- Open access
- Published: 04 July 2015

Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates
- Gilbert Abotisem Abiiro 1 , 2 &
- Manuela De Allegri 1
BMC International Health and Human Rights volume 15 , Article number: 17 ( 2015 ) Cite this article
22k Accesses
76 Citations
18 Altmetric
Metrics details
There is an emerging global consensus on the importance of universal health coverage (UHC), but no unanimity on the conceptual definition and scope of UHC, whether UHC is achievable or not, how to move towards it, common indicators for measuring its progress, and its long-term sustainability. This has resulted in various interpretations of the concept, emanating from different disciplinary perspectives. This paper discusses the various dimensions of UHC emerging from these interpretations and argues for the need to pay attention to the complex interactions across the various components of a health system in the pursuit of UHC as a legal human rights issue.
The literature presents UHC as a multi-dimensional concept, operationalized in terms of universal population coverage, universal financial protection, and universal access to quality health care, anchored on the basis of health care as an international legal obligation grounded in international human rights laws. As a legal concept, UHC implies the existence of a legal framework that mandates national governments to provide health care to all residents while compelling the international community to support poor nations in implementing this right. As a humanitarian social concept, UHC aims at achieving universal population coverage by enrolling all residents into health-related social security systems and securing equitable entitlements to the benefits from the health system for all. As a health economics concept, UHC guarantees financial protection by providing a shield against the catastrophic and impoverishing consequences of out-of-pocket expenditure, through the implementation of pooled prepaid financing systems. As a public health concept, UHC has attracted several controversies regarding which services should be covered: comprehensive services vs. minimum basic package, and priority disease-specific interventions vs. primary health care.
As a multi-dimensional concept, grounded in international human rights laws, the move towards UHC in LMICs requires all states to effectively recognize the right to health in their national constitutions. It also requires a human rights-focused integrated approach to health service delivery that recognizes the health system as a complex phenomenon with interlinked functional units whose effective interaction are essential to reach the equilibrium called UHC.
Peer Review reports
Universal health coverage (UHC) has been acknowledged as a priority goal of every health system [ 1 – 5 ]. The importance of this goal is reflected in the consistent calls by the World Health Organization (WHO) for its member states to implement pooled prepaid health care financing systems that promote access to quality health care and provide households with the needed protection from the catastrophic consequences of out-of-pocket (OOP) health-related payments [ 2 , 6 – 8 ]. This call has also been endorsed by the United Nations [ 5 ].
In the existing literature, different conceptual terminology, such as universal health care [ 9 ], universal health care coverage [ 10 , 11 ], universal health system, universal health coverage, or simply universal coverage, have been used to refer to basically the same concept [ 9 , 12 – 14 ]. Stuckler et al. [ 15 ] noted that “universal health care” is often used to describe health care reforms in high income countries while “universal health coverage” is associated with health system reforms within low- and middle-income countries (LMICs). Given that the poor, marginalized and most vulnerable populations mostly reside in LMICs, this paper places relatively high emphasis on such settings. Hence, we adopt the term universal health coverage (UHC) [ 2 ] throughout the paper.
It is argued that health system reforms aimed at UHC can be traced back to the emergence of organized health care in the 19th century, in response to labor agitations calling for the implementation of social security systems [ 16 – 18 ]. This phenomenon first started in Germany under the leadership of Otto von Bismarck, and later spread throughout other parts of Europe such as Britain, France and Sweden [ 16 – 18 ]. Later in 1948, the concept of UHC was implicitly enshrined in the WHO constitution which recognized that “the enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, and political belief, economic or social condition ” [ 19 ]. This fundamental human right was reaffirmed in the “ Health for all ” declaration of the Alma Ata conference on primary health care in 1978 [ 20 ].
In 2005, the concept of UHC was once again acknowledged and for the first time explicitly endorsed by the World Health Assembly (WHA) as the goal of sustainable health care financing [ 6 ]. The World Health Assembly resolution (WHA58.33) explicitly called for the implementation of health care financing systems centered on prepaid and pooling mechanisms aimed at achieving UHC [ 6 ]. Based on this Resolution, WHO defined UHC as “access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost, thereby achieving equity in access” [ 6 ] . The 2008 World Health Report re-emphasized prepayment and pooling systems as essential instruments for UHC by categorically stating that UHC entails “ pooling pre-paid contributions collected on the basis of ability to pay, and using these funds to ensure that services are available, accessible and produce quality care for those who need them, without exposing them to the risk of catastrophic expenditures” [ 7 ] . In 2010, the World Health Report, further stressed the role of health system financing for UHC by arguing that “ countries must raise sufficient funds, reduce the reliance on direct payments to finance services, and improve efficiency and equity” [ 2 ] . The concept of UHC as reflected in these WHO reports seems to be focused more on improving the health care financing function of a health system. The 2013 World Health Report built on prior work resulting in a call for research evidence to facilitate the transition of countries towards UHC [ 8 ]. The United Nations, the World Bank, the Gates Foundation, Oxfam, United States Agency for International Development (USAID), the International Labour Organization, United Nations Children’s Fund (UNICEF), Rockefeller Foundation, Results for Development Institute, the Joint Learning Network, among other international and regional development organizations have also in various ways recently endorsed and promoted the move towards UHC [ 5 , 21 – 25 ]. Considering the key role of the WHO and these other global actors in shaping the health policy debate at the global level, this recent history demonstrates a consistent and increasing international interest in the concept and debates surrounding UHC [ 2 , 26 ].
To date, the literature continues to present a clear consensus on the importance of UHC [ 23 , 27 – 29 ]. UHC was described by the Director General of WHO as “ the single most powerful concept that public health has to offer” [ 30 ]. Its potential to improve the health of the population, especially for the poor, has been demonstrated [ 31 , 32 ]. It is viewed as the phenomenon that will result in the third global transition and hence greatly influence the (re-) organization and financing of global health systems [ 29 ]. As an essential catalyst for poverty reduction and economic growth [ 14 , 33 , 34 ], UHC is regarded as a prerequisite for sustainable development [ 35 ]. It has therefore been advocated for as an important health goal in the post-2015 global development agenda [ 35 – 40 ]. The Lancet Commission on Investing in Health reports that this goal can be progressively attained by 2035 [ 34 ].
Despite the global consensus on its importance, consensus on the conceptual definition, meaning, and scope of UHC are still missing [ 12 , 26 , 41 ]. Likewise, no consensus exists on whether UHC is achievable or not; on how to move towards it [ 3 , 22 , 42 , 43 ]; on common indicators for measuring progress towards it [ 13 , 24 , 28 , 29 , 44 ]; and on its long-term sustainability [ 27 ]. The absence of a clear consensus on the conceptual definition of UHC has resulted in various interpretations of the concept, emanating from different disciplinary perspectives. These different interpretations reveal distinct, but interlinked dimensions of UHC [ 2 ]. This paper seeks to explore these various interpretations and representations of the concept of UHC from a multidimensional perspective and to discuss the various dimensions of UHC emerging from these interpretations. The arguments presented in this paper are based on a synthesis of the literature emerging from recent global debates on UHC. We adapted the WHO framework [ 2 ] to guide the presentation of our synthesis of the conceptual debates currently being advanced in the literature. Inspired by the WHO framework, our conceptual reasoning is that advancing UHC requires a healthy interaction across the three coverage dimensions: population coverage, financial protection and access to health services, held together by the view of health as a legal human right.
Discussions
Universal health coverage as a legal right to health.
A group of scholars, building their opinions from a legal and human rights perspective, enshrined in various international covenants and treaties [ 45 – 49 ], argue that the concept of UHC implies the existence of a legal framework to ensure that every resident gets access to affordable health care [ 15 , 50 , 51 ]. This portrays UHC as a reformulation of the “ health for all” goal of the Alma Ata Declaration [ 15 , 22 , 52 – 54 ]. The view of UHC as a legal obligation imposed on all states that ratified the convention on the right to health [ 45 ], implies that UHC calls for all States to create legal entitlements to health care for all their residents [ 50 , 55 , 56 ], thereby placing the responsibility for the delivery of UHC on national governments [ 5 , 17 , 57 ]. To guarantee a comprehensive right to health, the legal obligation of the state needs to reach beyond mere health service provision to include deliberate efforts to advance improvements in structures which are recognized to act as important social determinants of health such as, education, housing, sanitation and portable water as well as equitable gender and power relations [ 58 – 60 ]. The goal of UHC and the responsibility of moving towards it, therefore, need to be mandated by national laws [ 4 , 61 , 62 ]. Backman et al. [ 63 ] report that only 56 states have constitutional provisions that legally recognize the right to health and argue that even within these states, much work is still needed to ensure that this right is guaranteed in actual practice for all. Kingston et al. [ 55 ] also argue that even the state-centered view of the right to health is based on a false assumption that all people have legal nationalities. They insist that this false assumption is the cause for the medical exclusion of some migrants, especially illegal immigrants, from accessing institutionalized health care within their countries of residence. This situation is even more serious in LIMCs, where states find it difficult to raise sufficient revenues to finance health care for their legal citizenry. The vague definition of the right to health for non-nationals premised on the individual state’s economic ability and willingness to guarantee it [ 46 ], is therefore a potential recipe for social exclusion on the basis of nationality. Current debates on UHC therefore need to seriously reflect on ways by which the rights of stateless individuals to health care can also be guaranteed within the framework of UHC.
Acknowledging financial constraints to enforcing the right to health within poor-resource settings, some scholars explicitly call for international assistance for health as a way of strengthening the right to health component of UHC [ 62 , 64 ]. This, they argue, can be implemented through the establishment of a global fund to finance UHC [ 65 ] thereby presenting health as a global public good [ 66 ]. The notion of creating a common fund for UHC also recognizes the transnational nature of emerging global health problems and the inherent global interdependency needed to deal with such problems [ 67 ]. The possibility of funding global efforts towards UHC from this global fund is being explored. Initial results reveal conflicting expectations and interests between the potential donors/financiers and beneficiary countries [ 65 ]. The rights-based arguments for UHC therefore suggest a shift on the ethical spectrum of international assistance for health, from the concept of international health, where international assistance for health is viewed as a form of charity, towards that of global health [ 62 , 67 – 69 ] which is driven by the cosmopolitan ethical preposition that states should assist each other on the basis of humanitarian responsibility [ 68 , 69 ] and solidarity [ 67 ]. This cosmopolitan ethical view has the potential of facilitating efforts at raising more international assistance to facilitate UHC within its broader dimensions currently being advanced by WHO and other global experts.
Population coverage as a dimension of universal health coverage
Another group of scholars [ 22 , 61 ], also supportive of the rights-based perspective, argue that UHC implies “ equal or same entitlements” to the benefits of a health system. This reflects the notion of universal enrollment into health-related social security or risk protection systems [ 17 , 70 ] or population coverage under public health financing systems [ 2 ]. This notion therefore puts people (population) at the center of UHC [ 71 ]. Universal population coverage is to be understood in relation to the tenets of the right to health [ 45 ] as the absence of systemic exclusion of certain population groups (especially the poor and vulnerable) from the coverage of public prepaid funds and the ability of all residents to enjoy the same entitlements to the benefits of such public funding, irrespective of their nationality, race, sexual orientation, gender, political affiliations, socio-economic status or geographic locations [ 2 , 12 , 22 , 53 , 55 , 61 , 72 – 74 ].
To distinguish between aggregate and equity-based measures of population coverage, both WHO & the World Bank [ 24 ] have defined population coverage along two dimensions. Thus; achieving a 100 % coverage of the total population as an aggregate measure, or ensuring a relatively good proportion of coverage of the poorest 40 % compared to the rest of the population as an equity-based measure [ 24 ]. The overall notion of equity, defined as progressive income-rated contributions to health financing and need-based entitlements to health services, is embedded in almost all conceptual definitions of universal population coverage [ 2 , 4 , 75 – 77 ]. Implicit in the notion of equity is the concept of income and risk cross-subsidization [ 78 ], whereby the rich cross-subsidize the poor, whilst the healthy cross-subsidize the sick [ 61 ]. Notwithstanding this, other scholars have warned that universal population coverage, although desirable, must be carefully pursued to avoid creating a situation of which official entitlements will be offered to all people yet the existing health system may not have sufficient capacity to deliver quality health care for all the population [ 79 , 80 ]. This is referred to as adverse incorporation or inclusion [ 79 ].
Financial protection as a dimension of universal health coverage
From the perspective of health economics, UHC is viewed as a means of protection against the economic consequences of ill health [ 81 , 82 ]. A guaranteed financial protection requires the implementation of a health care financing mechanism that does not require direct (substantial) out-of-pocket (OOP) payments, official or informal, such as user fees, copayments and deductibles, for health care at the point of use [ 23 , 74 , 81 , 83 ]. This is the reason why the international community has endorsed financing health care from pooled prepaid mechanisms such as tax (general or dedicated) revenue, and contributions from social health insurance (usually for formal sector employees), private health insurance, and micro health insurance as essential pre-requisites for moving towards universal financial protection [ 6 ]. The existing literature does not reveal a consensus on the best prepayment mechanism or the right mix of prepayment systems that will guarantee adequate financial protection [ 22 , 84 ]. A report by Oxfam [ 22 ] suggests that within the context of LMICs, different development partners each promote their ideologically favored prepayment mechanisms as a strategy towards achieving UHC. Both the WHO and the academic community, however, recommend that such ideological prescriptions should be abandoned in favor of mixed pooling systems that can coordinate funds from different prepaid sources, in a manner that reflects context-specific UHC needs [ 2 , 28 ]. This recommendation is also rooted in the recognition that no country, not even high income ones, has achieved complete coverage, relying solely on one single financing strategy [ 4 ]. Within a mixed pooling system, there is the need to ensure proper monitory of both private and public inputs that go into the financing system.
The WHO recommends two measures for assessing progress towards financial protection: the incidence of catastrophic health care expenditure and the incidence of impoverishment resulting from OOP payments for health care [ 25 ]. The proportion of total health care expenditure incurred through OOP payments is normally used as an indicator of financial protection at the national level [ 2 ]. WHO recommends a maximum OOP expenditure threshold of 15–20 % of total health care expenditure as a requirement for financial protection [ 2 ]. At the household level, a quantitative measure of financial protection is the proportion of households incurring OOP healthcare expenditure exceeding 40 % of their household’s non-subsistence (i.e., non-food) expenditure [ 85 ] or 10 % of total household expenditure [ 86 ]. It must be noted that direct medical cost of seeking health care is not the only barrier to financial protection. A good estimate of catastrophic health care expenditure must therefore reflect all relevant costs including non-medical costs such as the cost of travelling to a health facility and loss of earnings while being treated among others. These quantitative measures, estimated on the basis of actual health care cost incurred, however, only reflect the true situation of financial risk protection if all those who need care can actually utilize health services [ 87 ]. It is argued that, such utilization-focused quantitative cost estimates are often not able to capture the quantum of needed healthcare that is forgone due to fear of impoverishment associated with utilization [ 87 ]. Effective universal financial protection can, therefore, be attained not only if the population does not incur (substantial) OOP payments and critical income losses due to payment for health care, but if there are no fears of and delays in seeking healthcare due to financial reasons, no borrowing and sale of valuable assets to pay for healthcare, and no detentions in hospitals for non-payment of bills [ 2 , 61 , 80 , 86 , 88 – 90 ].
Access to services as a dimension of universal health coverage
From the perspective of public health, it is argued that a UHC package should include a comprehensive spectrum of health services in line with the WHO’s conceptualization of UHC as “ access to key promotive, preventive, curative and rehabilitative health interventions … ” [ 2 , 6 ]. From a feasibility view point, other scholars, however, argue that the focus should be on the provision of a minimum basic package to cover priority health needs for which there are effective low-cost interventions [ 91 ] . Some of these scholars insist that this package should include priority services in line with the health-related Millennium Development Goals (MDGs) [ 14 , 24 ], thereby suggesting a continuous focus on vertical disease-specific interventions. While some of these scholars argue that the expansion and effective implementation of disease-specific interventions, especially those focused on prevention, can improve health and reduce health system costs, opponents insist that all disease-specific interventions create fragmentation and undermine broader efforts aimed at system-wide strengthening [ 92 , 93 ]. The opposing scholars call for a focus on primary health care [ 7 , 15 , 94 ], to the extent that Yates [ 74 ] calls for a clear timetable, proposing 2015 as deadline, for the achievement of universal access to primary health care.
A number of authors further distinguish between official health service coverage, defined in terms of entitlement to services, and actual effective coverage, defined in terms of real access and utilization of health services according to need [ 13 , 44 , 51 ]. It follows that attempts to measure UHC should focus on indicators that measure actual effective service coverage in relation to people’s ability to obtain real access to services, without facing barriers on both the demand and the supply side [ 13 , 51 , 70 ]. Real access, is further defined as access in relation to the availability of health services, personnel and facilities; geographical accessibility of health services; acceptability defined in relation to appropriate client-provider interactions, timeliness, appropriateness and quality of services; and affordability in terms of medical and transport costs of services relative to clients’ ability-to-pay [ 73 , 80 , 95 – 106 ]. A guaranteed sufficient capacity of the local health system, in terms of adequate health infrastructure, qualified human resources, equipment and tools, to deliver quality health care is therefore an essential component of the access dimension of UHC [ 2 , 11 , 107 ]. It is interesting to note that “ Availability, Acceptability, Affordability and Quality (AAAQ)” of health services as essential sub-components of real access are directly rooted in the human rights conceptual framework and captured in broader discussions on the right to health [ 45 , 63 ].
Considering its interactive facets, it can be concluded that UHC emerges from the literature as a multi-dimensional concept, operationalized in terms of population coverage of health-related social security systems, financial protection, and access to quality health care according to need [ 17 ], and pursued within the framework of health care as an international legal obligation grounded in international human rights laws [ 45 , 46 , 48 , 49 ]. As an essential pre-condition for moving towards UHC in LMICs, there is therefore the need for all states to abide by the international human rights obligation imposed on them and thereby legally recognize the right to health in their national constitutions. It is only on this basis that the needed national and political commitment can be enhanced for a successful move towards universal population coverage of health-related social security systems, financial protection and access to services, which are essential components of a guaranteed comprehensive right to health and hence UHC. UHC can thus be understood as a broad legal, rights-based, social humanitarian, health economics and public health concept [ 15 , 17 , 27 , 42 ]. As such, it transcends a mere legal extension of the coverage of prepaid financing systems such as health insurance or tax-based systems to all residents, to ensuring that other financial and health system bottlenecks are removed to enhance effective financial protection and equitable access to services for all. As an overall health system strengthening tool, UHC can only be achieved through a human rights-focused integrated approach that recognizes the health system as a complex phenomenon with interlinked functional units whose effective interaractions are essential to reach the equilibrium called UHC. It follows that in LMICs, interventions aimed at strengthening health systems need to attract as much attention and funding as currently being deployed towards disease-specific interventions within the framework of the MDGs. Such an action has the capability of improving local service delivery capacity and hence of building resilient and responsive health systems to facilitate the move towards UHC. The move towards UHC should therefore be conceptualized as a continuous process of identifying gaps in the various interactive UHC dimensions, and designing context-specific strategies to address these gaps in accordance with the international legal obligations imposed on states by international agreements on the right to health. As a global issue, international assistance based on the principle of global solidarity is indispensable in the move towards UHC in LMICs.
Abbreviations
Availability, Acceptability, Affordability, Quality
Low - and Middle-Income Countries
Millennium Development Goals
Out-of-pocket
Universal Health coverage
United Nations Children’s Fund
United States Agency for International Development
World Health Assembly
World Health Organization
Garrett L, Chowdhury AMR, Pablos-Méndez A. All for universal health coverage. Lancet. 2009;374:1294–9.
Article PubMed Google Scholar
WHO. The World Health Report 2010 - Health Systems Financing: the path to universal coverage. Geneva: World Health Organization; 2010.
Google Scholar
Mills A, Ally M, Goudge J, Gyapong J, Mtei G. Progress towards universal coverage: the health systems of Ghana, South Africa and Tanzania. Health Policy Plan. 2012;27 suppl 1:i4–12.
Kutzin J. Health financing for universal coverage and health system performance: concepts and implications for policy. Bull World Health Organ. 2013;91:602–11.
Article PubMed PubMed Central Google Scholar
United Nations’ General Assembly. Global Health and Foreign policy. Agenda item 123. The Sixty-seventh session (A/67/L.36). New York: United Nations; 2012.
World Health Organization. Sustainable health financing, universal coverage and social health insurance. Geneva: World Health Organization; 2005.
WHO. World Health Report 2008 - primary health care - now more than ever. Geneva: World Health Organization; 2008.
WHO. WHO | World Health Report 2013: research for universal health coverage. Genena: World Health Organization; 2013.
Reddy KS, Patel V, Jha P, Paul VK, Kumar AKS, Dandona L. Towards achievement of universal health care in India by 2020. A call to action. Lancet. 2011;377:760–8.
Gorin S. Universal health care coverage in the United States: Barriers, prospects, and implications. Health Soc Work. 1997;22:223–30.
Article CAS PubMed Google Scholar
Collet T-H, Salamin S, Zimmerli L, Kerr EA, Clair C, Picard-Kossovsky M, et al. The quality of primary care in a country with universal health care coverage. J Gen Intern Med. 2011;26:724–30.
O’Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? Lancet. 2013;6736:13–5.
de Noronha JC. Universal health coverage: how to mix concepts, confuse objectives, and abandon principles. Cad Saúde Pública. 2013;29:847–9.
Kieny M-P, Evans DB. Universal health coverage. East Mediterr Health J. 2013;19:305-6.
Stuckler D, Feigl AB, Basu S, McKee M. The political economy of universal health coverage. In: Background paper for the global symposium on health systems research. Geneva: World Health Organization; 2010.
Bärnighausen T, Sauerborn R. One hundred and eighteen years of the German health insurance system. Are there any lessons for middle-and low-income countries. Soc Sci Med. 2002;54:1559–87.
Savedoff W, de Ferranti D, Smith A, Fan V. Political and economic aspects of the transition to universal health coverage. Lancet. 2012;380:924–32.
McKee M, Balabanova D, Basu S, Ricciardi W, Stuckler D. Universal health coverage: a quest for all countries but under threat in some. Value Health. 2013;16(1, Supplement):S39–45.
WHO. Constitution of the World Health Organization. Geneva: World Health Organisation; 1948.
Declaration of Alma-Ata. International Conference on Primary Health Care, Al ma-Ata, USSR, 6–12 September 1978. http://www.euro.who.int/__data/assets/pdf_file/0009/113877/E93944.pdf . Accessed 4 May, 2015.
Bristol N. Global action towards Universal health coverage: a report for the CSIS Global Health Policy Center. Washington DC: Centre for strategic and International Studies; 2014.
Oxfam. Universal Health Coverage : Why health insurance schemes are leaving the poor behind. Oxford: Oxfam International; 2013.
World Bank WHO. WHO/World Bank Ministerial-level Meeting on Universal Health Coverage 18–19 February 2013. Geneva: World Health Organization’s headquarters; 2013.
WHO, World Bank. Monitoring Progress towards Universal Health Coverage at Country and Global Levels: A Framework. Joint WHO/World Bank Group Discussion Paper. Geneva: World Health Organization; 2013.
World Bank, WHO. Towards Universal Health Coverage by 2030. Washington DC: World Bank Group; 2014.
Latko B, Temporão JG, Frenk J, Evans TG, Chen LC, Pablos-Mendez A, et al. The growing movement for universal health coverage. Lancet. 2011;377:2161–3.
Borgonovi E, Compagni A. Sustaining universal health coverage: the interaction of social, political, and economic sustainability. Value Health. 2013;16(1, Supplement):S34–8.
Kutzin J. Anything goes on the path to universal health coverage? No. Bull World Health Organ. 2012;90:867–8.
Rodin J, de Ferranti D. Universal health coverage. The third global health transition? Lancet. 2012;380:861–2.
Chan M. Best days for public health are ahead of us, says WHO Director-General. Geneva, Switzerland: Address to the 65th World Health Assembly; 2012.
Lee Y-C, Huang Y-T, Tsai Y-W, Huang S-M, Kuo KN, McKee M, et al. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res. 2010;10:225.
Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet. 2012;380:917–23.
The World Bank. World Development Report 1993. Investing in Health. New York: Oxford University Press; 1993.
Book Google Scholar
Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382:1898–955.
Evans DB, Marten R, Etienne C. Universal health coverage is a development issue. Lancet. 2012;380:864–5.
D’Ambruoso L. Global health post-2015: the case for universal health equity. Global Health Action. 2013;6:19661.
Sheikh M, Cometto G, Duvivier R. Universal health coverage and the post 2015 agenda. Lancet. 2013;381:725–6.
United Nations. Adopting consensus text, General Assembly encourages member states to plan, pursue transition of National Health Care Systems towards Universal Coverage. In: Sixty-seventh General Assembly Plenary 53rd Meeting (AM). New York: Department of Public Information • News and Media Division; 2012.
Vega J. Universal health coverage. The post-2015 development agenda. Lancet. 2013;381:179–80.
Victora C, Saracci R, Olsen J. Universal health coverage and the post-2015 agenda. Lancet. 2013;381:726.
Sengupta M. Universal Health Coverage: Beyond rhetoric. In: McDonald DA, Ruiters G, editors. Municipal Services Project, Occasional Paper No 20 - November 2013. http://www.alames.org/documentos/uhcamit.pdf . Accessed 14 May, 2015.
Holmes D. Margaret Chan: committed to universal health coverage. Lancet. 2012;380:879.
Horton R, Das P. Universal health coverage: not why, what, or when—but how? Lancet. 2014;384:2101.
Article Google Scholar
Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. 2012;380:933–43.
Office of the United Nations High Commissioner for Human Rights, WHO. The Right to Health: Joint Fact Sheet WHO/OHCHR/323. Geneva: World Health Organization; 2007.
United Nations’ General Assemby. International Covenant on Economic, Social and Cultural Rights: Adopted and opened for signature, ratification and accession by General Assembly resolution 2200A (XXI) of 16 December 1966 entry into force 3 January 1976, in accordance with article 27. New York: United Nations; 1966.
Young S, The U.S. Fund for UNICEF Education Department. The United Nations Convention on the Rights of the Child: An Introduction -A Middle School Unit (Grades 6–8). U.S. Malawi: Fund for UNICEF/Mia Brandt; 2006.
United Nations. Convention on the Rights of Persons with Disabilities. New York: United Nations; 2006.
United Nations General Assemby. Convention on the Elimination of All Forms of Discrimination against Women. New York: United Nations; 1979.
Bárcena A. Health protection as a citizen’s right. Lancet. 2014;6736:61771–2.
Scheil-Adlung X, Bonnet F. Beyond legal coverage: assessing the performance of social health protection. Int Soc Secur Rev. 2011;64:21–38.
Forman L, Ooms G, Chapman A, Friedman E, Waris A, Lamprea E, et al. What could a strengthened right to health bring to the post-2015 health development agenda?: interrogating the role of the minimum core concept in advancing essential global health needs. BMC Int Health Hum Rights. 2013;13:48.
Fried ST, Khurshid A, Tarlton D, Webb D, Gloss S, Paz C, et al. Universal health coverage: necessary but not sufficient. Reprod Health Matters. 2013;21:50–60.
Hammonds R, Ooms G. The emergence of a global right to health norm - the unresolved case of universal access to quality emergency obstetric care. BMC Int Health Hum Rights. 2014;14:4.
Kingston LN, Cohen EF, Morley CP. Debate: limitations on universality: the “right to health” and the necessity of legal nationality. BMC Int Health Hum Rights. 2010;10:11.
Yamin AE, Frisancho A. Human-rights-based approaches to health in Latin America. Lancet. 2014;6736(14):61280.
Rosen G. A History of Public Health. Maryland: John Hopkins University Press; 1993.
Wilkinson R, Marmot M. Social determinants of health. The solid facts. Copenhagen: World Health Organization; 1998.
Marmot M, Wilkinson R. Social determinants of health. New York: Oxford University Press; 2005.
WHO. Social determinants of health: report by the Secretariat EB132/14. Geneva: World Health Organization; 2012.
McIntyre D. Health service financing for universal coverage in east and southern Africa, EQUINET Discussion Paper 95. Harare: Regional Network for Equity in Health in East and Southern Africa (EQUINET); 2012.
Ooms G. From international health to global health: how to foster a better dialogue between empirical and normative disciplines. BMC Int Health Hum Rights. 2014; 14:36.
Backman G, Hunt P, Khosla R, Jaramillo-Strouss C, Fikre BM, Rumble C, et al. Health systems and the right to health: an assessment of 194 countries. Lancet. 2008;372:2047–85.
Ooms G, Latif LA, Waris A, Brolan CE, Hammonds R, Friedman EA, et al. Is universal health coverage the practical expression of the right to health care? BMC Int Health Hum Rights. 2014; 14:3.
Ooms G, Hammonds R. Financing Global Health Through a Global Fund for Health? Working Group on Financing | PAPER 4. London: CHATHAM HOUSE (The Royal Institute of International Affairs); 2014.
Chen LC, Evans T, Cash R. Health as a global public good. In: Kaul I, Stern M, Grunberg I, editors. Global public goods: international cooperation in the 21st century. New York: Oxford University Press; 1999. p. 284–304.
Chapter Google Scholar
Frenk J, Gómez-Dantés O, Moon S. From sovereignty to solidarity: a renewed concept of global health for an era of complex interdependence. Lancet. 2014;383:94–7.
Stuckler D, McKee M. Five metaphors about global-health policy. Lancet. 2008;372:95–7.
Lencucha R. Cosmopolitanism and foreign policy for health: ethics for and beyond the state. BMC Int Health Hum Rights. 2013;13:29.
Knaul FM, González-Pier E, Gómez-Dantés O, García-Junco D, Arreola-Ornelas H, Barraza-Lloréns M, et al. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet. 2012;380:1259–79.
The Lancet. Universal health coverage post-2015: putting people first. Lancet. 2014;384:2083.
Allotey P, Verghis S, Alvarez-Castillo F, Reidpath DD. Vulnerability, equity and universal coverage – a concept note. BMC Public Health. 2012;12 Suppl 1:S2.
Ravindran TS. Universal access: making health systems work for women. BMC Public Health. 2012;12 Suppl 1:S4.
Yates R. Universal health care and the removal of user fees. Lancet. 2009;373:2078–81.
McIntyre D. What healthcare financing changes are needed to reach universal coverage in South Africa? SAMJ: S Afr Med J. 2012;102:489–90.
Mills A, Ataguba JE, Akazili J, Borghi J, Garshong B, Makawia S, et al. Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet. 2012;380:126–33.
Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health. 2014;13:1–72.
Goudge J, Akazili J, Ataguba J, Kuwawenaruwa A, Borghi J, Harris B, et al. Social solidarity and willingness to tolerate risk- and income-related cross-subsidies within health insurance: experiences from Ghana, Tanzania and South Africa. Health Policy Plan. 2012;27 suppl 1:i55–63.
Hickey S, Du Toit A. Adverse incorporation, social exclusion and chronic poverty, CPRC Working Paper 81. Chronic Poverty Research Centre: Manchester, UK; 2007.
Abiiro GA, Mbera GB, De Allegri M. Gaps in universal health coverage in Malawi: a qualitative study in rural communities. BMC Health Serv Res. 2014;14:234.
Palmer N, Mueller DH, Gilson L, Mills A, Haines A. Health financing to promote access in low income settings—how much do we know? Lancet. 2004;364:1365–70.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure. A multicountry analysis. Lancet. 2003;362:111–7.
McIntyre D, Ranson MK, Aulakh BK, Honda A. Promoting universal financial protection: evidence from seven low-and middle-income countries on factors facilitating or hindering progress. Health Res Policy Syst. 2013;11:36.
Kutzin J, Ibraimova A, Jakab M, O’Dougherty S. Bismarck meets Beveridge on the Silk Road: coordinating funding sources to create a universal health financing system in Kyrgyzstan. Bull World Health Organ. 2009;87:549–54.
Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Affair. 2007;26:972–83.
Cleary S, Birch S, Chimbindi N, Silal S, McIntyre D. Investigating the affordability of key health services in South Africa. Soc Sci Med. 2013;80:37–46.
Moreno-Serra R, Millett C, Smith PC. Towards improved measurement of financial protection in health. PLoS Med. 2011;8, e1001087.
Dekker M, Wilms A. Health insurance and other risk-coping strategies in Uganda. The case of Microcare Insurance Ltd. World Dev. 2009;38:369–78.
Kruk ME, Goldmann E, Galea S. Borrowing and selling to pay for health care in low- and middle-income countries. Health Aff. 2009;28:1056–66.
Leive A, Xu K. Coping with out-of-pocket health payments: empirical evidence from 15 African countries. Bull World Health Organ. 2008;86:849–56.
Sachs JD. Achieving universal health coverage in low-income settings. Lancet. 2012;380:944–7.
Adam T, Hsu J, de Savigny D, Lavis JN, Røttingen J-A, Bennett S. Evaluating health systems strengthening interventions in low-income and middle-income countries: are we asking the right questions? Health Policy Plan. 2012;27 suppl 4:iv9–19.
PubMed Google Scholar
Rao KD, Ramani S, Hazarika I, George S. When do vertical programmes strengthen health systems? A comparative assessment of disease-specific interventions in India. Health Policy Plan. 2014;29:495–505.
Sustainable Development Solutions Network. Health in the framework of development: Technical Report for the Post-2015 Development Agenda. New York: Sustainable Development Solutions Network: Global Inititative for the United Nation; 2014.
Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–20.
CAS PubMed PubMed Central Google Scholar
Arnold C, Theede J, Gagnon A. A qualitative exploration of access to urban migrant healthcare in Nairobi, Kenya. Soc Sci Med. 2014;110:1–9.
Dillip A, Alba S, Mshana C, Hetzel MW, Lengeler C, Mayumana I, et al. Acceptability – a neglected dimension of access to health care: findings from a study on childhood convulsions in rural Tanzania. BMC Health Serv Res. 2012;12:113.
Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19:69–79.
Evans DB, Hsu J, Boerma T. Universal health coverage and universal access. Bull World Health Organ. 2013;91:546–546A.
Goudge J, Gilson L, Russell S, Gumede T, Mills A. Affordability, availability and acceptability barriers to health care for the chronically ill: longitudinal case studies from South Africa. BMC Health Serv Res. 2009;9:75.
Jacobs B, Ir P, Bigdeli M, Annear PL, Damme WV. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012;27:288–300.
Macha J, Harris B, Garshong B, Ataguba JE, Akazili J, Kuwawenaruwa A, et al. Factors influencing the burden of health care financing and the distribution of health care benefits in Ghana, Tanzania and South Africa. Health Policy Plan. 2012;27 suppl 1:i46–54.
McIntyre D, Thiede M, Birch S. Access as a policy-relevant concept in low- and middle-income countries. Health Econ Policy Law. 2009;4(Pt 2):179–93.
O’Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saúde Pública. 2007;23:2820–34.
Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–40.
Silal SP, Penn-Kekana L, Harris B, Birch S, McIntyre D. Exploring inequalities in access to and use of maternal health services in South Africa. BMC Health Serv Res. 2012;12:120.
Meessen B, Malanda B. No universal health coverage without strong local health systems. Bull World Health Organ. 2014;92:78–78A.
Download references
Acknowledgement
GAA was funded by a scientific contract from the Institute of Public Health, University of Heidelberg, Germany, and a senior research assistant contract from the University for Development Studies, Ghana. MDA is fully funded by a core position in the Medical Faculty of the University of Heidelberg, Germany.
Author information
Authors and affiliations.
Institute of Public Health, Medical Faculty, University of Heidelberg, Heidelberg, Germany
Gilbert Abotisem Abiiro & Manuela De Allegri
Department of Planning and Management, Faculty of Planning and Land Management, University for Development Studies, University Post Box 3, Wa, Upper West Region, Ghana
Gilbert Abotisem Abiiro
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Gilbert Abotisem Abiiro .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
GAA conceptualized and designed the study, undertook the literature search, data extraction and analysis, and drafted the paper. MDA supported the conceptualization and design of the study and paper drafting, and critically reviewed the drafts and contributed to its finalization. Both authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Abiiro, G.A., De Allegri, M. Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates. BMC Int Health Hum Rights 15 , 17 (2015). https://doi.org/10.1186/s12914-015-0056-9
Download citation
Received : 15 January 2015
Accepted : 29 June 2015
Published : 04 July 2015
DOI : https://doi.org/10.1186/s12914-015-0056-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Universal health coverage
- Multi-dimensional concept
- Rights-based
- Population coverage
- Financial protection
- Access to health services
- Health system
- Conceptual literature
- Global debates
BMC International Health and Human Rights
ISSN: 1472-698X
- General enquiries: [email protected]
- Open access
- Published: 23 March 2023
Quality of care in the context of universal health coverage: a scoping review
- Bernice Yanful ORCID: orcid.org/0000-0002-6824-6694 1 ,
- Abirami Kirubarajan 2 ,
- Dominika Bhatia 2 ,
- Sujata Mishra 2 ,
- Sara Allin 2 &
- Erica Di Ruggiero 1 , 2 , 3
Health Research Policy and Systems volume 21 , Article number: 21 ( 2023 ) Cite this article
8646 Accesses
2 Citations
7 Altmetric
Metrics details
Introduction
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries. The primary objective of this scoping review was to summarize the existing conceptual and empirical literature on quality of care within the context of UHC and identify knowledge gaps.
We conducted a scoping review using the Arksey and O’Malley framework and further elaborated by Levac et al. and applied the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines. We systematically searched MEDLINE, EMBASE, CINAHL-Plus, PAIS Index, ProQuest and PsycINFO for reviews published between 1 January 1995 and 27 September 2021. Reviews were eligible for inclusion if the article had a central focus on UHC and discussed quality of care. We did not apply any country-based restrictions. All screening, data extraction and analyses were completed by two reviewers.
Of the 4128 database results, we included 45 studies that met the eligibility criteria, spanning multiple geographic regions. We synthesized and analysed our findings according to Kruk et al.’s conceptual framework for high-quality systems, including foundations, processes of care and quality impacts. Discussions of governance in relation to quality of care were discussed in a high number of studies. Studies that explored the efficiency of health systems and services were also highly represented in the included reviews. In contrast, we found that limited information was reported on health outcomes in relation to quality of care within the context of UHC. In addition, there was a global lack of evidence on measures of quality of care related to UHC, particularly country-specific measures and measures related to equity.
There is growing evidence on the relationship between quality of care and UHC, especially related to the governance and efficiency of healthcare services and systems. However, several knowledge gaps remain, particularly related to monitoring and evaluation, including of equity. Further research, evaluation and monitoring frameworks are required to strengthen the existing evidence base to improve UHC.
Peer Review reports
According to the World Health Organization, universal health coverage (UHC) is achieved when ‘all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship’ [ 1 ]. UHC has gained renewed attention from researchers and policymakers following its inclusion in the 2030 Agenda for Sustainable Development (SDGs). SDG target 3.8 calls for achieving ‘universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all’ [ 2 ].
While there is growing evidence linking UHC to different health, economic and social outcomes, recent estimates suggest that about 800 million people globally still do not have access to full financial coverage of essential health services, including but not limited to high-income countries [ 3 ]. The WHO’s well-established UHC cube identifies three dimensions of UHC: (1) population (who is covered); (2) services (services that are covered); (3) direct costs (the proportion of the costs that are covered) [ 4 ]. Absent from the cube is the explicit inclusion of quality of care. However, without attention to the quality of care provided, increasing service coverage alone is unlikely to produce better health outcomes. As such, quality of care is critical to the achievement of UHC. A high-quality health system has been defined as one ‘that optimises health care in a given context by consistently delivering care that improves or maintains health outcomes, by being valued and trusted by all people, and by responding to changing population needs’ [ 5 , p. e1200].
Current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries (LMICs) [ 6 ]. While the era of the Millennium Development Goals (MDGs) expanded access to essential health services in LMICs, poor quality of care remains a significant problem, and explains persistently high levels of maternal and child mortality [ 6 ]. In addition, poor quality of care is estimated to cause between 5.7 and 8.4 million deaths yearly in LMICs [ 7 ]. Low-quality services are also an issue in high-income countries (HICs), particularly for disadvantaged populations such as immigrant and Indigenous groups [ 6 , 8 ].
As such, efforts to achieve UHC focused solely on expanding access to care are insufficient. Achieving UHC will require a more deliberate focus on quality of care across its various dimensions including effectiveness, safety, people-centredness, timeliness, equity, integration of care and efficiency [ 6 ]. However, existing literature synthesizing evidence on the quality of care within the context of UHC is more limited.
The primary objective of this scoping review is to synthesize and analyse the existing conceptual and empirical literature on quality of care within the context of UHC. The secondary objective is to identify knowledge gaps on quality of care within the context of advancing UHC and highlight areas for further inquiry.
We conducted a scoping review using the five-stage scoping review framework proposed by Arksey and O’Malley [ 9 ] and further elaborated by Levac et al. with the following stages [ 10 ]: (1) formulating the research question; (2) searching for relevant studies; (3) selection of eligible studies; (4) data extraction and (5) analysing and describing the results. In addition, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines [ 11 ]. In accordance with the guidelines, our protocol is publicly available through Open Science Forum [ 12 ]. The scoping review methodology was selected due to its relevance to both identifying emerging and established content areas, and integration of diverse study methodologies [ 13 ]. As such, our methodology was well-aligned with the exploratory aims of our study.
To synthesize the existing knowledge on quality of care within the context of UHC, we focused on retrieving and analysing relevant reviews (as opposed to primary research studies). Bennett et al. [ 14 ] applied this overview of reviews approach in identifying health policy and system research priorities for the SDGs.
Information sources and search strategy
We developed the search strategy in consultation with a research librarian with expertise in public health and health systems. After finalizing our search in MEDLINE (Ovid) through an iterative process involving pilot tests, we completed a systematic search of MEDLINE (Ovid), EMBASE (Ovid), CINAHL-Plus (EBSCO), PAIS Index, ProQuest and PsycINFO (Ovid) for articles published from 1 January 1995 to 27 September 2021. The date cut-off of 1995 was selected to capture articles published during the period leading up to the adoption of the MDGs. We applied adapted search filters from the InterTASC Information Specialists’ Subgroup Search Filter Resource for each database [ 15 ].
Our searches combined terms related to the concepts of (1) UHC (e.g. universal health insurance, universal coverage) and (2) quality of care and its seven dimensions (e.g. equity, safety, people-centredness). Our search strategy is available in Appendix A. Figure 1 outlines the eligibility criteria we used to assess studies for inclusion in the review.
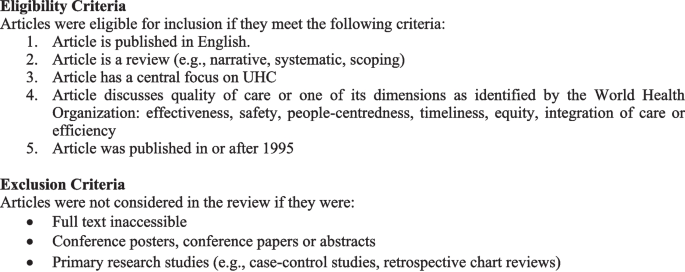
Eligibility and exclusion criteria
Data management
Results from database searches were managed through Covidence ( www.covidence.org ) for deduplication and screening.
Study selection
Two reviewers (BY&AK) independently assessed studies against the eligibility criteria in two phases: (1) titles and abstracts and (2) full-text articles. A pilot test of the title and abstract screening was completed for approximately the first 100 search results. The two reviewers discussed disagreements to revise eligibility criteria as required. Any disagreements were resolved via consensus and in consultation with senior co-authors.
Data extraction
BY & AK independently completed data extraction for the first 10 articles using a standardized form. Following the pilot, the full data extraction was completed by the two reviewers in parallel. We extracted data on key study characteristics and according to each domain and subcomponent identified in Kruk et al.’s [ 5 ] framework described in the following section. The process of data extraction was iterative, with the form subject to revisions. Geographic regions were classified either by WHO regions [ 16 ] or through self-identification by the articles, such as a global focus, LMICs, HICs, ‘developing’ or ‘developed’.
Data synthesis
We synthesized the results through both a descriptive summary and a qualitative, narrative synthesis. We anchored our narrative synthesis in Kruk et al.’s [ 5 ] conceptual framework for high-quality health systems. The framework draws from Donabedian’s well-known conceptual model of quality of care, which was first developed in the 1960s and identifies structures, processes and outcomes as three components of quality of care. Kruk et al. [ 5 ] offer a new evidence-based framework relevant to present-day health systems, recognizing the heterogeneity of health systems across HIC and LMIC contexts.
They define three key domains of a high-quality health system, which they argue should be at the core of implementing and advancing UHC: foundations, processes of care and quality impacts. Foundations refer to the context and resources required to lead a high-quality health system. Processes of care include competent care and systems, relating to evidence-based effective care and health systems’ ability to respond to patient needs. Quality impacts include both patient and provider-reported health outcomes and client confidence in the health system, as well as economic benefits such as a reduction of resource waste and financial risk protection. The Kruk et al. [ 5 ] framework does not explicitly address equity; however, the authors state that equity in the quality of healthcare is critical, which they define as ‘the absence of disparities in the quality of health services between individuals and groups with different levels of underlying social disadvantage [p. e1214].’ When compared with Donabedian’s model for evaluating the quality of care [ 17 ], Kruk et al. [ 5 ] offer a much more elaborated framework that explicitly names a range of subcomponents to guide quality measurement and improvement (e.g. governance, positive user experience, etc.).
As our scoping review examines the existing literature on quality of care within the context of UHC and identifies knowledge gaps, Kruk et al.’s [ 5 ] framework provided a useful analytic tool by which to organize and interpret our findings.
We organized the results from our narrative synthesis according to each component of the framework (foundations, processes of care and quality impacts), addressing equity as a cross-cutting theme across these components. Table 1 summarizes the components and subcomponents of the framework.
Description of included reviews
The database searches yielded 4128 results after deduplication. Following screening, 45 articles that met eligibility criteria were included in the review. The search results are shown in Appendix A and a summary of each article is presented in Table 2 . Narrative reviews comprised 40.0% of the studies ( n = 18), 35.6% were systematic reviews (n = 16), while 20.0% were scoping reviews ( n = 9), and 4.4% were overviews of systematic reviews ( n = 2). Of the 45 reviews, 28 covered multiple WHO regions (62.2%). This included reviews with a broad global focus, reviews focused on LMICs, ‘developing’ or ‘developed’ countries, as well as reviews with an explicit focus on more than one of six WHO regions. Regarding the dimensions of quality of care, equity was the most well represented, examined by 40 of the studies (88.9%). Integration of care and safety were the least represented across the studies, each examined by 11 of the reviews (24.4%). We did not formally appraise the quality of studies included in our review, which is not required for a scoping review given its overarching aim to map the scope and size of the available literature on a given topic.
Narrative synthesis of results
Conceptualizing universal healthcare/coverage and quality of care.
The included studies highlighted varying definitions of UHC and quality of care. A common definition of UHC was that all people who require any essential healthcare services, including but not limited to promotion, prevention and treatment, are able to access services without financial stress [ 18 , 19 , 20 ]. One study further expanded this definition to include that UHC was the desired outcome of health system performance [ 18 ]. Some studies specified the definition was outlined in the Alma Ata declaration [ 21 , 22 ].
Definitions of quality of care also varied. One study distinguished between service quality (e.g. patient satisfaction, responsiveness) and technical quality (e.g. adherence to clinical guidelines) [ 23 ]. Another study defined high-quality healthcare as ‘providing the highest possible level of health with the available resources’ [ 24 , p. 142]. However, most studies did not provide a working definition of quality of care, and instead used proxy indicators such as infant mortality [ 25 ] to highlight quality-related outcomes.
Synthesis according to Kruk et al. Conceptual framework
Below, we synthesize findings from the studies according to the components of Kruk et al.’s [ 5 ] conceptual framework (foundations, processes of care and impacts). We highlight the most common themes that we identified in the literature for each domain and provide illustrative examples. Unless specified, findings were not specific to LMIC or HIC contexts.
Foundations
Governance: leaders, policies, processes and procedures providing direction and oversight of health system(s).
A common theme across the literature was health system governance at local, regional and national scales, and its relationship to quality of care within the context of UHC. Naher et al. [ 26 ] identified transparency, accountability, laws and regulations, and citizen engagement as critical components of governance. The articles discussed both poor and good governance, their underlying determinants and drivers, as well as interventions to improve governance and thus quality of care [ 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ].
The literature suggests that poor governance is a common issue across health systems, and is both a cause and indicator of poor-quality care. Causes and forms of poor governance include weak supervision of, and inadequate incentives and remuneration for healthcare providers; lack of transparency and accountability in decision-making; and insufficient financial capacity; in addition to fragmented regulations and policies. Poor governance has also been found to result in low patient trust and confidence in the health system, wasted resources and poor patient outcomes [ 26 , 40 , 44 ]. In contrast, the reviewed literature described strong governance as critical to effective healthcare services [ 26 ] and the basis for achieving UHC [ 32 ].
Interventions to improve governance described by the reviewed literature include decentralization, social accountability mechanisms, such as social audits, and policy reforms to strengthen provider incentives and service integration [ 26 , 28 , 31 , 45 , 47 , 53 ]. However, the evidence regarding the effectiveness of these interventions on governance and quality of care was largely inconclusive. Regarding integration, White [ 45 ] noted the need to ensure adequate leadership and organizational capacity before integrating services, as a key determinant of success.
Quality of care measures
Six studies identified measures and/or measurement instruments to assess quality of care or its various dimensions within the context of UHC [ 19 , 22 , 27 , 30 , 42 , 51 ]. These measures differed based on their service areas of focus (e.g. family planning, primary care), the geographic contexts for which they are intended and whether they assessed foundations, processes of care or quality impacts. The reviewed literature identified a lack of standardized quality assessment tools as a significant barrier to the realization of UHC [ 22 , 42 ]. However, researchers also noted the need for country-specific indicators reflective of a country’s unique social, political and economic circumstances, and population needs and expectations [ 18 , 22 , 30 , 39 , 51 ]. Studies also emphasized the importance of integrating equity as an explicit component in the measurement and monitoring of UHC through for example, disaggregation of data by key socioeconomic and demographic variables including place of residence, occupation, religion, ethnicity and migration status [ 18 , 27 , 30 , 35 ]. Table 3 maps the measures identified in the studies according to the domains and subdomains of Kruk et al.’s framework.
Skills and availability of health system workers
Several studies also identified critical health workforce shortages and inequities in the distribution of appropriately qualified staff between urban and rural areas as significant constraints to the provision of high-quality, equitable care within the context of UHC, particularly in LMIC contexts [ 21 , 23 , 25 , 29 , 31 , 38 , 40 , 43 , 44 , 46 , 47 , 48 , 49 , 50 , 53 ]. Strategies discussed to address these concerns included (i) improving recruitment and retention of health system staff for rural and remote areas [ 21 , 46 , 47 , 50 ]; (ii) recruiting and training community health workers, while increasing the skills of lay health workers [ 21 ]; (iii) training traditional medicine practitioners in conventional medicine and utilizing them as community health workers [ 49 ]; and (iv) increasing task shifting, through delegating tasks to less specialized health workers [ 21 , 31 ], for which supportive supervision and adequate training is required [ 21 ].
Processes of care
Access to competent care and systems, incentives to improve quality of care delivery.
Evidence from the reviewed studies suggests that poor provider competence across a range of health services remains an ongoing issue, particularly in LMICs, posing a considerable barrier to the provision of timely, safe and effective quality of care [ 22 , 23 , 29 , 31 , 33 , 39 , 40 , 46 , 47 , 49 ]. For example, in China, a study with standardized patients found that providers in village hospitals provided correct treatment for tuberculosis only 28% of the time [ 47 ].
Within health systems seeking to provide UHC, significant inequities remain in both LMICs and HICs regarding the quality of care received by different populations. Vulnerable populations, who are more likely to receive care from lower-level health facilities, such as health centres, are disproportionately impacted by incompetent care and systems, having already constrained access to care [ 26 ], fewer options regarding providers and being more likely to receive inappropriate referrals [ 40 ], all indicators of lower-quality care.
Four studies described organizational factors influencing provider competence, including performance appraisal, continuing education, incentives, and remuneration and payment mechanisms [ 27 , 31 , 40 , 46 ]. For example, Sanogo et al. [ 40 ] discussed how delays in provider reimbursement as observed in Ghana, can demotivate healthcare providers, which Agarwal et al. [ 27 ] noted may decrease providers’ willingness to exert maximum effort on assigned tasks, compromising the quality of care.
Regarding incentives to improve motivation and quality of care delivery, Yip et al. [ 47 ] suggested a pay-for-performance system in China, as physicians are traditionally incentivized for treatment-based care through fee-for-service. However, the systematic review from Wiysonge et al. [ 46 ] noted a lack of evidence to support whether financial incentives for healthcare providers would improve quality of care in low-income countries.
User experience: wait times and people centredness
Wait times, a core component of quality of care, were noted as ongoing concerns in HICs and LMICs [ 21 , 23 , 33 , 39 , 40 , 47 , 48 , 55 , 56 ]. In HICs such as Norway and the United Kingdom, long wait times have been found to increase the demand for duplicative voluntary private health insurance, which Kiil argues may threaten the overall quality of public-sector driven UHC and exacerbate inequities [ 56 ]. In LMICs, evidence has shown that service quality is often superior in the private sector compared with the public sector, defined in relation to shorter wait times, better hospitality and increased time spent with providers [ 23 ].
Several studies described the relationship between positive user experience and people-centred care, which focuses on the needs and preferences of populations served while engaging them in shaping health policies and services. In addition, people centredness has been linked to improved mental and physical health, and reduced health inequities among other outcomes [ 20 , 22 , 31 , 35 , 57 ].
One study presented a people-centred care partnership model intended to support the work of advanced practice nurses in sustaining UHC, identifying nine attributes of people centredness including mutual trust and shared decision-making [ 20 ].
Several studies also discussed strategies aimed at increasing patient/community voice and engagement and the people centredness of health systems. These strategies included citizenship endorsement groups in Mexico [ 34 ] and various public forums to foster accountability and transparency [ 26 ]. However, McMichael et al. [ 35 ] cautioned that approaches to increase the voice of patients and communities risk excluding the most vulnerable, as those facing the greatest barriers to participation in such initiatives are often the most disadvantaged in their access and use of health services.
Quality impacts
Quality of care outcomes.
A few of the reviewed articles reported on empirical studies that analyzed patient and population health outcomes in relation to quality of care in the context of UHC. Where reported, these outcomes were discussed in reference to (i) specific programmes intended to improve quality of care and advance UHC, (ii) the impacts of health insurance schemes or health system reforms, (iii) private versus public sector provision of healthcare and/or (iv) the effects of specific service delivery models.
Regarding programmes intended to improve the quality of care, a community health extension programme in Ethiopia was associated with increased perinatal survival and decreased prevalence of communicable diseases. Though resource constraints such as inadequate medical supplies and limited supervision of health extension workers were noted as challenges, a key success factor included strong community engagement [ 29 ].
Another six studies examined health outcomes in relation to health insurance schemes or health system reforms [ 25 , 40 , 46 , 47 , 48 , 55 ]. Some improvements in health outcomes were noted. For example, in China, health system reforms aimed at achieving UHC have been associated with decreased maternal mortality rates [ 25 ]. However, the burden of noncommunicable diseases such as diabetes is rising amid significant gaps in their detection and treatment [ 47 ].
Studies also compared patient outcomes in relation to private versus public sector healthcare provision [ 24 , 56 , 58 ]. How the private sector was conceptualized varied across the studies, both in terms of how it was categorized (e.g. for-profit versus not-for-profit), as well as its role in healthcare financing and delivery. Given this heterogeneity, whether the public or private sector leads to higher-quality care and consequently, better health outcomes, is unclear in the reviewed literature. However, the private sector, when financed through out-of-pocket payments, is more likely to exacerbate inequities in access to healthcare.
Finally, two studies examined integrated models of care and their relationship to health outcomes [ 52 , 54 ]. According to these studies, different forms of service integration may positively impact health, for example, through slowed disease progression [ 54 ] and decreased preterm births [ 52 ].
Patient-reported satisfaction and trust in health system
Reports of poor perceived quality of care and low patient satisfaction as barriers to healthcare uptake and enrollment in health insurance schemes were common across the reviewed studies [ 26 , 28 , 36 , 40 , 44 , 47 , 55 , 56 ]. For instance, Alhassan et al. [ 28 ] found that perceived low quality of care, long wait times and poor treatment by healthcare providers reduced clients’ trust in Ghana’s National Health Insurance Scheme, reducing subsequent re-enrollment rates. In Ghana, perceived quality of care was found to exert a greater influence on men’s decisions regarding care uptake than on women’s decisions [ 36 , 44 ]. O’Connell et al. [ 36 ] suggested this gendered difference may be due to men’s care being more likely to be prioritized within household financial decisions, affording them the opportunity to be more discerning regarding the quality of care.
Several studies also discussed the effects of health system reforms and different service delivery models on patient satisfaction and trust in healthcare systems [ 23 , 28 , 29 , 31 , 38 , 43 , 47 , 54 , 57 ]. Yip et al. noted that despite reforms aimed at expanding access to care across China, many patients have chosen to forgo care at primary healthcare facilities altogether due to a lack of trust and dissatisfaction with quality of care [ 47 ]. Similarly, Ravaghi et al. identified contradictory results regarding the effects of hospital autonomy reforms on patient satisfaction. Two studies in Indonesia cited in Ravaghi’s review reported improvements, while others noted decreased or no change in patient satisfaction [ 38 ]. In contrast, four reviews found that integrated, people-centred health services may positively impact patient satisfaction [ 29 , 31 , 54 , 57 ].
Efficiency of healthcare services and systems
Twenty-seven studies addressed the efficiency of healthcare systems and services, which the review by Morgan et al., defined as ‘the extent to which resources are used effectively or are wasted’ [ 23 , p. 608]. These studies discussed inefficiencies in health systems [ 22 , 26 , 28 , 29 , 44 , 48 ], the possible effects of health reforms and other interventions on efficiency [ 21 , 25 , 31 , 37 , 38 , 41 , 44 , 45 , 46 , 47 , 50 , 53 , 54 , 55 , 58 , 59 ], efficiency as a criterion in health policymaking [ 32 ], and the measurement of efficiency [ 22 , 30 , 42 , 51 ], an example of which, as cited in Rezapour et al.’s study, was the percentage of prescriptions including antibiotics in health centres and health posts [ 51 ].
Additionally, some studies compared the efficiency of public and private sector healthcare provision, reporting mixed results [ 23 , 24 , 48 , 58 , 61 ]. For example, higher overhead costs and lower quality of care outcomes, including higher death rates, have been observed in private hospitals compared with public hospitals in the United States [ 24 ]. In contrast, research on the National Health Service in England has suggested that privatization and market-oriented reforms have improved the efficiency of hospital care through cost cutting without evidence of reduced quality [ 58 ].
In LMICs, the private sector has been linked to increased service costs related to overprescribing and use of unnecessary and expensive procedures [ 23 ]. However, Morgan et al. noted that studies assessing private sector performance in LMICs have often focused on unqualified or informal small private providers, such as small drug shops, operating amid weak public health systems and poor regulation, providing an incomplete picture of the role of the private sector in progress towards UHC [ 23 ]. Table 4 captures a high-level overview of the key highlights related to each domain and subdomain of Kruk et al.’s [ 5 ] framework discussed in the studies.
Identified evidence gaps and priorities for future research
Substantial evidence gaps that were identified in the reviewed literature are grouped thematically below. Themes are ordered by how frequently they were discussed by the reviewed studies.
Gap 1: How to measure and monitor UHC, with particular attention to quality of care and equity
Several studies identified the need for additional research to inform the development, selection and use of monitoring and evaluation frameworks and measures to assess quality of care and equity in relation to UHC in various geographic contexts at multiple levels of the health system, including facility and institutional levels [ 22 , 30 , 31 , 34 , 39 , 42 ]. For example, Rodney et al. stressed that countries should select contextually relevant indicators, and pay particular attention to the measurement of equity within UHC, cautioning that measuring equity based solely on wealth quintiles may mask inequities related to other factors such as race or disability [ 39 ]. In addition, two studies discussed the lack of client-reported measurements and advocated for further research to integrate data from household surveys and user-experience surveys [ 22 , 30 ].
Gap 2: Comparative information on the efficiency and effectiveness of public and private health provision and appropriate mix of public and private healthcare
Researchers noted the need for more conclusive evidence comparing the efficiency and effectiveness of public and private health sector provision, and the role of the private sector in contributing to UHC [ 21 , 23 , 56 , 57 , 62 ]. For example, Morgan et al. highlighted the need for greater evidence on how system-level influences such as regulations, may be used to create a public–private healthcare mix that promotes high-quality care and supports the achievement of UHC [ 23 ].
Gap 3: Effects of financial and insurance schemes on quality-of-care delivery and patient outcomes
The reviewed literature identified a lack of evidence regarding the impacts of different financial and insurance schemes on quality-of-care delivery and patient outcomes, particularly for vulnerable groups including women-headed households, children with special needs and migrants [ 34 , 46 , 55 , 62 ]. For example, van Hees et al. noted a lack of evidence regarding the impacts of financial schemes, such as pooling of funds and cost sharing, on equity [ 55 ].
Gap 4: Effects of integrated service delivery models
Studies identified the need for more robust evidence related to the effects of integrated service delivery models on access to quality care, as well as patient and population health outcomes [ 22 , 37 , 52 , 54 ]. Lê et al. specifically highlighted the lack of evidence on equity outcomes related to service integration, suggesting the need for further research in this area [ 54 ].
Gap 5: Mechanisms and contexts that enable and hinder implementation of quality-related interventions
Finally, researchers called for additional evidence regarding the mechanisms and contextual factors such as societal stigma that influence the effectiveness of interventions related to quality of care in the context of UHC [ 34 , 37 , 55 ]. To this aim, van Hees et al. recommended realist evaluations to surface what works, for whom, and in what contextual circumstances [ 55 ]. For example, Palagyi et al. identified a need for further research on task shifting, particularly how the skills gained by health workers can be maintained, and its implications for team dynamics and the delivery of existing programmes [ 37 ].
This scoping review aimed to characterize the existing conceptual and empirical literature on quality of care within the context of UHC. As noted in our results, in the reviewed literature, quality of care was often ill defined or defined inconsistently. A lack of conceptual clarity compromises the development of a robust evidence base able to inform the design and implementation of effective quality-related policies and interventions.
The 45 articles we reviewed for our study reveal a heterogeneous body of literature when compared with Kruk et al.’s quality of care framework. While some framework components including governance and the efficiency of healthcare services and systems were highly represented in the included literature, others were less represented such as physical and technological resources and tools, and patient and population health outcomes.
We also noted in the reviewed literature a lack of clarity regarding how the studies distinguished between private sector involvement in financing and/or delivery of care. This lack of clarity limits our understanding of the implications of private sector engagement for the quality of care and the achievement of UHC in various geographical contexts. Research is required to provide greater clarity of the role and impacts of private sector involvement in financing and/or delivery of health services, to help inform countries’ decision-making regarding private sector engagement. In addition, further research is needed regarding the interactions between the public and private sector and their effects on the sustainability of UHC. For example, studies have noted a concern that the availability of concierge services can create downstream implications for people who cannot afford private insurance, such as an imbalance in resource distribution [ 57 ].
Overall, the identified evidence gaps pointed to the need to build a stronger evidence base about what works, for whom, and under what contextual circumstances, and with what effects on equity to improve quality of care in LMICs and HICs. This includes a need for further evidence on the effects of integrated service delivery models, as well as how regulation can be used to create a public–private healthcare mix promoting high-quality and equitable care. The literature further highlighted the urgent need for additional research to inform the creation of robust monitoring and evaluation frameworks prioritizing equity that could support improvements to quality of care. This includes further research to help support the inclusion and use of disaggregated data, such as by wealth, sex and ethnicity to monitor and inform efforts to increase equity in access, utilization and outcomes for vulnerable populations. Beyond the above-noted research priorities, we also recommend additional research comparing quality related outcomes before and after UHC implementation, and how they intersect with health equity.
Strengths of our scoping review include the use of a broad search methodology and validated search filters in consultation with an expert librarian, and the use of a conceptual framework to guide analysis of findings. Further, our search was not constrained based on country of origin. In our search of the literature, we did not find other published reviews of similar scope about quality of care within the context of UHC.
The primary limitation of our review is the small number of included studies that met our eligibility criteria. This highlights that quality-related research in UHC remains an emerging field. In addition, many of the included studies were narrative reviews, which may not have captured the full breadth of the literature. Another limitation of our review is that we included only English-language studies. Future reviews should attempt to search and synthesize evidence in additional languages to provide more global relevance. Further, the conceptual framework we applied to the analysis of findings does not consider various factors that render health systems more fragile such as pandemics, disasters and conflicts, which may compromise the quality of care and realization of UHC. As our study did not include search terms for specific vulnerable populations such as Indigenous or racialized groups, there is also need for future research related to LMICs and communities experiencing marginalization and discrimination within HICs.
In addition, there may be limited applicability of findings across studies to different geographic regions. Finally, due to the heterogeneity and qualitative nature of the included studies, meta-analysis and synthesis beyond thematic analysis were not feasible.
This review summarized the existence of available evidence on quality of care within the context of UHC, identifying strategies aimed at improving quality of care as well as diverse knowledge gaps. Further research, evaluation and monitoring frameworks including those that attend to equity are required to strengthen the existing evidence base.
Availability of data and materials
This work analyzed secondary sources, which are cited and are publicly accessible or with academic institutional credentials. Authors can confirm that all other relevant data are included in the article and/or its additional files.
Abbreviations
African Region
Region of the Americas
Community Health Worker
Eastern Mediterranean Region
European Region
High-Income Countries
Low- and Middle-Income Countries
Millennium Development Goals
National Health Insurance Scheme
National Health Service
Primary Healthcare
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Sustainable Development Goals
South-East Asian Region
Universal Health Coverage
Western Pacific Region
World Health Organization. Regional Office for the Eastern Mediterranean. Universal health coverage. WHO; 2023. Available from: https://www.emro.who.int/health-topics/uhc/index.html .
United Nations. SDG indicators. Metadata repository. UN; 2023. Available from: https://unstats.un.org/sdgs/metadata/?Text=&Goal=3&Target=3.8SDG .
World Health Organization. Primary health care on the road to universal health coverage. WHO; 2019. Available from: https://www.who.int/docs/default-source/documents/2019-uhc-report-executive-summary .
World Health Organization. The world health report: health systems financing: the path to universal coverage. WHO; 2010. Available from: https://apps.who.int/iris/handle/10665/44371 .
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–252. https://doi.org/10.1016/S2214-109X(18)30386-3 .
Article PubMed PubMed Central Google Scholar
World Health Organization, OECD, International Bank for Reconstruction and Development/The World Bank. Delivering quality health services: a global imperative for universal health coverage. WHO, OECD, World Bank Group; 2018. Available from: https://www.worldbank.org/en/topic/universalhealthcoverage/publication/delivering-quality-health-services-a-global-imperative-for-universal-health-coverage .
National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Care Services, Board on Global Health, Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: improving health care worldwide. National Academies Press; 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535653/ .
Canadian Institute for Health Information. Hospital care for heart attacks among First Nations, Inuit and Métis. CIHI; 2013. Available from: https://publications.gc.ca/site/eng/439389/publication.html .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616 .
Article Google Scholar
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. https://doi.org/10.1186/1748-5908-5-69 .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7);467–73. https://doi.org/10.7326/M18-0850 .
Yanful B, Kirubarajan A, Mishra S, Bhatia D, Allin S, Di Ruggiero E. Quality in universal health coverage: protocol for a scoping review. Open Science Framework; 2020. Available from: https://osf.io/f8vb6/ .
Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4. https://doi.org/10.1016/j.jclinepi.2014.03.013 .
Article PubMed Google Scholar
Bennett S, Jessani N, Glandon D, Qiu M, Scott K, Meghani A, et al. Understanding the implications of the Sustainable Development Goals for health policy and systems research: results of a research priority setting exercise. Global Health. 2020;16(1):5. https://doi.org/10.1186/s12992-019-0534-2 .
The InterTASC Information Specialists’ Sub-Group. The ISSG search filter resource. ISSG; 2022. Available from: https://sites.google.com/a/york.ac.uk/issg-search-filters-resource/home .
World Health Organization. WHO regional offices. WHO; 2023. Available from: https://www.who.int/about/who-we-are/regional-offices .
Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(3):166. https://doi.org/10.1111/j.1468-0009.2005.00397.x .
Boerma T, Eozenou P, Evans D, Evans T, Kieny MP, Wagstaff A. Monitoring progress towards universal health coverage at country and global levels. PLoS Med. 2014;11(9):e1001731. https://doi.org/10.1371/journal.pmed.1001731 .
Gupta RD, Shahabuddin A. Measuring progress toward universal health coverage: does the monitoring framework of Bangladesh need further improvement? Cureus. 2018; 10(1):e2041. https://doi.org/10.7759/cureus.2041 .
Kamei T, Takahashi K, Omori J, Arimori N, Hishinuma M, Asahara K, et al. Toward advanced nursing practice along with people-centered care partnership model for sustainable universal health coverage and universal access to health. Rev Lat Am Enfermagem. 2017; 25:1–10. https://doi.org/10.1590/1518-8345.1657.2839 .
Blanchet K, Gordon I, Gilbert CE, Wormald R, Awan H. How to achieve universal coverage of cataract surgical services in developing countries: lessons from systematic reviews of other services. Ophthalmic Epidemiol. 2012;19(6):329–39. https://doi.org/10.3109/09286586.2012.717674 .
Bresick G, Christians F, Makwero M, Besigye I, Malope S, Dullie L. Primary health care performance: a scoping review of the current state of measurement in Africa. BMJ Glob Health. 2019;4(Suppl 8):e001496. https://doi.org/10.1136/bmjgh-2019-001496 .
Morgan R, Ensor T, Waters H. Performance of private sector health care: implications for universal health coverage. Lancet. 2016;388(10044):606–12. https://doi.org/10.1016/s0140-6736(16)00343-3 .
Petrou P, Samoutis G, Lionis C. Single-payer or a multipayer health system: a systematic literature review. Public Health. 2018;163:141–52. https://doi.org/10.1016/j.puhe.2018.07.006 .
Article CAS PubMed Google Scholar
Li H, Liu K, Gu J, Zhang Y, Qiao Y, Sun X. The development and impact of primary health care in China from 1949 to 2015: a focused review. Int J Health Plann Manage. 2017;32(3):339–50. https://doi.org/10.1002/hpm.2435 .
Naher N, Hoque R, Hassan MS, Balabanova D, Adams AM, Ahmed SM. The influence of corruption and governance in the delivery of frontline health care services in the public sector: a scoping review of current and future prospects in low and middle-income countries of south and south-east Asia. BMC Public Health. 2020;20(1), 880. https://doi.org/10.1186/s12889-020-08975-0 .
Agarwal S, Sripad P, Johnson C, Kirk K, Bellows B, Ana J, et al. A conceptual framework for measuring community health workforce performance within primary health care systems. Hum Resour Health. 2019;17(1):86. https://doi.org/10.1186/s12960-019-0422-0 .
Alhassan RK, Nketiah-Amponsah E, Arhinful DK. A review of the national health insurance scheme in Ghana: what are the sustainability threats and prospects? PLoS ONE. 2016;11(11):e0165151. https://doi.org/10.1371/journal.pone.0165151 .
Article CAS PubMed PubMed Central Google Scholar
Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):24. https://doi.org/10.1186/s12992-019-0470-1 .
Báscolo E, Houghton N, del Riego A. Construcción de un marco de monitoreo para la salud universal. Rev Panam Salud Pública. 2018. https://doi.org/10.26633/rpsp.2018.81 .
Bitton A, Fifield J, Ratcliffe H, Karlage A, Wang H, Veillard JH, et al. Primary healthcare system performance in low-income and middle-income countries: a scoping review of the evidence from 2010 to 2017. BMJ Glob Health. 2019;4(Suppl 8):e001551. https://doi.org/10.1136/bmjgh-2019-001551 .
Farzaneh A, Ravaghi H. Fanaei A. The ethical framework for policy-making of universal health coverage: a systematic review. J Clin Diagn Res. 2020;14(3):IE01–6. https://doi.org/10.7860/jcdr/2019/43038.13589 .
Ansu-Mensah M, Danquah FI, Bawontuo V, Ansu-Mensah P, Kuupiel D. Maternal perceptions of the quality of care in the free maternal care policy in sub-Sahara Africa: a systematic scoping review. BMC Health Serv Res. 2020;20(1):911. https://doi.org/10.1186/s12913-020-05755-9 .
Mate KS, Sifrim ZK, Chalkidou K, Cluzeau F, Cutler D, Kimball M, et al. Improving health system quality in low- and middle-income countries that are expanding health coverage: a framework for insurance. Int J Qual Health Care. 2013;25(5):497–504. https://doi.org/10.1093/intqhc/mzt053 .
McMichael C, Healy J. Health equity and migrants in the Greater Mekong Subregion. Glob Health Action. 2017;10(1):1271594. https://doi.org/10.1080/16549716.2017.1271594 .
O’Connell TS, Bedford KJA, Thiede M, McIntyre D. Synthesizing qualitative and quantitative evidence on non-financial access barriers: implications for assessment at the district level. Int J Equity Health. 2015;14(1):54. https://doi.org/10.1186/s12939-015-0181-z .
Palagyi A, Dodd R, Jan S, Nambiar D, Joshi R, Tian M, et al. Organisation of primary health care in the Asia-Pacific region: developing a prioritised research agenda. BMJ Glob Health. 2019;4(Suppl 8):e001467. https://doi.org/10.1136/bmjgh-2019-001467 .
Ravaghi H, Foroughi Z, Nemati A, Bélorgeot VD. A holistic view on implementing hospital autonomy reforms in developing countries: a systematic review. Health Policy Plan. 2018;33(10):1118–27. https://doi.org/10.1093/heapol/czy095 .
Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health. 2014;13(1):72. https://doi.org/10.1186/s12939-014-0072-8 .
Sanogo NA, Fantaye AW, Yaya S. Universal health coverage and facilitation of equitable access to care in Africa. Front Public Health. 2019;26(7):102. https://doi.org/10.3389/fpubh.2019.00102 .
Sehngelia L, Pavlova M, Groot W. Impact of healthcare reform on universal coverage in Georgia: a systematic review. Divers Equal Health Care. 2016;13:5. https://doi.org/10.21767/2049-5471.100074 .
Sprockett A. Review of quality assessment tools for family planning programmes in low- and middle-income countries. Health Policy Plan. 2017;32(2):292-302. https://doi.org/10.1093/heapol/czw123 .
Teerawattananon Y, Luz A, Pilasant S, Tangsathitkulchai S, Chootipongchaivat S, Tritasavit N, et al. How to meet the demand for good quality renal dialysis as part of universal health coverage in resource-limited settings? Health Res Policy Syst. 2016;14(1):21. https://doi.org/10.1186/s12961-016-0090-7 .
Umeh CA. Challenges toward achieving universal health coverage in Ghana, Kenya, Nigeria, and Tanzania. Int J Health Plann Manage. 2018;33(4):794–805. https://doi.org/10.1002/hpm.2610 .
White F. Primary health care and public health: foundations of universal health system. Med Princ Pract. 2015;24(2):103–16. https://doi.org/10.1159/000370197 .
Wiysonge CS, Paulsen E, Lewin S, Ciapponi A, Herrera CA, Opiyo N, et al. Financial arrangements for health systems in low-income countries: an overview of systematic reviews. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD011084.pub2 .
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192–204. https://doi.org/10.1016/s0140-6736(19)32136-1 .
Christmals CD, Aidam K. Implementation of the National Health Insurance Scheme (NHIS) in Ghana: lessons for South Africa and low- and middle-income countries. Risk Manag Healthc Policy. 2020;13:1879–904. https://doi.org/10.2147/rmhp.s245615 .
Kim JK, Kim KH, Shin YC, Jang BH, Ko SG. Utilization of traditional medicine in primary health care in low- and middle-income countries: a systematic review. Health Policy Plan. 2020; 35(8):1070–83. https://doi.org/10.1093/heapol/czaa022 .
Mumghamba EG, Joury E, Fatusi O, Ober-Oluoch J, Onigbanjo RJ, Honkala S. Capacity building and financing oral health in the African and Middle East Region. Adv Dent Res. 2015;27(1):32–42. https://doi.org/10.1177/0022034515578909 .
Rezapour R, Tabrizi JS, Farahbakhsh M, Saadati M, Abdolahi HM. Developing Iranian primary health care quality framework: a national study. BMC Public Health. 2019;19(1):911. https://doi.org/10.1186/s12889-019-7237-8 .
Schmied V, Mills A, Kruske S, Kemp L, Fowler C, Homer C. The nature and impact of collaboration and integrated service delivery for pregnant women, children and families: collaboration in universal child and family health services. J Clin Nurs. 2010;19(23–24):3516–26. https://doi.org/10.1111/j.1365-2702.2010.03321.x .
Victora CG, Hanson K, Bryce J, Vaughan JP. Achieving universal coverage with health interventions. Lancet. 2004;364(9444):1541–8. https://doi.org/10.1016/s0140-6736(04)17279-6 .
Lê G, Morgan R, Bestall J, Featherstone I, Veale T, Ensor T. Can service integration work for universal health coverage? Evidence from around the globe. Health Policy. 2016;120(4):406–19. https://doi.org/10.1016/j.healthpol.2016.02.007 .
van Hees SGM, O’Fallon T, Hofker M, Dekker M, Polack S, Banks LM, et al. Leaving no one behind? Social inclusion of health insurance in low- and middle-income countries: a systematic review. Int J Equity Health. 2019;18(1):134. https://doi.org/10.1186/s12939-019-1040-0 .
Kiil A. What characterises the privately insured in universal health care systems? A review of the empirical evidence. Health Policy. 2012;106(1):60–75. https://doi.org/10.1016/j.healthpol.2012.02.019 .
Palumbo R. Keeping candles lit: the role of concierge medicine in the future of primary care. Health Serv Manage Res. 2017;30(2):121–8. https://doi.org/10.1177/0951484816682397 .
Almeida ÁS. The role of private non-profit healthcare organizations in NHS systems: implications for the Portuguese hospital devolution program. Health Policy. 2017;121(6):699–707. https://doi.org/10.1016/j.healthpol.2017.03.016 .
Hayati R, Bastani P, Kabir MJ, Kavosi Z, Sobhani G. Scoping literature review on the basic health benefit package and its determinant criteria. Glob Health. 2018;14(1):26. https://doi.org/10.1186/s12992-018-0345-x .
Schveitzer MC, Zoboli ELCP, Vieira MM da S. Nursing challenges for universal health coverage: a systematic review. Rev Lat Am Enfermagem. 2016(24):e2676. https://doi.org/10.1590/1518-8345.0933.2676 .
Fallah R, Bazrafshan A. Participation of delivering private hospital services in universal health coverage: a systematic scoping review of the developing countries’ evidence. J Educ Health Promot. 2021;31(10):113. https://doi.org/10.4103/jehp.jehp_957_20 .
Nandi S, Schneider H. Using an equity-based framework for evaluating publicly funded health insurance programmes as an instrument of UHC in Chhattisgarh State, India. Health Res Policy Syst. 2020;18(1):50. https://doi.org/10.1186/s12961-020-00555-3 .
Download references
Acknowledgements
Thank you to Vincci Lui from Gerstein Science Information Centre at the University of Toronto for her guidance and advice regarding the search strategy. We also would like to acknowledge Garry Aslanyan, Beverley Essue, Miguel Ángel González Block, Greg Marchildon and Jeremy Veillard, for their guidance.
This research was funded by the Canadian Institutes of Health Research (CIHR) (#407149) for the project titled ‘Towards Equitable Universal Health Coverage in a Globalized Era: A Research Agenda-Setting Workshop’.
Author information
Authors and affiliations.
Division of Social and Behavioural Health Sciences, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Bernice Yanful & Erica Di Ruggiero
Institute of Health Policy, Management and Evaluation, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Abirami Kirubarajan, Dominika Bhatia, Sujata Mishra, Sara Allin & Erica Di Ruggiero
Centre for Global Health, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Erica Di Ruggiero
You can also search for this author in PubMed Google Scholar
Contributions
All listed authors were involved in the study design. BY and AK performed title/abstract and full-text screening, data extraction, and data synthesis, as well as drafting the manuscript. All authors contributed to subsequent revisions. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Bernice Yanful .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sara Allin and Erica Di Ruggiero are co-senior authors.
APPENDIX A: Appendix: Search Strategy
Database: ovid medline: epub ahead of print, in-process & other non-indexed citations, ovid medline® daily and ovid medline®, 1946: september 27, 2021.
# | Searches | Results |
|---|---|---|
1 | Universal health insurance.mp or exp Universal Health Insurance/ | 4022 |
2 | (UHC or (universal adj2 (coverage or care or healthcare or healthcare or health-care)) or ((universal or population or public) adj2 (healthcare or health care or health-care or health coverage or healthcare coverage or health care coverage or health-care coverage or access to care or access to health or access to healthcare or access to health care or access to health-care or access to health service* or access to medicine* or health access or healthcare access or health care access or health-care access or health service* access or medicine* access or health insurance or healthcare insurance or health care insurance or health-care insurance))).mp | 34,774 |
3 | exp Quality Improvement/ or exp Quality Indicators, Health Care/ | 43,714 |
4 | quality.mp | 1,170,848 |
5 | ((integrat* adj2 care) or (consult* or participat* or collab* or partner*) or ((people or person) adj2 cent*) or effective* or timel* or safe* or efficien*).mp | 4,263,417 |
6 | (((systematic OR state-of-the-art OR scoping OR literature OR umbrella) ADJ (review* OR overview* OR assessment*)) OR "review* of reviews" OR meta-analy* OR metaanaly* OR ((systematic OR evidence) ADJ1 assess*) OR "research evidence" OR metasynthe* OR meta-synthe*).tw. OR exp Review Literature as Topic/ OR exp Review/ OR Meta-Analysis as Topic/ OR Meta-Analysis/ OR "systematic review"/ | 2,838,112 |
7 | 1 OR 2 | 34,774 |
8 | 3 OR 4 OR 5 | 5,042,750 |
9 | 6 AND 7 AND 8 | 1799 |
10 | limit 9 to yr = "1995 -Current" | 1612 |
Appendix B: Study Selection
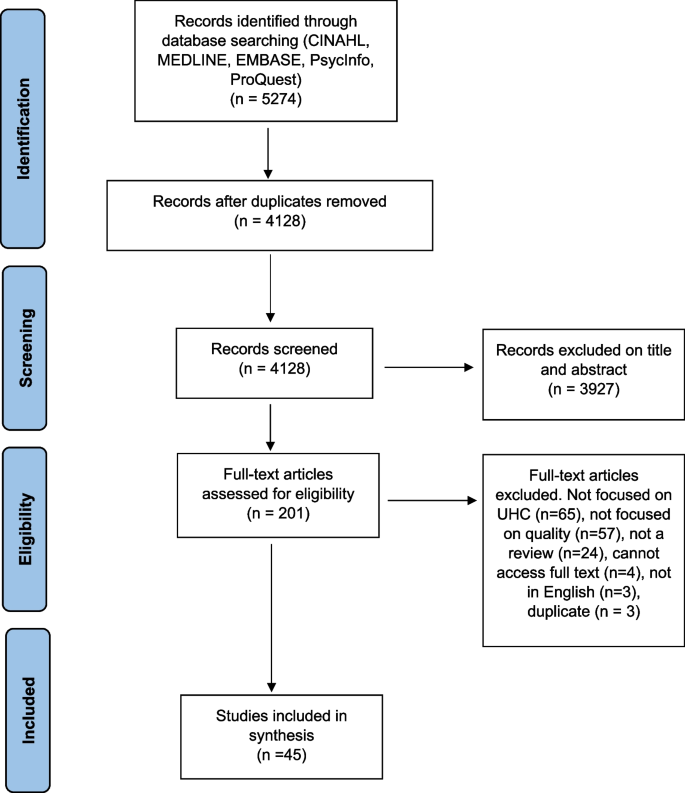
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yanful, B., Kirubarajan, A., Bhatia, D. et al. Quality of care in the context of universal health coverage: a scoping review. Health Res Policy Sys 21 , 21 (2023). https://doi.org/10.1186/s12961-022-00957-5
Download citation
Received : 21 June 2022
Accepted : 28 December 2022
Published : 23 March 2023
DOI : https://doi.org/10.1186/s12961-022-00957-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of care
- Universal health coverage
- Health systems
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Supplements
- Open Access Articles
- Research Collections
- Review Collections
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About Health Policy and Planning
- About the London School of Hygiene and Tropical Medicine
- HPP at a glance
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, limitations of the analysis, conclusions, acknowledgements.
- < Previous
The political economy of universal health coverage: a systematic narrative review
- Article contents
- Figures & tables
- Supplementary Data
Syed Shahiq Rizvi, Rundell Douglas, Owain D Williams, Peter S Hill, The political economy of universal health coverage: a systematic narrative review, Health Policy and Planning , Volume 35, Issue 3, April 2020, Pages 364–372, https://doi.org/10.1093/heapol/czz171
- Permissions Icon Permissions
The uptake and implementation of universal health coverage (UHC) is primarily a political, rather than a technical, exercise, with contested ideas and diverse stakeholders capable of facilitation or resistance—even veto—of the policy uptake. This narrative systematic review, undertaken in 2018, sought to identify all peer-reviewed publications dealing with concepts relating to UHC through a political economy framing. Of the 627 papers originally identified, 55 papers were directly relevant, with an additional eight papers added manually on referral from colleagues. The thematic analysis adapted Fox and Reich’s framework of ideas and ideologies, interests and institutions to organize the analysis. The results identified a literature strong in its exploration of the ideologies and ideas that underpin UHC, but with an apparent bias in authorship towards more rights-based, left-leaning perspectives. Despite this, political economy analyses of country case studies suggested a more diverse political framing for UHC, with the interests and institutions engaged in implementation drawing on pragmatic and market-based mechanisms to achieve outcomes. Case studies offered limited detail on the role played by specific interests, though the influence of global development trends was evident, as was the role of donor organizations. Most country case studies, however, framed the development of UHC within a narrative of national ownership, with steps in implementation often critical political milestones. The development of institutions for UHC implementation was predicated largely on available infrastructure, with elements of that infrastructure—federal systems, user fees, pre-existing insurance schemes—needing to be accommodated in the incremental progress towards UHC. The need for technical competence to deliver ideological promises was underlined. The review concludes that, despite the disparate sources for the analyses, there is an emerging shared narrative in the growing literature around the political economy of UHC that offers an increasing awareness of the political dimensions to UHC uptake and implementation.
Key Messages
Uptake and implementation of universal health coverage (UHC) is primarily a political, rather than technical, exercise.
The political economy of UHC arises from contested ideas and ideologies, diverse stakeholder interests and formal and informal institutions for its implementation.
A framework of analysis is needed to clarify concepts and identify obstacles and nodes of possibility for policy influence.
Universal health coverage… is intrinsically political and cannot be achieved without recognition of its dependence on, and consequences for, both governance and politics ( Greer and Méndez, 2015 ).
As Greer and Méndez (2015) suggest, even in contexts where universal health coverage (UHC) is being proposed for implementation, it will remain contested—policy advocates cannot presume on political consensus to support it. In this article, we use the current World Health Organization (WHO) definition of UHC:
Universal health coverage (UHC) means that all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship. This definition of UHC embodies three related objectives: • Equity in access to health services - everyone who needs services should get them, not only those who can pay for them; • The quality of health services should be good enough to improve the health of those receiving services; and • People should be protected against financial-risk, ensuring that the cost of using services does not put people at risk of financial harm ( WHO, 2019 ).
UHC incurs cost—and the commitment to increase coverage, ensure financial protection and enhance the scope and quality of services and access to medicines will require increased fiscal space in health expenditure. Recent global economic downturns have resulted in some countries moving away from their commitments to UHC as economic austerity bites ( McKee et al. , 2013 ). ‘Leaving no-one behind’—the promise of the Sustainable Development Goals, where UHC ‘cuts across all of the health-related SDGs’ ( WHO, 2019 )—will necessarily result in redistribution of resources, and in some cases reprioritization. Clearly, both political and economic factors will be at play—and a political economy approach, examining this interface among power, resources and their deployment, is necessary to inform advocacy and implementation. For this review:
Political economy analysis is concerned with the interaction of political and economic processes within a society: the distribution of power and wealth between different groups and individuals, and the processes that create, sustain and transform these relationships over time ( Collinson, 2003 ).
Krieger draws attention to the importance of political economy to the study of the determinants of disease, a perspective readily translated to the policy uptake and analysis of UHC, a health systems framework that is intimately engaged in those relationships and in shaping a health systems response to both disease and its social determinants:
Analysis of causes of disease distribution requires attention to the political and economic structures, processes and power relationships that produce societal patterns of health, disease, and wellbeing via shaping the conditions in which people live and work ( Krieger, 2011 ).
This article analyses the peer-reviewed literature to examine this interface between political economy and UHC, and uses a framework for research and development analysis. The value of a political economy analysis to health systems research, as Krieger (2011) points out, is in the explicit linkage of health to its social and political determinants. Given the relatively recent introduction of political economy to health systems and policy analysis, this systematic review has identified a literature that is divided between the theoretical exploration and implementation of UHC. The resultant analysis offers a deeper understanding that reaches beyond the technical implementation of UHC to identify factors in its political and social context that enable or constrain it, allowing both researchers and policy-makers to explore for themselves these complex factors as they engage UHC in its local context.
Fox and Reich (2015) , in their framework for evaluation and action, offer four variables that act to enable or obstruct the uptake and implementation of UHC: ‘interests’, ‘institutions’, ‘ideas’ and ‘ideology’. For the purposes of this analysis, we have combined ‘ideology’ and ‘ideas’, and changed the order of the variables. ‘Ideas and ideology' are logically linked to the ‘interests’ that embody them, and are shaped by them—and subsequently the ‘institutions’ that operationalize their policy directions:
‘Ideology’ is the higher-level political framing against which ideas are explored and establishes the political rationale and justification for the adoption and implementation of UHC. ‘Ideas’ become important because they embody the narratives, the metaphors that shape how UHC is perceived, and how it is discussed and popularly represented.
‘Interests’ expands the sense of stakeholders to include all individuals and groups who have a substantive interest in UHC—government ministries, political parties, private companies, professional organizations and unions, civil society organizations, donors and most importantly population groups, the direct beneficiaries of UHC.
‘Institutions’ necessarily include the formal political structures linked to UHC policy and its implementation, with particular attention to veto points—those conjunctures in the process that are entirely dependent on the support of specific individuals or agencies. They also extend to the informal institutions—cultural norms and expectations, precedent and existing structures—that shape (and may contest) that implementation ( Fox and Reich, 2015 ).
We have used these variables as headings in our analysis, seeking to explore within them their influence on the processes of UHC implementation.
This study uses a systematic narrative review process as articulated in the RAMESES guidelines ( Wong et al. , 2013 ). These are designed to combine both systematic comprehensiveness with the capacity to incorporate knowledge from a diverse range of disciplinary sources, making the sense of available evidence, and integrating it into an explanatory narrative. Following an exploratory search in Google, Google Scholar and Abstract reviews, the terms integral to UHC and political economy were exploded to identify alternative terminologies and are documented in Table 1 . From these exploded keywords, combinations were set out in six search strategies ( Table 2 ) across 14 health, economics and social and political science databases. The search period was limited by the development of the concept of UHC, commencing from 2005, when Universal Coverage was cited in a World Health Assembly resolution ( WHA, 2005 ), to February 2018.
Key terms and alternative terminology
| Terms . | Alternative terminology . |
|---|---|
| Political economy | Political economists, politics, economics, economic analysis, policy-making, policy implementation, political settlements analysis, science–policy interface |
| Universal health coverage | UHC, universal coverage, universal health care, universal care, universal access, social health insurance, socialized health care |
| Social health protection | Social welfare, public welfare services, health equity, social determinants of health, social protection in health, social protection, social health promotion, social security, public health security, global health security, social ecology health promotion, social health insurance |
| Health financing | Health systems financing, healthcare financing, health financing system, public health financing, health economics, health spending, healthcare finance, health expenditure, healthcare management |
| Stakeholder analysis | Stakeholder mapping, stakeholder value network, stakeholder management, stakeholder impact analysis, stakeholder interest |
| Terms . | Alternative terminology . |
|---|---|
| Political economy | Political economists, politics, economics, economic analysis, policy-making, policy implementation, political settlements analysis, science–policy interface |
| Universal health coverage | UHC, universal coverage, universal health care, universal care, universal access, social health insurance, socialized health care |
| Social health protection | Social welfare, public welfare services, health equity, social determinants of health, social protection in health, social protection, social health promotion, social security, public health security, global health security, social ecology health promotion, social health insurance |
| Health financing | Health systems financing, healthcare financing, health financing system, public health financing, health economics, health spending, healthcare finance, health expenditure, healthcare management |
| Stakeholder analysis | Stakeholder mapping, stakeholder value network, stakeholder management, stakeholder impact analysis, stakeholder interest |
Keyword combinations for searches
| 1. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘universal health coverage’ OR (‘universal health care’ OR ‘universal healthcare’) OR UHC OR healthcare OR ‘universal coverage’ OR ‘socialized health insurance’] |
| 2. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘social health protection’ OR ‘social welfare’ OR ‘social protection’ OR (equity or inequity) OR ‘social determinants of health’ OR ‘health security’ OR ‘public health security’ OR ‘social health insurance’ OR ‘financial risk protection’] |
| 3. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND (‘health financing’ OR ‘health systems financing’ OR ‘healthcare financing’ OR ‘health economics’ OR ‘health spending’ OR ‘healthcare finance’) |
| 4. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND (‘stakeholder mapping’ OR ‘stakeholder interest’ OR ‘stakeholder value network’) |
| 5. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘universal health coverage’ OR (‘universal health care’ OR ‘universal healthcare’) OR UHC OR healthcare OR ‘universal coverage’ OR ‘socialized health insurance’ OR ‘financial risk protection’] AND (‘stakeholder mapping’ OR ‘stakeholder interest’ OR ‘stakeholder value network’) |
| 6. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘universal health coverage’ OR (‘universal health care’ OR ‘universal healthcare’) OR UHC OR healthcare OR ‘universal coverage’ OR ‘socialized health insurance’] AND [‘social health protection’ OR ‘social welfare’ OR ‘social protection’ OR (equity or inequity) OR ‘social determinants of health’ OR ‘health security’ OR ‘public health security’ OR ‘social health insurance’] AND [‘social health protection’ OR ‘social welfare’ OR ‘social protection’ OR (equity or inequity) OR ‘social determinants of health’ OR ‘health security’ OR ‘public health security’ OR ‘social health insurance’ OR ‘financial risk protection’] AND (‘health financing’ OR ‘health systems financing’ OR ‘healthcare financing’ OR ‘health economics’ OR ‘health spending’ OR ‘healthcare finance’) AND (‘stakeholder mapping’ OR ‘stakeholder interest’ OR ‘stakeholder value network’) |
| 1. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘universal health coverage’ OR (‘universal health care’ OR ‘universal healthcare’) OR UHC OR healthcare OR ‘universal coverage’ OR ‘socialized health insurance’] |
| 2. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘social health protection’ OR ‘social welfare’ OR ‘social protection’ OR (equity or inequity) OR ‘social determinants of health’ OR ‘health security’ OR ‘public health security’ OR ‘social health insurance’ OR ‘financial risk protection’] |
| 3. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND (‘health financing’ OR ‘health systems financing’ OR ‘healthcare financing’ OR ‘health economics’ OR ‘health spending’ OR ‘healthcare finance’) |
| 4. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND (‘stakeholder mapping’ OR ‘stakeholder interest’ OR ‘stakeholder value network’) |
| 5. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘universal health coverage’ OR (‘universal health care’ OR ‘universal healthcare’) OR UHC OR healthcare OR ‘universal coverage’ OR ‘socialized health insurance’ OR ‘financial risk protection’] AND (‘stakeholder mapping’ OR ‘stakeholder interest’ OR ‘stakeholder value network’) |
| 6. [‘political econom*’ OR politic* OR ‘economic analysis’ OR (‘policy making’ OR policy-making) OR ‘policy implementation’ OR ‘political settlements’] AND [‘universal health coverage’ OR (‘universal health care’ OR ‘universal healthcare’) OR UHC OR healthcare OR ‘universal coverage’ OR ‘socialized health insurance’] AND [‘social health protection’ OR ‘social welfare’ OR ‘social protection’ OR (equity or inequity) OR ‘social determinants of health’ OR ‘health security’ OR ‘public health security’ OR ‘social health insurance’] AND [‘social health protection’ OR ‘social welfare’ OR ‘social protection’ OR (equity or inequity) OR ‘social determinants of health’ OR ‘health security’ OR ‘public health security’ OR ‘social health insurance’ OR ‘financial risk protection’] AND (‘health financing’ OR ‘health systems financing’ OR ‘healthcare financing’ OR ‘health economics’ OR ‘health spending’ OR ‘healthcare finance’) AND (‘stakeholder mapping’ OR ‘stakeholder interest’ OR ‘stakeholder value network’) |
A total of 1159 papers were identified in the search, with 627 papers remaining following the removal of duplicates. Inclusion criteria included English language publications, referring to UHC or one of the three related objectives in its definition ( WHO, 2019 ), and explicitly linked to a political economy perspective ( Collinson, 2003 ). Papers were excluded where they did not use a political economy framework, or where the details of their analysis were narrower than the three stated objectives. Following the screening of title and abstract, 127 papers were identified as likely to be relevant and two researchers (R.D. and P.S.H.) independently examining full text confirmed 55 publications for analysis, with the difference of opinion on five papers, which were discussed and subsequently included. An additional eight papers were added manually, identified as relevant by the researchers and their networks ( Figure 1 ). The analysis of the papers was undertaken manually, using the adapted Fox and Reich’s (2015) framework: the first tranche of thematic analysis examined ideologies and ideas. This explored accounts of the policy uptake and implementation of UHC but also examined the theoretical premises of political economy analyses applied to UHC. The second tranche of analysis identified the interests—the stakeholders in UHC analyses and, where possible, linked these to the framings already explored in the first tranche. The final tranche was into the institutions—the formal and informal agencies and processes that enable or obstruct the implementation of UHC. Following this analysis, a further exploration of those papers detailing political economy analysis of UHC initiatives in specific countries was undertaken, to be published independently.

Search and selection diagram for analysis
The search strategy used for this analysis focuses on the interface between political economy and UHC, identifying papers that have been filtered through peer review prior to publication. As a consequence of this specific focus on the intersection between political economy and UHC, the result is not a comprehensive representation of the literature on UHC, or of any single country’s progress to UHC, but only explores analyses of UHC where a political economy framing has been specifically used. The inclusion criteria, which required an explicit political economy perspective, meant that, in most cases, only one or two analyses of each country were available. To apply a political analysis to any individual country, a richer, more complex understanding would be achieved from the engagement of local expertise and the integration of a broader literature into the framework offered in this study.
The values of UHC—universality, service quality and access and financial protection and equity—are themselves politically framed, and there is a resultant bias towards social democratic perspectives both in the cases represented and in the analyses of them. Despite this, there is a wide range of political positions expressed in the implementation and analysis of UHC initiatives: it is not exclusively a ‘left’ agenda, and in many countries, UHC has been introduced and supported by a broad spectrum of political parties and philosophical and political positions.
The findings of the analysis of the selected literature have been organized using the four variables identified by Fox and Reich (2015) .
Ideology and ideas
Ideologies as defined by Fox and Reich (2015) are world views that may be drawn upon to justify or underpin change. They can be seen as the overarching logic or ‘cognitive background’ that guides an institution’s policy preferences ( Campbell, 1998 ). Within this study, ideologies advocated within social democracy, liberalism and conservatism are formed on the basis of values that are deemed important by the proponents of each respective world view—or in cases such as ‘neo-liberalism’, used by ideological opponents to characterize a perceived position. Values, such as solidarity, equality and autonomy, rest upon certain assumptions about human rights and behaviour, and Frenk and Gómez-Dantés (2015) point out that these assumptions are expressed either explicitly or implicitly through the distribution, delivery and financing of healthcare resources. This then gives us a framework to dissect the implied motivations and emotions that fuel specific positions and actions taken by actors and institutions, in influencing a state’s progress towards UHC. Similar values-based frameworks have also been proposed by Shiffman (2009) , Rushton and Williams (2012) and van Olmen et al. (2012) , among others.
The economic structures that these ideologies, values and assumptions act upon may be either private market oriented or public intervention oriented, or in most modern pluralistic health sectors, a combination of the two, necessary to appease all parties and to achieve comprehensive UHC ( McPake and Hanson, 2016 ). Levels of market regulation will vary even among countries that ascribe to the same political ideology. Identifying ideological elements and values at play at the beginning of the policy-making process is important for two reasons as described by McInnes and Lee (2012) . The first is to avoid proceeding with a mix of contradictory policies that will ultimately need to be reconciled; the second is to provide insight into opportunities for effective framing and priority setting during debate and negotiation processes.
Reeves et al. (2015) and McKee et al. (2013) suggest that governments led by left-leaning parties were more likely to implement UHC and tended to better utilize progressive sources to ultimately invest more money on healthcare than right-leaning parties. Raphael and Bryant (2006) overtly advocate social democratic policy models as a preferred platform for UHC, but it is clear that UHC implementation is formed by diverse political and historical narratives and other contextual factors. The literature offers examples of both success and failure from similar contextual backgrounds, as well as examples of achieving similar results from vastly different contextual backgrounds. The persistent imprint of colonialism continues to impact on Bangladesh through its highly centralized public administration, ultimately constraining the responsiveness of services to societal healthcare needs, though civil society initiatives have compensated for this, producing significant progress ( Osman and Bennett, 2018 ). Ichoku et al. (2013) , drawing light to the differences between the ideas of social solidarity embedded within traditional Sub-Saharan African institutions and the pseudo-capitalistic ideology that persisted after colonial domination, argue that historically injected values that once made sense might now conflict and restrict progress. Values can be instilled from a variety of sources: countries where the residual impacts of colonialism seem remote may now face economic policy practices similar to those experienced under colonialism as a result of the forced adoption of neoliberal values attached to conditional aid contacts, written by global developmental partners ( Ravindran, 2014 ).
Given the apparent bias of analysts in this space, and the selective narratives of policies used by countries to achieve UHC, the literature points to social democratic ideologies as most conducive to progress towards UHC—in particular those that utilize the values of equity, solidarity and welfare as a means of increasing worker productivity ( McKee et al. , 2013 ; Reeves et al. , 2015 ). In practice, there is a massive overlap between institutional ideologies, and at times, institutions may act in direct opposition to the ideology they lay claim to. Ghana’s social welfare cash transfer programme—Livelihood Empowerment against Poverty (LEAP)—was initiated by its free market-oriented ‘right of centre’ New Patriotic Party ( Abdulai, 2019 ). The contested political support—or resistance—around the US Affordable Health Care Act reflects current diversity and polarized extremes in political ideology ( Osman and Bennett, 2018 ), but political actors from all ends of the ideological spectrum can, and do, come together and find common ground in the pursuit of UHC.
Within the literature, ideologies, although presented as the background paradigms that underlie policies, also may be applied in a reductionist—and unhelpful—labelling of actors and institutions. Political ideologies usually comprise both a social set of values and an economic set of values. Social values embrace a range of values based on equity to those based on individualism. Economic values cover a continuum from private sector and free market oriented to public sector oriented—and complex combinations of both ( Figure 2 ). The evidence is that governments and their oppositions simultaneously utilize mechanisms from all ends of both social and economic spectrums and also draw from vastly different values, when dealing with different policies. It then follows that the ‘left-wing’ and ‘right-wing’ labels often used to describe governments are not only imprecise but also polarizing when seeking to explore the most politically appropriate interventions for the specific context ( Davidson, 2014 ).

Schematic diagram of political ideas
A more pragmatic approach would be to assess the nuance in what Fox and Reich (2015) term the ‘ideas’ truly represented and held by stakeholders, institutions and their proposed policies. Chemouni (2018) was able to illustrate this with the case of Rwanda and its community-based health insurance (CBHI). A superficial analysis might conclude that the Tutsi-dominant Rwandan regime had no interest in expanding social protection benefits to the majority-Hutu rural population, but with the implementation and commitment to CBHI, the government was able to achieve 86% population coverage. Further analysis shows that the prevailing values of a self-reliant nation, long-term regime legitimization and the role of the state in coordinating socio-economic progress allowed the Rwandan Patriotic Front to progress these reforms in apparently counterintuitive ways. The political construction of the ‘good Rwandan’—self-reliant, rejecting dependence—was critical to expanding the ‘mutuelles’ and resisting external donor pressure to increase co-payments ( Chemouni, 2018 ).
A key starting point for all interventions is being receptive to the tensions and congruencies between the implicit and explicit values held by stakeholders and institutions ( Borgonovi and Compagni, 2013 ; Lavers and Hickey, 2016 ). The links between ideologies and ideas are not necessarily linear: ideologies may be maintained in political rhetoric, but the operational ideas and values held by the parties might not be congruent with traditional understandings of the ideologies that these institutions lay claim to. While conflicts between claimed or implied ideologies might be difficult to reconcile, productive alliances can still be built around the operational ideas and goals. This capacity to find shared functional territory is absolutely vital, as political commitment from a wide variety of ministries, levels of government and industries is needed to progress towards UHC. Okech and Lelegwe (2016) , seeking to identify the key factors limiting Kenya’s progress towards UHC, cite the complete absence of collaboration as a result of self-serving interests, and the resulting lack of communication between interests in policy, research and practice. Korea and Taiwan’s multi-stakeholder approach to UHC policy planning and implementation presents contrasting perspectives: neither the strengths nor weaknesses of their UHC policies could be adequately explained by the apparently superficial political positions held by actors in the health governance space ( Kwon and Chen, 2008 ). Other factors were clearly at play.
Fox and Reich’s (2015) usage of ‘interests’ suggests an expanded definition of stakeholders—recognizing the importance not only of agencies but also of individuals and coalitions sharing ideologies or ideas, or invested in the institutions that would implement UHC. Analysis of these interests can make it clear as to which actors will impede or expedite progress through the policy cycle. It can also give a sense of how progress is perceived by interest groups, which can help during the agenda-setting process. Further analysis of the underlying values and assumptions of the institutions and interest groups involved, based on their previous actions and stated mandates, can identify points of tension and opportunity that might not be immediately apparent. This can also suggest which new institutions or multi-sectoral alliances need to be established, and how they might interact with the existing ecosystem. The positioning of analysts influences how interests are represented. Political economic analyses of the patterns of behaviour and political and economic histories of the institutions and interest groups may be explicitly represented through the political and theoretical prisms of the authors ( Ichoku et al. , 2013 ; Kelsall and Heng, 2016 ; Lavers and Hickey, 2016 ; Fouda and Paolucci, 2017 ) and may not reflect how stakeholders would represent themselves. In contrast, ‘technical’ analyses framed as exemplars of successful UHC implementation, may offer less overt political framing ( Bayarsaikhan et al. , 2015 ; Okech and Lelegwe, 2016 ; Frenk and Gómez-Dantés, 2015 ; Reich et al. , 2016 ; Lan, 2017 ). Despite this, the construction of a technical analysis as independent, ‘objective’ assessment brings its own inherent values framework, which may still be implicit in the text ( Carrin et al. , 2007 ; Carrin et al. , 2008 ; Minh et al. , 2014 ).
The case studies examined in this review are not consistent in the degree of granularity with which they identify stakeholders in their exploration of the political economy of UHC. The lessons from the African SHIELD project are quite explicit in their identification of domestic—and where relevant, international—institutions and their positions and support, though individuals and their influence are not specified ( Gilson et al. , 2012 ). Other studies may refer to selected individuals by name or title ( Krajewski-Siuda et al. , 2008 ; Basaza et al. , 2013 ; Chemouni, 2018 ), but specific identification of stakeholders is more frequent at the level of agencies—or networks and coalitions of interests.
Analysis of the reports of country case studies suggests that for high- or upper-middle-income countries, the coalitions of importance for UHC have been domestic, with political and popular alliances critical. Krajewski-Siuda et al. ’s (2008) analysis of the Polish National Health Fund credits its creation—despite substantial opposition—to key political alliances with union support, and an ambivalent media, and its demise to the collapse of that coalition. Despite that uncertain beginning, the initiative has served as a platform for subsequent developments in UHC. The review confirms that the political routes to UHC are diverse. Costa-Rica’s ‘Caja Costarricense de Seguro Social’ has been tracked across 7 decades towards UHC ( Vargas and Muiser, 2013 ), with critical shifts—and reversals—of coalitions of support and opposition over that period enabling UHC implementation. In this case, UHC implementation was driven by political support at the highest level and popular demand, despite the ‘the absence of real consensus among the policy elite’. Chee (2008) , examining the contested healthcare sector in Malaysia, documents the transition from a statist to more pluralist system, with incremental alliances between the state and private services counterbalanced by the response of civil society organizations. Lan (2017) identifies a path-dependent, incremental implementation of UHC in Taiwan, with progress constrained by a cultural–ideological framing shared by both political elites and the population, until fiscal crisis drove a resolution.
Lower-middle- or low-income country studies are more likely to make reference to international influences, though the extent to which this is explicit varies and makes tracking the influence of international agencies more difficult, with the extent of that influence often underplayed ( Lavers and Hickey, 2016 ). In their analysis of Uganda's national health insurance scheme, Basaza et al. (2013) directly acknowledge the policy advice of the Social Health Protection Network P4H (Providing for Health) through facilitating study visits of countries offering models UHC progress, and list bilateral and multilateral donor agencies as influential stakeholders, together with domestic actors. Reference to a ‘Joint Learning Network for UHC’ review of Mongolia’s Social Health Insurance suggests some significant level of engagement by WHO and the World Bank, but the key political drivers described are clearly domestic ( Bayarsaikhan et al. , 2015 ).
The interplay between domestic and international actors is complex. Abdulai (2019) revisits Ghana’s LEAP implementation and questions the extent to which donor conditionalities played in its implementation. Pisani et al. ’s tracking of UHC in Indonesia attributes the dominant impetus to domestic political imperatives but makes reference to the contribution of academics and civil society and the financial underpinnings of US, Australian and German bilateral assistance, ‘though no interviewees reported that the views of foreign development agencies significantly influenced the shape or outcome of domestic discussions’. In their presentation of Kenya’s social health insurance proposal, the authors—with multiple representatives from the Kenyan Ministry of Health (MoH) and the National Hospital Insurance Fund, technical advisors from both WHO and the International Labor Organization and UK and German bilateral development agencies—make only glancing reference to international support, though domestic stakeholder positions are carefully documented ( Carrin et al. , 2007 ). Chemouni’s (2018) account of Rwanda’s path to UHC documents the contribution of multiple multilateral, bilateral and global public–private partnerships over the past 2 decades, providing technical assistance in the analysis and development of proposals. He points to the unexpected success of a health systems strengthening bid submitted by the MoH and a coalition of then GTZ 1 and the United Nations Development Program and the Rwandan First Lady’s Protection and Care of Families against AIDS to the Global Fund to fight acquired immune deficiency syndrome, tuberculosis and malaria. The collapse of this alliance, in the face of MoH opposition, is one instance of Rwanda’s assertion of its own policy direction against external influences, even in coalition with significant internal interests. The review indicates that local ownership necessarily reframes the financial and technical contributions from international agencies to progress on UHC and that ownership is critical to the success of its implementation.
Institutions
The institutions that drive UHC—the formal political structures linked to UHC policy and its implementation—are key to translating the systematic review into a narrative that permits the identification of nodes of possible influence in the policy trajectory of UHC. They also influence the informal expectations and precedents that might shape UHC uptake but are shaped by the existing infrastructure from which they are developed. It is this local context that shapes the diversity of options in the institutions that build UHC, as evidenced in the political economy analyses from different country case studies. They are also vulnerable to political and economic changes in both global and domestic contexts. The inclusion of the achievement of UHC as one of the United Nations' Sustainable Development Goals targets (SDG3.8) provides a global commitment for translation into national institutions, though economic austerity has seen countries withdrawing from those same commitments, unpicking legislation and regulation relevant to UHC ( McKee et al. , 2013 ; Osman and Bennett, 2018 ). Politicization of the UHC agenda can expedite its progressive implementation into local institutions ( Borgonovi and Compagni, 2013 ), as in overt politicization as in the Ghanaian experience ( Fusheini, 2016 ), but then render it vulnerable to political reversal, as was also the case in Poland ( Krajewski-Siuda et al. , 2008 ).
Nigeria’s National Health Insurance System points to the dynamic nature of institutional roles and the complex interplay between federal and state responsibilities in a federal system. Onoka et al. ’s (2015) account unpacks these challenges, with inadequate clarification of the role of the states in the policy design stage, and consequent independent development by individual states of their own health insurance structure. With inclusion in the programme made voluntary, the inconsistencies between states significantly compromised effective coverage and uniform implementation. There were also tensions between private providers and state accountability, compounded by this divergence between state programmes, and a loosely managed incorporation of private providers into the scheme ( Onoka et al. , 2013 ). McPake and Hanson (2016) point to the common role of the private sector in pluralistic health systems to provide higher-level services to those who can afford them. Their potential for contracted provision of publically accessible services within UHC depends on effective government financial stewardship and the capacity for effective regulation.
The political dynamic in Cambodia has proved positive in the incremental progress in the development of institutions towards UHC, despite ambivalent assessments of the political economy of health, with Kelsall and Heng (2016) describing it as ‘an elite bargain in which both appropriating rents and delivering health outcomes are important’. Procurement of medications and a largely unregulated private sector continue to offer challenges in terms of the institutions necessary for the implementation of UHC, but the history of health sector reform and, in particular, the Health Coverage Plan that extended health infrastructure throughout Cambodia have laid down a solid basis of technical competence and ensured almost universal access to health service delivery.
The Health Equity Funds (HEFs) were initially introduced to overcome the obstacles of user fees for the poor but have been increasingly standardized in terms of their processes and aligned with health sector administration. The MoH has increased the domestic proportion of funding for the HEFs, enabling an expansion in their availability. The reimbursement of fees for the poor enhances the salaries of health professionals in an apparent virtuous cycle that guarantees sustainability, with both patients and providers benefitting in this scenario ( Kelsall and Heng, 2016 ). Kelsall and Heng (2016) identify two contrasting dynamics—health seeking and rent seeking—working together within the MoH, with health seen both as a desirable outcome in its own right, but also ‘increasingly seen as a good ‘gift’ for constituents in order to buy legitimacy at the ballot box’ ( Jones, 2013 ). The scale up of the HEF from its civil society roots has also enabled local cheques and balances against leakage to be institutionalized, a valuable mechanism as it is incorporated into the broader coverage of UHC. Ironically, the frank political settlement analyses offered by both Jones (2013) and Kelsall and Heng (2016) suggest that an explicit awareness of the political economy allows for a more pragmatic and realistic framing to build the institutions of UHC.
McKee et al. (2013) draw attention to the window of opportunity that presents politically for the implementation of UHC—the British National Health System providing the iconic example. Clarke and Le Masson (2017) point to the transformative possibilities in rebuilding institutions in response to national calamity, but the positive political window can also see UHC aligned with other larger political concepts, and the institutions of UHC their embodiment. For Mexico, the window was political: a shift from single-party domination to a democratized state that enabled a greater diversity of voices to be heard in the Mexican parliament and social policies that targeted a broader proportion of the population ( Gómez-Dantés et al. , 2015 ). These political shifts in power reflect broader progress in civil and political rights and provide a platform from which to establish a sense of urgency and demand for policies framed towards reducing inequalities ( Frenk et al. , 2006 ). The right to health care was framed as a mechanism for achieving social equality in Mexico, made concrete through implementing the General Health Law in 2003, and introducing the state-sponsored health insurance system Segura Popular, that achieved universal coverage by 2012 ( The Lancet, 2012 ). Recognizing the opportune moments that invite intervention can be especially effective for getting UHC-oriented policies onto the broader political agenda ( Grépin and Dionne, 2013 ).
But the strategic response to the window of opportunity is often predicated on the solid foundation of building institutions for the implementation of UHC. Having framed UHC in terms of rights, technical capacity to operationalize that claim is imperative. One of the greatest strengths of the Mexican reform effort was the technical capacity of the MoH, with the Minister of Health launching a small pilot programme to establish the proof of concept and garner support from the President. Pilots and other evidence gathering mechanisms provided data that alleviated speculative worries held by international actors and key national actors, such as the Minister of Finance ( Gómez-Dantés et al. , 2015 ). Positive results from the pilot provided the basis of discussions with the Minister of Finance for expansion to begin. The technical expertise and research capacity provided by these institutions not only directed the content of the proposed policies but also fuelled the political drive and framing process ( Frenk et al. , 2006 ).
The implementation of UHC is heavily dependent on institutional evolution ( Savedoff et al. , 2012 ; Reich et al. , 2016 ), and there is extensive available experience across both health and health financing systems ( Carrin et al. , 2008 ; Musango et al. , 2012 ; Meheus and McIntyre, 2017 ). The insights of political economy complement this with a deep understanding of the social, economic and political economy of the context within which UHC institutions operate. Path dependency is evident in the need to deal with the legacy of existing user-fees legislation and infrastructure, as in the Cambodian example ( Kelsall et al. , 2016 ), or in the transition into universal health insurance for Tanzania ( Pederson and Jacob, 2018 ). The role of the private sector is implicit in many health systems, with private provision (both for-profit and not-for-profit) filling state service gaps either formally through contracting or other regulated relationships, or the provision of insurance ( Chee, 2008 ). Attitudes in low- and middle-income countries (LMICs) towards engagement of the private sector in the institutions that implement UHC are divergent, ranging from the negative (prohibition or constraint) to the positive (encouragement, subsidizing and purchasing of services) ( Montagu and Goodman, 2016 ), and some concern expressed around UHC lies in perceptions of the ‘privatization’ of health and the redirection of resources away from public health priorities ( Schmidt et al. , 2015 ).
There has been an exponential growth in interest in political economy in health over the past 5 years: a simple search using ‘political economy’ as the search term in PubMed reveals 191 records in 2014, rising consistently to 831 in 2019. The Prince Mahidol Awards Conference (2019) in Bangkok had as its theme ‘The Political Economy of NCDs: A Whole of Society Approach’; in anticipation of the High Level Meeting on UHC, the monograph ‘Health: A Political Choice. Delivering Universal Health Coverage 2030’ has been recently released in collaboration with the WHO ( Kirton and Kickbusch, 2019 ) and the political economy of health is the focus of a recent special issue of the journal Health Systems and Reform ( Sparkes et al. , 2019 ; Campos and Reich, 2019 ). Sparkes et al. (2019) , seeking to develop a political economy analysis for health financing reform, conducted two systematic reviews, one on the technical aspects of health financing reforms, which provided ‘very little information about the political economy of the process’, and the second on political economy and health policy ‘similarly did not lead us to an existing framework or model that would suit our purposes’. Despite extensive mobilization towards UHC across a range of countries ( Monteira de Andrade et al. , 2015 ; Reeves et al. , 2015 ; Alami, 2017 ), the political economy prism has been applied only to a limited number of country experiences.
The experience encountered by Sparkes et al. (2019) is not dissimilar to our own, with an apparent divide between those papers that elaborate the ideologies and ideas around the political economy of UHC, and the more technically oriented papers dealing with the interests and institutions involved in its implementation, despite their interdependence in practice. This may arise because of the professional backgrounds of the analysts, with the political or technical perspectives preferenced, depending on discipline. Recognizing the imperative for the technical to engage the political—and vice versa—and faced with the failure of the literature to yield an appropriate framing, Sparkes et al. (2019) have adopted the framework developed by Campos and Reich (2019) based on the major categories of stakeholders in health policy in LMICs: interest group politics, bureaucratic politics, budget politics, leadership politics, beneficiary politics and donor politics. The classification is heuristic and allows a useful exploration of political dynamics in the case studies explored but is grounded in a theorized categorization of stakeholder orientation, rather than emerging directly from research. The juxtaposition of the technical and political that Sparkes et al. (2019) highlight is the critical interface of this dialogue and lies at the heart of the implicit recognition of the importance of political commitment to the achievement of UHC referred to in SDG3.8—but the apparent uncertainty about how to ensure this.
Despite the challenges outlined in the discussion, there is some evidence of an emergent narrative evident in this nascent literature around the intersection between political economy and UHC. The central variables identified by Fox and Reich (2015) —ideologies and ideas, interests and institutions—have been useful both for clarifying the areas of focus for any analysis and highlighting their porosity and interdependence. The systematic review of literature points to an increasing awareness of the significance of the political economy of health ( Greer and Méndez, 2015 ) and its direct application to the global uptake of UHC, and a growing body of critical case studies of UHC and national health systems from a political economy perspective.
But the current interest in—but limited research application of—political economy analysis for UHC, and the sharp divide between technical and political analyses, points to the need for further multidisciplinary research that will cast light on the obstacles to UHC uptake and implementation. This narrative systematic review has demonstrated a growing health systems and policy literature that explicitly claims a political economy perspective but provides only glimpses of how this perspective is being applied to specific country contexts. The thematic analysis of the case studies identified in this study points to the interfaces between the variables as point of possible influence in the UHC policy process: an awareness of where ideology and ideas can influence interests, where interests and their ideas can be aligned to optimize the development of institutions, where changes in ideas or interests shape new contexts for UHC implementation and where contextual change or external factors open windows of opportunity for new policy.
There is a need to build the theoretical and practical frameworks that would enable competent and consistent analysis, the necessary funding to expand that research and the policy preparedness to engage its findings and implications. A deeper exploration and theorizing of political economy is needed to complement the contribution of rapid reviews, and technical assessment in providing policy evidence towards UHC, outlining approaches that would enhance the rigour, accessibility and applicability of such evidence ( Langlois et al. , 2019 ), but rather than target specific evidence for policy-making, there is a need for a collaborative body of research that would provide an exploration of the political economy of UHC that would deeply inform its policy adoption and implementation—both in specific countries and across the broader international context. It would begin with the clarification of ideologies and ideas—beginning with reflective exercise for the analysts themselves, clarifying their own values and concepts—and map out the ideologies and ideas identified across stakeholder interests. It would trace the political influence of those ideologies and ideas through the stakeholder interests into the formal and informal institutions that enable UHC, identifying veto points and the nodes of possibility that catalyze UHC progress. From this base, the technical exploration of options for UHC becomes realistic, with the uncertainty around the political context of those largely clarified, alliances negotiated and challenges identified.
R.D. undertook the systematic review search as part of a WHO internship. S.S.R.’s primary analysis of the findings was funded through a University of Queensland Summer Research Scholarship. P.S.H.’s conceptualization and analysis were partially funded by a consultancy with the Social Health Protection Network P4H (Providing for Health).
The opinions expressed are those of the authors alone and do not reflect WHO or Social Health Protection Network P4H positions.
Ethical approval. None required.
Abdulai A.-G. 2019 . Rethinking Elite Commitment to Social Protection in Ghana: Insights from an Adapted Political Settlements Approach . Manchester : Effective States and Inclusive Development .
Google Scholar
Google Preview
Alami R. 2017 . Health financing systems, health equity and universal health coverage in Arab countries . Development and Change 48 : 146 – 79 .
Basaza RK , O’Connell TS , Chapčáková I. 2013 . Players and processes behind the national health insurance scheme: a case study of Uganda . BMC Health Services Research 13 : 357 .
Bayarsaikhan D , Kwon S , Chimeddagva D. 2015 . Social health insurance development in Mongolia: opportunities and challenges in moving towards Universal Health Coverage . International Social Security Review 68 : 93 – 113 .
Borgonovi E , Compagni A. 2013 . Sustaining universal health coverage: the interaction of social, political, and economic sustainability . Value in Health 16 : S34 – 8 .
Campbell JL. 1998 . Institutional analysis and the role of ideas in political economy . Theory and Society 27 : 377 – 409 .
Campos PA , Reich MR. 2019 . Political analysis for health policy implementation . Health Systems and Reform 5 : 224 – 35 .
Carrin G , James C , Adelhardt M et al. 2007 . Health financing reform in Kenya—assessing the social health insurance proposal . South African Medical Journal 97 : 130 – 5 .
Carrin G , Mathauer I , Xu K , Evans DB. 2008 . Universal coverage of health services: tailoring its implementation . Bulletin of the World Health Organization 86 : 857 – 63 .
Chee HL. 2008 . Ownership, control, and contention: challenges for the future of healthcare in Malaysia . Social Science & Medicine 66 : 2145 – 56 .
Chemouni B. 2018 . The political path to universal health coverage: power, ideas and community-based health insurance in Rwanda . World Development 106 : 87 – 98 .
Clarke L , Le Masson V. 2017 . Shocks, stresses and universal health coverage: pathways to address resilience and Health. Working Paper 526. London: Overseas Development Institute.
Collinson S. (ed). 2003 . Power, Livelihoods and Conflict: Case Studies in Political Economy Analysis for Humanitarian Action. London : Humanitarian Policy Group, Overseas Development Institute , 3 .
Davidson K. 2014 . A typology to categorize the ideologies of actors in the sustainable development debate . Sustainable Development 22 : 1 – 14 .
Fouda A , Paolucci F. 2017 . Path dependence and universal health coverage: the case of Egypt . Frontiers in Public Health 5 : 325 .
Fox AM , Reich MR. 2015 . The politics of universal health coverage in low and middle-income countries: a framework for evaluation and action . Journal of Health Politics, Policy and Law 40 : 1023 – 60 .
Frenk J , Gómez-Dantés O. 2015 . Ethical and human rights foundations of health policy: lessons from comprehensive reform in Mexico . Health and Human Rights 17 : 31 – 7 .
Frenk J , González-Pier E , Gómez-Dantés O , Lezana MA , Knaul FM. 2006 . Comprehensive reform to improve health system performance in Mexico . The Lancet 368 : 1524 – 34 .
Fusheini A. 2016 . The politico-economic challenges of Ghana’s national health insurance scheme implementation . International Journal of Health Policy and Management 5 : 543 – 52 .
Gilson L , Erasmus E , Borghi J et al. 2012 . Using stakeholder analysis to support moves towards universal coverage: lessons from the SHIELD project . Health Policy and Planning 27 : i64 – 76 .
Gómez-Dantés O , Reich MR , Garrido-Latorre F. 2015 . Political economy of pursuing the expansion of social protection in health in México . Health Systems & Reform 1 : 207 – 16 .
Greer SL , Méndez CA. 2015 . Universal health coverage: a political struggle and governance challenge . American Journal of Public Health 105 : S637 – 9 .
Grépin KA , Dionne KY. 2013 . Democratization and universal health coverage: a case comparison of Ghana, Kenya, and Senegal . Global Health Governance 6 : 2 .
Ichoku HE , Fonta WM , Ataguba JE. 2013 . Political economy and history: making sense of health financing in sub-Saharan Africa . Journal of International Development 25 : 297 – 309 .
Jones H. 2013 . Building political ownership and technical leadership. ODI Report. London: Overseas Development Institute.
Kelsall T , Heng S. 2016 . Inclusive healthcare and the political settlement in Cambodia . New Political Economy 21 : 238 – 55 .
Kelsall T , Hart T , Laws E. 2016 . Political settlements and pathways to universal health coverage. Working Paper 432. London: Overseas Development Institute.
Kirton J , Kickbusch I. 2019 . Health: A Political Choice. Delivering Universal Health Coverage 2030 . London : GT Media Group .
Krajewski-Siuda K , Romaniuk P , Gericke CA. 2008 . Political analysis of the conception of the Polish National Health Fund . Journal of Public Health 16 : 153 – 9 .
Krieger N. 2011 . Epidemiology and the People’s Health: Theory and Context . Oxford : Oxford University Press , 168 .
Kwon HJ , Chen FL. 2008 . Governing universal health insurance in Korea and Taiwan . International Journal of Social Welfare 17 : 355 – 64 .
Lan J-C. 2017 . Achieving and sustaining universal health coverage: fiscal reform of the national health insurance in Taiwan . Applied Health Economics and Health Policy 15 : 717 – 31 .
Langlois EV , Straus SE , Antony J et al. 2019 . Using rapid reviews to strengthen health policy and systems and progress towards universal health coverage . BMJ Global Health 4 : e001178 .
Lavers T , Hickey S. 2016 . Conceptualising the politics of social protection expansion in low income countries: the intersection of transnational ideas and domestic politics . International Journal of Social Welfare 25 : 388 – 98 .
McInnes C , Lee K. 2012 . Framing and global health governance: key findings . Global Public Health 7 : S191 – 8 .
McKee M , Balabanova D , Basu S , Ricciardi W , Stuckler D. 2013 . Universal health coverage: a quest for all countries but under threat in some . Value in Health 16 : S39 – 45 .
McPake B , Hanson K. 2016 . Managing the public-private mix to achieve universal health coverage . The Lancet 388 : 622 – 30 .
Meheus F , McIntyre D. 2017 . Fiscal space for domestic funding of health and other social services . Health Economics, Policy and Law 12 : 159 – 77 .
Minh HV , Pocock NS , Chaiyakunapruk N. 2014 . Progress toward universal health coverage in ASEAN . Global Health Action 7 : 25856 .
Montagu D , Goodman C. 2016 . Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector? The Lancet 388 : 613 – 21 .
de Andrade LOM , Filho AP , Solar O et al. 2015 . Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries . The Lancet 385 : 1343 – 51 .
Musango L , Orem JN , Elovainio R , Kirigia J. 2012 . Moving from ideas to action—developing health financing systems towards universal coverage in Africa . BMC International Health and Human Rights 12 : 30 .
Okech TC , Lelegwe SL. 2016 . Analysis of universal health coverage and equity on health care in Kenya . Global Journal of Health Science 8 : 218 .
Onoka CA , Hanson K , Hanefeld J. 2015 . Towards universal coverage: a policy analysis of the development of the National Health Insurance Scheme in Nigeria . Health Policy and Planning 30 : 1105 – 17 .
Onoka CA , Onwujekwe OE , Uzochukwu BS , Ezumah NN. 2013 . Promoting universal financial protection: constraints and enabling factors in scaling-up coverage with social health insurance in Nigeria . Health Research Policy and Systems 11 : 20 .
Osman F , Bennett S. 2018 . Political economy and quality of primary health service in rural Bangladesh and the United States of America: a comparative analysis . Journal of International Development 30 : 818 – 36 .
Pederson RH , Jacob T. 2018 . Social protection in an electorally competitive environment (2): the politics of health insurance in Tanzania. ESID Working Paper 10 . Manchester: Effective States and Inclusive Development.
Prince Mahidol Awards Conference. 2019 . The Political Economy of NCDs: A Whole of Society Approach . https://pmaconference.mahidol.ac.th/site/previosConference , accessed 19 August 2019.
Raphael D , Bryant T. 2006 . Maintaining population health in a period of welfare state decline: political economy as the missing dimension in health promotion theory and practice . Promotion & Education 13 : 236 – 42 .
Ravindran T. 2014 . Poverty, food security and universal access to sexual and reproductive health services: a call for cross-movement advocacy against neoliberal globalisation . Reproductive Health Matters 22 : 14 – 27 .
Reeves A , Gourtsoyannis Y , Basu S et al. 2015 . Financing universal health coverage—effects of alternative tax structures on public health systems: cross-national modelling in 89 low-income and middle-income countries . The Lancet 386 : 274 – 80 .
Reich MR , Harris J , Ikegami N et al. 2016 . Moving towards universal health coverage: lessons form 11 country studies . The Lancet 387 : 811 – 6 .
Rushton S , Williams OD. 2012 . Frames, paradigms and power: global health policy-making under neoliberalism . Global Society 26 : 147 – 67 .
Savedoff WD , de Ferranti D , Smith AL et al. 2012 . Political and economic aspects of the transition to universal health coverage . The Lancet 380 : 924 – 32 .
Schmidt H , Gostin LO , Emanuel EJ. 2015 . Public health, universal health coverage, and sustainable development goals: can they coexist? The Lancet 386 : 928 – 30 .
Shiffman J. 2009 . A social explanation for the rise and fall of global health issues . Bulletin of the World Health Organization 87 : 608 – 13 .
Sparkes SP , Bump JB , Özçelik EA , Kutzin J , Reich MR. 2019 . Political economy analysis for health financing reform . Health Systems and Reform 5 : 183 – 94 .
The Lancet. 2012 . Mexico: celebrating universal health coverage . The Lancet 380 : 622 .
van Olmen J , Marchal B , Van Damme W , Kegels G , Hill PS. 2012 . Health systems frameworks in their political context: framing divergent agendas . BMC Public Health 12 : 774 .
Vargas JF , Muiser J. 2013 . Promoting universal financial protection: a policy analysis of universal health coverage in Costa Rica (1940–2000) . Health Research Policy and Systems 11 : 28 .
WHA. 2005 . Resolution WHA58.33 Sustainable Health Financing, Universal Coverage and Social Health Insurance . Geneva : World Health Assembly .
WHO. 2019 . Universal Health Coverage and Health Financing. https://www.who.int/health_financing/universal_coverage_definition/en/ , accessed 19 August 2019.
Wong G , Greenhalgh T , Westhorp G , Buckingham J , Pawson R. 2013 . RAMESES publication standards: meta-narrative reviews . BMC Medicine 11 : 20 .
GTZ Deutsche Gesellschaft für Technische Zusammenarbeit, later GIZ Deutsche Gesellschaft für Internationale Zusammenarbeit.
- narrative discourse
| Month: | Total Views: |
|---|---|
| January 2020 | 166 |
| February 2020 | 47 |
| March 2020 | 27 |
| April 2020 | 105 |
| May 2020 | 30 |
| June 2020 | 37 |
| July 2020 | 105 |
| August 2020 | 201 |
| September 2020 | 200 |
| October 2020 | 184 |
| November 2020 | 158 |
| December 2020 | 118 |
| January 2021 | 181 |
| February 2021 | 150 |
| March 2021 | 169 |
| April 2021 | 152 |
| May 2021 | 179 |
| June 2021 | 167 |
| July 2021 | 69 |
| August 2021 | 81 |
| September 2021 | 130 |
| October 2021 | 147 |
| November 2021 | 152 |
| December 2021 | 96 |
| January 2022 | 154 |
| February 2022 | 69 |
| March 2022 | 157 |
| April 2022 | 144 |
| May 2022 | 132 |
| June 2022 | 91 |
| July 2022 | 84 |
| August 2022 | 96 |
| September 2022 | 115 |
| October 2022 | 131 |
| November 2022 | 150 |
| December 2022 | 126 |
| January 2023 | 101 |
| February 2023 | 111 |
| March 2023 | 131 |
| April 2023 | 148 |
| May 2023 | 125 |
| June 2023 | 72 |
| July 2023 | 90 |
| August 2023 | 146 |
| September 2023 | 126 |
| October 2023 | 147 |
| November 2023 | 192 |
| December 2023 | 232 |
| January 2024 | 209 |
| February 2024 | 166 |
| March 2024 | 217 |
| April 2024 | 203 |
| May 2024 | 193 |
| June 2024 | 123 |
Email alerts
Citing articles via.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1460-2237
- Copyright © 2024 The London School of Hygiene and Tropical Medicine and Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 02 April 2022
Is the healthcare provision in the Netherlands compliant with universal health coverage based on the right to health? A narrative literature review
- Thomas Kuipers 1 ,
- Remco van de Pas 2 &
- Anja Krumeich 3
Globalization and Health volume 18 , Article number: 38 ( 2022 ) Cite this article
5415 Accesses
4 Citations
11 Altmetric
Metrics details
Universal health coverage, as one of the targets of the Sustainable Development Goals, is the access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost. It is a practical expression of the concern for health equity and the right to health, and a goal for all countries. This review is a novel attempt to explore the healthcare provision in the Netherlands as an expression of universal health coverage based on the right to health.
The study adopted a narrative review approach using a framework that consists of 10 universal health coverage indicators which are derived from seven human rights principles. The techno-economic approach to healthcare provision by the Dutch state achieves a healthcare system where most of the population is covered for most of the services for most of the costs. The Dutch state complies with its minimum core obligations, while less attention is paid to participatory decision making and non-discrimination principles. However, with the fiscal sustainability of healthcare provision showing erosion, basing healthcare policy on values based on human rights principles might prevent a regressive policy.
- Universal health coverage
Inequalities in levels of income, opportunities and health outcomes remain a cause for concern in societies, including high-income countries (HICs), and even more so in light of the COVID-19 pandemic [ 1 , 2 , 3 ]. All countries have a moral obligation to address fairness and social justice in the distribution of collective goods like healthcare. Attempts within public health to properly address the societal factors that are relevant to complex health problems have been insufficient, which is partly exacerbated by the absence of a coherent conceptual framework [ 4 ]. One such framework is based on human rights, which have gained attention in global development policies such as the Sustainable Development Goals (SDGs). It has also gained attention in regional and national efforts to address inadequate access to healthcare [ 5 ].
In this context, the World Health Organization (WHO) proposed Universal Health Coverage (UHC) as a target for the health-related goal on the 2030 Agenda for Sustainable Development, which was unanimously adopted during the 2015 United Nations General Assembly [ 6 , 7 ]. The 2005 World Health Assembly (WHA) resolution on Sustainable health financing, Universal coverage and social health insurance defined UHC as the “ access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost, thereby achieving equity in access ” [ 8 ]. The 2010 World Health report on Health system financing: the path towards universal health coverage elaborated as to how countries can modify their health systems to achieve UHC by identifying the three UHC dimensions: what , who and the proportion of costs that is covered [ 9 ]. These dimensions concern the extent of services included, the population that is covered for these services, and the proportion of the costs that is covered by pooled funds versus out-of-pocket payments (OOPPs). OOPPs are direct costs that can result in financial hardship or even ‘catastrophic health expenditure’, the inability to pay for healthcare due to high costs in relation to income [ 9 ].
The right to health and health equity
In addition to these technical UHC dimensions, the WHO’s normative conceptualization indicates UHC to be “by definition, a practical expression of the concern for health equity and the right to health” [ 6 ]. Health equity and the right to health are terms that should be handled with care though, as their interpretations and implications are contended among scholars and subjected to debate. Firstly, health equity is a concept related to justice and qualifies some inequalities as inequities [ 10 ] . Health inequities are defined by “ differences which are unnecessary and avoidable but, in addition, are also considered unfair and unjust” [ 11 ] . These inequities are at the conceptual foundation of the right to health, and provide moral principles to resolve conflicts between human rights and to locate rights in relation to other social values and goals [ 12 , 13 ].
Secondly, the legal conceptualization of the right to health underpinning this review is based on the formulation in the 1966 International Covenant on Economic, Social, and Cultural Rights (ICESCR). General Comment 14, an explanatory document issued by the Committee on Economic, Social and Cultural Rights (CESCR), states that “ the right to health must be understood as a right to the enjoyment of a variety of facilities, goods, services and conditions necessary for the realization of the highest attainable standard of health” [ 14 ] . Furthermore, it normatively prescribes that health facilities, goods and services should be available , accessible , acceptable , and of good quality . UHC is intended to address these conditions of healthcare, generally referred to as the AAAQ framework, to advance the right to health [ 15 ]. It takes into account the limited resources of states, irrespective of their wealth, and requires states to take steps towards the realization of the right to health in a progressive manner [ 16 ].
To integrate the concepts of the right to health and UHC, Ooms et al . have identified seven important human rights principles that the Committee applies in their elaboration of the right to health in General Comment 14 [ 10 ]. The right to health demands states to abide by the principles of minimum core obligations , progressive realization , non-discrimination , cost-effectiveness , participatory decision making , shared responsibility , and the attention to vulnerable or marginalized groups . Table 1 portrays a synthesis of these seven human rights principles and the UHC components as proposed by Sridhar et al .. The result is a normative framework, consisting of 10 measurable and achievable indicators, that evaluates the extent to which UHC is based on the right to health (see Table 1 ) [ 17 ].
The healthcare landscape and key reforms in the Netherlands
Historically, the Dutch healthcare system included a mix of public and private health insurance schemes. By the end of the 1960’s, this formed a compromise between the faith-based socialistic norms of broad accessibility to a public healthcare system and principles rooted in liberalism of a private health system based on conditions set by the government [ 18 ]. It consisted of private insurance for the wealthy and social insurance for the rest. However, this two-tiered healthcare system exacerbated health inequalities between socio-economic groups in the Dutch society [ 19 ]. In addition, various major issues had been on the healthcare agenda for years: an increased tension between supply of and demand for health care, the need for cost-containment, upholding solidarity principles and the increasing pressure on accessibility [ 18 ].
A culmination of decades’ worth of deliberation and discussion to address these ‘maladies’ in the health system led eventually to a major health insurance reform for the curative care sector in 2006 by introducing market principles to the health insurance landscape [ 19 ]. Furthermore, a major reform of long-term care starting in 2015 due to pressing budget deficits after the financial crisis and an increasing demand for an ageing population. In order to improve efficiency and affordability, long-term care was decentralized to the municipalities or dispersed to health insurers, while care at home and self-reliance was promoted. Seemingly, municipalities are in a better position to more efficiently tailor care to the citizens’ needs. Table 2 outlines the current health finance and policy landscape for the various healthcare sectors in the Netherlands.
Universal health coverage in the Netherlands
It remains unclear to what extent healthcare provision in the Netherlands is compliant with UHC as an expression of the right to health. Although the universality in UHC ostensibly suggests that everyone should be covered, not a single country has achieved complete coverage. This provides the opportunity for all to make progress [ 24 , 25 , 26 ]. While the international community identified UHC as the way forward in strengthening resilient health systems, the discussion on the relevance of UHC seems to focus on low- and middle-income countries rather than HIC’s [ 24 ]. This is in part due to a common notion suggesting that many HIC’s have already fulfilled the targets of UHC. Also, the absence of a relevant UHC monitoring framework applicable to HIC’s plays a role, as Bergen et al. argues [ 24 ]. HIC’s like the Netherlands might be expected to meet higher standards in fulfilling the right to health when compared to low- and middle-income countries.
This review is therefore a novel attempt to relate UHC to a HIC such as the Netherlands, with the ‘UHC based on the Right to Health’ framework (see Table 1 ) as a lens to analyze the Dutch policy landscape. We acknowledge that the implementation of the right to health goes beyond the implementation of UHC, also in the Netherlands. It includes, amongst others, action on the Social Determinants of Health and should address the health(care) needs of specific marginalized groups, such as undocumented migrants. For this review, we follow Ooms et al. analyses that, in the context of the Sustainable Development agenda, UHC can be considered a practical expression of the right to health care , in essence a subset of the broader Right to Health concept. We explore the health service provision as an expression of UHC based on the right to health, and aim to contribute to the debate on UHC in HIC’s and the use of rights-based approaches to health systems’ financing and organization.
Methodology
Research design.
The study adopted a narrative literature review design. A narrative review is a type of non-systematic literature review that is used to for more general debates and can serve to provoke thought and dialectic exchange since it combines theory and context [ 27 ]. This review followed a methodological approach described in previous publications, which includes: a preliminary literature search, a description and synthesis of the available topical literature, and reports it using the necessary elements of a narrative review [ 27 , 28 , 29 ]. Predefined concepts are tested through the collection, aggregation, and triangulation of empirical data to synthesize empirical statements [ 30 ]. The review entails a narrative synthesis of previously published information on the subjects of UHC and the right to health in the Netherlands. Its purpose is to provide empirical and broader perspective on these subjects, and hence not to provide a comprehensive systemic review.
Data collection
Data was collected through the use of PubMed and Google Scholar or purposively collected from various (inter)governmental organizations. The data that this review utilizes is collected from both qualitative and quantitative academic research ( n = 31) and grey literature ( n = 42) sources, among which from governmental organizations ( n = 8), non-governmental organizations ( n = 20) and intergovernmental organizations ( n = 14). It includes various types of data such as academic research, policy briefs, reports, book chapters, websites, health information databases, legal documents and acts, and epidemiological and public health documentation. A specific search for case studies, including academic, legal and grey literature reporting on human rights violations in relation to health care provision in the Netherlands, complemented the data collection.
The data was purposively searched using key terms based on each of the frameworks indicators. The data was assessed for various inclusion criteria; accessibility in the public domain, either in print or digitally, written in English or Dutch, and the most recent documentation providing it to be no earlier than 2004. The data utilized is from the public domain, in print and accessible on the web or in a library. Through an iterative process, the executive summaries and abstracts of the literature were reviewed and critically appraised, and the literature relevant to the indicator was subsequently included until enough data saturation occurred to inform the indicator.
Theoretical framework
The ‘UHC based on the Right to Health’ framework (see Table 1 ) allows for a concise synthesis for each of the 10 indicators. Sridhar et al. described three major challenges with indicator development: data availability, universality of targets, and the adaptability of global goals to local populations. These indicators have been proposed to measure the achievement of UHC that captures the right to health principles in a measurable, achievable and sustainable manner [ 17 ].
The indicators from the right to health framework might not capture the priorities of the Netherlands. It should be recognized that the process of determining these targets involve political considerations. Therefore, while interpreting the results, emphasis should be placed on the right to health principles behind each indicator, rather than whether or not the Netherlands is explicitly compliant with each indicator. Also, the definition of UHC varies among experts. The WHO’s conceptualization of UHC is used in this review, as it is considered the international mandated authority on health. The covenant and the general comment 14 serves as the legal international framework on the definition of the right to health and its interpretation.
Furthermore, the right to health is broader than just health care and includes other determinants of health. The 10 indicators of the UHC framework based on in the right to health are about health care rather than health, and do not include other determinants of health. In the context of the Sustainable Development Goals, Sridhar et al . have proposed these 10 indicators to capture the achievement of the principles that flow from the right to health. yet can also be operationalized to generate measurable, achievable, sustainable indicators. The implementation of the SDG’s is a global responsibility, and is required to be likewise implemented in, and periodically reviewed for, high-income countries, including the Netherlands [ 31 ]. Given these global sustainable development requirements, this review focused on analyzing the right to healthcare using the 10 indicators proposed by Sridhar et al. [ 10 ].
UHC based on the right to health
The first five indicators of the framework deal with the minimum core obligations of a state and whether or not these obligations are realized in a progressive manner. The Netherlands has an implicit legal mandate for UHC ( Indicator 1 ) which consists of a vast variety of different acts and legislation within national, regional and global jurisdictions.
On an international level, the Netherlands is a signatory to the Universal Declaration of Human Rights and the United Nations Principles for Older Persons, and has also ratified the ICESCR and the Convention on the Rights of Persons with Disabilities [ 32 ]. The UHC mandate on a regional level is derived from the European Convention of Human Rights, the European Social Charter, and the Convention for the Protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine [ 32 ]. On a national level, the following five acts form the legal basis for healthcare provision: the Health Insurance Act for curative healthcare services, the Long-term Care Act for institutional care, the Social Support Act for domestic care and social support, the Youth Act for care for citizens under 18 years of age, and the Public Health Act for disease prevention, health promotion, and health protection (see Table 2 ) [ 21 ]. More than dozens of other domestic laws arrange how healthcare and its financing is shaped, including both legislation specific to health and more general legislation concerning health.
The next indicators relate to the three dimensions of UHC; what , who and the proportion of costs that are covered. The benefit package for basic health insurance under the 2006 Health Insurance Act covers a broad set of healthcare services ( Indicator 2 ), including but not limited to: care provided by hospitals, general practitioners, and medical specialists, midwifery care and maternity care assistance, medical aids and devices, transportation, pharmaceutical care, and primary and secondary ambulatory mental health care [ 33 ]. Most non-essential healthcare services (routine dentalcare, physiotherapy, complementary and alternative medicines etc.) and elective procedures are either partially covered or excluded from the basic health insurance coverage and included in supplementary insurance packages instead. Domestic care, youth care, prevention services and social support is founded in separate legal acts. These services are delivered on a decentral level by the municipalities and funded by the state budget and income dependent cost-sharing [ 21 ].
All residents in the Netherlands and Dutch citizens abroad who pay income tax to the Dutch state are obligated under the Health Insurance Act to be insured for this basic health benefit plan ( Indicator 3 ). Parallel health systems or arrangements exist for military personal, undocumented migrants and people that refuse to be insured based on religious beliefs or certain world views [ 21 ]. A small minority of the population (1.31%) is reported to be either uninsured or defaulting on their payments [ 34 ].
The Netherlands operates a complex cost-sharing system including mandatory and voluntary deductibles (a form of out-of-pocket payment that is paid per year before insurance covers the remaining expenses), own contributions, insurance premiums, and income taxation ( Indicator 4 ) [ 21 ]. The mandatory deductible is levied on all healthcare expenses with the exception of general practitioner consultations, maternity care, home nursing care, and integrated care. An additional voluntary deductible can by chosen by the insured which results in a discount on the insurance premium. The OOPPs have increased in the recent years, mainly due to an increase in the mandatory deductible and a cost shift from public to private sources by excluding services from the basic benefit package [ 21 ].
The Netherlands is among the world’s biggest healthcare spenders. Its health expenditure has risen considerably in the last decades due to greater propensity to use tertiary care, the introduction of new technologies, and the relaxation of fiscal restrictions on health expenditure ( Indicator 5 ) [ 35 , 36 ]. The majority of the expenditure is concentrated on the chronically ill, the elderly, and the dying.
Due to the rising healthcare costs in the Netherlands, there is much attention to the cost-effectiveness of healthcare interventions. While cost-effectiveness is an important principle of the insurance package, in practice it plays a substantial role mainly in the assessment of pharmaceuticals [ 37 , 38 ]. Cost-effectiveness is addressed by many research programs and initiatives invested in efficiency research, as well as by improving the use of cost-efficiency in healthcare by legal and economic incentives [ 21 , 39 , 40 , 41 ].
The 7 th and 8 th indicators concern the shared responsibility for UHC, as states and other actors that are in a position to assist must indeed do so to a minimum threshold [ 17 ]. They capture how much a state spend on official development assistance (ODA) and whether or not the right to health is stated in their foreign development policy. Due to shifting priorities, the Dutch government has not met the internationally accepted target of spending 0.7% of GDP on official development assistance in recent years ( Indicator 7 ) [ 42 ]. Nonetheless, health is a prominent area for the Dutch ODA with 8.5% of the ODA budget spend on Global health in 2015 [ 43 ]. The Netherlands has a long history in protecting and promoting human rights and is party to UN human rights covenants and nearly all human rights conventions. Sexual and reproductive health and rights (SRHR) is the dominant focus of international health policy, used by the Netherlands to invest in health system strengthening. Nevertheless, the Dutch international development policy does not explicitly promote and protect the right to health or UHC ( Indicator 8 ) [ 44 , 45 , 46 , 47 ].
The Netherlands has no SARA assessment on participatory decision making ( Indicator 9 ) [ 48 ]. Participatory decision making can vary in terms of its deliberativeness, perspective, and decision power. In the last decades, patients have been more involved in the decision-making process, mainly visible in the involvement of patient organizations in hearings, and research and protocol development. The increase of patient involvement has mostly been due to patients’ rights in patient-healthcare provider relationships and the freedom of choice in the healthcare market. Various mechanisms have a legal basis for patient participation on a more institutional and organizational level [ 49 ]. For example, patients can seek influence on the (budgeting) policies of long-term care facilities by the means of client councils. Also, health insurers are required under the Health Insurance act to involve patients in the decisions around the healthcare purchases. Nevertheless, public representation is often limited to the non-deliberative consultation of patients. Examples of involvement of citizens, rather than patients, in the decision-making process around the funding of interventions using collective means have been limited [ 41 ]. A recent initiative called Burgerforum, keuzes in de zorg utilizes a citizens panel to inform the ministry of health on which healthcare services citizens find important to be covered in the basic insurance package [ 50 ].
As with the previous indicator, the Netherlands has no SARA assessment on the prioritization of marginalized groups ( Indicator 10 ) [ 48 ]. Vulnerable and marginalized groups in the Netherlands are heterogeneous groups, among which people with (long term) physical and psychosocial problems, secluded elderly, addicts, homeless people, ethnic minorities, documented and undocumented migrants, and people of lower socioeconomic status. The insurance coverage and its impact can vary for some of these groups.
For example, some key articles indicate that the high-income class spends less than 1% of their income on healthcare in the form of OOPPs, compared to more than 4% for the low-income class [ 21 , 51 ]. Meanwhile, the difference of the amount of years perceived to be in good health between the lowest and highest income class has been 18.2 years [ 52 ]. Inequalities of the quality adjusted-life years expectancy between the low and highly educated have also widened [ 53 ].
Also, undocumented migrants and asylum seekers are excluded from health insurance under the Health Insurance Act and covered through parallel arrangements. In principle, undocumented migrants have access to the same healthcare services covered in the basic benefit package and providers are obliged to provide the services. However, OOPPs are required for the care they receive. As this relates to people who are often not able to pay, healthcare providers are partially reimbursed by the government if certain terms are met [ 21 ]. Furthermore, asylum seekers are covered for care that is comparable to the basic benefits package. The access to healthcare for asylum seekers is regulated through the Asylum Seekers Care Regulation ( Regeling Zorg Asielzoekers ). Asylum seekers are listed with special asylum seekers health centers and do not have to pay mandatory deductibles or insurance [ 21 ].
Minimum core obligations and progressive realization
The overall health financing and care policy environment in the Netherlands indicates that healthcare coverage is compliant with a conception of UHC based on the right to health. The first proportion of the UHC based on the right to health analysis provides an overall positive impression when it’s evaluated for its compliance with the legal principles as is set out in the ICESCR. The underlying legal principles behind these indicators are the state’s minimum core obligations and progressive realization . Embedded in a vast body of legislation, most essential and curative healthcare services are covered for most people living in the Netherlands. In other words, a large proportion of the costs are covered for most services for most people. While this might be expected in most HIC’s like the Netherlands, it would be useful to discuss the trends considering the rising healthcare costs. Although essential services are provided and accessible to most people, cost-containment of healthcare expenditure can potentially lead to retrogression in the realization of the right to health.
For example, the effects of the reforms privatizing the health insurance system are to be considered here [ 49 ]. In accordance with the 2006 Health Insurance Act, healthcare providers are incentivized to differentiate themselves by price and services via the selective contracting of health insurers [ 54 ]. Selective contracting in addition to the quality and quantity requirements can put pressure on the accessibility of care, especially in areas with low population density [ 49 ]. For example, multiple hospitals filed for bankruptcy in 2018 due to quality and quantity of care issues [ 55 ]. The introduction of market principles to the health insurance sector as well as the decentralization and reallocation of the long-term care (accompanied with large budget cuts), have contributed to slowdown the growth of the total health expenditure [ 21 , 56 ]. However, it remains to be seen the coming decades if these efforts for cost-containment are sustainable as the population continues to age [ 21 , 36 ]. Furthermore, trends and projections of health inequities show that they continue to persist or even increase [ 21 ]. These health inequalities are linked to societal determinants like income, work, education, urbanization, nationality, lifestyle, healthcare accessibility etc. For example, the adverse health effects due to unemployment after the recent economic recession are becoming apparent and mainly affect people with a lower income or other vulnerable groups [ 21 ]. The socio-economic consequences of the COVID-19 pandemic might also further exacerbate health inequalities.
Another example are the various austerity measures that were part of these cost-containment efforts. One of the them relates to the rise of OOPPs due to the gradual shift of public to private sources [ 21 ]. This is done by an ongoing limitation of services covered by the Health Insurance Act or the Long-Term Care Act [ 49 ]. For instance, various non-essential healthcare services like physiotherapy, routine dentistry care, occupational therapy, exercise therapy and dietary therapy are excluded from the basic insurance package or conditionally included [ 21 ]. They are subsequently covered by supplementary insurance plans for which (contrary to the basic insurance package) health insurers are allowed to differentiate the premiums according to a patient’s risk profile. So-called high-risk groups, like the chronically ill, elderly, disabled and psychiatric patients, can count on a higher premium in order to be insured for these services [ 49 ]. Furthermore, these services might only be accessible to people who are able to pay for it privately, raising all sorts of concerns regarding equity and the distribution of services.
Another austerity measure has been the gradual increase of the mandatory insurance deductible [ 49 ]. The mandatory deductible serves to reduce the moral hazard of being insured, which is the use of more or extra health services just because the expenses are covered by the insurance. It has been gradually raised form €150 (in 2008) to €385 (in 2020) and contributed to the increase of OOPPs [ 21 , 57 ]. In the Netherlands, OOPPs make up for a relatively small proportion of total spending compared to other OECD countries [ 36 ]. However, the insurance deductibles have not been included in the statistics for some reason. Furthermore, the burden of OOPPs are unequally distributed and tilted towards the people of lower socioeconomic status and the so-called high-risk groups. Data from household income and expenditure surveys identified by the WHO suggests that if OOP spending is reduced to levels lower than 15% of total health expenditure, few households would be engaged in catastrophic health expenditure [ 58 ]. Thus, while the minimum core obligations are largely fulfilled, the principle of progressive realization warrants caution and further study considering the impact of the cost-containment measures over time.
Shared responsibility, shared decision making, attention to vulnerable and marginalized groups and non-discrimination
The last set of the indicators underly the legal principles of shared responsibility, shared decision making, attention to vulnerable and marginalized groups and non-discrimination . They give a much more ambiguous impression of its accordance to the right to health principles. The extent to which they are implemented according to a rights-based approach, and as such integrated in the Dutch health system, does not seem to be as readily apparent as the first proportion of indicators previously discussed. While adequate resources to deliver UHC are being mobilized, it remains to be seen whether this level of spending and redistribution of public revenue proves to be sustainable in the context of the demographic changes in the coming decades [ 36 ].
Furthermore, the Netherlands is a significant proponent of human rights, which it promotes in both domestic and international policy. However, the right to health as it is integrated in the Dutch international development agenda is specific to SRHR. The policy puts sexual and reproductive health, as well as gender perspectives and inequities, forward as a fundamental human rights issue. The Netherlands takes a prominent role within the international community in advocating for these rights [ 45 , 47 ]. However, the health-related allocation of ODA on UHC or health system strengthening seem to be relatively insufficient compared to the spending on projects related to SRHR. This emphasis on SRHR that targets specific health services and programs might distract from investing in the more fundamental contributions to UHC and health system strengthening in low- and middle-income countries.
Lastly, the Netherlands does not implement an official SARA on the prioritization of marginalized groups. Asylum seekers are excluded from the Health Insurance Act and receive care through a parallel health system, with a central financial reimbursement policy for healthcare providers who provide services for undocumented migrants. While this policy ensures the availability of healthcare services for this group, it does not necessarily equate to adequate utilization of these services [ 59 , 60 , 61 ]. For example, the translation services have been defunded in an effort for cost-containment and to stimulate integration. This threatens the accessibility and acceptability of healthcare provision among patients with limited language proficiency (including but not limited to undocumented migrants) [ 62 ]. Therefore, a SARA should be implemented for undocumented migrants with special attention to the cultural access and gender and ethnic aspects. This is a vulnerable group that deserves careful attention in the context of UHC in HIC countries [ 25 ].
There is also no SARA implemented on participatory decision making in the Netherlands, neither in any of the other HIC’s [ 48 ]. A perspective of citizens in the decision-making process around the financing of health services from the collective funds is important yet limited. However, the recent non-governmental initiative Burgerforum, keuzes in de zorg aims to gather an insight into what society values concerning the financing of healthcare services from public funding [ 50 ]. This citizens panel is an attempt to address some important societal questions: which healthcare services are we willing to pay for each other and what do we value in making these choices? This deliberative panel is part of a larger societal debate on how resources for health can and should be distributed in the Netherlands [ 21 , 41 , 50 , 63 ]. A health system co-owned by the population, communities and civil society is critical to strengthen health governance for UHC [ 64 ].
Limitations
There are various comments and limitations to the design and findings of this review. A main limitation of a narrative literature review design is the less systematic and more iterative method of data searching. This can lead to a selection bias and subsequently influence the interpretation of the findings [ 27 , 28 ]. While considered by the authors, the aim of the review is to present a broad and reflective scope of the topics at hand. Given time and resources, a narrative and iterative literature review design provided to be the most suitable. While this review is not exhaustive, it provides a concise and high-yield overview of UHC and the Right to Health in the context of the Netherlands. A first rapid review via several academic search engines indicated that PubMed and Google Scholar yielded qualitatively the most results. Other search engines like Web of Science and LexisNexis provided mainly duplication of results and few relevant additional data sources. Also, a rapid assessment of (legal) case studies provided little specific information that altered the overall analysis of this paper. Another limitation of this review relates to its focus on healthcare provision and the complexity of the Dutch healthcare system. Table 2 merely provides a brief overview of the main components of the health provision landscape. The way UHC is measured under the SDG framework is to a significant extent captured in the healthcare provision under the 2006 Health Insurance act, hence the focus of the review. The pressing availability of expensive treatment and medicines is also on the policy agenda and merits its own analysis [ 65 , 66 ].
Also, the right to health requires greater attention to the realities of power dynamics, health and gender inequities and social determinants of health [ 67 ]. The Center for Economic and Social Rights addresses this issue through the OPERA framework; a tool designed to not only measure outcomes through indicators, but also by taking into account the policy efforts and commitments in monitoring the fulfillment of ECS rights. The OPERA framework has been developed to give a more comprehensive picture of compliance of states to the economic, cultural and social rights. It would be relevant to apply the OPERA framework to the Netherlands as to have a more complete image, from a specific health angle, of how it fulfills the ECS rights of its citizens.
As formulated in the ICESCR, the right to health mainly focuses on the equality of dignity, legal standing, and legal status, but lacks emphasis on the equality of social or economic positions. Inequalities in social class and economic status are hence, according the ICESR, of lesser significance, unless these interferes with the realization of the right to health. In other words, any inequalities above the minimum requirements to fulfilling the right to health are legally permitted. In addition, these underlying determinants of health tend to be considered individually and sequentially, and thus underestimate the interlinked and cumulative effects of the determinants [ 68 ]. While the right to health approach, as used this review, does address equity within the 10 indictors, a more thorough analysis of the concepts of fairness and equity of the health policy beyond the right to health is warranted. A path-dependency investigation of the observations made and an enquiry of the demands for health equity in relation to health care financing are interesting subjects for further studies.
Policy and research implications
What should we expect from the Dutch government to be a decent way to move healthcare financing forward with an rights-based approach? Generating a sustainable and equitable financial revenue remains of uttermost importance for the future health policy agenda. There should be a progressive realization to the inclusion of healthcare services in the basic health package. It is important that these services, as well as the services already included, are evaluated for their cost-effectiveness as well as societal relevance. It therefore requires adequate participation of citizens in the decision-making process. Furthermore, the Netherlands needs to take more responsibility to the achievement of UHC in low-income countries if is to play its part in achieving the SDGs. This can be done by increasing the provision of financial means, via ODA, to projects earmarked, directly or indirectly, for UHC implementation. While these issues are important, the sustainability of UHC is not only a matter of economic or financial considerations. Attention should also be paid to the social and political dimensions, especially in the context of HIC’s. The increasing neoliberal approach to healthcare policy is argued to put pressure on the progressive realization of UHC in many European countries [ 63 , 69 ]. When financial resources for healthcare are scarce, rooting healthcare provision in principles like the right to health might prevent a regressive policy [ 13 , 24 ]. It is therefore of extra importance to not only adequately address the health of vulnerable people and marginalized groups in health policies, but also in the policy process itself by involving them and other citizens in the decision making around financing healthcare from public resources. One might say that the ability to protect and respect minority rights is one of the determinants of the decency of a democratic society [ 70 ].
Finally, the overall policy landscape in the Netherlands shows that UHC is based to a great extent on the right to health. Nonetheless, it raises questions on the underlying values of how the right to health is and could be interpreted, and how the current political climate frames healthcare. An enquiry of the right to health as a moral right would reflect on ethical questions considering legitimate, relevant or obligatory actions in healthcare. How ought healthcare (or even health itself) to be distributed? And how can this distribution be achieved in a fair and just manner? The right to health serves as a reference point for both ethical principles guiding our actions and a legal obligation with varying levels of enforcement [ 12 ]. The UHC debate in the Netherlands falls somewhat short of an ethical and philosophical enquiry into health system financing policies. This debate seems to be rather rational techno-economic in nature with an approach based on resource-oriented values [ 71 ]. Perhaps health equity and fairness are not as dominant of values in Dutch health policy as might be expected. Future research could also focus on unpacking the synergies and tensions between the economic and normative dimensions of health system financing. The right to health as a moral concept could be explored in the context of health system financing [ 13 ]. As policies on health system financing takes the direction of decentralizing and shifting to the private sector, the research agenda is seemingly directed towards the implementation of cost-containment measures. Deliberating the entirety of health system financing, for example by a complex system approach, is needed to tackle the most pressing healthcare issues the coming decades [ 72 ].
The healthcare provision in the Netherlands is characterized by a techno-economic focus: all the essential services are covered, the mandatory nature of the insurance covers virtually the whole population, and pooled funding prevents catastrophic health expenditure. This approach towards achieving UHC is seen in the emphasis on the legal human rights principle of minimum core obligations . The shared-responsibility, non-discrimination and participatory decision-making aspects of public policy for UHC require more attention. However, the fiscal sustainability of healthcare is under pressure and the COVID-19 pandemic might exacerbate inequalities. A regressive healthcare policy might be prevented by basing it to principles and values of equity and fairness. Healthcare provision is a question of just distribution as much as cost-effectiveness.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
Committee on Economic, Social and Cultural Rights
Gross Domestic Product
High-income country
International Covenant on Economic, Social and Cultural Rights
Official Development Aid
Organization for Economic Co-operation and Development
Out-of-pocket payment
Service Availability and Readiness Assessment
Sustainable Development Goal
Universal Health Coverage
United Nations
World Health Assembly
World Health Organization
Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–9.
Article Google Scholar
UHC2030. State of commitment to universal health coverage: synthesis, 2020. 2020 p. 1–69. Available from: https://www.uhc2030.org/what-we-do/voices/accountability/the-state-of-uhc-commitment/
United Nations. World Social Report 2020: Inequality in a rapidly changing world [Internet]. 2020 p. 1–216. (World Social Report). Report No.: 978–92–1–130392–6. Available from: https://www.un-ilibrary.org/content/books/9789210043670
Gostin LO. Public Health, Ethics, and Human Rights: A Tribute to the Late Jonathan Mann. J Law Medicine Ethics. 2001;29(2):121–30.
Article CAS Google Scholar
London L. What Is a Human-Rights Based Approach to Health and Does It Matter? Health Hum Rights. 2008;10(1):65.
World Health Organization. Positioning Health in the Post-2015 Development Agenda: WHO Discussion Paper. Geneva: World Health Organization. 2012;1–4. Available from: https://www.who.int/topics/millennium_development_goals/post2015/WHOdiscussionpaper_October2012.pdf
United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. General Assembly Resolution 70/1, 25 September 2015. 2015;16301:1–40. Available from: http://unctad.org/meetings/es/SessionalDocuments/ares70d1_es.pdf
World Health Assembly. Resolution WHA58.20: Sustainable Health Financing, Universal Coverage and Social Health Insurance. [Internet]. 2005 p. 13–6. Available from: http://apps.who.int/iris/bitstream/10665/20302/1/A58_20-en.pdf?ua=1
World Health Organization. The world health report: health systems financing: the path to universal coverage. 2010. Available from: https://apps.who.int/iris/handle/10665/44371
Ooms G, Latif LA, Waris A, Brolan CE, Hammonds R, Friedman EA, et al. Is universal health coverage the practical expression of the right to health care? Bmc Int Health Hum R. 2014;14:3.
Whitehead M. The Concepts and Principles of Equity and Health. Int J Health Serv. 1992;22(3):429–45.
Backman G. The right to health: theory and practice. Backman G, editor. Vol. 1.1. 2012. 368 p.
Ruger JP. Toward a Theory of a Right to Health: Capability and Incompletely Theorized Agreements. Yale J Law Humanit. 2006;18:3.
PubMed PubMed Central Google Scholar
UN Committee on Economic, Social, and Cultural Rights. General Comment No. 14: The Right to the Highest Attainable Standard of Health (Art. 12 of the Covenant). UN Committee on Economic, Social and Cultural Rights (CESCR) [Internet]. 2000;2000:2,7,19. Available from: https://digitallibrary.un.org/record/425041?ln=en
World Health Organization. Anchoring universal health coverage in the Right to Health: What difference would it make? Policy brief [Internet]. 2015. Available from https://apps.who.int/iris/handle/10665/199548 .
International Covenant on Economic, Social, and Cultural Rights. Secur Dialogue [Internet]. 1977;8(3):279–82. Available from: http://www.ohchr.org/Documents/ProfessionalInterest/cescr.pdf
Sridhar D, McKee M, Ooms G, Beiersmann C, Friedman E, Gouda H, et al. Universal Health Coverage and the Right to Health: From Legal Principle to Post-2015 Indicators. Int J Health Serv. 2015;45:495–506.
Grinten T van der, Kasdrop J. 25 jaar sturing in de gezondheidszorg: Van Verstatelijking Naar Ondernemerschap. Den Haag: Sociaal en Cultureel Planburea; 1999. p. 1–67.
Daley BC, Gubb J. Healthcare Systems: The Netherlands. Civitas. 2013;1–15. Available from: http://www.civitas.org.uk/content/files/netherlands.pdf
Gress S, Manouguian M, Wasem J. Health Insurance Reform in the Netherlands. CESifo DICE Report. 2007;63–7.
Kroneman M, Boerma W, van den Berg M, Groenewegen P, de Jong J, van Ginneken E. The Netherlands: health system review. Health Syst Transit. 2016;18:1–239.
PubMed Google Scholar
Dijkhoff T. Long-Term Care in Europe A Juridical Approach. 2018. p. 309–52.
Book Google Scholar
RD F, MR B, ILW B, R DB, AJEH B, JF DG, et al. Eerste evaluatie Jeugdwet: Na de transitie nu de transformatie [First evaluation Youth Act: After the transition it’s time for the transformation]. 2018 p. 639. Available from: https://publicaties.zonmw.nl/eerste-evaluatie-jeugdwet/
Bergen N, Ruckert A, Id RL. Monitoring Frameworks for Universal Health Coverage: What About High-Income Countries ? Int J Heal Policy Management. 2019;8(7):387–93.
Aldridge RW, Miller AK, Jakubowski B, Pereira L, Fille F, Noret I. Falling through the Cracks: The Failure of Universal Healthcare Coverage in Europe, European Network to Reduce Vulnerabilities in Health Observatory Report. 2017; Available from: https://www.medecinsdumonde.org/en/actualites/publications/2017/11/08/falling-through-cracks-failure-universal-healthcare-coverage-europe
Chan M. Ten years in public health 2007–2017. 2017;6–12. Available from: https://www.who.int/publications/i/item/ten-years-in-public-health-2007-2017
Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J Chiropr Med. 2006;15:5–17.
Google Scholar
Ferrari R. Writing narrative style literature reviews. Medical Writ. 2015;24(4):230–5.
Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4(1):5.
Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev. 2012;1:28.
Gupta J, Vegelin C. Sustainable development goals and inclusive development. Int Environ Agreements Politics Law Econ. 2016;16(3):433–48.
Mens C voor de R van de. Juridisch kader: In de zorg. 2021. Available from: https://mensenrechten.nl/juridisch-kader-de-zorg
Rijksoverheid. Waarvoor ben ik verzekerd via het basispakket van de zorgverzekering? | Vraag en antwoord | Rijksoverheid.nl. 2021; Available from: https://www.rijksoverheid.nl/onderwerpen/zorgverzekering/vraag-en-antwoord/wat-zit-er-in-het-basispakket-van-de-zorgverzekering
Ministry of Health, Welfare, and Sport. VWS- Verzekerdenmonitor 2016. 2016;1–41. Available from: https://www.tweedekamer.nl/kamerstukken/brieven_regering/detail?id=2016Z18700&did=2016D38441
Bank W. World Bank Open Data. Data. 2021; Available from: https://data.worldbank.org/
Bakx P, O’Donnell O, van Doorslaer E. Spending on Health Care in the Netherlands: Not Going So Dutch. Fisc Stud. 2016;37:593–625.
Ligtenberg G, Staal PC, Goettsch WG, Knies S. Kosteneffectiviteit in de zorg. College voor Zorgverzekeringen. 2013;33. Available from: https://www.zorginstituutnederland.nl/publicaties/rapport/2013/09/30/kosteneffectiviteit-in-de-zorg
Zwaap J, Knies S, der CM van, Staal P, der LH van. Kosteneffectiviteit in de praktijk. 2015;64. Available from: https://www.zorginstituutnederland.nl/publicaties/rapport/2015/06/26/kosteneffectiviteit-in-de-praktijk
ZonMw. Health care efficiency research. 2017; Available from: https://www.zonmw.nl/en/research-and-results/efficiency-studies/programmas/programme-detail/health-care-efficiency-research/
Mot E, Aalbers R, Stuut K, Douven R. De introductie van dure technologie in de zorg. 2017;1–18. Available from: https://www.cpb.nl/publicatie/de-introductie-van-dure-technologie-in-de-zorg
Raad voor Volksgezondheid en Zorg. Zicht op zinnige en duurzame zorg. 2006; Available from: https://www.raadrvs.nl/documenten/publicaties/2006/06/07/zinnige-en-duurzame-zorg
Organisation for Economic Co-operation and Development. Health spending (indicator) as % of GDP. Health Spending. 2017; Available from: https://data.oecd.org/healthres/health-spending.htm
Donortracker. The Netherlands Donor Profile. 2017; Available from: https://donortracker.org/netherlands/globalhealth
Ministry of Foreign Affairs. Wat de wereld verdient: Een nieuwe agenda voor hulp, handel en investeringen. 2013;1–49. Available from: https://www.tweedekamer.nl/kamerstukken/detail?id=2013Z06915&did=2013D14362
Ministry of Foreign Affairs. Respect en recht voor ieder mens. 2013;1–31. Available from: https://www.tweedekamer.nl/kamerstukken/detail?id=2013Z12246&did=2013D25214
Review TNUP. National report submitted by the Kingdom of the Netherlands. 2017; Available from: http://www.ohchr.org/EN/HRBodies/UPR/Pages/NLindex.aspx
Netherlands K of the. Report on the implementation of the Sustainable Development Goals. 2017;1–53. Available from: https://sustainabledevelopment.un.org/content/documents/16109netherlands.pdf , https://gateway.sdgcharter.nl/sites/default/files/2017-07/16109Netherlands.pdf .
World Health Organization. Service Availability and Readiness Assessment (SARA). Available from: https://www.who.int/data/data-collection-tools/service-availability-and-readiness-assessment-(sara)/service-availability-and-readiness-assessment-(sara)-reports
Toebes B, Giorgi MS. The Right to Health, A Multi-Country Study of Law Policy and Practice. 2014. p. 403–36.
Baltussen R, Bijlmakers L, Jansen M. Draagvlak voor lastige keuzes: Eindrapport van het Burgerforum “Keuzes in de zorg.” 2018;112. Available from: https://www.radboudumc.nl/projecten/burgerforum/manifest
Raad voor Maatschappelijke Ontwikkeling. Kwetsbaar in kwadraat: Krachtige steun aan kwetsbare mensen. Raad voor Mataschappelijke Ontwikkeling; 2001 p. 1–112. Available from: https://www.raadrvs.nl/binaries/raadrvs/documenten/publicaties/2001/03/01/kwetsbaar-in-kwadraat/Kwetsbaar_in_kwadraat.pdf
National Institute for Public Health and Environment. Gezondheidsverschillen. Volksgezondheid Toekomst Verkenning. 2018; Available from: https://www.vtv2018.nl/gezondheidsverschillen
Gheorghe M, Wubulihasimu P, Peters F, Nusselder W, Baal PHMV. Health inequalities in the Netherlands: trends in quality-adjusted life expectancy (QALE) by educational level. European J Public Heal. 2016;26(5):794–9.
Bes RE, Curfs EC, Groenewegen PP, de Jong JD. Selective contracting and channelling patients to preferred providers: A scoping review. Health Policy. 2017;121(5):504–14.
Commissie onderzoek faillissementen ziekenhuizen. De aangekondigde ondergang: Onderzoek naar de faillissementen van het MC Slotervaart en de MC IJsselmeerziekenhuizen. 2020. Available from: https://www.eerstekamer.nl/overig/20200304/rapport_de_aangekondigde_ondergang/meta
Krabbe-Alkemade Y, Makai P, Shestalova V, Voesenek T. Containing or shifting? Health expenditure decomposition for the aging Dutch population after a major reform. Health Policy. 2020;124(3):268–74.
Esch TEM van, Brabers AEM, Dijk CV, Groenewegen PP, Jong JDD. Inzicht in zorgmijden: Aard, omvang, redenen en achtergrondkenmerken. 2015; Available from: https://www.nivel.nl/sites/default/files/bestanden/Inzicht-zorgmijden.pdf ?
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–7.
Gil-Salmerón A, Katsas K, Riza E, Karnaki P, Linos A. Access to Healthcare for Migrant Patients in Europe: Healthcare Discrimination and Translation Services. Int J Environ Res Pu. 2021;18(15):7901.
Rosa W, van Jos R, Linda J. Health care seeking practices of undocumented migrants in the Netherlands: a qualitative exploration of health care seeking behaviour. 2016.
Bloemen E. Toegang tot zorg voor ongedocumenteerde migranten: Wat helpt om zorg te krijgen? Pharos. 2019. p. 25.
Sheldon T. Protests mount to cuts in translation services in the Netherlands. Bmj. 2011;342(jun27 2):d4049.
Toebes B. The right to health and the privatization of national health systems: a case study of the Netherlands. Health Hum Rights. 2006;9(1):102–27.
Organization WH. Voice, agency, empowerment: Handbook on social participation for universal health coverage. 2021. Available from: https://www.who.int/publications/i/item/9789240027794
Volksgezondheid M van. Samenvatting Visie Geneesmiddelen. 2016. Available from: https://www.rijksoverheid.nl/documenten/kamerstukken/2016/01/29/kamerbrief-over-visie-op-geneesmiddelen
International HA. New and affordable medicines in the Netherlands: Tracing the Dutch government’s policy commitments and actions. 2018. Available from: https://haiweb.org/publication/report-new-and-affordable-medicines-in-the-netherlands-tracing-the-dutch-governments-policy-commitments-and-actions/
Chapman AR. The social determinants of health, health equity, and human rights. Health Hum Rights. 2010;12:17–30.
Neves-Silva P, Martins GI, Heller L. Human rights’ interdependence and indivisibility: a glance over the human rights to water and sanitation. Bmc Int Health Hum R. 2019;19:14.
Borgonovi E, Compagni A. Sustaining universal health coverage: The interaction of social, political, and economic sustainability. Value Health. 2013;16:S34–8.
Panichas GE. Rights, Respect, and the Decent Society. J Soc Philos. 2000;31(1):51–67.
Gerrits RG, van den Berg MJ, Klazinga NS, Kringos DS. Statistics in Dutch policy debates on health and healthcare. Health Res Policy Sy. 2019;17(1):55.
Wietmarschen HA, Wortelboer HM, Greef J. Grip on health: A complex systems approach to transform health care. J Eval Clin Pract. 2018;24(1):269–77.
Download references
Acknowledgements
We would like to acknowledge Gorik Ooms for his thoughtful comments on an initial version of the manuscript as well as the journal’s reviewers for their detailed and constructive feedback.
Not applicable.

Author information
Authors and affiliations.
National Institute of Public Health and Environment, Antonie van Leeuwenhoeklaan 9, 3721 MA, Bilthoven, The Netherlands
Thomas Kuipers
Department of Public Health, Institute of Tropical Medicine, Nationalestraat 155, 2000, Antwerp, Belgium
Remco van de Pas
Department of Health, Ethics, and Society, Maastricht University, Minderbroedersberg 4-6, 6211 LK, Maastricht, The Netherlands
Anja Krumeich
You can also search for this author in PubMed Google Scholar
Contributions
TK and RP conceptualized this manuscript. TK wrote the original draft. RP and AK participated in the revisions of the draft and provided final adjustments of the manuscript after critically revising it for intellectual content. All authors endorse the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Thomas Kuipers .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The views in this manuscript solely reflect the opinions of the authors and none of the institutions with which he/she is affiliated to.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kuipers, T., van de Pas, R. & Krumeich, A. Is the healthcare provision in the Netherlands compliant with universal health coverage based on the right to health? A narrative literature review. Global Health 18 , 38 (2022). https://doi.org/10.1186/s12992-022-00831-7
Download citation
Received : 05 May 2021
Accepted : 16 March 2022
Published : 02 April 2022
DOI : https://doi.org/10.1186/s12992-022-00831-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Right to health
- The Netherlands
- Health equity
- Health system financing
Globalization and Health
ISSN: 1744-8603
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
Call for experts for the Universal health and preparedness review (UHPR) Technical Advisory Group
Deadline: 14 july 2024.
The World Health Organization (WHO) is seeking experts to serve as members of the Universal Health and Preparedness Review Technical Advisory Group.
The COVID-19 pandemic has shown that no country was fully prepared to deal with a pandemic of such scale, severity, and impact. The Universal Health and Preparedness Review (UHPR) was proposed to increase accountability and transparency among Member States in gap identification and capacity building for better health emergency preparedness. The peer-review nature of the envisioned UHPR ensures that key issues identified will be acted upon at the highest political levels of government, and that relevant recommendations will be followed up upon and monitored on a regular basis.
To provide technical guidance and advice on the UHPR process, a group of global technical experts was convened to support WHO in the development of relevant technical documents including the methodology for reviewing countries’ preparedness status, and other indicators to be used by all Member States undergoing the review process.
Functions of the UHPR Technical Advisory Group
In its capacity as a technical advisory body to WHO, the UHPR Technical Advisory Group (TAG) shall provide expert inputs to WHO on the technical content of the UHPR, including draft processes for piloting, and ensure that relevant technical documents are evidence-based, logical, and appropriate. The TAG shall have the following functions:
- Support WHO strategies to ensure that the implementation of the UHPR adheres to its key principles and requirements while also considering the unique contexts and specific needs of countries.
- Provide feedback and outcomes to WHO from the UHPR pilots and refine technical content concluding in a final version to be presented by WHO at the 78th World Health Assembly in 2025.
Operations of the UHPR Technical Advisory Group
The UHPR TAG will normally meet at least four times each year. However, WHO may convene additional meetings as deemed necessary. TAG meetings may be held in person (at WHO headquarters in Geneva or another location, as determined by WHO) or virtually, via video or teleconference. The working language of the group will be English.
Who can express interest in being a TAG member?
The UHPR TAG will be multidisciplinary, with members who have a range of technical knowledge, skills and experience relevant to UHPR. Approximately 12 members will be selected.
WHO welcomes expressions of interest from senior level officials with expertise in the following areas:
- International Health Partnership and Multilateral Cooperation
- Health Planning and Financing
- Health Economics
- Peer-Review Mechanisms (UPR and no UPR)
- Universal Health Coverage
- Health Systems Strengthening
- Global Health Diplomacy
- Global Health Governance
- Health Security and Policy
- Parliamentarians
- CSO Engagement
Submitting your expression of interest
To register your interest in being considered for the UHPR technical advisory group members, please submit the following documents by 15 July 2024, 24:00h (midnight) Geneva time to [email protected] using the subject line “Expression of interest for the UHPR Technical Advisory Group:
A cover letter, indicating your motivation for applying and how you satisfy the selection criteria. Please note that, if selected, membership will be in a personal capacity. Therefore, do not use the letterhead or other identification of your employer or organization;
- Your curriculum vitae; and
- A signed and completed Declaration of Interests (DOI) form for WHO Experts, available at https://www.who.int/about/ethics/declarations-of-interest .
After submission, your expression of interest will be reviewed by WHO. Due to an expected high volume of interest, only selected individuals will be informed.
Important information about the selection processes and conditions of appointment
Members of WHO advisory groups must be free of any real, potential or apparent conflicts of interest. To this end, applicants are required to complete the WHO Declaration of Interests for WHO Experts. Selection as a member of the advisory groups is dependent on WHO determining that there is no conflict of interest or that any identified conflicts can be appropriately managed (in addition to WHO’s evaluation of an applicant’s experience, expertise and motivation and other criteria).
All TAG members will serve in their individual expert capacity and shall not represent any governments, commercial industries or entities, research, academic or civil society organizations, or any other bodies, entities, institutions, or organizations. Members are expected to fully comply with the Code of Conduct for WHO Experts ( https://www.who.int/about/ethics/declarations-of-interest ). TAG members will be expected to sign and return a completed confidentiality undertaking prior to the beginning of the first meeting.
Telephone interviews may be scheduled between an applicant and the WHO Secretariat at any point during the selection process to enable WHO to ask questions relating to an applicant’s experience and expertise and/or to assess whether the applicant meets the criteria for membership in the relevant TAG.
The selection of TAG members will be made by WHO in its sole discretion, taking into account the following (non-exclusive) criteria: relevant technical expertise; experience in international and country policy work; communication skills; and the ability to work constructively with people from different cultural backgrounds and orientations. The selection of TAG members will also take account of the need for diverse perspectives from different regions, especially from low and middle-income countries, as well as gender balance.
If selected by WHO, proposed members will be sent an invitation letter and a Memorandum of Agreement. Appointment as a member of a TAG will be subject to the proposed member returning the countersigned copy of these two documents to WHO.
WHO reserves the right to accept or reject any expression of interest, to annul the open call process and reject all expressions of interest at any time without incurring any liability to the affected applicant or applicants and without any obligation to inform the affected applicant or applicants of the grounds for WHO's action. WHO may also decide, at any time, to halt proceeding with the establishment of the TAG, disband an existing TAG or modify the work of the AG.
WHO shall not in any way be obliged to reveal, or discuss with any applicant, how an expression of interest was assessed or to provide any other information relating to the evaluation/selection process or to state the reasons for choosing or not choosing a member.
WHO may publish the names and a short biography of the selected individuals on the WHO website.
TAG members will not be remunerated for their services in relation to the TAG or otherwise. Travel and accommodation expenses of TAG members to participate in TAG meetings will be covered by WHO in accordance with its applicable policies, rules and procedures.
The appointment of TAG members will be limited in time as indicated in the letter of appointment.
If you have any questions about this “Call for experts”, please write to [email protected] before the applicable deadline.
Related Other
Learn more about the Technical Advisory Group (TAG) for Universal Health and Preparedness Review (UHPR)
Loading metrics
Open Access
Peer-reviewed
Research Article
Functional connectivity changes in the brain of adolescents with internet addiction: A systematic literature review of imaging studies
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Child and Adolescent Mental Health, Department of Brain Sciences, Great Ormond Street Institute of Child Health, University College London, London, United Kingdom
Roles Conceptualization, Supervision, Validation, Writing – review & editing
* E-mail: [email protected]
Affiliation Behavioural Brain Sciences Unit, Population Policy Practice Programme, Great Ormond Street Institute of Child Health, University College London, London, United Kingdom
- Max L. Y. Chang,
- Irene O. Lee

- Published: June 4, 2024
- https://doi.org/10.1371/journal.pmen.0000022
- Peer Review
- Reader Comments
Internet usage has seen a stark global rise over the last few decades, particularly among adolescents and young people, who have also been diagnosed increasingly with internet addiction (IA). IA impacts several neural networks that influence an adolescent’s behaviour and development. This article issued a literature review on the resting-state and task-based functional magnetic resonance imaging (fMRI) studies to inspect the consequences of IA on the functional connectivity (FC) in the adolescent brain and its subsequent effects on their behaviour and development. A systematic search was conducted from two databases, PubMed and PsycINFO, to select eligible articles according to the inclusion and exclusion criteria. Eligibility criteria was especially stringent regarding the adolescent age range (10–19) and formal diagnosis of IA. Bias and quality of individual studies were evaluated. The fMRI results from 12 articles demonstrated that the effects of IA were seen throughout multiple neural networks: a mix of increases/decreases in FC in the default mode network; an overall decrease in FC in the executive control network; and no clear increase or decrease in FC within the salience network and reward pathway. The FC changes led to addictive behaviour and tendencies in adolescents. The subsequent behavioural changes are associated with the mechanisms relating to the areas of cognitive control, reward valuation, motor coordination, and the developing adolescent brain. Our results presented the FC alterations in numerous brain regions of adolescents with IA leading to the behavioural and developmental changes. Research on this topic had a low frequency with adolescent samples and were primarily produced in Asian countries. Future research studies of comparing results from Western adolescent samples provide more insight on therapeutic intervention.
Citation: Chang MLY, Lee IO (2024) Functional connectivity changes in the brain of adolescents with internet addiction: A systematic literature review of imaging studies. PLOS Ment Health 1(1): e0000022. https://doi.org/10.1371/journal.pmen.0000022
Editor: Kizito Omona, Uganda Martyrs University, UGANDA
Received: December 29, 2023; Accepted: March 18, 2024; Published: June 4, 2024
Copyright: © 2024 Chang, Lee. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The behavioural addiction brought on by excessive internet use has become a rising source of concern [ 1 ] since the last decade. According to clinical studies, individuals with Internet Addiction (IA) or Internet Gaming Disorder (IGD) may have a range of biopsychosocial effects and is classified as an impulse-control disorder owing to its resemblance to pathological gambling and substance addiction [ 2 , 3 ]. IA has been defined by researchers as a person’s inability to resist the urge to use the internet, which has negative effects on their psychological well-being as well as their social, academic, and professional lives [ 4 ]. The symptoms can have serious physical and interpersonal repercussions and are linked to mood modification, salience, tolerance, impulsivity, and conflict [ 5 ]. In severe circumstances, people may experience severe pain in their bodies or health issues like carpal tunnel syndrome, dry eyes, irregular eating and disrupted sleep [ 6 ]. Additionally, IA is significantly linked to comorbidities with other psychiatric disorders [ 7 ].
Stevens et al (2021) reviewed 53 studies including 17 countries and reported the global prevalence of IA was 3.05% [ 8 ]. Asian countries had a higher prevalence (5.1%) than European countries (2.7%) [ 8 ]. Strikingly, adolescents and young adults had a global IGD prevalence rate of 9.9% which matches previous literature that reported historically higher prevalence among adolescent populations compared to adults [ 8 , 9 ]. Over 80% of adolescent population in the UK, the USA, and Asia have direct access to the internet [ 10 ]. Children and adolescents frequently spend more time on media (possibly 7 hours and 22 minutes per day) than at school or sleeping [ 11 ]. Developing nations have also shown a sharp rise in teenage internet usage despite having lower internet penetration rates [ 10 ]. Concerns regarding the possible harms that overt internet use could do to adolescents and their development have arisen because of this surge, especially the significant impacts by the COVID-19 pandemic [ 12 ]. The growing prevalence and neurocognitive consequences of IA among adolescents makes this population a vital area of study [ 13 ].
Adolescence is a crucial developmental stage during which people go through significant changes in their biology, cognition, and personalities [ 14 ]. Adolescents’ emotional-behavioural functioning is hyperactivated, which creates risk of psychopathological vulnerability [ 15 ]. In accordance with clinical study results [ 16 ], this emotional hyperactivity is supported by a high level of neuronal plasticity. This plasticity enables teenagers to adapt to the numerous physical and emotional changes that occur during puberty as well as develop communication techniques and gain independence [ 16 ]. However, the strong neuronal plasticity is also associated with risk-taking and sensation seeking [ 17 ] which may lead to IA.
Despite the fact that the precise neuronal mechanisms underlying IA are still largely unclear, functional magnetic resonance imaging (fMRI) method has been used by scientists as an important framework to examine the neuropathological changes occurring in IA, particularly in the form of functional connectivity (FC) [ 18 ]. fMRI research study has shown that IA alters both the functional and structural makeup of the brain [ 3 ].
We hypothesise that IA has widespread neurological alteration effects rather than being limited to a few specific brain regions. Further hypothesis holds that according to these alterations of FC between the brain regions or certain neural networks, adolescents with IA would experience behavioural changes. An investigation of these domains could be useful for creating better procedures and standards as well as minimising the negative effects of overt internet use. This literature review aims to summarise and analyse the evidence of various imaging studies that have investigated the effects of IA on the FC in adolescents. This will be addressed through two research questions:
- How does internet addiction affect the functional connectivity in the adolescent brain?
- How is adolescent behaviour and development impacted by functional connectivity changes due to internet addiction?
The review protocol was conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see S1 Checklist ).
Search strategy and selection process
A systematic search was conducted up until April 2023 from two sources of database, PubMed and PsycINFO, using a range of terms relevant to the title and research questions (see full list of search terms in S1 Appendix ). All the searched articles can be accessed in the S1 Data . The eligible articles were selected according to the inclusion and exclusion criteria. Inclusion criteria used for the present review were: (i) participants in the studies with clinical diagnosis of IA; (ii) participants between the ages of 10 and 19; (iii) imaging research investigations; (iv) works published between January 2013 and April 2023; (v) written in English language; (vi) peer-reviewed papers and (vii) full text. The numbers of articles excluded due to not meeting the inclusion criteria are shown in Fig 1 . Each study’s title and abstract were screened for eligibility.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmen.0000022.g001
Quality appraisal
Full texts of all potentially relevant studies were then retrieved and further appraised for eligibility. Furthermore, articles were critically appraised based on the GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) framework to evaluate the individual study for both quality and bias. The subsequent quality levels were then appraised to each article and listed as either low, moderate, or high.
Data collection process
Data that satisfied the inclusion requirements was entered into an excel sheet for data extraction and further selection. An article’s author, publication year, country, age range, participant sample size, sex, area of interest, measures, outcome and article quality were all included in the data extraction spreadsheet. Studies looking at FC, for instance, were grouped, while studies looking at FC in specific area were further divided into sub-groups.
Data synthesis and analysis
Articles were classified according to their location in the brain as well as the network or pathway they were a part of to create a coherent narrative between the selected studies. Conclusions concerning various research trends relevant to particular groupings were drawn from these groupings and subgroupings. To maintain the offered information in a prominent manner, these assertions were entered into the data extraction excel spreadsheet.
With the search performed on the selected databases, 238 articles in total were identified (see Fig 1 ). 15 duplicated articles were eliminated, and another 6 items were removed for various other reasons. Title and abstract screening eliminated 184 articles because they were not in English (number of article, n, = 7), did not include imaging components (n = 47), had adult participants (n = 53), did not have a clinical diagnosis of IA (n = 19), did not address FC in the brain (n = 20), and were published outside the desired timeframe (n = 38). A further 21 papers were eliminated for failing to meet inclusion requirements after the remaining 33 articles underwent full-text eligibility screening. A total of 12 papers were deemed eligible for this review analysis.
Characteristics of the included studies, as depicted in the data extraction sheet in Table 1 provide information of the author(s), publication year, sample size, study location, age range, gender, area of interest, outcome, measures used and quality appraisal. Most of the studies in this review utilised resting state functional magnetic resonance imaging techniques (n = 7), with several studies demonstrating task-based fMRI procedures (n = 3), and the remaining studies utilising whole-brain imaging measures (n = 2). The studies were all conducted in Asiatic countries, specifically coming from China (8), Korea (3), and Indonesia (1). Sample sizes ranged from 12 to 31 participants with most of the imaging studies having comparable sample sizes. Majority of the studies included a mix of male and female participants (n = 8) with several studies having a male only participant pool (n = 3). All except one of the mixed gender studies had a majority male participant pool. One study did not disclose their data on the gender demographics of their experiment. Study years ranged from 2013–2022, with 2 studies in 2013, 3 studies in 2014, 3 studies in 2015, 1 study in 2017, 1 study in 2020, 1 study in 2021, and 1 study in 2022.
https://doi.org/10.1371/journal.pmen.0000022.t001
(1) How does internet addiction affect the functional connectivity in the adolescent brain?
The included studies were organised according to the brain region or network that they were observing. The specific networks affected by IA were the default mode network, executive control system, salience network and reward pathway. These networks are vital components of adolescent behaviour and development [ 31 ]. The studies in each section were then grouped into subsections according to their specific brain regions within their network.
Default mode network (DMN)/reward network.
Out of the 12 studies, 3 have specifically studied the default mode network (DMN), and 3 observed whole-brain FC that partially included components of the DMN. The effect of IA on the various centres of the DMN was not unilaterally the same. The findings illustrate a complex mix of increases and decreases in FC depending on the specific region in the DMN (see Table 2 and Fig 2 ). The alteration of FC in posterior cingulate cortex (PCC) in the DMN was the most frequently reported area in adolescents with IA, which involved in attentional processes [ 32 ], but Lee et al. (2020) additionally found alterations of FC in other brain regions, such as anterior insula cortex, a node in the DMN that controls the integration of motivational and cognitive processes [ 20 ].
https://doi.org/10.1371/journal.pmen.0000022.g002
The overall changes of functional connectivity in the brain network including default mode network (DMN), executive control network (ECN), salience network (SN) and reward network. IA = Internet Addiction, FC = Functional Connectivity.
https://doi.org/10.1371/journal.pmen.0000022.t002
Ding et al. (2013) revealed altered FC in the cerebellum, the middle temporal gyrus, and the medial prefrontal cortex (mPFC) [ 22 ]. They found that the bilateral inferior parietal lobule, left superior parietal lobule, and right inferior temporal gyrus had decreased FC, while the bilateral posterior lobe of the cerebellum and the medial temporal gyrus had increased FC [ 22 ]. The right middle temporal gyrus was found to have 111 cluster voxels (t = 3.52, p<0.05) and the right inferior parietal lobule was found to have 324 cluster voxels (t = -4.07, p<0.05) with an extent threshold of 54 voxels (figures above this threshold are deemed significant) [ 22 ]. Additionally, there was a negative correlation, with 95 cluster voxels (p<0.05) between the FC of the left superior parietal lobule and the PCC with the Chen Internet Addiction Scores (CIAS) which are used to determine the severity of IA [ 22 ]. On the other hand, in regions of the reward system, connection with the PCC was positively connected with CIAS scores [ 22 ]. The most significant was the right praecuneus with 219 cluster voxels (p<0.05) [ 22 ]. Wang et al. (2017) also discovered that adolescents with IA had 33% less FC in the left inferior parietal lobule and 20% less FC in the dorsal mPFC [ 24 ]. A potential connection between the effects of substance use and overt internet use is revealed by the generally decreased FC in these areas of the DMN of teenagers with drug addiction and IA [ 35 ].
The putamen was one of the main regions of reduced FC in adolescents with IA [ 19 ]. The putamen and the insula-operculum demonstrated significant group differences regarding functional connectivity with a cluster size of 251 and an extent threshold of 250 (Z = 3.40, p<0.05) [ 19 ]. The molecular mechanisms behind addiction disorders have been intimately connected to decreased striatal dopaminergic function [ 19 ], making this function crucial.
Executive Control Network (ECN).
5 studies out of 12 have specifically viewed parts of the executive control network (ECN) and 3 studies observed whole-brain FC. The effects of IA on the ECN’s constituent parts were consistent across all the studies examined for this analysis (see Table 2 and Fig 3 ). The results showed a notable decline in all the ECN’s major centres. Li et al. (2014) used fMRI imaging and a behavioural task to study response inhibition in adolescents with IA [ 25 ] and found decreased activation at the striatum and frontal gyrus, particularly a reduction in FC at inferior frontal gyrus, in the IA group compared to controls [ 25 ]. The inferior frontal gyrus showed a reduction in FC in comparison to the controls with a cluster size of 71 (t = 4.18, p<0.05) [ 25 ]. In addition, the frontal-basal ganglia pathways in the adolescents with IA showed little effective connection between areas and increased degrees of response inhibition [ 25 ].
https://doi.org/10.1371/journal.pmen.0000022.g003
Lin et al. (2015) found that adolescents with IA demonstrated disrupted corticostriatal FC compared to controls [ 33 ]. The corticostriatal circuitry experienced decreased connectivity with the caudate, bilateral anterior cingulate cortex (ACC), as well as the striatum and frontal gyrus [ 33 ]. The inferior ventral striatum showed significantly reduced FC with the subcallosal ACC and caudate head with cluster size of 101 (t = -4.64, p<0.05) [ 33 ]. Decreased FC in the caudate implies dysfunction of the corticostriatal-limbic circuitry involved in cognitive and emotional control [ 36 ]. The decrease in FC in both the striatum and frontal gyrus is related to inhibitory control, a common deficit seen with disruptions with the ECN [ 33 ].
The dorsolateral prefrontal cortex (DLPFC), ACC, and right supplementary motor area (SMA) of the prefrontal cortex were all found to have significantly decreased grey matter volume [ 29 ]. In addition, the DLPFC, insula, temporal cortices, as well as significant subcortical regions like the striatum and thalamus, showed decreased FC [ 29 ]. According to Tremblay (2009), the striatum plays a significant role in the processing of rewards, decision-making, and motivation [ 37 ]. Chen et al. (2020) reported that the IA group demonstrated increased impulsivity as well as decreased reaction inhibition using a Stroop colour-word task [ 26 ]. Furthermore, Chen et al. (2020) observed that the left DLPFC and dorsal striatum experienced a negative connection efficiency value, specifically demonstrating that the dorsal striatum activity suppressed the left DLPFC [ 27 ].
Salience network (SN).
Out of the 12 chosen studies, 3 studies specifically looked at the salience network (SN) and 3 studies have observed whole-brain FC. Relative to the DMN and ECN, the findings on the SN were slightly sparser. Despite this, adolescents with IA demonstrated a moderate decrease in FC, as well as other measures like fibre connectivity and cognitive control, when compared to healthy control (see Table 2 and Fig 4 ).
https://doi.org/10.1371/journal.pmen.0000022.g004
Xing et al. (2014) used both dorsal anterior cingulate cortex (dACC) and insula to test FC changes in the SN of adolescents with IA and found decreased structural connectivity in the SN as well as decreased fractional anisotropy (FA) that correlated to behaviour performance in the Stroop colour word-task [ 21 ]. They examined the dACC and insula to determine whether the SN’s disrupted connectivity may be linked to the SN’s disruption of regulation, which would explain the impaired cognitive control seen in adolescents with IA. However, researchers did not find significant FC differences in the SN when compared to the controls [ 21 ]. These results provided evidence for the structural changes in the interconnectivity within SN in adolescents with IA.
Wang et al. (2017) investigated network interactions between the DMN, ECN, SN and reward pathway in IA subjects [ 24 ] (see Fig 5 ), and found 40% reduction of FC between the DMN and specific regions of the SN, such as the insula, in comparison to the controls (p = 0.008) [ 24 ]. The anterior insula and dACC are two areas that are impacted by this altered FC [ 24 ]. This finding supports the idea that IA has similar neurobiological abnormalities with other addictive illnesses, which is in line with a study that discovered disruptive changes in the SN and DMN’s interaction in cocaine addiction [ 38 ]. The insula has also been linked to the intensity of symptoms and has been implicated in the development of IA [ 39 ].
“+” indicates an increase in behaivour; “-”indicates a decrease in behaviour; solid arrows indicate a direct network interaction; and the dotted arrows indicates a reduction in network interaction. This diagram depicts network interactions juxtaposed with engaging in internet related behaviours. Through the neural interactions, the diagram illustrates how the networks inhibit or amplify internet usage and vice versa. Furthermore, it demonstrates how the SN mediates both the DMN and ECN.
https://doi.org/10.1371/journal.pmen.0000022.g005
(2) How is adolescent behaviour and development impacted by functional connectivity changes due to internet addiction?
The findings that IA individuals demonstrate an overall decrease in FC in the DMN is supported by numerous research [ 24 ]. Drug addict populations also exhibited similar decline in FC in the DMN [ 40 ]. The disruption of attentional orientation and self-referential processing for both substance and behavioural addiction was then hypothesised to be caused by DMN anomalies in FC [ 41 ].
In adolescents with IA, decline of FC in the parietal lobule affects visuospatial task-related behaviour [ 22 ], short-term memory [ 42 ], and the ability of controlling attention or restraining motor responses during response inhibition tests [ 42 ]. Cue-induced gaming cravings are influenced by the DMN [ 43 ]. A visual processing area called the praecuneus links gaming cues to internal information [ 22 ]. A meta-analysis found that the posterior cingulate cortex activity of individuals with IA during cue-reactivity tasks was connected with their gaming time [ 44 ], suggesting that excessive gaming may impair DMN function and that individuals with IA exert more cognitive effort to control it. Findings for the behavioural consequences of FC changes in the DMN illustrate its underlying role in regulating impulsivity, self-monitoring, and cognitive control.
Furthermore, Ding et al. (2013) reported an activation of components of the reward pathway, including areas like the nucleus accumbens, praecuneus, SMA, caudate, and thalamus, in connection to the DMN [ 22 ]. The increased FC of the limbic and reward networks have been confirmed to be a major biomarker for IA [ 45 , 46 ]. The increased reinforcement in these networks increases the strength of reward stimuli and makes it more difficult for other networks, namely the ECN, to down-regulate the increased attention [ 29 ] (See Fig 5 ).
Executive control network (ECN).
The numerous IA-affected components in the ECN have a role in a variety of behaviours that are connected to both response inhibition and emotional regulation [ 47 ]. For instance, brain regions like the striatum, which are linked to impulsivity and the reward system, are heavily involved in the act of playing online games [ 47 ]. Online game play activates the striatum, which suppresses the left DLPFC in ECN [ 48 ]. As a result, people with IA may find it difficult to control their want to play online games [ 48 ]. This system thus causes impulsive and protracted gaming conduct, lack of inhibitory control leading to the continued use of internet in an overt manner despite a variety of negative effects, personal distress, and signs of psychological dependence [ 33 ] (See Fig 5 ).
Wang et al. (2017) report that disruptions in cognitive control networks within the ECN are frequently linked to characteristics of substance addiction [ 24 ]. With samples that were addicted to heroin and cocaine, previous studies discovered abnormal FC in the ECN and the PFC [ 49 ]. Electronic gaming is known to promote striatal dopamine release, similar to drug addiction [ 50 ]. According to Drgonova and Walther (2016), it is hypothesised that dopamine could stimulate the reward system of the striatum in the brain, leading to a loss of impulse control and a failure of prefrontal lobe executive inhibitory control [ 51 ]. In the end, IA’s resemblance to drug use disorders may point to vital biomarkers or underlying mechanisms that explain how cognitive control and impulsive behaviour are related.
A task-related fMRI study found that the decrease in FC between the left DLPFC and dorsal striatum was congruent with an increase in impulsivity in adolescents with IA [ 26 ]. The lack of response inhibition from the ECN results in a loss of control over internet usage and a reduced capacity to display goal-directed behaviour [ 33 ]. Previous studies have linked the alteration of the ECN in IA with higher cue reactivity and impaired ability to self-regulate internet specific stimuli [ 52 ].
Salience network (SN)/ other networks.
Xing et al. (2014) investigated the significance of the SN regarding cognitive control in teenagers with IA [ 21 ]. The SN, which is composed of the ACC and insula, has been demonstrated to control dynamic changes in other networks to modify cognitive performance [ 21 ]. The ACC is engaged in conflict monitoring and cognitive control, according to previous neuroimaging research [ 53 ]. The insula is a region that integrates interoceptive states into conscious feelings [ 54 ]. The results from Xing et al. (2014) showed declines in the SN regarding its structural connectivity and fractional anisotropy, even though they did not observe any appreciable change in FC in the IA participants [ 21 ]. Due to the small sample size, the results may have indicated that FC methods are not sensitive enough to detect the significant functional changes [ 21 ]. However, task performance behaviours associated with impaired cognitive control in adolescents with IA were correlated with these findings [ 21 ]. Our comprehension of the SN’s broader function in IA can be enhanced by this relationship.
Research study supports the idea that different psychological issues are caused by the functional reorganisation of expansive brain networks, such that strong association between SN and DMN may provide neurological underpinnings at the system level for the uncontrollable character of internet-using behaviours [ 24 ]. In the study by Wang et al. (2017), the decreased interconnectivity between the SN and DMN, comprising regions such the DLPFC and the insula, suggests that adolescents with IA may struggle to effectively inhibit DMN activity during internally focused processing, leading to poorly managed desires or preoccupations to use the internet [ 24 ] (See Fig 5 ). Subsequently, this may cause a failure to inhibit DMN activity as well as a restriction of ECN functionality [ 55 ]. As a result, the adolescent experiences an increased salience and sensitivity towards internet addicting cues making it difficult to avoid these triggers [ 56 ].
The primary aim of this review was to present a summary of how internet addiction impacts on the functional connectivity of adolescent brain. Subsequently, the influence of IA on the adolescent brain was compartmentalised into three sections: alterations of FC at various brain regions, specific FC relationships, and behavioural/developmental changes. Overall, the specific effects of IA on the adolescent brain were not completely clear, given the variety of FC changes. However, there were overarching behavioural, network and developmental trends that were supported that provided insight on adolescent development.
The first hypothesis that was held about this question was that IA was widespread and would be regionally similar to substance-use and gambling addiction. After conducting a review of the information in the chosen articles, the hypothesis was predictably supported. The regions of the brain affected by IA are widespread and influence multiple networks, mainly DMN, ECN, SN and reward pathway. In the DMN, there was a complex mix of increases and decreases within the network. However, in the ECN, the alterations of FC were more unilaterally decreased, but the findings of SN and reward pathway were not quite clear. Overall, the FC changes within adolescents with IA are very much network specific and lay a solid foundation from which to understand the subsequent behaviour changes that arise from the disorder.
The second hypothesis placed emphasis on the importance of between network interactions and within network interactions in the continuation of IA and the development of its behavioural symptoms. The results from the findings involving the networks, DMN, SN, ECN and reward system, support this hypothesis (see Fig 5 ). Studies confirm the influence of all these neural networks on reward valuation, impulsivity, salience to stimuli, cue reactivity and other changes that alter behaviour towards the internet use. Many of these changes are connected to the inherent nature of the adolescent brain.
There are multiple explanations that underlie the vulnerability of the adolescent brain towards IA related urges. Several of them have to do with the inherent nature and underlying mechanisms of the adolescent brain. Children’s emotional, social, and cognitive capacities grow exponentially during childhood and adolescence [ 57 ]. Early teenagers go through a process called “social reorientation” that is characterised by heightened sensitivity to social cues and peer connections [ 58 ]. Adolescents’ improvements in their social skills coincide with changes in their brains’ anatomical and functional organisation [ 59 ]. Functional hubs exhibit growing connectivity strength [ 60 ], suggesting increased functional integration during development. During this time, the brain’s functional networks change from an anatomically dominant structure to a scattered architecture [ 60 ].
The adolescent brain is very responsive to synaptic reorganisation and experience cues [ 61 ]. As a result, one of the distinguishing traits of the maturation of adolescent brains is the variation in neural network trajectory [ 62 ]. Important weaknesses of the adolescent brain that may explain the neurobiological change brought on by external stimuli are illustrated by features like the functional gaps between networks and the inadequate segregation of networks [ 62 ].
The implications of these findings towards adolescent behaviour are significant. Although the exact changes and mechanisms are not fully clear, the observed changes in functional connectivity have the capacity of influencing several aspects of adolescent development. For example, functional connectivity has been utilised to investigate attachment styles in adolescents [ 63 ]. It was observed that adolescent attachment styles were negatively associated with caudate-prefrontal connectivity, but positively with the putamen-visual area connectivity [ 63 ]. Both named areas were also influenced by the onset of internet addiction, possibly providing a connection between the two. Another study associated neighbourhood/socioeconomic disadvantage with functional connectivity alterations in the DMN and dorsal attention network [ 64 ]. The study also found multivariate brain behaviour relationships between the altered/disadvantaged functional connectivity and mental health and cognition [ 64 ]. This conclusion supports the notion that the functional connectivity alterations observed in IA are associated with specific adolescent behaviours as well as the fact that functional connectivity can be utilised as a platform onto which to compare various neurologic conditions.
Limitations/strengths
There were several limitations that were related to the conduction of the review as well as the data extracted from the articles. Firstly, the study followed a systematic literature review design when analysing the fMRI studies. The data pulled from these imaging studies were namely qualitative and were subject to bias contrasting the quantitative nature of statistical analysis. Components of the study, such as sample sizes, effect sizes, and demographics were not weighted or controlled. The second limitation brought up by a similar review was the lack of a universal consensus of terminology given IA [ 47 ]. Globally, authors writing about this topic use an array of terminology including online gaming addiction, internet addiction, internet gaming disorder, and problematic internet use. Often, authors use multiple terms interchangeably which makes it difficult to depict the subtle similarities and differences between the terms.
Reviewing the explicit limitations in each of the included studies, two major limitations were brought up in many of the articles. One was relating to the cross-sectional nature of the included studies. Due to the inherent qualities of a cross-sectional study, the studies did not provide clear evidence that IA played a causal role towards the development of the adolescent brain. While several biopsychosocial factors mediate these interactions, task-based measures that combine executive functions with imaging results reinforce the assumed connection between the two that is utilised by the papers studying IA. Another limitation regarded the small sample size of the included studies, which averaged to around 20 participants. The small sample size can influence the generalisation of the results as well as the effectiveness of statistical analyses. Ultimately, both included study specific limitations illustrate the need for future studies to clarify the causal relationship between the alterations of FC and the development of IA.
Another vital limitation was the limited number of studies applying imaging techniques for investigations on IA in adolescents were a uniformly Far East collection of studies. The reason for this was because the studies included in this review were the only fMRI studies that were found that adhered to the strict adolescent age restriction. The adolescent age range given by the WHO (10–19 years old) [ 65 ] was strictly followed. It is important to note that a multitude of studies found in the initial search utilised an older adolescent demographic that was slightly higher than the WHO age range and had a mean age that was outside of the limitations. As a result, the results of this review are biased and based on the 12 studies that met the inclusion and exclusion criteria.
Regarding the global nature of the research, although the journals that the studies were published in were all established western journals, the collection of studies were found to all originate from Asian countries, namely China and Korea. Subsequently, it pulls into question if the results and measures from these studies are generalisable towards a western population. As stated previously, Asian countries have a higher prevalence of IA, which may be the reasoning to why the majority of studies are from there [ 8 ]. However, in an additional search including other age groups, it was found that a high majority of all FC studies on IA were done in Asian countries. Interestingly, western papers studying fMRI FC were primarily focused on gambling and substance-use addiction disorders. The western papers on IA were less focused on fMRI FC but more on other components of IA such as sleep, game-genre, and other non-imaging related factors. This demonstrated an overall lack of western fMRI studies on IA. It is important to note that both western and eastern fMRI studies on IA presented an overall lack on children and adolescents in general.
Despite the several limitations, this review provided a clear reflection on the state of the data. The strengths of the review include the strict inclusion/exclusion criteria that filtered through studies and only included ones that contained a purely adolescent sample. As a result, the information presented in this review was specific to the review’s aims. Given the sparse nature of adolescent specific fMRI studies on the FC changes in IA, this review successfully provided a much-needed niche representation of adolescent specific results. Furthermore, the review provided a thorough functional explanation of the DMN, ECN, SN and reward pathway making it accessible to readers new to the topic.
Future directions and implications
Through the search process of the review, there were more imaging studies focused on older adolescence and adulthood. Furthermore, finding a review that covered a strictly adolescent population, focused on FC changes, and was specifically depicting IA, was proven difficult. Many related reviews, such as Tereshchenko and Kasparov (2019), looked at risk factors related to the biopsychosocial model, but did not tackle specific alterations in specific structural or functional changes in the brain [ 66 ]. Weinstein (2017) found similar structural and functional results as well as the role IA has in altering response inhibition and reward valuation in adolescents with IA [ 47 ]. Overall, the accumulated findings only paint an emerging pattern which aligns with similar substance-use and gambling disorders. Future studies require more specificity in depicting the interactions between neural networks, as well as more literature on adolescent and comorbid populations. One future field of interest is the incorporation of more task-based fMRI data. Advances in resting-state fMRI methods have yet to be reflected or confirmed in task-based fMRI methods [ 62 ]. Due to the fact that network connectivity is shaped by different tasks, it is critical to confirm that the findings of the resting state fMRI studies also apply to the task based ones [ 62 ]. Subsequently, work in this area will confirm if intrinsic connectivity networks function in resting state will function similarly during goal directed behaviour [ 62 ]. An elevated focus on adolescent populations as well as task-based fMRI methodology will help uncover to what extent adolescent network connectivity maturation facilitates behavioural and cognitive development [ 62 ].
A treatment implication is the potential usage of bupropion for the treatment of IA. Bupropion has been previously used to treat patients with gambling disorder and has been effective in decreasing overall gambling behaviour as well as money spent while gambling [ 67 ]. Bae et al. (2018) found a decrease in clinical symptoms of IA in line with a 12-week bupropion treatment [ 31 ]. The study found that bupropion altered the FC of both the DMN and ECN which in turn decreased impulsivity and attentional deficits for the individuals with IA [ 31 ]. Interventions like bupropion illustrate the importance of understanding the fundamental mechanisms that underlie disorders like IA.
The goal for this review was to summarise the current literature on functional connectivity changes in adolescents with internet addiction. The findings answered the primary research questions that were directed at FC alterations within several networks of the adolescent brain and how that influenced their behaviour and development. Overall, the research demonstrated several wide-ranging effects that influenced the DMN, SN, ECN, and reward centres. Additionally, the findings gave ground to important details such as the maturation of the adolescent brain, the high prevalence of Asian originated studies, and the importance of task-based studies in this field. The process of making this review allowed for a thorough understanding IA and adolescent brain interactions.
Given the influx of technology and media in the lives and education of children and adolescents, an increase in prevalence and focus on internet related behavioural changes is imperative towards future children/adolescent mental health. Events such as COVID-19 act to expose the consequences of extended internet usage on the development and lifestyle of specifically young people. While it is important for parents and older generations to be wary of these changes, it is important for them to develop a base understanding of the issue and not dismiss it as an all-bad or all-good scenario. Future research on IA will aim to better understand the causal relationship between IA and psychological symptoms that coincide with it. The current literature regarding functional connectivity changes in adolescents is limited and requires future studies to test with larger sample sizes, comorbid populations, and populations outside Far East Asia.
This review aimed to demonstrate the inner workings of how IA alters the connection between the primary behavioural networks in the adolescent brain. Predictably, the present answers merely paint an unfinished picture that does not necessarily depict internet usage as overwhelmingly positive or negative. Alternatively, the research points towards emerging patterns that can direct individuals on the consequences of certain variables or risk factors. A clearer depiction of the mechanisms of IA would allow physicians to screen and treat the onset of IA more effectively. Clinically, this could be in the form of more streamlined and accurate sessions of CBT or family therapy, targeting key symptoms of IA. Alternatively clinicians could potentially prescribe treatment such as bupropion to target FC in certain regions of the brain. Furthermore, parental education on IA is another possible avenue of prevention from a public health standpoint. Parents who are aware of the early signs and onset of IA will more effectively handle screen time, impulsivity, and minimize the risk factors surrounding IA.
Additionally, an increased attention towards internet related fMRI research is needed in the West, as mentioned previously. Despite cultural differences, Western countries may hold similarities to the eastern countries with a high prevalence of IA, like China and Korea, regarding the implications of the internet and IA. The increasing influence of the internet on the world may contribute to an overall increase in the global prevalence of IA. Nonetheless, the high saturation of eastern studies in this field should be replicated with a Western sample to determine if the same FC alterations occur. A growing interest in internet related research and education within the West will hopefully lead to the knowledge of healthier internet habits and coping strategies among parents with children and adolescents. Furthermore, IA research has the potential to become a crucial proxy for which to study adolescent brain maturation and development.
Supporting information
S1 checklist. prisma checklist..
https://doi.org/10.1371/journal.pmen.0000022.s001
S1 Appendix. Search strategies with all the terms.
https://doi.org/10.1371/journal.pmen.0000022.s002
S1 Data. Article screening records with details of categorized content.
https://doi.org/10.1371/journal.pmen.0000022.s003
Acknowledgments
The authors thank https://www.stockio.com/free-clipart/brain-01 (with attribution to Stockio.com); and https://www.rawpixel.com/image/6442258/png-sticker-vintage for the free images used to create Figs 2 – 4 .
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. 5 ed. Washington, D.C.: American Psychiatric Publishing; 2013.
- 10. Stats IW. World Internet Users Statistics and World Population Stats 2013 [ http://www.internetworldstats.com/stats.htm .
- 11. Rideout VJR M. B. The common sense census: media use by tweens and teens. San Francisco, CA: Common Sense Media; 2019.
- 37. Tremblay L. The Ventral Striatum. Handbook of Reward and Decision Making: Academic Press; 2009.
- 57. Bhana A. Middle childhood and pre-adolescence. Promoting mental health in scarce-resource contexts: emerging evidence and practice. Cape Town: HSRC Press; 2010. p. 124–42.
- 65. Organization WH. Adolescent Health 2023 [ https://www.who.int/health-topics/adolescent-health#tab=tab_1 .
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 14, Issue 6
- Perceptions of families and healthcare providers about feeding preterm infants in the neonatal intensive care unit: protocol for a qualitative systematic review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0009-0008-5313-9272 Willow R Schanz 1 ,
- Aunum Akhter 2 ,
- Georgette Richardson 3 ,
- http://orcid.org/0000-0003-0229-966X William T Story 4 ,
- Riley Samuelson 5 ,
- http://orcid.org/0000-0002-7026-0006 Aamer Imdad 6
- 1 The University of Iowa Roy J and Lucille A Carver College of Medicine , Iowa City , Iowa , USA
- 2 Division of Neonatology , The University of Iowa Health Care, Stead Family Department of Pediatrics, Roy J and Lucille A Carver College of Medicine , Iowa City , Iowa , USA
- 3 Division of Pediatric Psychology , The University of Iowa Health Care, Stead Family Department of Pediatrics , Iowa City , Iowa , USA
- 4 Department of Community and Behavioral Health , The University of Iowa College of Public Health , Iowa City , Iowa , USA
- 5 University of Iowa Hardin Library for the Health Sciences , Iowa City , Iowa , USA
- 6 Division of Gastroenterology, Hepatology, Pancreatology and Nutrition , University of Iowa Health Care, Stead Family Department of Pediatrics, Roy J and Lucille A Carver College of Medicine , Iowa City , Iowa , USA
- Correspondence to Dr Aamer Imdad; aamer-imdad{at}uiowa.edu
Introduction The underdevelopment of preterm infants can lead to delayed progression through key early milestones. Demonstration of safe oral feeding skills, constituting proper suck-swallow reflex are requirements for discharge from the neonatal intensive care unit (NICU) to ensure adequate nutrition acquisition. Helping an infant develop these skills can be draining and emotional for both families and healthcare staff involved in the care of preterm infants with feeding difficulties. Currently, there are no systematic reviews evaluating both family and healthcare team perspectives on aspects of oral feeding. Thus, we first aim to evaluate the current knowledge surrounding the perceptions, experiences and needs of families with preterm babies in the context of oral feeding in the NICU. Second, we aim to evaluate the current knowledge surrounding the perceptions, experiences and needs of healthcare providers (physicians, advanced practice providers, nurses, dietitians, speech-language pathologists and occupational therapists) in the context of oral feeding in the NICU.
Methods and analysis A literature search will be conducted in multiple electronic databases from their inception, including PubMed, CINHAL, Embase, the Cochrane Central Register for Controlled Trials and PsycINFO. No restrictions will be applied based on language or data of publication. Two authors will screen the titles and abstracts and then review the full text for the studies’ inclusion in the review. The data will be extracted into a pilot-tested data collection sheet by three independent authors. To evaluate the quality, reliability and relevance of the included studies, the Critical Appraisal Skills Programme checklist will be used. The overall evidence will be assessed using the Grading of Recommendation Assessment, Development and Evaluation criteria. We will report the results of the systematic review by following the Enhancing Transparency in Reporting the synthesis of Qualitative research checklist.
Ethics and dissemination Ethical approval of this project is not required as this is a systematic review using published and publicly available data and will not involve contact with human subjects. Findings will be published in a peer-reviewed journal.
PROSPERO registration number CRD42023479288.
- Paediatric gastroenterology
- Systematic Review
- Percieved Social Support
- NEONATOLOGY
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2024-084884
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
This will be a systematic review evaluating both the perspectives of families and neonatal healthcare professionals on feeding practices of preterm infants in the neonatal intensive care unit (NICU).
Evaluating the perspectives of both family members and neonatal healthcare professionals involved in the care of preterm babies with feeding difficulties may uncover shared grievances and mutually beneficial opportunities for quality improvement in the NICU.
Included studies might be conducted in diverse settings, so generalisability to clinical practice may be affected by cultural, language and healthcare systems context.
Introduction
An estimated 13.4 million babies were born preterm (<37 weeks gestation) in 2020, which represented about 10% of all live births worldwide. 1 Preterm birth is a serious health event that contributes to significant morbidity, mortality and increased healthcare cost in neonates. Over 40% of premature infants will experience feeding difficulties, such as struggling to develop typical feeding reflexes (sucking, swallowing, appropriate breathing) and coordinated oesophageal bolus transport. 2 Consequently, feeding difficulties are associated with elevated healthcare costs due to increased length of stay in the neonatal intensive care unit (NICU) and invasive measures, such as a central line or other parenteral support, to supply the infant with adequate nutrients. 3 4 Poor feeding skills are associated with increased morbidity through malnutrition and growth restriction as well as increased mortality through oropharyngeal aspiration. 5 6
Despite the global prevalence, expense and severity of feeding difficulties, no universal guidelines function as the gold standard of care for feeding preterm infants. 7 The resulting high variability in approach may lead to dissatisfaction among NICU families and healthcare professionals. Families of preterm infants have been shown to express concerns about the technicality of feeding interventions, communication with providers regarding their child and feeling isolated from the feeding approaches in the NICU. 8 Tube feeding, a common feeding intervention for preterm infants, has been associated with increased cost, rehospitalisation, stress and anxiety for families. Due to the emotional nature of feeding a newborn, family members may struggle with learning to feed their infant in this manner. 8 Additionally, nurse perceptions of oral feeding in the NICU have emphasised the impactful role they hold in teaching feeding techniques and relieving emotional distress for the family, which has highlighted a need for greater collaboration between the family and care providers. 9 Family integrated care has been perceived to be helpful in the reduction of maternal stress by parents of preterm infants as well as a necessary and feasible care model by neonatologists and NICU nurses that has the potential to lower length of hospitalisation, decrease healthcare costs and improve breastfeeding rates in preterm infants. 10–12 The approach to feeding preterm infants requires a multidisciplinary effort, including the family, nurses, dietitians, occupational therapists, speech-language pathologists, social workers, advanced practice providers and physicians. Despite these experiences being reported, there is still limited understanding regarding the perceptions of families and caregivers on feeding preterm infants in the NICU. 13 14 This qualitative systematic review aims to analyse the current global knowledge of the perceptions, experiences and needs of families and healthcare staff (nurses, physicians, advanced practice providers, dietitians, occupational therapists, social workers and speech-language pathologists) involved in the feeding process of preterm infants in the NICU, as well as possible improvements to decrease barriers to high-quality care.
Methods and analysis
This systematic review will be conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and checklist. 15
Literature search
Systematic electronic queries, available in online supplemental appendix A , will be conducted in major databases, including PubMed, CINHAL, Embase, the Cochrane Central Register for Controlled Trials and PsycINFO from their inception to date of inquiry. Key terms used in the search are those related to population, context and phenomena of interest (perspectives, views, needs, experiences, perceptions, barriers, challenges). Studies will not be excluded based on the publication year, publication status, geographical location or language. Thus, this analysis will include studies from all countries. Studies evaluating specific racial, gender, geographic, age (of family or provider) differences will be included in this review as long as they evaluate qualitative aspects of our phenomena of interest. Bibliographic software (EndNote) will be used to combine database search results, and duplicates will be removed.
Supplemental material
Eligibility criteria.
The populations of interest include families of preterm infants (parents, mother, father, grandmother, grandfather and guardians) and neonatal healthcare professionals (nurses, physicians, advanced practice providers, caregivers, dietitians, speech-language pathologists, social workers and occupational therapists) involved in the feeding care of preterm infants. For this review, preterm birth will be defined as gestational age <37 weeks at birth. If relevant, additional definitions such as late preterm: 34–36 weeks, moderately preterm: 32–34 weeks, very preterm: 28–32 weeks, extremely preterm: <28 weeks gestational age at birth, will be used and clearly reported.
We are interested in the global state of enteral and oral feeding in preterm infants while in NICUs from the perspective of both families and healthcare providers.
Phenomena of interest
The main phenomena of interest are the experiences and perceptions of families with preterm infants and healthcare providers of preterm infants as outlined below:
Family experiences regarding NICU feeding practices.
Family perceptions of NICU feeding practices.
Family needs regarding care of infants with feeding difficulties.
Family barriers regarding care of infants with feeding difficulties.
Healthcare staff perceptions of the NICU feeding practices.
Healthcare staff needs regarding care of infants with feeding difficulties.
Healthcare staff barriers regarding care of infants with feeding difficulties.
Screening and selection of studies
Screening of studies will be conducted through systematic review software Covidence by three authors (WRS, GR and AI). The initial review will consist of title and abstract filtering for relevance to systematic review objective by three authors (WRS, GR and AI). For studies to progress to future screening, they must evaluate the perceptions regarding feeding practices of preterm infants in the NICU in one of our two populations of interest: (1) families and (2) healthcare providers. Studies deemed irrelevant or out of context will be excluded, such as those evaluating children in the paediatric intensive care unit and those evaluating NICU graduates following up in outpatient clinics. The second stage of study selection will include a complete text review of each potential article by three authors (WRS, GR and AI). Conflicts at all stages will be resolved by discussion and contacting a senior author. Additionally, the references of relevant reviews will be evaluated for inclusion in the review. In the case that only an abstract is available for a given study, authors will be contacted to obtain information on and evaluate methods and results. If we are unable to obtain additional information, the abstract will be evaluated exclusively by inclusion criteria. If a paper is published in a language other than English, we will attempt to translate the article for use in this review. If we are unable to translate the article, we will exclude it from this review.
Data extraction
Data extraction will occur independently by three authors (WRS, GR and AI) and subsequent comparison will occur. Conflicts will be resolved through discussion. To standardise data acquisition, a custom data extraction template will be piloted and used in Covidence. Information to be collected from each study will include:
Study design, study duration, study setting, setting country/region, study year and interventions.
Participants
Recruitment methods, including inclusion and exclusion criteria; group differences; sample size; sample size calculation; relevant baseline characteristics (family participants: maternal age, infant gestational age at birth, infant weight at birth, race/ethnicity, etc.; healthcare professional participants: role, experience, race/ethnicity, etc.); intervention groups.
Qualitative: Phenomena of interest (perceptions, experiences, change in satisfaction, change in feeding rate, etc); definitions of phenomena of interest.
Quantitative (if regarding phenomena of interest): variable type (continuous, dichotomous, qualitative); reporting measure (continuous variable: CIs, SD, SE, etc; dichotomous variable: the number of participants, percentage of participants, OR, etc; qualitative); statistical significance of outcome (p value).
Major themes addressed
Stress, anxiety, fear, needs, barriers, satisfaction, etc.
Other relevant constructs
First-order constructs (participant quotes); second-order constructs (author interpretations).
This data extraction protocol is modelled from thematic analysis principles of qualitative evidence synthesis and recommendations by the Cochrane Qualitative and Implementation Methods Group guidance for data extraction and data synthesis. 16 17 After data extraction, these data will be exported to Excel for synthesis and organised by relevant population.
Data synthesis
Data will be synthesised for each relevant population and outcome combination by three authors (WRS, GR and AI). Major themes will be described in a narrative fashion and simple descriptive statistics may be utilised for clarity. In the case of studies having quantitative measures of our qualitative interests, we will report the data as follows: If relevant, dichotomous data will be reported with OR, 95% CIs, and risk ratios, and continuous data will be reported as confidence intervals. Significant construct findings will be reported as quotes, percentages or other descriptive reports. Any inconsistencies or discrepancies between studies will be considered and reported. Data will be reported in narratives and tables for presentation.
Reporting results
Once the study analysis is complete, we will provide a narrative synthesis of all included studies and analysis between comparable studies. We will compare knowledge, beliefs, attitudes and perceptions of families with infants in the NICU within this population as well as compare these findings to the knowledge, beliefs, attitudes and perceptions knowledge of neonatal healthcare professionals. We will include all findings listed in the ‘Phenomena of interest’ section. Reporting of results will be in accordance with PRISMA and Enhancing Transparency in Reporting the synthesis of Qualitative research guidelines. 15 18
Critical appraisal of the studies
To evaluate the quality, reliability and relevance of the included studies, we plan to follow the Critical Appraisal Skills Programme checklist. 19 This tool is often used to appraise qualitative research and is adaptable to emphasise particular areas of interest within our research question. It is recommended by Cochrane and complements the use of the Grading of Recommendations Assessment, Development and Evaluation—Confidence in Evidence from Reviews of Qualitative Research (GRADE-CERQ) approach through evaluating the strengths and weaknesses of each study rather than on the basis of exclusion. This tool will be used by three members of the review team (WRS, GR and AI), and disagreements will be mediated through conversation.
Certainty of review findings
The GRADE-CERQ approach will be used to evaluate the overall certainty of evidence. 20 This approach is a comprehensive framework used to assess the overall certainty of the evidence for an outcome using study characteristics such as study design, inconsistency, indirectness of evidence, risk of bias, publication bias and imprecision estimates. We will include the GRADE-CERQ assessment results in an evidence profile that contains certainty ratings, including very low, low, moderate or high, based on the evidence across studies for primary outcomes. We will follow the GRADE-CERQ guidelines for assessing confidence in our qualitative evidence findings, which are based on four components: methodological limitations, relevance, adequacy and coherence. Based on analysis in each of these categories, the study will be given a score of either strong or weak. Concerns with any of the components may reduce our confidence in a review finding.
Patient and public involvement
Ethics and dissemination.
This is a qualitative systematic review that evaluates data present in the public domain through published studies and does not involve contact with human subjects. As a study of published literature, this study was not subject to formal IRB (Institutional Reviw Board) approval. We anticipate that the systematic review will be complete by fall of 2024 and will be submitted for publication in a peer-reviewed journal.
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
The authors would like to acknowledge Paul Casella for his help in editing the manuscript
- Moller A-B ,
- Bradley E , et al
- Yamasaki JT , et al
- Rolnitsky A ,
- Urbach D , et al
- Victora CG ,
- Walker SP , et al
- Jackson B ,
- Mörelius E ,
- Sahlén Helmer C ,
- Hellgren M , et al
- Zhu X , et al
- Li Y , et al
- Wang S , et al
- Osborn EK ,
- Alshaikh E ,
- Nelin LD , et al
- Gulati IK ,
- Jadcherla S
- McKenzie JE ,
- Bossuyt PM , et al
- Flemming K , et al
- Flemming K ,
- McInnes E , et al
- Glenton C , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors Conceptualisation: WRS, AA, GR and AI; Methodology: WRS, AA, GR, WTS, RS and AI; Writing–original draft preparation: WRS and AI; Writing–review and editing: WRS, AA, GR, WTS, RS and AI. All authors have read and agreed to the published version of the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Is the healthcare provision in the Netherlands compliant with universal health coverage based on the right to health? A narrative literature review
Affiliations.
- 1 National Institute of Public Health and Environment, Antonie van Leeuwenhoeklaan 9, 3721 MA, Bilthoven, The Netherlands. [email protected].
- 2 Department of Public Health, Institute of Tropical Medicine, Nationalestraat 155, 2000, Antwerp, Belgium.
- 3 Department of Health, Ethics, and Society, Maastricht University, Minderbroedersberg 4-6, 6211 LK, Maastricht, The Netherlands.
- PMID: 35366916
- PMCID: PMC8976435
- DOI: 10.1186/s12992-022-00831-7
Universal health coverage, as one of the targets of the Sustainable Development Goals, is the access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost. It is a practical expression of the concern for health equity and the right to health, and a goal for all countries. This review is a novel attempt to explore the healthcare provision in the Netherlands as an expression of universal health coverage based on the right to health.The study adopted a narrative review approach using a framework that consists of 10 universal health coverage indicators which are derived from seven human rights principles. The techno-economic approach to healthcare provision by the Dutch state achieves a healthcare system where most of the population is covered for most of the services for most of the costs. The Dutch state complies with its minimum core obligations, while less attention is paid to participatory decision making and non-discrimination principles. However, with the fiscal sustainability of healthcare provision showing erosion, basing healthcare policy on values based on human rights principles might prevent a regressive policy.
Keywords: Health equity; Health system financing; Right to health; The Netherlands; Universal health coverage.
© 2022. The Author(s).
PubMed Disclaimer
Conflict of interest statement
The authors declare that they have no competing interests.
Similar articles
- The missing link in Kenya's universal health coverage experiment: a preventive and promotive approach to SRHR. Owino L, Wangong'u A, Were N, Maleche A. Owino L, et al. Sex Reprod Health Matters. 2020 Dec;28(2):1851347. doi: 10.1080/26410397.2020.1851347. Sex Reprod Health Matters. 2020. PMID: 33393897 Free PMC article.
- Universal access to essential medicines as part of the right to health: a cross-national comparison of national laws, medicines policies, and health system indicators. Perehudoff K. Perehudoff K. Glob Health Action. 2020 Dec 31;13(1):1699342. doi: 10.1080/16549716.2019.1699342. Glob Health Action. 2020. PMID: 33131456 Free PMC article.
- Universal health coverage and key populations. Macdonald V, Verster A, Seale A, Baggaley R, Ball A. Macdonald V, et al. Curr Opin HIV AIDS. 2019 Sep;14(5):433-438. doi: 10.1097/COH.0000000000000570. Curr Opin HIV AIDS. 2019. PMID: 31241544 Review.
- Universal Health Coverage and Essential Packages of Care. Watkins DA, Jamison DT, Mills T., Atun T., Danforth K, Glassman A, Horton S, Jha P, Kruk ME, Norheim OF, Qi J, Soucat A, Verguet S, Wilson D, Alwan A. Watkins DA, et al. In: Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, Nugent R, editors. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017 Nov 27. Chapter 3. In: Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN, Nugent R, editors. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017 Nov 27. Chapter 3. PMID: 30212154 Free Books & Documents. Review.
- The role of insurance in the achievement of universal coverage within a developing country context: South Africa as a case study. van den Heever AM. van den Heever AM. BMC Public Health. 2012;12 Suppl 1(Suppl 1):S5. doi: 10.1186/1471-2458-12-S1-S5. Epub 2012 Jun 22. BMC Public Health. 2012. PMID: 22992410 Free PMC article.
- Cost-effectiveness analysis of antibiotic prophylaxis versus no antibiotic prophylaxis for acute cholecystectomy. Satheeskaran M, Hussan A, Anto A, de Preux L. Satheeskaran M, et al. BMJ Open Gastroenterol. 2023 Aug;10(1):e001162. doi: 10.1136/bmjgast-2023-001162. BMJ Open Gastroenterol. 2023. PMID: 37562856 Free PMC article. Clinical Trial.
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. - DOI - PubMed
- UHC2030. State of commitment to universal health coverage: synthesis, 2020. 2020 p. 1–69. Available from: https://www.uhc2030.org/what-we-do/voices/accountability/the-state-of-uh...
- United Nations. World Social Report 2020: Inequality in a rapidly changing world [Internet]. 2020 p. 1–216. (World Social Report). Report No.: 978–92–1–130392–6. Available from: https://www.un-ilibrary.org/content/books/9789210043670
- Gostin LO. Public Health, Ethics, and Human Rights: A Tribute to the Late Jonathan Mann. J Law Medicine Ethics. 2001;29(2):121–130. doi: 10.1111/j.1748-720X.2001.tb00330.x. - DOI - PubMed
- London L. What Is a Human-Rights Based Approach to Health and Does It Matter? Health Hum Rights. 2008;10(1):65. doi: 10.2307/20460088. - DOI - PubMed
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Universal healthcare coverage, patients' rights, and nurse-patient communication: a critical review of the evidence
Abukari kwame.
1 College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Pammla M. Petrucka
2 College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Associated Data
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
The Sustainable Development Goals adopted by world leaders on September 25, 2015, aimed to end poverty and hunger, promote gender equity, empower women and girls, and ensure human dignity and equality by all human beings in a healthy environment. These development goals were premised on international human rights norms and institutions, thereby acknowledging the relevance of human rights in achieving each goal. Particularly, sustainable development goal 3, whose objective is to achieve universal health coverage, enhance healthy lives, and promote well-being for all, implicitly recognizes the right to health as crucial. Our focus in this paper is to discuss how promoting patients’ rights and enhancing effective nurse-patient communication in the healthcare setting is a significant and necessary way to achieve universal health coverage. Through a critical review of the empirical research evidence, we demonstrated that enhancing patients’ rights and effect nurse-patient communication will promote people-centered care, improve patients’ satisfaction of care outcomes, increase utilization of care services, and empower individuals and families to self-advocate for their health. These steps directly impact primary healthcare strategies and the social determinants of health as core components to achieving universal health coverage. We argue that without paying attention to the human rights dimensions or employing human rights strategies, implementing the other efforts will be inadequate and unsustainable in protecting the poorest and most vulnerable populations in the achievement of goal 3.
On September 25, 2015, world leaders at the United Nations (UN) General Assembly adopted a set of 17 sustainable development goals (SDGs) and 69 targets in an agenda titled Transforming our World: The 2030 Agenda for Sustainable Development, in which global leaders pledged to take bold and transformative steps to free the world and all people from poverty and hunger, to promote gender equity and empower women and girls, and to ensure that human dignity and equality are enjoyed by all human beings in a healthy environment [ 1 ]. These far-reaching, people-centered, and transformative sets of goals and targets focused on ensuring that “no one is left behind” as the world forges ahead to achieve economic, social, and environmental sustainability in its development programs, practices, and policies by 2030.
Recognizing the values of human dignity and equality and the impact development programs, practices, and policies have on these values, the SDGs were anchored on international human rights law, norms, and provisions, as emphasized in the Preamble, the Declaration, and other sections of the agenda document. In particular, the significance of health as a human right and the need for universal access to health by all was captured in SDG3, whose focus is to "ensure healthy lives and promote well-being for all, at all ages." [ 1 , p. 14] Yet, despite recognizing the right to health in SDG3 and the significance of implementing the SGDs with attention to human rights principles as emphasized in the SDGs Agenda, the right to health is only implicitly referenced in targets 3.7 and 3.8 of SDG3.
Without much attention to human rights and the right to health principles in the universal health coverage (UHC) discourse or strategies to implement the targets, the approaches outlined in SDG3 will be inadequate to protect the poorest and most vulnerable populations in the achievement of SDG3 [ 2 , 3 ]. Implementing UHC ensures that all people can obtain the health services they desire without suffering significant financial hardship when accessing those services [ 4 ]. For UHC to thrive, there must be equity in access to care services so that all those who need these services can get them. In addition, care services must be of high quality to improve the health of the people receiving them, and accessing the services must guarantee financial-risk protection such that the cost of using the service does not put undue financial stress on the users [ 4 , 5 ].
Moreover, as a right to health issue, UHC recognizes the importance of the social determinants of health (SDH), the role of primary healthcare, and the impact of both internal and external healthcare institutional factors [ 5 – 8 ]. Furthermore, healthcare issues, such as coverage vs. access, access vs. quality, and care itself, are significant in the UHC discourses. These issues need to be critically examined, as Fried et al. [ 5 ] argued that access to healthcare services does not often guarantee quality services or satisfaction of care outcomes. We explore the question: How does a consideration of patient rights and the right to health contribute to achieving SDG3 and the global discourse of universal health coverage? Thus, we aim to present and discuss the UHC of SDG3 from a rights-based approach. Further, we will examine how effective nurse-patient communication and respect for patients' rights are crucial to achieving UHC; hence, emphasizing the right to health and patients' rights in the UHC discourse is desired now than ever. To achieve this paper's objectives, we will first discuss UHC as a human rights issue. Next, we examine the right to health and patients' rights, effective nurse-patient communication, and patient-centered care as crucial to achieving UHC. We then present a position statement for consideration in health policy, decision-making, and practice before concluding the paper.
Critical review methodology was adopted in this paper. Grant and Booth [ 9 ] argued that a critical literature review explores and evaluates the diverse body of previous research to take stock of what is significant which may result in a model or hypothesis building. Also, Pare´ et al. [ 10 ] argued that one strength of critical reviews is their ability to highlight problems and gaps in research about a topic with the aim of strengthening knowledge development by giving a focus and direction for studies or to improve practice. Scholars have noted that despite the relevance of critical reviews, it has “no formal requirement to present methods of the search, synthesis, and analysis explicitly” as done in systematic reviews, and that “the interpretative elements are necessarily subjective and the resulting product is the starting point for further evaluation” [ 9 , p. 97; 10 ]. Thus, we adopted a critical stance in this paper by engaging with the literature to argue that achieving universal healthcare access by 2030 depends on taking note of the issues we discuss into consideration in nursing care practices, health policy, education, and management.
Despite the limitations of a critical review methodology, some scientific literature review principles were implemented in this study. The paper originated from the first author’s doctoral comprehensive exams organized in February 2021. Included articles were recommended by four expert interdisciplinary doctoral committee members including the second author. Each committee member was asked to recommend at least ten relevant articles on the topic. The objective of the written exam was to discuss the relevance of patient rights and the right to health in advancing the global discourse on universal healthcare coverage (UHC) as crucial to achieving the health sustainable development goal. Recommendations were made by the committee members after a follow-up oral exam. The first author then conducted a further literature search using keywords such as patient rights, the right to health, universal healthcare coverage, SDG3, patient-centered care, patient-centered communication, and nurse-patient communication . CINAHL, PubMed, Medline, and Google Scholar databases were searched.
The aim of conducting a further literature search was to broaden the discussion to include the significance of patient-centered care practices in achieving universal healthcare access. All included studies in this critical review were empirical research that investigated the healthcare issues around the keyword in different care settings published in English and open access. All relevant articles were read, and findings relevant to our review question were identified, organized, and discussed in this paper.
Universal health coverage as a human rights issue
The right to health and respect for patient rights in healthcare practices are crucial to achieving health for all and universal healthcare access. Particularly, human rights principles of equity, respect for human dignity, non-discrimination, participation, and transparency in healthcare practice and management, health policy design, and implementation are significant to ensuring health for all by 2030 [ 11 ]. Human rights and the right to health are advocated for in many international human rights documents. For instance, Article 25(1) of the 1948 United Nations (UN) Universal Declaration of Human Rights (UDHR) and Articles 2.2 and 12 of the 1966 International Covenant on Economic, Social, and Cultural Rights (ICESCR) have all underscored health as a human right [ 11 , 12 ].
Furthermore, in nursing care, the revised Code of Ethics for Nurses observes that "inherent in nursing is a respect for human rights, including cultural rights, the right to life and choice, to dignity and to be treated with respect" [ 13 , p. 2]. It further states that the enjoyment of these rights must not be restricted by a person's "age, colour, creed, culture, disability or illness, gender, sexual orientation, nationality, political [affiliation], race or social status" [ 13 , p. 2]. And the significance of human rights in achieving UHC is further emphasized; “nurses value health care as a human right, affirming the right to universal access to health care for all” [ 13 , p. 18]. This assertion acknowledges the interrelatedness of health, human rights, and other socio-cultural dimensions of being human.
As noted earlier, furthering an SDH approach in UHC implementation will require examining the impact of culture and contextual factors on access to health and healthcare service utilization. In particular, care providers' respect for cultural diversity in care and displaying cultural competency and sensitivity to care can promote access [ 12 , 13 ]. Therefore, UHC as a human rights issue is essential, which we addressed further in the next section, under the right to health and patients' rights in the context of health for all by 2030.
Universal health coverage, the right to health, and patients' rights
The right to health is a global concern espoused in several international human rights norms, laws, protocols, and instruments, as indicated in the previous section. The right to health constitutes freedoms and entitlements and recognizes the impact of socio-cultural factors on health. Nonetheless, the right to health does not mean the right to be healthy, given that individual biological and socio-economic conditions differ [ 12 ]. The right to health is an inclusive right and privileges non-discrimination and human dignifying practices in healthcare access. It upholds crucial human rights principles, including respect for human dignity, informed consent, self-determination, and participation in healthcare decision-making [ 12 – 14 ]. For instance, General Comment No. 14 enjoins on State parties the responsibility of making healthcare facilities, services, and personnel available and accessible (easy to reach, affordable, informative). Care services must be acceptable (respectful of medical ethics and culturally appropriate) and of high-quality regarding the services provided, staff, medicines, and facilities/equipment [ 14 ].
Furthermore, patients' rights are human rights principles emanate from healthcare practices and interactions among care providers, patients, and caregivers. In the European Declaration on the Rights of Patients , patients' rights are defined as fundamental human rights in health care, aiming to protect patients' dignity and integrity and respect for the patient as a person [ 15 ]. Therefore, the right to health and patients' rights are collectively termed 'human rights in patient care' which outlines the core principles of respect for patients' dignity, privacy, informed consent, and self-determination as critical human rights that must be maintained in healthcare practices and interactions [ 13 , 16 ]. Per these rights, patients and their caregivers must be fully involved in their care needs, as the ICN Code of Ethics for Nurses [ 13 ] obligates care providers to provide care services that are person-centered, and respect and value patients' cultural and social characteristics and preferences. Thus, patients and their families must be treated uniquely based on their care needs and circumstances.
For instance, historical antecedents in health research, biomedical experiments, and healthcare practices have shown that communities and specific cultural groups were unethically treated. Moreover, happenings in many modern healthcare institutions are replete with abusive and discriminatory care practices, as cited studies in this and the subsequent sections will show. Hence, the right to health and patients' rights have become critical human rights issues in several countries. National patients' rights charter, service pledges, codes of ethics, and standards of practices for various healthcare professional groups are being developed to safeguard patients' rights. Examples of these documents include the Helsinki Declaration for medical research [ 17 ], the ICN Code of Ethics for Nurses , [ 13 ] the International Code of Ethics for Midwives , [ 18 ] and national patients' charters such as the Patients' Charter of Ghana , [ 19 ] the Charter of Patients' Rights in Egypt , [ 20 ] and patient charters of several other countries [ 21 ].
These national patients' rights charters have stipulated specific rights and responsibilities of patients that healthcare professionals must uphold and preserve in their care practices and the care process.
Patients' rights are essentially part of the right to health, which, when respected and upheld, can significantly contribute to UHC achievement. First, UHC advocates making healthcare accessible and affordable for all, however, healthcare practices that do not respect patients' rights could lead to inadequate care outcomes and care satisfaction [ 22 ]. Moreover, substandard and undignifying patient-provider interactions could prevent future access and utilization of healthcare services and facilities, despite these being available, as observed by Ojwang [ 23 ] and Ojwang et al. [ 24 ] in studies on patients' rights in Kenyan hospitals. These studies found that, although some patients were treated with dignity and respect, many others were often ignored, discriminated against, intimidated, grouped, and labeled based on their social status. Ojwang et al. [ 24 ] argued that these acts by nurses threatened patients' rights to dignity and humanness and often led to patients complaining, criticizing, protesting, and accusing nurses, as ways to assert their rights. These incidents can affect care quality and uptake, especially among vulnerable patients.
The value of patients' rights and effective patient-provider communication and interaction is crucial to achieving UHC. Following this argument, the critical questions to ask are how can effective nurse-patient communication and patient-centered care practices contribute to UHC? How can a study on nurse-patient communication and patients' rights contribute to the UHC discourse's advancement?
Universal healthcare coverage, healthcare systems, and patients' rights
We acknowledge that advocating a human-rights-based approach to UHC would have implications for healthcare policy implementation and care practices. First, achieving UHC means making healthcare services in all healthcare systems, including traditional medical systems (traditional complementary and alternative medical systems), available, accessible, affordable, and high quality. The traditional medical systems provide healthcare to over 60% of global populations in developing and developed countries. Hence, nation-states and their governments will need to embrace integrative healthcare systems and incorporate traditional medical systems practices and services into their national healthcare policies, planning, financing, and monitoring/evaluation practices [ 25 ]. The WHO has noticed that existing barriers, such as geographical and institutional barriers, “the predominance of curative, hospital-based, and disease-based healthcare services” are responsible for poor access to care services over the years [ 26 , p. 35]. Other studies have shown that differences in belief systems about health, illness, and healing between western biomedical and traditional indigenous practitioners constitute a significant barrier to medical system integrations [ 26 , 27 ].
Another critical factor is that funding for traditional medicine and services is low as governments and their health ministries have challenges budgeting and planning for health services provided by traditional healers [ 26 ]. For instance, Carrie et al. observed that “although the overall cost of delivering traditional medicines may be lower than the price of modern medicine, lack of sufficient funding and coverage to enable access may limit the use of traditional medicine in communities” [ 27 , p. 5]. Despite the challenges in achieving integrative healthcare systems, the WHO [ 25 ] argues that accessing qualified traditional and complementary medicine is a positive way to achieve universal health coverage.
Besides, issues of patients' rights, cultural sensitivity, and humility will need a holistic examination within different healthcare systems and practices to avoid the marginalization of specific cultural groups. Some societies, cultural groups, and vulnerable populations have had historical experiences of trauma, injustice, and discrimination with their national healthcare systems and healthcare providers. As a result, many of these cultural groups and populations have distrusted their national healthcare systems and care professionals. Hence, to achieve UHC, the historical experiences, unique circumstances, and medical worldviews of these cultural groups and societies must be considered when designing healthcare policies and practice guidelines to achieve health for all, a position taken strongly by the revised ICN Code of Ethics for Nurses [ 13 ].
Furthermore, the interpretation and application of patient rights principles in particular cultural contexts, medical systems, and healthcare practices (e.g., spiritual healing) may require critical lenses. Many patients' rights principles appear to honour individuality and individual autonomy. However, healthcare decision-making in many cultural contexts is a collective process, sometimes without engaging the patient. Care providers working with an individualistic understanding of human rights and patient rights (influenced mainly by Western ideals) will have to widen their knowledge of human and patient rights to embrace individual rights within collective values. Thus, the compatibility of cultural values, beliefs, and perspectives with Western notions of human rights and patient rights may need a rethink. Healthcare policymakers and care professionals need to reflect on the challenges in implementing UHC policies when collective values and norms overshadow individual rights in positive ways.
UHC, effective nurse-patient communication, and patient-centered care practices
Patient-centered care (PCC) is an approach to care and interpersonal interaction between care providers and patients during care. It embodies providing care services that respect and respond to patients' unique care needs and preferences [ 27 ]. In PCC, patients' experiences, stories, and knowledge must be valued and considered, and patients must engage in the care process as collaborators [ 27 , 28 ]. The first element of the ICN Code of Ethics for nurses––nurses and people––emphasized PCC in nursing care [ 13 ]. It focuses on nurses' interactions with people who access care in the healthcare setting and requires that nurses promote a conducive environment in which the human rights, values, customs, and spiritual beliefs of individuals, families, and communities are respected [ 13 , 29 , 30 ].
The nurse-patient dyad is crucial because nurses constitute a strong healthcare workforce and have more contact hours with patients [ 13 ]. They carry out various care functions, including recording patients' history and vital statistics, caring for patients' hygiene needs (e.g., bathing/washing and dressing patients), and maintaining ward hygiene [ 31 ]. Also, nurses perform some health administrative functions, such as logging cases, and completing forms for patient transfer or health insurance coverage [ 31 , 32 ].
As nurses continue to engage in medical teams and assume new roles with increasing expertise, their social positions and power dynamics also continue to evolve in the clinical space [ 33 , 34 ]. This emerging reality makes the social relationship between nurses and patients very complex across different care settings [ 33 ]. Due to patients’ varying healthcare needs, their dependence on health professionals for care and support, and the knowledge position nurses occupy, there can be a power imbalance in clinical interactions, mostly in favour of nurses. For instance, in a case study on patient involvement in routine palliative clinical care situations, Glasdam et al. [ 34 ] observed that nurses did not readily take up patients’ invitation to dialogue or the knowledge they provide about their body state. The authors argued that the “distribution of power and knowledge between patients and nurses condition nurses to set the agenda and assess when and at what level it is relevant to take up patients’ invitations to involve them in their own case” [ 35 , p. 1618]. According to Glasdam et al., “nurses have the power to define when and how the involvement of patients is going to happen in clinical routine care situations in nursing practice.” [35, p. 1624] Despite the findings by these scholars, we think that different care situations, patients’ contextual variables/backgrounds, and knowledge state could influence the power dimensions in nurse-patient clinical interactions. For details on power dynamics in nurse-patient interactions, see Glasdam et al. [ 34 ] and Mattar e Silva et al. [ 35 ] on physician-nurse power relationships.
Moreover, traditionally paternalizing perceptions about patients as passive participants in care routines are changing as patient empowerment principles are advocated in healthcare ethics and practice [ 36 ]. For instance, Delaney [ 36 ] noted that healthcare organizations and professionals have become more receptive to patient engagement in Australia with the knowledge that patient involvement in their care can enhance safety and care quality. Moreover, the ICN [ 37 ], in its position statement on informed patients, expects nurses, patients, and the public to get involved in research that explores the nature and quality of patient information and how it affects health outcomes and nursing care. Thus, nurses have responsibilities of respecting patients' unique values, needs, beliefs, and rights; disseminating appropriate information for effective decision-making; protecting patients' and caregivers' confidentiality. In addition, nurses must demonstrate professionalism, including "respectfulness, responsiveness, compassion, trustworthiness, and integrity" while providing care, as emphasized in empirical studies and the ICN code of ethics [ 13 , p. 2; 38 ]. The dynamism in nurse-patient communication and interaction makes it an imperative and fruitful ground for engaging in discourses of UHC and patients' rights.
Another essential issue in patient-provider interactions that borders on patient rights is patient autonomy in clinical interactions. As a reviewer rightly observed, patients’ expectation of their degree of autonomy could be compromised when traditional models of bioethics that socialize and position the patient as a passive participant in medical interactions are invoked. Hence, to encourage patient freedom in care, the ICN [ 39 ] position statement on nurses and human rights obligates nurses, and by extension, other care providers, to respect patients’ health rights at all times and in all places, including how they express their care needs, worries, and wishes. Nonetheless, several factors can affect patients' expectation of autonomy, including their health status, socio-cultural backgrounds, knowledge of their illness, and previous experiences with healthcare institutions and care providers. Furthermore, notions of “good and bad patient,” as observed by Campbell et al. [ 40 ], can influence patients’ expectations of their autonomy in clinical interactions.
Generally, however, studies have shown that when care is patient-centered and human dignity preserving, patient disclosure increases, length of stay in hospitals reduces, and patients become empowered to take care of their health [ 24 , 38 ]. Moreover, PCC fosters patients' and caregivers' active participation in healthcare decision-making to improve care quality, [ 41 ] an essential UHC component. PCC, as a patients' rights practice in care, reduces negative attitudes and personal behaviours from both care providers and patients, thereby reducing conflicts, discrimination, abuse, and disrespect, and increases the uptake of care services and positive nurse-patient relationships [ 32 , 42 ].
Communication in nurse-patient clinical interactions is effective if patients are (i) provided the needed information about their health conditions, (ii) engaged in the care processes as significant dialogic partners, (iii) listened to, or given the option to choose from alternative care plans and procedures [ 38 , 41 ]. Effective nurse-patient communication is therapeutic and forms an essential component of PCC. Therefore, the ICN position statement on cultural and linguistic competence recommends that nurses must communicate verbally and in writing in ways sensitive to patients' needs and in a language that patients can understand, if possible, through the use of trained interpreters and translators [ 43 ]. Moreover, effective communication in the nurse-patient dyad can reduce misunderstandings between care providers and patients. For instance, Crawford et al. [ 44 ] maintain that providing equitable and quality health care is compromised when communication difficulties are present, even when healthcare is accessible.
Care and clinical communication become patient-centered when nurses value patients' beliefs, respect patients' cultural backgrounds, and provide care according to patients' needs, preferences, and unique conditions [ 13 ]. It also entails communicating in ways that engage patients and their caretakers and actively listening to patients' concerns [ 13 , 37 , 39 ]. Patient-centered care practices will curtail patient stigmatization and discrimination, especially against people living with HIV/AIDS, mental health illnesses, and the poor, illiterate, and vulnerable patients [ 22 , 32 ]. Besides, effective nurse-patient communication can increase access to healthcare, patient disclosure, patients' participation in healthcare decision making, positive satisfaction of care outcomes, and accurate healthcare data, essential in promoting UHC [ 32 ].
A Note for consideration in health policy and decision-making
Universal health coverage and providing health for all have been a global agenda for decades and captured as the right to health in most international human rights norms and instruments, as highlighted in this paper. However, improving access to healthcare and ensuring better health for the world's poor, marginalized, and vulnerable populations (e.g., women, children, the elderly, people with disabilities, and Indigenous peoples) has never been vigorously pursued than in the twenty-first century. Starting from early 2000, world leaders at the United Nations agreed to eight development goals achievable within the next 15 years, as the 2015 UN Millennium Development Goals (MDGs). Three of these goals: MDG4 (reduce child mortality), MDG5 (reduce maternal mortality), and MDG6 (Combat HIV/AIDS, malaria, and other diseases), were primarily targeted at health and improving healthcare access to the most vulnerable global populations. Significant gains were made in these goals despite several different challenges. For example, governments were not strictly required to provide disaggregated data in monitoring and reporting the MDGs. Instead, they focused on achieving quantified targets without much emphasis on quality, and attention to human rights-based targets in the MDGs was lacking (see [ 2 ] for other critiques).
Following the MDGs' challenges, a more progressive, people-centered, and interdependent set of development goals was adopted again in September 2015, as Sustainable Development Goals (SDGs), achievable by 2030. An overarching health goal, the SDG3, has broader targets and indicators than were found in the health MDGs. Although achieving this particular goal and the rest require financial, logistics, and other resources, emphasizing the human rights dimensions and principles in their implementation process is paramount. Without this focus, the SDGs would likely suffer the same faith as the MDGs. Hence, in this section, critical recommendations are outlined for consideration of health policy and decision-making regarding taking a human rights and patients' rights approach to the UHC/SDG3.
First, awareness of patients' rights must be a critical healthcare decision priority in many countries through public health campaigns. Healthcare advocacy campaigns within healthcare institutions must include information on patients' rights and responsibilities. As a significant sector of the health workforce, nurses should verbally inform, explain to, and educate patients with poor health literacy about patient rights. When patients' rights to dignity, informed consent, participation, among others, are preserved during clinical interactions, abuse and discrimination are reduced, and patient disclosure and uptake of healthcare services increase, [ 36 , 37 , 45 ]. Without much attention to this quality aspect of care, access to available healthcare services will be affected. Many women often refuse facility-based delivery or accessing maternity care in hospitals due to abuse, discrimination, and disrespect. Instead, they prefer home delivery attended by traditional birth attendants [ 22 , 42 , 46 ]. Also, abuse of patients' rights and lack of privacy, confidentiality, and respect, coupled with other ethical dilemmas in HIV/AIDs care settings, affected the uptake of HIV/AIDS care services among this patient population [ 47 ].
Secondly, patients' rights regulatory schemes must be instituted in healthcare institutions to enforce patient rights charter regulations and the implementation of nursing ethical codes and standards of practice, and to promote equity and environmental justice when accessing healthcare, as emphasized in the ICN [ 13 , 39 ]. That is, upholding healthcare ethical standards and patients' rights in healthcare practices will significantly reduce abuse, discrimination, marginalization, and improve care outcomes [ 48 ].
Advocating and advancing patients’ rights in nursing practice and care must begin from healthcare educational institutions. Nursing educators must incorporate effective nurse-patient communication and patients' rights models as core components of nursing curricula for knowledge acquisition [ 13 ]. Thus, effective nurse-patient communication is crucial to promoting patient-centered care and patient rights in clinical interactions.
Also, healthcare managers can elevate patient rights responsibilities among care professionals by providing regular in-service training on approaches to preserve patients' rights and implement effective communication in practice [ 28 , 37 , 48 – 50 ]. These in-service training will bolster care professionals' quality, which is critical to achieving UHC [ 8 ] and a right to health obligation healthcare institutions must fulfil [ 12 , 14 , 39 ]. Nursing managers should continue to improve nurses' expertise, skills, cultural competence, and quality of care [ 13 , 32 , 51 ]. The active engagement of care managers in the nurse-patient dyad through monitoring and evaluation practices will further support better nurse-patient relationships, patient-centered care practices, and address nurses' personal and professional challenges [ 36 , 52 ]. For instance, Delaney [ 36 ] argues that traditional healthcare management styles focused on illness, intervention, and medication have limitations on optimizing health. Adjusting and aligning clinical care management that honour patients' needs and input have positive outcomes. Moreover, adopting transformational leadership, collaborative and innovative practices can support patients’ participation in, understanding of, and recovery from ill-health. The 21 st -century nurse faces many demands and challenges, including increasing patient needs, high patient turnout, added administrative duties (e.g., filling diverse forms), and limited time to interact with patients. As a result, there should be an ongoing dialogue between management level officers on how to support healthcare staff to provide quality and patient-centered care that is ethical and patients' dignity preserving.
Advocating for UHC is crucial and forms one route to healthcare access. Yet, improving care quality and patient satisfaction constitutes another significant matter that needs attention. Broadening UHC implementation processes to include discourses on effective nurse-patient communication, respecting patients' rights, and promoting the right to health is essential to achieving ‘Health for All’ by 2030. Shifting healthcare policy, education, decision-making, and practice to embody the socio-biology and social determinants of health approaches is a priority. The impact of culture and other contextual factors on healthcare access are significant and deserving in UHC discourse.
Healthcare institutional internal structures, hierarchies, and practices that hamper good nurse-patient communication and patients' rights need critical examination. Nurses and nursing managers have active roles to ensure that care is patient-centered and based on human rights, patients' rights, and the right to health principles. Without incorporating a human rights lens and approaches to the implementations of the SDG3, the targets and indicators may be inadequate to protect the poor and vulnerable populations in the global effort to achieve UHC access by 2030.
A limitation of this study, which generally applies to critical reviews is its methodology, which puts less emphasis on literature search and analysis criteria. Thus, the outcome of such a review might be interpreted by some scholars as less scientific. Nonetheless, our critical engagement with the literature and the recommendations made by the expert doctoral committee on both the included studies and an earlier version of the paper will overcome this limitation.
Acknowledgements
An earlier version of this study was submitted as part of author AK's written Ph.D. Comprehensive Exam, which AK's Ph.D. committee reviewed. We express our gratitude to the committee members for their valuable comments, suggestions, and critique.
Abbreviations
| AIDS | Acquire Immune Deficiency Syndrome |
| CESCR | Committee on Economic, Social, and Cultural Rights |
| HIV | Human Immunodeficiency Virus |
| ICESCR | International Covenant on Economic, Social and Cultural Rights |
| ICN | International Council of Nurses |
| MDG(s) | Millennium Development Goal(s) |
| NCD | Non-communicable diseases |
| PCC | Patient-centered care |
| PHC | Primary health care |
| SDGs | Sustainable Development Goals |
| SDG3 | Sustainable Development Goal 3 |
| SDH | Social determinants of health |
| TB | Tuberculosis |
| UDHR | Universal Declaration of Human Rights |
| UHC | Universal health coverage |
| UNICEF | United Nations International Children Emergency Fund |
| WHO | World Health Organization |
Authors’ contributions
PMP conceived the topic and recommended some relevant articles. AK conducted the literature search, read all the articles, and drafted the manuscript. PMP revised and reviewed the manuscript for intellectual content. Both authors read and approved the submitted version of the manuscript.
Authors’ information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan. Kwame holds a BA in Geography and Linguistics from the University of Ghana and two Master of Philosophy degrees in Indigenous Studies and English Linguistics from UiT, The Arctic University of Norway, Tromso. Kwame's research interests include patients’ rights in nurse-patient clinical communication, language use in social interaction, health communication, medical anthropology, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is Interim Associate Dean, Research & Graduate Studies, and professor in Nursing at the College of Nursing, University of Saskatchewan. She has extensive experience in qualitative and indigenous research methodologies and has published extensively in nursing. Pammla's research areas include child and maternal health, Indigenous peoples' health, global health, and vulnerable populations. Also, she is a co-editor of the BMC Nursing journal and a reviewer for many academic journals.
The authors have no financial obligations to declare.
Availability of data and materials
Declarations.
Not applicable.
The authors declare that there are no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
Literature showed that modern healthcare access and coverage were in extension stages during the PHC era flagshipped with "health for all (HFA)", prolifically achieving vaccination, communicable disease control, and the use of modern contraceptive methods. ... Historical review; Universal health coverage, health, healthcare access, equity ...
INTRODUCTION. In recent years, there has been an increased push for universal health coverage (UHC) at the global level. UHC is defined by the World Health Organization (WHO) as "ensuring that all people obtain the health services they need, of good quality, without suffering financial hardship when paying for them" [].This concept was initially created in 1883 after Germany introduced ...
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries.
Universal health coverage (UHC) has been acknowledged as a priority goal of every health system [1-5].The importance of this goal is reflected in the consistent calls by the World Health Organization (WHO) for its member states to implement pooled prepaid health care financing systems that promote access to quality health care and provide households with the needed protection from the ...
Discussion: The literature presents UHC as a multi-dimensional concept, operationalized in terms of universal population coverage, universal financial protection, and universal access to quality health care, anchored on the basis of health care as an international legal obligation grounded in international human rights laws. As a legal concept ...
Abstract. Introduction: Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries.
Article PDF Available Literature Review. Universal healthcare coverage, patients' rights, and nurse-patient communication: a critical review of the evidence. March 2022; BMC Nursing 21(54)
According to our literature review, we identified 15 articles that discussed the role of universal health coverage (UHC) on countries' health system performance in times of public health crises, none of which provided quantitative evidence to substantiate UHC's potential role in building health system resilience against external shocks like ...
Conclusions: This study provides a straightforward summary of previous studies that explored the challenges related to UHC and. conducted an in-depth analysis of viable solutions. Key words ...
Background: Resilient health system (RHS) is crucial to achieving universal health coverage (UHC) and health security. However, little is known about strategies towards RHS to improve UHC and health security. This systematic review aims to synthesise the literature to understand approaches to build RHS toward UHC and health security.
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries. The primary objective of this scoping review was to summarize the existing ...
The UN has declared universal health coverage an urgent global goal. Efforts to achieve this goal have been supported by rigorous research on the scientific, technical, and administrative aspects of health systems design. Yet a substantial portion of the world's population does not have access to essential health services. There is growing recognition that achieving universal health coverage ...
A scoping review of the studies on UHC and its dimensions is crucial to map and characterize the existing studies towards UHC. This will help to identify key concepts, gaps in the research, and types and sources of evidence to inform practice, policymaking, and research [ 11 ]. The goals of this scoping review towards universality of UHC were ...
Introduction. Universal health coverage… is intrinsically political and cannot be achieved without recognition of its dependence on, and consequences for, both governance and politics (Greer and Méndez, 2015).. As Greer and Méndez (2015) suggest, even in contexts where universal health coverage (UHC) is being proposed for implementation, it will remain contested—policy advocates cannot ...
Universal health coverage, as one of the targets of the Sustainable Development Goals, is the access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost. It is a practical expression of the concern for health equity and the right to health, and a goal for all countries. This review is a novel attempt to explore the healthcare provision ...
three prominent universal healthcare systems: the Canadian Healthcare System, the United Kingdom's National Health Service (NHS), and Sweden's healthcare model. These case studies provide tangible illustrations of the economic principles and outcomes associated with universal healthcare. 2. Literature Review 2.1 The Concept of Universal Healthcare
The attainment of the noble objective of Universal Health Coverage (UHC)- 'leaving no one behind' necessitates sufficient financial resources, an ample supply of skilled healthcare professionals, and the availability of essential services as part of a basic package This paper presents an analysis of the health system, health seeking behaviours and health service utilization en route to UHC ...
Background The progress of Universal health coverage (UHC) is measured using tracer indicators of key interventions, which have been implemented in healthcare system. UHC is about population, comprehensive health services and financial coverage for equitable quality services and health outcome. There is dearth of evidence about the extent of the universality of UHC in terms of types of health ...
UNIVERSAL HEALTH INSURANCE ACCESS EFFORTS IN MA: A Literature Review 1 Health Resources in Action II. Introduction The federal Patient Protection and Affordable Care Act (ACA) — passed in 2010 — was largely modeled after the Massachusetts (MA) 2006 Health Care Reform effort (Chapter 58). Given the strong parallels between the Affordable
Background: The Universal Health Coverage (UHC) is a very important and effective policy in the health system of countries worldwide.Using the experiences and learning from the best practices of successful countries in the UHC can be very helpful. Therefore, the aim of the present study is to provide a scoping review of successful global interventions and practices in achieving UHC.
Given the inconsistencies in the provision of psychological interventions identified in the literature and through reports, this report aimed to (1) review existing recommendations on psychosocial interventions to address UASC mental health needs, (2) examine the current mental health provision within health and social care in England from service providers' perspectives, and (3) synthesise ...
Our focus in this paper is to discuss how promoting patients' rights and enhancing effective nurse-patient communication in the healthcare setting is a significant and necessary way to achieve universal health coverage. Through a critical review of the empirical research evidence, we demonstrated that enhancing patients' rights and effect nurse ...
The Universal Health and Preparedness Review (UHPR) was proposed to increase accountability and transparency among Member States in gap identification and capacity building for better health emergency preparedness. The peer-review nature of the envisioned UHPR ensures that key issues identified will be acted upon at the highest political levels ...
Internet usage has seen a stark global rise over the last few decades, particularly among adolescents and young people, who have also been diagnosed increasingly with internet addiction (IA). IA impacts several neural networks that influence an adolescent's behaviour and development. This article issued a literature review on the resting-state and task-based functional magnetic resonance ...
Discussion. The literature presents UHC as a multi-dimensional concept, operationalized in terms of universal population coverage, universal financial protection, and universal access to quality health care, anchored on the basis of health care as an international legal obligation grounded in international human rights laws.
Methods and analysis A literature search will be conducted in multiple electronic databases from their inception, including PubMed, CINHAL, Embase, the Cochrane Central Register for Controlled Trials and PsycINFO. No restrictions will be applied based on language or data of publication. Two authors will screen the titles and abstracts and then review the full text for the studies' inclusion ...
This review is a novel attempt to explore the healthcare provision in the Netherlands as an expression of universal health coverage based on the right to health.The study adopted a narrative review approach using a framework that consists of 10 universal health coverage indicators which are derived from seven human rights principles.
A systematic literature review requires a rigorous and structured qualitative research approach that results in reliable and validated conclusions, giving credence and explanatory power to the findings (Alexander, 2020; Aveyard, 2018; Littell et al., 2008). The transdisciplinary focus of our review study addresses the benefits and opportunities ...
Despite the limitations of a critical review methodology, some scientific literature review principles were implemented in this study. The paper originated from the first author's doctoral comprehensive exams organized in February 2021. ... affirming the right to universal access to health care for all" [13, p. 18]. This assertion ...