Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

The relationship between workload and burnout among nurses: The buffering role of personal, social and organisational resources
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Institute of Occupational, Social and Environmental Medicine, University Medical Center of the Johannes Gutenberg University Mainz, Mainz, Germany
Roles Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Software, Writing – review & editing
Roles Conceptualization, Funding acquisition, Investigation, Resources, Writing – review & editing
Roles Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing
Affiliation Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf, Hamburg, Germany
Roles Conceptualization, Investigation, Methodology, Resources, Supervision, Writing – review & editing
Affiliations Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf, Hamburg, Germany, Department for Occupational Medicine, Hazardous Substances and Health Science, Institution for Accident Insurance and Prevention in the Health and Welfare Services (BGW), Hamburg, Germany
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing
¶ ‡ These authors are joint senior authors on this work.
Affiliations Institute of Occupational, Social and Environmental Medicine, University Medical Center of the Johannes Gutenberg University Mainz, Mainz, Germany, Federal Institute for Occupational Safety and Health (BAuA), Berlin, Germany
Roles Supervision, Writing – review & editing
* E-mail: [email protected]
- Elisabeth Diehl,
- Sandra Rieger,
- Stephan Letzel,
- Anja Schablon,
- Albert Nienhaus,
- Luis Carlos Escobar Pinzon,
- Pavel Dietz

- Published: January 22, 2021
- https://doi.org/10.1371/journal.pone.0245798
- Peer Review
- Reader Comments
Workload in the nursing profession is high, which is associated with poor health. Thus, it is important to get a proper understanding of the working situation and to analyse factors which might be able to mitigate the negative effects of such a high workload. In Germany, many people with serious or life-threatening illnesses are treated in non-specialized palliative care settings such as nursing homes, hospitals and outpatient care. The purpose of the present study was to investigate the buffering role of resources on the relationship between workload and burnout among nurses. A nationwide cross-sectional survey was applied. The questionnaire included parts of the Copenhagen Psychosocial Questionnaire (COPSOQ) (scale ‘quantitative demands’ measuring workload, scale ‘burnout’, various scales to resources), the resilience questionnaire RS-13 and single self-developed questions. Bivariate and moderator analyses were performed. Palliative care aspects, such as the ‘extent of palliative care’, were incorporated to the analyses as covariates. 497 nurses participated. Nurses who reported ‘workplace commitment’, a ‘good working team’ and ‘recognition from supervisor’ conveyed a weaker association between ‘quantitative demands’ and ‘burnout’ than those who did not. On average, nurses spend 20% of their working time with palliative care. Spending more time than this was associated with ‘burnout’. The results of our study imply a buffering role of different resources on burnout. Additionally, the study reveals that the ‘extent of palliative care’ may have an impact on nurse burnout, and should be considered in future studies.
Citation: Diehl E, Rieger S, Letzel S, Schablon A, Nienhaus A, Escobar Pinzon LC, et al. (2021) The relationship between workload and burnout among nurses: The buffering role of personal, social and organisational resources. PLoS ONE 16(1): e0245798. https://doi.org/10.1371/journal.pone.0245798
Editor: Adrian Loerbroks, Universtiy of Düsseldorf, GERMANY
Received: July 30, 2020; Accepted: January 7, 2021; Published: January 22, 2021
Copyright: © 2021 Diehl et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: According to the Ethics Committee of the Medical Association of Rhineland-Palatinate (Study ID: 837.326.16 (10645)), the Institute of Occupational, Social and Environmental Medicine of the University Medical Center of the University Mainz is specified as data holding organization. The institution is not allowed to share the data publically in order to guarantee anonymity to the institutions that participated in the survey because some institution-specific information could be linked to specific institutions. The data set of the present study is stored on the institution server at the University Medical Centre of the University of Mainz and can be requested for scientific purposes via the institution office. This ensures that data will be accessible even if the authors of the present paper change affiliation. Postal address: University Medical Center of the University of Mainz, Institute of Occupational, Social and Environmental Medicine, Obere Zahlbacher Str. 67, D-55131 Mainz. Email address: [email protected] .
Funding: The research was funded by the BGW - Berufsgenossenschaft für Gesundheitsdienst und Wohlfahrtspflege (Institution for Statutory Accident Insurance and Prevention in Health and Welfare Services). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: I have read the journal’s policy and the authors of this manuscript have the following competing interests: The project was funded by the BGW - Berufsgenossenschaft für Gesundheitsdienst und Wohlfahrtspflege (Institution for Statutory Accident Insurance and Prevention in Health and Welfare Services). The BGW is responsible for the health concerns of the target group investigated in the present study, namely nurses. Prof. Dr. A. Nienhaus is head of the Department for Occupational Medicine, Hazardous Substances and Health Science of the BGW and co-author of this publication. All other authors declare to have no potential conflict of interest. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
Introduction
Our society has to face the challenge of a growing number of older people [ 1 ], combined with an expected shortage of skilled workers, especially in nursing care [ 2 ]. At the same time, cancer patients, patients with non-oncological diseases, multimorbid patients [ 3 ] and patients suffering from dementia [ 4 ] are to benefit from palliative care. In Germany, palliative care is divided into specialised and general palliative care ( Table 1 ). The German Society for Palliative Medicine (DGP) estimated that 90% of dying people are in need of palliative care, but only 10% of them are in need of specialised palliative care, because of more complex needs, such as complex pain management [ 5 ]. The framework of specialised palliative care encompasses specialist outpatient palliative care, inpatient hospices and palliative care units in hospitals. In Germany, most nurses in specialised palliative care have an additional qualification [ 6 ]. Further, nurses in specialist palliative care in Germany have fewer patients to care for than nurses in other fields which results in more time for the patients [ 7 ]. Most people are treated within general palliative care in non-specialized palliative care settings, which is provided by primary care suppliers with fundamental knowledge of palliative care. These are GPs, specialists (e.g. oncologists) and, above all, staff in nursing homes, hospitals and outpatient care [ 8 ]. Nurses in general palliative care have basic skills in palliative care from their education. However, there is no data available on the extent of palliative care they provide, or information on an additional qualification in palliative care. Palliative care experts from around the world consider the education and training of all staff in the fundamentals of palliative care to be essential [ 9 ] and a study conducted in Italy revealed that professional competency of palliative care nurses was positively associated with job satisfaction [ 10 ]. Thus, it is possible that the extent of palliative care or an additional qualification in palliative care may have implications on the working situation and health status of nurses. In Germany, there are different studies which concentrate on people dying in hospitals or nursing homes and the associated burden on the institution’s staff [ 11 , 12 ], but studies considering palliative care aspects concentrate on specialised palliative care settings [ 6 , 13 , 14 ]. Because the working conditions of nurses in specialised and general palliative care are somewhat different, as stated above, this paper focuses on nurses working in general palliative care, in other words, in non-specialized palliative care settings.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0245798.t001
Burnout is a large problem in social professions, especially in health care worldwide [ 19 ] and is consistently associated with nurses intention to leave their profession [ 20 ]. Burnout is a state of emotional, physical, and mental exhaustion caused by a long-term mismatch of the demands associated with the job and the resources of the worker [ 21 ]. One of the causes for the alarming increase in nursing burnout is their workload [ 22 , 23 ]. Workload can be either qualitative (pertaining to the type of skills and/or effort needed in order to perform work tasks) or quantitative (the amount of work to be done and the speed at which it has to be performed) [ 24 ].
Studies analysing burnout in nursing have recognised different coping strategies, self-efficacy, emotional intelligence factors, social support [ 25 , 26 ], the meaning of work and role clarity [ 27 ] as protective factors. Studies conducted in the palliative care sector identified empathy [ 28 ], attitudes toward death, secure attachment styles, and meaning and purpose in life as protective factors [ 29 ]. Individual factors such as spirituality and hobbies [ 30 ], self-care [ 31 ], coping strategies for facing the death of a patient [ 32 ], physical activity [ 33 ] and social resources, like social support [ 33 , 34 ], the team [ 6 , 13 ] and time for patients [ 32 ] were identified, as effectively protecting against burnout. These studies used qualitative or descriptive methods or correlation analyses in order to investigate the relationship between variables. In contrast to this statistical approach, fewer studies examined the buffering/moderating role of resources on the relationship between workload and burnout in nursing. A moderator variable affects the direction and/or the strength of the relationship between two other variables [ 35 ]. A previous study has showed resilience as being a moderator for emotional exhaustion on health [ 36 ], and other studies revealed professional commitment or social support moderating job demands on emotional exhaustion [ 37 , 38 ]. Furthermore, work engagement and emotional intelligence was recognised as a moderator in the work demand and burnout relationship [ 39 , 40 ].
We have analysed the working situation of nurses using the Rudow Stress-Strain-Resources model [ 41 ]. According to this model, the same stressor can lead to different strains in different people depending on available resources. These resources can be either individual, social or organisational. Individual resources are those resources which are owned by an individual. This includes for example personal capacities such as positive thinking as well as personal qualifications. Social resources consist of the relationships an individual has, this includes for example relationships at work as well as in his private life. Organisational resources refer to the concrete design of the workplace and work organisation. For example, nurses reporting a good working team may experience workload as less threatening and disruptive because a good working team gives them a feeling of security, stability and belonging. According to Rudow, individual, social or organisational resources can buffer/moderate the negative effects of job demands (stressors) on, for example, burnout (strain).
Nurses’ health may have an effect on the quality of the services offered by the health care system [ 42 ], therefore, it is of great interest to do everything possible to preserve their health. This may be achieved by reducing the workload and by strengthening the available resources. However, to the best of our knowledge, we are not aware of any study which considers palliative care aspects within general palliative care in Germany. Therefore, the aim of the study was to investigate the buffering role of resources on the relationship between workload (‘quantitative demands’) and burnout among nurses. Palliative care aspects, such as information on the extent of palliative care were incorporated to the analyses as covariates.
Study design and participants
An exploratory cross-sectional study was conducted in 2017. In Germany, there is no national register for nurses. Data for this study were collected from a stratified 10% random sample of a database with outpatient facilities, hospitals and nursing homes in Germany from the Institution for Statutory Accident Insurance and Prevention in Health and Welfare Services in Germany. This institution is part of the German social security system. It is the statutory accident insurer for nonstate institutions in the health and welfare services in Germany and thus responsible for the health concerns of the target group investigated in the present study, namely nurses. Due to data protection rules, this institution was also responsible for the first contact with the health facilities. 126 of 3,278 (3.8%) health facilities agreed to participate in the survey. They informed the study team about how many nurses worked in their institution, and whether the nurses would prefer to answer a paper-and-pencil questionnaire (with a pre-franked envelope) or an online survey (with an access code ). 2,982 questionnaires/access codes were sent out to the participating health facilities (656 to outpatient care, 160 to hospitals and 2,166 to nursing homes), where they were distributed to the nurses ( S1 Table ). Participation was voluntary and anonymous. Informed consent was obtained written at the beginning of the questionnaire. Approval to perform the study was obtained by the ethics committee of the State Chamber of Medicine in Rhineland-Palatinate (Clearance number 837.326.16 (10645)).
Questionnaire
The questionnaire contained questions regarding i) nurse’s sociodemographic information and information on current profession as well as ii) palliative care aspects. Furthermore, iii) parts of the German version of the Copenhagen Psychosocial Questionnaire (COPSOQ), iv) a resilience questionnaire [RS-13] and v) single questions relating to resources were added.
i) Sociodemographic information and information on current profession.
The nurse’s sociodemographic information and information on current profession included the variables ‘age’, ‘gender’, ‘marital status’, ‘education’, ‘professional qualification’, ‘working area’, ‘professional experience’ and ‘extent of employment’.
ii) Palliative care aspects.
Palliative care aspects included self-developed questions on ‘additional qualification in palliative care’, the ‘number of patients’ deaths within the last month (that the nurses cared for personally)’ and the ‘extent of palliative care’. The latter was evaluated by asking: how much of your working time (as a percentage) do you spend with care of palliative patients? The first two items were already used in the pilot study. The pilot study consisted of a qualitative part, where interviews with experts in general and specialised palliative care were performed [ 43 ]. These interviews were used to develop a standardized questionnaire which was used for a cross-sectional pilot survey [ 6 , 44 ].
iii) Copenhagen Psychosocial Questionnaire (COPSOQ).
The questionnaire included parts of the German standard version of the Copenhagen Psychosocial Questionnaire (COPSOQ) [ 45 ]. The COPSOQ is a valid and reliable questionnaire for the assessment of psychosocial work environmental factors and health in the workplace [ 46 , 47 ]. The scales selected were ‘quantitative demands’ (four items, for example: “Do you have to work very fast?”) measuring workload, ‘burnout’ (six items, for example: “How often do you feel emotionally exhausted?”), ‘meaning of work’ (three items, for example: “Do you feel that the work you do is important?”) and ‘workplace commitment’ (four items, for example: “Do you enjoy telling others about your place of work?”).
iv) Resilience questionnaire RS-13.
The RS-13 questionnaire is the short German version of the RS-25 questionnaire developed by Wagnild & Young [ 48 ]. The questionnaire postulates a two-dimensional structure of resilience formed by the factors “personal competence” and “acceptance of self and life”. The RS-13 questionnaire measures resilience with 13 items on a 7-point scale (1 = I do not agree, 7 = I totally agree with different statements) and has been validated in representative samples [ 49 , 50 ]. The results of the questionnaire were grouped into persons with low, moderate or high resilience.
v) Questions on resources.
Single questions on personal, social and organizational resources assessed the nurses’ views of these resources in being helpful in dealing with the demands of their work. Further, single questions collected the agreement to different statements such as ‘Do you receive recognition for your work from the supervisor? ’ (see Table 4 ). These resources were frequently reported in the pilot study by nurses in specialised palliative care [ 6 ].
Data preparation and analysis
The data from the paper-and-pencil and online questionnaires were merged, and data cleaning was done (e.g. questionnaires without specification to nursing homes, hospitals or outpatient care were excluded). The scales selected from the COPSOQ were prepared according to the COPSOQ guidelines. In general, COPSOQ items have a 5-point Likert format, which are then transformed into a 0 to 100 scale. The scale score is calculated as the mean of the items for each scale, if at least half of the single items had valid answers. Nurses who answered less than half of the items in a scale were recorded as missing. If at least half of the items were answered, the scale value was calculated as the average of the items answered [ 46 ]. High values for the scales ‘quantitative demands‘ and ‘burnout‘ were considered negative, while high values for the scales ‘meaning of work’ and ‘workplace commitment’ were considered positive. The proportion of missing values for single scale items was between 0.5% and 2.7%. Cronbach’s Alpha was used to assess the internal consistency of the scales. A Cronbach’s Alpha > 0.7 was regarded as acceptable [ 35 ]. The score of the RS-13 questionnaire ranges from 13 to 91. The answers were grouped according to the specifications in groups with low resilience (score 13–66), moderate resilience (67–72) and high resilience (73–91) [ 49 ]. The categorical resource variables were dichotomised (example: not helpful/little helpful vs. quite helpful/very helpful).
The study was conceptualised as an exploratory study. Consequently, no prior hypotheses were formulated, so the p-values merely enable the recognition of any statistically noteworthy findings [ 51 ]. Descriptive statistics (absolute and relative frequency, M = mean, SD = standard deviation) were used to depict the data. Bivariate analyses (Pearson correlation, t-tests, analysis of variance) were performed to infer important variables for the regression-based moderation analysis. Variables which did not fulfil all the conditions for linear regression analysis were recoded as categorical variables [ 35 ]. The variable ‘extent of palliative care’ was categorised as ‘≤ 20 percent of working time’ vs. ‘> 20 percent of working time’ due to the median of the variable (median = 20).
The first step with regard to the moderation analysis was to determine the resource variables. Therefore all resource variables that reached a p-value < 0.05 in the bivariate analysis with the scale ‘burnout’ were further analysed (scale ‘meaning of work’, scale ‘workplace commitment’, variables presented in Table 4 ). The moderator analysis was conducted using the PROCESS program developed by Andrew F. Hayes. First, scales were mean-centred to reduce possible scaling problems and multicollinearity. Secondly, for all significant resource variables the following analysis were done: the ‘quantitative demand’, one resource (one per model) and the interaction term between the ‘quantitative demand’ and the resource, as well as the covariates ‘age’, ‘gender’, ‘working area’, ‘extent of employment’, the ‘extent of palliative care’ and the ‘number of patient deaths within the last month’ were added to the moderator analysis, in order to control for confounding influence. If the interaction term between the ‘quantitative demand’ and the resource accounted for significantly more variance than without interaction term (change in R 2 denoted as ΔR 2 , p < 0.05), a moderator effect of the resource was present. The interaction of the variables (± 1 SD the mean or variable manifestation such as yes and no) was plotted.
All the statistical calculations were performed using the Statistical Package for Social Science (SPSS, version 23.5) and the PROCESS macro for SPSS (version 3.5 by Hayes) for the moderator analysis.
Of the 2,982 questionnaires/access codes sent out, 497 were eligible for the analysis. The response rate was 16.7% (response rate of outpatient care 14.6%, response rate of hospitals 18.1% and response rate of nursing homes 16.0%). Since only n = 29 nurses from hospitals participated, these were excluded from data analysis. After data cleaning , the final number of participants was n = 437.
Descriptive results
The basic characteristics of the study population are presented in Table 2 . The average age of the nurses was 42.8 years, and 388 (89.6%) were female. In total, 316 nurses answered the question how much working time they spend caring for palliative patients. Sixteen (5.1%) nurses reported spending no time caring for palliative patients, 124 (39.2%) nurses reported between 1% to 10%, 61 (19.30%) nurses reported between 11% to 20% and 115 (36.4%) nurses reported spending more than 20% of their working time for caring for palliative patients. Approximately one-third (n = 121, 27.7%) of the nurses in this study did not answer this question. One hundred seventeen (29.5%) nurses reported 4 or more patient deaths, 218 (54.9%) reported 1 to 3 patient deaths and 62 (15.6%) reported 0 patient deaths within the last month.
https://doi.org/10.1371/journal.pone.0245798.t002
Table 3 presents the mean values and standard deviations of the scales ‘quantitative demands’, ‘burnout’, and the resource scales ‘meaning of work’ and ‘workplace commitment’. All scales achieved a satisfactory level of internal consistency.
https://doi.org/10.1371/journal.pone.0245798.t003
Bivariate analyses
There was a strong positive correlation between the ‘quantitative demands’ and ‘burnout’ scales (r = 0.498, p ≤ 0.01), and a small negative correlation between ‘burnout’ and ‘meaning of work’ (r = -0.222, p ≤ 0.01) and ‘workplace commitment’ (r = -0.240, p ≤ 0.01). Regarding the basic and job-related characteristics of the sample shown in Table 2 , ‘burnout’ was significantly related to ‘extent of palliative care’ (≤ 20% of working time: n = 199, M = 46.06, SD = 20.28; > 20% of working time: n = 115, M = 53.80, SD = 20.24, t(312) = -3.261, p = 0.001). Furthermore, there was a significant effect regarding the ‘number of patient deaths during the last month’ (F (2, 393) = 5.197, p = 0.006). The mean of the burnout score was lower for nurses reporting no patient deaths within the last month than for nurses reporting four or more deaths (n = 62, M = 42.47, SD = 21.66 versus n = 116, M = 52.71, SD = 20.03). There was no association between ‘quantitative demands’ and an ‘additional qualification in palliative care’ (no qualification: n = 328, M = 55.77, SD = 21.10; additional qualification: n = 103, M = 54.39, SD = 20.44, p = 0.559).
The association between ‘burnout’ and the evaluated (categorical) resource variables is presented in Table 4 . Nurses mostly had a lower value on the ‘burnout’ scale when reporting various resources. Only the resources ‘family’, ‘religiosity/spirituality’, ‘gratitude of patients’, ‘recognition through patients/relatives’ and an ‘additional qualification in palliative care’ were not associated with ‘burnout’.
https://doi.org/10.1371/journal.pone.0245798.t004
Moderator analyses
In total, 16 moderation analyses were conducted. Table 5 presents the results of the moderation analyses where a significant moderation was found. For ‘workplace commitment’, there was a positive and significant association between ‘quantitative demands’ and ‘burnout’ (b = 0.47, SE = 0.051, p < 0.001). An increase of one value on the scale ‘quantitative demands’ increased the scale ‘burnout’ by 0.47. ‘Workplace commitment’ was negatively related to ‘burnout’, meaning that a higher degree of ‘workplace commitment’ was related to a lower level of ‘burnout’ (b = -0.11, SE = 0.048, p = 0.030). A model with the interaction term of ‘quantitative demands’ and the resource ‘workplace commitment’ accounted for significantly more variance in ‘burnout’ than a model without interaction term (ΔR 2 = 0.021, p = 0.004). The impact of ‘quantitative demands’ on ‘burnout’ was dependent on ‘workplace commitment’ (b = -0.01, SE = 0.002 p = 0.004). The variables explained 31.9% of the variance in ‘burnout’.
https://doi.org/10.1371/journal.pone.0245798.t005
Regarding the ‘good working team’ resource, the variables ‘quantitative demands’ and ‘burnout’ were positively and significantly associated (b = 0.76, SE = 0.154, p < 0.001), and the variables ‘good working team’ and ‘burnout’ were not associated (b = -3.15, SE = 3.52, p = 0.372). A model with the interaction term of ‘quantitative demands’ and the ‘good working team’ resource accounted for significantly more variance in ‘burnout’ than a model without interaction term (ΔR 2 = 0.011, p = 0.040). The ‘good working team’ resource moderated the impact of ‘quantitative demands’ on ‘burnout’ (b = -0.34, SE = 0.165, p = 0.004). The variables explained 29.7% of the variance in ‘burnout’.
The associations between ‘quantitative demands’ and ‘burnout’ (b = 0.63, SE = 0.085, p < 0.001), between ‘recognition supervisor’ and ‘burnout’ (b = -7.29, SE = 2.27, p = 0.001), and the interaction term of ‘quantitative demands’ and the resource ‘recognition supervisor’ (b = -0.34, SE = 0.108, p = 0.002) were significant. Again, a model with the interaction term accounted for significantly more variance in ‘burnout’ than a model without interaction term (ΔR 2 = 0.024, p = 0.002). ‘Recognition from supervisor’ influenced the impact of ‘quantitative demands’ on burnout for -0.34 on the 0 to 100 scale. The variables explained 33.7% of the variance in ‘burnout’.
Figs 1 – 3 demonstrates simple slopes of the interaction effects of ‘workplace commitment’ predicting ‘burnout’ at high, average and low levels ( Fig 1 ) respectively with and without the resource ‘good working team’ ( Fig 2 ) and ‘recognition from supervisor’ ( Fig 3 ). Higher ‘quantitative demands’ were associated with higher levels of ‘burnout’. At low ‘quantitative demands’, the ‘burnout’ level was quite similar for all nurses. However, when ‘quantitative demands’ increased, nurses who confirmed that they had the resources stated a lower ‘burnout’ level than nurses who denied having them. This trend is repeated by the resources ‘workplace commitment’, ‘good working team’ and ‘recognition from supervisor’.
https://doi.org/10.1371/journal.pone.0245798.g001
https://doi.org/10.1371/journal.pone.0245798.g002
https://doi.org/10.1371/journal.pone.0245798.g003
The palliative care aspect ‘extent of palliative care’ showed that spending more than 20 percent of working time in care for palliative patients increased burnout significantly by a value of approximately 5 on a 0 to 100 scale ( Table 5 ).
The aim of the present study was to analyse the buffering role of resources on the relationship between workload and burnout among nurses. This was done for the first time by considering palliative care aspects, such as information on the extent of palliative care.
The study shows that higher quantitative demands were associated with higher levels of burnout, which is in line with other studies [ 37 , 39 ]. Furthermore, the results of this study indicate that working in a good team, recognition from supervisor and workplace commitment is a moderator within the workload—burnout relationship. Although the moderator analyses revealed low buffering effect values, social resources were identified once more as important resources. This is consistent with the results of a study conducted in the field of specialised palliative care in Germany, where a good working team and workplace commitment moderated the impact of quantitative demands on nurses burnout [ 52 ]. A recently published review also describes social support from co-workers and supervisors as a fundamental resource in preventing burnout in nurses [ 53 ]. Workplace commitment was not only reported as a moderator between workload and health in the nurse setting [ 37 ], but also as a moderator between work stress and burnout [ 54 ] and between work stress and other health related aspects outside the nurse setting [ 55 ]. In the present study, the effect of high workload on burnout was reduced with increasing workplace commitment. Nurses reporting a high work commitment may experience workload as less threatening and disruptive because workplace commitment gives them a feeling of belonging, security and stability. However, there are also some correlation studies which observed no direct relationship between workplace commitment and burnout for occupations in the health sector [ 56 ]. A study from Serbia assessed workplace commitment by nurses and medical technicians as a protective factor against patient-related burnout, but not against personal and work-related burnout [ 57 ]. Furthermore, a study conducted in Estonia reported no relationship between workplace commitment and burnout amongst nurses [ 58 ]. As there are indications that workplace commitment is correlated with patient safety [ 59 ], the development and improving of workplace commitment needs further scientific investigation.
This study observed slightly higher burnout rates among nurses who reported a ‘good working team’ for low workload. This fact is not decisive for the interpretation of the moderation effect of this resource because moderation is present. When workload increased, nurses who confirmed that they worked in a good working team stated a lower burnout level. However, the result of the current study showed that a good working team is particularly important when workload increases, in the most extreme cases team work in palliative care is necessary to save a person’s life. Because team work in today’s health care system is essential, health care organisations should foster team work in order to enhance their clinical outcomes [ 60 ], improve the quality of patient care as well as health [ 61 ] and satisfaction of nurses [ 62 ].
The bivariate analysis revealed that nurses who reported getting recognition from colleagues, through the social context, salary and gratitude from relatives of patients stated a lower value on the burnout scale. This is in accordance with the results of a qualitative study, which indicated that the feeling of recognition, and that one’s work is useful and worthwhile, is very important for nurses and a source of satisfaction [ 63 ]. Furthermore, self-care, self-reflection [ 64 ] and professional attitude/dissociation seem to play an important role in preventing burnout. The bivariate analysis also revealed a relationship between resilience and burnout. Nurses with high resilience reported lower values on the burnout scale, but a buffering role of resilience on burnout was not assessed. The present paper focuses solely on quantitative demands and burnout. In future studies, the different fields of nursing demands, like organisational or emotional demands, should be assessed in relation to burnout, job satisfaction and health.
Finally, we observed whether the consideration of palliative care aspects is associated with burnout. The bivariate analysis revealed a relationship between the extent of palliative care, number of patient deaths within the last month and burnout. Using regression analyses, only the extent of palliative care was associated with burnout. Since, to the best of our knowledge, the present study is the first study to consider palliative care aspects within general palliative care in Germany, these variables need further scientific investigation, not only within the demand—burnout relationship but also between the demand—health and the demand—job satisfaction relationship. Furthermore, palliative care experts from around the world considered the education and training of all members of staff in the fundamentals of palliative care to be essential [ 9 ]. One-fourth of the respondents in the present study had an additional qualification in palliative care, which was not obligatory. We assessed a relationship between quantitative demands and burnout but no relationship between an additional qualification and quantitative demands nor burnout. Nevertheless, we assessed a protective effect of the additional qualification within the pilot study in specialised palliative care, in relation both to organisational demands and demands regarding the care of relatives [ 6 ]. This suggests that the additional qualification is a resource, but one which depends on the field of demand. Further analyses would be required to review benefits achieved by additional qualifications in general palliative care.
The variable extent of palliative care is the one with the most missing values in the survey, thus future analyses should not only study larger samples but also reconsider the question on extent of palliative care.
Finally, it can be said that the main contribution of the present study is to make palliative care aspects in non-specialised palliative care settings a subject of discussion.
Limitations
The following potential limitations need to be stated: although a random sample was drawn, the sample is not representative for general palliative care in Germany due to a low participation rate of the health facilities, a low response rate of the nurses, the different responses of the health facilities and the exclusion of hospitals. One possible explanation for the low participation rate of the health facilities is the sampling procedure and data protection rules, which did not allowed the study team to contact the institutions in the sample. Due to the low participation rate, the results of the present study may be labelled as preliminary. Further, the data are based on a detailed and anonymous survey, and therefore the potential for selection bias has to be considered. It is possible that the institutions and nurses with the highest burden had no time for or interest in answering the questionnaire. It is also possible that the institutions which care for a high number of palliative patients may have taken particular interest in the survey. Additionally, some items of the questionnaire were self-developed and not validated but were considered valuable for our study as they answered certain questions that standardized questionnaires could not. The moderator analyses revealed low effect values and the variance explained by the interaction terms is rather low. However, moderator effects are difficult to detect, therefore, even those explaining as little as one percent of the total variance should be considered [ 65 ]. Consequently, the additional amount of variance explained by the interaction in the current study (2% for workplace commitment and recognition of supervisor and 1% for good working team) is not only statistically significant but also practically and theoretically relevant. When considering the results of the current study, it must be taken into account that the present paper focuses solely on quantitative demands and burnout. In future studies, the different fields of nursing demands have to be carried out on the role of resources. This not only pertains for burnout, but also for other outcomes such as job satisfaction and health. Finally, the cross-sectional design does not allow for casual inferences. Longitudinal and interventional studies are needed to support causality in the relationships examined.
Conclusions
The present study provides support to a buffering role of workplace commitment, good working teams and recognition from supervisors on the relationship between workload and burnout. Initiatives to develop or improve workplace commitment and strengthen collaboration with colleagues and supervisors should be implemented in order to reduce burnout levels. Furthermore, the results of the study provides first insights that palliative care aspects in general palliative care may have an impact on nurse burnout, and therefore they have gone unrecognised for too long in the scientific literature. They have to be considered in future studies, in order to improve the working conditions, health and satisfaction of nurses. As our study was exploratory, the results should be confirmed in future studies.
Supporting information
S1 table. number of questionnaires sent out to facilites and response rate..
https://doi.org/10.1371/journal.pone.0245798.s001
Acknowledgments
We thank the nurses and the health care institutions for taking part in the study. We thank D. Wendeler, O. Kleinmüller, E. Muth, R. Amma and C. Kohring who were helpful in the recruitment of the participants and data collection.
- 1. OECD. Health at a glance 2015: OECD indicators. 2015th ed. Paris: OECD Publishing; 2015.
- View Article
- PubMed/NCBI
- Google Scholar
- 5. Melching H. Palliativversorgung—Modul 2 -: Strukturen und regionale Unterschiede in der Hospiz- und Palliativversorgung. Gütersloh; 2015.
- 8. German National Academy of Sciences Leopoldina and Union of German Academies of Sciences. Palliative care in Germany: Perspectives for practice and research. Halle (Saale): Deutsche Akademie der Naturforscher Leopoldina e. V; 2015.
- 12. George W, Siegrist J, Allert R. Sterben im Krankenhaus: Situationsbeschreibung, Zusammenhänge, Empfehlungen. Gießen: Psychosozial-Verl.; 2013.
- 15. Deutsche Krebsgesellschaft, Deutsche Krebshilfe, Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Palliativmedizin für Patienten mit einer nicht heilbaren Krebserkrankung: Langversion 1.1; 2015.
- 16. Deutsche Gesellschaft für Palliativmedizin. Definitionen zur Hospiz- und Palliativversorgung. 2016. https://www.dgpalliativmedizin.de/images/DGP_GLOSSAR.pdf . Accessed 8 Sep 2020.
- 17. Deutscher Hospiz- und PalliativVerband e.V. Hospizarbeit und Palliativversorgung. 2020. https://www.dhpv.de/themen_hospiz-palliativ.html . Accessed 20 May 2020.
- 24. van Veldhoven Marc. Quantitative Job Demands. In: Peeters M, Jonge de J, editors. An introduction to contemporary work psychology. Chichester West Sussex UK: John Wiley & Sons; 2014. p. 117–143.
- 35. Field A. Discovering statistics using IBM SPSS statistics. 4th ed. Los Angeles, London, New Delhi, Singapore, Washington DC, Melbourne: SAGE; 2016.
- 41. Rudow B. Die gesunde Arbeit: Psychische Belastungen, Arbeitsgestaltung und Arbeitsorganisation. 3rd ed. Berlin, München, Boston: De Gruyter Oldenbourg; 2014.
- 45. Freiburger Forschungsstelle für Arbeits- und Sozialmedizin. Befragung zu psychosozialen Faktoren am Arbeitsplatz. 2016. https://www.copsoq.de/assets/COPSOQ-Standard-Fragebogen-FFAW.pdf . Accessed 6 Mar 2020.
- 60. O’Daniel M, Rosenstein AH. Patient Safety and Quality: An Evidence-Based Handbook for Nurses: Professional Communication and Team Collaboration. Rockville (MD); 2008.
- 61. Canadian Health Services Research Foundation. eamwork in healthcare: promoting effective teamwork in healthcare in Canada.: Policy synthesis and recommendations.; 2006.
- Open access
- Published: 08 October 2022
Workload and quality of nursing care: the mediating role of implicit rationing of nursing care, job satisfaction and emotional exhaustion by using structural equations modeling approach
- Fatemeh Maghsoud 1 ,
- Mahboubeh Rezaei 2 ,
- Fatemeh Sadat Asgarian 3 &
- Maryam Rassouli 4
BMC Nursing volume 21 , Article number: 273 ( 2022 ) Cite this article
11k Accesses
17 Citations
Metrics details
Nursing workload and its effects on the quality of nursing care is a major concern for nurse managers. Factors which mediate the relationship between workload and the quality of nursing care have not been extensively studied. This study aimed to investigate the mediating role of implicit rationing of nursing care, job satisfaction and emotional exhaustion in the relationship between workload and quality of nursing care.
In this cross-sectional study, 311 nurses from four different hospitals in center of Iran were selected by convenience sampling method. Six self-reported questionnaires were completed by the nurses. The data were analyzed by SPSS version 16. Structural equation modeling was used to determine the relationships between the components using Stata 14 software.
Except direct and mutual relationship between workload and quality of nursing care ( P ≥ 0.05), the relationship between other variables was statistically significant ( P < 0.05). The hypothesized model fitted the empirical data and confirmed the mediating role of implicit rationing of nursing care, job satisfaction and emotional exhaustion in the relationship between workload and the quality of nursing care (TLI, CFI > 0.9 and RMSEA < 0.08 and χ 2 /df < 3).
Workload affects the quality of the provided nursing care by affecting implicit rationing of nursing care, job satisfaction and emotional exhaustion. Nurse managers need to acknowledge the importance of quality of nursing care and its related factors. Regular supervision of these factors and provision of best related strategies, will ultimately lead to improve the quality of nursing care.
Peer Review reports
Care is the core of the nursing profession and the main factor which distinguishes nursing from other health-related professions [ 1 , 2 ]. High-quality nursing care means the provision of easy and accessible care by competent qualified nurses [ 3 ]. Nowadays, the maintenance and improvement of the quality of nursing care is the most important challenge for nursing care systems around the world [ 4 ]. The first step in improving the quality of nursing care is to evaluate and analyze the quality of provided care and examine the factors affecting on it [ 5 ].
Various variables can affect the quality of nursing care [ 6 , 7 , 8 ]; one of which is workload. Zuniga et al. (2015) indicated in Switzerland that increased workload and, subsequently, increased stress could reduce the quality of nursing care [ 9 ]. However, there are contradictory findings in this regard. It was shown in another study that there was a high level of nursing care quality despite the high workload and inadequate human resources and equipment [ 6 ]. In another study, the workload was measured by total direct nursing hours. The results showed a significant correlation between total direct nursing hours and some indicators of nursing care quality such as incidence of patient restraint, and mortality rate. Nevertheless, there was no significant correlation with other indicators of nursing care quality like incidence density of pressure sores, the incidence of falls, the incidence of tube self-extraction, and incidence density of infection [ 10 ].
In addition to the correlation between workload and the quality of nursing care, a number of other factors can also be involved in this relationship. For example, workload can lead to implicit rationing of nursing care, thereby can affect the quality of care. In a study conducted in Lebanon, the level of perceived workload in all shifts had a positive relationship with the level of rationing of nursing care [ 11 ]. Because of many reasons such as high workload, nurses may find themselves in situations where they are forced to omit the necessary cares, do them briefly or with delay [ 11 , 12 ]. Nurses are unable to provide comprehensive care in accordance with professional standards, and it can affect the quality of nursing care [ 13 ]. A study conducted in China showed that the nurses who had a higher score in rationing of nursing care, had a lower score of the quality of nursing care [ 14 ]. Moreover, while increased rationing in rehabilitation, care, supervision and social care in nursing homes, decreases the quality of nursing care, increased rationing in the field of documentation increases the quality of nursing care [ 9 ].
Job satisfaction seems to be another factor mediating the relationship between workload and the quality of nursing care. Inegbedion et al. (2020) indicated that increased workload could be associated with decreased job satisfaction among nurses [ 15 ]. Workload as a strong stressor can negatively affect the job satisfaction of nurses [ 16 ]. Job satisfaction is a multidimensional emotional concept which reflects the interaction between nurses' expectations and values, their environment and personal characteristics [ 17 ]. Perception of the significance of nurses' job satisfaction and its improvement is essential in providing high-quality care with optimal clinical outcomes. In the study of Aron et al. (2015), 87.6% of nurses believed that the quality of care provided by nurses was affected by their job satisfaction [ 18 ]. According to another study, job satisfaction was a significant predictor of the quality of nursing care [ 19 ].
Workload may also affect the quality of nursing care by causing emotional exhaustion in nurses. The results of a study revealed that 55.4% of Canadian nurses suffered from emotional exhaustion. The high workload in this study was a predictor of emotional exhaustion and there was a positive and significant correlation between workload and emotional exhaustion [ 20 ]. Additionally, the findings of Nantsupawat et al. (2016) were indicative of the effect of emotional exhaustion on the quality of nursing care. While increased emotional exhaustion of nurses in their study increased the incidence of medication errors and infections, it decreased the quality of nursing care [ 21 ]. Findings of another study showed that among the components of job burnout, emotional exhaustion had the strongest relationship with the quality of nursing care [ 22 ].
Previous studies have mainly investigated the relationship of one or two variables with the quality of nursing care and the simultaneous effect of several mediating variables on the quality of nursing care has not been examined [ 23 , 24 , 25 ]. Many of these studies have not used a comprehensive questionnaire to assess all aspects of the quality of nursing care or have been conducted in other settings except hospital units [ 6 , 9 , 26 , 27 ]. Assessing the quality of nursing care with an incomplete questionnaire or with only one question does not cover all dimensions of quality of nursing care such as the care-related activities, nursing care environment, nursing process, and strategies that empower patients and will provide incomplete findings [ 28 , 29 ].
Accordingly, to improve the quality of nursing care, we need to determine these variables and their mediating roles, in order to better control them through applying effective interventions. Using Structural Equation Modeling (SEM) is one powerful tool for mediation analysis [ 30 , 31 ], this study was conducted to investigate the mediating role of implicit rationing of nursing care, job satisfaction, and emotional exhaustion in the relationship between workload and the quality of nursing care in Iran.
The theoretical model in this study was developed by reviewing the related literature (Fig. 1 ) to test three hypotheses:
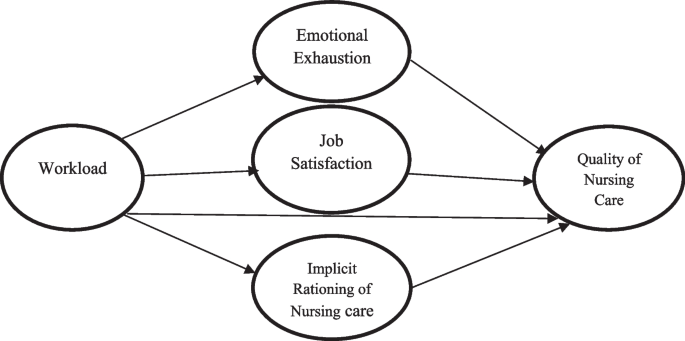
Hypothesized model
H1: Implicit rationing of nursing care plays a mediating role in the relationship between workload and the quality of nursing care.
H2: Job satisfaction plays a mediating role in the relationship between workload and the quality of nursing care.
H3: Emotional exhaustion plays a mediating role in the relationship between workload and the quality of nursing care.
Study design and participants
This cross-sectional study was conducted from October to December 2020 in inpatient units of four selected hospitals in central Iran, Kashan city. According to the guidelines of structural equation modeling, the study required at least 300 participants [ 32 ]. As such, 311 employed nurses participated in the study by using the convenience sampling method. Inclusion criteria were as follows: willingness to participate in the study, having at least six months of work experience, having experience of direct clinical care of patients, and having at least a bachelor's degree in nursing. Exclusion criteria were failure to complete the questionnaire and decline to answer the questionnaires in the process of the study.
Instrumentation
Six tools were used to collect data and analyze the variables of this study:
Nurse's demographic information questionnaire which contains questions about age, gender, marital status, current workplace unit, employment status, nursing work experience, duration of working in the current unit, having overtime, average salary per month, being a nurse as a second job, having a second job beside nursing and the level of interest in the nursing.
The NASA Task Load Index (NASA-TLX) includes six areas of mental demand, physical demand, temporal demand, performance, effort and, frustration. The final score is calculated to be between zero and 100, where scores higher than 50 are indicative of a high overall subjective workload [ 33 ]. Using Cronbach's alpha coefficient, the reliability of this questionnaire has been reported to be above 0.8 in previous studies [ 34 , 35 ].
Basel Extend of Rationing of Nursing Care (BERNCA) questionnaire which has 20 items based on a 4-point Likert scale. In this questionnaire, nurses assess themselves how many times in the past month they have not been able to perform the listed care activities and have been forced to ration them. The total mean score of rationing is 0–3, and the higher the score, the more will be the care that has been rationed. Cronbach's alpha coefficient was calculated to be 0.93 [ 36 ]. The reliability coefficient was calculated at 0.91 in the present study.
The Minnesota Satisfaction Questionnaire (MSQ) which was designed by Weiss et al. (1967) and has two long and short versions [ 37 ]. In this study, the short version of the questionnaire was used. This 18-item questionnaire is based on a 5-point Likert scale and higher scores are indicative of better job satisfaction. The reliability and validity of this questionnaire was determined in Iran [ 38 ]. Using Cronbach's alpha, the reliability of this questionnaire was calculated at 0.77 in the present study.
The emotional exhaustion subscale of the Maslach Burnout Inventory (MBI), includes nine items and is based on a 7-point Likert scale. Higher scores indicate higher emotional exhaustion [ 39 ]. The validity and reliability of this scale were examined in Iran and Cronbach's alpha coefficient was reported to be 0.88 [ 40 ]. Cronbach's alpha coefficient was calculated to be 0.90 in the study of Maslach et al. (1996) and 0.89 in the present study.
The Good Nursing Care Scale (GNCS) is a comprehensive questionnaire that examines all aspects of the quality of nursing care. It has two parallel versions for the nurse and the patient and the nurse's version was used in the present study. This questionnaire has 40 items and seven dimensions include nurses’ characteristics in providing care ( such as type of interaction with the patient, and accuracy ), care-related activities ( such as patient education, and emotional support ), care preconditions ( such as nurse’s knowledge, skill, and experience ), nursing care environment ( such as infection control, maintain patient safety, and patient privacy protection ), nursing process ( conditions related to patient’s admission, treatment and, discharge ), patient empowerment strategies in coping with the disease ( such as paying attention to the patient’s level of knowledge, answering the questions ), and collaboration with the patient's family and relatives ( such as providing sufficient information to the family, and family participation in treatment process ). The scale is based on a 5-point Likert scale and the higher the obtained score, the more will be the quality of provided care [ 28 , 29 ]. This scale has been psychometrically evaluated and used in different countries and Cronbach's alpha coefficient for the scale has been in the range of 0.80 to 0.94 in various studies [ 6 , 41 , 42 , 43 ]. Cronbach's alpha coefficient was calculated to be 0.93 in the present study.
Data collection
All six questionnaires were filled out by the participants based on their work performance in the past month. After obtaining the informed written and oral consent of the eligible nurses, they were explained how to complete the questionnaires. It order to prevent the nurses’ fatigue, the questionnaires were prepared in both online and paper format. The researcher asked each of the participants if they wanted to fill out the questionnaires online or on paper format. If the participants chose the paper format, the questionnaires were delivered to them and were collected at the appointed time. All of the questionnaires have been assessed immediately after the response of the participants and any missing data have been filled by them. But if the participants selected the online version, the link to the questionnaires was sent to their cellphone. This link was designed in such a way that a person could answer only once through the link of the questionnaire and until all the questions were answered, the questionnaire was not sent. Accordingly, there were no missing data. All data collection process was done by a researcher (first author).
Data analysis
Data were analyzed using SPSS version 16 and Stata version 14. Categorical data were described by frequencies and percentages, and quantitative continuous data by mean and standard deviation (SD). The correlation between the variables was determined by the Pearson correlation coefficient test. Structural equation modeling was used to capture the structure of relationships among a web of latent and observed components. To understand the relationships between the variables, according to the theoretical model of the study, all variables were analyzed using Stata software and the structural model was developed. In this study, three types of absolute, comparative and, parsimony fit indices were examined. The Root Mean Square Error of Approximation (RMSEA), the Comparative Fit Index (CFI) Tucker-Lewis Index (TLI), and the ratio of chi-square to the degrees of freedom (χ2 / df) were considered for the good fit of the model. A model is considered to have good fit if the (χ2 / df) value is lower than 3, CFI and TLI are 0.90 or greater, and the RMSEA value is less than 0.08 [ 44 , 45 ]
Participants’ characteristics
All of 311 distributed questionnaires were completed and analyzed. The mean age of the nurses participating in the study was 32.68 ± 6.73 years. The majority of the participants were female (86.5%) and married (76.2%). The complete demographic information of the participants can be seen in Table 1 .
Bivariate analysis
According to the scoring of the questionnaires, the workload of the nurses was at a high level, implicit rationing of nursing care happened rarely, the job satisfaction of nurses was at a moderate level and emotional exhaustion was at a low level. Moreover, the quality of the provided nursing care was at a good level (Table 2 ).
According to the result of Pearson correlation coefficient, there was a statistically significant correlation between the various variables of the study (except workload and quality of nursing care) (Table 3 ).
Structural equation model
Based on the results of this study, the direct effect of workload on implicit rationing of nursing care, job satisfaction and emotional exhaustion was statistically significant ( p < 0.05). Moreover, implicit rationing of nursing care, job satisfaction, and emotional exhaustion had an indirect statistically significant effect on the relationship between workload and quality of nursing care ( p < 0.05) (Table 4 ).
The obtained good fit indices confirmed the mediating role of implicit rationing of nursing care (TLI = 0.94; CFI = 0.95; RMSEA = 0.05), job satisfaction (TLI = 1; CFI = 1; RMSEA = 0.01) and emotional exhaustion (TLI = 0.96; CFI = 0.95; RMSEA = 0.01) in the relationship between workload and the quality of nursing care.
As shown in Fig. 2 , the model fit the data well and was consistent with the hypothesized model. By putting together the three variables of implicit rationing of nursing care, job satisfaction, and emotional exhaustion as mediators in the model, a good fit was obtained (TLI = 0.95; χ2/df = 2.3; CFI = 0.96; and RMSEA = 0.05).
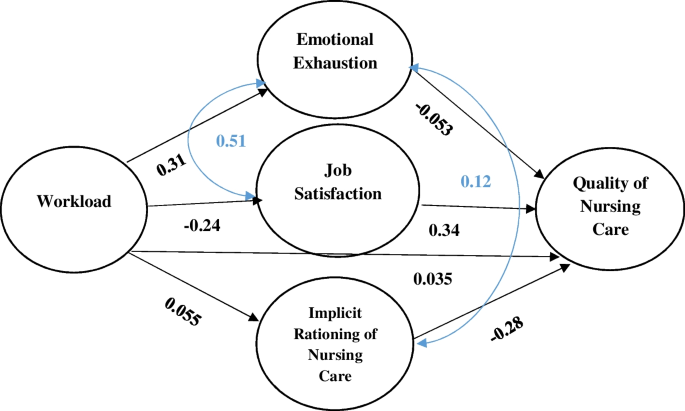
The final model
The results of this study supported the proposed hypothesized model. The findings shown in this structural equation model provided strong support for the study hypotheses.
Based on the findings, implicit rationing of nursing care played a mediating role in the relationship between workload and the quality of nursing care. Therefore, the H1 hypothesis was supported. When the nurses’ workload is high and they are responsible for caring for a large number of patients, they are inevitably forced to ration some important interventions which, in turn, can reduce the quality of nursing care [ 12 , 13 ]. An earlier study showed that implicit rationing of nursing care functions as a mediator between predictive variables such as workload and patient-related outcomes such as medication error and patients’ falling. These adverse events can reduce the quality of nursing care [ 20 ]. In other words, workload has an indirect effect on patient-related outcomes through care rationing and affecting the ability of nurses in completing their main tasks. In another study, nurse-to-patient ratio, as an important indicator in the workload of nurses, affected the quality of care and the incidence of adverse events through rationing of care. In other words, poor nurse staffing levels leads to the rationing of nursing care and, thereby, hinders the provision of high quality care [ 14 ]. Some other studies also referred to the mediating role of rationing of nursing care in the relationship between workload and patient safety [ 46 ] as well as in the relationship between workload and patients’ falling [ 47 ]. Accordingly, implicit rationing of nursing care seems to play a key role in the relationship between workload and the quality of nursing care.
In the present study, nurses’ job satisfaction was the second variable that mediated the relationship between workload and quality of nursing care. Hence, the H2 hypothesis was supported. When the workload is increased, nurses cannot meet some of the needs of patients despite the effort they make. So, nurses do not have a positive attitude toward their performances, leading to less job satisfaction [ 23 , 48 ]. In these circumstances, nurses do not have the necessary peace of mind and precision in the workplace which may negatively affect their efficiency and performance, decreasing the quality of the provided care [ 49 ]. Job satisfaction is an important variable that mediates the relationship between workload and other variables such as intention to leave the job and position [ 50 , 51 ]. Therefore, this is affecting the quality of nursing care indirectly. However, more research is required to investigate the mediating role of job satisfaction.
Emotional exhaustion was another mediating variable in the relationship between workload and quality of nursing care in this study. Therefore, the H3 hypothesis was supported. Emotional exhaustion is considered to be the most important component of job burnout and nurses who experience high levels of emotional exhaustion will suffer from job burnout and have a lower ability and tendency to provide high-quality care [ 39 , 52 ]. According to Van Bogaert et al. (2009), emotional exhaustion plays a mediating role in the relationship between nurses’ workplace conditions and the quality of nursing care [ 53 ]. Liu et al. (2018) also indicated that emotional exhaustion mediates the relationship between workload and patient safety. When nurses are constantly exposed to stressful work environments, their reactions become more chronic and serious, and they need more time to recover [ 46 ]. Additionally, because of high workload and regular attendance at the hospital, nurses do not have much opportunity to rest and regain their energy and, thus, will experience a perpetual emotional exhaustion [ 54 ].
It is noticed from this study that there was no significant correlation between workload and quality of nursing care. This finding is interesting and in line with an earlier study in which despite the high levels of workload and insufficiency of human resources and equipment, the quality of nursing care was at a high level [ 6 ]. Considering that both the nurse’s workload and the quality of nursing care have been investigated from the nurse's point of view, more reliable results have been obtained in this study. It should be noted that the final model in this study is a full mediation model, as the three variables (rationing of nursing care, job satisfaction, and emotional exhaustion) fully mediate the effect of workload on the quality of nursing care. So, after controlling for this mediation effect, there is no direct effect of workload on quality of nursing care [ 55 ].
Also, it seems that experience of high levels of workload for a long period of time and fall into the habit of these conditions lead to nurses can manage difficult situations. According to this finding, it is suggested that temporary or permanent high nursing workload should be taken into consideration in the next researches. Also, social desirability bias which is the tendency to respond in a pleasing way, in answering the questions related to quality of nursing care may also have been influential.
Study limitations
This study has several limitations: a) the present study was confined to frontline nurses in four selected governmental hospitals in a small city in the country; so, generalization of the findings may be limited; b) given the limited number of available participants, the convenience sampling method was used to provide the minimum sample size. It is suggested that future studies be conducted in different cities of the country and private and public hospitals with more participants, to be able to compare the findings; c) the use of self-report questionnaires and nurses’ perceptions to obtain data on the study variables may be a potential limitation because of social desirability bias [ 56 , 57 ]. It is recommended that future studies use more precise data collection strategies with observation or retrospective methodology; d) because the questionnaires filled out by the participants based on their work performance in the past month, recall bias may be another limitation of this study; e) although SEM approach was used in this study, causation cannot be established with the cross-sectional study design.
Implication for clinical practice
Nurse managers have a prominent position related to issues such as nursing workload, rationing of nursing care, job satisfaction and emotional exhaustion. Providing any intervention in these fields, will ultimately effect on the quality of nursing care. Nursing workload, which was at high level, is a major concern in this study. Some strategies such as staffing and resource adequacy assessment and hiring more nurses to increase staffing levels can be useful [ 58 ]. Moderate levels of job satisfaction and emotional exhaustion were another important finding of this study. Administering flexible work schedules, increasing monthly salary, suggesting some mental health resources, and modification of work environment may be improving nurses’ job satisfaction and decrease their emotional exhaustion. Regular supervision of clinical nursing care activities and provision of continuous feedback are important to ensure that essential nursing care tasks are provided and prevent any compromise of nursing care [ 59 ] .
Despite the limitations, this study highlighted that the three variables of implicit rationing of nursing care, job satisfaction and emotional exhaustion played a mediating role in the relationship between workload and quality of nursing care. In other words, the effect of workload was applied to the quality of nursing care through these three variables. Therefore, the assumed theoretical model was approved and provided a theoretical basis for quality of nursing care. Nurse managers should pay special attention to the three mediating variables and monitor them periodically and try to solve problems in these areas. Nurse managers should be aware that support of nurses means the support of high-quality care of the patients and overlooking the issues and problems of nurses will have negative effect on the patients.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Basel Extend of Rationing of Nursing Care
Comparative Fit Index
Good Nursing Care Scale
Maslach Burnout Inventory
Minnesota Satisfaction Questionnaire
NASA Task Load Index
Root Mean Square Error of Approximation
Standard Deviations
Tucker-Lewis Index
Labrague LJ, McEnroe-Petitte DM, Papathanasiou IV, Edet OB, Arulappan J, Tsaras K. Nursing students’ perceptions of their own caring behaviors: a multicountry mtudy. Int J Nurs Knowl. 2017;28(4):225–32. https://doi.org/10.1111/2047-3095.12108 .
Article PubMed Google Scholar
Ross-Kerr JC, Wood MJ. Canadian nursing: issues and perspectives. 5th ed. Canada: Mosby Publisher; 2010.
Google Scholar
Charalambous A, Papadopoulos IR, Beadsmoore A. Listening to the voices of patients with cancer, their advocates and their nurses: a hermeneutic-phenomenological study of quality nursing care. Eur J Oncol Nurs. 2008;12(5):436–42. https://doi.org/10.1016/j.ejon.2008.05.008 .
Vinckx MA, Bossuyt I, Dierckx de Casterlé B. Understanding the complexity of working under time pressure in oncology nursing: a grounded theory study. Int J Nurs Stud. 2018;87:60–8. https://doi.org/10.1016/j.ijnurstu.2018.07.010 .
Jaramillo Santiago LX, Osorio Galeano SP, Salazar Blandón DA. Quality of nursing care: perception of parents of newborns hospitalized in neonatal units. Invest Educ Enferm. 2018;36(1):e08. https://doi.org/10.17533/udea.iee.v36n1e08 .
Gaalan K, Kunaviktikul W, Akkadechanunt T, Wichaikhum OA, Turale S. Factors predicting quality of nursing care among nurses in tertiary care hospitals in Mongolia. Int Nurs Rev. 2019;66(2):176–82. https://doi.org/10.1111/inr.12502 .
Article CAS PubMed Google Scholar
Labrague LJ, De Los Santos JAA, Tsaras K, Galabay JR, Falguera CC, Rosales RA, et al. The association of nurse caring behaviors on missed nursing care, adverse patient events and perceived quality of care: A cross-sectional study. J Nurs Manag. 2020;28(8):2257–65. https://doi.org/10.1111/jonm.12894 .
Guirardello EB. Impact of critical care environment on burnout, perceived quality of care and safety attitude of the nursing team. Rev Lat Am Enfermagem. 2017;25:e2884. https://doi.org/10.1590/1518-8345.1472.2884 .
Article PubMed PubMed Central Google Scholar
Zúñiga F, Ausserhofer D, Hamers JP, Engberg S, Simon M, Schwendimann R. Are staffing, work environment, work stressors, and rationing of care related to care workers’ perception of quality of care? A cross-sectional study. J Am Med Dir Assoc. 2015;16(10):860–6. https://doi.org/10.1016/j.jamda.2015.04.012 .
Chang LY, Yu HH, Chao YC. The Relationship between nursing workload, quality of care, and nursing payment in intensive care units. J Nurs Res. 2019;27(1):1–9. https://doi.org/10.1097/jnr.0000000000000265 .
Article CAS PubMed PubMed Central Google Scholar
Dhaini SR, Simon M, Ausserhofer D, Al Ahad MA, Elbejjani M, Dumit N, et al. Trends and variability of implicit rationing of care across time and shifts in an acute care hospital: a longitudinal study. J Nurs Manag. 2020;28(8):1861–72. https://doi.org/10.1111/jonm.13035 .
Kalisch BJ, Landstrom GL, Hinshaw AS. Missed nursing care: a concept analysis. J Adv Nurs. 2009;65(7):1509–17. https://doi.org/10.1111/j.1365-2648.2009.05027.x .
Cho SH, Lee JY, You SJ, Song KJ, Hong KJ. Nurse staffing, nurses prioritization, missed care, quality of nursing care, and nurse outcomes. Int J Nurs Pract. 2020;26(1):e12803. https://doi.org/10.1111/ijn.12803 .
Zhu X, Zheng J, Liu K, You L. Rationing of nursing care and its relationship with nurse staffing and patient outcomes: the mediation effect tested by structural equation modeling. Int J Environ Res Public Health. 2019;16(10):1672. https://doi.org/10.3390/ijerph16101672 .
Article PubMed Central Google Scholar
Inegbedion H, Inegbedion E, Peter A, Harry L. Perception of workload balance and employee job satisfaction in work organizations. Heliyon. 2020;6(1):e03160. https://doi.org/10.1016/j.heliyon.2020.e03160 .
Bautista JR, Lauria PAS, Contreras MCS, Maranion MMG, Villanueva HH, Sumaguingsing RC, et al. Specific stressors relate to nurses’ job satisfaction, perceived quality of care, and turnover intention. Int J Nurs Pract. 2020;26(1):e12774. https://doi.org/10.1111/ijn.12774 .
Misener TR, Cox DL. Development of the Misener nurse practitioner job satisfaction scale. J Nurs Meas. 2001;9(1):91–108.
Article CAS Google Scholar
Aron S. Relationship between nurses’ job satisfaction and quality of healthcare they deliver [thesis]. Mankato: Minnesota State University; 2015.
Al-Hamdan Z, Smadi E, Ahmad M, Bawadi H, Mitchell AM. Relationship between control over nursing practice and job satisfaction and quality of patient care. J Nurs Care Qual. 2019;34(3):E1–6. https://doi.org/10.1097/NCQ.0000000000000390 .
MacPhee M, Dahinten VS, Havaei F. The impact of heavy perceived nurse workloads on patient and nurse outcomes. Adm Sci. 2017;7(1):1–17. https://doi.org/10.3390/admsci7010007 .
Article Google Scholar
Nantsupawat A, Nantsupawat R, Kunaviktikul W, Turale S, Poghosyan L. Nurse burnout, nurse-reported quality of care, and patient outcomes in Thai hospitals. J Nurs Scholarsh. 2016;48(1):83–90. https://doi.org/10.1111/jnu.12187 .
Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. 2017;32(4):475–82. https://doi.org/10.1007/s11606-016-3886-9 .
Farman A, Kousar R, Hussain M, Waqas A, Gillani SA. Impact of job satisfaction on quality of care among nurses on the public hospital of lahore, pakistan. Saudi J Med Pharm Sci. 2017;3(6):511–9.
Ball JE, Murrells T, Rafferty AM, Morrow E, Griffiths P. “Care left undone” during nursing shifts: associations with workload and perceived quality of care. BMJ Qual Saf. 2014;23(2):116–25. https://doi.org/10.1136/bmjqs-2012-001767 .
Starc J, Erjavec K. Impact of the dimensions of diversity on the quality of nursing care: the case of Slovenia. Open Access Maced J Med Sci. 2017;5(3):383–90. https://doi.org/10.3889/oamjms.2017.086 .
Boonpracom R, Kunaviktikul W, Thungjaroenkul P, Wichaikhum O. A causal model for the quality of nursing care in Thailand. Int Nurs Rev. 2019;66(1):130–8. https://doi.org/10.1111/inr.12474 .
Rochefort CM, Clarke SP. Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal units. J Adv Nurs. 2010;66(10):2213–24. https://doi.org/10.1111/j.1365-2648.2010.05376.x .
Leino-Kilpi H, Vuorenheimo J. The patient’s perspective on nursing quality: developing a framework for evaluation. Int J Qual Health Care. 1994;6(1):85–95. https://doi.org/10.1093/intqhc/6.1.85 .
Stolt M, Katajisto J, Anders Kottorp A, Leino-Kilpi H. Measuring the quality of care: a Rasch validity analysis of the good nursing care scale. J Nurs Care Qual. 2019;34(4):E1–6. https://doi.org/10.1097/NCQ.0000000000000391 .
Byrne BM. Structural equation modeling with AMOS: basic concepts, applications, and programming. New York, NY: Routledge; 2016.
Book Google Scholar
Gunzler D, Chen T, Wu P, Zhang H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch Psychiatry. 2013;25:390–4. https://doi.org/10.3969/j.issn.1002-0829.2013.06.009 .
Jackson DL. Revisiting sample size and number of parameter estimates: Some support for the N: q hypothesis. Struct Equ Modeling. 2003;10(1):128–41.
Hart SG, Staveland LE. Development of NASA-TLX (Task Load Index): Results of empirical and theoretical research. Adv Psychol. 1988;52:139–83.
Xiao YM, Wang ZM, Wang MZ, Lan YJ. The appraisal of reliability and validity of subjective workload assessment technique and NASA-task load index. Chin J Ind Hyg Dis. 2005;23(3):178–81.
Mohammadi M, Nasl Seraji J, Zeraati H. Developing and accessing the validity and reliability of a questionnaire to assess the mental workload among ICUs nurses in one of the Tehran University of medical sciences hospitals. J Sch Public Health Inst Public Health Res. 2013;11(2):87–96 ([in Persian]).
Schubert M, Glass TR, Clarke SP, Schaffert-Witvliet B, De Geest S. Validation of the basel extent of rationing of nursing care instrument. Nurs Res. 2007;56(6):416–24. https://doi.org/10.1097/01.NNR.0000299853.52429.62 .
Weiss DJ, Dawis RV, England GW. Manual for the Minnesota satisfaction questionnaire: Minnesota studies in vocational rehabilitation. University of Minnesota: Minneapolis: industrial relations center; 1967. p. 1–120.
Azadi R, Eydi H. The effects of social capital and job satisfaction on employee performance with organizational commitment mediation role. Organ Behav Manage Sport Stud. 2015;2(4):11–24 ([in Persian]).
Maslach C, Jackson S, Leiter M. The Maslach burnout inventory manual. 3rd ed. Palo Alto: Consulting Psychologists Press; 1996. p. 191–210.
Azizi L, Feyzabadi Z, Salehi M. Exploratory and confirmatory factor analysis of maslach burnout inventory among tehran universitys employees. J Psychol Stud. 2008;4(3):73–92 ([inPersian]).
Zhao SH, Akkadechanunt T, Xue XL. Quality nursing care as perceived by nurses and patients in a Chinese hospital. J Clin Nurs. 2009;18(12):1722–8. https://doi.org/10.1111/j.1365-2702.2008.02315.x .
Istomina N, Suominen T, Razbadauskas A, Martinkėnas A, Meretoja R, Leino-Kilpi H. Competence of nurses and factors associated with it. Medicina (Kaunas). 2011;47(4):230–7.
Esmalizadeh A, Heidarzadeh M, Karimollahi M. Translation and psychometric properties of good nursing care scale from nurses’ perspective in Ardabil educational centers, 2018. J Health Care. 2019;21(3):252–62 ([in Persian]).
Fabrigar LR, Porter RD, Norris ME. Some things you should know about structural equation modeling but never thought to ask. J Consum Psychol. 2010;20(2):221–5.
Sivo SA, Fan X, Witta EL, Willse JT. The search for “optimal” cutoff properties: Fit index criteria in structural equation modeling. J Exp Educ. 2006;74(3):267–88.
Liu X, Zheng J, Liu K, Baggs JG, Liu J, Wu Y, et al. Hospital nursing organizational factors, nursing care left undone, and nurse burnout as predictors of patient safety: a structural equation modeling analysis. Int J Nurs Stud. 2018;86:82–9. https://doi.org/10.1016/j.ijnurstu.2018.05.005 .
Kalisch BJ, Tschannen D, Lee KH. Missed nursing care, staffing, and patient falls. J Nurs Care Qual. 2012;27(1):6–12. https://doi.org/10.1097/NCQ.0b013e318225aa23 .
Semachew A, Belachew T, Tesfaye T, Adinew YM. Predictors of job satisfaction among nurses working in Ethiopian public hospitals, 2014: institution-based cross-sectional study. Hum Resour Health. 2017;15(1):31. https://doi.org/10.1186/s12960-017-0204-5 .
Safavi M, Abdollahi SM, Salmani Mood M, Rahimh H, Nasirizadeh M. Relationship between nurses’ quality performance and their job satisfaction. Q J Nurs Manag. 2017;6(1):53–61.
Chen YC, Guo YL, Chin WS, Cheng NY, Ho JJ, Shiao JS. Patient-nurse ratio is related to nurses’ intention to leave their job through mediating factors of burnout and job dissatisfaction. Int J Environ Res Public Health. 2019;16(23):4801. https://doi.org/10.3390/ijerph16234801 .
Holland P, Tham TL, Sheehan C, Cooper B. The impact of perceived workload on nurse satisfaction with work-life balance and intention to leave the occupation. Appl Nurs Res. 2019;49:70–6. https://doi.org/10.1016/j.apnr.2019.06.001 .
Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. 2010;33(4):288–98. https://doi.org/10.1002/nur.20383 .
Van Bogaert P, Meulemans H, Clarke S, Vermeyen K, Van de Heyning P. Hospital nurse practice environment, burnout, job outcomes and quality of care: test of a structural equation model. J Adv Nurs. 2009;65(10):2175–85. https://doi.org/10.1111/j.1365-2648.2009.05082.x .
Gillet N, Huyghebaert-Zouaghi T, Réveillère C, Colombat P, Fouquereau E. The effects of job demands on nurses’ burnout and presenteeism through sleep quality and relaxation. J Clin Nurs. 2020;29(3–4):583–92. https://doi.org/10.1111/jocn.15116 .
Ballen CJ, Salehi S. Mediation analysis in discipline-based education research using structural equation modeling: beyond “what works” to understand how it works, and for whom. J Microbiol Biol Educ. 2021;22:e00108-e121. https://doi.org/10.1128/jmbe.00108-21 .
Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. 10th ed: Wolters Kluwer; 2017.
Mondal H, Mondal SH. Social desirability bias: a confounding factor to consider in survey by self-administered questionnaire. Indian J Pharmacol. 2018;50(3):143–4. https://doi.org/10.4103/ijp.IJP_15_17 .
Lake ET, Riman KA, Sloane DM. Improved work environments and staffing lead to less missed nursing care: A panel study. J Nurs Manag. 2020;28(8):2157–65. https://doi.org/10.1111/jonm.12970 .
Jones TL, Hamilton P, Murry N. Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. Int J Nurs Stud. 2015;52(6):1121–37. https://doi.org/10.1016/j.ijnurstu.2015.02.012 .
Download references
Acknowledgements
The authors would like to express their gratitude to all the nurses who helped us in conducting this research. This article is extracted from the first author’s thesis in Master of Science in nursing. The thesis has been financially supported as a research project by the Vice Chancellor for Research and Technology of Kashan University of Medical Sciences (Registration Number: 99113 dated 19 Sep. 2020).
The article has been financially supported as a research project by the Vice Chancellor for Research and Technology of Kashan University of Medical Sciences (Registration Number: 99113 dated 19 Sep. 2020).
Author information
Authors and affiliations.
Medical Surgical Nursing, School of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran
Fatemeh Maghsoud
Trauma Nursing Research Center, School of Nursing and Midwifery, Kashan University of Medical Sciences, 5th of Qotb –e Ravandi Blvd, P.O.Box: 8715981151, Kashan, Iran
Mahboubeh Rezaei
Social Determinants of Health (SDH) Research Center, Kashan University of Medical Sciences, Kashan, Iran
Fatemeh Sadat Asgarian
Department of Pediatric and Reproductive Health, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Maryam Rassouli
You can also search for this author in PubMed Google Scholar
Contributions
FM, MR, FA and MR were responsible for the study conception/design. FM performed the data collection. FA, FM and MR analyzed and interpreted the participants’ data. FM and MR were significant contributors in writing the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Mahboubeh Rezaei .
Ethics declarations
Ethics approval and consent to participate.
In this study, all methods were carried out in accordance with the Declaration of Helsinki and approved by the ethics committee of Kashan University of Medical Sciences, with the ethics code of IR.KAUMS.NUHEPM.REC.1399.047. All participants signed written informed consent and were voluntarily enrolled to the study. Also, they could withdraw from the study at any time. All participants were assured that their information would remain confidential.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Maghsoud, F., Rezaei, M., Asgarian, F.S. et al. Workload and quality of nursing care: the mediating role of implicit rationing of nursing care, job satisfaction and emotional exhaustion by using structural equations modeling approach. BMC Nurs 21 , 273 (2022). https://doi.org/10.1186/s12912-022-01055-1
Download citation
Received : 02 May 2022
Accepted : 29 September 2022
Published : 08 October 2022
DOI : https://doi.org/10.1186/s12912-022-01055-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care rationing
- Job satisfaction
- Quality of nursing care
- Structural equation modeling
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Research article
- Open access
- Published: 13 June 2014
How nurses and their work environment affect patient experiences of the quality of care: a qualitative study
- Renate AMM Kieft 1 ,
- Brigitte BJM de Brouwer 1 ,
- Anneke L Francke 2 , 3 &
- Diana MJ Delnoij 4
BMC Health Services Research volume 14 , Article number: 249 ( 2014 ) Cite this article
481k Accesses
202 Citations
47 Altmetric
Metrics details
Healthcare organisations monitor patient experiences in order to evaluate and improve the quality of care. Because nurses spend a lot of time with patients, they have a major impact on patient experiences. To improve patient experiences of the quality of care, nurses need to know what factors within the nursing work environment are of influence. The main focus of this research was to comprehend the views of Dutch nurses on how their work and their work environment contribute to positive patient experiences.
A descriptive qualitative research design was used to collect data. Four focus groups were conducted, one each with 6 or 7 registered nurses in mental health care, hospital care, home care and nursing home care. A total of 26 nurses were recruited through purposeful sampling. The interviews were audiotaped, transcribed and subjected to thematic analysis.
The nurses mentioned essential elements that they believe would improve patient experiences of the quality of nursing care: clinically competent nurses, collaborative working relationships, autonomous nursing practice, adequate staffing, control over nursing practice, managerial support and patient-centred culture. They also mentioned several inhibiting factors, such as cost-effectiveness policy and transparency goals for external accountability. Nurses feel pressured to increase productivity and report a high administrative workload. They stated that these factors will not improve patient experiences of the quality of nursing care.
Conclusions
According to participants, a diverse range of elements affect patient experiences of the quality of nursing care. They believe that incorporating these elements into daily nursing practice would result in more positive patient experiences. However, nurses work in a healthcare context in which they have to reconcile cost-efficiency and accountability with their desire to provide nursing care that is based on patient needs and preferences, and they experience a conflict between these two approaches. Nurses must gain autonomy over their own practice in order to improve patient experiences.
Peer Review reports
In countries throughout the world, patient experiences are being monitored in order to obtain information about the delivery and quality of healthcare [ 1 ]. Patient experiences can be defined as a reflection of what actually happened during the care process and therefore provide information about the performance of healthcare workers [ 2 ]; it refers to the process of care provision [ 3 ]. In the United States [ 4 ] and many European countries [ 5 ], assessing patient experiences is part of a systematic survey programme. In the Netherlands, the government has implemented a national performance framework for comparing the quality of healthcare. This framework contains a set of quality indicators that include patient experiences. The Consumer Quality Index (CQI) is used as the measurement standard [ 6 ].
Assessing patient experiences of the quality of care not only provides information about the actual experiences, but also reveals which quality aspects patients regard as most important [ 7 ]. Many studies have been performed to analyse what patients consider essential within healthcare [ 8 – 10 ]. For example, a study by the Picker Institute Europe [ 11 ] revealed eight general quality aspects:
Involvement in decisions and respect for preferences
Clear, comprehensible information and support for self-care
Emotional support, empathy and respect
Fast access to reliable health advice
Effective treatment
Attention to physical and environmental needs
Involvement of, and support for, family and carers
Continuity of care and smooth transitions
The quality aspects are mostly reflected in questionnaires used to monitor patient experiences, such as the CQI [ 12 ] or the Consumer Assessment of Healthcare Providers and Systems (CAHPS) [ 4 ]. Patients are asked which aspects in receiving care are of importance and about their actual experiences [ 13 ].
Patient experiences have been identified as an indicator for evaluating and improving the quality of care [ 3 , 14 ]. When healthcare organisations assess patient experiences, professionals can use the results for internal quality improvements. Professionals use patient experiences and preferences to adjust their own practice and to make visible their contribution to patient outcomes [ 15 ].
Because nurses spend a lot of time with patients [ 16 ], they affect patient experiences of care [ 17 ]. Research has shown that the nursing work environment is a determining factor. It seems that when patients have positive experiences of nursing care, nurses also experience a good and healthy work environment [ 18 – 20 ]. A healthy work environment can be defined as a work setting in which nurses are able to both achieve the goals of the organisation and derive personal satisfaction from their work [ 21 ]. A healthy work environment fosters a climate in which nurses are challenged to use their expertise, skills and clinical knowledge. Furthermore, nurses who work in such an environment are encouraged to provide patients with excellent nursing care [ 21 ]. Research by Kramer and Schmalenberg revealed that several aspects are related to the work environment [ 22 ]. The researchers used grounded theory to identify eight ‘essentials of magnetism’ that define the nursing work environment and influence the quality of nursing care. From the perspective of nurses, the following eight ‘essentials’ are crucial in a work environment to the provision of high quality nursing care [ 22 ]:
Clinically competent nurses
Adequate staffing.
Good nurse–physician relationships
Autonomous nursing practice
Nurse manager support
Control over nursing practice
Support for education
A culture that values concern for patients
Relation between nursing work environment and patient experiences of the quality of care
The American Nurses Credentialing Center (ANCC) started the Magnet Recognition Program in the early 1990s. This programme was built upon the study carried out in 1983 by McClure et al. [ 23 ]. It is focused on improving patient care, patient safety and patient experiences by creating a good and healthy work environment for nurses. Research has shown that patient experiences in healthy work environments are significantly better [ 24 – 26 ].
The relationship between the nursing work environment and patient experiences was also investigated in a cross-sectional study carried out in 430 hospitals by Kutney-Lee et al. [ 18 ]. The researchers used data on patient experiences from the national CAHPS survey. The nursing work environment was measured with the PES-NWI tool, which includes items on nursing leadership and nurse–physician relationships. Data on 20,984 staff nurses were used in the study. The nursing work environment had significant relations with all ten CAHPS measures, indicating that the quality of the work environment has an influence on patient experiences of the quality of care.
This finding corresponds with the cross-sectional study by McHugh et al. [ 19 ] in which 428 hospitals and 95,499 registered nurses participated. The researchers used data from the PES-NWI and the CAHPS. They concluded that nurses’ dissatisfaction with their work environment was associated with a significantly lower quality of patient experiences.
In the RN4Cast project [ 20 ], 61,168 hospital nurses and more than 131,000 patients in Europe and the United States were questioned in a cross-sectional survey. The aim of this immense study was to determine whether the nursing work environment affected patient care. The PES-NWI was used to measure the nurses’ perceptions of their work environment. Patients’ overall satisfaction was measured with the national CAHPS survey. The perceptions of nurses and those of patients were found to be consistent, indicating that both patients and nurses had more positive experiences in hospitals with better work environments.
Although there is a relationship between the nursing work environment and patient experiences of the quality of care, it is not clear how this relationship is formed and characterised from the perspective of Dutch nurses, and which aspects in daily practice influence patient experiences. Could these aspects somehow be linked to the ‘essentials of magnetism’? Little is known about the underlying mechanisms and how these result in better patient experiences. In 2006, the Dutch government started to move towards a healthcare model of responsible consumer choice and care services competition [ 27 ]. Because of this entrepreneurial approach, healthcare organisations transformed their policy towards a cost-efficiency and productive care system (e.g. a shorter length of stay per patient) [ 28 ]. Furthermore, today’s patients tend to suffer from multiple disorders or illnesses, which results in a higher complexity of care and an increased nursing workload. The increasing complexity of patient care requires well-trained nurses who are capable of creating a safe and patient-centred environment [ 29 ]. In 2011, the Netherlands Institute for Health Services Research conducted a literature study to investigate the roles and positions of nurses in Belgium, Germany, the United Kingdom, the United States and Canada, and found differences in levels of education and nursing job profile or job description in all five countries [ 30 ].
Given the circumstances and changes with which Dutch nurses are confronted, it is important and relevant to examine and comprehend their views on how their work and work environment contribute to positive patient experiences.
Aim of study
The aim of this study was to understand from the perspective of nurses how the nursing work environment is related to positive patient experiences.
Research question
The central research question was: According to nurses, which elements of their work and work environment influence patient experiences of the quality of nursing care?
The sub-questions were:
Are these elements related to the eight essentials of magnetism?
What is the mechanism by which these elements lead to better patient experiences?
Research design
A phenomenological approach was applied to explore areas about which little is known or to gain an understanding of specific areas. Phenomenology is the study of subjective experience, feelings and behaviours of people [ 31 , 32 ].
Sample size, composition and data collection
To gain a deeper understanding of the influence of the nursing work environment on patient experiences, we conducted four focus groups. The purpose was to elicit ideas, thoughts and perceptions from nurses [ 31 ] about patient experiences and how nurses can improve those experiences. We recruited participants by purposeful sampling, using the following criteria:
Participants must be employed as registered nurses or certified nursing assistants.
Participants must have worked as nurses for at least two years.
Participants must be operative in mental health care, hospital care, home care or nursing home care.
Nurses are active in various settings and every setting has its specific dynamics. By gaining insight into their perspectives, we were able to compare possibly different views. In addition, we obtained an overall view of the total healthcare system.
The organisations we recruited are participating in a Dutch programme called Excellent Care. The programme is based on the eight essentials of magnetism and focuses on creating a dynamic, inspiring and innovative nursing work environment in order to improve the quality of care. We asked the programme director of each organisation to recruit nurses for the focus groups. A total of 26 registered nurses participated. Each focus group consisted of 6 or 7 registered nurses in mental health care, hospital care, home care and nursing home care, respectively. The nurses described their perceptions and views with respect to their own areas of expertise.
Each focus group discussion was led by two researchers. One researcher facilitated the interview, and the other had an observing role and monitored the process. After each focus group, the researchers evaluated and critically reflected on the process in order to examine the quality of the meetings. This investigator triangulation allowed the dissection of possibly different views.
The researchers used an interview guide with predefined topic areas (Table 1 , topic list). The sequencing of questions depended on the process of the group and the responses of the informants.
Each focus group lasted two hours. The researchers explained the procedures and introduced the topic to be debated. When the informants were discussing certain topics, the researchers applied a non-directive approach because of the dynamics of the group and the different perspectives that were being examined. When certain views were polarised, the researcher stimulated the discussion by introducing a new question or topic. All conversations were digitally recorded and then transcribed to improve transferability.
Ethical considerations
This was a qualitative study in competent subjects without any intervention. It did not involve any form of invasion of the participant's integrity, and in such cases no approval by an ethics committee is required in the Netherlands (according to the Medical Research Involving Human Subjects Act; see ccmo-online.nl). All respondents received written and verbal information about the aim and content of the study. Study participation was voluntary. Data were analysed in an anonymous way and the results were non-traceable to individual participants.
Data analysis
The transcribed data were open coded and categorised. Several themes were extracted by organising and structuring the categories. During the analytical process, interview fragments were constantly compared. The literally transcribed interviews were reviewed several times to check whether elements might have been overlooked. The final analysis was presented to the participants and they were asked to comment on the contents. This member check helped to determine whether we had adequately understood and interpreted the data. The analytical procedure and findings were discussed within the research team to improve the quality of analysis. MaxQDA software was used to support the coding ordering analyses.
The sample consisted of 26 registered nurses (6 male and 20 female nurses). The mean age of the participants and the mean length of nursing experience varied per focus group, as shown in Table 2 below.
Participants formulated several facilitating elements that they consider fundamental to improving patient experiences of the quality of care. They also mentioned such inhibiting factors as cost-effectiveness and transparency and accountability goals. These factors prevent them from improving patient experiences (Table 3 ).
Both facilitating elements and inhibiting factors are elaborated below.
Facilitating elements
Participants stated that in order to act in a professional manner, nurses need to have certain competencies, namely social skills, expertise & experience, and priority setting.
Social skills
Participants stated that social skills are an important competency to create a trustful care relationship. They indicated correct behaviour and attitude, composure, making time for patients, and listening and having empathy as essential nursing competencies. According to participants, these social skills convey a sense of commitment to the patient and play a major role in meeting patient expectations.
Nurses must have the ability to develop and maintain good relationships with patients. For patients, nursing care is about being heard and seen. Knowing that you’re in safe hands. You allay their fear and uncertainty. You give patients confidence and hope in return. You offer them several options from which they can choose. Someone who is dependent, and does not know what will happen, is more suspicious and anxious. (Respondent 21, hospital focus group)
Expertise & experience
Participants mentioned three key aspects related to expertise, namely knowledge, technical skills and communicative capabilities. According to participants, the first key aspect means that nurses must have substantive knowledge related to the nursing profession. They indicated that nurses should maintain and follow both existing developments and new insights. According to participants, nurses must continually invest in nursing knowledge and education. In their view, nurses ought to offer state-of-the-art interventions or activities that are in line with the agreed nursing policy.
As a second key aspect related to expertise, participants indicated that nurses must have technical skills in order to provide effective and safe care.
The third aspect mentioned by participants is that nurses must have communicative capabilities. Participants said that nurses serve as spokespersons for patients who are often in vulnerable positions. They stated that nurses are easily accessible and can act as a link between the patient and other professions. According to participants, nurses can use the right substantive arguments on behalf of a patient’s interests or needs. Participants mentioned that this expertise is important for patients because it is related to the quality of care.
If you can answer a care-related question, it gives the patient a certain peace of mind. It signals: she knows what she's talking about. I notice that patients really appreciate it when I share knowledge and offer them information that at the time they don’t yet have. Only then can patients make decisions about their own care. (Respondent 15, nursing home focus group)
In addition to substantive expertise, participants stated that nursing experience is also of influence. According to them, a junior nurse has too little experience to respond creatively to sometimes complex care situations. However, according to participants, junior and senior nurses can learn from each other: they should work as a team and collectively pursue their common objectives. In their view, experience is gained through practice. According to participants, this can be characterised as 'expertise'.
When you suspect someone is contemplating suicide, you need to know how serious this is. Is it just a cry of “I'm not feeling well” or are these serious thoughts? Has the patient already made plans, does the patient have a death wish, or is it an impulsive thought? In that sense you need to reflect on the signals very carefully. You can only learn this from practice. (Respondent 1, mental health care focus group)
Priority setting
As stated by participants, various activities can occur simultaneously during the daily care of patients. According to them, nurses should assess what care is needed and then flexibly coordinate diverse actions with each other. In the view of participants, prioritisation is about the organisation of nursing care. Patients need nurses who have clinical experience in order to coordinate care. Nurses must decide what choices to make, what is urgent and what is important. Those choices influence patient experiences.
Prioritisation is very important. It means that you have to coordinate the daily care and decide which activities have priority. Patients sometimes have to wait for help. If you’re in a hasty mood, you transmit that feeling to patients. It shows immediately. The restlessness affects the other patients. (Respondent 18, nursing home focus group)
Participants said that patients sometimes have to wait before they are taken care of, or that nurses are not immediately available to answer questions or deal with problems. According to participants, patients do not always obtain the right and needed care, especially when the nurses’ workload is high.
Collaborative working relationships
According to participants, it is important to develop and maintain collaborative working relationships with professionals, including those in their own field. In the view of participants, collaborative working relationships exist when all the involved professionals interact and operate in a complementary manner, and show mutual respect that is based on knowledge and expertise. Participants stated that all professionals need to discuss and influence patient care on the basis of their own expertise. Participants believe that problems will be solved sooner when ideas and thoughts are exchanged. In their view, it is about sharing information and communication. As stated by participants, communication and aligning with each other is needed so that no conflicting information is given and uniformity in care or treatment is provided. This generates, according to the participants, composure and clarity towards patients.
Participants believe that collaboration and communication affect how patients experience the quality and effectiveness of care.
We have a patient who is very compulsive. We made agreements about how to approach and handle this patient. We continually need to communicate with each other, physicians, psychologists, nurses. Clear communication is so important, and I miss that sometimes. When you have good relationships it is easier to review and discuss the treatment administered. It will not only increase your knowledge, but also be helpful in the communication with the patient and his family. It’s easier to explain why the specific treatment is being deployed. (Respondent 5, mental health care focus group)
Participants in all four focus groups stated that the scope of practice for which they are accountable influences patient experiences. The scope of practice, according to them, means that nurses can control their own work related to patient care and can make independent decisions about patient outcomes based on clinical judgements. Participants therefore believe it is essential to monitor and measure outcomes, as long as the monitoring is directly related to patient care. However, participants indicated that they did not have insight into care results obtained from assessments.
We participate in an annual national prevalence survey. We have to fill out a lot of forms. It’s an administrative burden and takes a lot of time – time we can’t spend on patient care. We get a pile of papers, screen patients and register them. It doesn’t contribute to the quality of care because we never get any feedback. And what does one measurement tell us? It doesn’t inform us whether we are doing well or not. I do not believe that. (Respondent 12, home care focus group)
According to participants, there is no policy to improve patient experiences on the basis of the information derived from assessments. Participants could not indicate whether the interventions deployed are actually leading to desired nursing care results, including patient experiences. Participants feel they have insufficient autonomy to influence this process.
Participants stated that the number of nurses available influences how patients experience the quality of care. Although they could not indicate what number they consider sufficient, they think that a sufficient nurse staffing level is linked to team composition or staff mix. For instance, participants indicated the proportion of registered nurses to student nurses, or the number of different nurse qualification levels in one team. Participants stated that several tasks and assignments have been transferred to nurses with a lower qualification in order to work as efficiently as possible and to achieve higher productivity. As a result, participants believe that nursing care is, in general, increasingly developing in the direction of task-centred care in which different working methods are applied. According to them, this affects patient experiences of the quality and effectiveness of nursing care.
Nurses provide care within certain theoretical frameworks that are designed to increase the self-reliance and self-management of the patient. Nurse assistants have a more practical focus and take over patient care at a point when they should not. These two ways of working are confusing for patients. And we think 'How come the patient is made to feel so nervous?’ and afterwards we notice two contradictory ways of working. (Respondent 3, mental health care focus group)
As stated by participants, a sufficient nurse staffing level determines whether patient wishes and needs are met. According to participants, an insufficient deployment of nursing staff has a direct negative impact on patient experience.
I work alone in a group. For example, when I’m in the bathroom with a patient, the other patients are alone. So I have to keep my eyes and ears open and must respond to what occurs. And that is not always easy. I constantly think: I must check if everything is all right. Because I’m responsible for the other patients. I always leave the bathroom door partly open, so I can see and listen to what is going on in the living room. I provide patient care too hastily. My patients obviously feel that. (Respondent 17, nursing home focus group)
The participants stated that control over nursing practice means that nurses are involved in nursing policy or nursing issues. In their view, nurses are not always in charge and cannot always make their own decisions about nursing issues. Participants feel that this affects the quality of nursing care.
In the past, I always made my own schedule. Now we have planners and they don’t have any experience with care. Efficient planning is more important than patient-centred planning. It doesn’t matter whether it suits the patient. The patient should be scheduled later if it fits better in the planned route. (Respondent 9, home care focus group)
The participants stated that if nurses were more involved in the development of nursing policies, this would have a positive influence on patient care. According to them, they would be able to reflect upon and discuss nursing issues related to the quality of patient care, which would improve the quality of care.
Managerial support
Participants indicated that a manager should pay attention to the team spirit and unity. In their view, a manager must be able to handle conflicts, and also be visible and approachable. Participants said that they believe that a manager should ask the opinion of nurses; therefore, in their opinion, regular contact is important.
A manager, according to the participants, must be able to create the right conditions and have the logistical ability to ensure continuity of care. In their view, this means arranging sufficient personnel, replacement staff and succession planning.
Participants find that managers critically examine the deployment of personnel. According to them, the nursing staff mix has drifted towards a model whereby higher-educated nurses are replaced with lower-educated ones. They noted that management is tied to a system that is dominated by controlling costs. Thus in their view, nurses may want to provide a patient with a specific form of care, while management limits care to a maximum number of minutes based on budgetary considerations. According to participants, nurses regularly experience a tension with management in shaping care that meets patient expectations.
We want to provide certain care, but that’s at the expense of something else. If we do one thing, we can’t do another. For instance, we plan 30 minutes for patient care. When a patient wants to go outside for a walk, this will cost him 10 minutes of this total time. So we really have to negotiate with the patient or his family. This leads, of course, to lots of misunderstandings. I understand that feeling. (Respondent 13, nursing home focus group)
Patient-centred care
According to participants, the focus of nurses is the provision of patient-centred care. They define this as nursing care that is focussed on patient needs and preferences and is intended to increase patient self-management and encourage improved health and recovery.
As participants stated, nurses are the first points of contact for patients. In the participants’ view, they are often with the patient for 24 hours/7 days a week (except for home care) and gather large amounts of information about them. They think that direct contact with patients is crucial to building and maintaining a relationship of trust. The participants believe that high quality nursing care is achieved when patients feel heard and understood, consider themselves to be in safe hands and know that their care problems have been noticed. This, according to the participants, results in positive patient experiences.
We listen to the patient and talk to him. We immerse ourselves in his background. What is important, how he copes and handles care problems. Based on this knowledge, we present the patient with a number of options so that he can decide upon a solution for his care problems. (Respondent 8, home care focus group)
Inhibiting factors
The participants talked about two inhibiting factors that prevent them from improving patient experiences: cost-effectiveness and transparency & accountability goals.
Cost-effectiveness
Participants stated that organisation policy is focused on the efficient and effective deployment of people and resources. They mentioned the transfer of tasks to less well qualified nurses in order to work as efficiently as possible and to achieve higher productivity. In their view, care is more and more standardised. At the same time, they noted that care has become increasingly complex. According to them, patients are generally older and have multiple age-related comorbidities. The participants experience an increasing workload and work-associated pressure.
In recent years, patient turnover has increased. It means that patients are discharged quicker. As soon as they recover, they’re sent home. However, patients sometimes also have chronic disorders. I sometimes think it is irresponsible [to send these patients home so quickly]. Patients get less attention because the work pressure is high. (Respondent 22, hospital focus group)
Transparency & accountability goals
Participants reported an increasing administrative workload to account for the quality and costs of care.
So many forms. Entering the data means a double administrative workload. We use different programs. We first have to register in program X. Then we have to register our measurements and enter all kinds of codes in another program. Log in and log out. The registrations and coding are needed for the government and health insurers. It is not always patient related and does not inform us about the health status of patients. (Respondent 23, hospital focus group)
The administrative workload is, according to participants, out of balance. They said that this means that monitoring and registration is aimed not at improving nursing care, but at serving an external accountability goal to inform health insurers and the government.
The participants stated that they have little autonomy to change this policy. According to them, monitoring care results should help nurses to improve their own practice. For them, it means that nurses can reflect upon and discuss nursing issues related to quality of patient care, including the results of patient experiences.
We interviewed 26 nurses working in various Dutch healthcare settings in order to ascertain their views on how their work and their work environment contribute to positive patient experiences. Using an open approach, we obtained insights into their perceptions and noted what they said. Participants stated that a diverse range of elements are essential to providing high-quality nursing care. When these elements are incorporated into daily nursing practice, the participants expect it will result in more positive patient experiences of nursing care. The elements are: clinically competent nurses, collaborative relationships, autonomous nursing practice, adequate staffing, control over nursing practice, managerial support and patient-centred care.
One of the sub-questions was whether the identified elements are related to the eight essentials of magnetism defined by Kramer and Schmalenberg [ 22 ]. We found that they are. The essential of magnetism ‘nurse–physician relationships’ is, in our opinion, not totally applicable in a modern healthcare system. Although physicians are represented in all settings, also other professionals, such as psychologists, social workers or physical therapists, are part of a healthcare team. The participants stated that a good relationship must be based on collaboration and clear communication not only with physicians, but with all involved healthcare workers. The participants stated that patient wellbeing must be the common aim of all the involved professionals and that communication and collaboration must support this shared goal. We therefore replaced ‘nurse–physician relationships’ with ‘collaborative working relationships’.
Competing policies in the nursing setting
The other sub-question concerned mechanisms by which these elements lead to better patient experiences. By analysing the data it became clear that nurses operate in a complex healthcare context. These different views control the manner in which nurses can practise their profession. We noticed that nurses are confronted with organisation policies that are focussed on cost-efficiency, transparency and accountability goals. According to participants, this has led to a more productive care system. It also became clear that nurses flourish within a patient-centred care system. Such a system supports individual patients in their need to make decisions and participate in their own care. This means that organisations should facilitate a culture where nurses can professionally support patients by practising high-quality nursing care [ 33 ].
Each view is defendable on its own, but collectively they contradict each other. The context in which nurses work is almost paradoxical: they have to offer patient-centred care in a standardised and productive care system.
In the Dutch context, healthcare insurers, the government and healthcare providers are responsible and accountable for providing good quality care. However, these parties have different foci. Each year, healthcare insurers make agreements with healthcare providers about which care will be delivered. These agreements are defined in a healthcare procurement contract [ 28 ]. Individuals who legally live in the Netherlands are obliged to take out individual health insurance [ 27 ]. In order to make well-considered choices, individuals need to be informed about the quality of care provided by healthcare workers. Healthcare insurers are therefore driven by accountability goals, because they need to determine whether healthcare organisations or professionals meet the minimum standard of performance, as agreed upon in the healthcare procurement contract [ 34 ]. The government is the supervisory authority that ensures the proper functioning of the healthcare system and is therefore responsible for the transparency process [ 35 ]. In the Netherlands, a national performance framework for comparing the quality of healthcare is implemented under the supervision of the government [ 36 ]. This framework contains a set of quality indicators and related measures, including patient experiences [ 6 , 37 ]. Healthcare insurers and the government collect data for external accountability goals [ 38 ]. Healthcare providers and professionals themselves are also responsible for the quality of care. Their aim is more internally driven, namely to improve the quality of care and to make visible their contribution to patient outcomes [ 39 , 40 ]. However, our research showed that nurses do not receive feedback on their scores and they are not aware that they could – and even should – use these data to monitor and improve the quality of their work.
It could be argued that the dominance of cost-effective policy and transparency determines the manner in which nurses can practise their profession and that this influences patient experiences of care. Ancarani [ 41 ] showed that patient satisfaction was negatively associated with management-controlled wards that are under pressure to produce. Open, collaborative, innovative wards and wards that are focused on the welfare and involvement of nurses and that provide supervisory support and training were positively associated with patient satisfaction. This confirms that the environment in which nurses operate influences patient experiences of the quality of care. This corresponds with the findings of our research, in which participants stated that the dominance of policies focussed on cost-effectiveness and transparency lead to more pressure to produce and a high administrative workload. The participants feel that they have insufficient autonomy to influence this policy.
Strong nursing practice
To incorporate the identified elements into nursing practice, cost-effectiveness, transparency and patient-centred care policy need to be connected. For example, the registration and monitoring of outcomes should be used not only to quantify achievements against transparency goals, but also for overall nursing quality improvement. Nurses should be able to decide which issues are of importance to improve patient care.
Connecting the different policies requires the participation and commitment of both nurses and nursing management. Nurses need to be challenged to shape their own environment and create a strong nursing practice [ 42 ], which will result in more positive patient experiences [ 43 ].
Limitations of this study
We conducted four focus groups, one each with nurses in mental health care, hospital care, home care and nursing home care. Although we gained a broader insight into the perspectives of nurses, every sector has its specific dynamics and context. Therefore, one focus group per sector might have been insufficient. However, we reached data saturation as new information did not appear and similar themes emerged within the focus groups.
This study was limited to nurses, but to fully understand the nuances of this relation, it might be interesting to analyse patients’ views.
The knowledge obtained from this research has resulted in a better understanding of how nurses regard their role in achieving positive patient experiences. From the viewpoint of the interviewed nurses, several elements are essential in relation to patient experiences of the quality of nursing care: clinically competent nurses, collaborative working relationships, autonomous nursing practice, adequate staffing, control over nursing practice, managerial support and patient-centred culture. These elements correspond to the eight ‘essentials of magnetism’. If these elements are incorporated into the nursing practice, it will most likely result in more positive patient experiences of nursing care.
This research revealed several factors that nurses find inhibiting when it comes to improving patient experiences of the quality of nursing care. Current nursing policy is heavily focussed on cost-effectiveness and transparency for external accountability, which creates a high administrative workload and pressure to increase productivity. However, despite all the registrations that take place for external accountability, the participating nurses stated that they do not monitor care results to improve their own practice. They felt they insufficient autonomy to influence this. They believe it is important to reflect upon and discuss nursing issues related to the quality of patient care, including patient experiences.
Recommendation
Further research is recommended to examine whether the elements of a healthy work environment are statistically related to patient experiences in the Dutch healthcare setting. In the Netherlands, patient experiences are measured with the Consumer Quality Index (CQI) [ 6 ].
Nurses’ perceptions of their work environment are measured using the Essentials of Magnetism Tool II (EOMII) questionnaire [ 44 ]. Further research should focus on the statistical relations between CQI and EOMII.
Abbreviations
American Nurses Credentialing Center
Practice environment scale of the nursing work index
Essential of magnetism tool II
Consumer quality index
Consumer assessment of healthcare providers and systems.
World Health Organization: The world health report 2000: health systems: improving performance. 2000, Chapter 2: 31-35.
Google Scholar
Jenkinson C, Coulter A, Bruster S, Richards N, Chandola T: Patients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Qual Saf Health Care. 2002, 11 (4): 335-339. 10.1136/qhc.11.4.335.
Article CAS PubMed PubMed Central Google Scholar
Suhonen R, Papastavrou E, Efstathiou G, Tsangari H, Jarosova D, Leino-Kilpi H, Patiraki E, Karlou C, Balogh Z, Merkouris A: Patient satisfaction as an outcome of individualised nursing care. Scand J Caring Sci. 2012, 26 (2): 372-380. 10.1111/j.1471-6712.2011.00943.x.
Article PubMed Google Scholar
Giordano LA, Elliott MN, Goldstein E, Lehrman WG, Spencer PA: Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010, 67 (1): 27-37. 10.1177/1077558709341065.
Delnoij DM: Measuring patient experiences in Europe: what can we learn from the experiences in the USA and England?. Eur J Public Health. 2009, 19 (4): 354-356. 10.1093/eurpub/ckp105.
Framework for quality indicators: A framework for the development and management of quality indicators for the Dutch Health Care Transparency Programme. http://www.zichtbarezorg.nl/mailings/FILES/htmlcontent/Programma%20Zichtbare%20Zorg/DEF_Framework%20for%20quality%20indicators_EN.pdf .
Rademakers J, Delnoij D, de Boer D: Structure, process or outcome: which contributes most to patients' overall assessment of healthcare quality?. BMJ Quality & Safety. 2011, 20 (4): 326-331. 10.1136/bmjqs.2010.042358.
Article Google Scholar
Damman OC, Hendriks M, Sixma HJ: Towards more patient centred healthcare: A new Consumer Quality Index instrument to assess patients’ experiences with breast care. Eur J Cancer. 2009, 45 (9): 1569-1577. 10.1016/j.ejca.2008.12.011.
Bridges J, Flatley M, Meyer J: Older people's and relatives’ experiences in acute care settings: Systematic review and synthesis of qualitative studies. Int J Nurs Stud. 2010, 47 (1): 89-107. 10.1016/j.ijnurstu.2009.09.009.
Attree M: Patients’ and relatives’ experiences and perspectives of ‘good’ and ‘not so good’ quality care. J Adv Nurs. 2001, 33 (4): 456-466. 10.1046/j.1365-2648.2001.01689.x.
Article CAS PubMed Google Scholar
Our mission and values. http://www.pickereurope.org/our-mission-and-values.html .
Zuiddijk M: Measuring and improving the quality of care from the healthcare user perspective: the Consumer Quality Index. 2011, Tilburg: Tilburg University
Triemstra M, Winters S, Kool RB, Wiegers TA: Measuring client experiences in long-term care in the Netherlands: a pilot study with the Consumer Quality Index Long-term Care. BMC Health Serv Res. 2010, 10 (1): 95-10.1186/1472-6963-10-95.
Article PubMed PubMed Central Google Scholar
Mainz J: Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003, 15 (6): 523-530. 10.1093/intqhc/mzg081.
Hendriks M, Spreeuwenberg P, Rademakers J, Delnoij D: Dutch healthcare reform: did it result in performance improvement of health plans? A comparison of consumer experiences over time. BMC Health Serv Res. 2009, 9 (1): 167-10.1186/1472-6963-9-167.
Westbrook J, Duffield C, Li L, Creswick N: How much time do nurses have for patients? A longitudinal study quantifying hospital nurses' patterns of task time distribution and interactions with health professionals. BMC Health Serv Res. 2011, 11 (1): 319-10.1186/1472-6963-11-319.
Teng CI, Hsiao FJ, Chou TA: Nurse-perceived time pressure and patient-perceived care quality. J Nurs Manag. 2010, 18 (3): 275-284. 10.1111/j.1365-2834.2010.01073.x.
Kutney-Lee A, McHugh MD, Sloane DM, Cimiotti JP, Flynn L, Neff DF, Aiken LH: Nursing: a key to patient satisfaction. Health Aff. 2009, 28 (4): w669-w677. 10.1377/hlthaff.28.4.w669.
McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH: Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff. 2011, 30 (2): 202-210. 10.1377/hlthaff.2010.0100.
Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, Bruyneel L, Rafferty AM, Griffiths P, Moreno-Casbas MT, Tishelman C, Scott A, Brzostek T, Kinnunen J, Schwendimann R, Heinen M, Zikos D, Sjetne IS, Smith HL, Kutney-Lee A: Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012, 344.
Disch J: Creating healthy work environments. Creat Nurse. 2002, 8 (2): 3-4.
Kramer M, Schmalenberg C: Staff nurses identify essentials of magnetism. Magnet hospitals revisited: Attraction and retention of professional nurses Washington, DC: American Nurses Publishing. Edited by: McClure ML, Hinshaw AS. 2002, Washington DC: American Nurses Association, 25-59. 2
McClure ML, Poulin MA, Sovie MD AWM: Magnet Hospitals: Attraction and Retention of Professional Nurses (The original study). Magnet Hospitals Revisited: Attraction and Retention of Professional Nurses. Edited by: McClure ML, Hinshaw AS. 2002, Washington DC: American Nurses Association, 1-24. 2
Aiken LH, Sloane DM, Lake ET, Sochalski J, Weber AL: Organization and outcomes of inpatient AIDS care. Med Care. 1999, 37 (8): 760-772. 10.1097/00005650-199908000-00006.
Aiken LH: Superior outcomes for Magnet Hospitals: The Evidence Base. Magnet Hospitals Revisited: Attraction and Retention of Professional Nurses. Edited by: McClure ML, Hinshaw AS. 2002, Washington DC: American Nurses Association, 61-81. 2
Gardner JK, Thomas-Hawkins C, Fogg L, Latham CE: The relationship between nurses' perceptions of the hemodialysis unit work environment and nurse turnover, patient satisfaction, and hospitalizations. Nephrol Nurs J. 2007, 34 (3): 271.
PubMed Google Scholar
Enthoven AC, van de Ven WP: Going Dutch—managed-competition health insurance in the Netherlands. N Engl J Med. 2007, 357 (24): 2421-2423. 10.1056/NEJMp078199.
Helderman JK, Schut FT, van der Grinten TE, van de Ven WP: Market-oriented health care reforms and policy learning in the Netherlands. J Health Polit Policy Law. 2005, 30 (1–2): 189-209.
Velden LFJ, Francke AL, Batenburg RS: Vraag- en aanbodontwikkelingen in de verpleging en verzorging in Nederland: een kennissynthese van bestaande literatuur en gegevensbronnen. Nederlands Instituut voor onderzoek van de gezondheidszorg. 2011
Mistiaen P, Kroezen M, Triemstra M, Francke AL: Verpleegkundigen en verzorgenden in internationaal perspectief. Een literatuurstudie naar rollen en posities van beroepsbeoefenaren in de verpleging en verzorging. Nederlands Instituut voor onderzoek van de gezondheidszorg (NIVEL). 2011
Holloway I, Wheeler S: Qualitative Research in Nursing. 2002, Blackwell Science Ltd, 2
Creswell JW: Research design. Qualitative, Quantitative, and mixed methods approaches. Vol. 2nd edition. 2003, Thousand Oaks: Sage publication
Shaller D: Patient-centered care: what does it take?. The Commonwealth Fund. 2007
Tawfik-Shukor AR, Klazinga NS, Arah OA: Comparing health system performance assessment and management approaches in the Netherlands and Ontario, Canada. BMC Health Serv Res. 2007, 7 (1): 25-10.1186/1472-6963-7-25.
Arah OA, Klazinga N, Delnoij D, Ten Asbroek A, Custers T: Conceptual frameworks for health systems performance: a quest for effectiveness, quality, and improvement. Int J Qual Health Care. 2003, 15 (5): 377-398. 10.1093/intqhc/mzg049.
Ten Asbroek A, Arah O, Geelhoed J, Custers T, Delnoij D, Klazinga N: Developing a national performance indicator framework for the Dutch health system. Int J Qual Health Care. 2004, 16 (suppl 1): i65-i71.
Lauriks S, Buster MC, de Wit MA, Arah OA, Klazinga NS: Performance indicators for public mental healthcare: a systematic international inventory. BMC Public Health. 2012, 12 (1): 214-10.1186/1471-2458-12-214.
Delnoij DM, Rademakers JJ, Groenewegen PP: The Dutch Consumer Quality Index: an example of stakeholder involvement in indicator development. BMC Health Serv Res. 2010, 10 (1): 88-10.1186/1472-6963-10-88.
Zuidgeest M, Delnoij DM, Luijkx KG, de Boer D, Westert GP: Patients' experiences of the quality of long-term care among the elderly: comparing scores over time. BMC Health Serv Res. 2012, 12 (1): 26-10.1186/1472-6963-12-26.
Zuidgeest M, Strating M, Luijkx K, Westert G, Delnoij ED: Using client experiences for quality improvement in long-term care organizations. Int J Qual Health Care. 2012, 24 (3): 224-229. 10.1093/intqhc/mzs013.
Ancarani A, Di Mauro C, Giammanco MD: How are organisational climate models and patient satisfaction related? A competing value framework approach. Soc Sci Med. 2009, 69 (12): 1813-1818. 10.1016/j.socscimed.2009.09.033.
Mensik JS, Martin DM, Scott KA, Horton K: Development of a Professional Nursing Framework: The Journey Toward Nursing Excellence. J Nurs Adm. 2011, 41 (6): 259-264. 10.1097/NNA.0b013e31821c460a.
Donahue MO, Piazza IM, Griffin MQ, Dykes PC, Fitzpatrick JJ: The relationship between nurses' perceptions of empowerment and patient satisfaction. Appl Nurs Res. 2008, 21 (1): 2-7. 10.1016/j.apnr.2007.11.001.
de Brouwer B: Measuring the nursing work environment: Translation and psychometric evaluation of the Essentials of Magnetism. Int Nurs Rev. 2014, In Press
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1472-6963/14/249/prepub
Download references
Acknowledgements
The authors should like to thank all the nurses who participated in the focus groups. We also want to thank the programme directors who helped to recruit the participants and who facilitated the interviews by providing an interview room. This paper represents independent research that was not funded by a grant.
Author information
Authors and affiliations.
Dutch Nurses’ Association, PO Box 8212, 3503, RE, Utrecht, The Netherlands
Renate AMM Kieft & Brigitte BJM de Brouwer
1/ NIVEL, Netherlands Institute for Health Services Research, PO Box 1568, 3500, BN, Utrecht, The Netherlands
Anneke L Francke
2/ EMGO+/VU medical center, Van der Boechorststraat 7, 1081, BT, Amsterdam, The Netherlands
Professor of Transparency in Healthcare from the Patient's Perspective, Tranzo, Tilburg University, PO Box 90153, 5000, LE, Tilburg, The Netherlands
Diana MJ Delnoij
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Renate AMM Kieft .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
RK participated in the design of the study, conducted the focus groups and analyses, and drafted the manuscript. BdB participated in the data collection (two focus groups) and revised the manuscript. DD participated in formulating the research questions, designing the study, and collecting and analysing the data (two focus groups), and helped to draft the manuscript. ALF participated in the design of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Kieft, R.A., de Brouwer, B.B., Francke, A.L. et al. How nurses and their work environment affect patient experiences of the quality of care: a qualitative study. BMC Health Serv Res 14 , 249 (2014). https://doi.org/10.1186/1472-6963-14-249
Download citation
Received : 06 November 2013
Accepted : 06 June 2014
Published : 13 June 2014
DOI : https://doi.org/10.1186/1472-6963-14-249
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient experiences
- Quality improvement
- Nursing work environment
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

How do you read organization’s silence over rise of Nazism?

Got milk? Does it give you problems?

Cancer risk, wine preference, and your genes
Photos by Stephanie Mitchell/Harvard Staff Photographer
Love, death, fear, guilt, pride, hope, friendship, alienation, and so much sorrow. Through it all, they kept showing up.
14 nurses on life and work during COVID
Colleen Walsh
Harvard Staff Writer
Since early 2020, when the pandemic exploded around the world, Massachusetts has seen nearly 19,000 COVID deaths and more than 840,000 cases. If a line graph of hospital admissions over the past 20 months looks like a series of peaks and valleys, the initial surge was Mount Everest for the state’s medical facilities, with patient loads and death rates that have not been matched since. To understand how the crisis has felt for frontline workers caring for the sick and dying, the Gazette reached out to 14 nurses at four Harvard-affiliated hospitals, many of whom work in intensive-care units. When the pandemic began, some had just started their careers, while others had been on the job for years. They risked their lives to stand by their patients, and their stories are marked by hope, heartbreak, and resilience.
“It’s never easy to witness my patients suffering, but I never gave up on any of them. I held out hope and prayed that each would survive.”
Afomia bekele.
Brigham & Women’s Hospital, Boston
I work on the gynecology surgical oncology inpatient floor, but during the pandemic, the entire floor converted into a COVID-19 inpatient unit. Working with these patients brought extraordinary challenges. First, I went through extreme anxiety and fear of being exposed to the virus and carrying it home to my family. In addition, the work was incredibly taxing. Nurses jumped in on many other job duties on the COVID floor in order to reduce the use of personal protective equipment. We fed patients, cleaned up after them, made video and audio calls with their loved ones. Through all this, seeing these patients deteriorate and having several heartbreaking discussions with family members was an emotional roller-coaster. The patients in this unit had low oxygen levels and could suddenly become critically ill. Of course, it’s never easy to witness my patients suffering, but I never gave up on any of them. I held out hope and prayed that each would survive. I cheered each patient that I discharged home, and seeing them reunite with a family member put a smile on my face. Most of all, I appreciated the support I received from my family. That encouraged me to keep going.
“The unknown was frightening, but the urgency the pandemic placed on health care workers all over the world didn’t allow us to sit in that fear or uncertainty for too long.”
Rachel bresilla.
Beth Israel Deaconess Medical Center, Boston
March 2020, my fast-paced medical-surgical unit came to an abrupt halt. John Ryan, our nursing director, informed us that our unit would be transitioning to a 36-bed COVID intensive-care unit. We were then whisked away to a four-hour crash course on “how to be a critical-care support nurse.” What I remember next is a unit filled with ventilated COVID patients. I vividly remember the fear that banded my co-workers and myself together and a sense of uncertainty that was felt throughout the medical center. The unknown was frightening, but the urgency the pandemic placed on health care workers all over the world didn’t allow us to sit in that fear or uncertainty for too long. Our patients needed us, their families were trusting us, and we were called to act, adapt, and help save as many of those precious lives we cared for as possible. I look back to that time with great pride. Pride in the devoted care we provided for each person in those hospital beds. Pride in how the Beth Israel Deaconess Medical Center community came together to support and encourage us in every way imaginable. Great pride in every hospital staff member who showed up every day despite the unknown. The year 2020 undoubtedly marked us all in a unique, defining way. For me, it’s the year I silenced fear, rose to the challenge, persevered, and embodied the year of the nurse.
“The intensive-care units were unrecognizable, with large numbers of very sick patients. … With all the personal protective equipment we were wearing, you could not identify who a person was or their role on the unit.”
Michelle covell.
Brigham & Women’s Hospital
As a medical intensive care unit nurse, I have been working through the pandemic in the same capacity from the start. The most stressful time was opening the first special pathogens unit (SPU). The intensive-care units were unrecognizable, with large numbers of very sick patients. Nurses, doctors, respiratory therapists, and physical therapists were pooled together from all over the hospital to help care for the patients. With all the personal protective equipment we were wearing, you could not identify who a person was or their role on the unit, so we put tape with our names and roles on our scrubs and instituted a shift huddle so people could briefly get to know each other and what was happening with their patients. As a charge nurse, I had to figure out who were the sickest patients needing the most support. I would try to keep morale going by assigning breaks and lunches. When my spouse, also a Brigham nurse, was deployed to the SPU, we worked opposite shifts so one of us could be home to manage remote learning for our eighth-grade twins. Members of our community wanted so desperately to help that a group of parents delivered dinners to our house three days a week for two months! Whether a homemade meal or just pizza delivery, it always arrived with a lovely note of support or some flowers, something positive and encouraging that helped us get through this time. These meals lifted a huge weight off our shoulders, and we are forever grateful to everyone for their support. The selfless acts that seem small but have a huge impact for the greater good are what bring me hope.
“We would go home to shower not just because we didn’t want to risk exposing loved ones, but to attempt to wash off trauma, wash away the guilt of wondering if we could do more.”
Grace defrank.
Mount Auburn Hospital, Cambridge
During the beginning of the pandemic there was no questioning — we showed up, we did what we had to do. We would go home to shower not just because we didn’t want to risk exposing loved ones, but to attempt to wash off trauma, wash away the guilt of wondering if we could do more and not spending quality time with our patients in their last moments. Death became commonplace. Nevertheless, sad and defeating. I had lost sight of myself as a nurse. If anything, the pandemic opened my eyes to how incredible health care workers are. We truly had each other’s backs and kept each other going. While working through COVID-19 will always affect me as a nurse, I refuse to let it define my nursing career. I’d like to think it pushed me into wanting more for myself in my career. I craved something new, something I hope to find more fulfilling. I am all of three shifts into a new job in the nursery and I can’t even try to explain how good it feels to hear, “Time of birth, 5:39 p.m.”
“The effects of the pandemic on the lives of mothers giving birth under these extreme conditions and the impact on their babies is something I still struggle to process.”
Sonya elenbaas.
Beth Israel Deaconess Medical Center
The pandemic shook our world, and the health care community in particular over these past 18 months. The effects of the pandemic on the lives of mothers giving birth under these extreme conditions and the impact on their babies is something I still struggle to process. As a neonatal intensive care unit (NICU) nurse at Beth Israel for the past 21 years, I have never experienced a crisis quite like this, despite the life-and-death nature of my job. There is a layer of complexity in treating moms and infants during a pandemic that necessitated the collaboration of clinicians from all areas of expertise in the NICU and labor and delivery units to minimize the risks of transmission of the virus and the potentially grave effects on our patients. My role as a nurse never felt more important or more valued than during this time. The innumerable gestures of gratitude from patients’ families, from our own families and friends, and from the world outside of the hospital were astounding and incredibly uplifting for all of us as health care workers. Reflecting on the past 18 months, I feel a sense of pride at having been part of a team of health care workers who found creative solutions to how we could safely care for high-risk infants born to COVID-positive mothers while not diminishing our responsibility to provide life-saving care. I see the progress that science and the understanding of the virus has brought to our level of care and the lives of our patients, and their families, and it gives me a feeling of relief as well as hope.
“These patients were parents, grandparents, sons, daughters, neighbors, and friends, all fighting this horrible virus alone in an isolated room.”
Michael ferrazzi.
I transferred to the medical intensive care unit from one of the medical step-down units during the beginning of the second surge back in the fall of 2020. I had no idea what I was getting myself into. To say I was overwhelmed and scared is an understatement. Seeing with my own eyes how critically ill with COVID-19 these patients were was truly eye-opening. These patients were parents, grandparents, sons, daughters, neighbors, and friends, all fighting this horrible virus alone in an isolated room. We utilized FaceTime and Zoom so our patients could see and communicate with their loved ones on a screen before we had to use a breathing tube to treat their deteriorating respiratory status. Unfortunately, for many this was the last time they saw their loved ones. Through all this hardship, I witnessed extraordinary teamwork with disciplines across the Brigham. Caregivers were working in unfamiliar areas with a common goal to care for and support these critical patients during an unprecedented time. I’m afraid we could experience another surge again, but I remain hopeful for a light at the end of this very dark tunnel.
“At first we were all fearful, worried about bringing COVID home to our families. But once we started taking care of these incredibly sick patients, we just did what needed to get done.”
Lisa mcneil.
Massachusetts General Hospital, Boston
I treated COVID-19 patients during both surges. I tried to make calls twice a day to update family members. In the beginning, we used our own phones to help them FaceTime, and later, the hospital was able to get a computer in every room, just so they could hear their voices. After 30 years in the intensive care unit, I’ve learned I’m here to help the patient, and the patient’s family. I lost my mother when I was young, and I’ve never forgotten how an incredible team of nurses and doctors helped me through. Their support ensured I wouldn’t carry that tragedy as a burden for the rest of my life. I try to bring that approach to the families I work with. Mass General has also supported us in every way. In the early days, volunteers from other parts of the hospital ensured we were putting on and taking off our protective equipment correctly to avoid any contamination. That was crucial in the beginning, and I am so grateful to them. I liken it to what the military must go through when something bad happens. Everyone just steps up to help. At first we were all fearful, worried about bringing COVID home to our families. But once we started taking care of these incredibly sick patients, we just did what needed to get done.
“To the family members who lost loved ones to COVID and were not able to be at their bedsides, please know they were not alone. We held their hands, we wiped their tears as we wiped our own, and we prayed for them as well as for you.”
Jane postizzi.
For most of my nursing career, I have worked on an intermediate medical unit that treats patients with a multitude of complex and chronic issues. These patients can become critically ill, and as medical professionals, we rely on our experience and education to help support them through such difficult times. It wasn’t until I worked directly with patients infected with COVID-19 in the special pathogens unit that I felt all that gained experience and intuition were essentially useless. I learned to accept the harsh unpredictability of COVID and harnessed my energy toward what I felt I could control: patient comfort and care. It was never lost on us that these patients were more alienated than the greater hospital population. The hospital provided means for patients to virtually communicate with their loved ones and, although this was deeply appreciated, it did not replace the importance of holding that person’s hand when it was needed most. We witnessed patients say goodbye to their families over Zoom and then we stayed by their sides. To the family members who lost loved ones to COVID and were not able to be at their bedsides, please know they were not alone. We held their hands, we wiped their tears as we wiped our own, and we prayed for them as well as for you.
“I never imagined I would begin my nursing career during a pandemic. Although I was excited to see what I could do as a nurse, I was also nervous as my floor became a COVID unit within a week.”
Madelin puleo.
Massachusetts General Hospital
I never imagined I would begin my nursing career during a pandemic. Although I was excited to see what I could do as a nurse, I was also nervous as my floor became a COVID unit within a week. One of the hardest things was seeing how quickly patients deteriorated. The worst part was that they could not have their loved ones at their bedsides. It was difficult to watch patients suffer physically and emotionally. Luckily, we were able to facilitate Zoom calls, allowing patients to see and speak to their families even if it was on a screen. In the beginning, we had little information about this disease. Hospitals saw a shortage of personal protective equipment and that terrified health care workers. We were afraid of getting COVID and spreading it to our loved ones. Months later this fear came true. I got sick with COVID despite having followed protocol. Luckily, I only experienced mild symptoms, and I got through it with the help of family and my husband, who was my rock. I am also extremely thankful for my co-workers’ support. From the beginning, everybody was so wonderful, teaching me how to become a great nurse, despite facing one of the scariest times in their careers. It was such a relief knowing no matter how unprepared I felt, they made sure I was ready to take care of these patients; I knew I was not alone in this fight. The year 2020 was not what any of us expected, but it taught me to be thankful for the small things and to appreciate life more.
“As we tackled this, we went from being hailed as heroes to being utterly overwhelmed by the constantly evolving policies, procedures, and guidelines that the pandemic created.”
Catie raftery.
Working as a nurse during a pandemic has been a humbling experience. What I presumed would be a smooth intro to intermediate medical nursing quickly shifted when the pandemic hit four months into my first hospital job. All of a sudden, we were immersed in this deadly pandemic, and a few months later, I was relocated to the COVID unit. There, our task was to treat patients with an illness marked by enigmatic spread and elusive cure, one which threatened to upend the lives of all those in its path. As we tackled this, we went from being hailed as heroes to being utterly overwhelmed by the constantly evolving policies, procedures, and guidelines that the pandemic created. In addition, we juggled comforting families only able to see their loved ones through the screens of iPads; holding the hands of those who feared for their lives; consciously deciding to spend additional time with patients who expressed feelings of loneliness and seclusion; and battling the constant fear and anxiety of exposing ourselves or our families. Although it may take years to process all these events, I know that every day I show up, give my all, and strive to bring hope, peace, comfort, and joy to every single person I encounter. It has been my greatest honor to be able to be a registered nurse in a time like this.
“These hard times have molded me into a more patient, caring, and empathetic person, both at my workplace and in my everyday life.”
Tatiana raufi.
Mount Auburn Hospital
I have been a nurse for two years now and over the last year alone, I have had experiences I never expected to have so early in my career. To put it bluntly, it’s been an emotional roller-coaster. I cannot emphasize enough how much I value the powerful bonds that I have created with my co-workers, my second family. Being at the bedside of those sick with COVID-19 has been psychologically and physically exhausting, but I’ve learned how critical my role as a nurse is in bridging a connection, with consistent communication with patients and their loved ones. There are many times I had to be the voice of my patient, whether it was relaying what was needed from the medical team or providing continuous updates to those they care about but who were unable to come into the hospital. These hard times have molded me into a more patient, caring, and empathetic person, both at my workplace and in my everyday life. Despite the tragedies I have witnessed, I am grateful for all I have learned and for who I have become.
“I had a 6-month-old at the time. Then, five days before our peak surge numbers in the hospital, I found out I was pregnant.”
Caitlin sullivan.
In my 12 years as a nurse, I never anticipated anything like this. Being scared and overwhelmed are the feelings that really stand out to me from March and April of 2020 — going to work every day not knowing if I was going to get sick or bring COVID-19 home. I had a 6-month-old at the time. Then, five days before our peak surge numbers in the hospital, I found out I was pregnant. I remember holding my son after a shift and thinking, “I can’t get this. I have to stay well for you.” I also remember the complete devastation the virus caused among our most vulnerable, and how ruthless it was. At first, we saw older patients with comorbidities. Then we started seeing people in their 40s and 50s who were otherwise healthy. Our most intensive therapies were no match for the virus. In the beginning, no families were allowed to visit, so we were the only ones with patients in their final moments, holding their hands. That stays with you. To cope, we relied on our co-workers. We cried together, supported each other, and just rallied together and found strength in one another because we shared that unique bond. The people I work with are truly incredible. We really couldn’t do what we do, or what we have done, without each other.
“How do I tell a neonatal intensive care unit nurse her assignment today is to hold the iPad for the family of a dying adult intensive-care unit patient so they can say goodbye?”
Mary tenney.
To the non-nursing community, I am the head nurse, the supervisor of nurses, the one who takes care of things like staffing and budgeting, but it’s actually so much more than that. On Feb. 28, 2020, I attended a hospital leadership meeting where we learned of a confirmed case of COVID-19 in California. My immediate thought was, “Just like Ebola, we’ll painstakingly make sure staff know how to use personal protective equipment but then never actually need it.” Within two weeks, I realized how naive that notion really was. To say supporting the nurses who reported to me was a challenge is a gross understatement. My job as their nurse manager is to make sure they are providing safe and quality care, but to also educate to protect them from harm. How do I teach them new ways of utilizing PPE, to extend the lifespan of their PPE? How do I tell a neonatal intensive care unit nurse her assignment today is to hold the iPad for the family of a dying adult intensive-care unit patient so they can say goodbye? I did it with empathy, encouragement, and positive reminders of why we all became nurses.
“The tears from my colleagues were real. The fear in their eyes was real. The compassionate care they provided to every patient coming into our emergency department was real. And the pride I have for my colleagues is real.”
Roxane white.
The end of 2019 was difficult, bringing us many challenges in the emergency department — and this was before COVID hit. While we were devising a plan to turn things around, 2020 reared its ugly head and brought us COVID. We didn’t know what to expect and were understandably afraid, however, it took a pandemic to help bring our team together. Every staff member in our department banded together to get through this thing together. We ensured each of us wore the proper personal protective equipment, despite the frequent changes to protocol. We listened to one another’s fears and raised each other’s spirits every day. We worked equally hard for the COVID patients who came in. The tears from my colleagues were real. The fear in their eyes was real. The compassionate care they provided to every patient coming into our emergency department was real. And the pride I have for my colleagues is real. This togetherness could be felt throughout the medical center, and it was a good feeling. Once you’ve been through a pandemic with your colleagues, you have a special bond that will last a lifetime.
Share this article
You might like.
Medical historians look to cultural context, work of peer publications in wrestling with case of New England Journal of Medicine

Biomolecular archaeologist looks at why most of world’s population has trouble digesting beverage that helped shape civilization

Biologist separates reality of science from the claims of profiling firms
Epic science inside a cubic millimeter of brain
Researchers publish largest-ever dataset of neural connections
How far has COVID set back students?
An economist, a policy expert, and a teacher explain why learning losses are worse than many parents realize
Pop star on one continent, college student on another
Model and musician Kazuma Mitchell managed to (mostly) avoid the spotlight while at Harvard
Increased Workload on Nurses During COVID-19 Essay
Description.
One of the national problems worth paying attention to is the COVID-19 pandemic within a hospital. In fact, this is a terrible phenomenon that has no definite limits and boundaries. For instance, dozens and hundreds of cases of infection occur every day in the US and several countries’ hospitals and the number of deaths has an imposing figure (Spinelli & Pellino, 2020). Coronavirus is spreading to people at an unprecedented rate, but, unfortunately, there is no universal, “magic” cure for all the ailments and symptoms. Hence, due to the intractability and ambiguity of the situation, such an issue is not only national but also global.
The problem has already affected the current work setting and environment in several hospitals. However, it can further aggravate such a situation and bring great “inconvenience.” COVID-19 may lead to an even greater workload, an irregular work schedule, and a change in work format (Diab-Bahman & Al-Enzi, 2020). For example, in the Infusion Center, a relatively wide range of work responsibilities has changed and expanded compared to the pre-pandemic period. From now on, visits to patients are strictly regulated, and their activities, behavior, and actions are carefully and thoroughly taken into account and recorded.
The organization has joined forces to combat the pandemic based on the national issue. For example, doctors and nurses work together, help and support each other, and perform not only their immediate duties but also secondary ones. According to Norful et al. (2018), the joint management of medics is considered from the point of view of respect, trust, effective communication, and a common philosophy of treatment. Consequently, the work has been greatly facilitated, burnout has been prevented, and patients, in turn, are satisfied with the quality of care and treatment.
Nevertheless, it is most likely that one should make the following changes. For instance, it is recommended to distribute the degree of load on physicians rationally, change the schedule and improve the reward system. According to Jacobs et al. (2018), this will result in the welfare and well-being of employees, involvement and motivation for success are key factors that allow a medical organization to achieve specific goals. Therefore, introducing these changes makes it possible to achieve high-quality services provided, efficiency, and effectiveness of the health organization.
Diab-Bahman, R., & Al-Enzi, A. (2020). The impact of the COVID-19 pandemic on conventional work settings. International Journal of Sociology and Social Policy, 40 (9/10), pp. 909-927. Web.
Jacobs, B., McGovern, J., Heinmiller, J., & Drenkard, K. (2018). Engaging employees in well-being: Moving from the Triple Aim to the Quadruple Aim. Nursing Administration Quarterly, 42 (3), pp. 231–245. Web.
Norful, A. A., de Jacq, K., Carlino, R., & Poghosyan, L. (2018). Nurse practitioner–physician comanagement: A theoretical model to alleviate primary care strain. Annals of Family Medicine, 16 (3), pp. 250–256. Web.
Spinelli, A., & Pellino, G. (2020). COVID-19 pandemic: Perspectives on an unfolding crisis. Journal of British Surgery, 107 (7), pp. 785-787. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, May 23). Increased Workload on Nurses During COVID-19. https://ivypanda.com/essays/increased-workload-on-nurses-during-covid-19/
"Increased Workload on Nurses During COVID-19." IvyPanda , 23 May 2023, ivypanda.com/essays/increased-workload-on-nurses-during-covid-19/.
IvyPanda . (2023) 'Increased Workload on Nurses During COVID-19'. 23 May.
IvyPanda . 2023. "Increased Workload on Nurses During COVID-19." May 23, 2023. https://ivypanda.com/essays/increased-workload-on-nurses-during-covid-19/.
1. IvyPanda . "Increased Workload on Nurses During COVID-19." May 23, 2023. https://ivypanda.com/essays/increased-workload-on-nurses-during-covid-19/.
Bibliography
IvyPanda . "Increased Workload on Nurses During COVID-19." May 23, 2023. https://ivypanda.com/essays/increased-workload-on-nurses-during-covid-19/.
- Electronic Health Record Change and Infusion Pumps Response
- Harriet Ann Jacobs’ Narrative
- Postoperative Care of Mr. Johnston
- Clinical Skills Self-Assessment
- Body Clock and Patient Scheduling
- How I Will Use My Nursing Degree
- Aspects of Nursing Care Process
- Teach-Back Method in Education on Hypertension
How to Write a Nursing Essay with a Quick Guide

Ever felt the blank-page panic when assigned a nursing essay? Wondering where to start or if your words will measure up to the weight of your experiences? Fear not, because today, we're here to guide you through this process.
Imagine you're at your favorite coffee spot, armed with a cup of motivation (and maybe a sneaky treat). Got it? Great! Now, let's spill the secrets on how to spin your nursing tales into words that not only get you that A+ but also tug at the heartstrings of anyone reading. We've got your back with nursing essay examples that'll be your inspiration, an outline to keep you on the right path, and more!
What Is a Nursing Essay
Let's start by dissecting the concept. A nursing essay serves as a focused exploration of a specific aspect of nursing, providing an opportunity for students to demonstrate their theoretical knowledge and its practical application in patient care settings.
Picture it as a journey through the challenges and victories of a budding nurse. These essays go beyond the classroom, tackling everything from tricky ethical dilemmas to the impact of healthcare policies on the front lines. It's not just about grades; it's about proving, 'I'm ready for the real deal.'
So, when you read or write a nursing essay, it's not just words on paper. It's like looking into the world of someone who's about to start their nursing career – someone who's really thought about the ins and outs of being a nurse. And before you kick off your nursing career, don't shy away from asking - write my essay for me - we're ready to land a professional helping hand.
How to Start a Nursing Essay
When you start writing a nursing essay, it is like gearing up for a crucial mission. Here's your quick guide from our nursing essay writing service :

Choosing Your Topic: Select a topic that sparks your interest and relates to real-world nursing challenges. Consider areas like patient care, ethical dilemmas, or the impact of technology on healthcare.
Outline Your Route : Plan your essay's journey. Create a roadmap with key points you want to cover. This keeps you on track and your essay on point.
Craft a Strong Thesis: Assuming you already know how to write a hook , kick off your writing with a surprising fact, a thought-provoking quote, or a brief anecdote. Then, state your main argument or perspective in one sentence. This thesis will serve as the compass for your essay, guiding both you and your reader through the rest of your writing.
How to Structure a Nursing Essay
Every great essay is like a well-orchestrated performance – it needs a script, a narrative that flows seamlessly, capturing the audience's attention from start to finish. In our case, this script takes the form of a well-organized structure. Let's delve into the elements that teach you how to write a nursing essay, from a mere collection of words to a compelling journey of insights.

Nursing Essay Introduction
Begin your nursing essay with a spark. Knowing how to write essay introduction effectively means sharing a real-life scenario or a striking fact related to your topic. For instance, if exploring patient care, narrate a personal experience that made a lasting impression. Then, crisply state your thesis – a clear roadmap indicating the direction your essay will take. Think of it as a teaser that leaves the reader eager to explore the insights you're about to unfold.
In the main body, dive into the heart of your essay. Each paragraph should explore a specific aspect of your topic. Back your thoughts with examples – maybe a scenario from your clinical experience, a relevant case study, or findings from credible sources. Imagine it as a puzzle coming together; each paragraph adds a piece, forming a complete picture. Keep it focused and let each idea flow naturally into the next.
Nursing Essay Conclusion
As writing a nursing essay nears the end, resist the urge to introduce new elements. Summarize your main points concisely. Remind the reader of the real-world significance of your thesis – why it matters in the broader context of nursing. Conclude with a thought-provoking statement or a call to reflection, leaving your reader with a lasting impression. It's like the final scene of a movie that leaves you thinking long after the credits roll.
Nursing Essay Outline
Before diving into the essay, craft a roadmap – your outline. This isn't a rigid skeleton but a flexible guide that ensures your ideas flow logically. Consider the following template from our research paper writing service :
Introduction
- Opening Hook: Share a brief, impactful patient care scenario.
- Relevance Statement: Explain why the chosen topic is crucial in nursing.
- Thesis: Clearly state the main argument or perspective.
Patient-Centered Care:
- Definition: Clarify what patient-centered care means in nursing.
- Personal Experience: Share a relevant encounter from clinical practice.
- Evidence: Integrate findings from reputable nursing literature.
Ethical Dilemmas in Nursing Practice
- Scenario Presentation: Describe a specific ethical challenge faced by nurses.
- Decision-Making Process: Outline steps taken to address the dilemma.
- Ethical Frameworks: Discuss any ethical theories guiding the decision.
Impact of Technology on Nursing
- Current Trends: Highlight technological advancements in nursing.
- Case Study: Share an example of technology enhancing patient care.
- Challenges and Benefits: Discuss the pros and cons of technology in nursing.
- Summary of Key Points: Recap the main ideas from each section.
- Real-world Implications: Emphasize the practical significance in nursing practice.
- Closing Thought: End with a reflective statement or call to action.
A+ in Nursing Essays Await You!
Ready to excel? Let us guide you. Click now for professional nursing essay writing assistance.
Nursing Essay Examples
Here are the nursing Essay Examples for you to read.
Writing a Nursing Essay: Essential Tips
When it comes to crafting a stellar nursing essay, a few key strategies can elevate your work from ordinary to exceptional. Here are some valuable tips from our medical school personal statement writer :

Connect with Personal Experiences:
- Approach: Weave personal encounters seamlessly into your narrative.
- Reasoning: This not only adds authenticity to your essay but also serves as a powerful testament to your firsthand understanding of the challenges and triumphs in the nursing field.
Emphasize Critical Thinking:
- Approach: Go beyond describing situations; delve into their analysis.
- Reasoning: Nursing essays are the perfect platform to showcase your critical thinking skills – an essential attribute in making informed decisions in real-world healthcare scenarios.
Incorporate Patient Perspectives:
- Approach: Integrate patient stories or feedback into your discussion.
- Reasoning: By bringing in the human element, you demonstrate empathy and an understanding of the patient's experience, a core aspect of nursing care.
Integrate Evidence-Based Practice:
- Approach: Support your arguments with the latest evidence-based literature.
- Reasoning: Highlighting your commitment to staying informed and applying current research underscores your dedication to evidence-based practice – a cornerstone in modern nursing.
Address Ethical Considerations:
- Approach: Explicitly discuss the ethical dimensions of your topic.
- Reasoning: Nursing essays provide a platform to delve into the ethical complexities inherent in healthcare, showcasing your ability to navigate and analyze these challenges.
Balance Theory and Practice:
- Approach: Connect theoretical concepts to real-world applications.
- Reasoning: By bridging the gap between theory and practice, you illustrate your capacity to apply academic knowledge effectively in the dynamic realm of nursing.
Highlight Interdisciplinary Collaboration:
- Approach: Discuss collaborative efforts with other healthcare professionals.
- Reasoning: Acknowledging the interdisciplinary nature of healthcare underscores your understanding of the importance of teamwork – a vital aspect of successful nursing practice.
Reflect on Lessons Learned:
- Approach: Conclude with a thoughtful reflection on personal growth or lessons from your exploration.
- Reasoning: This not only provides a satisfying conclusion but also demonstrates your self-awareness and commitment to continuous improvement as a nursing professional.
As we wrap up, think of your essay as a story about your journey into nursing. It's not just about getting a grade; it's a way to share what you've been through and why you want to be a nurse.
Imagine the person reading it – maybe a teacher, a future coworker, or someone starting their nursing journey. They're trying to understand your passion and why you care about nursing.
So, when you write, remember it's more than just an assignment. It's your chance to show why nursing matters to you. And if you ever need help – there's always support from our essay writer online .
Ready to Excel in Your Nursing School Essay?
Order now and experience the expertise of our professional writers!
How to Write a Nursing Essay?
How can a nursing essay effectively address ethical considerations, what are some examples of evidence-based practices in nursing essays.

Daniel Parker
is a seasoned educational writer focusing on scholarship guidance, research papers, and various forms of academic essays including reflective and narrative essays. His expertise also extends to detailed case studies. A scholar with a background in English Literature and Education, Daniel’s work on EssayPro blog aims to support students in achieving academic excellence and securing scholarships. His hobbies include reading classic literature and participating in academic forums.

is an expert in nursing and healthcare, with a strong background in history, law, and literature. Holding advanced degrees in nursing and public health, his analytical approach and comprehensive knowledge help students navigate complex topics. On EssayPro blog, Adam provides insightful articles on everything from historical analysis to the intricacies of healthcare policies. In his downtime, he enjoys historical documentaries and volunteering at local clinics.
Related Articles
%20(3).webp)
Nursing Essay Examples

Nursing Essay Examples That Will Help You Write a Stellar Paper
Published on: May 6, 2023
Last updated on: Jan 29, 2024

Share this article
Many nursing students struggle with writing effective nursing essays, which are an essential part of their education and professional development.
Poor essay writing skills can lead to low grades and an inability to effectively communicate important information.
This blog provides a comprehensive guide to writing nursing essays with examples and tips for effective writing. Whether you are a nursing student or a professional looking to improve your writing skills, this blog has something for you.
By following the tips and examples provided, you can write compelling nursing essays that showcase your dedication to the field.
Let’s get started.
On This Page On This Page -->
What is a Nursing Essay?
A nursing essay is a type of academic writing that aims to explore a particular topic related to nursing. It also presents a clear and concise argument or viewpoint supported by evidence.
Nursing essays can take many forms, including:
- Descriptive essays
- Reflective essays
- Analytical essays
- Persuasive essays
What is the Importance of the Nursing Essay?
Nursing essays are important for several reasons. First, they help nursing students develop critical thinking skills by requiring them to analyze and evaluate information.
Second, they help students develop research skills by requiring them to locate and use credible sources to support their arguments.
Third, nursing essays help students develop communication skills by requiring them to present their ideas clearly and concisely in writing. Finally, nursing essays are important for nursing education because they prepare students for the types of writing.
Paper Due? Why Suffer? That's our Job!
To help students better understand how to write nursing essays, it can be helpful to review examples.
Below are some examples of nursing essays.
Nursing School Essay Examples
College Nursing Essay Examples
Graduate Nursing Essay Examples
Nursing Scholarship Essay Examples
Nursing Essay Conclusion Examples
Nursing Essay Examples of Different Fields
Nursing is a diverse field with many different specialties and areas of focus. As a result, nursing essays can take many different forms and cover a wide range of topics.
Given below are some examples of different types of nursing essays:
Personal Philosophy Of Nursing - Essay Examples
Cal State Fullerton Nursing Essay Examples
Evidence Based Practice Nursing In Medical Field - Essay Examples
Leadership In Nursing And Healthcare Professionals - Essay Examples
Principles Of Professional Practice Of Nursing Professionals And Pharmacists
If you're seeking additional examples of nursing essays, you're in luck!
Below are some more examples that can help you gain a better understanding of nursing essays:
Health Care And Reflective Models For Nursing - Essay Examples
History Of Nursing Essay Examples
Ethical Dilemma In Nurses Work - Essay Examples
Mental Health Nursing Essay Examples
Why I Want To Be A Nurse Essay
Working In A Team And Collaboration In Nursing
How to Write a Nursing Essay
Writing a nursing essay can seem daunting, but with the right approach, it can be a rewarding experience.
Here are the key steps involved in writing a nursing essay:
Understanding the Topic and Question
The first step in writing a nursing essay is to carefully read and understand the topic and question.
This will help you determine what information you need to research and include in your essay. Make sure you understand any key terms or concepts related to the topic. Consider different perspectives or viewpoints that may be relevant.

Researching the Topic
Once you have a clear understanding of the topic and question, it's time to research.
Start by gathering information from credible sources such as academic journals, textbooks, and government websites.
Consider both primary and secondary sources, and make sure to take detailed notes as you read.
Organizing and Outlining the Essay
Once you have completed your research, it's time to organize your ideas and create an outline for your essay.
Start by identifying the main points or arguments you want to make, and then organize them into a logical order that flows well.
Your outline should include an introduction, body paragraphs, and a conclusion.
Writing the Essay
With your outline in place, it's time to start writing your essay. Make sure to follow your outline closely, and use clear and concise language that effectively communicates your ideas.
Use evidence from your research to support your arguments, and cite your sources appropriately.
Editing and Revising the Essay
Once you have completed a first draft of your essay, take some time to edit and revise it. Look for any errors in grammar, spelling, or punctuation, and make sure your essay is well-organized and flows well.
Consider asking a peer or instructor to review your essay and provide feedback.
What To Include In Your Nursing Essay
When writing a nursing essay, there are several key elements that you should include. Here are some important things to keep in mind:
- Introduction
Your introduction should provide a brief overview of the topic and purpose of your essay. It should also include a clear thesis statement that presents your main argument or point of view.
- Background Information
Provide some background information on the topic to help the reader better understand the context of your essay. This can include relevant statistics, historical information, or other contextual details.
- Evidence and Examples
Use evidence and examples from your research to support your arguments and demonstrate your knowledge of the topic. Make sure to cite your sources appropriately and use a variety of sources to strengthen your argument.
- Analysis and Evaluation
Provide analysis and evaluation of the evidence and examples you've presented. This can include discussing strengths and weaknesses, comparing and contrasting different viewpoints, or offering your own perspective on the topic.
Your conclusion should summarize the main points of your essay and restate your thesis statement. It should also offer some final thoughts or suggestions for further research or action.
Nursing Essay Topic Ideas
Choosing a topic for your nursing essay can be challenging, but there are many areas in the field that you can explore. Here are some nursing essay topic ideas to consider:
- The role of technology in nursing practice
- The impact of cultural diversity on healthcare delivery
- Nursing leadership and management in healthcare organizations
- Ethical issues in nursing practice
- The importance of patient-centered care in nursing practice
- The impact of evidence-based practice on nursing care
- The role of nursing in promoting public health
- Nursing education and the importance of lifelong learning
- The impact of nursing shortages on healthcare delivery
- The importance of communication in nursing practice
These are just a few ideas to get you started. You can also explore other topics related to nursing that interest you or align with your academic or professional goals.
Remember to choose a topic that is relevant, interesting, and feasible to research and write about.
Tips for Writing an Effective Nursing Essay
Writing a successful nursing essay requires careful planning, research, and attention to detail. Here are some tips to help you write an effective nursing essay:
- Writing Concisely and Clearly
Nursing essays should be written in clear and concise language, avoiding unnecessary jargon or technical terms. Use simple language and short sentences to help ensure that your ideas are communicated clearly and effectively.
- Stating a Clear Thesis Statement
Your thesis statement should clearly state your main argument and provide a roadmap for the rest of your essay. It should be clear, concise, and located at the end of your introduction.
- Using Proper Citation and Referencing
Citing and referencing your sources is crucial in any academic writing, including nursing essays. Make sure to use proper citation and referencing styles, such as APA or MLA. Include a reference list or bibliography at the end of your essay.
- Seeking Feedback and Revising
Before submitting your nursing essay, seek feedback from peers, professors, or writing tutors. Use their feedback to revise and improve your essay. Make sure that it is well-structured, coherent, and effectively communicates your point of view.
By following these tips, you can write a nursing essay that demonstrates your knowledge and skills in the field.
In conclusion, writing a successful nursing essay requires careful planning, research, and attention to detail.
To showcase your knowledge in the field of nursing, it is important to have a clear understanding of the topic at hand. When writing your nursing essay, be sure to include relevant examples, incorporate current research, and use proper citation and referencing.
And remember , seeking feedback and revising your essay is key to ensuring that it effectively communicates your ideas and arguments.
If you need help with your nursing essay or any other type of academic writing, consider using our AI essay writer .
Our nursing essay writing service can provide personalized support to help you succeed in your academic goals.
So, why wait? Contact us to get college essay writing help today!
Cathy A. (Literature)
For more than five years now, Cathy has been one of our most hardworking authors on the platform. With a Masters degree in mass communication, she knows the ins and outs of professional writing. Clients often leave her glowing reviews for being an amazing writer who takes her work very seriously.
Paper Due? Why Suffer? That’s our Job!
Legal & Policies
- Privacy Policy
- Cookies Policy
- Terms of Use
- Refunds & Cancellations
- Our Writers
- Success Stories
- Our Guarantees
- Affiliate Program
- Referral Program
- AI Essay Writer
Disclaimer: All client orders are completed by our team of highly qualified human writers. The essays and papers provided by us are not to be used for submission but rather as learning models only.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier Sponsored Documents
Nursing workload, nurse staffing methodologies and tools: A systematic scoping review and discussion
Peter griffiths.
a University of Southampton, Health Sciences, United Kingdom
b National Institute for Health Research Applied Research Collaboration (Wessex), United Kingdom
c Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Sweden
Christina Saville
Jeremy jones, natalie pattison.
d University of Hertfordshire, School of Health and Social Work, United Kingdom
e East & North Hertfordshire NHS Trust, United Kingdom
Thomas Monks
f University of Exeter, College of Medicine and Health, United Kingdom
Associated Data
The importance of nurse staffing levels in acute hospital wards is widely recognised but evidence for tools to determine staffing requirements although extensive, has been reported to be weak. Building on a review of reviews undertaken in 2014, we set out to give an overview of the major approaches to assessing nurse staffing requirements and identify recent evidence in order to address unanswered questions including the accuracy and effectiveness of tools.
We undertook a systematic scoping review. Searches of Medline, the Cochrane Library and CINAHL were used to identify recent primary research, which was reviewed in the context of conclusions from existing reviews.
The published literature is extensive and describes a variety of uses for tools including establishment setting, daily deployment and retrospective review. There are a variety of approaches including professional judgement, simple volume-based methods (such as patient-to-nurse ratios), patient prototype/classification and timed-task approaches. Tools generally attempt to match staffing to a mean average demand or time requirement despite evidence of skewed demand distributions. The largest group of recent studies reported the evaluation of (mainly new) tools and systems, but provides little evidence of impacts on patient care and none on costs. Benefits of staffing levels set using the tools appear to be linked to increased staffing with no evidence of tools providing a more efficient or effective use of a given staff resource. Although there is evidence that staffing assessments made using tools may correlate with other assessments, different systems lead to dramatically different estimates of staffing requirements. While it is evident that there are many sources of variation in demand, the extent to which systems can deliver staffing levels to meet such demand is unclear. The assumption that staffing to meet average need is the optimal response to varying demand is untested and may be incorrect.
Conclusions
Despite the importance of the question and the large volume of publication evidence about nurse staffing methods remains highly limited. There is no evidence to support the choice of any particular tool. Future research should focus on learning more about the use of existing tools rather than simply developing new ones. Priority research questions include how best to use tools to identify the required staffing level to meet varying patient need and the costs and consequences of using tools.
Tweetable abstract
Decades of research on tools to determine nurse staffing requirements is largely uninformative. Little is known about the costs or consequences of widely used tools.
What is already known about the topic?
- • There are many studies showing adverse effects of low nurse staffing on patient outcomes.
- • There has been a longstanding interest in developing systems to determine the required staffing level.
- • Despite decades of research and a large number of tools, previous reviews have highlighted limited evidence about their use.
What this paper adds
- • Recent years continue to see reports of new staffing tools and systems.
- • Important sources of variability are neglected in published reports.
- • Benefits are associated with increased staffing levels but the costs and benefits of using a tool, as opposed to simply increasing staffing, remain unknown.
1. Introduction
Multiple reviews of research have established that higher registered nurse staffing levels in hospitals are associated with better patient outcomes and improved care quality, including lower risks of in-hospital mortality, shorter lengths of stay and fewer omissions of necessary care (e.g. Brennan et al., 2013 ; Griffiths et al., 2016 , 2018b ; Kane et al., 2007 ; Shekelle, 2013 ). However, beyond providing an injunction to invest in ‘more’ staff, such studies rarely indicate directly how many staff are required. The ability to determine the ‘right’ number of staff, both to employ and to deploy on any given shift, is an imperative from the perspective of both quality and efficiency of care ( Saville et al., 2019 ). In this paper, we consider the evidence base for approaches to measuring nursing workload and tools used to determine the number of nurses that are required for general acute-care hospital wards.
1.1. Nurse staffing levels and outcomes
Low nurse staffing is associated with omissions of essential nursing care ( Griffiths et al., 2018b ), identified as a key mechanism leading to adverse patient outcomes ( Recio-Saucedo et al., 2018 ). Building on the extensive evidence from cross-sectional studies, recent studies have shown associations at a patient- rather than hospital- or unit-level ( Griffiths et al., 2018a , 2019 ; Needleman et al., 2011b ). These include studies involving direct observation of care delivery ( Bridges et al., 2019 ) and studies showing that omissions in care mediate associations between staffing levels and outcomes ( Ball et al., 2018 ; Bruyneel et al., 2015 ; Griffiths et al., 2018a ). While cause and effect cannot be directly inferred from observational studies, the case for a conclusion that low nurse staffing causes harm to patients is increasingly compelling. Perhaps the case is best made by considering the alternative proposition. It seems highly unlikely that there are no adverse outcomes caused by low nurse staffing levels.
Partly as a response to this evidence, policies of mandatory staffing minimums have been much discussed and implemented in a number of jurisdictions, most notably California, USA ( Donaldson and Shapiro, 2010 ; Mark et al., 2013 ; Royal College of Nursing, 2012 ). Yet, even where mandatory staffing policies are implemented, patient care needs that cannot be met by the minimum must be identified, and staffing adjusted accordingly. The question of how best to identify the required nurse staffing level remains unanswered.
1.2. Staffing tools and methodologies
Determination of appropriate nurse staffing levels and measurement of workload have been studied since the earliest days of research into nursing (e.g. Lewinski-Corwin, 1922 ). Over the years, there have been many reviews focussing on methods for determining nurse staffing requirements. All have highlighted major deficits in the evidence. The problem is not a simple lack of published literature. One early review of nurse staffing methodologies, published in 1973, included a bibliography of over 1000 studies ( Aydelotte, 1973 ). However, finding no evidence concerning the relative costs or effectiveness of different staffing methods and little evidence for validity or reliability, the authors concluded “Although the intent of the methodologies is admirable, all are weak” (p. 57) ( Aydelotte, 1973 ).
Subsequent reviews have had to embrace an ever-growing body of research and an increasing number of systems. A review undertaken for the then Department of Health and Social Services (DHSS) in the UK in 1982 identified over 400 different systems for determining staffing requirements ( DHSS Operational Research Service, 1982 ). Despite the volume of writing, evidence to judge the merits of these systems has remained elusive. Writing in 1994, Edwardson and Giovanetti noted the absence of published scientific evidence for a number of systems, such as GRASP or Medicus, which were in widespread use in North America ( Edwardson and Giovannetti, 1994 ). They also noted that although different systems tended to produce results that were highly correlated, they could nonetheless produce substantially different estimates of the required level of nursing staff for a given patient or unit ( Edwardson and Giovannetti, 1994 ).
Fasoli and Haddock reviewed 63 sources (primary research, theoretical articles and reviews) and again found that there was insufficient evidence for the validity of many current systems for measuring nursing workload and staffing requirements, concluding that systems are not sufficiently accurate for resource allocation or decision-making ( Fasoli et al., 2011 ; Fasoli and Haddock, 2010 ). Other reviews reinforce this pervasively negative picture of the evidence ( Arthur and James, 1994 ; Butler et al., 2011 ; Hurst, 2002 ; Twigg and Duffield, 2009 ). The field is dominated by descriptive reports of locally developed approaches and none of these reviews found any evidence for the impact of implementation of a tool on outcomes for quality of care, patients or staff ( Griffiths et al., 2016 ).
However, the topic remains important. Identifying low staffing as a significant contributor to “conditions of appalling care ”, a key recommendation of the Francis Inquiry into the failings of the Mid Staffordshire General Hospital in the United Kingdom was the development of guidance for nurse staffing including:
“…evidence-based tools for establishing what each service is likely to require as a minimum in terms of staff numbers and skill mix.”(p. 1678) ( Francis, 2013 )
In this paper we aim to give an overview of approaches to measuring nurse staffing requirements for general acute hospital wards, drawing primarily on existing reviews, before presenting a more comprehensive overview of more recent primary research to determine whether (and how) evidence has changed in recent years.
2. Review methods and scope
2.1. search strategy and approach to review.
The sheer volume of material and unanswered questions identified in other reviews makes this a daunting area to summarise. We describe the current review as systematic in the sense that we aim to be explicit about the approach to identification and selection of literature. However, as we primarily aim to map the literature, identifying recent developments, key features and areas of relative strength and weakness, without necessarily giving each study an in-depth critical appraisal, we consider this a scoping review, serving to summarise findings and identify gaps in the knowledge ( Arksey and O'Malley, 2005 ).
We draw selectively on older authoritative sources and reviews to give a general overview and background to the evidence (including the reviews already cited), using the results of our comprehensive searches and review of reviews undertaken for the National Institute for Health and Care Excellence, NICE ( Griffiths et al., 2014 ) as a key source.
In order to identify more recent studies, we searched Medline, CINAHL (key word only) and The Cochrane Library using the terms “Workload”[key word, MESH] or “Patient Classification”[key word] AND “Personnel Staffing and Scheduling” AND “Nurs*”[key word] or “Nursing”[MESH] and limited results using the OVID Medline sensitive limits for reviews, therapy, clinical prediction guides, costs or economics. We checked the sensitivity of this search, which was designed to be specific, using the results of our earlier more comprehensive search ( Griffiths et al., 2014 ) as a test set. We performed additional searches for citations to existing reviews and for other works by the authors of those reviews (since such reviews might be conducted as a prelude to new empirical research). We also undertook focussed searches on databases for works by key authors and searched the World Wide Web using the names of widely used tools. Searches were completed in mid-December 2018. We looked specifically for new reviews published after 2014 (when searches for our 2014 review of reviews were completed) and primary studies published from 2008 onwards, because the most recent review in our review of reviews was published in 2010 ( Fasoli and Haddock, 2010 ). After removing duplicates, we had 392 recent sources to consider.
2.2. Selection of primary research
Consistent with the aims of a scoping review, we took a liberal approach to inclusion for material to review. We included primary studies that described the development, reliability or validity testing of systems/ tools for measuring nursing workload/ predicting staffing requirements; studies that compared the workload as assessed by different measures, or which used a tool as part of a wider study in such a way that it might provide some insight into the validity of tools or another aspect of the determination of nurse staffing requirements; and studies that reported the costs and/or consequences of using a tool, including the impact on patient outcomes. We also included descriptive papers that might not merit the label ‘study’, provided that they included some data. We only included studies that were of direct relevance to staffing on general acute adult inpatient units and so excluded studies focussing exclusively on (for example) intensive or maternity care. However, had we identified material that demonstrated a significant methodological advance or other insight we were open to including it for illustrative purposes.
3.1. Overview of approaches to determining nurse staffing levels
There are many methods for determining nurse staffing requirements described in the literature. They are generally classified into several broad types ( Fig. 1 ) although the distinction between these approaches is less absolute than it may appear and terminology varies.

Major approaches for determining nurse staffing requirements.
Telford's professional judgement method ( Telford, 1979 ), first formally described in the UK in the 1970s, provides a way of converting the shift-level staffing plan, decided using expert opinion, into the number of staff to employ. The method describes calculation of the number of nurses to employ (generally referred to in the UK literature as the nursing ‘establishment’) in order to reliably fill the daily staffing plan (planned roster), making allowance for holidays, study leave and sickness/absence. Conversely, this method can be used to infer the daily staffing plan from the whole time equivalent staff employed by a ward, as illustrated by Hurst (2002 ). The full ‘Telford’ method provides a framework for wider deliberation, but the judgement of required staffing does not require the use of objective measures to determine need ( Arthur and James, 1994 ), hence it is an example of a ‘ professional judgement’- based approach . In recent years, this deliberative approach without formal measurement is reflected in the United States Veteran's Administration staffing methodology ( Taylor et al., 2015 ).
‘Benchmarking approaches ’ involve using expert judgements to identify suitable comparators, with the staffing levels compared between similar units to establish requirements. For many years this approach was used by the audit commission in the UK ( Audit Commission, 2001 ) to compare nursing establishments and expenditure between units across hospitals. Although characterised by Hurst (2002) as a distinct method, like professional judgement, benchmarking does not involve any formal assessment of patient requirements for nursing care. Rather, consensus methods and expert professional judgement are often used in selecting appropriate benchmarks and so it could be characterised as a particular form of the professional judgement approach, although such characterisation requires that such a judgement is applied. Furthermore, while the process of comparison with similar wards gives the appearance of objectivity, much depends on how the initial staffing levels were arrived at, and there is ample evidence that perceptions of staffing requirements are often anchored to historical staffing levels ( Ball et al., 2019 ; Twigg and Duffield, 2009 ).
While accounts of professional judgement and benchmarking exercises often focus on determining establishments, both can also be used to determine a daily staffing plan or shift-level nurse-patient ratio or equivalent (such as nursing hours per patient). In this way they assign a target number of nursing staff or hours per patient or bed ( Hurst, 2002 ), informing staff deployment decisions. Such approaches specify unit types to which a particular staffing level applies, although categories tend to be broad (e.g. intensive care, general medical surgical and rehabilitation). Some more recent approaches to monitoring workload (see below) extend this approach to take a wider view of activity, for example adding in admissions and discharges over and above the patient census, and therefore we term these patient-nurse ratio approaches ‘volume-based’ approaches .
Approaches that appear to set minimum staffing levels per patient, an example of a volume-based approach, are sometimes explicit in stating that additional staffing may be required to meet peaks in demand. For example, the legislation that established mandatory nurse-patient ratios in California includes a stipulation that hospitals also use a system for determining individual patient care requirements to identify the need for staffing above the specified minimum ( State of California, 1999 ). Thus, approaches which seek to determine staffing requirements accounting for individual patient variation in need or other factors driving workload can be used as alternatives to, or in conjunction with, minimum staffing levels based purely on patient volumes.
Whereas volume-based approaches measure variation in workload determined by patient counts, other approaches recognise that patients in a given type of ward may have different care requirements. Edwardson and Giovannetti (1994) , offer a typology of three main approaches for determining individual patient need: prototype, task and indicator systems. Hurst also describes three main types: Patient Classification Systems, timed-task and regression-based ( Hurst et al., 2002 ).
Prototype or Patient Classification Systems group patients according to their nursing care needs and assign a required staffing level for each ( Fasoli and Haddock, 2010 ; Hurst, 2002 ). They use either pre-existing categorisations, e.g. diagnosis-related groups ( Fasoli and Haddock, 2010 ), or bespoke categorisations, e.g. classifications based on levels of acuity and/or dependency groups. The Safer Nursing Care Tool ( The Shelford Group, 2014 ), the most widely used method for determining staffing requirements in England ( Ball et al., 2019 ), is one such system. Patients are allocated to one of five acuity/dependency categories with a weighting (described as a ‘multiplier’) to indicate the required staff to employ associated with patients in each category.
In task (or timed-task ) approaches, a detailed care plan, consisting of specific ‘tasks’, is constructed for each new patient and used to determine the required staffing ( Hurst, 2002 ). Each task is assigned an amount of time. The commercial GRASP system, still widely used in the United States, is an example of such a system ( Edwardson and Giovannetti, 1994 ).
As with prototype approaches, indicator approaches ultimately assign patients to categories, in this case based upon ratings across a number of factors that are related to the time required to deliver patient care. These can include broad assessments of condition (e.g. ‘unstable’), states (e.g. ‘non ambulatory’), specific activities (e.g. complex dressings) or needs (e.g. for emotional support or education) ( Edwardson and Giovannetti, 1994 ). The Oulu Patient Classification, part of the RAFAELA system, is one such example. Patients are assigned to one of four classifications, representing different amounts of care required, based upon a weighted rating of care needs across six dimensions ( Fagerström and Rainio, 1999 ). However, the inclusion of some specific activities in Edwardson and Giovennetti's definition of indicator approaches makes it clear that the distinction from task / activity-based systems is not an absolute one. Typically, though, task-based systems take many more elements into account: over 200 in some cases ( Edwardson and Giovannetti, 1994 ).
Hurst also identified regression -based approaches, which model the relationship between patient-, ward- and hospital-related variables, and the establishment in adequately-staffed wards ( Hurst, 2002 ). To obtain the recommended establishment for a particular ward, coefficients derived from the regression models are used to estimate the required staffing. There are relatively few examples, although Hoi and colleagues provide one recent example, the Workload Intensity Measurement System ( Hoi et al., 2010 ). In some respects, regression-based models simply represent a particular approach to allocating time across a number of factors within an indicator-based system, rather than directly observing or estimating time linked to specific activities or patient groups. The RAFAELA system, widely used in the Nordic countries, although based on a relatively simple indicator system, uses a regression-based approach to determine the staffing required to deliver an acceptable intensity of nursing work for a given set of patients in a given setting ( Fagerström and Rainio, 1999 ; Fagerstrom and Rauhala, 2007 ; Rauhala and Fagerström, 2004 ).
In these more tailored approaches, the method for determining the required times for patient groups or tasks varies. The literature describes the use of both empirical observations and expert opinion to determine the average time associated with tasks or patient classifications ( De Cordova et al., 2010 ; Myny et al., 2014 ; Myny et al., 2010 ). In some cases, there is an explicit attempt to make workload/time allocations based on reaching some threshold of quality. For example, wards contributing to the database from which the multipliers for the Safer Nursing Care Tool are derived must meet a predefined standard for care quality ( Smith et al., 2009 ). Non-patient contact time, for example care planning and documentation or other activities that take place away from the bedside (which are not always easily attributable to individual patients), is dealt with in different ways. All approaches consider this, often assigning a fixed percentage time allocation over and above direct care that has been measured.
While some approaches appear to be more precise than others, using detailed patient care plans at one extreme (timed-task) and apparently assuming all patients have similar needs (volume-based) at the other, all use average time allocations, with an unstated assumption that when summed across tasks and patients, individual variation can be accommodated.
3.1.1. Staffing decisions and the use of tools
A number of different decisions can be made using staffing systems and tools, with decisions operating in different time frames ( Table 1 ). Nursing managers must decide in advance how many nursing staff to employ (often referred to as the nursing establishment ) and how many nursing staff to deploy each shift, either as a fixed daily staffing plan or in response to immediate demand. Accounts of indicator and task approaches often focus on measuring immediate need (and implicitly deploying staff to meet such need) rather than determining an establishment to fill planned rosters. These are separate but inter-related decisions, which all rely on being able to quantify nursing workload. The distinction is sometimes unclear in published accounts and the relationship between these uses tends to be implicit rather than explicit.
Uses of staffing systems and tools.
For example, the Safer Nursing Care Tool was designed to support decisions about the total nursing establishment required on a ward based on meeting the daily needs of a sample of patients ( The Shelford Group, 2014 ). More recently, its core acuity-dependency scoring system has been used to plan and review daily staffing levels, supporting deployment and real-time redeployment decisions, for example using the SafeCare system from the commercial rostering system provider Allocate ( Allocate Software, 2017 ).
There are also examples of tools specifically to balance workload within a unit, which thus focussed primarily on immediate assignments for staff members ( Brennan and Daly, 2015 ; Brennan et al., 2012 ). Finally, tools can be used retrospectively to review the success of staffing plans (how well the plan met needs) or as a measure of resource use for pricing, budgeting or billing purposes ( Kolakowski, 2016 ).
3.1.2. Overlap between approaches
While the classifications are useful to distinguish broad approaches, the differences are not absolute. For example, professional judgement-based approaches might involve benchmarking to set a fixed establishment for a ward based on an underlying staffing model that aims for a given nurse-patient ratio on each shift and so resembles a volume-based approach. The original determination of the staffing requirement might have involved a detailed appraisal of patient need on a given ward involving many factors similar to those considered in other systems, without a formal calculation of workload based on measurements.
On the other hand, prototype or indicator systems set establishments or daily staffing plans based on a measurement of a sample of individual patient needs, assuming that this can be used to generalise to the patient population as a whole. The establishment, once set, implies that care needs are then met by a fixed nurse-to-patient ratio or number of hours per day, although these ratios may differ between wards. Indeed, a prototype classification system, such as the Safer Nursing Care Tool, resembles a volume-based mandatory minimum staffing policy supplemented by assessment of variation above the base requirement, such as that implemented in California, because there is an implied absolute minimum staffing level per patient, associated with the prototype with the lowest staffing requirement.
3.1.3. Choice of tools
The reviews cited earlier made it clear that there was little basis to prefer any one approach over another based on the available evidence. Professional judgement-based approaches, despite being open to accusations of subjectivity, cannot be readily dismissed without evidence that moving from a judgement-based staffing model to one informed by a tool has improved any outcomes or made more efficient staffing allocations. Existing reviews present no such evidence ( Arthur and James, 1994 ; Aydelotte, 1973 ; DHSS Operational Research Service, 1982 ; Fasoli and Haddock, 2010 ; Griffiths et al., 2016 ; Hurst, 2002 ; Twigg and Duffield, 2009 ). Professional judgement remains central and indeed is incorporated into some tools. One of the most comprehensively researched systems determines the staffing requirement by titration against a subjective report of work intensity ( Fagerström and Rainio, 1999 ; Rauhala and Fagerström, 2004 ).
The use of subjective judgements would matter little if different approaches gave similar results, but this is not the case. While direct comparisons are relatively rare, it is clear from the available evidence that different systems can give vastly different estimates of required staffing (e.g. Jenkins-Clarke, 1992 ; O'Brien-Pallas et al., 1991 , 1992 , 1989 ). In one study, the five systems tested provided estimates that correlated highly. However, they offered a wide range of average staffing requirements for the same sample of 256 patients, from 6.65 h per patient per day to 11.18 ( O'Brien-Pallas et al., 1992 ).
3.2. Recent evidence
From our searches for primary studies we found 37 recent sources to consider. They were diverse in their methods although all were observational studies. We classified the sources according to the main purposes of the articles, although some articles did not clearly sit in a single category and were given a dual classification (see Table 2 for classifications and Table 4 in Supplemental material for fuller descriptions).
Recent studies/sources used in the review.
3.2.1. Descriptions
These descriptive studies illustrate the currency of a range of approaches including professional judgement ( Taylor et al., 2015 ), prototype ( Fenton and Casey, 2015 ; The Shelford Group, 2014 ) and indicator systems ( Fagerström et al., 2014 ; Kolakowski, 2016 ), with at least one explicitly combining approaches ( Fagerström et al., 2014 ). Studies demonstrate variation between wards and from day to day and month to month (e.g. Gabbay and Bukchin, 2009 ; Smith et al., 2009 ), arising from the number of patients, the numbers of admissions and discharges, individual patient characteristics and their specific needs (e.g. Fagerström et al., 2014 ; Hurst, 2009 ; Smith et al., 2009 ), as well as contextual factors such as the physical arrangement of the ward ( Hurst, 2008 ).
While demonstrating that measured demand for nursing care can vary considerably, none of the descriptive studies provided a measure that allowed the variation to be directly quantified in terms of variability in the staff required from day to day. Knowledge of this variability would help determine whether a fixed staffing plan is liable to meet patient need on a regular basis. This lack of direct quantification is an important limitation given that tools are used to guide fixed staffing plans.
3.2.2. Comparisons
The findings of earlier studies, showing that different methods can give very different results, are reflected in recent research. Differences between alternative approaches to counting patients for methodologies using hours per patient day appear to be of marginal practical significance ( Beswick et al., 2010 ; Simon et al., 2011 ), but other factors can make a substantial difference to estimated staffing requirements. Methods that take into account more factors appear to arrive at higher workloads. An unquantified statistically significant increase to workload from including patient turnover in a volume-based measure was noted in one study ( Beswick et al., 2010 ). An acuity- and dependency-based indicator system identified an additional six hours of care per day compared to a standard (fixed) hours per patient day method ( Rivera, 2017 ). A new multifactorial indicator system with additional care categories and revised timings resulted in an estimated nursing requirement that was double that determined by an existing simpler system ( Hoi et al., 2010 ).
3.2.3. Tool development
Many studies (thirteen) report the development of new measures or adaptation of existing measures. Most system types, including professional judgement, volume-based approaches and timed-task feature on this list, adding to the range considered in recent descriptions (above). The measures were often developed for local use only. Typically, papers identify time or some weighting associated with aspects of care or particular groups of patients ‘on average’. However, they generally fail to report or consider variability in the underlying estimates.
That variation around the average time could be important is illustrated in the work of Myny and colleagues in Belgium ( Myny et al., 2014 , 2010 ), which as well as being an exception by reporting variability, also represents one of the few examples of a sustained programme of research in recent years. Although the reports were focussed on demonstrating the precision of the mean time estimates they derived, the degree of variation associated with a particular task is well illustrated. The estimated standard time for “partial help with hygienic care in bed” had a 95% confidence interval from 7.6 to 21.2 min. The underlying sample of observations could not be easily determined but the wide confidence intervals appear to result from intrinsic variability rather than simply a small sample. “Settling a bed ridden patient” had an interquartile range from 5 to 25.75 min ( Myny et al., 2010 ).
It may be that prototype approaches, where measures are based on typical care needs of patients fitting a particular profile, are less subject to variation between individuals with the same classification because multiple care needs ‘average out’, but we found no equivalent estimates of variation for such systems. One reason that measures of variability rarely appear may be that despite the external appearance of ‘objectivity’, the times or weights assigned within systems are often wholly or partly arrived at through an expert consensus exercise, for example , Brennan et al. (2012) and Hurst et al. (2008) . In part this is likely due to the volume of observation required to obtain reliable time estimates ( Myny et al., 2010 ). It is clear that professional judgement remains an important source of information and validation for any system.
3.2.4. Evaluation
Correlations between measures of staffing requirement or workload have been used to establish validity (e.g. Brennan et al., 2012 ; Hurst et al., 2008 ; Larson et al., 2017 ; Morales-Asencio et al., 2015 ; Smith et al., 2009 ). In all but one of these examples, the criterion used to establish validity is, in effect, a professional judgement of demand for nursing care. The centrality of professional judgement as a criterion is demonstrated by the RAFAELA system, in which the Oulu Patient Classification (OPC) weighting that is associated with nurses’ judgements that staffing is ‘optimal’ is used to set target staffing ( Fagerström et al., 2014 ).
Successful implementation of any system requires significant investment to engage and train staff. Taylor and colleagues describe the substantial challenges faced in implementing a professional judgement-based system for the US Veteran's Administration ( Taylor et al., 2015 ). While concluding that their system can be successfully implemented, they highlighted nursing leadership and front line staff buy-in as essential. They also emphasised the importance of staff training and the risk of cynicism if staff invest effort in a new system but see little tangible outcome. Even in the face of broad staff support, a pre-implementation study found that there was insufficient engagement with the measures of staffing adequacy required by the RAFAELA system, and satisfactory reliability also proved hard to achieve ( van Oostveen et al., 2016 ). Nurses can make reliable assessments using a number of systems ( Brennan et al., 2012 ; Liljamo et al., 2017 ; Perroca, 2013 ), although achieving inter-rater agreement is not always straightforward and the reliability of ratings in a new setting should not be assumed, even for tools where reliability has been established previously ( van Oostveen et al., 2016 ). Reliability of assessment in “real life” may be considerably lower than that achieved under controlled conditions and there are potential adverse effects on engagement when items that end users consider to be important aspects of care are omitted because of less desirable psychometric properties ( Brennan and Daly, 2015 ).
Given the importance of nurse staffing levels for maintaining the quality of patient care and the significant proportion of hospital budgets spent on staffing wards, there has been remarkably little attention given to the impact of tools or systems. Nonetheless recent years have seen the appearance of some evidence linking a mismatch between staff deployed and a calculated staffing requirement to adverse outcomes. This evidence does not clearly point to any particular measurement system and instead tends to align with evidence showing the benefits of higher staffing levels. These studies give some further indication of the validity of some tools as workload measures, but do not, in general, support conclusions that the tools give ‘optimal’ staffing levels, in the sense of identifying a level at which adverse outcomes are minimised or there are diminishing returns from further increase.
A US study using an unspecified commercial Patient Classification System found that the hazard of death was increased by 2% on every occasion a patient was exposed to a shift with 8 or more hours below the target defined by the system ( Needleman et al., 2011a ). Mortality was also increased by exposure to shifts with unusually high patient turnover, suggesting that this might be generating additional workload unmeasured by the system.
In Finland, nursing workload above the ‘optimal’ level measured using the OPC was associated with adverse patient outcomes, including increased mortality ( Fagerstrom et al., 2018 ; Junttila et al., 2016 ). However, nursing workload below the optimal level (higher staffing) was associated with improvements in outcomes ( Fagerstrom et al., 2018 ; Junttila et al., 2016 ), challenging the notion of this staffing level as ‘optimal’. Furthermore, the OPC workload measure was not clearly superior to a simple patient per nurse measure based on analysis of decision curves ( Fagerstrom et al., 2018 ).
More recently, a UK study found that registered nurse staffing below the level planned using the Safer Nursing Care Tool was associated with a 9% increase in the hazard of death in one English hospital trust, although low assistant staffing according to this criterion was not associated with mortality increases ( Griffiths et al., 2018a ). This study also explored staffing level as a continuous variable and found that the relationship between mortality and registered nurse staffing levels appeared to be linear, with no clear threshold effect at the Safer Nursing Care Tool-recommended level.
After implementing a ‘Nursing Hours per Patient Day’ methodology in three hospitals in Australia, there were increases in staffing levels and improvements in several patient outcomes over time, including mortality ( Twigg et al., 2011 ). This volume-based methodology assigns a minimum staffing level (measured in hours per patient day) for six different ward types, based on the patient case mix and complexity. An accompanying economic analysis estimated the cost per life year gained was AUD$8907 ( Twigg et al., 2013 ).
3.2.5. Operational research
Studies emanating from the tradition of operational research are examples of a larger body of literature that focuses on nurse rostering rather than workload measurement tools ( Saville et al., 2019 ). These studies highlight that rosters based on average staffing requirement may not provide an optimal solution to meet varying patient need.
Two studies determined that optimal staffing in the face of varying patient demand was higher than a level determined by staffing to meet the mean demand ( Davis et al., 2014 ; Harper et al., 2010 ). In one case, apparent ‘overstaffing’ was associated with net cost savings in modelling, in part because of the potential value of ‘excess’ staff who were available for redeployment to understaffed units ( Davis et al., 2014 ). Other studies modelled the effects of the use of varying configurations of ‘float’ pools to meet fluctuation in demand arising from multiple sources ( Kortbeek et al., 2015 ; Maenhout and Vanhoucke, 2013 ). These two studies again demonstrate the myriad of sources of variation in demand, and the challenge of matching supply of nursing care to that demand, particularly with an establishment based on the ‘average’ demand, while providing little insight into how demand for nursing care should be measured in the first place.
4. Discussion
Writing in 1994, Edwardson and Giovanetti concluded that a number of key questions about nursing workload systems remained unanswered:
- • Do the results of workload measurement systems depart significantly from the professional judgements of practicing nurses?
- • Does the implementation of a staffing methodology or tool lead to altered staffing levels or, conversely, do historical staffing levels influence the assessment of need?
- • Do workload measurement systems improve the quality of care?
- • Do workload measurement systems result in more efficient use of nursing personnel?
While recent years have seen a continued interest and a significant number of publications, these questions remain largely unanswered. There is evidence that some systems are reliable, that workload measured by a system correlates with other (largely subjective) measures, that low staffing relative to a measured requirement is associated with worse patient outcomes and that increased staffing levels associated with use of a system is associated with improved patient outcomes. However, there is no basis on which to determine that any system gives the ‘correct’ staffing levels.
The results of several workload measurement systems correlate with the professional judgement of practicing nurses, but the correspondence is not perfect and the significance of any discrepancies in estimated staffing requirements is unclear. Despite correlations, different systems can give dramatically different results and so it is clear that there can be no single answer to the questions of whether workload measurement systems result in improvements in the utilisation of nursing personnel . The advantage of complex systems over simpler systems is unclear. There is some evidence that the more aspects of care are included in otherwise similar indicator or volume-based systems, the higher the estimated staffing requirement. However, there is little basis on which to judge which is correct other than an evidence base showing higher staffing is associated with better outcomes.
Patient outcomes have been shown to improve when staffing is increased above levels identified as ‘optimal’ using professional judgements and a widely used prototype system. Such a finding is consistent with historical staffing levels and expectations influencing perceptions of what is required. So although professional judgement remains central and no system has been shown to be superior, it too may be systematically biased. Although there are perceptions of benefits from using staffing methodologies, the effect on the costs or quality of care remains unclear and the resources involved in running the systems are unquantified, although the required investments could be considerable ( Ball et al., 2019 ).
Given the significant body of evidence that emphasises the specific association between registered nurse staffing levels or skill mix and outcomes (e.g. Aiken et al., 2017 ) it is perhaps surprising that the mix of staff is rarely addressed directly in this literature. This may be because many systems have their origins in settings where the contribution of support staff to direct patient care is lower, e.g. the USA ( Aiken et al., 2017 ). The issue of determining skill mix is compounded by the fact that the involvement of support staff in the delivery of nursing care can vary widely ( Kessler et al., 2010 ). Some tools consider only registered or licensed nurses while others, such as the Safer Nursing Care Tool ( The Shelford Group, 2014 ), plan the total nursing team size and defer the skill mix decision to professional judgement.
4.1. Sources of variation
The methods described in the literature generally match staffing levels to the average (mean) demand associated with a particular patient group, factor or aspect of care when attempting to estimate current or future staffing requirements. Yet in the face of variable demand, simplistic responses based on the average may not be the best way to use the results of measurement systems. While much of the literature is concerned with measurement and identification of sources of variation, it is poor at quantifying such variation in a way that allows its impact on decision-making to be understood.
When workload distributions are approximately normal with small standard deviations, the mean may be an appropriate basis for planning, as the workload will vary from the mean by a relatively small amount. Assuming some degree of flexibility in the work capacity of a given group of staff, most patients’ needs might be safely accommodated most of the time. While some systems such as RAFAELA are explicit about an acceptable degree of variation from the mean ( Fagerström et al., 2014 ), this is rare, and the impact on safety of small deviations has not been widely researched.
However, both substantial variability and skewed distributions seem more plausible. Reports rarely provide estimates of variation in time required for specific aspects of care, but the few that do show that variation around the mean is considerable ( Myny et al., 2014 ). Left (negatively) skewed ward occupancy distributions have been reported ( Davis et al., 2014 ). When this is the case, mean staffing requirements are lower than the median, leading to relative understaffing more than 50% of the time if the mean is used.
Even where a mean adequately allows staff to meet variable demand, it is often unclear how much care needs to be observed to establish a reliable mean. As is clear from Myny et al. (2010) , estimating reliable means can be challenging even in a large scale study. The basis on which recommended observation periods were determined for widely used systems such as the Safer Nursing Care Tool is unclear because variation is not reported.
Variation in demand arises at multiple levels, for example patient census, need per patient and time taken to deliver care for a patient with a given set of needs. While some systems account for these factors to some extent, they rarely consider that the averages they use to determine staffing requirements, associated with a given factor, are also subject to variation. So while a task-based system may recognise that different patients require very different care, in assigning an average time it does not account for the variability in time taken to complete a task. In Table 3 , we summarise some major sources of variation. Variation around the average may be compounded as multiple aspects of care are considered, or may tend to ‘average out’, but this is simply unknown.
Sources of variation in demand for and supply of nursing care.
While task-based systems are challenged by the need to specify and time all aspects of nursing work, prototype systems cannot account for variation associated with activities that are not directly linked to the patient prototype. For example, patient turnover generates substantial nursing work ( Myny et al., 2012 ), which is highly variable between and within wards, with some predictable sources of variation (such as day of the week) ( Griffiths et al., 2018a ). Such variation is not easy to account for in a patient prototype because patients are admitted or discharged at points in time, while the prototype does not change.
Few systems formally consider non-patient factors that may influence workload. For example, while evidence that ward layout may alter staffing requirements is limited ( Hurst, 2008 ), simple factors influenced by layout such as travel distances and opportunity for patient surveillance are recognised as having the potential to generate considerable variation in workload ( Maben et al., 2016 , 2015 ). While variation arising from factors such as layout can be accommodated if times required are estimated for each unit, this does raise a final issue.
Variation is often systematic and just as demand is variable, so is the supply of staff to meet that demand (see Table 3 ). This is a particular issue when planning establishments and advance rosters to meet need. As an example, in order to ensure that there are sufficient staff available to provide cover on wards, the literature describes the need to add an “uplift” to establishments to allow for staff sickness ( Hurst, 2002 ; Telford, 1979 ). However, staff sickness does not occur uniformly. Rather it occurs in clusters, with clear seasonal patterns and variation by day of the week ( Barham and Begum, 2005 ). Allowing a small percentage of additional staff based on the average percentage of time lost does not mean that sufficient staff are available to cover days or weeks when staff are actually absent.
4.2. ‘Optimal’ staffing
Each staffing method makes an underlying assumption about what constitutes ‘adequate’, ‘safe’ or ‘quality’ staffing, although these are often implicit. The staffing to deliver the ‘right’ frequency and length of nursing tasks in the timed-task approach, and the ‘right’ amount of care per patient in the nurse-patient ratio approach must be decided upon. These parameters are generally obtained from expert judgement, from observations of care provided or from existing establishments, ideally in settings deemed to meet some quality criteria ( Hurst, 2002 ). The question of whether this staffing level is ‘optimal’, or what criteria might define an optimal staffing level is rarely, if ever, addressed.
There is evidence that staffing to the ‘optimal’ level defined by the RAFAELA tool is associated with reduced mortality when compared to lower staffing ( Junttila et al., 2016 ) but since mortality is further reduced by staffing at higher levels, it is hard to conclude that this staffing level is, truly, optimal. It is, in effect, a professional judgement about what constitutes reasonable staffing, which is, in turn, bounded by historical expectations ( Taylor et al., 2015 ; Telford, 1979 ). While this question arises in relation to the RAFAELA tool, because it explicitly identifies an optimum staffing level, the issue applies to all systems. While tools can motivate staffing increases it is also possible that they could restrict staffing at a level that is not clearly ‘optimal’.
The appropriate response to variation in the productivity of staff, related to factors such as experience or efficient deployment of a team, also makes any definition of an ‘optimal’ staffing level a challenge. While it seems important to recognise that (for example) less experienced staff may be less able to meet a given level of demand and thus require some additional support, setting a lower staffing level based on the relative efficiency of a team may appear to be punishing success. Furthermore, while most systems emphasise measurement of demand, optimal management of staffing involves achieving an appropriate balance between supply and demand. ‘Optimal’ staffing levels may be lower if peaks in demand can be reduced ( Litvak et al., 2005 ; Litvak and Laskowski-Jones, 2011 ). Nursing services do not operate in isolation and the demand for nursing care and the required level of staff may also change as inputs from other staff groups vary. Perhaps, above all, this illustrates that there is a limit to what can be achieved through measurement, both because of the fallible nature of the measures, but also because of the complex judgements that are required.
4.3. Limitations
The volume of literature considered for this review and the wide range of questions addressed means that we have not focussed on critiquing specific studies or attempting to draw conclusions about any particular approach. We may have missed some recent studies or older studies about some of the tools featuring in the more recent research. However, our approach of building on existing reviews and our extensive searches means that it is unlikely that we have missed substantial volumes of research that would lead to an overall different conclusion.
4.4. Future research
Staff costs and patient outcomes using different systems have rarely been compared. Controlled trials comparing outcomes of staffing guided by tools with other approaches may be challenging to undertake, but are by no means impossible to conceive. Cluster randomised trials may be feasible and controlled before-and-after studies of staffing systems have been reported or are underway ( Drennan et al., 2018 ). Because there are so many unanswered questions much progress can be made outside a trial framework. Natural variation around target staffing levels (for example due to staff sickness) provide further opportunity to study the association of target staffing levels with outcomes using quasi-experimental methods. Questions that remain unanswered about many tools include the extent to which they truly identify a level of staffing sufficient to meet the needs of a ward of patients, and the number of observations required to get an accurate baseline to estimate average need. The apparently simple assumption, that staffing to meet average need is the optimal response to varying demand, is also untested empirically, although research reviewed here suggests this assumption is likely to be incorrect. For systems designed to determine ward establishments, the extent to which the establishments efficiently or effectively deliver staffing levels to match varying patient need (either with or without additional flexible staffing) can be addressed in observational and simulation studies.
5. Conclusions
The volume of literature on staffing methodologies is vast and growing. However, there is no substantial evidence base on which to select any particular method or tool. There has been a repeated pattern whereby new tools are developed with little programmatic research addressed at existing tools, even when they are widely used. The extensive research reporting the development of the RAFAELA system stands out as an honourable exception in this regard, although neither costs nor effects of using the tool compared to another tool or no tool at all have been reported. Benefits associated with tools appear to be based on increased staffing levels.
Despite the lack of evidence, an appetite for formal systems and tools exists. While professional judgement remains the nearest to a gold standard, the desire to use a tool or other formal system to support and indeed justify such a judgement has remained a constant theme that can be traced back to Telford's work in the 1970s in the UK, and no doubt beyond. While limitations in tools have continually motivated the development of new approaches, limited evidence means it is hard to determine if existing approaches may be ‘good enough’ or if new approaches are any better in practice. The lack of discernible progress in building an evidence base leads us to conclude that rather than continue to develop new tools, it is time to take a much closer look at those already in use and to investigate the best way to use them and the costs and the consequences of doing so.
Conflict of interest
Other than the project funding, the authors declare no competing interests that might be perceived as influencing the results of this paper.
Acknowledgements and funding
This research was funded by the National Institute for Health Research’s Health Services & Delivery Research programme (grant number 14/194/21).
The views expressed are those of the author(s) and not necessarily those of the National Institute for Health Research, the Department of Health and Social Care, ‘arms-length’ bodies or other government departments.
The Safer Nursing Care Study Group comprises: Jane Ball (University of Southampton), Rosemary Chable (University Hospital Southampton National Health Service Foundation Trust), Andrew Dimech (Royal Marsden National Health Service Foundation Trust), Peter Griffiths (University of Southampton), Yvonne Jeffrey (Poole Hospital National Health Service Foundation Trust), Jeremy Jones (University of Southampton), Thomas Monks (University of Southampton), Natalie Pattison (University of Hertfordshire/East & North Herts NHS Trust), Alexandra Recio Saucedo (University of Southampton), Christina Saville (University of Southampton) and Nicky Sinden (Portsmouth Hospitals National Health Service Trust).
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.ijnurstu.2019.103487 .
Appendix. Supplementary materials
Essay on Nurse – 10 Lines, 100, 500, 1000 Words
Essay on Nurse: Explore the critical role and diverse responsibilities of nurses in this insightful Essay . From providing compassionate patient care to navigating complex healthcare systems, the article of Essay on Nurse delves into the challenges and rewards of the nursing profession.
Essay on Nurse highlights the evolving role of nurses as advocates, educators, and integral members of the healthcare team. Gain a deeper understanding of the impact of nursing on patient outcomes and the broader healthcare landscape, emphasizing the indispensable contributions of nurses in promoting well-being and ensuring quality healthcare delivery.
Table of Contents
Essay on Nurse in English in 10 Lines
This Essay on Nurse delves into the multifaceted role of nurses, exploring their vital contributions to healthcare, compassionate patient care, and the evolving dynamics of the nursing profession.
- Nurses play a pivotal role in healthcare, providing essential patient care and support.
- Their responsibilities range from administering medications to monitoring vital signs.
- Nurses serve as advocates, ensuring patients’ needs and concerns are addressed.
- Compassion is a hallmark of nursing, fostering a healing and supportive environment.
- Continuous education is integral, as nurses stay updated on medical advancements.
- Nurses collaborate with healthcare teams, contributing to comprehensive patient care.
- The nursing profession encompasses diverse specialties, from pediatrics to critical care.
- Nurses navigate challenging situations, demonstrating resilience and adaptability.
- The evolving role of nurses includes health promotion, disease prevention, and patient education.
- Their commitment to humanity makes nurses unsung heroes in the healthcare system.
Also See – If I were a Doctor Essay – 100, 500, 1000 Words, 10 Lines
Short Essay on Nurse in 100 Words
This Essay on Nurse explores the indispensable role of nurses in healthcare, emphasizing their compassionate patient care, advocacy, continuous education, and pivotal contributions to the evolving dynamics of the nursing profession in a concise 100-word description.
Nurses are the heartbeat of healthcare, providing essential care with unwavering compassion. Their role extends beyond administering treatments to embodying empathy, offering solace to patients.
Advocates for patient rights, nurses navigate complex medical landscapes, ensuring holistic care. Continuous education keeps them abreast of medical advancements. Nurses are pivotal collaborators within healthcare teams, contributing expertise to enhance patient outcomes.
From critical care to pediatrics, the diverse specialties within nursing reflect their versatility. Facing challenges with resilience, nurses are unsung heroes, embodying the human touch in the healthcare system and making an immeasurable impact on individual well-being and the broader healthcare landscape.
Essay on Nurse in 500 Words
This Essay on Nurse delves into the multifaceted world of nursing, exploring the pivotal role of nurses, their compassionate patient care, advocacy, continuous learning, and contributions to the dynamic healthcare landscape within a comprehensive 500-word description.
The Essence of Nursing: A Compassionate Journey in Healthcare
Nursing stands as the heartbeat of healthcare, a profession that transcends clinical duties to embody compassion, dedication, and versatile expertise. At its core, nursing is about providing fundamental care that shapes the patient experience.
From administering medications with precision to vigilantly monitoring vital signs, nurses execute diverse responsibilities that form the bedrock of quality healthcare. The essence of nursing, however, goes beyond technical skills; it’s the ability to infuse these tasks with unwavering compassion, creating an environment conducive to healing and support.
Beyond their clinical roles, nurses take on the mantle of patient advocates. In the labyrinth of the healthcare system, they ensure the voice of the patient is not lost. Advocacy is not just a component of nursing; it’s a commitment to safeguarding the well-being and dignity of those under their care. A nurse’s role extends far beyond the administration of treatments; it involves being a steadfast advocate, navigating the complexities of healthcare on behalf of the patient.
Compassion is the hallmark of nursing. In the emotionally charged realm of illness, nurses provide not only medical care but also emotional support. Their compassionate touch becomes a source of solace in moments of vulnerability, fostering a healing environment that transcends medical treatments. This empathetic connection with patients is what sets nursing apart, turning it into not just a profession but a calling driven by the innate desire to alleviate suffering and promote well-being.
Nursing is a dynamic profession that necessitates continuous education and adaptability. Staying abreast of the latest medical advancements, mastering cutting-edge technologies, and evolving with the ever-changing landscape of healthcare are inherent to nursing practice. The commitment to ongoing education ensures that nurses provide care at the forefront of medical knowledge, contributing to positive patient outcomes in an increasingly complex healthcare environment.
Nurses function as integral collaborators within interdisciplinary healthcare teams. Their expertise extends beyond bedside care; they actively contribute to comprehensive patient management. Effective communication and collaboration with physicians, therapists, and other healthcare professionals are fundamental aspects of nursing practice. This collaborative approach ensures a holistic, patient-centered care model that addresses the myriad dimensions of health and well-being.
The nursing profession spans a vast array of specialties, underscoring its versatility. From critical care units to pediatric wards, nurses adapt their skills to meet the unique demands of various healthcare settings. This diversity in specialties emphasizes the breadth and depth of their impact on patient outcomes, showcasing the adaptability of nursing professionals to different medical contexts.
Despite its rewarding aspects, nursing is not without its challenges. Nurses navigate demanding work hours, emotionally taxing situations, and high-stress environments with resilience. The ability to face adversity with poise and adaptability is a testament to the strength of character inherent in nursing professionals. Their commitment to patient well-being remains unwavering, even in the face of formidable challenges.
In essence, nurses are the unsung heroes of the healthcare system. Their contributions extend beyond the clinical realm, embodying the human touch that distinguishes healthcare from mere medical interventions. While often working behind the scenes, nurses bridge the gap between medical expertise and compassionate, empathetic care. They exemplify the profound difference that compassionate care can make in the journey to health and healing, positioning nursing as an indispensable pillar of the healthcare system.
1000 Words Essay on Nurse in English
This 1000-word Essay on Nurse explores the multifaceted role of nurses, delving into their compassionate patient care, advocacy, continuous learning, collaborative contributions to healthcare teams, and the evolving dynamics within the nursing profession.
The Heart of Healthcare: Exploring the Profound Role of Nurses
Introduction
The nursing profession stands as the heartbeat of healthcare, embodying compassion, expertise, and resilience. This essay delves into the multifaceted world of nursing, exploring its pivotal role, the challenges faced, and the evolving dynamics within the healthcare spectrum.
The Essence of Nurse: Providing Fundamental Care
At the core of nurse lies the provision of fundamental care that shapes the patient experience. This Essay on Nurse explores the diverse responsibilities of nurses, from administering medications to vigilantly monitoring vital signs. The essence of nurse goes beyond technical skills; it is about infusing these tasks with unwavering compassion, creating an environment conducive to healing and support.
Advocacy: Ensuring the Patient’s Voice is Heard
Nurses are not only caregivers but also advocates for patients within the complex healthcare system. This Essay on Nurse delves into how nurses navigate the labyrinth of healthcare to ensure the patient’s voice is not lost. Advocacy is not just a component of nursing; it is a commitment to safeguarding the well-being and dignity of those under their care.
Compassion as a Hallmark: Fostering a Healing Environment
Compassion is the hallmark of nursing, turning it from a profession into a calling. This Essay on Nurse explores how nurses, in the emotionally charged realm of illness, provide not only medical care but also emotional support. Their compassionate touch becomes a source of solace in moments of vulnerability, fostering a healing environment that transcends medical treatments.
Continuous Education and Adaptability
Nurse is a dynamic profession that demands continuous education and adaptability. This Essay on Nurse delves into the necessity of staying abreast of the latest medical advancements, mastering cutting-edge technologies, and evolving with the ever-changing landscape of healthcare. The commitment to ongoing education ensures that nurses provide care at the forefront of medical knowledge.
Collaborators in Healthcare Teams: Enhancing Patient Management
Nurses function as integral collaborators within interdisciplinary healthcare teams. This Essay on Nurse explores how their expertise extends beyond bedside care, actively contributing to comprehensive patient management. Effective communication and collaboration with physicians, therapists, and other healthcare professionals are fundamental aspects of nursing practice, ensuring a holistic, patient-centered care model.
Diverse Specialties, Versatile Roles: Adapting to Healthcare Settings
The nursing profession encompasses a myriad of specialties, showcasing its versatility. This Essay on Nurse delves into how nurses adapt their skills to meet the unique demands of various healthcare settings. From critical care units to pediatric wards, the diversity in specialties emphasizes the breadth and depth of their impact on patient outcomes.
Facing Challenges with Resilience
Despite its rewarding aspects, nursing is not without its challenges. This Essay on Nurse explores how nurses navigate demanding work hours, emotionally taxing situations, and high-stress environments with resilience. The ability to face adversity with poise and adaptability is a testament to the strength of character inherent in nursing professionals.
Unsung Heroes in Healthcare: Bridging the Gap with Compassion
This Essay on Nurse highlights the often-overlooked contributions of nurses as the unsung heroes of the healthcare system. Their impact extends beyond the clinical realm, embodying the human touch that distinguishes healthcare from mere medical interventions. While often working behind the scenes, nurses bridge the gap between medical expertise and compassionate, empathetic care.
In conclusion, nursing stands as an indispensable pillar of the healthcare system. This essay has explored the multifaceted role of nurses, from providing fundamental care to advocating for patients, fostering a healing environment with compassion, and actively contributing to patient management within healthcare teams.
Their adaptability to diverse specialties and resilience in facing challenges exemplify the strength of character inherent in nursing professionals. As the unsung heroes of healthcare, nurses embody the human touch, making a profound difference in the journey to health and healing.
In conclusion, the essay on nurse has illuminated the multifaceted role of nurses in healthcare. From compassionate patient care to critical decision-making, nurses play a pivotal role in promoting well-being. The essay emphasizes the significance of their skills, dedication, and adaptability in a dynamic healthcare landscape. As integral members of the healthcare team, nurses not only provide essential medical services but also contribute to the overall patient experience. This exploration underscores the importance of recognizing and appreciating the tireless efforts of nurses in fostering a healthier society.
Related Essays
Essay on Modern Indian Woman – 100, 500, 1000 Words, 10 Lines

Essay on Future of English in India – 10 Lines, 500 & 1000 Words
Essay on Bhai Dooj – 10 Lines, 100, 500, 1000 Words
Essay About Ooty – 10 Lines, 500 & 1000 Words

Draupadi Murmu Essay – 10 Lines, 100, 500, 1000 Words
Computer Essay – Short Essay, 10 Lines, 500 & 1000 Words
Leave a comment cancel reply.
Save my name, email, and website in this browser for the next time I comment.
Essay Sample on Why I Want to Be A Nurse
Nursing is a rewarding and challenging career that has the power to make a real difference in people’s lives. Whether your motivation is to help others, attain financial freedom, or both, writing a “Why I Want To Be A Nurse” essay is an excellent opportunity to express your passion and commitment to the field.
In this article, we’ll explore the reasons why you might want to become a nurse and provide you with helpful tips and inspiration for writing a powerful and persuasive essay .
Why I Want to Be A Nurse (Free Essay Sample)
Nursing is a career that offers a unique combination of hands-on care and emotional support to those in need. There are many reasons why someone might choose to become a nurse, including:
The Empathy and Altruism of Nursing
I have a strong desire to help people and hope to become a nurse. I think nursing is the best way for me to make a difference in other people’s lives because it combines my natural empathy and desire to help people. Nursing gives me a chance to positively touch people’s lives, which has always attracted me to the thought of doing so.
I saw the beneficial effects that nurses may have on people’s life as a child. I have always been moved by the kindness and concern they have for their patients. The small gestures of kindness, like holding a patient’s hand or speaking encouraging words, have always touched me. I think nurses have a special power to change people’s lives and leave a lasting impression, and I want to contribute to that.
Additionally, I think that becoming a nurse is a great and selfless job. To provide for their patients and ensure they are secure and comfortable, nurses put their own needs on hold. I absolutely respect this kind of dedication to helping others, and I aim to exhibit it in my own nursing career.
The Economic Benefits of Nursing
The financial stability that comes with being a nurse is one of the reasons I wish to pursue this career. Nursing is a field that is in high demand, which translates to a wealth of job opportunities and competitive salaries. This profession offers the chance for a stable income, which makes it a good choice for people who want to secure their financial future.
Nursing not only gives economic freedom but also a flexible work schedule that promotes a healthy work-life balance. Many nurses can choose to work part-time or in a variety of places, such as clinics, hospitals, and schools..
A Love for the Science and Art of Nursing
To succeed in the unique field of nursing, one must have both artistic talent and scientific knowledge. This mix is what initially drew me to the thought of becoming a nurse. The human body and its mechanisms have always captivated me, and I enjoy learning about the science that underpins healthcare. But nursing requires more than just a scientific knowledge of the body. It also requires an artistic understanding of the patient and their needs.. Nursing is a demanding and fulfilling job since it combines science and art, which is why I’m drawn to it.
I saw as a child the effect nurses had on patients and their families. Their compassion and understanding have motivated me to seek a profession in nursing because they frequently offer comfort and help in the hardest of situations. My enthusiasm for the science and art of nursing will undoubtedly help me to have a good influence on other people’s lives. I want to work as a nurse and improve the lives of the people I take care of, whether it be by giving medication, educating patients, or just being a reassuring presence.
Continuous Professional Development in Nursing
I think the nursing industry is dynamic and always changing, which gives people a lot of chances to learn and grow. I would have the chance to continuously advance my knowledge and abilities in this sector if I choose to become a nurse. In turn, this would enable me to better care for my patients and stay abreast of professional developments.
There are several different nursing specialties available as well. There are many options, including critical care, pediatrics, gerontology, and surgical nursing. Because of the variety of disciplines available, nurses have the chance to develop their interests and find their niche.
I am certain that a career in nursing will provide me the chance to pursue my passion for healthcare while also allowing me to grow professionally.
Nursing is a fulfilling and noble career that offers a mix of hands-on care, emotional support, and professional growth. I am inspired by the positive impact nurses have on patients and their families and aim to offer my own empathy and compassion. The nursing industry is constantly changing, providing ample opportunities for growth and job prospects with financial stability. The ultimate reward in a nursing career is the satisfaction of making a difference in people’s lives.
Tips for Writing A Compelling Why I Want To Be A Nurse Essay
Now that you understand the reasons why someone might want to become a nurse, it’s time to learn how to write a compelling essay. Here are some tips and strategies to help you get started:
Create an Outline
Before you start writing, it’s important to identify the main points you’ll discuss in your essay. This will help you stay organized and make your essay easier to read.
Start with an Attention-grabbing Introduction
Your introduction is your chance to make a good first impression and engage the reader. Start with a hook that captures the reader’s attention, such as a surprising statistic or personal story .
Be Specific and Personal
Rather than making general statements about why you want to become a nurse, be specific and personal. Share your own experiences, motivations, and passions, and explain why nursing is the right career choice for you.
Highlight your Skills and Qualifications
Nursing is a demanding and complex profession that requires a wide range of skills and qualifications. Be sure to highlight your relevant skills, such as compassion, communication, and problem-solving, and explain how they make you a good fit for the nursing field.
Related posts:
- The Great Gatsby (Analyze this Essay Online)
- Pollution Cause and Effect Essay Sample
- Essay Sample on How Can I Be a Good American
- The Power of Imaging: Why I am Passionate about Becoming a Sonographer
Improve your writing with our guides

Youth Culture Essay Prompt and Discussion

Why Should College Athletes Be Paid, Essay Sample

Reasons Why Minimum Wage Should Be Raised Essay: Benefits for Workers, Society, and The Economy
Get 15% off your first order with edusson.
Connect with a professional writer within minutes by placing your first order. No matter the subject, difficulty, academic level or document type, our writers have the skills to complete it.
100% privacy. No spam ever.

- Account Settings
FEATURED INSIGHTS
- Site-of-care shifts
- Specialty care
- State of the healthcare industry
- The workforce crisis
- Value-based care
- View all featured insights
RESOURCES BY SECTOR
- Digital health
- Health plans
- Hospitals and health systems
- Medical device
- Physicians and medical groups
- Professional services
- View all sectors
NEWS & INSIGHTS
- Daily Briefing
- Radio Advisory
- Advisory Board tools
PRODUCTS & SERVICES
- Research Membership
- Custom Research
- Expert Support
- Advisory Board Fellowship
- On-Demand Courses
- Sponsorship
FEATURED CONTENT
Truly personalized care is possible. here's how to make it a reality..
Learn to navigate 4 key obstacles to improve patient access to innovative care.

- AskAdvisory
Our direct-to-expert service is here to help you navigate your membership, our research, and your most pressing challenges in healthcare. No question is too big or too small.
Nurses Week 2024: Support and celebrate your staff
For Nurses Week 2024, we're celebrating the remarkable impact nurses have on the organizations and communities they serve . Advisory Board 's Allyson Paiewonsky explains how nursing leaders can support their staff and provides resources to help leaders address key challenges facing the nursing workforce today.
3 underlying causes of nurse recruitment and retention challenges
Today marks the first day of Nurses Week 2024 — an annual commitment established by the American Nurses Association (ANA) to recognize the invaluable contributions of nurses.
This year's theme, "Nurses Make the Difference," coincides with the ongoing efforts of C-suite leaders to stabilize their nursing workforces. Despite significant time and resource investments, overall RN turnover remains too high and first-year turnover is particularly challenging. As a result, nursing leaders are understandably concerned about the RN workforce shortage and focused on addressing urgent challenges.
As nursing leaders navigate the challenges facing their workforces, it is vital for them to provide support and guidance. Here are three key opportunities nursing leaders can leverage in 2024 and beyond.
1. Prioritize making improvements to nursing work environments
The workforce crisis has highlighted the undeniable difference nurses make in care teams and the overall success of their organizations. Nurses' contributions extend far beyond patient care — they play a central part in driving the success of healthcare organizations, influencing patient outcomes and satisfaction, and maintaining operational excellence.
It is crucial that hospitals and health systems recognize their importance by prioritizing improvements to nurses' work environments. This includes ensuring adequate staffing levels, manageable workloads, and access to necessary emotional health and wellbeing resources. By investing in nurses' work environments, we can enhance job satisfaction, reduce burnout, and improve patient safety and quality of care.
We've put together resources to help healthcare leaders honor nurses by making meaningful impacts in their work environments:
- 5 ongoing challenges of the workforce crisis — and what to do about them
- How Allegheny Health Network's Blended Nursing Model Addresses Staffing Shortages
2. Deploy AI and technology to streamline workflows
Nurse workflows have become inundated with repetitive administrative tasks that detract from their clinical training. In an era of technological advancements, artificial intelligence (AI) has the potential to revolutionize nursing workflows. By leveraging AI-powered tools, nurses can streamline administrative tasks, allowing them to focus more on direct patient care. For instance, AI-assisted triaging, automated vital sign data entry, and clinical decision support can augment nursing workflows, thereby freeing up valuable time for nurses to spend with their patients.
While AI is well-positioned to support nurses, it should not be a replacement for nurses. AI can't comprehensively fulfill a nurse's full scope of practice — nursing is much more than completing tasks, as it involves building relationships and critical thinking. Nurses and their unique expertise make a difference in patient care.
When leaders are thinking about implementing AI and other technologies, it is crucial to include nurses in selecting and implementing technology that will impact their day-to-day work. Nurses should actively be involved in tech decision-making and implementation if we want those investments to succeed.
While leaders should not leverage technology to replace nurses, they should use it to help nurses practice at the top of their licenses. Here are a few resources to help leaders understand how technology can streamline workflows and address workforce challenges:
- AI nurses? Inside Nvidia, Hippocratic AI's new partnership
- 3 ways AI can help nurses
- How technology can help solve the workforce crisis
3. Leverage virtual nursing to ease workforce shortage pain points
Virtual nursing offers a transformative solution that not only addresses a shortage of nurses but also provides crucial support to novice nurses. By offloading administrative tasks or delegating specific care responsibilities to a virtual nurse, bedside nurses receive more time for direct patient interaction.
Additionally, through virtual platforms, novice nurses can collaborate with experienced mentors, seek guidance, and receive real-time feedback. This virtual support system helps bridge the experience gap and empowers novice nurses to gain confidence and competence in their practice. We compiled a list of resources to help leaders understand the benefits of virtual nursing, with guidance on how to implement a virtual nursing program:
A detailed look at the top 2 models for virtual nursing care
- Virtual nursing: What it is, and why we need it
- Your how-to guide for implementing a virtual nursing program
Ultimately, nurse leaders shouldn't act alone in addressing these concerns — other members of the C-suite at hospitals and health systems need to lend their support as well. The best way to do this is to give nursing leaders the ability to implement innovative solutions to best support their nurses. To learn more about how health systems can help address nursing leaders' concerns, read our take on what health systems should know about nurse leaders' priorities.
On May 9, join us for a transformative webinar that challenges the conventional wisdom on leadership development. Also, tune into Radio Advisory on May 7 for our podcast episode celebrating Nurses Week.
Is this content helpful?

Allyson Paiewonsky, MPH
Posted on May 06, 2024
Updated on May 06, 2024

4 key concerns of nurse leaders — and how the rest of the C-suite can help

4 essential EOY conversations to have with your nursing team
We help leaders and future leaders in the healthcare industry work smarter and faster by providing provocative insights, actionable strategies, and practical tools to support execution.
- All Resources
- Our History
- Legal Disclaimer
- Privacy Policy
- Terms of Use
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:

- About About IWF The Women of IWF Champion Women Board of Directors Join Our Team Fellowship Program Affiliated Websites Code of Ethics Shop Media Requests Member Login
- Policy Center Center for Economic Opportunity Center for Energy and Conservation Education Freedom Center Independent Women's Law Center
- Programs She Thinks Podcast High Noon Podcast Bespoke Podcast At The Bar Students Over Systems Event
- Real Stories Women's Prisons Stories Identity Crisis Stories Female Athlete Stories Dissident Stories Stand With Women Stories ESA Stories Kids First Stories Healthcare Price Transparency Stories Chasing Work Stories
- Economy Government Spending Jobs Mobility Regulations Socialism Taxes
- Culture Community Family Feminism Media & Entertainment Personal Freedom Political Correctness Sex & Gender
- Health Costs & Accessiblity Drugs Health Care Wellness
- Environment Conservation Progress
- Innovation Agriculture Safety Tech
- Education Higher Ed K-12 School Choice Title-IX Transparency Divisive Ideology
- Law 1st Amendment Administrative State Civil Justice Reform Criminal Justice Reform Electoral College Judiciary Sex Discrimination
- Security Foreign Affairs United Nations Immigration National Defense
- Work Career Advice Child Care ERA Gender Quotas Harassment Paid Leave Wage Gap
How a New Charter School Model Puts Rural High Schoolers on Path to Nursing
Last Friday, a public charter school in rural West Virginia graduated its first-ever class of high school seniors. For some of the newly-minted graduates of WIN Academy , their college graduation is only one year away.
This new charter school has students earn a year’s worth of college credits toward a nursing degree while completing the requirements for their high school diplomas. The new alumni are now only two semesters away from an associate’s degree in nursing, which will allow them to start their careers in less time and at less expense than they would through a traditional pathway.
The WIN Academy model, created by BridgeValley Community and Technical College president Dr. Casey Sacks, was designed to help meet the needs of students and the communities they will go on to serve. The country needs more nurses; the U.S. Chamber of Commerce forecasts there will be 193,100 job openings for registered nurses every year between 2022 and 2032. But only 177,400 people will join the nursing workforce over those same ten years, according to the Bureau of Labor Statistics .
In West Virginia, the need for nurses is especially acute . And to stave off a workforce crisis, a systemic change must make the profession more accessible than it is now.
WIN Academy graduates say they are thankful for the opportunity to fast-track their path to a college degree. Allyson Randolph, class of 2024, said, “I feel like I just got that jump-start” by choosing to attend WIN Academy rather than her government-assigned high school for her senior year.
Though transferring schools meant leaving her friends and the typical high school traditions, Randolph says her decision helped her hone in on what future career she wants. “I always knew I wanted to go into the medical field,” she said, “I just didn’t know what part of the medical field.”
Kaden Thaxton graduated with Randolph last weekend. He said, “You’re given all the resources to excel” in the unique educational model, including resources other schools do not provide. Among the most meaningful opportunities for Thaxton were clinicals, which are day-long shadowing experiences in the medical field. Thaxton participated in clinicals at a day care, a nursing home, and a hospital. In the fall, Kaden will continue working towards an associate’s degree at BridgeValley.
Graduates of the high school are admitted automatically to BridgeValley, where they can complete their associate’s degree in nursing in one year or work toward transferring to a four-year college. (Someone can become a Registered Nurse with an associate’s degree, though a bachelor’s degree opens up more opportunities for leadership and career advancement.)
Dr. Sacks sees the potential for this educational model to extend into other industries. In the fall, she’ll launch WIN Academy Advanced Manufacturing, which replicates the same concept to prepare students for a different in-demand industry.
Disclaimer: The author of this piece worked with WIN Academy founder Dr. Casey Sacks at the U.S. Department of Education and works with Dr. Sacks to spread awareness of BridgeValley Community and Technical College and WIN Academy.
Stay Connected
Stay up-to-date with everything IWF! Sign up for our newsletter:
Celebrating and Connecting with Our Elders
Jennifer oliver o’connell | $(document).ready( function() { // or shorthand of $( function () { $.each($(".latest-author"), function(index, value ) { if($( this ).text().indexof("’") >= 0){ $author_name = $( this ).text(); $new_text = $author_name.replace("’", "'"); $( this ).text($new_text); } }); }); blog, los angeles teachers union members skip school to demand more money, ginny gentles | $(document).ready( function() { // or shorthand of $( function () { $.each($(".latest-author"), function(index, value ) { if($( this ).text().indexof("’") >= 0){ $author_name = $( this ).text(); $new_text = $author_name.replace("’", "'"); $( this ).text($new_text); } }); }); blog, the problem with ‘scouting america’, elizabeth grace matthew | $(document).ready( function() { // or shorthand of $( function () { $.each($(".latest-author"), function(index, value ) { if($( this ).text().indexof("’") >= 0){ $author_name = $( this ).text(); $new_text = $author_name.replace("’", "'"); $( this ).text($new_text); } }); }); blog, carbon offsetting can’t escape controversy, gabriella hoffman | $(document).ready( function() { // or shorthand of $( function () { $.each($(".latest-author"), function(index, value ) { if($( this ).text().indexof("’") >= 0){ $author_name = $( this ).text(); $new_text = $author_name.replace("’", "'"); $( this ).text($new_text); } }); }); blog, sign up for updates.
- Cell (optional)
- Become a Mobile Insider. Text WOMAN to 40442 to opt in. Sign up for recurring informational messages from IWF. Msg&data rates may apply. Terms & Privacy Policy.
- Phone This field is for validation purposes and should be left unchanged.
- Share full article
Advertisement
Supported by
Women at Work, and With Their Families Too
More from our inbox:, mythologizing trump, mentally ill and in prison, say no to more offshore drilling.

To the Editor:
Re “ An Act of Defiance Can Improve Things for Working Moms ,” by Toby Kiers (Opinion guest essay, May 4):
I am a woman nearing the completion of my B.A. in philosophy, and I have the absurd hopes of going on to get my Ph.D. and work in academia and also have a family.
Dr. Kiers’s essay both shed light on the frustrating reality of the discrimination that mothers face in the world of academic research, and provided a shining beacon of hope to counteract it.
The false binary that women are presented and that so many people (including Dr. Kiers’s own child, she noted) assume is that we must decide: our research, our careers, our academic endeavors, or our children. One or the other.
Dr. Kiers has called this out; this is not actually a choice we have to make. Motherhood is not a detriment to our academic abilities and research contributions; it actually strengthens it in new and unexpected ways.
Dr. Kiers, in her refusal to choose between her research pursuits and her family, is helping to forge an exciting path forward. It is a path to a world where women can be celebrated, respected and supported with all that they are and all that they contribute, including their children.
That is the academic world I hope to enter into someday.
Megan Clancy Washington
Kudos to Dr. Toby Kiers! Her story is shared not only by fellow scientists, but by women at large. I admire her courage in bringing her 3-week-old son to work, and in pondering the advice of an older woman who discouraged her from being self-deprecating.
“What can feel like an inconvenience is often a blessing in disguise,” she writes. Amen to that! As far as detachment and vulnerability creating meaning? I now see vulnerability being valued and detachment being questioned in health care, via narrative prose and poetry by nurses and physicians.
I am a seasoned nurse. This article brought me back to the AIDS epidemic. In terms of science, we really had no idea what we were dealing with. I was on maternity leave and had come to know “brain fog” intimately. I received a call asking if I would open a new department for AIDS. After a day thinking about it, I accepted. My two boys went with me into the wilderness of men dying of a virus we knew little about.
My sons are now 40 and 50. The older one still recounts stories of things he learned and joy he felt at a party that those dying men held for us nurses on Mother’s Day. Vulnerability informing the work? You bet!
Pamela Mitchell Bend, Ore.
Since I am a woman who walked across the medical school graduation stage holding my toddler, while eight months pregnant with No. 2, I can certainly identify with Toby Kiers’s essay about managing a career as a scientist while parenting.
It was extremely trying for me to charge into residency with very small children at home. But I am blessed to have a wonderful husband who loved fathering, and was able to take a sabbatical for some of my residency.
As a result, our two daughters, now young adults, are very close to their father. I think that this is the real win in how things are evolving for women in the workplace. Partners get to join in on the nitty-gritty as well as the glorious moments of parenting.
I do believe I missed out on the sort of lovely parenting my mother gave me as a stay-at-home mom. But I was also able to show our daughters what commitment to an intellectual and humanistic goal looks like.
I certainly think medical residency programs are over the top in terms of workload and emotional toll; this needs to evolve. But I think enjoying the participation of both parents in the up-close-and-personal part of child-rearing makes all of our children stronger.
Susan Ferguson Berkeley, Calif.
Re “ Trump Embraces Lawlessness in the Name of a Higher Law ,” by Matthew Schmitz (Opinion guest essay, April 4):
Mythologizing Donald Trump — either Mr. Schmitz fancifully comparing him to outlaws like Robin Hood, Billy the Kid and Jesse James, who titillated people with their challenges to authority, or Christian evangelicals’ even more far-fetched casting of Mr. Trump as King Cyrus or even Jesus — fails because most of us see him for what he is, a narcissist with no positive agenda and no respect for the law.
If we must make comparisons, it’s to David Duke, the Klansman who ran for president, or Gov. George Wallace, standing in the schoolhouse door to block integration. The only people who saw them as rebels with a cause were themselves defending a lost cause, much like those who flock to MAGA now.
Steve Horwitz Moraga, Calif.
Re “ Inmate’s Death Highlights Failures in Mental Health ” (front page, May 6), about the troubled life and death of a prisoner, Markus Johnson:
As a social worker who has worked in the field of mental health for more than 50 years, I read with interest and sadness yet another article about a mentally ill individual who was not provided with adequate treatment and subsequently died in prison.
This article highlights the failure of deinstitutionalization. It demonstrates how our prisons have become the institutions replacing those that formerly housed the mentally ill. Not only are the mentally ill being ill served, but so too is the public, which is at risk of harm from those hallucinating on the streets.
Our shelter system is also not in a position to manage needed services and supervision. The last resort is a cell. I believe that providing long-term residential programs with highly supervised step-down programs would provide a solution to the tragedies we currently read about daily. Certainly the cost would be less than incarceration.
Let’s look to providing real help rather than punishment for our mentally ill population.
Helen Rubel Irvington, N.Y.
“ Offshore Oil Production Expands as Companies Cite Energy Needs ” (Business, May 10) lays out Big Oil’s plan for the Gulf of Mexico. Let’s be real: We’re in a global climate crisis. The last thing we need is for the fossil fuel industry to expand offshore drilling.
If climate change, rising ocean temperatures and the risk of horrific events like the Deepwater Horizon disaster weren’t enough reason to stop offshore oil expansion, we also know that this industry cannot be counted on to clean up its mess when the wells have run dry.
There is a huge backlog when it comes to plugging defunct or abandoned wells, removing old oil platforms and remediating the seafloor damaged by drilling operations. Oil and gas companies have already littered the Gulf of Mexico with more than 18,000 miles of disused pipeline and over 14,000 unplugged wells , which can leak chemicals like methane into the ocean.
It also comes with financial risks: If offshore oil and gas operators file for bankruptcy (as 37 have done since 2009 ), U.S. taxpayers could be forced to foot the bill for cleanup.
Enough is enough: We cannot afford more offshore drilling.
Andrew Hartsig Anchorage The writer is senior director, Arctic conservation, for Ocean Conservancy.
Manitoba taking steps to increase oversight of private nursing agencies, premier says
Province issuing rfp for agencies to become validated, allowing them to work with service providers: kinew.

Social Sharing
The Manitoba government wants to have more oversight over private nursing agencies in the province and is taking steps toward that, Premier Wab Kinew says.
The province is issuing a request for proposals for private nursing agencies to become validated by the province, allowing them to work with service providers in Manitoba, Kinew said during his inaugural state of the province address with the Brandon Chamber of Commerce on Thursday.
Nurses have been leaving Manitoba's public health-care system in droves for private agencies amid growing frustrations with things like mandatory overtime, nurse to patient ratios, working conditions and growing violence combined with a lack of scheduling flexibility, Kinew said.
"What it means for our provincial health-care system is we still have to staff these health-centres … but now we're paying [agency nurses] more than ever to do so," he said.
"We're trying to be fiscally responsible … and we're looking at the situation with agencies, and thinking we have to take action."
- Manitoba spent $3.9M in 1 year on private nurses to fill shortages in Winnipeg, Opposition NDP says
- Nursing agencies are staffing hospitals at 'huge cost' to health-care system, experts say
The province spent $56 million on agency nurses in the first three quarters of the 2023-24 fiscal year, according to preliminary data from Shared Health, of which $21 million was spent in Prairie Mountain Health, the health authority in southwestern Manitoba.
Kinew says that number shows "an increasing reliance on agency nurses" across Prairie Mountain. The province is also hearing concerns about the conditions those nurses are working under, he said.
"One of the anecdotes is a nurse [who] works in one centre, drives to a different centre where they're picking up an agency shift, [and] sleeps in the car on the side of the road in between," he said.
"Do you want to be the patient — or do you want your loved one, your kid, your parent — to be the patient for the nurse that's being run off their feet travelling from one site to the other?"

Manitoba has agreements with 75 different private nursing agencies that were signed by the previous Progressive Conservative government, Kinew said.
He drew a comparison to British Columbia, which has nearly four times the population of Manitoba but just 19 private nursing agencies, he said.
"I think the case is pretty clear that we need to have greater oversight. We need to take some action."
'Necessary,' nurses union president says
Manitoba Nurses Union president Darlene Jackson says she's pleased by the announcement.
Holding private and for-profit nursing agencies to the same standard as nurses employed in Manitoba's public health-care system "is not only reasonable, but necessary," she said in a Thursday statement to CBC.
A resolution passed at the Manitoba Federation of Labour's annual convention last week pledged that the nurses' union would work in collaboration with the federation to lobby the provincial government to start regulating the use of agency nurses.
- Manitoba's nurses reach tentative contract with employers only weeks after last contract expired
- Manitoba's rural emergency departments closed for 80,000 hours in 2023: data
Kinew said the work behind Thursday's announcement began before the resolution was passed, but he hopes it addresses the concerns raised by the labour federation and the union.
The province cannot realistically introduce a mandate targeting nursing agencies, he said, because they're being used to keep some of its health-care facilities open.
However, validating agencies means "we'll be able to ensure that there are standards in place, that there are … health and safety regulations being put into place," he said.
"And most importantly…. we're going to start to put an incentive structure in place here in Manitoba that will make the public health-care system that you rely on a more attractive place to work, while also being more self-sustaining from a cost perspective."
Corrections
- An earlier version of this story reported that Kinew said Manitoba spent $56 million on agency nurses in the 2023-24 fiscal year. Shared Health later clarified that preliminary data shows the province spent that amount of money in the first three quarters of the fiscal year. May 16, 2024 6:26 PM CT
With files from Chelsea Kemp
Related Stories
- Former Manitoba premier Heather Stefanson resigning as MLA
- N.B. premier wrong to blame immigration for housing crisis, advocates say
- Nova Scotia premier believes Northern Pulp plant will never reopen
- P.E.I. premier withdraws unparliamentary comment during heated exchange
- Feds give Manitoba $19.2M to boost wildfire fighting capacity, province matches for $38.4M total
Need help organizing for summer? We tapped 'The Home Edit' stars for their recommendations
- TODAY Plaza
- Share this —

- Watch Full Episodes
- Read With Jenna
- Inspirational
- Relationships
- TODAY Table
- Newsletters
- Start TODAY
- Shop TODAY Awards
- Citi Concert Series
- Listen All Day
Follow today
More Brands
- On The Show
It’s Nurses Appreciation Week! 16 deals to show those superheroes some love

Long hours in the hospital, last-minute shifts and running through emergency rooms are things superheroes do — AKA nurses! National Nurses Week celebrates the healthcare staff and is blessing them with discounts across different categories.
From May 6 to May 12, all nurses can take advantage and save on skincare, wellness, food, clothing and more. And if you’re a nurse or have a caregiver in your life who's looking for comfort, this is the time to splurge on a pair of high-quality sneakers and thank them for their hard work.
So whether they need a new set of scrubs or should upgrade their Stanley Quencher , there are plenty of deals and highlights that fit their work lifestyle. You'll need to have your work identification handy to take advantage of the best offers. (Some of these deals also apply to the U.S. military, first responders and teachers , too.)
Discounts for Nurses Appreciation Week | Year-round discounts and deals for nurses
Discounts for Nurses Appreciation Week
America's favorite coffee chain is offering a free cup of Joe at participating restaurants during Nurse Appreciation Week.

Catarina One-Pocket Scrub Top
Nurses can score 20% off sitewide on new items for men and women.
NursesMates

Dove Slip-on
Looking for a shoe that withstands a 12-hour shift? This brand is offering 25% off site-wide when you use the code NURSE25 .

European Linen Sheet Set
This affordable brand is offering nurses 10% off their first purchase including one of Quince's best sellers, the European Linen Sheet Set.
Year-round discounts for nursep

Adidas Country OG Shoes
All verified medical professionals, first responders, nurses, teachers and military members can get an exclusive discount of 30% online and 15% at factory outlets.

This shoe brand is loved by many medical professionals and nurses, and they can get a 25% discount across eligible items online.

Comrad Compression Socks
This brand offers compression socks made for all-day support and comfort. Healthcare workers can get a special discount up to 35% off when they sign up.

Crocs Classic Clog
Nurses and healthcare workers receive 15% off all full-priced styles after registering with ID.me.

e.l.f. Cosmetics Sheer Slick Lipstick in Black Cherry
You might be saving lives but that doesn't mean your beauty routine has to pivot. Essential workers can get 25% off on e.l.f. cosmetics through their discount program .
Factor Meals

Sometimes taking a break during work is hard. This brand offers nurses 55% off on the first box and 15% off on your next boxes for over a year.
Hello Fresh

Hello Fresh Meal Delivery Kit
Nurses can get 60% off on their first box of easy-to-make meals , and 15% off for 51 weeks.

Iconic Western Denim Shirt
Whether you need a new tee or a pair of jeans, nurses can score up to 15% off site-wide when they verify their license.

Lululemon Align High-Rise Short 6"
This athleisure brand is raved by many athletes and healthcare workers, so if you're on the field you can get 15% discount year-round.

Stanley The Quencher H2.0 FlowState Tumbler
Hospital employees and other workers can receive 20% off site-wide by verifying their eligibility through ID.me .

Theragun Relief
Once you get verified through ID.me you can get up to 20% off on this fan-favorite massage gun .

Yeti Stainless Steel Tumbler (20 Ounce)
Maybe Yeti is the tumbler of your choice to stay hydrated throughout your work shift. Nurses can get 20% to 40% off on eligible drinkware when they verify their ID.
Jannely is the SEO Writer for Shop TODAY.
Find anything you save across the site in your account
In the campus protests over the war in Gaza, language and rhetoric are—as they have always been when it comes to Israel and Palestine—weapons of mass destruction.
By Zadie Smith
A philosophy without a politics is common enough. Aesthetes, ethicists, novelists—all may be easily critiqued and found wanting on this basis. But there is also the danger of a politics without a philosophy. A politics unmoored, unprincipled, which holds as its most fundamental commitment its own perpetuation. A Realpolitik that believes itself too subtle—or too pragmatic—to deal with such ethical platitudes as thou shalt not kill. Or: rape is a crime, everywhere and always. But sometimes ethical philosophy reënters the arena, as is happening right now on college campuses all over America. I understand the ethics underpinning the protests to be based on two widely recognized principles:
There is an ethical duty to express solidarity with the weak in any situation that involves oppressive power.
If the machinery of oppressive power is to be trained on the weak, then there is a duty to stop the gears by any means necessary.
The first principle sometimes takes the “weak” to mean “whoever has the least power,” and sometimes “whoever suffers most,” but most often a combination of both. The second principle, meanwhile, may be used to defend revolutionary violence, although this interpretation has just as often been repudiated by pacifistic radicals, among whom two of the most famous are, of course, Mahatma Gandhi and Martin Luther King, Jr . In the pacifist’s interpretation, the body that we must place between the gears is not that of our enemy but our own. In doing this, we may pay the ultimate price with our actual bodies, in the non-metaphorical sense. More usually, the risk is to our livelihoods, our reputations, our futures. Before these most recent campus protests began, we had an example of this kind of action in the climate movement. For several years now, many people have been protesting the economic and political machinery that perpetuates climate change, by blocking roads, throwing paint, interrupting plays, and committing many other arrestable offenses that can appear ridiculous to skeptics (or, at the very least, performative), but which in truth represent a level of personal sacrifice unimaginable to many of us.
I experienced this not long ago while participating in an XR climate rally in London. When it came to the point in the proceedings where I was asked by my fellow-protesters whether I’d be willing to commit an arrestable offense—one that would likely lead to a conviction and thus make travelling to the United States difficult or even impossible—I’m ashamed to say that I declined that offer. Turns out, I could not give up my relationship with New York City for the future of the planet. I’d just about managed to stop buying plastic bottles (except when very thirsty) and was trying to fly less. But never to see New York again? What pitiful ethical creatures we are (I am)! Falling at the first hurdle! Anyone who finds themselves rolling their eyes at any young person willing to put their own future into jeopardy for an ethical principle should ask themselves where the limits of their own commitments lie—also whether they’ve bought a plastic bottle or booked a flight recently. A humbling inquiry.
It is difficult to look at the recent Columbia University protests in particular without being reminded of the campus protests of the nineteen-sixties and seventies, some of which happened on the very same lawns. At that time, a cynical political class was forced to observe the spectacle of its own privileged youth standing in solidarity with the weakest historical actors of the moment, a group that included, but was not restricted to, African Americans and the Vietnamese. By placing such people within their ethical zone of interest, young Americans risked both their own academic and personal futures and—in the infamous case of Kent State—their lives. I imagine that the students at Columbia—and protesters on other campuses—fully intend this echo, and, in their unequivocal demand for both a ceasefire and financial divestment from this terrible war, to a certain extent they have achieved it.
But, when I open newspapers and see students dismissing the idea that some of their fellow-students feel, at this particular moment, unsafe on campus, or arguing that such a feeling is simply not worth attending to, given the magnitude of what is occurring in Gaza, I find such sentiments cynical and unworthy of this movement. For it may well be—within the ethical zone of interest that is a campus, which was not so long ago defined as a safe space, delineated by the boundary of a generation’s ethical ideas— it may well be that a Jewish student walking past the tents, who finds herself referred to as a Zionist, and then is warned to keep her distance, is, in that moment, the weakest participant in the zone. If the concept of safety is foundational to these students’ ethical philosophy (as I take it to be), and, if the protests are committed to reinserting ethical principles into a cynical and corrupt politics, it is not right to divest from these same ethics at the very moment they come into conflict with other imperatives. The point of a foundational ethics is that it is not contingent but foundational. That is precisely its challenge to a corrupt politics.
Practicing our ethics in the real world involves a constant testing of them, a recognition that our zones of ethical interest have no fixed boundaries and may need to widen and shrink moment by moment as the situation demands. (Those brave students who—in supporting the ethical necessity of a ceasefire—find themselves at painful odds with family, friends, faith, or community have already made this calculation.) This flexibility can also have the positive long-term political effect of allowing us to comprehend that, although our duty to the weakest is permanent, the role of “the weakest” is not an existential matter independent of time and space but, rather, a contingent situation, continually subject to change. By contrast, there is a dangerous rigidity to be found in the idea that concern for the dreadful situation of the hostages is somehow in opposition to, or incompatible with, the demand for a ceasefire. Surely a ceasefire—as well as being an ethical necessity—is also in the immediate absolute interest of the hostages, a fact that cannot be erased by tearing their posters off walls.
Part of the significance of a student protest is the ways in which it gives young people the opportunity to insist upon an ethical principle while still being, comparatively speaking, a more rational force than the supposed adults in the room, against whose crazed magical thinking they have been forced to define themselves. The equality of all human life was never a self-evident truth in racially segregated America. There was no way to “win” in Vietnam. Hamas will not be “eliminated.” The more than seven million Jewish human beings who live in the gap between the river and the sea will not simply vanish because you think that they should. All of that is just rhetoric. Words. Cathartic to chant, perhaps, but essentially meaningless. A ceasefire, meanwhile, is both a potential reality and an ethical necessity. The monstrous and brutal mass murder of more than eleven hundred people, the majority of them civilians, dozens of them children, on October 7th, has been followed by the monstrous and brutal mass murder (at the time of writing) of a reported fourteen thousand five hundred children. And many more human beings besides, but it’s impossible not to notice that the sort of people who take at face value phrases like “surgical strikes” and “controlled military operation” sometimes need to look at and/or think about dead children specifically in order to refocus their minds on reality.
To send the police in to arrest young people peacefully insisting upon a ceasefire represents a moral injury to us all. To do it with violence is a scandal. How could they do less than protest, in this moment? They are putting their own bodies into the machine. They deserve our support and praise. As to which postwar political arrangement any of these students may favor, and on what basis they favor it—that is all an argument for the day after a ceasefire. One state, two states, river to the sea—in my view, their views have no real weight in this particular moment, or very little weight next to the significance of their collective action, which (if I understand it correctly) is focussed on stopping the flow of money that is funding bloody murder, and calling for a ceasefire, the political euphemism that we use to mark the end of bloody murder. After a ceasefire, the criminal events of the past seven months should be tried and judged, and the infinitely difficult business of creating just, humane, and habitable political structures in the region must begin anew. Right now: ceasefire. And, as we make this demand, we might remind ourselves that a ceasefire is not, primarily, a political demand. Primarily, it is an ethical one.
But it is in the nature of the political that we cannot even attend to such ethical imperatives unless we first know the political position of whoever is speaking. (“Where do you stand on Israel/Palestine?”) In these constructed narratives, there are always a series of shibboleths, that is, phrases that can’t be said, or, conversely, phrases that must be said. Once these words or phrases have been spoken ( river to the sea, existential threat, right to defend, one state, two states, Zionist, colonialist, imperialist, terrorist ) and one’s positionality established, then and only then will the ethics of the question be attended to (or absolutely ignored). The objection may be raised at this point that I am behaving like a novelist, expressing a philosophy without a politics, or making some rarefied point about language and rhetoric while people commit bloody murder. This would normally be my own view, but, in the case of Israel/Palestine, language and rhetoric are and always have been weapons of mass destruction.
It is in fact perhaps the most acute example in the world of the use of words to justify bloody murder, to flatten and erase unbelievably labyrinthine histories, and to deliver the atavistic pleasure of violent simplicity to the many people who seem to believe that merely by saying something they make it so. It is no doubt a great relief to say the word “Hamas” as if it purely and solely described a terrorist entity. A great relief to say “There is no such thing as the Palestinian people” as they stand in front of you. A great relief to say “Zionist colonialist state” and accept those three words as a full and unimpeachable definition of the state of Israel, not only under the disastrous leadership of Benjamin Netanyahu but at every stage of its long and complex history, and also to hear them as a perfectly sufficient description of every man, woman, and child who has ever lived in Israel or happened to find themselves born within it. It is perhaps because we know these simplifications to be impossible that we insist upon them so passionately. They are shibboleths; they describe a people, by defining them against other people—but the people being described are ourselves. The person who says “We must eliminate Hamas” says this not necessarily because she thinks this is a possible outcome on this earth but because this sentence is the shibboleth that marks her membership in the community that says that. The person who uses the word “Zionist” as if that word were an unchanged and unchangeable monolith, meaning exactly the same thing in 2024 and 1948 as it meant in 1890 or 1901 or 1920—that person does not so much bring definitive clarity to the entangled history of Jews and Palestinians as they successfully and soothingly draw a line to mark their own zone of interest and where it ends. And while we all talk, carefully curating our shibboleths, presenting them to others and waiting for them to reveal themselves as with us or against us—while we do all that, bloody murder.
And now here we are, almost at the end of this little stream of words. We’ve arrived at the point at which I must state clearly “where I stand on the issue,” that is, which particular political settlement should, in my own, personal view, occur on the other side of a ceasefire. This is the point wherein—by my stating of a position—you are at once liberated into the simple pleasure of placing me firmly on one side or the other, putting me over there with those who lisp or those who don’t, with the Ephraimites, or with the people of Gilead. Yes, this is the point at which I stake my rhetorical flag in that fantastical, linguistical, conceptual, unreal place—built with words—where rapes are minimized as needs be, and the definition of genocide quibbled over, where the killing of babies is denied, and the precision of drones glorified, where histories are reconsidered or rewritten or analogized or simply ignored, and “Jew” and “colonialist” are synonymous, and “Palestinian” and “terrorist” are synonymous, and language is your accomplice and alibi in all of it. Language euphemized, instrumentalized, and abused, put to work for your cause and only for your cause, so that it does exactly and only what you want it to do. Let me make it easy for you. Put me wherever you want: misguided socialist, toothless humanist, naïve novelist, useful idiot, apologist, denier, ally, contrarian, collaborator, traitor, inexcusable coward. It is my view that my personal views have no more weight than an ear of corn in this particular essay. The only thing that has any weight in this particular essay is the dead. ♦
New Yorker Favorites
The day the dinosaurs died .
What if you started itching— and couldn’t stop ?
How a notorious gangster was exposed by his own sister .
Woodstock was overrated .
Diana Nyad’s hundred-and-eleven-mile swim .
Photo Booth: Deana Lawson’s hyper-staged portraits of Black love .
Fiction by Roald Dahl: “The Landlady”
Sign up for our daily newsletter to receive the best stories from The New Yorker .
By signing up, you agree to our User Agreement and Privacy Policy & Cookie Statement . This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

By Ruth Margalit

By Keeanga-Yamahtta Taylor
By Jay Caspian Kang

By Susan B. Glasser

COMMENTS
The impact of nurses' working conditions on patients' care is a major concern for the health system. The reviewed articles identified a relationship between the variables included in this paper. Nurses' workload was related to burnout and decreased safety and quality of care.
The issue of nurse work overload depends on the perspective that one chooses. References. Carayon, P., & Gurses, A. P. (2008). Nursing workload and patient safety - A human factors engineering perspective. In H. R. G (Ed.), Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcase Research and ...
Workload in the nursing profession is high, which is associated with poor health. Thus, it is important to get a proper understanding of the working situation and to analyse factors which might be able to mitigate the negative effects of such a high workload. In Germany, many people with serious or life-threatening illnesses are treated in non-specialized palliative care settings such as ...
When workload increased, nurses who confirmed that they worked in a good working team stated a lower burnout level. However, the result of the current study showed that a good working team is particularly important when workload increases, in the most extreme cases team work in palliative care is necessary to save a person's life. ...
This review identifies the body of nursing workload research and establishes the need to include a subjective perception of the nurse as part of any workload measure. Keywords: nursing workload, human factors, subjective mental workload, cognitive workload T he demands in nursing and health care have received increasing attention in recent years.
Background Nursing is considered a hard job and their work stresses can have negative effects on health and quality of life. The aim of this study was to investigate the correlation between job stress with quality of life and care behaviors in nurses. Methods This cross-sectional survey design study was performed with the participation of 115 nurses working in two hospitals. The nurses were ...
Background Nursing workload and its effects on the quality of nursing care is a major concern for nurse managers. Factors which mediate the relationship between workload and the quality of nursing care have not been extensively studied. This study aimed to investigate the mediating role of implicit rationing of nursing care, job satisfaction and emotional exhaustion in the relationship between ...
The modern health care delivery system is complex and rapidly changing and it is therefore important for nursing staff to work together to secure patient safety (Jomaa et al., 2021) and quality of care (Kalisch et al., 2007; Zeleníková et al., 2020).Teamwork and team-based care are identified as key contributors to patient safety and quality patient care (Mitchell et al., 2012; WHO, 2016).
Background Healthcare organisations monitor patient experiences in order to evaluate and improve the quality of care. Because nurses spend a lot of time with patients, they have a major impact on patient experiences. To improve patient experiences of the quality of care, nurses need to know what factors within the nursing work environment are of influence. The main focus of this research was ...
ABSTRACT Many outcomes in nurses' work lives are influenced by their job satisfaction. Background: One of the tools that measures nurses' job satisfaction is the McCloskey/Mueller Job Satisfaction tool. Several databases were accessed to identify studies published after 2002 that measured nurses' job satisfaction using the McCloskey/Mueller Job Satisfaction tool and identified an outcome ...
14 nurses on life and work during COVID. Colleen Walsh. Harvard Staff Writer. November 2, 2021 long read. Since early 2020, when the pandemic exploded around the world, Massachusetts has seen nearly 19,000 COVID deaths and more than 840,000 cases. If a line graph of hospital admissions over the past 20 months looks like a series of peaks and ...
Objective 1: Evaluate the workplace wellness program's impact on nurse burnout (Ernawati et al., 2022). Objective 2: Boost nurse engagement by involving them in decision-making (Fitzpatrick et al., 2019). Objective 3: Improve nurse work-life balance with flexible arrangements and resources for stress management.
COVID-19 pandemic: Perspectives on an unfolding crisis. Journal of British Surgery, 107 (7), pp. 785-787. Web. This essay, "Increased Workload on Nurses During COVID-19" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper.
Here's your quick guide from our nursing essay writing service: Choosing Your Topic: Select a topic that sparks your interest and relates to real-world nursing challenges. Consider areas like patient care, ethical dilemmas, or the impact of technology on healthcare. Outline Your Route: Plan your essay's journey.
The more than 1,140 U.S. nurses who lost their lives in the first year of the pandemic knew the risks to themselves and their families. And yet they stayed in harm's way. They cared for their ...
Nursing practice is rapidly evolving, and patient pathways are becoming more efficient and cost-effective. The last decades have seen growing complexity of the healthcare environment due to advanced technological and medical developments as well as a stronger focus on standardization and the logic of production that permeate today's hospital cultures. 1 This means that nurses not only have ...
As a result, nursing essays can take many different forms and cover a wide range of topics. Given below are some examples of different types of nursing essays: Personal Philosophy Of Nursing - Essay Examples. Cal State Fullerton Nursing Essay Examples. Evidence Based Practice Nursing In Medical Field - Essay Examples.
We included primary studies that described the development, reliability or validity testing of systems/ tools for measuring nursing workload/ predicting staffing requirements; studies that compared the workload as assessed by different measures, or which used a tool as part of a wider study in such a way that it might provide some insight into ...
This 1000-word Essay on Nurse explores the multifaceted role of nurses, delving into their compassionate patient care, advocacy, continuous learning, collaborative contributions to healthcare teams, and the evolving dynamics within the nursing profession. The Heart of Healthcare: Exploring the Profound Role of Nurses.
Explore the reasons why you want to become a nurse and learn how to write a compelling Why I Want To Be A Nurse essay. Get inspiration from a free example. ... Many nurses can choose to work part-time or in a variety of places, such as clinics, hospitals, and schools.. A Love for the Science and Art of Nursing.
Here are three key opportunities nursing leaders can leverage in 2024 and beyond. 1. Prioritize making improvements to nursing work environments. The workforce crisis has highlighted the undeniable difference nurses make in care teams and the overall success of their organizations.
Therefore, your "why I want to be a nurse" essay should emphasize your ability to be caring, empathetic, patient, and comforting to others. Share examples that showcase your natural inclination for caregiving: "Volunteering at the Red Cross shelter after the wildfires by comforting displaced families demonstrated my patience and ...
The country needs more nurses; the U.S. Chamber of Commerce forecasts there will be 193,100 job openings for registered nurses every year between 2022 and 2032. ... where they can complete their associate's degree in nursing in one year or work toward transferring to a four-year college. (Someone can become a Registered Nurse with an ...
The National Commission to Address Racism in Nursing (the Commission) and the American Nurses Association (ANA) celebrate the achievement of awareness, advocacy and recognition that is SHIFT's documentary film "Everybody's Work: Healing What Hurts Us All," which examines the hidden disease of systemic racism plaguing health care in the United States.
Re " An Act of Defiance Can Improve Things for Working Moms ," by Toby Kiers (Opinion guest essay, May 4): I am a woman nearing the completion of my B.A. in philosophy, and I have the absurd ...
Manitoba spent $3.9M in 1 year on private nurses to fill shortages in Winnipeg, Opposition NDP says. Nursing agencies are staffing hospitals at 'huge cost' to health-care system, experts say. The ...
Yeti Stainless Steel Tumbler (20 Ounce) $ 35.00. YETI. Maybe Yeti is the tumbler of your choice to stay hydrated throughout your work shift. Nurses can get 20% to 40% off on eligible drinkware ...
In the campus protests over the war in Gaza, language and rhetoric are—as they have always been when it comes to Israel and Palestine—weapons of mass destruction. By Zadie Smith. May 5, 2024 ...