Critical Thinking, Clinical Reasoning, and Clinical Judgment
A practical approach.
7th Edition - July 23, 2019
Author: Donna D. Ignatavicius
Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Pract… Read more


Purchase options
LIMITED OFFER
Save 50% on book bundles
Immediately download your ebook while waiting for your print delivery. No promo code is needed.
Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 7th Edition brings these concepts to life through engaging text, diverse learning activities, and real-life examples. Easy-to-understand language and a "how-to" approach equip you to become a sensible, resilient critical thinker with the clinical reasoning skills you need to think think through complex issues and make sound clinical decisions. This edition emphasizes readiness for clinical practice and the Next Generation NCLEX exam, with a focus on systems thinking, interprofessional practice, nursing skills for the 21st century, and Quality and Safety for Nursing Education (QSEN) competencies.
- Clear, straightforward approach and motivational writing style
- Focus on application ("how to") with supporting rationales (theory) makes difficult concepts easy to learn.
- Critical Thinking Indicators feature evidence-based descriptions of behaviors that foster critical thinking in nursing practice.
- Highlighted features and sections that promote deep learning include: This Chapter at a Glance , Learning Outcomes, Key Concepts, Guiding Principle boxes, Critical Moments boxes, Other Perspectives features, Think-Pair-Share activities, H.M.O. (Help Me Out) cartoons, real-life clinical scenarios, Key Points, Critical Thinking Exercises , and more!
- Cultural, spiritual, and lifespan content explores the nurse’s role in hospitals, long-term care settings, and entire communities, presenting a broad approach to critical thinking.
- Inclusion of ethics- and standards-based professional practice reflects the increased demand for accountability in today’s professional climate.
- Timely coverage of the latest in nursing education and critical thinking includes concept-based learning; QSEN and IOM standards; problem-focused versus outcome-focused thinking; prioritization and delegation; developing a culture of safe, healthy work environments; expanding roles related to diagnosis and management; improving grades and passing tests the first time; NCLEX exam preparation; ensuring that documentation reflects critical thinking; communication and interpersonal skills; strategies for common workplace challenges; and more.
1. What are Critical Thinking, Clinical Reasoning, and Clinical Judgment? 2. Becoming a Critical Thinker 3. Critical Thinking and Learning Cultures: Teaching, Learning, and Taking Tests 4. Interprofessional Clinical Reasoning, Decision Making, and Judgment 5. Ethical Reasoning, Professionalism, Evidence-Based Practice, and Quality Improvement 6. Practicing Clinical Reasoning, Clinical Judgment, and Decision-making Skills 7. Interprofessional Practice Skills: Communication, Teamwork, and Self-Management NEW interprofessional collaboration focus!
Appendix A. Concept Mapping Appendix B. Nursing Process Summary Appendix C. Examples of CTIs within 4-Circle Model (New) Appendix D. Patient’s Rights and Nurses’ Rights Appendix E. DEAD ON Game Appendix F. Key Brain Parts Involved in Thinking Appendix G. Example SBAR Tool Appendix H. Results of Two Studies Describing Critical Thinking Skills Appendix I. Example Responses for Critical Thinking and Clinical Reasoning Exercises
- No. of pages : 268
- Language : English
- Edition : 7
- Published : July 23, 2019
- Imprint : Elsevier
- Paperback ISBN : 9780323676922
- Paperback ISBN : 9780323581257
- eBook ISBN : 9780323594721
Donna D. Ignatavicius
JavaScript seems to be disabled in your browser. For the best experience on our site, be sure to turn on Javascript in your browser.
15% off Personal Digital Subscriptions

- Need Help ?
- Free Shipping *
- Secure Payment
- Direct from Elsevier
- Europe (ENG) (€)
- Germany (€)
- Latin America ($)
- Middle East ($)
- Create an Account
- Compare Products
- Bestsellers
- Digital Subscriptions
Shop by Category
- Fundamentals and Skills
Sale Disclaimer
Critical Thinking, Clinical Reasoning, and Clinical Judgment, 7th Edition
- Share to receive a discount off your next order
- Share on Twitter
VitalSource Bookshelf gives you access to content when, where, and how you want. When you read an eBook on VitalSource Bookshelf, enjoy such features as:
- Access online or offline, on mobile or desktop devices.
- Bookmarks, highlights and notes sync across all your devices.
- Smart study tools such as note sharing and subscription, review mode, and Microsoft OneNote integration.
- Search and navigate content across your entire Bookshelf library.
- Interactive notebook and read-aloud functionality.
- Look up additional information online by highlighting a word or phrase.
- NEW! Spotlight on systems thinking teaches you to consider how things are related, while coverage of conceptual thinking helps you focus on big ideas first.
- NEW! Information on effective clinical simulations encourages learning through practice and debriefing.
- NEW! Clinical reasoning principles are highlighted throughout to ensure you are practice ready.
- NEW! Current critical judgment models are illustrated and explained in a clear, engaging style.
- NEW! Expanded content on growing nursing trends addresses competency assessment, electronic charting (informatics) and "thinking beyond the EHR," clinical evaluation, and preceptor and learner strategies.
- NEW! Strong emphasis on interprofessional collaboration includes new content on its growing importance in health care.
- Clear, straightforward approach and motivational writing style provides vivid examples, memorable anecdotes, and real-life case scenarios to make content come alive.
- Focus on application ("how to") with supporting rationales (theory) makes difficult concepts easy to learn.
- Critical Thinking Indicators feature evidence-based descriptions of behaviors that foster critical thinking in nursing practice.
- Highlighted features and sections that promote deep learning include: This Chapter at a Glance , Learning Outcomes, Key Concepts, Guiding Principle boxes, Critical Moments boxes, Other Perspectives features, Think-Pair-Share activities, H.M.O. (Help Me Out) cartoons, real-life clinical scenarios, Key Points, Critical Thinking Exercises , and more!
- Cultural, spiritual, and lifespan content explores the nurse’s role in hospitals, long-term care settings, and entire communities, presenting a broad approach to critical thinking.
- Inclusion of ethics- and standards-based professional practice reflects the increased demand for accountability in today’s professional climate.
- Timely coverage of the latest in nursing education and critical thinking includes concept-based learning; QSEN and IOM standards; problem-focused versus outcome-focused thinking; prioritization and delegation; developing a culture of safe, healthy work environments; expanding roles related to diagnosis and management; improving grades and passing tests the first time; NCLEX exam preparation; ensuring that documentation reflects critical thinking; communication and interpersonal skills; strategies for common workplace challenges; and more.
| ISBN Number | 9780323581257 |
|---|---|
| Main Author | By Rosalinda Alfaro-Lefevre |
| Copyright Year | 2020 |
| Edition Number | 7 |
| Format | Book |
| Trim | 191w x 235h |
| Illustrations | 50 illustrations (50 in full color) |
| Imprint | Elsevier |
| Page Count | 268 |
| Publication Date | 24 Sep 2019 |
| Stock Status | IN STOCK |
1. What are Critical Thinking, Clinical Reasoning, and Clinical Judgment? 2. Becoming a Critical Thinker 3. Critical Thinking and Learning Cultures: Teaching, Learning, and Taking Tests 4. Interprofessional Clinical Reasoning, Decision Making, and Judgment 5. Ethical Reasoning, Professionalism, Evidence-Based Practice, and Quality Improvement 6. Practicing Clinical Reasoning, Clinical Judgment, and Decision-making Skills 7. Interprofessional Practice Skills: Communication, Teamwork, and Self-Management NEW interprofessional collaboration focus!
Appendix A. Concept Mapping Appendix B. Nursing Process Summary Appendix C. Examples of CTIs within 4-Circle Model (New) Appendix D. Patient’s Rights and Nurses’ Rights Appendix E. DEAD ON Game Appendix F. Key Brain Parts Involved in Thinking Appendix G. Example SBAR Tool Appendix H. Results of Two Studies Describing Critical Thinking Skills Appendix I. Example Responses for Critical Thinking and Clinical Reasoning Exercises
Related Products
Marios Loukas
Edited by Joseph Iannotti
William F. Young
Roger Smith
Edited by David A. Kaminsky
Alan R. Crossman
Edited by Joseph P Iannotti
Edited by Roshan Patel
* Elsevier is a leading publisher of health science books and journals, helping to advance medicine by delivering superior education, reference information and decision support tools to doctors, nurses, health practitioners and students. With titles available across a variety of media, we are able to supply the information you need in the most convenient format.
Copyright © 2024, its licensors, and contributors.
All rights are reserved, including those for text and data mining, AI training, and similar technologies.
For problems or suggestions regarding this site, please visit our Support Hub .
JavaScript seems to be disabled in your browser. For the best experience on our site, be sure to turn on Javascript in your browser.

- 01865 844 640
- Free UK Delivery
- Secure Payment
- Direct from Elsevier
- Europe (ENG) (€)
- Germany (€)
- Latin America ($)
- Middle East ($)
- Create an Account
- Compare Products
- Bestsellers
- Nursing Month
Shop by Category
- Nursing & Midwifery
- General Nursing
Critical Thinking, Clinical Reasoning, and Clinical Judgment, 7th Edition
- Share to receive a discount off your next order
- Share on Twitter

- NEW! Spotlight on systems thinking teaches you to consider how things are related, while coverage of conceptual thinking helps you focus on big ideas first.
- NEW! Information on effective clinical simulations encourages learning through practice and debriefing.
- NEW! Clinical reasoning principles are highlighted throughout to ensure you are practice ready.
- NEW! Current critical judgment models are illustrated and explained in a clear, engaging style.
- NEW! Expanded content on growing nursing trends addresses competency assessment, electronic charting (informatics) and "thinking beyond the EHR," clinical evaluation, and preceptor and learner strategies.
- NEW! Strong emphasis on interprofessional collaboration includes new content on its growing importance in health care.
- Clear, straightforward approach and motivational writing style provides vivid examples, memorable anecdotes, and real-life case scenarios to make content come alive.
- Focus on application ("how to") with supporting rationales (theory) makes difficult concepts easy to learn.
- Critical Thinking Indicators feature evidence-based descriptions of behaviors that foster critical thinking in nursing practice.
- Highlighted features and sections that promote deep learning include: This Chapter at a Glance , Learning Outcomes, Key Concepts, Guiding Principle boxes, Critical Moments boxes, Other Perspectives features, Think-Pair-Share activities, H.M.O. (Help Me Out) cartoons, real-life clinical scenarios, Key Points, Critical Thinking Exercises , and more!
- Cultural, spiritual, and lifespan content explores the nurse’s role in hospitals, long-term care settings, and entire communities, presenting a broad approach to critical thinking.
- Inclusion of ethics- and standards-based professional practice reflects the increased demand for accountability in today’s professional climate.
- Timely coverage of the latest in nursing education and critical thinking includes concept-based learning; QSEN and IOM standards; problem-focused versus outcome-focused thinking; prioritization and delegation; developing a culture of safe, healthy work environments; expanding roles related to diagnosis and management; improving grades and passing tests the first time; NCLEX exam preparation; ensuring that documentation reflects critical thinking; communication and interpersonal skills; strategies for common workplace challenges; and more.
| ISBN Number | 9780323676922 |
|---|---|
| Author Information | By Rosalinda Alfaro-Lefevre |
| Copyright Year | 2020 |
| Edition Number | 7 |
| Format | Book |
| Format Size | Other |
| Imprint | Elsevier |
| Page Count | 0 |
| Publication Date | 02-10-2019 |
| Stock Status | IN STOCK |

VitalSource eBooks for practitioners and students

Bring it with you - The Bookshelf app allows you to access books on your laptop, tablet or mobile, so your ebooks go where ever you are - online or offline.
Take notes - Highlight, bookmark and take notes and highlights automatically stay in sync no matter where you make them.

Listen to eBooks - When you need to go screenless, the Text-to-speech tool will read your book aloud.

Powerful search - The searching capabilities allow you to search keywords through all your eBooks, the entire Bookshelf Library and well as on Wikipedia.

Ecological - Manage your environmental impact with paperless books.
How to read your VitalSource eBooks
- Purchase your VitalSource eBook on the Elsevier Health site
- Download VitalSource Bookshelf , the best app for smarter reading, studying, and learning
- Redeem your redeption code you received via email, and download your eBook
- Access your VitalSource eBook on any laptop, tablet, or smartphone device with VitalSource Bookshelf
Copyright © 2024, its licensors, and contributors.
All rights are reserved, including those for text and data mining, AI training, and similar technologies.
Cookies are used by this site. To decline or learn more, visit our Cookies page. Cookie Settings
JavaScript seems to be disabled in your browser. For the best experience on our site, be sure to turn on Javascript in your browser.

- Need Help ?
- Free Shipping *
- Secure Payment
- Direct from Elsevier
- Europe (ENG) (€)
- Germany (€)
- Latin America ($)
- Middle East ($)
- Create an Account
- Compare Products
- Flash Cards
- Online Resources
- Complete Anatomy
- Australian Titles
- Student Corner
Shop by Category
Critical Thinking, Clinical Reasoning, and Clinical Judgment, 7th Edition
- Share to receive a discount off your next order
- Share on Twitter
- NEW! Spotlight on systems thinking teaches you to consider how things are related, while coverage of conceptual thinking helps you focus on big ideas first.
- NEW! Information on effective clinical simulations encourages learning through practice and debriefing.
- NEW! Clinical reasoning principles are highlighted throughout to ensure you are practice ready.
- NEW! Current critical judgment models are illustrated and explained in a clear, engaging style.
- NEW! Expanded content on growing nursing trends addresses competency assessment, electronic charting (informatics) and "thinking beyond the EHR," clinical evaluation, and preceptor and learner strategies.
- NEW! Strong emphasis on interprofessional collaboration includes new content on its growing importance in health care.
- Clear, straightforward approach and motivational writing style provides vivid examples, memorable anecdotes, and real-life case scenarios to make content come alive.
- Focus on application ("how to") with supporting rationales (theory) makes difficult concepts easy to learn.
- Critical Thinking Indicators feature evidence-based descriptions of behaviors that foster critical thinking in nursing practice.
- Highlighted features and sections that promote deep learning include: This Chapter at a Glance , Learning Outcomes, Key Concepts, Guiding Principle boxes, Critical Moments boxes, Other Perspectives features, Think-Pair-Share activities, H.M.O. (Help Me Out) cartoons, real-life clinical scenarios, Key Points, Critical Thinking Exercises , and more!
- Cultural, spiritual, and lifespan content explores the nurse’s role in hospitals, long-term care settings, and entire communities, presenting a broad approach to critical thinking.
- Inclusion of ethics- and standards-based professional practice reflects the increased demand for accountability in today’s professional climate.
- Timely coverage of the latest in nursing education and critical thinking includes concept-based learning; QSEN and IOM standards; problem-focused versus outcome-focused thinking; prioritization and delegation; developing a culture of safe, healthy work environments; expanding roles related to diagnosis and management; improving grades and passing tests the first time; NCLEX exam preparation; ensuring that documentation reflects critical thinking; communication and interpersonal skills; strategies for common workplace challenges; and more.
| ISBN Number | 9780323676922 |
|---|---|
| Description Author List | By |
| Copyright Year | 2020 |
| Edition Number | 7 |
| Format | Book |
| Trim | Other |
| Imprint | Elsevier |
| Page Count | 0 |
| Publication Date | 26 Sep 2019 |
| Stock Status | IN STOCK |
1. What are Critical Thinking, Clinical Reasoning, and Clinical Judgment? 2. Becoming a Critical Thinker 3. Critical Thinking and Learning Cultures: Teaching, Learning, and Taking Tests 4. Interprofessional Clinical Reasoning, Decision Making, and Judgment 5. Ethical Reasoning, Professionalism, Evidence-Based Practice, and Quality Improvement 6. Practicing Clinical Reasoning, Clinical Judgment, and Decision-making Skills 7. Interprofessional Practice Skills: Communication, Teamwork, and Self-Management NEW interprofessional collaboration focus!
Appendix A. Concept Mapping Appendix B. Nursing Process Summary Appendix C. Examples of CTIs within 4-Circle Model (New) Appendix D. Patient’s Rights and Nurses’ Rights Appendix E. DEAD ON Game Appendix F. Key Brain Parts Involved in Thinking Appendix G. Example SBAR Tool Appendix H. Results of Two Studies Describing Critical Thinking Skills Appendix I. Example Responses for Critical Thinking and Clinical Reasoning Exercises
* Elsevier is a leading publisher of health science books and journals, helping to advance medicine by delivering superior education, reference information and decision support tools to doctors, nurses, health practitioners and students. With titles available across a variety of media, we are able to supply the information you need in the most convenient format.
Copyright © 2024, its licensors, and contributors.
All rights are reserved, including those for text and data mining, AI training, and similar technologies.
Cookies are used by this site. Cookie Settings
For problems or suggestions regarding this site, please visit our Support Hub .
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 6 clinical reasoning, decisionmaking, and action: thinking critically and clinically.
Patricia Benner ; Ronda G. Hughes ; Molly Sutphen .
Affiliations
This chapter examines multiple thinking strategies that are needed for high-quality clinical practice. Clinical reasoning and judgment are examined in relation to other modes of thinking used by clinical nurses in providing quality health care to patients that avoids adverse events and patient harm. The clinician’s ability to provide safe, high-quality care can be dependent upon their ability to reason, think, and judge, which can be limited by lack of experience. The expert performance of nurses is dependent upon continual learning and evaluation of performance.
- Critical Thinking
Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years. There are several key definitions for critical thinking to consider. The American Philosophical Association (APA) defined critical thinking as purposeful, self-regulatory judgment that uses cognitive tools such as interpretation, analysis, evaluation, inference, and explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations on which judgment is based. 2 A more expansive general definition of critical thinking is
. . . in short, self-directed, self-disciplined, self-monitored, and self-corrective thinking. It presupposes assent to rigorous standards of excellence and mindful command of their use. It entails effective communication and problem solving abilities and a commitment to overcome our native egocentrism and sociocentrism. Every clinician must develop rigorous habits of critical thinking, but they cannot escape completely the situatedness and structures of the clinical traditions and practices in which they must make decisions and act quickly in specific clinical situations. 3
There are three key definitions for nursing, which differ slightly. Bittner and Tobin defined critical thinking as being “influenced by knowledge and experience, using strategies such as reflective thinking as a part of learning to identify the issues and opportunities, and holistically synthesize the information in nursing practice” 4 (p. 268). Scheffer and Rubenfeld 5 expanded on the APA definition for nurses through a consensus process, resulting in the following definition:
Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, openmindedness, perseverance, and reflection. Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge 6 (Scheffer & Rubenfeld, p. 357).
The National League for Nursing Accreditation Commission (NLNAC) defined critical thinking as:
the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research 7 (p. 8).
These concepts are furthered by the American Association of Colleges of Nurses’ definition of critical thinking in their Essentials of Baccalaureate Nursing :
Critical thinking underlies independent and interdependent decision making. Critical thinking includes questioning, analysis, synthesis, interpretation, inference, inductive and deductive reasoning, intuition, application, and creativity 8 (p. 9).
Course work or ethical experiences should provide the graduate with the knowledge and skills to:
- Use nursing and other appropriate theories and models, and an appropriate ethical framework;
- Apply research-based knowledge from nursing and the sciences as the basis for practice;
- Use clinical judgment and decision-making skills;
- Engage in self-reflective and collegial dialogue about professional practice;
- Evaluate nursing care outcomes through the acquisition of data and the questioning of inconsistencies, allowing for the revision of actions and goals;
- Engage in creative problem solving 8 (p. 10).
Taken together, these definitions of critical thinking set forth the scope and key elements of thought processes involved in providing clinical care. Exactly how critical thinking is defined will influence how it is taught and to what standard of care nurses will be held accountable.
Professional and regulatory bodies in nursing education have required that critical thinking be central to all nursing curricula, but they have not adequately distinguished critical reflection from ethical, clinical, or even creative thinking for decisionmaking or actions required by the clinician. Other essential modes of thought such as clinical reasoning, evaluation of evidence, creative thinking, or the application of well-established standards of practice—all distinct from critical reflection—have been subsumed under the rubric of critical thinking. In the nursing education literature, clinical reasoning and judgment are often conflated with critical thinking. The accrediting bodies and nursing scholars have included decisionmaking and action-oriented, practical, ethical, and clinical reasoning in the rubric of critical reflection and thinking. One might say that this harmless semantic confusion is corrected by actual practices, except that students need to understand the distinctions between critical reflection and clinical reasoning, and they need to learn to discern when each is better suited, just as students need to also engage in applying standards, evidence-based practices, and creative thinking.
The growing body of research, patient acuity, and complexity of care demand higher-order thinking skills. Critical thinking involves the application of knowledge and experience to identify patient problems and to direct clinical judgments and actions that result in positive patient outcomes. These skills can be cultivated by educators who display the virtues of critical thinking, including independence of thought, intellectual curiosity, courage, humility, empathy, integrity, perseverance, and fair-mindedness. 9
The process of critical thinking is stimulated by integrating the essential knowledge, experiences, and clinical reasoning that support professional practice. The emerging paradigm for clinical thinking and cognition is that it is social and dialogical rather than monological and individual. 10–12 Clinicians pool their wisdom and multiple perspectives, yet some clinical knowledge can be demonstrated only in the situation (e.g., how to suction an extremely fragile patient whose oxygen saturations sink too low). Early warnings of problematic situations are made possible by clinicians comparing their observations to that of other providers. Clinicians form practice communities that create styles of practice, including ways of doing things, communication styles and mechanisms, and shared expectations about performance and expertise of team members.
By holding up critical thinking as a large umbrella for different modes of thinking, students can easily misconstrue the logic and purposes of different modes of thinking. Clinicians and scientists alike need multiple thinking strategies, such as critical thinking, clinical judgment, diagnostic reasoning, deliberative rationality, scientific reasoning, dialogue, argument, creative thinking, and so on. In particular, clinicians need forethought and an ongoing grasp of a patient’s health status and care needs trajectory, which requires an assessment of their own clarity and understanding of the situation at hand, critical reflection, critical reasoning, and clinical judgment.
Critical Reflection, Critical Reasoning, and Judgment
Critical reflection requires that the thinker examine the underlying assumptions and radically question or doubt the validity of arguments, assertions, and even facts of the case. Critical reflective skills are essential for clinicians; however, these skills are not sufficient for the clinician who must decide how to act in particular situations and avoid patient injury. For example, in everyday practice, clinicians cannot afford to critically reflect on the well-established tenets of “normal” or “typical” human circulatory systems when trying to figure out a particular patient’s alterations from that typical, well-grounded understanding that has existed since Harvey’s work in 1628. 13 Yet critical reflection can generate new scientifically based ideas. For example, there is a lack of adequate research on the differences between women’s and men’s circulatory systems and the typical pathophysiology related to heart attacks. Available research is based upon multiple, taken-for-granted starting points about the general nature of the circulatory system. As such, critical reflection may not provide what is needed for a clinician to act in a situation. This idea can be considered reasonable since critical reflective thinking is not sufficient for good clinical reasoning and judgment. The clinician’s development of skillful critical reflection depends upon being taught what to pay attention to, and thus gaining a sense of salience that informs the powers of perceptual grasp. The powers of noticing or perceptual grasp depend upon noticing what is salient and the capacity to respond to the situation.
Critical reflection is a crucial professional skill, but it is not the only reasoning skill or logic clinicians require. The ability to think critically uses reflection, induction, deduction, analysis, challenging assumptions, and evaluation of data and information to guide decisionmaking. 9 , 14 , 15 Critical reasoning is a process whereby knowledge and experience are applied in considering multiple possibilities to achieve the desired goals, 16 while considering the patient’s situation. 14 It is a process where both inductive and deductive cognitive skills are used. 17 Sometimes clinical reasoning is presented as a form of evaluating scientific knowledge, sometimes even as a form of scientific reasoning. Critical thinking is inherent in making sound clinical reasoning. 18
An essential point of tension and confusion exists in practice traditions such as nursing and medicine when clinical reasoning and critical reflection become entangled, because the clinician must have some established bases that are not questioned when engaging in clinical decisions and actions, such as standing orders. The clinician must act in the particular situation and time with the best clinical and scientific knowledge available. The clinician cannot afford to indulge in either ritualistic unexamined knowledge or diagnostic or therapeutic nihilism caused by radical doubt, as in critical reflection, because they must find an intelligent and effective way to think and act in particular clinical situations. Critical reflection skills are essential to assist practitioners to rethink outmoded or even wrong-headed approaches to health care, health promotion, and prevention of illness and complications, especially when new evidence is available. Breakdowns in practice, high failure rates in particular therapies, new diseases, new scientific discoveries, and societal changes call for critical reflection about past assumptions and no-longer-tenable beliefs.
Clinical reasoning stands out as a situated, practice-based form of reasoning that requires a background of scientific and technological research-based knowledge about general cases, more so than any particular instance. It also requires practical ability to discern the relevance of the evidence behind general scientific and technical knowledge and how it applies to a particular patient. In dong so, the clinician considers the patient’s particular clinical trajectory, their concerns and preferences, and their particular vulnerabilities (e.g., having multiple comorbidities) and sensitivities to care interventions (e.g., known drug allergies, other conflicting comorbid conditions, incompatible therapies, and past responses to therapies) when forming clinical decisions or conclusions.
Situated in a practice setting, clinical reasoning occurs within social relationships or situations involving patient, family, community, and a team of health care providers. The expert clinician situates themselves within a nexus of relationships, with concerns that are bounded by the situation. Expert clinical reasoning is socially engaged with the relationships and concerns of those who are affected by the caregiving situation, and when certain circumstances are present, the adverse event. Halpern 19 has called excellent clinical ethical reasoning “emotional reasoning” in that the clinicians have emotional access to the patient/family concerns and their understanding of the particular care needs. Expert clinicians also seek an optimal perceptual grasp, one based on understanding and as undistorted as possible, based on an attuned emotional engagement and expert clinical knowledge. 19 , 20
Clergy educators 21 and nursing and medical educators have begun to recognize the wisdom of broadening their narrow vision of rationality beyond simple rational calculation (exemplified by cost-benefit analysis) to reconsider the need for character development—including emotional engagement, perception, habits of thought, and skill acquisition—as essential to the development of expert clinical reasoning, judgment, and action. 10 , 22–24 Practitioners of engineering, law, medicine, and nursing, like the clergy, have to develop a place to stand in their discipline’s tradition of knowledge and science in order to recognize and evaluate salient evidence in the moment. Diagnostic confusion and disciplinary nihilism are both threats to the clinician’s ability to act in particular situations. However, the practice and practitioners will not be self-improving and vital if they cannot engage in critical reflection on what is not of value, what is outmoded, and what does not work. As evidence evolves and expands, so too must clinical thought.
Clinical judgment requires clinical reasoning across time about the particular, and because of the relevance of this immediate historical unfolding, clinical reasoning can be very different from the scientific reasoning used to formulate, conduct, and assess clinical experiments. While scientific reasoning is also socially embedded in a nexus of social relationships and concerns, the goal of detached, critical objectivity used to conduct scientific experiments minimizes the interactive influence of the research on the experiment once it has begun. Scientific research in the natural and clinical sciences typically uses formal criteria to develop “yes” and “no” judgments at prespecified times. The scientist is always situated in past and immediate scientific history, preferring to evaluate static and predetermined points in time (e.g., snapshot reasoning), in contrast to a clinician who must always reason about transitions over time. 25 , 26
Techne and Phronesis
Distinctions between the mere scientific making of things and practice was first explored by Aristotle as distinctions between techne and phronesis. 27 Learning to be a good practitioner requires developing the requisite moral imagination for good practice. If, for example, patients exercise their rights and refuse treatments, practitioners are required to have the moral imagination to understand the probable basis for the patient’s refusal. For example, was the refusal based upon catastrophic thinking, unrealistic fears, misunderstanding, or even clinical depression?
Techne, as defined by Aristotle, encompasses the notion of formation of character and habitus 28 as embodied beings. In Aristotle’s terms, techne refers to the making of things or producing outcomes. 11 Joseph Dunne defines techne as “the activity of producing outcomes,” and it “is governed by a means-ends rationality where the maker or producer governs the thing or outcomes produced or made through gaining mastery over the means of producing the outcomes, to the point of being able to separate means and ends” 11 (p. 54). While some aspects of medical and nursing practice fall into the category of techne, much of nursing and medical practice falls outside means-ends rationality and must be governed by concern for doing good or what is best for the patient in particular circumstances, where being in a relationship and discerning particular human concerns at stake guide action.
Phronesis, in contrast to techne, includes reasoning about the particular, across time, through changes or transitions in the patient’s and/or the clinician’s understanding. As noted by Dunne, phronesis is “characterized at least as much by a perceptiveness with regard to concrete particulars as by a knowledge of universal principles” 11 (p. 273). This type of practical reasoning often takes the form of puzzle solving or the evaluation of immediate past “hot” history of the patient’s situation. Such a particular clinical situation is necessarily particular, even though many commonalities and similarities with other disease syndromes can be recognized through signs and symptoms and laboratory tests. 11 , 29 , 30 Pointing to knowledge embedded in a practice makes no claim for infallibility or “correctness.” Individual practitioners can be mistaken in their judgments because practices such as medicine and nursing are inherently underdetermined. 31
While phronetic knowledge must remain open to correction and improvement, real events, and consequences, it cannot consistently transcend the institutional setting’s capacities and supports for good practice. Phronesis is also dependent on ongoing experiential learning of the practitioner, where knowledge is refined, corrected, or refuted. The Western tradition, with the notable exception of Aristotle, valued knowledge that could be made universal and devalued practical know-how and experiential learning. Descartes codified this preference for formal logic and rational calculation.
Aristotle recognized that when knowledge is underdetermined, changeable, and particular, it cannot be turned into the universal or standardized. It must be perceived, discerned, and judged, all of which require experiential learning. In nursing and medicine, perceptual acuity in physical assessment and clinical judgment (i.e., reasoning across time about changes in the particular patient or the clinician’s understanding of the patient’s condition) fall into the Greek Aristotelian category of phronesis. Dewey 32 sought to rescue knowledge gained by practical activity in the world. He identified three flaws in the understanding of experience in Greek philosophy: (1) empirical knowing is the opposite of experience with science; (2) practice is reduced to techne or the application of rational thought or technique; and (3) action and skilled know-how are considered temporary and capricious as compared to reason, which the Greeks considered as ultimate reality.
In practice, nursing and medicine require both techne and phronesis. The clinician standardizes and routinizes what can be standardized and routinized, as exemplified by standardized blood pressure measurements, diagnoses, and even charting about the patient’s condition and treatment. 27 Procedural and scientific knowledge can often be formalized and standardized (e.g., practice guidelines), or at least made explicit and certain in practice, except for the necessary timing and adjustments made for particular patients. 11 , 22
Rational calculations available to techne—population trends and statistics, algorithms—are created as decision support structures and can improve accuracy when used as a stance of inquiry in making clinical judgments about particular patients. Aggregated evidence from clinical trials and ongoing working knowledge of pathophysiology, biochemistry, and genomics are essential. In addition, the skills of phronesis (clinical judgment that reasons across time, taking into account the transitions of the particular patient/family/community and transitions in the clinician’s understanding of the clinical situation) will be required for nursing, medicine, or any helping profession.
Thinking Critically
Being able to think critically enables nurses to meet the needs of patients within their context and considering their preferences; meet the needs of patients within the context of uncertainty; consider alternatives, resulting in higher-quality care; 33 and think reflectively, rather than simply accepting statements and performing tasks without significant understanding and evaluation. 34 Skillful practitioners can think critically because they have the following cognitive skills: information seeking, discriminating, analyzing, transforming knowledge, predicating, applying standards, and logical reasoning. 5 One’s ability to think critically can be affected by age, length of education (e.g., an associate vs. a baccalaureate decree in nursing), and completion of philosophy or logic subjects. 35–37 The skillful practitioner can think critically because of having the following characteristics: motivation, perseverance, fair-mindedness, and deliberate and careful attention to thinking. 5 , 9
Thinking critically implies that one has a knowledge base from which to reason and the ability to analyze and evaluate evidence. 38 Knowledge can be manifest by the logic and rational implications of decisionmaking. Clinical decisionmaking is particularly influenced by interpersonal relationships with colleagues, 39 patient conditions, availability of resources, 40 knowledge, and experience. 41 Of these, experience has been shown to enhance nurses’ abilities to make quick decisions 42 and fewer decision errors, 43 support the identification of salient cues, and foster the recognition and action on patterns of information. 44 , 45
Clinicians must develop the character and relational skills that enable them to perceive and understand their patient’s needs and concerns. This requires accurate interpretation of patient data that is relevant to the specific patient and situation. In nursing, this formation of moral agency focuses on learning to be responsible in particular ways demanded by the practice, and to pay attention and intelligently discern changes in patients’ concerns and/or clinical condition that require action on the part of the nurse or other health care workers to avert potential compromises to quality care.
Formation of the clinician’s character, skills, and habits are developed in schools and particular practice communities within a larger practice tradition. As Dunne notes,
A practice is not just a surface on which one can display instant virtuosity. It grounds one in a tradition that has been formed through an elaborate development and that exists at any juncture only in the dispositions (slowly and perhaps painfully acquired) of its recognized practitioners. The question may of course be asked whether there are any such practices in the contemporary world, whether the wholesale encroachment of Technique has not obliterated them—and whether this is not the whole point of MacIntyre’s recipe of withdrawal, as well as of the post-modern story of dispossession 11 (p. 378).
Clearly Dunne is engaging in critical reflection about the conditions for developing character, skills, and habits for skillful and ethical comportment of practitioners, as well as to act as moral agents for patients so that they and their families receive safe, effective, and compassionate care.
Professional socialization or professional values, while necessary, do not adequately address character and skill formation that transform the way the practitioner exists in his or her world, what the practitioner is capable of noticing and responding to, based upon well-established patterns of emotional responses, skills, dispositions to act, and the skills to respond, decide, and act. 46 The need for character and skill formation of the clinician is what makes a practice stand out from a mere technical, repetitious manufacturing process. 11 , 30 , 47
In nursing and medicine, many have questioned whether current health care institutions are designed to promote or hinder enlightened, compassionate practice, or whether they have deteriorated into commercial institutional models that focus primarily on efficiency and profit. MacIntyre points out the links between the ongoing development and improvement of practice traditions and the institutions that house them:
Lack of justice, lack of truthfulness, lack of courage, lack of the relevant intellectual virtues—these corrupt traditions, just as they do those institutions and practices which derive their life from the traditions of which they are the contemporary embodiments. To recognize this is of course also to recognize the existence of an additional virtue, one whose importance is perhaps most obvious when it is least present, the virtue of having an adequate sense of the traditions to which one belongs or which confront one. This virtue is not to be confused with any form of conservative antiquarianism; I am not praising those who choose the conventional conservative role of laudator temporis acti. It is rather the case that an adequate sense of tradition manifests itself in a grasp of those future possibilities which the past has made available to the present. Living traditions, just because they continue a not-yet-completed narrative, confront a future whose determinate and determinable character, so far as it possesses any, derives from the past 30 (p. 207).
It would be impossible to capture all the situated and distributed knowledge outside of actual practice situations and particular patients. Simulations are powerful as teaching tools to enable nurses’ ability to think critically because they give students the opportunity to practice in a simplified environment. However, students can be limited in their inability to convey underdetermined situations where much of the information is based on perceptions of many aspects of the patient and changes that have occurred over time. Simulations cannot have the sub-cultures formed in practice settings that set the social mood of trust, distrust, competency, limited resources, or other forms of situated possibilities.
One of the hallmark studies in nursing providing keen insight into understanding the influence of experience was a qualitative study of adult, pediatric, and neonatal intensive care unit (ICU) nurses, where the nurses were clustered into advanced beginner, intermediate, and expert level of practice categories. The advanced beginner (having up to 6 months of work experience) used procedures and protocols to determine which clinical actions were needed. When confronted with a complex patient situation, the advanced beginner felt their practice was unsafe because of a knowledge deficit or because of a knowledge application confusion. The transition from advanced beginners to competent practitioners began when they first had experience with actual clinical situations and could benefit from the knowledge gained from the mistakes of their colleagues. Competent nurses continuously questioned what they saw and heard, feeling an obligation to know more about clinical situations. In doing do, they moved from only using care plans and following the physicians’ orders to analyzing and interpreting patient situations. Beyond that, the proficient nurse acknowledged the changing relevance of clinical situations requiring action beyond what was planned or anticipated. The proficient nurse learned to acknowledge the changing needs of patient care and situation, and could organize interventions “by the situation as it unfolds rather than by preset goals 48 (p. 24). Both competent and proficient nurses (that is, intermediate level of practice) had at least two years of ICU experience. 48 Finally, the expert nurse had a more fully developed grasp of a clinical situation, a sense of confidence in what is known about the situation, and could differentiate the precise clinical problem in little time. 48
Expertise is acquired through professional experience and is indicative of a nurse who has moved beyond mere proficiency. As Gadamer 29 points out, experience involves a turning around of preconceived notions, preunderstandings, and extends or adds nuances to understanding. Dewey 49 notes that experience requires a prepared “creature” and an enriched environment. The opportunity to reflect and narrate one’s experiential learning can clarify, extend, or even refute experiential learning.
Experiential learning requires time and nurturing, but time alone does not ensure experiential learning. Aristotle linked experiential learning to the development of character and moral sensitivities of a person learning a practice. 50 New nurses/new graduates have limited work experience and must experience continuing learning until they have reached an acceptable level of performance. 51 After that, further improvements are not predictable, and years of experience are an inadequate predictor of expertise. 52
The most effective knower and developer of practical knowledge creates an ongoing dialogue and connection between lessons of the day and experiential learning over time. Gadamer, in a late life interview, highlighted the open-endedness and ongoing nature of experiential learning in the following interview response:
Being experienced does not mean that one now knows something once and for all and becomes rigid in this knowledge; rather, one becomes more open to new experiences. A person who is experienced is undogmatic. Experience has the effect of freeing one to be open to new experience … In our experience we bring nothing to a close; we are constantly learning new things from our experience … this I call the interminability of all experience 32 (p. 403).
Practical endeavor, supported by scientific knowledge, requires experiential learning, the development of skilled know-how, and perceptual acuity in order to make the scientific knowledge relevant to the situation. Clinical perceptual and skilled know-how helps the practitioner discern when particular scientific findings might be relevant. 53
Often experience and knowledge, confirmed by experimentation, are treated as oppositions, an either-or choice. However, in practice it is readily acknowledged that experiential knowledge fuels scientific investigation, and scientific investigation fuels further experiential learning. Experiential learning from particular clinical cases can help the clinician recognize future similar cases and fuel new scientific questions and study. For example, less experienced nurses—and it could be argued experienced as well—can use nursing diagnoses practice guidelines as part of their professional advancement. Guidelines are used to reflect their interpretation of patients’ needs, responses, and situation, 54 a process that requires critical thinking and decisionmaking. 55 , 56 Using guidelines also reflects one’s problem identification and problem-solving abilities. 56 Conversely, the ability to proficiently conduct a series of tasks without nursing diagnoses is the hallmark of expertise. 39 , 57
Experience precedes expertise. As expertise develops from experience and gaining knowledge and transitions to the proficiency stage, the nurses’ thinking moves from steps and procedures (i.e., task-oriented care) toward “chunks” or patterns 39 (i.e., patient-specific care). In doing so, the nurse thinks reflectively, rather than merely accepting statements and performing procedures without significant understanding and evaluation. 34 Expert nurses do not rely on rules and logical thought processes in problem-solving and decisionmaking. 39 Instead, they use abstract principles, can see the situation as a complex whole, perceive situations comprehensively, and can be fully involved in the situation. 48 Expert nurses can perform high-level care without conscious awareness of the knowledge they are using, 39 , 58 and they are able to provide that care with flexibility and speed. Through a combination of knowledge and skills gained from a range of theoretical and experiential sources, expert nurses also provide holistic care. 39 Thus, the best care comes from the combination of theoretical, tacit, and experiential knowledge. 59 , 60
Experts are thought to eventually develop the ability to intuitively know what to do and to quickly recognize critical aspects of the situation. 22 Some have proposed that expert nurses provide high-quality patient care, 61 , 62 but that is not consistently documented—particularly in consideration of patient outcomes—and a full understanding between the differential impact of care rendered by an “expert” nurse is not fully understood. In fact, several studies have found that length of professional experience is often unrelated and even negatively related to performance measures and outcomes. 63 , 64
In a review of the literature on expertise in nursing, Ericsson and colleagues 65 found that focusing on challenging, less-frequent situations would reveal individual performance differences on tasks that require speed and flexibility, such as that experienced during a code or an adverse event. Superior performance was associated with extensive training and immediate feedback about outcomes, which can be obtained through continual training, simulation, and processes such as root-cause analysis following an adverse event. Therefore, efforts to improve performance benefited from continual monitoring, planning, and retrospective evaluation. Even then, the nurse’s ability to perform as an expert is dependent upon their ability to use intuition or insights gained through interactions with patients. 39
Intuition and Perception
Intuition is the instant understanding of knowledge without evidence of sensible thought. 66 According to Young, 67 intuition in clinical practice is a process whereby the nurse recognizes something about a patient that is difficult to verbalize. Intuition is characterized by factual knowledge, “immediate possession of knowledge, and knowledge independent of the linear reasoning process” 68 (p. 23). When intuition is used, one filters information initially triggered by the imagination, leading to the integration of all knowledge and information to problem solve. 69 Clinicians use their interactions with patients and intuition, drawing on tacit or experiential knowledge, 70 , 71 to apply the correct knowledge to make the correct decisions to address patient needs. Yet there is a “conflated belief in the nurses’ ability to know what is best for the patient” 72 (p. 251) because the nurses’ and patients’ identification of the patients’ needs can vary. 73
A review of research and rhetoric involving intuition by King and Appleton 62 found that all nurses, including students, used intuition (i.e., gut feelings). They found evidence, predominately in critical care units, that intuition was triggered in response to knowledge and as a trigger for action and/or reflection with a direct bearing on the analytical process involved in patient care. The challenge for nurses was that rigid adherence to checklists, guidelines, and standardized documentation, 62 ignored the benefits of intuition. This view was furthered by Rew and Barrow 68 , 74 in their reviews of the literature, where they found that intuition was imperative to complex decisionmaking, 68 difficult to measure and assess in a quantitative manner, and was not linked to physiologic measures. 74
Intuition is a way of explaining professional expertise. 75 Expert nurses rely on their intuitive judgment that has been developed over time. 39 , 76 Intuition is an informal, nonanalytically based, unstructured, deliberate calculation that facilitates problem solving, 77 a process of arriving at salient conclusions based on relatively small amounts of knowledge and/or information. 78 Experts can have rapid insight into a situation by using intuition to recognize patterns and similarities, achieve commonsense understanding, and sense the salient information combined with deliberative rationality. 10 Intuitive recognition of similarities and commonalities between patients are often the first diagnostic clue or early warning, which must then be followed up with critical evaluation of evidence among the competing conditions. This situation calls for intuitive judgment that can distinguish “expert human judgment from the decisions” made by a novice 79 (p. 23).
Shaw 80 equates intuition with direct perception. Direct perception is dependent upon being able to detect complex patterns and relationships that one has learned through experience are important. Recognizing these patterns and relationships generally occurs rapidly and is complex, making it difficult to articulate or describe. Perceptual skills, like those of the expert nurse, are essential to recognizing current and changing clinical conditions. Perception requires attentiveness and the development of a sense of what is salient. Often in nursing and medicine, means and ends are fused, as is the case for a “good enough” birth experience and a peaceful death.
- Applying Practice Evidence
Research continues to find that using evidence-based guidelines in practice, informed through research evidence, improves patients’ outcomes. 81–83 Research-based guidelines are intended to provide guidance for specific areas of health care delivery. 84 The clinician—both the novice and expert—is expected to use the best available evidence for the most efficacious therapies and interventions in particular instances, to ensure the highest-quality care, especially when deviations from the evidence-based norm may heighten risks to patient safety. Otherwise, if nursing and medicine were exact sciences, or consisted only of techne, then a 1:1 relationship could be established between results of aggregated evidence-based research and the best path for all patients.
Evaluating Evidence
Before research should be used in practice, it must be evaluated. There are many complexities and nuances in evaluating the research evidence for clinical practice. Evaluation of research behind evidence-based medicine requires critical thinking and good clinical judgment. Sometimes the research findings are mixed or even conflicting. As such, the validity, reliability, and generalizability of available research are fundamental to evaluating whether evidence can be applied in practice. To do so, clinicians must select the best scientific evidence relevant to particular patients—a complex process that involves intuition to apply the evidence. Critical thinking is required for evaluating the best available scientific evidence for the treatment and care of a particular patient.
Good clinical judgment is required to select the most relevant research evidence. The best clinical judgment, that is, reasoning across time about the particular patient through changes in the patient’s concerns and condition and/or the clinician’s understanding, are also required. This type of judgment requires clinicians to make careful observations and evaluations of the patient over time, as well as know the patient’s concerns and social circumstances. To evolve to this level of judgment, additional education beyond clinical preparation if often required.
Sources of Evidence
Evidence that can be used in clinical practice has different sources and can be derived from research, patient’s preferences, and work-related experience. 85 , 86 Nurses have been found to obtain evidence from experienced colleagues believed to have clinical expertise and research-based knowledge 87 as well as other sources.
For many years now, randomized controlled trials (RCTs) have often been considered the best standard for evaluating clinical practice. Yet, unless the common threats to the validity (e.g., representativeness of the study population) and reliability (e.g., consistency in interventions and responses of study participants) of RCTs are addressed, the meaningfulness and generalizability of the study outcomes are very limited. Relevant patient populations may be excluded, such as women, children, minorities, the elderly, and patients with multiple chronic illnesses. The dropout rate of the trial may confound the results. And it is easier to get positive results published than it is to get negative results published. Thus, RCTs are generalizable (i.e., applicable) only to the population studied—which may not reflect the needs of the patient under the clinicians care. In instances such as these, clinicians need to also consider applied research using prospective or retrospective populations with case control to guide decisionmaking, yet this too requires critical thinking and good clinical judgment.
Another source of available evidence may come from the gold standard of aggregated systematic evaluation of clinical trial outcomes for the therapy and clinical condition in question, be generated by basic and clinical science relevant to the patient’s particular pathophysiology or care need situation, or stem from personal clinical experience. The clinician then takes all of the available evidence and considers the particular patient’s known clinical responses to past therapies, their clinical condition and history, the progression or stages of the patient’s illness and recovery, and available resources.
In clinical practice, the particular is examined in relation to the established generalizations of science. With readily available summaries of scientific evidence (e.g., systematic reviews and practice guidelines) available to nurses and physicians, one might wonder whether deep background understanding is still advantageous. Might it not be expendable, since it is likely to be out of date given the current scientific evidence? But this assumption is a false opposition and false choice because without a deep background understanding, the clinician does not know how to best find and evaluate scientific evidence for the particular case in hand. The clinician’s sense of salience in any given situation depends on past clinical experience and current scientific evidence.
Evidence-Based Practice
The concept of evidence-based practice is dependent upon synthesizing evidence from the variety of sources and applying it appropriately to the care needs of populations and individuals. This implies that evidence-based practice, indicative of expertise in practice, appropriately applies evidence to the specific situations and unique needs of patients. 88 , 89 Unfortunately, even though providing evidence-based care is an essential component of health care quality, it is well known that evidence-based practices are not used consistently.
Conceptually, evidence used in practice advances clinical knowledge, and that knowledge supports independent clinical decisions in the best interest of the patient. 90 , 91 Decisions must prudently consider the factors not necessarily addressed in the guideline, such as the patient’s lifestyle, drug sensitivities and allergies, and comorbidities. Nurses who want to improve the quality and safety of care can do so though improving the consistency of data and information interpretation inherent in evidence-based practice.
Initially, before evidence-based practice can begin, there needs to be an accurate clinical judgment of patient responses and needs. In the course of providing care, with careful consideration of patient safety and quality care, clinicians must give attention to the patient’s condition, their responses to health care interventions, and potential adverse reactions or events that could harm the patient. Nonetheless, there is wide variation in the ability of nurses to accurately interpret patient responses 92 and their risks. 93 Even though variance in interpretation is expected, nurses are obligated to continually improve their skills to ensure that patients receive quality care safely. 94 Patients are vulnerable to the actions and experience of their clinicians, which are inextricably linked to the quality of care patients have access to and subsequently receive.
The judgment of the patient’s condition determines subsequent interventions and patient outcomes. Attaining accurate and consistent interpretations of patient data and information is difficult because each piece can have different meanings, and interpretations are influenced by previous experiences. 95 Nurses use knowledge from clinical experience 96 , 97 and—although infrequently—research. 98–100
Once a problem has been identified, using a process that utilizes critical thinking to recognize the problem, the clinician then searches for and evaluates the research evidence 101 and evaluates potential discrepancies. The process of using evidence in practice involves “a problem-solving approach that incorporates the best available scientific evidence, clinicians’ expertise, and patient’s preferences and values” 102 (p. 28). Yet many nurses do not perceive that they have the education, tools, or resources to use evidence appropriately in practice. 103
Reported barriers to using research in practice have included difficulty in understanding the applicability and the complexity of research findings, failure of researchers to put findings into the clinical context, lack of skills in how to use research in practice, 104 , 105 amount of time required to access information and determine practice implications, 105–107 lack of organizational support to make changes and/or use in practice, 104 , 97 , 105 , 107 and lack of confidence in one’s ability to critically evaluate clinical evidence. 108
When Evidence Is Missing
In many clinical situations, there may be no clear guidelines and few or even no relevant clinical trials to guide decisionmaking. In these cases, the latest basic science about cellular and genomic functioning may be the most relevant science, or by default, guestimation. Consequently, good patient care requires more than a straightforward, unequivocal application of scientific evidence. The clinician must be able to draw on a good understanding of basic sciences, as well as guidelines derived from aggregated data and information from research investigations.
Practical knowledge is shaped by one’s practice discipline and the science and technology relevant to the situation at hand. But scientific, formal, discipline-specific knowledge are not sufficient for good clinical practice, whether the discipline be law, medicine, nursing, teaching, or social work. Practitioners still have to learn how to discern generalizable scientific knowledge, know how to use scientific knowledge in practical situations, discern what scientific evidence/knowledge is relevant, assess how the particular patient’s situation differs from the general scientific understanding, and recognize the complexity of care delivery—a process that is complex, ongoing, and changing, as new evidence can overturn old.
Practice communities like individual practitioners may also be mistaken, as is illustrated by variability in practice styles and practice outcomes across hospitals and regions in the United States. This variability in practice is why practitioners must learn to critically evaluate their practice and continually improve their practice over time. The goal is to create a living self-improving tradition.
Within health care, students, scientists, and practitioners are challenged to learn and use different modes of thinking when they are conflated under one term or rubric, using the best-suited thinking strategies for taking into consideration the purposes and the ends of the reasoning. Learning to be an effective, safe nurse or physician requires not only technical expertise, but also the ability to form helping relationships and engage in practical ethical and clinical reasoning. 50 Good ethical comportment requires that both the clinician and the scientist take into account the notions of good inherent in clinical and scientific practices. The notions of good clinical practice must include the relevant significance and the human concerns involved in decisionmaking in particular situations, centered on clinical grasp and clinical forethought.
The Three Apprenticeships of Professional Education
We have much to learn in comparing the pedagogies of formation across the professions, such as is being done currently by the Carnegie Foundation for the Advancement of Teaching. The Carnegie Foundation’s broad research program on the educational preparation of the profession focuses on three essential apprenticeships:
To capture the full range of crucial dimensions in professional education, we developed the idea of a three-fold apprenticeship: (1) intellectual training to learn the academic knowledge base and the capacity to think in ways important to the profession; (2) a skill-based apprenticeship of practice; and (3) an apprenticeship to the ethical standards, social roles, and responsibilities of the profession, through which the novice is introduced to the meaning of an integrated practice of all dimensions of the profession, grounded in the profession’s fundamental purposes. 109
This framework has allowed the investigators to describe tensions and shortfalls as well as strengths of widespread teaching practices, especially at articulation points among these dimensions of professional training.
Research has demonstrated that these three apprenticeships are taught best when they are integrated so that the intellectual training includes skilled know-how, clinical judgment, and ethical comportment. In the study of nursing, exemplary classroom and clinical teachers were found who do integrate the three apprenticeships in all of their teaching, as exemplified by the following anonymous student’s comments:
With that as well, I enjoyed the class just because I do have clinical experience in my background and I enjoyed it because it took those practical applications and the knowledge from pathophysiology and pharmacology, and all the other classes, and it tied it into the actual aspects of like what is going to happen at work. For example, I work in the emergency room and question: Why am I doing this procedure for this particular patient? Beforehand, when I was just a tech and I wasn’t going to school, I’d be doing it because I was told to be doing it—or I’d be doing CPR because, you know, the doc said, start CPR. I really enjoy the Care and Illness because now I know the process, the pathophysiological process of why I’m doing it and the clinical reasons of why they’re making the decisions, and the prioritization that goes on behind it. I think that’s the biggest point. Clinical experience is good, but not everybody has it. Yet when these students transition from school and clinicals to their job as a nurse, they will understand what’s going on and why.
The three apprenticeships are equally relevant and intertwined. In the Carnegie National Study of Nursing Education and the companion study on medical education as well as in cross-professional comparisons, teaching that gives an integrated access to professional practice is being examined. Once the three apprenticeships are separated, it is difficult to reintegrate them. The investigators are encouraged by teaching strategies that integrate the latest scientific knowledge and relevant clinical evidence with clinical reasoning about particular patients in unfolding rather than static cases, while keeping the patient and family experience and concerns relevant to clinical concerns and reasoning.
Clinical judgment or phronesis is required to evaluate and integrate techne and scientific evidence.
Within nursing, professional practice is wise and effective usually to the extent that the professional creates relational and communication contexts where clients/patients can be open and trusting. Effectiveness depends upon mutual influence between patient and practitioner, student and learner. This is another way in which clinical knowledge is dialogical and socially distributed. The following articulation of practical reasoning in nursing illustrates the social, dialogical nature of clinical reasoning and addresses the centrality of perception and understanding to good clinical reasoning, judgment and intervention.
Clinical Grasp *
Clinical grasp describes clinical inquiry in action. Clinical grasp begins with perception and includes problem identification and clinical judgment across time about the particular transitions of particular patients. Garrett Chan 20 described the clinician’s attempt at finding an “optimal grasp” or vantage point of understanding. Four aspects of clinical grasp, which are described in the following paragraphs, include (1) making qualitative distinctions, (2) engaging in detective work, (3) recognizing changing relevance, and (4) developing clinical knowledge in specific patient populations.
Making Qualitative Distinctions
Qualitative distinctions refer to those distinctions that can be made only in a particular contextual or historical situation. The context and sequence of events are essential for making qualitative distinctions; therefore, the clinician must pay attention to transitions in the situation and judgment. Many qualitative distinctions can be made only by observing differences through touch, sound, or sight, such as the qualities of a wound, skin turgor, color, capillary refill, or the engagement and energy level of the patient. Another example is assessing whether the patient was more fatigued after ambulating to the bathroom or from lack of sleep. Likewise the quality of the clinician’s touch is distinct as in offering reassurance, putting pressure on a bleeding wound, and so on. 110
Engaging in Detective Work, Modus Operandi Thinking, and Clinical Puzzle Solving
Clinical situations are open ended and underdetermined. Modus operandi thinking keeps track of the particular patient, the way the illness unfolds, the meanings of the patient’s responses as they have occurred in the particular time sequence. Modus operandi thinking requires keeping track of what has been tried and what has or has not worked with the patient. In this kind of reasoning-in-transition, gains and losses of understanding are noticed and adjustments in the problem approach are made.
We found that teachers in a medical surgical unit at the University of Washington deliberately teach their students to engage in “detective work.” Students are given the daily clinical assignment of “sleuthing” for undetected drug incompatibilities, questionable drug dosages, and unnoticed signs and symptoms. For example, one student noted that an unusual dosage of a heart medication was being given to a patient who did not have heart disease. The student first asked her teacher about the unusually high dosage. The teacher, in turn, asked the student whether she had asked the nurse or the patient about the dosage. Upon the student’s questioning, the nurse did not know why the patient was receiving the high dosage and assumed the drug was for heart disease. The patient’s staff nurse had not questioned the order. When the student asked the patient, the student found that the medication was being given for tremors and that the patient and the doctor had titrated the dosage for control of the tremors. This deliberate approach to teaching detective work, or modus operandi thinking, has characteristics of “critical reflection,” but stays situated and engaged, ferreting out the immediate history and unfolding of events.
Recognizing Changing Clinical Relevance
The meanings of signs and symptoms are changed by sequencing and history. The patient’s mental status, color, or pain level may continue to deteriorate or get better. The direction, implication, and consequences for the changes alter the relevance of the particular facts in the situation. The changing relevance entailed in a patient transitioning from primarily curative care to primarily palliative care is a dramatic example, where symptoms literally take on new meanings and require new treatments.
Developing Clinical Knowledge in Specific Patient Populations
Extensive experience with a specific patient population or patients with particular injuries or diseases allows the clinician to develop comparisons, distinctions, and nuanced differences within the population. The comparisons between many specific patients create a matrix of comparisons for clinicians, as well as a tacit, background set of expectations that create population- and patient-specific detective work if a patient does not meet the usual, predictable transitions in recovery. What is in the background and foreground of the clinician’s attention shifts as predictable changes in the patient’s condition occurs, such as is seen in recovering from heart surgery or progressing through the predictable stages of labor and delivery. Over time, the clinician develops a deep background understanding that allows for expert diagnostic and interventions skills.
Clinical Forethought
Clinical forethought is intertwined with clinical grasp, but it is much more deliberate and even routinized than clinical grasp. Clinical forethought is a pervasive habit of thought and action in nursing practice, and also in medicine, as clinicians think about disease and recovery trajectories and the implications of these changes for treatment. Clinical forethought plays a role in clinical grasp because it structures the practical logic of clinicians. At least four habits of thought and action are evident in what we are calling clinical forethought: (1) future think, (2) clinical forethought about specific patient populations, (3) anticipation of risks for particular patients, and (4) seeing the unexpected.
Future think
Future think is the broadest category of this logic of practice. Anticipating likely immediate futures helps the clinician make good plans and decisions about preparing the environment so that responding rapidly to changes in the patient is possible. Without a sense of salience about anticipated signs and symptoms and preparing the environment, essential clinical judgments and timely interventions would be impossible in the typically fast pace of acute and intensive patient care. Future think governs the style and content of the nurse’s attentiveness to the patient. Whether in a fast-paced care environment or a slower-paced rehabilitation setting, thinking and acting with anticipated futures guide clinical thinking and judgment. Future think captures the way judgment is suspended in a predictive net of anticipation and preparing oneself and the environment for a range of potential events.
Clinical forethought about specific diagnoses and injuries
This habit of thought and action is so second nature to the experienced nurse that the new or inexperienced nurse may have difficulty finding out about what seems to other colleagues as “obvious” preparation for particular patients and situations. Clinical forethought involves much local specific knowledge about who is a good resource and how to marshal support services and equipment for particular patients.
Examples of preparing for specific patient populations are pervasive, such as anticipating the need for a pacemaker during surgery and having the equipment assembled ready for use to save essential time. Another example includes forecasting an accident victim’s potential injuries, and recognizing that intubation might be needed.
Anticipation of crises, risks, and vulnerabilities for particular patients
This aspect of clinical forethought is central to knowing the particular patient, family, or community. Nurses situate the patient’s problems almost like a topography of possibilities. This vital clinical knowledge needs to be communicated to other caregivers and across care borders. Clinical teaching could be improved by enriching curricula with narrative examples from actual practice, and by helping students recognize commonly occurring clinical situations in the simulation and clinical setting. For example, if a patient is hemodynamically unstable, then managing life-sustaining physiologic functions will be a main orienting goal. If the patient is agitated and uncomfortable, then attending to comfort needs in relation to hemodynamics will be a priority. Providing comfort measures turns out to be a central background practice for making clinical judgments and contains within it much judgment and experiential learning.
When clinical teaching is too removed from typical contingencies and strong clinical situations in practice, students will lack practice in active thinking-in-action in ambiguous clinical situations. In the following example, an anonymous student recounted her experiences of meeting a patient:
I was used to different equipment and didn’t know how things went, didn’t know their routine, really. You can explain all you want in class, this is how it’s going to be, but when you get there … . Kim was my first instructor and my patient that she assigned me to—I walked into the room and he had every tube imaginable. And so I was a little overwhelmed. It’s not necessarily even that he was that critical … . She asked what tubes here have you seen? Well, I know peripheral lines. You taught me PICC [peripherally inserted central catheter] lines, and we just had that, but I don’t really feel comfortable doing it by myself, without you watching to make sure that I’m flushing it right and how to assess it. He had a chest tube and I had seen chest tubes, but never really knew the depth of what you had to assess and how you make sure that it’s all kosher and whatever. So she went through the chest tube and explained, it’s just bubbling a little bit and that’s okay. The site, check the site. The site looked okay and that she’d say if it wasn’t okay, this is what it might look like … . He had a feeding tube. I had done feeding tubes but that was like a long time ago in my LPN experiences schooling. So I hadn’t really done too much with the feeding stuff either … . He had a [nasogastric] tube, and knew pretty much about that and I think at the time it was clamped. So there were no issues with the suction or whatever. He had a Foley catheter. He had a feeding tube, a chest tube. I can’t even remember but there were a lot.
As noted earlier, a central characteristic of a practice discipline is that a self-improving practice requires ongoing experiential learning. One way nurse educators can enhance clinical inquiry is by increasing pedagogies of experiential learning. Current pedagogies for experiential learning in nursing include extensive preclinical study, care planning, and shared postclinical debriefings where students share their experiential learning with their classmates. Experiential learning requires open learning climates where students can discuss and examine transitions in understanding, including their false starts, or their misconceptions in actual clinical situations. Nursing educators typically develop open and interactive clinical learning communities, so that students seem committed to helping their classmates learn from their experiences that may have been difficult or even unsafe. One anonymous nurse educator described how students extend their experiential learning to their classmates during a postclinical conference:
So for example, the patient had difficulty breathing and the student wanted to give the meds instead of addressing the difficulty of breathing. Well, while we were sharing information about their patients, what they did that day, I didn’t tell the student to say this, but she said, ‘I just want to tell you what I did today in clinical so you don’t do the same thing, and here’s what happened.’ Everybody’s listening very attentively and they were asking her some questions. But she shared that. She didn’t have to. I didn’t tell her, you must share that in postconference or anything like that, but she just went ahead and shared that, I guess, to reinforce what she had learned that day but also to benefit her fellow students in case that thing comes up with them.
The teacher’s response to this student’s honesty and generosity exemplifies her own approach to developing an open community of learning. Focusing only on performance and on “being correct” prevents learning from breakdown or error and can dampen students’ curiosity and courage to learn experientially.
Seeing the unexpected
One of the keys to becoming an expert practitioner lies in how the person holds past experiential learning and background habitual skills and practices. This is a skill of foregrounding attention accurately and effectively in response to the nature of situational demands. Bourdieu 29 calls the recognition of the situation central to practical reasoning. If nothing is routinized as a habitual response pattern, then practitioners will not function effectively in emergencies. Unexpected occurrences may be overlooked. However, if expectations are held rigidly, then subtle changes from the usual will be missed, and habitual, rote responses will inappropriately rule. The clinician must be flexible in shifting between what is in background and foreground. This is accomplished by staying curious and open. The clinical “certainty” associated with perceptual grasp is distinct from the kind of “certainty” achievable in scientific experiments and through measurements. Recognition of similar or paradigmatic clinical situations is similar to “face recognition” or recognition of “family resemblances.” This concept is subject to faulty memory, false associative memories, and mistaken identities; therefore, such perceptual grasp is the beginning of curiosity and inquiry and not the end. Assessment and validation are required. In rapidly moving clinical situations, perceptual grasp is the starting point for clarification, confirmation, and action. Having the clinician say out loud how he or she is understanding the situation gives an opportunity for confirmation and disconfirmation from other clinicians present. 111 The relationship between foreground and background of attention needs to be fluid, so that missed expectations allow the nurse to see the unexpected. For example, when the background rhythm of a cardiac monitor changes, the nurse notices, and what had been background tacit awareness becomes the foreground of attention. A hallmark of expertise is the ability to notice the unexpected. 20 Background expectations of usual patient trajectories form with experience. Tacit expectations for patient trajectories form that enable the nurse to notice subtle failed expectations and pay attention to early signs of unexpected changes in the patient's condition. Clinical expectations gained from caring for similar patient populations form a tacit clinical forethought that enable the experienced clinician to notice missed expectations. Alterations from implicit or explicit expectations set the stage for experiential learning, depending on the openness of the learner.
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses’ continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
This section of the paper was condensed and paraphrased from Benner, Hooper-Kyriakidis, and Stannard. 23 Patricia Hooper-Kyriakidis wrote the section on clinical grasp, and Patricia Benner wrote the section on clinical forethought.
- Cite this Page Benner P, Hughes RG, Sutphen M. Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinically. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 6.
- PDF version of this page (147K)
In this Page
- Clinical Grasp
Other titles in this collection
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Nurses' reasoning process during care planning taking pressure ulcer prevention as an example. A think-aloud study. [Int J Nurs Stud. 2007] Nurses' reasoning process during care planning taking pressure ulcer prevention as an example. A think-aloud study. Funkesson KH, Anbäcken EM, Ek AC. Int J Nurs Stud. 2007 Sep; 44(7):1109-19. Epub 2006 Jun 27.
- Registered nurses' clinical reasoning skills and reasoning process: A think-aloud study. [Nurse Educ Today. 2016] Registered nurses' clinical reasoning skills and reasoning process: A think-aloud study. Lee J, Lee YJ, Bae J, Seo M. Nurse Educ Today. 2016 Nov; 46:75-80. Epub 2016 Aug 15.
- Combining the arts: an applied critical thinking approach in the skills laboratory. [Nursingconnections. 2000] Combining the arts: an applied critical thinking approach in the skills laboratory. Peterson MJ, Bechtel GA. Nursingconnections. 2000 Summer; 13(2):43-9.
- Review About critical thinking. [Dynamics. 2004] Review About critical thinking. Hynes P, Bennett J. Dynamics. 2004 Fall; 15(3):26-9.
- Review The 'five rights' of clinical reasoning: an educational model to enhance nursing students' ability to identify and manage clinically 'at risk' patients. [Nurse Educ Today. 2010] Review The 'five rights' of clinical reasoning: an educational model to enhance nursing students' ability to identify and manage clinically 'at risk' patients. Levett-Jones T, Hoffman K, Dempsey J, Jeong SY, Noble D, Norton CA, Roche J, Hickey N. Nurse Educ Today. 2010 Aug; 30(6):515-20. Epub 2009 Nov 30.
Recent Activity
- Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinical... Clinical Reasoning, Decisionmaking, and Action: Thinking Critically and Clinically - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Critical Thinking, Clinical Reasoning, and Clinical Judgment 7th Edition A Practical Approach
- Author(s) Rosalinda Alfaro-LeFevre
- Publisher Saunders
Programmatic Assessment of Clinical Reasoning: New Opportunities to Meet an Ongoing Challenge.
- Dario Torre , Michelle Daniel , +3 authors Lambert Schuwirth
- Published in Teaching and learning in… 25 May 2024
- Education, Medicine
45 References
Clinical reasoning performance assessment: using situated cognition theory as a conceptual framework, programmatic assessment of competency-based workplace learning: when theory meets practice, fairness in assessment: identifying a complex adaptive system, where the rubber meets the road — an integrative review of programmatic assessment in health care professions education, embedding a coaching culture into programmatic assessment, assessment of clinical reasoning: three evolutions of thought, grounding judgement in context: a conceptual learning model of clinical reasoning, assessment of clinical competence: written and computer-based simulations, the medical council of canada's key features project: a more valid written examination of clinical decision‐making skills, how to improve the teaching of clinical reasoning: a narrative review and a proposal, related papers.
Showing 1 through 3 of 0 Related Papers
- Open access
- Published: 24 May 2024
Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial
- Jian Zhao 1 na1 ,
- Xin Gong 1 na1 ,
- Jian Ding 1 ,
- Kepin Xiong 2 ,
- Kangle Zhuang 3 ,
- Rui Huang 1 ,
- Shu Li 4 &
- Huachun Miao 1
BMC Medical Education volume 24 , Article number: 571 ( 2024 ) Cite this article
326 Accesses
Metrics details
Case-based learning (CBL) methods have gained prominence in medical education, proving especially effective for preclinical training in undergraduate medical education. Tetralogy of Fallot (TOF) is a congenital heart disease characterized by four malformations, presenting a challenge in medical education due to the complexity of its anatomical pathology. Three-dimensional printing (3DP), generating physical replicas from data, offers a valuable tool for illustrating intricate anatomical structures and spatial relationships in the classroom. This study explores the integration of 3DP with CBL teaching for clinical medical undergraduates.
Sixty senior clinical medical undergraduates were randomly assigned to the CBL group and the CBL-3DP group. Computed tomography imaging data from a typical TOF case were exported, processed, and utilized to create four TOF models with a color 3D printer. The CBL group employed CBL teaching methods, while the CBL-3DP group combined CBL with 3D-printed models. Post-class exams and questionnaires assessed the teaching effectiveness of both groups.
The CBL-3DP group exhibited improved performance in post-class examinations, particularly in pathological anatomy and TOF imaging data analysis ( P < 0.05). Questionnaire responses from the CBL-3DP group indicated enhanced satisfaction with teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities ( P < 0.05). These findings underscore the potential of 3D printed models to augment the effectiveness of CBL, aiding students in mastering instructional content and bolstering their interest and self-confidence in learning.
The fusion of CBL with 3D printing models is feasible and effective in TOF instruction to clinical medical undergraduates, and worthy of popularization and application in medical education, especially for courses involving intricate anatomical components.
Peer Review reports
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease(CHD) [ 1 ]. Characterized by four structural anomalies: ventricular septal defect (VSD), pulmonary stenosis (PS), right ventricular hypertrophy (RVH), and overriding aorta (OA), TOF is a focal point and challenge in medical education. Understanding anatomical spatial structures is pivotal for learning and mastering TOF [ 2 ]. Given the constraints of course duration, medical school educators aim to provide students with a comprehensive and intuitive understanding of the disease within a limited timeframe [ 3 ].
The case-based learning (CBL) teaching model incorporates a case-based instructional approach that emphasizes typical clinical cases as a guide in student-centered and teacher-facilitated group discussions [ 4 ]. The CBL instructional methods have garnered widespread attention in medical education as they are particularly appropriate for preclinical training in undergraduate medical education [ 5 , 6 ]. The collection of case data, including medical records and examination results, is essential for case construction [ 7 ]. The anatomical and hemodynamic consequences of TOF can be determined using ultrasonography, computed tomography (CT), and magnetic resonance imaging techniques. However, understanding the anatomical structures from imaging data is a slow and challenging psychological reconstruction process for undergraduate medical students [ 8 ]. Three-dimensional (3D) visualization is valuable for depicting anatomical structures [ 9 ]. 3D printing (3DP), which creates physical replicas based on data, facilitates the demonstration of complex anatomical structures and spatial relationships in the classroom [ 10 ].
During the classroom session, 3D-printed models offer a convenient means for hands-on demonstration and communication, similar to facing a patient, enhancing the efficiency and specificity of intra-team communication and discussion [ 11 ]. In this study, we printed TOF models based on case imaging data, integrated them into CBL teaching, and assessed the effectiveness of classroom instruction.
Research participants
The study employed a prospective, randomized controlled design which received approval from the institutional ethics committee. Senior undergraduate students majoring in clinical medicine at Wannan Medical College were recruited for participation based on predefined inclusion criteria. The researchers implemented recruitment according to the recruitment criteria by contacting the class leaders of the target classes they had previously taught. Notably, these students were in their third year of medical education, with anticipation of progressing to clinical courses in the fourth year, encompassing Internal Medicine, Surgery, Obstetrics, Gynecology, and Pediatrics. Inclusion criteria for participants encompassed the following: (1) proficient communication and comprehension abilities, (2) consistent attendance without absenteeism or truancy, (3) absence of failing grades in prior examinations, and (4) capability to conscientiously fulfill assigned learning tasks. Exclusion criteria were (1) absence from lectures, (2) failure to complete pre-and post-tests, and (3) inadequate completion of questionnaires. For their participation in the study, Students were provided access to the e-book “Localized Anatomy,” authored by the investigators, as an incentive for their participation. Voluntary and anonymous participation was emphasized, with participants retaining the right to withdraw from the study at any time without providing a reason.
The study was conducted between May 1st, 2023, and June 30, 2023, from recruitment to completion of data collection. Drawing upon insights gained from a previous analogous investigation which yielded an effect size of 0.95 [ 10 ]. Sample size was computed, guided by a statistical consultant, with the aim of 0.85 power value, predicated on an effect size of 0.8 and a margin of error set at 0.05. A minimum of 30 participants per group was calculated using G*Power software (latest ver. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), resulting in the recruitment of a total of 60 undergraduate students. Each participant was assigned an identification number, with codes placed in boxes. Codes drawn from the boxes determined allocation to either the CBL group or the CBL-3DP group. Subsequently, participants were randomly assigned to either the CBL group, receiving instruction utilizing the CBL methodology, or the CBL-3DP group, which received instruction integrating both CBL and 3D Printed models.
Printing of TOF models
Figure 1 A shows the printing flowchart of the TOF models. A typical TOF case was collected from the Yijishan Hospital of Wannan Medical College. The CT angiography imaging data of the case was exported. Mimics Research 20.0 software (Mimics Innovation Suite version 20, Materialize, Belgium) was used for data processing. The cardiovascular module of the CT-Heart tool was employed to adjust the threshold range, independently obtain the cardiac chambers and vessels, post-process the chambers and vessels to generate a hollow blood pool, and merge it with the myocardial volume to construct a complete heart model. The file was imported into Magics 24.0 software (version 24.0; Materialize, Belgium) for correction using the Shell tool page. After repairs, the model entered the smoothing page, where tools such as triangular surface simplification, local smoothing, refinement and smoothing, subdivision of components, and mesh painting were utilized to achieve varying degrees of smoothness. Finally, optimized data were obtained and exported as stereolithography (STL) files. An experienced cardiothoracic surgeon validated the anatomical accuracy of the digital model.
The STL files were imported into a 3D printer (J401Pro; Sailner 3D Technology, China) for model printing. This printer can produce full-color medical models using different materials. The models were fabricated using two distinct materials: rigid and flexible. Both materials are suitable for the observational discussion of the teaching objectives outlined in our study. From the perspective of observing pathological changes in the TOF, there is no significant difference between the two materials.
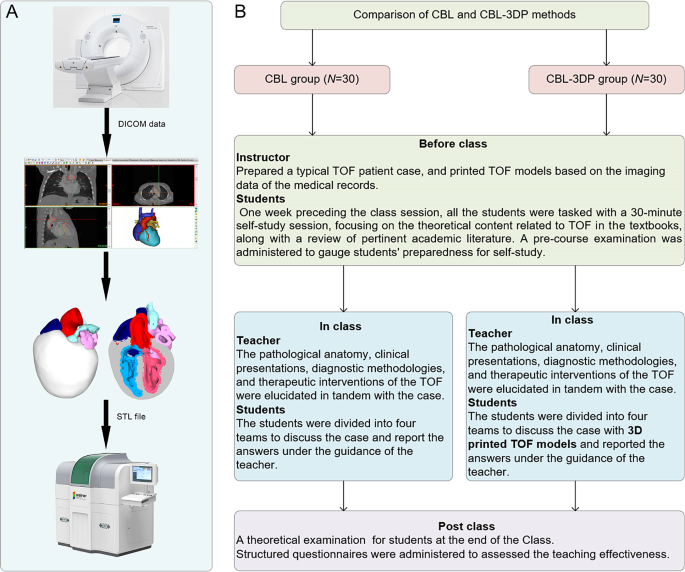
Experimental flow chart of this study. A TOF model printing flow chart. B The instructional framework
Teaching implementation
Figure 1 B illustrates the instructional framework employed in this study. One week preceding the class session, all the students were tasked with a 30-minute self-study session, focusing on the theoretical content related to TOF as outlined in the Pediatrics and Surgery textbooks, along with a review of pertinent academic literature. Both groups received co-supervision from two basic medicine lecturers boasting over a decade of teaching experience, alongside a senior cardiothoracic surgeon. Teaching conditions remained consistent across groups, encompassing uniform assessment criteria and adherence to predefined teaching time frames, all conducted in a Project-Based Learning (PBL) classroom at Wannan Medical College. Additionally, a pre-course examination was administered to gauge students’ preparedness for self-study.
In adherence to the curriculum guidelines, the teaching objectives aimed to empower students to master TOF’s clinical manifestations, diagnostic modalities, and differential diagnoses, while acquainting them with treatment principles and surgical methodologies. Additionally, the objectives sought to cultivate students’ clinical reasoning abilities and problem-solving skills. the duration of instruction for the TOF theory session was standardized to 25 min. The didactic content was integrated with the TOF case study to construct a coherent pedagogical structure.
During the instructional session, both groups underwent teaching utilizing the CBL methodology. Clinical manifestations and case details of TOF cases were presented to stimulate students’ interest and curiosity. Subsequently, the theory of TOF, including its etiology, pathogenesis, pathologic anatomy, clinical manifestations, diagnostic methods, and therapeutic interventions, was briefly elucidated. Emphasis was then placed on the case, wherein selected typical TOF cases were explained, guiding students in analysis and discussion. Students were organized into four teams under the instructors’ supervision, fostering cooperative learning and communication, thereby deepening their understanding of the disease through continuous inquiry and exploration (Fig. 2 L). In the routinely equipped PBL classroom with standard heart models (Fig. 2 J, K), all students had prior exposure to human anatomy and were familiar with these models. Both groups were provided with four standard heart models for reference, while the CBL-3DP group received additional four 3D-printed models depicting TOF anomalies, enriching their learning experience (Fig. 2 D, G). After the lesson, summarization, and feedback sessions were conducted to consolidate group discussions’ outcomes, evaluate teaching effectiveness, and assess learning outcomes.
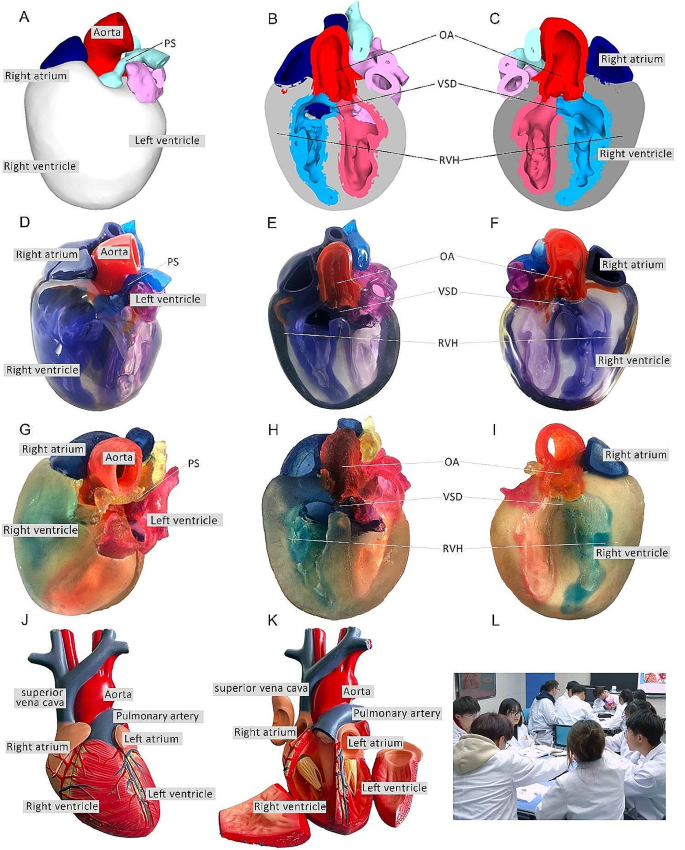
Heart models utilized in instructional sessions. A External perspective of 3D digital models. B, C Cross-sectional views following trans-septal sagittal dissection of the 3D digital model (PS: Pulmonary Stenosis; OA: Overriding Aorta; VSD: Ventricular Septal Defect; RVH: Right Ventricular Hypertrophy). D External depiction of rigid 3D printed model. E, F Sagittal sections of the rigid 3D printed model. G External portrayal of flexible 3D printed model. H, I Sagittal sections of the flexible 3D printed model. J, K The normal heart model employed in the instruction of the CBL group. L Ongoing classroom session
Teaching effectiveness assessment
Following the instructional session, participants from the two groups underwent a theoretical examination to assess their comprehension of the taught material. This assessment covered domains such as pathological anatomy, clinical manifestations, imaging data interpretation, diagnosis, and treatment relevant to TOF. Additionally, structured questionnaires were administered to evaluate the efficacy of the pedagogical approach employed. The questionnaire consisted of six questions designed to gauge participants’ understanding of the teaching content, enhancement of diagnostic skills, cultivation of critical thinking and clinical reasoning abilities, bolstering of confidence in managing TOF cases, satisfaction with the teaching mode, and satisfaction with the CBL methodology.
The questionnaire employed a 5-point Likert scale to gauge responses, with 5 indicating “strongly satisfied/agree,” 4 for “satisfied/agree,” 3 denoting “neutral,” 2 reflecting “dissatisfied/disagree,” and 1 indicating “strongly dissatisfied/disagree.” It comprised six questions, with the initial two probing participants’ knowledge acquisition, questions 3 and 4 exploring satisfaction regarding enhanced competence, and the final two assessing satisfaction with teaching methods and modes. Additionally, participants were encouraged to provide suggestions at the end of the questionnaire. To ensure the questionnaire’s validity, five esteemed lecturers in basic medical sciences with more than 10 years of experience verified its content and assessed its Content Validity Ratio and Content Validity Index to ensure alignment with the study’s objectives.
Statistical analysis
Statistical analyses were conducted utilizing GraphPad Prism 9.0 software. Aggregate score data for both groups were presented as mean ± standard deviation (x ± s). The gender comparisons were analyzed with the chi-square (χ2) test, while the other variables were compared using the Mann-Whitney U test. The threshold for determining statistical significance was set at P < 0.05.
Three-dimensional printing models
After configuring the structural colors of each component (Fig. 2 A, B, C), we printed four color TOF models using both rigid and flexible materials, resulting in four life-sized TOF models. Two color TOF models were created using rigid materials (Fig. 2 D, E, F). These models, exhibiting resistance to deformation, and with a firm texture, smooth and glossy surface, and good transparency, allowing visibility of the internal structures, were deemed conducive to teaching and observation. We also fabricated two color TOF models using flexible materials (Fig. 2 G, H, I), characterized by soft texture, opacity, and deformability, allowing for easy manipulation and cutting. It has potential utility beyond observational purposes. It can serve as a valuable tool for simulating surgical interventions and may be employed to create tomographic anatomical specimens. In this study, both material models were suitable for observation in the classroom. The participants were able to discern the four pathological changes characteristic of TOF from surface examination or cross-sectional analysis.
Baseline characteristics of the students
In total, 60 students were included in this study. The CBL group comprised 30 students (14 males and 16 females), with an average age of (21.20 ± 0.76) years. The CBL-3DP group consisted of 30 students (17 males and 13 females) with an average age of 20.96 years. All the students completed the study procedures. There were no significant differences in age, sex ratio, or pre-class exam scores between the two groups ( P > 0.05), indicating that the baseline scores between the two groups were comparable (Table 1 ).
Theoretical examination results
All students completed the research procedures as planned. The post-class theoretical examination encompassed assessment of pathological anatomy, clinical presentations, imaging data interpretation, diagnosis, and treatment pertinent to TOF. Notably, no statistically significant disparities were observed in the scores on clinical manifestations, diagnosis and treatment components between the cohorts, as delineated in Table 2 . Conversely, discernible distinctions were evident whereby the CBL-3DP group outperformed the CBL group notably in pathological anatomy, imaging data interpretation, and overall aggregate scores ( P < 0.05).
Results of the questionnaires
All the 60 participants submitted the questionnaire. Comparing the CBL and CBL-3DP groups, the scores from the CBL-3DP group showed significant improvements in many areas. This included satisfaction with the teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities (Fig. 3 B, C, D, E). All of which improved significantly ( P < 0.05 for the first aspects and P < 0.01 for the rest). However, the two groups were not comparable ( P > 0.05) in terms of understanding of the teaching content and Satisfaction with the CBL methodology (Fig. 3 A, F).
Upon completion of the questionnaires, participants were invited to proffer recommendations. Notably, in the CBL group, seven students expressed challenges in comprehending TOF and indicated a need for additional time for consolidation to enhance understanding. Conversely, within the CBL-3DP group, twelve students advocated for the augmentation of model repertoire and the expansion of disease-related data collection to bolster pedagogical efficacy across other didactic domains.
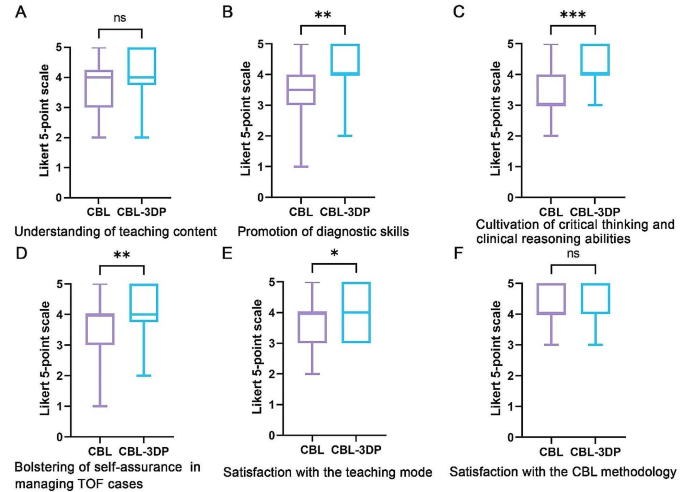
Five-point Likert scores of students’ attitudes in CBL ( n = 30) and CBL-3DP ( n = 30) groups. A Understanding of teaching content. B Promotion of diagnostic skills. C Cultivation of critical thinking and clinical reasoning abilities. D Bolstering of self-assurance in managing TOF cases. E Satisfaction with the teaching mode. F Satisfaction with the CBL methodology. ns No significant difference, * p < 0.05, ** p < 0.01, *** p < 0.001
TOF presents a significant challenge in clinical practice, necessitating a comprehensive understanding for effective diagnosis and treatment [ 12 ]. Traditional teaching methods in medical schools have relied on conventional resources such as textbooks, 2D illustrations, cadaver dissections, and radiographic materials to impart knowledge about complex conditions like TOF [ 13 ]. However, the limitations of these methods in fully engaging students and bridging the gap between theoretical knowledge and practical application have prompted a need for innovative instructional approaches.
CBL has emerged as a valuable tool in medical education, offering students opportunities to engage with authentic clinical cases through group discussions and inquiry-based learning [ 14 ]. By actively involving students in problem-solving and decision-making processes, CBL facilitates the application of theoretical knowledge to real-world scenarios, thus better-preparing students for future clinical practice [ 15 ]. Our investigation revealed that both groups of students exhibited comparable levels of satisfaction with the CBL methodology, devoid of discernible disparities.
CHD presents a formidable challenge due to the intricate nature of anatomical anomalies, the diverse spectrum of conditions, and individual variations [ 16 ]. Utilizing 3D-printed physical models, derived from patient imaging data, can significantly enhance comprehension of complex anatomical structures [ 17 ]. These models have proven invaluable in guiding surgical planning, providing training for junior or inexperienced pediatric residents, and educating healthcare professionals and parents of patients [ 18 ]. Studies indicate that as much as 50% of pediatric surgical decisions can be influenced by the insights gained from 3D printed models [ 19 ]. By providing tangible, anatomically accurate models, 3D printing offers a unique opportunity for people to visualize complex structures and enhance their understanding of anatomical intricacies. Our study utilized full-color, to-scale 3D printed models to illustrate the structural abnormalities associated with TOF, thereby enriching classroom sessions and facilitating a deeper comprehension of the condition.
Comparative analysis between the CBL-3DP group and the CBL group revealed significant improvements in post-test performance, particularly in pathological anatomy and imaging data interpretation. Additionally, questionnaire responses indicated higher levels of satisfaction and confidence among students in the CBL-3DP group, highlighting the positive impact of incorporating 3D printed models into the learning environment, improving the effectiveness of CBL classroom instruction. Despite the merits, our study has limitations. Primarily, participants were exclusively drawn from the same grade level within a single college, possibly engendering bias owing to shared learning backgrounds. Future research could further strengthen these findings by expanding the sample size and including long-term follow-up to assess the retention of knowledge and skills. Additionally, the influence of the 3D models depicting a normal heart on the learning process and its potential to introduce bias into the results warrants consideration, highlighting a need for scrutiny in subsequent studies.
As medical science continues to advance, the need for effective teaching methods becomes increasingly paramount. Our study underscores the potential of combining active learning approaches like CBL with innovative technologies such as 3D printing to enhance teaching effectiveness, improve knowledge acquisition, and foster students’ confidence and enthusiasm in pursuing clinical careers. Moving forward, further research and integration of such methodologies are essential for meeting the evolving demands of medical education, especially in areas involving complex anatomical understanding.
Conclusions
Integrating 3D-printed models with the CBL method is feasible and effective in TOF instruction. The demonstrated success of this method warrants broad implementation in medical education, particularly for complex anatomical topics.
Data availability
All data supporting the conclusions of this research are available upon reasonable request from the corresponding author.
Apitz C, Webb GD, Redington AN. Tetralogy of Fallot. Lancet. 2009;374:1462–71.
Article Google Scholar
Ghosh RM, Jolley MA, Mascio CE, Chen JM, Fuller S, Rome JJ, et al. Clinical 3D modeling to guide pediatric cardiothoracic surgery and intervention using 3D printed anatomic models, computer aided design and virtual reality. 3D Print Med. 2022;8:11.
Chakrabarti R, Wardle K, Wright T, Bennie T, Gishen F. Approaching an undergraduate medical curriculum map: challenges and expectations. BMC Med Educ. 2021;21:341.
Donkin R, Yule H, Fyfe T. Online case-based learning in medical education: a scoping review. BMC Med Educ. 2023;23:564.
Novack JP. Designing cases for case-based immunology teaching in large medical school classes. Front Immunol. 2020;11:995.
Chen HC, Van Den Broek WES, Ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90:431–6.
Wang M, Sun Z, Jia M, Wang Y, Wang H, Zhu X, et al. Intelligent virtual case learning system based on real medical records and natural language processing. BMC Med Inf Decis Mak. 2022;22:60.
Yoo S-J, Thabit O, Kim EK, Ide H, Yim D, Dragulescu A, et al. 3D printing in medicine of congenital heart diseases. 3D Print Med. 2015;2:3.
Yammine K, Violato C. A meta-analysis of the educational effectiveness of three-dimensional visualization technologies in teaching anatomy. Anat Sci Educ. 2015;8:525–38.
Miao H, Ding J, Gong X, Zhao J, Li H, Xiong K, et al. Application of 3D-printed pulmonary segment specimens in experimental teaching of sectional anatomy. BMC Surg. 2023;23:109.
Sun Z, Wong YH, Yeong CH. Patient-specific 3D-printed low-cost models in medical education and clinical practice. Micromachines (Basel). 2023;14:464.
Downing TE, Kim YY. Tetralogy of Fallot: general principles of management. Cardiol Clin. 2015;33:531–41. vii–viii.
Jia X, Zeng W, Zhang Q. Combined administration of problem- and lecture-based learning teaching models in medical education in China: a meta-analysis of randomized controlled trials. Med (Baltim). 2018;97:e11366.
McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD.S20377.
Zeng N, Lu H, Li S, Yang Q, Liu F, Pan H, et al. Application of the combination of CBL teaching method and SEGUE framework to improve the doctor-patient communication skills of resident physicians in otolaryngology department. Bmc Med Educ. 2024;24:201.
Sun Z. Patient-specific 3D-printed models in pediatric congenital heart disease. Children. 2023;10:319.
Meyer-Szary J, Luis MS, Mikulski S, Patel A, Schulz F, Tretiakow D, et al. The role of 3D printing in planning complex medical procedures and training of medical professionals—cross-sectional multispecialty review. IJERPH. 2022;19:3331.
Sun Z, Wee C. 3D printed models in cardiovascular disease: an exciting future to deliver personalized medicine. Micromachines-basel. 2022;13:1575.
Valverde I, Gomez-Ciriza G, Hussain T, Suarez-Mejias C, Velasco-Forte MN, Byrne N, et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicentre study. Eur J Cardio-thorac. 2017;52:1139–48.
Download references
Acknowledgements
We extend our sincere appreciation to the instructors and students whose invaluable participated in this study.
This paper received support from the Education Department of Anhui Province, China (Grant Numbers 2022jyxm1693, 2022jyxm1694, 2022xskc103, 2018jyxm1280).
Author information
Jian Zhao and Xin Gong are joint first authors.
Authors and Affiliations
Department of Human Anatomy, Wannan Medical College, No.22 West Wenchang Road, Wuhu, 241002, China
Jian Zhao, Xin Gong, Jian Ding, Rui Huang & Huachun Miao
Department of Cardio-Thoracic Surgery, Yijishan Hospital of Wannan Medical College, Wuhu, China
Kepin Xiong
Zhuhai Sailner 3D Technology Co., Ltd., Zhuhai, China
Kangle Zhuang
School of Basic Medical Sciences, Wannan Medical College, Wuhu, China
You can also search for this author in PubMed Google Scholar
Contributions
Jian Zhao and Huachun Miao designed the research. Jian Zhao, Xin Gong, Jian Ding, Kepin Xiong designed the tests and questionnaires. Kangle Zhuang processed the imaging data and printed the models. Xing Gong and Kepin Xiong implemented the teaching. Jian Zhao and Rui Huang collected the data and performed the statistical analysis. Jian Zhao and Huachun Miao prepared the manuscript. Shu Li and Huachun Miao revised the manuscript. Shu Li provided the Funding acquisition. All authors reviewed and approved the final manuscript.
Corresponding authors
Correspondence to Shu Li or Huachun Miao .
Ethics declarations
Ethics approval and consent to participate.
This investigation received ethical approval from the Ethical Committee of School of Basic Medical Sciences, Wannan Medical College (ECBMSWMC2022-1-12). All methodologies adhered strictly to established protocols and guidelines. Written informed consent was obtained from the study participants to take part in the study.
Consent for publication
Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.

Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhao, J., Gong, X., Ding, J. et al. Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial. BMC Med Educ 24 , 571 (2024). https://doi.org/10.1186/s12909-024-05583-z
Download citation
Received : 03 March 2024
Accepted : 21 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s12909-024-05583-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Case-based learning
- 3D printing
- Tetralogy of fallot
- Medical undergraduates
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Search with any image
Unsupported image file format.
Image file size is too large..
Drag an image here
- Medical Books
Sorry, there was a problem.

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player

Follow the author

Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach 7th Edition
Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 7th Edition brings these concepts to life through engaging text, diverse learning activities, and real-life examples. Easy-to-understand language and a "how-to" approach equip you to become a sensible, resilient critical thinker with the clinical reasoning skills you need to think think through complex issues and make sound clinical decisions. This edition emphasizes readiness for clinical practice and the Next Generation NCLEX exam, with a focus on systems thinking, interprofessional practice, nursing skills for the 21st century, and Quality and Safety for Nursing Education (QSEN) competencies.
- Clear, straightforward approach and motivational writing style provides vivid examples, memorable anecdotes, and real-life case scenarios to make content come alive.
- Focus on application ("how to") with supporting rationales (theory) makes difficult concepts easy to learn.
- Highlighted features and sections that promote deep learning include: This Chapter at a Glance , Learning Outcomes, Key Concepts, Guiding Principle boxes, Critical Moments boxes, Other Perspectives features, Think-Pair-Share activities, H.M.O. (Help Me Out) cartoons, real-life clinical scenarios, Key Points, Critical Thinking Exercises , and more!
- Cultural, spiritual, and lifespan content explores the nurse’s role in hospitals, long-term care settings, and entire communities, presenting a broad approach to critical thinking.
- Inclusion of ethics- and standards-based professional practice reflects the increased demand for accountability in today’s professional climate.
- Timely coverage of the latest in nursing education and critical thinking includes concept-based learning; QSEN and IOM standards; problem-focused versus outcome-focused thinking; prioritization and delegation; developing a culture of safe, healthy work environments; expanding roles related to diagnosis and management; improving grades and passing tests the first time; NCLEX exam preparation; ensuring that documentation reflects critical thinking; communication and interpersonal skills; strategies for common workplace challenges; and more.
- NEW! Spotlight on systems thinking teaches you to consider how things are related, while coverage of conceptual thinking helps you focus on big ideas first.
- NEW! Information on effective clinical simulations encourages learning through practice and debriefing.
- NEW! Clinical reasoning principles are highlighted throughout to ensure you are practice ready.
- NEW! Current critical judgment models are illustrated and explained in a clear, engaging style.
- NEW! Expanded content on growing nursing trends addresses competency assessment, electronic charting (informatics) and "thinking beyond the EHR," clinical evaluation, and preceptor and learner strategies.
- NEW! Strong emphasis on interprofessional collaboration includes new content on its growing importance in health care.
- ISBN-10 0275972356
- ISBN-13 978-0323581257
- Edition 7th
- Publisher Elsevier
- Publication date October 9, 2019
- Language English
- Dimensions 7.5 x 0.5 x 9 inches
- Print length 268 pages
- See all details

Customers who bought this item also bought

Editorial Reviews
Learn the critical thinking and clinical judgment skills you need to provide safe, effective patient care.
Product details
- ASIN : 0323581250
- Publisher : Elsevier; 7th edition (October 9, 2019)
- Language : English
- Paperback : 268 pages
- ISBN-10 : 0275972356
- ISBN-13 : 978-0323581257
- Item Weight : 1.36 pounds
- Dimensions : 7.5 x 0.5 x 9 inches
- #25 in Nursing Fundamentals & Skills (Books)
- #5,709 in Unknown
About the author
Rosalinda alfaro-lefevre.
A passionate nurse and educator with over 30 years experience, I’m committed to making difficult content easy to understand. My work is used throughout the world in 7 languages. I’m honored to have received the AJN Book of the Year and Sigma Theta Tau Best Pick awards.
Customer reviews
| 2 star | 0% | |
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
- Sort reviews by Top reviews Most recent Top reviews
Top reviews from the United States
There was a problem filtering reviews right now. please try again later..
Top reviews from other countries
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell on Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Become an Amazon Hub Partner
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- Open access
- Published: 04 June 2024
Clinical competency of nurses trained in competency-based versus objective-based education in the Democratic Republic of the Congo: a qualitative study
- Mari Nagai ORCID: orcid.org/0000-0001-6731-5064 1 ,
- Miyuki Oikawa 2 ,
- Tomoko Komagata 3 ,
- Josué Désiré Bapitani Basuana 4 ,
- Gérard Kahombo Ulyabo 4 ,
- Yui Minagawa 1 ,
- Sadatoshi Matsuoka 1 ,
- Yuriko Egami 1 ,
- Mari Honda 1 &
- Toyomitsu Tamura 1
Human Resources for Health volume 22 , Article number: 38 ( 2024 ) Cite this article
89 Accesses
2 Altmetric
Metrics details
Designing competency-based education (CBE) programmes is a priority in global nursing education for better nursing care for the population. In the Democratic Republic of the Congo (DRC), object-based education (OBE) remains mainstream in pre-service nursing education programmes. Recently, the Ministry of Health developed a self-assessment tool and quantitatively compared the clinical competency of CBE- and OBE-trained nurses. This study aimed to qualitatively triangulate the results of self-evaluation by exploring perception of supervisors, incumbent CBE-, and OBE-trained nurses in comparison with the competence of the two types of nurses, and to identify influential factors or barriers to their competence in clinical settings.
A qualitative descriptive approach with conventional content analysis was applied. Twenty interviews with clinical supervisors who oversaw both CBE- and OBE-trained nurses, 22 focus group discussions (FGDs) with CBE-trained nurses, and 21 FGDs with OBA-trained nurses currently working in health facilities were conducted. Participants of the FGDs were selected from the participants of the DRC self-assessment competency comparison study where there was no statistically significance between CBE- and OBE-trained nurses in the demographic characteristics. Data were analysed in terms of the competencies identified by the Ministry of Health.
The supervisors recognised that the CBE-trained nurses had stronger competencies in professional communication, making decisions about health problems, and engaging in professional development, but were weak in clinical skills. This study identified challenges for supervisors in assuring standardised care in health facilities with OBE- and CBE-trained nurses, as well as barriers for CBE-trained nurses as a minority in the workplace in demonstrating their competencies.
Conclusions
The study results support the Ministry of Health’s policy to expand CBE in pre-service education programmes but reveal that its slow implementation impedes full utilisation of the acquired competencies at health facilities. Implementation could be accelerated by strengthening cooperation among the Ministry of Health’s three human resource departments, and developing and implementing a well-planned, legally binding, long-term CBE reform strategy, including an approach to the Continuing Professional Development system.
Peer Review reports
Primary healthcare (PHC) is the cornerstone of universal health coverage (UHC). Its implementation requires a diverse workforce, including nurses who have acquired competencies to address people’s health needs [ 1 ]. As an outcome-based and learner-centric approach, competency-based education (CBE) enhances the clinical performance of healthcare providers [ 2 ]. CBE is expected to produce a health workforce that can provide optimal care by making comprehensive decisions based on acquired competencies [ 3 ]. The shift from traditional object-based education (OBE) to CBE has been a key trend in health professional education worldwide [ 4 , 5 ]. The Global Strategic Direction for Nursing and Midwifery also identifies CBE as a priority in creating policies in the global nursing education sector [ 6 ].
The achievement of UHC is a salient health policy in the Democratic Republic of the Congo (DRC) [ 7 ]. There, PHC is primarily available in health districts where health centres (HCs) provide frontline health services and general hospitals (GHs) serve as referrals. Most of the health service provisions in health facilities, especially at HCs, rely on nurses, as the health workforce regulation does not require allocation of a doctor due to shortages. Pre-service nursing education is provided through different systems by two ministries; the Ministry of Higher and University Education governs bachelor’s and advanced diploma courses in nursing education, while the Ministry of Public Health (MoH) governs secondary nursing education institutions and certificate courses for secondary nurses. As of 2019, nurses accounted for 47.1% (93,218) of all health personnel registered by the MoH, of which 37.0% (34,449) of nurses were secondary nurses [ 8 ]. While primary nurses are expected to work in health administration or take managerial responsibility in health facilities, secondary nurses play a critical role in the DRC to perform multiple nursing tasks, including providing PHC in lower-level health facilities [ 9 ]. Based on a 2002 survey which identified the gap between the outcomes of pre-service secondary nursing education and the competencies required for clinical practice [ 7 ], the MoH issued a ministerial decree in 2005 for introducing CBE in secondary nursing education institutions to strengthen pre-service education and provide secondary nurses with the competencies required for providing PHC [ 10 ]. Twenty-six decentralised provincial health departments are responsible for managing the health workforce, including secondary nursing education institutions. As of 2019, only 110 (21%) of the 526 secondary nursing education institutions nationwide implement CBE [ 8 ]. Despite support from external partners such as a nursing education partnership initiative to expand access to CBE programmes [ 11 ], seven out of the 26 provinces have not introduced CBE at all. In the provinces that partially introduced CBE, some nursing education institutions continued to offer OBE simultaneously. Thus, in some HCs and GHs, both newly qualified CBE- and OBE-secondary nurses work together. CBE implementation challenges have been reported in the DRC and other African countries, with obstacles including lack of teachers, capital, and planning [ 11 , 12 ].
Secondary nurses in the DRC must have five competencies for clinical practice: (1) establishing professional communication, (2) making decisions about health problems, (3) performing nursing interventions, (4) managing resources, and (5) engaging in professional development. Nursing students must acquire skills such as collecting patient data, identifying the patient's health problems, and planning a nursing care plan [ 13 ]. The scope of CBE goes beyond mere skill development; it entails mastering comprehensive nursing skills [ 5 ]. It integrates acquired knowledge, skills, and attitudes, which can enhance clinical performance [ 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 ]. The CBE programmes in secondary nursing education institutions allocate 358 h to integrate vertical knowledge and skills into optimal care over four years, whereas OBE programmes do not provide this opportunity [ 22 ].
After more than 10 years since CBE-trained secondary nurses started working in health facilities in the DRC, the MoH developed a DRC self-assessment competency scale and compared the competencies of CBE-trained with those of OBE-trained secondary nurses, both having 2–5 years of clinical experience. The result showed that the former has statistically higher competency in communication, decision making, and nursing interventions [ 23 ]. However, it was unclear how their supervisors perceive their competence, and how these two types of nurses interact with each other in clinical settings [ 24 ]. This study aimed to qualitatively triangulate the results of self-evaluation by exploring perception of supervisors, incumbent CBE-, and OBE nurses in comparison with the competence of the two types of nurses, as well as to identify influential factors or barriers to their competence in clinical settings.
Design, setting, and participants
A qualitative descriptive approach with conventional content analysis was applied to achieve the aims of the study. The target population and the selection criteria were: (1) secondary nurses with 2–5 years of clinical experience, who had graduated after 2012 from nursing education institutions using CBE in the DRC and currently worked in lower level health facilities such as HCs or GHs providing PHC (CBE-nurses); (2) secondary nurses with 2–5 years of clinical experience, who had graduated after 2012 from nursing education institutions using OBE and currently worked in lower level health facilities such as HCs or GHs providing PHC (OBE-nurses); and (3) clinical supervisors who oversaw both the CBE- and OBE-nurses in the health facilities. For this qualitative study, we randomly selected CBE- and OBE-nurses from participants of the DRC self-assessment competency comparison study [ 23 ] where there was no statistically significance between the two groups in demographic characteristics such as gender, age, years of experience, type of health facility, and position in the health facilities. For the comparison study, nine of the 26 provinces in DRC (Sud-Kivu, Nord-Kivu, Kasai-Central, Kongo-Central, Lualaba, Haut-Katanga, Kwilu, Kasai-Oriental, and Kinshasa) were selected based on transport accessibility and safety considerations for the research team to visit from Kinshasa [ 25 ]. Next, to compare OBE and CBE in similar conditions, a total of 10 cities (two from Kwilu and one from other 8 provinces) were selected where nursing education institutions applying OBE and CBE co-exist in both urban and rural areas, using the graduates list provided by the MoH. Then, health facilities where those two types of graduates were working were identified with the help of each city’s education institutions and provincial and district health offices. We identified the clinical supervisors who oversaw both CBE- and OBE- nurses in those health facilities.
Study participants had to be accessible at the time of the study, be able to travel to the interview site, and provide their consent to participate in the study. Most clinical supervisors were trained in OBE when they were nursing students. Sampling was discontinued when theoretical saturation was reached.
Data collection
Open-ended questionnaires were administered. Individual interviews were conducted for supervisors, while focus group discussions (FGDs) were conducted with CBE- and OBE-nurses separately. The research team (six authors) who had strong local contextual knowledge and experience in research in low- and middle-income countries including the DRC developed interview guides for the individual interviews and FGDs in French. The interview guides comprised questions regarding respondents’ demographics, their perceptions of the competence of secondary nurses in general, the differences between the competence of CBE- and OBE-nurses, and their views on improving nursing care. The questionnaires and guides were pilot-tested and finalised. Prior to data collection, the chief officer of the Department of Health Science Education in the MoH trained 10 MoH officers and two provincial health officers per province on the interview guide to conduct quality interviews in the provinces. Between January and September 2021, 10 interview teams (eight of which were gender-mixed), each comprising one MoH officer from Kinshasa and two officers from the target provinces, collected data. All interviews and FGDs were conducted face-to-face in a private setting at nursing education institutions or district health offices to ensure a favourable and private interview environment. Each interview and FGD lasted between 30–60 min and were recorded using an audio recorder. Participants were informed of their right to refuse study participation and assured of the confidentiality of the information they provided. They were paid travel allowances from their workplace to the interview venue. Twenty supervisors were interviewed (11 males, 9 females, 10 working at public health facilities, 2 in private health facilities, 5 in religious health facilities and 3 in others), and 22 FGDs with CBE-nurses and 21 FGDs with OBE-nurses (6–8 participants per each FGD) were conducted.
Ethical consideration
The authors obtained ethical approval from the Ethics Committees of the MoH of the DRC (No. 137/CNES/BN/PMMF/2019 du 21/09/2019) and the National Center for Global Health and Medicine in Japan (NCGM-G-004023-00). All participants provided written informed consent.
Data analysis
The authors transcribed the audio-recorded interviews into Microsoft Word in French, then manually analysed the transcripts and read and reread them to familiarise themselves with the data. In accordance with the qualitative descriptive methodology, perceptions of the differences between CBE and OBE nurses and challenges in health facilities were identified, extracted and coded. A total of 26 codes were further analysed to identify similarities and differences, then categorised into nine themes and matched with the five competencies required for clinical practice, as well as influential factors or barriers to competency in the clinical setting.
Trustworthiness
Credibility of the findings was enhanced through data source, methodological and investigator triangulations [ 26 ]. Data were collected from three sources, namely CBE-nurses, OBE-nurses, and their supervisors. Both individual interviews and FGDs were used to collect data. An individual interview allows the interviewee to speak freely and frankly and allows the interviewer to probe topics in certain depth without interruption [ 27 ]. FGDs are useful for assessment purposes because researchers can obtain wider opinions and perceptions from participants who build on each other’s ideas through ‘piggybacking’ [ 28 ]. During the interviews and FGDs, interviewers noted key points and restated them to participants to confirm accuracy or credibility. Furthermore, credibility was supported through the analysis and interpretation by all authors. The primary coding, categorisation of key phrases, and interpretation of the qualitative data were initially undertaken by the second author who had lived in the DRC for a significant period of time and had strong local contextual knowledge. The analysis was separately conducted by the first author with a qualitative research background of more than a decade, and the last author with the same background as the second author. These three authors presented initial analyses to the remaining authors to discuss interpretations and seek clarification and alternate explanations, which led to the enhancement of confirmability [ 26 ]. Transferability and dependability were boosted through description of the research context, and study procedures including data collection and analysis [ 26 ].
Strength of CBE-nurses
Most of the supervisors recognised the CBE-nurses to be better, particularly at three competencies required for nurses in the DRC (i.e., establishing professional communication, making decisions about health problems, and engaging in professional development) which aligns with the findings of the quantitative study using the self-evaluation scale.
CBE allows nurses, in addition to the theory learned in school, to be confronted with realities on the ground... They try to solve problems in relation to the needs of the patients. (Supervisor 9 in Kasaï-Oriental Province)
Supervisors recognised that CBE-nurses communicate with patients and the community better than OBE-nurses, especially respecting patients and community habits, using understandable language, informing patients and communities about health services, and checking that given information was understood.
CBE-nurses communicate with patients before providing nursing care. They introduce themselves to the patient and start a conversation like ‘Where are you from?’ But OBE-nurses struggle to communicate with patients. (Supervisor 8 in Sud-Kivu Province) OBE-nurses prescribe medicine and say, ‘Take it at home’. That’s it. CBE-nurses explain how to take the medicine, what the results will be, and observe whether the patient understood that information, then say ‘Come back to the health centre if you don’t feel better, I am happy to see how you are doing’. (Supervisor 8 in Kasaï-Central Province, Supervisor 8 in Sud-Kivu Province) CBE-nurses go into the community, see how the community is suffering, and encourage them to visit the health centre. (Supervisor 8 in Kasaï-Central Province)
Supervisors also identified CBE-nurses’ superiority in data gathering from different sources to identify health problems, analysing them to plan nursing interventions, and assessing the results to improve the nursing plan. These are components to making decisions about health problems.
OBE-nurses are not interested in the root cause. CBE-nurses go out to understand the community and use that knowledge when they see patients at a health facility. (Supervisor 3 in Kwilu Province) I found that CBE-nurses are very focused, can identify issues and priority needs of patients, and plan nursing care more effectively than OBE-nurses. (Supervisor 1 in Sud-Kivu Province)
However, some supervisors who did not know about the introduction of a competency-based programme criticised CBE-nurses as they try to share and discuss patients’ health issues with colleagues and supervisors, which is in fact one of the components of the competency to make decisions about health problems.
I find that the OBE-nurses can decide and work alone, but CBE-nurses always consult and involve other staff to make decisions. (Supervisor 7 in Sud-Kivu Province)
One supervisor identified the strength of CBE-nurses with their habit of active learning to update their knowledge, which is the competency to engage in professional development.
I think the education reform has done something. The CBE-nurses adapt better to the context and perform better in their duties. They are motivated and active. The CBE- nurses ask me questions to develop themselves, while OBE-nurses who graduated in the same year pretend they know everything, and don’t try to learn. (Supervisor 13 in Kongo Central Province)
Weakness of CBE-nurses
Supervisors identified that CBE-nurses’ relative weakness is their clinical skills.
I don't know if it's because of the teacher or school curriculum, but I see that there is a problem with the CBE-nurses in terms of practical clinical skills. (Supervisor 2 in Lualaba Province) I find that the CBE-nurses have some insufficiency, for example, they don't have the capacity of reading flowcharts or using partogrammes. I suspect that the school teacher or the supervisor of clinical practice did not teach enough about how to use those tools. (Supervisor 7 in Sud-Kivu Province)
FGDs separately organised with OBE- and CBE-nurses supported this supervisor’s observation about the novice of CBE nurses’ clinical skills.
CBE-nurses have shortcomings in practice. It seems they have not received enough practical training before graduation. For example, they are not good at attending delivery or calculating the doses of medicines and infusions for children. (FGD with OBE-nurses in Kinshasa) Sometimes there are techniques that we still need to learn in-depth. Our knowledge and experience are limited. There are practices we didn’t confront during clinical training when we were students. (FGD with CBE-nurses in Bukavu province)
Challenges in health facilities
Some supervisors recognise the difficulty of having OBE-nurses and CBE-nurses work together in the same health facility and the importance of the supervisor's role.
[With my mediation,] CBE- and OBE-nurses in my health facility share information to understand their differences and complement each other. (Supervisor 3 in Kwilu Province) I ask CBE-nurses to mentor OBE-nurses so that the OBE-nurses can work like the CBE nurses. (Supervisor 8 in Kasaï-Central Province) We, the supervisors, need to understand the new education, to be able to put ourselves in the shoes of those who give the current care [CBE-nurses] so that, between the two [OBE- and CBE-nurses], things can smoothly move forward. (Supervisor 3 in Haut-Katanga Province)
FGDs with the CBE-nurses supported the supervisor's statement that CBE-nurses were committed to improving care in healthcare facilities.
When I first came to work, OBE-nurses thought that I was going to fight with them. It was like a war. But by integrating them into everything I already knew, they are now able to provide care with the competency-based approach, too. I showed them that I am trained in five competencies in my school, and how to solve a problem by integrating several resources. (FGD with CBE-nurses in Bukavu province)
However, not all CBE-nurses have such positive experiences in their workplace. Rather, they struggle to get support and understanding from colleagues.
There are not a lot of CBE-nurses in my health facility. So, it's difficult... There are some people who accept my way of working, but others don't. They don’t know the new competency-based approach, so they criticise me. (FGD with CBE nurses in Kinshasa) OBE-nurses criticised us saying that we are too proud because we studied with a competency base. They say we're going to replace them. We need to say, no, we didn’t come to replace you. (FGD with CBE nurses in Bukavu province) Our way of working with the new approaches creates a conflict in the workplace. (FGD with CBE nurses in Kinshasa)
In such a work environment, CBE-nurses experience difficulties in utilising their competencies.
OBE-nurses tell me to follow their way. I’m the only CBE-nurse in my workplace. It's a difficult situation. ...Their work experience is greater than mine, so they say they know better than me. (FGD with CBE nurses in Kinshasa) Where I work, the majority of the staff received OBE. They don’t know what I learned. Sometimes they treat me like a servant, and that causes conflicts between us. (FGD with CBE nurses in Kinshasa)
Based on such problematic situations in health facilities, both supervisors and CBE-nurses expressed the need for competency-based in-service training as recurrent programmes for experienced OBE-nurses/supervisors.
Most supervisors received OBE, so, they don’t know well about the competency-based approach. Training should be conducted for such supervisors so that all of us can have the same commitment. (Supervisor 1 in Sud-Kivu Province) There is something we don't know about new education. When the education reform is applied at the school, we, who are in the health facilities, must also be briefed on this, to speak the same language with newly graduated nurses. (Supervisor 6 in Kasaï- Central Province) I hope OBE-nurses get an opportunity to receive competency-based training. Then OBE- and CBE-nurses can work better together. (FGD with CBE nurses in Kinshasa)
Some supervisors noted that for CBE-nurses to demonstrate their competency, comprehensive health system strengthening is needed, including tackling the workforce shortage in health facilities.
Because of the shortage of staff, one nurse needs to cover several positions in my health facility and continuously work without the rest. We try to prioritise providing more or less satisfactory care for the patients. In this situation, when we find any issue in a nurse, it is difficult to judge if the nurse doesn’t have the competency, or is overwhelmed by the heavy workload. When the working conditions don't meet the standards, the judgement can be biased. Once the working condition meets the standards, then we can really reap the benefits of this new education approach in health facilities. (Supervisor 9 in Kasaï-Oriental Province)
Increasing the availability and quality of the health workforce and strengthening PHC are essential for achieving UHC in the DRC [ 7 ], and nurses are expected to play a particularly important role [ 9 ]. This is the first qualitative study to explore the effectiveness of CBE in secondary nurses who are working in lower level health facilities where there is no doctor, playing a critical role in providing PHC in the DRC [ 29 ]. The results show that supervisors in health facilities recognised that CBE-nurses have stronger competencies than OBE-nurses, especially in the areas of establishing professional communication, making decisions about health problems , and engaging in professional development. These results are aligned with the findings of the quantitative study in which the CBE- and OBE-nurses evaluated their own competencies using a DRC-specific self-assessment nurse competence scale [ 23 ]. The better performance by CBE-nurses in comparison with OBE-nurses has been proven in high- and upper-middle-income countries [ 30 , 31 , 32 ]. A review from China found that CBE-nurses performed better than OBE-nurses in terms of critical thinking, interpersonal communication, and professional development [ 33 ]. Our study showed that even in low-income countries such as the DRC, CBE can improve nursing care at health facilities.
Our study findings support the policy of the MoH in the DRC, which introduced CBE into the pre-service education system to achieve UHC through PHC. It also encourages other resource-limited countries to confidently promote CBE. However, the progress to shift from OBE to CBE has been slow. Fifteen years after the issuance of a ministerial decree, only 21% of the nursing education institutions have introduced CBE in the DRC. This study identified that the simultaneous implementation of the two approaches causes multiple challenges in health facilities, such as the feud between OBE- and CBE-nurses and the provision of unstandardised nursing care. The MoH continues preparing and conducting annual graduation examinations with different questions for CBE- and OBE-trained students, which places a heavy burden on the MoH in terms of finances, time, and human resources.
Some sub-Saharan African countries face the same challenges in implementing policies once they are enforced [ 34 ]. The successful transition from OBE to CBE in Rwanda highlights the importance of medium- and long-term reform plans [ 12 ]. In the DRC, the ministerial decree from the MoH to introduce CBE in 2005 was not legally binding, and the enforcement thereof was left to the provincial governments in a decentralised system, relying on each province’s leadership and capacity. A well-planned, legally binding CBE reform strategy will be helpful to speed up the transition to CBE. The MoH could consider abolishing the national standardised final examinations for OBE-trained students by a certain year. Strengthening the legally binding accreditation system for nursing education institutions could also be considered to close poor-quality ones, such as those having no capacity to introduce CBE curricula.
This study also revealed the importance of approaching the continuing professional development (CPD) system in CBE reform. Until all education institutions introduce CBE and all clinical nurses who graduated with OBE retire from their work, CBE- and OBE-nurses will continue to work together in health facilities across the country. This makes each health facility struggle to systematically provide standardised nursing care, as this study has identified. CBE-nurses expressed their challenges in demonstrating their competencies at their workplace where most supervisors and colleagues do not know about CBE. In fact, some supervisors who lack an understanding of CBE consider the performance of CBE-nurses, such as careful decision-making by consulting with other staff, as a shortfall and indicative of not being able to make decisions by themselves. This implies that supervisors lack a thorough understanding of the new education approach and cannot properly evaluate staff performance. To transfer the results of CBE to clinical practice, it is critical that all health facility staff, including supervisors and OBE-nurses, have a thorough knowledge of CBE through the CPD system so that CBE-nurses can effectively demonstrate their acquired competence in clinical settings [ 31 ].
The clinical skills of CBE-nurses were identified as relatively weak by supervisors. FGDs supported this observation and contradicts the curriculum of CBE in the fourth year which allocates longer hours in situational simulation and clinical training than the OBE curriculum (2498 h vs 2300 h) [ 23 ]. One of the reasons for this weakness could be the inadequate quality of clinical training provided for nurse students in health facilities, which is an issue in nursing education in many lower income countries [ 35 , 36 , 37 , 38 ]. In the DRC, provincial health departments have a role to monitor secondary nursing education institutions three times a year. However, no concrete monitoring tool for the provincial department exists to assess the quality of clinical training at health facilities. In the medium- and long-term plans for CBE reform, a concrete strategy to monitor and improve clinical training should be included. The collaboration between nursing education institutions, healthcare facilities, and officers at health departments at provincial and district levels is key to ensure highly competent future nurses.
Strong MoH leadership is critical in the comprehensive medium- and long-term strategic plan for a smoother transition from OBE to CBE both in the pre-service and in-service education system. In the DRC, three separate departments in the MoH manage human resources. The Department of Human Resources for Health is responsible for the recruitment and placement of personnel, the Department of Health Science Education is responsible for the pre-service education of secondary nurses, and the Department of Continuing Education is responsible for CPD. Although CBE reform is one of the priorities in the MoH [ 7 ], the three departments have no concrete plan to proceed with the reform in synergy. It is imperative to strengthen the cooperation between the three departments to accomplish the MoH’s priority to provide quality PHC at lower-level health facilities through competent nurses.
This study has several limitations. Although a 360-degree evaluation approach with each nurse is a more comprehensive methodology [ 39 , 40 ], being a low-income country with a vast territory and limited resources, it has been difficult for the MoH to apply it. The results from our study, using interviews and FGDs to carefully sampled nurses, are still informative for policy implications in the DRC; thus, our methodology could be useful for other resource-limited countries. This study did not explore the broader challenges and constraints such as the working environment, and possible solutions in the wider health system. A more comprehensive health system analysis could be considered in future studies.
The supervisors recognised that CBE-nurses have stronger competencies in professional communication, making decisions about health problems, and engaging in professional development, which supports the MoH policy to expand CBE in nationwide pre-service education. However, challenges exist for supervisors to assure standardised care at health facilities with two types of nurses, and for CBE-nurses to fully demonstrate their competencies at health facilities where they are a minority. The development and implementation of a well-planned, legally binding, longer-term CBE reform strategy, including an approach to the CPD system with strong cooperation among the three departments of the MoH, would be the key to accelerating the provision of PHC by competent nurses.
Availability of data and materials
The datasets used and/or analysed during this study are available from the corresponding author on reasonable request.
Abbreviations
- Competency-based education
Continuing professional development
- Democratic Republic of the Congo
Focus group discussion
General hospital
Health centre
Ministry of Public Health
National Center for Global Health and Medicine
Object-based education
Primary healthcare
Universal health coverage
World Health Organization and United Nations Children’s Fund (UNICEF). A vision for primary health care in the 21st century: towards universal health coverage and Sustainable Development Goals. Geneva. 2018
Imanipour M, Ziarat MH, Mohammadi MM. The effect of competency-based education on clinical performance of health care providers: a systematic review and meta-analysis. Int J Nurs Pract. 2022;28: e13003. https://doi.org/10.1111/ijn.13003 .
Article PubMed Google Scholar
Lewis LS, Rebeschi LM, Hunt E. Nursing education practice update 2022: competency-based education in nursing. SAGE Open Nurs. 2022;2022:8. https://doi.org/10.1177/23779608221140774 .
Article Google Scholar
Frenk J, Chen L, Bhutta ZA, et al. Health professionals for new century: transforming education to strengthen health system in an interdependent world. The Lancet. 2010;376:1923–58. https://doi.org/10.1016/S0140-6736(10)61854-5 .
Palermo C, Aretz HT, Hlnboe ES. Editorial: competency frameworks in health professions education. Front Med. 2022;9:1034729. https://doi.org/10.3389/fmed.2022.1034729 .
World Health Organization. Global strategic directions for nursing and midwifery 2021–2025. 2021.
Ministère de la Santé. Plan National de Développement Sanitaire recadre pour la période 2019-2022: vers la couverture sanitaire universelle. Ministry of Public Health, Democratic Republic of the Congo. 2018 (in French).
Ministère de la Santé. Annuaire statistiques des ressources humaines de la sante. Ministry of Public Health, Democratic Republic of the Congo. August 2019 (in French).
Parent F, Lemenu D, Lejeune C. Référentien de Compétences Infirmières En RD du Congo Dans Le Cadre du Renforcement des Ressources Humaines En Santé. Santé Publique. 2006;18:459–73 ( in French ).
Article CAS PubMed Google Scholar
Ministère de la Santé. Arreté Ministériel, portant mise en application du nouveau programme de formation de base des infirmiers du niveau Sécondaire et de son mode d'evaluation en RDC. Ministry of Public Health, Democratic Republic of the Congo. 2005 (in French)
Michaels-Strasser S, Smith J, Khanyola J, Sutton R, Price T, El Sadr WM. Strengthening the quality and quantity of the nursing and midwifery workforce: report on eight years of the NEPI project. Ann Glob Health. 2018;84(1):31–5.
Article PubMed PubMed Central Google Scholar
Muraraneza C, Mtshali GN. Planning reform to competency based curricula in undergraduate nursing and midwifery education: a qualitative study. Nurse Edu Today. 2021;106: 105066. https://doi.org/10.1016/j.nedt.2021.105066 .
Ministère de la Santé. Référentiel de Compétences infirmières du niveau secondaire, version révisée. Ministry of Public Health, Democratic Republic of the Congo. 2009 (in French).
Cowan DT, Norman I, Coopamah VP. Competence in nursing practice: a controversial concept—a focused review of literature. Accid Emerg Nurs. 2007;15:20–6.
Cowin LS. Competency measurements: testing convergent validity for two measures. J Adv Nurs. 2008;64:272–7.
Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287:226–35.
Lenburg CB, Klein C, Abdur-Rahman V, Spencer T, Boyer S. The COPA model: a comprehensive framework designed to promote quality care and competence for patient safety. Nurs Educ Perspect. 2009;30:312–7.
PubMed Google Scholar
Scott Tilley DD. Competency in nursing: a concept analysis. J Contin Educ Nurs. 2008;39:58–64 ( quiz 65–56, 94 ).
Ten Cate O, Scheele F. Competency-based postgraduate training: can we bridge the gap between theory and clinical practice? Acad Med. 2007;82:542–7.
Fisher C, Cusack G, Cox K, Feigenbaum K, Wallen GR. Developing competency to sustain evidence-based practice. J Nurs Adm. 2016;46:581–5.
Pijl-Zieber EM, Barton S, Konkin J, Awosoga O, Caine V. Competence and competency-based nursing education: finding our way through the issues. Nurse Edu Today. 2014;34:676–8.
Ministère de la Santé. Planification annuelle de cours, semaines d’integration et stage des Infirmiers. Ministry of Public Health, Democratic Republic of the Congo. 2019 (in French).
Tamura T, Bapitani D, Kahombo G, Minagawa Y, Matsuoka S, Oikawa M, Egami Y, Honda M, Nagai M. Comparison of the clinical competency of nurses trained in competency-based and object-based approaches in the Democratic Republic of the Congo: a cross-sectional study. Global Health Med. 2023;5(3):142–50.
Hudelson, Patricia M. Division of Mental Health, World Health Organization. Qualitative research for health programmes. Geneva. 1994. https://iris.who.int/handle/10665/62315
Ministère du Plan. Annuaire statistique RDC 2020. https://www.undp.org/sites/g/files/zskgke326/files/migration/cd/UNDP-CD-ANNUAIRE-STAT.-2020-pdf (accessed August 6, 2023) (in French).
Chowdhury AI. Issue of quality in a qualitative research: an overview. Innovat Issues Approach Soc Sci. 2015;8(1):142–62.
Google Scholar
Carolyn B, Palena N. Conducting in-depth interviews: a guide for designing and conducting in-depth interviews for evaluation input. USA: Pathfinder International; 2006.
Leung FH, Savithiri R. Spotlight on focus groups. Can Fam Physician. 2009;55(2):218–9.
PubMed PubMed Central Google Scholar
Ministère de la Santé. Recueil des normes de création, d'organisation et de fonctionnement des structures du zome de santé en République Démocratique du Congo, 2019 (in French).
Nguyen D-Q, Blais J-G. Approche par objectifs ou approche par compétences ? Repères conceptuels et implications pour les activités d’enseignement, d’apprentissage et d’évaluation au cours de la formation clinique. Pédagogie Médicale. 2007;8:232–51. https://doi.org/10.1051/pmed:2007026 .
Yanhua C, Watson R. A review of clinical competence assessment in nursing. Nurse Educ Today. 2011;31:832–6. https://doi.org/10.1016/j.nedt.2011.05.003 .
Gruppen LD, Mangrulkar RS, Kolars JC. The promise of competency-based education in the health professions for improving global health. Human Resour Health. 2012;10:43. https://doi.org/10.1186/1478-4491-10-43 .
Chen S, Zhang C, Li W. The effects of competency-based training model in the training of new nurses: a meta-analysis and systematic review. PLoS ONE. 2022;17(11): e02277484. https://doi.org/10.1371/journal.pone.0277484 .
Article CAS Google Scholar
Muraraneza C, Mtshali GN, Mukamana D. Issues and challenges of curriculum reform to competency-based curricula in Africa: a meta-synthesis. Nurs Health. 2016;19:5–12.
Merry L, Castiglione SA, Rouleau G, Letourneau D, Larue C, Deschenes MF, Gonsalves DM, Ahmed L. Continuing professional development (CPD) system development, implementation, evaluation and sustainability for healthcare professionals in low- and lower-middle-income countries: a rapid scoping review. BMC Med Educ. 2023;23:498. https://doi.org/10.1186/s12909-023-04427-6 .
Bvumbwe T. Enhancing nursing education via academic–clinical partnership: an integrative review. Int J Nurs Sci. 2016;3:314–22.
Kablan BNG. Obstacles to the functioning of the competency-based approach. Int J Edu Res. 2021; 9(11).
Younas A, Rasheed SP, Sommer J. Current situation and challenges concerning nursing education in Pakistan. Nurse Educ Pract. 2019;41: 102638.
Sadeghi T, Loripoor M. Usefulness of 360 degree evaluation in evaluating nursing students in Iran. Korean J Med Educ. 2016;28(2):195–200.
Gonzalez-Gil MT, Parro-Moreno AI, Oter-Quintana C, Gonzalez-Blazquez C, Martinez-Marcos M, Casillas-Santana M, et al. 360-Degree evaluation: towards a comprehensive, integrated assessment of performance on clinical placement in nursing degree: a descriptive observational study. Nurse Educ Today. 2020;95: 104594.
Download references
Acknowledgements
The authors would like to express their profound gratitude to the fieldwork team especially for the following MoH officers: Adolphe Ilondo Ngamashi, Angèlique Mukomba Muzinga, Beatrice Bobo Musesu, Elisabeth Akatshi Lushima, Jacob Mputu Tshiondo, Léonie Lubuimi Benge, Marcel Baroani Bunzuki, Marie-Thérèse Tshabu Bukasa, and Séverin Bushiri Mutupeke and to the health professionals who participated in the study.
This study was supported by a Research Grant for International Health (19A10 and 20A04) from Japan's Ministry of Health, Labour and Welfare. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Bureau of International Health Cooperation, National Center for Global Health and Medicine, Tokyo, Japan
Mari Nagai, Yui Minagawa, Sadatoshi Matsuoka, Yuriko Egami, Mari Honda & Toyomitsu Tamura
National College of Nursing, National Center for Global Health and Medicine, Tokyo, Japan
Miyuki Oikawa
School of Nursing, Tokyo Women’s Medical University, Tokyo, Japan
Tomoko Komagata
Department of Health Science Education, Ministry of Public Health, Kinshasa, Democratic Republic of the Congo
Josué Désiré Bapitani Basuana & Gérard Kahombo Ulyabo
You can also search for this author in PubMed Google Scholar
Contributions
MN, MO, TK, GUK, SM, YM and TT developed the study design and data collection tools in consultation with DBJB, YE and MH. MO, DBJB, GUK, and YM supervised the field data collection discussion with MN, SM, TK and TT. MN, MO, SM, and TT undertook the data analysis. All authors contributed to the preparation of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mari Nagai .
Ethics declarations
Ethics approval and consent to participate.
The authors obtained ethical approval from the Ethics Committees of the MoH of the DRC (No. 137/CNES/BN/PMMF/2019 du 21/09/2019) and the NCGM in Japan (NCGM-G-004023-00). All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nagai, M., Oikawa, M., Komagata, T. et al. Clinical competency of nurses trained in competency-based versus objective-based education in the Democratic Republic of the Congo: a qualitative study. Hum Resour Health 22 , 38 (2024). https://doi.org/10.1186/s12960-024-00921-0
Download citation
Received : 17 October 2023
Accepted : 16 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1186/s12960-024-00921-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical nurses
- Clinical supervisors
- Resource-limited countries
- Standardized nursing care
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Get the Reddit app
A subreddit for those who enjoy learning about flags, their place in society past and present, and their design characteristics
Flag of Elektrostal, Moscow Oblast, Russia

- Bahasa Indonesia
- Eastern Europe
- Moscow Oblast
Elektrostal
Elektrostal Localisation : Country Russia , Oblast Moscow Oblast . Available Information : Geographical coordinates , Population, Altitude, Area, Weather and Hotel . Nearby cities and villages : Noginsk , Pavlovsky Posad and Staraya Kupavna .
Information
Find all the information of Elektrostal or click on the section of your choice in the left menu.
- Update data
| Country | |
|---|---|
| Oblast |
Elektrostal Demography
Information on the people and the population of Elektrostal.
| Elektrostal Population | 157,409 inhabitants |
|---|---|
| Elektrostal Population Density | 3,179.3 /km² (8,234.4 /sq mi) |
Elektrostal Geography
Geographic Information regarding City of Elektrostal .
| Elektrostal Geographical coordinates | Latitude: , Longitude: 55° 48′ 0″ North, 38° 27′ 0″ East |
|---|---|
| Elektrostal Area | 4,951 hectares 49.51 km² (19.12 sq mi) |
| Elektrostal Altitude | 164 m (538 ft) |
| Elektrostal Climate | Humid continental climate (Köppen climate classification: Dfb) |
Elektrostal Distance
Distance (in kilometers) between Elektrostal and the biggest cities of Russia.
Elektrostal Map
Locate simply the city of Elektrostal through the card, map and satellite image of the city.
Elektrostal Nearby cities and villages
Elektrostal Weather
Weather forecast for the next coming days and current time of Elektrostal.
Elektrostal Sunrise and sunset
Find below the times of sunrise and sunset calculated 7 days to Elektrostal.
| Day | Sunrise and sunset | Twilight | Nautical twilight | Astronomical twilight |
|---|---|---|---|---|
| 8 June | 02:43 - 11:25 - 20:07 | 01:43 - 21:07 | 01:00 - 01:00 | 01:00 - 01:00 |
| 9 June | 02:42 - 11:25 - 20:08 | 01:42 - 21:08 | 01:00 - 01:00 | 01:00 - 01:00 |
| 10 June | 02:42 - 11:25 - 20:09 | 01:41 - 21:09 | 01:00 - 01:00 | 01:00 - 01:00 |
| 11 June | 02:41 - 11:25 - 20:10 | 01:41 - 21:10 | 01:00 - 01:00 | 01:00 - 01:00 |
| 12 June | 02:41 - 11:26 - 20:11 | 01:40 - 21:11 | 01:00 - 01:00 | 01:00 - 01:00 |
| 13 June | 02:40 - 11:26 - 20:11 | 01:40 - 21:12 | 01:00 - 01:00 | 01:00 - 01:00 |
| 14 June | 02:40 - 11:26 - 20:12 | 01:39 - 21:13 | 01:00 - 01:00 | 01:00 - 01:00 |
Elektrostal Hotel
Our team has selected for you a list of hotel in Elektrostal classified by value for money. Book your hotel room at the best price.
| Located next to Noginskoye Highway in Electrostal, Apelsin Hotel offers comfortable rooms with free Wi-Fi. Free parking is available. The elegant rooms are air conditioned and feature a flat-screen satellite TV and fridge... | from | |
| Located in the green area Yamskiye Woods, 5 km from Elektrostal city centre, this hotel features a sauna and a restaurant. It offers rooms with a kitchen... | from | |
| Ekotel Bogorodsk Hotel is located in a picturesque park near Chernogolovsky Pond. It features an indoor swimming pool and a wellness centre. Free Wi-Fi and private parking are provided... | from | |
| Surrounded by 420,000 m² of parkland and overlooking Kovershi Lake, this hotel outside Moscow offers spa and fitness facilities, and a private beach area with volleyball court and loungers... | from | |
| Surrounded by green parklands, this hotel in the Moscow region features 2 restaurants, a bowling alley with bar, and several spa and fitness facilities. Moscow Ring Road is 17 km away... | from | |
Elektrostal Nearby
Below is a list of activities and point of interest in Elektrostal and its surroundings.
Elektrostal Page
| Direct link | |
|---|---|
| DB-City.com | Elektrostal /5 (2021-10-07 13:22:50) |

- Information /Russian-Federation--Moscow-Oblast--Elektrostal#info
- Demography /Russian-Federation--Moscow-Oblast--Elektrostal#demo
- Geography /Russian-Federation--Moscow-Oblast--Elektrostal#geo
- Distance /Russian-Federation--Moscow-Oblast--Elektrostal#dist1
- Map /Russian-Federation--Moscow-Oblast--Elektrostal#map
- Nearby cities and villages /Russian-Federation--Moscow-Oblast--Elektrostal#dist2
- Weather /Russian-Federation--Moscow-Oblast--Elektrostal#weather
- Sunrise and sunset /Russian-Federation--Moscow-Oblast--Elektrostal#sun
- Hotel /Russian-Federation--Moscow-Oblast--Elektrostal#hotel
- Nearby /Russian-Federation--Moscow-Oblast--Elektrostal#around
- Page /Russian-Federation--Moscow-Oblast--Elektrostal#page
- Terms of Use
- Copyright © 2024 DB-City - All rights reserved
- Change Ad Consent Do not sell my data

COMMENTS
Description. Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 7th Edition brings these concepts to life through engaging text, diverse learning activities, and real-life examples. Easy-to-understand ...
Simple approach and motivational writing style include vivid examples, memorable anecdotes, and real case scenarios to make content come alive. Practical strategies to promote critical thinking, clinical reasoning, and clinical judgment are incorporated along with supporting evidence as to why the strategies work.
Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 5th Edition, provides the tools you need to become a safe, competent nurse. Using an inspiring, insightful, "how-to" approach, this book helps you develop critical thinking, clinical reasoning, and test-taking skills in preparation for the NCLEX® Examination ...
Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 7th Edition brings these concepts to life through engaging text, diverse learning activities, and real-life examples. Easy-to-understand language and a "how-to" approach equip you to become a sensible ...
Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 7 th Edition brings these concepts to life through engaging text, diverse learning activities, and real-life examples. Easy-to-understand language and a "how-to" approach equip you to become a sensible ...
Critical Thinking, Clinical Reasoning and Clinical Judgment: A Practical Approach, Pageburst E-book on Kno. ... Clinical Reasoning and Clinical Judgment: A Practical Approach, Pageburst E-book on Kno: Contributor: Rosalinda Alfaro-Lefevre: Publisher: Elsevier Health Sciences, 2016: ISBN: 0323358934, 9780323358934:
Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 7 th Edition brings these concepts to life through engaging text, diverse learning activities, and real-life examples. Easy-to-understand language and a "how-to" approach equip you to become a sensible ...
What's behind every healed patient? Critical thinking! Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 5th Edition, provides the tools you need to become a safe, competent nurse. Using an inspiring, insightful, "how-to" approach, this book helps you develop critical thinking, clinical reasoning, and test-taking skills in preparation for the NCLEX(R ...
In the nursing education literature, clinical reasoning and judgment are often conflated with critical thinking. The accrediting bodies and nursing scholars have included decisionmaking and action-oriented, practical, ethical, and clinical reasoning in the rubric of critical reflection and thinking.
Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach 7th Edition is written by Rosalinda Alfaro-LeFevre and published by Saunders. The Digital and eTextbook ISBNs for Critical Thinking, Clinical Reasoning, and Clinical Judgment are 9780323594721, 0323594727 and the print ISBNs are 9780323581257, 0323581250. Save up to 80% versus print by going digital with ...
Simple approach and motivational writing style include vivid examples, memorable anecdotes, and real case scenarios to make content come alive. Practical strategies to promote critical thinking, clinical reasoning, and clinical judgment are incorporated along with supporting evidence as to why the strategies work.
Clinical reasoning (CR) is a universal ability that mobilizes integration of necessary fundamental knowledge while delivering high-quality patient care in a variety of contexts in a timely and effective way [1, 2].Daniel et al. [] define it as a "skill, process or outcome wherein clinicians observe, collect, and interpret data to diagnose and treat patients".
A programmatic assessment model of clinical reasoning that is developmentally oriented, optimizes learning though feedback and coaching, uses multiple assessment methods, and provides opportunity for meaningful triangulation of data can help address some of the challenges of clinical reasoning assessment. Issue: Clinical reasoning is essential to physicians' competence, yet assessment of ...
Simple approach and motivational writing style include vivid examples, memorable anecdotes, and real case scenarios to make content come alive. Practical strategies to promote critical thinking, clinical reasoning, and clinical judgment are incorporated along with supporting evidence as to why the strategies work.
Comparing the CBL and CBL-3DP groups, the scores from the CBL-3DP group showed significant improvements in many areas. This included satisfaction with the teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities (Fig. 3B, C, D
Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 5th Edition, provides the tools you need to become a safe, competent nurse. Using an inspiring, insightful, "how-to" approach, this book helps you develop critical thinking, clinical reasoning, and test-taking skills in preparation for the NCLEXª Examination ...
Both online and campus-based accelerated BSN Chicago prepare students for the challenges and opportunities of modern nursing practice, instill critical thinking and clinical reasoning skills, and fulfill the educational requirements for licensure as a registered nurse (RN). Read on to explore school spotlights, and ABSN-specific considerations ...
Develop the critical thinking and reasoning skills you need to make sound clinical judgments! Alfaro-LeFevre's Critical Thinking, Clinical Reasoning, and Clinical Judgment: A Practical Approach, 7th Edition brings these concepts to life through engaging text, diverse learning activities, and real-life examples. Easy-to-understand language and a "how-to" approach equip you to become a sensible ...
Background Designing competency-based education (CBE) programmes is a priority in global nursing education for better nursing care for the population. In the Democratic Republic of the Congo (DRC), object-based education (OBE) remains mainstream in pre-service nursing education programmes. Recently, the Ministry of Health developed a self-assessment tool and quantitatively compared the ...
3 Institute for the Study of War and AEI's Critical Threats Project 2024 migrant workplaces and increase crackdowns at border crossings to temporarily placate emotional cries for retribution following the March 22 attack as the Kremlin continues to develop a cogent and practical response. Key Takeaways:
601K subscribers in the vexillology community. A subreddit for those who enjoy learning about flags, their place in society past and present, and…
Elektrostal Geography. Geographic Information regarding City of Elektrostal. Elektrostal Geographical coordinates. Latitude: 55.8, Longitude: 38.45. 55° 48′ 0″ North, 38° 27′ 0″ East. Elektrostal Area. 4,951 hectares. 49.51 km² (19.12 sq mi) Elektrostal Altitude.
Just answer a few questions to get matched with a local General Contractor. Or browse through the list of trusted General Contractors in Elektrostal' on Houzz: See Elektrostal' Ge