
Herb-drug interactions: A literature review
- Children's Medical Center Research Institute At Ut Southwestern
Research output : Contribution to journal › Review article › peer-review
Herbs are often administered in combination with therapeutic drugs, raising the potential of herb-drug interactions. An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations. Cases have been published reporting enhanced anticoagulation and bleeding when patients on long-term warfarin therapy also took Salvia miltiorrhiza (danshen). Allium sativum (garlic) decreased the area under the plasma concentration-time curve (AUC) and maximum plasma concentration of saquinavir, but not ritonavir and paracetamol (acetaminophen), in volunteers. A. sativum increased the clotting time and international normalised ratio of warfarin and caused hypoglycaemia when taken with chlorpropamide. Ginkgo biloba (ginkgo) caused bleeding when combined with warfarin or aspirin (acetylsalicylic acid), raised blood pressure when combined with a thiazide diuretic and even caused coma when combined with trazodone in patients. Panax ginseng (ginseng) reduced the blood concentrations of alcohol (ethanol) and warfarin, and induced mania when used concomitantly with phenelzine, but ginseng increased the efficacy of influenza vaccination. Scutellaria baicalensis (huangqin) ameliorated irinotecan-induced gastrointestinal toxicity in cancer patients. Piper methysticum (kava) increased the 'off' periods in patients with parkinsonism taking levodopa and induced a semicomatose state when given concomitantly with alprazolam. Kava enhanced the hypnotic effect of alcohol in mice, but this was not observed in humans. Silybum marianum (milk thistle) decreased the trough concentrations of indinavir in humans. Piperine from black (Piper nigrum Linn) and long (P. longum Linn) peppers increased the AUC of phenytoin, propranolol and theophylline in healthy volunteers and plasma concentrations of rifamipicin (rifampin) in patients with pulmonary tuberculosis. Eleutheroccus senticosus (Siberian ginseng) increased the serum concentration of digoxin, but did not alter the pharmacokinetics of dextromethorphan and alprazolam in humans. Hypericum perforatum (hypericum; St John's wort) decreased the blood concentrations of ciclosporin (cyclosporin), midazolam, tacrolimus, amitriptyline, digoxin, indinavir, warfarin, phenprocoumon and theophylline, but did not alter the pharmacokinetics of carbamazepine, pravastatin, mycophenolate mofetil and dextromethorphan. Cases have been reported where decreased ciclosporin concentrations led to organ rejection. Hypericum also caused breakthrough bleeding and unplanned pregnancies when used concomitantly with oral contraceptives. It also caused serotonin syndrome when used in combination with selective serotonin reuptake inhibitors (e.g. sertraline and paroxetine). In conclusion, interactions between herbal medicines and prescribed drugs can occur and may lead to serious clinical consequences. There are other theoretical interactions indicated by preclinical data. Both pharmacokinetic and/or pharmacodynamic mechanisms have been considered to play a role in these interactions, although the underlying mechanisms for the altered drug effects and/or concentrations by concomitant herbal medicines are yet to be determined. The clinical importance of herb-drug interactions depends on many factors associated with the particular herb, drug and patient. Herbs should be appropriately labeled to alert consumers to potential interactions when concomitantly used with drugs, and to recommend a consultation with their general practitioners and other medical carers.
| Original language | English (US) |
|---|---|
| Pages (from-to) | 1239-1282 |
| Number of pages | 44 |
| Journal | |
| Volume | 65 |
| Issue number | 9 |
| DOIs | |
| State | Published - 2005 |
ASJC Scopus subject areas
- Pharmacology (medical)
Access to Document
- 10.2165/00003495-200565090-00005
Other files and links
- Link to publication in Scopus
Fingerprint
- Herb-Drug Interactions Medicine & Life Sciences 100%
- Warfarin Medicine & Life Sciences 58%
- Kava Medicine & Life Sciences 53%
- Hypericum Medicine & Life Sciences 47%
- Garlic Medicine & Life Sciences 43%
- Panax Medicine & Life Sciences 41%
- Milk Thistle Medicine & Life Sciences 34%
- Scutellaria baicalensis Medicine & Life Sciences 32%
T1 - Herb-drug interactions
T2 - A literature review
AU - Hu, Zeping
AU - Yang, Xiaoxia
AU - Ho, Paul Chi Lui
AU - Sui, Yung Chan
AU - Heng, Paul Wan Sia
AU - Chan, Eli
AU - Duan, Wei
AU - Hwee, Ling Koh
AU - Zhou, Shufeng
N2 - Herbs are often administered in combination with therapeutic drugs, raising the potential of herb-drug interactions. An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations. Cases have been published reporting enhanced anticoagulation and bleeding when patients on long-term warfarin therapy also took Salvia miltiorrhiza (danshen). Allium sativum (garlic) decreased the area under the plasma concentration-time curve (AUC) and maximum plasma concentration of saquinavir, but not ritonavir and paracetamol (acetaminophen), in volunteers. A. sativum increased the clotting time and international normalised ratio of warfarin and caused hypoglycaemia when taken with chlorpropamide. Ginkgo biloba (ginkgo) caused bleeding when combined with warfarin or aspirin (acetylsalicylic acid), raised blood pressure when combined with a thiazide diuretic and even caused coma when combined with trazodone in patients. Panax ginseng (ginseng) reduced the blood concentrations of alcohol (ethanol) and warfarin, and induced mania when used concomitantly with phenelzine, but ginseng increased the efficacy of influenza vaccination. Scutellaria baicalensis (huangqin) ameliorated irinotecan-induced gastrointestinal toxicity in cancer patients. Piper methysticum (kava) increased the 'off' periods in patients with parkinsonism taking levodopa and induced a semicomatose state when given concomitantly with alprazolam. Kava enhanced the hypnotic effect of alcohol in mice, but this was not observed in humans. Silybum marianum (milk thistle) decreased the trough concentrations of indinavir in humans. Piperine from black (Piper nigrum Linn) and long (P. longum Linn) peppers increased the AUC of phenytoin, propranolol and theophylline in healthy volunteers and plasma concentrations of rifamipicin (rifampin) in patients with pulmonary tuberculosis. Eleutheroccus senticosus (Siberian ginseng) increased the serum concentration of digoxin, but did not alter the pharmacokinetics of dextromethorphan and alprazolam in humans. Hypericum perforatum (hypericum; St John's wort) decreased the blood concentrations of ciclosporin (cyclosporin), midazolam, tacrolimus, amitriptyline, digoxin, indinavir, warfarin, phenprocoumon and theophylline, but did not alter the pharmacokinetics of carbamazepine, pravastatin, mycophenolate mofetil and dextromethorphan. Cases have been reported where decreased ciclosporin concentrations led to organ rejection. Hypericum also caused breakthrough bleeding and unplanned pregnancies when used concomitantly with oral contraceptives. It also caused serotonin syndrome when used in combination with selective serotonin reuptake inhibitors (e.g. sertraline and paroxetine). In conclusion, interactions between herbal medicines and prescribed drugs can occur and may lead to serious clinical consequences. There are other theoretical interactions indicated by preclinical data. Both pharmacokinetic and/or pharmacodynamic mechanisms have been considered to play a role in these interactions, although the underlying mechanisms for the altered drug effects and/or concentrations by concomitant herbal medicines are yet to be determined. The clinical importance of herb-drug interactions depends on many factors associated with the particular herb, drug and patient. Herbs should be appropriately labeled to alert consumers to potential interactions when concomitantly used with drugs, and to recommend a consultation with their general practitioners and other medical carers.
AB - Herbs are often administered in combination with therapeutic drugs, raising the potential of herb-drug interactions. An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations. Cases have been published reporting enhanced anticoagulation and bleeding when patients on long-term warfarin therapy also took Salvia miltiorrhiza (danshen). Allium sativum (garlic) decreased the area under the plasma concentration-time curve (AUC) and maximum plasma concentration of saquinavir, but not ritonavir and paracetamol (acetaminophen), in volunteers. A. sativum increased the clotting time and international normalised ratio of warfarin and caused hypoglycaemia when taken with chlorpropamide. Ginkgo biloba (ginkgo) caused bleeding when combined with warfarin or aspirin (acetylsalicylic acid), raised blood pressure when combined with a thiazide diuretic and even caused coma when combined with trazodone in patients. Panax ginseng (ginseng) reduced the blood concentrations of alcohol (ethanol) and warfarin, and induced mania when used concomitantly with phenelzine, but ginseng increased the efficacy of influenza vaccination. Scutellaria baicalensis (huangqin) ameliorated irinotecan-induced gastrointestinal toxicity in cancer patients. Piper methysticum (kava) increased the 'off' periods in patients with parkinsonism taking levodopa and induced a semicomatose state when given concomitantly with alprazolam. Kava enhanced the hypnotic effect of alcohol in mice, but this was not observed in humans. Silybum marianum (milk thistle) decreased the trough concentrations of indinavir in humans. Piperine from black (Piper nigrum Linn) and long (P. longum Linn) peppers increased the AUC of phenytoin, propranolol and theophylline in healthy volunteers and plasma concentrations of rifamipicin (rifampin) in patients with pulmonary tuberculosis. Eleutheroccus senticosus (Siberian ginseng) increased the serum concentration of digoxin, but did not alter the pharmacokinetics of dextromethorphan and alprazolam in humans. Hypericum perforatum (hypericum; St John's wort) decreased the blood concentrations of ciclosporin (cyclosporin), midazolam, tacrolimus, amitriptyline, digoxin, indinavir, warfarin, phenprocoumon and theophylline, but did not alter the pharmacokinetics of carbamazepine, pravastatin, mycophenolate mofetil and dextromethorphan. Cases have been reported where decreased ciclosporin concentrations led to organ rejection. Hypericum also caused breakthrough bleeding and unplanned pregnancies when used concomitantly with oral contraceptives. It also caused serotonin syndrome when used in combination with selective serotonin reuptake inhibitors (e.g. sertraline and paroxetine). In conclusion, interactions between herbal medicines and prescribed drugs can occur and may lead to serious clinical consequences. There are other theoretical interactions indicated by preclinical data. Both pharmacokinetic and/or pharmacodynamic mechanisms have been considered to play a role in these interactions, although the underlying mechanisms for the altered drug effects and/or concentrations by concomitant herbal medicines are yet to be determined. The clinical importance of herb-drug interactions depends on many factors associated with the particular herb, drug and patient. Herbs should be appropriately labeled to alert consumers to potential interactions when concomitantly used with drugs, and to recommend a consultation with their general practitioners and other medical carers.
UR - http://www.scopus.com/inward/record.url?scp=22844441147&partnerID=8YFLogxK
UR - http://www.scopus.com/inward/citedby.url?scp=22844441147&partnerID=8YFLogxK
U2 - 10.2165/00003495-200565090-00005
DO - 10.2165/00003495-200565090-00005
M3 - Review article
C2 - 15916450
AN - SCOPUS:22844441147
SN - 0012-6667
Advertisement
Herb-Drug Interactions
A Literature Review
- Review Article
- Published: 17 September 2012
- Volume 65 , pages 1239–1282, ( 2005 )
Cite this article

- Zeping Hu 1 ,
- Xiaoxia Yang 1 ,
- Paul Chi Lui Ho 1 ,
- Sui Yung Chan 1 ,
- Paul Wan Sia Heng 1 ,
- Eli Chan 1 ,
- Wei Duan 2 ,
- Hwee Ling Koh 1 &
- Shufeng Zhou 1
6717 Accesses
470 Citations
32 Altmetric
Explore all metrics
Herbs are often administered in combination with therapeutic drugs, raising the potential of herb-drug interactions. An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations.
Cases have been published reporting enhanced anticoagulation and bleeding when patients on long-term warfarin therapy also took Salvia miltiorrhiza (danshen). Allium sativum (garlic) decreased the area under the plasma concentration-time curve (AUC) and maximum plasma concentration of saquinavir, but not ritonavir and paracetamol (acetaminophen), in volunteers. A. sativum increased the clotting time and international normalised ratio of warfarin and caused hypoglycaemia when taken with chlorpropamide. Ginkgo biloba (ginkgo) caused bleeding when combined with warfarin or aspirin (acetylsalicylic acid), raised blood pressure when combined with a thiazide diuretic and even caused coma when combined with trazodone in patients. Panax ginseng (ginseng) reduced the blood concentrations of alcohol (ethanol) and warfarin, and induced mania when used concomitantly with phenelzine, but ginseng increased the efficacy of influenza vaccination. Scutellaria baicalensis (huangqin) ameliorated irinotecan-induced gastrointestinal toxicity in cancer patients.
Piper methysticum (kava) increased the ‘off’ periods in patients with parkinsonism taking levodopa and induced a semicomatose state when given concomitantly with alprazolam. Kava enhanced the hypnotic effect of alcohol in mice, but this was not observed in humans. Silybum marianum (milk thistle) decreased the trough concentrations of indinavir in humans. Piperine from black ( Piper nigrum Linn ) and long ( P. longum Linn ) peppers increased the AUC of phenytoin, propranolol and theophylline in healthy volunteers and plasma concentrations of rifamipicin (rifampin) in patients with pulmonary tuberculosis. Eleutheroccus senticosus (Siberian ginseng) increased the serum concentration of digoxin, but did not alter the pharmacokinetics of dextromethorphan and alprazolam in humans. Hypericum perforatum (hypericum; St John’s wort) decreased the blood concentrations of ciclosporin (cyclosporin), midazolam, tacrolimus, amitriptyline, digoxin, indinavir, warfarin, phenprocoumon and theophylline, but did not alter the pharmacokinetics of carbamazepine, pravastatin, mycophenolate mofetil and dextromethorphan. Cases have been reported where decreased ciclosporin concentrations led to organ rejection. Hypericum also caused breakthrough bleeding and unplanned pregnancies when used concomitantly with oral contraceptives. It also caused serotonin syndrome when used in combination with selective serotonin reuptake inhibitors (e.g. sertraline and paroxetine).
In conclusion, interactions between herbal medicines and prescribed drugs can occur and may lead to serious clinical consequences. There are other theoretical interactions indicated by preclinical data. Both pharmacokinetic and/or pharmacodynamic mechanisms have been considered to play a role in these interactions, although the underlying mechanisms for the altered drug effects and/or concentrations by concomitant herbal medicines are yet to be determined. The clinical importance of herb-drug interactions depends on many factors associated with the particular herb, drug and patient. Herbs should be appropriately labeled to alert consumers to potential interactions when concomitantly used with drugs, and to recommend a consultation with their general practitioners and other medical carers.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Psychiatric adverse events associated with semaglutide, liraglutide and tirzepatide: a pharmacovigilance analysis of individual case safety reports submitted to the EudraVigilance database
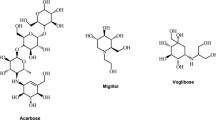
A review of alpha-glucosidase inhibitors from plants as potential candidates for the treatment of type-2 diabetes
Together or Apart? Revealing the Impact of Dietary Interventions on Bioavailability of Quinolones: A Systematic Review with Meta-analyses
Izzo AA, Ernst E. Interactions between herbal medicines and prescribed drugs: a systematic review. Drugs 2001; 61(15): 2163–75
Article PubMed CAS Google Scholar
Fugh-Berman A. Herbal medicinals: selected clinical considerations, focusing on known or potential drug-herb interactions. Arch Intern Med 1999; 159(16): 1957–8
Fugh-Berman A. Herb-drug interactions. Lancet 2000; 355(9198): 134–8
Fugh-Berman A, Ernst E. Herb-drug interactions: review and assessment of report reliability. Br J Clin Pharmacol 2001; 52(5): 587–95
Heck AM, DeWitt BA, Lukes AL. Potential interactions between alternative therapies and warfarin. Am J Health System Pharm 2000; 57(13): 1221–7
CAS Google Scholar
Elvin-Lewis M. Should we be concerned about herbal remedies. J Ethnopharmacol 2001; 75(2–3): 141–64
Wilkinson GR. The effects of diet, aging and disease-states on presystemic elimination and oral drug bioavailability in humans. Adv Drug Deliv Rev 1997; 27(2–3): 129–59
Evans AM. Influence of dietary components on the gastrointestinal metabolism and transport of drugs. Ther Drug Monit 2000; 22(1): 131–6
Ioannides C. Pharmacokinetic interactions between herbal remedies and medicinal drugs. Xenobiotica 2002; 32(6): 451–78
Zhou SF, Gao YH, Wen QJ, et al. Interactions of herbs with cytochrome P450. Drug Metab Rev 2003; 35(1): 35–98
Walter-Sack I, Klotz U. Influence of diet and nutritional status on drug metabolism. Clin Pharmacokinet 1996; 31: 47–64
Kolars JC, Awni WM, Merion RM, et al. First-pass metabolism of cyclosporin by the gut. Lancet 1991; 338: 1488–90
Paine MF, Shen DD, Kunze KL, et al. First-pass metabolism of midazolam by the human intestine. Clin Pharmacol Ther 1996; 60: 14–24
Kim RB, Fromm MF, Wandel C, et al. The drug transporter P-glycoprotein limits oral absorption and brain entry of HIV-1 protease inhibitors. J Clin Invest 1998; 101(2): 289–94
Fromm MF, Busse D, Kroemer HK, et al. Differential induction of prehepatic and hepatic metabolism of verapamil by rifampin. Hepatology 1996; 24: 796–801
Greiner B, Eichelbaum M, Fritz P, et al. The role of intestinal P-glycoprotein in the interaction of digoxin and rifampin. J Clin Invest 1999; 104: 147–53
Westphal K, Weinbrenner A, Zschiesche M, et al. Induction of P-glycoprotein by rifampin increases intestinal secretion of talinolol in human beings: a new type of drug/drug interaction. Clin Pharmacol Ther 2000; 68: 345–55
Eisenberg DM, Kessler RC, Foster C, et al. Unconventional medicine in the United States: prevalence, costs, and patterns of use. N Engl J Med 1993; 328: 246–52
Goldman P. Herbal medicines today and the roots of modern pharmacology. Ann Intern Med 2001; 135 (8 Pt 1): 594–600
PubMed CAS Google Scholar
Shaw D, Leon C, Kolev S, et al. Traditional remedies and food supplements: a 5-year toxicological study (1991–1995). Drug Saf 1997; 17(5): 342–56
WHO. WHO monographs on selected medicinal plants. Vol. 2. Geneva: World Health Organization, 2002
Google Scholar
WHO. WHO monographs on selected medicinal plants. Vol. 1. Geneva: World Health Organization, 1999
Hoffmann D. The information sourcebook of herbal medicine. Freedom (CA): Crossing Press, 1994
Ernst E. Herbal medicine: a concise overview for professionals. Boston (MA): Butterworth-Heinemann, 1999
Ross IA. Medicinal plants of the world: chemical constituents, traditional, and modern medicinal uses. Totowa (NJ): Humana Press, 2001
Fetrow CW, Avila JR. The complete guide to herbal medicines. Springhouse (PA): Springhouse Corp., 2000
Huang KC. The pharmacology of Chinese herbs. Boca Raton (FL): CRC Press, 1998
Book Google Scholar
Yang YF. Chinese herbal medicines: comparisons and characteristics. Edinburgh: Churchill Livingstone, 2002
Izzo AA, Borrelli F, Capasso R. Herbal medicine: the dangers of drug interaction. Trends Pharmacol Sci 2002; 23(8): 358–91
Scott GN, Elmer GW. Update on natural product-drug interactions. Am J Health Syst Pharm 2002; 59(4): 339–47
PubMed Google Scholar
Klepser TB, Klepser ME. Unsafe and potentially safe herbal therapies. Am J Health Syst Pharm 1999; 56(2): 125–38
Abebe W. Herbal medication: potential for adverse interactions with analgesic drugs. J Clin Pharm Ther 2002; 27(6): 391–401
Brazier NC, Levine MA. Drug-herb interaction among commonly used conventional medicines: a compendium for health care professionals. Am J Ther 2003; 10(3): 163–9
Article PubMed Google Scholar
Zhou S, Chan E, Pan SQ, et al. Pharmacokinetic interactions of drugs with St John’s wort. J Psychopharmacol 2004; 18(2): 262–76
Izzo AA, Di Carlo G, Borrelli F, et al. Cardiovascular pharmacotherapy and herbal medicines: the risk of drug interaction. Int J Cardiol 2005; 98(1): 1–14
Sparreboom A, Cox MC, Acharya MR, et al. Herbal remedies in the United States: potential adverse interactions with anti-cancer agents. J Clin Oncol 2004; 22(12): 2489–503
Izzo AA. Herb-drug interactions: an overview of the clinical evidence. Fundam Clin Pharmacol 2005; 19(1): 1–16
Harris JC, Cottrell SL, Plummer S, et al. Antimicrobial properties of Allium sativum (garlic). Appl Microbiol Biotechnol 2001; 57(3): 282–6
Kyo E, Uda N, Kasuga S, et al. Immunomodulatory effects of aged garlic extract. J Nutr 2001; 131(3s): S1075–9
Standish LJ, Greene KB, Bain S, et al. Alternative medicine use in HIV-positive men and women: demographics, utilization patterns and health status. AIDS Care 2001; 13(2): 197–208
Dausch JG, Nixon DW. Garlic: a review of its relationship to malignant disease. Prev Med 1990; 19(3): 346–61
Singh UP, Prithiviraj B, Sarma BK, et al. Role of garlic (Allium sativum L.) in human and plant diseases. Indian J Exp Biol 2001; 39(4): 310–22
Amagase H, Petesch BL, Matsuura H, et al. Intake of garlic and its bioactive components. J Nutr 2001; 131 Suppl. 3: 955S–62S
Markowitz JS, Devane CL, Chavin KD, et al. Effects of garlic (Allium sativum L.) supplementation on cytochrome P450 2D6 and 3A4 activity in healthy volunteers. Clin Pharmacol Ther 2003; 74(2): 170–7
Gurley BJ, Gardner SF, Hubbard MA, et al. Cytochrome P450 phenotypic ratios for predicting herb-drug interactions in humans. Clin Pharmacol Ther 2002; 72(3): 276–87
Fitzsimmons ME, Collins JM. Selective biotransformation of the human immunodeficiency virus protease inhibitor saquinavir by human small-intestinal cytochrome P450 3A4: potential contribution to high first-pass metabolism. Drug Metab Dispos 1997; 25(2): 256–66
Foster BC, Foster MS, Vandenhoek S, et al. An in vitro evaluation of human cytochrome P450 3A4 and P-glycoprotein inhibition by garlic. J Pharm Pharm Sci 2001; 4(2): 176–84
Piscitelli SC, Burstein AH, Weiden N, et al. The effect of garlic supplements on the pharmacokinetics of saquinavir. Clin Infect Dis 2002; 34(2): 234–8
Kim AE, Dintaman JM, Waddell DS. Saquinavir, an HIV protease inhibitor, is transported by P-glycoprotein. J Pharmacol Exp Ther 1998; 286: 143–9
Gisolf EH, van Heeswijk RP, Hoetelmans RW, et al. Decreased exposure to saquinavir in HIV-1infected patients after long-term antiretroviral therapy including ritonavir and saquinavir. AIDS 2000; 14: 801–5
Gallicano K, Foster B, Choudhri S. Effect of short-term administration of garlic supplements on single-dose ritonavir pharmacokinetics in healthy volunteers. Br J Clin Pharmacol 2003; 55(2): 199–202
Hsu A, Granneman GR, Bertz RJ. Ritonavir: clinical pharmacokinetics and interactions with other anti-HIV agents. Clin Pharmacokinet 1998; 35(4): 275–91
Laroche M, Choudhri S, Gallicano K, et al. Severe gastrointestinal toxicity with concomitant ingestion of ritonavir and garlic [abstract]. Can J Infect Dis 1998; 9 Suppl. A: 471P
Ernst E. Complementary AIDS therapies: the good, the bad, and the ugly. Int J STD AIDS 1997; 8(5): 281–5
Sussman E. Garlic supplements can impede HIV medication [letter]. AIDS 2002; 16(9): N5
Article Google Scholar
Sunter WH. Warfarin and garlic [letter]. Pharm J 1991; 246: 772
Evans V. Herbs and the brain: friend or foe? The effects of ginkgo and garlic on warfarin use. J Neurosci Nurs 2000; 32(4): 229–32
German K, Kumar U, Blackford HN. Garlic and the risk of TURP bleeding. Br J Urol 1995; 76(4): 518
Petry JJ. Garlic and postoperative bleeding. Plast Reconstr Surg 1995; 96(2): 483–4
Rose KD, Croissant PD, Parliament CF, et al. Spontaneous spinal epidural hematoma with associated platelet dysfunction from excessive garlic ingestion: a case report. Neurosurgery 1990; 26(5): 880–2
Fedder SL. Spinal epidural hematoma and garlic ingestion [letter]. Neurosurgery 1990; 27(4): 659
Briggs WH, Xiao H, Parkin KL, et al. Differential inhibition of human platelet aggregation by selected Allium thiosulfinates. J Agric Food Chem 2000; 48(11): 5731–5
Rahman K, Billington D. Dietary supplementation with aged garlic extract inhibits ADP-induced platelet aggregation in humans. J Nutr 2000; 130(11): 2662–5
MacDonald JA, Langler RF. Structure-activity relationships for selected sulfur-rich antithrombotic compounds. Biochem Biophys Res Commun 2000; 273(2): 421–4
Bordia A, Verma SK, Srivastava KC. Effect of garlic (Allium sativum) on blood lipids, blood sugar, fibrinogen and fibrinolytic activity in patients with coronary artery disease. Prostaglandins Leukot Essent Fatty Acids 1998; 58(4): 257–63
Aslam M, Stockley IH. Interaction between curry ingredient (karela) and drug (chlorpropamide) [letter]. Lancet 1979; I(8116): 607
Sheela CG, Kumud K, Augusti KT. Anti-diabetic effects of onion and garlic sulfoxide amino acids in rats. Planta Med 1995; 61(4): 356–7
Sheela CG, Augusti KT. Antidiabetic effects of S-allyl cysteine sulphoxide isolated from garlic Allium sativum Linn . Indian J Exp Biol 1992; 30(6): 523–6
Mathew PT, Augusti KT. Studies on the effect of allicin (diallyl disulphide-oxide) on alloxan diabetes. I: hypoglycaemic action and enhancement of serum insulin effect and glycogen synthesis. Indian J Biochem Biophys 1973; 10(3): 209–12
Zhang XH, Lowe D, Giles P, et al. Gender may affect the action of garlic oil on plasma cholesterol and glucose levels of normal subjects. J Nutr 2001; 131(5): 1471–8
Sitprija S, Plengvidhya C, Kangkaya V, et al. Garlic and diabetes mellitus phase II clinical trial. J Med Assoc Thai 1987; 70 Suppl. 2: 223–7
Day C, Cartwright T, Provost J, et al. Hypoglycaemic effect of Momordica charantia extracts. Planta Med 1990; 56(5): 426–9
Gwilt PR, Lear CL, Tempero MA, et al. The effect of garlic extract on human metabolism of acetaminophen. Cancer Epidemiol Biomarkers Prev 1994; 3(2): 155–60
Lin MC, Wang EJ, Patten C, et al. Protective effect of diallyl sulfone against acetaminophen-induced hepatotoxicity in mice. J Biochem Toxicol 1996; 11(1): 11–20
Manyike PT, Kharasch ED, Kalhorn TF, et al. Contribution of CYP2E1 and CYP3A to acetaminophen reactive metabolite formation. Clin Pharmacol Ther 2000; 67(3): 275–82
Li H, Dai Y, Zhang H, et al. Pharmacological studies on the Chinese drug radix Angelicae dahuricae. Zhongguo Zhong Yao Za Zhi 1991; 16(9): 560–76
Kim CM, Heo MY, Kim HP, et al. Pharmacological activities of water extracts of Umbelliferae plants. Arch Pharm Res 1991; 14(1): 87–92
Saiki Y, Morinaga K, Okegawa O, et al. On the coumarins of the roots of Angelica dahurica Benth. et Hook. Yakugaku Zasshi 1971; 91(12): 1313–7
Baek NI, Ahn EM, Kim HY, et al. Furanocoumarins from the root of Angelica dahurica. Arch Pharm Res 2000; 23(5): 467–70
Qiao SY, Yao XS, Wang ZY. Coumarins of the roots of Angelica dahurica [abstract]. Planta Med 1996; 62(6): 584
Ishihara K, Kushida H, Yuzurihara M, et al. Interaction of drugs and Chinese herbs: pharmacokinetic changes of tolbutamide and diazepam caused by extract of Angelica dahurica. J Pharm Pharmacol 2000; 52(8): 1023–9
Bergendorff O, Dekermendjian K, Nielsen M, et al. Furanocoumarins with affinity to brain benzodiazepine receptors in vitro. Phytochemistry 1997; 44(6): 1121–11124
Dekermendjian K, Ai JL, Nielsen M, et al. Characterisation of the furanocoumarin phellopterin as a rat brain benzodiazepine receptor partial agonist in vitro. Neurosci Lett 1996; 219(3): 151–4
Cai Y, Bennett D, Nair RV, et al. Inhibition and inactivation of murine hepatic ethoxy- and pentoxyresorufin O-dealkylase by naturally occurring coumarins. Chem Res Toxicol 1993; 6(6): 872–9
Kleiner HE, Vulimiri SV, Reed MJ, et al. Role of cytochrome P450 1A1 and 1B1 in the metabolic activation of 7,12-dimethylbenz[a]anthracene and the effects of naturally occurring furanocoumarins on skin tumor initiation. Chem Res Toxicol 2002; 15(2): 226–35
Kleiner HE, Reed MJ, DiGiovanni J. Naturally occurring coumarins inhibit human cytochromes P450 and block benzo[a]pyrene and 7,12-dimethylbenz[a]anthracene DNA adduct formation in MCF-7 cells. Chem Res Toxicol 2003; 16(3): 415–22
Maenpaa J, Sigusch H, Raunio H, et al. Differential inhibition of coumarin 7-hydroxylase activity in mouse and human liver microsomes. Biochem Pharmacol 1993; 45(5): 1035–42
Guo LQ, Taniguchi M, Chen QY, et al. Inhibitory potential of herbal medicines on human cytochrome P450-mediated oxidation: properties of Umbelliferous or Citrus crude drugs and their relative prescriptions. Jpn J Pharmacol 2001; 85(4): 399–408
Zhu DP. Dong quai . Am J Chin Med 1987; 15(3–4): 117–25
Lin LZ, He XG, Lian LZ, et al. Liquid Chromatographic electrospray mass spectrometric study of the phthalides of Angelica sinensis and chemical changes of Z-ligustilide. J Chromatogr 1998; 810(1–2): 71–9
Zhao KJ, Dong TT, Tu PF, et al. Molecular genetic and chemical assessment of Radix Angelica (Danggui) in China. J Agric Food Chem 2003; 51(9): 2576–83
Huang WH, Song CQ. Research progresses in the chemistry and pharmacology of Angelica sinensis (Oliv.) Diel [in Chinese]. Zhongguo Zhong Yao Za Zhi 2001; 26(3): 147–51
Mao X, Kong L, Luo Q, et al. Screening and analysis of permeable compounds in Radix Angelica Sinensis with immobilized liposome chromatography. J Chromatogr B Analyt Technol Biomed Life Sci 2002; 779(2): 331–9
Ji SG, Chai YF, Wu YT, et al. Determination of ferulic acid in Angelica sinensis and Chuanxiong by capillary zone electrophoresis. Biomed Chromatogr 1999; 13(5): 333–4
Guo T, Sun Y, Sui Y, et al. Determination of ferulic acid and adenosine in Angelicae Radix by micellar electrokinetic chromatography. Anal Bioanal Chem 2003; 375(6): 840–3
Yang Q, Populo SM, Zhang J, et al. Effect of Angelica sinensis on the proliferation of human bone cells. Clin Chim Acta 2002; 324(1–2): 89–97
Mei QB, Tao JY, Cui B. Advances in the pharmacological studies of radix Angelica sinensis (Oliv) Diels (Chinese Danggui). Chin Med J (Engl) 1991; 104(9): 776–81
Russell L, Hicks GS, Low AK, et al. Phytoestrogens: a viable option? Am J Med Sci 2002; 324(4): 185–8
He ZP, Wang DZ, Shi LY, et al. Treating amenorrhea in vital energy-deficient patients with angelica sinensis-astragalus membranaceus menstruation-regulating decoction. J Tradit Chin Med 1986; 6(3): 187–90
Hardy ML. Herbs of special interest to women. J Am Pharm Assoc (Wash) 2000; 40(2): 234–42
Hirata JD, Swiersz LM, Zeil B, et al. Does dong quai have estrogenic effects in postmenopausal women? A double-blind, placebo-controlled trial. Fertil Steril 1997; 68(6): 981–6
Page 2nd RL, Lawrence JD. Potentiation of warfarin by dong quai. Pharmacotherapy 1999; 19(7): 870–6
Yin ZZ, Zhang LY, Xu LN. The effect of Dang-Gui (Angelica sinensis) and its ingredient ferulic acid on rat platelet aggregation and release of 5-HT (author’s transi) [in Chinese]. Yao Xue Xue Bao 1980; 15(6): 321–6
Lo ACT, Chan K, Yeung JHK, et al. Danggui (Angelica sinensis) affects the pharmacodynamics but not the pharmacokinetics of warfarin in rabbits. Eur J Drug Metab Pharmacokinet 1995; 20(1): 55–60
Teel RW, Huynh H. Modulation by phytochemicals of cytochrome P450-linked enzyme activity. Cancer Lett 1998; 133(2): 135–41
Li T. Siberian ginseng. Horttechnology 2001; 11: 79–84
Gaffney B, Hugel H, Rich P. The effects of Eleutherococcus senticosus and Panax ginseng on steroidal hormone indices of stress and lymphocyte subset numbers in endurance athletes. Life Sci 2001; 70(4): 431–42
Davydov M, Krikorian AD. Eleutherococcus senticosus (Rupr. & Maxim.) Maxim. (Araliaceae) as an adaptogen: a closer look. J Ethnopharmacol 2000; 72(3): 345–93
Hou JP. The chemical constituents of ginseng plants. Comp Med East West 1977; 5(2): 123–45
Donovan JL, DeVane CL, Chavin KD, et al. Siberian ginseng (Eleutheroccus senticosus) effects on CYP2D6 and CYP3A4 activity in normal volunteers. Drug Metab Dispos 2003; 31(5): 519–22
Budzinski JW, Foster BC, Vandenhoek S, et al. An in vitro evaluation of human cytochrome P450 3A4 inhibition by selected commercial herbal extracts and tinctures. Phytomedicine 2000; 7(4): 273–82
Medon PJ, Ferguson PW, Watson CF. Effects of Eleuthewcoccus senticosus extracts on hexobarbital metabolism in vivo and in vitro. J Ethnopharmacol 1984; 10(2): 235–41
Knodell RG, Dubey RK, Wilkinson GR, et al. Oxidative metabolism of hexobarbital in human liver: relationship to polymorphic S-mephenytoin 4-hydroxylation. J Pharmacol Exp Ther 1988; 245(3): 845–9
McRae S. Elevated serum digoxin levels in a patient taking digoxin and Siberian ginseng. CMAJ 1996; 155(3): 293–5
Dasgupta A, Wu S, Actor J, et al. Effect of Asian and Siberian ginseng on serum digoxin measurement by five digoxin immunoassays: significant variation in digoxin-like immunoreactivity among commercial ginsengs. Am J Clin Pathol 2003; 119(2): 298–303
Oken BS, Storzbach DM, Kaye JA. The efficacy of Ginkgo biloba on cognitive function in Alzheimer disease. Arch Neurol 1998; 55(11): 1409–15
McKenna DJ, Jones K, Hughes K. Efficacy, safety, and use of ginkgo biloba in clinical and preclinical applications. Altern Ther Health Med 2001; 7(5): 70–86
Wesnes KA, Ward T, McGinty A, et al. The memory enhancing effects of a Ginkgo biloba/Panax ginseng combination in healthy middle-aged volunteers. Psychopharmacology 2000: 152(4): 353–61
Mahady GB. Ginkgo biloba for the prevention and treatment of cardiovascular disease: a review of the literature}. J Cardiovasc Nurs 2002; 16(4): 21–32
Diamond BJ, Shiflett SC, Feiwel N, et al. Ginkgo biloba extract: mechanisms and clinical indications. Arch Phys Med Rehabil 2000; 81(5): 668–78
Andrieu S, Gillette S, Amouyal K, et al. Association of Alzheimer’s disease onset with ginkgo biloba and other symptomatic cognitive treatments in a population of women aged 75 years and older from the EPIDOS study. J Gerontol A Biol Sci Med Sci 2003; 58(4): 372–7
Ponto LL, Schultz SK. Ginkgo biloba extract: review of CNS effects. Ann Clin Psychiatry 2003; 15(2): 109–19
Tang YP, Lou FC, Wang JH, et al. Coumaroyl flavonol glycosides from the leaves of Ginkgo biloba. Phytochemistry 2001; 58(8): 1251–6
Krieglstein J, Ausmeier F, Elabhar H, et al. Neuroprotective effects of Ginkgo biloba constituents. Eur J Pharm Sci 1995; 3(1): 39–48
Article CAS Google Scholar
van Beek TA. Chemical analysis of Ginkgo biloba leaves and extracts. J Chromatogr A 2002; 967(1): 21–55
Lichtblau D, Berger JM, Nakanishi K. Efficient extraction of ginkgolides and bilobalide from Ginkgo biloba leaves. J Nat Prod 2002; 65(10): 1501–4
Jaggy H, Koch E. Chemistry and biology of alkylphenols from Ginkgo biloba L. Pharmazie 1997; 52(10): 735–8
Baron-Ruppert G, Luepke NP. Evidence for toxic effects of alkylphenols from Ginkgo biloba in the hen’s egg test (HET). Phytomedicine 2001; 8(2): 133–8
Ahlemeyer B, Selke D, Schaper C, et al. Ginkgolic acids induce neuronal death and activate protein phosphatase type-2C. Eur J Pharmacol 2001; 430(1): 1–7
Koch E, Jaggy H, Chatterjee SS. Evidence for immunotoxic effects of crude Ginkgo biloba L. leaf extracts using the popliteal lymph node assay in the mouse. Int J Immunopharmacol 2000; 22(3): 229–36
Lepoittevin JP, Benezra C, Asakawa Y. Allergic contact dermatitis to Ginkgo biloba L. : relationship with urushiol. Arch Dermatol Res 1989; 281(4): 227–30
Galluzzi S, Zanetti O, Binetti G, et al. Coma in a patient with Alzheimer’s disease taking low dose trazodone and Ginkgo biloba . J Neurol Neurosurg Psychiatry 2000; 68(5): 679–80
Sasaki K, Hatta S, Haga M, et al. Effects of bilobalide on gamma-aminobutyric acid levels and glutamic acid decarboxylase in mouse brain. Eur J Pharmacol 1999; 367 (2–3): 165–73
Sasaki K, Hatta S, Wada K, et al. Bilobalide prevents reduction of gamma-aminobutyric acid levels and glutamic acid decarboxylase activity induced by 4-O-methylpyridoxine in mouse hippocampus. Life Sci 2000; 67(6): 709–15
Shinozuka K, Umegaki K, Kubota Y, et al. Feeding of Ginkgo biloba extract (GBE) enhances gene expression of hepatic cytochrome P-450 and attenuates the hypotensive effect of nicardipine in rats. Life Sci 2002; 70(23): 2783–92
Umegaki K, Saito K, Kubota Y, et al. Ginkgo biloba extract markedly induces pentoxyresorufin O-dealkylase activity in rats. Jpn J Pharmacol 2002; 90(4): 345–51
Sasaki K, Wada K, Hatta S, et al. Bilobalide, a constituent of Ginkgo biloba L. , potentiates drug-metabolizing enzyme activities in mice: possible mechanism for anticonvulsant activity against 4-O-methylpyridoxine-induced convulsions. Res Commun Mol Pathol Pharmacol 1997; 96(1): 45–56
Vaes LP, Chyka PA. Interactions of warfarin with garlic, ginger, ginkgo, or ginseng: nature of the evidence. Ann Pharmacother 2000; 34(12): 1478–82
Matthews Jr MK. Association of Ginkgo biloba with intracerebral hemorrhage. Neurology 1998; 50(6): 1933–4
Rosenblatt M, Mindel J. Spontaneous hyphema associated with ingestion of Ginkgo biloba extract [letter]. N Engl J Med 1997: 336(15): 1108
Meisel C, Johne A, Roots I. Fatal intracerebral mass bleeding associated with Ginkgo biloba and ibuprofen. Atherosclerosis 2003; 167(2): 367
Engelsen J, Nielsen JD, Hansen KF. Effect of coenzyme Q10 and Ginkgo biloba on warfarin dosage in patients on long-term warfarin treatment: a randomized, double-blind, placebo-controlled cross-over trial [in Danish]. Ugeskr Laeger 2003; 165(18): 1868–71
Kim YS, Pyo MK, Park KM, et al. Antiplatelet and antithrombotic effects of a combination of ticlopidine and Ginkgo biloba ext (EGb 761). Thromb Res 1998; 91(1): 33–8
Lamant V, Mauco G, Braquet P, et al. Inhibition of the metabolism of platelet activating factor (PAF-acether) by three specific antagonists from Ginkgo biloba. Biochem Pharmacol 1987; 36(17): 2749–52
Fessenden JM, Wittenborn W, Clarke L. Gingko biloba : a case report of herbal medicine and bleeding postoperatively from a laparoscopic cholecystectomy. Am Surg 2001; 67(1): 33–5
Skogh M. Extracts of Ginkgo biloba and bleeding or haemorrhage. Lancet 1998; 352(9134): 1145–6
Vale S. Subarachnoid haemorrhage associated with Ginkgo biloba [letter]. Lancet 1998; 352(9121): 36
Rowin J, Lewis SL. Spontaneous bilateral subdural hematomas associated with chronic Ginkgo biloba ingestion. Neurology 1996; 46(6): 1775–6
Bal Dit Sollier C, Caplain H, Drouet L. No alteration in platelet function or coagulation induced by EGb761 in a controlled study. Clin Lab Haematol 2003; 25(4): 251–3
Mauro VF, Mauro LS, Kleshinski JF, et al. Impact of ginkgo biloba on the pharmacokinetics of digoxin. Am J Ther 2003; 10(4): 247–51
Yin OQ, Tomlinson B, Waye MM, et al. Pharmacogenetics and herb-drug interactions: experience with Ginkgo biloba and omeprazole. Pharmacogenetics 2004; 14(12): 841–50
Ohnishi N, Kusuhara M, Yoshioka M, et al. Studies on interactions between functional foods or dietary supplements and medicines. I: effects of Ginkgo biloba leaf extract on the pharmacokinetics of diltiazem in rats. Biol Pharm Bull 2003; 26(9): 1315–20
Kalus JS, Piotrowski AA, Fortier CR, et al. Hemodynamic and electrocardiographic effects of short-term ginkgo biloba. Ann Pharmacother 2003; 37(3): 345–9
Mehlsen J, Drabaek H, Wiinberg N, et al. Effects of a Ginkgo biloba extract on forearm haemodynamics in healthy volunteers. Clin Physiol Funct Imaging 2002; 22(6): 375–8
Jezova D, Duncko R, Lassanova M, et al. Reduction of rise in blood pressure and cortisol release during stress by Ginkgo biloba extract (EGb 761) in healthy volunteers. J Physiol Pharmacol 2002; 53(3): 337–48
Kudolo GB. The effect of 3-month ingestion of Ginkgo biloba extract on pancreatic beta-cell function in response to glucose loading in normal glucose tolerant individuals. J Clin Pharmacol 2000; 40(6): 647–54
Zhang J, Fu S, Liu S, et al. The therapeutic effect of Ginkgo biloba extract in SHR rats and its possible mechanisms based on cerebral microvascular flow and vasomotion. Clin Hemorheol Microcirc 2000; 23(2–4): 133–8
Umegaki K, Shinozuka K, Watarai K, et al. Ginkgo biloba extract attenuates the development of hypertension in deoxycorticosterone acetate-salt hypertensive rats. Clin Exp Pharmacol Physiol 2000; 27(4): 277–82
Chermat R, Brochet D, DeFeudis FV, et al. Interactions of Ginkgo biloba extract (EGb 761), diazepam and ethyl betacarboline-3-carboxylate on social behavior of the rat. Pharmacol Biochem Behav 1997; 56(2): 333–9
Nordberg A, Svensson AL. Cholinesterase inhibitors in the treatment of Alzheimer’s disease: a comparison of tolerability and pharmacology. Drug Saf 1998; 19(6): 465–80
Yasui-Furukori N, Furukori H, Kaneda A, et al. The effects of Ginkgo biloba extracts on the pharmacokinetics and pharmacodynamics of donepezil. J Clin Pharmacol 2004; 44(5): 538–42
Jann MW, Shirley KL, Small GW. Clinical pharmacokinetics and pharmacodynamics of cholinesterase inhibitors. Clin Pharmacokinet 2002; 41(10): 719–39
Wada K, Ishigaki S, Ueda K, et al. Studies on the constitution of edible and medicinal plants. I: isolation and identification of 4-O-methylpyridoxine, toxic principle from the seed of Ginkgo biloba L. Chem Pharm Bull (Tokyo) 1988; 36(5): 1779–82
Scott PM, Lau BP, Lawrence GA, et al. Analysis of Ginkgo biloba for the presence of ginkgotoxin and ginkgotoxin 5’-glucoside. J AOAC Int 2000; 83(6): 1313–20
Zhang XY, Zhou DF, Su JM, et al. The effect of extract of Ginkgo biloba added to haloperidol on Superoxide dismutase in inpatients with chronic schizophrenia. J Clin Psychopharmacol 2001; 21(1): 85–8
Zhang XY, Zhou DF, Zhang PY, et al. A double-blind, placebocontrolled trial of extract of Ginkgo biloba added to haloperidol in treatment-resistant patients with schizophrenia. J Clin Psychiatry 2001; 62(11): 878–83
Kudolo GB. The effect of 3-month ingestion of Ginkgo biloba extract (EGb 761) on pancreatic beta-cell function in response to glucose loading in individuals with non-insulin-dependent diabetes mellitus. J Clin Pharmacol 2001; 41(6): 600–11
Sugiyama T, Kubota Y, Shinozuka K, et al. Ginkgo biloba extract modifies hypoglycemic action of tolbutamide via hepatic cytochrome P450 mediated mechanism in aged rats. Life Sci 2004; 75(9): 1113–22
Hatano T, Fukuda T, Miyase T, et al. Phenolic constituents of licorice. III: structures of glicoricone and licofuranone, and inhibitory effects of licorice constituents on monoamine oxidase. Chem Pharm Bull (Tokyo) 1991; 39(5): 1238–43
Hatano T, Fukuda T, Liu YZ, et al. Phenolic constituents of licorice. IV: correlation of phenolic constituents and licorice specimens from various sources, and inhibitory effects of licorice extracts on xanthine oxidase and monoamine oxidase. Yakugaku Zasshi 1991; 111(6): 311–21
Li C, Homma M, Oka K. Characteristics of delayed excretion of flavonoids in human urine after administration of Shosaiko-to, a herbal medicine. Biol Pharm Bull 1998; 21(12): 1251–7
Shon JH, Park JY, Kim MS, et al. Effect of licorice ( Radix glycyrrhizae ) on the pharmacokinetics and pharmacodynamics of midazolam in healthy subjects [abstract]. Clin Pharmacol Ther 2001; 69: P78
Gorski JC, Hall SD, Jones DR, et al. Regioselective biotransformation of midazolam by members of the human cytochrome P450 3A (CYP3A) subfamily. Biochem Pharmacol 1994; 47(9): 1643–53
Kent UM, Aviram M, Rosenblat M, et al. The licorice root derived isoflavan glabridin inhibits the activities of human cytochrome P450S 3A4, 2B6, and 2C9. Drug Metab Dispos 2002; 30(6): 709–15
Paolini M, Pozzetti L, Sapone A, et al. Effect of licorice and glycyrrhizin on murine liver CYP-dependent monooxygenases. Life Sci 1998; 62(6): 571–82
Homma M, Oka K, Ikeshima K, et al. Different effects of traditional Chinese medicines containing similar herbal constituents on prednisolone pharmacokinetics. J Pharm Pharmacol 1995; 47(8): 687–92
Akao T, Terasawa T, Hiai S, et al. Inhibitory effects of glycyrrhetic acid derivatives on 11 beta- and 3 alpha-hydroxysteroid dehydrogenases of rat liver. Chem Pharm Bull (Tokyo) 1992; 40(11): 3021–4
Ojima M, Satoh K, Gomibuchi T, et al. The inhibitory effects of glycyrrhizin and glycyrrhetinic acid on the metabolism of cortisol and prednisolone: in vivo and in vitro studies. Nippon Naibunpi Gakkai Zasshi 1990; 66(5): 584–96
Davis EA, Morris DJ. Medicinal uses of licorice through the millennia: the good and plenty of it. Mol Cell Endocrinol 1991; 78(1–2): 1–6
Teelucksingh S, Mackie AD, Burt D, et al. Potentiation of hydrocortisone activity in skin by glycyrrhetinic acid. Lancet 1990; 335(8697): 1060–3
Souness GW, Morris DJ. The antinatriuretic and kaliuretic effects of the glucocorticoids corticosterone and cortisol following pretreatment with carbenoxolone sodium (a liquorice derivative) in the adrenalectomized rat. Endocrinology 1989; 124(3): 1588–90
Elinav E, Chajek-Shaul T. Licorice consumption causing severe hypokalemic paralysis. Mayo Clin Proc 2003; 78(6): 767–8
Lin SH, Yang SS, Chau T, et al. An unusual cause of hypokalemic paralysis: chronic licorice ingestion. Am J Med Sci 2003; 325(3): 153–6
Nishimura N, Naora K, Hirano H, et al. Effects of sho-saiko-to (xiao chai hu tang), a Chinese traditional medicine, on the gastric function and absorption of tolbutamide in rats. Yakugaku Zasshi 2001; 121(2): 153–9
Nishimura N, Naora K, Hirano H, et al. Effects of Sho-saiko-to on the pharmacokinetics and pharmacodynamics of tolbutamide in rats. J Pharm Pharmacol 1998; 50(2): 231–6
Bilia AR, Gallori S, Vincieri FF. St John’s wort and depression: efficacy, safety and tolerability: an update. Life Sci 2002; 70(26): 3077–96
Obach RS. Inhibition of human cytochrome P450 enzymes by constituents of St John’s wort, an herbal preparation used in the treatment of depression. J Pharmacol Exp Ther 2000; 294(1): 88–95
Erdelmeier CAJ. Hyperforin, possibly the major non-nitrogenous secondary metabolite of Hypericum perforatum L. Pharmacopsychiatry 1998; 31S: 2–6
Moore LB, Goodwin B, Jones SA, et al. St John’s wort induces hepatic drug metabolism through activation of the pregnane X receptor. Proc Natl Acad Sci U S A 2000; 97(13): 7500–2
Kerb R, Brockmoller J, Staffeldt B, et al. Single-dose and steady-state pharmacokinetics of hypericin and pseudohypericin. Antimicrob Agents Chemother 1996; 40(9): 2087–93
Schulz HU, Schurer M, Bassler D, et al. Investigation of the bioavailability of hypericin, pseudohypericin, hyperforin and the flavonoids quercetin and isorhamnetin following single and multiple oral dosing of a hypericum extract containing tablet. Arzneimittelforschung 2005; 55(1): 15–22
Johne A, Schmider J, Brockmoller J, et al. Decreased plasma levels of amitriptyline and its metabolites on comedication with an extract from St John’s wort (Hypericum perforatum). J Clin Psychopharmacol 2002; 22(1): 46–54
Venkatakrishnan K, Schmider J, Harmatz JS, et al. Relative contribution of CYP3A to amitriptyline clearance in humans: in vitro and in vivo studies. J Clin Pharmacol 2001; 41(10): 1043–54
Venkatakrishnan K, Greenblatt DJ, von Moltke LL, et al. Five distinct human cytochromes mediate amitriptyline N-demethylation in vitro: dominance of CYP 2C19 and 3A4. J Clin Pharmacol 1998; 38(2): 112–21
Venkatakrishnan K, von Moltke LL, Greenblatt DJ. Nortriptyline E-10-hydroxylation in vitro is mediated by human CYP2D6 (high affinity) and CYP3A4 (low affinity): implications for interactions with enzyme-inducing drugs. J Clin Pharmacol 1999; 39(6): 567–77
von Moltke LL, Greenblatt DJ, Harmatz JS, et al. Triazolam biotransformation by human liver microsomes in vitro: effects of metabolic inhibitors and clinical confirmation of a predicted interaction with ketoconazole. J Pharmacol Exp Ther 1996; 276(2): 370–9
Markowitz JS, DeVane CL, Boulton DW, et al. Effect of St John’s wort (Hypericum perforatum) on cytochrome P-450 2D6 and 3A4 activity in healthy volunteers. Life Sci 2000; 66(9): PL133–9
Wang ZQ, Gorski C, Hamman MA, et al. The effects of St John’s wort (Hypericum perforatum) on human cytochrome P450 activity. Clin Pharmacol Ther 2001; 70(4): 317–26
Dresser GK, Schwarz UI, Wilkinson GR, et al. Coordinate induction of both cytochrome P4503A and MDR1 by St John’s wort in healthy subjects. Clin Pharmacol Ther 2003; 73(1): 41–50
Burstein AH, Horton RL, Dunn T, et al. Lack of effect of St John’s wort on carbamazepine pharmacokinetics in healthy volunteers. Clin Pharmacol Ther 2000; 68(6): 605–12
Pelkonen O, Myllynen P, Taavitsainen P, et al. Carbamazepine: a ‘blind’ assessment of CYP-associated metabolism and interactions in human liver-derived in vitro systems. Xenobiotica 2001; 31(6): 321–43
Kerr BM, Thummel KE, Wurden CJ, et al. Human liver carbamazepine metabolism: Role of CYP3A4 and CYP2C8 in 10, 11-epoxide formation. Biochem Pharmacol 1994; 47(11): 1969–79
Tateishi T, Asoh M, Nakura H, et al. Carbamazepine induces multiple cytochrome P450 subfamilies in rats. Chem Biol Interact 1999; 117(3): 257–68
Kudriakova TB, Sirota LA, Rozova GI, et al. Autoinduction and steady-state pharmacokinetics of carbamazepine and its major metabolites. Br J Clin Pharmacol 1992; 33(6): 611–5
Owen A, Pirmohamed M, Tettey JN, et al. Carbamazepine is not a substrate for P-glycoprotein. Br J Clin Pharmacol 2001; 51(4): 345–9
Ohnishi N, Nakasako S, Okada K, et al. Studies on interactions between traditional herbal and western medicines. IV: lack of pharmacokinetic interactions between Saiko-ka-ryukotsuborei-to and carbamazepine in rats. Eur J Drug Metab Pharmacokinet 2001; 26(1–2): 129–35
Akhlaghi F, Trull AK. Distribution of cyclosporin in organ transplant recipients. Clin Pharmacokinet 2002; 41(9): 615–37
Lown KS, Mayo RR, Leichtman AB, et al. Role of intestinal P-glycoprotein (mdr1) in interpatient variation in the oral bioavailability of cyclosporine. Clin Pharm Ther 1997; 62(3): 248–60
Christians U, Strohmeyer S, Kownatzki R, et al. Investigations on the metabolic pathways of cyclosporine. II: elucidation of the metabolic pathways in vitro by human liver microsomes. Xenobiotica 1991; 21(9): 1199–210
Kronbach T, Fischer V, Meyer UA. Cyclosporine metabolism in human liver: identification of a cytochrome P-450III gene family as the major cyclosporine-metabolizing enzyme explains interactions of cyclosporine with other drugs. Clin Pharmacol Ther 1988; 43(6): 630–5
Combalbert J, Fabre I, Fabre G, et al. Metabolism of cyclosporin A. IV: purification and identification of the rifampicin-inducible human liver cytochrome P-450 (cyclosporin A oxidase) as a product of P450IIIA gene subfamily. Drug Metab Dispos 1989; 17(2): 197–207
Jurima-Romet M, Crawford K, Cyr T, et al. Terfenadine metabolism in human liver: in vitro inhibition by macrolide antibiotics and azole antifungals. Drug Metab Dispos 1994; 22(6): 849–57
Fahr A. Cyclosporin clinical pharmacokinetics. Clin Pharmacokinet 1993; 24: 472–95
Christians U, Strohmeyer S, Kownatzki R, et al. Investigations on the metabolic pathways of cyclosporine: I. Excretion of cyclosporine and its metabolites in human bile: isolation of 12 new cyclosporine metabolites. Xenobiotica 1991; 21(9): 1185–98
Maurer G, Lemaire M. Biotransformation and distribution in blood of cyclosporine and its metabolites. Transplant Proc 1986; 18: 25–34
Ruschitzka F, Meier PJ, Turina M, et al. Acute heart transplant rejection due to Saint John’s wort. Lancet 2000; 355(9203): 548–9
Barone GW, Gurley BJ, Ketel BL, et al. Drug interaction between St John’s wort and cyclosporine. Ann Pharmacother 2000; 34(9): 1013–6
Mai I, Kruger H, Budde K, et al. Hazardous pharmacokinetic interaction of Saint John’s wort ( Hypericum perforatum ) with the immunosuppressant cyclosporin. Int J Clin Pharmacol Ther 2000; 38(10): 500–2
Karliova M, Treichel U, Malago M, et al. Interaction of Hypericum perforatum (St John’s wort) with cyclosporin A metabolism in a patient after liver transplantation. J Hepatol 2000; 33(5): 853–5
Breidenbach T, Kliem V, Burg M, et al. Profound drop of cyclosporin A whole blood trough levels caused by St John’s wort (Hypericum perforatum). Transplantation 2000; 69(10): 2229–30
Bauer S, Stornier E, Johne A, et al. Alterations in cyclosporin A pharmacokinetics and metabolism during treatment with St John’s wort in renal transplant patients. Br J Clin Pharmacol 2003; 55(2): 203–11
Wieling J, Tamminga WJ, Sakiman EP, et al. Evaluation of analytical and clinical performance of a dual-probe phenotyping method for CYP2D6 polymorphism and CYP3A4 activity screening. Ther Drug Monit 2000; 22(4): 486–96
Bradford LD. CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics 2002; 3(2): 229–43
Johne A, Brockmoller J, Bauer S, et al. Pharmacokinetic interaction of digoxin with an herbal extract from St John’s wort (Hypericum perforatum). Clin Pharmacol Ther 1999; 66(4): 338–45
Lacarelle B, Rahmani R, de Sousa G, et al. Metabolism of digoxin, digoxigenin digitoxosides and digoxigenin in human hepatocytes and liver microsomes. Fundam Clin Pharmacol 1991; 5(7): 567–82
Salphati L, Benet LZ. Metabolism of digoxin and digoxigenin digitoxosides in rat liver microsomes: involvement of cytochrome P4503A. Xenobiotica 1999; 29(2): 171–85
Durr D, Stieger B, Kullak-Ublick GA, et al. St John’s wort induces intestinal P-glycoprotein/MDR1 and intestinal and hepatic CYP3A4. Clin Pharmacol Ther 2000; 68: 598–604
Schinkel AH, Wagenaar E, van Deemter L, et al. Absence of the mdr1a P-Glycoprotein in mice affects tissue distribution and pharmacokinetics of dexamethasone, digoxin, and cyclosporin A. J Clin Invest 1995; 96(4): 1698–705
Drescher S, Glaeser H, Murdter T, et al. P-glycoprotein-mediated intestinal and biliary digoxin transport in humans. Clin Pharmacol Ther 2003; 73(3): 223–31
Gault H, Longerich L, Dawe M, et al. Digoxin-rifampin interaction. Clin Pharmacol Ther 1984; 35(6): 750–4
Rameis H. On the interaction between phenytoin and digoxin. Eur J Clin Pharmacol 1985; 29(1): 49–53
Conseil G, Baubichon-Cortay H, Dayan G, et al. Flavonoids: a class of modulators with bifunctional interactions at vicinal ATP: and steroid-binding sites on mouse P-glycoprotein. Proc Natl Acad Sci U S A 1998; 95(17): 9831–6
Markham A, Wagstaff AJ. Fexofenadine. Drugs 1998; 55(2): 269–74
Cvetkovic M, Leake B, Fromm MF, et al. OATP and P-glycoprotein transporters mediate the cellular uptake and excretion of fexofenadine. Drug Metab Dispos 1999; 27(8): 866–71
Tian R, Koyabu N, Takanaga H, et al. Effects of grapefruit juice and orange juice on the intestinal efflux of P-glycoprotein substrates. Pharm Res 2002; 19(6): 802–9
Lippert C, Ling J, Brown P, et al. Mass balance and pharmacokinetics of MDL 16455A in healthy male volunteers [abstract]. Pharm Res 1995; 12: S390
Woosley RL, Chen Y, Freiman JP, et al. Mechanism of the cardiotoxic actions of terfenadine. JAMA 1993; 269: 1532–6
Wang ZQ, Hamman MA, Huang SM, et al. Effect of St John’s wort on the pharmacokinetics of fexofenadine. Clin Pharmacol Ther 2002; 71(6): 414–20
Johnson JR, Bross P, Cohen M, et al. Approval summary: imatinib mesylate capsules for treatment of adult patients with newly diagnosed Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase. Clin Cancer Res 2003; 9(6): 1972–9
Cohen MH, Williams G, Johnson JR, et al. Approval summary for imatinib mesylate capsules in the treatment of chronic myelogenous leukemia. Clin Cancer Res 2002; 8(5): 935–42
Cohen MH, Johnson JR, Pazdur R. U.S. Food and Drug Administration Drug Approval Summary: conversion of imatinib mesylate (STI571; Gleevec) tablets from accelerated approval to full approval. Clin Cancer Res 2005; 11(1): 12–9
Frye RF, Fitzgerald SM, Lagattuta TF, et al. Effect of St John’s wort on imatinib mesylate pharmacokinetics. Clin Pharmacol Ther 2004; 76(4): 323–9
Smith P. The influence of St. John’s wort on the pharmacokinetics and protein binding of imatinib mesylate. Pharmacotherapy 2004; 24(11): 1508–14
Bolton AE, Peng B, Hubert M, et al. Effect of rifampicin on the pharmacokinetics of imatinib mesylate (Gleevec, STI571) in healthy subjects. Cancer Chemother Pharmacol 2004; 53(2): 102–6
Mathijssen RH, Verweij J, de Bruijn P, et al. Effects of St John’s wort on irinotecan metabolism. J Natl Cancer Inst 2002; 94(16): 1247–9
Eich-Hochli D, Oppliger R, Golay KP, et al. Methadone maintenance treatment and St John’s wort: a case report. Pharmacopsychiatry 2003; 36(1): 35–7
Moody DE, Alburges ME, Parker RJ, et al. The involvement of cytochrome P450 3A4 in the N-demethylation of L-alpha-acetylmethadol (LAAM), norLAAM, and methadone. Drug Metab Dispos 1997; 25(12): 1347–53
Wang JS, De Vane CL. Involvement of CYP3A4, CYP2C8, and CYP2D6 in the metabolism of (R)- and (S)-methadone in vitro. Drug Metab Dispos 2003; 31(6): 742–7
Borgelt-Hansen L. Oral contraceptives: an update on health benefits and risks. J Am Pharm Assoc (Wash) 2001; 41(6): 875–86
Burkman RT, Collins JA, Shulman LP, et al. Current perspectives on oral contraceptive use. Am J Obstet Gynecol 2001; 185 (2 Suppl.): S4–12
Thummel KE, Wilkinson GR. In vitro and in vivo drug interactions involving human CYP3A. Annu Rev Pharmacol Toxicol 1998; 38: 389–430
Guengerich FP. Oxidation of 17-ethynylestradiol by human liver cytochrome P450. Mol Pharmacol 1988; 33(5): 500–8
Murphy PA. St John’s wort and oral contraceptives: reasons for concern? J Midwifery Womens Health 2002; 47(6): 447–50
Shader RI, Greenblatt DJ. More on oral contraceptives, drug interactions, herbal medicines, and hormone replacement therapy. J Clin Psychopharmacol 2000; 20(4): 397–8
Ernst E. Second thoughts about safety of St John’s wort. Lancet 1999; 354(9195): 2014–6
Bolt HM. Interactions between clinically used drugs and oral contraceptives. Environ Health Perspect 1994; 102 Suppl. 9: 35–8
Yue QY, Bergquist C, Gerden B. Safety of St John’s wort (Hypericum perforatum). Lancet 2000; 355: 548–9
Schwarz UI, Buschel B, Kirch W. Unwanted pregnancy on self-medication with St John’s wort despite hormonal contraception. Br J Clin Pharmacol 2003; 55(2): 112–3
Kaufeler R, Meier B, Brattstrom A. Ze 117: clinical efficacy and safety [abstract]. In: Roots I, Kemper FH, editors. Abstract book symposium on Phytopharmaka VII. Research and clinical applications. Berlin: Symposium Organising Committee, 2001 Oct 12–13
Piscitelli SC, Burstein AH, Chaitt D, et al. Indinavir concentrations and St John’s wort. Lancet 2000; 355(9203): 547–8
Chiba M, Hensleigh M, Nishime JA, et al. Role of cytochrome P450 in human metabolism of MK-639, a potent human immunodeficiency virus protease inhibitor. Drug Metab Dispos 1996; 24: 307–14
Decker CJ, Laitinen LM, Bridson GW, et al. Metabolism of amprenavir in liver microsomes: role of CYP3A4 inhibition for drug interactions. J Pharm Sci 1998; 87(7): 803–7
de Maat MM, Hoetelmans RM, Mathot RA, et al. Drug interaction between St John’s wort and nevirapine. AIDS 2001; 15(3): 420–1
Erickson DA, Mather G, Trager WF, et al. Characterization of the in vitro biotransformation of the HIV-1 reverse transcriptase inhibitor nevirapine by human hepatic cytochromes P-450. Drug Metab Dispos 1999; 27(12): 1488–95
Kawaguchi A, Ohmori M, Tsuruoka S, et al. Drug interaction between St John’s Wort and quazepam. Br J Clin Pharmacol 2004; 58(4): 403–10
Vaswani M, Linda FK, Ramesh S. Role of selective serotonin reuptake inhibitors in psychiatric disorders: a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry 2003; 27(1): 85–102
Lantz MS, Buchalter E, Giambanco V. St John’s wort and antidepressant drug interactions in the elderly. J Geriatr Psychiatry Neurol 1999; 12(1): 7–10
Gordon JB. SSRIs and St John’s wort: possible toxicity? Am Fam Physician 1998; 57(5): 950–3
Barbenel DM, Yusufi B, O’Shea D, et al. Mania in a patient receiving testosterone replacement postorchidectomy taking St John’s wort and sertraline. J Psychopharmacol 2000; 14(1): 84–6
Spinella M, Eaton LA. Hypomania induced by herbal and pharmaceutical psychotropic medicines following mild traumatic brain injury. Brain Inj 2002; 16(4): 359–67
Dannawi M. Possible serotonin syndrome after combination of buspirone and St John’s wort [letter]. J Psychopharmacol 2002; 16(4): 401
Cookson J. Side-effects of antidepressants. Br J Psychiatry 1993; 163 Suppl. 20: 20–4
Roz N, Mazur Y, Hirshfeld A, et al. Inhibition of vesicular uptake of monoamines by hyperforin. Life Sci 2002; 71(19): 2227–37
Wonnemann M, Singer A, Siebert B, et al. Evaluation of synaptosomal uptake inhibition of most relevant constituents of St John’s wort. Pharmacopsychiatry 2001; 34 Suppl. 1: S148–51
Butterweck V, Bockers T, Korte B, et al. Long-term effects of St John’s wort and hypericin on monoamine levels in rat hypothalamus and hippocampus. Brain Res 2002; 930(1–2): 21–9
Nathan P J. Hypericum perforatum (St John’s wort): a non-selective reuptake inhibitor? A review of the recent advances in its pharmacology . J Psychopharmacol 2001; 15(1): 47–54
Parker V, Wong AH, Boon HS, et al. Adverse reactions to St John’s wort. Can J Psychiatry 2001; 46(1): 77–9
Beckman SE, Sommi RW, Switzer J. Consumer use of St John’s wort: a survey on effectiveness, safety, and tolerability. Pharmacotherapy 2000; 20(5): 568–74
Sugimoto K, Ohmori M, Tsuruoka S, et al. Different effects of St John’s Wort on the pharmacokinetics of simvastatin and pravastatin. Clin Pharmacol Ther 2001; 70(6): 518–24
Bolley R, Zulke C, Kammerl M, et al. Tacrolimus-induced nephrotoxicity unmasked by induction of the CYP3A4 system with St John’s wort [letter]. Transplantation 2002; 73(6): 1009
Mai I, Stornier E, Bauer S, et al. Impact of St John’s wort treatment on the pharmacokinetics of tacrolimus and mycophenolic acid in renal transplant patients. Nephrol Dial Transplant 2003; 18(4): 819–22
Nebel A, Schneider BJ, Baker RK, et al. Potential metabolic interaction between St John’s wort and theophylline [letter]. Ann Pharmacother 1999; 33(4): 502
Sarkar MA, Hunt C, Guzelian PS, et al. Characterization of human liver cytochromes P-450 involved in theophylline metabolism. Drug Metab Dispos 1992; 20(1): 31–7
Maurer A, Johne A, Bauer S. Interaction of St John’s wort extract with phenprocoumon [abstract]. Eur J Clin Pharmacol 1999; 55: A22
He M, Korzekwa KR, Jones JP, et al. Structural forms of phenprocoumon and warfarin that are metabolized at the active site of CYP2C9. Arch Biochem Biophys 1999; 372(1): 16–28
Kaminsky LS, Zhang ZY. Human P450 metabolism of warfarin. Pharmacol Ther 1997; 73(1): 67–74
Goodwin B, Moore LB, Stoltz CM, et al. Regulation of the human CYP2B6 gene by the nuclear pregnane X receptor. Mol Pharmacol 2001; 60(3): 427–31
Wentworth JM, Agostini M, Love J, et al. St John’s wort, a herbal antidepressant, activates the steroid X receptor. J Endocrinol 2000; 166(3): R11–6
Bray BJ, Perry NB, Menkes DB, et al. St John’s wort extract induces CYP3A and CYP2E1 in the Swiss Webster mouse. Toxicol Sci 2002; 66(1): 27–33
Roby CA, Anderson GD, Kantor E, et al. St John’s wort: effect on CYP3A4 activity. Clin Pharmacol Ther 2000; 67(5): 451–7
Hennessy M, Kelleher D, Spiers JP, et al. St John’s wort increases expression of P-glycoprotein: implications for drug interactions. Br J Clin Pharmacol 2002; 53(1): 75–82
Perloff MD, von Moltke LL, Stornier E, et al. Saint John’s wort: an in vitro analysis of P-glycoprotein induction due to extended exposure. Br J Pharmacol 2001; 134(8): 1601–8
Xie R, Tan LH, Polasek EC, et al. CYP3A and P-glycoprotein activity induction with St. John’s wort in healthy volunteers from 6 ethnic populations. J Clin Pharmacol 2005; 45(3): 352–6
Moschella C, Jaber BL. Interaction between cyclosporine and Hypericum perforatum (St John’s wort) after organ transplantation. Am J Kidney Dis 2001; 38(5): 1105–7
Kane GC, Lipsky JJ. Drug-grapefruit juice interactions. Mayo Clin Proc 2000; 75(9): 933–42
Bailey DG, Malcolm J, Arnold O, et al. Grapefruit juice-drug interactions. Br J Clin Pharmacol 1998; 46(2): 101–10
Hunter J, Hirst BH. Intestinal secretion of drugs: the role of p-glycoprotein and related drug efflux systems in limiting oral drug absorption. Adv Drug Deliver Rev 1997; 25: 129–57
Zhang YC, Benet LZ. The gut as a barrier to drug absorption: combined role of cytochrome P450 3A and P-glycoprotein. Clin Pharmacokinet 2001; 40(3): 159–68
Wang MQ, Guilbert LJ, Ling L, et al. Immunomodulating activity of CVT-E002, a proprietary extract from North American ginseng (Panax quinquefolium). J Pharm Pharmacol 2001; 53(11): 1515–23
Liao BS, Newmark H, Zhou RP. Neuroprotective effects of ginseng total saponin and ginsenosides Rb1 and Rg1 on spinal cord neurons in vitro. Exp Neurol 2002; 173(2): 224–34
Deyama T, Nishibe S, Nakazawa Y. Constituents and pharmacological effects of Eucommia and Siberian ginseng. Acta Pharmacol Sin 2001; 22(12): 1057–70
Chi JG. Cancer chemoprevention of INSAM (Ginseng): foreword [abstract]. J Korean Med Sci 2001; 16 Suppl. S: S1
Nishino H, Tokuda H, Li T, et al. Cancer chemoprevention by ginseng in mouse liver and other organs. J Korean Med Sci 2001; 16 Suppl. S: S66–9
Han BH, Han YN, Park MH, et al. Chemistry and biochemistry of ginseng components: ginsenosides and antioxidants. In: Mori A, Satoh A, editors. Emerging drugs: molecular aspects of Asian medicines. Singapore: World Scientific Publisher, 2001: 387–98
Kitagawa I, Yoshikawa M, Yoshihara M, et al. Chemical studies of crude drugs (1): constituents of Ginseng radix rubra [in Japanese]. Yakugaku Zasshi 1983; 103: 612–22
Bae EA, Han MJ, Choo MK, et al. Metabolism of 20 (S)- and 20 (R)-ginsenoside R-g3 by human intestinal bacteria and its relation to in vitro biological activities. Biol Pharm Bull 2002; 25(1): 58–63
Coon JT, Ernst E. Panax ginseng : a systematic review of adverse effects and drug interactions. Drug Saf 2002; 25(5): 323–44
Lee FC, Ko JH, Park JK, et al. Effects of Panax ginseng on blood alcohol clearance in man. Clin Exp Pharmacol Physiol 1987; 14(6): 543–6
Agarwal DP. Genetic polymorphisms of alcohol metabolizing enzymes. Pathol Biol (Paris) 2001; 49(9): 703–9
Ashmarin IP, Danilova RA, Obukhova MF, et al. Main ethanol metabolizing alcohol dehydrogenases (ADH I and ADH IV): biochemical functions and the physiological manifestation. FEBS Lett 2000; 486(1): 49–51
Koo MW. Effects of ginseng on ethanol induced sedation in mice. Life Sci 1999; 64(2): 153–60
Petkov V, Koushev V, Panova Y. Accelerated ethanol elimination under the effect of Ginseng (experiments on rats). Acta Physiol Pharmacol Bulg 1977; 3(1): 46–50
Lee YJ, Pantuck CB, Pantuck EJ. Effect of ginseng on plasma levels of ethanol in the rat. Planta Med 1993; 59(1): 17–9
Shader RI, Greenblatt DJ. Phenelzine and the dream machine: ramblings and reflections. J Clin Psychopharmacol 1985; 5(2): 65
Jones BD, Runikis AM. Interaction of ginseng with phenelzine. J Clin Psychopharmacol 1987; 7(3): 201–2
Shader RI, Greenblatt DJ. Bees, ginseng and MAOIs revisited. J Clin Psychopharmacol 1988; 8(4): 235
Sala F, Mulet J, Choi S, et al. Effects of ginsenoside Rg2 on human neuronal nicotinic acetylcholine receptors. J Pharmacol Exp Ther 2002; 301(3): 1052–9
Toda N, Ayajiki K, Fujioka H, et al. Ginsenoside potentiates NO-mediated neurogenic vasodilatation of monkey cerebral arteries. J Ethnopharmacol 2001; 76(1): 109–13
Liu D, Li B, Liu Y, et al. Voltage-dependent inhibition of brain Na (+) channels by American ginseng. Eur J Pharmacol 2001: 413(1): 47–54
Kim S, Ahn K, Oh TH, et al. Inhibitory effect of ginsenosides on NMDA receptor-mediated signals in rat hippocampal neurons. Biochem Biophys Res Commun 2002; 296(2): 247–54
Baker GB, Urichuk LJ, McKenna KF, et al. Metabolism of monoamine oxidase inhibitors. Cell Mol Neurobiol 1999; 19(3): 411–26
Janetzky K, Morreale AP. Probable interaction between warfarin and ginseng. Am J Health Syst Pharm 1997; 54(6): 692–3
Jiang X, Williams KM, Liauw WS, et al. Effect of St John’s wort and ginseng on the pharmacokinetics and pharmacodynamics of warfarin in healthy subjects. Br J Clin Pharmacol 2004; 57(5): 592–9
Yuan CS, Wei G, Dey L, et al. Brief communication: American ginseng reduces warfarin’s effect in healthy patients: a randomized, controlled trial. Ann Intern Med 2004; 141(1): 23–7
Cui X, Sakaguchi T, Shirai Y, et al. Orally administered Panax ginseng extract decreases platelet adhesiveness in 66% hepatectomized rats. Am J Chin Med 1999; 27(2): 251–6
Yun YP, Do JH, Ko SR, et al. Effects of Korean red ginseng and its mixed prescription on the high molecular weight dextraninduced blood stasis in rats and human platelet aggregation. J Ethnopharmacol 2001; 77(2–3): 259–64
Jung KY, Kim DS, Oh SR, et al. Platelet activating factor antagonist activity of ginsenosides. Biol Pharm Bull 1998; 21(1): 79–80
Kuo SC, Teng CM, Lee JC, et al. Antiplatelet components in Panax ginseng. Planta Med 1990; 56(2): 164–7
Zhu M, Chan KW, Ng LS, et al. Possible influences of ginseng on the pharmacokinetics and pharmacodynamics of warfarin in rats. J Pharm Pharmacol 1999; 51(2): 175–80
Nguyen TD, Villard PH, Barlatier A, et al. Panax vietnamensis protects mice against carbon tetrachloride-induced hepatotoxicity without any modification of CYP2E1 gene expression. Planta Med 2000; 66(8): 714–9
Chang TKH, Chen J, Benetton SA. In vitro effect of standardized ginseng extracts and individual ginsenosides on the catalytic activity of human CYP1A1, CYP1A2, and CYP1B1. Drug Metab Dispos 2002; 30(4): 378–84
Henderson GL, Harkey MR, Gershwin ME, et al. Effects of ginseng components on c-DNA-expressed cytochrome P450 enzyme catalytic activity. Life Sci 1999; 65(15): PL209–14
Furutsu M, Koyama Y, Kusakabe M, et al. Preventive effect of the extract of Du-zhong (Tochu) leaf and ginseng root on acute toxicity of chlorpyrifos. Jpn J Toxicol Environ Health 1997; 43(2): 92–100
Kim HJ, Chun YJ, Park JD, et al. Protection of rat liver micro-somes against carbon tetrachloride-induced lipid peroxidation by red ginseng saponin through cytochrome P450 inhibition. Planta Med 1997; 63(5): 415–8
Scaglione F, Cattaneo G, Alessandria M, et al. Efficacy and safety of the standardised Ginseng extract G115 for potentiating vaccination against the influenza syndrome and protection against the common cold [corrected; published erratum appears in Drugs Exp Clin Res 1996; 22 (6): 338]}. Drugs Exp Clin Res 1996; 22(2): 65–72
Rivera E, Hu S, Concha C. Ginseng and aluminium hydroxide act synergistically as vaccine adjuvants. Vaccine 2003; 21(11–12): 1149–57
Hu S, Concha C, Lin F, et al. Adjuvant effect of ginseng extracts on the immune responses to immunisation against Staphylococcus aureus in dairy cattle. Vet Immunol Immunopathol 2003; 91(1): 29–37
Rivera E, Daggfeldt A, Hu S. Ginseng extract in aluminium hydroxide adjuvanted vaccines improves the antibody response of pigs to porcine parvovirus and Erysipelothrix rhusiopathiae . Vet Immunol Immunopathol 2003; 91(1): 19–27
Singh YN, Singh NN. Therapeutic potential of kava in the treatment of anxiety disorders. CNS Drugs 2002; 16(11): 731–43
Volz HP, Kieser M. Kava-kava extract WS 1490 versus placebo in anxiety disorders: a randomized placebo-controlled 25-week outpatient trial. Pharmacopsychiatry 1997; 30(1): 1–5
Pittler MH, Ernst E. Efficacy of kava extract for treating anxiety: systematic review and meta-analysis. J Clin Psychopharmacol 2000; 20(2): 84–9
Rouse J. Kava: a South Pacific herb for anxiety, tension and insomnia. Clin Nutr Insights 1998; 96: 3900–5
Wheatley D. Stress-induced insomnia treated with kava and valerian: singly and in combination. Hum Psychopharmacol 2001; 16(4): 353–6
Stevinson C, Huntley A, Ernst E. A systematic review of the safety of kava extract in the treatment of anxiety. Drug Saf 2002; 25(4): 251–61
Bilia AR, Gallon S, Vincieri FF. Kava-kava and anxiety: growing knowledge about the efficacy and safety. Life Sci 2002; 70(22): 2581–97
Lebot V, Lévesque J. The origin and distribution of kava (Piper methysticum Forst, f. and Piper wichmannii C. DC, Piperaceae): a phytochemical approach. Allertonia 1989; 5: 223–80
Zou L, Harkey MR, Henderson GL. Effects of herbal components on cDNA-expressed cytochrome P450 enzyme catalytic activity. Life Sci 2002; 71(13): 1579–89
Anke J, Ramzan I. Pharmacokinetic and pharmacodynamic drug interactions with Kava (Piper methysticum Forst, f.) J Ethnopharmacol 2004; 93(2–3): 153–60
Herberg KW. Effect of Kava-Special Extract WS 1490 combined with ethyl alcohol on safety-relevant performance parameters [in German]. Blutalkohol 1993; 30(2): 96–105
Jamieson DD, Duffield PH. Positive interaction of ethanol and kava resin in mice. Clin Exp Pharmacol Physiol 1990; 17(7): 509–14
Almeida JC, Grimsley EW. Coma from the health food store: interaction between Kava and alprazolam. Ann Intern Med 1996; 125(11): 940–1
Yuan CS, Dey L, Wang A, et al. Kavalactones and dihydrokavain modulate GABAergic activity in a rat gastric-brainstem preparation. Planta Med 2002; 68(12): 1092–6
Jussofie A, Schmiz A, Hiemke C. Kavapyrone enriched extract from Piper methysticum as modulator of the GABA binding site in different regions of rat brain. Psychopharmacology (Berl) 1994; 116(4): 469–74
Gorski JC, Jones DR, Hamman MA, et al. Biotransformation of alprazolam by members of the human cytochrome P4503A subfamily. Xenobiotica 1999; 29(9): 931–44
Herberg KW. Safety-related performance after intake of kava-extract, bromazepam and their combination. Z Allgemeinmed 1996; 72: 973–7
Schelosky L, Raffauf C, Jendroska K, et al. Kava and dopamine antagonism. J Neurol Neurosurg Psychiatry 1995; 58(5): 639–40
Baum SS, Hill R, Rommelspacher H. Effect of kava extract and individual kavapyrones on neurotransmitter levels in the nucleus accumbens of rats. Prog Neuropsychopharmacol Biol Psychiatry 1998; 22(7): 1105–20
Meseguer E, Taboada R, Sanchez V, et al. Life-threatening parkinsonism induced by kava-kava. Mov Disord 2002; 17(1): 195–6
Bajad S, Bedi KL, Singla AK, et al. Piperine inhibits gastric emptying and gastrointestinal transit in rats and mice. Planta Med 2001; 67(2): 176–9
Hiwale AR, Dhuley JN, Naik SR. Effect of co-administration of piperine on pharmacokinetics of beta-lactam antibiotics in rats. Indian J Exp Biol 2002; 40(3): 277–81
Gupta SK, Bansal P, Bhardwaj RK, et al. Comparative anti-nociceptive, anti-inflammatory and toxicity profile of nimesulide vs nimesulide and piperine combination. Pharm Res 2000; 41(6): 657–62
Mujumdar AM, Dhuley JN, Deshmukh VK, et al. Effect of piperine on pentobarbitone induced hypnosis in rats. Indian J Exp Biol 1990; 28(5): 486–7
Shoba G, Joy D, Joseph T, et al. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med 1998; 64(4): 353–6
Badmaev VV, Majeed M, Prakash L. Piperine derived from black pepper increases the plasma levels of coenzyme q10 following oral supplementation. J Nutr Biochem 2000; 11(2): 109–13
Bano G, Raina RK, Zutshi U, et al. Effect of piperine on bioavailability and pharmacokinetics of propranolol and theophylline in healthy volunteers. Eur J Clin Pharmacol 1991; 41(6): 615–7
Johnson JA, Herring VL, Wolfe MS, et al. CYP1A2 and CYP2D6 4-hydroxylate propranolol and both reactions exhibit racial differences. J Pharmacol Exp Ther 2000; 294(3): 1099–105
Ching MS, Bichara N, Blake CL, et al. Propranolol 4- and 5-hydroxylation and N-desisopropylation by cloned human cytochrome P4501A1 and P4501A2. Drug Metab Dispos 1996; 24(6): 692–4
Yoshimoto K, Echizen H, Chiba K, et al. Identification of human CYP isoforms involved in the metabolism of propranolol enantiomers: N-desisopropylation is mediated mainly by CYP1A2. Br J Clin Pharmacol 1995; 39(4): 421–31
Singh J, Reen RK. Modulation of constitutive, benz[a]anthracene- and phenobarbital-inducible cytochromes-P450 activities in rat hepatoma H4IIEC3/G-cells by piperine. Curr Sci 1994; 66(5): 365–9
Dalvi RR, Dalvi PS. Comparison of the effects of piperine administered intragastrically and intraperitoneally on the liver and liver mixed-function oxidases in rats. Drug Metabol Drug Interact 1991; 9(1): 23–30
Kang MH, Won SM, Park SS, et al. Piperine effects on the expression of P4502E1, P4502B and P4501A in rat. Xenobiotica 1994; 24(12): 1195–204
Zutshi RK, Singh R, Zutshi U, et al. Influence of piperine on rifampicin blood levels in patients of pulmonary tuberculosis. J Assoc Physicians India 1985; 33: 223–4
Schuetz EG, Schinkel AH, Relling MV, et al. P-glycoprotein: a major determinant of rifampicin-inducible expression of cytochrome P4503A in mice and humans. Proc Natl Acad Sci U S A 1996; 93: 4001–5
Bhardwaj RK, Glaeser H, Becquemont L, et al. Piperine, a major constituent of black pepper, inhibits human P-glycoprotein and CYP3A4. J Pharmacol Exp Ther 2002; 302(2): 645–50
Atal CK, Zutshi U, Rao PG. Scientific evidence on the role of Ayurvedic herbals on bioavailability of drugs. J Ethnopharmacol 1981; 4: 229–32
Dalvi RR, Dalvi PS. Differences in the effects of piperine and piperonyl butoxide on hepatic drug-metabolizing enzyme system in rats. Drug Chem Toxicol 1991; 14(1–2): 219–29
Tjia JF, Colbert J, Back DJ. Theophylline metabolism in human liver microsomes: inhibition studies. J Pharmacol Exp Ther 1996; 276(3): 912–7
Ha HR, Chen J, Freiburghaus AU, et al. Metabolism of theophylline by cDNA-expressed human cytochromes P-450. Br J Clin Pharmacol 1995; 39(3): 321–6
Velpandian T, Jasuja R, Bhardwaj RK, et al. Piperine in food: interference in the pharmacokinetics of phenytoin. Eur J Drug Metab Pharmacokinet 2001; 26(4): 241–7
Bano G, Amla V, Raina RK, et al. The effect of piperine on pharmacokinetics of phenytoin in healthy volunteers. Planta Med 1987; 53(6): 568–9
Tsukamoto S, Cha BC, Ohta T. Dipiperamides A, B, and C: bisalkaloids from the white pepper Piper nigrum inhibiting CYP3A4 activity. Tetrahedron 2002; 58(9): 1667–71
Veronese ME, Mackenzie PI, Doecke CJ, et al. Tolbutamide and phenytoin hydroxylations by cDNA-expressed human liver cytochrome P4502C9. Biochem Biophys Res Commun 1991; 175(3): 1112–8
Bajpai M, Roskos LK, Shen DD, et al. Roles of cytochrome P4502C9 and cytochrome P4502C19 in the stereoselective metabolism of phenytoin to its major metabolite. Drug Metab Dispos 1996; 24(12): 1401–14
Cuttle L, Munns AJ, Hogg NA, et al. Phenytoin metabolism by human cytochrome P450: involvement of P450 3A and 2C forms in secondary metabolism and drug-protein adduct formation. Drug Metab Dispos 2000; 28(8): 945–50
Munns AJ, De Voss JJ, Hooper WD, et al. Bioactivation of phenytoin by human cytochrome P450: characterization of the mechanism and targets of covalent adduct formation. Chem Res Toxicol 1997; 10(9): 1049–58
Komatsu T, Yamazaki H, Asahi S, et al. Formation of a dihydroxy metabolite of phenytoin in human liver microsomes/cytosol: roles of cytochromes P4502C9, 2C19, and 3A4. Drug Metab Dispos 2000; 28(11): 1361–8
Schinkel AH, Wagenaar E, Mol CA, et al. P-glycoprotein in the blood-brain barrier of mice influences the brain penetration and pharmacological activity of many drugs. J Clin Invest 1996; 97: 2517–24
Cummins CL, Jacobsen W, Benet LZ. Unmasking the dynamic interplay between intestinal P-glycoprotein and CYP3A4. J Pharmacol Exp Ther 2002; 300(3): 1036–45
Ji XY, Tan BK, Zhu YZ. Salvia miltiorrhiza and ischemic diseases. Acta Pharmacol Sin 2000; 21(12): 1089–94
Lee AR, Wu WL, Chang WL, et al. Isolation and bioactivity of new tanshinones. J Nat Prod 1987; 50(2): 157–60
Chan TY. Interaction between warfarin and danshen (Salvia miltiorrhiza). Ann Pharmacother 2001; 35(4): 501–4
Yu CM, Chan JC, Sanderson JE. Chinese herbs and warfarin potentiation by ‘danshen’. J Intern Med 1997; 241(4): 337–9
Au-Yeung KK, Zhu DY, O K, et al. Inhibition of stress-activated protein kinase in the ischemic/reperfused heart: role of magnesium tanshinoate B in preventing apoptosis. Biochem Pharmacol 2001; 62(4): 483–93
Zhou W, Ruigrok TJ. Protective effect of danshen during myocardial ischemia and reperfusion: an isolated rat heart study. Am J Chin Med 1990; 18(1–2): 19–24
Wu TW, Zeng LH, Fung KP, et al. Effect of sodium tanshinone IIA sulfonate in the rabbit myocardium and on human cardiomyocytes and vascular endothelial cells. Biochem Pharmacol 1993; 46(12): 2327–32
Kim SY, Moon TC, Chang HW, et al. Effects of tanshinone I isolated from Salvia miltiorrhiza bunge on arachidonic acid metabolism and in vivo inflammatory responses. Phytother Res 2002; 16(7): 616–20
Oh SH, Nan JX, Sohn DW, et al. Salvia miltiorrhiza inhibits biliary obstruction-induced hepatocyte apoptosis by cytoplasmic sequestration of p53. Toxicol Appl Pharmacol 2002; 182(1): 27–33
Lee TY, Mai LM, Wang GJ, et al. Protective mechanism of Salvia miltiorrhiza on carbon tetrachloride-induced acute hepatotoxicity in rats. J Pharmacol Sci 2003; 91(3): 202–10
Peng Y, Liu F, Luo J, et al. Effects of danshen and shengmaiye on glomerulosclerosis by adriamycin in rats [in Chinese]. Hunan Yi Ke Da Xue Xue Bao 1999; 24(4): 332–4
Sato M, Sato T, Ose Y, et al. Modulating effect of tanshinones on mutagenic activity of Trp-P-1 and benzo[a]pyrene in Salmonella typhimurium. Mutat Res 1992; 265(2): 149–54
Abd-Elazem IS, Chen HS, Bates RB, et al. Isolation of two highly potent and non-toxic inhibitors of human immunodeficiency virus type 1 (HIV-1) integrase from Salvia miltiorrhiza. Antiviral Res 2002; 55(1): 91–106
Kang BY, Chung SW, Kim SH, et al. Inhibition of interleukin-12 and interferon-gamma production in immune cells by tanshinones from Salvia miltiorrhiza. Immunopharmacology 2000; 49(3): 355–61
Ryu SY, Oak MH, Kim KM. Inhibition of mast cell degranulation by tanshinones from the roots of Salvia miltiorrhiza. Planta Med 1999; 65(7): 654–5
O K, Lynn EG, Vazhappilly R, et al. Magnesium tanshinoate B (MTB) inhibits low density lipoprotein oxidation. Life Sci 2001; 68(8): 903–12
Zhao BL, Jiang W, Zhao Y, et al. Scavenging effects of salvia miltiorrhiza on free radicals and its protection for myocardial mitochondrial membranes from ischemia-reperfusion injury. Biochem Mol Biol Int 1996; 38(6): 1171–82
Kang DG, Yun YG, Ryoo JH, et al. Anti-hypertensive effect of water extract of danshen on renovascular hypertension through inhibition of the renin angiotensin system. Am J Chin Med 2002; 30(1): 87–93
Wang GZ, Ru X, Ding LH, et al. Short term effect of Salvia miltiorrhiza in treating rat acetic acid chronic gastric ulcer and long term effect in preventing recurrence. World J Gastroenterol 1998; 4(2): 169–70
Lay IS, Chiu JH, Shiao MS, et al. Crude extract of Salvia miltiorrhiza and salvianolic acid B enhance in vitro angiogenesis in murine SVR endothelial cell line. Planta Med 2003; 69(1): 26–32
Liu J, Shen HM, Ong CN. Role of intracellular thiol depletion, mitochondrial dysfunction and reactive oxygen species in Salvia miltiorrhiza-induced apoptosis in human hepatoma HepG2 cells. Life Sci 2001; 69(16): 1833–50
Wu WL, Chang WL, Chen CF. Cytotoxic activities of tanshinones against human carcinoma cell lines. Am J Chin Med 1991; 19(3–4): 207–16
Izzat MB, Yim APC, El-Zufari MH. A taste of Chinese medicine! Ann Thorac Surg 1998; 66: 941–942
Cheng TO. Warfarin danshen interaction [letter]. Ann Thorac Surg 1999; 67(3): 894
Lo AC, Chan K, Yeung JH, et al. The effects of danshen ( Salvia miltiorrhiza ) on pharmacokinetics and pharmacodynamics of warfarin in rats. Eur J Drug Metab Pharmacokinet 1992; 17(4): 257–62
Petitpas I, Bhattacharya AA, Twine S, et al. Crystal structure analysis of warfarin binding to human serum albumin: anatomy of drug site I. J Biol Chem 2001; 276(25): 22804–9
Fitos I, Visy J, Kardos J. Stereoselective kinetics of warfarin binding to human serum albumin: effect of an allosteric interaction. Chirality 2002; 14(5): 442–8
Gupta D, Jalali M, Wells A, et al. Drug-herb interactions: unexpected suppression of free Danshen concentrations by salicylate. J Clin Lab Anal 2002; 16(6): 290–4
Makino T, Wakushima H, Okamoto T, et al. Pharmacokinetic interactions between warfarin and kangen-karyu, a Chinese traditional herbal medicine, and their synergistic action. J Ethnopharmacol 2002; 82(1): 35–40
Tang W, Eisenbrand G. Scutellaria baicalensis Georgi: Chinese drugs of plant original. Heidelberg: Springer-Verlag, 1992
Qi L, Zhou R, Wang YF, et al. Study of major flavonoids in crude Scutellariae Radix by micellar electrokinetic capillary chromatography. J Capillary Electrophor 1998; 5(5–6): 181–4
Taniguchi C, Homma M, Takano O, et al. Pharmacological effects of urinary products obtained after treatment with saiboku-to, a herbal medicine for bronchial asthma, on type IV allergic reaction. Planta Med 2000; 66(7): 607–11
Hou YN, Zhu XY, Cheng GF. Effects of baicalin on liver microsomal cytochrome P450 system [in Chinese]. Yao Xue Xue Bao 2000; 35(12): 890–2
Lin CC, Shieh DE. The anti-inflammatory activity of Scutellaria rivularis extracts and its active components, baicalin, baicalein and wogonin. Am J Chin Med 1996; 24(1): 31–6
Shieh DE, Liu LT, Lin CC. Antioxidant and free radical scavenging effects of baicalein, baicalin and wogonin. Anticancer Res 2000; 20(5A): 2861–5
Gao Z, Huang K, Yang X, et al. Free radical scavenging and antioxidant activities of flavonoids extracted from the radix of Scutellaria baicalensis Georgi. Biochim Biophys Acta 1999; 1472(3): 643–50
Ikemoto S, Sugimura K, Yoshida N, et al. Antitumor effects of Scutellariae radix and its components baicalein, baicalin, and wogonin on bladder cancer cell lines. Urology 2000; 55(6): 951–5
Akao T, Kawabata K, Yanagisawa E, et al. Baicalin, the predominant flavone glucuronide of scutellariae radix , is absorbed from the rat gastrointestinal tract as the aglycone and restored to its original form. J Pharm Pharmacol 2000; 52(12): 1563–8
Wakui Y, Yanagisawa E, Ishibashi E, et al. Determination of baicalin and baicalein in rat plasma by high-performance liquid chromatography with electrochemical detection. J Chromatogr 1992; 575(1): 131–6
Lai MY, Hsiu SL, Tsai SY, et al. Comparison of metabolic pharmacokinetics of baicalin and baicalein in rats. J Pharm Pharmacol 2003; 55(2): 205–9
Lai MY, Hsiu SL, Chen CC, et al. Urinary pharmacokinetics of baicalein, wogonin and their glycosides after oral administration of Scutellariae Radix in humans. Biol Pharm Bull 2003; 26(1): 79–83
Canal P, Gay C, Dezeuze A, et al. Pharmacokinetics and pharmacodynamics of irinotecan during a phase II clinical trial in colorectal cancer: Pharmacology and Molecular Mechanisms Group of the European Organization for Research and Treatment of Cancer. J Clin Oncol 1996; 14(10): 2688–95
Gupta E, Mick R, Ramirez J, et al. Pharmacokinetic and pharmacodynamic evaluation of the topoisomerase inhibitor irinotecan in cancer patients. J Clin Oncol 1997; 15(4): 1502–10
Kudoh S, Fujiwara Y, Takada Y, et al. Phase II study of irinotecan combined with cisplatin in patients with previously untreated small-cell lung cancer. West Japan Lung Cancer Group. J Clin Oncol 1998; 16(3): 1068–74
Humerickhouse R, Lohrbach K, Li L, et al. Characterization of CPT-11 hydrolysis by human liver carboxylesterase isoforms hCE-1 and hCE-2. Cancer Res 2000; 60(5): 1189–92
Bencharit S, Morton CL, Howard-Williams EL, et al. Structural insights into CPT-11 activation by mammalian carboxylesterases. Nat Struct Biol 2002; 9(5): 337–42
Rivory LP, Bowles MR, Robert J, et al. Conversion of irinotecan (CPT-11) to its active metabolite, 7-ethyl-10-hydroxy-camptothecin (SN-38), by human liver carboxylesterase. Biochem Pharmacol 1996; 52(7): 1103–11
Hanioka N, Ozawa S, Jinno H, et al. Human liver UDP-glucuronosyltransferase isoforms involved in the glucuronidation of 7-ethyl-10-hydroxycamptothecin. Xenobiotica 2001; 31(10): 687–99
Mathijssen RHJ, van Alphen RJ, Verweij J, et al. Clinical pharmacokinetics and metabolism of irinotecan (CPT-11). Clin Cancer Res 2001; 7(8): 2182–94
Santos A, Zanetta S, Cresteil T, et al. Metabolism of irinotecan (CPT-11) by CYP3A4 and CYP3A5 in humans. Clin Cancer Res 2000; 6(5): 2012–20
Sugiyama Y, Kato Y, Chu X. Multiplicity of biliary excretion mechanisms for the camptothecin derivative irinotecan (CPT-11), its metabolite SN-38, and its glucuronide: role of canalicular multispecific organic anion transporter and P-glycoprotein. Cancer Chemother Pharmacol 1998; 42 Suppl.: S44–9
Gupta E, Lestingi TM, Mick R, et al. Metabolic fate of irinotecan in humans: correlation of glucuronidation with diarrhea. Cancer Res 1994; 54(14): 3723–5
Xie R, Mathijssen RH, Sparreboom A, et al. Clinical pharmacokinetics of irinotecan and its metabolites in relation with diarrhea. Clin Pharmacol Ther 2002; 72(3): 265–75
Mori K, Kondo T, Kamiyama Y, et al. Preventive effect of Kampo medicine (Hangeshashin-to) against irinotecan-induced diarrhea in advanced non-small-cell lung cancer. Cancer Chemother Pharmacol 2003; 51(5): 403–6
Takasuna K, Kasai Y, Kitano Y, et al. Protective effects of kampo medicines and baicalin against intestinal toxicity of a new anticancer camptothecin derivative, irinotecan hydrochloride (CPT-11), in rats. Jpn J Cancer Res 1995; 86(10): 978–84
Kase Y, Hayakawa T, Aburada M, et al. Preventive effects of Hange-shashin-to on irinotecan hydrochloride-caused diarrhea and its relevance to the colonic prostaglandin E2 and water absorption in the rat. Jpn J Pharmacol 1997; 75(4): 407–13
Kase Y, Hayakawa T, Togashi Y, et al. Relevance of irinotecan hydrochloride-induced diarrhea to the level of prostaglandin E2 and water absorption of large intestine in rats. Jpn J Pharmacol 1997; 75(4): 399–405
Narita M, Nagai E, Hagiwara H, et al. Inhibition of betaglucuronidase by natural glucuronides of kampo medicines using glucuronide of SN-38 (7-ethyl-10-hydroxy-camptothecin) as a substrate. Xenobiotica 1993; 23(1): 5–10
Chu XY, Suzuki H, Ueda K, et al. Active efflux of CPT-11 and its metabolites in human KB-derived cell lines. J Pharmacol Exp Ther 1999; 288(2): 735–41
Chu XY, Kato Y, Ueda K, et al. Biliary excretion mechanism of CPT-11 and its metabolites in humans: involvement of primary active transporters. Cancer Res 1998; 58(22): 5137–43
Chu XY, Kato Y, Niinuma K, et al. Multispecific organic anion transporter is responsible for the biliary excretion of the camptothecin derivative irinotecan and its metabolites in rats. J Pharmacol Exp Ther 1997; 281(1): 304–14
Wallace S, Carrier D, Clausen E. Extraction of nutraceuticals from milk thistle: part II. Extraction with organic solvents. Appl Biochem Biotechnol 2003; 108(1–3): 891–904
Barreto J, Wallace S, Carrier D, et al. Extraction of nutraceuticals from milk thistle. I: hot water extraction. Appl Biochem Biotechnol 2003; 108(1–3): 881–90
Wellington K, Jarvis B. Silymarin: a review of its clinical properties in the management of hepatic disorders. Biodrugs 2001; 15(7): 465–89
Quaglia MG, Bossu E, Donati E, et al. Determination of silymarine in the extract from the dried silybum marianum fruits by high performance liquid chromatography and capillary electrophoresis. J Pharm Biomed Anal 1999; 19(3–4): 435–42
Kvasnicka F, Biba B, Sevcik R, et al. Analysis of the active components of silymarin. J Chromatogr A 2003; 990(1–2): 239–45
Ding T, Tian S, Zhang Z, et al. Determination of active component in silymarin by RP-LC and LC/MS. J Pharm Biomed Anal 2001; 26(1): 155–61
Lorenz D. Untersuchungen zur elimination von silymarin bei cholezystektomiertan patientsten 2. Mitteilung: Biliaere elimination nach mehrfacher oraler Gabe. Planta Med 1982; 45: 216–23
Kren V, Ulrichova J, Kosina P, et al. Chemoenzymatic preparation of silybin beta-glucuronides and their biological evaluation. Drug Metab Dispos 2000; 28(12): 1513–7
Weyhenmeyer R, Mascher H, Birkmayer J. Study on doselinearity of the pharmacokinetics of silibinin diastereomers using a new stereospecific assay. Int J Clin Pharmacol Ther Toxicol 1992; 30(4): 134–41
Gatti G, Perucca E. Plasma concentrations of free and conjugated silybin after oral intake of a silybin-phosphatidylcholine complex (silipide) in healthy volunteers. Int J Clin Pharmacol Ther 1994; 32(1): 614–7
Schandalik R, Gatti G, Perucca E. Pharmacokinetics of silybin in bile following administration of silipide and silymarin in cholecystectomy patients. Arzneimittelforschung 1992; 42(7): 964–8
Salmi HA, Sarna S. Effects of silymarin on chemical functional and morphological alterations of the liver. Scand J Gastroenterol 1982; 17: 517–21
Piscitelli SC, Formentini E, Burstein AH, et al. Effect of milk thistle on the pharmacokinetics of indinavir in healthy volunteers. Pharmacotherapy 2002; 22(5): 551–6
DiCenzo R, Shelton M, Jordan K, et al. Coadministration of milk thistle and indinavir in healthy subjects. Pharmacotherapy 2003; 23(7): 866–70
Beckmann-Knopp S, Rietbrock S, Weyhenmeyer R, et al. Inhibitory effects of silibinin on cytochrome P-450 enzymes in human liver microsomes. Pharmacol Toxicol 2000; 86(6): 250–6
Venkataramanan R, Ramachandran V, Komoroski BJ, et al. Milk thistle, a herbal supplement, decreases the activity of CYP3A4 and uridine diphosphoglucuronosyl transferase in human hepatocyte cultures. Drug Metab Dispos 2000; 28(11): 1270–3
Sridar C, Goosen TC, Kent UM, et al. Silybin inactivates cytochromes P450 3A4 and 2C9 and inhibits major hepatic glucuronosyltransferases. Drug Metab Dispos 2004; 32(6): 587–94
Schandalik R, Perucca E. Pharmacokinetics of silybin following oral administration of silipide in patients with extrahepatic biliary obstruction. Drugs Exp Clin Res 1994; 20(1): 37–42
Gurley BJ, Gardner SF, Hubbard MA, et al. In vivo assessment of botanical supplementation on human cytochrome P450 phenotypes: Citrus aurantium, Echinacea purpurea , milk thistle, and saw palmetto. Clin Pharmacol Ther 2004; 76(5): 428–40
Zhang S, Morris ME. Effects of the flavonoids biochanin A, morin, phloretin, and silymarin on P-glycoprotein-mediated transport. J Pharmacol Exp Ther 2003; 304(3): 1258–67
Tyagi AK, Singh RP, Agarwal C, et al. Silibinin strongly synergizes human prostate carcinoma DU145 cells to doxorubicin-induced growth Inhibition, G2-M arrest, and apoptosis. Clin Cancer Res 2002; 8(11): 3512–9
Maitrejean M, Comte G, Barron D, et al. The flavanolignan silybin and its hemisynthetic derivatives, a novel series of potential modulators of P-glycoprotein. Bioorg Med Chem Lett 2000; 10(2): 157–60
Schlichting J, Leuschner U. Drug therapy of primary biliary diseases: classical and modern strategies. J Cell Mol Med 2001; 5(1): 98–115
Paumgartner G, Beuers U. Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited. Hepatology 2002; 36(3): 525–31
Angulo P, Patel T, Jorgensen RA, et al. Silymarin in the treatment of patients with primary biliary cirrhosis with a suboptimal response to ursodeoxycholic acid. Hepatology 2000; 32(5): 897–900
Ellis GR, Stephens MR. Untitled [photograph and brief case report]. BMJ 1999; 319: 650
Deahl M. Betel nut-induced extrapyramidal syndrome: an unusual drug interaction. Mov Disord 1989; 4(4): 330–2
Mathews Jr MK. Association of Ginkgo biloba with intracerebral haemorrhage [letter]. Neurology 1998; 50(6): 1933–4
Rey JM, Walter G. Hypericum perforatum (St John’s wort) in depression: pest or blessing? Med J Aust 1998; 169(11–12): 583–6
Bon S, Hartmann K, Kubn M. Johanniskraut: ein enzyminduktor? Schweitz Apoth Ztg 1999; 16: 535–6
Breidenbach T, Hoffmann MW, Becker T, et al. Drug interaction of St John’s wort with cyclosporin [letter]. Lancet 2000: 355(9218): 1912
Roots I, Johne A, Maurer A. Arzneimittel interaktionen von hypericum-extract [abstract]. In: Roots I, Kemper FH, editors. Proc Germ Soc Pharmacol. Berlin: Conference Organising Committee, 2000 Jun 16–17
Barone GW, Gurley BJ, Ketel BL, et al. Herbal supplements: a potential for drug interactions in transplant recipients. Transplantation 2001; 71(2): 239–41
Khawaja IS, Marotta RF, Lippmann S. Herbal medicines as a factor in delirium. Psychiatr Serv 1999; 50(7): 969–70
Valenzuela A, Bustamante JC, Videla C, et al. Effect of silybin dihemisuccinate on the ethanol metabolizing systems of the rat liver. Cell Biochem Funct 1989; 7(3): 173–8
Comoglio A, Tomasi A, Malandrino S, et al. Scavenging effect of silipide, a new silybin-phospholipid complex, on ethanol-derived free radicals. Biochem Pharmacol 1995; 50(8): 1313–6
Varga M, Buris L, Fodor M. Ethanol elimination in man under influence of hepatoprotective silibinin. Blutalkohol 1991; 28(6): 405–8
Gyonos I, Agoston M, Kovacs A, et al. Silymarin and vitamin E do not attenuate and vitamin E might even enhance the antiarrhythmic activity of amiodarone in a rat reperfusion arrhythmia model. Cardiovasc Drugs Ther 2001; 15(3): 233–40
Gill J, Heel RC, Fitton A. Amiodarone: an overview of its pharmacological properties, and review of its therapeutic use in cardiac arrhythmias. Drugs 1992; 43(1): 69–110
Trivier J–M, Libersa C, Belloc C, et al. Amiodarone N-deethylation in human liver microsomes: involvement of cytochrome P4503A enzymes (first report). Life Sci 1993; 52(10): 91–6
Fabre G, Julian B, Saint-Aubert B, et al. Evidence for CYP3A-mediated N-deethylation of amiodarone in human liver microsomal fractions. Drug Metab Dispos 1993; 21(6): 978–85
Ohyama K, Nakajima M, Nakamura S, et al. A significant role of human cytochrome P4502C8 in amiodarone N-deethylation: an approach to predict the contribution with relative activity factor. Drug Metab Dispos 2000; 28(11): 1303–10
Scambia G, De Vincenzo R, Ranelletti FO, et al. Antiproliferative effect of silybin on gynaecological malignancies: synergism with cisplatin and doxorubicin. Eur J Cancer 1996; 32A(5): 877–82
Giacomelli S, Gallo D, Apollonio P, et al. Silybin and its bioavailable phospholipid complex (IdB 1016) potentiate in vitro and in vivo the activity of cisplatin. Life Sci 2002; 70(12): 1447–59
Bokemeyer C, Fels LM, Dunn T, et al. Silibinin protects against cisplatin-induced nephrotoxicity without compromising cisplatin or ifosfamide anti-tumour activity. Br J Cancer 1996; 74(12): 2036–41
Gaedeke J, Fels LM, Bokemeyer C, et al. Cisplatin nephrotoxicity and protection by silibinin. Nephrol Dial Transplant 1996: 11(1): 55–62
Shelley MD, Burgon K, Mason MD. Treatment of testicular germ-cell cancer: a cochrane evidence-based systematic review. Cancer Treat Rev 2002; 28(5): 237–53
Sandercock J, Parmar MK, Torri V, et al. First-line treatment for advanced ovarian cancer: paclitaxel, platinum and the evidence. Br J Cancer 2002; 87(8): 815–24
Piccart MJ, Lamb H, Vermorken JB. Current and future potential roles of the platinum drugs in the treatment of ovarian cancer. Ann Oncol 2001; 12(9): 1195–203
Go RS, Adjei AA. Review of the comparative pharmacology and clinical activity of cisplatin and carboplatin. J Clin Oncol 1999; 17(1): 409–22
Zima T, Kamenikova L, Janebova M, et al. The effect of silibinin on experimental cyclosporine nephrotoxicity. Ren Fail 1998; 20(3): 471–9
von Schonfeld J, Weisbrod B, Muller MK. Silibinin, a plant extract with antioxidant and membrane stabilizing properties, protects exocrine pancreas from cyclosporin A toxicity. Cell Mol Life Sci 1997; 53(11–12): 917–20
Dresser GK, Spence JD, Bailey DG. Pharmacokinetic-pharmacodynamic consequences and clinical relevance of cytochrome P450 3A4 inhibition. Clin Pharmacokinet 2000; 38(1): 41–57
Zhou S, Gao Y, Jiang W, et al. Interactions of herbs with cytochrome P450. Drug Metab Rev 2003; 35(1): 35–98
Zhou S, Lim LY, Chowbay B. Herbal modulation of P-glycoprotein. Drug Metab Rev 2004; 36(1): 57–104
Zhou S, Chan E, Li SC, et al. Predicting pharmacokinetic herbdrug interactions. Drug Metabol Drug Interact 2004; 20(3): 143–58
Download references
Acknowledgements
The authors appreciate the support by the National University of Singapore Academic Research Funds.
The authors have provided no information on conflicts of interest directly relevant to the content of this review.
Author information
Authors and affiliations.
Department of Pharmacy, Faculty of Science, National University of Singapore, Science Drive 4, Singapore, 117543
Zeping Hu, Xiaoxia Yang, Paul Chi Lui Ho, Sui Yung Chan, Paul Wan Sia Heng, Eli Chan, Hwee Ling Koh & Shufeng Zhou
Department of Biochemistry, Faculty of Medicine, National University of Singapore, Singapore
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Shufeng Zhou .
Rights and permissions
Reprints and permissions
About this article
Hu, Z., Yang, X., Ho, P.C.L. et al. Herb-Drug Interactions. Drugs 65 , 1239–1282 (2005). https://doi.org/10.2165/00003495-200565090-00005
Download citation
Published : 17 September 2012
Issue Date : June 2005
DOI : https://doi.org/10.2165/00003495-200565090-00005
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Cardiovascular effects of herbal products and their interaction with antihypertensive drugs—comprehensive review.

Share and Cite
Nyulas, K.-I.; Simon-Szabó, Z.; Pál, S.; Fodor, M.-A.; Dénes, L.; Cseh, M.J.; Barabás-Hajdu, E.; Csipor, B.; Szakács, J.; Preg, Z.; et al. Cardiovascular Effects of Herbal Products and Their Interaction with Antihypertensive Drugs—Comprehensive Review. Int. J. Mol. Sci. 2024 , 25 , 6388. https://doi.org/10.3390/ijms25126388
Nyulas K-I, Simon-Szabó Z, Pál S, Fodor M-A, Dénes L, Cseh MJ, Barabás-Hajdu E, Csipor B, Szakács J, Preg Z, et al. Cardiovascular Effects of Herbal Products and Their Interaction with Antihypertensive Drugs—Comprehensive Review. International Journal of Molecular Sciences . 2024; 25(12):6388. https://doi.org/10.3390/ijms25126388
Nyulas, Kinga-Ilona, Zsuzsánna Simon-Szabó, Sándor Pál, Márta-Andrea Fodor, Lóránd Dénes, Margit Judit Cseh, Enikő Barabás-Hajdu, Bernadett Csipor, Juliánna Szakács, Zoltán Preg, and et al. 2024. "Cardiovascular Effects of Herbal Products and Their Interaction with Antihypertensive Drugs—Comprehensive Review" International Journal of Molecular Sciences 25, no. 12: 6388. https://doi.org/10.3390/ijms25126388
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Open access
- Published: 20 May 2021
Current perspectives in herbal and conventional drug interactions based on clinical manifestations
- Ajaykumar Rikhabchand Surana ORCID: orcid.org/0000-0002-3855-4602 1 ,
- Shivam Puranmal Agrawal 1 ,
- Manoj Ramesh Kumbhare 1 &
- Snehal Balu Gaikwad 1
Future Journal of Pharmaceutical Sciences volume 7 , Article number: 103 ( 2021 ) Cite this article
4777 Accesses
8 Citations
Metrics details
Herbs are an important source of pharmaceuticals. Herbs are traditionally used by millions of peoples for medicine, food and drink in developed and developing nations considering that they are safe. But, interaction of herbs with other medicines may cause serious adverse effects or reduces their efficacy. The demand for “alternative” medicines has been increased significantly, which include medicine derived from plant or herbal origin. The objective of this review article mainly focuses on drug interactions of commonly used herbs along with possible mechanisms. The method adopted for this review is searching of herb-drug interactions in online database.
Herb-drug interaction leads to pharmacological modification. The drug use along with herbs may show pharmacodynamic and pharmacokinetic interactions. Pharmacokinetic interaction causes alteration in absorption, distribution, metabolism and elimination. Similarly, pharmacodynamic interaction causes additive or synergistic or antagonist effect on the drugs or vice versa. Researchers had demonstrated that herbs show the toxicities and drug interactions like other pharmacologically active compounds. There is lack of knowledge amongst physician, pharmacist and consumers related to pharmacological action and mechanism of herb-drug interaction. This review article focuses on the herb-drug interaction of danshen ( Salvia miltiorrhiza ), Echinacea ( Echinacea purpurea ), garlic ( Allium sativum ), ginkgo ( Ginkgo biloba ), goldenseal ( Hydrastis canadensis ), green tea ( Camellia sinensis ), kava ( Piper methysticum ), liquorice ( Glycyrrhiza glabra ), milk thistle ( Silybum marianum ) and St. John’s wort ( Hypericum perforatum ) along with probable mechanisms and clinical manifestation based on case studies reported in literature.
Herb-drug interactions may lead to serious side effects. Physician, pharmacist and patients must be more cautious while prescribing and or consuming these herbs.
Interaction is referred to as when the effect of one drug is changed due to the presence of another compound (food, herbal or drug) [ 1 ]. The demand for “alternative” medicines has been raised significantly, which include medicine derived from plant, animal and mineral source, i.e. herbal origin [ 2 ]. Herbal medications comprise of many phytochemicals, thus, may increase the chances of herb-drug interactions (HDIs) [ 3 ]. The global dietary supplement market size in 2019 was expected to reach about USD 123.28 billion. The same was projected to increase at a CAGR of 8.2% during the span of 2020–2027 [ 4 ]. Fifty-two million Americans (40% adults) accounted for use of complementary and alternative medicines reported in the survey of Centers for Disease Control and Prevention USA [ 5 ]. A 2011 survey by the Harvard Opinion Research Program revealed that most Americans regularly consume dietary supplements for boosting the immune system [ 6 ]. Herbals are considered to be the best option as alternative medicine all around the world due to less cost, easy availability and less side effects as compared to synthetic medicines. People should be sure of herbal drugs, owing synthetic drug has adverse effects not only in developed nations but also in developing nations. The consumption of herbal products and food supplements is not reported by people to their physicians or pharmacist. Almost all herbal products are easily available (OTC) in the market. The herbs contain various pharmacological properties due to the presence of multiple chemical constituents. Many times, the label of herbal products contain half-truth or misleading information. Given above are the major factors for HDIs, thereby increasing the likelihood of the HDIs not being identified and resolved in time. Furthermore, clinical trials addressing the safety and risk of coadministered drugs with certain herbal products showed that the outcomes are greatly affected by pharmacogenetics and/or individual.
There is lack of information about use of herbals by patients to physician and pharmacist. Many physicians are unaware about of the possible risks of HDIs. There appears to be dearth of knowledge amongst physician, pharmacist and consumers related to pharmacological action and mechanism of HDIs [ 7 ]. As HDIs occur between conventional drugs and herbal products, identification and awareness of exact HDIs become necessary. This review article focuses on the HDIs along with probable mechanisms and clinical manifestation based on case studies reported in the literature.
To collect all cases of HDIs and adverse effects, a selective literature search using publicly available electronic databases (especially the PubMed database, Scopus, and Korean databases) was performed. We used the search items including “Herbal Drug Interactions”, “drug safety pharmacology”, “Danshen Interaction”, “Echinacea Interactions”, “Garlic Interactions”, “ Ginkgo Biloba Interactions”, “Goldenseal Interactions”, “Green Tea Interactions”, “Kava Interactions”, “Liqcorice Interactions”, “Milk Thistle Interactions”, “St. Jhon’s Wort Interactions” alone and combined with the terms “herbal hepatotoxicity”, or “herb induced liver injury”. The search was primarily focused on English-language case reports, case series and clinical reviews, published till Nov. 2020. The literature with language other than English was used by converting them into English.
Mechanism involved in herb-drug interactions
Mechanism of HDIs is often clinically significant since it influences both the time course and methods of circumventing the interaction. Different mechanisms of HDIs were reported. It mainly includes the change in the gastrointestinal functions which leads to overall changes in transportation of the drug in the body. The HDI mechanism is broadly classified into pharmacokinetic and pharmacodynamic interactions.
Pharmacokinetic interactions
Inhibition and induction of transport and efflux proteins.
The absorption, distribution and elimination of drugs is widely affected by the ATP-binding cassette family which are required for drug transportation.
P-Glycoprotein (P-gp)
The absorption, distribution and elimination/reabsorption of many clinically important therapeutic substances are regulated by P-gp family proteins. Direct interaction with binding sites on the P-gp molecule takes place through competitive or non-competitive inhibition or induction of the efflux of drugs, due to modulation of P-gp by herbal constituents. The pharmacokinetic interaction based on P-gp occurs mainly by depletion of energy required for driving the translocation of P-gp-bound drug substrate, which takes place due to inhibition of ATP binding, hydrolysis or coupling of ATP-hydrolysed molecules by the phytochemicals present in herbs [ 8 ].
Multidrug resistance-associated protein-2 (MRP2)
MRP2 family is ATP-dependent, which is responsible for the transport of hydrophobic anionic conjugates and extrudes hydrophobic neutral molecules. MRP2 from liver cells exports bulky hydrophilic compounds like glutathione, glucuronide, sulfate conjugates, camptothecin and paracetamol into the bile [ 9 ].
Alteration of gastrointestinal functions
Alteration of absorption of concomitantly administered medicines along with herbal medicines takes place through several mechanisms: alteration in gastric pH, formation of insoluble complexes due to complexation and chelation, alteration in gastrointestinal motility and alteration in gastrointestinal transit time [ 10 ].
Herb-drug interactions at metabolism level
The enzymes responsible for the metabolism of synthetic drugs or their transporters are either inhibited or induced by herbal products, which cause HDIs. The enzyme degrades, deactivates or conjugates to drugs before excretion. The inhibition or induction of this enzyme by herbs causes HDIs.
I.Enzyme inhibition
The half-lives of drugs can be prolonged by inhibition of drug-metabolizing enzymes. Due to increase in half-lives of drug, plasma concentration of drug may hike unexpectedly after more doses which results into prolonged action or toxicity. Efficacy of drug may be lowered by inhibiting drug transporters, which decreases absorption of therapeutic agents. Inhibition can be of two types, viz. reversible inhibition and irreversible inhibition. The systemic exposure of the victim drug due to a decrease in metabolic clearance and/or increase in bioavailability is manifested by reversible inhibition. Competitive inhibition occurs when herb binds to the active sites of the enzyme and prevents the binding of synthetic drug and enzyme [ 8 , 11 ]. Irreversible inhibition or quasi-irreversible inhibition is characterised by time-dependent inhibition or mechanism-based inhibition. Irreversible noncovalent binding of an herb to the enzyme takes place in irreversible inhibition. Unlike reversible inhibition, the interaction can continue after removal of the perpetrator since recovery of enzyme activity depends on de novo protein synthesis [ 12 ].
II.Enzyme induction
Due to enzyme induction, plasma concentration of drug reaches subtherapeutic levels. Toxicity may be due to enhanced blood levels caused by induction of drug transporter. The enzyme induction by herbs may result in a reduction of serum drug concentrations. If metabolite is active, it may result in toxicity [ 13 ].
Metabolism occurs in two phases. Phase I reactions involve conversion to a newly formed derivative or cleavage of original drug via oxidation, reduction and hydrolysis reactions. In phase I, P450 enzymes and their subfamilies CYP1A, CYP1B, CYP2C, CYP2D, CYP2E and CYP3A play an important role. These enzymes naturally are present in the liver endoplasmic reticulum and also in the intestine [ 14 ]. Phase II reactions involve conjugation with an endogenous substance like glucuronic acid and sulfate. UDP-glucuronosyltransferase and sulfotransferase enzymes catalyse phase II conjugation reaction. Donation of a cofactor through a reaction which is catalysed by transferase causes conjugation of a substrate with a nucleophilic group (amino, hydroxyl, thiol, etc.) [ 15 ].
Alteration in renal elimination
Herbal products interact with renal functioning, leading to alteration in elimination of drug via inhibition of tubular secretion, tubular reabsorption or interference with glomerular filtration [ 16 ]. Certain herbal diuretics increase the glomerular filtration rate, and few act as direct tubular irritants [ 17 ].
Pharmacodynamic interactions
Pharmacodynamic interactions are either additive (or synergetic) or antagonistic. Additive or synergistic interaction potentiates the action of synthetic drug. Antagonistic interaction reduces the efficacy of synthetic drugs [ 18 ].
Herbal-drug interactions
The herbs which were frequently used by physicians and also as home remedies for various ailments in alternative system of medicines are selected for this review.
Danshen ( Salvia miltiorrhiza )
Danshen is used as an antibacterial, antioxidative, antineoplastic, anticoagulation and anti-inflammatory. Danshen contains diterpenoids (tanshinones and royleanones) and phenolic acids including danshensu, caffeic acid, protocatechuic aldehyde, protocatechuic acid, salvianolic acid A−E, lithospermic acid and rosmarinic acid. Danshen also contains essential oils, triterpenoids, flavone, amino acids, metallic elements and many others [ 19 ].
Danshen shows haemostasis effects like platelet aggregation inhibition, interference with the extrinsic blood coagulation, antithrombin III-like activity and promotion of fibrinolytic activity. Danshen has reported to increase area under the plasma drug concentration-time curve (AUC), elimination half-lives (t 1/2 ) and maximum plasma concentrations (C max ) and decrease total body clearance (CL) and apparent volume of distribution (V d ) of R- and S- isoform of warfarin in rats. In humans, there was increase in international normalized ratio (INR) after taking danshen and warfarin together [ 20 ]. Case report reported interaction between warfarin and danshen, leading to increase in INR, which potentiated anticoagulant effect of warfarin and increased risk of bleeding [ 21 ]. Another case was reported which lead to abnormalities of clotting in patient having rheumatic heart disease, caused by danshen and warfarin concomitant use [ 22 ].
A sequential pharmacokinetic interaction study reported induction of CYP3A4 enzyme in the gut by danshen. The confidence intervals of C max , t 1/2 , oral clearance (CL/F) and AUC zero to infinity (AUC ∞ ) of midazolam before and after oral administration of danshen tablets were (0.559, 0.849), (0.908, 1.142), (1.086, 1.688) and (0.592, 0.921), respectively, was to be 90%. There was a decline in bioavailability of midazolam due to danshen use [ 23 ].
Echinacea ( Echinacea purpurea )
Echinacea contains alkamides, caffeic acid derivative, cichoric acid, flavonoids and phenolic acids. Echinacea is worldwide used for its immunomodulatory and anti-inflammatory properties. The plant is also reported to show larvicidal activity and antibacterial and antiviral activities, especially against influenza viruses [ 24 ].
In in vivo clinical studies, 12 healthy subjects were dosed 1600 mg/day with E. purpurea extracts (for 8 days) along with caffeine, tolbutamide and midazolam to evaluate CYP1A2, CYP2C9 and CYP3A enzyme activities, respectively. The results obtained showed Echinacea extract inhibited hepatic CYP1A2 and CYP2C9, and induced CYP3A4 enzyme activity, which lead to 27% decrease in caffeine CL/F, 12% decrease in tolbutamide CL/F and 42% increase in the systematic clearance and reduced AUC by 23% of midazolam respectively [ 25 ]. Similarly, another in vivo assessment showed that E. purpurea extract inhibited CYP1A2 and induced CYP3A4 [ 26 ]. Thus, it is recommended not to use drugs that are substrate of CYP1A2, CYP2C9 and CYP3A4 enzyme along with concomitant use of Echinacea extract.
Garlic ( Allium sativum )
Garlic mainly contains organosulfur compounds such as allicin, diallyl disulfide, diallyl trisulfide and S-allyl cysteine. Garlic is used as antihyperlipidemic, antimicrobial, anti-inflammatory, antiprotozoal, anticancer and immunomodulatory activity. Garlic has been reported to show toxicity at higher doses. In contrast, some studies also showed intoxication after consumption of garlic [ 27 ].
The two in vivo pharmacokinetic trials were conducted to study the effect of garlic on the antiviral drug saquinavir. The study found that ingestion of garlic increased expression of duodenal P-gp to 131% in subjects. The average AUC and C max of saquinavir was decreased by garlic up to 51% and 54% respectively, in subjects with concomitant use along with garlic. The AUC values and C max values returned up to 60–70% of their values after the 10-day washout period. Saquinavir is metabolised by the enzyme cytochrome P450 (CYP3A4) and is also a substrate of P-gp. Thus, increased clearance and decreased bioavailability of saquinavir are possible due to induction of P-gp along with concomitant use of garlic [ 28 , 29 ].
Clinical study shows that the intake of S-allyl cysteine (active constituent of garlic) inhibits platelet aggregation [ 30 ]. A human survey found that a significant number of patients who used herbs in conjunction with warfarin had higher INR levels, indicating that this combination had potential or additive effects. Thus, inhibition of platelet aggregation shows an additive anticoagulant effect, which is a possible mechanism for warfarin and garlic interaction, which ultimately increases the anticoagulant effect. Increased anticoagulant may increase the risk of bleeding [ 31 ].
The randomized clinical trial of garlic-chlorzoxazone cocktails was given for 28 days on healthy subjects. The pre-supplementation and post-supplementation effect of garlic on CYP2E1 enzyme was evaluated by measuring 6-hydroxychlorzoxazone/chlorzoxazone serum ratio. A controlled trial showed a decrease in 6-hydroxychlorazoxazone/chlorzoxazone serum ratio by about 22%, which suggests inhibition of CYP2E1 activity by garlic [ 32 ]. Similarly, another study showed a 40% decrease in 6-hydroxychlorzoxazone/chlorzoxazone serum ratio [ 33 ].
A case report showed abnormal INR level in patients using a cocktail of fluindione-garlic. Garlic has been previously reported to inhibit some cytochrome P450 isoforms. Thus, garlic can putatively increase fluindione metabolism, thereby garlic acting as an enzymatic inducer. INR level decreased from 2.4 to 1.8 (post-supplementation of garlic for 12 days), and INR level increased to 2.8 (7 days after stopping garlic). A low INR level reduces the anticoagulant effect, increasing the risk of blood clotting (the cause of stroke). Another mechanism could be inhibition of fluindione binding to plasma proteins, but no such studies have been reported [ 34 ]. It is thus suggested that concomitant use of saquinavir, warfarin, chlorzoxazone and fluindione with garlic should be prevented.
Gingko ( Ginkgo biloba )
Ginkgo biloba leaf contains flavonol glycosides (kaempferol, quercetin, myricetin, apigenin, isorhamnetin, luteolin and tamarixetin) and terpene trilactones (ginkgolide A, B, C, J, K, L, M, P, and Q and bilobalide), proanthocyanidins and organic acids. G. biloba leaf extract is used in the treatment of Alzheimer’s disease, neurodegenerative disease, cerebral insufficiency, neurosensory problems, eye ailments, vascular insufficiencies, age-related memory deficit and oxidative stress. In addition, G. biloba is leaf used as anti-angiogenesis, anti-inflammatory, and anti-asthmatic [ 35 ].
In in vivo clinical trials, 10 healthy volunteers were given G. biloba extract (GBE) to test its effect on CYP2C9 using tolbutamide as a probe. The AUC for tolbutamide after taking GBE was reduced by 16% as compared to AUC before use of garlic along with tolbutamide. Although the interaction is considered minor, caution must be taken during concomitant use [ 36 ].
An open-label study in healthy volunteers showed a decrease in the AUC and C max of midazolam by 34% and 31% respectively when used along with GBE. This research found that GBE induces CYP3A metabolism, which leads to a decrease in midazolam concentrations [ 37 ].
In a comparative clinical study, the C max of nifedipine was nearly doubled in two subjects when GBE was taken at the same time. The probable mechanism of action is inhibition of CYP3A by GBE. Increased nifedipine causes severe and longer-lasting headaches, with dizziness or hot flushes [ 38 ].
The human trial reported significantly reduced C max of omeprazole (from 0.69 ± 0.27 to 0.48 ± 0.27 mg/ml) and omeprazole sulfone (from 0.20 ± 0.07 to 0.13 ± 0.06 mg/ml) and an increase in C max of 5-hydroxyomeprazole (from 0.28 ± 0.14 to 0.45 ± 0.21mg/ml) post-administration of G. biloba with omeprazole. Omeprazole is metabolized to 5-hydroxyomeprazole in the body. Also, after post-administration of G. biloba , renal clearance of 5-hydroxyomeprazole was significantly decreased (from 2.70 ± 1.17 to 1.53 ± 0.79 mL/min/kg). The mechanism for this interaction is increased hydroxylation of omeprazole by induction of CYP2C19 [ 39 ].
A single oral dose of GBE did not show any change in the pharmacokinetics of talinolol in 10 healthy, non-smoking male volunteers. C max of talinolol was raised by 36%, AUC (0–24) by 26% and AUC ∞ by 22% respectively. A study suggests that long-term use of GBE prejudiced talinolol disposition in humans, by affecting the activity of drug transporters like P-gp [ 40 ].
Randomized controlled trials showed elevation in AUC and C max of fexofenadine by 55% and 68% respectively. Probable mechanism for this is inhibition of P-gp-mediated efflux in humans by GBE. The AUC and C max of fexofenadine were expressively increased after coadministration quercetin (constituent of gingko) as compared to that of the placebo treatment.
A case report suggested that fatal cerebral haemorrhage was associated with concomitant use of G. biloba and ibuprofen intake in healthy men. Potential inhibition of platelet-activating factor takes place due to ginkgolide B that is a component of G. biloba . G. biloba has been reported with bleeding complications. The interaction takes place possibly due to the additive effect of GBE on ibuprofen by the inhibition of the TXA2-dependent platelet aggregation [ 41 ].
A case study showed that there was an increase in BP in a man, with coadministration of thiazide diuretics and GBE. The blood pressure increased further for a few weeks. BP returned to normal level when both diuretics and GBE were stopped. Due to the severity of complication of the interaction, the responses were not rechallenged. Diuretics are known to lower the BP, but use of GBE leads to the opposite pharmacodynamic effect (increased blood pressure). The possible mechanism for this interaction could be agonism. There are no clinical trials recorded for increase in blood pressure by GBE, but the combination should be prevented [ 42 ].
In a case study, fatal seizures were reported with anticonvulsant medications like valproic acid. GBE has been reported to induce CYP2C19 enzyme activity. The CYP450 enzyme is reported to metabolise valproate, chiefly by CYP2C9 and CYP2C19. Thus, this coadministration of valproic acid and Ginkgo biloba extract should be prevented [ 43 ].
A case study reported that a man with a persistent and painful erection of the penis that had lasted for 4 h was admitted to a hospital. Metabolism of risperidone by CYP2D6 and CYP3A4 has been recorded in literature. Both the enzymes CYP2D6 and CYP3A4 are inhibited by GBE, which is a mechanism or interaction between risperidone and GBE. Simultaneous use of GBE and risperidone increases the serum concentration of risperidone and increases the hazard of adverse effects, such as priapism [ 44 ].
Negative pharmacokinetic interaction of efavirenz was reported, in a case study (47-year-old HIV infected patient), with terpenoids (component of G. biloba ). The probable mechanism of interaction was either by induction of CYP3A4 and P-gp. Induction of CYP3A4 and P-gp by terpenoids lowers the efavirenz plasma level in patients (from 1.26 to 0.48 mg/l). The lowering of human plasma efavirenz level results in virological failure. So, it is recommended that the combination should be avoided [ 45 ].
Flavonoids are a component of G. biloba bound to benzodiazepine binding site, which possess GABAergic activity. Trazadone is used to treat behavioural disturbances as it possesses hypnotic and sedative activity. The CYP3A4 enzyme is responsible for metabolism of trazodone into active compound 1-(m-chlorophenyl) piperazine (mCPP). Flavonoids increase the activity of CYP3A4 in humans. A case study reported that flavonoids act on benzodiazepine receptors and increase the GABAergic activity by increasing mCPP production (mCPP enhances the release of GABA), which leads to increased GABAergic activity and leads to coma in patients [ 46 ].
Goldenseal ( Hydrastis canadensis )
Goldenseal mainly contains berberine, 3,4-dimethoxy-2-(methoxycarbonyl) benzoic acid, 3,5,30 -trihydroxy-7,40 -dimethoxy-6,8-C-dimethyl-flavone, chilenine, (2R)-5,40 -dihydroxy-6-C-methyl -7-methoxy-flavanone, 5,40 -dihydroxy-6,8-di-C-methyl-7-methoxy-flavanone, noroxyhydrastinine, oxyhydrastinine and 40,50-dimethoxy-4-methyl-30-oxo-(1,2,5,6-tetrahydro-4H-1,3-dioxolo-[40 ,50 :4,5] -benzo [1,2-e]-1,2-oxazocin)-2-spiro-10-phtalan [ 47 ]. Goldenseal is reported in folk medicine for the treatment of urinary disorders, gastrointestinal disturbances and skin ailments [ 48 ].
In vivo clinical study was performed for the action of goldenseal on CYP isoform enzyme, which reported inhibition of CYP2D6 and CYP3A4/5 by 40% [ 49 ].
A study on humans was performed to determine CYP2D6 activity using debrisoquine. By evaluating debrisoquine urinary recovery ratios, 50% inhibition of CYP2D6 activity was observed by post-supplementation of goldenseal along with debrisoquine, which lead to a decrease in debrisoquine urinary recovery ratios [ 50 ].
Randomized clinical trials in healthy humans showed that AUC ∞ and C max increased from 107.9 ± 43.3 to 175.3 ± 74.8 ng.h/ml and from 50.6 ± 26.9 to 71.2 ± 50.5 ng/ml respectively for midazolam, with concomitant use of goldenseal. AUC and C max of midazolam were increased by inhibition of CYP3A4/5 [ 51 ].
Berberine is a chemical found in goldenseal extract. A clinical trial was performed on humans to check the effect of berberine on pharmacokinetics of cyclosporin A. The results obtained from this trial showed an increase in AUC of cyclosporin A from 104 to 123 mg/l. This study proves berberine mediated increase in cyclosporin A bioavailability by inhibition of CYP3A4 [ 52 ].
Green tea ( Camellia sinensis )
Green tea mainly contains catechins, polyphenols and epigallocatechin-3-gallate. Green tea possesses antioxidant, antimutagenic, antidiabetic, anti-inflammatory, antibacterial and antiviral properties. Green tea is used for weight loss and preventing ageing and prostate and other cancers [ 53 ].
An in vivo study reported that catechins (present in green tea extract) inhibit folic acid uptake. Catechins are competitive inhibitors of DHFR, which adversely affect folate uptake. DHFR is responsible for folate intestinal absorption. Folate is reduced to tetrahydrofolate and methylated to 5-methyltetrahydrofolate during intestinal absorption of folate before it is absorbed in the blood [ 54 ]. In vivo studies in humans reported reduction in C max and AUC of folic acid by 58.4% and 43.9%, during concomitant use of folic acid and green tea, leading to a decrease in bioavailability of folic acid. The probable mechanism of interaction is inhibition of carrier-mediated absorption of folates [ 55 ].
A clinical trial in humans reported that green tea weakly inhibits CYP450 3A4, which is the main metabolizing enzyme of simvastatin [ 56 ]. A study showed that consumption of green tea with simvastatin leads to increase in C max of simvastatin lactone (metabolite of simvastatin lactone prodrug) from 3.70 to 7.21ng/mL, before and after supplementation of green tea. Similarly, the AUC of simvastatin lactone increased from 6.3 to 12.5 ng.h/mL. The subject improved tolerance to simvastatin after the patient stopped drinking green tea and simvastatin [ 57 ].
Green tea is a source of vitamin K [ 58 ]. Green tea products accentuate the anticoagulant effect of warfarin, leading to bleeding complications. Exogenous intake of vitamin K antagonises the effect of warfarin. A study on humans showed a decrease in INR level from 3.79 to 1.14 (after 1 month) on concomitant consumption of green tea and warfarin. The INR level increased to 2.55 on the discontinuation of green tea [ 59 ].
Kava ( Piper methysticum )
Kava contains kavain, dihydrokavain, methysticin, dihydromethysticin, demethoxyyangonin, and yangonin. Kava has a beneficial effect in euphoria, analgesia, neuroprotection, and anticonvulsant properties. Kava is also used in the treatment of anxiety [ 60 ].
The active components of kava (pyrones) are reported to have neuropharmacologic interactions with the central nervous system receptors. Kava also has weak effects on GABA or benzodiazepine receptors [ 61 ]. A study showed additive pharmacodynamic effects between a-pyrones and other GABA-active sedatives [ 62 ]. A case study showed a lethargic and disoriented state in patients during concomitant use of kava and alprazolam (benzodiazepine) [ 63 ]. Previous studies showed that this interaction is possible due to the additive effect of kava on benzodiazepine receptors, leading to life-threatening conditions.
Kava inhibits CYP2E1, and chlorzoxazone is a CYP2E1 probe. Clinical trials reported that kava showed a significant reduction in 6-hydroxychlorzoxazone/chlorzoxazone serum ratios by 40%. It is, thus, suggested that kava should not be taken simultaneously with chlorzoxazone [ 49 ].
Kava is reported to have dopamine antagonism property. A case report in a 76-year-old Parkinson’s disease patient showed reduced activity of levodopa (a precursor of dopamine). On further investigation, it was reported that the patient simultaneously consumed kava and dopamine, which lead to decrease in dopamine efficacy (decreased dopamine level) due to an antagonising property of kava [ 64 ].
Liquorice ( Glycyrrhiza glabra )
Biologically active compounds present in liquorice are glycosides (glycyrrhizic acid), flavonoids (chalcones, liquiritin, isoliquiritin, liquiritin apioside and isoprenoid-substituted flavonoids), chromenes (coumarins and dihydrostilbenes) and saponins (triterpenoid saponins). Liquorice is reported for wide-ranging biological activities like antiviral, antimicrobial, antioxidant, antiallergic, hepatoprotective, neuroprotective, anti-inflammatory and dermatological activities [ 65 ].
Glycyrrhizin is a potent inducer of the CYP3A4-metabolizing enzyme. CYP3A4 catalyses sulfoxidation of omeprazole. A study reported that glycyrrhizin induces CYP3A4-catalysed sulfoxidation of omeprazole leading to a decrease in C max of omeprazole, during simultaneous use of liquorice and omeprazole [ 66 ].
Glycyrrhizin induces CYP3A4 enzyme (which catalyses midazolam 11-hydroxylation), leading to a reduction in plasma concentrations of midazolam. This inhibition was confirmed by an in vivo study, where mRNA expression of CYP3A4 and other CYP450 family members in mice was decreased significantly by liquorice. Human study confirmed an interaction between midazolam and liquorice [ 67 ].
Milk thistle ( Silybum marianum )
Silybin A and B, isosilybin A and B, silychristin A, silyhermin, neosilyhermine A, neosilyhermine B, mariamides A and B, quercetin, morin, chlorogenic acid and caffeic acid are some of the major chemical constituents present in milk thistle. Milk thistle is widely used in jaundice and calculi of the liver and gallbladder and is useful in controlling haemorrhages [ 68 ].
Metronidazole is a substrate of CYP3A4-metabolizing enzyme. A clinical trial on 12 human subjects confirmed increased CL of metronidazole (by 29.51%) with concomitant use of milk thistle. It also decreased t½, C max and AUC, as a cause of induction of both intestinal P-gp and CYP3A4 [ 69 ].
Milk thistle decreased the AUC of E-3174 (active metabolite of losartan) and increased the AUC of losartan, reported in a clinical trial on 12 healthy men. The study reported that the decrease in losartan AUC is dependent on inhibition of CYP2C9 [ 70 ].
Talinolol C max increased potentially from 172.68 ± 61.53 to 219.20 ± 52.77 ng/ml (after 14 days) after simultaneous administration of milk thistle as compared to placebo treatment, in human studies. AUC of talinolol increased by 36.2%, and oral clearance of talinolol decreased by 23.1% during milk thistle-talinolol coadministration, by inhibition of P-gp [ 71 ].
St. John’s wort ( Hypericum perforatum )
The major active constituents present in St. John’s wort are hyperforin and hypericin (pseudohypericin, isohypericin, protohypericin, protopseudohypericin, Cyclopseudohypericin) and also flavonoids (kaempferol, quercetin, luteolin, biapigenin), tannins and volatile oils. St. John’s wort is used as an antidepressant, antiviral and antibacterial. It also shows sedative and astringent properties. It is used traditionally for the treatment of excitability, neuralgia, sciatica, fibrositis, anxiety, menopausal neurosis and depression and as a nerve tonic and topical application for wound treatment [ 72 ].
The study confirmed that long-term use of SJW may cause reduced clinical effectiveness of CPY3A4 substrate drugs by CPY3A4 induction, which may lead to an increase in dosage of the drug [ 73 ]. The study showed direct induction of intestinal P-gp/MDR1 by SJW in humans [ 74 ].
CYP2C19 carries out demethylation of amitriptyline to nortriptyline, at low amitriptyline concentration. When the concentration of amitriptyline is higher, the CYP3A4 enzyme carries out its demethylation [ 75 , 76 ]. P-gp is a drug transporter which is responsible for efflux of amitriptyline from gut epithelial cells to the gut lumen, which causes co-regulation of systemic availability. Increase activity of P-gp causes reduced systemic availability [ 77 ]. A clinical trial showed that concomitant use of amitriptyline and SJW extract LI160 decreases the AUC of amitriptyline (by 22%) and nortriptyline (by 41%), which is a metabolite of amitriptyline in humans. The pharmacokinetics of St. John’s wort is affected by induction of CYP3A4 and/or induction of P-gp [ 78 ].
Atorvastatin is a substrate of CYP3A4 and P-gp; thus, its use with SJW should be prevented. In a human trial, concomitant treatment with a SJW product reduced the efficacy and effect of atorvastatin, resulting in an increase in LDL cholesterol levels of 0.32 mmol/l, or about 30% of the expected treatment. The possible mechanism of action is increased in CYP3A4 and P-gp activity [ 79 ].
Cyclosporine is widely used to prevent rejection of organs after organ transplantation. Various case reports have reported of serious organ rejection after transplantation due to simultaneous use of cyclosporine with SJW [ 80 , 81 , 82 , 83 ]. The efficacy of cyclosporine is decreased, which causes rejection of organs [ 73 , 74 ]. Thus, serious and potentially fatal interactions between cyclosporine and SJW are likely to occur via induction of CYP3A4 and/or P-gp by St. John’s wort.
MDR1/P-gp mediates the intestinal absorption and distribution and renal excretion of digoxin. SJW is reported to induce P-gp drug transporter. Clinical trials showed that concomitant use of SJW and digoxin lead to an increase in efflux function of P-gp into the intestinal lumen, which lead to a decrease of digoxin AUC by 25% [ 84 , 85 ].
A case report on four patients showed a median decrease of 47% of the original methadone concentration, during concomitant use of methadone and SJW [ 86 ].
A study on humans showed a two-fold increase in CL of alprazolam after administration of alprazolam with SJW for 14 days. The increase in CL of alprazolam was observed due to CYP3A4 enzyme induction. The increased CL leads to a decrease in alprazolam blood concentration [ 73 ].
Imatinib is predominantly metabolized by cytochrome CYP3A4. Concomitant use of SJW and imatinib lead to increased imatinib CL by 43% (12.5 to 17.9 l/h), imatinib AUC was decreased by 30% (from 34.5 to 24.2 mg. h/ml) and C max was also significantly decreased [ 87 , 88 ].
HIV-1 protease inhibitors are substrates of the CYP3A4 enzyme. A clinical trial was performed to evaluate the effect of SJW on plasma concentrations of the HIV-1 protease inhibitor (indinavir), which was found to decrease plasma levels of indinavir in 8 volunteers by an average of 57% [ 89 ].
A trial performed in 5 cancer patients showed decreased plasma levels of SN-38 (active metabolite of irinotecan) by 42% on post-supplementation of SJW and irinotecan as compared to the placebo treatment [ 90 ].
NNRTI and nevirapine are substrates of multidrug transporter P-gp and are extensively metabolized via the cytochrome CYP3A4 enzyme system. A human study showed a decrease in blood concentration of nevirapine by increasing its oral clearance by 35%, due to induction of CYP3A4 enzyme [ 91 ].
In a human subject, it was found that SJW significantly induced the activity of CYP2E1 (approximately 140%) on comparing pre-supplementation and post-supplementation ratios. The two clinical trials found that SJW extract lead to increase in the hydroxychlorzoxazone/chlorzoxazone serum ratios. This increase in ratio is due to induction of CYP2E1 enzyme [ 32 , 33 ].
Serotonin reuptake in the central nervous system is inhibited by bupropion [ 92 ]. Serotonin reuptake is weakly inhibited by SJW. Various reports of SJW interacting with SSRIs have been reported, leading to various side effects, including serotonin syndrome. The side effect is due to an additive effect of two similarly acting drugs [ 93 ]. Dystonia is a syndrome which causes sustained muscle contractions, producing twisting and repetitive movements and postures. Dystonia syndrome is a very well-recognised side-effect of many medicines (antipsychotics and serotonin reuptake inhibitor drugs) affecting dopamine concentrations. A 58-year-old female reported prolonged orofacial dystonia. On evaluation, it was found that the woman was consuming bupropion and St. John’s wort together. Both bupropion and St. John’s wort are reported to inhibit the reuptake of dopamine, potentially resulting in additive effects on dopaminergic transmission and hence causing dopaminergic side effects such as dystonia [ 94 ].
Buspirone is a partial agonist at 5-HT1A receptors. St. John’s wort is testified to be a non-selective 5-HT reuptake inhibitor, which upregulated the postsynaptic 5-HT1A and 5-HT2A receptors. A case study reported that the concomitant administration of buspirone and St. John’s wort medications leads to overstimulation of the 5-HT1A receptors, therefore leading to the development of serotonin syndrome and hypomanic episode [ 95 ].
A systematic representation of herb-drug interactions of herbs with possible mechanism, outcome and level of HDIs is given in Table 1 .
Herb-drug interactions may lead to serious side effects. The reviewed studies clearly indicate that herbal medicines can interact with allopathic or modern medicines and show unwanted effects. Most of the interaction may have negligible clinical significance, but some may lead to life-threatening effect on public health. Our review suggests to physician, pharmacist and common people to avoid such combination in practice. Patients should be aware of the herb-drug interactions for their safety. In this review, we have discussed in details herb-drug interaction of most commonly used herbs in a regular practice by physicians all over the world. It is, therefore, important that health care professionals should take into account of herb-drug interactions when prescribing drugs to patients.
Availability of data and materials
Not applicable
Abbreviations
5-hydroxy tryptamine
Adenosine triphosphate
Area under plasma drug concentration-time curve
AUC zero to infinity
Compound annual growth rate
Oral clearance
Body clearance
Maximum plasma concentrations
Cytochrome-P
Dihydrofolate reductase
Gamma-aminobutyric acid
G. biloba extract
- Herb-drug interactions
International normalized ratio
1-(m-chlorophenyl) piperazine
Multidrug resistance
Multidrug resistance-associated protein-2
Non-nucleoside reverse transcriptase inhibitors
Over the counter
P-Glycoprotein
St. John’s wort
Elimination half-lives
Thromboxane A2
Uridine diphosphate
United States dollar
Apparent volume of distribution
Williamson E, Driver S, Baxter K (2002) Stockley’s herbal medicines interactions, 6th ed. pharmaceutical press, London.
Pasi AK (2013) Herb-drug interaction: an overview. Int J Pharm Sci Res 4:3770–3774. https://doi.org/ https://doi.org/10.13040/IJPSR.0975-8232.4(10).3770-74
Izzo AA, Borrelli F, Capasso R (2002) Herbal medicine: the dangers of drug interaction. Trends Pharmacol Sci 23(8):358–359. https://doi.org/10.1016/s0165-6147(02)02059-x
Article CAS PubMed Google Scholar
(2021) Dietary Supplements Market Size | Industry Analysis Report 2027 Dietary supplements market size, share & trends analysis report by ingredient (vitamins, minerals), by form, by application, by end user, by distribution channel, by region, and segment forecasts, 2020 – 2027.
Barnes PM, Bloom B, Nahin RL (2008) Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 12:1–23
Google Scholar
Blendon RJ, Benson JM, Botta MD, Weldon KJ (2013) Users’ views of dietary supplements. JAMA Intern Med 173 1:74–76. https://doi.org/ https://doi.org/10.1001/2013.jamainternmed.311 .
Fasinu PS, Bouic PJ, Rosenkranz B (2012) An Overview of the Evidence and Mechanisms of Herb–Drug Interactions. Front Pharmacol 3:1–19. https://doi.org/ https://doi.org/10.3389/fphar.2012.00069
Lin JH, Lu AYH (1998) Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet 35 5:361–390. https://doi.org/ https://doi.org/10.2165/00003088-199835050-00003 .
Takano M, Yumoto R, Murakami T (2006) Expression and function of efflux drug transporters in the intestine. Pharmacol Ther 109 1-2:137–161. https://doi.org/ https://doi.org/10.1016/j.pharmthera.2005.06.005 .
Fugh-Berman A (2000) Herb-drug interactions. Lancet 355 9198:134–138. https://doi.org/ https://doi.org/10.1016/S0140-6736(99)06457-0 .
Hollenberg PF (2002) Characteristics and common properties of inhibitors, inducers, and activators of CYP enzymes. Drug Metab Rev 34 1-2:17–35. https://doi.org/ https://doi.org/10.1081/DMR-120001387 .
Grimm SW, Einolf HJ, Hall SD, He K, Lim HK, Ling KHJ, Lu C, Nomeir AA, Seibert E, Skordos KW, Tonn GR, Van Horn R, Wang RW, Wong YN, Yang TJ, Obach RS (2009) The conduct of in vitro studies to address time-dependent inhibition of drug-metabolizing enzymes: a perspective of the pharmaceutical research and manufacturers of America. Drug Metab Dispos 37 7:1355–1370. https://doi.org/ https://doi.org/10.1124/dmd.109.026716 .
Wienkers LC, Heath TG (2005) Predicting in vivo drug interactions from in vitro drug discovery data. Nat Rev Drug Discov 4 10:825–833. https://doi.org/ https://doi.org/10.1038/nrd1851 .
Ortiz de Montellano PR (1995) Cytochrome P450: structure, mechanism, and biochemistry, 2nd edn. Kluwer Academic / Plenum Press, New York. https://doi.org/10.1007/978-1-4757-2391-5
Book Google Scholar
Tsai HH, Lin HW, Simon Pickard A, Tsai HY, Mahady GB (2012) Evaluation of documented drug interactions and contraindications associated with herbs and dietary supplements: a systematic literature review. Int J Clin Pract 66 11:1056–1078. https://doi.org/ https://doi.org/10.1111/j.1742-1241.2012.03008.x
Bagnis CI, Deray G, Baumelou A, Le Quintrec M, Vanherweghem JL (2004) Herbs and the kidney. Am J Kidney Dis 44 1:1–11. https://doi.org/ https://doi.org/10.1053/j.ajkd.2004.02.009
Al-Ali M, Wahbi S, Twaij H, Al-Badr A (2003) Tribulus terrestris: preliminary study of its diuretic and contractile effects and comparison with Zea mays. J Ethnopharmacol 85 2-3:257–260. https://doi.org/ https://doi.org/10.1016/S0378-8741(03)00014-X
Izzo AA (2005) Herb-drug interactions: an overview of the clinical evidence. Fundam Clin Pharmacol 19 1:1–16. https://doi.org/ https://doi.org/10.1111/j.1472-8206.2004.00301.x
MEIm XD, Cao YF, Che YY, Li J, Shang ZP, Zhao WJ, Qiao YJ, Zhang JY (2019) Danshen: a phytochemical and pharmacological overview. Chin J Nat Med 17 1:59–80. https://doi.org/ https://doi.org/10.1016/S1875-5364(19)30010-X
Chan TYK (2001) Interaction between warfarin and danshen (salvia miltiorrhiza). Ann Pharmacother 35 4:501–504. https://doi.org/ https://doi.org/10.1345/aph.19029
Izzat MB, Yim APC, El-Zufari MH (1998) A taste of Chinese medicine! Ann Thorac Surg 66 3:941–942. https://doi.org/ https://doi.org/10.1016/S0003-4975(98)00624-9
Yu CM, Chan JCN, Sanderson JE (1997) Chinese herbs and warfarin potentiation by “Danshen.” J Intern Med 241:337–339. https://doi.org/ https://doi.org/10.1046/j.1365-2796.1997.134137000.x
Qiu F, Wang G, Zhang R, Sun J, Jiang J, Ma Y (2010) Effect of danshen extract on the activity of CYP3A4 in healthy volunteers. Br J Clin Pharmacol 69 6:656–662. https://doi.org/ https://doi.org/10.1111/j.1365-2125.2010.03624.x
Manayi A, Vazirian M, Saeidnia S (2015) Echinacea purpurea: pharmacology, phytochemistry and analysis methods. Pharmacogn Rev 9 17:63–72. https://doi.org/ https://doi.org/10.4103/0973-7847.156353
Gorski JC, Huang S-M, Pinto A, Hamman MA, Hilligoss JK, Zaheer NA, Desai M, Miller M, Hall SD (2004) The effect of echinacea (Echinacea purpurea root) on cytochrome P450 activity in vivo. Clin Pharmacol Ther 75 1:89–100. https://doi.org/ https://doi.org/10.1016/j.clpt.2003.09.013
Gurley B, Gardner S, Hubbard M, Williams D, Gentry W, Carrier J, Khan I, Edwards D, SHAH AB, Gurley B, Gardner S, Hubbard M, Williams D, Gentry W, Carrier J, Khan I, Edwards D, Shah A (2004) In vivo assessment of botanical supplementation on human cytochrome P450 phenotypes: Citrus aurantium, Echinacea purpurea, milk thistle, and saw palmetto. Clin Pharmacol Ther 76:428–440. https://doi.org/ https://doi.org/10.1016/j.clpt.2004.07.007
Mikaili P, Maadirad S, Moloudizargari M, Aghajanshakeri S, Sarahroodi S (2013) Therapeutic uses and pharmacological properties of garlic, shallot, and their biologically active compounds. Iran J Basic Med Sci 16:1031–1048. https://doi.org/ https://doi.org/10.22038/ijbms.2013.1865 , 10
Hajda J, Rentsch KM, Gubler C, Steinert H, Stieger B, Fattinger K (2010) Garlic extract induces intestinal P-glycoprotein, but exhibits no effect on intestinal and hepatic CYP3A4 in humans. Eur J Pharm Sci 41:729–735. https://doi.org/ https://doi.org/10.1016/j.ejps.2010.09.016 , 5
Piscitelli SC, Burstein AH, Welden N, Gallicano KD, Falloon J (2002) The effect of garlic supplements on the pharmacokinetics of saquinavir. Clin Infect Dis 34 2:234–238. https://doi.org/ https://doi.org/10.1086/324351
Macan H, Uykimpang R, Alconcel M, Takasu J, Razon R, Amagase H, Niihara Y (2006) Aged garlic extract may be safe for patients on warfarin therapy. J Nutr 136 3:793S-795S. https://doi.org/ https://doi.org/10.1093/jn/136.3.793s
Djuv A, Nilsen OG, Steinsbekk A (2013) The co-use of conventional drugs and herbs among patients in Norwegian general practice: a cross-sectional study. BMC Complement Altern Med 13 1:1–11. https://doi.org/ https://doi.org/10.1186/1472-6882-13-295
Gurley B, Gardner S, Hubbard M, Williams D, Gentry W, Khan I, Shah A (2005) Clinical assessment of effects of botanical supplementation on cytochrome P450 phenotypes in the elderly: St John’s wort, garlic oil, Panax ginseng and Ginkgo biloba. Drugs Aging 22 6:525–539. https://doi.org/ https://doi.org/10.2165/00002512-200522060-00006
Gurley BJ, Gardner SF, Hubbard MA, Williams DK, Gentry WB, Cui Y, Ang CYW (2002) Cytochrome P450 phenotypic ratios for predicting herb-drug interactions in humans. Clin Pharmacol Ther 72 3:276–287. https://doi.org/ https://doi.org/10.1067/mcp.2002.126913
Pathak A, Léger P, Bagheri H, Senard JM, Boccalon H, Montastruc JL (2003) Garlic interaction with fluindione: a case report. Therapies 58 4:380–381. https://doi.org/ https://doi.org/10.2515/therapie:2003060
Mohanta TK, Tamboli Y, Zubaidha PK (2014) Phytochemical and medicinal importance of Ginkgo biloba L. Nat Prod Res 28 10:746–752. https://doi.org/ https://doi.org/10.1080/14786419.2013.879303
Uchida S, Yamada H, Li XD, Maruyama S, Ohmori Y, Oki T, Watanabe H, Umegaki K, Ohashi K, Yamada S (2006) Effects of Ginkgo biloba extract on pharmacokinetics and pharmacodynamics of tolbutamide and midazolam in healthy volunteers. J Clin Pharmacol 46 11:1290–1298. https://doi.org/ https://doi.org/10.1177/0091270006292628
Robertson SM, Davey RT, Voell J, Formentini E, Alfaro RM, Penzak SR (2008) Effect of Ginkgo biloba extract on lopinavir, midazolam and fexofenadine pharmacokinetics in healthy subjects. Curr Med Res Opin 24:591–599. https://doi.org/ https://doi.org/10.1185/030079908X260871 , 2
Yoshioka M, Ohnishi N, Koishi T, Obata Y, Nakagawa M, Matsumoto T, Tagagi K, Takara K, Ohkuni T, Yokoyama T, Kuroda K (2004) Studies on interactions between functional foods or dietary supplements and medicines. IV. Effects of Ginkgo biloba leaf extract on the pharmacokinetics and pharmacodynamics of nifedipine in healthy volunteers. Biol Pharm Bull 27 12:2006–2009. https://doi.org/ https://doi.org/10.1248/bpb.27.2006
Ophelia Y, Brian T, Mary W, Albert C, Mosess C (2004) Pharmacogenetics and herb–drug interactions: experience with Ginkgo biloba and omeprazole. Pharmacogenetics 14:841–850
Article Google Scholar
Fan L, Tao GY, Wang G, Chen Y, Zhang W, He YJ, Li Q, Lei HP, Jiang F, Hu DL, Huang YF, Zhou HH (2009) Effects of Ginkgo biloba extract ingestion on the pharmacokinetics of talinolol in healthy Chinese volunteers. Ann Pharmacother 43 5:944–949. https://doi.org/ https://doi.org/10.1345/aph.1L656
Meisel C, Johne A, Roots I (2003) Fatal intracerebral mass bleeding associated with Ginkgo biloba and ibuprofen . Atherosclerosis 167 2:367. https://doi.org/ https://doi.org/10.1016/S0021-9150(03)00015-7
Shaw D, Leon C, Kolev S, Murray V (1997) Traditional remedies and food supplements. A 5-year toxicological study (1991-1995). Drug Saf 17 5:342–356. https://doi.org/ https://doi.org/10.2165/00002018-199717050-00006
Kupiec T, Raj V (2005) Fatal seizures due to potential herb-drug interactions with Ginkgo biloba. J Anal Toxicol 29 7:755–758. https://doi.org/ https://doi.org/10.1093/jat/29.7.755
Lin YY, Chu SJ, Tsai SH (2007) Association between priapism and concurrent use of risperidone and Ginkgo biloba . Mayo Clin Proc 82 10:1289–1290. https://doi.org/ https://doi.org/10.4065/82.10.1289
Wiegman D-J, Brinkman K, Franssen EJ (2009) Interaction of Ginkgo biloba with efavirenz. AIDS 23 9:1184–1185. https://doi.org/ https://doi.org/10.1097/QAD.0b013e32832c412b
Galluzzi S, Zanetti O, Binetti G, Trabucchi M, Frisoni G (2000) Coma in a patient with Alzheimer’s disease taking low dose trazodone and ginkgo biloba. J Neurol Neurosurg Psychiatry 68:679-6680. https://doi.org/ https://doi.org/10.1136/jnnp.68.5.679a
Leyte-Lugo M, Britton ER, Foil DH, Brown AR, Todd DA, Rivera-Chávez J, Oberlies NH, Cech NB (2017) Secondary metabolites from the leaves of the medicinal plant goldenseal (Hydrastis canadensis). Phytochem Lett 20:54–60. https://doi.org/ https://doi.org/10.1016/j.phytol.2017.03.012
Ernst E (2006) Complementary therapies for pain management: an evidence-based approach, 2nd edn. Mosby Elsevier, Philadelphia
Gurley B, Gardner S, Hubbard M, Williams D, Gentry W, Khan I, Shah A (2005) In vivo effects of goldenseal, kava kava, black cohosh, and valerian on human cytochrome P450 1A2, 2D6, 2E1, and 3A4/5 phenotypes. Clin Pharmacol Ther 77:415–426. https://doi.org/ https://doi.org/10.1016/j.clpt.2005.01.009 , 5
Gurley BJ, Swain A, Hubbard MA, Williams DK, Barone G, Hartsfield F, Tong Y, Carrier DJ, Cheboyina S, Battu SK (2008) Clinical assessment of CYP2D6-mediated herb-drug interactions in humans: effects of milk thistle, black cohosh, goldenseal, kava kava, St. John’s wort, and Echinacea. Mol Nutr Food Res 52(7):755–763. https://doi.org/ https://doi.org/10.1002/mnfr.200600300
Gurley B, Swain A, Hubbard M, Hartsfield F, Thaden J, Williams DK, Gentry WB, Tong Y (2008) Supplementation with goldenseal (Hydrastis canadensis), but not kava kava (Piper methysticum), inhibits human CYP3A activity in vivo. Clin Pharmacol Ther 83(1):61–69. https://doi.org/ https://doi.org/10.1038/sj.clpt.6100222
Xin HW, Wu XC, Li Q, Yu AR, Zhong MY, Liu YY (2006) The effects of berberine on the pharmacokinetics of ciclosporin a in healthy volunteers. Methods Find Exp Clin Pharmacol 28(1):25–29. https://doi.org/ https://doi.org/10.1358/mf.2006.28.1.962774
Rani R, Nagpal D, Gullaiya S, Madan S, Agrawal S (2014) Phytochemical, pharmacological and beneficial effects of green tea. Artic Int J Pharmacogn Phytochem Res 6:420–426
Alemdaroglu NC, Wolffram S, Biossel J-P, Closs E, Spahn-Langguth H, Langguth P (2007) Inhibition of folic acid uptake by catechins and tea extracts in Caco-2 cells. Planta Med 73(01):27–32. https://doi.org/https://doi.org/ https://doi.org/10.1055/s-2006-951745
Alemdaroglu NC, Dietz U, Wolffram S, Spahn-Langguth H, Langguth P (2008) Influence of green and black tea on folic acid pharmacokinetics in healthy volunteers: potential risk of diminished folic acid bioavailability. Biopharm Drug Dispos 29(6):335–348. https://doi.org/ https://doi.org/10.1002/bdd.617
Chow HHS, Hakim IA, Vining DR, Crowell JA, Cordova CA, Chew WM, Xu MJ, Hsu CH, Ranger-Moore J, Alberts DS (2006) Effects of repeated green tea catechin administration on human cytochrome P450 activity. Cancer Epidemiol Biomark Prev 15(12):2473–2476. https://doi.org/ https://doi.org/10.1158/1055-9965.EPI-06-0365
Werba JP, Giroli M, Cavalca V, Nava MC, Tremoli E, Bo LD (2008) The effect of green tea on simvastatin tolerability. Ann Intern Med 149:286–287. https://doi.org/ https://doi.org/10.7326/0003-4819-149-4-200808190-00019 , 4
Booth SL, Sadowski JA, Pennington JAT (1995) Phylloquinone (vitamin K1) content of foods in the U.S. Food and Drug Administration’s Total diet study. J Agric Food Chem 43(6):1574–1579. https://doi.org/ https://doi.org/10.1021/jf00054a030
Taylor JR, Wilt VM (1999) Probable antagonism of warfarin by green tea. Ann Pharmacother 33(4):426–428. https://doi.org/ https://doi.org/10.1345/aph.18238
Cote CS, Kor C, Cohen J, Auclair K (2004) Composition and biological activity of traditional and commercial kava extracts. Biochem Biophys Res Commun 322(1):147–152. https://doi.org/ https://doi.org/10.1016/j.bbrc.2004.07.093
Davies LP, Drew CA, Duffield P, Johnston GAR, Jamieson DD (1992) Kava pyrones and resin: studies on GABAA, GABAB and benzodiazepine binding sites in rodent brain. Pharmacol Toxicol 71(2):120–126. https://doi.org/ https://doi.org/10.1111/j.1600-0773.1992.tb00530.x
Jussofie A, Schmiz A, Hiemke C (1994) Kavapyrone enriched extract from Piper methysticum as modulator of the GABA binding site in different regions of rat brain. Psychopharmacology 116(4):469–474. https://doi.org/ https://doi.org/10.1007/BF02247480
Almeida JC, Grimsley EW (1996) Coma from the health food store: interaction between kava and alprazolam. Ann Intern Med 125(11):940–941. https://doi.org/ https://doi.org/10.7326/0003-4819-125-11-199612010-00023
Schelosky L, Raffauf C, Jendroska K, Poewe W (1995) Kava and dopamine antagonism. J Neurol Neurosurg Psychiatry 58(5):639–640. https://doi.org/10.1136/jnnp.58.5.639
Article CAS PubMed PubMed Central Google Scholar
Mamedov NA, Egamberdieva D (2019) Phytochemical constituents and pharmacological effects of licorice: a review. In: Ozturk M, Hakeem KR (eds) Plant and human health, Pharmacology and therapeutics uses, vol 3. Springer, Switzerland, pp 1–21
Tu JH, Hu DL, Dai LL, Sun Y, Fan L, Zhang M, Tan ZR, Chen Y, Li Z, Zhou HH (2010) Effect of glycyrrhizin on CYP2C19 and CYP3A4 activity in healthy volunteers with different CYP2C19 genotypes. Xenobiotica 40(6):393–399. https://doi.org/ https://doi.org/10.3109/00498251003748095
Lv Q-L, Wang G-H, Chen S-H, Hu L, Zhang X, Ying G, Qin C-Z, Zhou H-H (2016) In vitro and in vivo inhibitory effects of glycyrrhetinic acid in mice and human cytochrome P450 3A4. Int J Environ Res Public Health 13(1):84. https://doi.org/ https://doi.org/10.3390/ijerph13010084
Porwal O, Mohammed Ameen MS, Anwer ET, Uthirapathy S, Ahamad J, Tahsin A (2019) Silybum marianum (Milk Thistle): review on its chemistry, morphology, ethnomedical uses, phytochemistry and pharmacological activities. J Drug Deliv Ther 9: 5199–206. https://doi.org/ https://doi.org/10.22270/jddt.v9i5.3666
Rajnarayana K, Reddy M, Vidyasagar J, Krishna D (2004) Study on the influence of silymarin pretreatment on metabolism and disposition of metronidazole. Arzneimittelforschung 54(02):109–113. https://doi.org/ https://doi.org/10.1055/s-0031-1296944
Han Y, Guo D, Chen Y, Chen Y, Tan ZR, Zhou HH (2009) Effect of silymarin on the pharmacokinetics of losartan and its active metabolite E-3174 in healthy Chinese volunteers. Eur J Clin Pharmacol 65(6):585–591. https://doi.org/ https://doi.org/10.1007/s00228-009-0624-9
Han Y, Guo D, Chen Y, Tan ZR, Zhou HH (2009) Effect of continuous silymarin administration on oral talinolol pharmacokinetics in healthy volunteers. Xenobiotica 39(9):694–699. https://doi.org/ https://doi.org/10.1080/00498250903060077
Barnes J, Anderson LA, Phillipson JD (2001) St John’s wort (Hypericum perforatum L.): a review of its chemistry, pharmacology and clinical properties. J Pharm Pharmacol 53(5):583–600. https://doi.org/ https://doi.org/10.1211/0022357011775910
Markowitz JS, Donovan JL, DeVane CL, Taylor RM, Ruan Y, Wang JS, Chavin KD (2003) Effect of St John’s wort on drug metabolism by induction of cytochrome P450 3A4 enzyme. J Am Med Assoc 290(11):1500–1504. https://doi.org/ https://doi.org/10.1001/jama.290.11.1500
Durr D, Stieger B, Kullak-Ublick GA, Rentsh KM, Steinert HC, Meier PJ, Fattinger K (2000) St John’s wort induces intestinal P-glycoprotein/MDR1 and intestinal and hepatic CYP3A4. Clin Pharmacol Ther 68(6):598–604. https://doi.org/ https://doi.org/10.1067/mcp.2000.112240
Venkatakrishnan K, Greenblatt DJ, Von Moltke LL, Schmider J, Harmatz JS, Shader RI (1998) Five distinct human cytochromes mediate amitriptyline N-demethylation in vitro: dominance of CYP 2C19 and 3A4. J Clin Pharmacol 38(2):112–121. https://doi.org/ https://doi.org/10.1002/j.1552-4604.1998.tb04399.x
Schmider J, Greenblatt DJ, Harmatz JS, Shader RI (1996) Enzyme kinetic modelling as a tool to analyse the behaviour of cytochrome P450 catalysed reactions: application to amitriptyline N-demethylation. Br J Clin Pharmacol 41(6):593–604. https://doi.org/ https://doi.org/10.1046/j.1365-2125.1996.35717.x
Uhr M, Steckler T, Yassouridis A, Holsboer F (2000) Penetration of amitriptyline, but not of fluoxetine, into brain is enhanced in mice with blood-brain barrier deficiency due to Mdr1a P-glycoprotein gene disruption. Neuropsychopharmacology 22(4):380–387. https://doi.org/ https://doi.org/10.1016/S0893-133X(99)00095-0
Andreas J, Jurgen S, Jurgen B, Andreas S, Elke S, Steffen B, Gudrun S, Matthias L, Ivar R (2002) Decreased plasma levels of amitriptyline and its metabolites on comedication with an extract from St. John’s wort (Hypericum perforatum). J Clin Psychopharmacol 22:46–54
Andren L, Andreasson A, Eggertsen R (2007) Interaction between a commercially available St. John’s wort product (Movina) and atorvastatin in patients with hypercholesterolemia. Eur J Clin Pharmacol 63(10):913–916. https://doi.org/ https://doi.org/10.1007/s00228-007-0345-x
Dresser G, Schwarz UL, Wilkinson GR, Kim RB (2003) Coordinate induction of both cytochrome P4503A and MDR1 by St John’s wort in healthy subjects. Clin Pharmacol Ther 73(1):41–50. https://doi.org/ https://doi.org/10.1067/mcp.2003.10
Mai I, Bauer S, Perloff E, Johne A, Uehleke B, Frank B, Budde K, Roots I (2004) Hyperforin content determines the magnitude of the St John’s wort–cyclosporine drug interaction. Clin Pharmacol Ther 76(4):330–340. https://doi.org/ https://doi.org/10.1016/j.clpt.2004.07.004
Barone GW, Gurley BJ, Ketel BL, Lightfoot ML, Abul-Ezz SR (2000) Drug interaction between St. John’s wort and cyclosporine. Ann Pharmacother 34(9):1013–1016. https://doi.org/ https://doi.org/10.1345/aph.10088
Moschella C, Jaber BL (2001) Interaction between cyclosporine and Hypericum perforatum (St. John’s wort) after organ transplantation. Am J Kidney Dis 38(5):1105–1107. https://doi.org/ https://doi.org/10.1053/ajkd.2001.28617
Johne A, Brockmoller J, Bauer S, Maurer A, Langheinrich M, Roots I (1999) Pharmacokinetic interaction of digoxin with an herbal extract from St John’s wort (Hypericum perforatum). Clin Pharmacol Ther 66(4):338–345. https://doi.org/ https://doi.org/10.1053/cp.1999.v66.a101944
Mueller SC, Uehleke B, Woehling H, Petzsch M, Majcher-Peszynska J, Hehl E-M, Sievers H, Frank B, Riethling A-K, Drewelow B (2004) Effect of St John’s wort dose and preparations on the pharmacokinetics of digoxin. Clin Pharmacol Ther 75(6):546–557. https://doi.org/ https://doi.org/10.1016/j.clpt.2004.01.014
Eich-Hochli D, Oppliger R, Golay KP, Baumann P, Eap CB (2003) Methadone maintenance treatment and St. John’s wort: a case report Pharmacopsychiatry 36(1):35–37. https://doi.org/ https://doi.org/10.1055/s-2003-38090
Frye R, Fitzgerald S, Lagattuta T, Hruska M, Egorin M (2004) Effect of St John’s wort on imatinib mesylate pharmacokinetics. Clin Pharmacol Ther 76(4):323–329. https://doi.org/ https://doi.org/10.1016/j.clpt.2004.06.007
Smith P, Bullock J, Booker B, Hass C, Berenson C, Jusko W (2004) The influence of St. John’s wort on the pharmacokinetics and protein binding of imatinib mesylate. Pharmacotherapy 24(11):1508–1514. https://doi.org/ https://doi.org/10.1592/phco.24.16.1508.50958
Piscitelli SC, Burstein AH, Chaitt D, Alfaro RM, Falloon J (2000) Indinavir concentrations and St John’s wort. Lancet 355(9203):547–548. https://doi.org/ https://doi.org/10.1016/S0140-6736(99)05712-8
Mathijssen RHJ, Verweij J, De Bruijn P, Loos WJ, Sparreboom A (2002) Effects of St. John’s wort on irinotecan metabolism. J Natl Cancer Inst 94(16):1247–1249. https://doi.org/ https://doi.org/10.1093/jnci/94.16.1247
de Maat MM, Hoetelmans RM, Mathôt RA, van Gorp EC, Meenhorst PL, Mulder JW, Beijnen JH (2001) Drug interaction between St John’s wort and nevirapine. AIDS 15:420–421
Roddy E (2004) Bupropion and other non-nicotine pharmacotherapies. BMJ 328(7438):509–511. https://doi.org/ https://doi.org/10.1136/bmj.328.7438.509
Fugh-Berman A, Ernst E (2001) Herb-drug interactions: review and assessment of report reliability. Br J Clin Pharmacol 52(5):587–595. https://doi.org/ https://doi.org/10.1046/j.0306-5251.2001.01469.x
Parker V, Wong AHC, Boon HS, Seeman MV (2001) Adverse reactions to St John’s wort. Can J Psychiatr 46(1):77–79. https://doi.org/ https://doi.org/10.1177/070674370104600112
Dannawi M (2002) Possible serotonin syndrome after combination of buspirone and St John’s wort. J Psychopharmacol 16(4):401. https://doi.org/10.1177/026988110201600420
Article PubMed Google Scholar
Kim KA, Park PW, Park JY (2009) Short-term effect of quercetin on the pharmacokinetics of fexofenadine, a substrate of P-glycoprotein, in healthy volunteers. Eur J Clin Pharmacol 65 6:609–614. https://doi.org/ https://doi.org/10.1007/s00228-009-0627-6
Download references
Acknowledgements
Authors are also thankful to the Principal, S.M.B.T. College of Pharmacy, Dhamangaon, India, for providing necessary facilities.
No funding was available for this work.
Author information
Authors and affiliations.
S.M.B.T. College of Pharmacy, Dhamngaon Tal Igatpuri, Dist Nashik, M.S., 422403, India
Ajaykumar Rikhabchand Surana, Shivam Puranmal Agrawal, Manoj Ramesh Kumbhare & Snehal Balu Gaikwad
You can also search for this author in PubMed Google Scholar
Contributions
SAP and SBG collected the reference material and prepared the draft of manuscript. ARS and MRK conceptualized, designed, and concluded the work and prepared the final version for submission. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Ajaykumar Rikhabchand Surana .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Surana, A.R., Agrawal, S.P., Kumbhare, M.R. et al. Current perspectives in herbal and conventional drug interactions based on clinical manifestations. Futur J Pharm Sci 7 , 103 (2021). https://doi.org/10.1186/s43094-021-00256-w
Download citation
Received : 15 January 2021
Accepted : 10 May 2021
Published : 20 May 2021
DOI : https://doi.org/10.1186/s43094-021-00256-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Herb-Drug Interactions: A Literature Review

2005, Drugs
Related Papers
Alternative & Complementary Therapies
Eric L Yarnell
Journal of Alternative Medical Research
Sonia Singla
Pankaj Agrawa
International Journal of Pharmaceutical Sciences and Nanotechnology
Dr. Sujatha Samala
Alternative medicine is becoming popular worldwide and this is clearly evident from the rapidly escalating sales figures. The time tested and clinically proven herbal medicines like St. John’s wort, Ginkgo biloba, Garlic, Ephedra, Echinacea etc., make up most of the world’s market as for as alternative medicine is concerned. In spite of its increasing popularity, global criticism regarding the safety of herbal medicines is gaining importance. The surfacing of the adverse effects/adverse events due to concomitant use of herbs and prescription medicines undermine the safety of herbal medicines. The safety of herbal medicines still remains a daunting task. The herbs like St. John’s wort, Ginkgo biloba, Garlic, Ephedra, Echinacea etc., have been reported to interact pharmacokinetically and pharmacodynamically with several prescription medicines. The available literature also bolsters that concomitant use of herbs and drugs can lead to several adverse effects/adverse events. This articl...
To evaluate the pharmacokinetics and adverse effects of medicinal herbs, as well as clinical evidence of herb-drug interactions. Electronic searches were conducted in multiple databases, including MEDLINE, EMBASE, the Cochrane Library, CINAHL, NAPRALERT, International Pharmaceutical Abstracts, CANCERLIT, CISCOM, and HerbMed. Search terms used included common names, scientific names, and synonyms for the herbs and their primary active constituents. Bibliographies of relevant articles were also searched by hand to obtain additional references. No restrictions were placed on language or quality of publications. All literature collected pertained to adverse effects, pharmacokinetics, and suspected or confirmed cases of herb-drug interactions. Over 80 herbs or bo-tanicals (including plants, fungi, algae, and common constituents) were identified that had clinically significant interactions with prescription and over-the-counter drugs. Interestingly, herbs beginning with the letter " g " (garlic, ginger, ginkgo, and grapefruit) were among the herbs most commonly involved in herb-drug interactions. Drugs with anticoagulant/antiplatelet activity (e.g. warfarin, aspirin) were frequently implicated in herb-drug interactions, with documented interactions with over 30 herbs and herbal products. Because many herbs have demonstrated adverse effects on the liver, the potential for interaction with hepatotoxic agents (such as acetaminophen) is also significant. Clinical outcomes of reported herb-drug interactions ranged from mild to severe. Of note, fatalities (though rare) have occurred with concomitant ephedra and caffeine use. As herbal products (and dietary supplements in general) continue to grow in popularity , patients and health care providers should be vigilant of potential herb-drug interactions.
MARMARA PHARMACEUTCAL JOURNAL
F.Gul DÜLGER
Frontiers in Pharmacology
Patrick Bouic
Joko Rinanto
Clinical Pharmacokinetics
Abdelhamid Zaid
Bangladesh Journal of Medical Science
Rashid Bhikha
This review examines the interaction between herbal remedies and conventional (orthodox) drugs. There has been a substantial increase in the consumption of herbal remedies in recent times for various reasons. They are often combined with one another, and are often used simultaneously with conventional drugs that are taken for a wide range of disorders, both acute and chronic. The probability of a real and substantial interaction between the therapeutic agents originating from different medical paradigms is likewise expanding. Whilst most of the herb-drug interactions are undoubtedly minor, benign, and harmless, there are reports of more serious interactions. Possible reasons for specific herb-drug interactions are examined, particularly from the pharmacokinetic and pharmacodynamic perspectives.
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.

RELATED PAPERS
Life Sciences
Pedro Chávez
Adriane Fugh-Berman
edzard E Ernst
John Neustadt
Critical Reviews in Food Science and Nutrition
Mahadi Hasan
jerry M cott
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Open access
- Published: 02 June 2024
Neuroleptic malignant syndrome and serotonin syndrome: a comparative bibliometric analysis
- Waleed M. Sweileh 1
Orphanet Journal of Rare Diseases volume 19 , Article number: 221 ( 2024 ) Cite this article
234 Accesses
1 Altmetric
Metrics details
This study aimed to analyze and map scientific literature on Neuroleptic Malignant Syndrome (NMS) and Serotonin Syndrome (SS) from prestigious, internationally indexed journals. The objective was to identify key topics, impactful articles, prominent journals, research output, growth patterns, hotspots, and leading countries in the field, providing valuable insights for scholars, medical students, and international funding agencies.
A systematic search strategy was implemented in the PubMed MeSH database using specific keywords for NMS and SS. The search was conducted in the Scopus database, renowned for its extensive coverage of scholarly publications. Inclusion criteria comprised articles published from 1950 to December 31st, 2022, restricted to journal research and review articles written in English. Data were analyzed using Microsoft Excel for descriptive analysis, and VOSviewer was employed for bibliometric mapping.
The search yielded 1150 articles on NMS and 587 on SS, with the majority being case reports. Growth patterns revealed a surge in NMS research between 1981 and 1991, while SS research increased notably between 1993 and 1997. Active countries and journals differed between NMS and SS, with psychiatry journals predominating for NMS and pharmacology/toxicology journals for SS. Authorship analysis indicated higher multi-authored articles for NMS. Top impactful articles focused on review articles and pathogenic mechanisms. Research hotspots included antipsychotics and catatonia for NMS, while SS highlighted drug interactions and specific medications like linezolid and tramadol.
Conclusions
NMS and SS represent rare but life-threatening conditions, requiring detailed clinical and scientific understanding. Differential diagnosis and management necessitate caution in prescribing medications affecting central serotonin or dopamine systems, with awareness of potential drug interactions. International diagnostic tools and genetic screening tests may aid in safe diagnosis and prevention. Reporting rare cases and utilizing bibliometric analysis enhance knowledge dissemination and research exploration in the field of rare drug-induced medical conditions.
Introduction
Neuroleptic malignant syndrome (NMS) and serotonin syndrome (SS) are drug-induced, potentially life-threatening conditions that are infrequently encountered in medical practice, necessitating prompt intervention [ 1 , 2 , 3 , 4 ]. Neuroleptic Malignant Syndrome is characterized by a decrease in dopamine activity in the brain, often associated with the use of dopamine antagonists, primarily neuroleptic or antipsychotic medications [ 5 , 6 ]. While the exact pathophysiology of NMS remains incompletely understood, it is believed to involve dopamine dysregulation in the basal ganglia and hypothalamus. This dysregulation, particularly the blockade of dopamine receptors, especially D2 receptors, leads to a state of dopamine deficiency, manifesting in symptoms such as muscle rigidity, hyperthermia, and autonomic instability. Furthermore, withdrawal from dopamine agonists, such as L-Dopa, can also precipitate NMS in susceptible individuals. Serotonin Syndrome is characterized by an excess of serotonin (5-HT) in the central nervous system, typically stemming from the use of serotonergic medications or substances that elevate serotonin levels [ 7 , 8 ]. These drugs encompass antidepressants, notably selective serotonin reuptake inhibitors (SSRIs), opioids, specific psychedelics, serotonin agonists, and herbal supplements. The pathophysiology of SS revolves around the excessive stimulation of serotonin receptors, particularly the 5-HT2A receptors. This heightened stimulation precipitates a spectrum of symptoms, ranging from agitation, confusion, hyperthermia, muscle rigidity, to autonomic dysfunction. The severity of SS can vary widely, from mild manifestations to life-threatening conditions, contingent upon the extent of serotonin excess and individual susceptibility factors.
Both NMS and SS exhibit shared clinical manifestations, including hyperthermia, hypertension, hypersalivation, diaphoresis, and altered mental status [ 4 ], with instances of coexistence reported in some patients [ 9 ]. However, they diverge in their etiologies and clinical presentations. For instance, individuals with NMS typically display hyporeflexia, normal pupil size, and normal bowel sounds, contrasting with SS patients who often present with hyperreflexia, dilated pupils, and hyperactive bowel activity [ 10 ]. NMS is typified by lead-pipe muscle rigidity, whereas SS manifests with increased muscle tone, particularly in the lower extremities [ 11 , 12 ]. Given these distinctions, treatment strategies for NMS and SS diverge based on their underlying causes [ 2 ]. The mechanisms driving these syndromes differ significantly; while NMS involves diminished dopamine activity in the brain, SS is characterized by elevated serotonin levels [ 13 ]. Dopamine antagonists, such as neuroleptics or antipsychotics, are commonly implicated in NMS [ 14 , 15 , 16 ], although other triggers like withdrawal from dopamine agonists, like L-Dopa, can also induce NMS [ 17 , 18 ]. Conversely, SS can result from various drug classes, including antidepressants, opioids, psychedelics, serotonin agonists, and certain herbs [ 7 , 19 , 20 , 21 , 22 , 23 ]. Consequently, distinct medications are employed for their management; benzodiazepines and serotonin antagonists are standard therapy for SS, whereas dopaminergic agents and dantrolene are preferred for NMS [ 10 ]. While the incidence of NMS remains low, particularly among patients receiving newer generation antipsychotics [ 24 , 25 ], recent studies on SS incidence are lacking. However, a 1999 study reported an incidence of 0.4 cases per 1000 patient-months with nefazodone [ 26 ], while SS incidence reaches 14–16% in cases of selective serotonin reuptake inhibitor (SSRI) overdose [ 27 ].
Research context and objectives
The landscape of psychiatric pharmacotherapy has evolved over time, witnessing a surge in the number of approved drugs and the introduction of novel classes into clinical practice [ 28 , 29 , 30 , 31 ]. This trend is particularly notable in the treatment of depression and schizophrenia, where the absence of universally safe and effective drugs persists [ 32 , 33 , 34 , 35 , 36 ]. Additionally, off-label utilization of antidepressants and antipsychotics has been observed among patients with dementia and other neuro-cognitive disorders [ 37 , 38 , 39 , 40 , 41 ], contributing to an upward trajectory in psychiatric drug consumption [ 42 , 43 ]. The risk of SS is linked to any medication or herb augmenting the central serotonergic pathway, necessitating vigilant monitoring by healthcare professionals due to the potential for adverse effects, whether as a primary mechanism or side effect [ 20 ]. A concerning trend of unsupported polypharmacy in psychiatric medications has also emerged [ 44 ], along with significant prescribing of antidepressants and antipsychotics to dementia patients without documented indications of depression or psychosis [ 45 , 46 ], mirroring similar trends among individuals with intellectual disabilities [ 47 ]. The escalating demand for psychiatric therapy raises apprehensions regarding the likelihood of adverse medication effects [ 48 ], exacerbated by increased prescribing rates, polypharmacy, and off-label usage, which heighten the incidence of drug-induced toxicities, including NMS and SS. Analyzing published literature on drug-induced NMS and SS provides valuable insights into these rare yet severe toxicities, aligning with the pressing global public health burden of depression, schizophrenia, and related conditions, accentuated by the fatal toxicities associated with specific psychiatric medications. This scientific literature on NMS and SS is ripe for analysis and mapping to delineate current research hotspots [ 49 , 50 , 51 , 52 , 53 , 54 , 55 ], addressing the gap in the literature. Accordingly, the present study aims to analyze and map scientific research on NMS and SS published in prestigious, internationally indexed journals. Through this analysis, the study seeks to identify key topics, impactful articles, prominent journals, research output, growth patterns, hotspots, and leading countries in the field, providing valuable insights for scholars, medical students, and international funding agencies to discern research trajectories, bibliographic trends, and knowledge structures pertaining to NMS and SS. Ultimately, this endeavor aims to invigorate scholarly discourse and inform clinical practice in the field.
Database and keywords
In this study, we employed a systematic search strategy to extract relevant scientific literature on NMS and SS from the PubMed MeSH database. Specifically, we utilized the following keywords:
Malignant neuroleptic syndrome: “malignant neuroleptic syndrome”.
Serotonin syndrome: “serotonin syndrome” or “serotonin toxicity”.
To ensure comprehensive coverage, we conducted our search in Scopus, a prestigious scientific database owned by Elsevier, which has previously been utilized for analyzing research in psychiatry [ 56 , 57 ]. Scopus is renowned for its extensive coverage, encompassing a vast array of scholarly publications in the field. Notably, Scopus encompasses over 95% of the content included in other databases such as PubMed and Web of Science, rendering it an ideal platform for our study [ 58 ].
Inclusion and exclusion criteria
We restricted our search to articles published from 1950 to December 31st, 2022, and focused exclusively on journal research and review articles written in English. Excluded from our analysis were editorials, notes, letters, and conference abstracts. Additionally, articles pertaining to non-human subjects were excluded, ensuring the relevance of our findings. We meticulously reviewed the titles and abstracts of over 100 articles to eliminate irrelevant publications, such as those mentioning NMS or SS only marginally, thereby refining the scope of our analysis.
Our search strategy yielded results indicative of its validity, as evidenced by the prominent presence of leading scientists and journals in the fields of psychiatry and pharmacology. This reaffirmed the robustness of our search criteria and the relevance of the retrieved literature to our study objectives.
Data management, analysis, and mapping
The dataset comprising the retrieved articles was subjected to descriptive analysis using Microsoft Excel. Subsequently, we employed VOSviewer, a freely available online tool, for bibliometric mapping purposes [ 59 ]. VOSviewer maps offer researchers a visual tool for exploring bibliometric data, revealing patterns, relationships, and trends within a dataset. Interpretation of these maps involves understanding several key elements. Firstly, node size indicates the prominence or frequency of an item, with larger nodes representing more significant themes or influential publications. Secondly, node color categorizes items into clusters, with similar colors indicating thematic groupings. Thirdly, the thickness of connecting lines between nodes signifies the strength of associations, with thicker lines indicating stronger connections. Lastly, the distance between nodes reflects the similarity or dissimilarity between items, with closer nodes indicating stronger relationships. Overall, VOSviewer maps provide a comprehensive visual overview of bibliometric data, enabling researchers to identify clusters, influential publications, and emerging trends within their field of study by considering the interplay between node size, color, line thickness, and spatial relationships. Within the descriptive analysis, we presented lists of active countries and journals, alongside a linear graph illustrating the growth of publications over time. In the keyword visualization map generated using VOSviewer, node size corresponded to the frequency of occurrence of each keyword, enabling visual identification of prominent themes. Similarly, in the journal visualization map, node size reflected the normalized citation count received by each journal, providing insights into publication impact within the field.
Number of publications
The search strategy yielded a total of 1150 articles on NMS and 587 on SS. Among the articles on NMS, 791 (68.8%) were case reports, while 384 (65.4%) of the articles on SS took the form of case reports.
Growth of publications
The earliest scientific publication on NMS dates back to 1973 [ 60 ], while publications on SS emerged in 1979 [ 61 ]. Research on NMS experienced a notable surge between 1981 and 1991, followed by a fluctuating decline. Conversely, research on SS saw a steep increase between 1993 and 1997, followed by a fluctuating rise. Figure 1 illustrates the growth trends of research on NMS and SS.
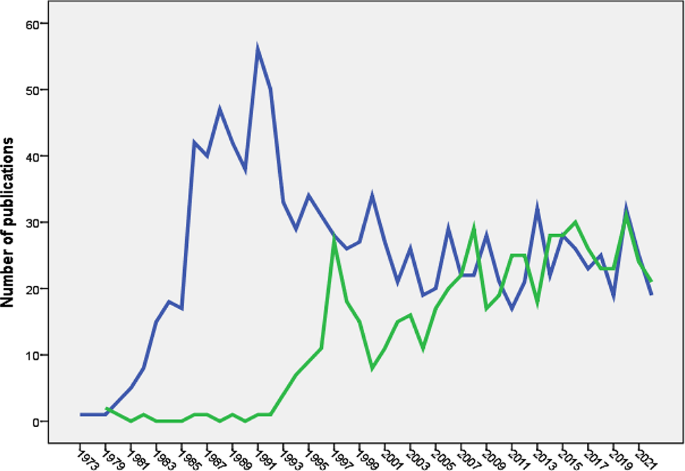
Annual growth of publications of NMS (blue line) and SS (green line). The Figure was created by SPSS program
Active countries and journals
Table 1 outlines the top five countries contributing articles on NMS and SS. Japan ranked second in NMS publications but fifth in SS publications. Table 2 presents the top five active journals for both NMS and SS, with NMS publications primarily within psychiatry journals and SS publications within pharmacology/toxicology journals.
Authorship analysis
Articles on NMS involved 3820 authors (mean = 3.1 authors per article), with 89 (7.3%) single-authored and 171 (14.1%) multi-authored articles. Similarly, articles on SS included 2105 authors (mean = 3.0 authors per article), with 102 (16.0%) single-authored and 41 (7.1%) multi-authored articles.
Most impactful articles
The top five impactful articles on NMS comprised mainly review articles and a research article focusing on the pathogenic role of dopamine antagonists [ 62 ]. For SS, the top five impactful articles included review articles and research articles discussing the Hunter diagnostic criteria [ 63 ] and the role of monoamine oxidase inhibitors (MAO-I) and opioid analgesics in serotonin toxicity [ 64 ].
Research hotspots
Research hotspots were identified by mapping author keywords with a minimum occurrence of five times (Figs. 2 and 3 ). Notable hotspots for SS included antidepressants, SSRIs, tramadol, linezolid, cyproheptadine, and drug interactions. For NMS, hotspots included antipsychotics (various drug names), catatonia, and rhabdomyolysis.
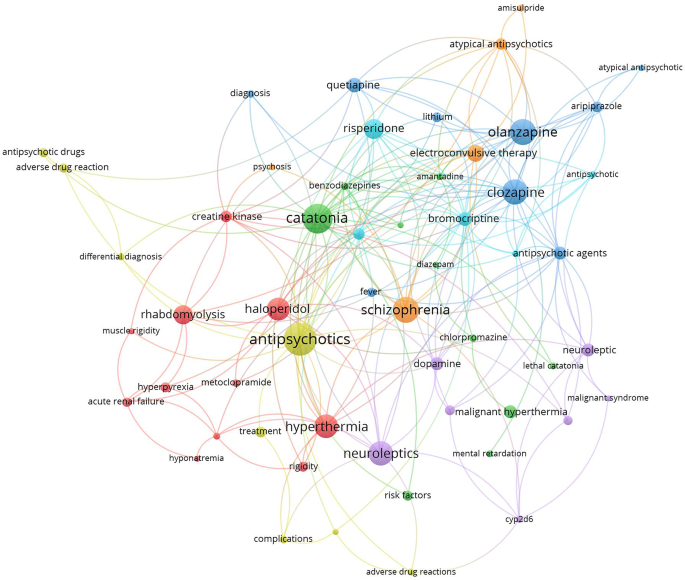
Network visualization map of author keywords with minimum occurrences of five times. Large nodes represent research hotspots on NMS. The term NMS was not shown to make other keywords more visible
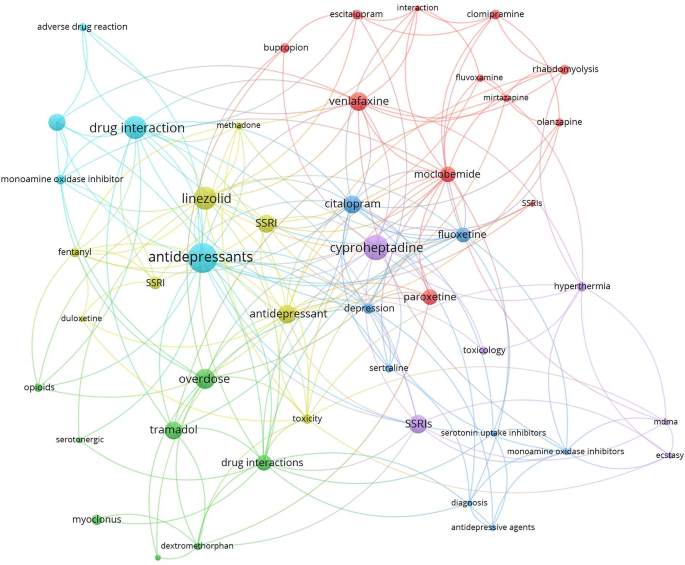
Network visualization map of author keywords with minimum occurrences of five times. Large nodes represent research hotspots on SS. The term SS was not shown to make other keywords more visible
Journal citation analysis
The top 15 active journals in publishing articles on NMS and SS were mapped (Figs. 4 and 5 ). Notably, articles on NMS published in the American Journal of Psychiatry and the Journal of Clinical Psychiatry received the highest number of citations per article. Similarly, articles on SS published in Clinical Toxicology and the Annals of Pharmacotherapy garnered the most citations per article.
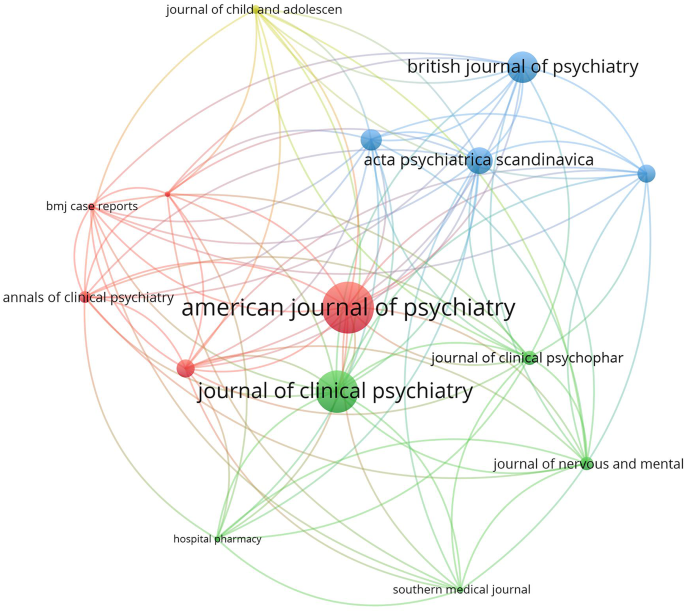
Network visualization map of the top 15 journals in the field of NMS. Large node sized indicates higher normalized citation count
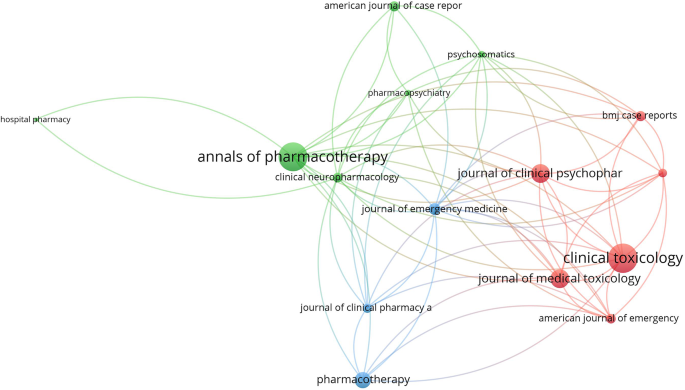
Network visualization map of the top 15 journals in the field of SS. Large node sized indicates higher normalized citation count
Geographic mapping
The geographic distribution of research publications on NMS and SS was illustrated on a worldwide map (Fig. 6 ), with the majority of contributions originating from the US. Several countries in specific regions showed minimal to no research output on either NMS or SS.
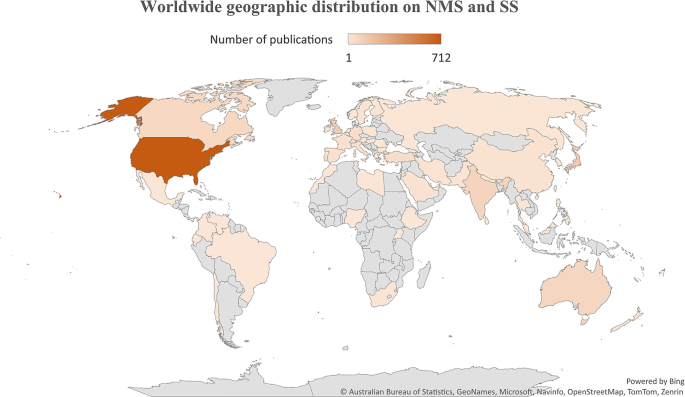
Worldwide distribution of research publications on NMS and SS. Figure was created by Microsoft Excel
Molecular genetics
The retrieved literature on NMS has 20 articles that discussed the potential link between NMS and certain genetics. Ten articles discussed the potential linkage between Cytochrome 2D6 and potential risk for NMS [ 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 ]. Five articles discussed the potential linkage between dopamine receptor 2 gene polymorphism and NMS [ 75 , 76 , 77 , 78 , 79 ]. Four articles discussed the linkage between ryanodine receptor gene mutations and susceptibility to NMS [ 80 , 81 , 82 , 83 ]. No association was found between NMS and serotonin receptor gene variation [ 84 ]. The literature on SS has few articles that discussed the genetic predisposition of patients to SS such as the 5-HT receptor gene or the CYP 2D6 gene polymorphism [ 85 , 86 ].
Drug interactions
Serious drug-drug interactions leading to NMS were mentioned in a limited number of articles and involved the administration of two dopamine antagonists [ 87 ] or two atypical antipsychotic drugs [ 88 ]. However, there were many articles discussing potential SS caused by drug-drug interactions, which included SSRI–methylene blue [ 89 ], SSRI–metoclopramide [ 89 ], sertraline–phenelzine [ 90 ], anti-depressants–opioids [ 91 ], citalopram-fentanyl [ 92 ], a combination of two anti-depressants [ 93 ], SSRI-linezolid [ 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 ], sertraline–phenelzine [ 90 ], citalopram-buspirone [ 103 ], venlafaxine-tranylcypromine [ 104 ], and many others [ 92 , 105 , 106 , 107 , 108 , 109 ].
Non-psychiatric causative agents
The retrieved literature on SS, showed that several drugs and drug classes not related to antidepressants can induce SS. Examples of such drugs included Linezolid, CNS stimulants (amphetamine), hallucinogens (LSD), opioids (fentanyl), ondansetron, sumatriptan, and certain herbs (St. John’s wort), metoclopramide, ritonavir, and others [ 5 , 20 , 110 , 111 ]. The retrieved literature on NMS showed that drug-induced NMS is limited to antipsychotics and withdrawal of dopamine agonists [ 112 , 113 , 114 ].
Diagnostic criteria
For NMS, there were 30 articles that discussed issues related to diagnosis. In 2011, an international panel tried to develop NMS diagnostic criteria [ 115 , 116 ]. The neutrophil-lymphocyte ratio was suggested by certain researchers as a diagnostic test for NMS [ 117 , 118 ]. The differential diagnosis for NMS compared to SS and catatonia was also published [ 13 , 118 , 119 ]. For SS, there were 17 articles that discussed issues related to diagnosis of SS. The Hunter diagnostic criteria was one of these articles [ 63 ]. Other articles discussed controversies and the importance of differential diagnosis in SS [ 120 ].
The current study analyzed and compared the scientific literature on two rare drug-induced conditions with certain overlapping clinical features. Both syndromes are mainly caused by medications used in psychiatry, such as those for schizophrenia and depression. The name “NMS” implies that the syndrome is correlated with the use of neuroleptic medications, while the name “SS” implies that it is correlated with any medication or herb that raises serotonin centrally.
The analysis showed that the volume of research publications on NMS was larger and started earlier than research publications on SS. The NMS is associated with the use of dopamine antagonists (neuroleptics). The history of using old-generation antipsychotics for the treatment of schizophrenia dates back to the 1950s [ 121 , 122 , 123 , 124 , 125 ]. On the other hand, the introduction of the SSRI drug class, the main causative agent of SS, dates back to the late 1980s [ 126 ]. The difference in the history of introduction into clinical practice explains the differences between SS and NMS in growth patterns. The difference in the volume of literature between the two syndromes could be due to diagnostic uncertainty [ 127 ] for NMS versus SS, the seriousness of medical complications, or debate regarding whether an atypical antipsychotic drug class causes NMS in a similar way to conventional antipsychotics [ 13 , 30 , 128 , 129 , 130 ]. The current study showed that the number of research publications on NMS started to decline after 1991 but the number of publications on SS started to increase after 1997. The introduction of atypical antipsychotics with lesser dopaminergic side effects than conventional antipsychotics decreased the incidence of NMS and therefore decreased the number of publications with time. On the other hand, the increased number of SS publications after 1997 could be explained by the many reported drug interactions at serotonin level leading to more cases of SS with time.
The current study showed that journals in the field of psychiatry ranked highest in publishing articles on NMS, while those in the field of pharmacology/toxicology ranked highest in publishing articles on SS. The reason for this difference is difficult to explain. However, NMS is primarily limited to schizophrenia patients taking antipsychotic drugs, while SS might occur in normal people taking SSRIs for depression or any other condition. Furthermore, the potentially large numbers of drug- or drug-herb interactions make the SS interesting to pharmacology/toxicology journals [ 22 ]. Actually, SS has been termed “serotonin toxicity” implying relatedness to toxicology [ 131 ].
The findings of the current study regarding active countries were not surprising. The English-speaking countries, the US, the UK, Australia, and Canada showed leading roles in many scientific disciplines and ranked first in several studies that analyzed research activity [ 132 , 133 , 134 , 135 ]. This is due to advancements in technology, medicine, clinical practice, and research funding in high-income countries relative to other countries. However, there are also reasons related to the nature of journals indexed in Scopus. The vast majority of Scopus-indexed journals publish articles in English, and the vast majority of the journals are issued by publishers and institutions based in the US, Europe, or Australia. Therefore, Scopus might be biased toward scholars in English-speaking countries. The finding that research articles on NMS tend to be multi-authored while those on SS are not is not easy to explain. However, it is possible that cases of NMS tend to involve a larger medical team due to the nature of complications that might involve renal and blood complications. Furthermore, the treatment of NMS requires medications and follow-up. All this makes the number of authors in a case study of NMS higher than those involved in SS cases [ 13 , 136 , 137 ].
Of the retrieved articles on SS and NMS, the research article “The hunter serotonin toxicity criteria: Simple and accurate diagnostic decision rules for serotonin toxicity” [ 63 ] received the highest number of citations excluding the review articles. The diagnosis of SS is based on the clinical symptoms and the medical history of the patient. Harvey Sternbach introduced the first diagnostic criteria for SS in 1991 and the Hunter Diagnostic Criteria tool was introduced in 2003 [ 63 , 138 ].
Mapping the retrieved literature on NMS showed that rhabdomyolysis and catatonia constituted distinct research hotspots in addition to those related to antipsychotic medications and schizophrenia. However, mapping the author keywords of SS research publications showed that linezolid, drug interactions, and tramadol constituted research hotspots in addition to antidepressants and SSRIs. Rhabdomyolysis has been reported as a consequence of NMS even among children and adolescents [ 139 , 140 ]. However, reports of rhabdomyolysis among patients taking antipsychotics were published, suggesting that rhabdomyolysis could be a side effect of antipsychotics even in the absence of NMS [ 139 , 140 ]. Catatonia is, as NMS, a consequence of neuroleptic drugs, and there is an overlap in clinical features between the symptoms of catatonia and those of NMS, which makes the distinction between them difficult [ 141 ]. Linezolid is an antibiotic that was originally designed to be used as an anti-depressant by virtue of its MAO enzyme inhibition property [ 142 ]. This explains the many cases of SS induced by drug interactions with Linezolid [ 141 ]. The relatively higher number of research articles on drug/herb interactions leading to SS is attributed to the presence of many and different drug classes that affect and increase serotonergic pathways in the brain [ 90 , 105 , 109 , 143 ]. The scientific controversy about the potential ability of tramadol to cause SS received a high number of citations. Current scientific evidence supports the ability of tramadol to cause SS due to its molecular pharmacological effects on both the opioid and serotonergic systems [ 105 , 107 , 144 , 145 , 146 , 147 ]. Cyproheptadine was also a research hotspot in the field of SS. Cyproheptadine has anti-histaminic, anticholinergic, and anti-serotonergic properties and that is why it has been used to counter the symptoms of SS [ 148 , 149 , 150 ].
The current study showed that SS has a wide range of possible drug/herb interactions due to the many drugs that affect the serotonin system. Of particular interest is the one with opioid analgesics, since they are commonly used in hospital settings. Opioids, including fentanyl and even dextromethorphan in cough syrups, were reported to increase serotonin levels, and therefore caution should be practiced when given to patients with SSRIs in their medical records [ 19 , 22 , 109 , 151 ].
Limitations
Limitations arise in this study from various factors. Firstly, the reliance on the Scopus database for literature retrieval could potentially limit the inclusivity of articles from low- and middle-income countries. Although Scopus offers extensive coverage, the possibility exists that some relevant journals from these regions may not be indexed, thereby leading to a potential underestimation of publications from certain geographic areas. Secondly, despite efforts to employ a comprehensive search strategy, the use of a title-abstract search method might have resulted in the retrieval of some false-positive results. While validation tests were conducted to mitigate this issue, the possibility of false positives cannot be entirely ruled out. Thirdly, the analysis focused solely on articles published in English-language journals, which could introduce a language bias and limit the generalizability of findings. This exclusion of literature published in other languages may have led to the omission of relevant data from non-English sources. Lastly, diagnostic uncertainty poses a challenge in distinguishing between neuroleptic malignant syndrome (NMS) and serotonin syndrome (SS) due to overlapping clinical features and the absence of definitive diagnostic tests. Misdiagnosis or underreporting of cases may have occurred, potentially impacting the accuracy of the literature analysis and conclusions drawn from it.
In conclusion, NMS and SS represent rare but potentially life-threatening conditions associated with drug-induced dysregulation of dopamine and serotonin systems, respectively. The study analyzed and compared the scientific literature on these syndromes, revealing distinct growth patterns, research hotspots, and publication trends. The findings underscored the evolving landscape of psychiatric pharmacotherapy and the complexities involved in diagnosing and managing NMS and SS. While NMS research exhibited a longer history and a decline in publications over time, SS research witnessed a notable increase in publications, reflecting advancements in pharmacological understanding and the recognition of SS as a significant clinical entity. Identified research hotspots provided valuable insights into emerging areas of interest, including drug interactions, molecular genetics, and diagnostic criteria. Understanding these trends is essential for informing clinical practice, guiding future research endeavors, and promoting collaboration among scholars and healthcare professionals. Despite the study’s contributions, several limitations warrant consideration, including database restrictions, potential publication bias, and diagnostic uncertainties. Addressing these limitations through expanded literature search strategies, international collaboration, and improved diagnostic tools is crucial for advancing knowledge and enhancing patient care in the field of rare drug-induced syndromes. Moving forward, efforts to develop standardized diagnostic criteria, genetic screening tools, and international reporting mechanisms for NMS and SS are warranted. Additionally, continued bibliometric analysis and mapping of literature on rare medical conditions can facilitate ongoing research and contribute to the dissemination of knowledge across global healthcare communities.
Data availability
All data present in this article can be retrieved from Scopus using keywords listed in the methodology.
Abbreviations
- Neuroleptic malignant syndrome
Serotonin Syndrome/ Serotonin toxicity
Darracq MA, Comment. Neuroleptic malignant syndrome versus serotonin syndrome: the search for a diagnostic tool. Ann Pharmacother. 2012;46(4):611–2. https://doi.org/10.1345/aph.1P787a . author reply 3.
Article PubMed Google Scholar
Sokoro AA, Zivot J, Ariano RE. Neuroleptic malignant syndrome versus serotonin syndrome: the search for a diagnostic tool. Ann Pharmacother. 2011;45(9):e50. https://doi.org/10.1345/aph.1P787 .
Fernández M, Lago L, Alonso MG, Guede A, Benavente JL, Olivares JM. Serotonin syndrome versus neuroleptic malignant syndrome: a case report. Actas Esp Psiquiatr. 2018;46(2):68–74.
PubMed Google Scholar
Dosi R, Ambaliya A, Joshi H, Patell R. Serotonin syndrome versus neuroleptic malignant syndrome: a challenging clinical quandary. BMJ Case Rep. 2014. https://doi.org/10.1136/bcr-2014-204154 . 2014.
Article PubMed PubMed Central Google Scholar
Tormoehlen LM, Rusyniak DE. Neuroleptic malignant syndrome and serotonin syndrome. Handb Clin Neurol. 2018;157:663–75. https://doi.org/10.1016/b978-0-444-64074-1.00039-2 .
Ware MR, Feller DB, Hall KL. Neuroleptic malignant syndrome: diagnosis and management. Prim Care Companion CNS Disord. 2018;20(1). https://doi.org/10.4088/PCC.17r02185 .
Maitland S, Baker M. Serotonin syndrome. Drug Ther Bull. 2022;60(6):88–91. https://doi.org/10.1136/dtb.2021.000032 .
Mikkelsen N, Damkier P, Pedersen SA. Serotonin syndrome-A focused review. Basic Clin Pharmacol Toxicol. 2023;133(2):124–9. https://doi.org/10.1111/bcpt.13912 .
Article CAS PubMed Google Scholar
Prakash S, Lodha D, Rawat KS. Coexistence of serotonin syndrome and neuroleptic malignant syndrome: does it exist? BMJ Case Rep. 2021;14(8). https://doi.org/10.1136/bcr-2021-241578 .
Katus LE, Frucht SJ. Management of Serotonin Syndrome and neuroleptic malignant syndrome. Curr Treat Options Neurol. 2016;18(9):39. https://doi.org/10.1007/s11940-016-0423-4 .
Hadad E, Weinbroum AA, Ben-Abraham R. Drug-induced hyperthermia and muscle rigidity: a practical approach. Eur J Emerg Med. 2003;10(2):149–54. https://doi.org/10.1097/00063110-200306000-00018 .
Haddad PM, Dursun SM. Neurological complications of psychiatric drugs: clinical features and management. Hum Psychopharmacol. 2008;23(Suppl 1):15–26. https://doi.org/10.1002/hup.918 .
Perry PJ, Wilborn CA. Serotonin syndrome vs neuroleptic malignant syndrome: a contrast of causes, diagnoses, and management. Ann Clin Psychiatry. 2012;24(2):155–62.
Pileggi DJ, Cook AM. Neuroleptic malignant syndrome. Ann Pharmacother. 2016;50(11):973–81. https://doi.org/10.1177/1060028016657553 .
Hasan S, Buckley P. Novel antipsychotics and the neuroleptic malignant syndrome: a review and critique. Am J Psychiatry. 1998;155(8):1113–6. https://doi.org/10.1176/ajp.155.8.1113 .
Belvederi Murri M, Guaglianone A, Bugliani M, Calcagno P, Respino M, Serafini G, et al. Second-generation antipsychotics and neuroleptic malignant syndrome: systematic review and case report analysis. Drugs R D. 2015;15(1):45–62. https://doi.org/10.1007/s40268-014-0078-0 .
Article CAS PubMed PubMed Central Google Scholar
Mizuno Y, Takubo H, Mizuta E, Kuno S. Malignant syndrome in Parkinson’s disease: concept and review of the literature. Parkinsonism Relat Disord. 2003;9(Suppl 1). https://doi.org/10.1016/s1353-8020(02)00125-6 . :S3-9.
Rainer C, Scheinost NA, Lefeber EJ. Neuroleptic malignant syndrome. When levodopa withdrawal is the cause. Postgrad Med. 1991;89(5):175–8. https://doi.org/10.1080/00325481.1991.11700900 .
Baldo BA, Rose MA. The anaesthetist, opioid analgesic drugs, and serotonin toxicity: a mechanistic and clinical review. Br J Anaesth. 2020;124(1):44–62. https://doi.org/10.1016/j.bja.2019.08.010 .
Bartlett D. Drug-Induced Serotonin Syndrome. Crit Care Nurse. 2017;37(1):49–54. https://doi.org/10.4037/ccn2017169 .
Hu Z, Yang X, Ho PC, Chan SY, Heng PW, Chan E, et al. Herb-drug interactions: a literature review. Drugs. 2005;65(9):1239–82. https://doi.org/10.2165/00003495-200565090-00005 .
Baldo BA. Opioid analgesic drugs and serotonin toxicity (syndrome): mechanisms, animal models, and links to clinical effects. Arch Toxicol. 2018;92(8):2457–73. https://doi.org/10.1007/s00204-018-2244-6 .
Scotton WJ, Hill LJ, Williams AC, Barnes NM. Serotonin syndrome: pathophysiology, clinical features, management, and potential future directions. Int J Tryptophan Res. 2019;12:1178646919873925. https://doi.org/10.1177/1178646919873925 .
Velamoor VR. Neuroleptic malignant syndrome. Recognition, prevention and management. Drug Saf. 1998;19(1):73–82. https://doi.org/10.2165/00002018-199819010-00006 .
Berman BD. Neuroleptic malignant syndrome: a review for neurohospitalists. Neurohospitalist. 2011;1(1):41–7. https://doi.org/10.1177/1941875210386491 .
Mackay FJ, Dunn NR, Mann RD. Antidepressants and the serotonin syndrome in general practice. Br J Gen Pract. 1999;49(448):871–4.
CAS PubMed PubMed Central Google Scholar
Isbister GK, Bowe SJ, Dawson A, Whyte IM. Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose. J Toxicol Clin Toxicol. 2004;42(3):277–85. https://doi.org/10.1081/clt-120037428 .
Adell A. Brain NMDA receptors in Schizophrenia and Depression. Biomolecules. 2020;10(6). https://doi.org/10.3390/biom10060947 .
Laszlovszky I, Barabássy Á, Németh G, Cariprazine. A broad-spectrum antipsychotic for the treatment of Schizophrenia: Pharmacology, Efficacy, and Safety. Adv Ther. 2021;38(7):3652–73. https://doi.org/10.1007/s12325-021-01797-5 .
Orzelska-Górka J, Mikulska J, Wiszniewska A, Biała G. New atypical antipsychotics in the treatment of Schizophrenia and Depression. Int J Mol Sci. 2022;23(18). https://doi.org/10.3390/ijms231810624 .
Marwaha S, Palmer E, Suppes T, Cons E, Young AH, Upthegrove R. Novel and emerging treatments for major depression. Lancet. 2023;401(10371):141–53. https://doi.org/10.1016/s0140-6736(22)02080-3 .
Preda A, Shapiro BB. A safety evaluation of aripiprazole in the treatment of schizophrenia. Expert Opin Drug Saf. 2020;19(12):1529–38. https://doi.org/10.1080/14740338.2020.1832990 .
Solmi M, Murru A, Pacchiarotti I, Undurraga J, Veronese N, Fornaro M, et al. Safety, tolerability, and risks associated with first- and second-generation antipsychotics: a state-of-the-art clinical review. Ther Clin Risk Manag. 2017;13:757–77. https://doi.org/10.2147/tcrm.S117321 .
Cheniaux E, Nardi AE. Evaluating the efficacy and safety of antidepressants in patients with bipolar disorder. Expert Opin Drug Saf. 2019;18(10):893–913. https://doi.org/10.1080/14740338.2019.1651291 .
Sommer BR, Fenn H, Pompei P, DeBattista C, Lembke A, Wang P, et al. Safety of antidepressants in the elderly. Expert Opin Drug Saf. 2003;2(4):367–83. https://doi.org/10.1517/14740338.2.4.367 .
Carvalho AF, Sharma MS, Brunoni AR, Vieta E, Fava GA. The Safety, Tolerability and Risks Associated with the use of newer generation antidepressant drugs: a critical review of the literature. Psychother Psychosom. 2016;85(5):270–88. https://doi.org/10.1159/000447034 .
Yunusa I, Rashid N, Demos GN, Mahadik BS, Abler VC, Rajagopalan K. Comparative outcomes of commonly used off-label atypical antipsychotics in the treatment of dementia-related psychosis: a Network Meta-analysis. Adv Ther. 2022;39(5):1993–2008. https://doi.org/10.1007/s12325-022-02075-8 .
Scheltema Beduin A, de Haan L. Off-label second generation antipsychotics for impulse regulation disorders: a review. Psychopharmacol Bull. 2010;43(3):45–81.
Hefner G, Wolff J, Toto S, Reißner P, Klimke A. Off-label use of antidepressants, antipsychotics, and mood-stabilizers in psychiatry. J Neural Transm (Vienna). 2022;129(11):1353–65. https://doi.org/10.1007/s00702-022-02542-0 .
Haw C, Stubbs J. Off-label use of antipsychotics: are we mad? Expert Opin Drug Saf. 2007;6(5):533–45. https://doi.org/10.1517/14740338.6.5.533 .
Maher AR, Theodore G. Summary of the comparative effectiveness review on off-label use of atypical antipsychotics. J Manag Care Pharm. 2012;18(5 Suppl B):S1–20. https://doi.org/10.18553/jmcp.2012.18.s5-b.1 .
González-López MDC, Díaz-Calvo V, Ruíz-González C, Nievas-Soriano BJ, Rebollo-Lavado B, Parrón-Carreño T. Consumption of Psychiatric drugs in Primary Care during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(8). https://doi.org/10.3390/ijerph19084782 .
Heald AH, Stedman M, Farman S, Khine C, Davies M, De Hert M, et al. Links between the amount of antipsychotic medication prescribed per population at general practice level, local demographic factors and medication selection. BMC Psychiatry. 2020;20(1):528. https://doi.org/10.1186/s12888-020-02915-3 .
Mojtabai R, Olfson M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch Gen Psychiatry. 2010;67(1):26–36. https://doi.org/10.1001/archgenpsychiatry.2009.175 .
Drummond N, McCleary L, Freiheit E, Molnar F, Dalziel W, Cohen C, et al. Antidepressant and antipsychotic prescribing in primary care for people with dementia. Can Fam Physician. 2018;64(11):e488–97.
PubMed PubMed Central Google Scholar
Luo H, Lau WCY, Chai Y, Torre CO, Howard R, Liu KY, et al. Rates of antipsychotic drug prescribing among people living with Dementia during the COVID-19 pandemic. JAMA Psychiatry. 2023;80(3):211–9. https://doi.org/10.1001/jamapsychiatry.2022.4448 .
Henderson A, McSkimming P, Kinnear D, McCowan C, McIntosh A, Allan L, et al. Changes over a decade in psychotropic prescribing for people with intellectual disabilities: prospective cohort study. BMJ Open. 2020;10(9):e036862. https://doi.org/10.1136/bmjopen-2020-036862 .
Rogers K, Spring B. Mental Health professionals are in high demand as the pandemic enters a Second Year. CNBC; 2022.
Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: findings from the Global Burden of Disease study. J Psychiatr Res. 2020;126:134–40. https://doi.org/10.1016/j.jpsychires.2019.08.002 .
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86–92. https://doi.org/10.1016/j.jad.2017.05.003 .
Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–73. https://doi.org/10.2147/ndt.S96649 .
Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global Epidemiology and burden of Schizophrenia: findings from the global burden of Disease Study 2016. Schizophr Bull. 2018;44(6):1195–203. https://doi.org/10.1093/schbul/sby058 .
Global, regional, and, national, burden, of, 12, mental, disorders, in, 204, countries, and, territories, 1990–2019, a, systematic, analysis, for, the, Global, Burden, of, Disease, Study, 2019. Lancet Psychiatry. 2022;9(2):137–50. https://doi.org/10.1016/s2215-0366(21)00395-3 .
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–41. https://doi.org/10.1001/jamapsychiatry.2014.2502 .
Hany M, Rehman B, Azhar Y, Chapman J. Schizophrenia. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2023. StatPearls Publishing LLC.; 2023.
Sweileh WM. Analysis of global research output on diabetes depression and suicide. Ann Gen Psychiatry. 2018;17:44. https://doi.org/10.1186/s12991-018-0214-2 .
Sweileh WM. Contribution of researchers in the arab region to peer-reviewed literature on mental health and well-being of university students. Int J Ment Health Syst. 2021;15(1):50. https://doi.org/10.1186/s13033-021-00477-9 .
Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, web of Science, and Google Scholar: strengths and weaknesses. FASEB Journal: Official Publication Federation Am Soc Experimental Biology. 2008;22(2):338–42. https://doi.org/10.1096/fj.07-9492LSF .
Article CAS Google Scholar
van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–38. https://doi.org/10.1007/s11192-009-0146-3 .
Meltzer HY. Rigidity, hyperpyrexia and coma following fluphenazine enanthate. Psychopharmacologia. 1973;29(4):337–46. https://doi.org/10.1007/bf00429281 .
Silbergeld EK, Hruska RE. Lisuride and LSD: dopaminergic and serotonergic interactions in the serotonin syndrome. Psychopharmacology. 1979;65(3):233–7. https://doi.org/10.1007/bf00492209 .
Henderson VW, Wooten GF. Neuroleptic malignant syndrome: a pathogenetic role for dopamine receptor blockade? Neurology. 1981;31(2):132–7. https://doi.org/10.1212/wnl.31.2.132 .
Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96(9):635–42. https://doi.org/10.1093/qjmed/hcg109 .
Gillman PK. Monoamine oxidase inhibitors, opioid analgesics and serotonin toxicity. Br J Anaesth. 2005;95(4):434–41. https://doi.org/10.1093/bja/aei210 .
Ueno S, Otani K, Kaneko S, Koshiro K, Kondoh K, Kotani Y, et al. Cytochrome P-450 2D6 gene polymorphism is not associated with neuroleptic malignant syndrome. Biol Psychiatry. 1996;40(1):72–4. https://doi.org/10.1016/0006-3223(95)00427-0 .
Ochi S, Kawasoe K, Abe M, Fukuhara R, Sonobe K, Kawabe K, et al. A case study: neuroleptic malignant syndrome with risperidone and CYP2D6 gene variation. Gen Hosp Psychiatry. 2011;33(6):640. https://doi.org/10.1016/j.genhosppsych.2011.03.003 . .e1-2.
Article Google Scholar
Kato D, Kawanishi C, Kishida I, Furuno T, Matsumura T, Hasegawa H, et al. CYP2D6 gene deletion allele in patients with neuroleptic malignant syndrome: preliminary report. Psychiatry Clin Neurosci. 2005;59(4):504–7. https://doi.org/10.1111/j.1440-1819.2005.01405.x .
Iwahashi K, Yoshihara E, Nakamura K, Ameno K, Watanabe M, Tsuneoka Y, et al. CYP2D6 HhaI genotype and the neuroleptic malignant syndrome. Neuropsychobiology. 1999;39(1):33–7. https://doi.org/10.1159/000026557 .
Iwahashi K, Nakamura K, Suwaki H, Tsuneoka Y, Ichikawa Y. CYP2D6 Hhal genotype and the neuroleptic malignant syndrome (NMS). Clin Chim Acta. 1997;265(1):143–4. https://doi.org/10.1016/s0009-8981(97)00113-7 .
Kato D, Kawanishi C, Kishida I, Furuno T, Suzuki K, Onishi H, et al. Effects of CYP2D6 polymorphisms on neuroleptic malignant syndrome. Eur J Clin Pharmacol. 2007;63(11):991–6. https://doi.org/10.1007/s00228-007-0355-8 .
Kawanishi C, Shimoda Y, Fujimaki J, Onishi H, Suzuki K, Hanihara T, et al. Mutation involving cytochrome P450IID6 in two Japanese patients with neuroleptic malignant syndrome. J Neurol Sci. 1998;160(1):102–4. https://doi.org/10.1016/s0022-510x(98)00238-x .
Kawanishi C, Hanihara T, Maruyama Y, Matsumura T, Onishi H, Inoue K, et al. Neuroleptic malignant syndrome and hydroxylase gene mutations: no association with CYP2D6A or CYP2D6B. Psychiatr Genet. 1997;7(3):127–9. https://doi.org/10.1097/00041444-199723000-00007 .
Butwicka A, Krystyna S, Retka W, Wolańczyk T. Neuroleptic malignant syndrome in an adolescent with CYP2D6 deficiency. Eur J Pediatr. 2014;173(12):1639–42. https://doi.org/10.1007/s00431-013-2208-z .
Zivković M, Mihaljević-Peles A, Sagud M, Silić A, Mihanović M. The role of CYP2D6 and TaqI a polymorphisms in malignant neuroleptic syndrome: two case reports with three episodes. Psychiatr Danub. 2010;22(1):112–6.
Mihara K, Kondo T, Suzuki A, Yasui-Furukori N, Ono S, Sano A, et al. Relationship between functional dopamine D2 and D3 receptors gene polymorphisms and neuroleptic malignant syndrome. Am J Med Genet B Neuropsychiatr Genet. 2003;117b(1):57–60. https://doi.org/10.1002/ajmg.b.10025 .
Kishida I, Kawanishi C, Furuno T, Kato D, Ishigami T, Kosaka K. Association in Japanese patients between neuroleptic malignant syndrome and functional polymorphisms of the dopamine D(2) receptor gene. Mol Psychiatry. 2004;9(3):293–8. https://doi.org/10.1038/sj.mp.4001422 .
Kishida I, Kawanishi C, Furuno T, Matsumura T, Hasegawa H, Sugiyama N, et al. Lack of association in Japanese patients between neuroleptic malignant syndrome and the TaqI a polymorphism of the dopamine D2 receptor gene. Psychiatr Genet. 2003;13(1):55–7. https://doi.org/10.1097/00041444-200303000-00010 .
Ram A, Cao Q, Keck PE Jr., Pope HG Jr., Otani K, Addonizio G, et al. Structural change in dopamine D2 receptor gene in a patient with neuroleptic malignant syndrome. Am J Med Genet. 1995;60(3):228–30. https://doi.org/10.1002/ajmg.1320600311 .
Akihito Suzuki MD, Tsuyoshi Kondo PD,, MDPD, Koichi Otani MD,, PD, Kazuo Mihara MD,, PD, Norio, Yasui-Furukori MD,, PD, Sano A,, MDPD et al. Association of the TaqI A Polymorphism of the Dopamine D2 Receptor Gene With Predisposition to Neuroleptic Malignant Syndrome. 2001;158(10):1714-6. https://doi.org/10.1176/appi.ajp.158.10.1714 .
Matsusue A, Hara K, Kageura M, Kashiwagi M, Lu W, Ishigami A, et al. Genetic analysis of ryanodine receptor 1 gene and carnitine palmitoyltransferase II gene: an autopsy case of neuroleptic malignant syndrome related to vegetamin. Leg Med (Tokyo). 2009;11(Suppl 1):S570–2. https://doi.org/10.1016/j.legalmed.2009.01.074 .
Miyatake R, Iwahashi K, Matsushita M, Nakamura K, Suwaki H. No association between the neuroleptic malignant syndrome and mutations in the RYR1 gene associated malignant hyperthermia. J Neurol Sci. 1996;143(1–2):161–5. https://doi.org/10.1016/s0022-510x(96)00015-9 .
Sato T, Nishio H, Iwata M, Kentotsuboi, Tamura A, Miyazaki T, et al. Postmortem molecular screening for mutations in ryanodine receptor type 1 (RYR1) gene in psychiatric patients suspected of having died of neuroleptic malignant syndrome. Forensic Sci Int. 2010;194(1–3):77–9. https://doi.org/10.1016/j.forsciint.2009.10.014 .
Russell T, Riazi S, Kraeva N, Steel AC, Hawryluck LA. Ecstacy-induced delayed rhabdomyolysis and neuroleptic malignant syndrome in a patient with a novel variant in the ryanodine receptor type 1 gene. Anaesthesia. 2012;67(9):1021–4. https://doi.org/10.1111/j.1365-2044.2012.07226.x .
Kawanishi C, Hanihara T, Shimoda Y, Suzuki K, Sugiyama N, Onishi H, et al. Lack of association between neuroleptic malignant syndrome and polymorphisms in the 5-HT1A and 5-HT2A receptor genes. Am J Psychiatry. 1998;155(9):1275–7. https://doi.org/10.1176/ajp.155.9.1275 .
Kaneda Y, Kawamura I, Fujii A, Ohmori T. Serotonin syndrome - ‘potential’ role of the CYP2D6 genetic polymorphism in asians. Int J Neuropsychopharmacol. 2002;5(1):105–6. https://doi.org/10.1017/s1461145701002723 .
Calmy KIL, Ambrosioni A, Assouline J, Daali B, Fathi Y. Serotonin syndrome following drug-drug interactions and CYP2D6 and CYP2C19 genetic polymorphisms in an HIV-infected patient. Aids. 2012;26(18):2417–8. https://doi.org/10.1097/QAD.0b013e32835a11ba .
Agarwal P, Omoruyi A, Perai KG, MacDaid K, Burton A. Neuroleptic malignant syndrome (NMS) on clozapine with a potential atypical Interaction with Paliperidone. Case Rep Psychiatry. 2021;2021:5584104. https://doi.org/10.1155/2021/5584104 .
Mazhar F, Akram S, Haider N, Ahmed R. Overlapping of Serotonin Syndrome with neuroleptic malignant syndrome due to Linezolid-Fluoxetine and Olanzapine-Metoclopramide interactions: a Case Report of two serious adverse drug effects caused by Medication Reconciliation failure on Hospital Admission. Case Rep Med. 2016;2016:7128909. https://doi.org/10.1155/2016/7128909 .
Gillman PK. CNS toxicity involving methylene blue: the exemplar for understanding and predicting drug interactions that precipitate serotonin toxicity. J Psychopharmacol. 2011;25(3):429–36. https://doi.org/10.1177/0269881109359098 .
Graber MA, Hoehns TB, Perry PJ. Sertraline-phenelzine drug interaction: a serotonin syndrome reaction. Ann Pharmacother. 1994;28(6):732–5. https://doi.org/10.1177/106002809402800610 .
Gnanadesigan N, Espinoza RT, Smith R, Israel M, Reuben DB. Interaction of serotonergic antidepressants and opioid analgesics: is serotonin syndrome going undetected? J Am Med Dir Assoc. 2005;6(4):265–9. https://doi.org/10.1016/j.jamda.2005.04.012 .
Ailawadhi S, Sung KW, Carlson LA, Baer MR. Serotonin syndrome caused by interaction between citalopram and fentanyl. J Clin Pharm Ther. 2007;32(2):199–202. https://doi.org/10.1111/j.1365-2710.2007.00813.x .
Chan BS, Graudins A, Whyte IM, Dawson AH, Braitberg G, Duggin GG. Serotonin syndrome resulting from drug interactions. Med J Aust. 1998;169(10):523–5. https://doi.org/10.5694/j.1326-5377.1998.tb123399.x .
Clark DB, Andrus MR, Byrd DC. Drug interactions between linezolid and selective serotonin reuptake inhibitors: case report involving sertraline and review of the literature. Pharmacotherapy. 2006;26(2):269–76. https://doi.org/10.1592/phco.26.2.269 .
Bai AD, McKenna S, Wise H, Loeb M, Gill SS. Association of Linezolid with Risk of Serotonin Syndrome in patients receiving antidepressants. JAMA Netw Open. 2022;5(12):e2247426. https://doi.org/10.1001/jamanetworkopen.2022.47426 .
Karkow DC, Kauer JF, Ernst EJ. Incidence of Serotonin Syndrome with Combined Use of Linezolid and Serotonin Reuptake inhibitors compared with Linezolid Monotherapy. J Clin Psychopharmacol. 2017;37(5):518–23. https://doi.org/10.1097/jcp.0000000000000751 .
Gupta V, Karnik ND, Deshpande R, Patil MA. Linezolid-induced serotonin syndrome. BMJ Case Rep. 2013;2013. https://doi.org/10.1136/bcr-2012-008199 .
Mitwally H, Saad MO, Alkhiyami D, Fahmi AM, Mahmoud S, Hmoud EA, et al. Risk of serotonin syndrome in acutely ill patients receiving linezolid and opioids concomitantly: a retrospective cohort study. IJID Reg. 2022;5:137–40. https://doi.org/10.1016/j.ijregi.2022.09.008 .
Huang V, Gortney JS. Risk of serotonin syndrome with concomitant administration of linezolid and serotonin agonists. Pharmacotherapy. 2006;26(12):1784–93. https://doi.org/10.1592/phco.26.12.1784 .
Gatti M, Raschi E, De Ponti F. Serotonin syndrome by drug interactions with linezolid: clues from pharmacovigilance-pharmacokinetic/pharmacodynamic analysis. Eur J Clin Pharmacol. 2021;77(2):233–9. https://doi.org/10.1007/s00228-020-02990-1 .
Masbough F, Roshanzamiri S, Rahimi M, Sahraei Z, Evini PET. Serotonin syndrome due to concomitant use of linezolid and methadone. Clin Case Rep. 2022;10(11):e6341. https://doi.org/10.1002/ccr3.6341 .
Essakow J, Jin L, Marupudi N, Wattier R, McQuillen P, Franzon D. Serotonin Syndrome in an infant Associated with Linezolid and Opioid Use. J Pediatr Pharmacol Ther. 2022;27(6):564–8. https://doi.org/10.5863/1551-6776-27.6.564 .
Spigset O, Adielsson G. Combined serotonin syndrome and hyponatraemia caused by a citalopram-buspirone interaction. Int Clin Psychopharmacol. 1997;12(1):61–3. https://doi.org/10.1097/00004850-199701000-00010 .
Brubacher JR, Hoffman RS, Lurin MJ. Serotonin syndrome from venlafaxine-tranylcypromine interaction. Vet Hum Toxicol. 1996;38(5):358–61.
CAS PubMed Google Scholar
Nelson EM, Philbrick AM. Avoiding serotonin syndrome: the nature of the interaction between tramadol and selective serotonin reuptake inhibitors. Ann Pharmacother. 2012;46(12):1712–6. https://doi.org/10.1345/aph.1Q748 .
Aboukarr A, Giudice M. Interaction between Monoamine oxidase B inhibitors and selective serotonin reuptake inhibitors. Can J Hosp Pharm. 2018;71(3):196–207.
Gray R, Moore Iii A, Berry F, Afroze F, Cherukupalli D. Serotonin Syndrome after PACU Administration of Tramadol and Meperidine. Turk J Anaesthesiol Reanim. 2022;50(4):309–11. https://doi.org/10.5152/tjar.2022.21355 .
Mateo-Carrasco H, Muñoz-Aguilera EM, García-Torrecillas JM, Abu Al-Robb H. Serotonin syndrome probably triggered by a morphine-phenelzine interaction. Pharmacotherapy. 2015;35(6):e102–5. https://doi.org/10.1002/phar.1581 .
Declercq PL, Eraldi JP, Beuzelin M, Gélinotte S, Marchalot A, Bougerol F, et al. Severe serotonin syndrome caused by an interaction between an antidepressant and a cough syrup. Therapie. 2021;76(3):249–52. https://doi.org/10.1016/j.therap.2020.02.020 .
Foong AL, Grindrod KA, Patel T, Kellar J. Demystifying serotonin syndrome (or serotonin toxicity). Can Fam Physician. 2018;64(10):720–7.
Sun-Edelstein C, Tepper SJ, Shapiro RE. Drug-induced serotonin syndrome: a review. Expert Opin Drug Saf. 2008;7(5):587–96. https://doi.org/10.1517/14740338.7.5.587 .
Chan TC, Evans SD, Clark RF. Drug-induced hyperthermia. Crit Care Clin. 1997;13(4):785–808. https://doi.org/10.1016/s0749-0704(05)70369-9 .
Horseman M, Panahi L, Udeani G, Tenpas AS, Verduzco R Jr., Patel PH, et al. Drug-Induced Hyperth Rev Cureus. 2022;14(7):e27278. https://doi.org/10.7759/cureus.27278 .
Savvidou A, Jennions E, Wikström S, Olsson-Engman M, Sofou K, Darin N. Drug-induced hyperthermia with rhabdomyolysis in CLN3 disease. Eur J Paediatr Neurol. 2022;39:74–8. https://doi.org/10.1016/j.ejpn.2022.06.007 .
Gurrera RJ, Caroff SN, Cohen A, Carroll BT, DeRoos F, Francis A, et al. An international consensus study of neuroleptic malignant syndrome diagnostic criteria using the Delphi method. J Clin Psychiatry. 2011;72(9):1222–8. https://doi.org/10.4088/JCP.10m06438 .
Gurrera RJ, Mortillaro G, Velamoor V, Caroff SN. A validation study of the International Consensus Diagnostic Criteria for neuroleptic malignant syndrome. J Clin Psychopharmacol. 2017;37(1):67–71. https://doi.org/10.1097/jcp.0000000000000640 .
Karamustafalioglu N, Kalelioglu T, Celikel G, Genc A, Emul M. Clinical utility of neutrophil-lymphocyte ratio in the diagnosis of neuroleptic malignant syndrome. Nord J Psychiatry. 2019;73(4–5):288–92. https://doi.org/10.1080/08039488.2019.1623315 .
Kalelioglu T, Celikel G, Balaban OD, Karamustafalioglu N, Penberthy JK. Can Neutrophil-Lymphocyte ratio be a useful Criterion for neuroleptic malignant syndrome in the absence of Leukocytosis? Iran J Psychiatry. 2021;16(3):370–3. https://doi.org/10.18502/ijps.v16i3.6264 .
Védie C, Poinso F, Hemmi F, Rivet B. Major symptoms and differential diagnosis of neuroleptic malignant syndrome: three case reports. Eur Psychiatry. 2000;15(5):334–7. https://doi.org/10.1016/s0924-9338(00)00403-x .
Uddin MF, Alweis R, Shah SR, Lateef N, Shahnawaz W, Ochani RK, et al. Controversies in serotonin syndrome diagnosis and management: a review. J Clin Diagn Res. 2017;11(9):Oe05–7. https://doi.org/10.7860/jcdr/2017/29473.10696 .
Jašović-Gašić M, Vuković O, Pantović M, Cvetić T, Marić-Bojović N. Antipsychotics–history of development and field of indication, new wine–old glassess. Psychiatr Danub. 2012;24(Suppl 3):S342–4.
Danilov DS. [A current view on the history of atypical antipsychotics]. Zh Nevrol Psikhiatr Im S S Korsakova. 2017;117(5):85–93. https://doi.org/10.17116/jnevro20171175185-93 .
De Risio A, Lang AP. History and therapeutic rationale of long acting antipsychotics. Curr Clin Pharmacol. 2014;9(1):39–52. https://doi.org/10.2174/15748847113089990057 .
Shen WW. A history of antipsychotic drug development. Compr Psychiatry. 1999;40(6):407–14. https://doi.org/10.1016/s0010-440x(99)90082-2 .
Ramachandraiah CT, Subramaniam N, Tancer M. The story of antipsychotics: past and present. Indian J Psychiatry. 2009;51(4):324–6. https://doi.org/10.4103/0019-5545.58304 .
Perez-Caballero L, Torres-Sanchez S, Bravo L, Mico JA, Berrocoso E. Fluoxetine: a case history of its discovery and preclinical development. Expert Opin Drug Discov. 2014;9(5):567–78. https://doi.org/10.1517/17460441.2014.907790 .
Margetić B, Aukst-Margetić B. Neuroleptic malignant syndrome and its controversies. Pharmacoepidemiol Drug Saf. 2010;19(5):429–35. https://doi.org/10.1002/pds.1937 .
Saha KB, Bo L, Zhao S, Xia J, Sampson S, Zaman RU. Chlorpromazine versus atypical antipsychotic drugs for schizophrenia. Cochrane Database Syst Rev. 2016;4(4):Cd010631. https://doi.org/10.1002/14651858.CD010631.pub2 .
Divac N, Prostran M, Jakovcevski I, Cerovac N. Second-generation antipsychotics and extrapyramidal adverse effects. Biomed Res Int. 2014;2014:656370. https://doi.org/10.1155/2014/656370 .
Meltzer HY. Update on typical and atypical antipsychotic drugs. Annu Rev Med. 2013;64:393–406. https://doi.org/10.1146/annurev-med-050911-161504 .
Talton CW. Serotonin Syndrome/Serotonin toxicity. Fed Pract. 2020;37(10):452–9. https://doi.org/10.12788/fp.0042 .
Sweileh WM, Sawalha AF, Al-Jabi SW, Zyoud SH, Shraim NY, Abu-Taha AS. A bibliometric analysis of literature on malaria vector resistance: (1996–2015). Globalization Health. 2016;12(1):76. https://doi.org/10.1186/s12992-016-0214-4 .
Zyoud SH, Shakhshir M, Abushanab AS, Al-Jabi SW, Koni A, Shahwan M, et al. Mapping the global research landscape on nutrition and the gut microbiota: visualization and bibliometric analysis. World J Gastroenterol. 2022;28(25):2981–93. https://doi.org/10.3748/wjg.v28.i25.2981 .
Sweileh WM. Bibliometric analysis of peer-reviewed literature on climate change and human health with an emphasis on infectious diseases. Globalization Health. 2020;16(1):44. https://doi.org/10.1186/s12992-020-00576-1 .
Sweileh WM. Global research trends of World Health Organization’s top eight emerging pathogens. Globalization Health. 2017;13(1):9. https://doi.org/10.1186/s12992-017-0233-9 .
Bilanakis N, Peritogiannis V, Kalampokis G. Infections as complications of neuroleptic malignant syndrome. World J Biol Psychiatry. 2009;10(4 Pt 3):973–6. https://doi.org/10.1080/15622970801935578 .
Taniguchi N, Tanii H, Nishikawa T, Miyamae Y, Shinozaki K, Inoue Y, et al. Classification system of complications in neuroleptic malignant syndrome. Methods Find Exp Clin Pharmacol. 1997;19(3):193–9.
Hegerl U, Bottlender R, Gallinat J, Kuss HJ, Ackenheil M, Möller HJ. The serotonin syndrome scale: first results on validity. Eur Arch Psychiatry Clin Neurosci. 1998;248(2):96–103. https://doi.org/10.1007/s004060050024 .
Modi S, Dharaiya D, Schultz L, Varelas P. Neuroleptic malignant syndrome: complications, outcomes, and Mortality. Neurocrit Care. 2016;24(1):97–103. https://doi.org/10.1007/s12028-015-0162-5 .
Park JI, Park TW. Rhabdomyolysis and Neuroleptic Malignant Syndrome Associated with very low-dose antipsychotics in children and adolescent. Clin Psychopharmacol Neurosci. 2019;17(3):450–2. https://doi.org/10.9758/cpn.2019.17.3.450 .
Desai S, Hirachan T, Toma A, Gerolemou A. Malignant Catatonia Versus neuroleptic malignant syndrome. Cureus. 2021;13(6):e15818. https://doi.org/10.7759/cureus.15818 .
Shouan A, Kumar R, Lal V, Grover S. Linezolid-induced serotonin syndrome. Ind Psychiatry J. 2020;29(2):345–8. https://doi.org/10.4103/ipj.ipj_37_19 .
Keltner N, Harris CP. Serotonin syndrome: a case of fatal SSRI/MAOI interaction. Perspect Psychiatr Care. 1994;30(4):26–31. https://doi.org/10.1111/j.1744-6163.1994.tb00446.x .
Park SH, Wackernah RC, Stimmel GL. Serotonin syndrome: is it a reason to avoid the use of tramadol with antidepressants? J Pharm Pract. 2014;27(1):71–8. https://doi.org/10.1177/0897190013504957 .
Beakley BD, Kaye AM, Kaye AD, Tramadol. Pharmacology, Side effects, and Serotonin Syndrome: a review. Pain Physician. 2015;18(4):395–400.
Hassamal S, Miotto K, Dale W, Danovitch I. Tramadol: understanding the risk of serotonin syndrome and seizures. Am J Med. 2018;131(11):1382. e1-.e6 https://doi.org/10.1016/j.amjmed.2018.04.025 .
Ruiz de Villa A, Jones T, Lleshi A, Macahuachi M, Lamar K, Bazikian Y. Serotonin toxicity precipitated by Tramadol in the setting of polypharmacy: a case of Serotonin Syndrome. Cureus. 2021;13(11):e20059. https://doi.org/10.7759/cureus.20059 .
Graudins A, Stearman A, Chan B. Treatment of the serotonin syndrome with cyproheptadine. J Emerg Med. 1998;16(4):615–9. https://doi.org/10.1016/s0736-4679(98)00057-2 .
Deardorff OG, Khan T, Kulkarni G, Doisy R, Loehr C. Serotonin Syndrome: Prophylactic Treatment with Cyproheptadine. Prim Care Companion CNS Disord. 2016;18(4). https://doi.org/10.4088/PCC.16br01966 .
Lappin RI, Auchincloss EL. Treatment of the serotonin syndrome with cyproheptadine. N Engl J Med. 1994;331(15):1021–2. https://doi.org/10.1056/nejm199410133311514 .
Baldo BA. Toxicities of opioid analgesics: respiratory depression, histamine release, hemodynamic changes, hypersensitivity, serotonin toxicity. Arch Toxicol. 2021;95(8):2627–42. https://doi.org/10.1007/s00204-021-03068-2 .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Biomedical Sciences, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
Waleed M. Sweileh
You can also search for this author in PubMed Google Scholar
Contributions
W.S initiated the idea, did the analysis, writing, and submission.
Corresponding author
Correspondence to Waleed M. Sweileh .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that he has no financial or non-financial competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sweileh, W.M. Neuroleptic malignant syndrome and serotonin syndrome: a comparative bibliometric analysis. Orphanet J Rare Dis 19 , 221 (2024). https://doi.org/10.1186/s13023-024-03227-5
Download citation
Received : 20 April 2023
Accepted : 27 May 2024
Published : 02 June 2024
DOI : https://doi.org/10.1186/s13023-024-03227-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Serotonin syndrome
- Research publications, comparative analysis
Orphanet Journal of Rare Diseases
ISSN: 1750-1172
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- For Consumers
- Consumer Updates
FDA 101: Dietary Supplements
Dietary supplements can help improve health but can also have risks. Get the facts on supplements and how the FDA regulates them to help keep you safe.

Multivitamins, vitamin D, echinacea, and fish oil are among the many dietary supplements lining store shelves or available online. Perhaps you already take a supplement or are thinking about using one. Dietary supplements can be beneficial to your health, but they can also involve health risks. So, it’s important that you talk with a health care professional to help you decide if a supplement is right for you.
Read on to learn what dietary supplements are (and are not), what role the U.S. Food and Drug Administration has in regulating them, and how to make sure you and your family use supplements safely.
What Are Dietary Supplements?
Dietary supplements are intended to add to or supplement the diet and are different from conventional food. Generally, to the extent a product is intended to treat, diagnose, cure, or prevent diseases, it is a drug, even if it is labeled as a dietary supplement. Supplements are ingested and come in many forms, including tablets, capsules, soft gels, gel caps, powders, bars, gummies, and liquids.
Common supplements include:
- Vitamins (such as multivitamins or individual vitamins like vitamin D and biotin).
- Minerals (such as calcium, magnesium, and iron).
- Botanicals or herbs (such as echinacea and ginger).
- Botanical compounds (such as caffeine and curcumin).
- Amino acids (such as tryptophan and glutamine).
- Live microbials (commonly referred to as “probiotics”).
What Are the Benefits of Dietary Supplements?
Dietary supplements can help you improve or maintain your overall health, and supplements can also help you meet your daily requirements of essential nutrients.
For example, calcium and vitamin D can help build strong bones, and fiber can help to maintain bowel regularity. While the benefits of some supplements are well established, other supplements need more study. Also, keep in mind that supplements should not take the place of the variety of foods that are important for a healthy diet.
What Are the Risks of Dietary Supplements?
Before buying or taking a dietary supplement, talk with a health care professional—such as your doctor, nurse, registered dietician, or pharmacist—about the benefits and risks.
Many supplements contain ingredients that can have strong effects in the body. Additionally, some supplements can interact with medications, interfere with lab tests, or have dangerous effects during surgery. Your health care professional can help you decide what supplement, if any, is right for you.
When taking dietary supplements, be alert to the possibility of a bad reaction or side effect (also known as an adverse event).
Problems can occur especially if you:
- Combine supplements.
- Mix medicines and supplements .
- Take too much of some supplements.
- Take supplements instead of medications.
If you experience an adverse event while taking a dietary supplement, immediately stop using the supplement, seek medical care or advice, and report the adverse event to the FDA .
How Are Dietary Supplements Regulated?
The Federal Food, Drug, and Cosmetic Act (FD&C Act) was amended in 1994 by the Dietary Supplement Health and Education Act (often referred to as DSHEA), which defined “dietary supplement” and set out FDA’s authority regarding such products. Under existing law:
- The FDA does NOT have the authority to approve dietary supplements for safety and effectiveness, or to approve their labeling, before the supplements are sold to the public.
- Under the FD&C Act, it is the responsibility of dietary supplement companies to ensure their products meet the safety standards for dietary supplements and are not otherwise in violation of the law.
- Dietary supplement labels are required to have nutrition information in the form of a Supplement Facts label that includes the serving size, the number of servings per container, a listing of all dietary ingredients in the product, and the amount per serving of those ingredients. They also must have a statement on the front of the product identifying it as a “dietary supplement” or similar descriptive term (e.g., “herbal supplement” or “calcium supplement”).
In general, even if a product is labeled as a dietary supplement, a product intended to treat, prevent, cure, or alleviate the symptoms of a disease is a drug, and subject to all requirements that apply to drugs.
The FDA’s Role and Actions to Help Keep You Safe
Even though the FDA does not approve dietary supplements, there are roles for the agency in regulating them.
- Since companies can often introduce a dietary supplement to the market without notifying the FDA, the agency's role in regulating supplements primarily begins after the product enters the marketplace.
- The FDA periodically inspects dietary supplement manufacturing facilities to verify companies are meeting applicable manufacturing and labeling requirements.
- The FDA also reviews product labels and other labeling information, including websites, to ensure products are appropriately labeled and that they do not include claims that may render the products drugs (e.g., claims to treat, diagnose, cure, or prevent diseases).
- The FDA monitors adverse event reports submitted by dietary supplement companies, health care professionals, and consumers as well as other product complaints for valuable information about the safety of products once they are on the market.
- Work with the company to bring the product into compliance.
- Ask the company to voluntarily recall the product.
- Take action to remove a dangerous product from the market.
Tips to Be a Safe and Informed Consumer
Before taking a dietary supplement, talk with your health care professional. They can help you decide which supplements, if any, are right for you. You can also contact the manufacturer for information about the product.
- Take only as described on the label. Some ingredients and products can be harmful when consumed in high amounts, when taken for a long time, or when used in combination with certain drugs or foods.
- Do not substitute a dietary supplement for a prescription medicine or for the variety of foods important to a healthy diet.
- Do not assume that the term "natural" to describe a product ensures that it is safe.
- Be wary of hype. Sound health advice is generally based upon research over time, not a single study.
- Learn to spot false claims. If something sounds too good to be true, it probably is.
Why Is It Important to Report an Adverse Event?
If you experience adverse event, also known as a side effect or bad reaction, the FDA encourages both you and your health care professional to report the adverse event to the FDA.
You can help the FDA, yourself, and other consumers by reporting an adverse event. A single adverse event report can help us identify a potentially dangerous product and possibly remove it from the market.
For a list of potential serious reactions to watch for, and to learn how to report an adverse event, please see the FDA’s webpage, How to Report a Problem with Dietary Supplements .
Adverse events can also be reported to the product's manufacturer or distributor through the address or phone number listed on the product's label. Dietary supplement firms are required to report serious adverse events they receive about their dietary supplements to FDA within 15 days.
For a general, nonserious complaint or concern about dietary supplements, contact your local FDA Consumer Complaint Coordinator .
Additional Resources:
- Dietary Supplements , FDA
- Information for Consumers on Using Dietary Supplements , FDA
- Dietary Supplement Fact Sheets , National Institutes of Health
Get regular FDA email updates delivered on this topic to your inbox.
- Español (Spanish)
HIV Treatment
What is a drug interaction.
- A drug interaction is a reaction between two (or more) drugs or between a drug and a food, beverage, or supplement. Taking a drug while having certain medical conditions can also cause a drug interaction. For example, taking a nasal decongestant if you have high blood pressure may cause an unwanted reaction.
A drug interaction can affect how a drug works or cause unwanted side effects.
- Treatment with HIV medicines (called antiretroviral therapy or ART ) helps people with HIV live longer, healthier lives and reduces the risk of HIV transmission . But drug interactions can complicate HIV treatment.
- Health care providers carefully consider potential drug interactions before recommending an HIV treatment regimen . Before taking HIV medicines, tell your health care provider about all prescription and nonprescription medicines, vitamins, nutritional supplements, and herbal products you are taking or plan to take.
What is a drug interaction?
Medicines help us feel better and stay healthy. But sometimes drug interactions can cause problems. There are three types of drug interactions:
- Drug-drug interaction : A reaction between two (or more) drugs.
- Drug-food interaction : A reaction between a drug and a food or beverage.
- Drug-condition interaction: A reaction that occurs when taking a drug while having a certain medical condition. For example, taking a nasal decongestant if you have high blood pressure may cause an unwanted reaction.
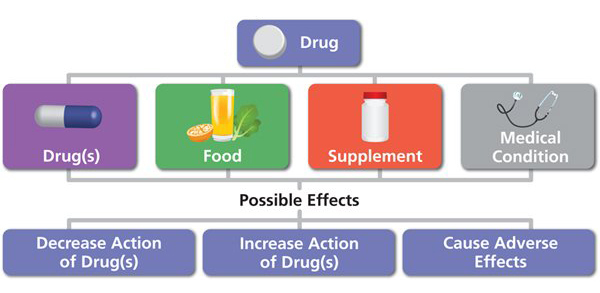
Do HIV medicines ever cause drug interactions?
Treatment with HIV medicines (called antiretroviral therapy or ART ) helps people with HIV live longer, healthier lives and reduces the risk of HIV transmission . But drug interactions, especially drug-drug interactions, can complicate HIV treatment.
Drug-drug interactions between different HIV medicines and between HIV medicines and other medicines are common. Before recommending an HIV treatment regimen , health care providers carefully consider potential drug-drug interactions between HIV medicines. They also ask about other medicines a person may be taking. For example, some HIV medicines may make hormonal birth control less effective, so women using hormonal contraceptives may need to use an additional or different method of birth control to prevent pregnancy. For more information about using birth control and HIV medicines at the same time, view the HIV and Birth Control infographic from HIVinfo.
Can drug-food interactions and drug-condition interactions affect people taking HIV medicines?
Yes, the use of HIV medicines can lead to both drug-food interactions and drug-condition interactions.
Food can affect the absorption of some HIV medicines and increase or reduce the concentration of the medicine in the blood. Depending on the HIV medicine, the change in concentration may be helpful or harmful. Directions on how to take HIV medicines specify whether to take the medicine with food or on an empty stomach. Some HIV medicines can be taken with or without food, because food does not affect their absorption.
Conditions, such as kidney disease, hepatitis, and pregnancy, can affect how the body processes HIV medicines. The dosing of some HIV medicines may need to be adjusted in people with certain medical conditions.
How can a person avoid drug interactions?
You can take the following steps to avoid drug interactions:
- Tell your health care provider about all prescription and nonprescription medicines you are taking or plan to take. Also tell your health care provider about any vitamins, nutritional supplements, and herbal products you take.
- Tell your health care provider about any other conditions you may have, such as high blood pressure or diabetes.
- What is the medicine used for?
- How should I take the medicine?
- While taking the medicine, should I avoid any other medicines or certain foods or beverages?
- Can I take this medicine safely with the other medicines that I am taking? Are there any possible drug interactions I should know about? What are the signs of those drug interactions?
- In the case of a drug interaction, what should I do?
- Take medicines according to your health care provider's instructions. Always read the information and directions that come with a medicine. Drug labels and package inserts include important information about possible drug interactions.
This fact sheet is based on information from the following sources:
From the Department of Health and Human Services:
- Drug-Drug Interactions
- Considerations for Antiretroviral Use in Special Patient Populations: HIV and the Older Person , Transgender People with HIV , and Women with HIV
From the U.S. Food and Drug Administration:
- Drug Interactions: What You Should Know
From the National Institute on Aging:
- Safe Use of Medicines for Older Adults
Also see the HIV Source collection of HIV links and resources.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Herb-drug interactions: a mechanistic approach
Affiliation.
- 1 School of Pharmaceutical Sciences, Shoolini University, Solan, India.
- PMID: 32160796
- DOI: 10.1080/01480545.2020.1738454
In India, traditional herbal medicines have been an essential part of therapy for the last centuries. However, a large portion of the general populace is using these therapies in combination with allopathy lacking a proper understanding of possible interactions (synergistic or antagonistic) between the herbal product and the allopathic drug. This is based on the assumption that herbal drugs are relatively safe, i.e. without side effects. We have established a comprehensive understanding of the possible herb-drug interactions and identified interaction patterns between the most common herbs and drugs currently in use in the Indian market. For this purpose, we listed common interactors (herbs and allopathic drugs) using available scientific literature. Drugs were then categorized into therapeutic classes and aligned to produce a recognizable pattern present only if interactions were observed between a drug class and herb in the scientific literature. Interestingly, the top three categories (with highest interactors), antibiotics, oral hypoglycemics, and anticonvulsants, displayed synergistic interactions only. Another major interactor category was CYP450 enzymes, a natural component of our metabolism. Both activation and inhibition of CYP450 enzymes were observed. As many allopathic drugs are known CYP substrates, inhibitors or inducers, ingestion of an interacting herb could result in interaction with the co-administered drug. This information is largely unavailable for the Indian population and should be studied in greater detail to avoid such interactions. Although this information is not absolute, the systematic literature review proves the existence of herb-drug interactions in the literature and studies where no interaction was detected are equally important.
Keywords: CYP450; Herb–drug interaction; Indian traditional medicine; synergism.
PubMed Disclaimer
Similar articles
- Interactions of herbs with cytochrome P450. Zhou S, Gao Y, Jiang W, Huang M, Xu A, Paxton JW. Zhou S, et al. Drug Metab Rev. 2003 Feb;35(1):35-98. doi: 10.1081/dmr-120018248. Drug Metab Rev. 2003. PMID: 12635815 Review.
- Drug-herb interactions: eliminating toxicity with hard drug design. Yang XX, Hu ZP, Duan W, Zhu YZ, Zhou SF. Yang XX, et al. Curr Pharm Des. 2006;12(35):4649-64. doi: 10.2174/138161206779010440. Curr Pharm Des. 2006. PMID: 17168768 Review.
- Herbal interactions involving cytochrome p450 enzymes: a mini review. Delgoda R, Westlake AC. Delgoda R, et al. Toxicol Rev. 2004;23(4):239-49. doi: 10.2165/00139709-200423040-00004. Toxicol Rev. 2004. PMID: 15898829 Review.
- Herb-drug interaction studies of herbs used in treatment of cardiovascular disorders-A narrative review of preclinical and clinical studies. Shaikh AS, Thomas AB, Chitlange SS. Shaikh AS, et al. Phytother Res. 2020 May;34(5):1008-1026. doi: 10.1002/ptr.6585. Epub 2020 Jan 6. Phytother Res. 2020. PMID: 31908085 Review.
- Drug-herb interactions between Scutellaria baicalensis and pharmaceutical drugs: Insights from experimental studies, mechanistic actions to clinical applications. Zhou X, Fu L, Wang P, Yang L, Zhu X, Li CG. Zhou X, et al. Biomed Pharmacother. 2021 Jun;138:111445. doi: 10.1016/j.biopha.2021.111445. Epub 2021 Mar 10. Biomed Pharmacother. 2021. PMID: 33711551 Review.
- Pharmaceutical Prospects of Curcuminoids for the Remedy of COVID-19: Truth or Myth. Fu YS, Ho WY, Kang N, Tsai MJ, Wu J, Huang L, Weng CF. Fu YS, et al. Front Pharmacol. 2022 Apr 14;13:863082. doi: 10.3389/fphar.2022.863082. eCollection 2022. Front Pharmacol. 2022. PMID: 35496320 Free PMC article. Review.
- Cytoprotective Potential of Aged Garlic Extract (AGE) and Its Active Constituent, S-allyl-l-cysteine, in Presence of Carvedilol during Isoproterenol-Induced Myocardial Disturbance and Metabolic Derangements in Rats. Asdaq SMB, Challa O, Alamri AS, Alsanie WF, Alhomrani M, Almutiri AH, Alshammari MS. Asdaq SMB, et al. Molecules. 2021 May 27;26(11):3203. doi: 10.3390/molecules26113203. Molecules. 2021. PMID: 34071846 Free PMC article.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Taylor & Francis
Other Literature Sources
- figshare - Data
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
VIDEO
COMMENTS
Herbs are often administered in combination with therapeutic drugs, raising the potential of herb-drug interactions. An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations. Cas …
Herbs are often administered in combination with therapeutic drugs, raising the potential of herb-drug interactions. An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations.
A pharmacodynamic herb-drug interaction may occur when taking one or more herbal substances of equal or opposing pharmacological effects to the drug. ... herbal medicines start appearing consistently in review articles on drug interactions [9,10,11] as well as in ... Metabolism is perhaps the most scrutinised aspect in literature, followed by ...
An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations. Cases have been ...
This review examines three bodies of literature related to herb-drug interactions: case reports, clinical studies, evaluations found in six drug interaction checking resources.
Herbs are often administered in combination with therapeutic drugs, raising the potential of herb-drug interactions. An extensive review of the literature identified reported herb-drug interactions with clinical significance, many of which are from case reports and limited clinical observations.Cases have been published reporting enhanced anticoagulation and bleeding when patients on long-term ...
A Review on Herbal Drug Interaction. ... Literature searches were performed using the following . ... Because drug-herb interactions can significantly affect circulating levels of drug and, hence ...
The present review includes an evaluation of the cardioprotective and antihypertensive effects of garlic, Aloe vera, green tea, Ginkgo biloba, berberine, ginseng, Nigella sativa, Apium graveolens, thyme, cinnamon and ginger, and their possible interactions with antihypertensive drugs. A literature search was undertaken via the PubMed, Google ...
In 10 SRs, herb-drug interactions were hypothetical as the primary research was based on in vitro and/or animal studies. This overview suggests that the quality of research on herb−drug interactions is often wanting.
The objective of this review article mainly focuses on drug interactions of commonly used herbs along with possible mechanisms. The method adopted for this review is searching of herb-drug interactions in online database. Herb-drug interaction leads to pharmacological modification.
All literature collected pertained to adverse effects, pharmacokinetics, and suspected or confirmed cases of herb-drug interactions. Over 80 herbs or bo-tanicals (including plants, fungi, algae, and common constituents) were identified that had clinically significant interactions with prescription and over-the-counter drugs.
The current study showed that SS has a wide range of possible drug/herb interactions due to the many drugs that affect the serotonin system. Of particular interest is the one with opioid analgesics, since they are commonly used in hospital settings. ... Heng PW, Chan E, et al. Herb-drug interactions: a literature review. Drugs. 2005;65(9):1239 ...
Read on to learn what dietary supplements are (and are not), what role the U.S. Food and Drug Administration has in regulating them, and how to make sure you and your family use supplements safely ...
This review examines three bodies of literature related to herb-drug interactions: case reports, clinical studies, evaluations found in six drug interaction checking resources. The aim of the study is to examine the congruity of resources and to assess the degree to which case reports signal for fur …
A drug interaction is a reaction between two (or more) drugs or between a drug and a food, beverage, or supplement. Taking a drug while having certain medical conditions can also cause a drug interaction. For example, taking a nasal decongestant if you have high blood pressure may cause an unwanted reaction.
We have established a comprehensive understanding of the possible herb-drug interactions and identified interaction patterns between the most common herbs and drugs currently in use in the Indian market. For this purpose, we listed common interactors (herbs and allopathic drugs) using available scientific literature.