in Every Page.

In order to continue enjoying our site, we ask that you confirm your identity as a human. Thank you very much for your cooperation.
Academic Support for Nursing Students
No notifications.
Disclaimer: This essay has been written by a student and not our expert nursing writers. View professional sample essays here.
View full disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this essay are those of the author and do not necessarily reflect the views of NursingAnswers.net. This essay should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
Evidence Based Practice Impact Of Nurses Nursing Essay
Info: 2399 words (10 pages) Nursing Essay Published: 11th Feb 2020
Reference this
Tagged: evidence-based practice
If you need assistance with writing your nursing essay, our professional nursing essay writing service is here to help!
Gethin, G. & Cowman, S. (2008) Manuka honey vs. hydrogel – a prospective, open label, multicentre, randomised controlled trial to compare desloughing efficacy and healing outcomes in venous ulcers. Journal of Clinical Nursing. 18 (3) p.466-474.
Our nursing and healthcare experts are ready and waiting to assist with any writing project you may have, from simple essay plans, through to full nursing dissertations.
Hancock, H. C. & Easen, P. R. (2006) The decision-making processes of nurses when extubating patients following cardiac surgery: An ethnographic study. International Journal of Nursing Studies. [Online] 43 (6) p.693-705.
Cite this work.
To export a reference to this article please select a referencing stye below:
Related Services

- Nursing Essay Writing Service

- Nursing Dissertation Service

- Reflective Writing Service
Related Content
Content relating to: "evidence-based practice"
Evidence based practice refers to all the clinical judgments that are prepared on the basis of investigation and scientific studies which facilitates in the distribution of the high quality care to the patient to make better results. Evidence-based health care practices are accessible for a number of circumstances such as diabetes, heart failure, kidney failure, and asthma.
Related Articles

Benefits of Evidence Based Practice (EBP)
Evidence Based Practice, also known as EBP according to (Liamputtong, 2013) is a “process that requires the practitioner to find best empirical evidence...
Evidence Based Practice in Child Health Care
Tamara J. Hall APN Role Utilize evidence based practice guidelines to manage the comprehensive health care needs of children ages birth to 19 years in a culturally sensitive manner within the medi...
Literature Review of Reflexivity in Qualitative Studies
Every research study needs to be contextualised, understood within the background and context of its place within the theoretical and practice spectrum (Fink, 2005). ...
DMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on the NursingAnswers.net website then please:
Our academic writing and marking services can help you!
- Marking Service
- Samples of our Work
- Full Service Portfolio
Related Lectures
Study for free with our range of nursing lectures!
- Drug Classification
- Emergency Care
- Health Observation
- Palliative Care
- Professional Values

Write for Us
Do you have a 2:1 degree or higher in nursing or healthcare?
Study Resources
Free resources to assist you with your nursing studies!
- APA Citation Tool
- Example Nursing Essays
- Example Nursing Assignments
- Example Nursing Case Studies
- Reflective Nursing Essays
- Nursing Literature Reviews
- Free Resources
- Reflective Model Guides
- Nursing and Healthcare Pay 2021
Fall 2024 Semester
Undergraduate courses.
Composition courses that offer many sections (ENGL 101, 201, 277 and 379) are not listed on this schedule unless they are tailored to specific thematic content or particularly appropriate for specific programs and majors.
- 100-200 level
ENGL 151.S01: Introduction to English Studies
Tuesday and Thursday, 11 a.m.-12:15 p.m.
Sharon Smith
ENGL 151 serves as an introduction to both the English major and the discipline of English studies. In this class, you will develop the thinking, reading, writing and research practices that define both the major and the discipline. Much of the semester will be devoted to honing your literary analysis skills, and we will study and discuss texts from several different genres—poetry, short fiction, the novel, drama and film—as well as some literary criticism. As we do so, we will explore the language of the discipline, and you will learn a variety of key literary terms and concepts. In addition, you will develop your skills as both a writer and researcher within the discipline of English.
ENGL 201.ST1 Composition II: The Mind/Body Connection
In this section of English 201, students will use research and writing to learn more about problems that are important to them and articulate ways to address those problems. The course will focus specifically on issues related to the mind, the body and the relationship between them. The topics we will discuss during the course will include the correlation between social media and body image; the efficacy of sex education programs; the degree to which beliefs about race and gender influence school dress codes; and the unique mental and physical challenges faced by college students today. In this course, you will be learning about different approaches to argumentation, analyzing the arguments of others and constructing your own arguments. At the same time, you will be honing your skills as a researcher and developing your abilities as a persuasive and effective writer.
ENGL 201.S10 Composition II: Environmental Writing
Monday/Wednesday/Friday 1-1:50 p.m.
Gwen Horsley
English 201 will help students develop the ability to think critically and analytically and to write effectively for other university courses and careers. This course will provide opportunities to develop analytical skills that will help students become critical readers and effective writers. Specifically, in this class, students will:
- Focus on the relationships between world environments, land, animals and humankind.
- Read various essays by environmental, conservational and regional authors.
- Produce student writings.
Students will improve their writing skills by reading essays and applying techniques they witness in others’ work and those learned in class. This class is also a course in logical and creative thought. Students will write about humankind’s place in the world and our influence on the land and animals, places that hold special meaning to them or have influenced their lives and stories of their own families and their places and passions in the world. Students will practice writing in an informed and persuasive manner, in language that engages and enlivens readers by using vivid verbs and avoiding unnecessary passives, nominalizations and expletive constructions.
Students will prepare writing assignments based on readings and discussions of essays included in "Literature and the Environment " and other sources. They may use "The St. Martin’s Handbook," as well as other sources, to review grammar, punctuation, mechanics and usage as needed.
ENGL 201.13 Composition II: Writing the Environment
Tuesday and Thursday 9:30-10:45 a.m.
Paul Baggett
For generations, environmentalists have relied on the power of prose to change the minds and habits of their contemporaries. In the wake of fires, floods, storms and droughts, environmental writing has gained a new sense of urgency, with authors joining activists in their efforts to educate the public about the grim realities of climate change. But do they make a difference? Have reports of present and future disasters so saturated our airwaves that we no longer hear them? How do writers make us care about the planet amidst all the noise? In this course, students will examine the various rhetorical strategies employed by some of today’s leading environmental writers and filmmakers. And while analyzing their different arguments, students also will strengthen their own strategies of argumentation as they research and develop essays that explore a range of environmental concerns.
ENGL 201 Composition II: Food Writing
S17 Tuesday and Thursday 12:30-1:45 p.m.
S18 Tuesday and Thursday 2-3:15 p.m.
Jodi Andrews
In this composition class, students will critically analyze essays about food, food systems and environments, food cultures, the intersections of personal choice, market forces and policy and the values underneath these forces. Students will learn to better read like writers, noting authors’ purpose, audience organizational moves, sentence-level punctuation and diction. We will read a variety of essays including research-intensive arguments and personal narratives which intersect with one of our most primal needs as humans: food consumption. Students will rhetorically analyze texts, conduct advanced research, reflect on the writing process and write essays utilizing intentional rhetorical strategies. Through doing this work, students will practice the writing moves valued in every discipline: argument, evidence, concision, engaging prose and the essential research skills for the 21st century.
ENGL 221.S01 British Literature I
Michael S. Nagy
English 221 is a survey of early British literature from its inception in the Old English period with works such as "Beowulf" and the “Battle of Maldon,” through the Middle Ages and the incomparable writings of Geoffrey Chaucer and the Gawain - poet, to the Renaissance and beyond. Students will explore the historical and cultural contexts in which all assigned reading materials were written, and they will bring that information to bear on class discussion. Likely themes that this class will cover include heroism, humor, honor, religion, heresy and moral relativity. Students will write one research paper in this class and sit for two formal exams: a midterm covering everything up to that point in the semester, and a comprehensive final. Probable texts include the following:
- The Norton Anthology of English Literature: The Middle Ages. Ed. Alfred David, M. H. Abrams, and Stephen Greenblatt. 9th ed. New York: W. W. Norton & Company, 2012.
- The Norton Anthology of English Literature: The Sixteenth Century and Early Seventeenth Century. Ed. George M. Logan, Stephen Greenblatt, Barbara K Lewalski, and M. H. Abrams. 9th ed. New York: W. W. Norton & Company, 2012.
- The Norton Anthology of English Literature: The Restoration and the Eighteenth Century. Ed. George M. Logan, Stephen Greenblatt, Barbara K Lewalski, and M. H. Abrams. 9th ed. New York: W. W. Norton & Company, 2012.
- Gibaldi, Joseph. The MLA Handbook for Writers of Research Papers. 6th ed. New York: The Modern Language Association of America, 2003.
- Any Standard College Dictionary.
ENGL 240.S01 Juvenile Literature Elementary-5th Grade
Monday, Wednesday and Friday noon-12:50 p.m.
April Myrick
A survey of the history of literature written for children and adolescents, and a consideration of the various types of juvenile literature. Text selection will focus on the themes of imagination and breaking boundaries.
ENGL 240.ST1 Juvenile Literature Elementary-5th Grade
Randi Anderson
In English 240 students will develop the skills to interpret and evaluate various genres of literature for juvenile readers. This particular section will focus on various works of literature at approximately the K-5 grade level. We will read a large range of works that fall into this category, as well as information on the history, development and genre of juvenile literature.
Readings for this course include classical works such as "Hatchet," "Little Women", "The Lion, the Witch and the Wardrobe" and "Brown Girl Dreaming," as well as newer works like "Storm in the Barn," "Anne Frank’s Diary: A Graphic Adaptation," "Lumberjanes," and a variety of picture books. These readings will be paired with chapters from "Reading Children’s Literature: A Critical Introduction " to help develop understanding of various genres, themes and concepts that are both related to juvenile literature and also present in our readings.
In addition to exposing students to various genres of writing (poetry, historical fiction, non-fiction, fantasy, picture books, graphic novels, etc.) this course will also allow students to engage in a discussion of larger themes present in these works such as censorship, race and gender. Students’ understanding of these works and concepts will be developed through readings, research, discussion posts, exams and writing assignments designed to get students to practice analyzing poetry, picture books, informational books and transitional/easy readers.
ENGL 241.S01: American Literature I
Tuesday and Thursday 12:30-1:45 p.m.
This course provides a broad, historical survey of American literature from the early colonial period to the Civil War. Ranging across historical periods and literary genres—including early accounts of contact and discovery, narratives of captivity and slavery, poetry of revolution, essays on gender equality and stories of industrial exploitation—this class examines how subjects such as colonialism, nationhood, religion, slavery, westward expansion, race, gender and democracy continue to influence how Americans see themselves and their society.
Required Texts
- The Norton Anthology of American Literature: Package 1, Volumes A and B Beginnings to 1865, Ninth Edition. (ISBN 978-0-393-26454-8)
ENGL 283.S01 Introduction to Creative Writing
Steven Wingate
Students will explore the various forms of creative writing (fiction, nonfiction and poetry) not one at a time in a survey format—as if there were decisive walls of separation between then—but as intensely related genres that share much of their creative DNA. Through close reading and work on personal texts, students will address the decisions that writers in any genre must face on voice, rhetorical position, relationship to audience, etc. Students will produce and revise portfolios of original creative work developed from prompts and research. This course fulfills the same SGR #2 requirements ENGL 201; note that the course will involve a research project. Successful completion of ENGL 101 (including by test or dual credit) is a prerequisite.
ENGL 283.S02 Introduction to Creative Writing
Jodilyn Andrews
This course introduces students to the craft of writing, with readings and practice in at least two genres (including fiction, poetry and drama).
ENGL 283.ST1 Introduction to Creative Writing
Amber Jensen, M.A., M.F.A.
This course explores creative writing as a way of encountering the world, research as a component of the creative writing process, elements of craft and their rhetorical effect and drafting, workshop and revision as integral parts of writing polished literary creative work. Student writers will engage in the research practices that inform the writing of literature and in the composing strategies and writing process writers use to create literary texts. Through their reading and writing of fiction, poetry and creative nonfiction, students will learn about craft elements, find examples of those craft elements in published works and apply these elements in their own creative work, developed through weekly writing activities, small group and large group workshop and conferences with the instructor. Work will be submitted, along with a learning reflection and revision plan in each genre and will then be revised and submitted as a final portfolio at the end of the semester to demonstrate continued growth in the creation of polished literary writing.
- 300-400 level
ENGL 424.S01 Language Arts Methods grades 7-12
Tuesday 6-8:50 p.m.
Danielle Harms
Techniques, materials and resources for teaching English language and literature to middle and secondary school students. Required of students in the English education option.
AIS/ENGL 447.S01: American Indian Literature of the Present
Thursdays 3-6 p.m.
This course introduces students to contemporary works by authors from various Indigenous nations. Students examine these works to enhance their historical understanding of Indigenous peoples, discover the variety of literary forms used by those who identify as Indigenous writers, and consider the cultural and political significance of these varieties of expression. Topics and questions to be explored include:
- Genre: What makes Indigenous literature indigenous?
- Political and Cultural Sovereignty: Why have an emphasis on tribal specificity and calls for “literary separatism” emerged in recent decades, and what are some of the critical conversations surrounding such particularized perspectives?
- Gender and Sexuality: What are the intersecting concerns of Indigenous Studies and Women, Gender and Sexuality Studies, and how might these research fields inform one another?
- Trans-Indigeneity: What might we learn by comparing works across different Indigenous traditions, and what challenges do such comparisons present?
- Aesthetics: How do Indigenous writers understand the dynamics between tradition and creativity?
- Visual Forms: What questions or concerns do visual representations (television and film) by or about Indigenous peoples present?
Possible Texts
- Akiwenzie-Damm, Kateri and Josie Douglas (eds), Skins: Contemporary Indigenous Writing. IAD Press, 2000. (978-1864650327)
- Erdrich, Louise, The Sentence. Harper, 2021 (978-0062671127)
- Harjo, Joy, Poet Warrior: A Memoir. Norton, 2021 (978-0393248524)
- Harjo, Sterlin and Taika Waititi, Reservation Dogs (selected episodes)
- Talty, Morgan. Night of the Living Rez, 2022, Tin House (978-1953534187)
- Wall Kimmerer, Robin. Braiding Sweet Grass, Milkweed Editions (978-1571313560)
- Wilson, Diane. The Seed Keeper: A Novel. Milkweed Editions (978-1571311375)
- Critical essays by Alexie, Allen, Cohen, Cox, King, Kroeber, Ortiz, Piatote, Ross and Sexton, Smith, Taylor, Teuton, Treuer, Vizenor, and Womack.
ENGL 472.S01: Film Criticism
Tuesdays 2-4:50 p.m.
Jason McEntee
Do you have an appreciation for, and enjoy watching, movies? Do you want to study movies in a genre-oriented format (such as those we typically call the Western, the screwball comedy, the science fiction or the crime/gangster, to name a few)? Do you want to explore the different critical approaches for talking and writing about movies (such as auteur, feminist, genre or reception)?
In this class, you will examine movies through viewing and defining different genres while, at the same time, studying and utilizing different styles of film criticism. You will share your discoveries in both class discussions and short writings. The final project will be a formal written piece of film criticism based on our work throughout the semester. The course satisfies requirements and electives for all English majors and minors, including both the Film Studies and Professional Writing minors. (Note: Viewing of movies outside of class required and may require rental and/or streaming service fees.)
ENGL 476.ST1: Fiction
In this workshop-based creative writing course, students will develop original fiction based on strong attention to the fundamentals of literary storytelling: full-bodied characters, robust story lines, palpable environments and unique voices. We will pay particular attention to process awareness, to the integrity of the sentence, and to authors' commitments to their characters and the places in which their stories unfold. Some workshop experience is helpful, as student peer critique will be an important element of the class.
ENGL 479.01 Capstone: The Gothic
Wednesday 3-5:50 p.m.
With the publication of Horace Walpole’s "The Castle of Otranto " in 1764, the Gothic officially came into being. Dark tales of physical violence and psychological terror, the Gothic incorporates elements such as distressed heroes and heroines pursued by tyrannical villains; gloomy estates with dark corridors, secret passageways and mysterious chambers; haunting dreams, troubling prophecies and disturbing premonitions; abduction, imprisonment and murder; and a varied assortment of corpses, apparitions and “monsters.” In this course, we will trace the development of Gothic literature—and some film—from the eighteenth-century to the present time. As we do so, we will consider how the Gothic engages philosophical beliefs about the beautiful and sublime; shapes psychological understandings of human beings’ encounters with horror, terror, the fantastic and the uncanny; and intervenes in the social and historical contexts in which it was written. We’ll consider, for example, how the Gothic undermines ideals related to domesticity and marriage through representations of domestic abuse, toxicity and gaslighting. In addition, we’ll discuss Gothic texts that center the injustices of slavery and racism. As many Gothic texts suggest, the true horrors of human existence often have less to do with inexplicable supernatural phenomena than with the realities of the world in which we live.
ENGL 485.S01: Undergraduate Writing Center Learning Assistants
Flexible Scheduling
Nathan Serfling
Since their beginnings in the 1920s and 30s, writing centers have come to serve numerous functions: as hubs for writing across the curriculum initiatives, sites to develop and deliver workshops and resource centers for faculty as well as students, among other functions. But the primary function of writing centers has necessarily and rightfully remained the tutoring of student writers. This course will immerse you in that function in two parts. During the first four weeks, you will explore writing center praxis—that is, the dialogic interplay of theory and practice related to writing center work. This part of the course will orient you to writing center history, key theoretical tenets and practical aspects of writing center tutoring. Once we have developed and practiced this foundation, you will begin work in the writing center as a tutor, responsible for assisting a wide variety of student clients with numerous writing tasks. Through this work, you will learn to actively engage with student clients in the revision of a text, respond to different student needs and abilities, work with a variety of writing tasks and rhetorical situations, and develop a richer sense of writing as a complex and negotiated social process.
Graduate Courses
Engl 572.s01: film criticism, engl 576.st1 fiction.
In this workshop-based creative writing course, students will develop original fiction based on strong attention to the fundamentals of literary storytelling: full-bodied characters, robust story lines, palpable environments and unique voices. We will pay particular attention to process awareness, to the integrity of the sentence and to authors' commitments to their characters and the places in which their stories unfold. Some workshop experience is helpful, as student peer critique will be an important element of the class.
ENGL 605.S01 Seminar in Teaching Composition
Thursdays 1-3:50 p.m.
This course will provide you with a foundation in the pedagogies and theories (and their attendant histories) of writing instruction, a foundation that will prepare you to teach your own writing courses at SDSU and elsewhere. As you will discover through our course, though, writing instruction does not come with any prescribed set of “best” practices. Rather, writing pedagogies stem from and continue to evolve because of various and largely unsettled conversations about what constitutes effective writing and effective writing instruction. Part of becoming a practicing writing instructor, then, is studying these conversations to develop a sense of what “good writing” and “effective writing instruction” might mean for you in our particular program and how you might adapt that understanding to different programs and contexts.
As we read about, discuss and research writing instruction, we will address a variety of practical and theoretical topics. The practical focus will allow us to attend to topics relevant to your immediate classroom practices: designing a curriculum and various types of assignments, delivering the course content and assessing student work, among others. Our theoretical topics will begin to reveal the underpinnings of these various practical matters, including their historical, rhetorical, social and political contexts. In other words, we will investigate the praxis—the dialogic interaction of practice and theory—of writing pedagogy. As a result, this course aims to prepare you not only as a writing teacher but also as a nascent writing studies/writing pedagogy scholar.
At the end of this course, you should be able to engage effectively in the classroom practices described above and participate in academic conversations about writing pedagogy, both orally and in writing. Assessment of these outcomes will be based primarily on the various writing assignments you submit and to a smaller degree on your participation in class discussions and activities.
ENGL 726.S01: The New Woman, 1880–1900s
Thursdays 3–5:50 p.m.
Katherine Malone
This course explores the rise of the New Woman at the end of the nineteenth century. The label New Woman referred to independent women who rebelled against social conventions. Often depicted riding bicycles, smoking cigarettes and wearing masculine clothing, these early feminists challenged gender roles and sought broader opportunities for women’s employment and self-determination. We will read provocative fiction and nonfiction by New Women writers and their critics, including authors such as Sarah Grand, Mona Caird, George Egerton, Amy Levy, Ella Hepworth Dixon, Grant Allen and George Gissing. We will analyze these exciting texts through a range of critical lenses and within the historical context of imperialism, scientific and technological innovation, the growth of the periodical press and discourse about race, class and gender. In addition to writing an argumentative seminar paper, students will complete short research assignments and lead discussion.
ENGL 792.ST1 Women in War: Female Authors and Characters in Contemporary War Lit
In this course, we will explore the voices of female authors and characters in contemporary literature of war. Drawing from various literary theories, our readings and discussion will explore the contributions of these voices to the evolving literature of war through archetypal and feminist criticism. We will read a variety of short works (both theoretical and creative) and complete works such as (selections subject to change): "Eyes Right" by Tracy Crow, "Plenty of Time When We Get Home" by Kayla Williams, "You Know When the Men are Gone" by Siobhan Fallon, "Still, Come Home" by Katie Schultz and "The Fine Art of Camouflage" by Lauren Johnson.

IMAGES
VIDEO
COMMENTS
The importance of evidence based practice is to enable nurses to provide high quality care, improve outcomes for patient and families and to run a more efficient health service. Therefore other agencies within the health service will benefit when interventions and care is based on research (Burns & Grove 2007).
Steps of Writing an EBP Research Paper in Nursing. Once you have been assigned to write an evidence-based paper, you need to follow the steps below to write the best essay. 1. Choose a Topic for your Paper. There are many methods you can use when choosing an EBP topic.
Evidence-based practice (EBP) refers to the integration of the best available research evidence, clinical expertise, and patient preferences or values to guide healthcare decision-making and improve patient outcomes (ANA, 2023). According to the ANA, there are five key steps in implementing EBP: ask a clinical question, acquire the evidence ...
1. Evidence-based practice in nursing provides nurses with scientifically supported research to help them make well-educated decisions. 2. EBP in nursing helps nurses stay up-to-date about new nursing interventions and protocols used in patient care. 3.
Evidence-based clinical practice or evidence-based medicine is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients" (Sackett et al., 1996). The beginning of Evidence-Based Practice (EBP), formerly known as evidence-based medicine, was initiated by Archie Cochrane in ...
1. Title page. The first part of an EBP paper is the title page. Like every other academic paper, an EBP research paper must have a title page, and the title page must be formatted appropriately. Ensuring your title page is formatted correctly is vital so you do not get penalized during grading.
Research studies show that evidence-based practice (EBP) leads to higher quality care, improved patient outcomes, reduced costs, and greater nurse satisfaction than traditional approaches to care. 1-5 Despite these favorable findings, many nurses remain inconsistent in their implementation of evidence-based care. Moreover, some nurses, whose education predates the inclusion of EBP in the ...
Step 1. Collect internal data on current practice. Link problems, interventions, and outcomes. Step 3. Appraise the value of the evidence. Synthesize the best evidence. Assess the risks and benefits of the new practice. Step 2. Identify sources of evidence.
APA Tutorial. In October 2019, the American Psychological Association made radical changes its style, especially with regard to the format and citation rules for students writing academic papers. Use this guide to learn how to format and cite your papers using APA Style, 7th edition. You can start by viewing the video tutorial.
Table 1: Developing evidence‐based practice guidelines and a nursing illustration (adapted from Proctor and Rosen, 2004) Step Illustration Step 1: Locate evidence‐based interventions relevant to the outcomes of interest. The nurse is interested in helping patients to manage their asthma better. Three
EBP and Quadruple Aim. EBP, or evidence-based practice, is a methodical strategy for making healthcare decisions incorporating the best available evidence, clinical knowledge, and patient values and preferences (Jolley, 2020). It displays the application of scientific ideas to improve healthcare productivity and offer high-quality services.
The Johns Hopkins Nursing Evidence-Based Practice: Implementing Change Project. The expected outcome is eliminating the risk of falls, reducing the number of falls, and preventing the falls-related injuries. We will write. a custom essay specifically for you by our professional experts. 182 writers online.
7. Offer suggestions for future research on evidence-based practice in nursing. EBP Research Paper Literature Review Writing- Evidence-Based Practice (EBP) Evidence-based practice (EBP) is an approach to nursing that focuses on using evidence to guide clinical decisions. EBP is effective in improving patient outcomes and reducing healthcare costs.
evidence and assumptions and thinking through the logic of arguments, you will begin to figure out what you think about complicated or controversial topics. Your goal when you write an essay should not be only to show readers what you know, but to learn more about something that you're genuinely curious about.
Evidence Based Practice (EBP) has proven to be a reliable framework for making these types of important decisions. EBP provides a sequential and structured approach for integrating the best available evidence into the decision-making process. Typically, this process entails formulating an answerable question, searching for the best available ...
EBP is a process used to review, analyze, and translate the latest scientific evidence. The goal is to quickly incorporate the best available research, along with clinical experience and patient preference, into clinical practice, so nurses can make informed patient-care decisions ( Dang et al., 2022 ). EBP is the cornerstone of clinical practice.
The authors describe a new course (Evidence-Based Nursing 1) that was implemented as part of an undergraduate nursing program. The researchers observed that the targeted learners were willing to make evidence-based practices part of their nursing philosophies after completing the course. The practice can encourage practitioners to integrate EBP ...
A literature review is an integrated analysis of scholarly writings that are related directly to your research question. Put simply, it's a critical evaluation of what's already been written on a particular topic.It represents the literature that provides background information on your topic and shows a connection between those writings and your research question.
Steps of Evidence-Based Practice. Steps of promoting adoption of EBPs can be viewed from the perspective of those who conduct research or generate knowledge, 23, 37 those who use the evidence-based information in practice, 16, 31 and those who serve as boundary spanners to link knowledge generators with knowledge users. 19 Steps of knowledge transfer in the AHRQ model 37 represent three major ...
You use evidence (big 'E' research evidence and little 'e' industry-based evidence/anecdotal evidence based on experience/practice) to support your position and convince readers of your argument's validity (i. the extent to which your opinion and argument is well founded).
An evidence based practice paper can take a lot of forms, from a standard essay or case report to coursework or even a thesis. Regardless of the name, mastering the art of writing such a paper is crucial for any nursing school student. ... Opt for Nursing Evidence Based Practice Writing Services. We are available to assist you 24/7. Our team ...
The impact of team-based care on patient outcomes in primary care settings. The use of music therapy to improve sleep quality in hospitalized patients. The effectiveness of nurse-led interventions in reducing falls in older adults. The impact of nurse-led care on maternal and infant outcomes in low-resource settings.
Evidence-based writing calls for you to use outside sources to support your own ideas. This gives your writing credibility, and can strengthen an argument. In this lesson, we will learn more about ...
Evidence Based Practice Impact Of Nurses Nursing Essay. Evidence-based practice (EBP) is widely recognised within the role of nursing. Its implementation and purpose in the delivery of care is seen as an important driver for nursing practice and clinical outcomes (Cullen & Adams 2010). It has been defined as the:
Students will practice writing in an informed and persuasive manner, in language that engages and enlivens readers by using vivid verbs and avoiding unnecessary passives, nominalizations and expletive constructions.Students will prepare writing assignments based on readings and discussions of essays included in "Literature and the Environment ...