The HCCI Home-Based Primary Care Implementation Model
According to estimates from the Small Business Administration, approximately 50% of small businesses fail within the first five years. Only 25% make it to 15 years or more. While a house call program isn’t an IT firm or subscription-based clothing firm, the challenges facing those organizations – that often prove insurmountable – are not all that different.
Research suggests that organizations, and practices, fail due to shortcomings in the following:
- Assessing the market
- Creating a viable business and financial plan
- Hiring enough of the right people
- Patient and caregiver satisfaction
- Flexibility and changing with the environment
Many well-intentioned practitioners who see a need in their area – patients who are no longer able to access traditional primary care – jump in with good intentions of meeting that need. They bring a much-needed model of care to a vulnerable population. What happens too often, however, is those same practitioners find themselves struggling months later, encountering issues with staffing, staff retention, and revenue generation. They work tireless hours for little financial return. The intrinsic rewards of home-based primary care are notable, and the care provided is life-changing for many patients and caregivers. But if the practice isn’t sustainable, all those good intentions and good work are at risk.
HCCI has developed a model for implementing and growing house call programs. Starting with the fundamentals of establishing a business, including researching the market and creating a business plan, the HCCI House Call Implementation Model guides practitioners through the multiple aspects of building and leading a successful practice. While the initial phases of the model are critical and not to be overlooked, the Model is interactive by design, and can be entered at any level. HCCI has developed a rich array of learning opportunities and tools to support practices as they grow and can provide expert assistance whenever additional guidance is requested.
HCCI is dedicated to increasing access to home-based primary care for the millions of chronically ill, medically complex patients who need it. The HCCI House Call Implementation Model supports the work of practitioners who seek to do that, helping them create thriving and sustainable house call practices equipped to provide long-term solutions for their patients.
Click here to download a copy of the model. Contact us to learn how HCCI can support your practice.

Categories:
- Benefits of HBPC
- Caregiver Stories
- CMS Updates
- Data Insights
- General Features
- Practice Management
- Practice Spotlight
- Training & Education
- February 2023
- December 2022
- November 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- February 2021
- December 2020
- October 2020
- August 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- February 2019
- January 2019
- November 2018
- October 2018
- September 2018
- August 2018

Interest in home-based primary care is growing as payments increase, technology improves, and the population ages.
THOMAS CORNWELL, MD, FAAFP, AND BRIANNA PLENCNER, CPC, CPMA
Fam Pract Manag. 2021;28(3):22A-22G
Author disclosures: no relevant financial affiliations disclosed.

The United States is experiencing a resurgence of home-based primary care (HBPC) after a rapid decline during the last century. Steady growth in physician house calls started with the doubling of house call payment rates in 1998 and a doubling and tripling of domiciliary payment rates in 2006. Other factors include the aging of our society; increased technology that allows X-rays, ultrasounds, electrocardiograms, and lab tests to be done in the home; and new CPT payments that target complex patients such as those who need chronic care management, remote patient monitoring, and advance care planning.
HBPC's value has been demonstrated through improved outcomes and reduced costs for complex patients. Medicare's Independence at Home house call program improved outcomes and decreased costs by $2,000 per patient per year, and the U.S. Department of Veterans Affairs' HBPC program reduced hospital days by 60%, readmissions by 21%, and nursing home use by an astounding 89%. 1 The data generated support for HBPC on Capitol Hill, at the Centers for Medicare & Medicaid Services (CMS), from Medicare Advantage plans, and from investors.
More recently, the COVID-19 public health emergency (PHE) brought virtual care into patients' homes in a remarkable way. But telehealth is beyond the scope of this article. Currently, Congressional action is needed to enable telehealth to continue in the home after the PHE.
Still, family physicians can take advantage of the growing support for HBPC. This article outlines steps for adding house calls to an office-based practice. Reasons to do so include the following:
Continuity of care for patients who have difficulty getting to the office, ensuring they are not lost in the system.
Better quality of care, increased time with patients, and improved doctor-patient-caregiver relationships, resulting in increased patient satisfaction scores, increased referrals from family members, increased physician satisfaction, and decreased burnout.
Improved end-of-life care, fulfilling the wishes of the majority of patients who desire to be at home surrounded by loved ones at the time of death.
Improved value-based care performance from superior risk capture, reducing gaps in care, improving quality, and lowering the total cost of care.
Increased reimbursement for complex patient care.
Increased payment, improved technology, and the aging of the population have all contributed to steady growth in physician house calls.
House calls have been shown to improve patient outcomes and decrease costs by $2,000 per patient per year.
When adding house calls to an office-based practice, three ingredients necessary to success are patients, processes, and payments.
THREE INGREDIENTS FOR SUCCESS
A successful house call program requires three ingredients: patients, processes, and payments.
Patients . There is some flexibility in choosing which patients should receive home visits. Medicare has never required house call patients to meet the homebound definition that it requires for receiving skilled nursing and therapy services in the home. But until January 2019, Medicare required additional documentation of medical necessity for every home visit, describing why a house call was needed in “lieu of an office visit.” The 2019 Medicare Physician Fee Schedule Final Rule removed this requirement as of Jan. 1, 2019.
Still, most house call programs focus on complex patients who have difficulty getting to the office. Some practices use data analytics to identify and target high-risk patients. Common candidates for HBPC include the following:
Frail older adults with multiple (often five or more) chronic conditions and deficiencies in activities of daily living (ADL).
Younger homebound patients, usually with one principal neuromuscular condition such as multiple sclerosis, amyotrophic lateral sclerosis, or cervical spine injuries (some on ventilators).
Patients with high-risk diagnoses like congestive heart failure and chronic obstructive pulmonary disease.
Patients with high hospital and emergency department (ED) utilization in the past six to 12 months.
Patients with hierarchical condition category (HCC) scores greater than 2.0.
Another group well-suited for HBPC is post-acute, transitional care management (TCM) patients. During the high-risk transition period, these patients benefit from a short course of HBPC that reduces complications and readmissions. Payments for TCM (CPT codes 99495 and 99496) have increased more than 20% over the past two years. CMS has also unbundled virtually all care management services that previously were not billable within the 30-day TCM period. These include chronic care management, care plan oversight for home health and hospice services, face-to-face and non-face-to-face prolonged services, and more when reasonable and necessary. Numerous hospitals are partnering with HBPC programs to reduce their readmission rates.
Logistical considerations for choosing house call patients include the following:
Geography: A geographic radius should be determined for home visits based on driving time (e.g., no more than 20 minutes from the physician's office or home). Telehealth, at least while it is allowed under the PHE, is an excellent way to provide care for more distant patients.
Established vs. new house call patients: Some practices may decide to limit house calls to established patients. But if you desire to grow a house call practice, the largest referral source tends to be home health agencies, followed by hospital and rehabilitation discharge planners, social services, and word of mouth.
Place of service: Practices may offer house calls to patients at home or in domiciliary settings (e.g., assisted living facilities or group homes). There are economies of scale in domiciliary care because you can see multiple patients in the same location on the same day, and the payments are roughly the same as home visits.
Capacity: A good way to start is with a half day or one full day of house calls per week, and then increase that time as volume demands.
Operational processes . Practices will need to address operational issues such as scheduling, visit preparation, staffing, supply management, and safety.
Efficient scheduling is critical to reduce travel time, and can be achieved through the following steps:
Schedule patients in close proximity. This is facilitated by assigning days to specific geographic areas and using mapping/routing software.
Map and route patients one to two days before the visit, notify patients or caregivers of the approximate visit time (usually providing a two- to four-hour window or simply indicating morning or afternoon), and verify the address (sometimes the address on file is for mailing the bill and is not the patient's physical location).
Use electronic health record flags/alerts for travel notes, communication preferences, and patient preferences. Special visit instructions should be noted on the schedule (e.g., “call daughter ahead,” “go in back door,” or “dogs need to be secured”).
Call when en route to the visit so the patient is ready and has medication out.
Give patients follow-up timeframes (e.g., four to six weeks or two to three months) instead of exact dates to allow the schedule to be fluid, to facilitate scheduling patients within the same geographic area, and to enable last-minute schedule changes based on patient acuity.
Make sure that clerical tasks are done before the visit, including obtaining signed forms and medical records (e.g., HIPAA forms, consent for treatment, or medical history forms) when possible.
Staffing considerations include the following:
Medical assistant (MA) support: Many physicians choose to do house calls solo, mainly because of the cost of including an MA. But having an MA route and drive saves the physician significant time and allows charting and phone calls while in transit. During the house call, the MA can check vitals, do immunizations, draw blood, assist with medication reconciliation and refills, get forms signed, review gaps in care, do assessments (such as PHQ-2/9, Mini-Cog, nutritional, and safety surveys), assist with wound care, help with orders (e.g., durable medical equipment, home health, and hospice), and increase safety. Making one extra house call a day covers the MA's cost, and the time savings more than allow for that one extra call.
Advanced practice provider visits: Nurse practitioner and physician assistant house calls have dramatically increased over the past decade; they are now the largest provider group making house calls. This is a cost-effective model with good outcomes, when provided with physician support.
Supply management involves keeping track of what supplies are used and restocking at the end of the day. Unlike in the office, you cannot walk down the hall to a storage closet if you run out of something during a home visit. Ensure equipment is sanitized and charged. Have a container in the car for standard supplies that are not damaged by temperature extremes (e.g., wound care items). Review schedules in advance to identify any special supply needs (e.g., a cooler for storing and transporting drawn labs).
Safety concerns include higher crime areas and homes with potentially dangerous patients, caregivers, or pets. Safety and emergency plans should include the following:
Handling car accidents and other incidents such as falls with injuries, needle-sticks, etc.
Handling pets in the home. Some HBPC programs require pets be caged during visits. Others leave it to the discretion of the pet owner and the physician.
Sitting on a hard surface chair to avoid unseen soiling, bedbugs, etc.
Washing or sanitizing hands before, during, and after the visit.
Noting safety issues on the schedule, including a history of multi-resistant organisms, bed bugs, or firearms (which should always be locked). During the PHE, conduct COVID-19 screening questions when notifying the patient of the appointment time and again when en route to the patient's home.
Seeing patients in higher crime areas during daylight hours. There is debate among HBPC clinicians about wearing clothing that identifies them as health care workers, such as a lab jacket. Some think it's better to avoid drawing attention to themselves. Others believe it is good for people to know they are there to provide care. Determine which is more comfortable for you.
Turning on smartphone location service apps, which enable the office to know the physician's location and allow the physician to quickly call in an emergency through a simple touch or verbal command.
Planning for inclement weather or natural disasters. Patients may need to be rescheduled.
Exiting the premises if the physician feels unsafe. Consider having a code word to alert staff if you need assistance.
Clinical processes . The Institute for Healthcare Improvement's Age-Friendly Health Systems' "4Ms" framework is an excellent approach to complex house call patients. The 4Ms are what matters , medication , mentation , and mobility. What matters is determined through conversations with patients about their goals of care, leading to advance directives. The home is an ideal setting to have these conversations. It is also the best place to reconcile and optimize medications , which often includes deprescribing in frail older adults. Mentation refers to diagnosing and managing dementia, depression, and delirium. Mobility focuses on ADLs, maintaining function, gait, safety, and independence. (See “ Common assessments in HBPC .”)
A house call's main clinical difference is that the exam room is in the patient's home. This requires bringing the office to the patient. The table below shows the modern-day “black bag.” The supply list will vary somewhat depending on what the physician is comfortable doing in the home. The home also provides tremendous information about the patient, including diet, safety (are there grab bars, fall hazards, etc.), social determinants of health, and what matters to the patient (pictures, religious objects, etc.). It is important to be culturally sensitive in patients' homes, which is best accomplished by asking about patient and caregiver preferences.
It is wise to review charts the day before the home visit to see if fasting blood work or any unique supplies are needed, such as injections, immunizations, or gastrostomy tubes. It also helps to review charts for complex, new, and TCM patients ahead of the visit and start pre-charting. Extensive prep time (more than 30 minutes) can be billed using CPT codes for prolonged evaluation and management (E/M) services. (See “ Commonly used CPT codes in home-based primary care .”)
House call practices commonly have 20% to 25% mortality rates, so it is critical to discuss goals of care such as the patient's desired medical decision-maker if needed, level of hospital care, cardiopulmonary resuscitation (CPR), and end-of-life wishes (e.g., desired place of death, hospice services, and funeral arrangements). These advance care planning (ACP) discussions can be billed with CPT code 99497 if a minimum of 16 minutes is spent and the patient consents to the conversation voluntarily (be sure to note this in your documentation). These discussions often take place over several visits, and there is no limit on how often ACP can be billed. Copays are waived for ACP done during annual wellness visits, but co-pays will apply if performed with another service.
House call patients are best served by an interdisciplinary team providing a range of services, often virtually, including the following:
Ancillary service providers (mobile X-ray, ultrasound, and phlebotomy).
Home health and hospice (Medicare pays physicians for the certification and recertification of home health and care plan oversight if they spend 30 minutes in a calendar month overseeing home health or hospice).
Care coordination departments (such as ED or hospital discharge planning).
Durable medical equipment companies.
Community organizations (Area Agencies on Aging can assist with Meals on Wheels, utilities, home maintenance, etc.; other community organizations may provide behavioral health, private duty, or respite care; and websites such as findhelp.org by Aunt Bertha list resources by ZIP code).
Other professionals making house calls (audiologists, dentists, optometrists, podiatrists, etc.).
PAYMENT FOR HOUSE CALLS
Medicare fee-for-service (FFS) payments fund most house call programs. The 2021 changes in office outpatient E/M documentation requirements do not apply to home or domiciliary visit codes, so you are still required to use the 1995 or 1997 E/M documentation guidelines for these visits. Billing by time still requires that more than 50% of the visit be spent in counseling and/or coordination of care. (See “ Home and domiciliary E/M codes and payment rates .”) Other commonly used CPT codes in HBPC and their payment rates are listed in the table above. Most of these CPT codes are new in the past decade.
Value-based care (VBC) payments are fueling the growth of house calls. Payments can vary, from shared savings with only upside potential and no downside risk, to global capitation with full risk for all patient care. Three things are essential for success: 1) capturing risk scores for accurate payment, 2) improving quality and the patient experience and closing gaps in care, and 3) lowering costs principally by reducing acute care utilization. House calls do all three exceedingly well and lower acute-care usage more than any other intervention. For family practices involved in Accountable Care Organizations or other forms of VBC, house calls can significantly contribute to the bottom line.
American Academy of Family Physicians Home-based Primary Care Member Interest Group (AAFP members only)
Rerucha CM, Salinas R, Shook J, Duane M. House calls . Am Fam Physician . 2020;102(4):211–220.
Home Centered Care Institute
HCCIntelligence™ Resource Center
American Academy of Home Care Medicine
Cornwell T. House calls are reaching the tipping point — now we need the workforce. J Patient Cent Res Rev . 2019;6(3):188-191.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Don't bother with copy and paste.
Get this complete sample business plan as a free text document.
Home Health Care Business Plan
Start your own home health care business plan
CaringCompanion
Value proposition.
CaringCompanion provides high-quality, personalized home health care services to seniors and individuals with disabilities, letting them maintain independence and comfort within their own homes.
The Problem
Demand for reliable, high-quality and affordable home health care services is growing. Many seniors and individuals with disabilities face challenges in finding home health care providers that can effectively address their specific needs while also offering the necessary support to ensure a high quality of life at home.
The Solution
CaringCompanion offers a comprehensive and holistic approach to home health care by connecting clients with experienced, certified caregivers who possess the skills and expertise to provide personalized care and support. Our services include personalized care plans that ensure each client receives the appropriate level of assistance.
Target Market
The primary market for CaringCompanion is seniors and individuals with disabilities who want to maintain their independence while receiving assistance with daily living activities in the comfort of their own homes. This may include individuals recovering from surgery, facing chronic health conditions or dealing with cognitive impairments such as Alzheimer’s or dementia.
Competitors & Differentiation
Current alternatives.
- Traditional home health care agencies
- Independent caregivers
- Assisted living facilities and nursing homes
CaringCompanion stands out by offering personalized care plans and a thorough caregiver vetting process. Our customized care plans allow us to address each client’s specific needs and preferences, and our dedication to ongoing caregiver training and support ensures that our team stays up-to-date with the latest best practices while maintaining open communication with patients and their families.
Funding Needs
CaringCompanion requires $250,000 in initial funding to cover operating expenses, caregiver salaries, marketing efforts, insurance, and other startup costs.
Sales Channels
- Official CaringCompanion website
- Social media platforms
- Local senior centers and community organizations
- Referrals from existing clients
Marketing Activities
- Content marketing through blog posts and articles
- Social media campaigns
- Local advertising and sponsorships
- Networking with healthcare professionals and senior organizations
Financial Projections
2023: $180,000
2024: $250,000
2025: $325,000
Expenses/Costs
2023: $130,000
2024: $175,000
2025: $210,000
2023: $50,000
2024: $75,000
2025: $115,000
- Secure initial funding – June 1, 2023
- Launch official CaringCompanion website – July 1, 2023
- Hire and train first team of caregivers – August 1, 2023
- Acquire first 10 clients – September 30, 2023
- Establish partnerships with local healthcare providers – December 31, 2023
- Reach 50 active clients – June 30, 2024
- Expand service offerings and geographic reach – January 1, 2025
Team and Key Roles
Founder & ceo.
Responsible for overall business operations, client management, and strategic growth initiatives.
Care Coordinator
Oversees client intake, caregiver assignments, and care plan development.
Caregiver Team
Provides in-home care services, ensuring clients’ needs are met with compassion and professionalism.
Marketing Manager
Develops and executes marketing strategies to attract new clients and enhance brand visibility.
Partnerships & Resources
Local healthcare providers.
Collaborate with physicians, therapists, and other healthcare professionals to ensure coordinated care and support for our clients.
Senior Organizations
Partner with local senior centers, community organizations, and advocacy groups to provide resources, educational materials, and support to seniors and their families.
Insurance Companies
Establish relationships with insurance providers to offer our services as a covered benefit, making home health care more accessible and affordable for clients.

The quickest way to turn a business idea into a business plan
Fill-in-the-blanks and automatic financials make it easy.
No thanks, I prefer writing 40-page documents.

Discover the world’s #1 plan building software
Non-Medical Home care Business Plan Guide + Example

July 6, 2023
Adam Hoeksema
The in-home healthcare industry has been experiencing remarkable growth over the past few years, propelled by an aging population, increased life expectancy, and a growing preference for care within the comfort of one's own home. The Global In-Home Health Care market size was valued at around USD 305.9 billion in 2021 and is expected to reach approximately USD 629.3 billion by 2028, according to data from Fortune Business Insights. Key driving factors include the prevalence of chronic diseases, increased need for cost-effective healthcare delivery systems, technological advancements, and government initiatives promoting home healthcare. Moreover, the recent COVID-19 pandemic has put a spotlight on the importance and feasibility of home healthcare, further catalyzing its growth. The industry's trajectory suggests a promising future for businesses aiming to provide high-quality, personalized care services within a patient's home.
Read more: 9 Home Healthcare Industry Financial Stats
Based on the industry growth, there is no surprise that many are starting new businesses or considering starting a new home healthcare business.
There are two basic types of businesses that you could start:
- In Home Healthcare Business
- In Home Non-Medical Care Business
In this blog post I am going to guide you through the process of creating a business plan for a non medical home care business. You can also download our free non-medical home care business plan template and start creating your custom plan as you follow along. I plan to cover the following:
- Why Write a Business Plan for a Non-Medical Home Care Business?
What Should be Included in a Non-Medical Home Care Business Plan?
- Non-Medical Home Care Business Plan Outline
How to Analyze the Market Demand for a Non-Medical Home Care Business?
How to find and retain employees for a non-medical home care business, how to find customers for a non-medical home care business.
- How Much Working Capital is Needed for a Non-Medical Home Care Business?
- How to create financial projections for your non-medical home care business
- Non-Medical Home Care Example Business Plan
Non-Medical Home Care Business Plan FAQs
With that as the guide, let’s dive in!
Why Write a Business Plan for a Non-Medical Home Care Business?
I could say something like “if you fail to plan you plan to fail” or give you a long list of reasons why the business planning exercise could be beneficial for you, but at the end of the day, most people write a business plan because the people with the money ask for it. Your potential investors or lenders probably are asking for your business plan, so you just have to roll up your sleeves and get it done.
A non-medical home care business plan should include a Company Description, Market Analysis, Service Offerings, Marketing and Sales Strategy and Financial Projections. Our business plan template has the following outline.
Non-Medical Home Business Plan Outline
I. executive summary.
II. Business Concept
III. Market Analysis
IV. Competition Analysis
V. Marketing Strategy
VI. Menu and Kitchen Operations
VII. Service and Hospitality
VIII. Financial Plan
- Startup Costs:
Projected Financial Summary:
Annual sales, gross profit and net profit:, key financial ratios:, income statement:, balance sheet:, cash flow statement:.
IX. Organizational Structure
X. Conclusion
In order to analyze the market demand for a non-medical home care business, you first need to determine what services you might provide.
Non-Medical Home Care Services
Non-medical home care services focus on helping individuals with their daily activities and needs, improving their quality of life without necessarily providing healthcare-specific treatments. Here are some examples:
Personal Care: This includes assistance with activities of daily living (ADLs) such as bathing, dressing, grooming, toileting, and feeding.
Companionship: This involves providing social interaction to prevent loneliness and depression. Companions may engage the individual in conversations, read books, play games, or accompany them to social events.
Meal Preparation: Some non-medical care services involve preparing meals for individuals who may have difficulty cooking for themselves. They may also assist with grocery shopping.
Light Housekeeping: This can include help with tasks like doing laundry, dishes, taking out the trash, and general tidying up around the home.
Transportation Services: Non-medical home care providers can offer non-emergency medical transportation to and from appointments, social engagements, shopping trips, or other errands.
Medication Reminders: While non-medical home care providers do not administer medication, they can remind individuals to take their medication at the appropriate times to ensure adherence to their regimen.
Respite Care: These services provide temporary relief to primary caregivers, allowing them time off for rest, personal errands, or vacations.
Mobility Assistance: Helping individuals move around, whether it's transferring from the bed to a chair or assisting with ambulation around the house or outdoors.
Once you decide what services you might want to provide, you can use Google Keyword Planner Tool to search for keyword phrases related to those services in your area and get an estimate of the number of people searching for those services each month. This can really help analyze which services might be the most popular. For example, I did a search for home care in Chicago and found that there are roughly 320 monthly searches for that keyword phrase. There are roughly 90 monthly search for non-emergency medical transportation in Chicago and only 10 searches per month for companionship services in Chicago.

This should help you get a feel for the most in demand services in your area.
One of the biggest challenges for most non-medical home care businesses is finding and retaining employees. You will likely need some unique plans to recruit and retain good employees. Here are some ideas:
Recruitment:
Clear Job Descriptions: Ensure that the roles and responsibilities are clearly stated in your job advertisements. This way, potential employees will understand exactly what is expected of them.
Strong Online Presence: A well-designed website and active social media accounts can enhance your business's credibility and reach. Post job vacancies on your website, LinkedIn, job boards, and social media platforms to attract potential employees.
Partnerships with Local Institutions: Build relationships with vocational schools, nursing schools, and community colleges. They can provide a steady stream of potential candidates.
Employee Referral Program: Your current employees might know others who would be a good fit for your business. Offering incentives for successful referrals can be a productive recruitment tool.
Competitive Pay and Benefits: Offering competitive salaries and benefits, such as health insurance, retirement plans, paid time off, can significantly increase employee retention.
Employee Recognition and Rewards: Regularly acknowledge and reward the hard work and dedication of your employees. This could be through an "Employee of the Month" program, performance bonuses, or simply a thank you note.
Professional Development: Offer ongoing training and development opportunities. This will not only improve the quality of your services but will also show your employees that you value their personal and professional growth.
Supportive Work Environment: Create a culture that supports work-life balance. This could include flexible scheduling, mental health resources, and supportive management.
Open Communication: Foster a culture of open communication where employees feel comfortable voicing their ideas and concerns. Regularly ask for feedback and be responsive to it.
Career Advancement Opportunities: Provide clear pathways for career progression within your company. This gives employees something to work towards and helps them see a future with your organization.
By combining these effective recruitment and retention strategies, your non-medical home care business can build and maintain a reliable, motivated, and highly-skilled team.
Finding customers for your non-medical home care business is all about understanding your target audience, building awareness, and establishing trust in your services. Here are several strategies to help attract clients:
Referral Networks: Build strong relationships with healthcare professionals, such as doctors, nurses, physical therapists, social workers, and hospital discharge planners. They can refer patients to your service. Also, consider forming partnerships with senior centers, retirement communities, and organizations that cater to your target demographic.
Online Marketing: Ensure your business has a robust online presence. Create a professional website detailing your services, customer testimonials, pricing, and contact information. Utilize SEO strategies to ensure your site ranks highly in search results related to home care in your area. Also, leverage social media platforms to connect with potential clients and their families.
Community Outreach: Participate in local events and sponsor activities that resonate with your target audience. Giving talks on elder care topics or offering free workshops can help establish your business as an authority in the field.
Content Marketing: Write blogs or create videos on topics that your potential clients might search for online, such as "How to choose a home care provider" or "Benefits of non-medical home care." This helps position your business as a trusted resource.
Direct Mail and Brochures: Despite the digital age, direct mail campaigns can still be effective, particularly as many seniors may not be as internet-savvy. Distribute brochures or flyers in areas frequented by your target demographic.
Customer Testimonials and Reviews: Encourage satisfied customers to share their experiences online. Positive testimonials and reviews can be powerful tools for attracting new clients.
Networking: Attend industry-related events and join professional organizations to meet others in the field who might refer clients to you.
Paid Advertising: Consider paid advertising options like Google Ads or Facebook Ads targeting your local area and specific demographics.
Follow-up Services: If a client discontinues your service (e.g., because of hospitalization), ensure to follow up. They might need your service again when they are discharged.
Remember, trust and reliability are key in this industry. By delivering high-quality service, maintaining professional standards, and putting your clients' needs first, you can build a strong reputation that will attract and retain customers.
How Much Working Capital is Needed for a Non-Medical Home Care Business?
As we soon move into the financial projections section, one of the key questions for a non-medical home care business is how much working capital will be needed. I spent over 10 years leading an SBA Microloan Program and we funded many loans for home care services that needed working capital. The basic challenge was that companies often got paid through Medicare or Medicaid which could potentially have a significant delay between the time the service is provided and when you get paid. In the meantime you have to pay your employees. So the more clients you get the more working capital you actually need to float. I would expect that you should have at least 45 days worth of payroll available as working capital. So if your employees cost $50,000 per month, you should have access to a line of credit for at least $75,000 and you should be careful about how fast you grow.
Watch: How growing too fast can lead to bankruptcy even if you are profitable
How to Create Financial Projections for a Home Healthcare Business Plan
Just like in any industry, the in-home healthcare business has its unique factors that influence financial projections, such as client acquisition, reimbursement rates, and regulatory compliance. Utilizing an in-home healthcare financial projection template can simplify the process and increase your confidence. Creating accurate financial projections goes beyond showcasing your ability to provide in-home healthcare services; it's about illustrating the financial path to profitability and the realization of your mission to deliver quality care. To develop precise projections, consider the following key steps:
- Estimate startup costs for your in-home healthcare business, including licensing and certifications, insurance, office space or administrative setup, equipment, and initial marketing efforts.
- Forecast revenue based on projected client volume, reimbursement rates, and potential growth in service offerings or specialty areas.
- Project costs related to employee wages, training and development, supplies and equipment, transportation, and administrative expenses.
- Estimate operating expenses like rent, utilities, insurance premiums, software subscriptions, and marketing costs.
- Calculate the capital needed to launch and sustain your in-home healthcare business, covering initial expenses and providing working capital for continued growth and operations.
While financial projections are a vital component of your in-home healthcare business plan, seek guidance from experienced professionals in the industry. Adapt your projections based on real-world insights, leverage industry resources, and stay informed about regulatory changes, industry standards, and evolving healthcare models to ensure your financial plan aligns with your goals and positions your business for long-term success in providing exceptional in-home care.
Example Non-Medical Care Business Plan
Explore our comprehensive Non-Medical Home Care Business Plan Guide below, complete with an example template to jumpstart your planning process. Download the editable Google Doc version and follow our video walkthrough to tailor the plan to your unique business concept.
Table of Contents
Ii. company description, iv. service offerings, v. marketing and sales strategy, vi. financial projections, use of startup funds:, vii. conclusion.
Our non-medical home care business, named "Compassionate Care", aims to provide high-quality and affordable in-home care services to seniors and people with disabilities in the Dallas-Fort Worth area. Our mission is to help people live with dignity and independence in the comfort of their own homes, by providing compassionate and trustworthy care to meet their physical, emotional, and social needs.
The home care industry has experienced significant growth in recent years, driven by the aging of the population and the increasing demand for alternatives to institutional care. Compassionate Care will differentiate itself from competitors by offering a comprehensive suite of services, including personal care, homemaking, transportation, and companionship, tailored to the individual needs and preferences of each client. Our services will be delivered by a team of experienced and qualified caregivers, who will undergo rigorous background checks and training, and be bonded and insured.
Based on market research and financial projections, we expect Compassionate Care to generate $1 million in revenue in its first year of operations, and to achieve a net profit margin of 22% by the end of year three. To finance the business, we will seek a combination of debt and equity financing, from banks, angel investors, and family and friends.
Compassionate Care was founded by two friends, Jane Doe and John Doe, who have a combined 20 years of experience in the health care and social services industries. Jane has a Bachelor's degree in Nursing and has worked as a registered nurse for 10 years, while John has a Master's degree in Social Work and has been a social worker for 10 years. Both have a passion for helping people and a vision to create a company that provides compassionate and high-quality care to seniors and people with disabilities.
Compassionate Care will be incorporated as a Limited Liability Company (LLC) and will be headquartered in Dallas, Texas. The company will be owned and operated by Jane and John, who will act as the CEO and COO, respectively. The company will employ a team of 15 caregivers, who will be supervised by a director of nursing and a director of operations. The company will also have an office manager and a marketing and sales coordinator, who will handle administrative and marketing tasks.
The home care industry is a growing and dynamic market, with an estimated value of $100 billion in the United States. The demand for home care services is driven by the aging of the population, the increasing prevalence of chronic conditions, and the preference for home-based care over institutional care. According to the U.S. Census Bureau, the number of people aged 65 and older is projected to increase from 56 million in 2020 to 84 million in 2050, representing a 50% increase. Moreover, the number of people with disabilities who require assistance with daily activities is also expected to grow, as a result of improved medical care and increased longevity.
Compassionate Care's target market will be seniors and people with disabilities in the Dallas-Fort Worth area, who need assistance with activities of daily living and desire to maintain their independence and quality of life at home. The target market will include individuals who live alone, as well as those who live with family or friends, who need additional support and companionship. The target market will also include those who are transitioning from hospital to home, who need short-term or intermittent care.
Compassionate Care will face competition from other home care agencies, as well as from informal care providers, such as family members, friends, and neighbors. However, Compassionate Care will differentiate itself from competitors by offering a comprehensive and customized approach to care, by involving clients and their families in the care planning process, and by ensuring that the caregivers are well-trained and compassionate. Our services will also be priced competitively, while maintaining high quality standards.
Compassionate Care will offer a range of in-home care services to meet the diverse needs and preferences of its clients. Our services will include the following:
- Personal Care: Assistance with activities of daily living, such as bathing, dressing, grooming, toileting, and transferring.
- Homemaking: Assistance with household tasks, such as light housekeeping, laundry, meal preparation, and shopping.
- Transportation: Assistance with errands, appointments, and recreational activities, using the client's or the company's vehicle.
- Companionship: Socialization and emotional support, through conversation, games, reading, and other activities of interest.
All of our services will be tailored to the individual needs and preferences of each client, and will be provided in accordance with a care plan that is developed in collaboration with the client and the caregiver. The care plan will be reviewed and updated regularly, based on the client's changing needs and preferences.
Compassionate Care will employ a multi-channel marketing strategy, to reach its target audience and generate leads. Our marketing and sales efforts will include the following:
- Website: A professional and user-friendly website, which will provide information about the company and its services, testimonials, and a contact form.
- Referral Network: Collaboration with hospitals, rehabilitation centers, senior centers, and other organizations that serve seniors and people with disabilities, to promote our services and receive referrals.
- Direct Mail: A targeted direct mail campaign, using mailing lists of seniors and people with disabilities in the Dallas-Fort Worth area, to introduce our services and offer a special promotion.
- Social Media: Active presence on social media platforms, such as Facebook, Twitter, and Instagram, to engage with our target audience and promote our services.
- Referral Program: A referral program, which will offer incentives to clients, caregivers, and referral sources who refer new clients to the company.
Compassionate Care expects to generate $1 million in revenue in its first year of operations, and to grow its revenue by 100% in each subsequent year. The revenue will come from the sale of home care services, which will be priced competitively, based on the number and type of services provided.
Compassionate Care expects to achieve a profit margin of 10% by the end of year three, and to reinvest a portion of the profits into the business to support its growth and expansion.
All of the unique financial projections you see below were generated using ProjectionHub’s Home Healthcare financial projection template . Use PH20BP to enjoy a 20% discount on the template.

Watch how to create financial projections for your very own home care business:

Compassionate Care is poised to capture a significant share of the home care market in the Dallas-Fort Worth area, by providing high-quality and customized care services to seniors and people with disabilities. The company's experienced and dedicated management team, its commitment to excellence, and its focus on client satisfaction, will set it apart from competitors and ensure its success. We look forward to serving the needs of our clients and their families, and to making a positive impact on their lives.
Compassionate Care will also be committed to giving back to the community, by participating in volunteer and fundraising activities, and by supporting organizations that serve seniors and people with disabilities. Our goal is to be not only a trusted and respected provider of home care services, but also a responsible and engaged member of the community.
With this comprehensive business plan, we are confident that Compassionate Care will become a leading provider of non-medical home care services in the Dallas-Fort Worth area. We are eager to launch this business and to make a positive difference in the lives of our clients and the community.
How do I start a non-medical home care business?
To start an non-medical home care business, obtain the necessary licenses and certifications, establish legal and regulatory compliance, develop policies and procedures, hire qualified caregivers or nurses, establish relationships with healthcare providers, and create a marketing strategy to reach potential clients.
What types of non-medical home care services can I offer?
Non-medical home care services can include personal care assistance, medication management, medical monitoring, wound care, physical therapy, occupational therapy, speech therapy, respite care, and end-of-life care, among others.
How can I attract clients to my non-medical home care business?
To attract clients, establish relationships with hospitals, nursing homes, churches, and healthcare professionals for referrals, create a professional website with informative content, participate in local healthcare events or fairs, network with community organizations, and provide exceptional and compassionate care.
What legal and regulatory requirements do I need to comply with in the non-medical home care industry?
Legal and regulatory requirements in the non-medical home care industry can include obtaining proper licensing, complying with privacy regulations (such as HIPAA in the United States), following state and federal guidelines for caregiver qualifications, and adhering to safety and health regulations.
About the Author
Adam is the Co-founder of ProjectionHub which helps entrepreneurs create financial projections for potential investors, lenders and internal business planning. Since 2012, over 50,000 entrepreneurs from around the world have used ProjectionHub to help create financial projections.
Other Stories to Check out
How to know if your financial projections are realistic.
It is important for financial projections for a small business or startup to be realistic or else an investor or lender may not take them seriously. More importantly, the founder may make a financial mistake without a reliable plan.
How to Finance a Small Business Acquisition
In this article we are going to walk through how to finance a small business acquisition and answer some key questions related to financing options.
How to Acquire a Business in 11 Steps
Many people don't realize that acquiring a business can be a great way to become a business owner if they prefer not to start one from scratch. But the acquisition process can be a little intimidating so here is a guide helping you through it!
Have some questions? Let us know and we'll be in touch.
Everything that you need to know to start your own business. From business ideas to researching the competition.
Practical and real-world advice on how to run your business — from managing employees to keeping the books.
Our best expert advice on how to grow your business — from attracting new customers to keeping existing customers happy and having the capital to do it.
Entrepreneurs and industry leaders share their best advice on how to take your company to the next level.
- Business Ideas
- Human Resources
- Business Financing
- Growth Studio
- Ask the Board
Looking for your local chamber?
Interested in partnering with us?
Start » business ideas, how to start a home care business.
Starting a home care business can be a lucrative opportunity for anyone with health care experience. Learn the seven steps you’ll need to take to get started.

Home care businesses provide a valuable service to the community, which is why the industry is expected to double in size over the next 15 years. But the job is demanding, and it’s essential to perform your due diligence before getting started.
What is a home care business?
Home care businesses offer home health and medical services to aging or sick individuals. It’s an umbrella term used to refer to multiple types of services.
A home care business could provide the following services:
- Companionship to seniors.
- Assisting clients with daily activities like housekeeping and cooking.
- Home therapy services, like physical and occupational therapy.
- Hospice care.
7 tips to starting a home care business
Find out what certifications you need.
Before starting a home care business, you must certify your business through the state and obtain a license. It’s also a good idea to check your local health department to find out if you need any additional licenses. This is not an overnight process and could take as long as a year to complete.
Decide what services you’ll offer
Home care businesses can cover a wide variety of services. You want to decide which type of services you will provide based on your experience and your staff.
If you’re not sure what service you want to offer, spend some time researching the top growing trends in the health care field. This can be an excellent way to match your skills with the current market demand.
As a home care worker, you cannot discuss health records with family or friends.
Identify your target market
Next, you’ll want to spend some time thinking about your target market. This is not necessarily the clients you’ll be serving, but the individuals who will be hiring you. For instance, if you offer hospice services, your target market is the adult children who will hire you to care for their parents.
Create a business plan
The best way to set yourself up for success is by coming up with a detailed business plan. A business plan will outline your target market, your financial plan and how you plan to market your business.
Having a business plan can make it easier to qualify for a small business loan. A loan can help you get your business off the ground faster and let you avoid having to dip into your savings.
[ Read more: How to Write a One-Page Business Plan in a Hurry ]
Make sure you understand HIPAA laws
HIPAA compliance can be one of the most challenging aspects of starting a home care business. HIPAA laws protect the patient's privacy and ensure that third parties can’t access their records without their consent.
As a home care worker, you cannot discuss health records with family or friends. This could frustrate some family members and friends and make it harder for you to do your job. Make sure you have a thorough understanding of HIPAA laws before starting your business.
Come up with a marketing plan
Once you have your business set up and have applied for the appropriate licenses, you should begin marketing your business. You can promote your business on social media and invest in local advertising.
And don’t forget to ask current clients for referrals. Referrals are an excellent―and free―way to grow your business.
[ Read more: The Difference Between Sales and Marketing ]
Hire your staff
If you want to grow your home care business, then at some point you’ll have to bring on staff. You should choose your employees carefully since they directly represent the quality care you will provide.
Conduct a thorough interview process and run background checks on all employees. You can find potential employees through a staffing agency or through personal recommendations.
[ Read more: The Best Interview Questions to Ask, According to Franchise Owners ]
CO— aims to bring you inspiration from leading respected experts. However, before making any business decision, you should consult a professional who can advise you based on your individual situation.
Follow us on Instagram for more expert tips & business owners’ stories.
CO—is committed to helping you start, run and grow your small business. Learn more about the benefits of small business membership in the U.S. Chamber of Commerce, here .

Subscribe to our newsletter, Midnight Oil
Expert business advice, news, and trends, delivered weekly
By signing up you agree to the CO— Privacy Policy. You can opt out anytime.
For more business ideas
11 self-care business ideas for entrepreneurs, how to start a brewery, how to start your own real estate business.
By continuing on our website, you agree to our use of cookies for statistical and personalisation purposes. Know More
Welcome to CO—
Designed for business owners, CO— is a site that connects like minds and delivers actionable insights for next-level growth.
U.S. Chamber of Commerce 1615 H Street, NW Washington, DC 20062
Social links
Looking for local chamber, stay in touch.
Healthcare Business Plan Template
Written by Dave Lavinsky
Healthcare Business Plan
You’ve come to the right place to create your Healthcare business plan.
We have helped over 10,000 entrepreneurs and business owners create business plans and many have used them to start or grow their Healthcare companies.
Below is a template to help you create each section of your Healthcare business plan.
Executive Summary
Business overview.
Riverside Medical is a family medical clinic located in San Francisco, California. Our goal is to provide easy access to quality healthcare, especially for members of the community who have low to moderate incomes. Our clinic provides a wide range of general and preventative healthcare services, including check-ups, minor surgeries, and gynecology. Anyone of any age or group is welcome to visit our clinic to get the healthcare that they need.
Our medical practitioners and supporting staff are well-trained and have a passion for helping improve the health and well-being of our clients. We serve our patients not just with our knowledge and skills but also with our hearts. Our clinic was founded by Samantha Parker, who has been a licensed doctor for nearly 20 years. Her experience and compassion will guide us throughout our mission.
Product Offering
Riverside Medical will provide extensive general care for all ages, creating a complete healthcare solution. Some of the services included in our care include the following:
- Primary care: annual checkups, preventative screenings, health counseling, diagnosis and treatment of common conditions
- Gynecology: PAP tests, annual well-woman exam, and family planning
- Pediatrics: infant care, annual physicals, and immunizations
- Minor procedures: stitches, casts/splints, skin biopsies, cyst removals, and growth lacerations
- Health and wellness: weight loss strategies, nutrition guidance, hormone balance, and preventive and routine services
The costs will depend upon the materials used, the physician’s time, and the amount designated for each procedure. Medical bills will be billed either directly to the patient or to their insurance provider.
Customer Focus
Riverside Medical will primarily serve the community living and working within the San Francisco bay area. The city is diverse and growing and includes people of all ages, ethnicities, and backgrounds. Everyone is welcome to visit our clinic to receive the health care they need.
Management Team
Riverside Medical’s most valuable asset is the expertise and experience of its founder, Samantha Parker. Samantha has been a licensed family doctor for 20 years now. She spent the most recent portion of her career on medical mission trips, where she learned that many people are not privileged to have access to quality medical services. Samantha will be responsible for ensuring the general health of her patients and creating a viable and profitable business medical practice.
Riverside Medical will also employ nurses, expert medical staff, and administrative assistants that also have a passion for healthcare.
Success Factors
Riverside Medical will be able to achieve success by offering the following competitive advantages:
- Location: Riverside Medical’s location is near the center of town. It’s visible from the street with many people walking to and from work on a daily basis, giving them a direct look at our clinic, most of which are part of our target market.
- Patient-oriented service: Riverside Medical will have a staff that prioritizes the needs of the patients and educates them on the proper way how to take care of themselves.
- Management: Samantha Parker has a genuine passion for helping the community, and because of her previous experience, she is fully equipped and overqualified to open this practice. Her unique qualifications will serve customers in a much more sophisticated manner than our competitors.
- Relationships: Having lived in the community for 25 years, Samantha Parker knows many of the local leaders, newspapers, and other influences. Furthermore, she will be able to draw from her ties to previous patients from her work at other clinics to establish a starting clientele.
Financial Highlights
Riverside Medical is seeking a total funding of $800,000 of debt capital to open its clinic. The capital will be used for funding capital expenditures and location build-out, acquiring basic medical supplies and equipment, hiring initial employees, marketing expenses, and working capital.
Specifically, these funds will be used as follows:
- Clinic design/build: $100,000
- Medical supplies and equipment: $150,000
- Six months of overhead expenses (rent, salaries, utilities): $450,000
- Marketing: $50,000
- Working capital: $50,000
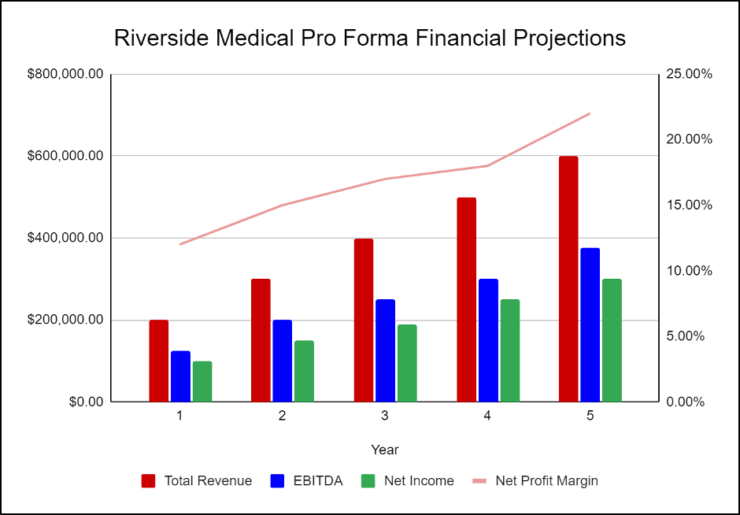
The following graph below outlines the pro forma financial projections for Riverside Medical.
Company Overview
Who is riverside medical, riverside medical history.
Samantha Parker started the clinic with the goal of providing easy access to good quality health service, especially to those members of the community with low to moderate income. After years of planning, she finally started to build Riverside Medical in 2022. She gathered a group of professionals to fund the project and was able to incorporate and register Riverside Medical with their funding support.
Since its incorporation, Riverside Medical has achieved the following milestones:
- Found clinic space and signed Letter of Intent to lease it
- Developed the company’s name, logo, and website
- Hired a contractor for the office build-out
- Determined equipment and fixture requirements
- Began recruiting key employees with previous healthcare experience
- Drafted marketing campaigns to promote the clinic
Riverside Medical Services
Industry analysis.
The global healthcare market is one of the largest and highest-valued industries in the world. According to Global Newswire, the global healthcare services market is currently valued at $7548.52 billion and is expected to reach $10414.36 billion in 2026. This growth is expected to continue for the foreseeable future.
The biggest drivers of industry growth throughout the next decade will be a continual increase in illnesses and diseases as well as a quickly aging population. With more people aging and needing daily/frequent care, hospitals and medical clinics are bound to be in even more demand than they already are.
One obstacle for the industry is the rising cost of care. Though this results in greater profits, more and more Americans cannot afford basic medical care. Therefore, they are opting out of procedures they believe are unnecessary or unimportant.
Despite the challenges of the next decade, the industry is still expected to see substantial growth and expansion.

Customer Analysis
Demographic profile of target market.
Riverside Medical will serve the residents of the San Francisco bay area as well as those who work in the area.
The population of the area experiences a large income gap between the highest earners and the lowest earners. Therefore, it is hard for middle and lower-class families to find quality care that is affordable. As a result, they are in need of the services that we offer and are looking for accessible medical care.
The precise demographics of San Francisco are as follows:
Customer Segmentation
Our clinic is a general family practice and will treat patients of all ages, incomes, physical abilities, races, and ethnicities. As such, there is no need to create marketing materials targeted at only one or two of these groups, but we can appeal to all with a similar message.
Competitive Analysis
Direct and indirect competitors.
Riverside Medical will face competition from other companies with similar business profiles. A description of each competitor company is below.
City Medical
Founded in 2008, City Medical is a membership-based, primary-care practice in the heart of the city. City Medical offers a wide range of primary care services for patients who subscribe to the practice for an annual fee. Patients enjoy personalized care, including office visits, as well as the diagnosis and treatment of common health problems. The patient membership fee covers the services listed below, and most care is received in-office. However, some additional services, such as lab testing and vaccinations, are billed separately. Furthermore, though the annual fee is convenient for some, it is too high for many families, so many are priced out of care at this facility.
Bay Doctors
Bay Doctors is a primary care practice that provides highly personalized medical care in the office or patients’ homes. Bay Doctors includes a team of dedicated healthcare professionals with dual residency in Emergency Medicine and Internal Medicine. The practice offers same-day/next-day appointments, telemedicine, office visits, and home visits. Some of the medical care services they provide are primary care, urgent care, emergency care, gynecology, pediatrics, and minor procedures.
Community Care
Established in 1949, Community Care is a non-profit regional healthcare provider serving the city and surrounding suburbs. This facility offers a wide variety of medical services, including 24-hour emergency care, telemedicine, primary care, and more. In addition to their medical care, they have a wide variety of fundraising activities to raise money to operate the hospital and help families cover the costs of their care.
Competitive Advantage
Riverside Medical enjoys several advantages over its competitors. These advantages include:
Marketing Plan
Brand & value proposition.
The Riverside Medical brand will focus on the company’s unique value proposition:
- Client-focused healthcare services, where the company’s interests are aligned with the customer
- Service built on long-term relationships
- Big-hospital expertise in a small-clinic environment
Promotions Strategy
The promotions strategy for Riverside Medical is as follows:
Riverside Medical understands that the best promotion comes from satisfied customers. The company will encourage its patients to refer their friends and family by providing healthcare benefits for every new client produced. This strategy will increase in effectiveness after the business has already been established.
Direct Mail
The company will use a direct mail campaign to promote its brand and draw clients, as well. The campaign will blanket specific neighborhoods with simple, effective mail advertisements that highlight the credentials and credibility of Riverside Medical.
Website/SEO
Riverside Medical will invest heavily in developing a professional website that displays all of the clinic’s services and procedures. The website will also provide information about each doctor and medical staff member. The clinic will also invest heavily in SEO so the brand’s website will appear at the top of search engine results.
Social Media
Riverside Medical will invest heavily in a social media advertising campaign. The marketing manager will create the company’s social media accounts and invest in ads on all social media platforms. It will use targeted marketing to appeal to the target demographics.
Riverside Medical’s pricing will be lower than big hospitals. Over time, client testimonials will help to maintain our client base and attract new patients. Furthermore, we will be able to provide discounts and incentives for lower-income families by connecting with foundations and charities from people who are interested in helping.
Operations Plan
The following will be the operations plan for Riverside Medical.
Operation Functions:
- Samantha Parker is the founder of Riverside Medical and will operate as the sole doctor until she increases her patient list and hires more medical staff. As the clinic grows, she will operate as the CEO and take charge of all the operations and executive aspects of the business.
- Samantha is assisted by Elizabeth O’Reilly. Elizabeth has experience working as a receptionist at a fast-paced hospital and will act as the receptionist/administrative assistant for the clinic. She will be in charge of the administrative and marketing aspects of the business.
- Samantha is in the process of hiring doctors, nurses, and other medical staff to help with her growing patient list.
Milestones:
The following are a series of path steps that will lead to the vision of long-term success. Riverside Medical expects to achieve the following milestones in the following twelve months:
3/202X Finalize lease agreement
5/202X Design and build out Riverside Medical location
7/202X Hire and train initial staff
9/202X Kickoff of promotional campaign
11/202X Reach break-even
1/202X Reach 1000 patients
Financial Plan
Key revenue & costs.
Riverside Medical’s revenues will come primarily from medical services rendered. The clinic will either bill the patients directly or their insurance providers.
The major cost drivers for the clinic will include labor expenses, lease costs, equipment purchasing and upkeep, and ongoing marketing costs.
Funding Requirements and Use of Funds
Key assumptions.
Below are the key assumptions required to achieve the revenue and cost numbers in the financials and to pay off the startup business loan.
- Year 1: 120
- Year 2: 150
- Year 3: 200
- Year 4: 275
- Year 5: 400
- Annual lease: $50,000
Financial Projections
Income statement, balance sheet, cash flow statement, healthcare business plan faqs, what is a healthcare business plan.
A healthcare business plan is a plan to start and/or grow your healthcare business. Among other things, it outlines your business concept, identifies your target customers, presents your marketing plan and details your financial projections.
You can easily complete your Healthcare business plan using our Healthcare Business Plan Template here .
What are the Main Types of Healthcare Businesses?
There are a number of different kinds of healthcare businesses , some examples include: Nursing care, Physical home health care, or Home health care aides:
How Do You Get Funding for Your Healthcare Business Plan?
Healthcare businesses are often funded through small business loans. Personal savings, credit card financing and angel investors are also popular forms of funding.
What are the Steps To Start a Healthcare Business?
Starting a healthcare business can be an exciting endeavor. Having a clear roadmap of the steps to start a business will help you stay focused on your goals and get started faster.
1. Develop A Healthcare Business Plan - The first step in starting a business is to create a detailed healthcare business plan that outlines all aspects of the venture. This should include potential market size and target customers, the services or products you will offer, pricing strategies and a detailed financial forecast.
2. Choose Your Legal Structure - It's important to select an appropriate legal entity for your healthcare business. This could be a limited liability company (LLC), corporation, partnership, or sole proprietorship. Each type has its own benefits and drawbacks so it’s important to do research and choose wisely so that your healthcare business is in compliance with local laws.
3. Register Your Healthcare Business - Once you have chosen a legal structure, the next step is to register your healthcare business with the government or state where you’re operating from. This includes obtaining licenses and permits as required by federal, state, and local laws.
4. Identify Financing Options - It’s likely that you’ll need some capital to start your healthcare business, so take some time to identify what financing options are available such as bank loans, investor funding, grants, or crowdfunding platforms.
5. Choose a Location - Whether you plan on operating out of a physical location or not, you should always have an idea of where you’ll be based should it become necessary in the future as well as what kind of space would be suitable for your operations.
6. Hire Employees - There are several ways to find qualified employees including job boards like LinkedIn or Indeed as well as hiring agencies if needed – depending on what type of employees you need it might also be more effective to reach out directly through networking events.
7. Acquire Necessary Healthcare Equipment & Supplies - In order to start your healthcare business, you'll need to purchase all of the necessary equipment and supplies to run a successful operation.
8. Market & Promote Your Business - Once you have all the necessary pieces in place, it’s time to start promoting and marketing your healthcare business. This includes creating a website, utilizing social media platforms like Facebook or Twitter, and having an effective Search Engine Optimization (SEO) strategy. You should also consider traditional marketing techniques such as radio or print advertising.
Other Helpful Business Plan Templates
Nonprofit Business Plan Template Non-Emergency Medical Transportation Business Plan Template Medical Practice Business Plan Template Home Health Care Business Plan Template

Healthcare Business Plan Template
Written by Dave Lavinsky
There are several types of Healthcare businesses, from family medicine practices to urgent care centers to home health care agencies. Regardless of the type of healthcare business you have, a business plan will keep you on track and help you grow your healthcare business in an organized way. In addition, if you plan to seek funding, investors and lenders will use your business plan to determine the level of risk.
Download our Ultimate Business Plan Template here >
Below is the business plan outline you should use to create a business plan for your healthcare company. Also, here are links to several healthcare business plan templates:
- Assisted Living Business Plan
- Counseling Private Practice Business Plan Template
- Dental Business Plan
- Home Health Care Business Plan
- Medical Practice Business Plan Template
- Medical Spa Business Plan Template
- Non Medical Home Care Business Plan Template
- Nursing Home Business Plan Template
- Pharmacy Business Plan
- Urgent Care Business Plan
Finish Your Business Plan Today!
Healthcare business plan example outline, executive summary.
Although it serves as the introduction to your business plan, your executive summary should be written last. The first page helps financiers decide whether to read the full plan, so provide the most important information. Give a clear and concise description of your healthcare company. Provide a summary of your market analysis that proves the need for another healthcare business, and explain your company’s unique qualifications to meet that need.
Company Analysis
Your company analysis explains your healthcare business as it exists right now. Describe the company’s founding, current stage of business, and legal structure. Highlight any past milestones, such as lining up clients or hiring healthcare providers with a proven track record. Elaborate on your unique qualifications, such as expertise in a currently underserved niche market.
Industry Analysis
The healthcare industry is incredibly large and diverse, but your analysis should focus on your specific segment of the market. Do you specialize in pediatric healthcare? senior healthcare? emergency medicine? family medicine? Figure out where your healthcare company fits in, and then research the current trends and market projections that affect your niche. Create a detailed strategy for overcoming any obstacles that you uncover.
Customer Analysis
Who will your healthcare company serve? Are they families? The elderly? What is important to them in a healthcare business? How do they select a healthcare provider? Narrow down their demographics as closely as you can, and then figure out what their unique needs are and how you can fulfill them.
Finish Your Healthcare Business Plan in 1 Day!
Don’t you wish there was a faster, easier way to finish your business plan?
With Growthink’s Ultimate Business Plan Template you can finish your plan in just 8 hours or less!
Competitive Analysis
Your direct competitors are those healthcare companies that fulfill the same needs for the same target market as yours. Your indirect competitors are healthcare businesses that target a different market, or other companies that fulfill a different need for your target market. Describe each of your direct competitors individually, and talk about the things that set your healthcare company apart. Categorize your indirect competitors as a group and talk about them as a whole.
Marketing Plan
A solid marketing plan is based on the four P’s: Product, Price, Promotion, and Place. The Product section describes the healthcare you sell along with any other services you provide. Price will change according to the specifics of the property, but you can delineate your fees here. Promotion is your means of getting new business. Place is your physical office location, along with your web presence and the areas where you sell. Another category, Customer retention, refers to the ways you will build loyalty.
Operations Plan
Your operations plan explains your methods for meeting the goals you set forth. Everyday short-term processes include all of the daily tasks involved in servicing clients. Long-term processes are the ways you will meet your defined business goals, such as expanding into new markets or new types of service.
Management Team
The management team section highlights the backgrounds of the key members of your team. Focus on those aspects that prove your team’s ability to build and run a successful company. A business mentor or advisor can help fill in any gaps, provided you can identify the specific ways that your advisor will influence your company’s growth.
Financial Plan
Investors and lenders heavily scrutinize the financial plan, but it is often the most challenging part of the business plan to write. Healthcare is a strong market, it usually not subject to economic turns. The financial plan requires you to detail your individual revenue streams by implementation timeline and relative importance, and disclose any sources of outside funding. You also need to summarize your past and future Income Statements, Cash Flow Statements, and Balance Sheets, based on key assumptions that must be both reasonable and verifiable based on an analysis of similar companies. You should also provide a solid exit strategy that shows your understanding of the market and your desire to capitalize on profitability.
Your full financial projections should be attached in the appendix along with any other documents that support your claims, such as letters from key partners.
Healthcare Business Plan FAQs
What is the easiest way to complete my healthcare business plan.
Growthink's Ultimate Business Plan Template allows you to quickly and easily complete your Healthcare Business Plan.
What is the Goal of a Business Plan's Executive Summary?
The goal of your Executive Summary is to quickly engage the reader. Explain to them the type of healthcare business you are operating and the status; for example, are you a startup, do you have a healthcare business that you would like to grow, or are you operating a chain of healthcare businesses?
Don’t you wish there was a faster, easier way to finish your Healthcare business plan?
OR, Let Us Develop Your Plan For You
Since 1999, Growthink has developed business plans for thousands of companies who have gone on to achieve tremendous success. Click here to see how our professional business plan writers can create your business plan for you.
Other Helpful Business Plan Articles & Templates

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- VA Author Manuscripts

Adapting a Whole Health Model to Home-Based Primary Care: Bridging Person-Driven Priorities With Veteran and Family-Centered Geriatric Care
Anne k. schwabenbauer.
1 Erie Veterans Affairs Medical Center, Erie, Pennsylvania, United States
Cynthia M. Knight
2 Veterans Affairs Boston Healthcare System, Boston, Massachusetts, United States
Nicole Downing
Michelle morreale-karl.
3 Department of Medicine, Harvard Medical School
Michelle E. Mlinac
4 Department of Psychiatry, Harvard Medical School
Anne K. Schwabenbauer contributed to the conceptualization, project administration, visualization, writing of the original draft, and reviewing and editing of the manuscript. Cynthia M. Knight contributed to the conceptualization, writing of the original draft, and reviewing and editing of the manuscript. Nicole Downing contributed to the writing of the original draft. Michelle Morreale-Karl contributed to the conceptualization, supervision, and review and editing of the manuscript. Michelle E. Mlinac contributed to the conceptualization, project administration, visualization, supervision, writing of the original draft, and reviewing and editing of the manuscript.
Through the integration of Whole Health for Life into the Department of Veterans Affairs (VA) health care system, the VA aims to transform health care delivery from a disease management approach to one that embraces person-centered care. The home-based primary care (HBPC) program is a care model that, within the VA, provides holistic primary care services to homebound veterans with multiple chronic medical conditions, mental health issues, and functional declines. These veterans may have limited access to VA programs delivered in a traditional outpatient format. This article describes adaptations to the whole health model of care that could improve its accessibility and applicability to HBPC veterans, caregivers, and the interdisciplinary teams that serve this population. These modifications are informed by whole-person geriatric and gerontological and family-systems theories and address population-based differences in the focus and approach to care. The focus on care is expanded to (a) reflect the importance of attending to caregiver needs and well-being and (b) shift from a preventative model to one that prioritizes resilience and maintenance. The approach to care emphasizes alternative modes of delivery, adaptations to interventions, and integration of geriatric-specific medical considerations into the self-care domains and more directly centers the collaboration between family, the VA, and community partners. This adapted model also addresses the unique needs of health care teams providing in-home services to medically complex veterans and offers suggestions for enhancing self-care and preventing burnout.
Whole Health for Life (WH) is an emerging model of practice redesign with the Department of Veterans Affairs (VA), broadening and refocusing traditional care to center instead on patient values, empowering veterans to set and meet personal health goals ( Kligler et al., 2018 ; Krejci et al., 2014 ). This shift in perspective incorporates patient and provider wellness, peer support, and complementary and integrative health strategies (CIH). The WH model can be illustrated using the Circle of Health ( U.S. Department of Veterans Affairs, 2020 ; see Figure 1 ), which positions the veteran at the center of the circle, surrounded by domains of self-care. Mindfulness permeates all aspects of the Circle of Health as it guides veterans’ path to living a fulfilling life in accordance with their values ( Kligler et al., 2017 ).

Note. See U.S. Department of Veterans Affairs (2020) . See the online article for the color version of this figure.
WH is championed in the primary care setting where veterans work with their team in identifying what is most important to them in reaching their goals. This model aims to be implemented beyond primary care as well, including referrals to special classes (e.g., group tai chi), engaging veterans as WH peer partners, and attention to veteran wellness. WH is not specifically aimed at any one type of veteran patient, and it is unclear how the model may fit those older veterans with more complex chronic illnesses who may not be able to engage in traditional outpatient care. This group of veterans often depends on friends or family serving as caregivers, who are also not explicitly addressed in this model. An early finding from an initial WH rollout at one flagship site suggested that older veterans in general were less likely to be referred for specialty WH programming ( Marchand et al., 2020 ).
The home-based primary care (HBPC) model has also developed within VA and non-VA health care settings in recent years ( Edes, 2010 ). This patient-aligned care team provides in-home holistic care to veterans with multiple advanced chronic health problems (e.g., heart failure, renal disease, COPD, dementia, and often depression and anxiety) and functional declines, helping them to age in place and reduce emergency room visits and hospitalizations. Interprofessional HBPC teams serve veterans who, for reasons of age, disability, or complexity, have difficulty getting their care needs met through traditional outpatient primary care. HBPC teams within the VA typically include nurse care managers, social workers, pharmacists, primary care providers, physical and occupational therapists, dieticians, and mental health providers (most commonly psychologists).
In comparison with older adults broadly, those served in HBPC setting are generally sicker and more frail and have more barriers accessing usual outpatient care ( Totten et al., 2016 ), although many more older adults could potentially benefit from HBPC than presently receive it due to lack of provider availability, reimbursement issues, and other barriers ( Edes, 2019 ; Ritchie & Leff, 2018 ). Many HBPC veterans have comorbid mental health issues such as depression, anxiety, or posttraumatic stress disorder ( Edes, 2010 ). Older veterans who utilize VA services in general may have psychiatric trends that differ in important ways from the general older veteran population and older adults as a whole, including having a higher incidence of alcohol use disorder ( Williamson et al., 2018 ) and in displaying risk and resiliency factors that may affect their treatment needs given many (but not all) have lived through prior combat exposure ( Karel et al., 2020 ). While differences exist, some characteristics of HBPC veterans are generalizable to nonveterans that receive home care. Older adults who utilize home care across the United States have high rates of depression and anxiety ( Xiang et al., 2018 ). Older adults electing to remain in place in general face similar issues and goals that those receiving HBPC do, including staying socially connected, engaging in activities, maintaining health and quality of life, and preserving independence and autonomy ( Chum et al., 2020 ).
Family or friends serving as caregivers play a significant role in patient care for this seriously ill veteran population, though not all veterans have someone available or willing to fill this need. Chronic illness impacts not only the veteran but also their caregivers and, in many cases, also the larger family unit. Consistent with the family systems illness model ( Rolland, 2017 ), HBPC teams provide longitudinal health care that addresses the varying needs of the veteran, caregiver, and family across time. Caregivers in home care settings are particularly well suited to being partners in care collaboration ( Ris et al., 2019 ) and in care receipt ( Smith-Carrier et al., 2018 ). While paid or formal caregivers (e.g., those working for home health agencies) can play key roles in health care provision for HBPC patients ( Reckrey, 2020 ), this article will specifically focus on informal caregivers who have family or friend relationships with veterans receiving care. These caregivers may also include medical foster home caregivers who provide care to veterans living in their homes ( Haverhals et al., 2016 ); veterans residing in medical foster homes receive their primary care through HBPC. One important role that HBPC plays is to support veterans and their informal caregivers through facilitating access to care, developing shared goals, care coordination, and providing emotional support ( Shafir et al., 2016 ; Smith-Carrier et al., 2018 ; Wool et al., 2019 ). Family caregivers are also critical partners in service delivery for older adults as there is a significant shortage of geriatrics-trained health care providers ( Foley & Luz, 2020 ).
This article describes how the WH model can be meaningfully adapted to the unique needs of HBPC veterans and their caregivers, informed by whole-person state-of-the-art geriatric and gerontological theory (e.g., the geriatric 5Ms: mobility, medications, multicomplexity, mind, what matters most, Tinetti et al., 2017 ; preference-based care, Van Haitsma et al., 2019 ). For example, WH centers on “what matters to you, not what is the matter with you,” an approach consistent with the geriatric 5Ms’ tenet of aligning care to what matters most to older patients. Use of person-centered and family-centered approaches for the types of veterans served by HBPC, including values-based goal setting (e.g., Feder et al., 2019 ), caregiver support and family interventions (e.g., Nichols et al., 2017 ; Pillemer & Gilligan, 2018 ), CIH (e.g., Kogan et al., 2017 ; Mbizo et al., 2018 ), and telephone-based peer support (e.g., Lauckner & Hutchinson, 2016 ; Tomasino et al., 2017 ) have been shown to be achievable. As this large system change unfolds within the VA, we consider ways to modify the WH model to fit with the needs of HBPC veterans, caregivers, and the teams that serve them. This adapted model may also be meaningful for HBPC or home care teams outside of the VA system as they consider ways to provide person-centered care to patients in their homes.
Adaptations of the Whole Health Model
We have adapted the circle of health for use in HBPC as shown in Figure 2 , a modification with two main differences from the original. First, the caregiver (when available) joins the patient at the center of the circle, emphasizing both the caregiver’s integrated role in the patient’s health care and the importance of attending to the caregiver’s own needs and goals. Repositioning the caregiver alongside the veteran is a key element of care in primary care ( Epperly et al., 2019 ; Parmar et al., 2020 ) and in care for those with serious illness ( Sperber, 2019 ) and is consistent with recommendations by the VA and non-VA organizations such as the Elizabeth Dole Foundation’s (2017) Campaign for Inclusive Care; the National Academies of Sciences, Engineering, and Medicine (2016) ; the AARP and the National Alliance for Caregiving (2020) . The centrality of the caregiver makes it imperative that a HBPC WH approach includes tools that also directly benefit the caregiver’s health and well-being. Therefore, an HBPC WH approach recognizes caregivers as essential to the circle of health and incorporates holistic tools specific to the caregiver’s own health. Including the caregivers in the center of the circle underlines their importance as vital partners in care delivery, particularly in light of the geriatric workforce shortage ( Flaherty & Bartles, 2019 ).

Note. The me and my caregiver; values and preferences; family and community supports; mobility; adaptation; family and friends; and preventions, treatment, and management components of the adapted circle of health are modifications from the original figure. The power of the mind self-care component was not included in the adapted circle of health. See online article for the color version of this figure.
Second, the focus of WH shifts from a preventative health promotion orientation to one of resilience and maintenance of functioning, blending WH principles with those from gerontological theory and geriatrics practice. The wider social system encompassing family and community supports replaces the emphasis on mindful awareness, underlying the critical role that loved ones and social systems play in supporting the veteran and their caregiver. Appreciating the family-system context can help HBPC teams understand how a family’s dynamics, health illness beliefs, and collective strengths impact health care provision ( Steinglass, 2006 ). HBPC teams are well suited to deliver family-system-informed whole health care as they offer collaborative primary care with an integrated mental health provider and are freer from financial reimbursement challenges faced when providing geriatric care in the community. Community supports (e.g., home-delivered meals, homemaking services) provide additional foundation for the patient to remain at home. Community care outside the VA (e.g., assisted living or nursing home) is available when a higher level of care is needed.
We modified the outer circles to include a shift from “prevention and treatment” to “prevention, treatment, and management.” Prevention of disease is recontextualized and shares an emphasis with maintenance of function in this population of older adults with complex illnesses. Prevention is congruent with the veteran’s and caregiver’s values and may be focused on conditions that may emerge in the context of advanced medical illness or disability, such as preventing falls or skin breakdown, minimizing caregiver burnout, or reducing the likelihood of hospitalization or need for long-term care. HBPC’s approach includes both conventional and complementary medicine and is evident throughout the domains of self-care. However, access to both types of treatment approaches can be challenging, particularly in rural areas with limited access to internet or other resources. Correspondingly, Tables 1 and and2 2 describe specific WH interventions that HBPC teams can utilize to support veterans and caregivers, respectively.
Suggested HBPC Team Interventions to Adapt the Component of Whole Health for HBPC Veterans
Suggested Whole-Health-Consistent HBPC Team Interventions to Support Informal Caregivers
Note . HBPC = home-based primary care.
Me and Caregiver
Both veterans and caregivers can be empowered by a WH approach to care. For many HBPC veterans, caregivers are necessary to access and engage with the components of self-care serving as a liaison between providers and community resources, coach in the implementation of WH tools, and partner in many therapeutic interventions. Caregivers provide the basic daily care that is essential for HBPC veterans, helping them toward maintaining current abilities, preventing or slowing further decline, and optimizing quality of life. The centrality of the caregiver makes it imperative that a HBPC WH approach include tools that also directly benefit the caregiver’s health and well-being. Therefore, it is recommended that an HBPC WH approach not only recognize caregivers as core to the circle of health and implementation of the personal health plan but also incorporate holistic tools specific to caregiver whole health. The HBPC team should assess the goals of both the veteran and the caregiver and adjust the care plan to meet those goals.
It is important to note that the relationship between informal caregiver and care recipient generally is not the only kind of relationship they may have with one another. A family-systems lens also takes into account other roles (e.g., partner, parent–child, close friend) and how the veteran’s health issues and need for care affect those roles and those of the broader family or social network. In VA HBPC, family-systems issues are regularly evaluated by the team’s social workers as part of a comprehensive psychosocial assessment, taking into consideration family processes and dynamics as they evolve over the course of serious illness. Interventions offered by HBPC social workers and mental health providers can address the family unit as a whole and support individual relationships within the family. For example, integrative behavioral couples therapy delivered in the home can support relationship continuity for a veteran and caregiver who are in a partnered relationship ( Riley, 2019 ; Wetherell et al., 2020 ).
Values and Preferences
Values represent the aspects of ourselves, our families, our communities, and our environment that are most important to us. They are foundational to goal selection and attainment as well as the internal motivation that facilitates this process. While variability exists, individuals with characteristics similar to HBPC veterans tend to place the greatest value on activities and relationships that are presently meaningful ( Fredrickson & Carstensen, 1990 ; Saajanaho et al., 2016 ; Shaw et al., 2007 ). In turn, the goals stemming from these values are centered on maintaining these activities and relationships and avoiding future loss in these areas ( Baltes & Baltes, 1990 ; Baltes & Carstensen, 1996 ; Remillard, 2019 ; Zhang & Radhakrishnan, 2018 ).
HBPC teams may support veterans’ values in many ways. For example, independence may be something highly valued by a veteran who does not want her daughter to move in to help her. In contrast, the daughter may value her mother’s safety and is willing to forego some of her own independence to provide care for her mother. The nurse observes the escalating tension between the veteran and her daughter and asks the social worker to evaluate the situation. The team may work collaboratively to help resolve this conflict by identifying other resources to promote home safety while still promoting independence for the veteran.
Given the reliance of many HBPC veterans on caregivers and the broad impact that chronic illness and debility have on caregivers and the larger family system, it is equally as important to understand their values and preferences and the dynamics that shape them. Factors such as family legacy of illness and loss, communication patterns, and organization can impact the patient’s and caregiver’s decisions and ability to adapt to illness-related changes (i.e., level of need, relational dynamics, roles) and cope with illness-related stressors ( Rolland, 2017 ). Providing values-driven care from this standpoint requires evaluating these critical family-system variables as well as eliciting and understanding the veteran’s and caregiver’s values and preferences, educating the veteran and caregiver about health care decisions consistent with their goals and preferences, accepting veteran’s and caregiver’s decisions regarding treatment, and resolving differences within the veteran-caregiver dyad in a manner that is consistent with their preferences ( Boyd et al., 2019 ; Institute for Healthcare Improvement, 2018 ; Rolland et al., 2017 ; Tinetti et al., 2019 ). An HBPC-WH approach must not only consider the veteran’s and caregiver’s values and preferences but also appreciate the familial context and history that shapes them. A common task for HBPC teams is to conduct goals-of-care conversations with veterans and their families, a process that may evolve over time and can be a source of conflict and stress within the family system. This tension may be driven by conflicting values, a lack of communication with in the family, or confusion about illness course and prognosis ( Rolland, 2017 ; Rolland et al., 2017 ).Using a family-systems lens, the HBPC team may support this process through assessing the family’s values and dynamics and facilitating healthy communication between all parties at each phase of the illness.
Domains of Self Care
Adaptation and coping.
The self-care domain of “personal development” as described in the original WH model encompasses multiple areas including developing talents and potential, building social capital, nurturing positive emotions, fostering lifelong learning, enhancing creativity, improving quality of life, and contributing to the realization of dreams and aspirations ( Mirgain, 2014 ).While the aspects of personal development intrinsic to the individual may still apply in late life, those that are temporally distant and emphasize growth and productivity are less relevant ( Carstensen et al., 1999 ; Fung et al., 2020 ; Korff & Biemann, 2020 ). For HBPC veterans, the focus may shift from skill development and achievement to reflecting on past experiences and repurposing existing skills and strengths to face current challenges ( Baltes & Baltes, 1990 ; Carpentieri et al., 2017 ; Joly-Burra et al., 2020 ; Remillard et al., 2019 ). Though not explicitly described in the WH model, cultural factors may drive great variation in what goals in adaptation and coping look like in late life over time. Goals may extend beyond the self and across life domains (i.e., familial, social) and may often be motivated by what is meaningful to them today even if not achievable within their lifetime. For example, older veterans may wish to share their unique life experiences with the medical team, their families, and other veterans through the “My Life, My Story” project ( Ringler et al., 2015 ), reflecting both the wish to make an immediate connection with these individuals and the wish to share their stories as part of their legacies. The priorities may be two-fold: (a) adaptation to current circumstances in a manner that maintains a cohesive sense of social usefulness consistent with lifelong values and ideals and (b) establishing a legacy and benefitting current and future generations ( Erikson & Erikson, 1997 ; Gottlieb & Sevigny, 2016 ). Given this shift in the focus of development, we propose that a self-care domain focused on enhancing adaptation and coping would be more congruent with the health and wellness goals of HBPC veterans.
Coping and adaptation also occur within the context of the caregiving relationship. As the veteran’s health and associated needs evolve over the time, the caregiving system supporting the veteran must also adapt. In order to successfully navigate these transitions, the caregiver needs to understand the nature of the demands at each phase of the illness and have the psychological, emotional, and instrumental resources to meet them ( Rolland, 2017 ). A WH model that fully incorporates the caregiver must include strategies that support caregivers through these transitions and help them adaptively cope with the implications these changes have for all domains of the veteran’s and caregiver’s lives ( Branson et al., 2019 ).
The domain known as “working the body” is renamed “mobility.” For veterans in HBPC, physical activity remains an important aspect of self-care, with benefits including management of chronic illness, cognitive health, mobility, muscle integrity, fall prevention, range of motion, and emotional health ( Elsawy & Higgins, 2010 ). However, the level of cognitive and physical debility in this population necessitates that physical activity goals shift from improving fitness to maintaining mobility, fostering resilience, and slowing future decline ( Whitson et al., 2016 ). HBPC veterans’ often limited mobility and degree of disability may inhibit participation in outpatient WH physical activity programs in multiple ways. This population is largely homebound and therefore unable to access VA or community-based resources such as yoga classes or exercise groups. Furthermore, the level of physical ability required to safely perform many of these activities far exceeds that of most HBPC veterans. In order to be accessible to this population, WH programming must take into account the mobility and ability levels of these veterans and provide activities that are accessible and consistent with veterans’ physical capabilities. Caregiving is also often physically demanding (and many may have their own health issues), particularly when veterans need assistance with activities of daily living, and caregivers may not prioritize time for exercise as self-care. Physically demanding caregiving may contribute to burnout ( Orgeta & Miranda-Castillo, 2014 ). Virtual visits or exercise classes may be useful to both veterans and caregivers.
Getting adequate sleep and feeling well rested are vital for the health and well-being of HBPC veterans and their caregivers. Sleep promotes healing, improves coping, and is necessary to be at one’s cognitive best. In this patient population, insomnia may be driven by many issues such as pain, changing sleep patterns, timing of bodily functions, medical ailments, medication side effects, decreased daytime activity, sedentary lifestyle, sleep environment, and psychiatric issues ( Foley et al., 1999 ; Gooneratne & Vitiello, 2014 ; Moraes et al., 2014 ). The complexity of the HBPC population also limits the utility of many treatments for insomnia. The risk of polypharmacy, potential adverse side effects of many sleep medications for older adults, and patient aversion to taking additional medications often preclude the use of prescribed medication and herbal supplements. Cognitive impairment and physical debility may require modification to psychotherapeutic (cognitive behavioral therapy for insomnia) and self-care-based (physical activity, mindfulness) interventions. Obstacles to recharging also exist for the caregivers of HBPC veterans. Caregiver stress, nocturnal activities of the care recipient, and caregiver’s own medical and psychiatric conditions can place the caregiver and care recipient at risk for negative outcomes ( Creese et al., 2008 ; Leggett et al., 2018 ; McCurry et al., 2009 ).
Food and Drink
Achieving adequate nutrition and hydration are essential to promoting and maintaining physical, cognitive, and emotional health in HBPC veterans who are at risk of malnutrition ( Win et al., 2017 ). Additionally, maintaining cultural and personal food preferences can greatly enhance quality of life. While supporting cultural food preferences can improve quality of life, it may also not be consistent with dietary recommendations. There are a variety of considerations and challenges when addressing this goal including medication and illness-based dietary restrictions, the need to adapt food viscosity and texture based on swallowing and dentition, age-related changes to appetite and taste, and the limited ability to independently access and prepare healthy foods ( Locher et al., 2009 ; Mudge et al., 2011 ; Roberts et al., 2019 ). The diversity and complexity of potential obstacles requires an HBPC-WH approach that is broad and inclusive and incorporates the patient, caregiver, interdisciplinary care team, and community resources. HBPC veterans and caregivers often require assistance with every step of accessing and preparing balanced meals. Given the physical and cognitive limitations of many HBPC veterans, successful interventions should incorporate, and in some cases center on, caregivers as they often execute most of these tasks and monitor safe eating practices (i.e., use of thickeners, rate of consumption, eating technique).Caregivers’ stress level, financial resources, or own functional issues may complicate access to nutritious and comforting meals for both them and those for whom they care. HBPC teams should address the role that food and nutrition play in the family structure—for example, routinely evaluating the family’s risk for food insecurity or incorporating cultural preferences into dietary recommendations as much as is feasible.
Family and Friends
For HBPC veterans, a WH approach to maintaining connections with family and friends must reflect the scope, focus, and challenges of this population’s interpersonal relationships. Positive social relationships have a significant impact on emotional and physical health and can serve an adaptive coping function ( Heckhausen et al., 2010 ). The size of many HBPC veterans’ social networks may have been reduced through illness, death, or distance. Widowhood and the loss of friends and family members occurs more frequently in late life. The loss of family and friends due to estrangement may further contribute to this decline, particularly given that these are more likely to be intimate relationships (parent–child, sibling, old friends) that would typically remain a source of positive emotional support. This involuntary diminishment in social network in conjunction with the physical dependency and limited mobility of many HBPC veterans leaves the HBPC population more vulnerable to the negative impact of social isolation and loneliness as well as gaps in instrumental resources often provided by family and friends.
Thus, a WH approach to family and friends will need to incorporate tools to assist veterans in reconnecting with those they wish to reconnect with and compensate for these losses. Support from the HBPC social worker and mental health provider can help veterans access instrumental supports and repair relationships with family and friends that may have fractured or strained over time and assist them in accepting and grieving lost relationships that cannot be regained. New social connections may form if veterans begin to attend senior centers or adult day health centers ( Brown et al., 2014 ) or if they receive in-home help. In some cases, veterans are unwilling to utilize these resources due to a lack of interest in investing the time and emotional energy into new relationships, feeling unwelcome or socially rejected by staff and other attendees of these facilities, discomfort with an unknown individual in the home providing personal care, and needs that are beyond the scope of an outside agency.
Friends and family often serve as the primary or supplementary caregivers whose daily support is essential to maintaining current levels of health and independence. While critical to the health and well-being of HBPC veterans, the caregiver’s dual role (i. e., being both caregiver and child/partner/friend) has the potential to cause discord for both parties ( Heckhausen et al., 2010 ; Savundranayagam & Montgomery, 2010 ). This conflict becomes increasingly likely as greater dependency forces a shift in the nature of the original family/friend relationship toward that of caregiver-care recipient ( Montgomery & Kosloski, 2013 ). The care recipient may feel they are becoming burdensome due to many factors including increased physical dependency, empathy, and concern for the loved one facing the challenges of caregiving, a sense of personal responsibility or guilt about the caregiver’s hardship, inequity in the relationship, and the inability to fulfill their own roles and responsibilities ( Kowal et al., 2012 ; McPherson et al., 2010 , ; McPherson et al., 2007 ). Distress related to feelings of burdensomeness is associated with reduced quality of life, loss of personal dignity, decreased self-esteem, greater hopelessness, risk of suicide, and increased rates of depression, anxiety, and adjustment disorder ( Akechi et al., 2004 ; Chio et al., 2005 ; Kwak et al., 2014 ; Nieuwenhuis et al., 2018 ; Wilson et al., 2005 ). In the HBPC veteran/caregiver dyad, these phenomena can drive conflict between caregiver and care recipient (e.g., through refusal to allow family caregivers to complete tasks such as bathing or toileting [ Mournet et al., 2020 ; Newsom, 1999 ]).
The stressors associated with caregiving place the caregiver at risk of experiencing negative emotional and physical outcomes. Multiple factors such as circumstances directly related to the caregiver’s situation or caregiving responsibilities (i.e., care recipient’s level of dependence, managing behavioral issues), the caregiver’s subjective experience of these demands (i.e., role overload), impact of caregiving on other life domain (i.e., financial strain, job stress), or internal strain related to caregiving (i.e., loss of self-concept) can be sources of caregiver stress ( Pearlin et al., 1990 ). Whether a caregiver experiences significant strain as a result of these is a dynamic process influenced by the number of stressors, the characteristics of the caregiver (i.e., age, gender, socioeconomic status), the nature and quality of the relationship with the care recipient, intrinsic coping ability, and the availability of support services and resources. While many caregivers do not report significant strain related to caregiving, those that do have higher rates of depression and poorer health outcomes ( Pinquart & Sörensen, 2003 ; Roth et al., 2009 ). The degree of caregiver strain also directly impacts the care recipients as high levels of caregiver strain are associated with increased risk of abuse, placement in long-term care, and poorer health outcomes for the care recipient( Beach et al., 2005 ; Elliott & Pezent, 2008 ).
Although caregiving is associated with potential negative outcomes, it is also important to recognize the positive psychological impact of being a caregiver. Caregiving can provide a sense of fulfillment, satisfaction, enhanced self-efficacy, and competence ( Kim et al., 2007 ; Loyd et al., 2016 ; Lynch et al., 2018 ; Pierce et al., 2007 ). Additionally, caregiving is associated with personal growth and a greater satisfaction with life ( Haley et al., 2009 ; Jones et al., 2011 ; National Opinion Research Center, 2014 ). Many caregivers have these positive experiences while also struggling with the strain of caregiving ( Harmell et al., 2011 ).
Tending to the health of the care recipient, the caregiver, and their relationship are essential components of a HBPC-WH model, and interventions to support each of these must be emphasized throughout the model. While the caregiver and care recipient may individually benefit from different interventions, it is also necessary to view those involved in providing care as a system and consider the needs of this partnership ( Rolland, 2019 ). Given the importance of the caregiver-care recipient relationship, a HBPC-WH model should strongly emphasize tools that support the health of this relationship. This may include family-based consultation both as family member(s) first move into the role of caregiver and then on an ongoing basis as the dynamics of these relationships shift.
Spirit and Meaning
In late life, spirituality may mean gaining understanding, finding meaning, and accepting past experiences and current realities ( Brown & Lowis, 2003 ; Erikson & Erikson, 1997 ; Tornstam, 1997 ). This process provides a sense of purpose in late life and the opportunity to rise above any distress that may have been associated with past experiences. Spiritual engagement is often a source of strength and resiliency and has been associated with better physical and mental health ( Agli et al., 2015 ; Buco et al., 2018 ; Contrada et al., 2004 ; Daaleman et al., 2004 ; Hosseini et al., 2019 ; Koenig et al., 2014 ; Wachholtz & Pargament, 2008 ; Whitehead & Bergeman, 2019 ). Spirituality helps buffer against loss and adversity by promoting human virtues (e.g., forgiveness, patience, gratitude) and a cognitive framework that instills meaning in loss and difficult life events ( Damianakis & Marziali, 2012 ; Koenig et al., 2014 ). The potential benefits of spirituality extend to the caregiver, where it may play an important role in managing the strain of caregiving, finding meaning in caregiving work, and coping with grief and loss ( Damianakis & Marziali, 2012 ; Damianakis et al., 2018 ; Lai et al., 2018 ; McLennon et al., 2011 ). As excursions outside the home are curtailed, home or virtual visits by chaplains or clergy can provide meaningful connections.
Surroundings
The home is the predominant environment for the mostly homebound HBPC population. The home may reinforce a sense of personal continuity, providing a link between one’s past and present self ( Rowles & Bernard, 2013 ). It can also act as a physical representation of the individual’s independence and autonomy, as a connection to emotionally salient memories, and as an anchor to a social support network ( Wiles et al., 2012 ). Many HBPC veterans say that remaining in their home is their primary goal, but at times, the home may no longer meet their needs, sometimes necessitating a move to a more supportive living environment. This new environment may be living with the caregiver (or having the caregiver move in) or moving to a formal setting such as assisted living or a nursing home. Each transition brings its own benefits and challenges. For example, in the case of an adult child caregiver moving in with a parent, longstanding familial conflicts may reemerge. The shared living space may also spur memories of earlier times in the family, harmonious or otherwise. The veteran’s internal resources and the circumstances surrounding relocation can affect whether they successfully adjust to their new environment. Those who relocate against their will may feel they have lost control, have difficulty adjusting to the relocation, and experience poorer health outcomes ( Chen et al., 2007 ; Laughlin et al., 2007 ). In contrast, those who relocate willingly may be better able to maintain a sense of personal control. These individuals also adjust better to relocation and experience greater overall well-being ( Bekhet et al., 2008 , 2009 ). For lesbian, gay, bisexual, and transgender (LGBT) veterans who may lack a loved one to provide needed care ( Czaja et al., 2016 ), concern around entering a communal living environment may be based on a lifetime of societal and institutional discrimination. The LGBT community faces ongoing stigma and bias that can limit access to services and generate increased distress due to experiences of heterosexism, cissexism, transphobia, and homophobia from residents and staff ( Donaldson & Vacha-Haase, 2016 ; Hiedemann & Brodoff, 2013 ; Fredriksen-Goldsen et al., 2013 ; National Senior Citizens Law Center, 2015 ). A WH model that supports all aspects of HBPC veterans’ well-being will need to include tools focused on both supporting veterans in their home and supporting relocation adjustment when necessary.
Additional Whole Health Components
Peer support.
Given the isolation of both veterans and caregivers served by HBPC, there is a prime opportunity to provide peer support to both groups. Home visits, telephone calls, or televideo visits made to veterans by peers may help to provide important social connection, advice, and support. Additionally, with expanded access to virtual care, interventions such as multifamily groups may be innovative strategies for use in this population (e.g., Sherman et al., 2011 ; Steinglass et al., 2011 ). For example, one of our sites is currently piloting a brief televideo group intervention for HBPC veterans with Parkinson’s disease and their families. Programs such as VA Video Connect, Home Telehealth, and the Digital Divide, which provide access to equipment and assistance for veterans in the operation of the equipment, have been implemented to support care access and reduce social isolation during the COVID-19 pandemic. The use of non-VA applications such as Doximity, FaceTime, and Zoom as well as home telehealth through community VA services has also provided additional means of contact with home-based health care teams.
Patient and Caregiver Feedback
Receiving regular input from veterans and their caregivers is key to informing the type of person-centered and family-centered care encompassed by the WH model. HBPC teams can conduct regular surveys of veterans and caregivers to ensure quality care is being delivered with their input. See Table 3 for an example of survey questions that can be completed by both the veteran and the caregiver whenever possible. Veterans and caregivers may have differing perceptions of care, but both provide important feedback to HBPC teams. While these surveys may be completed by mail, surveys done by phone can minimize burden on caregivers and allow probing for additional information when needed.
HBPC Patient Satisfaction Survey Sample Questions
Provider Self-Care
Provider self-care is critical for HBPC team members who face long hours driving in traffic or far distances, haul heavy bags in and out of homes, enter unpredictable home environments, encounter logistical and technological challenges, and risk burnout while managing veterans with complex medical and emotional needs ( O’Brien et al., 2019 ). Providers are often in the home alone with the patient and thus need to independently triage and manage when anything goes awry. Providers are often drawn to this valuable work because home-delivered care is meaningful and unlike anything else in health care. Provider self-care is critical in retaining this vital workforce. Suggested WH interventions for HBPC providers themselves are offered in Table 4 .
HBPC Provider-Focused Whole Health Interventions to Improve Wellness and Reduce Burnout Risk
The WH model of patient care is an opportunity to strengthen veteran-centered and family-centered care for a vulnerable population. As WH rolls out across the VA (first to flagship facilities in each VA region, then to other medical centers within that region) and simultaneously holistic geriatric care models are spreading, HBPC teams can think creatively about how to carry these principles into the home and, when applicable, into the family context. Recognizing and including the caregiver as being central to the overall care approach is vital with this population of older chronically ill patients. More fully integrating the family into the WH model extends its usefulness, likely even to veterans of later service eras (e.g., veterans of Iraq and Afghanistan) and with HBPC patients outside the VA. There are ample opportunities for research and quality improvement work in this area—for example, identifying HBPC veterans’ preferences around CIH approaches, determining feasibility of the WH model within this population, as well as identifying HBPC veteran, caregiver, and provider experiences with the WH model. These adjustments to the WH model align it with other emerging geriatric care models in the community, such as the essential care model ( Golden et al., 2019 ), and can help the VA continue to drive innovation in health care ( Edes, 2019 ). Beyond the VA, many of these whole-person interventions can be applied to older adults or others dealing with chronic illness and disability in outpatient primary care, rehab, palliative care, hospice, or long-term care settings, including values-based goal setting, family-systems orientation, CIH approaches, and evidence-based support for caregivers.
Public Significance Statement
This article describes modifications to the Department of Veterans Affairs’ whole health model of care to increase its accessibility and applicability to the older adults and their caregivers who are served by home-based primary care programs. The needs and goals of these medically complex older adults may differ from those of younger, more active patients. The article emphasizes the importance of caregivers as part of the whole health model and outlines strategies for adapting whole health practices to integrated geriatric health care settings.
Acknowledgments
This material is the result of work supported with resources and the use of the facilities of the Veterans Affairs Boston Healthcare System and the Erie Veterans Affairs Medical Center. These contents do not represent the views of the U.S. Department of Veterans Affairs or the U.S. government.
We have no conflicts of interest to disclose.
- AARP and the National Alliance for Caregiving. (2020). Caregiving in the United States 2020 . 10.26419/ppi.00103.001 [ CrossRef ]
- Agli O, Bailly N, & Ferrand C (2015). Spirituality and religion in older adults with dementia: A systematic review . International Psychogeriatrics , 27 ( 5 ), 715–725. 10.1017/S1041610214001665 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Akechi T, Okuyama T, Sugawara Y, Nakano T, Shima Y, & Uchitomi Y (2004). Major depression, adjustment disorders, and post-traumatic stress disorder in terminally ill cancer patients . Journal of Clinical Oncology , 22 ( 10 ), 1957–1965. 10.1200/JCO.2004.08.149 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baltes PB, & Baltes MM (Eds.). (1990). Psychological perspectives on successful aging: The model of selective optimization with compensation. In Baltes PB & Baltes MM, Successful aging: Perspectives from the behavioral sciences (pp. 1–34). Cambridge University Press. [ Google Scholar ]
- Baltes M, & Carstensen L (1996). The process of successful aging . Ageing and Society , 16 ( 4 ), 397–422. 10.1017/S0144686X00003603 [ CrossRef ] [ Google Scholar ]
- Beach SR, Schulz R, Williamson GM, Miller LS, Weiner MF, & Lance CE (2005). Risk factors for potentially harmful informal caregiver behavior . Journal of the American Geriatrics Society , 53 ( 2 ), 255–261. 10.1111/j.1532-5415.2005.53111.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beaudreau SA, Gould CE, Mashal N, Huh JWT, & Fairchild JK (2019). Application of problem solving therapy for late-life anxiety . Cognitive and Behavioral Practice , 26 ( 2 ), 381–394. 10.1016/j.cbpra.2018.05.003 [ CrossRef ] [ Google Scholar ]
- Bekhet AK, Zauszniewski JA, & Nakhla WE (2009). Reasons for relocation to retirement communities: A qualitative study . Western Journal of Nursing Research , 31 ( 4 ), 462–479. 10.1177/0193945909332009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bekhet AK, Zauszniewski JA, & Wykle ML (2008). Midwest nursing research society sage best paper award: Milieu change and relocation adjustment in elders . Western Journal of Nursing Research , 30 ( 1 ), 113–129. 10.1177/0193945907309309 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boyd C, Smith CD, Masoudi FA, Blaum CS, Dodson JA, Green AR, Kelley A, Matlock D, Ouellet J, Rich MW, Schoenborn NL, & Tinetti ME (2019). Decisions making for older adults with multiple chronic conditions: Executive summary for the American Geriatrics Society guiding principles on the care of older adults with multimorbidity . Journal of the American Geriatrics Society , 67 ( 4 ), 665–673. 10.1111/jgs.15809 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Branson J, Branson A, Pozniak K, Tookes J, & Schmidt M (2019). The role of family during older adults’ living transitions: Implications for helping professionals and family counselors . The Family Journal , 27 ( 1 ), 75–83. 10.1177/1066480718809418 [ CrossRef ] [ Google Scholar ]
- Brown C, & Lowis MJ (2003). Psychosocial development in the elderly: An investigation into Erikson’s ninth stage . Journal of Aging Studies , 17 ( 4 ), 415–426. 10.1016/S0890-4065(03)00061-6 [ CrossRef ] [ Google Scholar ]
- Brown EL, Friedemann M-L, & Mauro AC (2014). Use of adult day care service centers in an ethnically diverse sample of older adults . Journal of Applied Gerontology , 33 ( 2 ), 189–206. 10.1177/0733464812460431 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buco CEAM, Buenviaje KAC, Bulan RBC, Cabaña RJL, Cabuhat MKS, Bongar MVV, & Macindo JRB (2018). Developing and testing a model of quality of life among chronically-ill, community-dwelling older adults: A structural equation model . Archives of Gerontology and Geriatrics , 78 , 261–268. 10.1016/j.archger.2018.07.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carpentieri JD, Elliott J, Brett CE, & Deary IJ (2017). Adapting to aging: Older people talk about their use of selection, optimization, and compensation to maximize well-being in the context of physical decline . Journals of Gerontology: Series B , 72 ( 2 ), 351–361. 10.1093/geronb/gbw132 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carstensen LL, Isaacowitz DM, & Charles ST (1999). Taking time seriously: A theory of socioemotional selectivity . American Psychologist , 54 ( 3 ), 165–181. 10.1037/0003-066X.54.3.165 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen CK, Zimmerman S, Sloane PD, & Barrick AL (2007). Assisting living policies promoting autonomy and their relationship to depressive symptoms . The American Journal of Geriatric Psychiatry , 15 ( 2 ), 122–129. 10.1097/01.JGP.0000247163.49665.5b [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chio A, Gauthier A, Calvo A, Ghiglione P, & Mutani R (2005). Caregiver burden and patients’ perception of being a burden in ALS . Neurology , 6 ( 10 ), 1780–1792. 10.1212/01.WNL.0000162034.06268.37 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chum K, Fitzhenry G, Robinson K, Murphy M, Phan D, Alvarez J, Hand C, Laliberte Rudman D, & McGrath C (2020). Examining community-based housing models to support aging in place: A scoping review . The Gerontologist . Advance online publication. 10.1093/geront/gnaa142 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Contrada RJ, Goyal TM, Cather C, Rafalson L, Idler EL, & Krause TJ (2004). Psychosocial factors in outcomes of heart surgery: The impact of religious involvement and depressive symptoms . Health Psychology , 23 ( 3 ), 227–238. 10.1037/0278-6133.23.3.227 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Creese J, Bédard M, Brazil K, & Chambers L (2008). Sleep disturbances in spousal caregivers of individuals with Alzheimer’s disease . International Psychogeriatrics , 20 ( 1 ), 149–161. 10.1017/S1041610207005339 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Czaja SJ, Sabbag S, Lee CC, Schulz R, Lang S, Vlahovic T, Jaret A, & Thurston C (2016). Concerns about aging and caregiving among middle-aged and older lesbian and gay adults . Aging & Mental Health , 20 ( 11 ), 1107–1118. 10.1080/13607863.2015.1072795 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Daaleman TP, Perera S, & Studenski SA (2004). Religion, spirituality, and health status in geriatric outpatients . Annals of Family Medicine , 2 ( 1 ), 49–53. 10.1370/afm.20 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Damianakis T, & Marziali E (2012). Older adults’ response to the loss of a spouse: The function of spirituality in understanding the grieving process . Aging & Mental Health , 16 ( 1 ), 57–66. 10.1080/13607863.2011.609531 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Damianakis T, Wilson K, & Marziali E (2018). Family caregiver support groups: Spiritual reflections’ impact on stress management . Aging & Mental Health , 22 ( 1 ), 70–76. 10.1080/13607863.2016.1231169 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donaldson WV, & Vacha-Haase T (2016). Exploring staff clinical knowledge and practice with LGBT residents in long-term care: A grounded theory of cultural competency and training needs . Clinical Gerontologist , 39 ( 5 ), 389–409. 10.1080/07317115.2016.1182956 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Edes T (2010). Innovations in homecare: VA home-based primary care . Generations: Journal of the American Society on Aging , 34 ( 2 ), 29–34. Retrieved August 1, 2019, from https://www.jstor.org/stable/26555725 [ Google Scholar ]
- Edes T (2019). Connecting social, clinical, and home care services: Where healthcare needs to go . Journal of the American Geriatrics Society , 67 ( S2 ), S419–S422. 10.1111/jgs.15933 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elizabeth Dole Foundation. (2017, November16). The Elizabeth Dole Foundation, VA and USAA launch new alliance to integrate caregivers into veterans medical care [Press release]. http://www.prweb.com/releases/2017/11/prweb14927896.htm
- Elliott TR, & Pezent GD (2008). Family caregivers of older persons in rehabilitation . NeuroRehabilitation , 23 ( 5 ), 439–446. 10.3233/NRE-2008-23507 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elsawy B, & Higgins KE (2010). Physical activity guidelines for older adults . American Family Physician , 31 ( 1 ), 55–59. [ PubMed ] [ Google Scholar ]
- Epperly T, Bechtel C, Sweeney R, Greiner A, Grumbach K, Schilz J, Stream G, & O’Connor M (2019). The shared principles of primary care: A multistakeholder initiative to find a common voice . Family Medicine , 51 ( 2 ), 179–184. 10.22454/FamMed.2019.925587 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Erikson EH, & Erikson JM (1997). The life cycle completed: Extended version with new chapters on the ninth stage of development . Norton. [ Google Scholar ]
- Feder SL, Kiwak E, Costello D, Dindo L, Hernandez-Bigos K, Vo L, Geda M, Blaum C, Tinetti ME, & Naik AD (2019). Perspectives of patients in identifying their values-based health priorities . Journal of the American Geriatrics Society , 67 ( 7 ), 1379–1385. 10.1111/jgs.15850 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flaherty E, & Bartles SJ (2019). Addressing the community-based geriatric healthcare workforce shortage by leveraging the potential of interprofessional teams . Journal of the American Geriatrics Society , 67 ( S2 ), S400–S408. 10.1111/jgs.15924 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Foley DJ, Monjan A, Simonsick EM, Wallace RB, & Blazer DG (1999). Incidence and remission of insomnia among elderly adults: An epidemiological study of 6,800 persons over three years . Sleep , 22 ( 2 ), S366–S372. https://psycnet.apa.org/record/1999-03090-003 [ PubMed ] [ Google Scholar ]
- Foley KT, & Luz CC (2020). Retooling the healthcare workforce for an aging America: A current perspective . The Gerontologist . Advance online publication. 10.1093/geront/gnaa163 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fredrickson BL, & Carstensen LL (1990). Choosing social partners: How old age and anticipated endings make people more selective . Psychology and Aging , 5 ( 3 ), 335–347. 10.1037/0882-7974.5.3.335 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fredriksen-Goldsen KI, Kim H-J, Barkan SE, Muraco A, & Hoy-Ellis CP (2013). Health disparities among lesbian, gay, & bisexual older adults: Results from population–based study . American Journal of Public Health , 103 ( 10 ), 1802–1809. 10.2105/AJPH.2012.301110 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fung HH, Chu ST, Jiang D, Chen AX, & Ng CC (2020). Contrasting the effects of mortality salience and future time limitation on goal prioritization in older and younger adults . Journals of Gerontology: Series B , 75 ( 10 ), 2112–2121. 10.1093/geronb/gbz133 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Golden RL, Emery-Tiburcio EE, Post S, Ewald B, & Newman M (2019). Connecting social, clinical, and home care services for persons with serious illness in the community . Journal of the American Geriatrics Society , 67 ( S2 ), S412–S418. 10.1111/jgs.15900 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gooneratne NS, & Vitiello MV (2014). Sleep in older adults: Normative changes, sleep disorders, and treatment options . Clinics in Geriatric Medicine , 30 ( 3 ), 591–627. 10.1016/j.cger.2014.04.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gottlieb BH, & Sevigny A (2016). Social usefulness: Theory and evidence concerning a late life identity construct . International Journal of Aging & Human Development , 83 ( 4 ), 333–365. 10.1177/0091415016655165 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haley WE, Allen JY, Grant JS, Clay JO, Perkins M, & Roth DL (2009). Problems and benefits reported by stroke family caregivers: Results from a prospective epidemiological study . Stroke , 40 ( 6 ), 2129–2133. 10.1161/STROKEAHA.108.545269 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Harmell AL, Chattillion EA, Roepke SK, & Mausbach BT (2011). A review of the psychobiology of dementia caregiving: A focus on resilience factors . Current Psychiatry Reports , 13 ( 3 ), 219–224. 10.1007/s11920-011-0187-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haverhals LM, Manheim CE, Gilman CV, Jones J, & Levy C (2016). Caregivers create a veteran-centric community in VHA medical foster homes . Journal of Gerontological Social Work , 59 ( 6 ), 441–457. 10.1080/01634372.2016.1231730 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heckhausen J, Wrosch C, & Schulz R (2010). A motivational theory of life-span development . Psychological Review , 117 ( 1 ), 32–60. 10.1037/a0017668 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hiedemann B, & Brodoff L (2013). Increased risk of needing long-term care among older adults living with same-sex partners . American Journal of Public Health , 103 ( 8 ), e27–e33. 10.2105/AJPH.2013.301393 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hosseini S, Chaurasia A, & Oremus M (2019). The effect of religion and spirituality on cognitive function: A systematic review . The Gerontologist , 59 ( 2 ), e76–e85. 10.1093/geront/gnx024 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Institute for Healthcare Improvement. (2018). No place like home: Advancing the care of safety in the home . http://www.ihi.org/resources/pp./Publications/No-Place-Like-Home-Advancing-Safety-of-Care-in-the-Home.aspx
- Joly-Burra E, Linden Van der M, Ghisletta P, & Van der Linden M (2020). A mixed-method study on strategies in everyday personal goals among community-dwelling older adults . Gerontology , 66 ( 5 ), 484–493. 10.1159/000508824 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jones PS, Winslow BW, Lee JW, Burns M, & Zhang XE (2011). Development of a caregiver empowerment model to promote positive outcomes . Journal of Family Nursing , 17 ( 1 ), 11–28. 10.1177/1074840710394854 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karel MJ, Wray LO, Adler G, Hannum AO, Luci K, Brady LA, & McGuire MH (2020). Mental health needs of aging veterans: Recent evidence and clinical recommendations . Clinical Gerontologist . Advance online publication. 10.1080/07317115.2020.1716910 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karlin BE, Trockel M, Taylor CB, Gimeno J, & Manber R (2013). National dissemination of cognitive behavioral therapy for insomnia in veterans: Therapist- and patient-level outcomes . Journal of Consulting and Clinical Psychology , 81 ( 5 ), 912–917. 10.1037/a0032554 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kim Y, Baker F, & Spillers RL (2007). Cancer caregivers’ quality of life: Effects of gender, relationship, and appraisal . Journal of Pain and Symptom Management , 34 ( 3 ), 294–304. 10.1016/j.jpainsymman.2006.11.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kligler B, Cotter A, Roca H, & Saenger M (2017). Whole health/integrative health in the VA: Focusing on what matters to the veteran rather than what is the matter with them . EXPLORE: The Journal of Science and Healing , 13 ( 4 ), 274–276. 10.1016/j.explore.2017.04.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kligler B, Niemtzow RC, Drake DF, Ezeji-Okoye SC, Lee RA, Olson J, & Reddy KP (2018). The current state of integrative medicine with the U.S. Department of Veterans Affairs . Medical Acupuncture , 30 ( 5 ), 230–234. 10.1089/acu.2018.29087-rtl [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koenig HG, Berk LS, Daher NS, Pearce MJ, Bellinger DL, Robins CJ, Nelson B, Shaw SF, Cohen HJ, & King MB (2014). Religious involvement is associated with greater purpose, optimism, generosity and gratitude in persons with major depression and chronic medical illness . Journal of Psychosomatic Research , 77 ( 2 ), 135–143. 10.1016/j.jpsychores.2014.05.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kogan M, Cheng S, Rao S, Democker S, & Nelson MK (2017). Integrative medicine for geriatric and palliative care . The Medical Clinics of North America , 101 ( 5 ), 1005–1029. 10.1016/j.mcna.2017.04.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Korff J, & Biemann T (2020). Adjusting the lookout: Subjective health, loneliness, and life satisfaction predict future time perspective . Psychology and Aging , 35 ( 8 ), 1170–1183. 10.1037/pag0000513 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kowal J, Wilson KG, McWilliams LA, Péloquin K, & Duong D (2012). Self-perceived burden in chronic pain: Relevance, prevalence, and predictors . Pain , 153 ( 8 ), 1735–1741. 10.1016/j.pain.2012.05.009 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krejci LP, Carter K, & Gaudet T (2014). Whole health: The vision and implementation of personalized, proactive, patient-driven healthcare for veterans . Medical Care , 52 ( 12, Suppl. 5 ), S5–S8. 10.1097/MLR.0000000000000226 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kwak M, Ingersoll-Dayton B, & Burgard S (2014). Receipt of care and depressive symptoms later in life: The importance of self-perceptions of aging . Journals of Gerontology: Series B , 69 ( 2 ), 325–335. 10.1093/geronb/gbt128 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lai C, Luciani M, Di Mario C, Galli F, Morelli E, Ginobbi P, Aceto P, & Lombardo L (2018). Psychological impairments burden and spirituality in caregivers of terminally ill cancer patients . European Journal of Cancer Care , 27 ( 1 ), Article e12674. 10.1111/ecc.12674 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lauckner H, & Hutchinson SL (2016). Peer support for people with chronic conditions in rural areas: A scoping review . Rural and Remote Health , 16 ( 1 ), Article 3601. 10.22605/RRH3601 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Laughlin A, Parsons M, Kosloski KD, & Bergman-Evans B (2007). Predictors of mortality following involuntary interinstitutional relocation . Journal of Gerontological Nursing , 33 ( 9 ), 20–26. 10.3928/00989134-20070901-04 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leggett A, Polenick CA, Maust DT, & Kales HC (2018). What hath night to do with sleep? The caregiving context and dementia caregivers’ nighttime awakenings . Clinical Gerontologist , 41 ( 2 ), 158–166. 10.1080/07317115.2017.1352057 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Locher JL, Ritchie CS, Roth DL, Sen B, Vickers KS, & Vailas LI (2009). Food choice among homebound older adults: Motivations and perceived barriers . The Journal of Nutrition, Health & Aging , 13 ( 8 ), 659–664. 10.1007/s12603-009-0194-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Loyd J, Patterson T, & Muers J (2016). The positive aspects of caregiving in dementia: A critical review of the qualitative literature . Dementia , 15 ( 6 ), 1534–1561. 10.1177/1471301214564792 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lynch SH, Shuster G, & Lobo ML (2018). The family caregiver experience – Examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes . Journal of Aging and Mental Health , 22 ( 11 ), 1424–1431. 10.1080/13607863.2017.1364344 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marchand WR, Beckstrom J, Nazarenko E, Sweeny RU, Hermann T, Yocus MR, Romesser J, Roper J, Yabko B, & Parker A (2020). The Veterans Health Administration whole health model of care: Early implementation and utilization at a large healthcare system . Military Medicine , 185 ( 11–12 ), e2150–e2157. 10.1093/milmed/usaa198 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mbizo J, Okafor A, Sutton MA, Leyva B, Stone LM, & Olaku O (2018). Complementary and alternative medicine use among persons with multiple chronic conditions: Results from the 2012 National Health Interview Survey . BMC Complementary and Alternative Medicine , 18 , Article 281. 10.1186/s12906-018-2342-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McCurry SM, Gibbons LE, Logsdon RG, Vitiello MV, & Teri L (2009). Insomnia in caregivers of persons with dementia: Who is at risk and what can be done about it? Sleep Medicine Clinics , 4 ( 4 ), 519–526. 10.1016/j.jsmc.2009.07.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McLennon SM, Habermann B, & Rice M (2011). Finding meaning as a mediator of burden on the health of caregivers of spouses with dementia . Aging & Mental Health , 15 ( 4 ), 522–530. 10.1080/13607863.2010.543656 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McPherson CJ, Wilson KG, Chyurlia L, & Leclerc C (2010). The balance of give and take in caregiver–partner relationships: An examination of self-perceived burden, relationship equity, and quality of life from the perspective of care recipients following stroke . Rehabilitation Psychology , 55 ( 2 ), 194–203. 10.1037/a0019359 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McPherson CJ, Wilson KG, & Murray MA (2007). Feeling like a burden to others: A systematic review focusing on the end of life . Palliative Medicine , 21 ( 2 ), 115–128. 10.1177/0269216307076345 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mirgain SA (2014). Personal development . University of Wisconsin-Madison. https://wholehealth.wisc.edu/overviews/personal-development/ [ Google Scholar ]
- Montgomery RJV, & Kosloski K (2013). Pathways to caregiver and identity and implications for support services. In Talley RC & Montgomery RJV (Eds.), Caregiving across the lifespan: Research, practice, and policy (pp. 131–156). Springer. [ Google Scholar ]
- Moraes W, Piovezan R, Poyares D, Bittencourt LR, Santos-Silva R, & Tufik S (2014). Effects of aging on sleep structure throughout adulthood: A population-based study . Sleep Medicine , 14 ( 4 ), 401–409. 10.1016/j.sleep.2013.11.791 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morey MC, Lee CC, Castle S, Valencia WM, Katzel L, Giffuni J, Kopp T, Cammarata H, McDonald M, Oursler KA, Wamsley T, Jain C, Bettger JP, Pearson M, Manning KM, Intrator O, Veazie P, Sloane R, Li J, & Parker DC (2018). Should structured exercise be promoted as a model of care? Dissemination of the Department of Veterans Affairs Gerofit program . Journal of the American Geriatrics Society , 66 ( 5 ), 1009–1016. 10.1111/jgs.15276 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mournet AM, Bower E, & Van Orden KA (2020). Domains of functional Impairment and their association with thwarted belonging and perceived burden in older adults . Clinical Gerontologist , 43 ( 1 ), 95–103. 10.1080/07317115.2019.1650406 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mudge AM, Ross LJ, Young AM, Isenring EA, & Banks MD (2011). Helping understand nutritional gaps in the elderly (HUNGER): A prospective study of patient factors associated with inadequate nutritional intake in older medical patients . Clinical Nutrition , 30 ( 3 ), 320–325. 10.1016/j.clnu.2010.12.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Academies of Sciences, Engineering, and Medicine. (2016). Families caring for an aging America . The National Academies Press. 10.17226/23606 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Opinion Research Center. (2014). Long-term care in America: Expectations and realities. The Long-Term Care Poll . https://www.longtermcarepoll.org/project/long-term-care-in-america-expectations-and-reality/
- National Senior Citizens Law Center. (2015). LGBT older adults in long-term care facilities: Stories from the field. LGBT Long Term Care . www.lgbtlongtermcare.org
- Newsom JT (1999). Another side to caregiving: Negative reactions to being helped . Current Directions in Psychological Science , 8 ( 6 ), 183–187. 10.1111/1467-8721.00043 [ CrossRef ] [ Google Scholar ]
- Nezu CM, Palmatier AD, & Nezu AM (2004). Problem solving therapy for caregivers. In Chang EC, D’Zurilla TJ, & Sanna LJ (Eds.), Social problem solving: Theory, research, and training (pp. 223–238). American Psychological Association. [ Google Scholar ]
- Nichols LO, Martindale-Adams J, Zhu CW, Kaplan EK, Zuber JK, & Waters TM (2017). Impact of the REACH II and REACH VA dementia caregiver intervention on healthcare costs . Journal of the American Geriatrics Society , 65 ( 5 ), 931–936. 10.1111/jgs.14716 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nieuwenhuis AV, Beach SR, & Schulz R (2018). Care recipient concerns about being a burden and unmet needs for care . Innovation in Aging , 2 ( 3 ), Article igy026. 10.1093/geroni/igy026 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O’Brien K, Bradley S, Ramirez-Zohfeld V, & Lindquist L (2019). Stressors facing home-based primary care providers . Geriatrics , 4 ( 1 ), Article 17. 10.3390/geriatrics4010017 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Orgeta V, & Miranda-Castillo C (2014). Does physical activity reduce burden in careers of people with dementia? A literature review . International Journal of Geriatric Psychiatry , 29 ( 8 ), 771–783. 10.1002/gps.4060 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Parmar J, Anderson S, Abbasi M, Ahmadinejad S, Brémault-Phillips S, Chan K, Charles L, Dobbs BM, Khera AS, Stickney-Lee J, & Tian PGJ (2020). Support for family caregivers: A scoping review of family physician’s perspectives on their role in supporting family caregivers . Health & Social Care in the Community , 28 ( 3 ), 716–733. 10.1111/hsc.12928 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the stress process: An overview of concepts and their measures . The Gerontologist , 30 ( 5 ), 583–594. 10.1093/geront/30.5.583 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pierce LL, Steiner V, Govoni A, Cervantez-Thompson T, & Friedemann ML (2007). Two sides to the caregiving story . Topics in Stroke Rehabilitation , 14 ( 2 ), 13–20. 10.1310/tsr1402-13 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pillemer K, & Gilligan M (2018). Translating basic research on the aging family to caregiving intervention: The case of within-family differences . Innovation in Aging , 2 ( 1 ), Article igx035. 10.1093/geroni/igx035 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pinquart M, & Sörensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis . Psychology and Aging , 18 ( 2 ), 250–267. 10.1037/0882-7974.18.2.250 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qualls SH (2000). Therapy with aging families: Rationale, opportunities and challenges . Aging & Mental Health , 4 ( 3 ), 191–199. 10.1080/713649925 [ CrossRef ] [ Google Scholar ]
- Reckrey J (2020). COVID-19 confirms it: Paid caregivers are essential members of the healthcare team . Journal of the American Geriatrics Society , 68 ( 8 ), 1679–1680. 10.1111/jgs.16566 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Remillard ET, Fausset CB, & Fain WB (2019). Aging with long-term mobility impairment: Maintaining activities of daily living via selection, optimization, and compensation . The Gerontologist , 59 ( 3 ), 559–569. 10.1093/geront/gnx186 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Riley GA (2019). Relationship continuity/discontinuity – A framework for investigating the role of relationships in the experience of living with dementia . American Journal of Alzheimer’s Disease and Other Dementias , 34 ( 3 ), 145–147. 10.1177/1533317518813557 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ringler T, Ahearn EP, Wise M, Lee ER, & Krahn D (2015). Using life stories to connect veterans and providers . Federal Practitioner , 32 ( 6 ), 8–14. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ris I, Schnepp W, & Imhof RM (2019). An integrative review on family caregivers’ involvement in care of home-dwelling elderly . Health & Social Care in the Community , 27 ( 3 ), e95–e111. 10.1111/hsc.12663 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ritchie C, & Leff B (2018). Population health and tailored medical care in the home: The roles of home-based primary care and home-based palliative care . Journal of Pain and Symptom Management , 55 ( 3 ), 1041–1046. 10.1016/j.jpainsymman.2017.10.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts HC, Lim S, Cox NJ, & Ibrahim K (2019). The challenge of managing undernutrition in older people with frailty . Nutrients , 11 ( 4 ), Article 808. 10.3390/nu11040808 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robinson JB, & Wetherell JL (2018). An interdisciplinary intervention for fear of falling: Lessons learned from two case studies . Clinical Gerontologist , 41 ( 4 ), 366–373. 10.1080/07317115.2017.1325423 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rolland JS (2017). Neurocognitive impairment: Addressing couple and family challenges . Family Process , 56 ( 4 ), 799–818. 10.1111/famp.12316 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rolland JS (2019). CFHA Don Bloch award acceptance speech . Families, Systems & Health , 37 ( 1 ), 95–97. 10.1037/fsh0000401 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rolland JS, Emanuel LL, & Torke AM (2017). Applying a family systems lens to proxy decision making in clinical practice and research . Families, Systems & Health , 35 ( 1 ), 7–17. 10.1037/fsh0000250 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roth DL, Perkins M, Wadley VG, Temple EM, & Haley WE (2009). Family caregiving and emotional strain: Associations with quality of life in a large national sample of middle-aged and older adults . Quality of Life Research , 18 ( 6 ), 679–688. 10.1007/s11136-009-9482-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rowles G, & Bernard M (2013). The meaning and significance of place in old age. In Rowles G & Bernard M (Eds.), Environmental gerontology: Making meaningful places in old age (pp. 3–24). Springer. [ Google Scholar ]
- Saajanaho M, Viljanen A, Read S, Eronen J, Kaprio J, Jylhä M, & Taina R (2016). Mobility limitation and changes in personal goals among older women . The Journals of Gerontology: Series B , 71 ( 1 ), 1, 1–10. 10.1093/geronb/gbu094 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Savundranayagam MY, & Montgomery RJV (2010). Impact of role discrepancy on caregiver burden among spouses . Research on Aging , 32 ( 2 ), 175–199. 10.1177/0164027509351473 [ CrossRef ] [ Google Scholar ]
- Shafir A, Garrigues SK, Schenker Y, Leff B, Neil J, & Ritchie C (2016). Homebound patient and caregiver perceptions of quality of care in home-based primary care: A qualitative study . Journal of the American Geriatrics Society , 64 ( 8 ), 1622–1627. 10.1111/jgs.14244 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shaw BA, Krause N, Liang J, & Bennett J (2007). Tracking changes in social relationships throughout late life . The Journals of Gerontology: Series B , 62 ( 2 ), S90–S99. 10.1093/geronb/62.2.s90 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sherman MD, Fischer EP, Sorocco K, & McFarlane WR (2011). Adapting the multifamily group model to the Veterans Affairs system: The REACH program . Couple and Family Psychology: Research and Practice , 1 ( S ), 74–84. 10.1037/2160-4096.1.S.74 [ CrossRef ] [ Google Scholar ]
- Smith-Carrier T, Pham T, Akhtar S, Seddon G, Nowaczynski M, Sinha SK (2018). ‘It’s not just the word care, it’s the meaning of the word… (they) actually care’: Caregivers’ perceptions of home-based primary care in Toronto, Ontario . Ageing and Society , 38 ( 10 ), 2019–2040. 10.1017/S0144686X1700040X [ CrossRef ] [ Google Scholar ]
- Sperber NR, Boucher NA, Delgado R, Shepherd-Banigan ME, McKenna K, Moore M, Barrett R, Kabat M, & Van Houtven CH (2019). Including family caregivers in seriously ill veterans’ care: A mixed-methods study . Health Affairs , 38 ( 6 ), 957–963. 10.1377/hlthaff.2019.00012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Steinglass P (2006). The future of family systems medicine: Challenges and opportunities . Families, Systems & Health , 24 ( 4 ), 396–411. 10.1037/1091-7527.24.4.396 [ CrossRef ] [ Google Scholar ]
- Steinglass P, Ostroff JS, & Steinglass AS (2011). Multiple family groups for adult cancer survivors and their families: A 1-day workshop model . Family Process , 50 ( 3 ), 393–409. 10.1111/j.1545-5300.2011.01359.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tinetti M, Dindo L, Smith CD, Blaum C, Costello D, Ouellet G, Rosen J, Hernandez-Bigos K, Geda M, & Naik A (2019). Challenges and strategies in patients’ health priorities – Aligned decision making for older adults with multiple chronic conditions . PLoS ONE , 14 ( 6 ), Article e0218249. 10.1371/journal.pone.0218249 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tinetti M, Huang A, & Molnar F (2017). The geriatric 5M’s: A new way of communicating what we do . Journal of the American Geriatrics Society , 65 ( 9 ), Article 2115. 10.1111/jgs.14979 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tomasino KN, Lattie EG, Ho J, Palac HL, Kaiser SM, & Mohr DC (2017). Harnessing peer support in an online intervention for older adults with depression . The American Journal of Geriatric Psychiatry , 25 ( 10 ), 1109–1119. 10.1016/j.jagp.2017.04.015 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tornstam L (1997). Gerotranscendence: The contemplative dimension of aging . Journal of Aging Studies , 11 ( 2 ), 143–154. 10.1016/S0890-4065(97)90018-9 [ CrossRef ] [ Google Scholar ]
- Totten AM, White-Chu EF, Wasson N, Morgan E, Kansagara D, Davis-O’Reilly C, & Goodin S (2016). Home-based primary care interventions (Comparative Effectiveness Reviews, No. 164) . Agency for Healthcare Research and Quality. [ PubMed ] [ Google Scholar ]
- U.S. Department of Veterans Affairs. (2020, March30). Whole health: The circle of health . https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
- Van Haitsma K, Abbott KM, Arbogast A, Bangerter LR, Heid AR, Behrens LL, & Madrigal C (2019). A preference-based model of care: An integrative theoretical model of the role of preferences in person-centered care . The Gerontologist , 60 ( 3 ), 376–384. 10.1093/geront/gnz075 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wachholtz AB, & Pargament KI (2008). Migraines and meditation: Does spirituality matter? Journal of Behavioral Medicine , 31 ( 4 ), 351–366. 10.1007/s10865-008-9159-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Walker PH, Pock A, Ling CG, Kwon KN, & Vaughan M (2016). Battlefield acupuncture: Opening the door for acupuncture in Department of Defense/Veteran’s Administration health care . Nursing Outlook , 64 ( 5 ), 491–1119. 10.1016/j.outlook.2016.07.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wetherell JL, Steiner ARW, & Sisco S (2020). Implementing evidence-based therapy in the home. In Terry DJ, Mlinac ME, & Steadman-Wood PL (Eds.), Providing home care for older adults: A professional guide for mental health practitioners (pp. 132–148). 10.4324/9780429326363 [ CrossRef ] [ Google Scholar ]
- Whitehead BR, & Bergeman CS (2019). Daily religious coping buffers the stress–effect relationship and benefits overall metabolic health in older adults . Psychology of Religion and Spirituality , 12 ( 4 ), 393–399. 10.1037/rel0000251 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whitson HE, Duan-Porter W, Schmader KE, Morey MC, Cohen HJ, & Colón-Emeric CS (2016). Physical resilience in older adults: Systematic review and development of an emerging construct . Journals of Gerontology A: Biological and Medical Sciences , 71 ( 4 ), 489–495. 10.1093/gerona/glv202 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wiles JL, Leibing A, Guberman N, Reeve J, & Allen RES (2012). The meaning of “aging in place” to older people . The Gerontologist , 52 ( 3 ), 357–366. 10.1093/geront/gnr098 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Williamson V, Stevelink SAM, Greenberg K, & Greenberg N (2018). Prevalence of mental health disorders in elderly U.S. military veterans: A meta-analysis and systematic review . The American Journal of Geriatric Psychiatry , 26 ( 5 ), 534–545. 10.1016/j.jagp.2017.11.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wilson KG, Curran D, & McPherson CJ (2005). A burden to others: A common source of distress for the terminally ill . Cognitive Behaviour Therapy , 34 ( 2 ), 115–123. 10.1080/16506070510008461 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Win AZ, Ceresa C, Arnold K, & Allison TA (2017). High prevalence of malnutrition among elderly veterans in home based primary care . The Journal of Nutrition, Health & Aging , 21 ( 6 ), 610–613. 10.1007/s12603-017-0918-z [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wool E, Shotwell JL, Slaboda J, Kozikowski A, Smith KL, Abrashkin K, Rhodes KV, Norman GJ, & Pekmezaris R (2019). A qualitative investigation of the impact of home-based primary care on family caregivers . Journal of Frailty and Aging , 8 ( 4 ), 210–214. 10.14283/jfa.2019.19 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wray LO, Shulan MD, Toseland RW, Freeman KE, Vasquez BE, & Gao J (2010). The effect of telephone support groups on costs of care for veterans with dementia . The Gerontologist , 50 ( 5 ), 623–631. 10.1093/geront/gnq040 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Xiang X, Leggett A, Himle JA, & Kales HC (2018). Major depression and subthres-hold depression among older adults receiving home care . The American Journal of Geriatric Psychiatry , 26 ( 9 ), 939–949. 10.1016/j.jagp.2018.05.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhang W, & Radhakrishnan K (2018). Evidence on selection, optimization, and compensation strategies to optimize aging with multiple chronic conditions: A literature review . Geriatric Nursing , 39 ( 5 ), 534–542. 10.1016/j.gerinurse.2018.02.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
How to draft a business plan for a new DPC practice

An independent practice is a business. A direct care practice, in particular, needs a solid business plan that addresses the details of operating productively. A business plan includes financial projections as well as plans and goals for patient panel size, practice location, and other logistics necessary to run a successful practice. Drafting a business plan for your new practice requires research, forecasts, and realistic objectives.
Given the financial structure of the direct care practice, careful planning can help ensure the practice’s success. Elements of a business include:
- Practice location
- Membership pricing structure
- Patient panel requirements
- Staffing requirements / plans
- Marketing plan
- Partnerships with other healthcare providers
- Financial projections
- Short-term and long-term goals
Be sure to include a plan for optimizing technology, especially electronic health records ( EHRs ) in your new practice.
As you draft a business plan for a new direct care practice you will need to determine where you want your practice to be located. Is there an area in your community that has a need for your services? What is convenient for your target patient population ?
Setting your membership pricing structure will require financial planning and projections. Some factors to consider are time, variable costs, and overhead (including the cost of growing the practice). Will you offer reduced fees for children and the elderly? You will also need to determine whether you will accept any type of insurance, including whether to accept Medicare patients. Pricing and financial projections will also need to include your ideal patient panel size, both now and when growing your practice.
The marketing section of your business plan will include a section on how to educate patients about the direct care model. Include how you will create a website, how often you will post on social media, and if you need to contract with a professional to help you with outreach and promotional efforts.
The key to drafting a business plan is to be realistic and to treat the plan as a living, usable document. Be realistic about the potential patient base in the location you’ve chosen for your practice as well as in your financial projections and planning. There will be a ramp-up period for a new practice, so include realistic start-up costs, promotional costs, and staffing costs. Then project your growth based on comparisons with other independent practices in your area and on the population you will serve.
Use the business plan to track and manage your business on an ongoing basis. It is not a document to be completed and put on a shelf. Your business plan will be your guide to managing a successful practice and to planning your growth as a direct care practice.

© 2024 Elation. All Rights Reserved
Collection Home-Based Primary Care

With an estimated two million homebound adults in the U.S. today and the nation’s older adult population increasing, home-based primary care is putting a new face on the “house calls” of yesteryear. As the shift to home- and community-based care continues, health care organizations are seeking new options for providing health care services in the comfort of the home. Home-based primary care is particularly valuable for frail older adults and people with disabilities who have multiple chronic conditions, functional impairments, and/or social challenges that make office or hospital visits difficult. The COVID-19 pandemic further accelerated opportunities to test and spread this approach.
Many home-based primary care models care include interdisciplinary care teams to identify and address social needs, comprehensive care coordination, and innovative technology to track and share information. High-quality home-based primary care options can serve as a critical tool to help provide more person-centered care to underserved populations, reduce health care disparities, and curb spiraling costs associated with unnecessary hospital visits or nursing home admissions.
Health care stakeholders can use this Playbook Collection to understand the latest evidence behind home-based primary care models and explore practical tools and case studies to learn considerations and effective strategies for implementing these programs.
What works in home-based primary care?
Following are summaries of peer-reviewed research, evaluations, and reports on home-based primary care programs. Many of these programs have demonstrated positive results, such as improved health and quality of life for patients and their caregivers and reduced acute care use and costs across different populations and settings.
Outcomes of Home-Based Primary Care for Homebound Older Adults: A Randomized Clinical Trial (Journal of American Geriatrics Society)
“eyes in the home”: addressing social complexity in veterans affairs home-based primary care (journal of general internal medicine), evaluation of the independence at home demonstration: an examination of the first five years (center for medicare & medicaid innovation), integrated home- and community-based services improve community survival among independence at home medicare beneficiaries without increasing medicaid costs (journal of the american geriatrics society), dedicated to the mission: strategies us department of veterans affairs home-based primary care teams apply to keep veterans at home (journal of the american geriatrics society), the effects of home-based primary care on medicare costs at spectrum health/priority health from 2012-present: a matched cohort study (bmc health services research), operation and challenges of home-based medical practices in the us: findings from six aggregated case studies (bmc health services research), preventing hospitalization with veterans affairs home-based primary care: which individuals benefit most (journal of the american geriatrics society), reduced emergency room and hospital utilization in persons with multiple chronic conditions and disability receiving home-based primary care (disability and health journal), home-based primary care interventions (agency for healthcare research and quality), better access, quality, and cost for clinically complex veterans with home-based primary care (journal of the american geriatrics society), a mixed-methods evaluation of home-based primary care in dementia within an integrated system (journal of the american geriatrics society), what do these models look like in practice.
Below find case studies and on-the-ground perspectives on specific home-based primary care programs. Case studies detail each program’s population, care team structure, payment model, lessons and preliminary outcomes, and other care model features that may be useful to organizations interested in implementing these or similar models.
Landmark Health: Providing Comprehensive In-Home Care to Older Adults
- Rush@Home: Meeting People with Complex Needs Where They Are
- Keeping Veterans Healthy at Home: Lessons from the VA’s Home-Based Primary Care Program
“At Home, with Care”: Lessons from New York City Home-Based Primary Care Practices Managing COVID-19 (Journal of the American Geriatrics Society)
Medical care at home comes of age (california health care foundation), providing primary care to homebound patients: ucsf health's care at home program (centers for medicare & medicaid services), how can my organization implement this approach.
Following are practical tools and strategies that health systems, providers, and payers can use when seeking to build or augment a home-based primary care program.
HCCIntelligence: Tools and Tip Sheets (Home Centered Care Institute)
A practical guide to expanding home-based primary care with telehealth (west health), home-based primary care resources: a toolkit for health partners (american academy of home care medicine), home-based primary care fall prevention and management toolkit (veterans health administration national center for patient safety), re-envisioning care for people with involved disabilities (center for consumer engagement in health innovation).
Share your success : Let us know about your innovations in home-based primary care for people with complex needs.
Related Playbook Blog Posts
- Advancing Health Equity for People Who Are Homebound
- Public Health’s Role in Vaccinating People who are Homebound
- Cleveland Clinic Paramedic Telehealth Program: Incorporating In-Home Acute Care to Meet the Needs of Homebound Older Adults
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Johns Hopkins Care at Home
In-home primary care.

For some people over 65, it can be challenging to get to the doctor’s office for proper care. But missing out on medical appointments can increase your risk of going to the emergency room or being hospitalized. Johns Hopkins Medicine provides in-home primary care for people age 65 or older who have difficulty leaving home because of medical conditions or physical limitations.
Our experienced geriatricians, nurse practitioners and other health professionals provide compassionate care in the comfort of your home. We offer in-home primary care throughout Howard County and parts of Baltimore City and Baltimore County. To get started, call us at 410-550-0931 , or apply for the program with our online application .
Who might benefit from in-home primary care?
With in-home primary care, also called home-based primary care, we bring health care to you. Our goal is to provide regular doctor or nurse practitioner visits ranging from once a month to every three months. We are also available to handle urgent medical needs as they come up.
Our home-based primary care services may be appropriate if you:
- Cannot get to your primary care provider without large effort, either by you or a loved one
- Need someone to come with you to your appointments or need special transportation
- Use oxygen or assistive devices such as a cane or walker
- Have difficulty walking or shortness of breath with exertion
- Have had multiple hospitalizations or emergency room visits over the past few years
- Have difficulty with activities of daily living, such as bathing or moving around your home
- Require multiple days to recover from trips outside the home
- Have cognitive or behavioral impairment
We treat and help people manage a wide range of chronic, complex conditions, including:
- Alzheimer’s disease and other types of dementia
- Chronic obstructive pulmonary disease (COPD)
- Heart disease, including heart failure and coronary artery disease
- Movement disorders such as Parkinson’s disease and amyotrophic lateral sclerosis (ALS)
- Recovery after stroke
- Bedsores and chronic wounds
- Conditions requiring home ventilator support
Am I eligible for in-home primary care?
If you can answer “yes” to these questions, you may be eligible for our services:
- Do you live in Howard County or one of these ZIP codes in central Maryland: 21202, 21205, 21213, 21215, 21219, 21222, 21224 or 21231?
- Are you 65 or older?
- Do you have a chronic disease or physical limitation that prevents you from driving or leaving home without significant help?
- Do you or a caregiver have access to a phone for scheduling appointments?
When you contact us to register for care, we may ask additional questions to check your eligibility.
Johns Hopkins Home-based Medicine Helps Fill Community’s Primary Care Gaps
When Florence Gundlach needed additional help for her dementia, her doctor recommended she get medical support at home. Since 2019, home care physicians have been providing care to Florence, improving the quality of life for her and her two adult sons.

In-Home Primary Care Services We Offer
If you qualify, you can receive our in-home primary care services for as long as you need them. Our services include:
- 24/7/365 support by phone with on-call doctors
- Primary care to address your specific health needs
- Coordination for home medical equipment, including recommending, ordering and having equipment delivered to your home
- Management of chronic conditions
- Medication review
- Referrals to community resources (For Howard County residents, we work with the Community Care Team at Howard County General Hospital.)
- Palliative care and end-of-life care
- Regular visits during standard business hours
- Urgent home visits to address health needs that can’t wait for the next regular visit
- Telehealth visits by phone or video
You can also email us at [email protected] . Apply for the program today with our online application .
Why Choose Johns Hopkins Medicine for In-Home Primary Care?
We make it easy for you to get the care you need, when you need it. Highlights of our home-based primary care include:
Multidisciplinary team
You have access to a team of health care providers from several fields of medicine. We work together to develop care plans that address a wide range of physical, emotional and social health needs. We help families navigate some of the challenges of caring for their loved one with chronic medical conditions.
Urgent house calls
If you need urgent care, we send a provider to your home the same day you call us. With our urgent house calls, you receive the care you need without going to the hospital.
Palliative care services
For people adjusting to loss of independence and ability and in need for care toward the end of life, we provide compassionate health care. Caregivers feel supported and often relieved by having medical care for a loved one provided in the home.
Expertise in geriatric primary care
Our team includes geriatricians, nurse practitioners, registered nurses, social workers and community health workers who have specialized training and experience in gerontology (care for older adults). We focus on primary care for people who have complex or multiple chronic conditions, and we personalize your care based on your goals and preferences.
Same provider for routine visits
Whenever possible, the same provider comes to your home for your regular visits, every four to eight weeks. We build a close relationship with you, learning your health needs and preferences so we can provide better care.
In-Home Primary Care: What to Expect
You can become our patient with a provider’s referral, or you or a loved one can call us to get started. After we receive your referral, here’s what you can expect:
- Referral and intake call: When we receive your referral, we call you to make sure you qualify for in-home care. We then schedule your first in-home visit with a provider, usually within four weeks of your referral.
- Your first visit: Our provider conducts a thorough physical exam and asks you about your medical history, symptoms and other details to fully understand your health and your home environment. We take the time to understand what’s most important to you, and get to know you as a person.
- Ongoing visits: For your ongoing care, we create a personalized care plan based on your health needs. You should expect care similar to what you would have at your primary care doctor’s office, except we’ll be coming to your home.
Learn more about our program and how we can help you:
Call Us: 410-550-0931
Interpreter Services
If English is not your primary language or if you have partial or total hearing loss, our trained, qualified medical interpreters speak more than 230 languages, including sign language. Learn more about language services available through Johns Hopkins Medicine.

IMAGES
VIDEO
COMMENTS
Our Home Care business plan is designed to address all vital elements necessary for a detailed and effective operational strategy. This plan encompasses the scope of our home care services, marketing approaches, the environment in which we operate, an analysis of our competitors, the structure of our management team, and financial projections.
The intrinsic rewards of home-based primary care are notable, and the care provided is life-changing for many patients and caregivers. But if the practice isn't sustainable, all those good intentions and good work are at risk. ... including researching the market and creating a business plan, the HCCI House Call Implementation Model guides ...
Industry Analysis. According to Grand View Research, the global home health care industry was valued at $336 billion USD in 2021. It is also expected to grow at a compound annual growth rate of 7.93% from 2022 to 2030 and reach a value of $666.9 billion USD by 2030.
But you don't want them to get bored with an overly lengthy statement. You can always go into greater detail about your services in the products and services section of your business plan. 2. Be specific about your service offering. As a home health care business, you will likely provide a variety of services.
Steps To Start A Home Care Business. Starting a home care business is like creating a sourdough starter. It takes plenty of patience, the right ingredients and a tried-and-true formula. Here's a basic roadmap to help you embark on your home care business journey. Create a Plan. Planning is essential to the success of any new venture.
Interest in home-based primary care is growing as payments increase, technology improves, and the population ages. THOMAS CORNWELL, MD, FAAFP, AND BRIANNA PLENCNER, CPC, CPMA Fam Pract Manag. 2021 ...
Insurance Companies. Establish relationships with insurance providers to offer our services as a covered benefit, making home health care more accessible and affordable for clients. Download This Plan. Download a free home health care sample business plan template. Part of our library of over 550 industry-specific sample business plans.
In developing your Income Statement and Balance Sheets be sure to include several of the key costs needed in starting or growing a home health care business: Cost of equipment like standard nursing supplies, sanitary products, and emergency medications. Payroll or salaries paid to staff. Business insurance.
This toolkit details the benefits of home-based primary care to help providers demonstrate the need for these programs. ... Payers and providers can use this toolkit to learn more about home-based primary care and make the business case for their own organizations to adopt HBPC programs. VIEW THE RESOURCE. Posted to The Playbook on. June 26, 2019.
The Global In-Home Health Care market size was valued at around USD 305.9 billion in 2021 and is expected to reach approximately USD 629.3 billion by 2028, according to data from Fortune Business Insights. Key driving factors include the prevalence of chronic diseases, increased need for cost-effective healthcare delivery systems, technological ...
A business plan will outline your target market, your financial plan and how you plan to market your business. Having a business plan can make it easier to qualify for a small business loan. A loan can help you get your business off the ground faster and let you avoid having to dip into your savings. [Read more: How to Write a One-Page Business ...
Once the office site, EHR, and staff are chosen, the direct care practice needs to determine the services that will be offered and the monthly cost to cover those services. The monthly fee range depends on the age of the patient and can be anywhere from $25 to $85 per month, with the 2015 average just under $78.
PlanBuildr's Healthcare business plan template will help you to quickly and easily complete your Healthcare business plan. ... City Medical is a membership-based, primary-care practice in the heart of the city. City Medical offers a wide range of primary care services for patients who subscribe to the practice for an annual fee. ... Home Health ...
3. From the Brink of Extinction. HBPC is making a comeback in the U.S. after a precipitous decline in the 20th century. While 40% of all U.S. medical care in 1930 occurred in the home [], by 1950, this number dropped to 10%, and to only 0.6% of all patient encounters by 1980 [].The New England Journal of Medicine (NEJM) documented a further decline in their ominously entitled 1997 article ...
In addition, if you plan to seek funding, investors and lenders will use your business plan to determine the level of risk. Download our Ultimate Business Plan Template here >. Below is the business plan outline you should use to create a business plan for your healthcare company. Also, here are links to several healthcare business plan templates:
Home-based primary care (HBPC) interventions move the delivery of primary care from an office to the patient's home. HBPC programs have roots in the house call and community health outreach practices of earlier eras. In the past, house calls were a standard part of medical care and community health. Forty percent of physicians made house calls ...
Through the integration of Whole Health for Life into the Department of Veterans Affairs (VA) health care system, the VA aims to transform health care delivery from a disease management approach to one that embraces person-centered care. The home-based primary care (HBPC) program is a care model that, within the VA, provides holistic primary ...
One estimate suggests that 90% of health care spending can be influenced by primary care, even though it only accounts for 5%-6% of overall spending. For this reason, primary care is especially well-suited to value-based reimbursements tied to overall health outcomes or total cost of care. 6. Primary care physicians (PCPs) and their care teams ...
Drafting a business plan for your new practice requires research, forecasts, and realistic objectives. Given the financial structure of the direct care practice, careful planning can help ensure the practice's success. Elements of a business include: Practice location. Membership pricing structure.
With an estimated two million homebound adults in the U.S. today and the nation's older adult population increasing, home-based primary care is putting a new face on the "house calls" of yesteryear. As the shift to home- and community-based care continues, health care organizations are seeking new options for providing health care services in the comfort of the home.
Our experienced geriatricians, nurse practitioners and other health professionals provide compassionate care in the comfort of your home. We offer in-home primary care throughout Howard County and parts of Baltimore City and Baltimore County. To get started, call us at 410-550-0931, or apply for the program with our online application.
PCS Business Plan 2020/21 | Our Practices & Priorities 05 Research in Primary Care We have already begun to establish a research function within PCS. This work aims to set Sheffield as a centre of primary care excellence and draw funding into general practice, opening up opportunities to progress into commercial studies in the future.
Home Based Primary Care is health care services provided to Veterans in their home. The program is for Veterans who need team based in-home support for ongoing diseases and illnesses that affect their health and daily activities. Veterans usually have difficulty making and keeping clinic visits because of the severity of their illness and are ...
Medicare.gov Care Compare is a new tool that helps you find and compare the quality of Medicare-approved providers near you. You can search for nursing homes, doctors, hospitals, hospice centers, and more. Learn how to use Care Compare and make informed decisions about your health care. Official Medicare site.