- Study protocol
- Open access
- Published: 19 November 2019

Optimising the use of caesarean section: a generic formative research protocol for implementation preparation
- Meghan A. Bohren ORCID: orcid.org/0000-0002-4179-4682 1 , 2 ,
- Newton Opiyo 2 ,
- Carol Kingdon 3 ,
- Soo Downe 3 &
- Ana Pilar Betrán 2
Reproductive Health volume 16 , Article number: 170 ( 2019 ) Cite this article
12 Citations
3 Altmetric
Metrics details
Caesarean section rates are rising across all geographical regions. Very high rates for some groups of women co-occur with very low rates for others. Both extremes are associated with short and longer term harms. This is a major public health concern. Making the most effective use of caesarean section is a critical component of good quality, sustainable maternity care. In 2018, the World Health Organization published evidence-based recommendations on non-clinical interventions to reduce unnecessary caesarean section. The guideline identified critical research gaps and called for formative research to be conducted ahead of any interventional research to define locally relevant determinants of caesarean birth and factors that may affect implementation of multifaceted optimisation strategies. This generic formative research protocol is designed as a guide for contextual assessment and understanding for anyone planning to take action to optimise the use of caesarean section.
This formative protocol has three main components: (1) document review; (2) readiness assessment; and (3) primary qualitative research with women, healthcare providers and administrators. The document review and readiness assessment include tools for local mapping of policies, protocols, practices and organisation of care to describe and assess the service context ahead of implementation. The qualitative research is organized according to twelve identified interventions that may optimise use of caesarean section. Each intervention is designed as a “module” and includes a description of the intervention, supporting evidence, theory of change, and in-depth interview/focus group discussion guides. All study instruments are included in this protocol.
This generic protocol is designed to underpin the formative stage of implementation research relating to optimal use of caesarean section. We encourage researchers, policy-makers and ministries of health to adapt and adopt this design to their context, and share their findings as a catalyst for rapid uptake of what works.
Antecedentes
El uso de la cesárea está aumentando en todo el mundo. Tasas muy altas de cesárea en algunos grupos de mujeres coexisten con tasas muy bajas en otros grupos. Ambos extremos conllevan riesgos a corto y a largo plazo y constituyen un importante problema de salud pública. Un uso adecuado de la cesárea es crucial para proveer una atención clínica sostenible de calidad durante el embarazo y el parto. En 2018 la Organización Mundial de la Salud publicó recomendaciones de base fáctica para reducir las cesáreas innecesarias a través de intervenciones no clínicas. Dicha guía detecta importantes lagunas en la investigación e insta a que se realice una investigación formativa previa a la implementación de estrategias destinadas a reducir u optimizar el uso de cesáreas, investigación que tiene como objetivo identificar los determinantes del uso de la cesárea y otros factores que pueden afectar la implementación de dichas estrategias a nivel local. El presente artículo ofrece un protocolo genérico de investigación formativa que puede ser utilizado como guía por todos aquellos que quieran planificar una intervención para optimizar el uso de la cesárea. Tiene como objetivo evaluar y entender el contexto en el que se piensa actuar.
Este protocolo de investigación formativa tiene tres componentes: (1) examen de la documentación; (2) evaluación de la factibilidad; y (3) investigación cualitativa con las mujeres, los proveedores de servicios de salud y la administración de los centros. Los dos primeros componentes incluyen herramientas para llevar a cabo un mapeo local de las políticas de salud, las prácticas y los protocolos clínicos, y la organización de la atención que se ofrece, lo que permite describir y evaluar el contexto local antes de empezar a actuar. La investigación cualitativa está organizada en torno a 12 intervenciones que podrían reducir las cesáreas innecesarias. Cada una de ellas se presenta en un «módulo» que contiene la descripción de la intervención y las pruebas que la refrendan, la teoría del cambio y la planilla para las entrevistas o los grupos de debate. Todos los instrumentos necesarios están incluidos en el protocolo.
Este protocolo genérico esta diseñado para llevar a cabo una investigación formativa previa a la realización de intervenciones destinadas a optimizar el uso de la cesárea a nivel local. Investigadores, responsables de la formulación de políticas y ministerios de salud en todo el mundo pueden adoptar y adaptar el protocolo para usarlo en su contexto particular. Alentamos a que se compartan los resultados obtenidos a fin de catalizar la investigación y promover el acceso a intervenciones efectivas.
Les taux de césariennes sont en hausse dans toutes les régions du monde. Des taux très élevés dans certains groupes de femmes coexistent avec des taux très bas dans d’autres. Ces deux extrêmes sont associés à des conséquences négatives à court et à long terme. Ceci constitue un problème de santé publique majeur. Optimiser l’utilisation de la césarienne est crucial pour des soins de santé maternelle durables et de bonne qualité. En 2018, sur la base des recherches réalisées, l’Organisation Mondiale de la Santé a publié des recommandations d’interventions non-cliniques pour la réduction des césariennes non nécessaires. Ce guide a identifié des lacunes notables en matière de recherche et a appelé à la réalisation de recherches formatives avant la réalisation d’une intervention, afin de définir les déterminants locaux des naissances par césarienne et les facteurs qui pourraient affecter la mise en œuvre de stratégies d’optimisation multidimensionnelles. Ce protocole de recherche formative original a été créé comme un guide pour l’évaluation et la compréhension du contexte à l’attention de ceux qui prévoient d’agir pour optimiser l’utilisation de la césarienne.
Ce protocole de recherche formative inclut trois composantes principales: (1) une revue de la littérature; (2) une évaluation rapide de l’état de préparation; (3) une recherche qualitative initiale avec les femmes, les prestataires de soins de santé et les administratifs. La revue de la littérature et l’évaluation rapide de l’état de préparation incluent des outils pour la cartographie de la mise en œuvre de politiques locales, de protocoles, de pratiques et d’organisation des soins afin de décrire et d’évaluer le contexte avant toute mise en œuvre. La recherche qualitative est organisée en 12 interventions susceptibles de réduire les césariennes non nécessaires. Chaque intervention est conçue comme un « module » et comprend une description de l’intervention, des éléments de revue de la littérature, une théorie du changement, ainsi que des guides pour des entretiens approfondis et des discussions de groupe. Tous les outils d’études sont inclus dans ce protocole.
Ce protocole original a été conçu pour venir en appui d’une recherche formative qui constitue une étape d’une recherche de mise en œuvre visant à une utilisation optimale de la césarienne. Nous encourageons les chercheurs, les responsables de politiques et les ministres de la santé à adopter et adapter ce protocole à leur contexte, ainsi qu’à partager et utiliser leurs résultats comme un catalyseur pour l’adoption rapide de mesures efficaces.
Peer Review reports
Plain English summary
Many women across the world give birth by caesarean section, which can be a life-saving intervention for both the woman and her baby. However, some women have a caesarean section even if there is not a medical need to have one. This can lead to short- and long-term risks for the woman and her baby. We use the term “optimising the use of caesarean section” to refer to making the best possible use of caesarean section to improve the health and well-being of women and their babies.
There are many factors contributing to high caesarean section rates including incentives for healthcare providers, a culture of intervention in the hospital setting, healthcare providers’ fear of blame, beliefs about provider-patient relationships, perceptions about the convenience about different types of birth, and social norms around birth. These multiple factors need to be addressed when designing research, evaluation or health services to optimise the use of caesarean section.
In this paper, we propose a research protocol that can be used by researchers, ministries of health, or others to understand and address caesarean section. We propose to start with formative research. Formative research refers to gathering data that might be useful to understand the issue and people the issue is affecting, then use this data to develop programs or further research. We provide a template for how this research could be conducted, including the research protocol (background, rationale, objectives, design, methods and logistics) and study tools (a document review, readiness assessment, and qualitative research guides).
Caesarean section is a surgical procedure that can prevent maternal and newborn mortality when used for medically indicated reasons [ 1 ]. However, there is no evidence of benefits for women or babies who do not have a medical indication [ 2 ]. As with all surgical procedures, caesarean section is associated with short and long-term risks for women, children, and future pregnancies, as well as substantial healthcare costs [ 2 , 3 , 4 , 5 ]. These risks are higher in settings where women have limited access to comprehensive obstetric and post-surgical care. Rapid rises in caesarean section without concurrent decreases in maternal or perinatal morbidity or mortality suggest that a large proportion of caesarean sections are unnecessary. Across 150 countries, 18.6% of all births are estimated to occur by caesarean section, ranging from 1.4 to 56.4% across different countries [ 6 ]. The global caesarean section rate increased by 12.4% (from 6.7 to 19.1%) from 1990 to 2014 [ 6 ].
Rising caesarean section rates are a global challenge that affects high-, middle-, and low-income countries across all geographical regions [ 1 , 6 , 7 ]. The causes of increased rates vary across and within contexts, and may include differences in professional practices, fear of medical litigation and associated professional risk-aversion, changes to the characteristics of the population (e.g.: increasing prevalence of obesity, or increasing proportion of older women or multiple births), as well as economic, organisational, and sociocultural factors such as generational shifts in work and family responsibilities, women’s increasing desire to determine how and when their babies are born, and physician preferences [ 1 , 8 , 9 , 10 ]. Sustained increases in caesarean section rates are a major public health concern and there is an urgent need for evidence-based guidance to address this trend [ 1 ]. Optimising caesarean section rates (i.e. making the best or most effective use of caesarean section to improve the health and well-being of women and their babies) is also a critical component of improving the quality of care during childbirth [ 11 ]. This includes ensuring the availability, accessibility and affordability of caesarean section when needed by a woman and/or her baby. However women give birth, providers should ensure that care is provided with respect, maintaining dignity, and that women understand and consent to both what is happening in the moment and to what may happen in the future [ 11 ].
In 2018, the World Health Organization (WHO) published evidence-based recommendations on non-clinical interventions to reduce unnecessary caesarean section [ 1 ]. Evidence for the effectiveness of interventions was derived from an updated Cochrane review of 29 studies [ 12 ]. This was complemented by an analysis of values, acceptability, equity, resource implications, and feasibility of the included interventions, derived from three qualitative evidence syntheses [ 13 , 14 , 15 ]. The guideline contains five recommendations on non-clinical interventions to reduce unnecessary caesarean section (Table 1 ), which are designed to inform the development of national and subnational policies and protocols in this area, and should be implemented in conjunction with other interventions to improve the quality of care during childbirth [ 1 ].
The WHO guideline highlighted key research gaps around uncertainty in the effects of interventions, applicability of evidence to other settings, and limited evidence contributing to the guideline questions [ 1 ]. In line with implementation science principles for complex interventions, the WHO guideline also highlighted that future intervention and implementation research in this area should be preceded by formative research to define locally relevant determinants of caesarean birth and potential interventions [ 1 ]. Given the complex factors contributing to rising caesarean section rates, implementation research is a useful approach to engage key stakeholders across multiple disciplines to better understand and design interventions. Using an implementation research approach is particularly useful for changing organisational structures and individual behaviours around practices that may be resistant to change, including sub-optimal use of caesarean section.
In this paper, WHO is proposing a generic formative research protocol that can be adapted and implemented in different contexts to guide the design and implementation of interventions to reduce unnecessary caesarean section rates. This protocol is designed as a generic protocol for the formative stage in preparation for the implementation of targeted interventions and/or trials, and is expected to be adapted and adopted by different sites (by WHO, ministries of health, or other research partners). The protocol provides guidance and a range of tools to assist teams in this endeavour, and can be tailored for what works in different settings. Local findings based on this protocol could be used to design implementation studies and to frame implementation strategies, including formal baseline and endline assessment of the effectiveness of the implementation process as a whole. Theoretically, this formative research would represent the first phase in a multi-phase project, using different methods and approaches:
Phase 1: formative phase consisting of a document review, readiness assessment and primary qualitative research
Phase 2: intervention design and preparation of implementation strategy
Phase 3: intervention implementation and evaluation, including baseline and endline assessment
The objective of the overall project would be to design and implement a multifaceted strategy that is locally relevant, culturally accepted by women and providers and can be implemented effectively to reduce unnecessary caesarean sections. This protocol outlines Phase 1 of this project only (formative phase), to inform the development of interventions.
Conceptual framework
The WHO guideline proposes a new ecological framework for understanding the different levels of factors affecting caesarean section rates (Fig. 1 ) [ 1 ]. This includes influences from clinical factors, women and their families, communities, health professionals and larger organisational and systems factors [ 1 ]. Women receive information about pregnancy and childbirth from multiple informal and formal information sources, including their friends, families, media and internet. This information can shape their opinions and choices about their preferred mode of childbirth, where to give birth, and how to take care of their babies [ 17 , 18 ]. Women’s networks can provide them with emotional support and empowerment, and can influence their levels of fear, anxiety and uncertainty. Likewise, women’s own previous birth experiences may influence her choices and preferences for subsequent pregnancies. Discussing a woman’s previous birth experiences with a healthcare provider may help to provide more individualised care for a woman and ensure that she has a meaningful dialogue with her care team. These influences and experiences ultimately shape women’s preferences for her preferred mode of childbirth [ 13 ].
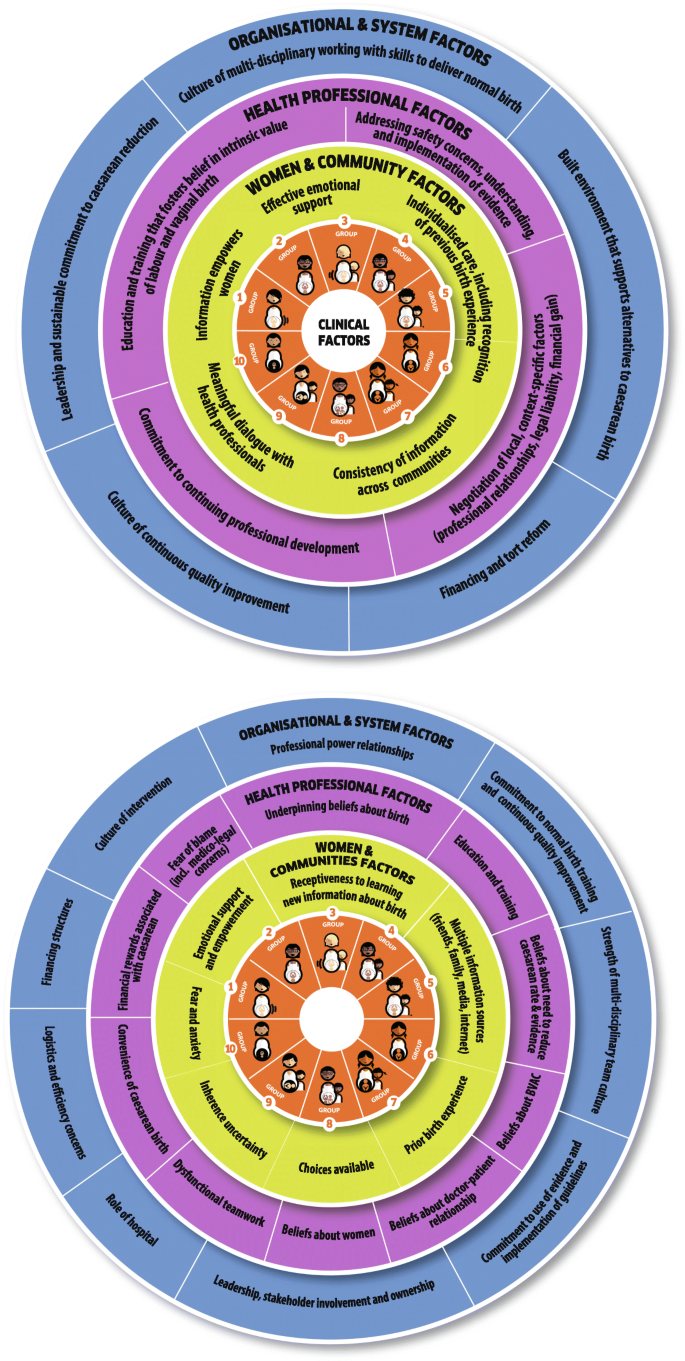
Ecological model to understand factors influencing caesarean section rates related to women, society, health providers, and healthcare organizations that affect caesarean section use at the local level. These factors surround the obstetric and clinical factors that also affect the frequency of births by caesarean section, which are represented in the middle by the Robson 10-group classification (reproduced with permission from [ 16 ])
Health professionals working on maternity wards also shape the context of women’s mode of childbirth. Providers have sets of beliefs developed from their own training and experiences regarding the intrinsic value of different modes of birth and childbirth practices [ 13 , 14 , 15 ]. Likewise, their training and education shapes their skillset for managing different modes of birth, their opinions regarding the necessity of reducing caesarean section rates, and their opinions and skills for managing vaginal birth after caesarean section. Providers work within the structures of care and teams within the health facility, which may impact the perceived convenience and financial rewards of caesarean birth. They must navigate decisions about patient care within the context of locally-relevant factors such as professional relationships, legal liability, and financial gain.
Organisational culture also influences caesarean section. A culture of continuous quality improvement may promote the identification of potential issues and promote action to resolve issues, such as high or increasing caesarean section rates. Committing to a practice of evidence-based childbirth care and local implementation of guidelines and protocols may influence the use of caesarean section. Leadership and promoting team-based care can improve skills to manage vaginal birth and provide a supportive learning environment. The built environment of the facility, such as the available bed space and structure of the labour ward, plays an important role in the organisation of care. A culture of medicalisation of childbirth may lead to higher than necessary rates of caesarean section, among other unnecessary interventions. Lastly, legal liability for the health outcomes of women and babies may influence the level of intervention or risk that providers are comfortable with [ 14 , 15 ].
Interventions to reduce unnecessary caesarean section should consider these multi-level influences on the decision-making process for mode of birth. Given the multiple levels of influences, this protocol includes formative research about a package of interventions that addresses different factors contributing to unnecessary caesarean section. This protocol is designed to help local teams to select intervention(s) that are most likely to work in their settings and provide critical information on how to implement them.
To explore how national, sub-national and facility-level policies and practices influence the feasibility, availability, and implementability of interventions to reduce unnecessary caesarean section;
To explore the readiness of health facilities to implement interventions to reduce unnecessary caesarean sections;
To explore how different interventions to reduce unnecessary caesarean section should be implemented in a specific context;
To explore implementation considerations, including expectations, preferences, feasibility and acceptability of different interventions to reduce unnecessary caesarean section, from the perspectives of the following stakeholders:
Women (nulliparous, and multiparous with and without previous caesarean section)
Providers (midwives, nurses, doctors, administrators working on the maternity ward)
Policy-makers; and
To assess potential facilitators and barriers to the implementation of different interventions to reduce unnecessary caesarean section in a specific context.
Project description
This study protocol outlines the formative phase activities to inform the development of interventions to reduce unnecessary caesarean section. Table 2 provides an overview of how to use this protocol, and Fig. 2 depicts a flow chart to determine where to begin reducing unnecessary caesarean section in a specific context. The formative phase of this project has three main components: (1) document review; (2) readiness assessment; and (3) primary qualitative research. Detailed overviews of each component are described in the following sections.
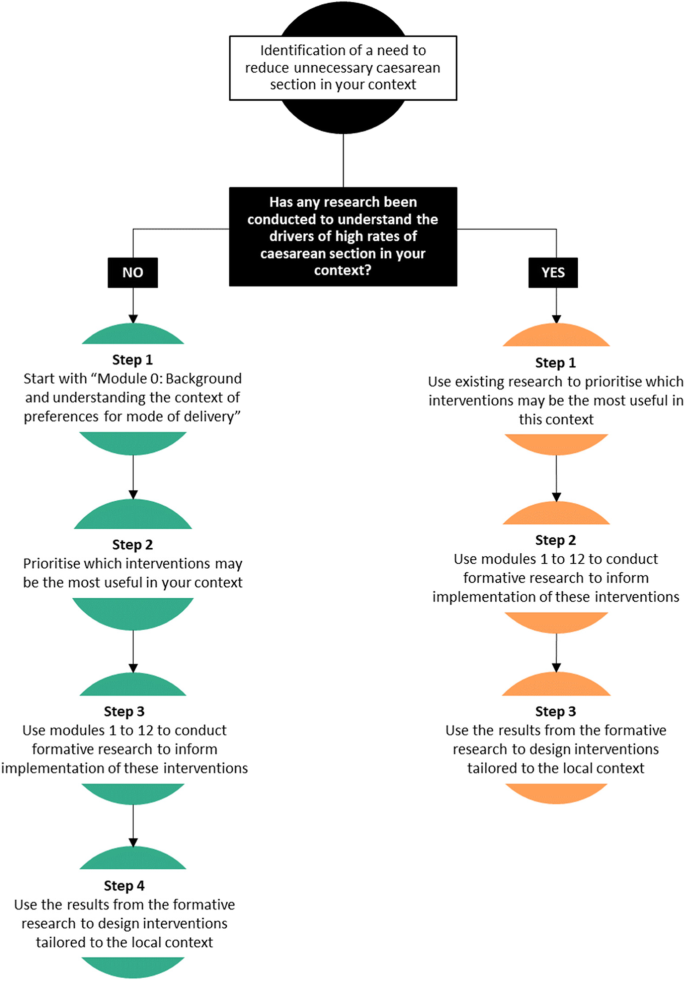
Flow chart to determine where to begin reducing unnecessary caesarean section in your context
Twelve potential interventions that may influence use of caesarean section were identified through the guideline development process (see Additional file 1 for a description of each intervention, theory of change, and supporting evidence). The document review (Additional file 2 ), readiness assessment (Additional file 3 ) and qualitative research focus on the potential for implementation of these interventions, as well as a background module to understand the context of preferences for mode of birth (Additional file 4 ). The twelve interventions are:
Prenatal education and support (Additional file 5 )
Decision-aids for mode of birth (Additional file 6 )
Psychosocial support for women with a fear of childbirth (Additional file 7 )
Labour companionship (Additional file 8 )
Public dissemination of caesarean rates at a facility-level (Additional file 9 )
Audit and feedback (including Robson classification and external review of labour and delivery records) (Additional file 10 )
Mandatory second opinion for caesarean birth (Additional file 11 )
In-service training and implementation of clinical protocols (Additional file 12 )
Equalizing physician pay for vaginal and caesarean birth (Additional file 13 )
Opinion leader education (Additional file 14 )
Setting a goal for caesarean section rate at a facility-level (Additional file 15 )
Policies limiting legal liability and malpractice lawsuits (Additional file 16 )
Study sites
This study will be conducted in a set of health facilities where interventions to reduce unnecessary caesarean section are planned to be implemented. This protocol is designed to be applied to both public and private health facility contexts. The recruitment of participants (particularly women) may need to be modified if this protocol is implemented in contexts with a large private health sector, as it is possible that women may attend public facilities for antenatal care (where recruitment would take place) but give birth in a private facility. These considerations should be discussed with the country research team prior to implementation and addressed in site specific protocols. Some changes may be required to ensure the protocol is relevant for specific sites.
Document review
Using a structured approach to identify important barriers and enablers to implementing interventions to reduce unnecessary caesarean section will help to ensure that important barriers are not overlooked, and that important enablers are considered in the implementation plan [ 19 ]. These barriers and enablers may be national, regional, or contextually-specific, and therefore dependent on local circumstances to inform judgments about what decisions and actions to take for implementation [ 20 ]. For the purposes of this study, “local” refers to facility, district, subnational and national levels, and the goal is to identify important factors for implementation considerations [ 20 ]. For example, this could include national guidelines, professional policies, professional responsibilities (which cadre of providers make decisions about interventions), capacity of the health facilities and system, the availability of providers and equipment, political traditions or other cultural norms, costs of implementation, and the characteristics of the implementation area and of those who reside there [ 20 ]. This information is useful to assess the applicability and use of global reviews of effectiveness to the local context [ 12 ]. Furthermore, this information can inform assessments of the impact of the intervention, inform judgments about the likely values and preferences of users and providers, determine what resources are available and what might need to be sourced, and suggest how the sustainability of the intervention(s) may be maintained after the end of the formal implementation project [ 20 ]. Local information to address these topics may be obtained from several different sources, such as reviewing policy documents and existing research on caesarean section conducted in a similar context [ 13 , 14 ], as well as through qualitative research with key stakeholders (explained in detail in this protocol).
For this study, the starting point for exploring the local context is through a document review of the relevant resources to answer key questions about the context of maternity care and caesarean section (full document review form located in Additional file 2 ). The document review should be conducted systematically in order to ensure that important data are not omitted or overlooked. The protocol follows the principles of evidence-informed policy-making outlined in the SUPPORT tools to ensure that information from the local context is adequately considered [ 20 ].
Readiness assessment
After the document review, the local team will be better informed to conduct the readiness assessment. The readiness assessment will allow the team to describe and assess the service delivery context ahead of implementation, and may be carried out concurrently with the qualitative research in each study site. Providing a systematic approach to assessing readiness will ensure that the local situation informs and tailors the intervention(s) in a way that is suitable for implementation in that context. Responses to the domains in the readiness assessment will be combined with the findings from the qualitative research to identify and prioritise barriers and to develop potential multifaceted interventions and considerations for implementation. The readiness assessment template is available in Additional file 3 .
- Qualitative research
To meet the study objectives, qualitative research methods will be used, specifically in-depth interviews (IDIs) and focus group discussions (FGDs) among different cadres of stakeholders, including (at a minimum) women, healthcare providers, and administrators. It may be appropriate to include other key stakeholders, such as partners, husbands, family members, community influencers or service funders, depending on the local drivers for caesarean section rates. The appropriate mix of stakeholders will be identified by the local research team in consultation with clinical staff and community members. The purpose of these IDIs and FGDs is to explore implementation considerations for interventions to reduce unnecessary caesarean section (expectations, preferences, feasibility, and acceptability), facilitators and barriers to successful implementation, and what the components of the intervention should look like in a specific context.
Participants and recruitment
The following participants are proposed:
Maternity service users , including:
Pregnant nulliparous women
Pregnant multiparous women with a previous caesarean section
Pregnant multiparous women without a previous caesarean section
Maternity service providers , including:
Obstetricians and other doctors working on the maternity ward, including trainees, medical officers
Midwives and/or nurses
Other skilled birth attendants as appropriate
Facility administrators , including:
Matron-in-charge of the labour ward
Head of obstetrics
Medical director
Other administrators such as head of finance, legal director.
In each site, we suggest that all three main groups of participants are included, though specific sub-groups may vary depending on who is most likely to influence the use of caesarean section locally. For example, in some contexts it might be appropriate to include other groups of maternity service users such as partners/husbands, other family members, or community leaders.
Pregnant women aged 18 to 49 years who attend antenatal care will be invited to participate in FGDs. If appropriate in a given context, pregnant adolescents (e.g. aged 15 to 17 years) may also be included, for example in settings where adolescent pregnancy rates are high, or where pregnant minors are considered emancipated. The local research team will ensure that a diverse group of women are included, including a mix of urban/rural, parity, age, ethnicity and religion, in order to account for the views of multiple end users. The research teams will facilitate contact with women during their visit to the health facility for antenatal care. In the appropriate area of the health facility (e.g.: antenatal care waiting area and patient rooms) informational materials (in appropriate local languages) about the study will be displayed, such as posters and pamphlets using visual information to ensure accessibility of information. The informational materials will contain information about the study, eligible participants, and how to participate. To help facilitate recruitment and participation, at least one researcher will be on site, and they will not be a part of the staff taking care of the patient (and ideally, not a clinician). This will help to ensure that consent to participate is not influenced by power imbalances.
We have defined providers as doctors, nurses, midwives, and other skilled birth attendants working on the maternity ward in the study facilities. These providers will be invited to participate in IDIs. The research team will ensure that, to the extent possible given health workforce constraints, a diverse group of providers are interviewed in each facility, including by age, gender, and years of experience. We have defined administrators as those working as managers on the maternity ward or health facility (e.g.: medical/clinical director, head of obstetrics, matron-in-charge, and finance/legal officers). These administrators will be invited to participate in IDIs. Given the small number of people in these leadership positions, we do not expect that it will be possible to stratify by additional sociodemographic characteristics. Providers and administrators will be contacted at their place of work in the study hospital. In the appropriate area of the health facility (e.g.: staff break room or resting area), informational materials about the study will be displayed, such as posters and pamphlets. The informational materials will contain information about the study, eligible participants, and how to participate. Potentially eligible participants who are providers or administrators may also be identified from staff records, then contacted on an individual basis to participate (e.g.: via email or telephone).
Each individual will be provided with information about the study and invited to participate. If they agree to participate, they will be asked to provide consent. All IDIs and FGDs will take place in a private setting and will be audio recorded. IDIs are anticipated to last from 20 to 60 min (depending on the number of modules/interventions included), and FGDs are anticipated to last approximately 60 min (although this may be longer in some contexts). IDIs and FGDs will be facilitated by the research teams. For the FGDs conducted with women, the research assistants will be female.
Maximum variation sampling will be used to achieve a diverse sample of participants, to make sure that the findings are a reasonable reflection of the views and experiences of local stakeholders. This method uses pre-specified parameters to stratify the sample [ 21 ] and encourages recruitment and sampling based on diversity. Table 3 outlines the sampling grid with the stratification proposed for conducting IDIs with providers and service users, for each facility included in the study. In each of the study facilities, healthcare providers will be sampled based on their cadre, such as nurse/midwives or doctors/specialists. In each facility, facility administrators will be selected based on the managerial organization of the facility. We expect the type or designation of facility administrators to vary by facility, but at the minimum would include the medical administrative head of the facility, the head of the obstetrics and gynaecology department, and relevant administrative staff responsible for financial and legal matters.
Depending on the scale of implementation, IDIs with users (women) may either be conducted in all of the study facilities, or in a subset of the study facilities. For example, if ten facilities are included in this study, then it may be more feasible to conduct IDIs with users in four or five facilities, provided that there is not expected to be substantial variation in the characteristics of users (for example, if two or more facilities are located in the same city). This subset of facilities should be chosen to ensure diversity between facilities, such as by geographical region, urban/rural location, or level of care (e.g.: secondary/tertiary or district/state levels). Efforts will be taken to have a diverse sample of users, including nulliparous and multiparous women, older and younger women, and women of different religions or ethnicities.
The proposed sampling grids (Table 3 ) will guide the data collection process; however it is advisable for data collection to continue until no new insights emerge (the point of data saturation). If this point is not reached after data collection with the pre-specified number of participants, more participants should be recruited until the team agrees that saturation has been reached. Sampling may also need to be adjusted if minority groups (e.g. based on religion, ethnicity, migration status, Indigeneity, etc) are specified as key populations. These adjustments will be made on a site-specific basis. Once the IDIs and FGDs are conducted, the study participants will not be followed up on an individual basis, unless member-checking occurs.
Follow-up procedures
After the completion of data collection, transcription and translation (if necessary), a data analysis workshop will be held in order to facilitate analysis and interpretation of findings at a local level. This workshop should be facilitated by the research teams and include key stakeholders such as hospital staff, community members, and women's groups. The workshops will assist in refining which interventions and approaches may work best and how they could be put into practice. The emerging findings from the providers and administrators will be fed back to and discussed with the facility teams during the data analysis process to improve trustworthiness of the interpretation. The findings will be discussed with different stakeholders and these findings will be used to inform the development of the implementation research intervention. The research findings will also be communicated back to the community members, for example through presentations, group meetings, posters in the facility, or (when available) through mobile technologies and social media..
Study instruments
The instruments include a document review form, readiness assessment form, and semi-structured interview guides. Eligible individuals will also complete a consent form prior to participation. The instruments are available in Additional files 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 and 16 .
Data management and quality assurance
Prior to data collection, a training session will be conducted for all the research teams. We suggest that this training workshop is up to 3-5 days in duration to cover the background of the project, research design, manual of operations, review and pilot the study tools, ethical considerations, informed consent, and project implementation plan. Depending on the composition of the research team, this may include country PIs, social scientists, research coordinators, research assistants, transcribers/translators and any other relevant team members. This training session will ideally build the research capacity in each site, guide all involved in the study in to the objectives of the study, ethical and governance considerations and data collection procedures. It will cover practice sessions with the tools, as well with undertaking recruitment and consent procedures appropriately.
During the data collection period, principal investigators will be in constant communication with the research assistants in the field in order to respond to any issues that arise during data collection. Ideally, transcription will occur in parallel to data collection and will be shared on an on-going basis with the study team to ensure the quality of the data and to determine if certain themes need to be further explored. This may include providing feedback on topics that could be probed more deeply during future interviews, identification of areas for improvement, and facilitating dialogue with the country teams regarding saturation of data.
All digitally recorded qualitative data will first be transcribed verbatim in the original language used for collection using a structured format. Verbatim transcription will be performed close to the time of completion of the interviews to maintain the originality of the interview without loss of themes. Ideally, the person transcribing the data will be the same person who conducted the interview to improve trustworthiness of the data. If translation is needed, the research team will collectively decide on the most appropriate time to translate, which will depend on the study context, considering the following options:
Translate all study transcripts into a mutually intelligible language prior to analysis : in situations where the research may have been conducted in dialects or local languages that are not fully understood by all members of the research team.
Conduct analyses in local or contextually-relevant language and translate final themes and key quotations for dissemination : in situations where the research team fully understands the language(s) used for data collection, in order to help preserve the linguistic nuances.
Back translation should be conducted on a subset of transcripts or analytic units in order to validate the translations. Observations and assessments during interviews will be written up as field notes. The transcripts will be complemented with notes taken during the interviews. Data transcription will be performed under the supervision of the designated social scientist who will review all transcripts for completeness.
Data analysis
It is recommended that the qualitative data are analysed and interpreted using a thematic analysis approach [ 22 ]. A thematic analysis approach was chosen to identify, analyse and report patterns and themes within the data [ 22 ]. The thematic analysis will be performed according to the following steps: (1) organizing the data; (2) generating categories, themes, and patterns; (3) testing emergent hypothesis; and (4) searching for alternative explanations. The research team will conduct a thematic analysis to explore findings related to the objectives of the study. The team will explore common themes that span geographic and cultural differences while noting important differences across settings that need to be accounted for during the implementation phase. Throughout data collection, data analysis will take place in parallel to the point of data saturation. This close collaboration between the qualitative research team, the lead social scientists, and the data collectors will ensure quality analysis and interpretation of the data across sites and has proven to be an efficient process in previous studies coordinated by WHO [ 23 , 24 , 25 , 26 , 27 , 28 , 29 ].
Researcher reflexivity
Throughout the study design, analysis and interpretation process, the research team should reflect and discuss how their own training, life experiences, and perspectives may influence the analysis process (reflexivity). Considering reflexivity of the research team is a key component of conducting qualitative research, and should be reflected on throughout the project on an ongoing basis (including research design, selection of co-investigators, data collection training, analysis, interpretation and write-up). Given the expected multi-disciplinary nature of the research team (which may include, for example, obstetricians, social scientists, and maternal health researchers), we expect that the process of reflexive dialogue will yield enriching discussions about how to best design the interventions to reduce unnecessary caesarean section in a manner that accounts for the preferences and needs of women, healthcare providers, and healthcare administrators.
Research team composition
In all cases, teams should involve project staff who are skilled at both quantitative and qualitative data collection, analysis, and interpretation, and stakeholders who can take the standpoint of local service users, community influencers. To ensure feasibility, reliability, and validity of the project, we suggest a diverse research team composition consisting of the following individuals. A principal/lead investigator whose responsibility is overall coordination and leadership. A lead social scientist with experience in qualitative data collection and analysis to coordinate the qualitative component and understand social science implications of findings. Facility-level research coordinators at each study site to act as the gate-keeper for the facility-based data collection (for example, this may be an obstetrics trainee, medical officer, or midwife/nurse). Research assistants to conduct the qualitative interviews (ideally female research assistants with a non-clinical background for data collection with women, and research assistants with some clinical knowledge or experience for data collection with providers). The team may also need transcribers and translators for the qualitative component, or research assistants may also be able to do these tasks.
Gender, social equity and rights
All women have the right to high quality, respectful care during childbirth, and healthcare services need to be structured and organized in a fashion that helps protect and promote these rights. Overuse of interventions that are not needed undermines these rights, as does underuse of required interventions. This protocol is offered to those who aim to understand and improve how to implement interventions to reduce unnecessary caesarean section. Feminist and gender theories on human reproduction have historically struggled to understand and explain why some women actively pursue medical interventions during childbirth, including caesarean section. Contemporary feminist engagement with the medicalization of childbirth may view women who seek caesarean sections as relinquishing control to medical professionals, or consider why some women feel positive and empowered by relinquishing control [ 30 , 31 ]. For example, a study conducted in India found that young women may seek caesarean birth as a means of gaining control over their bodies during the postnatal period, as their in-laws allowed them to have a longer recovery period after the birth [ 32 ]. In other settings, such as Brazil, women may view caesarean birth as the norm, and place value on caesarean birth as the highest quality of care attainable to them [ 33 ]. In Taiwan, women have conceptualised caesarean birth as a means to avoid “suffering twice” from the pain of labour and childbirth, and potential complications of vaginal birth on future sexual pleasure [ 34 ]. Therefore, some women may seek caesarean birth as a means to manipulate societal structures of power and gender inequality [ 33 ].
Public health research has demonstrated that women’s preferences for and knowledge of caesarean section is highly influenced by their sociocultural contexts, including the perspectives of their peers, families, religious communities, and the healthcare systems that they interact with [ 35 , 36 ]. These entities can shape the way that women feel about their own bodies before, during and after pregnancy, such as the expectation of “returning to normal” after birth. This suggests that some women’s preferences for caesarean birth may be influenced by implicit socialisation by dominant values [ 34 ]. Feminist arguments emphasize the need to understand these influences and values, but also allow space for women to make choices over their bodies. A key challenge is ensuring that women can make informed choices based on adequate and accurate information of the benefits and risks of caesarean section, and to understand how these choices can be influenced by hospital or provider interests that may be rooted in patriarchal structures of medicine [ 37 ].
Research has demonstrated the existence of substantial within country economic inequalities in caesarean section across 72 low- and middle-income countries, where caesarean section rates were lowest in the poorest wealth quintile (median 3.7%) and highest in the richest wealth quintile (median 18.4%) [ 7 ]. Boatin and colleagues hypothesized that these inequalities may be due to inadequate access in emergency obstetric care among the poorest groups, and higher use of caesarean section without medical indication among the richest groups [ 7 ]. The protocol we offer in this paper will contribute to addressing these inequalities by providing foundational evidence on how to best design and implement interventions to reduce unnecessary caesarean sections, from the perspective of all relevant stakeholders, including pregnant and postnatal women, and junior front-line staff. Many of the proposed interventions have the potential to reduce inequalities, and promote health equity, although this has not yet been explored in the literature. For example, audit and feedback cycles may help to ensure that all women who have a medical indication for caesarean section receive one. Likewise, group therapy and decision aids for women may be particularly useful to women with a fear of childbirth or women with a previous caesarean section.
For each context that this project is implemented in, the intention is for the research team to consider how to include participants with different backgrounds and experiences. For example, when identifying groups of women to participate in the qualitative research, care should be taken to include women from different ethnic/racial groups, religions, and geographical residence. This will help to ensure that diverse perspectives are included when developing future interventions, which may help to reduce any existing inequalities in use of or access to caesarean section. Broad participation criteria should also ensure the inclusion, as far as possible, of all cadres of healthcare providers and women with different life situations (including religion, sexual orientation, socioeconomic status, ethnicity, age). Sub-groups of healthcare providers or women could include adolescents, unmarried women, women of different ethnicities, migrant women, women who are HIV positive, and junior staff who are not in positions of power. We consider it important to ensure the selection of participants does not discriminate against any group, as women in this category may be at greater risk of receiving poor quality care in the facility. If such women are included, they will be protected by the universal standards of confidentiality and privacy that apply to all participants. However, all women, including these vulnerable groups, should be free to refuse to participate, both confidentially and without prejudice.
Ethical considerations
All potential participants will receive information about the study in their language of choice, conforming to ethical requirements for research involving human subjects. The language should be easy to understand and free of technical jargon. Participants will be given sufficient time to reflect on the information and ask questions. Those who consent to participate in the study will be requested to sign the informed consent form, and it will be made clear that they are free to withdraw from the study at any stage without risk of any negative consequences. For women with low levels of literacy, an impartial witness will be present during the entire informed consent process. Both the witness and the individual discussing the consent will sign and date the consent form. The contact details of the local investigators, including telephone numbers, will be made available to the participants should they require further information and assistance.
The study does not involve any intervention. Participants will not experience any direct and/or immediate benefits for participating in the study. However, this study aims to collection information to inform the implementation phase of a project to reduce unnecessary caesarean section which ultimately has the potential to improve the quality of care around childbirth in the future. Study participants and other women using or intending to use facilities for childbirth will benefit from the increased scientific knowledge on this topic, which will ultimately promote high-quality, woman-centred care in the facilities. Improving societal knowledge on this topic will improve the awareness of quality of care in maternity services.
Other safeguards include the use of unique participant numbers on all study forms, and ensuring that interviewers and data collectors are not current or previous employees of the study facility. Study participants will receive a reimbursement to cover their transportation to the venue of the interview, if applicable. The value of this payment will be determined in consultation with the research teams, to ensure that it does not constitute an inducement. Refreshments will be available during focus group discussions.
This protocol has been adapted for implementation in Argentina, Burkina Faso, Thailand, and Viet Nam as part of the "Appropriate use of Caesarean section through QUALI ty DEC ision-making by women and providers" (QUAL-DEC) project [ 38 ]. In the QUALI-DEC project, we have used the readiness assessment, document review, and adapted the qualitative modules specific to the intervention components: (1) opinion leader education to implement clinical practice guidelines, (2) labour companionship, (3) decision-analysis tool for mode of birth, and (4) caesarean section audit and feedback.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
Focus group discussion
In-depth interview
World Health Organization
World Health Organization. WHO recommendations on non-clinical interventions to reduce unnecessary caesarean sections. Geneva, Switzerland: World Health Organization; 2018.
World Health Organization. WHO Statement on Caesarean Section Rates. Geneva, Switzerland; 2015.
Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: systematic review and meta-analysis. PLoS Med. 2018;15(1):e1002494.
Article Google Scholar
Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review Am J Obstet Gynecol. 2012;207(1):14–29.
Cook JR, Knight M, Dhanjal MK. Multiple repeat caesarean section in the UK: incidence and consequences to mother and child. A national, prospective cohort study—authors’ reply. Bjog. 2013;120(9):1155.
Article CAS Google Scholar
Betran AP, Ye J, Moller AB, Zhang J, Gulmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and National Estimates: 1990-2014. PLoS One. 2016;11(2):e0148343.
Boatin AA, Schlotheuber A, Betran AP, Moller AB, Barros AJD, Boerma T, Torloni MR, Victora CG, Hosseinpoor AR. Within country inequalities in caesarean section rates: observational study of 72 low and middle income countries. Bmj. 2018;360:k55.
Mi J, Liu F. Rate of caesarean section is alarming in China. Lancet. 2014;383(9927):1463–4.
Zwecker P, Azoulay L, Abenhaim HA. Effect of fear of litigation on obstetric care: a nationwide analysis on obstetric practice. Am J Perinatol. 2011;28(4):277–84.
Lin HC, Xirasagar S. Institutional factors in cesarean delivery rates: policy and research implications. Obstet Gynecol. 2004;103(1):128–36.
Tuncalp O, Were WM, Maclennan C, Oladapo OT, Gulmezoglu AM, Bahl R, Daelmans B, Mathai M, Say L, Kristensen F, Temmerman M, Bustreo F. Quality of care for pregnant women and newborns - the WHO vision. BJOG: An International Journal of Obstetrics and Gynaecology. 2015;122(8):1045–9.
Chen I, Opiyo N, Tavender E, Mortazhejri S, Rader T, Petkovic J, Yogasingam S, Taljaard M, Agarwal S, Laopaiboon M, Wasiak J, Khunpradit S, Lumbiganon P, Gruen RL, Betran AP. Non-clinical interventions for reducing unnecessary caesarean section. The Cochrane database of systematic reviews. 2018;9:Cd005528.
PubMed Google Scholar
Kingdon C, Downe S, Betran AP. Women’s and communities’ views of targeted educational interventions to reduce unnecessary caesarean section: a qualitative evidence synthesis. Reprod Health. 2018;15(1):130.
Kingdon C, Downe S, Betran AP. Non-clinical interventions to reduce unnecessary caesarean section targeted at organisations, facilities and systems: systematic review of qualitative studies. PLoS One. 2018;13(9):e0203274.
Kingdon C, Downe S, Betran AP. Interventions targeted at health professionals to reduce unnecessary caesarean sections: a qualitative evidence synthesis. BMJ Open. 2018;8(12):e025073.
Betrán AP, Temmerman M, Kingdon C, Mohiddin A, Opiyo N, Torloni MR, Zhang J, Musana O, Wanyonyi SZ, Gülmezoglu AM, Downe S. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018;392(10155):1358–68.
Torloni MR, Betran AP, Montilla P, Scolaro E, Seuc A, Mazzoni A, Althabe F, Merzagora F, Donzelli GP, Merialdi M. Do Italian women prefer cesarean section? Results from a survey on mode of delivery preferences. BMC Pregnancy Childbirth. 2013;13:78.
Torloni MR, Campos Mansilla B, Merialdi M, Betran AP. What do popular Spanish women's magazines say about caesarean section? A 21-year survey. Bjog. 2014;121(5):548–55.
The SURE Collaboration. SURE Guides for preparing and using evidence-based policy briefs. Version 2.1 [updated November 2011]. 2011.
Lewin S, Oxman AD, Lavis JN, Fretheim A, Garcia Marti S, Munabi-Babigumira S. SUPPORT tools for evidence-informed policymaking in health 11: Finding and using evidence about local conditions. Health research policy and systems / BioMed Central. 2009;7 Suppl 1:S11.
Bernard RH. Sampling III: Nonprobability samples and choosing informants. Research methods in anthropology: qualitative and quantitative approaches. 5th ed. United Kingdom: AltaMiraPress; 2011.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Balde MD, Bangoura A, Diallo BA, Sall O, Balde H, Niakate AS, Vogel JP, Bohren MA. A qualitative study of women’s and health providers’ attitudes and acceptability of mistreatment during childbirth in health facilities in Guinea. Reprod Health. 2017;14(1):4.
Balde MD, Diallo BA, Bangoura A, Sall O, Soumah AM, Vogel JP, Bohren MA. Perceptions and experiences of the mistreatment of women during childbirth in health facilities in Guinea: a qualitative study with women and service providers. Reprod Health. 2017;14(1):3.
Bohren MA, Vogel JP, Tuncalp O, Fawole B, Titiloye MA, Olutayo AO, Ogunlade M, Oyeniran AA, Osunsan OR, Metiboba L, Idris HA, Alu FE, Oladapo OT, Gulmezoglu AM, Hindin MJ. Mistreatment of women during childbirth in Abuja, Nigeria: a qualitative study on perceptions and experiences of women and healthcare providers. Reprod Health. 2017;14(1):9.
Bohren MA, Vogel JP, Tuncalp O, Fawole B, Titiloye MA, Olutayo AO, Oyeniran AA, Ogunlade M, Metiboba L, Osunsan OR, Idris HA, Alu FE, Oladapo OT, Gulmezoglu AM, Hindin MJ. “by slapping their laps, the patient will know that you truly care for her”: a qualitative study on social norms and acceptability of the mistreatment of women during childbirth in Abuja, Nigeria. SSM - population health. 2016;2:640–55.
Kyaddondo D, Mugerwa K, Byamugisha J, Oladapo OT, Bohren MA. Expectations and needs of Ugandan women for improved quality of childbirth care in health facilities: a qualitative study. Int J Gynecol Obstet. 2017;139(Suppl 1):38–46.
Maya ET, Adu-Bonsaffoh K, Dako-Gyeke P, Badzi C, Vogel J, Bohren M, Adanu R. Women’s perspectives of mistreatment during childbirth at health facilities in Ghana: findings from a qualitative study. Reproductive Health Matters. 2018;26(53):70–87.
Ojelade OA, Titiloye MA, Bohren MA, Olutayo AO, Olalere AA, Akintan A, Oladapo OT, Fawole B. The communication and emotional support needs to improve women's experience of childbirth care in health facilities in Southwest Nigeria: a qualitative study. Int J Gynecol Obstet. 2017;139(Suppl 1):27–37.
Fox B, Worts D. Revisting the critique of medicalized childbirth: A contribution to the sociology of birth. Gend Soc. 1999;13(3):326–46.
McAra-Couper J, Jones M, Smythe L. Caesarean-section, my body, my choice: the construction of ‘informed choice’ in relation to intervention in childbirth. Fem Psychol. 2011;22(1):81–97.
Donner H. The place of birth: childbearing and kinship in Calcutta middle-class families. Med Anthropol. 2003;22(4):303–41.
Behague DP. Beyond the simple economics of cesarean section birthing: women's resistance to social inequality. Cult Med Psychiatry. 2002;26(4):473–507.
Kuan CI. “Suffering twice”: the gender politics of cesarean sections in Taiwan. Med Anthropol Q. 2014;28(3):399–418.
Litorp H, Mgaya A, Kidanto HL, Johnsdotter S, Essén B. ‘What about the mother?’ Women’s and caregivers’ perspectives on caesarean birth in a low-resource setting with rising caesarean section rates. Midwifery. 2015;31(7):713–20.
Long Q, Kingdon C, Yang F, Renecle MD, Jahanfar S, Bohren MA, Betran AP. Prevalence of and reasons for women’s, family members’, and health professionals’ preferences for cesarean section in China: a mixed-methods systematic review. PLoS Med. 2018;15(10):e1002672.
Beckett K. Choosing cesarean: feminism and the politics of childbirth in the United States. Fem Theory. 2005;6(3):251–75.
Zamboni L, Schellenberg J, Hanson C, Betran AP, Dumont A. Assessing scalability of an intervention: why, how and who? Health Policy Plan. 2019;34(7):544-52.
Download references
Acknowledgements
We appreciate the contributions from women and healthcare providers in Kenya and India for piloting the tools, and the support from the Bangalore Birth Network to recruit and facilitate pilot FGDs.
Funding to develop this protocol was received from the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research, World Health Organization.
Author information
Authors and affiliations.
Gender and Women’s Health Unit, Centre for Health Equity, University of Melbourne School of Population and Global Health, 207 Bouverie St, Carlton, VIC, Australia
Meghan A. Bohren
UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research, World Health Organization, 20 Avenue Appia, Genève, Switzerland
Meghan A. Bohren, Newton Opiyo & Ana Pilar Betrán
School of Community Health and Midwifery, Faculty of Health and Wellbeing, University of Central Lancashire, Preston, UK
Carol Kingdon & Soo Downe
You can also search for this author in PubMed Google Scholar
Contributions
MAB and APB conceptualized the study and drafted the protocol. NO, CK and SD piloted the study tools for content and face validity in Kenya and India, and provided feedback on the draft and tools. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Meghan A. Bohren .
Ethics declarations
Ethics approval and consent to participate.
Scientific and technical approval was obtained from the WHO Human Reproduction Programme (HRP) Review Panel on Research Projects (RP2) and ethics approval was received from the WHO Ethics Review Committee (protocol ID, 004571).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Interventions that may reduce the rate of unnecessary caesarean sections. Twelve potential interventions that may influence use of caesarean section were identified through the WHO guideline development. This file provides a description of each intervention, theory of change, and supporting evidence for each potential intervention.
Additional file 2.
Data collection form: document review.
Additional file 3.
Data collection form: readiness form assessment.
Additional file 4.
Qualitative module 0: Background and understanding context of preferences for mode of delivery.
Additional file 5.
Qualitative module 1: Prenatal education and support.
Additional file 6.
Qualitative module 2: Decision-aids for mode of birth.
Additional file 7.
Qualitative module 3: Psychosocial support for women with fear of childbirth.
Additional file 8.
Qualitative module 4: Labour companionship.
Additional file 9.
Qualitative module 5: Public dissemination of caesarean section rates at a facility-level.
Additional file 10.
Qualitative module 6: Audit and feedback including external review of labour and delivery records and use of Robson classification as a feedback too.
Additional file 11.
Qualitative module 7: Mandatory second opinion before conducting a caesarean section.
Additional file 12.
Qualitative module 8: In-service training and implementation of clinical practice guidelines.
Additional file 13.
Qualitative module 9: Equalising physician pay for vaginal and caesarean birth.
Additional file 14.
Qualitative module 10: Opinion leader education.
Additional file 15.
Qualitative module 11: Setting a goal for caesarean section rate at a facility-level.
Additional file 16.
Qualitative module 12: Policies limiting legal liability and malpractice lawsuits.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Bohren, M.A., Opiyo, N., Kingdon, C. et al. Optimising the use of caesarean section: a generic formative research protocol for implementation preparation. Reprod Health 16 , 170 (2019). https://doi.org/10.1186/s12978-019-0827-1
Download citation
Received : 29 August 2019
Accepted : 18 October 2019
Published : 19 November 2019
DOI : https://doi.org/10.1186/s12978-019-0827-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Caesarean section
- Implementation science
- Complex intervention
- Formative research
- Behavioural change
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Prevalence and determinants of caesarean section in South and South-East Asian women
Roles Conceptualization, Writing – original draft
Affiliation Departments of Neurology, All India Institute of Medical Sciences, New Delhi, India
Roles Formal analysis
Affiliations Department of Biostatistics, King Abdullah International Medical Research Center, Riyadh, Saudi Arabia, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia, Ministry of the National Guard—Health Affairs, Riyadh, Saudi Arabia
Roles Data curation
Affiliation Assam University, Silchar, Assam, India
Roles Writing – review & editing
* E-mail: [email protected]
Affiliation The Graduate School, University of West London, London, United Kingdom
Roles Methodology
Affiliation Department of Quality Assurance Unit, Eurofins Therapeutics Limited, Bangalore, India
Roles Resources
Affiliations King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia, Ministry of the National Guard—Health Affairs, Riyadh, Saudi Arabia, Department of Population Health Research, King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
- Vivek Verma,
- Ramesh K. Vishwakarma,
- Dilip C. Nath,
- Hafiz T. A. Khan,
- Ram Prakash,

- Published: March 12, 2020
- https://doi.org/10.1371/journal.pone.0229906
- Reader Comments
Caesarean section is considered a relatively preferable and safe method of delivery as compared to normal delivery. Since the last decade, its prevalence has increased in both developed and developing countries. In the context of developing countries viz., South Asia (the highest populated region) and South-East Asia (the third-highest populated region), where a significant proportion of home deliveries were reported,however, the preference for, caesarean delivery and its associated factors are not well understood.
To study the caesarean delivery in the South and South-East Asian countries and to determine the factors associated with the preference for caesarean delivery.
Methodology
Demographic and Health Survey Data on from ever-married women of nine developing countries of South and South-East Asia viz., Vietnam, India, Maldives, Timor-Leste, Nepal, Indonesia, Pakistan, Bangladesh, and Cambodia have been considered. Both bivariate and binary logistic regression models were used to estimate the propensity of a woman undergoing for caesarean delivery and to assess the influence of maternal socioeconomic characteristics towards the preference for caesarean delivery.
Obtained results have shown an inclination of caesarean delivery among urban than rural women and are quite conspicuous, but is found to be underestimated mostly among rural women. Caesarean delivery in general is mostly predisposed among women whose baby sizes are either very large or smaller than average, have a higher level of education and place of delivery is private medical institutions. The logistic regression also revealed the influence of maternal socioeconomic characteristics towards the preference for caesarean delivery. Based on nine South and South-East Asian countries an overall C-section prevalence of 13%, but based on institutional births its increase to 19%. The forest plot demonstrated that a significant inclination of C-section among urban than rural regions. In Meta-Analysis, very high and significant heterogeneity among countries is observed, but confirms that in terms of prevalence of C-section all of the countries follow independent pattern.
Study of seven urban and four rural regions of nine South and South- East Asian countries showed, a significant inclination towards the caesarean delivery above the more recent outdated WHO recommended an optimal range of 10–15%and are associated maternal socioeconomic characteristics. In order to control unwanted caesarean delivery, the government needs to develop better healthcare infrastructure and along with more antenatal care related schemes to reduce the risks associated with increased caesarean delivery.
Citation: Verma V, Vishwakarma RK, Nath DC, Khan HTA, Prakash R, Abid O (2020) Prevalence and determinants of caesarean section in South and South-East Asian women. PLoS ONE 15(3): e0229906. https://doi.org/10.1371/journal.pone.0229906
Editor: Russell Kabir, Anglia Ruskin University, UNITED KINGDOM
Received: January 18, 2020; Accepted: January 28, 2020; Published: March 12, 2020
Copyright: © 2020 Verma et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are from The DHS Program ( https://dhsprogram.com/data/ ).
Funding: Eurofins Limited provided support in the form of salary for author: RP. The specific role of this author is articulated in the ‘author contributions’ section.
Competing interests: The authors have read the journal's policy and the authors of this study have the following competing interests: RP is a paid employee of Eurofins Limited ( https://www.eurofins.com/agroscience-services/about-us/latest-news/eurofins-scientific-to-acquire-advinus-therapeutics/ ). There are no patents, products in development or marketed products associated with this research to declare. This does not alter our adherence to PLOS ONE policies on sharing data and materials.
1. Introduction
Caesarean section in developed and developing countries[ 1 – 3 ], are considered as the mostpreferred method of childbirth. The preference of caesarean section is found to be comparatively high in the last decade[ 4 ], and one of the significant reason is attributed to the reduction in mortality risk of death to mother and child during delivery[ 5 ],[ 6 ]. There are various factors causing an increase in C-section. In most of the developing countries, demographic changes, social and educational improvement have led to an increase in the number of women delaying their pregnancies until getting on their end of fertile life[ 7 ]. This social development pooled with accessibility to birth control and infertility treatment has increased the number of women experiencing their first pregnancy only after 35 years of age[ 8 ]. The Caesarean section or C-section is a surgical procedure, where delivery proceeds through the abdominal and uterine incision. This procedure is appropriate in situations where vaginal (or normal) delivery is considered life-threatening for the mother and the baby. Although caesarean delivery is considered a relatively safe delivery method but has complications[ 9 ] as compared to vaginal birth or a natural method of birth. One of the major issues with the caesarean deliveries other than post-delivery risks and complication is the cost. It increases due to operation and longer stay in hospitals, and that result in an increased financial burden to the families[ 10 ]. The most frequently occurring complications during and after a caesarean to mothers and children have already been discussed [ 11 – 14 ]. In thepast, the World Health Organization[ 15 ] had suggested that although caesarean section is a safe method, if caesarean rate exceeds the limit of 10–15%, it may not lead to better outcomes. However, that previous suggestion had come under criticism for multiple reasons. The WHO may have changed it's view as it released a statement in 2015 with the headline. WHO recommends that every effort should be made to provide caesarean sections to women in need rather than to achieve any specific rate. Earlier works[ 16 – 18 ] have suggested that if caesarean rate increases above WHO recommended the range, then as a consequence the risk of manifestation of other public health-related problems for both mothers and children will also increase. Some of work[ 19 ] have more recently concluded that the 1985 WHO document[ 15 ] looked at studies that were incomplete because they examined data from limited sets of countries and often examined outcomes in wealthier countries. In addition, many studies used data from varying years without accounting for heterogeneity across years.
Furthermore, what is being overlooked is that the WHO document[ 15 ] looked at correlation only with mortality. Fetal and maternal morbidities were not taken into account for these rates. It is essential to keep foremost in mind that fetal morbidity should be weighed much higher than maternal morbidity as failure to do C-section when indicated can result in babies with profound brain damage which are catastrophic not only for the babies entire future life but also catastrophic for the parental caregivers and the rest of the family.
The rate of caesarean section is usually defined as the fraction of women who adopted caesarean delivery procedure among total childbirths in a specified time period in a specific geographic area. Under the assumption that in this selected area almost all deliveries took place in medical institutions, as the procedure of caesarean delivery is possible their only, then the existing models and estimates of the caesarean rate discussed in the literatures are appropriate. But in developing countries of South and South-East Asia viz., Vietnam, India, Maldives, Timor-Leste, Nepal, Indonesia, Pakistan, Bangladesh and Cambodia, a considerable proportion of child deliveries are carried out at home,known as non-institutional birth( Table 1 ) and are completely free of risks and complications associated with caesarean deliveries.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0229906.t001
The countries of South and South-East Asia are regions of great social, economic and political diversity. Despite their diversity, countries in this region are attempting to reduce their regional health challenges ([ 20 ] and [ 21 ]) and promoting safe and healthy maternal and child health, and also encourage deliveries in the supervision of trained health professionals[ 22 ], under proper hygienic conditions.
As the caesarean is a surgical procedure and is only possible at medical institutions. Therefore, the present study have focused on the prevalence of caesarean section among women from different South and South-East Asian countries, who have experienced the institutional deliveries, have been investigated. In this study, an attempt has been made to provide a better understanding of the behavioral pattern of among women of these countries towards caesarean section by comparing their residence, educational status, birth parity and choice of place of delivery. Through this study, the dependency and importance of the socio-economic factors on the caesarean section preference for delivery have also been explored.
Data for this study was obtained from Demographic and Health Surveys (DHS) database on maternal deliveries occurred in nine developing countries viz., Vietnam, India, Mal- dives, Timor-Leste, Nepal, Indonesia, Pakistan, Bangladesh and Cambodia. DHS is a series of nationally representative household surveys that provide information on population, health and nutritional status of mother and child. The study dataset includes only the latest round of data of each selected country. List of selected South and South-East Asian countries and the corresponding survey years are given in Table 1 . In the present study, it is assumed that woman corresponding to each country has equal possibility of being experiencing the caesarean delivery; therefore, the analysis is done without incorporating the weight variable.
2. Study parameters
The relationship with incidences of caesarean section with some of the associated maternal socio-economic characteristics viz., maternal age, place of residence, level of maternal education, birth order of the child, and type of medical facility that opted for delivery and size of the baby has been modeled. Age as reported subjectively by mother, and grouped into 6 subgroups: 15–19, 20–24, …,40–44. The 45 to 49 age group was not taken into account due to a lack of sufficient data. The type of place of residence is classified as rural and urban. The educational qualification is classified into three classes, primary, secondary and higher. Birth order of the born child is grouped into first, second, third, fourth and fifth or more. The medical institutions that opted for the delivery are grouped as government or private facilities. The size of the child was classified as below average, average and above average, and large. Our interest lies in finding the prevalence of caesarean section in the countries of South and South-East Asia.
Statistical analyses
Both bivariate logistic regressions and multivariate logistic regression models have constructed separately to estimate the prevalence of caesarean section to a woman based on her socio-economic characteristics, viz., maternal age, place of residence, level of maternal education, birth order of the child, and type of medical facility that opted for delivery and size of the baby. The results obtained from the regression analyses have been presented in terms of the odds ratios (ORs) with 95% confidence interval (CI). Statistical analyses were performed using the Statistical Analysis System (SAS) package, (university edition) and SAS version 9.4, and all other computation is carried out using R (version-3.0.3). Corresponding to each of the associated maternal socio-economic characteristics, the associations with the prevalence of caesarean sections have been examined using binary logistic regression analyses, to examine the effect of socio-economic factors on the odds of caesarean birth and non-caesarean birth. The event of caesarean section during delivery is considered as a dichotomous variable, where if caesarean then denotes'1' and '0' for otherwise.
The database considered for the present study does not contain any individual identifiable information. Due to the unidentified nature of the dataset and no human subject were directly involved in the present study; therefore, this study was exempt from any ethical or Institutional Review Board clearance.

3. Results and discussion
Prevalence of caesarean section.
Table 2 presents the rate of caesarean section based on both institutional and non-institutional births, separated by place of residences viz.,rural and urban regions, of South and South-East Asian Countries. A substantial inter-region variation in caesarean rates corresponding to each country has been observed. Obtained results have shown an inclination of caesarean delivery among urban than rural women and are quite conspicuous. Even with additional non-institutional births ( Table 2 ) to institutional births, the rate of caesarean delivery was found in urban part is highest in women of Maldives (39.07%) followed by India (23.64%), Bangladesh (21.82%), Vietnam (21.72%), Pakistan (17.75%) and Indonesia (17.25%), which have crossed the WHO recommended range of 10–15%[ 19 ]. The caesarean rate in the rural women of Maldives (30.70%) has only crossed the WHO recommended range. The caesarean rate in women residing in urban regions is five times of rural women in Nepal; three times of rural women of Vietnam, Timor-Leste, Indonesia and Cambodia, and twice of the rural women of India, Pakistan and Bangladesh.
https://doi.org/10.1371/journal.pone.0229906.t002
To obtain a better estimate for the prevalence of caesarean deliveries in each of the selected South and South-East Asian Countries, the population is classified into two disjointed sub-populations based on their place of delivery viz., institutional or non-institutional. Here, institutional deliveries referred to those deliveries occurred at any private or government medical institutions, whereas births occurred other than any medical institutions, are considered as non-institutional births. To visualize the prevalence of caesarean section and the population at risk, only institutional deliveries have been taken into account for investigation.
Results based on institutional delivery, Table 3 shows that the rate of caesarean delivery found is highest among the urban women of Bangladesh (62.88%) followed by Maldives (39.18%), Pakistan (27.79%), India (27.28%), Indonesia (22.49%), Vietnam (22.05%), and Nepal (17.47%) that have crossed the WHO recommended range of 10–15%. Among the rural women, the caesarean rate is on the higher side of Bangladesh (54.78%) followed by Maldives (32.21%), Pakistan (20.46%) and Indonesia (18.79%), which have crossed the WHO recommended range. The overall caesarean rate in women of five countries viz., India, Maldives, Indonesia, Pakistan, andBangladesh, have found more than 15%.
https://doi.org/10.1371/journal.pone.0229906.t003
The percentage distribution of caesarean section among women based on their socio- demographic characteristics has been depicted in Figs 1 – 6 . Fig 1 is showing a positive association of caesarean rate with the 15–39 age-grouped women, but on the contrary the caesarean rate among women belongs to 40–44 is comparatively low as compared to those belongs to 35–39. It also shows that the caesarean rates are more than 15% (WHO recommended) among the women aged 30 and above in all countries except Timor-Leste and Cambodia. Fig 2 depicts a negative association between the prevalence of caesarean delivery and the birth order of the child, i.e., chance to get caesarean section is high to women having birth order less than four. In countries Maldives and Bangladesh, caesarean rates are very high and found for all birth orders. From Fig 3 , it has been found that caesarean is more preferred to women whose baby sizes are either very large or smaller than average. Irrespective of the size of the baby, caesarean rates in Maldives, Nepal, and Bangladesh have been found to be very high. Fig 4 depicts a positive association between caesarean section and women's education level. It is found in all countries that women who have a higher level of education are more predisposed towards caesarean childbirth. Caesarean sections among urban women, as depicted in Fig 5 , were very high as compared to those of rural women except in Bangladesh, where rates are very high in women from both regions. Fig 6 , depicts the caesarean sections among the women whose delivery occurred at private medical institutions which are very high compared to those delivered at government medical institutions.
https://doi.org/10.1371/journal.pone.0229906.g001
https://doi.org/10.1371/journal.pone.0229906.g002
https://doi.org/10.1371/journal.pone.0229906.g003
https://doi.org/10.1371/journal.pone.0229906.g004
https://doi.org/10.1371/journal.pone.0229906.g005
https://doi.org/10.1371/journal.pone.0229906.g006
Determinants of prevalence of caesarean section
Tables 4 and 5 show the results of the bivariate and multivariate logistic regression analysis, respectively. The unadjusted analysis of multivariate logistic regression has revealed that maternal age, mother's education (except Vietnam and Maldives), choice of medical institutions (government and private) for childbirth (except Vietnam and the Maldives), birth order and place of residence (except the Maldives, Timor-Leste, and Bangladesh) have a significant effect on caesarean section. The variable baby size" has a significant effect on the prevalence of caesarean delivery (except Timor-Leste, Nepal, Indonesia, Bangladesh and Cambodia). The bivariate analyses applied in the study showed that maternal age, mother's education (except Timor-Leste), choice of medical facility for childbirth (except the Maldives), birth order and place of residence (except the Maldives) have a significant effect on the prevalence of caesarean section. The variable 'size of the baby' had been found to be insignificant in Timor-Leste, Nepal, Indonesia, Bangladesh, and Cambodia, while in the remaining countries viz.,Vietnam, Maldives, Pakistan, and India revealed a significant effect on the prevalence of caesarean delivery.
https://doi.org/10.1371/journal.pone.0229906.t004
https://doi.org/10.1371/journal.pone.0229906.t005
Women with higher education were more likely to have a caesarean section compared to those who have less education. Women who have opted for private institutions for delivery, compared to governmental medical institutions, were more likely to undergo a caesarean section. The order of birth showed a constant decrease in caesarean section. The place of residence showed that urban women, compared to their rural counterparts, have seen to be more likely to experience caesarean sections. The size of the infants has been found significant associated with caesarean section in countries viz., Vietnam, Maldives, Pakistan and India,which shows that women in these countries with a baby size outside of average reference size are more likely to give birth by caesarean section.
As caesarean is a surgical procedure and is possible in medical institutions, whereas women, whose delivery is not institutional, cannot be considered to be exposed for caesarean delivery and are not part of the population of interest. Corresponding to each selected country, the results revealed a shift towards institutional delivery over those of non-institutional deliveries, which indicate the effectiveness of health programs and mothers' increasing awareness of the importance of institutional delivery. It should also be noted regarding the Maldives that the prevalence of caesarean sections based on the total number of deliveries was 31.78%, which is quite close to the prevalence based on births in institutions, 33.14%. The reason for this closeness of estimates is that in the Maldives, 95.94% of births are institutional. In the case of Timor-Leste and Bangladesh, respectively, where 19.21% and 23.52% of births are in institutions. The prevalence based on the institutional births in Timor-Leste and Bangladesh has found to 4.45 and 5.2 times higher than those rates based on the total number of births, respectively. Our findings suggest that women with higher education are more likely to undergo caesarean as compared to uneducated women. The age of women was found to have a weak positive impact (the odds are slightly higher than one) on the risk of caesarean (i.e., every one-year increment on women's age, the risk of caesarean is approximately 1.1 times in women as compared to women with normal delivery). There are positive trends found for caesarean delivery in private hospitals. Our results indicate that odds for caesarean delivery in private hospitals as compared to government hospitals are very high. Results suggest that women with higher education are more likely to have caesarean sections than women who are uneducated. The age of women with low impact (odds are slightly higher than 1) on the risk of caesarean section. Results have indicated that odds for caesarean delivery in private hospitals as compared to government hospitals are very high.
Based on nine South and South-East Asian countries, where 3,24,708 births reported (both institutional and non-institutional) who had an overall C-section prevalence of 13% in Fig 7 . All of the selected nine countries with an overall odds ratio (OR) of caesarean prevalence in urban as compared to rural was 2.60 (95% CI 2.54–2.65). Among 2,28,055 institutional births reported ( Fig 8 ), with an overall prevalence of C-section 19%, except in Timor-Leste, the OR of caesarean prevalence in urban as compared to rural was more than one and are significant. Here, using Figs 7 and 8 , we also meta-analysed caesarean data to demonstrate the pattern of C-section among urban and rural regions of different countries, by using the odds ratios and forest plot. Fig 7 examined the prevalence pattern of C-section in urban regions as compared to rural regions. The heterogeneity in the pattern of caesarean prevalence in urban and rural regions among countries can be confirmed by a high I 2 value, which was found to be 88% based on combined institutional and non-institutional birth records, and 96% based on institutional births, and both of them have significant p-value. Due to this large and significant heterogeneity, pooled estimated of C-section in South and South-East Asian countries will not be appropriate, but confirms that in terms of prevalence of C-section all of the countries follow independent pattern.
https://doi.org/10.1371/journal.pone.0229906.g007
https://doi.org/10.1371/journal.pone.0229906.g008
There is a significant inclination in institutional deliveries in all selected countries, which indicates the effectiveness of women's awareness programs and programs. The main reason for this transition is that it reduces the risks and complications that occur during deliveries. This increase in the number of deliveries may be an important reason for caesarean delivery bias in countries viz., Maldives, Indonesia, Pakistan, Bangladesh and India,above the previous WHO recommended an optimal range of 10–15%. Having said this, the recommended rate might be higher if preventing serious morbidity is also taken into account. The prevalence of caesarean section is also examined for different socioeconomic covariate markers. The analysis shows that maternal age, maternal education, and birth order are significantly associated with caesarean delivery.
Of all the other determinants of the prevalence of caesarean delivery in any medical facility, the choice of place of birth viz., Government and private facilities may be a strong influence on the choice to undergo a caesarean section. Increases in the caesarean rates create a heavy burden on the health system[ 15 ] and also increases the risk of other health problems to both mother and baby, and unwanted caesarean delivery also puts a huge financial burden on the family economic status.
The limitations of the present study are that non-institutional births have not been taken into account to determine the extent of normal birth. The reason for non-institutional births could be attributed to fear of surgical proceeding involved in C-section or poor economical status or unavailability well equipped medical facility. Moreover, to under- stand the priority of C-section deliveries for further investigation of the reasons behind the prevalence, more relevant data on women and doctors' decision-making process for the safe child delivery and related risks, are needed. Due to unavailability of the reason for opting C-section among women having institutional births, further analysis about the situation where C-section is more preferable remained unexplored.
4. Conclusions
This study examines the prevalence of caesarean section in selected countries of South and South-East Asia, which is the top and third-largest populous region in the world. To represent the difference between rural and urban areas, the DHS datasets are considered so that the variation between the various facilities and the health and demographic indicators can be examined according to their place of residence. Both the logistic regression and the meta-analysis have shown a behavior change in rural and urban areas towards the adoption of a caesarean procedure. But in urban areas, rates are comparatively higher than in therural areas. The results showed that despite the disparity in the prevalence of caesarean section among rural and urban women, the percentages based on institutional births are completely different from those obtained using the information on total births. As a result, the government needs to develop better healthcare infrastructure and along with more antenatal care related schemes to reduce the risks associated with increased caesarean delivery.
Supporting information
https://doi.org/10.1371/journal.pone.0229906.s001
Acknowledgments
The authors would like express their deepest gratitude and sincerely thank to the Demographic and Health Surveys (DHS) programme, to provide access of data for this study. Also the authors would like to thank all of the anonymous reviewers for their valuable comments and suggestions that helped us to improve the quality of the article.
- View Article
- Google Scholar
- 2. Chavan Niranjan. "Caesarean Delivery." In Labour Room Emergencies , pp. 297–303. Springer, Singapore, 2020.
- PubMed/NCBI
Effect of previous caesarean section on reproductive and pregnancy outcomes after assisted reproductive technology: A systematic review and meta‑analysis
Affiliations.
- 1 Department of Gynaecology, Huzhou Maternity and Child Care Hospital, Huzhou, Zhejiang 313000, P.R. China.
- 2 Reproductive Center, Huzhou Maternity and Child Care Hospital, Huzhou, Zhejiang 313000, P.R. China.
- PMID: 38800052
- PMCID: PMC11117117
- DOI: 10.3892/etm.2024.12572
Pregnancies following previous caesarean section (CS) are associated with higher incidence of infections, postpartum haemorrhage and obstetric complications. The present study aimed to explore the effect of previous CS on reproductive, maternal and neonatal outcomes in women who underwent assisted reproductive techniques (ART). A systematic review and meta-analysis were conducted to assess reproductive and pregnancy outcomes following ART in women with and without a previous CS. Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines were followed. Eligible language articles written in English, published up to October 2023, were identified in Medline, Google Scholar and Science Direct databases. The quality of the included studies was assessed using the Newcastle Ottawa Scale. A total of 19 articles, reporting on 13 different outcomes met the inclusion criteria. It was revealed that women with previous CS had 9% lower clinical pregnancy rates, 13% lower live birth rates, 11% lower implantation rates and 28% lower multiple pregnancy rates compared with women who had prior natural vaginal deliveries. Additionally, previous CS was associated with an 8-fold higher risk of difficult embryo transfers. No significant differences were noted in ectopic pregnancy rates, miscarriage rates or biochemical pregnancy rates. The present systematic review and meta-analysis demonstrated that previous CS is associated with decreased prospects of clinical pregnancy, live birth and successful embryo implantation during ART. The findings of the present study underscored the need to counsel women with prior CS regarding its potential impact on ART outcomes.
Keywords: assisted reproductive techniques; caesarean section; pregnancy outcomes; reproductive outcomes; vaginal delivery.
Copyright: © 2024 Cao and Chen.
Grants and funding
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.11(5); 2021

Original research
Caesarean sections and health financing: a global analysis.
1 Kolegji Heimerer, Pristina, Kosovo
2 The Dartmouth Institute for Health Policy and Clinical Practice, Lebanon, New Hampshire, USA
Günther Fink
3 Swiss Tropical and Public Health Institute, Basel, Switzerland
4 University of Basel, Basel, Switzlerland
Associated Data
bmjopen-2020-044383supp001.pdf
Data are available in a public, open access repository. The data used for this study are freely available from the WHO’s Global Health Expenditure Database and Global Health Observatory, and from the World Bank Open Data.
The objective of this study is to explore the association of health financing indicators with the proportion of births by caesarean section (CS) across countries.
Ecological cross-country study.
This study examines CS proportions across 172 countries.
Main outcome measures
The primary outcome was the percentage excess of CS proportion, defined as CS proportions above the global target of 19%. We also analysed continuous CS proportions, as well as excess proportion with a more restrictive 9% global target. Multivariable linear regressions were performed to test the association of health financing factors with the percentage excess proportions of CS. The health financing factors considered were total available health system resources (as percentage of gross domestic product), total contributions from private households (out-of-pocket, compulsory and voluntary health insurance contributions) and total national income.
We estimate that in 2018 there were a total of 8.8 million unnecessary CS globally, roughly two-thirds of which occurred in upper middle-income countries. Private health financing was positively associated with percentage excess CS proportion. In models adjusted for income and total health resources as well as human resources, each 10 per cent increase in out-of-pocket expenditure was associated with a 0.7 per cent increase in excess CS proportions. A 10 per cent increase in voluntary health insurance was associated with a 4 per cent increase in excess CS proportions.
Conclusions
We have found that health system finance features are associated with CS use across countries. Further monitoring of these indicators, within countries and between countries will be needed to understand the effect of financial arrangements in the provision of CS.
Strengths and limitations of this study
- Our study benefits from a large sample size, using information from 172 countries.
- The ecological nature of our study means that we cannot make definitive statements about causality in considering the relationship between the variables of interest.
- Although we used some of most reliable internationally available data sources, the quality of such data may not be entirely uniform across countries included in the analysis.
- We have been able to adjust only for some confounders in our statistical models. There are other macro level factors that do play a role that we could not account for in our analysis.
Introduction
Caesarean section (CS) rates have been increasing rapidly over the past decades at the global scale, with remarkable variation both within and between countries. 1–15 Such medical practice variation, in general, implies inefficient use of resources, that is, patients may not get what they need (underuse) or will get medically unnecessary care (overuse). 16 17 Empirically, CS rates between 9 to 19 per cent have been associated with improved health outcomes for mother and babies. 5 18–20 As such, rates below 9 per cent are likely to represent underuse, while rates above 19 per cent likely represent overuse and may cause more harm than benefits to mothers and children, leaving aside the substantial additional cost and burden to the health system. 1 5 6 21 22 Overuse of procedures like CS is likely to take away resources that could be used for other beneficial procedures and care.
As with all healthcare utilisation measures, overuse of delivery-related resources is a manifestation of the effect of a range of factors influencing health system performance, including health system structure and financing, medical practice patterns and patient preferences and behaviours. 1 23 On the supply side, it can be a manifestation of availability of resources, that is, supply sensitive care, 17 where more resources available mean more care provided, and/or provider behaviour, that is, supplier induced demand. 24 Recent studies have highlighted the relevance of financing and incentives to the overuse of CS. 25–27 In many settings, payment mechanisms or reimbursement systems provide a financial incentive for providers to deliver by CS rather than vaginally. 25–27 For example, hospitals incentivise, via time-pressures 28 29 or scheduling policies, 30 31 insurers via payment models like fee for service 32–34 or higher reimbursements rates for CS. 35 36 In developing countries, this can also happen via informal rewards. 37
Health sector financing approaches are complex and highly heterogeneous across countries, ranging from full government financing to mandatory insurance contribution and direct out-of-pocket payments. Modalities through which health sectors are financed affect how resources are spent, and how care is delivered. It is also likely that patients have more influence on provider behaviour in settings where the majority of healthcare costs are paid out-of-pocket than in settings where the entire health sector is centrally controlled and paid by government resources. In this paper, we explore the association of health financing indicators with caesarean proportions across countries using the most recent data on CS proportions and financial indicators. Our primary hypothesis was that reliance on private payment mechanisms would increase pressure on providers to use CS through one of two main mechanisms: first, by reducing governmental control over the services provided and second, by increasing entitlement and relative bargaining power of patients who may have personal preferences for CS.
We used data from several sources including Global Health Expenditure Database and Global Health Observatory (GHO) data from the WHO as well as the World Bank Open Data. The Global Health Expenditure Database of the WHO provides data on health spending for close to 190 member countries from 2000 to 2018. This is an annually updated database where the WHO works collaboratively with member countries. The GHO is also a WHO gateway to health-related statistics for its 194 member countries. GHO country data includes all country statistics and health profiles that are available within the WHO. The World Bank’s data catalogue provides access to over 3000 data sets and 14 000 indicators and includes microdata, time series statistics and geospatial data. A list of all data sources is provided in the online supplemental appendix .
Supplementary data
Outcome variable.
The primary outcome variable was the percentage excess of CS. Based on the most recent estimates, 5 we used a CS proportion of 19 per cent as our reference, and considered all births delivered via CS above this level as excess. Specifically, we coded percentage excess CS (the proportion of deliveries in 2019 that exceeded 19% CS) as zero if a country has a proportion ≤19 per cent, and as the actual proportion minus 19 per cent when the proportion exceeds this target. We also analysed percentage excess of CS using a 9 per cent benchmark 20 and (continuous) CS proportions as secondary outcomes.
Exposure variables
Our primary exposure variables of interest are private contributions to health financing. Private contributions comprise three types of private health-related expenditures: (1) mandatory contributions to health insurance schemes; (2) voluntary contributions to (additional) insurance schemes and (3) out-of-pocket payments. We first considered a variable that combines all three variables, and thus measured total private contributions as percentage of total current health expenditure. In a second step, we analysed each of these three components separately, that is, included separate variables for mandatory contributions, voluntary contributions and out-of-pocket payments, all expressed as per cent of total current health expenditure. Mandatory contributions to health insurance are the primary source of health financing in insurance-based systems such as the ones in Germany, Switzerland or the USA, and most typically directly collected through employers in high-income settings. Voluntary insurance schemes are largely absent in countries such as Cuba, Jordan or Norway, but play a significant role in other settings. In many European countries such as Austria and Switzerland, voluntary insurance covers between 5 and 10 per cent of health expenditure—in Brazil, voluntary insurance contracts cover over one-third of total expenditure. Voluntary insurance generally covers premium services (such as fast access to doctors and private rooms) but in some cases can also reduce out-of-pocket co-payments. Out-of-pocket payments exist in all countries but range from less than 1 per cent in Kiribati and Nauru to close to 80 per cent in Armenia and Azerbaijan. The full data used in the analysis is provided in the online supplemental appendix .
Statistical analysis
We started by presenting the global distribution of CS proportions graphically. In a second step, we showed CS proportions as well as the estimated total CS percentage excess relative to the 19 and 9 per cent targets. Following the World Bank’s country classification, we divided countries into high, upper middle, lower middle and low income countries and separately computed excess shares and number for each country-income group. In a third step, we examined the association of CS percentage excess with health financing mechanisms. We first estimated ordinary least squares regression models with percentage excess CS, using 19 and 9 per cent as benchmarks, as well the overall CS proportion as outcome and total private contributions as exposure variable. We then estimated a similar model where we included separate variables for compulsory, voluntary and out-of-pocket payments. In both models, we controlled for income per capita and general size of the health sector to reduce potential confounding biases. To further address residual confounding concerns, we estimated two additional models that also controlled for the proportion of deliveries made by skilled birth attendants (model 3) as well as the health systems human resources (model 4). All confounding variables included have been shown to predict variation in medical practice, 1 17 such as variation in CS provision. 1 To address missing data on some of the control variables, we used Stata’s multiple imputation with chained equations algorithm.
Sensitivity analysis
To ensure the results are not disproportionately shaped by specific regions, we estimate separate models by country-income group in our sensitivity analysis. All analysis was conducted using the Stata V.15 SE statistical software package.
Patient and public involvement statement
Our study does not directly use data from patients. We used only the WHO and the World Bank data published online.
Figure 1 shows the distribution of caesarean proportions for the 172 countries with data available. CS proportions varied between 0.5 per cent in South Sudan and 58.1 per cent in the Dominican Republic. At the regional level, lowest proportions were observed for the WHO Africa region (mean 7 per cent) and highest proportions were found for the Americas, with an average proportion of 31.8 per cent. Ninety countries (52 per cent) had CS proportions ≤19%, and 82 countries (48 per cent) had proportions above the target range.

Global distribution of caesarean birth proportions. CS, caesarean section.
Table 1 provides summary statistics for our sample. Countries with CS proportions >19% were on average substantially wealthier, and had higher obstetrician and midwife densities, while overall health expenditure as percentage of gross domestic product (GDP) was relatively similar in the two subgroups (6.5 vs 7.2%, p value 0.112). Countries with CS proportions >19% had substantially higher average rates of out-of-pocket expenditures as well as mandatory and voluntary insurance contributions. The correlation between all variables used is shown in the online supplemental appendix . The highest bivariate correlation was found between midwife density and GDP per capita (0.79)—no evidence of multicollinearity was found in the regression models.
Descriptive statistics by excess category
Table shows mean and SD for all variables for the full sample, as well as for countries with a CS proportion ≤9% and 19%, and countries with a CS proportion >9% and 19%.
*P values are based on a zero-mean-difference test between the two subsamples.
CHE, current health expenditure as percentage of GDP; CS, caesarean section; GDP, gross domestic product.
Overall, using a 19 per cent benchmark, we estimate that there were 8.8 million unnecessary CS in 2018. Table 2 summarises the global distribution of CS and percentage excess CS using the World Bank’s country income classification for the 172 countries in our sample. Given that most countries with missing data in the GHO have low populations, the 172 countries in our sample covered 97 per cent of the global births in 2018. While low-income countries did not contribute at all to percentage excess provision of CS in that year, overprovision was common in lower middle-income countries. Overall, lower middle-income countries accounted for 48 per cent of all births in 2018, and for 18 per cent of all percentage excess CS. Upper middle-income countries account for 25 per cent of all births, but for 67 per cent of all percentage excess CS. Using 9 per cent as a benchmark, we estimate a total of 17 million of unnecessary CS. Trends across country income groups mimic the main findings with 19 per cent benchmark.
Distribution of birth, percentage excess of CS across country income groups
CS, caesarean section.
Table 3 shows the main regression results. There are three sets of results. We first show results for our main outcome measure, that is, percentage excess using 19 per cent benchmark. The other two sets included results for additional outcomes, that is, percentage excess using 9 per cent benchmark and the absolute CS proportion. When we pooled all private contributions in column 1, we found a small positive association between private contributions and CS excess. A coefficient of 0.08 implies that countries with 100 per cent private financing have on average 8 per cent higher excess CS proportions than countries relying fully on government financing. When we split private contributions into their three components in column 2, we found that this overall association is primarily driven by voluntary insurance mechanisms. When controlling only for GDP per capita and the size of the health sector in table 3 , column 2, we found no associations for out-of-pocket expenditure, a moderate sized coefficient for compulsory contributions and a rather large coefficient for voluntary health insurance: each 10 per cent increase in voluntary health insurance contributions is associated with a 5.6 per cent increase in excess CS proportions. These associations change only marginally when adjusting for general reproductive and health access variables in table 3 , columns 3 and 4. Effects are similar or even more pronounced if we use percentage excess with 9 per cent benchmark or continuous CS proportions.
Associations between health financing variables and CS proportions
Estimated coefficients are based on ordinary least squares regressions with heteroscedasticity-robust SEs in parenthesis. Missing values on predictor were imputed using Stata’s mi impute algorithm. *P values <0.10; **P value <0.05; ***P value <0.01. Column 1 uses the combined private expenditure variable as primary exposure variable. Columns 2–4 show separate results for out-of-pocket, voluntary and compulsory insurance contributions. All models control for GDP per capita and current health expenditure (percentage of GDP). Column 3 further controls for the percentage of births attended by a skilled birth attendant. Column 4 also control for the obstetrician and midwife densities. Descriptive statistics and definitions of all variables are provided in table 1 .
Table 4 shows the main results of our sensitivity analysis. When we split our sample by country income groups, we find the largest associations in all categories for the upper-middle income group, and the weakest in the low-income group. Due to the small sample sizes the precision of these estimates is however very low (all p values >0.1) for all outcome measures we used.
Sensitivity analysis: associations by country income group
Estimated coefficients are based on ordinary least squares regressions with heteroscedasticity-robust SEs in parenthesis. Missing values on predictor were imputed using Stata’s mi impute algorithm. Total private expenditure is defined as the sum of out-of-pocket expenditure, mandatory and voluntary insurance contributions. Columns 1–4 show multivariable estimates using CS proportion as outcomes. Columns 5–8 use proportion >9% as outcome. Columns 9–11 use proportion >19% as outcome. No estimates are shown for lower income countries for CS >19% due to lack of variation. *P values <0.10; **P value <0.05; ***P value <0.01.
Consistent with previous papers highlighting the increasing global trend of increasing CS proportions 2–9 we have found a striking number of CS that seem unnecessary. Using a relatively conservative 19 per cent CS rate benchmark, we estimate that 8.8 million unnecessary CS were carried out in 2018. The vast majority of these percentage excess CS occurred in upper-middle income countries. Belizán et al using a 15 per cent benchmark, with data between 1993 and 1997 estimated that over 850 000 unnecessary CS are performed each year in Latin America. 8 Gibbons et al looking at 137 countries, using a 15 per cent benchmark and data from 2008, estimated that 6.2 million unnecessary CS are performed each year, with China and Brazil accounting for close to 50% of this global total. With a 20 per cent benchmark rate, there was an estimate of 4 million of unnecessary CS a year. 6 Our estimates are about 30 per cent higher than these previous numbers may represents both a growing number of births each year and a continued rise in CS rates in middle-income settings.
Studies looking at global CS trends have highlighted the associations between CS and maternal and newborn mortality, 5 18–20 socioeconomic status of women, 3 9 private sector care 8 9 38 and economic growth. 4 8 Our results suggests that health financing mechanisms may play a key role in explaining the large differences across countries. We show that, on average, countries relying on private financing have higher CS rates. These associations are particularly pronounced for voluntary health insurance schemes, which generally are used to ‘top up’ basic health plans and allow users to use premium features. Health insurance, by incentivising healthcare providers, 1 25–27 is known to encourage the overuse of CS. 26 39
In general, higher CS rates should be expected in higher income countries due to increased resources 17 40 or supply sensitive care. 17 40 Similar to previous studies, 4 8 we find that national CS rates increase with income. We find however that this positive gradient is only observable up to the middle-income category, and flat or even declining in higher income settings. The generally positive trends can be attributed to a large number of factors, including an increasing proportion of births occurring in health facilities 9 or attended by trained health personnel, 7 different work force composition 41–45 and different technology. 46
Increases in CS rates are a result of multitude of factors 1 23 that interact in complex ways. As such, results of ecological studies should be interpreted with caution, and in the context of the specific systems analysed. For example, private insurance and private sector care often overlap at the country level, and both are likely to contribute to the use of care in general and CS in particular. 25–27 Studies looking at cross-country comparisons have documented the impact of private care. Belizán et al looking at 19 Latin American countries, observed a positive correlation between private hospitals and the rate of CS. 8 Boerma et al , on the basis of data from 169 countries, 9 and Benova et al looking at 57 countries, 38 concluded similarly. Another example of complexities in interaction of health system factors as they influence service delivery, is explanation of social inequalities in CS rates. Social inequalities in CS rates highlighted by Boatin et al 3 and Boerma et al 9 also suggest the important influences of economic and cultural issues. 37 47–51 Supply factors, such as hospital beds, equipment and human resources (ie, obstetricians and midwives) are also known to influence CS rates. 1 52 53 The lack of decreasing CS rates with lower numbers of skilled birth attendants in Latin American countries, as compared with other countries with lower skilled birth attendant numbers, 7 may reflect cultural and social trends in such countries, and is an useful example to illustrate the complexity of the interplay and influence of health system factors in CS rates.
The ecological nature of study design is the main limitation of this study, as we cannot establish a causal relationship between our variables of interest. Although we used some of most reliable internationally available data sources from the WHO and the World Bank, we should be aware that the quality of such data may not be entirely uniform across countries included in the analysis. Finally, we have been able to adjust only for some confounders in our statistical models. There are many other macro level factors (ie, societal and cultural factors) that do play a role and we have not accounted in our analysis.
The exploratory results in this paper should be viewed as a first step towards an in-depth analysis of current health financing systems and their implications for sustainable provision of care in the future. Several pathways forward seem possible. First, global studies with larger and more detailed data on health system characteristics generated from global monitoring systems. Second, performing systematic reviews of individual studies looking at CS rates and health system factors. CS is one of the most studied procedures globally. Evidence synthesis in the form of systematic reviews could serve not just the cause of addressing CS increase and variation but can also prove to be a reference point in the general cause of examining health system influence on under and overuse of medical care. Finally, country specific analysis or even regional or facility level analysis looking at individual case data will be able to establish conclusive links of health system features with CS provision. 25 27 This information can inform national policy efforts as well as global efforts for improvement of health system financing arrangements. Not all nations may be able to engage in research on optimal financial incentives despite persisting problems with CS. 54 Global collaborations to support countries struggling with these issues might be beneficial.
The results presented in this study suggest that, on average, countries relying more heavily on private contributions and voluntary health insurance have higher proportions of excess CS. Further research will be needed to better understand features driving these results and to help countries move towards more efficient use of health system resources.
Supplementary Material
Acknowledgments.
We thank Riaz Agahi for editing this manuscript and Arber Lama for support with literature search.
Contributors: IH and GF developed and designed the study, retrieved the data from the indicated sources, analysed and interpreted the data and jointly drafted the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
- Open access
- Published: 22 May 2024
Factors conditioning pain control and reduction in post-cesarean section parturients: a cross-sectional study
- Anna Bogusława Pilewska-Kozak 1 ,
- Magdalena Dziurka 2 ,
- Agnieszka Bałanda –Bałdyga 3 ,
- Marta Joanna Monist 4 ,
- Ewelina Kopiel 5 ,
- Krzysztof Jurek 6 ,
- Anna Francesca Łęcka 7 &
- Beata Dobrowolska 2
BMC Pregnancy and Childbirth volume 24 , Article number: 382 ( 2024 ) Cite this article
Metrics details
Pain experienced by women in the perinatal period constitutes a complex and multifaceted phenomenon. The aim of the study was to assess conditions of pain locus of control and pain reduction in post-cesarean section parturients.
Materials and methods
A cross-sectional quantitative study with convenience sampling was performed among 175 hospitalized post-cesarean section women in hospitals in Eastern Poland in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement. A self-design questionnaire regarding general information and obstetrics/gynaecology medical interview, The Pain Coping Strategies Questionnaire (CSQ) and The Beliefs about Pain Control Questionnaire (BPCQ) were used. The inclusion criteria were as follows (1) age of ⩾ 18 years old; (2) cesarean section (CS); (3) period from the 13th hour to the end of the 72nd hour after the procedure; and (4) informed consent. The data was analyzed with IBM SPSS Statistics.
Internal locus of control (M = 14.02) was provided the highest value by the parturients and followed by chance events (M = 12.61) and doctors’ power (M = 12.18). Dominant coping with pain strategies in the post-cesarean parturients were coping self-statements (M = 19.06), praying or hoping (M = 18.86). The parturients assessed their pain coping (M = 3.31) strategies along with pain reduction (M = 3.35) at the moderate level. Higher pain control was correlated with cognitive pain coping strategies (β = 0.305; t = 4.632; p < 0.001), internal pain control β = 0.191; t = 2.894; p = 0.004), cesarean section planning (β = -0.240; t = -3.496; p = 0.001) and past medical history of CS (β = 0.240; t = 3.481; p = 0.001). The skill of reduction of pain was positively associated with cognitive pain coping strategies (β = 0.266; t = 3.665; p < 0.001) and being in subsequent pregnancy (β = 0.147; t = 2.022; p = 0.045). Catastrophizing and hoping were related to lower competences of coping with pain (B = − 0.033, SE = 0.012, β = − 0.206, T = -2.861).
Conclusions
The study allowed for identification and better comprehension of factors conditioning pain control and pain reduction in parturients after the cesarean section. Furthermore, a stronger belief that pain can be dealt with is found in the parturients characterized by cognitive pain coping strategies and internal pain locus of control. The skill of reduction of pain is related to cognitive coping strategy and procreation status.
Peer Review reports
Pain according to Revised International Association for the Study of Pain (IASP) force definition (2020, p. 1976–1982) is “an unpleasant emotional and sensory experience for human beings that is or can be related to potential or actual tissue damage which is affected by psychological, social and biological factors” [ 1 ]. In healthcare, pain should be constantly assessed and monitored as well as respected if reported by patients. Fulfilling an adaptive role, pain can influence psycho-social well-being of people. It can be manifested by both verbal and non-verbal signs. However, lack of verbal communication of pain should be remembered not to exclude experiencing of pain [ 1 ]. Pain that occurs in labour is a particular type of pain since it constitutes a complex and multifaceted phenomenon. An increase in pain intensity aids the physiologic process of labour progress [ 2 , 3 ]. Giving birth is an exhilarating event for mothers that even though they experience pain they describe it as both a tearing apart or excruciating and pleasing feeling [ 4 ]. A lot of different factors have an impact on severity of pain. Psychological factors are one of them and they comprise a competence of using pain reduction techniques by patients as well as their beliefs about pain control [ 5 ].
Locus of control is a factor associated with individual perception of pain by patients and their ability of dealing with pain [ 6 ]. Individuals with internal pain locus of control are responsible and believe that they control pain and interpret their experiences as a result of activities undertaken by them. However, individuals directed at others, namely with external locus of control feel that they are less responsible and thus they usually refer more to external factors such as other people’s activities, luckiness or chance [ 7 ]. Dependence between health locus of control and health behaviours have been indicated [ 6 ]. Internal locus of control is related to more common health promoting behaviors undertaken due to individuals’ beliefs about their influence on the course of disease; thus increasing their sense of efficiency in this way [ 8 ].
In turn, coping strategies are defined as individuals’ attempts (cognitive and behavioral) aimed at establishing control and dealing with the situation perceived by the individuals as threat, to some extent, in the emotional and physical aspect [ 9 ]. According to Hamilton et al. [ 10 ] emotions play the main role in coping with pain (energizing force in self-regulation).
Caesarean section (CS) in 2020 in Europe was performed at least 1.12 million times [ 11 ]. One out of five (21%) of deliveries worldwide are completed with a C-Sect. [ 12 ]. Moreover, the global rates of CS have significantly increased. The World Health Organisation (WHO) predicts that it will grow to 29% till 2030 [ 12 ]. Countries in which there are more cesarean sections than normal vaginal birth deliveries are as follows Brazil, Cyprus, the Dominican Republic, Egypt and Turkey. A high percentage of CSs also remains in Romania (44.1%), Bulgaria (43.1%), Poland (39.3%), Hungary (37.3%) and the USA (3.2%) [ 12 , 13 , 14 , 15 ]. To compare the lowest percentage of CSs performed is found in France (19.7%), Lithuania and Estonia (19.4%), Sweden (16.6%), and Finland (16.5%) [ 12 , 14 ].
An essential measure taken by the WHO in 2018 was the issue of recommendations concerning non-clinical activities aimed at diminishing the number of unnecessary cesarean Sect. [ 15 ]. Therefore, a crucial element of perinatal care was highlighted as the focus on women’s education covered by: (1) child birth training workshops; (2) nurse-led applied relaxation training programme; (3) psychosocial couple-based prevention programme; (4) psychoeducation [ 15 ]. In the case of psychoeducation directed to women suffering from anxiety before labour and conducted by a midwife/therapist, it should encompass, among other things, information about anxiety, restlessness prior to labour, normalization of individual behaviours and responses during labour, stages and process of labour, hospital procedures and ways of anaesthetizing labour pain [ 15 ]. Midwives work regarding preparing women for the experience of pre-labour anxiety provides clinical short- and long-term benefits. Those women who had anxiety prior to labour and had participated in psychoeducation on the subject, they less frequently had stressful retrospections of labour and endeavoured to natural vaginal birth in the future [ 16 ]. Furthermore, participation in psychoeducation on pre-labour anxiety in nulliparous women was associated with a diminished number of symptoms of post-partum depression and better preparation for labour and maternity [ 17 ].
Therefore, the objective of the work was to assess conditioning of pain locus of control and pain reduction in hospitalized parturients after the cesarean section in the first days following delivery.
Assessment of conditioning of pain locus of control and pain reduction in post-cesarean section (post-CS) parturients.
Study design
A cross-sectional descriptive study was carried in hospitals in Eastern Poland. The study was conducted in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement, (see S1.File) [ 18 ].
Study participants
Raosoft Sample Size Calculator was used to determine the sample size. For a confidence level of 0.90, a margin of error of 0.05, and a response distribution of 0.70, a sample size of 227 was required (based on 1.12 million cesarean section performed in Europe in 2020 as a population size indicator [ 11 ]). A convenience sample of 230 respondents in the puerperium hospitalized in maternity wards were asked to take part in the study. Consent to participation in the study was provided by 175 hospitalized post-CS parturients. The research was performed in two hospitals in city Lublin. The inclusion criteria were as follows (1) age of ⩾ 18 years old; (2) cesarean section; (3) period from the 13th hour after the surgical procedure to the end of the 72nd hour after the procedure; and (4) informed consent to take part in the research. Exclusion criteria: (1) lack of informed consent, (2) health status not allowing to give informed consent, (3) age below 18 years old, (4) period before 13th hour after CS, (5) 4th and subsequent postoperative day.
According to Nilson et al. [ 19 ] CS typically implies a hospital stay for 2–3 days. In order to obtain informed consent to participate in the study, the authors decided to include participants in the period from the 13th hour after the surgical procedure to the end of the 72nd hour after the procedure to allow uninterrupted skin-to-skin contact between mother and child in the first hours after CS. In addition, pain treatment is administered immediately after the caesarean section, which could affect the results of the investigation performed immediately after CS.
Instruments
To collect data the following research instruments were utilized:
The authors’ own questionnaire comprising 38 questions. The author’ self-designed survey questions were developed on the basis of a literature review [ 20 , 21 , 22 ] carried out by the researchers. The questionnaire was pilot-tested with a small sample group to identify any ambiguities or unclear items. Feedback from this pilot test was used to refine and improve the questionnaire. The first part of the questionnaire included open-ended and closed-ended questions of one choice concerning sociodemographic data like age, body weight, height, marital status, place of residence, education, material situation, professional status, and a type of work performed. The second part constituted closed-ended questions of one or multiple choice, semi-open questions and open-ended questions. They regarded the obstetrics and gynaecology medical interview, a category of emergency CS, reasons for CS, knowledge on CS, a type of an aesthesia, the course of the first days in the puerperium – complaints of pain and other possible problems/complications, methods of alleviating pain and the condition of a newborn.
The Pain Coping Strategies Questionnaire (CSQ) compiled by Anne C. Rosenstiel and Frances J. Keefe from the University of Colorado Health Sciences Center in 1983, in the Polish adaptation by Zygfryd Juczyński [ 23 ]. It is used to assess pain coping strategies and their effectiveness in pain management. It is aimed at assessment of adults, patients and individuals complaining of pain, though completely healthy people can also be researched. The CSQ allows for prediction of adjustment to complaints of chronic pain. Moreover, it is used to assess individual competences of applying different strategies to alleviate pain and deal with it [ 23 ]. The questionnaire consists of 42 items describing ways of coping with pain and two questions provided to evaluate individual’s own skills of dealing with pain and relieving it. The statements are attributed to each of the seven pain coping strategies – six cognitive and one behavioural – strategy of increasing behavioural activity. Among the cognitive strategies the following ones are distinguished: diverting attention, reinterpreting pain sensations, coping self-statements, ignoring pain sensations, praying or hoping, and catastrophizing. The aforementioned strategies belong to the following three factors: cognitive coping, diverting attention and restructuring as well as catastrophizing and hoping. The respondents assessed frequency of their behaviours in relation to pain felt by means of the 7-point Likert scale ranging from 0 - never do that to 6 – always do that. To assess pain management, the following items were rated from 0 – no control/no ability to 6 – complete control/complete ability. Whereas the assessment of degree of pain decrease ranged from 0 - no ability to reduce pain to 6 – complete ability to reduce pain. In each category of pain coping strategies, the results obtained were added. The range of the result in each strategy was from 0 to 36 points. The higher the result, the more significant the way of dealing with pain [ 23 ]. Separate interpretation was performed for two questions concerning the degree of pain control and pain reduction. The result ranged 0–6 points, the higher the result, the greater the significance of individual competences of coping with pain and diminishing it. The structure of factors can also be used to interpret the questionnaire. The factors distinguished (cognitive coping, diverting attention and restructuring as well as catastrophizing and hoping) can have a relationship with basic styles of coping with stress such as problem-focused coping, escape coping and emotion-focused coping [ 23 ]. The questionnaire does not contain any norms of interpreting it; thus, the application of other research results seem to be useful for comparison. The internal consistency of the Polish version of the CSQ was estimated by means of Cronbach alpha for the entire questionnaire of 0.80, though for particular strategies it exceeded 0.80 apart from diverting attention (0.64) and increasing behavioural activity (0.63).
The Beliefs about Pain Control Questionnaire (BPCQ) compiled by Suzanne Skevingtonfrom the School of Social Sciences, University of Bath in 1990, in the Polish adaptation by Zygfryd Juczyński [ 8 ]. It refers to scales assessing health locus of control and is used to assess beliefs about pain control in adult individuals who are ill or healthy and complain of pain. The BPCQ can be applied supportively in the diagnosis and therapy of pain patients [ 8 ]. The questionnaire encompasses 13 items divided into 3 factors. The factors assess the intensity of individual beliefs about managing pain (internal factors), an influence or power of doctors and chance events. The respondents completed the questionnaire on their own assessing to what extent they agree with the statement given by means of the 6-point Likert scale of 1 - no, I completely disagree; 2 –I disagree; 3- I rather disagree; 4 – I rather agree; 5 – I agree; 6 – yes, I completely agree. The BPCQ results are depicted in three dimensions. For each dimension, the sum of the results is calculated according to the diagnostic key provided – particular items are attributed to each dimension of pain locus of control. Each dimension indicates power of beliefs in the individuals researched concerning the influence of internal factors (W), doctors (L) and chance events on pain (P). The range of points obtained regarding internal control is 5–30 and for the rest two dimensions 4–24. The higher the result, the more powerful the belief that pain is managed by the influence of a particular factor [ 8 ]. The internal consistency of the Polish version of the BPCQ was estimated by means of Cronbach alpha of 0.75 for the entire scale. For particular dimensions of pain locus of control, power of doctors (L) it was 0.86, internal pain locus of control (W) 0.82 and chance events (P) 0.58.
Data collection
After permission for data collection from managers of hospitals, the researchers provided the questionnaires on the wards where inpatients stayed after caesarean section. The questionnaires were completed by the respondents after obtaining verbal informed consent to participate in the study and following instructions how to fill them out provided by researchers. Each paper version of the questionnaire included introduction with aim of the study, information of the study procedure and statement that filling in questionnaire is understood as giving consent to participate in the study, and that every respondent has right to resign from the study at any time during filling in questionnaire. The questionnaires filled in were collected and put into envelopes to be provided for individuals responsible for the research.
Statistical analysis
The data was analyzed with IBM SPSS Statistics for Windows, version 27 (IBM Corp., Armonk, NY, USA). Multiple linear regression analysis (the stepwise method) was used to identify independent variables which predicted pain control and pain reduction. The assumptions of linearity and homogeneity of variance were checked using scatter plots and no heteroscedasticity/no clear pattern was found in the plots. Skewness was within ± 1. Multicollinearity was checked and the minimum and maximum variable inflation factor (VIF) were 1.009 and 1.158 for pain control and 1.003 and 1.016 for pain reduction, respectively, indicating that there was no risk of multicollinearity. A general F-test and adjusted R-square were performed. Standardized Beta coefficients (β) were calculated to assess the level of association and statistical significance in the multiple regression analysis.
To assess potential predictors of pain control in the post-CS parturients, multiple linear regression was conducted by means of the stepwise method by introducing sociodemographic variables (age, marital status, place of residence, education, occupational and financial situation), obstetric history variables (planning of the pregnancy, number of pregnancies, CS planning, number of CS, breastfeeding, post-CS complications, medical complications, preparation for care of the baby, obtaining information about CS, attending antenatal classes, being with the baby after the delivery), variables regarding coping with pain and variables concerning health locus of control. To assess potential predictors of pain reduction in the parturients, the same set of variables was applied as in the case of pain control.
The results obtained of the analysis were assumed to be statistically significant at p < 0.05.
Ethical issues
The research was carried out following the approval of the Bioethics Committee of the Medical University of Lublin (KE-0254/114/2016) and in accordance with the Helsinki Declaration principles. The respondents were informed about their anonymity in the research, voluntary choice to participate or refuse to participate, aim of the study, course of data collection and their right of resigning from taking part in the study at any time. Verbal informed consent to participate in the study was obtained to avoid any signature from the respondents and protect their anonymity. Filled in questionnaires were put into separate envelops to ensure respondent’ privacy.
The study encompassed 175 post-CS parturients. The mean age of the respondents was 30 years old. The majority of the participants lived in the urban area ( n = 118; 67%), were married ( n = 142; 81.1%) and had higher education ( n = 134; 76.6%). Over a half of the respondents ( n = 96; 54.9%) had the caesarean section for the first time in the planned mode ( n = 89; 51%). Table 1 depicts sociodemographic data of the participants researched and their obstetric history along with their newborns’ condition.
The majority of the respondents had post-operative wound pain ( n = 171; 97.7%) and thus they needed the administration of analgesics ( n = 168; 96.0%). Over a quarter of the participants had pain on micturition ( n = 45; 25.7%), a total of 37 of them had pain on defecation (21.1%). Table 2 shows data on the experience of pain on the first day following the surgery and the use of analgesics by the parturients.
Pain locus of control and strategies of coping with pain
The highest value was attributed to internal pain locus of control (M = 14.02) among the respondents. Whereas, power of doctors (M = 12.18) and chance events (M = 12.61) were given similar values (Table 3 ).
The dominant strategy of coping with pain in the post-CS parturients was coping self-statements (M = 19.06) and praying and hoping (M = 18.86) (Table 4 ). The lowest value was found in the domain of reinterpreting pain sensations (M = 7.51). Moreover, the respondents assessed their abilities to cope with pain (M = 3.31) and reduce pain (M = 3.35) at the moderate level. Table 4 indicates the in-depth characteristics of coping with pain strategies in the research group.
Predictors of pain management
In the case of pain control, the final model (F (5.168) = 15.284; p < 0.001) predicted 30% of the variance (Adj. R2 = 0.296).The model meets the criteria for homoscedasticity of variances, and the residuals are normally distributed. Table 5 presents the summary model for the pain control score due to the stepwise multiple regression analysis.
The model obtained includes 5 essential predictors: cognitive coping with pain (β = 0.305; t = 4.632; p < 0.001), catastrophizing and hoping (β = -0.266; t = -4.137; p < 0.001), internal pain locus of control (β = 0.191; t = 2.894; p = 0.004), planning CS (β = -0.240; t = -3.496; p = 0.001) and past medical history of CS (β = 0.240; t = 3.481; p = 0.001). A higher control of pain was associated with cognitive coping with pain, internal pain locus of control, CS planning, history of CS. Catastrophizing and hoping were correlated with a lower pain control. Table 6 shows multiple regression analysis predicting the control pain score (final model).
Predictors of pain reduction
To investigate potential predictors of pain reduction in the respondents, the same set of variables was taken into account as in the case of pain control. The in-depth data on the issue are depicted in Tables 7 and 8 .
The final model (F (3.170) = 7.684; p < 0.001) predicted 10% of variance (Adj. R2 = 0.104). The model meets the criteria for homoscedasticity of variances, and the residuals are normally distributed (Table 7 ).
The model obtained includes three essential predictors: cognitive coping with pain (β = 0.266; t = 3.665; p < 0.001), catastrophizing and hoping (β = -0.206; t = -2.861; p < 0.001), being in subsequent pregnancy (β = 0.147; t = 2.022; p = 0.045). The ability to decrease pain was positively correlated with cognitive coping with pain and subsequent pregnancy. Catastrophizing and hoping was associated with lower competences to cope with pain (Table 8 ).
The variables such as: occupation, breastfeeding, post-CS complications, medical complications, preparation for care of the baby, obtaining information about CS, attending antenatal classes, being with the baby after the delivery did not demonstrate a statistical correlation with pain control and pain reduction among respondents.
Both pain locus of control after delivery and coping with pain strategies are midwifery issues of great significance which require more attention because of constantly increasing percentage of CSs performed [ 12 ]. In women predictors of labour pain experience are associated with having a sense of self-efficacy during the previous labour [ 24 ], their tendency to catastrophize pain [ 25 ] and sensitivity to anxiety and restlessness [ 26 ].
The research shows the need for further investigations and comprehension of labour pain, ways of dealing with it, promoting natural vaginal delivery as well as having positive experience during labour [ 27 ]. Therefore, the objective of the work was to assess conditioning of pain locus of control and pain reduction in the post-CS parturients.
Firstly, the results obtained can be summarized in the following way the parturients attributed the highest value to internal pain locus of control, then chance events and last but not least power of doctors. Different results were reported by Czerw et al. [ 28 ] where oncological patients suffering from ovarian cancer, breast cancer and endometrial cancer attributed pain locus of control to power of doctors. However, this diversity can result from different characteristics of the research groups, specificity of the perinatal and post-operative periods as well as specificity of oncological treatment. The results suggest that preparation for labour and delivery in pregnant women is of great significance mainly due to pain locus of control after the caesarean section. The literature reports also confirms positive impact of psychoeducation on perinatal women in their further performance in the new reality following the delivery [ 16 , 17 ].
Secondly, the dominant strategy of coping with pain found in the post-CS parturients was coping self-statements along with praying and hoping. Similar results were obtained in the research of oncological patients [ 28 , 29 , 30 ], coronary heart disease patients [ 31 ], patients with internal diseases [ 32 ] and females suffering from endometriosis [ 33 ]. Therefore, support of women after labour and delivery provided by healthcare professionals seems to be essential and it should include women’s needs and spirituality, for example women should be enabled to have a contact and talk with a priest, close relatives and friends in the postpartum period. The research indicates that patients expressed their needs of being cared for by medical professionals who are aware of their patients’ spiritual and religious needs [ 34 ]. Caesarean section as a surgery requires from the midwives to carefully monitor both infant and mother health condition [ 35 ]. Skin-to-skin contact after CS provides a number of possible positive outcomes for the woman [ 35 ]. Result of the study Salomończyk et al. (2022) showed a duration of the sin to skin contact after caesarean section last 1 to 5 min in 30.10% of the cases [ 35 ]. A crucial aspect of the appropriate care is also systematic pain assessment performed by nurses/midwives. Insufficient administration of analgesics may result in a high level of post-operative pain in post-CS parturients [ 36 ].
Thirdly, as far as coping with pain strategies are concerned, the lowest value was found in reinterpreting pain sensations. Moreover, the parturients assessed their competences of dealing with pain and relieving it moderately. Similar findings were provided in the case of patients with endometriosis who rarely used the strategies of reinterpreting pain sensations and ignoring pain [ 33 ]. In order to improve the results regarding post-CS parturients’ own competences of dealing with pain and relieving it, healthcare professionals should pay greater attention to the issue for instance during preparing women for labour and delivery. Such preparation would encompass encouragement to pregnant women to start education provided on antennal classes, participate in prenatal education on coping with pain along with non-pharmacological therapy in pain management, and such education would be delivered during appointments and check-ups with doctors/midwives [ 15 ].
Fourthly, the final model comprises five essential predictors of pain control such as cognitive coping with pain, catastrophizing and hoping, internal pain locus of control, CS planning and history of CS. The literature review highlights that self-confidence and positive attitude towards pain in patients contribute to diminishing the level of perceived pain and decreasing use of analgesics [ 37 ]. Women who had a high level of their self-efficacy in pain management had lower frequency of analgesics administration and asked for painkillers/anaesthesia at more advanced stages of labour [ 38 ]. In order to improve post-operative patients’ performance, healthcare professionals are encouraged to use cognitive and behavioural activities related to patients beliefs about pain management [ 39 ].
Furthermore, the research results obtained revealed that catastrophizing and hoping were correlated with lower pain control in the parturients researched. To sum up, the results suggest that past medical history of CS, CS planning and having knowledge of CS/perinatal management seem to be of great importance in raising awareness of pain in the parturients. Similar results were obtained by Tabriz et al. [ 40 ] where patients’ catastrophizing was associated with a lower level of pain control. Patients who are of the opinion that health is dependent on external factors such as faith, coincidence or other people have tendency to use passive strategies of coping with pain (e.g. catastrophizing) that are characterized by a feeling of helplessness and dependence on others [ 41 ]. In turn, the research indicates that individuals who have beliefs that they are able to control their health [ 41 ], experience lower intensity of pain [ 34 ] and use active strategies of coping with pain. Moreover, passive coping with pain strategies are more frequently found in patients with higher intensity of pain [ 42 , 43 ], patients with worse mental health and disability [ 43 ].
Fifthly, the model obtained encompasses three crucial predictors that reduce pain, namely cognitive coping with pain, catastrophizing and hoping, procreation status The ability to alleviate pain was positively correlated with cognitive coping with pain and procreation status. Catastrophizing and hoping were associated with lower competences of coping with pain. Internal pain locus of control was related to being responsible for decisions and activities taken [ 44 ]. This approach has been indicated to decrease the level of experienced pain-related stress [ 44 , 45 ]. Moreover, it increases pain tolerance, which improves patient-healthcare relationship and their collaboration, and abilities of coping with pain [ 44 , 45 ]. Interestingly, Christiaens et al. (2010) presented that Dutch post-CS females having positive attitude towards labour pain and controlling their use of analgesics required rarer administration of analgesics [ 46 ]. In turn, in the case of women from Belgium, their negative attitude to labour and delivery constituted predisposing factor for more frequent administration of analgesics [ 46 ]. Waldenstrom et al. (1996) found that more severe labour pain was felt by females with negative attitude towards pain and more frequently they were anxious during labour. Lesser emotional suffering in women was caused by acceptance of pain, and lack of pain acceptance more frequently led to requirement for pain reduction [ 47 ]. Sak et al. (2016) suggest that appropriate psychological preparation concerning beliefs about pain control may be linked to improvement of healthcare outcomes for patients in the future [ 48 ]. The application of perinatal psychoeducation regarding cognitive strategies for women who tend to catastrophize may contribute to identification and better comprehension of their individual strategies of coping with pain [ 49 ]. Having negative beliefs in the perinatal period has been proven to increase frequency of experiencing anxiety, having obstetric complications and intensity of pain [ 50 ]. An interesting outcome of the study was presented by Tułacz et al. (2021) where only 11.8% of respondents did not feel fear during pregnancy or postpartum period [ 51 ]. Among the reasons for concern women mentioned fear of separation of mother and child after childbirth [ 51 ]. Kanadys et al. (2022) suggest there is a need to increase individualized holistic psychoprophylactic care to postpartum women in poor and average financial situation and to those who are learning or studying by promoting the concept of self-care preferably already in the period before the conception [ 52 ].
Research limitations
The first research limitation can result from the fact that the research group represented solely Eastern Poland; thus, it cannot be representative for the entire population of post-CS women in Poland. The second research limitation can result from lack of pain severity assessment in the post-CS parturients by means of the pain assessment scale. Another research limitation constitutes the fact that a cross-sectional study was used with convenience sampling which may imply that the results of the study cannot be generalised. Therefore, no constructive conclusions can be drawn to indicate explicitly dependences between the particular variables. Additionally, although the research shows significant p-values in the stepwise multiple regression analysis on the model summary for the pain control score the R2s are considered as low. The results of our study demonstrates the need for further investigations and comprehension of this issue which requires a comparison of our findings with other authors’ results and implies a conservative interpretation of the study findings.
The research allowed for identification and better comprehension of factors conditioning pain control and pain reduction in the post-CS parturients. The past obstetric medical history of CS and planning CS in advance affect a higher level of pain locus of control. Moreover, a stronger belief that pain can be managed is found in the respondents who are characterized by cognitive coping with pain strategies and internal pain locus of control. However, the ability to manage pain, namely reduce pain is related to cognitive pain coping strategies, and procreation status since women in the postpartum period in subsequent pregnancy are better at reducing pain. Post-CD women who are characterized by catastrophizing and hoping have weaker beliefs about their abilities to deal with pain and lower competencies to cope with pain.
Implications
The research results obtained indicate the necessity for the application of an individual approach to women concerning coping with pain strategies after the cesarean section as well as their own pain locus of control during women’s psychoeducation conducted by midwives and other healthcare professionals, for instance on antenatal classes. Furthermore, the results obtained suggest further investigations regarding the subject, for example referring to the degree of pain experience. Medical professionals’ comprehension of determinants of pain perception and ways of coping with pain used by parturients can have a positive influence on the quality of post-operative care on maternity wards.
Data availability
All data generated and analysed during the current study are not publicly available due to protect participants’ privacy and confidentiality, but are available from the corresponding author on reasonable request.
Abbreviations
- Cesarean section
International Association for the Study of Pain
World Health Organisation
Post-cesarean section
Strengthening the Reporting of Observational studies in Epidemiology statement
Pain Coping Strategies Questionnaire
Beliefs about Pain Control Questionnaire
Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, Keefe FJ, Mogil JS, Ringkamp M, Sluka KA, Song XJ, Stevens B, Sullivan MD, Tutelman PR, Ushida T, Vader K. The revised International Association for the study of pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–82.
Article PubMed PubMed Central Google Scholar
Lowe NK. Critical predictors of sensory and affective pain during four phases of labor. J Psychosom Obstet Gynecol. 1991;12:193–208.
Article Google Scholar
Whitburn LY, Jones LE, Davey MA, Small R. Women׳s experiences of labour pain and the role of the mind: an exploratory study. Midwifery. 2014;30(9):1029–35.
Article PubMed Google Scholar
Lundgren IK. Dahlberg Women׳s experience of pain during childbirth midwifery 1998; 14: 105–10.
Bylinka J, Oniszczenko W, Temperament. Beliefs about Pain Control, and Pain Intensity in Endometriosis patients. J Clin Psychol Med Settings. 2016;23:410–9.
Arraras JI, Wright SJ, Jusue G, Tejedor M, Calvo JI. Coping style, locus of control, psychological distress and pain-related behaviours in cancer and other diseases. Psychol Health Med. 2002;7(2):181–7.
Przybyłko K, Walesa CZ. Psychological problems of pain. Horyz Psychol. 2016;6:105–27.
Google Scholar
Skevington SM. A standardized scale to measure beliefs about controlling pain (BPCQ): a preliminary study. Psychol Health. 1990;4:221–32.
Ablin JN, Cohen H, Neumann L, Kaplan Z, Buskila D. Coping styles in fibromyalgia: Effect of co-morbid posttraumatic stress disorder. Rheumatol Int. 2008;28:649–56.
Hamilton NA, Karoly P, Kitzman H. Self-regulation and chronic pain: the role of emotion. Cogn Therapy Res. 2004;28:559–76.
Eurostat Statistics Explained. Surgical operations and procedures statistics. https://ec.europa.eu/eurostat/statistics-explained/index.php .
World Health Organization. Caesarean section rates continue to rise, amid growing inequalities in access: Rising rates suggest increasing numbers of medically unnecessary, potentially harmful procedures. https://www.who.int/news/item/16-06-2021-caesarean-section-rates-continue-to-rise-amid-growing-inequalities-in-access .
Hamilton BE, Martin JA, Osterman MJK, Births. Provisional data for 2022. Vital Statistics Rapid Release; Report no 28. Hyattsville, MD: National Center for Health Statistics 2023. https://stacks.cdc.gov/view/cdc/127052 .
Eurostat Statistics Explained. Large differences in share of caesarean births. https://ec.europa.eu/eurostat/en/web/products-eurostat-news/-/ddn-20191217-1 .
WHO recommendations non-clinical interventions to reduce unnecessary caesarean sections. Web annex 2. Web annex 2: Description of included interventions. Geneva: World Health Organization. 2018 (WHO/RHR/18.21). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. http://apps.who.int/iris .
Fenwick J, Toohill J, Gamble J, Creedy DK, Buist A, Turkstra E, Sneddon A, Scuffham PA, Ryding EL. Effects of a midwife psycho-education intervention to reduce childbirth fear on women’s birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth. 2015;15:284.
Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmäki E, Ryding EL, Saisto T. Group psychoeducation with relaxation for severe fear of childbirth improves maternal adjustment and childbirth experience–a randomised controlled trial. J Psychoso Obstet Gynaecol. 2015;36(1):1–9.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative the strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Nilsson IM, Kronborg H, Knight CH, Strandberg-Larsen K. Early discharge following birth – what characterises mothers and newborns? Sex Reprod Healthc. 2017;11:60–8.
Mascarello KC, Horta BL, Silveira MF. Maternal complications and cesarean section without indication: systematic review and meta-analysis. Rev Saude Publica. 2017;51:105.
Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: systematic review and meta-analysis. PLoS Med. 2018;15(1):e1002494. https://doi.org/10.1371/journal.pmed.1002494 .
Stadnicka G, Łepecka-Klusek C, Pilewska-Kozak A, Pawłowska-Muc A. The sexual satisfaction of women after labour — part II. Nurs Probl / Problemy Pielęgniarstwa. 2015;23(3):362–6. https://doi.org/10.5603/PP.2015.0059 .
Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17(1):33–44.
Berentson-Shaw J, Scott KM, Jose PE. Do self-efficacy beliefs predict the primiparous labour and birth experience? A longitudinalstudy J. Reprod. Infant Psychol. 2009;27:357–73.
Fenwick Y, Hauck J, Downie J. Butt the childbirth expectations of a self-selected cohort of western Australian women. Midwifery. 2005;21:23–35.
Beebe R, Lee KA, Carrieri-Kohlman V, Humphreys J. The effects of childbirth self-efficacy and anxiety during pregnancy on prehospitalization labor. J Obstet Gynecol Neonat Nurs. 2007;36:410–8.
Declercq E, Young R, Cabral H, Ecker J. Is a rising cesarean delivery rate inevitable? Trends in industrialized countries, 1987 to 2007. Birth. 2011;38(2):99–104.
Czerw A, Religioni U, Sygit K, Nieradko-Heluszko A, Mękal D, Partyka O, Mikos M, Eid M, Strzępek Ł, Banaś T. Pain Control, Acceptance and Adjustment to the Disease among patients with ovarian, endometrial and breast Cancer in Poland. Int J Environ Res Public Health. 2021;18(22):12148.
Utne I, Miaskowski C, Bjordal K, Cooper BA, Valeberg BT, Rustøen T. Confirmatory Factor Analysis of the coping strategies questionnaire-revised in samples of Oncology outpatients and inpatients with Pain. Clin J Pain. 2009;25:391–400.
Krajewski W, Mazur M, Poterek A, Pastuszak A, Halska U, Tukiendorf A, Rymaszewska J, Zdrojowy R. Assessment of Pain Management, Acceptance of illness, and Adjustment to Life with Cancer in patients with nonmuscle invasive bladder Cancer. Biomed Res Int 2018: 7598632.
Nasiłowska-Barud A. Differences in the course of coronaryheartdisease in women in the context of selectedpersonalitytraits. IgnatianumPhilos Yearb. 2016;22:90–113.
Baczewska B, Kropornicka B, Dobrzyńska K, Block B, Krzyżanowska E, Łuczyk R, Olszak C, Nowicka E, Lorencowicz R, Muraczyńska B. Strategies of coping with pain in patients with chronicinternaldisease. J Educ Health Sport. 2016;6:281–98.
Łuczak-Wawrzyniak J, Szczepanska M, Skrzypczak J. Evaluation of quality of life in women with endometriosis and management method with side effects of the disease. Menopause Rev. 2007;6:329–33.
Akeredolu AP, Harbinson MT, Bell D. Incorporation of spiritual care as a component of healthcare and medical education: viewpoints of healthcare providers and trainees in Nigeria. Nigerian Health J. 2017;13:90–104.
Hesse T, Julich A, Paul J, Hahnenkamp K, Usichenko TI. Disparity between high satisfaction and severe pain in patients after caesarean section: a prospective observational-controlled investigation. Anesthesiol Res Pract. 2018; 2634768.
Salamończyk M, Błachnio M. Implementation of the first skin-to-skin contact after cesarean sections in maternity hospitals in Warsaw. Nurs 21st Century. 2022;21(3):169–73.
Crowe K, Vonbaeyer C. Predictors of a positive childbirth experience. Birth-Issues Perinat Care. 1989;16:59–63.
Article CAS Google Scholar
Manning MM, Wright TL. Self-efficacy expectancies, outcome expectancies, and the persistence of pain control in childbirth. J Personal Soc Psychol. 1983;45(2):421–31.
Jankowski R, Misterska E, Latuszewska J, Bogajewska B, Glowacki J. Differences in beliefs about pain control after surgery due to lumbar or cervical discopathy and degenerative spine disease. J Back Musculoskelet Rehabil. 2019;2:779–95.
Tabriz ER, Mohammadi R, Roshandel GR, Talebi R. Pain beliefs and perceptions and their relationship with coping strategies, stress, anxiety, and Depression in patients with Cancer. Indian J Palliat Care. 2019;25(1):61–5.
PubMed PubMed Central Google Scholar
Sengul Y, Kara B, Arda MN. The relationship between health locus of control and quality of life in patients with chronic low back pain. Turk Neurosurg. 2010;20(2):180–5.
PubMed Google Scholar
Prasertsri N, Holden J, Keefe FJ, Wilkie DJ. Repressive coping style: relationships with depression, pain, and pain coping strategies in lung cancer outpatients. Lung Cancer. 2011;71:235–40.
Benyon K, Muller S, Hill S, Mallen C. Coping strategies as predictors of pain and disability in older people in primary care: a longitudinal study. BMC Fam Pract. 2013;14:67.
van Dijk JF, Schuurmans MJ, Alblas EE, Kalkman CJ, van Wijck AJ. Postoperative pain: knowledge and beliefs of patients and nurses. J Clin Nurs. 2017;26:3500–10.
Milte CM, Luszcz MA, Ratcliffe J, Masters S, Crotty M. Influence of health locus of control on recovery of function in recently hospitalized frail older adults. Geriatr Gerontol Int. 2015;15:341–9.
Christiaens W, Verhaeghe M, Bracke P. Pain acceptance and personal control in pain relief in two maternity care models: a cross-national comparison of Belgium and the Netherlands. BMC Health Serv Res. 2010;10:268.
Waldenstrom U, Bergman V, Vasell G. The complexity of labor pain: experiences of 278 women. J Psychosom Obstet Gynecol. 1996;17:215–28.
Sak JJ, Sagan D, Pawlikowski J, Wiechetek M, Jarosz M. Impact of beliefs about pain control on perceptions of illness in surgical patients. Ann Agric Environ Med. 2016;2:144–7.
Escott D, Slade P, Spiby H. Preparation for pain management during childbirth: the psychological aspects of coping strategy development in antenatal education. Clin Psychol Rev. 2009;29(7):617–22.
Wuitchik M, Bakal D, Lipshitz J. Relationships between pain, cognitive activity and epidural analgesia during labor. Pain. 1990;41(2):125–32.
Tułacz K, Wierzbicka B, Berghausen-Mazur M. Concerns of pregnant women and women in childbed during the pandemic. Nurs 21st Century. 2021;20(1):15–21.
Kanadys K, Giermasińska A, Pytka MB, Pilewska-Kozak AB. Maternal quality of life in the postpartum period. Nurs 21st Century. 2022;21(1):34–44.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Obstetrics and Gynaecology Nursing, Chair of Obstetrics and Gynecology, Faculty of Health Sciences, Medical University in Lublin, Lublin, Poland
Anna Bogusława Pilewska-Kozak
Department of Holistic Care and Nursing Management, Faculty of Health Sciences, Medical University of Lublin, Lublin, Poland
Magdalena Dziurka & Beata Dobrowolska
Integrated Medical Care Department, Medical Faculty, Collegium Medicum, Cardinal Stefan Wyszynski University in Warsaw, Warsaw, Poland
Agnieszka Bałanda –Bałdyga
2nd Chair and Clinic of Gynecology, Faculty of Medicine, Medical University in Lublin, Lublin, Poland
Marta Joanna Monist
The Neonatal Unit of the University Clinical Hospital, No. 1 in Lublin, Lublin, Poland
Ewelina Kopiel
Sociology of Culture, Religion and Social Participation Institute of Sociological Sciences, The John Paul II Catholic University of Lublin, Lublin, Poland
Krzysztof Jurek
Saint Lazarus Hospice, The Society of Friends to People in Disease, Cracow, Poland
Anna Francesca Łęcka
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: A.B. P-K; collection of the data: E.K.; statistical analysis: K.J.; investigation: A.B. P-K., M.D., B.B.; methodology: A.B. P-K.; writing – original draft: A.B. P-K., M.D., A. B–B., M.J. M., A.F. Ł., B.D.; writing – review & editing: A.B. P-K., M.D., B.D. All authors reviewed the manuscript.
Corresponding author
Correspondence to Magdalena Dziurka .
Ethics declarations
Ethics approval and consent to participate.
The research was carried out following the approval of the Bioethics Committee of the Medical University of Lublin (KE-0254/114/2016) and in accordance with the Helsinki Declaration principles. The respondents were informed about their anonymity in the research, voluntary participation in the study, aim of the study, course of data collection and their right of resigning from taking part in the study at any time.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pilewska-Kozak, A.B., Dziurka, M., Bałanda –Bałdyga, A. et al. Factors conditioning pain control and reduction in post-cesarean section parturients: a cross-sectional study. BMC Pregnancy Childbirth 24 , 382 (2024). https://doi.org/10.1186/s12884-024-06579-9
Download citation
Received : 03 January 2024
Accepted : 13 May 2024
Published : 22 May 2024
DOI : https://doi.org/10.1186/s12884-024-06579-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pain control
- Pain coping strategies
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Introduction
- Conclusions
- Article Information
eTable. Indications for Cesarean Delivery and General Anesthesia
eFigure. Rates of General Anesthesia in Laboring Patients by Race and Ethnicity
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Thomas CL , Lange EMS , Banayan JM, et al. Racial and Ethnic Disparities in Receipt of General Anesthesia for Cesarean Delivery. JAMA Netw Open. 2024;7(1):e2350825. doi:10.1001/jamanetworkopen.2023.50825
Manage citations:
© 2024
- Permissions
Racial and Ethnic Disparities in Receipt of General Anesthesia for Cesarean Delivery
- 1 Department of Anesthesiology and Critical Care, University of Chicago Medical Center, Chicago, Illinois
- 2 Department of Anesthesia, Emory University, Atlanta, Georgia
- 3 Department of Anesthesiology, Northwestern University, Chicago, Illinois
- 4 Feinberg School of Medicine, Northwestern University, Chicago, Illinois
- 5 Department of Public Health Services, University of Chicago, Chicago, Illinois
- 6 Department of Obstetrics and Gynecology, The Ohio State University Wexner Medical Center, Columbus
- 7 Department of Anesthesia and Critical Care, University of Chicago Medical Center, Chicago, Illinois
- 8 Department Obstetrics & Gynecology, University of Chicago Medical Center, Chicago, Illinois
- 9 Department of Anesthesiology, Perioperative Medicine and Pain Management, University of Miami Miller School of Medicine, Miami, Florida
Question Do rates of general anesthesia use for cesarean delivery differ by race or ethnicity?
Findings In this cross-sectional study including 35 117 patients undergoing cesarean delivery, rates of general anesthesia use were higher among Black and Hispanic individuals. However, among patients who labored with an epidural catheter in situ, there were no significant differences in rates of general anesthesia use by race or ethnicity.
Meaning This study suggests that use of neuraxial labor analgesia may mitigate racial or ethnic disparities in general anesthesia use for cesarean delivery.
Importance General anesthesia for cesarean delivery is associated with increased maternal morbidity, and Black and Hispanic pregnant patients have higher rates of general anesthesia use compared with their non-Hispanic White counterparts. It is unknown whether risk factors and indications for general anesthesia differ among patients of differing race and ethnicity.
Objective To evaluate differences in general anesthesia use for cesarean delivery and the indication for the general anesthetic by race and ethnicity.
Design, Setting, and Participants In this retrospective, cross-sectional, single-center study, electronic medical records for all 35 117 patients who underwent cesarean delivery at Northwestern Medicine’s Prentice Women’s Hospital from January 1, 2007, to March 2, 2018, were queried for maternal demographics, clinical characteristics, obstetric and anesthetic data, the indication for cesarean delivery, and the indication for general anesthesia when used. Data analysis occurred in August 2023.
Exposure Cesarean delivery.
Main Outcomes and Measures The rate of general anesthesia for cesarean delivery by race and ethnicity.
Results Of the 35 117 patients (median age, 33 years [IQR, 30-36 years]) who underwent cesarean delivery, 1147 (3.3%) received general anesthesia; the rates of general anesthesia were 2.5% for Asian patients (61 of 2422), 5.0% for Black patients (194 of 3895), 3.7% for Hispanic patients (197 of 5305), 2.8% for non-Hispanic White patients (542 of 19 479), and 3.8% (153 of 4016) for all other groups (including those who declined to provide race and ethnicity information) ( P < .001). A total of 19 933 pregnant patients (56.8%) were in labor at the time of their cesarean delivery. Of those, 16 363 (82.1%) had neuraxial labor analgesia in situ. Among those who had an epidural catheter in situ, there were no racial or ethnic differences in the rates of general anesthesia use vs neuraxial analgesia use (Asian patients, 34 of 503 [6.8%] vs 1289 of 15 860 [8.1%]; Black patients, 78 of 503 [15.5%] vs 1925 of 15 860 [12.1%]; Hispanic patients, 80 of 503 [15.9%] vs 2415 of 15 860 [15.2%]; non-Hispanic White patients, 255 of 503 [50.7%] vs 8285 of 15 860 [52.2%]; and patients of other race or ethnicity, 56 of 503 [11.1%] vs 1946 of 15 860 [12.3%]; P = .16). Indications for cesarean delivery and for general anesthesia were not different when stratified by race and ethnicity.
Conclusions and Relevance Racial disparities in rates of general anesthesia continue to exist; however, this study suggests that, for laboring patients who had labor epidural catheters in situ, no disparity by race or ethnicity existed. Future studies should address whether disparities in care that occur prior to neuraxial catheter placement are associated with higher rates of general anesthesia among patients from ethnic and racial minority groups.
Widespread adoption of neuraxial analgesia and anesthesia into clinical obstetric anesthesia practice has resulted in a reduction in anesthesia-related maternal morbidity and mortality in the peripartum period. 1 , 2 As rates of general anesthesia for cesarean delivery have decreased, there has been a coincident decrease in anesthesia-related morbidity and mortality. 1 , 3 , 4 Compared with neuraxial anesthesia, general anesthesia for cesarean delivery is associated with higher rates of cardiac arrest, aspiration of gastric contents, airway management complications, surgical site infections, postpartum hemorrhage, and maternal mortality. 1 , 5 - 8 Furthermore, neuraxial anesthesia techniques allow for the administration of neuraxial opioids for postoperative pain control, thus minimizing systemic opioid use and improving maternal ambulation and return of bowel function while also decreasing opioid exposure to the fetus. 5 , 9 - 11
Reasons for general anesthesia use in modern clinical practice might include rescue general anesthesia for inadequate neuraxial anesthesia, general anesthesia during emergency circumstances in which there is not time to safely provide neuraxial anesthesia, or patient refusal of neuraxial anesthesia. Reducing rates of potentially avoidable use of general anesthesia has been proposed as an actionable clinical intervention to improve maternal morbidity and outcomes. 12 Rates of preventable general anesthetics are high (up to 44%) and are associated with anesthetic complications, surgical site infections, and venous thromboembolic events.
Racial disparities exist in the rates of neuraxial labor analgesia use, as well as in the use of neuraxial anesthesia for cesarean delivery. 13 - 16 Non-Hispanic Black (hereafter, Black) and Hispanic patients have higher odds of undergoing general anesthesia for cesarean delivery compared with non-Hispanic White (hereafter, White) patients. 17 , 18 There is a paucity of literature addressing why this disparity exists, and most studies evaluating racial and ethnic disparities in anesthetic techniques for cesarean delivery have been performed on a population level, lacking granularity.
Consequently, it is uncertain whether risk factors and indications for general anesthesia for cesarean delivery differ among racial and ethnic groups. 12 , 18 Identifying and addressing the cause of racial and ethnic anesthetic disparities may improve maternal outcomes and lessen disparity gaps. The objective of this study was to evaluate differences in general anesthesia use for cesarean delivery and its indications by race and ethnicity.
The study was approved by the Northwestern University institutional review board. A waiver of consent was granted for retrospective medical record review. Electronic medical record data for all pregnant patients who underwent a cesarean delivery at Northwestern Medicine’s Prentice Women’s Hospital between January 1, 2007, and March 2, 2018, were evaluated using the Northwestern University Enterprise Data Warehouse. The start date was selected based on the date on which electronic medical record data were first available for neuraxial labor analgesia. The end date was chosen as the date the hospital migrated to a new electronic medical record system. The only exclusion criterion was perimortem cesarean delivery. This report followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline for cross-sectional studies. 19
Demographic data extracted from the medical record using an electronic medical record query included maternal age, race and ethnicity, body mass index, insurance status (private insurance, Medicaid or public insurance, or unknown insurance status or none), and maternal comorbidities including diagnoses of anemia, diabetes, and hypertensive disorders of pregnancy. Race and ethnicity information was self-identified and provided by the patient on admission. At the time of data entry, there was not an option for a multiracial or multiethnic self-identification.
Race and ethnicity were then queried from the medical record. Data were classified as Asian, Black, Hispanic, White, and other. The “other” category included data for patients with low study representation (ie, American Indian or Alaska Native and Native Hawaiian or Pacific Islander) and patients without information on race or ethnicity.
Obstetric data included parity, gestational age, indication for the cesarean delivery, and whether the patient was laboring prior to the cesarean delivery. Information regarding laboring vs nonlaboring status was obtained from nursing documentation. Information regarding postpartum hemorrhage was queried from delivery notes; postpartum hemorrhage was defined as an estimated blood loss of greater than 1 L. Data regarding maternal comorbidities, such as diabetes or anemia, were obtained from a combination of billing codes from the hospital discharge summary, nursing flowsheets, and physician documentation.
Anesthetic data included the American Society of Anesthesiologists physical status classification, including emergency designation, anesthetic technique for cesarean delivery, and the presence of existing neuraxial labor analgesia. Patients who received both neuraxial and general anesthesia were classified as having received general anesthesia. For patients who received general anesthesia, both the indication for the cesarean delivery and the indication for general anesthesia were manually extracted via medical record review and were categorized using criteria modified from prior studies (eTable in Supplement 1 ). 18 , 20
Manual extraction of the indication for cesarean delivery and the indication for general anesthesia for each patient who underwent general anesthesia was performed by 2 of us (C.L.T. and Y.Z.). Failed neuraxial anesthesia was defined as either a failed initiation of spinal anesthesia or a failed intrapartum extension of an in situ catheter, not in the setting of fetal or obstetric emergency. Neuraxial anesthesia failure could have occurred for a number of reasons (eg, inadequate dermatomal coverage prior to cesarean delivery, intraoperative discomfort necessitating conversion to general anesthesia, or inability to place a spinal or epidural catheter).
Additional data collected included neonatal outcome (live birth vs fetal demise), postpartum hemorrhage, maternal blood transfusion, maternal postoperative intensive care unit admission, and severe maternal morbidity. For severe maternal morbidity, we used a composite of 21 conditions defined by the Centers for Disease Control and Prevention. 21
The primary outcome was the rate of general anesthesia use stratified by race and ethnicity. Statistical analysis was performed in August 2023. Normal distribution of continuous variables was evaluated with the Shapiro-Wilk test. Categorical data were compared using the Pearson χ 2 test or the Fisher exact test, and continuous data were compared using the Mann-Whitney test. Univariate and multivariable mixed-effects logistic regression analyses were performed to evaluate the associations between general anesthesia use and all risk factors. Potential risk factors identified in univariate analysis with P ≤ .10 were incorporated into a multivariable mixed-effects logistic regression model to create adjusted odds ratios (AORs) for general anesthesia use, in which the random effect was multiple deliveries by the same patient. Variables in the final multivariable mixed-effects logistic regression model included maternal age, race and ethnicity, insurance status, parity, multiple pregnancy, and preeclampsia. All P values were from 2-sided tests and results were deemed statistically significant at P < .05. Data were analyzed using Stata/SE, version 18 (StataCorp LP).
A total of 35 117 individuals (median age, 33 years [IQR, 30-36 years]) who underwent cesarean deliveries were identified; none were excluded because of perimortem status. Of patients undergoing cesarean delivery, 2422 were Asian (6.9%), 3895 were Black (11.1%), 5305 were Hispanic (15.1%), 19 479 were White (55.5%), and 4016 (11.4%) had other racial or ethnic identities or did not provide race and ethnicity information ( Table 1 ). Patients who received general anesthesia were more likely than those who received neuraxial anesthesia to have public insurance, be parous, have multiple gestations, and carry a maternal diagnosis of gestational hypertension or preeclampsia. They also had a higher American Society of Anesthesiologists physical status classification and were more likely to be designated as requiring emergency delivery. General anesthesia was performed in 1147 of cases (3.3%). A total of 19 933 pregnant patients (56.8%) were in labor immediately prior to their cesarean delivery. The rates of general anesthesia differed by race and ethnicity and were 2.5% for Asian patients (61 of 2422), 5.0% for Black patients (194 of 3895), 3.7% for Hispanic patients (197 of 5305), 2.8% for White patients (542 of 19 479), and 3.8% for all other patients (153 of 4016) ( P < .001).
Patients undergoing general anesthesia had higher rates of composite severe maternal morbidity, more intensive care unit admissions, higher rates of fetal demise, and higher rates of blood transfusion ( Table 2 ). After controlling for covariates, Black patients’ odds of undergoing general anesthesia were 1.42 times that of White patients (AOR, 1.42 [95% CI, 1.15-1.75]) ( Table 3 ). Other independent risk factors for general anesthesia included public insurance status (AOR, 1.31 [95% CI, 1.12-1.55]), multiple gestations (AOR, 1.47 [95% CI, 1.19-1.82]), and a diagnosis of preeclampsia (AOR, 2.61 [95% CI, 2.03-3.37]). Older age was a protective factor against general anesthesia (AOR, 0.96 [95% CI, 0.94-0.97]).
There were racial and ethnic differences between the general anesthesia rates and neuraxial anesthesia rates among patients in labor (eFigure in Supplement 1 ); however, there were no differences among the laboring patients who had an epidural catheter in situ (Asian patients, 34 of 503 [6.8%] vs 1289 of 15 860 [8.1%]; Black patients, 78 of 503 [15.5%] vs 1925 of 15 860 [12.1%]; Hispanic patients, 80 of 503 [15.9%] vs 2415 of 15 860 [15.2%]; White patients, 255 of 503 [50.7%] vs 8285 of 15 860 [52.2%]; and patients of other race or ethnicity, 56 of 503 [11.1%] vs 1946 of 15 860 [12.3%]; P = .16) ( Table 2 ). Of laboring patients, 16 363 (82.1%) had a preexisting epidural catheter in situ at the time of cesarean delivery.
The 3 most common indications for cesarean delivery being performed with general anesthesia were obstetric or fetal emergency, arrest of labor, and maternal hemorrhage ( Table 4 ). The 3 most common indications for general anesthesia use were obstetric or fetal emergency, failed neuraxial anesthesia, and maternal contraindications to neuraxial anesthesia. Neither the indications for cesarean delivery nor the indications for general anesthesia use differed by race or ethnicity.
This study demonstrates that racial and ethnic disparities exist in the use of general anesthesia for cesarean delivery. These findings are consistent with other studies showing that Black patients are nearly twice as likely to undergo general anesthesia for cesarean delivery as White patients. 17 , 18 This study extends those findings by demonstrating that there is no racial or ethnic disparity when labor epidural analgesia is provided prior to intrapartum cesarean delivery. The reduction of racial and ethnic disparities among patients with neuraxial catheters in situ for labor is a novel and clinically important finding, as the presence of a catheter in situ for labor allows for the ability to convert labor analgesia to surgical anesthesia for cesarean delivery. In the event that an urgent or intrapartum cesarean delivery is required, timely conversion of neuraxial labor analgesia to anesthesia is one strategy for avoiding a preventable general anesthetic. 22 , 23
Disparities do exist in neuraxial labor analgesia use, and Black and Hispanic patients are less likely than White patients to receive neuraxial analgesia. 15 , 24 , 25 Black individuals are less likely to have private insurance and more likely to have no insurance compared with White individuals, 25 and insurance coverage is associated with significant improvements in access to care, condition-specific outcomes, and self-reported health. 26 - 28 It is likely that a combination of systemic factors, social determinants of health, clinician factors such as implicit and/or explicit bias, and communication barriers are associated with the disparity in rates of neuraxial analgesia use. 29 , 30
While the optimal rate of general anesthesia for cesarean delivery is unknown, national societies such as the Society for Obstetric Anesthesia and Perinatology have established benchmarks and recommendations, with a proposed goal of less than 5% of cesarean deliveries being performed under general anesthesia. 31 Given that neuraxial labor analgesia may act as a safety mechanism to prevent use of general anesthesia, it is imperative that disparities in neuraxial labor analgesia use be further investigated and addressed. It is possible that early explanation of labor analgesic options and identification of patient preferences in regard to neuraxial analgesia may be key to mitigating disparities in neuraxial labor anesthesia care. 32 , 33 In addition, because having an epidural in situ for an intrapartum cesarean delivery was associated with a similar general anesthesia rate stratified by race and ethnicity, future studies may consider evaluating intrapartum vs nonintrapartum cesarean deliveries for obstetrical indications. Nonintrapartum cesarean deliveries might have other actionable factors that should be examined with a health care equity lens.
Given that we manually reviewed each case of an individual receiving general anesthesia, we are able to provide granular data about the clinical indication for the cesarean delivery and general anesthesia. These types of data are challenging to obtain from large databases that rely on administrative data or registries. We found no significant disparities in indications for cesarean delivery performed under general anesthesia or in the indications for general anesthesia.
Our study has some limitations. Due to the single-center nature of the data, the results may not be generalizable to maternal care in the US. The labor analgesia use rate at Northwestern Medicine’s Prentice Women’s Hospital is, on average, above 95%, indicating that the risk of avoidable general anesthesia for our patient cohort may be lower than other institutions where labor analgesia is used less often. 12 In addition, our data are retrospective; thus, we cannot infer causality. Our data lacked information that could categorize the urgency of cesarean delivery, which precluded our ability to evaluate general anesthetics for preventability. Because this study investigates only patients who underwent cesarean delivery, we are unable to provide rates of labor analgesia by race and ethnicity for all laboring patients at our institution.
These findings have both clinical and public health implications. The data suggest that the racial and ethnic disparities in general anesthesia rates exist in association with neuraxial catheter placement and that once a neuraxial catheter is in situ, these disparities no longer existed for the subset of patients undergoing intrapartum cesarean delivery. We speculate that the cause of this finding may be complex and may involve both patient-related and clinician-related factors. Future studies are needed to further elucidate the cause of the discrepancy in the administration of general anesthesia and neuraxial analgesia and strategies to eliminate it. Attention should focus on patient-centered, timely administration of neuraxial labor analgesia and on identifying actionable items among patients without epidural labor analgesia. In addition, future studies should attempt to replicate our findings to improve generalizability. These findings underscore the need to identify modifiable risk factors for general anesthesia use, to mitigate risk.
Accepted for Publication: November 19, 2023.
Published: January 9, 2024. doi:10.1001/jamanetworkopen.2023.50825
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Thomas CL et al. JAMA Network Open .
Corresponding Author: Caroline Leigh Thomas, MD, Department of Anesthesiology and Critical Care, University of Chicago Medical Center, 5841 S Maryland Ave, Room I-440, MC4028, Chicago, IL 60637 ( [email protected] ).
Author Contributions: Dr Thomas had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Thomas, Lange, Banayan, Peralta, Scavone, Toledo.
Acquisition, analysis, or interpretation of data: Thomas, Banayan, Zhu, Liao, Grobman, Scavone, Toledo.
Drafting of the manuscript: Thomas, Peralta, Toledo.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Liao, Toledo.
Obtained funding: Toledo.
Administrative, technical, or material support: Thomas, Zhu, Toledo.
Supervision: Lange, Grobman, Scavone, Toledo.
Conflict of Interest Disclosures: Dr Toledo reported receiving speaker’s fees from Pacira BioSciences Inc outside the submitted work. No other disclosures were reported.
Funding/Support: Dr Toledo has received funding from the National Institute on Minority Health and Health Disparities (grant R03MD011628), the Anesthesia Patient Safety Foundation, and the Shane Foundation.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Minority Health and Health Disparities, the Anesthesia Patient Safety Foundation, or the Shane Foundation.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

IMAGES
VIDEO
COMMENTS
A total of 150 women with cesarean section were enrolled in the study. Out of them, 88% were elective cesareans and 62% were emergency cesarean sections. Table 1 shows the sociodemographic and obstetric characteristics of the study participants. The maternal age for women undergoing cesarean section ranges from 19 years to 35 years.
The relation between caesarean section and asthma in offspring was performed in meta-analysis based on 11 studies. The study by Lavin et al. analyzed caesarean section within two populations, India and Vietnam which were analyzed separately. Total number of included children delivered by caesarean section were 1,791,855 and 1,277,620 vaginally ...
A caesarean section (CS) can be a life-saving intervention when medically indicated, but this procedure can also lead to short-term and long-term health effects for women and children. Given the increasing use of CS, particularly without medical indication, an increased understanding of its health effects on women and children has become crucial, which we discuss in this Series paper.
Cesarean section is a fetal delivery through an open abdominal incision (laparotomy) and an incision in the uterus (hysterotomy). The first cesarean documented occurred in 1020 AD, and since then, the procedure has evolved tremendously.[1] It is now the most common surgery performed in the United States, with over 1 million women delivered by cesarean every year. The cesarean delivery rate ...
Financial strategies that equalize the fees charged for vaginal births and caesarean sections. Notes to editors. About the study. The study, Trends and projections of caesarean section rates: global and regional estimates, is published in the BMJ Global Health. It is based on nationally-representative data from countries worldwide from 1990 to ...
Two studies (9,072 participants) investigated the development of adulthood asthma in children delivered by cesarean section (from 15 years) [74,75], and no statistically significant association between cesarean delivery and adulthood asthma was seen, although one of these studies was graded as low quality ; excluding this study changed the ...
Background: Cesarean section is one of the most commonly performed surgeries in obstetric practice for saving the lives of women and their newborns from pregnancy- and childbirth-related complications. Its prevalence has increased alarmingly in the last few years, which has motivated this research to identify the indications and determinants, influencing cesarean section delivery in the study ...
In this Series paper, we describe the frequency of, trends in, determinants of, and inequalities in caesarean section (CS) use, globally, regionally, and in selected countries. On the basis of data from 169 countries that include 98·4% of the world's births, we estimate that 29·7 million (21·1%, 95% uncertainty interval 19·9-22·4) births occurred through CS in 2015, which was almost ...
Therefore, the accompanying research study by Paixao and colleagues published in PLOS Medicine, looking at CS and associated child mortality in Brazil, provides further valuable evidence on the balance of benefits and risks [].. CS rates are rising worldwide: Boerma and colleagues, on the basis of data from 169 countries including 98.4% of the world's births, estimated that 29.7 million (21. ...
Introduction. The proportion of births by caesarean section (CS) continues to increase worldwide [1-3].Latest trends analysis shows that between 2000 and 2015, the global average CS rate increased by 9.0% (from 12.1% to 21.1%) [].Although the use is not growing in all regions at the same pace and inequalities within and between countries exist, the rise is not constrained to high- and middle ...
The Series shows that the global rate of caesarean birth has doubled in the past 15 years to 21%, and is increasing annually by 4%. While in southern Africa use of caesarean section is less than 5%, the rate is almost 60% in some parts of Latin America, including in Brazil where we will launch the Lancet Series at the World Congress of Gynecology and Obstetrics (FIGO) on Oct 18.
Introduction. The proportion of births by caesarean section (CS) continues to increase worldwide [1-3].Latest trends analysis shows that between 2000 and 2015, the global average CS rate increased by 9.0% (from 12.1% to 21.1%) [].Although the use is not growing in all regions at the same pace and inequalities within and between countries exist, the rise is not constrained to high- and middle ...
Background and methods: Caesarean section (C-section) is a major obstetric intervention for saving lives of women and their newborns from pregnancy and childbirth related complications. Un-necessary C-sections may have adverse impact upon maternal and neonatal outcomes. In Bangladesh there is paucity of data on clinical indication of C-section at population level.
A Cochrane review study (41 studies and 5046 patients) demonstrated that 5-HT 3 antagonists (eg, ondansetron, granisetron), dopamine antagonists (eg, metoclopramide, ... Post-operative urinary tract infection and wound infection in women undergoing cesarean section: a comparison of two study periods in 1985 and 1987. J Hosp Infect. 1989; 13: ...
Summary Caesarean section is associated with moderate-to-severe postoperative pain, ... Apart from one study , all studies noted that TAP blocks improved pain relief, increased patient satisfaction and resulted in a reduction of rescue analgesia. A comparison between lateral and posterior approaches concluded that the posterior approach ...
Background Caesarean section rates are rising across all geographical regions. Very high rates for some groups of women co-occur with very low rates for others. Both extremes are associated with short and longer term harms. This is a major public health concern. Making the most effective use of caesarean section is a critical component of good quality, sustainable maternity care. In 2018, the ...
Abstract. Caesarean section as a means of delivering babies has been around for centuries with numerous references to the procedure appearing in ancient writings (Simm & Matthew 2008). It is now the most common major surgical intervention carried out on women in the world, with between 23% and 30% of deliveries in the UK performed by caesarean ...
Background Caesarean section is considered a relatively preferable and safe method of delivery as compared to normal delivery. Since the last decade, its prevalence has increased in both developed and developing countries. In the context of developing countries viz., South Asia (the highest populated region) and South-East Asia (the third-highest populated region), where a significant ...
5. The effects of caesarean section rates on other outcomes, such as maternal and perinatal morbidity, paediatric outcomes, and psychological or social well-being are still unclear. More research is needed to understand the health effects of caesarean section on immediate and future outcomes. WHO Statement on Caesarean Section Rates
There have been three follow-up studies of existing trials of caesarean section techniques. 12-14 The sample sizes of these studies are small, and included only 18% of the women randomised into the original trials for two studies, 12,13 and 51% for the third. 14 In the only study comparing single- versus double-layer uterine closure, no ...
This section presents the research findings of this study to assess the factors associated with the high rates of caesarean delivery in Mengo Hospital. These findings were presented as per the objectives of the study, in which a total of 200 postpartum mothers were enrolled for primary data that was collected from 24/5/2019 to 19/7/2019.
During an emergency cesarean section (C-section) in 2016, Rachel Somerstein's anesthesia failed. ... The reviewer is at the Department of Ancient Mediterranean and Near Eastern Studies, University of British Columbia, Vancouver, BC, Canada. ... Subscribe to ScienceAdviser to get the latest news, commentary, and research, free to your inbox ...
Pregnancies following previous caesarean section (CS) are associated with higher incidence of infections, postpartum haemorrhage and obstetric complications. The present study aimed to explore the effect of previous CS on reproductive, maternal and neonatal outcomes in women who underwent assisted reproductive techniques (ART).
Background The prevalence of C-sections in India increased from 17.2% in 2016 to 21.5% in 2021. This study examines the variations in C-section prevalence and the factors correlating to these variations in Tamil Nadu (TN) and Chhattisgarh (CG). Methods Delivery by C-section as the outcome variable and several demographic, socio-economic, and clinical variables were considered as explanatory ...
Introduction. Caesarean section (CS) rates have been increasing rapidly over the past decades at the global scale, with remarkable variation both within and between countries. 1-15 Such medical practice variation, in general, implies inefficient use of resources, that is, patients may not get what they need (underuse) or will get medically unnecessary care (overuse). 16 17 Empirically, CS ...
Pain experienced by women in the perinatal period constitutes a complex and multifaceted phenomenon. The aim of the study was to assess conditions of pain locus of control and pain reduction in post-cesarean section parturients. A cross-sectional quantitative study with convenience sampling was performed among 175 hospitalized post-cesarean section women in hospitals in Eastern Poland in ...
This study explored women's perceptions and experiences of childbirth by unplanned Caesarean section. In-depth Interviews with 10 Caucasian women (mean age=28; SD=1.97) explored their lived ...
Key Points. Question Do rates of general anesthesia use for cesarean delivery differ by race or ethnicity?. Findings In this cross-sectional study including 35 117 patients undergoing cesarean delivery, rates of general anesthesia use were higher among Black and Hispanic individuals. However, among patients who labored with an epidural catheter in situ, there were no significant differences in ...
with >20 weeks of gestation who underw ent caesarean section with referral note. Results: A total 64% patients were referred from community health center. 63.5% patients were referred due to lack ...
Caesarean section (CS) rates are rising globally [1-8] with the leading indication being a previous CS, accounting for up to half of CS performed [5,9]. Northern Ireland (NI) had the highest CS rate in the United Kingdom (UK) between 2012 and 2013 at 29.8 % [2] however, more recent UK statistics reveal CS rates for England, Scotland, Wales and NI to be 40 % [10], 36.7 % [11], 35 % [12] and ...