- Patient Care & Health Information
- Diseases & Conditions
- Alcohol use disorder
Alcohol use disorder is a pattern of alcohol use that involves problems controlling your drinking, being preoccupied with alcohol or continuing to use alcohol even when it causes problems. This disorder also involves having to drink more to get the same effect or having withdrawal symptoms when you rapidly decrease or stop drinking. Alcohol use disorder includes a level of drinking that's sometimes called alcoholism.
Unhealthy alcohol use includes any alcohol use that puts your health or safety at risk or causes other alcohol-related problems. It also includes binge drinking — a pattern of drinking where a male has five or more drinks within two hours or a female has at least four drinks within two hours. Binge drinking causes significant health and safety risks.
If your pattern of drinking results in repeated significant distress and problems functioning in your daily life, you likely have alcohol use disorder. It can range from mild to severe. However, even a mild disorder can escalate and lead to serious problems, so early treatment is important.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Alcohol use disorder can be mild, moderate or severe, based on the number of symptoms you experience. Signs and symptoms may include:
- Being unable to limit the amount of alcohol you drink
- Wanting to cut down on how much you drink or making unsuccessful attempts to do so
- Spending a lot of time drinking, getting alcohol or recovering from alcohol use
- Feeling a strong craving or urge to drink alcohol
- Failing to fulfill major obligations at work, school or home due to repeated alcohol use
- Continuing to drink alcohol even though you know it's causing physical, social, work or relationship problems
- Giving up or reducing social and work activities and hobbies to use alcohol
- Using alcohol in situations where it's not safe, such as when driving or swimming
- Developing a tolerance to alcohol so you need more to feel its effect or you have a reduced effect from the same amount
- Experiencing withdrawal symptoms — such as nausea, sweating and shaking — when you don't drink, or drinking to avoid these symptoms
Alcohol use disorder can include periods of being drunk (alcohol intoxication) and symptoms of withdrawal.
- Alcohol intoxication results as the amount of alcohol in your bloodstream increases. The higher the blood alcohol concentration is, the more likely you are to have bad effects. Alcohol intoxication causes behavior problems and mental changes. These may include inappropriate behavior, unstable moods, poor judgment, slurred speech, problems with attention or memory, and poor coordination. You can also have periods called "blackouts," where you don't remember events. Very high blood alcohol levels can lead to coma, permanent brain damage or even death.
- Alcohol withdrawal can occur when alcohol use has been heavy and prolonged and is then stopped or greatly reduced. It can occur within several hours to 4 to 5 days later. Signs and symptoms include sweating, rapid heartbeat, hand tremors, problems sleeping, nausea and vomiting, hallucinations, restlessness and agitation, anxiety, and occasionally seizures. Symptoms can be severe enough to impair your ability to function at work or in social situations.
What is considered 1 drink?
The National Institute on Alcohol Abuse and Alcoholism defines one standard drink as any one of these:
- 12 ounces (355 milliliters) of regular beer (about 5% alcohol)
- 8 to 9 ounces (237 to 266 milliliters) of malt liquor (about 7% alcohol)
- 5 ounces (148 milliliters) of wine (about 12% alcohol)
- 1.5 ounces (44 milliliters) of hard liquor or distilled spirits (about 40% alcohol)
When to see a doctor
If you feel that you sometimes drink too much alcohol, or your drinking is causing problems, or if your family is concerned about your drinking, talk with your health care provider. Other ways to get help include talking with a mental health professional or seeking help from a support group such as Alcoholics Anonymous or a similar type of self-help group.
Because denial is common, you may feel like you don't have a problem with drinking. You might not recognize how much you drink or how many problems in your life are related to alcohol use. Listen to relatives, friends or co-workers when they ask you to examine your drinking habits or to seek help. Consider talking with someone who has had a problem with drinking but has stopped.
If your loved one needs help
Many people with alcohol use disorder hesitate to get treatment because they don't recognize that they have a problem. An intervention from loved ones can help some people recognize and accept that they need professional help. If you're concerned about someone who drinks too much, ask a professional experienced in alcohol treatment for advice on how to approach that person.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Genetic, psychological, social and environmental factors can impact how drinking alcohol affects your body and behavior. Theories suggest that for certain people drinking has a different and stronger impact that can lead to alcohol use disorder.
Over time, drinking too much alcohol may change the normal function of the areas of your brain associated with the experience of pleasure, judgment and the ability to exercise control over your behavior. This may result in craving alcohol to try to restore good feelings or reduce negative ones.
Risk factors
Alcohol use may begin in the teens, but alcohol use disorder occurs more frequently in the 20s and 30s, though it can start at any age.
Risk factors for alcohol use disorder include:
- Steady drinking over time. Drinking too much on a regular basis for an extended period or binge drinking on a regular basis can lead to alcohol-related problems or alcohol use disorder.
- Starting at an early age. People who begin drinking — especially binge drinking — at an early age are at a higher risk of alcohol use disorder.
- Family history. The risk of alcohol use disorder is higher for people who have a parent or other close relative who has problems with alcohol. This may be influenced by genetic factors.
- Depression and other mental health problems. It's common for people with a mental health disorder such as anxiety, depression, schizophrenia or bipolar disorder to have problems with alcohol or other substances.
- History of trauma. People with a history of emotional trauma or other trauma are at increased risk of alcohol use disorder.
- Having bariatric surgery. Some research studies indicate that having bariatric surgery may increase the risk of developing alcohol use disorder or of relapsing after recovering from alcohol use disorder.
- Social and cultural factors. Having friends or a close partner who drinks regularly could increase your risk of alcohol use disorder. The glamorous way that drinking is sometimes portrayed in the media also may send the message that it's OK to drink too much. For young people, the influence of parents, peers and other role models can impact risk.
Complications
Alcohol depresses your central nervous system. In some people, the initial reaction may feel like an increase in energy. But as you continue to drink, you become drowsy and have less control over your actions.
Too much alcohol affects your speech, muscle coordination and vital centers of your brain. A heavy drinking binge may even cause a life-threatening coma or death. This is of particular concern when you're taking certain medications that also depress the brain's function.
Impact on your safety
Excessive drinking can reduce your judgment skills and lower inhibitions, leading to poor choices and dangerous situations or behaviors, including:
- Motor vehicle accidents and other types of accidental injury, such as drowning
- Relationship problems
- Poor performance at work or school
- Increased likelihood of committing violent crimes or being the victim of a crime
- Legal problems or problems with employment or finances
- Problems with other substance use
- Engaging in risky, unprotected sex, or experiencing sexual abuse or date rape
- Increased risk of attempted or completed suicide
Impact on your health
Drinking too much alcohol on a single occasion or over time can cause health problems, including:
- Liver disease. Heavy drinking can cause increased fat in the liver (hepatic steatosis) and inflammation of the liver (alcoholic hepatitis). Over time, heavy drinking can cause irreversible destruction and scarring of liver tissue (cirrhosis).
- Digestive problems. Heavy drinking can result in inflammation of the stomach lining (gastritis), as well as stomach and esophageal ulcers. It can also interfere with your body's ability to get enough B vitamins and other nutrients. Heavy drinking can damage your pancreas or lead to inflammation of the pancreas (pancreatitis).
- Heart problems. Excessive drinking can lead to high blood pressure and increases your risk of an enlarged heart, heart failure or stroke. Even a single binge can cause serious irregular heartbeats (arrhythmia) called atrial fibrillation.
- Diabetes complications. Alcohol interferes with the release of glucose from your liver and can increase the risk of low blood sugar (hypoglycemia). This is dangerous if you have diabetes and are already taking insulin or some other diabetes medications to lower your blood sugar level.
- Issues with sexual function and periods. Heavy drinking can cause men to have difficulty maintaining an erection (erectile dysfunction). In women, heavy drinking can interrupt menstrual periods.
- Eye problems. Over time, heavy drinking can cause involuntary rapid eye movement (nystagmus) as well as weakness and paralysis of your eye muscles due to a deficiency of vitamin B-1 (thiamin). A thiamin deficiency can result in other brain changes, such as irreversible dementia, if not promptly treated.
- Birth defects. Alcohol use during pregnancy may cause miscarriage. It may also cause fetal alcohol spectrum disorders (FASDs). FASDs can cause a child to be born with physical and developmental problems that last a lifetime.
- Bone damage. Alcohol may interfere with making new bone. Bone loss can lead to thinning bones (osteoporosis) and an increased risk of fractures. Alcohol can also damage bone marrow, which makes blood cells. This can cause a low platelet count, which may result in bruising and bleeding.
- Neurological complications. Excessive drinking can affect your nervous system, causing numbness and pain in your hands and feet, disordered thinking, dementia, and short-term memory loss.
- Weakened immune system. Excessive alcohol use can make it harder for your body to resist disease, increasing your risk of various illnesses, especially pneumonia.
- Increased risk of cancer. Long-term, excessive alcohol use has been linked to a higher risk of many cancers, including mouth, throat, liver, esophagus, colon and breast cancers. Even moderate drinking can increase the risk of breast cancer.
- Medication and alcohol interactions. Some medications interact with alcohol, increasing its toxic effects. Drinking while taking these medications can either increase or decrease their effectiveness, or make them dangerous.
Early intervention can prevent alcohol-related problems in teens. If you have a teenager, be alert to signs and symptoms that may indicate a problem with alcohol:
- Loss of interest in activities and hobbies and in personal appearance
- Red eyes, slurred speech, problems with coordination and memory lapses
- Difficulties or changes in relationships with friends, such as joining a new crowd
- Declining grades and problems in school
- Frequent mood changes and defensive behavior
You can help prevent teenage alcohol use:
- Set a good example with your own alcohol use.
- Talk openly with your child, spend quality time together and become actively involved in your child's life.
- Let your child know what behavior you expect — and what the consequences will be for not following the rules.
Alcohol use disorder care at Mayo Clinic
- Nguyen HT. Allscripts EPSi. Mayo Clinic. May 5, 2022.
- What is A.A.? Alcoholics Anonymous. https://www.aa.org/what-is-aa. Accessed April 1, 2022.
- Mission statement. Women for Sobriety. https://womenforsobriety.org/about/#. Accessed April 1, 2022.
- Al-Anon meetings. Al-Anon Family Groups. https://al-anon.org/al-anon-meetings/. Accessed April 1, 2022.
- Substance-related and addictive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed April 26, 2018.
- Rethinking drinking: Alcohol and your health. National Institute on Alcohol Abuse and Alcoholism. https://www.rethinkingdrinking.niaaa.nih.gov/. Accessed April 1, 2022.
- Treatment for alcohol problems: Finding and getting help. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/treatment-alcohol-problems-finding-and-getting-help. Accessed April 1, 2022.
- Alcohol's effect on the body. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body. Accessed April 1, 2022.
- Understanding the dangers of alcohol overdose. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-dangers-of-alcohol-overdose. Accessed April 1, 2022.
- Frequently asked questions: About alcohol. Centers for Disease Control and Prevention. https://www.cdc.gov/alcohol/faqs.htm. Accessed April 1, 2022.
- Harmful interactions: Mixing alcohol with medicines. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/harmful-interactions-mixing-alcohol-with-medicines. Accessed April 1, 2022.
- Parenting to prevent childhood alcohol use. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/parenting-prevent-childhood-alcohol-use. Accessed April 1, 2022.
- Tetrault JM, et al. Risky drinking and alcohol use disorder: Epidemiology, pathogenesis, clinical manifestations, course, assessment, and diagnosis. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Holt SR. Alcohol use disorder: Pharmacologic management. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Saxon AJ. Alcohol use disorder: Psychosocial treatment. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Charness ME. Overview of the chronic neurologic complications of alcohol. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- Chen P, et al. Acupuncture for alcohol use disorder. International Journal of Physiology, Pathophysiology and Pharmacotherapy. 2018;10:60.
- Ng S-M, et al. Nurse-led body-mind-spirit based relapse prevention intervention for people with diagnosis of alcohol use disorder at a mental health care setting, India: A pilot study. Journal of Addictions Nursing. 2020; doi:10.1097/JAN.0000000000000368.
- Lardier DT, et al. Exercise as a useful intervention to reduce alcohol consumption and improve physical fitness in individuals with alcohol use disorder: A systematic review and meta-analysis. Frontiers in Psychology. 2021; doi:10.3389/fpsyg.2021.675285.
- Sliedrecht W, et al. Alcohol use disorder relapse factors: A systematic review. Psychiatry Research. 2019; doi:10.1016/j.psychres.2019.05.038.
- Thiamin deficiency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency,-dependency,-and-toxicity/thiamin-deficiency. Accessed April 2, 2022.
- Alcohol & diabetes. American Diabetes Association. https://www.diabetes.org/healthy-living/medication-treatments/alcohol-diabetes. Accessed April 2, 2022.
- Marcus GM, et al. Acute consumption of alcohol and discrete atrial fibrillation events. Annals of Internal Medicine. 2021; doi:10.7326/M21-0228.
- Means RT. Hematologic complications of alcohol use. https://www.uptodate.com/contents/search. Accessed April 1, 2022.
- What people recovering from alcoholism need to know about osteoporosis. NIH Osteoporosis and Related Bone Diseases National Resource Center. https://www.bones.nih.gov/health-info/bone/osteoporosis/conditions-behaviors/alcoholism. Accessed April 2, 2022.
- How to tell if your child is drinking alcohol. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/talk-they-hear-you/parent-resources/how-tell-if-your-child-drinking-alcohol. Accessed April 2, 2022.
- Smith KE, et al. Problematic alcohol use and associated characteristics following bariatric surgery. Obesity Surgery. 2018; doi:10.1007/s11695-017-3008-8.
- Fairbanks J, et al. Evidence-based pharmacotherapies for alcohol use disorder: Clinical pearls. Mayo Clinic Proceedings. 2020; doi:10.1016/j.mayocp.2020.01.030.
- U.S. Preventive Services Task Force. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2018; doi:10.1001/jama.2018.16789.
- Hall-Flavin DK (expert opinion). Mayo Clinic. April 25, 2022.
- Celebrate Recovery. https://www.celebraterecovery.com/. Accessed April 26, 2022.
- SMART Recovery. https://www.smartrecovery.org/. Accessed April 26, 2022.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 22 December 2022
Hazardous drinking and alcohol use disorders
- James MacKillop ORCID: orcid.org/0000-0002-8695-1071 1 , 2 ,
- Roberta Agabio ORCID: orcid.org/0000-0001-7395-6845 3 , 4 ,
- Sarah W. Feldstein Ewing 5 , 6 ,
- Markus Heilig 7 ,
- John F. Kelly 8 ,
- Lorenzo Leggio 9 , 10 ,
- Anne Lingford-Hughes 11 , 12 ,
- Abraham A. Palmer 13 ,
- Charles D. Parry 14 , 15 ,
- Lara Ray 16 &
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 17 , 18 , 19 , 20 , 21 , 22
Nature Reviews Disease Primers volume 8 , Article number: 80 ( 2022 ) Cite this article
3918 Accesses
30 Citations
89 Altmetric
Metrics details
- Human behaviour
- Translational research
Alcohol is one of the most widely consumed psychoactive drugs globally. Hazardous drinking, defined by quantity and frequency of consumption, is associated with acute and chronic morbidity. Alcohol use disorders (AUDs) are psychiatric syndromes characterized by impaired control over drinking and other symptoms. Contemporary aetiological perspectives on AUDs apply a biopsychosocial framework that emphasizes the interplay of genetics, neurobiology, psychology, and an individual’s social and societal context. There is strong evidence that AUDs are genetically influenced, but with a complex polygenic architecture. Likewise, there is robust evidence for environmental influences, such as adverse childhood exposures and maladaptive developmental trajectories. Well-established biological and psychological determinants of AUDs include neuroadaptive changes following persistent use, differences in brain structure and function, and motivational determinants including overvaluation of alcohol reinforcement, acute effects of environmental triggers and stress, elevations in multiple facets of impulsivity, and lack of alternative reinforcers. Social factors include bidirectional roles of social networks and sociocultural influences, such as public health control strategies and social determinants of health. An array of evidence-based approaches for reducing alcohol harms are available, including screening, pharmacotherapies, psychological interventions and policy strategies, but are substantially underused. Priorities for the field include translating advances in basic biobehavioural research into novel clinical applications and, in turn, promoting widespread implementation of evidence-based clinical approaches in practice and health-care systems.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
92,52 € per year
only 92,52 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Determinants of behaviour and their efficacy as targets of behavioural change interventions

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Psilocybin microdosers demonstrate greater observed improvements in mood and mental health at one month relative to non-microdosing controls
Dudley, R. Evolutionary origins of human alcoholism in primate frugivory. Q. Rev. Biol. 75 , 3–15 (2000).
Article CAS Google Scholar
Dudley, R. & Maro, A. Human evolution and dietary ethanol. Nutrients 13 , 2419 (2021).
World Health Organization. Global status report on alcohol and health 2018 (WHO, 2018).
Humphreys, K. & Kalinowski, A. Governmental standard drink definitions and low-risk alcohol consumption guidelines in 37 countries. Addiction 111 , 1293–1298 (2016).
Article Google Scholar
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (American Psychiatric Association, 2013).
World Health Organization. International statistical classification of diseases and related health problems. World Health Organization https://icd.who.int/ (2018).
Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B. & Monteiro, M. G. AUDIT. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care (WHO, 2001).
Volkow, N. D. Stigma and the toll of addiction. N. Engl. J. Med. 382 , 1289–1290 (2020).
Kilian, C. et al. Stigmatization of people with alcohol use disorders: an updated systematic review of population studies. Alcohol. Clin. Exp. Res. 45 , 899–911 (2021).
Volkow, N. D., Gordon, J. A. & Koob, G. F. Choosing appropriate language to reduce the stigma around mental illness and substance use disorders. Neuropsychopharmacology 46 , 2230–2232 (2021).
Saitz, R., Miller, S. C., Fiellin, D. A. & Rosenthal, R. N. Recommended use of terminology in addiction medicine. J. Addict. Med. 15 , 3–7 (2021).
White, A. et al. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcohol. Clin. Exp. Res. 39 , 1712–1726 (2015).
Grant, B. F. et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 72 , 757–766 (2015).
Kittirattanapaiboon, P. et al. Prevalence of mental disorders and mental health problems: Thai national mental health survey 2013. J. Ment. Health Thail. 25 , 1–19 (2017).
Google Scholar
Rehm, J., Room, R., van den Brink, W. & Jacobi, F. Alcohol use disorders in EU countries and Norway: an overview of the epidemiology. Eur. Neuropsychopharmacol. 15 , 377–388 (2005).
Rehm, J. et al. Prevalence of alcohol use disorders in primary health-care facilities in Russia in 2019. Addiction 117 , 1640–1646 (2022).
World Health Organization. ICD-11 for mortality and morbidity statistics. WHO https://icd.who.int/browse11/l-m/en (2018).
Puddephatt, J. A., Irizar, P., Jones, A., Gage, S. H. & Goodwin, L. Associations of common mental disorder with alcohol use in the adult general population: a systematic review and meta-analysis. Addiction 117 , 1543–1572 (2022).
National Institute on Drug Abuse. Why is there comorbidity between substance use disorders and mental illnesses? National Institute on Drug Abuse https://www.drugabuse.gov/publications/research-reports/common-comorbidities-substance-use-disorders/why-there-comorbidity-between-substance-use-disorders-mental-illnesses (2020).
Chassin, L., Sher, K. J., Hussong, A. & Curran, P. The developmental psychopathology of alcohol use and alcohol disorders: research achievements and future directions. Dev. Psychopathol. 25 , 1567–1584 (2013).
Kendler, K. S., Prescott, C. A., Myers, J. & Neale, M. C. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch. Gen. Psychiatry 60 , 929–937 (2003).
Hicks, B. M., Krueger, R. F., Iacono, W. G., McGue, M. & Patrick, C. J. Family transmission and heritability of externalizing disorders: a twin-family study. Arch. Gen. Psychiatry 61 , 922–928 (2004).
Dick, D. M. & Agrawal, A. The genetics of alcohol and other drug dependence. Alcohol. Res. Health 31 , 111–118 (2008).
Barr, P. B. & Dick, D. M. The genetics of externalizing problems. Curr. Top. Behav. Neurosci. 47 , 93–112 (2020).
Rehm, J., Rovira, P., Llamosas-Falcon, L. & Shield, K. D. Dose-response relationships between levels of alcohol use and risks of mortality or disease, for all people, by age, sex and specific risk factors. Nutrients 13 , 2652 (2021).
Eckardt, M. J. et al. Effects of moderate alcohol consumption on the central nervous system. Alcohol. Clin. Exp. Res. 22 , 998–1040 (1998).
Morojele, N. K., Shenoi, S. V., Shuper, P. A., Braithwaite, R. S. & Rehm, J. Alcohol use and the risk of communicable diseases. Nutrients 13 , 3317 (2021).
Rehm, J. et al. The relationship between different dimensions of alcohol use and the burden of disease – an update. Addiction 112 , 968–1001 (2017).
Rehm, J. et al. The role of alcohol use in the aetiology and progression of liver disease: a narrative review and a quantification. Drug Alcohol. Rev. 40 , 1377–1386 (2021).
Wild, C. P., Weiderpass, E. & Stewart, B. W. (eds) World Cancer Report: Cancer Research for Cancer Prevention (International Agency for Research on Cancer, 2020).
White, I. R., Altmann, D. R. & Nanchahal, K. Alcohol consumption and mortality: modelling risks for men and women at different ages. BMJ 325 , 191 (2002).
Shield, K. et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public. Health 5 , e51–e61 (2020).
Zahr, N. M., Kaufman, K. L. & Harper, C. G. Clinical and pathological features of alcohol-related brain damage. Nat. Rev. Neurol. 7 , 284 (2011).
Sullivan, E. V., Harris, R. A. & Pfefferbaum, A. Alcohol’s effects on brain and behavior. Alcohol. Res. Health 33 , 127–143 (2010).
Sullivan, E. V. & Pfefferbaum, A. Alcohol use disorder: neuroimaging evidence for accelerated aging of brain morphology and hypothesized contribution to age-related dementia. Alcohol https://doi.org/10.1016/J.ALCOHOL.2022.06.002 (2022).
Schwarzinger, M. et al. Contribution of alcohol use disorders to the burden of dementia in France 2008-13: a nationwide retrospective cohort study. Lancet Public Health 3 , e124–e132 (2018).
Lange, S. et al. Global prevalence of fetal alcohol spectrum disorder among children and youth: a systematic review and meta-analysis. JAMA Pediatr. 171 , 948–956 (2017).
Traccis, F. et al. Alcohol-medication interactions: a systematic review and meta-analysis of placebo-controlled trials. Neurosci. Biobehav. Rev. 132 , 519–541 (2021).
Laslett, A.-M., Room, R., Waleewong, O., Stanesby, O. & Callinan, S. (eds) Harm to Others from Drinking: Patterns in Nine Societies (WHO, 2019).
Nutt, D. J., King, L. A. & Phillips, L. D. Drug harms in the UK: a multicriteria decision analysis. Lancet 376 , 1558–1565 (2010).
Manthey, J. et al. What are the economic costs to society attributable to alcohol use? A systematic review and modelling study. Pharmacoeconomics 39 , 809–822 (2021).
Cloninger, C. R., Bohman, M. & Sigvardsson, S. Inheritance of alcohol abuse. Cross-fostering analysis of adopted men. Arch. Gen. Psychiatry 38 , 861–868 (1981).
Cloninger, C. R. Etiologic factors in substance abuse: an adoption study perspective. NIDA Res. Monogr. 89 , 52–72 (1988).
CAS Google Scholar
Heath, A. C. Genetic influences on alcoholism risk: a review of adoption and twin studies. Alcohol. Health Res. World 19 , 166 (1995).
Verhulst, B., Neale, M. C. & Kendler, K. S. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol. Med. 45 , 1061–1072 (2015).
True, W. R. et al. Common genetic vulnerability for nicotine and alcohol dependence in men. Arch. Gen. Psychiatry 56 , 655–661 (1999).
Bierut, L. J. Genetic vulnerability and susceptibility to substance dependence. Neuron 69 , 618 (2011).
Morozova, T. V., Goldman, D., Mackay, T. F. C. & Anholt, R. R. H. The genetic basis of alcoholism: multiple phenotypes, many genes, complex networks. Genome Biol. 13 , 239 (2012).
Zhou, H. et al. Genome-wide meta-analysis of problematic alcohol use in 435,563 individuals yields insights into biology and relationships with other traits. Nat. Neurosci. 23 , 809–818 (2020).
Edenberg, H. J., Gelernter, J. & Agrawal, A. Genetics of alcoholism. Curr. Psychiatry Rep. 21 , 26 (2019).
Luczak, S. E., Glatt, S. J. & Wall, T. L. Meta-analyses of ALDH2 and ADH1B with alcohol dependence in Asians. Psychol. Bull. 132 , 607–621 (2006).
Luo, H. R. et al. Origin and dispersal of atypical aldehyde dehydrogenase ALDH2487Lys. Gene 435 , 96–103 (2009).
Higuchi, S. et al. Aldehyde dehydrogenase genotypes in Japanese alcoholics. Lancet 343 , 741–742 (1994).
Brooks, P. J., Enoch, M. A., Goldman, D., Li, T. K. & Yokoyama, A. The alcohol flushing response: an unrecognized risk factor for esophageal cancer from alcohol consumption. PLoS Med. 6 , 0258–0263 (2009).
Edenberg, H. J. & McClintick, J. N. Alcohol dehydrogenases, aldehyde dehydrogenases, and alcohol use disorders: a critical review. Alcohol. Clin. Exp. Res. 42 , 2281–2297 (2018).
Ray, L. A. & Hutchison, K. E. Effects of naltrexone on alcohol sensitivity and genetic moderators of medication response: a double-blind placebo-controlled study. Arch. Gen. Psychiatry 64 , 1069–1077 (2007).
Ray, L. A. & Hutchison, K. E. A polymorphism of the µ,-opioid receptor gene (OPRM1) and sensitivity to the effects of alcohol in humans. Alcohol. Clin. Exp. Res. 28 , 1789–1795 (2004).
Schuckit, M. A. A critical review of methods and results in the search for genetic contributors to alcohol sensitivity. Alcohol. Clin. Exp. Res. 42 , 822–835 (2018).
Ramchandani, V. A. et al. A genetic determinant of the striatal dopamine response to alcohol in men. Mol. Psychiatry 16 , 809–817 (2011).
King, A. C., de Wit, H., McNamara, P. J. & Cao, D. Rewarding, stimulant, and sedative alcohol responses and relationship to future binge drinking. Arch. Gen. Psychiatry 68 , 389–399 (2011).
King, A. C., Hasin, D., O’Connor, S. J., McNamara, P. J. & Cao, D. A prospective 5-year re-examination of alcohol response in heavy drinkers progressing in alcohol use disorder. Biol. Psychiatry 79 , 489–498 (2016).
King, A. et al. Subjective responses to alcohol in the development and maintenance of alcohol use disorder. Am. J. Psychiatry 178 , 560–571 (2021).
Sanchez-Roige, S., Palmer, A. A. & Clarke, T. K. Recent efforts to dissect the genetic basis of alcohol use and abuse. Biol. Psychiatry 87 , 609–618 (2020).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
Walters, R. K. et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat. Neurosci. 21 , 1656–1669 (2018).
Kranzler, H. R. et al. Genome-wide association study of alcohol consumption and use disorder in 274,424 individuals from multiple populations. Nat. Commun. 10 , 1499 (2019).
Sanchez-Roige, S. et al. Genome-wide association study of alcohol use disorder identification test (AUDIT) scores in 20 328 research participants of European ancestry. Addiction Biol. 24 , 121–131 (2019).
Sanchez-Roige, S. et al. Genome-wide association study meta-analysis of the alcohol use disorders identification test (AUDIT) in two population-based cohorts. Am. J. Psychiatry 176 , 107–118 (2019).
Mallard, T. T. et al. Item-level genome-wide association study of the alcohol use disorders identification test in three population-based cohorts. Am. J. Psychiatry 179 , 58–70 (2022).
Kuo, S. I. C. et al. Mapping pathways by which genetic risk influences adolescent externalizing behavior: the interplay between externalizing polygenic risk scores, parental knowledge, and peer substance use. Behav. Genet. 51 , 543 (2021).
Dodge, N. C., Jacobson, J. L. & Jacobson, S. W. Effects of fetal substance exposure on offspring substance use. Pediatr. Clin. North. Am. 66 , 1149–1161 (2019).
Hughes, K. et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2 , e356–e366 (2017).
Pilowsky, D. J., Keyes, K. M. & Hasin, D. S. Adverse childhood events and lifetime alcohol dependence. Am. J. Public Health 99 , 258–263 (2009).
Capusan, A. J. et al. Re-examining the link between childhood maltreatment and substance use disorder: a prospective, genetically informative study. Mol. Psychiatry 26 , 3201–3209 (2021).
Lee, R. S., Oswald, L. M. & Wand, G. S. Early life stress as a predictor of co-occurring alcohol use disorder and post-traumatic stress disorder. Alcohol Res. 39 , 147–159 (2018).
Price, A., Cook, P. A., Norgate, S. & Mukherjee, R. Prenatal alcohol exposure and traumatic childhood experiences: a systematic review. Neurosci. Biobehav. Rev. 80 , 89–98 (2017).
Hemingway, S. J. A. et al. Twin study confirms virtually identical prenatal alcohol exposures can lead to markedly different fetal alcohol spectrum disorder outcomes–fetal genetics influences fetal vulnerability. Adv. Pediatr. Res. 5 , 23 (2018).
Rossow, I., Keating, P., Felix, L. & Mccambridge, J. Does parental drinking influence children’s drinking? A systematic review of prospective cohort studies. Addiction 111 , 204–217 (2016).
Sharmin, S. et al. Parental supply of alcohol in childhood and risky drinking in adolescence: systematic review and meta-analysis. Int. J. Environ. Res. Public. Health 14 , 287 (2017).
Ryan, S. M., Jorm, A. F. & Lubman, D. I. Parenting factors associated with reduced adolescent alcohol use: a systematic review of longitudinal studies. Aust. NZ J. Psychiatry 44 , 774–783 (2010).
Resnick, M. D. et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA 278 , 823–832 (1997).
Johnson, V. & Pandina, R. J. Effects of the family environment on adolescent substance use, delinquency, and coping styles. Am. J. Drug Alcohol Abus. 17 , 71–88 (1991).
Bailey, J. A., Hill, K. G., Oesterle, S. & Hawkins, J. D. Parenting practices and problem behavior across three generations: monitoring, harsh discipline, and drug use in the intergenerational transmission of externalizing behavior. Dev. Psychol. 45 , 1214–1226 (2009).
Iacono, W. G., Malone, S. M. & McGue, M. Behavioral disinhibition and the development of early-onset addiction: common and specific influences. Annu. Rev. Clin. Psychol. 4 , 325–348 (2008).
Hussong, A. M., Jones, D. J., Stein, G. L., Baucom, D. H. & Boeding, S. An internalizing pathway to alcohol use and disorder. Psychol. Addict. Behav. 25 , 390–404 (2011).
Khoury, J. E., Jamieson, B. & Milligan, K. Risk for childhood internalizing and externalizing behavior problems in the context of prenatal alcohol exposure: a meta-analysis and comprehensive examination of moderators. Alcohol. Clin. Exp. Res. 42 , 1358–1377 (2018).
Johnston, L. D., O’Malley, P. M. & Miech, R. A. Monitoring the Future national survey results on drug use, 1975–2013: overview, key findings on adolescent drug use (ERIC, 2014).
Lee, M. R. & Sher, K. J. ‘Maturing out’ of binge and problem drinking. Alcohol. Res. 39 , 31–42 (2018).
Maimaris, W. & McCambridge, J. Age of first drinking and adult alcohol problems: systematic review of prospective cohort studies. J. Epidemiol. Community Health 68 , 268–274 (2014).
Prescott, C. A. & Kendler, K. S. Age at first drink and risk for alcoholism: a noncausal association. Alcohol. Clin. Exp. Res. 23 , 101–107 (1999).
Bachman, J. G. et al. The Decline of Substance Use in Young Adulthood: Changes in Social Activities, Role, and Beliefs (Erlbaum, 2002).
Gotham, H. J., Sher, K. J. & Wood, P. K. Alcohol involvement and developmental task completion during young adulthood. J. Stud. Alcohol 64 , 32–42 (2003).
Wood, M. D., Sher, K. J. & McGowan, A. K. Collegiate alcohol involvement and role attainment in early adulthood: findings from a prospective high-risk study. J. Stud. Alcohol 61 , 278–289 (2000).
Lee, M. R., Chassin, L. & MacKinnon, D. P. Role transitions and young adult maturing out of heavy drinking: evidence for larger effects of marriage among more severe premarriage problem drinkers. Alcohol. Clin. Exp. Res. https://doi.org/10.1111/acer.12715 (2015).
Lee, M. R., Chassin, L. & Villalta, I. K. Maturing out of alcohol involvement: transitions in latent drinking statuses from late adolescence to adulthood. Dev. Psychopathol. 25 , 1137–1153 (2013).
Dawson, D. A., Grant, B. F., Stinson, F. S. & Chou, P. S. Maturing out of alcohol dependence: the impact of transitional life events. J. Stud. Alcohol 67 , 195–203 (2006).
Spanagel, R. Alcoholism: a systems approach from molecular physiology to addictive behavior. Physiol. Rev. 89 , 649–705 (2009).
Holmes, A., Spanagel, R. & Krystal, J. H. Glutamatergic targets for new alcohol medications. Psychopharmacology 229 , 539–554 (2013).
Heilig, M., Egli, M., Crabbe, J. C. & Becker, H. C. Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked? Addiction Biol. 15 , 169–184 (2010).
Heilig, M. et al. Reprogramming of mPFC transcriptome and function in alcohol dependence. Genes Brain Behav. 16 , 86–100 (2017).
Xiao, P. R. et al. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 153 , 22–28 (2015).
Wise, R. A. & Bozarth, M. A. A psychomotor stimulant theory of addiction. Psychol. Rev. 94 , 469–492 (1987).
Spanagel, R., Herz, A. & Shippenberg, T. S. Opposing tonically active endogenous opioid systems modulate the mesolimbic dopaminergic pathway. Proc. Natl Acad. Sci. USA 89 , 2046–2050 (1992).
Tanda, G. & di Chiara, G. A dopamine-mu1 opioid link in the rat ventral tegmentum shared by palatable food (Fonzies) and non-psychostimulant drugs of abuse. Eur. J. Neurosci. 10 , 1179–1187 (1998).
Koob, G. F. Drugs of abuse: anatomy, pharmacology and function of reward pathways. Trends Pharmacol. Sci. 13 , 177–184 (1992).
Martin, C. S., Earleywine, M., Musty, R. E., Perrine, M. W. & Swift, R. M. Development and validation of the Biphasic Alcohol Effects Scale. Alcohol. Clin. Exp. Res. 17 , 140–146 (1993).
Pohorecky, L. A. Biphasic action of ethanol. Biobehav. Rev. 1 , 231–240 (1977).
Koob, G. F. & le Moal, M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat. Neurosci. 8 , 1442–1444 (2005).
Gilpin, N. W., Herman, M. A. & Roberto, M. The central amygdala as an integrative hub for anxiety and alcohol use disorders. Biol. Psychiatry 77 , 859–869 (2015).
Koob, G. & Kreek, M. J. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am. J. Psychiatry 164 , 1149–1159 (2007).
Koob, G. F. Alcoholism, corticotropin-releasing factor, and molecular genetic allostasis. Biol. Psychiatry 63 , 137–138 (2008).
Augier, E. et al. A molecular mechanism for choosing alcohol over an alternative reward. Science 360 , 1321–1326 (2018).
Domi, E. et al. A neural substrate of compulsive alcohol use. Sci. Adv. 7 , eabg9045 (2021).
Seif, T. et al. Cortical activation of accumbens hyperpolarization-active NMDARs mediates aversion-resistant alcohol intake. Nat. Neurosci. 16 , 1094–1100 (2013).
Siciliano, C. A. et al. A cortical-brainstem circuit predicts and governs compulsive alcohol drinking. Science 366 , 1008–1012 (2019).
Heilig, M., Goldman, D., Berrettini, W. & O’Brien, C. P. Pharmacogenetic approaches to the treatment of alcohol addiction. Nat. Rev. Neurosci. 12 , 670–684 (2011).
Goldstein, R. Z. & Volkow, N. D. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat. Rev. Neurosci. 12 , 652–669 (2011).
Sullivan, E. V. & Pfefferbaum, A. Brain-behavior relations and effects of aging and common comorbidities in alcohol use disorder: a review. Neuropsychology 33 , 760–780 (2019).
Fritz, M., Klawonn, A. M. & Zahr, N. M. Neuroimaging in alcohol use disorder: from mouse to man. J. Neurosci. Res. 100 , 1140–1158 (2019).
Lees, B. et al. Promising vulnerability markers of substance use and misuse: a review of human neurobehavioral studies. Neuropharmacology 187 , 10850 (2021).
Schumann, G. et al. The IMAGEN study: reinforcement-related behaviour in normal brain function and psychopathology. Mol. Psychiatry 15 , 1128–1139 (2010).
Volkow, N. D. et al. The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev. Cogn. Neurosci. 32 , 4–7 (2018).
Brown, S. A. et al. The National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA): a multisite study of adolescent development and substance use. J. Stud. Alcohol Drugs 76 , 895–908 (2015).
Schacht, J. P., Anton, R. F. & Myrick, H. Functional neuroimaging studies of alcohol cue reactivity: a quantitative meta-analysis and systematic review. Addict. Biol. 18 , 121–133 (2013).
Courtney, K. E., Schacht, J. P., Hutchison, K., Roche, D. J. & Ray, L. A. Neural substrates of cue reactivity: association with treatment outcomes and relapse. Addict. Biol. 21 , 3–22 (2016).
Bach, P. et al. Incubation of neural alcohol cue reactivity after withdrawal and its blockade by naltrexone. Addict. Biol. 25 , e12717 (2020).
Karl, D. et al. Nalmefene attenuates neural alcohol cue-reactivity in the ventral striatum and subjective alcohol craving in patients with alcohol use disorder. Psychopharmacology 238 , 2179–2189 (2021).
Wrase, J. et al. Dysfunction of reward processing correlates with alcohol craving in detoxified alcoholics. Neuroimage 35 , 787–794 (2007).
Murphy, A. et al. Acute D3 antagonist GSK598809 selectively enhances neural response during monetary reward anticipation in drug and alcohol dependence. Neuropsychopharmacology 42 , 1049–1057 (2017).
Zhang, R. & Volkow, N. D. Brain default-mode network dysfunction in addiction. Neuroimage 200 , 313–331 (2019).
Orban, C. et al. Chronic alcohol exposure differentially modulates structural and functional properties of amygdala: a cross-sectional study. Addiction Biol. 26 , e12980 (2021).
Urban, N. B. L. et al. Sex differences in striatal dopamine release in young adults after oral alcohol challenge: a positron emission tomography imaging study with [11C]raclopride. Biol. Psychiatry 68 , 689–696 (2010).
Hansson, A. C. et al. Dopamine and opioid systems adaptation in alcoholism revisited: convergent evidence from positron emission tomography and postmortem studies. Neurosci. Biobehav. Rev. 106 , 141–164 (2019).
Erritzoe, D. et al. In vivo imaging of cerebral dopamine D3 receptors in alcoholism. Neuropsychopharmacology 39 , 1703–1712 (2014).
Heinz, A. et al. Correlation of stable elevations in striatal mu-opioid receptor availability in detoxified alcoholic patients with alcohol craving: a positron emission tomography study using carbon 11-labeled carfentanil. Arch. Gen. Psychiatry 62 , 57–64 (2005).
Hermann, D. et al. Low mu-opioid receptor status in alcohol dependence identified by combined positron emission tomography and post-mortem brain analysis. Neuropsychopharmacology 42 , 606–614 (2017).
Turton, S. et al. Blunted endogenous opioid release following an oral dexamphetamine challenge in abstinent alcohol-dependent individuals. Mol. Psychiatry 25 , 1749–1758 (2020).
Verplaetse, T. L., Cosgrove, K. P., Tanabe, J. & McKee, S. A. Sex/gender differences in brain function and structure in alcohol use: a narrative review of neuroimaging findings over the last 10 years. J. Neurosci. Res. 99 , 309–323 (2021).
Grace, S. et al. Sex differences in the neuroanatomy of alcohol dependence: hippocampus and amygdala subregions in a sample of 966 people from the ENIGMA Addiction Working Group. Transl Psychiatry 11 , 156 (2021).
Qi, S. et al. Reward processing in novelty seekers: a transdiagnostic psychiatric imaging biomarker. Biol. Psychiatry 90 , 529–539 (2021).
Bigelow, G. E. in Inter nationa l Handb ook of Alcohol Dependence and Problems (eds Heather, N., Peters, T. J. & Stockwell, T.) 299–315 (Wiley, 2001).
Higgins, S. T., Heil, S. H. & Lussier, J. P. Clinical implications of reinforcement as a determinant of substance use disorders. Annu. Rev. Psychol. 55 , 431–461 (2004).
Bickel, W. K., Johnson, M. W., Koffarnus, M. N., MacKillop, J. & Murphy, J. G. The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annu. Rev. Clin. Psychol. 10 , 641–677 (2014).
Mello, N. K. & Mendelson, J. H. Operant analysis of drinking patterns of chronic alcoholics. Nature 206 , 43–46 (1965).
Mendelson, J. H. & Mello, N. K. Experimental analysis of drinking behavior of chronic alcoholics. Ann. NY Acad. Sci. 133 , 828–845 (1966).
Petry, N. M. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology 154 , 243–250 (2001).
MacKillop, J. et al. Alcohol demand, delayed reward discounting, and craving in relation to drinking and alcohol use disorders. J. Abnorm. Psychol. 119 , 106–114 (2010).
Mackillop, J. The behavioral economics and neuroeconomics of alcohol use disorders. Alcohol. Clin. Exp. Res. 40 , 672–685 (2016).
MacKillop, J. et al. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology 216 , 305–321 (2011).
Amlung, M., Vedelago, L., Acker, J., Balodis, I. & MacKillop, J. Steep delay discounting and addictive behavior: a meta-analysis of continuous associations. Addiction 112 , 51–62 (2017).
Martínez-Loredo, V., González-Roz, A., Secades-Villa, R., Fernández-Hermida, J. R. & MacKillop, J. Concurrent validity of the Alcohol Purchase Task for measuring the reinforcing efficacy of alcohol: an updated systematic review and meta-analysis. Addiction 116 , 2635–2650 (2021).
Acuff, S. F., Dennhardt, A. A., Correia, C. J. & Murphy, J. G. Measurement of substance-free reinforcement in addiction: a systematic review. Clin. Psychol. Rev. 70 , 79–90 (2019).
Carter, B. L. & Tiffany, S. T. Meta-analysis of cue-reactivity in addiction research. Addiction 94 , 327–340 (1999).
MacKillop, J. et al. Behavioral economic analysis of cue-elicited craving for alcohol. Addiction 105 , 1599–1607 (2010).
Acuff, S. F., Amlung, M., Dennhardt, A. A., MacKillop, J. & Murphy, J. G. Experimental manipulations of behavioral economic demand for addictive commodities: a meta-analysis. Addiction 115 , 817–831 (2020); erratum 117, 2367 (2022).
Bouton, M. E., Maren, S. & McNally, G. P. Behavioral and neurobiological mechanisms of pavlovian and instrumental extinction learning. Physiol. Rev. 101 , 611–681 (2021).
Bouton, M. E. Context, attention, and the switch between habit and goal-direction in behavior. Learn. Behav. 49 , 349–362 (2021).
Hogarth, L. Addiction is driven by excessive goal-directed drug choice under negative affect: translational critique of habit and compulsion theory. Neuropsychopharmacology 45 , 720–735 (2020).
Brown, S. A., Christiansen, B. A. & Goldman, M. S. The Alcohol Expectancy Questionnaire: an instrument for the assessment of adolescent and adult alcohol expectancies. J. Stud. Alcohol 48 , 483–491 (1987).
Darkes, J., Greenbaum, P. E. & Goldman, M. S. Alcohol expectancy mediation of biopsychosocial risk: complex patterns of mediation. Exp. Clin. Psychopharmacol. 12 , 27–38 (2004).
Smith, G. T., Goldman, M. S., Greenbaum, P. E. & Christiansen, B. A. Expectancy for social facilitation from drinking: the divergent paths of high-expectancy and low-expectancy adolescents. J. Abnorm. Psychol. 104 , 32–40 (1995).
Christiansen, B. A., Smith, G. T., Roehling, P. V. & Goldman, M. S. Using alcohol expectancies to predict adolescent drinking behavior after one year. J. Consult. Clin. Psychol. 57 , 93–99 (1989).
Cooper, M. L., Frone, M. R., Russell, M. & Mudar, P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. J. Pers. Soc. Psychol. 69 , 990–1005 (1995).
Simons, J., Correia, C. J. & Carey, K. B. A comparison of motives for marijuana and alcohol use among experienced users. Addict. Behav. 25 , 153–160 (2000).
Kuntsche, E., Knibbe, R., Gmel, G. & Engels, R. Why do young people drink? A review of drinking motives. Clin. Psychol. Rev. 25 , 841–861 (2005).
Rooke, S. E., Hine, D. W. & Thorsteinsson, E. B. Implicit cognition and substance use: a meta-analysis. Addict. Behav. 33 , 1314–1328 (2008).
Cox, W. M., Hogan, L. M., Kristian, M. R. & Race, J. H. Alcohol attentional bias as a predictor of alcohol abusers’ treatment outcome. Drug Alcohol Depend. 68 , 237–243 (2002).
Rettie, H. C., Hogan, L. M. & Cox, W. M. Negative attentional bias for positive recovery-related words as a predictor of treatment success among individuals with an alcohol use disorder. Addict. Behav. 84 , 86–91 (2018).
Jarmolowicz, D. P. et al. in The Wiley-Blackwell Handbook of Addiction Psychopharmacology (eds MacKillop, J. & de Wit, H.) 27–61 (Wiley, 2013).
Ray, L. A., MacKillop, J., Leventhal, A. & Hutchison, K. E. Catching the alcohol buzz: an examination of the latent factor structure of subjective intoxication. Alcohol. Clin. Exp. Res. 33 , 2154–2161 (2009).
Quinn, P. D. & Fromme, K. Subjective response to alcohol challenge: a quantitative review. Alcohol. Clin. Exp. Res. https://doi.org/10.1111/j.1530-0277.2011.01521.x (2011).
Schuckit, M. A. A longitudinal study of children of alcoholics. Recent Dev. Alcohol. 9 , 5–19 (1991).
Schuckit, M. A. Biological, psychological and environmental predictors of the alcoholism risk: a longitudinal study. J. Stud. Alcohol 59 , 485–494 (1998).
Hendershot, C. S., Wardell, J. D., McPhee, M. D. & Ramchandani, V. A. A prospective study of genetic factors, human laboratory phenotypes, and heavy drinking in late adolescence. Addict. Biol. https://doi.org/10.1111/adb.12397 (2016).
Sher, K. J. & Trull, T. J. Personality and disinhibitory psychopathology: alcoholism and antisocial personality disorder. J. Abnorm. Psychol. 103 , 92–102 (1994).
Malouff, J. M., Thorsteinsson, E. B., Rooke, S. E. & Schutte, N. S. Alcohol involvement and the five-factor model of personality: a meta-analysis. J. Drug Educ. 37 , 277–294 (2007).
Malouff, J. M., Thorsteinsson, E. B. & Schutte, N. S. The five-factor model of personality and smoking: a meta-analysis. J. Drug Educ. 36 , 47–58 (2006).
Kotov, R., Gamez, W., Schmidt, F. & Watson, D. Linking ‘big’ personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol. Bull. 136 , 768–821 (2010).
Maclaren, V. V., Fugelsang, J. A., Harrigan, K. A. & Dixon, M. J. The personality of pathological gamblers: a meta-analysis. Clin. Psychol. Rev. 31 , 1057–1067 (2011).
Dick, D. M. et al. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biol. 15 , 217–226 (2010).
Patton, J. H., Stanford, M. S. & Barratt, E. S. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 51 , 768–774 (1995).
Whiteside, S. P. & Lynam, D. R. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Pers. Individ. Dif. 30 , 669–689 (2001).
Cyders, M. A., Littlefield, A. K., Coffey, S. & Karyadi, K. A. Examination of a short English version of the UPPS-P impulsive behavior scale. Addictive Behav. 39 , 1372–1376 (2014).
Coskunpinar, A., Dir, A. L. & Cyders, M. A. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcohol. Clin. Exp. Res. 37 , 1441–1450 (2013).
MacKillop, J. et al. The latent structure of impulsivity: impulsive choice, impulsive action, and impulsive personality traits. Psychopharmacology 233 , 3361–3370 (2016).
Fernie, G. et al. Multiple behavioural impulsivity tasks predict prospective alcohol involvement in adolescents. Addiction 108 , 1916–1923 (2013).
Sanchez-Roige, S. et al. Genome-wide association study of delay discounting in 23,217 adult research participants of European ancestry. Nat. Neurosci. 21 , 16–18 (2018).
MacKillop, J. et al. The brief alcohol social density assessment (BASDA): convergent, criterion-related and incremental validity. J. Stud. Alcohol Drugs 74 , 810–815 (2013).
Borgatti, S. P., Mehra, A., Brass, D. J. & Labianca, G. Network analysis in the social sciences. Science 323 , 892–895 (2009).
Rosenquist, J. N. Lessons from social network analyses for behavioral medicine. Curr. Opin. Psychiatry 24 , 139–143 (2011).
Burt, R. S., Kilduff, M. & Tasselli, S. Social network analysis: foundations and frontiers on advantage. Annu. Rev. Psychol. 64 , 527–547 (2013).
Rosenquist, J. N., Murabito, J., Fowler, J. H. & Christakis, N. A. The spread of alcohol consumption behavior in a large social network. Ann. Intern. Med. 152 , 426–433 (2010).
Bullers, S., Cooper, M. L. & Russell, M. Social network drinking and adult alcohol involvement: a longitudinal exploration of the direction of influence. Addict. Behav. 26 , 181–199 (2001).
Lau-Barraco, C., Braitman, A. L., Leonard, K. E. & Padilla, M. Drinking buddies and their prospective influence on alcohol outcomes: alcohol expectancies as a mediator. Psychol. Addict. Behav. 26 , 747–758 (2012).
Fortune, E. E. et al. Social density of gambling and its association with gambling problems: an initial investigation. J. Gambl. Stud. 29 , 329–342 (2013).
Fujimoto, K. & Valente, T. W. Social network influences on adolescent substance use: disentangling structural equivalence from cohesion. Soc. Sci. Med. 74 , 1952–1960 (2012).
Ennett, S. T. et al. The peer context of adolescent substance use: findings from social network analysis. J. Res. Adolesc. 16 , 159–186 (2006).
Meisel, M. K. et al. Egocentric social network analysis of pathological gambling. Addiction 108 , 584–591 (2013).
Stout, R. L., Kelly, J. F., Magill, M. & Pagano, M. E. Association between social influences and drinking outcomes across three years. J. Stud. Alcohol Drugs 73 , 489–497 (2012).
Longabaugh, R., Wirtz, P. W., Zywiak, W. H. & O’Malley, S. S. Network support as a prognostic indicator of drinking outcomes: the COMBINE study. J. Stud. Alcohol Drugs 71 , 837–846 (2010).
Kelly, J. F., Stout, R. L., Magill, M. & Tonigan, J. S. The role of Alcoholics Anonymous in mobilizing adaptive social network changes: a prospective lagged mediational analysis. Drug Alcohol Depend. 114 , 119–126 (2011).
Litt, M. D., Kadden, R. M., Kabela-Cormier, E. & Petry, N. Changing network support for drinking: initial findings from the Network Support Project. J. Consult. Clin. Psychol. 75 , 542–555 (2007).
Litt, M. D., Kadden, R. M., Kabela-Cormier, E. & Petry, N. M. Changing network support for drinking: network Support Project 2-year follow-up. J. Consult. Clin. Psychol. 77 , 229–242 (2009).
Agrawal, A. et al. Assortative mating for cigarette smoking and for alcohol consumption in female Australian twins and their spouses. Behav. Genet. 36 , 553–566 (2006).
Grant, J. D. et al. Spousal concordance for alcohol dependence: evidence for assortative mating or spousal interaction effects? Alcohol. Clin. Exp. Res. 31 , 717–728 (2007).
Leonard, K. E. & Eiden, R. D. Marital and family processes in the context of alcohol use and alcohol disorders. Annu. Rev. Clin. Psychol. 3 , 285–310 (2007).
AlMarri, T. S. K. & Oei, T. P. S. Alcohol and substance use in the Arabian Gulf region: a review. Int. J. Psychol. 44 , 222–233 (2009).
Russell, A. M., Yu, B., Thompson, C. G., Sussman, S. Y. & Barry, A. E. Assessing the relationship between youth religiosity and their alcohol use: a meta-analysis from 2008 to 2018. Addict. Behav. 106 , 106361 (2020).
Lin, H. C., Hu, Y. H., Barry, A. E. & Russell, A. Assessing the associations between religiosity and alcohol use stages in a representative U.S. sample. Subst. Use Misuse 55 , 1618–1624 (2020).
Roberts, S. C. M. Macro-level gender equality and alcohol consumption: a multi-level analysis across U.S. states. Soc. Sci. Med. 75 , 60–68 (2012).
Wagenaar, A. C., Salois, M. J. & Komro, K. A. Effects of beverage alcohol price and tax levels on drinking: a meta-analysis of 1003 estimates from 112 studies. Addiction 104 , 179–190 (2009).
Xuan, Z., Blanchette, J., Nelson, T. F., Heeren, T. & Oussayef, N. The alcohol policy environment and policy subgroups as predictors of binge drinking measures among US adults. Am. J. Public Health 105 , 816–822 (2015).
Subbaraman, M. S. et al. Relationships between US state alcohol policies and alcohol outcomes: differences by gender and race/ethnicity. Addiction 115 , 1285–1294 (2020).
Lamb, S., Greenlick, M. R. & McCarty, D (eds) Bridging the Gap between Practice and Research: Forging Partnerships with Community-Based Drug and Alcohol Treatment (National Academy Press, 1998).
Oliva, E. M., Maisel, N. C., Gordon, A. J. & Harris, A. H. S. Barriers to use of pharmacotherapy for addiction disorders and how to overcome them. Curr. Psychiatry Rep. 13 , 374–381 (2011).
Carroll, K. M. Lost in translation? Moving contingency management and cognitive behavioral therapy into clinical practice. Ann. NY Acad. Sci. 1327 , 94–111 (2014).
Room, R. Stigma, social inequality and alcohol and drug use. Drug Alcohol Rev. 24 , 143–155 (2005).
Xu, Y. et al. The socioeconomic gradient of alcohol use: an analysis of nationally representative survey data from 55 low-income and middle-income countries. Lancet Glob . Health 10 , e1268–e1280 (2022).
Roche, A. et al. Addressing inequities in alcohol consumption and related harms. Health Promot. Int. 30 (Suppl. 2), ii20–ii35 (2015).
American Psychiatric Association. Structured Clinical Interview for DSM-5: Research Version (American Psychiatric Association Publishing, 2015).
Schneider, L. H. et al. The diagnostic assessment research tool in action: a preliminary evaluation of a semistructured diagnostic interview for DSM-5 disorders. Psychol. Assess. 34 , 21–29 (2022).
Hallgren, K. A. et al. Practical assessment of alcohol use disorder in routine primary care: performance of an alcohol symptom checklist. J. Gen. Intern. Med. 37 , 1885–1893 (2022).
Hallgren, K. A. et al. Practical assessment of DSM-5 alcohol use disorder criteria in routine care: high test-retest reliability of an alcohol symptom checklist. Alcohol. Clin. Exp. Res. 46 , 458–467 (2022).
Levitt, E. E. et al. Optimizing screening for depression, anxiety disorders, and post-traumatic stress disorder in inpatient addiction treatment: a preliminary investigation. Addict. Behav. 112 , 106649 (2021).
Spanakis, P. et al. Problem drinking recognition among UK military personnel: prevalence and associations. Soc. Psychiatry Psychiatr. Epidemiol. https://doi.org/10.1007/S00127-022-02306-X (2022).
Roberts, E. et al. The prevalence of wholly attributable alcohol conditions in the United Kingdom hospital system: a systematic review, meta-analysis and meta-regression. Addiction 114 , 1726–1737 (2019).
Curry, S. J. et al. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force recommendation statement. JAMA 320 , 1899–1909 (2018).
McNeely, J. et al. Comparison of methods for alcohol and drug screening in primary care clinics. JAMA Netw. Open 4 , E2110721 (2021).
Singh, J. A. & Cleveland, J. D. Trends in hospitalizations for alcohol use disorder in the US from 1998 to 2016. JAMA Netw. Open 3 , e2016580 (2020).
Sword, W. et al. Screening and intervention practices for alcohol use by pregnant women and women of childbearing age: results of a Canadian survey. J. Obstet. Gynaecol. Can. 42 , 1121–1128 (2020).
Brothers, T. D. & Bach, P. Challenges in prediction, diagnosis, and treatment of alcohol withdrawal in medically ill hospitalized patients: a teachable moment. JAMA Intern. Med. 180 , 900–901 (2020).
Göransson, M., Magnusson, Å. & Heilig, M. Identifying hazardous alcohol consumption during pregnancy: implementing a research-based model in real life. Acta Obstet. Gynecol. Scand. 85 , 657–662 (2006).
Anderson, P., O’Donnell, A. & Kaner, E. Managing alcohol use disorder in primary health care. Curr. Psychiatry Rep. 19 , 79 (2017).
Bobb, J. F. et al. Evaluation of a pilot implementation to integrate alcohol-related care within primary care. Int. J. Environ. Res. Public Health 14 , 1030 (2017).
Chan, P. S.-f et al. Using Consolidated Framework for Implementation Research to investigate facilitators and barriers of implementing alcohol screening and brief intervention among primary care health professionals: a systematic review. Implement. Sci. https://doi.org/10.1186/s13012-021-01170-8 (2021).
Vaca, F. E. & Winn, D. The basics of alcohol screening, brief intervention and referral to treatment in the emergency department. West. J. Emerg. Med. 8 , 88 (2007).
Solberg, L. I., Maciosek, M. V. & Edwards, N. M. Primary care intervention to reduce alcohol misuse ranking its health impact and cost effectiveness. Am. J. Prev. Med. 34 , 143–152.e3 (2008).
Miller, W. R. & Rollnick, S. Motivational Interviewing: Helping People Change (Guilford Press, 2013).
Glass, J. E. et al. Specialty substance use disorder services following brief alcohol intervention: a meta-analysis of randomized controlled trials. Addiction 110 , 1404–1415 (2015).
Frost, M. C., Glass, J. E., Bradley, K. A. & Williams, E. C. Documented brief intervention associated with reduced linkage to specialty addictions treatment in a national sample of VA patients with unhealthy alcohol use with and without alcohol use disorders. Addiction 115 , 668–678 (2020).
Leggio, L. & Lee, M. R. Treatment of alcohol use disorder in patients with alcoholic liver disease. Am. J. Med. 130 , 124–134 (2017).
Litten, R. Z., Bradley, A. M. & Moss, H. B. Alcohol biomarkers in applied settings: recent advances and future research opportunities. Alcohol Clin. Exp. Res. 34 , 955–967 (2010).
Fairbairn, C. E. & Bosch, N. A new generation of transdermal alcohol biosensing technology: practical applications, machine-learning analytics and questions for future research. Addiction 116 , 2912–2920 (2021).
Walsham, N. E. & Sherwood, R. A. Ethyl glucuronide and ethyl sulfate. Adv. Clin. Chem. 67 , 47–71 (2014).
Philibert, R. et al. Genome-wide and digital polymerase chain reaction epigenetic assessments of alcohol consumption. Am. J. Med. Genet. B Neuropsychiatr. Genet. 177 , 479–488 (2018).
Miller, S., Mills, J. A., Long, J. & Philibert, R. A comparison of the predictive power of DNA methylation with carbohydrate deficient transferrin for heavy alcohol consumption. Epigenetics 16 , 969 (2021).
World Health Organization. The SAFER technical package. WHO https://www.who.int/publications/i/item/the-safer-technical-package (2019).
Stockwell, T., Giesbrecht, N., Vallance, K. & Wettlaufer, A. Government options to reduce the impact of alcohol on human health: obstacles to effective policy implementation. Nutrients 13 , 2846 (2021).
Sandmo, A. in The New Palgrave Dictionary of Economics (eds Durlauf, S. & Blume, L. E.) 1–4 (Palgrave Macmillan, 2008).
Chaloupka, F. J., Powell, L. M. & Warner, K. E. The use of excise taxes to reduce tobacco, alcohol, and sugary beverage consumption. Annu. Rev. Public Health 40 , 187–201 (2019).
Cabinet Secretary for Health and Social Care. Alcohol and drugs: minimum unit pricing. Scottish Government https://www.gov.scot/policies/alcohol-and-drugs/minimum-unit-pricing/ (2018).
Boniface, S., Scannell, J. W. & Marlow, S. Evidence for the effectiveness of minimum pricing of alcohol: a systematic review and assessment using the Bradford Hill criteria for causality. BMJ Open 7 , e013497 (2017).
Jones-Webb, R. et al. The effectiveness of alcohol impact areas in reducing crime in Washington neighborhoods. Alcohol. Clin. Exp. Res. 45 , 234–241 (2021).
Nepal, S. et al. Effects of extensions and restrictions in alcohol trading hours on the incidence of assault and unintentional injury: systematic review. J. Stud. Alcohol Drugs 81 , 5–23 (2020).
Wagenaar, A. C. & Toomey, T. L. Effects of minimum drinking age laws: review and analyses of the literature from 1960 to 2000. J. Stud. Alcohol Suppl. 63 , 206–225 (2002).
Green, R., Jason, H. & Ganz, D. Underage drinking: does the minimum age drinking law offer enough protection? Int. J. Adolesc. Med. Health 27 , 117–128 (2015).
Inchley, J. et al. Spotlight on Adolescent Health and Well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) Survey in Europe and Canada . International report. Vol. 1. Key findings. (WHO, 2020).
Johnston, L. D. et al. Monitoring the Future national survey results on drug use 2015 (ERIC, 2015).
The Lancet. Russia’s alcohol policy: a continuing success story. Lancet 394 , 1205 (2019).
Lynam, D. R. et al. Project DARE: no effects at 10-year follow-up. J. Consult. Clin. Psychol. 67 , 590–593 (1999).
Burton, R. et al. A rapid evidence review of the effectiveness and cost-effectiveness of alcohol control policies: an English perspective. Lancet 389 , 1558–1580 (2017).
Agabio, R. et al. Alcohol consumption is a modifiable risk factor for breast cancer: are women aware of this relationship? Alcohol Alcohol . https://doi.org/10.1093/ALCALC/AGAB042 (2021).
Sigfúsdóttir, I. D., Thorlindsson, T., Kristjánsson, A. L., Roe, K. M. & Allegrante, J. P. Substance use prevention for adolescents: the Icelandic Model. Health Promot. Int. 24 , 16–25 (2009).
D’Amico, E. J. & Feldstein Ewing, S. W. in The Ox f ord H andbook of Adolescent Substance Abuse (eds Zucker, R. A. & Brown, S. A.) 627–654 (Oxford Univ. Press, 2016).
Fachini, A., Aliane, P. P., Martinez, E. Z. & Furtado, E. F. Efficacy of brief alcohol screening intervention for college students (BASICS): a meta-analysis of randomized controlled trials. Subst. Abus. Treat. Prev. Policy 7 , 40 (2012).
Edalati, H. & Conrod, P. J. A review of personality-targeted interventions for prevention of substance misuse and related harm in community samples of adolescents. Front. Psychiatry 9 , 770 (2019).
National Institute on Alcohol Abuse and Alcoholism. NIAAA Recovery Research Definitions. NIAAA https://www.niaaa.nih.gov/research/niaaa-recovery-from-alcohol-use-disorder/definitions (2022).
Witkiewitz, K. et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol. Clin. Exp. Res. 41 , 179–186 (2017).
Hartwell, E. E., Feinn, R., Witkiewitz, K., Pond, T. & Kranzler, H. R. World Health Organization risk drinking levels as a treatment outcome measure in topiramate trials. Alcohol. Clin. Exp. Res. https://doi.org/10.1111/acer.14652 (2021).
Preusse, M., Neuner, F. & Ertl, V. Effectiveness of psychosocial interventions targeting hazardous and harmful alcohol use and alcohol-related symptoms in low- and middle-income countries: a systematic review. Front. Psychiatry 11 , 768 (2020).
Day, E. & Daly, C. Clinical management of the alcohol withdrawal syndrome. Addiction 117 , 804–814 (2022).
Reus, V. I. et al. The American Psychiatric Association practice guideline for the pharmacological treatment of patients with alcohol use disorder. Am. J. Psychiatry 175 , 86–90 (2018).
Agabio, R. & Leggio, L. Thiamine administration to all patients with alcohol use disorder: why not? Am. J. Drug Alcohol. Abus. 47 , 651–654 (2021).
Skinner, M. D., Lahmek, P., Pham, H. & Aubin, H. J. Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis. PLoS ONE 9 , e87366 (2014).
Jørgensen, C. H., Pedersen, B. & Tønnesen, H. The efficacy of disulfiram for the treatment of alcohol use disorder. Alcohol. Clin. Exp. Res. 35 , 1749–1758 (2011).
Jonas, D. E. et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA 311 , 1889–1900 (2014).
Kranzler, H. R. & Soyka, M. Diagnosis and pharmacotherapy of alcohol use disorder: a review. JAMA 320 , 815–824 (2018).
Canidate, S. S., Carnaby, G. D., Cook, C. L. & Cook, R. L. A systematic review of naltrexone for attenuating alcohol consumption in women with alcohol use disorders. Alcohol. Clin. Exp. Res. 41 , 466–472 (2017).
Ray, L. A. et al. Combined pharmacotherapy and cognitive behavioral therapy for adults with alcohol or substance use disorders: a systematic review and meta-analysis. JAMA Netw . Open 3 , e208279 (2020).
Garbutt, J. C. et al. Clinical and biological moderators of response to naltrexone in alcohol dependence: a systematic review of the evidence. Addiction 109 , 1274–1284 (2014).
Rubio, G. et al. Clinical predictors of response to naltrexone in alcoholic patients: who benefits most from treatment with naltrexone? Alcohol Alcohol. 40 , 227–233 (2005).
Fucito, L. M. et al. Cigarette smoking predicts differential benefit from naltrexone for alcohol dependence. Biol. Psychiatry 72 , 832–838 (2012).
Agabio, R., Pani, P. P., Preti, A., Gessa, G. L. & Franconi, F. Efficacy of medications approved for the treatment of alcohol dependence and alcohol withdrawal syndrome in female patients: a descriptive review. Eur. Addict. Res. 22 , 1–16 (2016).
Pierce, M., Sutterland, A., Beraha, E. M., Morley, K. & van den Brink, W. Efficacy, tolerability, and safety of low-dose and high-dose baclofen in the treatment of alcohol dependence: a systematic review and meta-analysis. Eur. Neuropsychopharmacol. 28 , 795–806 (2018).
Rose, A. K. & Jones, A. Baclofen: its effectiveness in reducing harmful drinking, craving, and negative mood. A meta-analysis. Addiction 113 , 1396–1406 (2018).
Garbutt, J. C. et al. Efficacy and tolerability of baclofen in a U.S. community population with alcohol use disorder: a dose-response, randomized, controlled trial. Neuropsychopharmacology 46 , 2250–2256 (2021).
Agabio, R., Baldwin, D. S., Amaro, H., Leggio, L. & Sinclair, J. M. A. The influence of anxiety symptoms on clinical outcomes during baclofen treatment of alcohol use disorder: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 125 , 296–313 (2021).
Agabio, R. et al. Baclofen for the treatment of alcohol use disorder: the Cagliari Statement. Lancet Psychiatry 5 , 957–960 (2018).
Ray, L. A. et al. State-of-the-art behavioral and pharmacological treatments for alcohol use disorder. Am. J. Drug Alcohol. Abus. 45 , 124–140 (2019).
Leggio, L., Falk, D. E., Ryan, M. L., Fertig, J. & Litten, R. Z. Medication development for alcohol use disorder: a focus on clinical studies. Handb. Exp. 258 , 443–462 (2020).
Witkiewitz, K., Litten, R. Z. & Leggio, L. Advances in the science and treatment of alcohol use disorder. Sci. Adv. 5 , eaax4043 (2019).
Johnson, B. A. et al. Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Lancet 361 , 1677–1685 (2003).
Hägg, S., Jönsson, A. K. & Ahlner, J. Current evidence on abuse and misuse of gabapentinoids. Drug Saf. 43 , 1235–1254 (2020).
Simpson, T. L. et al. Double-blind randomized clinical trial of prazosin for alcohol use disorder. Am. J. Psychiatry 175 , 1216–1224 (2018).
Grodin, E. N. et al. Ibudilast, a neuroimmune modulator, reduces heavy drinking and alcohol cue-elicited neural activation: a randomized trial. Transl Psychiatry 11 , 355 (2021).
MacKillop, J. et al. D-cycloserine to enhance extinction of cue-elicited craving for alcohol: a translational approach. Transl Psychiatry 5 , e544 (2015).
Miller, W. R., Zweben, A., DiClemente, C. C. & Rychtarik, R. G. Motivational Enhancement Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals With Alcohol Abuse and Dependence . Project MATCH Monograph Series, Vol. 2 (National Institute on Alcohol Abuse and Alcoholism, 1999).
Hettema, J., Steele, J. & Miller, W. R. Motivational Interviewing. Annu. Rev. Clin. Psychol. 1 , 91–111 (2005).
Frost, H. et al. Effectiveness of Motivational Interviewing on adult behaviour change in health and social care settings: a systematic review of reviews. PLoS ONE 13 , e0204890 (2018).
Steele, D. W. et al. Brief behavioral interventions for substance use in adolescents: a meta-analysis. Pediatrics 146 , e20200351 (2020).
Hendershot, C. S., Witkiewitz, K., George, W. H. & Marlatt, G. A. Relapse prevention for addictive behaviors. Subst. Abus. Treat. Prev. Policy 6 , 17 (2011).
Monti, P. M. & O’Leary, T. A. Coping and social skills training for alcohol and cocaine dependence. Psychiatr. Clin. North Am. 22 , 447–470 (1999).
Magill, M. et al. A meta-analysis of cognitive-behavioral therapy for alcohol or other drug use disorders: treatment efficacy by contrast condition. J. Consult. 87 , 1093–1105 (2019).
Kiluk, B. D. et al. Technology-delivered cognitive-behavioral interventions for alcohol use: a meta-analysis. Alcohol. Clin. Exp. 43 , 2285–2295 (2019).
Bowen, S. et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders. JAMA Psychiatry 71 , 547–556 (2014).
Schwebel, F. J., Korecki, J. R. & Witkiewitz, K. Addictive behavior change and mindfulness-based interventions: current research and future directions. Curr. Addict. 7 , 117–124 (2020).
McCrady, B. S., Epstein, E. E., Cook, S., Jensen, N. & Hildebrandt, T. A randomized trial of individual and couple behavioral alcohol treatment for women. J. Consult. Clin. Psychol. 77 , 243–256 (2009).
Powers, M. B., Vedel, E. & Emmelkamp, P. M. G. Behavioral couples therapy (BCT) for alcohol and drug use disorders: a meta-analysis. Clin. Psychol. Rev. 28 , 952–962 (2008).
McCrady, B. S. et al. Alcohol-focused behavioral couple therapy. Fam. Process. 55 , 443–459 (2016).
Petry, N. M. A comprehensive guide to the application of contingency management procedures in clinical settings. Drug Alcohol Depend. 58 , 9–25 (2000).
Benishek, L. A. et al. Prize-based contingency management for the treatment of substance abusers: a meta-analysis. Addiction 109 , 1426–1436 (2014).
Petry, N. M., Alessi, S. M., Olmstead, T. A., Rash, C. J. & Zajac, K. Contingency management treatment for substance use disorders: how far has it come, and where does it need to go? Psychol. Addict. Behav. 31 , 897 (2017).
Meyers, R. J. & Smith, J. E. Clinical Guide to Alcohol Treatment: The Community Reinforcement Approach (Guilford Press, 1995).
Godley, S. H. et al. The Adolescent Community Reinforcement Approach for Adolescent Cannabis Users . CYT Cannabis Youth Treatment Series, Vol. 4 (US Department of Health and Human Services, 2001).
Venner, K. L. et al. Culturally tailored evidence-based substance use disorder treatments are efficacious with an American Indian Southwest tribe: an open-label pilot-feasibility randomized controlled trial. Addiction 116 , 949–960 (2021).
National Institute on Drug Abuse. Principles of drug treatment: a research-based guide (third edition). NIDA https://nida.nih.gov/sites/default/files/675-principles-of-drug-addiction-treatment-a-research-based-guide-third-edition.pdf (2014).
Kelly, J. & Yeterian, J. in Addictions: A Comprehensive Guidebook (eds McCrady, B. S. & Epstein, E. E.) 500–525 (Oxford Univ. Press, 2013).
Bergman, B. G., Claire Greene, M., Hoeppner, B. B. & Kelly, J. F. Expanding the reach of alcohol and other drug services: prevalence and correlates of US adult engagement with online technology to address substance problems. Addict. Behav. 87 , 74–81 (2018).
Alcoholics Anonymous. Estimates of A.A. groups and members as of December 31, 2021. Alcoholics Anonymous https://www.aa.org/sites/default/files/literature/SMF-53%20EstimatesofAAGroupsandMembers%20EN%200122.pdf (2022).
Moos, R. H. & Moos, B. S. Participation in treatment and Alcoholics Anonymous: a 16-year follow-up of initially untreated individuals. J. Clin. Psychol. 62 , 735–750 (2006).
Institute of Medicine (US) Committee on Treatment of Alcohol Problems. Broadening the Base of Treatment for Alcohol Problems (National Academies Press, 1990).
Kelly, J. F., Humphreys, K. & Ferri, M. Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database Syst. Rev. 3 , CD012880 (2020).
Tonigan, J. S., Pearson, M. R., Magill, M. & Hagler, K. J. AA attendance and abstinence for dually diagnosed patients: a meta-analytic review. Addiction 113 , 1970–1981 (2018).
Humphreys, K. & Moos, R. H. Encouraging posttreatment self-help group involvement to reduce demand for continuing care services: two-year clinical and utilization outcomes. Alcohol. Clin. Exp. Res. 31 , 64–68 (2007).
Kelly, J. F. & McCrady B. S. in Research on Alcoholics Anonymous and Spiritual Aspects of Recovery (ed. Galanter, M) 797–836 (Springer, 2009).
Kelly, J. F. Is Alcoholics Anonymous religious, spiritual, neither? Findings from 25 years of mechanisms of behavior change research. Addiction 112 , 929–936 (2017).
Horvath, A. T. & Yeterian, J. SMART recovery: self-empowering, science-based addiction recovery support. J. Groups Addict. Recover. 7 , 102–117 (2012).
Zemore, S. E., Kaskutas, L. A., Mericle, A. & Hemberg, J. Comparison of 12-step groups to mutual help alternatives for AUD in a large, national study: differences in membership characteristics and group participation, cohesion, and satisfaction. J. Subst. Abus. Treat. 73 , 16–26 (2017).
Anton, R. F. et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 295 , 2003–2017 (2006).
Priester, M. A. et al. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J. Subst. Abus. Treat. 61 , 47–59 (2016).
Kaner, E. F. S. et al. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. Cochrane Database Syst. Rev. 9 , CD011479 (2017).
Levola, J., Aalto, M., Holopainen, A., Cieza, A. & Pitkänen, T. Health-related quality of life in alcohol dependence: a systematic literature review with a specific focus on the role of depression and other psychopathology. Nord. J. Psychiatry 68 , 369–384 (2014).
Imtiaz, S., Loheswaran, G., le Foll, B. & Rehm, J. Longitudinal alcohol consumption patterns and health-related quality of life: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Rev. 37 , 48–55 (2018).
Pettinati, H. M., Gastfriend, D. R., Dong, Q., Kranzler, H. R. & O’Malley, S. S. Effect of extended-release naltrexone (XR-NTX) on quality of life in alcohol-dependent patients. Alcohol. Clin. Exp. Res. 33 , 350–356 (2009).
Flórez, G. et al. Using topiramate or naltrexone for the treatment of alcohol-dependent patients. Alcohol. Clin. Exp. Res. 32 , 1251–1259 (2008).
Neto, D., Lambaz, R., Aguiar, P. & Chick, J. Effectiveness of sequential combined treatment in comparison with treatment as usual in preventing relapse in alcohol dependence. Alcohol Alcohol. 43 , 661–668 (2008).
Rus-Makovec, M. & Čebašek-Travnik, Z. Long-term abstinence and well-being of alcohol-dependent patients after intensive treatment and aftercare telephone contacts. Croat. Med. J. 49 , 763–771 (2008).
Charlet, K. & Heinz, A. Harm reduction – a systematic review on effects of alcohol reduction on physical and mental symptoms. Addict. Biol. 22 , 1119–1159 (2017).
Witkiewitz, K. et al. Drinking risk level reductions associated with improvements in physical health and quality of life among individuals with alcohol use disorder. Alcohol. Clin. Exp. Res. 42 , 2453 (2018).
Maher, B. Personal genomes: the case of the missing heritability. Nature 456 , 18–21 (2008).
Ray, L. A., MacKillop, J. & Hutchison, K. E. Pharmacogenetics of the µ-opioid receptor and the treatment of addictions. Per. Med. 4 , 217–220 (2007).
McClearn, G. E. & Vandenbergh, D. J. Structure and limits of animal models: examples from alcohol research. ILAR J. 41 , 144–152 (2000).
Nieto, S. J., Grodin, E. N., Aguirre, C. G., Izquierdo, A. & Ray, L. A. Translational opportunities in animal and human models to study alcohol use disorder. Transl Psychiatry 11 , 496 (2021).
MacKillop, J. & Murphy, C. in The Wiley-Blackwell Handbook of Addiction Psychopharmacology (eds MacKillop, J. & de Wit, H.) 315–344 (Wiley, 2013).
Morris, Z. S., Wooding, S. & Grant, J. The answer is 17 years, what is the question: understanding time lags in translational research. J. R. Soc. Med. 104 , 510–520 (2011).
Kwako, L. E., Momenan, R., Litten, R. Z., Koob, G. F. & Goldman, D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol. Psychiatry 80 , 179–189 (2016).
Voon, V. et al. Addictions NeuroImaging Assessment (ANIA): towards an integrative framework for alcohol use disorder. Neurosci. Biobehav. Rev. 113 , 492–506 (2020).
Harel, M. et al. Repetitive transcranial magnetic stimulation in alcohol dependence: a randomized, double-blind, sham-controlled proof-of-concept trial targeting the medial prefrontal and anterior cingulate cortices. Biol. Psychiatry https://doi.org/10.1016/J.BIOPSYCH.2021.11.020 (2021).
Lewis, C. C. et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry 76 , 324–335 (2019).
Samokhvalov, A. V. et al. Outcomes of an integrated care pathway for concurrent major depressive and alcohol use disorders: a multisite prospective cohort study. BMC Psychiatry 18 , 189 (2018).
Morgenstern, J. et al. An efficacy trial of adaptive interventions for alcohol use disorder. J. Subst. Abus. Treat. 123 , 108264 (2021).
Ashton, C. M. & Wray, N. P. Comparative Effectiveness Research: Evidence, Medicine, and Policy (Oxford Univ. Press, 2013).
Hasin, D. S., Stinson, F. S., Ogburn, E. & Grant, B. F. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry 64 , 830–842 (2007).
Han, B., Jones, C. M., Einstein, E. B., Powell, P. A. & Compton, W. M. Use of medications for alcohol use disorder in the US: results from the 2019 National Survey on Drug Use and Health. JAMA Psychiatry 78 , 922–924 (2021).
Spithoff, S., Turner, S., Gomes, T., Martins, D. & Singh, S. First-line medications for alcohol use disorders among public drug plan beneficiaries in Ontario. Can. Fam. Physician 63 , e277 (2017).
Morley, K. C., Logge, W., Pearson, S. A., Baillie, A. & Haber, P. S. National trends in alcohol pharmacotherapy: findings from an Australian claims database. Drug Alcohol Depend. 166 , 254–257 (2016).
Thompson, A., Ashcroft, D. M., Owens, L., van Staa, T. P. & Pirmohamed, M. Drug therapy for alcohol dependence in primary care in the UK: a Clinical Practice Research Datalink study. PLoS ONE 12 , e0173272 (2017).
Mark, T. L. et al. Physicians’ opinions about medications to treat alcoholism. Addiction 98 , 617–626 (2003).
Abraham, A. J., Andrews, C. M., Harris, S. J. & Friedmann, P. D. Availability of medications for the treatment of alcohol and opioid use disorder in the USA. Neurotherapeutics 17 , 55–69 (2020).
Carroll, K. M. Dissemination of evidence-based practices: how far we’ve come, and how much further we’ve got to go. Addiction 107 , 1031–1033 (2012).
Knudsen, H. K., Abraham, A. J. & Roman, P. M. Adoption and implementation of medications in addiction treatment programs. J. Addict. Med. 5 , 21–27 (2011).
Roberts, E., Hotopf, M. & Drummond, C. The relationship between alcohol-related hospital admission and specialist alcohol treatment provision across local authorities in England since passage of the Health and Social Care Act 2012. Br. J. Psychiatry 218 , 230–232 (2020).
Strang et al. Opioid use disorder. Nat. Rev. Dis. Primers 6 , 3 (2020).
Koob, G. F., Everitt, B. J. & Robbins, T. W. in Fundamental Neuroscience 4th edn (eds Squire, L. R. et al.) 871–898 (Elsevier, 2013).
WHO ASSIST Working Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction 97 , 1183–1194 (2002).
Ewing, J. A. Detecting alcoholism. The CAGE questionnaire. JAMA 252 , 1905–1907 (1984).
Knight, J. R., Sherritt, L., Shrier, L. A., Harris, S. K. & Chang, G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch. Pediatr. Adolesc. Med. 156 , 607–614 (2002).
Chan, A. W. K., Pristach, E. A., Welte, J. W. & Russell, M. Use of the TWEAK test in screening for alcoholism/heavy drinking in three populations. Alcohol. Clin. Exp. Res. 17 , 1188–1192 (1993).
Sheehan, D. V. et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59 (Suppl. 20), 22–23 (1998).
Sobell, L. C. & Sobell, M. B. in Handbook of Psychiatric Measures 1st edn (American Psychiatric Association) 477–479 (American Psychiatric Association, 2000).
Sullivan, J. T., Sykora, K., Schneiderman, J., Naranjo, C. A. & Sellers, E. M. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br. J. Addict. 84 , 1353–1357 (1989).
Forcehimes, A. A., Tonigan, J. S., Miller, W. R., Kenna, G. A. & Baer, J. S. Psychometrics of the Drinker Inventory of Consequences (DrInC). Addict. Behav. 32 , 1699–1704 (2007).
Kirouac, M. & Witkiewitz, K. Revisiting the drinker inventory of consequences: an extensive evaluation of psychometric properties in two alcohol clinical trials. Psychol. Addict. Behav. 32 , 52–63 (2018).
Stockwell, T., Murphy, D. & Hodgson, R. The severity of alcohol dependence questionnaire: its use, reliability and validity. Br. J. Addict. 78 , 145–155 (1983).
Read, J. P., Kahler, C. W., Strong, D. R. & Colder, C. R. Development and preliminary validation of the young adult alcohol consequences questionnaire. J. Stud. Alcohol 67 , 169–177 (2006).
Download references
Acknowledgements
J.M. is supported by the Peter Boris Chair in Addictions Research, a Tier 1 Canada Research Chair in Translational Addiction Research, and grants from the Canadian Institutes of Health Research, Health Canada, and the National Institutes of Health (NIH; R01AA024930, R01AA025911, R21 AA027679, R01AA025849). S.W.F.E. is supported by NIH grant K24AA026876. M.H. is supported by the Swedish Research Council (2013-07434, 2019-01138) and is a Clinical Scholar supported by the Knut and Alice Wallenberg Foundation. J.F.K. is supported by NIH grants K24AA022136 and R01AA025849 L.L. is a US federal employee at the National Institutes of Health, and is supported by the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism. C.D.P. is supported by the South African Medical Research Council. A.A.P. is supported by NIH grants P50DA037844, R01AA02628 and R01AA029688. L.R. is supported by NIH grant K24AA025704. The views expressed herein are those of the authors and do not reflect the official policy or position of the funding sources.
Author information
Authors and affiliations.
Peter Boris Centre for Addictions Research, McMaster University & St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
James MacKillop
Homewood Research Institute, Guelph, ON, Canada
Department of Biomedical Sciences, Section of Neuroscience and Clinical Pharmacology, University of Cagliari, Cagliari, Italy
Roberta Agabio
Neuroscience Institute, Section of Cagliari, National Research Council, Cagliari, Italy
Department of Psychology, University of Rhode Island, Kingston, RI, USA
Sarah W. Feldstein Ewing
Department of Psychology and Behavioural Sciences, Centre for Alcohol and Drug Research, Aarhus University, Aarhus, Denmark
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Recovery Research Institute and Department of Psychiatry, Massachusetts General Hospital & Harvard Medical School, Boston, MA, USA
John F. Kelly
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health, Bethesda, MD, USA
Lorenzo Leggio
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse, National Institutes of Health, Bethesda, MD, USA
Division of Psychiatry, Imperial College London, London, UK
Anne Lingford-Hughes
Central North West London NHS Foundation Trust, London, UK
Department of Psychiatry & Institute for Genomic Medicine, University of California San Diego, La Jolla, CA, USA
Abraham A. Palmer
Alcohol, Tobacco and Other Drug Research Unit, South African Medical Research Council, Cape Town, South Africa
Charles D. Parry
Department of Psychiatry, Stellenbosch University, Stellenbosch, South Africa
Departments of Psychology and Psychiatry, University of California, Los Angeles, Los Angeles, CA, USA
Institute for Mental Health Policy Research, Campbell Family Mental Health Research Institute, PAHO/WHO Collaborating Centre, Centre for Addiction and Mental Health, Toronto, Canada
Jürgen Rehm
Dalla Lana School of Public Health; Institute of Health Policy, Management and Evaluation; & Department of Psychiatry, University of Toronto (UofT), Toronto, Canada
WHO European Region Collaborating Centre at Public Health Institute of Catalonia, Barcelona, Spain
Technische Universität Dresden, Klinische Psychologie & Psychotherapie, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russian Federation
Zentrum für Interdisziplinäre Suchtforschung der Universität Hamburg (ZIS), Universitätsklinikum Hamburg-Eppendorf, Hamburg, Germany
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (J.M., A.A.P. and M.H.); Epidemiology (J.M., C.D.P. and J.R.); Mechanisms/pathophysiology (J.M., A.L.-H., A.A.P. and M.H.); Diagnosis, screening and prevention (J.M., A.L.-H., L.L., R.A., S.W.F.E., J.R. and M.H.); Management (J.M., A.L.-H., L.L., R.A., S.W.F.E., L.R., J.F.K. and M.H.); Quality of life (J.M., A.A.P. and M.H.); Outlook (J.M., A.A.P. and M.H.); Overview of Primer (J.M.).
Corresponding author
Correspondence to James MacKillop .
Ethics declarations
Competing interests.
J.M. is a principal and senior scientist in BEAM Diagnostics, Inc. and a consultant to Clairvoyant Therapeutics, Inc.; no associated products or services are discussed in the article. Outside his federal employment, L.L. receives an honorarium from the UK Medical Council on Alcoholism (Editor-in-Chief for Alcohol and Alcoholism ) and royalties from Routledge for a textbook. A.A.P. is on the Scientific Advisory Board of Vivid Genomics and is listed as an inventor on US patent US20160038559A1. M.H. is a member of the scientific advisory council of the Swedish Medical Products Agency, and Scientific Advisor to the Board of Health and Social Welfare; his views expressed here do not represent those of these agencies; M.H. has received consulting fees, research support or other compensation from Indivior, Camurus, Molteni, BrainsWay, Aelis Farma, Lundbeck and Janssen Pharmaceuticals. A.L.-H. has received honoraria paid into her Institutional funds for speaking and chairing engagements from Lundbeck, Lundbeck Institute UK, Janssen-Cilag, Pfizer and Servier; has received honoraria to deliver training and education for the British Association for Psychopharmacology; has received research grants or support from Lundbeck and GSK, and unrestricted funding from Alcarelle for a PhD; has been consulted by but received no monies from Dobrin; and is a member of a group producing UK Alcohol Clinical Guidelines, UK Government (Office for Health Improvement and Disparities, Department of Health and Social Care). R.A., S.W.F.E., J.F.K., C.D.P., L.R. and J.R. declare no competing interests.
Peer review
Peer review information.
Nature Reviews Disease Primers thanks D. M. Dick, L. Goodwin, E. Williams and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
MacKillop, J., Agabio, R., Feldstein Ewing, S.W. et al. Hazardous drinking and alcohol use disorders. Nat Rev Dis Primers 8 , 80 (2022). https://doi.org/10.1038/s41572-022-00406-1
Download citation
Accepted : 01 November 2022
Published : 22 December 2022
DOI : https://doi.org/10.1038/s41572-022-00406-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
A practice quit model to test early efficacy of medications for alcohol use disorder in a randomized clinical trial.
- Lara A. Ray
- Wave-Ananda Baskerville
- Karen Miotto
Psychopharmacology (2024)
Connect To Care (C2C): protocol for two-site randomized controlled pilot trial to improve outcomes for patients with hazardous drinking and PTSD and/or depression symptoms
- Michael A. Cucciare
- Kathy Marchant
- Christine Timko
Addiction Science & Clinical Practice (2023)
The brain structure, immunometabolic and genetic mechanisms underlying the association between lifestyle and depression
Nature Mental Health (2023)
Seeking Pleasure, Finding Trouble: Functions and Dysfunctions of Trait Sensation Seeking
- Henry W. Chase
- Merage Ghane
Current Addiction Reports (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.

Binge drinking is a growing public health crisis − a neurobiologist explains how research on alcohol use disorder has shifted
Assistant Professor of Biology, Biomedical Engineering and Pharmacology, Penn State
Disclosure statement
Nikki Crowley receives funding from The National Institutes of Health, The Brain and Behavior Research Foundation, and the Penn State Huck Institutes of the Life Sciences endowment funds.
Penn State provides funding as a founding partner of The Conversation US.
View all partners
With the new Amy Winehouse biopic “Back to Black ” in U.S. theaters as of May 17, 2024, the late singer’s relationship with alcohol and drugs is under scrutiny again. In July 2011, Winehouse was found dead in her flat in north London from “death by misadventure” at the age of 27. That’s the official British term used for accidental death caused by a voluntary risk.
Her blood alcohol concentration was 0.416%, more than five times the legal intoxication limit in the U.S. – leading her cause of death to be later adjusted to include “alcohol toxicity” following a second coroner’s inquest.
Nearly 13 years later, alcohol consumption and binge drinking remain a major public health crisis , not just in the U.K. but also in the U.S.
Roughly 1 in 5 U.S. adults report binge drinking at least once a week, with an average of seven drinks per binge episode . This is well over the amount of alcohol thought to produce legal intoxication, commonly defined as a blood alcohol concentration over 0.08% – on average, four drinks in two hours for women, five drinks in two hours for men.
Among women, days of “heavy drinking” increased 41% during the COVID-19 pandemic compared with pre-pandemic levels , and adult women in their 30s and 40s are rapidly increasing their rates of binge drinking , with no evidence of these trends slowing down. Despite efforts to comprehend the overall biology of substance use disorders, scientists’ and physicians’ understanding of the relationship between women’s health and binge drinking has lagged behind.
I am a neurobiologist focused on understanding the chemicals and brain regions that underlie addiction to alcohol . I study how neuropeptides – unique signaling molecules in the prefrontal cortex , one of the key brain regions in decision-making, risk-taking and reward – are altered by repeated exposure to binge alcohol consumption in animal models.
My lab focuses on understanding how things like alcohol alter these brain systems before diagnosable addiction, so that we can better inform efforts toward both prevention and treatment.
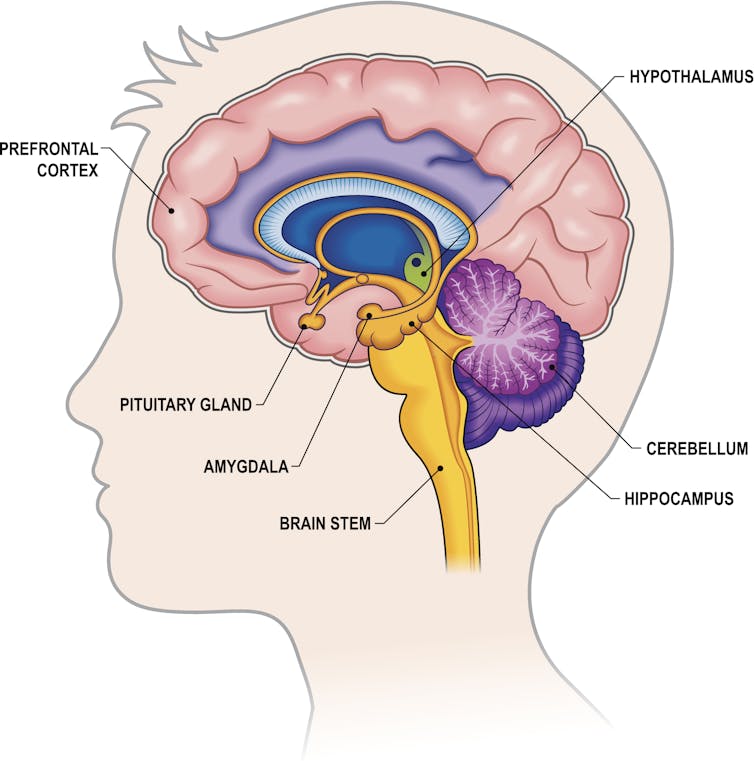
The biology of addiction
While problematic alcohol consumption has likely occurred as long as alcohol has existed, it wasn’t until 2011 that the American Society of Addiction Medicine recognized substance addiction as a brain disorder – the same year as Winehouse’s death. A diagnosis of an alcohol use disorder is now used over outdated terms such as labeling an individual as an alcoholic or having alcoholism.
Researchers and clinicians have made great strides in understanding how and why drugs – including alcohol, a drug – alter the brain. Often, people consume a drug like alcohol because of the rewarding and positive feelings it creates, such as enjoying drinks with friends or celebrating a milestone with a loved one. But what starts off as manageable consumption of alcohol can quickly devolve into cycles of excessive alcohol consumption followed by drug withdrawal.
While all forms of alcohol consumption come with health risks, binge drinking appears to be particularly dangerous due to how repeated cycling between a high state and a withdrawal state affect the brain. For example, for some people, alcohol use can lead to “ hangxiety ,” the feeling of anxiety that can accompany a hangover.
Repeated episodes of drinking and drunkenness, coupled with withdrawal, can spiral, leading to relapse and reuse of alcohol. In other words, alcohol use shifts from being rewarding to just trying to prevent feeling bad.
It makes sense. With repeated alcohol use over time, the areas of the brain engaged by alcohol can shift away from those traditionally associated with drug use and reward or pleasure to brain regions more typically engaged during stress and anxiety .
All of these stages of drinking, from the enjoyment of alcohol to withdrawal to the cycles of craving, continuously alter the brain and its communication pathways . Alcohol can affect several dozen neurotransmitters and receptors , making understanding its mechanism of action in the brain complicated.
Work in my lab focuses on understanding how alcohol consumption changes the way neurons within the prefrontal cortex communicate with each other. Neurons are the brain’s key communicator, sending both electrical and chemical signals within the brain and to the rest of your body.
What we’ve found in animal models of binge drinking is that certain subtypes of neurons lose the ability to talk to each other appropriately. In some cases, binge drinking can permanently remodel the brain. Even after a prolonged period of abstinence, conversations between the neurons don’t return to normal .
These changes in the brain can appear even before there are noticeable changes in behavior . This could mean that the neurobiological underpinnings of addiction may take root well before an individual or their loved ones suspect a problem with alcohol.
Researchers like us don’t yet fully understand why some people may be more susceptible to this shift, but it likely has to do with genetic and biological factors, as well as the patterns and circumstances under which alcohol is consumed.
Women are forgotten
While researchers are increasingly understanding the medley of biological factors that underlie addiction, there’s one population that’s been largely overlooked until now: women.
Women may be more likely than men to have some of the most catastrophic health effects caused by alcohol use, such as liver issues, cardiovascular disease and cancer . Middle-aged women are now at the highest risk for binge drinking compared with other populations.
When women consume even moderate levels of alcohol, their risk for various cancers goes up, including digestive, breast and pancreatic cancer , among other health problems – and even death. So the worsening rates of alcohol use disorder in women prompt the need for a greater focus on women in the research and the search for treatments.
Yet, women have long been underrepresented in biomedical research.
It wasn’t until 1993 that clinical research funded by the National Institutes of Health was required to include women as research subjects. In fact, the NIH did not even require sex as a biological variable to be considered by federally funded researchers until 2016. When women are excluded from biomedical research, it leaves doctors and researchers with an incomplete understanding of health and disease, including alcohol addiction.
There is also increasing evidence that addictive substances can interact with cycling sex hormones such as estrogen and progesterone . For instance, research has shown that when estrogen levels are high, like before ovulation, alcohol might feel more rewarding , which could drive higher levels of binge drinking. Currently, researchers don’t know the full extent of the interaction between these natural biological rhythms or other unique biological factors involved in women’s health and propensity for alcohol addiction.

Looking ahead
Researchers and lawmakers are recognizing the vital need for increased research on women’s health. Major federal investments into women’s health research are a vital step toward developing better prevention and treatment options for women.
While women like Amy Winehouse may have been forced to struggle both privately and publicly with substance use disorders and alcohol, the increasing focus of research on addiction to alcohol and other substances as a brain disorder will open new treatment avenues for those suffering from the consequences.
For more information on alcohol use disorder, causes, prevention and treatments, visit the National Institute on Alcohol Abuse and Alcoholism .
- Amy Winehouse
- Binge drinking
- Neurobiology
- Intoxication
- Alcohol consumption
- Alcohol use
- Alcohol use disorder
- COVID-19 pandemic

Senior Research Fellow - Women's Health Services

Senior Lecturer in Periodontics

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

Alcohol and Your Brain: The Latest Scientific Insights
Want to protect your brain here's what you need to know about alcohol consumption..
Posted March 18, 2024 | Reviewed by Devon Frye
- What Is Alcoholism?
- Find a therapist to overcome addiction
- Transient memory loss, “blackouts,” and hangovers related to alcohol consumption are brain health risks.
- Alcohol use disorder (alcoholism) is a risk factor for developing dementia.
- Heavy or excessive alcohol consumption is dangerous to the brain for a number of reasons.
- The impact of mild to moderate alcohol consumption (1-3 drinks a day) on brain function is less clear.
Depending on who you ask, you might be told to drink a few glasses of red wine a day or to avoid alcohol altogether. The reasons for such recommendations are many, but, by and large, they tend to stem from a study someone read about or saw reported in the news.
So why is it so hard to know whether alcohol is good or bad for us—especially for our brains? In this post, we’ll explore the current science and some practical ideas on how to approach the topic.
What Is Alcohol Anyway?
When people talk about drinking “alcohol,” they’re almost always referring to the consumption of ethanol. Ethanol is a natural product that is formed from the fermentation of grains, fruits, and other sources of sugar. It’s found in a wide range of alcoholic beverages including beer, wine, and spirits like vodka, whiskey, rum, and gin.
Evidence for human consumption of alcohol dates back over 10,000 years. Consumption of alcohol has and continues to serve major roles in religious and cultural ceremonies around the world. But unlike most food products, in the last century, alcohol has been wrapped up in nearly perpetual controversy over its moral effects and health implications.

How Does Alcohol Impact the Brain?
As anyone who’s consumed alcohol knows, ethanol can directly influence brain function. Ethanol is classified as a “depressant” because it has a generally slowing effect on brain activity through activation of γ-aminobutyric acid (GABA) pathways.
In an acute sense, consumption of alcohol can lead to uninhibited behavior, sedation, lapses in judgment, and impairments in motor function. At higher levels, the effects can progress to coma and even death.
The Known Brain-Damaging Effects of Excess Alcohol
There is no debate here: Excessively high levels of alcohol consumption over short periods of time are toxic and potentially deadly, specifically because of its effects on the brain.
One critical fact to understand about the overall and brain-specific effects of alcohol is that the entirety of the debate around the risk/benefit ratio concerns mild to moderate alcohol consumption. As it relates to the effects of high amounts of alcohol on the body and brain, the research is consistent: It’s a very bad choice.
High amounts of alcohol use are causal risk factors in the development of disease in the heart, liver, pancreas, and brain (including the brains of children in utero). In fact, 1 in 8 deaths in Americans aged 20-64 is attributable to alcohol use. When it comes to adults, excessive alcohol use can cause multiple well-defined brain issues ranging from short-term confusion to dementia .
What Is “Excessive” or “High” Alcohol Use?
Key to the nuance in the conversation about alcohol use are definitions. Across the board, “excessive” or “high” alcohol use is linked to worse overall and brain health outcomes. So what does that mean?
While definitions can be variable, one way to look at this is the consumption of 4 or more drinks on an occasion (for women) and 5 or more for men. Additionally, excess alcohol is defined as drinking more than 8 drinks a week (women) and 15 a week (men), or consuming alcohol if you are pregnant or younger than age 21.
Beyond this, by definition, consuming enough alcohol to cause a “brownout,” “blackout,” hangover, or other overt brain symptomatology is evidence that the alcohol you’ve consumed is creating problems in your brain. Alcohol use disorder (or alcoholism ) is also a clear issue for the brain. It has been linked to a higher risk for dementia, especially early-onset dementia in a study of 262,000 adults, as well as to smaller brain size .
Is There a “Safe” Amount of Alcohol for the Brain?
In a highly publicized article from Nature Communications , researchers looked at brain imaging data from nearly 37,000 middle-aged to older adults and cross-referenced their brain scans with their reported alcohol consumption. The findings were profound: People who drank more alcohol had smaller brains, even in people drinking only one or two alcoholic beverages a day.

Conversely, other recent data suggest a lower risk for dementia in people consuming a few alcoholic beverages a day. This includes a 2022 study showing that in around 27,000 people, consuming up to 40 grams of alcohol (around 2.5 drinks) a day was linked to a lower risk for dementia versus abstinence in adults over age 60. A much larger study of almost 4 million people in Korea noted that mild to moderate alcohol consumption was linked to a lower risk for dementia compared to non-drinking.
How Do We Make Sense of This Data?
When it comes to the bottom line as it relates to alcohol consumption and brain health, the data are rather solid on some fronts, and a bit less so on others. There’s also the potential for confounding variables, including the fact that many people like to drink alcohol to enjoy and enhance social bonds (which we know are beneficial for the brain). Here’s a summary of what the most recent research is telling us.
- Experiencing transient memory loss, “blackouts,” or hangovers related to alcohol consumption is overt evidence of threats to brain health.
- The impact of mild to moderate alcohol consumption (1-3 drinks a day) on brain function is less clear, but it seems unreasonable to start alcohol use for brain health.

Austin Perlmutter, M.D. , is a board-certified internal medicine physician and the co-author of Brain Wash .
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Alcohol Use and Your Health
- Underage Drinking
- Publications
- About Surveys on Alcohol Use
- About Standard Drink Sizes
- CDC Alcohol Program
- Alcohol Outlet Density Measurement Tools
- Resources to Prevent Excessive Alcohol Use
- Alcohol Applications and Online Tools
- Funding to Prevent Excessive Alcohol Use
- Alcohol-Related Disease Impact (ARDI) Application
- Check Your Drinking. Make a Plan to Drink Less.
- Controle su forma de beber. Haga un plan para beber menos.
- Deaths from Excessive Alcohol Use in the United States
- Addressing Excessive Alcohol Use: State Fact Sheets
- Excessive alcohol use can have immediate and long-term effects.
- Excessive drinking includes binge drinking, heavy drinking, and any drinking during pregnancy or by people younger than 21.
- Drinking less is better for your health than drinking more.
- You can lower your health risks by drinking less or choosing not to drink.

Why it's important
- The rest of the alcohol can harm your liver and other organs as it moves through the body.
- Using alcohol excessively on occasion or over time can have immediate and long-term health risks.
- By drinking less alcohol, you can improve your health and well-being.
Deaths from excessive alcohol use
Understanding alcohol use, excessive alcohol use.
Excessive alcohol use is a term used to describe four ways that people drink alcohol that can negatively impact health. Excessive drinking can also be deadly.
Excessive alcohol use includes:
- Binge drinking—Four or more drinks for women, or five or more drinks for men during an occasion.
- Heavy drinking—Eight or more drinks for women, or 15 or more drinks for men during a week.
- Underage drinking —any alcohol use by people younger than 21.
- Drinking while pregnant—any alcohol use during pregnancy .
Moderate alcohol use
Moderate drinking is having one drink or less in a day for women, or two drinks or less in a day for men.
Keep in mind
Effects of short-term alcohol use.
Drinking excessively on an occasion can lead to these harmful health effects:
- Injuries— motor vehicle crashes , falls, drownings, and burns.
- Violence—homicide, suicide, sexual violence, and intimate partner violence.
- Alcohol poisoning—high blood alcohol levels that affect body functions like breathing and heart rate.
- Overdose—from alcohol use with other drugs , like opioids.
- Sexually transmitted infections or unplanned pregnancy—alcohol use can lead to sex without protection, which can cause these conditions.
- Miscarriage, stillbirth, or fetal alcohol spectrum disorder (FASD) —from any alcohol use during pregnancy.
Effects of long-term alcohol use
Over time, drinking alcohol can have these effects:
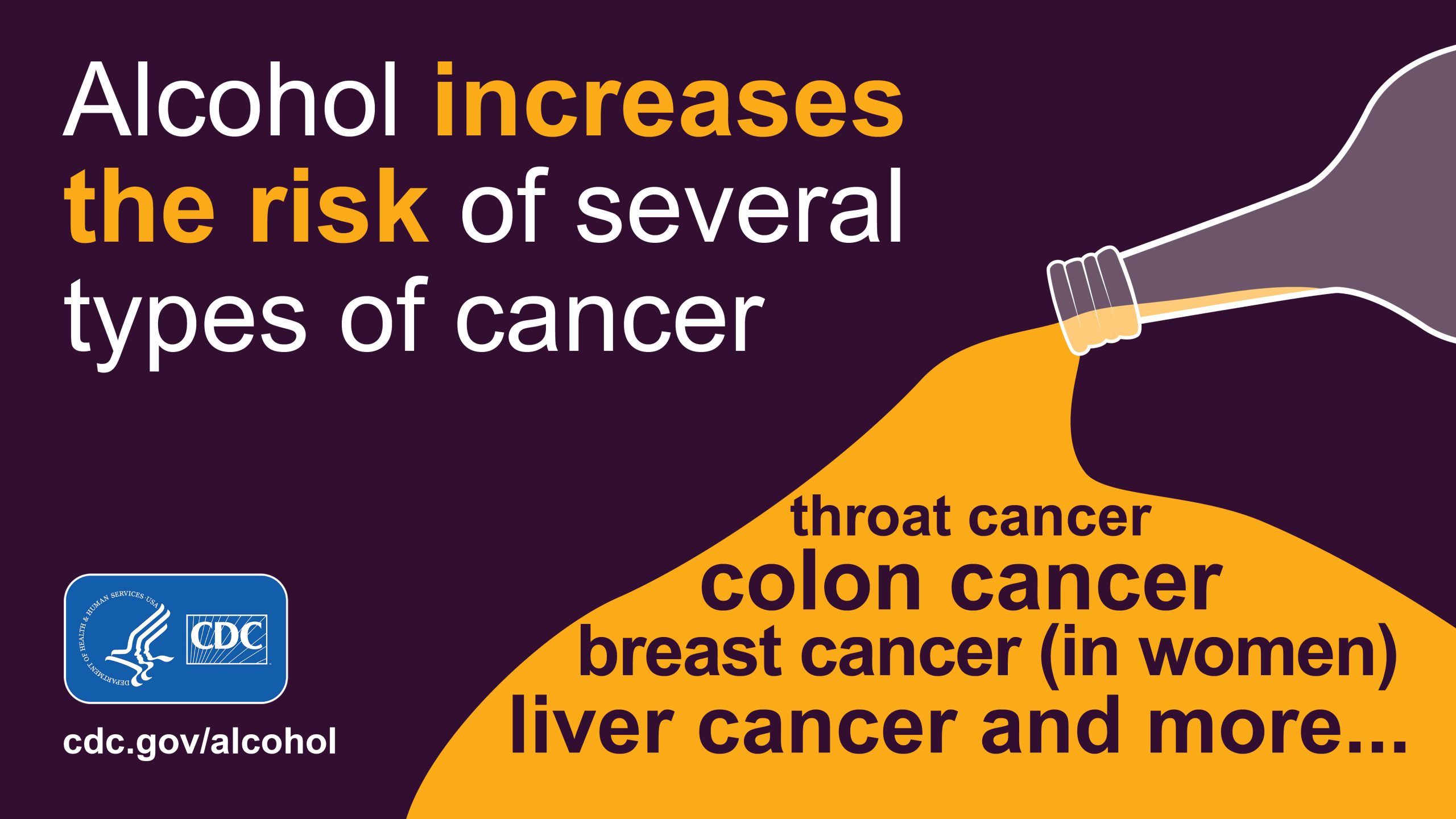
- The risk of some cancers increases with any amount of alcohol use. 2 This includes breast cancer (in women). 2 A
- More than 20,000 people die from alcohol-related cancers each year in the United States. 3
Other chronic diseases
Excessive alcohol use can lead to:
- High blood pressure.
- Heart disease.
- Liver disease.
- Alcohol use disorder—this affects both physical and mental health. B
- Digestive problems.
- Weaker immune system—increasing your chances of getting sick.
Social and wellness issues
- Mental health conditions, including depression and anxiety.
- Learning problems, and issues at school or work.
- Memory problems, including dementia.
- Relationship problems with family and friends.
You can take steps to lower your risk of alcohol-related harms.
The less alcohol you drink, the lower your risk for these health effects, including several types of cancer.
Check your drinking
- The risk of alcohol use leading to breast cancer in men has not been established.
- Most people who drink excessively do not have alcohol use disorder (also known as "alcohol dependence" or "alcoholism"). Many people who drink excessively can lower their alcohol use without specialized medical treatment. Facts about alcohol use disorder are available at: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder .
- Esser MB, Sherk A, Liu Y, Naimi TS. Deaths from excessive alcohol use — United States, 2016-2021. MMWR Morb Mortal Wkly Rep . 2024;73:154–161. doi: http://dx.doi.org/10.15585/mmwr.mm7308a1
- Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer . 2015;112(3):580-593. doi: 10.1038/bjc.2014.579
- Esser MB, Sherk A, Liu Y, Henley SJ, Naimi TS. Reducing alcohol use to prevent cancer deaths: estimated effects among U.S. adults. Am J Prev Med . 2024;66(4):725–729. doi: 10.1016/j.amepre.2023.12.003
Alcohol Use
Excessive alcohol use can harm people who drink and those around them. You and your community can take steps to improve everyone’s health and quality of life.
For Everyone
Public health.
- The Magazine
- Stay Curious
- The Sciences
- Environment
- Planet Earth
How Binge Drinking Shifted Research On Alcohol Use Disorders
"roughly 1 in 5 u.s. adults report binge drinking at least once a week.".

With the new Amy Winehouse biopic “Back to Black ” in U.S. theaters as of May 17, 2024, the late singer’s relationship with alcohol and drugs is under scrutiny again. In July 2011, Winehouse was found dead in her flat in north London from “death by misadventure” at the age of 27. That’s the official British term used for accidental death caused by a voluntary risk.
Her blood alcohol concentration was 0.416%, more than five times the legal intoxication limit in the U.S. – leading her cause of death to be later adjusted to include “alcohol toxicity” following a second coroner’s inquest.
Nearly 13 years later, alcohol consumption and binge drinking remain a major public health crisis , not just in the U.K. but also in the U.S.
Roughly 1 in 5 U.S. adults report binge drinking at least once a week, with an average of seven drinks per binge episode . This is well over the amount of alcohol thought to produce legal intoxication, commonly defined as a blood alcohol concentration over 0.08% – on average, four drinks in two hours for women, five drinks in two hours for men.
Among women, days of “heavy drinking” increased 41% during the COVID-19 pandemic compared with pre-pandemic levels , and adult women in their 30s and 40s are rapidly increasing their rates of binge drinking , with no evidence of these trends slowing down. Despite efforts to comprehend the overall biology of substance use disorders, scientists’ and physicians’ understanding of the relationship between women’s health and binge drinking has lagged behind.
I am a neurobiologist focused on understanding the chemicals and brain regions that underlie addiction to alcohol . I study how neuropeptides – unique signaling molecules in the prefrontal cortex , one of the key brain regions in decision-making, risk-taking and reward – are altered by repeated exposure to binge alcohol consumption in animal models.
My lab focuses on understanding how things like alcohol alter these brain systems before diagnosable addiction, so that we can better inform efforts toward both prevention and treatment.
The Biology Of Addiction
While problematic alcohol consumption has likely occurred as long as alcohol has existed, it wasn’t until 2011 that the American Society of Addiction Medicine recognized substance addiction as a brain disorder – the same year as Winehouse’s death. A diagnosis of an alcohol use disorder is now used over outdated terms such as labeling an individual as an alcoholic or having alcoholism.
Researchers and clinicians have made great strides in understanding how and why drugs – including alcohol, a drug – alter the brain. Often, people consume a drug like alcohol because of the rewarding and positive feelings it creates, such as enjoying drinks with friends or celebrating a milestone with a loved one. But what starts off as manageable consumption of alcohol can quickly devolve into cycles of excessive alcohol consumption followed by drug withdrawal.
While all forms of alcohol consumption come with health risks, binge drinking appears to be particularly dangerous due to how repeated cycling between a high state and a withdrawal state affect the brain. For example, for some people, alcohol use can lead to “ hangxiety ,” the feeling of anxiety that can accompany a hangover.
Repeated episodes of drinking and drunkenness, coupled with withdrawal, can spiral, leading to relapse and reuse of alcohol. In other words, alcohol use shifts from being rewarding to just trying to prevent feeling bad.
It makes sense. With repeated alcohol use over time, the areas of the brain engaged by alcohol can shift away from those traditionally associated with drug use and reward or pleasure to brain regions more typically engaged during stress and anxiety .
All of these stages of drinking, from the enjoyment of alcohol to withdrawal to the cycles of craving, continuously alter the brain and its communication pathways . Alcohol can affect several dozen neurotransmitters and receptors , making understanding its mechanism of action in the brain complicated.
Work in my lab focuses on understanding how alcohol consumption changes the way neurons within the prefrontal cortex communicate with each other. Neurons are the brain’s key communicator, sending both electrical and chemical signals within the brain and to the rest of your body.
What we’ve found in animal models of binge drinking is that certain subtypes of neurons lose the ability to talk to each other appropriately. In some cases, binge drinking can permanently remodel the brain. Even after a prolonged period of abstinence, conversations between the neurons don’t return to normal .
These changes in the brain can appear even before there are noticeable changes in behavior . This could mean that the neurobiological underpinnings of addiction may take root well before an individual or their loved ones suspect a problem with alcohol.
Researchers like us don’t yet fully understand why some people may be more susceptible to this shift, but it likely has to do with genetic and biological factors, as well as the patterns and circumstances under which alcohol is consumed.
Women are Forgotten
While researchers are increasingly understanding the medley of biological factors that underlie addiction, there’s one population that’s been largely overlooked until now: women.
Women may be more likely than men to have some of the most catastrophic health effects caused by alcohol use, such as liver issues, cardiovascular disease and cancer . Middle-aged women are now at the highest risk for binge drinking compared with other populations.
When women consume even moderate levels of alcohol, their risk for various cancers goes up, including digestive, breast and pancreatic cancer , among other health problems – and even death. So the worsening rates of alcohol use disorder in women prompt the need for a greater focus on women in the research and the search for treatments.
Yet, women have long been underrepresented in biomedical research.
It wasn’t until 1993 that clinical research funded by the National Institutes of Health was required to include women as research subjects. In fact, the NIH did not even require sex as a biological variable to be considered by federally funded researchers until 2016. When women are excluded from biomedical research, it leaves doctors and researchers with an incomplete understanding of health and disease, including alcohol addiction.
There is also increasing evidence that addictive substances can interact with cycling sex hormones such as estrogen and progesterone . For instance, research has shown that when estrogen levels are high, like before ovulation, alcohol might feel more rewarding , which could drive higher levels of binge drinking. Currently, researchers don’t know the full extent of the interaction between these natural biological rhythms or other unique biological factors involved in women’s health and propensity for alcohol addiction.
Looking Ahead
Researchers and lawmakers are recognizing the vital need for increased research on women’s health. Major federal investments into women’s health research are a vital step toward developing better prevention and treatment options for women.
While women like Amy Winehouse may have been forced to struggle both privately and publicly with substance use disorders and alcohol, the increasing focus of research on addiction to alcohol and other substances as a brain disorder will open new treatment avenues for those suffering from the consequences.
For more information on alcohol use disorder, causes, prevention and treatments, visit the National Institute on Alcohol Abuse and Alcoholism .
Nikki Crowley is an Assistant Professor of Biology, Biomedical Engineering and Pharmacology at Penn State. This article is republished from The Conversation under a Creative Commons license . Read the original article .
- drugs & addiction
Already a subscriber?
Register or Log In

Keep reading for as low as $1.99!
Sign up for our weekly science updates.
Save up to 40% off the cover price when you subscribe to Discover magazine.
Common Comorbidities with Substance Use Disorders Research Report Part 1: The Connection Between Substance Use Disorders and Mental Illness
Many individuals who develop substance use disorders (SUD) are also diagnosed with mental disorders, and vice versa. 2,3 Although there are fewer studies on comorbidity among youth, research suggests that adolescents with substance use disorders also have high rates of co-occurring mental illness; over 60 percent of adolescents in community-based substance use disorder treatment programs also meet diagnostic criteria for another mental illness. 4
Data show high rates of comorbid substance use disorders and anxiety disorders—which include generalized anxiety disorder, panic disorder, and post-traumatic stress disorder. 5–9 Substance use disorders also co-occur at high prevalence with mental disorders, such as depression and bipolar disorder, 6,9–11 attention-deficit hyperactivity disorder (ADHD), 12,13 psychotic illness, 14,15 borderline personality disorder, 16 and antisocial personality disorder. 10,15 Patients with schizophrenia have higher rates of alcohol, tobacco, and drug use disorders than the general population. 17 As Figure 1 shows, the overlap is especially pronounced with serious mental illness (SMI). Serious mental illness among people ages 18 and older is defined at the federal level as having, at any time during the past year, a diagnosable mental, behavior, or emotional disorder that causes serious functional impairment that substantially interferes with or limits one or more major life activities. Serious mental illnesses include major depression, schizophrenia, and bipolar disorder, and other mental disorders that cause serious impairment. 18 Around 1 in 4 individuals with SMI also have an SUD.
Data from a large nationally representative sample suggested that people with mental, personality, and substance use disorders were at increased risk for nonmedical use of prescription opioids. 19 Research indicates that 43 percent of people in SUD treatment for nonmedical use of prescription painkillers have a diagnosis or symptoms of mental health disorders, particularly depression and anxiety. 20
Youth—A Vulnerable Time
Although drug use and addiction can happen at any time during a person’s life, drug use typically starts in adolescence, a period when the first signs of mental illness commonly appear. Comorbid disorders can also be seen among youth. 21–23 During the transition to young adulthood (age 18 to 25 years), people with comorbid disorders need coordinated support to help them navigate potentially stressful changes in education, work, and relationships. 21
Drug Use and Mental Health Disorders in Childhood or Adolescence Increases Later Risk
The brain continues to develop through adolescence. Circuits that control executive functions such as decision making and impulse control are among the last to mature, which enhances vulnerability to drug use and the development of a substance use disorder. 3,24 Early drug use is a strong risk factor for later development of substance use disorders, 24 and it may also be a risk factor for the later occurrence of other mental illnesses. 25,26 However, this link is not necessarily causative and may reflect shared risk factors including genetic vulnerability, psychosocial experiences, and/or general environmental influences. For example, frequent marijuana use during adolescence can increase the risk of psychosis in adulthood, specifically in individuals who carry a particular gene variant. 26,27
It is also true that having a mental disorder in childhood or adolescence can increase the risk of later drug use and the development of a substance use disorder. Some research has found that mental illness may precede a substance use disorder, suggesting that better diagnosis of youth mental illness may help reduce comorbidity. One study found that adolescent-onset bipolar disorder confers a greater risk of subsequent substance use disorder compared to adult-onset bipolar disorder. 28 Similarly, other research suggests that youth develop internalizing disorders, including depression and anxiety, prior to developing substance use disorders. 29
Untreated Childhood ADHD Can Increase Later Risk of Drug Problems
Numerous studies have documented an increased risk for substance use disorders in youth with untreated ADHD, 13,30 although some studies suggest that only those with comorbid conduct disorders have greater odds of later developing a substance use disorder. 30,31 Given this linkage, it is important to determine whether effective treatment of ADHD could prevent subsequent drug use and addiction. Treatment of childhood ADHD with stimulant medications such as methylphenidate or amphetamine reduces the impulsive behavior, fidgeting, and inability to concentrate that characterize ADHD. 32
That risk presents a challenge when treating children with ADHD, since effective treatment often involves prescribing stimulant medications with addictive potential. Although the research is not yet conclusive, many studies suggest that ADHD medications do not increase the risk of substance use disorder among children with this condition. 31,32 It is important to combine stimulant medication for ADHD with appropriate family and child education and behavioral interventions, including counseling on the chronic nature of ADHD and risk for substance use disorder. 13,32

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Genetics of alcohol use disorder.
How do genes influence alcohol use disorder?
Alcohol use disorder (AUD) often seems to run in families, and we may hear about scientific studies of an “alcoholism gene.” Genetics certainly influence our likelihood of developing AUD, but the story isn’t so simple.
Research shows that genes are responsible for about half of the risk for AUD. Therefore, genes alone do not determine whether someone will develop AUD. Environmental factors, as well as gene and environment interactions account for the remainder of the risk.
Multiple genes play a role in a person’s risk for developing AUD. There are genes that increase a person’s risk, as well as those that may decrease that risk, directly or indirectly. For instance, some people of Asian descent carry a gene variant that alters their rate of alcohol metabolism, causing them to have symptoms like flushing, nausea, and rapid heartbeat when they drink. Many people who experience these effects avoid alcohol, which helps protect them from developing AUD.**
As we have learned more about the role genes play in our health, researchers have discovered that different factors can alter the expression of our genes. This field is called epigenetics. Scientists are learning more and more about how epigenetics can affect our risk for developing AUD.
Can our genes affect alcohol treatment?
Scientists are also exploring how genes may influence the effectiveness of treatments for AUD. For instance, the drug naltrexone has been shown to help some, but not all, patients with AUD to reduce their drinking. Research has shown that patients with AUD who also have variations in a specific gene respond positively to treatment with the drug, while those without the specific gene do not. A fuller understanding of how genes influence treatment outcomes will help doctors prescribe the treatment that is most likely to help each patient.***
What is NIAAA doing to learn more?
NIAAA has funded the Collaborative Studies on Genetics of Alcoholism (COGA) since 1989, with the goal of identifying the specific genes that influence alcohol use disorder. In addition, NIAAA funds investigators’ research in this important field, and also has an in-house research emphasis on the interaction of genes and the environment. NIAAA is committed to learning more about how genes affect AUD so that treatment—and prevention efforts—can continue to be developed and improved.
* Spectrum 1: 1 .
** AR&H Volume 31, Number 4, 2008
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Are the Long-Term Effects of Alcohol on the Body?
- Effects on Body
- Long-Term Risks
- Psychological Effects
- Consequences
- Addiction and Withdrawal
From a glass of wine with dinner to a night out with friends or a celebratory toast, alcohol consumption is deeply ingrained in many social practices and cultural traditions worldwide. In the United States, over 84% of adults report drinking alcohol at least once in their lifetime.
While casual to moderate drinking may be a part of life for some, excessive or chronic alcohol consumption can significantly impact your body and long-term health.
This article discusses the long-term effects of alcohol, including the risks to your physical health and mental well-being.
Morsa Images / Getty Images
How Alcohol Affects the Body
Alcohol is a central nervous system depressant that has immediate effects on the body, like intoxication (feeling drunk) and hangovers (unpleasant aftereffects from drinking). While these effects are short-lived, long-term alcohol use can trigger systemic (bodywide) inflammation , which damages the body's tissues and vital organs over time.
Cardiovascular System
Alcohol use impacts the cardiovascular system in several ways. In the short term, drinking alcohol increases your heart rate, and even moderate alcohol consumption can increase your blood pressure.
Chronic alcohol use and binge drinking damage the heart muscle, making it harder for the heart to pump blood effectively. Alcohol can also contribute to arrhythmias (irregular heartbeats) and hypertension (high blood pressure), increasing the risk of heart attack, stroke, and heart failure.
The liver metabolizes most of the alcohol you consume, breaking it down into acetaldehyde . Acetaldehyde is a toxin that can damage the body's organs and tissues before it is further broken down into acetate. This damage is most evident in the liver. Years of moderate to heavy drinking can cause liver scarring (fibrosis), increasing the risk of liver diseases like cirrhosis, alcoholic hepatitis, fatty liver disease, and liver cancer.
Gastrointestinal (GI) System
Alcohol consumption irritates the lining of the stomach and intestines. A night of drinking can cause uncomfortable symptoms like diarrhea, nausea, and vomiting. Chronic and excessive alcohol use disrupts the balance of bacteria in the gut microbiome (dysbiosis). Over time, this imbalance triggers chronic gastrointestinal inflammation, leading to a higher risk of gastrointestinal diseases.
Excess alcohol use can also impair nutrient absorption in the small intestine and increase the risk of malnutrition.
The brain is highly vulnerable to the damaging effects of alcohol, which disrupts communication between brain cells. Excessive or chronic alcohol use can lead to a steady decline in cognitive function, causing memory problems, difficulty learning new information, mood changes, and behavior changes.
Long-term alcohol use is associated with a higher risk of progressive cognitive decline and age-related neurological conditions like dementia.
Reproductive System
Alcohol use can cause sexual dysfunction, such as difficulty achieving or maintaining an erection and decreased sexual sensations. The impact alcohol has on the reproductive system extends beyond these temporary effects. Chronic alcohol use causes hormone imbalances in both men and women and leads to problems with fertility.
In people assigned male at birth, alcohol consumption can decrease testosterone production and sperm quality. In people assigned female at birth, alcohol use can interfere with regular ovulation and menstrual cycles and make it difficult to get pregnant.
Long-Term Health Risks
Alcohol is one of the leading causes of death in the United States, contributing to approximately 178,000 deaths annually. Over time, alcohol use takes a toll on your body and increases your risk of over 200 health conditions.
While the risk of health problems is higher in people who drink excessively, there is no safe level of alcohol consumption, and even light to moderate drinking comes with health risks. Long-term health risks associated with alcohol include:
- Heart disease : Alcohol consumption raises blood pressure and narrows the heart's arteries, decreasing blood flow and increasing the risk of heart disease, heart attack, and stroke.
- Liver disease : Alcohol use damages the liver over time, increasing the risk of liver diseases like fatty liver disease, alcohol-associated hepatitis, cirrhosis, and liver failure.
- Gastrointestinal disease : Alcohol damages the lining of the GI tract, causing inflammation that can impair gut function, cause GI bleeding, and increase the risk of GI diseases, such as gastroesophageal reflux disease (GERD).
- Cancer : Alcohol is a carcinogen that damages cellular DNA, impairs the absorption of essential nutrients, and triggers systemic inflammation. Research shows that alcohol consumption is associated with an increased risk of head and neck cancers, esophageal cancer, liver cancer, breast cancer, and colorectal cancer.
- Weakened immune system : Alcohol use can impair the body's immune response and alter signaling between immune cells. This, in turn, can increase the risk of infection, slow wound healing time, and trigger systemic inflammation (inflammation throughout the body) that contributes to organ damage and disease.
Moderate and Excessive Drinking Defined
The National Institute on Alcohol Abuse and Alcoholism defines moderate drinking as two or fewer drinks in a day for men and one or less in a day for women. Excessive (binge) drinking is defined as four or more drinks on a single occasion for women and five or more drinks on a single occasion for men.
Mental Health and Psychological Effects
While alcohol is seen as a way to relax or cope with stress, it can have severe effects on your mental health and well-being in the long run, including:
- Alcohol and mental health disorders : Some people use alcohol to self-medicate mood disorders like anxiety or depression, but this can lead to an unhealthy dependence on alcohol and worsening symptoms. Alcohol disrupts the brain's chemistry, leading to mood swings, irritability, and difficulty regulating emotions. Alcohol use also increases the risk of developing mood disorders, including anxiety, depression, and bipolar disorder.
- Alcohol use disorder (AUD) : Regular and excessive alcohol use can lead to AUD, a condition characterized by an inability to control alcohol consumption despite adverse consequences. People with AUD experience intense cravings and difficulty stopping drinking and may prioritize alcohol use over responsibilities and relationships.
- Cognitive function decline : Chronic alcohol consumption disrupts communication pathways in the brain and damages brain cells. Over time, this can lead to a decrease in cognitive function and increase the risk of alcohol-related dementia , which causes problems with memory, learning, focus, and concentration.
- Decision-making : Alcohol impairs judgment and decision-making abilities, increasing the likelihood of engaging in risky behaviors and making poor choices. Chronic alcohol use or misuse diminishes your ability to weigh the consequences of your actions and exercise self-control, leading to a cycle of destructive behaviors and adverse outcomes.
Social and Interpersonal Consequences
From strained family dynamics to work-related and financial troubles, the social and interpersonal consequences of alcohol use can be profound and far-reaching, such as:
- Relationships : Alcohol misuse often leads to strained relationships with family members, friends, and romantic partners. Alcohol-related conflicts, unpredictable behavior, and mood swings can erode trust and communication within relationships, leading to feelings of resentment, sadness, and fear. Children of parents who struggle with alcohol misuse are particularly vulnerable, experiencing emotional distress and psychological and behavioral problems.
- Work performance and productivity : Alcohol misuse can have a significant impact on your work performance. You may experience fatigue, trouble focusing, or difficulty completing your work tasks effectively. Chronic absenteeism due to alcohol-related issues can also jeopardize job security and career advancement.
- Finances : Financial troubles are common in people with AUD. Making impulsive purchases, spending excessive amounts on alcohol, having additional healthcare expenses, or losing wages due to decreased work productivity can contribute to significant financial burdens.
- Legal troubles : Driving under the influence (DUI), public intoxication, and other drinking-related behaviors can have lasting legal repercussions that affect employment opportunities, housing options, and personal freedoms.
Alcohol Addiction and Withdrawal
Alcohol addiction, or alcohol use disorder , is a complex and chronic brain disorder characterized by compulsive alcohol use, loss of control over drinking, and an intense craving for alcohol despite negative consequences.
AUD develops gradually. Over time, your brain's structure and function change, leading to tolerance, meaning you may require higher amounts of alcohol to achieve the desired effects. These brain changes contribute to the compulsive nature of addiction, making it difficult to abstain from alcohol.
If you have AUD and stop drinking, you may experience withdrawal symptoms that can affect your physical and mental health, including:
- Hand tremors (shakes)
- Irritability
- Loss of appetite
- Mood swings
- Nausea and vomiting
- Pale, clammy skin
- Rapid heart rate
- Trouble sleeping
At this point, you may have alcohol cravings or drink to avoid the low feelings withdrawal causes rather than for the pleasurable feelings alcohol consumption may offer.
A Word From Verywell
Life is a matter of moderation. It's not human to be perfect. The same concept applies to alcohol intake. It's been proven that alcohol isn't healthy to consume. If you can appreciate this fact and limit yourself, then you generally will keep your risk of alcohol-associated diseases low. If you feel you can't limit yourself despite this information, then you need to rethink your relationship with alcohol.
How Alcohol Use Disorder Is Treated
Treatment for AUD addresses the physical, psychological, and social impacts of alcohol addiction to help people with AUD achieve and maintain sobriety. If you are concerned about your alcohol use—or that of someone you care for—talk to a healthcare provider. They can assess your drinking pattern and help develop a treatment plan that may include:
- Behavioral treatments : Individual and group counseling sessions help develop the skills and strategies needed to manage cravings, cope with triggers, and prevent relapse. Common forms of behavioral counseling for alcohol addiction include cognitive behavioral therapy (CBT) and motivational enhancement therapy (MET).
- Medications : Several prescription medications can effectively help reduce cravings, manage withdrawal symptoms, and prevent relapse. These medications interfere with how the body processes alcohol or regulates brain chemicals involved in reward and motivation.
- Support groups : Groups like Alcoholics Anonymous (AA) and other 12-step programs provide a sense of community and connection for people cutting back or quitting alcohol and those who are in recovery. Sharing experiences, offering encouragement, and holding each other accountable can be a powerful way to maintain sobriety.
- Inpatient and outpatient treatment programs : Treatment programs can help people quit drinking and maintain sobriety. Inpatient programs offer intensive therapy and support in a residential setting, while outpatient programs allow people to continue living at home while receiving treatment.
Alcohol use, especially excessive alcohol consumption, can harm your physical and mental health. From damaging vital organs to impairing brain function and jeopardizing relationships, the negative consequences of excessive alcohol use are far-reaching. Chronic alcohol use raises your risk for health problems, including heart disease, liver disease, cancer, and mental health disorders.
If you choose to drink, do so in moderation: one drink per day or less for women and people assigned female at birth and two drinks or less daily for men and people assigned male at birth.
Talk to a healthcare provider if you are concerned about your drinking or that of a loved one. Professional treatments and support can help you overcome alcohol misuse and alcohol use disorder and improve your overall health and well-being.
Social Issues Research Center. Social and cultural aspects of drinking .
National Institute on Alcohol Abuse and Alcoholism. Alcohol use in the United States: Age groups and demographic characteristics . 2023.
MedlinePlus. Alcohol . January 3, 2024.
Tasnim S, Tang C, Musini VM, Wright JM. Effect of alcohol on blood pressure . Cochrane Database Syst Rev . 2020;7(7):CD012787. doi:10.1002/14651858.CD012787.pub2
American Heart Association. Is drinking alcohol part of a healthy lifestyle? December 30, 2019.
National Institute on Alcohol Abuse and Alcoholism. Alcohol metabolism . May 2022.
Osna NA, Donohue TM Jr, Kharbanda KK. Alcoholic liver disease: pathogenesis and current management . Alcohol Res . 2017;38(2):147-161.
Haber PS, Kortt NC. Alcohol use disorder and the gut . Addiction . 2021;116(3):658-667. doi:10.1111/add.15147
Barve S, Chen SY, Kirpich I, Watson WH, Mcclain C. Development, prevention, and treatment of alcohol-induced organ injury: the role of nutrition . Alcohol Res . 2017;38(2):289-302.
National Institute on Alcohol Abuse and Alcoholism. Alcohol and the brain: An overview .
Wiegmann C, Mick I, Brandl EJ, Heinz A, Gutwinski S. Alcohol and Dementia - What is the Link? A Systematic Review . Neuropsychiatr Dis Treat . 2020;16:87-99. doi:10.2147/NDT.S198772
Centers for Disease Control and Prevention. Excessive alcohol use is a risk to men’s health . February 29, 2024.
Salari N, Hasheminezhad R, Almasi A, et al. The risk of sexual dysfunction associated with alcohol consumption in women: a systematic review and meta-analysis . BMC Womens Health . 2023;23(1):213. doi:10.1186/s12905-023-02400-5
MedlinePlus. Reproductive hazards . March 22, 2024.
National Institute on Alcohol Abuse and Alcoholism. Medical complications: common alcohol-related concerns . March 13, 2024.
Centers for Disease Control and Prevention. What is excessive drinking? February 29, 2024.
National Cancer Institute. Alcohol and cancer risk . July 14, 2021.
National Institute on Alcohol Abuse and Alcoholism. Drinking levels defined . 2023.
National Institute on Alcohol Abuse and Alcoholism. Mental health issues: alcohol use disorder and common co-occuring conditions . January 12, 2024.
National Institute on Alcohol Abuse and Alcoholism. Understanding alcohol use disorder . January 2024.
Ridley NJ, Draper B, Withall A. Alcohol-related dementia: an update of the evidence . Alzheimers Res Ther . 2013;5(1):3. doi:10.1186/alzrt157
The JED Foundation. Understanding the mental health and drinking connection .
McCrady BS, Flanagan JC. The role of the family in alcohol use disorder recovery for adults . Alcohol Res . 2021;41(1):06. doi:10.35946/arcr.v41.1.06
Thørrisen MM, Bonsaksen T, Hashemi N, Kjeken I, van Mechelen W, Aas RW. Association between alcohol consumption and impaired work performance (presenteeism): a systematic review . BMJ Open . 2019;9(7):e029184. doi:10.1136/bmjopen-2019-029184
Collins SE. Associations Between Socioeconomic Factors and Alcohol Outcomes . Alcohol Res . 2016;38(1):83-94.
National Crime Prevention Council. Alcohol and drugs: Legal consequences .
National Institute on Alcohol Abuse and Alcoholism. The cycle of alcohol addiction .
MedlinePlus. Alcohol withdrawal . February 28, 2023.
National Institute on Alcohol Abuse and Alcoholism. Treatment for alcohol problems: finding and getting help . September 2023.
By Lindsay Curtis Curtis is a writer with over 20 years of experience focused on mental health, sexual health, cancer care, and spinal health.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Alcohol Res
- v.40(1); 2019

Alcohol Use Disorder and Depressive Disorders
Alcohol use disorder (AUD) and depressive disorders are among the most prevalent psychiatric disorders and co-occur more often than expected by chance. The aim of this review is to characterize the prevalence, course, and treatment of co-occurring AUD and depressive disorders. Studies have indicated that the co-occurrence of AUD and depressive disorders is associated with greater severity and worse prognosis for both disorders. Both pharmacologic and behavioral treatments have demonstrated efficacy for this population. However, treatment response is somewhat modest, particularly for drinking outcomes, highlighting the importance of further research on the etiology and treatment of co-occurring AUD and depressive disorders. Key future directions include studies to understand the heterogeneity of both AUD and depressive disorders, research on novel treatment approaches to enhance outcomes, and better understanding of sex and gender differences.
Introduction
Psychiatric disorders, such as anxiety and mood disorders, commonly co-occur with alcohol use disorder (AUD). Depressive disorders are the most common psychiatric disorders among people with AUD. 1 The co-occurrence of these disorders is associated with greater severity and worse prognosis than either disorder alone, 2 , 3 including a heightened risk for suicidal behavior. 4 This review provides an overview of the literature on the co-occurrence of AUD and depressive disorders and includes data on prevalence, course, and treatment outcomes. High-priority future research directions are suggested to better understand the co-occurrence of these conditions and to improve treatments.
Much of the published literature on the co-occurrence of AUD and depressive disorders uses the classifications from the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). 5 Where possible, this review specifies if the cited literature used the DSM-IV classifications for diagnosis (alcohol abuse or alcohol dependence) or the fifth edition (DSM-5) classification for diagnosis (AUD). 6 If a study reported results based on the combined DSM-IV diagnoses (i.e., included participants with alcohol abuse and participants with alcohol dependence), this review refers to the diagnosis as “DSM-IV AUD.” Although DSM-IV and DSM-5 AUD share many symptoms, the diagnoses are defined differently. In the DSM-5, AUD requires at least two symptoms, whereas DSM-IV alcohol abuse required only one symptom. Also, from DSM-IV to DSM-5, modifications were made to the symptoms that were included as diagnostic criteria. For example, the criterion of legal problems related to alcohol was removed, and the criterion of alcohol craving was added. Thus, where possible, this review identifies which version of the DSM was used in a study.
Overview of Depressive Disorders
Depressive disorders are complex and heterogeneous syndromes. These disorders are characterized by disrupted mood (e.g., low, numb, or irritable), along with an array of cognitive (e.g., feelings of worthlessness and difficulty concentrating) and physical (e.g., fatigue and lack of energy) symptoms. The DSM-5 includes seven distinct disorders under the category of depressive disorders, including major depressive disorder, persistent depressive disorder (dysthymia), premenstrual dysphoric disorder, substance/medication-induced depressive disorder, disruptive mood dysregulation disorder, other specified depressive disorder, and unspecified depressive disorder. 6 This review focuses on major depressive disorder, dysthymia, and substance-induced depressive disorder, which are the depressive disorders that have been studied most often in both the general population and among people with AUD.
Major depressive disorder is characterized by the presence of five or more symptoms that are present for at least 2 weeks. One of these symptoms must include depressed mood or anhedonia (significant loss of interest or pleasure in activities). Other symptoms are disturbances in appetite, sleep, psychomotor behaviors, energy, concentration, and decision-making; beliefs about worthlessness or guilt; and thoughts of suicide or suicide attempt. Dysthymia is more chronic than major depressive disorder, yet it is typically a milder disorder, characterized by at least 2 years of depressed mood and at least two additional symptoms, including dysfunction in appetite, sleep, energy, self-esteem, concentration, or decision-making, and feelings of hopelessness. Alcohol-induced depressive disorder refers to a depressive-like syndrome (characterized by depressed mood or anhedonia) that occurs only during and shortly after alcohol intoxication or withdrawal, remits after 3 to 4 weeks of alcohol abstinence, and is associated with significant distress and impairment.
Prevalence of depressive disorders and AUD
Major depressive disorder is the most common psychiatric disorder, affecting an estimated 10% to 15% of people in their lifetime, according to U.S. and international population-based surveys. 7 , 8 Dysthymia is less common than major depressive disorder, affecting less than 2% of people in their lifetime. 9
Likewise, major depressive disorder is the most common co-occurring psychiatric disorder among people with DSM-IV AUD. 1 Considering the prevalence of major depressive disorder and AUD in the general population, co-occurrence of these disorders is more frequent than can be expected based on chance, with odds ratios indicating a small effect size. Specifically, people with DSM-IV AUD, relative to those with no AUD, are 2.3 times more likely to also have major depressive disorder in the previous year, and they are 1.7 times more likely to have dysthymia in the previous year. 1 The prevalence of depressive disorders is greater among those with alcohol dependence, as compared to those diagnosed with alcohol abuse, with high prevalence of depression reported among treatment-seekers. People with DSM-IV alcohol dependence are 3.7 times more likely to also have major depressive disorder, and 2.8 times more likely to have dysthymia, in the previous year. Among people in treatment for DSM-IV AUD, almost 33% met criteria for major depressive disorder in the past year, and 11% met criteria for dysthymia. However, major depressive disorder is the most common co-occurring disorder among people who have AUD, partly because it is among the most common disorders in the general population.
Data from large population-based surveys suggest that the prevalence of alcohol-induced depression is small. For example, among people who also had a substance use disorder, less than 1% of their depressive disorders were classified as substance induced. 1 Studies have found a much higher prevalence of substance-induced depressive disorder among patients with AUD who were in treatment settings, when compared with studies of general population samples. One study reported that more than 25% of patients experienced a substance-induced depressive episode in their lifetime. 10 Nonetheless, studies have found that many cases initially diagnosed as substance-induced depression were later reclassified as independent depression (i.e., not substance induced) because the condition persisted after a period of abstinence. 11
Disproportionately affected populations
Several groups are disproportionately affected by co-occurring AUD and depressive disorders. For example, women are 1.5 to 2 times more likely in their lifetime to experience major depressive disorder than men. 12 Likewise, women with DSM-IV AUD are more likely than men with DSM-IV AUD to meet the criteria for major depressive disorder or dysthymia. 13 , 14 Sex differences are not limited to prevalence; they also are observed in the course of depressive disorders. A longitudinal study of young adults found that depression predicted alcohol problems in women but not in men. 15 This finding is consistent with reports from retrospective studies that examined relative age of onset for AUD and depressive disorders, in which women were more likely to experience depression before AUD, whereas men were more likely to develop AUD before depression. 16 , 17
Although race and ethnicity are clearly factors in the risk for developing AUD or depressive disorders, studies examining racial and ethnic differences in the prevalence of co-occurring AUD and depressive disorders have been hampered by small sample sizes, which make group comparisons difficult. 18 Nonetheless, data strongly support significant disparities in health care for co-occurring AUD and depressive disorders among racial and ethnic minority groups. The likelihood of receiving AUD care is similar across racial and ethnic groups, but people who identify as Black or Latino are significantly less likely than people who identify as White to receive services for mood and anxiety disorders or to receive integrated mental health and substance use disorder care. 19 , 20
Pathways to Co-Occurrence
Several potential developmental pathways have been proposed to explain the high rate of co-occurring AUD and depressive disorders, including: (1) depressive disorders increase risk for AUD, (2) AUD increases risk for depressive disorders, and (3) both conditions share pathophysiology or have common risk factors. Although evidence supports all three of these pathways, much research is still needed to understand the development of co-occurrence.
Much of the research on the development of co-occurring AUD and depressive disorders has relied on retrospective and longitudinal studies that examine the age of onset of the disorders. These studies have yielded mixed evidence. Some studies indicate that depressive disorders typically precede the onset of AUD, 21 others suggest that AUD generally precedes depressive disorders, 22 and still others report that the order of onset varies by gender (with women more likely to have earlier onset of depression than men). 17
Literature on the onset of substance use among youth and young adults has indicated that internalizing symptoms (e.g., depression and anxiety) generally protect against the onset of alcohol misuse in adolescents. 23 However, the association between internalizing symptoms and risk for alcohol use and misuse is influenced by key moderating factors, such as the presence of both internalizing and externalizing symptoms (e.g., impulsivity and aggression), 23 motives for substance use, 24 and gender. 25 For example, research has indicated that internalizing symptoms are a risk factor for the development of AUD in women but not in men. 25
AUD has been associated with risk for the onset of depressive symptoms and disorders. In one review, regular or heavy drinking in adolescents was shown to be associated with the risk for developing depressive symptoms and disorders. 26 In studies of adults, DSM-IV AUD was associated with risk for the onset of major depressive disorder and with dysthymia. 22 , 27
Research on the possibility of a common pathophysiology of co-occurring AUD and depressive disorders is limited, yet it is a growing area of inquiry. Studies of genetic liability have identified some evidence that AUD and depressive disorders share susceptibility. 28 – 30 Although much remains to be understood about the possible shared pathophysiology for these conditions, a number of candidate systems and processes have been identified, such as dysfunction in the reward and stress systems. 31
Data from studies of depressive disorders suggest that specific symptom profiles may reflect distinct pathophysiology. For example, different symptom types have been associated with electrical activity (measured by electroencephalogram) in the brain while patients are at rest. 32 A diagnosis of major depressive disorder can involve 227 unique symptom combinations; 6 thus, the combination of symptoms from AUD and depressive disorders can take many forms. Consideration of disorder heterogeneity is essential to better understand the development of the co-occurring disorders.
Course and prognosis
The prognosis of co-occurring AUD and depression is highly variable and depends on several factors, such as age of onset and the severity of the disorders. For example, DSM-IV alcohol dependence (particularly severe dependence) has been associated with persistence of depressive disorders, whereas alcohol abuse has not. 33 Furthermore, the association between depressive disorders and AUD outcomes depends on how depression was measured. A diagnosis of major depressive disorder typically has been associated with worse AUD treatment outcomes, 2 , 3 whereas more severe depressive symptoms alone have not been associated with worse AUD treatment outcomes, when compared to less severe depressive symptoms. 2 Depressive symptoms have been shown to significantly improve after a period of abstinence from alcohol (typically 3 to 4 weeks), 34 which may explain the lack of association between symptoms and drinking outcomes outside of the context of a depressive disorder.
Evidence from longitudinal data on whether AUD worsens depression outcomes is somewhat mixed, with some studies finding evidence for worse outcomes and others finding no difference. 35 However, large studies have suggested that recovery from both conditions is linked, with remission from one condition strongly related to remission from the other. 36 For example, results from a large ( N = 2,876) multisite trial of treatment for depressive disorders found that patients who had co-occurring substance use disorder had a lower likelihood of depressive disorder remission and had a longer time to remission, when compared to patients with no substance use disorder. 37
Although alcohol-induced depressive disorder is defined by remission of the depression after discontinuation of alcohol, the disorder has been associated with risk for onset of later major depressive disorder. 11 Another study reported that patients with alcohol-induced depressive disorders experienced worse alcohol-related outcomes than patients with alcohol dependence who had other types of depressive disorders. 38
Treatment of Co-Occurring AUD and Depressive Disorders
Many randomized trials have investigated treatments for co-occurring AUD and depressive disorders. In this section, trials that used medication and psychotherapy treatments are discussed, as are the effects of those treatments on depressive symptoms and AUD symptoms.
Medication trials
Medication trials for co-occurring AUD and depressive disorders have focused mostly on antidepressant medications. Several meta-analyses have integrated these findings. 39 – 42 In general, the research shows that for people with co-occurring AUD and depressive disorders, antidepressants are more effective than placebo at reducing symptoms of depression. The magnitude of the benefit of medication over placebo is similar to the benefit reported in studies of people diagnosed with depression alone. 40 , 41 Few medication trials have compared treatments directly; most trials compare a single medication with a placebo. Thus, little is known about the comparative effectiveness of active treatments. 39 However, meta-analyses have suggested that older antidepressant medications, such as tricyclic antidepressants, are more effective at reducing depressive symptoms than newer agents, such as selective serotonin reuptake inhibitors (SSRIs). 40 , 42 These results may be attributable—at least in part—to a large placebo response reported in studies of SSRIs. 41
The effects of antidepressants on drinking outcomes are modest. 40 , 42 However, the effect of antidepressant medications on drinking outcomes may be dependent on how those medications affect depression. Some evidence indicates that depression mediates the effect of antidepressants on drinking outcomes. 43 Consistent with these findings, a meta-analysis of trials of antidepressant treatment for people with AUD only (i.e., without co-occurring depression) did not demonstrate a significant effect on drinking outcomes when compared to treatment with placebo. 42
Studies of patients with co-occurring AUD and depressive disorders have demonstrated that treatments using medications (e.g., naltrexone) for AUD are safe and effective for reducing drinking and depression symptoms. 44 , 45 A meta-analysis of studies that used acamprosate to treat AUD found similar effects among people with and without depression, but these researchers also found a strong effect of alcohol abstinence on remission of depression. 46 Combinations of antidepressants and AUD medications (e.g., sertraline with naltrexone and acamprosate with escitalopram) 47 , 48 have also shown some promise for the treatment of these co-occurring disorders, with positive outcomes for both AUD and depressive symptoms.
Psychosocial treatments and mutual help
Researchers have examined the effects of behavioral and psychosocial therapies on co-occurring AUD and depressive disorders, although many of these studies have had small sample sizes. A meta-analysis of 12 studies that examined combined motivational interviewing and cognitive behavioral therapy for AUD and depression found significant, but modest, improvements in both depression and drinking outcomes. 49 These results are consistent with an earlier meta-analysis of several psychotherapies (e.g., interpersonal psychotherapy and cognitive behavioral therapy) that also indicated relatively modest, but positive, effects for depression and drinking outcomes. 50
Several studies have examined a transdiagnostic behavioral approach to treatment, which integrates the treatments for AUD and depressive symptoms. Behavioral activation is a behavioral therapy that specifically targets reward dysfunction to improve mood through better engagement with natural reinforcers. Treatment with behavioral activation therapy has demonstrated efficacy for depressive disorders 51 and for AUD; 52 thus, it may be particularly promising for treating the co-occurring disorders. A therapy called “life enhancement treatment for substance use,” or “LETS ACT,” is a modification of behavioral activation therapy for people with substance use disorders. This therapy has been shown to reduce substance-related consequences and improve likelihood of abstinence in samples of adults with substance dependence (including alcohol dependence). 52 In another study, an integrated cognitive behavioral therapy treatment for depressive disorders and substance use disorders was associated with greater reduction in alcohol use, but similar reductions in depression, when compared with the control condition, which was a 12-step facilitation therapy. 53
Some researchers have suggested that the effects of psychotherapy may account for some of the pill placebo response observed in medication studies. Specifically, for medication trials in which all participants also received some form of psychotherapy, pill placebo response rates were higher than they were for studies that did not include psychotherapy in the pill placebo condition. 41 Likewise, in a study of sertraline and naltrexone in which all participants received weekly psychotherapy, sertraline had no additive benefit. 54 These findings suggest that the psychotherapies used in these trials may have provided some antidepressant effect, either directly or through their effects on drinking.
Mutual-help groups also can be effective elements of treatment for co-occurring AUD and depressive disorders. Attendance at Alcoholics Anonymous (AA) meetings has been shown to decrease symptoms of depression. 55 In one study, researchers found that a reduction in depression mediated the effect that AA meeting attendance had on drinking outcomes, 56 indicating that a change in depression symptoms may be a mechanism through which attendance at AA meetings improves drinking outcomes.
Future Research Directions
Research has substantially improved understanding of the etiology, course, and treatment of co-occurring AUD and depressive disorders. However, significant gaps remain in our understanding of these two disorders, and these gaps present important opportunities for future research.
More knowledge about optimal treatments for co-occurring AUD and depressive disorders is needed. Although medication and behavioral therapy have both shown promise, response rates have been somewhat modest. Efforts to enhance treatment outcomes would benefit from investigation into the characteristics of people who do not respond to existing treatments. A better understanding of the heterogeneity within this population will inform more personalized treatment approaches and might ultimately improve treatment response.
The substantial variability in the course of co-occurring AUD and depressive disorders may reflect discrete underlying mechanisms, requiring distinct treatment approaches. For example, AUD that develops after the onset of a depressive disorder and is characterized by coping motives for alcohol use may differ critically from a depressive disorder that develops following chronic alcohol administration. Data from studies of depression indicate that the substantial variability in the symptoms presented reflects a heterogeneous pathophysiology, 32 yet research on heterogeneity in co-occurring AUD and depressive disorders remains limited. Although little is known about the possible shared pathophysiology of AUD and depressive disorders, preclinical research has identified common disruptions in reward and stress processing that are important candidates for further research. 31 Efforts to better characterize the mechanistic processes that may underlie observed clinical presentations will help identify more precise and personalized interventions.
Future research that leverages novel technologies, such as ecological momentary assessment and multimodal neuroimaging, will enhance our understanding of the interactions between mood and alcohol use and how those interactions may influence the nature, course, and treatment of co-occurring AUD and depressive disorders. Assessment of co-occurring AUD and depressive disorders using dimensional measures rather than discrete, categorical measures will be critical to understanding the full spectrum of severity of these conditions, including subclinical presentations.
Finally, the etiology, course, and treatment of both AUD and depression differ substantially by gender. Women have been underrepresented in much of the research on co-occurring AUD and depressive disorders, particularly in the early research on this topic. The research needs more representation of women to increase understanding of the sex differences and to better characterize the mechanisms underlying women’s heightened vulnerability for depressive disorders. For example, an important area for future research could be women who have co-occurring AUD and premenstrual dysphoric disorder, which is a depressive disorder characterized by a fluctuation of mood symptoms across the menstrual cycle. 6 Likewise, research is urgently needed to better understand co-occurring AUD and depressive disorders among racial and ethnic minorities. These populations experience disparities in access to care for AUD and depressive disorders but are underrepresented in studies of these disorders.
People with AUD have a heightened risk for depressive disorders, which are the most common co-occurring psychiatric disorders for this population. AUD and depressive disorders appear to share some behavioral, genetic, and environmental risk factors, yet these shared risks remain poorly understood.
Diagnosis and treatment of the commonly co-occurring AUD and depressive disorders have many challenges. Diagnosis is particularly challenging because of overlapping symptoms, such as the depressant effects of alcohol, and because of features that are common to both alcohol withdrawal and depressive disorders, such as insomnia and psychomotor agitation. The DSM-5 distinguishes a substance-induced disorder from a primary depressive disorder based on whether “the substance is judged to be etiologically related to the symptoms.” 6 (p180) Accordingly, any diagnosis of depression during active periods of drinking or during acute alcohol withdrawal should be made provisionally. Attempts to diagnose depression should focus on identifying periods of depression outside periods of drinking or withdrawal and should use collateral information (e.g., reports from family members or significant others) when possible. If depressive symptoms persist after a period of abstinence—4 weeks is the typical recommendation—a diagnosis of an independent (i.e., not substance-induced) depressive disorder can be made with more confidence. 6
Nonetheless, substance-induced depression is also associated with the risk for independent depressive disorders. Thus, treatment of depression should be considered, along with close monitoring of mood, for people who have substance-induced depression. 11 Treatment studies have supported the effects of both AUD medications (e.g., naltrexone) 44 and antidepressants 47 for the treatment of co-occurring AUD and depressive disorders. However, because of a lack of comparative trials on effectiveness (i.e., studies comparing more than one active treatment), the most effective approach is unknown. Behavioral therapy is understudied in this population despite evidence supporting the therapy as treatment for depressive disorders 51 and AUD 57 separately. Indeed, in placebo-controlled studies of medications for co-occurring AUD and depression, the inclusion of behavioral therapy as part of the standard treatment may explain the small effect sizes often observed. Behavioral activation therapy—a treatment that targets disruption in reward functioning, which is a common dysfunction in both AUD and depressive disorders—may have particular promise for treating the co-occurring disorders. 52
Despite the availability of several evidence-based medications and behavioral therapy approaches for treating co-occurring AUD and depressive disorders, improvements in treatment for this population are clearly needed. Consideration of disorder heterogeneity and key subgroup differences may help develop more targeted and personalized treatments to improve outcomes for this population.
Acknowledgments
This article was supported by the Charles Engelhard Foundation and National Institute on Drug Abuse grants K23DA035297 and K24DA022288.
Financial Disclosure
Dr. McHugh declares no competing financial interests. Dr. Weiss has been a consultant to Alkermes, Braeburn, Daiichi-Sankyo, GW Pharmaceuticals, Indivior, Janssen, and US WorldMeds.
- Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004; 61 (8):807–816. [ PubMed ] [ Google Scholar ]
- Greenfield SF, Weiss RD, Muenz LR, et al. The effect of depression on return to drinking: A prospective study. Arch Gen Psychiatry. 1998; 55 (3):259–265. [ PubMed ] [ Google Scholar ]
- Hasin D, Liu X, Nunes E, et al. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002; 59 (4):375–380. [ PubMed ] [ Google Scholar ]
- Conner KR, Gamble SA, Bagge CL, et al. Substance-induced depression and independent depression in proximal risk for suicidal behavior. J Stud Alcohol Drugs. 2014; 75 (4):567–572. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [ Google Scholar ]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [ Google Scholar ]
- Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005; 62 (10):1097–1106. [ PubMed ] [ Google Scholar ]
- Kessler RC, Ormel J, Petukhova M, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. 2011; 68 (1):90–100. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005; 62 (6):617–627. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schuckit MA, Tipp JE, Bergman M, et al. Comparison of induced and independent major depressive disorders in 2,945 alcoholics. Am J Psychiatry. 1997; 154 (7):948–957. [ PubMed ] [ Google Scholar ]
- Nunes EV, Liu X, Samet S, et al. Independent versus substance-induced major depressive disorder in substance-dependent patients: Observational study of course during follow-up. J Clin Psychiatry. 2006; 67 (10):1561–1567. [ PubMed ] [ Google Scholar ]
- Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003; 74 (1):5–13. [ PubMed ] [ Google Scholar ]
- Kessler RC, Crum RM, Warner LA, et al. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997; 54 (4):313–321. [ PubMed ] [ Google Scholar ]
- Khan S, Okuda M, Hasin DS, et al. Gender differences in lifetime alcohol dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res. 2013; 37 (10):1696–1705. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moscato BS, Russell M, Zielezny M, et al. Gender differences in the relation between depressive symptoms and alcohol problems: A longitudinal perspective. Am J Epidemiol. 1997; 146 (11):966–974. [ PubMed ] [ Google Scholar ]
- Hanna EZ, Grant BF. Gender differences in DSM-IV alcohol use disorders and major depression as distributed in the general population: Clinical implications. Compr Psychiatry. 1997; 38 (4):202–212. [ PubMed ] [ Google Scholar ]
- Prescott CA, Aggen SH, Kendler KS. Sex-specific genetic influences on the comorbidity of alcoholism and major depression in a population-based sample of U.S. twins. Arch Gen Psychiatry. 2000; 57 (8):803–811. [ PubMed ] [ Google Scholar ]
- Smith SM, Stinson FS, Dawson DA, et al. Race/ethnic differences in the prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006; 36 (7):987–998. [ PubMed ] [ Google Scholar ]
- Hatzenbuehler ML, Keyes KM, Narrow WE, et al. Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008; 69 (7):1112–1121. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nam E, Matejkowski J, Lee S. Racial/ethnic differences in contemporaneous use of mental health and substance use treatment among individuals experiencing both mental illness and substance use disorders. Psychiatr Q. 2017; 88 (1):185–198. [ PubMed ] [ Google Scholar ]
- Abraham HD, Fava M. Order of onset of substance abuse and depression in a sample of depressed outpatients. Compr Psychiatry. 1999; 40 (1):44–50. [ PubMed ] [ Google Scholar ]
- Fergusson DM, Boden JM, Horwood LJ. Tests of causal links between alcohol abuse or dependence and major depression. Arch Gen Psychiatry. 2009; 66 (3):260–266. [ PubMed ] [ Google Scholar ]
- Colder CR, Frndak S, Lengua LJ, et al. Internalizing and externalizing problem behavior: A test of a latent variable interaction predicting a two-part growth model of adolescent substance use. J Abnorm Child Psychol. 2018; 46 (2):319–330. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crum RM, Mojtabai R, Lazareck S, et al. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry. 2013; 70 (7):718–726. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Foster KT, Hicks BM, Iacono WG, et al. Gender differences in the structure of risk for alcohol use disorder in adolescence and young adulthood. Psychol Med. 2015; 45 (14):3047–3058. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pedrelli P, Shapero B, Archibald A, et al. Alcohol use and depression during adolescence and young adulthood: A summary and interpretation of mixed findings. Curr Addict Rep. 2016; 3 (1):91–97. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Falk DE, Yi HY, Hilton ME. Age of onset and temporal sequencing of lifetime DSM-IV alcohol use disorders relative to comorbid mood and anxiety disorders. Drug Alcohol Depend. 2008; 94 (1–3):234–245. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Andersen AM, Pietrzak RH, Kranzler HR, et al. Polygenic scores for major depressive disorder and risk of alcohol dependence. JAMA Psychiatry. 2017; 74 (11):1153–1160. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kuo PH, Gardner CO, Kendler KS, et al. The temporal relationship of the onsets of alcohol dependence and major depression: Using a genetically informative study design. Psychol Med. 2006; 36 (8):1153–1162. [ PubMed ] [ Google Scholar ]
- Zhou H, Polimanti R, Yang BZ, et al. Genetic risk variants associated with comorbid alcohol dependence and major depression. JAMA Psychiatry. 2017; 74 (12):1234–1241. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Renoir T, Pang TY, Lanfumey L. Drug withdrawal-induced depression: Serotonergic and plasticity changes in animal models. Neurosci Biobehav Rev. 2012; 36 (1):696–726. [ PubMed ] [ Google Scholar ]
- Webb CA, Dillon DG, Pechtel P, et al. Neural correlates of three promising endophenotypes of depression: Evidence from the EMBARC study. Neuropsychopharmacology. 2016; 41 (2):454–463. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Boschloo L, Vogelzangs N, van den Brink W, et al. Alcohol use disorders and the course of depressive and anxiety disorders. Br J Psychiatry. 2012; 200 (6):476–484. [ PubMed ] [ Google Scholar ]
- Liappas J, Paparrigopoulos T, Tzavellas E, et al. Impact of alcohol detoxification on anxiety and depressive symptoms. Drug Alcohol Depend. 2002; 68 (2):215–220. [ PubMed ] [ Google Scholar ]
- Sullivan LE, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: A systematic review. Am J Med. 2005; 118 (4):330–341. [ PubMed ] [ Google Scholar ]
- Hasin DS, Tsai WY, Endicott J, et al. Five-year course of major depression: Effects of comorbid alcoholism. J Affect Disord. 1996; 41 (1):63–70. [ PubMed ] [ Google Scholar ]
- Davis LL, Wisniewski SR, Howland RH, et al. Does comorbid substance use disorder impair recovery from major depression with SSRI treatment? An analysis of the STAR*D level one treatment outcomes. Drug Alcohol Depend. 2010; 107 (2–3):161–170. [ PubMed ] [ Google Scholar ]
- Samet S, Fenton MC, Nunes E, et al. Effects of independent and substance-induced major depressive disorder on remission and relapse of alcohol, cocaine and heroin dependence. Addiction. 2013; 108 (1):115–123. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Agabio R, Trogu E, Pani PP. Antidepressants for the treatment of people with co-occurring depression and alcohol dependence. Cochrane Database Syst Rev. 2018; 4 :CD008581. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Iovieno N, Tedeschini E, Bentley KH, et al. Antidepressants for major depressive disorder and dysthymic disorder in patients with comorbid alcohol use disorders: A meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011; 72 (8):1144–1151. [ PubMed ] [ Google Scholar ]
- Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence: A meta-analysis. JAMA. 2004; 291 (15):1887–1896. [ PubMed ] [ Google Scholar ]
- Torrens M, Fonseca F, Mateu G, et al. Efficacy of antidepressants in substance use disorders with and without comorbid depression. A systematic review and meta-analysis. Drug Alcohol Depend. 2005; 78 (1):1–22. [ PubMed ] [ Google Scholar ]
- Nunes EV, Quitkin FM, Donovan SJ, et al. Imipramine treatment of opiate-dependent patients with depressive disorders. A placebo-controlled trial. Arch Gen Psychiatry. 1998; 55 (2):153–160. [ PubMed ] [ Google Scholar ]
- Petrakis I, Ralevski E, Nich C, et al. Naltrexone and disulfiram in patients with alcohol dependence and current depression. J Clin Psychopharmacol. 2007; 27 (2):160–165. [ PubMed ] [ Google Scholar ]
- Salloum IM, Cornelius JR, Thase ME, et al. Naltrexone utility in depressed alcoholics. Psychopharmacol Bull. 1998; 34 (1):111–115. [ PubMed ] [ Google Scholar ]
- Lejoyeux M, Lehert P. Alcohol-use disorders and depression: Results from individual patient data meta-analysis of the acamprosate-controlled studies. Alcohol Alcohol. 2011; 46 (1):61–67. [ PubMed ] [ Google Scholar ]
- Pettinati HM, Oslin DW, Kampman KM, et al. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry. 2010; 167 (6):668–675. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Witte J, Bentley K, Evins AE, et al. A randomized, controlled, pilot study of acamprosate added to escitalopram in adults with major depressive disorder and alcohol use disorder. J Clin Psychopharmacol. 2012; 32 (6):787–796. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Riper H, Andersson G, Hunter SB, et al. Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: A meta-analysis. Addiction. 2014; 109 (3):394–406. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hesse M. Integrated psychological treatment for substance use and co-morbid anxiety or depression vs. treatment for substance use alone. A systematic review of the published literature. BMC Psychiatry. 2009; 9 :6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dimidjian S, Hollon SD, Dobson KS, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006; 74 (4):658–670. [ PubMed ] [ Google Scholar ]
- Daughters SB, Magidson JF, Anand D, et al. The effect of a behavioral activation treatment for substance use on post-treatment abstinence: A randomized controlled trial. Addiction. 2018; 113 (3):535–544. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lydecker KP, Tate SR, Cummins KM, et al. Clinical outcomes of an integrated treatment for depression and substance use disorders. Psychol Addict Behav. 2010; 24 (3):453–465. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Farren CK, Scimeca M, Wu R, et al. A double-blind, placebo-controlled study of sertraline with naltrexone for alcohol dependence. Drug Alcohol Depend. 2009; 99 (1–3):317–321. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kelly TM, Daley DC, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addict Behav. 2012; 37 (1):11–24. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wilcox CE, Tonigan JS. Changes in depression mediate the effects of AA attendance on alcohol use outcomes. Am J Drug Alcohol Abuse. 2018; 44 (1):103–112. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- National Institute on Alcohol Abuse and Alcoholism. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997; 58 (1):7–29. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Alcohol use disorder is a pattern of alcohol use that involves problems controlling your drinking, being preoccupied with alcohol or continuing to use alcohol even when it causes problems. ... Some research studies indicate that having bariatric surgery may increase the risk of developing alcohol use disorder or of relapsing after recovering ...
Alcohol is the most commonly used substance in the United States, with 84% of people 18 and older reporting lifetime use, according to data from the 2022 National Survey on Drug Use and Health. Alcohol use exists along a spectrum from low risk to alcohol use disorder (AUD). The intervening category, known as risky drinking, includes heavy drinking as well as binge drinking.[1] AUD is a chronic ...
It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism. Considered a brain disorder, AUD can be mild, moderate, or severe. Lasting changes in the brain caused by alcohol misuse perpetuate AUD and make individuals vulnerable to relapse.
alcohol-related causes annually, making alcohol the third leading preventable cause of death in ... • Research indicates that alcohol use during the teenage years could interfere with normal ... Table 5.4B—Alcohol Use Disorder in Past Year among Persons Aged 12 or Older, by Age Group and Demographic Characteristics: Percentages, 2017 and ...
1. Introduction. Alcohol use disorder (AUD) can be defined as a chronically relapsing disorder characterized by the compulsion to ingest alcohol, the loss of control in limiting alcohol intake despite adverse health, social, and occupational consequences, and the emergence of a negative emotional state that can involve feelings of anxiety, irritability, and dysphoria when access to alcohol is ...
Takeaways. Alcohol use disorder (AUD) is defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as "a problematic pattern of alcohol use leading to clinically significant impairment or distress," and is diagnosed as mild, moderate, or severe based on the number of symptoms, out of a possible 11, in the past 12 months.; As it progresses in severity, AUD can cause brain ...
Introduction. Alcohol Use Disorders (AUDs) are serious psychiatric conditions often leading to major adverse consequences. The 2018 World Health Organization's (WHO) Global Status Report on Alcohol and Health determined that in 2016 harmful use of alcohol caused approximately 3 million deaths (or 5.3% of all deaths), more than hypertension and diabetes combined.
Chronic diseases and cancer. The chronic medical risks of alcohol use include gastrointestinal disease, cardiovascular disease and cancer 28. Alcohol-attributable gastrointestinal disease includes ...
So the worsening rates of alcohol use disorder in women prompt the need for a greater focus on women in the research and the search for treatments. Yet, women have long been underrepresented in ...
Alcohol is regularly consumed throughout most of the world, including by nearly half the U.S. population age 12 or older. Heavy drinking, which is also common, contributes to multiple adverse medical, psychiatric, and social outcomes and more than 140,000 deaths annually in the United States. It is the major risk factor for alcohol use disorder (AUD), whose current U.S. prevalence is 11% ...
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), 6.2 percent of adults in the United States aged 18 and older had alcohol use disorder. 1 For example, a government survey revealed that about one in five individuals aged 12 to 20 were current alcohol users and about two in five young adults, aged 18 to 25, were binge ...
Alcohol use disorders consist of disorders characterised by compulsive heavy alcohol use and loss of control over alcohol intake. Alcohol use disorders are some of the most prevalent mental disorders globally, especially in high-income and upper-middle-income countries; and are associated with high mortality and burden of disease, mainly due to medical consequences, such as liver cirrhosis or ...
Alcohol consumption causes death and disability relatively early in life. In people aged 20-39 years, approximately 13.5% of total deaths are attributable to alcohol. There is a causal relationship between harmful use of alcohol and a range of mental and behavioural disorders, other noncommunicable conditions and injuries.
Alcohol use disorder (or alcoholism) is also a clear issue for the brain. It has been linked to a higher risk for dementia, especially early-onset dementia in a study of 262,000 adults, as well as ...
Mid-stage alcohol use disorder: Your alcohol use is now out of control and causes problems with daily life (work, family, financial, physical and mental health). Organ damage can be seen on lab tests and scans. End-stage alcohol use disorder: Drinking is now the main focus of your life, to the exclusion of food, intimacy, health and happiness ...
Effects of short-term alcohol use. Drinking excessively on an occasion can lead to these harmful health effects: Injuries— motor vehicle crashes, falls, drownings, and burns. Violence—homicide, suicide, sexual violence, and intimate partner violence. Alcohol poisoning—high blood alcohol levels that affect body functions like breathing and ...
Alcohol Use Disorder (AUD): AUD is a chronic relapsing brain disease characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. AUD can to severe, and recovery is possible regardless of severity. The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders
Almost one-third of the U.S. population meets alcohol use disorder (AUD) criteria on a lifetime basis. This review provides an overview of recent research on the prevalence and patterns of alcohol-related improvement and selectively reviews nationally representative surveys and studies that followed risk groups longitudinally with a goal of informing patients with AUD and AUD researchers ...
Introduction. Alcohol use disorder (AUD) is one of the leading causes of the global burden of disease and injury (WHO), despite the continuous discovery of novel pharmacotherapeutic agents (Pakri Mohamed et al., 2018).Various factors such as environmental, social, situational, and cultural context have distinctive consequences toward substance use and its effects on individuals (Latkin et al ...
Learn up-to-date facts and statistics on alcohol consumption and its impact in the United States and globally. Explore topics related to alcohol misuse and treatment, underage drinking, the effects of alcohol on the human body, and more. Find up-to-date statistics on lifetime drinking, past-year drinking, past-month drinking, binge drinking ...
DISCUSSION. Research on the epidemiology of recovery from AUD is somewhat uneven in scope and methods, and gaps remain in the knowledge base. Nonetheless, the bulk of evidence converges in showing that (1) improvements in alcohol-related problems, including recovery from AUD, are commonplace; (2) natural recovery is the dominant pathway; (3 ...
Topic: Alcohol Use. AHRQ has research focused on unhealthy alcohol use. About 18 million adult Americans have an alcohol use disorder. This means that their drinking causes distress and harm. It includes alcoholism and alcohol abuse. Implementing Screening and Treatment of Unhealthy Alcohol Use During COVID-19.
Roughly 1 in 5 U.S. adults report binge drinking at least once a week, with an average of seven drinks per binge episode. This is well over the amount of alcohol thought to produce legal intoxication, commonly defined as a blood alcohol concentration over 0.08%- on average, four drinks in two hours for women, five drinks in two hours for men.
Many individuals who develop substance use disorders (SUD) are also diagnosed with mental disorders, and vice versa. 2,3 Although there are fewer studies on comorbidity among youth, research suggests that adolescents with substance use disorders also have high rates of co-occurring mental illness; over 60 percent of adolescents in community-based substance use disorder treatment programs also ...
Alcohol is a leading cause of morbidity and mortality, with harms related to both acute and chronic effects of alcohol contributing to about 5 million emergency department visits and 99,000 deaths in the U.S. each year. There is no perfectly safe level of alcohol consumption, as current research points to health risks including cancer and cardiovascular risks even at low levels of consumption ...
Alcohol use disorder (AUD) often seems to run in families, and we may hear about scientific studies of an "alcoholism gene.". Genetics certainly influence our likelihood of developing AUD, but the story isn't so simple. Research shows that genes are responsible for about half of the risk for AUD. Therefore, genes alone do not determine ...
Alcohol use can cause sexual dysfunction, such as difficulty achieving or maintaining an erection and decreased sexual sensations. The impact alcohol has on the reproductive system extends beyond these temporary effects. Chronic alcohol use causes hormone imbalances in both men and women and leads to problems with fertility.
Alcohol use disorder (AUD) and depressive disorders are among the most prevalent psychiatric disorders and co-occur more often than expected by chance. The aim of this review is to characterize the prevalence, course, and treatment of co-occurring AUD and depressive disorders. Studies have indicated that the co-occurrence of AUD and depressive ...