Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

Understanding the impacts of health information systems on patient flow management: A systematic review across several decades of research
Roles Conceptualization, Data curation, Formal analysis, Resources, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Human-Centred Computing, Faculty of Information Technology, Monash University, Melbourne, Australia
Roles Conceptualization, Supervision, Writing – review & editing
Roles Supervision, Writing – review & editing
Affiliation Office of Research and Ethics, Eastern Health, Melbourne, Australia
Affiliation Monash Centre for Health Research and Implementation, Monash University, Melbourne, Australia
- Quy Nguyen,
- Michael Wybrow,
- Frada Burstein,
- David Taylor,
- Joanne Enticott

- Published: September 12, 2022
- https://doi.org/10.1371/journal.pone.0274493
- Peer Review
- Reader Comments
Patient flow describes the progression of patients along a pathway of care such as the journey from hospital inpatient admission to discharge. Poor patient flow has detrimental effects on health outcomes, patient satisfaction and hospital revenue. There has been an increasing adoption of health information systems (HISs) in various healthcare settings to address patient flow issues, yet there remains limited evidence of their overall impacts.
To systematically review evidence on the impacts of HISs on patient flow management including what HISs have been used, their application scope, features, and what aspects of patient flow are affected by the HIS adoption.
A systematic search for English-language, peer-review literature indexed in MEDLINE and EMBASE, CINAHL, INSPEC, and ACM Digital Library from the earliest date available to February 2022 was conducted. Two authors independently scanned the search results for eligible publications, and reporting followed the PRISMA guidelines. Eligibility criteria included studies that reported impacts of HIS on patient flow outcomes. Information on the study design, type of HIS, key features and impacts was extracted and analysed using an analytical framework which was based on domain-expert opinions and literature review.
Overall, 5996 titles were identified, with 44 eligible studies, across 17 types of HIS. 22 studies (50%) focused on patient flow in the department level such as emergency department while 18 studies (41%) focused on hospital-wide level and four studies (9%) investigated network-wide HIS. Process outcomes with time-related measures such as ‘length of stay’ and ‘waiting time’ were investigated in most of the studies. In addition, HISs were found to address flow problems by identifying blockages, streamlining care processes and improving care coordination.
HIS affected various aspects of patient flow at different levels of care; however, how and why they delivered the impacts require further research.
Citation: Nguyen Q, Wybrow M, Burstein F, Taylor D, Enticott J (2022) Understanding the impacts of health information systems on patient flow management: A systematic review across several decades of research. PLoS ONE 17(9): e0274493. https://doi.org/10.1371/journal.pone.0274493
Editor: Yong-Hong Kuo, University of Hong Kong, HONG KONG
Received: May 17, 2022; Accepted: August 28, 2022; Published: September 12, 2022
Copyright: © 2022 Nguyen et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data is provided in the article and in the supporting file S3. Copies of the included studies are freely available online.
Funding: QDN was supported by a Ph.D. scholarship jointly funded by the Monash University Graduate Research Industry Partnership (GRIP) program and by Eastern Health. The Funders of this work did not have any direct role in the design of the study, its execution, analyses, interpretation of the data, or decision to submit results for publication.
Competing interests: No authors have competing interests
1. Introduction
Patient flow refers to the progressive movement of patients through different units or departments of the care setting. The aim of patient flow management is to provide safe and efficient patient care while assuring the best use of resources [ 1 ]. Hospitals around the world have undertaken several efforts and strategies to tackle patient flow problems and to provide high-quality care at the right time and right place. Meanwhile, there is an extensive stream of research reporting methods and interventions addressing patient flow problems. A recent umbrella review [ 2 ] found that over 25 different interventions have been used by hospitals around the world to solve the overcrowding issues in the emergency department (ED). However, previous studies focused primarily on interventions for a single, isolated hospital unit or ward with ED being the most frequently mentioned [ 3 , 4 ]. While many systematic reviews related to patient flow interventions have been done, a summary of these systematic reviews shows that most of these reviews have focused on traditional, non-IT interventions such as triage, streaming, and fast track. Systematic reviews on using health information systems (HISs) to tackle patient flow problems exist; however, they are often limited to a single specific system, such as computer provider order entry (CPOE) system [ 5 ]; methods such as computer simulation modelling [ 6 ]; or measures such as length of stay (LOS) [ 7 ].
HISs have been adopted by health providers to improve patient flow in various healthcare settings. For example, in emergency care, the automatic push notification system was used to address ED congestion, reduce LOS, and decrease patient load by providing updated information and improving patient navigation [ 8 ]. Dashboard systems were adopted to coordinate ambulance services and improve access to emergency services across multiple hospitals [ 9 ]. HISs provides data about ED visits which were used to create a robust prediction about hospital admissions and increase logistical efficiency [ 10 ]. In addition, Blaya et al. [ 11 ] investigated the use of HISs in improving access to laboratory results and the quality of care. These are a few examples illustrating the impacts of HISs on patient flow management.
In recent patient flow research, it has been suggested that utilising advanced data analytics techniques for patient flow management can be achieved by adopting HISs. For example, Rutherford et al. [ 12 ] claim that data analytics is essential in achieving improvement in systematic-wide flows through its capabilities in matching patient demand and hospital supply. Real-time demand capacity has been successfully implemented in many healthcare organisations to predict and match supply and demand [ 13 ]. Similarly, Berg et al. [ 14 ] called for a shift in the research paradigm from predicting and controlling to analysing and managing to achieve better flow outcomes. This can be done through the application of information technology in analysing data to proactively manage patient flows. Despite the rich tradition of inquiry in research about the use of HISs in patient flow management, to date, to the best of our knowledge, no systematic review has been conducted to assess the impacts of a broad range of HISs on patient flow management, highlighting an evidence gap in the literature. Therefore, a systematic review of this topic will provide more complete insights as to how HISs have been adopted for and impacted patient flow management practice.
2. Objectives
This systematic literature review aimed to examine and summarise information from published studies on the use of HISs in healthcare settings to manage and improve patient flows. We are interested in exploring what information systems have been adopted for managing patient flow and solving flow problems such as blockages, delays, and overcrowding, and their effectiveness. We examined studies that focused on department-level (e.g., ED), hospital-wide, and network-wide interventions. Particularly, our objectives are to provide critical analysis on:
- Study characteristics: Chronological and geographical distribution of the studies, study settings, and research designs.
- Study contents: What types and features of information system have been used for patient flow management, their results and effectiveness on patient flow outcomes.
3. Research questions
This review addresses the following research questions:
- What HISs have been used for hospitals’ patient flow management?
- What are the impacts of HISs on patient flow outcomes?
- In what ways, have HISs been used to manage patient flow?
4.1 Search strategy
We searched for peer-reviewed journal articles published in English from MEDLINE and EMBASE via Ovid, CINAHL, INSPEC, and ACM Digital Library from the earliest date available to February 2022. In addition, we examined the reference lists of the search results to retrieve further eligible papers. The search was conducted from June 2020 to July 2020 and then re-run in February 2022 before the data extraction process.
With the assistance of a subject librarian, we developed a systematic search strategy for this review ( S1 File ). To obtain the most comprehensive search results, we employed medical subject headings (MeSH) keywords when they are available in combination with free text keywords from the PICOS framework. We combined the following terms ( Table 1 ) in our search for relevant studies.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0274493.t001
4.2 Eligibility
Table 2 specifies the inclusion and exclusion criteria used in the title and abstract screening process for this review.
https://doi.org/10.1371/journal.pone.0274493.t002
We included studies that described the impacts of HISs that were actually implemented and adopted for managing patient flow or solving patient flow problems. We excluded papers describing prototype systems, systems that were not implemented in practice or papers without real impacts of HISs on patient flow management such as those just reporting simulated results, simulation tests, or prediction models. Studies that focused on measures such as length of stay (LOS), and waiting time for clinical purposes without any relation to or discussion of patient flow management purposes were also excluded from this review.
Type of studies.
Apart from excluding simulation studies and review papers, we imposed no restrictions on the study’s design or publication date as long as the studies examined the effects of HIS on patient flow management.
Participants.
We included studies that were conducted in various healthcare settings including teaching hospitals, specialist hospitals and general hospitals (both public and private) and clinical centres. As long as the studies were conducted in these settings, we imposed no restrictions on the number of departments, units or wards involved. We also selected studies that addressed patient flow management at the network level, i.e., between different hospital sites and hospital centres. Studies investigating interventions in services not directly related to patient flow and patient access (such as financial services or insurance) were excluded from our review.
Type of intervention.
Health information system is a broad concept and hospitals generally adopt and use several types of information systems to manage their operations. In this review, we selected studies that addressed any type of computerised information systems that have been implemented and had impacts on patient flow outcomes. We also excluded paper-based information management systems, personal digital assistance devices, and medical tools such as surgery robots, CT scanners, heart rate measuring devices.
4.3 Study selection
To assist the selection of eligible studies for this review, we used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines with four key phases [ 16 ].
Initially, the first author searched through the pre-identified online databases by using combinations of the keywords to identify related studies. Duplicates were subsequently removed by using a tool called Covidence [ 17 ] and manually double checking by the first author. In the second step, two reviewers scanned the abstract of all studies to remove irrelevant or ineligible studies based on the predefined inclusion and exclusion criteria. The remaining studies went into the third step in which two reviewers assessed the full-text studies and further eliminated irrelevant papers. The final phase involved extracting data from included studies. We endeavoured to look for full-text files of the eligible papers in all resources available including using intra-library service to retrieve as many as possible
4.4 Data extraction and quality assessment
Information from the papers was extracted in the final list using an electronic data extraction form. Each study was given a unique identification number to ensure a consistent way of identifying studies between the two reviewers. The following data were extracted: authors, journals where the studies were published, year of publication, hospital’s country, the study settings, study objectives, study design, description of the information systems used, factors affecting the adoption of HISs for patient flow management, the effects of HISs on patient flow outcomes, study results, study limitation and research gaps ( S4 File , Example of data extraction form).
The GRADE [ 18 ] approach was adopted to assess the overall quality level of the evidence based on their design. GRADE approach provides particular useful guidelines for assessing health technology studies with heterogeneous study designs. Using the guidelines, the quality of evidence would be assessed as follows:
- High quality for randomized trial studies without serious limitations
- Low quality for observational studies
- ‘0’ level of quality for studies where quality is not assessable such as expert opinion and studies without objective evidence.
4.5 Analytic frameworks
We adopted literature review and expert opinion to develop frameworks that describe types of HISs, their functional capabilities, and associated benefits ( Table 3 ). We also used the conceptual model of Donabedian [ 19 ] as a framework for the analysis on patient flow outcomes. Donabedian’s model categorises care quality into three groups: structure, process, and outcomes.
https://doi.org/10.1371/journal.pone.0274493.t003
The literature search returned 5996 studies and the removal of duplicates reduced the number to 5095. After the first level of screening in which we screened the titles and abstracts and applied the exclusion criteria, 4824 studies were removed. We then proceeded to screen the full-text of 271 studies and 231 of them were excluded. In addition, four studies were added to the final pool through the reverse snowballing technique. Details of the screening process is summarised in Fig 1 , following the PRISMA flow diagram [ 16 ].
From : Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi: 10.1371/journal.pmed1000097 .
https://doi.org/10.1371/journal.pone.0274493.g001
We included 44 studies for our systematic review. The included studies reported mixed impacts of HISs on patient flow management, which can be categorised as follows:
- 33 studies reported positive impacts [ 9 , 20 – 51 ]
- 7 studies reported negative impacts [ 52 – 58 ] and 4 studies reported no impacts of ISs [ 59 – 62 ]. However, among the seven studies with negative impacts, two [ 55 , 58 ] found that the negative effects were temporary and the patient flow measures returned back at pre-implementation baselines.
5.1 Types and features of the HIS
The included 44 studies reported the impacts of 17 different types of HIS on patient flow: eight EHR systems, eight EMR systems, seven patient tracking systems, four computerised provider order entry systems (CPOE), three patient flow dashboard systems, three departmental information systems including ED (1) and Radiology (2), and one each for workflow management, admission prediction, documentation management, patient scheduling, medical prescribing, patient discharge management, patient referral management system, bed management, consultation management, clinical information management, and Asthma management. Table 4 summarises details of the study site and publication profile of the included studies (publication year, country and study settings).
https://doi.org/10.1371/journal.pone.0274493.t004
Research on the application of HISs to patient flow management can be dated back to the 1980s; however, it has gained prominence over the last decade. A majority of included studies were published in the period 2011–2020 (63.6%), compared to 29.5% of the 2001–2010 period and 6.8% of the 1988–2000 period. In addition, most of the studies selected for this review were published in developed countries where their governments have implemented promotional programs to increase the adoption of HISs in the healthcare sector. The number of studies from the USA was the highest with 24 studies, followed by Australia with nine studies. Canada and South Korea contributed three and two studies, respectively. One study was conducted in each of the followings: England, Italy, Japan, Portugal, Uganda, and Taiwan.
In terms of settings, 20 of the reviewed studies discussed the impacts of HIS interventions at the department level, while eleven studies addressed hospital-wide level and three studies address network-wide level. Within the department level, 15 studies focused on EDs, three in Radiology and two in Paediatrics. Studies focused on hospital-wide patient flow when they include the coordination between several departments or units. For example, Westbrook et al. [ 51 ] discussed the impacts of CPOE on the flow of patients between ED and Pathology departments in Australian hospitals. In addition, we found that four studies described the impacts of HISs on patient flow across hospital networks [ 9 , 31 , 39 , 42 ]. Fig 2 depicts where the reported HIS were studied in the care continuum and the number of studies.
The numbers in the circles correspond to the number of relevant studies reviewed.
https://doi.org/10.1371/journal.pone.0274493.g002
Specific functions of the 17 types of HIS that were described in the 44 studies included patient or event tracking (12 studies), clinical documentation management (12 studies), order entry (8 studies), patient registration (3 studies). Bed management, decision support, discharge management, patient flow reporting and prescription management were each included in three studies. Alert, disease detection, picture archiving, staff performance management, referral management, and reminder, were each discussed in one study. Almost all of the included HISs had the capability to integrate data from other systems. Twelve studies did not describe system features. Details of the HIS features and reported benefits are provided in S2 File .
5.2 Impacts on patient flow measures
Table 5 provides a summary of how key patient flow measures were grouped into three categories based on Donabedian model [ 19 ] and the number of studies that included these measures. Details of the included studies and HISs’ impacts on patient flow measures are provided in S3 File , Characteristics of all included studies and their findings.
https://doi.org/10.1371/journal.pone.0274493.t005
Impacts on outcome measures.
Outcomes measures were the most studied measures in the included papers. This is not surprising because health outcomes are the end products of care and the target of health interventions. Studies examined two main types of outcome measures: individual outcomes and organisational outcomes. Almost all studies focused on individual outcome measures in which time-related measures included LOS (25), waiting time (13), treatment time (6), test turnaround time (TAT) (6), and boarding time (2). The effects of HISs on these time related measures were mixed. With regard to LOS, following the use of HISs: 14 studies [ 22 – 25 , 29 , 32 , 33 , 36 , 38 , 39 , 41 , 43 , 45 , 51 ] reported a decrease in LOS, 7 studies [ 9 , 52 – 55 , 57 , 62 ] reported an increased LOS and 4 studies [ 58 – 61 ] found no difference. While most of these studies measured LOS in the ED, five studies [ 25 , 39 , 41 , 43 , 45 ] measured inpatient LOS and two studies [ 23 , 59 ] reported changes in patient LOS at paediatrics centres. The ED LOS was not consistently defined. ED LOS was defined as the difference between ED exit time and the recorded arrival time [ 52 ]. Whereas some studies [ 22 , 59 ] calculated detailed components which constitute the total LOS including time from arrival to triage, arrival to doctor, doctor to disposition, most other studies just reported the mean LOS.
Similarly, 14 studies reported impacts of HISs on waiting time. The results were mixed with 10 positive changes (reduction in waiting time), 2 negative and one with no statistically significant difference. Waiting time measures included waiting for the doctor, waiting for medical treatment, waiting for consultation and for examination. Three studies [ 43 , 58 , 59 ] examined impacts of EHRs on patients waiting for doctor time. In one study [ 59 ], investigators measured the mean patient flow time in a paediatric practice in the USA and found that although the mean patient flow time increased from 56.24 min to 81.43 min one month after the EHR implementation and to 64.60 min 12 months later, patients’ waiting time (check-in to front desk and front desk to triage) actually dropped down by 1.51 and 9.33 min. Their findings suggested the EHR led to more positive results than negative because it reduced waiting for administrative works, allowing more time to be spent on treatment activities. Two studies [ 54 , 56 ] reported negative impacts of HIS on the waiting time of ED patients. Gray and Fernandes [ 54 ] examined the adoption of CPOE in an ED in London Health Sciences Centre with around 100,000 patients per year to determine that CPOE caused an average increase of 5 min in waiting time. A more significant increase in waiting time from 40 to 78 min was observed in a 54,000 patient-per-year ED with the EMR system by Mohan, Bishop, and Mallows [ 56 ].
Treatment time is an important component of LOS and it directly influences health outcomes. However, in this review, we could only identify six studies that used this measure to assess the effectiveness of HIS. Unfortunately, these studies did not provide detailed explanation how the HIS affected treatment time. Three studies [ 22 , 23 , 44 ] found that health providers reduced treatment time when using an ED information system and a patient tracking system for their practice. The patient tracking system was used in a paediatric centre with 24,000 visits annually and it reduced the time of faculty paediatricians spent in Exam room from 11.33 to 6.53 min [ 23 ]. Meanwhile Baumlin et al. [ 22 ] determined a dramatic decrease by 1.90 h in the doctor-to-disposition time after an ED information system was implemented. Two studies about the EHR systems [ 58 , 59 ] and an asthma management system [ 60 ] did not identify a significant difference in treatment caused by the interventions.
TAT is another time-related measure and it was investigated in 6 studies [ 21 , 22 , 38 , 41 , 48 , 51 ]. TAT is defined as the time lapse between when the test is ordered and when the result is available [ 41 ]. Four studies [ 21 , 22 , 39 , 41 ] examined TAT of the radiology examinations and laboratory results; one study [ 48 ] investigated TAT of housekeeping services and one study [ 51 ] reported pathology examinations. All of the studies reported impressive reductions in TAT after the implementation of a HIS. For example, Nitrosi et al. [ 41 ] noted a decrease in the mean chest exam TAT from 33.9 to 9.62 h.
Finally, boarding time is an important patient flow measure that is often referred to as access block or bed block and it is a main patient flow problem [ 63 ]. Two studies [ 22 , 52 ] examined this measure although Pyron and Carter-Templeton [ 43 ] investigated provider discharge-to-nurse discharge time, which can be related to boarding time, but they did not explain or describe how this measure was calculated. Baumlin et al. [ 22 ] reported that the use of an ED information system reduced boarding time for the patient by 28% from 6.77 h to 4.90 h. By contrast, Feblowitz et al. [ 52 ] noticed an increase in the mean boarding time per patient from 211.2 min to 221.4 min in the long term (1 year after the implementation of an electronic documentation system) in an ED. However, neither study provided a causal relationship between HIS implementation and the changes in boarding time.
In addition to time-related measures, included studies also investigated other important individual outcomes including: four studies on the percentage of patients who left without being seen (LWBS), three studies on patient satisfaction, one each for mortality rate, and readmission rate. LWBS was studied in the ED setting. Three studies [ 54 , 56 , 61 ] reported increases of LWBS percentage with the most significant increase being reported in the study about a CPOE system from 24.3% to 42.0% [ 54 ], while Jensen [ 33 ] determined a reduction of 7.6%, but this study did not provide any subjective evidence. Patient satisfaction was measured in three studies with one positive result [ 35 ], one negative [ 62 ], and one neutral result [ 58 ]. The EHR system was found to reduce ED patient satisfaction because it increased LOS; however, the negative impacts lasted for only eight weeks before returning to the baseline from before the intervention implementation [ 62 ]. One study reported that the use of a patient discharging system [ 37 ] was associated with improvement in LOS for early discharge patients without higher rates of readmission. In another study, Inokuchi et al. [ 32 ] investigated the impacts of a newly-developed EMR system on the mortality rate at 28 days after hospitalisation and found no changes resulting from the intervention, which is a positive outcome.
Apart from the patient-related outcome measures above, studies also examined organisational outcomes including four studies about hospital costs, and one each for staff satisfaction, film saving and staff stress level. Three studies [ 33 , 47 , 53 ] calculated the reduction in LOS as hospital cost saving. The first study found that EMR systems were associated with 5.9% to 10.3% higher cost per discharge while with the implementation of a patient flow system, Jensen [ 33 ] reported that the hospital saved between 67,800 and 214,200 USD. The transition from traditional into digital radiology room through the implementation of a PACS system was found to reduce 90% of the film [ 41 ]. Staff satisfaction was examined in a study [ 49 ] which reported positive outcomes after the implementation of an electronic prescribing system. In a study about a workflow management system, Li et al. [ 35 ] found that the intervention greatly improved sonographers’ productivity while reducing their stress level, which was measured by a 5-point Likert scale. Measures related to organisational outcome are an interesting part of the HIS literature because most of the evidence in patient flow intervention focused primarily on patient-related outcome measures.
Impacts on process measures.
Studies examined a variety of measures related to staff productivity in clinical processes, and medical guideline adherence. Four studies examined the effect of HIS on the number of medical services performed by the staff. Two studies showed increased number of surgeries [ 31 ] and radiology tests [ 41 ]. Nitrosi and colleagues [ 41 ] studied the impacts of a PACS and found that the number of imaging procedures increased by 7% although the number of technologies and radiologists remained unchanged. An increase of 37% in the number of surgeries after a surgery information system was observed by Gomes and Lapao [ 31 ]. However, EHR implementation was found to decrease the number of patients that clinical staff could see [ 55 ] although the negative impact was only temporary and resolved three months post-implementation. The implementation of HIS did not change the medical guideline adherence of the staff when they are already providing care that adheres to the relevant guideline [ 60 ]. The number of patients seen per shift by medical staff was measured by Mohan, Bishop, and Mallows [ 56 ] in an investigation of the effectiveness of an EMR system and the impact was negative. Mathews et al. [ 37 ] and Tran et al. [ 49 ] both measured the impact of HIS on the percentage of early discharged patients and show positive outcomes. Finally, Tran et al. [ 49 ] reported an increase in the number of prescriptions prepared the day before discharge as a positive effect of a prescription system.
Impacts on structure measures.
Evidence on the impact of HIS on structure measures was more limited than data on process and outcome measures. Six of the 44 studies reported some data on structure measures. These structure measures are related to flow problems facing healthcare organisations and they were studied in ED settings. Almost all of the six studies reported positive impacts of HIS on these structure measures including the number of patient diversions and the number of ED patients with LOS over 12h [ 33 ], the proportion of early discharged patients [ 37 ], ED avoidance percentage [ 38 ], and the number and proportion of access blocks and hospital occupancy rates [ 27 ]. The study of Crilly et al. [ 27 ] found that the number of access blocks and hospital occupancy rates did not change after the implementation of a patient admission prediction system, but this is actually a positive outcome because the hospital presentations were increasing during the study period. By contrast, in one study, Mohan, Bishop, and Mallows [ 56 ] investigated the effect of an EMR system on the percentage of ambulance offloading time of more than 30 min which is also known as ambulance boarding and they found that the percentage went up from 10.5% to 13.3%.
5.3 Quality assessment of the included studies
Using the GRADE approach to assess the quality level of the evidence through their study design, two RCT studies [ 32 , 60 ] were assessed as high quality and 38 observational studies using retrospective or prospective data were rated low quality. Four studies including three expert opinions and one stating improvement without figures did not provide objective evidence and they were rated ‘0’ (the lowest rating). Two studies using multi-method design with both qualitative and quantitative components were rated low quality, based on the assessment of their quantitative component. Details of the quality assessment are provided in S5 File , Quality assessment of the included studies.
6. Discussion
6.1 summary of key findings.
This systematic review summarised and synthesised evidence from studies about HISs that have been applied to improve patient flow in both inpatient and outpatient settings. Overall, 33 out of the 44 included studies reported positive impacts of HIS on patient flow measures while 7 determined negative impacts, and 4 studies reported no significant impact. Half of the studies focused on patient flow at the departmental level; however, 18 studies reported the impact of HIS on the hospital-wide level and 4 studies reported network-wide impacts on HIS. Healthcare settings adopted at least 17 types of HIS to address patient flow problems and improve care efficiency.
We found that core features of the HIS interventions, that affected patient flow, included patient tracking, documentation management, order entry, patient registration, bed management, decision support, discharge management, prescription management and patient flow reporting. When it comes to the impacts of HIS on specific patient flow measures, most studies focused on outcome measures at both: patient (individual) and organisational level. Changes in individual outcomes were evident in time-related measures including length of stay (LOS), waiting time, treatment time, test turnaround time (TAT), and boarding time, and other measures such as left without being seen and patient satisfaction. Organisational outcome measures were noted in hospital costs, film saving, staff satisfaction, and staff stress level. Process measures and structure measures, although less examined in the included studies than outcome measures, are important measures. While process measures related to staff productivity and guideline adherence, structure measures included flow problems such as patient diversion, access block, hospital occupancy, ambulance offloading time, and ED patient with LOS over 12 h.
Noted HIS benefits included improvements in various patient flow aspects: access to needed information, staff communication, care coordination, work processes, and decision support. Ineffective interaction between hospital units is one of the most common causes of poor patient flow [ 64 ]. HISs were effective in fostering care coordination and collaboration among multidisciplinary teams by imposing a common set of flow key performance indicators (KPIs), and metrics into practice. The application of these common, sometimes “simple”, rules help develop common understandings and it is a key to governing complex systems [ 12 ]. In addition, the involvement of all team members in the development process of HIS is critical to achieving shared understandings. In this review, the effectiveness of HIS in care coordination was evident in many care processes such as patient check-in [ 59 ], elective waiting list management [ 31 ], bed management [ 36 , 48 ], ambulance distribution [ 38 ], and discharge [ 36 , 37 , 49 ]. By integrating information from multiple siloed systems, patient flow-related HIS reduce the time needed for care providers to acquire sufficient information to make critical decisions. Real-time data, notifications, and alerts functions are key features that enabled users to get the most updated information in a timely manner. The development of HISs often included redesigning the embedded care process or processes, an opportunity for care settings to eliminate redundant steps and apply best practices to their care processes. Streamlined work processes helped reduce waiting time for test results and free up staff from redundant information [ 22 , 34 ]. In addition, high degree of automation resulting from the HIS adoption contributed to the reduction in human errors, which can cause medical and health complications, and cognitive workload for hospital staff as they were not required to remember complex rules.
However, it still remains unclear how and why these interventions produced or did not produce positive or negative impacts. Most of the included studies were observational, before and after studies, making it challenging to establish the cause and effect link between HIS interventions and changes in patient flow measures. This has important implications because without a thorough understanding of why and how HIS affected patient flow, it is difficult to generalise the findings to other healthcare settings.
6.2 Strength and limitations
To date, several systematic reviews have been conducted to investigate interventions addressing patient flow problems; however, they focused mostly on operational methods such as triage, fast track, streaming [ 2 ]. Systematic reviews on the impact of HIS on patient flow are small in number and limited to single specific systems such as CPOE [ 5 ]. To the best of our knowledge, this review was the first attempt to evaluate a broad range of HISs applied in patient flow management. The novelty of this review lies in its research aim, and inclusion criteria, unlike most previous reviews on patient flow interventions, here, we included different types of HISs and broad scope of healthcare settings including departmental, organisational and network levels. Our findings provide different stakeholders with important insights for their implementation and adoption of HISs to optimise patient flow.
However, this review has several limitations. The first relates to the heterogeneous nature of the search terminology and the quantity and scope of the evidence. Although we conducted a comprehensive search, in many important domains, we could only identify a limited number of studies. The second limitation relates to the synthesis of varied outcomes and a broad range of HISs. In this review, we attempted to address this limitation by adopting analytic frameworks, which were based on domain experts and published literature, and by synthesising not only the health information system but also their functional features. Third, descriptions of the HIS interventions and the implementation process were often very limited, making it challenging to fully assess the system features and associated benefits. Fourth, most of the included studies are before-and-after, observational studies and therefore understanding of how and why HISs affected patient flow outcomes was very limited. Finally, we decided not to include a meta-analysis because of the diverse, heterogeneous outcomes reported in the included studies. A meta-analysis, in this case, is inappropriate and can be more of a hindrance than a help [ 65 ].
6.3 Implications for patient flow management practice
Hospitals and care centres have implemented several interventions to tackle patient flow problems to deliver optimal care. However, up until recently, most of the efforts were focused on addressing ED overcrowding problems [ 3 , 66 , 67 ]. It is evident in the literature that focusing solely on ED problems will not likely achieve optimal flow because EDs do not operate separately, rather they are part of an interconnected system [ 68 ]. Therefore, literature has urged that patient flow needs to be viewed from the whole system of care viewpoint and called for a shift from ED-focused to system-wide or hospital-wide interventions [ 12 , 69 ]. However, the gap between understanding the problem and having solutions to solve the problem seems still far. For example, even a holistic approach like Lean healthcare was still attached to a specific department or care process [ 4 ]. The frequently reported intervention to improve inpatient flow was implementing a specialised staff or team to coordinate patient flow across hospital units; however, the solution still posed significant challenges [ 3 ]. This systematic review found that apart from 22 studies focusing on department level, many studies reported hospital-wide or even network-wide level. HISs’ potential to address patient flow at the hospital-wide level were noted in their ability to improve communication between multidisciplinary teams [ 25 , 36 ], enhance care coordination [ 36 , 49 ], improve access to needed information [ 41 , 43 ], and streamline care processes [ 25 , 59 ]. One of the prominent causes of admission bottleneck is inefficient discharges [ 68 ] because any delays in inpatient discharge will increase hospital occupancy and ED overcrowding [ 69 ]. HISs showed their effectiveness in discharge prediction and established standardised discharge criteria for improving the discharge process [ 37 ]. These “medical-readiness criteria” have been shown to facilitate efficient planning and care coordination [ 37 ]. Addressing patient flow problems sometimes goes beyond hospital scope to a higher level of network-wide scope. A dashboard system was developed in Alberta, Canada to address ED overcrowding by coordinating emergency services between different emergency rooms within the region [ 9 ]. HISs were also used within a network of different hospitals to address the need for rehabilitation care services and improve the consultation process [ 42 ]. HISs can be scalable to a nationwide level to reduce waiting time for elective surgical patients [ 31 ]. By providing information about capacity, occupancy and demand, they can be highly effective in addressing the mismatch between supply and demand to improve patient flow.
6.4 Implications for future research
Moving forward, this review suggests important areas for future research in the field. First, additional studies need to explore barriers and facilitators of the HISs related to patient flow management. This will offer valuable implications for healthcare organisations to drive their HIS project to success and derive the most from their investment. Second, learning about the effectiveness of HISs on patient flow and associated factor during the post-implementation phase could help to advance the field. This is because of the evolutionary nature of HIS development in which factors associated with the application of HIS can be captured and used as lessons learned for the next evolution of the HIS [ 70 ]. In this review, only the study of Inokuchi et al. [ 32 ] addressed this topic. Patient flow is often negatively affected during the implementation of HIS because of changes in the workflow and human resources. Although the effect seemed temporary, learning about these periods and associated factors will bring implications for researchers and policymakers when considering the project timeline and expected challenges. Furthermore, although HISs are found to help healthcare organisations address patient flow management areas such as care coordination, timely access to information, and communication barriers, understanding why and how HIS could enhance each of these aspects can be extremely helpful. Part of the reasons to explain this is because most of the selected studies in this review did not include adequate details of the underlining technologies of the HIS interventions such as: what are the technical supports and architectures, what are the input and output data, or how the output data are represented in the user interface. The lack of technical specifications of the HIS interventions made it hard to fully comprehend how they contributed to the changes in patient flow management. Finally, during the last two years, the COVID-19 pandemic has completely disrupted patient flow management all over the world. Yet, we could not identify any studies on the role of HIS in remedying the impacts of the pandemic on patient flow.
7. Conclusion
Health information systems (HISs) provide clear benefits in managing patient flow over traditional paper record management systems. However, without a systematic evaluation and summary of the available evidence, stakeholders interested in adopting HISs in healthcare settings for patient low management might be lost in the ocean of information. This is especially true when it comes to the questions of what HIS to invest, what benefits and impacts to expect and how to maximize the values from their investment. This systematic review has revealed an increasing interest in adopting HIS to address patient flow issues in healthcare settings in the last decade. HISs can be effective solutions for patient flow management at the organisational-wide or even network-wide levels due to their great scalability and integrability. HISs were often found to be effective in improving communication and care coordination between team members, providing timely access to high quality information for decision making, and streamlining care processes. These improvements contributed to more efficient patient flow throughout the care continuum. As more healthcare and health-related data are generated, there are great opportunities for HISs such as decision support systems, and dashboard systems to help healthcare organisations harness the power of big-data analytics and achieve optimal patient flow. This review shows that HISs can impact various aspects of patient flow at different levels of care; however, how and why they delivered the impacts will require further research.
Supporting information
S1 file. search strategy..
https://doi.org/10.1371/journal.pone.0274493.s001
S2 File. Reported benefits of HISs on patient flow management.
https://doi.org/10.1371/journal.pone.0274493.s002
S3 File. Table of all included studies and findings.
https://doi.org/10.1371/journal.pone.0274493.s003
S4 File. Example of data extraction form.
https://doi.org/10.1371/journal.pone.0274493.s004
S5 File. Quality assessment of the included studies.
https://doi.org/10.1371/journal.pone.0274493.s005
S6 File. PRISMA checklist.
https://doi.org/10.1371/journal.pone.0274493.s006
Acknowledgments
We would like to thank the Faculty of Information Technology (Monash University) subject librarian, Mario Sos for his great expertise and valuable feedback in developing the search strategy. We are grateful for generous help from Quang H Vo in screening the titles, abstracts and full-text papers in our review. Also, Angela Melder from Monash Centre for Health Research and Implementation, Monash University and Monash Health gave us valuable feedback on the inclusion/exclusion criteria during the screening process.
- View Article
- PubMed/NCBI
- Google Scholar
- 12. Rutherford PA, Provost LP, Kotagal UR, Luther K, Anderson A. Achieving hospital-wide patient flow. IHI White Paper. Cambridge: Institute for Healthcare Improvement. 2017.
- 17. Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org .
To read this content please select one of the options below:
Please note you do not have access to teaching notes, methods for evaluating hospital information systems: a literature review.
EuroMed Journal of Business
ISSN : 1450-2194
Article publication date: 16 May 2008
It is widely accepted that the use of information and communication technology (ICT) in the healthcare sector offers great potential for improving the quality of services provided, the efficiency and effectiveness of personnel, and also reducing organizational expenses. This paper seeks to examine various hospital information system (HIS) evaluation methods.
Design/methodology/approach
In this paper a comprehensive search of the literature concerning the evaluation of complex health information systems is conducted and used to generate a synthesis of the literature around evaluation efforts in this field. Three approaches for evaluating hospital information systems are presented – user satisfaction, usage, and economic evaluation.
The main results are that during the past decade, computers and information systems, as well as their resultant products, have pervaded hospitals worldwide. Unfortunately, methodologies to measure the various impacts of these systems have not evolved at the same pace. To summarize, measurement of users' satisfaction with information systems may be the most effective evaluation method in comparison with the rest of the methods presented.
Practical implications
The methodologies, taxonomies and concepts presented in this paper could benefit researchers and practitioners in the evaluation of HISs.
Originality/value
This review points out the need for more thorough evaluations of HISs that look at a wide range of factors that can affect the relative success or failure of these systems.
- Information systems
- Customer satisfaction
- Economic performance
Aggelidis, V.P. and Chatzoglou, P.D. (2008), "Methods for evaluating hospital information systems: a literature review", EuroMed Journal of Business , Vol. 3 No. 1, pp. 99-118. https://doi.org/10.1108/14502190810873849
Emerald Group Publishing Limited
Copyright © 2008, Emerald Group Publishing Limited
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
- Research article
- Open access
- Published: 04 September 2014
Implementing electronic health records in hospitals: a systematic literature review
- Albert Boonstra 1 ,
- Arie Versluis 2 &
- Janita F J Vos 1
BMC Health Services Research volume 14 , Article number: 370 ( 2014 ) Cite this article
94k Accesses
169 Citations
55 Altmetric
Metrics details
The literature on implementing Electronic Health Records (EHR) in hospitals is very diverse. The objective of this study is to create an overview of the existing literature on EHR implementation in hospitals and to identify generally applicable findings and lessons for implementers.
A systematic literature review of empirical research on EHR implementation was conducted. Databases used included Web of Knowledge, EBSCO, and Cochrane Library. Relevant references in the selected articles were also analyzed. Search terms included Electronic Health Record (and synonyms), implementation, and hospital (and synonyms). Articles had to meet the following requirements: (1) written in English, (2) full text available online, (3) based on primary empirical data, (4) focused on hospital-wide EHR implementation, and (5) satisfying established quality criteria.
Of the 364 initially identified articles, this study analyzes the 21 articles that met the requirements. From these articles, 19 interventions were identified that are generally applicable and these were placed in a framework consisting of the following three interacting dimensions: (1) EHR context, (2) EHR content, and (3) EHR implementation process.
Conclusions
Although EHR systems are anticipated as having positive effects on the performance of hospitals, their implementation is a complex undertaking. This systematic review reveals reasons for this complexity and presents a framework of 19 interventions that can help overcome typical problems in EHR implementation. This framework can function as a reference for implementers in developing effective EHR implementation strategies for hospitals.
Peer Review reports
In recent years, Electronic Health Records (EHRs) have been implemented by an ever increasing number of hospitals around the world. There have, for example, been initiatives, often driven by government regulations or financial stimulations, in the USA [ 1 ], the United Kingdom [ 2 ] and Denmark [ 3 ]. EHR implementation initiatives tend to be driven by the promise of enhanced integration and availability of patient data [ 4 ], by the need to improve efficiency and cost-effectiveness [ 5 ], by a changing doctor-patient relationship toward one where care is shared by a team of health care professionals [ 5 ], and/or by the need to deal with a more complex and rapidly changing environment [ 6 ].
EHR systems have various forms, and the term can relate to a broad range of electronic information systems used in health care. EHR systems can be used in individual organizations, as interoperating systems in affiliated health care units, on a regional level, or nationwide [ 1 , 2 ]. Health care units that use EHRs include hospitals, pharmacies, general practitioner surgeries, and other health care providers [ 7 ].
The implementation of hospital-wide EHR systems is a complex matter involving a range of organizational and technical factors including human skills, organizational structure, culture, technical infrastructure, financial resources, and coordination [ 8 , 9 ]. As Grimson et al. [ 5 ] argue, implementing information systems (IS) in hospitals is more challenging than elsewhere because of the complexity of medical data, data entry problems, security and confidentiality concerns, and a general lack of awareness of the benefits of Information Technology (IT). Boonstra and Govers [ 10 ] provide three reasons why hospitals differ from many other industries, and these differences might also affect EHR implementations. The first reason is that hospitals have multiple objectives, such as curing and caring for patients, and educating new physicians and nurses. Second, hospitals have complicated and highly varied structures and processes. Third, hospitals have a varied workforce including medical professionals who possess high levels of expertise, power, and autonomy. These distinct characteristics justify a study that focuses on the identification and analysis of the findings of previous studies on EHR implementation in hospitals.
Study aim, theoretical framework, and terminology
In dealing with the complexity of EHR implementation in hospitals, it is helpful to know which factors are seen as important in the literature and to capture the existing knowledge on EHR implementation in hospitals. As such, the objective of this research is to identify, categorize, and analyze the existing findings in the literature on EHR implementation processes in hospitals. This could contribute to greater insight into the underlying patterns and complex relationships involved in EHR implementation and could identify ways to tackle EHR implementation problems. In other words, this study focusses on the identification of factors that determine the progress of EHR implementation in hospitals. The motives behind implementing EHRs in hospitals and the effects on performance of implemented EHR systems are beyond the scope of this paper.
To our knowledge, there have been no systematic reviews of the literature concerning EHR implementation in hospitals and this article therefore fills that gap. Two interesting related review studies on EHR implementation are Keshavjee et al. [ 11 ] and McGinn et al. [ 12 ]. The study of Keshavjee et al. [ 11 ] develops a literature based integrative framework for EHR implementation. McGinn et al. [ 12 ] adopt an exclusive user perspective on EHR and their study is limited to Canada and countries with comparable socio-economic levels. Both studies are not explicitly focused on hospitals and include other contexts such as small clinics and national or regional EHR initiatives.
This systematic review is explicitly focused on hospital-wide, single hospital EHR implementations and identifies empirical studies (that include collected primary data) that reflect this situation. The categorization of the findings from the selected articles draws on Pettigrew’s framework for understanding strategic change [ 13 ]. This model has been widely applied in case study research into organizational contexts [ 14 ], as well as in studies on the implementation of health care innovations [ 15 ]. It generates insights by analyzing three interactive dimensions – context , content , and process – that together shape organizational change. Pettigrew’s framework [ 13 ] is seen as applicable because implementing an EHR artefact is an organization-wide effort. This framework was specifically selected for its focus on organizational change, its ease of understanding, and its relatively general dimensions allowing a broad range of findings to be included. The framework structures and focusses the analysis of the findings from the selected articles.
An organization’s context can be divided into internal and external components. External context refers to the social, economic, political, and competitive environments in which an organization operates. The internal context refers to the structure, culture, resources, capabilities, and politics of an organization. The content covers the specific areas of the transformation under examination. In an EHR implementation, these are the EHR system itself (both hardware and software), the work processes, and everything related to these (e.g. social conditions). The process dimension concerns the processes of change, made up of the plans, actions, reactions, and interactions of the stakeholders, rather than work processes in general. It is important to note that Pettigrew [ 13 ] does not see strategic change as a rational analytical process but rather as an iterative, continuous, multilevel process. This highlights that the outcome of an organizational change will be determined by the context, content, and process of that change. The framework with its three categories, shown in Figure 1 , illustrates the conceptual model used to categorize the findings of this systematic literature review.
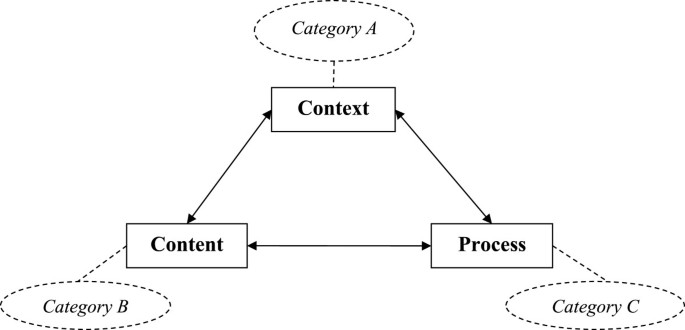
Pettigrew ’ s framework [ 13 ] ] and the corresponding categories.
In the literature, several terms are used to refer to electronic medical information systems. In this article, the term Electronic Health Record (EHR) is used throughout. Commonly used terms identified by ISO (the International Organization for Standardization) [ 16 ] plus another not identified by ISO are outlined below and used in our search. ISO considers Electronic Health Record (EHR) to be an overall term for “ a repository of information regarding the health status of a subject of care , in computer processable form ” [ 16 ], p. 13. ISO uses different terms to describe various types of EHRs. These include Electronic Medical Record (EMR), which is similar to an EHR but restricted to the medical domain. The terms Electronic Patient Record (EPR) and Computerized Patient Record (CPR) are also identified. Häyrinen et al. [ 17 ] view both terms as having the same meaning and referring to a system that contains clinical information from a particular hospital. Another term seen is Electronic Healthcare Record (EHCR) which refers to a system that contains all the available health information on a patient [ 17 ] and can thus be seen as synonymous with EHR [ 16 ]. A term often found in the literature is Computerized Physician Order Entry (CPOE). Although this term is not mentioned by ISO [ 16 ] or by Häyrinen et al. [ 17 ], we included CPOE for three reasons. First, it is considered by many to be a key hospital-wide function of an EHR system e.g. [ 8 , 18 ]. Second, from a preliminary analysis of our initial results, we found that, from the perspective of the implementation process, comparable issues and factors emerged from both CPOEs and EHRs. Third, the implementation of a comprehensive electronic medical record requires physicians to make direct order entries [ 19 ]. Kaushal et al. define a CPOE as “ a variety of computer - based systems that share the common features of automating the medication ordering process and that ensure standardized , legible , and complete orders ” [ 18 ], p. 1410. Other terms found in the literature were not included in this review as they were considered either irrelevant or too broadly defined. Examples of such terms are Electronic Client Record (ECR), Personal Health Record (PHR), Digital Medical Record (DMR), Health Information Technology (HIT), and Clinical Information System (CIS).
Search strategies
In order for a systematic literature review to be comprehensive, it is essential that all terms relevant to the aim of the research are covered in the search. Further, we need to include relevant synonyms and related terms, both for electronic medical information systems and for hospitals. By adding an * to the end of a term, the search engines pick out other forms, and by adding “ “ around words one ensures that only the complete term is searched for. Further, by including a ? as a wildcard character, every possible combination is included in the search.
The search used three categories of keywords. The first category included the following terms as approximate synonyms for hospital: “hospital*”, “healthcare”, and “clinic*”. The second category concerned implementation and included the term “implement*”. For the third category, electronic medical information systems, the following search terms were used: “Electronic Health Record*”, “Electronic Patient Record*”, “Electronic Medical Record*”, “Computeri?ed Patient Record*”, “Electronic Healthcare Record*”, “Computeri?ed Physician Order Entry”.
This relatively large set of keywords was necessary to ensure that articles were not missed in the search, and required a large number of search strategies to cover all those keywords. As we were seeking papers about the implementation of electronic medical information systems in hospitals , the search strategies included the terms shown in Table 1 .
The following three search engines were chosen based on their relevance to the field and their accessibility by the researcher: Web of knowledge, EBSCO, and The Cochrane Library. Most search engines use several databases but not all of them were relevant for this research as they serve a wide range of fields. Appendix A provides an overview of the databases used. The reference lists included in articles that met the selection criteria were checked for other possibly relevant studies that had not been identified in the database search.
The articles identified from the various search strategies had to be academic peer-reviewed articles if they were to be included in our review. Further, they were assessed and had to satisfy the following criteria to be included: (1) written in English, (2) full text available online, (3) based on primary empirical data, (4) focused on hospital-wide EHR implementation, and (5) meeting established quality criteria. A long list of abstracts was generated, and all of them were independently reviewed by two of the authors. They independently reviewed the abstracts, eliminated duplicates and shortlisted abstracts for detailed review. When opinions differed, a final decision over inclusion was made following a discussion between the researchers.
Data analysis
The quality of the articles that survived this filtering was assessed by the first two authors using the Standard Quality Assessment Criteria for Evaluating Primary Research Papers [ 18 ]. In other words, the quality of the articles was jointly assessed by evaluating whether specific criteria had been addressed, resulting in a rating of 2 (fully addressed), 1 (partly addressed), or 0 (not addressed) for each criteria. Different questions are posed for qualitative and quantitative research and, in the event of a mixed-method study, both questionnaires were used. Papers were included if they received at least half of the total possible points, admittedly a relatively liberal cut-off point given comments in the Standard Quality Assessment Criteria for Evaluating Primary Research Papers [ 20 ].
The next step was to extract the findings of the reviewed articles and to analyze these with the aim of reaching general findings on the implementation of EHR systems in hospitals. Categorizing these general findings can increase clarity. The earlier introduced conceptual model, based on Pettigrew’s framework for understanding strategic change, includes three categories: context (A), content (B), and process (C). As our review is specifically aimed at identifying findings related to the implementation process, possible motives for introducing such a system, as well as its effects and outcomes, are outside its scope. The authors held frequent discussions between themselves to discuss the meaning and the categorization of the general findings.
Paper selection
Applying the 18 search strategies listed in Table 1 with the various search engines resulted in 364 articles being identified. The searches were carried out on 12 March 2013 for search strategies 1–15 and on 18 April 2013 for search strategies 16–18. The latter three strategies were added following a preliminary analysis of the first set of results which highlighted several other terms and descriptions for information technology in health care. Not surprisingly, many duplicates were included in the 364 articles, both within and between search engines. Using the Refworks functions for identifying exact and close duplicates, 160 duplicates were found. However, this procedure did not identify all the duplicates present and the second author carried out a manual check that identified an additional 23 duplicates. When removing duplicates, we retained the link to the first search engine that identified the article and, as the Web of Knowledge was the first search engine used, most articles appear to have stemmed from this search engine. This left 181 different articles which were screened on title and abstract to check whether they met the selection criteria. When this was uncertain, the contents of the paper were further investigated. This screening resulted in just 13 articles that met all the selection criteria. We then performed two additional checks for completeness. First, checking the references of these articles identified another nine articles. Second, as suggested by the referees of this paper, we also used the term “introduc*” instead of “implement*”, together with the other two original categories of terms, and the term “provider” instead of “physician”, as part of CPOE. Each of these two searches identified one additional article (see Table 1 ). Of these resulting 24 articles, two proved to be almost identical so one was excluded, resulting in 23 articles for a final quality assessment.The results of the quality assessment can be found in Appendix B. The results show that two articles failed to meet the quality threshold and so 21 articles remained for in-depth analysis. Figure 2 displays the steps taken in this selection procedure.
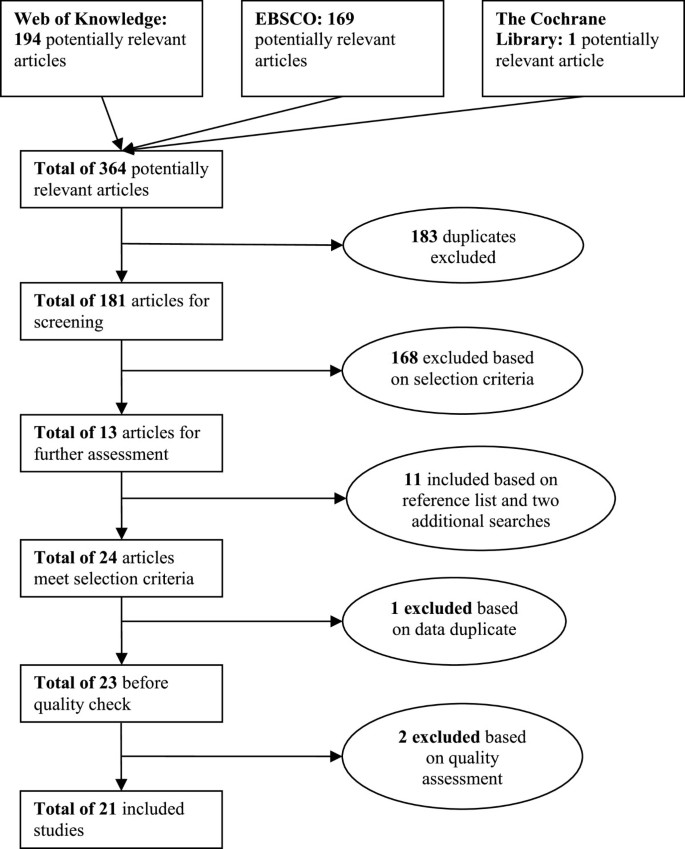
Selection procedure.
To provide greater insight into the context and nature of the 21 remaining articles, an overview is provided in Table 2 . All the studies except one were published after 2000. This reflects the recent increase in effort to implement organization-wide information systems, such as EHR systems, and also increasing incentives from governments to make use of EHR systems in hospitals. Of the 21 studies, 14 can be classified as qualitative, 6 as quantitative, and 1 as a mixed-method study. Most studies were conducted in the USA, with eight in various European countries. Teaching and non-teaching hospitals are almost equally the subject of inquiry, and some researchers have focused on specific types of hospitals such as rural, critical access, or psychiatric hospitals. Ten of the articles were in journals with a five-year impact factor in the Journal Citation Reports 2011 database. There is a huge difference in the number of citations but one should never forget that newer studies have had fewer opportunities to be cited.
Theoretical perspectives of reviewed articles
In research, it is common to use theoretical frameworks when designing an academic study [ 41 ]. Theoretical frameworks provide a way of thinking about and looking at the subject matter and describe the underlying assumptions about the nature of the subject matter [ 42 ]. By building on existing theories, research becomes focused in aiming to enrich and extend the existing knowledge in that particular field [ 42 ]. To provide a more thorough understanding of the selected articles, their theoretical frameworks, if present, are outlined in Table 3 .
It is striking that no specific theoretical frameworks have been used in the research leading to 13 of the 21 selected articles. Most articles simply state their objective as gaining insight into certain aspects of EHR implementation (as shown in Table 1 ) and do not use a particular theoretical approach to identify and categorize findings. As such, these articles add knowledge to the field of EHR implementation but do not attempt to extend existing theories.
Aarts et al. [ 21 ] introduce the notion of the sociotechnical approach: emphasizing the importance of focusing both on the social aspects of an EHR implementation and on the technical aspects of the system. Using the concept of emergent change, they argue that an implementation process is far from linear and predictable due to the contingencies and the organizational complexity that influences the process. A sociotechnical approach and the concept of emergent change are also included in the theoretical framework of Takian et al. [ 37 ]. Aarts et al. [ 21 ] elaborate on the sociotechnical approach when stating that the fit between work processes and the information technology determines the success of the implementation. Aarts and Berg [ 22 ] introduce a model of success or failure in information system implementation. They see creating synergy among the medical work practices, the information system, and the hospital organization as necessary for implementation, and argue that this will only happen if sufficient people accept a change in work practices. Cresswell et al.’s study [ 26 ] is also influenced by sociotechnical principles and draws on Actor-Network Theory. Gastaldi et al. [ 28 ] perceive Electronic Health Records as knowledge management systems and question how such systems can be used to develop knowledge assets. Katsma et al. [ 31 ] focus on implementation success and elaborate on the notion that implementation success is determined by system quality and acceptance through participation. As such, they adopt more of a social view on implementation success rather than a sociotechnical approach. Rivard et al. [ 34 ] examine the difficulties in EHR implementation from a cultural perspective. They not only view culture as a set of assumptions shared by an entire collective (an integration perspective) but also expect subcultures to exist (a differentiation perspective), as well as individual assumptions not shared by a specific (sub-) group (fragmentation perspective). Ford et al. [ 27 ] focus on an entirely different topic and investigate the IT adoption strategies of hospitals using a framework that identifies three strategies. These are the single-vendor strategy (in which all IT is purchased from a single vendor), the best-of-breed strategy (integrating IT from multiple vendors), and the best-of-suit strategy (a hybrid approach using a focal system from one vendor as the basis plus other applications from other vendors).
To summarize, the articles by Aarts et al. [ 21 ], Aarts and Berg [ 22 ], Cresswell et al. [ 26 ], and Takian et al. [ 37 ] apply a sociotechnical framework to focus their research. Gastaldi et al. [ 28 ] see EHRs as a means to renew organizational capabilities. Katsma et al. [ 31 ] use a social framework by focusing on the relevance of an IT system as perceived by the user and the participation of users in the implementation process. Rivard et al. [ 34 ] analyze how organizational cultures can be receptive to EHR implementation. Ford et al. [ 27 ] look at adoption strategies, leading them to focus on the selection procedure for Electronic Health Records. The 13 other studies did not use an explicit theoretical lens in their research.
Implementation-related findings
The process of categorization started by assessing whether a specific finding from a study should be placed in Category A, B, or C. Thirty findings were placed in Category A (context), 31 in Category B (content), and 66 in Category C (process). Comparing and combining the specific findings resulted in several general findings within each category. The general findings are each given a code (category character plus number) and the related code is indicated alongside each specific finding in Appendix C. Findings that were only seen in one article, and thus were lacking support, were discarded.
Category A - context
The context category of an EHR implementation process includes both internal variables (such as resources, capabilities, culture, and politics) and external variables (such as economic, political, and social variables). Six general findings were identified, all but one related to internal variables. An overview of the findings and corresponding articles can be found in Table 4 . The lack of general findings related to external variables reflects our decision to exclude the underlying reasons (e.g. political or social pressures) for implementing an EHR system from this review. Similarly, internal findings related to aspects such as perceived financial benefits or improved quality of care, are outside our scope.
A1: Large (or system-affiliated), urban, not-for-profit, and teaching hospitals are more likely to have implemented an EHR system due to having greater financial capabilities, a greater change readiness, and less focus on profit
The research reviewed shows that larger or system-affiliated hospitals are more likely to have implemented an EHR system, and that this can be explained by their easier access to the large financial resources required. Larger hospitals have more financial resources than smaller hospitals [ 30 ] and system-affiliated hospitals can share costs [ 27 ]. Hospitals situated in urban areas more often have an EHR system than rural hospitals, which is attributed to less knowledge of EHR systems and less support from medical staff in rural hospitals [ 29 ]. The fact that not-for-profit hospitals more often have an EHR system fully implemented and teaching hospitals slightly more often than private hospitals is attributed to the latter’s more wait-and-see approach and the more progressive change-ready nature of public and teaching hospitals [ 27 , 32 ].
A2: EHR implementation requires the selection of a mature vendor who is committed to providing a system that fits the hospital’s specific needs
Although this finding is not a great surprise, it is relevant to discuss it further. A hospital selecting its own vendor can ensure that the system will match the specific needs of that hospital [ 32 ]. Further, it is important to deal with a vendor that has proven itself on the EHR market with mature and successful products. The vendor must also be able to identify hospital workflows and adapt its product accordingly, and be committed to a long-term trusting relationship with the hospital [ 33 ]. With this in mind, the initial price of the system should not be the overriding consideration: the organization should be willing to avoid purely cost-oriented vendors [ 28 ], as costs soon mount if problems arise.
A3: The presence of hospital staff with previous experience of health information technology increases the likelihood of EHR implementation as less uncertainty is experienced by the end-users
In order to be able to work with an EHR system, users must be capable of using information technology such as computers and have adequate typing skills [ 19 , 32 ]. Knowledge of, and previous experience with, EHR systems or other medical information systems reduces uncertainty and disturbance for users, and this results in a more positive attitude towards the system [ 29 , 32 , 37 , 38 ].
A4: An organizational culture that supports collaboration and teamwork fosters EHR implementation success because trust between employees is higher
The influence of organizational culture on the success of organizational change is addressed in almost all the popular approaches to change management, as well as in several of the articles in this literature review. Ash et al. [ 23 , 24 ] and Scott et al. [ 35 ] highlight that a strong culture with a history of collaboration, teamwork, and trust between different stakeholder groups minimizes resistance to change. Boyer et al. [ 25 ] suggest creating a favorable culture that is more adaptive to EHR implementation. However, creating a favorable culture is not necessarily easy: a comprehensive approach including incentives, resource allocation, and a responsible team was used in the example of Boyer et al. [ 25 ].
A5: EHR implementation is most likely in an organization with little bureaucracy and considerable flexibility as changes can be rapidly made
A highly bureaucratic organizational structure hampers change: it slows the process and often leads to inter-departmental conflict [ 19 ]. Specifically, appointing a multidisciplinary team to deal with EHR-related issues can prevent conflict and stimulate collaboration [ 25 ].
A6: EHR system implementation is difficult because cure and care activities must be ensured at all times
During the process of implementing an EHR system, it is of the utmost importance that all relevant information is always available [ 28 , 34 , 39 ]. Ensuring the continuity of quality care while implementing an EHR system is difficult and is an important distinction from many other IT implementations.
Category B - content
The content of the EHR implementation process consists of the EHR system and the corresponding objectives, assumptions, and complementary services. Table 5 lists the five extracted general findings. These focus on both the hardware and software of the EHR system, and its relation to work practices and privacy.
B1: Creating a fit by adapting both the technology and work practices is a key factor in the implementation of EHR
This finding elaborates on the sociotechnical approach identified in the earlier section on the theories adopted in the articles. Several authors [ 21 , 26 , 31 , 37 ] make clear that creating a fit between the EHR system and the existing work practices requires an initial acknowledgement that an EHR implementation is not just a technical project and that existing work practices will change due to the new system. By customizing and adapting the system to meet specific needs, users will become more open to using it [ 19 , 26 , 28 ].
B2: Hardware availability and system reliability, in terms of speed, availability, and a lack of failures, are necessary to ensure EHR use
In several articles, authors highlight the importance of having sufficient hardware. A system can only be used if it is available to the users, and a system will only be used if it works without problems. Ash et al. [ 24 ], Scott et al. [ 35 ], and Weir et al. [ 19 ] refer to the speed of the system as well as to the availability of a sufficient number of adequate terminals see also [ 40 ] in various locations. Systems must be logically structured [ 29 ], reliable [ 32 ], and provide safe information access [ 37 ]. Boyer et al. [ 25 ] also mention the importance of technical aspects but add that these are not sufficient for EHR implementation.
B3: To ensure EHR implementation, the software needs to be user-friendly with regard to ease of use, efficiency in use, and functionality
Some authors distinguish between technical availability and reliability, and the user-friendliness of the software [ 19 , 24 , 32 ]. They argue that it is not sufficient for a system to be available and reliable, it should also be easy and efficient in use, and provide the functionality required for medical staff to give good care. If a system fails to do this, staff will not use the system and will stick to their old ways of working.
B4: An EHR implementation should contain adequate safeguards for patient privacy and confidentiality
Concerns over privacy and confidentiality are recognized by Boyer et al. [ 25 ] and Houser and Johnson [ 29 ] and are considered as a barrier to EHR implementation. Yoon-Flannery et al. [ 40 ] and Takian et al. [ 37 ] also recognize the importance of patient privacy and the need to address this issue by providing training and creating adequate safeguards.
B5: EHR implementation requires a vendor who is willing to adapt its product to hospital work processes
A vendor must be responsive and enable the hospital to develop its product to ensure a good and usable EHR system [ 32 , 33 ]. By so doing, dependence on the vendor decreases and concerns that arise within the hospital can be addressed [ 32 ]. This finding is related to A2 in the sense that an experienced, cooperative, and flexible vendor is needed to deal with the range of interest groups found in hospitals.
Category C - process
This category refers to the actual process of implementing the EHR system. Variables considered are time, change approach, and change management. In our review, this category produced the largest number of general findings (see Table 6 ), as might be expected given our focus on the implementation process. EHR implementation often leads to anxiety, uncertainty, and concerns about a possible negative impact of the EHR on work processes and quality. The process findings, including leadership, resource availability, communication and participation are explicitly aimed at overcoming resistance to EHR implementation. These interventions help to create a positive atmosphere of goal directedness, co-creation and partnership.
C1: Due to their influential position, management’s active involvement and support is positively associated with EHR implementation, and also counterbalances the physicians’ medical dominance
Several authors note the important role that managers play in EHR implementation. Whereas some authors refer to supportive leadership [ 19 , 24 ], others emphasize that strong and active management involvement is needed [ 25 , 32 – 35 ]. Strong leadership is relevant as it effectively counterbalances the physicians’ medical dominance. For instance, Rivard et al. [ 34 ] observe that physicians’ medical dominance and the status and autonomy of other health professionals hinder collaboration and teamwork, and that this complicates EHR implementation. Poon et al. [ 33 ] acknowledge this aspect and argue for strong leadership in order to deal with the otherwise dominant physicians. They also claim that leaders have to set an example and use the system themselves. At the same time, it is motivating that the implementation is managed by leaders who are recognized by the medical staff, for instance by head nurses and physicians or by former physicians and nurses [ 25 , 33 ]. Ovretveit et al. [ 32 ] argue that it helps the implementation if senior management repeatedly declares the EHR implementation to be of the highest priority and supports this with sufficient financial and human resources. Poon et al. [ 33 ] add to this by highlighting that, especially during uncertainties and setbacks, the common vision that guides the EHR implementation has to be communicated to hospital staff. Sufficient human resources include the selection of competent and experienced project leaders who are familiar with EHR implementation. Scott et al. [ 35 ] identify leadership styles for different phases: participatory leadership is valued in selection decisions, whereas a more hierarchical leadership style is preferable in the actual implementation.
C2: Participation of clinical staff in the implementation process increases support for and acceptance of the EHR implementation
Participation of end-users (the clinical staff) generates commitment and enables problems to be quickly solved [ 25 , 26 , 36 ]. Especially because it is very unlikely that the system will be perfect for all, it is important that the clinical staff become the owner, rather than customers, of the system. Clinical staff should participate at all levels and in all steps [ 19 , 28 , 32 , 36 ] from initial system selection onwards [ 35 ]. Ovretveit et al. [ 32 ] propose that this involvement should have an extensive timeframe, starting in the early stages of implementation, when initial vendor requirements are formulated (‘consultation before implementation’), through to the beginning of the use phase. Creating multidisciplinary work groups which determine the content of the EHR and the rules regarding the sharing of information contributes to EHR acceptance [ 25 ] and ensures realistic approaches acceptable to the clinical staff [ 36 ].
C3: Training end-users and providing real-time support is important for EHR implementation success
Frequently, the end-users of a new EHR system lack experience with the specific EHR system or with EHR systems in general. Although it is increasingly hard to imagine society or workplaces without IT, a large specific system, such as an EHR, still requires considerable training on how to use it properly. The importance of training is often underestimated, and inadequate training will create a barrier to EHR use [ 19 , 29 ]. Consequently, adequate training, of appropriate quantity and quality, must be provided at the right times and locations [ 19 , 32 , 36 ]. Simon et al. [ 36 ] add to this the importance of real-time support, preferably provided by peers and super-users.
C4: A comprehensive implementation strategy, offering both clear guidance and room for emergent change, is needed for implementing an EHR system
Several articles highlight aspects of an EHR implementation strategy. A good strategy facilitates EHR implementation [ 19 , 25 ] and consists of careful planning and preparation [ 36 ], a sustainable business plan, effective communication [ 28 , 40 ] and mandatory implementation [ 19 ]. Emergent change is perceived as a key characteristic of EHR implementation in complex organizations such as hospitals [ 21 ], and this suggests an implementation approach based on a development paradigm [ 31 ], which may initially even involve parallel use of paper [ 26 ]. The notion of emergent change has been variously applied, including in the theoretical frameworks of Aarts et al. [ 21 ] and Katsma et al. [ 31 ]. These studies recognize that EHR implementation is relatively unpredictable due to unforeseen contingencies for which one cannot plan. With their emphasis on emergent change with unpredictable outcomes, Aarts et al. [ 21 ] make a case for acknowledging that unexpected and unplanned contingencies will influence the implementation process. They argue that the changes resulting from these contingencies often manifest themselves unexpectedly and must then be dealt with. Additionally, Takian et al. [ 37 ] state that it is crucial to contextualize an EHR implementation so as to be better prepared for unexpected changes.

C5: Establishing an interdisciplinary implementation group consisting of developers, members of the IT department, and end-users fosters EHR implementation success
In line with the arguments for management support and for the participation of clinical staff, Ovretveit et al. [ 32 ], Simon et al. [ 36 ] and Weir et al. [ 19 ] build a case for using an interdisciplinary implementation group. By having all the direct stakeholders working together, a better EHR system can be delivered faster and with fewer problems.
C6: Resistance of clinical staff, in particular of physicians, is a major barrier to EHR implementation, but can be reduced by addressing their concerns
Clinical staff’s attitude is a crucial factor in EHR implementation [ 36 ]. Particularly, the physicians constitute an important group in hospitals. As such, their possible resistance to EHR implementation will form a major barrier [ 29 , 33 ] and may lead to workarounds [ 26 ]. Whether physicians accept or reject an EHR implementation depends on their acceptance of their work practices being transformed [ 22 ]. The likelihood of acceptance will be increased if implementers address the concerns of physicians [ 24 , 28 , 32 , 33 ], but also of other members of clinical staff [ 36 ].
C7: Identifying champions among clinical staff reduces resistance
The previous finding already elaborated on clinical staff resistance and suggested reducing this by addressing their concerns. Another way to reduce their resistance is related to the process of implementation and involves identifying physician champions, typically physicians that are well respected due to their knowledge and contacts [ 32 , 33 ]. Simon et al. [ 36 ] emphasize the importance of identifying champions among each stakeholder group. These champions can provide reassurance to their peers.
C8: Assigning a sufficient number of staff and other resources to the EHR implementation process is important in adequately implementing the system
Implementing a large EHR system requires considerable resources, including human ones. Assigning appropriate people, such as super-users [ 36 ] and a sufficient number of them to that process will increase the likelihood of success [ 19 , 32 , 33 , 36 ]. Further, it is important to have sufficient time and financial resources [ 26 , 32 ]. This finding is also relevant in relation to finding A6 (ensuring good care during organizational change).
These 19 general findings have been identified from the individual findings within the 20 analyzed articles. These findings are all related to one of the three main and interacting dimensions of the framework: six to context, five to content, and eight to process. This identification and explanation of the general findings concludes the results section of this systematic literature review and forms the basis for the discussion below.
This review of the existing academic literature sheds light on the current knowledge regarding EHR implementation. The 21 selected articles all originate from North America or Europe, perhaps reflecting a greater governmental attention to EHR implementation in these regions and, of course, our inclusion of only articles written in English. Two articles were rejected for quality reasons [ 43 , 44 ], see Appendix B. All but one of the selected articles have been published since 2000, reflecting the growing interest in implementing EHR systems in hospitals. Eight articles built their research on a theoretical framework, four of which use the same general lens of the sociotechnical approach [ 21 , 22 , 26 , 37 ]. Katsma et al. [ 31 ] and Rivard et al. [ 34 ] focus more on the social and cultural aspects of EHR implementation, the former on the relevance for, and participation of, users, the latter on three different cultural perspectives. Ford et al. [ 27 ] researched adoption strategies for EHR systems and Gastaldi et al. [ 26 ] consider them as a means to renew organizational capabilities. It is notable that the other reviewed articles did not use a theoretical framework to analyze EHR implementation and made no attempt to elaborate on existing theories.
A total of 127 findings were extracted from the articles, and these findings were categorized using Pettigrew’s framework for strategic change [ 13 ] as a conceptual model including the three dimensions of context, content, and process. To ensure a tight focus, the scope of the review was explicitly limited to findings related to the EHR implementation process, thus excluding the reasons for, barriers to, and outcomes of an EHR implementation.
Some of the findings require further interpretation. Contextual finding A1 relates to the demographics of a hospital. One of the assertions is that privately owned hospitals are less likely than public hospitals to invest in an EHR. The former apparently perceive the costs of EHR implementation to outweigh the benefits. This seems remarkable given that there is a general belief that information technology increases efficiency and reduces process costs, so more than compensating for the high initial investments. It is however important to note that the literature on EHR is ambivalent when it comes to efficiency; several authors record a decrease in the efficiency of work practices [ 25 , 33 , 35 , 38 ], whereas others mention an increase [ 29 , 31 ]. Finding A2 is a reminder of the importance of carefully selecting an appropriate vendor, taking into account experience with the EHR market and the maturity of their products rather than, for example, focussing on the cost price of the system. Given the huge investment costs, the price of an EHR system tends to have a major influence on vendor selection, an aspect that is also promoted by the current European tendering regulations that oblige (semi-) public institutions, like many hospitals, to select the lowest bidder, or the bidder that is economically the most preferable [ 45 ]. The finding that EHR system implementation is difficult because good medical care needs to be ensured at all times (A6) also deserves mention. Essentially, many system implementations in hospitals are different from IT implementations in other contexts because human lives are at stake in hospitals. This not only complicates the implementation process because medical work practices have to continue, it also requires a system to be reliable from the moment it is launched.
The findings regarding the content of the EHR system (Category B) highlight the importance of a suitable software product. A well-defined selection process of the software package and its associated vendor (discussed in A2) is seen as critical (B5). Selection should be based on a careful requirements analysis and an analysis of the experience and quality of the vendor. An important requirement is a sufficient degree of flexibility to customize and adapt the software to meet the needs of users and the work practices of the hospital (finding B1). At the same time the software product should challenge the hospital to rethink and improve its processes. A crucial condition for the acceptance by the diverse user groups of hospitals is the robustness of the EHR system in terms of availability, speed, reliability and flexibility (B2). This also requires adequate hardware in terms of access to computers, and mobile equipment to enable availability at all the locations of the hospital. Perceived ease of use of the system (B4) and the protection of patients’ privacy (B4) are other content factors that can make or break EHR implementation in hospitals.
The findings on the implementation process, our Category C, highlight four aspects that are commonly mentioned in change management approaches as important success factors in organizational change. The active involvement and support of management (C1), the participation of clinical staff (C2), a comprehensive implementation strategy (C4), and using an interdisciplinary implementation group (C5) correspond with three of the ten guidelines offered by Kanter et al. [ 46 ]. These three guidelines are: (1) support a strong leader role; (2) communicate, involve people, and be honest; and (3) craft an implementation plan. As the implementation of an EHR system is an organizational change process it is no surprise that these commonalities are identified in several of the analyzed articles. Three Category C findings (C2, C6, and C7) concern dealing with clinical staff given their powerful positions and potential resistance. Physicians are the most influential medical care providers, and their resistance can delay an EHR implementation [ 23 ], lead to at least some of it being dropped [ 21 , 22 , 34 ], or to it not being implemented at all [ 33 ]. Thus, there is ample evidence of the crucial importance of physicians’ acceptance of an EHR for it to be implemented. This means that clinicians and other key personnel should be highly engaged and motivated to contribute to EHR. Prompt feedback on requests, and high quality support during the implementation, and an EHR that clearly supports clinical work are key issues that contribute to a motivated clinical staff.
Analyzing and comparing the findings enables us to categorize them in terms of subject matter (see Table 7 ). By categorizing the findings in terms of subject, and by totaling the number of articles related to the individual findings on that subject, one can deduce how much attention has been given in the literature to the different topics. This analysis highlights that the involvement of physicians in the implementation process, the quality of the system, and a comprehensive implementation strategy are considered the crucial elements in EHR implementation.
Notwithstanding the useful results, this review and analysis has some limitations. Although we carefully developed and executed the search strategy, we cannot be sure that we found all the relevant articles. Since we focused narrowly on keywords, and these had to be part of an article’s title, we could have excluded relevant articles that used different terminology in their titles. Although searching the reference lists of identified articles did result in several additional articles, some relevant articles might still have been missed. Another limitation is the exclusion of publications in languages other than English. Further, the selection and categorization of specific findings, and the subsequent extraction of general findings, is subjective and depends on the interpretations of the authors, and other researchers might have made different choices. A final limitation is inherent to literature reviews in that the authors of the studies included may have had different motives and aims, and used different methods and interpretative means, in drawing their conclusions.
The existing literature fails to provide evidence of there being a comprehensive approach to implementing EHR systems in hospitals that integrates relevant aspects into an ‘EHR change approach’. The literature is diffuse, and articles seldom build on earlier ones to increase the theoretical knowledge on EHR implementation, notable exceptions being Aarts et al. [ 21 ], Aarts and Berg [ 22 ], Cresswell et al. [ 26 ], and Takian et al. [ 37 ]. The earlier discussion on the various results summarizes the existing knowledge and reveals gaps in the knowledge associated with EHR implementation. The number of EHR implementations in hospitals is growing, as well as the body of literature on this subject. This systematic review of the literature has produced 19 general findings on EHR implementation, which were each placed in one of three categories. A number of these general findings are in line with the wider literature on change management, and others relate to the specific nature of EHR implementation in hospitals.
The findings presented in this article can be viewed as an overview of important subjects that should be addressed in implementing an EHR system. It is clear that EHR systems have particular complexities and should be implemented with great care, and with attention given to context, content, and process issues and to interactions between these issues. As such, we have achieved our research goal by creating a systematic review of the literature on EHR implementation. This paper’s academic contribution is in providing an overview of the existing literature with regard to important factors in EHR implementation in hospitals. Academics interested in this specific field can now more easily access knowledge on EHR implementation in hospitals and can use this article as a starting point and build on the existing knowledge. The managerial contribution lies in the general findings that can be applied as guidelines when implementing EHR in hospitals. We have not set out to provide a single blueprint for implementing an EHR system, but rather to provide guidelines and to highlight points that deserve attention. Recognizing and addressing these aspects can increase the likelihood of getting an EHR system successfully implemented.
Appendix A - List of databases
This appendix provides an overview of all databases included in the used search engines. The databases in italic were excluded for the research as these databases focus on fields not relevant for the subject of EHR implementations.
Web of Knowledge
Web of Science
Biological Abstracts
Journal Citation Reports
Academic Search Premier
AMED - The Allied and Complementary Medicine Database
America : History & Life
American Bibliography of Slavic and East European Studies
Arctic & Antarctic Regions
Art Full Text ( H.W. Wilson )
Art Index Retrospective ( H.W. Wilson )
ATLA Religion Database with ATLASerials
Business Source Premier
Communication & Mass Media Complete
eBook Collection ( EBSCOhost )
Funk & Wagnalls New World Encyclopedia
Historical Abstracts
L ’ Annéephilologique
Library, Information Science & Technology Abstracts
MAS Ultra - School Edition
Military & Government Collection
MLA Directory of Periodicals
MLA International Bibliography
New Testament Abstracts
Old Testament Abstracts
Philosopher ’ s Index
Primary Search
PsycARTICLES
PsycCRITIQUES
Psychology and Behavioral Sciences Collection
Regional Business News
Research Starters - Business
RILM Abstracts of Music Literature
The Cochrane Library
Cochrane Database of Systematic Reviews
Cochrane Central Register of Controlled Trials
Cochrane Methodology Register
Database of Abstracts of Reviews of Effects
Health Technology Assessment Database
NHS Economic Evaluation Database
About The Cochrane Collaboration
Appendix B - Quality assessment
The quality of the articles was assessed with the Standard Quality Assessment Criteria for Evaluating Primary Research Papers [ 18 ]. Assessment was done by questioning whether particular criteria had been addressed, resulting in a rating of 2 (completely addressed), 1 (partly addressed), or 0 (not addressed) points. Table 8 provides the overview of the scores of the articles, (per question) for qualitative studies; Table 9 for quantitative studies; and Table 10 for mixed methods studies. Articles were included if they scored 50% or higher of the total amount of points possible. Based on this assessment, two articles were excluded from the search.
Appendix C - All findings
Table 11 displays all findings from the selected articles. The category number is related to the general finding as discussed in the Results section.
Abramson EL, McGinnis S, Edwards A, Maniccia DM, Moore J, Kaushal R: Electronic health record adoption and health information exchange among hospitals in New York State. J Eval Clin Pract. 2011, 18: 1156-1162.
Article PubMed Google Scholar
Robertson A, Cresswell K, Takian A, Petrakaki D, Crowe S, Cornford T, Sheikh A: Implementation and adoption of nationwide electronic health records in secondary care in England: qualitative analysis of interim results from a prospective national evaluation. Br Med J. 2010, 341: c4564-10.1136/bmj.c4564.
Article Google Scholar
Rigsrevisionen: Extract from the report to the Public Accounts Committee on the implementation of electronic patient records at Danish hospitals. 2011, http://uk.rigsrevisionen.dk/media/1886186/4-2010.pdf , 2011
Google Scholar
Hartswood M, Procter R, Rouncefield M, Slack R: Making a Case in Medical Work: Implications for the Electronic Medical Record. Comput Supported Coop Work. 2003, 12: 241-266. 10.1023/A:1025055829026.
Grimson J, Grimson W, Hasselbring W: The SI Challenge in Health Care. Commun ACM. 2000, 43 (6): 49-55.
Mantzana V, Themistocleous M, Irani Z, Morabito V: Identifying healthcare actors involved in theadoption of information systems. Eur J Inf Syst. 2007, 16: 91-102. 10.1057/palgrave.ejis.3000660.
Boonstra A, Boddy D, Bell S: Stakeholder management in IOS projects: analysis of an attempt to implement an electronic patient file. Eur J Inf Syst. 2008, 17 (2): 100-111. 10.1057/ejis.2008.2.
Jha A, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TF, Shields A, Rosenbaum S, Blumenthal D: Use of Electronic Health Records in US hospitals. N Engl J Med. 2009, 360: 1628-1638. 10.1056/NEJMsa0900592.
Article CAS PubMed Google Scholar
Heeks R: Health information systems: Failure, success and improvisation. Int J Med Inform. 2006, 75: 125-137. 10.1016/j.ijmedinf.2005.07.024.
Boonstra A, Govers MJ: Understanding ERP system implementation in a hospital by analysing stakeholders. N Technol Work Employ. 2009, 24 (2): 177-193. 10.1111/j.1468-005X.2009.00227.x.
Keshavjee K, Bosomworth J, Copen J, Lai J, Kucukyazici B, Liani R, Holbrook AM: Best practices in EMR implementation: a systematic review. Proceed of the 11th International Symposium on Health Information Mangement Research – iSHIMR. 2006, 1-15.
McGinn CA, Grenier S, Duplantie J, Shaw N, Sicotte C, Mathieu L, Leduc Y, Legare F, Gagnon MP: Comparison of use groups perspectives of barriers and facilitator to implementing EHR – a systematic review. BMC Med. 2011, 9: 46-10.1186/1741-7015-9-46.
Article PubMed PubMed Central Google Scholar
Pettigrew AM: Context and action in the transformation of the firm. J Manag Stud. 1987, 24 (6): 649-670. 10.1111/j.1467-6486.1987.tb00467.x.
Hartley J: Case Study Research. Chapter 26. Essential Guide to Qualitative Methods in Organizational Research. Edited by: Cassel C, Symon G. 2004, London: Sage
Hage E, Roo JP, Offenbeek MAG, Boonstra A: Implementation factors and their effect on e-health service adoption in rural communities: a systematic literature review. BMC Health Serv Res. 2013, 13 (19): 1-16.
ISO: Health informatics: Electronic health record - Definition, scope and context. Draft Tech Report. 2004, 03-16. ISO/DTR 20514. available at https://www.iso.org/obp/ui/#iso:std:iso:tr:20514:ed-1:v1:en
Häyrinen K, Saranto K, Nykänen P: Definition, structure, content, use and impacts of electronic health records: A review of the research literature. Int J Med Inform. 2008, 77: 291-304. 10.1016/j.ijmedinf.2007.09.001.
Kaushal R, Shojania KG, Bates DW: Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003, 163 (12): 1409-1416. 10.1001/archinte.163.12.1409.
Weir C, Lincoln M, Roscoe D, Turner C, Moreshead G: Dimensions associated with successful implementation of a hospital based integrated order entry system. Proc Annu Symp Comput Appl [Sic] in Med Care Symp Comput Appl Med Care. 1994, 653: 7.
Kmet LM, Lee RC, Cook LS: Standard quality assessment criteria for evaluating primary research papers from a variety of fields. 2004, Alberta Heritage Foundation for Medical Research, http://www.ihe.ca/documents/HTA-FR13.pdf .
Aarts J, Doorewaard H, Berg M: Understanding implementation: The case of a computerized physician order entry system in a large dutch university medical center. J Am Med Inform Assoc. 2004, 11 (3): 207-216. 10.1197/jamia.M1372.
Aarts J, Berg M: Same systems, different outcomes - Comparing the implementation of computerized physician order entry in two Dutch hospitals. Methods Inf Med. 2006, 45 (1): 53-61.
CAS PubMed Google Scholar
Ash J, Gorman P, Lavelle M, Lyman J, Fournier L: Investigating physician order entry in the field: lessons learned in a multi-center study. Stud Health Technol Inform. 2001, 84 (2): 1107-1111.
Ash JS, Gorman PN, Lavelle M, Payne TH, Massaro TA, Frantz GL, Lyman JA: A cross-site qualitative study of physician order entry. J Am Med Inform Assoc. 2003, 10 (2): 188-200. 10.1197/jamia.M770.
Boyer L, Samuelian J, Fieschi M, Lancon C: Implementing electronic medical records in a psychiatric hospital: A qualitative study. Int J Psychiatry Clin Pract. 2010, 14 (3): 223-227. 10.3109/13651501003717243.
Cresswell KM, Worth A, Sheikh A: Integration of a nationally procured electronic health record system into user work practices. BMC Med Inform Decis Mak. 2012, 12: 15-10.1186/1472-6947-12-15.
Ford EW, Menachemi N, Huerta TR, Yu F: Hospital IT Adoption Strategies Associated with Implementation Success: Implications for Achieving Meaningful Use. J Healthc Manag. 2010, 55 (3): 175-188.
PubMed Google Scholar
Gastaldi L, Lettieri E, Corso M, Masella C: Performance improvement in hospitals: leveraging on knowledge assets dynamics through the introduction of an electronic medical record. Meas Bus Excell. 2012, 16 (4): 14-30. 10.1108/13683041211276410.
Houser SH, Johnson LA: Perceptions regarding electronic health record implementation among health information management professionals in Alabama: a statewide survey and analysis. Perspect Health Inf Manage/AHIMA, Am Health Inf Manage Assoc. 2008, 5: 6-6.
Jaana M, Ward MM, Bahensky JA: EMRs and Clinical IS Implementation in Hospitals: A Statewide Survey. J Rural Health. 2012, 28: 34-43. 10.1111/j.1748-0361.2011.00386.x.
Katsma CP, Spil TAM, Ligt E, Wassenaar A: Implementation and use of an electronic health record: measuring relevance and participation in four hospitals. Int J Healthc Technol Manag. 2007, 8 (6): 625-643. 10.1504/IJHTM.2007.014194.
Ovretveit J, Scott T, Rundall TG, Shortell SM, Brommels M: Improving quality through effective implementation of information technology in healthcare. Int J Qual Health Care. 2007, 19 (5): 259-266. 10.1093/intqhc/mzm031.
Poon EG, Blumenthal D, Jaggi T, Honour MM, Bates DW, Kaushal R: Overcoming barriers to adopting and implementing computerized physician order entry systems in US hospitals. Health Aff. 2004, 23 (4): 184-190. 10.1377/hlthaff.23.4.184.
Rivard S, Lapointe L, Kappos A: An Organizational Culture-Based Theory of Clinical Information Systems Implementation in Hospitals. J Assoc Inf Syst. 2011, 12 (2): 123-162.
Scott JT, Rundall TG, Vogt TM, Hsu J: Kaiser Permanente’s experience of implementing an electronic medical record: a qualitative study. Br Med J. 2005, 331 (7528): 1313-1316. 10.1136/bmj.38638.497477.68.
Simon SR, Keohane CA, Amato M, Coffey M, Cadet M, Zimlichman E: Lessons learned from implementation of computerized provider order entry in 5 community hospitals: a qualitative study. BMC Med Inform Decis Mak. 2013, 13: 67-10.1186/1472-6947-13-67.
Takian A, Sheikh A, Barber N: We are bitter, but we are better off: case study of the implementation of an electronic health record system into a mental health hospital in England. BMC Health Serv Res. 2012, 12: 484-10.1186/1472-6963-12-484.
Ward MM, Vartak S, Schwichtenberg T, Wakefield DS: Nurses’ Perceptions of How Clinical Information System Implementation Affects Workflow and Patient Care. Cin-Comput Inform Nurs. 2011, 29 (9): 502-511. 10.1097/NCN.0b013e31822b8798.
Ward MM, Vartak S, Loes JL, O’Brien J, Mills TR, Halbesleben JRB, Wakefield DS: CAH Staff Perceptions of a Clinical Information System Implementation. Am J Manage Care. 2012, 18 (5): 244-252.
Yoon-Flannery K, Zandieh SO, Kuperman GJ, Langsam DJ, Hyman D, Kaushal R: A qualitative analysis of an electronic health record (EHR) implementation in an academic ambulatory setting. Inform Prim Care. 2008, 16 (4): 277-284.
Van Aken J, Berends H, Van der Bij H: Problem solving in organizations. 2012, New York, USA: Cambridge University Press
Book Google Scholar
Botha ME: Theory development in perspective: the role of conceptual frameworks and models in theory development. J Adv Nurs. 1989, 14 (1): 49-55. 10.1111/j.1365-2648.1989.tb03404.x.
Spetz J, Keane D: Information Technology Implementation in a Rural Hospital: A Cautionary Tale. J Healthc Manag. 2009, 54 (5): 337-347.
Massaro TA: Introducing Physician Order Entry at a Major Academic Medical-Center. Impact Organ Culture Behav Acad Med. 1993, 68 (1): 20-25.
CAS Google Scholar
Lundberg S, Bergman M: Tender evaluation and supplier selection methods in public procurement. J Purch Supply Manage. 2013, 19 (2): 73-83. 10.1016/j.pursup.2013.02.003.
Kanter RM, Stein BA, Jick TD: The Challenge of Organizational Change. 1992, New York, USA: Free Press
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1472-6963/14/370/prepub
Download references
Acknowledgement
We acknowledge the Master degree program Change Management at the University of Groningen for supporting this study. We also thank the referees for their valuable comments.
Author information
Authors and affiliations.
Faculty of Economics and Business, University of Groningen, Groningen, The Netherlands
Albert Boonstra & Janita F J Vos
Deloitte Consulting, Amsterdam, The Netherlands
Arie Versluis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Albert Boonstra .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
AB and JV established the research design and made significant contributions to the interpretation of the results. They supervised AV throughout the study, and participated in writing the final version of this paper. AV contributed substantially to the selection and analysis of included papers, and wrote a preliminary draft of this article. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Boonstra, A., Versluis, A. & Vos, J.F.J. Implementing electronic health records in hospitals: a systematic literature review. BMC Health Serv Res 14 , 370 (2014). https://doi.org/10.1186/1472-6963-14-370
Download citation
Received : 23 September 2013
Accepted : 11 August 2014
Published : 04 September 2014
DOI : https://doi.org/10.1186/1472-6963-14-370
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical Staff
- Electronic Health Record
- Electronic Patient Record
- Health Information Technology
- Computerize Physician Order Entry
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Maturity Models of Healthcare Information Systems and Technologies: a Literature Review
- Systems-Level Quality Improvement
- Published: 15 April 2016
- Volume 40 , article number 131 , ( 2016 )
Cite this article

- João Vidal Carvalho 1 ,
- Álvaro Rocha 2 &
- António Abreu 1
4530 Accesses
90 Citations
3 Altmetric
Explore all metrics
The maturity models are instruments to facilitate organizational management, including the management of its information systems function. These instruments are used also in hospitals. The objective of this article is to identify and compare the maturity models for management of information systems and technologies (IST) in healthcare. For each maturity model, it is identified the methodology of development and validation, as well as the scope, stages and their characteristics by dimensions or influence factors. This study resulted in the need to develop a maturity model based on a holistic approach. It will include a comprehensive set of influencing factors to reach all areas and subsystems of health care organizations.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Information Systems and Technologies Maturity Models for Healthcare: A Systematic Literature Review

Maturity Models for Hospital Information Systems Management: Are They Mature?

Hospital Information Systems Management: Towards a Comprehensive Maturity Model
Freixo, J., and Rocha, Á., Arquitetura de Informação de Suporte à Gestão da Qualidade em Unidades Hospitalares. RISTI - Revista Ibérica de Sistemas e Tecnologias de Informação 14:1–18, 2014.
Google Scholar
Sharma, B., Electronic Healthcare Maturity Model (eHMM). Quintegra Solutions Limited, 2008.
Rocha, Á., Evolution of information systems and technologies maturity in healthcare. Int. J. Healthc. Inf. Syst. Inform. 6(2):28–36, 2011.
Article Google Scholar
Carvalho, J. V., Rocha, A., and Vasconcelos, J. B., Towards an encompassing Maturity Model for the Management of Hospital Information Systems. J. Med. Syst. 39(9):1–9, 2015.
Rocha, Á., and Vasconcelos, J., Os Modelos de Maturidade na Gestão de Sistemas de Informação. Revista da Faculdade de Ciência e Tecnologia da Universidade Fernando Pessoa. 1:93–107, 2004.
Mutafelija, B., and Stromberg, H., Systematic Process Improvement Using ISO 9001:2000 and CMMI . Artech House, Boston, 2003.
Nolan, R., Managing de computer resource: A stage hypotesis. Commun. ACM 16(7):399–405, 1973.
Nolan, R., Managing the crisis in data processing. Harv. Bus. Rev. 57(2):115–126, 1979.
McKenney, J. L., and McFarlan, F. W., The information archipelago - Maps and bridges. Harv. Bus. Rev. 60(5):109–119, 1982.
King, J., and Kraemer, K., Evolution and organizational information systems: An assessment of Nolan’s stage model. Commun. ACM 27(5):466–475, 1984.
Huff, S. L., Munro, M. C., and Martin, B. H., Growth stages of end-user computing. Commun. ACM 31(5):542–550, 1998.
Earl, M. J., Management Strategies for Information Technologies . Prentice Hall, Upper Saddle River, 1989.
Galliers, R. D., and Sutherland, A. R., Information systems management and strategy formulation: The ‘stages of growth’ model revised. J. Inf. Syst. 1(2):89–114, 1991.
Auer, T., Beyond IS Implemention: A Skill-Based Aproach to IS Use. 3rd European Conference on Information Systems, Athens, Greece., 1995.
Khandelwal, V., and Ferguson, J., Critical Success Factors (CSFs) and the Growth of IT in Selected Geographic Regions. Proceedings of 32nd Hawaii International Conference on Systems Sciences (HICSS-32), USA., 1999.
King, W. R., and Teo, T. S. H., Integration between business planning and information systems planning: Validating a stage hypothesis. Decis. Sci. 28(2):279–307, 1997.
Mutsaers, E., Zee, H., and Giertz, H., The evolution of information technology. Inform. Manag. Comput. Secur. 6(3):115–126, 1998.
Nolan, R., and Koot, W., Nolan stages theory today: A framework for senior and IT management to manage information technology. Holland Manag. Rev. 31:1–24, 1992.
Damsgaard, J., and Scheepers, R., Managing the crises in intranet implementation: A stage model. Inf. Syst. J. 10(2):131–149, 2000.
Holland, C., and Light, B., A stage maturity model for enterprise resource planning systems. Data Base Adv. Inf. Syst. 32(2):34–45, 2001.
SEI Software Eng Institute, CMMI® for Development, Version 1.3, Improving processes for developing better products and services. Tech. Rep. No. CMU/SEI-2010-TR-033), Carnegie Mellon University, 2010.
SPICE, SPICE Project: Software Process Assessment: Part 2 - A model for process management, Version 1.0. 1995.
April, A., Abran, A., and Dumke, R., Assessment of software maintenance capability: A model and its architecture. Proceedings of the 8th European Conference on Software Maintenance and Reengineering (CSMR2004), Los Alamitos CA: IEEE Computer Society Press, 2004: p. 243–248.
Levin, G., and Nutt, H., Achieving Excellence in Business Development: The Business Development Capability Maturity Model. 2005. Available from: http://www.maturityresearch.com/novosite/biblio/CMM_Achieving%20Excellence%20in%20Business%20Development.pdf . Accessed Sep 2014.
Kerzner, H., Using the Project Management Maturity Model: Strategic Planning for Project Management , 2nd edition. Wiley, New York, 2005.
Brookes, N., and Clark, R., Using Maturity Models to Improve Project Management Practice. POMS 20th Annual Conference. Orlando Florida USA., 2009.
Murray, A., Capability Maturity Models - Using P3M3 to Improve Performance. Outperform: MakingStrategy Reality, 2006. 2.
Venkatesh, V., et al., User acceptance of information technology: Toward a unified view. MIS Q. 27(3):425–478, 2003.
Renken, J., Developing an IS/ICT management capability maturity framework. . Research conference of the South African Institute for Computer Scientists and Information Technologists (SAICSIT). Stellenbosch, 2004: p. 53–62.
Earl, M. J., Evolving the EBusiness. Bus. Strateg. Rev. 11:33–38, 2000.
Gardler, R., and Mehandjiev, N., Supporting Component-Based Software Evolution . In Aksit, M., Mezini, M. & Unland, R. (Eds.), Objects, Components, Architectures, Services, and Applications for a Networked World, 2003, Series: Lecture Notes in Computer Science , 2591. Springer Verlag., 2003: p. 103–120.
Ludescher, G., and Usrey, M., Towards an ECMM (E-Commerce Maturity Model). Proceedings of the First International Research Conference on Organizational Excellence in the Third Millennium. Estes Park: Colorado State University, 2000.
Marshall, S., E-Learning maturity model. Process descriptions . Victoria University of Wellington, New Zealand, 2007.
Berztiss, A.T., Capability Maturity for Knowledge Management. DEXA Workshop, IEEE Computer Society, 2002: p. 162–166.
Maybury, M.T., Knowledge Management at the MITRE Corporation. The MITRE Corporation, 2002. https://www.researchgate.net/publication/228858770_Knowledge_Management_at_The_MITRE_Corporation .
Rosemann, M., and deBruin, T., Business Process Management Maturity - A Model for Progression. Proceedings of the 13th ECIS, Regensburg, 2005.
Nascio, NASCIO Enterprise Architecture Maturity Model, Version 1.3. National Association of State Chief Information Officers, 2003.
DOC, IT Architecture Capability Maturity Model. Department of Commerce, USA Government Introduction, 2003.
Webster, J., and Watson, R. T., Analyzing the past to prepare for the future: Writing a literature review. MIS Q. 26(2):13–23, 2002.
Tranfield, D., Denyer, D., and Smart, P., Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br. J. Manag. 14:207–222, 2003.
Mettler, T., and Blondiau, A., HCMM – A Maturity Model for Measuring and Assessing the Quality of Cooperation between and within Hospitals. 25th IEEE International Symposium on Computer-Based Medical Systems (CBMS), 2012.
Holland, M., Dunbrack, L., and Piai, S., Healthcare IT Maturity Model: Western European Hospitals - The Leading Countries. European IT Opportunity: Healthcare Healthcare Provider IT Strategies Health Industry Insights, an IDC Company, 2008.
HIMSS, The EMR Adoption Model. HIMSS Analytics: Innovative Research/Informed Decisions, 2008.
Etin, D., Quality of Care with IDC & HIMSS models - Where are eHealth projects going in EMEA? EMC Spark, 2014. Available: http://sparkblog.emc.com/2014/05/quality-care-idc-himss-models-ehealth-projects-going-emea/ . Accessed Sep 2015.
Priestman, W., ICT Strategy 2007–2011 for The Royal Liverpool and Broadgreen University Hospitals NHS Trust. Trust Board Meeting 6th November 2007., 2007. Document Number: V1.4.
Clair, C.L., Electronic Medical Records Need More To Support “Meaningful Use”. Forrester Research Inc, 2010.
NEHTA, Interoperability Maturity Model: Version 2.0 . National E-Health Transition Authority Ltd, Sydney, 2007.
NHS, National Infrastructure Maturity Model [Online]. Available: http://systems.hscic.gov.uk/nimm . Accessed 16 Sep 2015. 2011.
Wetering, R., and Batenburg, R., A PACS maturity model: A systematic meta-analytic review on maturation and evolvability of PACS in the hospital enterprise. Int. J. Med. Inform. 78:127–140, 2009.
Article PubMed Google Scholar
HIMSS, Promoting Usability in Health Organizations: Initial Steps and Progress Toward a Healthcare Usability Maturity Model. Healthcare Information and Management Systems Society, 2011
Sanders, D., Burton, D.A., and Protti, D., The Healthcare Analytics Adoption Model: A Framework and Roadmap (white paper). 2013. Available from: https://www.healthcatalyst.com/whitepaper/healthcare-analytics-adoption-model/ . Accessed Oct 2015.
van Dick, L., and Schutte, C.S.L., The Telemedicine Service Maturity Model: A Framework for the Measurement and Improvement of Telemedicine Services. INTECH: open science/open minds, 2013. Chapter 10: 217–238.
Dunbrack, L. and L. Hand, A Maturity Model for Mobile in Healthcare. IDC Health Insights: Business Strategy, 2013. Doc # HI241777.
Garets, D., and Davis, M., Electronic Medical Records vs. Electronic Health Records: Yes, There Is a Difference. A HIMSS AnalyticsTM White Paper, 2006.
Sanders, D., A Model for Measuring Industry-Wide Adoption and Capability of Healthcare Analytics and Data Warehousing in the USA . ElectronicHealthcare 11(2), 2012.
Wetering, R., and Batenburg, R., Towards a Theory of PACS Deployment: An Integrative PACS Maturity Framework. J Digit Imaging . 27(3):337–350, 2014.
Staggers, N. and M. Rodney, Promoting Usability in Organizations with a New Health Usability Model: Implications for Nursing Informatics. NI 2012: Proceedings of the 11th International Congress on Nursing Informatics, 396, 2012.
Nielsen, J., Corporate Usability Maturity Stages: 1–4 and 5–8. 2006. Available from: https://www.nngroup.com/articles/usability-maturity-stages-1-4/ . Accessed Nov 2015.
Earthy, J., Usability Maturity Model: Human-Centredness Scale. IE2016 INUSE Deliverable D5.1.4s, 1998.
Schaffer, E., Instituionalization of Usability: A Step-By-Step Guide . Addison-Wesley, Boston, 2004.
Becker, J., Niehaves, B. et al., Maturity Models in IS Research. 18th European Conference on Information Systems, 2010.
Download references
Author information
Authors and affiliations.
Instituto Politécnico do Porto, ISCAP, S. Mamede de Infesta, Matosinhos, Portugal
João Vidal Carvalho & António Abreu
Departamento de Engenharia Informática, Universidade de Coimbra, Coimbra, Portugal
Álvaro Rocha
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to João Vidal Carvalho .
Additional information
This article is part of the Topical Collection on Systems-Level Quality Improvement
Rights and permissions
Reprints and permissions
About this article
Carvalho, J.V., Rocha, Á. & Abreu, A. Maturity Models of Healthcare Information Systems and Technologies: a Literature Review. J Med Syst 40 , 131 (2016). https://doi.org/10.1007/s10916-016-0486-5
Download citation
Received : 13 February 2016
Accepted : 31 March 2016
Published : 15 April 2016
DOI : https://doi.org/10.1007/s10916-016-0486-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Stages of growth
- Maturity models
- Hospital information systems
Advertisement
- Find a journal
- Publish with us
- Track your research
Hospital information systems applications and potential: a literature review revisited, 1982-1992
Affiliation.
- 1 School of Health and Rehabilitation Sciences, University of Pittsburgh, PA.
- PMID: 10139108
Although this article has addressed the many advancements in administrative and clinical applications of hospital information systems, there are many other issues that have affected and will continue to affect the development and transition of hospital information systems that are beyond its scope. A few of the more critical of these issues are the emergence of local area networks and wide area networks, more widespread use of graphical user interfaces (such as Windows), the powerful technology afforded by workstations and personal computers built with the 486 microchip, legal issues, and the always present obligation of ensuring data confidentiality and system security.
Publication types
- Clinical Medicine
- Databases, Factual / trends
- Diffusion of Innovation
- Expert Systems
- Hospital Administration
- Hospital Information Systems / trends*
- Medical Records Systems, Computerized
- United States
- Open access
- Published: 10 May 2024
A rare case of TFEB /6p21/ VEGFA -amplified renal cell carcinoma diagnosed by whole-exome sequencing: clinicopathological and genetic feature report and literature review
- Ruiqi Zhang 1 na1 ,
- Meili Ding 2 na1 ,
- Xingyao Zhu 1 ,
- Xiang Li 3 ,
- Lin Tao 4 ,
- Wenhao Hu 4 &
- Hong Zou 1
Diagnostic Pathology volume 19 , Article number: 66 ( 2024 ) Cite this article
171 Accesses
Metrics details
TFEB /6p21/ VEGFA -amplified renal cell carcinoma (RCC) is rare and difficult to diagnose, with diverse histological patterns and immunohistochemical and poorly defined molecular genetic characteristics.
Case presentation
We report a case of a 63-year-old male admitted in 2017 with complex histomorphology, three morphological features of clear cell, eosinophilic and papillary RCC and resembling areas of glomerular and tubular formation. The immunophenotype also showed a mixture of CD10 and P504s. RCC with a high suspicion of collision tumors was indicated according to the 2014 WHO classification system; no precise diagnosis was possible. The patient was diagnosed at a different hospital with poorly differentiated lung squamous cell carcinoma one year after RCC surgery. We exploited molecular technology advances to retrospectively investigate the patient’s molecular genetic alterations by whole-exome sequencing. The results revealed a 6p21 amplification in VEGFA and TFEB gene acquisition absent in other RCC subtypes. Clear cell, papillary, chromophobe, TFE3 -translocation, eosinophilic solid and cystic RCC were excluded. Strong TFEB and Melan-A protein positivity prompted rediagnosis as TFEB /6p21/ VEGFA -amplified RCC as per 2022 WHO classification. TMB-L (low tumor mutational load), CCND3 gene acquisition and MRE11A and ATM gene deletion mutations indicated sensitivity to PD-1/PD-L1 inhibitor combinations and the FDA-approved targeted agents Niraparib (Grade C), Olaparib (Grade C), Rucaparib (Grade C) and Talazoparib (Class C). GO (Gene Ontology) and KEGG enrichment analyses revealed major mutations and abnormal CNVs in genes involved in biological processes such as the TGF-β, Hippo, E-cadherin, lysosomal biogenesis and autophagy signaling pathways, biofilm synthesis cell adhesion substance metabolism regulation and others. We compared TFEB /6p21/ VEGFA -amplified with TFEB -translocated RCC; significant differences in disease onset age, histological patterns, pathological stages, clinical prognoses, and genetic characteristics were revealed.
We clarified the patient’s challenging diagnosis and discussed the clinicopathology, immunophenotype, differential diagnosis, and molecular genetic information regarding TFEB /6p21/ VEGFA -amplified RCC via exome analysis and a literature review.
1. For the first time, the molecular genetics of TFEB /6p21/ VEGFA -amplified renal cell carcinoma were completely and systematically characterized by exon sequencing.
2. The first case of TFEB /6p21/ VEGFA -amplified renal cell carcinoma with genomic instability was reported, presenting a new outlook on the treatment and prognosis of this tumor.
3. A systematic review and differentiation of TFEB /6p21/ VEGFA -amplified renal cell carcinoma and TFEB -translocated renal cell carcinoma in clinicopathological, histological, immunophenotypic, and molecular genetic features was performed.
TFEB /6p21/ VEGFA -amplified renal cell carcinoma is a rare subtype of renal cell carcinoma that was first proposed as a separate subtype by Argani et al. in 2016 (ref. [ 1 , 2 ]) and was not included in the WHO until 2022 due to its unique and rare nature. The interpretation of this tumor is imprecise; it is described as a relatively rare and highly aggressive tumor with a specific rate of recurrence and metastasis that tends to occur in middle-aged and older adults [ 3 , 4 ]. The tissue morphology of the tumor is diverse, mostly resembling papillary renal cell carcinoma (PRCC) with clear cell renal cell carcinoma (CCRCC)- or chromophobe renal cell carcinoma (CHRCC)-like morphology. These tumors demonstrate similar immunohistochemistry results to TFEB translocation renal cell carcinoma, commonly expressing pigment differentiation-related markers (Melan-A, HMB45, and cathepsin k). Molecular genetics suggests the presence of altered polyploid amplification in the region where the TFEB gene is located (6p21 region), including amplification of the critical genes VEGFA and CCND3 , suspected to be highly associated with the aggressive clinical course of this tumor in the absence of TFEB gene translocations [ 5 , 6 ].
The rare case we report with a mixture of clear cell carcinoma, eosinophilic carcinoma, and papillary renal carcinoma morphology phenotypes and characteristics was found in 2017 and initially diagnosed with renal cell carcinoma by regular morphology and immunohistochemistry analyses due to the limited molecular pathology available at the time [ 7 , 8 ]. Collision tumor was highly suspected in this patient; one year later, he developed poorly differentiated squamous cell carcinoma of the lung. As second-generation sequencing methods had matured, we continued evaluating this case by whole-exome sequencing and obtained hints of diagnostic value after obtaining in-depth mining sequencing results. Then, through immunohistochemical analysis and an extensive literature review, we differentiated the patient’s tumor from various types of renal cancer and diagnosed it as TFEB /6p21/ VEGFA -amplified renal cell carcinoma. The in-depth analysis of the molecular genetic changes in this case combined with a literature review to explore the relationships of these changes with diagnosis, prognosis, treatment and differential diagnosis with TFEB translocation renal cell carcinoma deepens our understanding of such tumors.
A 63-year-old male, was admitted to the hospital for right-sided low back pain in 2017. Fatty liver and a solid mass of the left kidney (internal partial liquefaction) were shown by abdominal ultrasonography, and a space-occupying lesion in the middle and lower part of the left kidney was observed by urinary CT, suggesting the possibility of renal carcinoma. A CT scan of the right kidney, bilateral ureters, and bladder showed no definite abnormal changes, though the rectal wall was slightly thickened. Lung CT showed no obvious abnormality. After admission, the patient underwent laparoscopic radical resection of left renal cancer under general anesthesia, and the operation went smoothly. The patient was diagnosed with poorly differentiated lung squamous cell carcinoma one year after RCC surgery, as shown in Fig. 1 h. After receiving two cycles of the "Docetaxel + Cis-platinum + Endo star" systemic intravenous chemotherapy regimen,the patient died. The postoperative survival time of patients with renal cancer was less than three years.
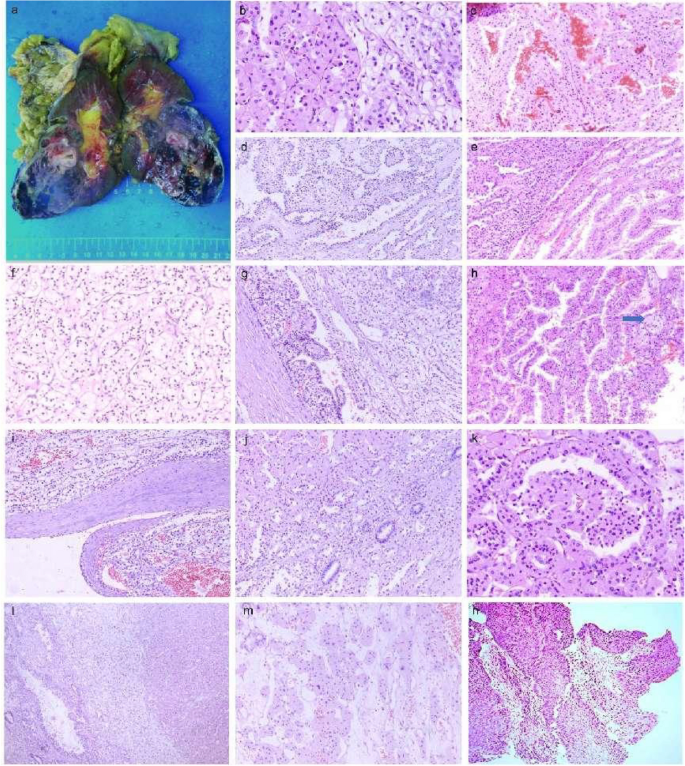
Gross images of the patient and HE staining of the tumor tissue. a The left kidney and surrounding fatty tissue were sent for examination, with a total size of 19 × 13 × 7 cm, and the size of the incised kidney was 13.5 × 8 × 6 cm. Most areas of the perirenal fat capsule were easy to peel off, and the focal renal epithelium was adherent to the adipose tissue, with a multicolored appearance and partial dark red necrosis. No lymph nodes were detected in the fatty tissue at the renal hilum. b The tumor tissue was biphasic, with areas of eosinophilic and clear cell coexistence. c Hemorrhagic and necrotic areas. d , e The tumor cells are arranged in a nested papillary pattern, and the papillae have a slender fibrovascular axis. f Tumor cells had abundant cytoplasm and clear cytoplasm. g The tumor cells were arranged in a striated papillary pattern. h Foam cell. i A fibrous pseudoenvelope is seen around the tumor. J , k Pseudo papillae and similar glomerular and tubular-like structures. l The tumor tissue was biphasic, with areas of eosinophilic and clear cell coexistence. m Tumor cells have abundant cytoplasm and eosinophilic cytoplasm. n Poorly differentiated squamous cell carcinoma of the lung
One left kidney with its surrounding adipose tissue was sent for examination, with a total size of 19 × 13 × 7 cm, and the kidney was dissected to a length of 13.5 × 8 × 6 cm. Most areas of the perirenal fat capsule were easy to peel off, and the focal renal epithelium adhered to the fatty tissue. A mass of 8.3 × 5.8 × 6 cm in size was seen in the middle and lower poles of the kidney, with a colorful external appearance, partly dark red necrosis, partially protruding into the renal pelvis, with a sebaceous thickness of 0.5 cm, and a medullary thickness of 2.8 cm. The ureter was 5 cm long and 0.4–0.5 cm in length. No lymph nodes were detected in the adipose tissue at the renal hilum (Fig. 1 a). Microscopically, a fibrous pseudocapsule was observed around the tumor (Fig. 1 i), and the tumor cells had a complex composition and diverse morphology (Fig. 1 b, l). Some cells were typical of clear cell carcinoma with nested and tubular distribution (Fig. 1 d), and some cells resembled eosinophilic papillary carcinoma with a fine fibrous vascular axis in the papilla (Fig. 1 e). Foam cells were observed in the focal interstitium (Fig. 1 h). In addition, pseudopapillaries and structures resembling glomeruli and renal tubules (Fig. 1 j, k) were observed, shift areas were observed in clear cells and the papillary regions, hemorrhage and necrosis were observed in some areas (Fig. 1 c), and focal interstitial edema was observed. There was no prominent cell atypia, and mitosis was rare. PAX-8 ( +) and AE1/3 (focal +) were positively expressed in the tumor cells overall, and CD10 ( +) (Fig. 2 d) and CA9 (focal + , cancer cells were positive in the clear differentiation area and negative in the tubular differentiation area) were positively expressed in the clear cell area (Fig. 2 g). CD31 staining showed strong positive epithelial AMACR (diffuse +) in the papillary carcinoma area except for in the clear cell area with more abundant interstitial vessels (Fig. 2 e). There was no loss of SDHB expression in the tumor cells (Fig. 2 i). The cells were all negative for CK20, TFE3 (Fig. 2 c), CD117 (Fig. 2 f), and CK7 (Fig. 2 h), and the tumor and had a low Ki-67 proliferation index of approximately 3–5% (Fig. 2 l). RCC with a high suspicion of collision tumors was indicated according to the 2014 WHO classification system; no precise diagnosis was possible.
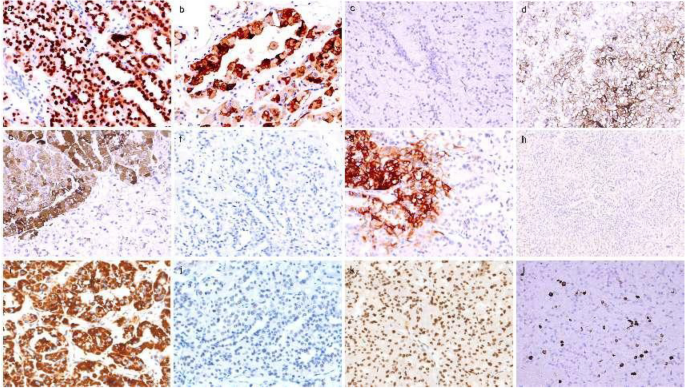
Immunohistochemistry results. a Tumor cell nuclei were strongly positive for TFEB × 20 ( b ) Melan-A positive × 20 ( c ) TFE3 negative × 20 ( d ) CD10( +) positive in the clear cell area × 20 ( e ) AMACR diffuse positive in the papillary carcinoma area × 20 ( f ) CD117 negative × 20 ( g ) CA9 focally positive with cancer cells positive in clear differentiation areas and negative in tubular differentiation areas × 20 ( h ) CK7 negative × 20 ( i ) SDHB positive × 20 ( j ) MSH6 negative × 20 and ( k ) MSH2 positive × 20 ( l ) The proliferation index of Ki67 was less than 10% × 20
To determine the molecular genetic alterations in the tumor, we extracted DNA from the patient’s normal tissue and parafn-embedded tumor tissue, performed exon sequencing in 2020. The summary of global mutations in the molecular genetics of this patient was shown in Supplementary Table 1 . Given the mutational advantage of CNV in cancer species and overall characteristics, high-frequency CNV analysis was performed on samples to obtain diagnostic information, as shown in Fig. 3 . CNVs were concentrated on chromosomes 6, 18, 19, and 21, and the patient demonstrated six significant regions of acquisition, including 6p21.1, 6p12.3, 18q12.1-18q23, 19p13.2, 19q13.2, 19q13.31 and six critical areas of deletion, including 6p21.1–21.3, 6p22.1–22.3, 11q11-11q25, 11p11-11p13, 17q25.1–25.3, and 18q12.1-18q23. Amplification of TFEB , VEGFA , and CCND3 genes located on the chromosome 6p21.1 segment (amplification fold > 2) was present, and the E2F3 gene was lost on the chromosome 6p22.3 segment. The somatic copy number variation (SCNA) characteristics of this patient were further combined and compared with classical oncogenes to find significantly associated driver genes. The DCC tumor suppressor gene was absent at 45,100,000–50460000 on chromosome 18. Genetic abnormalities associated with prognosis and treatment shows that the patient had TMB-L (low tumor mutation burden). The amplification mutation of CCND3 in somatic mutations suggested that the patient would be relatively sensitive to abemaciclib (grade D), palbociclib (grade D), and ribociclib (grade D). The MRE11A deletion mutation suggested relative sensitivity to niraparib (grade C), olaparib (grade C), rucaparib (grade C), and talazoparib (grade C). The ATM deletion mutation indicated relative sensitivity to Niraparib (grade C), Olaparib (grade C), Rucaparib (grade C), and Talazoparib (grade C) (Table 1 ).
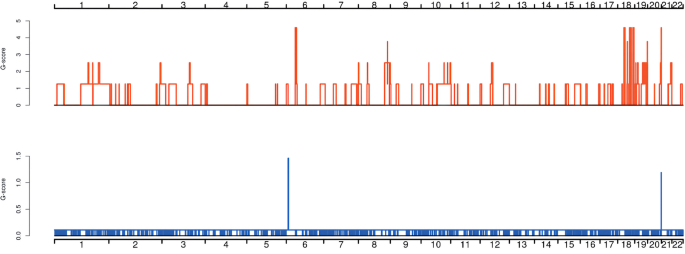
Distribution diagram of high-frequency CNV. The horizontal coordinates are chromosomes 1–22, and sex chromosomes were not considered in this analysis. The vertical coordinates indicate the scores of high-frequency CNV segments by GISTIC software, and higher scores indicate a higher frequency of CNV in this segment. Red indicates an increase in copy number, and blue indicates a decrease in copy number
To further understand the molecular genetic abnormalities of patients, germline mutations were screened by combining SNP comparisons with normal tissues to derive possible tumor susceptibility genes, as shown in Fig. 4 a ( MED23, PTPRB, ZFHX3, TSC1, AXIN2, CDK12, NFE2L2, AHNAK, ACNA1D, MN1, NRG1 BRCA2, IDH2, FGFR2, IRF2, DIS3, TP53, CEP290, RHBDF2 ). We identified 19 significant mutant genes for somatic variants in the exon coding region: MRE11A, ATM, NOTCH2, ATOH8, ASCC1, DOPEY2, HIST2H2AC, APC, ZCWPW1, POU2F3, CTC1, EXOC1, SLC5A12, MEN1, ATP12A, MNX1, SERPINB3, SERPINB4 , and BCL2 . On this basis, the somatic mutation of the patient was compared with the known driver genes in the database. The possible driver genes in the tumor sample were screened as ARID1B, MAX, NOTCH2 and APC (Fig. 4 b), in which a missense mutation of base C instead of base T occurred in the NOTCH2 gene located at position 120,471,691 on chromosome 1. Finally, 220 differential genes were screened among single nucleotide polymorphisms (SNPs) between tumor tissues and normal control tissues. These 220 genes were classified into 229 functional categories using the Gene Ontology (GO) database, as shown in Fig. 5 a, mainly involving biological processes such as biofilm synthesis, cell adhesion, regulation of substance metabolism, regulation of enzyme activity, rRNA processing, and biotransformation. Furthermore, 35 significant pathways related to this tumor were obtained by KEGG pathway enrichment analysis, as shown in Fig. 5 b, of which tumor-related routes accounted for 11.4% (4/35), metabolic pathways and other pathways accounted for 25.7% (9/35) and 62.9% (22/35), respectively. Inspired by the patient's lung cancer status during the last follow-up, investigated the microsatellite status. We identified a missense mutation in the exon region of the PMS2 gene located at 6,026,775 on chromosome 7, in which base C replaced base T.
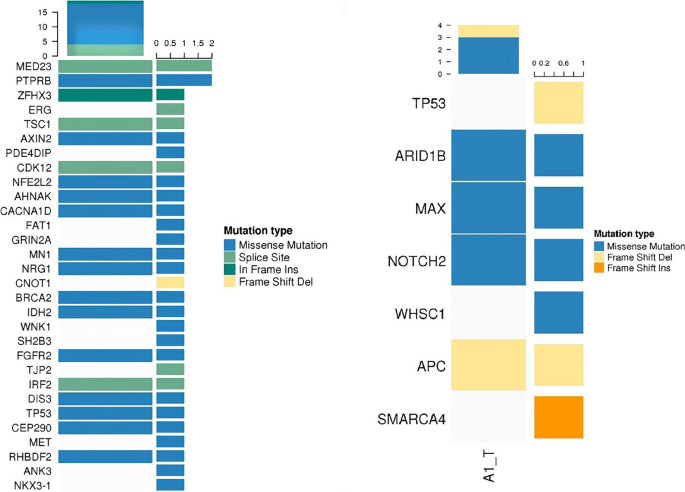
a Landscape map of susceptibility genes. b Landscape of known driver genes
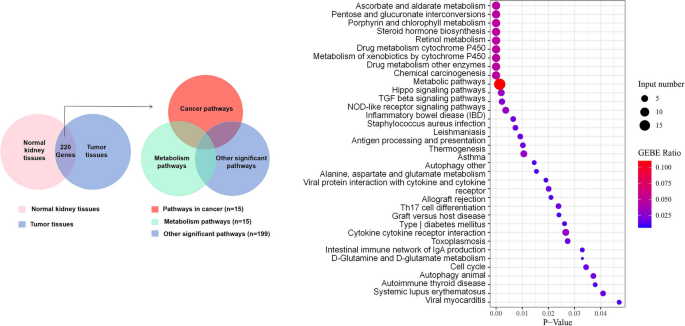
a Venn diagram of differentially expressed genes with missense mutations in SNPs of tumor samples versus normal samples. b Major pathways involved in SNPs differ between tumor tissue and control tissue in this patient
After exon sequencing, we used IHC technology to verify some genes that showed key changes in the sequencing results. Tumor cell nuclei were strongly positive for TFEB ( +) (Fig. 2 a), positive for Melan-A, MSH2 (present +) (Fig. 2 k), MLH1 (present +), and PMS2 (present + , focal -), and negative for MSH6 and HMB45.
TFEB /6p21/ VEGFA -amplified RCC defined by the 6p21.1 chromosomal region is a rare and gradually recognized RCC subtype that exists independently of TFEB -translocated RCC and has been included in the molecularly defined renal cancer subtypes by the World Health Organization in 2022 [ 9 ]. Our knowledge of this tumor is mainly derived from the preliminary studies of Gupta et al. [ 2 , 3 , 4 , 5 , 6 ], and the overall understanding of its biology is minimal. The lack of diagnosis and treatment guidelines makes this tumor challenging to treat, and 40% of cases experience aggressive metastasis or death.
We retrieved 8 papers with complete information about 50 cases of TFEB -amplified renal cell carcinoma (Supplementary Table 2 ) patients whose main characteristics were as follows: (1) Sex: there were 30 cases in males and 20 cases in females, with a male to female ratio of 3:2. (2) Age: the patients’ age ranged from 23 to 80 years, with a mean age of 63.46 and a median age of 65.00. (3) Tumor size: the average tumor size was 8.73 cm. (4) TNM stage: The percentage of TNM stage ≥ pT3 was 30/50. (5) ISUP grading: there was 1 case with a low grade, accounting for 1/40; 3 cases with grade 2, accounting for 3/40; 24 cases with grade 3, accounting for 24/40; 12 cases with grade 4, accounting for 12/40. (6) The presence of distant or regional metastases was confirmed at diagnosis or follow-up: there were 20 cases with complete follow-up information, of which 15 had metastases, representing a metastasis rate of 15/20. (7) Morphological features: microscopically, the tumor cells were morphologically diverse, with cells in nested (12/45), papillary (14/45), pseudopapillary (6/45), tubular papillary (18/45), and clear cell areas (20/45), and such tumors had an overall increase in cytoplasmic eosinophils, accounting for 27/45, some with cell necrosis (7/45). (8) Immunohistochemistry: the analyses revealed positivity for TFEB (+ , 5/7), cathepsin k(+ , 16/27), Melan-A (+ , 28/36) and HMB45 (+ , 6/30) (9) FISH: TFEB FISH revealed breaks & GT (10 signals, 32/33); VEGFA FISH revealed breaks & GT (10 signals; 14/14). (10) The other molecular genetic features observed were loss of chromosome 3p (6/12), loss of chromosome 7 (2/9), loss of chromosome 17 (4/9), occasional missense mutations in the SMARCB1 gene, and nonsense mutations in the FH gene.
In the 2022 WHO classification of renal cancer, in addition to TFEB amplifying renal cancer, TFEB -translocated renal cell carcinoma is included, which is a relatively rare subtype of kidney cancer typified by a translocation between the TFEB gene on chromosome 6 and the MALAT1/Alpha gene on chromosome 11 [ 10 ]. In a review of 40 cases of TFEB translocated renal cell carcinoma reported in the literature [ 3 , 6 , 11 , 12 ] (Supplementary Table 3 ), combined with the studies of Gupta and Qiuyang Lu et al. [ 3 , 6 , 10 , 13 ], we found significant differences between TFEB translocation and TFEB -amplified tumors in terms of age of disease onset, histological morphology, melanocyte markers, expression of cathepsin k, VEGFA/CCND3 gene expression, and aggressive behavior. The above differences contribute to the differential diagnosis of the two, as described in detail below (Table 2 ): 1. Clinicopathological features: there was no noticeable sex difference between the two groups. The former tumor occurred in adults and was small; the latter tumor developed at an older age and occurred in older patients, and the tumor volume was more prominent. 2. Histologic features: both tumors are primarily nonspecific, generally well-defined, and reddish-brown on the cut surface. The typical biphasic histopathological features of "large epithelioid cells and small cells clustered around clear basement membrane-like tissue" are more common in translocated RCC. More extensive morphological features, such as sclerosis and ossification, are occasionally seen in TFEB -translocated RCC. Amplified tumors were morphologically diverse, with cytoplasmic eosinophilia ( p = 0.013) and pseudopapillary, necrotic and true papilla, the characteristics of the amplified tumor. RCC with aberrant TFEB expression was a highly graded RCC, and TFEB -amplified renal cell carcinoma had a higher proportion of ≥ pT3 in TNM staging ( p = 0.047). 3. Immunophenotypic features: overexpression of TFEB genes frequently drives abnormal expression of melanocyte-associated antigens (HMB45, Melan-A) and osteoblast histone k (cathepsin k); overexpression of cathepsin k ( p < 0.000), HMB45 ( p < 0.000), and Melan-A ( p = 0.028) is more commonly found in TFEB -translocated renal cell carcinoma. 4. TFEB expression assay: the results of the TFEB gene expression assay are correlated with the immunohistochemistry results [ 2 , 3 , 6 , 14 ], but at the genetic level, amplified renal tumors have a low tendency to express TFEB , which is often accompanied by VEGFA gene amplification. Several studies suggest that the low expression of TFEB in amplified renal tumors may be attributed to their lack of typical biphasic morphology. 5. Prognosis: translocated RCC had an excellent clinical prognosis with a low recurrence and distant metastasis rate (1/8). Renal tumors with amplifications had a more aggressive clinical course, a higher recurrence and distant metastasis rate (15/20, p = 0.004), and a poorer clinical prognosis.
In sequencing, the CNV mutation in this case was consistent with the already reported by our team [ 15 ]. High-frequency CNV analysis yielded diagnostically significant alterations on chromosome 6. The CNV results further suggested that the gain in chromosomes 1q, 2p, 4q, 6p, 16p, 17q, 18q, 19q, 22q and loss in chromosome 18q were consistent with previous findings in TFEB -amplified renal cell carcinoma [ 3 , 4 , 16 ]. Nevertheless, the amplification of chromosomes 1p, 4p, 10q, 18q, 19p, and 21p and the loss of chromosome 17q in the present case has not been previously reported.
Subsequently, the germline mutations in this case were analyzed. The susceptibility of TP53 to mutation in normal tissues adjacent to cancer revealed the instability of the patient's tumor. Single nucleotide polymorphisms (SNPs) between tumor tissues and normal control tissues were analyzed, and the obtained differentially expressed genes were mapped to the KEGG and GO databases. The results are shown in Fig. 5 . The results can be interpreted from three levels. First, classical pathways associated with cancer, such as the TGF-β signaling pathway [ 17 , 18 ] and Hippo signaling pathway [ 19 ], were involved. Metabolism-related courses accounted for 25.7%, which was in line with results from previous studies that showed that kidney cancer is a metabolism-driven disease [ 20 ]. After enrichment, some pathways were associated with biological dysfunction and abnormal behavior caused by aberrant overexpression of TFEB genes, such as E-cadherin, an essential regulator of tumor cell-to-cell interactions, lysosomal biogenesis [ 21 ], and autophagy of tumor cells [ 22 , 23 ]. Given the close correlation between the above partial enrichment pathway and amplified mutations of the TFEB gene, which was consistent with our previous CNV results suggesting the presence of TFEB amplification, the rationale supporting the diagnosis of TFEB -amplified renal cell carcinoma was more robust. Among the genes with somatic missense mutations, NOTCH2 , NR3C1 , NT5E , PLAGL1 , and ACAT2 correlate with the occurrence and development of renal tumors. Among them, the NOTCH2 gene was related to cell stemness [ 24 ], which could induce and regulate the occurrence and apoptosis of tumor cells; NT5E could inhibit the growth, EMT process, and AKT/GSK-3β signaling pathway of sunitinib-resistant cells in renal cell carcinoma [ 25 ]. It has also been proposed that PLAGL1 protein levels in CCRCC tissues are positively correlated with distant metastasis and worse patient prognosis [ 26 , 27 ]; the ACAT2 gene was related to lipid metabolism [ 28 ], and its downregulation could lead to a poor tumor-specific survival prognosis. The remaining genes with missense mutations suggest changes associated with cell proliferation and differentiation, amino acid metabolism, nucleotide metabolism, and signal transduction pathways. In this case, a frameshift deletion occurred in the APC gene on chromosome 5, which encodes a tumor suppressor protein that acts as an antagonist of the Wnt signaling pathway and is also involved in other processes, including cell migration and adhesion. Transcriptional activation and apoptosis have also been reported in CHRCC metastatic chromophobe renal cell carcinoma with APC mutation [ 26 ].
During interpreting data, we obtained the diagnosis of TFEB -amplified RCC after summarizing the molecular genetic alterations of common and rare subtypes of kidney cancer by the latest guidelines and literature [ 8 , 29 ]. The development of molecular pathology has constantly advanced our understanding of kidney cancer, and some tumor subtypes based on specific molecular alterations, such as "translocation-associated renal cell carcinoma," were first introduced in the WHO classification in 2004 [ 7 ]. However, these molecularly defined tumors have shown a broad morphological spectrum in some recent studies, and whether there is a clear correlation between genotype and phenotype is worth discussing; thus, it is crucial to broaden the idea of differential diagnosis of tumors with the help of molecular tests such as second-generation sequencing [ 7 , 8 , 9 ].
During the follow-up, the patient developed poorly differentiated squamous cell carcinoma in the lung one year after kidney cancer surgery; the secondary lung malignancy led us to speculate whether there were some specific alterations at the genetic level in the patient. We first examined tumor mutation burden (TMB) and microsatellite instability (MSI), which are predictors of the efficacy of immune checkpoint inhibitor therapy. The results showed that the TMB was low. Regarding MSI, we first noticed the expression of MMR mismatch repair (MMR) protein and obtained the impact of low expression of MSH6 protein. Meanwhile, seven common loci in MSI were detected by next-generation sequencing technology, and the results suggested that they were microsatellite stable (MMS). However, we found in the exon sequencing results that there was a missense mutation in the exon region of the PMS2 gene on chromosome [ 7 ], in which base C replaced base T. Could the above situation suggest microsatellite instability in this patient? Considering the heterogeneity of the tumor during the assay and the methodology of the assay, the results of this patient's MSI status need to be further discussed and analyzed in the context of the literature.
This patient has multiple tumor characteristics, which was another interesting aspect of this case. Analyzing the expression of genes associated with homologous recombination repair could be beneficial in guiding the patient's clinical treatment. The sequencing results suggested that this patient had a homologous recombination-deficient (HRD) tumor, with the loss of ATM and MRE11A , which are key genes involved in the process of homologous recombination (HR) repair, suggesting that we could try targeted therapy with poly ADP ribose polymerase (PARP) inhibitors: this patient was relatively sensitive to niraparib (class C), olaparib (class C), rucaparib (class C), and talazoparib (class C). Olaparib, an inhibitor of oral poly ADP-ribose polymerase (PARP), is increasingly being demonstrated in clinical studies to be effective in HRD gene-deficient cell lines, such as those lacking ATM , in addition to providing sensitization in combination with chemotherapeutic agents and killing BRCA1 or BRCA2 gene-mutated tumor cells. Clinical trials are underway in patients with renal clear cell carcinoma, urothelial carcinoma, and prostate cancer. Talazoparib is a next-generation PARP inhibitor with a dual mechanism of action that stimulates tumor cell death by blocking PARP enzyme activity and binding PARP enzyme to DNA damage sites, and clinical trials of its use in patients with renal clear cell carcinoma are ongoing. The targeting effects of these drugs still need to be explored in depth. Sequencing results can guide targeted dosing, and the loss of these 2 genes may improve the benefit rate of PD-1/PD-L1 inhibitors; thus, this patient may benefit from immunotherapy.
The above findings help explain the complex pathogenesis of lung cancer secondary to kidney cancer two years after the initial patient diagnosis and provide some guidance for the clinical treatment of this disease; unfortunately, the patient developed the disease early and did not have a chance to receive the treatment with relevant drugs. By describing this case, we hope that more patients with a similar disease will have the option to try HRD-related targeted therapy and immunotherapy.
Kidney cancer is a complex disease with unpredictable clinical progression due to typical intertumor and intratumor heterogeneity and high genomic variability [ 30 , 31 ], which makes it difficult for traditional radiotherapy, chemotherapy, and targeted therapy to overcome the tumor. With the advent of the immune checkpoint inhibitor (ICI) era, a new generation of comprehensive treatment for kidney cancer has emerged [ 32 , 33 ]. In pre-kidney cancer studies, the mTOR inhibitors everolimus and tesilimus have been approved by the FDA for treating advanced metastatic renal cell carcinoma. These drugs are effective for metastatic TFEB-translocated renal cell carcinoma [ 34 ]. Pembrolizumab (Keytruda or pembrolizumab), approved by the US Food and Drug Administration (FDA), is a PD-L1 inhibitor for the treatment of patients with solid tumors, which has brought some clinical benefits to some patients [ 35 , 36 , 37 ]. Studies have further shown that TFEB affects the biological progression of renal cancer by acting on the mTOR pathway and positively correlates with the expression of PD-L1. In this case, the amplification of TFEB and the evaluation of genomic stability provide new opportunities for the combination of targeted therapy and immunotherapy for this type of cancer. Could MSI be a relevant immunotherapeutic marker for kidney cancer treatment? Can mTOR/PARP inhibitors be combined with PD-L1 inhibitors such as pembrolizumab in TFEB /6p21/ VEGFA -amplified RCC? Given the rarity of TFEB /6p21/ VEGFA -amplified renal cell carcinoma, pathologists and clinicians have not reported it domestically or internationally, and the above ideas need to be validated.
Whole-exome molecular genetic analysis of TFEB /6p21/ VEGFA -amplified renal cell carcinoma has enhanced our understanding of this type of tumor. For the first time, we reported possible tumor-related driver genes, alterations in specific chromosomal regions of CNV, and critical genes associated with targeted therapy in TFEB /6p21/ VEGFA -amplified renal cell carcinoma (Table 1 ), which deepened our understanding of the diagnosis and molecular genetic alterations of TFEB /6p21/ VEGFA -amplified renal cell carcinoma and provided new information for their prognosis and treatment.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Gene ontology
Kyoto Encyclopedia of Genes and Genomes
Biological Process
Cellular Component
Molecular Function
Somatic copy number variation
Papillary renal cell carcinoma
Clear cell renal cell carcinoma
Chromophobe renal cell carcinoma
Acquired cystic kidney disease-associated renal cell carcinoma
Tubulocystic renal cell carcinoma
Hereditary leiomyomatosis and renal cell carcinoma-associated renal cell carcinoma
Immunohistochemistry
Transcription Factor EB
Paired box protein 8
A-methylacyl-CoA racemase
Cytokeratin protein 7
Cluster of differentiation 10
Cluster of differentiation 117
Cluster of differentiation 31
Melanoma antigen recognized by T cell-1
Melanoma-related marker
Cytokeratin 20
Carbonic anhydrase IX
Succinate dehydrogenase B
MutL homolog 1
MutS homolog 2
MutS homolog 6
PMS1 homolog 2
Single nucleotide polymorphism
Insertion and deletion
Copy number variation
Single nucleotide variant
Microsatellite instability
Microsatellite instability-high
Mismatch repair
Deficient mismatch repair
Homologous Recombination Deficiency
Poly ADP ribose polymerase
Immune checkpoint inhibitor
Tumor mutation burden
Human leukocyte antigen class 1
Fluorescence in situ hybridization
Amin MB, Amin MB, Tamboli P, Javidan J, Stricker H, Venturina DP, et al. Prognostic impact of histologic subtyping of adult renal epithelial neoplasms: an experience of 405 cases. Am J Surg Pathol. 2002;26:281–91.
Article PubMed Google Scholar
Argani P, Ning Y, Antonescu CR, et al. TFEB -amplified renal cell carcinomas an aggressive molecular subset demonstrating variable melanocytic marker expression and morphologic heterogeneity. Am J Surg Pathol. 2016;40:1484–95.
Article PubMed PubMed Central Google Scholar
Gupta S, Argani P, Jungbluth AA, Chen YB, Reuter VE, editors. TFEB Expression Profiling in Renal Cell Carcinomas: Clinicopathologic Correlations; 2019.
Mendel L, Ambrosetti D, Bodokh Y, Ngo-Mai M, Durand M, Simbsler-Michel C, et al. Comprehensive study of three novel cases of TFEB-amplified renal cell carcinoma and review of the literature: evidence for a specific entity with poor outcome. Genes Chromosomes Cancer. 2018;57(3):99–113. https://doi.org/10.1002/gcc.22513 .
Article CAS PubMed Google Scholar
Gupta S, Johnson SH, Vasmatzis G, Porath B, Sukov WR. TFEB-VEGFA (6p21.1) co-amplified renal cell carcinoma: a distinct entity with potential implications for clinical management. Mod Pathol. 2017;30:998–1012.
Wyvekens N, Rechsteiner M, Fritz C, Wagner U, Tchinda J, Wenzel C, et al. Histological and molecular characterization of TFEB -rearranged renal cell carcinomas. Virchows Arch. 2019;474:625–31.
Theresa, Y., Chan. World Health Organization classification of tumours: Pathology & genetics of tumours of the urinary system and male genital organs | Edited by John N. Eble, Guido Sauter, Jonathan I. Epstein, and Isabell A. Sesterhenn World Health Organization: International Agency for Research on Cancer, Lyon, France, 2004, $75.00, ISBN 92–832–2415–9 - ScienceDirect. Urol. 2005;65:214–15.
Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO classification of tumours of the urinary system and male genital organs-part A: renal, penile, and testicular tumours. Eur Urol. 2016;70(1):93–105. https://doi.org/10.1016/j.eururo.2016.02.029 .
Moch H, Amin MB, Berney DM, Compérat EM, Gill AJ, Hartmann A, et al. The 2022 world health organization classification of Tumours of the urinary system and male genital organs-part a: renal, penile, and testicular Tumours. European urol. 2022;82:458–68.
Article Google Scholar
Caliò A, Harada S, Brunelli M, Pedron S, Segala D, Portillo SC, et al. TFEB rearranged renal cell carcinoma. A clinicopathologic and molecular study of 13 cases. Tumors harboring MALAT1-TFEB, ACTB-TFEB, and the novel NEAT1-TFEB translocations constantly express PDL1. Mod Pathol. 2021;34:842–50.
Skala SL, Xiao H, Udager AM, Dhanasekaran SM, Shukla S, Zhang Y, et al. Detection of 6 TFEB-amplified renal cell carcinomas and 25 renal cell carcinomas with MITF translocations: systematic morphologic analysis of 85 cases evaluated by clinical TFE3 and TFEB FISH assays. Mod Pathol. 2018;31(1):179–97. https://doi.org/10.1038/modpathol.2017.99 .
Kuroda N, Yorita K, Sasaki N, Ishihara A, Matsuura K, Daa T, et al. Clinicopathological study of 5 cases of renal cell carcinoma with t(6;11)(p21;q12). Pol J Pathol. 2017;68:66.
Mansueto G, Armani A, Viscomi C, D’Orsi L, De Cegli R, Polishchuk EV, et al. Transcription factor EB controls metabolic flexibility during exercise. Cell Metab. 2017;25(1):182–96. https://doi.org/10.1016/j.cmet.2016.11.003 .
Article CAS PubMed PubMed Central Google Scholar
Caliò A, Brunelli M, Segala D, Pedron S, Doglioni C, Argani P, et al. VEGFA amplification/increased gene copy number and VEGFA mRNA expression in renal cell carcinoma with TFEB gene alterations. Mod Pathol. 2019;32(2):258–68. https://doi.org/10.1038/s41379-018-0128-1 .
Kang XL, Zou H, Pang LJ, Hu WH, Li F. Chromosomal imbalances revealed in primary renal cell carcinomas by comparative genomic hybridization. Int J Clin Exp Pathol. 2015;8:3636.
PubMed PubMed Central Google Scholar
Peckova K, Vanecek T, Martinek P, Spagnolo D, Kuroda N, Brunelli M, et al. Aggressive and nonaggressive translocation t(6;11) renal cell carcinoma: comparative study of 6 cases and review of the literature. Ann Diagn Pathol. 2014;18:351–7.
Song W, He D, Chen Y, Yeh C, Hsu I, Huang Q, et al. Targeting newly identified ERβ/TGF-β1/SMAD3 signals with the FDA-approved anti-estrogen Faslodex or an ERβ selective antagonist in renal cell carcinoma. Mol Oncol. 2018;12:2055–71.
Nam H, Kundu A, Karki S, Brinkley G, Sudarshan S. TGF-B signaling suppresses TCA cycle metabolism in renal cancer. 2021.
Book Google Scholar
Yang WH, Ding CC, Sun T, Rupprecht G, Lin CC, Hsu D, et al. The Hippo Pathway Effector TAZ regulates Ferroptosis in renal cell carcinoma. Cell Rep. 2019;28(10):2501–2508.e4. https://doi.org/10.1016/j.celrep.2019.07.107 .
Linehan WM, Srinivasan R, Schmidt LS. The genetic basis of kidney cancer: a metabolic disease. Nat Rev Urol. 2010;7:277–85.
Nakamura S, Akayama S, Yoshimori T. Autophagy-independent function of lipidated LC3 essential for TFEB activation during the lysosomal damage responses. Autophagy. 2021;17(2):581–3. https://doi.org/10.1080/15548627.2020.1846292 .
Ide S, Beroza G, Kanamori M, Kikuchi A, Huynh T. TFEB links autophagy to lysosomal biogenesis. Science. 2011;1429:24–6303.
Google Scholar
Bahrami A, Bianconi V, Pirro M, Orafai HM, Sahebkar A. The role of TFEB in tumor cell autophagy: diagnostic and therapeutic opportunities. Life Sci. 2020;244:117341.
Xiao W, Gao Z, Duan Y, Yuan W, Ke Y. Notch signaling plays a crucial role in cancer stem-like cells maintaining stemness and mediating chemotaxis in renal cell carcinoma. J Exp Clin Cancer Res. 2017;36:41.
Peng D, Hu Z, Wei X, Ke X, Shen Y, Zeng X. NT5E inhibition suppresses the growth of sunitinib-resistant cells and EMT course and AKT/GSK-3β signaling pathway in renal cell cancer. IUBMB Life. 2019;71:113–24.
Abbosh P, Sundararajan S, Millis SZ, Hauben A, Reddy S, Geynisman DM, et al. Molecular and genomic profiling to identify actionable targets in Chromophobe renal cell cancer. Eur Urol Focus. 2018;4:969–71.
Godlewski J, Krazinski BE, Kowalczyk AE, Kiewisz J, Kiezun J, Kwiatkowski P, et al. PLAGL1 (ZAC1/LOT1) Expression in clear cell renal cell carcinoma: correlations with disease progression and unfavorable prognosis. Anticancer Res. 2016;36:617–24.
CAS PubMed Google Scholar
Zhao Z, Lu J, Han L, Wang X, Man Q, Liu S. Prognostic significance of two lipid metabolism enzymes, HADHA and ACAT2 , in clear cell renal cell carcinoma. Tumour. 2016;37:8121–30.
Article CAS Google Scholar
Piva F, Santoni M, Matrana MR, Satti S, Giulietti M, Occhipinti G, et al. BAP1, PBRM1 and SETD2 in clear-cell renal cell carcinoma: molecular diagnostics and possible targets for personalized therapies. Expert Rev Mol Diagn. 2015;15:1201–10.
Guarch R, Lawrie CH, Larrinaga G, Angulo JC, Pulido R, López JI. High levels of intratumor heterogeneity characterize the expression of epithelial-mesenchymal transition markers in high-grade clear cell renal cell carcinoma. Ann Diagn Pathol. 2018;34:27–30.
Turajlic S, Xu H, Litchfield K, Rowan A, Horswell S, Chambers T, et al. Deterministic Evolutionary Trajectories Influence Primary Tumor Growth: TRACERx Renal. Cell. 2018;173:595-610.e11.
Gill DM, Agarwal N. Cancer immunotherapy: a paradigm shift in the treatment of advanced urologic cancers. Urol Oncol. 2017;35:676–7.
Hammers HJ, Plimack ER, Infante JR, Rini BI, McDermott DF, Lewis LD, et al. Safety and efficacy of Nivolumab in combination with Ipilimumab in metastatic renal cell carcinoma: the CheckMate 016 Study. J Clin Oncol. 2017;35:3851–8.
Archetti M, Pienta KJ. Cooperation among cancer cells: applying game theory to cancer. Nat Rev Cancer. 2019;19(2):110–7. https://doi.org/10.1038/s41568-018-0083-7 .
Johnston KA, Lopez KM. Lysyl oxidase in cancer inhibition and metastasis. Cancer Lett. 2018;417:174–81. https://doi.org/10.1016/j.canlet.2018.01.006 .
Gaikwad S, Agrawal M, Kaushik I, Ramachandran S, Srivastava S. Immune checkpoint proteins: Signaling mechanisms and molecular interactions in cancer immunotherapy. Semin Cancer Biol. 2022;86:137–50.
Akinboro O, Larkins E, Pai-Scherf L, Mathieu L, Ren Y, Cheng J, et al. FDA Approval Summary: Pembrolizumab, Atezolizumab, and Cemiplimab-rwlc as single agents for first-line treatment of advanced/metastatic PD-L1 high NSCLC. Clinical Cancer Res. 2022;28:2221–8.
Download references
Acknowledgements
Not applicable.
This research was funded by the National Natural Science Foundation of China (grant numbers 81660411, 81460383) and the International Cooperation Project of Xinjiang Production and Construction Corps of China (grant number 2019BC001). The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Ruiqi Zhang and Meili Ding are co-first authors and contributed equally to this work.
Authors and Affiliations
Department of Pathology, The Second Affiliated Hospital of Zhejiang University School of Medicine, Zhejiang, 310009, China
Ruiqi Zhang, Xingyao Zhu & Hong Zou
Department of Pathology, The Yangxin County People’s Hospital, Binzhou, 251800, China
Department of Pathology, People’s Hospital of Xinjiang Uygur Autonomous Region, Xinjiang, 830001, China
Department of Pathology, The First Affiliated Hospital, Shihezi University School of Medicine, Xinjiang, 832002, China
Qi Hu, Lin Tao & Wenhao Hu
You can also search for this author in PubMed Google Scholar
Contributions
All authors conceived this research. RZ and MD collected and analyzed clinical samples and data. XZ and MD completed the construction of the tissue microarray and the production of HE slices. HZ designed and supervised the entire project scientifically. RZ and HZ are major contributors in writing the manuscript, QH participated in the manuscript writing and submission, HW and LT reviewed and edited the paper. HZ had final responsibility for the decision to submit for publication. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Hong Zou .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Institutional Ethics Review Board (IRB) of the First Affiliated Hospital of the School of Medicine, Shihezi University. And the study was conducted in accordance with the standards and ethics of the Declaration of Helsinki, and written informed consent was obtained from the patients.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhang, R., Ding, M., Zhu, X. et al. A rare case of TFEB /6p21/ VEGFA -amplified renal cell carcinoma diagnosed by whole-exome sequencing: clinicopathological and genetic feature report and literature review. Diagn Pathol 19 , 66 (2024). https://doi.org/10.1186/s13000-024-01476-3
Download citation
Received : 29 March 2023
Accepted : 02 March 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s13000-024-01476-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- TFEB /6p21/ VEGFA -amplified renal cell carcinoma
- Whole exome sequencing
- Differential diagnosis of molecular genetic changes
Diagnostic Pathology
ISSN: 1746-1596
- Submission enquiries: [email protected]
- Share full article
Advertisement
Supported by
Solar Storm Intensifies, Filling Skies With Northern Lights
Officials warned of potential blackouts or interference with navigation and communication systems this weekend, as well as auroras as far south as Southern California or Texas.

By Katrina Miller and Judson Jones
Katrina Miller reports on space and astronomy and Judson Jones is a meteorologist.
A dramatic blast from the sun set off the highest-level geomagnetic storm in Earth’s atmosphere on Friday that is expected to make the northern lights visible as far south as Florida and Southern California and could interfere with power grids, communications and navigations system.
It is the strongest such storm to reach Earth since Halloween of 2003. That one was strong enough to create power outages in Sweden and damage transformers in South Africa.
The effects could continue through the weekend as a steady stream of emissions from the sun continues to bombard the planet’s magnetic field.
The solar activity is so powerful that the National Oceanic and Atmospheric Administration, which monitors space weather, issued an unusual storm watch for the first time in 19 years, which was then upgraded to a warning. The agency began observing outbursts on the sun’s surface on Wednesday, with at least five heading in the direction of Earth.
“What we’re expecting over the next couple of days should be more significant than what we’ve seen certainly so far,” Mike Bettwy, the operations chief at NOAA’s Space Weather Prediction Center, said at a news conference on Friday morning.
For people in many places, the most visible part of the storm will be the northern lights, known also as auroras. But authorities and companies will also be on the lookout for the event’s effects on infrastructure, like global positioning systems, radio communications and even electrical power.
While the northern lights are most often seen in higher latitudes closer to the North Pole, people in many more parts of the world are already getting a show this weekend that could last through the early part of next week.

As Friday turned to Saturday in Europe, people across the continent described skies hued in a mottling of colors.
Alfredo Carpineti , an astrophysicist, journalist and author in North London, saw them with his husband from the rooftop of their apartment building.
“It is incredible to be able to see the aurora directly from one’s own backyard,” he said. “I was hoping to maybe catch a glimpse of green on the horizon, but it was all across the sky in both green and purple.”
Here’s what you need to know about this weekend’s solar event.
How will the storm affect people on Earth?
A geomagnetic storm watch or warning indicates that space weather may affect critical infrastructure on or orbiting near Earth. It may introduce additional current into systems, which could damage pipelines, railroad tracks and power lines.
According to Joe Llama, an astronomer at Lowell Observatory, communications that rely on high frequency radio waves, such as ham radio and commercial aviation , are most likely to suffer. That means it is unlikely that your cellphone or car radio, which depend on much higher frequency radio waves, will conk out.
Still, it is possible for blackouts to occur. As with any power outage, you can prepare by keeping your devices charged and having access to backup batteries, generators and radio.
The most notable solar storm recorded in history occurred in 1859. Known as the Carrington Event, it lasted for nearly a week, creating aurora that stretched down to Hawaii and Central America and impacting hundreds of thousands of miles of telegraph lines.
But that was technology of the 19th century, used before scientists fully understood how solar activity disrupted Earth’s atmosphere and communication systems.
“That was an extreme level event,” said Shawn Dahl, a forecaster at NOAA’s Space Weather Prediction Center. “We are not anticipating that.”
Unlike tornado watches and warnings, the target audience for NOAA’s announcements is not the public.
“For most people here on planet Earth, they won’t have to do anything,” said Rob Steenburgh, a space scientist at NOAA’s Space Weather Prediction Center.
The goal of the announcements is to give agencies and companies that operate this infrastructure time to put protection measures in place to mitigate any effects.
“If everything is working like it should, the grid will be stable and they’ll be able to go about their daily lives,” Mr. Steenburgh said.

Will I be able to see the northern lights?
It is possible that the northern lights may grace the skies this week over places that don’t usually see them. The best visibility is outside the bright lights of cities.
Clouds or stormy weather could pose a problem in some places. But if the skies are clear, even well south of where the aurora is forecast to take place, snap a picture or record a video with your cellphone. The sensor on the camera is more sensitive to the wavelengths produced by the aurora and may produce an image you can’t see with the naked eye.
Another opportunity could be viewing sunspots during the daytime, if your skies are clear. As always, do not look directly at the sun without protection. But if you still have your eclipse glasses lying around from the April 8 event, you may try to use them to try to spot the cluster of sunspots causing the activity.
How strong is the current geomagnetic storm?
Giant explosions on the surface of the sun, known as coronal mass ejections, send streams of energetic particles into space. But the sun is large, and such outbursts may not cross our planet as it travels around the star. But when these particles create a disturbance in Earth’s magnetic field, it is known as a geomagnetic storm.
NOAA classifies these storms on a “G” scale of 1 to 5, with G1 being minor and G5 being extreme. The most extreme storms can cause widespread blackouts and damage to infrastructure on Earth. Satellites may also have trouble orienting themselves or sending or receiving information during these events.
The current storm is classified as G5, or “extreme.” It is caused by a cluster of sunspots — dark, cool regions on the solar surface — that is about 16 times the diameter of Earth. The cluster is flaring and ejecting material every six to 12 hours.
“We anticipate that we’re going to get one shock after another through the weekend,” said Brent Gordon, chief of the space weather services branch at NOAA’s Space Weather Prediction Center.
Why is this happening now?
The sun’s activity ebbs and flows on an 11-year cycle, and right now, it is approaching a solar maximum. Three other severe geomagnetic storms have been observed so far in the current activity cycle, which began in December 2019, but none were predicted to cause effects strong enough on Earth to warrant a watch or warning announcement.
The cluster of sunspots generating the current storm is the largest seen in this solar cycle, NOAA officials said. They added that the activity in this cycle has outperformed initial predictions .
More flares and expulsions from this cluster are expected, but because of the sun’s rotation the cluster will be oriented in a position less likely to affect Earth. In the coming weeks, the sunspots may appear again on the left side of the sun, but it is difficult for scientists to predict whether this will cause another bout of activity.
“Usually, these don’t come around packing as much of a punch as they did originally,” Mr. Dahl said. “But time will tell on that.”
Jonathan O’Callaghan contributed reporting from London.
An earlier version of this article misstated the radio frequencies used by cellphones and car radios. They are higher frequencies, not low.
How we handle corrections
Katrina Miller is a science reporting fellow for The Times. She recently earned her Ph.D. in particle physics from the University of Chicago. More about Katrina Miller
Judson Jones is a meteorologist and reporter for The Times who forecasts and covers extreme weather. More about Judson Jones
What’s Up in Space and Astronomy
Keep track of things going on in our solar system and all around the universe..
Never miss an eclipse, a meteor shower, a rocket launch or any other 2024 event that’s out of this world with our space and astronomy calendar .
A dramatic blast from the sun set off the highest-level geomagnetic storm in Earth’s atmosphere, making the northern lights visible around the world .
With the help of Google Cloud, scientists who hunt killer asteroids churned through hundreds of thousands of images of the night sky to reveal 27,500 overlooked space rocks in the solar system .
A celestial image, an Impressionistic swirl of color in the center of the Milky Way, represents a first step toward understanding the role of magnetic fields in the cycle of stellar death and rebirth.
Scientists may have discovered a major flaw in their understanding of dark energy, a mysterious cosmic force . That could be good news for the fate of the universe.
Is Pluto a planet? And what is a planet, anyway? Test your knowledge here .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC11084135

Severe fever with thrombocytopenia syndrome with central nervous system symptom onset: a case report and literature review
Department of Neurology, Xuanwu Hospital, Capital Medical University, Beijing, 100053 China
Huimin Zhang
Shuting chai, associated data.
No datasets were generated or analysed during the current study.
Severe fever with thrombocytopenia syndrome (SFTS) is a natural focal disease transmitted mainly by tick bites, and the causative agent is SFTS virus (SFTSV). SFTS can rapidly progress to severe disease, with multiple-organ failure (MOF) manifestations such as shock, respiratory failure, disseminated intravascular coagulation (DIC) and death, but cases of SFTS patients with central nervous system (CNS) symptoms onset and marked persistent involuntary shaking of the perioral area and limbs have rarely been reported.
Case presentation
A 69-year-old woman with fever and persistent involuntary shaking of the perioral area and limbs was diagnosed with SFTS with CNS symptom onset after metagenomic next-generation sequencing (mNGS) of cerebrospinal fluid (CSF) and peripheral blood identified SFTSV. The patient developed a cytokine storm and MOF during the course of the disease, and after aggressive antiviral, glucocorticoid, and gamma globulin treatments, her clinical symptoms improved, her laboratory indices returned to normal, and she had a good prognosis.
This case gives us great insight that when patients with CNS symptoms similar to those of viral encephalitis combined with thrombocytopenia and leukopenia are encountered in the clinic, it is necessary to consider the possibility of SFTS involving the CNS. Testing for SFTSV nucleic acid in CSF and blood (mNGS or polymerase chain reaction (PCR)) should be carried out, especially in critically ill patients, and treatment should be given accordingly.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12883-024-03664-6.
Severe fever with thrombocytopenia syndrome (SFTS) is a natural focal disease transmitted mainly by tick bites, and the causative agent is a novel Bunyavirus, also known as SFTS virus (SFTSV), belonging to the Phenuiviridae family and the Bandavirus genus, which was first isolated from patient serum by the Chinese Centre for Disease Control and Prevention in 2010 [ 1 ]. The main features of SFTS include fever, thrombocytopenia, leukopenia and gastrointestinal symptoms, and in severe cases, patients may present with multiple‑organ failure (MOF) symptoms such as shock, respiratory failure, disseminated intravascular coagulation (DIC) and death, with a mortality rate of 5–30% in East Asia [ 2 , 3 ]. SFTS may also present with central nervous system (CNS) involvement, which can severely affect the patient’s disease progression and prognosis and is manifested by seizures, psychiatric symptoms, cognitive impairment, and disorders of consciousness [ 4 , 5 ]. However, reports of patients who present with CNS symptoms as the first symptom and with marked persistent involuntary shaking of the perioral area and limbs are rare.
A 69-year-old female patient was admitted to the hospital with fever for 4 days, involuntary shaking around the mouth and limbs for 3 days, and mental abnormalities for 1 day. The patient was admitted to the emergency department of another hospital 4 days before admission because of fever, where her body temperature reached 38.7 °C and she showed poor mental status, less talking, a loss of appetite, but no headache, vomiting, and limb twitching. A routine blood examination showed a white blood cell (WBC) count of 2.28 × 10 9 /L and a platelet count of 165 × 10 9 /L. When given a cooling infusion for symptomatic treatment, her body temperature would temporarily return to normal. Three days before admission, she experienced persistent involuntary trembling around the mouth and lips, as well as trembling of the tongue and extremities. The trembling of the lips, mouth, and both distal upper limbs was especially bothersome and was aggravated by emotional excitement and accompanied by slurred speech. Two days before admission, she had persistent fever, with a body temperature up to 39.6 °C, and the effect of antipyretic drugs was not good. A routine blood examination performed in another hospital showed a WBC count of 1.78 × 10 9 /L and a platelet count of 81 × 10 9 /L, which was significantly decreased compared with the count from the previous examination. One day prior to admission, the patient experienced babbling, restlessness, irritability, and a decline in time and place orientation and calculation power.
The patient had a many-year history of hypertension, diabetes mellitus and hyperlipidaemia; denied a history of working and living in hilly, forested and mountainous areas and travelling; denied a recent history of mosquito bites; and reported a history of close contact with a pet dog in the last month.
Neurological examination after admission showed that the patient had normal arousal but had unclear speech, hyperactivity, irritability. Her time and place orientation and calculation power decreased. The patient was uncooperative in the pharyngeal reflex examination, and involuntary tongue twitching could be seen when the tongue was stretched out. The remaining cranial nerve examination did not show any abnormalities. Perioral and limb involuntary shaking was obvious and persistent, especially in the perioral area and distal part of both upper limbs. Bilateral tendon reflexes were symmetrical, bilateral pathological signs were negative, and meningeal irritation signs were negative.
On admission, viral encephalitis was considered, and intravenous acyclovir antiviral therapy (0.5 g, q8h) was empirically administered. A comprehensive examination revealed that the patient had MOF: (1) Her platelet count further decreased to 63 × 10 9 /L (normal: 100–300 × 10 9 /L), toxic granules were seen in some granulocytes of the peripheral blood smear, and heterogeneous lymphocytes accounted for 21% of the total. (2) She had impaired liver function with elevated liver enzymes (alanine aminotransferase (ALT), 76 IU/L (normal: 5–40 IU/L); aspartate aminotransferase (AST), 188 IU/L (normal: 8–40 IU/L); and gamma-glutamyl transpeptidase (γ-GT), 177 IU/L (normal: 7–50 IU/L)), which was treated with magnesium isoglycyrrhizinate injection and vitamin C for liver protection. (3) She had acute myocardial injury, with an increased heart rate of > 120 beats/minute and markedly elevated myocardial enzyme and B-type natriuretic peptide levels (myoglobin, 299 ng/mL (normal: 25–58 ng/mL); troponin T, 209 ng/L (normal: 0–14 ng/L); and B-type natriuretic peptide, 9,355 pg/mL (normal: 0-125 pg/mL)). Electrocardiograms (ECGs) showed various atypical manifestations, such as short PR intervals; atrial premature, mild ST-segment depression in leads V2V3; and T-wave changes in multiple leads. Cardiac ultrasound showed a normal left ventricular ejection fraction but abnormal segmental motion of the left ventricular wall, biventricular diastolic insufficiency and a small amount of pericardial effusion. Coenzyme Q10 and trimetazidine were given to improve myocardial energy metabolism, and fluid intake and output were closely monitored. (4) The patient had a bacterial infection of the lungs, combined with type I respiratory failure, which were treated with tracheal intubation and mechanical ventilation immediately to assist respiration and antibiotic antimicrobial therapy. The patient did not have prolonged hypoxic injury. (5) She had impaired renal function, with elevated blood urea nitrogen (BUN) (17.33 mmol/L) (normal: 1.7–8.3 mmol/L) and urinary protein. We administered measures to ensure fluid intake and without the use of nephrotoxic drugs. (6) She had impaired pancreatic function, with elevated lipase (56.5 U/L) (normal: 5.6–51.3 U/L); we administered acid-suppressing drugs to inhibit pancreatic secretion and reduce the load and damage to pancreatic tissue. (7) She had abnormal coagulation, with a prolonged prothrombin time (PT) and thrombin time (TT) (15.7 s (normal: 11–15 s) for PT and 22.6 s (normal: 14–21 s) for TT), decreased fibrinogen (1.8 g/L) (normal: 2–4 g/L), and markedly elevated plasma D-dimer (9.01 µg/mL) (normal: 0.01–0.5 µg/mL) and fibrinogen degradation products (FDPs) (28.36 µg/mL) (normal: 0–5 µg/mL). (8) A thrombus had formed in her right peroneal vein and the intermuscular veins of the right and left calves, for which low molecular heparin anticoagulation was given. (9) Her muscle enzyme profiles were variably elevated (creatine kinase (CK), 335 IU/L (normal: 24–195 IU/L); lactate dehydrogenase (LDH), 1347 IU/L (normal: 109–245 IU/L); and alpha-hydroxybutyrate dehydrogenase (α-HBDH), 645 IU/L (normal: 72–182 IU/L)), correlating with inflammatory response-mediated organ damage. (10) The patient experienced a cytokine storm, with significantly increased inflammatory factors (ferritin > 1500 ng/mL (normal: 11-306.8 ng/mL), interleukin (IL)-6 = 49.88 pg/mL (normal: 0–20 pg/mL), IL-8 = 45.99 pg/mL (normal: 0-21.4 pg/mL), and IL-10 = 25.67 pg/mL (normal: 0-5.9 pg/mL), interferon (IFN)-α = 9.76 pg/mL (normal: 0-7.9 pg/mL), and IFN-γ = 18.7 pg/mL (normal: 0-17.3 pg/mL)) in serum (Table 1 ). (11) Finally, the patient showed an electrolyte balance disorder, as evidenced by hypernatremia (154 mmol/L) (normal: 135–145 mmol/L), hyperchloremia (119 mmol/L) (normal: 96–108 mmol/L), hypocalcaemia (1.92 mmol/L) (normal: 2.03–2.67 mmol/L), and hypophosphatemia (0.54 mmol/L) (normal: 0.84–1.65 mmol/L), and treatments included calcium supplementation, phosphorus supplementation, nasal administration of plain water, and a reduction of sodium and chlorine intake.
Summary of cytokine levels in CSF and blood
CSF , cerebrospinal fluid; IL , interleukin; TNF , tumour necrosis factor; IFN , interferon
Lumbar puncture was performed on the second day after admission (Table 2 ). Cerebrospinal fluid (CSF) was colourless and clear, with a pressure of 190 mmH 2 O (normal: 80–180 mmH 2 O) and a WBC count of 3 × 10 6 /L. CSF cytology showed scattered lymphocytes and a few mononuclear cells. The glucose level and protein counts were normal, chloride was slightly elevated (134 mmol/L) (normal: 118–128 mmol/L), immunoglobulins (Ig) were slightly elevated (IgA, 1.03 mg/dL (normal: 0-0.2 mg/dL); IgM, 0.22 mg/dL (normal: 0-0.2 mg/dL); and IgG, 6.68 mg/dL (normal: 0.48–5.86 mg/dL)), and CSF cytokine levels of IL-6 (27.46 pg/mL) (normal: 0–20 pg/mL) and IL-8 (546.93 pg/mL) (normal: 0-21.4 pg/mL) were elevated. CSF was negative for an autoimmune encephalitis antibody profile (NMDAR, CASPR2, AMPAR1, AMPAR2, LGI1, GABABR, DPPX, and IgLON5), neuroparaneoplastic syndrome antibody profile (Hu, Ri, Yo, CV2, Amphiphysin, GAD65, PNMA2, Recoverin, SOX1, Titin, Tr, and Zic4), and CNS demyelination antibody profile (AQP4, GFAP, MBP, and MOG). Metagenomic next-generation sequencing (mNGS) showed that the number of sequences of a novel Bunyavirus of the Bandavirus genus was 59 in the blood and 12 in the CSF. We also excluded acute febrile illnesses by serum and CSF mNGS, such as dengue fever, chikungunya fever, EB virus infection, renal syndrome hemorrhagic fever, and rickettsial disease.
Summary of the CSF tests
CSF , cerebrospinal fluid; Ig , immunoglobulin; NMDAR , N-methyl-D-aspartate receptor; CASPR2 , contactin associated protein 2; AMPAR , α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor; LGI1 , leucine-rich glioma inactivated 1; GABABR , gamma aminobutyric acid receptor type b; DPPX , dipeptidyl-peptidase-like protein-6; IgLON5 , immunoglobulin-like cell adhesion molecule 5; GAD65 , glutamic acid decarboxylase 65; PNMA2 , paraneoplastic antigen MA2; SOX1 , sex-determining region of Y chromosome-related high mobility group box 1; AQP4 , aquaporin protein-4; GFAP , glial fibrillary acidic protein; MBP , myelin basic protein; MOG , myelin oligodendrocyte glycoprotein
A diagnosis of SFTS that started with symptoms of CNS and encephalitis due to a novel Bunyavirus was considered based on the patient’s clinical presentation and laboratory test results. With immediate effect, acyclovir was adjusted to the broad-spectrum antiviral drug Foscarnet sodium (3 g, q8h); intravenous infusion of dexamethasone (10 mg qd for five days) and intravenous immunoglobulin (IVIG) (0.4 g/kg for five days) were administered to regulate immune function and inhibit the cytokine storm; nifedipine and benidipine hydrochloride were given to reduce the viral-induced calcium inflow to inhibit viral replication, reduce the viral load and increase the platelet count; clonazepam (1 mg, q8h) was given to relieve the patient’s obvious symptoms of involuntary shaking; and adequate symptomatic supportive therapy was given to ensure adequate calorie and protein intake and to maintain water, electrolyte, blood glucose and acid‒base balance.
After 3 days of hospitalization, the patient’s platelet and WBC counts began to rise gradually and returned to normal levels. After 5 days of hospitalization, the patient’s involuntary shaking and psychiatric symptoms were less severe than before, but compliance with activities was still poor, and her cognitive level still had not returned to normal. After 11 days of hospitalization, the lung infection was better than before, and ventilator withdrawal training was started. After 12 days of hospitalization, cranial magnetic resonance imaging (MRI) was performed, which showed slightly high signals in the bilateral anterior temporal lobe, temporal lobe hook gyrus, insular cortex, and bilateral thalamus on fluid attenuated inversion recovery (FLAIR) and diffusion weighted imaging (DWI) (Fig. 1 a-f). After 13 days of hospitalization, a blood sample was negative for novel Bunyavirus nucleic acid. After 16 days of hospitalization, her condition was significantly better than before, she could perform activities as instructed and answer questions correctly, her time and place orientation returned to normal, and her cognitive level was better than before. A electroencephalogram (EEG) was performed, and a full-lead low-wave amplitude state was observed (Fig. 2 ). After 17 days of hospitalization, the ventilator was completely withdrawn, and the tracheal tube was removed. A repeat lumbar puncture 3 weeks after hospitalization showed a pressure of 110 mmH 2 O, a WBC count of 4 × 10 6 /L, a normal protein count, a slightly elevated glucose level (5.19 mmol/L, compared with a glucose of 7.9 mmol/L over the same period), a slightly elevated chlorine level (130 mmol/L), and a return of Ig to normal. The levels of cytokines IL-6 (4.35 pg/mL) and IL-8 (96.17 pg/mL) decreased significantly compared with the previous levels, and the levels of whole-blood cytokines returned to the normal range (IL-6, 12.22 pg/mL; IL-8, 4.62 pg/mL; IL-10, 1.27 pg/mL; IFN-α, 0 pg/mL; and IFN-γ, 1.14 pg/mL) in serum (Table 1 ). No further novel Bunyaviruses were detected by mNGS of the CSF. Meanwhile, MOF gradually recovered, and liver, heart, lung, kidney, pancreas and coagulation function; the muscle enzyme profile; inflammatory factors; and electrolyte levels gradually returned to normal levels.

Cranial MRI of the patient 12 days after admission. Bilateral anterior temporal lobe (a and d) , temporal lobe leptomeningeal gyrus (a and d) , insular cortex (b and e) , and bilateral thalamus (c and f) FLAIR and DWI sequences with slightly high signals

Sixteen-lead resting-state EEG of the patient 16 days after admission. Simultaneous display an EEG record in monopolar and bipolar montages. A low-amplitude state can be seen in all leads. (a) monopolar montage EEG, (b) bipolar montage EEG
After antiviral therapy, immunotherapy, life support and symptomatic treatment, the patient’s vital signs were stable 3 weeks after admission, with clear speech and normal higher cortical function to perform tasks correctly on command. The muscle strength of all four limbs was grade 5, muscle tone was normal, bilateral tendon reflexes existed symmetrically, an ataxia test was normal, bilateral pathological signs were negative, and meningeal irritation signs were negative. She was discharged from the hospital in 23 days after admission. The patient was followed up 1 month after she was discharged from the hospital and is now back to her normal living conditions, with normal functioning of the higher cortex, the ability to take care of herself, and the ability to perform all of the activities she regularly engages in.
Discussion and conclusions
SFTS is an infectious disease caused by SFTSV infection. The epidemic period is mainly in May-August, and SFTSV is mainly transmitted by tick bites to humans. In recent years, interpersonal and human-animal transmission has also been found. An epidemiological survey of SFTS found that 48% of the patients had had close contact with their pets within two weeks of the onset of the disease [ 6 ]. The general population is susceptible, with a higher risk of infection in residents living in areas such as hills, mountains and forests and in people who spend time outdoors. In this case, SFTSV was isolated from blood and CSF. There was no history of tick bites or travel in the wild, but there was a history of close contact with a pet dog within the past month, and we hypothesized that the infected dog might have been the source of SFTSV in this patient.
The pathogenesis of CNS involvement in SFTS patients is unclear. Previous studies have demonstrated that Bunyaviruses have neurological properties of attack, and Park et al. found viral transcripts of novel Bunyaviruses in the brain and spinal cord of an aged model ferret. It is hypothesized that novel Bunyaviruses also involve the CNS, with consequent symptoms [ 7 ]. Possible mechanisms by which SFTSV attacks the CNS include direct invasion, cytokine storms, and impaired immune function. Kaneko et al. [ 8 ] performed an autopsy on a patient with SFTS with rapid CNS involvement, and the pathological findings revealed a massive infiltration of macrophages with high haematoxylin content and inflammatory cells around the microvessels of the cerebral pontine, fibrin deposition in the vessels, and focal degenerative lesions in some neuronal cells. In a variety of brain tissues, positive SFTSV nucleocapsid protein antigens were observed in the immunoblasts infiltrating the vascular lumen, suggesting that SFTSV can invade the CNS directly for disease development. The availability of agents that recognize these antigens also suggest immunoassays are possible and available for serodiagnosis. For example, serum enzyme linked immunosorbent assay or immunofluorescence to determine SFTSV antigens and antibodies have been used for clinical diagnosis [ 9 ]. Several studies [ 10 – 15 ] have found that the blood levels of several cytokines, including IFN-α, IFN-γ, IL-6, IL-8, IL-10, tumour necrosis factor (TNF)-α, and monocyte chemotactic protein (MCP)-1, are elevated in patients with SFTS, and IL-8 and MCP-1 levels in the CSF are significantly higher than the blood of those who present with CNS symptoms [ 10 ], suggesting that a cytokine storm may increase vascular permeability and prompt SFTSV to cross the blood‒brain barrier (BBB) and invade the CNS. SFTSV was found in the CSF of this patient, suggesting that the virus had invaded the patient’s CNS. The patient’s blood levels of IL-6, IL-8, IL-10, IFN-α, and IFN-γ were markedly elevated compared with normal ranges; IL-6 and IL-8 were elevated in the CSF; and CSF IL-8 levels were significantly higher than the blood levels, which was consistent with the results of a previous study [ 10 – 15 ], further suggesting that the cytokine storms induced by multiple elevated cytokines may increase BBB vascular permeability and contribute to the SFTSV invasion of the CNS. In patients with SFTS complicated by neurological involvement, protein and glucose levels in the CSF are normal and that an increase in leukocytes in the CSF may be uncommon. However, in the case of a high suspicion both on a clinical and epidemiological level in countries where the infection exists, in these patients the search for MCP-1 and IL-8 in the CSF and serum is indicated and CSF viral RNA detection are recommended.
According to the course of infection, SFTS can be divided into four periods: the incubation period, the febrile period, the MOF period, and the recovery period [ 1 – 3 , 16 ]. Patients with SFTS can present with neurological symptoms, which usually appear approximately 5 days after the onset of the disease (Table 3 ) and are often regarded as a complication of SFTS, which has been referred to as SFTS-associated encephalopathy/encephalitis (SFTSAE) [ 10 ]. SFTSAE mainly manifests as headache, seizures, mental abnormality, irritability, limb convulsions, cognitive impairment, and impaired consciousness, with an incidence of approximately 19.1-57.02% [ 4 , 5 , 11 , 17 ]. Most patients with SFTSAE develop impaired consciousness, such as coma, before their condition is taken seriously, which leads to a poor prognosis for the patients [ 4 , 18 ]. Most clinicians rely on the clinical manifestations to make the clinical diagnosis. SFTSV has rarely been isolated from CSF. We screened studies and case reports of SFTS with CNS involvement and found no reports of disease onset with CNS symptoms such as marked persistent involuntary shaking of the perioral area and extremities. In this case, the patient first presented with fever, followed by persistent involuntary tremors of the perioral area and limbs and mental behavioural abnormalities such as rambling, irritability and agitation; furthermore, the whole-genome sequence of SFTSV was found by mNGS of blood and CSF. The case reported here is a case of SFTS with CNS symptoms onset, accompanied by perioral and extremity persistent involuntary shaking, which has not been previously reported in the literature. It has been reported in the literature that SFTS patients can have tremors of limbs and muscles [ 8 , 17 , 19 ], but most of them occurred in the middle and late stages of the disease, and the tremor amplitude was small. In this case, the patient had large-amplitude involuntary shaking of the limbs that was persistent and intensified during agitation, which immediately attracted the clinician’s attention. An additional movie file shows this in more detail [see Additional file 1 ]. However, the specific underlying mechanism is not clear, and a description of similar symptoms of viral encephalitis and an analysis of the underlying mechanism have not been found before; therefore, further studies are needed. The course of the disease in this patient was consistent with the general pattern, with the clinical experience of the febrile period, the MOF period, and the recovery period. The febrile period lasted approximately 4 days, followed by MOF involving the liver, heart, lungs, kidneys, and pancreas, and then the recovery period began approximately 2 weeks after the disease onset, with clinical symptoms gradually returning to normal.
CNS involvement in relation to the timing of the clinical onset of SFTS
CNS , central nervous system; SFTS , severe fever with thrombocytopenia syndrome
There are fewer reports on neurological-related ancillary investigations (CSF, cranial imaging, and EEG) in SFTS patients with CNS involvement, and we analyse this because SFTS patients rarely start with CNS symptoms and go directly to the neurology department and because such patients are generally more severely ill, making it difficult for them to cooperate in completing the relevant investigations. In a few previous studies, lumbar puncture CSF tests in SFTS patients with CNS symptoms were mostly normal, with few abnormal changes in leukocyte counts, sugars and proteins [ 10 , 20 ]. Park et al. [ 10 ] analysed head imaging and EEG in a series of SFTS patients presenting with CNS symptoms, and no new focal lesions were seen on imaging in any of the brain parenchyma, suggesting that the imaging was not specific and that the EEG in the majority of the patients showed a slow-wave background rhythm (δ-θ), a common feature of encephalitis/encephalopathy. In this patient, two lumbar punctures were performed successively, and no CSF leukocyte abnormalities were observed in any of them either; it was presumed that SFTSV infection was less likely to involve the meninges. We performed cranial MRI and EEG on the patient 12 and 16 days after admission, respectively, and slightly high signals were observed in the bilateral anterior temporal lobes, temporal lobe hook gyrus, insular cortex, and bilateral thalamus in the FLAIR and DWI sequences of cranial MRI, all of which were consistent with the general imaging manifestations of viral encephalitis and were presumed to be related to viral invasion. In addition, we should consider the similarities and differences between the above MRI changes and cortical laminar necrosis associated with hypoxia or hypotension. We found that both had MRI high signals distributed along the cortex. However, this patient’s cranial MRI showed cortical high signals only in FLAIR and DWI sequences, and no abnormal signal was found in T1WI, which was the most obvious difference from cortical laminar necrosis. Furthermore, the patient did not show hypotension or significant hypoxic injury, so the changes on cranial MRI were more likely to be inflammatory changes of viral encephalitis and less relevant to cortical laminar necrosis. The background rhythm of the EEG was an α rhythm, and the whole leads were in low amplitude, which was different from previous studies [ 10 ]. It was presumed that the patient’s brain inflammation had tended to recover at that time, but the suppression of cortical function was remained.
There are no specific drugs for the treatment of CNS symptoms in SFTS, and symptomatic supportive treatment is the mainstay. In vitro and ex vivo studies have found that nifedipine or benidipine hydrochloride can inhibit SFTSV replication, reduce viral load, increase platelet counts, and reduce morbidity and mortality, as confirmed in a retrospective clinical study [ 21 , 22 ]. Glucocorticoids can inhibit the cytokine storms caused by the overproduction of cytokines and reduce patient mortality [ 12 , 13 , 23 ], and a Japanese report documented that three SFTS patients with impaired consciousness recovered without any neurological sequelae after short-term glucocorticoid treatment. However, the authors also suggested that the dosage should be minimized and the duration of administration should be shortened to inhibit cytokine storms and provide systemic benefit, rather than high doses or prolonged use, to avoid side effects [ 24 ]. Gamma globulin, which triggers complement activation and viral neutralization and influences the differentiation process of Schwann cells to increase their regenerative potential [ 25 ], has been used to treat other virus-induced encephalitides and can be used for the treatment of CNS symptoms in SFTS. Two successful cases of combined glucocorticoid and IVIG therapy were reported in Korea [ 26 ]. Two case reports documented that plasma exchange therapy reduced cytokine levels but not viral load, presumably making plasma exchange more effective at an early stage [ 27 , 28 ]. However, these are case reports, and the findings should be confirmed by large-scale randomized controlled studies. In this case, the patient was given the broad-spectrum antiviral drug foscarnet sodium, intravenous infusion of dexamethasone and IVIG to regulate the immune function of the body and inhibit the inflammatory storm, nifedipine and benidipine hydrochloride to inhibit viral replication and reduce the viral load, and other symptomatic treatments. The patient’s clinical manifestations and laboratory indicators gradually improved.
The prognosis of patients with SFTS is related to numerous factors, and studies have shown that advanced age; significant elevations in ALT, AST, CK, CK-MB, LDH, γ-GT, and BUN; low platelet count; persistent lowering of blood calcium; and the presence of CNS symptoms are all important influences that can lead to a poor prognosis [ 29 – 34 ]. Most of these are commonly used to monitor cardiac, hepatic and renal function, and significant abnormalities in their results indicate more severe organ damage and dysfunction. In addition, there is a statistically significant difference in serum viral copy number between deceased and non-dead patients. The mean viral copy number was higher in deceased patients than in surviving patients, and patients with higher copy numbers had higher mortality rates [ 35 , 36 ]. It was shown that the serum viral load detected by polymerase chain reaction (PCR) on admission was higher in SFTSAE patients than in non-encephalitis patients [ 11 ]. The above suggests a relationship between patient serum number of SFTSV RNA copies and encephalitis CNS symptoms and mortality in SFTS patients. CNS symptoms are often considered to be associated with fatal outcomes in patients with SFTS [ 33 ], and early diagnosis and treatment of neurological symptoms can help reduce mortality. Advanced age; long intervals between onset and admission; comorbid diabetes mellitus or subcutaneous haemorrhage; pulmonary rales; low platelet count; elevated neutrophil percentages and LDH, CK, and C-reactive protein (CRP) levels; and decreased chloride concentrations are significantly associated with the development of CNS symptoms and should be taken into consideration in clinical practice [ 11 , 17 ]. We believe that changes in platelet count and CK-MB should be monitored in patients with SFTSAE. As shown in previous, decreased platelet counts and high CK-MB levels are risk factors for poor prognosis in patients with SFTS. The presence of encephalitis is evidence of a more critical condition. Monitoring changes in platelet counts may provide an initial indication of the direction of the patient’s regression. It has been found that in cardiac enzyme profiles, patients presenting with CNS symptoms have elevated CK levels earlier than LDH and AST levels, and elevated liver enzyme levels later than cardiac enzymes [ 17 ]. Therefore, early monitoring of CK-MB levels may have a predictive effect on the development of CNS symptoms in patients. Although the mortality rate of SFTS patients presenting with CNS symptoms is significantly higher [ 11 ], several studies have found [ 11 , 37 , 38 ] that the long-term prognosis of surviving patients is good, with no obvious sequelae after active treatment. In this case, the patient’s laboratory indicators were consistent with the factors leading to a poor prognosis, and the CNS symptoms were prominent, suggesting that the condition was critical, but with timely administration of treatment, the patient’s condition eventually returned to normal.
In summary, we report a case of SFTS in a patient who started with CNS symptoms accompanied by marked persistent involuntary perioral and extremity shaking, and the whole-genome sequence of SFTSV was found by mNGS of both serum and CSF (It is important to note that hospitals where mNGS analysis is unavailable should use real-time fluorescent quantitative PCR to detect SFTS-specific nucleic acids in serum and CSF.). This has given us great insight into the fact that SFTS should be considered a possible cause when patients present with common CNS symptoms of viral encephalitis, such as mental behavioural abnormalities, convulsions, and cognitive deficits, or rare symptoms, such as persistent involuntary shaking of the perioral area and limbs in the rare case of this patient, combined with thrombocytopenia and leukopenia. Prompt lumbar puncture examination for SFTSV should be performed, and appropriate treatment should be given aggressively to reduce mortality.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
Author contributions.
Dawei Shan and Yan Zhang contributed to the conception and design of the manuscript. Dawei Shan collected the data and drafted the manuscript. Yan Zhang, Weibi Chen, Gang Liu, Huimin Zhang and Shuting Chai reviewed and modified the manuscript. All authors contributed to manuscript revision and read and approved the final submitted version.
This project was supported by National Key Research and Development Program of China (2020YFC2005403), and by China Association for Promotion of Health Science and Technology (JKHY2023001).
Data availability
Declarations.
Informed consent was obtained from the patient to publish this case, and approval for this study was provided by Research Ethics Committee of the Xuanwu Hospital of Capital Medical University.
Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the Editor of this journal.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
Health information systems (HIS) are critical systems deployed to help organizations and all stakeholders within the healthcare arena eradicate disjointed information and modernize health processes by integrating different health functions and departments across the healthcare arena for better healthcare delivery [1,2,3,4,5,6].Over time, the HIS has transformed significantly amidst several ...
Thus, through a comprehensive review of the extant literature, this study presents a critique of the health information system for healthcare to supplement the gap created as a result of the lack of an in-depth outlook of the current health information system from a holistic slant. From the studies, the health information system was ascertained ...
Abstract: Health information system deployment has been driven by the transformation and digital-. ization currently confronting healthcare. The need and potential of these systems within ...
E.g. Ball [4] presented perspectives on problems and prospects for hospital information systems. ... with more detail. Kumar et al. [24] identified research gaps in routine health information systems by means of a literature review for low- and middle-income countries. From 316 studies they identified obstacles related to data quality, data use ...
Abstract: The literature on the topic of health information systems (HISs) is reviewed in this paper. Specifically, the paper. reviews the literature on (i) the theoretical concept o f HISs (The ...
The following keywords were used in step 1: "Health information systems" OR "Health information technology" OR "Informatics" AND "Evaluation framework". Scopus, Science Direct, PubMed, CINAHL+, and Web of science (ISI) databases were chosen to conduct the systematic review. In step (2), we went through the title of identified ...
Background Patient flow describes the progression of patients along a pathway of care such as the journey from hospital inpatient admission to discharge. Poor patient flow has detrimental effects on health outcomes, patient satisfaction and hospital revenue. There has been an increasing adoption of health information systems (HISs) in various healthcare settings to address patient flow issues ...
Background Accelerated by the coronavirus disease 2019 (Covid-19) pandemic, major and lasting changes are occuring in healthcare structures, impacting people's experiences and value creation in all aspects of their lives. Information systems (IS) research can support analysing and anticipating resulting effects. Aim The purpose of this study is to examine in what areas health information ...
2.2 Smart Hospital Equipment and Systems. The following components were found to synthesize a smart hospital: Connected Medical Devices. Mobile devices interconnected with identification systems and clinical information systems, enable remote monitoring of patients, which results to an increasing automation and decision making.
In this paper a comprehensive search of the literature concerning the evaluation of complex health information systems is conducted and used to generate a synthesis of the literature around evaluation efforts in this field. Three approaches for evaluating hospital information systems are presented - user satisfaction, usage, and economic ...
Introduction. The quality of information systems represents the set of qualities and properties that characterize and determine the usefulness and existence of these systems [] (eg, security, usability, scalability, and others).Quality can be interpreted as a set of characteristics that a product or service possesses, as well as its capacity to satisfy new and complex user requirements (eg ...
The literature on the topic of health information systems (HISs) is reviewed in this paper. Specifically, the paper reviews the literature on (i) the theoretical concept of HISs (The What), (ii ...
The traditional healthcare system is facing various challenges. Chronic diseases are one of the big threats to human health, and are becoming a challenge to healthcare systems all over the world. 1 The rapidly growing aging population is becoming another challenge. The proportion of the world's population aged 60 years or above is expected to reach 21 percent in 2050. 2 Therefore, the ...
Background The literature on implementing Electronic Health Records (EHR) in hospitals is very diverse. The objective of this study is to create an overview of the existing literature on EHR implementation in hospitals and to identify generally applicable findings and lessons for implementers. Methods A systematic literature review of empirical research on EHR implementation was conducted ...
The maturity models identified in the literature review as the most relevants are the Quintegra Maturity Model for electronic Healthcare [] and the Healthcare IT (HIT) Maturity Model developed by IDC Health Industry Insights.They present a wide scope on Hospital IST [].The HIMSS Maturity Model for Electronic Medical Record [] and the Continuity of Care Maturity Model [] are examples of ...
Therefore, literature has urged that patient flow needs to be viewed from the whole system of care viewpoint and called for a shift from ED-focused to system-wide or hospital-wide interventions [12, 69]. However, the gap between understanding the problem and having solutions to solve the problem seems still far.
Hospital information systems applications and potential: a literature review revisited, 1982-1992. Hospital information systems applications and potential: a literature review revisited, 1982-1992. Top Health Inf Manage. 1993 May;13 (4):1-14.
For the systematic review, a literature search of the PubMed, CINAHL, Embase, and Cochrane Library databases was conducted to retrieve original articles published between 1970 and 2014. ... As the number of hospital information systems (HISs) have rapidly increased, systems for nursing also have increased. Since nursing care is a major ...
The lineage of systems librarianship has been traced in the literature from the first catalog cards that were typewritten instead of completed by hand1; ... Systems librarianship, when merged with the position of informationist, evolves into the identity of the systems informationist in the hospital setting. The Health Sciences Library at ...
Background/Objectives: The newly emergent COVID-19 pandemic involved primarily the respiratory system and had also major cardiovascular system (CVS) implications, revealed by acute myocardial infarction (AMI), arrhythmias, myocardial injury, and thromboembolism. CVS involvement is done through main mechanisms—direct and indirect heart muscle injury, with high mortality rates, worse short ...
fajar farhan, "Literature Review Evaluation of Hospital Management Information System (SIMRS) Implementation Using Hot-Fit Method," vol. 10, no. April, 2022, doi: 10.47794/jkhws.
The literature review identified 13 major categories of PHR ... Although primarily aimed at health information systems researchers, implications listed in this study can be further extended to health practitioners, insurance providers, and policy makers. ... Cooley Dickinson Hospital Improving transitions cuts HF readmissions. Hosp Case Manag ...
Background: This study aimed to systematically review case reports documenting rare adverse events in patients with small cell lung cancer (SCLC) following the administration of immune checkpoint inhibitors (ICIs). Methods: A systematic literature review was conducted to identify case reports detailing previously unreported adverse drug reactions to ICIs in patients with SCLC. The scope of the ...
The characteristics that facilitate the adoption of Accounting Information Systems in Small and Medium Enterprises (SMEs) and their influence on corporate performance are investigated to ensure the long-term viability of SMEs in the face of business challenges and advancements. The viability of Small and Medium Enterprises is heavily reliant on effectively managed firm finance management.
Information management plays an important role in the provision of care and it can be improved by information and communication technology. The purpose of this literature review is to describe ...
Background TFEB/6p21/VEGFA-amplified renal cell carcinoma (RCC) is rare and difficult to diagnose, with diverse histological patterns and immunohistochemical and poorly defined molecular genetic characteristics. Case presentation We report a case of a 63-year-old male admitted in 2017 with complex histomorphology, three morphological features of clear cell, eosinophilic and papillary RCC and ...
The development of hospital information systems (HISs) has a significant effect on care processes. ... The data collection tool was a researcher-made questionnaire based on valid scientific literature [2,13,], medical informatics expert's opinion, health IT, ... Online Information Review. 2009; 34 (4):660-662.
maturity models for management of hospitals, using the analytical model of organizational dimensions. proposed Morton (1994), adapted to hospitals. As highlighted by Frega et al. (2017), this ...
A dramatic blast from the sun set off the highest-level geomagnetic storm in Earth's atmosphere on Friday that is expected to make the northern lights visible as far south as Florida and ...
Severe fever with thrombocytopenia syndrome with central nervous system symptom onset: a case report and literature review ... We took this video on day 2 after the patient was admitted to the hospital. The patient develops persistent involuntary shaking of the perioral area and limbs, especially in the perioral area and distal limbs, which is ...