- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Effectiveness of...
Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials
- Related content
- Peer review
- Claire D Madigan , senior research associate 1 ,
- Henrietta E Graham , doctoral candidate 1 ,
- Elizabeth Sturgiss , NHMRC investigator 2 ,
- Victoria E Kettle , research associate 1 ,
- Kajal Gokal , senior research associate 1 ,
- Greg Biddle , research associate 1 ,
- Gemma M J Taylor , reader 3 ,
- Amanda J Daley , professor of behavioural medicine 1
- 1 Centre for Lifestyle Medicine and Behaviour (CLiMB), The School of Sport, Exercise and Health Sciences, Loughborough University, Loughborough LE11 3TU, UK
- 2 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
- 3 Department of Psychology, Addiction and Mental Health Group, University of Bath, Bath, UK
- Correspondence to: C D Madigan c.madigan{at}lboro.ac.uk (or @claire_wm and @lboroclimb on Twitter)
- Accepted 26 April 2022
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care.
Design Systematic review and meta-analysis of randomised controlled trials.
Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary care compared with no treatment, attention control, or minimal intervention and weight change at ≥12 months follow-up.
Data sources Trials from a previous systematic review were extracted and the search completed using the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021.
Data extraction and synthesis Two reviewers independently identified eligible studies, extracted data, and assessed risk of bias using the Cochrane risk of bias tool. Meta-analyses were conducted with random effects models, and a pooled mean difference for both weight (kg) and waist circumference (cm) were calculated.
Main outcome measures Primary outcome was weight change from baseline to 12 months. Secondary outcome was weight change from baseline to ≥24 months. Change in waist circumference was assessed at 12 months.
Results 34 trials were included: 14 were additional, from a previous review. 27 trials (n=8000) were included in the primary outcome of weight change at 12 month follow-up. The mean difference between the intervention and comparator groups at 12 months was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, P<0.001), favouring the intervention group. At ≥24 months (13 trials, n=5011) the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, P<0.001) favouring the intervention. The mean difference in waist circumference (18 trials, n=5288) was −2.5 cm (−3.2 to −1.8 cm, I 2 =69%, P<0.001) in favour of the intervention at 12 months.
Conclusions Behavioural weight management interventions for adults with obesity delivered in primary care are effective for weight loss and could be offered to members of the public.
Systematic review registration PROSPERO CRD42021275529.
Introduction
Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality. 1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19. 4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight. 6
Primary care is an ideal setting for delivering weight management services, and international guidelines recommend that doctors should opportunistically screen and encourage patients to lose weight. 7 8 On average, most people consult a primary care doctor four times yearly, providing opportunities for weight management interventions. 9 10 A systematic review of randomised controlled trials by LeBlanc et al identified behavioural interventions that could potentially be delivered in primary care, or involved referral of patients by primary care professionals, were effective for weight loss at 12-18 months follow-up (−2.4 kg, 95% confidence interval −2.9 to−1.9 kg). 11 However, this review included trials with interventions that the review authors considered directly transferrable to primary care, but not all interventions involved primary care practitioners. The review included interventions that were entirely delivered by university research employees, meaning implementation of these interventions might differ if offered in primary care, as has been the case in other implementation research of weight management interventions, where effects were smaller. 12 As many similar trials have been published after this review, an updated review would be useful to guide health policy.
We examined the effectiveness of weight loss interventions delivered in primary care on measures of body composition (weight and waist circumference). We also identified characteristics of effective weight management programmes for policy makers to consider.
This systematic review was registered on PROSPERO and is reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. 13 14
Eligibility criteria
We considered studies to be eligible for inclusion if they were randomised controlled trials, comprised adult participants (≥18 years), and evaluated behavioural weight management interventions delivered in primary care that focused on weight loss. A primary care setting was broadly defined as the first point of contact with the healthcare system, providing accessible, continued, comprehensive, and coordinated care, focused on long term health. 15 Delivery in primary care was defined as the majority of the intervention being delivered by medical and non-medical clinicians within the primary care setting. Table 1 lists the inclusion and exclusion criteria.
Study inclusion and exclusion criteria
- View inline
We extracted studies from the systematic review by LeBlanc et al that met our inclusion criteria. 11 We also searched the exclusions in this review because the researchers excluded interventions specifically for diabetes management, low quality trials, and only included studies from an Organisation for Economic Co-operation and Development country, limiting the scope of the findings.
We searched for studies in the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021 (see supplementary file 1). Reference lists of previous reviews 16 17 18 19 20 21 and included trials were hand searched.
Data extraction
Results were uploaded to Covidence, 22 a software platform used for screening, and duplicates removed. Two independent reviewers screened study titles, abstracts, and full texts. Disagreements were discussed and resolved by a third reviewer. All decisions were recorded in Covidence, and reviewers were blinded to each other’s decisions. Covidence calculates proportionate agreement as a measure of inter-rater reliability, and data are reported separately by title or abstract screening and full text screening. One reviewer extracted data on study characteristics (see supplementary table 1) and two authors independently extracted data on weight outcomes. We contacted the authors of four included trials (from the updated search) for further information. 23 24 25 26
Outcomes, summary measures, and synthesis of results
The primary outcome was weight change from baseline to 12 months. Secondary outcomes were weight change from baseline to ≥24 months and from baseline to last follow-up (to include as many trials as possible), and waist circumference from baseline to 12 months. Supplementary file 2 details the prespecified subgroup analysis that we were unable to complete. The prespecified subgroup analyses that could be completed were type of healthcare professional who delivered the intervention, country, intensity of the intervention, and risk of bias rating.
Healthcare professional delivering intervention —From the data we were able to compare subgroups by type of healthcare professional: nurses, 24 26 27 28 general practitioners, 23 29 30 31 and non-medical practitioners (eg, health coaches). 32 33 34 35 36 37 38 39 Some of the interventions delivered by non-medical practitioners were supported, but not predominantly delivered, by GPs. Other interventions were delivered by a combination of several different practitioners—for example, it was not possible to determine whether a nurse or dietitian delivered the intervention. In the subgroup analysis of practitioner delivery, we refer to this group as “other.”
Country —We explored the effectiveness of interventions by country. Only countries with three or more trials were included in subgroup analyses (United Kingdom, United States, and Spain).
Intensity of interventions —As the median number of contacts was 12, we categorised intervention groups according to whether ≤11 or ≥12 contacts were required.
Risk of bias rating —Studies were classified as being at low, unclear, and high risk of bias. Risk of bias was explored as a potential influence on the results.
Meta-analyses
Meta-analyses were conducted using Review Manager 5.4. 40 As we expected the treatment effects to differ because of the diversity of intervention components and comparator conditions, we used random effects models. A pooled mean difference was calculated for each analysis, and variance in heterogeneity between studies was compared using the I 2 and τ 2 statistics. We generated funnel plots to evaluate small study effects. If more than two intervention groups existed, we divided the number of participants in the comparator group by the number of intervention groups and analysed each individually. Nine trials were cluster randomised controlled trials. The trials had adjusted their results for clustering, or adjustment had been made in the previous systematic review by LeBlanc et al. 11 One trial did not report change in weight by group. 26 We calculated the mean weight change and standard deviation using a standard formula, which imputes a correlation for the baseline and follow-up weights. 41 42 In a non-prespecified analysis, we conducted univariate and multivariable metaregression (in Stata) using a random effects model to examine the association between number of sessions and type of interventionalist on study effect estimates.
Risk of bias
Two authors independently assessed the risk of bias using the Cochrane risk of bias tool v2. 43 For incomplete outcome data we defined a high risk of bias as ≥20% attrition. Disagreements were resolved by discussion or consultation with a third author.
Patient and public involvement
The study idea was discussed with patients and members of the public. They were not, however, included in discussions about the design or conduct of the study.
The search identified 11 609 unique study titles or abstracts after duplicates were removed ( fig 1 ). After screening, 97 full text articles were assessed for eligibility. The proportionate agreement ranged from 0.94 to 1.0 for screening of titles or abstracts and was 0.84 for full text screening. Fourteen new trials met the inclusion criteria. Twenty one studies from the review by LeBlanc et al met our eligibility criteria and one study from another systematic review was considered eligible and included. 44 Some studies had follow-up studies (ie, two publications) that were found in both the second and the first search; hence the total number of trials was 34 and not 36. Of the 34 trials, 27 (n=8000 participants) were included in the primary outcome meta-analysis of weight change from baseline to 12 months, 13 (n=5011) in the secondary outcome from baseline to ≥24 months, and 30 (n=8938) in the secondary outcome for weight change from baseline to last follow-up. Baseline weight was accounted for in 18 of these trials, but in 14 24 26 29 30 31 32 44 45 46 47 48 49 50 51 it was unclear or the trials did not consider baseline weight. Eighteen trials (n=5288) were included in the analysis of change in waist circumference at 12 months.

Studies included in systematic review of effectiveness of behavioural weight management interventions in primary care. *Studies were merged in Covidence if they were from same trial
- Download figure
- Open in new tab
- Download powerpoint
Study characteristics
Included trials (see supplementary table 1) were individual randomised controlled trials (n=25) 24 25 26 27 28 29 32 33 34 35 38 39 41 44 45 46 47 50 51 52 53 54 55 56 59 or cluster randomised controlled trials (n=9). 23 30 31 36 37 48 49 57 58 Most were conducted in the US (n=14), 29 30 31 32 33 34 35 36 37 45 48 51 54 55 UK (n=7), 27 28 38 41 47 57 58 and Spain (n=4). 25 44 46 49 The median number of participants was 276 (range 50-864).
Four trials included only women (average 65.9% of women). 31 48 51 59 The mean BMI at baseline was 35.2 (SD 4.2) and mean age was 48 (SD 9.7) years. The interventions lasted between one session (with participants subsequently following the programme unassisted for three months) and several sessions over three years (median 12 months). The follow-up period ranged from 12 months to three years (median 12 months). Most trials excluded participants who had lost weight in the past six months and were taking drugs that affected weight.
Meta-analysis
Overall, 27 trials were included in the primary meta-analysis of weight change from baseline to 12 months. Three trials could not be included in the primary analysis as data on weight were only available at two and three years and not 12 months follow-up, but we included these trials in the secondary analyses of last follow-up and ≥24 months follow-up. 26 44 50 Four trials could not be included in the meta-analysis as they did not present data in a way that could be synthesised (ie, measures of dispersion). 25 52 53 58 The mean difference was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, τ 2 =3.38; P<0.001) in favour of the intervention group ( fig 2 ). We found no evidence of publication bias (see supplementary fig 1). Absolute weight change was −3.7 (SD 6.1) kg in the intervention group and −1.4 (SD 5.5) kg in the comparator group.

Mean difference in weight at 12 months by weight management programme in primary care (intervention) or no treatment, different content, or minimal intervention (control). SD=standard deviation
Supplementary file 2 provides a summary of the main subgroup analyses.
Weight change
The mean difference in weight change at the last follow-up was −1.9 kg (95% confidence interval −2.5 to −1.3 kg, I 2 =81%, τ 2 =2.15; P<0.001). Absolute weight change was −3.2 (SD 6.4) kg in the intervention group and −1.2 (SD 6.0) kg in the comparator group (see supplementary figs 2 and 3).
At the 24 month follow-up the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, τ 2 =3.13; P<0.001) (see supplementary fig 4). As the weight change data did not differ between the last follow-up and ≥24 months, we used the weight data from the last follow-up in subgroup analyses.
In subgroup analyses of type of interventionalist, differences were significant (P=0.005) between non-medical practitioners, GPs, nurses, and other people who delivered interventions (see supplementary fig 2).
Participants who had ≥12 contacts during interventions lost significantly more weight than those with fewer contacts (see supplementary fig 6). The association remained after adjustment for type of interventionalist.
Waist circumference
The mean difference in waist circumference was −2.5 cm (95% confidence interval −3.2 to −1.8 cm, I 2 =69%, τ 2 =1.73; P<0.001) in favour of the intervention at 12 months ( fig 3 ). Absolute changes were −3.7 cm (SD 7.8 cm) in the intervention group and −1.3 cm (SD 7.3) in the comparator group.

Mean difference in waist circumference at 12 months. SD=standard deviation
Risk of bias was considered to be low in nine trials, 24 33 34 35 39 41 47 55 56 unclear in 12 trials, 25 27 28 29 32 45 46 50 51 52 54 59 and high in 13 trials 23 26 30 31 36 37 38 44 48 49 53 57 58 ( fig 4 ). No significant (P=0.65) differences were found in subgroup analyses according to level of risk of bias from baseline to 12 months (see supplementary fig 7).

Risk of bias in included studies
Worldwide, governments are trying to find the most effective services to help people lose weight to improve the health of populations. We found weight management interventions delivered by primary care practitioners result in effective weight loss and reduction in waist circumference and these interventions should be considered part of the services offered to help people manage their weight. A greater number of contacts between patients and healthcare professionals led to more weight loss, and interventions should be designed to include at least 12 contacts (face-to-face or by telephone, or both). Evidence suggests that interventions delivered by non-medical practitioners were as effective as those delivered by GPs (both showed statistically significant weight loss). It is also possible that more contacts were made with non-medical interventionalists, which might partially explain this result, although the metaregression analysis suggested the effect remained after adjustment for type of interventionalist. Because most comparator groups had fewer contacts than intervention groups, it is not known whether the effects of the interventions are related to contact with interventionalists or to the content of the intervention itself.
Although we did not determine the costs of the programme, it is likely that interventions delivered by non-medical practitioners would be cheaper than GP and nurse led programmes. 41 Most of the interventions delivered by non-medical practitioners involved endorsement and supervision from GPs (ie, a recommendation or checking in to see how patients were progressing), and these should be considered when implementing these types of weight management interventions in primary care settings. Our findings suggest that a combination of practitioners would be most effective because GPs might not have the time for 12 consultations to support weight management.
Although the 2.3 kg greater weight loss in the intervention group may seem modest, just 2-5% in weight loss is associated with improvements in systolic blood pressure and glucose and triglyceride levels. 60 The confidence intervals suggest a potential range of weight loss and that these interventions might not provide as much benefit to those with a higher BMI. Patients might not find an average weight loss of 3.7 kg attractive, as many would prefer to lose more weight; explaining to patients the benefits of small weight losses to health would be important.
Strengths and limitations of this review
Our conclusions are based on a large sample of about 8000 participants, and 12 of these trials were published since 2018. It was occasionally difficult to distinguish who delivered the interventions and how they were implemented. We therefore made some assumptions at the screening stage about whether the interventionalists were primary care practitioners or if most of the interventions were delivered in primary care. These discussions were resolved by consensus. All included trials measured weight, and we excluded those that used self-reported data. Dropout rates are important in weight management interventions as those who do less well are less likely to be followed-up. We found that participants in trials with an attrition rate of 20% or more lost less weight and we are confident that those with high attrition rates have not inflated the results. Trials were mainly conducted in socially economic developed countries, so our findings might not be applicable to all countries. The meta-analyses showed statistically significant heterogeneity, and our prespecified subgroups analysis explained some, but not all, of the variance.
Comparison with other studies
The mean difference of −2.3 kg in favour of the intervention group at 12 months is similar to the findings in the review by LeBlanc et al, who reported a reduction of −2.4 kg in participants who received a weight management intervention in a range of settings, including primary care, universities, and the community. 11 61 This is important because the review by LeBlanc et al included interventions that were not exclusively conducted in primary care or by primary care practitioners. Trials conducted in university or hospital settings are not typically representative of primary care populations and are often more intensive than trials conducted in primary care as a result of less constraints on time. Thus, our review provides encouraging findings for the implementation of weight management interventions delivered in primary care. The findings are of a similar magnitude to those found in a trial by Ahern et al that tested primary care referral to a commercial programme, with a difference of −2.7 kg (95% confidence interval −3.9 to −1.5 kg) reported at 12 month follow-up. 62 The trial by Ahern et al also found a difference in waist circumference of −4.1 cm (95% confidence interval −5.5 to −2.3 cm) in favour of the intervention group at 12 months. Our finding was smaller at −2.5 cm (95% confidence interval −3.2 to −1.8 cm). Some evidence suggests clinical benefits from a reduction of 3 cm in waist circumference, particularly in decreased glucose levels, and the intervention groups showed a 3.7 cm absolute change in waist circumference. 63
Policy implications and conclusions
Weight management interventions delivered in primary care are effective and should be part of services offered to members of the public to help them manage weight. As about 39% of the world’s population is living with obesity, helping people to manage their weight is an enormous task. 64 Primary care offers good reach into the community as the first point of contact in the healthcare system and the remit to provide whole person care across the life course. 65 When developing weight management interventions, it is important to reflect on resource availability within primary care settings to ensure patients’ needs can be met within existing healthcare systems. 66
We did not examine the equity of interventions, but primary care interventions may offer an additional service and potentially help those who would not attend a programme delivered outside of primary care. Interventions should consist of 12 or more contacts, and these findings are based on a mixture of telephone and face-to-face sessions. Previous evidence suggests that GPs find it difficult to raise the issue of weight with patients and are pessimistic about the success of weight loss interventions. 67 Therefore, interventions should be implemented with appropriate training for primary care practitioners so that they feel confident about helping patients to manage their weight. 68
Unanswered questions and future research
A range of effective interventions are available in primary care settings to help people manage their weight, but we found substantial heterogeneity. It was beyond the scope of this systematic review to examine the specific components of the interventions that may be associated with greater weight loss, but this could be investigated by future research. We do not know whether these interventions are universally suitable and will decrease or increase health inequalities. As the data are most likely collected in trials, an individual patient meta-analysis is now needed to explore characteristics or factors that might explain the variance. Most of the interventions excluded people prescribed drugs that affect weight gain, such as antipsychotics, glucocorticoids, and some antidepressants. This population might benefit from help with managing their weight owing to the side effects of these drug classes on weight gain, although we do not know whether the weight management interventions we investigated would be effective in this population. 69
What is already known on this topic
Referral by primary care to behavioural weight management programmes is effective, but the effectiveness of weight management interventions delivered by primary care is not known
Systematic reviews have provided evidence for weight management interventions, but the latest review of primary care delivered interventions was published in 2014
Factors such as intensity and delivery mechanisms have not been investigated and could influence the effectiveness of weight management interventions delivered by primary care
What this study adds
Weight management interventions delivered by primary care are effective and can help patients to better manage their weight
At least 12 contacts (telephone or face to face) are needed to deliver weight management programmes in primary care
Some evidence suggests that weight loss after weight management interventions delivered by non-medical practitioners in primary care (often endorsed and supervised by doctors) is similar to that delivered by clinician led programmes
Ethics statements
Ethical approval.
Not required.
Data availability statement
Additional data are available in the supplementary files.
Contributors: CDM and AJD conceived the study, with support from ES. CDM conducted the search with support from HEG. CDM, AJD, ES, HEG, KG, GB, and VEK completed the screening and full text identification. CDM and VEK completed the risk of bias assessment. CDM extracted data for the primary outcome and study characteristics. HEJ, GB, and KG extracted primary outcome data. CDM completed the analysis in RevMan, and GMJT completed the metaregression analysis in Stata. CDM drafted the paper with AJD. All authors provided comments on the paper. CDM acts as guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: AJD is supported by a National Institute for Health and Care Research (NIHR) research professorship award. This research was supported by the NIHR Leicester Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. ES’s salary is supported by an investigator grant (National Health and Medical Research Council, Australia). GT is supported by a Cancer Research UK fellowship. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: This research was supported by the National Institute for Health and Care Research Leicester Biomedical Research Centre; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
The lead author (CDM) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported, and that no important aspects of the study have been omitted.
Dissemination to participants and related patient and public communities: We plan to disseminate these research findings to a wider community through press releases, featuring on the Centre for Lifestyle Medicine and Behaviour website ( www.lboro.ac.uk/research/climb/ ) via our policy networks, through social media platforms, and presentation at conferences.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- Renehan AG ,
- Heller RF ,
- Bansback N ,
- Birmingham CL ,
- Abdullah A ,
- Peeters A ,
- de Courten M ,
- Stoelwinder J
- Aghili SMM ,
- Ebrahimpur M ,
- Arjmand B ,
- KETLAK Study Group
- ↵ Department of Health and Social Care. New specialised support to help those living with obesity to lose weight UK2021. www.gov.uk/government/news/new-specialised-support-to-help-those-living-with-obesity-to-lose-weight [accessed 08/02/2021].
- U.S. Preventive Services Task Force
- ↵ National Institute for Health and Care Excellence. Maintaining a Healthy Weight and Preventing Excess Weight Gain in Children and Adults. Cost Effectiveness Considerations from a Population Modelling Viewpoint. 2014, NICE. www.nice.org.uk/guidance/ng7/evidence/evidence-review-2-qualitative-evidence-review-of-the-most-acceptable-ways-to-communicate-information-about-individually-modifiable-behaviours-to-help-maintain-a-healthy-weight-or-prevent-excess-weigh-8733713.
- ↵ The Health Foundation. Use of primary care during the COVID-19 pandemic. 17/09/2020: The Health Foundation, 2020.
- ↵ Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings, 2017-18. 2019 ed. Canberra, Australia, 2018. www.abs.gov.au/AUSSTATS/[email protected]/Lookup/4839.0Main+Features12017-18?OpenDocument.
- LeBlanc ES ,
- Patnode CD ,
- Webber EM ,
- Redmond N ,
- Rushkin M ,
- O’Connor EA
- Damschroder LJ ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- McKenzie JE ,
- Bossuyt PM ,
- ↵ WHO. Main terminology: World Health Organization; 2004. www.euro.who.int/en/health-topics/Health-systems/primary-health-care/main-terminology [accessed 09.12.21].
- Aceves-Martins M ,
- Robertson C ,
- REBALANCE team
- Glasziou P ,
- Isenring E ,
- Chisholm A ,
- Wakayama LN ,
- Kettle VE ,
- Madigan CD ,
- ↵ Covidence [program]. Melbourne, 2021.
- Welzel FD ,
- Carrington MJ ,
- Fernández-Ruiz VE ,
- Ramos-Morcillo AJ ,
- Solé-Agustí M ,
- Paniagua-Urbano JA ,
- Armero-Barranco D
- Bräutigam-Ewe M ,
- Hildingh C ,
- Yardley L ,
- Christian JG ,
- Bessesen DH ,
- Christian KK ,
- Goldstein MG ,
- Martin PD ,
- Dutton GR ,
- Horswell RL ,
- Brantley PJ
- Wadden TA ,
- Rogers MA ,
- Berkowitz RI ,
- Kumanyika SK ,
- Morales KH ,
- Allison KC ,
- Rozenblum R ,
- De La Cruz BA ,
- Katzmarzyk PT ,
- Martin CK ,
- Newton RL Jr . ,
- Nanchahal K ,
- Holdsworth E ,
- ↵ RevMan [program]. 5.4 version: Copenhagen, 2014.
- Sterne JAC ,
- Savović J ,
- Gomez-Huelgas R ,
- Jansen-Chaparro S ,
- Baca-Osorio AJ ,
- Mancera-Romero J ,
- Tinahones FJ ,
- Bernal-López MR
- Delahanty LM ,
- Tárraga Marcos ML ,
- Panisello Royo JM ,
- Carbayo Herencia JA ,
- Beeken RJ ,
- Leurent B ,
- Vickerstaff V ,
- Hagobian T ,
- Brannen A ,
- Rodriguez-Cristobal JJ ,
- Alonso-Villaverde C ,
- Panisello JM ,
- Conroy MB ,
- Spadaro KC ,
- Takasawa N ,
- Mashiyama Y ,
- Pritchard DA ,
- Hyndman J ,
- Jarjoura D ,
- Smucker W ,
- Baughman K ,
- Bennett GG ,
- Steinberg D ,
- Zaghloul H ,
- Chagoury O ,
- Leslie WS ,
- Barnes AC ,
- Summerbell CD ,
- Greenwood DC ,
- Huseinovic E ,
- Leu Agelii M ,
- Hellebö Johansson E ,
- Winkvist A ,
- Look AHEAD Research Group
- LeBlanc EL ,
- Wheeler GM ,
- Aveyard P ,
- de Koning L ,
- Chiuve SE ,
- Willett WC ,
- ↵ World Health Organization. Obesity and Overweight, 2021, www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Starfield B ,
- Sturgiss E ,
- Dewhurst A ,
- Devereux-Fitzgerald A ,
- Haesler E ,
- van Weel C ,
- Gulliford MC
- Fassbender JE ,
- Sarwer DB ,
- Brekke HK ,

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics
Obesity Research
Language switcher.
Over the years, NHLBI-supported research on overweight and obesity has led to the development of evidence-based prevention and treatment guidelines for healthcare providers. NHLBI research has also led to guidance on how to choose a behavioral weight loss program.
Studies show that the skills learned and support offered by these programs can help most people make the necessary lifestyle changes for weight loss and reduce their risk of serious health conditions such as heart disease and diabetes.
Our research has also evaluated new community-based programs for various demographics, addressing the health disparities in overweight and obesity.
NHLBI research that really made a difference
- In 1991, the NHLBI developed an Obesity Education Initiative to educate the public and health professionals about obesity as an independent risk factor for cardiovascular disease and its relationship to other risk factors, such as high blood pressure and high blood cholesterol. The initiative led to the development of clinical guidelines for treating overweight and obesity.
- The NHLBI and other NIH Institutes funded the Obesity-Related Behavioral Intervention Trials (ORBIT) projects , which led to the ORBIT model for developing behavioral treatments to prevent or manage chronic diseases. These studies included families and a variety of demographic groups. A key finding from one study focuses on the importance of targeting psychological factors in obesity treatment.
Current research funded by the NHLBI
The Division of Cardiovascular Sciences , which includes the Clinical Applications and Prevention Branch, funds research to understand how obesity relates to heart disease. The Center for Translation Research and Implementation Science supports the translation and implementation of research, including obesity research, into clinical practice. The Division of Lung Diseases and its National Center on Sleep Disorders Research fund research on the impact of obesity on sleep-disordered breathing.
Find funding opportunities and program contacts for research related to obesity and its complications.
Current research on obesity and health disparities
Health disparities happen when members of a group experience negative impacts on their health because of where they live, their racial or ethnic background, how much money they make, or how much education they received. NHLBI-supported research aims to discover the factors that contribute to health disparities and test ways to eliminate them.
- NHLBI-funded researchers behind the RURAL: Risk Underlying Rural Areas Longitudinal Cohort Study want to discover why people in poor rural communities in the South have shorter, unhealthier lives on average. The study includes 4,000 diverse participants (ages 35–64 years, 50% women, 44% whites, 45% Blacks, 10% Hispanic) from 10 of the poorest rural counties in Kentucky, Alabama, Mississippi, and Louisiana. Their results will support future interventions and disease prevention efforts.
- The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is looking at what factors contribute to the higher-than-expected numbers of Hispanics/Latinos who suffer from metabolic diseases such as obesity and diabetes. The study includes more than 16,000 Hispanic/Latino adults across the nation.
Find more NHLBI-funded studies on obesity and health disparities at NIH RePORTER.

Read how African Americans are learning to transform soul food into healthy, delicious meals to prevent cardiovascular disease: Vegan soul food: Will it help fight heart disease, obesity?
Current research on obesity in pregnancy and childhood
- The NHLBI-supported Fragile Families Cardiovascular Health Follow-Up Study continues a study that began in 2000 with 5,000 American children born in large cities. The cohort was racially and ethnically diverse, with approximately 40% of the children living in poverty. Researchers collected socioeconomic, demographic, neighborhood, genetic, and developmental data from the participants. In this next phase, researchers will continue to collect similar data from the participants, who are now young adults.
- The NHLBI is supporting national adoption of the Bright Bodies program through Dissemination and Implementation of the Bright Bodies Intervention for Childhood Obesity . Bright Bodies is a high-intensity, family-based intervention for childhood obesity. In 2017, a U.S. Preventive Services Task Force found that Bright Bodies lowered children’s body mass index (BMI) more than other interventions did.
- The NHLBI supports the continuation of the nuMoM2b Heart Health Study , which has followed a diverse cohort of 4,475 women during their first pregnancy. The women provided data and specimens for up to 7 years after the birth of their children. Researchers are now conducting a follow-up study on the relationship between problems during pregnancy and future cardiovascular disease. Women who are pregnant and have obesity are at greater risk than other pregnant women for health problems that can affect mother and baby during pregnancy, at birth, and later in life.
Find more NHLBI-funded studies on obesity in pregnancy and childhood at NIH RePORTER.
Learn about the largest public health nonprofit for Black and African American women and girls in the United States: Empowering Women to Get Healthy, One Step at a Time .
Current research on obesity and sleep
- An NHLBI-funded study is looking at whether energy balance and obesity affect sleep in the same way that a lack of good-quality sleep affects obesity. The researchers are recruiting equal numbers of men and women to include sex differences in their study of how obesity affects sleep quality and circadian rhythms.
- NHLBI-funded researchers are studying metabolism and obstructive sleep apnea . Many people with obesity have sleep apnea. The researchers will look at the measurable metabolic changes in participants from a previous study. These participants were randomized to one of three treatments for sleep apnea: weight loss alone, positive airway pressure (PAP) alone, or combined weight loss and PAP. Researchers hope that the results of the study will allow a more personalized approach to diagnosing and treating sleep apnea.
- The NHLBI-funded Lipidomics Biomarkers Link Sleep Restriction to Adiposity Phenotype, Diabetes, and Cardiovascular Risk study explores the relationship between disrupted sleep patterns and diabetes. It uses data from the long-running Multiethnic Cohort Study, which has recruited more than 210,000 participants from five ethnic groups. Researchers are searching for a cellular-level change that can be measured and can predict the onset of diabetes in people who are chronically sleep deprived. Obesity is a common symptom that people with sleep issues have during the onset of diabetes.
Find more NHLBI-funded studies on obesity and sleep at NIH RePORTER.

Learn about a recent study that supports the need for healthy sleep habits from birth: Study finds link between sleep habits and weight gain in newborns .
Obesity research labs at the NHLBI
The Cardiovascular Branch and its Laboratory of Inflammation and Cardiometabolic Diseases conducts studies to understand the links between inflammation, atherosclerosis, and metabolic diseases.
NHLBI’s Division of Intramural Research , including its Laboratory of Obesity and Aging Research , seeks to understand how obesity induces metabolic disorders. The lab studies the “obesity-aging” paradox: how the average American gains more weight as they get older, even when food intake decreases.
Related obesity programs and guidelines
- Aim for a Healthy Weight is a self-guided weight-loss program led by the NHLBI that is based on the psychology of change. It includes tested strategies for eating right and moving more.
- The NHLBI developed the We Can! ® (Ways to Enhance Children’s Activity & Nutrition) program to help support parents in developing healthy habits for their children.
- The Accumulating Data to Optimally Predict obesity Treatment (ADOPT) Core Measures Project standardizes data collected from the various studies of obesity treatments so the data can be analyzed together. The bigger the dataset, the more confidence can be placed in the conclusions. The main goal of this project is to understand the individual differences between people who experience the same treatment.
- The NHLBI Director co-chairs the NIH Nutrition Research Task Force, which guided the development of the first NIH-wide strategic plan for nutrition research being conducted over the next 10 years. See the 2020–2030 Strategic Plan for NIH Nutrition Research .
- The NHLBI is an active member of the National Collaborative on Childhood Obesity (NCCOR) , which is a public–private partnership to accelerate progress in reducing childhood obesity.
- The NHLBI has been providing guidance to physicians on the diagnosis, prevention, and treatment of obesity since 1977. In 2017, the NHLBI convened a panel of experts to take on some of the pressing questions facing the obesity research community. See their responses: Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents (PDF, 3.69 MB).
- In 2021, the NHLBI held a Long Non-coding (lnc) RNAs Symposium to discuss research opportunities on lnc RNAs, which appear to play a role in the development of metabolic diseases such as obesity.
- The Muscatine Heart Study began enrolling children in 1970. By 1981, more than 11,000 students from Muscatine, Iowa, had taken surveys twice a year. The study is the longest-running study of cardiovascular risk factors in children in the United States. Today, many of the earliest participants and their children are still involved in the study, which has already shown that early habits affect cardiovascular health later in life.
- The Jackson Heart Study is a unique partnership of the NHLBI, three colleges and universities, and the Jackson, Miss., community. Its mission is to discover what factors contribute to the high prevalence of cardiovascular disease among African Americans. Researchers aim to test new approaches for reducing this health disparity. The study incudes more than 5,000 individuals. Among the study’s findings to date is a gene variant in African Americans that doubles the risk of heart disease.
Explore more NHLBI research on overweight and obesity
The sections above provide you with the highlights of NHLBI-supported research on overweight and obesity . You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
- Research article
- Open access
- Published: 05 July 2019
Obesity prevention and the role of hospital and community-based health services: a scoping review
- Claire Pearce ORCID: orcid.org/0000-0003-2129-467X 1 , 2 , 3 ,
- Lucie Rychetnik 1 , 2 , 4 ,
- Sonia Wutzke 1 an1 &
- Andrew Wilson 1 , 2
BMC Health Services Research volume 19 , Article number: 453 ( 2019 ) Cite this article
31k Accesses
31 Citations
5 Altmetric
Metrics details
Control of obesity is an important priority to reduce the burden of chronic disease. Clinical guidelines focus on the role of primary healthcare in obesity prevention. The purpose of this scoping review is to examine what the published literature indicates about the role of hospital and community based health services in adult obesity prevention in order to map the evidence and identify gaps in existing research.
Databases were searched for articles published in English between 2006 and 2016 and screened against inclusion and exclusion criteria. Further papers were highlighted through a manual search of the reference lists. Included papers evaluated interventions aimed at preventing overweight and obesity in adults that were implemented within and/or by hospital and community health services; were an empirical description of obesity prevention within a health setting or reported health staff perceptions of obesity and obesity prevention.
The evidence supports screening for obesity of all healthcare patients, combined with referral to appropriate intervention services but indicates that health professionals do not typically adopt this practice. As well as practical issues such as time and resourcing, implementation is impacted by health professionals’ views about the causes of obesity and doubts about the benefits of the health sector intervening once someone is already obese. As well as lacking confidence or knowledge about how to integrate prevention into clinical care, health professional judgements about who might benefit from prevention and negative views about effectiveness of prevention hinder the implementation of practice guidelines. This is compounded by an often prevailing view that preventing obesity is a matter of personal responsibility and choice.
Conclusions
This review highlights that whilst a population health approach is important to address the complexity of obesity, it is important that the remit of health services is extended beyond medical treatment to incorporate obesity prevention through screening and referral. Further research into the role of health services in obesity prevention should take a systems approach to examine how health service structures, policy and practice interrelationships, and service delivery boundaries, processes and perspectives impact on changing models of care.
Peer Review reports
Chronic diseases place a significant burden on the Australian healthcare system. They account for 90% of all deaths [ 1 ] and significantly reduce quality of life [ 2 ]. Being obese is a major risk factor for many chronic diseases including heart disease, cancer, kidney failure, pulmonary disease and diabetes [ 3 , 4 ]. Being overweight can impede the management of chronic conditions and is the second highest contributor to burden of disease. Obesity has been shown to reduce quality-adjusted life expectancy [ 5 ].
The World Health Organisation (WHO) highlights prevention of obesity as an important priority to reduce the impact of non-communicable disease. Both supporting people who are currently overweight to attain modest weight loss as well as preventing further increases in weight may eventually see a decrease in overall rates of obesity and a reduction in the rates of chronic diseases [ 6 ] and therefore a decrease in associated costs [ 7 ].
International guidelines recommend that preventive care be provided across the whole health system, integrated into ‘curative’ or disease management focused consultations, regardless of age or health status [ 8 ]. For obesity prevention, there are specific guidelines for the role of the general practitioner, for example the Royal Australian College of General Practitioners ‘Guidelines for preventive activities in general practice’ [ 9 ]. However, the prevention role of hospital and community health services is not as clearly articulated, particularly in relation to an adult population.
In this research we present a review of published literature investigating the role of hospital and community based health services in adult obesity prevention. The aim is to improve understanding of the role for hospital and community based health services in prevention as well as the potential enablers and barriers to the delivery of preventive health services in order to inform future research to support the development of obesity prevention guidelines applicable to a range of health service settings.
A scoping review [ 10 ] was conducted to map evidence and identify gaps in the extent, range, and nature of research undertaken in relation to the role of health services in obesity prevention. The focus of the review was on hospital and community based health services as unlike primary care, the roles of these services in obesity prevention are not clearly outlined in clinical guidelines.
Research question
The overarching question for this scoping study was: What does the peer reviewed literature reveal about the role of adult health services (excluding general practice) in the provision of obesity prevention and what are the key elements of implementation?
Data sources and search
Three databases (CINAHL and Medline concurrently and PubMed) were searched for references containing the words “obese” AND “prevent*” AND “healthcare/ health services” AND “adult”. Medline and CINAHL were searched concurrently to cover medical, nursing and allied health research. PubMed was searched to pick up those articles not yet assigned MESH headings. For practical reasons, the scope was limited to articles published in English between 2006 and 2016 (November). The Cochrane database was searched using the phrase “Prevention of overweight and obesity” to include systematic reviews conducted in the last 10 years.
Inclusion and exclusion criteria
As the aim of the review was to highlight clinical interventions as well as issues relating to implementation, papers were included if they fell into any of the following categories: (1) Evaluation of a specific hospital or community health based obesity prevention intervention; (2) Clinical guidelines featuring obesity prevention; (3) Systematic or scoping reviews of health service based obesity prevention or (4) Empirical description of obesity prevention within a health setting. A fifth category was identified in the process of undertaking the review: (5) Health staff or health service consumer perceptions of and beliefs about obesity and obesity prevention. For each of these categories, the focus of the intervention was on services for adults. We included primary studies as well as literature reviews.
Articles that were excluded were those that:
focused on prevention of childhood obesity;
were medical treatments aimed solely at weight loss, such as surgical or pharmaceutical interventions;
described an intervention that did not take place in a health setting or if that setting was focused solely on the role of general practitioners.
Papers were also excluded if they described obesity or associated disease but did not focus on interventions with a goal of prevention or if the focus was on population health initiatives that were not within the remit of health services, such as introducing food taxes. Opinion pieces and editorials were not included.
Data extraction
All articles were reviewed and divided into the categories described above. Information was summarised using a standardised extraction form developed for the review (see Tables 1 , 2 , 3 , 4 , 5 ) to identify the clinical areas where prevention is effective and the fundamental elements of implementation.
The primary aim of analysis was to determine the main factors in delivering adult obesity prevention within a health setting. Analysis commenced with an examination of intervention type, sample size, setting and duration. Studies were then grouped into categories that were empirically derived from the type of studies identified as summarised in Tables 1 , 2 , 3 , 4 , 5 . Analysis has been framed with the 5As framework [ 9 ] which is utilised as a preventative healthcare tool to identify risk factors for chronic disease. It originated as a smoking cessation tool but has been adapted for use with obesity.
Literature search
An initial PubMed search using the search terms “obese” AND “prevent*” AND “healthcare/ health services” AND “adult”, produced 710 articles. The first 40 of these articles were screened and found to be highly irrelevant. Subsequently, the PubMed search was changed to a title search “The Role of Health Services in the Prevention of Overweight and Obesity in Adults”. This produced 240 references, which on initial scan appeared to highlight more relevant documents. CINAHL and Medline searches using the same search terms produced 584 articles which on screening appeared to hold relevant studies. The Cochrane database search resulted in 151 references.
All references were then screened for duplicates before being assessed against the specific inclusion/ exclusion criteria. Further references were highlighted through a manual search of the reference list of those references which met the inclusion criteria. In all, 43 articles were included for review. Figure 1 presents the review flow chart.
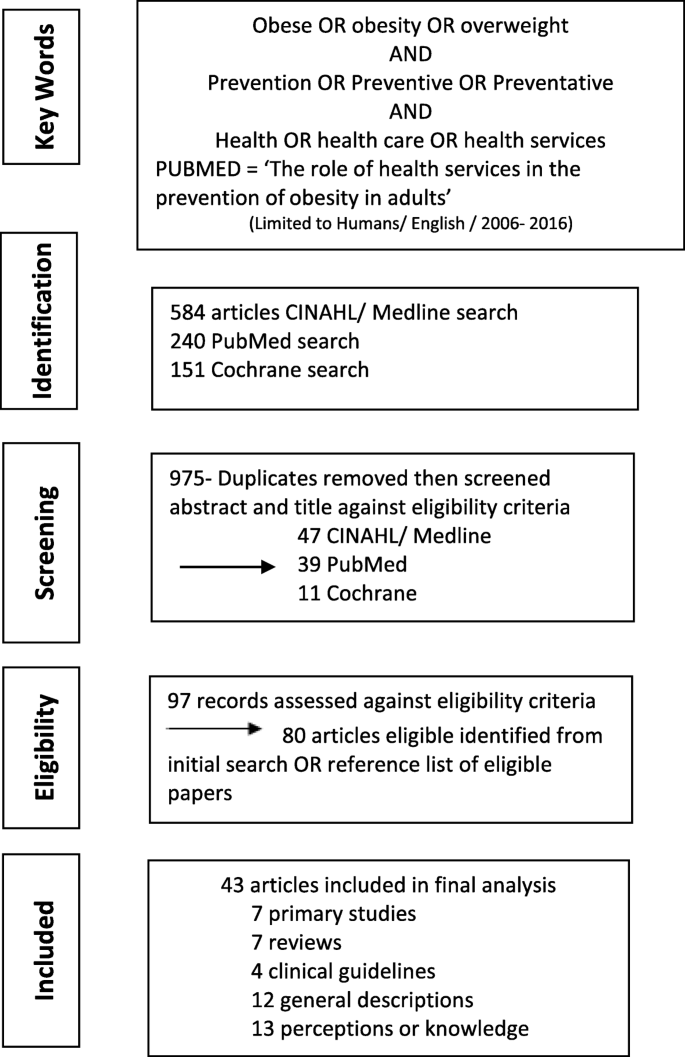
Scoping review flow chart
Scope of literature by category
Of the 43 papers included in the review, seven were primary studies of a specific health based obesity prevention intervention (Category 1) and seven were scoping or systematic reviews of specific health based obesity prevention interventions (Category 2). Four clinical guidelines were included (Category 3); two specific to the Australian context [ 9 , 41 ], one from the United States [ 42 ] and one from the United Kingdom [ 43 ]. One guideline, the Royal Australian Council of General Practitioners (RACGP) Red Book [ 44 ] focussed on primary healthcare but was included as it does examine implementation of the 5As framework. This framework is frequently utilised in preventive care and though most commonly used in primary care, is one which is applicable to a range of health services. The other three focus on primary healthcare, but also consider other health services. A group of 12 papers (Category 4) provided general descriptions of obesity prevention interventions within health settings. Thirteen papers (Category 5) surveyed health professionals or consumers about their perceptions or knowledge of obesity and/or obesity prevention. A summary of the papers in each category, and the extracted data can be found in Tables 1 , 2 , 3 , 4 , 5 .
How the 5A framework informs obesity prevention
The specific health based obesity prevention interventions (Category 1 and 2), were examined using the 5As framework [ 44 ]. The 5As framework is used to identify risk factors for chronic disease, including obesity, and to plan interventions to take into account the behavioural and physiological elements to be addressed [ 45 ]. The 5As refer to Ask (about risk factors); Assess (level of risk factors, health literacy and readiness to change); Advise/ Agree (use motivational interviewing to agree goals); Assist (develop a plan to address goals) and Arrange (organise support to achieve goals and maintain change) [ 44 ].
Whilst not all the papers explicitly referred to the 5As, elements of the framework were noted in each of the seven primary studies and three of the six literature reviews concerned with health service based prevention interventions. In the section below we apply the 5A framework to consider different elements of obesity prevention and how these have been reported in the literature.
Ask and assess
For this review, Ask and Assess have been considered together as both focus on gathering the initial information which will determine the next step. A focus on screening is supported by evidence which shows that weighing people and discussing the risks associated with putting on excess weight has an impact on individual knowledge and readiness for change which are basic factors if obesity prevention is to be effective [ 36 , 46 ]. The US Preventive Task Force and the National Heart, Lung, and Blood Institute guidelines recommend health services screen all adults for obesity [ 42 ].
Screening should include not only identifying risk factors but also ascertaining if a person is wanting to make changes to address the risk factors and their ability to do so based on factors such as health literacy, which is an individual’s ability to understand, interpret and apply information to their own health and healthcare [ 47 ]. In the included studies, there was a focus on determining risk factors but not on establishing an individual’s health literacy. The seven evaluation based papers identified a need to assess for obesity risk factors and the potential impact of these on health but only one [ 12 ] specifically concluded that there is a need to train staff in issues such as health literacy and readiness for change. This factor was missing all together from the systematic review summarising best practice in applying the framework [ 23 ].
All the primary study papers (Category 1) concluded that there is a role for health professionals in the provision of prevention advice and five of these seven studies discussed providing specific training to support this role [ 12 , 13 , 15 , 16 , 17 ]. However, targeted training does not automatically change practice. Two studies, one with community health staff and one with mental health clinicians, found that training changed practice in terms of assessment of risk factors but did not change practice in relation to providing advice [ 16 , 17 ]. In studies which reported that clinicians did provide advice, in most cases patients could recall that advice but these papers did not report on whether the people receiving the advice changed their behaviour or on the long term retention of that advice [ 11 , 12 , 13 , 15 ]. One systematic review [ 23 ] framed ‘advise’ in terms of telling people they needed to lose weight and how they should do that on the basis that sustained weight loss has the most significant impact on health. It did not consider supporting people to set their own goals around their weight or risk factors. The remaining six literature reviews did not report on health professionals providing advice.
The next step of the 5As framework is providing intervention aimed at assisting people to set goals to self-manage lifestyle changes. The primary studies (category 1) did not address this element, instead framing the role of health services not as providing support but instead referring to other agencies to provide this support. One literature review concluded that intensive long term support was required to assist people to embed changes but did not provide specific details of what this might look like [ 23 ]. Another concluded that assisting people to set goals related to weight management achieves better outcomes than linking goals to more general improvements in health [ 20 ]. The remaining literature reviews did not address the ‘assist’ element.
The final step of the 5As framework recommends providing support to help people achieve and maintain their weight goals. Three of the Category 1 health service evaluations focussed specifically on this step. All were unsuccessful in increasing health professional’s rate of referral to support services. [ 15 , 16 , 17 ]. For example, a recent study undertaken across several community health centres focussed on supporting community health staff to incorporate assessment, brief advice and referral in relation to addressing chronic disease risk factors, including obesity risk factors. The intervention was well supported over the 12 months of implementation by a range of initiatives including pre-intervention policy change, electronic resources and staff training. The intervention was successful in getting staff to undertake more assessments for risk factors but did not change practice in relation to brief advice or referral for intervention [ 17 ] . Similar results were obtained within a community mental health setting, concluding that even when clinical guidelines explicitly direct clinicians to incorporate preventive care into interactions, rates of care given around issues such as fruit and vegetable intake or physical activity remain low [ 16 ]. The study concluded that prevention may need to be delivered within a different model of care [ 16 ]. Two of the systematic reviews concluded that successful obesity prevention needs to include the provision of or referral to intensive, multicomponent behavioural interventions which aim to support weight loss and management [ 21 , 23 ].
Clinical areas in which obesity prevention may be warranted
The National Health and Medical Research Council (NHMRC) Clinical Practice Guidelines [ 6 ] identify different life stages where there is a greater risk of weight gain. The empirical studies were therefore analysed to identify the clinical areas where prevention may have the most significant impact and the specific elements key to working with these clinical groups. Fifteen of the papers included in the review focused on a particular life stage or cohort of patients. The clinical areas identified were maternity, which has received the most focus but has not been rigorously evaluated [ 13 , 14 , 26 , 27 , 31 , 33 , 34 , 36 , 48 ] and mental health [ 37 ]. Definitive evidence of how obesity prevention should be delivered in mental health services was not available.
The papers which focussed on maternity based services highlight the immediate consequences of maternal obesity including higher rates of gestational diabetes, high blood pressure and pre-eclampsia and higher risk births. Excess weight gain in pregnancy combined with not losing the weight after pregnancy are predictors of long-term maternal obesity and increases the risk of the child developing obesity whilst mothers with gestational diabetes are more likely to develop type 2 diabetes later in life [ 36 ]. Along with the individual risks to mother and child, there is an increased demand for services and a requirement for more specialised services to support woman and baby both during and after the birth [ 18 , 26 , 30 , 31 , 33 , 34 ].
Only one of the papers targeting obesity prevention in maternity care settings reported on a specific intervention. This found that women at risk of gestational diabetes who receive advice in relation to limiting weight gain during pregnancy are less likely to develop diabetes despite no significant difference in weight gain compared with a control group [ 13 ]. The other maternity focussed papers were more descriptive, providing a broad overview of implementation factors including the need for a multidisciplinary approach to reinforce the benefits of diet and physical activity beyond weight management. For example, obese pregnant women who are physically active have been shown to experience less depressive symptoms and report higher quality of life to obese women who are not physically active in pregnancy [ 14 ]. Two papers stated that discussions about safe weight gain and weight management needs to be done in a way that does not stigmatise or cause feelings of shame [ 27 , 33 ].
Only one paper looked at a life stage other than child bearing years, namely older adults [ 29 ]. This paper summarised the results of a large survey, focussing specifically on older persons’ perceptions of receiving weight management advice. As with similar studies looking at the adult population more generally [ 28 ], it was found that older adults were more likely to receive lifestyle advice if they were already obese or had a number of chronic conditions [ 29 ]. The disadvantage of many of the survey based studies was the reliance on self-reported weight and height.
In terms of specific clinical areas, studies have been conducted in mental health and community health services. It was reported that it is very difficult to change the practice of mental health staff to include a focus of physical health risk factors [ 16 ] with mental health clinicians not necessarily seeing this as their role [ 37 ] despite the fact that people with mental illness do want to reduce their risk factors [ 40 ]. Similarly in services delivering general community health care, despite the presence of risk factors and an openness by clients to receive preventive advice, community health staff do not deliver opportunistic prevention, particularly in relation to diet [ 8 , 17 ].
Perceptions and beliefs towards obesity prevention in health services
This review found that along with practical barriers to changing practice including a lack of time, resources or clinical guidelines [ 34 , 38 , 39 , 49 ], a key barrier to healthcare based obesity prevention is the perceptions and beliefs of health professionals towards obesity. As well as lacking confidence or knowledge about how to integrate prevention into clinical care, health professionals may simply not see it is their role [ 37 ]. There is also an issue with judgements being made in relation to who might benefit from prevention along with a negative view of the effectiveness of prevention, compounded by a view that preventing obesity is a matter of personal responsibility and choice [ 25 , 38 ].
The 13 studies which specifically looked at this issue are summarised in Category 5 of Tables 1 , 2 , 3 , 4 , 5 . These papers used a range of methods to ascertain attitudes, including questionnaires or surveys [ 8 , 32 , 36 , 37 , 39 , 40 , 46 , 49 , 50 ] and semi-structured interviews or focus groups [ 33 , 34 , 35 , 38 ] and were conducted with health professionals [ 33 , 34 , 35 , 37 , 38 , 39 , 49 , 50 ] and consumers [ 8 , 32 , 36 , 40 , 46 ]. Due to the range of methods and small numbers of many of the studies the results are not necessarily generalisable but a recurrence of themes indicates that perceptions and beliefs should be considered when incorporating obesity prevention into health care services.
The view of health professionals, that prevention is not their role, may be reinforced by the fact that they will probably not have had specific training in assessment and advice [ 16 ]. They may make judgements on who would benefit from preventive advice and tend to only raise the issue of weight if they know the patient [ 38 ]. Whilst health professionals are aware of the health implications of excess weight there may be a perception that they cannot be effective in their role due to a lack of patient motivation to enact change [ 25 ]. Other studies have shown that patients may not be told they are overweight or have the health consequences of being overweight discussed [ 21 , 32 ]. This is despite evidence to suggest that being told firstly they are overweight and secondly the health risks of excess weight can impact on an individual’s readiness to make changes to diet and levels of physical activity [ 28 ]. When discussions do occur, they are more likely to be with people who are already obese [ 24 , 28 ] or who have more frequent health encounters indicating that they have more complex health problems [ 29 ]. By clinicians not discussing weight and lifestyle with people before it becomes a significant problem there is a missed opportunity to prevent illness development based on known risk factors.
The uptake of prevention may also be impacted by a view that obesity is an issue of lifestyle choice and personal responsibility and therefore not the responsibility of health services unless linked to the treatment of a specific clinical condition [ 35 , 38 ]. Clinical guidelines may not be consistently followed because of a lack of knowledge of the guidelines existence or a belief that the guidelines will be ineffective due to pre-conceived ideas about the group of clients being targeted or a lack of confidence in the guidelines [ 19 , 35 ] . Specific to maternity services, clinicians acknowledge that weight gain in pregnancy is an issue but do not perceive that their patients see it as a problem [ 30 ]. In some instances, health professionals don’t feel confident talking to their patients about excess weight [ 35 , 38 , 39 , 51 ]. These findings occur even in areas where policy is in place directing clinicians to incorporate prevention, highlighting the need for more comprehensive, multi component change management strategies to enable health professionals to develop their practice to incorporate prevention routinely into interventions [ 8 ].
Without further training, baseline knowledge on appropriate interventions to support obesity prevention is generally poor [ 39 ] and advice may be given based on the clinicians own experience of weight management [ 38 ]. Educating staff about prevention may lead to an increase in assessment of risk but not a significant increase in brief advice or referral to other services for prevention intervention [ 15 , 17 ]. Both of these later elements are key to impacting on an individual’s chronic disease risk profile [ 16 ]. Training of staff may need to extend beyond principles of prevention and also include training on communicating complex information to people with low health literacy. This should include teaching techniques to ensure health professionals clarify their patient has understood information, [ 12 ] as this is a significant element in someone being able to adopt and follow preventive care advice [ 45 ].
However, the evidence of what education strategies are most effective, particularly in relation to increasing assessment and referral across all risk factors, is limited [ 52 ]. A systematic review of interventions to change the behaviour of health professionals found just six randomised control trials and the combined results of these were ambiguous [ 19 ]. When specifically looking at factors influencing health professionals decision to provide counselling regarding physical activity, the health professionals own levels of physical activity, whether or not they have specific training, knowing the patient well and the patient having risk factors for chronic disease were all influencing factors [ 22 ].
This review examined the literature in order to ascertain the role of hospital and community- based health services in adult obesity prevention as well as the potential enablers and barriers to the delivery of preventive health services. Whilst it is acknowledged that the health care system alone is not the answer to reducing the population impact of obesity [ 53 ], there is evidence that health services can significantly contribute to obesity prevention commencing with screening all patients for risk factors and providing brief advice. This should be followed up with referral to a service which provides long term follow-up with a focus on lifestyle change rather than just weight loss and should include consideration of an individual’s health literacy [ 41 , 42 , 43 , 44 ].
However, the reviewed evidence indicates that existing clinical guidelines, including the application of the 5As framework, are not being fully implemented. Where training and resources have focussed on prevention, there is an increase in the rate of screening provided but only a limited change in the rates of brief advice or referral to an intervention service [ 12 , 15 , 16 , 17 ]. Whilst assessment of risk factors may offer some benefits, greater change is achieved when this is followed up by advice and clear, individualised input to assist people to apply the advice to their own circumstances [ 54 ].
In taking a scoping approach to the role of health services, this review was able to draw out that a significant barrier to the implementation of prevention guidelines are the perceptions of health professionals. They may not see prevention as their role [ 16 ], make judgements about the causes of and responsibility for an individual’s weight, or make subjective decisions about who will benefit from their advice [ 25 , 35 , 38 ]. Health professionals may also not feel sufficiently confident to raise the issue of weight because of the social meanings attached or lack of knowledge [ 35 , 38 , 39 , 51 ]. Our review reveals these issues are common to nursing, allied health and medical staff.
Health care is predominantly delivered within a reactive model of care which is at odds with the concept of prevention [ 55 ]. Whilst there are obesity prevention guidelines which highlight the need to apply a framework such as the 5As, this fundamentally linear tool is designed to work within a traditional health care approach which focusses on the diagnosis and treatment of acute disease. As has been shown by this review, health professionals’ willingness or ability to change practice may be influenced by a range of factors, including their personal perceptions of obesity and of the potential value of prevention. So, whilst at a macro level policy and guidelines may be in place, implementation is hindered at a meso level by the mismatch between the medical model and the multifactorial causes of obesity and at a micro level by the impact of personal beliefs on patient interaction. Each of the factors dynamically influence the others so need should not be considered in isolation [ 53 ].
Changing the health system to implement effective action for the prevention of obesity therefore calls for an examination of the issues through a systems lens rather than taking a simple problem-solution driven approach. Health services are a complex system, constituted of a range of people, processes, activities, settings and structures. The interrelationships, boundaries, processes and perspectives connect in dynamic and non-linear ways which may result in emergent self-organised behaviour [ 56 ]. Importantly it should be acknowledged that systems are often nested within other systems with their own dynamics at play. Consequently, a search for solutions means identifying multiple causes as well as multiple points for intervention and being aware of unintended consequences [ 2 , 57 ]. The studies identified by this review focussed on a linear approach to implementing guidelines or examined the perspectives of just one clinical team or group within a system. There is a need for research to be undertaken which, using a systems approach, examines the opportunities and threats to prevention from the perspective of a range of players within the system and considers how these perspectives might be influenced by policy and guidelines, as well as each other. This could include looking at moving beyond traditional structural boundaries to look at alternative models of care to the medical model including the use of support roles outside of those typically considered to be health professionals, particularly in the role of ongoing support [ 56 , 58 ].
Obesity is often described as a ‘wicked’ problem due to the multifactorial causes requiring complex solutions. Whilst a population health approach is important to address this complexity, it is important that the remit of health services is extended beyond medical treatment to incorporate obesity prevention. [ 59 ]. Though this scoping review has demonstrated that there is evidence for incorporating obesity prevention into clinical care, research to date has taken a linear approach to the implementation of guidelines without explicitly factoring in the impact of the perceptions of clinicians and managers to the prevention role or addressing the individual responsibility discourse. Further research into the role of health services in obesity prevention should take a systems approach to examine the impacts of changing models of care whilst also taking into account the perceptions of health staff towards obesity and obesity prevention and the breadth of issues impacting on each individual’s ability to make lifestyle changes.
Strengths and limitations of the reviews
This review contributes to an understanding of the role of health services in obesity prevention by specifically focussing on services outside of primary health. The use of a scoping review allowed for broad coverage of the literature in order that the main issues could be highlighted in order to inform health policy, clinical practice and future research. The broad aims of the review may impact on attempts to replicate the review. Limiting the review to English language references may have excluded some evidence.
Availability of data and materials
Not applicable
Abbreviations
National Health and Medical Research Council
Royal Australian College of General Practitioners
World Health Organisation
Australian Institute of Health and Welfare. Premature mortaility from chronic disease. Canberra: AIHW; 2010.
Google Scholar
Wutzke, S., et al., Systems approaches for chronic disease prevention: sound logic and empirical evidence, but is this view shared outside of academia? Public health research & practice. n.d.. 2016.
Demattia R. Involve physicians and the local community in obesity initiatives. Manag Healthc Exec. 2013;23(3):48–9.
Brown WV, et al. Obesity: why be concerned? Am J Med. 2009;122(4 Suppl 1):S4–S11.
Article Google Scholar
Mastellos N, et al. Transtheoretical model stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst Rev. 2014;(2):1–88.
Wolf AM, Woodworth KA. Obesity prevention: recommended strategies and challenges. Am J Med. 2009;122(4 Suppl 1):S19–23.
Mitchell N, et al. Obesity: overview of an epidemic. Psychiatr Clin North Am. 2011;34(4):717–32.
McElwaine K, et al. The delivery of preventive care to clients of community health services. BioMed Central Health Serv Res. 2013;13:167.
The Royal Australian College of General Practitioners. Guidelines for preventive activities in general practice. 9th ed. East Melbourne; 2016.
Brien SE, et al. Overview of a formal scoping review on health system report cards. Implement Sci. 2010;5(1):2.
Jackson C, et al. Specialist health visitor-led weight management intervention in primary care: exploratory evaluation. J Adv Nurs. 2007;58(1):23–34 12p.
Davis TC, et al. Provider and patient intervention to improve weight loss: a pilot study in a public hospital clinic. Patient Educ Couns. 2008;72(1):56–62.
Mustila T, et al. Pragmatic controlled trial to prevent childhood obesity in maternity and child health care clinics: pregnancy and infant weight outcomes (the VACOPP study). BMC Pediatr. 2013;13(1):80.
Claesson IM, et al. Physical activity and psychological well-being in obese pregnant and postpartum women attending a weight-gain restriction programme. Midwifery. 2014;30(1):11–6.
McElwaine K, et al. Increasing preventive care by primary care nursing and allied health clinicians : a non-randomized, controlled trial. Am J Prev Med. 2014;47:424.
Bartlem KM, et al. Effectiveness of an intervention in increasing the provision of preventive care by community mental health services: a non-randomized, multiple baseline implementation trial. Implement Sci. 2016;11(1):1–12.
Wiggers J, et al. Increasing the provision of preventive care by community healthcare services: a stepped wedge implementation trial. Implement Sci. 2017;12(1):105.
Smith SA, Hulsey T, Goodnight W. Effects of obesity on pregnancy. JOGNN. 2008;37(2):176–84.
Flodgren G, et al. Interventions to change the behaviour of health professionals and the organisation of care to promote weight reduction in overweight and obese adults. Cochrane Database Syst Rev. 2010;(12):1–175
Kremers S, et al. Systematic prevention of overweight and obesity in adults: a qualitative and quantitative literature analysis. Obes Rev. 2010;11(5):371–9.
Article CAS Google Scholar
Kirk SF, et al. Effective weight management practice: a review of the lifestyle intervention evidence. Int J Obes. 2012;36(2):178–85.
Vuori IM, Lavie CJ, Blair SN. Physical activity promotion in the health care system. Mayo Clin Proc. 2013;88(12):1446–61.
Kushner RF, Ryan DH. Assessment and lifestyle management of patients with obesity: clinical recommendations from systematic reviews. Jama. 2014;312(9):943–52.
Lutfiyya MN, et al. Primary prevention of overweight and obesity: an analysis of national survey data. J Gen Intern Med. 2008;23(6):821–3.
Kemper KA. Stratifying patients for weight loss counseling. Nurs Pract. 2010;35(8):33–8 6p.
Phelan S. Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202(2):135.e1–8.
Heslehurst N. Identifying ‘at risk’ women and the impact of maternal obesity on National Health Service maternity services. Proc Nutr Soc. 2011;70(4):439–49.
Post RE, et al. The influence of physician acknowledgment of patients’ weight status on patient perceptions of overweight and obesity in the United States. Arch Intern Med. 2011;171(4):316–21.
Ahn S, Smith ML, Ory MG. Physicians’ discussions about body weight, healthy diet, and physical activity with overweight or obese elderly patients. J Aging Health. 2012;24(7):1179–202.
Oken E, et al. A qualitative study of gestational weight gain counseling and tracking. Matern Child Health J. 2013;17(8):1508–17.
Miller M, et al. Preventing maternal and early childhood obesity: the fetal flaw in Australian perinatal care. Aust J Prim Health. 2014;20(2):123–7.
Durant NH, et al. Patient provider communication about the health effects of obesity. Patient Educ Couns. 2009;75(1):53–7.
Heslehurst N, et al. How can maternity services be developed to effectively address maternal obesity? A qualitative study. Midwifery. 2011;27(5):e170–7.
Smith SA, et al. Community-based service provision for the prevention and management of maternal obesity in the north east of England: a qualitative study. Public Health. 2011;125(8):518–24.
Gunther S, et al. Barriers and enablers to managing obesity in general practice: a practical approach for use in implementation activities. Qual Prim Care. 2012;20(2):93–103.
PubMed Google Scholar
Leslie WS, Gibson A, Hankey CR. Prevention and management of excessive gestational weight gain: a survey of overweight and obese pregnant women. BMC Pregnancy Childbirth. 2013;13:10.
Robson D, et al. Mental health nursing and physical health care: a cross sectional study of nurses’ attitudes, practice and perceived training needs for the physical health care of people with severe mental illness. Int J Ment Health Nurs. 2013;22:409.
Schauer GL, et al. A qualitative inquiry about weight counseling practices in community health centers. Patient Educ Couns. 2014;97(1):82–7.
Kable A, et al. Nurse provision of healthy lifestyle advice to people who are overweight or obese. Nurs Health Sci. 2015;17(4):451–9.
Bartlem K, et al. Acceptability and receipt of preventive care for chronic-disease health risk behaviours reported by clients of community mental health services. Psychiatr Serv. 2015;66:857.
National Health and Medical Research Council, editor. Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. National Health and Medical Research Council, Editor. Melbourne; 2013.
Moyer VA, U.S.P.S.T. Force. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. [Summary for patients in Ann Intern Med. 2012 Sep 4;157(5):I-32; PMID: 22733111]. Ann Intern Med. 2012;157(5):373–8.
National Institute for Health and Clinical Excellence, Obesity prevention clinical guideline (CG43). 2006.
Royal Australian College of General Practitioners. Guidelines for preventive activities in general practice. 9th ed. RACGP, Editor. East Melbourne; 2016.
Harris M, Lloyd J. The role of Australian primary health care in the prevention of chronic disease. Australian National Preventive Health Agency, Editor; 2012.
Tol J, et al. Overweight and obese adults have low intentions of seeking weight-related care: a cross-sectional survey. BMC Public Health. 2014;14:582.
Australian Commission on Safety and Quality in Health Care. Health literacy: taking action to improve safety and quality. ACSQHC, Editor. Sydney; 2014.
Olson CM, et al. The healthy start partnership: an approach to obesity prevention in young families. Fam Community Health. 2014;37(1):74–85.
Brown I, Thompson J. Primary care nurses’ attitudes, beliefs and own body size in relation to obesity management. J Adv Nurs. 2007;60(5):535–43.
Nahm E-S, et al. Nurses’ self-care behaviors related to weight and stress. Nurs Outlook. 2012;60(_5):e23–31.
Brown I, et al. Management of obesity in primary care: nurses’ practices, beliefs and attitudes. J Adv Nurs. 2007;59(4):329–41.
McElwaine KM, et al. Systematic review of interventions to increase the delivery of preventive care by primary care nurses and allied health clinicians. Implement Sci. 2016;11(1):1–15.
World Health Organisation. Innovative care for chronic conditions: building blocks for action: global report. Geneva; 2002.
Aveyard P, et al. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction. 2012;107(6):1066–73.
Bauer UE, et al. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52.
Lipsitz LA. Understanding health care as a complex system: the foundation for unintended consequences. JAMA. 2012;308(3):243–4.
The Health Foundation. Evidence scan: Complex adaptive systems. London; 2010.
Dietz WH, et al. An integrated framework for the prevention and treatment of obesity and its related chronic diseases. Health Aff (Millwood). 2015;34(9):1456–63.
Kirk SF, et al. Blame, shame, and lack of support: a multilevel study on obesity management. Qual Health Res. 2014;24(6):790–800.
Lindstrom, J., Peltonen, M., Tuomilehto, J. Lifestyle strategies for weight control: experience from the Finnish Diabetes Prevention Study. Proceedings of the Nutririon Society, 2005;64:81–88
Ma, J., Xiao, L., Stafford, R.S. Adult Obesity and Office-based Quality of Care in the United States. Obesity 2009;17(5):1077–1085
Aronne, L.J., Wadden, T., Keenan Isoldi, K., Woodworth, K.A. When prevention fails: obesity treatment strategies. The American Journal of Medicine, 2019;122(4)I–CO4
Hernandez-Boussard, T., Ahmed, S M., Morton, J M. Obesity disparities in preventive care: findings from teh National Ambulatory Medical Care Survey, 2005-2007. Obesity. 2012;20(8):1639–44.
Download references
Acknowledgements
The primary author, Claire Pearce, receives a scholarship from the Australian Prevention Partnership Centre (TAPPC) to support her PhD candidacy. The co-authors all have an affiliation with TAPPC. The funding body was not involved directly in the design or completion of the study or in the writing of the manuscript.
Author information
Authors and affiliations.
The Australian Prevention Partnership Centre, Sydney, NSW, Australia
Claire Pearce, Lucie Rychetnik, Sonia Wutzke & Andrew Wilson
Menzies Centre for Health Policy, University of Sydney, Sydney, NSW, Australia
Claire Pearce, Lucie Rychetnik & Andrew Wilson
Canberra Health Services, Canberra, ACT, Australia
Claire Pearce
School of Medicine, University of Notre Dame, Sydney, Australia
Lucie Rychetnik
Author notes
Sonia wutzke is deceased. this paper is dedicated to her memory..
- Sonia Wutzke
You can also search for this author in PubMed Google Scholar
Contributions
CP conceived the study, screened citations and full-text articles, analysed and interpreted the data, and wrote and edited the manuscript. LR reviewed the analysis.
AW, SW and LR conceptualised and edited the manuscript. SW developed the results section and edited the initial drafts of the manuscript. CP, LR and AW have read and approved the final manuscript (not applicable for SW).
Corresponding author
Correspondence to Claire Pearce .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Pearce, C., Rychetnik, L., Wutzke, S. et al. Obesity prevention and the role of hospital and community-based health services: a scoping review. BMC Health Serv Res 19 , 453 (2019). https://doi.org/10.1186/s12913-019-4262-3
Download citation
Received : 03 April 2019
Accepted : 14 June 2019
Published : 05 July 2019
DOI : https://doi.org/10.1186/s12913-019-4262-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health services
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Strategic Plan
Strategic Plan for NIH Obesity Research
The Purpose of the Strategic Plan
The Strategic Plan for NIH Obesity Research serves as a guide to accelerate a broad spectrum of research toward developing new and more effective approaches to address the tremendous burden of obesity, so that people can look forward to healthier lives.
The Plan was originally published in 2011. In 2018-2019, the Obesity Research Task Force confirmed that the challenges and opportunities identified in the Plan reflect the current research landscape and should continue to guide obesity research.
- Full Report for the scientific community (PDF, 716.76 KB)
- Summary Report non-technical (PDF, 627.47 KB)
- View a video of former NIH Director Dr. Francis Collins discussing the Strategic Plan
Development of the Strategic Plan
The Strategic Plan was developed by the NIH Obesity Research Task Force with crucial input from researchers external to the NIH, professional and other health-focused organizations, and others through a public comment period. Research challenges and opportunities identified at meetings and workshops also helped shape the Strategic Plan, and will continue to inform NIH research planning.
Major Themes for Research Highlighted in the Strategic Plan
Research Opportunities:
- Discover fundamental biological processes that regulate body weight and influence behavior
- Understand the factors that contribute to obesity and its consequences
- Design and test new interventions for achieving and maintaining a healthy weight
- Evaluate promising strategies for obesity prevention and treatment in real-world settings and diverse populations
- Harness technology and tools to advance obesity research and improve healthcare delivery
Application of Research Findings:
- Facilitate integration of research results into community programs and medical practice
Questions and Answers
What are the goals of the plan.
The efforts of many individuals and institutions are essential to reducing the prevalence of obesity – including government, businesses, community organizations, healthcare professionals, schools, and families. Research can provide the foundation for these efforts. As the country's medical research agency, the NIH funds a spectrum of research to reduce the prevalence and burden of obesity. Research can lead to a better understanding of the causes and consequences of obesity and will give us the evidence for what works to prevent and treat obesity. In addition, research will help us reduce health disparities and inform policies.
Researchers seek to answer many questions, for example:
- How can we increase and use our knowledge of human biology and behavior to develop new and more effective prevention and treatment approaches?
- What aspects of our community environments and daily lives contribute to unhealthy eating and insufficient physical activity–and what can we change to make it easier for people to achieve a healthy weight?
- How can we rigorously evaluate interventions–whether based on individual lifestyle changes, pharmacological or surgical approaches, community-based programs, policy changes, or other environmental changes–to determine which really work?
- How do we scale up the approaches that show promise and expand those proven effective, in order to reach more people?
- Given that no single intervention will solve this complex problem, how can we continue to develop new and innovative approaches?
We hope that the plan will serve as a guide to accelerate progress in obesity research, and that this research will ultimately help extend healthy life and reduce the burdens of illness and disability.
Why create a strategic plan for obesity research?
Obesity is highly prevalent in the United States. Obesity increases a person’s chance of developing many health problems, including type 2 diabetes, heart disease, high blood pressure, fatty liver disease, respiratory problems (e.g., asthma and sleep apnea), and some cancers. Obesity adversely affects people's quality of life and exacts a substantial economic toll on the nation.
Obesity arises from a complex interplay of forces and affects some populations disproportionately. We need to take a multifaceted approach to combat it. Simply telling people to "eat less and exercise more" is not enough.
Research is the foundation for finding viable solutions. Research allows us to explore the roles that genetics and biology, our environment, and our lifestyles play in obesity – and to transform that knowledge into better prevention and treatment strategies. Through research, we rigorously evaluate interventions to see which ones really work and who can benefit most.
How can scientists apply to the NIH for funding for obesity-related research?
Information on funding opportunities , including lists of NIH obesity-related research solicitations, is available.
The strategic plan identifies and encourages a broad range of research opportunities and priorities to accelerate obesity research.
Researchers can obtain information about applying for NIH funding, and about the peer review system through which applications are evaluated, on the NIH Grants and Funding website . NIH publishes Notices of Funding Opportunities to solicit research on topics specific to many diseases and conditions, including obesity. Additionally, researchers are invited to submit applications independent of these topic-specific solicitations. View complete listings of all NIH research solicitations .
Grant applications that fall within the areas covered in the strategic plan are considered under the same review processes as other NIH research applications.
Who can be involved in implementing the strategic plan?
Advancing the progress of obesity research requires a strong pool of researchers with diverse areas of expertise who are dedicated to understanding and ameliorating obesity and its many adverse outcomes.
But researchers alone can't solve the obesity problem. We need the commitment of policymakers, healthcare practitioners, businesses, communities, families, and individuals to partner in research and implement what we learn. The NIH works with groups across the country and around the world—including universities, medical centers, businesses, schools, and communities—to study obesity, develop and evaluate strategies for prevention and treatment, train researchers, and teach people about science-based interventions to improve their health.
How can people act on the plan?
Everyone can play a role in enhancing obesity research and moving research results to longer and healthier lives. For example:
- Researchers can submit obesity-related grant applications that align with the areas of opportunity highlighted in the plan.
- When taking actions to reduce obesity—such as adding sidewalks or playgrounds to increase opportunities for physical activity or improving access to fresh, healthy foods—policymakers, community organizations, and others can participate in research to evaluate these efforts, to determine what is working, and how successful approaches could be expanded.
- The public can participate in clinical research studies to help inform the science of obesity – helping scientists to identify contributing factors and evaluate new prevention and treatment strategies.
- Open access
- Published: 21 June 2021

The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies
- Emma Farrell ORCID: orcid.org/0000-0002-7780-9428 1 ,
- Marta Bustillo 2 ,
- Carel W. le Roux 3 ,
- Joe Nadglowski 4 ,
- Eva Hollmann 1 &
- Deirdre McGillicuddy 1
Systematic Reviews volume 10 , Article number: 181 ( 2021 ) Cite this article
6324 Accesses
9 Altmetric
Metrics details
Obesity is a prevalent, complex, progressive and relapsing chronic disease characterised by abnormal or excessive body fat that impairs health and quality of life. It affects more than 650 million adults worldwide and is associated with a range of health complications. Qualitative research plays a key role in understanding patient experiences and the factors that facilitate or hinder the effectiveness of health interventions. This review aims to systematically locate, assess and synthesise qualitative studies in order to develop a more comprehensive understanding of the lived experience of people with obesity.
This is a protocol for a qualitative evidence synthesis of the lived experience of people with obesity. A defined search strategy will be employed in conducting a comprehensive literature search of the following databases: PubMed, Embase, PsycInfo, PsycArticles and Dimensions (from 2011 onwards). Qualitative studies focusing on the lived experience of adults with obesity (BMI >30) will be included. Two reviewers will independently screen all citations, abstracts and full-text articles and abstract data. The quality of included studies will be appraised using the critical appraisal skills programme (CASP) criteria. Thematic synthesis will be conducted on all of the included studies. Confidence in the review findings will be assessed using GRADE CERQual.
The findings from this synthesis will be used to inform the EU Innovative Medicines Initiative (IMI)-funded SOPHIA (Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy) study. The objective of SOPHIA is to optimise future obesity treatment and stimulate a new narrative, understanding and vocabulary around obesity as a set of complex and chronic diseases. The findings will also be useful to health care providers and policy makers who seek to understand the experience of those with obesity.
Systematic review registration
PROSPERO CRD42020214560 .
Peer Review reports
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health and quality of life, increases the risk of long-term medical complications and reduces lifespan [ 1 ]. Operationally defined in epidemiological and population studies as a body mass index (BMI) greater than or equal to 30, obesity affects more than 650 million adults worldwide [ 2 ]. Its prevalence has almost tripled between 1975 and 2016, and, globally, there are now more people with obesity than people classified as underweight [ 2 ].
Obesity is caused by the complex interplay of multiple genetic, metabolic, behavioural and environmental factors, with the latter thought to be the proximate factor which enabled the substantial rise in the prevalence of obesity in recent decades [ 3 , 4 ]. This increased prevalence has resulted in obesity becoming a major public health issue with a resulting growth in health care and economic costs [ 5 , 6 ]. At a population level, health complications from excess body fat increase as BMI increases [ 7 ]. At the individual level, health complications occur due to a variety of factors such as distribution of adiposity, environment, genetic, biologic and socioeconomic factors [ 8 ]. These health complications include type 2 diabetes [ 9 ], gallbladder disease [ 10 ] and non-alcoholic fatty liver disease [ 11 ]. Excess body fat can also place an individual at increased cardiometabolic and cancer risk [ 12 , 13 , 14 ] with an estimated 20% of all cancers attributed to obesity [ 15 ].
Although first recognised as a disease by the American Medical Association in 2013 [ 16 ], the dominant cultural narrative continues to present obesity as a failure of willpower. People with obesity are positioned as personally responsible for their weight. This, combined with the moralisation of health behaviours and the widespread association between thinness, self-control and success, has resulted in those who fail to live up to this cultural ideal being subject to weight bias, stigma and discrimination [ 17 , 18 , 19 ]. Weight bias, stigma and discrimination have been found to contribute, independent of weight or BMI, to increased morbidity or mortality [ 20 ].
Thomas et al. [ 21 ] highlighted, more than a decade ago, the need to rethink how we approach obesity so as not to perpetuate damaging stereotypes at a societal level. Obesity research then, as now, largely focused on measurable outcomes and quantifiable terms such as body mass index [ 22 , 23 ]. Qualitative research approaches play a key role in understanding patient experiences, how factors facilitate or hinder the effectiveness of interventions and how the processes of interventions are perceived and implemented by users [ 24 ]. Studies adopting qualitative approaches have been shown to deliver a greater depth of understanding of complex and socially mediated diseases such as obesity [ 25 ]. In spite of an increasing recognition of the integral role of patient experience in health research [ 25 , 26 ], the voices of patients remain largely underrepresented in obesity research [ 27 , 28 ].
Systematic reviews and syntheses of qualitative studies are recognised as a useful contribution to evidence and policy development [ 29 ]. To the best of the authors’ knowledge, this will be the first systematic review and synthesis of qualitative studies focusing on the lived experience of people with obesity. While systematic reviews have been carried out on patient experiences of treatments such as behavioural management [ 30 ] and bariatric surgery [ 31 ], this review and synthesis will be the first to focus on the experience of living with obesity rather than patient experiences of particular treatments or interventions. This focus represents a growing awareness that ‘patients have a specific expertise and knowledge derived from lived experience’ and that understanding lived experience can help ‘make healthcare both effective and more efficient’ [ 32 ].
This paper outlines a protocol for the systematic review of qualitative studies based on the lived experience of people with obesity. The findings of this review will be synthesised in order to develop an overview of the lived experience of patients with obesity. It will look, in particular, at patient concerns around the risks of obesity and their aspirations for response to obesity treatment.
The review protocol has been registered within the PROSPERO database (registration number: CRD42020214560) and is being reported in accordance with the reporting guidance provided in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement [ 33 , 34 ] (see checklist in Additional file 1 ).
Information sources and search strategy
The primary source of literature will be a structured search of the following electronic databases (from January 2011 onwards—to encompass the increase in research focused on patient experience observed over the last 10 years): PubMed, Embase, PsycInfo, PsycArticles and Dimensions. There is no methodological agreement as to how many search terms or databases out to be searched as part of a ‘good’ qualitative synthesis (Toye et al. [ 35 ]). However, the breadth and depth of the search terms, the inclusion of clinical and personal language and the variety within the selected databases, which cover areas such as medicine, nursing, psychology and sociology, will position this qualitative synthesis as comprehensive. Grey literature will not be included in this study as its purpose is to conduct a comprehensive review of peer-reviewed primary research. The study’s patient advisory board will be consulted at each stage of the review process, and content experts and authors who are prolific in the field will be contacted. The literature searches will be designed and conducted by the review team which includes an experienced university librarian (MB) following the methodological guidance of chapter two of the JBI Manual for Evidence Synthesis [ 36 ]. The search will include a broad range of terms and keywords related to obesity and qualitative research. A full draft search strategy for PubMed is provided in Additional file 2 .
Eligibility criteria
Studies based on primary data generated with adults with obesity (operationally defined as BMI >30) and focusing on their lived experience will be eligible for inclusion in this synthesis (Table 1 ). The context can include any country and all three levels of care provision (primary, secondary and tertiary). Only peer-reviewed, English language, articles will be included. Studies adopting a qualitative design, such as phenomenology, grounded theory or ethnography, and employing qualitative methods of data collection and analysis, such as interviews, focus groups, life histories and thematic analysis, will be included. Publications with a specific focus, for example, patient’s experience of bariatric surgery, will be included, as well as studies adopting a more general view of the experience of obesity.
Screening and study selection process
Search results will be imported to Endnote X9, and duplicate entries will be removed. Covidence [ 38 ] will be used to screen references with two reviewers (EF and EH) removing entries that are clearly unrelated to the research question. Titles and abstracts will then be independently screened by two reviewers (EF and EH) according to the inclusion criteria (Table 1 ). Any disagreements will be resolved through a third reviewer (DMcG). This layer of screening will determine which publications will be eligible for independent full-text review by two reviewers (EF and EH) with disagreements again being resolved by a third reviewer (DMcG).
Data extraction
Data will be extracted independently by two researchers (EF and EH) and combined in table format using the following headings: author, year, title, country, research aims, participant characteristics, method of data collection, method of data analysis, author conclusions and qualitative themes. In the case of insufficient or unclear information in a potentially eligible article, the authors will be contacted by email to obtain or confirm data, and a timeframe of 3 weeks to reply will be offered before article exclusion.
Quality appraisal of included studies
This qualitative synthesis will facilitate the development of a conceptual understanding of obesity and will be used to inform the development of policy and practice. As such, it is important that the studies included are themselves of suitable quality. The methodological quality of all included studies will be assessed using the critical appraisal skills programme (CASP) checklist, and studies that are deemed of insufficient quality will be excluded. The CASP checklist for qualitative research comprises ten questions that cover three main issues: Are the results of the study under review valid? What are the results? Will the results help locally? Two reviewers (EF and EH) will independently evaluate each study using the checklist with a third and fourth reviewer (DMcG and MB) available for consultation in the event of disagreement.
Data synthesis
The data generated through the systematic review outlined above will be synthesised using thematic synthesis as described by Thomas and Harden [ 39 ]. Thematic synthesis enables researchers to stay ‘close’ to the data of primary studies, synthesise them in a transparent way and produce new concepts and hypotheses. This inductive approach is useful for drawing inference based on common themes from studies with different designs and perspectives. Thematic synthesis is made up of a three-step process. Step one consists of line by line coding of the findings of primary studies. The second step involves organising these ‘free codes’ into related areas to construct ‘descriptive’ themes. In step three, the descriptive themes that emerged will be iteratively examined and compared to ‘go beyond’ the descriptive themes and the content of the initial studies. This step will generate analytical themes that will provide new insights related to the topic under review.
Data will be coded using NVivo 12. In order to increase the confirmability of the analysis, studies will be reviewed independently by two reviewers (EF and EH) following the three-step process outlined above. This process will be overseen by a third reviewer (DMcG). In order to increase the credibility of the findings, an overview of the results will be brought to a panel of patient representatives for discussion. Direct quotations from participants in the primary studies will be italicised and indented to distinguish them from author interpretations.
Assessment of confidence in the review findings
Confidence in the evidence generated as a result of this qualitative synthesis will be assessed using the Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research (GRADE CERQual) [ 40 ] approach. Four components contribute to the assessment of confidence in the evidence: methodological limitations, relevance, coherence and adequacy of data. The methodological limitations of included studies will be examined using the CASP tool. Relevance assesses the degree to which the evidence from the primary studies applies to the synthesis question while coherence assesses how well the findings are supported by the primary studies. Adequacy of data assesses how much data supports a finding and how rich this data is. Confidence in the evidence will be independently assessed by two reviewers (EF and EH), graded as high, moderate or low, and discussed collectively amongst the research team.
Reflexivity
For the purposes of transparency and reflexivity, it will be important to consider the findings of the qualitative synthesis and how these are reached, in the context of researchers’ worldviews and experiences (Larkin et al, 2019). Authors have backgrounds in health science (EF and EH), education (DMcG and EF), nursing (EH), sociology (DMcG), philosophy (EF) and information science (MB). Prior to conducting the qualitative synthesis, the authors will examine and discuss their preconceptions and beliefs surrounding the subject under study and consider the relevance of these preconceptions during each stage of analysis.
Dissemination of findings
Findings from the qualitative synthesis will be disseminated through publications in peer-reviewed journals, a comprehensive and in-depth project report and presentation at peer-reviewed academic conferences (such as EASO) within the field of obesity research. It is also envisaged that the qualitative synthesis will contribute to the shared value analysis to be undertaken with key stakeholders (including patients, clinicians, payers, policy makers, regulators and industry) within the broader study which seeks to create a new narrative around obesity diagnosis and treatment by foregrounding patient experiences and voice(s). This synthesis will be disseminated to the 29 project partners through oral presentations at management board meetings and at the general assembly. It will also be presented as an educational resource for clinicians to contribute to an improved understanding of patient experience of living with obesity.
Obesity is a complex chronic disease which increases the risk of long-term medical complications and a reduced quality of life. It affects a significant proportion of the world’s population and is a major public health concern. Obesity is the result of a complex interplay of multiple factors including genetic, metabolic, behavioural and environmental factors. In spite of this complexity, obesity is often construed in simple terms as a failure of willpower. People with obesity are subject to weight bias, stigma and discrimination which in themselves result in increased risk of mobility or mortality. Research in the area of obesity has tended towards measurable outcomes and quantitative variables that fail to capture the complexity associated with the experience of obesity. A need to rethink how we approach obesity has been identified—one that represents the voices and experiences of people living with obesity. This paper outlines a protocol for the systematic review of available literature on the lived experience of people with obesity and the synthesis of these findings in order to develop an understanding of patient experiences, their concerns regarding the risks associated with obesity and their aspirations for response to obesity treatment. Its main strengths will be the breadth of its search remit—focusing on the experiences of people with obesity rather than their experience of a particular treatment or intervention. It will also involve people living with obesity and its findings disseminated amongst the 29 international partners SOPHIA research consortium, in peer reviewed journals and at academic conferences. Just as the study’s broad remit is its strength, it is also a potential challenge as it is anticipated that searchers will generate many thousands of results owing to the breadth of the search terms. However, to the best of the authors’ knowledge, this will be the first systematic review and synthesis of its kind, and its findings will contribute to shaping the optimisation of future obesity understanding and treatment.
Availability of data and materials
Not applicable.
Abbreviations
Body mass index
Critical appraisal skills programme
Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research
Innovative Medicines Initiative
Medical Subject Headings
Population, phenomenon of interest, context, study type
Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. Can Med Assoc J. 2020;192(31):E875–91. https://doi.org/10.1503/cmaj.191707 .
Article Google Scholar
World Health Organisation. Fact sheet: obesity and overweight. Geneva: World Health Organisation; 2020.
Google Scholar
Mechanick J, Hurley D, Garvey W. Adiposity-based chronic disease as a new diagnostic term: the American Association of Clinical Endocrinologists and American College Of Endocrinology position statement. Endocrine Pract. 2017;23(3):372–8. https://doi.org/10.4158/EP161688.PS .
Garvey W, Mechanick J. Proposal for a scientifically correct and medically actionable disease classification system (ICD) for obesity. Obesity. 2020;28(3):484–92. https://doi.org/10.1002/oby.22727 .
Article PubMed Google Scholar
Biener A, Cawley J, Meyerhoefer C. The high and rising costs of obesity to the US health care system. J Gen Intern Med. 2017;32(Suppl 1):6–8. https://doi.org/10.1007/s11606-016-3968-8 .
Article PubMed PubMed Central Google Scholar
Department of Health and Social Care. Healthy lives, healthy people: a call to action on obesity in England. London: Department of Health and Social Care; 2011.
Di Angelantonio E, Bhupathiraju SN, Wormser D, Gao P, Kaptoge S, de Gonzalez AB, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86. https://doi.org/10.1016/S0140-6736(16)30175-1 .
Sharma AM. M, M, M & M: a mnemonic for assessing obesity. Obesity Reviews. 2010;11(11):808–9. https://doi.org/10.1111/j.1467-789X.2010.00766.x .
Article PubMed CAS Google Scholar
Asnawi A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract 2010;89:309-19. Diab Res Clin Pract. 2010;89:309–19.
Dagfinn A, Teresa N, Lars JV. Body mass index, abdominal fatness and the risk of gallbladder disease. 2015;30(9):1009.
Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20(9).
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. 2003;289(2):187-193.
Grover SA, Kaouache M, Rempel P, Joseph L, Dawes M, Lau DCW, et al. Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: a modelling study. 2015;3(2):114-122.
Ackerman S, Blackburn O, Marchildon F, Cohen P. Insights into the link between obesity and cancer. Curr Obes Rep. 2017;6(2):195–203. https://doi.org/10.1007/s13679-017-0263-x .
Wolin K, Carson K, Colditz G. Obesity and cancer. Oncol. 2010;15(6):556–65. https://doi.org/10.1634/theoncologist.2009-0285 .
Resolution 420: Recognition of obesity as a disease [press release]. 05/16/13 2013.
Brownell KD. Personal responsibility and control over our bodies: when expectation exceeds reality. 1991;10(5):303-10.
Puhl RM, Latner JD, O'Brien K, Luedicke J, Danielsdottir S, Forhan M. A multinational examination of weight bias: predictors of anti-fat attitudes across four countries. 2015;39(7):1166-1173.
Browne NT. Weight bias, stigmatization, and bullying of obese youth. 2012;7(3):107-15.
Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. 2015;26(11):1803-11.
Thomas SL, Hyde J, Karunaratne A, Herbert D, Komesaroff PA. Being “fat” in today’s world: a qualitative study of the lived experiences of people with obesity in Australia. 2008;11(4):321-30.
Ogden K, Barr J, Rossetto G, Mercer J. A “messy ball of wool”: a qualitative study of the dimensions of the lived experience of obesity. 2020;8(1):1-14.
Ueland V, Furnes B, Dysvik E, R¯rtveit K. Living with obesity-existential experiences. 2019;14(1):1-12.
Avenell A, Robertson C, Skea Z, Jacobsen E, Boyers D, Cooper D, et al. Bariatric surgery, lifestyle interventions and orlistat for severe obesity: the REBALANCE mixed-methods systematic review and economic evaluation. 2018;22(68).
The PLoS Medicine Editors. Qualitative research: understanding patients’ needs and experiences. Plos Med. 2007;4(8):1283–4.
Boulton M, Fitzpatrick R. Qualitative methods for assessing health care doi:10.1136/qshc.3.2.107. Qual Health Care. 1994;3:107–13.
Johnstone J, Herredsberg C, Lacy L, Bayles P, Dierking L, Houck A, et al. What I wish my doctor really knew: the voices of patients with obesity. Ann Fam Med. 2020;18(2):169–71. https://doi.org/10.1370/afm.2494 .
Brown I, Thompson J, Tod A, Jones G. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract. 2006;56(530):666–72.
PubMed PubMed Central Google Scholar
Brown I, Gould J. Qualitative studies of obesity: a review of methodology. Health. 2013;5(8A3):69–80.
Garip G, Yardley L. A synthesis of qualitative research on overweight and obese people’s views and experiences of weight management. Clin Obes. 2011;1(2-3):10–126.
Coulman K, MacKichan F, Blazeby J, Owen-Smith A. Patient experiences of outcomes of bariatric surgery: a systematic review and qualitative synthesis. Obes Rev. 2017;18(5):547–59. https://doi.org/10.1111/obr.12518 .
European Patients’ Forum. “Patients’ Perceptions of Quality in Healthcare”: Report of a survey conducted by EPF in 2016 Brussels: European Patients’ Forum; 2017.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349(jan02 1):g7647. https://doi.org/10.1136/bmj.g7647 .
Toye F, et al. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol. 2014;14(80).
Lockwood C, Porrit K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, et al. Chapter 2: Systematic reviews of qualitative evidence. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis: JBI; 2020, doi: https://doi.org/10.46658/JBIMES-20-03 .
Methley AM, et al. PICO, PICOS and SPIDER: a comparison study of spcificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Services Res. 2014;14.
Covidence. Cochrane Community; 2020. Available from: https://www.covidence.org .
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. https://doi.org/10.1186/1471-2288-8-45 .
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13(1):2. https://doi.org/10.1186/s13012-017-0688-3 .
Download references
Acknowledgements
Any amendments made to this protocol when conducting the study will be outlined in PROSPERO and reported in the final manuscript.
This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking (JU) under grant agreement No 875534. The JU receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA and T1D Exchange, JDRF and Obesity Action Coalition. The funding body had no role in the design of the study and will not have a role in collection, analysis and interpretation of data or in writing the manuscript.
Author information
Authors and affiliations.
School of Education, University College Dublin, Belfield, Dublin 4, Ireland
Emma Farrell, Eva Hollmann & Deirdre McGillicuddy
University College Dublin Library, Dublin, Ireland
Marta Bustillo
Diabetes Complications Research Centre, University College Dublin, Dublin, Ireland
Carel W. le Roux
Obesity Action Coalition, Tampa, USA
Joe Nadglowski
You can also search for this author in PubMed Google Scholar
Contributions
EF conceptualised and designed the protocol with input from DMcG and MB. EF drafted the initial manuscript. EF and MB defined the concepts and search items with input from DmcG, CleR and JN. MB and EF designed and executed the search strategy. DMcG, CleR, JN and EH provided critical insights and reviewed and revised the protocol. All authors have approved and contributed to the final written manuscript.
Corresponding author
Correspondence to Emma Farrell .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:..
PRISMA-P (Preferred Reporting Items for Systematic review and Meta-Analysis Protocols) 2015 checklist: recommended items to address in a systematic review protocol*.
Additional file 2: Table 1
. Search PubMed search string.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Farrell, E., Bustillo, M., le Roux, C.W. et al. The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies. Syst Rev 10 , 181 (2021). https://doi.org/10.1186/s13643-021-01706-5
Download citation
Received : 28 October 2020
Accepted : 14 May 2021
Published : 21 June 2021
DOI : https://doi.org/10.1186/s13643-021-01706-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lived experience
- Patient experience
- Obesity treatment
- Qualitative
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Overweight and obesity: effectiveness of interventions in adults
Affiliations.
- 1 Centro de Salud San Carlos, San Lorenzo de El Escorial, Madrid, España. Electronic address: [email protected].
- 2 Sección Departamental de Enfermería, Facultad de Medicina, Universidad Autónoma de Madrid, Madrid, España.
- PMID: 29274691
- DOI: 10.1016/j.enfcli.2017.06.005
Objective: To identify the most effective interventions in overweight and obese adults.
Method: A narrative review through a search of the literature in databases PubMed, Cochrane, Joanna Briggs Institute, EMBASE, Cuiden y Cinahl with free and controlled language (MeSH terms) using Boolean operators AND and NOT. The research was limited to articles published between 2007 and 2015. Eighteen articles were selected based on the established inclusion and exclusion criteria.
Results: Different types of interventions were identified based on the modification of lifestyles, mainly diet, physical activity and behavior. Major differences were found in specific content, degree of intensity of interventions, time tracking and elements evaluated. Most of studies found statistically significant weight loss but this was limited in terms of weight and number of people. Web-based interventions have no uniform effect on weight loss but achieve similar levels to face-to-face interventions in maintaining weight loss.
Conclusions: The combination of personalised diet, exercise and cognitive behavioural therapy is the most effective form of intervention in overweight and obesity. There is insufficient data to indicate whether group or individual interventions are more effective. Online intervention allows greater accessibility and lower cost.
Keywords: Adulto; Adults; Intervención; Intervention; Obesidad; Obesity.
Copyright © 2017 Elsevier España, S.L.U. All rights reserved.
Publication types
- Obesity / therapy
- Overweight / therapy*
- Treatment Outcome
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 11, Issue 6
- Changing the narrative around obesity in the UK: a survey of people with obesity and healthcare professionals from the ACTION-IO study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-9560-7873 Carly A Hughes 1 , 2 ,
- Amy L Ahern 3 ,
- Harsha Kasetty 4 ,
- Barbara M McGowan 5 ,
- Helen M Parretti 2 ,
- Ann Vincent 6 ,
- Jason C G Halford 7
- 1 Fakenham Weight Management Service, Fakenham Medical Practice , Fakenham , UK
- 2 Norwich Medical School, University of East Anglia , Norwich , UK
- 3 MRC Epidemiology Unit , University of Cambridge , Cambridge , UK
- 4 Novo Nordisk Ltd , Gatwick , UK
- 5 Institute of Diabetes, Endocrinology and Obesity, Guy’s and St Thomas’ NHS Foundation Trust , London , UK
- 6 Department of Medicine , University College London , London , UK
- 7 School of Psychology, University of Leeds , Leeds , UK
- Correspondence to Dr Carly A Hughes; carly.hughes{at}nhs.net
Objectives To investigate the perceptions, attitudes, behaviours and potential barriers to effective obesity care in the UK using data collected from people with obesity (PwO) and healthcare professionals (HCPs) in the Awareness, Care, and Treatment In Obesity maNagement–International Observation (ACTION-IO) study.
Design UK’s PwO (body mass index of ≥30 kg/m 2 based on self-reported height and weight) and HCPs who manage patients with obesity completed an online survey.
Results In the UK, 1500 PwO and 306 HCPs completed the survey. Among the 47% of PwO who discussed weight with an HCP in the past 5 years, it took a mean of 9 years from the start of their struggles with weight until a discussion occurred. HCPs reported that PwO initiated 35% of weight-related discussions; PwO reported that they initiated 47% of discussions. Most PwO (85%) assumed full responsibility for their own weight loss. The presence of obesity-related comorbidities was cited by 76% of HCPs as a top criterion for initiating weight management conversations. The perception of lack of interest (72%) and motivation (61%) in losing weight was reported as top reasons by HCPs for not discussing weight with a patient. Sixty-five per cent of PwO liked their HCP bringing up weight during appointments. PwO reported complex and varied emotions following a weight loss conversation with an HCP, including supported (36%), hopeful (31%), motivated (23%) and embarrassed (17%). Follow-up appointments were scheduled for 19% of PwO after a weight discussion despite 62% wanting follow-up.
Conclusions The current narrative around obesity requires a paradigm shift in the UK to address the delay between PwO struggling with their weight and discussing weight with their HCP. Perceptions of lack of patient interest and motivation in weight management must be challenged along with the blame culture of individual responsibility that is prevalent throughout society. While PwO may welcome weight-related conversations with an HCP, they evoke complex feelings, demonstrating the need for sensitivity and respect in these conversations.
Trial registration number NCT03584191 .
- general medicine (see internal medicine)
- public health
- epidemiology
- medical education & training
Data availability statement
Data are available upon reasonable request. De-identified participant data will be made available for this article on a specialised SAS data platform. Datasets from Novo Nordisk will be available permanently after completion of data analysis. Access to data can be made through a request proposal form and the access criteria can be found online (novonordisk-trials.com). Data will be shared with bona fide researchers submitting a research proposal requesting access to data. Data use is subject to approval by the independent review board.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-045616
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
Strengths include the scientific rigour in the study design and implementation.
The large number of UK respondents and the ability to directly compare the UK data to the equivalent global dataset is an additional strength.
Limitations of this study include possible response bias from the population sampled and recall bias.
The causes of obesity are complex and multifaceted, encompassing biological, genetic, environmental, economic, social and psychological factors. 1–3 The chronic and relapsing nature of obesity is associated with many serious physical and psychological comorbidities, reduced quality of life and increased healthcare costs. 2 4–8 The WHO has recognised obesity as a disease, and the National Institute for Health and Care Excellence provides guidance on its assessment and treatment. 9 More recently, it has been recognised as a risk factor for severity of COVID-19 infection. 5 6 The prevalence of overweight and obesity among adults in the UK has been increasing and was 63% in 2018. 7 This increase is thought to be primarily caused by people’s latent biological susceptibility interacting with a changing environment that includes more sedentary lifestyles and increased dietary abundance. 1 The prevalence of adiposity in the UK population is approaching similar levels to those reported in the US (71%), Chile (74%) and Mexico (75%), which are among the highest recorded adult overweight and obesity levels in the world. 8 The number of people with obesity (PwO) in the UK continues to rise, and severe and complex obesity (body mass index (BMI) ≥40 kg/m 2 ) increased from less than 1% of the total population in 1993 to nearly 4% in 2017. 10 The UK-wide National Health Service (NHS) costs attributable to overweight and obesity are projected to reach £9.7 billion by 2050, with wider societal costs estimated to reach £49.9 billion per year. 11 The significant increase in the prevalence of obesity has not been matched by a proportionate expansion of continuing education on the biological basis and clinical management of obesity and training provision for healthcare professionals (HCPs), irrespective of their discipline. 12 Moreover, little effort has been made to address weight stigma and societal effects of weight bias, which continue to be experienced in a consistently negative way by those who have excess weight or obesity. Current evidence demonstrates that weight stigma is widespread in the UK, 13 that weight stigma is experienced in many settings 14 15 and that experience of stigma is associated with negative psychosocial outcomes, increased eating, reduced engagement with physical activity and weight gain. 16
The variability of causal pathways of weight gain is inherently unsuited to a ‘one size fits all’ treatment approach. 1 There is a range of existing guidance to support practice and care throughout the obesity care pathway in the UK. 9 17 However, the extent and range of the provision of weight management services is inconsistent and geographically dependent. 18 The obesity care pathway has an important role within the whole systems approach to tackling obesity, as outlined in the Foresight’s report, 1 and endorsed in the Department of Health and Social Care’s (DHSC) Call to Action 19 and the Public Health England’s paper on a whole systems approach to obesity. 20 The DHSC clinical policy outlines a tiered system of obesity care with a focus on public health and community advice in tier 1; primary care, community interventions and pharmacotherapy in tier 2; multi-disciplinary weight management service in tier 3 and secondary care and bariatric surgery in tier 4. 21
Despite its wide global prevalence, obesity remains poorly understood by the general public and HCPs, and this contributes to the high levels of stigma associated with obesity. 22 Society is continually informed through intense media coverage that obesity is simple and easily manipulated. 23 This attitude contributes to greater perceptions of individual responsibility, contrary to evidence that suggests that many factors outside a person’s control influence obesity. 22 23 To improve the quality and accessibility of obesity care, a better understanding of the disease and the gaps between current and optimal obesity management strategies is required. The Awareness, Care, and Treatment In Obesity maNagement–International Observation (ACTION-IO) study assessed the perceptions, attitudes and behaviours of PwO and HCPs. 24 The global dataset 24 revealed a need to increase understanding of obesity and improve education concerning its aetiology. The aim of this subanalysis was to identify the perceptions, attitudes, behaviours and potential barriers to effective obesity care in the UK.
Study design and participants
The ACTION-IO study was a cross-sectional, non-interventional study that collected data via an online survey in Australia, Chile, Israel, Italy, Japan, Mexico, Saudi Arabia, South Korea, Spain, the UK and the United Arab Emirates. The full methods for the ACTION-IO study have been reported previously. 24 Eligible PwO in the UK were 18 years or older, with a current BMI of at least 30 kg/m 2 based on self-reported height and weight. The PwO sample was targeted for demographic representativeness based on gender, age, income, race/ethnicity and region. Therefore, PwO were excluded if they declined to provide any of these variables. Respondents were also excluded for non-obesity reasons, for high BMI or for dramatic weight loss, that is, if they were pregnant, participated in intense fitness or body building programmes, or had significant, unintentional weight loss in the past 6 months. Eligible UK’s HCPs were in practice for 2 years or more, with at least 70% of their time spent in direct patient care, and who had seen 100 or more patients in the past month, at least 10 of whom had a BMI of at least 30 kg/m 2 . HCPs specialising in general, plastic or bariatric surgery were excluded. Respondents were recruited via online panel companies (via email) to whom they had given permission to be contacted for research purposes, and completed the survey in English. All respondents provided electronic informed consent prior to initiation of the screening questions and survey. Preceding participation, PwO were only informed of the purpose of the study, and were blinded to the specific study goals.
Survey development and procedures
The study was designed by an international steering committee of obesity experts (representing primary care, endocrinology and psychology, and including three medical doctors employed by Novo Nordisk), with support from KJT Group (Honeoye Falls, New York, USA), and based on the ACTION US and Canada questionnaires. 25 26 KJT Group managed the acquisition and analysis of data; UK responses were collected between September 2018 and October 2018. Questionnaire items were carefully phrased and presented in identical order for each respondent. Items in a list were displayed in alphabetical, categorical, chronological or random order as relevant for each response. Respondents accessed the survey using a unique web link, details regarding the digital fingerprinting system used to assess unique site visitors has been previously described. 24 To prevent duplicate survey entries, unique site visitors were recorded via a user ID that was passed along the unique web link that respondents used to access the site. The system checked every respondent entering the survey against previous user IDs logged in its database. Respondents who began the survey and suspended were able to re-enter the survey while it was still open and finish the survey where they left off. Respondents who had already received a terminal status (complete, over-quota or terminate) were blocked from re-entering the survey. Following closure of the survey, no users were able to gain access. The user ID and data of suspended respondents were stored until the survey was closed and were then eliminated from the data analysis. The study was conducted in accordance with the Guidelines for Good Pharmacoepidemiology Practices. 27
To ensure representativeness to the general population, the final PwO sample was weighted to demographic targets within each country for age, gender, income, race/ethnicity and region. The HCP data were not weighted. Only data from those who completed the survey were included in the analyses.
Patient and public involvement
No patients or members of the public were involved in the design or conduct of the study. A patient representative was involved in the analysis and interpretation of the UK data and is an author on this article. She will also be involved in disseminating these findings to a wider audience.
Demographics
A total of 69 676 PwO and 2508 HCPs, in the UK, were invited. The response rate to the survey was 14% (9786/69 676) for PwO and 35% (886/2508) for HCPs, as expected for this type of study and in line with the target sample size. 24 Of those who completed the screening questions, the eligibility rate was 22% (2146/9779) for PwO and 53% (387/737) for HCPs. The final UK sample for the ACTION-IO survey was 1500 PwO and 306 HCPs, of whom 156 were primary care professionals (PCPs) and 150 were secondary care professionals (SCPs) ( table 1 ). Some differences were observed in the survey outcomes between PCPs and SCPs, which will be reported in full at a later date.
- View inline
Sample demographics and characteristics
Pre-consultation and initiation of weight management discussion
People with obesity.
Only about half (47%) of all PwO had discussed excess weight or losing weight with an HCP in the past 5 years. It took a median of 6 years and mean of 9 years (range: 0.0–56.0 years; IQR: 13 years) between the time when PwO said that they first started struggling with excess weight or obesity and when they first had a weight management conversation with an HCP ( figure 1A ). In comparison, globally it took a median of 3 years and a mean of 6 years (range: 0.0–68.0 years; IQR: 8 years ( figure 1A )). 24 Forty-seven per cent of PwO who discussed weight with an HCP reported that they initiated the conversation themselves. When PwO were asked to name the top five reasons why they may not discuss weight management with their HCP, the most common reason was the belief that it was their own responsibility to manage their weight (51% of PwO) ( figure 1B ). Indeed, when asked whether they agreed with the statement ‘my weight loss is completely my responsibility’, 85% of PwO agreed with the statement. Thirty-four per cent of PwO said that they were motivated to lose weight, and 36% provided a neutral response (neither agreed nor disagreed that they were motivated). Only 4% of PwO reported an indifference to losing weight as a reason for not discussing managing their weight with an HCP. Sixty-five per cent of PwO who previously had a weight conversation with their HCP liked that their HCP discussed their weight with them, and 58% who not previously had a conversation would have liked their HCP to bring up weight during their appointments. Most PwO (81%) believed that obesity has a large impact on overall health, similar to other chronic diseases such as diabetes (82%), stroke (88%), cancer (82%) or chronic obstructive pulmonary disease (COPD; 84%). The internet was cited as a source of information used by 31% of PwO for managing weight ( figure 2A ). Other sources of information were reported as family and friends (27%), weight loss programmes (26%), information from an HCP (23%) and media (books/magazines: 21%, television programmes: 20%) ( figure 2A ).
- Download figure
- Open in new tab
- Download powerpoint
Number of years between when struggle with weight began and first discussed with an HCP and PwO/HCP reasons for not discussing weight management. (A) Approximate number of years reported by the UK and global PwO (ACTION-IO study steering committee, personal communication) between the beginning of their struggle with weight and first discussion with an HCP. Calculated at respondent level from questions, ‘Approximately how old were you when you first remember struggling with excess weight or obesity?’ and ‘Approximately how old were you when a healthcare provider first discussed your excess weight or recommended that you lose weight?’. (B) Reasons reported by the UK’s PwO for not discussing managing their weight with an HCP. (C) Reasons reported by the UK’s HCPs for not discussing weight management with their patients. ACTION-IO, Awareness, Care, and Treatment In Obesity maNagement–International Observation; HCP, healthcare professional; PwO, people with obesity.
Sources of information and feelings after a weight discussion. (A) Sources of information most frequently used by the UK’s PwO for managing weight (reported by PwO). (B) Feelings reported by the UK’s PwO after their most recent weight or weight loss discussion with an HCP in the past 5 years. HCP, healthcare professional; PwO, people with obesity.
Healthcare professionals
Those HCPs who discussed weight with their patients reported that 35% of the time the patient initiated the conversation. Compared with PwO (85%), a smaller proportion of HCPs (33%) placed the responsibility for weight loss on PwO. Only 13% of HCPs thought that their patients were motivated to lose weight, and 42% provided a neutral response (neither agreed nor disagreed that their patients were motivated). The most commonly selected reason for not discussing weight management with a patient (selected by 72% of HCPs) was the perception that the patient was not interested in losing weight, and 61% of HCPs selected lack of patient motivation ( figure 1C ). Other reasons provided for not discussing obesity with a patient were that the appointments were not long enough and that they felt rushed (selected by 68% of HCPs), and that more important health issues/concerns were an impediment to discussing obesity with a patient (selected by 58% of HCPs). In addition, almost one-third of HCPs (31%) reported that the good health of a patient and the absence of weight-related comorbidities would be a reason for not discussing weight management. The most important criterion for initiating weight management conversations with a patient was the presence of obesity-related comorbidities, cited by 76% of HCPs. Only 68% of the UK’s HCPs (vs 76% of global HCPs 24 ) recognised the impact of obesity on health, and it was rated as less serious than diabetes, cancer, stroke or COPD by 40%, 65%, 62% and 43% of the UK’s HCPs, respectively.
Consultation
Eighty-one per cent of the PwO who had discussed weight with an HCP had had a discussion with a PCP, 42% with a nurse, 18% with a dietitian/nutritionist and 17% with a diabetes educator. PwO reported a complex mixture of feelings following a weight loss conversation with an HCP ( figure 2B ). PwO cited a combination of feelings such as supported 36%, hopeful 31%, motivated 23%, embarrassed 17%, indifferent 16%, discouraged 11%, relieved 10%, blamed 10%, rushed 10%, offended 4% and confused 4% ( figure 2B ).
Fifty-nine per cent of HCPs reported that they were extremely or very comfortable discussing weight, 30% were neither comfortable nor uncomfortable and 11% were a little or not at all comfortable discussing weight. On average, HCPs reported that they spent 10 min interacting with their patients when discussing weight (range: 1–20 min).
Consultation outcomes and follow-up
Among the 47% of PwO who had discussed their weight with an HCP in the past 5 years, 49% reported that they had been diagnosed with obesity in the past by an HCP (24% of all PwO, figure 3 ). Only 19% of PwO who had discussed their weight with an HCP had a follow-up appointment scheduled (9% of all PwO) ( figure 3 ). However, 62% of PwO would have liked a follow-up appointment and 96% reported attending or planning to attend a follow-up appointment if scheduled. The most frequent methods for managing weight tried by PwO were general improvements in eating habits/reducing calories (reported by 61% of PwO) and general increases in physical activity (55%), which were reported at a greater frequency than by global PwO (51% and 39% for general eating habits and physical activity, respectively; ACTION-IO study steering committee, personal communication). Bariatric surgery and behavioural therapy referral rates were reported in small numbers by the UK’s PwO (1% and 2%, respectively). Visits to a nutritionist/dietician and obesity specialist were reported less frequently by the UK’s PwO than global PwO (nutritionist/dietician: 11% UK, 24% global; obesity specialist: 2% UK, 9% global; ACTION-IO study steering committee, personal communication).
Obesity diagnoses and follow-up appointments with an HCP. Proportion of the UK’s PwO who discussed weight or weight loss with an HCP in the past 5 years and the frequency of obesity diagnoses and follow-up appointments. HCP, healthcare professional; PwO, people with obesity.
On average, HCPs scheduled follow-up appointments with 33% of their patients for obesity and 46% of HCPs said that patients kept these follow-up appointments always or most of the time. HCPs most frequently recommended general improvements in eating habits/reducing calories (reported by 61% of HCPs) and general increases in physical activity (65%). Referrals to obesity specialists were recommended less frequently by UK HCPs (12%) compared with the global dataset (23%). 24
PwO are faced with biological predispositions, and societal and environmental conditions that contribute to obesity, weight stigma and discrimination. Obesity prevention and management are key health priorities and require a whole systems approach. However, the national response for obesity focuses on individual responsibility regarding nutrition and lack of physical activity. In this study, multiple barriers to effective weight management were identified, which are summarised in figure 4 and discussed below.
A conceptual model of the obesity treatment pathway and barriers to obesity care in the UK. BMI, body mass index; HCP, healthcare professional; PwO, people with obesity.
Initiation of weight management discussion with HCPs
Fewer than half of PwO in the UK (47%) had a discussion with an HCP about their weight in the past 5 years, despite HCPs being the gateway to weight management care in the NHS. Moreover, for the PwO who did have a weight discussion, it took a mean of 9 years after they first started struggling with their weight before having the discussion (compared with 6 years globally). 24 This delay is particularly important as it may create an opportunity for significant obesity-related complications to develop. This long delay may also reflect a higher degree of obesity stigma in the UK 28 and a culture of individual responsibility for obesity. 29 30 Indeed, a focus on individual responsibility is reflected in UK government policy on obesity. 31 Reducing the time gap by initiating earlier weight management discussions may be an effective strategy for improving obesity treatment and preventing the development of comorbidities.
From the PwO perspective, a delay in seeking help could be linked to the high percentage (85%) of PwO who perceived their weight loss as completely their responsibility. From the HCP perspective, a delay in discussing obesity with a patient could be linked to reported perceptions that the patient was not interested or motivated in losing weight, consistent with previous research. 32 33 Other impediments to the discussion were HCPs’ views that there were more important health issues to discuss and that a weight management discussion is only required when weight-related comorbidities are present, as supported by other studies. 33 34 Moreover, HCPs in the UK underestimated the effect of obesity on health to a greater extent than the UK’s PwO and global HCPs. 24 For PwO, this will likely require a change in the narrative around obesity to lessen focus on individual responsibility, and for HCPs a need to increase the understanding of the health consequences of obesity and the desire of PwO for help and support. The internet, media, and family and friends formed a substantial source of information for PwO for managing weight. We need to change this from personal responsibility to recognising the aetiology of obesity and its implications for PwO.
Primary care is the gateway to obesity treatment, and most weight management discussions were held with a primary care physician or nurse. While many PwO welcomed weight discussions with HCPs, they also reported experiencing complex and varied emotions after these discussions. It is important to acknowledge the complexity of the experience for PwO. Studies have previously reported patients feeling that their obesity had been ignored, dismissed, distorted or attributed as the explanation of all their health problems by HCPs. 35–37 Negative experiences can contribute to depression, anxiety, low self-esteem and body dissatisfaction. 38 39 Dissatisfactory conversations with an HCP may discourage PwO from seeking further weight management help in the future and reinforce feelings of personal responsibility for weight management. The attitudes of health professionals towards obesity and its management have been generally reported to be negative, and knowledge and skills in managing obesity have been noted to be inconsistent. 40–45 Even well-intended acts can cause offence and humiliation, 46 and PwO often experience their weight in profoundly negative ways as a result of the pervasive stigmatisation of obesity. Patient experiences are valid indications of the strengths and shortcomings of the services they receive. 47 It is important to ensure that the narrative around obesity resonates with the lived experiences of those affected by it and encourages patients to engage with an HCP. 47 HCPs in turn should aim to provide compassionate care that is free of bias and use supportive communication and language to facilitate successful and meaningful conversations. 47
HCPs often have limited time and resources, and lack of time has previously been reported as a barrier to discussing obesity. 48 49 More HCPs in the UK (68%) than globally (54%) indicated that the limited appointment time would be a factor in not having a weight loss conversation. 24 This may be a reflection of the average primary care consultation time in the UK, which is 10 min and considerably shorter than in many other countries. 50 51 Other potential barriers described in the literature have included uncertainty about appropriate language, 48 concerns about compromising rapport 9 and concerns discussing a potentially upsetting and stigmatising topic. 22 50 52 However, in this study, relatively few HCPs reported discomfort with weight discussions.
Obesity diagnoses, follow-up appointments and referrals to specialists were infrequently reported by PwO, which could incorrectly reinforce the feeling of individual responsibility. Indeed, methods for managing weight reported by PwO, which relied largely on general improvements in eating habits and physical activity, suggest a lack of knowledge of effective treatment methods and/or a consequence of the availability of therapeutic options (see below).
The data from HCPs on the frequency of follow-up appointments and methods for obesity management largely aligned with the data from PwO. Barriers to effective weight management cited in the literature have included lack of effective and individualised treatment and/or referral options. 40 41 50 53 Weight management services in the UK exist as part of fragmented health and social care systems, which are geographically dependent. 49 54 55 The range of services and treatments, including pharmacotherapy and bariatric surgery, is limited in the UK, which may restrict HCPs in what they can offer patients. Indeed, HCPs report insufficient management options and scepticism about their efficacy. 56 57 This is further compounded by limited consultation times for the UK’s general practitioners. 50 51 The limited availability of weight management services, effective treatments and coherent, joined-up strategies in the UK health system are significant barriers to providing effective obesity care. 55
Strengths and limitations
Strengths of this study include scientific rigour in the study design (including carefully phrased and ordered questions to prevent biased responses, blinded purpose of the survey for PwO and determination of eligibility by initial screening questions to eradicate bias during recruitment) and implementation (including stratified sampling to provide a representative cohort of the general population and rigorous data analysis). Other strengths include the large number of UK’s PwO and HCP respondents and the ability to directly compare the UK data to the equivalent global dataset. Limitations include the cross-sectional design and reliance on accurate reporting from the PwO and HCP respondents, which could be perceived as recall bias. The self-reported height and weight could underestimate the BMI of the PwO. A higher proportion of HCPs than might be expected self-identified as obesity specialists using the broad criteria specified in table 1 . The low response rates could affect sample representativeness and is a known limitation for this type of study. Response bias from the population sampled cannot be ruled out. However, the PwO sample was representative of the demographics of the general population.
This study demonstrates the need to change the narrative around obesity, with less stigmatising focus on individual responsibility, for the government, commissioners, general public, PwO and HCPs. The findings identified areas that prevent PwO from seeking help and receiving appropriate care. In addition, the attitudes of HCPs prevent them from offering the support PwO require for obesity management. The consultation about weight with an HCP is the gateway to treatment in the NHS and improving the frequency and quality of PwO–HCP conversations is essential. Sufficient time should be given to HCPs to approach the topic of overweight and obesity sensitively and effectively. The current survey did not have high numbers of people with a BMI of over 40 kg/m 2 ; further research is required to understand whether people with higher BMIs have distinct experiences in the management of their obesity.
To conclude, a whole systems approach is required to address and eliminate weight bias and stigmatisation, to change the narrative around obesity in the UK, and to improve provision of NHS services. Educating the whole population, including PwO and HCPs, about the aetiology and psychology of obesity and the interaction with the obesogenic environment should help to ensure that patients access and receive quality care and effective weight treatment and management. Changing the narrative around obesity will allow for a more effective delivery framework for health service providers and greater access to effective treatment pathways and weight management services for PwO.
Ethics statements
Patient consent for publication.
Not required.
Ethics approval
The National Health Service Health Research Authority (Central Research Ethics Committee, London) advised that ethical approval was not needed in the UK.
Acknowledgments
We thank the participants of the study. Medical editorial assistance was provided by Anna Bacon from Articulate Science, and was funded by Novo Nordisk.
- Wilding JPH , et al
- Ralston J ,
- Brinsden H ,
- Buse K , et al
- Ghanemi A ,
- Yoshioka M ,
- Whitaker M , et al
- NHS Digital
- The Organization for Economic Cooperation and Development (OECD)
- National Institute of Health and Care Excellence (NICE)
- Public Health England
- Royal College of Physicians
- Codreanu SC , et al
- Vartanian LR ,
- Department of Health
- Obesity and Food Policy Branch
- Department of Health and Social Care
- Public Health England and NHS England
- Stanford FC ,
- Tauqeer Z ,
- Caterson ID ,
- Alfadda AA ,
- Auerbach P , et al
- Kaplan LM ,
- Jinnett K , et al
- Sharma AM ,
- Bélanger A ,
- Carson V , et al
- International Society for Pharmacoepidemiology (ISPE)
- Nadglowski J ,
- Salas RX , et al
- O'Keeffe M ,
- Watts K , et al
- Theis DRZ ,
- Hiddink G ,
- Koelen M , et al
- DiCicco-Bloom B , et al
- Merrill E ,
- Thomas SL ,
- Karunaratne A , et al
- Tuthill A ,
- O'Rahilly S , et al
- Psarou A , et al
- Leverence RR ,
- Williams RL ,
- Sussman A , et al
- Macdonald S ,
- Morrison D , et al
- Dewhurst A ,
- Devereux-Fitzgerald A , et al
- Henderson E
- World Health Organization
- Malterud K ,
- Ananthakumar T ,
- Hinton L , et al
- McPhillips R
- Gadsby EW ,
- Peckham S ,
- Coleman A , et al
- Gershlick B
- Puhl RM , et al
- Campbell K ,
- Timperio A , et al
- Claridge R ,
- Stubbe M , et al
Contributors CAH and JCGH are members of the ACTION-IO study steering committee and contributed to the design of the study. CAH, ALA, HK, BMM, HMP, AV and JCGH participated in the interpretation of data, and drafting and revision of the manuscript. All authors reviewed and approved the final, submitted version.
Funding This work and ACTION-IO was supported by Novo Nordisk. ALA is funded by the Medical Research Council through grant MC_UU_00006/6.
Competing interests CAH reports financial support from Novo Nordisk to attend an obesity conference during the conduct of the study, grants from the Rona Marsden Fund at Fakenham Medical Practice and personal fees from Orexigen Therapeutics, Consilient Health, Nestlé, Ethicon and Alva outside the submitted work. ALA reports grants from UKRI Medical Research Council and National Institute for Health Research, and non-financial support from WW (formerly Weight Watchers). HK is an employee of Novo Nordisk and owns shares in Novo Nordisk. BMM reports grants paid to her institution from Novo Nordisk and personal fees (consultancy and advisory board) from Novo Nordisk, Boehringer Ingelheim and Orexigen Therapeutics; and has received speaker fees for Eli Lilly, Novo Nordisk, Boehringer Ingelheim, Janssen, MSD and Sanofi. HMP reports grants from the National Institute for Health Research and Public Health England and an honorarium from Novo Nordisk (educational grant) outside the submitted work. AV acted as a speaker for Obesity Empowerment Network and is a board member of the Clinical Advisory Committee on the All Wales Obesity Strategy. JCGH reports fees (honoraria) paid to the University of Liverpool from Novo Nordisk, Orexigen and Boehringer Ingelheim during the conduct of the study.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:

The Obesity Society’s (TOS) grants program demonstrates our commitment to promote, reward, and encourage research in the field of obesity. The deadline to submit a Letter of Intent (LOIs) for the Early Career Research Grant has closed. Those selected for Phase 2 will be notified by June 21, 2024.
Applicants may apply for multiple grants.
A description of each grant and the instructions on how to apply are below.
If you have any questions, please email [email protected] .
Early Career Research Grant
The grant is offered by The Obesity Society as a member service to foster and stimulate new research ideas in any area of investigation related to obesity. The grant targets early-career investigators and post-doctoral fellows by funding proposals that demonstrate a high likelihood of resulting in new and innovative approaches in obesity research. Early-career investigators are defined as individuals who have received a PhD/DSc, DVM, MD or DO at the time of application. Investigators must also currently have a full-time, entry-level position (e.g., post-doctoral fellow, instructor, and up to Assistant Professor) at an established academic/research institution. Applicants may request up to $25,000. No indirect cost will be paid from this grant. Applicants invited to submit a full proposal will be notified approximately one month later. All applicants must be TOS members in good standing. This is a one-year grant and funding will begin the next calendar year.
Early Career Research Grant Eligibility Criteria:
The following applies to the Principal Investigator:
- Member of The Obesity Society (domestic and international)
- PhD/DSc, DVM, MD or DO at the time of application
- Post-doctoral fellows, junior faculty, and up to Assistant Professors who have not yet received an NIH K-award, equivalent career-development award, or R-level research project grant
- Assistant Professors do not require a mentor
- Applications from post-doctoral research fellows must have a mentor
- Potential to generate future funding
PhD/DSc, DVM or MD/DO degree must be obtained by date of application submission. Applicants may not be a post-doctoral fellow for more than five years.
How to Apply
- Submit a Letter of Intent Cover Page
- 1-page on institutional letterhead
- 1/2 inch margins
- 11-point font size
- Submit an NIH-style biosketch for the principal investigator. If the principal investigator is a post-doctoral fellow, the biosketch of the mentor should also be included
- The LOI and biosketch(es) must be collated and submitted as a single pdf
Applicants selected by The Obesity Society’s Science Development Committee will be notified and requested to submit a full proposal package. Required documents include:
- Original LOI and Biosketch(es), from the LOI submission
- Brief introduction to the proposed study and rationale for investigation (How will this work benefit the field?)
- Statement of specific aims and hypotheses
- Material and methods, feasibility
- Anticipated results, limitations, alternatives
- Future plans (How will the findings of this project be leveraged for future work? What are the next steps, next grants?)
- Budget Form (1-page) with justification (1-page limit)
- Salary for technical staff, supplies, core use, subject recruitment, patient care costs, and other research-related expenses.
- Equipment/capital expenses up to $5,000.
- Travel up to $2,000 (ObesityWeek® encouraged).
- If principal investigator requires salary support, a maximum of one month summer salary or 8% effort support is allowable.
- Mentor Letter of Support (1-page, for post-doctoral fellows and instructors)
Criteria for Evaluating Applications
- Significance – impact, innovation
- Investigator – potential in academic research, diversity/inclusion
- Research Plan – study design, methods, feasibility, alternatives/limitations
- Future Plans – (How will the findings of this project be leveraged for future work? What are the next steps, next grants?)
Thank you for your interest in joining a TOS Committee.
Your request has been sent..
Cookies on Obesity.org
By using Obesity.org, you agree to our use of cookies. We use cookies to provide you with a great experience and to help our website run effectively.
Your payment has been processed successfully!
We’re sorry. we could not process your payment..
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Addressing Obesity to Promote Healthy Aging
Meredith roderka.
a Section of Weight & Wellness, Department of Medicine, Dartmouth-Hitchcock, Lebanon, NH
Sadhana Puri
John a. batsis.
b Geisel School of Medicine at Dartmouth Hanover, NH
c The Dartmouth Institute for Health Policy & Clinical Practice, Lebanon, NH
d Dartmouth Centers for Health and Aging, Dartmouth College, Hanover, NH
e Section of General Internal Medicine, Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction
The population worldwide is aging and is not immune to the changing prevalence of obesity. Older adults with obesity are at risk for adverse events, including functional decline, institutionalization and mortality. Other consequences of obesity and changes in body composition with aging, are an increased risk of falls, fractures, reduced quality of life, and cognitive decline. This article will describe the epidemiology of obesity, its geriatric-specific consequences and the benefits and risks of intentional weight-loss.
Epidemiology of Obesity in Older Adults
It is projected that, over 83.7 million people in the US will be >65 years in the year 2050. 1 This demographic shift is largely due to an increase in baby boomers and improved medical care, all which have led to an increase in life expectancy. 1 The most recent National Health and Nutrition Examination Survey data highlights an obesity prevalence of ~41% in adults aged 60+, 2 that leads to consequences resulting in impaired physical function 3 decreased quality of life (QoL), institutionalization 4 and death. 5
Rates of obesity in older adults have also increased worldwide, 6 with rates tripling over the past 40 years. 7 Drivers of this epidemic include changes in the global food system, an increased intake of energy-dense foods and sedentary work, expanding urbanization, changes in transportation modalities, and the interactions of biological and environmental factors. There are important disparities observed in obesity rates in older adults including race/ethnicity 8 rural/urban 2 and socioeconomic status. 9 In 2007–2010, Hispanic men aged 75+ had a higher prevalence of obesity (27.9%) when compared with non-Hispanic white men (26.4%), 10 with different rates observed in women (49.4% in non-Hispanic black, 30.2% in Hispanic, and 27.5% in non-Hispanic white). 10 In the US, obesity prevalence was higher in rural than in urban residents. 9 Socioeconomic status (SES) influences the development of obesity in both developed and low-income countries. 11 Few studies demonstrate associations between SES and obesity in older adults. Individuals aged≥50 years with financial hardship in the EPIC-Norfolk study were at higher risk for obesity irrespective of education, social class or home ownership. 12
Changes in Body Composition
Aging is associated with body composition changes, including loss of skeletal muscle mass and redistribution of fat to the abdominal area and visceral organs. With age, there is a gradual increase in body fat; specifically visceral adipose tissue, 13 a trend continuing until extreme old age when fat mass may decrease. 14 Abdominal fat redistribution significantly contributes to insulin sensitivity and metabolic syndrome 15 and is a correlate of cardiometabolic disease. 16 Visceral fat promotes intramuscular fat infiltration that leads to pro-inflammatory cytokine production ultimately contributing to reduced muscle and physical function. 17
As muscle mass declines with age, 18 the amount of available insulin-responsive tissue drops which may also lead to insulin resistance. Starting at age 30, there is approximately a 20–40% decrease in muscle mass by age 70 that may lead to sarcopenia, 19 the age-related loss of muscle mass and strength. 20 The Health, Aging and Body Composition Study noted a loss of muscle mass was associated with a decline in strength in older adults, 21 but the decline in strength was more rapid than the loss of mass, suggesting a decline in muscle quality. 22 Changes in skeletal muscle mass and function is critically important as it affects older adults’ mobility and function.
While body mass index (BMI) is a simple and inexpensive method for assessing obesity, it lacks sensitivity and may underestimate adiposity in older adults. 18 This is, in part, due to its inability to discriminate between subcutaneous and visceral fat, and failing to account for muscle and bone mass. In contrast, waist circumference easily approximates increased intra-abdominal fat 23 with its sensitivity exceeding that of BMI, and is strongly associated with an increased morbidity risk. 24 Despite such limitations, BMI is valuable at the population-level by allowing health professionals to make comparisons across time, regions, and subgroups.
Consequences of Obesity
Consequences of obesity include cardiometabolic dysfunction, arthritis, pulmonary, urinary incontinence, cataracts, and cancer. 25 Specific to older adults include an increased risk of falls, cognitive decline, quality of life, and disability, which are reviewed below. 18
Obesity negatively impacts balance and increases postural sway, 26 predisposing to falling and negatively impacting activities of daily living. 27 Among middle-aged and older adults, obesity is associated with a higher prevalence of falls and stumbling during ambulation. 28 The prevalence of falls differs in men and women, with middle-aged women at a particularly higher risk, 29 which may be due to an increased rate of trip-related falls. 30 This has implications in sarcopenic obesity; in older men with obesity, for instance, the loss of muscle mass is associated with an increased risk of falls, 31 with rates higher in this population. 32 Participants with obesity that fall have a higher prevalence of pain and inactivity than fallers of a healthy weight. 28
The association between hip fractures and obesity is less understood with conflicting associations. 33 A prospective population-based study of sarcopenic obese men found a high risk of fracture. 31 Weight-loss leads to loss of bone density. Intentional weight-loss was strongly associated with an increased risk of hip fracture. The pathophysiology associated with such fractures and whether obesity impacts bone quality is unclear and requires further investigation. 33
Quality of Life
The presence of obesity in older adults negatively impacts quality of life (QoL), in part due to the loss of physical function that accompanies obesity. 34 Older obese adults were found to have a lower health-related QoL in the Medical Expenditure Panel Survey. 18 A study examining the relationship between BMI and QoL among adults aged ≥60 years old 35 found that overweight older females were more likely to have a lower scores andoverweight older males were less likely to have low visual analogue scale compared with normal BMI. Gaining an understanding of the differences in QoL in older obese adults could be helpful in tailoring specific interventions.
Cognitive Impairment
Several studies have explored the relationship between obesity and cognitive impairment. 36 – 38 Overweight and obesity demonstrated lower neuropsychological test scores than individuals with a normal BMI. Bischof 39 explored whether obesity in midlife or later life placed older adults at greater risk for cognitive decline and found that midlife obesity increased the risk for cognitive decline in late-life. Others demonstrated that conventional care plus nutritional counseling (vs. conventional care) in obese patients >60 years led to significant weight loss and improved global cognition, memory, semantic fluency, and Wisconsin categories. 37 Even a diet, exercise, and diet-exercise intervention in frail older obese adults age≥65 led to improved modified mini-mental status scores, trail making, and word fluency tests compared to controls at 1 year. 38 In contrast, the intensive lifestyle arm in Look-AHEAD 40 found no significant difference in the prevalence of cognitive impairment compared to controls. 36 There is promise that improved diet-exercise may positively impact cognition; further efficacy studies are needed.
Disability can be one of the most devastating consequences in older obese adults that leads to higher utilization, 41 institutionalization, 42 and death. 43 A number of factors promote the development of disablement process, both from a mechanical and inflammatory standpoint. Body fat redistribution promotes intramuscular fat infiltration leading to a vicious cycle of pro-inflammatory cytokine production and contributing to reduced muscle function. 17 ( Figure 3 ). Inflammatory-based lipotoxicity reduces the potential of muscular regeneration leading to muscle fibrosis, 44 promotes insulin resistance, and negatively impacts muscle strength. 17 Such tissue damage inhibits the regeneration of muscle mass in those with sarcopenic obesity that negatively impacts physical function. For example, greater muscle fat infiltration was associated with an increased risk of mobility limitation. 45 A meta-analysis found that a BMI ≥30 kg/m 2 with low muscle strength in older adults, and not low muscle mass, was associated with functional decline. 45 Persons with sarcopenic obesity have difficulty ascending and descending the stairs. 46 Applying newer sarcopenia definitions, the presence of sarcopenic obesity resulted in an increased risk of frailty, activity of daily living disability and instrumental activity of daily living disability. 47 Data from the Osteoarthritis Initiative also showed that a combination of low knee extensor strength and high BMI was associated with reduced gait speed, a lower degree of physical function, and decreased self-reported health status. 48 Considerable evidence exists to suggest that sarcopenia and obesity is strongly associated with reduced physical function in older adults.

From Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nat Rev Endocrinol. 2018;14(9):513–37; with permission.
The proposed interplay between adipose and muscle tissue, which is believed to contribute to the development of sarcopenic obesity, is shown. The black lines are stimulatory, while red lines with flat ends indicate inhibition. IGF1, insulin-like growth factor 1; TNF, tumor necrosis factor.
Nursing Home Admission
Older obese adults are at a higher risk for nursing home admission. A review suggested that obesity early in life is a risk factor for future admission, 42 even for middle-aged persons. 49 Separately, there was a greater rate of nursing home admission in whites with obesity compared to a normal BMI but no relationship in blacks. 50 Between 1992–2002, the proportion of newly admitted residents with obesity to nursing homes rose from 15% to 25%. 51 The distribution of residents with obesity was also unequal across different facilities, ranging from 0–40%, highlighting the inability of nursing homes to accommodate such residents. 51 The increased number of obese patients admitted to nursing homes can also impact the institution’s ability to accommodate such patients. Patient size was a barrier to admission, 52 but also led to increased time to accomplish care needs. 53 Nursing home administrators reported inadequate staffing for the care of morbidly obese residents in 31% of nursing homes and also reported concerns about having the proper equipment for individuals with obesity in 68% of nursing homes. 52
Obesity Paradox
A major challenge for clinical providers has been whether to recommend weight-loss interventions in older adults. This controversy, coined “the obesity paradox,” stems, in part, from the inverse correlation between higher adiposity and mortality observed from several epidemiological studies; data has been strongest amongst older adults.
Previous studies demonstrated that obesity is associated with increased survival in those with established cardiovascular disease (CVD). 54 There has also been support for the paradox in the context of type 2 diabetes, suggesting lower mortality in patients with type 2 diabetes and obesity than in normal or lower weight patients. 55 The paradox has been described in chronic obstructive pulmonary disease and in nursing home residents. 56 There are strong critics who believe the term ‘paradox’ is misleading as it was derived from biased observational studies. 57 A number of arguments dispel this paradox. Previous studies do not differentiate between unintentional weight loss associated with chronic illness and intentional weight loss. 57 , 58 The potential for bias increases with older age as the presence of chronic diseases accumulate, possibly explaining why this paradox is so prominent in older individuals. 58 Possible confounders are not accounted for (smoking, cardiorespiratory fitness or socioeconomic variables). 57 Last, mortality studies have stratified by smoking status which is associated with a lower BMI. 58
A key study refuting the obesity paradox analyzed the association between BMI and lifetime risk of cardiovascular disease. The study design accounted for measurement, selection, and survival bias and variable follow-up times by stratifying the risk for non-CVD death by age, sex, and BMI strata to observe the relationship between BMI and risk of mortality from CVD in an isolated fashion. Overweight and obesity were associated with a significantly increased risk for CVD, and obesity was associated with a shorter lifespan and a greater proportion of life lived with CVD. Incident CVD among middle-aged men and women with morbid obesity was accelerated by 7.5 and 7.1 years compared with middle-aged men and women with normal BMI. Men and women with normal BMI lived an average of 5.6 and 2.0 years, respectively, longer than those with morbid obesity. Future studies can learn from and build upon the methods of this study.
Benefits of Weight Loss in Older Adults
Guidelines support the role of intentional weight loss in older adults in improving physical function. 3 Clinicians need to individualize health promotion efforts and be aware of specific adverse events in this at-risk population. We briefly describe the risks/benefits of diet-exercise inducted weight-loss in older adults as there is a limited evidence base for pharmacotherapy and bariatric surgery. Other benefits are outlined in a recent review. 59
A review of weight-loss interventions in older adults 60 found a greater degree of weight loss in groups with a dietary component than in those with exercise alone. Exercise alone led to improved physical function and increased fat-free mass without significant weight loss. A combined diet/exercise approach led to the greatest improvement in physical performance and QoL, mitigating the reduction in muscle and bone mass observed in diet-only arms. More recently, a review assessed the impact of treating obesity in older persons 61 and found that lifestyle interventions resulted in similar weight-loss efficacy in older and younger people. Positive effects were observed on outcomes such as physical function and cardiovascular health. Weight-loss led to improved QoL of older adults in a 6-month study. 62 Weight loss plus the addition of any form of exercise (aerobic or resistance) has produced an improvement in QoL scores beyond those observed in the weight loss only conditions. 63 These findings suggest the importance in counseling patients in achieving their weight loss goals in order to help them improve their overall QoL.
Recent trials demonstrate the synergy of diet and exercise on improving physical function in older obese adults more than either separately. 64 Peak oxygen consumption increased more in the calorie restriction with aerobic/resistance training and diet-aerobic groups than in the diet-resistance group alone. Strength was higher in the diet-aerobic/resistance and resistance groups alone than in the aerobic group. Lean mass and hip bone mineral density decreased less in the diet-aerobic/resistance and resistance groups than in the aerobic group. Participants in LOOKAhead had improved gait speed over 4m and 400m walk tests and higher short performance physical battery scores over controls. 65
A meta-analysis showed that caloric restriction plus aerobic and resistance exercise helped preserve fat-free mass in older adults, supporting the role of these strategies in the treatment of sarcopenic obesity. 66 A randomized trial of a dietary intervention in older obese adults and hypertension resulted in a mean 3.5kg reduction in weight and a decreased need for anti-hypertensive medications by 30%. 67 Another study found that weight-loss via both diet and exercise effectively reduced pain and improved function and QoL in older adults with knee osteoarthritis in comparison to diet or exercise alone. 68 Hence, the optimal approach to improve physical function in older adults with obesity is a multi-component, caloric restriction combined with aerobic and resistance program.
Protein supplementation has been proposed to reduce the potential weight-loss induced muscle loss. Consumption throughout the day can reduce the likelihood of weight loss-induced sarcopenia by stimulating muscle protein synthesis. The PROT-Age group recommends 1.0–1.1 g/kg protein per day in divided doses, acknowledging that a ‘one size fits all protein recommendation’ fails to account for the complex physiological changes of ageing. 69 Of three studies evaluating the effects of high vs. low protein diets in older adults with obesity 70 , only one study 70 demonstrated a significant benefit of a high protein diet vs, normal protein diet on the short performance physical battery. While weight-loss was achieved at a comparable level in both groups, there were discrepancies in the age and sex of participants. 70 Future studies are critically needed.
Risks of Weight-Loss
There are inherent risks that healthcare providers should be mindful when counseling patients. Recognizing sarcopenia in the context of obesity is important 71 as reduction in caloric intake may lead to reduced adipose tissue, but also loss of muscle mass. Caloric restriction alone as a means of weight loss can increase the risk of sarcopenia, bone loss, and musculoskeletal injury in older adults. 59 , 48
We advise caloric restriction should be coupled with resistance-based exercises. In one systematic review, unopposed calorie restriction without resistance training led to the loss of muscle mass and handgrip strength of up to 4.6% and 1.7kg, respectively. 72 Diet-only interventions without exercise in older frail adults led to a marked loss of lean mass compared with diet-exercise, where the loss of lean mass was partially mitigated. 64 A review evaluating the effects of energy restriction on adults with a BMI≥25kg/m 2 showed that 81% of caloric restriction groups and 39% of caloric restriction with exercise led to ≥15% loss in fat-free mass, while exercise alone only led to modest loss in fat-free mass. Look-AHEAD participants showed significant reductions in total skeletal muscle mass in the intensive lifestyle group compared to controls. 73 In a 4-month trial, overweight and older adults in the caloric restriction group experienced a significant decrease in fat-free mass in contrast to the caloric restriction and exercise group. Recommendations for weight loss in older obese adults that allow for fat-free mass preservation include 150 min of aerobic exercise/week, 2–3 days of weight bearing exercises/week, protein supplementation 1.0–1.2 g/kg/day, and 1000 IU vitamin D or high-dose supplementation (if necessary). 59
Calorie restriction alone has also demonstrated reduced bone-mineral density. Soltani 74 reviewed 32 randomized trials in adults ≥18 years and found that weight-loss significantly led to reductions in hip and lumbar spine bone density. Hip bone density decline with weight-loss was more pronounced in participants with obesity. 74 A one-year study of older adults with obesity were randomized to caloric restriction, exercise, calorie restriction and exercise, or controls. 75 Participants in the caloric restriction group exhibited more bone density loss at total hip (−2.6%) compared with the caloric restriction-exercise and exercise groups (−1.1%, + 1.5%). 75 In Look-AHEAD, intensive lifestyle participants were at a 39% higher risk of fragility fractures. 73 The POUNDS LOST trial assessed diet-only effects of weight-loss in older adults with obesity on bone density, 76 demonstrating both weight loss and significant bone density loss at the spine, hip, and femoral neck. 76 Only women demonstrated a significant association between loss of bone density and loss of muscle mass. 76 Recommendations for weight-loss in older adults with obesity parallel those to mitigate muscle loss as outlined above but, in those indicated, consideration for osteoporosis therapy. 59
Other risks pertain to musculoskeletal injuries and hypoglycemia. The 12-month incidence of injuries related to exercises in older adults was roughly 13.8%. 77 Even in the LIFE study, the risk ratio between the exercise and the education group was no different. 78 Providers also must be mindful of alterations in metabolic variables, particularly hypoglycemia in participants on insulin as insulin sensitivity improves and reduces its need.
Importance of Treating Obesity to Promote Health Aging
Healthcare professionals can aid older patients with obesity in losing weight. The goal should be on improving physical function and QoL. The quality of care can be enhanced in its diagnosis and measurement. While BMI can be helpful, there may be improvements in accuracy by including waist circumference. Healthcare professionals can counsel patients by promoting multi-disciplinary lifestyle interventions. Concurrent dietary, behavioral, and exercise (aerobic/resistance) approaches should be prescribed and recommended as they lead to marked improvements in physical function, metabolic improvements, and can minimizes sarcopenia and osteoporosis. Caloric restriction without a concurrent resistance program may be detrimental; we advise against such an approach. Furthermore, there is a critical need to enhance delivery systems in the primary care setting by 79 changing policy structure and reimbursement mechanisms to permit non-physicians to deliver intensive behavioral therapy. 18 Monitoring of complications as a result of weight-loss induced metabolic improvements should be considered. We strongly advocate the need for additional community-based, pragmatic and effectiveness interventions to de-medicalize obesity in this population. Clinic-community partnerships are a potential way to help implement an easy, cost-effective method to improve weight management programs. 80 Promising preliminary data 81 shows that implementing a community-based weight management program are feasible and acceptable. Treating obesity in older adults can mitigate the significant public health crisis, reduce healthcare utilization and risk of long-term adverse events.

Data from the National Health and Nutrition Examination Survey demonstrating the changing demographics of older adults.

From DiMilia PR, Mittman AC, Batsis JA. Benefit-to-risk balance of weight loss interventions in older adults with obesity. Curr Diab Rep. 2019;19(11):114; with permission.
This figure represents the major risks associated with isolated calorie restricted, diet-induced weight loss on muscle, bone, and the cardiometabolic system and their impact on key outcomes of frailty, disability, quality of life, falls, and mortality. The interrelationships between these elements are presented through the arrows. Elements of the underlying pathophysiologic processes in aging in the older adult with obesity are presented. Aerobic and resistance exercises coupled with diet-induced weight loss mitigate the loss of muscle mass and strength, and bone mineral density (indicated by red line and prohibition symbol). This combination also stimulates enhancement of elements of the cardiometabolic system leading to improvements in glucose homeostasis and blood pressure, requiring providers to be cognizant of relative hypotension and hypoglycemia (indicated by green line and plus symbol). BMD, bone mineral density; BP, blood pressure; RAA, renin, angiotensin, aldosterone; QOL, quality of life; Rx, prescription medications; SNS, sympathetic nervous system.
- This article reviews epidemiology of obesity including increase in prevalence; race/ethnicity, and socioeconomic disparities.
- Consequences of obesity in older adults; falls, cognitive decline; fractures, quality of life, disability and nursing home admissions.
- There are specific benefits to intentional weight-loss on physical function and comorbidity but also key risks to muscle and bone loss that need to be understood
- Health care professionals should encourage older adults with obesity to try to implement healthy lifestyle behaviors that includes exercise and diet routine.
The population worldwide is aging. The prevalence of obesity in this population is also increasing. There are a range of consequences that effect these at-risk patients including increased risk of falls, fractures, reduced quality of life, and cognitive decline. This article will describe the epidemiology of obesity, the risks and benefits of weight loss, and the importance of treating obesity to help promote healthy aging.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE STATEMENT
The authors have nothing to disclose.

IMAGES
COMMENTS
In both children and adults, major consequences of obesity include the development of serious chronic disorders that further reduce quality of life and life span, such as type 2 diabetes, dyslipidemias, hypertension, and cardio‐ and cerebrovascular disease and their consequences in ischemic injuries. 7, 8 Furthermore, in 2020, the SARS‐CoV ...
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health, increases the risk of long-term medical complications and reduces lifespan. 1 Epidemiologic studies define obesity using the body mass index (BMI; weight/height 2), which can stratify obesity-related health risks at the population level.Obesity is operationally defined as a BMI exceeding 30 kg ...
Obesity research then, as now, largely focused on measurable outcomes and quantifiable terms such as body mass index [22, 23]. ... Studies based on primary data generated with adults with obesity ... Mechanick J. Proposal for a scientifically correct and medically actionable disease classification system (ICD) for obesity. ...
The obesity epidemic. The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a).A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2.It is well known that obesity and overweight are a growing problem globally with high rates in ...
Obesity is a prevalent, complex, progressive and relapsing chronic disease, characterized by abnormal or excessive body fat (adiposity), that impairs health. People living with obesity face ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
Introduction. Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality.1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19.4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight.6
See the 2020-2030 Strategic Plan for NIH Nutrition Research. The NHLBI is an active member of the National Collaborative on Childhood Obesity (NCCOR) external link. , which is a public-private partnership to accelerate progress in reducing childhood obesity. The NHLBI has been providing guidance to physicians on the diagnosis, prevention ...
Abstract and Figures. Abstract Obesity is a chronic metabolic disease characterized by an increase of body fat stores. It is a gateway to ill health, and has become one of the leading causes of ...
The estimated obesity-related health care costs are as high as $147. billion per year. Despite the alarming health risks and increasing health care costs, the. rates of screening and counseling for obesity in the primary care setting are merely 30%. This project outlines weight-management counseling strategies.
Control of obesity is an important priority to reduce the burden of chronic disease. Clinical guidelines focus on the role of primary healthcare in obesity prevention. The purpose of this scoping review is to examine what the published literature indicates about the role of hospital and community based health services in adult obesity prevention in order to map the evidence and identify gaps ...
A key element of the initial charge to the Task Force was the development of a Strategic Plan for NIH Obesity Research, published in 2004. In light of the rapid progress in obesity research highlighted above and the opportunity to capitalize on emerging scien-tific discoveries, the Task Force decided to update the Strategic Plan.
2.1. In Adults. Obesity can be defined as a condition of abnormal or excess fat accumulation in adipose tissue, to the extent that health may be impaired [].Body Mass Index (BMI), which is calculated as [(weight in kg) / (height in m) 2], is considered to be the most useful population-level measure of obesity, and it is a simple index to classify underweight, overweight and obesity in adults.
The Strategic Plan for NIH Obesity Research serves as a guide to accelerate a broad spectrum of research toward developing new and more effective approaches to address the tremendous burden of obesity, so that people can look forward to healthier lives. The Plan was originally published in 2011. In 2018-2019, the Obesity Research Task Force ...
Obesity is a prevalent, complex, progressive and relapsing chronic disease characterised by abnormal or excessive body fat that impairs health and quality of life. It affects more than 650 million adults worldwide and is associated with a range of health complications. Qualitative research plays a key role in understanding patient experiences and the factors that facilitate or hinder the ...
Objective: To identify the most effective interventions in overweight and obese adults. Method: A narrative review through a search of the literature in databases PubMed, Cochrane, Joanna Briggs Institute, EMBASE, Cuiden y Cinahl with free and controlled language (MeSH terms) using Boolean operators AND and NOT. The research was limited to articles published between 2007 and 2015.
Data will be shared with bona fide researchers submitting a research proposal requesting access to data. ... it has been recognised as a risk factor for severity of COVID-19 infection.5 6 The prevalence of overweight and obesity among adults in the UK has been increasing and was 63% in 2018.7 This increase is thought to be primarily caused by ...
The grant is offered by The Obesity Society as a member service to foster and stimulate new research ideas in any area of investigation related to obesity. The grant targets early-career investigators and post-doctoral fellows by funding proposals that demonstrate a high likelihood of resulting in new and innovative approaches in obesity research.
Overall, there was no significant change from 2003-2004 through 2011-2012 in high weight for recumbent length among infants and toddlers, obesity in 2- to 19-year-olds, or obesity in adults.
Prevalence of overweight (27.8% vs 21.8%) and obesity (21.9% vs 6.0%) were also significantly higher in women than men. About 45.6% of adult diabetes patients in Ghana are either overweight or obese. At the regional level, about 43.4%, 36.9%, 32.4% and 55.2% of residents in Ashanti, Central, Northern and Greater Accra region, respectively are ...
In draft guidance issued Tuesday, NICE signed off on Lilly's tirzepatide to help adults manage overweight and obesity alongside a change in diet and exercise. The endorsement paves the way for ...
Data will be shared with bona fide researchers submitting a research proposal requesting access to data. Data use is subject to approval by the independent review board. Ethics statements. Patient consent for publication. ... Health survey for England 2018. overweight and obesity in adults and children.
A 2008 report found that $1.00 in SNAP expenditures generates $1.73 in economic activity and that SNAP is among the most effective economic stimulus programs. Another study found that ...
The clinical significance of childhood obesity has a significant impact on both physical and mental health. 3 Child Obesity and Mental Health, Final Research Project Background of the problem: Childhood obesity is also associated with Mental health problems such as anxiety and depression. Low self-esteem and poor quality of life.
As shown in Figure 3-1, this weight gain was associated with substantial increases in the prevalence of overweight and obesity (body mass index [BMI] of 25 or greater) in both blacks and whites and both men and women: 52 percent to 76 percent of adults in these race/sex subgroups were in the healthy weight range (BMI 18.5 to 24.9) at the start ...
"This work remains relevant even in light of medical management of obesity, for example, with adults seeking treatment via bariatric surgeries and newer medications, such as Wegovy and Mounjaro. ... All faculty members with primary appointments in PHHP may submit proposals to the PHHP Research Innovation Fund. Priority is given to early ...
Epidemiology of Obesity in Older Adults. It is projected that, over 83.7 million people in the US will be >65 years in the year 2050. 1 This demographic shift is largely due to an increase in baby boomers and improved medical care, all which have led to an increase in life expectancy. 1 The most recent National Health and Nutrition Examination Survey data highlights an obesity prevalence of ...