Family planning among undergraduate university students: a CASE study of a public university in Ghana
Affiliations.
- 1 Department of Health Administration and Education, University of Education Winneba, Faculty of Science Education, P.O. Box 25, Winneba, Ghana. [email protected].
- 2 Department of Health Administration and Education, University of Education Winneba, Faculty of Science Education, P.O. Box 25, Winneba, Ghana.
- PMID: 30654787
- PMCID: PMC6337791
- DOI: 10.1186/s12905-019-0708-3
Background: Globally, the rate of unplanned pregnancies among students at institutions of higher education, continue to increase annually despite the universal awareness and availability of contraceptives to the general population. This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards contraception in the University of Education Winneba.
Methods: The study was a descriptive cross-sectional survey using a structured self-administered questionnaire. One hundred undergraduate students from the University of Education Winneba were selected using a multistage simple random sampling technique. A Likert scale was used to assess the attitude of the respondents towards family planning methods.
Results: Findings show that the respondents had a positive attitude towards family planning with an average mean score of about 4.0 using a contraceptive attitude Likert scale. Knowledge of contraception, awareness and benefits however do not commensurate contraceptive use among undergraduate students since availability, accessibility and preference influence usage. Emergency Contraception (Lydia) was reported as easy to get contraceptive, hence the most frequently used contraceptive (31%) among young female students aged 21-24 years who appeared as the most vulnerable in accessing and using contraceptives due to perceived social stigma.
Conclusion: The observation that levels of Family Planning awareness levels do not commensurate knowledge and usage levels calls for more innovative strategies for contraceptive promotion, and Education on the various university campus. The study recommends that public Universities in Ghana should consider a possible curriculum restructuring to incorporate family planning updates. In this regard, a nationwide mixed method study targeting other tertiary institutions including colleges of education in Ghana is required to explore the topic further to inform policy and programme decisions.
Keywords: Family planning; Ghana; Undergraduate students; University of Education; Winneba.
- Contraception Behavior / psychology
- Contraception Behavior / statistics & numerical data*
- Contraception, Postcoital
- Contraceptive Agents / therapeutic use
- Contraceptives, Oral, Combined / therapeutic use*
- Contraceptives, Postcoital / therapeutic use*
- Cross-Sectional Studies
- Family Planning Services / organization & administration
- Health Knowledge, Attitudes, Practice*
- Students / psychology
- Students / statistics & numerical data
- Universities
- Young Adult
- Contraceptive Agents
- Contraceptives, Oral, Combined
- Contraceptives, Postcoital
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.

Search life-sciences literature (44,094,942 articles, preprints and more)
- Free full text
- Citations & impact
- Similar Articles
Family planning among undergraduate university students: a CASE study of a public university in Ghana.
Author information, affiliations.
- Gbagbo FY 1
- Nkrumah J 1
ORCIDs linked to this article
- Gbagbo FY | 0000-0001-8441-6633
BMC Women's Health , 17 Jan 2019 , 19(1): 12 https://doi.org/10.1186/s12905-019-0708-3 PMID: 30654787 PMCID: PMC6337791
Abstract
Free full text .

Family planning among undergraduate university students: a CASE study of a public university in Ghana
Fred yao gbagbo.
Department of Health Administration and Education, University of Education Winneba, Faculty of Science Education, P.O. Box 25, Winneba, Ghana
Jacqueline Nkrumah
- Associated Data
The raw data and any material related to the study is available upon reasonable request from the corresponding author.
Globally, the rate of unplanned pregnancies among students at institutions of higher education, continue to increase annually despite the universal awareness and availability of contraceptives to the general population. This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards contraception in the University of Education Winneba.
The study was a descriptive cross-sectional survey using a structured self-administered questionnaire. One hundred undergraduate students from the University of Education Winneba were selected using a multistage simple random sampling technique. A Likert scale was used to assess the attitude of the respondents towards family planning methods.
The observation that levels of Family Planning awareness levels do not commensurate knowledge and usage levels calls for more innovative strategies for contraceptive promotion, and Education on the various university campus. The study recommends that public Universities in Ghana should consider a possible curriculum restructuring to incorporate family planning updates. In this regard, a nationwide mixed method study targeting other tertiary institutions including colleges of education in Ghana is required to explore the topic further to inform policy and programme decisions.
Electronic supplementary material
The online version of this article (10.1186/s12905-019-0708-3) contains supplementary material, which is available to authorized users.
Although national surveys on family planning [ 14 ] have extensively looked at contraceptive uptake in Ghana, little is known about contraceptive up take among students in Ghanaian Universities. This study therefore examines family planning acceptance among students of the University of Education, Winneba in Ghana to compliment national data on family planning.
A descriptive cross-sectional study design using a quantitative approach of data collection was adopted. This design was chosen because it fits studies in natural setting, explains phenomena from the view point of persons being studied and produces descriptive data from the respondent own written or spoken words [ 15 ].
The study was conducted in the main campus of the University of Education, Winneba. The university was established in 1992 to train middle and top-level manpower for the educational sector of Ghana. It has four main satellite campuses, (Winneba and Ajumako in the Central Region of Ghana, Kumasi, and Mampong campuses in Ashanti Region of Ghana). The Winneba campus has three smaller campuses with five faculties (Faculty of social science education, Faculty of languages, Faculty of science education, Faculty of educational studies and School of creative Arts).
A multistage sampling technique was used to select these respondents for the study. The first stage involved half day orientation of 2 field assistants (male and female) the estimation of the undergraduate students’ population who falls in this category during the period of the study. The second stage involved sample size calculation using an online Raosoft sample size calculator at 95% confidence interval, 5% margin of error and 50% response distribution [ 16 ]. In terms of the figures, the sample size n and margin of error E are given by:
Where N is the population size (134), R is the fraction of responses that the study is interested in, and Z(c/100) is the critical value for the confidence level c. The estimated number of respondents were then randomly sampled and contacted for participating in the in the third stage of the study. The fourth stage of the study involved distributing the developed questionnaires to consented students.
A Structured Questionnaire (See Additional file 1 ), designed by the authors was used to solicit responses from respondents. The questionnaire was exploratory in nature with both opened and closed ended questions to help respondents easily share their views. The questionnaire was pre-tested among 20 potential respondents from a different university. The Contraceptive Attitude Likert scales was used to measure attitudes by asking people to respond to series of statements about the topic, in terms of the extent to which they agree or disagree with them. Thus, tapping into the cognitive and affective components of attitudes [ 17 ]. The Contraceptive Attitude Scale presented positive and negative statements to elicit for responses that portray participants’ attitudes relating to contraception.
One hundred questionnaires were administered, and all the answers to a particular question were arranged, numbered and responses were coded. The responses were again listed and grouped, putting those with the same code together. Data analysis was done after data had been collected and checked for completeness and accuracy. The Statistical Package for Social Sciences (SPSS) software version 23 was used for data analysis. Frequencies, percentages and bar charts were used to describe the data in multivariable tables.
- Ethics approval and consent to participate
An approval was obtained from the University prior to data collection. Written consent for participation and publication of findings were also obtained from respondents after the purpose, objectives and potential risk and benefits inherent in the study had been explained to them. Prior to the commencement of the study, the research protocol was presented at the bi-weekly academic research seminars of the Faculty of Science Education, University of Education, Winneba. The seminar brought together lectures of the Faculty (equivalent to an ethical review meeting) who critiqued and reviewed the study protocol for ethical suitability and sound methodology. All participants in the study were given the opportunity to ask questions about the study at any stage, and to withdraw from the study at any time. All data collected were kept confidential and data was analysed anonymously to ensure that results were not traceable to individual respondent.
Background characteristics of respondents
Source: Field data 2017
Table Table2 2 present results of students’ knowledge, information sources and reasons for accepting or not accepting family planning. Family planning awareness and knowledge among students was a key consideration in the study.
Family Planning Knowledge, Information Sources and Reasons for Family Planning Acceptance among Student
Source: Field data 2017
About 94% of respondents answered yes to whether they have ever heard about family planning. Although majority (61%) of the respondents believed FP is helpful, about (67.0%) knew that one could get pregnant by relying on the withdrawal method. It appears most students would be committed to family planning uptake if services are made available. This is evident by 69% of them responding in the affirmative when asked whether they will encourage their family or friends to use family planning services in the University.
Having knowledge of family planning does not necessarily translate into utilization since the respondents had varied reasons for and against using family planning. Respondents who were of the view that FP was not helpful (25.0%) had either not used any family planning method before (28.0%) or had ever suffered unpleasant negative side effects (20.0%) following family planning usage or believed the bible is against family planning (2.0%).
Figure Figure1 1 presents respondents’ attitudes towards family planning as estimated using the Contraceptive Attitude Scale. The overall population surveyed had a positive attitude towards family planning (average mean attitude score was about 4.0 out of 5.0).

Attitude towards Family Planning
There were however some divergent responses to the questions relating to contraceptive use. Some of these include:
‘I will not have sexual intercourse if no contraceptive method was available’
‘I will use contraceptives even if my partner does not want me to use it’
‘I will not use contraceptives because they encourage promiscuity’
Source of Family planning services, Utilization and effects of FP methods
Table 4 documents the various family planning choices and reasons for the choices. About 65.0% of respondents reported that they primarily use contraceptives to prevent pregnancy and usually use a contraceptive before sexual intercourse (34.0%). When asked to select the primary methods of contraception frequently used, Emergency Contraception was the most reported frequently used (51%) contraceptive followed by male condoms (34.0%). Various side effects associated with some FP methods were also reported. Some respondents were of the view that there should be education for students on the risk and benefits of FP methods for effective use. Others believed FP should not be tolerated among students because it can be abused leading to major health problems that could affect studies. Knowledge of contraception, awareness and benefits however do not commensurate contraceptive use among undergraduate students since availability, accessibility, preference and cost of contraceptives hinders use.
Family planning choices and reasons for the choices
This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards family planning in the University of Education Winneba. The study was a descriptive cross-sectional survey using a structured self-administered questionnaire for data collection. Various findings obtained from the study had reproductive health programme and policy implications. Informal sources of family planning information such as friends, peers and relatives were common information sources for young people [ 18 ] but yet prone to misconceptions, distortions and half-truths. Other studies ranked the family (parents, brothers and sisters) as the lowest source of information on sexuality [ 19 – 21 ]. These findings are similar to those reported in the current study that high level of awareness (94.0%) of contraceptives is noted among university students.
At the tertiary level, one would have expected that all respondents would have known the implications of unprotected sexual intercourse. However the study finding that about (61%) of the respondents believed family planning is helpful implies that there are some other students who don’t belief in family planning hence having unprotected sexual intercourse. Although accessibility to family planning methods on campus in this study was very high (66.0%), results from other similar studies were to the contrary [ 29 , 30 ]. This therefore suggests that if students know the benefits and how to use contraceptives, they will not experience unwanted pregnancies and its associated consequences of unsafe abortion complications, disruption in academic work and possible death. Contraceptive education is a component of sex education and is one of the proven approaches to prevent risky sexual behaviour and must be introduced on university campuses to guide students’ family planning choices.
Additionally, findings also shows that there are some students about (67.0%) at the university who knew that one could get pregnant by relying on the withdrawal method yet that is their preferred family planning methods. Various studies [ 31 , 32 ] have explained this observation further by indicating that some adolescents girls feel that a partner’s use of condom suggest that they (the girls) might be classified as unclean, likened to commercial sex workers or seen as engaging in extra-relationship sexual activities if they negotiate for condom use during sexual intercourse. The perception of ‘ I trust my partner so no need for condom use’ further explains the frequency of withdrawal methods being a regular family planning method on campus.
Generally, it appears most students were committed to family planning uptake if services are made available as evident by about 69% of them responding in affirmative when asked whether they will encourage their family or friends to use family planning services in the University. This observation is positive for enhanced family planning service delivery on university campuses to meet the needs of students. Contrary to this observation are those of similar studies which reported that Student frown on invasive family planning methods [ 33 , 34 ]. The distinction between invasive and non-invasive methods bothers on factors such as availability of method, ease of use and adherence to instructions of a health professional to use the method.
Respondents outlined various sources of family planning information of which television adverts constituted the most reported (31%) source of information. This observation is quite worrying since anecdotal evidence from university campuses shows that majority of student rarely have and watch televisions whist on the various campuses. It will therefore be very important and useful to devise innovative ways of educating students on family planning methods whilst on campus.
A finding that having knowledge of family planning does not necessarily translate into usage is very revealing and of public health importance. As it would have been expected, using a method is the surest way of explaining its relevance. However in this study, respondents who were of the view that family planning was not helpful had never used any family planning method before (28.0%). It is there important to use of family planning satisfied client for contraceptive education and promotion on University campuses to ensure the desired positive results. These are students who are likely to positively influence their sexually active peers on contraceptive use since they are likely to say: ‘ I will not have sexual intercourse if no contraceptive method was available’ or ‘I will use contraceptives even if my partner does not want me to use it’ as reported in the study.
Regarding information on source of family planning services if required, most of the respondents (85%) knew where to get family planning services in their communities. For availability of family planning services when needed, about 64.0% of the respondents indicated that family planning services are always available in chemical shops and from colleges on campus when needed. The obvious indicated sources of contraceptives on campus (i.e., chemical shops and peers) do not provide varying choice of services there by limiting students to short term and less effective family planning methods. It is encouraging noting that about 58% of respondents will use FP methods in future. This is an indication of them understanding the importance of family planning to studies as about 65.0% of respondents reported primarily using contraceptives to prevent pregnancy and usually use a method before sexual intercourse (34.0%) despite the various side effects associated with some FP methods reported.
The following recommendations are therefore being suggested to chart a way forward:
Public Universities in Ghana should consider a possible curriculum restructuring to incorporate family planning lessons in the academic programme for students to acquire current knowledge in this area. The reproductive health education programs should include the importance of using dual contraceptive methods as a means to prevent HIV transmission and pregnancy, as well as information on how to make an informed decision relating to contraceptive choices.
The Winneba Municipal Health Directorate should incorporate family planning education on campuses into their public health programs.
The university health service should also create friendly environment for student to access family planning services and also collaborate with the student body to organise programmes to educate the students on family planning methods.
The student representative council (SRC) should also make family planning education a part of their programs and in collaboration with the university health services organise free STI testing and family planning counselling at least once yearly.
A nationwide mixed method study targeting other tertiary institutions particularly colleges of education in Ghana is required to explore the topic further for a national decision on contraceptive security in tertiary institutions in Ghana.
- Conclusions
- Additional file
Appendix I-Questionaire. The appendix I contains the structured question developed by the authors and used for data collection in the study. (DOCX 23 kb)
- Acknowledgements
The authors are grateful to the University of Education Winneba, Faculty of Science Education for the valuable inputs in shaping the manuscript. Many thanks also to the respondents for their corporation during data collection.
The entire study was jointly funded by the authors.
Availability of data and materials
- Abbreviations
- Authors’ contributions
FYG conceptualized and designed the study. JN supervised the data collection, analysis and drafted the initial report. Both authors discussed the report, edited it together and approved the manuscript for final submission.
The research protocol was first presented at the Faculty of Science Education, University of Education, Winneba periodic academic seminars for review and approval for methodology and ethical suitability. This seminar, brings together senior members and research fellows of the University to review research protocols and papers meant for publication and conferences. Approval for data collection and publication were subsequently granted following the full incorporation of comments received from the seminar presentation.
Prior to data collection, verbal and written permissions were sought from the respondents to participate in the study. The permission was granted after the objectives and nature of the study were satisfactorily explained to the respondents.
- Consent for publication
The respondents consented for the study to be published but assured of anonymity before administering the questionnaire. The respondents were also given the opportunity to ask questions about the study at any stage, and to withdraw from the study at any time.
- Competing interests
The authors declare that they have no competing interests in this study.
- Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Contributor Information
Fred Yao Gbagbo, Phone: +233243335708, Email: ku.oc.oohay@2002oayderfobgabg , Email: hg.ude.weu@obgabgyf .
Jacqueline Nkrumah, Phone: +233242507293, Email: hg.ude.weu@hamurknj , Email: moc.oohay@nenileuqcajj .
Full text links
Read article at publisher's site: https://doi.org/10.1186/s12905-019-0708-3
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Smart citations by scite.ai Smart citations by scite.ai include citation statements extracted from the full text of the citing article. The number of the statements may be higher than the number of citations provided by EuropePMC if one paper cites another multiple times or lower if scite has not yet processed some of the citing articles. Explore citation contexts and check if this article has been supported or disputed. https://scite.ai/reports/10.1186/s12905-019-0708-3
Article citations, sexual and reproductive health experiences, access to services, and sources of information among university students in ethiopia..
Chekol BM , Sheehy G , Siraneh Y
Front Reprod Health , 5:1271685, 14 Dec 2023
Cited by: 0 articles | PMID: 38162013 | PMCID: PMC10755960
Assessing motivators for utilizing family planning services among youth students in higher learning institutions in Dodoma, Tanzania: Protocol for analytical cross sectional study.
Munuo U , Moshi FV
PLoS One , 18(3):e0282249, 10 Mar 2023
Cited by: 0 articles | PMID: 36897915 | PMCID: PMC10004694
Contraceptive and abortion practices of young Ghanaian women aged 15-24: evidence from a nationally representative survey.
Keogh SC , Otupiri E , Castillo PW , Li NW , Apenkwa J , Polis CB
Reprod Health , 18(1):150, 18 Jul 2021
Cited by: 2 articles | PMID: 34275462 | PMCID: PMC8286596
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
- http://www.ebi.ac.uk/biostudies/studies/S-EPMC6337791?xr=true
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Perception of university students in Ghana about emergency contraception.
Baiden F , Awini E , Clerk C
Contraception , 66(1):23-26, 01 Jul 2002
Cited by: 22 articles | PMID: 12169377
The emergency contraceptive pill: a survey of knowledge and attitudes among students at Princeton University.
Harper CC , Ellertson CE
Am J Obstet Gynecol , 173(5):1438-1445, 01 Nov 1995
Cited by: 47 articles | PMID: 7503182
Use of non-emergency contraceptive pills and concoctions as emergency contraception among Nigerian University students: results of a qualitative study.
Ajayi AI , Nwokocha EE , Akpan W , Adeniyi OV
BMC Public Health , 16(1):1046, 04 Oct 2016
Cited by: 24 articles | PMID: 27716213 | PMCID: PMC5050919
The knowledge and perceptions of the first year medical students of an International University on family planning and emergency contraception in Nicosia (TRNC).
Asut O , Ozenli O , Gur G , Deliceo E , Cagin B , Korun O , Turk O , Vaizoglu S , Cali S
BMC Womens Health , 18(1):149, 15 Sep 2018
Cited by: 4 articles | PMID: 30219057 | PMCID: PMC6139172
Knowledge and perception of emergency contraception among female Nigerian undergraduates.
Aziken ME , Okonta PI , Ande AB
Int Fam Plan Perspect , 29(2):84-87, 01 Jun 2003
Cited by: 45 articles | PMID: 12783772
Europe PMC is part of the ELIXIR infrastructure
- Open access
- Published: 09 October 2015
Assessing the knowledge, attitude and practice of family planning among women living in the Mbouda health district, Cameroon
- Jobert Richie N. Nansseu 1 , 2 ,
- Emmanuel Choffor Nchinda 3 ,
- Jean-Claude Katte 4 ,
- Fatima M. Nchagnouot 1 &
- Guylaine D. Nguetsa 5
Reproductive Health volume 12 , Article number: 92 ( 2015 ) Cite this article
43k Accesses
9 Citations
Metrics details
Background and objective
Promotion of family planning has been shown to reduce poverty, hunger, maternal and infant mortality, and contribute to women’s empowerment. But many resource-limited countries still have very low rates of contraceptive use. The present study aimed to assess the knowledge, attitude and practice of family planning among women living in a resource-poor rural setting.
We conducted a cross-sectional study in January 2010 in the Mbouda Health District, Cameroon. After a multistage random selection, 120 households were selected. Participants were women aged at least 15 years old, sexually active, and who volunteered to participate in the study. Data were collected during an anonymous interview using a structured pre-tested questionnaire.
A total of 101 women were enrolled, their ages ranging from 18–58 years with a mean of 31.7 ± 8.8 years. Ninety-six percent of these women had already heard about family planning. Almost all respondents (98 %) were aware of at least one contraceptive method, the most cited being the male condom (96 %), the safe period (86.1 %), injectables (76.2 %) and oral pills (75.2 %), Sixty-six women (65.3 %) were currently practicing at least one contraceptive method, and the three prevailing methods used were: the safe period (50 %), the male condom (34.8 %), and injectables (12.1 %). The main reasons precluding women from practicing contraception were lack of knowledge (31.4 %), uselessness (31.4 %) and unbearable side effects (8.6 %). Fourteen of these women (42.4 %) expressed the willingness to start practicing contraception if they received more information about the subject. Decision on the number of children to have was made by both the man and the woman in 59.5 % of cases. The practice of contraception had been decided by the couple in 39.6 % of cases, and 9.4 % of men were not aware that their wives were currently practicing contraception.
Although the level of awareness about family planning and contraceptive methods is quite satisfactory, the level of contraceptive use is not optimal in our setting. Consequently, more adapted educational and counseling interventions should be undertaken among women, and family planning messages directed to men need to be included too.
Peer Review reports
Introduction
There is convincing evidence that poverty incidence is always higher among larger households. Indeed, Orbeta A. [ 1 ] figured out an enduring positive association between family size and poverty incidence and severity. He also showed how a large family size creates the conditions leading to greater poverty through its negative impact on household savings, labor force participation, and earnings of parents, as well as on the human capital investment in children [ 1 ]. Besides, we read from Renjhen et al. [ 2 ] that uncontrolled population growth is recognized as the single most important impediment to national development. Therefore, the promotion of family planning, especially in countries with high birth rates, has the potential to reduce poverty and hunger, and avert 32 % of all maternal deaths and nearly 10 % of childhood deaths [ 3 ]. It may also substancially contribute to women’s empowerment, achievement of universal primary schooling, and long-term environmental sustainability [ 3 ].
Programmes to promote family planning in developing countries began in the 1960s, with the number of countries with official policies to support family planning rising from only two in 1960–74 by 1975 and 115 by 1996 [ 4 ]. Between 1960 and 2000, the proportion of married women in developing regions using contraception increased from less than 10 to about 60 %, though with huge variations from one area to another [ 5 ]. However, many of today’s poorest countries, mainly in sub-Saharan Africa (SSA), still have high fertility and high unmet needs for family planning, and their populations are projected to double in the next few decades [ 3 ]. Moreover, in most African countries, high fertility and rapid population growth represent a bigger threat to achievement of the Millennium Development Goals than infectious diseases such as HIV/AIDS [ 3 ].
In 1986, the Cameroonian Government officially clarified its position about promoting the practice of family planning in the country, though there is dearth of information in this regard all over the country. Data from the Demographic and Health Survey (DHS) revealed a 26 and 24 % prevalence of contraceptive uptake respectively in 2004 and 2011 [ 6 ], hence a very low number of women using contraception. The present study aimed at assessing the knowledge, attitude and practice of family planning among women of a Cameroonian health district, specifically in a rural setting, and investigating male participation in family planning from the point of view of their female partner.
Study design and participants
This was a cross-sectional study conducted in January 2010 in the Mbouda Health District, Cameroon. This is one of the 19 health districts of the West Region of Cameroon, extending over 455 km 2 , and comprising nearly 227,448 inhabitants in 2010. The district is divided into 12 health areas among which 4 were randomly selected for recruitment: the Mbouda-West, Mbouda-North, Bafounda, and Toumaka health areas. In each of these zones, we randomly selected three neighborhoods among each of which ten households to be visited were subsequently retained, hence a total of 120 households. We were helped in this process by the sanitary authorities of the district alongside the heads of each selected health area with whom we visited each selected household in their respective zones.
Participants were women aged at least 15 years old, irrespective of their marital status and educational level, currently residing in the district, and who volunteered to take part in the study. Data were collected during an interview using a structured pre-tested questionnaire recording socio-demographic background (age, level of education, occupation, religion, marital status, type of household, family size, birth interval, number of children per bedrooms, and number of meals per day), knowledge on family planning, current method of contraception used, and the level of implication of the husband. Nineteen of the 120 households visited were not included in the study because the woman was absent when the investigator visited (10), or because of refusal to participate (9).
End-point definitions
We defined family planning as all the measures undertaken to limit and space births. In this regard, “limitation of births” referred to controlling the number of births, whereas “stopping births” meant ending deliveries by a definite or permanent method. On another hand, contraception was defined as prevention of conception, i.e. any method used not to become pregnant.
Statistical analysis
Data were coded, entered and analyzed using Epi info version 3.3.2 (Center for Disease Control, Atlanta, USA). Results are presented as mean ± standard deviation (SD) for quantitative variables, and count (percentage) for qualitative variables. Qualitative variable comparisons used the chi-square test or equivalents where appropriate. Odds ratios (OR) with 95 % confidence intervals were used to examine the impact of contraception on various outcomes. Results were considered statistically significant if p value < 0.05.
Ethical considerations
Before carrying-out this study, authorizations were obtained from the administrative and sanitary authorities of the study site, acting as ethical review board. Participants were informed of the various aspects of the study, and were anonymously included in the survey after they had signed the informed consent form. The study was conducted in accordance with the revised Helsinki Declaration.
We enrolled a total of 101 participants. Table 1 depicts the main socio-demographic characteristics of the study population. Ages varied between 18 and 58 years, with a mean of 31.7 ± 8.8 years. The most encountered age group was 20–24 years (21.8 %, see Table 1 ). Fifty nine women (58.4 %) had a secondary educational level, 51 (50.5 %) were housewives, and nearly two thirds of respondents (65.3 %) belonged to monogamic households (see Table 1 ).
The large majority of women (96 %) had already heard about family planning, nearly half of them (58.8 %) during educative sessions as part of antenatal care delivered in health facilities, but only 4 women (4.1 %) gave the right definition of family planning (see Table 2 ). Eighty women (79.2 %) had never visited a family planning centre. About two thirds of participants (60.3 %) had already heard about contraception, the exact definition being given by 38 (62.5 %) of them (see Table 2 ).
Table 2 spells out among others, the different methods of contraception known by our respondents. The most cited ones were: the male condom (96 %), the safe period (86.1 %), injectables (76.2 %) and oral pills (75.2 %). Five point nine percent of women cited one method, 8.9 % two methods, 7.9 % three methods, 5.9 % four methods, 15.8 % five methods, and 53.4 % of women cited more than 5 methods, but 2 % of participants were not aware of any contraceptive method (see Table 2 ).
Sixty-six women (65.3 %) were currently practicing at least one contraceptive method. Figure 1 presents a comparison between women practicing contraception or not with regard to their level of education. There was no relation between these two variables ( p > 0.05), as well as with age, marital status and occupation (all p values > 0.05). Among the women not practicing contraception, 14 (42.4 %) expressed the willingness to start doing so in the near future if they received more information about the subject. Figure 2 depicts the different methods used by women currently practicing contraception. The three main methods used were: the safe period (50 %), the male condom (34.8 %), and injectables (12.1 %). More than one method could be used by the same participant, the prevailing combination being safe period + male condom.
Comparison between women practicing contraception ( on the left ) and those not practicing contraception ( on the right ) with regard to educational level; no influence of the level of education on the practice or not of contraception ( p > 0.05)
Different contraceptive methods used by women currently on contraception. (The overall percentage >100 % because one woman could be using a combination of two or several contraceptive methods)
Among the women actively practicing contraception, 18 (27.7 %) were not satisfied with the current method used, the reasons being: ineffectiveness (55.6 %), side effects (22.2 %), and difficult usage (22.2 %). Of these women, 8 (44.4 %) were on the safe period, 7 (38.9 %) used the male condom, 2 (11.1 %) on injectables, and 1 (5.6 %) on the association safe period + male condom. Ten women (15.2 %) practicing contraception had undesirably become pregnant sometime in the past, among which 7 (70 %) used the safe period, 1 (10 %) the male condom, 1 (10 %) the injectables, and 1 (10 %) used the combination safe period + male condom.
The number of persons in the household varied from 2–40, with a mean of 7.3 ± 5.4 persons. The number of children per household varied between 1 and 18 with a mean of 4.5 ± 3.1 children. The number of children per woman ranged from 1–9, with a mean of 3.7 ± 2.1 children. Figure 3 is representative of the average number of children per age-group of the women interviewed. Women aged 40–44 had 6.1 children compared to women aged 35–39 who had 4.6 children, hence the inference that around or after 40 years old, the women of our study population continue to give birth. The dominating birth interval was 2 years (39.8 %); with the mean equal to 2.8 ± 0.9 years.
Average number of children with respect to age-groups. Intriguingly, women seem to continue delivering even into advanced ages (≥40 years)
In households not under family planning, there was a significant 3.2 increased likelihood to have less than three meals per day (95 % CI: 1.3-8.2; p < 0.05). Children living in households under family planning had a 1.2 fold increased risk of being more than 2 per bedroom, though statistically non-significant (95 % CI: 0.5-2.7; p > 0.05).
Decision on the number of children to have was made by both the man and the woman in 59.5 % of cases, whereas this discussion had never existed in 23 % of cases. The practice of contraception had been decided by the couple in 39.6 % of cases, only by the woman in 40 % of cases, and only by the man in 23.1 % of cases. Nine point four percent of men were not aware that their wives were currently practicing contraception.
The introduction of modern contraceptive techniques over the recent decades and the increasing availability of safer and more effective methods of preventing pregnancy have permitted people around the world to exercise their choice, make responsible decisions with respect to their reproduction and enjoy the benefits of family planning [ 7 ]. The current prevalence of contraceptive use is thus approaching 60 % worldwide, and in the less developed countries, almost 53 % of couples are using some form of contraception [ 4 , 5 , 8 ]. Results from the present study, conducted in a typical rural SSA setting, reveal a 65.3 % prevalence of contraception practice, highly superior to the 24 % reported by the 2011 Cameroon DHS, and nearly two times the specific prevalence in the West Region of the country (33.7 %) [ 6 ]. Besides, the overall prevalence of contraception practice in Cameroon has not changed from 2004–2011: 26 and 24 % respectively [ 6 ], questioning therefore the efforts that have been made so far to vulgarize such a practice around the country during the last decade. Presumably, a lot of work still needs to be done in this regard. For instance, more educational and counseling interventions should be undertaken everywhere (media, churches, schools, health centers among others), with special emphasis on the advantages of modern contraceptives.
Ninety six percent of our respondents had already heard about family planning, the main source of information being the health personnel (58.8 %). This finding corroborates that of Ghazal-Aswad et al. [ 7 ] where primary health care physicians were cited as main source of information. Contrariwise, school and friends/relatives [ 9 , 10 ], or media [ 2 ] were the main sources of information reported by other authors. Therefore, our primary health care providers have a major role to play in improving the women’s knowledge of family planning and awareness of different contraceptive methods available alongside their respective advantages and inconveniences. In this regard, primary health care providers’ knowledge and skills must be continuously enhanced and reinforced to deliver the right and sound advice about contraception. Besides, although the large majority of women had heard about family planning, very few of them (4.1 %) knew exactly what it refers to, and 60.3 % had heard about contraception before. This finding raises the issue of the content of information transmitted to women on family planning, contraception and contraceptive usage, stressing perhaps the need to adapt the message to be passed, may be by delivering it in appropriate words and in the women’s mother tongues. We have seen indeed that the large majority of our women had a secondary or less level of education, presumably hindering their capacity of understanding if scientific or complicated words are used.
Though some women had never heard about contraception (39.7 %), we found that, after the investigator explained what it refers to, 98 % of participants were aware of at least one contraceptive method, with more than half of them (53.4 %) being able to cite more than 5 contraceptive methods. The most cited methods were the modern ones (mainly condom, injectables, pills, implants, intrauterine device, and sterilization), followed by the traditional ones (mostly the safe period and coitus interruptus). Concurring our results, the 2011 Cameroon DHS revealed that 94 % of women were able to cite at least one contraceptive method, the most cited being the modern ones (the male condom at first as in our study) [ 6 ]. Likewise, Omo-Aghoja et al. [ 9 ] reported, in a rural Nigerian setting, a 92.3 % level of contraceptive awareness, the most widely known contraceptive methods being injectables, condoms and pills. It is worth noticing that the level of knowledge of contraceptive methods has increased over time in Cameroon: 73 % in 1991, 81 % in 1998, 90 % in 2004, and 94 % in 2011 [ 6 ].
However, this evolution contrasts with that of the practice of contraception which remains very low: 16 % in 1991, 19 % in 1998, 26 % in 2004 and 24 % in 2011 [ 6 ]. There is thus a large gap between contraceptive knowledge, approval and practice in our context. In our study, 39.7 % of women were not currently practicing contraception, and the prevailing reasons precluding this practice were lack of information (31.4 %), uselessness (31.4 %), and fear of side effects (14.3 %). In Nigeria, the factors associated with low contraceptive usage were: poor level of training and ineffective conveyance of relevant information to women by health personnel, low literacy levels, extremes of reproductive age and extremes of parity, fear of side effects, lack of knowledge and lack of spousal consent [ 9 ]. Other important factors affecting the use of contraceptive methods are unsatisfactory sexual life, inaccessibility of contraceptives, socioeconomic status, cultural background and religious belief [ 2 , 7 , 11 , 12 ]. These barriers have therefore to be taken into consideration when carrying the education and communication programmes in order to enhance contraception uptake and usage in our settings, especially that of modern contraceptives. For instance, 14 out of 35 women currently not practicing contraception expressed the willingness to do so if they received more information. Besides, more studies dedicated at a thorough investigation of the different reasons pertaining the nonuse of contraception and how these can be addressed, are urgently warranted in our milieu.
The dominating contraceptive methods used were the traditional ones (safe period, coitus interruptus, and abstinence: 60.6 %), followed by modern methods (male condom, pills, injectables, implants and female sterilization: 39.4 %), corroborating Ghazal-Aswad et al. [ 7 ] findings. By contrast, the 2011 Cameroon DHS showed that modern methods were more used than traditional ones [ 6 ]. In the same line, results from Omo-Aghoja et al. [ 9 ] showed that modern methods were those mostly used by women of the Amukpe community, Nigeria. Unfortunately, we did not search for the reasons forcing our women to choose one contraceptive method instead of another one. It is therefore difficult to explain why the traditional methods, which by the way are less reliable and need more efforts, outweighed the modern ones in our study. We can guess that, due to low educational and socioeconomic levels, cultural and religious beliefs, and lack of roads, modern contraceptives are perhaps unavailable, inaccessible or unaffordable. Studies targeting the cost-benefit and acceptance of each of the contraceptive methods should be conducted to address the right message during educative sessions in our settings. These sessions must focus on the advantages of modern contraceptives methods to demystify them and increase thereby their uptake.
Regrettably, the cross-sectional design of the present study precluded us from further investigations. Additionally, the self-reporting of information could have introduced some bias. Nonetheless, interviews were anonymous and confidential to make sure that none of the participants could feel uncomfortable while answering the questions. Although our findings cannot be generalized to the entire Cameroonian female population, we used a rigorous multistage random sampling method to recruit our respondents, enabling us to generalize our results to the entire female population of the Mbouda health district, though our sample size could be seen as relatively low.
While investigating male participation in family planning and contraceptive use, we found that there is a lack of male–female communication regarding the number of children to have and the practice of contraception, in line with Kaida et al. findings in Mpigi district, Uganda [ 13 ]. On the contrary, Lasee and Becker [ 14 ] reported that husband-wife communication about family planning was effective in 82 % of their couples. In the large majority of SSA settings, men have suffered from limited involvement in either receiving or providing reproductive health information, hence they are generally uninformed about contraceptive methods [ 13 , 15 ]. Additionally, it has been bolstered that women who did not discuss family planning with their male partner had a 2.8-fold increased risk for an unplanned pregnancy [ 16 ]. There is body of evidence that partner communication about family planning is associated with and is often essential to increase levels of knowledge, improve attitudes, and enhance the use of family planning methods [ 13 – 15 , 17 , 18 ]. Consequently, it clearly appears of urgent need to broaden the scope of family planning programmes by including family planning messages directed to men.
Although the level of awareness about family planning and contraceptive methods is quite satisfactory, the level of contraceptive uptake is not optimal in our setting. In this regard, more adapted educational and counseling interventions should be undertaken among women, and family planning messages directed to men need to be included too. Furthermore, primary health care providers’ knowledge and skills have to be continuously enhanced and strengthened to deliver the right and sound advice about family planning and contraception. Moreover, more studies dedicated at a thorough investigation of the different reasons pertaining the nonuse of contraception and how these can be addressed, are warranted. Additionally, future studies assessing the cost-benefit and acceptance of each of the contraceptive methods should be conducted to address the right message during educative sessions.
Orbeta A. Poverty, vulnerability and family size: evidence from the Philippines. ADBI Discussion Paper No. 29. Tokyo: Asian Development Bank Institute; 2005.
Google Scholar
Renjhen P, Kumar A, Pattanshetty S, Sagir A, Samarasinghe CM. A study on knowledge, attitude and practice of contraception among college students in Sikkim. India J Turk Ger Gynecol Assoc. 2010;11(2):78–81.
Article PubMed Google Scholar
Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: the unfinished agenda. Lancet. 2006;368(9549):1810–27.
UN Department of Social Affairs Population Division: World population policies 2003. In . New York: United Nations; 2004
UN Department of Social & Economic Affairs Population Division: Levels and trends in contraceptive use: 2003 Revision. In . New York: United Nations; 2004
National Intitute of Statistics and ICF International. Demographic and Health Survey and at multiple indicators (DHS-MICS) 2011 (2012) [ http://slmp-550-104.slc.westdc.net/~stat54/downloads/EDS-MICS/EDSMICS2011.pdf ] Accessed 05 April, 2015.
Ghazal-Aswad S, Rizk DE, Al-Khoori SM, Shaheen H, Thomas L. Knowledge and practice of contraception in United Arab Emirates women. J Fam Plann Reprod Health Care. 2001;27(4):212–6.
Article CAS PubMed Google Scholar
Huezo CM. Current reversible contraceptive methods: a global perspective. Int J Gynaecol Obstet. 1998;62 Suppl 1:S3–15.
Omo-Aghoja LO, Omo-Aghoja VW, Aghoja CO, Okonofua FE, Aghedo O, Umueri C, et al. Factors associated with the knowledge, practice and perceptions of contraception in rural southern Nigeria. Ghana Med J. 2009;43(3):115–21.
CAS PubMed PubMed Central Google Scholar
Aggarwal O, Sharma AK, Chhabra P. Study in sexuality of medical college students in India. J Adolesc Health. 2000;26(3):226–9.
Blanc AK, Way AA. Sexual behavior and contraceptive knowledge and use among adolescents in developing countries. Stud Fam Plann. 1998;29(2):106–16.
Hennink M, Cooper P, Diamond I. Asian women’s use of family planning services. Br J Fam Plann. 1998;24(2):43–52.
CAS PubMed Google Scholar
Kaida A, Kipp W, Hessel P, Konde-Lule J. Male participation in family planning: results from a qualitative study in Mpigi District. Uganda J Biosoc Sci. 2005;37(3):269–86.
PubMed Google Scholar
Lasee A, Becker S. Husband-Wife Communication About Family Planning and Contraceptive Use in Kenya. Int Fam Plan Perspect. 1997;23(1):15–20+33.
Article Google Scholar
Hulton L, Falkingham J. Male contraceptive knowledge and practice: what do we know? Reprod Health Matters. 1996;7(4):90–100.
Mbizvo MT, Bonduelle MM, Chadzuka S, Lindmark G, Nystrom L. Unplanned pregnancies in Harare, Zimbabwe: what is the contraceptive history and awareness of the mothers? Cent Afr J Med. 1997;43(7):200–5.
Chipfakacha VG. Attitudes of males on contraception: a KAPE survey. East Afr Med J. 1993;70(2):82–4.
Agyei WK, Migadde M. Demographic and sociocultural factors influencing contraceptive use in Uganda. J Biosoc Sci. 1995;27(1):47–60.
Download references
Acknowledgments
The authors are grateful to the administrative and health authorities of the Mbouda health district, to all the chiefs of the health areas selected for the study, and to all the women who have accepted to participate in this survey.
Author information
Authors and affiliations.
Department of Public Health, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, PO Box 1364, Yaoundé, Cameroon
Jobert Richie N. Nansseu & Fatima M. Nchagnouot
Sickle Cell Disease Unit, Mother and Child Centre of the Chantal Biya Foundation, Yaoundé, Cameroon
Jobert Richie N. Nansseu
Department of ENT and Head and Neck Surgery, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Yaoundé, Cameroon
Emmanuel Choffor Nchinda
Diabetes and Hypertension Treatment Centre, Bafoussam Regional Hospital, Bafoussam, Cameroon
Jean-Claude Katte
Pediatric Unit, Bertoua Regional Hospital, Bertoua, Cameroon
Guylaine D. Nguetsa
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jobert Richie N. Nansseu .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
JRNN, JCK, ENC and FNM conceived and designed the study, collected, analyzed and interpreted the data. JRNN drafted the manuscript. JRNN, ECN, JCK, FNM, and GDN critically revised the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Nansseu, J.R.N., Nchinda, E.C., Katte, JC. et al. Assessing the knowledge, attitude and practice of family planning among women living in the Mbouda health district, Cameroon. Reprod Health 12 , 92 (2015). https://doi.org/10.1186/s12978-015-0085-9
Download citation
Received : 17 April 2015
Accepted : 06 October 2015
Published : 09 October 2015
DOI : https://doi.org/10.1186/s12978-015-0085-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Contraception
- Family planning
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
- Research article
- Open access
- Published: 27 January 2016
Contraceptive use, knowledge, attitude, perceptions and sexual behavior among female University students in Uganda: a cross-sectional survey
- Henry Nsubuga 1 ,
- Juliet N. Sekandi 2 , 3 ,
- Hassard Sempeera 2 &
- Fredrick E. Makumbi 2
BMC Women's Health volume 16 , Article number: 6 ( 2015 ) Cite this article
66k Accesses
35 Citations
10 Altmetric
Metrics details
In Uganda, the risk of unintended pregnancies and unsafe abortions remains high due to relatively low contraceptive use. There is paucity of data on knowledge, attitudes, perceptions and practices towards modern contraceptives and, sexual and reproductive health especially among the young female university students.
A survey was conducted at Makerere University main campus in Kampala, Uganda during April 2014. A team of well-trained and experienced research assistants interviewed female undergraduate students who provided data on socio-demographic characteristics, knowledge, perceptions and attitudes and use of contraceptives, as well as other sexual and reproductive health practices. Users of any contraceptive method in the past 12 months were coded as ‘1’ and none users as ‘0’. The prevalence of contraceptive use was determined as the number of users divided by all female participants. Prevalence ratios (PRs) with their corresponding 95 % confidence intervals were used as measures of association between contraceptive use and associated factors. The PRs were obtained via a modified Poisson regression model using a generalized linear model with Poisson as family and a log link without an offset but including robust standard errors. All analyses were conducted with Stata version 13.
A total of 1,008 females responded to the survey; median (IQR) age was 21(20, 21) years, 38.6 % in year 2 of study, and nearly three quarters (72.3 %) were of Christian faith. Knowledge of any contraceptives was almost universal (99.6 %) but only 22.1 % knew about female condoms. Perceived acceptability of contraceptive use at the university (93 %) or being beneficial to male partners too (97.8 %) were high. Nearly 70 % had ever engaged in sexual intercourse and 62.1 % reported sexual intercourse in the past 12 months. Overall, 46.6 % reported current contraceptive use, with male condoms (34.5 %) being the commonest methods. Factors associated with higher contraceptive use were being in year 2, consensual union or perception that contraceptives are for females only. However, being evangelical/SDA or perception that contraceptive use is wrong was associated with lower contraceptive use. Overall, 9 % reported ever being pregnant, 2 % were pregnant at the time of the survey and a third (33.8 %) knew of a pregnant friend. About 40 % of ever pregnant respondents reported ever trying to terminate the pregnancy.
Conclusions
Knowledge, perceived acceptability and benefits of contraceptive use were nearly universal, but contraceptive use was suboptimal in this setting. Ever trying to terminate a pregnancy was common and a clear indicator of unintended pregnancies.
Peer Review reports
The proportion of young women reporting unintended pregnancy and unmet need for contraception remains high in developing countries [ 1 ]. Unintended pregnancies are associated with increased risk of unsafe abortions, maternal morbidity and mortality [ 2 ]. In order to avert the unintended pregnancies and consequent adverse outcomes, contraceptive use has been prioritized as a key intervention [ 3 ]. Improving the universal access to sexual and reproductive health services including contraceptives was a key target of the Millennium Development Goals (MDG) [ 4 , 5 ].
In developing countries, one in three women give birth before the age of 20 and pregnancy-related death during child birth is two times higher compared to women older than 20 years [ 5 ]. A quarter of the estimated 20 million unsafe abortions and 70,000 related deaths each year occur among women aged 15–19 years [ 5 ]. In sub-Saharan Africa alone, it is estimated that 14 million unintended pregnancies occur every year, with almost half occurring among women aged 15–24 years [ 6 ]. It is evident that use of effective contraceptive methods would potentially prevent 90 % of abortions, 20 % pregnancy-related morbidity and a third (32 %) of maternal deaths worldwide [ 4 ].
In Uganda, an estimated 1.2 million unintended pregnancies occurred in 2008, representing more than half of the country’s 2.2 million pregnancies [ 2 ]. The risk of pregnancy increases with a widening gap between sexual debut and age of first marriage [ 7 , 8 ]. In Uganda nearly two thirds (64 %) of women aged 25–49 years reported early sexual debut before the age of 18 years [ 9 ]. At the time of enrolling into Universities, women are at an age of about two years above the median age of sexual debut in Uganda suggesting that they are usually sexually active.
Overall, the use of contraceptives is not openly discussed among young unmarried women due to strong cultural and religious beliefs, which exposes the young women to the increased risk of unwanted/unintended pregnancies. In many African traditional culture settings, pregnancy before marriage is often viewed as an abomination. As such, many unmarried females who get unintended pregnancies seek abortions services for fear of societal judgment. Abortion in Uganda being illegal increases the risk of maternal deaths because it is usually unsafe and at times conducted by traditional herbalists.
According to the two major surveys conducted among university students in Uganda, findings indicated that students did not have access to sexual and reproductive health services and HIV/AIDS-related programmes despite their engagement in high-risk sexual behaviours [ 10 , 11 ]. Findings also showed that a quarter (25 %) of the university students had unmet need for contraceptives yet their level of awareness about contraceptives was high [ 1 , 12 ]. Knowledge, attitudes and perceptions (KAP) about sexual and reproductive health may influence contraceptive use suggesting that interventions based on KAP may lead to reduced rates of unintended pregnancies [ 13 ].
This study was motivated by the continued anecdotal reports showing a common occurrence of unintended pregnancies and sexually transmitted infections among students seeking services at the University’s Counseling and Guidance Centre. However, there was paucity of data on the knowledge, attitudes, and perceptions, access to and use of contraceptives and sexual and reproductive health services/information among Makerere University female students. Data generated from this study will inform and enhance the design of student-centered programs to improve contraceptive knowledge and use, and thus potentially avert the unintended pregnancies and the consequent adverse outcomes in teaching institutions such as Makerere University.
Design, study setting and population
Across-sectional survey was conducted among female undergraduate students at Makerere University main campus. Makerere University is the oldest and largest public institution of higher education in Uganda. The University offers both undergraduate and graduate programs to approximately 40,000 students, half of who are females. The main university campus is located about 2.5 km from the capital city, Kampala.
Data were collected from April 1 st to April 30 th 2014 among 1,008 students selected on the basis of halls of residence using quantitative data collection tools. All registered undergraduate students aged 18–30 years were eligible to participate in the study. Some female students resided at the three halls of residence at the main campus while majority resided off-campus at private hostels and a few were commuting from their parents’/guardians’ homes.
The study outcomes included knowledge, perception/attitudes towards contraception, and reported contraceptive use in the 12 months following the survey. The independent variables were age, year of study, religion/faith, marital status and source of health information about family planning services and commodities.
Knowledge was defined as the state of awareness of contraceptive methods, any specific types and the source of contraceptives. Attitude or perception was defined as respondent’s opinion or view, whether positive or negative towards a practice or behavior such as contraceptive use. Knowledge was operationalized based on the following question “ Have you ever heard about contraceptives? ” Affirmative responses (yes) led to subsequent questions on the reasons for use of contraceptives, methods and the sources known to her. Then the respondent was considered knowledgeable if they correctly provided responses based on the listed options on the tool. The perceptions/attitudes of respondents about contraceptives were assessed using a 5 point-likert scale consisting of a range of responses from strongly agree (1), agree (2), neutral (3), disagree (4) and strongly disagree (5). Statements such as “ It is not easy for me to discuss with my partner about sexual matters ”, “ Family planning is for females only and not males ”, “ Family planning is acceptable in our community ” were used to elicit respondent’s views/options so as to determine their perceptions or attitudes towards family planning.
Sample size estimation
A total of 973 female students were estimated as the appropriate sample size for this survey using the modified Kish-Leslie formula (Leslie Kish, 1965) for cross sectional studies. The sample size determination assumed 21.5 % of female students using modern contraceptives, a 5 % margin of error for the estimated p, 95 % confidence interval around the estimates, a design-effect of 3 to account for multistage sampling conducted through use of residential halls as clusters, and a survey response rate of 80 %. However, a total of 1,008 students were interviewed creating an excess of 35 respondents because interviews were conducted simultaneously at the multiple sites within the University.
Participant recruitment
The initial participant recruitment plan included a sampling frame of about 22,000 female registered students as of April 2014, which was obtained from the university academic registrar’s office. The list included each student’s assigned hall of residence, year of study, faculty where registered for the studies, and telephone contacts. A sample of 973 students was randomly selected from this sampling frame. However, only eighty-five students could be reached via the registered telephone contacts. Reasons for none accessibility was primarily due to incorrectly registered telephone numbers or use of the next of kin telephone number who was not aware of the student’s whereabouts at the time of the survey. Although three callbacks were conducted, this approach did not result into any improvement in response rates. The research team thereafter made a protocol amendment to recruit participants using convenience sampling. Interviewers were therefore assigned or stationed at the various academic units within the university during daytime (8 hours) to request students to participant in the study.
Data collection and quality assurance
The data collection tools were pre-tested and the study protocol piloted using twenty (20) questionnaires at a university within Kampala with similar characteristics as Makerere University. Research assistants/Interviewers were trained in data collection, research ethics, interviewer skills, seeking and administering informed consent. All the interviewers were graduates because the undergraduate participants were perceived to respond to persons who were senior in academic training. The interviews were conducted in English which both the interviewers and participants were knowledgeable. All completed questionnaires were reviewed by the field supervisors and checked for completeness by data editor at Makerere University School of Public Health data management centre. Interviewers were only allowed to interview another respondent after the field supervisor had completed reviewing the completed questionnaire.
Ethics statement
This study was reviewed and received ethical approval from the Higher Degrees Research and Ethics Committee at Makerere University School of Public Health and the Uganda National Council for Science and Technology. Permission to conduct the study was granted by the Makerere University administration. Written informed consent was obtained from all study participants.
Statistical analysis
Exploratory data analysis was conducted on all key variables. Descriptive statistics were generated with proportions (or percentages) for categorical data, and mean (standard deviation) for normally distributed data or median (inter-quartile range) if continuous data were skewed. Also bar graphs for categorical data such as reported contraceptive use by year of study were constructed. The main outcome of this study was current use of any contraceptive method, measured as a binary variable: “non-users” coded as “0” or “users” coded as “1”. Current use of contraception was calculated as the proportion of students who reported to have used any method of contraception in the past 12 months prior to the survey. Cross tabulations of knowledge, perceptions and attitudes towards contraceptive use and sexual behavior stratified by year of study were generated. The prevalence of contraceptive use was determined as the number of users divided by all female participants. Prevalence ratios (PRs) with their corresponding 95 % confidence intervals were used as measures of association between contraceptive use and associated factors. The PRs were obtained via a modified Poisson regression model using a generalized linear model with Poisson as family and a log link without an offset but including robust standard errors. The log-binomial model could not converge to provide an estimate of the PRs. Odds ratio could not be used as a measure of association because of the potential to overestimate the effect due to the high prevalence of the primary outcome. The year of study was considered as the main exposure variable, and adjusted for other variables including age, marital status, residence of student, religion, history of pregnancy and, beliefs and attitudes about contraceptives as potential confounders. All statistical analyses were performed in Stata version 12.1 (Statacorp, College Station. Texas).
Table 1 shows the characteristics of the study participants. A total of 1008 students were enrolled in the study. The recruitment of participants at the multiple independent academic units resulted into 35 extra participants, which was reported to the Institutional Review Board (IRB) as a protocol deviation. The mean (SD) age was 21.7 (2.3) years, with majority (87.5 %) aged 20–24 years, 38.6 % in year 2 of study, and Christian faith (Catholics 33.6 %, protestant 38.7 %) as the major reported religion. Most students were not married (87 %), just over a third (36.6 %) were resident in hostels, followed by homes (28.6 %), and only 18 % were staying at the halls of residence at the university campus.
Knowledge of contraceptive and sexual reproductive health
Table 2 shows Percentage distributions of Knowledge of Contraceptive Methods and Sexual Reproductive Health. Knowledge of contraceptives was nearly universal (99.6 %). The most commonly known modern methods were pills (86.7 %) and male condoms (88.4 %), followed by injectables (50.3 %), IUDs (35 %) and implants (26.7 %), female condom (22.1 %), while withdraw (34.2 %) was the most commonly mentioned traditional methods. The commonest sources of contraceptives were Hospitals (government, 64.3 %; private, 53.6 %), clinics (general 24 %, or Contraceptives 27.4 %) and pharmacy/drugs shops (36 %). The level of knowledge was also very high regarding sexually transmitted infections (98.7 %), HIV/AIDS (99.3 %) and prevention of HIV/AIDs (98.8 %) as well as its treatment (96 %). However, the proportions of students who knew about availability of treatment for HIV and STIs within their environs was low; 44.2 % and 59.2 % respectively.
Perceptions and attitudes towards contraceptive methods by year of study
Table 3 shows perceptions and attitudes towards contraceptive methods by year of study. Overall, nearly a quarter (23.6 %) perceived that modern contraceptive services and commodities were not accessible, or that it is not easy to discuss sexual matters with partner (24.4 %). About one in five students perceived that contraceptives were not for poor people (21.3 %) or that it is wrong to use contraceptives (20.1 %). However, only 6 % believed that contraceptives were for females only. Attitudes to contraceptives being acceptable in the student community (93 %), being beneficial for males too (97.8 %), and couple counseling being able to increase male involvement in contraceptive use (96.2 %) were highly rated as "agreed". All assessed perceptions and attitudes did not significantly differ by year of study.
Contraceptive use, sexual behavior and pregnancy
Table 4 shows contraceptive use, sexual behavior and pregnancy rates. Overall half (51.2 %) of the students were currently in sexual relationships, with slight increments in the proportions across the year of study. Nearly 70 % had ever engaged in sexual intercourse while 62.1 % reported sexual intercourse in the past 12 months. Over half (55.1 %) had ever used any method to prevent pregnancy while only 46.6 % were currently using contraceptives with male condoms being the most commonly mentioned methods used (34.5 %). Ever being pregnant or knowledge of a pregnant friend significantly varied by year of study; overall, 9 % reported ever being pregnant, 4.1 % (year-1), 9.8 % (year2) and 13.1% (year3+); (p = 0.003) while a third (33.8 %) knew of a pregnant friend 16.3 % (year-1), 38.9 % (year2) and 46.0 % (year3+), p < 0.001. Only 2 % of students reported being pregnant; higher among year 3+ compared to those in year-1. About 40 % of ever pregnant respondents reported ever trying to terminate a pregnancy.
Current contraceptive use by sexual active students
Figure 1 shows distribution of current contraceptive use by year of study. Among the sexually active students, male condoms 58 %, (n = 363) or other modern contraceptives 15 % (n = 93) where the most commonly mentioned methods, while 6 % (n = 37) only reported use of a traditional method. This pattern was similar across year of study. Although respondents were sexually active, about 1 in 5 (22 %) did not use any contraceptive, and this was most common in year-3+ (27.5 %) compared to either year 1 (18.4 %) or year 2 (18.3 %).
Current Use of Contraceptive Methods by 626 Sexually Active Students
Factors associated with contraceptive use
Table 5 shows the modified Poisson multivariable regression analysis of factors associated with contraceptive use. Compared to year-1, year-2 had a 22 % higher prevalence of contraceptive use. Contraceptive use was 3 % higher if a student was one year older than their counter-part adjusting for other factors.
The prevalence of contraceptive use was 75 % higher among married compared to none married, and 35 % lower in the Evangelical or SDAs compared to the Roman Catholic students. Perception of contraceptive methods being for females only was associated with a 41 % higher prevalence of contraceptive use relative too those who disagreed, while students who perceived it as being wrong to use contraceptives has a 33 % lower prevalence of use relative to those who had a favourable perception.
The study assessed the knowledge, attitudes, perceptions and use of contraceptives among female undergraduate students of Makerere University. Our findings show that knowledge was universal, but contraceptive use was suboptimal. The most commonly known and used methods were the male condoms and oral pills, but knowledge of the female condom was very low. Positive perceptions and attitudes were strongest on couple counseling acceptability of contraceptives at the university and benefits of contraceptives to males. Negative perceptions about contraceptives being for the poor or their use being wrong were mentioned. High level of contraceptive knowledge does not translate into actual use in this study or from other studies [ 14 , 15 ]. Religious beliefs as evidenced by lower use of contraceptives by evangelicals or Seventh Day Adventist have a clear negative influence of utilization; this has also been shown in other university setting in western Uganda [ 16 ]. Religious and moral beliefs clearly overlap and need further exploration in a University setting.
The level of knowledge about contraceptives was found to be lower in similar African university settings, ranging 53.3 % to 86.3 % [ 17 – 21 ]. It is possible that even though students were universally aware of a range of contraceptive methods and knew where to get the services, they may have faced other obstacles that we did not directly measure in our study. For example, previous studies done in Uganda have highlighted social-cultural factors as critical barriers to contraceptive use in young females [ 15 , 22 ]. Nalwadda and colleagues (2010) conducted a study in rural Uganda that specifically showed that societal norms such as condemning early engagement in sex, pregnancy and use of contraceptives among young unmarried girls presents a major obstacle to contraceptive use [ 23 ]. In our urban-based study, similar socio-cultural factors still have a lot influences leading to poor uptake of contraceptive among female students. In designing youth-friendly interventions it is imperative that efforts should be geared towards disseminating specific contraceptive information and education that is culturally-sensitive to the local setting.
Students knew the main sources of contraceptives services as government hospitals and private clinics but we did not verify if these were there major sources of contraceptive information. Awareness of sources was shown to reduce barriers and improve contraceptive use among female students in the University of Lesotho [ 1 ]. However, a study done in Ethiopia that evaluated major sources of information about contraceptives found out that a high knowledge of sources was not enough to result into actual use, rather the students needed more information about freely available contraceptive services [ 19 , 24 ]. These observations suggest that reproductive health education programs should offer accurate and comprehensive information while building skills for negotiating safer sexual behaviours [ 7 ].
Overall the students had positive attitudes and perceptions towards using contraceptives. However, negative perceptions and attitudes existed about accessibility to contraceptive services; these included discussion of sexual issues with partner, contraceptives being for the poor and wrong perceptions about contraceptive use. A study in Nigeria reported that a high proportion of students perceived contraceptive use as bad because they believed it caused infertility [ 25 ]. However, studies have reported positive attitudes specifically toward emergency contraceptives among students at Jimma and Adama university in Ethiopia [ 26 , 27 ] and negative attitudes toward emergency contraceptives increasing promiscuity in female students of Trinidad and Tobago [ 28 ].
Sexual activity among adolescents and young females is often associated with a greater risk for unintended pregnancies [ 2 ]. In our study, nearly 70 % of the students were sexually active in the past 12 months. This finding supports results from the Uganda demographic health survey showing that premarital sex is common, with at least one in five young females aged 15–24 being sexually active [ 9 ]. Young females joining universities often become sexually active partly due to peer-pressures, alcohol use, or as result of a perceived sense of being in control of their social lives [ 26 ]. Similar levels of sexual activity were reported from other studies done among female university students of the same age group [ 29 ]. In contrast, some earlier studies done in Africa showed lower levels of sexual activity among university students, these ranged from 14 % to 48 % [ 20 , 25 , 26 , 30 , 31 ]. The differences in levels of sexual activity may be due to temporal events like increased sexual reproductive health over time or could be explained by differences in religious and cultural beliefs surrounding premarital sex [ 32 ].
Contraceptive use of any method among the university students was 46.6 % which is nearly twice as high as the contraceptive prevalence of Uganda. On the other hand, the rate of use is lower than 79 % contraceptive used among females that was reported from a study done in Mbarara University in Uganda [ 16 ] and in other university students in Lesotho, Kenya and Ethiopia [ 1 , 14 , 33 ]. Factors that were significantly associated with contraceptive use in this study are consistent with findings from a recent survey in a nationally representative in Ugandan women [ 22 ]. The high level of sexual activity and the risk of unintended pregnancies point to a need to promote sexual and reprodcutive health sevices in this setting. Male condoms were the most common contraceptive methods followed by oral pills among the sexually active students. Similar findings have been obseved elsewhere in both the developed [ 13 , 31 , 34 ] or developing countries [ 1 , 25 , 27 , 28 , 35 ]. However methods such as oral pills and injectable contraceptives have also been mentioned as being common in some settings such as Adama University, Ethiopia [ 27 ].
Among the sexually active students, one in five were engaging in unsafe sex suggesting high risk to unintended pregnancies and sexually transmitted diseases including HIV infection. Unsafe sexual practices are common among young adults especially in universities and other higher educational institutions [ 10 , 11 , 13 ]. The reported prevalence of unsafe sex may be higher in this setting if some students also use emergency contraceptives for prevention of pregnancy. Previous studies elsewhere have shown high level of unsafe sex [ 31 , 33 ] in similar settings. However, our study did not specifically evaluate the use of emergency contraceptives.
The prevalence of reported pregnancy at the time of survey was low (2 %) but probably under-reported due to associated stigma among unmarried pregnant women. However, 9 % of the sexual active students reported being ever pregnant. Among the ever-pregnant females, 40 % had ever tried to terminate the pregnancy suggesting a high level of both unmet need for contraceptive and unintended pregnancy in this setting. The reported 40 % ever pregnant who tried to terminate a pregnancy may be an under estimate because abortion is illegal in Uganda, and can be very stigmatizing. Similar findings about abortion have been observed in Mexico public university among first year medical students where half (52 %) of the ever been pregnant female students performed unsafe abortions [ 36 ], and in Addis Ababa University Ethiopia 9 in 10 (90 %) of the ever pregnant students terminated their pregnancies with induced abortion [ 20 ].
Study strengths and limitations
Although the findings from this study are consistent with results from other university settings, we encountered some limitations. The planned random sampling based on the sampling frame from the University’s academic registrar was dropped in favor of convenience sampling. However, interviewers were assigned/stationed at multiple academic units and asked to as much as possible randomly select participants without any specific characteristics. Some of the information especially on issues such as abortion may be under-reported because abortion is illegal and stigmatizing. Also pregnancy among unmarried females is culturally unacceptable thus leading to a potential for under-reporting. However, the study team recruited and trained experienced interviewers within the age range of the respondents as a way of minimizing reporting bias. The consistence in the contraceptive use indicators with other studies and the nationally representative samples such as the Uganda demographical and health surveys provide credence and strength to findings observed in this study.
Knowledge, perceived acceptability and benefits of contraceptive use were nearly universal, but contraceptive use was suboptimal in this setting. Ever trying to terminate a pregnancy was common and a clear indicator of unintended pregnancies. Religious beliefs and misconceptions of need for contraceptive are key determinants of poor uptake of contraceptives.
Recommendations
Interventions that promote translation of knowledge into proper sexual and reproductive health practices are urgently needed. The high rate of unintended pregnancy as measured by ever-attempt to terminate a pregnancy needs to be addressed through increased counseling and information about contraceptives, and accessible and of contraceptive services to students who desire to use them.
Religious leaders may have to be engaged to discuss issues of sexual and reproductive health and how to avert the unintended pregnancies. The leadership of evangelical and SDA faith can be an important stakeholder in this endeavor.
Akintade OL, Pengpid S, Peltzer K. Awareness and use of and barriers to family planning services among female university students in Lesotho. South African Journal of Obstetrics and Gynaecology. 2011;17(2):36–42.
Google Scholar
Summers C, Guttmacher Institute. Unintended Pregnancy and Abortion in Uganda; 2013. https://www.guttmacher.org/presentations/unintended-pregnancy-abortion-Uganda.pdf downloaded January 26 2015.
World Health Organisation: Making Pregnancy Safer: Annual Report 2007. In . : World Health Organization, Geneva; 2008.
Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: the unfinished agenda. Lancet. 2006;368(9549):1810–27.
Article PubMed Google Scholar
United Nations Population Fund: State of the world population 2004. The Cairo consensus at ten: population, reproductive health and the global effort to end poverty. In . : UNFPA, New York; 2004.
Hubacher D, Mavranezouli I, McGinn E. Unintended pregnancy in sub-Saharan Africa: magnitude of the problem and potential role of contraceptive implants to alleviate it. Contraception. 2008;78(1):73–8.
Bearinger LH, Sieving RE, Ferguson J, Sharma V. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. 2007;369(9568):1220–31.
Mensch BS, Grant MJ, Blanc AK. The changing context of sexual initiation in sub-Saharan Africa. Popul Dev Rev. 2006;32:699–727.
Article Google Scholar
Uganda Bureau of Statistics (UBOS) and ICF International Inc. Uganda Demographic and Health Survey 2011. Kampala, Uganda: UBOS and Calverton, Maryland: ICF International Inc.; 2012.
Mayega RW: HIV/AIDS Sero-behavioral Survey in Six Universities in Uganda. In . : East Afrcian Community-African Medical and Research Foundation, AMREF; 2010.
Rutherford GW, Anglemyer A, Bagenda D, Muyonga M, Lindan CP, Barker JL, et al. University students and the risk of HIV and other sexually transmitted infections in Uganda: the Crane survey. International journal of adolescent medicine and health. 2014;26(2):209–15.
Orji EO, Adegbenro CA, Olalekan AW. Prevalence of sexual activity and family-planning use among undergraduates in Southwest Nigeria. Eur J Contracept Reprod Health Care. 2005;10(4):255–60.
Article CAS PubMed Google Scholar
Heisler K and Van Eron DM. "A descriptive study of undergraduate contraceptive attitudes among students at the University of New Hampshire". 2012. Honors Theses. Paper 8. http://scholars.unh.edu/cgi/viewcontent.cgi?article=1007&context=honors downloaded January 26 2016.
Ochako R, Mbondo M, Aloo S, Kaimenyi S, Thompson R, Temmerman M, et al. Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. BMC public health. 2015;15(1):118.
Article PubMed PubMed Central Google Scholar
Agyei WK, Migadde M. Demographic and sociocultural factors influencing contraceptive use in Uganda. Journal of biosocial science. 1995;27(1):47–60.
Mehra D, Agardh A, Petterson KO, Ostergren PO. Non-use of contraception: determinants among Ugandan university students. Global health action. 2012;5:18599.
Somba M, Mbonile M, Obure J, Mahande M. Sexual behaviour, contraceptive knowledge and use among female undergraduates' students of Muhimbili and Dar es Salaam Universities, Tanzania: a cross-sectional study. BMC women's health. 2014;14(1):94.
Ijirigho MI. "Use of Reproductive Health Information on Contraception among Female Undergraduates of University of Ibadan". 2010. Library Philosophy and Practice (e-journal). Paper 360. http://digitalcommons.unl.edu/libphilprac/360 downloaded January 26 2016
Lenjisa JL, Ulfina D, Tamme E, Kaba G, Berehe H, et al. Knowledge and Practice of Emergency Contraceptives among Students at Ambo Techniques College Ethiopia. Reprod Syst Sex Disord. 2014;3:136. doi:10.4172/2161-038X.1000136
Tolossa E, Meshesha B, Alemu Abajobir A. Assessment of level of knowledge and utilization of emergency contraception among female students of Hawassa University, south Ethiopia. Advances in Reproductive Sciences. 2013;1:51–6.
Hoque ME, Ghuman S. Knowledge, practices, and attitudes of emergency contraception among female university students in KwaZulu-Natal. South Africa PloS one. 2012;7(9), e46346.
Asiimwe JB, Ndugga P, Mushomi J, Manyenye Ntozi JP. Factors associated with modern contraceptive use among young and older women in Uganda; a comparative analysis. BMC public health. 2014;14:926.
Nalwadda G, Mirembe F, Byamugisha J, Faxelid E. Persistent high fertility in Uganda: young people recount obstacles and enabling factors to use of contraceptives. BMC public health. 2010;10:530.
Hooja N, Mital P. Knowledge, Attitude And Practices Relating To Emergency Contraception Among College Girls And Their Mothers. Internet Journal of Gynecology and Obstetrics. 2012 Volume 16 Number 1
Cadmus E, Owoaje E. Patterns Of Contraceptive Use Among Female Undergraduates In The University Of Ibadan, Nigeria. Internet Journal of Health. 2009 Volume 10 Number 2.
Tura G, Alemseged F, Dejene S. Risky Sexual Behavior and Predisposing Factors among Students of Jimma University, Ethiopia. Ethiopian journal of health sciences. 2012;22(3):170–80.
PubMed PubMed Central Google Scholar
Tilahun D, Assefa T, Belachew T. Knowledge, attitude and practice of emergency contraceptives among adama university female students. Ethiopian journal of health sciences. 2010;20(3):195–202.
Parey B, Addison L, Mark JK, Maurice B, Tripathi V, Wahid S, et al. Knowledge, attitude and practice of emergency contraceptive pills among tertiary level students in Trinidad: a cross-sectional survey. The West Indian medical journal. 2010;59(6):650–5.
CAS PubMed Google Scholar
Moser AM, Reggiani C, Urbanetz A. [Risky sexual behavior among university students in health science courses]. Revista da Associacao Medica Brasileira. 2007;53(2):116–21.
Adinew YM, Worku AG, Mengesha ZB. Knowledge of reproductive and sexual rights among University students in Ethiopia: institution-based cross-sectional. BMC Int Health Hum Rights. 2013 Feb 13;13:12. doi: 10.1186/1472-698X-13-12.
Simbar M, Tehrani FR, Hashemi Z. Reproductive health knowledge, attitudes and practices of Iranian college students. Eastern Mediterranean health journal. 2005;11(5–6):888–97.
Srikanthan A, Reid RL. Religious and cultural influences on contraception. J Obstet Gynaecol Can. 2008;30(2):129–37.
Erena GM, Kerbo AA. Unwanted pregnancy and associated factors among female students of Madawalabu University Bale Zone, Oromia Region south east, Ethiopia. Science Journal of Public Health. 2015;3(1):50–5.
Dinas K, Hatzipantelis E, Mavromatidis G, Zepiridis L, Tzafettas J. Knowledge and practice of contraception among Greek female medical students. Eur J Contracept Reprod Health Care. 2008;13(1):77–82.
Abiodun OM, Baloqun OR. Sexual activity and contraceptive use among young female students of tertiary educational institutions in Ilorin, Nigeria. Contraception. 2009;79(2):146–9.
Ortiz-Ortega A, De La Torre GG, Galvan F, Cravioto P, Paz F, Diaz-Olavarrieta C, et al. Abortion, contraceptive use, and adolescent pregnancy among first-year medical students at a major public university in Mexico City. Rev Panam Salud Publica. 2003;14(2):125–30.
Download references
Acknowledgements
The work was supported by a grant from The Family Health Research and Development Centre (FHRDC) Uganda Supported by Bill & Melinda Gates Institute for Population & Reproductive Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA. We thank the study participants and acknowledge the team of research assistants and the staff at the Makerere University, Counseling and Guidance Centre. We are grateful for the administrative support from Ms. Christine Muhumuza, the center Coordinator, FHRDC.
Author information
Authors and affiliations.
Makerere University, Counseling and Guidance Centre, Kampala, Uganda
Henry Nsubuga
Makerere University, College of Health Sciences, School of Public Health, Kampala, Uganda
Juliet N. Sekandi, Hassard Sempeera & Fredrick E. Makumbi
Department of Epidemiology and Biostatistics, College of Public Health, University of Georgia, Athens, Georgia, USA
Juliet N. Sekandi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Henry Nsubuga .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contribution
HN: Designed the study, coordinated recruitment of participants and assured quality of data collection, participated in data analysis, and in writing of all drafts and the final manuscript JNS: Designed the study, coordinated recruitment of participants and assured quality of data collection, participated in data analysis and in writing of all drafts and the final manuscript. HS: Designed the study, participated in data analysis, and writing of drafts and the final manuscript. FEM: Participated in study design, led data analysis, and manuscript writing. All authors read and approved the final manuscript.
Authors’ information
Henry Nsubuga and Juliet N. Sekandi shared first authorship.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Nsubuga, H., Sekandi, J.N., Sempeera, H. et al. Contraceptive use, knowledge, attitude, perceptions and sexual behavior among female University students in Uganda: a cross-sectional survey. BMC Women's Health 16 , 6 (2015). https://doi.org/10.1186/s12905-016-0286-6
Download citation
Received : 29 April 2015
Accepted : 23 January 2016
Published : 27 January 2016
DOI : https://doi.org/10.1186/s12905-016-0286-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Contraceptives
- Female undergraduates
- Perceptions
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research note
- Open access
- Published: 13 August 2018
Knowledge, attitude and practice towards family planning among reproductive age women in a resource limited settings of Northwest Ethiopia
- Ayele Semachew Kasa ORCID: orcid.org/0000-0003-3320-8329 1 ,
- Mulu Tarekegn 1 &
- Nebyat Embiale 2
BMC Research Notes volume 11 , Article number: 577 ( 2018 ) Cite this article
69k Accesses
33 Citations
Metrics details
To assess the knowledge and attitude regarding family planning and the practice of family planning among the women of reproductive age group in South Achefer District, Northwest Ethiopia, 2017.
The study showed that the overall proper knowledge, attitude and practice of women towards family planning (FP) was 42.3%, 58.8%, and 50.4% respectively. Factors associated with the practice of FP were: residence, marital status, educational status, age, occupation, and knowledge, and attitude, number of children and monthly average household income of participants. In this study, the level of knowledge and attitude towards family planning was relatively low and the level of family planning utilization was quite low in comparison with many studies. Every health worker should teach the community on family planning holistically to increase the awareness so that family planning utilization will be enhanced. Besides, more studies are needed in a thorough investigation of the different reasons affecting the non-utilizing of family planning and how these can be addressed are necessary.
Introduction
Family planning (FP) is defined as a way of thinking and living that is adopted voluntary upon the bases of knowledge, attitude, and responsible decisions by individuals and couples [ 1 ]. Family planning refers to a conscious effort by a couple to limit or space the number of children they have through the use of contraceptive methods [ 2 ].
Family planning deals with reproductive health of the mother, having adequate birth spacing, avoiding undesired pregnancies and abortions, preventing sexually transmitted diseases and improving the quality of life of mother, fetus and family as a whole [ 3 , 4 ].
The Federal Ministry of Health (FMOH) has undertaken many initiatives to reduce maternal mortality. Among these initiatives, the most important is the provision of family planning at all levels of the healthcare system [ 5 , 6 ]. Currently, short-term modern family planning methods are available at all levels of governmental and private health facilities, while long-term method is being provided in health centers, hospitals and private clinics [ 6 ].
The study done in Jimma Zone, Ethiopia showed that good knowledge on contraceptives did not match with the high contraceptive practice [ 7 ]. Different researchers showed that the highest awareness but low utilization of contraceptives making the situation a serious challenge [ 8 , 9 ].
Most of reproductive age women know little or incorrect information about family planning methods. Even when they know some names of contraceptives, they don’t know where to get them or how to use it. These women have negative attitude about family planning, while some have heard false and misleading information [ 10 , 11 ] and the current study aimed in assessing the knowledge, attitude and practice (KAP) of FP among women of reproductive age group in South Achefer District, Northwest Ethiopia.
Methods and materials
Study design and setup.
A community-based cross-sectional study was conducted in South Achefer District, Amhara Region, Northwest Ethiopia from March 01–April 01, 2017. Systematic sampling technique was used to recruit the sampled reproductive age women (15–49 years old). Based on the number of households obtained from the Kebele’s (Smallest administrative division) health post, the sample size (389) was distributed to the households. The sampling interval was determined based on the total number of 4431 households in the kebele. The first household was taken by lottery method and if there were more than one eligible individual in the same household one was selected by lottery method.
The data collection questionnaire was developed after reviewing different relevant literatures. The questionnaire, first developed in English language and then translated to Amharic (local language). Pretest was done on 5% of the total sample size at Ashuda kebele. After the pretest, necessary modifications and correction took place to ensure validity.
Those reproductive age women who answered ≥ 77% from knowledge assessing questions were considered as having good knowledge, those women who scored ≥ 90% from attitude assessing questions were considered as having favorable attitude and those women who scored ≥ 64% from practice assessing questions were considered as having good over all practice towards FP [ 7 ].
Data processing and analysis
The collected data was cleaned, entered and analyzed using SPSS version 21 software. Descriptive statistics were employed to describe socio-demographic, knowledge, attitude and practice variables. Chi squared (χ 2 ) test was used to determine association between variables. Associations were considered statistically significant when P-value was, < 0.05.
Socio-demographic characteristics of participants
The response rate in this study was 97.9%. Among 381 participants included, 185 (49%) were from rural villages. About 47% of the participants were illiterate and 52% were completed primary education. The monthly household income of the majority (42.5%) of the participants was between 1000 and 3000 Ethiopian birr. Regarding the family size of the participant’s, majority (48.3%) of them had ≥ 3 children.
The mean age of participants was 29.7 ± 6.4. Two hundred forty six (64.6%) and 133 (34.9%) were house wife’s and farmers respectively by their occupation. Almost two-third (65.4%) of participants were married, 24.9% were divorced by their marital status (Table 1 ).
Knowledge status of participants
All of participants ever heard about family planning methods. The major sources of information were from health workers (57.5%) and radio (41.5%). Regarding perceived side effects of using family planning, 13.1%, 24.9%, 9.7% and 52.2% of participants were responded heavy bleeding, irregular bleeding, an absence of menstrual cycle and abdominal cramp respectively were mentioned as a side effect. Among those who have children; 24.6% gave their last birth at home and 75.5% gave their last birth at the health institution. Regarding the overall knowledge of study participants, 161 (42.3%) had good knowledge towards family planning and the rest 220 (57.7%) had poor knowledge.
Attitude status of participants
The majority (88.5%) of the respondents ever discussed on family planning issues with their partners and wants to use it in the future. About 24.5% of the participants reported that they believe family planning exposes to infertility. Almost 23 (22.8%) of study participants reported that using family planning contradicts with their religion and culture. Regarding the overall attitude, 224 (58.8%) of the participants had favorable attitude and 157 (41.2%) had unfavorable attitude towards family planning.
Practice on family planning
Three fourth (75.3%) of study participants ever used contraceptive methods. The main types were pills (7.4%) and injectable (77.2%). The most common current reasons for not using were a desire to have a child (53.2%) and preferred method not available (46.8%). Almost half (50.4%) of study participants had good practice and the rest 49.6% had poor practice.
Factors associated with family planning practice
Study participants’ religion was not included in the analysis due to lack of variance, since almost all (99.2%) of participants were Orthodox Christians by their religion.
Women who had good knowledge were more likely to practice FP than those who have low knowledge (χ 2 = 117.995, d.f. = 1, P < 0.001) and women who had favorable attitude towards FP were more likely to practice FP (χ 2 = 106.696, d.f. = 1, P < 0.001). It was also seen that residence, age, educational status, occupation, marital status, number of children and monthly income of the were significantly associated with the practice of FP [(χ 2 = 69.723, d.f. = 1, P < 0.001), (χ 2 = 104.252, d.f. = 2, P < 0.002), (χ 2 = 119.264, d.f. = 1, P < 0.001), (χ 2 = 41.519, d.f. = 1, P < 0.001), (χ 2 = 39.050, d.f. = 1, P < 0.001), (χ 2 = 144,400, d.f = 3, P < 0.001) and (χ 2 = 179.366, d.f. = 1, P < 0.002)] respectively (Table 2 ).
Increasing program coverage and access of family planning will not be enough unless all eligible women have adequate awareness for favorable attitude and correctly and consistently practicing as per their need. Increasing awareness/knowledge and favorable attitude for practicing FP activities at all levels of eligible women are strongly recommended [ 6 ].
The results of the present study showed that 42.3% of study participants had good knowledge, 58.8% had favorable attitude, and 50.4% had good practice towards family planning. This finding was lower than a study conducted in Jimma zone, Southwest Ethiopia [ 7 ], Sudan [ 9 ], Tanzania [ 12 ] and another study done in Rohtak district, India [ 13 ]. The difference may be due to; studies done in Jimma zone, Sudan, Tanzania and Rohtak district involve only those coupled/married women. Married women might have good knowledge and attitude for practicing family planning. But in the current study, all women of reproductive age group regardless of their marital status were studied and this may lower their knowledge and attitude.
The current study showed that, 50.4% of reproductive age women were practicing family planning which was almost in line with a study done in Cambodia [ 14 ] and higher than a study done in rural part of Jordan [ 15 ] and India [ 16 ]. But it was lower than studies conducted in Jimma zone, Ethiopia [ 7 ], Rohtak district, India [ 13 ], urban slum community of Mumbai [ 17 ] and in Sikkim [ 18 ] in which 64%, 62%, 65.6% and 62% of participants respectively used family planning. The difference might be due to that study participants in Jimma zone, Rohtak and Mumbi were relatively residing in large city/town and this may help them to have a better access for family planning compared to the study done in South Achefer District.
In the current study, urban residents were more likely to use family planning methods (71.4%) than their rural counterparts (28.1%). This finding was in line with the findings from Ethiopian Demographic Health Survey (EDHS) [ 2 ]. This might be due to the reason that urban residents are more aware of family planning and hence practicing better.
It has also found that women who completed primary & secondary education were practicing family planning than those who were uneducated (77.1% and 20.6%) respectively. This finding was in line with a study done in Jimma, Ethiopia [ 19 ]. This might be due to the fact that women who were able to read and write would think in which FP activities are useful to be economically, self-sufficient and more likely to acquire greater confidence and personal control in marital relationships including the discussion of family size and contraceptive use.
This study showed that, age of the study participants had an association with practicing FP. Those reproductive age women’s whose age > 30 years were practicing family planning better than those whose age < 18 years. This finding was in line with a study done in India [ 20 ]. This might be due to the reason that, when age increases mothers awareness, attitude and practice towards family planning may increase. In addition, as age increases the chance of practicing sexual intercourse increases and as a result they would be interested to utilize family planning in one or another way.
It has also revealed that women’s average monthly household income has an association with their FP practicing habit. Those study participants whose average monthly income < 1000 ETB were using FP better than whose average monthly income > 3000 ETB. This is might be because those relatively who had better income may need more children and those with low income may not want to have more children beyond their income.
The current study also showed that knowledge and attitude of reproductive age women were related to FP utilization. Those reproductive age women who had good knowledge were utilized FP better than from those who were less knowledgeable. Those participants with favorable attitude were practicing better than those who had unfavorable attitude. This is might be due to the fact that knowledge and attitude for specific activities are the key factors to start behaving and maintaining it continuously.

Conclusion and recommendation
The level of knowledge and attitude towards family planning was relatively low and the level of family planning utilization was quite low in comparison with many studies.
Study participant’s residence, marital status, educational level, occupation, age, knowledge, attitude, their family size and their monthly average income were associated with FP utilization habit of reproductive age women.
Every health worker should teach the community on family planning holistically to increase the awareness so that family planning utilization will be enhanced.
Besides, more studies are needed in a thorough investigation of the different reasons affecting the non-utilizing of family planning and how these can be addressed are necessary.
Limitation of the study
As the data were collected using interviewer administered questionnaire, mothers might not felt free and the reported KAP might be overestimated or underestimated.
We do not used qualitative method of data collection to gather study participant’s internal feeling about family planning, so that triangulation was possible. In addition, barriers for utilizing contraception not addressed.
Abbreviations
Ethiopian Demographic Health Survey
Ethiopian birr
Federal Ministry of Health
family planning
knowledge, attitude and practice
World Health Organization. Standards for maternal and neonatal care. Geneva: World Health Organization; 2006.
Google Scholar
Central Statistical Agency. Ethiopian Demographic and Health Survey 2016 key indicators report. Addis Ababa and Maryland, Ethiopia; 2016.
World Health Organization. Fact sheets on family planning, World Health Organization. https://www.cycletechnologies.com/single-post/2017/02/14/World-Health-Organization-Updated-Family-Planning-Contraception-Fact-Sheet . Accessed 8 Feb 2018.
United Nations. World contraceptive use, 2009 wall chart. New York United Nations Population Division: United Nations; 2009. http://www.un.org/esa/population/publications/contraceptive2009/contracept2009_wallchart_front.pdf . Accessed 3 Mar 2018.
Central Statistical Agency. Ethiopia Mini Demographic and Health Survey 2014. Addis Ababa; 2014. http://www.dktethiopia.org/publications/ethiopia-mini-demographic-and-health-survey-2014 . Accessed 12 Feb 2018.
Federal Ministry of Health. National Guideline for Family Planning Services in Ethiopia; 2011. http://www.moh.gov.et/documents/20181/21665/National+Family+Planning+Guideline_Ethiopia_2011.pdf/ . Accessed 17 Feb 2018.
Tilahun T, Coene G, Luchters S, Kassahun W, Leye E. Family planning knowledge, attitude and practice among married couples in Jimma Zone, Ethiopia. PLoS ONE. 2013;8(4):e61335.
Article PubMed PubMed Central CAS Google Scholar
Menhaden AL, Khalil AO, Hamdan-Mansour AM, Sato T, Imoto A. Knowledge, attitudes, and practices towards family planning among women in the rural southern region of Jordan. East Mediterr Heal J. 2012;18(6):1–6.
Handady SO, Naseralla K, Sakin HH, Alawad AAM. Knowledge, attitude, and practice of family planning among married women attending primary health centerin Sudan. Int J Public Heal Res. 2015;3(5):243–7.
Gaur DR, Goel MK, Goel M. Contraceptive practices and related factors among female in predominantly rural Muslim area of North India. Internet J World Heal Soc Polit. 2008;5(1):1–5.
Oyedokun AO. Determinants of contraceptive Usage: lessons from Women in Osun State, Nigeria. J Humanit Soc Sci. 2007;1:1–14.
Lwelamira J, Mnyamagola G, Msaki MM. Knowledge, attitude and practice (KAP) towards modern contraceptives among married women of reproductive age in Mpwapwa District, Central Tanzania. Curr Res J Soc Sci. 2012;4(3):235–45. https://www.researchgate.net/publication/299488265 . Accessed 9 Feb 2018.
Gupta V, Mohapatra D, Kumar V. Family planning knowledge, attitude, and practices among the currently married women (aged 15–45 years) in an urban area of Rohtak district, Haryana. Int J Med Sci Public Heal. 2016;5(4):627–32.
Article Google Scholar
Sreytouch Vong. Knowledge, attitude and practice (KAP) of Family planningamong married women in BanteayMeanchey. Cambodia: Ritsumeikan Asia Pacifi c University; 2006.
Mahadeen AI, Khalil AO, Sato T, Imoto A. Knowledge, attitudes and practices towards family planning among women in the rural southern region of Jordan. East Mediterr Heal J. 2012;18(6):567–72.
Article CAS Google Scholar
Quereishi MJ, Mathew AK, Sinha A. Knowledge, attitude and practice of family planning methods among the rural females of Bagbahara block Mahasamund district in Chhattishgarh State, India. Glob J Med Public Heal. 2017;6(2):1–7. http://www.gjmedph.com . Accessed 5 Mar 2018.
Khan MM, Shaikh STSA. Study of knowledge and practice of contraception in urban slum community, Mumbai. Int J Curr Med Appl Sci. 2014;3(2):35–41.
Prachi R, Das GS, Ankur B, Shipra J, Binita K. A study of knowledge, attitude and practice of family planning among the women of reproductive age group in Sikkim. J Obs Gynecol India. 2008;58(1):63–7. https://www.researchgate.net/publication/228480182 . Accessed 16 Apr 2018.
Beekle AT. Awareness and determinants of family planning practice in Jima, Ethiopia. Int Nurs Rev. 2006;53:269.
Article PubMed CAS Google Scholar
Mohanan P, Kamath ASB. Fertility pattern and family planning practices in rural area in dakshina Kannada. Indian J Com Med. 2003;28:15–28.
Download references
Authors’ contributions
AS: approved the proposal with some revisions, participated in data analysis. MT: wrote the proposal, participated in data collection analyzed the data and drafted the paper. NE: approved the proposal with some revisions, participated in data analysis. All authors read and approved the final manuscript.
Acknowledgements
We are very grateful to all study participants for their commitment in responding to our questionnaires.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent to publish
Ethics approval and consent to participate.
Ethical clearance was obtained from the Ethical Review Committee of Bahir Dar University, College of Medicine & Health Sciences, and School of Nursing. The objective and purpose of the study were explained to officials at the Woreda and Kebele (smallest governmental administrative division) and a written permission consent was obtained from the study participants. For those study participants whose age is below 18 years consent to participate in the study was obtained from their parent during the data collection time.
No fund was received.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Department of Nursing, College of Medicine & Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Ayele Semachew Kasa & Mulu Tarekegn
Department of Surgery, School of Medicine, College of Medicine & Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Nebyat Embiale
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ayele Semachew Kasa .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Semachew Kasa, A., Tarekegn, M. & Embiale, N. Knowledge, attitude and practice towards family planning among reproductive age women in a resource limited settings of Northwest Ethiopia. BMC Res Notes 11 , 577 (2018). https://doi.org/10.1186/s13104-018-3689-7
Download citation
Received : 28 June 2018
Accepted : 06 August 2018
Published : 13 August 2018
DOI : https://doi.org/10.1186/s13104-018-3689-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family planning
BMC Research Notes
ISSN: 1756-0500
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Perceptions of family planning services and its key barriers among adolescents and young people in Eastern Nepal: A qualitative study
Roles Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation B.P. Koirala Institute of Health Sciences, Dharan, Nepal
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
Affiliation Department of Health Services, Ministry of Health and Population, Kathmandu, Nepal
Roles Data curation, Formal analysis, Writing – original draft, Writing – review & editing
Affiliation Nepal Health Sector Support Programme (NHSSP)/DFID/Ministry of Health and Population, Kathmandu, Nepal
Roles Formal analysis, Writing – original draft, Writing – review & editing
Affiliation Central Department of Public Health, Institute of Medicine, Kathmandu, Nepal
Roles Data curation, Formal analysis, Writing – review & editing
Affiliation Department of Electronics and Computer Engineering, Institute of Engineering, Tribhuvan University, Lalitpur, Nepal
Affiliation Department of Community Health Sciences, School of Public Health, Patan Academy of Health Sciences, Lalitpur, Nepal
Affiliation School of Public Health and Community Medicine, B.P. Koirala Institute of Health Sciences, Dharan, Nepal
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliation Department of Primary Care and Public Health, School of Public Health, Imperial College London, London, United Kingdom
- Navin Bhatt,
- Bandana Bhatt,
- Bandana Neupane,
- Ashmita Karki,
- Tribhuwan Bhatta,
- Jeevan Thapa,
- Lila Bahadur Basnet,
- Shyam Sundar Budhathoki

- Published: May 26, 2021
- https://doi.org/10.1371/journal.pone.0252184
- Reader Comments
Introduction
Family planning methods are used to promote safer sexual practices, reduce unintended pregnancies and unsafe abortion, and control population. Young people aged 15–24 years belong to a key reproductive age group. However, little is known about their engagement with the family planning services in Nepal. Our study aimed to identify the perceptions of and barriers to the use of family planning among youth in Nepal.
A qualitative explorative study was done among adolescents and young people aged 15–24 years from the Hattimuda village in eastern Nepal. Six focus group discussions and 25 in-depth interviews were conducted with both male and female participants in the community using a maximum variation sampling method. Data were analyzed using a thematic framework approach.
Many individuals were aware that family planning measures postpone pregnancy. However, some young participants were not fully aware of the available family planning services. Some married couples who preferred ’birth spacing’ received negative judgments from their family members for not starting a family. The perceived barriers to the use of family planning included lack of knowledge about family planning use, fear of side effects of modern family planning methods, lack of access/affordability due to familial and religious beliefs/myths/misconceptions. On an individual level, some couples’ timid nature also negatively influenced the uptake of family planning measures.
Women predominantly take the responsibility for using family planning measures in male-dominated decision-making societies. Moreover, young men feel that the current family planning programs have very little space for men to engage even if they were willing to participate. Communication in the community and in between the couples seem to be influenced by the presence of strong societal and cultural norms and practices. These practices seem to affect family planning related teaching at schools as well. This research shows that both young men and women are keen on getting involved with initiatives and campaigns for supporting local governments in strengthening the family planning programs in Nepal.
Citation: Bhatt N, Bhatt B, Neupane B, Karki A, Bhatta T, Thapa J, et al. (2021) Perceptions of family planning services and its key barriers among adolescents and young people in Eastern Nepal: A qualitative study. PLoS ONE 16(5): e0252184. https://doi.org/10.1371/journal.pone.0252184
Editor: Mary Hamer Hodges, Helen Keller International, SIERRA LEONE
Received: June 27, 2020; Accepted: May 12, 2021; Published: May 26, 2021
Copyright: © 2021 Bhatt et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: BPKIHS, B. P. Koirala Institute of Health Sciences; FP, Family Planning; FGD, Focus Group Discussion; IDI, In-Depth Interview; mCPR, Modern Contraceptive Prevalence Rate; SRH, Sexual and Reproductive Health
An unmet need for family planning results in unintended pregnancies and illegal abortions. This has major health and social implications and is often the leading cause of maternal and child mortality in low-income countries [ 1 , 2 ]. An estimated 214 million women of reproductive age lack access to contraception resulting in an estimated 67 million unintended pregnancies, 36 million induced abortions, and 76,000 maternal deaths each year [ 3 ]. Family planning (FP) is a key intervention to limit these adverse health outcomes [ 4 – 6 ]. Such interventions can prevent 90% of abortions, 32% of maternal deaths, 20% of pregnancy-related morbidity globally, and reduce 44% of maternal mortality in low-income countries [ 1 , 7 ]. FP reduces adolescent pregnancies, prevents pregnancy-related health risks, and helps to prevent HIV/AIDS [ 8 ]. Access to contraception promotes education, raises the economic status of women, and gradually empowers them resulting in improved health outcomes and better quality of life [ 3 , 5 , 9 , 10 ].
Global data show that only 32% of married women from low-income countries currently use modern contraceptives [ 9 ]. According to the Nepal Demographic Health Survey 2016, the total fertility rate was 2.3 births per woman, which is declining and approaching replacement fertility. This is an important achievement. However, the modern contraceptive prevalence rate (mCPR), which is 43%, is still below the target in Nepal [ 11 ]. Nepal has consistently failed to reach the target of mCPR for the past 20 years. The future projection of mCPR for 2030 is 60% [ 5 ], which may be a distant dream if the barriers and enablers are not identified on time to strengthen the current efforts.
Expanding the coverage and access to effective contraceptive methods are essential to meet the Sustainable Development Goals and to achieve universal access to reproductive healthcare services by 2030 [ 11 , 12 ]. For this, the government of Nepal has started a FP program with a focus on increasing the use of FP services and reducing the unmet need [ 5 , 11 ]. However, various factors negatively influence the delivery of FP services including lack of information, limited awareness of dissemination activities, lack of trained staff, and various cultural and religious factors [ 13 ].
Family planning is a choice for many youth, but they often experience barriers such as negative provider attitudes, long distances to healthcare facilities, and inadequate stock of preferred contraceptives [ 13 , 14 ]. Nepali youth are reluctant to use modern contraceptives due to misconceptions about long-term fertility risks, fear of side effects and overall lack of deeper knowledge [ 15 , 16 ]. Besides, FP decisions are mostly dependent on male household members, including husbands and other elder members [ 17 , 18 ]. Married women whose husbands are away as migrant workers face unique contraceptive challenges. When their husbands return home for a few weeks in a year, these women are not prepared with their contraceptives, which can result in unwanted pregnancies [ 18 ].
The extrapolation of the available literature on FP use among adults from Nepal and elsewhere suggests that youth is an under-researched population when it comes to FP There is also a dearth of evidence on perception and key barriers to the use of FP measures in this population. Hence, this study aims to identify the perceptions of the FP services and barriers to the use of FP among the youth in Nepal to assist policymakers in designing appropriate interventions to strengthen the family planning programs in Nepal.
Material and methods
Ethical considerations.
The study received ethical approval from the Institutional Review Committee of B.P. Koirala Institute of Health Sciences, Dharan, Nepal as per the Undergraduate Research Proposal review process (URPRB/01/015). We obtained informed written consent from all participants aged 18 and above. For minors, we obtained assent from the parents of the participants with the participants’ permission. For those who could not read, the information sheet was read aloud by a volunteer, verbal consent was given, and a thumbprint, in the presence of a witness, was used in place of a signature. To maintain the confidentiality of the information and the privacy of the participants, only selected participants and the moderators attended the sessions. Personal identifiers and locator information were not collected, and any identifying information accidentally mentioned was removed from the text before the analysis.
Study setting
The study was conducted among the participants from Hattimuda village of Morang district in Province One of Nepal. Hattimuda village is a community service area of B.P. Koirala Institute of Health Sciences (BPKIHS), Dharan, Nepal. BPKIHS is a public-funded health sciences university, which follows a teaching district concept adopted as a part of its community-based medical education curriculum. BPKIHS also runs a tertiary hospital service for the population of eastern Nepal [ 19 ]. There is a public health facility in Hattimuda village that provides primary health care services including FP services such as the distribution of contraceptives. The nearest secondary and tertiary levels of healthcare services are available 18 kilometers away in Biratnagar, which is the provincial capital and the headquarters of Morang district. According to the 2017/18 annual report of the Department of Health Services, the contraceptive prevalence rate of Morang district is 54.6% [ 5 ] whereas the unmet need for FP in Province One as per the Nepal Demographic Health Survey 2016 is 25% [ 11 ].
Study design
This was a qualitative study with an exploratory design to gather a deeper understanding of the perception of FP and its barriers. Focus group discussions (FGD) and in-depth interview (IDI) methods were used. The overall study lasted from November 2017 to October 2018.
Study population and sampling technique
Adolescents and young people between 15 and 24 years of age from Hattimuda were included in the study. We used the maximum variation sampling method to enroll participants. Pretesting, including one FGD and four IDIs, was conducted among residents in another village of the same district. The pretesting guided the selection of participants for FGDs and IDIs. Accordingly, FGDs were conducted among adolescents and young people, separately for male and female participants to allow for free expression of views during the discussion of potentially sensitive issues. Moreover, the respondents recommended that people at the forefront of the community such as the village leaders, schoolteachers, community health volunteers, religious leaders, youth leaders, and students be selected for the interviews to gather more information. Along with the recommendations from the pretesting, brainstorming was done with community volunteers to generate a list of people who understood the issues of adolescents and young people. More volunteers were added to the list upon the recommendation of the initial respondents. Thus, participants representing diverse backgrounds in terms of gender, profession, education, and social status, were selected. The IDIs were done among 25 prominent people in the community, which included leaders, school teachers, female community health volunteers, healthcare professionals working at the health post and FP service centers, and youth leaders from youth clubs. Health care providers were included in the interviews as their views would be invaluable due to their experience as FP service providers and as witnessing the health issues faced by youth. The teachers are regarded highly for their knowledge and opinions in Nepali communities. So, they were selected for the IDI to provide more insight into the educational barriers to FP and to help in youth mobilization for FP activities. Considering the vital role of local leaders in influencing the implementation and regulation of population-level activities in the village, they were selected for IDI. Six focus groups were conducted with a total of 48 respondents ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0252184.g001
Data collection
The Focus Group Discussions (FGD) and In-depth interviews (IDI) were conducted by the researchers within the team with prior experience in qualitative research methods. The interview team included an undergraduate medical student, two postgraduate resident doctors, a public health graduate, and a public health academic researcher. Before data collection, an orientation session was conducted for the interviewers using the interview schedule and the topic guide. The IDI guidelines and interview schedules were developed from the literature review and were modified after pretesting. Validation of the tools was ensured by using the Item Objective Congruence (IOC) index and consultation with academics with experience in FP research. Using a semi-structured open-ended questionnaire, the participants were assessed on their knowledge and perceptions regarding sexual and reproductive health (SRH) and FP, SRH problems faced by youth, challenges and barriers to use of FP services, the role of youth in combating the perceived challenges, and suggestions for enhancing the use of services. Data were considered to have reached saturation when the responses from participants became repetitive and/or no new responses were received.
Focus group discussions.
A representative group of youth from diverse backgrounds who could provide credible information about practices and factors affecting the use of FP in the community was selected. Separate FGDs were held for girls and boys to allow for free expression. A moderator was responsible for guiding the discussion and a note-taker for taking the notes, including recording non-verbal responses and ensuring the audio recording. A total of 6 FGDs, each containing 8 homogenous participants, were conducted. Each individual participated once in the FGD. Every member of the group could make their contribution to any question posed before proceeding to another question. Each FGD lasted for 60–90 minutes on average. The discussion was done in the Nepali language as preferred by participants and later translated into English during transcription.
In-depth interviews.
In-depth interviews with the key stakeholders were conducted using the Interview Schedule after obtaining the informed consent and audio-recorded with participant permission. A total of 25 IDIs were conducted for the average duration of 30–45 minutes, at a location convenient to the participant, which included their homes and offices.
Data management and analysis
A framework method of thematic analysis was used. The analysis included stages of transcription, familiarization with the interview, coding, developing a working analytical framework, applying the analytical framework, charting the data into the framework matrix, and interpretation of the data. The data collected from the focus groups and interviews were transcribed verbatim. The notes taken were used as a guide to segregate the responses by different respondents during the discussion. An independent researcher conversant in the Nepali and English languages cross-checked the transcripts for accuracy and preservation of original meaning during translation. Preliminary codes were assigned to the available data and then organized into thematic units that were continually revisited and revised as necessary. To ensure consistency of data and findings, two authors were involved in data analysis and reporting. The recordings were stored and accessed by the research team only and were destroyed after the analysis and final report preparation.
Operational definition
According to UNFPA, all persons within the age of 15–24 years are considered youth [ 20 ].
The baseline characteristics of the participants can be seen in Table 1 .
https://doi.org/10.1371/journal.pone.0252184.t001
The responses from the IDIs and FGDs revealed four broad themes. Within each broad theme were several substantive sub-themes that emerged from the data. The themes and subthemes are summarized in Table 2 below.
https://doi.org/10.1371/journal.pone.0252184.t002
Theme 1: Knowledge and perceptions of FP
A) knowledge and sources of information on fp..
Participants demonstrated awareness of some form of FP. However, some knew nothing about it. Health workers were commonly referred to as the sources of information, while some also mentioned peers, radio, television, and books. Male participants openly disclosed their sources of information on FP while some female participants were reluctant to share their sources.
b) Perceptions of FP.
Perceptions of FP varied among participants. Some male participants inferred FP measures as women’s business and did not show any interest in talking more about it. Some referred to FP as using condoms during intercourse, while others referred to oral pills and injectable hormones as FP. Some female participants looked at FP as a way of avoiding unwanted pregnancies.
“My sister used to say that she has been using injection (Depo-Provera) to control unwanted pregnancy . I think FP is about the same . ”- 19 years Female , FGD participant
Theme 2: Preference for FP methods and decision-making
Some female participants reported preference for traditional methods of contraception such as coitus interruptus and calendar method over modern methods. These people used modern methods of FP to start with, which they discontinued later due to the side effects. Participants also stated that the health facilities that provide FP services were far, and hence they had no alternative other than natural methods. Male participants hardly mentioned visiting any health facilities for FP purposes.
“Most of our clients who come for it (FP) are women. Even condoms are collected by women. Men rarely come alone or as couples for FP services.” - 35 years old Female, FP service provider, IDI participant
Yet husbands were responsible for the decision-making about FP and choices of methods for most couples. Some participants (both male and females) mentioned that women rather than men should use permanent FP measures. They believed that men being the breadwinner of the family, should not undergo sterilization, for example, as it would make them physically weak.
“Though I love my wife and I am concerned about her. But I have no options. I must work in a factory. I need to lift heavy weights there. All the major house chores are also done by me. These things (sterilization) would make me weak. How can I earn my livelihood then?”- 22 years Male, FGD participant
Some female participants expressed their concerns regarding the use of permanent FP methods. They mentioned that they had already been through various phases of pain, be it during menstruation, pregnancy, or delivery which has made them weak. Thus, they prefer their husbands to undertake any measures.
In contrast, unmarried participants stated that they would rather discuss and decide together with their partners regarding which method to choose in the future. Despite this interest, women were not sure how to engage their husbands in discussion. Some female participants said that they could not persuade their future husbands to use contraceptives as it would be disrespectful, whereas a few male participants believed it was a woman’s responsibility to use FP methods.
“It (FP) is stuff to be done by the women . So , there is no doubt about who would be doing it . Moreover , people would laugh at me if I do it -20 years Male , FGD participant “ Women have already gone through much pain in bringing up and taking care of the children and again keeping this stuff (FP) in their head is unjustifiable . As such, in comparison to the female operative procedure, I have heard that the male one is simple, less time consuming, and does not bring many complications . So, why not we men take the lead on this? ” -25 years Male, Youth leader, IDI participant
Theme 3: Barriers and challenges in the use of FP
A) supply-side barriers and challenges..
Participants indicated that contraceptive services are not always accessible nor affordable in rural areas. Health facilities are far, and many people feel reluctant to travel in a hot climate. Participants who were reluctant to travel said they were doubtful that the health facilities would have the methods in stock even if they managed to walk the distance. Others who were reluctant said they would be unable to afford the contraceptives from a private medical store regularly. A few participants raised the issue of privacy and unavailability of all services at the health centers. Similarly, young males from the community complained that the services at the health post were focused only on mothers and married couples, while the boys and the unmarried people were not given much attention. For this, they suggested changing the term to something other than FP because they believed that FP should include not only those who had families.
Participants expressed their frustration that FP and SRH services in their village had not been running well for more than a year. They felt that the government was not doing anything about it either. Some students expressed the need for an integrated curriculum at school covering every aspect of SRH and FP that would ensure adequate and proper knowledge of such crucial subjects. Despite the students’ desire to learn and understand FP, their teachers are often reluctant to talk about FP in detail. The participants also indicated that family members, in general, forbid girls and women from getting involved in FP awareness activities.
“Though we are eager to learn about those lessons (reproductive organs and health), our teacher skips them. They tell us to read it by ourselves.” -18 years Female, FGD participant
b) Demand-side barriers and challenges.
A few participants were confused about which method to choose, how to use it properly and did not even know where to seek FP services locally.
“My husband works abroad. Last year, when he came home during Dashain (festival), we had (intercourse). Later, he returned to his workplace. Meanwhile, I came to know that I was pregnant, after 3 months. I was shocked to hear that. We already had 3 children; 2 of them were unplanned. I did not have enough information about contraceptive measures in this situation. Had I known about them; I would have used them. I had serious trouble travelling to get it aborted.” - 24 years Female, FGD participant
Some female participants expressed their reluctance to use FP methods due to their own or other people’s past experiences and the fear of side effects, including vaginal bleeding, spotting, abdominal pain, nausea, vomiting, headache, acne, and infertility. These female participants expressed the need for a single-use FP method with fewer side effects for women which could be used without their husbands’ consent. The male participants were worried about the risk of unwanted pregnancy due to the breaking of condoms and a few participants also expressed concern that they experienced allergic reactions after the use of condoms. Moreover, they were concerned about not having any alternative methods of contraception other than condoms.
“I have a much bitter experience. I was using Depo injection before. But I started having over bleeding for which I was admitted to the hospital for a few days. Later, I was switched to implants but they also did not suit me. In between I also used pills, but they aggravated my acne and I was feeling nauseated every day. Uff…. I am fed up now. I swear, I won’t ever use any methods.” - 19 years Female, FGD participant “I have heard that keeping these things (Copper-T) in the uterus can cause cancer. Better to avoid it.” - 20 years Female, FGD participant “There aren’t many choices for men. I think using a condom during sex is like tying plastic around the tongue and eating food.” - 21 years Male, IDI participant
Religious and ethnic variation affected use of FP. Participants reported that people belonging to upper caste groups used FP measures more than lower caste groups. Likewise, people who had migrated from the hilly areas used FP services, whereas people from the local ethnic community did not use as they were less aware of it. FP decisions among young people seem to be influenced largely by religious beliefs, stigma, and the perceived role of men and women based on existing social norms. Some participants regarded children as a gift from God and denied using any FP methods. Some believed using FP was going against the law of nature, religion, and culture; thus, they would not avoid childbirth, but rather celebrate every birth. Some indicated that if couples did not have children within 1–2 years of marriage, then people would question the woman’s fertility. Most couples preferred sons to daughters as they believed sons would look after them and their property, while the daughters would be married and sent away, resulting in avoidance of FP measures until they have a son. Some couples even wished to have two sons because if anything unfortunate happened to one, the other son would still be with them to carry the generation forward.
“My aunt gave birth to a son after 5 successive daughters. She is pregnant again this time in the hope to have a son. She says that she cannot trust to have only one son because if anything happens to their only son, then she will have no one to pay tribute after her death.”- 22 years Female, FGD participant
Participants also said that people felt shy talking about FP openly. Female participants also felt uncomfortable asking for contraceptives with male health personnel at the health post. Similarly, teachers felt uncomfortable teaching about reproductive health and FP as their children and relatives could be present as students in the classroom. Participants indicated that some students would laugh and smile, making it difficult for the teachers to run the classroom sessions smoothly.
It was reported by a FP service provider that some men opposed their wives using any FP measures as they perceived that the use of FP measures allowed their wives to become promiscuous when they go abroad for work.
“Some husbands working abroad forbid their wives from using any FP measures because they fear the use of FP measures may provoke a sexual relationship with someone else in their absence”- 30 years Female, Health professional providing medical abortion services, IDI participant
Theme 4: Role of youth and suggestions to improve FP
The youth were interested in getting involved in a “peer to peer education” approach to increase awareness among the community about FP use. This approach would include peer training programs, role-plays/dramas, and counseling sessions to break the key barriers linked with such services. Activities ranging from redesigning the school’s curriculum to strengthening FP services in primary care centers, and from launching mobile outreach clinics to facilitating “spousal communication” were intended to change attitudes and support gender equality in sexual and reproductive health. Participants emphasized forming youth centers and collaborating with other youth clubs in the village. Furthermore, they suggested bringing religious leaders, teachers, doctors, and politicians as advisors of the youth centers would be beneficial as they are influential members of the community.
“I feel bad for my sister who is not given much importance from my parents. She got married against her choice due to her parents’ pressure. Now, they are forcing her to have kids. She is just 15 and if she gets pregnant, what will happen to her health and her child, how can she take care of a baby? I had a long debate with my father yesterday. I have now decided to start a youth club to promote awareness regarding FP and preventing early marriage and teenage pregnancies.” - 23 years Male, FGD participant
Male participants indicated that family planning programs are effective only when men prioritize women’s autonomy. Moreover, they expressed disappointment with the local government for not encouraging the involvement of men in FP programs in their village. To help address this issue, they expressed their interest in supporting the local government in bringing inclusive FP programs to their village.
“For a long time, women have been using those (Contraceptives) by hiding. We are always in fear about what others would say if they came to know about us using it. This can be addressed through male involvement and support.” -24 years Female, FGD participant
This qualitative study provides in-depth information on the understanding and perceptions of youth in Eastern Nepal regarding FP. This study generated findings regarding knowledge and perceptions of rural residents regarding FP and its methods; decision-making and preference among participants; supply-side and demand-side barriers and challenges regarding the use of FP measures; steps that can be taken to improve their use; and the role of youth in increasing FP coverage. Although most participants knew something about FP, a few female participants were completely unaware of it. And while some participants agreed that all married couples should be using FP measures, some unmarried male participants believed that those measures should be exclusively for women. These men said that they would let their wives use them after getting married. Current FP methods for men are either coitus-dependent, such as condoms or withdrawal, or permanent, such as vasectomy. Limited choices for men may have resulted in misconceptions that contraceptives are mostly for women.
Men often claimed to be the sole decision-maker of the family on important matters, including those related to family health and contraception. In most circumstances, men solely decide the FP measure to be used without having a discussion with their partner. This might be one of the reasons why women are bound to adopt a FP method that is not necessarily their choice. Besides, this problem is further reinforced by the limited options of FP methods available for men other than condoms and permanent sterilization. These findings are supported by other studies in South Asia, where family planning measures are mostly considered women’s responsibility [ 21 – 24 ]. Health workers, peers, and mass media were the most common sources of information regarding FP similar to prior studies in India [ 21 , 24 ] and Nepal [ 22 ]. Participants in this study seemed to assign FP responsibility to the other gender in terms of using FP. This could mean that there is a gap in communication within the couples when deciding about FP. There is a need for further research to identify ways to improve communication among couples.
Religious and ethnic variation influence FP use. People belonging to privileged ethnic groups used FP measures more than underprivileged groups. This is despite family planning services being free for all citizens in Nepal. In this study, people who had migrated from hilly regions knew about and used FP services more than those belonging to the ethnic community in the local region. This is an area for further research to understand differences in knowledge and perceptions regarding FP between the population groups. This can be argued as a limitation of the current FP promotion programs, which may not have considered the different needs of people from different religious and ethnic backgrounds [ 25 ]. A few participants reported that their holy scriptures forbade them from using FP methods as they viewed children as a gift from God; any artificial process interrupting pregnancy or preventing the possibility of life is a religious offense for them [ 26 ]. Previous studies from Nepal have shown that this belief has long been rooted in some communities [ 27 – 29 ].
Apart from religious beliefs, fear of side effects, having experienced adverse health consequences after using hormonal contraceptives, and fear of potential infertility in the future are reasons for reluctance using FP methods among women [ 30 ]. Besides, we can speculate that language and cultural barriers, and fear of discrimination especially by male counterparts negatively influence the use of FP measures among some women despite their strong interest in using them. The use of IEC materials in raising awareness and empowering married couples for shared decision-making could help generate demand [ 28 , 29 ]. Local cultural taboos restrict open communication about safer sex measures and sexual health in Nepal, prohibiting young girls and boys from receiving adequate information and guidance regarding sexual and reproductive health and FP [ 31 ].
Most of the married women and men stated that the decision-makers of the family are men. The husband decides whether or not to use contraception, or more specifically, whether or not to let their wives use it. However, unmarried participants expressed their willingness to decide mutually with their spouse regarding FP use in the future [ 21 , 32 ]. Most women in this study seemed comfortable letting their male partners decide on contraceptives. This attitude could be explained by the patriarchal dominance in decision-making [ 19 , 33 , 34 ].
Some men mentioned that condoms inhibit their sexual pleasure, which is why they prefer women to use other methods instead. A study conducted in Far West Nepal and another nationwide study reported similar concerns among men [ 31 , 35 ]. Adolescent girls stated that they were not comfortable talking to a male health worker about FP or to a female worker in the presence of a male health worker, which has also been reported elsewhere [ 36 ]. Some women said that their husbands forbade the use of contraceptives because they thought that contraceptives would allow their wives to become promiscuous and that using FP was a sign of infidelity. This issue, however, was not raised by any men in the study. Some women reported violence as a consequence of using contraceptives without their husband’s consent. Prior qualitative studies also reported that women may suffer domestic violence for opposing their husbands. Studies suggest that a multi-sectoral action involving stakeholders from health, women’s rights, and education sectors is imperative to further research and address this issue [ 29 , 36 , 37 ].
Supply constraints (distance to a provider for getting contraceptives, out of stock, limited choices of contraceptives, unaffordable methods, etc.) could aggravate the unmet need for contraception. These constraints are similar to all regular supplies faced by the health system in Nepal. However, supply-side interventions such as increasing the number of health facilities distributing FP services, policy focusing on consistent operating hours, and full stock of a wide variety of FP methods could largely improve uptake and increase contraceptive coverage [ 18 , 38 ].
Most female participants did not speak up when asked about their perception of the role of men in FP. On the other hand, male participants explained that the role of the youth could be disseminating FP information, conducting awareness campaigns, organizing dramas and role-plays to educate people about the religious and cultural barriers of FP use, etc. With appropriate training, the young men said they would be willing to work for FP advocacy in the community.
Reproductive health leaders and planners should identify men who are willing to share decision-making authority with their wives and devise behavioral change interventions [ 39 ]. Male participation could support the FP programs and also help empower women [ 40 ]. The participants in the study expressed the need for the current FP programs to consider the community members as key stakeholders in planning FP programs. There is a need to further explore possible ways of working with the rural, marginalized communities and hard-to-reach or specific ethnic groups to improve their update of FP services [ 41 ]. There is evidence that mass media messages increase the likelihood of FP use, which could be considered by advocacy and dissemination programs [ 42 ]. Evidence from maternal and newborn health care research shows that interventions that engage men result in more equitable couple communication and shared decision-making. This may be a relatable concept to be considered for FP programs as well [ 43 ].
We urge those in charge of the health and sexual education curriculum to find ways to encourage teachers to give equal attention to these topics, including FP education, as they would to any other. It was reported that teachers were reluctant to teach about FP as they perceived the young students felt discomfort around this topic. Further research to identify innovative youth-friendly methods to teach sexual and reproductive health topics to students may be helpful. Youth groups should be regarded as important stakeholders in the redesign of school health curricula, particularly for their insight into culturally sensitive and otherwise effective ways for delivery. Health professionals, members of local organizations, and community leaders pointed to the necessity of addressing unmet FP needs and the stigma associated with FP use through community education approaches that take into account cultural norms and beliefs [ 44 ]. Interventions focusing on reproductive health education curricula involving school teachers could be considered [ 45 ]. Strengthening health systems, bridging service gaps, improving the integration of contraceptive services and counseling with routine health care are important strategies for increasing contraceptive uptake in eastern Nepal [ 22 ].
Among the study’s limitations was the fact that it was conducted in a single village in eastern Nepal. Our findings might differ if the sample had been drawn from other parts of the country. Although participants spoke fluent Nepali, some phrases used in local dialects could not be perfectly translated into Nepali or English. These responses could have been affected by social desirability as the participants may have felt constrained from speaking freely with people from health institutions. To help reduce these obstacles we held open meetings and drop-in sessions with the support of community youth to disseminate the purpose of the study and build rapport with the young people in the village before we approached them for the study. Moreover, participants were assured anonymity and confidentiality, which may have increased their willingness to participate in the research.
Conclusions
There appear to be information and communication gaps between women and men regarding FP services and programs. The information gap could be addressed by exploring ways to increase information uptake in schools through redesigning the curriculum delivery. Mass media may be used to disseminate appropriate health education regarding FP. Health institutions could consider approaches to create FP information and service centers that are male-friendly. The communication gap may be more deeply rooted in the culture and traditions of Nepalese society. In a mostly patriarchal society, further identification of motivations for men to participate in FP related activities could be challenging. However, it is promising that men may be willing to support their partners for FP decision-making and engage in strengthening FP programs through the “peer to peer” approach via youth-led centers and community clubs. Program managers and policy makers need to take into account the fact that youth are willing to contribute to ongoing FP programs. Doing so would help bridge the information and communication gaps between school education and practice. Innovative research to further explore perceived benefits by youth on the uptake of family planning, sexual and reproductive health services is needed.
Supporting information
https://doi.org/10.1371/journal.pone.0252184.s001
https://doi.org/10.1371/journal.pone.0252184.s002
Acknowledgments
We extend our sincere thanks and regards to Dr. Agata Parfieniuk, Kirsty Lunney, and Anu Regmi for their invaluable contributions to the manuscript. We acknowledge the support received from Dr. Meika Bhattachan, Dr. Avinash Kumar Sunny, and Dr. Pawan Upadhyaya during data collection. The authors acknowledge the support received from the BPKIHS and participants for their participation in the study. Special thanks to Dr. Bibisha Baaniya, Dr. Garima Pudasaini, Dr. Soniya Gurung, Dr. Shristi Nepal, Bisha Baaniya, and Arshpreet Kaur for their generous support throughout the study.
- View Article
- Google Scholar
- PubMed/NCBI
- 5. Department of Health Services. Annual Report. DoHS. 2019. Available from: https://dohs.gov.np/wp-content/uploads/2019/07/DoHS-Annual-Report-FY-2074-75-date-22-Ashad-2076-for-web-1.pdf
- 8. World Health Organizaton. Family planning/Contraception. WHO. 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception
- 12. United Nations Department of Economic and Social Affairs Population Division. Family Planning and the 2030 Agenda for Sustainable Development: Data Booklet. (ST/ESA/ SER.A/429). 2019.
- 31. Dahal G., Hennink M. & Hinde A. Risky sexual behaviour among young men in Nepal. Southampton Statistical Sciences Research Institute, University of Southampton, Southampton. 2005. Available from; http://eprints.soton.ac.uk/id/eprint/14213
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Turk Ger Gynecol Assoc
- v.11(2); 2010

Language: English | Turkish
A study on knowledge, attitude and practice of contraception among college students in Sikkim, India
Hindistan, sikkim’deki kolej öğrencilerinin kontrasepsiyon hakkındaki bilgileri, tavırları ve uygulamaları konusundaki bir çalışma, prachi renjhen.
1 Melaka Manipal Medical College, Melaka, Malaysia
Ashwini Kumar
2 Kasturba Medical College, Manipal, India
Sanjay Pattanshetty
Afrin sagir, charmaine minoli samarasinghe.
To assess the knowledge, attitude and practice of contraception among the college students.
Materials and Methods
A cross sectional study was conducted in the Government College, Gangtok, Sikkim, during the month of April 2009 to evaluate the knowledge, attitude and practice of contraception among 156 students enrolled in the first year bachelor course. Descriptive statistics was used for data analysis.
98% (153/156) of the students had knowledge about family planning and 86% (134/156) of them had heard about contraceptives. Most of them knew about condoms (85%) and contraceptive pills (40%) but knowledge about permanent methods and Cu-T was poor (average 12%). Most students thought contraceptives were to be used to prevent unwanted pregnancy (35%) and for birth spacing (30%). 11% of students had used some form of contraceptive in the past and 7% were currently users. The most commonly used contraceptives were condoms, followed by combined use of OCP and condom.
The study highlights the need to motivate the youth for effective and appropriate use of contraceptives when required and arrest the trend towards unwanted pregnancy.
Özet
Amaç.
Kolej öğrencilerinin kontrasepsiyon haklkındaki bilgi, tecrübe ve tavırlarını değerlendirmek.
Gereç ve Yöntemler
Sikkim, Gangtok’taki devlet kolejinde okuyan 156 ilk yıl öğrencisinin kontrasepsiyon hakkındaki bilgi, tecrübe ve davranışlarını belirlemek için Nisan 2009’da kesitsel bir çalışma yürütüldü. Betimleyici istatistik analizleri kullanıldı.
Öğrencilerinin %98’i (153/159) aile planlamısını biliyordu ve %86’sı (134/156) kontrasepsiyonu duymuştu. Çoğu kondommu biliyor (%85) ve doğum kontrol hapları hakkında fikir sahibi (%40) iken, kalıcı yöntemler ve bakırlı rahim içi araçlar hakkında bilgisi olan azdı (ortalama %12). Çoğu kontraseptiflerin istenmeyen gebeliği önlemek için (%35) veya doğum sayısını azaltmak için (%30) kullanıldığ ını biliyor ve öğrencilerin %11’i geçmişte bazı yöntemleri uygularken,%7 kadar şu an herhangi bir yöntemi kullanıyordu. En sık uygulanan yöntem Kondom ve onu doğum kontrol hapları takip ediyordu.
Sonuç
Çalışmamız, gençleri etkin ve uygun kontraseptif kullanımı hakkında bilgilendirmeye, motive etmek ve istenmeyen gebelik oranını düşürmeye dikkat çekmiştir.
Introduction
The global population today stands at over 6 billion, one-sixth of which is in India. Uncontrolled population growth is recognized as the single most important impediment to national development. Despite the fact that India was the first country in the world to implement a national population control programme in 1952, the country is still struggling to contain the baby boom. A lot of efforts and resources have gone into the National Family Welfare Programme but the returns are not commensurate with the inputs. The programme has targeted eligible couples in its efforts to control the population.
The United Nations Fund for Population Activities (UNFPA) notes that future population trends will hinge on the fertility decisions of today’s men and women aged 15–24 years and on their ability and freedom to act on those decisions ( 1 ). Concern about adolescent fertility arises from its health implications both for the mother and the child, its demographic implications in societies with rapid population growth and its social development implications. Because of the young age-structure of India’s population, the reproductive attitude and behaviour of teenagers are likely to have an important impact on overall reproductive health, demographic and social outcome. Adolescent sex and exposure to the risk of pregnancy has attracted considerable research attention to understand its magnitude and address it as a problem. Studies in developed countries have shown a high level of such exposure ( 2 – 5 ), as also in Latin America ( 6 , 7 ), China ( 8 ) and some African countries like Uganda and Nigeria ( 9 – 11 ), South Africa ( 12 – 14 ) and India ( 15 , 16 ).
These facts warrant an investigation into the knowledge and attitude of this age-group regarding fertility control and contraception.
Material and Methods
A cross sectional study was conducted in the Government College, Gangtok, the capital town of Sikkim, a small state in north-east India. A Knowledge Attitude Practice (KAP) study was conducted among 156 students during the month of April 2009. The inclusion criteria: Students enrolled in the first year bachelor course, who were willing to participate in the study.
The exclusion criteria: Those students who were not willing to participate in the study.
Purposive Sampling with snowball technique was used. The questionnaire was designed by the authors after an extensive review of available literature, and the questionnaire was pretested. After obtaining written informed consent, the questionnaire was administered for data collection on general information, knowledge and attitude regarding family planning methods, and contraceptive practices.
Ethical committee clearance and permission from the principal of Government College was obtained. The students were assured regarding the confidentiality and secrecy of the information provided by them. The data was collected through the questionnaire which was voluntarily filled out by the students. Variables were knowledge, attitude, and practice of students regarding family planning and contraception.
Descriptive statistics was used for data analysis. The collected data was analyzed with regard to the information given by the subjects according to the set questionnaire items and the analyzed data is presented in the following tables.
The study showed that 98% (153/156) of the students had knowledge about family planning and 86% (134/156) of them had heard about contraceptives. and 69% knew about the source of availability of contraceptives.
73% (115/156) had gained information about family planning and contraception from the media, 33% from newspapers, 32% from friends and 21% from health personnel.
Awareness regarding various methods of contraception
The majority of the students (85%) knew about condoms but only 40% had knowledge about contraceptive pills. However, knowledge about permanent methods and intra-uterine devices was poor (average 12%).
Concept regarding contraceptive use
Most students thought that contraceptives were used to prevent unwanted pregnancy (35%) and for birth spacing (30%). 26% thought that the contraceptives could be used to have a child when required and about 23% thought that they could be used to prevent infections. 71% (111/156) of students thought that contraceptive use was beneficial, 13% (21/156) thought otherwise. 78% of students wanted to adopt family planning in the future but only 52% (81/156) were willing to use some contraceptive method in the future.
Reasons for not using contraceptives, N=21
The most common reasons (23%) cited for not using contraceptives were that it was against their religious beliefs to use a contraceptive and that it would interfere with sexual pleasure. However 19% felt that use of contraceptives may cause weakness and nearly 10% felt that it may lead to obesity.
The most preferred contraceptive method among the college students
The most common methods of contraception used by the students were condoms (past users 70% and current users 81%), followed by combined OC pills and condoms (17%). Of those students who had used some method of contraception, 6% had used OC pills; however in the current user group about 9% were using OC pills.
Many studies have been conducted all over the world to study the knowledge, attitude and practice of contraception in adolescent and young adults. A study conducted among 991 senior students (15–17 years) in North Gondar in 1995 by Fantahun MI et al showed the level of knowledge of contraception to be 75% ( 17 ). Another study conducted in Nigeria itself in 1998 by Araoye et al in randomly selected 971 males and females aged 18–24 years in a Nigerian tertiary institution showed that 97.7% of males and 98.4% females respectively knew at least one method of contraception ( 18 ). Adinma JI et al. conducted two studies in 1995 and 1999 and reviewed contraception in 498 Nigerian Tertiary School Girls-228 from the Medical Discipline (MD) of study and 270 from the Non-Medical Discipline (NMD) in 1995 and in 314 teenage Nigerian school girls comprising 128 students at secondary and 186 at tertiary levels of institution in 1999. The overall mean awareness of contraception was 70.9% in the first group, however the mean level of contraceptive awareness for the various methods of contraception was 38.2% for the second survey group: 22.6% for the secondary school girls and 54.4% for the tertiary school girls ( 19 , 20 ).
In India, two such studies have been carried out in Delhi and Ludhiana in the past. Aggarwal O et al. in Delhi ( 21 ) conducted the survey in 500 undergraduate students of the medical colleges of Delhi and reported the knowledge regarding, contraception to be 83.5%, which was comparable to the study conducted in Ludhiana by Benjamin ( 22 ) et al. among 527 senior secondary school children, where 87% were aware of contraception. Similar results were reported by Arowojolu AO ( 23 ) et al. from Nigeria, where a survey of 2388 Nigerian undergraduate students showed the contraceptive knowledge level to be 87.5%. In the present study group 86% of the college students had knowledge of contraception and 69% knew about the source of availability
The source of knowledge about contraception in most of the studies, like that of Fantahun MI et al. in North Gonder by Adinma JI in Nigeria and Aggarwal O et al. in Delhi, was from school and friends respectively, whereas in the present study it was the media which had played the most important role in spreading awareness about contraceptive methods among the students. In the study done by Fantahun MI et al. among 991 senior high school students in north Gonder, the most common reason for not using modern contraceptive methods among sexually active respondents was little or lack of knowledge of contraceptives followed by no access to contraceptives and harmful effects of contraceptives. In the present study the most common reasons (23%) cited for not using contraceptives were that it was against their religious beliefs to use contraceptives and that their sexual life would not be happy respectively. However, 19% felt that use of contraceptives would result in weakness, and nearly 10% felt that it would result in obesity. Arowojolu AO et al. surveyed 2388 Nigerian undergraduate students and reported that 87% had experienced sex but only 34% had used some method of contraception. In the study done by Fantahun et al. about 30% of students had experienced sex but only 17% had used contraception. The two studies done by Adinma JI et al. also had similar results, where the number of students who experienced sex was 57% and 26.8% and the use of contraceptive was 23.5% and 17% respectively. Lowes et al. from USA reported that 68% of 283 unmarried school students (at average 19 years of age) had experienced sex and 44% had used contraception, which is the highest among all the studies documented so far ( 24 ). In the present study experience of sex was not analysed but the use of contraceptives was the lowest, being only 17%, which was the same as that of the study conducted by Fantahun MI et al. in North Gonder in 1995 and Adinma et al in Nigeria.
The most preferred method of contraception in young adults was the condom followed by OCPs as reported in the study conducted by Fantahun MI in North Gonder in 1995 and by Araoye MO et al. in Nigeria in 1998. However, OCPs were the most preferred method of emergency contraception (43.9%) in a study conducted by Tamire W ( 25 ) in Ethiopia in 2007. In the present study the condom was the most preferred method of contraception used by the students (past users 70% and current users 81%).
In India also there is evidence from studies amongst senior secondary school students that adolescents are becoming increasingly sexually active. A study in four public and two government schools of South Delhi conducted in 1992 showed that 63.3% of boys and 37.4% of girls were of the opinion that students of their age had sex; 17% boys and 9% girls agreed to take the risk of AIDS rather than miss the chance of having sex with an attractive stranger ( 15 ). In another study conducted in four senior secondary schools in rural Delhi (in 1992), 23.4% boys and 15.1% girls admitted to having had sex, while 5.7% boys and 9.6% girls did not deny it ( 16 ).
The use of contraceptives among adolescents is significantly different from that of older married couples, and it is influenced by educational, developmental, social, and psychological factors.
The study highlights that knowledge and awareness do not always lead to a positive attitude towards the use of contraceptives. Although in the present study the actual number of sexually active young adults was not known, there appears a need for continuing education about sexuality and contraception. Also there is a need to motivate the youth for effective and appropriate use of contraceptives and arrest the trend towards unwanted pregnancy and increase in population. The media as we see has played a pivotal role in spreading awareness among the college students regarding contraceptives in the state of Sikkim. This can thus be used for motivating the young adults to adopt family planning methods and use of contraception.

Knowledge of Family planning methods & Contraception among college students (N=156)

Source of Knowledge regarding Family planning and contraception among college students (N=156)
Attitude towards use of contraception (N=156)
Conflict of interest
None declared
- Open access
- Published: 14 May 2024
Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study
- Jocelyn Schroeder 1 ,
- Barbara Pesut 1 , 2 ,
- Lise Olsen 2 ,
- Nelly D. Oelke 2 &
- Helen Sharp 2
BMC Nursing volume 23 , Article number: 326 ( 2024 ) Cite this article
181 Accesses
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada’s legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses’ (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education; and bereavement care for family. Nurses have a right under the law to conscientious objection to participating in MAiD. Therefore, it is essential to prepare nurses in their entry-level education for the practice implications and moral complexities inherent in this practice. Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context.
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
During phase 1, a 56-item survey was developed from existing literature that included demographic items and items designed to measure experience with death and dying (including MAiD), education and preparation, attitudes and beliefs, influences on those beliefs, and anticipated future involvement. During phase 2, an expert faculty panel reviewed, modified, and prioritized the items yielding 51 items. During phase 3, a sample of nursing students further evaluated and modified the language in the survey to aid readability and comprehension. The final survey consists of 45 items including 4 case studies.
Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students’ attitudes toward MAiD in a Canadian context.
The survey is appropriate for use in education and research to measure knowledge and attitudes about MAiD among nurse trainees and can be a helpful step in preparing nursing students for entry-level practice.
Peer Review reports
Medical Assistance in Dying (MAiD) is permitted under an amendment to Canada’s Criminal Code which was passed in 2016 [ 1 ]. MAiD is defined in the legislation as both self-administered and clinician-administered medication for the purpose of causing death. In the 2016 Bill C-14 legislation one of the eligibility criteria was that an applicant for MAiD must have a reasonably foreseeable natural death although this term was not defined. It was left to the clinical judgement of MAiD assessors and providers to determine the time frame that constitutes reasonably foreseeable [ 2 ]. However, in 2021 under Bill C-7, the eligibility criteria for MAiD were changed to allow individuals with irreversible medical conditions, declining health, and suffering, but whose natural death was not reasonably foreseeable, to receive MAiD [ 3 ]. This population of MAiD applicants are referred to as Track 2 MAiD (those whose natural death is foreseeable are referred to as Track 1). Track 2 applicants are subject to additional safeguards under the 2021 C-7 legislation.
Three additional proposed changes to the legislation have been extensively studied by Canadian Expert Panels (Council of Canadian Academics [CCA]) [ 4 , 5 , 6 ] First, under the legislation that defines Track 2, individuals with mental disease as their sole underlying medical condition may apply for MAiD, but implementation of this practice is embargoed until March 2027 [ 4 ]. Second, there is consideration of allowing MAiD to be implemented through advanced consent. This would make it possible for persons living with dementia to receive MAID after they have lost the capacity to consent to the procedure [ 5 ]. Third, there is consideration of extending MAiD to mature minors. A mature minor is defined as “a person under the age of majority…and who has the capacity to understand and appreciate the nature and consequences of a decision” ([ 6 ] p. 5). In summary, since the legalization of MAiD in 2016 the eligibility criteria and safeguards have evolved significantly with consequent implications for nurses and nursing care. Further, the number of Canadians who access MAiD shows steady increases since 2016 [ 7 ] and it is expected that these increases will continue in the foreseeable future.
Nurses have been integral to MAiD care in the Canadian context. While other countries such as Belgium and the Netherlands also permit euthanasia, Canada is the first country to allow Nurse Practitioners (Registered Nurses with additional preparation typically achieved at the graduate level) to act independently as assessors and providers of MAiD [ 1 ]. Although the role of Registered Nurses (RNs) in MAiD is not defined in federal legislation, it has been addressed at the provincial/territorial-level with variability in scope of practice by region [ 8 , 9 ]. For example, there are differences with respect to the obligation of the nurse to provide information to patients about MAiD, and to the degree that nurses are expected to ensure that patient eligibility criteria and safeguards are met prior to their participation [ 10 ]. Studies conducted in the Canadian context indicate that RNs perform essential roles in MAiD care coordination; client and family teaching and support; MAiD procedural quality; healthcare provider and public education; and bereavement care for family [ 9 , 11 ]. Nurse practitioners and RNs are integral to a robust MAiD care system in Canada and hence need to be well-prepared for their role [ 12 ].
Previous studies have found that end of life care, and MAiD specifically, raise complex moral and ethical issues for nurses [ 13 , 14 , 15 , 16 ]. The knowledge, attitudes, and beliefs of nurses are important across practice settings because nurses have consistent, ongoing, and direct contact with patients who experience chronic or life-limiting health conditions. Canadian studies exploring nurses’ moral and ethical decision-making in relation to MAiD reveal that although some nurses are clear in their support for, or opposition to, MAiD, others are unclear on what they believe to be good and right [ 14 ]. Empirical findings suggest that nurses go through a period of moral sense-making that is often informed by their family, peers, and initial experiences with MAID [ 17 , 18 ]. Canadian legislation and policy specifies that nurses are not required to participate in MAiD and may recuse themselves as conscientious objectors with appropriate steps to ensure ongoing and safe care of patients [ 1 , 19 ]. However, with so many nurses having to reflect on and make sense of their moral position, it is essential that they are given adequate time and preparation to make an informed and thoughtful decision before they participate in a MAID death [ 20 , 21 ].
It is well established that nursing students receive inconsistent exposure to end of life care issues [ 22 ] and little or no training related to MAiD [ 23 ]. Without such education and reflection time in pre-entry nursing preparation, nurses are at significant risk for moral harm. An important first step in providing this preparation is to be able to assess the knowledge, values, and beliefs of nursing students regarding MAID and end of life care. As demand for MAiD increases along with the complexities of MAiD, it is critical to understand the knowledge, attitudes, and likelihood of engagement with MAiD among nursing students as a baseline upon which to build curriculum and as a means to track these variables over time.
Aim, design, and setting
The aim of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. We sought to explore both their willingness to be involved in the registered nursing role and in the nurse practitioner role should they chose to prepare themselves to that level of education. The design was a mixed-method, modified e-Delphi method that entailed item generation, item refinement through an expert faculty panel [ 24 , 25 , 26 ], and initial item validation through a cognitive focus group interview with nursing students [ 27 ]. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
Participants
A panel of 10 faculty from the two nursing education programs were recruited for Phase 2 of the e-Delphi. To be included, faculty were required to have a minimum of three years of experience in nurse education, be employed as nursing faculty, and self-identify as having experience with MAiD. A convenience sample of 5 fourth-year nursing students were recruited to participate in Phase 3. Students had to be in good standing in the nursing program and be willing to share their experiences of the survey in an online group interview format.
The modified e-Delphi was conducted in 3 phases: Phase 1 entailed item generation through literature and existing survey review. Phase 2 entailed item refinement through a faculty expert panel review with focus on content validity, prioritization, and revision of item wording [ 25 ]. Phase 3 entailed an assessment of face validity through focus group-based cognitive interview with nursing students.
Phase I. Item generation through literature review
The goal of phase 1 was to develop a bank of survey items that would represent the variables of interest and which could be provided to expert faculty in Phase 2. Initial survey items were generated through a literature review of similar surveys designed to assess knowledge and attitudes toward MAiD/euthanasia in healthcare providers; Canadian empirical studies on nurses’ roles and/or experiences with MAiD; and legislative and expert panel documents that outlined proposed changes to the legislative eligibility criteria and safeguards. The literature review was conducted in three online databases: CINAHL, PsycINFO, and Medline. Key words for the search included nurses , nursing students , medical students , NPs, MAiD , euthanasia , assisted death , and end-of-life care . Only articles written in English were reviewed. The legalization and legislation of MAiD is new in many countries; therefore, studies that were greater than twenty years old were excluded, no further exclusion criteria set for country.
Items from surveys designed to measure similar variables in other health care providers and geographic contexts were placed in a table and similar items were collated and revised into a single item. Then key variables were identified from the empirical literature on nurses and MAiD in Canada and checked against the items derived from the surveys to ensure that each of the key variables were represented. For example, conscientious objection has figured prominently in the Canadian literature, but there were few items that assessed knowledge of conscientious objection in other surveys and so items were added [ 15 , 21 , 28 , 29 ]. Finally, four case studies were added to the survey to address the anticipated changes to the Canadian legislation. The case studies were based upon the inclusion of mature minors, advanced consent, and mental disorder as the sole underlying medical condition. The intention was to assess nurses’ beliefs and comfort with these potential legislative changes.
Phase 2. Item refinement through expert panel review
The goal of phase 2 was to refine and prioritize the proposed survey items identified in phase 1 using a modified e-Delphi approach to achieve consensus among an expert panel [ 26 ]. Items from phase 1 were presented to an expert faculty panel using a Qualtrics (Provo, UT) online survey. Panel members were asked to review each item to determine if it should be: included, excluded or adapted for the survey. When adapted was selected faculty experts were asked to provide rationale and suggestions for adaptation through the use of an open text box. Items that reached a level of 75% consensus for either inclusion or adaptation were retained [ 25 , 26 ]. New items were categorized and added, and a revised survey was presented to the panel of experts in round 2. Panel members were again asked to review items, including new items, to determine if it should be: included, excluded, or adapted for the survey. Round 2 of the modified e-Delphi approach also included an item prioritization activity, where participants were then asked to rate the importance of each item, based on a 5-point Likert scale (low to high importance), which De Vaus [ 30 ] states is helpful for increasing the reliability of responses. Items that reached a 75% consensus on inclusion were then considered in relation to the importance it was given by the expert panel. Quantitative data were managed using SPSS (IBM Corp).
Phase 3. Face validity through cognitive interviews with nursing students
The goal of phase 3 was to obtain initial face validity of the proposed survey using a sample of nursing student informants. More specifically, student participants were asked to discuss how items were interpreted, to identify confusing wording or other problematic construction of items, and to provide feedback about the survey as a whole including readability and organization [ 31 , 32 , 33 ]. The focus group was held online and audio recorded. A semi-structured interview guide was developed for this study that focused on clarity, meaning, order and wording of questions; emotions evoked by the questions; and overall survey cohesion and length was used to obtain data (see Supplementary Material 2 for the interview guide). A prompt to “think aloud” was used to limit interviewer-imposed bias and encourage participants to describe their thoughts and response to a given item as they reviewed survey items [ 27 ]. Where needed, verbal probes such as “could you expand on that” were used to encourage participants to expand on their responses [ 27 ]. Student participants’ feedback was collated verbatim and presented to the research team where potential survey modifications were negotiated and finalized among team members. Conventional content analysis [ 34 ] of focus group data was conducted to identify key themes that emerged through discussion with students. Themes were derived from the data by grouping common responses and then using those common responses to modify survey items.
Ten nursing faculty participated in the expert panel. Eight of the 10 faculty self-identified as female. No faculty panel members reported conscientious objector status and ninety percent reported general agreement with MAiD with one respondent who indicated their view as “unsure.” Six of the 10 faculty experts had 16 years of experience or more working as a nurse educator.
Five nursing students participated in the cognitive interview focus group. The duration of the focus group was 2.5 h. All participants identified that they were born in Canada, self-identified as female (one preferred not to say) and reported having received some instruction about MAiD as part of their nursing curriculum. See Tables 1 and 2 for the demographic descriptors of the study sample. Study results will be reported in accordance with the study phases. See Fig. 1 for an overview of the results from each phase.
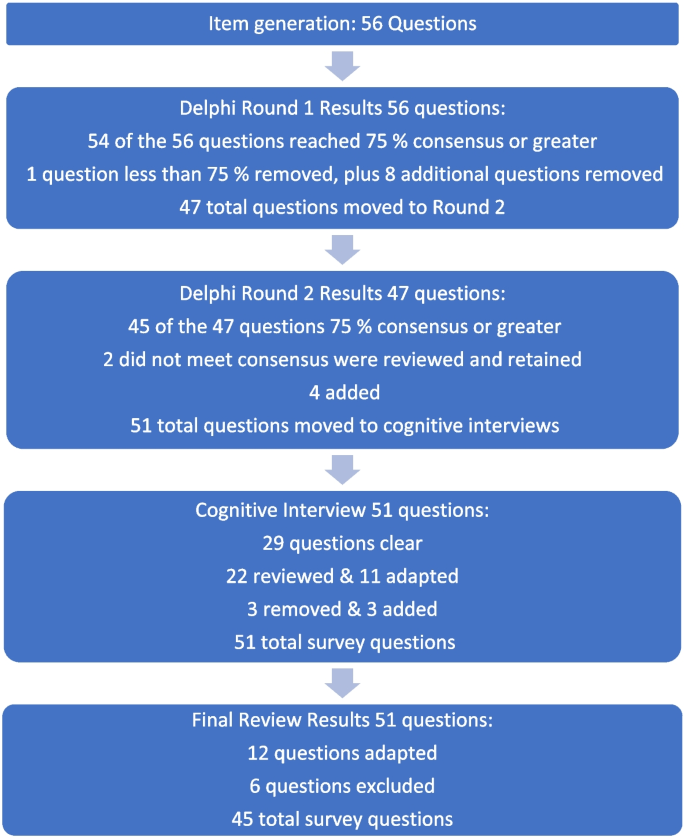
Fig. 1 Overview of survey development findings
Phase 1: survey item generation
Review of the literature identified that no existing survey was available for use with nursing students in the Canadian context. However, an analysis of themes across qualitative and quantitative studies of physicians, medical students, nurses, and nursing students provided sufficient data to develop a preliminary set of items suitable for adaptation to a population of nursing students.
Four major themes and factors that influence knowledge, attitudes, and beliefs about MAiD were evident from the literature: (i) endogenous or individual factors such as age, gender, personally held values, religion, religiosity, and/or spirituality [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], (ii) experience with death and dying in personal and/or professional life [ 35 , 40 , 41 , 43 , 44 , 45 ], (iii) training including curricular instruction about clinical role, scope of practice, or the law [ 23 , 36 , 39 ], and (iv) exogenous or social factors such as the influence of key leaders, colleagues, friends and/or family, professional and licensure organizations, support within professional settings, and/or engagement in MAiD in an interdisciplinary team context [ 9 , 35 , 46 ].
Studies of nursing students also suggest overlap across these categories. For example, value for patient autonomy [ 23 ] and the moral complexity of decision-making [ 37 ] are important factors that contribute to attitudes about MAiD and may stem from a blend of personally held values coupled with curricular content, professional training and norms, and clinical exposure. For example, students report that participation in end of life care allows for personal growth, shifts in perception, and opportunities to build therapeutic relationships with their clients [ 44 , 47 , 48 ].
Preliminary items generated from the literature resulted in 56 questions from 11 published sources (See Table 3 ). These items were constructed across four main categories: (i) socio-demographic questions; (ii) end of life care questions; (iii) knowledge about MAiD; or (iv) comfort and willingness to participate in MAiD. Knowledge questions were refined to reflect current MAiD legislation, policies, and regulatory frameworks. Falconer [ 39 ] and Freeman [ 45 ] studies were foundational sources for item selection. Additionally, four case studies were written to reflect the most recent anticipated changes to MAiD legislation and all used the same open-ended core questions to address respondents’ perspectives about the patient’s right to make the decision, comfort in assisting a physician or NP to administer MAiD in that scenario, and hypothesized comfort about serving as a primary provider if qualified as an NP in future. Response options for the survey were also constructed during this stage and included: open text, categorical, yes/no , and Likert scales.
Phase 2: faculty expert panel review
Of the 56 items presented to the faculty panel, 54 questions reached 75% consensus. However, based upon the qualitative responses 9 items were removed largely because they were felt to be repetitive. Items that generated the most controversy were related to measuring religion and spirituality in the Canadian context, defining end of life care when there is no agreed upon time frames (e.g., last days, months, or years), and predicting willingness to be involved in a future events – thus predicting their future selves. Phase 2, round 1 resulted in an initial set of 47 items which were then presented back to the faculty panel in round 2.
Of the 47 initial questions presented to the panel in round 2, 45 reached a level of consensus of 75% or greater, and 34 of these questions reached a level of 100% consensus [ 27 ] of which all participants chose to include without any adaptations) For each question, level of importance was determined based on a 5-point Likert scale (1 = very unimportant, 2 = somewhat unimportant, 3 = neutral, 4 = somewhat important, and 5 = very important). Figure 2 provides an overview of the level of importance assigned to each item.
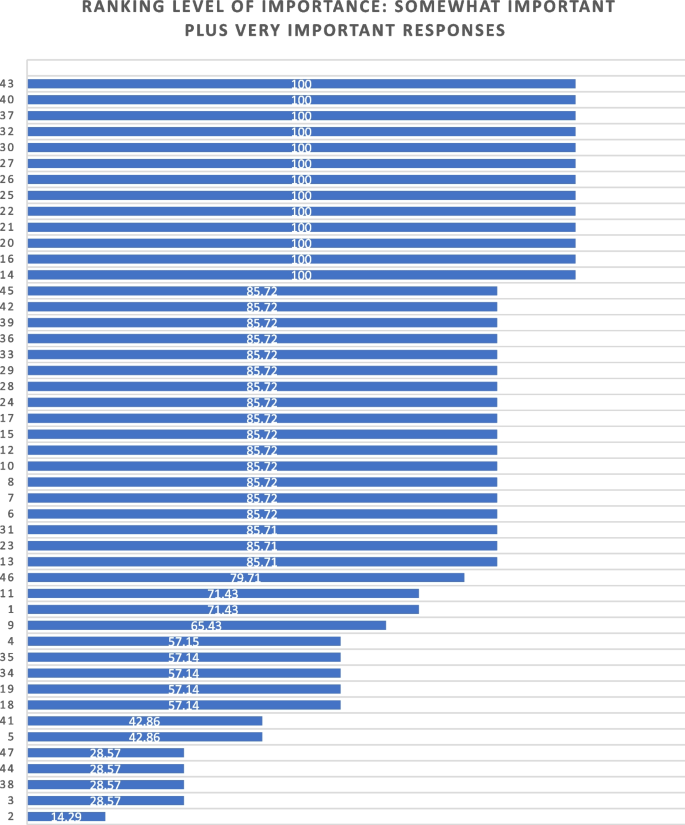
Ranking level of importance for survey items
After round 2, a careful analysis of participant comments and level of importance was completed by the research team. While the main method of survey item development came from participants’ response to the first round of Delphi consensus ratings, level of importance was used to assist in the decision of whether to keep or modify questions that created controversy, or that rated lower in the include/exclude/adapt portion of the Delphi. Survey items that rated low in level of importance included questions about future roles, sex and gender, and religion/spirituality. After deliberation by the research committee, these questions were retained in the survey based upon the importance of these variables in the scientific literature.
Of the 47 questions remaining from Phase 2, round 2, four were revised. In addition, the two questions that did not meet the 75% cut off level for consensus were reviewed by the research team. The first question reviewed was What is your comfort level with providing a MAiD death in the future if you were a qualified NP ? Based on a review of participant comments, it was decided to retain this question for the cognitive interviews with students in the final phase of testing. The second question asked about impacts on respondents’ views of MAiD and was changed from one item with 4 subcategories into 4 separate items, resulting in a final total of 51 items for phase 3. The revised survey was then brought forward to the cognitive interviews with student participants in Phase 3. (see Supplementary Material 1 for a complete description of item modification during round 2).
Phase 3. Outcomes of cognitive interview focus group
Of the 51 items reviewed by student participants, 29 were identified as clear with little or no discussion. Participant comments for the remaining 22 questions were noted and verified against the audio recording. Following content analysis of the comments, four key themes emerged through the student discussion: unclear or ambiguous wording; difficult to answer questions; need for additional response options; and emotional response evoked by questions. An example of unclear or ambiguous wording was a request for clarity in the use of the word “sufficient” in the context of assessing an item that read “My nursing education has provided sufficient content about the nursing role in MAiD.” “Sufficient” was viewed as subjective and “laden with…complexity that distracted me from the question.” The group recommended rewording the item to read “My nursing education has provided enough content for me to care for a patient considering or requesting MAiD.”
An example of having difficulty answering questions related to limited knowledge related to terms used in the legislation such as such as safeguards , mature minor , eligibility criteria , and conscientious objection. Students were unclear about what these words meant relative to the legislation and indicated that this lack of clarity would hamper appropriate responses to the survey. To ensure that respondents are able to answer relevant questions, student participants recommended that the final survey include explanation of key terms such as mature minor and conscientious objection and an overview of current legislation.
Response options were also a point of discussion. Participants noted a lack of distinction between response options of unsure and unable to say . Additionally, scaling of attitudes was noted as important since perspectives about MAiD are dynamic and not dichotomous “agree or disagree” responses. Although the faculty expert panel recommended the integration of the demographic variables of religious and/or spiritual remain as a single item, the student group stated a preference to have religion and spirituality appear as separate items. The student focus group also took issue with separate items for the variables of sex and gender, specifically that non-binary respondents might feel othered or “outed” particularly when asked to identify their sex. These variables had been created based upon best practices in health research but students did not feel they were appropriate in this context [ 49 ]. Finally, students agreed with the faculty expert panel in terms of the complexity of projecting their future involvement as a Nurse Practitioner. One participant stated: “I certainly had to like, whoa, whoa, whoa. Now let me finish this degree first, please.” Another stated, “I'm still imagining myself, my future career as an RN.”
Finally, student participants acknowledged the array of emotions that some of the items produced for them. For example, one student described positive feelings when interacting with the survey. “Brought me a little bit of feeling of joy. Like it reminded me that this is the last piece of independence that people grab on to.” Another participant, described the freedom that the idea of an advance request gave her. “The advance request gives the most comfort for me, just with early onset Alzheimer’s and knowing what it can do.” But other participants described less positive feelings. For example, the mature minor case study yielded a comment: “This whole scenario just made my heart hurt with the idea of a child requesting that.”
Based on the data gathered from the cognitive interview focus group of nursing students, revisions were made to 11 closed-ended questions (see Table 4 ) and 3 items were excluded. In the four case studies, the open-ended question related to a respondents’ hypothesized actions in a future role as NP were removed. The final survey consists of 45 items including 4 case studies (see Supplementary Material 3 ).
The aim of this study was to develop and validate a survey that can be used to track the growth of knowledge about MAiD among nursing students over time, inform training programs about curricular needs, and evaluate attitudes and willingness to participate in MAiD at time-points during training or across nursing programs over time.
The faculty expert panel and student participants in the cognitive interview focus group identified a need to establish core knowledge of the terminology and legislative rules related to MAiD. For example, within the cognitive interview group of student participants, several acknowledged lack of clear understanding of specific terms such as “conscientious objector” and “safeguards.” Participants acknowledged discomfort with the uncertainty of not knowing and their inclination to look up these terms to assist with answering the questions. This survey can be administered to nursing or pre-nursing students at any phase of their training within a program or across training programs. However, in doing so it is important to acknowledge that their baseline knowledge of MAiD will vary. A response option of “not sure” is important and provides a means for respondents to convey uncertainty. If this survey is used to inform curricular needs, respondents should be given explicit instructions not to conduct online searches to inform their responses, but rather to provide an honest appraisal of their current knowledge and these instructions are included in the survey (see Supplementary Material 3 ).
Some provincial regulatory bodies have established core competencies for entry-level nurses that include MAiD. For example, the BC College of Nurses and Midwives (BCCNM) requires “knowledge about ethical, legal, and regulatory implications of medical assistance in dying (MAiD) when providing nursing care.” (10 p. 6) However, across Canada curricular content and coverage related to end of life care and MAiD is variable [ 23 ]. Given the dynamic nature of the legislation that includes portions of the law that are embargoed until 2024, it is important to ensure that respondents are guided by current and accurate information. As the law changes, nursing curricula, and public attitudes continue to evolve, inclusion of core knowledge and content is essential and relevant for investigators to be able to interpret the portions of the survey focused on attitudes and beliefs about MAiD. Content knowledge portions of the survey may need to be modified over time as legislation and training change and to meet the specific purposes of the investigator.
Given the sensitive nature of the topic, it is strongly recommended that surveys be conducted anonymously and that students be provided with an opportunity to discuss their responses to the survey. A majority of feedback from both the expert panel of faculty and from student participants related to the wording and inclusion of demographic variables, in particular religion, religiosity, gender identity, and sex assigned at birth. These and other demographic variables have the potential to be highly identifying in small samples. In any instance in which the survey could be expected to yield demographic group sizes less than 5, users should eliminate the demographic variables from the survey. For example, the profession of nursing is highly dominated by females with over 90% of nurses who identify as female [ 50 ]. Thus, a survey within a single class of students or even across classes in a single institution is likely to yield a small number of male respondents and/or respondents who report a difference between sex assigned at birth and gender identity. When variables that serve to identify respondents are included, respondents are less likely to complete or submit the survey, to obscure their responses so as not to be identifiable, or to be influenced by social desirability bias in their responses rather than to convey their attitudes accurately [ 51 ]. Further, small samples do not allow for conclusive analyses or interpretation of apparent group differences. Although these variables are often included in surveys, such demographics should be included only when anonymity can be sustained. In small and/or known samples, highly identifying variables should be omitted.
There are several limitations associated with the development of this survey. The expert panel was comprised of faculty who teach nursing students and are knowledgeable about MAiD and curricular content, however none identified as a conscientious objector to MAiD. Ideally, our expert panel would have included one or more conscientious objectors to MAiD to provide a broader perspective. Review by practitioners who participate in MAiD, those who are neutral or undecided, and practitioners who are conscientious objectors would ensure broad applicability of the survey. This study included one student cognitive interview focus group with 5 self-selected participants. All student participants had held discussions about end of life care with at least one patient, 4 of 5 participants had worked with a patient who requested MAiD, and one had been present for a MAiD death. It is not clear that these participants are representative of nursing students demographically or by experience with end of life care. It is possible that the students who elected to participate hold perspectives and reflections on patient care and MAiD that differ from students with little or no exposure to end of life care and/or MAiD. However, previous studies find that most nursing students have been involved with end of life care including meaningful discussions about patients’ preferences and care needs during their education [ 40 , 44 , 47 , 48 , 52 ]. Data collection with additional student focus groups with students early in their training and drawn from other training contexts would contribute to further validation of survey items.
Future studies should incorporate pilot testing with small sample of nursing students followed by a larger cross-program sample to allow evaluation of the psychometric properties of specific items and further refinement of the survey tool. Consistent with literature about the importance of leadership in the context of MAiD [ 12 , 53 , 54 ], a study of faculty knowledge, beliefs, and attitudes toward MAiD would provide context for understanding student perspectives within and across programs. Additional research is also needed to understand the timing and content coverage of MAiD across Canadian nurse training programs’ curricula.
The implementation of MAiD is complex and requires understanding of the perspectives of multiple stakeholders. Within the field of nursing this includes clinical providers, educators, and students who will deliver clinical care. A survey to assess nursing students’ attitudes toward and willingness to participate in MAiD in the Canadian context is timely, due to the legislation enacted in 2016 and subsequent modifications to the law in 2021 with portions of the law to be enacted in 2027. Further development of this survey could be undertaken to allow for use in settings with practicing nurses or to allow longitudinal follow up with students as they enter practice. As the Canadian landscape changes, ongoing assessment of the perspectives and needs of health professionals and students in the health professions is needed to inform policy makers, leaders in practice, curricular needs, and to monitor changes in attitudes and practice patterns over time.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to small sample sizes, but are available from the corresponding author on reasonable request.
Abbreviations
British Columbia College of Nurses and Midwives
Medical assistance in dying
Nurse practitioner
Registered nurse
University of British Columbia Okanagan
Nicol J, Tiedemann M. Legislative Summary: Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying). Available from: https://lop.parl.ca/staticfiles/PublicWebsite/Home/ResearchPublications/LegislativeSummaries/PDF/42-1/c14-e.pdf .
Downie J, Scallion K. Foreseeably unclear. The meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhousie Law J. 2018;41(1):23–57.
Nicol J, Tiedeman M. Legislative summary of Bill C-7: an act to amend the criminal code (medical assistance in dying). Ottawa: Government of Canada; 2021.
Google Scholar
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf .
Council of Canadian Academies. The state of knowledge on advance requests for medical assistance in dying. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2019/02/The-State-of-Knowledge-on-Advance-Requests-for-Medical-Assistance-in-Dying.pdf .
Council of Canadian Academies. The state of knowledge on medical assistance in dying for mature minors. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-for-Mature-Minors.pdf .
Health Canada. Third annual report on medical assistance in dying in Canada 2021. Ottawa; 2022. [cited 2023 Oct 23]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2021.html .
Banner D, Schiller CJ, Freeman S. Medical assistance in dying: a political issue for nurses and nursing in Canada. Nurs Philos. 2019;20(4): e12281.
Article PubMed Google Scholar
Pesut B, Thorne S, Stager ML, Schiller CJ, Penney C, Hoffman C, et al. Medical assistance in dying: a review of Canadian nursing regulatory documents. Policy Polit Nurs Pract. 2019;20(3):113–30.
Article PubMed PubMed Central Google Scholar
College of Registered Nurses of British Columbia. Scope of practice for registered nurses [Internet]. Vancouver; 2018. Available from: https://www.bccnm.ca/Documents/standards_practice/rn/RN_ScopeofPractice.pdf .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Global Qual Nurs Res. 2020;7:2333393620938686. https://doi.org/10.1177/2333393620938686 .
Article Google Scholar
Pesut B, Thorne S, Schiller CJ, Greig M, Roussel J. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs. 2020;19:12. https://doi.org/10.1186/s12912-020-0404-5 .
Pesut B, Greig M, Thorne S, Burgess M, Storch JL, Tishelman C, et al. Nursing and euthanasia: a narrative review of the nursing ethics literature. Nurs Ethics. 2020;27(1):152–67.
Pesut B, Thorne S, Storch J, Chambaere K, Greig M, Burgess M. Riding an elephant: a qualitative study of nurses’ moral journeys in the context of Medical Assistance in Dying (MAiD). Journal Clin Nurs. 2020;29(19–20):3870–81.
Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2018;26(5):1337–49.
Wright DK, Chan LS, Fishman JR, Macdonald ME. “Reflection and soul searching:” Negotiating nursing identity at the fault lines of palliative care and medical assistance in dying. Social Sci & Med. 2021;289: 114366.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;54(4):511–20.
Bruce A, Beuthin R. Medically assisted dying in Canada: "Beautiful Death" is transforming nurses' experiences of suffering. The Canadian J Nurs Res | Revue Canadienne de Recherche en Sci Infirmieres. 2020;52(4):268–77. https://doi.org/10.1177/0844562119856234 .
Canadian Nurses Association. Code of ethics for registered nurses. Ottawa; 2017. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics .
Canadian Nurses Association. National nursing framework on Medical Assistance in Dying in Canada. Ottawa: 2017. Available from: https://www.virtualhospice.ca/Assets/cna-national-nursing-framework-on-maidEng_20170216155827.pdf .
Pesut B, Thorne S, Greig M. Shades of gray: conscientious objection in medical assistance in dying. Nursing Inq. 2020;27(1): e12308.
Durojaiye A, Ryan R, Doody O. Student nurse education and preparation for palliative care: a scoping review. PLoS ONE. 2023. https://doi.org/10.1371/journal.pone.0286678 .
McMechan C, Bruce A, Beuthin R. Canadian nursing students’ experiences with medical assistance in dying | Les expériences d’étudiantes en sciences infirmières au regard de l’aide médicale à mourir. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2019;5(1). https://doi.org/10.17483/2368-6669.1179 .
Adler M, Ziglio E. Gazing into the oracle. The Delphi method and its application to social policy and public health. London: Jessica Kingsley Publishers; 1996
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–12.
Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and health research. 1st ed. City: Wiley; 2011.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 1st ed. Thousand Oaks, Calif: Sage; 2005. ISBN: 9780761928041
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood EW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2017;26(1):37–49.
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood K. Nurses’ use of conscientious objection and the implications of conscience. J Adv Nurs. 2018;75(3):594–602.
de Vaus D. Surveys in social research. 6th ed. Abingdon, Oxon: Routledge; 2014.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149 .
Puchta C, Potter J. Focus group practice. 1st ed. London: Sage; 2004.
Book Google Scholar
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. Oxford: Oxford University Press; 2015.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Adesina O, DeBellis A, Zannettino L. Third-year Australian nursing students’ attitudes, experiences, knowledge, and education concerning end-of-life care. Int J of Palliative Nurs. 2014;20(8):395–401.
Bator EX, Philpott B, Costa AP. This moral coil: a cross-sectional survey of Canadian medical student attitudes toward medical assistance in dying. BMC Med Ethics. 2017;18(1):58.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53(4):511–20.
Brown J, Goodridge D, Thorpe L, Crizzle A. What is right for me, is not necessarily right for you: the endogenous factors influencing nonparticipation in medical assistance in dying. Qual Health Res. 2021;31(10):1786–1800.
Falconer J, Couture F, Demir KK, Lang M, Shefman Z, Woo M. Perceptions and intentions toward medical assistance in dying among Canadian medical students. BMC Med Ethics. 2019;20(1):22.
Green G, Reicher S, Herman M, Raspaolo A, Spero T, Blau A. Attitudes toward euthanasia—dual view: Nursing students and nurses. Death Stud. 2022;46(1):124–31.
Hosseinzadeh K, Rafiei H. Nursing student attitudes toward euthanasia: a cross-sectional study. Nurs Ethics. 2019;26(2):496–503.
Ozcelik H, Tekir O, Samancioglu S, Fadiloglu C, Ozkara E. Nursing students’ approaches toward euthanasia. Omega (Westport). 2014;69(1):93–103.
Canning SE, Drew C. Canadian nursing students’ understanding, and comfort levels related to medical assistance in dying. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2022;8(2). https://doi.org/10.17483/2368-6669.1326 .
Edo-Gual M, Tomás-Sábado J, Bardallo-Porras D, Monforte-Royo C. The impact of death and dying on nursing students: an explanatory model. J Clin Nurs. 2014;23(23–24):3501–12.
Freeman LA, Pfaff KA, Kopchek L, Liebman J. Investigating palliative care nurse attitudes towards medical assistance in dying: an exploratory cross-sectional study. J Adv Nurs. 2020;76(2):535–45.
Brown J, Goodridge D, Thorpe L, Crizzle A. “I am okay with it, but I am not going to do it:” the exogenous factors influencing non-participation in medical assistance in dying. Qual Health Res. 2021;31(12):2274–89.
Dimoula M, Kotronoulas G, Katsaragakis S, Christou M, Sgourou S, Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurs Educ Today. 2019;74:7–14.
Matchim Y, Raetong P. Thai nursing students’ experiences of caring for patients at the end of life: a phenomenological study. Int J Palliative Nurs. 2018;24(5):220–9.
Canadian Institute for Health Research. Sex and gender in health research [Internet]. Ottawa: CIHR; 2021 [cited 2023 Oct 23]. Available from: https://cihr-irsc.gc.ca/e/50833.html .
Canadian Nurses’ Association. Nursing statistics. Ottawa: CNA; 2023 [cited 2023 Oct 23]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics .
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47. https://doi.org/10.1007/s11135-011-9640-9 .
Ferri P, Di Lorenzo R, Stifani S, Morotti E, Vagnini M, Jiménez Herrera MF, et al. Nursing student attitudes toward dying patient care: a European multicenter cross-sectional study. Acta Bio Medica Atenei Parmensis. 2021;92(S2): e2021018.
PubMed PubMed Central Google Scholar
Beuthin R, Bruce A. Medical assistance in dying (MAiD): Ten things leaders need to know. Nurs Leadership. 2018;31(4):74–81.
Thiele T, Dunsford J. Nurse leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics. 2019;26(4):993–9.
Download references
Acknowledgements
We would like to acknowledge the faculty and students who generously contributed their time to this work.
JS received a student traineeship through the Principal Research Chairs program at the University of British Columbia Okanagan.
Author information
Authors and affiliations.
School of Health and Human Services, Selkirk College, Castlegar, BC, Canada
Jocelyn Schroeder & Barbara Pesut
School of Nursing, University of British Columbia Okanagan, Kelowna, BC, Canada
Barbara Pesut, Lise Olsen, Nelly D. Oelke & Helen Sharp
You can also search for this author in PubMed Google Scholar
Contributions
JS made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. JS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. BP made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. BP has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. LO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. LO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. NDO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. NDO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HS made substantial contributions to drafting and substantively revising the work. HS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
JS conducted this study as part of their graduate requirements in the School of Nursing, University of British Columbia Okanagan.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Selkirk College Research Ethics Board (REB) ID # 2021–011 and the University of British Columbia Behavioral Research Ethics Board ID # H21-01181.
All participants provided written and informed consent through approved consent processes. Research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schroeder, J., Pesut, B., Olsen, L. et al. Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study. BMC Nurs 23 , 326 (2024). https://doi.org/10.1186/s12912-024-01984-z
Download citation
Received : 24 October 2023
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12912-024-01984-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying (MAiD)
- End of life care
- Student nurses
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

COMMENTS
Background Globally, the rate of unplanned pregnancies among students at institutions of higher education, continue to increase annually despite the universal awareness and availability of contraceptives to the general population. This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards contraception in the University of ...
This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards family planning in the University of Education Winneba. The study was a descriptive cross-sectional survey using a structured self-administered questionnaire for data collection.
CALIFORNIA STATE UNIVERSITY SAN MARCOS THESIS SIGNATURE PAGE THESIS SUBMITTED IN PARTIAL FULFILLMENT . OF THE REQUIREMENTS FOR DEGREE MASTER OF PUBLIC HEALTH . THESIS TITLE: Examining Knowledge and Attitudes on Family Planning Among College Students . AUTHOR: Lizbet Vera . DATE OF SUCCESSFUL DEFENSE: Friday, April 26, 2019
ICRW's literature review in-cluded 24 systematic reviews published since 2000 that evaluated programs providing family planning information and services. All of these studies used experimental or quasi-experimental methods. While not every study focused specifically on adolescents and family planning (i.e., some included family planning for
Among these initiatives, the most important is the provision of family planning at all levels of the healthcare system [5, 6]. Currently, short-term modern family planning methods are available at all levels of governmental and private health facilities, while long-term method is being provided in health centers, hospitals and private clinics .
Use of family planning and related services. Two new studies from the updated review 14, 15 and eight from the prior review 22 - 24, 28, 31 - 34 addressed the use of family planning or related services, such as STI testing; of these ten studies, eight demonstrated a positive impact from community education interventions. 22 - 24, 28, 31 ...
The observation that levels of Family Planning awareness levels do not commensurate knowledge and usage levels calls for more innovative strategies for contraceptive promotion, and Education on the various university campus. BackgroundGlobally, the rate of unplanned pregnancies among students at institutions of higher education, continue to increase annually despite the universal awareness and ...
Family Planning, Fertility, and Medical School: A Survey of Students' Plans and Perceptions of Institutional Support ... The 30-question survey was developed based on extensive literature review of similar survey questions. ... and assisted reproductive technologies in the era of oocyte freezing among female and male university students. J ...
Background: Globally, the rate of unplanned pregnancies among students at institutions of higher education, continue to increase annually despite the universal awareness and availability of contraceptives to the general population. This study examined family planning among undergraduate university students focusing on their knowledge, use and attitudes towards contraception in the University ...
Europe PMC is an archive of life sciences journal literature. Family planning among undergraduate university students: a CASE study of a public university in Ghana. Sign in | Create an account. https://orcid.org. Europe PMC. Menu. About ...
Walden University ScholarWorks Walden Dissertations and Doctoral Studies Walden Dissertations and Doctoral Studies Collection 2021 Factors Influencing Family Planning Uptake Among Adolescents and Postpartum Women in Kenya ... Foundation of the Study and Literature Review . Introduction . Family planning (FP) refers to the preparation, knowledge ...
traditional family planning methods, such as withdrawal or periodic abstinence, were more effective (5). A study in Syrian refugees and two studies in Iraqi refugees found that knowledge of specific methods of family planning was almost non-existent among the young people in both populations (2,18,48). Misinformation and concerns over negative ...
Family Planning among University Students in Finland UNIVERSITY OF TAMPERE ACADEMIC DISSERTATION To be presented, with the permission of the Faculty of Medicine of the University of Tampere, for public discussion in the main auditorium of Building K, Medical School of the University of Tampere, Teiskontie 35, Tampere, on April 14th, 2007, at 12 ...
Introduction. The population growth rate for 2019 is projected at 1.08%. India will add a whopping 1.49 crores in 2019, contrary to the fact that India accounts for just 2.4 percent of the world surface area of 135.79 million square km yet it sustains 17.75 percent of the world population.[]WHO defines family planning as a way of thinking and living that is adopted voluntarily upon the basis ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on FAMILY PLANNING. Find methods information, sources, references or conduct a literature review on ...
Background and objective Promotion of family planning has been shown to reduce poverty, hunger, maternal and infant mortality, and contribute to women's empowerment. But many resource-limited countries still have very low rates of contraceptive use. The present study aimed to assess the knowledge, attitude and practice of family planning among women living in a resource-poor rural setting ...
This paper presents the findings of a qualitative assessment aimed at exploring knowledge, attitudes, and practices regarding family planning and factors that influence the need for and use of modern contraceptives. A descriptive exploratory study was conducted with married women and men aged between 15 and 40. Overall, 24 focus group discussions were conducted with male and female ...
The knowledge and perceptions of the first year medical students of an International University on family planning and emergency contraception in Nicosia (TRNC). BMC Womens Health . 2018; 18 ( 149 ):1-11. 10.1186/s12905-018-0641-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
This review is aimed to investigate family planning knowledge, attitudes, and practices in east African countries. through published papers.A re view was conducted on knowledge, attitude and ...
Background In Uganda, the risk of unintended pregnancies and unsafe abortions remains high due to relatively low contraceptive use. There is paucity of data on knowledge, attitudes, perceptions and practices towards modern contraceptives and, sexual and reproductive health especially among the young female university students. Methods A survey was conducted at Makerere University main campus ...
Objective To assess the knowledge and attitude regarding family planning and the practice of family planning among the women of reproductive age group in South Achefer District, Northwest Ethiopia, 2017. Result The study showed that the overall proper knowledge, attitude and practice of women towards family planning (FP) was 42.3%, 58.8%, and 50.4% respectively. Factors associated with the ...
Introduction Family planning methods are used to promote safer sexual practices, reduce unintended pregnancies and unsafe abortion, and control population. Young people aged 15-24 years belong to a key reproductive age group. However, little is known about their engagement with the family planning services in Nepal. Our study aimed to identify the perceptions of and barriers to the use of ...
98% (153/156) of the students had knowledge about family planning and 86% (134/156) of them had heard about contraceptives. ... The questionnaire was designed by the authors after an extensive review of available literature, and the questionnaire was pretested. ... and practice on emergency contraceptives among female university students in ...
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a ...