PERSPECTIVE article
The psychological and social impact of covid-19: new perspectives of well-being.
A commentary has been posted on this article:
Commentary: The psychological and social impact of COVID-19: New perspectives of well-being
- Read general commentary

- 1 Department of Human Sciences, Society and Health, University of Cassino and Southern Lazio of Cassino, Cassino, Italy
- 2 Independent Researcher, Milan, Italy
- 3 Department of Political and Social Studies, Sociology, University of Salerno, Fisciano, Italy
The recent Covid-19 pandemic has had significant psychological and social effects on the population. Research has highlighted the impact on psychological well-being of the most exposed groups, including children, college students, and health workers, who are more likely to develop post-traumatic stress disorder, anxiety, depression, and other symptoms of distress. The social distance and the security measures have affected the relationship among people and their perception of empathy toward others. From this perspective, telepsychology and technological devices assume important roles to decrease the negative effects of the pandemic. These tools present benefits that could improve psychological treatment of patients online, such as the possibility to meet from home or from the workplace, saving money and time and maintaining the relationship between therapists and patients. The aim of this paper is to show empirical data from recent studies on the effect of the pandemic and reflect on possible interventions based on technological tools.

Introduction
The Covid-19 pandemic led to a prolonged exposure to stress. As a consequence, researchers showed an increased interest in measuring social and community uneasiness in order to psychologically support the population. This increased attention might help in managing the current situation and other possible epidemics and pandemics. The security measures adopted in managing the pandemic had different consequences on individuals, according to the social role invested. Some segments of the population seem to be more exposed to the risk of anxious, depressive, and post-traumatic symptoms because they are more sensitive to stress.
The following article has two focuses of interest: (1) the evaluation of the psychological and social effects of the pandemic on the population, mostly children, college students, and health professionals; and (2) the identification of new perspectives of intervention based on digital devices and in line with the social security measures and mental health promotion. Telepsychology, for instance, is a valid tool, effective in taking charge of the psychological suffering caused by the pandemic and in preventing the chronicity of the disease. The prolonged stress could involve anxiety, depression, and the inability to manage traumatic and negative emotions. Furthermore, the constant fear of contagion affects daily life and leads to social isolation, modifying human relations.
COVID-19 and At-Risk Populations: Psychological and Social Impact of the Quarantine
Studies of pandemics faced over time, such as SARS, Ebola, H1N1, Equine Flu, and the current COVID-19, show that the psychological effects of contagion and quarantine is not limited on the fear of contracting the virus ( Barbisch et al., 2015 ). There are some elements related to the pandemic that affect more the population, such as separation from loved ones, loss of freedom, uncertainty about the advancement of the disease, and the feeling of helplessness ( Li and Wang, 2020 ; Cao et al., 2020 ). These aspects might lead to dramatic consequences ( Weir, 2020 ), such as the rise of suicides ( Kawohl and Nordt, 2020 ). Suicidal behaviors are often related to the feeling of anger associated with the stressful condition widely spread among people who lived/live in the most affected areas ( Miles, 2014 ; Suicide Awareness Voices of Education, 2020 ; Mamun and Griffiths, 2020 ). In light of these consequences, a carefully evaluation of the potential benefits of the quarantine is needed, taking into account the high psychological costs ( Day et al., 2006 ; Mazza et al., 2020 ).
As reported in a recent survey administered during the Covid-19 pandemic, children and young adults are particularly at risk of developing anxious symptoms ( Orgilés et al., 2020 ). The research involved a sample of 1,143 parents of Italian and Spanish children (range 3–18). In general, parents observed emotional and behavioral changes in their children during the quarantine: symptoms related to difficulty concentrating (76.6%), boredom (52%), irritability (39%), restlessness (38.8%), nervousness (38%), sense of loneliness (31.3%), uneasiness (30.4%), and worries (30.1%). From the comparison between the two groups—Spanish and Italian parents—it emerged that the Italian parents reported more symptoms in their children than the Spanish parents. Further data collected on a sample of college students at the time of the spread of the epidemic in China showed how anxiety levels in young adults are mediated by certain protective factors, such as living in urban areas, the economic stability of the family, and cohabitation with parents ( Cao et al., 2020 ). On the contrary, having infected relatives or acquaintances leads to a worsening in anxiety symptoms. Furthermore, the economic problems and the slowdown in academic activities are related with anxious symptoms ( Alvarez et al., 2020 ). In addition, an online survey conducted on the general population in China found that college students are more likely to experiencing stress, anxiety, and depression than others during the pandemic ( Li et al., 2020 ). These results suggest monitoring and promoting mental health of youths in order to reduce the negative impact of the quarantine ( CSTS, 2020 ; Fessell and Goleman, 2020 ; Li et al., 2020 ).
Health-care workers (HCWs) are another segment of population particularly affected by stress ( Garcia-Castrillo et al., 2020 ; Lai et al., 2020 ). HCWs are at risk to develop symptoms common in catastrophic situations, such as post-traumatic stress disorder, burnout syndrome, physical and emotional exhaustion, depersonalization, and dissociation ( Grassi and Magnani, 2000 ; Mache et al., 2012 ; Øyane et al., 2013 ). However, an epidemic presents different peculiarities compared to a catastrophic event, for instance, the stigmatizing attitudes in particular toward health professionals, who are in daily contact with the risk of infection ( Brooks et al., 2020 ). During SARS, up to 50% of health-care professionals suffered from acute psychological stress, exhaustion, and post-traumatic stress, caused by the fear of contagion of their family members and the prolonged social isolation ( Tam et al., 2004 ; Maunder et al., 2006 ).
As a consequence of the pandemic, the health professionals who were overworked suffered high level of psychophysical stress ( Mohindra et al., 2020 ). Health professionals also lived/live in daily life a traumatic condition called secondary traumatic stress disorder ( Zaffina et al., 2014 ), which describes the feeling of discomfort experienced in the helping relationship when treatments are not available for all patients and the professional must select who can access them and who cannot ( Roden-Foreman et al., 2017 ; Rana et al., 2020 ). Data from a survey on 1,257 HCWs who assisted patients in Covid-19 wards and in second- and third-line wards showed high percentages of depression (50%), anxiety (44.6%), insomnia (34%), and distress (71.5%) ( Lai et al., 2020 ). Also, the constant fear of contagion leads to obsessive thoughts ( Brooks et al., 2020 ), increasing the progressive closure of the person and reducing social relationships. In line with these results, Rossi et al. (2020) evaluated mental health outcomes among HCWs in Italy during the pandemic, confirming a high score of mental health issues, particularly among young women and front-line workers. Furthermore, Spoorthy et al. (2020) conducted a review on the gendered impact of Covid-19 and found that 68.7–85.5% of medical staff is composed of women, and the mean age ranged between 26 and 40 years. Also, women are more likely to be affect by anxiety, depression, and distress ( Lai et al., 2020 ; Zanardo et al., 2020 ). Liang et al. (2020) also found a relation between age and depressive symptoms associated with the pandemic. Indeed, the medical staff at younger ages (<30 years) reports higher self-rated depression scores and more concern about infecting their families than those of older age. Staff > 50 years of age reported increased stress due to patient’s death, the prolonged work hours, and the lack of personal protective equipment. Cai et al. (2020) also found that nurses felt more nervous compared to doctors.
As emerged by the recent literature, the promotion of psychological interventions on the specific population who is more likely to develop pathologies and suffering is needed. The Lancet Global Mental Health Commission’s observation ( Patel, 2018 ) reported that the use of digital technologies can provide mental health interventions in order to reduce anxiety and stress levels and increase self-efficacy ( Kang et al., 2020 ; Xiao et al., 2020 ).
Telepsychology: Training and Promotion of Psychological Well-Being
In order to reduce anxiety and depression symptoms widespread among the population, the World Health Organization (2019) and the Centers for Disease Control and Prevention (2020) proposed specific guidelines on the correct use of health protection with the aim to minimize the distress associated with health-care professions.
At the same time, as a consequence of the emerging issues, psychotherapists provided psychological support online, addressing the technological challenge ( Greenberg et al., 2020 ); Liu et al., 2020 ). In line with the technological progress, professional organizations promoted specific guidelines and policies related to customer protection, privacy, screening, evaluation, and development of self-help products ( Duan and Zhu, 2020 ; Zhou et al., 2020 ). Technological development in mental health foreshadows future trends that include “smart” mobile devices, cloud computing, virtual worlds, virtual reality, and electronic games in addition to the traditional psychotherapy tools. In this perspective, it is important to help future generations of psychologists and patients to collaborate in the potential growth areas, through education and training on the benefits and effectiveness of telepsychology ( Maheu et al., 2012 ).
Indeed, more awareness of the potentials of the online services is needed, exploring the main differences between the devices (chat, video-audio consultation, etc.) in order to use them in relation to the specific purposes identified by the professional. For example, the Italian Service of Online Psychology conducted a study based on a service of helpdesk on Facebook. This service guided people in asking for psychological help, working on their personal motivation. At the same time, another helpdesk on Skype provided some psychological sessions via webcam ( Gabri et al., 2015 ). In this line, telecounseling is a diffuse online method used by counselors and psychologists during the recent pandemic ( De Luca and Calabrò, 2020 ).
One of the future goals of public and private psychological organizations should be the promotion of specific training for psychologists and psychotherapists, with the following aims: (1) developing the basic skills in managing the effects of a pandemic and of emergency situations; and (2) sensitizing patients to online therapeutic relationship, providing the main rules and benefits of the process ( Stoll et al., 2020 ; Joint Task Force for the Development of Telepsychology Guidelines for Psychologists, 2013 ). On this line, a significant example is the Virginia Commonwealth University (VCU) which proposed PhDs in telepsychology, with the aim of training future psychologists in managing the psychological effects of the pandemic through an online psychology service ( Baylor et al., 2019 ). The service provided by the VCU had been effective in reducing anxiety, depression ( Sadock et al., 2017 ), and hospital recoveries ( Lanoye et al., 2017 ). As shown, telepsychology assumes a key role in the improvement of health care. Online psychological services avoid geographical barriers and are suitable to become a useful integrated tool in addition to traditional psychotherapy ( APS, 2020 ; Perrin et al., 2020 ).
Advantages of Psychological Support and Online Psychotherapy
Online psychological services provide several advantages, especially in the current situation of pandemic. First of all, online services help people in a short period of time, reducing the risk of contagion and the strong feeling of anxiety in both psychotherapists and patients, who feel uncomfortable in doing traditional psychotherapy due to the pandemic ( Békés and Aafjes-van Doorn, 2020 ). Furthermore, Pietrabissa et al. (2015) identified some of the main advantages of telepsychology, such as the decrease in waiting for the consultation, because it takes place from home or from the workplace, saving time and expense, less travel and rental costs for the office, for those who provide the service and for those who use it. As reported by the authors, online psychological services facilitate access to people who struggle to find support close to their social environment, avoiding difficulties related to mobility. Also, online services help people who have less confidence in psychotherapy. Indeed, mostly online psychotherapy takes place in one’s comfort zone, facilitating the expression of problems and feelings.
According to the situations, online services could provide a different medium. For instance, the chat is a useful tool to establish a first assessment of a person who feels uncomfortable in using video. Indeed, the online psychotherapy is perceived as more “acceptable.” Suler (2004) defined the term online disinhibition effect demonstrating how the web, unlike the real life, leads to the failure of the hierarchical relationship based on dominant-dominated among individuals; this aspect, according to the author, allows a greater sense of freedom in expressing oneself and less concern related to judgment ( ibid .). Other researchers ( Mantovani, 1995 ; Tosoni, 2004 ) have integrated to the construct of online disinhibition effect the concept of social space, emphasizing the role of the “situation,” of the “social norms” ( Brivio et al., 2010 , p. 811), of the tools (“artifacts”), and of the cyberplace, which allow different levels of interaction. Each person has a different experience of the network and several levels of disinhibition. For instance, a mild disinhibition could be a person who chooses to ask for help talking with a psychologist about their problems; while a high disinhibition could be represented by flaming, an expression of online bullying or cyberstalking.
Online psychological services should be integrated with the various territorial services in order to provide the patients local references in relation to the specific health and economic needs. Finally, the possibility for the therapist and for the patient to record the sessions via chat and in audio/video mode—with the informed consent of the participants ( Wells et al., 2015 )—provides another useful tool to compare the sessions and to underline the positive outcomes and the effectiveness of the therapeutic process. According to this perspective, online psychological support and psychotherapy become a resource for psychotherapists and patients in a co-build relationship ( Algeri et al., 2019 ).
Psychological and Social Suffering and the Empathic Process
In analyzing the psychological impact of the quarantine, the importance for individuals to feel integral part of the society emerged, an aspect often undervalued in psychological well-being. Experts of public health believe that social distancing is the better solution to prevent the spread of the virus. However, although it is not possible to predict the duration of the pandemic, we know very well the serious impact of these measures on the society, on relationships and interactions, in particular on the empathic process. In the early 90s, empathy was described as a form of identification in the psychological and physiological states of others. This definition led to a debate between the disciplines of philosophy of psychology and philosophy of the mind ( Franks, 2010 ). Willard Van Orman Quine (1908–2000) renewed attention to the debate on empathy with a thesis on the development of language and mind in the analytical philosophy. According to Quine, the attribution of the so-called intentional states, through which the psychology commonly explains human behavior, is based on empathy ( Treccani, 2020 ) and leads people to attribute beliefs, desires, and perceptions ( Quine, 1990 , 1992 , Pursuit of Truth: Revised Edition, 1992). Analyzing this aspect within the recent situation of the pandemic, an increment of antithetical positions and attitudes could be noticed. On the one hand, people identify themselves with those who suffer (neighbors, friends, relatives who are living stressful events), promoting activities such as the so-called “suspended expenses.” For instance, solidarity and humanitarian activities, food, and medicine delivery for people who are unable to go to the supermarket. On the other hand, there is a part of the population who experiences a feeling of “forced empathy.” This aspect could be also emphasized by the use of technological devices that might lead to a depersonalization of relationships, forcing the sense of closeness, at least virtually. The hyperconnection of feelings becomes a way to reduce the self-isolation and its consequences, representing the contrary of the idea of Durkheim (1858–1917), who considered society as a specific entity, built on social facts ( Durkheim, 1922 ). The sensation “to be forced to feel” could lead people to distance themselves from others after the emergency situation, incrementing social phobias.
Also, human communication is changing. The formal question “how are you?” at the beginning of a conversation is no longer just a formality, as before the pandemic. For example, the relationship between employee and the manager is different, leading to more responsibilities in listening and understanding feelings expressed during the video call, generating a forced reciprocity. Hence, the aforementioned “forced empathy” may be common in this period because the social distance and the emergency situation make people want to be heard and appreciated, and the simple question “how are you?” becomes an anchor to express fears and emotions ( Pasetti, 2020 ).
The Covid-19 pandemic has affected the way people live interpersonal relationships. The lockdown was characterized of a different organization of daily life, with an incrementation of time at home and a reduction of distance through digital devices. This period was also seen as an evolution in the concept of empathy, producing new perspectives in the study of the phenomenon according to a sociological and neurological points of view. Indeed, empathy—defined as the ability to understand and share the feelings of another—involves several elements, such as: (a) social context and historical period of the individual, (b) neurological mechanisms, and (c) psychological and behavioral responses to feelings of others. The neuro-sociological perspective analyzes the mechanisms involved in the empathic process, focusing on human communication and interpersonal relationships ( Singer and Lamm, 2009 ; Decety and Ickes, 2009 ). Specifically, in this historical period characterized by an increment in the man–machine relationship, neurosociology could become one of the principal sciences for the study of human relations and technology. “We live increasingly in a human–machine world. Anyone who doesn’t understand this, and who is not struggling to adapt to the new environment—whether they like that environment or not—is already being left behind. Adapting to the new, fast-changing, technologically enhanced context is one of the major challenges of our times. And that certainly goes for education” ( Prensky, 2012 , p. 64).
According to the abovementioned considerations, our suggestion consists in:
Primary prevention. Studying the impact of the pandemic toward an at-risk population to reduce symptoms related to stress and providing specific online psychological counseling based on the target (students, medical staff, parents, and teachers).
Secondary prevention. Overcoming the limitations of the human interaction based on digital devices: (1) developing new spaces of inter- and intrasocial communication and new tools of support and psychological treatment, reproducing the multisensory experienced during the face-to-face interaction (Virtual Reality, holograms, serious game etc.); (2) training the next generation of psychotherapists in managing online devices and in implementing their adaptive and personal skills; and (3) sensitizing the general population on telepsychology and its advantages.
Research according to the neurosociological perspective . Studying human interaction mediated by new technologies and the role of empathy, associating neuroscience, sociology, and psychology.
Author Contributions
VS, DA, and VA conceptualized the contribution. VS wrote the paper, reviewed the manuscript, and provided the critical revision processes as PI. All authors approved the submission of the manuscript.
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Algeri, D., Gabri, S., and Mazzucchelli, L. (2019). Consulenza psicologica online. Esperienze pratiche, linee guida e ambiti di intervento. Firenze: Giunti Editore.
Google Scholar
Alvarez, F., Argente, D., and Lippi, F. (2020). A simple planning problem for Covid-19 lockdown. Covid Econ. 14, 1–33. doi: 10.3386/w26981
CrossRef Full Text | Google Scholar
APS (2020). Psychologists welcome health fund telehealth support of Australians’ mental health during COVID-19 outbreak. Australia: Tratto da Australian Psuchology Society.
Barbisch, D., Koenig, K., and Shih, F. (2015). Is there a case for quarantine? Perspectives from SARS to Ebola . Dis. Med. Pub. Health Prepar. 9, 547–553. doi: 10.1017/dmp.2015.38
PubMed Abstract | CrossRef Full Text | Google Scholar
Baylor, C., Burns, M., McDonough, K., Mach, H., and Yorkstona, K. (2019). Teaching Medical Students Skills for Effective Communication With Patients Who Have Communication Disorders. Am. J. Spe. Lang. Pathol. 28, 155–164. doi: 10.1044/2018_ajslp-18-0130
Békés, V., and Aafjes-van Doorn, K. (2020). Psychotherapists’ attitudes toward online therapy during the COVID-19 pandemic. J. Psychother. Integr. 30, 238–247. doi: 10.1037/int0000214
Brivio, E., Ibarra, F., Galimberti, C., and Cilento. (2010). “An Integrated Approach to Interactions in Cyberplaces: The Presentation of Self in Blogs,” in Handbook of Research on Discourse Behavior and Digital Communication: Language Structures and Social Interaction , eds E. Brivio, F. Ibarra, and C. Galimberti (Pennsylvania: Information Science Reference/IGI Global), 810–829. doi: 10.4018/978-1-61520-773-2.ch052
Brooks, S., Webster, R. S., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395:10227. doi: 10.1016/S0140-6736(20)30460-8
Cai, H., Tu, B., Ma, J., Chen, L., Fu, L., Jiang, Y., et al. (2020). Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID19) in Hubei. China. Med. Sci. Monit. 2020:26. doi: 10.12659/MSM.924171
Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., et al. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psych. Res. 287:112934. doi: 10.1016/j.psychres.2020.112934
Centers for Disease Control and Prevention (2020). Preparedness Tools for Healthcare Professionals and Facilities Responding to Coronavirus (COVID-19) . Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/preparedness-checklists.html
CSTS (2020). Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Pub Health 17:1729. doi: 10.3390/ijerph17051729
Day, T., Park, A., Madras, N., Gumel, A., and Wu, J. (2006). When Is Quarantine a Useful Control Strategy for Emerging Infectious Diseases? Am. J. Epidemiol. 163, 479–485. doi: 10.1093/aje/kwj056
De Luca, R., and Calabrò, R. S. (2020). How the COVID-19 Pandemic is Changing Mental Health Disease Management: The Growing Need of Telecounseling in Italy. Innov. Clin. Neurosci. 17, 16–17.
Decety, J., and Ickes, W. (eds) (2009). The Social Neuroscience of Empathy. Cambridge, MA: MIT Press.
Duan, L., and Zhu, G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. Lancet. Psych. 7, 300–302. doi: 10.1016/s2215-0366(20)30073-0
Durkheim, E. (1922). Education et Sociologie. Milano: Ledizioni.
Fessell, D., and Goleman, D. (2020). How Healthcare Personnel Can Take Care of Themselves. US: HBR.
Franks, D. (2010). Neurosociology the nexus between neuroscience and social psychology. Londra. Springer.
Gabri, S., Mazzucchelli, S., and Algeri, D. (2015). The request for psychological help in the digital age: offering counseling through chat and video counseling. E J. Psychother. 2015, 2–10.
Garcia-Castrillo, L., Petrino, R., and Leach, R. (2020). European Society For Emergency Medicine position paper on emergency medical systems’ response to COVID-19. Eur. J. Emerg. Med. 27, 174–1777. doi: 10.1097/mej.0000000000000701
Grassi, L., and Magnani, K. (2000). Psychiatric Morbidity and Burnout in the Medical Profession: An Italian Study of General Practitioners and Hospital Physicians. Psychother. Psychosom. 69, 329–334. doi: 10.1159/000012416
Greenberg, N., Docherty, M., Gnanapragasam, S., and Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 368:m1211. doi: 10.1136/bmj.m1211
Joint Task Force for the Development of Telepsychology Guidelines for Psychologists (2013). Guidelines for the practice of telepsychology. Am. Psychol. 68, 791–800. doi: 10.1037/a0035001
Kang, L., Ma, S., and Chen, M. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 87, 11–17. doi: 10.1016/j.bbi.2020.03.028
Kawohl, W., and Nordt, C. (2020). COVID-19, unemployment, and suicide. Lancet Psych. 7, 389–390. doi: 10.1016/s2215-0366(20)30141-3
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., et al. (2020). Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
Lanoye, A., Stewart, K., Rybarczyk, B., Auerbach, S., Sadock, E., Aggarwal, A., et al. (2017). The impact of integrated psychological services in a safety net primary care clinic on medical utilization. J. Clin. Psychol. 73, 681–692. doi: 10.1002/jclp.22367
Li, L. Z., and Wang, S. (2020). Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psych. Res. 291, 0165–1781. doi: 10.1016/j.psychres.2020.113267
Li, S., Wang, Y., Yang, Y., Lei, X., and Yang, Y. (2020). Analysis of influencing factors of anxiety and emotional disorders in children and adolescents during home isolation during the epidemic of novel coronavirus pneumonia. Chin. J. Child Heal 2020, 1–9.
Liang, Y., Chen, M., Zheng, X., and Liu, J. (2020). Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 133, 1101–1102. doi: 10.1016/j.jpsychores.2020.110102
Liu, S., Yang, L., Zhang, C., Xiang, Y. T., Liu, Z., Hu, S., et al. (2020). Online mental health services in China during the COVID-19 outbreak. Lancet. Psych. 7, E17–E18. doi: 10.1016/S2215-0366(20)30077-8
Mache, S., Vitzthum, K., and Klapp, B. (2012). Stress, health and satisfaction of Australian and German doctors-a comparative study. World Hosp Health 48, 21–27.
Maheu, M. P., McMenamin, J., and Posen, L. (2012). Future of telepsychology, telehealth, and various technologies in psychological research and practice. Profess. Psychol. Res. Prac. 43, 613–621. doi: 10.1037/a0029458
Mamun, M. A., and Griffiths, M. D. (2020). First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian J. Psych. 51:102073. doi: 10.1016/j.ajp.2020.102073
Mantovani, G. (1995). Comunicazione e Identità: dalle situazioni quotidiane agli ambienti virtuali. Bologna: il Mulino.
Maunder, R. G., Lancee, W. J., Balderson, K. E., Bennett, J. P., and Borgundvaag, B. (2006). Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 12, 1924–1932. doi: 10.3201/eid1212.060584
Mazza, C., Ricci, E., Biondi, S., Colasanti, M., Ferracuti, S., Napoli, C., et al. (2020). Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Publ. Health 17:3165. doi: 10.3390/ijerph17093165
Miles, S. (2014). Kaci Hickox: Public Health and the Politics of Fear. Tratto da Bioethics . Available online at: http://www.bioethics.net/2014/11/kaci-hickox-public-health-and-the-politics-of-fear/ (accessed June 2, 2020).
Mohindra, R. R. R., Suri, V., Bhalla, A., and Singh, S. M. (2020). Issues relevant to mental health promotion in frontline health care providers managing quarantined/isolated COVID19 patients. Asian J. Psych. 51:102084. doi: 10.1016/j.ajp.2020.102084
Orgilés, M., Morales, A., Delvecchio, E., Mazzeschi, C., and Espada, J. (2020). Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. PsyArXiv 2020, 1–13. doi: 10.1017/s0033291720001841
Øyane, N. P. S., Elisabeth, M., Torbjörn, A., and Bjørn, B. (2013). Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One 2013:e70228. doi: 10.1371/journal.pone.0070228
Pasetti, J. (2020). Smart-working, costretti all’empatia da convenevoli forzati. Tratto da Sole24Ore . Available online at: https://alleyoop.ilsole24ore.com/2020/03/20/covid-19-empatia/?refresh_ce=1 (accessed June 3, 2020).
Patel, V. (2018). The Lancet Commission on global mental health and sustainable development. Lancet 392, 1553–1598. doi: 10.1016/S0140-6736(18)31612-X
Perrin, P., Rybarczyk, B., Pierce, B., Jones, H., Shaffer, C., and Islam, L. (2020). Rapid telepsychology deployment during the COVID-19 pandemic: A special issue commentary and lessons from primary care psychology training. Clin. Psychol. 76, 1173–1185. doi: 10.1002/jclp.22969
Pietrabissa, G., Manzoni, A., Algeri, D., Mazzucchelli, L., Carella, A., Pagnini, F., et al. (2015). Facebook Use as Access Facilitator for Consulting Psychology. Austr. Psychol. 50, 299–303. doi: 10.1111/ap.12139
Prensky, M. (2012). What ISN’T Technology Good At? Empathy for One Thing!. Educat. Technol. 52:64.
Quine, W. (1990). Pursuit of Truth. New York: Harvard University Press.
Quine, W. (1992). Pursuit of Truth: Revised Edition. New York: Harvard University Press.
Rana, W., Mukhtar, S., and Mukhtar, S. (2020). Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J. Psych. 51:102080. doi: 10.1016/j.ajp.2020.102080
Roden-Foreman, K., Solis, J., Jones, A., Bennett, M., Roden-Foreman, J., Rainey, E., et al. (2017). Prospective Evaluation of Posttraumatic Stress Disorder and Depression in Orthopaedic Injury Patients With and Without Concomitant Traumatic Brain Injury. J. Orthop. Trauma 31, e275–e280. doi: 10.1097/BOT.0000000000000884
Rossi, R., Socci, V., and Pacitti, F. (2020). Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw Open. 3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185
Sadock, E., Perrin, P., Grinnell, R., Rybarczyk, B., and Auerbach, S. (2017). Initial and follow-up evaluations of integrated psychological services for anxiety and depression in a safety net primary care clinic. Am. Psycol. Assoc. 73, 1462–1481. doi: 10.1002/jclp.22459
Singer, T., and Lamm, C. (2009). The Social Neuroscience of Empathy. Ann. N. Y. Acad. Sci. 2009, 81–96. doi: 10.1111/j.1749-6632.2009.04418.x
Spoorthy, M. S., Pratapa, S. K., and Mahant, S. (2020). Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psych. 51:1876. doi: 10.1016/j.ajp.2020.102119
Stoll, J., Müller, J., and Trachsel, M. (2020). Ethical Issues in Online Psychotherapy: A Narrative Review. Front. Psych. 10:993. doi: 10.3389/fpsyt.2019.00993
Suicide Awareness Voices of Education (2020). Preventing Suicide During and After the COVID-19 Pandemic . Available online at: https://save.org/blog/preventing-suicide-covid-19-pandemic (accessed June 5, 2020).
Suler, J. (2004). The Online Disinhibition Effect. Cyb. Psychol. Behav. 7, 321–326. doi: 10.1089/1094931041291295
Tam, C., Pang, E., Lam, L., and Chiu, H. (2004). Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 34, 1197–1204. doi: 10.1017/s0033291704002247
Tosoni, S. (2004). Identità virtuali: comunicazione mediata da computer e processi di costruzione dell’identità personale. Milano: FrancoAngeli.
Treccani (2020). Einfuhlung. Tratto da Treccani . Available online at: http://www.treccani.it/enciclopedia/einfuhlung/ (accessed June 10, 2020).
Weir, K. (2020). Grief and COVID-19: Mourning our bygonelives. Washington: American Psychological Association.
Wells, S. W., Moreno, L., Butler, E., and Glassman, L. (2015). “The informed consent process for therapeutic communication in clinical videoconferencing,” in Clinical videoconferencing in telehealth: Program development and practice , eds P. W. Tuerk and P. Shore (Berlin: Springer Inernational Publishing), 133–166. doi: 10.1007/978-3-319-08765-8_7
World Health Organization (2019). Emergency Global Supply Chain System (COVID-19) Catalogue . Available online at: https://www.who.int/publications/i/item/emergency-global-supply-chain-system-(covid-19)-catalogue (accessed June 10, 2020).
Xiao, H., Zhang, Y., Kong, D., Li, S., and Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 26:e923549. doi: 10.12659/MSM.923549
Zaffina, S., Camisa, V., Monducci, E., Vinci, M., Vicari, S., and Bergamaschi, A. (2014). Disturbo post traumatico da stress in operatori sanitari coinvolti in un incidente rilevante avvenuto in ambito ospedaliero. La Med. Del Lav. 105:2014.
Zanardo, V., Manghina, V., Giliberti, L., Vettore, M., Severino, L., and Straface, G. (2020). Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Gynechol. Obst. 150, 184–188. doi: 10.1002/ijgo.13249
Zhou, X., Snoswell, C. L., and Harding, L. E. (2020). The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. E Health. 26, 377–379. doi: 10.1089/tmj.2020.0068
Keywords : COVID-19, empathy, psychological disease, psychotherapy, social distancing, telepsychology
Citation: Saladino V, Algeri D and Auriemma V (2020) The Psychological and Social Impact of Covid-19: New Perspectives of Well-Being. Front. Psychol. 11:577684. doi: 10.3389/fpsyg.2020.577684
Received: 29 June 2020; Accepted: 03 September 2020; Published: 02 October 2020.
Reviewed by:
Copyright © 2020 Saladino, Algeri and Auriemma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Valeria Saladino, [email protected] ; [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
The psychological impact of COVID-19 on the mental health in the general population
Affiliations.
- 1 Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, Section of Psychiatry, University of Genoa, Genoa, Italy.
- 2 IRCCS Ospedale Policlinico San Martino, Genoa, Italy.
- 3 James J. Peters Veterans' Administration Medical Center, Bronx, NY, USA.
- 4 Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
- PMID: 32569360
- PMCID: PMC7337855
- DOI: 10.1093/qjmed/hcaa201
As a result of the emergence of coronavirus disease 2019 (COVID-19) outbreak caused by acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in the Chinese city of Wuhan, a situation of socio-economic crisis and profound psychological distress rapidly occurred worldwide. Various psychological problems and important consequences in terms of mental health including stress, anxiety, depression, frustration, uncertainty during COVID-19 outbreak emerged progressively. This work aimed to comprehensively review the current literature about the impact of COVID-19 infection on the mental health in the general population. The psychological impact of quarantine related to COVID-19 infection has been additionally documented together with the most relevant psychological reactions in the general population related to COVID-19 outbreak. The role of risk and protective factors against the potential to develop psychiatric disorders in vulnerable individuals has been addressed as well. The main implications of the present findings have been discussed.
Keywords: COVID-19 infection; mental health; preventive strategies; psychological distress.
© The Author(s) 2020. Published by Oxford University Press on behalf of the Association of Physicians. All rights reserved. For Permissions, please email: [email protected].
- Open access
- Published: 05 December 2022
“…It just broke me…”: exploring the psychological impact of the COVID-19 pandemic on academics
- Lynette Thompson ORCID: orcid.org/0000-0002-4472-0048 1 &
- Cindy Christian 1
BMC Psychology volume 10 , Article number: 289 ( 2022 ) Cite this article
4 Citations
2 Altmetric
Metrics details
The declaration of COVID-19 as a global pandemic by the World Health Organisation (WHO) in 2020 catapulted institutions of higher education into an emergency transition from face-to-face to online teaching. Given the nature of the COVID-19 pandemic and the continuing after-effects thereof, the study explored the psychological impact of the COVID-19 pandemic on academics.
A qualitative phenomenological research design was used to explore the psychological impact of the COVID-19 pandemic on academics. Data were collected by means of semi-structured interviews from a sample of 11 full-time academics permanently employed at six public and private higher education institutions in South Africa in 2020 and 2021. The data were analysed by means of thematic analysis.
The study found that the COVID-19 pandemic and lockdown restrictions had a largely negative psychological impact on academics in higher education. The most dominant negative emotions reported by participants included stress, anxiety, fear and guilt either due to the threat of the virus itself, potential for loss of life, lockdown restrictions, a new working environment, and/or their perceived inability to assist their students. Participants also reported feelings of emotional isolation and an increase in levels of emotional fatigue.
In conclusion, institutions of higher education need to be aware of the negative psychological impact of COVID-19 on academics, and ensure they create and foster environments that promote mental well-being. Institutions may offer psychological services and/or emotional well-being initiatives to their academic staff. They must create spaces and cultures where academics feel comfortable to request and seek well-being opportunities. In addition to mental and emotional well-being initiatives, institutions must provide academics with tangible teaching and learning support as this would go a long way in reducing much of the stress experienced by academics during the pandemic.
Peer Review reports
In March 2020, the World Health Organisation (WHO) declared COVID-19 a global pandemic [ 1 ]. In response to this declaration, the South African government announced a state of emergency and implemented lockdown measures for most citizens. Institutions of higher education were catapulted into an emergency transition from face-to-face contact teaching to online distance teaching. This change was implemented globally [ 2 ]. The lockdown, which meant working from home, and switching to online teaching, left many academics reeling as they tried to navigate their new working environment [ 3 ]. Given the nature of the COVID-19 pandemic and the continuing after-effects thereof, it is important to explore and understand the psychological impact of the COVID-19 pandemic on academics in higher education.
Research shows that university academics experienced the pandemic in phases, one of which was uncertainty and instability where they had to adjust to the demands of their new working environment [ 4 ]. Many academics experienced a fear of online teaching, increased workloads, and increased demands from students and university management. The study lists how academics experienced these stressors and the associated fatigue as the next phase in their experience of the pandemic [ 4 ]. Worry, fear, and fatigue were also experienced in response to other factors that accompanied living in a time of a pandemic. This finding is corroborated by a UK study that reported high levels of worry and fear in the early stages of the pandemic [ 5 ]. One of the main fears that academics had to contend with during the pandemic was the unexpected propulsion of academics and students into a new level of engagement with technology [ 2 , 6 ]. This transition occurred haphazardly but out of necessity. One author postulated that most academic staff at universities offering contact classes typically lacked the necessary experience in the pedagogy of online learning [ 6 ]. Many academics also reported anxiety over inadequate technological access and resources for themselves and their students [ 2 ]. This challenge was particularly pertinent to the South African context where most of the country’s population live in poverty.
The new work/life environment also brought about many new challenges. During the COVD-19 pandemic, the ability to differentiate between work and home life was demanding for academics. Meeting work deadlines, home-schooling their own children as well as running the household were challenging for many [ 3 ]. This compounded anxieties already experienced by the pandemic [ 7 ]. In addition to navigating their new work/life environment, studies show that academics were living with constant worry and fear over their health and that of their loved ones [ 8 ].
The United Nations has warned that the psychological effects of the pandemic, and lockdown restrictions, are underestimated and people should take care of their mental health and well-being [ 4 ]. The situation is even more dire in South Africa where many people have historic trauma and live in poverty, and the added burden of the pandemic exacerbated the risk of mental illness. It is also reported that mental health has been neglected during the pandemic as there has been an understandable focus on the physical well-being of populations [ 4 ]. The stress associated with the lack of technological and pedagogical readiness to teach completely in an online space, in conjunction with other stressors linked to the pandemic, led many academics to feel drained and emotionally depleted [ 7 ]. However, research shows that psychological impact is influenced by coping mechanisms employed by individuals [ 9 ], and that these coping mechanisms could account for decreased levels of worry and fear in the later stages of the pandemic [ 10 ].
Given the nature of the COVID-19 pandemic and the continuing after-effects thereof, the researchers explored the psychological impact on academics in higher education.
A cross-sectional, exploratory research study was conducted as it allowed the researchers to gather and explore data from multiple participants at a single point in time, based on appropriate inclusion criteria [ 11 ]. This allowed the researchers to explore the experiences of academic staff in public and private higher education institutions in South Africa.
This research was conducted through the lens of an interpretivist paradigm. The interpretivist paradigm argues that reality is fluid and not fixed; realities are therefore subjective where people are studied in their natural settings. According to one author [ 11 ], qualitative research can be used to better understand participants’ views and make meaning of their experiences, contexts and world. Thus, a qualitative phenomenological research design was used to explore the psychological impact of the COVID-19 pandemic on academics. A phenomenological research design was appropriate for this study as it allowed the researchers to access participants’ lived experiences of the COVID-19 pandemic.
Participants
The sample for the study was purposively selected based on specified inclusion criteria. The sample comprised 11 full-time academics employed at six different higher education institutions in the Western Cape (South Africa). During the recruitment process, each participant was asked to report their institution of employment. This information was securely stored. Selection criteria was as follows: being permanently employed at a South African higher education institution in 2020 and 2021. Three of the 11 participants were male and eight were female. The sample was drawn from the following academic disciplines: Psychology; IT; Commerce; Optometry and Law. Table 1 below outlines the participants’ demographics, depicting their discipline and job category:
Instruments
The interviews conducted in this study were guided by a semi-structured interview guide comprising seven questions. The broad domains that were explored during the interviews included: the impact of lockdown restrictions; operational changes to the teaching and learning environment; psychological impact and coping mechanisms. Examples of some of the semi-structured interview questions that participants were asked were as follows: “ What was your initial reaction to hearing about the lockdown restrictions associated with the COVID-19 pandemic?”, “Were there any changes to the teaching and learning environment and assessment strategy at your institution and what was the impact of these changes?” and “What does work-life balance mean to you?” and “How were you impacted by the pandemic emotionally and/or psychologically?”.
Participants were recruited using LinkedIn, a professional, business-oriented social networking platform used by professionals across various industries. This invitation was posted on both researchers’ personal LinkedIn profiles. An invitation to participate in the study was shared with prospective participants who met the inclusion criteria. In the invitation, participants were asked to complete an online consent form which was securely stored in a password-protected Drive that is only accessible by the co-researchers. Each researcher was assigned a set number of participants to initiate contact to set an appointment to conduct an online interview at a time convenient for the participants. Research interviews were split amongst the two researchers (one conducted six and the other conducted five interviews). The duration of the online interviews ranged between 12 and 45 min. All interviews were transcribed by a professional transcription company and the data were securely stored in the online Google Drive.
Data analysis
Data were analysed using thematic analysis (TA) [ 12 ]. When using TA, researchers try to identify, analyse and report on prominent themes or patterns within the data [ 12 ]. Thus, in this study, both the researchers identified and analysed the codes and themes related to the psychological impact of academics at higher education institutions.
This process was conducted manually using a Microsoft Excel spreadsheet to sort and colour-code the data. Undertaking this process manually allowed the researchers to engage in in-depth discussions about the data and ratify the process of assigning and naming of themes. Themes were assigned based on previous literature to ensure alignment in the data. Where new information emerged in the data, the researchers engaged in in-depth discussion to assign the most relevant theme.
Ethical considerations
Ethics approval to conduct the study was obtained from the Independent Institute of Education (IIE) which is the affiliated organisation of the researchers of this study. Participation in the study was voluntary and written informed consent was obtained from all participants. Participants were asked to complete an online confidentiality agreement which was stored in a password-protected location. All participants were informed about the purpose of the study and their right to withdraw at any point, without any consequences. Participants’ anonymity was upheld throughout the research process and all personal identifiers were removed. Participants were referred for counselling support if needed.
Legitimation and trustworthiness
In qualitative research, reality is a social construct. Therefore, the goal is rather to achieve a measure of trustworthiness as a form of legitimation of one’s research. To achieve a measure of trustworthiness in this study, the researchers applied Lincoln and Guba’s (1985) criteria [ 13 ]. Credibility was achieved in this study through the process of triangulation. Comparative analyses were conducted by both researchers who repeatedly identified patterns in the data. Patterns or themes that emerged from the data such as the impact of the lockdown restrictions or the psychological impact of the COVID-19 pandemic. Legitimacy and trustworthiness were also achieved through the transferability of the findings (patterns) in this study. The researchers conclude that the findings of this study may be transferred to other settings with similar contexts, such as academics in other universities during the time of the COVID-19 pandemic.
The researchers employed a process of reflexivity throughout the entire data collection and analysis process and aimed to ensure that their personal experiences did not impact or bias the findings of the study [ 14 ].
The study explored the psychological impact of COVID 19 on academics working in higher education institutions in South Africa. The following section entails the themes that emerged from the data analysis which include:
Impact of lockdown restrictions
A few participants shared that they experienced several emotions in relation to the announcement of the lockdown restrictions, which was largely related to the initial 21-day lockdown period. Participants responded as follows:
P4: “…daunting…horror…shock…anxiety”
P6: “Initially a lot of fear and anxiety around the unknown”
Many participants reported increased stress and anxiety. They reported that the stress and anxiety resulted mainly around the fear of the unknown in terms of the pandemic and the lockdown restrictions and worry about their health and that of their loved ones. The misinformation in the media further amplified the fear and anxiety.
P9: “so the anxiety now is coming from all those different sources around where you are, as you speak to your students and you wonder so what’s going to happen to me, given that…not just to say is this pandemic going to end or the loved ones that are passing away, but also economically you know, what’s going to happen. So those are some of the things that fed into the anxiety in my own personal experience."
Many of the participants shared their struggle of trying to implement boundaries in the workspace. The participants expressed their difficulty with switching off from work while working from home. One participant shared the following excerpt:
P3: “I found it really difficult to switch off because now your home is your office…boundaries are very difficult to maintain working from home, so fatigue was the order of the day”.
The participant shared that a consequence of blurring the lines was constant fatigue. This sentiment was shared by many other participants.
Participants also reported quite a lot of guilt as they felt that they were not spending enough quality time with family where they could give their undivided attention. They reported being unable to be emotionally available to their families as a result of the constant exhaustion and fatigue due to work and home responsibilities.
Some participants went as far as to self-diagnose and claimed to be suffering from depression. They did, however, acknowledge that they are self-diagnosed. While others reported that they were emotionally depleted due to the unending pandemic, underpinned by a false sense of hope that things would be better in 2021. They seemed to have held onto the new calendar year as the turning point for the end to the pandemic. When they realised this was not to be the case, the emotional depletion set in, and hope started to diminish. One participant even reported that their empathy for the students diminished due to mental exhaustion. This participant reported that due to their personal state of mental fatigue, their interest and care for the well-being of their students had reduced. Another participant reported that they had a pre-existing mental illness that was exacerbated by the pandemic:
P6: “I do suffer with anxiety and my anxiety was just pushed to the limit during the lockdown”.
Some participants reported that the pandemic and lockdown restrictions did not have any negative impact on their emotional and/or psychological well-being. They reported, however, that they experienced some financial impact albeit it was not always a direct impact - it was more related to extended family members. This, they claimed, did have an emotional impact on them though. Some reported that because they did not lose a loved one or “death was not close to home”, they were not conscious of any emotional and/or psychological impact on their well-being.
Thus, some participants reported that there was no emotional and/or psychological impact on their well-being. They considered themselves to be rather resilient during these adverse times:
P4: “I’m resilient, I can cope, I can…I’m able to deal with new challenges and I’ve grown because of it, ja and the adaptation, that agility for me was like a big boost to my self-confidence”.
For many participants, this is a positive side effect of the trials and tribulations of what they faced during the pandemic.
Changes to the teaching and learning environment
Most of the participants reported that a major change to the teaching and learning environment at their institution was centred around the move from predominantly face-to-face (i.e. contact) teaching and learning solely online. A few participants mentioned experiencing a sense of emotional isolation due to a lack of support from their institution. They felt unsupported by the institution in terms of the way changes were managed, unrealistic expectations (spoken and unspoken) and a lack of regard for personal wellbeing. This resulted in the participants feeling alone, experiencing panic and a heightened feeling of anxiety related to how best to navigate the implications that the lockdown restrictions had on the teaching and learning environment. The participants reported their experiences of 2020 as follows:
P1: “2020 was a rough year” and P7: “It was a very traumatic year”
This upheaval and disruption impacted lecturers and students in various ways. Both lecturers and students had to navigate technology and learning management systems in ways they did not need to in the days before the pandemic. The adaptation to online teaching left some lecturers feeling ill-prepared and anxious at the daunting task ahead:
P5: “…the switch to online was nerve-wracking”
Participants also reported feeling troubled and burdened when they could not assist their students with technological barriers, especially those that were due to socio-economic reasons, such as lack of connectivity, lack of efficient fibre, lack of devices.
Participants reported an increase in workload that was due to the adaptation to a new unfamiliar teaching and learning mode of delivery, supporting students as well as supporting fellow lecturers. One participant relayed the experience as follows:
P8: “it just broke me…the admin behind it was insane”
The participant explained that the marking load associated with the changes in the assessment strategy was exponential, resulting in increased stress levels. Participants also reported that the ever-changing, reactive nature of institutional decisions was rather stress-inducing and meant that the initial weeks and months of the lockdown were profoundly taxing - emotionally and physically.
P7: “Things changed very fast…. everything was so fluid” and “I even forgot what it feels to relax and what it feels to be at peace, what it feels to be happy…where there’s calmness…”.
One participant reported experiencing feelings of guilt related to all the changes that took place in terms of the lockdown restrictions. This guilt was also linked to the implications thereof for the way the participants had to disperse working hours throughout the day. Additionally, this sense of guilt was related to the different roles that the participant needed to fulfil (i.e., related to work and family). One participant explained that the severity of the stress associated with the day-to-day challenges was further exacerbated by the lockdown restrictions and the constant threat of contracting the coronavirus. This resulted in a negative impact on the participant’s physical and mental health.
The psychological impact of the pandemic on academics
Participants felt that there was no real demarcation between 2020 and 2021. Participants’ perceived lack of ‘closure’ of 2020 felt like 2021 was merely an extension of 2020. This had real implications for academics’ emotional fatigue and exhaustion levels. Many reported that they were emotionally depleted from the negative impact of the pandemic and ensuing lockdown restrictions.
P6: “I feel like this year sort of rolled on from 2020, again there was no real break, there was no switching off…”. P8: “The students are tired, and I am tired…because none of us could recover from 2020”.
This emotional fatigue was compounded by the fact that participants felt that in 2021 their institution did not adequately address the challenges and issues that were encountered in 2020; they felt there was a missed opportunity in 2021 to reflect on lessons learned from 2020 and ensure a less traumatic experience for lecturers and students alike. They felt as if there was a sense of institutional denial in what had occurred in 2020. One participant shared the following excerpt:
P1: “our socio-economic culture that we have in South Africa, and obviously we have quite a big divide between students who financially are able to afford internet and laptops and all of that, and students who aren’t.“
This participant expressed concern for students who did not have the financial resources to adapt to the online learning environment. Further to this, the participant also shared a feeling of helplessness related to not knowing whether students were accessing the content and their understanding of the content.
Coping mechanisms employed by academics
One participant shared that not dealing with the reality of the situation was a means of coping. The following excerpt was shared:
P8: “I adapted to that by not dealing with it”
The participants experienced a sense of avoidance in relation to all the changes which were implemented at their institution. Other participants reported using different coping mechanisms since the start of the pandemic. One participant shared that employing self-reflection practices such as daily positive affirmations was very helpful. The participant explained that it was important to reinforce boundaries with themselves and others, especially given that the physical demarcation of work and home became enmeshed. The participant shared that this meant choosing not to answer work emails after a particular time in order to safeguard quality time with family. The following quote demonstrates this:
P6: "I try to reinforce boundaries with myself”
One participant used faith/spirituality (i.e. prayer) as a coping mechanism while navigating many difficult challenges related to the pandemic. A few participants mentioned that accepting the situation and the realities associated with the pandemic and lockdown restrictions helped them to process what was happening and cope.
Some participants relied on the following coping mechanisms: increased alcohol consumption, listening to music, watching Netflix and reading. For some of these participants, these were new coping mechanisms employed at the start of the pandemic and for others, the coping mechanisms were already used but were used more intently. Many of the participants reported that they implemented physical activity (i.e. yoga and exercise at home) as a coping mechanism. A participant reported that consciously getting sufficient sleep in the evening as a means of coping with the daily responsibilities and changes that occurred at a rapid pace. One participant shared that they tracked the number of COVID-19 infections and deaths on a daily basis as a means of coping. The participant explained that this helped with identifying the ‘enemy’ and understanding the reality of an unfolding situation. Another participant shared that their coping mechanism was undertaking personal studies to escape the reality of the pandemic. The participant explained that studying was very helpful as a means of maintaining a semblance of normalcy. There were also a few participants who did not consciously make use of any coping mechanisms during the lockdown period. There was one participant who shared that they were just focused on surviving till the end of the year (when the pandemic would presumably come to an end). The following quote demonstrates this:
P5: “we just had to make it to the end of the year”
A few participants shared that they found comfort by caring for others and helping their colleagues to navigate all the changes that occurred in their respective institutions. This was a way of coping as participants found that this instilled a sense of hope for them. Others explained that helping others inadvertently helped them find a sense of meaning and purpose. These eudaimonic acts provided these participants with a sense of validation. One participant shared the following experience:
P2: “I think I’m also getting used to it, although it’s not healthy for my side because I can support a lot of students as much as I can but what about me, what am I doing for myself”.
During the interview, the participant identified that helping students and availing themselves to students constantly throughout the period of transition was a means of coping, however, they realised that this was a sacrifice of personal wellbeing in the process.
A few participants shared that connecting with loved ones (i.e. virtually or face to face when allowed) was an important means of coping during the lockdown period. Another participant shared that engaging with therapy throughout the lockdown period was very helpful with managing anxiety associated with the pandemic. In order to cope, a participant shared that planning was helpful during the pandemic because the demarcation between work and home life was compromised by the lockdown restrictions. The following excerpt is evidence of this:
P6: “…it sort of gives me that sense of security knowing that this is what I can control and this is what I’m planning to do for the next”.
The participant went on to explain that planning the things that needed to be done on a daily basis helped them feel a sense of control and a sense of achievement once a task was complete.
On a positive note, however, for some participants, there was a definite acceptance of reality and the new order of things in the pandemic. They reported that they had learned to adapt to the new way of teaching, and they felt more adept in their ability to deliver quality online teaching.
P9: “here’s a marked difference in terms of the systems, routine pattern of doing things, things have sorted of liked settled in…”.
This gave them a sense of achievement as their confidence in being able to get students to engage in the online space grew. This was a real struggle for many participants in 2020 as they linked student disengagement to their identity as an effective lecturer.
This study aimed to explore and better understand the psychological impact of the COVID-19 pandemic on academics. Most participants reported that the COVID-19 pandemic and the associated lockdown restrictions had a significant psychological impact on them. The dominant emotional responses reported by participants included stress and anxiety, fear (of the unknown), worry (related to contracting the coronavirus and the wellbeing of family members), guilt (associated with blurring the lines between work and home life). Most participants shared this sentiment given the physical changes related to where they worked and having to adapt to online learning instantaneously. As seen in this study, the consequences of blurring the lines left some participants feeling guilty for not being emotionally available to those who needed them. This finding is corroborated by previous studies that also found that the participants struggled to demarcate work and home life and in trying to find this balance, many of them ended up feeling stressed [ 3 , 4 ].
The sudden change to online learning at higher education institutions occurred across the world [ 2 ]. The results of this study showed that most of the participants experienced the change as stressful. Having to adapt their teaching and learning strategy, while learning to use technology in a meaningful way significantly contributed to the psychological strain. Additionally, participants shared a deep sense of concern for the wellbeing of their students given the pre-existing challenges (i.e. lack of access to technological devices and internet services). These challenges were further exacerbated by the advent of the pandemic. Academics in this study reported a sense of helplessness associated with being unable to reach students. A study by one author [ 7 ] also revealed how academics’ levels of stress increased when the changes to online learning were implemented.
The results of the study highlighted the psychological impact of the COVID-19 pandemic by demonstrating that academics experienced emotional isolation because of the lockdown restrictions and having to adapt to the new working environment. Further to this, the lack of institutional support in terms of managing the changes (i.e. such as having to navigate technology and learning management system), significantly contributed to the isolation and heightened feelings of panic and anxiety. This is confirmed by a study conducted by [ 7 ]. Many academics reported feeling ill-prepared and anxious about the adaptation. Additionally, the increased workload was highlighted as significantly contributing to their levels of stress. Another author [ 4 ] confirmed this and added that academics reported that their stress was compounded by the fact that they had to teach themselves the new technologies.
The fears of the academics were not restricted to the new working environment; it transcended into their personal lives as well. The findings of this study are supported by another study that found academics to be quite fearful of their health as well as that of their loved ones [ 8 ]. This worry added to their fears and anxieties around navigating their new work/life environment.
Some participants in this study seemed to experience a sense of avoidance in relation to their new work/life environment. This is in line with other findings conducted that also reported on participants who tended to use avoidance as a means of coping with the stressors of the pandemic and resulting lockdown restrictions [ 4 , 8 ]. It must be noted here that their study reported on gender differences as they found this experience to be particular for females, however, this study does not report on gender differences in this regard.
A significant finding of this study was the increase in emotional fatigue reported by most academics. The lack of demarcation between 2020 and 2021 resulted in academics feeling hopeless and helpless in trying to navigate work and life and fulfill all their academic responsibilities. Institutional denial significantly added to this burden and many academics reported experiencing psychological strain because of this. Academics felt that the lack of willingness from institutions to reflect on the impact of the changes which were implemented at the onset of the pandemic directly impacted their ability to pause, take stock, recreate, and innovate. Even though a few academics reported that they tried to be proactive by putting systems in place to support students, they ended up emotionally fatigued. Similar results were reported in a study where their participants experienced emotional fatigue because of the increased workload brought about by additional demands from colleagues and students [ 4 ].
The COVID-19 pandemic and ensuing lockdown restrictions in 2020 and 2021 had a negative psychological impact on many academics in public and private institutions of higher education in South Africa. Institutions must use the lessons learned from 2020 to 2021 to respond to the needs of academics in years to come.
Limitations and future research
The study naturally had some limitations. The first limitation was the limited participation of male academics. Taking into consideration the interplay between gender, gender roles, mental health, coping mechanisms, and the role of gender in academia, it is recommended that future studies on this topic include equal representation of males and females to gain more insight into the experiences and coping mechanisms employed by male academics.
Another limitation is the small sample size of participants and higher education institutions in the study. A small sample size such as the one in this study potentially impacts the transferability of the findings to other academics at other institutions. It may be that academics in other institutions did not share the same experiences as their contexts may have been different from the ones in this study.
Since this was a cross-sectional research study, future research could be conducted longitudinally. It would be interesting to explore the experiences of academics potentially after six to twelve months after this study to ascertain if they are still experiencing any negative psychological impact of COVID-19, but more importantly, if participants are still employing the coping mechanism they utilised during the pandemic.
Implications for practice
Given that academics experience constant pressures to adapt to an ever-changing higher education landscape, engage with students, impart knowledge and skills, produce high-quality research and participate in scholarship activities regularly, it is important that institutions ensure that academics are equipped to deal with rapid change in future—assistance that will help ease the transition from one status quo to another—particularly in times of national and/or international turmoil and upheaval.
Institutions must strive to respond to the psychological and emotional needs of academic staff. Institutions must create working environments and foster cultures where the mental well-being of academics is encouraged and even protected. Institutional management and human resource departments at academic institutions can create support groups for academics where they can share common challenges, share examples of new teaching and learning methodologies, as well as organise wellness activities and events to support academics to overcome or reduce some of the negative psychological impact created by the COVID-19 pandemic.
Institutions must use the lessons learned from 2020 to 2021 to respond to the needs of academics in years to come. They must ensure that academics are equipped to deal with rapid change in the future—assistance that will help ease the transition from one status quo to another—particularly in times of national and/or international turmoil and upheaval.
Institutions must strive to respond to the psychological and emotional needs of academic staff (lecturers and researchers). Institutions must create working environments and foster cultures where the mental well-being of academics is encouraged and even protected. Institutional management and human resource departments at academic institutions can create support groups for academics where they can share common challenges, share examples of new teaching and learning methodologies, as well as organise wellness activities and events to support academics to overcome or reduce some of the negative psychological impact created by the COVID-19 pandemic.
Availability of data and materials
The data analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
World Health Organisation
The Independent Institute of Education
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–60.
Google Scholar
Pokhrel S, Chhetri R. A literature review on Impact of COVID-19 pandemic on teaching and learning. High Educ Future. 2021;8(1):133–41.
Article Google Scholar
Mahesh VJ, Kumar S. Work from home experiences during COVID-19 pandemic among IT employees. J Contemp Issues Bus Gov. 2020;26(2):640–5.
van Niekerk RL, van Gent MM. Mental health and well-being of university staff during the coronavirus disease 2019 levels 4 and 5 lockdown in an eastern cape university, South Africa. South Afr J Psychiatry. 2021;27:1–7.
Kleinberg B, van der Vegt I, Mozes M. Measuring emotions in the COVID-19 real world worry dataset. 2020 [cited 2022 Nov 17]. Available from: https://osf.io/awy7r/ .
Hedding DW, Greve M, Breetzke GD, Nel W, van Vuuren BJ. COVID-19 and the academe in South Africa: not business as usual. S Afr J Sci. 2020;116(8):1–3.
Rapanta C, Botturi L, Goodyear P, Guàrdia L, Koole M. Online university teaching during and after the Covid-19 crisis: refocusing teacher presence and learning activity. 2020. Available from: https://doi.org/10.1007/s42438-020-00155-y .
Al Miskry ASA, Hamid AAM, Darweesh AHM. The impact of COVID-19 pandemic on university faculty, staff, and students and coping strategies used during the lockdown in the United Arab Emirates. Front Psychol. 2021;12:682757.
Sebri V, Cincidda C, Savioni L, Ongaro G, Pravettoni G. Worry during the initial height of the COVID-19 crisis in an italian sample. J Gen Psychol. 2021;148(3):327–59.
Ongaro G, Cincidda C, Sebri V, Savioni L, Triberti S, Ferrucci R, et al. A 6-month follow-up study on worry and its impact on well-being during the first wave of covid-19 pandemic in an Italian sample. Front Psychol. 2021;12:703214.
Aspers P, Corte U. What is qualitative in qualitative research. Qual Sociol. 2019;42(2):139–60.
Braun V, Clarke V. Using thematic analysis in psychology. Psychiatric Q. 2014;0887(1):37–41.
Stahl NA, King JR. Expanding approaches for research: understanding and using trustworthiness in qualitative research. J Dev Educ. 2020;44(1):26–8.
Palaganas EC, Sanchez MC, Molintas MVP, Caricativo RD. Reflexivity inqualitative research a journey of learning. Qual Rep. 2017;22(2):426–38.
Download references
Acknowledgements
Not applicable.
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and affiliations.
School of Humanities and Social Sciences, Faculty of Humanities and Social Sciences, The Independent Institute of Education, Cape Town, South Africa
Lynette Thompson & Cindy Christian
You can also search for this author in PubMed Google Scholar
Contributions
LT and CC worked equally on all sections of the journal. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Lynette Thompson .
Ethics declarations
Ethics approval and consent to participate.
The authors sought and received ethical approval (R.15557) from The Independent Institute of Education’s ethical committee. Participants provided prior consent to participate in the study. Study participants were informed about the study objectives prior to the interviews being conducted. Voluntary written informed consent for study participation and storage, was obtained from each study participant. Participants were informed that they had the right to withdrawal participation or data at any time, without giving reasons. All study protocols were performed in accordance with the Declaration of Helsinki.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Thompson, L., Christian, C. “…It just broke me…”: exploring the psychological impact of the COVID-19 pandemic on academics. BMC Psychol 10 , 289 (2022). https://doi.org/10.1186/s40359-022-01008-y
Download citation
Received : 03 July 2022
Accepted : 30 November 2022
Published : 05 December 2022
DOI : https://doi.org/10.1186/s40359-022-01008-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological impact
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

The coronavirus ( COVID ‐19) pandemic's impact on mental health
Bilal javed.
1 Faculty of Sciences, PMAS Arid Agriculture University, Rawalpindi Pakistan
2 Roy & Diana Vagelos Laboratories, Department of Chemistry, University of Pennsylvania, Philadelphia Pennsylvania, USA
Abdullah Sarwer
3 Nawaz Sharif Medical College, University of Gujrat, Gujrat Pakistan
4 Department of General Medicine, Allama Iqbal Memorial Teaching Hospital, Sialkot Pakistan
Erik B. Soto
5 Graduate School of Public Health, University of Pittsburgh, Pittsburgh Pennsylvania, USA
Zia‐ur‐Rehman Mashwani
Throughout the world, the public is being informed about the physical effects of SARS‐CoV‐2 infection and steps to take to prevent exposure to the coronavirus and manage symptoms of COVID‐19 if they appear. However, the effects of this pandemic on one's mental health have not been studied at length and are still not known. As all efforts are focused on understanding the epidemiology, clinical features, transmission patterns, and management of the COVID‐19 outbreak, there has been very little concern expressed over the effects on one's mental health and on strategies to prevent stigmatization. People's behavior may greatly affect the pandemic's dynamic by altering the severity, transmission, disease flow, and repercussions. The present situation requires raising awareness in public, which can be helpful to deal with this calamity. This perspective article provides a detailed overview of the effects of the COVID‐19 outbreak on the mental health of people.
1. INTRODUCTION
A pandemic is not just a medical phenomenon; it affects individuals and society and causes disruption, anxiety, stress, stigma, and xenophobia. The behavior of an individual as a unit of society or a community has marked effects on the dynamics of a pandemic that involves the level of severity, degree of flow, and aftereffects. 1 Rapid human‐to‐human transmission of the SARS‐CoV‐2 resulted in the enforcement of regional lockdowns to stem the further spread of the disease. Isolation, social distancing, and closure of educational institutes, workplaces, and entertainment venues consigned people to stay in their homes to help break the chain of transmission. 2 However, the restrictive measures undoubtedly have affected the social and mental health of individuals from across the board. 3
As more and more people are forced to stay at home in self‐isolation to prevent the further flow of the pathogen at the societal level, governments must take the necessary measures to provide mental health support as prescribed by the experts. Professor Tiago Correia highlighted in his editorial as the health systems worldwide are assembling exclusively to fight the COVID‐19 outbreak, which can drastically affect the management of other diseases including mental health, which usually exacerbates during the pandemic. 4 The psychological state of an individual that contributes toward the community health varies from person‐to‐person and depends on his background and professional and social standings. 5
Quarantine and self‐isolation can most likely cause a negative impact on one's mental health. A review published in The Lancet said that the separation from loved ones, loss of freedom, boredom, and uncertainty can cause a deterioration in an individual's mental health status. 6 To overcome this, measures at the individual and societal levels are required. Under the current global situation, both children and adults are experiencing a mix of emotions. They can be placed in a situation or an environment that may be new and can be potentially damaging to their health. 7
2. CHILDREN AND TEENS AT RISK
Children, away from their school, friends, and colleagues, staying at home can have many questions about the outbreak and they look toward their parents or caregivers to get the answer. Not all children and parents respond to stress in the same way. Kids can experience anxiety, distress, social isolation, and an abusive environment that can have short‐ or long‐term effects on their mental health. Some common changes in children's behavior can be 8 :
- Excessive crying and annoying behavior
- Increased sadness, depression, or worry
- Difficulties with concentration and attention
- Changes in, or avoiding, activities that they enjoyed in the past
- Unexpected headaches and pain throughout their bodies
- Changes in eating habits
To help offset negative behaviors, requires parents to remain calm, deal with the situation wisely, and answer all of the child's questions to the best of their abilities. Parents can take some time to talk to their children about the COVID‐19 outbreak and share some positive facts, figures, and information. Parents can help to reassure them that they are safe at home and encourage them to engage in some healthy activities including indoor sports and some physical and mental exercises. Parents can also develop a home schedule that can help their children to keep up with their studies. Parents should show less stress or anxiety at their home as children perceive and feel negative energy from their parents. The involvement of parents in healthy activities with their children can help to reduce stress and anxiety and bring relief to the overall situation. 9
3. ELDERS AND PEOPLE WITH DISABILITIES AT RISK
Elderly people are more prone to the COVID‐19 outbreak due to both clinical and social reasons such as having a weaker immune system or other underlying health conditions and distancing from their families and friends due to their busy schedules. According to medical experts, people aged 60 or above are more likely to get the SARS‐CoV‐2 and can develop a serious and life‐threatening condition even if they are in good health. 10
Physical distancing due to the COVID‐19 outbreak can have drastic negative effects on the mental health of the elderly and disabled individuals. Physical isolation at home among family members can put the elderly and disabled person at serious mental health risk. It can cause anxiety, distress, and induce a traumatic situation for them. Elderly people depend on young ones for their daily needs, and self‐isolation can critically damage a family system. The elderly and disabled people living in nursing homes can face extreme mental health issues. However, something as simple as a phone call during the pandemic outbreak can help to console elderly people. COVID‐19 can also result in increased stress, anxiety, and depression among elderly people already dealing with mental health issues.
Family members may witness any of the following changes to the behavior of older relatives 11 ;
- Irritating and shouting behavior
- Change in their sleeping and eating habits
- Emotional outbursts
The World Health Organization suggests that family members should regularly check on older people living within their homes and at nursing facilities. Younger family members should take some time to talk to older members of the family and become involved in some of their daily routines if possible. 12
4. HEALTH WORKERS AT RISK
Doctors, nurses, and paramedics working as a front‐line force to fight the COVID‐19 outbreak may be more susceptible to develop mental health symptoms. Fear of catching a disease, long working hours, unavailability of protective gear and supplies, patient load, unavailability of effective COVID‐19 medication, death of their colleagues after exposure to COVID‐19, social distancing and isolation from their family and friends, and the dire situation of their patients may take a negative toll of the mental health of health workers. The working efficiency of health professionals may decrease gradually as the pandemic prevails. Health workers should take short breaks between their working hours and deal with the situation calmly and in a relaxed manner. 5
5. STIGMATIZATION
Generally, people recently released from quarantine can experience stigmatization and develop a mix of emotions. Everyone may feel differently and have a different welcome by society when they come out of quarantine. People who recently recovered may have to exercise social distancing from their family members, friends, and relatives to ensure their family's safety because of unprecedented viral nature. Different age groups respond to this social behavior differently, which can have both short‐ and long‐term effects. 1
Health workers trying to save lives and protect society may also experience social distancing, changes in the behavior of family members, and stigmatization for being suspected of carrying COVID‐19. 6 Previously infected individuals and health professionals (dealing pandemic) may develop sadness, anger, or frustration because friends or loved ones may have unfounded fears of contracting the disease from contact with them, even though they have been determined not to be contagious. 5
However, the current situation requires a clear understanding of the effects of the recent outbreak on the mental health of people of different age groups to prevent and avoid the COVID‐19 pandemic.
6. TAKE HOME MESSAGE
- Understanding the effects of the COVID‐19 outbreak on the mental health of various populations are as important as understanding its clinical features, transmission patterns, and management.
- Spending time with family members including children and elderly people, involvement in different healthy exercises and sports activities, following a schedule/routine, and taking a break from traditional and social media can all help to overcome mental health issues.
- Public awareness campaigns focusing on the maintenance of mental health in the prevailing situation are urgently needed.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
AUTHOR CONTRIBUTIONS
B.J. and A.S. devised the study. B.J. collected and analyzed the data and wrote the first draft. E.B.S. edited and revised the manuscript. A.S. and Z.M. provided useful information. All the authors contributed to the subsequent drafts. The authors reviewed and endorsed the final submission.
Javed B, Sarwer A, Soto EB, Mashwani Z‐R. The coronavirus (COVID‐19) pandemic's impact on mental health . Int J Health Plann Mgmt . 2020; 35 :993–996. 10.1002/hpm.3008 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Research article
- Open access
- Published: 09 January 2021
A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being
- Johannes H. De Kock ORCID: orcid.org/0000-0002-2468-5572 1 , 2 ,
- Helen Ann Latham 3 ,
- Stephen J. Leslie 4 ,
- Mark Grindle 1 ,
- Sarah-Anne Munoz 1 ,
- Liz Ellis 1 ,
- Rob Polson 1 &
- Christopher M. O’Malley 1
BMC Public Health volume 21 , Article number: 104 ( 2021 ) Cite this article
463 Citations
84 Altmetric
Metrics details
Health and social care workers (HSCWs) have carried a heavy burden during the COVID-19 crisis and, in the challenge to control the virus, have directly faced its consequences. Supporting their psychological wellbeing continues, therefore, to be a priority. This rapid review was carried out to establish whether there are any identifiable risk factors for adverse mental health outcomes amongst HSCWs during the COVID-19 crisis.
We undertook a rapid review of the literature following guidelines by the WHO and the Cochrane Collaboration’s recommendations. We searched across 14 databases, executing the search at two different time points. We included published, observational and experimental studies that reported the psychological effects on HSCWs during the COVID-19 pandemic.
The 24 studies included in this review reported data predominantly from China (18 out of 24 included studies) and most sampled urban hospital staff. Our study indicates that COVID-19 has a considerable impact on the psychological wellbeing of front-line hospital staff. Results suggest that nurses may be at higher risk of adverse mental health outcomes during this pandemic, but no studies compare this group with the primary care workforce. Furthermore, no studies investigated the psychological impact of the COVID-19 pandemic on social care staff. Other risk factors identified were underlying organic illness, gender (female), concern about family, fear of infection, lack of personal protective equipment (PPE) and close contact with COVID-19. Systemic support, adequate knowledge and resilience were identified as factors protecting against adverse mental health outcomes.
Conclusions
The evidence to date suggests that female nurses with close contact with COVID-19 patients may have the most to gain from efforts aimed at supporting psychological well-being. However, inconsistencies in findings and a lack of data collected outside of hospital settings, suggest that we should not exclude any groups when addressing psychological well-being in health and social care workers. Whilst psychological interventions aimed at enhancing resilience in the individual may be of benefit, it is evident that to build a resilient workforce, occupational and environmental factors must be addressed. Further research including social care workers and analysis of wider societal structural factors is recommended.
Peer Review reports
Health and social care workers (HSCWs) continue to play a vital role in our response to the COVID-19 pandemic. It is known that HSCWs exhibit high rates of pre-existing mental health (MH) disorders [ 1 , 2 , 3 ] which can negatively impact on the quality of patient care [ 4 ].
Studies from previous infectious outbreaks [ 5 , 6 ] suggest that this group may be at risk of experiencing worsening MH during an outbreak. Current evidence examining the psychological impact on similar groups [ 7 , 8 , 9 ], suggest that this group may be at risk of experiencing poor MH as a direct result of the COVID-19 pandemic. Compounding the concerns about these data are that HSCWs will be likely to not only be at a higher risk for experiencing MH problems during the pandemic, but also in its aftermath [ 5 ].
There are some specific features of the COVID-19 pandemic that may specifically heighten its potential to impact on the MH of HSCWs.
Firstly, the scale of the pandemic in terms of cases and the number of countries affected has left all with an impression that ‘no-one is safe’. Media reporting of the pandemic has repeatedly focused on the number of deaths in HSCWs and the spread of the disease within health and social care facilities which is likely to have amplified the negative effects on the MH of HSCWs.
Secondly, usual practice has been significantly disrupted and many staff have been asked to work outside of their usual workplace and have been redeployed to higher risk front line jobs.
Finally, the intense focus on personal protective equipment (PPE) is likely to have specifically heightened the impact of COVID-19 on the MH of HSCWs due to the uncertainty surrounding the quantity and quality of equipment, the frequently changing guidance on what PPE is appropriate in specific clinical situations and the uncertainty regarding the absolute risk of transmission posed. While other workers will have been impacted by COVID-19, it is highly likely that the above factors will have disproportionately affected the MH of HSCWs [ 9 , 10 ]. Indeed a British Medical Association survey on the 14th May 2020 during the pandemic showed that 45% of UK doctors are suffering from depression, anxiety, stress, burnout or other mental health conditions relating to, or made worse by, the COVID-19 crisis [ 11 ].
Although evidence based psychological interventions are available for this population [ 12 ], there is a paucity of evidence about interventions for the MH of HSCWs during pandemics. Recent calls to action mandated the need to provide high quality data on the psychological impacts of the COVID-19 pandemic [ 13 , 14 ]. This pandemic has rapidly changed the functioning of society at many levels which suggests that these data are not only needed swiftly, but also with caution and scientific rigour [ 13 , 14 ].
These data are needed in order to equip HSCWs to do their job effectively – high levels of stress and anxiety have been shown to decrease staff morale, increase absenteeism, lower levels of work satisfaction and quality of care [ 6 , 15 ]. It is therefore a priority to understand the psychological needs of our HSCWs in order to provide them with the appropriate tools to mitigate the negative effects of dealing with the COVID-19 pandemic.
While HSCWs have been identified as vulnerable to the negative psychological impact from the current pandemic, they do not form a homogeneous population. It may therefore be appropriate to identify particularly vulnerable groups within the larger population of HSCWs and target psychological support to them. This review seeks to understand whether any group of HSCWs could be confidently excluded from psychological support interventions because they are deemed to be at a low risk. Holmes et al. [ 14 ] have warned that a one-size-fits-all approach to supporting HSCWs might not be effective. This, together with the lack of evidence around tailoring psychological interventions during pandemics [ 1 ], highlights the importance of identifying vulnerable groups, to ensure appropriately personalised interventions are made available.
Aim of the review
The aim of this review is to identify the psychological impact of the COVID-19 pandemic on the health and social care professions, more specifically to identify which sub-groups are most vulnerable to psychological distress and to identify the risk and protective factors associated with this population’s mental health.
This review, looking exclusively at the psychological impact of the COVID-19 pandemic on HSCWs will therefore contribute to informing where mental health interventions, together with organisational and systemic efforts to support this population’s mental health could be focussed in an effort to support psychological well-being [ 14 ]. Rapid but robust gathering of evidence to inform health decision-makers is vital and in circumstances such as these, the WHO recommends rapid reviews [ 16 ].
Search strategy
Planning, conducting and reporting of this study was based on the guidelines for rapid reviews [ 17 ], set by the WHO [ 16 ] and the recent COVID-19 Cochrane Collaboration’s recommendations [ 18 ].
Data sources and searches
Two authors (CoM & RP) searched across a broad range of databases to capture research from potentially relevant fields, including health, mental health and health management. Within the OVID platform of databases Medline, EMBase, HMIC and PsychInfo were searched. Within the EbscoHost platform of databases, CINAHL, Medline, APA PsychInfo, Business Source Elite, Health Source and Academic Search Complete were searched. Beyond the OVID and EbscoHost platforms, SCOPUS, the King’s Fund Library, Social Care Online, PROSPERO and Google Advanced were also searched, making 16 databases searched (14 unique databases and two having been searched twice on separate platforms).
Owing to the rapidly changing landscape of the COVID-19 pandemic, and in an effort to include as many eligible papers as possible, the search strategy was executed on 23 April 2020 and again 2 weeks later on 6 May 2020 using a combination of subject headings and keyword searching (see Additional file 1 ). The bibliographical database was created with EndNote X7™.
Search criteria
The design of the search criteria was intended to draw together research both for this rapid review, and to contribute to the design of a digital mental health intervention to enhance the psychological well-being of HSCWs. The design of the search criteria is discussed in further detail in the Additional file 1 .
Types of participants
Participants were restricted to HSCWs during the COVID-19 pandemic.
Types of studies included
Published observational and experimental studies that reported the psychological effects on HSCWs during the COVID-19 pandemic were included. The study designs included quantitative and qualitative primary studies. Studies relating to previous pandemics and epidemics (such as SARS, MERS, H1N1, H5N1, Zika, Ebola, West Nile Fever) were excluded as these results have been reported elsewhere [ 7 ]. Reviews, theses, position papers, protocol papers, and studies published in languages other than English were excluded.
Screening and selection of studies
Searches were screened according to the selection criteria by JDK. The full text of potentially relevant papers was retrieved for closer examination. The reviewer erred on the side of inclusion where there was any doubt, to ensure no potentially relevant papers were missed. The inclusion criteria were then applied against full text versions of the papers (where available) independently by JDK and HL. Disagreements regarding eligibility of studies were resolved by discussion and consensus. Where the two reviewers were still uncertain about inclusion, the other reviewers (RP, CoM) were asked to provide input to reach consensus.
Data extraction and quality assessment
Relevant data were extracted into structured tables including country, setting, population, study design, number of participants, mental health conditions and their measurement tools and main study results. Where available, we extracted risk factors and protective factors. HL, LE and JDK extracted all the data while JDK checked for accuracy and completeness.
Table 2 presents an overview of the validated tools used per study type to assess study quality and risk of bias. JDK and HL assessed the quality of cross-sectional studies with the Joanna Briggs Institute tool [ 48 ] and JDK assessed their risk of bias using the Evidence Partners [ 49 ] appraisal tool. JDK assessed the risk of bias for the longitudinal study with the Critical Appraisal Skills Programme (CASP) appraisal tool [ 50 ] and the uncontrolled before-after study with the ROBINS – I [ 51 ]. SAM utilised Joanna Briggs Institute tool to assess the qualitative studies [ 38 ] and the Mixed methods appraisal tool (MMAT) [ 41 ] to assess mixed methods studies.
Data synthesis and analysis
Current best practice guided the tabulated and narrative synthesis of the results [ 52 , 53 ]. The studies’ outcomes were categorised according to the psychological impact of COVID-19 on HSCWs of:
general psychological impacts
the risk factors associated with adverse mental health outcomes
the protective factors against adverse mental health outcomes
Previous studies’ logical syntheses [ 6 ] were adapted by organising the risk and protective factors into psychosocial, occupational, sociodemographic and environmental categories. The GRADE method from the Cochrane Collaboration [ 54 ] was used to assess the quality of evidence of outcomes included in this rapid review. Varied study quality, together with study type and outcome heterogeneity precluded performing a meta-analysis.
Patient and public involvement
Some members of the author team are frontline healthcare staff during the COVID-19 pandemic and contributed to the design of the review.
Search results
The 677 records of interest were found from the two searches (429 in search 1 and 529 in search 2). After 148 duplicates were removed, 529 records were screened. Of these, 82 full texts of potentially relevant studies were assessed for eligibility (see Fig. 1 ). Twenty-four published studies met the inclusion criteria for the rapid review.
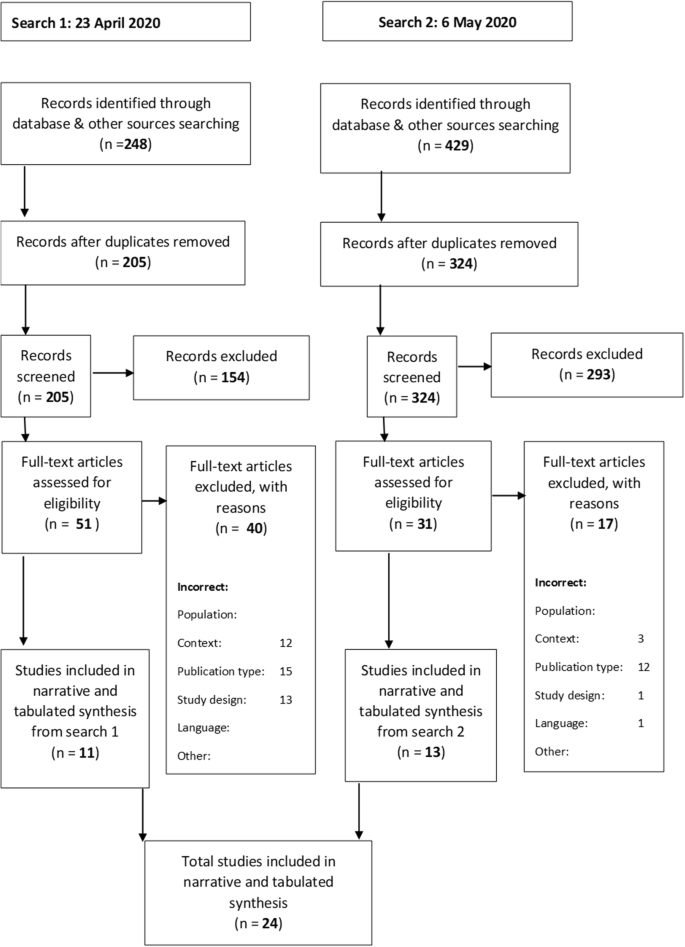
Prisma Flow Diagram
Study characteristics
The 24 studies included in this review consisted of 18 cross-sectional, 2 mixed methods, 2 qualitative, 1 longitudinal and 1 uncontrolled before-after study. The total number of participants in these studies was 13,731. In the cross-sectional studies, participant numbers ranged between 59 and 2299. Participant numbers in the two mixed method studies were 37 and 222 respectively, whilst the qualitative studies included 10 and 20 participants, respectively. The longitudinal study included 120 participants and the uncontrolled before-after study, 27 participants. See Table 1 for sampling methods within the included papers. The majority of papers utilised non-probability sampling methods, limiting generalisability of findings. One exception was Lai et al., who used region stratified 2-stage cluster sampling.
Eighteen of the studies were from China, of which 8 were based in Wuhan, where the COVID-19 outbreak began. The rest were from America (1), Israel (1), UK (1), Singapore (1), Pakistan (1), multicentre - Singapore & India (1), Global (1). Several validated measures were used to assess anxiety, depression, insomnia, stress and burnout. Table 1 provides an overview of the included studies.
Risk of bias assessment
The quality of the cross-sectional studies was fair, with 16 studies scoring 6 or higher on the JBI appraisal tool and eleven scoring 7 or higher (a score of 7 and above is an indicator of study quality). The majority of the studies indicated a low risk of bias when assessed with the Evidence Partners’ appraisal tool. The uncontrolled before-after study indicated a high risk of bias. The qualitative studies indicated a good level of quality (JBI scores of 9 & 10 respectively) while mixed methods studies showed varied quality. In the cross sectional studies, the most common problem affecting study quality was failure to deal with confounding factors. Failure to locate the researcher culturally or theoretically affected the qualitative papers, whilst the two mixed methods papers’ study quality was affected by lack of explicitly articulated research questions. A summary of the risk of bias and quality assessments are provided in Table 2 .
Psychological toll on healthcare workers
Of the 24 studies included, 22 directly assessed the psychological toll on healthcare workers and all found levels of anxiety, depression, insomnia, distress or Obsessive Compulsive Disorder (OCD) symptoms [ 24 , 25 , 26 , 27 , 29 , 30 , 31 , 33 , 34 , 35 , 36 , 37 , 39 , 40 , 42 , 43 , 44 , 46 , 47 , 58 , 59 , 60 ].
Psychological symptoms were assessed using various validated measures as outlined in Table 3 – the summary of included studies. The most common outcomes assessed were sleep, anxiety and depression. The prevalence of depressive symptoms varied greatly, ranging between 8.9% [ 39 ] to 50.4% [ 31 ]. These findings suggest marked differences in the prevalence of depressive symptoms across the studies. The prevalence of anxiety in cross-sectional studies ranged between 14.5% [ 39 ] to 44.6% [ 31 ]. Sleep was also assessed in several studies. Lai et al. [ 31 ] found the prevalence of sleep disturbances to be 34%, whilst another, nationwide survey in China found that HCWs had significantly worse sleep than the general population [ 29 ].
Risk factors associated with adverse mental health outcomes
Table 3 provides the GRADE evidence profile of the certainty of evidence for the risk factors associated with adverse MH outcomes during the COVID-19 pandemic identified through the review. These risk factors can be grouped into the three thematic areas of i) occupational, ii) psychosocial, iii) environmental.
Occupational factors
Medical hcws.
Two studies showed that medical HCWs (nurses and doctors) had significantly higher levels of MH risk in comparison to non-medical HCWs [ 34 , 47 ]. Zhang et al. [ 47 ] found that medical HCWs had significantly higher levels of insomnia, anxiety, depression, somatization and OCD symptoms in comparison to non-medical HCWs. This was also reflected in a large study in Fujian province, China, in which medical staff had significantly higher anxiety than admin staff [ 34 ]. In contrast, Tan et al. [ 39 ] found that in a population of 470 HCWs in Singapore, the prevalence of anxiety was significantly higher among non-medical HCWs than medical.
Healthcare groups
In three studies nurses were found to be at risk of worse MH outcomes than doctors [ 24 , 26 , 31 ]. One large study in China found nurses were at significant risk of more severe depression and anxiety than doctors [ 31 ]. Another found that nurses had significantly higher financial concerns than doctors and felt significantly more anxious on the ward when compared with other groups. There was no significant difference between professionals regarding stopping work or work overload [ 24 ]. A mixed method paper also showed that nurses had a higher rate of depressive symptoms than doctors. Whilst this was a small sample size, it echoes the findings from larger studies [ 26 ].
With regard to other HCWs, there were two studies which assessed dentists and other dental workers and found them to be at risk of anxiety and elevated distress. Neither study found any difference based on gender or educational level [ 36 , 59 ]. There were no studies comparing dental workers to other HCWs. We did not find any studies that focussed on the primary care workforce or that assessed social care workers.
With regard to seniority, one paper found that having an intermediate technical title was associated with more severe MH symptoms [ 31 ].
Frontline staff/direct contact with COVID-19
Four high-quality studies found being in a ‘frontline’ position or having direct contact with COVID-19 patients was associated with higher levels of psychological distress [ 30 , 31 , 34 , 42 ].
Increased direct exposure to COVID-19 patients increased the mental health risks in health care workers in one study in Wuhan [ 30 ]. This finding is backed by Lai et al. [ 31 ], who found that being a frontline worker was independently associated with more severe depression, anxiety and insomnia scores. In addition, a cross sectional survey of staff in a paediatric centre found that contact with COVID-19 patients was independently associated with increased risk of sleep disturbance [ 42 ]. Lu et al. [ 34 ] found that medical HCWs in direct contact with COVID-19 patients had almost twice the risk of anxiety and depression than non-medical staff with low risk of contact with COVID-19.
There were conflicting results found in two studies. A study in a cancer hospital in Wuhan found burnout frequency to be lower in frontline staff [ 43 ]. The authors identified confounding factors which may have led to this result, but it is of interest as it is one of the only studies that assessed HCWs outside of the acute general medicine setting. Li et al. [ 32 ], also found that frontline nurses had significantly lower levels of vicarious trauma scores than non-frontline workers and the general population.
Personal protective equipment (PPE)
PPE concerns were the most common theme brought up voluntarily in free-text feedback in a study by Chung & Yeung [ 60 ], and a survey in Pakistan revealed that 80% of participants expected provision of PPE [ 40 ]. H.Cai et al. [ 24 ] also found that PPE was protective when adequate, but a risk factor for stress when inadequate. This finding appears to be bolstered by a qualitative study of frontline nurses in Wuhan, which found that physical health and safety was one of their primary needs. This study also reported PPE as a protective factor [ 46 ].
Heavy workload
Longer working time per week was found to be a risk factor in a study by Mo et al. [ 35 ] This, together with increased work intensity or patient load per hour, were themes in a mixed methods study of 37 staff of a clinic in Beijing [ 26 ] and a qualitative study of nurses in China [ 37 ], also suggesting heavy workload as a risk factor.
Psychosocial factors
Fear of infection.
A fear of infection was a highlighted in a qualitative study by Cao et al., (2020, 31), and brought up as a theme in free-text feedback in a cross sectional survey by Chung & Yeung [ 60 ]. Ahmed et al. [ 59 ] found that 87% of dentists surveyed described a fear of being infected with COVID-19 from either a patient or a co-worker.
Concern about family
This was brought up as one of the main stress factors in a study by H.Cai et al. [ 24 ], particularly amongst staff in the 31–40 year age-group. Knowing that their family was safe was also the greatest stress reliever [ 24 ], whilst fear of infecting family was identified in 79.7% of 222 participants in a study in Pakistan [ 40 ]. It was also a theme highlighted in the qualitative data [ 26 , 37 ].
Sociodemographic factors
Younger age.
One Chinese web-based survey which included the general population and HCWs, showed that younger people had significantly higher anxiety and depression scores, but no difference in sleep quality. Conversely, the same study found that HCWs were significantly more likely to have poor sleep quality, but found no difference in anxiety or depressive symptoms based on occupation. The study did not examine the effect of age group on HCWs [ 29 ].
H. Cai et al. [ 24 ] suggested that age was more complex. They found that all age groups had concerns, but that the focus of their anxieties were different (for example: older staff were more likely to be anxious due to exhaustion from long hours and lack of PPE while younger staff were more likely to worry about their families).
Women were found to be at higher risk for depression, anxiety and insomnia by Lai et al. [ 31 ] This was also found to be an independent risk factor for anxiety in another large nationwide Chinese study [ 47 ]. However, a global survey of dentists found no differences based on gender [ 59 ].
Underlying illness
We found two studies which identified that having an underlying organic illness as an independent risk factor for poor psychological outcomes. A study of dentists in Israel found an increase in psychological distress in those with background illnesses as well as an increased fear of contracting COVID-19 and higher subjective overload [ 36 ]. In medical HCWs in China, organic illness was found to be an independent risk factor for insomnia, anxiety, OCD, somatising symptoms and depression in medical HCWs [ 47 ].
Being an only child
This was independently associated with sleep disturbance in paediatric HCWs in Wuhan [ 42 ]. Being an only child was also found to be significantly associated with stress by Mo et al. [ 35 ].
There was also a significant association between physical symptoms and poor psychological outcomes in a large multicentre study based in India and Singapore. It is unclear if this represented somatization or organic illness and the authors suggest the relationship between physical symptoms and psychological aspects was bi-directional [ 27 ].
Environmental factors
Point in pandemic curve.
One longitudinal study carried out in China in a surgical department, found that anxiety and depression scores during the ‘outbreak’ period were significantly higher when compared to a similar group assessed after the outbreak period [ 58 ]. This was a small sample of 120 and only assessed surgical staff, but this longitudinal data was supported by a qualitative study in China which suggested that anxiety peaks at the start of the outbreak and reduces with time [ 37 ].
Living in a rural area was only assessed by one study which showed that it was an independent risk factor for insomnia and anxiety in medical HCWs [ 47 ]. This may reflect a need to further investigate the effect of rurality on psychological wellbeing during this pandemic.

Protective factors against adverse mental health outcomes
The review identified protective factors against adverse mental health outcomes during COVID-19. Table 4 provides the GRADE evidence profile of the certainty of evidence for this. The protective factors can be grouped into the three thematic areas of: i) occupational, ii) psychosocial and iii) environmental.
W. Cai et al. [ 25 ] found that previous experience in a public health emergency (PHE) was protective against adverse mental health outcomes. Staff that had no previous experience were also more likely to have low rates of resilience, and social support.
A small cohort study of 27 surgeons, who were given pre and post training surveys, suggested that training alleviates psychological stress [ 22 ]. Good hospital guidance was identified to relieve stress in a study by H.Cai et al. [ 24 ], and increasing self-knowledge was a coping strategy deployed by staff. Dissemination of knowledge was also mentioned in a qualitative study by Yin & Zeng [ 46 ]; participants described subjective stress reduction after their seniors explained relevant knowledge to them.
Adequate PPE
As mentioned above, PPE was found to be a protective factor when adequate and a risk factor for poor mental health outcomes when deemed to be inadequate [ 24 , 46 ].
One study assessed self-efficacy in dental staff and found that it was a protective factor [ 36 ]. Self-efficacy was also found to improve sleep quality by Xiao et al. [ 44 ], whilst W.Cai et al. [ 25 ] measured resilience using a validated measure and found it to be a protective factor against adverse MH outcomes.
Being in a committed relationship
This was found to be protective by Shacham et al. [ 36 ] This was not directly assessed in other studies.
Safety of family
This had the biggest impact in reducing stress in a cross-sectional study by H. Cai et al. [ 24 ] This was also not assessed in other studies.
Support and recognition from the health care team, government and community was identified as a protective theme in several studies. Social support, measured using the Social Support Rate Scale (SSRS) was found to indirectly affect sleep by directly reducing anxiety and stress and increasing self-efficacy [ 44 ].
Team support was identified as a protective factor in a qualitative study by Sun et al. [ 37 ] Good hospital guidance was also identified as a stress reliever by H. Cai et al. [ 24 ], who found that HCWs expected recognition from the hospital authorities. This was echoed in a qualitative study of nurses in Wuhan where the desire for community concern was a strong need and tightly linked to the need for PPE and knowledge [ 46 ]:
‘ To be honest, I was very apprehensive before coming to the infectious department as support staff, but on the first day here, the head nurse personally explained relevant knowledge such as disinfection and quarantine, and that helped me calm down a lot . ”
“I hope that our society and government pay more attention to lack of personal protective equipment’ [ 46 ] .
As a communicable disease, and now a global public health emergency (PHE), COVID-19 places a unique challenge on our health and social care workforce that will disrupt not just their usual workplace duties but also their social context [ 62 ]. As we adjust to new ways of living and working, HSCWs are likely to continue to face challenges ahead. Our review confirms that the psychological impact of COVID-19 on health care workers is considerable, with significant levels of anxiety, depression, insomnia and distress. Studies revealed a prevalence of depressive symptoms between 8.9–50.4% and anxiety rates between 14.5–44.6% [ 31 , 39 ]. This is in keeping with other reviews and findings from previous viral outbreaks [ 7 , 8 , 63 ]. The majority of studies published to date come from China, particularly Wuhan - the epicentre of COVID-19. There is minimal evidence published to date on the psychological impact on HCWs in Europe or the US, which have been highly impacted by the pandemic. The studies included in this review were predominantly concerned with hospital settings – we found no studies relating to social care staff or primary care staff. This is a concern, as we have increasing evidence that a large proportion of Western deaths are happening in the community and specifically in care homes [ 64 ].
Our review aimed to identify whether there were any groups particularly vulnerable to poor mental health outcomes during COVID-19. We found some evidence that nurses may be at a higher risk than doctors [ 24 , 26 , 31 ]. This is similar to findings which take into account previous viral outbreaks [ 7 ]. Confounding factors were not robustly addressed however, and there were no studies that compared nurses with the primary care workforce or social care workers. There was some evidence that clinical HCWs may be at higher risk of psychological distress than non-clinical HCWs [ 34 , 47 ], but this was not absolute. Tan et al. [ 39 ] found a higher prevalence of anxiety among non-medical HCWs in Singapore. The prevalence of poor MH outcomes varied between countries. Chew et al. [ 27 ] revealed that in data from India and Singapore, there was an overall lower prevalence of anxiety and depression than similar cross-sectional data from China [ 27 , 31 , 39 , 60 ]. This suggests that different contexts and cultures may reveal different findings. It is possible that being at different points in their respective countries’ outbreak curve may have played a part, as there was evidence that this may be influential [ 58 ]. Tan et al. [ 39 ] postulated that the medical HCWs in Singapore had experienced a SARS outbreak in the past and thus were well prepared for COVID-19 both psychologically and in their infection control measures. What we can deduce is that context and cultural factors are likely to play a role, not just cadre or role of healthcare worker. It also highlights the importance of reviewing the evidence as more data emerges from other countries.
Several risk factors emerged, many in keeping with what has been found in other reviews [ 7 , 8 ]. Those with the strongest evidence were inadequate PPE [ 24 , 40 , 46 , 60 ], fear of infection [ 26 , 59 , 60 ] and heavy workload [ 26 , 35 , 37 ]. Consistent with prior outbreak data [ 7 , 63 ], there was also good evidence that close contact with COVID-19 cases was a predictor of higher levels of anxiety, depression and insomnia [ 30 , 31 , 34 , 42 ], although two studies appeared to show conflicting results [ 32 , 43 ]. Studies suggested that being younger in age [ 24 , 29 , 33 ] or being female [ 31 , 47 , 59 ] may be a risk factor, however this should be treated with caution. An alternative explanation for this study’s findings may be greater risk of frontline exposure amongst women, who are predominantly employed in lower status roles within healthcare globally according to the WHO [ 65 ]. It is important to note that respondents to all studies, when disaggregated by gender, were predominantly female and this may have impacted findings. The consistently higher mortality rate and risk of severe COVID-19 disease amongst men would suggest that the full picture regarding gender and MH during this pandemic is incomplete [ 66 , 67 ]. Although other risk factors were also identified, their certainty of evidence was deemed to be low.
The majority of cross-sectional studies focussed on measuring adverse MH outcomes which explains the lack of quantitative data on protective factors or coping mechanisms. Of the studies that did assess this, there were protective factors which were associated with adaptive psychological outcomes. Experience of prior infectious disease outbreaks and training were protective against poor mental health outcomes [ 22 , 24 , 25 , 46 ]. Adequate PPE was a protective factor when adequate and a risk factor when inadequate [ 24 , 46 , 60 ]. There was good evidence that resilience (measured by self-efficacy or resilience scales) was protective against poor mental health outcomes [ 25 , 36 , 44 ]. This is of importance when assessing how to positively contribute to reducing the psychological burden on our health and social care staff. There was strong evidence that community support was a protective factor [ 24 , 37 , 44 , 46 ]. Community support was important in a number of studies, referring to social support as well as recognition and support from the healthcare team, government and wider community [ 24 , 37 , 44 , 46 , 68 ]. Other adaptive behaviours emerged from qualitative data, including gratitude and the ability to find purpose and growth from the situation [ 37 ]. These findings are in keeping with a recent study which identified key domains of risk for burnout in healthcare. They highlighted that being part of a supportive team community is a strong protective factor as are clear values and meaningful work [ 69 ]. They advise that organisational-level interventions creating a healthy workplace are the key to preventing burnout [ 69 ]. This is echoed in a recent systematic review and meta-analysis of the effectiveness of interventions designed to reduce symptoms and prevalence of MH disorders and suicidal behaviour among physicians. This review concluded that, whilst individually directed interventions are associated with some reduction in symptoms of common MH disorders, there needs to be increased focus on organisational-level interventions that improve the work environment [ 2 ].
Whilst our findings showed evidence that occupational and environmental factors at the workplace level played a key role for MH outcomes, there was no mention of wider societal structural issues that have been emerging during this pandemic. Of particular importance is the evidence that black and ethnic minority people of all ages in the global north are at greater risk of contracting and dying from COVID-19 [ 70 , 71 , 72 ]. A recent large study in the US found that non-white HCWs were at increased risk of contracting COVID-19 and were disproportionately affected by inadequate PPE and close exposure to COVID-19 patients [ 3 ]. This suggests wider structural factors are at play and need to be investigated.
The paucity of empirical studies investigating the mental health of social care and primary care staff during the COVID-19 pandemic should also be rectified. With the majority of studies taking place in China, where ageing in place rather than residential care is the norm [ 73 ], it is unsurprising that none investigated care homes, where it is estimated around 40–50% of all deaths related to COVID-19 occur in Europe and the US [ 64 ]. Moreover, there is evidence that front-line HCWs who work in nursing homes are among the highest at risk of contracting the virus [ 3 ]. With the majority of studies taking place in urban hospital settings, and particularly in Wuhan – the epicentre of the outbreak – the generalizability of findings to other settings may be limited, particularly as countries pass through different points in the outbreak curve. However, this review does highlight the considerable psychological impact that COVID-19 has played so far on health care workers and, therefore, adds to the recent calls to take notice of this important issue [ 14 ]. Yet the evidence also suggests that, although predictors for psychological distress exist, these are not absolute and context may play an important role on the manifestation of adverse MH outcomes.
Strengths and limitations
This rapid review has synthesized and discussed the current literature on the psychological impact of the COVID-19 pandemic on health and social care workers. A major limitation was that no empirical studies investigating this impact on social care workers could be found – limiting generalisability to the population reviewed. Recent evidence also suggests that having an ongoing connection to a paid job, may be protective against poor MH outcomes during the pandemic [ 74 ]. It would therefore be useful to compare MH outcomes amongst HCWs, or the general population, who were not actively employed during the pandemic. Unfortunately, none of the studies included this data. Furthermore, job retention schemes have varied widely between countries worldwide, thus limiting the generalisability of findings if this data had been available [ 75 ].
However, to our knowledge, this is the first review investigating this population group in the context of COVID-19, without including prior viral outbreaks in its analysis and synthesis. We see this as a strength because this outbreak is different, and worth assessing in its own right. It has affected every country across the globe and disrupted everyday living in a way no other outbreak has in living memory [ 14 ]. A major strength of our review is that it endeavoured towards greater inclusion, during the rapidly changing COVID-19 landscape, by completing two runs of the search strategy spaced 2 weeks apart. Whilst we adhered to high methodological standards by assessing study quality and risk of bias, together with using the GRADE approach to evaluate the certainty evidence and following best practice principles [ 52 , 53 ] to present a narrative and tabulated synthesis, our review remains a rapid one with further clear limitations. The majority of the studies included in this review, for example, were from China and our selection criteria did not include studies from low-income countries or studies in languages other than English - limiting the generalizability of our findings. Being a rapid review, the protocol was not registered on PROSPERO and only one reviewer was responsible for the initial screening of papers and for several of the quality assessments. Finally, as the current review’s searches were carried out early in the pandemic, it will be valuable to consider emerging research from the global arena in the light of this review’s findings.
This rapid review confirms that front line HCWs are at risk of significant psychological distress as a direct result of the COVID-19 pandemic. Published studies suggest that symptoms of anxiety, depression, insomnia, distress and OCD are found within the healthcare workforce. However, most studies draw only from work in secondary care and none draw from the primary care or social care setting. Published studies so far are predominantly from China (18 out of 24 included studies) and most of these have sampled hospital staff in Wuhan - the epicentre. Findings in this review suggest that the study of different contexts and cultures may reveal different findings and we recommend more research in primary care and social care settings and to monitor rapidly emerging evidence from across the world. This should include analysis of wider societal factors including gender, racial and socio-economic disparities that may influence mental health outcomes in HCWs.
Although risk factors did emerge that were in keeping with evidence from other infectious disease outbreaks, our findings were not absolute. This review suggests that nurses may be at higher risk of adverse MH outcomes during this pandemic, but there were no studies comparing them with social care workers or the primary care workforce. Other risk factors that recurred in the data were heavy workload, lack of PPE, close contact with COVID-19, being female and underlying organic illness. Inconsistencies in findings and lack of data on staff outside hospital settings, suggest that targeting a specific group within health and social care staff with psychological interventions may be misplaced – as both presence of psychological distress and risk factors are spread across the healthcare workforce, rather than associated with particular sub-groups.
A recent call to action for mental health science during COVID-19 recommends research be undertaken to identify interventions that can be delivered under pandemic conditions to mitigate deteriorations in psychological well-being and support mental health. This call to action advised that personalised psychological approaches are likely to be a key [ 14 ]. Data from this review suggests that interventions which bolster psychological resilience may be of benefit because this was found to protect against adverse mental health outcomes. Due to the nature of the pandemic which prevents face-to-face interventions, this is likely to be digitally based. A recent systematic review, pre-dating COVID-19, suggested that individualised interventions can have modest effect on reducing adverse mental health outcomes amongst physicians [ 2 ]. However, our findings suggest that occupational and environmental factors in the workplace play a key role as risk factors and protective factors for mental health outcomes during this pandemic. Heavy workload, proximity to COVID-19 and inadequate PPE were risk factors for poor mental health, whereas good knowledge of COVID-19, a supportive work environment and adequate PPE were protective factors. It would appear from our findings that adequate PPE may be protective not just against infection, but also against adverse mental health outcomes. Individually targeted digital interventions are unlikely to address these factors [ 2 ]. We postulate that strengthening psychological resilience in a personalised approach may be effective in protecting our health and social care workers from adverse mental health outcomes but this must not defer responsibility from wider organisations and systems. We suggest that a holistic approach to HCWs psychological wellbeing is needed that includes personalised interventions alongside necessary structural changes to create a healthy, safe and supportive work environment. Further research including social care workers and analysis of wider societal structural factors is recommended.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
Connor-Davidson Resilience Scale
Centre for Epidemiologic Studies Depression Scale (CES-D)
Coronavirus disease 2019
Depression, Anxiety and Stress Scale
Generalised Anxiety Disorder Questionnaire
The Grades of Recommendation, Assessment, Development and Evaluation Working Group
Generalised self-efficacy scale
Hamilton Anxiety Rating Scale
Hamilton Depression Rating Scale
Healthcare workers
Health and social care workers
Impact of Event Scale
Insomnia Severity Index
Maslach Burnout Inventory (MBI)
- Mental health
Public Health Emergency
Patient Health Questionnaire-4
Patient Health Questionnaire
Personal protective equipment
Pittsburgh Sleep Quality Index
Zung Self-Rating Anxiety Scale
The Stanford Acute Stress Reaction questionnaire
Symptom checklist depression scale
The Symptom Checklist-90-R
Zung Self-Rating Depression Scale
Short Form Health Survey (SF-36)
Stress Overload Scale
Social Support Rating Scale
World Health Organisation
Gold JA. Covid-19: adverse mental health outcomes for healthcare workers. BMJ. 2020;369:m1815 https://doi-org.knowledge.idm.oclc.org/10.1136/bmj.m1815 .
Article PubMed Google Scholar
Petrie K, Crawford J, Baker STE, Dean K, Robinson J, Veness BJ, et al. Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(3):225–34 https://doi.org/10.1016/S2215-0366(18)30509-1 .
Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–83. https://doi.org/10.1016/S2468-2667(20)30164-X .
Article PubMed PubMed Central Google Scholar
Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171(8):555–67. https://doi.org/10.7326/M19-1152 .
Maunder R, Lancee W, Balderson K, Bennett J, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infect Dis. 2006;12(12):1924–32. https://doi.org/10.3201/eid1212.060584 .
Article Google Scholar
Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. 2018;60(3):248–57. https://doi.org/10.1097/JOM.0000000000001235 .
Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. https://doi-org.knowledge.idm.oclc.org/10.1136/bmj.m1642 .
Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–a review. Asian J Psychiatr. 2020;51:102119. https://doi.org/10.1016/j.ajp.2020.102119 .
Reger MA, Piccirillo ML, Buchman-Schmitt J. COVID-19, mental health, and suicide risk among health care workers: looking beyond the crisis. J Clin Psychiatry. 2020;81(5). https://doi.org/10.4088/JCP.20com13381 .
Neto MLR, Almeida HG, Esmeraldo JD, Nobre CB, Pinheiro WR, de Oliveira C, et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res. 2020;288:112972. https://doi.org/10.1016/j.psychres.2020.112972 .
Article PubMed PubMed Central CAS Google Scholar
British Medical Association. The mental health and wellbeing of the medical workforce – now and beyond COVID-19. 2020. Available from URL: https://www.bma.org.uk/media/2475/bma-covid-19-and-nhs-staff-mental-health-wellbeing-report-may-2020.pdf .
Google Scholar
Melnyk BM, Kelly SA, Stephens J, Dhakal K, McGovern C, Tucker S, et al. Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: a systematic review. Am J Health Promot. 2020:089011712092045 https://doi-org.knowledge.idm.oclc.org/10.1177/0890117120920451 .
United Nations. Policy Brief: COVID-19 and the need for action on mental health. 2020. Available from URL: https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf .
Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60 https://doi.org/10.1016/S2215-0366(20)30168-1 .
Brooks SK, Gerada C, Chalder T. Review of literature on the mental health of doctors: are specialist services needed? J Ment Health. 2011;20(2):146–56 https://doi-org.knowledge.idm.oclc.org/10.3109/09638237.2010.541300 .
Tricco AC, Langlois EV, Straus SE. Rapid reviews to strengthen health policy and systems: a practical guide. Geneva: World Health Organisation; 2017. Available from URL: https://apps.who.int/iris/bitstream/handle/10665/258698/9789241512763-eng.pdf;sequence=1 .
Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. Syst Rev. 2012;1(1):10. https://doi.org/10.1186/2046-4053-1-10 .
Garritty C, Gartlehner G, Kamel C, King V, Nussbaumer-Streit B, Stevens A., et al. Cochrane rapid reviews. interim guidance from the Cochrane Rapid Reviews Methods Group. 2020. Available from URL: https://methods.cochrane.org/rapidreviews/sites/methods.cochrane.org.rapidreviews/files/public/uploads/cochrane_rr_-_guidance-23mar2020-final.pdf .
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: systematic reviews of etiology and risk. In: Joanna Briggs Institute Reviewer's Manual The Joanna Briggs Institute; 2017. p. 2019–05.
Evidence Partners. Tool to Assess Risk of Bias. Contributed by the CLARITY Group at McMaster University: McMaster University; [Available from: https://www.evidencepartners.com/resources/methodological-resources/ .
Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(8):2821.
Article CAS PubMed Central Google Scholar
Balakumar C, Rait J, Montauban P, Zarsadias P, Iqbal S, Fernandes R. COVID-19: are frontline surgical staff ready for this? Br J Surg. 2020;107(7):e195. https://doi.org/10.1002/bjs.11663 .
Article CAS PubMed PubMed Central Google Scholar
Jüni P, Loke Y, Pigott T, Ramsay C, Regidor D, Rothstein H, et al. Risk of bias in non-randomized studies of interventions (ROBINS-I): detailed guidance. 2016.
Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and march 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:e924171. https://doi.org/10.12659/MSM.924171 .
Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona virus disease 2019. Asian J Psychiatr. 2020;51:102111. https://doi.org/10.1016/j.ajp.2020.102111 .
Cao J, Wei J, Zhu H, Duan Y, Geng W, Hong X, et al. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 Outbreak. Psychother Psychosom. 2020;89(4):252–4. https://doi.org/10.1159/000507453 .
Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–65. https://doi.org/10.1016/j.bbi.2020.04.049 .
Chung JPY, Yeung WS. Staff Mental Health Self-Assessment During the COVID-19 Outbreak. East Asian Arch Psychiatry. 2020;30(1):34.
Article CAS PubMed Google Scholar
Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288(112954):1–6. https://doi.org/10.1016/j.psychres.2020.112954 .
Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–7. https://doi.org/10.1016/j.bbi.2020.03.028 .
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 .
Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916–9. https://doi.org/10.1016/j.bbi.2020.03.007 .
Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. 2020;133:110102. https://doi.org/10.1016/j.jpsychores.2020.110102 .
Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. https://doi.org/10.1016/j.psychres.2020.112936 .
Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, et al. Work stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic. J Nurs Manage. 2020;28:1002–9. https://doi.org/10.1111/jonm.13014 .
Shacham M, Hamama-Raz Y, Kolerman R, Mijiritsky O, Ben-Ezra M, Mijiritsky E. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int J Environ Res Public Health. 2020;17(8):2900. https://doi.org/10.3390/ijerph17082900 .
Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;48(6):592–8. https://doi.org/10.1016/j.ajic.2020.03.018 .
Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179–87. https://doi.org/10.1097/XEB.0000000000000062 .
Tan BY, Yeo LL, Sharma VK, Chew NW, Jing M, Goh Y, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–20. https://doi.org/10.7326/M20-1083 .
Urooj U, Ansari A, Siraj A, Khan S, Tariq H. Expectations, fears and perceptions of doctors during Covid-19 pandemic. Pak J Med Sci. 2020;36:S37–42. https://doi.org/10.12669/pjms.36.COVID19-S4.2643 .
Bartlett G, Vedel I, Hong QN, Pluye P, Rousseau M, Fàbregues S, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91. https://doi.org/10.3233/EFI-180221 .
Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med (Lond ). 2020;70(5):364–9. https://doi-org.knowledge.idm.oclc.org/10.1093/occmed/kqaa074 .
Wu Y, Wang J, Luo C, Hu S, Lin X, Anderson AE, Bruera E, Yang X, Wei S, Qian Y. A comparison of burnout frequency among oncology physicians and nurses working on the front lines and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage. 2020;60(1):e60–5. https://doi.org/10.1016/j.jpainsymman.2020.04.008 .
Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. https://doi.org/10.12659/MSM.923549 .
Critical Appraisal Skills Programme. Cohort Study Checklist: Critical Appraisal Skills Programme (CASP); [Available from: https://casp-uk.net/casp-tools-checklists/ .
Yin X, Zeng L. A study on the psychological needs of nurses caring for patients with coronavirus disease 2019 from the perspective of the existence, relatedness, and growth theory. Int J Nurs Sci. 2020;7(2):157–60. https://doi.org/10.1016/j.ijnss.2020.04.002 .
Zhang W, Wang K, Yin L, Zhao W, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):1–9. https://doi.org/10.1159/000507639 .
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis [Adelaide]: Joanna Briggs Institute; 2020. https://doi.org/10.46658/JBIMES-20-08 .
Evidence Partners, CLARITY Group at McMaster University. Methodological resources: tools to assess risk of bias. 2020; Available from URL: https://www.evidencepartners.com/resources/methodological-resources/ .
CASP. Cohort Study Checklist. 2020. Available from URL: https://casp-uk.net/casp-tools-checklists/ .
Sterne JAC, Hernán M, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;i4919:355. https://doi.org/10.1136/bmj.i4919 .
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme 2006. Available from URL: https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf .
Campbell M, Katikireddi SV, Sowden A, McKenzie JE, Improving Conduct TH. Reporting of narrative synthesis of quantitative data (ICONS-quant): protocol for a mixed methods study to develop a reporting guideline. BMJ Open. 2018;8(2):e020064. https://doi.org/10.1136/bmjopen-2017-020064 .
Article PubMed Central Google Scholar
Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Paul Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane handbook for systematic reviews of interventions. 2nd ed; 2019. p. 403–31. https://doi.org/10.1002/9781119536604.ch15 .
Chapter Google Scholar
Cao J, Wei J, Zhu H, Duan Y, Geng W, Hong X, Jiang J, Zhao X, Zhu B. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychother Psychosom. 2020;89(4):252–54. https://doi.org/10.1159/000507453 .
Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. 2020;110102:133.
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729.
Xu J, Xu Q, Wang C, Wang J. Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res. 2020;288:112955. https://doi.org/10.1016/j.psychres.2020.112955 .
Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(8):2821. https://doi.org/10.3390/ijerph17082821 .
Chung JP, Yeung WS. Staff mental health self-assessment during the COVID-19 outbreak [Letter to editor]. East Asian Arch Psychiatry. 2020;30(1):34. https://doi.org/10.12809/eaap2014 .
Cai W, Lian B, Song X, Hou T, Deng G, Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona virus disease 2019. Asian J Psychiatr. 2020;102111:51.
Markwell A, Mitchell R, Wright AL, Brown AF. Clinical and ethical challenges for emergency departments during communicable disease outbreaks: can lessons from Ebola virus disease be applied to the COVID-19 pandemic? Emerg Med Australas. 2020;32(3):520–4 https://doi-org.knowledge.idm.oclc.org/10.1111/1742-6723.13514 .
Grace SL, Hershenfield K, Robertson E, Stewart DE. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics. 2005;46(5):385–91 https://doi.org/10.1176/appi.psy.46.5.385 .
Comas-Herrera A, Zalakain J, Litwin C, Hsu AT, Lane N, Fernández J. Mortality associated with COVID-19 outbreaks in care homes: early international evidence. 2020. Available from URL: https://ltccovid.org/2020/04/12/mortality-associated-with-covid-19-outbreaks-in-care-homes-early-international-evidence/ .
Boniol M, McIsaac M, Xu L, Wuliji T, Diallo K, Campbell J. Gender equity in the health workforce: analysis of 104 countries. 2019. Available from URL: https://www.who.int/hrh/resources/gender_equity-health_workforce_analysis/en/ .
Ortolan A, Lorenzin M, Felicetti M, Doria A, Ramonda R. Does gender influence clinical expression and disease outcomes in COVID-19? A systematic review and meta-analysis. Int J Infect Dis. 2020;99:496–504. https://doi.org/10.1016/j.ijid.2020.07.076 .
Pérez-López FR, Tajada M, Savirón-Cornudella R, Sánchez-Prieto M, Chedraui P, Terán E. Coronavirus disease 2019 and gender-related mortality in European countries: A meta-analysis. Maturitas. 2020;141:59–62 https://doi.org/10.1016/j.maturitas.2020.06.017 .
Al Knawy BA, Al-Kadri H, Elbarbary M, Arabi Y, Balkhy HH, Clark A. Perceptions of postoutbreak management by management and healthcare workers of a Middle East respiratory syndrome outbreak in a tertiary care hospital: a qualitative study. BMJ Open. 2019;9(5):e017476. https://doi.org/10.1136/bmjopen-2017-017476 .
Montgomery A, Panagopoulou E, Esmail A, Richards T, Maslach C. Burnout in healthcare: the case for organisational change. BMJ. 2019;366:l4774 https://doi.org/10.1136/bmj.l4774 .
Aldridge RW, Lewer D, Katikireddi SV, Mathur R, Pathak N, Burns R, et al. Black, Asian and Minority Ethnic groups in England are at increased risk of death from COVID-19: indirect standardisation of NHS mortality data. Wellcome Open Res. 2020;5:88. https://doi.org/10.12688/wellcomeopenres.15922.2 .
Tai DB, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2020. https://doi-org.knowledge.idm.oclc.org/10.1093/cid/ciaa815 .
APM Research Lab. The color of coronavirus: COVID-19 deaths by race and ethnicity in the US. 2020. Available from URL: https://www.apmresearchlab.org/covid/deaths-by-race .
Zhang X, Clarke CL. Rhynas SJ. A thematic analysis of Chinese people with dementia and family caregivers’ experiences of home care in China. Dementia (London, England). 2019:147130121986146 https://doi-org.knowledge.idm.oclc.org/10.1177/1471301219861466 .
Burchell B, Wang S, Kamerāde D, Bessa I, Rubery J. Cut hours, not people: no work, furlough, short hours and mental health during the COVID-19 pandemic in the UK. 2020. Available from URL: https://www.cbr.cam.ac.uk/fileadmin/user_upload/centre-for-business-research/downloads/working-papers/wp521.pdf .
Gentilini U, Almenfi M, Orton I, Dale P. Social Protection and Jobs Responses to COVID-19: A Real-Time Review of Country Measures. 2020. Available from URL: https://openknowledge.worldbank.org/handle/10986/33635 .
Download references
Acknowledgements
Thank you to Abbie Oman (University of Aberdeen) for critically reviewing our manuscript.
This project is funded by the Chief Science Office of the Scottish Government: RAPID RESEARCH IN COVID-19 PROGRAMME REF: COV/UHI/Portfolio. The funding sources had no role in the design or conduct of the study nor in the collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and affiliations.
University of the Highlands and Islands, Institute for Health Research and Innovation, University of the Highlands and Islands, Old Perth Road, Inverness, IV2 3JH, UK
Johannes H. De Kock, Mark Grindle, Sarah-Anne Munoz, Liz Ellis, Rob Polson & Christopher M. O’Malley
NHS Highland, Department of Clinical Psychology, New Craigs Hospital, Inverness, IV3 8NP, UK
Johannes H. De Kock
NHS Highland, Nairn Healthcare Group, Cawdor Rd, Nairn, IV12 5EE, UK
Helen Ann Latham
NHS Highland, NHS Highland Cardiac Unit Raigmore Hospital, Inverness, IV2 3UJ, UK
Stephen J. Leslie
You can also search for this author in PubMed Google Scholar
Contributions
JDK, SAM and HL had the idea for the study. JDK, RP, CoM designed the search strategy. JDK, HL, LE screened abstracts and full texts. JDK, HL, LE, SAM, acquired data, and assessed risk of bias in studies. MG contributed to interpreting the data. JDK, HL and SL wrote the manuscript. SL made substantial contributions to the revision of the manuscript. The corresponding author attests that all listed authors meet authorship criteria. All authors have approved the submitted version and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Correspondence to Johannes H. De Kock .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search Strategy. This additional file provides a comprehensive overview of the search criteria design as well as the search strategy and pattern.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
De Kock, J.H., Latham, H.A., Leslie, S.J. et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 21 , 104 (2021). https://doi.org/10.1186/s12889-020-10070-3
Download citation
Received : 26 May 2020
Accepted : 14 December 2020
Published : 09 January 2021
DOI : https://doi.org/10.1186/s12889-020-10070-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Intervention
- Social care
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

Coronavirus Disease 2019
The psychological impact of covid-19, new research provides insight into the psychological impact of covid-19..
Posted September 30, 2020 | Reviewed by Jessica Schrader

As the COVID-19 pandemic sweeps the globe bringing uncertainty, fear , loss, isolation, and hardship, individuals find themselves in a time of collective trauma. Situations like COVID-19 that can elicit collective trauma may lead to a number of psychological, relational, physiological, and spiritual consequences for those impacted (Aydin, 2017; Saul, 2014; for more information on collective trauma and its effects see " What is Collective Trauma? "). As the COVID-19 pandemic continues to uproot the lives of millions, current research seeks to understand the impact of the pandemic and how to mitigate the negative consequences that may be surfacing in response.
Since the onset of the COVID-19 pandemic in 2019, research has noted a variety of mental health consequences that have been experienced in response. Some of these consequences have included: stress , depression , anxiety , feelings of panic, feelings of hopelessness, frustration, feelings of desperation, and struggles with suicidal ideation and behavior, insomnia , irritability, emotional exhaustion, grief , and traumatic stress symptoms. Although the impact of COVID-19 is individual-specific and based on a number of factors (e.g. the length of quarantine, risk factors, trauma history, mental health history, etc.), some trends in mental health consequences have begun to emerge among the general population (Serafini et al., 2020).

According to a recent article by Serafini et al. (2020), although there may be varied responses to the COVID-19 pandemic, there are several common psychological reactions to COVID-19 that are surfacing amongst the general population. These reactions include intense and uncontrolled fear related to infection, pervasive anxiety, frustration, boredom , and disabling loneliness . Understandably, psychological consequences included in these findings may impair an individual’s well-being and quality of life. Although this is the case, Serafini et al. (2020) note that an individual’s resilience and social support may be factors that can aid them in adapting to this crisis.
The recent findings of Serafini et al. (2020) provide further insight into the ways in which the COVID-19 pandemic may be impacting many. Although these findings may be challenging to acknowledge, these findings provide important information as we continue to battle the COVID-19 crisis. These findings may provide a source of important validation to many about their experiences and increase awareness about what steps may need to be taken on individual and societal levels to minimize the psychological consequences of the COVID-19 pandemic. As discussed by Serafini et al. (2020) the recognition of these findings or the “the psychological impact of fear and anxiety induced by the rapid spread of pandemic needs to be clearly recognized as a public health priority for both authorities and policymakers” to reduce the mental health consequences of this pandemic.
Aydin, C. (2017). How to Forget the Unforgettable? On Collective Trauma, Cultural Identity, and Mnemotechnologies, Identity, 17:3, 125-137, DOI: 10.1080/15283488.2017.1340160
Saul, J. (2014). Collective trauma, collective healing: Promoting resilience in the aftermath of disaster. New York, NY: Routledge.
Serafini, G., Parmigian, B., Amerio, A., Aguglia, A., Sher, L., & Amore, M. (2020). The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine, 529-535, doi: 10.1093/qjmed/hcaa201 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337855/pdf/hcaa201.pdf

Danielle Render Turmaud, Ph.D., NCC , is a Counseling Professional who specializes in working with survivors of trauma and complex trauma; specifically, sexual trauma, childhood trauma, and interpersonal violence.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 May 2024
The effects of social support and parental autonomy support on the mental well-being of university students: the mediating role of a parent–child relationship
- Arif Jameel 1 ,
- Zhiqiang Ma 1 ,
- Mingxing Li 1 , 2 ,
- Abid Hussain 1 ,
- Muhammad Asif 1 &
- Yan Wang 1
Humanities and Social Sciences Communications volume 11 , Article number: 622 ( 2024 ) Cite this article
2 Altmetric
Metrics details
- Business and management
The COVID-19 pandemic, as well as the complex response techniques employed to halt its spread, are both detrimental to mental and emotional well-being. Students’ lives have been damaged by social alienation and self-isolation. These effects must be detected, analyzed, and dealt with to make sure the well-being of individuals, specifically students. This research examines the impact of parent–child relationships, parental autonomy support, and social support on enhancing students’ mental well-being using data collected from post-COVID-19. The Potential participants were students from several universities in Pakistan. For this reason, we chose Pakistan’s Punjab province, with 8 prominent institutions, as the primary focus for data collection. A questionnaire was created to gather information from 355 students. For descriptive statistics, SPSS was used, while AMOS structural equation modeling was used to test hypotheses. The findings revealed that social support on mental well-being (standardized β = 0.43, t = 7.57, p < 0.01) and parental autonomy support was significant and positively related to mental well-being (standardized β = 0.31, t = 5.016, p < 0.01), and predicted parent–child relationships. Furthermore, the parent–child relationship strongly mediated the association between social support, parental autonomy support, and students’ mental well-being. This research proposes that good social support and parental autonomy support improve parent–children relationships and contribute to students’ mental well-being.
Similar content being viewed by others

Determinants of behaviour and their efficacy as targets of behavioural change interventions
Mechanisms linking social media use to adolescent mental health vulnerability

Participatory action research
Introduction.
COVID-19 has grown increasingly concerned with mental health and well-being in the past few years. Many research investigations have found that students have higher levels of psychological suffering than the overall people. This psychological tension of this virus among students has had significant and longer-term mental health repercussions, leading to low physical well-being results, including an increase in cardiovascular illnesses and lowly mental health (MH) results. Students suffer from the mental load of this impact more than grownups because they lack the grownup’s ways to cope and physical growth (Rawat and Sehrawat, 2021 ). Students who have a history of MH difficulties are more likely to suffer MH problems amid a crisis (Gavin et al., 2020 ). On the advice of the Emergency Committee, the head of the “World Health Organization (WHO)” stated the novel Coronavirus, also identified as “COVID-19”, is a Health Emergency of Worldwide Distress. COVID-19 has catastrophic impacts on the global business environment, schooling, and humanity (Priya et al., 2021 ). Health professionals designed a complex response plan to stem the spread of COVID-19 from the pandemic’s start. Being isolated or home quarantined was an essential part of the approach. One of the measures authorities have attempted to sluggish the spread of the virus is isolation from society. Isolation from society can affect mental health, increasing symptoms of anxiety, depression, and stress (Robb et al., 2020 ). There has been a surge in the number of students reporting mental health difficulties in the present years at colleges and universities. The underlying explanation might be university students’ inexperience, as they often struggle to handle stress, mainly when confronted with educational, social, and career-related challenges. Following research, the COVID-19 pandemic increases students’ chances of developing unhappiness and suicidality (Xiong et al., 2021 ). Following the closure of university campuses, students tended to see their educational future as bleak. Isolation from society and a lack of adequate and effective MH assistance exacerbated students’ fragile status. Because of these factors, young individuals pursuing university are now at a higher risk of acquiring MH disorders (Su et al., 2021 ).
Social support is instinctively understood, but ideas about definitions conflict when specific questions are raised. Family practitioners believe that social support is one of the possible keys to an individual’s well-being, especially for those going through significant life transitions or crises (Kaplan et al., 1977 ). The definition of “social support” varies usually among those who have studied it. It has been discussed in a general way as support that is “provided by other people and arises within the context of interpersonal relationships” Cooke et al. ( 1988 ) and as “support accessible to an individual through social ties to other individuals, groups, and the larger community” (Lin et al., 1979 ). Parent–children relations are interpersonal interactions formed by the interaction of parents and Child in blood and genetically related families. Parent–children ties are the first social associations to which individuals are exposed. It influences many facets of personality development, social cognition, and mental well-being (Lu et al., 2020 ). A lower degree of social support, in particular, is connected to greater levels of depressive symptoms (Wang and Peck, 2013 ). Social support refers to the standard of emotional assistance provided by others.
Furthermore, research shows that social support levels are closely related to measures of reduced stress and psychological discomfort, as well as improved well-being (Wang and Peck, 2013 ). Nevertheless, most research on youths’ social support focuses on their families, with relatively little research on their peers’ social support (Oktavia et al., 2019 ). Based on the gaps in existing knowledge, this research intended to determine whether there is a link between parent–child relationships during social seclusion caused by the pandemic and MH. This study additionally explored how social support (SS), parental autonomy support (PAS), and parent–child relationships are related to students’ mental health and well-being. It also looks into the role of the parent–child relationship as a mediator. The outcomes of this investigation are expected to increase understanding of the topic. Despite several research in the field of MH, there is still a literature gap on the roles and linkages of parent–child relationships and their mediator behaviors. This research provides a model for simultaneously investigating the roles and intervening factors. The focus of this investigation is on the following research questions. How can social and parental autonomy support affect students’ MH following COVID-19? How does the parent–children relationship mediate this relationship? Following an exhaustive assessment of the pertinent literature (Akram et al., 2022 ; Li et al., 2022 ), it was discovered that numerous research has been conducted to evaluate parents–children relationships and MH-associated issues, but to the best of our knowledge no research has been performed in Pakistan yet to determine the answers to these study topics will be provided utilizing a single theoretical model. Based on the available literature, the present study initially posits that social and parental autonomy support favorably promotes the student’s mental well-being and positively connects with a parent–child relationship in Pakistan. The study also hypothesizes that the parent–child relationship impacts the mental well-being of the students and mediates the connection between social support, parental autonomy support, and mental well-being. The research could have subsequent contributions: To begin, the research provides a detailed and systematic investigation of the concepts of the parents–children relationship, social support, parental autonomy support, and mental well-being. Second, by integrating the parents–children relationship, the study enhances the comprehensive analytical model that investigates the association between SS, PAS, and mental well-being. The model of the research describes the theoretical viewpoint in an innovative manner. Furthermore, the work has both practical and theoretical ramifications.
Literature review
Social support and mental well-being of students.
Social support is instinctively understood, but ideas about definitions conflict when specific questions are raised. Family practitioners believe that social support is one of the possible keys to an individual’s well-being, especially for those going through significant life transitions or crises (Kaplan et al., 1977 ; Wilcox and Vernberg, 1985 ). The definition of “social support” varies usually among those who have studied it. It has been discussed in a general way as support that is “provided by other people and arises within the context of interpersonal relationships” Cooke et al. ( 1988 ) and as “support accessible to an individual through social ties to other individuals, groups, and the larger community” (Lin et al., 1979 ).
Multiple research investigations have revealed that several internal elements influence young students’ mental well-being, notably the temperament of the students Ypsilanti et al. ( 2020 ), parental style Rinaldi and Howe ( 2012 ), and peer interaction (Holmes et al., 2016 ). One of the most significant macrosocial elements impacting students’ mental health is social support, which relates to the subjective and objective support they get from their circle of friends and how they utilize it (Shen, 2009 ). “Family support, friend support, and other support” are common sources of social support (Dahlem et al., 1991 , p. 760). Through social bonding, social support may reduce psychological stress and maintain or enhance a person’s mental and physical well-being (Cohen and McKay, 2020 ; Tao et al., 2022 ). Prior studies have found that social support can make parents more positive, enhance their mental and physical wellness, and improve their parenting efficacy (Yan et al., 2023 ). Once parents believe they have access to support and networks of friends, their psychological well-being rises (Chatters et al., 2015 ). Parents with higher social support are more nurturing and consistent in their parenting and less likely to use harsh parenting behaviors across a range of child ages Byrnes and Miller ( 2012 ), and social support may assist parents in managing how they react emotionally to their kids (Marroquín, 2011 ). Social support may also give parents developmental knowledge and advice on proper parenting practices, allowing them to adapt to their expectations and enhance their parenting abilities (Ayala-Nunes et al., 2017 ). A lack of or insufficient social support, on the other hand, maybe an indicator of risk for parental psychological wellness, leading to incorrect parenting behaviors (Belsky and Jaffee, 2015 ; Hu et al., 2023 ). Parents with psychological problems have fewer beneficial relationships with their kids, experience more instances of not positive interactions and enmity, express less efficiently, and are less responsive to their children’s actions (Herwig et al., 2004 ). As a result, parents’ perceived social support influences parenting ideas and conduct, which can impact children’s mental well-being development. As a result, parents’ perceived social support may be favorably related to the mental well-being of their children.
H1: Social support positively related to the mental well-being of students
Parental autonomy support and mental well-being of students
Following the self-determination theory Ryan and Deci ( 2000 ), “autonomy” is the fundamental cognitive or emotional need that leads to optimum growth and functioning, for instance, higher levels of educational accomplishment and improved psychological well-being of students (Vasquez et al., 2016 ). Parental support has been proven in studies to increase autonomy in young people (Inguglia et al., 2015 ). Parental autonomy support (PAS) refers to parents promoting emerging adolescents’ growing desires for independence, like liberty of expression, pondering, and making decisions (Soenens et al., 2007 ). Numerous research concentrating on European societies have found that parental autonomy support is connected with positive psychosocial adjustment in individuals (Froiland, 2011 ; Soenens et al., 2007 ). An empirical study, for example, has shown that autonomy support in intimate associations is an important predictor of mental well-being (Arslan and Asıcı, 2022 ; Shamir and Shamir Balderman, 2023 ). Likewise, Kins et al. ( 2009 ) found that PAS is related to greater mental well-being in Belgian young adults. Surprisingly, cross-cultural research found that parental autonomy support is connected to mental well-being in “Chinese and North American” teenagers Lekes et al. ( 2010 ), indicating that PAS benefits people working in a group environment.
Furthermore, according to the latest meta-analysis, the parental autonomy support association is greater when it reflects both parents instead of just moms and dads (Vasquez et al., 2016 ). Accepting this viewpoint, the present research emphasizes PAS. Whereas various research in Western cultures indicates the relationship between PAS and mental well-being, nothing is known about the advantages of “parental autonomy support” in a communal community or the fundamental connection between PAS and mental well-being. Through self-regulatory processes, culture can influence mental well-being, impacting how individuals think, feel, and conduct themselves in pursuit of mental well-being (Siu, Spector, Cooper, and Lu, 2005 ). Thus, we posit that PAS impacts the mental well-being of university students.
H2: Parental autonomy support positively related to the mental well-being of the students
Mediating effect of parent–children relationship
Parent–children connections are interpersonal interactions formed by the interaction of parents and Child in blood and genetically related families. Parent–children ties are the first social associations to which individuals are exposed. It influences many facets of personality development, social cognition, and mental well-being (Lu et al., 2020 ). Greater social interaction has been shown to improve parent–children interactions, increase parent–children warmth, and decrease parent–children animosity (Lippold et al., 2018 ). This might be attributed to two factors. On the one hand, social assistance may significantly enhance children’s quality of family life (Balcells-Balcells et al., 2019 ; Feng et al., 2022 ). Parents might have more time to dedicate to parenting, resulting in improved parent–children interactions. On the other hand, social support has been shown to lower parental stress, promote mental well-being, and favorably affect how parents act (Avila et al., 2015 ; Östberg and Hagekull, 2000 ). Social support can help parents get good parenting counsel and assistance (Dominguez and Watkins, 2003 ). Social support may assist parents in managing their feelings about their children, which leads to improved parenting practices and more parental warmth (Byrnes and Miller, 2012 ). Parent–children relationships and children’s mental well-being are inextricably linked. Parent–children connections are crucial in the development of children. Parent–children connections have a greater influence on the Child than other interpersonal interactions in the family and have a significant impact on the growth of a person’s personality, mental well-being, and adjustment (Nock et al., 2009 ).
Parent–children attachment and intimacy are significant manifestations of parent–children interactions. In the long run, the continuing emotional link between a kid and a caregiver is known as parent–children bonding. A strong bond is a vital basis for children’s healthy development and integration into society, and parent–children bonds remain stable as adolescents age (Juffer et al., 2012 ). It has been demonstrated that young people with solid parent–children bonds acquire more beneficial social abilities, have greater cognitive functioning, and have greater mental and physical wellness (Ranson and Urichuk, 2008 ). Parent–children attachment is the tight, warm relationship between parents and kids, which may be shown in positive interaction behaviors and close sentiments about one another (Chen et al., 2015 ). According to several types of research, the parent–children connection is the foundation of proper child development and the most consistent safeguard for healthy personal growth (Barber et al., 2005 ). Li et al. ( 2022 ) used the parent–child relationship as a mediator in their study to explore the impact of parental mediation on internet addiction. In a nutshell, students who have close, warm parent–children connections experience less externalizing and internalizing difficulties Lamborn and Felbab ( 2003 ), have a lower incidence of suicide ideation Harris and Molock ( 2000 ), and have improved psychological well-being. Thus, parent–children relationships may act as a mediating variable between SS, PAS, and the mental well-being of students.
H3: Parents–children relationship mediates the association between social support and the mental well-being of the students
H4: Parents–children relationship mediates the association between parental autonomy support and the mental well-being of the students
Figure 1 depicts the hypothesized study model. The direct impacts of SS and PAS on the mental well-being of university students were investigated first, followed by studying the other linkages and indirect effects among social support, parental autonomy support, parent–children relationships, and the mental well-being of the students.
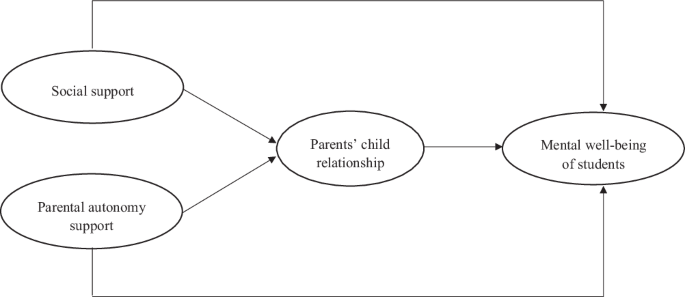
Hypothesized model.
Materials and methods
Sampling technique and data collection.
The Potential participants were students from several universities in Pakistan. For this reason, we chose Pakistan’s Punjab province, with 8 prominent institutions as the primary focus. Due to Covid 19, it was projected that the majority of the students would remain at home and endure some form of psychological disorder with their families. To gather data on the research variables, we employed a validated questionnaire that was distributed to assistance desks/information desks of the selected institutions for self-rated replies. The datagathering period was from April to May (2023). Data were collected on-site. We used snowball sampling since the datagathering was connected to extremely subtle and individual concerns, such as mental well-being, social support, and parent–child relationships.
Furthermore, we requested assistance from the directorates of student affairs at the respective institutions in determining the target participants. We accompanied the recommendations offered by different scholars, such as those who recommended: “every item must be represented employing five samples,” that “samples of three hundred shall be regarded as appropriate,” who suggested that “the size of it ought to be twenty times bigger than the expected factors,” and who suggested that “ N = 100–150” is adequate for conducting SEM (Anderson and Gerbing, 1988 ). Based on these scholars’ suggestions and the usual response percentage, we selected a sample size of 467 out of 355 that were found legitimate (response percentage of 76%). Male respondents comprised 55 percent, whereas female participants comprised 45 percent. Obtained surveys were utilized for research.
Measurement development
Each scale utilized in this investigation was taken and slightly modified from prior studies and had previously been authenticated by the researchers. Teti and Gelfand ( 1991 ) established the “Parent–Child Relationship” Scale, which is commonly used to measure the closeness of adolescents to their parents (Chen et al., 2015 ). It is made up of ten questions that relate to teenagers’ sentiments about their parents. Adolescents in this study were given questions like, “How openly do you talk with your parents?” The questions about perceived friend support were modified, and the sample construct was “I can count on my friends when things go wrong.”
Similarly, the study’s scale constructs of other people’s support were changed, and its example construct was “There is a special person in my life who cares about my feelings.” In this research, we assessed parental autonomy support developed by Soenens et al. ( 2007 ). It has five items: “My parents let me plan for things I want to do.” Furthermore, the assessment questions of mental well-being are measured by the five‐item scale of the World Health Organization. This scale was adapted from the study of (De Wit et al., 2007 ). Its three aspects, namely cognitive, emotional, and psychological health, were altered, and its construct was “I’ve been feeling optimistic about the future.” All of the constructs were measured on a “five-point Likert scale.” The Alpha for social support was 0.93. The Alpha value for parental autonomy support was 0.92. The Alpha for parent–child relationship was 0.90, and for mental well-being was 0.90.
Common method bias (CMB)
Since the data is collected all at once from a single source, bias concerns might surface and cast doubt on the study’s validity. The Harman single-factor test investigated the bias problem (Harman and Harman, 1976 ). The results demonstrated that each element of the suggested model could be separated into four variables, the first of which only explained 38.78% of the variation. According to this statistical value, normal biases must be lower than 50%. Therefore, our statistical data are free from prejudice.
Data analysis
We used Analysis of moment structures 25.0 to asses study hypotheses utilizing structural equation modeling (Shaffer et al., 2016 ). We used the two-step SEM technique Anderson and Gerbing ( 1988 ) recommended, beginning with CFA, to guarantee model adequacy. After that, an ultimate theoretical model was evaluated to evaluate the connections among every variable. Several fit indicators, such as 2/df, the CFI, TLI, the standardized root mean square residual (SRMR), and the root mean square error of approximation (RMSEA), were employed in the confirmatory factor analysis.
Descriptive statistics
The values for the mean, standard deviation, AVE, and Pearson’s correlations for each observed variable are displayed in Table 1 . The standard deviations ranged from 0.84 to 1.31, whereas the mean values were 1.43 to 2.94. Table 1 further reveals that the relationships between all variables analyzed are positive and substantial. Table 2 also indicates the DV of every factor for which the numerical values of average variance extracted are greater than the inter-correlational values, and the values of average variance extracted are also higher than 0.5 (Shaffer et al., 2016 ).
Measurement model
The measurement model in this work was evaluated using CFA Kline ( 2015 ), and Table 3 displays the standard factor loadings, Alpha, and CR of each component.
Social support, Parental autonomy support, Parent–child relationship, and mental well-being of students have Alpha of 0.92, 0.91, 0.90, and 0.88, respectively. These alphas exceed the suggested 0.70 threshold (Hair et al., 1998 ). The standardized factor loadings for Social support ranged from 0.78 to 0.86 for Parental autonomy support, 0.71 to 0.84 for the Parents–children relationship, 0.70 to 0.82, and 0.71 to 0.81 for the mental well-being of students. All factor loadings exceed 0.50 (Hair et al., 1998 ). The composite reliability (CR) ranges from 0.87 to 0.92 for Social support, Parental autonomy support, Parents–children relationship, and mental well-being of students, which is above the recommended value of 0.60 (Bagozzi et al., 1991 ).
In addition, we ran a serial-wise confirmatory factor analysis to ensure the model recognized different structures. The hypothesized 4-factor measurement model (Social support, Parental autonomy support, Parents–children relationship, and mental well-being of students) offered an appropriate fit to the data: χ 2 = 2693.55, Df = 946, χ 2 /df = 2.847, CFI = 0.92, TLI = 0.91, RMSEA = 0.05 and SRMR 0.04 (Table 3 ). The hypothesized 4-factor measurement model is the most suitable in each other models in Table 3 .
Table 3 shows that all observed items load the respective latent variables significantly. Other CFA models were contrasted with the proposed four-factor model. The validities are demonstrated by Table 4 ’s fit indices, providing a strong basis for evaluating the proposed four-factor model.
Hypotheses testing
We utilized a thorough structural equation modeling model with maximum likelihood estimation to analyze momentum structures and assess the study’s hypotheses. Simultaneously, hypotheses 1–2 (shown in Table 5 ) were supported by correlations (provided in Table 1 ) and SEM findings.
There is a strong positive correlation between students’ mental health and social support, as Hypothesis 1 suggests. Tables 1 and 5 provide the evidence we discovered supporting H1 (standardized β = 0.43, t = 7.57, p < 0.01). According to the second hypothesis, there will be a beneficial correlation between students’ mental health and PAS. With standardized β = 0.31, t = 5.016, and p < 0.01, H2 was supported.
H3 of our research uncovers that the ‘parents–children relationship significantly performs a mediating role in the association between social support and mental well-being of the students.’ Table 6 shows that when parent–child relationships are present, the β coefficient from social support and students’ mental health turns insignificant ( β = 0.041; S.E. = 0.060; t = 0.683; CI = −0.061, 1.012), but the indirect beta coefficient has a significant value ( β = 0.149; S.E. = 0.063; t = 2.365; CI = 0.337, 0.589). These findings demonstrate the mediating function of the parent–child bond in the association between students’ mental health and social support. The parent–child bond also acts as a mediator in the link between PAS and mental health, according to hypothesis 4. Table 6 shows a substantial mediating mechanism and a significant value for the beta coefficient. For H4, there is a substantial indirect correlation ( β = 0.163; S.E. = 0.062; t = 2.629; CI = 0.259, 0.352). Parental autonomy support and mental well-being have a direct link that eventually becomes negligible ( β = 0.008; S.E. = 0.060; t = 0.133; CI = −0.001, 0.013).
All formulated hypotheses of our study are accepted.
Mental health problems affect 10%–20% of students worldwide. Students’ susceptibility during the COVID-19 pandemic will likely influence this statistic. Poor mental health causes undesirable effects, including suicidal inclinations, behavioral disorders, and psychological abnormalities; hence, studies to remove or decrease the effects of bad mental health are critical. COVID-19 has made the already difficult state of youths and their mental health even more insecure. In the aftermath of a pandemic, the scale of COVID-19 the necessity for excellent research to fight MH concerns has grown exponentially. Keeping this information in mind, we developed our study subject and research questions and included parent–child relationships and linkages with students’ post-COVID-19 mental well-being of the pupils. The current research reviewed the literature on PAS, PSS, and people’s mental well-being after the COVID-19 pandemic. The literature study provided a vision of previous studies on the parent–child connection for mental well-being. According to research, the pandemic and its associated elements, such as quarantine, social isolation, and travel limitations, have been tense for students and other populations. Stress and worry caused by events such as closing schools, joblessness, poor healthcare, and uncertainty in education, job, and individual life have substantially influenced human mental and physical wellness (Pfefferbaum and North, 2020 ). We chose a paradigm that may serve the literature theoretically and practically, considering the significance of parent–child relationships after the pandemic. Prior study on the parent–child relationship has not investigated their role as a mediating variable in a unified model. The present research covers this gap in the literature by assuming that SS is positively linked with the mental well-being of students. The data analysis revealed that SS is substantially and highly positively associated with mental well-being; hence, H1 is accepted, in line with Cohen and McKay ( 2020 ), who discovered that social bonding and social support reduce psychological stress and enhance a person’s mental well-being.
Similarly, H2 investigated the association between parental autonomy support and mental well-being. It is also consistent with previous study findings that parental support has been proven to increase autonomy in young people, ultimately improving mental well-being (Inguglia et al., 2015 ). Because the conclusions indicated substantial values for each of these variables, H2 was also acceptable.
The mediation analysis was performed to determine if H3 and H4 were accepted or rejected. As previously stated in the findings section, mediating analysis was undertaken to check if the mediator increased the influence of independent variables on the dependent variable. Our research findings uncover that the ‘parents–children relationship significantly mediates the association between SS and mental well-being of the students.’ It can be viewed in the results section that the β coefficient from SS and mental well-being of the students turns insignificant in the attendance of the parent–children relationship, whereas the indirect beta coefficient has a significant value; this exhibits that the parent–children relationship plays a mediating role in the association between social support and the mental well-being of the students. Similarly, hypothesis 4 reveals that the parent–child relationship mediates the association between PAS and mental well-being. Table 6 shows that the beta value is significant, indicating a considerable mediation. The indirect association for hypothesis 4 is substantial, but the direct association between PAS and mental well-being turns insignificant. The H3 and H4 of our study are accepted.
Our findings reveal that all the proposed hypotheses were accepted, implying that SS has a good effect on the mental well-being of students and is related to a positive parent–child relationship. The findings then show that parent–child relationships positively influence mental well-being and play the role of mediating variable in the association between SS, PAS, and students’ mental well-being, which is in line with study findings that show that parent–child relationships mitigate the adverse influences of stress and foster mental wellness (Dam et al., 2023 ).
Implications
Our findings have far-reaching implications for medical practitioners, research organizations, and healthcare policymakers. Educational organizations should first become more aware of their students’ extra needs and mental health challenges. Future research should include people from various countries and ethnicities as COVID-19 control tactics and epidemic extent vary per country. Finally, the impacts of COVID-19 on students’ mental health have been overlooked. We urge instructors, higher education organizations, and mental health professionals to provide enough assistance to their students through the pandemic. Providing pupils with education to aid them in building self-efficacy, healthy parent–child relationships, and practical tools to cope with problems could help them handle the amplified stress that COVID-19 involves. It has been observed that durable and successful parent–child relationships were quite beneficial in helping pupils manage their stress. Administrators must appreciate MH practitioners’ function in supporting students seeking mental health support. Students’ capacity to tackle stress and create social support can assist them in escaping the harmful psychological impacts of the coronavirus outbreak. As a result, family, friends, and instructors should develop emotional resilience and enhance positive coping strategies among adolescents by adopting theory-tested treatments or programs. Because of constraints such as social isolation and lockdown, these treatments might be carried out in novel modes, for instance, webinars, online courses, and on-demand movies. Inter-professional probing programs and online mental behavior treatment boost students’ endurance and confidence (Schmutz, 2022 ). Furthermore, increasing social support could offer people a sense of higher psychological stability, reducing their fears and anxiety and helping them to function regularly during the pandemic. If students are urged to directly communicate their experiences and obstacles in their schooling after COVID-19, their morale will grow, and their MH will be preserved.
Limitations and future study
Our study has numerous limitations. For instance, this study relied on quantitative research; future research could use a qualitative or blended methodology to provide more intriguing outcomes. Secondly, the findings of this study were obtained by investigating eight educational institutions in Punjab province. Thirdly, because of the time limitation, we only carried out this study in one provincial unit. This research study might be broadened to other provincial units or nations in the future to generalize the study’s findings. Fourth, we obtained data from eight institutions; next, data from more institutions to be gathered to conduct the study. Finally, the current study included a mediating effect. Still, future studies may focus on using parent–child relationships as moderating variables. We suggest studying the reason for integrating PSS into the cognitive vulnerability model. As a result, new concerns have developed regarding the viability and significance of progressing to an integrative model, etiological paradigms, and innovative prospects for study and practical implementations.
The COVID-19 pandemic and the complex reaction techniques to halt its spread harm psychological and emotional well-being. Students’ lives have been damaged by social alienation and self-isolation. These effects must be detected, analyzed, and dealt with to guarantee the well-being of people like students. As a result, the present research sought to examine the influence of parental-child relationships, PAS, and SS in enhancing students’ mental well-being by gathering data from post-COVID-19. Students enrolling in Pakistani universities provided data. A survey for the survey was created to collect information from 355 students. SPSS was used to compute descriptive statistics, whereas AMOS structural equation modeling was employed to test hypotheses. These findings underlined the importance of the parent–child connection in dealing with complicated unfavorable conditions since it influences their mental results, particularly their psychological health. Optimistic and adverse relationships are opposed. Students who utilized primarily constructive relationship mechanisms with their parents experienced less emotional distress than those who employed more detrimental connection mechanisms with their parents (Budimir et al., 2021 ). Furthermore, the research emphasized the need for social support, such as friends and family, as well as parental autonomy support, in the fight against mental disorders. The findings also revealed that students require not only family support but also help from friends and others to create good relationships with parents to deal with psychological difficulties and stress produced by numerous sources.
Data availability
According to the confidential agreements with the participants, the dataset analyzed during the current study is not publicly available. The raw data supporting the conclusions of this article will be made available by the corresponding author upon reasonable request.
Akram AR, Abidin FA, Lubis FY(2022) Parental autonomy support and psychological well-being in university students during the COVID-19 pandemic: the role of autonomy satisfaction. Open Psychol J 15(1):1–8
Article Google Scholar
Anderson J, Gerbing D (1988) Structural equation modelling in practice: a review and recommended two-step approach. Psychol Bull 103(3):411–423
Arslan Ü, Asıcı E (2022) The mediating role of solution focused thinking in relation between mindfulness and psychological well-being in university students. Curr Psychol 41(11):8052–8061
Avila C, Holloway AC, Hahn MK, Morrison KM, Restivo M, Anglin R, Taylor VH (2015) An overview of links between obesity and mental health. Curr Obes Rep 4:303–310
Article PubMed Google Scholar
Ayala-Nunes L, Nunes C, Lemos I (2017) Social support and parenting stress in at-risk Portuguese families. J Soc Work 17(2):207–225
Bagozzi RP, Yi Y, Phillips LW(1991) Assessing construct validity in organizational research. Adm Sci Q 15(1):421–458
Balcells-Balcells A, Giné C, Guàrdia-Olmos J, Summers JA, Mas JM (2019) Impact of supports and partnership on family quality of life. Res Dev Disabilit 85:50–60
Barber BK, Stolz HE, Olsen JA, Collins WA, Burchinal M (2005) Parental support, psychological control, and behavioral control: assessing relevance across time, culture, and method. Monogr Soc Res Child Dev i–147(8)
Belsky J, Jaffee SR (2015) The multiple determinants of parenting. In: Developmental psychopathology: volume three: risk, disorder, and adaptation. Willey publishers, pp. 38–85
Budimir S, Probst T, Pieh C (2021) Coping strategies and mental health during COVID-19 lockdown. J Ment Health 30(2):156–163
Byrnes HF, Miller BA (2012) The relationship between neighborhood characteristics and effective parenting behaviors: the role of social support. J Fam Issue 33(12):1658–1687
Chatters LM, Taylor RJ, Woodward AT, Nicklett EJ (2015) Social support from church and family members and depressive symptoms among older African Americans. Am J Geriatr Psychiatry 23(6):559–567
Chen W, Li D, Bao Z, Yan Y, Zhou Z (2015) The impact of parent-child attachment on adolescent problematic Internet use: a moderated mediation model. Acta Psychol Sinica 47(5):611
Cohen S, McKay G (2020) Social support, stress and the buffering hypothesis: a theoretical analysis. In: Handbook of psychology and health (volume IV). Routledge, pp. 253–267
Cooke BD, Rossmann MM, McCubbin HI, Patterson JM (1988) Examining the definition and assessment of social support: a resource for individuals and families. Fam Relat (3):211–216
Dahlem NW, Zimet GD, Walker RR (1991) The multidimensional scale of perceived social support: a confirmation study. J Clin Psychol 47(6):756–761
Article CAS PubMed Google Scholar
Dam VAT, Do HN, Vu TBT, Vu KL, Do HM, Nguyen NTT, … Auquier P (2023) Associations between parent-child relationship, self-esteem, and resilience with life satisfaction and mental wellbeing of adolescents. Front Public Health 1–11
De Wit M, Pouwer F, Gemke RJ, Delemarre-Van De Waal HA, Snoek FJ (2007) Validation of the WHO-5 Well-Being Index in adolescents with type 1 diabetes. Diab Care 30(8):2003–2006
Dominguez S, Watkins C (2003) Creating networks for survival and mobility: social capital among African-American and Latin-American low-income mothers. Soc Prob 50(1):111–135
Feng Y, Zhou X, Qin X, Cai G, Lin Y, Pang Y, Zhang L (2022) Parental self-efficacy and family quality of life in parents of children with autism spectrum disorder in China: the possible mediating role of social support. J Pediatr Nurs 63:159–167
Froiland JM (2011) Parental autonomy support and student learning goals: a preliminary examination of an intrinsic motivation intervention. Paper presented at the Child & Youth Care Forum
Gavin B, Lyne J, McNicholas F (2020) Mental health and the COVID-19 pandemic. Irish J Psychol Med 37(3):156–158
Hair JF, Black WC, Babin BJ, Anderson RE, Tatham RL (1998) Multivariate data analysis. 5th edn. vol. 5, no. 3. Upper Saddle River, pp. 207–219
Harman HH, Harman HH (1976) Modern factor analysis. University of Chicago press
Harris TL, Molock SD (2000) Cultural orientation, family cohesion, and family support in suicide ideation and depression among African American college students. Suicide Life‐Threat Behav 30(4):341–353
Herwig JE, Wirtz M, Bengel J (2004) Depression, partnership, social support, and parenting: interaction of maternal factors with behavioral problems of the Child. J Affect Disord 80(2-3):199–208
Holmes CJ, Kim-Spoon J, Deater-Deckard K (2016) Linking executive function and peer problems from early childhood through middle adolescence. J Abnorm Child Psychol 44:31–42
Article PubMed PubMed Central Google Scholar
Hu J, Chiang JTJ, Liu Y, Wang Z, Gao Y (2023) Double challenges: How working from home affects dual‐earner couples’ work‐family experiences. Pers Psychol 76(1):141–179
Inguglia C, Ingoglia S, Liga F, Lo Coco A, Lo Cricchio MG (2015) Autonomy and relatedness in adolescence and emerging adulthood: Relationships with parental support and psychological distress. J Adult Dev 22(1):1–13
Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH (2012) Promoting positive parenting: an introduction. In: Promoting positive parenting. Routledge, pp. 1–10
Kaplan BH, Cassel JC, Gore S (1977) Social support and health. Med Care 15(5):47–58
Kins E, Beyers W, Soenens B, Vansteenkiste M (2009) Patterns of home leaving and subjective well-being in emerging adulthood: the role of motivational processes and parental autonomy support. Dev Psychol 45(5):1416
Kline RB (2015) Principles and practice of structural equation modeling. Guilford publications
Lamborn SD, Felbab AJ (2003) Applying ethnic equivalence and cultural values models to African-American teens’ perceptions of parents. J Adolesc 26(5):601–618
Lekes N, Gingras I, Philippe FL, Koestner R, Fang J (2010) Parental autonomy-support, intrinsic life goals, and well-being among adolescents in China and North America. J Youth Adolesc 39:858–869
Li J, Huang J, Hu Z, Zhao X (2022) Parent–child relationships and academic performance of college students: chain-mediating roles of gratitude and psychological capital. Front Psychol 13:794201
Li X, Ding Y, Bai X, Liu L (2022) Associations between parental mediation and adolescents’ internet addiction: the role of parent–child relationship and adolescents’ grades. Front Psychol 13:1061631
Lin N, Ensel WM, Simeone RS, Kuo W (1979) Social support, stressful life events, and illness: a model and an empirical test. J Health Soc Behav (2)108–119
Lippold MA, Glatz T, Fosco GM, Feinberg ME (2018) Parental perceived control and social support: linkages to change in parenting behaviors during early adolescence. Fam Process 57(2):432–447
Lu J, Lin L, Roy B, Riley C, Wang E, Wang K, Zhou X (2020) The impacts of parent-child communication on left-behind children’s mental health and suicidal ideation: a cross sectional study in Anhui. Child Youth Serv Rev 110:104785
Marroquín B (2011) Interpersonal emotion regulation as a mechanism of social support in depression. Clin Psych Rev 31(8):1276–1290
Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, De Girolamo G (2009) Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med 6(8):e1000123
Oktavia W, Urbayatun S, Mujidin Z (2019) The role of peer social support and hardiness personality toward the academic stress on students. Int J Sci Technol Res 8(12):2903–2907
Google Scholar
Östberg M, Hagekull B (2000) A structural modeling approach to the understanding of parenting stress. J Clin Child Psychol 29(4):615–625
Pfefferbaum B, North CS (2020) Mental health and the Covid-19 pandemic. N Engl J Med 383(6):510–512
Priya SS, Cuce E, Sudhakar K (2021) A perspective of COVID 19 impact on global economy, energy and environment. Int J Sustain Eng 14(6):1290–1305
Ranson KE, Urichuk LJ (2008) The effect of parent–child attachment relationships on Child biopsychosocial outcomes: a review. Early Child Dev Care 178(2):129–152
Rawat M, Sehrawat A (2021) Effect of COVID-19 on mental health of teenagers. Asian J Pediatr Res (3):28–32
Rinaldi CM, Howe N (2012) Mothers’ and fathers’ parenting styles and associations with toddlers’ externalizing, internalizing, and adaptive behaviors. Early Child Res Q 27(2):266–273
Robb CE, De Jager CA, Ahmadi-Abhari S, Giannakopoulou P, Udeh-Momoh C, McKeand J, Ward H (2020) Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: a survey of older adults in London, UK. Front Psychiatry 11:591120
Ryan RM, Deci EL (2000) Intrinsic and extrinsic motivations: Classic definitions and new directions. Contemp Educ Psychol 25(1):54–67
Schmutz JB (2022) Institutionalizing an interprofessional simulation education program: an organizational case study using a model of strategic change. J Interprof Care 36(3):402–412
Shaffer JA, DeGeest D, Li A (2016) Tackling the problem of construct proliferation: A guide to assessing the discriminant validity of conceptually related constructs. Organ Res Method 19(1):80–110
Shamir M, Shamir Balderman O (2023) Attitudes and feelings among married mothers and single mothers by choice during the Covid-19 crisis. J Fam Issue 45(3):0192513X231155661
Shen YE (2009) Relationships between self‐efficacy, social support and stress coping strategies in Chinese primary and secondary school teachers. Stress Health J Int Soc Investig Stress 25(2):129–138
Siu O-L, Spector PE, Cooper CL, Lu C-Q (2005) Work stress, self-efficacy, Chinese work values, and work well-being in Hong Kong and Beijing. Int J Stress Manag 12(3):274
Soenens B, Vansteenkiste M, Lens W, Luyckx K, Goossens L, Beyers W, Ryan RM (2007) Conceptualizing parental autonomy support: adolescent perceptions of promotion of independence versus promotion of volitional functioning. Dev Psychol 43(3):633
Su Z, McDonnell D, Wen J, Kozak M, Abbas J, Šegalo S, Cai Y (2021) Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Glob Health 17(1):1–8
Tao Y, Yu H, Liu S, Wang C, Yan M, Sun L, Zhang L (2022) Hope and depression: the mediating role of social support and spiritual coping in advanced cancer patients. BMC Psychiatry 22(1):345
Teti DM, Gelfand DM (1991) Behavioral competence among mothers of infants in the first year: the mediational role of maternal self‐efficacy. Child Dev 62(5):918–929
Vasquez AC, Patall EA, Fong CJ, Corrigan AS, Pine L (2016) Parent autonomy support, academic achievement, and psychosocial functioning: a meta-analysis of research. Educ Psychol Rev 28:605–644
Wang M-T, Peck SC (2013) Adolescent educational success and mental health vary across school engagement profiles. Dev Psychol 49(7):1266
Wilcox BL, Vernberg EM (1985) Conceptual and theoretical dilemmas facing social support research. In: Social support: theory, research and applications. Springer, pp. 3–20
Xiong J, Lipsitz O, Chen-Li D, Rosenblat JD, Rodrigues NB, Carvalho I, Mansur RB (2021) The acute antisuicidal effects of single-dose intravenous ketamine and intranasal esketamine in individuals with major depression and bipolar disorders: a systematic review and meta-analysis. J Psychiatr Res 134:57–68
Yan Z, Yu S, Lin W (2023) Parents’ perceived social support and children’s mental health: the chain mediating role of parental marital quality and parent‒child relationships. Curr Psychol (12):1–13
Ypsilanti A, Robson A, Lazuras L, Powell PA, Overton PG (2020) Self-disgust, loneliness and mental health outcomes in older adults: an eye-tracking study. J Affect Disord 266:646–654
Download references
This research is supported by the Jiangsu Funding Program for Excellent Postdoctoral Talent (No. 2022ZB643).
Author information
Authors and affiliations.
School of Management, Jiangsu University, Zhenjiang, 212013, People’s Republic of China
Arif Jameel, Zhiqiang Ma, Mingxing Li, Abid Hussain, Muhammad Asif & Yan Wang
Research Center for Green Development and Environmental Governance, Jiangsu University, Zhenjiang, 212013, China
Mingxing Li
You can also search for this author in PubMed Google Scholar
Contributions
AJ, MZ, YW, and ML conceptualized the study; MA and AH conducted the surveys and performed the Analysis; AJ and MZ wrote the first draft of the manuscript; all authors critically discussed the results, revised the manuscript, and have read and approved the manuscript.
Corresponding authors
Correspondence to Zhiqiang Ma or Yan Wang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
Ethical approval was obtained from the Jiangsu University Institutional Review Board (No. JUIRB/13178/2023). The survey process and procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Before data collection, all eligible respondents were informed about the aims of the study, voluntary participation, and the right to withdraw at any time without giving any reason. They were also assured of the confidentiality of the information to be collected.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Jameel, A., Ma, Z., Li, M. et al. The effects of social support and parental autonomy support on the mental well-being of university students: the mediating role of a parent–child relationship. Humanit Soc Sci Commun 11 , 622 (2024). https://doi.org/10.1057/s41599-024-03088-0
Download citation
Received : 15 August 2023
Accepted : 22 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1057/s41599-024-03088-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
COVID-19 and psychological distress: Lessons for India
Contributed equally to this work with: Vaijayanthee Anand, Luv Verma, Aekta Aggarwal, Priyadarshini Nanjundappa, Himanshu Rai
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Humanities and Social Sciences, Indian Institute of Management, Indore, Madhya Pradesh, India
Affiliation School of Aeronautics, Neemrana, Rajasthan, India
Affiliation Operations Management and Quantitative Techniques, Indian Institute of Management, Indore, Madhya Pradesh, India
Roles Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Management Studies, Indian Institute Of Technology, Chennai, Tamil Nadu, India
Affiliation Human Resources and Organizational Behaviour, Indian Institute of Management, Indore, Madhya Pradesh, India
- Vaijayanthee Anand,
- Luv Verma,
- Aekta Aggarwal,
- Priyadarshini Nanjundappa,
- Himanshu Rai

- Published: August 4, 2021
- https://doi.org/10.1371/journal.pone.0255683
- Reader Comments
The COVID-19 pandemic has undoubtedly altered the routine of life and caused unanticipated changes resulting in severe psychological responses and mental health crisis. The study aimed to identify psycho-social factors that predicted distress among Indian population during the spread of novel Coronavirus.
An online survey was conducted to assess the predictors of distress. A global logistic regression model was built, by identifying significant factors from individual logistic regression models built on various groups of independent variables. The prediction capability of the model was compared with the random forest classifier.
The respondents ( N = 1060) who are more likely to be distressed, are in the age group of 21-35 years, are females (OR = 1.425), those working on site (OR = 1.592), have pre-existing medical conditions (OR = 1.682), do not have health insurance policy covering COVID-19 (OR = 1.884), have perceived seriousness of COVID-19 (OR = 1.239), have lack of trust in government (OR = 1.246) and whose basic needs’ fulfillment are unsatisfactory (OR = 1.592). The ones who are less likely to be distressed, have higher social support and psychological capital. Random forest classifier correctly classified 2.3% and 17.1% of people under lower and higher distress respectively, with respect to logistic regression.
Conclusions
This study confirms the prevalence of high distress experienced by Indians at the time of COVID-19 and provides pragmatic implications for psychological health at macro and micro levels during an epidemiological crisis.
Citation: Anand V, Verma L, Aggarwal A, Nanjundappa P, Rai H (2021) COVID-19 and psychological distress: Lessons for India. PLoS ONE 16(8): e0255683. https://doi.org/10.1371/journal.pone.0255683
Editor: Ritesh G. Menezes, Imam Abdulrahman Bin Faisal University, SAUDI ARABIA
Received: March 6, 2021; Accepted: July 22, 2021; Published: August 4, 2021
Copyright: © 2021 Anand et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
1 Introduction
The COVID-19 pandemic has been affecting the world at an alarming rate, leaving it in shambles. According to the World Health Organization(WHO), in the month of March 2020, over 14, 000 people died due to the novel Coronavirus, with more than 3, 34, 000 being infected [ 1 ]. In India, 1, 251 confirmed COVID cases and 32 death cases were reported when nationwide lockdown was declared on 23rd March, 2020. The cases have risen sharply since then, and currently more than 10 million confirmed cases and nearing 1, 56000 death cases have been reported till date.
The spread of the disease was followed with a series of lockdown and stringent quarantine measures in various parts of the world, such as the travel restrictions, closure of educational institutions, offices, and commercial activities in India. Strict quarantine measures were prescribed to reduce the rate of infections in the country. India currently stands 2nd in the global index for the most number of infections after the USA ( https://COVID19.who.int/ ). Over the months, the cases of COVID-19 have been under control and a series of un-lockdowns were observed in India. However, the current statistics show that despite the nation-wide strategic implementation of the vaccination, there is a resurgence of COVID-19 infections, which may result in the various government imposed curbs and lockdowns.
The disease brought along several complications which were novel to the society. Along with the high mortality rates, this pandemic has severe physical, emotional and psychological ramifications. Globally, scientists have invested efforts in diagnosis and treatment of COVID-19. The breadth of the current research on COVID-19 focuses more on its clinical characteristics [ 2 ], likelihood of survival [ 3 ], genomic characterization of the virus [ 4 ] and drug and therapeutic options [ 5 ]. Additionally, growing incidences of anxiety, pain, insomnia and distress have been reported widely across nations [ 6 ]. Despite the spike in these cases, the myriad psychological impacts of COVID-19 on mental health have not received adequate attention [ 7 ]. Similarly, studies in India have been more conceptual in nature and paucity of empirical evidence on assessing the psychological effects and response to COVID-19 has been observed, [ 8 – 10 ].
Psychological distress is defined as a state of emotional suffering typically characterized by symptoms of depression and anxiety, which is recognized as a common mental health problem in the community [ 11 ]. In general, mental health and related issues are not recognized in public, and with the global pandemic, these ‘silent’ and insidious issues can go unnoticed. Confinement to physical spaces, lack of mobility, panic buying, fear of contraction, loss of income, adaptation to the new normal and the growing ambiguity were some of the observed collective experiences, affecting the overall well-being during the lockdown [ 12 ]. The COVID-19 outbreak has introduced additional stressors that further impinges the mental health status of the general population, making them vulnerable to psychological disorders. Studies have revealed that high distress and anxiety due to COVID-19 has resulted in poor psychological well-being [ 13 ], increase in suicidal tendencies [ 14 ], exasperated pre-existing mental health conditions [ 15 ] to name a few. It has also severely affected the family relationships and social dynamics [ 16 ], increase in cases of domestic violence [ 17 ], and abuse of alcohol [ 18 ].
A rapid increase in the COVID cases and its debilitating impact on the psychological health necessitates an empirical investigation to explore the prevalence and determinants of psychological distress. Such an investigation will help identify the vulnerable groups at risk. This will enable policy makers to design interventions with a targeted approach. Further, the insights of such a study will aid in promoting the protective and minimizing the risk factors. With the impending uncertainty about the end of the pandemic and the emergence of a new strain of the virus, there is a potential for yet another wave, which demands preparedness at the individual and community level. Thus, the objective of the present study is to investigate the psycho-social risk and protective factors to predict distress among general population in India during the COVID-19 pandemic. The findings of the study will contribute in prescribing measures to better manage the psychological crisis and further strengthen mental immunity during a public health emergency.
In the current study, the researchers identified various sources of distress encountered during the ongoing pandemic through interviews with Indian citizens of varied demographics. The interview responses were analysed and various themes were developed that represented different psycho-social stressors (risk and protective factors), which were mapped to the social-ecological model of public health behaviour. This model proposed by Bronfenbrenner (see [ 19 ] and references therein), recognizes individuals as embedded within the larger social systems and describes the interactive characteristics of individuals and environments that underlie public health behaviours [ 20 ]. This model is popularly used as a conceptual framework for guiding interventions in public mental health [ 21 ]. Additionally, this framework provides a holistic perspective to understand health and mental health behaviours.
Thus, the present study based on the tenets of the socio-ecological model, organises the psycho-social stressors as individual (socio-demographics and psychological capital), health-related risk (pre-existing medical conditions, health insurance, and perceived seriousness of COVID-19) and community factors (trust in government, social support and fulfillment of basic needs). The conceptual framework of the study is presented in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0255683.g001
This study adopted a cross-sectional survey approach and a country-wide data was collected. A snowball method of sampling was employed, promoting the study through existing networks and mailing lists. An invitation to participate in an online form was sent through various social media platforms.
2.1 Study participants
A total of 1543 respondents from across the country participated in the survey, and designed in the language of English. Among the filled responses, 1060 were considered for the analysis, who largely represented Indian middle to upper socio-economic status (SES)(who could follow English). The study was approved by the Research Review Board, School of Aeronautics, Neemrana, India. Participants were informed about the voluntary participation prior to filing the forms. The participants were informed about the background of involved researchers and about the motive/objective of the survey. The participation was completely voluntary and no intervention of any kind from the researchers conducting the study was involved. The participant was also given an option to skip answering any question(s), if s/he may wish to. The above was done to maintain the most salient ethical values such as beneficence, non-maleficence, trust within the investigator/participant and the privacy of personal information. To control the selection and response bias at respondents level, the survey was floated in various states to get the varied demographics. An easy escape route was provided to the participants as they could exit the survey at their will. To tackle the duplication of the response, the option of not being allowed to fill the survey from the same device more than once, was enabled. Finally, to remove the bias from the responses, a statistical procedure was followed. For an individual respondent, if the correlation values were above 0.75 or lower than -0.75 among all the independent variables, the corresponding response was removed, as highly correlated variables signify biased response [ 22 , 23 ]. Incomplete forms were determined as the another exclusion criteria. The information regarding the participants email was deleted to preserve anonymity. The demographic profiling of the participants is presented in Table 1 .
https://doi.org/10.1371/journal.pone.0255683.t001
2.2 Measures
2.2.1 socio-demographic factors..
The first part covered the socio-demographic details, which included age, gender, marital status, occupational status, family structure, number of economic dependents, educational level, and the place of residence.
2.2.2 Other factors.
The second part included questions anchored to the constructs of the study. Following are the measures used for the present study.
2.2.2.1 Health-related risk factors . Pre-existing medical condition was assessed by a single item in which respondents were asked to report if they were suffering from any chronic medical condition. The construct of Health Insurance was also measured by one item in which respondents reported if they possessed a health insurance policy that covered COVID related expenses. The degree of perceived seriousness of COVID-19, was measured by a single item on a 5-point scale (1 = not serious to 5 = extremely serious) which was adapted from the standardized questionnaire on risk perception of an infectious disease outbreak [ 24 ].
2.2.2.2 Community factors . Trust in Government (lack) was assessed to gauge the level of trust in Government’s capability in managing the crisis. 5 items were used to measure this construct on a 5-point scale (1 = strongly agree to 5 = strongly disagree). 2 items were adapted from Ma et al [ 25 ], while the other 3 items were self-developed based on the verbatim interview responses. The degree of social support in terms of availability of others to talk about one’s problems during the crisis was measured by employing 4 items from the appraisal subscale of Interpersonal Support Evaluation List-12 [ 26 ]. The items were responded on a 4-point rating scale (1 = definitely false to 4 = definitely true). To measure the (dis)satisfaction with the fulfillment of basic needs, the participants were asked to report the extent to which they were satisfied with the availability and accessibility of basic resources which included water, food, medicines, electricity and internet connection. This was measured on a 5-point scale (1 = unsatisfactory and 5 = extremely satisfactory).
2.2.2.3 Intrapersonal factors . Psychological capital defined as an individual’s positive psychological resource was measured through a standardized scale-PCQ-12 [ 27 ] that assessed the four integrating dimensions, namely, self-efficacy (3 items), hope (4 items), optimism (2 items) and resilience (3 items) on a 6-point scale (1 = strongly disagree to 6 = strongly agree). A summated score was considered for the study.
2.2.2.4 Psychological distress . It was assessed using 6 items Kessler Distress scale (K6) [ 28 ]. The items are used for screening major depression and generalised anxiety disorder and asks respondents how frequently they have experienced relevant symptoms during the past month. Each item had five options ranging from 0 (never) to 4 (all of the time).
The instruments designed for this study included items, that were self-developed exclusively for the study, while some were adapted from standardized scales, available and open for academic purposes. Prior permission to use standardized scales was sought by sending an email to the scale developers/ paper authors. The psychometric properties of the instrument were established. For the variables under study, the items were factor analyzed using principal components analysis with promax rotation which yielded an 6-factor structure explaining 67% of the total variance. The Kaiser–Meyer–Olkin (0.883) and Bartlett’s Test of Sphericity (18626, p>0.01) indicated that the factor model is appropriate. Confirmatory Factor Analysis was performed to test the validity measures. Construct validity of the measures was assessed by Factor Loading, Composite Reliability (CR) and Average Variance Extracted (AVE) [ 29 ]. All factor loadings were found to be significant and ranged from 0.70–0.82. Reliability results for all constructs were above 0.70, indicating satisfactory reliability [ 29 ]. Convergent validity was measured using the average variance extracted (AVE). All constructs exhibited an AVE greater than 0.50, indicating convergent validity. Discriminant validity was confirmed as the square roots of the AVE were larger than the coefficients of the bivariate correlation. Further, to check for the common method bias, Harman’s single-factor test was performed, where all constructs were subjected to Exploratory Factor Analysis with an unrotated factor solution to determine the number of factors necessary to account for the variance. The results revealed a total variance of 20% indicating an absence of common method bias.
2.3 Data analysis
The data analysis and modelling were performed using machine learning libraries based on statsmodels in Python. To test the multi-collinearity among considered variables, variance inflation factor (VIF) was calculated. None of the independent variables were dropped as their VIF was found to be less than 10 [ 30 – 32 ]. To explore the relationship of dependent variable (psychological distress) with independent variables, bivariate analyses were performed, including chi-squared test for discrete and independent t -test for continuous variables, which have been reported in Table 1 . The factors with p values equal to or less than 0.05 were considered to be significant. In the bivariate analysis, all the variables had p value less than 0.05 and hence no conclusion could be drawn about insignificance of any factor. To further investigate the statistical relevance of the predictors of distress, four logistic regression models were built [ 33 ], model 1 with socio-demographic variables, model 2 with health-related risk variables, model 3 with community variables, and model 4 with intrapersonal factor. Finally, a global model (Model 5) was constructed with only variables which had p value ≤ 0.05 in each of the individual models. In order to quantify the magnitude of the effect produced by independent variables with respect to the psychological distress, the effect size was measured through their odds Ratios (ORs) with a 95% confidence interval [ 34 , 35 ]. Accuracy, specificity and sensitivity were used as performance metrics for the models, since accuracy alone is not a good metric to indicate the correctly classified individuals under both low and higher distress [ 36 ]. The coefficient of determination, R 2 value, was considered as a measure of the goodness-of-fit of the model. As the accuracy of the logistic regression classifier on the global model was found to be less than 85%, thus random forest classifier was also employed to increase the overall accuracy of classification. K -fold cross validation, with K = 5, was employed so that the reported accuracy scores were not higher due to the over-fitting [ 37 , 38 ].
3.1 Psychological distress
Psychological distress which was initially categorized into a five point scale was re-categorized into two categories, low distress and high distress using median as a cut-off point [ 39 ]. Evaluating a cut-off point of 3 for distress, the results showed that 53.86% of the people considered for analysis were under high distress.
3.2 Independent variables and distress
Table 1 represents the descriptive statistical analysis of the various independent variables, in relation to the response variable distress.
3.3 Prediction of distress
This section details the results of the logistic regression models, which were built across the various predictors of the survey. The results indicate that the global regression model (Model 5) is able to explain the variability of the data to 42.4%. Logistic regression models are displayed in Table 2 . All the models had p -value less than 0.001.
https://doi.org/10.1371/journal.pone.0255683.t002
Model 1 (Sociodemographic variables) had an R 2 value of 35.5% with χ 2 = 809. It correctly classified 80.1% of respondents with specificity and sensitivity being 72% and 84%, respectively. The participants in the age group of 36–50 years (OR = 0.410, 95% CI = (0.289, 0.581)) and the ones with nuclear family structure (OR = 0.23, 95% CI = (0.151, 0.351)) were less likely to be distressed as compared to the ones in the age group of 21–35 years and the ones living alone respectively. The participants living in joint family structure (OR = 2.089, 95% CI = (1.228, 3.554)), the female participants (OR = 2.0023, 95% CI = (1.507, 2.660)), the ones working on site (OR = 2.428, 95% CI = (1.713, 3.441)) and the ones with only one dependent (OR = 2.380, 95% CI = (1.777, 3.187)) were more likely to be distressed than the ones living alone, males, the ones working from home and the ones with no dependents respectively.
Model 2(Health-related risk variables) had an R 2 value of 26.63% with χ 2 = 224. The participants with pre-existing medical conditions(OR = 3.066, 95% CI = (2.223, 4.228)) and the ones with no health insurance (OR = 3.352, 95% CI = (2.058, 5.462)) were more likely to be distressed than the ones who were unsure about their medical history, and who were not sure if they had a health insurance for COVID-19, respectively. The model correctly classified 67.5% of respondents with specificity and sensitivity being 67% and 65%, respectively.
Model 3 (Community variables) showed a predictive ability of 34.47% with χ 2 = 73.28, correctly classified 79.3% of respondents with specificity and sensitivity being 85% and 71%, respectively. The participants with lack of trust in government (OR = 1.497, 95% CI = (1.285, 1.745)), and the ones who were dissatisfied with the fulfillment of basic needs (OR = 3.235, 95% CI = (2.497, 4.190)) were more likely to be distressed. Those with high social support (OR = 0.387, 95% CI = (0.333, 0.449)) were less likely to be distressed.
Model 4 (Intrapersonal variable/Psychological Capital) showed a predictive ability of 6.23% with χ 2 and correctly classified 61.1% of respondents with specificity and sensitivity being 49% and 57%, respectively. The participants with psychological capital (OR = 0.689, 95% CI = (0.623, 0.761)) were less likely to be distressed.
Model 5 (Global Model), had a predictive ability of 42.4% and high chi-squared value ( χ 2 = 619), which represents good fit to the global model [ 33 ]. The significant predictive variables that showed the greater weight, with OR greater than 1, were gender, specifically female (OR = 1.425, 95% CI = (1.011, 2.008)), occupational status as working on site (OR = 1.592, 95% CI = (1.131, 2.241)), awareness about pre-existing medical conditions (OR = 1.682, 95% CI = (1.056, 2.680)), absence of health insurance policy (OR = 1.884, 95% CI = (1.105, 3.214)), high perceived seriousness of COVID-19 (OR = 1.239, 95% CI = (1.013, 1.515)), lack of trust in government (OR = 1.246, 95% CI = (1.020, 1.521)) and dissatisfaction with fulfillment of basic needs (OR = 1.592, 95% CI = (1.004, 2.524)). The predictors with OR less than 1 were psychological capital, social support and age group of 36–50 years. The remaining variables, family structure, number of dependents and absence of pre-existing medical conditions were insignificant.
The final model had a predictive ability of 42.4%, correctly classifying 82.2% of respondents with specificity and sensitivity being 77.5% and 86% respectively when modelled through logistic regression. In order to increase classification performance, random forest classifier was employed on the predictors of the global model (Model 5). The accuracy of this model was 92%, with specificity and sensitivity of 94.5% and 88.3% respectively. Even though, the correct classification of people under high distress increased by 2.3%, in comparison to logistic regression, the accuracy of the random forest classifier was 17.1% higher for people with low distress.
4 Discussion
The present study aimed at identifying the psycho-social factors predicting psychological distress, experienced amongst the general population in India, in the times of COVID-19 pandemic. As mentioned in §3.1, prevalence of distress was observed. The results of the study indicate that the socio-demographic, health-related risk, community and intrapersonal factors have a significant influence on distress.
Within the socio-demographic factors, the respondents in the age group of 21–35 years were found to be more prone to distress (40.98%) as compared to the other age groups considered for the study. These findings are consistent with those from previous studies during an epidemic [ 40 – 42 ], which showed that younger population was associated with an increased risk of distress. The studies have also shown that older adults have increased resilience to psychopathologies such as post-traumatic stress disorder after an emergency due to natural disasters, indicating that older population are better equipped to handle stressful situations. [ 43 – 46 ]. Studies suggest that younger population experiences higher anxiety due to proximity to contamination, information overload through social media and a poor tolerance of uncertainty, which might explain the findings of the present study [ 47 ]. This study reported that the females experienced higher distress (66.02%) than their counterparts, which is in line with the previously available extensive epidemiological literature. In accordance with other studies carried out in China during COVID-19 pandemic [ 7 , 48 , 49 ], women and young adults were the ones that suffered the greater psychological impact. Generally, women are the informal caregivers within families, and with the additional restrictive measures (such as closure of the educational institutions and care for elderly), might have led to an increased burden at home, thereby explaining higher distress [ 50 ]. Increased domestic responsibilities could further impact their work performance, whether working onsite or remotely, compounding their levels of distress [ 51 ]. Yet another reason could be increased occurrences of domestic violence against women that were recorded during times of crisis and quarantines [ 40 , 51 , 52 ]. This study found that the respondents who were working on site were more distressed (50.96%) than those working from home or not working. Similar results were found in a research amongst general adult population in Spain [ 53 ]. Perceived inadequate workplace protective equipment supply, fear of contracting the disease and the stigma associated with it, during COVID-19 pandemic significantly led to employee stress which explains why employees working on site were highly likely to be distressed [ 54 ]. Hence, fearing the consequences, employees preferred working from home during the COVID-19 pandemic.
Amongst the health-related risk factors evaluated in this study, all three sub-factors were found to be significantly contributing to distress. Extensive review of literature suggests that the following sub-factor, is rarely explored in the epidemiological literature. The findings revealed that people who had no health insurance were more stressed (46.94%) than the ones who were not sure if their insurance covered COVID-19 related expenses. The limited available literature showed that having difficulties in covering monthly expenses in non-pandemic times was positively correlated with distress, and it is of no surprise that the crisis situation could aggravate the stress levels [ 55 ]. Those with a history of pre-existing medical conditions reported higher distress (54.99%) than the ones who were not sure if they ever suffered from one. Similar findings suggest that poor perception of physical health [ 56 ] and a history of pre-existing medical conditions or illnesses [ 7 ] can lead to higher stress.
Previous literature has also asserted that perceived risk of contracting the disease is a significant stressor. The results of this study further validate the past findings as the respondents who perceived COVID-19 more seriously reported higher levels of distress(M = 4.38, SD = 0.49). An Asian study [ 57 ] further highlighted and confirmed the significant role of this factor in explaining poor mental health during COVID-19, in addition to other factors such as misinformation and social isolation in contributing to stress and mental morbidity. Perhaps, lack of authentic information, ambiguity about the novel Coronoavirus along with less confidence in healthcare fraternity to treat COVID-19 could explain higher stress [ 58 , 59 ].
The community factors assessed in the present paper showed higher association with the experience of distress. The first sub-factor i.e. lack of trust in the government initiatives to combat COVID-19 positively predicted high levels of distress(M = 4.26, SD = 0.44), much in line with the recent studies that suggest public’s trust in the government is critical for community mental health. Infact, [ 60 ] reports that the lack of trust can also hamper emergency and recovery procedures, harming general public during any given crisis situation, like COVID-19 pandemic. The resulting unrest and chaos, may probably, lead to an increase in distress. The second sub-factor, social support is well established as a protective factor, buffering the harmful effects of distress. Previous studies have highlighted the role of social support in reducing anxiety and stress, [ 61 ], with which the results of this study resonate (M = 4.31, SD = 0.46). The final sub-factor, the (dis)satisfaction with fulfillment of basic needs during the pandemic, which included food, water, electricity, medicine and internet, was found to have a positive significant influence on distress (M = 4.44, SD = 0.50). A paucity of research concerning availability or lack thereof in determining distress was observed. Limited research findings exhibited that availability of local medical facilities influenced levels of distress among Chinese population [ 62 ]. In fact, the basic underlying assumptions of need theories also state that only when human needs are fulfilled sufficiently, people experience happiness [ 63 ]. Due to stringent lockdown measures, panic buying due to perceived shortage of basic resources was reported, which could accentuate the stress levels [ 8 ].
The final factor for the study was psychological capital(PsyCap) and it was found that the respondents with higher PsyCap were less likely to be distressed(M = 2.53, SD = 0.59). This factor has been explored to a very limited extent during a pandemic or crisis, in the literature, which reflects a very pertinent gap in terms of research in intrapersonal factors. A meta-analytic study [ 64 ] on PsyCap states that those low in PsyCap are more prone to stress. The review further suggested that PsyCap’s agentic thinking has a motivating impact that can enhance internalization, determination, and pathways thinking, which contradict with the ‘giving up’ and despair associated with cynicism, thereby protecting an individual, from the toxic effects of stress. The extant literature [ 65 ] has established that the more positive capacities one uses, the ability to deal with stressful situations improves considerably.
5 Conclusion
This study confirms the prevalence of distress experienced by the citizens of India during the pandemic and provides pragmatic implications for stress management at macro and microlevels during an epidemiological crisis. Based on the findings it is suggested that public health machinery must conduct mental health audits during epidemiological emergencies, which are critical for effective management of community mental health. This can further aid in delivering targeted psycho-social interventions for the identified vulnerable groups (which includes females, 21–35 years old citizens, the ones with pre-existing medical conditions, and those working on site). Several initiatives are currently being undertaken by the Government such as providing tollfree helplines and tele counselling services for mental health assistance during the COVID-19 pandemic. Similarly, resource materials and manuals on managing stress during COVID, yoga and meditation, etc. are available to the public on the MOHFW-GOI website [ 66 ]. However, for effective reachability of such interventions, the services and facilities need to be curated to the specific needs of the identified susceptible groups.
Since the study revealed that those who did not possess an insurance policy for treatment of COVID-19 are more prone to distress, thus, it is recommended that the Government regulates and mandates the insurance companies to provide diagnostic and treatment coverage for the disease in the form of protective care. This will help to deal with any medical emergency with hopes of leading a worry-free life ahead. Further, the insurance companies must make efforts to communicate the coverage in their basic plans.
As public’s lack of trust towards the Government policies and initiatives around COVID-19 was identified as a significant predictor of distress, thus a constant attempt by the public authorities to understand the community’s perception of their policies must be undertaken. This will aid in employing effective strategies to inform, educate and communicate the public about such initiatives, thereby fostering trust in the Government. People’s perception of the seriousness of the disease which was also identified as major source of distress, is highly influenced by Government and social media communication. In this regard, greater caution needs to be exercised while devising risk communication strategies which can include preparedness, response, and recovery phases of a serious public health crisis, rather than just reporting on the number of infected, recovered and death cases. Dissatisfaction with fulfillment of basic needs was found to contribute to distress. Therefore, it is proposed that local authorities invest in assessing the basic needs and reallocating the distribution of basic resources during the crisis.
Human beings are gregarious in nature and we always need social connection in our lives. As reported in the study, social support during crisis, is paramount to cope with stressful situations. Thus, public health measures may focus on promoting a supportive environment: and provide resources to cultivate and maintain a sense of community belongingness. It is well known that external resources are not in our control, and thus it becomes imperative to focus on building and strengthening our internal resources to tide through these times. As the present study recognized positive capacities of resilience, hope, optimism and self-efficacy that constitute PsyCap as a protective factor during stressful situations, hence the Government, and systemic organizations/institutes such as schools, organizations and non-governmental organizations should invest in development of positive capacities for sustainable well-being in the community.
6 Limitations
Although the study contributed to the literature of mental health during COVID-19, it also has certain limitations. Since the sample comprised of respondents from restrictive socio-economic status, limited geographical coverage and poor representation from red-zone cities, the results cannot be generalized. The non-probability sampling method(snowball sampling) employed for the study may have potentially affected the generalizability and sample representativeness. As the study followed a cross-sectional approach, it could not capture the changing trends during multiple lockdowns observed in India. Hence, future studies can follow a longitudinal approach to identify and understand the changes which could have occurred over a period of time. Interpersonal factors like family dynamics and relationship with others, could be potential factors influencing distress which can be analyzed in future studies.
Supporting information
https://doi.org/10.1371/journal.pone.0255683.s001
- 1. Organization, W. & Others COVID-19 weekly epidemiological update, 25 May 2021. (World Health Organization, 2021)
- View Article
- Google Scholar
- PubMed/NCBI
- 19. Bronfenbrenner U. Making human beings human: Bioecological perspectives on human development. (Sage,2005)
- 30. Hair J., Black W., Babin B., Anderson R. & Tatham R. Multivariate data analysis. Uppersaddle River. (NJ: Pearson Prentice Hall,2006)
- 31. Mason R., Gunst R. & Hess J. Designs and analyses for fitting response surfaces. Statistic Design And Analysis Of Experiments: With Applications To Engineering And Science , 2nd Edn. Wiley, New York, 568–606 (1989)
- 60. OECD & OECD Trust in government, policy effectiveness and the governance agenda. Government At A Glance 2013 . (2013)
Impact of Covid-19 Pandemic on the Small Medium Entity Growth: Evidence from GCC
- First Online: 29 May 2024
Cite this chapter
- Azzam Hannoon 3 &
- Abdalmuttaleb Al-Sartawi 4
Part of the book series: Studies in Systems, Decision and Control ((SSDC,volume 528))
The paper intends to understand the research trends in Covid-19 and SMEs through a literature review and explores the most affected areas of SMEs during the Covid-19 pandemic. The study attempts to highlight the struggles of SMEs during Covid-19 crisis in the GCC. This paper gives a clear understanding of the current state of the research regarding the topic, i.e., the impact of COVID-19 on SMEs in the GCC, being investigated in a comprehensive platform. This paper calls for crisis management during turbulent times such as pandemics. More particularly this paper suggests developing strategies for employee engagement and voice that would lead to solidarity behavior and comradery among employees and managers of SMEs under crisis.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Qalati, S.A., Ostic, D., Sulaiman, M.A.B.A., Gopang, A.A., Khan, A.: Social media and SMEs’ performance in developing countries: effects of technological-organizational-environmental factors on the adoption of social media. SAGE Open 12 (2), 21582440221094590 (2022)
Article Google Scholar
Thorgren, S., Williams, T.A.: Staying alive during an unfolding crisis: How SMEs ward off impending disaster. J. Bus. Ventur. Insights 14 , e00187 (2020)
Zutshi, A., Mendy, J., Sharma, G.D., Thomas, A., Sarker, T.: From challenges to creativity: enhancing SMEs’ resilience in the context of COVID-19. Sustainability 13 (12), 6542 (2021)
Khalil, A., Abdelli, M.E.A., Mogaji, E.: Do digital technologies influence the relationship between the COVID-19 crisis and SMEs’ resilience in developing countries? J. Open Innovat.: Tech. Market, Complex. 8 (2), 100 (2022)
Burhan, M., Salam, M.T., Abou Hamdan, O., Tariq, H.: Crisis management in the hospitality sector SMEs in Pakistan during COVID-19. Int. J. Hosp. Manag. 98 , 103037 (2021)
Baker, S.R., Bloom, N., Davis, S.J., Terry, S.J.: COVID-Induced Economic Uncertainty. NBER Work. Pap (2020)
Google Scholar
Hermann, C.F.: Some consequences of crisis which limit the viability of organizations. Adm. Sci. Q. 61–82 (1963)
Prouska, R., Nyfoudi, M., Psychogios, A., Szamosi, L.T., Wilkinson, A.: Solidarity in action at a time of crisis: the role of employee voice in relation to communication and horizontal solidarity behaviour. Br. J. Manag. 34 (1), 91–110 (2023)
Kato, M., Charoenrat, T.: Business continuity management of small and medium sized enterprises: evidence from Thailand. Int. J. Disaster Risk Reduct. 27 , 577–587 (2018)
Stecke, K.E., Kumar, S.: Sources of supply chain disruptions, factors that breed vulnerability, and mitigating strategies. J. Mark. Channels 16 (3), 193–226 (2009)
Vogl, G.: Work as community: narratives of solidarity and teamwork in the contemporary workplace, who owns them? Sociol. Res. Online 14 (4), 27–36 (2009)
Download references
Author information
Authors and affiliations.
American University in the Emirates, Dubai, United Arab Emirates
Azzam Hannoon
Ahlia University, Manama, Kingdom of Bahrain
Abdalmuttaleb Al-Sartawi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Abdalmuttaleb Al-Sartawi .
Editor information
Editors and affiliations.
College of Business and Finance, Ahlia University, Manama, Bahrain
Abdalmuttaleb M. A. Musleh Al-Sartawi
An-Najah National University, Nablus, Palestine, State of
Abdulnaser Ibrahim Nour
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Hannoon, A., Al-Sartawi, A. (2024). Impact of Covid-19 Pandemic on the Small Medium Entity Growth: Evidence from GCC. In: Musleh Al-Sartawi, A.M.A., Nour, A.I. (eds) Artificial Intelligence and Economic Sustainability in the Era of Industrial Revolution 5.0. Studies in Systems, Decision and Control, vol 528. Springer, Cham. https://doi.org/10.1007/978-3-031-56586-1_46
Download citation
DOI : https://doi.org/10.1007/978-3-031-56586-1_46
Published : 29 May 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-56585-4
Online ISBN : 978-3-031-56586-1
eBook Packages : Engineering Engineering (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

COMMENTS
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
Terminology on Quarantine, Social Isolation, and Social Distancing. In the context of COVID-19 pandemic, the terms "social distancing," "social isolation," and "quarantine" have been used mostly as synonyms in the media, in communication with the public and even in scientific papers (Brooks et al., 2020).However, there are great differences between these designations, even though ...
2.1. Search process. To perform a systematic review and meta-analysis on studies evaluating the psychological and mental impact of COVID-19, we followed the Preferred reporting items for systematic reviews and meta-analyses guideline (Liberati et al., 2009).We conducted a comprehensive literature search on original articles published from 1 Nov 2019 to 25 May 2020 in electronic databases of ...
We included all papers related to the psychological impact of the COVID-19 outbreak published in English until 15 March 2021 related to young adults. However, we excluded reports that were not published in scientific peer-reviewed journals, reviews and studies in which the sample target (age range 18-30 years old) was not young people.
Furthermore, Spoorthy et al. (2020) conducted a review on the gendered impact of Covid-19 and found that 68.7-85.5% of medical staff is composed of women, and the mean age ranged between 26 and 40 years. Also, women are more likely to be affect by anxiety, depression, and distress ( Lai et al., 2020; Zanardo et al., 2020 ).
The psychological impact of COVID-19 lockdowns is small in magnitude and highly heterogeneous, suggesting that lockdowns do not have uniformly detrimental effects on mental health and that most people are psychologically resilient to their effects. ... (COVID-19) lockdowns from prior research, because the COVID-19 lockdowns have marked ...
Investigating the Prevalence of COVID-19-Related Sleep Disorders Among Individuals Recovering from COVID-19: A Cross-Sectional Analytical Study, Jundishapur Journal of Health Sciences, 15, 4 ...
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact.
The COVID-19 pandemic and associated countermeasures had an immensely disruptive impact on people's lives. Due to the lack of systematic pre-pandemic data, however, it is still unclear how ...
The COVID-19 pandemic has disrupted many aspects of life at a global scale. Mental health and psychological well-being have subsequently emerged as key research foci in healthcare and public ...
The psychological impact of COVID-19 lockdowns is small in magnitude and highly heterogeneous, suggesting that lockdowns do not have uniformly detrimental effects on mental health and that most people are psychologically resilient to their effects. ... (COVID-19) lockdowns from prior research, because the COVID-19 lockdowns have marked ...
The coronavirus disease (COVID-19) outbreak has affected not only physical health but also mental health and psychological wellbeing. This narrative review aimed to map the literature on the psychological impact on the young generation of the COVID-19 pandemic, social restrictions, and extraordinary measures to curb the spread of coronavirus.
Various psychological problems and important consequences in terms of mental health including stress, anxiety, depression, frustration, uncertainty during COVID-19 outbreak emerged progressively. This work aimed to comprehensively review the current literature about the impact of COVID-19 infection on the mental health in the general population ...
The coronavirus disease 2019 (COVID-19) pandemic is having a profound effect on all aspects of society, including mental health and physical health. We explore the psychological, social, and neuroscientific effects of COVID-19 and set out the immediate priorities and longer-term strategies for mental health science research.
Objective: A scoping review of studies published in the first year of the COVID-19 pandemic focused on individuals with pre-existing symptoms of depression, anxiety, and specified stressor-related disorders, with the objective of mapping the research conducted. Eligibility criteria: (1) direct study of individuals with pre-existing depressive, anxiety, and/or specified stressor-related (i.e ...
Recent loss through death, divorce, separation, even loss of interest in friends, hobbies and activities previously enjoyed. Changes in personality like sadness, withdrawal, irritability or anxiety. Changes in behavior, sleep patterns and eating habits. Erratic behavior, harming self or others. Low self-esteem including feelings of ...
The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely ...
The declaration of COVID-19 as a global pandemic by the World Health Organisation (WHO) in 2020 catapulted institutions of higher education into an emergency transition from face-to-face to online teaching. Given the nature of the COVID-19 pandemic and the continuing after-effects thereof, the study explored the psychological impact of the COVID-19 pandemic on academics.
Physical distancing due to the COVID‐19 outbreak can have drastic negative effects on the mental health of the elderly and disabled individuals. Physical isolation at home among family members can put the elderly and disabled person at serious mental health risk. It can cause anxiety, distress, and induce a traumatic situation for them.
The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely ...
Background The COVID-19 pandemic triggered vast governmental lockdowns. The impact of these lockdowns on mental health is inadequately understood. On the one hand such drastic changes in daily routines could be detrimental to mental health. On the other hand, it might not be experienced negatively, especially because the entire population was affected. Methods The aim of this study was to ...
Health and social care workers (HSCWs) continue to play a vital role in our response to the COVID-19 pandemic. It is known that HSCWs exhibit high rates of pre-existing mental health (MH) disorders [1,2,3] which can negatively impact on the quality of patient care [].Studies from previous infectious outbreaks [5, 6] suggest that this group may be at risk of experiencing worsening MH during an ...
The December, 2019 coronavirus disease outbreak has seen many countries ask people who have potentially come into contact with the infection to isolate themselves at home or in a dedicated quarantine facility. Decisions on how to apply quarantine should be based on the best available evidence. We did a Review of the psychological impact of quarantine using three electronic databases. Of 3166 ...
Since the onset of the COVID-19 pandemic in 2019, research has noted a variety of mental health consequences that have been experienced in response. Some of these consequences have included ...
The impact of the COVID-19 pandemic on the mental health of children is not yet fully understood. NIH-supported research is investigating factors that may influence the cognitive, social, and emotional development of children during the pandemic, including: Changes to routine. Virtual schooling. Mask wearing.
COVID-19 has grown increasingly concerned with mental health and well-being in the past few years. Many research investigations have found that students have higher levels of psychological ...
Purpose The COVID-19 pandemic has undoubtedly altered the routine of life and caused unanticipated changes resulting in severe psychological responses and mental health crisis. The study aimed to identify psycho-social factors that predicted distress among Indian population during the spread of novel Coronavirus. Method An online survey was conducted to assess the predictors of distress. A ...
There is limited research on the psychological motivators of support for disease control measures that do not require personal action. Focusing on the travel restrictions imposed on foreigners by the U.S. government during the early phases of the COVID-19 pandemic, the current study explored whether the Health Belief Model and the heuristic of multilevel institutional trust would help explain ...
This research demonstrates how an intrasectional lens can help better understand how different forms of mutually reinforcing inequities exist at all levels within the healthcare workforce and how these impact HCWs from certain backgrounds who face greater disadvantage, discrimination and disempowerment, particularly during times of crisis like the COVID-19 pandemic.
The COVID-19 pandemic has affected SMEs more than large firms, with these effects including a reduction in labor supply and customer demand, human mobility restrictions, interruptions in supply chains, and self-isolation [ 1 ]. The paper intends to understand the research trends in Covid-19 and SMEs through a literature review and explores the ...