- Summary of Recommendations
- USPSTF Assessment of Magnitude of Net Benefit
- Practice Considerations
- Update of Previous USPSTF Recommendations
- Supporting Evidence
- Research Needs and Gaps
- Recommendations of Others
- Article Information
USPSTF indicates US Preventive Services Task Force.
eFigure. US Preventive Services Task Force (USPSTF) Grades and Levels of Evidence
- USPSTF Recommendation: Depression and Suicide Risk Screening in Children and Adolescents JAMA US Preventive Services Task Force October 18, 2022 This 2022 Recommendation Statement from the US Preventive Services Task Force recommends screening for major depressive disorder (MDD) in adolescents aged 12 to 18 years (B recommendation) and concludes that current evidence is insufficient to assess the balance of benefits and harms of screening for MDD in children 11 years or younger (I statement) and of screening for suicide risk in children and adolescents (I statement). US Preventive Services Task Force; Carol M. Mangione, MD, MSPH; Michael J. Barry, MD; Wanda K. Nicholson, MD, MPH, MBA; Michael Cabana, MD, MA, MPH; David Chelmow, MD; Tumaini Rucker Coker, MD, MBA; Karina W. Davidson, PhD, MASc; Esa M. Davis, MD, MPH; Katrina E. Donahue, MD, MPH; Carlos Roberto Jaén, MD, PhD, MS; Martha Kubik, PhD, RN; Li Li, MD, PhD, MPH; Gbenga Ogedegbe, MD, MPH; Lori Pbert, PhD; John M. Ruiz, PhD; Michael Silverstein, MD, MPH; James Stevermer, MD, MSPH; John B. Wong, MD
- USPSTF Report: Screening for Depression and Suicide Risk in Children and Adolescents JAMA US Preventive Services Task Force October 18, 2022 This systematic review to support the 2022 US Preventive Services Task Force Recommendation Statement on screening for depression and suicide risk in children and adolescents summarizes published evidence on the benefits and harms of screening for and treatment of depression and suicide risk in children and adolescents 18 years or younger. Meera Viswanathan, PhD; Ina F. Wallace, PhD; Jennifer Cook Middleton, PhD; Sara M. Kennedy, MPH; Joni McKeeman, PhD; Kesha Hudson, PhD; Caroline Rains, MPH; Emily B. Vander Schaaf, MD, MPH; Leila Kahwati, MD, MPH
- USPSTF Review: Depression and Suicide Risk Screening JAMA US Preventive Services Task Force June 20, 2023 This systematic review to support the 2023 US Preventive Services Task Force Recommendation Statement on depression and suicide risk screening summarizes published evidence on the benefits and harms of screening for, and treatment of, depression and suicide risk in primary care settings, including during pregnancy and postpartum. Elizabeth A. O’Connor, PhD; Leslie A. Perdue, MPH; Erin L. Coppola, MPH; Michelle L. Henninger, PhD; Rachel G. Thomas, MPH; Bradley N. Gaynes, MD, MPH
- Reframing the Key Questions Regarding Screening for Suicide Risk JAMA Editorial June 20, 2023 Gregory E. Simon, MD, MPH; Julie E. Richards, PhD, MPH; Ursula Whiteside, PhD
- Screening for Depression and Suicide Risk in Adults JAMA JAMA Patient Page June 20, 2023 This JAMA Patient Page describes the pros and cons of screening for depression and suicide risk in adults. Jill Jin, MD, MPH
- Suicidality Screening Guidelines Highlight the Need for Intervention Studies JAMA Network Open Editorial June 20, 2023 Roy H. Perlis, MD, MSc

See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
US Preventive Services Task Force. Screening for Depression and Suicide Risk in Adults : US Preventive Services Task Force Recommendation Statement . JAMA. 2023;329(23):2057–2067. doi:10.1001/jama.2023.9297
Manage citations:
© 2024
- Permissions
Screening for Depression and Suicide Risk in Adults : US Preventive Services Task Force Recommendation Statement
- Editorial Reframing the Key Questions Regarding Screening for Suicide Risk Gregory E. Simon, MD, MPH; Julie E. Richards, PhD, MPH; Ursula Whiteside, PhD JAMA
- Editorial Suicidality Screening Guidelines Highlight the Need for Intervention Studies Roy H. Perlis, MD, MSc JAMA Network Open
- US Preventive Services Task Force USPSTF Recommendation: Depression and Suicide Risk Screening in Children and Adolescents US Preventive Services Task Force; Carol M. Mangione, MD, MSPH; Michael J. Barry, MD; Wanda K. Nicholson, MD, MPH, MBA; Michael Cabana, MD, MA, MPH; David Chelmow, MD; Tumaini Rucker Coker, MD, MBA; Karina W. Davidson, PhD, MASc; Esa M. Davis, MD, MPH; Katrina E. Donahue, MD, MPH; Carlos Roberto Jaén, MD, PhD, MS; Martha Kubik, PhD, RN; Li Li, MD, PhD, MPH; Gbenga Ogedegbe, MD, MPH; Lori Pbert, PhD; John M. Ruiz, PhD; Michael Silverstein, MD, MPH; James Stevermer, MD, MSPH; John B. Wong, MD JAMA
- US Preventive Services Task Force USPSTF Report: Screening for Depression and Suicide Risk in Children and Adolescents Meera Viswanathan, PhD; Ina F. Wallace, PhD; Jennifer Cook Middleton, PhD; Sara M. Kennedy, MPH; Joni McKeeman, PhD; Kesha Hudson, PhD; Caroline Rains, MPH; Emily B. Vander Schaaf, MD, MPH; Leila Kahwati, MD, MPH JAMA
- US Preventive Services Task Force USPSTF Review: Depression and Suicide Risk Screening Elizabeth A. O’Connor, PhD; Leslie A. Perdue, MPH; Erin L. Coppola, MPH; Michelle L. Henninger, PhD; Rachel G. Thomas, MPH; Bradley N. Gaynes, MD, MPH JAMA
- JAMA Patient Page Screening for Depression and Suicide Risk in Adults Jill Jin, MD, MPH JAMA
Importance Major depressive disorder (MDD), a common mental disorder in the US, may have substantial impact on the lives of affected individuals. If left untreated, MDD can interfere with daily functioning and can also be associated with an increased risk of cardiovascular events, exacerbation of comorbid conditions, or increased mortality.
Objective The US Preventive Services Task Force (USPSTF) commissioned a systematic review to evaluate benefits and harms of screening, accuracy of screening, and benefits and harms of treatment of MDD and suicide risk in asymptomatic adults that would be applicable to primary care settings.
Population Asymptomatic adults 19 years or older, including pregnant and postpartum persons. Older adults are defined as those 65 years or older.
Evidence Assessment The USPSTF concludes with moderate certainty that screening for MDD in adults, including pregnant and postpartum persons and older adults, has a moderate net benefit. The USPSTF concludes that the evidence is insufficient on the benefit and harms of screening for suicide risk in adults, including pregnant and postpartum persons and older adults.
Recommendation The USPSTF recommends screening for depression in the adult population, including pregnant and postpartum persons and older adults. (B recommendation) The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of screening for suicide risk in the adult population, including pregnant and postpartum persons and older adults. (I statement)
See the Summary of Recommendations figure.
Pathway to Benefit
To achieve the benefit of depression screening and reduce disparities in depression-associated morbidity, it is important that persons who screen positive are evaluated further for diagnosis and, if appropriate, are provided or referred for evidence-based care.
The US Preventive Services Task Force (USPSTF) makes recommendations about the effectiveness of specific preventive care services for patients without obvious related signs or symptoms to improve the health of people nationwide.
It bases its recommendations on the evidence of both the benefits and harms of the service and an assessment of the balance. The USPSTF does not consider the costs of providing a service in this assessment.
The USPSTF recognizes that clinical decisions involve more considerations than evidence alone. Clinicians should understand the evidence but individualize decision-making to the specific patient or situation. Similarly, the USPSTF notes that policy and coverage decisions involve considerations in addition to the evidence of clinical benefits and harms.
The USPSTF is committed to mitigating the health inequities that prevent many people from fully benefiting from preventive services. Systemic or structural racism results in policies and practices, including health care delivery, that can lead to inequities in health. The USPSTF recognizes that race, ethnicity, and gender are all social rather than biological constructs. However, they are also often important predictors of health risk. The USPSTF is committed to helping reverse the negative impacts of systemic and structural racism, gender-based discrimination, bias, and other sources of health inequities, and their effects on health, throughout its work.
Major depressive disorder (MDD), a common mental disorder in the US, can have a substantial impact on the lives of affected individuals. 1 , 2 If left untreated, MDD can interfere with daily functioning and can be associated with an increased risk of cardiovascular events, exacerbation of comorbid conditions, or increased mortality. 1 , 3 - 5 In 2019, 7.8% (19.4 million) of adults in the US experienced at least 1 major depressive episode; 5.3% (13.1 million) experienced a major depressive episode with severe impairment. 1 , 6 Depression can be a chronic condition characterized by periods of remission and recurrence, often beginning in adolescence or early adulthood. However, full recovery may occur. 1 There is overwhelming evidence of racial and ethnic disparities in depression treatment and outcomes. 7
Depression is common in postpartum and pregnant persons and affects both the parent and infant. Depression during pregnancy increases the risk of preterm birth and low birth weight or small-for-gestational age. 8 , 9 Postpartum depression may interfere with parent-infant bonding. 10 Data from the Pregnancy Risk Assessment Monitoring System has shown a recent increase in self-reported depression during pregnancy, from 11.6% in 2016 to 14.8% in 2019. 11
Suicide is the 10th leading cause of death in US adults (45 390 deaths [2019 data]). 12 From 2001 to 2017, there was a 31% increase in suicide deaths. 13 Over the last decade, there has been an increase; however, in recent years, suicide rates have declined. 14 In 2020, provisional suicide deaths numbered 45 855, which was 3% less than in 2019 (47 511 deaths). 15 , 16 However, rates did not decline among Black and Hispanic/Latino persons. 17 Rates of suicide attempts and deaths vary by sex, age, and race and ethnicity. 1 Psychiatric disorders and previous suicide attempts increase the risk of suicide. 1
The USPSTF concludes with moderate certainty that screening for MDD in adults, including pregnant and postpartum persons, as well as older adults, has a moderate net benefit .
The USPSTF concludes that the evidence is insufficient on the benefit and harms of screening for suicide risk in adults, including pregnant and postpartum persons, as well as older adults. As a result, the balance of benefits and harms cannot be determined.
See Table 1 and Table 2 for more information on the USPSTF recommendation rationale and assessment and the eFigure in Supplement for information on the recommendation grade. See the Figure for a summary of the recommendations for clinicians. For more details on the methods the USPSTF uses to determine the net benefit, see the USPSTF Procedure Manual. 18
This recommendation applies to adults 19 years or older who do not have a diagnosed mental health disorder or recognizable signs or symptoms of depression or suicide risk. Older adults are defined as those 65 years or older. This recommendation focuses on screening for MDD and does not address screening for other depressive disorders, such as minor depression or dysthymia.
The Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) defines MDD as having at least 2 weeks of mild to severe persistent feelings of sadness or a lack of interest in everyday activities. Depression can also present with irritability, poor concentration, and somatic complaints (eg, difficulty sleeping, decreased energy, and changes in appetite). 19
Perinatal depression is defined as depressive episodes that occur during pregnancy and the postpartum period (the first 12 months following delivery). 20 In addition to common symptoms of depressive disorders (eg, feeling sad or loss of interest in activities), other symptoms during the perinatal period may include difficulty bonding with the infant, persistent doubt in parenting abilities, and parental thoughts of death, suicide, self-harm, or harm to the infant. 21
Suicidal behavior includes suicidal ideation, suicide attempts, and suicide completion. Suicidal ideation refers to thinking about, considering, or planning suicide. Suicide attempts refer to nonfatal, self-directed, and potentially injurious behavior that is intended to result in death. Suicide completion is defined as a death caused by self-inflicted injurious behavior with the intent to cause death. 22
The USPSTF recommends screening for depression in all adults regardless of risk factors. Risk factors for depression include a combination of genetic, biological, and environmental factors, 1 , 23 such as a family history of depression, prior episode of depression or other mental health condition, a history of trauma or adverse life events, or a history of disease or illness (eg, cardiovascular disease). 24 - 30
Prevalence rates vary by sex, age, race, ethnicity, education, marital status, geographic location, poverty level, and employment status. 1 , 23 Women have twice the risk of depression compared with men. 31 , 32 Young adults, multiracial individuals, and Native American/Alaska Native individuals have higher rates of depression. 33
Risk factors for perinatal depression include life stress, low social support, history of depression, marital or partner dissatisfaction, and a history of abuse. 34
Many brief tools have been developed that screen for depression and are appropriate for use in primary care. All positive screening results should lead to additional assessments to confirm the diagnosis, determine symptom severity, and identify comorbid psychological problems.
Commonly used depression screening instruments include the Patient Health Questionnaire (PHQ) in various forms in adults, the Center for Epidemiologic Studies Depression Scale (CES-D), the Geriatric Depression Scale (GDS) in older adults, and the Edinburgh Postnatal Depression Scale (EPDS) in postpartum and pregnant persons. 1
Screening instruments for suicide risk include the Beck Hopelessness Scale, the SAD PERSONS Scale (Sex, Age, Depression, Previous attempt, Ethanol abuse, Rational thinking loss, Social supports lacking, Organized plan, No spouse, Sickness), and the SAFE-T (Suicide Assessment Five-step Evaluation and Triage). 1 Some depression screening instruments, such as the PHQ-9, incorporate questions that ask about suicidal ideation. 1
There is little evidence regarding the optimal timing for screening for depression; more evidence is needed in both perinatal and general adult populations. In the absence of evidence, a pragmatic approach might include screening adults who have not been screened previously and using clinical judgment while considering risk factors, comorbid conditions, and life events to determine if additional screening of patients at increased risk is warranted. Ongoing assessment of risks that may develop during pregnancy and the postpartum period is also a reasonable approach.
Effective treatment of depression in adults generally includes antidepressant medication or psychotherapy (eg, cognitive behavioral therapy or brief psychosocial counseling), alone or in combination. 1 Clinicians are encouraged to consider the unique balance of benefits and harms in the perinatal period when deciding the best treatment for depression for a pregnant or breastfeeding person.
Adequate systems and clinical staff are needed to ensure that patients are screened and, if they screen positive, are appropriately diagnosed and treated with evidence-based care or referred to a setting that can provide the necessary care. Inadequate support and follow-up may result in treatment failures or harm, including those indicated by the US Food and Drug Administration boxed warning for selective serotonin reuptake inhibitors (SSRIs). 1 These essential functions can be provided through a wide range of different arrangements of clinician types and settings, including primary care clinicians, mental health specialists, or both working collaboratively, such as within a collaborative care model. 1 , 35 Collaborative care is a multicomponent, health care system–level intervention that uses care managers to link primary care clinicians, patients, and mental health specialists. 1 , 35 Additional components of support include training and materials to improve clinicians’ knowledge and skills surrounding diagnosis and treatment of depression, facilitation or improvement of the referral process, and patient-specific treatment materials. 1 , 35
Potential barriers to screening include clinician knowledge and comfort level with screening, inadequate systems to support screening or to manage positive screening results, and impact on care flow, given the time constraints faced by primary care clinicians. Clinicians should be cognizant of stigma issues associated with mental health diagnoses and should aim to develop trusting relationships with patients, free of implicit bias, by being sensitive to cultural issues. 1
Clinicians should also be cognizant of the barriers that keep individuals with depression, particularly those identified through screening, from receiving adequate treatment. It is estimated that only 50% of patients with major depression are identified. 36 Only 35% of adults in the US with a depressive disorder receive care within the first year of condition onset. 37 Systemic barriers also exist, including lack of connection between mental health and primary care, patient hesitation to initiate treatment, and nonadherence to medication and therapy. 38 , 39
Racism and structural policies have contributed to wealth inequities in the US, 40 which can affect mental health services in underserved communities. 1 For example, wealth inequities may result in barriers to receiving mental health services, such as treatment costs and lack of insurance, which tend to have a greater impact on Black persons and other racial and ethnic groups than on White persons. 41 Black and Hispanic/Latino primary care patients are less likely to be diagnosed with depression or anxiety compared with White patients. 37 , 42 - 44 Black and Hispanic/Latino patients are also less likely to receive mental health services than Asian American or White patients. 45 , 46
Suicide is the second-leading cause of death in individuals aged 10 to 34 years. 2 Eighty-three percent of individuals who die by suicide were seen in primary care in the previous year; 24% had any mental health diagnosis in their medical records in the month prior to death. 47
Factors resulting in increased risk for suicide attempts include severe psychological distress, major depressive episodes, alcohol use disorder, marital status of being divorced or separated, or being unemployed. Important risk factors for suicide deaths include previous suicide attempts (strongest predictor of future suicide death), mental health disorders and substance abuse, family history of suicide or mental health disorders, life stressors, family violence or abuse, incarceration or legal problems, certain medical conditions, chronic pain, or being a military veteran. 1
Suicide risk varies by age, sex, and race and ethnicity. 1 Men are more than 3 times more likely to die by suicide than women. 48 The highest suicide rates for women occur between the ages of 45 and 54 years, while for men the highest rates occur after age 65 years. 48 In the US, the highest suicide rates occur among White adults, followed by Native American/Alaska Native adults. Between 2014 and 2019, suicide rates increased in Asian or Native Hawaiian/Pacific Islander individuals by 16% and in Black individuals by 30%. 49
Although evidence on harms of screening for suicide risk is limited, potential harms of screening include false-positive screening results that may lead to unnecessary referrals and treatment (and associated time and economic burden), labeling, anxiety, and stigma. Studies of suicide prevention interventions generally demonstrate that they are no more effective than usual care 1 ; however, 1 large pragmatic trial demonstrated an increased risk of self-harm with a dialectical behavioral therapy skills-building intervention. 50
Evidence is limited on the implementation of routine mental health screening in primary care settings in the US. No information on screening rates for depression and suicide risk in the US was identified. Suicide screening likely occurs as part of depression screening within settings that screen for suicide risk.
Screening instruments for suicide risk usually include components related to current suicidal ideation, self-harm behaviors, and assessments of past attempts and behaviors. It is unknown how often primary care clinicians detect elevated suicide risk in adults. Thirty-six percent of US primary care clinicians discussed suicide in encounters with patients showing symptoms of major depression or adjustment disorders or seeking antidepressants. 51
The Community Preventive Services Task Force (CPSTF) has several recommendations related to mental health conditions in adults. The CPSTF recommends collaborative care for managing depressive disorders. It recommends both home-based depression care and depression care management in primary care clinics for older adults. The CPSTF also recommends mental health benefits legislation in increasing appropriate utilization of mental health services for persons with mental health conditions. More information about the CPSTF and its recommendations on depression interventions is available on its website ( https://www.thecommunityguide.org ).
The Substance Abuse and Mental Health Services Administration maintains a national registry of evidence-based programs and practices for substance abuse and mental health interventions ( https://www.samhsa.gov/resource-search/ebp ) that may be helpful for clinicians looking for models of how to implement depression screening. The Suicide Prevention Resource Center, supported by the Substance Abuse and Mental Health Services Administration, offers various resources on suicide prevention ( https://sprc.org/ ).
In 2021, the US Surgeon General released a Call to Action that seeks progress toward full implementation of the National Strategy for Suicide Prevention ( https://www.hhs.gov/surgeongeneral/reports-and-publications/suicide-prevention/index.html ).
Perinatal Psychiatry Access Programs are population-based programs that aim to increase access to perinatal mental health care ( https://www.umassmed.edu/lifeline4moms/Access-Programs/ ). These programs build the capacity of medical professionals to address perinatal mental health and substance use disorders.
The USPSTF has recommendations on other mental health topics pertaining to adults, including screening for anxiety, 52 preventive counseling interventions for perinatal depression, 53 screening for unhealthy drug use, 54 and screening and behavioral counseling interventions for alcohol use. 55
This recommendation will replace the 2014 USPSTF recommendation statement on screening for suicide risk in adults 56 and the 2016 recommendation statement on screening for MDD in adults. 57 Previously, the USPSTF concluded that there was insufficient evidence to assess the balance of benefits and harms of screening for suicide risk in adults and older adults in primary care (I statement). The USPSTF recommended screening for MDD in in the general adult population, including pregnant and postpartum persons, noting that screening should be implemented with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow-up (B recommendation). The current recommendation statement is consistent with these previous recommendations.
The USPSTF commissioned a systematic review 1 , 58 to evaluate the benefits and harms of screening, accuracy of screening, and benefits and harms of treatment of MDD and suicide risk in asymptomatic adults that would be applicable to primary care settings.
The USPSTF examined evidence on the most widely used or recommended screening tools for depression: PHQ, any version; CES-D; EPDS for perinatal persons; and GDS for older adults. 1 , 58
The USPSTF found 14 primary studies (n = 8819) and 10 existing systematic reviews (n ≈ 75 000) on accuracy of screening tests for detecting depression. 1 , 58 The existing systematic reviews assessed different versions of the PHQ, 2- and 3-item Whooley screening questions, CES-D, and EPDS. 1 , 58 One study conducted a series of individual patient data meta-analyses to compare several versions of the PHQ with structured or semistructured interviews. In the individual patient data meta-analyses, the PHQ-9 identified 85% of participants with major depression and 85% of those without major depression, at the standard cutoff of 10 or greater, when compared with a semistructured interview reference standard (sensitivity, 0.85 [95% CI, 0.79-0.89]; specificity, 0.85 [95% CI, 0.82-0.87]; 47 studies [n = 11 234]). 1 , 58
At the standard cutoff of 2 or greater and when compared with a semistructured interview, the PHQ-2 was more sensitive than the PHQ-9, identifying 91% of participants with major depression (sensitivity, 0.91 [95% CI, 0.88-0.94]; 48 studies [n = 11 703]). However, specificity at that cutoff was lower, identifying 67% of participants without depression (specificity, 0.67 [95% CI, 0.64-0.71]; 48 studies [n = 11 703]). The Whooley screening questions and the CES-D demonstrated accuracy comparable with the PHQ-2. 1 , 58 The accuracy of the EPDS was also similar to that of the PHQ-2, with sensitivity ranging from 81% to 90% and specificity ranging from 83% to 88% at cutoffs of 11 and 12, compared with a fully structured diagnostic interview. 1 , 58
The 14 primary studies covered multiple versions of the GDS; the GDS-15 was the most common version. In the studies, participants were 55 years or older (mean age, 69-85 years). Fifty percent to 70% of participants were women. Race or ethnicity was reported in only 4 studies. In these 4 studies, patients were primarily White, although 1 study from the UK included only Afro-Caribbean participants. 1 , 58 The standard cutoff of 5 or greater had an acceptable balance of sensitivity and specificity. In a pooled analysis, the GDS-15 accurately identified participants with major depression (sensitivity, 0.94 [95% CI, 0.85-0.98]; I 2 = 85.7%; specificity, 0.81 [95% CI, 0.70-0.89]; I 2 = 99.2%), with a cutoff score of 5. 1 , 58
Three studies (n = 1801) assessed screening instruments for suicidal ideation. 1 , 58 - 61 Two studies evaluated general adult populations and 1 study evaluated older adults. The study with the most events was limited to older adults. 1 , 58 Individual screening tests (GDS-15, GDS-SI [GDS–Suicide Ideation], and SDDS-PC [Symptom Driven Diagnostic System for Primary Care]) were not examined in more than 1 study. Most screening instruments reported sensitivity and specificity above 0.80 for at least 1 reported cutoff score. 1 , 58
None of the studies on the accuracy of screening tests defined optimal screening timing or intervals for either general adult or perinatal populations.
Seventeen screening trials (n = 18 437 participants) directly addressed the benefits of screening for depression on health outcomes. Four trials included unscreened control groups. The remaining trials screened all participants but provided the screening results only to the intervention groups’ clinicians. 1 Trial participants included adults of all ages and perinatal populations; 6 studies included general adult populations, 4 studies were limited to older adults, 6 studies were limited to postpartum patients (between 2 and 12 weeks postpartum), and 1 study was limited to pregnant patients. 1 , 58
Nine of the studies were conducted in the US. The remaining studies were conducted in the UK, Hong Kong, and Northern European countries. 1 , 58 All studies took place in primary care, general practice, obstetrics-gynecology, or other maternal or child wellness settings. 1 , 58 The mean age of trial participants was 38.2 years. Across all studies, 93% of all participants were women. Women also comprised a majority of participants in studies focused on general adult populations (73% women) and older adults (66% women). Among studies conducted in the US, the proportion of Black participants ranged from 7.1% to 51.2% (6 studies); of Hispanic/Latino study participants, from 4.5% to 59.3% (4 studies); and of White study participants, from 29% to 94.1% (6 studies). Only 1 study reported the percentage of participants of Asian descent, and none reported the percentage who were Native American/Alaska Native. 1 , 58 Depression outcomes included the proportion of participants meeting criteria for depression or who were above a prespecified depression symptom score (“prevalence”), the proportion who no longer met criteria for depression or were below a prespecified symptom score (“remission”), the proportion whose depression symptoms were reduced by a specified amount (“response”), and mean symptom scores.
The direct evidence from the 17 screening trials demonstrated increased rates of depression remission or scoring below a specified symptom severity threshold after 6 to 12 months in general adult and perinatal populations. 1 , 58 Screening interventions, most of which also included other care management components, were associated with a lower prevalence of depression or clinically important depressive symptomatology at 6 months postbaseline or postpartum (or the closest follow-up to 6 months) (odds ratio [OR], 0.60 [95% CI, 0.50-0.73]; 8 randomized clinical trials [RCTs] [n = 10 244]; I 2 = 0%). Among participants scoring above a predefined symptom level at baseline, screening interventions were associated with a greater likelihood of remission or scoring below a specified level of depression symptomatology (OR, 1.58 [95% CI, 1.23-2.02]; 8 RCTs [n = 2302]; I 2 = 0%) after 6 months (or the closest follow-up to 6 months). However, no benefit in symptom severity measures was found (pooled mean difference in change, −1.0 [95% CI, −2.3 to 0.3]; 9 studies [n = 5543]; I 2 = 74.4%). 1 , 58
The evidence in older adult populations demonstrated smaller effects. Four trials examined screening only in older adults and only 1 trial used a depression measure that was specifically designed for older adults. Trials among general adult populations included older adults; however, none of the trials reported subgroup effects by age. 1 , 58 There was also a lack of evidence on the optimal time to screen or screening intervals.
Forty existing systematic reviews evaluated treatment for depression; 30 (≈346 RCTs [n ≈ 45 078]) addressed psychological treatment and 10 addressed pharmacologic treatment (≈522 studies [n ≈ 116 477]). One existing systematic review reported both psychological and pharmacotherapy treatment. 1 , 58 Psychotherapy treatment improved depression and other health outcomes such as anxiety symptoms, hopelessness, quality of life, and functioning in primary care patients, perinatal populations, and older adults. The broadest analysis (any type of psychotherapy compared with any kind of control condition, measuring the depression outcome immediately after treatment [typically 2-6 months postbaseline]) demonstrated a moderate to large effect on depression (standardized mean difference [SMD], −0.72 [95% CI, −0.78 to −0.67]; 385 studies [N not reported but estimated at ≈33 000]). The effect was smaller but still statistically significant when limited to studies in primary care patients (SMD, −0.42 [95% CI, −0.56 to −0.29]; 59 studies [N not reported]). 1 , 58 Remission and response to treatment were rarely reported. There were limited data for populations according to racial or ethnic group or whether participants were socially or economically disadvantaged. The limited evidence available suggested benefits of psychological treatment in these populations. 1 , 58
Pooled analyses of antidepressant medications demonstrated increased rates of remission and response to treatment and small but statistically significant reductions in depressive symptom severity in the short term (typically 8 weeks). 1 , 58 Fluoxetine (117 studies) was associated with a small reduction in symptom severity (SMD, −0.23 [95% CI, −0.28 to −0.19]), an increase in the odds of remission (OR, 1.46 [95% CI, 1.34-1.60]), and an increase in the odds of treatment response (OR, 1.52 [95% CI, 1.40-1.66]). 1 , 58 Limited evidence was available on the longer-term impact of antidepressants and on the benefits of pharmacologic treatment in older adults and pregnant persons. 1 , 58
Only 1 short-term RCT (n = 443) examined screening for suicide risk, which was limited to primary care patients who had screened positive for depression. 1 , 58 This trial reported no statistically significant group differences in suicidal ideation at 2 weeks’ follow-up, with 1 suicide attempt among all study participants. 1 , 58
Twenty-three RCTs (n = 22 632) of suicide prevention among persons at increased risk of suicide were included. 1 , 58 One trial evaluated lithium; the remaining trials studied behavioral interventions. The effectiveness of psychological interventions for suicide prevention on suicide deaths and suicide attempts could not be determined due to the small number of events. One suicide death was reported. Most studies reported 5 or fewer suicide attempts per study group, and the pooled effect was not statistically significant (OR, 0.94 [95% CI, 0.73-1.22]; 12 RCTs [n = 14 573]; I 2 = 11.2%) 1 , 58 Pooled analyses did not demonstrate improvement over usual care for suicidal ideation, self-harm, or depression symptom severity. 1 , 58
One depression screening RCT (n = 462) evaluated harms. This trial was among postpartum patients, and no adverse events were reported in the intervention and placebo groups. Across all other depression screening studies that evaluated the benefits of screening, there was no pattern of effects indicating that screening might paradoxically worsen any outcomes the interventions were intending to benefit. 1 , 58
Four existing systematic reviews (≈63 RCTs [n ≈ 8466]) addressed the harms of psychotherapy in the general adult and perinatal populations. Psychological interventions with any psychological treatment, self-guided internet-based cognitive behavioral therapy, or guided internet-based interventions did not increase the risk of harm, measured as a worsening of depressive symptoms. 1 , 58 In 3 existing systematic reviews, the deterioration rates were lower with psychological interventions or did not differ statistically from the control group. In an existing systematic review of older adults, 14 included trials did not report safety data. 1 , 58
Twenty-two existing systematic reviews (≈522 RCTs and 175 observational studies [n > 9 million]) and 1 cohort study (n = 358 351) addressed the harms of pharmacotherapy in adults of all ages and perinatal persons. 1 , 58 Two existing systematic reviews assessed perinatal patients, 4 evaluated older adults, and the remaining reviews included adults of any age. 1 , 58 Pharmacologic agents evaluated included SSRIs and other second-generation antidepressants. Harm outcomes included any adverse events, dropout due to adverse events, serious adverse events, suicide deaths, suicide attempts, and suicidal ideation. 1 , 58
Pharmacologic treatment was associated with a higher risk of dropout due to adverse events. There was also an increased risk of serious adverse events with SSRI use compared with placebo (OR, 1.39 [95% CI 1.12-1.72]; 44 RCTs [n not reported]; I 2 = 0%). The absolute risk of serious adverse events was low, and evidence for specific serious adverse events was limited. There were too few suicide deaths to examine the association between antidepressant use and suicide death. However, RCT and observational evidence demonstrated a small absolute increase in risk of suicide attempts with second-generation antidepressant use among adults up to age 65 years (OR, 1.53 [95% CI, 1.09-2.15] [n = 41 861]; 0.7% of antidepressants users vs 0.3% of placebo users). Evidence of other harmful outcomes (eg, cardiovascular-related, bleeding, mortality, risk of falls, fractures, or dementia) was limited and mostly included observational evidence. Evidence was also almost entirely limited to observational studies for serious harms of pharmacotherapy in pregnant or postpartum persons (eg, preeclampsia, gestational diabetes, postpartum hemorrhage, and spontaneous abortion). 1 , 58
A short-term study (2 weeks’ follow-up) among primary care patients (n = 443) who screened positive for depression assessed the harms of suicide risk screening. 62 Although absolute scores were higher on 2 of the 3 suicidal ideation measures, compared with no screening, the findings were not statistically significant. 1 , 58
Two RCTs of suicide prevention treatment reported on harms. There were no differences between groups at follow-up on an instrument developed to evaluate the perceived level of coercion experienced by service users during hospital admission. 63 , 64 A lithium trial found a higher rate of nonserious adverse events (75.7% with lithium, 69% with placebo; P value not reported) and of serious adverse events (38.8% with lithium, 34.1% with placebo; P value not reported). 64 However, there was no difference in withdrawals due to adverse events (1.2% with lithium, 1.5% with placebo; P value not reported). Treatment trials did not show results indicating paradoxical harms.
One large trial (n = 18 882) assessed 2 suicide prevention interventions among adults with an elevated risk of suicide based on the PHQ-9 (question 9). 65 A care management intervention, compared with usual care, had no impact on the rate of suicide attempts (hazard ratio, 1.07 [97.5% CI, 0.84 to 1.37]; P = .52). A low-intensity online skills training intervention was associated with an increased risk of suicide attempts (hazard ratio, 1.29 [97.5% CI, 1.02 to 1.64]; P = .02). 1 , 50 , 58
A draft version of this recommendation statement was posted for public comment on the USPSTF website from September 20, 2022, to October 17, 2022. In response to comments, the USPSTF added text in the Practice Considerations section to address barriers to screening such as lack of clinician training, time constraints, and lack of systems to ensure adequate follow-up. The USPSTF added language about treatment harms of suicide interventions to the Suggestions for Practice Regarding the I Statement and Supporting Evidence sections. The USPSTF incorporated additional language regarding screening intervals into the Practice Considerations section and highlighted it as an evidence gap. The USPSTF addressed the use of pharmacotherapy in pregnant and postpartum persons in the Practice Considerations section and added a resource to help clinicians in the Additional Tools and Resources section.
More evidence on whether and how screening for suicide risk can improve health outcomes is needed. There are several critical evidence gaps; more research is needed on the following.
Epidemiology and natural history of suicide risk. Persons who attempt suicide and survive and those who die by suicide are overlapping populations. More research is needed to understand these groups and to determine how primary care can improve health outcomes in these groups.
Foundational research is needed in primary care populations and pregnant and postpartum persons, including determining which tools should be used and how screening for suicide risk should be implemented.
Accuracy of single-item suicide screeners within depression screening instruments among patients who have screened positive for depression.
Whether more individuals with screen-detected suicidal ideation could be helped before they act.
Treatment studies in populations with screen-detected suicide risk in all age groups.
Potential harms of suicide risk interventions.
Benefits and potential harms of targeted vs general screening for suicide risk.
Targeting persons at high risk for suicide, such as Hispanic/Latino and Native American/Alaska Native persons or persons with depression, may help determine whether tailored therapies are more effective in these populations.
Although the evidence is clear that providing depression screening in adults and pregnant and postpartum patients is beneficial, more research is needed to ensure that all patients receive depression screening equitably. Studies are needed that provide more information on the following.
The effect of depression screening and the most accurate screening tools among Asian American, Black, Hispanic/Latino, and Native American/Alaska Native communities and other underrepresented groups (eg, populations defined by sex, race and ethnicity, sexual orientation, and gender identity).
Barriers to establishing adequate systems of care and how these barriers can be addressed; there are also limitations to understanding the direct effect of screening relative to other depression management supports.
Rigorous examination of implementation programs is needed that reports the percentage of patients being screened, referred, and treated for depression, as well as patient health outcomes.
The American College of Physicians recommends depression screening in all adults. It defines adults who are postpartum, have a personal or family history of depression, or have comorbid medical illnesses as being at increased risk. 66 The American College of Preventive Medicine recommends universal screening for depression for all adults. 67 The Institute for Clinical Systems Improvement recommends universal screening for suspected depression based on patient presentation, risk factors, and special populations (eg, pregnant and postpartum persons and individuals with cognitive impairment). 68 The American College of Obstetricians and Gynecologists recommends screening patients at least once during the perinatal period for depression and anxiety symptoms using a standardized, validated tool. 20 It also recommends that clinicians complete a full assessment of mood and emotional well-being (including screening for postpartum depression and anxiety with a validated instrument) during the comprehensive postpartum visit for each patient. 20 The US Department of Veterans Affairs recommends universal screening for suicide risk in veterans. 69
Accepted for Publication: May 12, 2023.
Corresponding Author: Michael J. Barry, MD, Informed Medical Decisions Program, Massachusetts General Hospital, 50 Staniford St, Boston, MA 02114 ( [email protected] )
The US Preventive Services Task Force (USPSTF) Members: Michael J. Barry, MD; Wanda K. Nicholson, MD, MPH, MBA; Michael Silverstein, MD, MPH; David Chelmow, MD; Tumaini Rucker Coker, MD, MBA; Karina W. Davidson, PhD, MASc; Esa M. Davis, MD, MPH; Katrina E. Donahue, MD, MPH; Carlos Roberto Jaén, MD, PhD, MS; Li Li, MD, PhD, MPH; Gbenga Ogedegbe, MD, MPH; Lori Pbert, PhD; Goutham Rao, MD; John M. Ruiz, PhD; James J. Stevermer, MD, MSPH; Joel Tsevat, MD, MPH; Sandra Millon Underwood, PhD, RN; John B. Wong, MD.
Affiliations of The US Preventive Services Task Force (USPSTF) Members: Harvard Medical School, Boston, Massachusetts (Barry); George Washington University, Washington, DC (Nicholson); Brown University, Providence, Rhode Island (Silverstein); Virginia Commonwealth University, Richmond (Chelmow); University of Washington, Seattle (Coker); Feinstein Institutes for Medical Research at Northwell Health, Manhasset, New York (Davidson); University of Pittsburgh, Pittsburgh, Pennsylvania (Davis); University of North Carolina at Chapel Hill (Donahue); The University of Texas Health Science Center, San Antonio (Jaén, Tsevat); University of Virginia, Charlottesville (Li); New York University, New York, New York (Ogedegbe); University of Massachusetts Medical School, Worcester (Pbert); Case Western Reserve University, Cleveland, Ohio (Rao); University of Arizona, Tucson (Ruiz); University of Missouri, Columbia (Stevermer); University of Wisconsin, Milwaukee (Underwood); Tufts University School of Medicine, Boston, Massachusetts (Wong).
Author Contributions: Dr Barry had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The USPSTF members contributed equally to the recommendation statement.
Conflict of Interest Disclosures: Authors followed the policy regarding conflicts of interest described at https://www.uspreventiveservicestaskforce.org/Page/Name/conflict-of-interest-disclosures . Dr Silverstein reported receiving a research grant on a community-based approach to maternal depression. All members of the USPSTF receive travel reimbursement and an honorarium for participating in USPSTF meetings.
Funding/Support: The USPSTF is an independent, voluntary body. The US Congress mandates that the Agency for Healthcare Research and Quality (AHRQ) support the operations of the USPSTF.
Role of the Funder/Sponsor: AHRQ staff assisted in the following: development and review of the research plan, commission of the systematic evidence review from an Evidence-based Practice Center, coordination of expert review and public comment of the draft evidence report and draft recommendation statement, and the writing and preparation of the final recommendation statement and its submission for publication. AHRQ staff had no role in the approval of the final recommendation statement or the decision to submit for publication.
Disclaimer: Recommendations made by the USPSTF are independent of the US government. They should not be construed as an official position of AHRQ or the US Department of Health and Human Services.
Additional Contributions: We thank Iris Mabry-Hernandez, MD, MPH (AHRQ), who contributed to the writing of the manuscript, and Lisa Nicolella, MA (AHRQ), who assisted with coordination and editing.
Additional Information: Published by JAMA®—Journal of the American Medical Association under arrangement with the Agency for Healthcare Research and Quality (AHRQ). ©2023 AMA and United States Government, as represented by the Secretary of the Department of Health and Human Services (HHS), by assignment from the members of the United States Preventive Services Task Force (USPSTF). All rights reserved.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
What is depression?
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working.
To be diagnosed with depression, the symptoms must be present for at least 2 weeks.
There are different types of depression, some of which develop due to specific circumstances.
- Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.
- Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe symptoms of depression that last much longer, usually for at least 2 years.
- Perinatal depression is depression that occurs during pregnancy or after childbirth. Depression that begins during pregnancy is prenatal depression, and depression that begins after the baby is born is postpartum depression.
- Seasonal affective disorder is depression that comes and goes with the seasons, with symptoms typically starting in the late fall or early winter and going away during the spring and summer.
- Depression with symptoms of psychosis is a severe form of depression in which a person experiences psychosis symptoms, such as delusions (disturbing, false fixed beliefs) or hallucinations (hearing or seeing things others do not hear or see).
People with bipolar disorder (formerly called manic depression or manic-depressive illness) also experience depressive episodes, during which they feel sad, indifferent, or hopeless, combined with a very low activity level. But a person with bipolar disorder also experiences manic (or less severe hypomanic) episodes, or unusually elevated moods, in which they might feel very happy, irritable, or “up,” with a marked increase in activity level.
Other depressive disorders found in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5-TR) include disruptive mood dysregulation disorder (diagnosed in children and adolescents) and premenstrual dysphoric disorder (that affects women around the time of their period).
Who gets depression?
Depression can affect people of all ages, races, ethnicities, and genders.
Women are diagnosed with depression more often than men, but men can also be depressed. Because men may be less likely to recognize, talk about, and seek help for their feelings or emotional problems, they are at greater risk of their depression symptoms being undiagnosed or undertreated.
Studies also show higher rates of depression and an increased risk for the disorder among members of the LGBTQI+ community.
What are the signs and symptoms of depression?
If you have been experiencing some of the following signs and symptoms, most of the day, nearly every day, for at least 2 weeks, you may have depression:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration, or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Not everyone who is depressed experiences all these symptoms. Some people experience only a few symptoms, while others experience many. Symptoms associated with depression interfere with day-to-day functioning and cause significant distress for the person experiencing them.
Depression can also involve other changes in mood or behavior that include:
- Increased anger or irritability
- Feeling restless or on edge
- Becoming withdrawn, negative, or detached
- Increased engagement in high-risk activities
- Greater impulsivity
- Increased use of alcohol or drugs
- Isolating from family and friends
- Inability to meet the responsibilities of work and family or ignoring other important roles
- Problems with sexual desire and performance
Depression can look different in men and women. Although people of all genders can feel depressed, how they express those symptoms and the behaviors they use to cope with them may differ. For example, men (as well as women) may show symptoms other than sadness, instead seeming angry or irritable. And although increased use of alcohol or drugs can be a sign of depression in anyone, men are more likely to use these substances as a coping strategy.
In some cases, mental health symptoms appear as physical problems (for example, a racing heart, tightened chest, ongoing headaches, or digestive issues). Men are often more likely to see a health care provider about these physical symptoms than their emotional ones.
Because depression tends to make people think more negatively about themselves and the world, some people may also have thoughts of suicide or self-harm.
Several persistent symptoms, in addition to low mood, are required for a diagnosis of depression, but people with only a few symptoms may benefit from treatment. The severity and frequency of symptoms and how long they last will vary depending on the person, the illness, and the stage of the illness.
If you experience signs or symptoms of depression and they persist or do not go away, talk to a health care provider. If you see signs or symptoms of depression in someone you know, encourage them to seek help from a mental health professional.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
What are the risk factors for depression?
Depression is one of the most common mental disorders in the United States . Research suggests that genetic, biological, environmental, and psychological factors play a role in depression.
Risk factors for depression can include:
- Personal or family history of depression
- Major negative life changes, trauma, or stress
Depression can happen at any age, but it often begins in adulthood. Depression is now recognized as occurring in children and adolescents, although children may express more irritability or anxiety than sadness. Many chronic mood and anxiety disorders in adults begin as high levels of anxiety in childhood.
Depression, especially in midlife or older age, can co-occur with other serious medical illnesses, such as diabetes, cancer, heart disease, chronic pain, and Parkinson’s disease. These conditions are often worse when depression is present, and research suggests that people with depression and other medical illnesses tend to have more severe symptoms of both illnesses. The Centers for Disease Control and Prevention (CDC) has also recognized that having certain mental disorders, including depression and schizophrenia, can make people more likely to get severely ill from COVID-19.
Sometimes a physical health problem, such as thyroid disease, or medications taken for an illness cause side effects that contribute to depression. A health care provider experienced in treating these complicated illnesses can help determine the best treatment strategy.
How is depression treated?
Depression, even the most severe cases, can be treated. The earlier treatment begins, the more effective it is. Depression is usually treated with psychotherapy , medication , or a combination of the two.
Some people experience treatment-resistant depression, which occurs when a person does not get better after trying at least two antidepressant medications. If treatments like psychotherapy and medication do not reduce depressive symptoms or the need for rapid relief from symptoms is urgent, brain stimulation therapy may be an option to explore.
Quick tip : No two people are affected the same way by depression, and there is no "one-size-fits-all" treatment. Finding the treatment that works best for you may take trial and error.
Psychotherapies
Several types of psychotherapy (also called talk therapy or counseling) can help people with depression by teaching them new ways of thinking and behaving and helping them change habits that contribute to depression. Evidence-based approaches to treating depression include cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT). Learn more about psychotherapy .
The growth of telehealth for mental health services , which offers an alternative to in-person therapy, has made it easier and more convenient for people to access care in some cases. For people who may have been hesitant to look for mental health care in the past, virtual mental health care might be an easier option.
Medications
Antidepressants are medications commonly used to treat depression. They work by changing how the brain produces or uses certain chemicals involved in mood or stress. You may need to try several different antidepressants before finding the one that improves your symptoms and has manageable side effects. A medication that has helped you or a close family member in the past will often be considered first.
Antidepressants take time—usually 4–8 weeks—to work, and problems with sleep, appetite, and concentration often improve before mood lifts. It is important to give a medication a chance to work before deciding whether it’s right for you. Learn more about mental health medications .
New medications, such as intranasal esketamine , can have rapidly acting antidepressant effects, especially for people with treatment-resistant depression. Esketamine is a medication approved by the U.S. Food and Drug Administration (FDA) for treatment-resistant depression. Delivered as a nasal spray in a doctor’s office, clinic, or hospital, it acts rapidly, typically within a couple of hours, to relieve depression symptoms. People who use esketamine will usually continue taking an oral antidepressant to maintain the improvement in their symptoms.
Another option for treatment-resistant depression is to take an antidepressant alongside a different type of medication that may make it more effective, such as an antipsychotic or anticonvulsant medication. Further research is needed to identify the role of these newer medications in routine practice.
If you begin taking an antidepressant, do not stop taking it without talking to a health care provider . Sometimes people taking antidepressants feel better and stop taking the medications on their own, and their depression symptoms return. When you and a health care provider have decided it is time to stop a medication, usually after a course of 9–12 months, the provider will help you slowly and safely decrease your dose. Abruptly stopping a medication can cause withdrawal symptoms.
Note : In some cases, children, teenagers, and young adults under 25 years may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. The FDA advises that patients of all ages taking antidepressants be watched closely, especially during the first few weeks of treatment.
If you are considering taking an antidepressant and are pregnant, planning to become pregnant, or breastfeeding, talk to a health care provider about any health risks to you or your unborn or nursing child and how to weigh those risks against the benefits of available treatment options.
To find the latest information about antidepressants, talk to a health care provider and visit the FDA website .
Brain stimulation therapies
If psychotherapy and medication do not reduce symptoms of depression, brain stimulation therapy may be an option to explore. There are now several types of brain stimulation therapy, some of which have been authorized by the FDA to treat depression. Other brain stimulation therapies are experimental and still being investigated for mental disorders like depression.
Although brain stimulation therapies are less frequently used than psychotherapy and medication, they can play an important role in treating mental disorders in people who do not respond to other treatments. These therapies are used for most mental disorders only after psychotherapy and medication have been tried and usually continue to be used alongside these treatments.
Brain stimulation therapies act by activating or inhibiting the brain with electricity. The electricity is given directly through electrodes implanted in the brain or indirectly through electrodes placed on the scalp. The electricity can also be induced by applying magnetic fields to the head.
The brain stimulation therapies with the largest bodies of evidence include:
- Electroconvulsive therapy (ECT)
- Repetitive transcranial magnetic stimulation (rTMS)
- Vagus nerve stimulation (VNS)
- Magnetic seizure therapy (MST)
- Deep brain stimulation (DBS)
ECT and rTMS are the most widely used brain stimulation therapies, with ECT having the longest history of use. The other therapies are newer and, in some cases, still considered experimental. Other brain stimulation therapies may also hold promise for treating specific mental disorders.
ECT, rTMS, and VNS have authorization from the FDA to treat severe, treatment-resistant depression. They can be effective for people who have not been able to feel better with other treatments; people for whom medications cannot be used safely; and in severe cases where a rapid response is needed, such as when a person is catatonic, suicidal, or malnourished.
Additional types of brain stimulation therapy are being investigated for treating depression and other mental disorders. Talk to a health care provider and make sure you understand the potential benefits and risks before undergoing brain stimulation therapy. Learn more about these brain stimulation therapies .
Natural products
The FDA has not approved any natural products for treating depression. Although research is ongoing and findings are inconsistent, some people use natural products, including vitamin D and the herbal dietary supplement St. John’s wort, for depression. However, these products can come with risks. For instance, dietary supplements and natural products can limit the effectiveness of some medications or interact in dangerous or even life-threatening ways with them.
Do not use vitamin D, St. John’s wort, or other dietary supplements or natural products without talking to a health care provider. Rigorous studies must be conducted to test whether these and other natural products are safe and effective.
Daily morning light therapy is a common treatment choice for people with seasonal affective disorder (SAD). Light therapy devices are much brighter than ordinary indoor lighting and considered safe, except for people with certain eye diseases or taking medications that increase sensitivity to sunlight. As with all interventions for depression, evaluation, treatment, and follow-up by a health care provider are strongly recommended. Research into the potential role of light therapy in treating non-seasonal depression is ongoing.
How can I find help for depression?
A primary care provider is a good place to start if you’re looking for help. They can refer you to a qualified mental health professional, such as a psychologist, psychiatrist, or clinical social worker, who can help you figure out next steps. Find tips for talking with a health care provider about your mental health.
You can learn more about getting help on the NIMH website. You can also learn about finding support and locating mental health services in your area on the Substance Abuse and Mental Health Services Administration (SAMHSA) website.
Once you enter treatment, you should gradually start to feel better. Here are some other things you can do outside of treatment that may help you or a loved one feel better:
- Try to get physical activity. Just 30 minutes a day of walking can boost your mood.
- Try to maintain a regular bedtime and wake-up time.
- Eat regular, healthy meals.
- Break up large tasks into small ones; do what you can as you can. Decide what must get done and what can wait.
- Try to connect with people. Talk with people you trust about how you are feeling.
- Delay making important decisions, such as getting married or divorced, or changing jobs until you feel better. Discuss decisions with people who know you well.
- Avoid using alcohol, nicotine, or drugs, including medications not prescribed for you.
How can I find a clinical trial for depression?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions, including depression. The goal of a clinical trial is to determine if a new test or treatment works and is safe. Although people may benefit from being part of a clinical trial, they should know that the primary purpose is to gain new scientific knowledge so that others can be better helped in the future.
Researchers at NIMH and around the country conduct many studies with people with and without depression. We have new and better treatment options today because of what clinical trials have uncovered. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- Clinical Trials – Information for Participants : Information about clinical trials, why people might take part in a clinical trial, and what people might experience during a clinical trial
- Clinicaltrials.gov: Current Studies on Depression : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Depression—Adults : List of studies currently recruiting adults with depression being conducted on the NIH campus in Bethesda, MD
- Join a Study: Depression—Children : List of studies currently recruiting children with depression being conducted on the NIH campus in Bethesda, MD
- Join a Study: Perimenopause-Related Mood Disorders : List of studies on perimenopause-related mood disorders being conducted on the NIH campus in Bethesda, MD
- Join a Study: Postpartum Depression : List of studies on postpartum depression being conducted on the NIH campus in Bethesda, MD
Where can I learn more about depression?
Free brochures and shareable resources.
- Chronic Illness and Mental Health: Recognizing and Treating Depression : This fact sheet provides information about the link between depression and chronic disease. It describes what a chronic disease is, symptoms of depression, and treatment options, and presents resources to find help for yourself or someone else.
- Depression : This brochure provides information about depression, including different types of depression, signs and symptoms, how it is diagnosed, treatment options, and how to find help for yourself or a loved one.
- Depression in Women: 4 Things to Know : This fact sheet provides information about depression in women, including signs and symptoms, types of depression unique to women, and how to get help.
- Perinatal Depression : This brochure provides information about perinatal depression, including how it differs from “baby blues,” causes, signs and symptoms, treatment options, and how to find help for yourself or a loved one.
- Seasonal Affective Disorder : This fact sheet provides information about seasonal affective disorder, including signs and symptoms, how it is diagnosed, causes, and treatment options.
- Seasonal Affective Disorder (SAD): More Than the Winter Blues : This infographic provides information about how to recognize the symptoms of SAD and what to do to get help.
- Teen Depression: More Than Just Moodiness : This fact sheet is for teens and young adults and provides information about how to recognize the symptoms of depression and what to do to get help.
- Digital Shareables on Depression : These digital resources, including graphics and messages, can be used to spread the word about depression and help promote depression awareness and education in your community.
Federal resources
- Depression (MedlinePlus - also en español )
- Moms’ Mental Health Matters: Depression and Anxiety Around Pregnancy ( Eunice Kennedy Shriver National Institute of Child Health and Human Development)
Research and statistics
- Journal Articles : This webpage provides articles and abstracts on depression from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Major Depression : This webpage provides the statistics currently available on the prevalence and treatment of depression among people in the United States.
- Depression Mental Health Minute : Take a mental health minute to watch this video on depression.
- NIMH Experts Discuss the Menopause Transition and Depression : Learn about the signs and symptoms, treatments, and latest research on depression during menopause.
- NIMH Expert Discusses Seasonal Affective Disorder : Learn about the signs and symptoms, treatments, and latest research on seasonal affective disorder.
- Discover NIMH: Personalized and Targeted Brain Stimulation Therapies : Watch this video describing repetitive transcranial magnetic stimulation and electroconvulsive therapy for treatment-resistant depression. Brain stimulation therapies can be effective treatments for people with depression and other mental disorders. NIMH supports studies exploring how to make brain stimulation therapies more personalized while reducing side effects.
- Discover NIMH: Drug Discovery and Development : One of the most exciting breakthroughs from research funded by NIMH is the development of a fast-acting medication for treatment-resistant depression based on ketamine. This video shares the story of how ketamine infusions meaningfully changed the life of a participant in an NIMH clinical trial.
- Mental Health Matters Podcast: Depression: The Case for Ketamine : Dr. Carlos Zarate Jr. discusses esketamine—the medication he helped discover—for treatment-resistant depression. The podcast covers the history behind the development of esketamine, how it can help with depression, and what the future holds for this innovative line of clinical research.
Last Reviewed: March 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Stanford Medicine-led research identifies a subtype of depression
Using surveys, cognitive tests and brain imaging, researchers have identified a type of depression that affects about a quarter of patients. The goal is to diagnose and treat the condition more precisely.
June 22, 2023 - By Emily Moskal

Knowing what type of depression a patient has can help clinicians provide the best treatment. Yurchanka Siarhei/Shutterstock.com
Scientists at Stanford Medicine conducted a study describing a new category of depression — labeled the cognitive biotype — which accounts for 27% of depressed patients and is not effectively treated by commonly prescribed antidepressants.
Cognitive tasks showed that these patients have difficulty with the ability to plan ahead, display self-control, sustain focus despite distractions and suppress inappropriate behavior; imaging showed decreased activity in two brain regions responsible for those tasks.
Because depression has traditionally been defined as a mood disorder, doctors commonly prescribe antidepressants that target serotonin (known as selective serotonin reuptake inhibitors or SSRIs), but these are less effective for patients with cognitive dysfunction. Researchers said that targeting these cognitive dysfunctions with less commonly used antidepressants or other treatments may alleviate symptoms and help restore social and occupational abilities.
The study , published June 15 in JAMA Network Open , is part of a broader effort by neuroscientists to find treatments that target depression biotypes, according to the study’s senior author, Leanne Williams , PhD, the Vincent V.C. Woo Professor and professor of psychiatry and behavioral sciences.
“One of the big challenges is to find a new way to address what is currently a trial-and-error process so that more people can get better sooner,” Williams said. “Bringing in these objective cognitive measures like imaging will make sure we’re not using the same treatment on every patient.”
Finding the biotype
In the study, 1,008 adults with previously unmedicated major depressive disorder were randomly given one of three widely prescribed typical antidepressants: escitalopram (brand name Lexapro) or sertraline (Zoloft), which act on serotonin, or venlafaxine-XR (Effexor), which acts on both serotonin and norepinephrine. Seven hundred and twelve of the participants completed the eight-week regimen.

Leanne Williams
Before and after treatment with the antidepressants, the participants’ depressive symptoms were measured using two surveys one, clinician-administered, and the other, a self-assessment, which include questions related to changes in sleep and eating. Measures on social and occupation functioning, as well as quality of life, were tracked as well.
The participants also completed a series of cognitive tests, before and after treatment, measuring verbal memory, working memory, decision speed and sustained attention, among other tasks.
Before treatment, scientists scanned 96 of the participants using functional magnetic resonance imaging as they engaged in a task called the “GoNoGo” that requires participants to press a button as quickly as possible when they see “Go” in green and to not press when they see “NoGo” in red. The fMRI tracked neuronal activity by measuring changes in blood oxygen levels, which showed levels of activity in different brain regions corresponding to Go or NoGo responses. Researchers then compared the participants’ images with those of individuals without depression.
The researchers found that 27% of the participants had more prominent symptoms of cognitive slowing and insomnia, impaired cognitive function on behavioral tests, as well as reduced activity in certain frontal brain regions — a profile they labeled the cognitive biotype.
“This study is crucial because psychiatrists have few measurement tools for depression to help make treatment decisions,” said Laura Hack , MD, PhD, the lead author of the study and an assistant professor of psychiatry and behavioral sciences. “It’s mostly making observations and self-report measures. Imaging while performing cognitive tasks is rather novel in depression treatment studies.”
Pre-treatment fMRI showed those with the cognitive biotype had significantly reduced activity in the dorsolateral prefrontal cortex and dorsal anterior cingulate regions during the GoNoGo task compared with the activity levels in participants who did not have the cognitive biotype. Together, the two regions form the cognitive control circuit, which is responsible for limiting unwanted or irrelevant thoughts and responses and improving goal selection, among other tasks.

After treatment, the researchers found that for the three antidepressants administered, the overall remission rates — the absence of overall depression symptoms — were 38.8% for participants with the newly discovered biotype and 47.7% for those without it. This difference was most prominent for sertraline, for which the remission rates were 35.9% and 50% for those with the biotype and those without, respectively.
“Depression presents in different ways in different people, but finding commonalities — like similar profiles of brain function — helps medical professionals effectively treat participants by individualizing care,” Williams said.
Depression isn’t one size fits all
Williams and Hack propose that behavior measurement and imaging could help diagnose depression biotypes and lead to better treatment. A patient could complete a survey on their own computer or in the doctor’s office, and if they are found to display a certain biotype, they might be referred to imaging for confirmation before undergoing treatment.
Researchers at the Stanford Center for Precision Mental Health and Wellness , which Williams directs, in partnership with the Stanford Translational Precision Mental Health Clinic, which Hack directs, are studying another medication — guanfacine — that specifically targets the dorsolateral prefrontal cortex region with support from Stanford University Innovative Medicines Accelerator . They believe this treatment could be more effective for patients with the cognitive subtype.
Williams and Hack hope to conduct studies with participants who have the cognitive biotype, comparing different types of medication with treatments such as transcranial magnetic stimulation and cognitive behavioral therapy. In transcranial magnetic stimulation, commonly referred to as TMS, magnetic fields stimulate nerve cells; in cognitive behavioral therapy, patients are taught to use problem-solving strategies to counter negative thoughts that contribute to both emotional dysregulation and loss of social and occupational abilities.
“I regularly witness the suffering, the loss of hope and the increase in suicidality that occurs when people are going through our trial-and-error process,” Hack said. “And it’s because we start with medications that have the same mechanism of action for everyone with depression, even though depression is quite heterogeneous. I think this study could help change that.”
Researchers from the Sierra-Pacific Mental Illness Research, Education and Clinical Center; the Veterans Affairs Palo Alto Health Care System; Brain Dynamic Centre, Westmead Institute for Medical Research; and the University of Sydney, Westmead, contributed to the work.
The study was funded through Brain Resource Company Operations Pty Ltd. and Stanford University’s Clinical and Translation Science Award Program overseen by the National Center for Advancing Translational Sciences at the National Institutes of Health (grant UL1TR003142-01).

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

Advertisement
Where in the Brain Is Depression?
- Mood Disorders (SM Strakowski, Section Editor)
- Published: 11 October 2012
- Volume 14 , pages 634–642, ( 2012 )
Cite this article

- Mayur Pandya 1 ,
- Murat Altinay 1 ,
- Donald A. Malone Jr. 1 &
- Amit Anand 2 , 3
9604 Accesses
192 Citations
78 Altmetric
12 Mentions
Explore all metrics
Major depressive disorder is a serious medical illness which is responsible for considerable morbidity and disability. Despite decades of research, the neural basis for depression is still incompletely understood. In this review, evidence from neuroimaging, neuropsychiatric and brain stimulations studies are explored to answer the question regarding the localization of depression in the brain. Neuroimaging studies indicate that although many regions of the brain have been repeatedly implicated in the pathophysiology of depression, not many consistent findings have been found until present. In recent times, the focus of neuroimaging has shifted from regional brain abnormalities to circuit level connectivity abnormalities. However, connectivity models are inherently more complicated, and the validity of these models remains to be tested. Neuropsychiatric studies of illnesses such as Parkinson’s disease and stroke provide promising clues regarding areas involved in depression, but again consistent findings are rare. Similarly, stimulation of a variety of brain regions and circuits has been reported as being effective in depression. Therefore, the current knowledge indicates that the pathophysiology of depression may be distributed across many brain regions and circuits. In future studies, this distributed nature of depression needs to be further investigated, primary and secondary areas affected need to be identified, and new paradigms to explain complex mental functions need to be explored.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications

The advances of post-stroke depression: 2021 update

Comorbid Anxiety and Depression: Clinical and Conceptual Consideration and Transdiagnostic Treatment
Papers of particular interest, published recently, have been highlighted as: •• of major importance.
First MB. Diagnostic and Statsitical Manual 4th Edition - Text Revision (DSM-IV-TR). Washington DC: American Psychiatric Publishing; 2000.
Google Scholar
Maclean PD. Evolutionary psychiatry and the triune brain. Psychol Med. 1985;15(02):219–21.
Article PubMed CAS Google Scholar
Rigucci S, Serafini G, Pompili M, Kotzalidis GD, Tatarelli R. Anatomical and functional correlates in major depressive disorder: the contribution of neuroimaging studies. World J Biol Psychiatr. 2009;11(2 Pt 2):165–80.
Kimbrell TA, Ketter TA, George MS, Little JT, Benson BE, Willis MW, et al. Regional cerebral glucose utilization in patients with a range of severities of unipolar depression. Biol Psychiatry. 2002;51(3):237–52.
Desmyter S, van Heeringen C, Audenaert K. Structural and functional neuroimaging studies of the suicidal brain. Prog Neuropsychopharmacol Biol Psychiatr. 2011;35(4):796–808.
Article CAS Google Scholar
George MS. Transcranial magnetic stimulation for the treatment of depression. Expert Rev Neurother. 2010;10(11):1761–72.
Article PubMed Google Scholar
Mayberg HS, Brannan SK, Tekell JL, Silva JA, Mahurin RK, McGinnis S, et al. Regional metabolic effects of fluoxetine in major depression: serial changes and relationship to clinical response. Biol Psychiatry. 2000;48(8):830–43.
Coffey CE, Wilkinson WE, Weiner RD, Parashos IA, Djang WT, Webb MC, et al. Quantitative cerebral anatomy in depression. A controlled magnetic resonance imaging study. Arch Gen Psychiatry. 1993;50(1):7–16.
Kumar A, Bilker W, Jin Z, Udupa J. Atrophy and high intensity lesions: complementary neurobiological mechanisms in late-life major depression. Neuropsychopharmacology. 2000;22(3):264–74.
Schweitzer I, Tuckwell V, Ames D, O'Brien J. Structural neuroimaging studies in late-life depression: a review. World J Biol Psychiatr. 2001;2(2):83–8.
Bremner JD, Vythilingam M, Vermetten E, Nazeer A, Adil J, Khan S, et al. Reduced volume of orbitofrontal cortex in major depression. Biol Psychiatry. 2002;51(4):273–9.
Drevets WC, Price JL, Simpson Jr JR, Todd RD, Reich T, Vannier M, et al. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386(6627):824–7.
Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, et al. Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am J Psychiatry. 1999;156(5):675–82.
PubMed CAS Google Scholar
Vogt BA, Finch DM, Olson CR. Functional heterogeneity in cingulate cortex: the anterior executive and posterior evaluative regions. Cerebr Cortex. 1992;2(6):435–43.
CAS Google Scholar
Critchley HD. The human cortex responds to an interoceptive challenge. Proc Natl Acad Sci U S A. 2004;101(17):6333–4.
Etkin A, Egner T, Peraza DM, Kandel ER, Hirsch J. Resolving emotional conflict: a role for the rostral anterior cingulate cortex in modulating activity in the Amygdala. Neuron. 2006;51(6):871–82.
Deen B, Pitskel NB, Pelphrey KA. Three systems of insular functional connectivity identified with cluster analysis. Cerebr Cortex. 2010.
Phillips ML, Young AW, Senior C, Brammer M, Andrew C, Calder AJ, et al. A specific neural substrate for perceiving facial expressions of disgust. Nature. 1997;389(6650):495–8.
Modinos G, Ormel J, Aleman A. Activation of anterior insula during self-reflection. PLoS One. 2009;4(2):e4618.
Critchley HD, Wiens S, Rotshtein P, Ohman A, Dolan RJ. Neural systems supporting interoceptive awareness. Nat Neurosci. 2004;7(2):189–95.
Surguladze SA, El-Hage W, Dalgleish T, Radua J, Gohier B, Phillips ML. Depression is associated with increased sensitivity to signals of disgust: a functional magnetic resonance imaging study. J Psychiatr Res. 2010;44(14):894–902.
Anand A, Li Y, Wang Y, Wu J, Gao S, Kalnin A, et al. Activity and connectivity of mood regulating circuit in depression: a functional magnetic resonance study. Biol Psychiatry. 2005;15(10):1079–88.
Article Google Scholar
Sprengelmeyer R, Steele JD, Mwangi B, Kumar P, Christmas D, Milders M, et al. The insular cortex and the neuroanatomy of major depression. J Affect Disord. 2011;133(1–2):120–7.
Davidson RJ, Irwin W, Anderle MJ, Kalin NH. The neural substrates of affective processing in depressed patients treated with venlafaxine. Am J Psychiatry. 2003;160(1):64–75.
Lorenzetti V, Allen NB, Fornito A, Yucel M. Structural brain abnormalities in major depressive disorder: a selective review of recent MRI studies. J Affect Disord. 2009;117(1–2):1–17.
MacQueen GM, Yucel K, Taylor VH, Macdonald K, Joffe R. Posterior hippocampal volumes are associated with remission rates in patients with major depressive disorder. Biol Psychiatry. 2008;64(10):880–3.
Kronmuller KT, Pantel J, Kohler S, Victor D, Giesel F, Magnotta VA, et al. Hippocampal volume and 2-year outcome in depression. Br J Psychiatry. 2008;192(6):472–3.
Sheline YI, Gado MH, Price JL. Amygdala core nuclei volumes are decreased in recurrent major depression. Neuroreport. 1998;9(9):2023–8.
Bremner JD, Narayan M, Anderson ER, Staib LH, Miller HL, Charney DS. Hippocampal volume reduction in major depression. Am J Psychiatry. 2000;157(1):115–8.
Bremner JD, Randall P, Scott TM, Bronen RA, Seibyl JP, Southwick SM, et al. MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152(7):973–81.
Vythilingam M, Heim C, Newport J, Miller AH, Anderson E, Bronen R, et al. Childhood trauma associated with smaller hippocampal volume in women with major depression. Am J Psychiatry. 2002;159(12):2072–80.
Duman RS. Synaptic plasticity and mood disorders. Mol Psychiatr. 2002;7 Suppl 1:S29–34.
Anand A, Charney DS. Norepinephrine dysfunction in depression. J Clin Psychiatr. 2000;61 Suppl 10:16–24.
Drevets WC. Neuroimaging and neuropathological studies of depression: implications for the cognitive-emotional features of mood disorders. Curr Opin Neurobiol. 2001;11(2):240–9.
Ketter TA. Functional brain imaging, limbic function, and affective disorders. Neuroscientist. 1996;2:55–65.
Soares JC, Mann JJ. The functional neuroanatomy of mood disorders. J Psychiatr Res. 1997;31(4):393–432.
Drevets WC, Price JL, Bardgett ME, Reich T, Todd RD, Raichle ME. Glucose metabolism in the amygdala in depression: relationship to diagnostic subtype and plasma cortisol levels. Pharmacol Biochem Behav. 2002;71(3):431–47.
Sheline YI, Barch DM, Donnelly JM, Ollinger JM, Snyder AZ, Mintun MA. Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI study. Biol Psychiatry. 2001;50(9):651–8.
Thomas KM, Drevets WC, Dahl RE, Ryan ND, Birmaher B, Eccard CH, et al. Amygdala response to fearful faces in anxious and depressed children. Arch Gen Psychiatry. 2001;58(11):1057–63.
Siegle GJ, Steinhauer SR, Thase ME, Stenger VA, Carter CS. Can't shake that feeling: event-related fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biol Psychiatry. 2002;51(9):693–707.
Kumari V, Mitterschiffthaler MT, Teasdale JD. Neural abnormalities during cognitive generation of affect in treatment resistant depression. Biol Psychiatry. 2003;54:777–91.
Fu CHY, Williams SCR, Cleare AJ, Brammer MJ, Walsh ND, Kim J, et al. Attenuation of the neural response to sad faces in major depression by antidepressant treatment: a prospective, event-related functional magnetic resonance imaging study. Arch Gen Psychiatry. 2004;61(9):877–89.
Krishnan KR, McDonald WM, Escalona PR, Doraiswamy PM, Na C, Husain MM, et al. Magnetic resonance imaging of the caudate nuclei in depression. Preliminary observations. Arch Gen Psychiatry. 1992;49(7):553–7.
Knutson B, Bhanji JP, Cooney RE, Atlas LY, Gotlib IH. Neural responses to monetary incentives in major depression. Biol Psychiatry. 2008;63(7):686–92.
Remijnse PL, Nielen MMA, van Balkom AJLM, Hendriks G-J, Hoogendijk WJ, Uylings HBM, et al. Differential frontal-striatal and paralimbic activity during reversal learning in major depressive disorder and obsessive-compulsive disorder. Psychol Med. 2009;39(09):1503–18.
Kumari V, Mitterschiffthaler MT, Teasdale JD, Malhi GS, Brown RG, Giampietro V, et al. Neural abnormalities during cognitive generation of affect in treatment-resistant depression. Biol Psychiatry. 2003;54(8):777–91.
Surguladze S, Brammer MJ, Keedwell P, Giampietro V, Young AW, Travis MJ, et al. A differential pattern of neural response toward sad versus happy facial expressions in major depressive disorder. Biol Psychiatry. 2005;57(3):201–9.
Malison RT, Price LH, Berman R, van Dyck CH, Pelton GH, Carpenter L, et al. Reduced brain serotonin transporter availability in major depression as measured by [123I]-2 beta-carbomethoxy-3 beta-(4-iodophenyl)tropane and single photon emission computed tomography. Biol Psychiatry. 1998;44(11):1090–8.
Kugaya A, Seneca NM, Snyder PJ, Williams SA, Malison RT, Baldwin RM, et al. Changes in human in vivo serotonin and dopamine transporter availabilities during chronic antidepressant administration. Neuropsychopharmacology. 2003;28(2):413–20.
Anand A, Shekhar A. Brain imaging studies in mood and anxiety disorders: special emphasis on the amygdala. Ann N Y Acad Sci. 2003;985:370–88.
Drevets WC, Videen TO, Price JL, Preskorn SH, Carmichael ST, Raichle ME. A functional anatomical study of unipolar depression. J Neurosci. 1992;12(9):3628–41.
Andreasen NC, Paradiso S, O'Leary DS. "Cognitive dysmetria" as an integrative theory of schizophrenia: a dysfunction in cortical-subcortical-cerebellar circuitry? Schizophr Bull. 1998;24(2):203–18.
McIntosh AR, Gonzalez-Lima F. Large-scale functional connectivity in associative learning: interrelations of the rat auditory, visual, and limbic systems. J Neurophysiol. 1998;80(6):3148–62.
Lawrie SM, Buechel C, Whalley HC, Frith CD, Friston KJ, Johnstone EC. Reduced frontotemporal functional connectivity in schizophrenia associated with auditory hallucinations. Biol Psychiatry. 2002;51(12):1008–11.
Friston K. Beyond phrenology: what can neuroimaging tell us about distributed circuitry? Annu Rev Neurosci. 2002;25:221–50.
Anand A, Mathews VP, Bukhari L, Wang Y, Shirely JA, Lightfoot J, et al. Functional connectivity within the mood regulating circuit in depression - an fMRI study. Biol Psychiatry. 2003;53(8S):95S.
Mayberg HS. Modulating dysfunctional limbic-cortical circuits in depression: towards development of brain-based algorithms for diagnosis and optimised treatment. Br Med Bull. 2003;65:193–207.
•• Price JL, Drevets WC. Neurocircuitry of mood disorders. Neuropsychopharmacology. 2009;35(1):192–216. An excellent recent review of basic and clinical studies of neuroanatomy of depression.
Heinz A, Braus DF, Smolka MN, Wrase J, Puls I, Hermann D, et al. Amygdala-prefrontal coupling depends on a genetic variation of the serotonin transporter. Nat Neurosci. 2005;8(1):20–1.
Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry. 2007;62(5):429–37.
Greicius M. Resting-state functional connectivity in neuropsychiatric disorders. Curr Opin Neurol. 2008;21(4):424–30. doi: 10.1097/WCO.0b013e328306f2c5 .
•• Lui S, Wu Q, Qiu L, Yang X, Kuang W, Chan RCK, et al. Resting-state functional connectivity in treatment-resistant depression. Am J Psychiatr. 2011;appi.ajp.2010.10101419. This study investigates connectivity of mood related brain regions in treatment responsive and treatment-resistant depression.
Sheline YI, Price JL, Yan Z, Mintun MA. Resting-state functional MRI in depression unmasks increased connectivity between networks via the dorsal nexus. Proc Natl Acad Sci. 2010;107(24):11020–5.
Cummings JL. Depression and Parkinson's disease: a review. Am J Psychiatry. 1992;149(4):443–54.
Benoit M, Robert PH. Imaging correlates of apathy and depression in Parkinson's disease. J Neurol Sci. 2011;310(1–2):58–60.
Kostic VS, Filippi M. Neuroanatomical correlates of depression and apathy in Parkinson's disease: magnetic resonance imaging studies. J Neurol Sci. 2011;310(1–2):61–3.
Paulsen JS, Nehl C, Hoth KF, Kanz JE, Benjamin M, Conybeare R, et al. Depression and stages of Huntington's disease. J Neuropsychiatry Clin Neurosci. 2005;17(4):496–502.
Paulsen JS, Ready RE, Hamilton JM, Mega MS, Cummings JL. Neuropsychiatric aspects of Huntington's disease. J Neurol Neurosurg Psychiatry. 2001;71(3):310–4.
Hobbs NZ, Pedrick AV, Say MJ, Frost C, Dar Santos R, Coleman A, et al. The structural involvement of the cingulate cortex in premanifest and early Huntington's disease. Mov Disord. 2011;26(9):1684–90.
Thiruvady DR, Georgiou-Karistianis N, Egan GF, Ray S, Sritharan A, Farrow M, et al. Functional connectivity of the prefrontal cortex in Huntington's disease. J Neurol Neurosurg Psychiatry. 2007;78(2):127–33.
Mayberg HS, Starkstein SE, Peyser CE, Brandt J, Dannals RF, Folstein SE. Paralimbic frontal lobe hypometabolism in depression associated with Huntington's disease. Neurology. 1992;42(9):1791–7.
Thieben MJ, Duggins AJ, Good CD, Gomes L, Mahant N, Richards F, et al. The distribution of structural neuropathology in pre-clinical Huntington’s disease. Brain. 2002;125(8):1815–28.
Singh A, Herrmann N, Black SE. The importance of lesion location in poststroke depression: a critical review. Can J Psychiatr. 1998;43(9):921–7.
Starkstein SE, Robinson RG, Honig MA, Parikh RM, Joselyn J, Price TR. Mood changes after right-hemisphere lesions. Br J Psychiatry. 1989;155:79–85.
Santos M, Kovari E, Gold G, Bozikas VP, Hof PR, Bouras C, et al. The neuroanatomical model of post-stroke depression: towards a change of focus? J Neurol Sci. 2009;283(1–2):158–62.
Provinciali L, Coccia M. Post-stroke and vascular depression: a critical review. Neurol Sci. 2002;22(6):417–28.
Ferro JM, Caeiro L, Santos C. Poststroke emotional and behavior impairment: a narrative review. Cerebrovasc Dis. 2009;27 Suppl 1:197–203.
Alexopoulos GS. The vascular depression hypothesis: 10 years later. Biol Psychiatry. 2006;60(12):1304–5.
Kanner AM. Mood disorder and epilepsy: a neurobiologic perspective of their relationship. Dialogues Clin Neurosci. 2008;10(1):39–45.
PubMed Google Scholar
Paradiso S, Hermann BP, Blumer D, Davies K, Robinson RG. Impact of depressed mood on neuropsychological status in temporal lobe epilepsy. J Neurol Neurosurg Psychiatry. 2001;70(2):180–5.
Archer J, Hutchison I, Korszun A. Mood and malignancy: head and neck cancer and depression. J Oral Pathol Med. 2008;37(5):255–70.
Litofsky NS, Resnick AG. The relationships between depression and brain tumors. J Neurooncol. 2009;94(2):153–61.
Rooney AG, Carson A, Grant R. Depression in cerebral glioma patients: a systematic review of observational studies. J Natl Canc Inst. 2010;103(1):61–76.
George MS. New methods of minimally invasive brain modulation as therapies in psychiatry: TMS, MST, VNS and DBS. 2002;349–60, 2002 Aug.
Carpenter LL, Janicak PG, Aaronson ST, Boyadjis T, Brock DG, Cook IA, et al. Transcranial magnetic stimulation (TMS) for major depression: a multisite, naturalistic, observational study of acute treatment outcomes in clinical practice. Depress Anxiety. 2012;29(7):587–96.
Connolly RK, Helmer A, Cristancho MA, Cristancho P, O'Reardon JP. Effectiveness of transcranial magnetic stimulation in clinical practice post-FDA approval in the United States: results observed with the first 100 consecutive cases of depression at an academic medical center. J Clin Psychiatr. 2012;73(4):e567–73.
Schutter DJLG. Quantitative review of the efficacy of slow-frequency magnetic brain stimulation in major depressive disorder. Psychol Med. 2010;40(11):1789–95.
Fox MD, Buckner RL, White MP, Greicius MD, Pascual-Leone A. Efficacy of transcranial magnetic stimulation targets for depression is related to intrinsic functional connectivity with the subgenual cingulate. Biol Psychiatr. 2012.
George MS, Nahas Z, Bohning DE, Kozel FA, Anderson B, Chae JH, et al. Vagus nerve stimulation therapy: a research update. Neurology. 2002;59(6 Suppl 4):S56–61.
Ko D, Heck C, Grafton S, Apuzzo ML, Couldwell WT, Chen T, et al. Vagus nerve stimulation activates central nervous system structures in epileptic patients during PET H2(15)O blood flow imaging. Neurosurgery. 1996;39(2):426–30. discussion 30–1.
Chae JH, Nahas Z, Lomarev M, Denslow S, Lorberbaum JP, Bohning DE, et al. A review of functional neuroimaging studies of vagus nerve stimulation (VNS). J Psychiatr Res. 2003;37(6):443–55.
Conway CR, Sheline YI, Chibnall JT, George MS, Fletcher JW, Mintun MA. Cerebral blood flow changes during vagus nerve stimulation for depression. Psychiatr Res. 2006;146(2):179–84. 2006 Mar 31.
•• Malone DA Jr, Dougherty DD, Rezai AR, Carpenter LL, Friehs GM, Eskandar EN, et al. Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biological Psychiatry. 2009;65(4):267–75. An important study of deep brain stimulation in a specific region for treatment of depression.
Schlaepfer TE, Cohen MX, Frick C, Kosel M, Brodesser D, Axmacher N, et al. Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression. Neuropsychopharmacology. 2007;33(2):368–77.
Kennedy SH, Giacobbe P, Rizvi SJ, Placenza FM, Nishikawa Y, Mayberg HS, et al. Deep brain stimulation for treatment-resistant depression: follow-up after 3 to 6 years. Am J Psychiatry. 2011;168(5):502–10.
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45(5):651–60.
Anderson RJ, Frye MA, Abulseoud OA, Lee KH, McGillivray J, Berk M, et al. Deep brain stimulation for treatment-resistant depression: efficacy, safety and mechanisms of action. Neurosci Biobehav Rev. 2012.
Lozano AM, Mayberg HS, Giacobbe P, Hamani C, Craddock RC, Kennedy SH. Subcallosal cingulate gyrus deep brain stimulation for treatment-resistant depression. Biol Psychiatry. 2008;64(6):461–7.
Baker KB, Kopell BH, Malone D, Horenstein C, Lowe M, Phillips MD, et al. Deep brain stimulation for obsessive-compulsive disorder: using functional magnetic resonance imaging and electrophysiological techniques: technical case report. Neurosurgery. 2007;61(5):E367–8. doi: 10.1227/01.neu.0000303995.66902.36 .
Bewernick BH, Hurlemann R, Matusch A, Kayser S, Grubert C, Hadrysiewicz B, et al. Nucleus accumbens deep brain stimulation decreases ratings of depression and anxiety in treatment-resistant depression. Biol Psychiatry. 2010;67(2):110–6.
Download references
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and affiliations.
Department of Psychiatry and Center for Behavioral Health, Neurological Institute, Cleveland Clinic, Cleveland, OH, USA
Mayur Pandya, Murat Altinay & Donald A. Malone Jr.
Department of Radiology, Indiana University Center for Neuroimaging, 950 West Walnut Street, E124, Indianapolis, IN, 46202, USA
Adult Outpatient Clinic, Department of Psychiatry, Indiana University School of Medicine, 550 University Blvd, Indianapolis, IN, 46202, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Amit Anand .
Rights and permissions
Reprints and permissions
About this article
Pandya, M., Altinay, M., Malone, D.A. et al. Where in the Brain Is Depression?. Curr Psychiatry Rep 14 , 634–642 (2012). https://doi.org/10.1007/s11920-012-0322-7
Download citation
Published : 11 October 2012
Issue Date : December 2012
DOI : https://doi.org/10.1007/s11920-012-0322-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Major depressive disorder
- Unipolar depression
- Limbic system
- Resting state connectivity
- Neuroimaging
- Parkinson’s disease
- Deep brain stimulation
- Transcranial magnetic stimulation
- Vagus nerve stimulation
- Mood disorders
- Find a journal
- Publish with us
- Track your research
More than just social media use may be causing depression in young adults, study shows
Over the past few decades, there has been a significant increase in the prevalence of depression in adolescents and young adults -- and a simultaneous uptick in the inclusion of technology and social media in everyday life. However, it is unclear how exactly social media use and depression are associated and relate to other behaviors, such as physical activity, green space exposure, cannabis use and eveningness (the tendency to stay up late).
In a study published May 15 in the International Journal of Mental Health and Addiction , a team of researchers, led by experts at Johns Hopkins Children's Center, investigated the association among social media use, depression and other health-related behaviors of young adults over time.
"Research shows that when social media use is high, depression is also high. But the question is -- is that because social media caused that person to be depressed? Or is it because people who are depressed tend to also use social media more, and spend less time exercising and being in green spaces? That is what we wanted to understand," says Carol Vidal, M.D., Ph.D., M.P.H., the first author of the study, a child and adolescent psychiatrist at Johns Hopkins Children's Center and an assistant professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine.
In their study, 376 young adults in Canada (82.4% women) were asked to complete three online questionnaires between May 2021 and January 2022. At each point, participants self-reported depressive symptoms based on the Patient Health Questionnaire (PHQ-9) -- a nine-item scale that is commonly used to measure depression -- as well as social media use, greenspace exposure, physical activity and cannabis use.
The researchers found that most study participants had at least mild depressive symptoms. Findings showed that participants who had higher social media use tended to be more depressed, and people who were more depressed also tended to use social media more. However, researchers found that social media use did not cause an increase or decrease in depressive symptom levels over time.
"We found that if you tended to be a person who was depressed, you were a person also spending more time on social media," explains Vidal.
Researchers also found that higher levels of social media use and higher levels of depressive symptoms were associated with lower levels of green space exposure. In addition, cannabis use and higher eveningness were also associated with higher depressive levels.
The study authors say these results show social media use and depression are associated, but do not provide evidence that greater social media use predicts an increase in depressive symptoms over time. The team also says these findings indicate people who suffer from depression should be cautious about the amount of time they spend on social media and should be encouraged to incorporate other healthy habits into their lifestyle.
"Being indoors and not exercising, staying up late and using cannabis has its risks," says Vidal. "It is important for providers to educate patients and for parents to instill healthy habits in their kids -- having a balance of moderate social media use and other outdoor activities and exercise is what people should strive for in today's digital age."
Vidal and other investigators believe there are many aspects to social media, and there are important next steps to learn more about its impact on the mental health of people of all ages, including younger children and adolescents.
- Mental Health
- Media and Entertainment
- Popular Culture
- STEM Education
- Social Issues
- Clinical depression
- Social psychology
- Adult attention-deficit disorder
- Cognitive bias
- Social inequality
- Public health
- Mental illness
Story Source:
Materials provided by Johns Hopkins Medicine . Note: Content may be edited for style and length.
Journal Reference :
- Carol Vidal, Frederick L. Philippe, Marie-Claude Geoffroy, Vincent Paquin. The Role of Social Media Use and Associated Risk and Protective Behaviors on Depression in Youth Adults: A Longitudinal and Network Perspective . International Journal of Mental Health and Addiction , 2024; DOI: 10.1007/s11469-024-01313-0
Cite This Page :

Explore More
- Computer Vision, Machine Learning Aid Driving
- Most Distant Known Galaxy
- A New Dinosaur from Zimbabwe
- The Case of the Missing Black Holes
- Adjusting Sunglasses for Your Windows
- Novel Gene-Editing Tool Created
- How Hummingbirds Hover With Such Accuracy
- Complete X and Y Chromosomes of Great Apes
- Moonlets Stuck Together Orbit 'Dinky' Asteroid
- Orchids Aid Seedlings Through Fungal Networks
Trending Topics
Strange & offbeat.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 29 May 2024
Temporal and spatial trend analysis of all-cause depression burden based on Global Burden of Disease (GBD) 2019 study
- Junjiao Liu 1 ,
- Yueyang Liu 2 ,
- Wenjun Ma 1 ,
- Yan Tong 1 &
- Jianzhong Zheng 1
Scientific Reports volume 14 , Article number: 12346 ( 2024 ) Cite this article
Metrics details
- Health care
- Medical research
Depression has been reported as one of the most prevalent psychiatric illnesses globally. This study aimed to obtain information on the global burden of depression and its associated spatiotemporal variation, by exploring the correlation between the global burden of depression and the social development index (SDI) and associated risk factors. Using data from the Global Burden of Disease study from 1990 to 2019, we described the prevalence and burden of disease in 204 countries across 21 regions, including sex and age differences and the relationship between the global disease burden and SDI. The age-standardized rate and estimated annual percentage change were used to assess the global burden of depression. Individuals with documented depression globally ranged from 182,183,358 in 1990 to 290,185,742 in 2019, representing an increase of 0.59%. More patients experienced major depressive disorder than dysthymia. The incidence and disability-adjusted life years of depression were the highest in the 60–64 age group and much higher in females than in males, with this trend occurring across all ages. The age-standardized incidence and adjusted life-years-disability rates varied with different SDI levels. Relevant risk factors for depression were identified. National governments must support research to improve prevention and treatment interventions.
Similar content being viewed by others

The burden of mental disorders in Asian countries, 1990–2019: an analysis for the global burden of disease study 2019
Incidence, prevalence, and global burden of ADHD from 1990 to 2019 across 204 countries: data, with critical re-analysis, from the Global Burden of Disease study
The burden of schizophrenia in the Middle East and North Africa region, 1990–2019
Introduction.
Mental disorders are a major contributor to the global burden of disease. It commonly results in a higher incidence of physical decline 1 , 2 , 3 , 4 and early death compared with normal age-related deaths 5 . The WHO Mental Health Action Plan 2013–2020 states that individuals suffering from mental illness have elevated rates of disability and death 6 . Individuals with depression and schizophrenia are 40–60% more likely to die suddenly compared to the general population, mainly because of undetected and untreated physical health problems they may be suffering from, such as cancer, cardiovascular disease, diabetes, and HIV infection and even suicide. Suicide is the second most common cause of death for young people in the world 7 .
There is evidence that depression predisposes individuals to myocardial infection and diabetes and having these illnesses increases the chances of developing depression. Many risk factors, such as low social status, alcohol abuse, and stress, are responsible for the development of mental illnesses 8 . Overall, mental illnesses, neurological disorders, and substance use disorders account for 13% of the global disease burden, with depression accounting for 4.3% of the total. Further, these are considered to be one of the main causes of disability worldwide, especially for female.
The economic costs of these health problems are enormous. According to a new study, the total financial costs of mental illness worldwide will reach $16.3 trillion between 2011 and 2030 9 . The Action Plan targets mental illness, stating that by 2020 countries’ suicide rates will have dropped by 10% and there will be a 20% increase in health care services for serious mental illnesses, including psychosis, bipolar disorder, and moderate-to-severe depression 10 .
Mental disorders are recognized as a major contributor to the global burden of disease, accounting for 1566.2 disability-adjusted life years (DALYs) per 100,000 of the global population in 2019. Among these, depressive disorders (major depressive disorder [MDD] and dysthymia) constituted the most significant proportion of mental disorder DALYs (37.3%) 11 . Depression can impair normal body functions and lead to depressive thoughts, which seriously affects people’s quality of life and is one of the most prevalent chronic mental illnesses worldwide. Its main symptoms are depressed emotions, declining interest, slowed thinking, sleep and eating disorders, and even suicidal thoughts in severe cases 12 , 13 , 14 . Around the world, in excess of 300 million people experience depression, which the WHO ranks it as the greatest contributor to global disability 15 . Most concerning of all, youth suffering from major depression have a 30 times higher likelihood of taking their own lives 16 . Despite the fact that depression have become one of the foremost health problems globally, little is known about their complex pathogenesis 17 , 18 .
The Global Burden of Disease (GBD) study offers detailed data on a wide range of diseases for 204 countries in 21 different regions worldwide 19 . The GBD database provides extensive information on the incidence of depression worldwide and categorizes depression into two broad groups: MDD and dysthymia 20 . We explored temporal trends and spatial distributions of depressive disorders, age and sex distributions, and the relationship between the Social Development Index (SDI) and risk factors affecting depression using data on depressive disorders in the GBD database from 1990 to 2019 20 . We described incidence and DALY rates, as well as estimated annual percentage change (EAPC) in incidence and DALY cases. The age-standardized rate (ASR) was considered to be increasing if the EAPC and the corresponding 95% CI were > 0, and the opposite were < 0. Outcomes of this study will contribute to our understanding of the global disease burden of depression, which is of great societal value in controlling and combating depression, and scientifically important for the development of psychology and neuroscience 21 .
Data sources
The data utilized in this study are available on the Global Health Data Exchange GBD Results Tool ( http://ghdx.healthdata.org/gbd-results-tool ) . GBD 2019 estimated incidence, prevalence, mortality, years lived with disability (YLDs), years of life lost (YLLs), and DALYs for 369 diseases and injuries, for males and females, 23 age groups, 204 countries and territories that were geographically grouped into 21 regions from 1990 onwards 11 . All measures are presented as quantities, ratios, and percentages; they can be selected by sex, age group, and region according to the needs of the study 10 . In this study, we extracted data on depression across all age groups and sexes from 21 GBD regions and 204 countries from 1990 to 2019. As not all diseases were estimated for all countries, the GBD 2019 study used the Bayesian meta-regression tool DisMod-MR 2.1 as the principal method to ensure that the incidence, prevalence, and mortality rates for each disease were consistent 22 , 23 .
Classification and definitions
Depressive disorders, mdd, and dysthymia.
In the International Classification of Diseases Tenth Revision (ICD-10), depressive disorders were categorised into two main groups: major depressive disorder (MDD) and dysthymia. Therefore, in the GBD study, both MDD and dysthymia were included in the category of depressive disorders. MDD is an episodic depressive disorder that may recur throughout an individual’s life, with each recurrence varying in severity. Dysthymia is a slow and mild persistent depressive disorder with symptoms less severe than those of MDD, but with a course characterised by persistence. Cases that met the diagnostic criteria for MDD and dysthymia according to the DSM (Diagnostic and Statistical Manual) and ICD (Diagnostic and Statistical Manual) were included in the GBD research disease model 24 .
The SDI is an aggregative metric that measures the development of a country or region, combining data on the total fertility rate for females under 25, the average level of education of females aged 15 and over, and per capita income. The GBD 2019 database categorises the world into five types of regions based on the SDI index: low-SDI (0–0.45), low-middle-SDI (0.45–0.61), middle-SDI (0.61–0.69), high-middle-SDI (0.69–0.81), and high-SDI (0.81–1) 10 , 24 .
Human development index (HDI)
HDI is an aggregative indicator that measure the level of economic and social development of United Nations Member States and consists of three basic variables: life expectancy, educational attainment, and quality of life. We obtained the 2019 HDI data from the United Nations Development Program’s Human Development Report to explore the association of the HDI and the EAPC for incidence and DALYs ( https://hdr.undp.org/en/composite/HDI , accessed on March 27, 2022) 25 .
Age-standardized rate (ASR) is a common indicator in epidemiology. When the composition of age structure is different between several comparison groups, the crude rate of direct comparison groups will lead to bias because it does not indicate whether the high incidence rate in a particular area is due to differences in age composition, and it is usually necessary to compare rates after standardization 26 . Therefore, the age-standardized incidence rate reflects the incidence level that is not affected by age factors, and does not represent the absolute incidence rate, but only to facilitate the comparison of incidence data in different regions or different periods.
The age-standardized rate was calculated on the basis of the following formula:
The age-standardized rate per 100,000 population is equal to the sum of the products of age-specific rates (wi, where i denotes the i th age class) and number of cases (or weight; wi) in the same age subgroup i of the selected reference standard population and then divided by the sum of the standard population weights 27 . Age-standardized rates were calculated considering the GBD world population. In this study, ASR was used to quantify the incidence of two types of depression and the trend of DALYs 28 .
The EAPC provides a well-recognized approach of characterizing ASR using a regression model that quantifies the average annual rate of change during a specific period, with the plus and minus signs representing the direction of change. The regression line was used to estimate the natural logarithm of the rate (i.e., y = α + βx + ϵ, where y = ln(ASR) and x = calendar year). The EAPC was calculated as 100 × (exp (β) − 1), with a 95% CI derived from a linear regression model. All statistics were analysed using R version 4.2.3, and a two-sided P < 0.05 was considered statistically significant 28 . The ASR was decreasing when both the EAPC and the upper limit of its 95% CI were ≤ 0; conversely, the ASR was increasing when both were ≥ 0; otherwise the ASR was stable. All statistical analyses were made with R software 19 .
Analytic strategy
We depicted changes in the prevalence and burden of disease of depression in 204 nations covering 21 distinct regions during the study period. The analysis indices included incidence and DALYs. The ASR was calculated considering the average population structure of the world from 2000 to 2025 as the standard population structure 25 . DALYs = YLDs + YLLs. Because depressive disorders are non-fatal diseases, YLDs are equivalent to DALYs in this instance. This study highlights the state of the burden of disease for depression and temporal and spatial trends from 1990 to 2019 24 . First, the incidence and DALYs of depressive disorders worldwide since 1990 to 2019 were odellin. The burden of depression was then evaluated according to age, sex, country, and region. The extent to which differing development levels affected the burden of depressive disorders was then assessed using the SDI and risk factors for depression 10 . In the result, we present 95% UI for every metric based on the 25th and 975th ordered values of 1000 draws of the posterior distribution. Uncertainty interval (UI) is the interval estimated by GBD research calculation method DisMod-MR, a Bayesian meta-regression tool. It takes into account the differences between different calculation methods in different countries, as well as the uncertainty of multiple filling of missing data values in different countries, which is obtained by repeated sampling calculation through the correlation matrix. Unlike confidence intervals, the UI not only adjusts for sampling error, but also captures uncertainty in multiple stages of analysis modelling and adjusts for the type and quality of data sources 28 .
Ethical committee
The study was compliant with the Guidelines for Accurate and Transparent Health Estimates Reporting, and the University of Washington Institutional Review Board reviewed and approved the waiver of informed consent for GBD 2019.
Since 1990 to 2019, depressive disorder cases have grown from 182,183,358 (95% UI 159,598,111–207,533,227) to 290,185,742 (95% UI 256,024,052–328,260,553), with a 0.59% (95% UI 0.55–0.64) increase in cases of depression for both male and female (see Supplementary Table S1 a). In 2019, 46,863,642 (95% UI 32,929,363–63,797,315) DALYs resulting from depression were documented with an upward trend of 0.61% since 1990 (see Table 1 , Supplementary Table S1 b). The incidence of depression was greater among females than males from 1990 to 2019, as were associated DALYs (see Fig. 1 , Table 1 ). In 2019, depression caused 110,123,422 (95% UI 96,668,365–124,305,433) incidence cases in males globally, and 180,062,320 (95% UI 159,076,846–204,131,417) incidence cases in females, resulting in 18,183,102 (95% UI 12,682,047–24,947,035) DALYs in males, and 28,680,540 (95% UI 20,155,773–39,319,358) DALYs in females. The age-standardised incidence rate (ASIR) of depressive disorders is found to grow with age, reaching a peak during the 60–64 year age group for females and the 80–84 year age group for males. However, there was a small decrease in the 25–29 years age group across both sexes. The age-standardized adjusted life-year disability rate (ASDR) of depression also showed an increasing trend with age. It began to decline in females after reaching a peak in the 55–59 age group. And for males, it peaks in the 60–64 age group and then begins to decline. ASDR for males and females were 452.17 (95% UI 316.79–618.13) and 702.08 (95% UI 492.3–963.58), respectively (see Fig. 2 , Table 1 ). Over all, Females develop a greater ASIR and ASDR than males in the same age group. However, during the period 1990–2019, the DALYs change was higher in males than in females, 0.65% in males (95% UI 0.61–0.69) compared to 0.59% in females (95% UI 0.54–0.63) (see Supplementary Table S1 b).

Temporal trend of global incidence ( a ) and DALYs ( b ) number of depressive disorders.

Age-standardized incidence rate ( a ) and age-standardized DALYs rate ( b ) trends of sex and age distribution.
In terms of the subtypes of depression, the incidence of MDD was much more prevalent than dysthymia at 2,784,803,790 (95% UI 241,280,545–312,774,423) and 15,381,951(95% UI 12,782,128–18,474,451) respectively in 2019. The same was true for DALYs, which were 37,202,742 (95% UI 25,650,205–51,217,042) and 9,660,901 (95% UI 6,311,566–14,421,787) respectively (see Table 1 ). During the period 1990–2019, the global depression ASIR has decreased significantly (EAPC = − 0.29%, 95% UI − 0.38 to − 0.21), whereas the ASDR has markedly increased (EAPC = 0.61%, 95% UI 0.57–0.65) (see Table 1 ).
Global burden and EAPC of depressive disorders by 21 GBD regions
Individuals with depressive disorders increased in all five SDI regions from 1990 through 2019 (see Supplementary Table S1 a). However, the ASIR decreased in the high-middle-SDI (EAPC = − 0.5%, 95% UI − 0.57 to − 0.43), middle-SDI (EAPC = − 0.2%, 95% UI − 0.28 to − 0.13), low-middle-SDI (EAPC = − 0.62%, 95% UI − 0.79 to − 0.44), and low-SDI regions (EAPC = − 0.38%, 95% UI − 0.5 to − 0.26), only increasing in the high-SDI regions (EAPC = 0.31%, 95% UI 0.18–0.44) (see Table 1 ). The same is true for DALYs cases and ASDR (Table 1 , Supplementary Table S1 b). ASDR decreased in the high-middle-SDI (EAPC = − 0.4%, 95% UI − 0.46 to − 0.34), middle-SDI (EAPC = − 0.18%, 95% UI − 0.24 to − 0.13), low-middle-SDI (EAPC = − 0.51%, 95% UI − 0.66 to − 0.36) and low-SDI regions (EAPC = − 0.3%, 95% UI − 0.4 to − 0.2), only increasing in the high-SDI regions (EAPC = 0.23%, 95% UI 0.14–0.33) (see Table 1 , Supplementary Table S1 b).
The incidence of depressive disorders grew in all regions, with a decline only in Central and Eastern Europe (see Fig. 3 a). Central Sub-Saharan Africa saw the maximum rate of increase (1.4%, 95% UI 1.29–1.51), followed by Western Sub-Saharan Africa (1.25%, 95% UI 1.22–1.28) and Eastern Sub-Saharan Africa (1.17%, 95% UI 1.13–1.21), with the decline being most marked in Eastern Europe (− 0.08%, 95% UI − 0.1 to − 0.05) (see Supplementary Table S1 a). There was a marked rise in ASR across high-income North America (EAPC = 0.62, 95% UI 0.32–0.92) and a marked drop in South Asia (EAPC = − 0.85, 95% UI − 1.1 to − 0.6) (see Table 1 ).
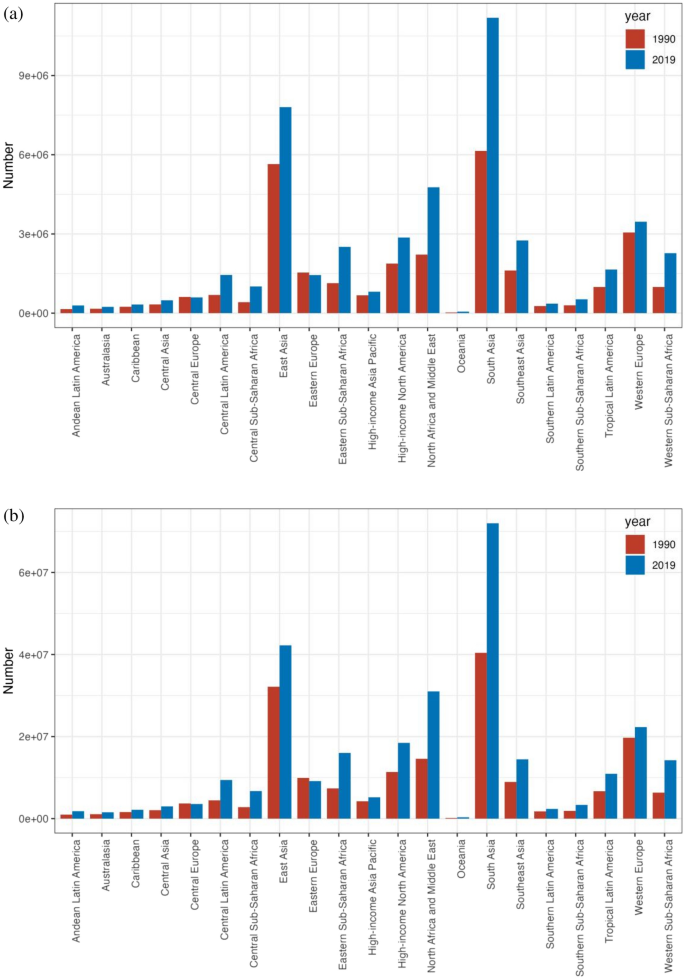
The incident cases ( a ) and DALYs ( b ) of depression at a regional level. The left column in each group is case data in 1990 and the right column in 2019.
DALYs corresponding to depressive disorders grown in all geographical regions, with a decline only in Central and Eastern Europe (see Fig. 3 b). The largest increase was occurred in Central Sub-Saharan Africa (1.43%, 95% UI 1.33–1.54), followed by Western Sub-Saharan Africa (1.29%, 95% UI 1.26–1.32) and Eastern Sub-Saharan Africa (1.21%, 95% UI 1.17–1.25), with the decline being most marked in Eastern Europe (− 0.06%, 95% UI − 0.08 to − 0.04) (Supplementary Table S1 b). There was a marked rise in ASR in Central Sub-Saharan Africa (EAPC = 1.43, 95% UI 1.33–1.54) and a decline in South Asia (EAPC = − 0.71, 95% UI − 0.92 to − 0.5) (see Table 1 ).
Global burden and EAPC of depressive disorders across 204 countries and territories
The ASIR for depression varied dramatically across 204 countries and territories in 2019 (see Fig. 4 a, Supplementary Table S2 a). The ASIR was highest in Uganda (8062.76, 95% UI 6946.5–9436.97), followed by Palestine (7864.2, 95% UI 6719.71–9216.83) and the Central African Republic (7230.55, 95% UI 6121.98–8465.86), and was lowest in Myanmar (1393.92, 95% UI 1188.1–1612.65), followed by Brunei Darussalam (1,575.58, 95% UI 1346.16 to 1854.56) and Indonesia (1794.07, 95% UI 1557.18–2060.02). Of the 204 countries and territories under analysed, the ASDR for depressive disorders in 2019 differed considerably (see Fig. 4 a, Supplementary Table S2 b), with the highest being in Uganda (1212.09, 95% UI 824.6–1696.26), followed by Palestine (1168.68, 95% UI 802.95–1624.31) and Greenland (1098.69, 95% UI 750.76–1540.82), and the lowest in Brunei Darussalam (260.29, 95% UI 177.62–360.71), followed by Myanmar (298.19, 95% UI 203.44–421.71) and Indonesia (350.26, 95% UI–242.89–488.45).

The global disease burden of depression for both sexes in 204 countries and territories. ( a1 ) The ASIR of depression in 2019; ( a2 ) the ASDR of depression in 2019; ( b1 ) the relative change in incident cases of depression between 1990 and 2019; ( b2 ) the relative change in DALYs number of depression between 1990 and 2019; ( c1 ) the EAPC of depression ASIR from 1990 to 2019; ( c2 ) the EAPC of depression ASDR from 1990 to 2019. ASIR age-standardized incidence rate, ASDR age-standardized DALYs rate, EAPC estimated annual percentage change (Image generated in R software version 4.2.3 ( https://cran.r-project.org )).
The global incidence of depression grew by 0.59% from 182,183,358 in 1990 to 290,185,742 in 2019. Qatar had the greatest growth (5.89%, 95% UI 5.34–6.51), followed by the United Arab Emirates (4.81%, 95% UI 4.09–5.53) and Equatorial Guinea (2.42%, 95% UI 2.19–2.67) (see Fig. 4 b, Supplementary Table S2 a). From 1990 to 2019, depression declined in 23 nations, with Latvia experiencing the largest reduction (− 0.32%, 95% UI − 0.38 to − 0.24), followed by Bosnia and Herzegovina (− 0.3%, 95% UI − 0.38 to − 0.21) and Estonia (− 0.27%, 95% UI − 0.34 to − 0.19). The DALYs for depression worldwide rose from 29,089,267 in 1990 to 46,863,642 in 2019, which is a 0.61% increase. Qatar had the most significant growth (5.99%, 95% UI 5.45–6.57), followed by the United Arab Emirates (4.91%, 95% UI 4.24 to 5.65) and Equatorial Guinea (2.48%, 95% UI 2.26 to 2.73) (see Fig. 4 b, Supplementary Table S2 b). DALYs for depression declined in 21 countries, with Latvia experiencing the largest decline from 1990 to 2019 (− 0.31%, 95% UI − 0.37 to − 0.24), followed by Bosnia and Herzegovina (− 0.29%, 95% UI − 0.36 to − 0.21) and Estonia (− 0.26%, 95% UI − 0.33 to − 0.19).
Among the 204 countries and territories, the greatest rise of ASIR occurred in Spain (EAPC = 1.05, 95% UI 0.78–1.31), next is Mexico (EAPC = 0.81, 95% UI 0.73 to 0.89) and Malaysia (EAPC = 0.79, 95% UI 0.59–1.00) (see Fig. 4 c, Supplementary Table S2 a). The most significant drop in ASR was Singapore (EAPC = − 1.97, 95% UI − 2.22 to − 1.73), then Sri Lanka (EAPC = − 1.23, 95% UI − 1.4 to − 1.06) and Slovenia (EAPC = − 1.15, 95% UI − 1.23 to − 1.07). Among all 204 countries and territories, Spain had the greatest rise in ASDR (EAPC = 0.94, 95% UI 0.69–1.18), then Mexico (EAPC = 0.74, 95% UI 0.67–0.81) and Malaysia (EAPC = 0.69, 95% UI 0.53–0.86) (see Fig. 4 c, Supplementary Table S2 b). The greatest decline in ASR was in Singapore (EAPC = − 1.83, 95% UI − 2.06 to − 1.59), next is Cuba (EAPC = − 1.23, 95% UI − 1.36 to − 1.1) and Estonia (EAPC = − 1.23, 95% UI − 1.36 to − 1.1).
The correlation of SDI with the global burden of depressive disorders
Substantial correlation was observed among the SDI and depression prevalence and also among the SDI and DALYs, as illustrated in Fig. 5 . A number of regions exceeded the expected levels of prevalence, including Central Sub-Saharan Africa and Australasia, while a number of regions fell below the expected levels of prevalence, including South-East Asia and the high-income regions Asia and the Pacific (see Fig. 5 a).

Age-standardized incidence rate ( a ) and age-standardized DALYs rate ( b ) for depression for 21GBD regions and 204 countries and territories ( c , d ) by Socio-demographic Index(SDI),1990–2019 (the black line indicates the correlation between all SDI regions and the incidence rate or DALY expected value).
Of the 204 countries and territories whose association with the 2019 SDI was recognised, most had a negative association with the SDI, with a few countries significantly above or below the expected level. Uganda and Palestine were significantly higher than expected, while Myanmar and Brunei were significantly lower than expected (see Fig. 5 c).
DALYs declined in many areas as the SDI became higher, with the exception of certain regions. For instance, the DALYs rate in Western Sub-Saharan Africa fell briefly, then rose, and then kept falling, forming an inverted U-curve. The DALYs rate of Tropical Latin America, which has a low-middle SDI rank, remained stable at first, then increased, before declining sharply. The rate of Southern Latin America, which has a middle SDI rank, remained stable at first, then decreased, and then continued to remain stable. The DALYs rate of Eastern Europe, which has a high-middle SDI, rose slightly, then fell sharply, remained stable for a period, and then fell slightly. High SDI ratios in high-income Asia–Pacific regions fell briefly and then rose, before falling slightly (see Fig. 5 b).
Since 1990 to 2019, the DALY rates obtained in high SDI-ranking regions, such as Western Europe, were mostly consistent with expectations. However, during the study period, some regions (e.g., high-income Asia–Pacific) continued to have DALYs far lower than expected, while others (e.g., Australasia and high-income North America) continued to have DALYs higher than expected (see Fig. 5 b). At the country level during 2019, following a similar pattern to the association of morbidity and SDI, there was a marked adverse correlation between DALYs and SDI, with a few exceptions (R = − 0.375, p < 0.001) (see Fig. 5 d) 28 .
The relationship between the HDI and the global burden of depressive disorders
No significant relationship was found between the EAPC for 1990 morbidity and morbidity (ρ = − 0.064, p = 0.363). An inverse association was identified with EAPC in DALYs and DALYs in 1990 (ρ = − 0.057, p = 0.014) (see Fig. 6 a). In view of the fact that the EAPC was below zero, the number of DALYs attributable to depressive disorders decreased more rapidly in countries with higher DALYs in 1990. In addition, a significant negative correlation was identified for EAPC with the 2019 HDI, suggesting that prevalence rates declined more rapidly in areas with higher HDI. The same association was identified with DALYs rate and HDI (ρ = − 0.213, p = 0.007) (see Fig. 6 b).

The EAPCs of depressive disorders at global, regional and national level. ( a ) The correlation between EAPC and age-standardized rate of depressive disorders incidence and ( b ) DALYs rate in 1990. ( c , d ) The correlation between EAPC and HDI in 2019. The circles represent countries that were available on HDI data. The size of circle is increased with the cases of depressive disorders cases. The ρ indices and p values presented were derived from Pearson correlation analysis. ( a ) ρ = − 0.064, p = 0.363 ( b ) ρ = − 0.057, p = 0.014 ( c ) ρ = − 0.198, p = 0.013 ( d ) ρ = − 0.213, p = 0.007.
Risk factors of depressive disorders
For the world as a whole, a small fraction of DALYs were ascribed to the three risk factors for which GBD estimates were obtainable, of which 6.7% attributable to intimate partner violence, 3.6% to bullying victimisation, and 4.4% to childhood sexual abuse (see Fig. 7 ). There is regional variation in the contributions of these risk factors. For instance, intimate partner violence had the greatest impact in Central Sub-Saharan Africa (9.6% of DALYs were attributable to intimate partner violence) and Southern Sub-Saharan Africa (9.1%), where intimate partner violence remains prevalent, and is lowest in Southeast Asia (3.8%). As well, the contribution of bullying vicitimisation was greatest in Central Sub-Saharan Africa (6.2% of DALYs attributable to bullying victimisation) and high-income North America (5.6%), and was lowest in Central Asia, where bullying victimisation is relatively low. In addition, the impact of childhood sexual abuse was greatest in Western Sub-Saharan Africa (8.5% of DALYs were attributable to childhood sexual abuse) and lowest in Central Asia. However, given that there were only three risk factors relevant to depressive disorders among the GBD study, the percentage of DALYs resulting from these three risk factors remains small when viewed as a whole, which means that there is a need for further study on the key influences of depression.

Proportion of depressive disorders DALYs attributable to intimate partner violence, bullying victimization, and childhood sexual abuse, for 21 GBD regions, 2019.
Depression, as a serious public health problem, is associated with adverse health outcomes and reduced life-expectancy 30 . This study presents the global burden of depression through GBD data, focusing on the temporal trends and spatial distribution of depression from 1990 to 2019, with a specific focus on EAPC. The outcome of the study offers an important reference value for all regional governments when formulating relevant prevention and treatment measures for depression 19 .
The outcomes of this study suggest that the overall burden of depression has increased rapidly within three decades, but the increase has not been uniform across age groups, sexes, or regions 10 . The further increase in the burden of depression observed in our study is in agreement with the outcomes by Liu et al. 29 . This is likely driven by the increasing social pressure brought about by economic development and population growth, and the serious aging of the population. In addition, with the economic development and the gradual improvement of people’s living standards, the demand for medical services is also rising, especially the increasing emphasis on mental health, in this case, the search for mental health services has also increased. It is also important to note that the continuous improvement of depression screening tools has made it possible for medical institutions and government agencies to obtain more comprehensive and accurate data. Our research suggests that MDD accounts for a large proportion of depression cases and is the most prevalent psychiatric category of depression, a finding which aligns with those of a 2022 study by Li et al. 31 .
Our research shows that females have higher rates of depression and DALYs than males across all age groups. The prevalence and DALYs rates of depression were highest in people aged 60–64 years. There are many reasons for this. The psychological characteristics of people in this age group undergo a major shift from concern for external things to their own bodies, the feeling of loneliness and isolation increases, and the intellect begins to diminish, which leads to emotional instability. Females are more prone to experience negative events and emotions, including postpartum mood swings, domestic violence, sexual abuse, and bullying, all of which may contribute to higher rates of depression 32 , 33 , 34 . Additionally, related reports have found that females are more selfless than males and are thus more prone to depression 35 . This finding partly explains sex differences in the onset of depression.
Our reports indicate that the rates of the two subtypes of depression, dysthymia and major depressive disorders, have remained largely stable globally and regionally over the study period, with the majority of patients suffering from MDD. The World Mental Health Survey estimated the annual prevalence of MDD to be 4.4% and the lifetime prevalence to be approximately 10% -15% 36 , 37 . With the continuous development of the social economy, accelerated pace of life, and increasingly fierce social competition, people’s psychological pressure is gradually increasing, and the incidence of MDD is increasing annually. MDD not only seriously affects the psychological condition and quality of life of patients, but also imposes tremendous mental and economic burdens to families and society 38 . In 2008, the WHO listed MDD as the third largest contributor to the global disease burden and predicted that MDD would be the leading contributor to the burden of disease by 2030 39 . Currently, about 300 million people worldwide suffer from MDD; therefore, effective control of major depressive disorders is an effective approach to preventing and managing depression 40 .
The findings suggest that Uganda’s relatively concentrated population and high prevalence of tropical diseases, malaria, AIDS, Ebola virus, sleeping sickness, viral hepatitis, and tuberculosis may be associated with its highest global ASR and ASDR for depression. Although the peak of the epidemic in Uganda, which had one of the world’s highest HIV prevalence rates, has passed and the rate of new cases has diminished in recent years, the number of people infected with the virus and living with the disease remains high, especially in rural areas. People living with HIV experience social prejudice and discrimination, which can lead to unemployment, poverty, family disintegration, and physical and psychological problems that can lead to low self-esteem, low mood, and even depression 41 , 42 . This shows that the prevention and control of HIV can affect depression.
The most significant rise in depression and DALYs was identified in Qatar, with the United Arab Emirates and Equatorial Guinea next. Significant increases in depression and DALYs were observed in the medium–high SDI and high-SDI regions. It could be because the level of economic development and education in these regions is relatively high, and the social pressure generated by residents is greater, leading to the increased prevalence of depression. Studies have found that individuals with different education levels have different levels of cognitive ability. Education level influences depression in individuals and can also impact spouses 43 . It is also true that social stress is an acknowledged risk factor for depression, and research have indicated that the higher the level of economic development, the more social stress people experience. Notably, the country with the most decline in depression and DALYs was Latvia, followed by Bosnia and Herzegovina, and Estonia 19 .
The ASIR and ASDR increased the most in Spain, followed by Mexico and Malaysia. These countries are reported to have higher economic incomes and sociodemographic indices, which confirm our statistics. However, in terms of ASR, the greatest decline in ASIR was in Singapore, then Sri Lanka and Slovenia; and the maximum decline in ASDR was in Singapore, Cuba, and Estonia 19 .
Further analysis of the relationship between illness and sociodemographic and geographic factors suggests that depression is more pronounced in terms of incidence in high-SDI and high-income countries, while the burden of depression is significantly higher in low-income and low-SDI countries.
In conclusion, the burden of depression varies across regions for a number of reasons. These include each region’s level of economic development, level of education, level of medical development and capacity to diagnose the illness, as well as the level of importance that governments attach to the illness 44 , 45 , 46 . Additionally, there are cultural differences that contribute to the different burdens of depression in different regions, such as customs and religious beliefs. The incidence of depression is still high, and the burden of the disease remains heavy, but the pathogenesis is unclear, which is an obstacle to the effective prevention and control of depression. This study nalysed the possible risk factors, such as domestic violence, bullying victimisation, and childhood sexual abuse. However, the GBD data show that the implication of these three risk factors on depression is small; that is, these three risk factors are not likely to be key risk factors for depression, indicating that this requires further investigation 47 .
To effectively prevent and control depression, governments must support depression-related research while taking appropriate steps to effectively address depression. For example, they should strengthen education on prevention and treatment, improve the capacity for early diagnosis and standardised treatment, establish mental health service measures for key populations, and carry out psychological intervention in a timely manner 19 .
This study performed the most comprehensive assessment of the depression burden to date. All the data used in this study were obtained from the GBD database, which offers a large sample size and high data quality, offering this study a distinct advantage in terms of data reliability. While numerous research have been conducted on the prevalence of depression in GBD 2019, the majority of these studies evaluate the condition using the age-period-cohort analytic approach, and their study regions, study objects, and focus subtypes of depression vary. Li et al., for instance, used the age-period cohort analytic approach to study the prevalence of depression among teenagers in the Western Pacific region 48 . In addition, Xu Y et al. used the age-period-cohort analytic method and limited their research to the incidence of depression across all areas, leaving unfinished business regarding studies on the burden of disorders like DALY 49 . Major depression is a subtype of depression, and Li et al. focused on examining gender variations in its illness burden. They discovered that women are more likely than males to experience major depression 31 . The disease burden of anxiety and major depression caused by bullying was examined by Hong C et al. as a risk factor. The findings indicated that from 1990 to 2019, there was a rising trend in both the DALY number and DALY rate of anxiety and major depression caused by bullying. Adopting effective techniques is necessary to eradicate bullying among children and adolescents 50 . Additionally, Yang F et al. used the age-period-cohort analysis method to conduct a thorough study on the prevalence of depression in 204 countries from 1990 to 2019. Findings from our study, such as the nations with the greatest and lowest incidence and DALY of depression, are in line with their conclusions. Moreover, the connection between the regional SDI and the depression incidence trend. But there isn’t any research on the prevalence and DALY of two distinct subtypes of depression, or on the connection between the HDI and depression burden, as well as the risk factors of depression 51 . This study comprehensively analysed the impact of depression and the temporal and spatial changes in disease burden at the global, 21 regional and 204 national levels. These include age-specific differences in the burden of depression, sex differences, and disease burden differences between the two subtypes of depression. Incidence, DALYs, ASIR, ASDR and EAPC (the change rate of ASIR and ASDR) are used to comprehensively describe the burden of disease from different perspectives and provide specific quantified values respectively. And most importantly, this study nalysed the relationship between the burden of depression and HDI, this is what is missing from all the relevant studies above. Finally, this study examined the depression risk factor data that was accessible in the GBD database. This will offer a crucial foundation for upcoming research on depression and its risk factors. All of the linked research mentioned above lack the analysis of risk variables. Nonetheless, this study possesses limitations. First, the GBD data used in this study were collected from a large amount of epidemiological survey data, processed, and integrated using corresponding statistical methods. The lack of original data in many countries and regions may have led to a bias in the differences in disease burden. Second, the comorbidity of MDD and dysthymia was excluded in this study. We hope that in the future the GBD database can further distinguish these disorders to facilitate a more complete analysis 52 , 53 .
Depression remains a serious challenge worldwide, and its burden of disease remains heavy. By analysing the global burden of depression, this study clarifies the current situation of depression in various countries and provides a scientific reference basis for governments to formulate active and effective prevention and treatment strategies. Countries, especially those with a high burden of depression, must vigorously strengthen mental health education, actively prevent risk factors, and adopt targeted interventions to raise the level of awareness of depression among their populations, and concurrently, call for the reform of the relevant systems and the elimination of policy barriers to better prevent and treat mental health disorders 54 , 55 .
Data availability
The dataset generated for this study can be found in the GBD at http://ghdx.healthdata.org/gbd-results-tool .
Lawrence, D., Kisely, S. & Pais, J. The epidemiology of excess mortality in people with mental illness. Can. J. Psychiatry . 55 , 752–760. https://doi.org/10.1177/070674371005501202 (2010).
Scott, K. M. et al . Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 73 , 150–158. https://doi.org/10.1001/jamapsychiatry.2015.2688 (2016).
Wahlbeck, K., Westman, J., Nordentoft, M., Gissler, M. & Laursen, T. M. Outcomes of Nordic mental health systems: Life expectancy of patients with mental disorders. Br. J. Psychiatry 199 , 453–458. https://doi.org/10.1192/bjp.bp.110.085100 (2011).
Scott, K. M. et al. Associations between DSM-IV mental disorders and subsequent heart disease onset: beyond depression. Int. J. Cardiol. 168 , 5293–5299 (2013).
Article PubMed Google Scholar
Piao, J. et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: A systematic analysis for the Global Burden of Disease study. Eur. Child Adolesc. Psychiatry. 31 (1827–1845), 14. https://doi.org/10.1007/s00787-022-02040-4(2022)(Epub (2022).
Article Google Scholar
Thomas, S. P. World Health Assembly adopts comprehensive Mental Health Action Plan for 2013–2020. Issues Ment. Health Nurs. 34 , 723–724. https://doi.org/10.3109/01612840.2013.831260 (2013).
Upthegrove, R., Marwaha, S. & Birchwood, M. Depression and schizophrenia: Cause, consequence, or trans-diagnostic issue?. Schizophr. Bull. 43 , 240–244. https://doi.org/10.1093/schbul/sbw097 (2017).
Kessler, R. C. et al. The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiol. Psichiatr. Soc. 18 , 23–33. https://doi.org/10.1017/s1121189x00001421 (2009).
Article PubMed PubMed Central Google Scholar
Wang, P. S. et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 370 , 841–850. https://doi.org/10.1016/S0140-6736(07)61414-7 (2007).
Piao, J. et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: A systematic analysis for the Global Burden of Disease study. Eur. Child Adolesc. Psychiatry 31 , 1827–1845. https://doi.org/10.1007/s00787-022-02040-4.[Epub2022July14] (2022).
GBD. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 9 , 137–150. https://doi.org/10.1016/S2215-0366(21)00395-3 (2022).
Cui, R. Editorial: A systematic review of depression. Curr. Neuropharmacol. 13 , 480. https://doi.org/10.2174/1570159x1304150831123535 (2015).
Article CAS PubMed Google Scholar
Luo, Y., Zhang, S., Zheng, R., Xu, L. & Wu, J. Effects of depression on heart rate variability in elderly patients with stable coronary artery disease. J. Evid. Based Med. 11 , 242–245. https://doi.org/10.1111/jebm.12310 (2018).
Seligman, F. & Nemeroff, C. B. The interface of depression and cardiovascular disease: Therapeutic implications. Ann. N. Y. Acad. Sci. 1345 , 25–35. https://doi.org/10.1111/nyas.12738 (2015).
Article ADS CAS PubMed Google Scholar
Smith, K. Mental health: A world of depression. Nature 515 , 181. https://doi.org/10.1038/515180a (2014).
Stringaris, A. Editorial: What is depression?. J. Child. Psychol. Psychiatr. 58 , 1287–1289. https://doi.org/10.1111/jcpp.12844 (2017).
Gross, M. Silver linings for patients with depression?. Curr. Biol. 24 , R851–R854. https://doi.org/10.1016/j.cub.2014.08.059 (2014).
Ménard, C., Hodes, G. E. & Russo, S. J. Pathogenesis of depression: Insights from human and rodent studies. Neuroscience 321 , 138–162. https://doi.org/10.1016/j.neuroscience.2015.05.053 (2016).
Solmi, M. et al. Incidence, prevalence, and global burden of autism spectrum disorder from 1990 to 2019 across 204 countries. Mol. Psychiatry 27 , 4172–4180 (2022).
Liu, Q. et al. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J. Psychiatr. Res. 126 , 134–140. https://doi.org/10.1016/j.jpsychires.2019.08.002 (2020).
Peng, H. et al. The global, national, and regional burden of dysthymia from 1990 to 2019: Insights from the Global Burden of Disease 2019 study. J. Affect. Disord. 333 , 524–526. https://doi.org/10.1016/j.jad.2023.04.024 (2023).
GBD. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2 (2020).
Hong, C. et al. Global trends and regional differences in the burden of anxiety disorders and major depressive disorder attributed to bullying victimisation in 204 countries and territories, 1999–2019: an analysis of the Global Burden of Disease Study. Epidemiol. Psychiatr. Sci. 31 , e85. https://doi.org/10.1017/S2045796022000683 (2022).
Article CAS PubMed PubMed Central Google Scholar
Ren, X. et al. Burden of depression in China, 1990–2017: Findings from the global burden of disease study 2017. J. Affect. Disord. 268 , 95–101. https://doi.org/10.1016/j.jad.2020.03.011 (2020).
Dai, H. et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLOS Med. 17 , e1003198. https://doi.org/10.1371/journal.pmed.1003198 (2020).
Hankey, B. F. et al. Partitioning linear trends in age-adjusted rates. Cancer Causes Control 11 , 31–35. https://doi.org/10.1023/a:1008953201688 (2000).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet . 396 , 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
Yue, T., Zhang, Q., Li, G. & Qin, H. Global burden of nutritional deficiencies among children under 5 years of age from 2010 to 2019. Nutrients 14 , 2685. https://doi.org/10.3390/nu14132685 (2022).
Liu, Q. et al. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J. Psychiatr Res. 126 , 134–140. https://doi.org/10.1016/j.jpsychires.2019.08.002 (2019).
Ogbo, F. A., Mathsyaraja, S., Koti, R. K., Perz, J. & Page, A. The burden of depressive disorders in South Asia, 1990–2016: findings from the global burden of disease study. BMC Psychiatry 18 , 333. https://doi.org/10.1186/s12888-018-1918-1 (2018).
Li, S. et al. Sex difference in global burden of major depressive disorder: Findings from the global burden of disease study 2019. Front. Psychiatry. 21 (13), 789305. https://doi.org/10.3389/fpsyt.2022.789305 (2022).
Keita, G. P. Psychosocial and cultural contributions to depression in women: Considerations for women midlife and beyond. J. Manag. Care Pharm. 13 (Supp 9), 12–15 (2007).
Google Scholar
Patel, V., Rodrigues, M. & DeSouza, N. Gender, poverty, and postnatal depression: A study of mothers in Goa India. Am. J. Psychiatr. 159 (1), 43–47 (2002).
Trivedi, J. K., Sareen, H. & Dhyani, M. Rapid urbanization-its impact on mental health: A south Asian perspective. Indian J. Psychiatry. 50 (3), 161 (2008).
Ahmad, O. B. et al . Age standardization of rates: a new WHO standard. GPE Discussion Paper Series: No 31, 10–12. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf (2001).
Ferrari, A. J. et al. Burden of depressive disorders by country, sex, age, and year: Findings from the global burden of disease study 2010. PLOS Med. 10 , e1001547. https://doi.org/10.1371/journal.pmed.1001547 (2013).
Bachner-Melman, R., Watermann, Y., Lev-Ari, L. & Zohar, A. H. Associations of self-repression with disordered eating and symptoms of other psychopathologies for men and women. J. Eat. Disord. 10 , 41. https://doi.org/10.1186/s40337-022-00569-y (2022).
Kessler, R. C. et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA 289 , 3095–3105. https://doi.org/10.1001/jama.289.23.3095 (2003).
Bromet, E. et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 9 , 90 (2011).
Sheehan, D. V. et al. Restoring function in major depressive disorder: A systematic review. J. Affect. Disord. 215 , 299–313 (2017).
Malhi, G. S. & Mann, J. J. Depression. Lancet 392 , 2299–2312 (2018).
Yang, L. et al. The effects of psychological stress on depression. Curr. Neuropharmacol. 13 , 494–504. https://doi.org/10.2174/1570159x1304150831150507 (2015).
Ironson, G., Henry, S. M. & Gonzalez, B. D. Impact of stressful death or divorce in people with HIV: A prospective examination and the buffering effects of religious coping and social support. J. Health Psychol. 25 , 606–616. https://doi.org/10.1177/1359105317726151 (2020).
Junqueira, P., Bellucci, S., Rossini, S. & Reimão, R. Women living with HIV/AIDS: Sleep impairment, anxiety and depression symptoms. Arq. Neuropsiquiatr. 66 , 817–820. https://doi.org/10.1590/s0004-282x2008000600008 (2008).
Lee, J. Pathways from education to depression. J. Cross. Cult. Gerontol. 26 , 121–135. https://doi.org/10.1007/s10823-011-9142-1 (2011).
Alonso, J. et al. Treatment gap for anxiety disorders is global: Results of the World Mental Health Surveys in 21 countries. Depress. Anxiety 35 , 195–208. https://doi.org/10.1002/da.22711 (2018).
Perez, M. I. et al. Obsessive-compulsive disorder misdiagnosis among mental healthcare providers in Latin America. J. Obsessive Compuls. Relat. Disord. 32 , 100693. https://doi.org/10.1016/j.jocrd.2021.100693 (2022).
Li, Z. B. et al. Burden of depression in adolescents in the Western Pacific Region from 1990 to 2019: An age-period-cohort analysis of the Global Burden of Disease study. Psychiatry Res. 336 , 115889. https://doi.org/10.1016/j.psychres.2024.115889 (2024).
Xu, Y. et al. Global, regional, and national incidence trends of depressive disorder, 1990–2019: An age-period-cohort analysis based on the Global Burden of Disease 2019 study. Gen. Hosp. Psychiatry. 88 , 51–60. https://doi.org/10.1016/j.genhosppsych.2024.03.003 (2024) ( Epub 2024 Mar 16 ).
Hong, C. et al. Global trends and regional differences in the burden of anxiety disorders and major depressive disorder attributed to bullying victimisation in 204 countries and territories, 1999–2019: An analysis of the Global Burden of Disease Study. Epidemiol. Psychiatr. Sci. 28 (31), e85. https://doi.org/10.1017/S2045796022000683 (2022).
Yang, F. et al. Thirty-year trends of depressive disorders in 204 countries and territories from 1990 to 2019: An age-period-cohort analysis. Psychiatry Res. 328 , 115433. https://doi.org/10.1016/j.psychres.2023.115433 (2023) ( Epub 2023 Aug 27 ).
Baca, E., Lázaro, J. & Hernández-Clemente, J. C. Historical perspectives of the role of Spain and Portugal in today’s status of psychiatry and mental health in Latin America. Int. Rev. Psychiatry 22 , 311–316. https://doi.org/10.3109/09540261.2010.501165 (2010).
Mullins, N. & Lewis, C. M. Genetics of depression: Progress at last. Curr. Psychiatry Rep. 19 , 43. https://doi.org/10.1007/s11920-017-0803-9 (2017).
McGrath, J. J. et al. Comorbidity within mental disorders: A comprehensive analysis based on 145 990 survey respondents from 27 countries. Epidemiol. Psychiatr. Sci. 29 , e153. https://doi.org/10.1017/S2045796020000633 (2020).
Article MathSciNet CAS PubMed PubMed Central Google Scholar
Plana-Ripoll, O. et al. Nature and prevalence of combinations of mental disorders and their association with excess mortality in a population-based cohort study. World Psychiatry 19 , 339–349. https://doi.org/10.1002/wps.20802 (2020).
Download references
Author information
Authors and affiliations.
College of Public Health, Shanxi Medical University, Taiyuan, Shanxi, China
Junjiao Liu, Wenjun Ma, Yan Tong & Jianzhong Zheng
Second Clinical Medical College, Nanchang University, Nanchang, Jiangxi, China
Yueyang Liu
You can also search for this author in PubMed Google Scholar
Contributions
JL performed the statistical analyses and wrote the manuscript. YL solved technical problems during the statistical analyses and participated in the conceptualization and design of the study, and the interpretation of the results. WM contributed to the conceptualization and design of the study.YT and JZ participated in the design of the study and critically evaluated and revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Yan Tong or Jianzhong Zheng .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Liu, J., Liu, Y., Ma, W. et al. Temporal and spatial trend analysis of all-cause depression burden based on Global Burden of Disease (GBD) 2019 study. Sci Rep 14 , 12346 (2024). https://doi.org/10.1038/s41598-024-62381-9
Download citation
Received : 20 September 2023
Accepted : 16 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1038/s41598-024-62381-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(8); 2022 Aug

Prevalence and Impact of Diagnosed and Undiagnosed Depression in the United States
1 Biology, Detroit Country Day School, Detroit, USA
Rohan Mangal
2 Medicine, University of Miami Miller School of Medicine, Miami, USA
Thor S Stead
3 Medicine, The Warren Alpert Medical School of Brown University, Providence, USA
R. Lane Coffee, Jr.
4 Internal Medicine, University of Central Florida, Orlando, USA
Latha Ganti
5 Emergency Medicine, HCA Florida Ocala Hospital, Ocala, USA
6 Emergency Medicine, Envision Physician Services, Plantation, USA
7 Emergency Medicine, University of Central Florida College of Medicine, Orlando, USA
Background: The objectives of this study were: 1) estimate the impact and severity of both diagnosed and undiagnosed depression in the general US population 2) explore the demographics of depression based on its common symptoms 3) interpret Patient Health Questionnaire-9 (PHQ-9) scores to improve accuracy in identifying individuals with depression.
Methods: A random sample of 200 individuals was selected from a general US adult population to complete the Patient Health Questionnaire-9 (PHQ-9).
Results: Only 39.4% of respondents indicated that they had a formal diagnosis of depression. In contrast, 53% of participants have considered seeking help from a mental health professional. More importantly, 31.45% of respondents without a formal diagnosis had a PHQ-9 score of over 10 (moderate to severe depression).
Conclusions: The results indicate that undiagnosed depression exists in the US population and suggest that access to mental health services needs to expand across the nation.
Introduction
Clinical depression is a mood disorder that causes a persistent feeling of sadness and loss of interest that can affect ones thinking and behavior. This condition can lead to a variety of physical and emotional problems and often requires long-term treatment [ 1 ]. In a normal brain, neurotransmitters successfully send chemical messages through electrical signals released and received by neuron synapses. Dopamine is responsible for regulating one’s motivation for reward [ 2 ]. When comparing the brain of a depressed patient, there are several abnormalities including brain shrinkage (atrophy), a loss of grey matter volume, and reduced functional activity in the hippocampus. There is also a depletion of the neurotransmitters in the central nervous system including serotonin, norepinephrine, or dopamine [ 3 ]. Personality traits such as low self-esteem, a family history of depression, childhood depression, or traumatic life events such as sexual or emotional abuse have also been associated with an increased risk for depression. In addition, individuals ages 18-25 years old, those who identify as two or more races, and women are more prone to depression [ 4 ]. Several forces interact to cause depression including faulty mood regulation by the brain, genetic vulnerability, and stimuli from traumatic events [ 5 ]. As the global coronavirus pandemic took place, depression cases in adults jumped from 8.5% before the pandemic to a staggering 27.8%. Research from the Boston University School of Public Health reveals that elevated depression rates have persisted into 2021, climbing to 32.8%, thus affecting one in three adults [ 6 ]. Depression typically occurs in multiple episodes, with signs and symptoms reoccurring often. Some of these symptoms include feelings of sadness and emptiness, frustration, sleep insomnia, lack of energy, reduced appetite and weight loss, anxiety, slow thinking, trouble concentrating, unexplained physical issues, and suicidal thoughts and actions [ 7 ]. Three of the more common methods used in depression treatment include cognitive behavioral therapy, which is a psychosocial intervention, interpersonal therapy, a form of therapy to improve interpersonal functioning, and psychodynamic therapy, an approach to facilitate a deeper understanding of one's emotions [ 8 ].
The Patient Health Questionnaire-9 (PHQ-9) is a self-administered questionnaire designed to screen, diagnose, and monitor the severity of depression. This assessment was derived from the original PHQ which aimed to address multiple health concerns including depression, panic, anxiety, etc. The PHQ-9 was developed by Spitzer, Williams, and Kroenke under a grant from Pfizer. This self-administered nine-question questionnaire assesses each criterion of depression in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and is commonly administered at therapists’ or doctors’ offices to monitor and evaluates a patient’s mental health [ 9 ].
The objectives of this study were: 1) estimate the impact and severity of both diagnosed and undiagnosed depression in the general US population; 2) explore the demographics of depression based on its common symptoms; 3) interpret PHQ-9 scores to improve accuracy in identifying individuals with depression.
Materials and methods
A cross-sectional study was conducted in July of 2022. Data were collected through an anonymous questionnaire using an online survey platform. A convenience sample of 200 respondents included all adults in the general US population regardless of age, sex, race, or ethnicity. This study was given an exempt determination by our institutional review board (2022-578).
Data collection
The survey consisted of three parts: First, it inquired about participants' demographics including their age, gender, level of education, and income. Then the PHQ-9 assessment with a few follow-up questions regarding their diagnosis of Depression. For each of the nine questions on the Patient Health Questionnaire, the respondent was asked: “Over the last 2 weeks, how often have you been bothered by the following problems?” Each question had only four choices including “Not at all” (0 points), “Several days” (1 point), “More than half the days” (2 points), or “Nearly every day” (3 points). The scores from all nine questions were added together to compute a total score. The interpretation of the depression severity is as follows: 0-4 points indicates none-minimal depression, 5-9 indicates mild depression, 10-14 indicates moderate depression, 15-19 indicates moderate-severe depression and 20-27 indicates severe depression. A few follow-up questions were asked regarding whether the patient had been formally diagnosed with depression, thought of seeing a mental health professional, what prevents them from seeing a mental health professional, and a final open-response question allowing them to express any concerns about their depression that hadn’t previously been expressed.
Statistical analysis
Statistical analysis was performed using JMP version 16 (SAS Institute Inc., Cary, NC, USA). Parametric tests were used for normally distributed variables and non-parametric tests were used for skewed data. Chi-square testing was performed to assess correlation between a high PHQ-9 score and having a formal diagnosis of depression. A p-value of <0.05 was considered statistically significant.
The cohort comprised of 200 individuals with 57.7% females and 42.3% males. The age distribution was 14% between the ages of 18-24, 29% between the ages of 25-24, 32% between 35-44, 10% between 45-54, and 13% of adults over the ages of 54 years old. The median age was 38, with an interquartile range of 30 to 44, and a range from 18-77 years. 31% of respondents’ highest level of education was high school, 28% university, 23% postgraduate, 15% vocational technical college, and 2% middle school. The distribution of race in the US population was: 60% White, 17% Latino, 12% Black, 6% Asian, 3% multiracial, 1% Native American and 1% other. Race was approximately proportional to the US population with 63% of respondents indicating they were White, 12% Black, 9% Hispanic, 7% Asian, 3% multiracial, with 2% preferring not to say and 4% composed of various other ethnicities. The distribution of annual household income was <$25,00 (21%), $25,000-50,000 (21%), $50,000-75,000 (16%), and $75,000-100,000 (15%), and >$100,00 (27%). In terms of marital status, 33% of participants were single, 39% were married, and 16% were living with a partner. Forty-two percent of respondents had no children, 17% had one child, 20% had two children, 12% had three children, and 4% had four children.
How often do you experience little interest or pleasure in socializing?
Only 22.3% indicated that they never experience little interest or pleasure in socializing. 38.3% indicated that they experience this several days, 24.4% indicated more than half the days, and 14.9% every day.
How often do you feel down, depressed, or hopeless?
Only 27.9% indicated that they never feel down, depressed, or hopeless, a majority of 45.3% of respondents on several days, 18.9% on more than half of the days, and 8% feeling this nearly every day.
How often do you have trouble falling asleep, staying asleep, or sleeping?
This question had a relatively even distribution with 37.8% of respondents saying they have trouble falling asleep on several days, 20.4% saying not at all, 20.9% indicating more than half the days, and 20.9% indicating nearly every day.
How often do you feel tired or have little energy?
A majority of 47.3% felt tired/had little energy on several occasions, with 12.4% never/rarely feeling tired, 17.9% more than half of the days and 22.4% nearly every day.
How often do you have a poor appetite or overeating?
Most participants did not seem to have any severe appetite issues with 31.8% indicating no issues, 41.3% indicating some days, 15.4% saying more than half the days and 11.4% indicating nearly every day.
How often do you feel bad about yourself - or that you’re a failure or have let yourself or your family down?
31.8% of participants indicated that they never/rarely feel bad about themselves or a failure to their daily. 41.3% indicated that they feel this on several days, 15.4% on more than half of the days, and 11.4% nearly every day.
How often do you have trouble concentrating on things, such as reading?
37.3% of respondents indicated that they do not have trouble concentrating on tasks such as reading, 39.8% indicating several days, 14.4% on more than half of the days, and 8.4% nearly every day.
How often do you speak so slowly that other people could have noticed. Or the opposite - being so fidgety or restless that you have been moving around a lot more than usual?
55.2% of participants indicated that they do not move too slowly or restlessly. 24.9% indicated these actions on several days, 10.9% indicating more than half the days, and 9% indicating nearly every day.
How often do you have thoughts that you would be better off dead or of hurting yourself in some way?
Of the most severe question asked in the survey, a majority of 65.7% indicated no thoughts of being better off dead or hurting themselves, however 22.4% indicated that they have had these thoughts on several days, 8% on more than half of the days, and a dangerous 4% on nearly every day. This marks the final question of the PHQ-9 Survey.
Additional questions
Interestingly, only 39.4% of respondents have indicated that they have had a formal diagnosis of depression and 60.6% have not. In contrast, 53% of participants have considered seeking help from a mental health professional while 47% have not considered such a course of action. To account for this disparity, a follow-up question asked: “Has anything prevented you from seeking help from a mental health professional?” with the answer choices ranging from “I don’t need it”, “Too busy”, and “Can’t afford it” to “Afraid of stigma”, “Other”, or “None of the above”. The largest proportion of respondents claimed that they did not need it (32.1%) and the second highest proportion chose “None of the above” (23.9%). The final open-ended question had a wide range of responses. Some examples include: “I have been feeling very down and just tired all the time I can get more irritated very easily and I get frustrated I get annoyed easily to where I don’t want to deal with no one”, “I’ve been denied for social security 3 times already”. Notably, many responses called for the need to expand access to mental healthcare and drive down these costs. Some examples include: “Wish there were more access to free mental healthcare”, and “Mental health care should be more accessible in the USA”.
PHQ-9 scores
The distribution of PHQ-9 Scores was skewed with a mean score of 9.74 points. The minimum score reported was 0, with the 25th percentile being 5, the median was 9, the 75th percentile was 13.5, and the maximum score was 26.
A statistical model was created to see whether the PHQ-9 score, age, or gender had an impact or not on whether the respondent had previously been diagnosed with depression. A high PHQ-9 score was significantly associated with a prior diagnosis of depression (P=0.0004). Age, gender, and race were not significant predictors. The adjusted R-Squared value is 0.184, meaning that 18.4% of the variation in a patient’s diagnoses can be explained by the model, indicating a solid statistical model. A separate column was generated analyzing those who had a PHQ-9 score of 10 or greater (moderate-severe depression). Almost half of the cohort (46.8%) screened positive. They were significantly more likely to have a formal diagnosis of depression when compared to those with lower scores (P<0.0001). More concerning was the 31.5% who did not have a formal diagnosis of depression but did have PHQ-9 scores >10 (Figure (Figure1 1 ).

Our survey suggests that Americans continue to face numerous external and internal crises that can lead to negative thoughts, feelings, emotions, and eventually depression. The burdens and costs of having depression are the most severe of any disease (increased medical care use, lower quality of life, and decreased workplace productivity) [ 10 ]. Depression continues to be undiagnosed because its signs and symptoms are misunderstood. As noted, many people are reluctant to act towards seeing a mental health professional due to the stigma attached to this disorder. As of 2020, more than 21 million Americans, almost 8.4%, experienced at least one major depressive episode [ 11 ]. In fact, during the COVID-19 pandemic, depression and anxiety rates increased by more than 25% worldwide, impacting almost every stratum of society, including adolescents [ 12 ], college students [ 13 ], healthcare workers [ 14 ], and physicians [ 15 ]. Millions more will suffer from recurring depression in their lifetime. In addition, children are having an increased pressure for conformity in our modern society, especially in a rapidly evolving digital world. This danger imposes a risk of developing low self-esteem, one of the risk factors for depression. From this survey, it is evident that depression needs to be better identified. In the open-ended responses, many individuals noted that there is a shortage of mental health counseling in their community, that their insurance does not cover it, or they simply can’t access these facilities. However, nearly half of all respondents screened positive for moderate to severe depression.
Limitations
Some racial/ethnic groups such as Hispanics were not as well represented as they should have been. A majority of participants were in the two lower income brackets (less than $25,000 and $25,000-50,000 annual income respectively), with less participation from the middle and upper classes. Additionally, only adults over the age of 18 were surveyed, so the prevalence of undiagnosed depression in teenagers could not be measured. One other factor to note is that many individuals suffering from depression may have declined to respond meaningfully to the survey due to personal issues. One major limitation is much of the survey was multiple choice with only four answer choices. As a result, some respondents may have had to underestimate or overestimate their responses to choose an answer. In the future, more in-depth assessments and surveys within specific demographic groups, such as lesbian, gay, bisexual, transgender, queer and intersex (LGBTQI) may facilitate more targeted and effective treatment.
Conclusions
Our data suggests depression is ongoing, and under-diagnosed. Increasing access to affordable care may be beneficial in diagnosis, treatment, and prevention. Overall, depression continues to be an ongoing problem in America and across the globe, and healthcare access and innovative solutions are imperative for improving our nation’s mental health and quality of life.
Acknowledgments
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. HCA Centralized Algorithms for Research Rules on IRB Exemptions (CARRIE)/ IRB issued approval 2022-578. Based on the information provided and attested as true, the research plan described does not require IRB oversight. This is because the investigators are either a) not engaging in research with human subjects as defined by federal regulations; b) engaging in research with human subjects deemed excluded from IRB oversight per 45CFR46.102(l) OR c) engaging in research with sufficient human subject protections in the design to meet one or more IRB exemption criteria set forth in 45CFR46.104.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.

IMAGES
VIDEO
COMMENTS
The depression process and related brain changes, however, have also been linked to the hyperactivity or dysregulation of the HPA axis [127,130,131,182,212]. One review indicates that a potential underpinning mechanism of depression relates to "HPA axis abnormalities involved in chronic stress" .
Worldwide, the incidence of major depressive disorder (MDD) is increasing annually, resulting in greater economic and social burdens. Moreover, the pathological mechanisms of MDD and the ...
Depression is a prevalent psychiatric disorder that often leads to poor quality of life and impaired functioning. Treatment during the acute phase of a major depressive episode aims to help the patient reach a remission state and eventually return to their baseline level of functioning. Pharmacotherapy, especially selective serotonin reuptake ...
The current speed of progress in depression research is simply remarkable. We have therefore been able to create a second special issue of Molecular Psychiatry, 2020, focused on depression, with ...
Major depression is a common illness that severely limits psychosocial functioning and diminishes quality of life. In 2008, WHO ranked major depression as the third cause of burden of disease worldwide and projected that the disease will rank first by 2030.1 In practice, its detection, diagnosis, and management often pose challenges for clinicians because of its various presentations ...
R. McShaneN Engl J Med 2023;389:1333-1334. Depression can become self-perpetuating as occupational, relationship, and social losses accrue. Sustained remission is achieved in less than half of ...
The causes of depression are manifold and complex. But biologically definable factors are starting to come to light. One theory that is gaining support is that the culprit might be a slowdown in ...
There are two common types of depression. Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.; Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe depression symptoms that last much longer, usually for at least 2 years.
Potential Preventable Burden. Suicide is the second-leading cause of death in individuals aged 10 to 34 years. 2 Eighty-three percent of individuals who die by suicide were seen in primary care in the previous year; 24% had any mental health diagnosis in their medical records in the month prior to death. 47.
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least 2 ...
This study, based on large and representative datasets and a valid and reliable screening tool for the assessment of depression, indicates that the point prevalence of clinically relevant depressive symptoms in Europe from 2013 to 2020 remains relatively stable, with wide variability between countries. These findings could be considered a baseline for monitoring the prevalence of clinically ...
Introduction. Major depressive disorder (MDD) is one of the most prevalent mental disorders worldwide, as well as one of the most disabling. According to the Global Burden of Disease study, depression is the fourth leading cause of disability (measured in disability adjusted life years), and it is expected to be the second by 2020.1 MDD has a greater impact on public health than physical ...
Abstract. One of the most consistent findings in the depression literature is that stressful life events predict the onset and course of depressive episodes. Cognitive and biological responses to life stressors have both been identified, albeit largely independently, as central to understanding the association between stress and depression.
Most of the studies included at least 1,000 people. The depression rate recorded between January and May 2020 — after the COVID-19 outbreak had begun in each country — ranged from 7% to 48% ...
Scientists at Stanford Medicine conducted a study describing a new category of depression — labeled the cognitive biotype — which accounts for 27% of depressed patients and is not effectively treated by commonly prescribed antidepressants. Cognitive tasks showed that these patients have difficulty with the ability to plan ahead, display ...
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest.[1][2] The American Psychiatric Association's Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies the depressive disorders into: ... Research indicates that MBCT is effective in reducing the risk of relapse in ...
Major depressive disorder is a serious medical illness which is responsible for considerable morbidity and disability. Despite decades of research, the neural basis for depression is still incompletely understood. In this review, evidence from neuroimaging, neuropsychiatric and brain stimulations studies are explored to answer the question regarding the localization of depression in the brain ...
Depression: The Latest Research. If you're one of more than 17 million adults or 3.2 million teens in the United States with major depression, you may know that treatment often falls short. The ...
The Role of Social Media Use and Associated Risk and Protective Behaviors on Depression in Youth Adults: A Longitudinal and Network Perspective. International Journal of Mental Health and ...
In addition, Xu Y et al. used the age-period-cohort analytic method and limited their research to the incidence of depression across all areas, leaving unfinished business regarding studies on the ...
The scores from all nine questions were added together to compute a total score. The interpretation of the depression severity is as follows: 0-4 points indicates none-minimal depression, 5-9 indicates mild depression, 10-14 indicates moderate depression, 15-19 indicates moderate-severe depression and 20-27 indicates severe depression.
Study with Quizlet and memorize flashcards containing terms like Psychiatrists and psychologists label behavior as disordered when it is A. aggressive, persistent, and intentional. B. selfish, habitual, and avoidable. C. deviant, distressful, and dysfunctional. D. biologically influenced, unconsciously motivated, and difficult to change., Ongoing patterns of behavior that are different from ...