Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- June 01, 2024 | VOL. 181, NO. 6 CURRENT ISSUE pp.461-564
- May 01, 2024 | VOL. 181, NO. 5 pp.347-460
- April 01, 2024 | VOL. 181, NO. 4 pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Devastating Clinical Consequences of Child Abuse and Neglect: Increased Disease Vulnerability and Poor Treatment Response in Mood Disorders
- Elizabeth T.C. Lippard , Ph.D. ,
- Charles B. Nemeroff , M.D., Ph.D.
Search for more papers by this author
A large body of evidence has demonstrated that exposure to childhood maltreatment at any stage of development can have long-lasting consequences. It is associated with a marked increase in risk for psychiatric and medical disorders. This review summarizes the literature investigating the effects of childhood maltreatment on disease vulnerability for mood disorders, specifically summarizing cross-sectional and more recent longitudinal studies demonstrating that childhood maltreatment is more prevalent and is associated with increased risk for first mood episode, episode recurrence, greater comorbidities, and increased risk for suicidal ideation and attempts in individuals with mood disorders. It summarizes the persistent alterations associated with childhood maltreatment, including alterations in the hypothalamic-pituitary-adrenal axis and inflammatory cytokines, which may contribute to disease vulnerability and a more pernicious disease course. The authors discuss several candidate genes and environmental factors (for example, substance use) that may alter disease vulnerability and illness course and neurobiological associations that may mediate these relationships following childhood maltreatment. Studies provide insight into modifiable mechanisms and provide direction to improve both treatment and prevention strategies.
“It is not the bruises on the body that hurt. It is the wounds of the heart and the scars on the mind.” —Aisha Mirza
“We can deny our experience but our body remembers.” —Jeanne McElvaney, Spirit Unbroken: Abby’s Story
It is now well established that childhood maltreatment, or exposure to abuse and neglect in children under the age of 18, has devastating consequences. Over the past two decades, research has begun not only to define the consequences in the context of health and disease but also to elucidate mechanisms underlying the link between childhood maltreatment and medical, including psychiatric, outcomes. Research has begun to shed light on how childhood maltreatment mediates disease risk and course. Childhood maltreatment increases risk for developing psychiatric disorders (e.g., mood and anxiety disorders, posttraumatic stress disorder [PTSD], antisocial and borderline personality disorders, and substance use disorders). It is associated with an earlier age at onset and a more severe clinical course (i.e., greater symptom severity) and poorer treatment response to pharmacotherapy or psychotherapy. Early-life adversity is also associated with increased vulnerability to several major medical disorders, including coronary artery disease and myocardial infarction, cerebrovascular disease and stroke, type 2 diabetes, asthma, and certain forms of cancer. The net effect is a significant reduction in life expectancy in victims of child abuse and neglect. The focus of this review is to expand on previous reviews by synthesizing the literature and integrating much recent data, with a focus on investigating childhood maltreatment interactions with risk for mood disorders, disease onset, and early disease heterogeneity, as well as emerging data suggesting modifiable mechanisms that could be targeted for early intervention and prevention strategies. A major emphasis of this review is to provide a clinically relevant update to practicing mental health practitioners.
Prevalence and Consequences of Childhood Maltreatment
It is estimated that one in four children will experience child abuse or neglect at some point in their lifetime, and one in seven children have experienced abuse over the past year. In 2016, 676,000 children were reported to child protective services in the United States and identified as victims of child abuse or neglect ( 1 ). However, it is widely accepted that statistics on such reports represent a significant underestimate of the prevalence of childhood maltreatment, because the majority of abuse and neglect goes unreported. This is especially true for certain types of childhood maltreatment (notably emotional abuse and neglect), which may never come to clinical attention but have devastating consequences on health independently of physical abuse and neglect or sexual abuse. Although rates of children being reported to child protective services have remained relatively consistent over recent decades ( Figure 1 ), our understanding of the devastating medical and clinical consequences of childhood maltreatment has grown, and childhood maltreatment is now well established as a major risk factor for adult psychopathology. In this review, we seek to summarize the burgeoning literature on childhood maltreatment, specifically focusing on the link between childhood maltreatment and mood disorders (depression and bipolar disorder). The data converge to point toward future directions for education, prevention, and treatment to decrease the consequences of childhood maltreatment, especially in regard to mood disorders.
FIGURE 1. National estimates of childhood maltreatment in the United States a
a Panel A graphs the prevalence of maltreatment (calculated national estimate/rounded number of victims by year, and panel B graphs rates of victimization per 1,000 children, between 1999 and 2016, as reported by the Children’s Bureau, which produces an annual Child Maltreatment report including data provided by the United States to the National Child Abuse and Neglect Data Systems. Estimated rates of maltreatment have remained high over the past two decades. The asterisk calls attention to the fact that before 2007, the national estimates were based on counting a child each time he or she was the subject of a child protective services investigation. In 2007, unique counts started to be reported. The unique estimates are based on counting a child only once regardless of the number of times he or she is found to be a victim during a reporting year. (Information obtained from https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment .)
Childhood Maltreatment Increases Risk for Illness Severity and Poor Treatment Response in Mood Disorders
The link between childhood maltreatment and risk for mood disorders and differences in disease course following illness onset has been well documented ( 2 – 8 ). Multiple studies have demonstrated greater rates of childhood maltreatment in patients with major depression and bipolar disorder ( 9 – 11 ). Indeed, a recent meta-analysis revealed that 46% of individuals with depression report childhood maltreatment ( 12 ). Patients with bipolar disorder also report high levels of childhood maltreatment ( 13 , 14 ), with estimates as high as 57% ( 15 ). Childhood maltreatment is associated with an increased risk and earlier onset of unipolar depression, with syndromal depression occurring on average 4 years earlier in individuals with a history of childhood maltreatment compared with those without such a history ( 12 ). Childhood maltreatment is also associated with a more pernicious disease course, including a greater number of lifetime depressive episodes and greater depression severity, with the majority of studies showing more recurrence and greater persistence of depressive episodes ( 16 – 18 ). For example, Wiersma et al. ( 19 ), in an analysis of 1,230 adults with major depressive disorder drawn from the Netherlands Study of Depression and Anxiety, found that childhood maltreatment (measured with the Childhood Trauma Interview) was associated with chronicity of depression, defined as being depressed for ≥24 months over the past 4 years, independent of comorbid anxiety disorders, severity of depressive symptoms, or age at onset. Increased risk for suicide attempts and comorbidities, including increased rates of anxiety disorders, PTSD, and substance use disorders, are reported in individuals with depression who experience childhood maltreatment. Individuals with major depressive disorder and atypical features report significantly more traumatic life events (including physical abuse, sexual abuse, and other forms of trauma) both before and after their first depressive episode, independently of sex, age at onset, or duration of depression ( 20 ). Additionally, childhood maltreatment has consistently been shown to be associated with poor treatment outcome (after psychotherapy, pharmacotherapy, and combined treatment) in depression, as assessed by lack of remission or response or longer time to remission ( 12 , 18 , 21 , 22 ).
Although the studies cited above describe a link between childhood maltreatment and a more pernicious depression course, most studies have been cross-sectional, and the possibility of recall bias and mood effects (owing to the retrospective investigation of childhood maltreatment in individuals who are currently depressed) cannot be ruled out. However, studies over the past few years comparing retrospective and prospective measurement of childhood maltreatment suggest consistency between retrospective reports and prospective designs ( 23 , 24 ), although a recent meta-analysis ( 25 ) suggested poor agreement between these measures, with better agreement observed when retrospective measures were based on interviews and in studies with smaller samples. Longitudinal and prospective studies are emerging that have further confirmed and extended our understanding of the devastating consequences of childhood maltreatment on illness course ( 5 , 7 ). Ellis et al. ( 26 ) recently reported that childhood maltreatment increased risk for more severe trajectories of depressive symptoms during a 7-year longitudinal study in 243 adolescents in the Orygen Adolescent Development Study. Gilman et al. ( 27 ) reported that childhood maltreatment increased the risk for recurrent depressive episodes and suicidal ideation by 20%−30% during a 3-year follow-up of 2,497 participants diagnosed with major depressive disorder in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Additionally, Widom et al. ( 7 ), in a study that followed a cohort of 676 children with documented childhood maltreatment and compared risk for major depression in adulthood between them and a cohort of 520 children matched on age, race, sex, and family social class who were not exposed to childhood maltreatment, found a clear association between childhood maltreatment and both increased risk for depression and earlier onset of the disorder.
Although more research has been reported investigating the link between childhood maltreatment and disease onset and course in unipolar depression, more recent evidence supports the link between childhood maltreatment and disease onset and course in bipolar disorder ( 28 ). Childhood maltreatment is associated with increased disease vulnerability and earlier age at onset of bipolar disorder ( 29 ). Jansen et al. ( 30 ) sought to determine whether childhood maltreatment mediated the effect of family history on diagnosis of a mood disorder. The findings indicated that one-third of the effect of family history on risk for mood disorders was mediated by childhood maltreatment. As with depression, studies on bipolar disorder with a prospective or longitudinal approach are few, but they are informative. Using data from the NESARC (N=33,375), Gilman et al. ( 31 ) found that childhood physical and sexual abuse were associated with increased risk for first-onset and recurrent mania independently of recent life stress. An association between childhood maltreatment and prodromal symptoms has also been reported in bipolar disorder ( 32 ), suggesting that childhood maltreatment may contribute to disease vulnerability before onset of the first manic episode. Childhood maltreatment in the context of bipolar disorder is also associated with a more pernicious disease course, including greater frequency and severity of mood episodes (both depressive and manic), greater severity of psychosis symptoms, and greater risk for comorbidities (i.e., anxiety disorders, PTSD, substance use disorders), rapid cycling, inpatient hospitalizations, and suicide attempts ( 28 , 33 – 41 ). Studies are beginning to emerge investigating treatment response in bipolar disorder following childhood maltreatment. Such studies remain few, but they suggest that childhood maltreatment is associated with a poor response to benzodiazepines ( 42 ) and anticonvulsants ( 41 ) in bipolar disorder. The concatenation of findings in depression and bipolar disorder are concordant in that childhood maltreatment increases risk for, and early onset of, first mood episode and episode recurrence. Childhood maltreatment affects disease trajectories, including in its association with more insidious mood episodes, poor treatment response, a greater risk for comorbidities, and a greater risk for suicide ideation, attempts, and completion. The link between childhood maltreatment and increased prevalence of suicide-related behaviors is of particular importance given the high rate of suicide ideation, attempts, and completion in depression and bipolar disorder. Despite many prevention strategies (e.g., education and outreach and clinical studies to identify risk factors for impending suicide attempts in individuals with mood disorders), suicide rates have not decreased but in fact have increased in the United States. The link between childhood maltreatment and suicide-related behavior has been reviewed by several groups ( 21 , 33 , 43 – 47 ). Dube et al. ( 48 ) reported that adverse childhood experiences, including childhood maltreatment, increased the risk for suicide attempts twofold to fivefold in 17,337 adults in the now classic Adverse Childhood Experiences Study. Gomez et al. ( 49 ) reported that physical or sexual abuse increased the odds of suicide ideation, planning, and attempts among the 9,272 adolescents in the U.S. National Comorbidity Survey Adolescent Supplement. Miller et al. ( 50 ) examined the relationship between childhood maltreatment and prospective suicidal ideation in a cohort of 682 youths followed over a 3-year period. Emotional maltreatment predicted suicidal ideation, independently of previous suicidal ideation and depressive symptom severity. Childhood maltreatment is also associated with earlier age at first suicide attempt ( 51 ). Additionally, an association between childhood maltreatment and suicide risk in 449 individuals age 60 or older was recently reported from the Multidimensional Study of the Elderly, in the Family Health Strategy in Porto Alegre, Brazil ( 52 ). The effect was independent of depressive symptom severity. These findings suggest that childhood maltreatment increases risk for suicide-related behavior across the lifespan. More work is warranted in investigating the biological mechanisms that may mediate the association between childhood maltreatment and suicide-related behaviors.
Timing of Childhood Maltreatment: Are There Periods of Heightened Sensitivity?
Although childhood maltreatment at any age can result in long-lasting consequences ( 53 ), there is evidence that the timing, duration, and severity of maltreatment mediate the risk for later psychopathology ( 54 ). Childhood maltreatment that occurs earlier in life and continues for a longer duration is associated with the worst outcomes ( 55 ). This is supported by preclinical models (rodent and nonhuman primate) that investigated maternal separation ( 56 , 57 ), a paradigm more similar to neglect in humans. One study in rodents found that maternal separation during the early postnatal period (days 2–15) but not the later postnatal period (days 7–20) is associated with anxious and depressive-like behaviors in adulthood ( 57 ). Although this postnatal period coincides with in utero development in humans, there is evidence that in utero insults in the form of stress can have consequences similar to early-life trauma ( 58 , 59 ), supporting the translational validity of these models. Clinical studies also support the importance of timing of childhood maltreatment in moderating risk for psychopathology. Cowell et al. ( 60 ) investigated the timing and duration of childhood maltreatment in 223 maltreated children between the ages of 3 and 9 and found that children who were maltreated during infancy and those who experienced chronic maltreatment had poorer inhibitory control and working memory. Dunn et al. ( 61 ) investigated the relationship between timing of childhood maltreatment and depression and suicidal ideation in early adulthood among 15,701 participants in the National Longitudinal Study of Adolescent Health, and found that exposure to early maltreatment, especially during the preschool years (between ages 3 and 5), was most strongly associated with depression. Additionally, sexual abuse occurring during early childhood, compared with adolescence, was reported to be more strongly associated with suicidal ideation ( 61 ). While these studies suggest that childhood maltreatment that occurs earlier in development may further increase risk for developing mood disorders and associated behaviors in adulthood, it is important to emphasize that evidence suggests that exposure to maltreatment during later childhood and adolescence also independently increases risk for mood disorders. Emotional abuse and neglect, especially if it occurs between ages 8 and 9, increases depressive symptoms ( 62 ). Emotional abuse during adolescence also increases risk for depression ( 63 ).
More work is emerging investigating the negative consequences of bullying. A study of 1,420 participants (ages 9–16) revealed that victims of bullying showed an increased prevalence of generalized anxiety disorder, depression, and suicide-related behavior ( 64 ). A recent study of more than 5,000 children that comprised a longitudinal data set (the Avon Longitudinal Study of Parents and Children in England and the Great Smoky Mountains Study in the United States) ( 65 ) found an increased risk for mental health problems, including anxiety, depression, and self-harm, in individuals who experienced bullying, but not other maltreatment. Additionally, an association between childhood bullying by peers and risk for suicide-related behaviors (ideation, planning, attempting, and onset of plan among ideators), independent of childhood maltreatment by adults, was reported in a sample of U.S. Army soldiers ( 66 ).
Some studies suggest that differential periods of sensitivity to different subtypes of maltreatment are distinctly associated with an increased risk for mood disorders. Recently, a stronger relationship was reported between adult depression and early childhood sexual abuse (occurring at age 5 or earlier) and later childhood physical abuse (occurring at age 13 or later), compared with maltreatment that occurred during other developmental periods ( 67 ). Harpur et al. ( 68 ) reported that early childhood maltreatment (between birth and age 4) predicted more anxiety symptoms, and maltreatment that occurred in late childhood or early adolescence (between ages 10 and 12) predicted more depressive symptoms in adolescence. Taken together, these studies suggest that maltreatment at any age and across different contexts (physical and emotional, familial- and peer-induced) often result in long-lasting and severe consequences and that there may be specific sensitive periods in development when exposure to distinct types of maltreatment may differentially increase risk for affective disorders in adulthood. To date, the majority of research investigating the impact of childhood maltreatment timing on illness risk and course in mood disorders has focused on depression. One study ( 69 ) reported that early sexual or physical abuse (before age 11) in 225 early psychosis patients (6.7% with a bipolar disorder diagnosis) coincided with lower scores on the Global Assessment of Functioning Scale and the Social and Occupational Functioning Assessment Scale during a 3-year follow-up period, whereas late sexual or physical abuse (between ages 12 and 15) did not. More work investigating timing of maltreatment and associated clinical outcomes is warranted.
Experiencing Single Subtypes of Abuse and Neglect Versus Experiencing Multiple Types
Several groups have sought to determine the impact of single types of childhood maltreatment on mood disorders. Although all types of childhood maltreatment (physical, emotional, and sexual) increase disease vulnerability and risk for more severe illness course in mood disorders, including increased risk for suicide ( 52 ), there may be some distinctions between individual subtypes and associated outcomes ( 70 ). An association between sexual abuse and lifetime risk for anxiety disorders, depression, and suicide attempts independent of other types of maltreatment has been reported ( 2 , 71 , 72 ). In bipolar disorder, physical abuse and sexual abuse independently increase risk for illness vulnerability and more severe course ( 13 ). One study of 446 youths (ages 7 to 17) found that physical abuse was independently associated with a longer duration of illness in bipolar disorder, a greater prevalence of comorbid PTSD and psychosis, and a greater prevalence of family history of a mood disorder when compared with sexual abuse, which was only associated with a greater prevalence of PTSD ( 13 ). Recent life stress in adulthood was found to increase risk for first-onset mania in individuals with a history of childhood physical maltreatment, but not individuals with a history of sexual maltreatment ( 31 ). However, it should be noted that early-life sexual abuse in the study was a strong risk factor for mania even in the absence of recent life stress.
Neglect is the least studied form of early-life adversity, and emerging data suggest differential consequences following neglect as compared with abuse ( 73 ). Similarly, long-lasting consequences following emotional maltreatment, independently of other forms of maltreatment, have also been reported ( 47 , 74 , 75 ). In a 2015 meta-analysis, emotional abuse showed the strongest association with depression, followed by neglect and sexual abuse ( 76 ), a finding supported by another recent meta-analysis ( 77 ). Spertus et al. ( 78 ) reported that emotional abuse and neglect predicted depressive symptoms even after controlling for physical and sexual abuse, further suggesting emotional abuse and neglect to be independently related to illness severity in depression. Parental “verbal aggression” was found to increase risk for depression and anxiety in adolescents, with risk suggested to be greater following verbal aggression compared with physical abuse ( 79 ). Khan et al. ( 63 ) recently reported that nonverbal emotional abuse in males and peer emotional abuse in females are important predictors of lifetime history of major depression and are more predictive than number of types of maltreatment experienced. Another recent meta-analysis ( 12 ) reported that in individuals with depression, emotional neglect was the most common reported form of childhood maltreatment, and emotional abuse was most closely related to symptom severity. High prevalence of emotional maltreatment is also reported in bipolar disorder (approximately 40%), with emotional maltreatment associated with disease vulnerability and more severe illness course, including rapid cycling, comorbid anxiety or stress disorders, suicide attempts or ideation, and cannabis use ( 80 ).
Although studies on subtypes of maltreatment are only now burgeoning, they are concordant in implicating emotional maltreatment, in addition to physical and sexual maltreatment, in increasing risk for, and differences in disease course of, mood disorders. Emotional maltreatment and neglect are clearly the least studied of all forms of childhood adversity. This is in part because they are often overlooked and least likely to come to clinical attention, as compared with physical and sexual abuse, which can, of course, result in physical injury. Because emotional maltreatment and neglect are likely the most prevalent forms of childhood maltreatment in psychiatric populations ( 81 ), and given findings suggesting that independent of other forms of maltreatment, emotional maltreatment has long-lasting consequences that increase risk for mood disorders and illness outcome ( 74 , 75 ), more research on the role of emotional maltreatment and neglect are urgently needed.
Although the findings described above suggest the hypothesis that different subtypes of early-life adversity may independently increase risk for mood disorders and that some subtypes may be more closely related to specific differences in illness course and severity, it is clear that subtypes of abuse and neglect, as a rule, do not occur in isolation but instead occur together in the same individuals. For example, individuals experiencing physical or sexual abuse likely also experience emotional maltreatment. Some studies have investigated the impact of multiple types of childhood maltreatment. A recent meta-analysis reported that 19% of individuals with major depression report more than one form of childhood maltreatment and, while all childhood maltreatment subtypes have been shown to increase the risk of depression, experiencing multiple forms of childhood maltreatment further elevates this risk ( 12 ). The Adverse Childhood Experiences study provided evidence of an additive effect of eight early-life stress events (including abuse but also other early-life stressors, such as divorce, domestic violence, household substance abuse, and parental loss) on adult psychopathology. Specifically, individuals with four or more early-life stress events had significantly increased risk for depression, anxiety, suicide attempts, substance use disorders, and other detrimental outcomes ( 82 , 83 ). An additive or cumulative effect of early-life stress on increased risk for mood, anxiety, and substance use disorders has also been reported by others ( 5 , 6 ). Multiple adverse childhood experiences (maltreatment plus other forms of stressful events) also result in higher rates of comorbidities ( 7 , 82 ). Likewise, a dose-response relationship between number of types of childhood maltreatment and illness severity in bipolar disorder has been suggested, including increased risk for comorbid anxiety disorders and substance use disorders ( 84 ).
Underlying Mechanisms by Which Childhood Maltreatment Increases Risk for Mood Disorders and Contributes to Disease Course
As depicted in Figure 2 , several putative biological mechanisms by which childhood maltreatment may increase the risk for mood disorders and disease progression have been described ( 21 , 85 ). These include, but are not limited to, inflammation and other immune system perturbations, alterations in the hypothalamic-pituitary-adrenal (HPA) axis, and genetic and epigenetic processes as well as structural and functional brain imaging changes. These studies provide insight into modifiable targets and provide direction to improve both treatment and prevention strategies.
FIGURE 2. Child maltreatment, its consequences, and windows for intervention across development a
a The gray arrow represents the development of disease vulnerability, disease onset, and variations in disease course and treatment. Exposure to childhood maltreatment at any point during development (red bar) can result in long-lasting consequences, including increasing disease vulnerability and illness severity in mood disorders. There may be optimal windows (black arrows) across development when interventions could decrease disease burden by decreasing disease vulnerability and improving illness course; these include before and after birth (parenting classes and parenting support groups), at the time of maltreatment, when prodromal symptoms begin to emerge, immediately following disease onset, and during disease course (e.g., improving treatment response). Modifiable targets are beginning to emerge (green arrows and text) and point to behavioral and environmental factors, as well as genetic and other molecular factors, that could be focused on for interventions.
Biological Abnormalities Associated With Childhood Maltreatment
Several persistent biological alterations associated with childhood maltreatment may mediate the increased risk for development of mood and other disorders. Childhood maltreatment is associated with systemic inflammation ( 86 , 87 ) as assessed by measurements of C-reactive protein (CRP) and inflammatory cytokines including tumor necrosis factor-alpha and interleukin-6. Childhood maltreatment was found to be associated with increased plasma CRP levels and increased body mass index in 483 participants identified as being on the psychosis spectrum ( 88 ). Patients with depression and bipolar disorder have also been reported to exhibit increased levels of inflammatory markers ( 89 – 92 ). It is unclear whether childhood maltreatment–associated inflammation is responsible for the observations in patients with mood disorders. Anti-inflammatory drugs are a promising novel therapeutic strategy in the subgroup of depressed patients with elevated inflammation ( 93 ), although the findings thus far are preliminary, and further study on inflammation as a modifiable target is warranted.
Another mechanism through which childhood maltreatment may increase risk for mood disorders is through alterations of the HPA axis and corticotropin-releasing factor (CRF) circuits that regulate endocrine, behavioral, immune, and autonomic responses to stress. Research documenting how childhood maltreatment contributes to altered HPA axis and CRF circuit activity in preclinical and clinical studies has been reviewed in detail elsewhere ( 21 ). Childhood adversity likely increases sensitivity to the effects of recent life stress on the course of both unipolar and bipolar disorder. Soldiers exposed to childhood maltreatment have a greater risk for depression or anxiety following recent life stressors ( 94 ). Likewise, individuals exposed to childhood maltreatment have a greater risk of mania following recent life stressors compared with individuals without childhood maltreatment ( 31 , 34 ). Individuals with depression or bipolar disorder and early-life stress report lower levels of stress prior to recurrence of a mood episode compared with individuals with depression or bipolar disorder without early-life stress ( 34 , 95 ); this suggests that less stress is required to induce a mood episode in individuals who were exposed to childhood maltreatment. These findings support theoretical sensitization frameworks on the role of stress in unipolar depression and bipolar disorder ( 96 – 99 ). Alterations in the HPA axis and CRF circuits following childhood maltreatment are mechanisms that likely contribute to increased risk for mood episodes following stressful life events and may be modifiable targets. Indeed, Abercrombie et al. ( 100 ) recently reported that therapeutics targeting cortisol signaling may show promise in the treatment of depression in adults with a history of emotional abuse.
In addition to the biological mechanisms noted above, genetic predisposition undoubtedly also plays a role in the pathogenesis of mood disorders following early-life stress. As previously reviewed ( 21 ), studies support the interaction of genetic predisposition and childhood maltreatment in increasing risk for mood disorders and affecting disease course. Indeed, this is now considered a prototype of how gene-by-environment interactions influence disease vulnerability. Polymorphisms in genes comprising components of the HPA axis and CRF circuits increase the risk for adult mood disorders in adults exposed to childhood maltreatment. For example, polymorphisms in the FK506 binding protein 5 (FKBP5) gene interact with childhood maltreatment to increase risk for major depression, suicide attempts, and PTSD ( 101 – 105 ). Caspi et al. ( 106 ) found that adults exposed to childhood maltreatment who carried the short arm allele of the serotonin transporter promoter polymorphism (heterozygotes and homozygotes) exhibited an increased risk for a depressed episode, greater depressive symptoms, and greater risk for suicidal ideation and attempts compared with homozygotes with two long arm alleles. A large number of studies now support the interaction between early-life stress, the serotonin transporter promoter, and other serotonergic gene polymorphisms and disease vulnerability and illness course in depression and bipolar disorder ( 107 – 111 ), although conflicting findings have also been reported ( 112 ). Childhood maltreatment has also been reported to interact with corticotropin-releasing hormone receptor 1 gene (CRHR1) polymorphisms to predict syndromal depression and increase risk for suicide attempts in adults ( 113 – 115 ). Early-life stress interactions with other genetic polymorphisms to influence risk for mood disorders and illness course include, but are not limited to, brain-derived neurotrophic factor (BDNF) Val66Met polymorphism ( 116 , 117 ), toll-like receptors ( 118 ), the oxytocin receptor ( 119 ), inflammation pathway genes ( 120 ), and methylenetetrahydrofolate reductase ( 121 ), although negative findings have also been reported ( 122 ). Studies employing polygenic risk score (PRS) analyses, an approach assessing the combined impact of multiple genotyped single-nucleotide polymorphisms, have reported that PRS is differentially related to risk for depression in individuals with a history of childhood maltreatment compared with those without maltreatment ( 123 , 124 ), although negative findings have also been reported ( 125 ).
Studies investigating the role of epigenetics (e.g., the modification of gene expression through DNA methylation and acetylation) in mediating detrimental outcomes following early-life stress have recently appeared ( 126 ). For example, a recent study reported that hypermethylation of the first exon of a monoamine oxidase A (MAOA) gene region of interest mediated the association between sexual abuse and depression ( 127 ). Childhood maltreatment is also associated with epigenetic modifications of the glucocorticoid receptor ( 128 ), the FKBP5 gene ( 101 ), and the serotonin 3A receptor ( 129 ), with these modifications associated with suicide completion, altered stress hormone systems, and illness severity, respectively. Childhood maltreatment–associated epigenetic changes in individuals who died by suicide have been identified in human postmortem studies ( 130 ). These studies, and others not cited here, support gene–by–childhood maltreatment interactions, including epigenetic modifications, in risk for mood disorders and in illness course.
Epigenetics may also be one mechanism that contributes to the intergenerational transmission of trauma ( 131 – 133 ), although it is important to note that nongenomic mechanisms are also implicated in the intergenerational transmission of behavior ( 134 ). There is a robust literature in rodent models supporting the intergenerational transmission of maternal behavior—maternal traits being passed to offspring—including abuse-related phenotypes ( 132 , 135 ). Intergenerational transmission of behavior is also implicated in humans. Yehuda et al. ( 136 , 137 ) investigated risk for psychopathology in offspring of Holocaust survivors. These pivotal studies identified increased risk for PTSD, mood disorders, and substance use disorders in offspring. These offspring also reported having higher levels of emotional abuse and neglect, which correlated with severity of PTSD in the parent ( 136 , 137 ), implicating early-life stress in transmission of psychopathology. While there is evidence that children with developmental disabilities are at a higher risk for neglect ( 138 – 140 ), there is a paucity of studies investigating whether offspring of individuals with mental illness are more liable to abuse. However, as discussed above, higher rates of maltreatment are reported in individuals with mood disorders, but whether and what familial factors may drive these elevated rates, or whether these interactions contribute to the intergenerational transmission of psychopathology, are not known. In light of the emerging data on intergenerational transmission of trauma, this is an important, complex area in need of further study. There have not been many genetic studies in this area. In a study investigating early-life maltreatment in a rodent model, early-life abuse (defined as stepping on, dropping, or dragging offspring, and active avoidance) was associated with altered BDNF expression and methylation in the prefrontal cortex in adult offspring, with adult offspring also showing poorer maternal care patterns when rearing their own offspring ( 135 ). Altered expression and methylation of BDNF is reported in individuals with mood disorders ( 141 , 142 ). These studies highlight the importance of understanding the intergenerational transmission of trauma and psychopathology to identify modifiable targets to improve outcomes, for example, the family unit and interpersonal relationships. It is noteworthy that while the majority of research has focused on intergenerational transmission of maternal traits, research is also emerging that supports the important role of paternal care on intergenerational transmission of behavior ( 131 ). More study on intergenerational transmission of trauma is needed.
Pathways to Mood Disorder Outcomes
More work on mechanisms and pathways by which childhood maltreatment increases risk for and ultimately results in adult mood disorders is essential for early intervention. Childhood maltreatment is associated with a marked increase in medical morbidities and an array of physical symptoms, and in general it predicts poor health and a shorter lifespan ( 143 , 144 ). Higher rates of comorbid substance use disorders in individuals with mood disorders who report experiencing childhood maltreatment is of particular interest. Childhood maltreatment has consistently been associated with a number of high-risk health behaviors, including smoking and alcohol and drug use—behaviors thought to contribute to the association between childhood maltreatment and poor health ( 145 – 148 ). These behaviors on their own increase risk for, and alter disease course in, mood disorders ( 149 – 153 ). More study on the relationship between early-life adversity, substance use disorders, and mood disorders is therefore warranted. For example, childhood maltreatment is associated with increased risky alcohol use, alcohol-related problems, and alcohol use disorders ( 154 , 155 ), and alcohol use disorders are an established risk factor for both depression and bipolar disorder ( 149 – 151 ) in addition to increasing risk for a more severe clinical course, such as further increasing risk for suicide ( 152 , 153 ). A recent study reported that depression mediates the relationship between childhood maltreatment and alcohol abuse ( 156 ). Another study recently reported that sexual abuse increased risk of alcohol use and depression in adolescence, which then influenced risk for adult depression, anxiety, and substance abuse ( 157 ). In a longitudinal study investigating changes in patterns of substance use over time in 937 adolescents, childhood maltreatment was associated with an increased progression toward heavy polysubstance use ( 158 ). More research is needed looking at the interactions between childhood maltreatment and other drugs of abuse. This is especially true in light of the current opioid epidemic, as increased rates of childhood maltreatment are also reported in individuals with opioid use disorders ( 159 – 161 ), and greater reported childhood maltreatment is associated with faster transmission from use to dependence ( 162 ) and with higher rates of suicide attempts in this population ( 163 ).
Interestingly, certain genes described above that exhibit gene–by–childhood maltreatment interactions on risk for mood disorders, including FKBP5 and the serotonin transporter promoter polymorphisms, also exhibit gene-by-childhood maltreatment interactions on risk for alcohol use disorders ( 164 – 168 ). Alterations in the stress hormone system are also associated with an increased risk for alcohol use disorders in individuals with a history of childhood maltreatment ( 169 ), and past-year negative life events have been reported to increase drinking and drug use, an effect that is dependent on genetic variation in the serotonin transporter gene ( 170 ). Childhood maltreatment has been found to be associated with an earlier age at initiation of alcohol and marijuana use, with this association mediated by externalizing behaviors ( 171 ). Impulsivity may mediate the relationship between childhood maltreatment and increased risk for developing alcohol or cannabis abuse ( 172 ). Etain et al. ( 173 ) conducted a path analysis in 485 euthymic patients with bipolar disorder and uncovered a significant association between impulsivity and emotional abuse, and impulsivity was associated with an increased risk for substance use disorders. These studies suggest that in some individuals with a history of childhood maltreatment, although not all, interventions that focus on alcohol or drug use problems, and specifically externalizing behaviors that may mediate the link between childhood maltreatment and alcohol or drug use problems (e.g., impulsivity), could decrease disease burden by decreasing risk for developing mood disorders or by improving illness course (e.g., decreasing symptom severity and risk for suicide).
Substance use disorders are also associated with increases in inflammatory markers ( 174 , 175 ). Inflammation is suggested to contribute to comorbid alcohol use disorders and mood disorders ( 176 ), and it contributes to a variety of medical morbidities ( 177 ), and these in turn are associated with an increased risk for mood disorders ( 177 ). Speculatively, inflammation may be one mechanism by which childhood maltreatment increases risk for medical morbidity and through that pathway increases risk for mood disorders. While there is a paucity of studies on the pathways described above, the associations between childhood maltreatment, risky health behaviors, inflammation, and medical morbidities warrant more study, as identifying pathways (mediators and moderators) to illness outcomes could foster the development of more effective interventions and treatment strategies.
It should be noted that not all individuals who experience childhood maltreatment develop mood disorders. This may be related in part to genetics. However, other resiliency factors are likely of importance. In a recent meta-analysis, Braithwaite et al. ( 178 ) identified interpersonal relationships, cognitive vulnerabilities, and behavioral difficulties as modifiable predictors of depression following childhood maltreatment. Specifically, social support and secure attachments were reported to exert a buffering effect on risk for depression, brooding was suggested to be a cognitive marker of risk, and externalizing behavior was suggested to be a behavioral marker of risk. Other researchers have also reported that social support may be protective and that interventions directed toward enhancing social support may decrease disease vulnerability and improve illness course ( 179 ). Metacognitive beliefs, or beliefs about one’s own cognition, are suggested to mediate the relationship between childhood maltreatment and mood-related and positive symptoms in individuals with psychotic or bipolar disorders ( 180 ). Specifically, beliefs about thoughts being uncontrollable or dangerous mediated the relationship between emotional abuse and depression or anxiety and positive symptom subscale score on the Positive and Negative Syndrome Scale. Affective lability was found to mediate the relationship between childhood maltreatment and several clinical features in bipolar disorder, including suicide attempts, anxiety, and mixed episodes ( 181 ), and social cognition was suggested to moderate the relationship between physical abuse and clinical outcome in an inpatient psychiatric rehabilitation program ( 182 ).
Childhood Maltreatment and Associated Alterations in Neural Structure and Function
Research on neurobiological consequences that may mediate the relationship between childhood maltreatment and risk for, and affect disease course in, mood disorders is clearly integral to addressing the question of whether the consequences of early-life stress are reversible. Although a comprehensive review of neuroimaging findings is beyond the scope of this review, over the past 5 years, review articles summarizing the neurobiological associations with childhood maltreatment have emphasized the long-lasting neurobiological structural and functional changes in the brain following maltreatment ( 21 , 83 , 183 , 184 ). In brief, while null and conflicting findings have been reported, data are converging to suggest that childhood maltreatment is associated with lower gray matter volumes and thickness in the ventral and dorsal prefrontal cortex, including the orbitofrontal and anterior cingulate cortices, hippocampus, insula, and striatum, with more recent studies also suggesting an association with decreased white matter structural integrity within and between these regions ( 185 – 194 ). Smaller hippocampal and prefrontal cortical volumes following childhood maltreatment are consistently reported in unipolar depression and other psychiatric disorders ( 189 , 195 – 199 ), with gene-by-environment interactions suggested ( 200 – 202 ). These studies suggest mechanisms that may cross diagnostic boundaries in conferring risk for psychopathology and genetic variation that may link neurobiology, childhood maltreatment, and vulnerability for detrimental outcomes.
Studies investigating differences in function within, and functional connectivity between, these regions following childhood maltreatment are emerging, with more recent results suggesting that these changes may relate to risk for psychopathology. It was recently reported that decreased prefrontal responses during a verbal working memory task mediated the relationship between childhood maltreatment and trait impulsivity in young adult women ( 203 ). In a study investigating functional responses to emotional faces in 182 adults with a range of anxiety symptoms ( 204 ), the authors found that increased amygdala and decreased dorsolateral prefrontal activity to fearful and angry faces—as well as increased insula activity to fearful and increased ventral but decreased dorsal and anterior cingulate activity to angry faces—mediated the relationship between childhood maltreatment and anxiety symptoms. Differences in functional connectivity, measured with multivariate network-based approaches, within the dorsal attention network and between task-positive networks and sensory systems have been reported in unipolar depression following childhood maltreatment ( 205 ). Altered reward-related functional connectivity between the striatum and the medial prefrontal cortex has also been reported in individuals with greater recent life stress and higher levels of childhood maltreatment, with increased connectivity associated with greater depressive symptom severity ( 206 ). Childhood maltreatment–associated changes in functional connectivity between the amygdala and the dorsolateral and rostral prefrontal cortex have been suggested to contribute to altered stress response and mood in adults ( 207 ). Additionally, childhood maltreatment has been reported to moderate the association between inhibitory control, measured with a Stroop color-word task, and activation in the anterior cingulate cortex while listening to personalized stress cues, an individual’s recounting of his or her own stressful events ( 208 ). As discussed above, it has been hypothesized that childhood maltreatment may increase risk for mood disorders through alterations of the HPA axis and CRF circuits in the brain. Therefore, research aimed at identifying neurobiological changes in function of CRF circuits in the brain that may mediate the relationship between childhood maltreatment and risk for mood disorders and affect disease course, including interactions with recent life stress, is a promising area of investigation.
Recent studies investigating altered function could suggest neurobiological mechanisms of risk but may also suggest possible mechanisms underlying resilience ( 183 ). Functional studies, such as those discussed above, that link functional changes in the brain following childhood maltreatment to mood-related symptoms can provide some clues to help identify mechanisms underlying risk. However, in the absence of longitudinal study of outcomes, these results must still be interpreted with caution. While the majority of studies have been cross-sectional, longitudinal studies are beginning to emerge. Opel et al. ( 209 ) recently reported that reduced insula surface area mediated the association between childhood maltreatment and relapse of depression among 110 patients with unipolar depression followed prospectively. A longitudinal study incorporating structural MRI in 51 adolescents (37% of whom had a history of childhood maltreatment) found that reduced cortical thickness in prefrontal and temporal cortices was associated with psychiatric symptoms at follow-up ( 210 ). Swartz et al. ( 211 ) followed 157 adolescents over a 2-year period and reported results suggesting that early-life stress is associated with amygdala hyperactivity during threat processing, with this finding preceding syndromal mood or anxiety. Longitudinal study of outcomes following childhood maltreatment and underlying neurobiology (predictors and trajectories) is critically needed to identify modifiable targets that confer risk and disentangle mechanisms of risk and resilience.
Only recently have studies investigating childhood maltreatment in bipolar disorder and neurobiological associations begun to emerge. Similar to unipolar depression and other psychiatric disorders, decreased ventral and dorsolateral prefrontal, insula, and hippocampal gray matter volume are reported in individuals with bipolar disorder with a history of childhood maltreatment compared with individuals with bipolar disorder without childhood maltreatment ( 202 , 212 , 213 ). Decreased white matter structural integrity across the whole brain, including lower structural integrity in the corpus callosum and uncinate fasciculus, have been reported in individuals with bipolar disorder who reported having experienced child abuse compared with those who did not and a healthy comparison group ( 214 , 215 ). Interestingly, one study ( 214 ) found that the effects of childhood maltreatment on white matter structural integrity were specific to individuals with bipolar disorder; decreased structural integrity was not observed in healthy comparison individuals with a history of childhood maltreatment compared with healthy individuals without maltreatment. In light of this finding, along with recently published data from other groups ( 216 – 218 ), it is possible that some consequences following childhood maltreatment may be more robust or distinct in some individuals—or that perhaps individuals with a genetic predisposition for mood disorders may be more vulnerable to the detrimental effects of childhood maltreatment.
Altered amygdala and hippocampal volumes are suggested to be differentially modulated following childhood maltreatment in patients with bipolar disorder compared with a healthy comparison group ( 216 ), although interactions with history of treatment (e.g., duration of lithium exposure) cannot be ruled out, as this was not investigated. Souza-Queiroz et al. ( 217 ) found that childhood maltreatment was associated with decreased amygdala volume, decreased ventromedial prefrontal connectivity with the amygdala and hippocampus, and decreased structural integrity in the uncinate fasciculus—the main white matter fiber tract connecting these regions. The bipolar group primarily drove these effects, with only smaller amygdala volume associated with childhood maltreatment in the healthy comparison group. While these findings could be driven by higher rates of maltreatment reported in the bipolar disorder group, or other clinical factors such as medication exposure and history of depressed or manic episodes, they could also suggest interactions between genetic vulnerability to bipolar disorder (or other environmental factors) and neurobiological consequences following childhood maltreatment.
More research is needed to identify genes that may influence neurobiological vulnerability following childhood maltreatment. An example of a potential gene that may mediate this relationship is the serotonin transporter promoter. Genetic variation in the serotonin transporter promoter is associated with differences in structural integrity of white matter in bipolar disorder ( 219 ). Because a large number of studies support the interaction between early-life stress, the serotonin transporter promoter, and disease vulnerability and illness course in depression and bipolar disorder ( 106 – 111 ), this example highlights the potential of genes to contribute to long-lasting structural consequences in the brain following childhood maltreatment in mood disorders. Genetic imaging studies are emerging and suggest gene-by-environment interactions on structural and functional alterations following childhood maltreatment. For example, one study found that hippocampal volume differences following childhood maltreatment are mediated by genetic variation in bipolar disorder ( 202 ). Additionally, polymorphisms in stress system genes, including FKBP5 and NR3C1, are suggested to moderate the effects of childhood maltreatment on amygdala reactivity ( 220 – 222 ) and hippocampal volumes ( 223 ). Studies investigating interactions between familial risk for mood disorders and childhood maltreatment and associated structural and functional changes in the brain would be useful to test whether familial factors (genetic and environmental vulnerability) may interact with childhood maltreatment to alter brain structure and function while avoiding confounders such as medication exposure.
Limitations and Future Directions
A sizable percentage of patients with mood disorders have a history of childhood maltreatment. While the devastating consequences of childhood maltreatment cannot be disavowed, several limitations in research should be noted. Research groups often assess childhood maltreatment differently, and this can result in a measurement bias. Demographic characteristics and differences in assessments (age and sex ratio of participants; clinical versus nonclinical populations being studied; observer-rated versus self-rated depression measures) are all suggested to contribute to differences in prevalence of childhood maltreatment and relation with illness severity ( 12 ). For example, studies using the Childhood Trauma Questionnaire report higher rates of emotional abuse compared with studies using other measures to investigate childhood maltreatment ( 12 ). Further study is warranted investigating the neurobiological mechanisms, underlying genetics, familial factors, and modifiable targets that may drive development of mood disorders following childhood maltreatment. A promising area is network-based approaches to understand this link ( 224 ). Additionally, consequences following different types of maltreatment require further investigation, as different forms of childhood maltreatment may be associated with distinct neural consequences, and a better understanding of these relations is critical for the development of more effective interventions and prevention strategies. For example, Heim et al. ( 225 ) reported that victims of sexual abuse exhibit more alterations in the somatosensory area, whereas victims of emotional abuse exhibit differences in areas mediating emotional processing and self-awareness, including the anterior cingulate and parahippocampal gyrus. More work is needed to investigate whether there are sensitive periods in development when maltreatment has more robust consequences on neurobiology. Humphreys et al. ( 226 ) recently reported that hippocampal volume differences were associated with stress severity during early childhood (≤5 years of age), but there was no association between hippocampal volumes and stress occurring during later childhood. Studies investigating interactions between childhood maltreatment and genetic variation or familial risk for mood disorders could identify mechanisms underlying risk and resiliency in the absence of some study-related confounders (e.g., medication).
Longitudinal studies are critically needed to distinguish what behaviors and mechanisms (genetic and neurobiological) may contribute to risk and whether alterations in behaviors or neurobiology are secondary to mood disorder onset. It is important to emphasize that sex differences likely contribute to outcomes following childhood maltreatment ( 227 ). These include females, compared with males, having a higher risk for internalizing disorders (depression and anxiety) ( 228 , 229 ), greater deficits in neural systems underlying emotional regulation ( 187 , 230 ), and being more susceptible to stress-induced changes in the HPA axis ( 231 ) following maltreatment. Males, compared with females, may be more vulnerable to developing externalizing disorders (conduct disorders and substance use disorders) ( 232 ). However, few studies have investigated sex differences following childhood maltreatment. More research on sex differences is critically needed, including on the underlying neurobiology. As previously reviewed ( 21 ), early-life adversity is associated with increased vulnerability to several major medical disorders, including coronary artery disease and myocardial infarction, cerebrovascular disease and stroke, type 2 diabetes, asthma, and certain forms of cancer. More work is needed on medical morbidities that may increase risk for early mortality following early-life adversity. Additionally, more research is needed on disparities that contribute to, and minority communities that show, elevated rates of early-life adversity. As discussed above, rates of early-life adversity are higher among individuals with developmental disabilities ( 138 – 140 ). Rates of trauma are also higher in youths in the lesbian, gay, bisexual, transgender, and questioning (LGBTQ) community ( 233 ). Few studies have been published in this area. Youths in the LGBTQ community show higher rates of mood disorders, anxiety, suicide, and alcohol and drug use ( 234 ). In a recent study, Rhoades et al. ( 235 ) investigated the relationship between parental rejection, homelessness, and mental health outcomes in LGBTQ youths. Parental rejection was associated with higher rates of homelessness, with experience of homelessness associated with greater feelings of hopelessness, PTSD and depressive symptoms, and greater prevalence of past suicide attempts and more individuals saying they are likely to attempt suicide in the future. More work is critically needed in vulnerable populations, including work focused on interventions that may improve mental health outcomes, for example, interventions that focus on the family unit and interpersonal relationships to foster support and educational interventions, which may decrease peer victimization and cyberbullying ( 236 , 237 ).
In summary, studies converge on and consistently support the finding that childhood maltreatment increases disease vulnerability for mood disorders, as well as a more pernicious disease course. A reduction in the prevalence of childhood maltreatment would have a substantial impact on decreasing disease burden ( 238 ). Studies suggesting modifiable targets are only just beginning to emerge and point to behavioral and environmental factors that could be focused on for early interventions.
Dr. Nemeroff has served as a consultant for Bracket (Clintara), Fortress Biotech, EMA Wellness, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen Research and Development, Magstim, Navitor Pharmaceuticals, Sunovion Pharmaceuticals, Taisho Pharmaceutical, Takeda, TC MSO, and Xhale; he holds stock in AbbVie, Antares, BI Gen Holdings, Celgene, Corcept Therapeutics Pharmaceuticals Company, EMA Wellness, OPKO Health, Seattle Genetics, TC MSO, Trends in Pharma Development, and Xhale; he is a member of the scientific advisory boards of the Anxiety Disorder Association of America (ADAA), the American Foundation for Suicide Prevention (AFSP), Bracket (Clintara), the Brain and Behavior Research Foundation, the Laureate Institute for Brain Research, Skyland Trail, and Xhale and on the boards of directors of ADAA, AFSP, Gratitude America, and Xhale Smart; he has had income sources or equity of $10,000 or more from American Psychiatric Publishing, Bracket (Clintara), CME Outfitters, EMA Wellness, Intra-Cellular Therapies, Magstim, Takeda, TC-MSO, and Xhale; he holds patents on a method and devices for transdermal delivery of lithium (US 6,375,990B1), a method of assessing antidepressant drug therapy via transport inhibition of monoamine neurotransmitter by ex vivo assay (US 7,148,027B2), and compounds, compositions, methods of synthesis, and methods of treatment (CRF receptor binding ligand) (US 8,551,996 B2). Dr. Lippard reports no financial relationships with commercial interests.
Dr. Lippard’s research is supported by NIH grant K01AA027573. Dr. Nemeroff’s research is supported by NIH grants MH117293 and AA-024933.
1 US Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau: Child Maltreatment 2016. Washington, DC, US Department of Health and Human Services, 2018 ( https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment) Google Scholar
2 Maniglio R : Child sexual abuse in the etiology of depression: a systematic review of reviews . Depress Anxiety 2010 ; 27 : 631 – 642 Crossref , Medline , Google Scholar
3 Maniglio R : Prevalence of child sexual abuse among adults and youths with bipolar disorder: a systematic review . Clin Psychol Rev 2013 ; 33 : 561 – 573 Crossref , Medline , Google Scholar
4 Lindert J , von Ehrenstein OS , Grashow R , et al. : Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis . Int J Public Health 2014 ; 59 : 359 – 372 Crossref , Medline , Google Scholar
5 Scott KM , Smith DR , Ellis PM : Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults . Arch Gen Psychiatry 2010 ; 67 : 712 – 719 Crossref , Medline , Google Scholar
6 Green JG , McLaughlin KA , Berglund PA , et al. : Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: associations with first onset of DSM-IV disorders . Arch Gen Psychiatry 2010 ; 67 : 113 – 123 Crossref , Medline , Google Scholar
7 Widom CS , DuMont K , Czaja SJ : A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up . Arch Gen Psychiatry 2007 ; 64 : 49 – 56 Crossref , Medline , Google Scholar
8 Benjet C , Borges G , Medina-Mora ME : Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence, and adulthood . J Psychiatr Res 2010 ; 44 : 732 – 740 Crossref , Medline , Google Scholar
9 Chapman DP , Whitfield CL , Felitti VJ , et al. : Adverse childhood experiences and the risk of depressive disorders in adulthood . J Affect Disord 2004 ; 82 : 217 – 225 Crossref , Medline , Google Scholar
10 Zavaschi ML , Graeff ME , Menegassi MT , et al. : Adult mood disorders and childhood psychological trauma . Br J Psychiatry 2006 ; 28 : 184 – 190 Crossref , Google Scholar
11 Kessler RC : The effects of stressful life events on depression . Annu Rev Psychol 1997 ; 48 : 191 – 214 Crossref , Medline , Google Scholar
12 Nelson J , Klumparendt A , Doebler P , et al. : Childhood maltreatment and characteristics of adult depression: meta-analysis . Br J Psychiatry 2017 ; 210 : 96 – 104 Crossref , Medline , Google Scholar
13 Romero S , Birmaher B , Axelson D , et al. : Prevalence and correlates of physical and sexual abuse in children and adolescents with bipolar disorder . J Affect Disord 2009 ; 112 : 144 – 150 Crossref , Medline , Google Scholar
14 Hyun M , Friedman SD , Dunner DL : Relationship of childhood physical and sexual abuse to adult bipolar disorder . Bipolar Disord 2000 ; 2 : 131 – 135 Crossref , Medline , Google Scholar
15 Post RM , Altshuler L , Leverich G , et al. : More stressors prior to and during the course of bipolar illness in patients from the United States compared with the Netherlands and Germany . Psychiatry Res 2013 ; 210 : 880 – 886 Crossref , Medline , Google Scholar
16 Bernet CZ , Stein MB : Relationship of childhood maltreatment to the onset and course of major depression in adulthood . Depress Anxiety 1999 ; 9 : 169 – 174 Crossref , Medline , Google Scholar
17 Comijs HC , van Exel E , van der Mast RC , et al. : Childhood abuse in late-life depression . J Affect Disord 2013 ; 147 : 241 – 246 Crossref , Medline , Google Scholar
18 Nanni V , Uher R , Danese A : Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis . Am J Psychiatry 2012 ; 169 : 141 – 151 Link , Google Scholar
19 Wiersma JE , Hovens JG , van Oppen P , et al. : The importance of childhood trauma and childhood life events for chronicity of depression in adults . J Clin Psychiatry 2009 ; 70 : 983 – 989 Crossref , Medline , Google Scholar
20 Withers AC , Tarasoff JM , Stewart JW : Is depression with atypical features associated with trauma history? J Clin Psychiatry 2013 ; 74 : 500 – 506 Crossref , Medline , Google Scholar
21 Nemeroff CB : Paradise lost: the neurobiological and clinical consequences of child abuse and neglect . Neuron 2016 ; 89 : 892 – 909 Crossref , Medline , Google Scholar
22 Quilty LC , Marshe V , Lobo DS , et al. : Childhood abuse history in depression predicts better response to antidepressants with higher serotonin transporter affinity: a pilot investigation . Neuropsychobiology 2016 ; 74 : 78 – 83 Crossref , Medline , Google Scholar
23 Scott KM , McLaughlin KA , Smith DA , et al. : Childhood maltreatment and DSM-IV adult mental disorders: comparison of prospective and retrospective findings . Br J Psychiatry 2012 ; 200 : 469 – 475 Crossref , Medline , Google Scholar
24 Fergusson DM , Horwood LJ , Boden JM : Structural equation modeling of repeated retrospective reports of childhood maltreatment . Int J Methods Psychiatr Res 2011 ; 20 : 93 – 104 Crossref , Medline , Google Scholar
25 Baldwin JR , Reuben A , Newbury JB , et al. : Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis . JAMA Psychiatry ( Epub ahead of print, March 20, 2019 ) Google Scholar
26 Ellis RER , Seal ML , Simmons JG , et al. : Longitudinal trajectories of depression symptoms in adolescence: psychosocial risk factors and outcomes . Child Psychiatry Hum Dev 2017 ; 48 : 554 – 571 Crossref , Medline , Google Scholar
27 Gilman SE , Trinh NH , Smoller JW , et al. : Psychosocial stressors and the prognosis of major depression: a test of axis IV . Psychol Med 2013 ; 43 : 303 – 316 Crossref , Medline , Google Scholar
28 Daruy-Filho L , Brietzke E , Lafer B , et al. : Childhood maltreatment and clinical outcomes of bipolar disorder . Acta Psychiatr Scand 2011 ; 124 : 427 – 434 Crossref , Medline , Google Scholar
29 Anand A , Koller DL , Lawson WB , et al. : Genetic and childhood trauma interaction effect on age of onset in bipolar disorder: an exploratory analysis . J Affect Disord 2015 ; 179 : 1 – 5 Crossref , Medline , Google Scholar
30 Jansen K , Cardoso TA , Fries GR , et al. : Childhood trauma, family history, and their association with mood disorders in early adulthood . Acta Psychiatr Scand 2016 ; 134 : 281 – 286 Crossref , Medline , Google Scholar
31 Gilman SE , Ni MY , Dunn EC , et al. : Contributions of the social environment to first-onset and recurrent mania . Mol Psychiatry 2015 ; 20 : 329 – 336 Crossref , Medline , Google Scholar
32 Noto MN , Noto C , Caribé AC , et al. : Clinical characteristics and influence of childhood trauma on the prodrome of bipolar disorder . Br J Psychiatry 2015 ; 37 : 280 – 288 Crossref , Google Scholar
33 Agnew-Blais J , Danese A : Childhood maltreatment and unfavourable clinical outcomes in bipolar disorder: a systematic review and meta-analysis . Lancet Psychiatry 2016 ; 3 : 342 – 349 Crossref , Medline , Google Scholar
34 Dienes KA , Hammen C , Henry RM , et al. : The stress sensitization hypothesis: understanding the course of bipolar disorder . J Affect Disord 2006 ; 95 : 43 – 49 Crossref , Medline , Google Scholar
35 Leverich GS , McElroy SL , Suppes T , et al. : Early physical and sexual abuse associated with an adverse course of bipolar illness . Biol Psychiatry 2002 ; 51 : 288 – 297 Crossref , Medline , Google Scholar
36 Erten E , Funda Uney A , Saatçioğlu Ö , et al. : Effects of childhood trauma and clinical features on determining quality of life in patients with bipolar I disorder . J Affect Disord 2014 ; 162 : 107 – 113 Crossref , Medline , Google Scholar
37 Carballo JJ , Harkavy-Friedman J , Burke AK , et al. : Family history of suicidal behavior and early traumatic experiences: additive effect on suicidality and course of bipolar illness? J Affect Disord 2008 ; 109 : 57 – 63 Crossref , Medline , Google Scholar
38 Park YM : Relationship between childhood maltreatment, suicidality, and bipolarity: a retrospective study . Psychiatry Investig 2017 ; 14 : 136 – 140 Crossref , Medline , Google Scholar
39 Pavlova B , Perroud N , Cordera P , et al. : Anxiety disorders and childhood maltreatment as predictors of outcome in bipolar disorder . J Affect Disord 2018 ; 225 : 337 – 341 Crossref , Medline , Google Scholar
40 Pavlova B , Perroud N , Cordera P , et al. : Childhood maltreatment and comorbid anxiety in people with bipolar disorder . J Affect Disord 2016 ; 192 : 22 – 27 Crossref , Medline , Google Scholar
41 Cakir S , Tasdelen Durak R , Ozyildirim I , et al. : Childhood trauma and treatment outcome in bipolar disorder . J Trauma Dissociation 2016 ; 17 : 397 – 409 Crossref , Medline , Google Scholar
42 Post RM , Leverich GS , Kupka R , et al. : Clinical correlates of sustained response to individual drugs used in naturalistic treatment of patients with bipolar disorder . Compr Psychiatry 2016 ; 66 : 146 – 156 Crossref , Medline , Google Scholar
43 Short AT , Nemeroff CB : Early life trauma and suicide , in Suicide: Phenomenology and Neurobiology . Edited by Cannon KE , Hudzik TJ . Basel, Springer , 2014 , pp 187– 205 Crossref , Google Scholar
44 Castellví P , Miranda-Mendizábal A , Parés-Badell O , et al. : Exposure to violence, a risk for suicide in youths and young adults: a meta-analysis of longitudinal studies . Acta Psychiatr Scand 2017 ; 135 : 195 – 211 Crossref , Medline , Google Scholar
45 Liu J , Fang Y , Gong J , et al. : Associations between suicidal behavior and childhood abuse and neglect: a meta-analysis . J Affect Disord 2017 ; 220 : 147 – 155 Crossref , Medline , Google Scholar
46 Miller AB , Esposito-Smythers C , Weismoore JT , et al. : The relation between child maltreatment and adolescent suicidal behavior: a systematic review and critical examination of the literature . Clin Child Fam Psychol Rev 2013 ; 16 : 146 – 172 Crossref , Medline , Google Scholar
47 Norman RE , Byambaa M , De R , et al. : The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis . PLoS Med 2012 ; 9 : e1001349 Crossref , Medline , Google Scholar
48 Dube SR , Anda RF , Felitti VJ , et al. : Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study . JAMA 2001 ; 286 : 3089 – 3096 Crossref , Medline , Google Scholar
49 Gomez SH , Tse J , Wang Y , et al. : Are there sensitive periods when child maltreatment substantially elevates suicide risk? Results from a nationally representative sample of adolescents . Depress Anxiety 2017 ; 34 : 734 – 741 Crossref , Medline , Google Scholar
50 Miller AB , Jenness JL , Oppenheimer CW , et al. : Childhood emotional maltreatment as a robust predictor of suicidal ideation: a 3-year multi-wave, prospective investigation . J Abnorm Child Psychol 2017 ; 45 : 105 – 116 Crossref , Medline , Google Scholar
51 Peyre H , Hoertel N , Stordeur C , et al. : Contributing factors and mental health outcomes of first suicide attempt during childhood and adolescence: results from a nationally representative study . J Clin Psychiatry 2017 ; 78 : e622 – e630 Crossref , Medline , Google Scholar
52 Behr Gomes Jardim G , Novelo M , Spanemberg L , et al. : Influence of childhood abuse and neglect subtypes on late-life suicide risk beyond depression . Child Abuse Negl 2018 ; 80 : 249 – 256 Crossref , Medline , Google Scholar
53 Dunn EC , Nishimi K , Powers A , et al. : Is developmental timing of trauma exposure associated with depressive and post-traumatic stress disorder symptoms in adulthood? J Psychiatr Res 2017 ; 84 : 119 – 127 Crossref , Medline , Google Scholar
54 Teicher MH , Samson JA : Annual research review: enduring neurobiological effects of childhood abuse and neglect . J Child Psychol Psychiatry 2016 ; 57 : 241 – 266 Crossref , Medline , Google Scholar
55 Dunn EC , Nishimi K , Gomez SH , et al. : Developmental timing of trauma exposure and emotion dysregulation in adulthood: are there sensitive periods when trauma is most harmful? J Affect Disord 2018 ; 227 : 869 – 877 Crossref , Medline , Google Scholar
56 Sanchez MM : The impact of early adverse care on HPA axis development: nonhuman primate models . Horm Behav 2006 ; 50 : 623 – 631 Crossref , Medline , Google Scholar
57 Roque S , Mesquita AR , Palha JA , et al. : The behavioral and immunological impact of maternal separation: a matter of timing . Front Behav Neurosci 2014 ; 8 : 192 Crossref , Medline , Google Scholar
58 Goldstein JM , Holsen L , Huang G , et al. : Prenatal stress-immune programming of sex differences in comorbidity of depression and obesity/metabolic syndrome . Dialogues Clin Neurosci 2016 ; 18 : 425 – 436 Crossref , Medline , Google Scholar
59 Heim CM , Entringer S , Buss C : Translating basic research knowledge on the biological embedding of early-life stress into novel approaches for the developmental programming of lifelong health . Psychoneuroendocrinology 2019 ; 105 : 123 – 137 Crossref , Medline , Google Scholar
60 Cowell RA , Cicchetti D , Rogosch FA , et al. : Childhood maltreatment and its effect on neurocognitive functioning: timing and chronicity matter . Dev Psychopathol 2015 ; 27 : 521 – 533 Crossref , Medline , Google Scholar
61 Dunn EC , McLaughlin KA , Slopen N , et al. : Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: results from the National Longitudinal Study of Adolescent Health . Depress Anxiety 2013 ; 30 : 955 – 964 Medline , Google Scholar
62 Schalinski I , Teicher MH , Nischk D , et al. : Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative, and depressive symptoms in adult inpatients . BMC Psychiatry 2016 ; 16 : 295 Crossref , Medline , Google Scholar
63 Khan A , McCormack HC , Bolger EA , et al. : Childhood maltreatment, depression, and suicidal ideation: critical importance of parental and peer emotional abuse during developmental sensitive periods in males and females . Front Psychiatry 2015 ; 6 : 42 Crossref , Medline , Google Scholar
64 Copeland WE , Wolke D , Angold A , et al. : Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence . JAMA Psychiatry 2013 ; 70 : 419 – 426 Crossref , Medline , Google Scholar
65 Lereya ST , Copeland WE , Costello EJ , et al. : Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries . Lancet Psychiatry 2015 ; 2 : 524 – 531 Crossref , Medline , Google Scholar
66 Campbell-Sills L , Kessler RC , Ursano RJ , et al. : Associations of childhood bullying victimization with lifetime suicidal behaviors among new US Army soldiers . Depress Anxiety 2017 ; 34 : 701 – 710 Crossref , Medline , Google Scholar
67 Jaye Capretto J : Developmental timing of childhood physical and sexual maltreatment predicts adult depression and post-traumatic stress symptoms . J Interpers Violence ( Epub ahead of print, April 1, 2017 ) Google Scholar
68 Harpur LJ , Polek E , van Harmelen AL : The role of timing of maltreatment and child intelligence in pathways to low symptoms of depression and anxiety in adolescence . Child Abuse Negl 2015 ; 47 : 24 – 37 Crossref , Medline , Google Scholar
69 Alameda L , Ferrari C , Baumann PS , et al. : Childhood sexual and physical abuse: age at exposure modulates impact on functional outcome in early psychosis patients . Psychol Med 2015 ; 45 : 2727 – 2736 Crossref , Medline , Google Scholar
70 Carr CP , Martins CM , Stingel AM , et al. : The role of early life stress in adult psychiatric disorders: a systematic review according to childhood trauma subtypes . J Nerv Ment Dis 2013 ; 201 : 1007 – 1020 Crossref , Medline , Google Scholar
71 Chen LP , Murad MH , Paras ML , et al. : Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis . Mayo Clin Proc 2010 ; 85 : 618 – 629 Crossref , Medline , Google Scholar
72 Maniglio R : The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury . Acta Psychiatr Scand 2011 ; 124 : 30 – 41 Crossref , Medline , Google Scholar
73 Humphreys KL , Zeanah CH : Deviations from the expectable environment in early childhood and emerging psychopathology . Neuropsychopharmacology 2015 ; 40 : 154 – 170 Crossref , Medline , Google Scholar
74 Shaffer A , Yates TM , Egeland BR : The relation of emotional maltreatment to early adolescent competence: developmental processes in a prospective study . Child Abuse Negl 2009 ; 33 : 36 – 44 Crossref , Medline , Google Scholar
75 Wright MO , Crawford E , Del Castillo D : Childhood emotional maltreatment and later psychological distress among college students: the mediating role of maladaptive schemas . Child Abuse Negl 2009 ; 33 : 59 – 68 Crossref , Medline , Google Scholar
76 Mandelli L , Petrelli C , Serretti A : The role of specific early trauma in adult depression: a meta-analysis of published literature: childhood trauma and adult depression . Eur Psychiatry 2015 ; 30 : 665 – 680 Crossref , Medline , Google Scholar
77 Infurna MR , Reichl C , Parzer P , et al. : Associations between depression and specific childhood experiences of abuse and neglect: a meta-analysis . J Affect Disord 2016 ; 190 : 47 – 55 Crossref , Medline , Google Scholar
78 Spertus IL , Yehuda R , Wong CM , et al. : Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice . Child Abuse Negl 2003 ; 27 : 1247 – 1258 Crossref , Medline , Google Scholar
79 Teicher MH , Samson JA , Polcari A , et al. : Sticks, stones, and hurtful words: relative effects of various forms of childhood maltreatment . Am J Psychiatry 2006 ; 163 : 993 – 1000 Link , Google Scholar
80 Dualibe AL , Osório FL : Bipolar disorder and early emotional trauma: a critical literature review on indicators of prevalence rates and clinical outcomes . Harv Rev Psychiatry 2017 ; 25 : 198 – 208 Crossref , Medline , Google Scholar
81 Saleptsi E , Bichescu D , Rockstroh B , et al. : Negative and positive childhood experiences across developmental periods in psychiatric patients with different diagnoses: an explorative study . BMC Psychiatry 2004 ; 4 : 40 Crossref , Medline , Google Scholar
82 Putnam KT , Harris WW , Putnam FW : Synergistic childhood adversities and complex adult psychopathology . J Trauma Stress 2013 ; 26 : 435 – 442 Crossref , Medline , Google Scholar
83 Anda RF , Felitti VJ , Bremner JD , et al. : The enduring effects of abuse and related adverse experiences in childhood: a convergence of evidence from neurobiology and epidemiology . Eur Arch Psychiatry Clin Neurosci 2006 ; 256 : 174 – 186 Crossref , Medline , Google Scholar
84 Sala R , Goldstein BI , Wang S , et al. : Childhood maltreatment and the course of bipolar disorders among adults: epidemiologic evidence of dose-response effects . J Affect Disord 2014 ; 165 : 74 – 80 Crossref , Medline , Google Scholar
85 McCrory E , De Brito SA , Viding E : Research review: the neurobiology and genetics of maltreatment and adversity . J Child Psychol Psychiatry 2010 ; 51 : 1079 – 1095 Crossref , Medline , Google Scholar
86 Danese A , Pariante CM , Caspi A , et al. : Childhood maltreatment predicts adult inflammation in a life-course study . Proc Natl Acad Sci USA 2007 ; 104 : 1319 – 1324 Crossref , Medline , Google Scholar
87 Toft H , Neupane SP , Bramness JG , et al. : The effect of trauma and alcohol on the relationship between level of cytokines and depression among patients entering psychiatric treatment . BMC Psychiatry 2018 ; 18 : 95 Crossref , Medline , Google Scholar
88 Aas M , Dieset I , Hope S , et al. : Childhood maltreatment severity is associated with elevated C-reactive protein and body mass index in adults with schizophrenia and bipolar diagnoses . Brain Behav Immun 2017 ; 65 : 342 – 349 Crossref , Medline , Google Scholar
89 Berk M , Kapczinski F , Andreazza AC , et al. : Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress, and neurotrophic factors . Neurosci Biobehav Rev 2011 ; 35 : 804 – 817 Crossref , Medline , Google Scholar
90 Leboyer M , Soreca I , Scott J , et al. : Can bipolar disorder be viewed as a multi-system inflammatory disease? J Affect Disord 2012 ; 141 : 1 – 10 Crossref , Medline , Google Scholar
91 Danese A , Moffitt TE , Pariante CM , et al. : Elevated inflammation levels in depressed adults with a history of childhood maltreatment . Arch Gen Psychiatry 2008 ; 65 : 409 – 415 Crossref , Medline , Google Scholar
92 Syed SA , Beurel E , Loewenstein DA , et al. : Defective inflammatory pathways in never-treated depressed patients are associated with poor treatment response . Neuron 2018 ; 99 : 914 – 924e3 Crossref , Medline , Google Scholar
93 Miller AH , Raison CL : Are anti-inflammatory therapies viable treatments for psychiatric disorders? Where the rubber meets the road . JAMA Psychiatry 2015 ; 72 : 527 – 528 Crossref , Medline , Google Scholar
94 Bandoli G , Campbell-Sills L , Kessler RC , et al. : Childhood adversity, adult stress, and the risk of major depression or generalized anxiety disorder in US soldiers: a test of the stress sensitization hypothesis . Psychol Med 2017 ; 47 : 2379 – 2392 Crossref , Medline , Google Scholar
95 La Rocque CL , Harkness KL , Bagby RM : The differential relation of childhood maltreatment to stress sensitization in adolescent and young adult depression . J Adolesc 2014 ; 37 : 871 – 882 Crossref , Medline , Google Scholar
96 Brietzke E , Mansur RB , Soczynska J , et al. : A theoretical framework informing research about the role of stress in the pathophysiology of bipolar disorder . Prog Neuropsychopharmacol Biol Psychiatry 2012 ; 39 : 1 – 8 Crossref , Medline , Google Scholar
97 Alloy LB , Abramson LY , Walshaw PD , et al. : A cognitive vulnerability-stress perspective on bipolar spectrum disorders in a normative adolescent brain, cognitive, and emotional development context . Dev Psychopathol 2006 ; 18 : 1055 – 1103 Crossref , Medline , Google Scholar
98 Heim C , Newport DJ , Mletzko T , et al. : The link between childhood trauma and depression: insights from HPA axis studies in humans . Psychoneuroendocrinology 2008 ; 33 : 693 – 710 Crossref , Medline , Google Scholar
99 Heim C , Newport DJ , Wagner D , et al. : The role of early adverse experience and adulthood stress in the prediction of neuroendocrine stress reactivity in women: a multiple regression analysis . Depress Anxiety 2002 ; 15 : 117 – 125 Crossref , Medline , Google Scholar
100 Abercrombie HC , Frost CP , Walsh EC , et al. : Neural signaling of cortisol, childhood emotional abuse, and depression-related memory bias . Biol Psychiatry Cogn Neurosci Neuroimaging 2018 ; 3 : 274 – 284 Crossref , Medline , Google Scholar
101 Klengel T , Mehta D , Anacker C , et al. : Allele-specific FKBP5 DNA demethylation mediates gene-childhood trauma interactions . Nat Neurosci 2013 ; 16 : 33 – 41 Crossref , Medline , Google Scholar
102 Binder EB , Bradley RG , Liu W , et al. : Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults . JAMA 2008 ; 299 : 1291 – 1305 Crossref , Medline , Google Scholar
103 Appel K , Schwahn C , Mahler J , et al. : Moderation of adult depression by a polymorphism in the FKBP5 gene and childhood physical abuse in the general population . Neuropsychopharmacology 2011 ; 36 : 1982 – 1991 Crossref , Medline , Google Scholar
104 Roy A , Gorodetsky E , Yuan Q , et al. : Interaction of FKBP5, a stress-related gene, with childhood trauma increases the risk for attempting suicide . Neuropsychopharmacology 2010 ; 35 : 1674 – 1683 Crossref , Medline , Google Scholar
105 Zimmermann P , Brückl T , Nocon A , et al. : Interaction of FKBP5 gene variants and adverse life events in predicting depression onset: results from a 10-year prospective community study . Am J Psychiatry 2011 ; 168 : 1107 – 1116 Link , Google Scholar
106 Caspi A , Sugden K , Moffitt TE , et al. : Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene . Science 2003 ; 301 : 386 – 389 Crossref , Medline , Google Scholar
107 Haberstick BC , Boardman JD , Wagner B , et al. : Depression, stressful life events, and the impact of variation in the serotonin transporter: findings from the National Longitudinal Study of Adolescent to Adult Health (Add Health) . PLoS One 2016 ; 11 : e0148373 Crossref , Medline , Google Scholar
108 Brezo J , Bureau A , Mérette C , et al. : Differences and similarities in the serotonergic diathesis for suicide attempts and mood disorders: a 22-year longitudinal gene-environment study . Mol Psychiatry 2010 ; 15 : 831 – 843 Crossref , Medline , Google Scholar
109 Karg K , Burmeister M , Shedden K , et al. : The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: evidence of genetic moderation . Arch Gen Psychiatry 2011 ; 68 : 444 – 454 Crossref , Medline , Google Scholar
110 Etain B , Lajnef M , Henrion A , et al. : Interaction between SLC6A4 promoter variants and childhood trauma on the age at onset of bipolar disorders . Sci Rep 2015 ; 5 : 16301 Crossref , Medline , Google Scholar
111 Provenzi L , Giorda R , Beri S , et al. : SLC6A4 methylation as an epigenetic marker of life adversity exposures in humans: a systematic review of literature . Neurosci Biobehav Rev 2016 ; 71 : 7 – 20 Crossref , Medline , Google Scholar
112 Culverhouse RC , Saccone NL , Horton AC , et al. : Collaborative meta-analysis finds no evidence of a strong interaction between stress and 5-HTTLPR genotype contributing to the development of depression . Mol Psychiatry 2018 ; 23 : 133 – 142 Crossref , Medline , Google Scholar
113 Bradley RG , Binder EB , Epstein MP , et al. : Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene . Arch Gen Psychiatry 2008 ; 65 : 190 – 200 Crossref , Medline , Google Scholar
114 Heim C , Bradley B , Mletzko TC , et al. : Effect of childhood trauma on adult depression and neuroendocrine function: sex-specific moderation by CRH receptor 1 gene . Front Behav Neurosci 2009 ; 3 : 41 Crossref , Medline , Google Scholar
115 Ben-Efraim YJ , Wasserman D , Wasserman J , et al. : Gene-environment interactions between CRHR1 variants and physical assault in suicide attempts . Genes Brain Behav 2011 ; 10 : 663 – 672 Crossref , Medline , Google Scholar
116 Gatt JM , Nemeroff CB , Dobson-Stone C , et al. : Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety . Mol Psychiatry 2009 ; 14 : 681 – 695 Crossref , Medline , Google Scholar
117 Savitz J , van der Merwe L , Stein DJ , et al. : Genotype and childhood sexual trauma moderate neurocognitive performance: a possible role for brain-derived neurotrophic factor and apolipoprotein E variants . Biol Psychiatry 2007 ; 62 : 391 – 399 Crossref , Medline , Google Scholar
118 Oliveira J , Etain B , Lajnef M , et al. : Combined effect of TLR2 gene polymorphism and early life stress on the age at onset of bipolar disorders . PLoS One 2015 ; 10 : e0119702 Google Scholar
119 Myers AJ , Williams L , Gatt JM , et al. : Variation in the oxytocin receptor gene is associated with increased risk for anxiety, stress, and depression in individuals with a history of exposure to early life stress . J Psychiatr Res 2014 ; 59 : 93 – 100 Crossref , Medline , Google Scholar
120 Cohen-Woods S , Fisher HL , Ahmetspahic D , et al. : Interaction between childhood maltreatment on immunogenetic risk in depression: discovery and replication in clinical case-control samples . Brain Behav Immun 2018 ; 67 : 203 – 210 Crossref , Medline , Google Scholar
121 Lok A , Bockting CL , Koeter MW , et al. : Interaction between the MTHFR C677T polymorphism and traumatic childhood events predicts depression . Transl Psychiatry 2013 ; 3 : e288 Crossref , Medline , Google Scholar
122 Tollenaar MS , Molendijk ML , Penninx BWJH , et al. : The association of childhood maltreatment with depression and anxiety is not moderated by the oxytocin receptor gene . Eur Arch Psychiatry Clin Neurosci 2017 ; 267 : 517 – 526 Crossref , Medline , Google Scholar
123 Peyrot WJ , Milaneschi Y , Abdellaoui A , et al. : Effect of polygenic risk scores on depression in childhood trauma . Br J Psychiatry 2014 ; 205 : 113 – 119 Crossref , Medline , Google Scholar
124 Mullins N , Power RA , Fisher HL , et al. : Polygenic interactions with environmental adversity in the aetiology of major depressive disorder . Psychol Med 2016 ; 46 : 759 – 770 Crossref , Medline , Google Scholar
125 Peyrot WJ , Van der Auwera S , Milaneschi Y , et al. : Does childhood trauma moderate polygenic risk for depression? A meta-analysis of 5765 subjects from the Psychiatric Genomics Consortium . Biol Psychiatry 2018 ; 84 : 138 – 147 Crossref , Medline , Google Scholar
126 Kundakovic M , Champagne FA : Early-life experience, epigenetics, and the developing brain . Neuropsychopharmacology 2015 ; 40 : 141 – 153 Crossref , Medline , Google Scholar
127 Checknita D , Ekström TJ , Comasco E , et al. : Associations of monoamine oxidase A gene first exon methylation with sexual abuse and current depression in women . J Neural Transm (Vienna) 2018 ; 125 : 1053 – 1064 Crossref , Medline , Google Scholar
128 McGowan PO , Sasaki A , D’Alessio AC , et al. : Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse . Nat Neurosci 2009 ; 12 : 342 – 348 Crossref , Medline , Google Scholar
129 Perroud N , Zewdie S , Stenz L , et al. : Methylation of serotonin receptor 3A in ADHD, borderline personality, and bipolar disorders: link with severity of the disorders and childhood maltreatment . Depress Anxiety 2016 ; 33 : 45 – 55 Crossref , Medline , Google Scholar
130 Brown A , Fiori LM , Turecki G : Bridging basic and clinical research in early life adversity, DNA methylation, and major depressive disorder . Front Genet 2019 ; 10 : 229 Crossref , Medline , Google Scholar
131 Braun K , Champagne FA : Paternal influences on offspring development: behavioural and epigenetic pathways . J Neuroendocrinol 2014 ; 26 : 697 – 706 Crossref , Medline , Google Scholar
132 Gudsnuk K , Champagne FA : Epigenetic influence of stress and the social environment . ILAR J 2012 ; 53 : 279 – 288 Crossref , Medline , Google Scholar
133 Galler J , Rabinowitz DG : The intergenerational effects of early adversity . Prog Mol Biol Transl Sci 2014 ; 128 : 177 – 198 Crossref , Medline , Google Scholar
134 Champagne F , Meaney MJ : Like mother, like daughter: evidence for non-genomic transmission of parental behavior and stress responsivity . Prog Brain Res 2001 ; 133 : 287 – 302 Crossref , Medline , Google Scholar
135 Roth TL , Lubin FD , Funk AJ , et al. : Lasting epigenetic influence of early-life adversity on the BDNF gene . Biol Psychiatry 2009 ; 65 : 760 – 769 Crossref , Medline , Google Scholar
136 Yehuda R , Halligan SL , Grossman R : Childhood trauma and risk for PTSD: relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion . Dev Psychopathol 2001 ; 13 : 733 – 753 Crossref , Medline , Google Scholar
137 Yehuda R , Bell A , Bierer LM , et al. : Maternal, not paternal, PTSD is related to increased risk for PTSD in offspring of Holocaust survivors . J Psychiatr Res 2008 ; 42 : 1104 – 1111 Crossref , Medline , Google Scholar
138 Ammerman RT , Hersen M , van Hasselt VB , et al. : Maltreatment in psychiatrically hospitalized children and adolescents with developmental disabilities: prevalence and correlates . J Am Acad Child Adolesc Psychiatry 1994 ; 33 : 567 – 576 Crossref , Medline , Google Scholar
139 McDonnell CG , Boan AD , Bradley CC , et al. : Child maltreatment in autism spectrum disorder and intellectual disability: results from a population-based sample . J Child Psychol Psychiatry 2019 ; 60 : 576 – 584 Crossref , Medline , Google Scholar
140 Perrigo JL , Berkovits LD , Cederbaum JA , et al. : Child abuse and neglect re-report rates for young children with developmental delays . Child Abuse Negl 2018 ; 83 : 1 – 9 Crossref , Medline , Google Scholar
141 Mill J , Tang T , Kaminsky Z , et al. : Epigenomic profiling reveals DNA-methylation changes associated with major psychosis . Am J Hum Genet 2008 ; 82 : 696 – 711 Crossref , Medline , Google Scholar
142 Brunoni AR , Lopes M , Fregni F : A systematic review and meta-analysis of clinical studies on major depression and BDNF levels: implications for the role of neuroplasticity in depression . Int J Neuropsychopharmacol 2008 ; 11 : 1169 – 1180 Crossref , Medline , Google Scholar
143 Springer KW , Sheridan J , Kuo D , et al. : Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women . Child Abuse Negl 2007 ; 31 : 517 – 530 Crossref , Medline , Google Scholar
144 Sachs-Ericsson NJ , Sheffler JL , Stanley IH , et al. : When emotional pain becomes physical: adverse childhood experiences, pain, and the role of mood and anxiety disorders . J Clin Psychol 2017 ; 73 : 1403 – 1428 Crossref , Medline , Google Scholar
145 Springer KW , Sheridan J , Kuo D , et al. : The long-term health outcomes of childhood abuse: an overview and a call to action . J Gen Intern Med 2003 ; 18 : 864 – 870 Crossref , Medline , Google Scholar
146 Hughes K , Bellis MA , Hardcastle KA , et al. : The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis . Lancet Public Health 2017 ; 2 : e356 – e366 Crossref , Medline , Google Scholar
147 Shin SH , Chung Y , Rosenberg RD : Identifying sensitive periods for alcohol use: the roles of timing and chronicity of child physical abuse . Alcohol Clin Exp Res 2016 ; 40 : 1020 – 1029 Crossref , Medline , Google Scholar
148 Anda RF , Croft JB , Felitti VJ , et al. : Adverse childhood experiences and smoking during adolescence and adulthood . JAMA 1999 ; 282 : 1652 – 1658 Crossref , Medline , Google Scholar
149 Marangoni C , Hernandez M , Faedda GL : The role of environmental exposures as risk factors for bipolar disorder: a systematic review of longitudinal studies . J Affect Disord 2016 ; 193 : 165 – 174 Crossref , Medline , Google Scholar
150 Faedda GL , Serra G , Marangoni C , et al. : Clinical risk factors for bipolar disorders: a systematic review of prospective studies . J Affect Disord 2014 ; 168 : 314 – 321 Crossref , Medline , Google Scholar
151 Merikangas KR , Gelernter CS : Comorbidity for alcoholism and depression . Psychiatr Clin North Am 1990 ; 13 : 613 – 632 Crossref , Medline , Google Scholar
152 Goldstein BI , Diamantouros A , Schaffer A , et al. : Pharmacotherapy of alcoholism in patients with co-morbid psychiatric disorders . Drugs 2006 ; 66 : 1229 – 1237 Crossref , Medline , Google Scholar
153 Goldstein BI , Velyvis VP , Parikh SV : The association between moderate alcohol use and illness severity in bipolar disorder: a preliminary report . J Clin Psychiatry 2006 ; 67 : 102 – 106 Crossref , Medline , Google Scholar
154 Potthast N , Neuner F , Catani C : The contribution of emotional maltreatment to alcohol dependence in a treatment-seeking sample . Addict Behav 2014 ; 39 : 949 – 958 Crossref , Medline , Google Scholar
155 Enoch MA : The role of early life stress as a predictor for alcohol and drug dependence . Psychopharmacology (Berl) 2011 ; 214 : 17 – 31 Crossref , Medline , Google Scholar
156 Salokangas RKR , From T , Luutonen S , et al. : Effect of childhood adversities on alcohol problems is mainly mediated by depression . Am J Addict ( Epub ahead of print, May 15, 2018 ) Google Scholar
157 Skinner ML , Hong S , Herrenkohl TI , et al. : Longitudinal effects of early childhood maltreatment on co-occurring substance misuse and mental health problems in adulthood: the role of adolescent alcohol use and depression . J Stud Alcohol Drugs 2016 ; 77 : 464 – 472 Crossref , Medline , Google Scholar
158 Hyucksun Shin S : A longitudinal examination of the relationships between childhood maltreatment and patterns of adolescent substance use among high-risk adolescents . Am J Addict 2012 ; 21 : 453 – 461 Crossref , Medline , Google Scholar
159 Garami J , Valikhani A , Parkes D , et al. : Examining perceived stress, childhood trauma and interpersonal trauma in individuals with drug addiction . Psychol Rep 2019 ; 122 : 433 – 450 Crossref , Medline , Google Scholar
160 Lei Y , Xi C , Li P , et al. : Association between childhood maltreatment and non-medical prescription opioid use among Chinese senior high school students: the moderating role of gender . J Affect Disord 2018 ; 235 : 421 – 427 Crossref , Medline , Google Scholar
161 Conroy E , Degenhardt L , Mattick RP , et al. : Child maltreatment as a risk factor for opioid dependence: comparison of family characteristics and type and severity of child maltreatment with a matched control group . Child Abuse Negl 2009 ; 33 : 343 – 352 Crossref , Medline , Google Scholar
162 Larance B , Gisev N , Cama E , et al. : Predictors of transitions across stages of heroin use and dependence prior to treatment-seeking among people in treatment for opioid dependence . Drug Alcohol Depend 2018 ; 191 : 145 – 151 Crossref , Medline , Google Scholar
163 Maloney E , Degenhardt L , Darke S , et al. : Suicidal behaviour and associated risk factors among opioid-dependent individuals: a case-control study . Addiction 2007 ; 102 : 1933 – 1941 Crossref , Medline , Google Scholar
164 Handley ED , Rogosch FA , Cicchetti D : From child maltreatment to emerging adult problem drinking: identification of a multilevel internalizing pathway among African American youth . Dev Psychopathol 2017 ; 29 : 1807 – 1821 Crossref , Medline , Google Scholar
165 Young-Wolff KC , Enoch MA , Prescott CA : The influence of gene-environment interactions on alcohol consumption and alcohol use disorders: a comprehensive review . Clin Psychol Rev 2011 ; 31 : 800 – 816 Crossref , Medline , Google Scholar
166 Keyes KM , Hatzenbuehler ML , Hasin DS : Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors . Psychopharmacology (Berl) 2011 ; 218 : 1 – 17 Crossref , Medline , Google Scholar
167 Kaufman J , Yang BZ , Douglas-Palumberi H , et al. : Genetic and environmental predictors of early alcohol use . Biol Psychiatry 2007 ; 61 : 1228 – 1234 Crossref , Medline , Google Scholar
168 Oo KZ , Aung YK , Jenkins MA , et al. : Associations of 5HTTLPR polymorphism with major depressive disorder and alcohol dependence: a systematic review and meta-analysis . Aust N Z J Psychiatry 2016 ; 50 : 842 – 857 Crossref , Medline , Google Scholar
169 Young-Wolff KC , Kendler KS , Prescott CA : Interactive effects of childhood maltreatment and recent stressful life events on alcohol consumption in adulthood . J Stud Alcohol Drugs 2012 ; 73 : 559 – 569 Crossref , Medline , Google Scholar
170 Covault J , Tennen H , Armeli S , et al. : Interactive effects of the serotonin transporter 5-HTTLPR polymorphism and stressful life events on college student drinking and drug use . Biol Psychiatry 2007 ; 61 : 609 – 616 Crossref , Medline , Google Scholar
171 Proctor LJ , Lewis T , Roesch S , et al. : Child maltreatment and age of alcohol and marijuana initiation in high-risk youth . Addict Behav 2017 ; 75 : 64 – 69 Crossref , Medline , Google Scholar
172 Kim ST , Hwang SS , Kim HW , et al. : Multidimensional impulsivity as a mediator of early life stress and alcohol dependence . Sci Rep 2018 ; 8 : 4104 Crossref , Medline , Google Scholar
173 Etain B , Lajnef M , Henry C , et al. : Childhood trauma, dimensions of psychopathology, and the clinical expression of bipolar disorders: a pathway analysis . J Psychiatr Res 2017 ; 95 : 37 – 45 Crossref , Medline , Google Scholar
174 Henriques JF , Portugal CC , Canedo T , et al. : Microglia and alcohol meet at the crossroads: microglia as critical modulators of alcohol neurotoxicity . Toxicol Lett 2018 ; 283 : 21 – 31 Crossref , Medline , Google Scholar
175 Nennig SE , Schank JR : The role of NFkB in drug addiction: beyond inflammation . Alcohol Alcohol 2017 ; 52 : 172 – 179 Crossref , Medline , Google Scholar
176 Neupane SP : Neuroimmune interface in the comorbidity between alcohol use disorder and major depression . Front Immunol 2016 ; 7 : 655 Crossref , Medline , Google Scholar
177 Kaptoge S , Di Angelantonio E , Lowe G , et al. : C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis . Lancet 2010 ; 375 : 132 – 140 Crossref , Medline , Google Scholar
178 Braithwaite EC , O’Connor RM , Degli-Esposti M , et al. : Modifiable predictors of depression following childhood maltreatment: a systematic review and meta-analysis . Transl Psychiatry 2017 ; 7 : e1162 Crossref , Medline , Google Scholar
179 Cheong EV , Sinnott C , Dahly D , et al. : Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor . BMJ Open 2017 ; 7 : e013228 Crossref , Medline , Google Scholar
180 Østefjells T , Lystad JU , Berg AO , et al. : Metacognitive beliefs mediate the effect of emotional abuse on depressive and psychotic symptoms in severe mental disorders . Psychol Med 2017 ; 47 : 2323 – 2333 Crossref , Medline , Google Scholar
181 Aas M , Henry C , Bellivier F , et al. : Affective lability mediates the association between childhood trauma and suicide attempts, mixed episodes and co-morbid anxiety disorders in bipolar disorders . Psychol Med 2017 ; 47 : 902 – 912 Crossref , Medline , Google Scholar
182 Choi KH , Davidson C , Spaulding WD : Social cognition moderates the influence of child physical abuse on inpatient psychiatric rehabilitation . J Nerv Ment Dis 2011 ; 199 : 465 – 470 Crossref , Medline , Google Scholar
183 Teicher MH , Samson JA , Anderson CM , et al. : The effects of childhood maltreatment on brain structure, function, and connectivity . Nat Rev Neurosci 2016 ; 17 : 652 – 666 Crossref , Medline , Google Scholar
184 Heany SJ , Groenewold NA , Uhlmann A , et al. : The neural correlates of Childhood Trauma Questionnaire scores in adults: a meta-analysis and review of functional magnetic resonance imaging studies . Dev Psychopathol 2018 ; 30 : 1475 – 1485 Crossref , Medline , Google Scholar
185 Hanson JL , Chung MK , Avants BB , et al. : Structural variations in prefrontal cortex mediate the relationship between early childhood stress and spatial working memory . J Neurosci 2012 ; 32 : 7917 – 7925 Crossref , Medline , Google Scholar
186 Cohen RA , Grieve S , Hoth KF , et al. : Early life stress and morphometry of the adult anterior cingulate cortex and caudate nuclei . Biol Psychiatry 2006 ; 59 : 975 – 982 Crossref , Medline , Google Scholar
187 Edmiston EE , Wang F , Mazure CM , et al. : Corticostriatal-limbic gray matter morphology in adolescents with self-reported exposure to childhood maltreatment . Arch Pediatr Adolesc Med 2011 ; 165 : 1069 – 1077 Crossref , Medline , Google Scholar
188 Van Dam NT , Rando K , Potenza MN , et al. : Childhood maltreatment, altered limbic neurobiology, and substance use relapse severity via trauma-specific reductions in limbic gray matter volume . JAMA Psychiatry 2014 ; 71 : 917 – 925 Crossref , Medline , Google Scholar
189 Sheffield JM , Williams LE , Woodward ND , et al. : Reduced gray matter volume in psychotic disorder patients with a history of childhood sexual abuse . Schizophr Res 2013 ; 143 : 185 – 191 Crossref , Medline , Google Scholar
190 Lim L , Hart H , Mehta M , et al. : Grey matter volume and thickness abnormalities in young people with a history of childhood abuse . Psychol Med 2018 ; 48 : 1034 – 1046 Crossref , Medline , Google Scholar
191 Lim L , Radua J , Rubia K : Gray matter abnormalities in childhood maltreatment: a voxel-wise meta-analysis . Am J Psychiatry 2014 ; 171 : 854 – 863 Link , Google Scholar
192 Yamada K , Suzuki Y , Okuyama M , et al. : Developmental abnormalities of the brain exposed to childhood maltreatment detected by diffusion tensor imaging . Neurol Res 2019 ; 41 : 19 – 25 Crossref , Medline , Google Scholar
193 McCarthy-Jones S , Oestreich LKL , Lyall AE , et al. : Childhood adversity associated with white matter alteration in the corpus callosum, corona radiata, and uncinate fasciculus of psychiatrically healthy adults . Brain Imaging Behav 2018 ; 12 : 449 – 458 Crossref , Medline , Google Scholar
194 Puetz VB , Parker D , Kohn N , et al. : Altered brain network integrity after childhood maltreatment: a structural connectomic DTI-study . Hum Brain Mapp 2017 ; 38 : 855 – 868 Crossref , Medline , Google Scholar
195 Bonne O , Vythilingam M , Inagaki M , et al. : Reduced posterior hippocampal volume in posttraumatic stress disorder . J Clin Psychiatry 2008 ; 69 : 1087 – 1091 Crossref , Medline , Google Scholar
196 Vythilingam M , Heim C , Newport J , et al. : Childhood trauma associated with smaller hippocampal volume in women with major depression . Am J Psychiatry 2002 ; 159 : 2072 – 2080 Link , Google Scholar
197 Driessen M , Herrmann J , Stahl K , et al. : Magnetic resonance imaging volumes of the hippocampus and the amygdala in women with borderline personality disorder and early traumatization . Arch Gen Psychiatry 2000 ; 57 : 1115 – 1122 Crossref , Medline , Google Scholar
198 Frodl T , Reinhold E , Koutsouleris N , et al. : Interaction of childhood stress with hippocampus and prefrontal cortex volume reduction in major depression . J Psychiatr Res 2010 ; 44 : 799 – 807 Crossref , Medline , Google Scholar
199 Opel N , Redlich R , Zwanzger P , et al. : Hippocampal atrophy in major depression: a function of childhood maltreatment rather than diagnosis? Neuropsychopharmacology 2014 ; 39 : 2723 – 2731 Crossref , Medline , Google Scholar
200 Frodl T , Skokauskas N , Frey EM , et al. : BDNF Val66Met genotype interacts with childhood adversity and influences the formation of hippocampal subfields . Hum Brain Mapp 2014 ; 35 : 5776 – 5783 Crossref , Medline , Google Scholar
201 Marusak HA , Kuruvadi N , Vila AM , et al. : Interactive effects of BDNF Val66Met genotype and trauma on limbic brain anatomy in childhood . Eur Child Adolesc Psychiatry 2016 ; 25 : 509 – 518 Crossref , Medline , Google Scholar
202 Poletti S , Locatelli C , Radaelli D , et al. : Effect of early stress on hippocampal gray matter is influenced by a functional polymorphism in EAAT2 in bipolar disorder . Prog Neuropsychopharmacol Biol Psychiatry 2014 ; 51 : 146 – 152 Crossref , Medline , Google Scholar
203 Hallowell ES , Oshri A , Liebel SW , et al. : The mediating role of neural activity on the relationship between childhood maltreatment and impulsivity . Child Maltreat ( Epub ahead of print, March 27, 2019 ) Google Scholar
204 Fonzo GA , Ramsawh HJ , Flagan TM , et al. : Early life stress and the anxious brain: evidence for a neural mechanism linking childhood emotional maltreatment to anxiety in adulthood . Psychol Med 2016 ; 46 : 1037 – 1054 Crossref , Medline , Google Scholar
205 Yu M , Linn KA , Shinohara RT , et al. : Childhood trauma history is linked to abnormal brain connectivity in major depression . Proc Natl Acad Sci USA 2019 ; 116 : 8582 – 8590 Crossref , Medline , Google Scholar
206 Hanson JL , Knodt AR , Brigidi BD , et al. : Heightened connectivity between the ventral striatum and medial prefrontal cortex as a biomarker for stress-related psychopathology: understanding interactive effects of early and more recent stress . Psychol Med 2018 ; 48 : 1835 – 1843 Crossref , Medline , Google Scholar
207 Kaiser RH , Clegg R , Goer F , et al. : Childhood stress, grown-up brain networks: corticolimbic correlates of threat-related early life stress and adult stress response . Psychol Med 2018 ; 48 : 1157 – 1166 Crossref , Medline , Google Scholar
208 Zhai ZW , Yip SW , Lacadie CM , et al. : Childhood trauma moderates inhibitory control and anterior cingulate cortex activation during stress . Neuroimage 2019 ; 185 : 111 – 118 Crossref , Medline , Google Scholar
209 Opel N , Redlich R , Dohm K , et al. : Mediation of the influence of childhood maltreatment on depression relapse by cortical structure: a 2-year longitudinal observational study . Lancet Psychiatry 2019 ; 6 : 318 – 326 Crossref , Medline , Google Scholar
210 Busso DS , McLaughlin KA , Brueck S , et al. : Child abuse, neural structure, and adolescent psychopathology: a longitudinal study . J Am Acad Child Adolesc Psychiatry 2017 ; 56 : 321 – 328.e1 Crossref , Medline , Google Scholar
211 Swartz JR , Williamson DE , Hariri AR : Developmental change in amygdala reactivity during adolescence: effects of family history of depression and stressful life events . Am J Psychiatry 2015 ; 172 : 276 – 283 Link , Google Scholar
212 Duarte DG , Neves MdeC , Albuquerque MR , et al. : Gray matter brain volumes in childhood-maltreated patients with bipolar disorder type I: a voxel-based morphometric study . J Affect Disord 2016 ; 197 : 74 – 80 Crossref , Medline , Google Scholar
213 Poletti S , Vai B , Smeraldi E , et al. : Adverse childhood experiences influence the detrimental effect of bipolar disorder and schizophrenia on cortico-limbic grey matter volumes . J Affect Disord 2016 ; 189 : 290 – 297 Crossref , Medline , Google Scholar
214 Stevelink R , Abramovic L , Verkooijen S , et al. : Childhood abuse and white matter integrity in bipolar disorder patients and healthy controls . Eur Neuropsychopharmacol 2018 ; 28 : 807 – 817 Crossref , Medline , Google Scholar
215 Benedetti F , Bollettini I , Radaelli D , et al. : Adverse childhood experiences influence white matter microstructure in patients with bipolar disorder . Psychol Med 2014 ; 44 : 3069 – 3082 Crossref , Medline , Google Scholar
216 Janiri D , Sani G , Rossi P , et al. : Amygdala and hippocampus volumes are differently affected by childhood trauma in patients with bipolar disorders and healthy controls . Bipolar Disord 2017 ; 19 : 353 – 362 Crossref , Medline , Google Scholar
217 Souza-Queiroz J , Boisgontier J , Etain B , et al. : Childhood trauma and the limbic network: a multimodal MRI study in patients with bipolar disorder and controls . J Affect Disord 2016 ; 200 : 159 – 164 Crossref , Medline , Google Scholar
218 Quidé Y , O’Reilly N , Rowland JE , et al. : Effects of childhood trauma on working memory in affective and non-affective psychotic disorders . Brain Imaging Behav 2017 ; 11 : 722 – 735 Crossref , Medline , Google Scholar
219 Benedetti F , Bollettini I , Poletti S , et al. : White matter microstructure in bipolar disorder is influenced by the serotonin transporter gene polymorphism 5-HTTLPR . Genes Brain Behav 2015 ; 14 : 238 – 250 Crossref , Medline , Google Scholar
220 White MG , Bogdan R , Fisher PM , et al. : FKBP5 and emotional neglect interact to predict individual differences in amygdala reactivity . Genes Brain Behav 2012 ; 11 : 869 – 878 Crossref , Medline , Google Scholar
221 Bogdan R , Williamson DE , Hariri AR : Mineralocorticoid receptor Iso/Val (rs5522) genotype moderates the association between previous childhood emotional neglect and amygdala reactivity . Am J Psychiatry 2012 ; 169 : 515 – 522 Link , Google Scholar
222 Di Iorio CR , Carey CE , Michalski LJ , et al. : Hypothalamic-pituitary-adrenal axis genetic variation and early stress moderates amygdala function . Psychoneuroendocrinology 2017 ; 80 : 170 – 178 Crossref , Medline , Google Scholar
223 Malhi GS , Das P , Outhred T , et al. : Effect of stress gene-by-environment interactions on hippocampal volumes and cortisol secretion in adolescent girls . Aust N Z J Psychiatry 2019 ; 53 : 316 – 325 Crossref , Medline , Google Scholar
224 Ho TC , Dennis EL , Thompson PM , et al. : Network-based approaches to examining stress in the adolescent brain . Neurobiol Stress 2018 ; 8 : 147 – 157 Crossref , Medline , Google Scholar
225 Heim CM , Mayberg HS , Mletzko T , et al. : Decreased cortical representation of genital somatosensory field after childhood sexual abuse . Am J Psychiatry 2013 ; 170 : 616 – 623 Link , Google Scholar
226 Humphreys KL , King LS , Sacchet MD , et al. : Evidence for a sensitive period in the effects of early life stress on hippocampal volume . Dev Sci 2019 ; 22 : e12775 Crossref , Medline , Google Scholar
227 Sweeney S , Air T , Zannettino L , et al. : Gender differences in the physical and psychological manifestation of childhood trauma and/or adversity in people with psychosis . Front Psychol 2015 ; 6 : 1768 Crossref , Medline , Google Scholar
228 Gallo EAG , De Mola CL , Wehrmeister F , et al. : Childhood maltreatment preceding depressive disorder at age 18 years: a prospective Brazilian birth cohort study . J Affect Disord 2017 ; 217 : 218 – 224 Crossref , Medline , Google Scholar
229 Gault-Sherman M , Silver E , Sigfúsdóttir ID : Gender and the associated impairments of childhood sexual abuse: a national study of Icelandic youth . Soc Sci Med 2009 ; 69 : 1515 – 1522 Crossref , Medline , Google Scholar
230 Herringa RJ , Birn RM , Ruttle PL , et al. : Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence . Proc Natl Acad Sci USA 2013 ; 110 : 19119 – 19124 Crossref , Medline , Google Scholar
231 Weiss EL , Longhurst JG , Mazure CM : Childhood sexual abuse as a risk factor for depression in women: psychosocial and neurobiological correlates . Am J Psychiatry 1999 ; 156 : 816 – 828 Link , Google Scholar
232 Kendler KS , Gardner CO : Sex differences in the pathways to major depression: a study of opposite-sex twin pairs . Am J Psychiatry 2014 ; 171 : 426 – 435 Link , Google Scholar
233 Andersen JP , Blosnich J : Disparities in adverse childhood experiences among sexual minority and heterosexual adults: results from a multi-state probability-based sample . PLoS One 2013 ; 8 : e54691 Crossref , Google Scholar
234 Rodgers SM : Transitional age lesbian, gay, bisexual, transgender, and questioning youth: issues of diversity, integrated identities, and mental health . Child Adolesc Psychiatr Clin N Am 2017 ; 26 : 297 – 309 Crossref , Medline , Google Scholar
235 Rhoades H , Rusow JA , Bond D , et al. : Homelessness, mental health, and suicidality among LGBTQ youth accessing crisis services . Child Psychiatry Hum Dev 2018 ; 49 : 643 – 651 Crossref , Medline , Google Scholar
236 Proulx CN , Coulter RWS , Egan JE , et al. : Associations of lesbian, gay, bisexual, transgender, and questioning-inclusive sex education with mental health outcomes and school-based victimization in US high school students . J Adolesc Health 2019 ; 64 : 608 – 614 Crossref , Medline , Google Scholar
237 Wiederhold BK : Cyberbullying and LGBTQ youth: a deadly combination . Cyberpsychol Behav Soc Netw 2014 ; 17 : 569 – 570 Crossref , Medline , Google Scholar
238 Li M , D’Arcy C , Meng X : Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions . Psychol Med 2016 ; 46 : 717 – 730 Crossref , Medline , Google Scholar
- Single cell transcriptomic representation of social dominance in prefrontal cortex and the influence of preweaning maternal and postweaning social environment 25 January 2024 | Scientific Reports, Vol. 14, No. 1
- Socioeconomic inequalities in child and adolescent mental health in Australia: the role of parenting style and parents’ relationships 21 February 2024 | Child and Adolescent Psychiatry and Mental Health, Vol. 18, No. 1
- Childhood maltreatment exposure is differentially associated with transdiagnostic perinatal depression symptoms Journal of Affective Disorders, Vol. 358
- Multimodal brain-derived subtypes of Major depressive disorder differentiate patients for anergic symptoms, immune-inflammatory markers, history of childhood trauma and treatment-resistance European Neuropsychopharmacology, Vol. 85
- Occipital connectivity networks mediate the neural effects of childhood maltreatment on depressive symptoms in major depressive disorder Asian Journal of Psychiatry, Vol. 97
- The Effectiveness of Child-Parent Psychotherapy on Traumatized Preschoolers and Their Caregivers: A Swedish Multi-Site Study 24 June 2024 | Evidence-Based Practice in Child and Adolescent Mental Health, Vol. 18
- Empowering parents of children with disabilities: assessing the impact of a child sexual abuse psychoeducation program in Türkiye 20 June 2024 | International Journal of Developmental Disabilities, Vol. 12
- When Laws Change: Ramifications and Implications for Child Custody Evaluations 19 June 2024 | Journal of Health Service Psychology, Vol. 2019
- The role of childhood cumulative trauma in the risk of lifetime PTSD: An epidemiological study Psychiatry Research, Vol. 336
- Compassion Focused Group Psychotherapy for attachment and relational trauma: Engaging people with a diagnosis of personality disorder 2 February 2024 | Psychology and Psychotherapy: Theory, Research and Practice, Vol. 97, No. 2
- An Explainable Framework to Predict Child Sexual Abuse Awareness in People Using Supervised Machine Learning Models 25 September 2023 | Journal of Technology in Behavioral Science, Vol. 9, No. 2
- Mentalisierungsbasierte Therapie mit Trauma-Fokus und tiergestützten Elementen 1 June 2024 | PDP - Psychodynamische Psychotherapie, Vol. 23, No. 2
- Mental Health Service Use in Children at Risk of Significant Harm: A Record Linkage Study of a Child Protection Register Social Science & Medicine, Vol. 52
- The Link Between Childhood Abuse Experiences and Homeless People’s Quality of Life: A Longitudinal Study 23 November 2023 | Journal of Child & Adolescent Trauma, Vol. 17, No. 2
- The Prevalence, Predictors, and Health Consequences of Disagreement in Reports of Child Maltreatment Exposure 30 May 2024 | Child Psychiatry & Human Development, Vol. 129
- Epigenetic mechanisms linking early-life adversities and mental health 9 May 2024 | Biochemical Journal, Vol. 481, No. 10
- Interpersonal Violence in Elite U.S. Athletes: Prevalence and Mental Health Correlates 16 May 2024 | Journal of Aggression, Maltreatment & Trauma
- Trauma history and course of therapy in a naturalistic cognitive behavior therapy outpatient sample: An archive data study 15 May 2024 | Journal of Clinical Psychology, Vol. 39
- Early life stress is associated with greater negative emotionality and peripheral inflammation in alcohol use disorder 13 May 2024 | Neuropsychopharmacology, Vol. 27
- Dissociative Amnesia: Remembrances Under Cover 10 May 2024 | Topics in Cognitive Science, Vol. 5
- Threat, safety, safeness and social safeness 30 years on: Fundamental dimensions and distinctions for mental health and well‐being 3 May 2024 | British Journal of Clinical Psychology, Vol. 2
- Childhood neglect, the neglected trauma. A systematic review and meta-analysis of its prevalence in psychiatric disorders Psychiatry Research, Vol. 335
- Childhood maltreatment patterns and suicidal ideation: mediating roles of depression, hope, and expressive suppression 20 April 2024 | European Child & Adolescent Psychiatry, Vol. 13
- Childhood maltreatment influences adult brain structure through its effects on immune, metabolic, and psychosocial factors 9 April 2024 | Proceedings of the National Academy of Sciences, Vol. 121, No. 16
- Symptom patterns in the co-occurrence of depressive and generalized anxiety symptoms: A network analysis of a Canadian nationally representative sample Journal of Affective Disorders, Vol. 351
- Facilitators and barriers to the implementation and sustainability of child-parent psychotherapy in Sweden: Clinicians’ experiences Children and Youth Services Review, Vol. 159
- Childhood Maltreatment and Adult Work Absenteeism: Work Meaningfulness as a Double-Edged Sword 7 April 2024 | International Journal of Environmental Research and Public Health, Vol. 21, No. 4
- An examination of questioning methods and the influence of child maltreatment on paediatric pain assessments: Perspectives of healthcare providers 7 December 2023 | Journal of Evaluation in Clinical Practice, Vol. 30, No. 3
- Longitudinal associations between child discipline methods and physical growth patterns across preschool years 17 January 2024 | Obesity, Vol. 32, No. 4
- Identification of factors associated with suicidal behavior in Colombian indigenous children and adolescents 29 March 2024 | International Journal of Mental Health, Vol. 42
- Development and Validation of the Mental Health Scale for Maltreated Children Psychiatry Investigation, Vol. 21, No. 3
- Alterations in the white matter structure of major depressive disorder patients and their link to childhood trauma 4 March 2024 | Frontiers in Psychiatry, Vol. 15
- The Dark and Comforting Side of Night Eating: Women’s Experiences of Trauma 3 January 2024 | Psychiatry International, Vol. 5, No. 1
- Practitioner Review: Neurobiological consequences of childhood maltreatment – clinical and therapeutic implications for practitioners 23 August 2023 | Journal of Child Psychology and Psychiatry, Vol. 65, No. 3
- Childhood emotional maltreatment and sensitivity to social rejection in emerging adults Child Abuse & Neglect, Vol. 149
- Beyond abuse and neglect: validation of the childhood interpersonal trauma inventory in a community sample of adults 29 February 2024 | Frontiers in Psychiatry, Vol. 15
- Grey matter abnormalities in major depressive disorder patients with suicide attempts: A systematic review of age-specific differences Heliyon, Vol. 10, No. 3
- Evaluation of the Treatment Programme for Families with Children in Andalusia: An analysis of the impact on the children 21 January 2024 | Child & Family Social Work, Vol. 237
- The impact of interpersonal traumas in Portuguese women’s psychological wellbeing: predictors of depression and post traumatic stress symptoms 19 January 2024 | Journal of Sexual Aggression, Vol. 34
- Efficacy of an internet-based written imagery rescripting intervention for survivors of institutional childhood abuse – A randomized controlled trial Child Abuse & Neglect, Vol. 147
- COVID‐19‐related stress exacerbates the effect of child maltreatment on negative affect via increased identity confusion during adolescence 18 September 2023 | Journal of Adolescence, Vol. 96, No. 1
- Resting‐state cerebral blood flow and functional connectivity abnormalities in depressed patients with childhood maltreatment: Potential biomarkers of vulnerability? 20 October 2023 | Psychiatry and Clinical Neurosciences, Vol. 78, No. 1
- A Glucocorticoid-Sensitive Hippocampal Gene Network Moderates the Impact of Early-Life Adversity on Mental Health Outcomes Biological Psychiatry, Vol. 95, No. 1
- Struggling Can Also Show on the Inside: Current Knowledge of the Impact of Childhood Maltreatment on Biomarkers in Mood Disorderss 1 March 2024 | Neuropsychiatric Disease and Treatment, Vol. Volume 20
- Stress, Crisis, and Trauma for Brazilian Youth and Their Families 23 February 2024
- Mental illness in children and its determinants in Ethiopia: A systematic review and meta-analysis, 2023 21 October 2023 | Clinical Child Psychology and Psychiatry, Vol. 29, No. 1
- Depressed patients with childhood maltreatment display altered intra- and inter-network resting state functional connectivity NeuroImage: Clinical, Vol. 43
- The role of the hypothalamic-pituitary-adrenal axis in depression across the female reproductive lifecycle: current knowledge and future directions 12 December 2023 | Frontiers in Endocrinology, Vol. 14
- High-throughput screening of glucocorticoid-induced enhancer activity reveals mechanisms of stress-related psychiatric disorders 27 November 2023 | Proceedings of the National Academy of Sciences, Vol. 120, No. 49
- The causal involvement of the BDNF-TrkB pathway in dentate gyrus in early-life stress-induced cognitive deficits in male mice 24 May 2023 | Translational Psychiatry, Vol. 13, No. 1
- Review of the Evidence for Neurofeedback Training for Children and Adolescents Who Have Experienced Traumatic Events 23 November 2022 | Trauma, Violence, & Abuse, Vol. 24, No. 5
- Topic Modeling as a Tool to Analyze Child Abuse from the Corpus of English Newspapers in Pakistan 7 October 2022 | Social Science Computer Review, Vol. 41, No. 6
- Psychometric properties of the Hungarian childhood trauma questionnaire short form and its validity in patients with adult attention-deficit hyperactivity disorder or borderline personality disorder 17 November 2023 | Borderline Personality Disorder and Emotion Dysregulation, Vol. 10, No. 1
- Effects of resilience and timing of adverse and adaptive experiences on interpersonal behavior: a transdiagnostic study in a clinical sample 24 October 2023 | Scientific Reports, Vol. 13, No. 1
- Suicide in a Colombian indigenous community: Beyond mental illness 30 June 2023 | International Journal of Social Psychiatry, Vol. 69, No. 8
- Interaction between childhood trauma experience and TPH2 rs7305115 gene polymorphism in brain gray matter volume 13 December 2023 | Behavioral and Brain Functions, Vol. 19, No. 1
- Adult human neurogenesis: A view from two schools of thought IBRO Neuroscience Reports, Vol. 15
- Digital mental health interventions for anxiety and mood disorders patients: A 24-week follow-up Clinical eHealth, Vol. 6
- Preventing mental illness in children that experienced maltreatment the efficacy of REThink online therapeutic game 5 June 2023 | npj Digital Medicine, Vol. 6, No. 1
- Parental overcontrol is associated with dysmorphic concern severity: A cross-sectional study Journal of Affective Disorders, Vol. 343
- Emerging adult college students' descriptions of exposure to childhood emotional abuse and associated factors: A qualitative exploration Child Abuse & Neglect, Vol. 146
- Childhood adversity predicts stronger premenstrual mood worsening, stress appraisal and cortisol decrease in women with Premenstrual Dysphoric Disorder 2 November 2023 | Frontiers in Endocrinology, Vol. 14
- Early sexual or physical abuse in female and male mood disorder patients Journal of Psychiatric Research, Vol. 167
- Theorie und Praxis der Trauma-fokussierten Mentalisierungsbasierten Therapie 20 September 2023 | Die Psychotherapie, Vol. 68, No. 6
- Transdiagnostic analysis of adverse childhood experiences and their association with psychopathology–A TRANS-D conform study Psychiatry Research, Vol. 329
- Effects of childhood neglect on regional brain activity and corresponding functional connectivity in major depressive disorder and healthy people: Risk factor or resilience? Journal of Affective Disorders, Vol. 340
- Day-to-day affect fluctuations in adults with childhood trauma history: a two-week ecological momentary assessment study 9 October 2023 | Psychological Medicine, Vol. 152
- Mood Disorders and Aggressive Traits Mediate Effects of Reported Childhood Adversity on Suicide Attempt Risk 1 September 2022 | Archives of Suicide Research, Vol. 27, No. 4
- Therapists' Perceived Competence in Delivering Trauma-Focused Cognitive Behavioral Therapy During Statewide Learning Collaboratives 7 July 2023 | The Journal of Behavioral Health Services & Research, Vol. 50, No. 4
- Comorbidity between major depressive disorder and physical diseases: a comprehensive review of epidemiology, mechanisms and management 15 September 2023 | World Psychiatry, Vol. 22, No. 3
- The mediation role of shame proneness in the association between perceived parenting and the severity of addictive behaviors: risk or protective factor? 16 September 2022 | Current Psychology, Vol. 42, No. 30
- The Timing Effect of Childhood Maltreatment in Depression: A Systematic Review and meta-Analysis 24 May 2022 | Trauma, Violence, & Abuse, Vol. 24, No. 4
- Psychosocial Factors and Parent-Infant Bonding Journal of Perinatal & Neonatal Nursing, Vol. 37, No. 4
- Effect of Childhood Trauma on Substance Users’ Attitudes of Coping with Stress 30 September 2023 | Bağımlılık Dergisi, Vol. 24, No. 3
- Impulsivity, Sensation-Seeking, Emotional Neglect, and Delinquent Behavior among Pakistani E-cigarette Users 30 September 2023 | Journal of Professional & Applied Psychology, Vol. 4, No. 3
- Mental Health Disorders and Psychotropic Medication: Prevalence and Related Characteristics Among Individuals in Foster Care 6 May 2023 | Journal of Child & Adolescent Trauma, Vol. 16, No. 3
- Child health care nurses' experience of language screening for 2.5‐year‐old children: A qualitative study 14 June 2023 | Nursing Open, Vol. 10, No. 9
- What Can the Health Humanities Contribute to Our Societal Understanding of and Response to the Deaths of Despair Crisis? 15 April 2023 | Journal of Medical Humanities, Vol. 44, No. 3
- Physical, sexual, and psychosocial health impacts of child abuse: Evidence from Ghana Advances in Life Course Research, Vol. 57
- Early-life adversity and later-life mental health: a conditional process analysis of sense of coherence and resilience-related resources 16 August 2023 | Frontiers in Child and Adolescent Psychiatry, Vol. 2
- Transdiagnostic evaluation of epigenetic age acceleration and burden of psychiatric disorders 17 April 2023 | Neuropsychopharmacology, Vol. 48, No. 9
- The Differential Relation of Emotional, Physical, and Sexual Abuse Histories to Antidepressant Treatment Remission and Persistence of Anhedonia in Major Depression: A CAN-BIND-1 Report 13 February 2023 | The Canadian Journal of Psychiatry, Vol. 68, No. 8
- Early adverse stress and depression severity: A pilot exploration of mediating psychological mechanisms 11 July 2023 | Development and Psychopathology, Vol. 121
- The separation distress hypothesis of depression – an update and systematic review 11 September 2023 | Neuropsychoanalysis, Vol. 25, No. 2
- Lifestyle Medicine Medical Clinics of North America, Vol. 270
- Cross-sectional study of retrospective self-reported childhood emotional neglect and inhibitory neurometabolite levels in the pregenual anterior cingulate cortex in adult humans Neurobiology of Stress, Vol. 2
- Psychometric validation of the French version of the adverse childhood experiences international questionnaire (ACE-IQ) Children and Youth Services Review, Vol. 150
- “When an Elephant Has Its Foot on the Tail of a Mouse…” Trauma-Focused Court Preparation Interventions for Sexually Abused Child Witnesses 2 February 2024 | Journal of Indian Association for Child and Adolescent Mental Health, Vol. 19, No. 3
- Childhood trauma and its influence on the clinical features of bipolar disorder Child Abuse & Neglect, Vol. 141
- The impacts of adverse childhood experiences on socioeconomic disadvantage by sexual and gender identity in the U.S. Child Abuse & Neglect, Vol. 141
- Risk Factors in Depression and Anxiety Disorders from the Framework of Developmental Psychopathology 30 June 2023 | Psikiyatride Güncel Yaklaşımlar, Vol. 15, No. 2
- Neurofeedback as neuroempowerment technique for affective regulation and interoceptive awareness in adolescence: preliminary considerations applied to a psychogenic pseudosyncope case 30 June 2023 | Frontiers in Rehabilitation Sciences, Vol. 4
- Childhood adversity and late-life depression: moderated mediation model of stress and social support 26 June 2023 | Frontiers in Psychiatry, Vol. 14
- Family environment and polygenic risk in the bipolar high‐risk context 16 March 2023 | JCPP Advances, Vol. 3, No. 2
- Subjective response to alcohol: Interactive effects of early life stress, parental risk for mood and substance use disorders, and drinking context Pharmacology Biochemistry and Behavior, Vol. 27
- Affective temperaments mediate the effect of childhood maltreatment on bipolar depression severity 10 May 2023 | Psychiatry and Clinical Neurosciences Reports, Vol. 2, No. 2
- Maternal depression and parenting stress in English-speaking Latina mothers with a history of adverse childhood experiences Children and Youth Services Review, Vol. 149
- The experience of mood disorder and substance use: An integrative review 8 October 2022 | Journal of Psychiatric and Mental Health Nursing, Vol. 30, No. 3
- The interplay of family history of depression and early trauma: associations with lifetime and current depression in the German national cohort (NAKO) 23 May 2023 | Frontiers in Epidemiology, Vol. 3
- Decreased cortical gyrification in major depressive disorder 8 May 2023 | Psychological Medicine, Vol. 2
- The serious health consequences of abuse and neglect in early life 3 May 2023 | BMJ
- Editorial: Synaptic plasticity and dysfunction, friend or foe? 3 May 2023 | Frontiers in Synaptic Neuroscience, Vol. 15
- Interventions for Posttraumatic Stress Disorder Arousal and Reactivity Symptoms in Adults with a History of Childhood Adversity: Scoping Review 12 July 2022 | Research on Social Work Practice, Vol. 33, No. 4
- Feasibility and Acceptability of Group Compassion-Focused Therapy to Treat the Consequences of Childhood Maltreatment in People With Psychiatric Disorders in France Journal of Nervous & Mental Disease, Vol. 211, No. 5
- Relationship between adverse childhood experiences, depression and suicidal behaviors in adulthood among young men who have sex with men: A prospective cohort study Journal of Psychiatric Research, Vol. 161
- Association between childhood maltreatment and social functioning in individuals with affective disorders: A systematic review and meta‐analysis 27 April 2023 | Acta Psychiatrica Scandinavica, Vol. 148
- The neurobiology of irritable bowel syndrome 2 February 2023 | Molecular Psychiatry, Vol. 28, No. 4
- The associations among childhood trauma, loneliness, mental health symptoms, and indicators of social exclusion in adulthood: A UK Biobank study 15 March 2023 | Brain and Behavior, Vol. 13, No. 4
- Stephen M. Strakowski , M.D.
- Trait self-acceptance mediates parental childhood abuse predicting depression and anxiety symptoms in adulthood Journal of Anxiety Disorders, Vol. 94
- Homotypical and Heterotypical Intergenerational Continuity of Child Maltreatment: Evidence from a Cohort of Families Involved with Child Protection Services 25 February 2023 | International Journal of Environmental Research and Public Health, Vol. 20, No. 5
- Childhood trauma and disruptive mood dysregulation disorder The Lancet Psychiatry, Vol. 10, No. 3
- Physical and social trauma: Towards an integrative transdiagnostic perspective on psychological trauma that involves threats to status and belonging Clinical Psychology Review, Vol. 99
- Childhood maltreatment disrupts HPA-axis activity under basal and stress conditions in a dose–response relationship in children and adolescents 16 July 2021 | Psychological Medicine, Vol. 53, No. 3
- A viewpoint on aldosterone and BMI related brain morphology in relation to treatment outcome in patients with major depression 20 December 2022 | Journal of Neuroendocrinology, Vol. 35, No. 2
- Elucidating the relations between adverse childhood experiences, age of exposure to adversity, and adult posttraumatic stress symptom severity in pregnant women Child Abuse & Neglect, Vol. 136
- Individualized Care in Person Centered Medicine 14 April 2023
- Self-Compassion: An Evolutionary, Biopsychosocial, and Social Mentality Approach 24 March 2023
- Self-Compassion in Adolescence 24 March 2023
- The Nucleus Accumbens CRH–CRHR1 System Mediates Early-Life Stress-Induced Sleep Disturbance and Dendritic Atrophy in the Adult Mouse 25 June 2022 | Neuroscience Bulletin, Vol. 39, No. 1
- The development of depression among youth
- Replication of distinct trajectories of antidepressant response to intravenous ketamine Journal of Affective Disorders, Vol. 321
- Trauma history in veterans with bipolar disorder and its impact on suicidality Journal of Psychiatric Research, Vol. 157
- Childhood abuse and cortical gray matter volume in patients with major depressive disorder Psychiatry Research, Vol. 319
- Severe Neglect: Fathers’ Neglect of Children 1 July 2023
- Neurobiological Foundations of Psychotherapies 13 July 2023
- ACE and its implication over the lifespan
- Interpersonal guilt and the working alliance in psychotherapy: The moderating role of childhood experience 17 September 2022 | Clinical Psychology & Psychotherapy, Vol. 30, No. 1
- Translation, cross-cultural adaptation and validity study of the “Play Nicely Program: The Healthy Discipline Handbook” for use in Brazil 1 January 2023 | Revista Brasileira de Enfermagem, Vol. 76, No. 6
- Tradução, adaptação transcultural e estudo de validação do “Play Nicely Program: The Healthy Discipline Handbook” 1 January 2023 | Revista Brasileira de Enfermagem, Vol. 76, No. 6
- The role of positive childhood experiences in the link between childhood maltreatment and affective lability in a sample of incarcerated men and women Child Abuse & Neglect, Vol. 135
- Childhood Sexual Abuse and Psychopathology 25 February 2024
- Leveraging North Carolina’s Assets to Prevent Child Trauma 1 September 2023 | North Carolina Medical Journal, Vol. 84, No. 5
- Effects of prenatal opioid exposure on synaptic adaptations and behaviors across development Neuropharmacology, Vol. 222
- Childhood sexual abuse and pervasive problems across multiple life domains: Findings from a five-decade study 23 December 2022 | Development and Psychopathology, Vol. 1
- Different perspective of the consequences of CAN syndrome Česko-slovenská pediatrie, Vol. 77, No. 6
- The role of childhood trauma, obesity and inflammatory biomarkers in the adherence to a digital intervention among bipolar disorder outpatients: A cluster analyses Journal of Affective Disorders Reports, Vol. 10
- Decreased brain network global efficiency after attachment memories retrieval in individuals with unresolved/disorganized attachment-related state of mind 18 March 2022 | Scientific Reports, Vol. 12, No. 1
- Combined effects of nitric oxide synthase 3 genetic variant and childhood emotional abuse on earlier onset of suicidal behaviours Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 119
- Sexual dimorphism in spatial learning and brain metabolism after exposure to a western diet and early life stress in rats Physiology & Behavior, Vol. 257
- Associations between childhood trauma and childhood psychiatric disorders in Brazil: a population-based, prospective birth cohort study The Lancet Psychiatry, Vol. 9, No. 12
- Identification of biopsychological trait markers in functional neurological disorders 23 November 2022 | Brain, Vol. 21
- Specific Associations Between Type of Childhood Abuse and Elevated C-Reactive Protein in Young Adult Psychiatric Rehabilitation Participants 18 September 2022 | International Journal of Neuropsychopharmacology, Vol. 25, No. 11
- Social media use and body image issues among adolescents in a vulnerable Louisiana community 3 November 2022 | Frontiers in Psychiatry, Vol. 13
- Factors associated with onset‐age in major affective disorders 15 September 2022 | Acta Psychiatrica Scandinavica, Vol. 146, No. 5
- Discrepancies between children's and caregivers' child maltreatment reporting and their associations with child wellbeing Child Abuse & Neglect, Vol. 133
- Is the end in the beginning? Child maltreatment increases the risk of non-suicidal self-injury and suicide attempts through impaired personality functioning Child Abuse & Neglect, Vol. 133
- Treatment efficacy and effectiveness in adults with major depressive disorder and childhood trauma history: a systematic review and meta-analysis The Lancet Psychiatry, Vol. 9, No. 11
- Pathological Dissociation in The National Comorbidity Survey Replication (NCS-R): Prevalence, Morbidity, Comorbidity, and Childhood Maltreatment 15 April 2022 | Journal of Trauma & Dissociation, Vol. 23, No. 5
- Longitudinal Associations Among Low-Income Mothers’ and Fathers’ Parenting and Relationships with Children and Adolescent Depression 18 March 2022 | Research on Child and Adolescent Psychopathology, Vol. 50, No. 10
- Experiencing Violence among Children and Adolescents with Depression in the Aspect of Polish Law 30 September 2022 | Journal of Clinical Medicine, Vol. 11, No. 19
- Gender-related association among childhood maltreatment, brain structure and clinical features in bipolar disorder European Neuropsychopharmacology, Vol. 63
- Interrelationships between childhood maltreatment, depressive symptoms, functional impairment, and quality of life in patients with major depressive disorder: A network analysis approach Child Abuse & Neglect, Vol. 132
- The neurobiology of childhood trauma—aldosterone and blood pressure changes in a community sample 14 January 2022 | The World Journal of Biological Psychiatry, Vol. 23, No. 8
- Childhood trauma and its impact on depressive and anxiety symptomatology in adulthood: A 6-year longitudinal study Journal of Affective Disorders, Vol. 312
- Rare variants implicate NMDA receptor signaling and cerebellar gene networks in risk for bipolar disorder 11 May 2022 | Molecular Psychiatry, Vol. 27, No. 9
- Trauma-Related Knowledge and Practice Changes among Brokers in a Community-Based Learning Collaborative 12 March 2022 | Research on Social Work Practice, Vol. 32, No. 6
- Tailoring Gratitude Interventions. How and for Whom Do They Work? The Potential Mediating Role of Reward Processing and the Moderating Role of Childhood Adversity and Trait Gratitude 12 May 2022 | Journal of Happiness Studies, Vol. 23, No. 6
- Adults Suffering from Violence Are at Risk of Poor Prognosis in Taiwan, 2000–2015 4 August 2022 | Healthcare, Vol. 10, No. 8
- Compassion Focused Group Therapy for People With a Diagnosis of Bipolar Affective Disorder: A Feasibility Study 20 July 2022 | Frontiers in Psychology, Vol. 13
- Childhood trauma, interleukin-17, C-reactive protein, metabolism, and psychosocial functioning in bipolar depression Journal of Affective Disorders Reports, Vol. 9
- Comorbidity and familial aggregation of back/neck pain in the NIMH Family Study of Affective Spectrum Disorders Journal of Psychosomatic Research, Vol. 158
- Modular-based psychotherapy (MoBa) versus cognitive–behavioural therapy (CBT) for patients with depression, comorbidities and a history of childhood maltreatment: study protocol for a randomised controlled feasibility trial 12 July 2022 | BMJ Open, Vol. 12, No. 7
- Reflecting on the enduring effects of childhood maltreatment Menopause, Vol. 29, No. 7
- The Chinese version of the Maltreatment and Abuse Chronology of Exposure (MACE) scale: Psychometric properties in a sample of young adults 30 June 2022 | PLOS ONE, Vol. 17, No. 6
- Early Life Adversity and Neuropsychiatric Disease: Differential Outcomes and Translational Relevance of Rodent Models 23 June 2022 | Frontiers in Systems Neuroscience, Vol. 16
- Insights from Expanded Adverse Childhood Experiences Screening in a Hospital-Based Outpatient Psychiatry Service 5 April 2022 | Psychiatric Quarterly, Vol. 93, No. 2
- No Sex Differences in Self-Reported Childhood Maltreatment in Major Depressive and Bipolar Disorders: A Retrospective Study 19 June 2022 | Brain Sciences, Vol. 12, No. 6
- Attachment insecurity partially mediates the relationship between childhood trauma and depression severity in bipolar disorder 10 March 2022 | Acta Psychiatrica Scandinavica, Vol. 145, No. 6
- School‐based child abuse prevention: The role of school climate in intervention outcomes for teachers 18 February 2022 | Psychology in the Schools, Vol. 59, No. 6
- Early Abusive Relationships–Influence of Different Maltreatment Types on Postpartum Psychopathology and Mother-Infant Bonding in a Clinical Sample 30 May 2022 | Frontiers in Psychiatry, Vol. 13
- Childhood Trauma, the HPA Axis and Psychiatric Illnesses: A Targeted Literature Synthesis 6 May 2022 | Frontiers in Psychiatry, Vol. 13
- Sex-Specific Brain Transcriptional Signatures in Human MDD and Their Correlates in Mouse Models of Depression 3 May 2022 | Frontiers in Behavioral Neuroscience, Vol. 16
- Risk of Personality disorders among childhood maltreatment victims: A nation-wide population-based study in Taiwan Journal of Affective Disorders, Vol. 305
- The association between child maltreatment and sleep disturbances among preschoolers Child Abuse & Neglect, Vol. 127
- Childhood adversity and adulthood major depressive disorder General Hospital Psychiatry, Vol. 76
- Investigating the Efficacy and Experiences With Narrative Exposure Therapy in Severe Mentally Ill Patients With Comorbid Post-traumatic Stress Disorder Receiving Flexible Assertive Community Treatment: A Mixed Methods Study 28 April 2022 | Frontiers in Psychiatry, Vol. 13
- Inflammation biomarkers in suicide attempts and their relation to abuse, global functioning and cognition 3 November 2021 | The World Journal of Biological Psychiatry, Vol. 23, No. 4
- A comparison of symptoms of bipolar and unipolar depression in postpartum women Journal of Affective Disorders, Vol. 303
- Early life stress and substance use disorders: The critical role of adolescent substance use Pharmacology Biochemistry and Behavior, Vol. 215
- Going beyond risk factor: Childhood maltreatment and associated modifiable targets to improve life-long outcomes in mood disorders Pharmacology Biochemistry and Behavior, Vol. 215
- Early adversity as the prototype gene × environment interaction in mental disorders? Pharmacology Biochemistry and Behavior, Vol. 215
- DNA Methylation as a Therapeutic and Diagnostic Target in Major Depressive Disorder 30 March 2022 | Frontiers in Behavioral Neuroscience, Vol. 16
- The Association of Abuse and Depression With Suicidal Ideation in Chinese Adolescents: A Network Analysis 28 March 2022 | Frontiers in Psychiatry, Vol. 13
- The Mediating Role of Forgiveness and Self-Efficacy in the Relationship Between Childhood Maltreatment and Treatment Motivation Among Malaysian Male Drug Addicts 11 March 2022 | Frontiers in Psychology, Vol. 13
- Lateral Habenula Beyond Avoidance: Roles in Stress, Memory, and Decision-Making With Implications for Psychiatric Disorders 3 March 2022 | Frontiers in Systems Neuroscience, Vol. 16
- Substance use disorders in bipolar disorders: Clinical correlates and treatment response to mood stabilizers Journal of Affective Disorders, Vol. 300
- Recognizing the importance of childhood maltreatment as a critical factor in psychiatric diagnoses, treatment, research, prevention, and education 4 November 2021 | Molecular Psychiatry, Vol. 27, No. 3
- Sex and sensitive period differences in potential effects of maltreatment on axial versus radial diffusivity in the corpus callosum 12 January 2022 | Neuropsychopharmacology, Vol. 47, No. 4
- Time for united action on depression: a Lancet–World Psychiatric Association Commission The Lancet, Vol. 399, No. 10328
- Cortisol trajectories measured prospectively across thirty years of female development following exposure to childhood sexual abuse: Moderation by epigenetic age acceleration at midlife Psychoneuroendocrinology, Vol. 136
- Effects of early life adversity on immediate early gene expression: Systematic review and 3-level meta-analysis of rodent studies 13 January 2022 | PLOS ONE, Vol. 17, No. 1
- Childhood adversities and mental disorders in first-year college students: results from the World Mental Health International College Student Initiative 11 January 2022 | Psychological Medicine, Vol. 91
- Bipolar Disorder
- Études expérimentales
- The influence of childhood trauma on the treatment outcomes of pharmacological and/or psychological interventions for adolescents and adults with bipolar disorder: A systematic review and meta-analysis Journal of Affective Disorders, Vol. 296
- Dissociative-Traumatic Dimension and Triple Network: An EEG Functional Connectivity Study in a Sample of University Students 17 November 2021 | Psychopathology, Vol. 55, No. 1
- Trascuratezza educativa, abbandono scolastico e disagio adolescenziale RIVISTA SPERIMENTALE DI FRENIATRIA, Vol. 146, No. 3
- Effect of a collaborative multidimensional approach versus usual care on the resolution of adult depression in primary care in Chile: study protocol for a single blinded cluster randomized controlled trial 17 February 2022 | F1000Research, Vol. 11
- Neuroinflammation, Early-Life Adversity, and Brain Development Harvard Review of Psychiatry, Vol. 30, No. 1
- Absence of a Healthy Parent: Mental and Physical Illness, Substance Misuse, and Trauma in the Life of Parents, Caregivers, and Significant Others 8 November 2022
- Overview of Psychological and Psychiatric Interventions After Trauma: Counseling, Psychotherapy, and Medications 8 November 2022
- Maltrato infantil y trastorno mental 29 December 2021 | Revista de Psiquiatría Infanto-Juvenil, Vol. 38, No. 4
- The Incredible Years Parenting and Child Treatment Programs: A Randomized Controlled Trial in a Child Welfare Setting in Spain Psychosocial Intervention, Vol. 31, No. 1
- Behavioral and pharmacological interventions for the prevention and treatment of psychiatric disorders with children exposed to maltreatment Pharmacology Biochemistry and Behavior, Vol. 211
- Fatty acid dysregulation in the anterior cingulate cortex of depressed suicides with a history of child abuse 18 October 2021 | Translational Psychiatry, Vol. 11, No. 1
- Feminism, gender medicine and beyond: a feminist analysis of "gender medicine" 3 August 2021 | International Journal for Equity in Health, Vol. 20, No. 1
- Age- and sex-specific effects of stress on parvalbumin interneurons in preclinical models: Relevance to sex differences in clinical neuropsychiatric and neurodevelopmental disorders Neuroscience & Biobehavioral Reviews, Vol. 131
- WITHDRAWN: The influence of psychological abuse on children's aggressive behaviour Aggression and Violent Behavior, Vol. 11
- The association of child neglect with lifestyles, depression, and self-esteem: Cross-lagged analyses in Chinese primary schoolchildren Behaviour Research and Therapy, Vol. 146
- Multiomic biological approaches to the study of child abuse and neglect Pharmacology Biochemistry and Behavior, Vol. 210
- Investigation of the Relationship between Premenstrual Syndrome, and Childhood Trauma and Mental State in Adolescents with Premenstrual Syndrome Journal of Pediatric Nursing, Vol. 61
- Mental disorders and cardiovascular disease: what should we be looking out for? 28 January 2021 | Heart, Vol. 107, No. 21
- BİR EĞİTİM FAKÜLTESİ ÖĞRENCİLERİNİN ÇOCUK HAKLARI, ÇOCUK İHMAL VE İSTİSMARI İLE İLGİLİ BİLGİ VE GÖRÜŞLERİNİN DEĞERLENDİRİLMESİ 31 October 2021 | ESTÜDAM Halk Sağlığı Dergisi, Vol. 6, No. 3
- Childhood trauma mediates repetitive transcranial magnetic stimulation efficacy in major depressive disorder 12 June 2021 | European Archives of Psychiatry and Clinical Neuroscience, Vol. 271, No. 7
- A retrospective study examining the adverse effect of childhood abuse among adult psychiatric service users in Britain 15 March 2021 | International Journal of Mental Health Nursing, Vol. 30, No. 5
- Perceived parental over-protection in non clinical young adults is associated with affective vulnerability: A cross-sectional study Journal of Affective Disorders, Vol. 292
- Daniel S. Pine , M.D. ,
- Steven P. Wise , Ph.D. ,
- Elisabeth A. Murray , Ph.D.
- Hypothalamic-Pituitary-Adrenal axis dysfunction by early life stress Neuroscience Letters, Vol. 759
- Cocaine-seeking behaviour is differentially expressed in male and female mice exposed to maternal separation and is associated with alterations in AMPA receptors subunits in the medial prefrontal cortex. Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 109
- Infective Messages 8 April 2021 | Journal of Nervous & Mental Disease, Vol. 209, No. 7
- Maria C. Pitharouli , M.Sc. ,
- Saskia P. Hagenaars , Ph.D. ,
- Kylie P. Glanville , Ph.D. ,
- Jonathan R.I. Coleman , Ph.D. ,
- Matthew Hotopf , Ph.D., F.R.C.Psych. ,
- Cathryn M. Lewis , Ph.D. ,
- Carmine M. Pariante , M.D., Ph.D.
- Serotonin-related rodent models of early-life exposure relevant for neurodevelopmental vulnerability to psychiatric disorders 11 May 2021 | Translational Psychiatry, Vol. 11, No. 1
- Adverse childhood experiences, adult depression, and suicidal ideation in rural Uganda: A cross-sectional, population-based study 12 May 2021 | PLOS Medicine, Vol. 18, No. 5
- Differential Alterations in Resting State Functional Connectivity Associated with Depressive Symptoms and Early Life Adversity 2 May 2021 | Brain Sciences, Vol. 11, No. 5
- Suicide Models and Treatment Models Are Separate Entities. What Does It Mean for Clinical Suicide Prevention? 17 May 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 10
- Implementing Child–Parent Psychotherapy (CPP) in Sweden: A Qualitative Study Exploring Experiences by Caregivers Taking Part of the Intervention with Their Child 24 May 2021 | Journal of Infant, Child, and Adolescent Psychotherapy, Vol. 20, No. 2
- Treatment‐resistant major depressive disorder: Canadian expert consensus on definition and assessment 2 February 2021 | Depression and Anxiety, Vol. 38, No. 4
- Retrospectively assessed trajectories of PTSD symptoms and their subsequent comorbidities Journal of Psychiatric Research, Vol. 136
- Childhood maltreatment history for guiding personalized antidepressant choice in major depressive disorder: Preliminary results from a systematic review Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 107
- How childhood trauma and recent adverse events are related to hair cortisol levels in a large adult cohort Psychoneuroendocrinology, Vol. 126
- Influence of childhood trauma on the treatment outcomes of pharmacological and/or psychological interventions for adolescents and adults with bipolar disorder: protocol for a systematic review and meta-analysis 29 April 2021 | BMJ Open, Vol. 11, No. 4
- Association of adverse childhood experiences with diabetes in adulthood: results of a cross-sectional epidemiological survey in Singapore 15 March 2021 | BMJ Open, Vol. 11, No. 3
- Maternal separation increases cocaine intake through a mechanism involving plasticity in glutamate signalling 24 April 2020 | Addiction Biology, Vol. 26, No. 2
- Creating a Compassionate World: Addressing the Conflicts Between Sharing and Caring Versus Controlling and Holding Evolved Strategies 10 February 2021 | Frontiers in Psychology, Vol. 11
- Staying alive: A 21st century agenda for mental health, child protection and forensic services 22 April 2021 | Human Systems: Therapy, Culture and Attachments, Vol. 1, No. 1
- Unexpected Peaks and Valleys: Navigating the Path to Adulthood with a Mood Disorder 11 March 2021
- Trauma and PTSD in Children Who Are Refugees or Immigrants 6 August 2021
- Genetic analyses of the endocannabinoid pathway in association with affective phenotypic variants Neuroscience Letters, Vol. 744
- Clinical features and risk factors of psychiatric disorders among maltreated children Taiwanese Journal of Psychiatry, Vol. 35, No. 1
- Prioritized Research for the Prevention, Treatment, and Reversal of Chronic Disease: Recommendations From the Lifestyle Medicine Research Summit 22 December 2020 | Frontiers in Medicine, Vol. 7
- Compassion: From Its Evolution to a Psychotherapy 9 December 2020 | Frontiers in Psychology, Vol. 11
- Childhood Trauma and Premenstrual Symptoms: The Role of Emotion Regulation Child Abuse & Neglect, Vol. 108
- Troubles anxieux, troubles dépressifs, conduites suicidaires et cannabis La Presse Médicale Formation, Vol. 1, No. 4
- The clinical characterization of the adult patient with depression aimed at personalization of management 15 September 2020 | World Psychiatry, Vol. 19, No. 3
- The Interactive Effects of Child Maltreatment and Adolescent Pregnancy on Late-Adolescent Depressive Symptoms 27 June 2020 | Journal of Abnormal Child Psychology, Vol. 48, No. 9
- Traumatic Events in Dual Disorders: Prevalence and Clinical Characteristics 6 August 2020 | Journal of Clinical Medicine, Vol. 9, No. 8
- Childhood experiences and adult health: the moderating effects of temperament Heliyon, Vol. 6, No. 5
- Anita Panayiotou , D.Psych. ,
- Stephen Wood , Ph.D., M.A. ,
- Alexandra Stainton , M.Sci. ,
- Tamsyn Van Rheenen , Ph.D. ,
- Kelly Allott , D.Psych. ,
- Christos Pantelis , M.D., F.R.C.Psych.
- Jerome Kagan , Ph.D.
- Taking up residence: A review of outcome studies examining residential treatment for youth with serious emotional and behavioural disorders Children and Youth Services Review, Vol. 111
- Early Life Stress and Substance Use Disorders: Underlying Neurobiology and Pathways to Adverse Outcomes 11 March 2020 | Adversity and Resilience Science, Vol. 1, No. 1
- Psychoanalysis and public health: Potential for integration? 5 March 2020 | International Journal of Applied Psychoanalytic Studies, Vol. 17, No. 1
- Ned H. Kalin , M.D.
- Childhood Maltreatment in Bipolar Disorders 12 July 2020
- Grant Report on the Effects of Childhood Maltreatment on Neurocircuitry in Adolescent Depression Journal of Psychiatry and Brain Science, Vol. 59
- Maltreatment
- Posttraumatic Stress
- Open access
- Published: 12 August 2021
The impact of childhood psychological maltreatment on mental health outcomes in adulthood: a protocol for a systematic review and meta-analysis
- Zhuoni Xiao ORCID: orcid.org/0000-0002-9715-174X 1 ,
- Mina Murat Baldwin 1 ,
- Franziska Meinck 2 , 3 ,
- Ingrid Obsuth 4 &
- Aja Louise Murray 1
Systematic Reviews volume 10 , Article number: 224 ( 2021 ) Cite this article
12k Accesses
11 Citations
12 Altmetric
Metrics details
Research suggests that childhood psychological maltreatment (i.e., emotional abuse and emotional neglect) is associated with mental health problems that persist into adulthood, for example anxiety, depression, post-traumatic stress disorder (PTSD), suicidal ideation, and aggression; however, a systematic review and meta-analysis of the existing literature would help clarify the magnitude and moderators of these associations, and the extent to which they may be affected by publication bias, as well as the methodological strengths and weakness of studies in this area.
The reporting of this protocol follows the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) Statement. Searches will be carried out via several databases, including Web of Science, Medline, PubMed, PsycINFO, Applied Social Science Index and Abstract, ERIC and EMBASE. Empirical peer-reviewed research articles that fit pre-specified eligibility criteria will be included in the review. Studies will be eligible if they include participants age 18 or over at time of mental health assessment, include information on childhood psychological maltreatment (emotional abuse and/or neglect) perpetrated by a primary caregiver or adult in the same household, and provide quantitative information on the association between these factors. Studies using prospective and retrospective designs and written in either English or Chinese will be eligible. Two independent reviewers will screen and assess studies for inclusion in the review as well as extract the data, with consensus reached through discussion in cases of discrepancy. A third reviewer will be consulted to resolve any discrepancies that remain. The relevant Newcastle–Ottawa scales will be used for assessing the quality of studies. If a sufficient number of comparable studies are retrieved, a meta-analysis will be conducted using a random effects model. Study-level moderators (i.e., year of publication, quality of the study and study geographical location) will be examined in the meta-analyses.
This systematic review will provide an understanding of the long-term effects of childhood psychological maltreatment on adult mental health, which adds to previous reviews focusing primarily on the effects of physical and sexual abuse. The results of the review will help inform clinical practice in approaches to treating those with a history of psychological maltreatment in childhood. The gaps and weaknesses in the evidence identified will also inform recommendations for future research.
Peer Review reports
Childhood abuse is significantly associated with adverse emotional, cognitive, behavioural and social outcomes for children [ 16 , 19 , 22 ], with difficulties frequently continuing into adulthood [ 7 ]. According to the World Health Organization (WHO) (2020), childhood abuse refers to all forms of abuse (e.g. physical, sexual, emotional, psychological and neglect) that result in potential or actual harm to a child’s physical or psychological health.
Childhood emotional abuse is the type of abuse least well-studied [ 1 ]. There has been one systematic review on the association between childhood emotional abuse and neglect in school-aged children [ 19 ],however, there has been no systematic review or meta-analysis on the long-term mental health effects of childhood psychological maltreatment on adults.
There are different definitions of psychological maltreatment, for example, Vega Castelo (2012) stated that psychological maltreatment refers to affective and cognitive aspects of child maltreatment. For the purpose of this review, psychological maltreatment is defined as including two specific concepts: childhood emotional abuse and childhood emotional neglect. Forms of psychological maltreatment may include rejecting, isolating, neglecting, exploiting, and terrorizing [ 12 ]. Emotional abuse in childhood refers to continual deliberate mistreatment of a child, which may include deliberately trying to scare, humiliate, ignore, and isolate the child. Emotional abuse is often a part of other forms of abuse,however, it can also happen on its own [ 4 ]. In contrast to emotional abuse, emotional neglect may be unintentional, and caregivers are sometimes unaware that they are emotionally neglecting their child. Emotional neglect in childhood refers to caregivers’ failure to recognize, understand or provide what a child really needs, and may sometimes refer to lack of attention to a child [ 4 ]. The primary distinction between childhood emotional neglect and childhood emotional abuse is that the former reflects indifferent parenting while the latter reflects hostile parenting [ 17 ].
This review will focus on psychological maltreatment perpetrated by primary caregivers or another adult in household specifically. This focus is motivated by the fact that in the traditional family model, primary caregivers and cohabiting adults are often the most important figures for a child. This is also reflected in commonly used measures of maltreatment. For example, in measures such as the Childhood Traumatic Questionnaire [ 5 ], Adverse Childhood Experience, etc., the items ask whether primary caregivers or adults living in the same household committed maltreatment. The focus on psychological maltreatment is motivated by the fact that it is currently the least-well studied form of abuse in terms of its effects on adult mental health. Part of the reason may be the challenges inherent in measuring psychological maltreatment. Compared with physical and sexual abuse, the assessment and identification of psychological maltreatment can be more difficult [ 2 ], since there is no physical evidence of its occurrence. However, the negative outcomes of it may manifest in numerous ways such as impaired emotional, cognitive, or social development, including outcomes such as depression [ 13 ], helplessness (Black, SlepAM, & Heyman, 2001), aggression (Diza, Simantov, & Rickert, 2002), emotional dysregulation (Burns, Jacksons, & Harding, 2010) delinquency, substance abuse, PTSD, anxiety, and low self-esteem (Kilpatrict, Saunders, & Smith, 2003).
Rationale for the current review
There are numerous systematic reviews on the associations between physical or sexual abuse and adult mental health [ 3 , 15 ],however—to the best of the authors’ knowledge—to date, no research has been carried out to synthesize current evidence on the relationships between childhood psychological maltreatment by primary caregivers (or adults living in the same household) and adult mental health. A systematic review on this topic can provide an understanding of the consistency and strength of the link between early childhood maltreatment and adult mental health outcomes at both the clinical and sub-clinical level. A systematic review and meta-analysis can help provide a more precise estimate of the association than has been provided by primary studies to date. It will also allow us to examine the factors that moderate the magnitude of this association, and to evaluate whether the field is affected by publication bias. Further, it will provide a characterization of the quality of empirical studies in this field and identify gaps in the literature.
The primary review questions will be:
What are the long-term effects of childhood psychological maltreatment on adult mental health?
What are the unique effects of childhood psychological maltreatment by caregivers on adult mental health after adjusting for other forms of abuse?
How do study-level moderators such as year of publication, quality of study and location of study affect these associations?
The Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) recommendations have been used to guide the reporting in this systematic review protocol and will be used to guide the reporting of the review itself [ 21 ]. This systematic review protocol has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42020197833.
Search strategy
To search the existing literature on childhood psychological maltreatment, the following keywords will be used: ‘child abuse’, ‘childhood psychological maltreatment’, ‘childhood emotional abuse’, ‘child neglect’, ‘childhood emotional neglect’, ‘psychological aggression’, ‘psychological violence’, ‘psychological domestic violence’ and ‘childhood psychological victimisation’. The Boolean operator ‘OR’ will be used to combine the search terms and with specific syntax be adapted to the different databases.
To capture the concept of mental health, these key search terms will be used: ‘mental health’, ‘generalised anxiety disorder’, ‘depression’, ‘major depression disorder’, ‘PTSD’, ‘personality disorder’, ‘eating disorder’, ‘bipolar disorder’, ‘schizophrenia’, ‘panic disorder’, ‘psychosis’, ‘social anxiety disorder’, ‘suicide ideation’, ‘suicide attempt’, ‘non-suicidal self-injury’ and ‘substance abuse’. The Boolean operator ‘OR’ will be used to combine these search terms, adapted to the syntax of different databases.
The Boolean operator (‘AND’) will be used to combine keywords from psychological maltreatment and mental health. In addition, the maltreatment terms will be combined with child* and the mental health terms with adult* using the AND operator in order to link the concepts to the relevant developmental stages.
Several databases will be used searching for relevant papers: Web of Science, Medline, PubMed, PsycINFO, Applied Social Science Index and Abstract, ERIC and EMBASE. For grey literature, several databases will be used: WHO database, PhD thesis/dissertation databases, and Open Grey.
For literature written in Chinese, ZhiWang which is a well-known database in China, and covers various journals written in Chinese, will be used for searching the literature.
Inclusion criteria
Participants aged over 18 at assessment of the mental health problems.
Measurement of abuse: studies that measured childhood psychological maltreatment using retrospective self-report, questionnaires, interviews, or police or social work records will be included.
Measurement of mental health: studies that measured mental health problems (standard diagnoses as listed in the DSM-V or ICD-10 or using mental health scores based on validated measures) using self-report, questionnaires or clinical interviews will be included.
Types of maltreatment: studies that only assessed childhood psychological maltreatment, childhood emotional neglect, childhood emotional abuse, or studies that assessed both childhood emotional abuse and childhood emotional neglect and other types of abuse (e.g., physical, or sexual) will be included. The abuse must have been committed by the primary caregivers, or the adult living in the same household.
Comparison: adults who experienced only childhood psychological maltreatment versus adults who experienced different forms of abuse during childhood, with or without psychological maltreatment versus adults who experienced no abuse during childhood will be compared.
Ascertainment of exposure to childhood psychological maltreatment by primary caregivers (or adults living in the same household): Studies using either retrospective or prospective data will be included.
Studies that reported odds ratio or other effect size: If the studies do not report the relevant effect size, they will be eligible for inclusion only if they provide the raw information such that the effect size could be calculated. When the raw information not available in the text, authors will contact the authors to request such data.
Additional inclusion criteria include:
Articles written in either English or Chinese will be included reflecting the language capabilities of the team.
Exclusion criteria
Any book chapters, case studies, letter, opinions, and editorials that do not present new data will be excluded.
Qualitative investigations will be excluded.
Studies that do not provide an analysis of childhood psychological maltreatment will be excluded.
Studies that focus on psychological maltreatment perpetrated by non-parental others or where data for primary caregivers or another adult in household cannot be disaggregated from data on abuse perpetrated by others will not be included.
Studies where different types of abuse are combined and not separately reported so that it is not possible to obtain an effect for childhood psychological maltreatment will be excluded.
Studies where the outcome is physical rather than mental illness will be excluded.
Review papers (narrative reviews, systematic reviews, and meta-analyses) will be excluded.
Study selection
The bibliographic software program Zotero will be used to manage and store relevant studies. Duplicate studies will be removed via this software. Two independent reviewers will scrutinise the electronic searches for eligibility and inclusion of studies into the systematic review based on their title and abstract. Full texts of potentially relevant papers will be retrieved and reviewed independently by two reviewers. A final determination of whether an article meets inclusion criteria will be made on examination of the full article, the reason for each excluded study will be documented. A third reviewer will be consulted to resolve any discrepancies that cannot be resolved through discussion between the original reviewers. Figure 1 presents the flow diagram to be adopted in the systematic review for study selection [ 20 ].
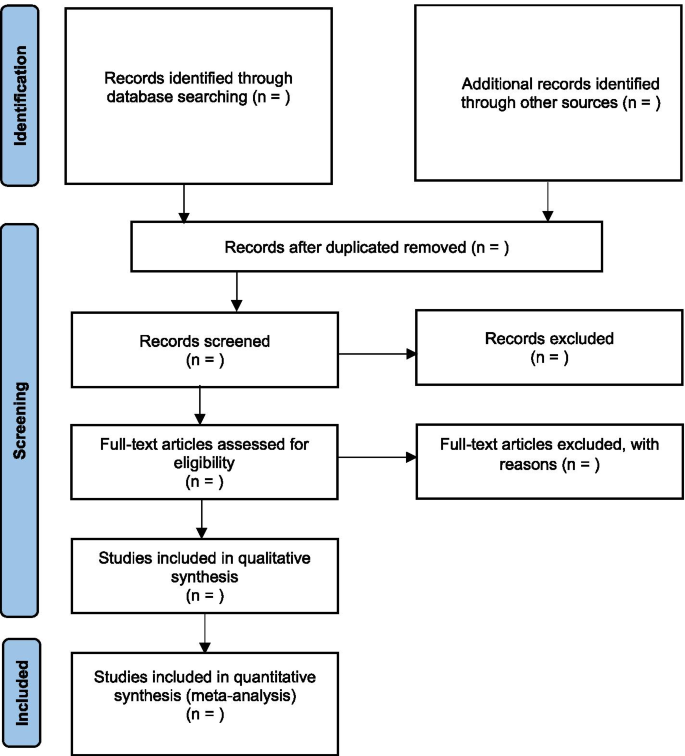
PRISMA flow diagram
Methodological appraisal of study
Classification of risk of bias as recommended by the Newcastle–Ottawa Quality Assessment Scale will be used to assess the quality of selected case–control for retrospective study or cohort studies for longitudinal studies [ 25 ]. Main domains of this assessment are selection (adequateness of case definition, representativeness of the cases, selection of controls and definition of controls), comparability (comparability of cases and controls based on the design or analysis) and exposure (ascertainment of exposure, same method of ascertainment for cases and control and non-response rate). A study can be awarded a maximum of four stars for selection, two stars for comparability and three stars for exposure. More stars represent lower risk of bias. Two reviewers will independently assess the studies for methodological quality with discrepancies being resolved through discussion and a third reviewer will be consulted where consensus cannot be reached through discussion.
Data extraction
Study findings will be extracted using a structured database. It will include pertinent information such as author name and date of publication, sample size, sample population, study geographical location, sample population demographic, study setting, study methodology, types of abuse, measurement of childhood psychological maltreatment, duration of abuse, measurement of various mental health outcomes, perpetrator of the maltreatment, age at exposure to maltreatment, the relation between childhood psychological maltreatment and mental health outcomes (as an odds ratio or risk ratio), and covariates adjusted for. When available, both adjusted and unadjusted statistics will be extracted. Two reviewers will independently conduct the data extraction with consensus reached through discussion in case of discrepancies. Where consensus is not reached through discussion, a third reviewer will be consulted. If any new categories are identified during the course of the review, they will be added, and the extraction database will be modified as needed. If there are any missing data or relevant information, authors will be contacted to supply the information. To detect the unique effects of childhood psychological maltreatment by caregivers on adult mental health after adjusting for other forms of abuse, researchers will extract the statistical information of the studies exploring the associations between childhood psychological maltreatment and adult mental health when adjusting for other types of abuse.
Data analysis
A narrative synthesis of the findings from the included studies will be presented. The narrative synthesis will focus on socio-demographic characteristics of the samples (duration of abuse, who the maltreatment was inflicted by, age at exposure to maltreatment), characteristic of the studies (study setting, sample size, study design), methodology (questionnaire, self-report, experimental design, clinical interview, police or social work records), types of mental health issues, effect size and odd/risk ratios.
A meta-analysis will be conducted if there are enough studies with information related to both childhood psychological maltreatment and mental health. Results will be summarized using a forest plot. Results from different study designs will not be pooled together (e.g., studies that assessed only childhood psychological maltreatment and studies that assessed different types of abuse) to prevent a misleading summary of the study effect; rather, they will be analysed separately. If possible, meta-analyses of both adjusted and unadjusted effects will be conducted and results compared. A random effects model will be utilized for the meta-analysis as it is likely that studies will not be homogeneous. Studies are expected to represent fairly substantial differences in method (i.e. types of participants, measurements) and are thus not anticipated to reflect a single underlying effect size. The ‘Metafor’ package for R statistical software will be used for meta-analysis [ 24 ].
The GRADE criteria will be used to assess the quality of the evidence provided by the observational studies in relation to the outcome (Higgins & Green, 2011). The quality of the evidence will be rated as very low, low, moderate, and high; and factors that may decrease the quality are risk of bias, imprecision, inconsistency and indirectness (Higgins & Green, 2011).
Assessment of heterogeneity and moderator analysis
Study heterogeneity will be assessed by examining the characteristics of studies and similarities between childhood psychological maltreatment and mental health outcomes. Statistical heterogeneity will be assessed by calculating Q and I 2 . Where there are sufficient numbers of studies in the meta-analysis, study-level moderators will be tested. These may include study quality (based on the quality assessment described above), study geographical location, year of publication, and sample size. Moderator analysis will be using the ‘Metafor’ package.
Assessment of reporting bias
In case of an appropriate number of studies ( n ≥ 10), publication bias will be assessed using a funnel plot for each outcome by plotting the effect size against study size (Higgins & Green, 2011). An Egger test [ 11 ] and the trim and fill method [ 10 ] will be used to statistically test for publication bias and its potential impact.
This protocol outlines the plan for a systematic review and, if applicable, a meta-analysis on the effects of childhood emotional abuse and childhood emotional neglect (collectively ‘psychological maltreatment’) perpetrated by primary caregivers or adults living in the same household in childhood on adult mental health outcomes. There is currently no systematic review and meta-analysis focusing specifically on the long-term effects of childhood psychological maltreatment on adult mental health outcomes, therefore, the review will help fill this important gap. The findings from this review could help illuminate the long-term impact of psychological maltreatment, in combination with and net of other forms of abuse. This can help inform prevention and intervention strategies to help target resources and minimise the impact of psychological maltreatment. It will also potentially provide insights into whether the impact of psychological maltreatment varies across contexts; which mental health outcomes it is most strongly related to; and whether its impact has changed over time. This review will also explore where the major gaps are in current evidence in other to make recommendations for future research. Finally, it will help provide an assessment of the quality of the work on the field and identify areas for improvement in future research to strengthen the evidence in the field.
Availability of data and materials
Not applicable.
Abbreviations
The Diagnostic and Statistical Manual of Mental Disorders (5th edition)
International Classification of Diseases, tenth revision
Preferred Reporting Items for Systematic Review and Meta-Analysis
Post-traumatic stress disorder
World Health Organization
Afroz S, Tiwari PSN. Psychological abuse: Impact on children. Ind J Health Wellbeing. 2015;6(5).
Aiosa-Karpas CJ, Karpas R, Pelcovitz D, Kaplan S. Gender identification and sex role attribution in sexually abused adolescent females. J Am Acad Child Adolesc Psychiatry. 1991;30(2):266–71.
Article CAS Google Scholar
Angelakis I, Austin J, Gooding P. Childhood maltreatment and suicide attempts in prisoners: A systematic meta-analytic review. Psychol Med. 2020;50(1):1–10.
Article Google Scholar
Baker A, Festinger T. Emotional abuse and emotional neglect subscales of the CTQ: Associations with each other, other measures of psychological maltreatment, and demographic variables. Child Youth Serv Rev. 2011;33(11):2297–302.
Bernstein DP, Fink L, Handelsman L, Foote J. Childhood trauma questionnaire. Assessment of family violence: A handbook for researchers and practitioners. 1998.
Black DA, Smith SlepAM, Heyman RE. Risk factors for psychological abuse. Aggression Violent Behavior. 2001;6:189–201.
Bor W, Collerson M, Cupit SC, McDermott B, Stallman HM, Walmsley KE. New directions in treatment of child physical abuse and neglect in Australia: MST-CAN a case study. Adv Mental Health. 2010;9:148–61.
Burns EE, Jackson JL, Harding HG. Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment & Trauma. 2010;19:801–19. https://doi.org/10.1080/10926771.2010.522947 .
Diaz A, Simantov E, Rickert VI. Effect of abuse on health: results of a national survey. Arch Pediatr Adolesc Med. 2002;156(8):811–7.
Duval S. The Trim and Fill Method. In Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments. Wiley; 2006. p. 127–44.
Egger M, Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Garbarino J, Guttman E, Seeley JW. The psychologically battered child. San Francisco, CA: Jossey-Bass; 1986.
Google Scholar
Gibb BE, Alloy LB, Abrahamson LY, Rose DT, Whitehouse WG, Donovan P, Tierney S. History of child maltreatment, negative cognitive styles and episodes of depression in adulthood. Cogn Ther Res. 2001;25:426–46. https://doi.org/10.1023/A:1005586519986 .
Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration: 2011. Available from www.cochrane-handbook.org . Accessed 29 Aug 2011.
Hovdestad W, Campeau A, Potter D, Tonmyr L. A systematic review of childhood maltreatment assessments in population-representative surveys since 1990. PloS One. 2015;10(5).
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Dunne MP. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–66.
Iwaniec D. The emotionally abused and neglect child: Identification, assessment, and intervention. New York: John Wiley and Sons; 1995.
Kilpatrick DG, Saunders BE, Smith DW. Youth victimization: Prevalence and implications. Research in brief. Washington, DC: US Department of Justice, Office of Justice Programs; 2003.
Maguire W, Naughton C, Tempest M, . . . Kemp. A systematic review of the emotional, behavioural and cognitive features exhibited by school‐aged children experiencing neglect or emotional abuse. Child Care Health Develop. 2015;41(5):641–53.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349.
Vega Castelo ADL. Outcomes of psychological maltreatment in children. 2013.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. NewCastle–Ottawa quality assessment scale—case control studies. 2012–06–15]. 2017. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
World Health Organization. Child Maltreatment. 2020. Retrieved from https://www.who.int/news-room/fact-sheets/detail/child-maltreatment .
Download references
Acknowledgements
FM received support from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme [Grant Agreement Number 852787] and the UK Research and Innovation Global Challenges Research Fund [ES/S008101/1].
Author information
Authors and affiliations.
Department of Psychology, University of Edinburgh, 7 George Square, Edinburgh, EH8 9JZ, UK
Zhuoni Xiao, Mina Murat Baldwin & Aja Louise Murray
School of Social and Political Science, University of Edinburgh, Edinburgh, UK
Franziska Meinck
Faculty of Health Sciences, North-West University, Vanderbijlpark, South Africa
Clinical Psychology Department, University of Edinburgh, Edinburgh, UK
Ingrid Obsuth
You can also search for this author in PubMed Google Scholar
Contributions
ZX is the guarantor of this review and has conceived the original research idea, has developed the selection criteria and search strategy, and will analyse the data. ZX and MMB will screen and extract the data from studies and will assess the risk of bias of each study. ALM will resolve any disagreements, make the final judgement, and will provide the guidance for interpreting the analysis. ALM, IO and FM guided the draft of the protocol, verified the selection criteria and search strategy, and contributed the revision of the protocol. ALM, IO and FM will also supervise the review process and will provide feedback if needed. All authors have read and approved the final manuscript of the review protocol.
Corresponding author
Correspondence to Zhuoni Xiao .
Ethics declarations
Ethics approval and consent to participate.
This study will based on the previous studies and will not collect new data or involve identifiable data. Therefore, ethical review is not required.
Competing interests
Additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Xiao, Z., Baldwin, M.M., Meinck, F. et al. The impact of childhood psychological maltreatment on mental health outcomes in adulthood: a protocol for a systematic review and meta-analysis. Syst Rev 10 , 224 (2021). https://doi.org/10.1186/s13643-021-01777-4
Download citation
Received : 02 November 2020
Accepted : 27 July 2021
Published : 12 August 2021
DOI : https://doi.org/10.1186/s13643-021-01777-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Last updated 27/06/24: Online ordering is currently unavailable due to technical issues. We apologise for any delays responding to customers while we resolve this. For further updates please visit our website: https://www.cambridge.org/news-and-insights/technical-incident
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert

- > Journals
- > The British Journal of Psychiatry
- > Volume 217 Issue 5
- > Emotional abuse and neglect: time to focus on prevention...

Article contents
The scale of the problem, unpacking mental health consequences, reversing adverse mental health effects, reducing harm through prevention strategies, conclusions, emotional abuse and neglect: time to focus on prevention and mental health consequences.
Published online by Cambridge University Press: 07 September 2020
- Supplementary materials
Emotional abuse and emotional neglect are among the most prevalent of childhood maltreatment types and associated with a range of poor mental health outcomes. We need to move beyond correlational research and shift our focus to sophisticated multimodal studies to fully understand the psychobiological mechanisms underlying these associations and to intervention studies.
Childhood maltreatment is commonly described as physical, sexual or emotional abuse and physical or emotional neglect by a parent, caregiver or other adult, with all kinds of abuse resulting from acts of commission, and neglect from acts of omission. There has been relatively less societal and research attention on emotional abuse and emotional neglect, compared with physical and sexual abuse and physical neglect. This might be explained, at least in part, by their less visible immediate impact (i.e. no physical injury or outward signs of abuse) and considerable regional and cultural variations in the definition of what constitutes emotional abuse or (emotional) neglect. Certain facets of emotional abuse, such as constant swearing, yelling, criticism or humiliation of a child, are easily noticeable, but others, such as unrealistic expectations or unreasonable demands on the child, or unfair treatment because of certain characteristics (e.g. physical disability, or appearance), are not always recognised. In some cases, these less apparent facets of emotional abuse may arise out of the childhood or lived experience of parents, caregivers, teachers and others, but nonetheless still cause (unintended) harm to the child. Emotional neglect, defined usually as a failure to attend to the child's emotional needs (e.g. never showing emotion while interacting with the child), can also be difficult to spot and quantify, as many parents or caregivers find it hard to provide a safe and loving environment for their children when facing relationship difficulties, mental health problems or addiction issues. In some settings, emotional abuse/neglect may also echo culturally accepted practices, for example the girl child neglect phenomenon seen in certain Asian communities, whereby girls receive less care and fewer resources than boys in the same family. Elimination of childhood maltreatment, if (at all) possible, is going to require efforts from many sections of society, including the government. Until these efforts completely succeed, psychiatry, psychology and neuroscience disciplines must continue to act to fully understand the psychobiological processes that explain mental health problems emerging in association with emotional abuse/neglect, alone or simultaneously with other kinds of maltreatment, and to develop and test suitable interventions to correct them.
Despite difficulties in recognising and measuring emotional abuse, meta-analyses of the global prevalence of maltreatment convincingly reveal that childhood emotional abuse is self-reported by a much larger proportion of the adult population (about 36%) compared with physical (about 18%) or sexual abuse (8–18%), or physical neglect (about 16%). Reference Stoltenborgh, Bakermans-Kranenburg, Alink and van IJzendoorn 1 , Reference Stoltenborgh, Bakermans-Kranenburg and Van Ijzendoorn 2 Interestingly, studies reliant on informants of abuse have documented a much lower prevalence of emotional abuse than those using self-reports. Childhood emotional neglect, which is likely to be underreported in some settings, is still reported by about 18% of the adult population. Reference Stoltenborgh, Bakermans-Kranenburg and Van Ijzendoorn 2 Children from any background can experience emotional abuse/neglect, although the prevalence rates may be higher in certain groups. For example, lesbian, gay, bisexual or transgender (LGBTQ+) youth may be more prone to experiencing emotional abuse, and possibly all types of abuse, because of societal ignorance or non-acceptance. Children from disadvantaged sectors of society, such as child workers or children displaced owing to war and other crises, may be subject to both inter- and intra-familial abuse and neglect as they spend time away from their families. At present, there are limited data on this topic from specific subgroups or low-resource countries.
Children who suffer maltreatment of any kind are known to experience poorer physical and mental health as adults, regardless of culture and geographical variations. Many people who suffered emotional abuse as children show feelings of hopelessness, poor self-esteem, reduced sense of social support, poor satisfaction with life, neurobiological changes in stress response systems, and structural and functional brain deficits; they are also at a heightened risk of developing psychiatric disorders. Problems such as depression, anxiety, eating disorders, suicidal symptomatology, psychosis, personality disorder and substance misuse often emerge in childhood and last through adulthood to old age. Importantly, a growing body of literature from both high- and low-income countries indicates that emotional abuse might have the most wide-ranging negative mental health impact of all childhood maltreatment types. Reference Pandey, Gupta, Upadhyay, Gupta, Shukla and Mishra 3 At present, there are few data addressing mental health consequences of emotional versus physical neglect. Nonetheless, both emotional abuse and emotional neglect seem to be a transdiagnostic risk factor for psychiatric disorders, especially anxiety and depression, perhaps mediated by dysfunctional (emotional) processing of self- and other-related information, accompanied with altered use or reduced availability of neural resources.
Further to simple association studies, there is now a pressing need for further research to fully examine the mental health consequences of emotional abuse and neglect at both ‘what’ and ‘how’ levels (i.e. what are the behavioural and brain changes following emotional abuse/neglect and how do they contribute to specific mental health outcomes?). A clear understanding of the psychobiological mechanisms that mediate between childhood emotional abuse and neglect and later vulnerability to specific mental disorders is critical for reducing such vulnerability and identifying targets for developing novel interventions. Although there have been some studies of neurophysiological correlates of childhood maltreatment (e.g. event-related brain potentials to facial expressions of anger or fear in maltreated versus non-maltreated children, or adults with and without a history of childhood maltreatment), they typically have not distinguished between different types of abuse and neglect. They have neither specifically focused on emotional abuse/neglect, which can be present with or without physical and sexual abuse and physical neglect, nor examined the observed neurophysiological changes in relation to the risk for particular disorders (e.g. depression versus psychosis). There is also a need for longitudinal studies examining the long-term impact of specific abuse and neglect, along with associated psychobiological changes, on prevalence of psychiatric disorders that usually emerge later in life. Lastly, future studies must proactively enquire about the protective factors that might promote resilience in the face of childhood emotional abuse/neglect.
With a paucity of studies empirically addressing the mechanisms underlying the association between emotional abuse/neglect and mental disorders, there are few clearly defined targets for reversing, or preventing the risks for, mental health problems in emotionally maltreated youth. However, it is already known that adults who suffered childhood maltreatment in general show a worse-than-usual response to standard pharmacological approaches to ameliorate their mental health problems, such as depressive symptoms, and respond relatively better to psychological interventions. This, taken together with evidence (e.g. Reference Pandey, Gupta, Upadhyay, Gupta, Shukla and Mishra 3 ) of the extensive and undesirable mental health impact of emotional abuse and neglect, encourages the development and use of psychological interventions, especially those targeting aberrant emotional processes, to reverse or even prevent (if applied in time) adverse mental health outcomes for maltreated children.
Encouragingly, there are early indications that psychological interventions aimed at correcting aberrant attentional processes or interpretational biases may be applied to improve mental health outcomes in maltreated youth. Reference Lau, Sharma, Bennett, Dhakal, Vaswani and Pandey 4 However, much of the research in this area has been correlational. The research focus and funding priorities now need to be expanded to include intervention studies Reference Berthelot, Lemieux and Maziade 5 and facilitate studies that would yield valuable information for identifying specific treatment targets (e.g. certain information processing or memory biases, unhelpful coping styles) for developing novel interventions and refining existing ones.
To minimise the short- and long-term harm associated with emotional abuse and neglect, child and adolescent psychiatrists, clinical psychologists and other professionals who routinely work with young people need to actively look for their signs and intervene to educate and safeguard where indicated. It is also important for these disciplines to interact with law makers and enforcement bodies to ensure that emotional abuse and (emotional) neglect, in the absence of visible signs, are appropriately acknowledged in governmental policies, and that no historically underserved populations (e.g. girls in certain societies) are ignored. Armed with empirical evidence, mental health professionals should also be encouraged and empowered to actively contribute to grass root campaigns to raise public awareness about the signs and consequences of these extremely harmful forms of childhood maltreatment.
Given the high prevalence rates and well-documented harmful mental health consequences of emotional abuse and neglect across countries and cultures, it is essential that we not only learn to recognise their signs but focus our efforts on clearly understanding the underlying mechanisms and on developing suitable interventions to minimise and prevent the risk of associated poor mental health outcomes. At present, the research on possible interventions for reversing the mental health problems associated with this kind of childhood maltreatment is in its infancy but shows promise. In parallel, we must also work towards raising public awareness about the signs and the mental health impact of emotional abuse and neglect and ensure that they are appropriately acknowledged in global child protection laws and policies.
V.K. reports a grant from Medical Research Council, UK (grant number: MR/N006194/1), for some of the research discussed in this editorial.
Declaration of interest
An ICMJE form is in the supplementary material, available online at https://doi.org/10.1192/bjp.2020.154 .
Kumari supplementary material

This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 217, Issue 5
- Veena Kumari (a1)
- DOI: https://doi.org/10.1192/bjp.2020.154
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
Advertisement
Childhood emotional neglect and adolescent depression: the role of self-compassion and friendship quality
- Published: 08 August 2022
- Volume 42 , pages 24451–24463, ( 2023 )
Cite this article

- Simeng Dong ORCID: orcid.org/0000-0002-0438-1512 1 ,
- Qinnan Dong 2 ,
- Haiyan Chen 3 &
- Shuai Yang 4
1523 Accesses
2 Citations
Explore all metrics
Numerous studies have shown that childhood emotional neglect experiences are an important risk factor for later physical and mental health problems. However, previous studies have not fully clarified the underlying mechanisms between childhood emotional neglect and depression, especially for adolescents in vocational schools. In the present study, we examined the mediating role of self-compassion in the association between childhood emotional neglect and depression and the moderating role of friendship quality in the direct and indirect relations involved. The participants were 848 vocational school adolescents, aged 14 to 20, who completed the questionnaires about childhood emotional neglect, self-compassion, depression, and friendship quality. The results showed that self-compassion partially mediated the relationship between childhood emotional neglect and adolescent depression. Importantly, friendship quality moderated the direct link between childhood emotional neglect and depression, and the indirect link between childhood emotional neglect and self-compassion, but not the indirect link between self-compassion and depression. Especially, adolescents in vocational school with high friendship quality displayed higher levels of self-compassion and lower levels of depression after experiencing childhood emotional neglect than those with low friendship quality. These findings highlight the mechanisms underlying the relationship between childhood emotional neglect and depression in vocational school adolescents.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

The Effect of Friendship Conflict on Depression, Anxiety and Stress in Chinese Adolescents: The Protective Role of Self-Compassion

The role of parenting, self-compassion and friendships in depressive symptoms among young people in the UK and China

Parental marital Relationship and depressive symptoms in adolescent boys and girls: The role of self-compassion and school connectedness
Afifi, T. O., Ford, D., Gershoff, E. T., Merrick, M., Grogan-Kaylor, A., Ports, K. A., MacMillan, H. L., Holden, G. W., Taylor, C. A., Lee, S. J., & Bennett, P., R (2017). Spanking and adult mental health impairment: The case for the designation of spanking as an adverse childhood experience. Child abuse & neglect , 71 , 24–31. https://doi.org/10.1016/j.chiabu.2017.01.014
Article Google Scholar
Abramson, D. M., Grattan, L. M., Mayer, B., Colten, C. E., Arosemena, F. A., Bedimo-Rung, A., et al. (2015). The resilience activation framework: a conceptual model of how access to social resources promotes adaptation and rapid recovery in post-disaster settings. Journal of Behavioral Health Services & Research , 42 (1), 42–57. https://doi.org/10.1007/s11414-014-9410-2
Alloy, L. B., & Abramson, L. Y. (1982). Learned helplessness, depression, and the illusion of control. Journal of Personality and Social Psychology , 42 (6), 1114–1126. https://doi.org/10.1037//0022-3514.42.6.1114
Article PubMed Google Scholar
Albertson, E.R., Neff, K.D. & Dill-Shackleford, K.E. (2015). Self-Compassion and Body Dissatisfaction in Women: A Randomized Controlled Trial ofa Brief Meditation Intervention. Mindfulness 6, 444–454. https://doi.org/10.1007/s12671-014-0277-3
Ban, J., & Oh, I. (2016). Mediating effects of teacher and peer relationships between parental abuse/neglect and emotional/behavioral problems. Child abuse & neglect , 61 , 35–42. https://doi.org/10.1016/j.chiabu.2016.09.010
Bernstein, D. P., & Fink, L. (1998). Childhood Trauma Questionnaire: A retrospective self-report manual San Antonio . TX: The Psychological Corporation
Google Scholar
Brooks, S. J., Krulewicz, S. P., & Kutcher, S. (2003). The kutcher adolescent depression scale: assessment of its evaluative properties over the course of an 8-week pediatric pharmacotherapy trial. Journal of Child & Adolescent Psychopharmacology , 13 (3), 337–349. https://doi.org/10.1089/104454603322572679
Beth, P. (1999). Childhood and adolescent abuse history, fear of negative evaluation, and social interaction self-statements: a correlational analysis. Child & Adolescent Social Work Journal , 16 (1), 47–65. https://doi.org/10.1023/A:1022265706650
Berndt, T. J. (1996). Transitions in friendship and friends’ influence. In J. A. Graber, J. Brooks-Gunn, & A. C. Petersen (Eds.), Transitions through adolescence: Interpersonal domains and context (pp. 57–84). Lawrence Erlbaum Associates, Inc.
Brummert Lennings, H. I., & Bussey, K. (2017). The mediating role of coping self-efficacy beliefs on the relationship between parental conflict and child psychological adjustment. Social Development , 26 (4), 753–766. https://doi.org/10.1111/sode.12241
Brown, R. C., Witt, A., Fegert, J. M., Keller, F., & Plener, P. L. (2017). Psychosocial interventions for children and adolescents after man-made and natural disasters: a meta-analysis and systematic review. Psychological Medicine , 47 (11), 1–13. https://doi.org/10.1017/S0033291717000496
Coolidge, F. L., Segal, D. L., Benight, C. C., & Danielian, J. (2004). The predictive power of horney’s psychoanalytic approach: an empirical study. American Journal of Psychoanalysis , 64 (4), 363–374. https://doi.org/10.1007/s11231-004-4324-z
Chinese National Mental Health Development Report (2019–2020). Chinese Academy of Sciences, 2021. Retrieved at https://www.cas.cn/yx/202103/t20210301_4779054.shtml . Accessed September 2, 2021.
Chu, X., Li, Z., Yan, B., Jing, H., & Fan, F. (2015). Comparative study of regular and vocational high school students on family socioeconomic status, social support, self-efficacy and well-being. Open Journal of Social Sciences , 03 (8), 61–68. https://doi.org/10.4236/jss.2015.38006
Collins, W. A., & Laursen, B. (2004). Changing relationships, changing youth: interpersonal contexts of adolescent development. Journal of Early Adolescence , 24 (1), 55–62. https://doi.org/10.1177/0272431603260882
Cohen, S., Be njuamin, H., Gottlieb, & Underwood, L. G. (2001). Review of : social relationships and health: challenges for measurement and intervention. Advances in mind-body medicine , 17 (2), 129–141. https://doi.org/10.1007/BF00844776
Chen, Y., Wang, L., & Zhao, J. (2021). Peer relationship profiles in rural Chinese adolescents: Longitudinal relations with subjective well-being. Journal of health psychology , 26 (11), 1803–1820. https://doi.org/10.1177/1359105319888278
Ding, H., Han, J., Zhang, M., Wang, K., Gong, J., & Yang, S. (2017). Moderating and mediating effects of resilience between childhood trauma and depressive symptoms in chinese children. Journal of Affective Disorders , 211 , 130–135. https://doi.org/10.1016/j.jad.2016.12.056
Diedrich, A., Grant, M., Hofmann, S. G., Hiller, W., & Berking, M. (2014). Self-compassion as an emotion regulation strategy in major depressive disorder. Behaviour research and therapy , 58 , 43–51. https://doi.org/10.1016/j.brat.2014.05.006
Evans, L. D., Kouros, C., Frankel, S. A., McCauley, E., Diamond, G. S., Schloredt, K. A., & Garber, J. (2015). Longitudinal relations between stress and depressive symptoms in youth: coping as a mediator. Journal of abnormal child psychology , 43 (2), 355–368. https://doi.org/10.1007/s10802-014-9906-5
Article PubMed PubMed Central Google Scholar
Epkins, C. C. , & Heckler, D. R. . (2011). Integrating etiological models of social anxiety and depression in youth: evidence for a cumulativeinterpersonal risk model. Clinical Child and Family Psychology Review, 14 (4), 329-376. https://doi.org/10.1007/s10567-011-0101-8
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine , 14 (4), 245–258. https://doi.org/10.1016/j.amepre.2019.04.001
Polanczyk, G. V., Salum, G. A., Sugaya, L. S., Caye, A., & Rohde, L. A. (2015). Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of child psychology and psychiatry and allied disciplines , 56 (3), 345–365. https://doi.org/10.1111/jcpp.12381
Gilbert, P. (2005). Compassion: Conceptualisations, research, and use in psychotherapy . London: Routledge. https://doi.org/10.1192/bjp.188.1.94-a
Book Google Scholar
Gilbert, P., & Procter, S. (2010). Compassionate mind training for people with high shame and self-criticism: overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy , 13 (6), 353–379. https://doi.org/10.1002/cpp.507
Gauze, C., Bukowski, W. M., & Sippola, A. A. K. (2010). Interactions between family environment and friendship and associations with self-perceived well-being during early adolescence. Child Development , 67 (5), 2201–2216. https://doi.org/10.1111/j.1467-8624.1996.tb01852.x
Gauze, C., Bukowski, W. M., Aquan-Assee, J., & Sippola, L. K. (1996). Interactions between Family Environment and Friendship and Associationswith Self-Perceived Well-Being during Early Adolescence. Child Development, 67 (5), 2201–2216. https://doi.org/10.2307/1131618
Hildyard, K. L., & Wolfe, D. A. (2002). Child neglect: developmental issues and outcomes☆. Child Abuse & Neglect , 26 (6–7), 679–695. https://doi.org/10.1016/s0145-2134(02)00341-1
Hammen, C., Henry, R., & Daley, S. E. (2000). Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of consulting and clinical psychology , 68 (5), 782–787. https://doi.org/10.1037/0022-006X.68.5.782
Havewala, M. , Felton, J. W. , & Lejuez, C. W. . (2019). Friendship quality moderates the relation between maternal anxiety and trajectories ofadolescent internalizing symptoms. Journal of Psychopathology and Behavioral Assessment, 41 (3), 495-506. https://doi.org/10.1007/s10862-019-09742-1
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach . New York, NY:Guilford Press.
Jt, A., Kai, H. B., & Jx, A. (2021). The mediating effect of self-compassion on the relationship between childhood maltreatment and depression. Journal of Affective Disorders , 291 , 288–293. https://doi.org/10.1016/j.jad.2021.05.019
Krieger, T., Altenstein, D., Baettig, I., Doerig, N., & Holtforth, M. G. (2013). Self-compassion in depression: associations with depressive symptoms, rumination, and avoidance in depressed outpatients. Behavior Therapy , 44 (3), 501–513. https://doi.org/10.1016/j.beth.2013.04.004
Kylie, B., Amanda, B., Patrick, M. E., & David, K. (2016). The influence of parental emotional neglect on assault victims seeking treatment for depressed mood and alcohol misuse: a pilot study. Journal of Clinical Medicine , 5 (10), https://doi.org/10.3390/jcm5100088
Li, F., Cui, Y., Li, Y., Guo, L., Ke, X., Liu, J., & Leckman, J. F. (2021). Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. Journal of Child Psychology and Psychiatry . https://doi.org/10.1111/jcpp.13445
Liu, J., Wan, Y. H., Yuan, C. J., Li, H., & Tao, Y., F. B (2016). Correlations between adverse childhood experiences and suicidal behavior among middle school students. Chinese Journal of School Health , 37 (4), 4. https://doi.org/10.16835/j.cnki.1000-9817.2016.04.027
Liu, Y., Tang, T., Sun, G., & Liu, Z., K, Y (2021). Research progress on self-compassion assessment tools. Chinese Journal of Modern Nursing , 27 (29), 5. https://doi.org/10.3760/cma.j.cn115682-20210106-00063
Lansford, J. E., Criss, M. M., Pettit, G. S., Dodge, K. A., & Bates, J. E. (2010). Friendship quality, peer group affiliation, and peer antisocial behavior as moderators of the link between negative parenting and adolescent externalizing behavior. Journal of Research on Adolescence , 13 (2), 161–184. https://doi.org/10.1111/1532-7795.1302002
Li, Q., Dong, Y., Zhang, Y., & Wang, K. (2020). The mediating effect of self – compassion between alexithymia and depressive symptoms in depression patients. Chinese Journal of Disease Control & Prevention , (11), 1308–1314. https://doi.org/10.16462/j.cnki.zhjbkz.2020.11.013
Larson, R. W., & Richards, M. H. (1991). Boredom in the Middle School Years: Blaming Schools versus Blaming Students. American Journal of Education , 99 (4), 418–443. https://doi.org/10.1086/443992
Lepore, S. J., Silver, R. C., Wortman, C. B., & Wayment, H. A. (1996). Social constraints, intrusive thoughts, and depressive symptoms among bereaved mothers. Journal of Personality and Social Psychology , 70 (2), 271–282. https://doi.org/10.1037//0022-3514.70.2.271
McLaughlin, K. A., Conron, K. J., Koenen, K. C., & Gilman, S. E. (2010). Childhood adversity, adult stressful life events, and risk of past-yearpsychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychological medicine, 40(10), 1647–1658. https://doi.org/10.1017/S0033291709992121
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking Rumination. Perspectives on Psychological Science , 3 (5), 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x
Neff, K. D. (2003a). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity , 2 (2), 85–101. https://doi.org/10.1080/15298860309032
Neff, K. D. (2003b). The development and validation of a scale to measure self- compassion. Self and Identity , 2 (3), 223–250. https://doi.org/10.1080/15298860309027
Neff, K. D., Kirkpatrick, K. L., & Rude, S. S. (2007). Self-compassion and adaptive psychological functioning. Journal of Research in Personality , 41 (1), 139–154. https://doi.org/10.1016/j.jrp.2006.03.004
Neff, K. D., & Vonk, R. (2008). Self-compassion versus global self-esteem: two different ways of relating to oneself. Journal of Personality , 77 (1), 23–50. https://doi.org/10.1111/j.1467-6494.2008.00537.x
Neff, K. D., Pisitsungkagarn, K., & Hsieh, Y. P. (2008). Self-compassion and self-construal in the united states, thailand, and taiwan. Journal of Cross-Cultural Psychology , 39 (3), 267–285. https://doi.org/10.1177/0022022108314544
Neff, K. D., & Mcgehee, P. (2010). Self-compassion and psychological resilience among adolescents and young adults. Self & Identity , 9 (3), 225–240. https://doi.org/10.1080/15298860902979307
Negriff, S., & Susman, E. J. (2011). Pubertal timing, depression, and externalizing problems: A framework, review, and examination of gender differences. Journal of Research on Adolescence , 21 (3), 717–746. https://doi.org/10.1111/j.1532-7795.2010.00708.x
Parker, J. G., & Asher, S. R. (1993). Friendship and friendship quality in middle childhood: Links with peer group acceptance and feelings of loneliness and social dissatisfaction. Developmental Psychology , 29 , 611–621. https://doi.org/10.1037/0012-1649.29.4.611
Post, R. M. (1992). Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. The American journal of psychiatry , 149 (8), 999–1010. https://doi.org/10.1176/ajp.149.8.999
Ross, N. D., Kaminski, P. L., & Herrington, R. (2019). From childhood emotional maltreatment to depressive symptoms in adulthood: The roles of self-compassion and shame. Child abuse & neglect , 92 , 32–42. https://doi.org/10.1016/j.chiabu.2019.03.016
Rehan, W., Antfolk, J., Johansson, A., & Santtila, P. (2016). Do Single Experiences of Childhood Abuse Increase Psychopathology Symptoms in Adulthood? Journal of interpersonal violence , 34 (5), 1021–1038. https://doi.org/10.1177/0886260516647004
Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the Self-Compassion Scale. Clinical psychology & psychotherapy , 18 (3), 250–255. https://doi.org/10.1002/cpp.702
Roy, A. (1999). Childhood trauma and depression in alcoholics: relationship to hostility. Journal of Affective Disorders , 56 (2–3), 215–218. https://doi.org/10.1016/S0165-0327(99)00044-0
Rueger, S. Y., Malecki, C. K., Pyun, Y., Aycock, C., & Coyle, S. (2016). A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychological Bulletin , 142 (10), 1017–1067. https://doi.org/10.1037/bul0000058
Rice, K. G., Cunningham, T. J., & Young, M. B. (1997). Attachment to parents, social competence, and emotional well-being: a comparison of black and white late adolescents. Journal of Counseling Psychology , 44 (1), 89–101. https://doi.org/10.1037/0022-0167.44.1.89
Sullivan, H. S. (1953). The interpersonal theory of psychiatry / harry stack sullivan; ed. helen swick perry. Social Service Review , 27 (4), https://doi.org/10.1086/639429
Shahar, B., Carlin, E. R., Engle, D. E., Hegde, J., Szepsenwol, O., & Arkowitz, H. (2012). A pilot investigation of emotion-focused two-chairdialogue intervention for self-criticism. Clinical psychology & psychotherapy , 19 (6), 496–507. https://doi.org/10.1002/cpp.762
Tylka, T. L., Russell, H. L., & Neal, A. A. (2015). Self-compassion as a moderator of thinness-related pressures’ associations with thin-ideal internalization and disordered eating. Eating Behaviors , 17 , 23–26. https://doi.org/10.1016/j.eatbeh.2014.12.009
Tarber, D. N., Cohn, T. J., Casazza, S., Hastings, S. L., & Steele, J. (2016). The Role of Self-compassion in Psychological Well-being for Male Survivors of Childhood Maltreatment. Mindfulness , 7 (5), 1193–1202. https://doi.org/10.1007/s12671-016-0562-4
WHO(2017). Depression and other common mental disorders: global health estimates (2017). Retrieved at https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/world-health-statistics . Accessed August 15, 2021.
Wekerle, C., Leung, E., Wall, A. M., Macmillan, H., Boyle, M., Trocme, N., et al. (2009). The contribution of childhood emotional abuse to teen dating violence among child protective services-involved youth. Child Abuse & Neglect , 33 (1), 45–58. https://doi.org/10.1016/j.chiabu.2008.12.006
Wang, Y., Lin, J., & Pan, J. (2015). The relationships among self-compassion, perfectionism, rumination and depression. Chinese Journal of Clinical Psychology , 23 (1), 120–123. https://doi.org/10.16128/j.cnki.1005-3611.2015.01.027.+128
Yang, W. J. , Pan, J. P. , & Yang, W. Y. . (2014). Situation of child neglect between left-behind children and living-with-parents children in ruralareas of china. Chinese Journal of School Health. 35 (2), 169–174. https://doi.org/10.16835/j.cnki.1000-9817.2014.02.005
Zhao, J., Sun, X., & Wang, Q. (2021). Emotional neglect and depressive symptoms of left-behind adolescents: The role of friendship quality and gender. Journal of Affective Disorders , 295 , 377–383. https://doi.org/10.1016/j.jad.2021.08.073
Zhou, H. M., Hao, N., Du, Y. S., et al. (2015). Validity and reliability of the Chinese version of the Kutcher Adolescent Depression Scale. Chinese Mental Health Journal , 29 (6), 413–418.
Download references
Author information
Authors and affiliations.
School of Economics and Management, Chongqing University of Posts and Telecommunications, Chongqing, China
Simeng Dong
School of Management, Chongqing College of International Business and Economics, Chongqing, China
Qinnan Dong
School of Economics, Chongqing Technology and Business University, Chongqing, China
Haiyan Chen
School of Marxism Studies, Chongqing University of Posts and telecommunications, Chongqing, China
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Simeng Dong .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Dong, S., Dong, Q., Chen, H. et al. Childhood emotional neglect and adolescent depression: the role of self-compassion and friendship quality. Curr Psychol 42 , 24451–24463 (2023). https://doi.org/10.1007/s12144-022-03539-4
Download citation
Received : 05 January 2022
Revised : 15 July 2022
Accepted : 18 July 2022
Published : 08 August 2022
Issue Date : October 2023
DOI : https://doi.org/10.1007/s12144-022-03539-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Childhood emotional neglect
- Self-compassion
- Friendship quality
- Find a journal
- Publish with us
- Track your research
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
How Childhood Emotional Neglect Can Show Up in Our Adult Life
Wendy Rose Gould is a lifestyle reporter with over a decade of experience covering health and wellness topics.
Yolanda Renteria, LPC, is a licensed therapist, somatic practitioner, national certified counselor, adjunct faculty professor, speaker specializing in the treatment of trauma and intergenerational trauma.
:max_bytes(150000):strip_icc():format(webp)/YolandaRenteria_1000x1000_tight_crop-a646e61dbc3846718c632fa4f5f9c7e1.jpg)
Delmaine Donson / Getty Images
How Do I Know If I Was Emotionally Neglected as a Child?
What are some examples of childhood emotional neglect, how does emotional neglect in childhood affect us as adults, how emotional neglect causes trauma, healing from childhood emotional neglect.
While everyone may perceive neglect differently, emotional neglect in childhood generally refers to when a child doesn’t experience emotional security or support from their guardian figures. Our emotions may have been completely ignored or invalidated —purposefully or unconsciously—or we might have been explicitly shamed for expressing our feelings.
Daniel Rinaldi, MHC
Emotional neglect is considered a form of trauma, as it can have long-lasting and profound effects on a person's emotional and psychological well-being.
This form of neglect can occur when a caregiver is not present, but when they are present they are emotionally unavailable, if the parent is ill-equipped to handle childhood emotions, or if the parent is purposefully dismissive .
“Emotional neglect is considered a form of trauma, as it can have long-lasting and profound effects on a person's emotional and psychological well-being,” says therapist Daniel Rinaldi , MHC. He adds that chronic emotional neglect can shape our emotional landscape as adults by affecting our self-esteem and impacting our interpersonal relationships.
Ongoing childhood emotional neglect is a form of child abuse and can lead to lasting trauma. This trauma can make it hard to develop a healthy relationship with others and with ourselves. We might even engage in self-sabotaging behaviors.
Therapy can teach us how to properly identify and label our emotions so that we can deal with them in a healthy way and begin to truly heal.
Raising children is highly nuanced and inherently difficult; there’s no doubt that our parents or caregivers made mistakes along the way. However, chronic emotional neglect is not the norm, and its ripple effects follow us well into adulthood.
“Emotional neglect can be hard to spot because it is not always visible—even to a professional,” says Aurisha Smolarski , LMFT, founder of Cooperative Coparenting. “It is also hard to spot because it tends to be based less on what a parent does and more on what they don’t do.”
Smolarski says that emotional neglect can be either intentional or unintentional, or even unconscious.
Some parents emotionally neglect their children because they’re uncomfortable with emotions in general and are unsure of how to respond to the complex feelings a child experiences.
Other parents are too overwhelmed with the stress in their own life—including struggles with addiction, work-life balance, child-rearing, and mental health issues. Smolarski also notes that parents who experienced abuse or neglect themselves may be more likely to neglect their own children.
Here are some signs of childhood emotional neglect. This isn’t an exhaustive list, but it provides a general idea of what emotional neglect looks like:
- Punishment for expressing negative emotions like sadness, frustration, or anger (e.g., being told to go to your room or be quiet)
- Lack of shared celebration or joy when experiencing a positive emotion like happiness or excitement (it might even present as zapping the positive emotion with a negative response)
- Being told your feelings or experiences aren’t valid or worth further examination (example phrases might include "You're too sensitive ," “Stop acting like a baby” or “Don’t worry about it.”)
- Dismissed or ignored feelings because the parent is focused on themselves or another situation
- Withholding or not showing affection , whether it is explicitly requested or not
- Failure to intervene or find a solution in situations when a child is under emotional stress
- Not acknowledging difficult emotions like grief after losing a pet or embarrassment after being bullied (often because the parent struggles to recognize or process these emotions themselves)
Those of us who were emotionally neglected as children often develop behavior patterns or coping mechanisms. Any of the following might be indicative of emotional neglect in childhood.
Emotional neglect can be either intentional or unintentional, or even unconscious.
Difficulty Expressing and Processing Emotions
Childhood emotional neglect can cause us to avoid emotions altogether in adulthood. We may struggle to identify our feelings or find it difficult to process big feelings.
There might also be a general sense of “numbness,” which is ultimately a form of self-protection. Smolarski adds, “They may choose to leave a relationship or situation instead of asking for something they need because that feels safer than the risk of rejection .”
Aurisha Smolarski, LMFT
They may withdraw or isolate from social or peer groups because they feel different and because they fear being asked to talk about how they feel.
People-Pleasing Tendencies
On the other side of the coin, Smolarski says that if we've been emotionally neglected as kids, we might end up becoming the “caretaker” or "burden holder" of our friends and family.
Essentially, addressing other people's emotions and needs allows us to feel worthy, loved, needed, and good enough. This can backfire if we end up focusing so much on others that we fail to prioritize ourselves.
We May Have a Super Hard Time Trusting Other People
Sometimes it feels safer to put up walls so that no one else can get in and potentially hurt us. We're simply trying to protect ourselves.
So, if we've experienced pain in the past we might end relationships the moment we feel threatened or avoid relationships completely.
Vulnerability and opening up to other people may feel scary too which limits the ability to connect with others. “They may withdraw or isolate from social or peer groups because they feel different and because they fear being asked to talk about how they feel,” Smolarski notes.
She adds that some might even self-sabotage their relationships to avoid feeling abandoned , rejected, or neglected. And those who find themselves in close relationships may struggle to access or voice their own emotions, which can negatively impact the relationship.
Our Self-Esteem May Take a Hit
Rinaldi says that chronic childhood neglect can often cause people to have low self-worth . If our self-esteem is low, we might write off our own emotions or even let people walk all over us.
Low self-esteem may also cause struggles with self-compassion and self-love.
We May Try to Cope in Some Not-So-Healthy Ways
In some cases, childhood emotional neglect can present with poor coping techniques as an adult. Bonnie Scott , LPC-S, founder of Mindful Kindness Counseling, says this is often because people who've been neglected have trouble trusting their own experience of emotions and needs.
“They may meet those needs in maladaptive ways, like becoming codependent on people who aren't good for them or showing people-pleasing behaviors to keep people around,” Scott says. They might also rely on drugs or alcohol to get them through a difficult emotion or become addicted to shopping, porn, online usage, risky sex, or food.
Rinaldi says that emotional neglect can impact someone’s life—even if it occurs only once or twice—though it is even more profound and complex when there’s a chronic pattern extended over a period of time.
Ongoing Neglect Is Child Abuse
Ongoing emotional neglect is considered a form of child abuse. According to the U.S. Department of Health & Human Services, it's a traumatic experience that, if severe or continued over a long period of time, can affect a child’s development.
“ Trauma can cause changes in the brain and nervous system that in turn lead to difficulty expressing emotions, lower self-esteem, shame, or guilt,” Smolarski says. “Children suffering from the trauma of neglect can have behavioral issues at home and in school and may struggle to form and maintain relationships in childhood and as adults.”
More severe neglect can lead to substance abuse, the tendency to engage in risky behavior, and long-term mental health issues, such as depression, anxiety, and post-traumatic stress disorder (PTSD) .
If you experienced childhood emotional neglect, know that you’re not alone. So many of us have survived this kind of abuse.
Making the effort to heal this wound is a sign of bravery, and can be done at any age.
Fortunately, healing is possible. There’s so much room for personal growth and a pathway to improved self-worth. Trust and emotional intimacy can be learned over time with patience and a strong support system. We can have and deserve fulfilling relationships.
“Remember that there is nothing wrong or bad about you or your emotions,” Smolarski says. “We all have emotions. It's just that you didn't have someone to reflect them back to you, to teach you that your emotions are welcome and valid, and to help you regulate them. Making the effort to heal this wound is a sign of bravery, and can be done at any age.”
Therapy Can Help
She adds that this process often requires professional support, such as therapy. Therapy allows us to explore past experiences, process unresolved emotions, and develop healthier coping strategies and communication skills.
In therapy, we can learn how to identify and label emotions accurately, develop self-compassion and self-acceptance, and figure out how to set and maintain healthy boundaries.
“Outside of professional settings, individuals can prioritize their emotional well-being through various self-care activities, such as engaging in activities that bring joy and fulfillment, practicing mindfulness and meditation to cultivate self-awareness, and journaling to express and process emotions,” Smolarski adds.
U.S. Department of Health & Human Services. " People Who Engage in Emotional or Psychological Abuse ."
National Institute of Mental Health. Post-traumatic stress disorder (PTSD) .
By Wendy Rose Gould Wendy Rose Gould is a lifestyle reporter with over a decade of experience covering health and wellness topics.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Long-term Effects of Child Abuse and Neglect on Emotion Processing in Adulthood
A key component of social competence is emotion processing, which includes emotion perception, communication, interpretation, and regulation of emotion ( Halberstadt, Denham, & Dunsmore, 2001 ). Emotions function to provide information about the environment and prepare for a behavioral response, triggering the appetitive or defensive systems, depending on the situation ( Bradley, Codispoti, Cuthbert, & Lang, 2001 ). Theories of emotion suggest that behavioral responses to emotions are directly related to emotion processing ( Halberstadt et al., 2001 ). This paper brings together research on child maltreatment, emotional development, and psychopathology to examine the consequences of child abuse and neglect for emotion processing in adulthood.
In general, child maltreatment has been found to disrupt the normal process of emotional development. First, studies of maltreating parents suggest that they show less positive emotion and more negative emotion than non-abusive parents ( Bugental, Blue, & Lewis, 1990 ; Kavanagh, Youngblade, Reid, & Fagot, 1988 ). It is also believed that maltreating parents tend to be isolated themselves and to isolate their children from interaction with others, providing fewer nonparental models of emotional communication ( Salzinger, Feldman, Hammer, & Rosario, 1993 ).
Second, a child who receives inconsistent or harsh caregiving has difficulty predicting the consequences of his/her behavior ( Dadds & Salmon, 2003 ) and this may be manifest in deficits in processing emotional information. For example, maltreated children have been found to show specific deficits in understanding ( Shipman & Zeman, 1999 ), recognizing ( Pollak, Cicchetti, Hornug, & Reed, 2000 ), and expressing emotion ( Gaensbauer, 1982 ) and are at risk for exhibiting social delays ( Kim & Cicchetti, 2010 ), deficits in empathy ( Beeghly & Cicchetti, 1994 ), and decreased engagement in prosocial behavior ( Koenig, Cicchetti, & Rogosch, 2004 ). These findings reveal general deficits in emotion processing in maltreated children, but the question remains about whether these deficits would persist into adulthood.
Using tests of facial emotion recognition (FER), Pollak and Sinha (2002) found that children with physical abuse histories were better able to identify facial displays of anger compared to controls. Several other studies using event-related potentials and behavioral evidence have found a sensitivity bias to perceive anger in physically abused children ( Pollak & Sinha, 2002 ; Pollak, Vardi, Pultzer-Bechner, & Curtin, 2005 ; Shackman, Shackman, & Pollak, 2007 ) and, more generally, in a sample of maltreated children ( Curtis & Cicchetti, 2011 , 2013 ; Leist & Dadds, 2009 ; Masten et al., 2008 ; Pollak, Klorman, Brumaghim, & Cicchetti, 2001 ). In an attempt to explain these findings, Pollak et al. (2005) suggested that in abusive home environments children learn to associate anger with threat of harm and therefore, they are hypervigilant to anger in their environment. Masten et al. (2008) elaborated on this theory to suggest that maltreated children become better prepared to identify threatening situations through hypervigilance of emotions. For example, these children may be more sensitive to anger in their abuser and fear of those around them because both sensitivities could help them identify threat quickly and potentially avoid additional abuse ( Masten et al., 2008 ). Consistent with these theories, Shackman et al. (2007) have shown that maltreated children show enhanced selective attention to angry facial expressions posed by their mothers. Thus, this body of research would suggest that individuals with histories of childhood physical abuse might be less likely to show deficits in processing negative emotional pictures and more likely to show deficits for pictures with positive or neutral valence.
Very little research has examined emotion recognition in neglected children. In earlier research, Bousha and Twentyman (1984) found that neglecting parents were less expressive and engaged with little exchange of affective information in interactions with their children and, thus, provided less support in learning to understand emotions more generally. Impoverished social and emotional environments, which are often present in cases of neglect, prevent the development of normal emotional skills ( Pollak et al., 2000 ) and may cause a blunted pattern of emotional reactivity ( Gilles, Berntson, Zipf, & Gunnar, 2000 ; van der Vegt, van der Ende, Kirschbaum, Verhulst, & Tiemeier, 2009 ). Pollak et al. (2000) reported that neglected children had more difficulty in recognizing emotional expressions in a vignette than a control group or physically abused children. When rating the similarity between facial expressions of different emotions, neglected children saw fewer distinctions between emotions compared to the other two groups ( Pollak et al., 2000 ). However, this is the only study to investigate emotion perception deficits specific to neglected children. Most studies have included only physically abused children or maltreated children (i.e. physically abused and/or neglected children). To our knowledge, no studies have focused on sexually abused children, and the existing literature is based almost exclusively on studies of children, with no research investigating the long-term effects of childhood abuse and neglect on adult emotion processing ability.
Potential Mechanisms Linking Childhood Maltreatment and Emotion Processing
If the impact of child abuse and neglect on emotion processing extends into adulthood, what might be some of mechanisms that lead to these outcomes? Research has increasingly shown that childhood abuse and neglect can result in a cascade of negative consequences across multiple domains of functioning ( Gilbert, Widom, Browne, Fergusson, Elspeth, & Janson, 2009 ; Widom, 2000 ) that might explain an increased risk for deficits in emotion processing abilities for individuals with histories of child abuse and/or neglect. Specifically, child abuse and neglect has been associated with cognitive deficits in general and various forms of psychopathology that may lead to emotion processing deficits.
First, several studies have reported that abused and neglected children are at increased risk for lower academic performance and intelligence in childhood ( Eckenrode, Laird, & Doris 1993 ; Jonson-Reid, Drake, Kim, Porterfield, & Han, 2004 ; Lansford, Dodge, Pettit, Bates, Crozier, & Kaplow, 2002 ) and that these effects of childhood maltreatment extend into young adulthood ( Perez & Widom, 1994 ). Thus, it is possible that deficits in intelligence lead to general deficits in performance on processing tasks, particularly those that involve memory, and this finding may help explain why maltreated children perform worse on these tasks.
It is also possible that some of the psychological consequences that have been associated with child abuse and neglect have a negative impact on performance on emotion processing tasks in adulthood. For example, individuals with histories of abuse have been found to exhibit more symptoms of anxiety disorders ( Springer, Sheridan, Kuo, & Carnes, 2007 ). A separate body of research reveals that individuals with higher levels of anxiety symptoms show deficits in emotion perception ( Mogg & Bradley, 1999 ) and emotion regulation ( Suveg, Morelen, Brewer, & Thomassin, 2010 ), and individuals with PTSD have shown an attentional bias to trauma-related stimuli ( Buckley, Blanchard, & Neill, 2000 ). In work by Pollak et al. (2001) , certain emotional cues become salient indicators of threat. Thus, in an emotion processing task, highly anxious individuals might be more likely to perform poorly on emotion processing tasks.
Childhood maltreatment has also been associated with increased risk for depression ( Cannon, Bonomi, Anderson, Rivara, & Thompson, 2010 ; Springer et al., 2007 ; Widom, DuMont, & Czaja, 2007 ). In turn, a separate body of research suggests that individuals with depression exhibit deficits in regulating emotions ( Joormann, Siemer, & Gotlib, 2007 ) and perceiving emotion in others ( Stuhrmann, Suslow, & Dannlowski, 2011 ). Therefore, it is possible that maltreated children may have difficulty recognizing emotions as a function of higher levels of depression ( Eberhart, Auerbach, Bigda-Peyton, & Abela, 2011 ).
At present, it is unclear whether the association between child maltreatment and deficits in processing of emotion would persist, independent of the effects of psychopathology. In one of the few studies to address this issue, Masten et al. (2008) focused on how PTSD might relate to maltreated children’s processing of emotions and found that maltreated children displayed a heightened ability (faster reaction time compared to controls) to identify fearful faces, independent of PTSD diagnosis. These findings with children suggest that maltreatment is uniquely related to emotion processing deficits, regardless of PTSD symptomatology.
In addition to internalizing consequences of child abuse and neglect, there is also a body of research that has linked childhood maltreatment to externalizing traits, including antisocial behavior and psychopathy ( Bernstein, Stein, & Handelsman, 1998 ; Kolla, Malcolm, Attard, Arenovich, Blackwood, & Hodgins, 2013 ; Lang, Klinteberg, & Alm, 2002 ; Weiler & Widom, 1996 ). A number of studies have also reported emotion processing deficits in individuals with antisocial and psychopathic traits ( Blair, Peschardt, Budhani, Mitchell, & Pine, 2006 ), including deficits in empathy ( Blair, 1995 ), experiencing of emotion ( Blair et al., 2006 ; Frick, Lilienfeld, Ellis, Loney, & Silverthorn, 1999 ), and identifying emotional expressions ( Blair et al., 2004 ; Deeley et al., 2006 ; Iria & Barbosa, 2009 ; Pham & Philippot, 2010 ). Antisocial individuals have been found to show specific deficits in perceiving negative emotions in facial expressions and to be less accurate in identifying emotions of fear or sadness than emotions of happiness or surprise ( Blair, Colledge, Murray, & Mitchell, 2001 ; Nichols, 2001 ). Maltreated children may show emotion processing deficits in adulthood through higher levels of psychopathic traits, reflecting greater desensitization, less empathy, or less responsiveness to the needs of others ( Weiler & Widom, 1996 ), critical characteristics of psychopaths. In sum, there are a number of plausible mechanisms that might explain deficits in emotional processing in adults with histories of childhood abuse and neglect and warrant investigation.
This study has several aims. The first goal is to assess emotion processing abilities in individuals with documented histories of childhood abuse and neglect and a matched control group who have been followed up into adulthood.
Hypothesis 1
Participants with a history of childhood maltreatment will be less accurate overall in recognizing affective pictures than controls, suggesting general deficits in processing emotional cues.
The second aim is to determine whether these emotion processing deficits vary by types of childhood maltreatment (physical and sexual abuse and neglect) and by emotional valance (positive, negative, or neutral). However, given the dearth of literature on the topic, no specific predictions are made about children who have been sexually abused.
Hypothesis 2
Based on earlier work suggesting that children growing up in abusive home environments will learn to associate anger with threat of harm ( Pollak et al., 2005 ), it is hypothesized that victims of childhood physical abuse will be more accurate in recognizing negative images (that is, physically abused children will not differ from controls), but less accurate in recognizing positive and neutral images, than matched controls.
Hypothesis 3
As a result of their impoverished social and emotional environments, it is predicted that neglected children will be less accurate in recognizing negative and positive images (emotionally valenced pictures) than controls.
A final aim is to examine whether the associations between childhood maltreatment and deficits in emotion processing abilities are, in part, a function of consequences of child maltreatment, specifically, IQ, psychopathology (Generalized Anxiety Disorder, PTSD, Dysthymia, and Major Depressive Disorder), and psychopathy or whether deficits are independent of these forms of psychopathology.
Hypothesis 4
It is hypothesized that IQ, psychopathology, and psychopathy will each mediate the relationship between child abuse and neglect and emotion processing accuracy.
The data used here are from a prospective cohort design study in which abused and neglected children were matched with non-abused, non-neglected children and followed into young adulthood. Because of the matching procedure, the participants are assumed to differ only in the risk factor (i.e., having experienced childhood sexual or physical abuse or neglect). Because it is not possible to assign participants to groups randomly, the assumption of equivalency for the groups is an approximation. The control group may also differ from the abused and neglected individuals on other variables associated with abuse or neglect. (For complete details of the study design and subject selection criteria, see Widom, 1989a .)
The initial phase of the study compared the abused and/or neglected children to the matched comparison group (N = 1,575) on juvenile and adult criminal arrest records ( Widom, 1989b ). The second phase involved tracking, locating, and interviewing both groups during 1989–1995, approximately 22 years after incidents of abuse and neglect (N = 1,196). This interview consisted of a series of structured and semi-structured questionnaires and rating scales, including the National Institute of Mental Health (NIMH) Diagnostic Interview Schedule - Revised (DIS-III-R), a standardized psychiatric assessment that yields Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) diagnoses ( Robins, Helzer, Cottler, & Goldring, 1989 ). Subsequent follow-up interviews were conducted in 2000–2002, 2003–2005, and in 2009–2010. The research presented in this paper uses information collected during all four interviews.
Participants and Design
The original sample of abused and neglected children (N = 908) was made up of court-substantiated cases of childhood physical and sexual abuse and neglect processed from 1967 to 1971 in the county juvenile (family) or adult criminal courts of a Midwestern metropolitan area. Cases of abuse and neglect were restricted to children 11 years of age or less at the time of the incident. A control group of children without documented histories of child abuse or neglect (N = 667) was matched with the abuse/neglect group on age, sex, race/ethnicity, and approximate family social class during the time that the abuse and neglect records were processed.
The control group represents a critical component of the study design. Children who were under school age at the time of the abuse and/or neglect were matched with children of the same sex, race, date of birth (±1 week), and hospital of birth through the use of county birth record information. For children of school age, records of more than 100 elementary schools for the same time period were used to find matches with children of the same sex, race, date of birth (±6 months), class in elementary school during the years 1967–1971, and home address, preferably within a five-block radius of the abused/neglected child. Overall, matches were found for 74% of the abused and neglected children. Non-matches occurred for a number of reasons. For birth records, non-matches occurred in situations when the abused and neglected child was born outside the county or state or when date of birth information was missing. For school records, non-matches occurred because of lack of adequate identifying information for the abused and neglected children or because the elementary school had closed and class registers were not available.
Of the original sample, 83% were located, and 1,196 (76%) participated in the 1989–1995 interview. Of those participants, 896 completed the second interview (2000–2002), 808 completed the third interview (2003–2005), and 649 completed the 2009–2010 interviews. The composition of the sample at the various waves of interviews has remained about the same. There were no significant differences in sex, race, age at initial abuse/neglect petition, or proportion who experienced overall abuse and/or neglect or any specific type of abuse or neglect across the four waves.
Of the 649 participants that completed the 2009–2010 interviews, 547 had complete information on the measures included here. Participants ranged in age from 38- to 55-years old ( M = 47.10; SD = 3.45), and 42.2% were male. Race/ethnic composition was 56.2% White, 35.3% African American, and 3.4% Hispanic. The overall abuse and neglect group represented 53.9% ( n = 295) of the sample [physical abuse 7.7% ( n = 42), sexual abuse 9% ( n = 49), and neglect 43% ( n = 235)]. These numbers add up to more than 295 because some participants had experienced more than one type of abuse or neglect). Table 1 presents demographic characteristics of the sample and descriptive statistics on each of the variables.
Demographic Information and Descriptive Statistics
| Overall ( =547) | Control ( =252) | Abuse/Neglect ( =295) | Any Physical Abuse ( =42) | Any Sexual Abuse ( =49) | Any Neglect ( =235) | ||
|---|---|---|---|---|---|---|---|
| Gender (% Male) | 42.20 | 46.80 | 38.30 | 45.20 | 12.20 | 41.30 | |
| Race (% White, non-Hispanic) | 59.20 | 59.50 | 59.00 | 78.60 | 55.10 | 58.30 | |
| Age (M, SD) | 47.10 (3.44) | 47.04 (3.46) | 47.15 (3.43) | 47.40 (3.62) | 48.12 (2.47) | 46.89 (3.52) | |
| MDD (M, SD) | 3.58 (2.75) | 3.22 (2.66) | 3.88 (2.80) | 3.90 (2.84) | 3.90 (3.04) | 3.88 (2.73) | |
| Dysthymia (M, SD) | 2.56 (2.12) | 2.22 (1.99) | 2.86 (2.19) | 2.79 (2.34) | 2.96 (2.42) | 2.82 (2.11) | |
| GAD (M, SD) | 4.32 (5.17) | 4.00 (4.81) | 4.60 (5.46) | 5.43 (5.64) | 5.14 (5.94) | 4.47 (5.34) | |
| PTSD (M, SD) | 7.65 (6.48) | 4.54 (5.39) | 6.54 (6.14) | 7.76 (5.88) | 8.92 (6.06) | 6.31 (6.10) | |
| PCL (M, SD) | 7.65 (6.48) | 6.37 (5.72) | 8.71 (6.88) | 8.97 (7.94) | 8.52 (6.62) | 8.57 (6.84) | |
| IQ (M, SD) | 89.90 (12.61) | 93.13 (12.50) | 87.19 (12.08) | 90.36 (13.58) | 88.80 (12.45) | 86.60 (12.05) | |
| IAPS (M, SD) | 41.45 (5.90) | 42.10 (5.78) | 40.91 (5.95) | 40.86 (6.66) | 40.65 (6.04) | 40.98 (5.77) | |
| SES (%) | Menial Service | 9.6 | 7.8 | 11.3 | 7.7 | 17.9 | 11.4 |
| Unskilled | 8.9 | 4.9 | 12.7 | 0 | 15.4 | 13.1 | |
| Semi-skilled | 26.5 | 21.5 | 31.2 | 19.2 | 20.5 | 33.5 | |
| Skilled Manual | 9.6 | 10.7 | 8.6 | 23.1 | 0 | 8.5 | |
| Clerical/Sales | 9.6 | 12.2 | 7.2 | 0 | 10.3 | 7.4 | |
| Technicians | 8.5 | 10.2 | 6.8 | 7.7 | 7.7 | 7.4 | |
| Managers | 12 | 13.7 | 10.4 | 11.5 | 15.4 | 9.1 | |
| Administrators | 7.7 | 8.3 | 7.2 | 11.5 | 7.7 | 6.3 | |
| Higher Executives | 7.5 | 10.7 | 4.5 | 19.2 | 5.1 | 3.4 | |
Note. M = Mean; SD = Standard Deviation; MDD = Major Depressive Disorder; GAD = Generalized Anxiety Disorder; PTSD = Posttraumatic Stress Disorder; PCL = Psychopathy Checklist- Revised; IAPS = International Affective Picture System; SES = Socioeconomic Status
Participants completed the interviews in their homes or, if preferred by the participant, another place appropriate for the interview. The interviewers were blind to the purpose of the study and to the inclusion of an abused and/or neglected group. Participants were also blind to the purpose of the study and were told that they had been selected to participate as part of a large group of individuals who grew up in the late 1960s and early 1970s. Institutional Review Board approval was obtained for the procedures involved in this study, and participants who participated gave written, informed consent. For individuals with limited reading ability, the consent form was presented and explained verbally.
Independent variable
Childhood abuse and neglect.
Childhood physical and sexual abuse and neglect were assessed through review of official records processed during the years 1967–1971. Physical abuse cases included injuries such as bruises, welts, burns, abrasions, lacerations, wounds, cuts, bone and skull fractures, and other evidence of physical injury. Sexual abuse charges included felony sexual assault, fondling or touching in an obscene manner, sodomy, incest, and rape. Neglect cases reflected a judgment that the parents’ deficiencies in childcare were beyond those found acceptable by community and professional standards at the time and represented extreme failure to provide adequate food, clothing, shelter, and medical attention to children. For the current study, abuse/neglect was coded (0 = no abuse history , 1 = history of physical, sexual abuse, and/or neglect ). Any Physical abuse was coded (0 = no physical abuse history , 1 = history of physical abuse ). Any Sexual abuse was coded (0 = no sexual abuse history , 1 = history of sexual abuse ). Any Neglect was coded (0 = no neglect history , 1 = history of neglect ). The specific type of abuse or neglect was coded as present, regardless of whether or not the person had experienced other types of abuse as well. Overall, 10.5% ( n = 31) of the abuse/neglect group experienced more than one type of maltreatment.
Outcome variable
International affective picture system (iaps, lang, bradley, & cuthbert, 2005 ).
The IAPS, a set of photos depicting positive, negative, or neutral content, has been used as a paradigm for studying the processing of emotional stimuli ( Bradley, Greenwald, Petry, & Lang, 1992 ). The IAPS has previously been used as a recall/recognition task to measure memory of affective information ( Blake, Varnhagen, & Parent, 2001 ; Bradley et al., 1992 ; Talmi, Schimmack, Paterson, & Moscovitch, 2007 ). Research suggests that attention is more likely to be directed to a stimulus with a motivational significance to an individual (e.g., an emotional stimulus) than a neutral, non-relevant stimulus (Sanchez-Navarro, Martinez-Selva, & Roman, 2005). In addition, several researchers have found that emotion has an enhancing effect on memory (e.g. Bradley et al, 1992 ). Therefore, in the IAPS recognition task, participants should be more accurate in recognizing positively and negatively valenced pictures compared to neutral pictures and deficits in recognizing emotionally valenced pictures may suggest that the participant failed to attend to the emotional cues in the picture. In this conceptualization, recognition is a marker of vigilance for emotional stimuli.
The latest version of the IAPS ( Lang et al. 2005 ) was used during the 2009–2010 in-person interview. The developers of the IAPS provide normative ratings on the valence (positive, negative, neutral) and dimensions of valence, ranging from 1 ( the most negative ) to 9 ( the most positive ) on a Likert-type rating scale. Out of the total 942 digital still photos that comprise the IAPS library, a total of 24 images, 8 neutral and 16 emotional (8 positive, 8 negative) were chosen using valence ratings obtained from prior validation studies (see Appendix A for the IAPS numbers, a brief title for the image, and image valences for all images used in this study). The pictures selected varied widely in content (including the neutral and mundane) and affective tone, from calm to arousing and pleasant to unpleasant. Each of these 24 images had a novel partner image similar in content and, when possible, matched on emotional valence that was used in the recognition task. Like the original images, the 24 matching, novel images were selected from the IAPS. The IAPS emotion valence scores for each group (negative, positive, and neutral) differed significantly from each other, F (2, 47) = 334.32, p < .01, with the valence of positive images averaging 7.48, neutral images 5.17, and negative images 2.92.
International Affective Picture System (IAPS) Number, Image Title, Image Valence, and Valance Score
| IAPS Number | Title | Valence Score | Valence | IAPS Number | Title | Valence Score | Valence |
|---|---|---|---|---|---|---|---|
| 2299 | Family at restaurant (AA) | 7.27 | Positive | 2395 | Family women (AA) | 7.49 | Positive |
| 2340 | Grandpa w/children (W) | 8.03 | Positive | 2360 | Family (W) | 7.60 | Positive |
| 5001 | Sunflower | 7.16 | Positive | 5200 | Flowers | 7.36 | Positive |
| 5760 | Nature | 8.05 | Positive | 5780 | Nature | 7.52 | Positive |
| 5836 | Couple on beach (W) | 7.25 | Positive | 4622 | People on beach (W) | 7.46 | Positive |
| 2222 | 2 boys reading | 7.11 | Positive | 2224 | Profile 3 kids | 7.24 | Positive |
| 1750 | Bunnies | 8.28 | Positive | 1610 | Rabbit | 7.82 | Positive |
| 1603 | Butterfly | 6.90 | Positive | 1604 | Butterfly on pink flower | 7.11 | Positive |
| 2205 | Elderly couple in hospital | 1.95 | Negative | 2590 | Elderly woman w/woman | 3.26 | Negative |
| 9220 | Couple in cemetery | 2.06 | Negative | 9001 | Cemetery | 3.10 | Negative |
| 9611 | Plane crash | 2.71 | Negative | 9050 | Plane crash w/people | 2.43 | Negative |
| 7360 | Pie with flies | 3.59 | Negative | 7380 | Pizza w/cockroaches | 2.46 | Negative |
| 9630 | Bomb | 2.96 | Negative | 8485 | Fire/explosion | 2.73 | Negative |
| 9342 | Pollution w/man | 2.85 | Negative | 9341 | Pollution w/boy | 3.38 | Negative |
| 2276 | Sad girl (AA) | 2.67 | Negative | 2271 | Sad girl (AA) | 4.20 | Negative |
| 2455 | Sad 3 teenage girls (W) | 2.96 | Negative | 2278 | Sad 2 girls (Hispanic) | 3.36 | Negative |
| 7283 | Fruit | 5.50 | Neutral | 7285 | Tomatoes | 5.67 | Neutral |
| 2513 | Woman w/scarf | 5.80 | Neutral | 2038 | Woman sitting in chair | 5.09 | Neutral |
| 7006 | Bowl | 4.88 | Neutral | 7009 | Mug | 4.93 | Neutral |
| 7100 | Fire hydrant | 5.24 | Neutral | 7710 | Bed | 5.42 | Neutral |
| 7025 | Stool | 4.63 | Neutral | 7235 | Chair | 4.96 | Neutral |
| 7224 | File cabinets | 4.45 | Neutral | 7700 | Messy office | 4.25 | Neutral |
| 2270 | Boy w/red shirt (AA) | 6.28 | Neutral | 9070 | Boy (AA) | 5.01 | Neutral |
| 5510 | Mushroom | 5.15 | Neutral | 5500 | Mushroom | 5.42 | Neutral |
Note . All pictures from the presentation section were shown again in the recognition section along with the 24 new pictures marked with double asterisks.
Before the IAPS was administered, participants were told that they would be viewing a series of images on the computer screen and to watch the images as they would a television. Administration consisted of two parts: a) an initial presentation phase in which the participant watched a series of 24 target images (positive, neutral, and negative) presented in random order for two seconds each (with no pause between images), and b) a recognition phase approximately 15 minutes later in which the participant watched a second series of 48 images (24 of which were the original target images from the presentation phase and 24 “novel partner” images) presented in random order. During the recognition phase, the participant was instructed to indicate whether or not he/she saw each image earlier. Each image appeared on the screen until the participant pressed a key to indicate whether he/she had seen the image before. Pictures were presented on a standard sized laptop PC. Recognition accuracy was calculated as the number of times the participant correctly indicated whether or not he/she had seen each of the positive, negative, and neutral pictures previously during the presentation phase.

Potential Mediators
Psychopathology.
The Diagnostic Interview Schedule - Revised (DIS-III-R), a standardized psychiatric assessment that yields Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) diagnoses ( Robins et al., 1989 ) was administered during the 1989–1995 in-person interviews to assess for Generalized Anxiety Disorder (GAD), Posttraumatic Stress Disorder (PTSD), Major Depressive Disorder (MDD), and Dysthymia. Continuous variables reflecting the number of lifetime symptoms reported for each of these disorders are used in analyses. The DIS-III-R demonstrates adequate reliability ( Robins, Helzer, Croughan, & Ratcliff, 1981 ). Table 1 presents the means and standard deviations for the number of lifetime symptoms for each of these disorders for these participants at approximate age 29.
Psychopathy
The Psychopathy Checklist- Revised (PCL-R; Hare, 1991 , 2003 ), the revised 20-item version, was used to determine psychopathy scores for the participants. Psychopathy ratings were based on information obtained from both official records and the 1989–1995 interviews (see Weiler & Widom, 1996 for details). Following Hare (1991) , items were scored as follows: 0 = the person does not meet the criteria for the item , 1 = the person meets the criteria to a certain extent , and 2 = the person clearly meets the criteria for the item . Because of the large number of participants and the massive amount of information, computer-generated PCL-R scores based on ratings from trained raters were calculated for each subject using SPSSX. A computerized scoring algorithm was developed after careful review and study of the criteria described in the PCL-R manual, discussion of the criteria and information available from our interview and files with PCL-R trainers. Using data from participants without excessive missing data, reliability analysis of the PCL-R in SPSS indicated that Cronbach’s Alpha was .80. In this sample, PCL-R scores ranged from 0 to 30 ( M = 7.65; SD = 6.48) with 6.4% scoring above 20, the top third of the distribution of scores (see Table 1 ).
The Quick Test (QT; Ammons & Ammons, 1962 ), a vocabulary test of intelligence that provides an index of overall cognitive functioning, was measured during the first interview that occurred during 1989–1995. The QT has been demonstrated to be a useful, reliable estimate of intellectual functioning ( Ammons & Ammons, 1962 ). Total scores were based on a raw count of items correct that were then recoded into scores ranging from 0 to 160 to be consistent with typical IQ test scoring with higher scores indicating higher intellectual functioning (see Table 1 ). The validity of the QT has been established through comparisons with other measures of IQ such as the Wechsler Adult Intelligence Scale, particularly with WAIS Verbal IQ ( Abidin & Byrne, 1967 ; Davis & Dizzonne, 1970 ).
Demographic Information
Control variables included sex ( male = 0, female = 1), race ( White, non-Hispanic = 1, others = 2), age, and socio-economic status (see Table 1 ). Age was a continuous variable representing the participant’s age during the 2009–2010 interviews. Occupational Code from the Hollingshead Four Factor Index of Socioeconomic Status (SES) ( Hollingshead, 1975 ) was used, with nine categories ranging from menial service workers to higher executives .
Prior to analysis, all variables in the study were assessed for univariate normality and multicollinearity. To assess univariate normality, skewness and kurtosis values were assessed using the guidelines for larger sample sizes ( DeCarlo, 1997 ; Tabachnick & Fidell, 2013 ). No variables in this study were determined to be skewed or kurtotic. Multicollinearity was assessed using the Variance Inflation Factor (VIF) criteria ( Tabachnick & Fidell, 2013 ) and no variables were determined to be multicollinear. (Correlation coefficients for all variables and measures are presented in Table 2 .)
Intercorrelation Matrix of All Variables
| PCL | GAD | PTSD | DYS | MDD | IQ | Age | Overall IAPS | Positive IAPS | Negative IAPS | Neutral IAPS | Sex | Race | SES | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PCL | 1.00 | 0.24 | 0.27 | 0.30 | 0.30 | −0.14 | −0.02 | −0.09 | −0.08 | −0.07 | −0.08 | −0.27 | −0.08 | 0.00 |
| GAD | 0.24 | 1.00 | 0.39 | 0.58 | 0.59 | 0.02 | −0.01 | 0.12 | 0.09 | 0.11 | 0.11 | 0.11 | 0.06 | 0.04 |
| PTSD | 0.27 | 0.39 | 1.00 | 0.46 | 0.46 | −0.07 | 0.02 | 0.00 | −0.01 | 0.00 | 0.01 | 0.18 | 0.03 | 0.01 |
| DYS | 0.30 | 0.58 | 0.46 | 1.00 | 0.90 | −0.05 | 0.02 | 0.05 | 0.04 | 0.07 | 0.04 | 0.16 | 0.01 | −0.01 |
| MDD | 0.30 | 0.59 | 0.46 | 0.90 | 1.00 | −0.01 | 0.01 | 0.09 | 0.07 | 0.10 | 0.08 | 0.14 | 0.03 | 0.00 |
| IQ | −0.14 | 0.02 | −0.07 | −0.05 | −0.01 | 1.00 | 0.09 | 0.31 | 0.30 | 0.29 | 0.23 | −0.11 | 0.16 | 0.04 |
| Age | −0.02 | −0.01 | 0.02 | 0.02 | 0.01 | 0.09 | 1.00 | −0.08 | −0.08 | −0.07 | −0.08 | 0.06 | −0.10 | 0.04 |
| IAPS: Overall | −0.09 | 0.12 | 0.00 | 0.05 | 0.09 | 0.31 | −0.08 | 1.00 | 0.87 | 0.90 | 0.89 | 0.09 | 0.15 | 0.00 |
| IAPS: Positive | −0.08 | 0.09 | −0.01 | 0.04 | 0.07 | 0.30 | −0.08 | 0.87 | 1.00 | 0.68 | 0.66 | 0.09 | 0.12 | 0.01 |
| IAPS: Negative | −0.07 | 0.11 | 0.00 | 0.07 | 0.10 | 0.29 | −0.07 | 0.90 | 0.68 | 1.00 | 0.71 | 0.08 | 0.12 | 0.01 |
| IAPS: Neutral | −0.08 | 0.11 | 0.01 | 0.04 | 0.08 | 0.23 | −0.08 | 0.89 | 0.66 | 0.71 | 1.00 | 0.06 | 0.15 | 0.00 |
| Sex | −0.27 | 0.11 | 0.18 | 0.16 | 0.14 | −0.11 | 0.06 | 0.09 | 0.09 | 0.08 | 0.06 | 1.00 | −0.07 | −0.08 |
| Race | −0.08 | 0.06 | 0.03 | 0.01 | 0.03 | 0.16 | −0.10 | 0.15 | 0.12 | 0.12 | 0.15 | −0.07 | 1.00 | 0.08 |
| SES | 0.00 | 0.04 | 0.01 | −0.01 | 0.00 | 0.04 | 0.04 | 0.00 | 0.01 | 0.01 | 0.00 | −0.08 | 0.08 | 1.00 |
Note. PCL = Psychopathy Checklist- Revised; GAD = Generalized Anxiety Disorder; PTSD = Posttraumatic Stress Disorder; DYS= Dysthymia; MDD = Major Depressive Disorder; IAPS = International Affective Picture System; Sex (Female = 1, Male = 0); Race (White = 1, Non-White = 0); SES = Socioeconomic Status (1 = menial service workers to 9 = higher executives ).
Ordinary Least Squares (OLS) regressions were conducted to determine whether child abuse and neglect predicted potential mediators (psychopathology and IQ) and recognition accuracy. Regressions are reported using standardized coefficients ( β) and all analyses controlled for age, sex, race, and SES. Separate regressions were performed to examine positive, negative, and neutral recognition accuracy.
Mplus Version 6.0 was used to conduct Structural Equation Modeling (SEM) to examine the role of potential mediators of the relationship between childhood abuse and neglect and picture recognition accuracy. All analyses controlled for age, sex, race, and SES, and matched controls were used as the comparison group in all analyses. For structural models, multiple indices of overall model fit (chi-square statistic [χ 2 ], comparative fit index [CFI], Tucker–Lewis index [TLI], Root-mean-square error of approximation [RMSEA], and standardized root mean square residual [SRMR]) were evaluated. A low chi-square and non-significance ( p < .05) are desirable, and a chi-square to degrees of freedom ( df ) ratio of less than 5 is considered adequate ( Bollen, 1989 ). A comparative fit index (CFI) and Tucker–Lewis index (TLI) of .90 or higher indicate good fit. Root-mean-square error of approximation (RMSEA) of less than .05 is considered a close fit, and a standardized root mean square residual (SRMR) of less than .08 is generally considered a good fit ( Hu & Bentler, 1999 ). Current recommendations support consideration of both the chi-square test and other indices of model fit ( Barrett, 2007 ).
Strength of mediational relationships was evaluated with tests of indirect effects ( MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002 ) and bias-corrected bootstrapped confidence intervals ( MacKinnon, Lockwood, & Williams, 2004 ). Full information maximum likelihood estimation was used to handle missing data on the SES variable. This method uses all data available for each case and thus avoids biases and loss of power associated with traditional approaches to missing data ( Allison, 2003 ; Schlomer, Bauman, & Card, 2010 ).
Child Abuse and Neglect and Recognition Accuracy
Table 3 presents findings regarding accuracy in emotion recognition by group (abuse/neglect vs. control) and type of maltreatment (any physical abuse, any sexual abuse, and any neglect vs. control). As hypothesized, childhood abuse and neglect significantly predicted overall recognition accuracy ( β =−0.11, p < .01) and this model explained 5% of the variance ( R 2 = .05, p < .01) indicating that individuals with a history of childhood abuse/neglect were less accurate in recognizing pictures than those without a history of childhood abuse/neglect. Neglect also significantly predicted overall recognition accuracy ( β = −0.10, p < .05) explaining 5% of the variance ( R 2 = .05, p < .05), but physical and sexual abuse did not. However, it should be noted physical and sexual abuse showed a similar non-significant trend. The effect size and the mean recognition accuracy scores for physical and sexual abuse groups were similar to those for the neglect group, suggesting that the lack of significant findings for overall picture recognition accuracy for the physical and sexual abuse groups may have been due to the small sample size of these two groups.
Regressions Predicting Picture Recognition Accuracy by Group (Abuse/Neglect vs. Control) and Type of Abuse/Neglect
| Overall | Positive Pictures | Negative Pictures | Neutral Pictures | |||||
|---|---|---|---|---|---|---|---|---|
| = 547; controls = 252; abuse/neglect = 295) | ||||||||
| Age | −0.07 | 0.04 | −0.07 | 0.04 | −0.06 | 0.04 | −0.07 | 0.04 |
| Sex | 0.11 | 0.04 | 0.11 | 0.04 | 0.10 | 0.04 | 0.08 | 0.04 |
| Race | 0.15 | 0.04 | 0.12 | 0.04 | 0.12 | 0.04 | 0.15 | 0.04 |
| SES | −0.01 | 0.05 | 0.00 | 0.05 | −0.00 | 0.05 | −0.01 | 0.05 |
| Abuse/neglect | −0.11 | 0.04 | −0.13 | 0.04 | −0.07 | 0.04 | −0.10 | 0.04 |
| 0.05 | 0.04 | 0.03 | 0.04 | |||||
| = 294; controls = 252, any physical abuse = 42) | ||||||||
| Age | −0.13 | 0.06 | −0.13 | 0.06 | −0.12 | 0.06 | −0.08 | 0.06 |
| Sex | 0.13 | 0.06 | 0.15 | 0.06 | 0.12 | 0.06 | 0.08 | 0.06 |
| Race | 0.09 | 0.06 | 0.05 | 0.06 | 0.10 | 0.06 | 0.09 | 0.06 |
| SES | 0.03 | 0.06 | 0.03 | 0.06 | 0.04 | 0.06 | 0.02 | 0.06 |
| Physical Abuse | −0.08 | 0.06 | −0.06 | 0.06 | −0.04 | 0.06 | −0.12 | 0.06 |
| 0.04 | 0.04 | 0.04 | 0.03 | |||||
| = 301; controls = 252, any sexual abuse = 49) | ||||||||
| Age | −0.14 | 0.06 | −0.15 | 0.06 | −0.11 | 0.06 | −0.12 | 0.06 |
| Sex | 0.15 | 0.06 | 0.14 | 0.06 | 0.16 | 0.06 | 0.10 | 0.06 |
| Race | 0.09 | 0.06 | 0.14 | 0.06 | 0.11 | 0.06 | 0.09 | 0.06 |
| SES | −0.02 | 0.06 | −0.02 | 0.06 | 0.00 | 0.06 | −0.03 | 0.06 |
| Sexual Abuse | −0.11 | 0.06 | −0.13 | 0.06 | −0.07 | 0.06 | −0.10 | 0.06 |
| 0.06 | 0.05 | 0.05 | 0.04 | |||||
| = 487; controls = 252, any neglect = 235) | ||||||||
| Age | −0.07 | 0.04 | −0.06 | 0.04 | −0.07 | 0.05 | −0.07 | 0.05 |
| Sex | 0.14 | 0.04 | 0.14 | 0.04 | 0.11 | 0.05 | 0.12 | 0.04 |
| Race | 0.12 | 0.04 | 0.11 | 0.04 | 0.09 | 0.05 | 0.13 | 0.04 |
| SES | −0.00 | 0.05 | 0.00 | 0.05 | 0.00 | 0.05 | −0.01 | 0.05 |
| Neglect | −0.10 | 0.04 | −0.13 | 0.04 | −0.07 | 0.05 | −0.08 | 0.04 |
| 0.05 | 0.05 | 0.03 | 0.04 | |||||
Note. N = number in analysis, includes abuse/neglect and control group participants; β= standardized regression coefficient; SE β = standard error of β ; R 2 = effect size; SES = socioeconomic status.
Picture Valence and Recognition Accuracy
Negative, neutral, and positive picture recognition accuracy scores were also compared for group (abuse/neglect vs. control) and type of maltreatment (see Table 3 ). Abuse/neglect overall ( β = −0.13, p < .01) and neglect ( β = −0.13, p < .01) each significantly predicted positive picture recognition accuracy, indicating less accuracy among these individuals in recognizing positive pictures, compared to controls. In addition, abuse/neglect overall ( β = −0.10, p < .05) and physical abuse ( β = −0.12, p < .05) each significantly predicted less accuracy in neutral picture recognition. Neither abuse/neglect in general or specific types of maltreatment predicted negative picture recognition accuracy. Interestingly, although not hypothesized, childhood sexual abuse predicted poorer performance on positive picture recognition, compared to controls ( β = −0.13, p < .05).
Child Abuse and Neglect and Potential Mediators: Psychopathology, Psychopathy, and IQ
The next set of results examined the extent to which the independent variables (overall abuse/neglect and type of maltreatment) predicted the hypothesized mediators (psychopathology, psychopathy, and IQ). The results in Table 4 indicate that a history of child abuse and neglect significantly predicted increased symptoms of MDD ( β = 0.11, p < .01), Dysthymia ( β = 0.14, p < .01), PTSD ( β = 0.16, p < .001), and Psychopathy ( β = 0.21, p < .001), and lower IQ ( β = −0.21, p < .001) compared to controls. This pattern of results was the same for the neglect group (see Table 4 ). A history of physical abuse predicted increased symptoms of PTSD ( β = 0.21, p < .001) and Psychopathy ( β = 0.17, p < .001), compared to controls, but not IQ ( β = −0.10, p = 0.08) or GAD ( β = 0.09, p = 0.14), MDD ( β = 0.10, p = 0.10), or Dysthymia symptoms ( β = 0.11, p = 0.07). The pattern of results for the sexual abuse group was the same as for the physical abuse group (see Table 4 ).
Group (Abuse/Neglect vs. Control) and Type of Abuse/Neglect as Predictors of Psychopathology and IQ
| Major Depressive Disorder | Dysthymia | Posttraumatic Stress Disorder | Generalized Anxiety Disorder | Psychopathy | IQ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| = 547; controls = 252; abuse/neglect = 295) | ||||||||||||
| Age | 0.02 | 0.04 | 0.03 | 0.04 | 0.04 | 0.04 | −0.02 | 0.04 | 0.02 | 0.04 | 0.25 | 0.04 |
| Sex | 0.14 | 0.04 | 0.15 | 0.04 | 0.17 | 0.04 | 0.12 | 0.04 | −0.29 | 0.04 | −0.08 | 0.04 |
| Race | 0.04 | 0.04 | 0.02 | 0.04 | 0.04 | 0.04 | 0.07 | 0.04 | −0.09 | 0.04 | 0.16 | 0.04 |
| SES | 0.03 | 0.05 | 0.02 | 0.05 | 0.03 | 0.05 | 0.06 | 0.05 | 0.01 | 0.05 | 0.02 | 0.05 |
| Group | 0.11 | 0.04 | 0.14 | 0.04 | 0.16 | 0.04 | 0.05 | 0.04 | 0.21 | 0.04 | −0.21 | 0.04 |
| 0.04 | 0.05 | 0.06 | 0.03 | 0.12 | 0.13 | |||||||
| = 294; controls = 252, any physical abuse = 42) | ||||||||||||
| Age | 0.01 | 0.06 | −0.01 | 0.06 | −0.03 | 0.06 | −0.06 | 0.06 | 0.03 | 0.06 | 0.35 | 0.05 |
| Sex | 0.13 | 0.06 | 0.12 | 0.06 | 0.14 | 0.06 | 0.19 | 0.06 | −0.32 | 0.06 | −0.12 | 0.06 |
| Race | −0.06 | 0.06 | −0.06 | 0.06 | −0.07 | 0.06 | 0.10 | 0.06 | −0.10 | 0.06 | 0.14 | 0.06 |
| SES | 0.01 | 0.07 | −0.02 | 0.07 | 0.01 | 0.07 | 0.11 | 0.07 | −0.02 | 0.07 | 0.00 | 0.09 |
| Physical Abuse | 0.10 | 0.06 | 0.11 | 0.06 | 0.21 | 0.06 | 0.09 | 0.06 | 0.17 | 0.06 | −0.10 | 0.05 |
| 0.03 | 0.03 | −0.07 | 0.06 | 0.13 | 0.15 | |||||||
| = 301; controls = 252, any sexual abuse = 49) | ||||||||||||
| Age | 0.05 | 0.06 | 0.04 | 0.06 | −0.01 | 0.06 | −0.02 | 0.06 | 0.03 | 0.06 | 0.34 | 0.05 |
| Sex | 0.13 | 0.06 | 0.12 | 0.06 | 0.17 | 0.06 | 0.17 | 0.06 | −0.33 | 0.06 | −0.14 | 0.06 |
| Race | −0.06 | 0.06 | −0.06 | 0.06 | −0.04 | 0.06 | 0.07 | 0.06 | −0.10 | 0.06 | 0.16 | 0.05 |
| SES | 0.02 | 0.07 | −0.03 | 0.07 | 0.01 | 0.06 | 0.07 | 0.07 | −0.06 | 0.06 | −0.02 | 0.05 |
| Sexual Abuse | 0.05 | 0.06 | 0.09 | 0.06 | 0.24 | 0.06 | 0.04 | 0.06 | 0.21 | 0.06 | −0.11 | 0.06 |
| 0.03 | 0.04 | 0.11 | 0.04 | 0.13 | 0.15 | |||||||
| = 487; controls = 252, any neglect = 235) | ||||||||||||
| Age | 0.03 | 0.05 | 0.04 | 0.05 | −0.01 | 0.05 | −0.02 | 0.05 | −0.01 | 0.04 | 0.27 | 0.04 |
| Sex | 0.12 | 0.05 | 0.13 | 0.04 | 0.15 | 0.04 | 0.09 | 0.05 | −0.31 | 0.04 | −0.09 | 0.04 |
| Race | 0.03 | 0.05 | 0.01 | 0.05 | 0.04 | 0.05 | 0.08 | 0.05 | −0.11 | 0.04 | 0.18 | 0.04 |
| SES | 0.04 | 0.05 | 0.03 | 0.05 | 0.03 | 0.05 | 0.05 | 0.05 | 0.01 | 0.05 | 0.02 | 0.05 |
| Neglect | 0.12 | 0.04 | 0.14 | 0.04 | 0.15 | 0.04 | 0.04 | 0.05 | 0.19 | 0.04 | −0.22 | 0.04 |
| 0.03 | 0.04 | 0.05 | 0.02 | 0.13 | 0.15 | |||||||
Note : β= standardized regression coefficient; SE β = standard error of β ; R 2 = effect size; SES = socioeconomic status.
Structural Equation Models
Overall picture recognition accuracy.
Separate models were tested for each potential mediator, with controls for age, race, sex, and SES (see Table 5 ) for abuse/neglect overall and for neglect specifically. We did not test these mediation models for physical and sexual abuse because the results of the earlier analyses indicated that they were not significant predictors of picture recognition accuracy.
Group (abuse/neglect overall vs. controls) and Neglect (IVs) as Predictors of Overall Picture Recognition Accuracy (DV) with Lifetime Symptoms of Major Depressive Disorder, Dysthymia, Generalized Anxiety Disorder, and Posttraumatic Stress Disorder, Psychopathy, and IQ as Potential Mediators (M,) each Modeled Separately
| Effect of IV on M | Effect of M on DV | Direct Effect of IV on DV | Indirect Effect of IV on DV | |||||
|---|---|---|---|---|---|---|---|---|
| β | SE | B | SE | β | SE | β | SE | |
| = 547; controls = 252; abuse/neglect = 295) | ||||||||
| Major Depressive Disorder | 0.11 | 0.04 | 0.10 | 0.04 | −0.10 | 0.04 | 0.01 | 0.01 |
| Dysthymia | 0.14 | 0.04 | 0.06 | 0.04 | −0.10 | 0.04 | 0.01 | 0.01 |
| Generalized Anxiety Disorder | 0.05 | 0.04 | 0.10 | 0.04 | −0.10 | 0.04 | 0.01 | 0.01 |
| Posttraumatic Stress Disorder | 0.16 | 0.04 | −0.01 | 0.04 | −0.09 | 0.04 | 0.00 | 0.01 |
| Psychopathy | 0.21 | 0.04 | −0.01 | 0.05 | −0.09 | 0.04 | 0.00 | 0.01 |
| IQ (Quick test) | −0.21 | 0.04 | 0.36 | 0.04 | −0.02 | 0.04 | −0.08 | 0.02 |
| = 487; controls = 252, any neglect = 235) | ||||||||
| Major Depressive Disorder | 0.12 | 0.04 | 0.07 | 0.05 | −0.09 | 0.04 | 0.01 | 0.01 |
| Dysthymia | 0.14 | 0.04 | 0.05 | 0.05 | −0.09 | 0.05 | 0.01 | 0.01 |
| Generalized Anxiety Disorder | 0.04 | 0.05 | 0.09 | 0.04 | −0.09 | 0.04 | 0.00 | 0.00 |
| Posttraumatic Stress Disorder | 0.15 | 0.04 | −0.03 | 0.05 | −0.08 | 0.05 | 0.00 | 0.01 |
| Psychopathy | 0.19 | 0.04 | −0.01 | 0.05 | −0.08 | 0.05 | 0.00 | 0.01 |
| IQ (Quick test) | −0.22 | 0.04 | 0.35 | 0.04 | 0.00 | 0.04 | −0.08 | 0.02 |
Note. β= standardized regression coefficient; SE = standard error of β .
For child abuse and neglect overall, the first column of Table 5 shows that the effect of child abuse/neglect on psychopathology and IQ was consistent with bivariate relationships described. Column 2 shows that MDD, GAD, and IQ predicted overall emotion processing, whereas the other variables did not. Looking at columns 3 and 4, it can be seen that the introduction of IQ had a significant mediation effect and reduced the effect of child maltreatment on overall accuracy in emotion processing to non-significance, suggesting that child abuse and neglect influences picture recognition accuracy through its effects on IQ. Goodness of fit indices for the model including child abuse and neglect overall and IQ as a mediator were χ 2 (4) = 8.40, p = .08, CFI = 0.96, TLI = 0.90, RMSEA = .05, SRMR = 0.02. This model explained 10% of the variance in recognition accuracy and the indirect effect was significant ( β = −0.07, p < .001). In contrast, the models that included other potential mediators (MDD, Dysthymia, PTSD, GAD, and Psychopathy) did not yield fit indices in the acceptable range, and therefore, paths are not interpretable.
For the neglect group specifically, the first column again shows that the effect of neglect on psychopathology and IQ was consistent with bivariate relationships described earlier. However, Column 2 shows that only GAD and IQ predicted emotion processing accuracy, whereas the other potential mediators did not. Again, the introduction of IQ produced a significant mediation effect and reduced the effect of child maltreatment on emotion processing to non-significance, suggesting that child abuse and neglect influences picture recognition accuracy through its effects on IQ. Goodness of fit indices for the model including only IQ were χ 2 (4) = 9.65, p < .05, CFI = 0.96, TLI = 0.90, RMSEA = .05, SRMR = 0.03. This model explained 15% of the variance in recognition accuracy and the indirect effect was significant ( β = −0.08, p < .001). In contrast, the models including each of the other potential mediators (MDD, Dysthymia, PTSD, GAD, and Psychopathy) did not yield fit indices in the acceptable range and, therefore, the paths were not interpretable.
This is the first prospective study of emotion processing accuracy in individuals with documented cases of childhood abuse and neglect who were followed up and assessed in middle adulthood. As hypothesized, these findings showed that individuals with a history of childhood abuse and/or neglect were less accurate in processing affective pictures than those without such a history. In addition, these results showed that childhood histories of abuse/neglect in general and neglect and sexual abuse in particular predicted deficits in positive, but not negative, picture recognition. These results were unexpected, but it is possible that these previously abused and neglected individuals have developed negative worldviews that might have prevented them from recognizing positive emotions. It is also possible that they have received and perceived less positive emotions during their lives, making it more difficult in adulthood to recognize and distinguish positive emotions.
In contrast to our hypotheses, the processing of negatively valenced pictures did not differ between maltreated and control groups and specifically for individuals with histories of physical abuse and neglect. It is possible that the task assessed here was substantially different than past studies of facial emotion perception. Facial emotion perception depends on facial expressions for emotion-related cues, whereas cues in the affective pictures presented here include those from facial expression, body posture, and contextual factors. Therefore, deficits may be more difficult to detect because more emotion-related cues are available. It is also possible that these extra cues enabled these individuals to compensate for deficits.
We had specifically hypothesized that physically abused children would have problems with negative emotion pictures, but the results did not support this hypothesis. On first glance, one might attribute this result to the smaller sample size for the physically abused group and interpret the lack of deficits in negative emotion processing as a power problem. However, inspection of the small effect size suggests that low power was not the case, and the significant finding that adults with a history of childhood physical abuse were less accurate in processing neutral affective pictures. Another possibility is that individuals with histories of physical abuse might have been more likely to identify neutral stimuli as negative, based on a negative attribution bias ( Dodge, Pettit, Bates, & Valente, 1995 ). This possibility is intriguing, but unfortunately, the current paradigm does not permit an examination of the type of errors made. Participants were only asked to indicate whether they had seen the picture previously or not. They were not asked to judge the positivity or negativity of the pictures as has been done in facial emotion recognition paradigms. Future research will need to examine these issues more carefully.
Although it was hypothesized that the emotion processing deficits in previously abused and neglected children might be the result of psychopathology (Generalized Anxiety Disorder, PTSD, Dysthymia, and Major Depressive Disorder) or psychopathy, we found that lifetime symptoms of MDD and GAD assessed at age 29 predicted overall emotion recognition accuracy at mean age 47. Interestingly, these new findings are consistent with the previous research on psychopathology and emotion perception in clinical samples. However, these two forms of psychopathology (MDD and GAD) did not account for the relationship between child abuse/neglect and picture recognition accuracy. These new findings are similar to the earlier work of Masten et al. (2008) with children that suggested that maltreatment is uniquely related to emotion processing deficits regardless of PTSD symptomatology.
It was also expected that psychopathy would predict deficits in emotion perception, although we did not find this to be the case. It may be that characteristics of much of the prior literature [a focus on incarcerated or forensic samples ( Blair et al., 2004 ; Deeley et al., 2006 ; Iria & Barbosa, 2009 ; Pham & Philippot, 2010 )] may in part explain the differences in findings. For example, one might wonder whether there is something about psychopaths who get caught and are incarcerated that influences the emotion perception findings.
These results indicated that only IQ played a significant role as a mediator between child maltreatment and emotion processing accuracy in adulthood. These new findings suggest that emotion processing studies need to control for participants’ IQ because it is clear from these results that IQ had a substantial impact on recognition accuracy. It is also possible that the task here may have demanded more cognitive skills than other types of emotion processing tasks and, therefore, maltreated individuals with lower IQs might have been particularly disadvantaged.
Although these findings provide important information about the effects of child abuse and neglect on emotion processing, some limitations should be noted. First, the findings are based on cases of childhood abuse and neglect drawn from official court records and most likely represent the most extreme cases processed in the system. Second, cases that came to the attention of the courts are skewed toward the lower end of the socio-economic spectrum and, therefore, these results cannot be generalized to abused and neglected children who grew up in middle- or upper-class homes. Third, the data were from cases of abuse and neglect that occurred in the late 1960s and early 1970s in the Midwest part of the United States. Research should attempt to replicate these findings in samples from other time periods and geographic regions. However, these cases of child abuse and neglect are from the late 1960s and early 1970s are comparable in demographic characteristics to the kinds of cases being processed by child protection services across the country. Fourth, a final limitation suggested by one anonymous reviewer is that IQ may not be stable over time (see Salthouse, 2001 ). Therefore, although the temporal relationship in the present study is appropriate to examine the mediating role of intelligence, it is possible that IQ assessed in childhood or adolescence may have shown a different relationship to emotion picture accuracy than IQ assessed in young adulthood. Unfortunately, we are not able to explore these possibilities with our existing data.
Despite these limitations, the present study builds on previous research on emotion processing and childhood maltreatment in several ways. First, by studying affective picture recognition rather than emotion perception ability, this study examines another aspect of emotion processing that involves more basic attentional processes to emotionally salient environmental cues. This aspect of emotion processing has broader implications for daily emotional functioning in that it suggests deficits in attending to various emotional cues in the environment rather than just faces in particular. Second, by studying an adult sample, this study showed that effects of childhood abuse/neglect on emotion processing extend until middle adulthood, although it would be worthwhile to have multiple assessments over time to rule out competing explanations for improvement (or lack thereof) in emotion processing skills. Third, this study examined effects of different types of maltreatment on emotion processing and found victims of childhood neglect and sexual abuse had difficulty processing positive pictures. Fourth, the current study suggests that psychopathology and psychopathy do not significantly mediate the relationship between childhood maltreatment and emotion processing, although it was clear that certain forms of psychopathology did have an impact on emotion processing accuracy. Lastly, this study adds to the existing literature by suggesting that intelligence may mediate the relationship between childhood maltreatment and emotion processing. Therefore, research and interventions that target emotional processing deficits in victims of childhood maltreatment must consider and take into account the possible presence of intellectual deficits.
Acknowledgments
This research was supported in part by grants from Eunice Kennedy Shriver NICHD (HD40774), NIMH (MH49467 and MH58386), NIJ (86-IJ-CX-0033 and 89-IJ-CX-0007), NIDA (DA17842 and DA10060), NIAAA (AA09238 and AA11108), and the Doris Duke Charitable Foundation to the second author. Points of view are those of the authors and do not necessarily represent the position of the United States Department of Justice.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
- Abidin RR, Byrne AB. Quick Test validation study and examination of form equivalency. Psychological Reports. 1967; 20 :735–739. [ PubMed ] [ Google Scholar ]
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003; 112 :545–557. doi: 10.1037/0021-843X.112.4.545. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ammons RB, Ammons CH. The Quick Test. Missoula, MT: Psychological Test Specialists; 1962. [ Google Scholar ]
- Barrett P. Structural equation modeling: Adjudging model fit. Personality and Individual Differences. 2007; 42 :815–824. doi: 10.1016/j.paid.2006.09.018. [ CrossRef ] [ Google Scholar ]
- Beeghly M, Cicchetti D. Child maltreatment, attachment, and the self system: Emergence of an internal state lexicon in toddlers at high social risk. Development and Psychopathology. 1994; 6 :5–30. [ PubMed ] [ Google Scholar ]
- Bernstein DP, Stein JA, Handelsman L. Predicting personality pathology among adult patients with substance use disorders: Effects of childhood maltreatment. Addictive Behaviors. 1998; 23 :855–868. [ PubMed ] [ Google Scholar ]
- Blair RJR. Facial expressions, their communicatory functions and neurocognitive substrates. Philosophical Transactions of the Royal Society of London B Biological Sciences. 2003; 358 :561–72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blair RJR. A cognitive developmental approach to morality: Investigating the psychopath. Cognition. 1995; 57 :1–29. [ PubMed ] [ Google Scholar ]
- Blair RJR, Colledge E, Murray L, Mitchell DG. A selective impairment in the processing of sad and fearful expressions in children with psychopathic tendencies. Journal of Abnormal Child Psychology. 2001; 29 :491–498. [ PubMed ] [ Google Scholar ]
- Blair RJR, Mitchell D, Peschardt K, Colledge E, Leonard R, Shine J, Perrett DI. Reduced sensitivity to others’ fearful expressions in psychopathic individuals. Personality and Individual Differences. 2004; 37 :1111–1122. doi: 10.1016/j.paid.2003.10.008. [ CrossRef ] [ Google Scholar ]
- Blair RJR, Peschardt KS, Budhani S, Mitchell DGV, Pine DS. The development of psychopathy. Journal of Child Psychology & Psychiatry. 2006; 47 :262–275. [ PubMed ] [ Google Scholar ]
- Blake TM, Varnhagen CK, Parent MB. Emotionally arousing pictures increase blood glucose levels and enhance recall. Neurobiology of Learning and Memory. 2001; 75 :262–273. [ PubMed ] [ Google Scholar ]
- Bollen KA. Structural equations with latent variables. New York, NY: Wiley; 1989. [ Google Scholar ]
- Bousha DM, Twentyman CT. Mother-child interaction style in abuse, neglect, and control groups: Naturalistic observations in the home. Journal of Abnormal Psychology. 1984; 93 :106–114. [ PubMed ] [ Google Scholar ]
- Bradley MM, Codispoti M, Cuthbert BN, Lang PJ. Emotion and motivation: I. Defensive and appetitive reactions in picture processing. Emotion. 2001; 1 :276–298. doi: 10.1037//1528-3542.1.3.276. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradley MM, Greenwald MK, Petry MC, Lang PJ. Remembering pictures: Pleasure and arousal in memory. Journal of Experimental Psychology: Learning, Memory, and Cognition. 1992; 18 :379–390. [ PubMed ] [ Google Scholar ]
- Buckley TC, Blanchard EB, Neill WT. Information processing and PTSD: A review of the empirical literature. Clinical Psychology Review. 2000; 28 :1041–1065. [ PubMed ] [ Google Scholar ]
- Bugental DB, Blue J, Lewis J. Caregiver beliefs and dysphoric affect directed to difficult children. Developmental Psychology. 1990; 26 :631–638. [ Google Scholar ]
- Cannon EA, Bonomi AE, Anderson ML, Rivara FP, Thompson RS. Adult health and relationship outcomes among women with abuse experiences during childhood. Violence and Victims. 2010; 25 :291–305. [ PubMed ] [ Google Scholar ]
- Curtis WJ, Cicchetti D. Affective facial expression processing in young children who have experienced maltreatment during the first year of life: An event-related potential study. Development and Psychopathology. 2011; 23 :373–395. doi: 10.1017/S0954579411000125. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Curtis WJ, Cicchetti D. Affective facial expression processing in 15-month-old infants who have experienced maltreatment: An event-related potential study. Child Maltreatment. 2013; 18 :140–154. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dadds MR, Salmon K. Punishment insensitivity and parenting: Temperament and learning as interacting risks for antisocial behavior. Clinical Child and Family Psychology Review. 2003; 6 :69–86. [ PubMed ] [ Google Scholar ]
- Davis WE, Dizzonne MF. Relationship between the QT and the WAIS. Psychological Reports. 1970; 26 :457–458. [ Google Scholar ]
- DeCarlo LT. On the meaning and use of kurtosis. Psychological Methods. 1997; 2 :292–307. [ Google Scholar ]
- Deeley Q, Daly E, Surguladze S, Tunstall N, Mezey G, Beer D, Murphy DG. Facial emotion processing in criminal psychopathy: Preliminary functional magnetic resonance imaging study. British Journal of Psychiatry. 2006; 189 :533–539. doi: 10.1192/bjp.bp.106.021410. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dodge KA, Pettit GS, Bates JE, Valente E. Social information- processing patterns partially mediate the effect of early physical abuse on later conduct problems. Journal of Abnormal Psychology. 1995; 104 :632–643. [ PubMed ] [ Google Scholar ]
- Eberhart NK, Auerbach RP, Bigda-Peyton J, Abela JRZ. Maladaptive schemas and depression: Tests of stress generation and diathesis-stress models. Journal of Social and Clinical Psychology. 2011; 30 :75–104. [ Google Scholar ]
- Eckenrode J, Laird M, Doris J. School performance and disciplinary problems among abused and neglected children. Developmental Psychology. 1993; 29 :53–62. [ Google Scholar ]
- Frick PJ, Lilienfeld S, Ellis M, Loney B, Silverthorn P. The association between anxiety and psychopathy dimensions in children. Journal of Abnormal Child Psychology. 1999; 27 :383–392. [ PubMed ] [ Google Scholar ]
- Gaensbauer TJ. Regulation of emotional expression in infants from two contrasting caretaking environments. Journal of the American Academy of Child Psychiatry. 1982; 21 :163–170. [ PubMed ] [ Google Scholar ]
- Gilbert R, Widom CS, Browne K, Fergusson DM, Elspeth W, Janson S. Child Maltreatment 1: Burden and consequences of child maltreatment in high-income countries. The Lancet. 2009; 373 :68–81. [ PubMed ] [ Google Scholar ]
- Gilles EE, Berntson GG, Zipf WB, Gunnar MR. Neglect is associated with a blunting of behavioral and biological stress responses in human infants. Paper presented at the International Conference of Infant Studies; Brighton, England. 2000. [ Google Scholar ]
- Halberstadt AG, Denham SA, Dunsmore JC. Affective social competence. Social Development. 2001; 10 :79–119. [ Google Scholar ]
- Hare RD. The Hare Psychopathy Checklist–Revised. Toronto, Ontario: Multi-Health Systems; 1991. [ Google Scholar ]
- Hare RD. The Hare Psychopathy Checklist–Revised. Toronto, Ontario: Multi-Health Systems; 2003. [ Google Scholar ]
- Hollingshead AA. Unpublished manuscript. Yale University; New Haven, CT: 1975. Four-factor index of social status. [ Google Scholar ]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling- A Multidisciplinary Journal. 1999; 6 :1–55. [ Google Scholar ]
- Iria C, Barbosa F. Perception of facial expressions of fear: Comparative research with criminal and non-criminal psychopaths. The Journal of Forensic Psychiatry and Psychology. 2009; 20 :66–73. doi: 10.1080/14789940802214218. [ CrossRef ] [ Google Scholar ]
- Jonson-Reid M, Drake B, Kim J, Porterfield S, Han L. A prospective analysis of the relationship between reported child maltreatment and special education eligibility among poor children. Child Maltreatment. 2004; 9 :382–94. [ PubMed ] [ Google Scholar ]
- Joormann J, Siemer M, Gotlib IH. Mood regulation in depression: Differential effects of distraction and recall of happy memories on sad mood. Journal of Abnormal Psychology. 2007; 116 :484–490. [ PubMed ] [ Google Scholar ]
- Kavanagh K, Youngblade L, Reid J, Fagot B. Interactions between children and abusive vs. control parents. Journal of Clinical Child Psychology. 1988; 17 :137–142. [ Google Scholar ]
- Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry. 2010; 51 :706–716. doi: 10.1111/j.1469-7610.2009.02202.x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koenig AL, Cicchetti D, Rogosch FA. Moral development: The association between maltreatment and young children’s prosocial behaviors and moral transgressions. Social Development. 2004; 13 :87–106. [ Google Scholar ]
- Kolla NJ, Malcolm C, Attard S, Arenovich T, Blackwood N, Hodgins S, Blackwood N. Childhood maltreatment and aggressive behaviour in violent offenders with psychopathy. Canadian Journal of Psychiatry. 2013; 58 :487–494. [ PubMed ] [ Google Scholar ]
- Lang PJ, Bradley MM, Cuthbert BN. Technical Report A-6. Gainesville: University of Florida; 2005. International Affective Picture System (IAPS): Affective ratings of pictures and instruction manual. [ Google Scholar ]
- Lang S, Klinteberg B, Alm P. Adult psychopathy and violent behavior in males with early neglect and abuse. Acta Psychiatrica Scandinavica. 2002; 412 :93–100. [ PubMed ] [ Google Scholar ]
- Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Archives of Pediatric Adolescent Medicine. 2002; 156 :824–30. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leist T, Dadds MR. Adolescents’ ability to read different emotional faces relates to their history of maltreatment and type of psychopathology. Clinical Child Psychology and Psychiatry. 2009; 14 :237–250. doi: 10.1177/1359104508100887. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002; 7 :83–104. doi: 10.1037/1082-989X.7.1.83. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004; 39 :99–128. doi: 10.1207/s15327906mbr3901_4. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Masten CL, Guyer AE, Hodgdon HB, McClure EB, Charney DS, Ernst M, et al. Recognition of facial emotions among maltreated children with high rates of post-traumatic stress disorder. Child Abuse & Neglect. 2008; 32 :139–153. doi: 10.1016/j.chiabu.2007.09.006. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mogg K, Bradley BP. Orienting of attention to threatening facial expressions presented under conditions of restricted awareness. Cognition & Emotion. 1999; 13 :713–740. [ Google Scholar ]
- Nichols S. Mindreading and the cognitive architecture underlying altruistic motivation. Mind and Language. 2001; 16 :425–455. [ Google Scholar ]
- Perez CM, Widom CS. Childhood victimization and long-term intellectual and academic outcomes. Child Abuse & Neglect. 1994; 18 :617–633. [ PubMed ] [ Google Scholar ]
- Pham TH, Philippot P. Decoding of facial expression of emotion in criminal psychopaths. Journal of Personality Disorders. 2010; 24 :445–459. [ PubMed ] [ Google Scholar ]
- Pollak SD, Cicchetti D, Hornug K, Reed A. Recognizing emotion in faces: Developmental effects of child abuse and neglect. Developmental Psychology. 2000; 36 :679–688. doi: 10.1037//0012-1649.36.5.679. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pollak SD, Klorman R, Brumaghim J, Cicchetti D. P3b reflects maltreated children’s reactions to facial displays of emotion. Psychophysiology. 2001; 38 :267–274. [ PubMed ] [ Google Scholar ]
- Pollak SD, Sinha P. Effects of early experience on children’s recognition of facial displays of emotion. Developmental Psychology. 2002; 38 :784–791. doi: 10.1037//0012-1649.38.5.784. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pollak SD, Vardi S, Pultzer Bechner AM, Curtin JJ. Physically abused children’s regulation of attention in response to hostility. Child Development. 2005; 76 :968–977. [ PubMed ] [ Google Scholar ]
- Robins LN, Helzer JE, Cottler L, Goldring E. National Institute of Mental Health Diagnostic Interview Schedule, Version III Revised (DIS-III-R) St. Louis, MO: Washington University; 1989. [ Google Scholar ]
- Robins LN, Helzer JE, Croughan JL, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics, and validity. Archives of General Psychiatry. 1981; 38 :381–389. doi: 10.1001/archpsyc.1981.01780290015001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Salthouse TA. Structural models of the relations between age and measures of cognitive functioning. Intelligence. 2001; 29 (2):93–115. [ Google Scholar ]
- Salzinger S, Feldman RS, Hammer M, Rosario M. The effects of physical abuse on children’s social relationships. Child Development. 1993; 64 :169–187. [ PubMed ] [ Google Scholar ]
- Sanchez-Navarro JP, Martinez-Selva JM, Roman F. Uncovering the relationship between defense and orienting in emotion: Cardiac reactivity to unpleasant pictures. International Journal of Psychophysiology. 2006; 61 :34–46. doi: 10.1016/j.ijpsycho.2005.10.023. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. Journal of Counseling Psychology. 2010; 57 :1–10. doi: 10.1037/a0018082. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shackman JE, Shackman AJ, Pollak SD. Physical abuse amplifies attention to threat and increases anxiety in children. Emotion. 2007; 7 :838–852. doi: 10.1037/1528-3542.7.4.838. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shipman KL, Zeman J. Emotional understanding: A comparison of physically maltreating and nonmaltreating mother–child dyads. Journal of Clinical Child Psychology. 1999; 28 :407–417. [ PubMed ] [ Google Scholar ]
- Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse & Neglect. 2007; 31 :517–530. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stuhrmann A, Suslow T, Dannlowski U. Facial emotion processing in major depression: A systematic review of neuroimaging findings. Biology of Mood & Anxiety Disorders. 2011; 1 :10–27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Suveg C, Morelen D, Brewer GA, Thomassin K. The emotion dysregulation model of anxiety: A preliminary path analytic examination. Journal of Anxiety Disorders. 2010; 24 :924–930. [ PubMed ] [ Google Scholar ]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 6. Boston, MA: Allyn and Bacon; 2013. [ Google Scholar ]
- Talmi D, Schimmack U, Paterson T, Moscovitch M. The role of attention and relatedness in emotionally enhanced memory. Emotion. 2007; 7 :89–102. [ PubMed ] [ Google Scholar ]
- van der Vegt EJM, van der Ende J, Kirschbaum C, Verhulst FC, Tiemeier H. Early neglect and abuse predict diurnal cortisol patterns in adults: A study of international adoptees. Psychoneuroendocrinology. 2009; 34 :660–669. [ PubMed ] [ Google Scholar ]
- Weiler BL, Widom CS. Psychopathy and criminal behavior in abused and neglected young adults. Criminal Behavior and Mental Health. 1996; 6 :253–271. [ Google Scholar ]
- Widom CS. Child abuse, neglect and adult behavior: Research design and findings on criminality, violence, and child abuse. American Journal of Orthopsychiatry. 1989a; 59 :355–367. [ PubMed ] [ Google Scholar ]
- Widom CS. The cycle of violence. Science. 1989b; 244 :160–166. doi: 10.1126/science.2704995. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Widom CS. Understanding the consequences for childhood victimization. In: Robert MD, Reese M, editors. Treatment of child abuse. Baltimore, MD: Johns Hopkins University Press; 2000. pp. 339–361. [ Google Scholar ]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007; 64 :49–56. [ PubMed ] [ Google Scholar ]
Childhood Emotional Neglect: 5 Hidden Consequences

Parents or guardians failed to meet their children’s basic emotional needs or were insensitive to their distress or developmental needs.
Known as childhood emotional neglect (CEN), it is a type of adverse childhood experience (ACE). ACEs are highly stressful and potentially traumatic events or situations that occur during childhood or adolescence.
Adverse childhood experiences include living with someone who has mental health or substance abuse problems; losing a parent to death, divorce, or abandonment; and physical, sexual, and emotional abuse.
But unlike abuse, CEN may happen because of a lack of awareness. Researchers have established that CEN can result in a variety of psychological disorders, including depression, anxiety, substance abuse, and impaired social functioning later in life (Derin et al., 2022; Haslam & Taylor, 2022; Müller et al., 2019; Rees, 2008).
How can we help clients recover from its effects? In this article, we share insights on the phenomenon and suggestions for evidence-based interventions that foster healing and growth.
Before you continue, we thought you might like to download our three Emotional Intelligence Exercises for free . These science-based exercises will enhance your ability to understand and work with your emotions and give you the tools to foster the emotional intelligence of your clients, students, or employees.
This Article Contains
What is childhood emotional neglect, what are the potential causes of emotional neglect, 5 consequences of childhood emotional neglect, 5 signs and symptoms of childhood emotional neglect in adults, tests for childhood emotional neglect.
- 4 Books on Childhood Maltreatment, Abuse & Neglect
Healing From Childhood Emotional Neglect
Resources from positivepsychology.com, a take-home message.
CEN refers to a failure to meet the basic emotional needs of a child, a lack of emotional responsiveness to a child’s distress, ignoring a child’s social and emotional developmental needs, and expecting children to deal with situations beyond their maturity or that are unsafe (Teicher & Samson, 2013).
Sadly, it is a very common phenomenon.
Meta-analyses have revealed that the global prevalence of childhood emotional neglect is around 18% (Stoltenborgh et al., 2013; Stoltenborgh et al., 2015).
CEN has been closely associated with psychological disorders, including depression, anxiety, and substance abuse, in young adults and later in life (Grummitt et al., 2022; Infurna et al., 2016; Salokangas et al., 2020).
In addition, CEN can have long-term effects on social functioning and result in social anxiety , poor interpersonal interactions, and reduced relationship quality (Derin et al., 2022; Haslam & Taylor, 2022; Müller et al., 2019; Rees, 2008).
Intentional vs. unintentional neglect
According to Jonice Webb (2012, p. 15), a psychologist who extensively researched the phenomenon and coined the term childhood emotional neglect, CEN is “the failure of parents to respond enough to a child’s emotional needs.”
Webb emphasizes that this neglect can be both intentional and unintentional. Intentional CEN occurs when parents purposefully dismiss or invalidate their child’s emotions. Unintentional childhood emotional neglect arises when parents, despite their love and care, overlook the significance of emotional connection or are unable to establish it.
How neglect differs from abuse and mistreatment
Differentiating between neglect and abuse is crucial in understanding CEN. While abuse often involves intentional harm or mistreatment, neglect can involve unintentional negligence.
Emotional neglect can be subtle. Parents may fail to notice, validate, or respond to a child’s emotions.
Jonice Webb provides a clear explanation of the distinction between abuse and neglect on her website, saying, “Emotional neglect is, in some ways, the opposite of mistreatment and abuse” (What is, para. 4).
Parental neglect refers to a parent’s inaction, while abuse and mistreatment are acts of the parent. It is the inability to identify, acknowledge, or react suitably to a child’s emotions. It is not evident, noteworthy, or memorable because it is an act of omission.

ACEs can breed more ACEs in the next generations. Ylitervo et al. (2023, p. 1) found that “childhood adversities are transferred from parents to children at least in some form.”
“If parents have experienced ACEs, they will have a higher risk of mental health problems, and since having a depressed parent, for example, is considered an adverse childhood event, the child of such a parent will be at risk, leading to a vicious cycle in which adversities can be passed on for generations” (Ylitervo et al., 2023, p. 1).
Emotionally neglectful parents
Emotionally neglectful parents may contribute to childhood emotional neglect due to a lack of awareness or understanding of their child’s emotional needs. “Emotionally neglectful parents often appear loving and caring on the surface but remain unaware of their child’s emotional world” (Webb, 2012, p. 87).
This unconscious neglect can result from the parents’ own emotional challenges, making it challenging for them to attune to their child’s feelings.
Uninvolved parenting
Uninvolved parenting, characterized by emotional detachment and a lack of responsiveness, is another potential cause of CEN. The absence of emotional engagement can leave children feeling overlooked, invisible, and unimportant and may hinder the development of crucial emotional skills .
Cold mother syndrome
The term “cold mother syndrome” refers to a pattern of maternal behavior characterized by emotional distance, coldness, and unresponsiveness. This syndrome highlights the significant role active maternal warmth plays in fostering emotional wellbeing during childhood (Streep, 2017).
Peg Streep has written several powerfully empathetic books on the effects of having cold, unloving, or narcissistic mothers. In Daughter Detox (Streep, 2017), for example, she writes movingly about how cold mothers can destroy our trust in the legitimacy of our feelings and our connectedness to our emotions. A thus injured sense of self can result in constant self-vigilance, in being distrustful of others, and in not feeling worthy of respect and love.
This kind of mothering can impact attachment style and generate fearful dismissive or fearful avoidant behaviors.
Childhood emotional neglect can cast a long shadow on emotional wellbeing, both for young adults and later in life. As mentioned, those who have experienced CEN are more likely to struggle with (Grummitt et al., 2022; Infurna et al., 2016; Salokangas et al., 2020):
- Depression,
- Substance abuse
In addition, CEN can also result in abandonment issues and severely impact a client’s attachment style. Clients may find it more difficult to trust others and establish intimate relationships (Derin et al., 2022; Haslam & Taylor, 2022; Müller et al., 2019; Rees, 2008).
Abandonment issues
Abandonment issues stem from the emotional void created by childhood emotional neglect. Webb (2012, p. 42) describes how CEN “leaves a child feeling unseen, unheard, and unimportant.” The absence of emotional validation and responsiveness during formative years can instigate a profound fear of abandonment in adulthood.
Individuals who experience CEN may develop hypersensitivity to perceived rejection or neglect, often attributing it to their inherent unworthiness. This heightened sensitivity can impact relationships, causing them to distance themselves emotionally or cling excessively to others, seeking constant reassurance.
Attachment styles
CEN significantly influences the development of personal attachment styles, which form the basis for interpersonal relationships. Bowlby (1958) has shown that secure attachments in childhood lay the foundation for healthy relationships in adulthood. CEN can give rise to insecure attachment styles.
Individuals with a history of emotional neglect may exhibit anxious, avoidant, or disorganized attachment styles. Anxious attachment manifests as a fear of abandonment, leading to clinginess and constant seeking of validation.
Avoidant attachment, on the other hand, is marked by emotional distance and an aversion to intimacy. Disorganized attachment combines elements of both, creating a complex interplay of approach and avoidance behaviors (Streep, 2017).
You may enjoy this video, which delves more deeply into the questions of the consequences of CEN.
CEN shapes the emotional landscape of individuals, often leaving a profound impact on their adult lives. Recognizing the signs and symptoms of CEN is a crucial step toward understanding and addressing the aftermath of emotional neglect.
1. Emotional detachment
One hallmark sign of CEN is emotional detachment. Because their emotions were ignored or invalidated as children, adults who experienced CEN may struggle to connect with their emotions, leading to a sense of emptiness or numbness. This emotional detachment may hinder the formation of meaningful relationships and impede personal growth (Webb, 2012).
2. Perfectionism and overachievement
Individuals who grew up with emotional neglect may develop perfectionistic tendencies as a coping mechanism. The pursuit of perfection becomes a way to seek external validation and compensate for the lack of emotional support (Streep, 2017).
3. Difficulty setting boundaries
Another subtle but pervasive symptom of childhood emotional neglect is difficulty setting and maintaining healthy boundaries . Adults who have experienced emotional neglect may struggle to assert their needs, fearing rejection or abandonment. Recognizing and addressing these challenges is vital for fostering healthy interpersonal connections (Streep, 2017).
4. Low self-esteem
CEN often gives rise to feelings of inadequacy and low self-esteem in adulthood. Individuals with a history of neglect may struggle with a persistent sense of not being good enough (Webb, 2012).
Unraveling the roots of low self-esteem involves acknowledging the impact of emotional neglect and working toward building a more positive self-perception (Webb, 2012).
5. Difficulty expressing needs
Adults who have experienced CEN may find it challenging to express their needs openly. Addressing the difficulty of expressing needs requires cultivating assertiveness skills and fostering a sense of self-worth (Webb, 2012; Streep, 2017).
Download 3 Free Emotional Intelligence Exercises (PDF)
These detailed, science-based exercises will help you or your clients understand and use emotions advantageously.
Download 3 Free Emotional Intelligence Tools Pack (PDF)
By filling out your name and email address below.
Mental health professionals may use various assessments and tools to explore and identify the presence of CEN. It is essential to recognize that CEN is often diagnosed through clinical interviews, self-report measures, and discussions about an individual’s emotional experiences. Some commonly used methods for assessing CEN include the following:
1. CEN Questionnaire
Developed by Jonice Webb, this questionnaire is a self-report questionnaire designed to assess the extent of emotional neglect experienced during childhood.
It includes questions related to emotional expression, validation, and parental responsiveness.
You can access the questionnaire here .
2. The Childhood Trauma Questionnaire (CTQ)
While not specific to CEN, the CTQ is a widely used tool that includes a section on emotional neglect. It assesses various forms of childhood trauma, including emotional neglect, and can provide insights into the individual’s experiences. You can find out more about it on this website and access the questionnaire here .
It is crucial to approach these assessments with the understanding that childhood emotional neglect is a nuanced and often subtle form of emotional neglect. Professionals typically use a combination of assessments and clinical judgment to make a diagnosis.
4 Books on Childhood Maltreatment, Abuse & Neglect
If you would like to read more about the topic or recommend self-help books to your clients who have suffered from CEN, you may find the following four books helpful.
1. Running on Empty: Overcome Your Childhood Emotional Neglect – Jonice Webb
The psychologist Jonice Webb coined the term childhood emotional neglect and was the first researcher to write a book about the topic in 2012.
In her book, Webb explores 12 types of parents who inadvertently neglected their children emotionally, 10 issues that emotionally neglected children struggle with as adults, and six clear strategies for how to overcome CEN.
Find the book on Amazon .
2. Daughter Detox: Recovering From an Unloving Mother and Reclaiming Your Life – Peg Streep
Daughter Detox is recommended for anyone who has experienced the challenges of having an unloving mother.
The author, Peg Streep, provides a compassionate and insightful exploration of this difficult dynamic, offering practical strategies and exercises for healing and reclaiming one’s life.
The book offers valuable guidance and support for those navigating the complexities of maternal relationships, and it can be a source of empowerment and transformation for readers seeking to heal from this experience.
3. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma – Bessel van der Kolk
This ground-breaking book by renowned psychiatrist Bessel van der Kolk explores the effects of trauma on the body and mind.
It delves into the ways trauma can be stored in the body and offers insights into innovative therapeutic approaches for healing. While it is not specifically about CEN, many of van der Kolk’s suggestions for therapeutics apply and can be helpful for CEN, too.
4. The Deepest Well: Healing the Long-Term Effects of Childhood Adversity – Nadine Burke Harris
The physician Nadine Burke Harris explores the science behind adverse childhood experiences and their impact on health.
The book emphasizes the importance of early intervention and resilience in mitigating the effects of childhood adversity.
The effects of CEN can be mitigated by self-reflection and therapy. Seeking the guidance of a mental health professional can be a crucial step in healing from CEN.
Therapists specializing in trauma and emotional neglect can provide a safe space for individuals to explore their emotions, identify patterns, and develop coping strategies. Psychodynamic therapy, Cognitive-Behavioral Therapy, Acceptance and Commitment Therapy, and Dialectical Behavior Therapy may all be useful therapeutic approaches.
Fostering self-compassion is perhaps the most important and helpful therapeutic intervention when working with a client who has experienced CEN. Deepening self-knowledge and helping clients develop a more compassionate self-story are crucial, as are identifying and changing negative core beliefs that revolve around unlovability and being bad or unworthy.
Mindfulness practices can also help clients tune in to their emotions, fostering a deeper understanding of their inner experiences. Mindfulness allows individuals to observe their thoughts and feelings without judgment, creating space for self-compassion and acceptance.
Learning to establish and maintain healthy boundaries is another crucial skill for individuals with a history of CEN.
In addition, Hartanto et al. (2020) found that purpose in life significantly moderates the link between childhood emotional neglect and adult depressive symptoms. Their study “highlights the important role played by purpose in life in building resilience, coping against adverse life events, and psychological wellbeing” (Hartanto et al., 2020, p. 1).
Purpose includes having a clear sense of meaningful direction in our lives. It entails working toward long-term life pursuits and goals and can help us persevere and continue to strive in spite of external difficulties. Having a purpose also provides a sense of coherence and helps us develop more helpful self-stories (Hartanto et al., 2020).
Given the importance of developing kinder, more compassionate stories about ourselves when we have suffered from CEN, you may find these articles on self-compassion helpful:
- 15 Most Interesting Self-Compassion Research Findings
- 8 Powerful Self-Compassion Exercises & Worksheets (+PDF)
You may also find these free tools for fostering self-compassion useful:
- Letter of Self-Compassion
- I Will Survive
You may also enjoy these tools for boundary setting:
- Visualizing Your Boundaries
- The Personal Boundary Continuum: A Self-Reflection Tool
Finally, why not have a look at this life purpose tool?
- Uncover Your Purpose
If you’re looking for more science-based ways to help others develop emotional intelligence, check out this collection of 17 validated EI tools for practitioners. Use them to help others understand and use their emotions to their advantage.
17 Exercises To Develop Emotional Intelligence
These 17 Emotional Intelligence Exercises [PDF] will help others strengthen their relationships, lower stress, and enhance their wellbeing through improved EQ.
Created by Experts. 100% Science-based.
Sadly, CEN is a very common experience. Much more subtle and harder to grasp than child abuse, it can nevertheless have serious negative consequences for mental health and attachment styles later in life.
The good news is that there are books, self-help strategies, and psychological interventions that can help clients process and make sense of these ACEs and begin to heal from them.
First and foremost, people who have experienced CEN should be encouraged and supported to develop more self-compassion, to take their emotions seriously, understand and reconnect with their emotions, and learn how to set healthy boundaries.
We hope you enjoyed reading this article. Don’t forget to download our three Emotional Intelligence Exercises for free .
- Bowlby, J. (1958). The nature of the child’s tie to his mother. International Journal of Psychoanalysis , 39 , 350–371.
- Derin, S., Selman, S. B., Alyanak, B., & Soylu, N. (2022). The role of adverse childhood experiences and attachment styles in social anxiety disorder in adolescents. Clinical Child Psychology and Psychiatry , 27 (3), 644–657.
- Grummitt, L. R., Kelly, E. V., Barrett, E. L., Lawler, S., Prior, K., Stapinski, L. A., & Newton, N. C. (2022). Associations of childhood emotional and physical neglect with mental health and substance use in young adults. The Australian and New Zealand Journal of Psychiatry , 56 (4), 365–375.
- Haslam, Z., & Taylor, E. P. (2022). The relationship between child neglect and adolescent interpersonal functioning: A systematic review. Child Abuse & Neglect , 125 .
- Hartanto, A., Ypng, J. C., Lee, S. T. H., Ng, W. Q., & Tong, E. M. W. (2020). Putting adversity in perspective: Purpose in life moderates the link between childhood emotional abuse and neglect and adulthood depressive symptoms. Journal of Mental Health , 29 (4), 473–482.
- Infurna, M. R., Reichl, C., Parzer, P., Schimmenti, A., Bifulco, A., & Kaess, M. (2016). Associations between depression and specific childhood experiences of abuse and neglect: A meta-analysis. Journal of Affective Disorders , 190 , 47–55.
- Müller, L. E., Bertsch, K., Bülau, K., Herpertz, S. C., & Buchheim, A. (2019). Emotional neglect in childhood shapes social dysfunctioning in adults by influencing the oxytocin and the attachment system: Results from a population-based study. International Journal of Psychophysiology , 136 , 73–80.
- Rees, C. (2008). The influence of emotional neglect on development. Paediatrics and Child Health , 18 (12), 527–534.
- Salokangas, R. K. R., Schultze-Lutter, F., Schmidt, S. J., Pesonen, H., Luutonen, S., Patterson, P., & Hietala, J. (2020). Childhood physical abuse and emotional neglect are specifically associated with adult mental disorders. Journal of Mental Health , 29 (4), 376–384.
- Stoltenborgh, M., Bakermans-Kranenburg, M. J., Alink, L. R. A., & van Ijzendoorn, M. H. (2015). The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Review , 24 (1), 37–50.
- Stoltenborgh, M., Bakermans-Kranenburg, M. J., & van Ijzendoorn, M. H. (2013). The neglect of child neglect: A meta-analytic review of the prevalence of neglect. Social Psychiatry and Psychiatric Epidemiology , 48 (3), 345–355.
- Streep, P. (2017). Daughter detox: Recovering from an unloving mother and reclaiming your life . Ile d’Espoir Press.
- Teicher, M. H., & Samson, J. A. (2013). Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. The American Journal of Psychiatry , 170 (10), 1114–1133.
- Webb, J. (2012). Running on empty: Overcome your childhood emotional neglect . Morgan James.
- What is childhood emotional neglect? (n.d.). https://drjonicewebb.com/
- Ylitervo, L., Veijola, J., & Halt, A.-H. (2023). Emotional neglect and parents’ adverse childhood events. European Psychiatry , 66 (1), 1–6.

Share this article:
Article feedback
Let us know your thoughts cancel reply.
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Dysregulation: Navigating Through Emotional Turmoil
As mental health professionals, we often find emotional dysregulation at the heart of our clients’ challenges. Like a yoyo, the ups and downs of emotions [...]

Neuroticism: 12 Emotion Regulation Skills & Worksheets
Neuroticism is a crucial aspect of personality and significantly impacts how we see ourselves and the world around us (Widiger & Oltmanns, 2017). Those of [...]
14 Anger Management Books & Workbooks for Therapists & Kids
Anger is a universal emotion. It can be a natural response to perceived threats, generating the energy required to protect ourselves and obtain justice. However, [...]
Read other articles by their category
- Body & Brain (54)
- Coaching & Application (58)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (23)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (27)
- Meditation (20)
- Mindfulness (44)
- Motivation & Goals (46)
- Optimism & Mindset (34)
- Positive CBT (30)
- Positive Communication (22)
- Positive Education (48)
- Positive Emotions (32)
- Positive Leadership (19)
- Positive Parenting (16)
- Positive Psychology (34)
- Positive Workplace (37)
- Productivity (18)
- Relationships (45)
- Resilience & Coping (39)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
3 Emotional Intelligence Exercises (PDF)
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About The British Journal of Social Work
- About the British Association of Social Workers
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Introduction, gaps in knowledge, limitations of this review, supplementary material, social workers’ perceptions of the nature of child neglect: a systematic literature review.
- Article contents
- Figures & tables
- Supplementary Data
Jennifer Gibbs, Barry Coughlan, Tessa Morgan, Arbenita Mikushnica, Samantha Phippard, Francesca Crozier-Roche, Taliah Drayak, David Graham, Jack Smith, Robbie Duschinsky, Social Workers’ Perceptions of the Nature of Child Neglect: A Systematic Literature Review, The British Journal of Social Work , 2024;, bcae102, https://doi.org/10.1093/bjsw/bcae102
- Permissions Icon Permissions
Neglect is the most common form of child maltreatment in the UK and the USA. This article reviews research about how child neglect is perceived by social workers. We conducted a systematic review and identified fifty relevant studies, using a range of methodologies, published since the 1989 Children Act. The themes were identified iteratively and synthesised using a narrative method. The review found that despite evidence that neglect is associated with several adverse outcomes, neglect is a lower priority for social work intervention compared to other forms of maltreatment. This is particularly true for emotional neglect and neglect of older children. The review found that social workers conceptualise poverty and neglect as being distinctly different and try to address poverty through practical, non-punitive interventions. However, assessments could better recognise how deprivation exacerbates other risk factors for neglect. The review found a lack of knowledge about perceptions of neglect in adolescents and children with a disability and about the threshold for intervention when neglect is cumulative. Practice may be improved by better recognising and addressing the societal context to neglect allegations and the risk of long-term harm. Achieving this may have resource and training implications.
Neglect is the most commonly documented form of child maltreatment in the UK ( Department for Education, 2023 ) and the USA ( US Department of Health & Human Services, 2023 ). Death or serious injury from neglect is rare ( Dickens et al. , 2022a ). Nonetheless, meta-analyses have shown that neglect, particularly emotional neglect, is moderately associated with adverse outcomes, including suicidal behaviour ( Liu et al. , 2017 ; Angelakis et al. , 2019 , 2020 ), depression ( Liu et al. , 2017 ; Nelson et al. , 2017 ; Humphreys et al. , 2020 ), borderline personality disorder ( Porter et al. , 2020 ), psychosis ( Peh et al. , 2019 ) and impaired educational achievement ( Romano et al. , 2015 ). The strength of the association is comparable to that of other forms of maltreatment ( Coughlan et al. , preprint ).
There has been a longstanding ‘neglect of neglect’ ( Wolock and Horowitz, 1984 ) in public consciousness and social work practice. Recent reviews of practice continue to observe a ‘normalisation’ ( Dickens et al. , 2022b , p. 52) and ‘desensitisation’ ( Brandon et al. , 2020 , p. 63) to neglect and insufficient professional curiosity ( Dickens et al. , 2023 ). There are also concerns that thresholds for intervention are too high ( Daniel, 2015 ; Stokes, 2016 ).
Research into neglect faces several challenges. First, definitions of neglect are inconsistent ( Horwath, 2007 ), with some considering only past harm and others future risk ( Dubowitz et al. , 1993 ; Zuravin, 1999 ). There is a shortage of evidence-based instruments with which to measure neglect ( Haworth et al. , 2024 ). Secondly, there is concern about the overlap between neglect and social disadvantage. The link to poverty is well documented ( Esposito et al. , 2022 ; Goldacre and Hood, 2022 ; Skinner et al. , 2023 ), with some authors alleging that neglect is ‘too often confused with poverty’ ( Dewan, 2018 ; Raz and Sankaran, 2019 , p. 1529). There are also concerns that mothers are judged harshly, overlooking the responsibilities of fathers ( Turney, 2000 ).
Given the above concerns, this review aims to explore social workers’ perceptions of neglect. This question is relevant to practice and academic scholarship, where informant reporting, particularly from social workers is used as an indicator of neglect ( Stoltenborgh et al. , 2015 ).
We are aware of only two previous systematic reviews on this topic. One is unpublished and does not include quality appraisal. These concentrated primarily on the views of other stakeholders ( Daniel et al. , 2010 ) and non-empirical papers ( Chaudhry, 2016 ).
A systematic review was completed according to PRISMA guidelines ( Page et al. , 2021 ) ( Supplementary Appendix 1 ).
Search strategy
Web of Science, Embase, PsychInfo, Scopus and Assia were searched on 7 July 2023 (see Supplementary Appendix 2 for search strategy). Filters identified articles in English, written after the 1989 Children Act (enacted 1991), in which current statutory thresholds are defined.
Snowballing added thirty-nine results, including one piece of ‘grey’ literature ( Horwath, 2001 ) containing supplementary data from published studies ( Horwath, 2004 , 2005 ). This search yielded 2,091 studies once duplicates were removed.
Inclusion criteria were drafted and refined following evidence mapping ( Popay et al. , 2006 ), with the addition of the fourth and fifth exclusion criteria (see Supplementary Appendix 3 for PRISMA flowchart). Figure 1 states the inclusion and exclusion criteria. We defined ‘neglect’ as harmful acts of omission by a caregiver (failure to do something necessary for a child’s wellbeing) and excluded acts of commission (proactively doing something harmful to the child; Zuravin, 1999 ). To ensure relevance, we included only empirical studies which reported discrete findings about neglect. We included the views of child welfare practitioners who had, or were working towards, a social work qualification and of child protection investigators, whatever their qualifications. We included empirical studies of any methodology which explored social workers’ responses to hypothetical situations, what might be termed their ‘espoused perceptions’, and studies exploring perceptions implicit in practitioners’ actions, their ‘enacted perceptions’. We excluded studies about the context of perceptions.

Title and abstract screening decision flow-chart. This flowchart shows the criteria used to decide which of the 2,091 items identified from database searches were relevant to the review’s question.
Using Rayyan, J.G. screened all titles and abstracts, identifying 108 potentially relevant articles from the total of 2,091. A.M. independently screened 10 per cent of these, with complete agreement. J.G. then extracted and screened full texts. J.G. and A.M. are both social workers.
Quality appraisal and synthesis
J.G. used the Mixed Methods Appraisal Tool ( Hong et al. , 2018 ) to evaluate the studies’ merit in their own right, and Gough’s Weight of Evidence framework ( Gough, 2007 ) to assess quality in relation to this review’s question. Supplementary Appendix 4 details data extraction and quality appraisal.
The selected studies used a wide range of methodologies. Several vignette studies ( Segal, 1992 ; Rose and Meezan, 1995 , 1996 ; Rose, 1999 ; Proctor, 2012 ) were inspired by the same study ( Giovannoni and Becerra, 1979 ) but instruments and reporting practices varied. Meta-analysis was not, therefore, feasible and we instead used an adapted form of narrative synthesis ( Popay et al. , 2006 ) (see Appendices 5 and 6). Recurrent themes were identified iteratively, and quantitative data were translated into themes. Themes were tabulated, alongside study characteristics to allow for comparison between studies. Relationships in the data were then explored to develop a preliminary synthesis.
To add rigour, J.G. discussed findings with social work (A.M. and S.P.) and non-social work collaborators (academics B.C., T.M. and R.D. and experts by experience, F.C.R., T.D., D.G. and J.S.) and reflected on how her positionality as a practising social worker shaped her interpretation.
Fifty articles, describing forty-six discrete studies, met the criteria.
Three studies were theses, one a report and the remainder was articles from peer-reviewed journals.
Twenty-four studies were rated as high-quality, and twenty-six as medium quality.
Most studies were conducted in the USA (nineteen) or the UK (eleven).
Respondents were predominantly female, in line with the demographics for the profession ( Department for Education, 2022 ). Two studies recruited students.
Thirteen papers used interviews and/or focus groups to look at social workers’ ‘espoused’ perceptions. Most were conducted in the UK (eleven) or Ireland (two); seven were conducted after 2010. Eleven of these were assessed as high quality. A further seventeen studies, of which two were from the same project ( Rose and Meezan, 1995 , 1996 ), used surveys containing case vignettes. The majority of these were completed in the USA (thirteen) and prior to 2000 (ten); five were rated as high quality.
Of studies of ‘enacted’ perceptions (perceptions implicit in practice decisions), seven studies conducted qualitative analyses of case files and one of serious case reviews. These were all conducted in the UK and Ireland. Seven were of high quality. Three reported findings from the same project ( Horwath, 2001 , 2004 , 2005 ). Finally, eleven analysed administrative records, of which six were high-quality. These were conducted in the USA, Canada and Australia. Finally, two studies, of which one high-quality study, observed social workers’ practice.
The main themes identified in the selected studies were:
Definitions of harmful neglect
Perceived risk factors for neglect.
The priority afforded to neglect.
Neglect is a multi-faceted issue
Qualitative studies selected found that social workers had complex and diverse understandings of neglect ( Stone, 1998 ; Coope and Theobald, 2006 ). Perceived components of neglect included child and parent factors, family dynamics, compliance and wider societal issues ( Stone, 1998 ). Neglect was perceived to manifest in relation to both physical and psychological needs ( Horwath, 2001 ; Coope and Theobald, 2006 ).
Definitions of neglect are not fixed
Several studies demonstrated that social workers’ views about neglect were not entirely consistent ( Ashton, 1999 ; Berrick et al. , 2020 ; Bolton et al. , 2021 ). The agreement was lowest, at one point as low as 16 per cent, about vignettes classified by an ‘expert’ as constituting moderate harm ( Arruabarrena and De Paúl, 2012 ; Bolton et al. , 2021 ) and about age-appropriate levels of supervision ( Youssef and Atta, 1998 ; Arruabarrena and De Paúl, 2012 ). Training in standardised assessment tools only partially improved consistency ( Arruabarrena and De Paúl, 2012 ).
Social workers recognised this complexity. Sixty-seven per cent agreed with the statement, ‘subjective information influences decision-making in cases of child neglect’ ( Horwath, 2001 , p. 58). Qualitative studies reported reflections such as ‘there are no systems to say when enough is enough’ ( Horwath, 2001 , p. 93) (see also Chaudhry, 2016 , p. 80; Casey and Hackett, 2021 , p. 2105).
Younger children are perceived to be more vulnerable
The selected studies did not test child variables systematically. Only three survey vignettes featured children over eleven and none depicted children over fourteen years. Results were sometimes reported in broad categories, for example, ‘6–17 s’ ( Bérubé et al. , 2017 ).
Nonetheless, there was evidence that age influences social workers’ perceptions of neglect. In their espoused and enacted perceptions, social workers were more likely to be concerned about basic care, emotional warmth and guidance ( Bérubé et al. , 2017 ) and recommend removal ( Mandel et al. , 1995 ) for younger children. Practitioners commented that teenagers could take some responsibility for their own needs ( Hicks and Stein, 2015 ).
Analysis of child protection services databases showed no significant difference in the likelihood that social workers would substantiate allegations of neglect for younger children and adolescents ( Raissian et al. , 2014 ). However, adolescents were less likely to be referred in the first place, so it is possible that any referrals were for particularly serious matters, explaining this difference.
Mothers are more frequently held to account for neglect than fathers
One study found that, once identified as perpetrators of neglect, males and females had comparable odds of their child being removed ( Crawford and Bradley, 2016 ). However, when first identifying perpetrators, there was evidence that assessments and interventions more frequently focused on the mother ( Horwath, 2004 , 2005 ; Farmer and Lutman, 2014 ; Bérubé et al. , 2017 ). One explanation is linked to the prioritisation of physical care needs (discussed below), which tradition depicts as a mother’s responsibility ( Scourfield, 2000 ). An alternative explanation is of pragmatism since attempts to engage fathers were not always successful ( Horwath, 2005 ; Farmer and Lutman, 2014 ); however, worryingly, sometimes no effort was evident ( Daniel and Baldwin, 2001 ; Horwath, 2005 ).
Parental substance misuse, mental ill-health and learning difficulties are perceived risk factors for neglect
The selected studies suggested that social workers believed that certain parental factors increased the risk of neglect including substance misuse ( Stone, 1998 ; Forrester, 2000 ; Horwath, 2001 ; Coope and Theobald, 2006 ; Bérubé et al. , 2017 ; Freisthler et al. , 2017 ), learning difficulties/disability ( Proctor, 2012 ; Tefre, 2017 ) and mental ill-health (no studies differentiated between mental illnesses). It was felt that these parental factors led to neglect through inadequate supervision, inadequate safety, stimulation, emotional warmth and guidance and boundaries ( Bérubé et al. , 2017 ), failure to meet immediate needs ( Roscoe et al. , 2021 ) and financial difficulties which made basic necessities unaffordable ( Horwath, 2001 ). There was also evidence that the social acceptability of parental behaviour influenced perceptions, with greater concern about misuse of illegal drugs than of alcohol or prescription drugs ( Forrester, 2000 ; Freisthler et al. , 2017 ).
Nonetheless, the studies found that social workers still felt sympathy towards parents with learning disabilities ( Proctor, 2012 ) and mental ill-health ( Tufford et al. , 2015 ). Indeed, one study found that student social workers over-identified with the parent and failed to address the risk to the child during a practice observation ( Tufford et al. , 2015 ).
In decision-making about neglect, social workers may place more weight on indicators of future risk, such as parental factors, than on harm that has already occurred
Two studies suggested that parental factors were the strongest influence on perceptions of neglect ( Stone, 1998 ; Tefre, 2017 ), one child factors ( Chaudhry, 2016 ). However, the latter study placed child factors at the top of a list of survey responses, which may have led respondents, whereas the former studies coded answers to open questions.
Although social workers stated that they would consider the impact on the child ( Hicks and Stein, 2015 ) there was little evidence of this in case files ( Daniel and Baldwin, 2001 ; Horwath, 2005 ; Horwath and Tarr, 2015 ). Rather, assessments often discussed parenting in a ‘vacuum’ ( Horwath and Tarr, 2015 , p. 1388) and treated siblings as an undifferentiated group ( Casey and Hackett, 2021 ). This may reflect a lack of recording or difficulty measuring the impact on a child.
Material deprivation of itself is not considered to constitute neglect. However, practitioners do not always fully recognise how poverty exacerbates other risk factors
In both high-income (UK) ( Stone, 1998 ) and low-income (Guatemala) ( Coope and Theobald, 2006 ) countries, social workers reported that poverty often coexisted with neglect.
In their ‘espoused’ perceptions, social workers stated that material deprivation did not itself amount to neglect, rather, a deficit of caregiving also had to be present ( Stone, 1998 ). Studies of ‘enacted’ perceptions (practice) confirmed that caregiver concerns were present in 99 per cent of neglect investigations ( Palmer et al. , 2022 ) and that the presence of such risk factors predicted social workers’ response better than poverty ( Gordon and Gibbons, 1998 ) or housing ( Hirsch et al. , 2015 ) alone. Some social workers also recognised that emotional neglect could occur within affluent families ( Bernard, 2019 ; Bernard and Greenwood, 2019 ).
In instances where the link between poverty and neglect was obvious, such as a lack of essentials, social workers exercised flexible thresholds: ’Is there no food in house because it is dole day…?’ ( Horwath, 2001 , p. 59). Furthermore, two older studies found that if all other factors were kept equal (including parental risk factors), social workers were less likely to escalate interventions when responding to case vignettes ( Mandel et al. , 1995 ) or actual cases ( Gordon and Gibbons, 1998 ) concerning children from certain low-income groups, for example, lone parents. This suggests that social workers were influenced by parental capacity and intent. Non-punitive interventions might be offered in such circumstances ( Coope and Theobald, 2006 ; Beck and Vornanen, 2019 ; Abdullah et al. , 2021 ). Indeed, there was evidence from serious case reviews that sometimes practitioners sometimes overcompensated, ‘normalising’ neglect in the context of poverty and overlooking more serious concerns ( Taylor et al. , 2024 ).
Thus, in their discourse, some social workers claimed to achieve a binary distinction between poverty and neglect, for example, ‘it is not because of a lack of will, but… a lack of resources’ ( Beck and Vornanen, 2019 , p. 23) (see also Coope and Theobald, 2006 , p. 531; Casey and Hackett, 2021 , p. 2105).
Nonetheless, there was evidence that in practice social workers did not always differentiate between poverty and neglect as neatly as they believed. They sometimes underestimated the prevalence of hardship ( Bérubé et al. , 2017 ) and failed to fully recognise how poverty contributed to parental risk factors. Comments in the ‘environmental’ section of assessments were often tokenistic and not integrated with the rest of the assessment ( Daniel and Baldwin, 2001 ; Casey and Hackett, 2021 ). Some social workers recognised this risk of perpetuating structural inequalities: ‘it does feel like you are … persecuting women for the inadequacies of society’ ( Scourfield, 2000 , p. 379). They were also frustrated by barriers when pursuing concerns about more affluent, powerful families ( Bernard, 2019 ; Bernard and Greenwood, 2019 ).
The priority afforded to neglect
The greatest concern is for physical and supervisory neglect.
Vignettes concerning physical needs featured in ten of the survey studies and inadequate supervision in nine (one did not break findings down into neglect subtypes). These were almost entirely rated towards the higher end of the severity scale ( Craft and Staudt, 1991 ; Segal, 1992 ; Rose and Meezan, 1995 ; 1996 ; Dubowitz et al. , 1998 ; Youssef and Atta, 1998 ; Ashton, 1999 ; Rose, 1999 ; Proctor, 2012 ). The only exception was a medium-quality study, which reported the average for a group of vignettes at slightly below the half-way mark ( Rose and Meezan, 1995 , 1996 ; Rose, 1999 ). Concern was highest when the risk of harm was imminent, such as failure to give essential medical care, and lowest when the harm was more distal, such as wearing ill-fitting clothing ( Craft and Staudt, 1991 ).
Emotional neglect was featured in seven vignette studies; two reported distinct findings about behavioural neglect. These were rated as slightly above the middle of the seriousness scale ( Segal, 1992 ; Rose and Meezan, 1995 , 1996 ; Dubowitz et al. , 1998 ; Rose, 1999 ), other than very extreme examples, for example, ‘… parents have kept their child locked in since birth…’ ( Segal, 1992 ). Fewer than 30 per cent of social workers thought the emotional neglect vignettes would meet the threshold for statutory intervention ( Craft and Staudt, 1991 ).
Only three studies included discrete findings about educational neglect ( Craft and Staudt, 1991 ; Segal, 1992 ; Youssef and Atta, 1998 ). More than half of social workers considered these to amount to maltreatment ( Segal, 1992 ; Youssef and Atta, 1998 ), yet a minority felt that concerns would meet the threshold for statutory intervention ( Craft and Staudt, 1991 ). Vignettes featuring non-school attendance were considered to be much more serious (28–50 per cent would substantiate) than a lack of toys (4 per cent) ( Craft and Staudt, 1991 ).
Comparing the relative priority of these neglect subtypes, two high-quality studies agreed that physical and supervisory neglect were perceived as the most serious and most likely to meet the threshold for substantiation, whilst emotional neglect was the lowest priority ( Craft and Staudt, 1991 ; Youssef and Atta, 1998 ). Three other studies found that emotional/psychological neglect was rated higher than physical ( Rose and Meezan, 1995 , 1996 ; Dubowitz et al. , 1998 ). However, the latter study’s data appear to contain an error. The quality of these studies was also impaired by including in this category vignettes which could equally be classified as inadequate supervision or physical abuse.
A slightly contrasting picture emerged when social workers were asked about their priorities in abstract terms. More agreed with the statement ‘the most damaging environment for children is one of high criticism and low warmth’ (53 per cent, n = 21) than ‘the essential aspect of parenting is providing for a child’s physical needs and safety’ (33 per cent, n = 13) ( Horwath, 2001 , 2004 ). This may reflect a disconnect between social workers’ values and their ability to respond to emotionally harmful actions in practice. Nonetheless, there remained a sizeable minority of participants who prioritised physical over emotional needs ( Horwath, 2004 ).
Unfortunately, few studies of perceptions ‘enacted’ in practice differentiated between neglect subtypes. Those which did suggest a similar order of priority: abandonment and lack of supervision were the most common reasons for investigations ( Palmer et al. , 2022 ) and court proceedings ( Farmer and Lutman, 2014 ). Educational neglect was the least likely ( Van Wert et al. , 2018 ). Two older studies found that emotional neglect was rarely mentioned in case files ( Horwath, 2004 ) and there was instead a ‘preoccupation with dirt, disorder and diet’ ( Scourfield, 2000 , p. 377). Unfortunately, we found no more recent evidence.
Neglect is a lower priority than other forms of maltreatment
The selected studies provided evidence of how social workers prioritise neglect in comparison to other forms of abuse. Only three such survey studies were rated as high quality ( Abner, 1996 ; Youssef and Atta, 1998 ; Stokes and Taylor, 2014 ) but the same trends were seen in medium-quality studies ( Ashton, 1999 ; Rossi et al. , 1999 ; Beck and Vornanen, 2019 ), namely that vignettes depicting neglect were consistently rated as less serious than those featuring physical or sexual abuse. Interestingly, this pattern held even when the physical consequences from neglect were more serious ( Abner, 1996 ), suggesting that parental intent influenced perceptions.
Studies of perceptions ‘enacted’ in practice showed a similar picture. High-quality analyses of administrative data showed that children investigated for neglect were less likely to be placed on the child protection register ( Gordon and Gibbons, 1998 ) and to be removed from their parents ( Crawford and Bradley, 2016 ) or referred for mental health support ( Fong et al. , 2018 ) than those investigated for other forms of abuse. Removal often only happened after a child had experienced a different form of maltreatment ( Barber and Delfabbro, 2009 ; Farmer and Lutman, 2014 ). One exception to this found that children investigated for neglect were more likely to receive ongoing child welfare services than those investigated for other forms of maltreatment once other variables were controlled for ( King et al. , 2021 ). This difference may be because the study area used an assessment tool which considered future as well as past harm.
This review is the first to explore how social workers define neglect. It contributes to the wider literature in several ways.
First, neglect is a complex, multi-faceted issue and practitioners’ definitions are not entirely consistent.
Secondly, there is evidence that social workers’ working definitions of neglect encompass the risk of future harm as well as past events, with particular emphasis on parental risk factors.
Thirdly, there is a suggestion that social workers consider parental intent when assessing neglect. This may reflect a belief that intent predicts recurrence and also anxiety about blaming vulnerable parents who cause harm unintentionally. Nevertheless, this concern with parental interests could mean that the child’s needs get overlooked.
Fourthly, this review suggests that, although social workers recognise children’s emotional needs, in practice, priority is afforded to the imminent physical needs of younger children. Sometimes, this may be a response to high-profile child deaths (e.g. in Scourfield, 2000 ) but it appears to be a wider issue which we suspect reflects the difficulty of evidencing emotional harm.
The review also suggests that social workers may not prioritise neglect as much as other forms of maltreatment. Given the adverse effects of neglect cited in the introduction, this review raises the possibility that children experiencing neglect, particularly emotional neglect, may receive insufficient support, especially at an early stage. Social workers may also be intervening unnecessarily with children who experience deprivation but are emotionally well ( Scourfield, 2000 ). Caution is needed, however, since much of the literature on the long-term sequelae of child neglect uses participant self-reporting, which carries recall bias ( Stoltenborgh et al. , 2015 ). To better understand whether social workers’ attitudes to neglect are proportionate, further evidence is needed about outcomes for children where neglect allegations are not substantiated, ideally from a prospective cohort study or administrative data.
A final contribution from this review is that social workers have good intentions in relation to poverty but may not always fully realise these. The review found a lack of discussion from social workers about how poverty relates to other perceived risk factors for neglect. This may be a product of the studies’ research design but there was some evidence that opportunities to consider structural factors were not always utilised optimally. The reasons for this are unclear but it is possible that social workers only documented factors that they could influence.
The review highlighted several gaps in knowledge of how social workers perceive neglect.
A first limitation is about emotional, educational and behavioural neglect, which featured infrequently in the selected studies. Additionally, since most knowledge comes from vignette studies published pre-2000, evidence is lacking about contemporary issues such as preventable childhood obesity, dental decay or online supervision.
A second limitation is about perceptions of neglect of older children and those with disabilities. This is at odds with the needs of practice. Epidemiological studies have shown that children with disabilities are more likely to be referred due to concerns about neglect ( Sullivan and Knutson, 2000 ). Furthermore, in 2021 in England, 38 per cent ( n = 9540) of children subject to a child protection plan for neglect were aged ten or over ( Department for Education, 2023 ). Academic literature is also increasingly recognising the link between adolescent neglect and exploitation ( Hicks and Stein, 2015 ; Raws, 2019 ).
A third limitation is about cumulative harm. Neglect is frequently a chronic problem ( Stone, 1998 ), yet the vignette studies only contributed to knowledge about isolated incidents or risk factors. This risks under-representing the perceived seriousness of neglect. Further information is needed about where the ‘tipping point’ is believed to be for intervention. Detailed analysis of case files would be beneficial here, as would questionnaires asking about responses to a series of vignettes.
A fourth limitation concerns differences in perceptions over time and between countries. Knowledge was hampered by the lack of a consistent instrument with which to measure perceptions and a change in dominant methodologies, from vignette survey studies prior to 2000 to qualitative methods since.
A final comment is about the overall quality of studies. Fewer than half of the studies selected were of high quality. Sampling strategies were a persistent weakness. Convenience methods dominated and their implications were not always adequately evaluated. This means that social workers’ views are likely to be more diverse than the selected studies suggest.
The search strategy only included articles in English, creating a geographical bias.
This review also only included studies with discrete findings about neglect yet as many as half of the children referred experienced more than one form of maltreatment ( Euser et al. , 2013 ). This may have resulted in some over-sharp distinctions in findings about neglect and limits generalisability to practice.
Only one researcher assessed the quality of studies and their subsequent weight of evidence, creating some risk of bias.
This review also did not consider the context to social workers’ perceptions.
For practice, this review leads to the following conclusions. First, social workers may need to give higher priority to neglect, particularly emotional neglect and neglect of older children. To achieve this, they need to recognise the risk of long-term harm and better evidence of how neglect affects individual children. Achieving this, whilst simultaneously responding to referrals concerning imminent physical risk, will have training and resource implications. Secondly, social workers should ensure that they explicitly capture information about the societal context to neglect allegations, including the role of poverty and gender. This will make assessments fairer and ensure that opportunities for intervention are not missed.
For child welfare researchers, the review implies that when administrative data state that an allegation of neglect was substantiated, this most likely involved physical or supervisory neglect, and an imminent risk of harm. Children may have experienced emotional, behavioural or educational neglect without this being substantiated. It also suggests that practitioners’ perceptions vary somewhat, which might help explain outlying results. Finally, there is evidence that social workers have good intentions regarding poverty and make some attempt to address this, within the limitations of resources.
Supplementary material is available at British Journal of Social Work Journal online.
Jennifer Gibbs currently receives funding via an National Institute for Health and Care Research Pre-Doctoral Fellowship, award number NIHR302735. The article was largely complete by the time that the fellowship commenced but some fellowship time was spent finishing the work.
Conflict of interest statement : None declared.
Abdullah A. , Ayim M. , Bentum H. , Emery C. R. ( 2021 ) ‘ Parental poverty, physical neglect and child welfare intervention: Dilemma and constraints of child welfare workers in Ghana ’, Children and Youth Services Review , 126 , 106036 .
Google Scholar
Abner J. P. ( 1996 ) Effects of Type of Maltreatment, Severity of Physical Consequence, and Respondent Variables on the Perceptions of Medical Neglect and Physical Abuse , Gainesville, FL , Graduate School, University of Florida .
Google Preview
Angelakis I. , Austin J. L. , Gooding P. ( 2020 ) ‘ Association of childhood maltreatment with suicide behaviors among young people: A systematic review and meta-analysis ’, JAMA Network Open , 3 ( 8 ), pp. e2012563 .
Angelakis I. , Gillespie E. L. , Panagioti M. ( 2019 ) ‘ Childhood maltreatment and adult suicidality: A comprehensive systematic review with meta-analysis ’, Psychological Medicine , 49 ( 7 ), pp. 1057 – 78 .
Arruabarrena I. , De Paúl J. ( 2012 ) ‘ Improving accuracy and consistency in child maltreatment severity assessment in child protection services in Spain: New set of criteria to help caseworkers in substantiation decisions ’, Children and Youth Services Review , 34 ( 4 ), pp. 666 – 74 .
Ashton V. ( 1999 ) ‘ Worker judgements of seriousness about and reporting of suspected child maltreatment ’, Child Abuse & Neglect , 23 ( 6 ), pp. 539 – 48 .
Barber J. G. , Delfabbro P. H. ( 2009 ) ‘ The profile and progress of neglected and abused children in long-term foster care ’, Child Abuse & Neglect , 33 ( 7 ), pp. 421 – 8 .
Beck K. F. , Vornanen R. ( 2019 ) ‘ Responding to child maltreatment: Comparison between school social work in Finland and Germany ’, Journal of Comparative Social Work , 14 ( 2 ), pp. 5 – 29 .
Bernard C. ( 2019 ) ‘ Recognizing and addressing child neglect in affluent families ’, Child & Family Social Work , 24 ( 2 ), pp. 340 – 7 .
Bernard C. , Greenwood T. ( 2019 ) ‘ We’re giving you the sack’—social workers’ perspectives of intervening in affluent families when there are concerns about child neglect ’, The British Journal of Social Work , 49 ( 8 ), pp. 2266 – 82 .
Berrick J. , Dickens J. , Pösö T. , Skivenes M. ( 2020 ) ‘ Are child protection workers and judges in alignment with citizens when considering interventions into a family? A cross-country study of four jurisdictions ’, Children and Youth Services Review , 108 , 104562 .
Bérubé A. , Lafantaisie V. , Clément M.-È. , Coutu S. , Dubeau D. , Caron J. , Lacharité C. ( 2017 ) ‘ Caseworkers' perspective on risk factors in the family environment influencing mothers' difficulties in meeting children's needs ’, Children and Youth Services Review , 82 , 365 – 72 .
Bolton A. , Gandevia S. , Newell B. R. ( 2021 ) ‘ Appropriate responses to potential child abuse: The importance of information quality ’, Child Abuse & Neglect , 117 , 105062 .
Brandon M. , Sidebotham P. , Belderson P. , Cleaver H. , Dickens J. , Garstang J. , Harris J. , Sorensen P. , Wate R. ( 2020 ) Complexity and Challenge: A Triennial Analysis of SCRs 2014–2017 , Department for Education. https://assets.publishing.service.gov.uk/media/5e5ce103e90e07110f9f6cab/TRIENNIAL_SCR_REPORT_2014_to_2017.pdf .
Casey B. , Hackett S. ( 2021 ) ‘ Deconstructing discourses in assessments of child neglect ’, The British Journal of Social Work , 51 ( 6 ), pp. 2097 – 115 .
Chaudhry M. N. ( 2016 ) The Identification of Child Neglect in Social Work Practice , Salford, England, School of Health and Social Care, University of Salford.
Coope C. M. , Theobald S. ( 2006 ) ‘ Children at risk of neglect: Challenges faced by child protection practitioners in Guatemala City ’, Child Abuse & Neglect , 30 ( 5 ), pp. 523 – 36 .
Coughlan B. , Duschinsky R. , Bakermans-Kranenburg M. , Bakkum L. , Skinner G. , Markham A. , Beckwith H. , van IJzendoorn M. H. (preprint). Sequelae of Child Maltreatment: Umbrella Synthesis on Mental Health Correlates in Over 11 Million Participants . https://doi.org/10.31234/osf.io/zj7kb .
Craft J. L. , Staudt M. M. ( 1991 ) ‘ Reporting and founding of child neglect in urban and rural communities ’, Child Welfare: Journal of Policy, Practice, and Program , 70 ( 3 ), pp. 359 – 70 .
Crawford B. , Bradley M. S. ( 2016 ) ‘ Parent gender and child removal in physical abuse and neglect cases ’, Children and Youth Services Review , 65 , 224 – 30 .
Daniel B. ( 2015 ) ‘ Why have we made neglect so complicated? Taking a fresh look at noticing and helping the neglected child ’, Child Abuse Review , 24 ( 2 ), pp. 82 – 94 .
Daniel B. , Baldwin N. ( 2001 ) ‘ Assessment practice in cases of child neglect: A developmental project ’, Practice , 13 ( 4 ), pp. 21 – 38 .
Daniel B. , Taylor J. , Scott J. ( 2010 ) ‘ Recognition of neglect and early response: Overview of a systematic review of the literature ’, Child & Family Social Work , 15 ( 2 ), pp. 248 – 57 .
Department for Education . ( 2022 ) Children’s Social Work Workforce , London, Department for Education.
Department for Education . ( 2023 ) Characteristics of Children in Need , London, Department for Education.
Dewan S. ( 2018 ) Family Separation: It’s a Problem for US Citizens, Too , New York, NY, The New York Times.
Dickens J. , Cook L. , Cossar J. , Okpokiri C. , Taylor J. , Garstang J. ( 2023 ) ‘ Re-envisaging professional curiosity and challenge: Messages for child protection practice from reviews of serious cases in England ’, Children and Youth Services Review , 152 , 107081 .
Dickens J. , Taylor J. , Cook L. , Cossar J. , Garstang J. , Hallett N. , Olloy E. , Rennolds N. , Rimmer J. , Sorensen P. , Wate R. ( 2022a ) Learning for the Future: Final Analysis of Serious Case Reviews, 2017 to 2019 . https://assets.publishing.service.gov.uk/media/639702918fa8f55307a28c61/Serious_case_reviews_1998_to_2019_-_continuities__changes_and_challenges.pdf .
Dickens J. , Taylor J. , Cook L. , Cossar J. , Garstang J. , Rimmer J. ( 2022b ) Serious Case Reviews 1998 to 2019: Continuities, Changes and Challenges . Department for Education.
Dubowitz H. , Black M. , Starr R. H. , Zuravin S. ( 1993 ) ‘ A conceptual definition of child neglect ’, Criminal Justice and Behavior , 20 ( 1 ), pp. 8 – 26 .
Dubowitz H. , Klockner A. , Starr R. H. , Black M. M. ( 1998 ) ‘ Community and professional definitions of child neglect ’, Child Maltreatment , 3 ( 3 ), pp. 235 – 43 .
Esposito T. , Chabot M. , Caldwell J. , Webb C. , Delaye A. , Fluke J. D. , Trocmé N. , Bywaters P. ( 2022 ) ‘ The differential association of socioeconomic vulnerabilities and neglect-related child protection involvement across geographies: Multilevel structural equation modeling ’, Children and Youth Services Review , 138 , 106505 .
Euser S. , Alink L. R. A. , Pannebakker F. , Vogels T. , Bakermans-Kranenburg M. J. , Van Ijzendoorn M. H. ( 2013 ) ‘ The prevalence of child maltreatment in the Netherlands across a 5-year period ’, Child Abuse & Neglect , 37 ( 10 ), pp. 841 – 51 .
Farmer E. , Lutman E. ( 2014 ) ‘ Working effectively with neglected children and their families—What needs to change ’, Child Abuse Review , 23 ( 4 ), pp. 262 – 73 .
Fong H.-F. , Alegria M. , Bair-Merritt M. H. , Beardslee W. ( 2018 ) ‘ Factors associated with mental health services referrals for children investigated by child welfare ’, Child Abuse & Neglect , 79 , 401 – 12 .
Forrester D. ( 2000 ) ‘ Parental substance misuse and child protection in a British sample: A survey of children on the Child Protection Register in an inner London district office ’, Child Abuse Review , 9 ( 4 ), pp. 235 – 46 .
Freisthler B. , Kepple N. J. , Wolf J. P. , Curry S. R. , Gregoire T. ( 2017 ) ‘ Substance use behaviors by parents and the decision to substantiate child physical abuse and neglect by caseworkers ’, Children and Youth Services Review , 79 , 576 – 83 .
Giovannoni , J. & Becerra , R. ( 1979 ). Defining child abuse. New York : Free Press .
Goldacre A. , Hood R. ( 2022 ) ‘ Factors affecting the social gradient in children’s social care ’, The British Journal of Social Work , 52 ( 6 ), pp. 3599 – 617 .
Gordon D. , Gibbons J. ( 1998 ) ‘ Placing children on child protection registers: Risk indicators and local authority differences ’, British Journal of Social Work , 28 ( 3 ), pp. 423 – 36 .
Gough D. ( 2007 ) ‘ Weight of evidence: A framework for the appraisal of the quality and relevance of evidence ’, Research Papers in Education , 22 ( 2 ), pp. 213 – 28 .
Haworth S. , Schaub J. , Kidney E. , Montgomery P. ( 2024 ) ‘ A systematic review of measures of child neglect ’, Research on Social Work Practice , 34 ( 1 ), pp. 17 – 40 .
Hicks L. , Stein M. ( 2015 ) ‘ Understanding and working with adolescent neglect: Perspectives from research, young people and professionals ’, Child & Family Social Work , 20 ( 2 ), pp. 223 – 33 .
Hirsch B. K. , Yang M.-Y. , Font S. , Slack K. S. ( 2015 ) ‘ Physically hazardous housing and risk for child protective services involvement ’, Child Welfare , 94 ( 1 ), pp. 87 – 104 .
Hong Q.N. , Pluye P. , Fàbregues S. , Bartlett G. , Boardman F. , Cargo M. , Dagenais P. , Gagnon M.-P. , Griffiths F. , Nicolau B. , O’Cathain A. , Rousseau M.-C. , Vedel I. ( 2018 ) Mixed Methods Appraisal Tool (MMAT) , Canada, Canadian Intellectual Property Office.
Horwath J. ( 2001 ) Child Neglect is My View Your View? Working with Cases of Child Neglect in the North Eastern Health Board . London: Jessica Kinglsey.
Horwath J. ( 2004 ). 'Is, this child neglect? The influence of differences in perceptions of child neglect on social work practice’, in Walker M. , Horwath J. , Macdonald G. , Turney D. , Buckley H. , Daniel B. , Taylor J. (eds), Child Neglect: Practice Issues for Health and Social Care , London , Jessica Kingsley Publishers .
Horwath J. ( 2005 ) ‘ Identifying and assessing cases of child neglect: learning from the Irish experience ’, Child & Family Social Work , 10 ( 2 ), pp. 99 – 110 .
Horwath J. ( 2007 ) Child Neglect: Identification and Assessment , Basingstoke , Palgrave Macmillan .
Horwath J. , Tarr S. ( 2015 ) ‘ Child visibility in cases of chronic neglect: Implications for social work practice ’, British Journal of Social Work , 45 ( 5 ), pp. 1379 – 94 .
Humphreys K. L. , LeMoult J. , Wear J. G. , Piersiak H. A. , Lee A. , Gotlib I. H. ( 2020 ) ‘ Child maltreatment and depression: A meta-analysis of studies using the Childhood Trauma Questionnaire ’, Child Abuse & Neglect , 102 , pp. 104361 – 20 .
King B. , Black T. , Fallon B. , Lung Y. ( 2021 ) ‘ The role of risk in child welfare decision-making: A prospective cohort examination of families transferred to ongoing child protection services after an investigation ’, Children and Youth Services Review , 125 , pp. 105983 .
Liu J. , Fang Y. , Gong J. , Cui X. , Meng T. , Xiao B. , He Y. , Shen Y. , Luo X. ( 2017 ) ‘ Associations between suicidal behavior and childhood abuse and neglect: A meta-analysis ’, Journal of Affective Disorders , 220 , pp. 147 – 55 .
Mandel D. R. , Lehman D. R. , Yuille J. C. ( 1995 ) ‘ Reasoning about the removal of a child from home- a comparison of police officers and social workers ’, Journal of Applied Social Psychology , 25 ( 10 ), pp. 906 – 21 .
Nelson J. , Klumparendt A. , Doebler P. , Ehring T. ( 2017 ) ‘ Childhood maltreatment and characteristics of adult depression: Meta-analysis ’, The British Journal of Psychiatry: The Journal of Mental Science , 210 ( 2 ), pp. 96 – 104 .
Page M. J. , McKenzie J. E. , Bossuyt P. M. , Boutron I. , Hoffmann T. C. , Mulrow C. D. , Shamseer L. , Tetzlaff J. M. , Akl E. A. , Brennan S. E. , Chou R. , Glanville J. , Grimshaw J. M. , Hróbjartsson A. , Lalu M. M. , Li T. , Loder E. W. , Mayo-Wilson E. , McDonald S. , McGuinness L. A. , Stewart L. A. , Thomas J. , Tricco A. C. , Welch V. A. , Whiting P. , Moher D. ( 2021 ) ‘ The PRISMA 2020 statement: an updated guideline for reporting systematic reviews ’, British Medical Journal , 372 , pp. n71 – n71 .
Palmer L. , Font S. , Eastman A. L. , Guo L. , Putnam-Hornstein E. ( 2022 ) ‘ What does child protective services investigate as neglect? A population-based study ’, Child Maltreatment , 29 ( 1 ), pp. 96 – 105 .
Peh O. H. , Rapisarda A. , Lee J. ( 2019 ) ‘ Childhood adversities in people at ultra-high risk (UHR) for psychosis: A systematic review and meta-analysis ’, Psychological Medicine , 49 ( 7 ), pp. 1089 – 101 .
Popay J. , Roberts H. , Sowden A. , Petticrew M. , Arai L. , Rodgers M. , Britten N. , Roen K. , Duffy S. ( 2006 ) Guidance on the Conduct of Narrative Synthesis in Systematic Reviews . https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf .
Porter C. , Palmier‐Claus J. , Branitsky A. , Mansell W. , Warwick H. , Varese F. ( 2020 ) ‘ Childhood adversity and borderline personality disorder: A meta‐analysis ’, Acta Psychiatrica Scandinavica , 141 ( 1 ), pp. 6 – 20 .
Proctor S. N. ( 2012 ) Implicit Bias, Attributions, and Emotions in Decisions about Parents with Intellectual Disabilities by Child Protection Workers’ , ProQuest Information & Learning. The Pennsylvania State University.
Raissian K. M. , Dierkhising C. B. , Geiger J. M. , Schelbe L. ( 2014 ) ‘ Child maltreatment reporting patterns and predictors of substantiation: Comparing adolescents and younger children ’, Child Maltreatment , 19 ( 1 ), pp. 3 – 16 .
Raws P. ( 2019 ) ‘ Adolescent neglect: Messages from research for policy and practice ’, Child Abuse Review , 28 ( 3 ), pp. 240 – 7 .
Raz M. , Sankaran V. ( 2019 ) ‘ Opposing family separation policies for the welfare of children ’, American Journal of Public Health , 109 ( 11 ), pp. 1529 – 30 .
Romano E. , Babchishin L. , Marquis R. , Fréchette S. ( 2015 ) ‘ Childhood maltreatment and educational outcomes ’, Trauma, Violence & Abuse , 16 ( 4 ), pp. 418 – 37 .
Roscoe J. N. , Lery B. , Thompson D. ( 2021 ) ‘ Child safety decisions and parental mental health problems: A new analysis of mediating factors ’, Child Abuse & Neglect , 120 , 105202 .
Rose S. J. ( 1999 ) ‘ Reaching consensus on child neglect: African American mothers and child welfare workers ’, Children and Youth Services Review , 21 ( 6 ), pp. 463 – 79 .
Rose S. J. , Meezan W. ( 1995 ) ‘ Child neglect: A study of the perceptions of mothers and child welfare workers ’, Children and Youth Services Review , 17 ( 4 ), pp. 471 – 86 .
Rose S. J. , Meezan W. ( 1996 ) ‘ Variations in perceptions of child neglect ’, Child Welfare: Journal of Policy, Practice, and Program , 75 ( 2 ), pp. 139 – 60 .
Rossi P. H. , Schuerman J. , Budde S. ( 1999 ) ‘ Understanding decisions about child maltreatment ’, Evaluation Review , 23 ( 6 ), pp. 579 – 98 .
Scourfield J. ( 2000 ) ‘ The rediscovery of child neglect ’, The Sociological Review (Keele) , 48 ( 3 ), pp. 365 – 82 .
Segal U. A. ( 1992 ) ‘ Child abuse in India: An empirical report on perceptions ’, Child Abuse & Neglect , 16 ( 6 ), pp. 887 – 908 .
Skinner G. C. M. , Bywaters P. W. B. , Kennedy E. ( 2023 ) ‘ A review of the relationship between poverty and child abuse and neglect: Insights from scoping reviews, systematic reviews and meta‐analyses ’, Child Abuse Review (Chichester, England: 1992) , 32 ( 2 ) , e2795 .
Stokes J. ( 2016 ) Child Neglect Decision-making: Missed Opportunities’, Child Maltreatment: Emerging Issues in Practice , Care and Prevention pp. 57-83. New York : Nova Science Publishers.
Stokes J. , Taylor J. ( 2014 ) ‘ Does type of harm matter? A factorial survey examining the influence of child neglect on child protection decision-making ’, Child Care in Practice , 20 ( 4 ), pp. 383 – 98 .
Stoltenborgh M. , Bakermans-Kranenburg M. J. , Alink L. R. A. , van Ijzendoorn M. H. ( 2015 ) ‘ The prevalence of child maltreatment across the globe: Review of a series of meta-analyses ’, Child Abuse Review , 24 ( 1 ), pp. 37 – 50 .
Stone B. ( 1998 ) ‘ Child neglect: Practitioners’ perspectives ’, Child Abuse Review , 7 ( 2 ), pp. 87 – 96 .
Sullivan P. M. , Knutson J. F. ( 2000 ) ‘ Maltreatment and disabilities: A population-based epidemiological study ’, Child Abuse & Neglect , 24 ( 10 ), pp. 1257 – 73 .
Taylor J. , Dickens J. , Garstang J. , Cook L. , Hallett N. , Molloy E. ( 2024 ) ‘ Tackling the ‘normalisation of neglect’: Messages from child protection reviews in England ’, Child Abuse Review , 33 ( 1 ), p. e2841 .
Tefre Ø. S. ( 2017 ) ‘ Maternal intellectual disability and infant neglect: Child welfare risk assessments in Norway, England and California, USA ’, British Journal of Social Work , 47 ( 7 ), pp. 2014 – 31 .
Tufford L. , Bogo M. , Asakura K. ( 2015 ) ‘ How do social workers respond to potential child neglect ’, Social Work Education , 34 ( 2 ), pp. 229 – 43 .
Turney D. ( 2000 ) ‘ The feminizing of neglect ’, Child & Family Social Work , 5 ( 1 ), pp. 47 – 56 .
US Department of Health & Human Services . ( 2023 ) A.F.C.A.F., Administration on Children, Youth and Families, Children’s Bureau , Child Maltreatment 2021 . Available from https://www.acf.hhs.gov/cb/data-research/child-maltreatment .
Van Wert M. , Fallon B. , Trocmé N. , Collin-Vézina D. ( 2018 ) ‘ Educational neglect: Understanding 20 years of child welfare trends ’, Child Abuse & Neglect , 75 , 50 – 60 .
Wolock I. , Horowitz B. ( 1984 ) ‘ Child maltreatment as a social problem: The neglect of neglect ’, The American Journal of Orthopsychiatry , 54 ( 4 ), pp. 530 – 43 .
Youssef R. M. , Atfa H. Y. ( 1998 ) ‘ Child abuse and neglect: Its perception by those who work with children ’, Eastern Mediterranean Health Journal , 4 ( 2 ), pp. 276 – 92 .
Zuravin , Susan J. ( 1999 ) “Child Neglect: A Review of Definitions and Measurement Research.” Neglected Children: Research, Practice, and Policy . pp. 24 – 46 . Thousand Oaks, California : SAGE Publications .
Supplementary data
| Month: | Total Views: |
|---|---|
| June 2024 | 77 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1468-263X
- Print ISSN 0045-3102
- Copyright © 2024 British Association of Social Workers
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
ORIGINAL RESEARCH article
Childhood emotional neglect and adolescent depression: assessing the protective role of peer social support in a longitudinal birth cohort.

- 1 Psychiatric and Neurodevelopmental Genetics Unit, Center for Genomic Medicine, Massachusetts General Hospital, Boston, MA, United States
- 2 Department of Psychiatry, Massachusetts General Hospital/Harvard Medical School, Boston, MA, United States
- 3 Center on the Developing Child at Harvard University, Cambridge, MA, United States
Introduction: Childhood adversities have been shown to increase psychopathology risk, including depression. However, the specific impact of childhood emotional neglect on later depression has been understudied. Moreover, few studies have investigated relational protective factors that may offset the risk of depression for children who experienced emotional neglect. Analyzing data ( n = 3,265) from the Avon Longitudinal Study of Parents and Children (ALSPAC) study, a longitudinal birth cohort of children born to pregnant women residing in Avon, UK from 1990 to 1992, we assessed the prospective relationship between childhood emotional neglect and depressive symptoms in late adolescence, and tested whether peer social support in mid-adolescence moderates this relationship.
Methods: Childhood emotional neglect, defined as the absence of parental attention and support, was measured across seven assessments from age 8 to 17.5. Peer social support was measured at age 15. Depressive symptoms were measured at age 18. We analyzed the associations between emotional neglect and depressive symptoms, and between peer support and depressive symptoms, and also tested interactive effects of peer support on the association between emotional neglect and depressive symptoms.
Results: Higher levels of emotional neglect were associated with increased depressive symptoms at 18. Conversely, strong peer social support was associated with reduced depressive symptoms, though no significant interaction with emotional neglect was detected.
Conclusion: Although childhood emotional neglect is a risk factor for later depression, our results suggest that strong peer social support at age 15 may generally reduce the risk of depressive symptoms by the time children reach late adolescence. Fostering strong peer support in youth may help offset depression risk for all youth, even among those who have experienced emotional neglect.
Introduction
At least one in five youth in the United States, the United Kingdom, and other developed countries ( 1 – 3 ) experience childhood adversities such as exposure to abuse, neglect, or other major life stressors, which can considerably impact their socio-emotional, cognitive, and physical development, while simultaneously increasing the long-term risk of mental health difficulties ( 4 , 5 ). In particular, exposure to childhood adversities can more than double the risk of depression in later childhood and adulthood and is also associated with increased suicide rates in adulthood ( 6 – 8 ).
One form of childhood adversity that has remained relatively understudied in its long-term mental health impact is emotional neglect ( 9 ). Emotional neglect can be defined as caregivers' persistent disregard of children's emotional needs, including failure to provide comfort when a child becomes scared or distressed ( 10 ). Importantly, exposure to childhood emotional neglect is associated with poor developmental outcomes such as increased maladaptive behaviors and lower self-esteem ( 5 , 10 ), as well as psychopathology in adulthood ( 11 ). However, few studies have focused specifically on childhood emotional neglect with regards to its impact on depression risk in late adolescence, a vulnerable developmental stage when the risk of developing depression is particularly high ( 12 ) and when the prevalence of depression has increased substantially over the past decade, according to national estimates from the United States ( 13 ).
Although childhood adversities such as emotional neglect can exert lasting consequences on mental health outcomes during development, these deleterious effects may be buffered by positive experiences. Understanding potential protective factors, particularly those that could be intervened upon earlier in development, could foster strategies to support the long-term mental health of youth facing adversities such as emotional neglect. While the protective factors that may help mitigate the effects of childhood emotional neglect remain largely unknown, one particularly promising factor that may buffer the negative effects of childhood emotional neglect on depression risk is social support ( 14 ). Social support, defined as the extent to which individuals may receive emotional or instrumental help from others, is a noteworthy predictor of children's positive psychosocial development such as increased self-esteem and confidence ( 15 , 16 ). Strong social support from close others can protect against negative mental health outcomes such as depression, both in general ( 17 ) and following childhood adversities such as emotional, physical, and sexual abuse in childhood and adulthood ( 14 , 18 ). Importantly, considerable research on childhood adversities has mostly focused on the supportive role of family members ( 19 , 20 ); however, children specifically experiencing emotional neglect at home may instead need to develop positive and strong relationships outside the home, with their peers ( 21 ).
Promising observational data suggest that strong peer social support is inversely associated with depressive symptoms among individuals with a history of childhood adversities ( 22 ) and that higher perceived peer social support may weaken the association between reported childhood adversities and depressive symptoms in adulthood ( 14 ). However, these studies have been conducted retrospectively in adults, who reported on their current peer support rather than support they may have received as children. By contrast, less is known about protective effects of peer social support during adolescence. Given that adolescence is a crucial time for peer bonding and relationship development ( 23 ), peer social support during this developmental period may be an important and intervenable protective factor that could promote long-term wellbeing and resilience to depression despite childhood adversities experienced at home. Importantly, the extent to which peer social support observed in mid-adolescence can prospectively influence depression risk and moderate the potentially deleterious effects of childhood emotional neglect remains unknown.
To address these knowledge gaps, we analyzed data from the Avon Longitudinal Study of Parents and Children (ALSPAC), a longitudinal birth cohort that followed mothers and their children residing in Avon, UK from before birth through the child's mid-twenties ( 24 , 25 ). This longitudinal cohort provides the unique opportunity to characterize childhood emotional neglect across multiple points during childhood and prospectively capture peer social support during adolescence in relation to later depression risk. Our study was informed by theories on emotional and behavioral development in children ( 14 , 26 , 27 ), which suggest childhood adversities, including deprivation from normative caregiver inputs, may increase risk for poor self-esteem, altered reward processing, and depression across development. Our study aimed to: (1) assess the relationship between childhood emotional neglect and depressive symptoms in adolescence, (2) investigate the association between peer social support and adolescent depressive symptoms, as well as (3) test the combined and interactive effects of peer social support and childhood emotional neglect on adolescent depressive symptoms. Given previous research linking childhood adversities to negative mental health outcomes and the role of increased social support as a protective factor for poor health outcomes in adolescence, we hypothesized that childhood emotional neglect would be associated with increased depressive symptoms and that strong peer social support would be associated with lower depressive symptoms. Further, we hypothesized that peer support would moderate the relationship between childhood emotional neglect and depressive symptoms, such that the association between emotional neglect and later depressive symptoms would be attenuated in children who experienced higher peer support in adolescence.
Materials and Methods
Women residing in Avon, UK, a city in the southwest of England, with expected delivery dates from April 1991 to December 1992 who were willing to participate in the study were recruited into ALSPAC ( n = 14,541 pregnancies) ( 24 , 25 , 28 ). Of the women who gave birth, there were 14,062 live births; the children alive at 1 year of age ( n = 13,988) were enrolled in the study. An additional 913 children were enrolled in the study after age 7, resulting in a total sample size of 14,901 children that were alive at 1 year of age. Compared to UK mothers and Avon mothers, ALSPAC mothers were more likely to be White, married, and own a house ( 24 ). Additional ALSPAC information can be found using a searchable data dictionary and variable search tool on the ALSPAC website: http://www.bristol.ac.uk/alspac/researchers/our-data/ . Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees. Informed consent for the use of data collected via questionnaires and clinics was obtained from participants following the recommendations of the ALSPAC Ethics and Law Committee at the time.
Childhood Emotional Neglect by Parents
We used repeated measures of parental attention and monitoring to create our emotional neglect variable; previous studies have shown that repeated measures of child maltreatment can minimize recall biases ( 29 ). Our emotional neglect variable is consistent with definitions from the World Health Organization ACE International Questionnaire and previous published studies from the ALSPAC cohort that have used a similar approach to define emotional neglect based on low levels of parental attention and monitoring reported by children over time ( 10 , 30 ). Specifically, children prospectively reported their experiences of parental attention and monitoring at eight separate assessments from 8 to 17.5 years of age (97, 116, 150, 162, 168, 186, 192, 210 months). Participants were asked to respond to statements such as “How often do your caretakers take the time to listen to you when you talk about what happened during your free time?” and “How often do your caretakers ask what happened at school, on a normal school day?” Response options were based on either a 4-point or 5-point Likert scale (more details for each response option can be found in Supplementary Table 1 ).
In line with previous approaches ( 10 ), each of these 23 items was then dichotomized with the most extreme response for each item coded as a 1 (exposed to emotional neglect), while all other responses were given a 0 (unexposed to emotional neglect). Conceptually, we determined that only the complete absence of monitoring and attention (e.g., response options indicated as “none”) should be taken to reflect a problematic situation of parental neglect, rather than this construct of neglect existing on a gradient opposite to parental monitoring. Therefore, and similar to studies elsewhere, we only took the most extreme response for each item as contributing to a total score reflecting emotional neglect. Previous research in the ALSPAC cohort has operationalized emotional neglect in a similar binary fashion based on the reported absence of parental attention and monitoring ( 10 ). See Supplementary Table 1 for the variables used and criteria. The 23 items that resulted from this binary classification strategy were summed to create one total quantitative score for emotional neglect, with values ranging from 0 to 14 in our study (maximum possible score of 23). There was moderately-strong internal consistency reliability for the 23 parental monitoring items used to construct the emotional neglect variable in our sample, a = 0.79. Based on a histogram of this total quantitative score, participants were then categorized into one of four levels of exposure to emotional neglect: none (total score = 0); mild (total score = 1); moderate (total score = 2); high (total score = 3 or more).
Perceived Peer Social Support
Perceived peer social support was reported by children at age 15 with the five-item shortened version of the Cambridge Hormones and Moods Project Friendship questionnaire ( 31 ). We chose to focus on children's perceived social support at age 15 because acceptance and support by peers at this age is a strong predictor of self-worth and self-esteem ( 32 ). This five-item friendship questionnaire asks youth respondents to report on their perceived peer social support using a 4-point Likert scale, with each item ranging from 0 to 3. Items included: “Overall how happy are you with your friends (3 = most of the time, 2 = sometimes, 1 = not often, 0 = not at all),” “Do your friends understand you (3 = most of the time, 2 = sometimes, 1 = not often, 0 = not at all),” “Do you talk to your friends about problems (3 = most of the time, 2 = sometimes, 1 = not often, 0 = not at all),” “Are you happy with the number of friends you've got (3 = very happy, 2 = quite happy, 1 = quite unhappy, 0 = unhappy),” and “Do you see your friends outside of school (3 = almost every day, 2 = at least once per week, 1 = less than once per week, 0 = hardly ever).” The five items were summed to create one total score ranging from 0 to 15, with greater scores indicating greater peer social support, as scored in previous research ( 33 ). The mean inter-item correlation for the five-item perceived social support questionnaire was modest ( r = 0.22), which is similar to previous research findings on this measure ( 34 ).
Depressive Symptoms
Depressive symptoms were reported by adolescents at age 18 using the Short Mood and Feelings Questionnaire (SMFQ); ( 35 , 36 ). The SMFQ includes 13 questions asking respondents to report on depressive symptoms in the past 2 weeks using a 3-point Likert scale, ranging from 0 to 2 (0 = not true, 1 = sometimes true, 2 = true). All items were summed to create one total score, ranging from 0 to 26 with higher scores indicating increased symptoms of depression. Some of the items are related to emotions, such as “I felt miserable or unhappy” or “I felt I was not good anymore,” whereas others were related to cognition and thoughts, such as “I found it hard to think properly and concentrate” or “I thought nobody really loved me.” We found strong internal consistency for SMFQ in our sample, α = 0.91. The SMFQ has previously shown strong validity and has been used in prior research with ALSPAC data as well as many other studies ( 37 ).
All models included the following covariates: the child's sex, race, and mother's age at child's birth, number of previous pregnancies, marital status, home ownership status, and education attainment at the time she gave birth. These covariates were selected as key sociodemographic characteristics from our work and prior literature that could potentially influence the relationship between exposure to emotional neglect and later depressive symptoms ( 38 , 39 ). We also included two potential childhood adversities—mother's psychopathology when the child was 8 months old, and being born into a one-parent household—as additional covariates in a sensitivity analysis.
Statistical Analyses
To prevent the loss of information, improve the statistical power to detect associations in the data, and reduce bias in our effect estimates, we performed multiple imputation using chained questions (MICE package in R, version 3.13.0) for missing data ( 40 ). Multiple imputation using chained questions is an iterative procedure for computing missing data. It operates by systematically calculating the missing values for each variable using a regression model containing the non-missing data from other specified variables available in the dataset. For our MICE procedure, we implemented this iterative process 25 times for each of the 20 imputed datasets we created. Each of the 20 datasets contained all ALSPAC participants with SMFQ scores available at age 18 ( n = 3,263). We then performed our inference using the pooled estimates from those 20 imputed datasets ( 41 ).
All confounders and exposures were imputed for in the imputation model. Data on the child's depressive symptoms at age 18 as well as variables pertaining to the child's friendships throughout adolescence, a strong predictor of social support levels ( 42 ), were included in the imputation procedure to provide additional information in an effort to yield more accurate estimates for missing covariate and exposure data.
Regression Models
We ran three linear regression models. Model 1 tested the association between levels of childhood emotional neglect and depressive symptom scores at 18. Model 2 added to Model 1 by including peer social support, allowing us to assess the effect of both emotional neglect and levels of peer social support on depressive symptoms at age 18. Using an interaction term between childhood neglect and the levels of social support, Model 3 added to Model 2 by assessing whether social support was an effect modifier of the relationship between childhood emotional neglect and depressive symptoms. To increase interpretability of the results, we standardized the SMFQ depression outcome variable with a mean of 0 and SD of 1, such that beta values for each of the independent variables in the model reflected standard deviation changes in the depressive symptoms. All models were adjusted for the covariates as described in the Measures (e.g., home ownership status, child sex, race).
Sample Description
Our analytic sample was composed of 3,263 singleton children with complete outcome data on depressive symptoms at age 18 ( Table 1 ). Demographics of the complete case sample prior to imputation are shown in Table 1 . Of the 3,263 participants, 64.4% identified as female, 96.1% identified as white, and most were first- or second-born children (48.9%, 34.8%, respectively). Eighty-nine percent of the mothers were 20–35 years old at the child's birth, 22.5% had a University degree or above, 83.9% were married, and 85.1% had a mortgage or owned a home.

Table 1 . Baseline characteristics of participants in the analytic sample ( n = 3,263).
Total depressive symptom scores, measured using the SMFQ, ranged from 0 to 26 ( M = 6.80, SD = 5.89) ( Table 2 ). Nearly 9% of children in our analytic sample could be classified as experiencing high exposure to emotional neglect, 10% with moderate exposure, 18% with low exposure, and 63% with no exposure. The distribution of the peer social support measure was left-skewed toward higher scores ( M = 12.94, SD = 1.69, ranged from 0 to 15), with individuals tending to endorse relatively high levels of peer social support.
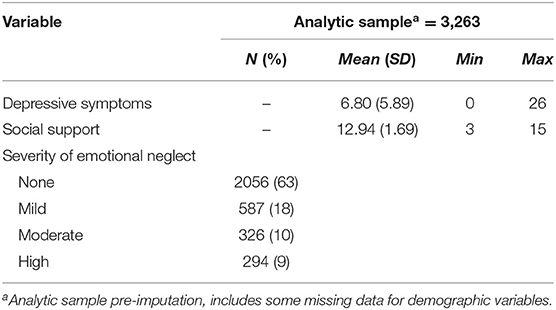
Table 2 . Descriptive statistics for depressive symptoms, social support, and childhood emotional neglect variables in the analytic sample ( n = 3,263).
Association Between Childhood Emotional Neglect and Depressive Symptoms at 18
To determine the influence of emotional neglect on depression risk, we next examined the relationship between childhood emotional neglect and depressive symptoms at age 18. Mild, moderate, and high levels of exposure to childhood emotional neglect, compared to those with no exposure, were significantly associated with increased depressive symptoms at age 18 (β = 0.15, p < 0.01; β = 0.31, p < 0.01; β = 0.38, p < 0.01) ( Table 3 , Model 1), with a Model 1 R 2 of 0.06.
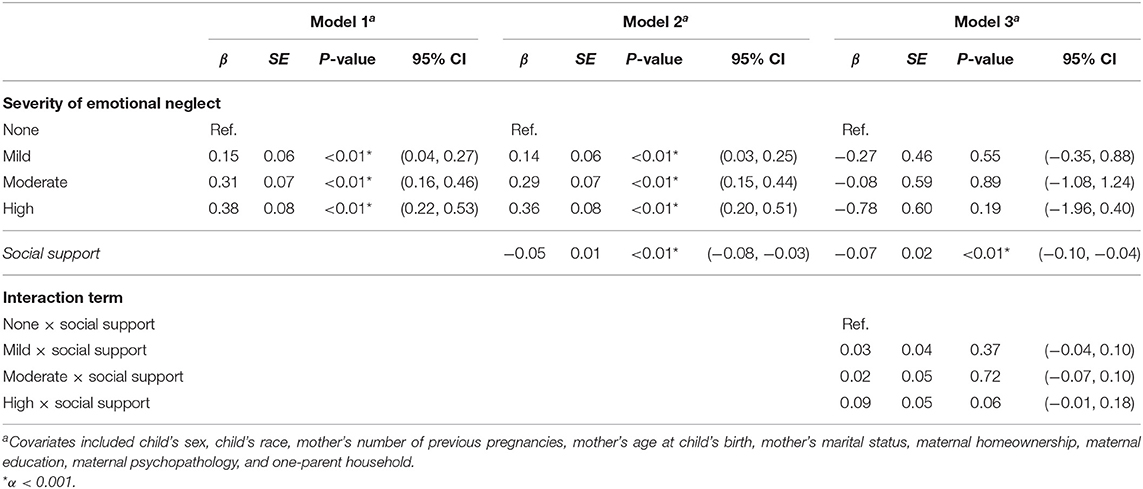
Table 3 . Results of linear regression analysis assessing the association between degree of severity of childhood emotional neglect on depressive symptoms at age 18, adjusting for covariates.
Association Between Emotional Neglect, Peer Support, and Depressive Symptoms at 18
We next examined the role of peer social support and emotional neglect on depressive symptoms by including both peer social support and emotional neglect as independent main effects in the same model. The overall Model 2 had a R 2 of 0.07. Here, we found that mild, moderate, and high levels of exposure to emotional neglect were still associated with significantly higher depressive symptoms at age 18 compared to no exposure (β = 0.14, p = 0.01; β = 0.29, p < 0.01; β = 0.36, p < 0.01, respectively) ( Table 3 , Model 2). We also found a significant negative association between perceived peer social support and depressive symptoms (β = −0.05, p < 0.01) indicating that as perceived peer social support increases, depressive symptoms decrease, even after adjusting for childhood emotional neglect ( Table 3 , Model 2). This adjusted association of peer social support is notable because preliminary analyses indicated that continuous social support and emotional neglect scores were negatively correlated to a statistically significant but modest extent ( r s = −0.09, p = 0.01 in non-imputed sample).
Interaction Between Peer Support and Emotional Neglect on Depressive Symptoms at 18
Finally, we examined the statistical interaction between social support and emotional neglect to determine whether peer social support moderated the relationship between emotional neglect and depressive symptoms. The overall Model 3 had a R 2 of 0.07. We did not detect any significant statistical interaction between levels of emotional neglect and social support on depressive symptoms (mild, p = 0.55, moderate, p = 0.89, high p = 0.19 at the α = 0.05 level) ( Table 3 , Model 3). In this model, social support maintained a significant independent main effect with fewer depressive symptoms (β = −0.07, p < 0.01), while emotional neglect no longer showed a significant main effect ( Table 3 , Model 3). Notably, the direction of effect and pattern of results in all three models remained consistent even in sensitivity analyses adjusting for other potential early adversities (i.e., maternal psychopathology, one-parent household).
In this prospective study, we found that childhood emotional neglect was significantly associated with depressive symptoms in late adolescence, whereas stronger peer social support in mid-adolescence was associated with reduced depressive symptoms, even after accounting for emotional neglect. Peer support did not show a statistical interaction with emotional neglect, suggesting that the protective effects of peer social support on depression held both for children who experienced emotional neglect as well as those who did not.
To date, limited research has focused specifically on the influences of childhood emotional neglect on mental health outcomes. Emotional neglect is less overt than other forms of maltreatment, such as physical abuse, making it a relatively challenging construct to assess ( 5 , 9 , 43 ). Informed by similar approaches in prior literature ( 8 ), we established a working empirical definition in which the presence of low levels of parental attention, support, and monitoring reported by children over time was aggregated into a quantitative index of emotional neglect exposure, and then categorized to reflect severity of this exposure. Per this definition, 19% of our study sample had experienced at least moderate to high levels of emotional neglect. This highlights the prevalence of emotional neglect experiences during childhood in a population-based birth cohort and the need to understand its long-term mental health consequences. Prior studies focusing on a broader range of childhood adversities have suggested that emotional forms of abuse and neglect have particularly strong associations with depression relative to other forms (e.g., physical abuse, sexual abuse, and physical neglect) ( 5 ). Our study focused specifically on emotional neglect provides further prospective support for its role as a risk factor for later depression. Further understanding about the mechanisms of this association—that is, how emotional neglect translates into depression risk—is needed. Some research has shown that emotional neglect often co-occurs with other forms of childhood maltreatment ( 9 ), and so it may be a marker of other adverse experiences.
In our study, we found that peer social support in mid-adolescence was significantly associated with reduced depressive symptoms in late adolescence. Our findings are similar to previous research in adult samples reporting that childhood adversity (including emotional neglect) was associated with later depression and that social support was linked to a decrease in adulthood depressive symptoms ( 14 ). While this result aligns with a robust and growing evidence base linking peer social support and depressive outcomes across the life course ( 44 ), our study contributes further evidence that peer social support is protectively associated with depressive symptoms in adolescence, a key time period for the emergence of depression, even after adjusting for exposure to childhood emotional neglect. Strong peer social support has been linked to academic achievement, positive self-worth, and quality of life across development ( 20 , 45 , 46 ). Importantly, our study suggests that strong perceived support from peers during mid-adolescence, a time when youth increasingly rely on relationships outside the home ( 47 ), is generally beneficial and could even offset the negative mental health impacts of emotional neglect from caregivers. Children with stronger peer support may receive the benefits of sharing similar experiences, distraction, and positive interactions that in turn, lead to lower likelihood of depression. Future studies should examine additional protective factors related to childhood adversity, such as participating in extracurricular activities and satisfaction with school, that could decrease depressive symptoms even in the context of emotional neglect ( 48 ).
Prior research has also suggested there may be specific developmental stages or sensitive periods when children are not just more vulnerable to developing psychopathology, but may also be more responsive to interventions ( 49 ). While we selected mid-adolescence based on developmental theory and available data, future research should aim to empirically determine whether there are specific sensitive periods in development where the strengthening of peer social support may be particularly helpful in offsetting risk for depression. Moreover, whether other forms of social support that may be available to youth, such as teacher and broader community support, can also mitigate depression risk in children exposed to emotional neglect is also a topic requiring further investigation.
In this study, we did not observe a statistical interaction between peer social support in mid-adolescence and emotional neglect, and so cannot conclude that peer support specifically buffers the effect of emotional neglect. This finding is somewhat contrary to retrospective studies in adult cohorts, which have found that peer social support, at least in adulthood, may buffer the effects of childhood adversities (e.g., emotional neglect, physical abuse, household substance abuse) on depressive symptoms ( 14 ). It is possible that peer support, or other forms of social support, only show an interactive buffering effect with other forms of childhood adversities and not emotional neglect. The absence of a significant statistical interaction may also be due to a modest sample size for testing statistical interactions, although this suggests that even if an interaction truly does exist, its magnitude is likely to be small in nature. However, we found that the effects of peer social support persisted even after adjusting for emotional neglect and other potential confounders, indicating that the protective influences of peer social support apply even in the context of emotional neglect exposure. As such, all children, even those who have experienced significant neglect from their caregivers, may experience a reduction in depression risk if they have strong relationships with their peers.
Limitations
One potential limitation of this study is our empirical definition of emotional neglect. Although we relied on existing approaches in defining emotional neglect on the basis of extreme low responses to measures that assess parental monitoring, support, and attention ( 10 ), future work may benefit from refining assessments for emotional neglect that specifically measure the extent of caregiver emotional responsiveness vs. unavailability to the child's emotional and psychological needs. Including more direct and comprehensive questions would likely result in a more accurate measurement of this important construct ( 10 ). Future studies should address cultural differences when designing a measure for emotional neglect, which may influence self-reporting and perceptions of maltreatment ( 9 ). While similar overall, there are some sociodemographic differences between mothers and children from the ALSPAC cohort in comparison to the UK population (e.g., race distribution, socioeconomic factors) that may limit the generalizability of our findings. The moderate sample size and the homogenous population were other limitations of this study, which may have limited our ability to detect significant interactive associations and extend interpretation of our findings to broader contexts, respectively. Further research might also assess the influence of peer social support on depression risk for children exposed to emotional neglect and other forms of maltreatment in more racially and ethnically diverse populations. Although our study focused primarily on emotional neglect independent from other childhood adversities and also accounted for two other childhood adversity exposures (i.e., maternal psychopathology, one-parent household), future studies may incorporate additional ACEs and contextual exposures as potential covariates in the model, because particularly for some groups childhood adversities often co-occur. Finally, our study focused on observational associations. Although our prospective design strengthens the inference that peer social support may indeed affect future risk of depression, rather than the other way around, adolescents who are vulnerable to depression may also have difficulties with building strong peer relationships for example, due to traits such as interpersonal sensitivity ( 50 ). Depression could also lead to decreases in peer support ( 51 ). More longitudinal studies with prospective measures of both depression and peer support across time may allow us to better disentangle these temporal relationships. Moreover, potential recall bias may have influenced participant's accurate self-reporting of childhood emotional neglect, whether through underreporting or overreporting ( 29 ).
Our findings suggest that strong social support at age 15 may be a protective factor linked to reduced depressive symptoms in youth, even among those who have been neglected emotionally. Schools, caretakers, and health professionals should be alert to the identification of emotional neglect because children who are affected are likely to be at higher risk for depressive symptoms later in life. These findings may well lead to clinicians and schools enhancing opportunities for socially supportive peer interventions that optimize mental health outcomes for vulnerable children.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: http://www.bristol.ac.uk/alspac/researchers/our-data/ .
Ethics Statement
The studies involving human participants were reviewed and approved by ALSPAC Ethics and Law Committee and the Local Research Ethics Committees. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
EG, KC, AL, BS, and ED contributed to conception and design of the study. All authors contributed to the article and approved the submitted version.
The UK Medical Research Council and Wellcome (Grant ref: 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors, who will serve as guarantors for the contents of this paper. This research was specifically funded by the National Institute of Mental Health of the National Institutes of Health (ED Award Number R01MH113930). KC was partially supported by a Kaplen Fellowship on Depression from the Harvard Medical School. A comprehensive list of grants funding is available on the ALSPAC website ( http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf ).
Author Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.681176/full#supplementary-material
1. Elmore AL, Crouch E. The association of adverse childhood experiences with anxiety and depression for children and youth, 8 to 17 years of age. Acad Pediatr. (2020) 20:600–8. doi: 10.1016/j.acap.2020.02.012
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. (2009) 373:68–81. doi: 10.1016/S0140-6736(08)61706-7
3. Hughes K, Ford K, Kadel R, Sharp CA, Bellis MA. Health and financial burden of adverse childhood experiences in England and Wales: a combined primary data study of five surveys. BMJ Open. (2020) 10:e036374. doi: 10.1136/bmjopen-2019-036374
4. Dunn EC, Nishimi K, Gomez SH, Powers A, Bradley B. Developmental timing of trauma exposure and emotion dysregulation in adulthood: are there sensitive periods when trauma is most harmful? J Affect Disord. (2018) 227:869–77. doi: 10.1016/j.jad.2017.10.045
5. Humphreys KL, LeMoult J, Wear JG, Piersiak HA, Lee A, Gotlib IH. Child maltreatment and depression: a meta-analysis of studies using the Childhood Trauma Questionnaire. Child Abuse Neglect. (2020) 102:104361. doi: 10.1016/j.chiabu.2020.104361
6. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. REPRINT of: relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med. (2019) 56:774–86. doi: 10.1016/j.amepre.2019.04.001
7. Haynes E, Crouch E, Probst J, Radcliff E, Bennett K, Glover S. Exploring the association between a parent's exposure to Adverse Childhood Experiences (ACEs) and outcomes of depression and anxiety among their children. Child Youth Serv Rev. (2020) 113:105013. doi: 10.1016/j.childyouth.2020.105013
CrossRef Full Text | Google Scholar
8. Houtepen LC, Heron J, Suderman MJ, Fraser A, Chittleborough CR, Howe LD. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: a prospective cohort study in the UK. PLoS Med. (2020) 17:e1003031. doi: 10.1371/journal.pmed.1003031
9. Kumari V. Emotional abuse and neglect: time to focus on prevention and mental health consequences. Brit J Psychiatry. (2020) 217:1–3. doi: 10.1192/bjp.2020.154
10. Houtepen LC, Heron J, Suderman MJ, Tilling K, Howe LD. Adverse childhood experiences in the children of the Avon Longitudinal Study of Parents and Children (ALSPAC). Wellcome Open Res. (2018) 3:106. doi: 10.12688/wellcomeopenres.14716.1
11. Kisely S, Abajobir AA, Mills R, Strathearn L, Clavarino A, Najman JM. Child maltreatment and mental health problems in adulthood: birth cohort study. Brit J Psychiatry. (2018) 213:698–703. doi: 10.1192/bjp.2018.207
12. Clayborne ZM, Varin M, Colman I. Systematic review and meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiatry. (2019) 58:72–9. doi: 10.1016/j.jaac.2018.07.896
13. Mojtabai R, Olfson M. National trends in mental health care for US adolescents. JAMA Psychiatry. (2020) 77:703–14. doi: 10.1001/jamapsychiatry.2020.0279
14. Cheong EV, Sinnott C, Dahly D, Kearney PM. Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open. (2017) 7:e013228. doi: 10.1136/bmjopen-2016-013228
15. Ikiz FE, Cakar FS. Perceived social support and self-esteem in adolescence. Proc Soc Behav Sci. (2010) 5:2338–42. doi: 10.1016/j.sbspro.2010.07.460
16. Pinquart M. Associations of parenting dimensions and styles with externalizing problems of children and adolescents: an updated meta-analysis. Dev Psychol. (2017) 53:873–932. doi: 10.1037/dev0000295
17. Choi KW, Stein MB, Nishimi KM, Ge T, Coleman JRI, Chen CY, et al. An exposure-wide and mendelian randomization approach to identifying modifiable factors for the prevention of depression. Am J Psychiatry. (2020) 177:944–54. doi: 10.1176/appi.ajp.2020.19111158
18. Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont). (2007) 4:35–40. Available online at: https://psycnet.apa.org/record/2007-07464-009
PubMed Abstract | Google Scholar
19. Muzik M, Umarji R, Sexton MB, Davis MT. Family social support modifies the relationships between childhood maltreatment severity, economic adversity and postpartum depressive symptoms. Matern Child Health J. (2017) 21:1018–25. doi: 10.1007/s10995-016-2197-4
20. Zhao J, Peng X, Chao X, Xiang Y. Childhood maltreatment influences mental symptoms: the mediating roles of emotional intelligence and social support. Front Psychiatry. (2019) 10:415. doi: 10.3389/fpsyt.2019.00415
21. Birkeland MS, Birkeland MS, Breivik K, Breivik K, Wold B, Wold B. Peer acceptance protects global self-esteem from negative effects of low closeness to parents during adolescence and early adulthood. J Youth Adolesc. (2014) 43:70–80. doi: 10.1007/s10964-013-9929-1
22. Brinker J, Cheruvu VK. Social and emotional support as a protective factor against current depression among individuals with adverse childhood experiences. Prevent Med Rep. (2016) 5:127–33. doi: 10.1016/j.pmedr.2016.11.018
23. Camara M, Bacigalupe G, Padilla P. The role of social support in adolescents: are you helping me or stressing me out? Int J Adolesc Youth. (2017) 22:123–36. doi: 10.1080/02673843.2013.875480
24. Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, et al. Cohort profile: the avon longitudinal study of parents and children: ALSPAC mothers cohort. Int J Epidemiol. (2013) 42:97–110. doi: 10.1093/ije/dys066
25. Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, et al. Cohort profile: the ‘children of the 90s'—the index offspring of the Avon longitudinal study of parents and children. Int J Epidemiol. (2013) 42:111–27. doi: 10.1093/ije/dys064
26. Hanson JL, Hariri AR, Williamson DE. Blunted ventral striatum development in adolescence reflects emotional neglect and predicts depressive symptoms. Biol Psychiatry. (2015) 78:598–605. doi: 10.1016/j.biopsych.2015.05.010
27. Stoltenborgh M, Bakermans-Kranenburg MJ, van Ijzendoorn MH. The neglect of child neglect: a meta-analytic review of the prevalence of neglect. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:345–55. doi: 10.1007/s00127-012-0549-y
28. Northstone K, Lewcock M, Groom A, Boyd A, Macleod J, Timpson NJ, et al. The Avon Longitudinal Study of Parents and Children (ALSPAC): an updated on the enrolled sample of index children in 2019. Wellcome Open Res. (2019) 4:51. doi: 10.12688/wellcomeopenres.15132.1
29. Baldwin JR, Reuben A, Newbury JB, Danese A. Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry. (2019) 76:584–93. doi: 10.1001/jamapsychiatry.2019.0097
30. WHO. Adverse Childhood Experiences International Questionnaire. Adverse Childhood Experiences International Questionnaire (ACE-IQ). (2018). Available online at: https://www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq) (accessed March 1, 2021).
31. Goodyer I, Wright C, Altham P. Recent achievements and adversities in anxious and depressed school age children. J Child Psychol Psychiatry. (1990) 31:1063–77. doi: 10.1111/j.1469-7610.1990.tb00846.x
32. Magro SW, Utesch T, Dreiskämper D, Wagner J. Self-esteem development in middle childhood: support for sociometer theory. Int J Behav Dev. (2018) 43:118–27. doi: 10.1177/0165025418802462
33. Singh SPDM, Winsper CP, Wolke DP, Bryson AP. School mobility and prospective pathways to psychotic-like symptoms in early adolescence: a prospective birth cohort study. J Am Acad Child Adolesc Psychiatry. (2014) 53:518.e1–27.e1. doi: 10.1016/j.jaac.2014.01.016
34. Pickard H, Happé F, Mandy W. Navigating the social world: the role of social competence, peer victimisation and friendship quality in the development of social anxiety in childhood. J Anxiety Disord. (2018) 60:1–10. doi: 10.1016/j.janxdis.2018.09.002
35. Angold A, Costello EJ, Pickles A, Messer SC, Winder F, Silva D. The development of a short questionnaire for use in epidemiological studies of depression in chidlren and adolescents. Int J Methods Psychiatr Res. (1995) 5:237–49.
Google Scholar
36. Messer SC, Angold A, Costello J, Loeber R, Van Kammen W, Stouthamer-Loeber M. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: factor composition and structure across development. Int J Methods Psychiatr Res. (1995) 5:251–62.
37. Turner N, Joinson C, Peters TJ, Wiles N, Lewis G. Validity of the short mood and feelings questionnaire in late adolescence. Psychol Assess. (2014) 26:752–62. doi: 10.1037/a0036572
38. Crawford KM, Choi K, Davis KA, Zhu Y, Soare TW, Smith AD, et al. Exposure to early childhood maltreatment and its effect over time on social cognition. Dev Psychopathol. (2020) 2020:1–11. doi: 10.1017/S095457942000139X
39. Hibbeln JR, Davis JM, Steer C, Emmett P, Rogers I, Williams C, et al. Maternal seafood consumption in pregnancy and neurodevelopmental outcomes in childhood (ALSPAC study): an observational cohort study. Lancet. (2007) 369:578–85. doi: 10.1016/S0140-6736(07)60277-3
40. Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatric Res. (2011) 20:40–9. doi: 10.1002/mpr.329
41. Little RJA, Rubin DB. Statistical Analysis with Missing Data . Newark: John Wiley and Sons, Incorporated (2019).
42. Lee C-YS, Goldstein SE. Loneliness, stress, and social support in young adulthood: does the source of support matter? J Youth Adolesc. (2016) 45:568–80. doi: 10.1007/s10964-015-0395-9
43. Cohen JR, McNeil SL, Shorey RC, Temple JR. Maltreatment subtypes, depressed mood, and anhedonia: a prospective study with adolescents. Psychol. Trauma. (2019) 11:704–12. doi: 10.1037/tra0000418
44. Stice E, Ragan J, Randall P. Prospective relations between social support and depression: differential direction of effects for parent and peer support? J Abnorm Psychol. (2004) 113:155–9. doi: 10.1037/0021-843X.113.1.155
45. Luo Y, Xiang Z, Zhang H, Wang Z. Protective factors for depressive symptoms in adolescents: interpersonal relationships and perceived social support. Psychol Sch. (2017) 54:808–20. doi: 10.1002/pits.22033
46. Alsubaie MM, Stain HJ, Webster LAD, Wadman R. The role of sources of social support on depression and quality of life for University students. Int J Adolesc Youth. (2019) 24:484–96. doi: 10.1080/02673843.2019.1568887
47. Lerner RM, Steinberg LD. Handbook of Adolescent Psychology . Hoboken, NJ: John Wiley and Sons (2009). doi: 10.1002/9780470479193
48. Khambati N, Mahedy L, Heron J, Emond A. Educational and emotional health outcomes in adolescence following maltreatment in early childhood: a population-based study of protective factors. Child Abuse Neglect. (2018) 81:343–53. doi: 10.1016/j.chiabu.2018.05.008
49. Dunn EC, Soare TW, Raffeld MR, Busso DS, Crawford KM, Davis KA, et al. What life course theoretical models best explain the relationship between exposure to childhood adversity and psychopathology symptoms: recency, accumulation, or sensitive periods? Psychol Med. (2018) 48:2562–72. doi: 10.1017/S0033291718000181
50. Hernandez EM, Trout ZM, Liu RT. Vulnerability-specific stress generation: childhood emotional abuse and the mediating role of depressogenic interpersonal processes. Child Abuse Neglect. (2016) 62:132–41. doi: 10.1016/j.chiabu.2016.10.019
51. Ren P, Qin X, Zhang Y, Zhang R. Is social support a cause or consequence of depression? A longitudinal study of adolescents. Front Psychol. (2018) 9:1634. doi: 10.3389/fpsyg.2018.01634
Keywords: emotional neglect, social support, depression, childhood adversity, ALSPAC
Citation: Glickman EA, Choi KW, Lussier AA, Smith BJ and Dunn EC (2021) Childhood Emotional Neglect and Adolescent Depression: Assessing the Protective Role of Peer Social Support in a Longitudinal Birth Cohort. Front. Psychiatry 12:681176. doi: 10.3389/fpsyt.2021.681176
Received: 16 March 2021; Accepted: 21 June 2021; Published: 09 August 2021.
Reviewed by:
Copyright © 2021 Glickman, Choi, Lussier, Smith and Dunn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erin C. Dunn, edunn2@mgh.harvard.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

- Child Development
8 Signs of Emotional Neglect in a Family
7. emotions are taboo, and not just negative ones..
Posted December 11, 2021 | Reviewed by Vanessa Lancaster
- Understanding Child Development
- Find a child or adolescent therapist near me
- You don't need a perfect family to be emotionally happy and healthy, but your family must be "good enough."
- People growing up in emotionally neglectful families may sense something is wrong but have no idea what it is.
- If your family is inattentive to feelings, there are things you can do to take care of yourself.
As adults, most of us tend to minimize the impact our birth families, or what therapists call the “family of origin,” have on our daily choices and lives. But, the reality is that the family you were born into and that raised you still lingers in your adult brain, influencing feelings, reactions, and choices.
In 1953, D.W. Winnicott first introduced the concept of “the good enough mother” in a groundbreaking book called Playing and Reality . His words changed the field of psychology and mental health forever by linking the way you experience your connection with your parents in childhood to the way you are as an adult. His essential concept was that you don’t need a perfect parent to turn out okay. You only need to have a parent that’s “good enough.”
A 2019 research study by Susan Woodhouse found that a parent only has to get it right 50 percent of the time to be a “good enough” parent.
Childhood Emotional Neglect
Childhood emotional neglect happens when your parents sufficiently neglect your emotions and emotional needs. Meaning, they do not notice what you are feeling, ask about your feelings, connect with you on an emotional level, or validate your feelings enough .
Emotionally neglectful parents usually have no idea they neglect their children’s emotions. They are typically folks who tend to turn a blind eye to feelings in general, including their own, friends’, family’s, co-workers’, and children’s. They may mean well and care for and want to do their best for their kids. They probably have no idea what they are missing.
This can make many emotionally neglectful families challenging to spot. They are indeed “good enough” in the most visible ways. They may provide you with a home, food, clothing, and rides to soccer practice. But they do not have frank talks with you about problems you’re facing, soothe you enough when your friends hurt your feelings, or teach you how to notice, name, or manage your emotions.
The one failure of the emotionally neglectful family is emotional. There may be enough hugs. There may be enough money. There may be enough food and clothing. But this family does not manage to provide enough emotional awareness, validation, compassion, or emotional care to the children.
This is what makes emotionally neglectful families difficult to see or identify. Unlike emotional abuse or physical neglect, emotional failures are difficult to see.
As a psychologist who works with adults who grew up with childhood emotional neglect, I have seen how it affects people’s relationships with their families of origin. It often results in adult children who sense that something is wrong with them but have no idea what that is and are also baffled by their feelings about their families.
8 Signs of Emotional Neglect to Watch For in Your Family
- Your family conversations tend to be on surface topics, meaning they are seldom about emotional, meaningful, painful, or negative things. This may even make it boring .
- You sometimes feel an unexplained resentment or anger toward your parents (which you may feel guilty about).
- You go to family events with hopes of enjoying yourself, but you often come away feeling empty or disappointed.
- Difficult or interpersonal problems in the family are generally ignored instead of addressed directly.
- It feels like your siblings are competing with each other, but you’re not sure for what.
- Affection in your family is expressed via action (doing things for people) and not so much by words or emotional expression.
- Emotion –perhaps only negative emotions, but maybe all –seems taboo in your family.
- You feel surprisingly lonely or left out when you’re with your family.
The members of an emotionally neglectful family do suffer. They suffer from what goes unsaid, unshared, undiscussed, unnoticed, and unvalidated. If your family is emotionally neglectful, and if you pay attention , you may notice some of the above signs whenever you spend time with them.
Like a beautiful cake baked without enough sugar, what may appear fine is not fine. The emotionally neglectful family suffers from an absence of enough of a key ingredient that may not be visible but matters greatly to enjoyment and quality. The feelings that should be sweetening the connections and warmth in the family are shoved underground.

This is why you may have felt bored, resentful, disappointed, stifled, or alone when it comes to your family. This is why it’s so important to name the problem of childhood emotional neglect and make a conscious decision to fight against it in your own life.
What You Can Do
You cannot fix your family, and you do not need to try. But you can start changing yourself. Choose an item from the list of eight above that applies to your family, and start behaving the opposite way in your own life.
Talk about meaningful things, fight against feeling guilty for your feelings, focus on self-care when with your family, talk about difficult problems, express your affection and warmth toward others in words, and face your negative emotions. You don’t have to do it perfectly. You only need to do it enough .
Scores of good people have been in your shoes and walked your path before you, and many more are walking with you now. Last but not least, and above all, please know that you are not alone.
© Jonice Webb
To determine whether you might be living with the effects of childhood emotional neglect, you can take the free Emotional Neglect Questionnaire. You'll find the link in my bio.
Facebook /LinkedIn image: fizkes/Shutterstock
Winnicott, D W. Playing and Reality. London: Routledge, 1989
U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. “Child Maltreatment 2018.” Accessed July 31, 2020. https://www.acf.hhs.gov/cb/research-data-technology /statistics-research/child-maltreatment
Susan S. Woodhouse, Julie R. Scott, Allison D. Hepworth, Jude Cassidy. Secure Base Provision: A New Approach to Examining Links Between Maternal Caregiving and Infant Attachment. Child Development, 2019; DOI: 10.1111/cdev.1322

Jonice Webb, Ph.D., is a licensed psychologist and author of two books, Running On Empty: Overcome Your Childhood Emotional Neglect and Running On Empty No More: Transform Your Relationships.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that could derail our entire day. Here’s how we can face triggers with less reactivity and get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
Introduction. At least one in five youth in the United States, the United Kingdom, and other developed countries (1-3) experience childhood adversities such as exposure to abuse, neglect, or other major life stressors, which can considerably impact their socio-emotional, cognitive, and physical development, while simultaneously increasing the long-term risk of mental health difficulties (4, 5).
Childhood maltreatment is commonly described as physical, sexual or emotional abuse and physical or emotional neglect by a parent, caregiver or other adult, with all kinds of abuse resulting from acts of commission, and neglect from acts of omission. There has been relatively less societal and research attention on emotional abuse and emotional ...
Research documenting how childhood maltreatment contributes to altered HPA axis and CRF circuit activity in preclinical and clinical studies has been reviewed in detail elsewhere ... Wong CM , et al.: Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice.
In terms of prevalence, a worldwide meta-analysis estimated rates of 12.7% for sexual abuse, 16.3% for physical neglect, 18.4% for emotional neglect, 22.6% for physical abuse, and 36.3% for emotional abuse . These data indicate that childhood maltreatment is globally widespread, affecting the lives of millions of children.
Research suggests that childhood psychological maltreatment (i.e., emotional abuse and emotional neglect) is associated with mental health problems that persist into adulthood, for example anxiety, depression, post-traumatic stress disorder (PTSD), suicidal ideation, and aggression; however, a systematic review and meta-analysis of the existing literature would help clarify the magnitude and ...
A systematic review of the emotional, behavioural and cognitive features exhibited by school-aged children experiencing neglect or emotional abuse. Child: Care, Health and Development, 41(5), 641-653 ... (2013). Translational research on child neglect: Progress and future needs introduction. Child Maltreatment, 18(1), 3-7. https://doi.org ...
1. Introduction. Childhood emotional neglect (CEN), a subtype of childhood maltreatment (including physical, sexual, or emotional abuse and physical or emotional neglect), refers to a failure to meet the basic emotional needs of a child, insensitivity to the child's distress, and ignoring the child's social and emotional development (Teicher & Samson, 2013).
The scale of the problem. Despite difficulties in recognising and measuring emotional abuse, meta-analyses of the global prevalence of maltreatment convincingly reveal that childhood emotional abuse is self-reported by a much larger proportion of the adult population (about 36%) compared with physical (about 18%) or sexual abuse (8-18%), or physical neglect (about 16%).
Childhood emotional neglect is positively correlated with adolescent depression. The stress-sensitization model (Post, 1992) proposes that the adversity encountered in childhood may increase the individual's sensitivity to future stressful events, and among various forms of childhood abuse, emotional neglect may be the most easily overlooked potential form of abuse.
For instance, research indicated that childhood emotional neglect negatively predicted the development of individual empathy skills, and this predictive effect was mediated by attachment avoidance (i.e., emotional neglect shapes the formation of an avoidant attachment pattern, leading to reduced cognitive empathy abilities in individuals) (Yang ...
tl;dr. Ongoing childhood emotional neglect is a form of child abuse and can lead to lasting trauma. This trauma can make it hard to develop a healthy relationship with others and with ourselves. We might even engage in self-sabotaging behaviors. Therapy can teach us how to properly identify and label our emotions so that we can deal with them ...
Background:Childhood neglect is a risk factor for subsequent mental health problems. However, research on the unique contribution of emotional and physical subtypes of neglect is lacking. ... mean age = 18.9, 70% female) responded in an online survey to questions on childhood emotional and physical neglect, childhood abuse, symptoms of ...
Perhaps least represented in existing treatment outcome research are the needs of adult survivors of childhood maltreatment experienced primarily in the form of severe emotional abuse and neglect during childhood. Frequently overlooked, minimized, or misunderstood is psychological maltreatment, defined as children's exposure to recurrent and severe forms of emotional abuse and emotional ...
Emotional neglect from childhood teaches adults to ignore, minimize, or be ashamed of their feelings. Current research establishes the importance of feelings when used effectively. People can ...
This paper brings together research on child maltreatment, emotional development, and psychopathology to examine the consequences of child abuse and neglect for emotion processing in adulthood. Childhood Maltreatment and Emotion Processing. In general, child maltreatment has been found to disrupt the normal process of emotional development.
1. Introduction. Childhood emotional neglect (CEN) is a form of childhood trauma (including physical/sexual/emotional abuse and physical/emotional neglect), referring to when a child's basic emotional needs are not met, distress is not treated sensitively, and social and emotional development is ignored (Teicher & Samson, Citation 2013).Meta-analyses revealed that the global prevalence of CEN ...
Child neglect globally. Child neglect is a major world health and social problem (Kubolsky et al., 2020). A meta-analysis estimated the worldwide prevalence of neglect to be 16% for physical neglect and 18% for emotional neglect, though globally there is paucity of research regarding child neglect (Stoltenborgh et al., 2013).
Childhood Emotional Neglect: 5 Hidden Consequences. Almost 1 in 5 adults globally may have been neglected as a child, and it most likely happened unintentionally (Stoltenborgh et al., 2013). Parents or guardians failed to meet their children's basic emotional needs or were insensitive to their distress or developmental needs.
This article reviews research about how child neglect is perceived by social workers. We conducted a systematic review and identified fifty relevant studies, using a range of methodologies, published since the 1989 Children Act. ... This is particularly true for emotional neglect and neglect of older children. The review found that social ...
The authors highlight research that suggests adults who experience childhood emotional neglect may: fear, or be hypersensitive to, perceived signs of rejection. overreact to stressful events ...
Childhood emotional neglect which has an important place among the neglect types, is a relationship pattern in which the emotional needs of child are constantly ignored, invalidated or appreciated ...
Methods: Childhood emotional neglect, defined as the absence of parental attention and support, was measured across seven assessments from age 8 to 17.5. Peer social support was measured at age 15. ... Some research has shown that emotional neglect often co-occurs with other forms of childhood maltreatment , ...
The members of an emotionally neglectful family do suffer. They suffer from what goes unsaid, unshared, undiscussed, unnoticed, and unvalidated. If your family is emotionally neglectful, and if ...
For this rapid review, child maltreatment is conceptualised as a category of violence against children encompassing physical abuse, emotional abuse, sexual abuse, and neglect, and exposure to family and domestic violence also known as interpersonal violence (UNICEF, 2023).Child maltreatment occurs within children's homes, education settings, workplaces, and communities (Pinherio, 2006).
Objective: There is poor understanding on health care utilization, productivity losses, and burden of adverse childhood experiences (ACEs) in multiethnic Asian populations. Part of this research gap stems from the limited epidemiological data on neglect, emotional abuse, bullying, and dysfunctional home environments. This study estimated health care utilization, productivity losses, and burden ...
Research has found that anxiety can sometimes be an indication of childhood emotional neglect. Growing up with emotionally unavailable parents can make it difficult to understand, process, and ...