We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 3: Examination of Sensory Function
Kevin K. Chui; Thomas J. Schmitz
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Introduction, sensory integration, sensation and movement.
- SENSORY INTEGRITY
- CLINICAL INDICATIONS
- AGE-RELATED SENSORY CHANGES
- PRELIMINARY CONSIDERATIONS
- CLASSIFICATION OF THE SENSORY SYSTEM
- TYPES OF SENSORY RECEPTORS
- PATHWAYS FOR TRANSMISSION OF SOMATIC SENSORY SIGNALS
- SOMATOSENSORY CORTEX
- PREPARATION FOR ADMINISTERING THE SENSORY EXAMINATION
- THE SENSORY EXAMINATION
- RELIABILITY
- QUANTITATIVE SENSORY TESTING AND SPECIALIZED TESTING INSTRUMENTS
- CRANIAL NERVE SCREENING
- SENSORY INTEGRITY WITHIN THE CONTEXT OF TREATMENT
- SUPPLEMENTAL READINGS
- APPENDIX 3.A: TWO-POINT DISCRIMINATION VALUES FOR HEALTHY SUBJECTS 20 TO 24 YEARS OF AGE
- Full Chapter
- Supplementary Content
Understand the purpose(s) of performing a sensory examination.
Understand the relationship between preliminary mental status screening and tests for sensory function.
Describe the classification and function of the receptor mechanisms involved in the perception of sensation.
Identify the spinal pathways that mediate sensation.
Understand the guidelines for administering an examination of sensory function.
Describe the testing protocol for each sensory modality.
Using the case study example, apply clinical decision-making skills to application of sensory examination data.
If all of the sensory stimuli which enter the central nervous system were allowed to bombard the higher centers of the brain, the individual would be rendered utterly ineffective. It is the brain's task to filter, organize, and integrate a mass of sensory information so that it can be used for the development and execution of the brain's functions. 1 , p. 25 —A. Jean Ayers, PhD
The human system is continually inundated with sensory information from a variety of environmental inputs as well as from movement, touch, awareness of the body in space, sight, sound, and smell. "In all higher order motor behaviors, the brain must correlate sensory inputs with motor outputs to accurately assess and control the body's interaction with the environment." 2 , p.32 Sensory integration is the ability of the brain to organize, interpret, and use sensory information. This integration provides an internal representation of the environment that informs and guides motor responses. 2 These sensory representations provide the foundation on which motor programs for purposeful movements are planned, coordinated, and implemented. 3 Ayers defined sensory integration as "the neurological process that organizes sensation from one's own body and from the environment and makes it possible to use the body effectively within the environment." 4 , p. 11 In an intact system, sensory integration occurs automatically without conscious effort.
Sensory integration is a theory developed by A. Jean Ayers (1920–1989), an occupational therapist whose work focused on examining the manner in which sensory integration develops, identifying patterns of dysfunction in children with learning disorders, and developing intervention strategies to improve processing of sensory information. The theory purports that disordered sensory integration directly affects both motor and cognitive learning and that interventions designed to enhance sensory integration will improve learning. 1 Bundy and Murray 5 suggest the value of the theory lies in its usefulness in (1) explaining behaviors of individuals with impaired sensory integration functions, (2) establishing a plan of care (POC) to address specific impairments, and (3) predicting expected outcomes of the selected interventions.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Arch Plast Surg
- v.49(3); 2022 May

Clinical Assessment of Pain and Sensory Function in Peripheral Nerve Injury and Recovery: A Systematic Review of Literature
Albin a. john.
1 Department of Orthopaedic Surgery, Texas Tech University Health Sciences Center, Lubbock, Texas
Stephen Rossettie
John rafael, cameron t. cox, ivica ducic.
2 Washington Nerve Institute, McLean, Virginia
Brendan J. Mackay
Peripheral nerve injuries (PNIs) often present with variable symptoms, making them difficult to diagnose, treat, and monitor. When neurologic compromise is inadequately assessed, suboptimal treatment decisions can result in lasting functional deficits. There are many available tools for evaluating pain and functional status of peripheral nerves. However, the literature lacks a detailed, comprehensive view of the data comparing the clinical utility of these modalities, and there is no consensus on the optimal algorithm for sensory and pain assessment in PNIs. We performed a systematic review of the literature focused on clinical data, evaluating pain and sensory assessment methods in peripheral nerves. We searched through multiple databases, including PubMed/Medline, Embase, and Google Scholar, to identify studies that assessed assessment tools and explored their advantages and disadvantages. A total of 66 studies were selected that assessed various tools used to assess patient's pain and sensory recovery after a PNI. This review may serve as a guide to select the most appropriate assessment tools for monitoring nerve pain and/or sensory function both pre- and postoperatively. As the surgeons work to improve treatments for PNI and dysfunction, identifying the most appropriate existing measures of success and future directions for improved algorithms could lead to improved patient outcomes.
Peripheral nerve injuries (PNIs) continue to present challenges for surgeons, and multiple novel techniques and products have been utilized to address shortcomings of nerve repair. 1 2 3 Pain and/or sensory deficits often develop after traumatic PNI or nerve surgery. 4 In traumatic PNIs, surrounding tissue damage is common and has been associated with suboptimal outcomes. 5 6 While treatment decisions in more severe injuries may be relatively straightforward, incomplete transections or nervous deficiency not caused by trauma can be difficult to diagnose, treat, and monitor given due to subtle symptoms and/or slow progression to functional deficits. If nerve function is not accurately assessed, diagnosis may be delayed or overlooked and could result in long-lasting functional deficits with impaired quality of life. 7 8 9
As understanding of nerve regeneration has improved, so have methods for evaluating nerve status both pre- and postoperatively. Given that nerve assessment algorithms can impact diagnosis, intervention, and recovery, a comprehensive view of the relevant literature may ultimately assist surgeons in improving patient outcomes.
Development Process
The authors performed a systematic review across multiple databases using a comprehensive combination of keywords and search algorithm according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. 10 The literature search focused on clinical data regarding the assessment of sensory and pain recovery after PNI was undertaken to define the utility of each assessment tool.
Literature Search
A systematic literature review was conducted to identify study abstracts for screening. The databases used included PubMed/Medline, Embase, Cochrane, and Google Scholar databases using the controlled terms: “Humans” and “Peripheral nerve injuries” and “sensory” or “pain” or “function” or “assessment” or “recovery” or “outcome.” Manual additions to our search query were made using the key terms: “sensory recovery,” “sensory outcomes,” “sensory assessment,” “sensory testing,” “sensation assessment,” “sensation assessment,” “nerve assessment,” “nerve sensory testing,” “sensory function testing,” and “nerve evaluation.” Search dates were from January 1960 to December 2020.
Study Eligibility
A minimum of two reviewers worked independently to further review and screen abstracts and titles. All articles that reported pathogenesis of sensory deficits secondary to nerve damage and those that assessed various tools used to measure sensory recovery and pain assessment tools were included. Only articles in English were reviewed. Full-text articles were assessed during screening if there was uncertainty on whether the article should be included. Article titles and abstracts that did not address our research question objective were excluded. Further full-text assessment of the selected articles was done, and articles that did not address peripheral nerve motor assessment and recovery were excluded. The PRISMA diagram in Fig. 1 further describes the literature evaluation process.

PRISMA 2009 flow diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Data Extraction
After assessment of eligibility, three authors extracted data from the marked articles. Important parameters that were recorded when available included the year of the study, number of patients in the study, sensitivity and specificity of the tools assessed, benefits and limitations of tools assessed, opportunities for improvement, and clinical roles in nerve recovery assessment.
Degree of peripheral nerve recovery can be assessed by testing the patient's postinjury sensory, pain, and motor function. Due to the breadth of information in each of these categories, the scope of this manuscript is limited to the monitoring of sensory recovery and pain attenuation. When assessing for peripheral nerve recovery, it is an important factor that there are multiple different types of nerves in the human body that vary based on size, myelination, conduction velocity, and function with larger and more heavily myelinated neurons, providing faster conduction velocities and carrying different types of information than smaller, unmyelinated neurons. 6 11 These nerves can carry information from mechanosensory organs found on nonhairy or glabrous skin, such as the Ruffini endings, Meissner corpuscles, Merkel discs, and Pacinian corpuscles, to provide sensory information about texture and shape. 11
Regardless of the types of receptors or nerve fibers, nerves can be damaged during trauma and are classed by Seddon based on the demyelination and the extent of damage incurred to various layers of the nerve sheath and connective tissues. The mildest forms of injury or neurapraxia are often inflammatory injuries whereby nerves are compressed or pulled by surrounding structures. Severe nerve injuries or neurotmesis can lead to complete damage of the nerve's function due to complete transection of axons. 6
Pain Assessment Tools
Pain is a critical factor in any nerve treatment algorithm. Poorly controlled pain has been linked to poor outcomes and long-term disability. 12 13 A study of 70 soldiers who had sustained combat-related injuries found that 23% of sidelined soldiers could have returned to active duty if not for nerve-related chronic pain that increased their disability rating. 14
Patients with upper extremity (UE) nerve injuries often have high pain disability (Pain Disability Index [PDI]), UE disability (Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire), and illness intrusiveness (the Illness Intrusiveness Rating Scale). 15 The disability that arises from pain can also lead to higher rates of reactive depression. 16
Numerical Rating Scale and Pain Visual Analog Scale
Aims/advantages.
The Numerical Rating Scale (NRS) and Visual Analog Scale (VAS) for pain are two methods of measuring patients' self-reported pain levels. 17 18 19 Pain intensity, while important, is deficient without the context of the patient's pain tolerance. The VAS scale directs patients to indicate their pain on a 10-cm horizontal line between “no pain” and “worst imaginable pain” at the ends of the line. The distance between “no pain” and the patient's mark is recorded as patient's perception of pain. 18 19 The NRS follows a similar method of identifying patient pain between “no pain” and “worst imaginable pain” but can be administered graphically or verbally. The VAS and NRS have excellent sensitivity and are reliable, with strong correlation between scores provided by the two tools. 18
Disadvantages/Criticisms
These scales incorrectly assume that pain is a linear phenomenon. Furthermore, experience of pain varies between individuals. 17 With respect to the VAS, patients who are cognitively impaired will not be able to provide an accurate assessment of their pain using the tool, and it has been shown that the majority of all patients (including unimpaired patients) do not prefer the VAS. 18 Older patients, similarly, can have difficulty completing the VAS due to impaired motor skills. This scale can only be administered in person (not via telephone). 19 20 While both tests help contextualize the pain intensity within what patients consider their unidimensional spectrum of pain, the tests do not convey information on the quality of the pain. 19
Improvements
The labels on either end of the VAS test should be standardized as differing terminology can skew responses. 20 The NRS also requires further standardization as the test has been performed with differing numbers of stratifications (11, 21, or 101 levels). 20
Role in Nerve Assessment Algorithm
This tool should be used to identify patient-perceived pain intensity. Additional tools must be used to determine pain quality.
McGill's Pain Questionnaire and Short-Form MPQ
The McGill's Pain Questionnaire (MPQ) incorporates sensory and pain response data, as well as pain intensity, to better understand the full spectrum of pain experienced by patients. 21 The questionnaire is a reliable and valid tool that can distinguish between nocioceptive pain and neuropathic pain and is sensitive to the effects of nerve interventions. 19 22
The length of the MPQ may place excessive burden on the respondent. The questionnaire also has complex vocabulary that can affect compliance. 19 As a result, this test can be difficult to standardize among different clinics or hospital groups. 17 19 22 Given its length, scoring of the MPQ can erroneously correlate quantity and quality such that high scores can be achieved with increased numbers of low quality responses. 22 While the Short-Form-MPQ (SF-MPQ) is both easier to take and less complex to understand, it still requires supervision and familiarity with questionnaire terminology. 19
Criticisms of the MPQ resulted in the creation of the SF-MPQ. By reducing complexity and length, the SF-MPQ decreased respondent burden. Both the MPQ and the SF-MPQ can assess multiple types of pain but neither was designed to assess neuropathic pain. 23 To incorporate neuropathic pain characterization, SF-MPQ-2 was developed with seven domains for neuropathic pain. The SF-MPQ-2 is a reliable tool that has increased generalizability without increasing respondent burden. 23
The MPQ is no longer recommended, as it has been succeeded by the SF-MPQ in understanding patient's dimensions of pain. This tool can be used to assess patient pain intensity, quality, and efficacy of treatment. The SF-MPQ-2 should be used when evaluating neuropathic pain.
Pain Disability Index
The PDI is a 7-item questionnaire that assesses the extent to which pain interferes with patients' daily life activities (family and home responsibilities, recreation, social activity, occupation, sexual behavior, self-care, and life-support activity). 24 Each item is ranked on a scale of no disability (0) to total disability 10 where disability is defined as limitations in fulfillment of a role that was once normal for that individual. The PDI has high internal consistency, sensitivity, modest test–retest reliability, and good concurrent validity. 15 25 26 Scores can also indicate psychological distress and other pain-related disabilities. 25
Pain behaviors (PBs) used in the PDI are not necessarily linked to disability. 25 Furthermore, there is a lack of standardization as some physicians use a one-factor PDI while others use a two-factor PDI. 26
The brevity and reliability of the PDI places it ahead of more comprehensive tools such as the Sickness Impact Profile, Wet Haven Yale Multiaxial Pain Inventory, and Chronic Illness Problem Inventory. However, it correlates well with the VAS tool. A one factor PDI may be used as an alternative to the VAS to understand both the intensity and the multidimensional experience of patients' pain. 26
Cold Intolerance Symptom Severity
Cold intolerance, characterized by pain, stiffness, or altered perception with cold exposure, is a prevalent symptom in many UE PNIs and can present throughout a patient's recovery course. 27 28 Using a cold intolerance severity scale, researchers have noted that 38% of patients with hand fractures are cold intolerant and that cold intolerance correlates with pain. 16 While the pathophysiology of cold intolerance is not fully understood, the severity of cold intolerance may indicate poor nerve recovery. 29 30 Unfortunately, patients do not report complete recovery from cold intolerance and may require lifestyle modifications. 29 31 32
The Cold Intolerance Symptom Severity (CISS) is a short questionnaire that assesses cold intolerance and how it affects daily function. Incidences of cold intolerance, sources of relief, and activities that may provoke cold intolerance are recorded using this questionnaire. The higher the score, the greater the cold intolerance. It is a highly reproducible and reliable test of cold intolerance in upper extremity injuries. 12 29 31 32 33 34
The CISS is a broad assessment of cold intolerance that sacrifices a focus on symptom-specific minutia to maximize compliance. 29 The CISS does not accurately characterize the size of cold intolerant area, nor does it record how quickly symptoms of cold intolerance precipitate on cold exposure. 32 Some have claimed that the grouping of the CISS scores into mild, moderate, severe, and extreme severe, is arbitrarily decided. 31 Other critics of the CISS note that the test combines location, severity, and activity; however, these variables are not independent. Furthermore, the scoring system gives unwarranted emphasis to the answer option “Other” in Questions 2 to 4. 32 34 The scoring system also gives more weight to activity impairments than symptom characteristics when determining overall score. 32 34
Critics of the CISS have proposed that the inclusion of answer options “not applicable” and “never” in Questions 2 and 3. 31
The CISS may be used as a screening tool to identify pathologic cold intolerance. 31
Patient-Reported Outcome Measurement Information System Pain Intensity
The Patient-Reported Outcome Measurement Information System (PROMIS) Pain Intensity form initially contained a single item assessing a patient's average pain on a self-reported scale (1 = no pain and 10 = worst pain imaginable). 35 36 The test has demonstrated excellent reliability and validity and can be used in a wide variety of clinical scenarios. 37
The PROMIS Pain Intensity offers little improvement over the traditional VAS and/or NRS.
A 3-item PROMIS Pain intensity form has been developed which includes ratings of worst pain and average pain in the past 7 days, as well as pain at the time of completing the questionnaire. 38
The PROMIS Pain Intensity can be used replacing NRS or VAS to evaluate pain intensity and may be preferred when simultaneously tracking other PROMIS scores (e.g., behavior and interference).
Patient-Reported Outcome Measurement Information System Pain Interference
The PROMIS Pain Interference form is a 9-item questionnaire developed to assess the degree in which pain negatively affects daily activities. 35 39 The form has been well validated with high reliability and independence of individual items/questions. 39 Scores can be compared with a baseline of the uninjured general population. 39
Validation studies were performed with a large range of individuals both healthy and with a variety of health problems. 39
The PROMIS Pain Interference form may be used to assess the degree in which nerve pain is impacting patients' daily activities and relationships. While it has been used in some peripheral nerve surgery studies, 40 41 more clinical data are needed to determine its place in a variety of nerve-related pathologies.
Patient-Reported Outcome Measurement Information System Pain Behavior
The PROMIS PB form is a 39-item questionnaire designed to comprehensively assess the behaviors performed by patients who communicate their pain to others (e.g., verbal complaints, facial expressions, gestures, posture, and activity limitations). 42 Responses may give insights into the intensity, cause, and coping mechanisms associated with pain, particularly in chronic conditions. 42
The complete PROMIS PB form has high respondent burden, and all questions may not be relevant to a particular clinical scenario. It is unable to distinguish between acute and chronic pain which are considered unique experiences from a patient's perspective. 43
The PROMIS-PB can be adapted to create a short form for a given clinical scenario. 42
While other pain assessments may be more valuable for assessing efficacy of interventions, the PROMIS PB form may assist in guiding nonsurgical treatment of chronic neuropathic pain.
Patient-Reported Outcome Measurement Information System Neuropathic Pain Quality Scale
The Neuropathic Pain Quality scale (PROMIS-PQ-Neuro) is a 5-item questionnaire developed specifically to assess the quality of neuropathic pain (as opposed to nociceptive pain). 38 It has good sensitivity and specificity and can be used to differentiate between neuropathic and nonneuropathic pain. 38
The PROMIS-PQ-Neuro was validated in patients with chronic conditions including osteoarthritis, rheumatoid arthritis, diabetic neuropathy, and cancer chemotherapy-induced peripheral neuropathy. 38 Other PROMIS forms have been developed to assess pain intensity, interference with daily activities, and behaviors expressed when in pain. 39 42 44 These were also developed and validated in patients with chronic conditions unrelated to peripheral nerve dysfunction.
While the PROMIS-PQ-Neuro is a reliable test for assessing pain quality, further clinical data are needed to determine its role in the context of peripheral nerve assessment.
Sensory Testing
In a clinical setting, sensation includes not only receptor detection of physical stimuli but also cortical mapping of inputs. Sensory impulses can be modulated via receptor field size and number. Furthermore, these receptors can be identified as quick or slow adapting. 45 While sensation is the subjective experience of stimuli, sensibility is the capacity to appreciate these stimuli. 46 Sensory testing most often measures sensation, and multiple tests can be used to address different parameters, including fast- or slow-acting receptors, innervation density, and/or distal versus proximal location of neurologic compromise. 45 47 A comparison of common sensory testing modalities is presented in Table 1 . 48 49 50 51 52 53 54 55
Abbreviation: SD, standard deviation.
Two-Point Discrimination
Developed in 1834 by E. H. Weber and refined in 1935 by Wilgis, the Two-Point Discrimination (2PD) measures the minimum distance between two stimuli at which a patient can correctly identify them as distinct points. 46 56 The test is used to assess tactile discrimination and reveals the number of reinnervated receptors. Either one or two probes are applied to a surface with pressure that causes minimal discomfort, and patients are asked to report the number of probes that they can feel. The smallest distance that a patient can effectively discriminate between the two separate stimuli is recorded.
There are two types of 2PD, static and moving. Static 2PD measures density of the slow-adapting receptors as they reinnervate. Moving 2PD measures, the quick-adapting receptors that recover sooner than other kinds of receptors. 17 Researchers, using various health care workers and 2PD tests at two distances, demonstrated that similar 2PD results were measured across all observers and that the variability did not significantly affect its validity. 57
While this measure is helpful in patients with acute, mild nerve injury, it may not be useful in patients with chronic or severe nerve injury, as the distance of discernment often is far greater than the width of a digit. 45 58 Other criticisms of the technique include the lack of standardization of the force applied. 28 45 59 60 Additionally, time between stimulus applications (from first to second point of 2PD) has been shown to affect the ability to discriminate between stimuli. 61 While some have supported the 2PD test for its high level of consistency, 62 others have consider it to be inherently inconsistent, largely due to the lack of control of application force, even within a single tester. 60 63 64 65 66 Despite its widespread use, the 2PD has been shown to have low validity in assessing the tactile spatial acuity of hands. 58 The 2PD test also shows a lack of correlation or predictive value with commonly used electrodiagnostic techniques such as nerve conduction studies. 67 Perhaps most importantly, 2PD has been criticized for poor responsiveness which may be related to its use of passive rather than active touch (e.g., patients are touched by an object versus actively touching an object). 28 68
One improvement of the 2PD test is the addition of orientation, resulting in a new two-point orientation discrimination (2POD) test. 56 This solves the problem of unintended nonspatial cues, an issue highlighted by critics who noted that at close distances, the brain may be able to detect a change in overall magnitude of pressure without truly detecting the two separate points of contact. 61 By requiring the patient to specify the orientation (horizontal vs. vertical) of the second stimulus relative to the first, this false detection can be avoided. 56 69 Spatial direction detection may also be enhanced using an adaptive stimulus. 69
Attempts to address the lack of applied force standardization in 2PD have resulted in multiple novel devices. These include the Absolute Digimatic caliper, 56 Dellon's Pressure-Specifying Sensory device, 17 and the Disk-Criminator, the last of which has been shown to have good intertester reliability when used in a consistent manner. 70 71
Criticisms of the 2PD's passive touch limitation have led to alternative discrimination testing modalities such as tactile acuity charts (74). These consist of raised dots or rings on a sheet which patients must actively touch to discern multiple points at a variety of spacing intervals. Tactile acuity charts have demonstrated superior test–retest reliability over a 1-week period compare with passive measures. 72
2PD is indicated for assessing tactile gnosis after nerve injury. 73 In a systematic review of peripheral nerve reconstruction functional outcomes, the most commonly used test was the static 2-point discrimination (S2PD) assessment for sensory assessment. 62 Given its limitations, results of 2PD should be corroborated by other tests and/or clinical findings, especially when subjective recovery does not align with 2PD findings.
Semmes–Weinstein Monofilament Test
Semmes–Weinstein monofilaments (SWM) assess cutaneous pressure threshold to reveal reinnervation status. 17 The filament exerts a constant force on the skin area for approximately 1 second, and threshold is defined as the lightest filament that patients responded to correctly. 58 Results of SWM are superior to those attained from a tuning fork (detailed in a later section) as they provide stratified and quantitative measures that can be followed through the patient's recovery process. 17 The test can also be used to identify sensory perception in all areas of the hand. It is a reliable, standardized, easily administered, and inexpensive method of obtaining quantitative sensory data. 73 Additionally, it has been shown to have significant associations with other evaluation tools, such as nerve conduction studies, particularly for carpal tunnel syndrome (CTS). 74 Unlike 2PD, the amount of force applied during SWM testing is controlled by the thickness of each filament. 63 64
The SWM test is a fragile test due to its use of small filaments, and it is also limited by its use of an ordinal scale rather than a continuous scale. 28 Additionally, it has been criticized for its inability to account for variables outside of nerve injury that increase threshold, such as skin callouses and increased age. 75 The SWM test is more time-consuming than the 2PD which may make it less feasible in a busy office. 76 77
The Weinstein Enhanced Sensory Test (WEST) is a more robust SWM test that focuses on consistent filament size across the filaments in a test kit. It also reports continuous force values rather than ordinal values. 28 Furthermore, it demonstrates the best responsiveness in all sensory tests, especially in children, and is easily administered and scored in the clinical setting. 59
SWM is indicated for assessing reinnervation after PNI. 73 It is often used alternatively to 2PD when there is adequate time in clinic to perform SWM. 76 Compared with 2PD, it has higher responsiveness to sensory function and can therefore be used to detect recovery sooner than 2PD.
Pick-Up Test
Initially developed by Moberg 78 in 1958 and then quantified by Omer, 79 the Pick-Up test assesses general sensibility and tactile gnosis. In this test, patients are timed as they pick up an object and place it in a designated area while blindfolded. This test not only assesses whether the patient can sense the object but also if they can combine the sensory input with motion. 46 Compared with 2PD, the Pick-Up test has shown higher sensitivity to changes in patients with median nerve injury. 68
The objects in this test have been specified as 10 small metal objects, but further specification does not exist. Without a standardized and/or commercially available set of metal objects for this test, clinicians must choose their own objects which adds heterogeneity between studies using this test. 78
Standardization of the objects would improve the consistency of the Pick-Up test among clinicians.
Since the 2PD test often does not detect early nerve recovery, the Pick-Up test may be used as a complement to the 2PD test, as it offers additional information to an examination in the early postoperative period. However, subsequent tests have been developed to fill this role (Shape Texture Identification [STI] test, detailed in a later section).
Vibration Assessment
Vibration thresholds of fast-adapting receptors are tested using a tuning fork. A low-frequency fork can be used to assess early damage to nerves (especially after compression injury), as well as early recovery and reinnervation of previously damaged nerves. 80 Much like thermal sensitivity (discussed in a later section), fast-adapting fibers for vibration typically respond quickly to injury. 46 For chronic nerve compression, a higher frequency fork should be used.
This test is highly subjective and based on patient recall. Tuning forks have been criticized for their low clinical value due to shortcomings, including low interrater and intrarater reliability, 81 variable application of force, and inconsistent performance of the fork due to the influence of the examiner's hand holding the instrument. 64
While vibration thresholds are variable with tuning forks, vibration thresholds can be quantified using a Vibrometer. Vibrometers have fixed many of the problems associated with tuning forks, delivery is standardized with controlled frequency, intensity, and ramp speed. 75 The Vibratron II (fixed frequency 120 Hz) has shown great intertester reliability. 82 83 Still, these are relatively, uncommonly used in clinic for evaluation of nerve recovery after neurotmesis as they have been noted to be expensive and have been mainly studied in compression syndromes and vibration-induced neuropathy. 83
Though they are highly reliable, traditional vibrometers can only assess a single frequency and may not be able to address the full spectrum of nerve deficiency. Newer vibrometers include multiple vibration threshold frequencies. 45
Role in Nerve Assessment Algorithm (Recommendations for Appropriate Use)
Tuning forks have very limited indications for clinical use. Vibrometers may be used to detect early nerve injury in patients that may need surgery for nerve repair, especially following nerve compression or vibration-induced neuropathy. 80 83
The Ten Test was initially described by Strauch et al as a quick and convenient way to assess light touch using an examiner's hand and patient's responses to the experience on a scale of 1 to 10, with 10 being normal. 84 This test compares touch on an affected limb versus that on the contralateral limb and can provide a quick screening of the large A-β nerve fibers. 84 It has good validity, reliability, and sensitivity, especially in CTS patients. In fact, it was found to be superior to the WEST and both forms of 2PD for detecting minimal loss of sensation in patients with CTS. 76 The Ten Test assesses patient perception of sensation on a scale of 0 to 10 and utilizes the healthy contralateral limb to understand sensory deficits. 45 This test can be used for adults and children over 5 years of age. 54 59
The Ten Test is more subjective than most other sensation tests and has been criticized for lacking a standardized method to document hyperesthesia. 76 85 Additionally, the test relies on one side of the body having full sensation. Many patients (especially older or diabetic patients) may be unaware of mild bilateral sensory loss which may confound results of this test.
Clinicians may use the Ten Test to understand a patient's perceived discomfort and sensory changes after an injury. These subjective findings represent one component of sensory function and should be corroborated by more objective measures when possible. 59
Shape Texture Identification Test (STI)
The STI test uses multiple objects of varying size and shape that the patient has to identify. This test is particularly useful in median nerve injury patients as it requires active manipulation. The STI differs from other tactile gnosis tests in that it specifically focuses on identifying shapes, objects, and textures. 59 The active manipulation is a key feature of the STI test that makes it a valuable complement to 2PD which does not take into account active touch. 63 This test has shown high sensitivity and specificity for measurement of tactile gnosis at follow-up assessments following nerve injury. 33 63 73 Unlike the previously described Pick-Up test, the STI is highly standardized. 86
Although the STI test is standardized and existing reports have shown its validity, the literature for the STI test is limited, given its relatively recent development and less-frequent clinical use compared with tests such as 2PD and SWM. 87 At present, the STI is typically used as a complement to the 2PD test rather than a stand-alone measure of sensory recovery.
The STI reliably detects change in previously injured nerve function and should be used as a complement or alternative to 2PD or SWM, particularly when these do not correlate with subjective findings. Further clinical data are needed to determine whether STI may replace 2PD or SWM in current assessment algorithms.
Manual Tactile Test
The manual tactile test (MTT) was developed as a result of need to refine and interpret sensory information through self-generated movements with greater precision. 88 Additionally, active hand sensation can facilitate better predictions for hand performance than those of traditional sensibility assessments. The MTT is comprised of three subtests which assess patients' ability to discern the weight (barognosis), roughness (roughness discrimination), and shape (stereognosis) of an object using active touch of the hand.
The MTT was developed to incorporate both cutaneous pressure and kinesthetic impulses transmitted through the hand. Given that more types of sensory information are included, the MTT may provide more comprehensive data on tactile gnosis following nerve injury. Among sensory tests for peripheral nerves, the inclusion of barognosis is unique to the MTT and has shown utility in monitoring functional sensibility of neuropathic hands both pre- and postoperatively. 58
The MTT is used primarily for patients with CTS. Since it requires the ability to manipulate the hand, the MTT cannot be executed with a patient lacking this capacity. 58 Although the test can be used to measure sensation in patients with CTS, it may not be superior to other, more commonly used sensory tests. In fact, Hsu et al found that both 2PD and SWM had better diagnostic power than MTT in CTS. 88 The test is currently lacking a measurement for tactile threshold sensibility which may need to be added if it is to stand on its own.
The MTT has been used in determining the impairment of manual touch sensibility for CTS with high reliability, accuracy, and validity. In addition to its use for patients with CTS, clinicians have begun using the test to track age-related degradation in sensorimotor control of the hand in the elderly population, and to monitor nerve recovery after injury. 58 88 While the SWM is currently considered a superior diagnostic tool, the MTT has been suggested as an adjunct to SWM in monitoring the progression of hand sensibility during the regeneration period. 58
Thermal Sensitivity Test (Excluding Cold Intolerance)
The Thermal Sensitivity Test was first described as a method of assessing thermal discrimination in patients with diabetic peripheral neuropathy. Thermal sensitivity is reliant on small fibers which are usually the first to be damaged in diabetic neuropathy. 89 More recently, however, the Thermal Sensitivity Test was used in a study to assess recovery after complete nerve laceration (neurotmesis). The 2015 retrospective study showed a correlation between thermal sensitivity and mechanosensory function, as measured by 2PD test and Semmes–Weinstein test. However, recovery of temperature differentiation was demonstrated in approximately half of the patients in this study, while 17% had normal 2PD test and only 7% had normal SW monofilament test. These results indicate that thermal sensitivity is recovered prior to full recovery and may be a better indicator of return of protective sensation rather than full functional recovery. 74
Although it correlates with better overall hand function, good temperature sensibility is seen in patients with poor touch sensibility as well. Therefore, the test may be a more sensitive but far less-specific measure of recovered hand function. Additionally, cold intolerance is thought to be a more determinant factor for hand function than temperature discrimination, and no significant relationship has been shown between these two variables. 74
Although the Thermal Sensitivity Test correlates with overall hand function, it is less clinically relevant than touch sensibility. It is not currently used often for nerve assessment following neurotmesis, although future studies may lead to increased usage of the assessment for this purpose, particularly in the early stages of recovery. 74
Selecting the optimal nerve test(s) is difficult and lacks standardization across the field. While a battery of tests may be ideal, there are practical considerations that prevent surgeons from performing every test at each visit. Thus, it is important to optimize the assessment algorithm to obtain the most accurate and relevant data regarding each patient's unique presentation. 90
Pain can be assessed both via cold intolerance and traditional pain assessments. Of the cold intolerance tools, the CISS is recommended as a screening tool to identify pathologic cold intolerance. Of the other pain assessments, the NRS and VAS, while simple to administer, provide only one dimension of pain. A multidimensional approach using SF-MPQ or PDI is recommended. Of the two multidimensional assessment tools, the MPQ will characterize pain while the PDI will give insight into how pain is affecting daily life.
While 2PD is widely used for sensory assessment, it lacks responsiveness and may require either a complementary test or an alternative. The Pick-Up test, Thermal Sensitivity Test, or vibration assessment are good complements to the 2PD test when the 2PD is not responsive. Alternatively, one may choose to use the SWM instead of the 2PD. The SWM is the most responsive tool and has high reliability; however, it can be time-consuming and is not always practical. Additional tests may be utilized to add functional perspective, including the STI test or the MTT test. The Ten Test, though highly subjective, may be used when time or instrumentation is lacking, as it is a simple, rapid assessment.
Limitations
Further studies are encouraged to assess the necessity and ideal combination of tools when assessing peripheral nerve sensory recovery and pain management. When assessing peripheral nerve sensory recovery and pain assessment, the various combinations of tools and idiosyncratic administration methods can lead to heterogeneity when performing a literature review on this topic. Furthermore, there is a paucity of data regarding clinically relevant differences regarding pain scores before and after treatment for PNI. To further standardize sensory and pain assessments, there is a need for increased research in these areas.
Despite advances in diagnosis and treatment of PNIs, there remains no consensus on the optimal assessment algorithm. This review may serve as a valuable resource for surgeons determining the appropriate sensory and pain assessments to monitor nerve function both pre- and postoperatively.
Conflict of Interest Though not directly funded, the authors would like to disclose the following support: I.D.: AxoGen Medical Director. B.J.M.: Paid teaching for TriMed. Paid teaching and consulting, as well as research support from AxoGen. Paid consulting for Baxter/Synovis and GLG. The remaining authors have nothing to disclose.
Author Contributions
A.A.J.: conceptualization, investigation, project administration, and manuscript preparation. S.R.: investigation, and manuscript preparation. J.R.: investigation, and manuscript preparation. C.T.C: conceptualization, project administration, and manuscript preparation. I.D.: supervision and validation. B.J.M.: conceptualization and validation.
- Português Br
- Journalist Pass
Case report: Stem cells a step toward improving motor, sensory function after spinal cord injury
Susan Barber Lindquist
Share this:

ROCHESTER, Minn. — Stem cells derived from a patient's own fat offer a step toward improving — not just stabilizing — motor and sensory function of people with spinal cord injuries , according to early research from Mayo Clinic .
A clinical trial enrolled 10 adults to treat paralysis from traumatic spinal cord injury. After stem cell injection, the first patient demonstrated improvement in motor and sensory functions, and had no significant adverse effects, according to a case report published in Mayo Clinic Proceedings .
Watch: Chris Barr's Mayo Clinic story .
Journalists: Broadcast-quality video (5:12) is in the downloads at the end of this post. Please "Courtesy: Mayo Clinic News Network." Read the script.
As a phase I multidisciplinary clinical trial, the study tests the safety, side effects and ideal dose of stem cells. Early trial findings show that patient response varies. The Mayo team plans to continue analyzing patient responses, and further results will be published on the other nine trial participants.
Read more from the study team in this Center for Regenerative Medicine blog post .
"In this case report, the first patient was a superresponder, but there are other patients in the trial who are moderate responders and nonresponders," says Mohamad Bydon, M.D. , a Mayo Clinic neurologic surgeon and first author of the report. "One of our objectives in this study and future studies is to better delineate who will be a responder and why patients respond differently to stem cell injections.
"The findings to date will be encouraging to patients with spinal cord injuries, as we are exploring an increasing array of options for treatment that might improve physical function after these devastating injuries."
Between 250,000 and 500,000 people worldwide suffer a spinal cord injury each year, often with life-changing loss of sensory and motor function, according to the World Health Organization . Up to 90% of these cases are from traumatic causes.
All subjects enrolled in this study received fat-derived stem cell treatment, which is experimental and is not approved by the Food and Drug Administration (FDA) for large-scale use. However, the FDA allowed its use in this research.
In the case report, the patient, then 53, injured the spinal cord in his neck in a 2017 surfing accident. He suffered a complete loss of function below the level of injury, meaning he could not move or feel anything below his neck. He had surgery to decompress and fuse his cervical vertebrae. Over the next few months, with physical and occupational therapy, he regained limited ability to use his arms and legs, and some sensory function improved. However, his progress plateaued at six months after his injury.
The patient enrolled in the study nine months after his injury. His stem cells were collected by taking a small amount of fat from his abdomen. Over eight weeks, the cells were expanded in the laboratory to 100 million cells. Then the stem cells were injected into the patient's lumbar spine, in the lower back, 11 months after his injury.
"We want to intervene when the physical function has plateaued, so that we do not allow the intervention to take credit for early improvements that occur as part of the natural history with many spinal cord injuries. In this case, the patient was injected with stem cells nearly one year after his injury," Dr. Bydon says.
The patient was observed at baseline and at regular intervals over 18 months following injection. His physical therapy scores improved. For example, in the 10-meter walk test, the patient's baseline of 57.72 seconds improved at 15 months to 23 seconds. And in the ambulation test, the patient's baseline of 635 feet for 12.8 minutes improved at 15 months to 2,200 feet for 34 minutes.
The patient's occupational therapy scores also improved, such as grip and pinch strength, and manual dexterity. His sensory scores improved, with pin prick and light touch tests, as did his mental health score.
The stem cells migrate to the highest level of inflammation, which is at the level of spinal cord injury, but the cells' mechanism of interacting with the spinal cord is not fully understood, Dr. Bydon says. As part of the study, investigators collected cerebrospinal fluid on all of the patients to look for biological markers that might give clues to healing. Biological markers are important because they can help identify the critical processes that lead to spinal cord injury at a cellular level and could lead to new regenerative therapies.
"Regenerative medicine is an evolving field," says Wenchun Qu, M.D., Ph.D. , a Mayo Clinic physiatrist and pain specialist, and senior author of the report. "Mayo's research and use of stem cells are informed by years of rigorous scientific investigation. We strive to ensure that patients who receive stem cells are fully educated in the risks, benefits, alternatives and unknowns about these therapies. Through our clinical trials with stem cells, we are learning from and improving these procedures."
Further study is needed to scientifically verify the effectiveness of stem cell therapy for paralysis from spinal cord injury, the authors note. It is uncertain when or if this procedure will have FDA approval for routine clinical care.
Other researchers involved in this study were Allan Dietz, Ph.D. ; Sandy Goncalves; F.M. Moinuddin, Ph.D.; Mohammed Ali Alvi, M.B.B.S.; Anshit Goyal, M.B.B.S.; Yagiz Yolcu, M.D.; Christine Hunt, D.O. ; Kristin Garlanger, D.O. ; Ronal d Reeves, M.D. ; Andre Terzic, M.D., Ph.D. ; and Anthony Windebank, M.D. — all from Mayo Clinic.
The cell product was developed and manufactured in the Mayo Clinic Immune, Progenitor and Cell Therapeutics (IMPACT) Lab directed by Dr. Dietz.
This research was funded by grants from Regenerative Medicine Minnesota and Mayo Clinic Transform the Practice and supported by Mayo Clinic Center for Regenerative Medicine .
The authors have no relevant disclosures or conflicts of interest to report.
About Mayo Clinic Proceedings Mayo Clinic Proceedings is a monthly peer-reviewed medical journal that publishes original articles and reviews dealing with clinical and laboratory medicine, clinical research, basic science research, and clinical epidemiology. Mayo Clinic Proceedings is sponsored by the Mayo Foundation for Medical Education and Research as part of its commitment to physician education. It publishes submissions from authors worldwide. The journal has been published for more than 90 years and has a circulation of 127,000. Visit the Mayo Clinic Proceedings website to view articles.
About Mayo Clinic Center for Regenerative Medicine Mayo Clinic Center for Regenerative Medicine seeks to integrate, develop and deploy new regenerative medicine products and services that continually differentiate Mayo's practice to draw patients from around the world for complex care. Learn more on the Center for Regenerative Medicine website .
About Mayo Clinic Mayo Clinic is a nonprofit organization committed to innovation in clinical practice, education and research, and providing compassion, expertise and answers to everyone who needs healing. Visit the Mayo Clinic News Network for additional Mayo Clinic news and An Inside Look at Mayo Clinic for more information about Mayo.
Media contact:
- Susan Barber Lindquist, Mayo Clinic Public Affairs, 507-284-5005, [email protected]
- E.coli infection linked to romaine lettuce Mayo Clinic to hold first Middle East Healthcare Social Media Summit in Dubai
Related Articles

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 25 November 2009
Neural reorganization following sensory loss: the opportunity of change
- Lotfi B. Merabet 1 &
- Alvaro Pascual-Leone 1
Nature Reviews Neuroscience volume 11 , pages 44–52 ( 2010 ) Cite this article
8359 Accesses
456 Citations
138 Altmetric
Metrics details
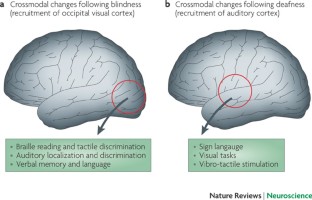
Sensory deprivation is associated with striking crossmodal neuroplastic changes in the brain.
Following sensory deprivation (for example, blindness or deafness), there is functional recruitment of brain areas that are normally associated with the processing of the lost sense by those sensory modalities that are spared.
These changes seem to underlie adaptive and compensatory behaviours in both blind and deaf individuals.
In the case of blindness, occipital cortical areas are recruited to process non-visual forms of sensory information such as touch, hearing and verbal memory.
In the case of deafness, auditory and language-related areas are recruited to process tactile as well as linguistic and non-linguistic visual information.
Experiments in animal models have helped to uncover potential mechanisms underlying these neuroplastic changes, such as the existence of direct cortico-cortical connections between relevant sensory processing areas.
Not all neuroplastic changes are beneficial. There is the possibility of maladaptive consequences, particularly in the context of rehabilitation and the restoration of lost sensory function.
There is growing evidence that sensory deprivation is associated with crossmodal neuroplastic changes in the brain. After visual or auditory deprivation, brain areas that are normally associated with the lost sense are recruited by spared sensory modalities. These changes underlie adaptive and compensatory behaviours in blind and deaf individuals. Although there are differences between these populations owing to the nature of the deprived sensory modality, there seem to be common principles regarding how the brain copes with sensory loss and the factors that influence neuroplastic changes. Here, we discuss crossmodal neuroplasticity with regards to behavioural adaptation after sensory deprivation and highlight the possibility of maladaptive consequences within the context of rehabilitation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
176,64 € per year
only 14,72 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Cross-modal motion aftereffects transfer between vision and touch in early deaf adults

Training-induced plasticity enables visualizing sounds with a visual-to-auditory conversion device

Sound suppresses earliest visual cortical processing after sight recovery in congenitally blind humans
Calvert, G. A. & Thesen, T. Multisensory integration: methodological approaches and emerging principles in the human brain. J. Physiol. Paris 98 , 191–205 (2004).
Article PubMed Google Scholar
Stein, B. E. & Stanford, T. R. Multisensory integration: current issues from the perspective of the single neuron. Nature Rev. Neurosci. 9 , 255–266 (2008).
Article CAS Google Scholar
Driver, J. & Noesselt, T. Multisensory interplay reveals crossmodal influences on 'sensory-specific' brain regions, neural responses, and judgments. Neuron 57 , 11–23 (2008).
Article CAS PubMed PubMed Central Google Scholar
Axelrod, S. Effects of Early Blindness; Performance of Blind and Sighted Children on Tactile and Auditory Tasks (American Foundation for the Blind, New York, 1959).
Google Scholar
Myklebust, H. R. & Brutten, M. A study of the visual perception of deaf children. Acta Otolaryngol. Suppl. 105 , 1–126 (1953).
CAS PubMed Google Scholar
Rauschecker, J. P. Compensatory plasticity and sensory substitution in the cerebral cortex. Trends Neurosci. 18 , 36–43 (1995).
Article CAS PubMed Google Scholar
Jones, E. G. Cortical and subcortical contributions to activity-dependent plasticity in primate somatosensory cortex. Annu. Rev. Neurosci. 23 , 1–37 (2000).
Kaas, J. H., Merzenich, M. M. & Killackey, H. P. The reorganization of somatosensory cortex following peripheral nerve damage in adult and developing mammals. Annu. Rev. Neurosci. 6 , 325–356 (1983).
Rossignol, S. Plasticity of connections underlying locomotor recovery after central and/or peripheral lesions in the adult mammals. Philos. Trans. R. Soc. Lond. B Biol. Sci. 361 , 1647–1671 (2006).
Carroll, T. J. Blindness: What It Is, What It Does, And How To Live With It (Little, Boston, 1961). References 10 and 11 give classic descriptions of rehabilitation in the blind and the 'folklore' associated with vision loss.
Wagner-Lampl, A. & Oliver, G. W. Folklore of blindness. J. Vis. Impair. Blind. 88 , 267–276 (1994).
Alary, F. et al. Tactile acuity in the blind: a closer look reveals superiority over the sighted in some but not all cutaneous tasks. Neuropsychologia 47 , 2037–2043 (2009). References 12–24 describe superior performance on sensory tasks in the blind.
Alary, F. et al. Tactile acuity in the blind: a psychophysical study using a two-dimensional angle discrimination task. Exp. Brain Res. 187 , 587–594 (2008).
Goldreich, D. & Kanics, I. M. Tactile acuity is enhanced in blindness. J. Neurosci. 23 , 3439–3445 (2003).
Van Boven, R. W., Hamilton, R. H., Kauffman, T., Keenan, J. P. & Pascual-Leone, A. Tactile spatial resolution in blind braille readers. Neurology 54 , 2230–2236 (2000).
Gougoux, F. et al. Neuropsychology: pitch discrimination in the early blind. Nature 430 , 309 (2004).
Gougoux, F., Zatorre, R. J., Lassonde, M., Voss, P. & Lepore, F. A functional neuroimaging study of sound localization: visual cortex activity predicts performance in early-blind individuals. PLoS Biol. 3 , e27 (2005).
Article PubMed PubMed Central CAS Google Scholar
Lessard, N., Pare, M., Lepore, F. & Lassonde, M. Early-blind human subjects localize sound sources better than sighted subjects. Nature 395 , 278–280 (1998).
Roder, B. et al. Improved auditory spatial tuning in blind humans. Nature 400 , 162–166 (1999).
Voss, P. et al. Early- and late-onset blind individuals show supra-normal auditory abilities in far-space. Curr. Biol. 14 , 1734–1738 (2004).
Fortin, M. et al. Wayfinding in the blind: larger hippocampal volume and supranormal spatial navigation. Brain 131 , 2995–3005 (2008).
Niemeyer, W. & Starlinger, I. Do the blind hear better? Investigations on auditory processing in congenital or early acquired blindness. II. Central functions. Audiology 20 , 510–515 (1981).
Amedi, A., Raz, N., Pianka, P., Malach, R. & Zohary, E. Early 'visual' cortex activation correlates with superior verbal memory performance in the blind. Nature Neurosci. 6 , 758–766 (2003).
Roder, B., Rosler, F. & Neville, H. J. Auditory memory in congenitally blind adults: a behavioral-electrophysiological investigation. Brain Res. Cogn. Brain Res. 11 , 289–303 (2001).
Pascual-Leone, A. & Torres, F. Plasticity of the sensorimotor cortex representation of the reading finger in Braille readers. Brain 116 , 39–52 (1993).
Sterr, A. et al. Perceptual correlates of changes in cortical representation of fingers in blind multifinger Braille readers. J. Neurosci. 18 , 4417–4423 (1998).
Sterr, A. et al. Changed perceptions in Braille readers. Nature 391 , 134–135 (1998).
Elbert, T. et al. Expansion of the tonotopic area in the auditory cortex of the blind. J. Neurosci. 22 , 9941–9944 (2002).
Stevens, A. A. & Weaver, K. E. Functional characteristics of auditory cortex in the blind. Behav. Brain Res. 196 , 134–138 (2009).
Burgess, N., Maguire, E. A. & O'Keefe, J. The human hippocampus and spatial and episodic memory. Neuron 35 , 625–641 (2002).
Veraart, C. et al. Glucose utilization in human visual cortex is abnormally elevated in blindness of early onset but decreased in blindness of late onset. Brain Res. 510 , 115–121 (1990).
Wanet-Defalque, M. C. et al. High metabolic activity in the visual cortex of early blind human subjects. Brain Res. 446 , 369–373 (1988).
Buchel, C. Functional neuroimaging studies of Braille reading: cross-modal reorganization and its implications. Brain 121 , 1193–1194 (1998).
Burton, H. et al. Adaptive changes in early and late blind: a fMRI study of Braille reading. J. Neurophysiol. 87 , 589–607 (2002).
Sadato, N. et al. Neural networks for Braille reading by the blind. Brain 121 , 1213–1229 (1998).
Sadato, N. et al. Activation of the primary visual cortex by Braille reading in blind subjects. Nature 380 , 526–528 (1996).
Pietrini, P. et al. Beyond sensory images: object-based representation in the human ventral pathway. Proc. Natl Acad. Sci. USA 101 , 5658–5663 (2004).
Ptito, M., Moesgaard, S. M., Gjedde, A. & Kupers, R. Cross-modal plasticity revealed by electrotactile stimulation of the tongue in the congenitally blind. Brain 128 , 606–614 (2005).
Voss, P., Gougoux, F., Zatorre, R. J., Lassonde, M. & Lepore, F. Differential occipital responses in early- and late-blind individuals during a sound-source discrimination task. Neuroimage 40 , 746–758 (2008).
Poirier, C. et al. Auditory motion perception activates visual motion areas in early blind subjects. Neuroimage 31 , 279–285 (2006).
Kujala, T. et al. The role of blind humans' visual cortex in auditory change detection. Neurosci. Lett. 379 , 127–131 (2005).
Weeks, R. et al. A positron emission tomographic study of auditory localization in the congenitally blind. J. Neurosci. 20 , 2664–2672 (2000).
Roder, B., Stock, O., Bien, S., Neville, H. & Rosler, F. Speech processing activates visual cortex in congenitally blind humans. Eur. J. Neurosci. 16 , 930–936 (2002).
Burton, H., Diamond, J. B. & McDermott, K. B. Dissociating cortical regions activated by semantic and phonological tasks: a FMRI study in blind and sighted people. J. Neurophysiol. 90 , 1965–1982 (2003).
Burton, H., Snyder, A. Z., Diamond, J. B. & Raichle, M. E. Adaptive changes in early and late blind: a FMRI study of verb generation to heard nouns. J. Neurophysiol. 88 , 3359–3371 (2002).
Amedi, A. et al. Shape conveyed by visual-to-auditory sensory substitution activates the lateral occipital complex. Nature Neurosci. 10 , 687–689 (2007).
Arno, P. et al. Occipital activation by pattern recognition in the early blind using auditory substitution for vision. Neuroimage 13 , 632–645 (2001).
Collignon, O., Lassonde, M., Lepore, F., Bastien, D. & Veraart, C. Functional cerebral reorganization for auditory spatial processing and auditory substitution of vision in early blind subjects. Cereb. Cortex 17 , 457–465 (2007).
De Volder, A. G. et al. Changes in occipital cortex activity in early blind humans using a sensory substitution device. Brain Res. 826 , 128–134 (1999).
Pascual-Leone, A., Walsh, V. & Rothwell, J. Transcranial magnetic stimulation in cognitive neuroscience—virtual lesion, chronometry, and functional connectivity. Curr. Opin. Neurobiol. 10 , 232–237 (2000).
Cohen, L. G. et al. Functional relevance of cross-modal plasticity in blind humans. Nature 389 , 180–183 (1997).
Hamilton, R. & Pascual-Leone, A. Cortical plasticity associated with Braille learning. Trends Cogn. Sci. 2 , 168–174 (1998).
Kupers, R. et al. rTMS of the occipital cortex abolishes Braille reading and repetition priming in blind subjects. Neurology 68 , 691–693 (2007).
Amedi, A., Floel, A., Knecht, S., Zohary, E. & Cohen, L. G. Transcranial magnetic stimulation of the occipital pole interferes with verbal processing in blind subjects. Nature Neurosci. 7 , 1266–1270 (2004).
Merabet, L. B. et al. Functional recruitment of visual cortex for sound encoded object identification in the blind. Neuroreport 20 , 132–138 (2009).
Article PubMed PubMed Central Google Scholar
Hamilton, R., Keenan, J. P., Catala, M. & Pascual-Leone, A. Alexia for Braille following bilateral occipital stroke in an early blind woman. Neuroreport 11 , 237–240 (2000).
Merabet, L. et al. Feeling by sight or seeing by touch? Neuron 42 , 173–179 (2004).
Levanen, S. & Hamdorf, D. Feeling vibrations: enhanced tactile sensitivity in congenitally deaf humans. Neurosci. Lett. 301 , 75–77 (2001). References 58–62 describe superior performance on sensory tasks in the deaf.
Arnold, P. & Murray, C. Memory for faces and objects by deaf and hearing signers and hearing nonsigners. J. Psycholinguist. Res. 27 , 481–497 (1998).
McCullough, S. & Emmorey, K. Face processing by deaf ASL signers: evidence for expertise in distinguished local features. J. Deaf Stud. Deaf Educ. 2 , 212–222 (1997).
Bavelier, D. et al. Visual attention to the periphery is enhanced in congenitally deaf individuals. J. Neurosci. 20 , RC93 (2000).
Dye, M. W., Hauser, P. C. & Bavelier, D. Is visual selective attention in deaf individuals enhanced or deficient? The case of the useful field of view. PLoS ONE 4 , e5640 (2009).
Neville, H. J. & Lawson, D. Attention to central and peripheral visual space in a movement detection task: an event-related potential and behavioral study. II. Congenitally deaf adults. Brain Res. 405 , 268–283 (1987).
Proksch, J. & Bavelier, D. Changes in the spatial distribution of visual attention after early deafness. J. Cogn. Neurosci. 14 , 687–701 (2002).
Bosworth, R. G. & Dobkins, K. R. Visual field asymmetries for motion processing in deaf and hearing signers. Brain Cogn. 49 , 170–181 (2002).
Bosworth, R. G. & Dobkins, K. R. The effects of spatial attention on motion processing in deaf signers, hearing signers, and hearing nonsigners. Brain Cogn. 49 , 152–169 (2002).
Fine, I., Finney, E. M., Boynton, G. M. & Dobkins, K. R. Comparing the effects of auditory deprivation and sign language within the auditory and visual cortex. J. Cogn. Neurosci. 17 , 1621–1637 (2005).
Levanen, S. Neuromagnetic studies of human auditory cortex function and reorganization. Scand. Audiol. Suppl. 49 , 1–6 (1998).
Auer, E. T. Jr, Bernstein, L. E., Sungkarat, W. & Singh, M. Vibrotactile activation of the auditory cortices in deaf versus hearing adults. Neuroreport 18 , 645–648 (2007).
MacSweeney, M. et al. Neural systems underlying British Sign Language and audio-visual English processing in native users. Brain 125 , 1583–1593 (2002).
Nishimura, H. et al. Sign language 'heard' in the auditory cortex. Nature 397 , 116 (1999).
Petitto, L. A. et al. Speech-like cerebral activity in profoundly deaf people processing signed languages: implications for the neural basis of human language. Proc. Natl Acad. Sci. USA 97 , 13961–13966 (2000).
Finney, E. M., Clementz, B. A., Hickok, G. & Dobkins, K. R. Visual stimuli activate auditory cortex in deaf subjects: evidence from MEG. Neuroreport 14 , 1425–1427 (2003).
Finney, E. M., Fine, I. & Dobkins, K. R. Visual stimuli activate auditory cortex in the deaf. Nature Neurosci. 4 , 1171–1173 (2001).
Bavelier, D. et al. Impact of early deafness and early exposure to sign language on the cerebral organization for motion processing. J. Neurosci. 21 , 8931–8942 (2001).
Neville, H. J. & Lawson, D. Attention to central and peripheral visual space in a movement detection task. III. Separate effects of auditory deprivation and acquisition of a visual language. Brain Res. 405 , 284–294 (1987).
Atkinson, J., Marshall, J., Woll, B. & Thacker, A. Testing comprehension abilities in users of British Sign Language following CVA. Brain Lang. 94 , 233–248 (2005).
Hickok, G., Love-Geffen, T. & Klima, E. S. Role of the left hemisphere in sign language comprehension. Brain Lang. 82 , 167–178 (2002).
Hickok, G., Klima, E., Kritchevsky, M. & Bellugi, U. A case of 'sign blindness' following left occipital damage in a deaf signer. Neuropsychologia 33 , 1597–1606 (1995).
Saito, K., Otsuki, M. & Ueno, S. Sign language aphasia due to left occipital lesion in a deaf signer. Neurology 69 , 1466–1468 (2007).
Kosslyn, S. M. et al. The role of area 17 in visual imagery: convergent evidence from PET and rTMS. Science 284 , 167–170 (1999).
McGuire, P. K. et al. Functional anatomy of inner speech and auditory verbal imagery. Psychol. Med. 26 , 29–38 (1996).
Obretenova, S., Halko, M. A., Plow, E. B., Pascual-Leone, A. & Merabet, L. B. Neuroplasticity associated with tactile language communication in a deaf-blind subject. Front. Hum. Neurosci. (in the press).
Bavelier, D. & Neville, H. J. Cross-modal plasticity: where and how? Nature Rev. Neurosci. 3 , 443–452 (2002).
Schroeder, C. E. et al. Anatomical mechanisms and functional implications of multisensory convergence in early cortical processing. Int. J. Psychophysiol. 50 , 5–17 (2003). References 85–94 report key findings from animal studies of crossmodal neuroplasticity.
Rauschecker, J. P. & Kniepert, U. Auditory localization behaviour in visually deprived cats. Eur. J. Neurosci. 6 , 149–160 (1994).
King, A. J. & Parsons, C. H. Improved auditory spatial acuity in visually deprived ferrets. Eur. J. Neurosci. 11 , 3945–3956 (1999).
Rauschecker, J. P. & Korte, M. Auditory compensation for early blindness in cat cerebral cortex. J. Neurosci. 13 , 4538–4548 (1993).
Korte, M. & Rauschecker, J. P. Auditory spatial tuning of cortical neurons is sharpened in cats with early blindness. J. Neurophysiol. 70 , 1717–1721 (1993).
Wallace, M. T., Carriere, B. N., Perrault, T. J. Jr, Vaughan, J. W. & Stein, B. E. The development of cortical multisensory integration. J. Neurosci. 26 , 11844–11849 (2006).
Wallace, M. T. & Stein, B. E. Early experience determines how the senses will interact. J. Neurophysiol. 97 , 921–926 (2007).
Carriere, B. N. et al. Visual deprivation alters the development of cortical multisensory integration. J. Neurophysiol. 98 , 2858–2867 (2007).
Rauschecker, J. P. Auditory cortical plasticity: a comparison with other sensory systems. Trends Neurosci. 22 , 74–80 (1999).
Weinberger, N. M. Dynamic regulation of receptive fields and maps in the adult sensory cortex. Annu. Rev. Neurosci. 18 , 129–158 (1995).
Kral, A., Schroder, J. H., Klinke, R. & Engel, A. K. Absence of cross-modal reorganization in the primary auditory cortex of congenitally deaf cats. Exp. Brain Res. 153 , 605–613 (2003).
Kral, A. Unimodal and cross-modal plasticity in the 'deaf' auditory cortex. Int. J. Audiol. 46 , 479–493 (2007).
King, A. J. & Nelken, I. Unraveling the principles of auditory cortical processing: can we learn from the visual system? Nature Neurosci. 12 , 698–701 (2009).
Hall, A. J. & Lomber, S. G. Auditory cortex projections target the peripheral field representation of primary visual cortex. Exp. Brain Res. 190 , 413–430 (2008).
Falchier, A., Clavagnier, S., Barone, P. & Kennedy, H. Anatomical evidence of multimodal integration in primate striate cortex. J. Neurosci. 22 , 5749–5759 (2002).
Rockland, K. S. & Ojima, H. Multisensory convergence in calcarine visual areas in macaque monkey. Int. J. Psychophysiol. 50 , 19–26 (2003).
Cappe, C. & Barone, P. Heteromodal connections supporting multisensory integration at low levels of cortical processing in the monkey. Eur. J. Neurosci. 22 , 2886–2902 (2005).
Wang, Y., Celebrini, S., Trotter, Y. & Barone, P. Visuo-auditory interactions in the primary visual cortex of the behaving monkey: electrophysiological evidence. BMC Neurosci. 9 , 79 (2008).
Fu, K. M. et al. Auditory cortical neurons respond to somatosensory stimulation. J. Neurosci. 23 , 7510–7515 (2003).
Wittenberg, G. F., Werhahn, K. J., Wassermann, E. M., Herscovitch, P. & Cohen, L. G. Functional connectivity between somatosensory and visual cortex in early blind humans. Eur. J. Neurosci. 20 , 1923–1927 (2004).
Zangaladze, A., Epstein, C. M., Grafton, S. T. & Sathian, K. Involvement of visual cortex in tactile discrimination of orientation. Nature 401 , 587–590 (1999).
Merabet, L. B. et al. Rapid and reversible recruitment of early visual cortex for touch. PLoS ONE 3 , e3046 (2008).
Pascual-Leone, A., Amedi, A., Fregni, F. & Merabet, L. B. The plastic human brain cortex. Annu. Rev. Neurosci. 28 , 377–401 (2005). Review comparing neuroplasticity in both sensory and motor systems, including a discussion of possible underlying neurophysiological mechanisms.
Wiesel, T. N. & Hubel, D. H. Single-cell responses in striate cortex of kittens deprived of vision in one eye. J. Neurophysiol. 26 , 1003–1017 (1963). Classic study of visual deprivation highlighting the importance of critical periods.
Hensch, T. K. Critical period plasticity in local cortical circuits. Nature Rev. Neurosci. 6 , 877–888 (2005).
Cohen, L. G. et al. Period of susceptibility for cross-modal plasticity in the blind. Ann. Neurol. 45 , 451–460 (1999).
Sadato, N., Okada, T., Honda, M. & Yonekura, Y. Critical period for cross-modal plasticity in blind humans: a functional MRI study. Neuroimage 16 , 389–400 (2002).
Fieger, A., Roder, B., Teder-Salejarvi, W., Hillyard, S. A. & Neville, H. J. Auditory spatial tuning in late-onset blindness in humans. J. Cogn. Neurosci. 18 , 149–157 (2006).
Harrison, R. V., Gordon, K. A. & Mount, R. J. Is there a critical period for cochlear implantation in congenitally deaf children? Analyses of hearing and speech perception performance after implantation. Dev. Psychobiol. 46 , 252–261 (2005).
Kos, M. I., Deriaz, M., Guyot, J. P. & Pelizzone, M. What can be expected from a late cochlear implantation? Int. J. Pediatr. Otorhinolaryngol. 73 , 189–193 (2009).
Zhou, X. & Merzenich, M. M. Intensive training in adults refines A1 representations degraded in an early postnatal critical period. Proc. Natl Acad. Sci. USA 104 , 15935–15940 (2007).
Zhou, X. & Merzenich, M. M. Developmentally degraded cortical temporal processing restored by training. Nature Neurosci. 12 , 26–28 (2009).
Sterr, A., Green, L. & Elbert, T. Blind Braille readers mislocate tactile stimuli. Biol. Psychol. 63 , 117–127 (2003).
Ptito, M. et al. TMS of the occipital cortex induces tactile sensations in the fingers of blind Braille readers. Exp. Brain Res. 184 , 193–200 (2008).
Kupers, R. et al. Transcranial magnetic stimulation of the visual cortex induces somatotopically organized qualia in blind subjects. Proc. Natl Acad. Sci. USA 103 , 13256–13260 (2006).
Gregory, R. L. Seeing after blindness. Nature Neurosci. 6 , 909–910 (2003). With reference 125, this paper describes historical and modern sight restoration surgeries and their behavioural consequences.
Senden, M. V. Space and Sight: the Perception of Space and Shape in the Congenitally Blind Before and After Operation (Free Press, Glencoe, Illinois, 1960).
Fine, I., Smallman, H. S., Doyle, P. & MacLeod, D. I. Visual function before and after the removal of bilateral congenital cataracts in adulthood. Vision Res. 42 , 191–210 (2002).
Fine, I. et al. Long-term deprivation affects visual perception and cortex. Nature Neurosci. 6 , 915–916 (2003).
Ostrovsky, Y., Andalman, A. & Sinha, P. Vision following extended congenital blindness. Psychol. Sci. 17 , 1009–1014 (2006).
Saenz, M., Lewis, L. B., Huth, A. G., Fine, I. & Koch, C. Visual motion area MT+/V5 responds to auditory motion in human sight-recovery subjects. J. Neurosci. 28 , 5141–5148 (2008).
Mandavilli, A. Visual neuroscience: look and learn. Nature 441 , 271–272 (2006).
Bavelier, D., Dye, M. W. & Hauser, P. C. Do deaf individuals see better? Trends Cogn. Sci. 10 , 512–518 (2006).
Giraud, A. L. & Lee, H. J. Predicting cochlear implant outcome from brain organisation in the deaf. Restor. Neurol. Neurosci. 25 , 381–390 (2007).
PubMed Google Scholar
Lee, D. S. et al. Cross-modal plasticity and cochlear implants. Nature 409 , 149–150 (2001).
Giraud, A. L., Price, C. J., Graham, J. M., Truy, E. & Frackowiak, R. S. Cross-modal plasticity underpins language recovery after cochlear implantation. Neuron 30 , 657–663 (2001).
Rouger, J. et al. Evidence that cochlear-implanted deaf patients are better multisensory integrators. Proc. Natl Acad. Sci. USA 104 , 7295–7300 (2007).
Champoux, F., Lepore, F., Gagne, J. P. & Theoret, H. Visual stimuli can impair auditory processing in cochlear implant users. Neuropsychologia 47 , 17–22 (2009).
Merabet, L. B., Rizzo, J. F., Amedi, A., Somers, D. C. & Pascual-Leone, A. What blindness can tell us about seeing again: merging neuroplasticity and neuroprostheses. Nature Rev. Neurosci. 6 , 71–77 (2005).
Fox, K. Experience-dependent plasticity mechanisms for neural rehabilitation in somatosensory cortex. Philos. Trans. R. Soc. Lond. B Biol. Sci. 364 , 369–381 (2009).
World Health Organization. Visual impairment and blindness. World Health Organization [ online ], (2009).
World Health Organization. Deafness and hearing impairment. World Health Organization [ online ], (2006).
Brennan, M. & Bally, S. J. Psychosocial adaptations to dual sensory loss in middle and late adulthood. Trends Amplif. 11 , 281–300 (2007).
Sadato, N., Okada, T., Kubota, K. & Yonekura, Y. Tactile discrimination activates the visual cortex of the recently blind naive to Braille: a functional magnetic resonance imaging study in humans. Neurosci. Lett. 359 , 49–52 (2004).
Collignon, O., Voss, P., Lassonde, M. & Lepore, F. Cross-modal plasticity for the spatial processing of sounds in visually deprived subjects. Exp. Brain Res. 192 , 343–358 (2009).
Download references
Acknowledgements
L.B.M. is supported by a K 23 EY016131 award from the National Eye Institute.
Author information
Authors and affiliations.
Department of Neurology, Berenson-Allen Center for Noninvasive Brain Stimulation, Beth Israel Deaconess Medical Center, Harvard Medical School, 330 Brookline Avenue, KS-158, Boston, 02215, Massachusetts, USA
Lotfi B. Merabet & Alvaro Pascual-Leone
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Lotfi B. Merabet .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
Related links
Further information.
Berenson-Allen Center for Noninvasive Brain Stimulation
With regards to multisensory integration, refers to the interaction of sensory information from the different sensory modalities that can lead to an enhanced perceptual experience.
The ability of the nervous system to change its functional and structural organization in response to development, experience, the environment, damage or insult.
A large negative-direction evoked potential (measured by electroencephalography) detected over the fronto-central region of the scalp and peaking between 80 and 120 ms after the onset of a stimulus (typically auditory). This potential has been found to be sensitive to features of sounds associated with speech.
(SSD). A device that transforms the characteristics of one sensory modality (for example, vision) into stimuli that can be perceived by another sensory modality (for example, touch or hearing). This strategy is often used in assistive technology to access sensory information normally perceived by an impaired sensory modality by using the remaining intact senses.
A neurological disorder characterized by the loss of the ability to read. Alexia typically occurs following damage to specific language-relevant areas of the brain (particularly within the left hemisphere) as well as the occipital and parietal lobes.
A neurological disorder characterized by impaired expression and understanding of language, as well as reading and writing. It is usually the result of damage to areas of the brain involved with language processing.
A relatively rare genetic disorder with clinical subtypes characterizing the degree of severity and a leading cause of combined deafness and blindness. Hearing loss is associated with a defective inner ear whereas the visual loss is associated with degeneration of retinal cell function.
Pertaining to information processing strategies, a top-down approach describes the flow of sensory information from higher-order cortical areas to lower-order processing levels. This is opposite to 'bottom-up' processing, in which information being processed from lower-order regions flows to higher-order areas of sensory cortex.
A surgically implanted electronic device that provides the sense of sound in individuals with profound hearing loss. The device works by electrically stimulating nerve fibres of the cochlea to transmit sensory information provided by external components including a microphone and speech processor.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Merabet, L., Pascual-Leone, A. Neural reorganization following sensory loss: the opportunity of change. Nat Rev Neurosci 11 , 44–52 (2010). https://doi.org/10.1038/nrn2758
Download citation
Published : 25 November 2009
Issue Date : January 2010
DOI : https://doi.org/10.1038/nrn2758
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
- Suddha Sourav
- Ramesh Kekunnaya
- Brigitte Röder
Communications Biology (2024)
Decoding auditory deprivation: resting-state fMRI insights into deafness and brain plasticity
- Uttam Kumar
- Kalpana Dhanik
Brain Structure and Function (2024)
An Inverse Relationship Between Gray Matter Volume and Speech-in-Noise Performance in Tinnitus Patients with Normal Hearing Sensitivity
- Somayeh Shahsavarani
- Fatima T. Husain
Journal of the Association for Research in Otolaryngology (2023)
Early Interplay of Smell and Sight in Human Development: Insights for Early Intervention With High-Risk Infants
- Giulia Purpura
- Stefania Petri
Current Developmental Disorders Reports (2023)
Comparing Presence and Absence of Initial In-Person Contact and Written Feedback in RE&CBT E-Supervision
- Ensad Miljkovic
Journal of Rational-Emotive & Cognitive-Behavior Therapy (2023)

Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
JavaScript seems to be disabled in your browser. For the best experience on our site, be sure to turn on Javascript in your browser.
SENSORY CLOTHING
- Weighted Vests & Outerwear
- Weighted Compression Vests
- Compression Tops & Bottoms
- Sensory Accessories
ACTIVE TOYS & TOOLS
- Outdoor Play
- Obstacle Course
- Scooters & Riding Toys
- Exercise & Therapy Balls
- Tunnels, Tents & Barrels
CALMING TOYS & TOOLS
- Body Socks & Sensory Sacks
- Weighted Toys & Animals
- Brushes & Rollers
- Sand & Snow
- Weighted Blankets
- Sleeping Bags & Sheets
SENSORY CLASSROOM
- Break Boxes & Kits
- Classroom Corners
- Sensory Hallways
- Classroom Tools
- Speech Tools
- Sensory Games
- Social Emotional Learning
SENSORY SEATING
- Flexible Seating
- Sensory Cushions
- Foot Fidgets
SENSORY ROOM EQUIPMENT
- Trampolines
- Crash Mats & Safety Mats
- Ball Pits & Accessories
- Furniture & Seating
- Floor Tiles & Spot Markers
- Activity Wall Panels
- Sensory Boards
- Bubble Tubes
- Fiber Optics
- LED Products
- Sensory Room Packages
EASY TO CLEAN
Hardware & accessories, training and courses.

- Shop All Sensory Clothing
- Shop All Active Toys & Tools
- Shop All Calming Toys & Tools
- Shop All Sleep
- Shop All Sensory Classroom
- Shop All Sensory Seating
- Easy to Clean
- Hardware & Accessories
- Training and Courses
- Cerebral Palsy
- Down Syndrome
- Fine Motor Delay
- Gross Motor Delay
- Learning Disabilities
- Sensory Processing Disorder
- Speech & Communication Delay
- Visual & hearing Impairment
- Social-Emotional Challenge
Flapping or Jumping? How to Cope with Sensory Overload
Mindfulness for Kids
SENSORY ROOMS
Sensory room videos, case studies, other sensory solutions.
- Sensory Corners & Hallways
- Sensory Equipment
- Break Boxes & Travel Kits
Get a glimpse of incredible sensory spaces in schools, clinics and private homes.
SENSORY ROOM PACKAGES
Browse our ready-to-go sensory spaces.
Sensory Rooms
Other Sensory Solutions
- Case Studies
- Sensory Room Videos
- Training & Courses
- Free Webinars and Videos
- ESSER Spending Options
- Free Templates & Printables
- Product Installation Manuals
- Sensory Room Research
THERAPIST DIRECTORY
Explore relevant sensory topics explained by our expert OT team.
View an online version of our catalog.
SENSORY COACH TRAINING VIDEOS
Learn Effective Strategies for SPD, ADHD and Autism
- Sensory Coach Training Videos
It all started with one struggling child. Today it’s a company committed to empowering different.
OUR EXPERT TEAM
Meet the dedicated team committed to celebrating the strengths of kids with special needs.
PRODUCT SAFETY
Learn about our commitment to safety, our number one priority.
MEDIA & AWARDS
Read about our products and resources as featured in The Wall Street Journal, Reuters and more.
- Our expert team
- Product Safety
- Media & Awards
- Compare Products
Sensory Room Case Studies
Every sensory room starts with a story.
Get a glimpse into the background, vision, and design process behind some of our best sensory spaces.
Fun and Function Sensory Room Case Studies

Heaven on Earth

Little Cave Man

Sensory Dream At Coal City

Noah's Sensory Gym

A Sensory Stadium Suite

Haddon Heights Haven

Sinai’s Sensory Sensation

Our Lady of Confidence

Order in the Court

Small Kids, Big Needs

Texas Tranquility

Recess Romp Around

A Spectacular Sensory Makeover

Double the Sensory Fun

Sensory Library In Session
Your sensory room can be the next success story.
- Open access
- Published: 16 January 2024
Effects of school-based occupational therapy program for children with disabilities in elementary school in Korea: a case study
- Eun-Hwa Jeong 1
BMC Psychology volume 12 , Article number: 26 ( 2024 ) Cite this article
1260 Accesses
Metrics details
The purpose of this case study was to explore the effects of a school-based occupational therapy on children’s attention, school adaptation, sensory processing, and motor function for children in special classes in elementary school in Korea.
Case presentation
The subjects of this study were a 7-year-old boy with autism spectrum disorder and a 9-year-old girl with intellectual disability. The school-based occupational therapy program consisted of 10 sessions and was conducted once a week for an hour and a half. The program consisted of classroom activities, use of school facilities, emotional management, and activities based on sensory integration, and was conducted as individual and group programs according to sessions. As a result of the study, all improved when the pre- and post-scores of the two children’s attention assessment, school adjustment scale, sensory processing evaluation tool for the children in school and BOT-2-SF were compared.
Conclusions
Although the results from two cases cannot be generalized, the findings suggest the school-based occupational therapy program may help a positive effect on the school life of children with disabilities. Further investigation is necessary.
Peer Review reports
Introduction
It is difficult for children with disabilities to properly perform learning activities, school rules, and social interactions due to physical difficulties, difficulty in controlling emotions, impulsivity, and poor attention in school life [ 1 ]. Also, when accompanied by sensory processing disorder, difficulty in following instructions, learning, and controlling behavior can cause school adaptation problems [ 2 ].
Occupational therapists prepare students for and participate in important learning and developmental activities within the school environment through school-based occupational therapy [ 3 ]. Occupational therapists can help children with disabilities prepare for learning and carry out other related activities in schools. It provides academic and non-academic interventions, including social skills, academic and behavior management, and athletic participation [ 4 ].
It has been reported that 90% of occupational therapists in school-based occupational therapy practices perform sensory integration interventions based on ‘Ayres’ theory [ 4 ]. Sensory integration is a way to help children improve their adaptive ability to interact with their environment. Therefore, the fundamental purpose is to prevent non-adaptive behaviors or difficulties and improve the quality of life and performance by appropriately interacting with the environment and the body [ 2 , 3 , 4 ]. However, when applying these sensory integration interventions to school-based occupational therapy, it is necessary to appropriately apply other intervention for improving school adaptation according to needs. And it is more reasonable to establish an intervention plan based on this after identifying students’ performance skills and non-adaptive behaviors [ 4 , 5 ].
School occupational therapists in Korea mainly provide intervention based on the medical model, focusing on improving children’s occupational performance problems by improving deficits in subcomponents such as cognitive, motor, and sensory. In previous studies, it was found that writing for learning skills, fine motor and visual motor integration were most often implemented as interventions of school-based occupational therapy [ 6 ]. However, most children with school adjustment problems need interventions for overall school performance, such as following rules and instructions, paying attention, and interacting with peers, rather than academic skills [ 7 ]. In other words, school-based occupational therapy requires occupational therapists to deal with non-adaptive behaviors that hinder children’s adaptation to school in the natural environment of the classroom. It can potentially lead to a positive impact on academic performance [ 4 , 5 , 6 ]. In developed countries where school based occupational therapy was implemented before Korea, school occupational therapists emphasize that therapy services should be provided in natural environments such as classrooms, playgrounds, cafeterias, and hallways in order to achieve academic and functional goals [ 8 ].
The role of occupational therapists in schools and educational systems is to facilitate students’ ability to perform tasks or perform meaningful and purposeful activities as students. Therefore, it is necessary for occupational therapists to cooperate with teachers to evaluate students’ functional performance problems in the classroom and to provide necessary interventions to students by discussing effective programs. In this respect, this case study was to confirm the effectiveness of a school-based occupational therapy program that applied a client-centered approach. Therefore, the purpose of this study was to explore the effects of a school-based occupational therapy intervention focusing on school adaptation on children’s the attention, school adaptation, sensory processing, and motor function for children in special classes in elementary school in Korea.
Participants
The subjects of this study were two children from a special class at Elementary School in Korea. Subject A was a 7-year-old male with autism, and subject B was a 9-year-old female with intellectual disability accompanied by autistic features. Subject A did not have social interaction including eye contact, frequently stared into space, and had a very short attention span. There were problems in that they often left their seats during class, showed stereotyped behaviors such as going around the classroom in a circle, and frequently made meaningless sounds such as shouting during class. In addition, he was unable to hold a pencil for writing and was unable to use a spoon for eating, so he had to eat with assistance. Subject B often expresses crying and anger when she is not allowed to do what he wants, and often leaves her seat during activities. These characteristics caused problems in peer relationships due to difficulties in controlling and expressing emotions during school life. In addition, problems with social interaction often occurred due to difficulties in conversations appropriate to the situation.
This study was designed to conduct pre- and post-tests on attention, motor function, school adaptation, and sensory processing function of each subject to confirm the effectiveness of the school-based occupational therapy program. This study used convenience sampling. Therefore, the criteria for selecting subjects were students from special classes at the elementary school where the experiment was conducted, who were able to participate in the study. Subjects in this study did not take any additional treatment or psychopharmacological medications.
The intervention program was implemented for 10 sessions from March to June 2022. During the intervention period, the intervention was conducted every Friday from 2:00 to 3:30 p.m.
The program was planned and executed by an intervention team composed of occupational therapists. The intervention goal for each subject was set by the elementary school special class teacher and the intervention team. The evaluation of attention, school adaptation, and sensory processing function was conducted by special class teachers. And The evaluation of motor function was conducted by the intervention team.
Pre- and post-assessments were conducted in sessions 1 and 10, respectively, and were included in the intervention session. Additionally, the evaluator and intervention provider were the same.
Intervention
The school-based occupational therapy program of this study was constructed based on the framework of sensory integration theory and the school-based occupational therapy model. There were two students in the group, three occupational therapists and one special education teacher running the sessions. The teacher only participated in goal setting, and direct intervention was conducted by occupational therapists. According to the purpose of each session, an individual program suitable for the intervention goal and a group program in which two children participated were conducted. The goal of this school-based occupational therapy program was to improve school adjustment, including learning activities, school rules, and interactions, by mediating each child’s problems. The intervention goal of subject A was to improve attention, and provide an experience of school assignments during activities for school adaptation. The intervention goal of subject B was to improve school adaptation and self-expression skills through school assignment experiences (Table 1 ).
Assessments
Attention assessment.
In this study, sub-items of the Korea-Child Behavior Checklist (K-CBCL) were used to evaluate the subject’s attention. K-CBCL is a standardized child and adolescent behavior assessment tool that translated the Child Behavior Checklist developed by Achenbach and Edelbrock (1983) into Korean [ 9 , 10 , 11 ]. The Cronbach alpha value of K-CBCL was 0.62-0.86. It is evaluated for children between the ages of 4 and 17, and is divided into a social ability scale and a problem behavior syndrome scale. The social ability scale consists of 13 items of 3 categories (sociality, academic performance, and total social ability). The problem behavior syndrome scale consists of 117 questions in 13 categories (deterioration, physical symptoms, anxiety/depression, social immaturity, thinking problems, attention problems, delinquency, aggression, internalization problems, externalization problems, total problem behavior, sexual problems, and emotional instability). Each item is on a 3-point scale (0 points; never, 1 point; occasionally or infrequently, 2 points; frequent or severe), with a score ranging from 0 to 234 points. Scoring and interpretation of results can be done by creating a profile to ensure that it falls within the clinical range [ 10 , 11 ]. In this study, 11 items of attention problem among the subscales of the Problem Behavior Syndrome scale were evaluated to evaluate children’s attention. It is interpreted that the higher the score, the lower the attention.
School adjustment scale
The school life adjustment scale consists of 4 areas: class attitude, friendship, positive personal behavior, and school rules, with a total of 20 questions [ 12 ]. The scale was a 4-point Likert scale of not at all (1 point), a little not (2 points), a little bit yes (3 points), and very yes (4 points). In this study, a total of 10 questions were evaluated by reorganizing them into questions suitable for school life adjustment of children in special classes. It is interpreted that the higher the score, the higher the adaptation to school life.
Sensory processing assessment tool for schools
A sensory processing assessment tool for schools was developed to evaluate behaviors related to sensory processing difficulties in school life of school-age children [ 13 ]. The evaluation items consisted of 42 items in the general learning activity area, and the detailed areas consisted of tactile processing, movement processing, visual processing, auditory processing, olfactory processing, and multisensory processing. In addition, the arts and sports activity area consist of 15 questions, and the meal time and break time activity area consists of 21 questions, totaling 78 questions [ 13 ]. The scale consists of three-point scales of 1 (not so), 2 (normal), and 3 (very so). The score can be calculated by summing the total score for each area and the total score. A higher score indicates difficulty in sensory processing.
Bruininks-Oseretsky test of motor proficiency-2-SF
The Bruininks-Oseretsky Test of Motor Proficiency-2-SF (BOT-2-SF) was used to measure children’s motor skills. In its short form, the assessment includes 14 items from eight subtests, reflecting different motor domains: (a) fine motor precision(drawing lines through crooked paths, folding papers), (b) fine motor integration(copying a square, copying a star), (c) manual dexterity(transferring pennies), (d) bilateral coordination(jumping in place—same sides synchronized, tapping feet and fingers—same sides synchronized), (e) balance(walking forward on a line, standing on one leg on a balance beam), (f) speed and agility(stationary hops), (g) upper-limb coordination(dropping and catching a ball with both hands, dribbling a ball with alternating hands), (h) strength(knee push‐ups, sit ups) [ 14 ]. The raw score of each item was converted according to the inspection manual, and the total score was obtained by adding the scores of these items.
According to the characteristics of this study, the pre- and post-change values of each subject were presented in a table and graphed. Attention assessment and school life adjustment scale were compared to check changes in variables related to each subject’s list of problems by comparing changes in all items. The analysis of the sensory processing evaluation for school aimed to identify the intervention effect on detailed factors by confirming the change in each area and the total score. BOT-2-SF compared the change in conversion score and total score for each item of the subject.
The changes in the pre- and post-scores of each subject’s attentions, school adaptation, sensory processing, and motor function are shown in the Table 2 . There was a positive change in scores for attention, school adaptation, and sensory processing of all subjects. Subject A was not performed in the BOT-2-SF because He had difficulty following instructions due to his symptoms. Subject B had a positive score change in the BOT-2-SF.
The change in scores for all items of each subject’s attention assessment is shown in Fig. 1 . Subject A had positive score changes in the items of hyperactivity, maladaptive daydreaming, impulsiveness, tension, and anxious gestures. Subject B had positive score changes in hyperactivity, stupor, maladaptive daydreaming, and poor motor function.
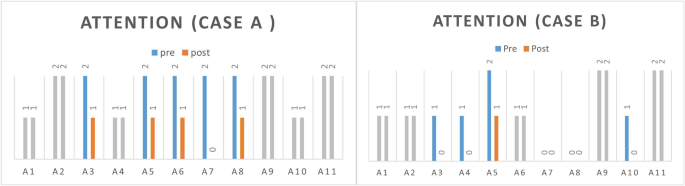
Results of attention assessment
A1: acting younger than one’s age, A2: attention problems, A3: hypercactivity, A4: stupor, A5: maladaptive daydreaming, A6: impulsiveness, A7: tension, A8: anxious gestures, A9: poor schoolwork, A10: poor motor function, A11: stare blankly into space
Gray means no change in pre-post scores
The change in scores for all items of each subject’s school life adjustment scale is shown in Fig. 2 . Subject A had positive score changes in the following items: ‘The student has relationships with several friends.’, ‘The student has appropriated physical contact with peers.’, ‘The student uses school facilities carefully.’, ‘The student is orderly when using the bathroom.’, ‘The student greets the teacher well.’ Subject B had positive score changes in the following items: ‘The student has relationships with several friends.’, ‘The student induces the other person’s interest in an appropriate way.’, ‘The student is good at controlling his mood.’, ‘The student uses school facilities carefully.’, ‘The student greets the teacher well.’
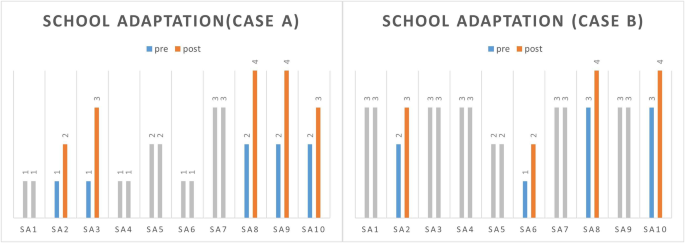
Results of school adjustment scale
SA1: The student listens attentively to the teacher’s assignment instructions or explanations. SA2: The student has relationships with several friends. SA3: The student has appropriated physical contact with peers. SA4: The student responds appropriately to praise, blame, and punishment. SA5: The student induces the other person’s interest in an appropriate way. SA6: The student is good at controlling his mood. SA7: The student keeps their school hours and class hours well. SA8: The student uses school facilities carefully. SA9: The student is orderly when using the bathroom. SA10: The student greets the teacher well. Gray means no change in pre-post scores
The results of each subject’s sensory assessment tool for schools are shown in Table 3 . According to the total score, there was a positive score change for sensory processing in both subjects. Negative score changes appeared in the arts and sports activity area of subject A, but positive changes in the pre- and post-scores of the two subjects were found in all other evaluation items.
Discussion and conclusion
This study explored the effects on children’s attention, school adaptation, sensory processing, and motor function through a school-based occupational therapy program consisting of classroom activities, use of school facilities, emotional management, and activities based on sensory integration. The concept of school adjustment is understood as a complex concept consisting of several sub-variables. In summarizing various studies, learning activities, school rules, peer relationships, and teacher relationships are classified as sub-variables [ 15 , 16 , 17 ]. In this study, a school-based occupational therapy program aimed at school adaptation was constructed, and the occupational therapy team and the special class teacher cooperated to identify each child’s problems. And it was composed of individual and group programs according to the session.
As a result of this study, both children showed positive change in attention. Both children showed improvement in hyperactivity and maladaptive daydreaming items. This is influenced by handicrafts and physical activities aimed at improving attention, based on previous studies that sensory integration-based activities can cause self-regulation and attention improvement [ 18 , 19 , 20 ]. Subject A showed a decrease in scores in the items of impulsivity, tension, and anxious gestures. ASD children like subject A are known to show high correlations with lack of sociability, negative emotions, and anxiety [ 20 ]. These factors manifest in the form of self-injurious behavior, aggression, and lack of self-control that negatively affect school life. Therefore, the results of this study can be supported based on previous studies that the process of regulating and processing senses in children with autism can affect the regulation of behavior and emotions [ 20 , 21 ] In addition, it is thought that not only sensory integration-based programs but also programs implemented for school assignment experience and adaptation to school facilities improved adaptability to activities and places. Subject B showed a positive score change in motor dullness in the attention assessment. Also, subject B showed improvement in the BOT-SF score. These results are considered to have been helpful through the group session applied physical activity, gross motor activity, and sensory integration-based physical activity.
Both children showed positive results on the school adjustment scale. After the intervention, both subjects had relationships with various friends, showed a tendency to use school facilities carefully, and greeted teachers better. In particular, subject A came to have proper physical contact with friends and was found to keep order better when using the bathroom. On the other hand, subject B showed improved emotional regulation. It may be due to the method in which this program identified problems of each subject through a client-centered approach and operated in individual and group sessions. These results are considered to have been induced by the effect of intervention programs aimed at adaptive behaviors for school life, such as school rules, social skills, and use of school facilities, rather than specific academic skills.
The total score of the two children’s sensory processing assessment tool for schools showed a positive change, but there were some differences in the scores of the detailed items. Subject A had relatively improved eye contact during classroom interaction, attention to visual stimuli, and recognition of visual stimuli. In addition, performance improved when lifting and moving the food tray, food or drink did not spill easily while eating, and hyperactivity decreased during breaks. Therefore, it was confirmed that the adaptation behavior in school life was improved. These results can be inferred that various sensory stimuli through fine and gross motor activities influenced visual processing and attention [ 22 ]. In addition, it is thought that the meal utensil training and school facility use program influenced the improvement of subject A’s adaptive behavior during meal and break time activities. Subject B showed some improvement in the movement processing score due to reduction in hyperactivity during class activities, improvement in postural control, improvement in both-handed task performance, and improvement in pencil grip. In addition, it showed improvement in visual processing scores by improve attention on visual stimuli and improved spatial arrangement organization during writing. And there was improvement in music and physical activity. These results are supported by previous studies that in the process of receiving and processing various sensory stimuli, motor function, self-regulation ability, and concentration are improved, which affects the performance of activities, cognitive function, and communication function [ 18 , 19 , 20 , 21 , 22 ].
Children with disabilities in special classes have different characteristics for each disease, and there are differences in school adaptation according to age, school type, and severity. Therefore, it can be considered to operate a school-based occupational therapy program by grouping and operating according to the child’s characteristics, age, or intervention goal, or dividing individual and group sessions as in this study. However, in Korea, occupational therapists often provide treatment support services in treatment rooms based on existing medical models rather than supporting students’ school life in a cooperative team with teachers in a school environment. In order for children to adapt to school, it is necessary for teachers to focus on the child’s educational aspects and for occupational therapists to cooperate based on the goal of improving children’s occupational skills [ 23 ]. In this regard, active efforts are needed for school occupational therapy through the development of educational programs and establishment of systems to enable interdisciplinary cooperation.
This study conducted a single group program as a case study, and it is very limited to generalize. Additionally, the effects of exogenous variables such as children’s maturation and development cannot be ruled out regarding the results of this study. Therefore, there is a need to expand randomized controlled trials using the school-based occupational therapy intervention program applied in this study. It could be a school-based occupational therapy program targeting all children in special classes or a group of children with a diagnosis different from the subjects of this study. There is also a need to standardize the procedures of school-based occupational therapy programs by organizing the process of evaluation-intervention-outcome and developing a protocol in which this process is progressively repeated.
Occupational therapists working at school need to cooperate with teachers to evaluate students’ functional performance problems in school and provide necessary interventions for students’ school adjustment. At this time, it can be effective that combined intervention of individual and group programs under the intervention goal of school adjustment. In addition, activities based on sensory integration can be helpful to improve non-adaptive behaviors such as hyperactivity, impulsivity, and reduced attention in children with disabilities. It is hoped that this study will emphasize the need for occupational therapy services in the educational field, thereby building a system for collaboration with teachers and demonstrating the expertise of occupational therapists in the school life of children with disabilities.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Barnes KJ, Beck AJ, Vogel KA, Grice KO, Murphy D. Perceptions regarding school-based occupational therapy for children with emotional disturbances. Am J Occup Ther. 2003;57(3):337–41. https://doi.org/10.5014/ajot.57.3.337
Article PubMed Google Scholar
Dunn W, Myles BS, Orr S. The sensory processing associated with asperger syndrome: a preliminary investigation. Am J Occup Ther. 2002;56(1):97–102. https://doi.org/10.5014/ajot.56.1.97
Bazyk S, Case-smith J. School-based occupational therapy. In: Case-smith J, O’Brien JC, editors. Occupational therapy for children. Philadelphia, USA: Elservier Inc; 2009.
Google Scholar
Ji SY, Lee SA, Park SY, Hong MK. Sensory integration and occupational therapy for elementary students collaborative group program: implementing school AMPS. J Kor Acad of Sens Integ. 2013;11(1):11–27.
Spencer KC, Turkett A, Vaughan R, Koenig S. School-based practice patterns: a survey of occupational therapists in Colorado. Am J Occup Ther. 2004;60(1):81–91. https://doi.org/10.5014/ajot.60.1.81
Article Google Scholar
Jung NH. (2014). A systematic review on effects of school-based occupational therapy. J Kor Acad of Sens Integ. 2014;12(1):25–38. https://doi.org/10.18064/JKASI.2014.12.1.025
Jeon SS, Kim EK. Teacher’s perception of the skills necessary for success in the general elementary school. Kor J Earl Child Spec Edu. 2007;7(1):1–20. https://doi.org/10.1177/0022466904038002040
Kim SY, Kim SJ. Using an intervention model for occupational therapy service specialist based on a special education supporting center. Jour of KoCon a. 2011;22(4):225–34. https://doi.org/10.5392/JKCA/2011.11.4.225
Achenbach TM, Edelbrock C. Manual for the child behavior checklist and revised child behavior profile. Burlington: University of Vermont, Department of Psychiatry. 1983, Available online: https://www.semanticscholar.org/paper/Manual-for-the-Child%3A-Behavior-Checklist-and-Child-Achenbach-Edelbrock/408859045620a 1a00dc2ad253a9c799cdef51eff.
Achenbach TM. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, University of Vermont, Department of Psychiatry; 1991.
Oh KJ, Lee HR, Hong KE, Ha EH. K-CBCL child and adolescent behavior assessment scale. JoongAng Jeokseong Publishing House: Seoul; 1997.
Kim HR, Lee WR. A study on the related variables on school life adjustment of students with disabilities: focusing on intellectual disabilities and ADHD. J Emot Behav Disord. 2018;34(4):337–58. https://doi.org/10.20993/JEBD.34.4.14
Cho SY. Development and validation of a sensory processing evaluation tool for the children in school., Thesis PD. Yonsei University, Wonju, Korea; 2019.
Bruininks RH, Bruininks BD. Bruininks–Oseretsky test of motor proficiency. 2nd ed. Pearson Assessment: Minneapolis, USA; 2005.
Ladd GW, Kochenderfer BJ, Coleman CC. Friendship quality as a predictor of young children’s early school adjustment. Child Dev. 1996;67(3):1103–18. https://doi.org/10.2307/1131882
Kim JN. Development and validation of school adjustment scale for middle school student and high school student - short form. Kor J Counsel Psycho. 2013;25(3):497–517.
Kim YR. Educational psychology for effective classes. Muneumsa: Seoul, Korea; 2000.
Kim HH, Hwang BG, Yoo BK. The effects of the hand-function training applied sensory integration group treatment program on the hand-function and ADL ability of children with developmental disability. Kor J Phys Multi Disabil. 2011;54(1):127–43. https://doi.org/10.20971/kcpmd.2011.54.1.127
Schaaf RC, Hunt J, Benevides T. Occupational therapy using sensory integration to improve participation of a child with autism: a case report. Am J Occup Ther. 2012;66(5):547–55. https://doi.org/10.5014/ajot.2012.004473
Schaaf RC, Benevides TW, Kelly D, Mailloux-Maggio Z. Occupational therapy and sensory integration for children with autism: a feasibility, safety, acceptability and fidelity study. Autism. 2012;16(3):321–7. https://doi.org/10.1177/1362361311435157
Pfeiffer BA, Koenig K, Kinnealey M, Sheppard M, Henderson L. Effectiveness of sensory integration interventions in children with autism spectrum disorders: a pilot study. Am J Occup Ther. 2011;65(1):76–85. https://doi.org/10.5014/ajot.2011.09205
Cham R, Iverson JM, Bailes AH, Jennings JR, Eack SM, Redfern MS. Attention and sensory integration for postural control in young adults with autism spectrum disorders. Exp Brain Res. 2021;239(5):1417–26. https://doi.org/10.1007/s00221-021-06058-z
O’Donoghue C, O’Leary J, Lynch H. Occupational therapy services in school-based practice: a pediatric occupational therapy perspective from Ireland. Occup Ther Int. 2021. https://doi.org/10.1155/2021/6636478
Article PubMed PubMed Central Google Scholar
Download references
Acknowledgements
Not applicable.
This work was supported by the 2022 Far East University Research Grant (FEU2022S05).
Author information
Authors and affiliations.
Dept. of Occupational Therapy, College of Health Science, Far East University, 76-32, Daehak-gil, Gamgok-myeon, Eumseong-gun, Chungcheongbuk-do, 27601, Republic of Korea
Eun-Hwa Jeong
You can also search for this author in PubMed Google Scholar
Contributions
Eun-Hwa Jeong: Conceptualization, Study design, Analysis, Writing-original draft, Writing-review & editing.
Corresponding author
Correspondence to Eun-Hwa Jeong .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted under mutual cooperation agreement between institutions (No.0002604 − 0001036). Ethical approval was sought and provided by Institutional Review Board of Far East University. This study performed in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Written Informed consent for publication was obtained from all subjects and their parents/legal guardians involved in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jeong, EH. Effects of school-based occupational therapy program for children with disabilities in elementary school in Korea: a case study. BMC Psychol 12 , 26 (2024). https://doi.org/10.1186/s40359-024-01520-3
Download citation
Received : 13 June 2023
Accepted : 04 January 2024
Published : 16 January 2024
DOI : https://doi.org/10.1186/s40359-024-01520-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- School adaptation
- School-based occupational therapy
- Sensory processing
- Sensory integration
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Sensory Alterations
Chapter 49 Sensory Alterations Objectives • Differentiate among the processes of reception, perception, and reaction to sensory stimuli. • Discuss the relationship of sensory function to an individual’s level of wellness. • Discuss common causes and effects of sensory alterations. • Discuss common sensory changes that normally occur with aging. • Identify factors to assess in determining a patient’s sensory status. • Identify nursing diagnoses relevant to patients with sensory alterations. • Develop a plan of care for patients with sensory deficits. • List interventions for preventing sensory deprivation and controlling sensory overload. • Describe conditions in a health care agency or patient’s home that you can modify to promote meaningful sensory stimulation. • Discuss ways to maintain a safe environment for patients with sensory deficits. Key Terms Aphasia, p. 1240 Auditory, p. 1233 Conductive hearing loss, p. 1245 Expressive aphasia, p. 1240 Gustatory, p. 1233 Hyperesthesia, p. 1246 Kinesthetic, p. 1233 Olfactory, p. 1233 Otolaryngologist, p. 1238 Ototoxic, p. 1241 Proprioceptive, p. 1236 Receptive aphasia, p. 1240 Refractive error, p. 1244 Sensory deficit, p. 1234 Sensory deprivation, p. 1234 Sensory overload, p. 1235 Stereognosis, p. 1233 Strabismus, p. 1244 Tactile, p. 1233 http://evolve.elsevier.com/Potter/fundamentals/ • Review Questions • Animations • Concept Map Creator • Case Study with Questions • Audio Glossary • Interactive Learning Activities • Key Term Flashcards • Content Updates Imagine the world without sight, hearing, or the ability to feel objects or sense aromas around you. Human beings rely on a variety of sensory stimuli to give meaning and order to events occurring in their environment. The senses form the perceptual base of our world. Stimulation comes from many sources in and outside the body, particularly through the senses of sight (visual), hearing (auditory), touch (tactile), smell (olfactory), and taste (gustatory). The body also has a kinesthetic sense that enables a person to be aware of the position and movement of body parts without seeing them. Stereognosis is a sense that allows a person to recognize the size, shape, and texture of an object. The ability to speak is not a sense but it is similar in that some patients lose the ability to interact meaningfully with other human beings. Meaningful stimuli allow a person to learn about the environment and are necessary for healthy functioning and normal development. When sensory function is altered, a person’s ability to relate to and function within the environment changes drastically. Many patients seeking health care have preexisting sensory alterations. Others develop them as a result of medical treatment (e.g., hearing loss from antibiotic use or hearing or visual loss from brain tumor removal) or hospitalization. The health care environment is a place of unfamiliar sights, sounds, and smells and minimal contact with family and friends. If patients feel depersonalized and are unable to receive meaningful stimuli, serious sensory alterations sometimes develop. As a nurse, you meet the needs of patients with existing sensory alterations and recognize patients most at risk for developing sensory problems. You also help patients who have partial or complete loss of a major sense to find alternate ways to function safely within their environment. Scientific Knowledge Base Normal Sensation Normally the nervous system continually receives thousands of bits of information from sensory nerve organs, relays the information through appropriate channels, and integrates the information into a meaningful response. Sensory stimuli reach the sensory organs to elicit an immediate reaction or present information to the brain to be stored for future use. The nervous system must be intact for sensory stimuli to reach appropriate brain centers and for an individual to perceive the sensation. After interpreting the significance of a sensation, the person is then able to react to the stimulus. Table 49-1 summarizes normal hearing and vision. TABLE 49-1 Normal Hearing and Vision FUNCTION ANATOMY AND PHYSIOLOGY Ear Transmits to the brain an accurate pattern of all sounds received from the environment, the relative intensity of these sounds, and the direction from which they originate Two ears provide stereophonic hearing to judge sound direction. The external ear canal shelters the eardrum and maintains relatively constant temperature and humidity to maintain elasticity. The middle ear is an air-containing space between the eardrum and oval window. It contains three small bones (ossicles). The eardrum and ossicles transfer sound to the fluid-filled inner ear. Movement of the stapes in the oval window creates vibrations in the fluid that bathes the membranous labyrinth, which contains the end organs of hearing and balance. The union of the vestibular (balance) and cochlear (hearing) portions of the labyrinth explains the combination of hearing and balance symptoms that occur with inner ear disorders. Vibration of the eardrum transmits through the bony ossicles. Vibrations at the oval window transmit in perilymph within the inner ear to stimulate hair cells that send impulses along the eighth cranial nerve to the brain. Eye Transmits to the brain an accurate pattern of light that is reflected from solid objects in the environment and becomes transformed into color and hue Light rays enter the convex cornea and begin to converge. Fine adjustment of light rays occurs as they pass through the pupil and lens. Change in the shape of the lens focuses light on the retina. The retina has a pigmented layer of cells to enhance visual acuity. The sensory retina contains the rods and cones (i.e., photoreceptor cells sensitive to stimulation from light). Photoreceptor cells send electrical potentials by way of the optic nerve to the brain. Reception, perception, and reaction are the three components of any sensory experience (see Chapter 43 ). Reception begins with stimulation of a nerve cell called a receptor, which is usually for only one type of stimulus such as light, touch, or sound. In the case of special senses, the receptors are grouped close together or located in specialized organs such as the taste buds of the tongue or the retina of the eye. When a nerve impulse is created, it travels along pathways to the spinal cord or directly to the brain. For example, sound waves stimulate hair cell receptors within the organ of Corti in the ear, which causes impulses to travel along the eighth cranial nerve to the acoustic area of the temporal lobe. Sensory nerve pathways usually cross over to send stimuli to opposite sides of the brain. The actual perception or awareness of unique sensations depends on the receiving region of the cerebral cortex, where specialized brain cells interpret the quality and nature of sensory stimuli. When a person becomes conscious of a stimulus and receives the information, perception takes place. Perception includes integration and interpretation of stimuli based on the person’s experiences. A person’s level of consciousness influences perception and interpretation of stimuli. Any factors lowering consciousness impair sensory perception. If sensation is incomplete such as blurred vision or if past experience is inadequate for understanding stimuli such as pain, the person can react inappropriately to the sensory stimulus. It is impossible to react to all stimuli entering the nervous system. The brain prevents sensory bombardment by discarding or storing sensory information. A person usually reacts to stimuli that are most meaningful or significant at the time. However, after continued reception of the same stimulus, a person stops responding, and the sensory experience goes unnoticed. For example, a person concentrating on reading a good book is not aware of background music. This adaptability phenomenon occurs with most sensory stimuli except for those of pain. The balance between sensory stimuli entering the brain and those actually reaching a person’s conscious awareness maintains a person’s well-being. If an individual attempts to react to every stimulus within the environment or if the variety and quality of stimuli are insufficient, sensory alterations occur. Sensory Alterations The most common types of sensory alterations are sensory deficits, sensory deprivation, and sensory overload. When a patient suffers from more than one sensory alteration, the ability to function and relate effectively within the environment is seriously impaired. Sensory Deficits A deficit in the normal function of sensory reception and perception is a sensory deficit. A person loses a sense of self with impaired senses. Initially he or she withdraws by avoiding communication or socialization with others in an attempt to cope with the sensory loss. It becomes difficult for the person to interact safely with the environment until he or she learns new skills. When a deficit develops gradually or when considerable time has passed since the onset of an acute sensory loss, a person learns to rely on unaffected senses. Some senses may even become more acute to compensate for an alteration. For example, a blind patient develops an acute sense of hearing to compensate for visual loss. Patients with sensory deficits often change behavior in adaptive or maladaptive ways. For example, a patient with a hearing impairment turns the unaffected ear toward the speaker to hear better, whereas another patient avoids people because he or she is embarrassed about not being able to understand what other people say. Box 49-1 summarizes common sensory deficits and their influence on those affected. Box 49-1 Common Sensory Deficits Visual Deficits Presbyopia: A gradual decline in the ability of the lens to accommodate or focus on close objects. Individual is unable to see near objects clearly. Cataract: Cloudy or opaque areas in part of the lens or the entire lens that interfere with passage of light through the lens, causing problems with glare and blurred vision. Cataracts usually develop gradually, without pain, redness, or tearing in the eye. Dry eyes: Result when tear glands produce too few tears, resulting in itching, burning, or even reduced vision. Glaucoma: A slowly progressive increase in intraocular pressure that, if left untreated, causes progressive pressure against the optic nerve, resulting in peripheral visual loss, decreased visual acuity with difficulty adapting to darkness, and a halo effect around lights. Diabetic retinopathy: Pathological changes occur in the blood vessels of the retina, resulting in decreased vision or vision loss caused by hemorrhage and macular edema. Macular degeneration: Condition in which the macula (specialized portion of the retina responsible for central vision) loses its ability to function efficiently. First signs include blurring of reading matter, distortion or loss of central vision, and distortion of vertical lines. Hearing Deficits Presbycusis: A common progressive hearing disorder in older adults. Cerumen accumulation: Buildup of earwax in the external auditory canal. Cerumen becomes hard and collects in the canal and causes conduction deafness. Balance Deficit Dizziness and disequilibrium: Common condition in older adulthood, usually resulting from vestibular dysfunction. Frequently a change in position of the head precipitates an episode of vertigo or disequilibrium. Taste Deficit Xerostomia: Decrease in salivary production that leads to thicker mucus and a dry mouth. Often interferes with the ability to eat and leads to appetite and nutritional problems. Neurological Deficits Peripheral neuropathy: Disorder of the peripheral nervous system, characterized by symptoms that include numbness and tingling of the affected area and stumbling gait. Stroke: Cerebrovascular accident caused by clot, hemorrhage, or emboli disrupting blood flow to the brain. Creates altered proprioception with marked incoordination and imbalance. Loss of sensation and motor function in extremities controlled by the affected area of the brain also occurs. A stroke affecting the left hemisphere of the brain results in symptoms on the right side such as difficulty with speech. A stroke on the right hemisphere has symptoms on the left side, which includes visual spatial alterations such as loss of half of a visual field or inattention and neglect, especially to the left side. Sensory Deprivation The reticular activating system in the brainstem mediates all sensory stimuli to the cerebral cortex; thus patients are able to receive stimuli even while sleeping deeply. Sensory stimulation must be of sufficient quality and quantity to maintain a person’s awareness. Three types of sensory deprivation are reduced sensory input (sensory deficit from visual or hearing loss), the elimination of patterns or meaning from input (e.g., exposure to strange environments), and restrictive environments (e.g., bed rest) that produce monotony and boredom ( Ebersole et al., 2008 ). There are many effects of sensory deprivation ( Box 49-2 ). In adults the symptoms are similar to psychological illness, confusion, symptoms of severe electrolyte imbalance, or the influence of psychotropic drugs. Therefore always be aware of a patient’s existing sensory function and the quality of stimuli within the environment. Box 49-2 Effects of Sensory Deprivation Cognitive • Reduced capacity to learn • Inability to think or problem solve • Poor task performance • Disorientation • Bizarre thinking • Increased need for socialization, altered mechanisms of attention Affective • Boredom • Restlessness • Increased anxiety • Emotional lability • Panic • Increased need for physical stimulation Perceptual • Changes in visual/motor coordination • Reduced color perception • Less tactile accuracy • Changes in ability to perceive size and shape • Changes in spatial and time judgment Modified from Ebersole P et al.: Toward healthy aging: human needs and nursing response, ed 7, St Louis, 2008, Mosby. Sensory Overload When a person receives multiple sensory stimuli and cannot perceptually disregard or selectively ignore some stimuli, sensory overload occurs. Excessive sensory stimulation prevents the brain from responding appropriately to or ignoring certain stimuli. Because of the multitude of stimuli leading to overload, a person no longer perceives the environment in a way that makes sense. Overload prevents meaningful response by the brain; the patient’s thoughts race, attention scatters in many directions, and anxiety and restlessness occur. As a result, overload causes a state similar to that produced by sensory deprivation. However, in contrast to deprivation, overload is individualized. The amount of stimuli necessary for healthy function varies with each individual. People are often subject to environmental overload more at one time than another. A person’s tolerance to sensory overload varies with level of fatigue, attitude, and emotional and physical well-being. The acutely ill patient easily experiences sensory overload. The patient in constant pain or who undergoes frequent monitoring of vital signs is at risk. Multiple stimuli combine to cause overload even if the nurse offers a comforting word or provides a gentle back rub. Some patients do not benefit from nursing intervention because their attention and energy are focused on more stressful stimuli. Another example is a patient who is hospitalized in an intensive care unit (ICU), where the activity is constant. Lights are always on. Patients can hear sounds from monitoring equipment, staff conversations, equipment alarms, and the activities of people entering the unit. Even at night an ICU is very noisy. It is easy to confuse the behavioral changes associated with sensory overload with mood swings or simple disorientation. Look for symptoms such as racing thoughts, scattered attention, restlessness, and anxiety. Patients in ICUs sometimes resort to constantly fingering tubes and dressings. Constant reorientation and control of excessive stimuli become an important part of a patient’s care. Nursing Knowledge Base Factors Influencing Sensory Function Many factors influence the capacity to receive or perceive stimuli. All are conditions or situations that you manage when delivering care. Age Infants and children are at risk for visual and hearing impairment because of a number of genetic, prenatal, and postnatal conditions. A concern with high-risk neonates is that early, intense visual and auditory stimulation can adversely affect visual and auditory pathways and alter the developmental course of other sensory organs ( Hockenberry and Wilson, 2011 ). Visual changes during adulthood include presbyopia and the need for glasses for reading. These changes usually occur from ages 40 to 50. In addition, the cornea, which assists with light refraction to the retina, becomes flatter and thicker. These aging changes lead to astigmatism. Pigment is lost from the iris, and collagen fibers build up in the anterior chamber, which increases the risk of glaucoma by decreasing the resorption of intraocular fluid. Other normal visual changes associated with aging include reduced visual fields, increased glare sensitivity, impaired night vision, reduced depth perception, and reduced color discrimination. Hearing changes begin at the age of 30. Changes associated with aging include decreased hearing acuity, speech intelligibility, and pitch discrimination. Low-pitched sounds are easiest to hear, but it is difficult to hear conversation over background noise. It is also difficult to discriminate the consonants (z, t, f, g) and high-frequency sounds (s, sh, ph, k). Vowels that have a low pitch are easiest to hear. Speech sounds are distorted, and there is a delayed reception and reaction to speech. A concern with normal age-related sensory changes is that older adults with a deficit are sometimes inappropriately diagnosed with dementia ( Ebersole et al., 2008 ). Gustatory and olfactory changes begin around age 50 and include a decrease in the number of taste buds and sensory cells in the nasal lining. Reduced taste discrimination and sensitivity to odors are common. Proprioceptive changes common after age 60 include increased difficulty with balance, spatial orientation, and coordination. Older adults cannot avoid obstacles as quickly, and the automatic response to protect and brace oneself when falling is slower. Older adults experience tactile changes, including declining sensitivity to pain, pressure, and temperature secondary to peripheral vascular disease and neuropathies. Meaningful Stimuli Meaningful stimuli reduce the incidence of sensory deprivation. In the home meaningful stimuli include pets, music, television, pictures of family members, and a calendar and clock. The same stimuli need to be present in health care settings. Note whether patients have roommates or visitors. The presence of others offers positive stimulation. However, a roommate who constantly watches television, persistently tries to talk, or continuously keeps lights on contributes to sensory overload. The presence or absence of meaningful stimuli influences alertness and the ability to participate in care. Amount of Stimuli Excessive stimuli in an environment causes sensory overload. The frequency of observations and procedures performed in an acute health care setting are often stressful. If a patient is in pain or restricted by a cast or traction, overstimulation frequently is a problem. In addition, a room that is near repetitive or loud noises (e.g., an elevator, stairwell, or nurses’ station) contributes to sensory overload. Social Interaction The amount and quality of social contact with supportive family members and significant others influence sensory function. The absence of visitors during hospitalization or residency in an extended care facility influences the degree of isolation a patient feels. This is a common problem in hospital intensive care settings, where visitation is often restricted. The ability to discuss concerns with loved ones is an important coping mechanism for most people. Therefore the absence of meaningful conversation results in feelings of isolation, loneliness, anxiety, and depression for a patient. Often this is not apparent until behavioral changes occur. Environmental Factors A person’s occupation places him or her at risk for hearing, visual, and peripheral nerve alterations. Individuals who have occupations involving exposure to high noise levels (e.g., factory or airport workers) are at risk for noise-induced hearing loss and need to be screened for hearing impairments. Hazardous noise is common in work settings and recreational activities. Noisy recreational activities that weaken hearing ability include target shooting and hunting, woodworking, and listening to loud music. Individuals who have occupations involving risk of exposure to chemicals or flying objects (e.g., welders) are at risk for eye injuries and need to be screened for visual impairments. Sports activities and consumer fireworks also place individuals at risk for visual alterations. Occupations that involve repetitive wrist or finger movements (e.g., heavy assembly line work) cause pressure on the median nerve, resulting in carpal tunnel syndrome. Carpal tunnel syndrome alters tactile sensation and is one of the most common industrial or work-related injuries. Patients at risk for carpal tunnel need to be carefully assessed for numbness, tingling, weakness, and pain. A hospitalized patient is sometimes at risk for sensory alterations as a result of exposure to environmental stimuli or a change in sensory input. Patients who are immobilized by bed rest or who have a chronic disability are unable to experience all of the normal sensations of free movement. Another group at risk includes patients isolated in a health care setting or at home because of conditions such as active tuberculosis (see Chapter 28 ). These patients stay in private rooms and are often unable to enjoy normal interactions with visitors. Cultural Factors Certain sensory alterations occur more commonly in select ethnic groups. Analysis of data from the African Descent and Glaucoma Evaluation study (ADAGES) showed that people of African ethnicity perform significantly worse than people of European descent on tests of visual function ( Racette et al., 2010 ). Cultural disparities in vision impairment are significant, in part because visual impairment may be indirectly associated with an increased risk of suicide through poor self-rated health ( Lam et al., 2008 ). Box 49-3 summarizes additional sensory alterations that are associated with a patient’s cultural heritage. Box 49-3 Cultural Aspects of Care Disparities in Sensory Alteration Studies indicate that differences in sensory impairments exist among ethnic groups. Non-Hispanic white and Mexican-American people have a higher prevalence of hearing problems than non-Hispanic black people ( Dillon et al., 2010 ). Latinos have higher rates of developing visual impairment, blindness, diabetic eye disease, and cataracts than non-Hispanic whites ( National Eye Institute, 2010a ). Whites have a higher incidence of age-related macular degeneration than people of African descent ( National Eye Institute, 2010b ). Although early diagnosis and treatment may slow the progression of sensory impairments, patients do not always volunteer information about impairments. They often focus on other symptoms or medical conditions, or they do not think that their primary care physician is the right person to talk to ( Rosenberg and Sperazza, 2008 ). Implications for Practice • Encourage patients to discuss sensory impairments by asking a few simple but focused questions. • Enhance your knowledge of the services available to patients with sensory impairments and educate patients about the organizations that exist to provide assistance. • Facilitate access to services to promote the early detection and treatment of sensory impairments. • Identify the patient’s preferred method of communication—use an interpreter service if needed. • Ensure that health information is available in the appropriate language and format (e.g., large print). Critical Thinking Successful critical thinking requires a synthesis of knowledge and information gathered from patients, experience, critical thinking attitudes, and intellectual and professional standards. Clinical judgments require you to anticipate the information necessary, analyze the data, and make decisions regarding patient care. Patients’ conditions are always changing. During assessment ( Fig. 49-1 ) consider all critical thinking elements that help you make appropriate nursing diagnoses. In the case of sensory alterations, integrate knowledge of the pathophysiology of sensory deficits, factors that affect sensory function, and therapeutic communication principles. This knowledge enables you to conduct appropriate assessments, anticipate what to recognize when a patient describes a sensory problem, and make judgments of any abnormalities. For example, knowing the typical symptoms caused by a cataract helps you recognize the pattern of visual changes that a patient with cataracts reports. FIG. 49-1 Critical thinking model for sensory alterations assessment. Previous experiences in caring for patients with sensory deficits enable nurses to recognize limitations in function in each new patient and how they affect the patient’s ability to carry out daily activities. For example, after caring for a patient with a hearing impairment, you are able to conduct a more effective assessment of the next patient by using approaches that promote the patient’s ability to hear your questions. When critical thinking attitudes and standards are applied during assessment, they ensure a thorough and accurate database from which to make decisions. For example, perseverance is necessary to learn details about how visual changes influence a patient’s ability to socialize. Evidence-based standards of care and practice such as those from the American Academy of Ophthalmology and the American Speech-Language-Hearing Association provide criteria for screening sensory problems and establishing standards for competent, safe, effective care and practice. Use critical thinking to conduct a thorough assessment and then plan, implement, and evaluate care that enables the patient to function safely and effectively ( Box 49-4 ). Box 49-4 Evidence-Based Practice Consequences of Waiting for Cataract Surgery PICO Question: Are adult patients who wait 6 months or longer for cataract surgery at increased risk for negative outcomes compared to patients who wait less than 6 months? Evidence Summary Cataracts are a major disease affecting vision. With appropriate evaluation this disease is readily diagnosed and treated. The high levels of efficacy and minimal complications associated with cataract surgery have led to a high demand for this procedure. Current literature shows that vision impairment is associated with impaired activities of daily living, social isolation, and decreased function ( Lam et al., 2008 ). Thus the development of evidence-based benchmarks for medically acceptable wait times has significant implications. Outcomes associated with wait times of less than 6 weeks are better than those associated with wait times more than 6 months. Patients who wait more than 6 months to have cataract surgery typically experience more vision loss, a reduced quality of life, and an increased rate of falls compared with patients who wait less than 6 weeks ( Hodge et al., 2007 ). Application to Nursing Practice • Facilitate the prompt referral of patients with cataracts to an ophthalmologist. • Before surgery provide all relevant information to patients about what happens before, during, and after surgery ( Wasfi and Abd-Elsayed, 2008 ). • Ensure that all patients receive written information to minimize anxiety ( Wasfi and Abd-Elsayed, 2008 ). • Encourage patients to access support from others with visual impairments. • During the wait period help to identify creative strategies to promote self-care. Nursing Process Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care for your patients. Assessment During the assessment process, thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care. Through the Patient’s Eyes When conducting an assessment, value the patient as a full partner in planning, implementing, and evaluating care. Patients are often hesitant to admit sensory losses. Therefore start gathering information by establishing a therapeutic rapport with the patient. Elicit his or her values, preferences, and expectations with regard to his or her sensory impairment. Many patients have a definite plan as to how they want their care delivered. Some patients expect caregivers to recognize and appropriately manage and adjust their environment to meet their sensory needs. This includes helping the patient learn and adapt to a changed lifestyle based on the specific sensory impairment. Determine from the patient which interventions have been helpful in the past in the management of limitations. Assess the patient’s expertise with his or her own health and symptoms. Always remember that patients with sensory alterations have strengthened their other senses and expect caregivers to anticipate their needs (e.g., for safety and security). When assessing a patient with or at risk for sensory alteration, first consider the pathophysiology of existing deficits and the factors influencing sensory function to anticipate how to approach his or her assessment. For example, if a patient has a hearing disorder, adjust your communication style and focus the assessment on relevant criteria related to hearing deficits. Collect a history that also assesses the patient’s current sensory status and the degree to which a sensory deficit affects the patient’s lifestyle, psychosocial adjustment, developmental status, self-care ability, health promotion habits, and safety. Also focus the assessment on the quality and quantity of stimuli within the patient’s environment. Persons at Risk Older adults are a high-risk group because of normal physiological changes involving sensory organs. However, be careful not to automatically assume that a patient’s sensory problem is related to advancing age. For example, adult sensorineural hearing loss is often caused by exposure to excess and prolonged noise or metabolic, vascular, and other systemic alterations. Some patients benefit from a referral to an audiologist or otolaryngologist if assessment reveals serious hearing problems. Other individuals at risk for sensory alterations include those living in a confined environment such as a nursing home. Although most quality nursing homes or centers offer meaningful stimulation through group activities, environmental design, and mealtime gatherings, there are exceptions. The individual who is confined to a wheelchair, suffers from poor hearing and/or vision, has decreased energy, and avoids contact with others is at significant risk for sensory deprivation. If the environment creates monotony, the individual is less able to learn and think. Patients who are acutely ill are also at risk because of an unfamiliar and unresponsive environment. This does not mean that all hospitalized patients have sensory alterations. However, you need to carefully assess patients subjected to continued sensory stimulation (e.g., ICU settings, long-term hospitalization, or multiple therapies). Assess the patient’s environment within both the health care setting and the home, looking for factors that pose risks or need adjustment to provide safety and more stimulation. Sensory Alterations History The nursing history includes assessment of the nature and characteristics of sensory alterations or any problem related to an alteration ( Box 49-5 ). When taking the history, consider the ethnic or cultural background of the patient because certain alterations are higher in some cultural groups. Box 49-5 Nursing Assessment Questions Nature of the Problem • What type of problem are you having with your vision/hearing? • What have you tried to correct the vision/hearing difficulty? • Do you use any devices to improve your vision/hearing? Signs and Symptoms • Ask a patient with visual alterations: Do you require books with large print or on audiotape? Are you able to prepare a meal or write a check? • Ask a patient with hearing alterations: What types of sounds or tones do you have difficulty hearing? Do people tell you that they have to “shout” for you to hear them? Do you have a ringing, crackling, or buzzing in your ears? • Is there pain: sharp, dull, burning, itching? • Have you noticed any redness, swelling, or drainage? Any signs of infection? Onset and Duration • When did you notice the problem? How long has this problem lasted? • Does it come and go, or is it constant? Predisposing Factors • Do you work or participate in any activities that have the potential for vision/hearing injury? If so, how do you protect your hearing and vision? • Do you have a family history of cataracts, glaucoma, macular degeneration, or hearing loss? • When was your last vision/hearing examination? Effect on Patient • What effect has your vision/hearing problem had on your work, family, or social life? • Have changes in your vision/hearing affected your feelings of independence? • How does your vision/hearing problem make you feel about yourself? • Do you have problems with routine care of glasses, contact lenses, or hearing aids? During the history it is useful to assess the patient’s self-rating for a sensory deficit by asking, “Rate your hearing as excellent, good, fair, poor, or bad.” Then, based on the patient’s self-rating, explore his or her perception of a sensory loss more fully. This provides an in-depth look at how the sensory loss influences the patient’s quality of life. In the case of hearing problems, a screening tool such as the Hearing Handicap Inventory for the Elderly (HHIE-S) effectively identifies patients needing audiological intervention. The HHIE-S is a 5-minute, 10-item questionnaire that assesses how the individual perceives the social and emotional effects of hearing loss. The higher the HHIE-S score, the greater the handicapping effect of a hearing impairment. A nursing history also reveals any recent changes in a patient’s behavior. Frequently friends or family are the best resources for this information. Ask the family the following questions: • Has your family member shown any recent mood swings (e.g., outbursts of anger, nervousness, fear, or irritability)? • Have you noticed the family member avoiding social activities? Mental Status Assessment of mental status is valuable when you suspect sensory deprivation or overload. Observation of a patient during history taking, during the physical examination (see Chapter 30 ), and while providing nursing care offers valuable data about key patient behaviors and his or her mental status. Observe the patient’s physical appearance and behavior, measure cognitive ability, and assess his or her emotional status. The Mini-Mental State Examination (MMSE) is a tool you can use to measure disorientation, change in problem-solving abilities, and altered conceptualization and abstract thinking (see Chapter 30 ). For example, a patient with severe sensory deprivation is not always able to carry on a conversation, remain attentive, or display recent or past memory. An important step toward preventing cognition-related disability is education by nurses about disease process, available services, and assistive devices. Physical Assessment To identify sensory deficits and their severity, use physical assessment techniques to assess vision, hearing, olfaction, taste, and the ability to discriminate light touch, temperature, pain, and position (see Chapter 30 ). Table 49-2 summarizes specific assessment techniques for identifying sensory deficits. You gather more accurate data if the examination room is private, quiet, and comfortable for the patient. In addition, rely on personal observation to detect sensory alterations. Patients with a hearing impairment may seem inattentive to others, respond with inappropriate anger when spoken to, believe people are talking about them, answer questions inappropriately, have trouble following clear directions, and have monotonous voice quality and speak unusually loud or soft. TABLE 49-2 Assessment of Sensory Function ASSESSMENT ACTIVITIES BEHAVIOR INDICATING DEFICIT (CHILDREN) BEHAVIOR INDICATING DEFICIT (ADULTS) Vision Ask patient to read newspaper, magazine, or lettering on menu. Ask patient to identify colors on color chart or crayons. Observe patients performing ADLs. Self-stimulation, including eye rubbing, body rocking, sniffing or smelling, arm twirling; hitching (using legs to propel while in sitting position) instead of crawling Poor coordination, squinting, underreaching or overreaching for objects, persistent repositioning of objects, impaired night vision, accidental falls Hearing Assess patient’s hearing acuity (see Chapter 30 ) using spoken word and tuning fork tests. Assess for history of tinnitus. Observe patient conversing with others. Inspect ear canal for hardened cerumen. Observe patient behaviors in a group.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Legal Implications in Nursing Practice
- Young and Middle Adults
- Nursing Diagnosis
- Stress and Coping
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Instructional Materials
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning
MyNSTA Community
- My Collections
Wearing on Her Nerves
Exploring the Interrelation between the Nervous and Muscular Systems
By Kathleen G. Brown, Sharon S. Ellerton
Share Start a Discussion
This case study is designed to integrate important aspects of the nervous and muscular system portions of an anatomy and physiology course. Students follow the story of “Kathy,” whose symptoms involve both sensory and motor components of the nervous system. The students must recognize the key factors of nerve transmission, examine where there could be interruption, and recognize how the interruption would affect body function. They also need to identify the role that the nervous system plays in muscular function. Through the case, students explore the relationship between both body systems, consider how one affects the other, and discover how function can be affected by external factors.
Download Case
Date Posted
- Understand the direction and components of a sensory impulse.
- Understand the direction and components of a motor impulse.
- Learn about the structure and function of myelin and Nodes of Ranvier.
- Learn about the anatomy and physiology of muscle contraction.
- Learn about the muscles involved in specific body movements.
- Learn about the symptoms, indicators, and diagnosis of multiple sclerosis.
Nervous system; muscular system; neurophysiology; neuron; axon; myelin; myelin sheath; Nodes of Ranvier; nerve transmission; sensory function; motor function; motor impulse; muscle fiber; muscle contraction; multiple sclerosis; degenerative disease
Subject Headings
EDUCATIONAL LEVEL
Undergraduate lower division, Professional, Clinical
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials, you may also like.
Web Seminar
Join us on Tuesday, June 4, 2024, from 7:00 PM to 8:30 PM ET, to learn about the free lesson plans and storyline units designed for high school studen...
Join us on Thursday, October 24, 2024, from 7:00 PM to 8:00 PM ET, to learn about all NSTA Teacher Awards available and how to apply.Did you come up w...
Brain mechanisms underlying sensory hypersensitivity in a mouse model of autism spectrum disorder
Sensory hypersensitivity in grin2b-mutant mice linked to acc hyperactivity and brain-wide hyperconnectivity.
A research team led by Director KIM Eunjoon of the Center for Synaptic Brain Dysfunctions and Director KIM Seong-Gi of the Center for Neuroscience Imaging Research within the Institute for Basic Science (IBS) has identified the primary cause of sensory hypersensitivity related to autism spectrum disorders (ASD).
Autism affects approximately 1 in 36 individuals and is marked by significant challenges in social interaction and communication. Around 90% of autism patients also suffer from abnormal sensory hypersensitivity that deeply affects their daily functioning. This hypersensitivity results in exaggerated or dampened responses to common sensory stimuli such as sound, light, and touch, which leads to considerable stress and further social withdrawal. The precise brain region responsible for this sensory dysfunction is unknown, which hinders treatment efforts.
The IBS researchers studied an ASD mouse model with a mutation in the Grin2b gene, which encodes the GluN2B subunit of NMDA receptors. NMDA receptors, a type of glutamate receptor in the brain, have garnered attention in the context of autism due to their crucial role in synaptic transmission and neural plasticity. It was hypothesized that the Grin2b gene mutation in mice would induce ASD-like phenotypes, including sensory abnormalities, and that certain brain mechanisms may play important roles.
The researchers monitored neural activity and functional connectivity in the brains of these mice using activity-dependent markers and functional magnetic resonance imaging (fMRI). In these mice, the researchers discovered increased neuronal activity in the anterior cingulate cortex (ACC). The ACC is one of the higher-order cortical regions that have been extensively studied for cognitive and emotional brain functions, but have been understudied for brain disease-related sensory abnormalities.
Interestingly, when the hyperactivity of ACC neurons was inhibited using chemogenetic methods, sensory hypersensitivity were normalized, indicating the pivotal role of ACC hyperactivity in sensory hypersensitivity associated with autism.
Director KIM Eunjoon states, "This new research demonstrates the involvement of the anterior cingulate cortex (ACC), which has been known for its deep association with cognitive and social functions, in sensory hypersensitivity in autism."
The hyperactivity of the ACC was also associated with the enhanced functional connectivity between the ACC and other brain areas. It is believed both hyperactivity and the hyperconnectivity of the ACC with various other brain regions are involved with sensory hypersensitivity in Grin2b-mutant mice.
Director KIM Seong-Gi states, "Past studies attributed peripheral neurons or primary cortical areas to be important for ASD-related sensory hypersensitivity. These studies often only focused on the activity of a single brain region. In contrast, our study investigates not only the activity of ACC but also the brain-wide hyperconnectivity between the ACC and various cortical/subcortical brain regions, which gives us a more complete picture of the brain."
The researchers plan to study the detailed mechanisms underlying the increased excitatory synaptic activity and neuronal hyperconnectivity. They suspect that the lack of Grin2b expression may inhibit the normal process of weakening and pruning synapses that are less active so that relatively more active synapses can participate in refining neural circuits in an activity-dependent manner. Other areas of research interest is studying the role of ACC in other mouse models of ASD.
This study was published in the journal Molecular Psychiatry.
- Nervous System
- Birth Defects
- Brain Tumor
- Neuroscience
- Learning Disorders
- Animal Learning and Intelligence
- Autistic spectrum
- Sensory system
- Asperger syndrome
- House mouse
Story Source:
Materials provided by Institute for Basic Science . Note: Content may be edited for style and length.
Journal Reference :
- Soowon Lee, Won Beom Jung, Heera Moon, Geun Ho Im, Young Woo Noh, Wangyong Shin, Yong Gyu Kim, Jee Hyun Yi, Seok Jun Hong, Yongwhan Jung, Sunjoo Ahn, Seong-Gi Kim, Eunjoon Kim. Anterior cingulate cortex-related functional hyperconnectivity underlies sensory hypersensitivity in Grin2b-mutant mice . Molecular Psychiatry , 2024; DOI: 10.1038/s41380-024-02572-y
Cite This Page :
Explore More
- Life Expectancy May Increase by 5 Years by 2050
- Toward a Successful Vaccine for HIV
- Highly Efficient Thermoelectric Materials
- Toward Human Brain Gene Therapy
- Whale Families Learn Each Other's Vocal Style
- AI Can Answer Complex Physics Questions
- Otters Use Tools to Survive a Changing World
- Monogamy in Mice: Newly Evolved Type of Cell
- Sustainable Electronics, Doped With Air
- Male Vs Female Brain Structure
Trending Topics
Strange & offbeat.

IMAGES
VIDEO
COMMENTS
HESI Case Study: Sensory Function. During the initial interview, the registered nurse inspects the external anatomy of the eye. the eye is a sensory organ of vision, and it is well protected by a bony orbital cavity and surrounded with a cushion of fat. the nurse notes that the cornea looks cloudy and an arcus senilis is seen around the cornea.
Disturbed sensory alteration (auditory). Clients with impaired hearing often smile and nod in agreement with the person conversing even though they are unable to clearly hear the conversation. Appearing to be inattentive, speaking loudly, and difficulty following directions are other indications of a disturbance in auditory sensory function.
The sensory system receives and processes information that generates an individual's awareness of their environment. ... each with their own specific function, generate the overall sense of touch, position in space, and pain. ... The role of glutamate in neuronal ion homeostasis: A case study of spreading depolarization. PLoS Comput Biol. 2017 ...
Schaaf RC, Nightlinger KM. Occupational therapy using a sensory integrative approach: A case study of effectiveness. American Journal of Occupational Therapy. 2007; 61:239-246. [Google Scholar] Shoener RF, Kinnealey M, Koenig KP. You can know me now if you listen: Sensory, motor, and communication issues in a nonverbal person with autism.
Using the case study example, apply clinical decision-making skills to application of sensory examination data. SENSORY INTEGRATION If all of the sensory stimuli which enter the central nervous system were allowed to bombard the higher centers of the brain, the individual would be rendered utterly ineffective.
Free Evolve Hesi Case Study Sensory Function Roger Caillois Lewis's Medical-Surgical Nursing Mariann M. Harding,Jeffrey Kwong,Debra Hagler,2022-09 Kinesiology David Paul Greene,Susan L. Roberts,2005-01-01 Approaching the subject of kinesiology from the perspective of occupational therapy, this unique text written by occupational therapists ...
Literature Search. A systematic literature review was conducted to identify study abstracts for screening. The databases used included PubMed/Medline, Embase, Cochrane, and Google Scholar databases using the controlled terms: "Humans" and "Peripheral nerve injuries" and "sensory" or "pain" or "function" or "assessment" or "recovery" or "outcome."
ROCHESTER, Minn. — Stem cells derived from a patient's own fat offer a step toward improving — not just stabilizing — motor and sensory function of people with spinal cord injuries, according to early research from Mayo Clinic. A clinical trial enrolled 10 adults to treat paralysis from traumatic spinal cord injury. After stem cell […]
Sensory Function Case Study- 93%. Study with Quizlet and memorize flashcards containing terms like Meet the Client A client visits the primary care health clinic where they tell the nurse that their vision is getting really bad. The client reports having to turn up the volume on the television pretty loud to hear clearly.
Admittedly, neuroplastic changes and associated behavioural gains in the case of late-onset sensory deprivation are less clear and relatively few studies have addressed this issue.
Fun and Function Sensory Room Case Studies. Every sensory room starts with a story. Get a glimpse into the background, vision, and design process behind some of our best sensory spaces. ...
The purpose of this case study was to explore the effects of a school-based occupational therapy on children's attention, school adaptation, sensory processing, and motor function for children in special classes in elementary school in Korea. The subjects of this study were a 7-year-old boy with autism spectrum disorder and a 9-year-old girl with intellectual disability.
Reception, perception, and reaction are the three components of any sensory experience (see Chapter 43).Reception begins with stimulation of a nerve cell called a receptor, which is usually for only one type of stimulus such as light, touch, or sound. In the case of special senses, the receptors are grouped close together or located in specialized organs such as the taste buds of the tongue or ...
Abstract. This case study is designed to integrate important aspects of the nervous and muscular system portions of an anatomy and physiology course. Students follow the story of "Kathy," whose symptoms involve both sensory and motor components of the nervous system. The students must recognize the key factors of nerve transmission, examine ...
HESI Case Study: Sensory Function. Fred Johnson, a 76-year-old retired farmer, visits the Health Clinic where he tells the nurse that his vision is getting "awful blurry lately" and that he finds he has to "have the television up pretty loud" to hear clearly. The nurse prepares to complete an assessment of Fred's sensory function.
and it is well pr. rn hesi case study - sensory function 1 assessment during the initial interview. the registered nurse inspects the external anatomy of the eye the eye is a sensory organ of vision.
Exam (elaborations) $20.49. Also available in package deal from $28.99. Add to cart Add to wishlist. 100% satisfaction guarantee. Immediately available after payment. Both online and in PDF. No strings attached. 23.
A case study demonstrates the usefulness of this approach. Functional neurological disorder (FND) is characterized by motor and sensory symptoms that are unexplained by traditional neurological or medical conditions. 1,2 Patients with FND do not demonstrate lesional disease. 1,2 They experience neurological symptoms involving the voluntary ...
Chronic middle ear infection is associated with hearing loss. Additionally, clients should be aware that medications, such as some antibiotics and large doses of aspirin, can be ototoxic. Week 10 Hesi Sensory Function Case Study Learn with flashcards, games, and more — for free.
Mar. 2, 2020 — A study reveals a neural circuit that appears to underlie sensory hypersensitivity in a mouse model of autism, offering a possible strategy for developing new ... Print Email Share