Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- June 01, 2024 | VOL. 181, NO. 6 CURRENT ISSUE pp.461-564
- May 01, 2024 | VOL. 181, NO. 5 pp.347-460
- April 01, 2024 | VOL. 181, NO. 4 pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Link , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
- Open access
- Published: 13 November 2021
Risk and protective factors of drug abuse among adolescents: a systematic review
- Azmawati Mohammed Nawi 1 ,
- Rozmi Ismail 2 ,
- Fauziah Ibrahim 2 ,
- Mohd Rohaizat Hassan 1 ,
- Mohd Rizal Abdul Manaf 1 ,
- Noh Amit 3 ,
- Norhayati Ibrahim 3 &
- Nurul Shafini Shafurdin 2
BMC Public Health volume 21 , Article number: 2088 ( 2021 ) Cite this article
139k Accesses
101 Citations
20 Altmetric
Metrics details
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was adopted for the review which utilized three main journal databases, namely PubMed, EBSCOhost, and Web of Science. Tobacco addiction and alcohol abuse were excluded in this review. Retrieved citations were screened, and the data were extracted based on strict inclusion and exclusion criteria. Inclusion criteria include the article being full text, published from the year 2016 until 2020 and provided via open access resource or subscribed to by the institution. Quality assessment was done using Mixed Methods Appraisal Tools (MMAT) version 2018 to assess the methodological quality of the included studies. Given the heterogeneity of the included studies, a descriptive synthesis of the included studies was undertaken.
Out of 425 articles identified, 22 quantitative articles and one qualitative article were included in the final review. Both the risk and protective factors obtained were categorized into three main domains: individual, family, and community factors. The individual risk factors identified were traits of high impulsivity; rebelliousness; emotional regulation impairment, low religious, pain catastrophic, homework completeness, total screen time and alexithymia; the experience of maltreatment or a negative upbringing; having psychiatric disorders such as conduct problems and major depressive disorder; previous e-cigarette exposure; behavioral addiction; low-perceived risk; high-perceived drug accessibility; and high-attitude to use synthetic drugs. The familial risk factors were prenatal maternal smoking; poor maternal psychological control; low parental education; negligence; poor supervision; uncontrolled pocket money; and the presence of substance-using family members. One community risk factor reported was having peers who abuse drugs. The protective factors determined were individual traits of optimism; a high level of mindfulness; having social phobia; having strong beliefs against substance abuse; the desire to maintain one’s health; high paternal awareness of drug abuse; school connectedness; structured activity and having strong religious beliefs.
The outcomes of this review suggest a complex interaction between a multitude of factors influencing adolescent drug abuse. Therefore, successful adolescent drug abuse prevention programs will require extensive work at all levels of domains.
Peer Review reports
Introduction
Drug abuse is a global problem; 5.6% of the global population aged 15–64 years used drugs at least once during 2016 [ 1 ]. The usage of drugs among younger people has been shown to be higher than that among older people for most drugs. Drug abuse is also on the rise in many ASEAN (Association of Southeast Asian Nations) countries, especially among young males between 15 and 30 years of age. The increased burden due to drug abuse among adolescents and young adults was shown by the Global Burden of Disease (GBD) study in 2013 [ 2 ]. About 14% of the total health burden in young men is caused by alcohol and drug abuse. Younger people are also more likely to die from substance use disorders [ 3 ], and cannabis is the drug of choice among such users [ 4 ].
Adolescents are the group of people most prone to addiction [ 5 ]. The critical age of initiation of drug use begins during the adolescent period, and the maximum usage of drugs occurs among young people aged 18–25 years old [ 1 ]. During this period, adolescents have a strong inclination toward experimentation, curiosity, susceptibility to peer pressure, rebellion against authority, and poor self-worth, which makes such individuals vulnerable to drug abuse [ 2 ]. During adolescence, the basic development process generally involves changing relations between the individual and the multiple levels of the context within which the young person is accustomed. Variation in the substance and timing of these relations promotes diversity in adolescence and represents sources of risk or protective factors across this life period [ 6 ]. All these factors are crucial to helping young people develop their full potential and attain the best health in the transition to adulthood. Abusing drugs impairs the successful transition to adulthood by impairing the development of critical thinking and the learning of crucial cognitive skills [ 7 ]. Adolescents who abuse drugs are also reported to have higher rates of physical and mental illness and reduced overall health and well-being [ 8 ].
The absence of protective factors and the presence of risk factors predispose adolescents to drug abuse. Some of the risk factors are the presence of early mental and behavioral health problems, peer pressure, poorly equipped schools, poverty, poor parental supervision and relationships, a poor family structure, a lack of opportunities, isolation, gender, and accessibility to drugs [ 9 ]. The protective factors include high self-esteem, religiosity, grit, peer factors, self-control, parental monitoring, academic competence, anti-drug use policies, and strong neighborhood attachment [ 10 , 11 , 12 , 13 , 14 , 15 ].
The majority of previous systematic reviews done worldwide on drug usage focused on the mental, psychological, or social consequences of substance abuse [ 16 , 17 , 18 ], while some focused only on risk and protective factors for the non-medical use of prescription drugs among youths [ 19 ]. A few studies focused only on the risk factors of single drug usage among adolescents [ 20 ]. Therefore, the development of the current systematic review is based on the main research question: What is the current risk and protective factors among adolescent on the involvement with drug abuse? To the best of our knowledge, there is limited evidence from systematic reviews that explores the risk and protective factors among the adolescent population involved in drug abuse. Especially among developing countries, such as those in South East Asia, such research on the risk and protective factors for drug abuse is scarce. Furthermore, this review will shed light on the recent trends of risk and protective factors and provide insight into the main focus factors for prevention and control activities program. Additionally, this review will provide information on how these risk and protective factors change throughout various developmental stages. Therefore, the objective of this systematic review was to determine the risk and protective factors of drug abuse among adolescents worldwide. This paper thus fills in the gaps of previous studies and adds to the existing body of knowledge. In addition, this review may benefit certain parties in developing countries like Malaysia, where the national response to drugs is developing in terms of harm reduction, prison sentences, drug treatments, law enforcement responses, and civil society participation.
This systematic review was conducted using three databases, PubMed, EBSCOhost, and Web of Science, considering the easy access and wide coverage of reliable journals, focusing on the risk and protective factors of drug abuse among adolescents from 2016 until December 2020. The search was limited to the last 5 years to focus only on the most recent findings related to risk and protective factors. The search strategy employed was performed in accordance with the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) checklist.
A preliminary search was conducted to identify appropriate keywords and determine whether this review was feasible. Subsequently, the related keywords were searched using online thesauruses, online dictionaries, and online encyclopedias. These keywords were verified and validated by an academic professor at the National University of Malaysia. The keywords used as shown in Table 1 .
Selection criteria
The systematic review process for searching the articles was carried out via the steps shown in Fig. 1 . Firstly, screening was done to remove duplicate articles from the selected search engines. A total of 240 articles were removed in this stage. Titles and abstracts were screened based on the relevancy of the titles to the inclusion and exclusion criteria and the objectives. The inclusion criteria were full text original articles, open access articles or articles subscribed to by the institution, observation and intervention study design and English language articles. The exclusion criteria in this search were (a) case study articles, (b) systematic and narrative review paper articles, (c) non-adolescent-based analyses, (d) non-English articles, and (e) articles focusing on smoking (nicotine) and alcohol-related issues only. A total of 130 articles were excluded after title and abstract screening, leaving 55 articles to be assessed for eligibility. The full text of each article was obtained, and each full article was checked thoroughly to determine if it would fulfil the inclusion criteria and objectives of this study. Each of the authors compared their list of potentially relevant articles and discussed their selections until a final agreement was obtained. A total of 22 articles were accepted to be included in this review. Most of the excluded articles were excluded because the population was not of the target age range—i.e., featuring subjects with an age > 18 years, a cohort born in 1965–1975, or undergraduate college students; the subject matter was not related to the study objective—i.e., assessing the effects on premature mortality, violent behavior, psychiatric illness, individual traits, and personality; type of article such as narrative review and neuropsychiatry review; and because of our inability to obtain the full article—e.g., forthcoming work in 2021. One qualitative article was added to explain the domain related to risk and the protective factors among the adolescents.
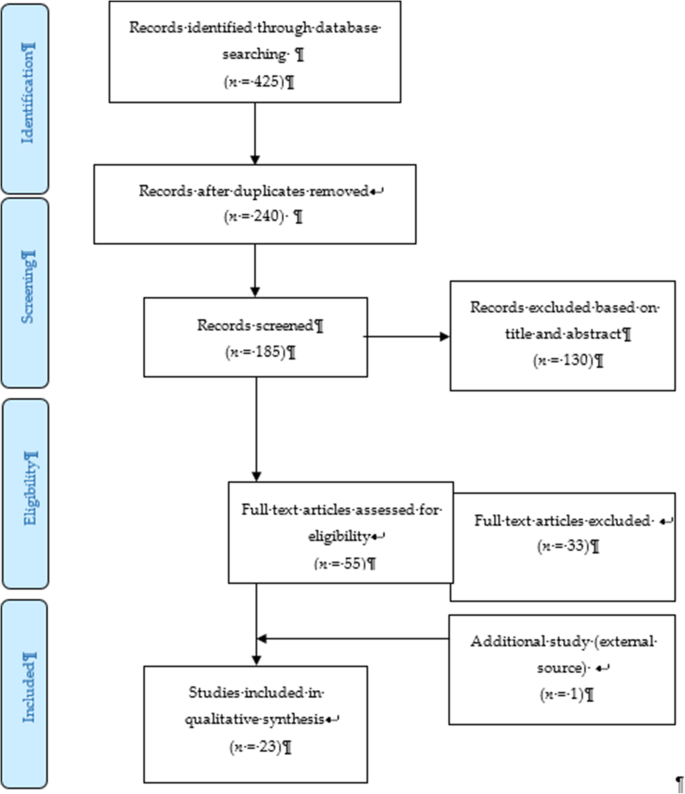
PRISMA flow diagram showing the selection of studies on risk and protective factors for drug abuse among adolescents.2.2. Operational Definition
Drug-related substances in this context refer to narcotics, opioids, psychoactive substances, amphetamines, cannabis, ecstasy, heroin, cocaine, hallucinogens, depressants, and stimulants. Drugs of abuse can be either off-label drugs or drugs that are medically prescribed. The two most commonly abused substances not included in this review are nicotine (tobacco) and alcohol. Accordingly, e-cigarettes and nicotine vape were also not included. Further, “adolescence” in this study refers to members of the population aged between 10 to 18 years [ 21 ].
Data extraction tool
All researchers independently extracted information for each article into an Excel spreadsheet. The data were then customized based on their (a) number; (b) year; (c) author and country; (d) titles; (e) study design; (f) type of substance abuse; (g) results—risks and protective factors; and (h) conclusions. A second reviewer crossed-checked the articles assigned to them and provided comments in the table.
Quality assessment tool
By using the Mixed Method Assessment Tool (MMAT version 2018), all articles were critically appraised for their quality by two independent reviewers. This tool has been shown to be useful in systematic reviews encompassing different study designs [ 22 ]. Articles were only selected if both reviewers agreed upon the articles’ quality. Any disagreement between the assigned reviewers was managed by employing a third independent reviewer. All included studies received a rating of “yes” for the questions in the respective domains of the MMAT checklists. Therefore, none of the articles were removed from this review due to poor quality. The Cohen’s kappa (agreement) between the two reviewers was 0.77, indicating moderate agreement [ 23 ].
The initial search found 425 studies for review, but after removing duplicates and applying the criteria listed above, we narrowed the pool to 22 articles, all of which are quantitative in their study design. The studies include three prospective cohort studies [ 24 , 25 , 26 ], one community trial [ 27 ], one case-control study [ 28 ], and nine cross-sectional studies [ 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. After careful discussion, all reviewer panels agreed to add one qualitative study [ 46 ] to help provide reasoning for the quantitative results. The selected qualitative paper was chosen because it discussed almost all domains on the risk and protective factors found in this review.
A summary of all 23 articles is listed in Table 2 . A majority of the studies (13 articles) were from the United States of America (USA) [ 25 , 26 , 27 , 29 , 30 , 31 , 34 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ], three studies were from the Asia region [ 32 , 33 , 38 ], four studies were from Europe [ 24 , 28 , 40 , 44 ], and one study was from Latin America [ 35 ], Africa [ 43 ] and Mediterranean [ 45 ]. The number of sample participants varied widely between the studies, ranging from 70 samples (minimum) to 700,178 samples (maximum), while the qualitative paper utilized a total of 100 interviewees. There were a wide range of drugs assessed in the quantitative articles, with marijuana being mentioned in 11 studies, cannabis in five studies, and opioid (six studies). There was also large heterogeneity in terms of the study design, type of drug abused, measurements of outcomes, and analysis techniques used. Therefore, the data were presented descriptively.
After thorough discussion and evaluation, all the findings (both risk and protective factors) from the review were categorized into three main domains: individual factors, family factors, and community factors. The conceptual framework is summarized in Fig. 2 .
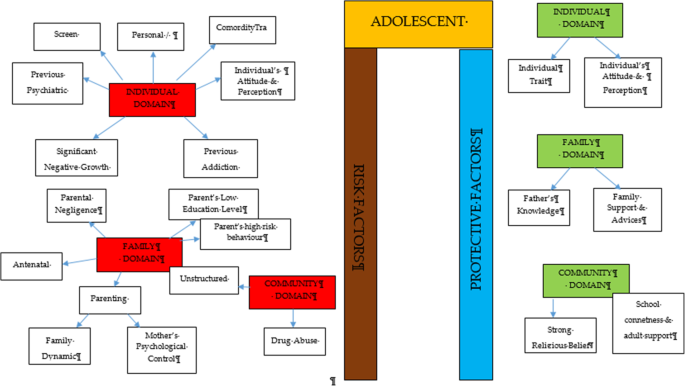
Conceptual framework of risk and protective factors related to adolescent drug abuse
DOMAIN: individual factor
Risk factors.
Almost all the articles highlighted significant findings of individual risk factors for adolescent drug abuse. Therefore, our findings for this domain were further broken down into five more sub-domains consisting of personal/individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance history, comorbidity and an individual’s attitude and perception.
Personal/individual traits
Chuang et al. [ 29 ] found that adolescents with high impulsivity traits had a significant positive association with drug addiction. This study also showed that the impulsivity trait alone was an independent risk factor that increased the odds between two to four times for using any drug compared to the non-impulsive group. Another longitudinal study by Guttmannova et al. showed that rebellious traits are positively associated with marijuana drug abuse [ 27 ]. The authors argued that measures of rebelliousness are a good proxy for a youth’s propensity to engage in risky behavior. Nevertheless, Wilson et al. [ 37 ], in a study involving 112 youths undergoing detoxification treatment for opioid abuse, found that a majority of the affected respondents had difficulty in regulating their emotions. The authors found that those with emotional regulation impairment traits became opioid dependent at an earlier age. Apart from that, a case-control study among outpatient youths found that adolescents involved in cannabis abuse had significant alexithymia traits compared to the control population [ 28 ]. Those adolescents scored high in the dimension of Difficulty in Identifying Emotion (DIF), which is one of the key definitions of diagnosing alexithymia. Overall, the adjusted Odds Ratio for DIF in cannabis abuse was 1.11 (95% CI, 1.03–1.20).
Significant negative growth exposure
A history of maltreatment in the past was also shown to have a positive association with adolescent drug abuse. A study found that a history of physical abuse in the past is associated with adolescent drug abuse through a Path Analysis, despite evidence being limited to the female gender [ 25 ]. However, evidence from another study focusing at foster care concluded that any type of maltreatment might result in a prevalence as high as 85.7% for the lifetime use of cannabis and as high as 31.7% for the prevalence of cannabis use within the last 3-months [ 30 ]. The study also found significant latent variables that accounted for drug abuse outcomes, which were chronic physical maltreatment (factor loading of 0.858) and chronic psychological maltreatment (factor loading of 0.825), with an r 2 of 73.6 and 68.1%, respectively. Another study shed light on those living in child welfare service (CWS) [ 35 ]. It was observed through longitudinal measurements that proportions of marijuana usage increased from 9 to 18% after 36 months in CWS. Hence, there is evidence of the possibility of a negative upbringing at such shelters.
Personal psychiatric diagnosis
The robust studies conducted in the USA have deduced that adolescents diagnosed with a conduct problem (CP) have a positive association with marijuana abuse (OR = 1.75 [1.56, 1.96], p < 0.0001). Furthermore, those with a diagnosis of Major Depressive Disorder (MDD) showed a significant positive association with marijuana abuse.
Previous substance and addiction history
Another study found that exposure to e-cigarettes within the past 30 days is related to an increase in the prevalence of marijuana use and prescription drug use by at least four times in the 8th and 10th grades and by at least three times in the 12th grade [ 34 ]. An association between other behavioral addictions and the development of drug abuse was also studied [ 29 ]. Using a 12-item index to assess potential addictive behaviors [ 39 ], significant associations between drug abuse and the groups with two behavioral addictions (OR = 3.19, 95% CI 1.25,9.77) and three behavioral addictions (OR = 3.46, 95% CI 1.25,9.58) were reported.
Comorbidity
The paper by Dash et al. (2020) highlight adolescent with a disease who needs routine medical pain treatment have higher risk of opioid misuse [ 38 ]. The adolescents who have disorder symptoms may have a risk for opioid misuse despite for the pain intensity.
Individual’s attitudes and perceptions
In a study conducted in three Latin America countries (Argentina, Chile, and Uruguay), it was shown that adolescents with low or no perceived risk of taking marijuana had a higher risk of abuse (OR = 8.22 times, 95% CI 7.56, 10.30) [ 35 ]. This finding is in line with another study that investigated 2002 adolescents and concluded that perceiving the drug as harmless was an independent risk factor that could prospectively predict future marijuana abuse [ 27 ]. Moreover, some youth interviewed perceived that they gained benefits from substance use [ 38 ]. The focus group discussion summarized that the youth felt positive personal motivation and could escape from a negative state by taking drugs. Apart from that, adolescents who had high-perceived availability of drugs in their neighborhoods were more likely to increase their usage of marijuana over time (OR = 11.00, 95% CI 9.11, 13.27) [ 35 ]. A cheap price of the substance and the availability of drug dealers around schools were factors for youth accessibility [ 38 ]. Perceived drug accessibility has also been linked with the authorities’ enforcement programs. The youth perception of a lax community enforcement of laws regarding drug use at all-time points predicted an increase in marijuana use in the subsequent assessment period [ 27 ]. Besides perception, a study examining the attitudes towards synthetic drugs based on 8076 probabilistic samples of Macau students found that the odds of the lifetime use of marijuana was almost three times higher among those with a strong attitude towards the use of synthetic drugs [ 32 ]. In addition, total screen time among the adolescent increase the likelihood of frequent cannabis use. Those who reported daily cannabis use have a mean of 12.56 h of total screen time, compared to a mean of 6.93 h among those who reported no cannabis use. Adolescent with more time on internet use, messaging, playing video games and watching TV/movies were significantly associated with more frequent cannabis use [ 44 ].
Protective factors
Individual traits.
Some individual traits have been determined to protect adolescents from developing drug abuse habits. A study by Marin et al. found that youth with an optimistic trait were less likely to become drug dependent [ 33 ]. In this study involving 1104 Iranian students, it was concluded that a higher optimism score (measured using the Children Attributional Style Questionnaire, CASQ) was a protective factor against illicit drug use (OR = 0.90, 95% CI: 0.85–0.95). Another study found that high levels of mindfulness, measured using the 25-item Child Acceptance and Mindfulness Measure, CAMM, lead to a slower progression toward injectable drug abuse among youth with opioid addiction (1.67 years, p = .041) [ 37 ]. In addition, the social phobia trait was found to have a negative association with marijuana use (OR = 0.87, 95% CI 0.77–0.97), as suggested [ 31 ].
According to El Kazdouh et al., individuals with a strong belief against substance use and those with a strong desire to maintain their health were more likely to be protected from involvement in drug abuse [ 46 ].
DOMAIN: family factors
The biological factors underlying drug abuse in adolescents have been reported in several studies. Epigenetic studies are considered important, as they can provide a good outline of the potential pre-natal factors that can be targeted at an earlier stage. Expecting mothers who smoke tobacco and alcohol have an indirect link with adolescent substance abuse in later life [ 24 , 39 ]. Moreover, the dynamic relationship between parents and their children may have some profound effects on the child’s growth. Luk et al. examined the mediator effects between parenting style and substance abuse and found the maternal psychological control dimension to be a significant variable [ 26 ]. The mother’s psychological control was two times higher in influencing her children to be involved in substance abuse compared to the other dimension. Conversely, an indirect risk factor towards youth drug abuse was elaborated in a study in which low parental educational level predicted a greater risk of future drug abuse by reducing the youth’s perception of harm [ 27 , 43 ]. Negligence from a parental perspective could also contribute to this problem. According to El Kazdouh et al. [ 46 ], a lack of parental supervision, uncontrolled pocket money spending among children, and the presence of substance-using family members were the most common negligence factors.
While the maternal factors above were shown to be risk factors, the opposite effect was seen when the paternal figure equipped himself with sufficient knowledge. A study found that fathers with good information and awareness were more likely to protect their adolescent children from drug abuse [ 26 ]. El Kazdouh et al. noted that support and advice could be some of the protective factors in this area [ 46 ].
DOMAIN: community factors
- Risk factor
A study in 2017 showed a positive association between adolescent drug abuse and peers who abuse drugs [ 32 , 39 ]. It was estimated that the odds of becoming a lifetime marijuana user was significantly increased by a factor of 2.5 ( p < 0.001) among peer groups who were taking synthetic drugs. This factor served as peer pressure for youth, who subconsciously had desire to be like the others [ 38 ]. The impact of availability and engagement in structured and unstructured activities also play a role in marijuana use. The findings from Spillane (2000) found that the availability of unstructured activities was associated with increased likelihood of marijuana use [ 42 ].
- Protective factor
Strong religious beliefs integrated into society serve as a crucial protective factor that can prevent adolescents from engaging in drug abuse [ 38 , 45 ]. In addition, the school connectedness and adult support also play a major contribution in the drug use [ 40 ].
The goal of this review was to identify and classify the risks and protective factors that lead adolescents to drug abuse across the three important domains of the individual, family, and community. No findings conflicted with each other, as each of them had their own arguments and justifications. The findings from our review showed that individual factors were the most commonly highlighted. These factors include individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance and addiction history, and an individual’s attitude and perception as risk factors.
Within the individual factor domain, nine articles were found to contribute to the subdomain of personal/ individual traits [ 27 , 28 , 29 , 37 , 38 , 39 , 40 , 43 , 44 ]. Despite the heterogeneity of the study designs and the substances under investigation, all of the papers found statistically significant results for the possible risk factors of adolescent drug abuse. The traits of high impulsivity, rebelliousness, difficulty in regulating emotions, and alexithymia can be considered negative characteristic traits. These adolescents suffer from the inability to self-regulate their emotions, so they tend to externalize their behaviors as a way to avoid or suppress the negative feelings that they are experiencing [ 41 , 47 , 48 ]. On the other hand, engaging in such behaviors could plausibly provide a greater sense of positive emotions and make them feel good [ 49 ]. Apart from that, evidence from a neurophysiological point of view also suggests that the compulsive drive toward drug use is complemented by deficits in impulse control and decision making (impulsive trait) [ 50 ]. A person’s ability in self-control will seriously impaired with continuous drug use and will lead to the hallmark of addiction [ 51 ].
On the other hand, there are articles that reported some individual traits to be protective for adolescents from engaging in drug abuse. Youth with the optimistic trait, a high level of mindfulness, and social phobia were less likely to become drug dependent [ 31 , 33 , 37 ]. All of these articles used different psychometric instruments to classify each individual trait and were mutually exclusive. Therefore, each trait measured the chance of engaging in drug abuse on its own and did not reflect the chance at the end of the spectrum. These findings show that individual traits can be either protective or risk factors for the drugs used among adolescents. Therefore, any adolescent with negative personality traits should be monitored closely by providing health education, motivation, counselling, and emotional support since it can be concluded that negative personality traits are correlated with high risk behaviours such as drug abuse [ 52 ].
Our study also found that a history of maltreatment has a positive association with adolescent drug abuse. Those adolescents with episodes of maltreatment were considered to have negative growth exposure, as their childhoods were negatively affected by traumatic events. Some significant associations were found between maltreatment and adolescent drug abuse, although the former factor was limited to the female gender [ 25 , 30 , 36 ]. One possible reason for the contrasting results between genders is the different sample populations, which only covered child welfare centers [ 36 ] and foster care [ 30 ]. Regardless of the place, maltreatment can happen anywhere depending on the presence of the perpetrators. To date, evidence that concretely links maltreatment and substance abuse remains limited. However, a plausible explanation for this link could be the indirect effects of posttraumatic stress (i.e., a history of maltreatment) leading to substance use [ 53 , 54 ]. These findings highlight the importance of continuous monitoring and follow-ups with adolescents who have a history of maltreatment and who have ever attended a welfare center.
Addiction sometimes leads to another addiction, as described by the findings of several studies [ 29 , 34 ]. An initial study focused on the effects of e-cigarettes in the development of other substance abuse disorders, particularly those related to marijuana, alcohol, and commonly prescribed medications [ 34 ]. The authors found that the use of e-cigarettes can lead to more severe substance addiction [ 55 ], possibly through normalization of the behavior. On the other hand, Chuang et al.’s extensive study in 2017 analyzed the combined effects of either multiple addictions alone or a combination of multiple addictions together with the impulsivity trait [ 29 ]. The outcomes reported were intriguing and provide the opportunity for targeted intervention. The synergistic effects of impulsiveness and three other substance addictions (marijuana, tobacco, and alcohol) substantially increased the likelihood for drug abuse from 3.46 (95%CI 1.25, 9.58) to 10.13 (95% CI 3.95, 25.95). Therefore, proper rehabilitation is an important strategy to ensure that one addiction will not lead to another addiction.
The likelihood for drug abuse increases as the population perceives little or no harmful risks associated with the drugs. On the opposite side of the coin, a greater perceived risk remains a protective factor for marijuana abuse [ 56 ]. However, another study noted that a stronger determinant for adolescent drug abuse was the perceived availability of the drug [ 35 , 57 ]. Looking at the bigger picture, both perceptions corroborate each other and may inform drug use. Another study, on the other hand, reported that there was a decreasing trend of perceived drug risk in conjunction with the increasing usage of drugs [ 58 ]. As more people do drugs, youth may inevitably perceive those drugs as an acceptable norm without any harmful consequences [ 59 ].
In addition, the total spent for screen time also contribute to drug abuse among adolescent [ 43 ]. This scenario has been proven by many researchers on the effect of screen time on the mental health [ 60 ] that leads to the substance use among the adolescent due to the ubiquity of pro-substance use content on the internet. Adolescent with comorbidity who needs medical pain management by opioids also tend to misuse in future. A qualitative exploration on the perspectives among general practitioners concerning the risk of opioid misuse in people with pain, showed pain management by opioids is a default treatment and misuse is not a main problem for the them [ 61 ]. A careful decision on the use of opioids as a pain management should be consider among the adolescents and their understanding is needed.
Within the family factor domain, family structures were found to have both positive and negative associations with drug abuse among adolescents. As described in one study, paternal knowledge was consistently found to be a protective factor against substance abuse [ 26 ]. With sufficient knowledge, the father can serve as the guardian of his family to monitor and protect his children from negative influences [ 62 ]. The work by Luk et al. also reported a positive association of maternal psychological association towards drug abuse (IRR 2.41, p < 0.05) [ 26 ]. The authors also observed the same effect of paternal psychological control, although it was statistically insignificant. This construct relates to parenting style, and the authors argued that parenting style might have a profound effect on the outcomes under study. While an earlier literature review [ 63 ] also reported such a relationship, a recent study showed a lesser impact [ 64 ] with regards to neglectful parenting styles leading to poorer substance abuse outcomes. Nevertheless, it was highlighted in another study that the adolescents’ perception of a neglectful parenting style increased their odds (OR 2.14, p = 0.012) of developing alcohol abuse, not the parenting style itself [ 65 ]. Altogether, families play vital roles in adolescents’ risk for engaging in substance abuse [ 66 ]. Therefore, any intervention to impede the initiation of substance use or curb existing substance use among adolescents needs to include parents—especially improving parent–child communication and ensuring that parents monitor their children’s activities.
Finally, the community also contributes to drug abuse among adolescents. As shown by Li et al. [ 32 ] and El Kazdouh et al. [ 46 ], peers exert a certain influence on other teenagers by making them subconsciously want to fit into the group. Peer selection and peer socialization processes might explain why peer pressure serves as a risk factor for drug-abuse among adolescents [ 67 ]. Another study reported that strong religious beliefs integrated into society play a crucial role in preventing adolescents from engaging in drug abuse [ 46 ]. Most religions devalue any actions that can cause harmful health effects, such as substance abuse [ 68 ]. Hence, spiritual beliefs may help protect adolescents. This theme has been well established in many studies [ 60 , 69 , 70 , 71 , 72 ] and, therefore, could be implemented by religious societies as part of interventions to curb the issue of adolescent drug abuse. The connection with school and structured activity did reduce the risk as a study in USA found exposure to media anti-drug messages had an indirect negative effect on substances abuse through school-related activity and social activity [ 73 ]. The school activity should highlight on the importance of developmental perspective when designing and offering school-based prevention programs [75].
Limitations
We adopted a review approach that synthesized existing evidence on the risk and protective factors of adolescents engaging in drug abuse. Although this systematic review builds on the conclusion of a rigorous review of studies in different settings, there are some potential limitations to this work. We may have missed some other important factors, as we only included English articles, and article extraction was only done from the three search engines mentioned. Nonetheless, this review focused on worldwide drug abuse studies, rather than the broader context of substance abuse including alcohol and cigarettes, thereby making this paper more focused.
Conclusions
This review has addressed some recent knowledge related to the individual, familial, and community risk and preventive factors for adolescent drug use. We suggest that more attention should be given to individual factors since most findings were discussed in relation to such factors. With the increasing trend of drug abuse, it will be critical to focus research specifically on this area. Localized studies, especially those related to demographic factors, may be more effective in generating results that are specific to particular areas and thus may be more useful in generating and assessing local control and prevention efforts. Interventions using different theory-based psychotherapies and a recognition of the unique developmental milestones specific to adolescents are among examples that can be used. Relevant holistic approaches should be strengthened not only by relevant government agencies but also by the private sector and non-governmental organizations by promoting protective factors while reducing risk factors in programs involving adolescents from primary school up to adulthood to prevent and control drug abuse. Finally, legal legislation and enforcement against drug abuse should be engaged with regularly as part of our commitment to combat this public health burden.
Data availability and materials
All data generated or analysed during this study are included in this published article.
Nation, U. World Drug Report 2018 (United Nations publication, Sales No. E.18X.XI.9. United Nation publication). 2018. Retrieved from https://www.unodc.org/wdr2018
Google Scholar
Degenhardt L, Stockings E, Patton G, Hall WD, Lynskey M. The increasing global health priority of substance use in young people. Lancet Psychiatry. 2016;3(3):251–64. https://doi.org/10.1016/S2215-0366(15)00508-8 Elsevier Ltd.
Article PubMed Google Scholar
Ritchie H, Roser M. Drug Use - Our World in Data: Global Change Data Lab; 2019. https://ourworldindata.org/drug-use [10 June 2020]
Holm S, Sandberg S, Kolind T, Hesse M. The importance of cannabis culture in young adult cannabis use. J Subst Abus. 2014;19(3):251–6.
Luikinga SJ, Kim JH, Perry CJ. Developmental perspectives on methamphetamine abuse: exploring adolescent vulnerabilities on brain and behavior. Progress Neuro Psychopharmacol Biol Psychiatry. 2018;87(Pt A):78–84. https://doi.org/10.1016/j.pnpbp.2017.11.010 Elsevier Inc.
Article CAS Google Scholar
Ismail R, Ghazalli MN, Ibrahim N. Not all developmental assets can predict negative mental health outcomes of disadvantaged youth: a case of suburban Kuala Lumpur. Mediterr J Soc Sci. 2015;6(1):452–9. https://doi.org/10.5901/mjss.2015.v6n5s1p452 .
Article Google Scholar
Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86(2):189–99. https://doi.org/10.1016/j.pbb.2006.12.001 .
Article CAS PubMed Google Scholar
Schulte MT, Hser YI. Substance use and associated health conditions throughout the lifespan. Public Health Rev. 2013;35(2). https://doi.org/10.1007/bf03391702 Technosdar Ltd.
Somani, S.; Meghani S. Substance Abuse among Youth: A Harsh Reality 2016. doi: https://doi.org/10.4172/2165-7548.1000330 , 6, 4.
Book Google Scholar
Drabble L, Trocki KF, Klinger JL. Religiosity as a protective factor for hazardous drinking and drug use among sexual minority and heterosexual women: findings from the National Alcohol Survey. Drug Alcohol Depend. 2016;161:127–34. https://doi.org/10.1016/j.drugalcdep.2016.01.022 .
Article PubMed PubMed Central Google Scholar
Goliath V, Pretorius B. Peer risk and protective factors in adolescence: Implications for drug use prevention. Soc Work. 2016;52(1):113–29. https://doi.org/10.15270/52-1-482 .
Guerrero LR, Dudovitz R, Chung PJ, Dosanjh KK, Wong MD. Grit: a potential protective factor against substance use and other risk behaviors among Latino adolescents. Acad Pediatr. 2016;16(3):275–81. https://doi.org/10.1016/j.acap.2015.12.016 .
National Institutes on Drug Abuse. What are risk factors and protective factors? National Institute on Drug Abuse (NIDA); 2003. Retrieved from https://www.drugabuse.gov/publications/preventing-drug-use-among-children-adolescents/chapter-1-risk-factors-protective-factors/what-are-risk-factors
Nguyen NN, Newhill CE. The role of religiosity as a protective factor against marijuana use among African American, White, Asian, and Hispanic adolescents. J Subst Abus. 2016;21(5):547–52. https://doi.org/10.3109/14659891.2015.1093558 .
Schinke S, Schwinn T, Hopkins J, Wahlstrom L. Drug abuse risk and protective factors among Hispanic adolescents. Prev Med Rep. 2016;3:185–8. https://doi.org/10.1016/j.pmedr.2016.01.012 .
Macleod J, Oakes R, Copello A, Crome PI, Egger PM, Hickman M, et al. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 2004;363(9421):1579–88. https://doi.org/10.1016/S0140-6736(04)16200-4 .
Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28. https://doi.org/10.1016/S0140-6736(07)61162-3 .
Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187–94. https://doi.org/10.1177/0269881105049040 .
Nargiso JE, Ballard EL, Skeer MR. A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the united states: A social ecological perspective. J Stud Alcohol Drugs. 2015;76(1):5–20. https://doi.org/10.15288/jsad.2015.76.5 .
Guxensa M, Nebot M, Ariza C, Ochoa D. Factors associated with the onset of cannabis use: a systematic review of cohort studies. Gac Sanit. 2007;21(3):252–60. https://doi.org/10.1157/13106811 .
Susan MS, Peter SA, Dakshitha W, George CP. The age of adolescence. Lancet Child Adolesc Health. 2018;2(Issue 3):223–8. https://doi.org/10.1016/S2352-4642(18)30022-1 .
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91. https://doi.org/10.3233/EFI-180221 .
McHugh ML. Interrater reliability: The kappa statistic. Biochem Med. 2012;22(3):276–82. https://doi.org/10.11613/bm.2012.031 .
Cecil CAM, Walton E, Smith RG, Viding E, McCrory EJ, Relton CL, et al. DNA methylation and substance-use risk: a prospective, genome-wide study spanning gestation to adolescence. Transl Psychiatry. 2016;6(12):e976. https://doi.org/10.1038/tp.2016.247 Nature Publishing Group.
Article CAS PubMed PubMed Central Google Scholar
Kobulsky JM. Gender differences in pathways from physical and sexual abuse to early substance use. Child Youth Serv Rev. 2017;83:25–32. https://doi.org/10.1016/j.childyouth.2017.10.027 .
Luk JW, King KM, McCarty CA, McCauley E, Stoep A. Prospective effects of parenting on substance use and problems across Asian/Pacific islander and European American youth: Tests of moderated mediation. J Stud Alcohol Drugs. 2017;78(4):521–30. https://doi.org/10.15288/jsad.2017.78.521 .
Guttmannova K, Skinner ML, Oesterle S, White HR, Catalano RF, Hawkins JD. The interplay between marijuana-specific risk factors and marijuana use over the course of adolescence. Prev Sci. 2019;20(2):235–45. https://doi.org/10.1007/s11121-018-0882-9 .
Dorard G, Bungener C, Phan O, Edel Y, Corcos M, Berthoz S. Is alexithymia related to cannabis use disorder? Results from a case-control study in outpatient adolescent cannabis abusers. J Psychosom Res. 2017;95:74–80. https://doi.org/10.1016/j.jpsychores.2017.02.012 .
Chuang CWI, Sussman S, Stone MD, Pang RD, Chou CP, Leventhal AM, et al. Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addict Behav. 2017;74:41–7. https://doi.org/10.1016/j.addbeh.2017.05.021 .
Gabrielli J, Jackson Y, Brown S. Associations between maltreatment history and severity of substance use behavior in youth in Foster Care. Child Maltreat. 2016;21(4):298–307. https://doi.org/10.1177/1077559516669443 .
Khoddam R, Jackson NJ, Leventhal AM. Internalizing symptoms and conduct problems: redundant, incremental, or interactive risk factors for adolescent substance use during the first year of high school? Drug Alcohol Depend. 2016;169:48–55. https://doi.org/10.1016/j.drugalcdep.2016.10.007 .
Li SD, Zhang X, Tang W, Xia Y. Predictors and implications of synthetic drug use among adolescents in the gambling Capital of China. SAGE Open. 2017;7(4):215824401773303. https://doi.org/10.1177/2158244017733031 .
Marin S, Heshmatian E, Nadrian H, Fakhari A, Mohammadpoorasl A. Associations between optimism, tobacco smoking and substance abuse among Iranian high school students. Health Promot Perspect. 2019;9(4):279–84. https://doi.org/10.15171/hpp.2019.38 .
Miech RA, O’Malley PM, Johnston LD, Patrick ME. E-cigarettes and the drug use patterns of adolescents. Nicotine Tob Res. 2015;18(5):654–9. https://doi.org/10.1093/ntr/ntv217 .
Schleimer JP, Rivera-Aguirre AE, Castillo-Carniglia A, Laqueur HS, Rudolph KE, Suárez H, et al. Investigating how perceived risk and availability of marijuana relate to marijuana use among adolescents in Argentina, Chile, and Uruguay over time. Drug Alcohol Depend. 2019;201:115–26. https://doi.org/10.1016/j.drugalcdep.2019.03.029 .
Traube DE, Yarnell LM, Schrager SM. Differences in polysubstance use among youth in the child welfare system: toward a better understanding of the highest-risk teens. Child Abuse Negl. 2016;52:146–57. https://doi.org/10.1016/j.chiabu.2015.11.020 .
Wilson JD, Vo H, Matson P, Adger H, Barnett G, Fishman M. Trait mindfulness and progression to injection use in youth with opioid addiction. Subst Use Misuse. 2017;52(11):1486–93. https://doi.org/10.1080/10826084.2017.1289225 .
Dash GF, Feldstein Ewing SW, Murphy C, Hudson KA, Wilson AC. Contextual risk among adolescents receiving opioid prescriptions for acute pain in pediatric ambulatory care settings. Addict Behav. 2020;104:106314. https://doi.org/10.1016/j.addbeh.2020.106314 Epub 2020 Jan 11. PMID: 31962289; PMCID: PMC7024039.
Osborne V, Serdarevic M, Striley CW, Nixon SJ, Winterstein AG, Cottler LB. Age of first use of prescription opioids and prescription opioid non-medical use among older adolescents. Substance Use Misuse. 2020;55(14):2420–7. https://doi.org/10.1080/10826084.2020.1823420 .
Zuckermann AME, Qian W, Battista K, Jiang Y, de Groh M, Leatherdale ST. Factors influencing the non-medical use of prescription opioids among youth: results from the COMPASS study. J Subst Abus. 2020;25(5):507–14. https://doi.org/10.1080/14659891.2020.1736669 .
De Pedro KT, Esqueda MC, Gilreath TD. School protective factors and substance use among lesbian, gay, and bisexual adolescents in California public schools. LGBT Health. 2017;4(3):210–6. https://doi.org/10.1089/lgbt.2016.0132 .
Spillane NS, Schick MR, Kirk-Provencher KT, Hill DC, Wyatt J, Jackson KM. Structured and unstructured activities and alcohol and marijuana use in middle school: the role of availability and engagement. Substance Use Misuse. 2020;55(11):1765–73. https://doi.org/10.1080/10826084.2020.1762652 .
Ogunsola OO, Fatusi AO. Risk and protective factors for adolescent substance use: a comparative study of secondary school students in rural and urban areas of Osun state, Nigeria. Int J Adolesc Med Health. 2016;29(3). https://doi.org/10.1515/ijamh-2015-0096 .
Doggett A, Qian W, Godin K, De Groh M, Leatherdale ST. Examining the association between exposure to various screen time sedentary behaviours and cannabis use among youth in the COMPASS study. SSM Population Health. 2019;9:100487. https://doi.org/10.1016/j.ssmph.2019.100487 .
Afifi RA, El Asmar K, Bteddini D, Assi M, Yassin N, Bitar S, et al. Bullying victimization and use of substances in high school: does religiosity moderate the association? J Relig Health. 2020;59(1):334–50. https://doi.org/10.1007/s10943-019-00789-8 .
El Kazdouh H, El-Ammari A, Bouftini S, El Fakir S, El Achhab Y. Adolescents, parents and teachers’ perceptions of risk and protective factors of substance use in Moroccan adolescents: a qualitative study. Substance Abuse Treat Prevent Policy. 2018;13(1):–31. https://doi.org/10.1186/s13011-018-0169-y .
Sussman S, Lisha N, Griffiths M. Prevalence of the addictions: a problem of the majority or the minority? Eval Health Prof. 2011;34(1):3–56. https://doi.org/10.1177/0163278710380124 .
Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. https://doi.org/10.1016/j.cpr.2009.11.004 .
Ricketts T, Macaskill A. Gambling as emotion management: developing a grounded theory of problem gambling. Addict Res Theory. 2003;11(6):383–400. https://doi.org/10.1080/1606635031000062074 .
Williams AD, Grisham JR. Impulsivity, emotion regulation, and mindful attentional focus in compulsive buying. Cogn Ther Res. 2012;36(5):451–7. https://doi.org/10.1007/s10608-011-9384-9 .
National Institutes on Drug Abuse. Drugs, brains, and behavior the science of addiction national institute on drug abuse (nida). 2014. Retrieved from https://www.drugabuse.gov/sites/default/files/soa_2014.pdf
Hokm Abadi ME, Bakhti M, Nazemi M, Sedighi S, Mirzadeh Toroghi E. The relationship between personality traits and drug type among substance abuse. J Res Health. 2018;8(6):531–40.
Longman-Mills S, Haye W, Hamilton H, Brands B, Wright MGM, Cumsille F, et al. Psychological maltreatment and its relationship with substance abuse among university students in Kingston, Jamaica, vol. 24. Florianopolis: Texto Contexto Enferm; 2015. p. 63–8.
Rosenkranz SE, Muller RT, Henderson JL. The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychol Trauma Theory Res Pract Policy. 2014;6(1):25–33. https://doi.org/10.1037/a0031920 .
Krishnan-Sarin S, Morean M, Kong G, et al. E-Cigarettes and “dripping” among high-school youth. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-3224 .
Adinoff B. Neurobiologic processes in drug reward and addiction. Harvard review of psychiatry. NIH Public Access. 2004;12(6):305–20. https://doi.org/10.1080/10673220490910844 .
Kandel D, Kandel E. The gateway hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatrica. 2014;104(2):130–7.
Dempsey RC, McAlaney J, Helmer SM, Pischke CR, Akvardar Y, Bewick BM, et al. Normative perceptions of Cannabis use among European University students: associations of perceived peer use and peer attitudes with personal use and attitudes. J Stud Alcohol Drugs. 2016;77(5):740–8.
Cioffredi L, Kamon J, Turner W. Effects of depression, anxiety and screen use on adolescent substance use. Prevent Med Rep. 2021;22:101362. https://doi.org/10.1016/j.pmedr.2021.101362 .
Luckett T, NewtonJohn T, Phillips J, et al. Risk of opioid misuse in people with cancer and pain and related clinical considerations:a qualitative study of the perspectives of Australian general practitioners. BMJ Open. 2020;10(2):e034363. https://doi.org/10.1136/bmjopen-2019-034363 .
Lipari RN. Trends in Adolescent Substance Use and Perception of Risk from Substance Use. The CBHSQ Report. Substance Abuse Mental Health Serv Admin. 2013; Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27656743 .
Muchiri BW, dos Santos MML. Family management risk and protective factors for adolescent substance use in South Africa. Substance Abuse. 2018;13(1):24. https://doi.org/10.1186/s13011-018-0163-4 .
Becoña E, Martínez Ú, Calafat A, Juan M, Fernández-Hermida JR, Secades-Villa R. Parental styles and drug use: a review. In: Drugs: Education, Prevention and Policy: Taylor & Francis; 2012. https://doi.org/10.3109/09687637.2011.631060 .
Berge J, Sundel K, Ojehagen A, Hakansson A. Role of parenting styles in adolescent substance use: results from a Swedish longitudinal cohort study. BMJ Open. 2016;6(1):e008979. https://doi.org/10.1136/bmjopen-2015-008979 .
Opara I, Lardier DT, Reid RJ, Garcia-Reid P. “It all starts with the parents”: a qualitative study on protective factors for drug-use prevention among black and Hispanic girls. Affilia J Women Soc Work. 2019;34(2):199–218. https://doi.org/10.1177/0886109918822543 .
Martínez-Loredo V, Fernández-Artamendi S, Weidberg S, Pericot I, López-Núñez C, Fernández-Hermida J, et al. Parenting styles and alcohol use among adolescents: a longitudinal study. Eur J Invest Health Psychol Educ. 2016;6(1):27–36. https://doi.org/10.1989/ejihpe.v6i1.146 .
Baharudin MN, Mohamad M, Karim F. Drug-abuse inmates maqasid shariah quality of lifw: a conceotual paper. Hum Soc Sci Rev. 2020;8(3):1285–94. https://doi.org/10.18510/hssr.2020.83131 .
Henneberger AK, Mushonga DR, Preston AM. Peer influence and adolescent substance use: a systematic review of dynamic social network research. Adolesc Res Rev. 2020;6(1):57–73. https://doi.org/10.1007/s40894-019-00130-0 Springer.
Gomes FC, de Andrade AG, Izbicki R, Almeida AM, de Oliveira LG. Religion as a protective factor against drug use among Brazilian university students: a national survey. Rev Bras Psiquiatr. 2013;35(1):29–37. https://doi.org/10.1016/j.rbp.2012.05.010 .
Kulis S, Hodge DR, Ayers SL, Brown EF, Marsiglia FF. Spirituality and religion: intertwined protective factors for substance use among urban American Indian youth. Am J Drug Alcohol Abuse. 2012;38(5):444–9. https://doi.org/10.3109/00952990.2012.670338 .
Miller L, Davies M, Greenwald S. Religiosity and substance use and abuse among adolescents in the national comorbidity survey. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1190–7. https://doi.org/10.1097/00004583-200009000-00020 .
Moon SS, Rao U. Social activity, school-related activity, and anti-substance use media messages on adolescent tobacco and alcohol use. J Hum Behav Soc Environ. 2011;21(5):475–89. https://doi.org/10.1080/10911359.2011.566456 .
Simone A. Onrust, Roy Otten, Jeroen Lammers, Filip smit, school-based programmes to reduce and prevent substance use in different age groups: what works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev. 2016;44:45–59. https://doi.org/10.1016/j.cpr.2015.11.002 .
Download references
Acknowledgements
The authors acknowledge The Ministry of Higher Education Malaysia and The Universiti Kebangsaan Malaysia, (UKM) for funding this study under the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). We also thank the team for their commitment and tireless efforts in ensuring that manuscript was well executed.
Financial support for this study was obtained from the Ministry of Higher Education, Malaysia through the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Community Health, Universiti Kebangsaan Malaysia, Cheras, 56000, Kuala Lumpur, Malaysia
Azmawati Mohammed Nawi, Mohd Rohaizat Hassan & Mohd Rizal Abdul Manaf
Centre for Research in Psychology and Human Well-Being (PSiTra), Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, 43600, Bangi, Selangor, Malaysia
Rozmi Ismail, Fauziah Ibrahim & Nurul Shafini Shafurdin
Clinical Psychology and Behavioural Health Program, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Noh Amit & Norhayati Ibrahim
You can also search for this author in PubMed Google Scholar
Contributions
Manuscript concept, and drafting AMN and RI; model development, FI, NI and NA.; Editing manuscript MRH, MRAN, NSS,; Critical revision of manuscript for important intellectual content, all authors. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Rozmi Ismail .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the Secretariat of Research Ethics, Universiti Kebangsaan Malaysia, Faculty of Medicine, Cheras, Kuala Lumpur (Reference no. UKMPPI/111/8/JEP-2020.174(2). Dated 27 Mac 2020.
Consent for publication
Not applicable.
Competing interests
The authors AMN, RI, FI, MRM, MRAM, NA, NI NSS declare that they have no conflict of interest relevant to this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nawi, A.M., Ismail, R., Ibrahim, F. et al. Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health 21 , 2088 (2021). https://doi.org/10.1186/s12889-021-11906-2
Download citation
Received : 10 June 2021
Accepted : 22 September 2021
Published : 13 November 2021
DOI : https://doi.org/10.1186/s12889-021-11906-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug abuse, substance, adolescent
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Substance Abuse A Literature Review of the Implications and Solutions

2019, International Journal of Scientific & Engineering Research Volume 10, Issue 10, October-2019
Substance or Drug abuse is a serious public health problem affecting usually adolescents and young adults. It affects both males and females and it is the major source of crimes in youth and health related problems in many communities. It harms unborn babies and destroys fami lies. As indicated by the Diagnostic and Statistical Manual of Mental Disorder, Fifth Edition, DSM DSM-5 “ The essent ial feature of substance use disorder is a cluster of cognitive, behavioral and physiological symptoms indicating the individual continues to use the substance despite significant substance related problems”. SubstanceSubstances that are abused are many and include alcohol, tobacco/nicotine, caffeine, cannabis, inhalants, opioids , sedatives, anti anti-anxiety and hypnotics, psychostimulants like cocaine, amphetamine, methamphethamine and hallucinogens.
Related Papers
Noorul Amin
Substance abuse is also known as drug abuse. It is a rapidly growing menace in India and so in the erstwhile princely state of Jammu and Kashmir. This problem places a huge burden on society as it generates loopholes in the physical, mental, familial, financial, legal and social fabrics of our life in the community. The common terms that are used to identify these maladaptive behaviors are drug addicts, substance user, alcoholic or more community based terms like baivda, charsi, drunkard, etc. These problems of substance abuse like alcohol, tobacco, opioids, cannabis etc. need to be stopped and ways are to identified to keep the younger generation away from this new and growing problem of drug addiction. Statistics have proved that youth in Kashmir are inclined to substances and are slowly and steadily going in the lap of substance use disorders.
Substance Abuse Disorders
Nicolas Clark , Vladimir Poznyak
Nicoletta Clementi
Siniša Franjić
The beginning of tobacco, alcohol and psychoactive drug use usually occurs during adolescence, and young people are, due to the specifics of growing up, relative inexperience and a certain youthful propensity to risk, the most vulnerable population group to adopt and develop addictive behavior. It is a well-known fact that drug abuse among children and young people has increased in recent years. Illegal drugs are abused-marijuana, hashish, LSD, amphetamines, ecstasy, heroin, cocaine, but also legal alcohol and tobacco, as well as household substances-glue, gasoline, gas and home pharmacies such as sedatives. The combination of all these substances is not uncommon. Young people start taking drugs very early, most often in high school, sometimes already in primary school, and the transition to high school is especially risky. Children and young people start taking drugs for a variety of reasons: out of a desire to feel like an adult, a desire to fit in and belong to a group, a desire to relax and feel good, a desire to rebel and take risks, out of curiosity. Many experiment with drugs, or take them just to taste, some become occasional or regular users, and some develop addictions. When it comes to traditional drugs such as alcohol and tobacco, many young people will start taking them believing that it is also a socially acceptable way of behaving even if they are aware of the possible harmful effects on health, they believe that, since this is done by a large number of adults, the consequences are not inevitable. Most young people, however, only experiment with various drugs that can be addictive, and during adolescence the habit stops or becomes established as moderate. In a number of cases, abuse develops to the point that it begins to interfere with schooling, family relationships, social life, and productivity in general. Then we talk about addiction.
International Journal of Psychiatry in Clinical Practice
Patrick Weledji
Substance misuse has a profound effect in terms of harm across all areas of society. This includes high costs in terms of healthcare provision, social and economic costs as well as the effect on individuals and their families. Maintaining abstinence via psychosocial interventions is the key to reducing the prevalence but also the most difficult to achieve because of the opposing neurophysiological forces. This paper briefly reviewed the sequelae of dependence with alcohol, opiates and stimulants and the dilemma in management. Methods: Electronic searches of the medline (PubMed) database, Cochrane library, and science citation index were performed to identify original published studies on substance abuse and drug dependence. Relevant articles were searched from relevant chapters in specialized texts and all included.
Journal of emerging technologies and innovative research
Dr.Anjali Sahai
Leonard Saxe
Journal of Nursing Ufpe on Line Jnuol Doi 10 5205 01012007
Giovana Gomes
Putul Mahanta
Drug abuse and dependence ‘represents different ends ’ the same disease processes. Over the long-term, this dependence results in physical harms, behavioral problems and association with people that have seen seems abused. The actions of drugs are misused in all fields. This misused is not limited to therapeutic purposes, but to terminate the frustrated lives as well. During the past few years, dramatic changes have occurred in the field of drugs abuse. Magnificent increases is everywhere in the number of drug users who are the member of dominant culture. These users turn to some form of crude amateur crime like burglary, robbery and even the prostitution to support their habits. Juvenile’s addiction in the larger cities has become a major problem causing substantial harm to the society. The medico legal, social, moral and ethical issues will be briefed here.
Journal of Advanced Research in Humanities and Social Sciences
Dr. J Balamurugan PhD
Reviews the literature and states that appropriate research describing initial use of illicit drugs suggests that disruption of normal child-parent relationships, lack of involvement in organized groups, and few effective peer relationships may have been predisposing factors in some individuals initiating use of illicit drugs. Research also suggests that socialization to nontraditional norms, parental modeling of licit and illicit drug use, involvement with drug-using peers, and positive experiences with drugs may have been important factors in initial use for other individuals. It is concluded that both theory and research need a clear distinction between the several paths leading to initial drug abuse, particularly since separate statistical analyses may be necessary for people in each path.
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
International Journal of Humanities and Social Science
JACKSON DECARVALHO
ISAIAH ABIERO
Peertechz Journals
المجلة العراقية للصيدلة
IP Innovative Publication Pvt. Ltd.
hannah appiah kubi
International Journal of Scientific and Research Publications (IJSRP)
CHUKWUNWIKE NWONU
The International Journal of Indian Psychology
Pradeep Gupta
asmita rannaware
Adolescent and Youth Health
Ifemed Journal
Archiv Euromedica
Lucretia Anghel
International Journal of Medical Reviews
Khodabakhsh Ahmadi
Clinical pharmacology and therapeutics
Rachel Tyndale
Azrah Hassan
American Journal of Psychiatry
James T Barter, MD
Derege Kebede
Ivor Ebenezer
Richard Hammersley
HSOA Journal of Addiction & Addictive Disorders
OGUCHE T H A N K G O D E Emmanuel
ibuathu njati
Kurt Michael
donna kirkby
Journal of the American Academy of Nurse Practitioners
Madeline Naegle
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
The use of drugs and medical students: a literature review
Affiliations.
- 1 4Th-year Medical Students fo the State University of Ponta Grossa (PR), Brazil.
- 2 Master in Science and Technology Teaching; Associate Professor of the Medical Program of the State University of Ponta Grossa (PR), Brazil.
- 3 PhD in Internal Medicine; Adjunct Professor of Medicine at the Ponta Grossa State University (UEPG), Ponta Grossa (PR), Brazil.
- PMID: 30304147
- DOI: 10.1590/1806-9282.64.05.462
Introduction: The consumption and abuse of alcohol and other drugs are increasingly present in the lives of university students and may already be considered a public health problem because of the direct impacts on the physical and mental health of these individuals. The requirements of the medical program play a vital role in the increasing rate of drug users.
Objectives: To carry out a systematic review of the literature on the use of drugs, licit or not, in Brazilian medical students.
Methods: A descriptive-exploratory study, in which the SciELO and MEDLINE databases were used. A total of 99 articles were found, of which 16 were selected for this review.
Results: Alcohol and tobacco were the most frequently used licit drugs among medical students. The most consumed illicit drugs were marijuana, solvents, "lança-perfume" (ether spray), and anxiolytics. The male genre presented a tendency of consuming more significant amounts of all kinds of drugs, with the exception of tranquilizers. It was found an increasing prevalence of drug consumption in medical students, as the program progressed, which may result from the intrinsic stress from medical school activities. Students who do not use psychoactive drugs are more likely to live with their parents, to disapprove drugs consumption, to practice religious beliefs and to be employed.
Conclusion: The prevalence of licit and illicit drug use among medical students is high, even though they understand the injuries it may cause.
PubMed Disclaimer
Similar articles
- Licit and illicit drug use in cluster headache. Govare A, Leroux E. Govare A, et al. Curr Pain Headache Rep. 2014 May;18(5):413. doi: 10.1007/s11916-014-0413-8. Curr Pain Headache Rep. 2014. PMID: 24715619 Review.
- Medical students: abuse of psychoactive substances and sexuality aspects. Carvalho KA, Sant'Anna MJ, Coates V, Omar HA. Carvalho KA, et al. Int J Adolesc Med Health. 2008 Jul-Sep;20(3):321-8. doi: 10.1515/ijamh.2008.20.3.321. Int J Adolesc Med Health. 2008. PMID: 19097570
- Use of licit and illicit drugs at the University of Alfenas. Fiorini JE, Alves AL, Ferreira LR, Fiorini CM, Durães SW, Santos RL, Nascimento LC, Geraldini AM, Ortiz Cde F. Fiorini JE, et al. Rev Hosp Clin Fac Med Sao Paulo. 2003 Jul-Aug;58(4):199-206. doi: 10.1590/s0041-87812003000400003. Epub 2003 Sep 30. Rev Hosp Clin Fac Med Sao Paulo. 2003. PMID: 14534672
- Use of the inhalant lança by Brazilian medical students. Mesquita AM, de Andrade AG, Anthony JC. Mesquita AM, et al. Subst Use Misuse. 1998 Jun;33(8):1667-80. doi: 10.3109/10826089809058949. Subst Use Misuse. 1998. PMID: 9680087
- Psychoactive drug use by medical students: a review of the national and international literature. Mesquita AM, Laranjeira R, Dunn J. Mesquita AM, et al. Sao Paulo Med J. 1997 Jan-Feb;115(1):1356-65. doi: 10.1590/s1516-31801997000100007. Sao Paulo Med J. 1997. PMID: 9293117 Review.
- Cigarette Smoking, Risky Alcohol Consumption, and Marijuana Smoking among University Students in Germany: Identification of Potential Sociodemographic and Study-Related Risk Groups and Predictors of Consumption. Hoff TA, Heller S, Reichel JL, Werner AM, Schäfer M, Tibubos AN, Simon P, Beutel ME, Letzel S, Rigotti T, Dietz P. Hoff TA, et al. Healthcare (Basel). 2023 Dec 16;11(24):3182. doi: 10.3390/healthcare11243182. Healthcare (Basel). 2023. PMID: 38132073 Free PMC article.
- Gender differences in alcohol abuse/dependence among medical undergraduates during the post-COVID‑19 pandemic period (October 20, 2020-April 5, 2021) in China. Wang X, Peng P, Liu Y, Yang WF, Chen S, Wang Y, Yang Q, Li M, Wang Y, Hao Y, He L, Wang Q, Zhang J, Ma Y, He H, Zhou Y, Long J, Qi C, Tang YY, Liao Y, Tang J, Wu Q, Liu T. Wang X, et al. BMC Psychiatry. 2023 Oct 16;23(1):753. doi: 10.1186/s12888-023-05260-3. BMC Psychiatry. 2023. PMID: 37845643 Free PMC article.
- Risk factors for cardiovascular diseases during medical academic training. Thiago Faé M, Vier Gambetta M, Ramos N, Cristiane Lopes S, Oliveira Fischer Bacca C. Thiago Faé M, et al. Am J Cardiovasc Dis. 2023 Aug 15;13(4):252-263. eCollection 2023. Am J Cardiovasc Dis. 2023. PMID: 37736354 Free PMC article.
- Drug use among medical students in São Paulo, Brazil: a cross-sectional study during the coronavirus disease 2019 pandemic. Lemos-Santos P, Blumrich L, Debia JB, Castaldelli-Maia JM, Suen PJC, Malbergier A. Lemos-Santos P, et al. Sao Paulo Med J. 2023 Sep 8;142(2):e2022493. doi: 10.1590/1516-3180.2022.0493.R1.150623. eCollection 2023. Sao Paulo Med J. 2023. PMID: 37703121 Free PMC article.
- Does medical school cause depression or do medical students already begin their studies depressed? A longitudinal study over the first semester about depression and influencing factors. Pelzer A, Sapalidis A, Rabkow N, Pukas L, Günther N, Watzke S. Pelzer A, et al. GMS J Med Educ. 2022 Aug 4;39(5):Doc58. doi: 10.3205/zma001579. eCollection 2022. GMS J Med Educ. 2022. PMID: 36540560 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Scientific Electronic Library Online
- MedlinePlus Consumer Health Information
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Drug Addiction - Science topic

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

An official website of the United States government, Department of Justice.
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Substance Use Treatment Programs
Youth substance use treatment programs aim to reduce alcohol and illicit drug use, and the misuse of licit drugs, in youths who have been clinically diagnosed with a substance use problem. These programs differ from prevention programs, which aim to promote abstinence in youths to prevent their initial or escalating use. [1] Treatment programs can take a multitude of approaches, such as court-based, residential-based, and family-inclusive programs to help youth develop skills and knowledge to reduce substance use (Drake, 2012; Van Ryzin et al., 2016; Winters, Botzet, and Fahnhorst, 2011).
Substance use disorder in youth is a prevalent problem. An estimated 2.8 percent (712,000) of youths ages 12 to 17 experienced an alcohol use disorder in the past year, and 6.3 percent (1.6 million) of youths ages 12 to 17 experienced a substance use disorder in the past year (SAMSHA, 2021). However, the rate of utilization of substance use treatment programs is low. According to a study by Haughwout and colleagues (2016), fewer than 12 percent of youths who have a substance use disorder participate in treatment.
This literature review focuses on substance use disorder among youths under 18 and on the utilization of substance use treatment programs. The review describes the scope of substance use among youth, the theoretical base of substance-use treatment programs, risk factors that can lead to substance use disorders, protective factors that can buffer against substance use disorders, various types of treatment programs and outcome evidence, limitations to treatment programs, and the research currently available.
[1] For more information, see the Model Programs Guide literature review on Substance Use Prevention Programs .
Scope of the Problem
Overview of substance use disorders.
Among youth in the United States, it is estimated that 8 percent will experience an alcohol use disorder, and 2 percent to 3 percent will experience an illicit drug use disorder before turning 18 Merikangas et al., 2010; Swendsen et al., 2012; SAMSHA, 2011). Several surveys collect information on youths' self-reported use of alcohol and their use of illicit [1] and licit [2] drugs. These self-reported data are then used to calculate the prevalence rates of youth substance use (such as 30-day prevalence in alcohol use or past-year use of narcotics). However, few surveys collect information specifically regarding the prevalence of substance use disorders in youth. Substance use disorder is a diagnosable condition of ongoing and habitual use, and is distinct from substance use, which refers to episodes of occasional use. Most of the information provided below on prevalence rates of youth substance use disorders (and specific disorders such as alcohol use disorder) come from one survey, the National Survey on Drug Use and Health ( NSDUH ), which is the most comprehensive and up-to-date federal survey.
The NSDUH is administered by the Substance Abuse and Mental Health Services Administration (SAMHSA) and collects national and state-level data annually from all 50 states and the District of Columbia. In 2020, more than 36,000 people ages 12 and older were surveyed, including 6,337 interviews conducted with youths ages 12 to 17. Findings pertaining to substance use disorders—including alcohol use disorder, illicit drug use disorder, and more-specific disorders resulting from marijuana, cocaine, heroin, prescription pain reliever, or opioid use—are presented in an annual report.
In general, rates of substance use disorder among youth have declined and leveled off since the first decade of the 2000s. Specifically, among 12- to 17-year-olds, past-year alcohol use disorder declined from 5.9 percent (or 1.5 million youths) in 2002 to 1.7 percent (or 414,000 youths) in 2019. Within the same age group, 3.4 percent (or 894,000 youths) had a past-year illicit drug use disorder in 2019, which was higher than estimates in 2017 and 2018, but similar to estimates in 2015 and 2016. [3
In 2020 the NSDUH used the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ( DSM–5 ) criteria to assess substance use disorder. The DSM-5 is the most current diagnostic tool published by the American Psychiatric Association (APA), and it serves as the principal authority for psychiatric diagnoses. Previous surveys used the DSM–4 criteria, meaning that the 2020 findings cannot be easily compared with previous years. In 2020, respondents were identified as having a substance use disorder if they met two or more of the following criteria in a 12-month period:
- Consuming the substance in larger amounts or over a longer period of time than intended.
- Desiring to cut back on or stop use of the substance but being unsuccessful in these attempts.
- Spending a significant amount of time obtaining, using, or recovering from using the substance.
- Experiencing cravings and urges to use the substance.
- Failing to meet school, home, or work obligations because of substance use.
- Continuing to use the substance despite problems it has caused.
- Giving up important social, occupational, or recreational activities because of substance use.
- Continuing to use substances, even in situations where it is physically dangerous.
- Continuing to use substances, despite having physical or psychological problems that may have been caused or made worse by the substance.
- Needing more of the substance to achieve the desired effect (increased tolerance).
- Development of withdrawal symptoms, which can be relieved by taking more of the substance.
Using these criteria, it was estimated that 6.3 percent (1.6 million) of youths ages 12 to 17 experienced a substance use disorder in the past year (SAMHSA, 2021).

Alcohol Use Disorder
Alcohol is the most commonly used drug among youth (NIAAA, 2022). According to the 2020 NSDUH, 8.2 percent of youths reported using alcohol in the past month, 4.1 percent reported binge alcohol use, and 0.6 percent reported heavy alcohol use [4] in the past month (SAMHSA, 2021). However, while any alcohol use by youths is problematic, not all youths who drink alcohol meet the criteria for an alcohol use disorder.
The NSDUH identified respondents as having alcohol use disorder if they had used alcohol on 6 or more days in the past 12 months and if they also met two or more of the DSM–5 criteria for alcohol use disorder. The criteria for alcohol use disorder are as follows:
- Used alcohol in larger amounts or for a longer time period than intended.
- Had a persistent desire or made unsuccessful attempts to cut down on alcohol use.
- Spent a great deal of time in activities to obtain, use, or recover from alcohol use.
- Felt a craving or strong desire to use alcohol.
- Engaged in recurrent alcohol use resulting in failure to fulfill major role obligations at work, school, or home.
- Continued to use alcohol despite social or interpersonal problems caused by the effects of alcohol.
- Gave up or reduced important social, occupational, or recreational activities because of alcohol use.
- Continued to use alcohol in physically hazardous situations.
- Continued to use alcohol despite physical or psychological problems caused by alcohol use.
- Developed tolerance (i.e., needed to use alcohol more than before to get desired effects or noticing that the same amount of alcohol had less effect than before.
- Experienced a required number of withdrawal symptoms after cutting back or stopping alcohol use.
Based on these requirements, the NSDUH estimated that 2.8 percent (712,000) of youths ages 12 to 17 experienced alcohol use disorder in the past year.
Illicit Drug Use Disorder
Many youths experiment with illicit drugs, in addition to alcohol. In 2020, 13.8 percent of youths who responded to the NSDUH indicated past-year illicit drug use (SAMHSA, 2021). However, not all youths who engage in illicit drug use will meet the criteria for an illicit drug use disorder.
The NSDUH identified respondents as having an illicit drug use disorder if they met the DSM–5 substance use disorder criteria (described above under Overview of Substance Use Disorders) for one or more of the following illicit drugs: marijuana, cocaine, heroin, hallucinogens, inhalants, methamphetamine, or prescription psychotherapeutic drugs (stimulants, tranquilizers or sedatives, and pain relievers). For respondents whose drug use concentrated on a certain substance, specific disorders (such as marijuana use disorder, opioid use disorder, prescription pain reliever use disorder, cocaine use disorder, and heroin use disorder) were included.
In 2020, using past-year use rates among 12- to 17-year-olds, the NSDUH (SAMHSA, 2021) estimated that 4.9 percent (1.4 million youths) met criteria for at least one illicit drug use disorder. Specifically:
- 4.1 percent (1 million youths) met criteria for marijuana use disorder.
- 0.3 percent (80,000 youths) met criteria for opioid use disorder.
- 0.3 percent (80,000 youths) met criteria for prescription pain reliever use disorder.
- 0.1 percent (28,000 youths) met criteria for cocaine use disorder.
- Estimates for heroin use disorder could not be calculated with sufficient precision.
Co-Occurring Mental Health Disorders and Substance Use Disorders Among Youth
Youth substance use and mental health problems are commonly experienced simultaneously; an estimated 60 percent to 75 percent of youths with substance use disorders also have a co-occurring mental health disorder (Torrens et al., 2012; Burkstein and Horner, 2010; Chan, Dennis, and Funk, 2008; Turner et al., 2004; Hoffman et al., 2004). Common co-occurring mental health problems include conduct disorder, Attention Deficit Hyperactivity Disorder (ADHD), mood disorders, and trauma-related disorders (Burkstein and Horner, 2010).
Youths may turn to alcohol or drugs to help alleviate symptoms associated with mental health disorders, such as hopelessness, anxiety, irritability, or negative thoughts. However, substance use can have the opposite effect, which can lead to exacerbating and/or worsening these symptoms (Ramo et al., 2005). As a result, co-occurring disorders are associated with more-severe substance use disorder symptoms (Chan, Dennis, and Funk, 2008; Wise, Cuffe, and Fischer, 2001).
Research on co-occurring substance use disorder and mental health disorders in youth has largely focused on mood disorders, or mental health disorders that largely affect one’s emotional state such as depression and anxiety. Youths who have experienced a major depressive episode (MDE) are twice as likely to engage in alcohol or illicit drug use, compared with youths who have not experienced one (SAMHSA, 2021). Using DSM–5 criteria, youths were identified as having experienced an MDE if in the past year if 1) they had at least one period of 2 weeks or longer when, for most of the day nearly every day, they felt depressed or lost interest or pleasure in daily activities, and 2) they also had problems with sleeping, eating, energy, concentration, or self-worth or had recurrent thoughts of death or recurrent suicidal ideation. In 2020, 2.7 percent of adolescents surveyed (644,000 people) experienced a substance use disorder and a major depressive episode in the same year (SAMHSA, 2021). The 2020 NSDUH examined rates of substance use disorder in youths who experienced MDE in the past year. Based on these criteria, an estimated 2.7 percent (644,000) of youths ages 12 to 17 experienced both MDE and substance use disorder in the past year (SAMHSA, 2021).
Overall Key Findings
Findings from the NSDUH showed that 2.8 percent of youths ages 12 to 17 met the criteria for alcohol use disorder and 4.9 percent met the criteria for at least one illicit drug use disorder. T he most common type of illicit drug use disorder was marijuana use disorder (4.1 percent), with well under 1 percent of youths experiencing opioid, prescription pain reliever, or cocaine use disorder. The NSDUH also found that 2.7 percent of youths experienced both a substance use disorder and a major depressive episode. Yet, substance use treatment use remained low among youths who met the criteria for substance use disorder and therefore demonstrated a need for treatment (SAMHSA, 2021).
Differences in Substance Use Disorder by Gender
While many studies have described the differences between adult men and women in the prevalence of substance use disorders (e.g., Vasilenko, Evans–Polce, and Lanza, 2017), and some research have focused on the differences between adolescent boys and girls in substance use and initiation (e.g., Johnston et al., 2020), there is limited research on the difference in the prevalence of substance use disorders between adolescent boys and girls (Aarons et al., 2001; Gau et al., 2007; McHugh et al., 2018). For example, a study of prevalence of adolescent substance use disorders among youth ages 13 to 18 across five sectors of care (e.g., juvenile justice system, mental health system, child welfare) found that rates of substance use disorder were higher among males (Aarons et al., 2001). Also, a study from Taiwan found that boys were more likely than girls to develop substance use disorders in adolescence (Gau et al., 2007). Studies of older youth (ages 16 to 25) have found that documented opioid use disorder was higher for males than females (Bagley et al., 2021). However, several sources find that there is more gender parity in problematic substance use in adolescence than in adulthood (e.g., Young et al., 2002; McHugh et al., 2018) and that the differences by gender that had existed in the past have been getting smaller.
[1] Illicit drugs include marijuana (in 40 states), opioids (e.g., heroin), certain stimulants (e.g., methamphetamine, cocaine), hallucinogens (e.g., LSD), and dissociative drugs (e.g., PCP) [NIDA, 2020].
[2] Licit drugs include alcohol, nicotine (e.g., cigarettes), marijuana (as of 2022, in Alaska, California, Colorado, the District of Columbia, Maine, Massachusetts, Michigan, Nevada, Oregon, and Washington), certain stimulants (e.g., coffee), medicines used for illnesses, over-the-counter drugs used as directed, and prescription medicines used by the person to whom the drugs were prescribed (NIDA, 2020).
[3] The 2015 NSDUH was the first year during which estimates were provided for any illicit drug use disorder among youths. Previous years collected data on specific illicit drug use disorders only (e.g., marijuana, cocaine, and heroin use disorders).
[4] The NSDUH defines binge drinking for males as having 5 or more drinks on the same occasion at least 1 day in the past 30 days. Binge drinking for females is defined as having 4 or more drinks on the same occasion at least 1 day in the past 30. Heavy alcohol use is defined as binge drinking on 5 or more days in the past 30 days based on the thresholds described (SAMHSA, 2021).
Theoretical Background
The various treatment approaches for youths experiencing substance use disorders are grounded in numerous theories. These theories inform treatment programming that works to encourage behavioral change and improve youths’ interpersonal relationships (Liddle et al., 2018, Slesnick and Prestopnik, 2009, Akers et al., 1979). Prevalent theories underlying substance use disorder treatment programs for youth include various learning theories (i.e., cognitive–behavioral), family-based theories, and therapeutic justice. Also, several authors use self-determination theory to examine the influence of motivation in treatment engagement among youths (Bowers et al., 2017; Cleverley, Grenville, and Henderson, 2018).
Learning Theories. Classical, operant, and social learning theories have been applied to understand youths' substance use behavior and to inform treatment programming. Within these theories, substance use is viewed as behavior that is learned in the context of social interactions (e.g., observing parents, siblings, or peers) and that persists depending on whether there are rewards or punishments for the behavior (Akers et al., 1979). These theories inform behavior or cognitive–behavioral models that conceptualize adolescent substance use as learned behaviors initiated and maintained in the context of environmental factors (Waldron and Kaminer, 2004) and that can be changed by modifying thought processes or reinforcing new behaviors (Winters et al., 2018). With this, the majority of individual and group-based cognitive–behavioral treatments have involved multicomponent approaches of cognitive strategies, such as identifying distorted thinking patterns, combined with behavioral strategies, such as problem-solving, coping with cravings, and substance refusal skills training, which teach strategies for avoiding high-risk drug use situations (Waldron and Turner, 2008). These treatments help build youths' motivation to change by providing incentives for abstinence (Winters et al., 2018). Often, cognitive–behavioral therapy for substance use will include components such as self-monitoring, avoidance of stimulus cues, altering reinforcement contingencies, and coping-skills training to manage and resist urges to use. The use of modeling, behavior rehearsal, feedback, and homework assignments are characteristic during treatment sessions (Waldron and Kaminer, 2004).
Self-Determination Theory. This is a theory of human motivation based on three basic psychological needs: 1) autonomy, 2) competence, and 3) relatedness (Deci and Ryan, 2012; Ryan and Deci, 2000). It has been applied in many life domains, including substance use treatment engagement (Bowers et al., 2017; Groshkova, 2010). The theory proposes that there are several types of external motivation and that levels of engagement in treatment are determined by how individuals subjectively perceive these external pressures (Cleverley, Grenville, and Henderson, 2018; Deci and Ryan, 1985; Wild and Enzle, 2002). For example, youths often are extrinsically motivated by their parents to enter treatment. This could result in youths’ resentfully complying out of fear of consequences or, by contrast, understanding and accepting that substance use is an instrumental step toward a better future. These differing patient perceptions lead to different treatment experiences (Cleverley, Grenville, and Henderson, 2018; Ryan and Deci, 2000).
Family Systems Theory . General systems theory, which focuses on how the parts of a system interact with one another, helped inform development of family systems theory, which was developed in the late 1960s and early 1970s. Key concepts in family systems theory are feedback, homeostasis, and boundaries (Lander, Howsare, and Byrne, 2013). Homeostasis refers to the idea that it is the tendency of a system to seek stability and equilibrium (Brown and Christensen, 1986), and in family systems theory this means that each family member tends to function in such a way that keeps the whole system in balance, even if it is not healthy for specific individuals (Lander, Howsare, and Byrne, 2013). Feedback refers to the circular way in which parts of the family system communicate with one another. Finally, boundaries regulate interpersonal contact, either in a healthy way (e.g., boundaries define healthy adult and child roles in the family) or an unhealthy way (e.g., maintaining secrets) [Lander, Howsare, and Byrne, 2013].
Multiple models of family therapy have been developed using the family systems theory and focusing on improving family functioning and social relationships (Waldron and Turner, 2008; Liddle et al., 2009; Liddle et al., 2018), including the multisystemic family systems therapy model. Some treatment programs incorporate concepts from the crisis intervention theory , which contends that families are more amenable to counseling and open to change during a crisis (e.g., youth running away, youth using alcohol or drugs) [Slesnick and Prestopnik, 2009]. Therefore, these programs start by bringing the family together to address the immediate issues the youth is experiencing. In general, approaches that involve family are based on the therapeutic premise that the family has the most significant and long-lasting influence on adolescent development (Winters et al., 2018).
Although family is an important part of a young person's social environment and often is essential to resolving a young person's substance use problems, interventions at the family system level alone may not be sufficient depending on the individual's situation (Liddle, 1999). Therefore, many family and individual treatment approaches address the multiple systems that maintain youths' substance use, including individual, familial, and extrafamilial systems (Liddle, 1999). Many substance-use-treatment programs for youth integrate multiple therapeutic strategies within their treatment service framework, incorporating elements from family-based treatment, group and individual cognitive–behavioral therapy, motivational approaches, among others to enhance outcomes (Gray and Squeglia, 2018). Common components among them are teaching skills to resist the triggers associated with a youth's substance use, addressing life functioning issues that may have contributed to both the onset and maintenance of the substance use (including mental health and family issues), and identifying and building on a young person's strengths (Winters et al., 2018).
Therapeutic Jurisprudence. In addition, courts-based treatment programs for youth are often grounded in the theoretical perspective of therapeutic jurisprudence, which integrates knowledge of mental health and behavioral change with the implementation of law (Wilson, Olaghere, and Kimbrell, 2019). Under therapeutic jurisprudence, it is argued that legal rules and procedures can be used to improve the mental and physical well-being of youths (that is, justice-involved juveniles often with drug-involved offenses) within the court system. The emphasis under this model is on the selection of a therapeutic option that promotes health but does not conflict with the normative values of the justice system, such as due process (Rottman and Casey, 1999). Principles of therapeutic justice include close monitoring of a youth's behavior, multidisciplinary involvement, and collaboration with community-based and governmental organizations (Wilson, Olaghere, and Kimbrell, 2019). Drug courts are a primary example of court-based programs that use the principles of therapeutic jurisprudence (BJA, 2003).
Risk Factors for Substance Use Disorder
Risk factors [1] consist of personal traits, characteristics of the environment, and conditions in the family, school, and community that are linked to a youth's likelihood of engaging in delinquency and other problem behaviors such as substance use (Murray and Farrington, 2010). These risk factors can exist at the individual, peer, school, family, and community levels. Research on risk factors that can affect youths' likelihood of success in substance use treatment programs is largely limited; therefore, the research discussed below focuses on risk factors that are linked to a youth's likelihood of developing a substance use disorder. However, this research is limited, as many studies focus on risk factors of substance use initiation rather than on specific disorders (Bacio et al., 2015). Additional information on substance use initiation can be found in the Substance Use Prevention Programs Literature Review .
Individual . These risk factors include any characteristic directly related to or within a youth that affect the likelihood of their engaging in a specific behavior, such as substance use. These risk factors can stem from genetics, early moral development, personality traits, temperament, and negative life events (Development Services Group, 2015; Wong, Slotboom, and Bijleveld, 2010; Dick et al., 2013; Hodgins, Kratzer, and McNeil, 2001). For example, research has found that genetics play a role in the development of a substance use disorder in youth, and some biobehavioral traits attributed to predisposition for substance use disorders are influenced by genetics (Dick et al., 2013). However, studies emphasize that parenting and environmental factors affect risk factors related to genetics (Hines et al., 2015; Sloboda, Glantz, and Tarter, 2012; Prom–Wormley et al., 2017); this is seen especially in studies involving twins (Dick et al., 2013).
Other researchers have examined the effect of personality profiles on youth substance use disorders. One study found that youths with substance use disorders had greater levels of neuroticism, lower agreeableness, and lower conscientiousness than siblings of similar ages without substance use disorders (Anderson et al., 2007; Kotov et al., 2010).
As previously mentioned, various mental health disorders, such as Attention Deficit Hyperactivity Disorder (ADHD), conduct disorders, and mood disorders, are associated with substance use disorders (Lee et al., 2011; Mason et al., 2019; Torrens et al., 2012; Wilens et al., 2011). A 3-year longitudinal study of adolescents in Taiwan found that conduct disorder and ADHD were two of the most significant predictive factors for adolescent substance use disorder (Gau et al., 2007). In addition, a meta-analysis of 37 longitudinal studies with more than 750,000 participants examining the relationship between childhood psychiatric disorders and subsequent substance abuse found that childhood ADHD, oppositional defiant disorder, conduct disorder, and depression increased the risk of developing substance-related disorders (Groenman, Janssen, and Oosterlaan, 2017). However, researchers in several different studies have emphasized that the relationship between mental health disorders and substance use disorders can be multidirectional, which means causation cannot necessarily be established (Wilens et al., 2004; Winters et al., 2014). In other words, it is difficult to determine whether the mental health disorder preceded the substance use disorder, or the other way around.
Peer. Research on peer influences and substance use disorder is limited. However, available research indicates many findings of the impact of peer influences on youth substance use and initiation. Peer risk factors for substance use include having friends who engage in delinquent behavior, having friends who use substances, and gang membership. Research demonstrates that an association with peers who engage in deviant behavior and use substances is one of the strongest risk factors for youth substance use and initiation (Coffman, Melde, and Esbensen, 2015; Ferguson and Meehan, 2011; Handren, Donaldson, and Crano, 2016; Whitesell et al., 2013). For example, a study of youths in Ohio found that association with delinquent peers was the strongest correlate to substance use, even when other relevant factors (such as family and neighborhood) were controlled for (Ferguson and Meehan, 2011). Peer influences also appear to affect frequency of substance use among youth. A study of 16- to 21-year-olds found that the perceived extent of peer substance involvement was statistically significantly correlated with frequency and intensity of cannabis use, and frequency of drinking alcohol (Boys et al., 1999).
As with studies on individual risk factors, research has shown that the causal pathway between peers and substance use is multidirectional (Winters et al., 2014). Youths choose their peers based on shared interests and behaviors, but interests and behaviors are shaped by peers. Evidence shows that youths who use substances seek friendships with other youths who use substances (Light et al., 2013, Osgood et al., 2013; Young and Rees, 2013). However, there is limited research on the development of youth substance use disorders and peer relationships, compared with the available research on the impact of peer relationships on substance use in general.
School. School risk factors can also affect the risk of developing a future substance use disorder. Poor performance in school, such as low grades and low academic motivation, is linked to initiation of substance use and substance use disorders in youth (Bugbee et al., 2019; Patte, Qian, and Leatherdale, 2017; Weinberg, 2001). Other school factors, such as truancy and suspension, also are associated with substance use disorders (Henry, Knight, and Thornberry, 2012; Flaherty, Sutphen, and Ely; 2012). A longitudinal study of 1,241 girls found that many school behaviors in youth were associated with later substance use disorders, such as low seventh and eighth grade standardized math scores, suspension from school, truancy, and not having a high school diploma (Fothergill et al., 2008). However, this is yet another area where the direction of association is unclear. Whether academic failure leads to substance use disorders or substance use disorders lead to academic failure cannot be determined clearly (Cooley–Strickland et al., 2009; Weinberg, 2001).
Family. Family-level risk factors, such as parental behaviors and family structure, can also affect a youth’s likelihood of developing a substance use disorder. Research has shown that neglect and abuse can make a strong impact on substance use and disorder on a youth. A study of more than 34,000 people found that physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect in youth were all associated with various substance use disorders later in life (Danielson, 2016; Afifi et al., 2012). While research has found that substance use disorders in parents also make a strong impact on youth substance use, there is little research on how parents' substance disorders influence disorders in their children (Biederman et al., 2000; Lucenko et al., 2015, Whitten et al., 2019). Some research indicates that family risk factors may differ by gender. For example, a study of 1,421 youths ages 10 to 16 found that family conflict was significantly associated with substance use disorder for girls but not for boys (Skeer et al., 2011).
Community. Community-level risk factors are another area where there is much research on youth substance use and initiation, but not a lot of research focused on the impact on youth substance use disorders. One study, using data from 38,115 youths ages 11 to 17, found that higher self-reported neighborhood disorganization (defined by the study as perceived levels of safety and crime) was associated with higher levels of substance use dependence as defined by the DSM–4, even after controlling for individual- and family-level risk factors. Youths who reported both medium and high levels of neighborhood disorganization had higher odds of both substance use and dependence, compared with youths who reported low levels of neighborhood disorganization (Winstanley et al., 2008).
[1] For more information, see the Model Programs Guide literature review on Risk Factors for Delinquency .
Protective Factors Against Substance Use Disorders
Protective factors [1] are factors in a youth's life that can prevent or mitigate the likelihood of substance use disorder. These factors are aspects of a youth's life that act as a buffer to reduce negative effects of adversity (Vanderbilt–Adriance and Shaw, 2008). Compared with risk factors, there is less research on protective factors regarding substance use. There is even less research focused on protective factors and substance use disorders or protective factors that increase the likelihood of success in substance use treatment programs (Cleveland et al., 2008).
Similar to risk factors, protective factors can occur on the individual, peer, school, family, and community level. As previously stated, protective factors mitigate the effect of adversity and other risk factors. For example, prosocial peers serve as a protective factor against many forms of deviant behavior, and against substance use and initiation (Osgood et al., 2013). The presence of close peers can also mitigate the effect that metal health disorders, such as depression, have on the likelihood of developing a substance use disorder (Mason et al., 2019).
Additionally, early-sustained abstinence following residential substance use treatment has been shown to be predictive of long-term abstinence, suggesting that even a short period of continuing-care posttreatment can significantly improve long-term abstinence rates (Godley et al., 2007).
Though research on community-level factors often focuses on substance use and initiation, it has been found also to make an impact on a youth’s likelihood of developing a substance use disorder. One study found that higher levels of social capital, defined as community engagement and involvement in various volunteering programs, decreased the likelihood of a youth’s using substances or developing a substance dependence as defined by the DSM–4 (Winstanley et al., 2008). Researchers have also found that family factors, such as living in a household with two parents (Gau et al., 2007), and school factors, such as good academic performance (Gau et al., 2007), can protect against developing a substance use disorder.
For youths with certain mental health disorders, there also is some research on the effect of treatments that use medications on later substance use. For example, some research on treatment for ADHD found that the use of medication as part of treatment reduced later substance use problems in adolescence (Hammerness et al., 2017; Wilens et al., 2003), though other researchers have found that this treatment did not influence substance use outcomes (Wise, Cuffe, and Fischer, 2001; Humphreys, Engs, and Lee, 2013).
[1] For more information, see the Model Programs Guide literature review on Protective Factors Against Delinquency .
Substance Use Treatment Utilization
Research indicates that treatment initiation, engagement, and completion among youths with substance use disorders is low—significantly lower than among adults (Alinsky et al., 2020; Brorson et al., 2013; Cummings et al., 2011; Merikangas et al., 2010). Because engagement and retention in treatment is one of the strongest predictors of improved outcomes among adolescents (Acevedo et al., 2020), examining utilization is important.
The NSDUH asks respondents who have used alcohol or illicit drugs in their lifetime whether they ever have received substance use treatment, and for those who have received treatment whether this treatment was received in the 12 months before completing the survey. Treatment includes care received at any location, such as a hospital (inpatient), a rehabilitation facility (inpatient or outpatient), a mental health center, an emergency room, a private doctor's office, prison or jail, or a self-help group (e.g., Alcoholics or Narcotics Anonymous). In acknowledgment of the COVID–19 pandemic, the NSDUH also asked respondents whether they had received professional counseling, medication, or treatment through virtual or telehealth services. The 2020 NSDUH additionally collected information on treatment received at specialty facilities, which was defined as treatment received at a hospital (inpatient only), a drug or alcohol rehabilitation facility (inpatient or outpatient), or a mental health center. Specialty facilities did not include any services received virtually (SAMHSA, 2021).
In 2020, 6.4 percent (1.6 million) of youths ages 12 to 17 demonstrated a need for substance use treatment (regardless of whether they met criteria for substance use disorder). This is defined by the NSDUH as if respondents indicated they felt they needed treatment. Among these youths, 3.5 percent previously received substance use treatment in a specialty facility. Among youths ages 12 to 17 who met the criteria for a substance use disorder, 7.6 percent received any kind of substance use treatment within the past year. The 2020 NSDUH found that 98.4 percent of youths ages 12 to 17 who did not receive treatment at a specialty facility cited that they did not feel they needed treatment (SAMHSA, 2021).
Among the 644,000 youths ages 12 to 17 in 2020 with a co-occurring substance use disorder and a major depressive episode in the past year, 69 percent (438,000 youths) received either substance use treatment at a specialty facility or mental health services in the past year, 66.8 percent (424,000 youths) received only mental health services, and 0.9 percent (6,000 youths) received both substance use treatment at a specialty facility and mental health services (SAMHSA, 2021).
Factors That Influence Participation in Treatment
Several factors influence participation in treatment programs. A small body of literature evaluates these factors, which include motivation, preexisting mental health disorders, diagnoses, family support, and demographic variables such as gender, race, ethnicity, and age (Haughwout et al., 2016; Settipani et al., 2018; Groshkova, 2010; McHugh et al., 2018). Studies examine various aspects of participation, including program initiation, program engagement, and program completion (Bowers, 2021; Haughwout et al., 2016; Becan et al., 2015).
Severity of the problem. Haughwout and colleagues (2016) used NSDUH findings from 2002 through 2013 to examine treatment-seeking behaviors among youth. They found that treatment utilization was higher among those youths who met criteria for a substance use disorder, compared with those youths who used substances but did not meet criteria for substance use disorder. Treatment engagement was greater for youths with illicit drug use disorders, such as marijuana dependence, compared with alcohol use disorder. Overall, findings indicated that, among youths with a substance use disorder, the severity of the problems caused by substance use (e.g., involvement in the criminal justice system) and the perceived need for treatment were associated with higher treatment utilization. Additionally, youths with illicit drug use disorders using more than one substance had an increased treatment utilization rate (Haughwout et al., 2016).
Family influence. Some studies examine family factors such as parental discipline styles, expectations, support, and socioeconomic status (e.g., Berridge et al., 2017; Dakof, Tejeda, and Liddle, 2001; Haughwout et al., 2016; Santisteban et al., 2015; Settipani et al., 2018). For example, a study of 224 youths ages 12 to 17 who were referred to drug treatment found that youths who had parents with higher expectations for their children’s educational attainment were more likely to participate in at least four drug abuse treatment sessions than youths who did not have parents with these high expectations (Dakof, Tejeda, and Liddle, 2001). Also, analysis of NSDUH data from 2002 through 2013 found that talking with parents about the need for treatment increased treatment utilization (Haughwout et al., 2016). A qualitative study of 31 youths and young adults ages 17 to 25 found that those who entered treatment indicated that pressure from parents to enter treatment, and parental support such as making appointments, providing financial support, and ensuring medication adherence were significant motivations for entering treatment (Cleverley, Grenville, and Henderson, 2018). A study of 110 Hispanic substance-misusing adolescents assessed parenting practices in five dimensions: 1) positive parenting, 2) discipline effectiveness, 3) discipline avoidance, 4) rules on having a set time to be home, and 5) extent of involvement. They found that youths who had parents with better discipline strategies and who felt effective and competent in their parenting were more likely to seek residential or outpatient treatment services (Santisteban et al., 2015). This study also found that youths with parents who had spent more years in the United States were more likely to use outpatient services (as compared with no services), and youths with parents who had lower parenting stress were more likely to use residential treatment services (compared with no services).
Finally, some studies have found that family financial and educational situations can influence treatment seeking behaviors. In a study of 189 youths seeking treatment for substance use concerns, 70 percent reported that they expected their finances to have an impact on their treatment (Settipani et al., 2018). Additionally, a longitudinal study of 358 adolescents in outpatient programs found that parental education was significantly associated with attendance at 12-step programs, meaning that adolescents whose parents had higher levels of education were more likely to attend the treatment program than those with parents with lower levels of education (Lui et al., 2017). However, the same study found no socioeconomic differences in treatment initiation or treatment retention. This may be due to everyone in the sample's having health insurance and to the near-full employment status of the adolescents' parents.
Other mental health diagnoses. Externalizing disorders have been identified as risk factors for not participating in or not successfully completing substance use treatment (Santisteban et al., 2015; Wise, Cuffe, and Fischer, 2001), while internalizing disorders have been identified as predictors of participating in treatment (Bowers, 2021). A study of 91 adolescents in a residential substance abuse treatment program examined factors associated with successful treatment, as defined by the treatment team at the time of discharge in terms of attendance, positive interactions in groups, level of denial, quality of projects, interactions with peers and staff, and meeting individualized treatment plan goals (Wise, Cuffe, and Fischer, 2001). They found that participants with Attention Deficit Hyperactivity Disorder (ADHD) or Conduct Disorder were less likely to participate successfully in treatment than those without ADHD or Conduct Disorder. Another study of more than 300 youths and young people ages 14 to 24 who were receiving outpatient services for concurrent disorders found that the strongest predictor of attending five or more sessions was having an internalizing problem (Bowers, 2021). In other words, individuals with higher levels of internalizing problems (such as depression) were more engaged in treatment than those with lower levels of internalizing problems.
Motivation. Motivation is considered a key factor in successfully engaging in substance use treatment (DiClemente, 1999; Groshkova, 2010). The role of motivation is particularly relevant to youth, since many enter treatment because it has been mandated or recommended, as opposed to self-referring (Bowers et al., 2017; Cleverley, Grenville, and Henderson, 2018; Knight et al., 2016). Several studies have examined the influence of motivation on participation in substance use treatment. A study of 547 youths from multiple substance use treatment programs found that participants with higher pretreatment motivation were more likely to have stronger relationships with program counselors, which predicted more successful outcomes after leaving the programs (Joe et al., 2014). Motivation also predicted stronger relationships with peers in the treatment program. A small qualitative study of 31 youths ages 17 to 25 in mental health treatment found that internal factors, such as wanting to better their academic, social, or financial situation, and external factors, such as familial pressure, were identified as motivating these young people to seek treatment (Bowers et al., 2017). Several interventions have been designed to increase youths' motivation to engage in treatment (Becan et al., 2015; Knight et al., 2016).
Gender. There is limited information on gender differences in treatment engagement for substance use disorders. Some research has found that adolescent girls are more likely than adolescent boys to receive treatment for alcohol use disorder, while boys are more likely than girls to receive treatment for marijuana use disorder, or for any type of illicit substance treatment overall (Haughwout et al., 2016; McHugh et al., 2018). Other studies have found no difference in treatment initiation or retention by gender (e.g., Lui et al., 2017). Several studies have found that girls have a higher comorbidity between substance use disorder and mental health disorders and greater histories of trauma than boys (e.g., Fernández-Artamendi, Martínez-Loredo, and López-Núñez, 2021; Yildiz, Ciftci, and Yalcin, 2020), which can affect engagement and success in treatment interventions. Once youths are in a treatment program, some studies have found that girls are more likely than boys to engage, succeed, and complete the program. For example, a study of 91 adolescents in a residential substance abuse treatment program (Wise, Cuffe, and Fischer, 2001, mentioned above) found that girls were more likely than boys to successfully participate in treatment.
Race and ethnicity. Several studies have examined racial and ethnic disparities among substance use treatment utilization. In their analyses of more than 140,000 adolescents from the NSDUH , Cummings and colleagues (2011) found that among youths with substance use disorders Black and Hispanic adolescents were less likely than white adolescents to receive treatment. A literature review of behavioral health services for youths of racial and ethnic minority groups found that, compared with non-Latino white adolescents with a substance use disorder, Black adolescents with a substance use disorder reported receiving less specialty and informal care, while Latinos with a substance use disorder reported receiving fewer informal services (Alegria et al., 2011). Several studies of youth in the juvenile justice system have found similar racial and ethnic disparities (e.g., Farenthold, 2010; Mansion and Chassin, 2016). A systematic literature review of studies examining juvenile justice system processing found that most studies examining referral to mental health or substance misuse treatment from within the juvenile justice system found at least some race effects disadvantaging youths of color (Spinney et al., 2016). For example, a study of about 600 juveniles on probation in New York found that, relative to white juveniles, Black and Hispanic juveniles who were screened and referred for mental health or substance use services were significantly less likely to access them (Wasserman et al., 2009). The study also found that Black juveniles were significantly less likely than others to participate in the initial screening. However, racial and ethnic disparities in referral to and utilization of substance use treatment are not always found (e.g., Mulvey, Schubert, and Chung, 2007; Yan and Dannerbeck, 2011).
Types of Substance Use Treatment Programs and Outcome Evidence
Treatment programs primarily focus on helping youths with existing substance use issues who have been clinically diagnosed with a substance use disorder by the Diagnostic and Statistical Manual for Mental Disorders criteria. However, some treatment programs serve youths without a formal diagnosis who exhibit or report risky substance use behavior or have come into contact with the justice system.
For youths currently experiencing substance use disorders, particularly youths involved in the juvenile justice system, more intensive services may be needed, compared with the programming youths may receive in prevention interventions. Treatment services typically are more comprehensive than prevention programs, owing to their retroactive (rather than proactive) focus. Specifically, treatment programs include components related to prosocial development as a means to address existing antisocial behaviors, negative peer relations, and poor family functioning (Development Services Group, 2015).
It is important to recognize that programs that have been shown to reduce adult substance use may not translate as well for youth. Substance-using youths seldom are dependent on substances in the traditional sense that adults experience addiction. Youths and adults may misuse drugs for different reasons, and there are differences in the psychology of juvenile and adult substance use disorders (Bureau of Justice Assistance, 2003). Adolescence is an important development phase that involves changes in cognitive, emotional, behavioral, and social skills necessary for a productive life that are influenced by important relationships, such as those with family, friends/peers, school, and the community (Development Services Group, 2015; Gray and Squeglia, 2018).
Various types of youth substance use treatment programs, including those featured in the Model Programs Guide, are discussed below.
Motivational Interviewing
Motivational interviewing (MI) is a counseling method that can be implemented as a standalone program or can be incorporated as an element of a larger program. MI uses collaborative, client-centered, goal-oriented communication to address hesitancy toward behavioral change by encouraging and evoking personal desires for transformation (Stein et al., 2006b, Naar–King, 2011). MI aims to increase an individual's perspective on the importance of change. When provided to youths with substance use issues, the long-term goal is to help them reduce or stop using drugs and alcohol. A youth's subtle desires for change are uncovered through a series of selective interviews guiding the youth to concentrate on their behaviors and explore overarching goals in regard to personal motivations, values, and opinions and reasons to change (Stein et al., 2006b; D’Amico et al., 2013).
Stein and colleagues (2006b) examined the effects of a standalone MI program for substance abuse issues of juveniles in a state facility . The program focused on youth engagement with substance use therapy and targeted youths who reported regular or binge marijuana or alcohol use or who were sentenced to a post-adjudication facility. For this program, motivational interviewing was designed to be modified as appropriate to be meaningful for each youth and their desire to change. This MI program was delivered by research counselors and consisted of four components: 1) establishing rapport, 2) assessing the youth’s motivation for change, 3) motivational enhancement, and 4) establishing goals for change. The study authors compared youths receiving MI with a control group of youths who did not receive MI. They found that the control group experienced statistically significantly more negative engagement with substance use therapy than the MI treatment group, meaning that youths who received MI were more likely than youth in the control group to take treatment seriously (Stein et al., 2006b). However, there was no statistically significant impact on positive treatment engagement, meaning juveniles who received MI were no more likely to actively participate in treatment sessions, compared with youths in the control group. Another study by Stein and colleagues (2006a), which examined the same sample of youths 3 months later, found the effectiveness of MI treatment appeared to be mediated by depressive symptoms. The authors found that, compared with the control group, the MI treatment group had statistically significantly lower self-reported measures of risky driving behavior (such as driving under the influence of alcohol and marijuana), but only for youths with low depressive symptoms. When examining youths with high depressive symptoms, researchers found the control group had statistically significantly lower self-reported measures of risky driving behavior, compared with the MI treatment group. The entire treatment group was statistically significantly less likely to report driving solo under the influence of alcohol, compared with the control group, but there were no statistically significant differences between the groups in driving alone under the influence of marijuana or being a passenger in a car operated by a driver under the influence of alcohol or marijuana (Stein et al., 2006b).
Juvenile Drug Courts/Court-Based Programs
Juvenile drug courts (JDCs)are specialized juvenile court dockets for youths with substance use problems and substance use disorders in need of specialized treatment services, allowing for intensive judicial supervision that is not ordinarily available in traditional juvenile courts (Latimer, Morton–Bourgon, and Chrétien, 2006; Mitchell et al., 2012; Shaffer, 2006; Drake, 2012). JDCs work conjointly with treatment providers, social services, school and vocational programs, law enforcement, probation, and other agencies (Latimer, Morton–Bourgon, and Chrétien, 2006; Mitchell et al., 2012; Shaffer, 2006; Drake, 2012). Core elements of JDCs include drug testing and treatment services, regular judicial contact, and meetings with a case manager and/or a probation officer. Additionally, most JDCs make referrals for educational programs, job training, and mental health services. [1]
Evaluations of programs have found mixed results with regard to the effectiveness of JDCs in both substance use and recidivism outcomes. For example, Juvenile Drug Courts in Utah operate with basic drug court components, including screening and assessment, individualized treatment plans, judicial supervision, community-based treatment, regular court hearings, accountability and compliance monitoring, comprehensive services, and a nonadversarial team approach (Hickert et al., 2011). An evaluation of the four largest JDCs in Utah by Hickert and colleagues (2011) found no statistically significant difference between youths who participated in the JDCs and youths in the probation comparison group for alcohol and other drug recidivism after 30 months. However, they did find that youths in the JDCs had statistically significantly fewer subsequent criminal offenses (i.e., recidivism of any offense), compared with youths in the comparison group. Other evaluations have shown more positive results. The Baltimore County (Md.) Juvenile Drug Court targets 13- to 17-year-olds who admit to drug or alcohol abuse. The program has four phases, each of which focuses on different aspects of treatment and services. The first two phases are highly structured and include frequent treatment sessions, supervision meetings, and drug testing. The last two phases are designed as aftercare phases, which involve decreasing supervision and treatment sessions and focus on relapse prevention. An evaluation by Mackin and colleagues (2010) showed youths in the program had statistically significantly lower average numbers of re-arrests for drug charges and total re-arrests (for any charge), compared with youths in the comparison group, at the 2-year follow-up.
Numerous meta-analyses examining the effectiveness of juvenile drug courts have also found mixed effects. When examining measures of general recidivism, Drake (2012) and Shaffer (2006) found small, statistically significant decreases in the recidivism of JDC participants, compared with nonparticipants. Conversely, Latimer and colleagues (2006) did not find a statistically significant impact of JDCs on recidivism measures. With regard to other outcomes, Mitchell and colleagues (2012) reviewed four studies that examined the effect of JDCs on drug use and found no statistically significant effect. Tanner–Smith and colleagues (2016) reviewed eight studies and also found an overall non–statistically significant effect on drug use, suggesting that JDCs have not been found to have a consistent effect on drug use.
An example of a court-based program is the Juvenile Breaking the Cycle (JBTC) Program in Lane County, Oregon . The program was a post-arrest effort designed to help substance-using youth, using a comprehensive approach. The primary goals of the program were to increase access to treatment, reduce substance use, and reduce delinquency among high-risk, antisocial youths through intensive case-management services. Youths ages 9 to 18 with alcohol or other drug problems and assessed as high risk for involvement in serious and chronic offenses were eligible for JBTC. Components of the model included substance abuse treatment, mental health services, judicial oversight (incorporating drug court for some participants), and case management that consisted of supervision by a probation counselor and service coordination by a service coordinator (along with urinalysis). Lattimore and colleagues (2004) found that participation in the JBTC program had no statistically significant effect on whether youths reported using alcohol or illicit drugs (other than marijuana), at the follow-up period. However, participation in the JBTC program was associated with a statistically significant reduction in marijuana use. Regarding recidivism outcomes, JBTC youths were statistically significantly less likely to be re-arrested, and participation in the JBTC program was associated with a statistically significant decrease in the number of re-arrests after 12 months (Lattimore et al., 2004).
Family-Inclusive Therapy
As previously discussed, research has shown that family dynamics often contribute to the development of youths' substance use disorders (Van Ryzin et al., 2016). The importance of family involvement and familial relationships in the recovery of substance-using youths is regularly reiterated throughout evaluation research of treatment programs (Christie, Cheetham, and Lubman, 2020). Other studies have shown family-based treatments to have higher retention rates, which may be related to positive treatment outcomes (Rowe and Liddle, 2003; Liddle et al., 2018). Further, intensive family-based treatments have been shown to reduce family and community environmental risk factors (such as familial conflict or association with negative peer groups) that contribute to adolescent substance use problems and disorders (Liddle et al., 2009; Liddle et al., 2018; Horigian, Anderson, and Szapocznik, 2016).
In general, family-based interventions can include a wide range of programs that are designed to decrease youths’ problem and antisocial behaviors, including substance use, by making positive changes in their familial and social environments (Dopp et al., 2017). Specifically, these interventions focus on establishing better communication and reducing conflict between parents and youths, improving parenting skills, and helping youths better engage with their families and in their school environment (Baldwin et al., 2012). Various therapies inform the specific treatment techniques used, including behavioral and cognitive–behavioral therapies. Dopp and colleagues (2017) conducted a meta-analysis of 24 effect sizes from 10 studies and found that family-based treatment had statistically significant positive effects on substance use for treatment group youths, compared with control group youths.
Numerous specific therapeutic models concentrate on including the family in treatment services for youth. Multidimensional Family Therapy (MDFT) is a well-established approach for youth substance use treatment (Liddle et al., 2001; Waldron and Turner, 2008; Rigter et al., 2013; van der Pol et al., 2018) that promotes communication among family members, targeting social competence and parental involvement/relationships. The MDFT approach is individualized, family based, and comprehensive, requiring collaboration across many social systems (Liddle et al., 2009). Using a multidimensional approach, the MDFT intervention emphasizes improving four major domains for youth, which are seen as contributing factors to the rise and decline of behavioral problems in a youth's life: 1) the youth, 2) parents, 3) family, and 4) the community (that is, peers, school, and so forth) [Liddle et al., 2018; Rigter et al., 2013; van der Pol, 2018]. Overall, the goal of the program is to improve individual and family functioning to reduce substance misuse and related problem behaviors (such as committing crimes). There have been numerous evaluations of MDFT. Rigter and colleagues (2013) evaluated the efficacy of MDFT on substance use and dependence among Western European youths ages 13 to 18 from five outpatient treatment sites. Eligible youths were diagnosed with a cannabis-use disorder by the DSM–4 guidelines and had at least one parent willing to participate. However, at the 12-month follow-up, there were no statistically significant differences in the prevalence of diagnosis of cannabis use disorder between youths in the MDFT intervention group and youths in the treatment-as-usual comparison group. Conversely, Liddle and colleagues (2018) evaluated the efficacy of MDFT in a sample of youths in the United States diagnosed with a substance use disorder and at least one comorbid psychiatric disorder. At the 18-month follow-up, youths in the MDFT intervention group reported a statistically significant decrease in substance use problems, compared with youths in the treatment-as-usual group.
Another example of an intervention that incorporates family into programming services is the Multisystemic Therapy | Family Integrated Transitions (MST–FIT) program, which provides integrated and family services to youths in a residential facility who have committed offenses and have co-occurring mental health and chemical dependency disorders (Trupin et al., 2011). Services are provided during a youth's transition from incarceration back into the community. The overall goal of MST–FIT is to provide necessary treatment to youths to reduce recidivism. The program also seeks to connect youths and families to appropriate community supports, increase youths' abstinence from alcohol and drugs, improve youths' mental health, and increase youths' prosocial behavior. Trupin and colleagues (2011) found that the MST–FIT program statistically significantly reduced felony recidivism at 36 months postrelease; however, the program did not have a statistically significant effect on measures of overall recidivism (i.e., felony and misdemeanors combined), misdemeanor recidivism, or violent felony recidivism. In addition, the program evaluation did not examine the impact on youths' substance use.
Multisystemic Therapy | Substance Abuse (MST for substance use) is a version of multisystemic therapy (MST) for youths with substance abuse and dependency issues who are diagnosed using the DSM–4 . Although the emphasis is on youths, MST operates by incorporating the youths' family and friends and addressing all potential spheres of behavioral influence. It aims to enhance a family's capacity to keep track of adolescent behavior and instill clear rewards and punishments for positive and negative/irresponsible behavior. Henggeler and colleagues (2002) found that youths who received MST for substance abuse showed statistically significantly higher rates of abstinence from marijuana, compared with control group youths who did not receive MST, at the 4-year follow-up. However, there were no statistically significant differences between groups on cocaine use. Another study by Henggeler and colleagues (2006) found no statistically significant difference in alcohol use between youths who participated in a drug court program and received MST for substance abuse and youths in the control group who received no services, at the 12-month follow-up. However, youths who received MST in a drug court program showed statistically significant reductions in heavy alcohol use, marijuana use, and multiple-/poly-drug use, compared with control group youths.
Some interventions specifically aim to treat youths' substance abuse after a family crisis. Ecologically Based Family Therapy (EBFT) is a home-based, family preservation model for families in crisis because a youth has run away from home. The model targets 12- to 17-year-olds who are staying in a runaway shelter and dealing with substance use issues. Treatment begins by preparing the youth and the family members, in individual sessions, to come together and talk about the issues that led to the runaway episode. After the individual sessions, the family and youth are brought together to address the issues associated with the dysfunctional interactions between family members and the continuation of problem behaviors. An evaluation by Slesnick and Prestopnik (2009) found that treatment group youths who participated in EBFT reported a statistically significant reduction in the percentage of days they used alcohol or drugs, compared with control group youths who received services as usual, at the 15-month follow-up.
Residential-Based Treatment
Youths may receive treatment while they are placed in a residential facility. The period of residential placement offers an opportunity to intervene in the cycle of youths' drug or alcohol use. Different types of residential-based substance use treatment programs are available, including therapeutic communities or group counseling (Mitchell, Wilson, and MacKenzie, 2012). Residential treatment is an important option for youths at high risk of overdose or suicide, those who present a public safety risk, or are without family members who can be involved in treatment (Liddle et al., 2018).
Incarceration-Based Therapeutic Communities (TC) for Juveniles employ a comprehensive, residential drug-treatment program model for substance-using youths who have committed offenses. The programs are designed to foster changes in attitudes, perceptions, and behaviors related to youth substance use. The TC for juveniles uses a developmentally appropriate comprehensive approach to a) address substance use and mental health issues and b) promote healthy development. Mitchell, Wilson, and MacKenzie (2012) synthesized four studies looking at the effectiveness of incarceration-based TCs for youths in reducing recidivism and found no statistically significant difference between treatment group and comparison group youths on recidivism postrelease. Drake (2012) analyzed the effect sizes from three studies on the efficacy of incarceration-based TCs for juveniles on recidivism and also found no statistically significant difference between treatment group and comparison group youths on recidivism postrelease. However, the results from both meta-analyses should be interpreted with caution, given the limited number of studies included. Further, neither meta-analysis examined the effectiveness of incarceration-based TCs in reducing substance use.
Brief Interventions
Brief interventions designed to address substance use in youth vary in terms of length and structure and can be delivered in an electronic format, in-person by a service provider (such as a counselor, physician, or nurse), or even self-administered by youth. In general, these are concise, convenient, and cost-effective interventions designed to motivate and provide resources to participants to help them change their alcohol or drug consumption behavior, and to seek more intensive treatment if needed (Tanner–Smith and Lipsey, 2015). However, one limitation to this type of program is that it usually is not targeted specifically toward substance use disorder, and therefore substance use disorder is not typically an outcome of interest. This is an area where more research is required (Smedslund et al., 2017).
Computerized Brief Interventions for Youth Alcohol Use are designed to appeal to younger generations who have grown up in the digital media age (Smedslund et al., 2017). Specifically, these interventions target individuals ages 15 to 25, who are high or risky consumers of alcohol but motivated to change. Risky consumption of alcohol is defined as consuming 1) at least 5 beverages during any one drinking session or more than 14 alcoholic beverages a week for males and 2) 4 beverages during any one drinking session or more than 7 alcoholic beverages a week for females. Computerized brief interventions usually consist of three components: 1) assessment, 2) feedback, and 3) decisionmaking. The assessment component classifies users as low-risk, medium-risk, high-risk, or very high-risk alcohol drinkers and provides the individuals with a recommendation on whether they would benefit from a more formalized treatment program than the computerized brief intervention. The feedback component provides the users with information on their scores after each assessment and responds to their reactions to their assessment. Finally, the decisionmaking component asks users to specify their motivation for behavioral change. Smedslund and colleagues (2017) aggregated the results of 15 studies (those that included both assessment and feedback components, but no decisionmaking component) and found that computerized brief interventions statistically significantly reduced short-term alcohol consumption for youths who participated, compared with youths who received no interventions.
Targeted Brief Alcohol Interventions (BAI) for Alcohol Use for Adolescents and Young Adults seek to reduce alcohol use or alcohol-related problems for youths and young adults using a short-term intervention (one to five sessions). BAIs can be delivered in a variety of settings such as primary care/student health centers, schools/universities, and emergency rooms; for youths, they can also be self-administered by participants. They typically include at least one of the following components: a discussion of alcohol consumption, feedback on risk or levels of alcohol use, comparisons with local or national norms, information on potential harms, or coping strategies and goal-setting plans for dealing with drinking situations. Tanner–Smith and Lipsey (2015) reviewed 24 studies that included adolescent samples (ages 11 to 17) and found that youths who participated in BAIs reported statistically significant reductions in levels of alcohol consumption and levels of alcohol-related problems, compared with control group youths.
Prevention Programming
Prevention programs are typically designed to deter adolescents from initial substance use. However, some early prevention programs are designed specifically with the goal of making a long-term impact on substance use disorders. These programs have a theoretical framework surrounding the goal of reducing early risk factors that can lead to later problem behaviors such as substance use disorders (Kellman et al., 2008).
Good Behavior Game is one such program. It is a classroom management strategy designed to reduce aggressive and disruptive classroom behavior. By preventing these early risk factors, it seeks to reduce future problem behaviors such as criminal activity and substance use. Good Behavior Game is a group-contingent reinforcement game, in which students work in teams and are rewarded as a team for following classroom rules. This creates an incentive for students to manage their own behavior through group reinforcement and mutual self-interest. Kellman and colleagues (2008) conducted a randomized controlled trial to examine the impact of Good Behavior Game on lifetime alcohol abuse or dependence disorders. The participants were ages 5 to 10 during the program and were surveyed 14 years after the program ended. The study authors found that treatment group participants had lower rates for lifetime alcohol abuse or dependence disorders, compared with the control group, at the 14-year follow-up. This difference was statistically significant.
[1] For more information, see the MPG literature review on Juvenile Drug Courts .
Limitations of Research on Treatment Programs
Although there is research on how well treatment programs can (or cannot) reduce youth substance use and/or improve substance use disorders, it has some limitations. Most substance use treatment programs evaluated within the juvenile justice system typically examine recidivism-based outcomes and often neglect to examine substance use outcomes fully (Trupin et al., 2011; Anspach and Ferguson, 2005; Hickert et al., 2011). In addition, because these programs are so closely linked with the juvenile justice system, they usually rely on one measure of substance use, such as one or more positive drug screen results (Anspach and Ferguson, 2005; Hickert et al., 2011). While instances of positive drug screens may be one way to measure substance use, this measure fails to incorporate self-reported drug or alcohol use, or substance use identified through other screening methods administered by service professionals.
Further, with research of youth substance use disorders and treatment programs, there often are barriers to conducting research with young people. It can be particularly challenging to follow up with youths who struggle to access services because of their inaccessibility, and there are ethical considerations related to consent in youth participants (Christie, Cheetham, and Lubman, 2020).
Other limitations exist when attempting to examine the specific components that make a program effective, particularly with regard to different types of illicit or licit substance use. If different family, courts-based, or residential-based programs incorporate similar elements, it is difficult to discern which specific program components successfully affect substance use (Trupin et al., 2011; Henggeler et al., 2006). For example, motivational interviewing can be implemented as a standalone program (Stein et al., 2006a; Stein et al., 2006b) or it may be included as a specific component in a juvenile drug court or as part of a specific program, such as Multidimensional Family Therapy. MDFT and juvenile drug court programs both incorporate some kind of family-based treatment (Waldron and Turner, 2008; Liddle et al., 2018; Liddle et al., 2009; Hickert et al., 2011; Anspach and Ferguson, 2005). Additionally, there is limited research into which types of programs are the most effective for different types of substances (McGovern and Carroll, 2013).
Further, there is little research on pharmacotherapy for youth licit and illicit substance use (Squeglia et al., 2019; Winters et al., 2018). Although research on adults with substance use disorders has shown positive results with treatments such as Methadone Maintenance Therapy and Buprenorphine Maintenance Therapy , especially when addressing opioid use disorders/dependence (Mattick et al., 2009; Mattick et al., 2014), this research has not be conducted much with youth, in part because a) federal regulations restrict methadone access for adolescents, b) training and U.S. Food and Drug Administration approval are required for prescribing buprenorphine, and c) there is stigma regarding medications for opioid use disorder (Chatterjee et al., 2019). However, there is some evidence that reception of medication-assisted treatments influences treatment duration among youths. Researchers examining a sample of more than 4,500 youths ages 13 to 22 found that youths who received opioid use disorder medication (e.g., buprenorphine, naltrexone) within 3 months of diagnosis with an opioid use disorder stayed in treatment longer than those who did not receive the medication (150 days of treatment, compared with 67 days of treatment) [Hadland et al., 2018]. Research indicates that the effect of pharmacotherapy for youth is unclear.
Additionally, most youths who participate in substance use treatment programs are not able to sustain long-term substance use reduction or cessation; some interventions do not see results related to continued substance use lasting more than 1 year posttreatment, including some of the programs discussed in the previous section (Tanner–Smith and Lipsey, 2015; Gray and Squeglia, 2018; Dennis et al., 2004). This has encouraged the development of aftercare or continuing care programs (Godley et al., 2007; Godley et al., 2014), usually after residential treatment or drug court participation. As stated previously, research shows that early-sustained abstinence is predictive of long-term abstinence (Godley et al., 2007). However, many substance use treatment programs for youth still lack this component, with youths returning to the community without the continued support needed to promote continued abstinence (Godley et al., 2007). Further research is needed regarding the effectiveness of aftercare or continuing care for youth following both outpatient and residential treatment, and on the best approaches for implementation (Kaminer, Burleson, and Burke, 2008; Godley et al., 2014; Gonzales et al., 2014).
Conclusions
Though rates of substance use disorder among youth have declined and leveled off since the first decade of the 2000s, it remains a prevalent issue, and research demonstrates a clear need for treatment programs directed toward adolescents (Chatterjee et al., 2019; SAMSHA, 2021).
There are a wide range of substance use treatment programs for adolescents, depending on their needs and situation. Family-inclusive therapies, for example, are common substance-use-disorder treatment programs, because family dynamics often make a strong impact on the development of substance use disorders (Van Ryzin et al., 2016). Residential-based treatment programs are also important in the field, as they are beneficial for youths with a substance use disorder who may not have family able to become involved with their treatment (Liddle et al., 2018).
Though 2.8 percent of youths ages 12 to 17 experienced alcohol use disorder in the past year, and 4.9 percent of 12- to 17-year-olds met criteria for at least one illicit drug use disorder, there is still limited research regarding specific risk factors, protective factors, and treatment options for youths diagnosed with a substance use disorder, according to DSM–4 criteria (Bacio et al., 2015; Cleveland et al., 2008; SAMSHA, 2021). Further research could overcome current limitations, such as examining substance use–related outcomes outside of the juvenile justice system, conducting studies on pharmacotherapy for youths' licit and illicit substance use, and exploring risk and protective factors specifically surrounding substance use disorders in youths.
Aarons, G.A., Brown, S.A., Hough, R.L., Garland, A.F., and Wood, P.A. 2001. Prevalence of adolescent substance use disorders across five sectors of care. Journal of the American Academy of Child & Adolescent Psychiatry 40(4):419–426.
Acevedo, A., Harvey, N, Kamanu, M., Tendulkar, S., and Fleary, S. 2020. Barriers, facilitators, and disparities in retention for adolescents in treatment for substance use disorders: A qualitative study with treatment providers. Substance Abuse Treatment, Prevention and Policy 15(42):1–13.
Afifi, T.O., Henriksen, C.A., Asmundson, G.J.G., and Sareen, J. 2012. Childhood maltreatment and substance use disorders among men and women in a nationally representative sample. Canadian Journal of Psychiatry 57(11):677–686.
Akers, R.L., Krohn, M.D., Lanza–Kaduce, L., and Radosevich, M. 1979. Social learning and deviant behavior: A specific test of a general theory. American Sociological Review 44(August):636–655.
Alegria, M., Carson, N.J., Goncalves, M., and Keefe, K. 2011. Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. Journal of the American Academy of Child and Adolescent Psychiatry 50(1):22–31.
Alinksy, R.H., Zima, B.T., Rodean, J., Matson, P.A., Larochelle, M.R., Adger, H, Bagley, S.M., and Hadland, S.E. 2020. Receipt of addiction treatment after opioid overdose among Medicaid-enrolled adolescents and young adults. Journal of the American Medical Association Pediatrics 174(3):1–10.
Anderson, K.G., Tapert, S.F., Moadab, I., Crowley, T.J., and Brown, S.A. 2007. Personality risk profile for conduct disorder and substance use disorders in youth. Addictive Behaviors, 32(10):2377–2382.
Anspach, D.F., and Ferguson, A.S. 2005. Part II: Outcome Evaluation of Main’s Statewide Juvenile Drug Treatment Court Program. Augusta, ME: University of Southern Maine.
Bacio, G.A., Estrada, Y., Huang, S., Martínez, M., Sardinas, K., and Prado, G. 2015. Ecodevelopmental predictors of early initiation of alcohol, tobacco, and drug use among Hispanic adolescents. Journal of School Psychology 53(3):195–208.
Bagley, S.M., Chavez, L., Braciszewski, J.M., Akolsile, M., Boudreau, D.M., Lapham, G., Campbell, C.I., Bart, G., Yarborough, B.J.H., Samet, J.H., Saxon, A.J., Rossom, R.C., Binswanger, I.A., Murphy, M.T., Glass, J.E., and Bradley, K.A. 2021. Receipt of medications for opioid use disorder among youth engaged in primary care: Data from six health systems. Addiction Science & Clinical Practice 16(1):1 – 18.
Baldwin, S.A., Christian, S., Berkeljon, A., Shadish, W.R., and Bean, R. 2012. The effects of family therapies for adolescent delinquency and substance abuse: A meta-analysis. Journal of Marital and Family Therapy 38(1):281–304.
Becan, J.E., Knight, D.K., Crawley, R.D., Joe, G.W., and Flynn, P.M. 2015. Effectiveness of the Treatment Readiness and Induction Program for increasing adolescent motivation for change. Journal of Substance Abuse Treatment 50:38 – 49.
Berridge, J., McCann, T.V., Lubman, D.I., and Cheetham, A. Perceived barriers and enablers of help-seeking for substance use problems during adolescence. SAGE Journals 19(1).
Biederman, J., Faraone, S.V., Monuteaux, M.C., and Feighner, J.A. 2000. Patterns of alcohol and drug use in adolescents can be predicted by parental substance use disorders. Pediatrics 106(4):792–797.
(BJA) Bureau of Justice Assistance. 2003. Juvenile Drug Court: Strategies in Practice. Washington, DC: U.S. Department of Justice (DOJ), Office of Justice Programs (OJP), BJA.
Bowers, A. 2021. Factors Influencing Service Engagement of Youth in Services for Concurrent Disorders: A Mixed-Methods Approach. Doctoral dissertation. Toronto, Ontario: University of Toronto.
Bowers, A., Cleverley, K., Di Clemente, C., and Henderson, J. 2017. Transitional-aged youth perceptions of influential factors for substance-use change and treatment seeking. Patient Preference and Adherence 11:1939–1948.
Boys, A., Marsden, J., Griffiths, P., Fountain, J., Stillwell, G., and Strang, J. 1999. Substance use among young people: The relationship between perceived functions and intentions. Addiction 94(7):1043–1050.
Brorson, H.H., Arnevik, E.A., Rand–Hendriksen, K., and Duckert, F. 2013. Dropout from addiction treatment: A systematic review of risk factors. Clinical Psychology Review 33:1010–1024.
Brown, J., and Christensen, D. 1986. Family Therapy Theory and Practice. Monterey, CA: Brooks/Cole.
Bugbee, B.A., Beck, K.H., Fryer, C.S., and Arria, A.M. 2019. Substance use, academic performance, and academic engagement among high school seniors. Journal of School Health 89(2):145–156.
Bukstein, O.G., and Horner, M.S. 2010. Management of the adolescent with substance use disorders and comorbid psychopathology. Child and Adolescent Psychiatric Clinics of North America 19(3):609–623.
Chan, Y.F., Dennis, M.L., and Funk, R.R. 2008. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment 34(1):14–24.
Chatterjee, A., Larochelle, M. R., Xuan, Z., Wang, N., Bernson, D., Silverstein, M., and Bagley, S.M. 2019. Nonfatal opioid-related overdoses among adolescents in Massachusetts 2012–14. Drug and Alcohol Dependence 194:28–31.
Christie, G.I.G., Cheetham, A., and Lubman, D.I. 2020. Interventions for alcohol and drug use disorders in young people: Ten key evidence-based approaches to inform service delivery. Current Addiction Reports 7:464–474.
Cleveland, M.J., Feinberg, M., Bontempo, D., and Greenberg, M. 2008. The role of risk and protective factors in substance use across adolescence. Journal of Adolescent Health 43(2):157–164.
Cleverley, K., Grenville, M., and Henderson, J. 2018. Youths perceived parental influence on substance use changes and motivation to seek treatment. Journal of Behavioral Health Services & Research. doi: 10.1007/s11414–018–9590–2
Coffman, D., Melde, C., and Esbensen, F.–A. 2015. Gang membership and substance use: Guilt as a gendered causal pathway. Journal of Experimental Criminology 11(1):71–95.
Cooley–Strickland, M., Quille, T.J., Griffin, R.S., Stuart, E.A., Bradshaw, C.P., and Furr–Holden, D. 2009. Community violence and youth: Affect, behavior, substance use, and academics. Clinical Child and Family Psychology Review 12(2):127–156.
Cummings, J.R., Wen, H., and Druss, B.G. 2011. Racial/ethnic differences in treatment for substance use disorders among U.S. adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 50(12):1265–1274.
Dakof, G.A., Tejeda, M., and Liddle, H.A. 2001. Predictors of engagement in adolescent drug abuse treatment. Journal of the American Academy of Child & Adolescent Psychiatry 40(3):274–281.
D’Amico, E.J., Hunter, S.B., Miles, J., Ewing, B.A., and Osilla, K.C. 2013. A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first-time alcohol or drug offense. Journal of Substance Abuse Treatment 45(5):1–21.
Danielson, C. 2016. Reducing risk for substance use problems among adolescents with a child maltreatment history. Journal of the American Academy of Child and Adolescent Psychiatry 55(10):S293.
Deci, E.L., and Ryan, R.M. 1985. The general causality orientations scale: Self-determination in personality. Journal of Research in Personality 19(2):109–134.
Deci, E.L., and Ryan, R.M. 2012. Self-determination theory. In Handbook of Theories of Social Psychology, edited by P.A.M. Van Lange, A.W. Kruglanski, and E.T. Higgins. Newbury Park, CA: SAGE Publications Ltd., pp. 416–436.
Dennis, M., Godley, S.H., Diamond, G., Tims, F.M. , Babor, T., Donaldson, J., and Liddle, H. 2004. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment 27:197–213.
Development Services Group, Inc. 2015. Protective Factors for Delinquency. Literature review. Washington, DC: DOJ, OJP, Office of Juvenile Justice and Delinquency Prevention (OJJDP). https://ojjdp.ojp.gov/model-programs-guide/literature-reviews/protective_factors.pdf
Dick, D.M., Aliev, F., Latendresse, S.J., Hickman, M., Heron, J., Macleod, J., Joinson, C., Maughan, B., Lewis, G., and Kendler, K.S. 2013. Adolescent alcohol use is predicted by childhood temperament factors before age 5, with mediation through personality and peers. Alcoholism: Clinical and Experimental Research 37:2108–2117.
DiClemente, C.C. 1999. Motivation for change: Implications for substance abuse treatment. Psychological Science 10(3):209–213.
Dopp, A.R., Borduin, C.M., White, M.H., and Kuppens, S. 2017. Family-based treatments for serious juvenile offenders: A multilevel meta-analysis. Journal of Consulting and Clinical Psychology 85(4):335–354.
Drake, E. 2012. Chemical Dependency Treatment for Offenders: A Review of the Evidence and Benefit–Cost Findings . Olympia, WA: Washington State Institute for Public Policy.
Farenthold, E.C. 2010. The Effect on Juvenile Re-Offending of Confining and Treating Juveniles With Substance Use Disorders in Harris County . Doctoral dissertation. Ann Arbor, MI: UMI Dissertation Publishing.
Ferguson, C.J., and Meehan, D.C. 2011. With friends like these…: Peer delinquency influences across age cohorts on smoking, alcohol, and illegal substance use. European Psychiatry 26(1):6–12.
Fernández–Artamendi, S., Martínez–Loredo, V., & López–Núñez, C. 2021. Sex differences in comorbidity between substance use and mental health in adolescents: Two sides of the same coin. Psicothema 33(1):36–43.
Flaherty, C.W., Sutphen, R.D., and Ely, G.E. 2012. Examining substance abuse in truant youths and their caregivers: Implications for truancy intervention. Children and Schools 34(4):201–211.
Fothergill, K.E., Ensminger, M.E., Green, K.M., Crum, R.M., Robertson, J., and Juon, H.–S. 2008. The impact of early school behavior and educational achievement on adult drug use disorders: A prospective study. Drug and Alcohol Dependence 92:191–199.
Gau, S.S.F., Chong, M.–Y., Yang, P., Yen, C.–F., Liang, K.–Y., and Cheng, A.T.A. 2007. Psychiatric and psychosocial predictors of substance use disorders among adolescents. British Journal of Psychiatry 190:42–48.
Godley, M.D., Godley, S.H., Dennis, M.L., Funk, R.R., and Passetti, L.L. 2007. The effect of assertive continuing care (ACC) on continuing care linkage, adherence, and abstinence following residential treatment for adolescents. Addiction 102:81–93.
Godley, M.D., Godley, S.H., Dennis, M.L., Funk, R.R., and Passetti, L.L. 2014. A randomized trial of assertive continuing care and contingency management for adolescents with substance use disorders. Journal of Consulting and Clinical Psychology 82(1):40–51.
Gonzales, R., Ang, A., Murphy, D.A., Glik, D.C., and Anglin, M.D. 2014. Substance use recovery outcomes among a cohort of youth participating in a mobile-based texting aftercare pilot program. Journal of Substance Abuse Treatment 47(1):20–26.
Gray, K.M., and Squeglia, L.M. 2018. Research review: What have we learned about adolescent substance use? Journal of Child Psychology and Psychiatry 59(6):618–627.
Groenman, A.P., Janssen, T.W.P., and Oosterlaan, J. 2017. Childhood psychiatric disorders as risk factor for subsequent substance abuse: A meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry 56(7):556–569.
Groshkova, T. 2010. Motivation in substance misuse treatment. Addiction Research & Theory 18(5):494–510.
Hadland, S.E., Bagley, S. M., Rodean, J., Silverstein, M., Levy, S., Larochelle, M.R., and Zima, B.T. 2018. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. Journal of the American Medical Association Pediatrics 172(11):1029–1037.
Hammerness, P., Petty, C., Faraone, S.V., and Biederman, J. 2017. Do stimulants reduce the risk for alcohol and substance use in youth with ADHD? A secondary analysis of a prospective, 24-month open-label study of osmotic-release methylphenidate. Journal of Attention Disorders 21(1):71–77.
Handren, L.M., Donaldson, C.D., and Crano, W.D. 2016. Adolescent alcohol use: Protective and predictive parent, peer, and self-related factors. Prevention Science 17(7):862–871.
Haughwout, S.P., Harford, T.C., Castle, I.J.P., and Grant, B.F. 2016. Treatment utilization among adolescent substance users: Findings from the 2002 to 2013 National Survey on Drug Use and Health. Alcoholism: Clinical and Experimental Research 40(8):1717–1727.
Henggeler, S.W., Flingempeel, W.G., Brondino, M.J., and Pickrel, S.G. 2002. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry 41:868–874.
Henggeler, S.W., Halliday–Boykins, C.A., Cunningham, P.B., Randall, J., Shapiro, S.B., and Chapman, J.E. 2006. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. Journal of Consulting and Clinical Psychology 74:42–54.
Henry, K.L., Knight, K., and Thornberry, T. 2012. School disengagement as a predictor of dropout, delinquency, and problem substance use during adolescence and early adulthood. Journal of Youth and Adolescence 41(2):156–166.
Hickert, A., Becker, E., Prospero, M., and Moleni, K. 2011. Impact of juvenile drug courts on drug use and criminal behavior. OJJDP Journal of Juvenile Justice 1(1):60–77.
Hines, L.A., Morley, K.I., Mackie, C., and Lynskey, M. 2015. Genetic and environmental interplay in adolescent substance use disorders. Current Addiction Reports 2:122–129.
Hodgins, S., Kratzer, L., and McNeil, T.F. 2001. Obstetric complications, parenting, and risk of criminal behavior. Archives of General Psychiatry 58(8):746–752.
Horigian, V.E., Anderson, A.R., and Szapocznik, J. 2016. Family-based treatments for adolescent substance use. Child and Adolescent Psychiatric Clinics of North America 25(4):603–628.
Humphreys, K. L., Eng, T., and Lee, S. S. 2013. Stimulant medication and substance use outcomes: A meta-analysis. Journal of the American Medical Association Psychiatry 70(7):740–749.
Joe, G.W., Knight, D.K., Becan, J.E., and Flynn, P.M. 2014. Recovery among adolescents: Models for posttreatment gains in drug abuse treatments. Journal of Substance Abuse Treatment 46(3):362–373.
Johnston, L.D., Miech, R.A., O’Malley, P.M., Bachman, J.G., Schulenberg, J.E., and Patrick, M.E. 2020. Monitoring the Future National Survey Results on Drug Use 1975–2019: 2019 Overview, Key Findings on Adolescent Drug Use. Ann Arbor, MI: University of Michigan, Institute for Social Research.
Kaminer, Y., Burleson, J.A., and Burke, R.H. 2008. The efficacy of aftercare for adolescents with alcohol-use disorders: A randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry 47(12):1405–1412.
Kellman, S.G., Hendricks Brown, C., Poduska, J.M., Ialongo, N.S., Wang, W., Toyinbo, P., Petras, H., Ford, C., Windham, A., and Wilcox, H.C. 2008. Effects of a universal classroom behavior management program in first and second grades on young adult behavioral, psychiatric, and social outcomes. Drug and Alcohol Dependence 95 (Supplement 1):S5–S28.
Knight, D.K., Joe, G.W., Crawley, R.D., Becan, J.E., Dansereau, D.F., and Flynn, P.M. 2016. The effectiveness of the Treatment Readiness and Induction Program (TRIP) for improving during-treatment outcomes. Journal of Substance Abuse Treatment 62:20–27.
Kotov, R., Gamex, W., Schmidt, F., and Watson, D. 2010. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136(5):768–821.
Lander, L., Howsare, J, and Byrne, M. 2013. The impact of substance use disorders on families and children: From theory to practice. Social Work and Public Health 28(0):194–205.
Latimer, J., Morton–Bourgon, K., and Chretien, J.–A. 2006. A meta-analytic examination of drug treatment courts: Do they reduce recidivism? Ottawa, Ontario: Department of Justice Canada.
Lattimore, P.K., Krebs, C.P., Graham, P., and Cowell, A.J. 2004. Evaluation of the Juvenile Breaking the Cycle Program. Research Triangle Park, NC: RTI International.
Lee, S.S., Humphreys, K.L., Flory, K., Liu, R., and Glass, K. 2011. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review 31(3):328–341.
Liddle, H.A. 1999. Theory development in a family-based therapy for adolescent drug abuse. Journal of Clinical and Child Psychology 28(4):521–532.
Liddle, H.A., Dakof, G.A., Parker, K., Diamond, G.S., Barrett, K., and Tejeda, M. 2001. Multidimensional Family Therapy for adolescent drug abuse: Results of a randomized clinical trial. American Journal of Drug and Alcohol Abuse 27(4):651–688.
Liddle, H.A., Dakof, G.A., Rowe, C.L., Henderson, C.E., Greenbaum, P., Wang, W., and Alberga, L. 2018. Multidimensional family therapy as a community-based alternative to residential treatment for adolescents with substance use and co-occurring mental health disorders. Journal of Substance Abuse Treatment 90:47–56.
Liddle, H.A., Rowe, C.L., Dakof, G.A., Henderson, C.E., and Greenbaum, P.E. 2009. Multidimensional Family Therapy for young adolescent substance abuse: Twelve-month outcomes of a randomized controlled trial. Journal of Consulting and Clinical Psychology 77(1):12–25.
Light J.M., Greenan, C.C., Rusby, J.C., Nies, K.M., and Snijders, T.A.B. 2013. Onset to first alcohol use in early adolescence: A network diffusion model . Journal of Adolescent Research 23:48–49.
Lucenko, B.A., Sharkova, I.V., Huber, A., Jemelka, R., and Mancuso, D. 2015. Childhood adversity and behavioral health outcomes for youth: An investigation using state administrative data. Child Abuse and Neglect 47:48–58.
Lui, C.K., Sterling, S.A., Chi, F. W., Lu, Y., and Campbell, C.I. 2017. Socioeconomic differences in adolescent substance abuse treatment participation and long-term outcomes. Addictive Behaviors 68:45–51.
Mackin, J.R., Lucas, L.M., Lambarth, C.H., Herrera, T.A., Wallter, M.S., Carey, S.M., and Finigan, M.W. 2010. Baltimore County Juvenile Drug Court Outcome and Cost Evaluation. Portland, OR: NPC Research.
Mansion, A.D., and Chassin, L.A. 2016. The effect of race/ethnicity on the relation between substance use disorder diagnosis and substance use treatment receipt among male serious adolescent offenders. Children and Youth Services Review 61:237–244.
Mason, M., Mennis, J., Russell, M., Moore, M., and Brown, A. 2019. Adolescent depression and substance use: The protective role of prosocial peer behavior. Journal of Abnormal Child Psychology 47:1065–1074.
Mattick, R.P., Breen, C., Kimber, J., and Davoli, M. 2009. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews (3):CD002209.
Mattick, R.P., Breen, C., Kimber, J., and Davoli, M. 2014. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database of Systematic Review (2):CD002207.
McGovern, M.P., and Carroll, K.M. 2013. Evidence-based practices for substance use disorders. Psychiatric Clinics of North America 26(4):991–1010.
McHugh, R.K., Votaw, V.R., Sugarman, D.E., and Greenfield, S.F. 2018. Sex and gender differences in substance use disorders. Clinical Psychology Review 66(December):12–23.
Merikangas, K.R., He, J.P., Burstein, M., Swanson, S.A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., and Swendsen, J. 2010. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication | Adolescent Supplement. Journal of the American Academy of Child and Adolescent Psychiatry 49(10):980–989.
Mitchell, O., Wilson, D., Eggers, A., and Mackenzie, D. 2012. Drug courts’ effects on criminal offending for juveniles and adults. Campbell Systematic Reviews 4.
Mulvey, E.P., Schubert, C.A., and Chung, H.L. 2007. Service use after court involvement in a sample of serious adolescent offenders. Children and Youth Services Review 29 (4):518–544.
Murray, J., and Farrington, D.P. 2010. Risk factors for conduct disorder and delinquency: Key findings from longitudinal studies. Canadian Journal of Psychiatry 55(10):633–642.
Naar–King, S. 2011. Motivational interviewing in adolescent treatment. Canadian Journal of Psychiatry 56(11):651–657.
NIAAA (National Institute on Alcohol Abuse and Alcoholism). 2022, October. Underage Drinking . Bethesda, MD: National Institutes of Health, NIAAA. Retrieved January 3, 2023, from the web: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/underage-drinking#:~:text=Underage%20drinking%20is%20a%20serious,enormous%20health%20and%20safety%20risks
NIDA (National Institute on Drug Abuse). 2014, January. Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide . Bethesda, MD: National Institutes of Health, NIDA. Retrieved January 5, 2023, from the web: https://nida.nih.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide/director
Osgood, D.W., Ragan, D.T., Wallace, L., Gest, S.D., Feinberg, M.E., and Moody, J. 2013. Peers and the emergence of alcohol use: Influence and selection processes in adolescent friendship networks. Journal of Research on Adolescence 23:500–512.
Patte, K.A., Qian, W., and Leatherdale, S.T. 2017. Marijuana and alcohol use as predictors of academic achievement: A longitudinal analysis among youth in the COMPASS study. Journal of School Health 87(5):310–318.
Prom–Wormley, E.C., Ebejer, J., Dick, D.M., and Bowers, M.S. 2017. The genetic epidemiology of substance use disorder: A review. Drug and Alcohol Dependence 180:241–259.
Ramo, D.E., Anderson, K.G., Tate, S.R., and Brown, S.A. 2005. Characteristics of relapse to substance use in comorbid adolescents. Addictive Behaviors 30:1811–1823.
Rigter, H., Henderson, C.E., Pelc, I., Tossmann, P., Phan, O., Hendrinks, V., Schaub, M., and Rowe, C.L. 2013. Multidimensional family therapy lowers the rate of cannabis dependence in adolescents: A randomized controlled trial in western European outpatient settings. Drug and Alcohol Dependence 130(1–3):85–93.
Rottman, D., and Casey, P. 1999. Therapeutic jurisprudence and the emergence of problem-solving courts. National Institute of Justice :12–19.
Rowe, C.L., and Liddle, H.A. 2003. Substance abuse. Journal of Marital and Family Therapy 29(1):97–120.
Ryan, R.M., and Deci, E.L. 2000a. Intrinsic and extrinsic motivations: Class definitions and new directions. Contemporary Education Psychology 25(1):54–67.
Ryan, R.M., and Deci, E.L. 2000b. Self-determination theory: Basic psychological needs in motivation, development, and wellness. American Psychologist 55(1):68–78.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2011. Results From the 2010 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H–41, HHS Publication No. (SMA) 11–4658. Rockville, MD: U.S. Department of Health and Human Services (HHS), SAMHSA.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2021. Key Substance Use and Mental Health Indicators in the United States: Results From the 2020 National Survey on Drug Use and Health. Publication No. PEP21–07–01–003. Rockville, MD: HHS, SAMHSA.
Santisteban, D. A., Mena, M. P., Muir, J., McCabe, B. E., Abalo, C., & Cummings, A. M. 2015. The efficacy of two adolescent substance abuse treatments and the impact of comorbid depression: Results of a small randomized controlled trial. Psychiatric Rehabilitation Journal 38(1):55–64.
Settipani, C.A., Hawke, L.D., Virdo, G., Yorke, E., Mehra, K., and Henderson, J. 2018. Social determinants of health among youth seeking substance use and mental health treatment. Journal of the Canadian Academy of Child and Adolescent Psychiatry 27(4):213–221.
Shaffer, D. 2006. Reconsidering Drug Court Effectiveness: A Meta-Analytic Review. Las Vegas, NV: University of Las Vegas Department of Criminal Justice.
Skeer, M.R., McCormick, M.C., Normand, S.–L. T., Mimiaga, M.J., Buka, S.L., and Gilman, S.E. 2011. Gender differences in the association between family conflict and adolescent substance use disorders. Journal of Adolescent Health 49(2):187–192.
Slesnick, N., and Prestopnik, J. 2009. Comparison of family therapy outcome with alcohol abusing, runaway adolescents. Journal of Marital and Family Therapy 35(3):255–277.
Sloboda, Z., Glantz, M.D., and Tarter, R.E. 2012. Revisiting the concepts of risk and protective factors for understanding the etiology and development of substance use and substance use disorders: Implications for prevention. Substance Use and Misuse 47:944–962.
Smedslund, G., Wollscheid, S., Fang, L., Nilsen, W., Steiro, A., and Larun, L. 2017. Effects of early, computerized brief interventions on risky alcohol use and risky cannabis use among young people. Campbell Collaboration 6.
Spinney, E., Yeide, M., Feyerherm, W., Cohen, M., Stephenson, R., and Thomas, C. 2016. Racial disparities in referrals to mental health and substance abuse services from the juvenile justice system: A review of the literature. Journal of Crime and Justice 39(1):153–573.
Squeglia, L.M., M.C., Fadus, McClure, E.A., Tomko, R.L., and Gray, K.M. 2019. Pharmacological treatment of youth substance use disorders. Journal of Child and Adolescent Psychopharmacology 29(7):559–572.
Stein, L.A.R., Colby, S.M., Barnett, N.P., Monti, P.M., Golembeske, C., and Lebeau–Craven, R. 2006a. Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. American Journal on Addictions 15:50–57.
Stein, L.A.R., Colby, S.M., Barnett, N.P., Monti, P.M., Golembeske, C., Lebeau–Craven, R., and Miranda, R. 2006b. Enhancing substance abuse treatment engagement in incarcerated adolescents. Psychological Services 3(1):25–34.
Swendsen, J., Burstein, M., Case, B., Conway, K., Dierker, L., He, J., and Merikangas, K.R. 2012. The use and abuse of alcohol and illicit drugs in U.S. adolescents: Results from the National Comorbidity Survey | Adolescent Supplement. Archives of General Psychiatry 69(4):390–398.
Tanner–Smith, E.E., and Lipsey, M.W. 2015. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment 51:1–18.
Tanner–Smith, E.E., Lipsey, M.W., and Wilson, D.B. 2016. Juvenile drug court effects on recidivism and drug use: A systematic review and meta-analysis. Journal of Experimental Criminology 12(4):477–513.
Torrens, M., Rossi, P.C., Martinez–Riera, R., Martinez–Sanvisens, D., and Bulbena, A. 2012. Psychiatric co-morbidity and Substance Use Disorders: Treatment in parallel systems or in one integrated system? Substance Use and Misuse 47(8–9):1005–1014.
Trupin, E.J., Kerns, S.E.U., Cusworth Walker, S., DeRobertis, M.T., and Steward, D.G. 2011. Family integrated transitions: A promising program for juvenile offenders with co-occurring disorders. Journal of Child and Adolescent Substance Abuse 20:421–436.
Turner, W.C., Muck, R.D., Muck, R.J., Stephens, R.L., and Sukumar, B. 2004. Co-occurring disorders in the adolescent mental health and substance abuse treatment systems. Journal of Psychoactive Drugs. 36(4):455–462.
Vanderbilt–Adriance, E., and Shaw, D. 2008. Conceptualizing and reevaluating resilience across levels of risk, time, and domains of competence. Clinical Child and Family Psychology Review 11(1–2):30–58.
van der Pol, T.M., Henderson, C.E., Hendriks, V., Schaud, M.P., and Rigter, H. 2018. Multidimensional family therapy reduces self-reported criminality among adolescents with a cannabis use disorder. International Journal of Offender Therapy and Comparative Criminology 62(6):1573–1588.
Van Ryzin, M.J., Roseth, C.J., Fosco, G.M., Lee, Y., and Che, I. 2016. A component-centered meta-analysis of family-based prevention programs for adolescent substance use. Clinical Psychology Review 45:72–80.
Vasilenko, S.A., Evans–Polce, R.J., and Lanza, S.T. 2017. Age trends in rates of substance use disorders across ages 18–90: Differences by gender and race/ethnicity. Drug and Alcohol Dependence 180:260–264.
Waldron, H.B., and Kaminer, Y. 2004. On the learning curve: The emerging evidence supporting cognitive–behavioral therapies for adolescent substance abuse. Addiction 99(Suppl 2):93–105.
Waldron, H.B., and Turner, C.W. 2008. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology 37(1):238–261.
Wasserman, G.A., McReynolds, L.S., Musabegovic, H., Whited, A.L., Keating, J.M., and Huo, Y. 2009. Evaluating project connect: Improving juvenile probationers’ mental health and substance use service access. Administration and Policy in Mental Health and Mental Health Services Research 36(6):393–405.
Weibnerg, N.Z. 2001. Risk factors for adolescent substance abuse. Journal of Learning Disabilities 34(4):343–351.
Whitesell, M., Bachand, A., Peel, J., and Brown, M. 2013. Familial, social, and individual factors contributing to risk for adolescent substance use. Journal of Addiction. doi: 10.1155/2013/579310
Whitten, T., Burton, M., Tzoumakis, S., and Dean, K. 2019. Parental offending and child physical health, mental health, and drug use outcomes: A systematic literature review. Journal of Child and Family Studies 28(5):1155–1168.
Wild, T.C., and Enzle, M.E. 2002. Social contagion of motivational orientations. In Handbook of Self-Determination, edited by E.L. Deci and R.M. Ryan. Rochester, NY: University of Rochester Press, pp. 141–157.
Wilens, T.E., Biederman, J., Kwon, A., Ditterline, J., Forkner, P., Moore, H., Swezey, A., Snyder, L., Henin, A., Wozniak, J. and Faraone, S.V. 2004. Risk of substance use disorders in adolescents with bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 43(11):1380–1386.
Wilens, T.E., Faracone, S., Biedermann, J., and Gunawardene, S. 2003. Does stimulant therapy of ADHD beget later substance abuse: A meta analytic review of the literature. Pediatrics 11:179–185.
Wilens, T.E., Martelon, M., Joshi, G., Bateman, C., Fried, R., Petty, C., and Biederman, J. 2011. Does ADHD predict substance use disorders? A 10-year follow-up study of young adults with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry 50(6):543–553.
Wilson, D.B., Olaghere, A., and Kimbrell, C.S. 2019. Implementing juvenile drug treatment courts: A meta-aggregation of process evaluations. Journal of Research in Crime and Delinquency 56(4).
Winstanley, E., Steinwachs, D., Ensminger, M., Latkin, C., Stitzer, M., and Olsen, Y. 2008. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug and Alcohol Dependence 92(1–3):173–182.
Winters, K.C., Botzet, A.M., and Fahnhorst, T. 2011. Advances in adolescent substance abuse treatment. Current Psychiatry Reports 13(5):416–421.
Winters, K.C., Botzet, A.M., Stinchfield, R., Gonzales–Castaneda, R., Finch, A.J., Piehler, T.F., Ausherbauer, K., Chalmers, K., and Hemze, A. 2018. Adolescent substance abuse treatment: A review of evidence-based research. In Adolescent Substance Abuse: Issues in Children’s and Families’ Lives, edited by C. Leukefeld and T. Gullotta. New York, NY: Springer.
Winters, K.C., Tanner–Smith, E.E., Bresani, E., and Meyers, K. 2014. Current advances in the treatment of adolescent drug use. Adolescent Health, Medicine, and Therapeutics 5:199–210.
Wise, B.K., Cuffe, S.P., and Fischer, T. 2001. Dual diagnosis and successful participation of adolescents in substance abuse treatment. Journal of Substance Abuse Treatment 21(3):161–165.
Wong, T., Slotboom, A.M., and Bijeveld, C. 2010. Risk factors for delinquency in adolescent and young adult females: A European review. European Journal of Criminology 7:266–284.
Yan, J., and Dannerbeck A. 2011. Exploring the relationship between gender, mental health needs, and treatment orders in a metropolitan juvenile court. Journal of Child & Family Studies 20(1):9–22.
Yildiz, D., Ciftci, A., and Yalcin, O. 2020. The association between trauma history, trauma-related psychopathology, and treatment completion at an adolescent inpatient substance abuse treatment center in turkey. Journal of Child & Adolescent Substance Abuse 29(1):58–67.
Young, S.E., Corley, R.P., Stallings, M.C., Rhee, S.H., Crowley, T.J., and Hewitt, J.K. 2002. Substance use, abuse and dependence in adolescence: Prevalence, symptom profiles and correlates. Drug and Alcohol Dependence 68:309–322.
Young, J.T., and Rees, C. 2013. Social networks and delinquency in adolescence: Implications for life-course criminology. In Handbook of Life-Course Criminology, edited by C.L. Gibson and M.D. Krohn. New York, NY: Springer, pp. 159–180.
About this Literature Review
Suggested Reference: Development Services Group, Inc. January 2023. "Substance Use Treatment Programs." Literature review. Washington, DC: Office of Juvenile Justice and Delinquency Prevention. https://ojjdp.ojp.gov/model-programs-guide/literature-reviews/Substance-Use-Treatment-Programs
Prepared by Development Services Group, Inc., under Contract Number: 47QRAA20D002V.
Last Update: January 2023
Advertisement
Adverse Drug Reactions to Opioids: A Study in a National Pharmacovigilance Database
- Original Research Article
- Published: 12 October 2023
- Volume 46 , pages 1133–1148, ( 2023 )
Cite this article

- Moa Gustafsson ORCID: orcid.org/0009-0009-8230-9485 1 , 2 ,
- Cristiano Matos ORCID: orcid.org/0000-0002-6279-1421 2 ,
- João Joaquim ORCID: orcid.org/0000-0001-9979-0062 2 ,
- Joep Scholl ORCID: orcid.org/0000-0002-9222-5965 3 &
- Florence van Hunsel ORCID: orcid.org/0000-0001-8965-3224 3
644 Accesses
4 Citations
9 Altmetric
Explore all metrics
Introduction
Opioids are commonly used as analgesics; however, like any medicine, they can produce adverse drug reactions (ADRs), including nausea, constipation, dependence, and respiratory depression, that result in harmful and fatal events. Therefore, it is essential to monitor the safety of these drugs in clinical practice.
This study aimed to characterize the safety profile of opioids by conducting a descriptive study based on a spontaneous reporting system (SRS) for ADRs in The Netherlands, focusing on abuse, misuse, medication errors, and differences between sexes.
Reports submitted to the Netherlands Pharmacovigilance Centre Lareb from January 2003 to December 2021 with an opioid drug as the suspected/interacting medicine were analyzed. Reporting odds ratios (RORs) for drug-ADR combinations were calculated, analyzed, and corrected for sex and drug utilization (expenditure) for the Dutch population.
A total of 8769 reports were analyzed. Tramadol was the opioid with the most reports during the period ( n = 2746), while oxycodone or tramadol had the highest number of reports per year in the study period. The most reported ADRs from opioid use were nausea, followed by dizziness and vomiting, independent of sex, and all of them were more often reported in women. Vomiting associated with tramadol (ROR females/males = 2.17) was significantly higher in women. Buprenorphine was responsible for most ADRs when corrected for expenditure, with high RORs observed with application site hypersensitivity, application site reaction, and application site rash. Fentanyl gave rise to most of the reports of ADRs concerning abuse, misuse, and medication errors.
Patients treated with opioids experienced ADRs, primarily nausea, dizziness, and vomiting. For those groups of drugs, no significant differences were found between the sexes, except for the vomiting associated with tramadol. In general, ADRs related to opioids presented higher RORs when uncorrected and corrected for sexes and expenditure than other drugs. There was more disproportionate reporting for ADRs concerning abuse, misuse, and medication errors for opioids than other drugs in the Dutch SRS.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Comparative rates of mortality and serious adverse effects among commonly prescribed opioid analgesics.

Reporting Rates of Opioid-Related Adverse Events Since 1965 in Canada: A Descriptive Retrospective Study

Preventability of adverse effects of analgesics: analysis of spontaneous reports
Pathan H, J Williams. Basic opioid pharmacology: an update. Br J Pain. 2012;6(1):11–6.
Bowdle TA. Adverse effects of opioid agonists and agonist-antagonists in anaesthesia. Drug Saf. 1998;19(3):173–89.
CAS PubMed Google Scholar
Oxycodone KE. J Pain Symptom Manag. 2005;29(5 Suppl):S47-56.
Google Scholar
Zöllner C, Stein C. Opioids. Analgesia. 2006:31–63.
National Institute on Drug Abuse. Prescription opioids DrugFacts. 2021. https://nida.nih.gov/publications/drugfacts/prescription-opioids .
Fields HL. The doctor’s dilemma: opiate analgesics and chronic pain. Neuron. 2011;69(4):591–4.
CAS PubMed PubMed Central Google Scholar
Leppert W, Krajnik M, Wordliczek J. Delivery systems of opioid analgesics for pain relief: a review. Curr Pharm Des. 2013;19(41):7271–93.
Packiasabapathy S, S. Sadhasivam. Gender, genetics, and analgesia: understanding the differences in response to pain relief. J Pain Res. 2018;11:2729–39.
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111(1):52–8.
Serdarevic M, Striley CW, Cottler LB. Sex differences in prescription opioid use. Curr Opin Psychiatry. 2017;30(4):238–46.
PubMed PubMed Central Google Scholar
Marie Preciado S, et al. National gender differences in the prescribing of opioid medications from 2006 to 2015. J Opioid Manag. 2020;16(3):197–208.
PubMed Google Scholar
Campbell CI, et al. Age and gender trends in long-term opioid analgesic use for noncancer pain. Am J Public Health. 2010;100(12):2541–7.
Samulowitz A, et al. “Brave Men” and “Emotional Women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. 2018;2018:6358624.
Amir C, et al. Test-retest reliability of an adaptive thermal pain calibration procedure in healthy volunteers. J Pain. 2022;23(9):1543–55.
Mogil JS, Chanda ML. The case for the inclusion of female subjects in basic science studies of pain. Pain. 2005;117(1–2):1–5.
United Nations Office on Drugs and Crime. World Drug Report 2019: 35 million people worldwide suffer from drug use disorders while only 1 in 7 people receive treatment. 2019. https://www.unodc.org/unodc/en/frontpage/2019/June/world-drug-report-2019_-35-million-people-worldwide-suffer-from-drug-use-disorders-while-only-1-in-7-people-receive-treatment.html .
World Health Organization. The selection and use of essential medicines: report of the WHO expert committee, 2017 (including the 20th WHO model list of essential medicines and the 6th model list of essential medicines for children). World Health Organization; 2017.
Cragg A, et al. Risk factors for misuse of prescribed opioids: a systematic review and meta-analysis. Ann Emerg Med. 2019;74(5):634–46.
Berterame S, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016;387(10028):1644–56.
Zin CS, Chen LC, Knaggs RD. Changes in trends and pattern of strong opioid prescribing in primary care. Eur J Pain. 2014;18(9):1343–51.
Ruscitto A, Smith BH, Guthrie B. Changes in opioid and other analgesic use 1995–2010: repeated cross-sectional analysis of dispensed prescribing for a large geographical population in Scotland. Eur J Pain. 2015;19(1):59–66.
Kalkman GA, et al. Trends in use and misuse of opioids in the Netherlands: a retrospective, multi-source database study. Lancet Public Health. 2019;4(10):e498–505.
Bedene A, et al. Opioid prescription patterns and risk factors associated with opioid use in the Netherlands. JAMA Netw Open. 2019;2(8): e1910223.
Degenhardt L, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–207.
Benyamin R, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105–20.
Trescot AM, et al. Opioid pharmacology. Pain Physician. 2008;11(2 Suppl):S133–53.
Inturrisi CE. Clinical pharmacology of opioids for pain. Clin J Pain. 2002;18(4 Suppl):S3-13.
Baldo P, Francescon S, Fornasier G. Pharmacovigilance workflow in Europe and Italy and pharmacovigilance terminology. Int J Clin Pharm. 2018;40(4):748–53.
National Institute on Drug Abuse. Misuse of prescription drugs research report. National Institute of Drug Abuse; 2020. https://nida.nih.gov/download/37630/misuse-prescription-drugs-research-report.pdf?v=add4ee202a1d1f88f8e1fdd2bb83a5ef .
Ferner RE, Easton C, Cox AR. Deaths from medicines: a systematic analysis of coroners’ reports to prevent future deaths. Drug Saf. 2018;41(1):103–10.
Frequently asked questions (FAQ): drug overdose deaths in Europe. European Monitoring Centre for Drugs and Drug Addiction; 2022.
Casati A, Sedefov R, Pfeiffer-Gerschel T. Misuse of medicines in the European Union: a systematic review of the literature. Eur Addict Res. 2012;18(5):228–45.
Giraudon I, et al. Prescription opioid abuse in the UK. Br J Clin Pharmacol. 2013;76(5):823–4.
Shah K, Barker KA. Out-of-hospital medication errors: a 6-year analysis of the national poison data system. Pharmacoepidemiol Drug Saf. 2009;18(11):1080–5.
Lavon O, Ben-Zeev A, Bentur Y. Medication errors outside healthcare facilities: a national poison centre perspective. Basic Clin Pharmacol Toxicol. 2014;114(3):288–92.
Mulac A, et al. Severe and fatal medication errors in hospitals: findings from the Norwegian Incident Reporting System. Eur J Hosp Pharm. 2021;28(e1):e56–61.
Jambrina AM, et al. Detection and prevention of medication errors by the network of sentinel pharmacies in a Southern European Region. J Clin Med. 2022;12(1):194.
Lobaugh LMY, et al. Medication errors in pediatric anesthesia: a report from the wake up safe quality improvement initiative. Anesth Analg. 2017;125(3):936–42.
Wang HW, et al. An experimental investigation of masking in the US FDA adverse event reporting system database. Drug Saf. 2010;33(12):1117–33.
MedDRA. Medical dictionary for regulatory activities. Maintenance and Support Services Organization; 2022.
World Health Organization. WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD index 2011. World Health Organization; 2011.
WHO Collaborating Centre for Drug Statistics Methodology. N02A opioids. 2023. https://www.whocc.no/atc_ddd_index/?code=n02a .
Nederland, Z., GIPdatabank. Aantal gebruikers 2013–2018 van Pijnstillers, 2019.
Szumilas M. Explaining odds ratios. J Can Acad Child Adolesc Psychiatry. 2010;19(3):227–9.
Schifano F, et al. The e-psychonaut drugs’ psychopharmacology. Curr Opin Pharmacol. 2021;57:165–74.
Schifano F, Chiappini S. Pregabalin: a range of misuse-related unanswered questions. CNS Neurosci Ther. 2019;25(5):659.
European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). European drug report 2022: trends and developments. EMCDDA; 2023.
Lessenger JE, Feinberg SD. Abuse of prescription and over-the-counter medications. J Am Board Fam Med. 2008;21(1):45–54.
Chiappini S, F Schifano. What about “pharming”? Issues regarding the misuse of prescription and over-the-counter drugs. Brain Sci. 2020;10(10):736.
Chiappini S, F. Schifano. What about “pharming”? Issues regarding the misuse of prescription and over-the-counter drugs. MDPI; 2020. p. 736.
Chiappini S, et al. Pharmacovigilance signals of the opioid epidemic over 10 years: data mining methods in the analysis of pharmacovigilance datasets collecting adverse drug reactions (ADRs) reported to EudraVigilance (EV) and the FDA Adverse Event Reporting System (FAERS). Pharmaceuticals. 2022;15(6):675.
Schifano F, et al. Assessing the 2004–2018 fentanyl misusing issues reported to an international range of adverse reporting systems. Front Pharmacol. 2019;10:46.
European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). Opioids: health and social responses. Lisbon: EMCDDA; 2021.
Centers for Disease Control and Prevention. Assessing benefits and harms of opioid therapy. https://www.cdc.gov/drugoverdose/pdf/assessing_benefits_harms_of_opioid_therapy-a.pdf .
Weesie Y, et al. Voorschrijven van opioïden in de huisartsenpraktijk. Utrecht: Netherlands Institute for Health Services Research (NIVEL); 2016.
Højsted J, Sjøgren P. Addiction to opioids in chronic pain patients: a literature review. Eur J Pain. 2007;11(5):490–518.
de Vries ST, et al. Sex differences in adverse drug reactions reported to the National Pharmacovigilance Centre in the Netherlands: an explorative observational study. Br J Clin Pharmacol. 2019;85(7):1507–15.
Holm L, Ekman E, Jorsäter Blomgren K. Influence of age, sex and seriousness on reporting of adverse drug reactions in Sweden. Pharmacoepidemiol Drug Saf. 2017. 26(3):335–43.
Zopf Y, et al. Women encounter ADRs more often than do men. Eur J Clin Pharmacol. 2008;64(10):999–1004.
Tran C, et al. Gender differences in adverse drug reactions. J Clin Pharmacol. 1998;38(11):1003–9.
Lopes GS, et al. Sex differences in type and occurrence of adverse reactions to opioid analgesics: a retrospective cohort study. BMJ Open. 2021;11(6): e044157.
de Vries ST, et al. Sex differences in adverse drug reactions of metformin: a longitudinal survey study. Drug Saf. 2020;43(5):489–95.
Ekhart C, et al. Sex Differences in Reported Adverse Drug Reactions of Selective Serotonin Reuptake Inhibitors. Drug Saf. 2018;41(7):677–83.
Mack KA, et al. Prescription practices involving opioid analgesics among Americans with Medicaid, 2010. J Health Care Poor Underserved. 2015;26(1):182–98.
Frenk SM, KS Porter, Paulozzi L. Prescription opioid analgesic use among adults: United States, 1999–2012. US Department of Health and Human Services, Centers for Disease Control and Prevention; 2015.
Schieber LZ, et al. Variation in adult outpatient opioid prescription dispensing by age and sex—United States, 2008–2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):298–302.
Johnson JL, L Greaves, R Repta. Better science with sex and gender: a primer for health research. Women's Health Res Netw. 2007.
Keefe FJ, et al. Coping with rheumatoid arthritis pain: catastrophizing as a maladaptive strategy. Pain. 1989;37(1):51–6.
Forsythe LP, et al. Race and sex differences in primary appraisals, catastrophizing, and experimental pain outcomes. J Pain. 2011;12(5):563–72.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191.
Jackson T, et al. Gender differences in pain perception: The mediating role of self-efficacy beliefs. Sex Roles. 2002;47:561–8.
Pleym H, et al. Gender differences in drug effects: implications for anesthesiologists. Acta Anaesthesiol Scand. 2003;47(3):241–59.
Berkley, K.J., Sex differences in pain. Behav Brain Sci. 1997. 20(3):371–80 (discussion 435–513) .
Craft RM. Sex differences in drug- and non-drug-induced analgesia. Life Sci. 2003;72(24):2675–88.
Inglis JM, et al. Documentation of adverse drug reactions to opioids in an electronic health record. Intern Med J. 2021;51(9):1490–6.
Napp Pharmaceuticals Ltd. OxyNorm 5 mg Hard Capsules SmPC. 1999. https://www.medicines.org.uk/emc/product/3850/smpc#UNDESIRABLE_EFFECTS . 2022.
Bristol Laboratories Ltd. Brimisol PR 100 mg Prolonged-Release Tablets SmPC. 2011. 2021. https://www.medicines.org.uk/emc/product/8550/smpc#UNDESIRABLE_EFFECTS . Cited 11 Jan 2023.
Kyowa Kirin Ltd. Abstral 200 microgram sublingual tablets SmPC. 2008. 2022. https://www.medicines.org.uk/emc/product/10265/smpc#UNDESIRABLE_EFFECTS . Cited 2022.
Ethypharm UK Ltd. Actimorph 20 mg Orodispersible tablets SmPC. 2021. https://www.medicines.org.uk/emc/product/13443/smpc#UNDESIRABLE_EFFECTS .
MedlinePlus. Nitroglycerin Spray. https://medlineplus.gov/druginfo/meds/a615006.html . Cited 12 Oct 2022.
Grunenthal Ltd. Tramacet 37.5 mg/ 325 mg film-coated tablets SmPC. 2003. 2022. https://www.medicines.org.uk/emc/product/6630/smpc#ORIGINAL . Cited 11 Jan 2023.
Yezierski RP. The effects of age on pain sensitivity: preclinical studies. Pain Med. 2012;13(Suppl 2):S27–36.
Lautenbacher S, et al. Age changes in pain perception: a systematic-review and meta-analysis of age effects on pain and tolerance thresholds. Neurosci Biobehav Rev. 2017;75:104–13.
Fayaz A, et al. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open. 2016;6(6): e010364.
Yancik R. Population aging and cancer: a cross-national concern. Cancer J. 2005;11(6):437–41.
Wilder-Smith OHG. Opioid use in the elderly. Eur J Pain. 2005;9(2):137–40.
Chiappini S, et al. Opioid painkiller dependence in a sample of elderly medical inpatients. Psychogeriatrics. 2021;21(3):265–71.
Olthoff MV, et al. Overgevoeligheid voor hulpstoffen in pleisters. Nederlands Tijdschrift voor Geneeskunde; 2019. p. 163.
Alqahtani MS, et al. Advances in oral drug delivery. Front Pharmacol. 2021;12: 618411.
Vander Hulst K, et al. Allergic contact dermatitis from transdermal buprenorphine. Contact Dermat. 2008;59(6):366–9.
Romita P, et al. Contact dermatitis due to transdermal therapeutic systems: a clinical update. Acta Biomed. 2018;90(1):5–10.
Chiappini S., et al., Pharmacovigilance signals of the opioid epidemic over 10 years: data mining methods in the analysis of pharmacovigilance datasets collecting adverse drug reactions (ADRs) Reported to EudraVigilance (EV) and the FDA Adverse Event Reporting System (FAERS). Pharmaceuticals (Basel). 2022;15(6).
Häkkinen M, Vuori E, Ojanperä I. Prescription opioid abuse based on representative postmortem toxicology. Forensic Sci Int. 2014;245:121–5.
Comer SD, Cahill CM. Fentanyl: Receptor pharmacology, abuse potential, and implications for treatment. Neurosci Biobehav Rev. 2019;106:49–57.
O’Connor AB. Is actiq use in noncancer-related pain really “a recipe for success”? Pain Med. 2008;9(2):258–60.
Passik SD, Kirsh KL. Weighing in on the off-label use of Actiq™ for noncancer-related pain: a recipe for success or a recipe for disaster? Pain Med. 2007;8(2):130–3.
Carreyrou J. Narcotic ‘lollipop’is big seller despite FDA curbs. Wall Street J; 2006:735399–114.
European Medicines Agency. Withdrawal Assessment report: Effentora. Amsterdam: European Medicines Agency; 2013.
European Medicines Agency. Questions and answers, Withdrawal of the application for a change to the marketing authorisation for Effentora (fentanyl). Amsterdam: European Medicines Agency; 2013.
Takeda Pharma A/S. Instanyl 50 micrograms/dose nasal spray, solution SmPC. 2009. https://www.ema.europa.eu/en/documents/product-information/instanyl-epar-product-information_en.pdf .
Teva B.V. Effentora 100 micrograms buccal tablets. 2008. https://www.ema.europa.eu/en/documents/product-information/effentora-epar-product-information_en.pdf .
Jain P, et al. Evaluation of opioid overdose reports in patients treated with extended-release naltrexone: postmarketing data from 2006 to 2018. Drug Saf. 2021;44(3):351–9.
Ekhart C, de Vries T, van Hunsel F. Psychiatric adverse drug reactions in the paediatric population. Arch Dis Child. 2020;105(8):749–55.
Hazell L, Shakir SA. Under-reporting of adverse drug reactions : a systematic review. Drug Saf. 2006;29(5):385–96.
Coleman JJ, Pontefract SK. Adverse drug reactions. Clin Med (Lond). 2016;16(5):481–5.
Lewer D, et al. Causes of death among people who used illicit opioids in England, 2001–18: a matched cohort study. Lancet Public Health. 2022;7(2):e126–35.
Güner MD, Ekmekci PE. Healthcare professionals’ pharmacovigilance knowledge and adverse drug reaction reporting behavior and factors determining the reporting rates. J Drug Assess. 2019;8(1):13–20.
Cheema E, et al. Barriers to reporting of adverse drugs reactions: a cross sectional study among community pharmacists in United Kingdom. Pharm Pract (Granada). 2017;15(3):931.
Joaquim J, et al. All-round approaches to increase adverse drug reaction reports: a scoping review. Drugs & Therapy Perspectives. 2023;39:249–61.
Matos C, Rodrigues L, Joaquim J. Attitudes and opinions of Portuguese community pharmacy professionals towards patient reporting of adverse drug reactions and the pharmacovigilance system. Drugs Ther Perspect. 2017;33:188–94.
Pande S. Causality or relatedness assessment in adverse drug reaction and its relevance in dermatology. Indian J Dermatol. 2018;63(1):18–21.
Wallerstedt SM, G Brunlöf, A. Sundström. Rates of spontaneous reports of adverse drug reactions for drugs reported in children. Drug Saf. 2011;34(8):669–82.
Download references
Author information
Authors and affiliations.
Department of Pharmacology, Institute of Neuroscience and Physiology, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
Moa Gustafsson
Polytechnic Institute of Coimbra, Coimbra Health School, Coimbra, Portugal
Moa Gustafsson, Cristiano Matos & João Joaquim
Netherlands Pharmacovigilance Centre Lareb, MH’s-Hertogenbosch, The Netherlands
Joep Scholl & Florence van Hunsel
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Moa Gustafsson .
Ethics declarations
No funding was received for this study.
Conflict of interest
Moa Gustaffson, Cristiano Matos, João Joaquim, Joep Scholl and Florence van Hunsel have no conflicts of interest to declare that are directly relevant to the contents of this study.
Ethical approval
Ethical approval was not needed for this study.
Consent to participate
No approval or consent was needed for this study.
Consent for publication
Availability of data and materials.
The datasets for this manuscript are not publicly available due to the data protection policy of the Pharmacovigilance Centre Lareb. Requests to access the datasets should be directed to the first author and will be granted on reasonable request.
Code availability
The SQL statements for the data used in this article are not publicly available due to the data protection policy of Lareb. Requests to access the datasets should be directed to the first author and will be granted on reasonable request.
Authors’ contributions
The original study protocol was designed by MG and CM with input from FvH. JS established the query and dataset. Data analysis was performed by MG and CM, and the design of the manuscript was determined by all authors. All authors contributed to the final data analysis and manuscript drafting and revision. All authors approved the final version to be published and agreed to be accountable for all aspects of the work.
Privacy statement
All personal data from the patient’s reporting form is handled in accordance with the General Data Protection Regulation (GDPR) and the general privacy regulation of the Pharmacovigilance Centre Lareb.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Gustafsson, M., Matos, C., Joaquim, J. et al. Adverse Drug Reactions to Opioids: A Study in a National Pharmacovigilance Database. Drug Saf 46 , 1133–1148 (2023). https://doi.org/10.1007/s40264-023-01351-y
Download citation
Accepted : 11 September 2023
Published : 12 October 2023
Issue Date : November 2023
DOI : https://doi.org/10.1007/s40264-023-01351-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

A review of tobacco abuse and its epidemiological consequences
Micah o. omare.
1 Department of Physical and Biological Sciences, Moi University, P.O Box 3900, Eldoret, 30100 Kenya
2 Africa Center of Excellence II in Phytochemicals, Textiles and Renewable Energy (ACE II PTRE), Moi University, P.O. Box 3900-30100, Eldoret, Kenya
Joshua K. Kibet
3 Department of Chemistry, Egerton University, P.O Box 536-20115, Egerton, Kenya
Jackson K. Cherutoi
Fredrick o. kengara.
4 Department of Chemistry, Maseno University, Private Bag, Maseno, Kenya
The economic burden caused by death and disease in the world is credited mainly to tobacco use—currently linked to approximately 8,000,000 deaths per year with approximately 80% of these faralities reported in low and middle income economies. The World Health Organization (WHO) estimates that nearly 7,000,000 deaths are attributed to direct tobacco use, while approximately 1,200,000 non-smokers exposed to second hand cigarette smoke die every year. Accordingly, tobacco use is a major threat to the public health infrastructure; therefore, proper cessation interventions must be put in place to curb tobacco abuse and ease economic and social burdens caused by the tobacco epidemic.
A systematic review was conducted to investigate how scientific efforts have been advanced towards harm reduction among smokers and non-smokers. Relevant articles published during the period 2010–2020 in PubMed, Crossref, Google scholar, and Web of Science were used in this study. The articles were selected based on health impacts of cigarette smoking, tobacco cessation and emerging diseases, including Covid−19. Various cessation strategies have been identified although their efficiency is yet to match the desired results.
A series of carcinogenic chemicals are generated during cigarette smoking resulting in serious health complications such as cancer and mutagenesis. The precursors for tobacco induced diseases are toxic and carcinogenic chemicals of the nitrosamine type, aldehydes, polonium-210 and benzo[a]pyrene, which bio-accumulate in the body system during cigarette smoking to cause disease. Rehabilitation facilities, use of drugs to diminish the desire to smoke, heavy taxation of tobacco products and warning labels on cigarettes are some of the cessation strategies employed towards curbing tobacco abuse.
The need for further research to develop better methods and research based policies for safe cigarette smoking and workable cessation strategies must be a priority in order to deal with the tobacco epidemic. Campaigns to promote tobacco cessation and abstinence are recommended in this review as a sure measure to mitigate against the deleterious impacts caused by cigarette smoking and tobacco abuse.
Introduction
Tobacco is one of the most notoriously abused drug substance among the rural and urban populations in the developing world—a pattern which may also be replicated across developed countries (Vellios et al. 2018 ). The National Institute on Drug Abuse (NIDA) of the United States of America approximates the cost of tobacco abuse, alcohol and banned drugs to be a costly undertaking in terms of crime, lost productivity and health care which is estimated to cost approximately 5% of the US gross domestic product (GDP) (NIDA 2020 ). Globally, a steady increase in the rate of consumption of tobacco products and the number of smokers in the past decade has been reported (Mishra et al. 2016 ; O'Connor et al. 2020 ). As a result, this trend has triggered serious concerns regarding cessation on the abuse of illegal drugs and cigarette smoking which is potentially harmful to human health. Cigarette smoking has been clearly established as a risk factor for various degenerative diseases such as lung cancer and cardiovascular diseases by various scientific and epidemiological surveys (Jha 2020 ; Omari et al. 2015 ). Nonetheless, tobacco cigarette smokers are believed to be highly susceptible to the novel respiratory disease, Covid-19, given that smoke from cigarettes is a precursor for alterations on the angiotensin converting enzyme-2 (ACE-2) receptor for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) (Brake et al. 2020 ). Consequently, the World Health Organization (WHO) has been on the forefront to educate the public worldwide on the dangers of tobacco use, which forms the basis of its Framework Convention on Tobacco Control (FCTC) guidelines (WHO 2019 ). In this review, scientific efforts directed towards the cessation of tobacco smoking and the perceived harm and impacts arising from the frequent use of this psychoactive drug are assessed by reviewing selected published articles from different journals and databases. The emerging chemicals from tobacco cigarette smoke and scientific efforts taken in order to reduce emitted toxins; use of catalysts, tobacco additives, temperature variations, heat not burn cigarettes, e-cigarettes, and other methods have been evaluated towards harm reduction. Findings from this review may direct further research in devising methods that can enhance cessation of cigarette smoking thereby promoting the healthy livelihood of cigarette smokers, and non-cigarette smokers who conventionally suffer from the effects of sidestream smoke. For the record, this work has considered literature that is published in the English language only. After the search on the multidisciplinary databases and google scholar, a number of published reports on the subject of interest, especially tobacco cigarettes smoking, toxicity and Covid-19, and carcinogenicity, were the primary focus of this review.
Methodology
A detailed literature search was conducted in PubMed, Google scholar, and scientific electronic libraries online from Jan 2020 to April 2020 in line with the procedures described in previous literature review study protocols (Palmatier et al. 2018 ). The literature search was self-sufficiently done in a selection of databases that comprised original published articles in peer-reviewed journals, patents, books, dissertations, and reports that addressed tobacco abuse. Accordingly, articles published between January 2012 and April 2020 were considered if they had information about tobacco ailments, such as respiratory diseases; asthma and emphysema. For search precision, information used in this work was picked from the google search engine by including general terms such as tobacco toxicity, cancer, and carcinogenicity, dangers, intake methods, throat cancer, smoking, cigarettes, SARS-CoV-2, Covid-19 vulnerability, and smoking cessation. The authors set the online databases to give notifications of search outputs that contained information relevant and matching the established search standards such as academia, science direct, Mendeley, and google scholar, which were saved on personal computers (PCs) for further reading and analysis.
Results and discussions
Tobacco use as a precursor for cancer.
Cigarette smoking is a well-established leading cause for cancer and mutagenesis, and the determinant factors are the duration of smoking, and the number of cigarettes smoked, which precipitate the risk for histologic types of lung cancer: squamous cell carcinoma, small cell carcinoma, adenocarcinoma, and large cell carcinoma (Babalık et al. 2018 ). Therefore, cigarette smoking is a precursor for transitional cell carcinomas of the bladder, ureter, and renal pelvis (Arora et al. 2018 ; Soliman 2018 ; Wojtczyk-Miaskowska and Schlichtholz 2019 ). Furthermore, cigarette smoke is known to raise the risk of sinonasal and nasopharyngeal cancer (Miligi et al. 2020 ). In addition, oropharyngeal and hypopharyngeal cancer have also been reported to be initiated by cigarette smoking (Liao et al. 2018 ). Additionally, liver cancer can be induced by cigarette smoking (Petrick et al. 2018 ). Therefore, most cancers are initiated by the carcinogenic chemicals present in cigarette smoke; the most common type of cancer being adenocarcinoma (Coleman et al. 2018 ).
Conventionally, tobacco can be used as either smoked tobacco or smokeless tobacco. When smoked, tobacco cigarettes emit smoke that has been linked to lung related deaths as evidenced by a number of scientific studies that emphasize that burning cigarettes release numerous chemicals that are biologically detrimental (Coleman et al. 2018 ; Shihadeh et al. 2015 ). Smoked tobacco products include but not limited to cigarettes, water pipes (Shihadeh et al. 2015 ), electronic cigarettes (Smith 2019 ), bidis, and krekets (Mishra et al. 2016 ). Alternatively, when tobacco is consumed in other forms apart from smoking, it consequently constitutes smokeless tobacco products such as loosely chewed tobacco leaves, snus, naswar, gutka snuffs, and tobacco paste (Hajek et al. 2019 ; Khan et al. 2019 ; Kindvall et al. 2019 ; Mohapatra 2019 ). Scientific analysis on these smokeless tobacco products have unraveled more than 20 chemical compounds known to be cancer causing agents, which include tobacco-specific nitrosamines, N-nitrosamine acids, volatile N-nitrosamines, polycyclic aromatic hydrocarbons, and aldehydes (McAdam et al. 2013 ; Warnakulasuriya and Straif 2018 ). The methods of tobacco intake and popularity trends are illustrated in Table Table1 1 .
Tobacco consumption methods and popularity trends
| Market product | Method of intake | Popularity percentage | Trend in the past two decades | References |
|---|---|---|---|---|
| smoked tobacco | cigarettes | 83% | increase | Mishra et al. |
| bidis | 13% | decrease | Mishra et al. | |
| krekets | 10% | decrease | Mishra et al. | |
| water pipes | 38% | increase | Shihadeh et al. | |
| smokeless tobacco | ||||
| loose leaf chewing | mouth chewing | 35% | decrease | Stepanov et al. |
| moist snuf (snus) | pinch put between gingival and buccal mucosa | 77% | increase | Kindvall et al. |
| dry snuf | nasal inhalation | 60% | decrease | Kindvall et al. |
| e-cigarettes | nasal inhalation | 80% | increase | Hajek et al. |
Loose leaf tobacco chewing is prepared from tobacco leaves that are air cured, crushed, and a flavoring agent added to improve its taste (Stepanov et al. 2014 ). On the other hand, moist snuff, snus, consist of fire and air-cured dark tobacco, while dry snuff comprises fermented and fire cured powder (Kindvall et al. 2019 ; Pillitteri et al. 2020 ). Apparently, the main motivating factor for an individual to use tobacco products is nicotine—a tobacco alkaloid constituting nearly 95% of tobacco chemicals (Ji et al. 2017 ; McKinney and Vansickel 2016 ). When tobacco enters the human biological system in the form of smoke, numerous compounds constituting tobacco smoke are taken in by the smoker (Tsai et al. 2018 ), which are initiators for generative and degenerative diseases including cancer and grave respiratory diseases, such as emphysema, asthma, cardio obstructive pulmonary disorder (COPD) (Ferrante and Conti 2017 ).
Tobacco smoke chemistry has been the subject of extensive investigation by various scientific research authorities and individual researchers for over a century (McAdam et al. 2016 ) and to date, over 7000 compounds have been established to be present in tobacco smoke, with more than 50 of these chemicals identified as carcinogenic by IARC (Warnakulasuriya and Straif 2018 ; Weng et al. 2018 ). During tobacco burning, compounds including carbon monoxide, benzene, formaldehyde, polycyclic aromatic hydrocarbons (PAHs), hydrogen cyanide, and nitrosamines are produced (Morgan et al. 2017 ; Nlemedim 2017 ). In the process, incomplete combustion reactions occur at the core of the burning cigarette which consequently results in the production of PAHs (Nlemedim 2017 ; Weng et al. 2018 ).
Tobacco effluents possesses toxic, mutagenic, and carcinogenic properties because they are extremely lipid soluble (Barnes et al. 2018 ), and therefore spontaneously adsorbed in the gastrointestinal tract in humans (Warnakulasuriya and Straif 2018 ). In addition, PAHs are rapidly distributed in the human biological tissues and deposited in fats where they bind to the DNA consequently initiating a series of disruptive effects that often end up as tumor progenitors (Warnakulasuriya and Straif 2018 ; Weng et al. 2018 ). For this reason, PAHs are listed among the highly human health threatening chemicals with a high potency that usually leads to cancer among the cigarette smoking community (Hecht 2012 ). Besides, PAHs have been reported to cause several other toxicological expressions in humans that include but are not limited to engorged liver with cell oedema and congestion of the liver connective tissues and blood vessels, loss in body weight, intoxication of male and female genital system, uterus development retardation, learning and lowered intelligent quotient (IQ), oocyte damage, and kidney cell infection (McAdam et al. 2016 ; O'Brien et al. 2016 ).
Some compounds, including tobacco specific nitrosamines (TSNAs) and nicotine, occur naturally in tobacco and are released during tobacco burning (Edwards et al. 2017 ; Konstantinou et al. 2018 ). Nicotine predominantly present in tobacco mainly exists in two forms—protonated nicotine and non-protonated nicotine—that are pH dependent (El-Hellani et al. 2015 ). Non-protonated nicotine is a free base and the more addictive form of nicotine, which is extremely bioavailable and freely absorbed into the blood system and is responsible for the pleasurable psychoactive effects (O'Connor et al. 2020 ). Scientifically, TSNAs have been recognized as the chief cancer causing agents in both smoked and smokeless tobacco (O'Connor et al. 2020 ; Xue et al. 2014 ). Tobacco is known to consist of four principle TSNA chemicals: N-nitrosonornicotine (NNN), 4-methyl-N-nitrosamino-1-(3-pyridyl)-1-butanone (NNK), N-nitrosoanatabine (NAT), and N-nitrosoanabasine (NAB) (Xue et al. 2014 ). Of these four, IARC marks NNN and NNK as the key cancer initiating agents in tobacco (Singhavi et al. 2018 ; Zamora and Hidalgo 2020 ). Nitrosamines form when secondary and tertiary amines react with nitriles to yield nitrosamine out of which over 70 nitrosamines have been confirmed scientifically as carcinogenic (Gunduz et al. 2016 ). Nitrosation of secondary amines is a very fast reaction process in which the hydrogen attached to the nitrogen is replaced by the –NO group in significantly high yields, although on the other hand, nitrosation of the tertiary amines is a slow process (Spahr et al. 2017 ). Therefore, nitrosation of secondary amines (nornicotine, anabasine, and anatabine) leads to the formation of tobacco explicit nitrosamines NNN, NAB, and NAT, while nornicotine, anabasine, and anatabine form part of the important alkaloids in tobacco (Cai et al. 2016 ). Nitrosation of tertiary amines nicotine yields NNN, which together with nicotine-derived NNK, have been identified to be strong carcinogens that have the potential to induce malignant and non-malignant tumors in humans depending on the route of administration or ingestion (De Flora et al. 2016 ). Fresh tobacco leaves contain low levels of TSNAs but the levels of these chemicals increase during tobacco curing (Wang et al. 2017 ). Accordingly, during cigarette smoking N-nitrosamines enters the smokers’ body system through inhalation of mainstream cigarette smoke and/or side stream cigarette smoke (Gunduz et al. 2016 ; Hang et al. 2018 ). As a result, both active smokers and passive smokers become vulnerable to nitrosamines that endogenously form from uptake of alkaloids and nitrogen oxides or nitriles (Barnes et al. 2018 ; Wang et al. 2017 ). Other cancer causing agents in tobacco smoke include benzo(a)pyrene (BaP), polonium−210, and cadmium (Omari et al. 2015 ; Shafik et al. 2019 ; IARC 2019 ). BaP has been classified by IARC as a group 2A cancer causing chemical and is therefore a risk chemical (IARC 2019 ; Vu et al. 2015 The introduction of electronic cigarettes was supposed to promise safer cigarettes suggested to deliver low nicotine levels (Carlsen and Skjerven 2018 ; Hajek et al. 2019 ). Contrary to this proposition, scientific research on the dangers of e-cigarettes has revealed that they are more toxic and yield potentially carcinogenic chemicals formed during the use of e-cigarettes (Armendáriz-Castillo et al. 2019 ), Table Table2. 2 . A number of compounds released from e-cigarettes have been reported to cause genetic mutation that subsequently leads to the growth of malignant cells and ultimately cancer (Barnes et al. 2018 ). Some of the molecular compounds suspected to be cancerous are presented in Fig. 1 .
Some carcinogenic chemicals reported in tobacco smoke
| Tobacco chemicals | Carcinogenicity level | Reference |
|---|---|---|
| carbon monoxide | group 1 | IARC |
| benzene | group 1 | Loomis et al. |
| formaldehyde | group 1 | d’Ettorre et al. |
| polycyclic aromatic hydrocarbons (PAHs) | group 1, group 2A, and group 2B | ARC |
| hydrogen cyanide | not listed | |
| lead | group 2B | Bjurlin et al. |
| tobacco specific nitrosamines (TSNAs) | group 1 | Bjurlin et al. |
| nicotine | not listed | |
| benzo(a)pyrene (BaP) | group 1 | Santonicola et al. |
| polonium−210 | group 1 | Stanfill |
| cadmium | group 1 | Stanfill |
| heterocyclic aromatic amines | group 2A | Bjurlin et al. |
| aldehydes | group 2B | |
| phenolic compounds | not listed | |
| volatile hydrocarbons | group 1 | IARC |
| nitro hydrocarbons | not listed | |
| toluene | group 2A | Warden et al. |
| furan | group 2A | IARC |
| 2-methylfuran | group 2B | IARC |

Tobacco specific nitrosamines identified from e-cigarettes (IARC 2019 )
Accordingly, Drazen et al. ( 2019 ) asserted that there is a potential likelihood of an e-cigarette user getting addicted to nicotine because of its increased concentration as a result of more frequent vaping than regular smoking, thereby subjecting the user to grave health risks. Based on this observation, it has been pointed out that the increasing rates of e-cigarette use among the youth, who are considered the major consumers of e-cigarette, can be credited to the highly addictive nature of nicotine, which has the capacity to cause a public health crisis, at least, according to scientific surveys (Kurgat et al. 2016 ; Singh et al. 2020 ). Aromatic amines, aldehydes, phenolic compounds, volatile hydrocarbons, nitro hydrocarbons, and various organic compounds present in tobacco smoke have also been proven carcinogenic through experimental studies on animals (CDC 2010 ; Zamora and Hidalgo 2020 ). IARC has classified these chemicals as group 2B, which are possibly carcinogenic to human beings, group 2A, which are probably carcinogenic to humans or group 1, which are carcinogenic to humans (IARC 2019 ; CDC 2010 ). Additionally, it has long been reported that benzene, toluene, furan, 2-methylfuran, and isobutylene are some of the components of gas-phase cigarette smoke considered detrimental to cigarette smokers (Hang et al. 2018 ; Sleiman et al. 2014 ). Nevertheless, these compounds are sighted as potential leads in initiating lung cancer (Warden et al. 2018 ). However, there is limited information documented in literature regarding their cancer causing mechanisms (Hang et al. 2018 ).
Emerging potent tobacco chemicals
Numerous scientific researchers have identified the chemical composition of tobacco smoke with significant efforts invested on establishing the suspected carcinogens and their connection between cigarette smoking and the associated adverse health effects (Armendáriz-Castillo et al. 2019 ; McAdam et al. 2018 ). Additionally, active chemical species predominantly present in cigarette smoke include hydroxyl radicals, hydrogen peroxide, and superoxide anion radicals, which are mostly generated during the tobacco burning (Assaf et al. 2016 ). Therefore, environmentally persistent free radicals are a subject of great interest in research with more focus being emphasized on the formation mechanisms and their related effects on human health. Free radicals have a major contribution to impairing the respiratory landscape by majorly causing chronic cardiopulmonary dysfunction owing to the fact that they can trigger the generation of reactive oxygen species (ROS) and are well-established precursors for oxidative stress and cardiac arrest (Panth et al. 2016 ).
Heterocyclic hydrocarbons have been reported to be predominantly present in cigarette smoke (Barnes et al. 2018 ). During the thermal degradation of tobacco biomass, dibenzofuran and their associated dioxins in their polychlorinated notoriously very toxic forms are produced (Rehman et al. 2019 ). On the other hand, furan can be classified as an endocrine disrupting chemical given that it has a higher ability to alter animal physiology by disrupting hormonal levels (Ferreira et al. 2019 ). During organ development, if organisms are exposed to endocrine disrupting chemicals, such as furan (C 4 H 4 O), they cause irreversible damage to the hormonal profile (Grill et al. 2015 ; Rehman et al. 2019 ). Therefore, furans can have highly devastating biological organizational effects on the developing fetus if exposed to cigarette smoke during pregnancy (Horinouchi et al. 2016 ; Rehman et al. 2019 ). Research conducted on heterocyclic aromatic compounds has revealed that they contribute to bacterial mutagenicity (Roemer et al. 2016 ). These compounds form through the conventional milliard reactions involving creatinine, free amino acids, and sugars (Barzegar et al. 2019 ; et al., 2020). For instance, heterocyclic aromatic hydrocarbons are activated metabolically by N-hydroxylation that forms the intermediate ion arylnitrenium, and have been reported to influence DNA damage and toxicity (Barzegar et al. 2019 ; Chen 2020 ). Similarly, aldehydes, phenolic compounds, volatile hydrocarbons, and nitro hydrocarbons are reported to be predominantly present in cigarette smoke in various concentration levels (CDC et al. 2010 ).
In one survey, it was reported that aldehydes can potentially undergo chemical reactions involving nucleophilic targets in body cells, lipids, and proteins and consequently form stable and unstable adducts (Sapkota and Wyatt 2015 ). Accordingly, pathological injuries in human beings are initiated in the lungs due to alterations of cellular functions in addition to damaged proteins, nucleic acids, and lipids thereby propagating vascular diseases (Phaniendra et al. 2015 ). Lately, there have been attempts to explore methods in which tobacco toxins can be reduced or destroyed during cigarette burning because of the observed reluctance in the smoking population to quit smoking, and the opposition of tobacco processing companies to adopt technologies that would lower harm as a result of cigarette use (Peeters and Gilmore 2015 ). Table Table2 2 presents selected carcinogenic chemicals classified as carcinogenic by IARC. On the other hand, Table Table3 3 reports the health effects of a variety of chemicals released from tobacco burning.
Chemicals present in e-cigarettes and their associated health effects (Armendáriz-Castillo et al. 2019 ; IARC 2019 )
| Name | Health effects | Carcinogenic potential |
|---|---|---|
| (+)-aromadendrene | cytotoxic/skin irritation | unknown |
| (z)-3-hexen-1-ol | eye irritation | unknown |
| 1-methyl phenanthrene | cytotoxic/eye irritation/skin irritation | group 3 |
| 1,3-butanediol | low concern based on experimental and modeled data | unknown |
| 1,3-propanediol | not a significant hazard via inhalation of either the gas phase or a gas/aerosol mixture | unknown |
| 2-acetylpyrrole | skin irritation | unknown |
| 2,3-dimethylpyrazine | cytotoxic | unknown |
| 2,3-pentanedione | skin irritation/eye irritation/systemic organ irritation | unknown |
| 2,3,5-trimethylpyrazine | cytotoxic | unknown |
| 3-methyl-1-butanol | cytotoxic/skin irritation/eye irritation/respiratory tract irritation | unknown |
| acetic acid | respiratory tract irritation | unknown |
| benzyl acetate | cytotoxic/eye irritation/respiratory tract irritation | group 3 |
| benzyl alcohol | cytotoxic | unknown |
| butyl butyrate | eye irritation/mild effects/behavioral Effects | unknown |
| camphor | cytotoxic/neurotoxic/systemic organ irritation/mild effects/ behavioral effects | unknown |
| cinnamaldehyde | eye irritation/respiratory tract irritation/systemic organ irritation | |
| cinnamyl alcohol | unknown effects in human health | group 2B |
| coumarin | behavioral effects/systemic organ irritation | group 3 |
| methyl cyclopentenolone | unknown effects in human health | |
| diacetyl | eye irritation/skin irritation | group 3 |
| diethylene glycol | systemic organ irritation/ skin irritation | |
| ethylbutyrate | mild effects/behavioral effects | |
| ethylmaltol | cytotoxic | unknown |
| ethylvanillin | unknown effects in human heal | unknown |
| ethylene glycol | harmful effects in animal model | unknown |
| glycerin | eye irritation/skin irritation/respiratory tract irritation | unknown |
| hydroxyacetone | cytotoxic | group 2B |
| i-butyric acid | respiratory tract irritation | |
| isobutyl acetate | eye irritation/skin irritation/respiratory tract irritation/mild effects | group 2B |
| isoamyl acetate | eye irritation/skin irritation/respiratory tract irritation | unknown |
| isopentyl isovalerate | harmful effects in animal models | unknown |
| l-menthyl acetate | respiratory tract irritation | unknown |
| limonene | no evidence of carcinogenic activity in rats or human | unknown |
| maltol | cytotoxic | unknown |
| menthone | harmful effects in animal models | unknown |
| methylanthranilate | unknown effects in human health | group 2B |
| methylcinnamate | unknown effects in human health | unknown |
| methylsalicylate | neurotoxin/cardiovascular effects | unknown |
| myosmine | carcinogenic | group 2B |
| n-hexanol | harmful effects in animal models | group 2B |
| nicotyrine | unknown effects in human health | |
| o-tolualdehyde | harmful effects in animal models/unknown effects in human health | unknown |
| -cymene | skin irritation/mild effects | group 2B |
| propylene glycol | respiratory tract irritation | unknown |
| safrole | harmful effects in animal models | group 2B |
| thujone (sum of α- and β-diastereomers) | harmful effects in animal models | unknown |
| trans-2-hexen-1-ol | unknown effects in human health | unknown |
| vanillin | cytotoxic | unknown |
| β–damascone | skin irritation | group 3 |
| γ–decalactone | respiratory tract irritation | unknown |
Designing methods that can successfully reduce toxins in tobacco will offer an effective strategy in minimizing mortality and morbidity among the cigarette smoking community (Abrams et al. 2018 ). With respect to this proposal, heat not burn methods have been preferably considered for use in consuming tobacco products (Abrams et al. 2018 ; Lachenmeier et al. 2018 ). These techniques involve inserting tobacco products into a tobacco heating system where they are heated at temperatures below the cigarette combustion temperatures as opposed to directly burning the cigarette (Lachenmeier et al. 2018 ). Such techniques when employed can significantly reduce the heat created toxins in the aerosol inhaled by the cigarette smoker (Smith et al. 2016 ). The desire for such techniques is aimed at lowering toxicants in cigarettes hence the manufacture of electronic cigarettes (e-cigarette), which are presumed to aid tobacco cessation (Pokhrel et al. 2015 ).
An e-cigarette is an electric device that allows an active smoker to inhale nicotine with supposedly fewer compounds responsible for most harmful smoking effects although the possibility of forming reactive free radical species that can cause oxidative stress and cardiac arrest cannot be ruled out (Smith 2019 ). Ideally, e-cigarettes serve as a nicotine replacement therapy that enhances the reduction towards the desire to smoke and eventually making it easier for smokers to quit smoking but on the contrary, research survey has found this to be untrue (Kindvall et al. 2019 ). In operational e-cigarettes, an e-liquid is heated to produce e-vapor in the form of aerosols with flavorings and nicotine, which are consequently delivered into the smoker (DeVito and Krishnan-Sarin 2018 ). Even though the use of e-cigarettes is presumed to be safer compared to ordinary cigarette (Hilton et al. 2016 ), they have been reported to contain toxins that induce toxicity, inflammation, and oxidative stress in smokers (Dasgupta and Klein 2014 ), as listed in Table Table3. 3 . During the use of e-cigarettes, factors leading to the synthesis of TSNAs are believed to be put under control (Farsalinos et al. 2015 ; Konstantinou et al. 2018 ). For instance, some farmers and manufacturers have employed strategies that lower the alkaloid content in tobacco in order to suppress NNN and nornicotine development given that NNN and NNK are the two TSNAs that have been classified by the IARC as carcinogenic to humans (Kumar et al. 2018 ). This has been achieved by removing the nitrate-reducing microbial activity, controlling the conditions of the temperature and humidity during curing, and employing heat exchange methods that lower nitrosamine concentration levels (Law et al. 2016 ; Riddick et al. 2017 ). Similarly, low yield “light” cigarettes and “ultra-light” cigarettes have been designed by different tobacco processing companies, and they are suggested to contain fewer toxins compared to the normal “heavy” cigarettes (Popova et al. 2018 ). Elsewhere, a study on nicotine reduction and its associated impacts has pointed out two required lines of action; preventing addiction and reduction or stoppage of tobacco consumption altogether, which never has an easy strategy towards tobacco cessation (Schmidt et al. 2018 ). Whereas the use of e-cigarettes and light cigarettes as alternative ways to reduce tobacco toxins may be a successful strategy, controlling thousands of other tobacco toxins released during tobacco burning cannot be achieved by these techniques, which are focused only in lowering nicotine concentration levels in a cigarette (Auer et al. 2017 ). Moreover, smokers may end up consuming more of these cigarettes in order to get the desired effect of smoking, leading to ingesting high levels of toxins, which may be injurious to the human biological environment (Benowitz et al. 2017 ; Morean et al. 2016 ).
Efforts have been advanced towards devising methods that can aid in lowering the concentrations of TSNAs in cigarette smoke which form as a result of microbes in tobacco decay during tobacco curing and thus produce nitrites and NOx precursors for TSNAs production when tobacco is burned (Warek et al. 2019 ). Further, it has been pointed out that the use of nitrite scavengers as additives can eliminate active microbes (Stanfill 2020 ). Accordingly, Shi and Yang ( 2017 ) have described a novel alternative technique that focuses on reducing bacteria and bacterial activities in tobacco extracts, which eventually reduce TSNAs in cigarette smoke. Furthermore, the method described by d’Ettorre et al. ( 2017 ) for the reduction of TSNAs and improving the leaf quality in tobacco during curing has been found to be effective in minimizing TSNAs health effects arising from cigarette smoking. It is important to note that tobacco soil treatment and spraying of tobacco plants prior to harvesting stimulates antioxidant production that interferes with the formation of TSNAs during curing (Li et al. 2008 ). In addition, the use of filters that can selectively remove TSNAs from cigarettes smoke has been suggested (Li et al. 2018 ) but still found to be ineffective especially in removing carbon monoxide to any acceptable degree. Because TSNAs are produced during curing and fermentation processes, an alternative method such as pasteurization of snus can be employed to produce tobacco products of minimal harm (Stanfill 2020 ).
Furthermore, a review on the interventions that promote harm reduction due to continued tobacco use is important in quitting cigarette smoking (Lindson-Hawley et al. 2016 ). The associated dangers of smoking can also be minimized by lowering the number of cigarettes smoked daily or consuming alternative tobacco products such as chewing tobacco or snus which constitute the necessary tobacco replacement therapy (Lindson-Hawley et al. 2016 ). The use of pharmaceuticals, including bupropion and varenicline, has also been evaluated to be helpful in reducing tobacco toxins (Jiloha 2014 ; Prochaska and Benowitz 2019 ), although there is a lack of precise evidence on their workability. For this reason, the use of smokeless tobacco products has been highly recommended as an alternative route to smoking on the argument that they are low tar yielding and presumably safer (Drazen et al. 2019 ). On the contrary, a number of chemicals have been identified (IARC 2019 ; Kumar et al. 2018 ), as listed in Table Table4, 4 , and IARC has classified these chemicals as carcinogenic.
Chemicals in smokeless tobacco and their IARC classification (IARC 2019 )
| Tobacco chemical | IARC classification | Tobacco chemical | IARC classification |
|---|---|---|---|
| NNN | 1 | chlordane | 2B |
| NNK | 1 | heptachlor | 2B |
| benzo (a)pyrene | 1 | 3-(methylnitrosamino)-propionitrile | 2B |
| formaldehyde | 1 | cobalt | 2B |
| beryllium | 1 | ochratoxin A | 2B |
| arsenic | 1 | aflatoxin M1 | 2B |
| cadmium | 1 | lead | 2B |
| N-nitrosodimethylamine | 2A | NAT | 3 |
| nitrosoacids (NA) | 2A | NAB | 3 |
| dibenz[a,h]anthracene | 2A | N-nitrosoproline | 3 |
| dichlorodiphenyltrichloroethane | 2A | N-hydroxyproline | 3 |
| nitrate | 2A | 3-(n-nitrosomethylamino)-propionaldehyde | 3 |
| nitrite | 2A | benzo[e]pyrene | 3 |
| hydrazine | 2A | triphenylene | 3 |
| ethyl carbamate | 2A | pyrene | 3 |
| n-nitrosodiethanolamine | 2B | fluoranthene | 3 |
| N-nitrososarcosine (NSAR) | 2B | acenaphthene | 3 |
| N-nitrosoethylmethylamine | 2B | fluorene | 3 |
| N-nitrosopyrrolidine | 2B | phenanthrene | 3 |
| N-nitrosopiperidine | 2B | anthracene | 3 |
| n-nitrosomorpholine | 2B | benzo[g,h,i]perylene | 3 |
| N-nitrosodiethanolamine | 2B | crotonaldehyde | 3 |
| benz[a]anthracene | 2B | acrolein | 3 |
| chrysene | 2B | endrin | 3 |
| benzoflouranthene (j) | 2B | maleic hydrazine | 3 |
| indeno[1,2,3-cd]pyrene | 2B | Natural gas liquids | 3 |
| 5-methylcytosine | 2B | n-nitrosoguvacine | 3 |
| naphthalene | 2B | euginol | 3 |
| benzo[b]fluoranthene | 2B | chromium | 3 |
| benzo[k]fluoranthene | 2B | mercury | 3 |
| dibenzo[a,i]pyrene | 2B | quercetin | 3 |
| acetaldehyde | 2B | morpholine | 3 |
Accordingly, even though the use of smokeless tobacco products is regarded as an alternative to reducing nicotine toxicology and their related risks in human health, the identification of these carcinogens in smokeless tobacco products renders them more dangerous to the cigarette smoking population (Lee et al. 2016 ). Meanwhile, a lack of policies for regulation and monitoring of the concentrations of chemicals in commercially available smokeless tobacco products may be considered as the major reason for quality control failures (Kumar et al. 2018 ). In order to address these challenges, efforts have been invested by relevant drug regulating authorities in many countries worldwide to evaluate the contents of these chemicals in tobacco and cigarettes before releasing a tobacco product into the market (Wright 2015 ).
The consequences of tobacco abuse
According to Mallock et al. ( 2018 ), cigarette smoke is highly toxic due to the generation of poisonous pyrolysis products during burning. For instance, a study carried out by Ivashynka et al. ( 2019 ) explored the effects of cigarette smoking and determined that it led to increased heart beat and a corresponding increase in blood pressure. Moreover, maternal smoking has been associated with decrease in intelligence test performance, poor cognitive achievements, memory impairment, hyperactivity and weak attention span (Kristjansson et al. 2018 ). Evidently from previous studies, ageing in humans has been linked to repeated inhalation of smoke from cigarettes during passive and active smoking (MacNee et al. 2014 ). Accordingly, smoking decreases biological ageing to approximately 55 years, especially among women (Skjodt et al. 2018 ). Subsequently, substance smoking speeds up the normal ageing process of the cigarette smoker’s skin, contributing to wrinkles and loss of skin’s aesthetic value and beauty (Clatici et al. 2017 ). These effects are prone to occur to a smoker after a period of about 10 years or less depending on the number of cigarettes an individual smokes, and the longer the smoking period (Fatani et al. 2020 ; Osman et al. 2017 . Notably, earlier skin damage as a result of smoking can be manifested on the smoker, but it is difficult for one to observe them immediately (Clatici et al. 2017 ). Moreover, facial wrinkles in human beings can be strongly projected from cigarette smoking and these can be attributed essentially to nicotine uptake, which causes thinning of blood vessels on the outermost skin layer, thereby impairing blood flow to the skin (Benowitz and Burbank 2016 ). As a result, the skin is starved of oxygen and nutrients, including vitamin A (Clatici et al. 2017 ). Moreover, fibers such as collagen and elastin, which are responsible for skin strength and elasticity, are destroyed by more than 7000 chemicals in tobacco smoke leading to skin sagging and premature wrinkles and haggard looks (Skjodt et al. 2018 ).
Additionally, scientific studies have reported the occurrence of chronic coughs and tuberculosis cases ignited by cigarette smoking, implying that increased tobacco consumption rates and exposure to second hand tobacco smoke promotes the risk of tuberculosis and death (Bisallah et al. 2018 ). Furthermore, coughs can serve as the first signature in cigarettes smokers of a respiratory concern (Ashok et al. 2017 ). The harmful effects of cigarette smoking are greatly magnified by HIV infected individuals who continue to smoke even when the disease is under control as a result of medication (Popova et al. 2018 ). More disturbing is that these groups of people lose more years of life to cigarette smoking than the disease itself since, other than the adverse health effects of smoking, cigarette smoking exposes HIV-positive individuals to threats for a host of grave HIV associated comorbidities and untimely deaths (Giles et al. 2018 ).
Nicotine addiction among the cigarette smoking community is a severe public health concern worldwide due to the genetic factors that contribute to disease vulnerability, and which also result in brain disorders and other harmful effects to the individual and economic burden to the society at large (Ji et al. 2017 ). Chromosomal complications arise as a result of harboring risk genes for addiction to various toxic compounds in cigarette smoke (Li and Burmeister 2009 ). As per studies performed for numerous addiction phenotypes, a prediction for linkage regions on chromosome 11 contributions towards addictive phenotypes has been undertaken previously (Bevilacqua and Goldman 2009 ). Habitual smoking therefore has been linked to chromosome 11q14 and the smoking behavior associated with chromosome 11q12 (Li 2018 ). A study by Pineles et al. ( 2014 ) determined that tobacco constituents can greatly damage the chromosomes in sperm or alter the morphological changes of the sperm, reduce the sperm density, sperm mobility and semen volume, thus affecting the male fertility capability.
The epidemiological impacts of Covid-19 on cigarette smokers
The worldwide outbreak of SARS-CoV-2, the precursor for the disease Covid-19, has been associated with more deaths among cigarette smokers compared to individuals who have never smoked (Vardavas and Nikitara 2020 ). Nicotine in cigarette smoke induces and causes alterations and responses in the human immune system, especially in the lungs, and thus initiates infections, allergy, tumor necrosis factor α- expression, mucosal inflammation, and other respiratory illnesses (Brake et al. 2020 ; Lippi and Henry 2020 ). However, contrary to this, there is no association between active smoking and the severity of Covid-19 (Lippi and Henry 2020 ) but a disputation of these sentiments is registered in a review study conducted by Vardavas and Nikitara ( 2020 ) who determined that individuals that were current smokers or former smokers exhibited severe symptoms of Covid-19 with higher chances of intensive care unit (ICU) admission in contrast with nonsmokers. Furthermore, a susceptibility analysis of Covid-19 on smokers based on ACE-2 receptors determined that the receptor expression in intrapulmonary airways and epithelial cells was higher in current smokers than former smokers, but significantly much higher than in people who have never smoked (Wang et al. 2020 ), therefore indicating a presumably higher probability for Covid-19 infection in smokers than individuals who have never smoked. Evidently, these observations are in agreement with findings from scientific experiments on ACE-2 expression in the small airways of Covid-19 patients, for both smokers and none smokers (Leung et al. 2020 ). The spread of Covid-19 is greatly through contact with infected surfaces even though it is also suspected to be airborne and highly contagious. Accordingly, it can be supposed that, smokers have a possibility of contracting the SARS-Cov-2 as a result of their fingers touching the cigarette stick and successfully pass it to their mouths through the lips biting the cigar stick. More so, water pipe smoked tobacco products are commonly communal and involve mouth piece sharing and the chances of spreading SARS-Cov-2 virus cannot be ignored. Therefore, these observations among cigarette smokers can result in high cases of Covid-19 infections.
Tobacco cessation strategies
Individual smokers are likely to quit smoking by shifting to lower tar and low nicotine cigarettes that are apparently less harmful or elect to use cigarettes that have reduced toxicity levels such as light cigarettes (Borrelli and O’Connor 2019 ). In the past few years, there have been significant innovative and effective behavioral and pharmacological smoking cessation methods such as use of heat not burn cigarettes including e-cigarettes and vaping (Singh et al. 2020 ). A systematic review on smokers and non-smokers perceptions of visually unappealing cigarette sticks concludes that an individual’s smoking behavior is influenced by the appearance of the cigarette (Drovandi et al. 2018 ), and therefore, normally from a marketing perspective, cigarettes may have physical attributes that are either appealing or non-appealing to consumers in terms of size, color, and health warnings written on the cigarette packs. Accordingly, a cigarette is appealing to the consumer based on visual, olfactory or other perceptual or cognitive signals that influence the user’s apparent taste, smell, and chemisthetic flavor (Da Ré et al. 2018 ; O'Connor et al. 2020 ).
In order to reduce the use of tobacco products, a control technique may possibly require modifications in size, color, and written health warnings on the cigarette sticks in order to render them unappealing and hence promote negative perception in cigarette smoking (Drovandi et al. 2018 ). This is very important given that in terms of size; smaller diameter cigarettes have been found to be attractive to the cigarette smoking population unlike those with large diameters (Drovandi et al. 2018 ; Moodie et al. 2017 ). On the same point, brighter colored cigarettes have been reported by Drovandi et al. 2018 to be more attractive to smokers. Therefore, irrespective of health warnings being labeled on cigarettes, there are reports that they are ineffective in successfully curbing cigarette smoking because smokers tend to ignore them or find them to be irrelevant when compared to their perceived cigarette smoking “benefits” (Moodie et al. 2017 ). Accordingly, in order to promote and achieve further reduction in tobacco use, new and deterent warnings that include the financial consequences and impact on individual appearance can be effective in discouraging smokers and/or otherwise increase taxation on cigarettes beyond the reach of a majority of cigarette smoking community (Langley 2019 ; Tynan et al. 2016 ). Lazard et al. ( 2018 ) and colleagues have emphasized that health warnings written on cigarette packages do not discourage smoking and are therefore ineffective in promoting tobacco cessation behavior, although previous research has found this argument to be obsolete and not authoritative. Nonetheless, this is mainly important given that it provides information and reminds the smokers of the health risks associated with tobacco abuse.
The introduction of e-cigarettes has become common among the youth and it is employed as a cessation strategy aimed at assisting adult smokers to quit cigarette smoking (Singh et al. 2020 ). On the contrary, a statement made by Food and Drug Administration (FDA), commissioner Scott Gottlieb on the use of e-cigarettes (UFDA 2018 ) asserts that e-cigarettes have been assessed as the leading cause of pulmonary diseases, and projects these types of cigarettes as potentials for dire health consequences. As a rejoinder, Schier et al. ( 2019 ) and colleagues recommend that all persons should refrain from using e-cigarettes until such a time when more research-based information will be available to address the dangers e-cigarettes and their associated lung injury among other ailments.
Legislative policies that have been passed by different countries with respect to tobacco use if strictly applied can help promote tobacco cessation (Hatoun et al. 2018 ). These measures include the implementation of policies such as the application of huge tobacco excise taxes which may have a significant potential to reduce tobacco abuse (Tynan et al. 2016 ). By enforcing huge excise taxes on tobacco products, the purchase prices are raised thereby decreasing the number of consumers that can afford the commodity and hence leading to a possible reduction in cigarette smoking (Tynan et al. 2016 ). Cessation on cigarette smoking has also been enhanced by implementing smoke free air laws, comprehensive marketing bans, and media campaigns that have impacted greatly in the reduction of cigarette smoking (Hatoun et al. 2018 ). Smokers’ advice to quit on medical grounds has been cited as a move in the right direction towards long term abstinence and opportunistic smoking cessation (Aveyard et al. 2012 ). Consequently, smoking cessation can be achieved through interaction with smokers by offering social and therapeutic assistance to quit smoking.
There is evidence that the use of drugs such as the antidepressant bupropion (zyban) can be helpful in cases of cigarette smoking (Reddy et al. 2020 ; Ng 2017 ). Nonetheless, research has revealed that the side effect of this drug on HIV patients because it interacts with some anti-HIV drugs such as ritonavir and efavirenz ( Sustiva ) to cause more health complications (Cirrincione and Scarsi 2018 ), and therefore this option is strongly advised against. Additionally, bupropion has been found to cause dry mouth, restlessness, insomnia, and headaches among certain users (Bhatia et al. 2017 ).
This review has highlighted the current trends in tobacco abuse and its potency as a cancer agent, emerging chemicals from tobacco smoke, efforts taken to reduce tobacco toxins, the health consequences, and epidemiological impacts of smoking on the prevalence of the novel Covid-19 pandemic. The increasing number of smokers and tobacco abuse worldwide has caused a grave concern on the associated deleterious health impacts given that there is a lack of control policies regulating and monitoring the concentrations of chemicals in commercially available smokeless tobacco products sold on the market. Accordingly, thousands of chemicals have been identified in both cigarette smoke and smokeless tobacco products and classified as carcinogenic by the International agency for research on cancer (IARC). As a result of this challenge, various methods have been suggested in order to promote “safe” smoking and minimize tobacco harm. These measures include but not limited to, the use of heat not burn cigarettes, lowering TSNAs in tobacco, use of pharmaceutical additives such as bupropion and varenicline, oleoresins and other chemical additives such as menthol, humectants and essential oils (chocolate, ginger, lavender, peppermint, vanilla, cinnamon) with the sole aim of reducing toxins and improving taste in cigarette smoking. Nevertheless, these techniques have not been effective in achieving the intended goal, and therefore, quitting cigarette smoking is suggested as the only sure option to reduce tobacco mortality and morbidity. Lately, the Covid-19 (SARS-Cov-2) pandemic has posed a serious health concern worldwide, especially for cigarette smokers whose immune system is compromised. This is likely to persist owing to the fact that there is no known definitive medication regimen designed towards countering the pandemic, at least as of the time of this review; however, several vaccines are currently being developed and tested, with distribution being planned for the near future. Various sanitation instructions have been suggested in order to help in mitigating the spread of the SARS-Cov-2 virus among the general public. On the other hand, smoking has been linked to severity of Covid-19 effects in smokers and eventually earlier stage deaths. Consequently, smoking cessation campaigns have been emphasized and include inscription of health warnings on cigarettes, laying down stringent laws prohibiting the use of tobacco products, media campaigns, use of antidepressants, and assisting smokers to quit smoking through advice and rehabilitation. Although smoking cessation has not been achieved to a significant degree, the current methods employed have proven to be quite effective.
Acknowledgements
The authors are thankful to the Africa Center of Excellence II in Phytochemicals, Textiles and Renewable Energy (ACE II PTRE) – Moi University, and Egerton University, Division of Research and Extension for facilitating the success of this review article.
Authors’ contributions
Micah O. Omare: Formal analysis, and writing original draft. Joshua K. Kibet: Conceptualization, methodology, formal analysis, writing & editing, validation & supervision. Jackson K. Cherutoi: Project administration, resources, review & editing. Fredrick O. Kengara: Writing & editing, validation & supervision.
The authors are grateful to the Africa Center of Excellence II in Phytochemicals, Textiles and Renewable Energy (ACE II PTRE) and Egerton University grant #EU/RE/DVC/072 for co-funding this research.
Compliance with ethical standards
The authors declare no conflict of interest.
Not applicable.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Micah O. Omare, Email: moc.liamg@hacimtimramo .
Joshua K. Kibet, Email: ek.ca.notrege@tebikj .
Jackson K. Cherutoi, Email: moc.oohay@noskcajioturehc .
Fredrick O. Kengara, Email: ek.ca.onesam@aragnekf .
- Abrams DB, Glasser AM, Pearson JL, Villanti AC, Collins LK, Niaura RS. Harm minimization and tobacco control: reframing societal views of nicotine use to rapidly save lives. Annu Rev Public Health. 2018; 39 :193–213. doi: 10.1146/annurev-publhealth-040617-013849. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- ARC (2010) Some non-heterocyclic polycyclic aromatic hydrocarbons and some related exposures. (Vol. 92). IARC Press, International Agency for Research on Cancer. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 92.). https://www.ncbi.nlm.nih.gov/books/NBK321712/ [ PMC free article ] [ PubMed ]
- Armendáriz-Castillo I, Guerrero S, Vera-Guapi A, Cevallos-Vilatuña T, García-Cárdenas JM, Guevara-Ramírez P et al. (2019) Genotoxic and carcinogenic potential of compounds associated with electronic cigarettes: a systematic review. Hindawi. 10.1155/2019/1386710 [ PMC free article ] [ PubMed ]
- Arora HC, Fascelli M, Zhang JH, Isharwal S, Campbell SC. Kidney, ureteral, and bladder cancer: a primer for the internist. Med Clin N. 2018; 102 (2):231–249. doi: 10.1016/j.mcna.2017.10.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ashok M, Girish R, Varsha N. Know your cough: a new index to assess effects of cough severity on patient’s health and overall symptoms–an Indian survey report. Prim Health Care. 2017; 7 (277):2167–1079. doi: 10.4172/2167-1079.1000277. [ CrossRef ] [ Google Scholar ]
- Assaf NW, Altarawneh M, Oluwoye I, Radny M, Lomnicki SM, Dlugogorski BZ. Formation of environmentally persistent free radicals on α-Al2O3. Environ Sci Technol. 2016; 50 (20):11094–11102. doi: 10.1021/acs.est.6b02601. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Auer R, Concha-Lozano N, Jacot-Sadowski I, Cornuz J, Berthet A. Heat-not-burn tobacco cigarettes: smoke by any other name. JAMA Intern Med. 2017; 177 (7):1050–1052. doi: 10.1001/jamainternmed.2017.1419. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aveyard P, Begh R, Parsons A, West R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction. 2012; 107 (6):1066–1073. doi: 10.1111/j.1360-0443.2011.03770.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Babalık M, Topaloğlu İ, Saltürk Z, Berkiten G, Atar Y, Tutar B, et al. The effects of exposure to environmental cigarette smoke on the vocal folds of rats. J Voice. 2018; 32 (6):652–654. doi: 10.1016/j.jvoice.2017.09.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barnes JL, Zubair M, John K, Poirier MC, Martin FL. Carcinogens and DNA damage. Biochem Soc Trans. 2018; 46 :1213–1224. doi: 10.1042/BST20180519. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barzegar F, Kamankesh M, Mohammadi A. Heterocyclic aromatic amines in cooked food: a review on formation, health risk-toxicology and their analytical techniques. Food Chem. 2019; 280 :240–254. doi: 10.1016/j.foodchem.2018.12.058. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Benowitz NL, Burbank AD. Cardiovascular toxicity of nicotine: implications for electronic cigarette use. Trends Cardiovasc Med. 2016; 26 (6):515–523. doi: 10.1016/j.tcm.2016.03.001. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Benowitz NL, Donny EC, Hatsukami DK. Reduced nicotine content cigarettes, e-cigarettes and the cigarette end game. SSA. 2017; 112 (1):6. doi: 10.1111/add.13534. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bevilacqua L, Goldman D. Genes and addictions. Clin Pharmacol Ther. 2009; 85 (4):359. doi: 10.1038/clpt.2009.6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bhatia SC, Petty F, Gabel T (2017) Substance and non substance related addiction disorders: diagnosis and treatment. Bentham Science, Sharjah. 10.2174/97816810834381170101
- Bjurlin MA, Matulewicz RS, Roberts TR, Dearing BA, Schatz D, Sherman S et al (2020) Carcinogen biomarkers in the urine of electronic cigarette users and implications for the development of bladder cancer: a systematic review. Eur Urol Oncol S2588-9311(20):30029–30028. 10.1016/j.euo.2020.02.004 [ PubMed ]
- Bisallah CI, Rampal L, Sidik SM, Iliyasu Z, Lye MS, Onyilo MO. Knowledge, attitude and preventive practices regarding tuberculosis and its predictors among HIV patients in general hospital, Minna, north-central, Nigeria. Mal J Med Health Sci. 2018; 14 (1):45–55. [ Google Scholar ]
- Borrelli B, O’Connor GT. E-cigarettes to assist with smoking cessation. N Engl J Med. 2019; 380 (7):678–679. doi: 10.1056/NEJMe1816406. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brake SJ, Barnsley K, Lu W, McAlinden KD, Eapen MS, Sohal SS. Smoking upregulates angiotensin-converting enzyme-2 receptor: a potential adhesion site for novel coronavirus SARS-CoV-2 (Covid-19) J Clin Med. 2020; 9 (3):E841. doi: 10.3390/jcm9030841. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cai B, Ji H, Fannin FF, Bush LP. Contribution of nicotine and nornicotine toward the production of N′-Nitrosonornicotine in air-cured tobacco (Nicotiana tabacum) J Nat Prod. 2016; 79 (4):754–759. doi: 10.1021/acs.jnatprod.5b00678. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carlsen KCL, Skjerven HO, Carlsen KH. The toxicity of E-cigarettes and children’s respiratory health. Paediatr Respir Rev. 2018; 28 :63–67. doi: 10.1016/j.prrv.2018.01.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- CDC (2010) Publications and reports of the surgeon general. In: Office of the Surgeon General (Ed) How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the surgeon general, Atlanta (GA): Centers for Disease Control and Prevention (US). Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/21452462 [ PubMed ]
- CDC, NCCDPHP, OSH (2010) How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2010. 3, Chemistry and Toxicology of Cigarette Smoke and Biomarkers of Exposure and Harm). https://www.ncbi.nlm.nih.gov/books/NBK53014/ [ PubMed ]
- Chen CH. Xenobiotic metabolic enzymes: bioactivation and antioxidant defense. Cham: Springer; 2020. Foreign compounds: foods, drugs, and other chemicals; pp. 11–22. [ Google Scholar ]
- Cirrincione LR, Scarsi KK. Drug interactions in infectious diseases: antimicrobial drug interactions. Cham: Humana; 2018. Drug interactions in HIV: nucleoside, nucleotide and nonnucleoside reverse transcriptase inhibitors and entry inhibitors; pp. 297–356. [ Google Scholar ]
- Clatici VG, Racoceanu D, Dalle C, Voicu C, Tomas-Aragones L, Marron SE, et al. Perceived age and life style. The specific contributions of seven factors involved in health and beauty. Maedica. 2017; 12 (3):191–201. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Coleman HG, Xie S-H, Lagergren J. The epidemiology of esophageal adenocarcinoma. Gastroenterology. 2018; 154 (2):390–405. doi: 10.1053/j.gastro.2017.07.046. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Da Ré AF, Gurgel LG, Buffon G, Moura WER, Marques Vidor DCG, Maahs MAP. Tobacco influence on taste and smell: systematic review of the literature. Int Arch Otorhinolaryngol. 2018; 22 (1):81–87. doi: 10.1055/s-0036-1597921. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dasgupta A, Klein K. Oxidative stress caused by cigarette smoking, alcohol abuse, and drug abuse. Sandiego: Elservier; 2014. pp. 59–75. [ Google Scholar ]
- De Flora S, Ganchev G, Iltcheva M, La Maestra S, Micale RT, Steele VE, et al. Pharmacological modulation of lung carcinogenesis in smokers: preclinical and clinical evidence. TIPS. 2016; 37 (2):120–142. doi: 10.1016/j.tips.2015.11.003. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- DeVito EE, Krishnan-Sarin S. E-cigarettes: impact of E-liquid components and device characteristics on nicotine exposure. Curr Neuropharmacol. 2018; 16 (4):438–459. doi: 10.2174/1570159X15666171016164430. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Drazen JM, Morrissey S, Campion EW (2019) The dangerous flavors of e-cigarettes. N Engl J Med. 10.1056/NEJMe1900484 [ PubMed ]
- Drovandi A, Teague P-A, Glass B, Malau-Aduli B (2018) A systematic review of smoker and non-smoker perceptions of visually unappealing cigarette sticks. Tob Induc Dis 16. 10.18332/tid/82191 [ PMC free article ] [ PubMed ]
- d’Ettorre G, Criscuolo M, Mazzotta M (2017) Managing formaldehyde indoor pollution in anatomy pathology departments. IOS Press, 56(3):397–402. 10.3233/WOR-172505 [ PubMed ]
- Edwards SH, Rossiter LM, Taylor KM, Holman MR, Zhang L, Ding YS, et al. Tobacco-specific nitrosamines in the tobacco and mainstream smoke of US commercial cigarettes. Chem Res Toxicol. 2017; 30 (2):540–551. doi: 10.1021/acs.chemrestox.6b00268. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- El-Hellani A, El-Hage R, Baalbaki R, Salman R, Talih S, Shihadeh A, et al. Free-base and protonated nicotine in electronic cigarette liquids and aerosols. Chem Res Toxicol. 2015; 28 (8):1532–1537. doi: 10.1021/acs.chemrestox.5b00107. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Farsalinos KE, Gillman G, Poulas K, Voudris V. Tobacco-specific nitrosamines in electronic cigarettes: comparison between liquid and aerosol levels. Int J Environ Res Public Health. 2015; 12 (8):9046–9053. doi: 10.3390/ijerph120809046. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fatani AZ, Alshamrani HM, Alshehri KA, Almaghrabi AY, Alzahrani YA, Abduljabbar MH. Awareness on the association between skin aging and smoking: impact on smoking quitting. Imam J Appl Sci. 2020; 5 (1):33. doi: 10.4103/ijas.ijas_17_19. [ CrossRef ] [ Google Scholar ]
- Ferrante M, Conti GO. Environment and neurodegenerative diseases: an update on miRNA role. Microrna. 2017; 6 (3):157–165. doi: 10.2174/2211536606666170811151503. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ferreira IM, Pinho O, Petisca C (2019) Potential effects of furan and related compounds on HealthCoffee, pp 520–540. 10.1039/9781788015028-00520
- Giles ML, Gartner C, Boyd MA. Smoking and HIV: what are the risks and what harm reduction strategies do we have at our disposal? AIDS Res Ther. 2018; 15 (1):26. doi: 10.1186/s12981-018-0213-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grill AE, Schmitt T, Gates LA, Lu D, Bandyopadhyay D, Yuan JM, Murphy SE, Peterson LA. Abundant rodent furan-derived urinary metabolites are associated with tobacco smoke exposure in humans. Chem Res Toxicol. 2015; 28 :1508–1516. doi: 10.1021/acs.chemrestox.5b00189. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gunduz I, Kondylis A, Jaccard G, Renaud JM, Hofer R, Ruffieux L, et al. Tobacco-specific N-nitrosamines NNN and NNK levels in cigarette brands between 2000 and 2014. RTP. 2016; 76 :113–120. doi: 10.1016/j.yrtph.2016.01.012. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N et al (2019) E-cigarettes compared with nicotine replacement therapy within the UK stop smoking services: the TEC RCT. Health Technol Assess. 10.3310/hta23430 [ PMC free article ] [ PubMed ]
- Hang B, Wang Y, Huang Y, Wang P, Langley SA, Bi L, et al. Short-term early exposure to thirdhand cigarette smoke increases lung cancer incidence in mice. Clin Sci. 2018; 132 (4):475–488. doi: 10.1042/CS20171521. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hatoun J, Davis-Plourde K, Penti B, Cabral H, Kazis L. Tobacco control laws and pediatric asthma. Pediatrics. 2018; 141 (Supplement 1):130–136. doi: 10.1542/peds.2017-1026P. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hecht SS. Lung carcinogenesis by tobacco smoke. Int J Cancer. 2012; 131 :2724–2732. doi: 10.1002/ijc.27816. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hilton S, Weishaar H, Sweeting H, Trevisan F, Katikireddi SV. E-cigarettes, a safer alternative for teenagers? A UK focus group study of teenagers' views. BMJ Open. 2016; 6 (11):e013271. doi: 10.1136/bmjopen-2016-013271. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Horinouchi T, Higashi T, Mazaki Y, Miwa S. Carbonyl compounds in the gas phase of cigarette mainstream smoke and their pharmacological properties. Biol Pharm Bull. 2016; 39 :909–914. doi: 10.1248/bpb.b16-00025. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- IARC . Air pollution and cancer. In: Straif K, Cohen A, Samet J, editors. IARC Scientific Publication No. 161. Lyon: IARC; 2013. [ Google Scholar ]
- IARC (2019) IARC monographs on the identification of carcinogenic hazards to humans List Classif. Agents Classif. IARC Monogr (vol 1). IARC, Lyon
- Ivashynka A, D’Alfonso S, Copetti M, Naldi P, Fontana A, Cucovici A, Leone M. Effects of cigarette smoking and smoking cessation on multiple sclerosis severity: a cross-sectional study (P4.6-008) Neurology. 2019; 92 :P4.6–P008. doi: 10.13140/RG.2.2.13408.84486. [ CrossRef ] [ Google Scholar ]
- Jha P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. Elife. 2020; 9 :e49979. doi: 10.7554/eLife.49979. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ji M, Zhang Y, Li N, Wang C, Xia R, Zhang Z, et al. Nicotine component of cigarette smoke extract (CSE) decreases the cytotoxicity of CSE in BEAS-2B cells stably expressing human cytochrome P450 2A13. Int J Environ Res Public Health. 2017; 14 (10):1221. doi: 10.3390/ijerph14101221. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jiloha RC. Pharmacotherapy of smoking cessation. Indian J Psychiatry. 2014; 56 (1):87–95. doi: 10.4103/0019-5545.124726. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Khan Z, Suliankatchi RA, Heise TL, Dreger S. Naswar (smokeless tobacco) use and the risk of oral cancer in Pakistan: a systematic review with meta-analysis. NTR. 2019; 21 (1):32–40. doi: 10.1093/ntr/ntx281. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kindvall M, Jonsson L, Schyberg M (2019) Freeze dried oral smokeless tobacco snuff or non-tobacco snuff product and method of manufacturing thereof. Retrieved from https://patents.google.com/patent/US10278416B2/en
- Konstantinou E, Fotopoulou F, Drosos A, Dimakopoulou N, Zagoriti Z, Niarchos A, et al. Tobacco-specific nitrosamines: a literature review. Food Chem Toxicol. 2018; 118 :198–203. doi: 10.1016/j.fct.2018.05.008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kristjansson AL, Thomas S, Lilly CL, Thorisdottir IE, Allegrante JP, Sigfusdottir ID. Maternal smoking during pregnancy and academic achievement of offspring over time: a registry data-based cohort study. Prev Med. 2018; 113 :74–79. doi: 10.1016/j.ypmed.2018.05.017. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kumar A, Bhartiya D, Kaur J, Kumari S, Singh H, Saraf D, et al. Regulation of toxic contents of smokeless tobacco products. Indian J Med Res. 2018; 148 (1):14. doi: 10.4103/ijmr.IJMR_2025_17. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kurgat C, Kibet J, Cheplogoi P. Molecular modeling of major tobacco alkaloids in mainstream cigarette smoke. Chem Cent J. 2016; 10 :43. doi: 10.1186/s13065-016-0189-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lachenmeier DW, Anderson P, Rehm J. Heat-not-burn tobacco products: the devil in disguise or a considerable risk reduction? Int J Alcohol Drug Res. 2018; 7 (2):8–11. doi: 10.7895/ijadr.250. [ CrossRef ] [ Google Scholar ]
- Langley TE. Tobacco harm reduction: making sure no one gets left behind. Nicotine Tob Res. 2019; 21 (1):1–2. doi: 10.1093/ntr/nty186. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Law AD, Fisher C, Jack A, Moe LA. Tobacco, microbes, and carcinogens: correlation between tobacco cure conditions, tobacco-specific nitrosamine content, and cured leaf microbial community. Microb Ecol. 2016; 72 (1):120–129. doi: 10.1007/s00248-016-0754-4. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lazard AJ, Kowitt SD, Huang L-L, Noar SM, Jarman KL, Goldstein AO. Believability of cigarette warnings about addiction: national experiments of adolescents and adults. NTR. 2018; 20 (7):867–875. doi: 10.1093/ntr/ntx185. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee DC, Crosier BS, Borodovsky JT, Sargent JD, Budney AJ (2016) Online survey characterizing vaporizer use among cannabis users. Drug Alcohol Depend 159:227–233. 10.1016/j.drugalcdep.2015.12.020 [ PMC free article ] [ PubMed ]
- Leung JM, Yang CX, Tam A, Shaipanich T, Hackett TL, Singhera GK et al (2020) ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur Respir J. 10.1183/13993003.00688-2020 [ PMC free article ] [ PubMed ]
- Li MD. Tobacco smoking addiction: epidemiology, genetics, mechanisms, and treatment. Singapore: Springer; 2018. Involvement of variants in gene clusters CHRNA5/A3/B4 on chromosome 15 to smoking behaviors and lung cancer; pp. 47–69. [ Google Scholar ]
- Li MD, Burmeister M. New insights into the genetics of addiction. Nat Rev Genet. 2009; 10 (4):225–231. doi: 10.1038/nrg2536. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Li Q, Hempfling WP, Krauss MR (2008) Spray and/or soil treatment of tobacco to reduce TSNAs. United States Patent Appl. Publ. within the TVPP US20080035228. http://europepmc.org/patents/PAT/US2008202538 . Accessed 24 May 2020
- Li SH, Sun XD, Wang Y-z, Shi CL, W-b G, Wang W-m, et al. Novel mesoporous composite with zeolite-like selectivity to capture tobacco specific nitrosamine NNK. Chem Eng. 2018; 332 :331–339. doi: 10.1016/j.cej.2017.09.090. [ CrossRef ] [ Google Scholar ]
- Liao YT, Tseng HD, Chang PMH, Chu PY, Kuo YJ, Liu CY. Second primary spindle cell carcinoma of oral cavity and oropharynx: a case report and literature review. Reports—Medical Cases, Images and Videos. 2018; 1 (2):16. doi: 10.3390/reports1020016. [ CrossRef ] [ Google Scholar ]
- Lindson-Hawley N, Hartmann-Boyce J, Fanshawe TR, Begh R, Farley A, Lancaster T (2016) Interventions to reduce harm from continued tobacco use. Cochrane Database Systemat Rev. 10.1002/14651858.CD005231 [ PMC free article ] [ PubMed ]
- Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19) Eur J Intern Med. 2020; 75 :107–108. doi: 10.1016/j.ejim.2020.03.014. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Loomis D, Guyton KZ, Grosse Y, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, et al. Carcinogenicity of benzene. Lancet Oncol. 2017; 18 (12):1574–1575. doi: 10.1016/S1470-2045(17)30832-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MacNee W, Rabinovich RA, Choudhury G. Ageing and the border between health and disease. Eur Respir J. 2014; 44 (5):1332–1352. doi: 10.1183/09031936.00134014. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mallock N, Böss L, Burk R, Danziger M, Welsch T, Hahn H, et al. Levels of selected analytes in the emissions of “heat not burn” tobacco products that are relevant to assess human health risks. Arch Toxicol. 2018; 92 (6):2145–2149. doi: 10.1007/s00204-018-2215-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McAdam KG, Faizi A, Kimpton H, Porter A, Rodu B. Polycyclic aromatic hydrocarbons in US and Swedish smokeless tobacco products. Chem Cent J. 2013; 7 (1):151. doi: 10.1186/1752-153X-7-151. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McAdam K, Eldridge A, Fearon IM, Liu C, Manson A, Murphy J, et al. Influence of cigarette circumference on smoke chemistry, biological activity, and smoking behaviour. Regul Toxicol Pharmacol. 2016; 82 :111–126. doi: 10.1016/j.yrtph.2016.09.010. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McAdam K, Murphy J, Eldridge A, Meredith C, Proctor C. Integrating chemical, toxicological and clinical research to assess the potential of reducing health risks associated with cigarette smoking through reducing toxicant emissions. Regul Toxicol Pharmacol. 2018; 95 :102–114. doi: 10.1016/j.yrtph.2018.03.005. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McKinney DL, Vansickel AR. Neuropathology of drug addictions and substance misuse. Richmond: RD&E, Altria Client Services; 2016. Nicotine chemistry, pharmacology, and pharmacokinetics; pp. 93–103. [ Google Scholar ]
- Miligi L, Buzzoni C, Piro S. Epidemiology of sinonasal cancer. In: Franchi A, editor. Pathology of sinonasal tumors and tumor-like lesions. Cham: Springer; 2020. pp. 3–17. [ Google Scholar ]
- Mishra S, Joseph RA, Gupta PC, Pezzack B, Ram F, Sinha DN, et al. Trends in bidi and cigarette smoking in India from 1998 to 2015, by age, gender and education. BMJ Glob Health. 2016; 1 (1):e000005. doi: 10.1136/bmjgh-2015-000005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mohapatra T. Gutkha and causative factors of gutkha addiction: a sociological study in “twin city” of Odisha. Int J Soc Sci Econ Res. 2019; 9 (3):476–513. doi: 10.5958/2249-6270.2019.00056.4. [ CrossRef ] [ Google Scholar ]
- Moodie C, MacKintosh AM, Gallopel-Morvan K, Hastings G, Ford A. Adolescents’ perceptions of an on-cigarette health warning. Nicotine Tob Res. 2017; 19 (10):1232–1237. doi: 10.1093/ntr/ntw165. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morean ME, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. Nicotine concentration of e-cigarettes used by adolescents. Drug Alcohol Depend. 2016; 1 (167):224–227. doi: 10.1016/j.drugalcdep.2016.06.031. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morgan JC, Byron MJ, Baig SA, Stepanov I, Brewer NT. How people think about the chemicals in cigarette smoke: a systematic review. J Behav Med. 2017; 40 (4):553–564. doi: 10.1007/s10865-017-9823-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ng QX. A systematic review of the use of bupropion for attention-deficit/hyperactivity disorder in children and adolescents. J Child Adolesc Psychopharmacol. 2017; 27 (2):112–116. doi: 10.1089/cap.2016.0124. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- NIDA (2020) Trends & statistics. Retrieved from https://www.drugabuse.gov/related-topics/trends-statistics
- Nlemedim ON (2017) Organic chemical compounds in different Brands of Cigarette Smoke. Dissertation, Texas Southern University
- O'Brien JL, Langlois PH, Lawson CC, Scheuerle A, Rocheleau CM, Waters MA, et al. Maternal occupational exposure to polycyclic aromatic hydrocarbons and craniosynostosis among offspring in the national birth defects prevention study. Birth Defects Res Part A Clin Mol Teratol. 2016; 106 (1):55–60. doi: 10.1002/bdra.23389. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O'Connor R, Watson CH, Swan GE, Nettles DS, Geisler RC, Hendershot TP. PhenX: agent measures for tobacco regulatory research. BMJ. 2020; 29 (1):20–26. doi: 10.1136/tobaccocontrol-2019-054976. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Omari M, Kibet J, Cherutoi J, Bosire J, Rono N. Heavy metal content in mainstream cigarette smoke of common cigarettes sold in Kenya, and their toxicological consequences. Int Res J Environ Sci. 2015; 4 (6):75–79. [ Google Scholar ]
- Osman OF, Elbashir RMI, Abbass IE, Kendrick C, Goyal M, Yap MH (2017). Automated assessment of facial wrinkling: a case study on the effect of smoking. In: 2017 IEEE international conference on systems, man, and cybernetics (SMC). 10.1109/SMC.2017.8122755
- Palmatier RW, Houston MB, Hulland J. Review articles: purpose, process, and structure. J Acad Mark Sci. 2018; 46 :1–5. doi: 10.1007/s11747-017-0563-4. [ CrossRef ] [ Google Scholar ]
- Panth N, Paudel KR, Parajuli K. Reactive oxygen species: a key hallmark of cardiovascular disease. Adv Med Sci. 2016; 2016 :9152732. doi: 10.1155/2016/9152732. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peeters S, Gilmore AB. Understanding the emergence of the tobacco industry’s use of the term tobacco harm reduction in order to inform public health policy. Tob Control. 2015; 24 :182. doi: 10.1136/tobaccocontrol-2013-051502. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Petrick JL, Campbell PT, Koshiol J, Thistle JE, Andreotti G, Beane-Freeman LE, et al. Tobacco, alcohol use and risk of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: the liver cancer pooling project. BJC. 2018; 118 (7):1005–1012. doi: 10.1038/s41416-018-0007-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Phaniendra A, Jestadi DB, Periyasamy L. Free radicals: properties, sources, targets, and their implication in various diseases. Ind J Clin Biochem. 2015; 30 (1):11–26. doi: 10.1007/s12291-014-0446-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pillitteri JL, Shiffman S, Sembower MA, Polster MR, Curtin GM (2020) Assessing comprehension and perceptions of modified-risk information for snus among adult current cigarette smokers, former tobacco users, and never tobacco users. Addict Behav Rep 11:100254. 10.1016/j.abrep.2020.100254 [ PMC free article ] [ PubMed ]
- Pineles BL, Park E, Samet JM. Systematic review and meta-analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. Am J Epidemiol. 2014; 179 :807–823. doi: 10.1093/aje/kwt334. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pokhrel P, Herzog TA, Muranaka N, Fagan P. Young adult e-cigarette users’ reasons for liking and not liking e-cigarettes: a qualitative study. Psychol Health. 2015; 30 (12):1450–1469. doi: 10.1080/08870446.2015.1061129. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Popova L, Lempert LK, Glantz SA. Light and mild redux: heated tobacco products’ reduced exposure claims are likely to be misunderstood as reduced risk claims. Tob Control. 2018; 27 :s87. doi: 10.1136/tobaccocontrol-2018-054324. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prochaska JJ, Benowitz NL. Current advances in research in treatment and recovery: nicotine addiction. Sci Adv. 2019; 5 (10):9763. doi: 10.1126/sciadv.aay9763. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reddy K, Kher S, Kathuria H. Prescription medications to help you stop smoking. Am J Respir Crit Care. 2020; 201 (6):11–12. doi: 10.1164/rccm.2016P11. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rehman H, Ullah I, David M, Ullah A, Jahan S. Neonatal exposure to furan alters the development of reproductive systems in adult male Sprague Dawley rats. Food Chem Toxicol. 2019; 130 :231–241. doi: 10.1016/j.fct.2019.05.020. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Riddick M, Marshall J, Parker R (2017) Systems and apparatus for reducing tobacco-specific nitrosamines in dark-fire cured tobacco through electronic control of curing conditions. US Patent US20170055565A1. Retrieved from https://patents.google.com/patent/US20170055565A1/en
- Roemer E, Meisgen T, Diekmann J, Conroy L, Stabbert R. Heterocyclic aromatic amines and their contribution to the bacterial mutagenicity of the particulate phase of cigarette smoke. J Toxlet. 2016; 243 :40–47. doi: 10.1016/j.toxlet.2015.12.008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Santonicola S, Albrizio S, Murru N, Ferrante MC, Mercogliano R. Study on the occurrence of polycyclic aromatic hydrocarbons in milk and meat/fish based baby food available in Italy. Chemosphere. 2017; 184 :467–472. doi: 10.1016/j.chemosphere.2017.06.017. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sapkota M, Wyatt TA. Alcohol, aldehydes, adducts and airways. Biomolecules. 2015; 5 (4):2987–3008. doi: 10.3390/biom5042987. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schier JG, Meiman JG, Layden J, Mikosz CA, VanFrank B, King BA, et al. Severe pulmonary disease associated with electronic-cigarette–product use—interim guidance. MMWR Morb Mortal Wkly Rep. 2019; 68 (36):787–790. doi: 10.15585/mmwr.mm6836e2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmidt HD, Rupprecht LE, Addy NA. Neurobiological and neurophysiological mechanisms underlying nicotine seeking and smoking relapse. Mol Neuropsychiatry. 2018; 4 :169–189. doi: 10.1159/000494799. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shafik SS, Shafeq OS, Salman MA. The annual inhalation radiation effective dose estimations for hookah tobacco smoking of Baghdad’s publics. J Phys Conf Ser. 2019; 1279 :012044. doi: 10.1088/1742-6596/1279/1/012044. [ CrossRef ] [ Google Scholar ]
- Shi X, Yang X (2017) Tobacco flavor extract with reduced tsnas. US Patent US20170231267A1. Retrieved from https://patents.google.com/patent/US20170231267A1/en
- Shihadeh A, Schubert J, Klaiany J, El Sabban M, Luch A, Saliba NA. Toxicant content, physical properties and biological activity of waterpipe tobacco smoke and its tobacco-free alternatives. BMJ. 2015; 24 (1):22–30. doi: 10.1136/tobaccocontrol-2014-051907. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singh S, Windle SB, Filion KB, Thombs BD, O'Loughlin JL, Grad R, Eisenberg MJ. E-cigarettes and youth: patterns of use, potential harms, and recommendations. Prev Med. 2020; 133 :106009. doi: 10.1016/j.ypmed.2020.106009. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singhavi H, Ahluwalia JS, Stepanov I, Gupta PC, Gota V, Chaturvedi P, et al. Tobacco carcinogen research to aid understanding of cancer risk and influence policy. Laryngoscope Investig Otolaryngol. 2018; 3 (5):372–376. doi: 10.1002/lio2.204. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Skjodt N, Mamoshina P, Kochetov K, Cortese F, Kovalchuk A, Aliper A, et al. Smoking causes early biological aging: a deep neural network analysis of common blood test results. Eur Respiratory Soc. 2018; 52 :OA3809. doi: 10.1183/13993003.congress-2018.OA3809. [ CrossRef ] [ Google Scholar ]
- Sleiman M, Logue JM, Luo W, Pankow JF, Gundel LA, Destaillats H. Inhalable constituents of thirdhand tobacco smoke: chemical characterization and health impact considerations. Environ Sci Technol. 2014; 48 (22):13093–13101. doi: 10.1021/es5036333. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith P (2019) E-cigarettes-Tobacco Prevention and Control-Minnesota Department of Health. Retrieved from https://www.health.state.mn.us/ecigarettes
- Smith MR, Clark B, Lüdicke F, Schaller J-P, Vanscheeuwijck P, Hoeng J, et al. Evaluation of the tobacco heating system 2.2. Part 1: description of the system and the scientific assessment program. Regul Toxicol Pharmacol. 2016; 81 :17–26. doi: 10.1016/j.yrtph.2016.07.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Soliman M (2018) Cancer causing chemicals, cancer causing substances. IntechOpen, pp 48–56. 10.5772/intechopen.71560
- Spahr S, Cirpka OA, Von Gunten U, Hofstetter TB. Formation of N-nitrosodimethylamine during chloramination of secondary and tertiary amines: role of molecular oxygen and radical intermediates. Environ Sci Technol. 2017; 51 (1):280–290. doi: 10.1021/acs.est.6b04780. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stanfill SB (2020) Chapter eight - reducing carcinogen levels in smokeless tobacco products. In: Pickworth WB (ed) Smokeless tobacco products. Elsevier, pp 167–187. 10.1016/B978-0-12-818158-4.00008-X
- Stepanov I, Biener L, Yershova K, Nyman AL, Bliss R, Parascandola M, et al. Monitoring tobacco-specific N-nitrosamines and nicotine in novel smokeless tobacco products: findings from round II of the new product watch. NTR. 2014; 16 (8):1070–1078. doi: 10.1093/ntr/ntu026. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tsai J, Homa DM, Gentzke AS, Mahoney M, Sharapova SR, Sosnoff CS, et al. Exposure to secondhand smoke among nonsmokers—United States, 1988–2014. Morb mortal Wkly Rep. 2018; 67 (48):1342. doi: 10.15585/mmwr.mm6748a3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tynan MA, Holmes CB, Promoff G, Hallett C, Hopkins M, Frick B. State and local comprehensive smoke-free laws for worksites, restaurants, and bars—United States, 2015. Morb Mortal Wkly Rep. 2016; 65 (24):623–626. doi: 10.15585/mmwr.mm6524a4. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- UFDA (2018) Statement from FDA Commissioner Scott Gottlieb, M.D., on new steps to address epidemic of youth e-cigarette use [Press release]. Retrieved from https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-new-steps-address-epidemic-youth-e-cigarette-use
- Vardavas CI, Nikitara K (2020) COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis 18:20. 10.18332/tid/119324 [ PMC free article ] [ PubMed ]
- Vellios N, Ross H, Perucic A-M. Trends in cigarette demand and supply in Africa. PLoS One. 2018; 13 (8):e0202467–e0202467. doi: 10.1371/journal.pone.0202467. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vu AT, Taylor KM, Holman MR, Ding YS, Hearn B, Watson CH. Polycyclic aromatic hydrocarbons in the mainstream smoke of popular US cigarettes. Chem Res Toxicol. 2015; 28 (8):1616–1626. doi: 10.1021/acs.chemrestox.5b00190. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang J, Yang H, Shi H, Zhou J, Bai R, Zhang M et al (2017) Nitrate and nitrite promote formation of tobacco-specific nitrosamines via nitrogen oxides intermediates during postcured storage under warm temperature. J Chem. 10.1155/2017/6135215
- Wang J, Luo Q, Chen R, Chen T, Li J (2020) Susceptibility analysis of COVID-19 in smokers based on ACE2. Preprints. 10.20944/preprints202003.0078.v1
- Warden H, Richardson H, Richardson L, Siemiatycki J, Ho V. Associations between occupational exposure to benzene, toluene and xylene and risk of lung cancer in Montréal. Occup Environ Med. 2018; 75 (10):696–702. doi: 10.1136/oemed-2017-104987. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Warek U, Nielsen MT, Xu D, Cui M, Luo X, Jin X et al. (2019) Nitrite-degrading and TSNA-degrading bacteria and methods of making and using. US Patent US10226064B2. Retrieved from https://patents.google.com/patent/US10226064B2/en
- Warnakulasuriya S, Straif K. Carcinogenicity of smokeless tobacco: evidence from studies in humans & experimental animals. IJMR. 2018; 148 (6):681. doi: 10.4103/ijmr.IJMR_149_18. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weng MW, Lee HW, Park SH, Hu Y, Wang HT, Chen LC, Rom WN, Huang WC, Lepor H, Wu XR, Yang CS, Tang MS. Aldehydes are the predominant forces inducing DNA damage and inhibiting DNA repair in tobacco smoke carcinogenesis. Proc Natl Acad Sci. 2018; 115 :E6152. doi: 10.1073/pnas.1804869115. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- WHO (2019) WHO report on the global tobacco epidemic 2019: offer help to quit tobacco use. Retrieved from https://escholarship.org/content/qt1g16k8b9/qt1g16k8b9.pdf
- Wojtczyk-Miaskowska A, Schlichtholz B. Tobacco carcinogens and the methionine metabolism in human bladder cancer. Mutat Res. 2019; 782 :108281. doi: 10.1016/j.mrrev.2019.06.001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wright C. Standardized methods for the regulation of cigarette-smoke constituents. Tob Regul Sci. 2015; 66 :118–127. doi: 10.1016/j.trac.2014.11.011. [ CrossRef ] [ Google Scholar ]
- Xue J, Yang S, Seng S. Mechanisms of cancer induction by tobacco-specific NNK and NNN. Cancers. 2014; 6 (2):1138–1156. doi: 10.3390/cancers6021138. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zamora R, Hidalgo FJ. Formation of heterocyclic aromatic amines with the structure of aminoimidazoazarenes in food products. Food Chem. 2020; 313 :126–128. doi: 10.1016/j.foodchem.2019.126128. [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Substance or Drug abuse is a serious public health problem affecting usually adolescents and young adults. It affects both males and females and it is. the major source of crimes in youth and ...
In addition to the effect on health, ... Wisdom of the Crowds (WOTC) method, and a published literature review to document the size of key populations . The sample size for this category of studies ranged from 42 ... Prevalence for drug abuse was 545 per 1000 children. Specific substance prevalence: tobacco 37.6%; sniffing glue 31.2%; alcohol ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
2. Substance Abuse and Different Social Groups. When researching substance abuse and its harmful effects, researchers predominantly focus on certain social groups with a higher tendency towards substance taking and misuse, such as adolescents and male adults [13,14,15,16,17,18].This is valid, as they may encounter various demanding life and social challenges, expectations, interpersonal ...
While an earlier literature review ... found exposure to media anti-drug messages had an indirect negative effect on substances abuse through school-related activity ... evidence on the risk and protective factors of adolescents engaging in drug abuse. Although this systematic review builds on the conclusion of a rigorous review of studies in ...
Substance-Related Disorders* / epidemiology. Insight refers to a person's understanding of themselves and the world around them. Recent literature has explored people's insight into their substance use disorder (SUD) and how this is linked to treatment adherence, abstinence rates, and comorbid mental health symptoms. The aim of this systematic ….
The amount of drug abuse research has increased since the 1960s because of grants by the National Institute on Drug Abuse and National Institute of Mental Health. ... From this literature review, ... Overall adverse effects. This narrative review provided a brief overview of the acute and chronic effects of cannabis. Adverse effects from higher ...
Drug use disorders (DUDs), refer to the forced and endless use of certain drugs with dependency characteristics in the pursuit of special psychological effects rather than medical purposes, can cause serious psychological, physiological consequences, and social problems [1,2,3], including cognitive impairment, suicidal tendencies, decreased quality of life, and risk of infectious diseases [4,5 ...
This review, synthesizing emerging findings on this complex topic, is intended to inform research and clinical care focused on adolescents. ... Literature searches were conducted using PubMed, yielding a cross-section of observational and interventional studies focused on adolescent substance use. Findings were organized and categorized to ...
The review, which consists of literature search of journals and chapters in books, provides an insight into common drugs and substances that are abused, causes of drug abuse, social effect ...
Cocaine abuse has been reported to cause devastating systemic and ocular side effects. Retinal vascular occlusion following cocaine abuse has been scarcely reported in the literature. Herein, we ...
Introduction and background. Drug misuse is a widespread issue; in 2016, 5.6% of people aged 15 to 26 reported using drugs at least once [].Because alcohol and illegal drugs represent significant issues for public health and urgent care, children and adolescents frequently visit emergency rooms [].It is well known that younger people take drugs more often than older adults for most drugs.
Implications and effects on parents and family. Zimic and Jackic (Citation 2012) aver that the impact that substance abuse has on the family and on the individual family members merit attention.Lander et al. (Citation 2013) maintains that family members are affected by the individual's substance abuse; however, each individual is affected differently together with, but not limited to, having ...
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA ...
The aim of the present review is to provide a contemporary comprehensible overview of exciting recent developments in the understanding of brain circuits related to the nature and effects of cannabis abuse and addiction as well as to highlight the current therapeutic approach to effective management. Method: A thorough manual literature and ...
Illicit substance/drug abuse is on a rising trend globally. Illicit drugs are classified as stimulants, depressants and hallucinogens. These drugs are categorized into two groups of hallucinogens including crystal (methamphetamine), ecstasy (3,4-methylenedioxy-methamphetamine), marijuana and Lysergic Acid Diethylamide (LSD) and non-hallucinogens including opium, heroin and crack.
A total of 99 articles were found, of which 16 were selected for this review. Results: Alcohol and tobacco were the most frequently used licit drugs among medical students. The most consumed illicit drugs were marijuana, solvents, "lança-perfume" (ether spray), and anxiolytics. The male genre presented a tendency of consuming more significant ...
2. Allostatic Model of Drug Use and Abuse. Given the multiple causes and consequences of drug use and abuse, understanding this complexity is critical to prevention and treatment strategies [].One comprehensive model of these issues has recently been presented by Koob and his colleagues who describe the various stages of drug use and abuse, the factors important in their display, and the ...
Drug abuse is a serious public health problem that affects almost every community and family in some way. Each year drug abuse causes millions of serious illnesses or injuries among Americans. ... The review of the research literature below outlines the association between substance use disorders ... desired effect, or markedly diminished ...
We review the still scarce but growing literature on resilience to the effects of social stress on the rewarding properties of drugs of abuse. We define the concept of resilience and how it is ...
A systematic literature review of studies examining juvenile justice system processing found that most studies examining referral to mental health or substance misuse treatment from within the juvenile justice system found at least some race effects disadvantaging youths of color (Spinney et al., 2016).
Drug and substance abuse have far reaching ramifications, for instance, according. to the survey by NACADA (2012) with a sample of 632 children, it was found out. that 6% have ever engaged in sex while on drugs ( 7.3% for boys and 4.4% for girls).The median age at sexual debut being estimated at 11 years.
Abstract. Substance use disorders (SUDs) are associated with numerous medical, psychiatric, psychological, spiritual, economic, social, family, and legal problems, creating a significant burden for affected individuals, their families, and society. This paper focuses on the effects of SUDs on family and social problems and emphasizes the need ...
Opioids are agents that can interact with the opioid receptors in the human body [].Examples of agonists of the opioid receptor include morphine, tramadol, fentanyl, [] and oxycodone [], while buprenorphine is a partial agonist and naloxone is an antagonist [].Activating the mu-opioid receptor is the primary known means of producing an analgesic effect; however, other opioid receptors may have ...
Conclusion. This review has highlighted the current trends in tobacco abuse and its potency as a cancer agent, emerging chemicals from tobacco smoke, efforts taken to reduce tobacco toxins, the health consequences, and epidemiological impacts of smoking on the prevalence of the novel Covid-19 pandemic.