Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

Trauma informed interventions: A systematic review
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations School of Nursing, The Johns Hopkins University, Baltimore, Maryland, United States of America, Bloomberg School of Public Health, The Johns Hopkins University, Baltimore, Maryland, United States of America
Roles Formal analysis, Writing – original draft, Writing – review & editing
Affiliation School of Nursing, Duke University, Durham, North Carolina, United States of America
Roles Data curation, Writing – original draft, Writing – review & editing
Affiliation School of Public Health, University of Minnesota, Minneapolis, Minnesota, United States of America
Roles Formal analysis, Writing – review & editing
Affiliation School of Nursing, The Johns Hopkins University, Baltimore, Maryland, United States of America
Roles Data curation, Writing – review & editing
Affiliation School of Nursing, Vanderbilt University, Nashville, Tennessee, United States of America
Affiliation Medstar Good Samaritan Hospital, Baltimore, Maryland, United States of America
Roles Data curation, Formal analysis, Writing – original draft, Writing – review & editing
- Hae-Ra Han,
- Hailey N. Miller,
- Manka Nkimbeng,
- Chakra Budhathoki,
- Tanya Mikhael,
- Emerald Rivers,
- Ja’Lynn Gray,
- Kristen Trimble,
- Sotera Chow,
- Patty Wilson

- Published: June 22, 2021
- https://doi.org/10.1371/journal.pone.0252747
- Reader Comments
Health inequities remain a public health concern. Chronic adversity such as discrimination or racism as trauma may perpetuate health inequities in marginalized populations. There is a growing body of the literature on trauma informed and culturally competent care as essential elements of promoting health equity, yet no prior review has systematically addressed trauma informed interventions. The purpose of this study was to appraise the types, setting, scope, and delivery of trauma informed interventions and associated outcomes.
We performed database searches— PubMed, Embase, CINAHL, SCOPUS and PsycINFO—to identify quantitative studies published in English before June 2019. Thirty-two unique studies with one companion article met the eligibility criteria.
More than half of the 32 studies were randomized controlled trials (n = 19). Thirteen studies were conducted in the United States. Child abuse, domestic violence, or sexual assault were the most common types of trauma addressed (n = 16). While the interventions were largely focused on reducing symptoms of post-traumatic stress disorder (PTSD) (n = 23), depression (n = 16), or anxiety (n = 10), trauma informed interventions were mostly delivered in an outpatient setting (n = 20) by medical professionals (n = 21). Two most frequently used interventions were eye movement desensitization and reprocessing (n = 6) and cognitive behavioral therapy (n = 5). Intervention fidelity was addressed in 16 studies. Trauma informed interventions significantly reduced PTSD symptoms in 11 of 23 studies. Fifteen studies found improvements in three main psychological outcomes including PTSD symptoms (11 of 23), depression (9 of 16), and anxiety (5 of 10). Cognitive behavioral therapy consistently improved a wide range of outcomes including depression, anxiety, emotional dysregulation, interpersonal problems, and risky behaviors (n = 5).
Conclusions
There is inconsistent evidence to support trauma informed interventions as an effective approach for psychological outcomes. Future trauma informed intervention should be expanded in scope to address a wide range of trauma types such as racism and discrimination. Additionally, a wider range of trauma outcomes should be studied.
Citation: Han H-R, Miller HN, Nkimbeng M, Budhathoki C, Mikhael T, Rivers E, et al. (2021) Trauma informed interventions: A systematic review. PLoS ONE 16(6): e0252747. https://doi.org/10.1371/journal.pone.0252747
Editor: Vedat Sar, Koc University School of Medicine, TURKEY
Received: July 1, 2020; Accepted: May 23, 2021; Published: June 22, 2021
Copyright: © 2021 Han et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: This is a systematic review. All relevant data were extracted from the published studies included in the review.
Funding: This study was supported, in part, by a grant from the Johns Hopkins Provost Discovery Award (HRH). Additional funding was received from the National Center for Advancing Translational Sciences (UL1TR003098, HRH), National Institute of Nursing Research (P30NR018093, HRH; T32NR012704, HM), National Institute on Aging (R01AG062649, HRH; F31AG057166, MN), Robert Wood Johnson Foundation Health Policy Research Scholar program (MN), and Substance Abuse and Mental Health Services Administration (5T06SM060559‐ 07, PW). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There was no additional external funding received for this study.
Competing interests: The authors have declared that no competing interests exist.
Despite the United States’ commitment to health equity, health inequities remain a pressing concern among some of the nation’s marginalized populations, such as racial/ethnic or gender minority populations. For example, according to the 2016 National Health and Nutrition Examination Survey (NHANES), 29.1% of Mexican Americans and 24.3% of African Americans with diabetes had hemoglobin A1C greater than 9% (the gold standard of glucose control with levels ≤ 7% deemed adequate), compared to 11% in non-Hispanic whites [ 1 ]. The 2016 survey also revealed that 40.9% and 41.5% of Mexican Americans and African Americans with hypertension, respectively, had their blood pressure under control, compared to 51.7% in non-Hispanic whites. In 2014, 83% of all new diagnoses of HIV infection in the United States occurred among gay, bisexual, and other men who have sex with men, with African American men having the highest rates [ 2 ].
Several factors have been discussed as root causes of health inequities. For example, Farmer et al. [ 3 ] noted structural violence—the disadvantage and suffering that stems from the creation and perpetuation of structures, policies and institutional practices that are innately unjust—as a major determinant of health inequities. According to Farmer et al., because systemic exclusion and disadvantage are built into everyday social patterns and institutional processes, structural violence creates the conditions which sustain the proliferation of health and social inequities. For example, a recent analysis [ 4 ] using a sample including 4,515 National Health and Nutrition Examination Survey participants between 35 and 64 years of age revealed that black men and women had fewer years of education, were less likely to have health insurance, and had higher allostatic load (i.e., accumulation of physiological perturbations as a result of repeated or chronic stressors such as daily racial discrimination) compared to white men (2.5 vs 2.1, p <.01) and women (2.6 vs 1.9, p <.01). In the analysis, allostatic load burden was associated with higher cardiovascular and diabetes-related mortality among blacks, independent of socioeconomic status and health behaviors.
Browne et al. [ 5 ] identified essential elements of promoting health equity in marginalized populations such as trauma-informed and culturally competent care. In particular, trauma-informed care is increasingly getting closer attention and has been studied in a variety of contexts such as addiction treatment [ 6 – 8 ] and inpatient psychiatric care [ 9 ]. While there is a growing body of the literature on trauma-informed care, no prior review has systematically addressed trauma-informed interventions; one published review of literature [ 10 ] limited its scope to trauma survivors in physical healthcare settings. As such, the purpose of this paper is to conduct a systematic review and synthesize evidence on trauma-informed interventions.
For the purpose of this paper, we defined trauma as physical and psychological experiences that are distressing, emotionally painful, and stressful and can result from “an event, series of events, or set of circumstances” such as a natural disaster, physical or sexual abuse, or chronic adversity (e.g., discrimination, racism, oppression, poverty) [ 11 , 12 ]. We aim to: 1) describe the types, setting, scope, and delivery of trauma informed interventions and 2) evaluate the study findings on outcomes in association with trauma informed interventions in order to identify gaps and areas for future research.
Five electronic databases—PubMed, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), SCOPUS and PsycINFO—were searched from the inception of the databases to identify relevant quantitative studies published in English. The initial literature search was conducted in January 2018 and updated in June 2019 using the same search strategy.
Review design
We conducted a systematic review of quantitative evidence to evaluate the effects of trauma informed interventions. Due to heterogeneity relative to study outcomes, designs, and statistical analyses approaches among the included studies, we qualitatively synthesized the study findings. Three trained research assistants extracted study data. Specifically, we used the PICO framework to extract and organize key study information. The PICO framework offers a structure to address the following questions for study evidence [ 13 ]: Patient problem or population (i.e., patient characteristics or condition); Intervention (type of intervention tested or implemented); Comparison or control (comparison treatment or control condition, if any), and Outcome (effects resulting from the intervention).
Eligibility
Inclusion criteria..
Articles were screened for their relevance to the purpose of the review. Articles were included in this review if the study was: about trauma informed approach (i.e., an approach to address the needs of people who have experienced trauma) or an aspect of this approach, published in English language and involved participants who were 18 years and older. Also, only quantitative studies conducted within a primary care or community setting were included.
Exclusion criteria.
Exclusion criteria were: studies in or with military populations, refugee or war-related trauma populations, studies with mental health experts and clinicians as research subjects or studies of incarcerated and inpatient populations. Conference abstracts that had limited information on study characteristics were also excluded.
Search strategy and selection of studies
Search strategy..
Following consultation with a health science librarian, peer-reviewed articles were searched in PubMed, Embase, CINAHL, SCOPUS and PsycINFO using MeSH and Boolean search techniques. Search terms included: "trauma focused" OR "trauma-focused" OR "trauma informed" OR "trauma-informed." We also searched for the term trauma within three words of informed or focus ((trauma W/3 informed) OR (trauma W/3 focused), or (traumaN3 (focused OR informed)). Detailed search terms for each database are provided in Appendix 1.
Study selection.
The initial electronic search yielded 7,760 references and the follow-up search yielded 5,207 which were all imported into the Covidence software for screening [ 14 ]. Screening of the references was conducted by 2 independent reviewers and disagreements were resolved through consensus. There were 4,103 duplicates removed from the imported articles and 8,864 studies were forwarded to the title and abstract screening stage. Eight thousand five hundred and twenty-one studies were excluded because they were irrelevant. Three hundred and forty-three abstracts were identified to be read fully. Following this, 311 articles were excluded for focusing on other psychological conditions (n = 120), were non-experimental studies (n = 78) and were in inpatient or incarcerated populations (n = 46). One additional companion article was identified during full text review. Therefore, thirty-three articles met the inclusion criteria and are reported in this review. Fig 1 provides details of the selection process and identifies the reasons why articles were excluded at each stage.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0252747.g001
Quality assessment
We used the Joanna Briggs Institute quality appraisal tools [ 15 ] for randomized controlled trials (RCTs), quasi-experimental studies, and retrospective studies to assess the rigor of each study included in this review. The Joanna Briggs Institute quality appraisal tools [ 15 ] include items asking about methodological elements that are critical to the rigor of each type of study designs. In particular, one of the items for RCTs addresses participant blinding to treatment assignment. Due to the nature of trauma-informed interventions included in our review, it was decided that participant blinding is not relevant and hence was removed from the appraisal list for RCTs. No studies were excluded on the basis of the quality assessment. The quality assessment process was conducted independently by two raters. Inter-rater agreement rates ranged from 56% to 100% with the resulting statistic indicating substantial agreement (average inter-rater agreement rate = 77%). Discrepancies between raters were resolved via inter-rater discussion.
Overview of studies
Table 1 summarizes the main characteristics of the 32 unique studies included in the review, with one companion article [ 16 ] for a study which was later reported with a more thorough examination of findings [ 17 ] totaling 33 articles. More than half (n = 19) of the 32 studies were RCTs [ 17 – 35 ] whereas twelve studies were quasi-experimental [ 36 – 47 ] and one was retrospective study [ 48 ]. Thirteen studies were conducted in the U.S. [ 17 – 19 , 22 , 26 , 27 , 29 , 35 , 39 – 41 , 45 , 47 ]; five in the Netherlands [ 30 , 31 , 33 , 38 , 48 ]; three in Canada [ 23 , 25 , 46 ]; two in Australia [ 21 , 24 ]; two in the United Kingdom [ 36 , 44 ]; two in Sweden [ 42 , 43 ]; on study in Chile [ 20 ]; Iran [ 32 ]; Haiti [ 37 ]; South Africa [ 34 ]; and Germany [ 28 ]. Fourteen of the studies only included females in their sample [ 18 , 20 , 21 , 23 – 25 , 27 , 28 , 38 – 41 , 45 , 48 ]. The average sample size was 78 participants, with a range from 10 participants [ 38 ] to 297 participants [ 48 ]. Of the studies included, 67% had a sample size above 50 [ 18 – 22 , 26 , 29 – 34 , 36 , 37 , 39 – 42 , 46 – 48 ].
https://doi.org/10.1371/journal.pone.0252747.t001
The studies included in this review recruited their study populations largely based on the type of trauma they were aiming to address, such as individuals that experienced interpersonal traumatic event such as child abuse, sexual assault, or domestic violence [ 16 – 18 , 20 – 22 , 24 – 26 , 35 , 40 – 43 , 45 , 46 ], individuals with substance abuse disorders [ 19 , 47 , 48 ], couples experiencing clinically significant marital issues [ 23 ], individuals with limb amputations [ 38 ], dental phobia [ 28 ], or fire service personnel suffering from post-traumatic stress disorder [ 44 ]. Trauma was self-reported in eight articles [ 16 , 17 , 20 , 22 , 26 , 34 , 35 , 47 ]. In contrast, nine studies clearly identified a measurement of trauma; the Trauma History Questionnaire [ 19 , 45 ], the Childhood Trauma Questionnaire [ 23 , 25 ], the Childhood Maltreatment Interview Schedule [ 23 ], the Revised Conflict Tactics Scale adapted for sex work [ 39 ], the Traumatic Events Screening Instrument for Adults [ 27 ], the Life Events Checklist [ 46 ], and the Adverse Childhood Experiences [ 18 ]. Two studies used a clinical tool (e.g. eye movement desensitization and reprocessing [ 38 ] and Diagnostic and Statistical Manual of Mental Disorders, 4 th edition [ 41 ] to identify or diagnose trauma. Fifteen studies did not include direct measurements for trauma [ 21 , 24 , 28 – 33 , 36 , 37 , 40 , 42 – 44 , 48 ].
Quality ratings
Tables 2 – 4 shows final scores of quality assessment. Quality of the 32 unique studies included in this review varied across individual studies. Twelve of 19 RCTs included in the review were of high quality (i.e., 9 to 11) [ 17 , 18 , 20 , 21 , 24 , 26 , 28 , 29 , 31 , 33 – 35 ] and six were of medium quality (i.e., 5 to 8) [ 19 , 22 , 23 , 25 , 27 , 30 ]. One study scored 4 of 12 [ 32 ]. The low rating study [ 32 ] lacked relevant information to adequately score its methodological rigor. Most RCTs clearly described randomization, group equivalence at baseline, rates and reasons for attrition, study outcomes, and analysis. Blinding of outcomes assessors to treatment assignment was used and described in several RCTs [ 17 , 20 , 21 , 24 , 27 , 35 ], whereas blinding of those delivering treatment was discussed clearly in only one study [ 25 ]. The majority of the quasi-experimental studies were of high quality (i.e., 7 or higher), except two, which scored 2 of 9 [ 37 ] and 6 of 9 [ 39 ], respectively. Six of twelve quasi-experimental studies [ 36 , 41 – 44 , 47 ] had a comparison group to strengthen internal validity of causal inferences by comparing intervention and control groups. Some of these studies, however, noted differences in baseline assessments between groups [ 36 , 43 , 44 ]. Finally, one retrospective study [ 48 ] scored 11 of 11 and hence was rated as high quality.
https://doi.org/10.1371/journal.pone.0252747.t002
https://doi.org/10.1371/journal.pone.0252747.t003
https://doi.org/10.1371/journal.pone.0252747.t004
Characteristics of trauma-informed interventions
Type of intervention..
Table 5 details the trauma informed intervention characteristics included in this review. The two most frequently used interventions were eye movement desensitization and reprocessing (EMDR) [ 28 , 30 , 31 , 33 , 36 , 38 ]—a multi-phase intervention using bilateral stimulation, such as left-to-right eyes movements or hand tapping, to desensitize individuals to a traumatic memory or image—and trauma-focused cognitive behavioral therapy or cognitive behavioral therapy (CBT) [ 26 , 27 , 32 , 46 , 48 ]—a psychological approach to introduce emotional regulation and coping strategies (e.g., deep muscle relaxation, yoga, thought discovery and breathing techniques) to deal with negative feelings and behaviors surrounding a trauma of interest [ 32 , 48 ]. The implementation of CBT varied on the trauma of interest. Other studies implemented interventions using general trauma focused therapy [ 22 , 43 ], emotion focused therapy [ 23 , 25 ], stress reduction programs [ 17 ], cognitive processing therapy [ 24 ], brief electric psychotherapy [ 31 ], present focused group therapy [ 26 ], compassion focused therapy [ 44 ], prolonged exposure [ 45 ], stress inoculation training [ 45 ], psychodynamic therapy [ 45 ], and visual schema displacement therapy [ 30 ]. A number of studies included more than one of these therapies [ 13 , 26 , 30 , 31 , 33 , 36 , 45 ].
https://doi.org/10.1371/journal.pone.0252747.t005
Setting, scope, and delivery of intervention.
Twenty of the interventions were identified to occur in an outpatient clinic/setting [ 19 – 21 , 24 , 25 , 27 – 29 , 31 – 34 , 36 , 39 , 40 , 42 , 43 , 46 – 48 ]. Four of the studies took place in a research lab or office [ 23 , 26 , 41 , 45 ], one study occurred in the community [ 17 ], and one study implemented therapy in three locations, two of which were outpatient and one of which was a residential treatment center [ 47 ]. Lastly, one study occurred in internally displaced people’s camps within a metropolitan area in Haiti [ 37 ]. The remaining studies did not identify a specific setting [ 22 , 35 , 38 , 44 ].
The interventions ranged in length and time, but most often occurred weekly. The longest intervention was done by Lundqvist and colleagues [ 43 ], which lasted a total length of 2-years and included 46 sessions. Several other studies included 20 sessions or more [ 18 , 22 , 23 , 25 , 26 ]. The interventions were most commonly delivered by medical professionals, including but not limited to: psychologists or psychiatrists, therapists, social workers, mental health clinicians and physicians [ 16 , 17 , 20 – 29 , 33 , 36 , 38 , 39 , 41 , 44 – 47 ]. The articles frequently noted that the interventionists were masters-level-prepared or higher in their profession [ 21 , 23 , 25 – 27 , 33 , 40 , 47 ]. In addition to standard education and licensure, many of the professionals implementing the interventions were required to obtain further training in the therapy of interest [ 23 – 25 , 27 – 30 , 33 , 36 , 38 – 40 , 46 , 47 ]. Two studies were identified to be delivered by lay persons [ 34 , 37 ].
Fidelity was addressed in 16 of the included articles [ 16 , 19 , 21 , 23 , 24 , 26 – 30 , 33 – 35 , 45 – 47 ]. The manner in which fidelity was addressed varied by study. Videotaping or audiotaping therapy sessions [ 21 , 23 , 24 , 28 – 30 , 33 , 35 ] were most common, followed by deploying regular supervision of the therapy sessions [ 21 , 23 , 27 , 29 , 33 , 46 ], using a training manual or intervention protocols [ 19 , 21 , 33 , 46 ], or having individuals unaffiliated with the study or blind to the intervention rate sessions [ 21 , 26 , 28 , 35 ]. Additionally, three articles utilized fidelity checks/checklists to ensure components of the intervention were addressed [ 16 , 30 , 47 ] or had patients and/or therapists rate therapy sessions [ 26 , 34 , 45 ]. Finally, one study had quality assurance worksheets completed after each session that were later reviewed by the study coordinator [ 34 ].
Effects of trauma-informed interventions
Trauma-informed interventions were tested to improve several psychological outcomes, such as post-traumatic stress disorder (PTSD), depression, and anxiety. The most frequently assessed psychological outcome was PTSD, which was examined in 23 out of the 32 studies [ 17 , 20 – 27 , 31 , 33 , 35 – 39 , 41 , 42 , 44 – 48 ]. Among the studies that assessed PTSD as an outcome, 11 found significant reductions in PTSD symptoms and severity following the trauma-informed intervention [ 17 , 20 , 21 , 24 , 26 , 28 , 34 , 42 , 45 – 47 ], however, one of these studies, which utilized outpatient psychoeducation, did not find significant differences in reduction between the intervention and control group [ 20 ]. Trauma-informed interventions that were associated with a significant reduction in PTSD were a mindfulness-based stress reduction program [ 16 ], two therapies using the Trauma Recovery and Empowerment Model (TREM) [ 47 ], CBT [ 26 , 46 ], EMDR [ 28 ], general trauma-focused therapy [ 42 ], psychodynamic therapy [ 45 ], stress inoculation therapy [ 45 ], present-focused therapy [ 26 ], and cognitive processing therapy [ 24 ]. In addition, an intervention designed to reduce stress and improve HIV care engagement improved PTSD symptoms; however, this intervention was not intended to treat PTSD [ 34 ].
Other commonly assessed psychological symptoms, including depression and anxiety, were examined in 16 [ 17 – 21 , 24 – 26 , 29 , 31 , 32 , 35 , 40 , 44 , 47 , 48 ] and 10 [ 21 , 24 , 25 , 28 , 29 , 35 , 36 , 44 , 47 , 48 ] studies, respectively. Among these, trauma-informed interventions were associated with decreased or improved depressive symptoms in 9 studies [ 17 , 18 , 20 , 21 , 24 , 32 , 35 , 47 , 48 ] and decreased or improved anxiety in 5 studies [ 21 , 28 , 35 , 47 , 48 ]. For example, Vitriol and colleagues found that outpatient psychoeducation resulted in improved depressive symptoms in women with severe depression and childhood trauma [ 20 ]. Similarly, Kelly and colleagues found that female survivors of interpersonal violence experienced a significantly greater reduction of depressive symptoms in the intervention group (mindfulness-based stress reduction) compared to the control group [ 16 , 17 ]. Other therapies that resulted in improved depressive symptoms were TREM [ 47 ], prolonged exposure therapy [ 21 ], CBT [ 32 , 46 ], psychoeducational cognitive restructuring [ 35 ], and financial empowerment education [ 18 ]. Cognitive processing therapy similarly resulted in large reductions in depression symptoms, however this reduction was also observed in the control group [ 24 ]. The same studies showed that TREM [ 47 ], prolonged exposure therapy [ 21 ], CBT [ 48 ], and psychoeducational cognitive restructuring [ 35 ] were associated with improved anxiety. Lastly, in a separate study than the one highlighted above, EMDR was associated with improved anxiety [ 28 ].
A select number of the studies found associations between trauma-informed interventions and other psychological outcomes such as attachment anxiety, attachment avoidance, psychiatric symptoms or dental distress. For example, the trauma-informed mindfulness-based reduction program implemented by Kelly and colleagues was associated with a greater decrease in anxious attachment, measured by the Relationship Structures Questionnaire, compared to the waitlist group [ 17 ]. Similarly, Masin-Moyer and colleagues found that TREM and an attachment-informed TREM (ATREM) were associated with significant reductions in group attachment anxiety, group attachment avoidance, and psychological distress in women with a history of interpersonal trauma [ 47 ]. Additionally, individuals in an outpatient substance abuse treatment program, consisting of psychoeducational seminars and trauma-informed addiction treatment, experienced significantly better outcomes of psychiatric severity, measured by the Global Appraisal of Individual Needs scale, compared to a control treatment group [ 19 ]. Doering and colleagues found that EMDR, compared to the control group, was associated with significantly greater improvement in dental stress, anxiety and fear in patients with dental-phobia [ 28 ].
There was a series of interpersonal, emotional and behavioral outcomes assessed in the included studies. For example, adult females that were sexually abused in childhood experienced a significant improvement in social interaction and social adjustment after receiving trauma focused group therapy [ 43 ]. Similarly, Dalton and colleagues found that couples that received emotion focused therapy experienced a significant reduction in relationship distress [ 23 ] and MacIntosh and colleagues found that individuals that received CBT reported lower interpersonal problems post-treatment [ 46 ]. Trauma-based interventions were also associated with emotional outcomes. Visual schema displacement therapy and EMDR both were superior to the control treatment in reducing emotional disturbance and vividness of negative memories [ 30 ]. In a separate study, CBT was found to reduce levels of emotional dysregulation in individuals that experienced childhood sexual abuse [ 46 ]. Lastly, trauma-informed interventions were associated with behavioral outcomes, including HIV risk reduction [ 26 ], decreased days of alcohol use [ 27 ], and improvements in avoidance of client condom negotiations, frequency of sex trade under influence of drugs or alcohol, and use of intimate partner violence support [ 40 ]. Interventions that were associated with these behavioral outcomes included trauma focused and present focused group therapy [ 26 ], CBT [ 27 ], and a trauma-informed support, validation, and safety-promotion dialogue intervention [ 40 ].
Publication bias
We analyzed three sets of outcome variables for publication bias: PTSD, depression, and anxiety. Based on Begg and Mazumdar test, there was no evidence of publication bias for PTSD (z = 1.55, p = 0.121) and anxiety (z = 0.29, p = 0.769). However, there was some evidence of publication bias for depression (z = 5.19, p<.001). The statistically significant publication bias for depression appears to be mainly due to large effect sizes in Nixon [ 24 ] and Bowland [ 35 ].
According to our database search, this is the first systematic review to critically appraise trauma-informed interventions using a comprehensive definition of trauma. In particular, our definition encompassed both physical and psychological experiences resulting from various circumstances including chronic adversity. Overall, there was inconsistent evidence to suggest trauma informed interventions in addressing psychological outcomes. We found that trauma-informed interventions were effective in improving PTSD [ 17 , 20 , 21 , 24 , 26 , 28 , 34 , 42 , 45 – 47 ] and anxiety [ 21 , 28 , 35 , 47 , 48 ] in less than half of the studies where these outcomes were included. We also found that depression was improved in less than about two thirds of the studies where the outcome was included [ 17 , 18 , 20 , 21 , 24 , 32 , 35 , 47 , 48 ]. Although limited in the number of published studies included this review, available evidence consistently supported trauma-informed interventions in addressing interpersonal [ 23 , 43 , 46 ], emotional [ 30 , 46 ], and behavioral outcomes [ 26 , 27 , 40 ].
Effective trauma informed intervention models used in the studies varied, encompassing CBT, EMDR, or other cognitively oriented approaches such as mindfulness exercises [ 16 , 24 , 26 , 28 , 32 , 35 , 45 , 46 , 48 ]. In particular, CBT was noted as an effective trauma informed intervention strategy which successfully led to improvements in a wide range of outcomes such as depression [ 32 , 48 ], anxiety [ 48 ], emotional dysregulation [ 46 ], interpersonal problems [ 23 , 46 ], and risky behaviors (e.g., days of alcohol use) [ 27 ]. While the majority of the studies included in the review were focused on interpersonal trauma such as child abuse, sexual assault, or domestic violence [ 16 – 18 , 20 – 22 , 24 – 26 , 35 , 40 – 43 , 45 , 46 ], growing evidence demonstrates perceived discrimination and racism as significant psychological trauma and as underlying factors in inflammatory-based chronic diseases such as cardiovascular disease or diabetes [ 4 ]. Future trauma informed interventions should consider a wide-spectrum of trauma types, such as racism and discrimination, by which racial/ethnic minorities are disproportionately affected from [ 49 ].
While the majority of the trauma informed interventions were delivered by specialized medical professionals trained in the therapy [ 16 , 17 , 20 – 29 , 33 , 36 , 38 – 41 , 44 – 47 ], several of the articles lacked full descriptions of interventionist training and fidelity monitoring [ 20 , 22 , 25 , 36 , 38 – 41 , 44 ]. Two studies were identified to be delivered by lay persons [ 34 , 37 ]. There is sufficient evidence to suggest that lay persons, upon training, can successfully cover a wide scope of work and produce the full impact of community-based intervention approaches [ 50 ]. Given such, there is a strong need for trauma informed intervention studies to clearly elaborate the contents and processes of lay person training such as competency evaluation and supervision to optimize the use of this approach.
There are methodological issues to be taken into consideration when interpreting the findings in this review. While twenty-three of 32 studies were of high quality [ 17 , 18 , 20 , 21 , 24 , 26 , 28 , 29 , 31 , 33 – 36 , 38 , 40 – 48 ], some studies lacked methodological rigor, which might have led to false negative results (no effects of trauma informed interventions). For example, about one-third (31%) had a sample size less than 50 [ 17 , 23 – 25 , 27 , 28 , 35 , 38 , 43 , 45 ]. In addition, half of the quasi-experimental studies [ 37 – 40 , 45 , 46 ] did not have a comparison group or when they had one, group differences were noted in baseline assessments [ 36 , 43 , 44 ]. In several studies, therapists took on both traditional treatment and research responsibilities (e.g., delivery of the intervention) [ 20 , 25 , 29 , 32 , 33 , 36 , 40 , 46 , 47 ], yet blinding of those delivering treatment was discussed clearly in only one study [ 25 ]. This dual role is likely to have led to the disclosure of group allocation, hence, threatening the internal validity of the results. Future studies should address these issues by calculating proper sample size a priori, using a comparison group, and concealing group assignments.
Review limitations
Several limitations of this review should be noted. First, by using narrowly defined search terms, it is possible that we did not extract all relevant articles in the existing literature. However, to avoid this, we conducted a systematic electronic search using a comprehensive list of MeSH terms, as well as similar keywords, with consultation from an experienced health science librarian. Additionally, we hand searched our reference collections, Second, the trauma informed interventions included in this review were implemented to predominantly address trauma related to sexual or physical abuse among women. Thus, our findings may not be applicable to trauma related to other types of incidence such as chronic adversity (e.g., racism or discrimination). Likewise, there were insufficient studies addressing a wider range of trauma impacts such as emotion regulation, dissociation, revictimization, non-suicidal self-injury or suicidal attempts, or post-traumatic growth. Future research is warranted to address these broader impacts of trauma. We included only articles written in English; therefore, we limited the generalizability of the findings concerning studies published in non-English languages. Finally, we used arbitrary cutoff scores to categorize studies as low, medium, and high quality (quality ratings of 0-4, 5-8, and 9+ for RCTs and 0-3, 4-6, 7+ for quasi-experimental studies, respectively). Using this approach, each quality-rating item was equally weighted. However, certain factors (e.g., randomization method) may contribute to the study quality more so than others.
Our review of 33 articles shows that there is inconsistent evidence to support trauma informed interventions as an effective intervention approach for psychological outcomes (e.g., PTSD, depression, and anxiety). With growing evidence in health disparities, adopting trauma informed approaches is a growing trend. Our findings suggest the need for more rigorous and continued evaluations of the trauma informed intervention approach and for a wide range of trauma types and populations.
Supporting information
S1 checklist..
https://doi.org/10.1371/journal.pone.0252747.s001
S1 Appendix. Search strategies.
https://doi.org/10.1371/journal.pone.0252747.s002
Acknowledgments
We would like to express our appreciation to a medical librarian, Stella Seal for her assistance with article search. Both Kristen Trimble and Sotera Chow were students in the Masters Entry into Nursing program and Hailey Miller and Manka Nkimbeng were pre-doctoral fellows at The Johns Hopkins University when this work was initiated.
- 1. Health disparities data. 2020 May 28 [cited 28 May 2020]. In healthypeople.gov [Internet]. Available from: https://www.healthypeople.gov/2020/data-search/health-disparities-data/health-disparities-widget .
- 2. HIV and AIDS. 2018 April [cited 28 May, 2020]. In: Agency for Healthcare Research and Quality [Internet]. Available from: https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/effectivetreatment/hiv.html .
- 3. Farmer P, Kim YJ, Kleinman A, Basilico M. Introduction: A biosocial approach to global health. In: Farmer P, Kim YJ, Kleinman A, Basilico M, editor. Reimagining global health: An introduction. Berkeley and Los Angeles, CA: University of California Press; 2013. p. 1–14.
- View Article
- PubMed/NCBI
- Google Scholar
- 11. National Institute of Mental Health. Helping children and adolescents cope with violence and disasters: What parents can do. U.S. Department of Health and Human Services; 2013.
- 12. Trauma and violence. 2019 [Last updated on August 2]. [Internet]. Available from: https://www.samhsa.gov/trauma-violence .
- 13. Evidence-based practice in health. 2020 Dec 21. [cited 21 December 2020]. [Internet]. Available from https://canberra.libguides.com/c.php?g=599346&p=4149722#s-lg-box-12888072 .
- 14. Covidence systematic review software, Veritas Health Innovation. 2019 [Last updated on February 4]. [Internet]. Available at: https://www.covidence.org/ .
- 15. Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: Systematic reviews of effectiveness. In: Aromataris E MZ, editor. Joanna Briggs Institute Reviewer’s Manual . The Joanna Briggs Institute; 2017.
- Open access
- Published: 14 September 2022
Trauma-informed care in the UK: where are we? A qualitative study of health policies and professional perspectives
- Elizabeth Emsley 1 ,
- Joshua Smith 1 ,
- David Martin 2 &
- Natalia V. Lewis 3
BMC Health Services Research volume 22 , Article number: 1164 ( 2022 ) Cite this article
13k Accesses
9 Citations
15 Altmetric
Metrics details
Trauma-informed (TI) approach is a framework for a system change intervention that transforms the organizational culture and practices to address the high prevalence and impact of trauma on patients and healthcare professionals, and prevents re-traumatization in healthcare services. Review of TI approaches in primary and community mental healthcare identified limited evidence for its effectiveness in the UK, however it is endorsed in various policies. This study aimed to investigate the UK-specific context through exploring how TI approaches are represented in health policies, and how they are understood and implemented by policy makers and healthcare professionals.
A qualitative study comprising of a document analysis of UK health policies followed by semi-structured interviews with key informants with direct experience of developing and implementing TI approaches. We used the Ready Extract Analyse Distil (READ) approach to guide policy document review, and the framework method to analyse data.
We analysed 24 documents and interviewed 11 professionals from healthcare organizations and local authorities. TI approach was included in national, regional and local policies, however, there was no UK- or NHS-wide strategy or legislation, nor funding commitment. Although documents and interviews provided differing interpretations of TI care, they were aligned in describing the integration of TI principles at the system level, contextual tailoring to each organization, and addressing varied challenges within health systems. TI care in the UK has had piecemeal implementation, with a nation-wide strategy and leadership visible in Scotland and Wales and more disjointed implementation in England. Professionals wanted enhanced coordination between organizations and regions. We identified factors affecting implementation of TI approaches at the level of organization (leadership, service user involvement, organizational culture, resource allocation, competing priorities) and wider context (government support, funding). Professionals had conflicting views on the future of TI approaches, however all agreed that government backing is essential for implementing policies into practice.
Conclusions
A coordinated, more centralized strategy and provision for TI healthcare, increased funding for evaluation, and education through professional networks about evidence-based TI health systems can contribute towards evidence-informed policies and implementation of TI approaches in the UK.
Peer Review reports
Individual, interpersonal and collective trauma is a highly prevalent and costly public health problem [ 1 ]. The WHO World Mental Health Survey identified that 70% of participants had experienced lifetime traumas, including physical violence, intimate partner sexual violence, and trauma related to war [ 2 ]. People experiencing socio-economic disadvantage, women, minoritized ethnic groups, and the LGBTQ + community are disproportionally affected by violence and trauma [ 3 , 4 ]. Adverse childhood experiences (ACEs) are stressful or traumatic events that occur during childhood or adolescence [ 5 ]. In England, a household survey found that nearly half of adults had experienced at least one ACE, including childhood sexual, physical or verbal abuse, as well as household domestic violence and abuse (DVA) [ 6 ]. DVA is considered to be a chronic and cumulative cause of complex trauma [ 7 ]. Up to 29% women and 13% men have experienced DVA in their lifetime, at a cost of £14 billion a year to the UK economy [ 7 , 8 , 9 ].
Cumulative trauma across the lifespan is associated with multiple health consequences [ 10 ]. The links between cumulative adversity from ACEs, DVA and other traumatic experiences are explained within the ecobiodevelopmental framework and the concept of toxic stress [ 11 ]. In a systematic review and meta-analysis of 37 observational studies of health behaviours and adult disease, patients with four or more ACEs were at higher risk of a range of poorer health outcomes including cardiovascular disease and mental ill health, versus those with no ACEs history [ 12 ]. Individuals and families who have experienced violence and trauma seek support from healthcare and other services for the physical, psychological and socioeconomic consequences of trauma [ 1 , 13 ]. In the household survey in England and Wales, adults who had experienced four ACEs were twice as likely to attend their general practice repeatedly, compared with those with no ACEs history, and incidence of health service use rose as the ACEs experiences increased [ 14 ]. In a systematic review 47% of patients in mental health services had experienced physical abuse and 37% had experienced sexual abuse [ 15 ].
If the high prevalence and negative impacts of trauma are not recognised and addressed in healthcare services, there may be negative consequences for patients and healthcare professionals. Patients may not disclose trauma or recognise the impact of trauma on their health [ 16 ]. Patients may also be at risk of re-triggering and re-traumatization, for example by the removal of choice regarding treatment, judgemental responses following a disclosure of abuse, seclusion and restraint [ 17 , 18 , 19 ]. Re-traumatization within health services can affect both patients and members of staff, with the latter experiencing vicarious trauma [ 20 ]. The resulting chronic stress may impact on staff members’ ability to empathise and support others [ 21 ]. Many healthcare staff themselves have lived experience of trauma. A recent systematic review of healthcare professionals’ own experience of DVA, reported a pooled lifetime prevalence of 31.3% (95% CI [24.7%, 38.7%] [ 22 ].
Over last 20 years, several frameworks for a trauma-informed (TI) approach at the health systems level have been developed [ 13 , 17 , 23 , 24 , 25 , 26 , 27 , 28 ]. These frameworks aim to prevent re-traumatization in healthcare services and mitigate the high prevalence and negative effects of violence and trauma on patients and healthcare professionals. A TI approach (synonyms TI care, TI service system) starts from the assumption that every patient and healthcare professional could potentially have been affected by trauma [ 13 ]. By realising and recognising these experiences and their impacts, we can respond by providing services in a trauma-informed way to improve healthcare experience and outcomes for both patients and staff. The process of becoming a TI system is guided by key principles of safety, trust, peer support, collaboration, empowerment and cultural sensitivity [ 13 ]. The most cited frameworks for a system-level TI approach are those by Harris and Fallot [ 29 ], and the US Substance Abuse and Mental Health Services Administration (SAMHSA) [ 13 ]. These frameworks highlight that it is necessary to, firstly, change organizational culture and environments (organizational domain) and then change clinical practices (clinical domain) by incorporating the four TI assumptions and six TI principles throughout the ten implementation domains within a health system [ 13 ] . Other authors proposed similar constructs for the framework of TI approach, often using slightly differing terminology [ 29 , 30 ]. The authors consistently highlighted that the framework of TI approach is not a protocol but rather high-level guidance applicable to any human service system and should be tailored to the organizational and wider contexts. The process of becoming a TI system is described as a transformation journey rather than a one-off activity.
Despite a 20-year history of the TI approach framework, several reviews have found limited evidence for their effectiveness in health systems, with most studies conducted in North America and only one qualitative study in the UK [ 31 , 32 , 33 ]. Despite little evidence of acceptability, effectiveness, and cost effectiveness in the UK context, policies and guidelines at national, regional and organisational levels recommend implementing TI approaches in healthcare organisations and systems. It is important to understand how TI approaches are being introduced into policy documents, and how these policies are being interpreted and applied within UK healthcare. This study aims to understand the UK-specific context for implementing a TI approach in healthcare by exploring:
How are TI approaches represented in UK health policies?
How are TI approaches understood by policy makers and healthcare professionals?
How are TI approaches implemented in the UK?
This study of UK policy and practice will help us understand what TI approaches mean for policy makers and professionals to inform future UK-specific policy and TI approaches in healthcare.
To answer our research questions, and consider perspectives from different standpoints, we conducted a multi-method qualitative study comprised of a document analysis of UK health policies followed by semi-structured interviews with key informants. Document analysis explored how TI approaches are represented in UK health policy while interviews explored professional views on how they are understood and implemented. We used the Ready Extract Analyse Distil (READ) approach [ 34 ], to guide the review of health policies and the framework method [ 35 ], to analyse data. The framework method is suitable for applied health research conducted by multi-disciplinary teams with varied experiences of qualitative analysis.
Data collection
Data collection occurred between October 2020 and June 2021, with researchers and interviewees based in remote settings due to social distancing restrictions during the COVID-19 pandemic. Sample size was informed by the concept of information power [ 36 ], and restricted by the available funding and a tight timeline.
Document search
We defined policy as ‘a statement of the government’s position, intent or action’ [ 37 ], and considered this definition at the level of a nation, local authority or organization. Two researchers (EE, NVL) identified key policy and related contextual documents, which provided background information on TI approaches. We identified documents through: (i) searches for peer reviewed and grey literature in our earlier systematic review on TI primary care and community mental healthcare [ 31 ], (ii) snowballing of references from included documents, (iii) signposting by interview participants and experts in the field of TI care. Researchers retrieved documents meeting the inclusion criteria: adult healthcare, UK-focus and discussion of TI approaches. We excluded documents on child healthcare, trauma-specific interventions and non-UK focus.
Qualitative interviews
We conducted virtual semi-structured interviews with professionals at decision making levels who have direct experience of developing and implementing TI approaches in the UK healthcare system. We agreed to recruit up to 10 professionals from national and local governments and healthcare organisations. Researchers sent an expression of interest letter via email and Twitter to: (i) individuals and professional networks of policy makers, (ii) authors of included policy documents, (iii) individuals recommended by interview participants. Interested individuals contacted study researchers who checked their eligibility, sent participant information leaflets, answered questions, and arranged interviews with those eligible and willing to proceed. Interviews were conducted over the Zoom video call platform. Researchers obtained verbal informed consent, asked demographic questions, and followed a flexible topic guide to ensure primary issues were covered during all interviews but allowing participants to introduce unanticipated issues. The topic guide explored participant experiences of developing and implementing TI approaches and their views on how TI approaches have come to be represented in policy and implementation (Additional file 1 ). The interviews were audio-recorded with consent, professionally transcribed verbatim, and anonymised.
Data analysis started alongside data collection, to help refine and guide further data collection [ 35 ]. We followed the four-step READ approach to document review in health policy research: 1) ‘Ready your materials’ which involves agreeing the type and quantity of documents to analyse, 2) ‘Extract data’ whereby key document information such as basic data and concepts are organized, 3)’Analyse data’ when data is interpreted and findings are developed, 4) ‘Distil your findings’ which involves assessing whether there is sufficient data to answer the research question and findings are refined into a narrative [ 34 ].
In step one, two researchers (EE, NVL) agreed to use purposive sampling to gather 24 documents representing a broad range of document categories including primary legislation, parliamentary documents, NHS and Public Health England strategy and planning documents, service-user perspectives, evaluation reports, and guidance on ‘how to do’ TI approach [ 38 ]. EE ordered included documents chronologically. In step two, EE read and re-read all included documents and used a customized Excel form to extract data on document title, authors, year, source, objectives, target audience, focus, key messages, referenced evidence, policies/guidelines, and recommendations. During data extraction, researchers made notes about how each document answered the following questions: What is TI care? TI care for whom? Why TI care? EE and NVL met regularly to discuss preliminary ideas for analysis.
In step three, we imported all included documents and interview transcripts into NVivo R project and applied the framework method [ 35 ]. To address variability in definitions and terminology regarding TI approaches, we included key concepts from the well-known SAMHSA system-level framework [ 13 ], as a basis for our coding frame, for example the six TI principles. First, all researchers read four documents and two interview transcripts and independently manually coded text relevant to our research questions using a combination of inductive and deductive coding [ 39 ]. Deductive coding helped to identify concepts related to TI care, even if the document itself did not specifically use the “trauma-informed” term. The researchers then met to compare initial thematic codes and agree on a ‘working analytical framework’ which was imported into NVivo and applied to the documents and interviews transcripts. We refined the framework by adding and merging thematic codes identified subsequently, ran matrix coding queries by data sub-sets (documents, interviews), and combined codes into final analytical themes that answered our research questions. During the analysis stage, researchers met bi-weekly to finalise the dataset, develop and refine coding frame and themes. We wrote reflective diaries and analytical notes and discussed how our clinical backgrounds in general practice and psychiatry, and varied experiences of qualitative research, could have influenced the analysis.
In step four, we stopped document review when we reached the pre-specified number of documents and discussed common findings. First, we illustrated how TI approaches have developed in the UK over time by creating an integrated timeline with document publication dates, the years when interview participants began working in this area, and broader contextual factors from national news and related media. Then we integrated findings from the analysis of documents and interviews through three iterative cycles of developing final analytical themes cutting across documents and interviews. Researchers produced written accounts of the themes, and tables with illustrative quotes that explained how TI approaches have been represented in policy documents, understood, and implemented in the UK.
Policy documents
We identified 50 documents and selected 24 policy documents at national, local, and organizational levels. The remaining 26 documents provided context and a background on TI approaches. The documents included were published over nine years (2012–2021) and considered all UK nations, multiple sectors, government policy and service-user voices. The documents either mentioned a TI approach or discussed related concepts such as a patient choice and safety of services (Table 1 ).
Mirroring the historical development of TI approaches from mental health services [ 13 , 29 ], across both documents and interviews, mental health was the most referenced sector ( n = 24), followed by women’s health ( n = 11), healthcare for rough-sleepers ( n = 7), primary care ( n = 4) and major incident management ( n = 1). The level of application of the TI approach varied from one organization [ 55 ], to a public health board [ 59 ], to NHS-wide [ 48 , 50 ]. The geographic coverage of policy documents ranged from UK wide ( n = 10) to regional application ( n = 24). Scotland emerged as a leading region with the TI knowledge and skills framework for the Scottish Workforce [ 25 ].
The timeline of TI approaches and related concepts in the UK showed a steady growth between 2012 and 2021 with parallel developments from top-down and bottom-up (Fig. 1 ).
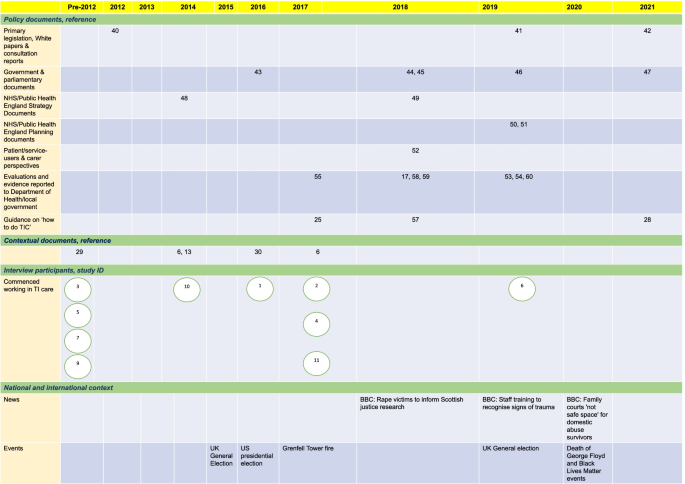
An integrated timeline of how TI approaches have developed in the UK. Document publication dates, the years when interview participants began working in this area, and broader contextual factors from national news and related media are captured. The number/s in each cell correspond to a document reference [ 6 , 13 , 17 , 25 , 28 , 29 , 30 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 59 , 60 ]
We identified few documents prior to 2012, with the Health and Social Care Act published in 2012. Although the Act did not specifically use the term TI care, it discussed related concepts of a greater voice for patients, enabling patient choice and safety of services. We found a noticeable clustering of documents in 2018 and 2019. Potential contributions could be the release of key contextual documents such as the US SAMHSA guidance and the National ACEs Study in the preceding years [ 13 , 14 ]. Other possible reasons could be the high-profile MeToo and Black Lives Matter movements and tragedies like Grenfell fire. Relevant news articles, including calls for rape victim support and professional training on trauma, came to the fore in 2018–2021. These events and activities have brought the issues of trauma, vulnerable populations, intersectionality, and racial justice to the foreground and may have helped achieve a focus on TI approaches as a responsive system-level framework.
In total, 21 professionals expressed interest, 2 did not have direct experience of TI approach at the system level, 8 did not respond by the deadline, 11 provided consent and were interviewed. Interviews lasted between 32 and 68 min (mean 52 min). We achieved a maximum variation sample representing diversity of gender (4 men, 7 women), organizations (public, private, third sector), professional role (frontline to leadership positions), and direct experience of developing and/or implementing TI approaches in healthcare (from 2 to 25 years). Most participants developed and implemented TI approaches in England, at the level of organizations and local authorities (Table 2 ).
Three out of ten interview participants had been involved in developing and implementing TI approaches prior to the release of the first document in 2012, with the rest becoming involved in 2017, just prior to the clustering of documents in 2018 and 2019 indicating a pivotal wave of popularity of the TI approach framework at this time. Participants explained that their clinical practice facilitated interest in the topic.
Our framework analysis has produced three analytical themes with seven sub-themes:
How TI approaches are represented in UK health policies
How ti approaches are understood, ti care as different from other practices, ti care as a contextually tailored organizational approach.
TI care as a remedy to challenges;
How TI approaches are implemented
Piecemeal implementation and a need for a shared vision, factors that facilitated or hindered implementation, the evidence-policy gap, the future of ti care in the uk.
We found that the TI approach is referenced in government initiatives and included in policies at a national level, as well as in NHS and non-NHS organizations, local authorities, and devolved nations; however, there was no dedicated strategy or a position statement, nor was there an agreed terminology and framework, or a robust evidence base in the UK. Despite growing endorsement of TI approaches in policy documents (Fig. 1 ), positive statements at the national and NHS level were not backed up with legislation, guidance, funding commitment, and resource allocation.
We found divergent interpretations of a TI approach versus other concepts related to trauma, such as ACEs, psychologically informed environments and standard good clinical practice. One participant unified concepts such as TI care, ACEs and psychologically informed environments in recognising past traumatic experiences. Another participant detached the terms ACEs and TI care, reflecting that ACEs have become well known in research whereas a TI approach is a pragmatic way of supporting those who have experienced trauma. All documents and most participants clearly differentiated between a TI approach at the system level and standalone TI practices (e.g., routine enquiry about ACEs, one-off training about trauma). However, some participants considered standalone TI practices to be a TI approach. Documents and most interviewees differentiated TI approach from a good clinical practice by incorporation of the TI assumptions and principles [ 25 ].
In line with the SAMHSA guidance [ 13 ], document and interview data showed that the framework of a TI approach needs to be tailored to the organizational and wider context. Policy documents advised organizations to clarify what TI care means for them, and that application of the framework should depend on the needs of service users and organisations [ 25 , 28 , 52 , 54 , 59 , 60 ]. Several documents suggested that this organizational tailoring should be informed by service-users through co-production and co-design of services [ 17 , 28 , 49 , 52 , 53 , 54 , 55 , 60 , 61 ].
TI care as a remedy to challenges
In all policy documents and in nine interviews, TI approaches were presented as a remedy to a variety of problems within health systems. Sixteen of twenty-five documents justified a TI approach as a way for addressing the high prevalence and negative impact of violence and trauma on patients, with eleven documents considering its impact on staff. The growing international evidence base for the impact of psychological trauma and the need for service response was used in documents and interviews to justify TI approaches as a pragmatic solution to these concerns. However, the documents and interview participants justified the need for TI care by citing US and Welsh epidemiological studies on ACEs, DVA and patient accounts of being re-traumatized in services. We found no references to intervention studies that demonstrated effectiveness, cost-effectiveness, or acceptability of TI approaches in the UK.
In the NHS Long Term Plan, TI care was also identified as a component of a new model of integrated care [ 50 ]. A TI approach has also been presented as a solution to addressing the collective trauma of the COVID-19 pandemic for patients and staff [ 62 ].
Interviewees confirmed the piecemeal implementation of TI approaches in the UK and felt that a shared national vision would be beneficial. Participants agreed that the implementation of TI approaches varied across the UK, with Scotland having more strategic coordinated implementation (additional file 2 , quote 1). We found that different regions and organizations reinvented the TI approach wheel, with interviewees expressing a need for national coordination. Participants expressed the need for adequate allocated resources and a more unified approach across organizations and sectors as a solution to the patchy implementation in England (additional file 2 , quote 2). They gave examples of the bottom-up networking initiatives driven by experts in TI care who created opportunities for sharing best practice and resources for implementing TI approaches. Participants cited a UK-wide Trauma Informed Community of Action and local TI care working groups.
One participant from England suggested that whilst the SAMSHA definition of TI approach was widely cited, they did not feel there was an agreed set of components and activities for implementing the framework in practice. This participant felt that a consensus on shared practice standards was a necessary next step for TI care in the UK.
At the organization level, some participants felt high level leadership support was needed, and if lacking is a barrier to implementing a TI approach. To achieve effective implementation leaders with power and those with passion were felt to be important. The concept of organizational champions garnered support when “ champions act as influencers and their credibility within services adds to the potential for buy-in from other staff ”, fostering sustainable change [ 53 ]. One participant warned against a reliance on top-down leadership, explaining that when a senior leader leaves an organization’s priorities can change. The participant also felt that change driven from the top-down, might lead to resistance from front-line staff (additional file 2 , quote 3). Some interviewees reaffirmed the view that people with lived experience should be involved in leading implementation of TI approaches (additional file 2 , quote 4).
Some interviewees felt that passionate individuals alone cannot create effective change without support at the organization level (additional file 2 , quote 5). Collective responsibility and organizational commitment were highlighted as an essential factor to support individuals with passion. In contrast, unsupportive organizational culture and high-pressure environments was perceived as a barrier (additional file 2 , quote 6). One document cited scarcity of resources and low staff morale, as well as a resistance to new initiatives and upheaval [ 52 ]. Competing demands and opportunity costs were also raised (additional file 2 , quote 7).
At the wider context level, documents highlighted the value of political support capable of influencing practice nationally [ 17 ]. Some interviewees explained disconnected and decentralized implementation of TI approaches across the UK by a shortage of political will and leadership in the central UK government, compared with those of the devolved administrations in Scotland and Wales (additional file 2 , quote 8). Proposed explanations included smaller territories, populations and governments, and “ more of a left-leaning social conscience politics” (Participant 3). Another interviewee called for a united parliamentary leadership recognised by government and capable of influencing policy.
Inadequate funding and commissioning of services was also described as a barrier, partly explaining regional differences in implementation of TI care (additional file 2 , quote 9). The COVID-19 pandemic was perceived as a barrier that contributed to the backlog of initiatives and work in the pipeline (additional file 2 , quote 10).
UK policies on implementation of TI approaches were not supported by UK-specific, methodologically robust, evidence for effectiveness, cost effectiveness and acceptability. Participants explained the policy-evidence gap by citing methodological challenges of evaluating system-level transformation and a need for commitment from commissioners and funders (additional file 2 , quote 11). In addition, participants who developed and implemented TI approaches in their organizations and regions did not have the capacity to evaluate their initiatives and disseminate the findings (additional file 2 , quote 12).
Participants had differing views on the future of TI care in the UK, although most agreed on its permanency. Some interviewees felt that TI approaches have already gained a critical momentum in the UK. In contrast to comments about TI care as a passing trend or ‘buzzword’ in the absence of in depth understanding, several interviewees voiced confidence that TI approach is here to stay, and will evolve, being incorporated into policy as well as being adopted more widely. Others were less optimistic and were concerned that insufficient political backing means policy endorsement will not translate to meaningful practice change.
Some participants thought that TI care should become a mandatory consideration with stronger central policy or monitoring by national watchdogs. They felt that the support of additional nation-wide regulatory measures could be beneficial. In contrast, some interviewees showed scepticism, fearing the creation of further ‘box-ticking’ measures. They feared that efforts to police or monitor providers could create a burden of empty bureaucracy without improving practice (additional file 2 , quote 13).
Our document analysis of health policies and interviews with professionals found differing representation, understanding, and implementation of TI approaches in the UK with wide variations between geographical areas, services, and individual professionals. Cross-sectoral endorsement of TI approaches in policies was not supported by high-level legislation or funding, and a UK-specific evidence base. Despite divergent and conflicting interpretations of TI approaches, the common understanding was that it differs from other practices by integrating TI principles at the organisational level and it should be tailored to the organization and wider contexts. It can also address NHS problems from integrated care to post-COVID recovery. We found more centralized implementation of TI approaches in Scotland and Wales versus piecemeal implementation in England. The implementation of TI approaches in England was driven from the bottom-up by passionate dedicated leaders at the level of organization or local authority, who called for more coordinated working supported by the UK government and NHS leaders. We identified factors that facilitated or hindered implementation of TI approaches at the level of organization (leadership, service user involvement, organizational culture, resource allocation, competing priorities) and wider context (government support, funding). The evidence-policy gap in TI care implementation can be explained by limited funding and evaluation capacity. Professionals had differing views on the future of TI approaches, however all agreed that without political backing at the government level, policy endorsement will not translate into meaningful implementation.
Our finding of a marked difference in the landscape of TI approaches in healthcare systems between the devolved nations, with evidence of a unified national strategy emerging in Scotland and Wales and notably absent in England could have several explanations. These include smaller territories, populations, and governments in devolved nations, with clear buy-in from government-level leadership in Scotland. Our analysis highlighted the initiatives of local decision-makers in England who have developed and implemented TI approaches in their own organizations and local authorities. The absence of a national strategy in England contributed to the piecemeal implementation, with some regions leading the way, and others silent. As local TI leads have been left to ‘find their own way’, they may not always have been aware of similar initiatives in other organizations and regions. A proposed solution was bottom-up initiatives aiming to bring the local TI leads together to share resources and good practice. This finding indicates the need for a leader on TI approaches within or linked to the UK government who can support and strengthen the bottom-up initiatives.
Another important finding is confirmation of the evidence-policy gap, with proposed reasons emerging in the analysis. Interview participants explained an absence of UK evidence on the effectiveness of TI approaches by a need for more interest from commissioners and funders, as well as a lack of physical and methodological capacity to evaluate system-level TI approaches. The former can be resolved through funding calls and comprehensive, transparent evaluation. The latter can be addressed by funding evaluations and raising awareness regarding available methodologies and tools for evaluating TI system change interventions [ 32 , 33 ].
Our finding of differing understanding of TI-approaches is in line with prior literature [ 63 ]. We found that some participants interpreted standalone TI practices (e.g., ACEs enquiry, one-off training about TI care) as a TI approach. Such interpretations are not supported by evidence. Authors of the ACEs study explained that the ACEs score is not a diagnostic tool, therefore care should be taken if used as part of community-wide screening, with rigorous evaluation of its use [ 64 ]. Recent reviews also found limited evidence on outcomes from routine enquiry, recommending further research [ 65 , 66 ]. Several systematic reviews demonstrated that standalone awareness raising did not result in change in behaviour and practices among healthcare professionals [ 67 , 68 ].
These misunderstandings can be explained by the conceptual mutability of a TI approach framework, lack of awareness about existing frameworks, and a need for coordinated working led by experts in TI approaches. The evidence of emerging working groups and UK-wide professional networks on TI care is promising. However, these initiatives require adequate funding and coordination to sustain momentum and develop further. These professional networks can become the platform for education about evidence-based TI approaches contributing to increasing value and reducing waste in research and implementation in this field.
This study is methodologically robust with perspectives drawn from UK policy documents and professionals, who have direct experience of developing and implementing TI approaches. Data analysis occurred alongside data collection, to help refine and guide further data collection. The limitations include no professional informants from devolved nations and no participants at the level of UK government. Due to time and funding restrictions, we could only recruit 11 professionals and did not interview patients including those with lived experience of trauma. Our small sample size could have resulted in underrepresentation of views of some stakeholders. Future research should recruit informants from these groups to draw a complete picture of the landscape of TI approaches in the UK.
Although health policies endorse implementation of TI approaches in the UK, they do not provide specific legislation, strategy or funding and are not supported by evidence of effectiveness. Understanding and implementation of TI approaches varies between regions, organizations, and individual professionals; however, all agree that if implemented at the system level and contextually tailored, TI approaches can mitigate varied problems withing NHS. The implementation of TI approaches in the UK is driven by local experts in TI care. A coordinated, more centralized strategy and enhanced provisioning for TI healthcare, including increased funding for evaluation and education through TI professional networks, can contribute towards evidence-informed policies and implementation of TI approaches in the UK.
Availability of data and materials
Data are available at the University of Bristol data repository, data.bris, at https://doi.org/10.5523/bris.2awc5pqkavac12d6jm1qp9wetm .
For reference: Lewis, N. (2022): TAPCARE policy review study. https://doi.org/10.5523/bris.2awc5pqkavac12d6jm1qp9wetm
All methods were performed in accordance with relevant guidelines and regulations as detailed here: https://www.biomedcentral.com/getpublished/editorial-policies#research+involving+human+embryos%2C+gametes%2C+and+stem+cells .
Abbreviations
Adverse childhood experiences
Coronavirus disease
Domestic violence and abuse
National Health Service
Substance Abuse and Mental Health Services Administration
Trauma-informed
United Kingdom
United States of America
Magruder KM, McLaughlin KA, Elmore Borbon DL. Trauma is a public health issue. Eur J Psychotraumatol. 2017;8(1):1375338.
Article Google Scholar
Kessler RC, et al. Trauma and PTSD in the who world mental health surveys. Eur J Psychotraumatol. 2017;8(sup5):1353383.
Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. Am J Community Psychol. 2007;40(3–4):313–32.
Ellis AE. Providing trauma-informed affirmative care: Introduction to special issue on evidence-based relationship variables in working with affectional and gender minorities. Pract Innov. 2020;5(3):179–88.
Prevention, C.f.D.C.a., Adverse Childhood Experiences (ACEs): preventing early trauma to improve adult health, in CDC Vital Signs. 2019.
Bellis MA, et al. National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Med. 2014;12:72.
Scottish government. NHS Education for Scotland, S.G. Domestic abuse- and trauma-informed practice: companion document.
Statistics, O.f.N., Percentage of adults aged 16 to 74 years who were victims of domestic abuse in the last year, by ethnic group: year ending March 2018 to year ending March 2020, in Crime Survey for England and Wales (CSEW). 2020.
Rhys Oliver, B.A., Stephen Roe, Miriam Wlasny The economic and social costs of domestic abuse. 2019. 77.
Sacchi L, Merzhvynska M, Augsburger M. Effects of cumulative trauma load on long-term trajectories of life satisfaction and health in a population-based study. BMC Public Health. 2020;20(1):1612.
Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–46.
Hughes K, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–66.
Administration, S.A.a.M.H.S., SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach . Department of Health and Human Services USA, 2014: p. 27.
Bellis M, et al. The impact of adverse childhood experiences on health service use across the life course using a retrospective cohort study. J Health Serv Res Policy. 2017;22(3):168–77.
Mauritz MW, et al. Prevalence of interpersonal trauma exposure and trauma-related disorders in severe mental illness . Eur J Psychotraumatol. 2013;4:4.
Heron RL, Eisma MC. Barriers and facilitators of disclosing domestic violence to the healthcare service: a systematic review of qualitative research. Health Soc Care Community. 2021;29(3):612–30.
Department of Health and Social Care, A. The Women’s Mental Health Taskforce: Final report. 2018. 73.
Sweeney A, et al. A paradigm shift: relationships in trauma-informed mental health services. BJPsych advances. 2018;24(5):319–33.
Schippert ACSP, Grov EK, Bjørnnes AK. Uncovering re-traumatization experiences of torture survivors in somatic health care: A qualitative systematic review. PLoS ONE. 2021;16(2):e0246074–e0246074.
Article CAS Google Scholar
Jimenez RR, et al. Vicarious trauma in mental health care providers. J Interprofessional Educ Pract. 2021;24:100451.
Sweeney A, et al. Trauma-informed mental healthcare in the UK: what is it and how can we further its development? Ment Health Rev J. 2016;21:174–92.
Dheensa, S., et al., Healthcare Professionals' Own Experiences of Domestic Violence and Abuse: A Meta-Analysis of Prevalence and Systematic Review of Risk Markers and Consequences. Trauma Violence Abuse, 2022: p. 15248380211061771.
Harris M, F.R., Using trauma theory to design service systems. San Francisco. CA: Jossey-Bass; 2001.
Google Scholar
S, H. Medical Directors' Recommendations on Trauma-informed Care for Persons with Serious Mental Illness. 2018. 1–20.
Scottish government. NHS Education for Scotland, S.G. Transforming psychological trauma: a knowledge and skills framework for the Scottish workforce. 2017. 124.
Government of Canada. Canada, G.o. Trauma and violence-informed approaches to policy and practice. 2018.
Kimberg L, W.M., Trauma and trauma-informed care. New York. NY: Springer, Berlin Heidelberg; 2019.
Clare Law, L.W., Mickey Sperlich, Julie Taylor, A good practice guide to support implementation of trauma-informed care in the perinatal period . 2021: p. 42.
Harris M, Fallot RD. Envisioning a trauma-informed service system: a vital paradigm shift. New Dir Ment Health Serv. 2001;89:3–22.
Bowen EA, Murshid NS. Trauma-informed social policy: a conceptual framework for policy analysis and advocacy. Am J Public Health. 2016;106(2):223–9.
Dawson S, et al. Trauma-informed approaches to primary and community mental health care: protocol for a mixed-methods systematic review. BMJ Open. 2021;11(2):e042112.
Purtle J. Systematic review of evaluations of trauma-informed organizational interventions that include staff trainings. Trauma Violence Abuse. 2020;21(4):725–40.
Heidi Melz, C.M., Erin Ingoldsby, Karen Cairone, Mary Mackrain Review of Trauma-Informed Initiatives at the Systems Level. Trauma-Informed Approaches: Connecting Research, Policy, and Practice to Build Resilience in Children and Families. 2019. 37.
Dalglish SL, Khalid H, McMahon SA. Document analysis in health policy research: the READ approach. Health Policy Plan. 2021;35(10):1424–31.
Gale NK, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Williams N. Government policy - a spotter’s guide. 2012.
Hughes G. New models of care: the policy discourse of integrated care. People, Place and Policy Online. 2017;11:72–89.
Virginia Braun, V.C., Successful Qualitative Research. A Practical Guide for Beginners. London: Sage Publishing; 2013.
Parliament, U., Health and Social Care Act. 2012: https://www.legislation.gov.uk/ukpga/2012/7/introduction/enacted .
Government H. Transforming the response to domestic abuse: consultation response and draft bill. 2019.
Government H. Integration and Innovation: working together to improve health and social care for all D.o.H.a.S. Care, Editor. 2021.
Office, H., Ending Violence against Women and Girls. 2016: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/522166/VAWG_Strategy_FINAL_PUBLICATION_MASTER_vRB.PDF .
Government S. Public Health Priorities for Scotland. 2018.
Government H. HM Government: Serious Violence Strategy. 2018.
Home Office. Ending violence against women and girls 2016–2020: refresh strategy H. Office, Editor. 2019.
Government H. C.O. Department of Health and Social Care, Editor. COVID-19 Mental Health and Wellbeing Recovery Action Plan. 2021.
NHS England. NHS Five Year Forward View. 2014. 41.
Health and Justice, A.F.a.S.A.R.C.S.T. Strategic Direction for Sexual Assault and Abuse Services: Lifelong care for victims and survivors: 2018 - 2023. 2018. 28.
NHS, The NHS Long Term Plan. 2019. p. 136.
NHS, NHS Mental Health Implementation Plan 2019/20–2023/24. 2019.
Jo Wilton, A.W. Engaging with complexity: Providing effective trauma-informed care for women. 2019. 26.
Lauren Bear, G.D., Jessica Southgate A sense of safety: Trauma-informed approaches for women. 2019. 24.
Bunting L, M., L, Mooney, S, MacDonald, M, Coulter, S, Hayes, D, Forbes, T, Developing trauma informed practice in Northern Ireland: Key messages. 2019, Queen’s University Belfast. p. 33.
Kennedy, A. Successes and struggles keeping trauma in mind: development of a trauma informed adult mental health service.
Royal College of Psychiatrists, C.C.f.Q.I. Ten evidence-based reasons for embedding values-based ‘Enabling Environments’ in health care.
S, R., Trauma-informed approaches. Trauma-informed care: implications for practice. 2018: https://www.nottinghamshire.gov.uk/media/1533199/traumainformedcare.pdf .
C, G., Trauma-informed care in response to adverse childhood experiences. Nursing Times, 2018. 114: 7, 46–49.
Highland N. The Annual Report of the Director of Public Health: Adverse Childhood Experiences. Resilience and Trauma Informed Care: A Public Health Approach to Understanding and Responding to Adversity; 2018. p. 82.
Network, N.E.C.N.a.t.N.E.a.N.C.A.H.S., Developing real world system capability in trauma informed care: learning from good practice . Trauma Informed Community of Action, 2020: p. 24.
Steven Thirkle, A.K., Paras Patel, Petia Sice ROOTS: A reflective framework for mapping the implementation journey of trauma-informed care 2021. 38.
Fenney D. The role of trauma-informed care during the Covid-19 pandemic. 2021.
Sweeney A, Taggart D. (Mis)understanding trauma-informed approaches in mental health. J Ment Health. 2018;27(5):383–7.
Anda RF, Porter LE, Brown DW. Inside the adverse childhood experience score: strengths, limitations, and misapplications. Am J Prev Med. 2020;59(2):293–5.
Ford K, et al. The evidence base for routine enquiry into adverse childhood experiences: a scoping review. Child Abuse Negl. 2019;91:131–46.
Gentry SV, Paterson BA, Does screening or routine enquiry for adverse childhood experiences (ACEs) meet criteria for a screening programme? A rapid evidence summary. J Public Health. 2021;fdab238.
Zaher E, Keogh K, Ratnapalan S. Effect of domestic violence training: systematic review of randomized controlled trials. Can Fam Physician. 2014;60(7):618-24-e340-7.
Kalra N, et al. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst Rev. 2021;5:CD012423.
PubMed Google Scholar
Download references
Acknowledgements
We would like to thank all the interview participants and those with an interest in TI approaches who kindly shared policy documents and background literature with the study group. We would like to acknowledge the contributions of Dr Sandi Dheensa in reviewing the draft manuscript.
This report is independent research funded by the National institute for Health and Care Research (NIHR), Research Capability Funding stream via NHS Bristol, North Somerset and South Gloucestershire Clinical Commissioning Group. NVL was also supported by the NIHR Bristol Biomedical Research Centre (grant BRC-1215-20011). The views expressed are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
Centre for Academic Primary Care, Bristol Medical School, University of Bristol, Bristol, UK
Elizabeth Emsley & Joshua Smith
Centre for Academic Mental Health, Bristol Medical School, University of Bristol, Bristol, UK
David Martin
NIHR Bristol Biomedical Research Centre, University Hospitals Bristol and Weston NHS Foundation Trust and University of Bristol, Bristol, UK
Natalia V. Lewis
You can also search for this author in PubMed Google Scholar
Contributions
NVL conceived, designed, and led the study. EE, NVL, JS and DM collected and analysed documents and interview data. EE and NVL wrote the first draft of the manuscript with input from DM and JS. All authors contributed to subsequent revision and approved the final version.
Corresponding author
Correspondence to Elizabeth Emsley .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Faculty of Health Sciences Research Ethics Committee at University of Bristol (Ref 114665, 11 February 2021). Interview participants provided verbal informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. .
Interview topic guide.
Additional file 2.
Analytical themes with subthemes and supporting quotes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Emsley, E., Smith, J., Martin, D. et al. Trauma-informed care in the UK: where are we? A qualitative study of health policies and professional perspectives. BMC Health Serv Res 22 , 1164 (2022). https://doi.org/10.1186/s12913-022-08461-w
Download citation
Received : 16 March 2022
Accepted : 05 August 2022
Published : 14 September 2022
DOI : https://doi.org/10.1186/s12913-022-08461-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological trauma
- Mental health
- Primary health care
- Public health
- Qualitative research
- Policy making
- Health policy
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 13 October 2015
Adverse childhood experiences and trauma informed care: the future of health care
- Resmiye Oral 1 ,
- Marizen Ramirez 2 ,
- Carol Coohey 3 ,
- Stephanie Nakada 4 ,
- Amy Walz 4 ,
- Angela Kuntz 4 ,
- Jenna Benoit 1 &
- Corinne Peek-Asa 2
Pediatric Research volume 79 , pages 227–233 ( 2016 ) Cite this article
97k Accesses
279 Citations
59 Altmetric
Metrics details
- Paediatric research
- Paediatrics
Adverse childhood experiences (ACEs) are related to short- and long-term negative physical and mental health consequences among children and adults. Studies of the last three decades on ACEs and traumatic stress have emphasized their impact and the importance of preventing and addressing trauma across all service systems utilizing universal systemic approaches. Current developments on the implementation of trauma informed care (TIC) in a variety of service systems call for the surveillance of trauma, resiliency, functional capacity, and health impact of ACEs. Despite such efforts in adult medical care, early identification of childhood trauma in children still remains a significant public health need. This article reviews childhood adversity and traumatic toxic stress, presents epidemiologic data on the prevalence of ACEs and their physical and mental health impacts, and discusses intervention modalities for prevention.
Similar content being viewed by others

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Investigating child sexual abuse material availability, searches, and users on the anonymous Tor network for a public health intervention strategy

Differences in childhood stress between Neanderthals and early modern humans as reflected by dental enamel growth disruptions
Childhood adversity: definition and scope.
Childhood adversity may potentially have detrimental effects on long-term health ( 1 ). Adversity may include discrete events or ongoing circumstances that are outside of the child’s control and are perceived as negative by the child ( 1 , 2 ). The cumulative burden of adverse experiences has been shown to cause negative effects on physiological, cognitive, behavioral, and psychological functions ( 2 ).
The Adverse Childhood Experiences (ACEs) study focused on most common types of adversity that are encountered in the United States. These 10 ACEs included child abuse (emotional, physical, or sexual), child neglect (emotional or physical), and household dysfunction (domestic violence, substance abuse, mental illness or criminal activity, or parental absence) ( 3 , 4 ). Subsequently, extreme economic adversity, bullying, school violence, and community violence have been described to be other commonly encountered ACEs ( 5 ). Other forms of adversity described in the literature include traumatic loss of a loved one, sudden and frequent relocations, serious accidents, life-threatening childhood illness/injury, pornography (exposure or participation), prostitution, natural disaster, kidnapping, torture, war, refugee camps, and terrorism ( 3 , 4 , 5 , 6 , 7 ). Other studies specifically focused on identifying ACEs in children in real time and reported that major childhood adversities, including growing up in poverty, peer rejection and lack of friends, poor school performance, property crime, and witnessing community violence, are associated with increased lifelong risk for negative life events and negative health outcomes as well. Measuring childhood adversities during childhood has been shown to offer improvements to the original ACE scale by examining more short-term behavioral and emotional symptoms that may serve as a link between ACEs and long-term health problems ( 8 , 9 ).
Traumatic Toxic Stress: How ACEs Affect Neurological Functioning
Health care professionals are becoming continually more aware of the social and environmental determinants of health, and the multiple effects of the environment on health outcomes are becoming increasingly better defined.
Physiologic/Positive Stress, Tolerable Stress, and Traumatic Toxic Stress
Stressors encountered throughout life may be experienced in different ways ( 1 , 2 ): When a dog barks at a child, or when preparing for an examination, “fight or flight” reaction may help the child generate the inner resources to deal with the stressor, which helps survival and growth. Such stressors are positive/physiological stressors. When a child experiences an illness that requires multiple invasive interventions, this stressor may be perceived as tolerable stress in the presence of supporting environmental factors such as nurturing relationships. Chronic/sustained stressors in the absence of a supportive environment on the other hand may lead to toxic stress as follows:
Stress response involves engagement of two primary systems: the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system ( 1 , 2 , 10 , 11 ). These systems work in collaboration to respond to both acute stressors and chronic/sustained stressors. The activation of the HPA axis begins in the hypothalamus by the release of proinflammatory cytokines that trigger corticotrophin-releasing hormone, which stimulates the release of adrenocorticotropin-releasing hormone from the anterior pituitary. Adrenocorticotropin-releasing hormone leads to the release of cortisol, norepinephrine, and epinephrine from the adrenal cortex. These stress hormones stimulate a myriad of responses from various organ systems including hepatic (gluconeogenesis), cardiovascular (increasing heart rate and blood pressure), respiratory (dilating the bronchioles), and many others ( 11 , 12 ). Once the HPA axis is activated and cortisol is released, a negative feedback loop works to mediate the response. This feedback loop acts as a moderator to keep the stress response from becoming harmful. In physiologic and tolerable stress response, this feedback loop, as well as the elimination of the environmental stressor, helps the spike in stress hormones return to baseline quickly and easily ( 11 , 12 ).
In traumatic toxic stress (TTS) however, chronic negative environmental factors can lead to chronic or sustained stress response system activation. This chronic activation has the ability to lead to the disruption of the structure and function of the neuroendocrine and immune systems ( 10 ). Thus, excess cortisol level in the circulation is sustained with subsequent chronic activation of the HPA axis ( 3 ). In the short term, this overactivation can result in an overload of cortisol, and in the long term, a relative lack of cortisol ( 2 ).
Both of these deviations may lead to negative health consequences ( 10 ). Too much cortisol suppresses the immune response and increases the chance of infection, while too little cortisol leads to the inflammatory response persisting after it is no longer needed ( 3 ). Animal studies have linked poorly responsive HPA axis to a variety of autoimmune diseases including rheumatoid arthritis, systemic lupus erythematosus, Sjogren’s syndrome, fibromyalgia, and chronic fatigue syndrome. In humans, TTS has been linked to prolonged wound healing, decreased antibody production after vaccination, and susceptibility to viral infection ( 2 , 13 ).
Neurologic Remodeling in the Context of TTS
The dysregulation of the HPA axis can also lead to long-term modifications on multiple organ systems, most notably in the brain ( 1 , 14 ). TTS has been shown to lead to changes, especially in the more susceptible young brain, which can lead to long-term effects on both physiology and behavior ( 2 , 14 , 15 ). The genes that determine how the body responds to stress are highly subject to epigenetic modifications ( 16 ). Epigenetic changes may occur via DNA methylation and histone acetylation that modify gene expression. While some of these modifications are transient, others are programmed early in life and will remain embedded throughout the child’s lifetime with the potential to be passed on to the next generation ( 16 ). It was also shown that the three regions of the brain that are most prominently affected by TTS are laden with glucocorticoid receptors. These regions are the hippocampus, the prefrontal cortex, and the amygdala ( 10 , 11 , 13 , 14 ).
The hippocampus, intimately involved in the formation of new memories and learning, undergoes proliferation throughout childhood. When the brain is subjected to remodeling via TTS in animals, hippocampal neuronal proliferation is significantly suppressed, which leads to significant long-term impairments in learning and new memory formation ( 11 , 14 , 15 ).
Children who are victims of chronic abuse may experience remodeling in the amygdala as well. The amygdala, part of the limbic system, is activated in response to stress and has been shown to generate impulsive behaviors ( 11 , 15 ). In the context of TTS, dendritic growth and proliferation in the amygdala lead to an increase in impulsive behavior ( 11 , 14 ). Conversely, TTS causes the prefrontal cortex, the part of the brain that is dedicated to planning and impulse control, to be underdeveloped and have fewer synaptic connections leading to poor impulse control ( 14 , 15 ).
These regional brain alterations can ultimately convert an individual’s physiologic stress responses into toxic stress responses, through which the person perceives benign experiences as life-threatening events ( 2 ). These alterations in brain architecture may also promote the development of social and behavioral coping “skills” that are maladaptive with subsequent health consequences ( 1 , 2 , 17 ).
Epidemiology of Childhood Adversity
The original ACEs study on more than 17,000 adult participants showed 64% of the population surveyed reported at least one ACE ( 4 ). In 2010, five states, including Arkansas, Louisiana, New Mexico, Tennessee, and Washington, found similar results ( 18 ): Of 26,229 subjects that were surveyed, 59% reported having experienced at least one ACE. A 2012 survey of Iowans revealed that 55% of Iowa adult population had experienced at least one ACE ( 19 ).
Studies also showed that ACEs are likely to co-occur ( 4 , 18 , 19 , 20 ). The original ACEs study revealed that 13% of the respondents had four or more ACEs during childhood compared to 15% of the respondents in both the 2010 Centers for Disease Control and Prevention multistate study and the Iowa study ( 4 , 18 , 19 ).
The International Society for the Prevention of Child Abuse and Neglect created child abuse screening tools for global use, which provide opportunity to screen for ACEs as well ( 21 , 22 ). These tools were used in the multinational Balkan Epidemiology of Child Abuse and Neglect study, which revealed the presence of at least one ACE in 65–83% of the 42,272 children surveyed in nine Balkan countries ( 22 ).
Impact of Childhood Adversity and TTS on Health
The original ACEs study by Felitti et al . in 1998 set out to test the cumulative and long-term effect of several types of ACEs, not just one type of childhood victimization, on adult well-being. This study, which has led to over 50 publications, has profoundly changed the focus of the child maltreatment field by shifting the focus from the effect of individual types of childhood victimization to the cumulative effect of ACEs on child and adult well-being ( 3 , 4 , 20 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 ).
Other researchers have also shown that ACEs predict higher rates of negative health outcome ( 3 , 4 , 20 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ). These outcomes can be loosely divided into (i) health risk behaviors (ii) leading causes of death and other chronic health problems, (iii) poor mental health, and (iv) other impacts ( 4 , 18 , 42 ).
Health Risk Behaviors
The number of ACEs has been found to be related to several health-risk behaviors, including substance abuse (alcohol and illicit substances) ( 4 , 18 , 19 , 20 , 28 , 29 , 30 ), tobacco use ( 4 , 18 , 19 , 28 , 30 ), sexual behaviors that contribute to unintended pregnancy and sexually transmitted diseases ( 28 , 32 ), and obesity ( 4 , 18 , 20 , 33 ). Having experienced four or more ACEs increases the rate of smoking (2.2 times), alcoholism (7.4 times), substance abuse (4.2 times), intravenous illicit substance abuse (11.3 times), severe obesity (1.6 times), and sexual intercourse with 50 or more partners (3.2 times) with a clear dose–response relationship between the number of ACEs and the adoption of these high-risk behaviors ( 4 , 18 , 19 , 20 ). These behaviors have been referred to as a “trauma organized” lifestyle and predispose individuals to mental and physical illness throughout life ( 23 , 45 ). Thus, the neurological changes that are mediated by TTS, a “trauma organized lifestyle,” and the circumstances that are associated with limited access to health care, together are believed to lead to increased risk of morbidity and mortality ( 4 , 34 , 44 ).
Leading Causes of Disease and Other Chronic Diseases
Childhood trauma can also lead to several leading causes of death among adults, including heart disease and stroke ( 25 , 28 ), liver disease ( 28 ), lung cancer ( 34 ), and chronic obstructive pulmonary disease ( 26 , 28 ), the relationship becoming more apparent with four or more ACEs. An increasing number of ACEs has also been found to be related to autoimmune diseases, such as rheumatoid arthritis ( 27 , 28 ), frequent headaches ( 35 , 40 ), primary insomnia ( 36 ), and several metabolic risk biomarkers (obesity, high blood pressure, high total cholesterol, low high-density lipoprotein cholesterol, high glycated hemoglobin) ( 37 ). Some of these health outcomes have also been found to be associated with changes in immune function as a result of TTS ( 2 , 3 , 13 ).
Mental Health
There is an extensive empirical literature on the relationship between the cumulative number of ACEs and mental health challenges. Researchers have found a relationship between the number of ACEs and learning and behavioral problems among children and adolescents ( 20 , 23 , 28 , 29 , 30 , 31 ), and somatic disorders ( 39 , 40 ), hallucinations ( 3 , 28 ), anxiety and obsessive–compulsive disorders ( 30 , 41 ), depression, and suicide attempts ( 28 , 29 , 30 , 31 ) among adults. Specifically, four or more ACEs increased the risk of depression (4.5 times) and suicide attempts (12.2 to 15.3 times) ( 4 , 19 ).
Individuals who have experienced multiple traumas and resultant emotional dysregulation may present with posttraumatic stress disorder characterized with dissociation and increased automatic reactivity ( 46 , 47 , 48 , 49 ). Patients with dissociative posttraumatic stress disorder also exhibit emotional under-engagement creating barriers in establishing and maintaining healthy and supportive relationships, which is the basis for recovery from stress. Thus, these individuals may have difficulties in responding to traditional treatment ( 47 ).
Other Impacts
Finally, researchers have found that people who reported more ACEs were more likely to report poor or fair health ( 33 , 42 ), or a lower sense of well-being ( 43 ), have poorer access to medical/mental health services ( 4 , 19 , 42 ), be less satisfied with their lives ( 30 ), have higher work-related problems/unemployment ( 4 ), and die prematurely by as much as 20 years earlier ( 4 , 34 , 43 ) than people who reported fewer ACEs. Finally, an increasing number of ACEs was found to be related to an increase in health care utilization/costs ( 28 , 42 ).
Approaches to Reducing the Burden of ACEs
The high population prevalence of ACEs and their association with a wide variety of negative outcomes support the need to prioritize ACEs prevention. Given the complex interplay between the individual, the family, the community, and the larger sociopolitical structure, the socio-ecological model provides a good conceptual framework to guide prevention. To have the desired multilevel effect, strategies to prevent the occurrence of ACEs and their adverse impacts are needed at every level ( 50 ).
Following the general public health approach, primary prevention includes efforts to prevent ACEs so that children grow up with less exposure to adversity and are less likely to have children of their own who experience ACEs ( Table 1 ) ( 51 ). Secondary prevention includes efforts immediately after an ACE to reduce the immediate and short-term consequences. Tertiary prevention includes efforts to treat and reduce long-term consequences of ACEs ( 51 ).
Understanding ACE prevalence and risk factors as well as identifying individuals who have experienced ACEs is a critical element in a comprehensive approach to prevention. However, a focus on primary prevention of ACEs, in which the incidence of ACEs is reduced at the population level, will have the greatest individual and societal impact ( 52 , 53 ). In order to accomplish this, the interventions should focus on strengthening individual and community resilience rather than solely identifying and responding to individual ACEs by strengthening communities and reducing resource disparity. For example, child abuse prevention programs such as emergency nurseries, programs that provide referrals to services such as homeless shelters and food pantries, and increased availability of mental health and substance abuse treatment can reduce the risk for ACE events at the population level.
An increasing number of prevention and intervention approaches are becoming available at various levels: At the individual and family levels, primary prevention programs such as Circle of Security that improve parent–child attachment can reduce ACE experiences such as child abuse and neglect ( 54 ). Other programs, such as the Period of Purple Crying prevent specific types of abuse, such as shaken baby syndrome ( 55 ).
Targeted primary prevention programs at the community and societal levels are rare. Three of 17 studies evaluating universal campaigns measured child abuse as an outcome, and of these, two of the three studies found significant decreases ( 52 ). Triple-P or Positive Parenting Program is an example of a universal program that supports positive parenting at the individual, family, community, and societal levels through targeted education and social campaigns ( 1 ).
Secondary strategies have been primarily focused at the individual and family levels. Child protective service agencies are one example, which are widespread but vary markedly in different countries and states and often address the most severe cases of child maltreatment. New programs that attempt to identify and respond to adverse experiences earlier, and before they are severe enough to require hospital treatment or an official agency response, are growing in priority such as home visiting programs that are found to be effective in reducing child abuse and neglect and improving family function ( 56 ).
Interventions such as psychological first aid (PFA) implemented in nonfamily settings, such as schools or health facilities, may provide the opportunity to identify effected children early and to increase program reach. Although originally developed as a response to disasters, PFA provides a framework that has been applied to other personal adverse experiences such as interpersonal violence and family trauma ( 57 ). PFA identifies children and their caregivers immediately after a life stressor and provides information, education, comfort, and support, which results in acceleration of recovery, promotion of mental health, and increased resiliency ( 58 , 59 ). Recently, the World Health Organization published “Psychological first aid: Guide for field workers,” which describes crises ranging from “war to natural disasters, accidents, fires, and interpersonal violence.” ( 60 ). Adults trained in PFA report increased knowledge, skills, and self-efficacy in applying skills to support youth with histories of trauma ( 61 , 62 ). One study also reported PFA being effective in improving connectedness and stress among youth traumatized by a disaster, bullying, death or illness of a family member, or injury ( 59 ). Thus, PFA is an ideal program that may be delivered by all members of a trauma-informed organization, even by those without advanced mental health training.
In addition, parent-child interaction therapy (PCIT) and child parent psychotherapy (CPP) are also emerging evidence-based treatment modalities to prevent and manage ACEs and their impact on the intrafamilial relationships as early as possible via a two-generational approach ( 63 , 64 ).
Cognitive behavioral therapy is the most common approach to reduce psychological symptoms from trauma that can be directed at all family members. Systematic reviews of the effectiveness of cognitive behavioral therapy on adults show that is has some effect on reducing symptoms of posttraumatic stress disorder, depression, and anxiety and has the potential to change dysfunctions of the nervous system ( 65 , 66 ). New evidence suggests that family approaches are best ( 67 ). Evidence for cognitive behavioral therapy for children is mixed, and increasing knowledge about the pediatric brain may help inform child-based approaches ( 68 ).
Other tertiary approaches are found predominantly in educational, medical, child welfare, and justice settings. TIC, which is being integrated in settings such as health care, service agencies for high-risk families, and in correctional facilities, help service providers become aware of the effects of ACEs and how to integrate compassionate care. Although TIC is among the most prevalent strategies to address ACEs, few outcome evaluation studies have been conducted ( 51 , 69 , 70 , 71 ).
Critical gaps exist in the evidence base for responding to ACEs, especially for primary prevention at the community and sociopolitical levels. Gaps in our foundational knowledge about the global prevalence and cultural differences in response to ACEs also hinder prevention.
Trauma Informed Care
TIC is considered a comprehensive multilevel approach that shifts the way organizations view and approach trauma. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) ( 72 ),
“A program, organization, or system that is trauma-informed realizes the widespread impact of trauma and understands potential paths for recovery; recognizes the signs and symptoms of trauma in clients, families, staff, and others involved with the system; and responds by fully integrating knowledge about trauma into policies, procedures, and practices, and seeks to actively resist re- traumatization.”
The impetus for TIC stems from a realization that systems of care that serve children are often unaware of trauma experiences of their clientele, which may lead to re-traumatization and failure to provide appropriate referrals ( 73 , 74 ). TIC involves validation and recognition of the effects of traumatic events, common coping strategies, and effective treatments. Transforming organizations into trauma-informed systems entails organizational changes and the development of culturally sensitive infrastructure that is responsive to the needs of traumatized individuals ( 74 ).
The SAMHSA promotes the use of six broad principles for TIC ( 74 ):
1. Safety. Promoting a sense of safety involves a conscious effort to ensure that all members and clients of an organization are physically and emotionally safe.
2. Trustworthiness and transparency. Organizations must approach decisions with transparency and engender trust of staff and their clientele.
3. Peer support. Peers, which include family of traumatized children as well as individuals who have lived with histories of trauma, can be critical resources for support.
4. Collaboration and mutuality. All members of an organization can equally contribute to the healing of children impacted by adverse experiences.
5. Empowerment, voice, and choice. Developing plans of action for clients requires patient-centered approaches that empower clients.
6. Cultural, historical and gender issues. Efforts must be culturally sensitive and free of prejudices based on biases and stereotypes.
Efforts to integrate these principles require support at the top levels of an organization and the implementation of policies and protocols to assure that trauma-informed activities are carried out by staff ( 51 ). As an example, the architecture of patient rooms and the physical environment must be inviting and pose no risk for re-traumatization.
Another essential component of TIC identified by SAMHSA and other researchers is the implementation of screening, assessment, and trauma treatment services to identify children who have experienced adversity ( 72 , 74 ). Adoption of trauma-screening procedures should be coupled with screening for resiliency, family functional capacity, community-based resources, behavioral and neuropsychological assessments, and previous interventions for trauma ( 74 ).
Trauma-informed organizations must adopt trauma-specific interventions that work in concert with screening for trauma. Although SAMHSA provides a list of known trauma-specific interventions, most of which are based on psychosocial educational empowerment principals and require professional therapists for delivery, none are currently being endorsed as for use in concert with TIC ( 75 ). Others, however, are discussing the need for integrating specific evidence-based strategies such as parent-child interaction therapy and child parent psychotherapy into trauma-informed systems that service youth who may have histories of trauma ( 64 , 72 ).
Implementation of TIC
A number of communities have embraced TIC to support children with adverse experiences. In 2000, Tarrant County in Texas formed a “mental health connection” collaboration of medical, county, city, and child health agencies and developed a strategic plan that involved the development of “learning communities” engaged in implementing local efforts in prevention, which included education and training; screening and referral through service agencies; and implementation of trauma-focused cognitive behavioral therapy sessions ( 33 ). The community State agencies are now beginning to adopt trauma-informed approaches, including the Oregon Health Authority and New York’s juvenile justice system ( 72 ).
In 2005, the National Center for Trauma Informed Care was created by SAMHSA to provide training and technical assistance to support communities and organizations interested in becoming trauma-informed via in-person consultation and through virtual networks, and by providing materials, curricula, and resources ( 75 ). The Child Welfare Information Gateway is another agency providing support specifically to child welfare agencies to develop trauma-informed systems ( 76 ).
New research is emerging on the effectiveness of TIC in improving health care delivery. One study reported that primary care providers trained in TIC had increased patient-centered interactions and patient satisfaction ( 69 ). Suarez et al . ( 77 ) reported early results of improved outcomes among at-risk girls serviced by Project Kealeahou in Hawaii. Centers from California, Massachusetts, Ohio, Wisconsin, Iowa, among others, are also implementing TIC in medical setting with promising positive outcome results ( 64 ). Additional research is needed to fully understand the impacts of trauma informed approaches on children.
Statement of Financial Support
The authors report no conflict of interest.
Garner AS, Shonkoff JP ; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics 2012; 129 :e224–31.
Article Google Scholar
Shonkoff JP, Garner AS, Siegel BS, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012; 129 :232–46.
Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA 2001; 286 :3089–96.
Article CAS Google Scholar
Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998; 14 :245–58.
National Child Traumatic Stress Network. Types of traumatic stress, 2015. ( http://www.nctsn.org/trauma-types . )
Center for the Study of Traumatic Stress. The impact of kidnapping, shooting and torture on children, 2015. ( http://www.cstsonline.org/assets/media/documents/CSTS_impact_kidnapping_shooting_torture_children.pdf .)
Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry 2010; 197 :378–85.
Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatr 2013; 167 :70–5.
Marie-Mitchell A, O’Connor TG. Adverse childhood experiences: translating knowledge into identification of children at risk for poor outcomes. Acad Pediatr 2013; 13 :14–9.
Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics 2013; 131 :319–27.
Elenkov IJ, Chrousos GP. Stress system–organization, physiology and immunoregulation. Neuroimmunomodulation 2006; 13 :257–67.
Carroll TB, Aron DC, Findling JW, Tyrrell B. Glucocorticoids and adrenal androgens. In: Gardner DG, Shoback D, eds. Greenspan’s Basic and Clinical Endocrinology, 9th edn . New York: McGraw-Hill, 2011:285–327.
Google Scholar
Webster JI, Tonelli L, Sternberg EM. Neuroendocrine regulation of immunity. Annu Rev Immunol 2002; 20 :125–63.
National Scientific Council on the Developing Child. Excessive stress disrupts the architecture of the developing brain: Working Paper 3. Updated Edition, 2015 . ( http://developingchild.harvard.edu/resources/reports_and_working_papers/working_papers/wp3/ .)
Brodal P. The Central Nervous System: Structure and Function, 3rd edn. New York: Oxford University Press, 2004.
National Scientific Council on the Developing Child. Early experiences can alter gene expression and affect long-term development: Working Paper No. 10, 2015. ( http://developingchild.harvard.edu/index.php/resources/reports_and_working_papers/working_papers/wp10/ .)
Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA 2009; 301 :2252–9.
Centers for Disease Control and Prevention. Adverse childhood experiences reported by adults --- five states, 2009. MMWR Morb Mortal Wkly Rep 2010; 59 :1609–13.
Iowa Aces 360. Adverse childhood experiences in Iowa: a new way of understanding lifelong health, 2015 . ( http://www.iowafoodandfitness.org/uploads/PDF_File_74101481.pdf .)
Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl 2011; 35 :408–13.
Zolotor AJ, Runyan DK, Dunne MP, et al. ISPCAN Child Abuse Screening Tool Children’s Version (ICAST-C): instrument development and multi-national pilot testing. Child Abuse Negl 2009; 33 :833–41.
CORDIS: Community Research and Development Information Service. Final Report Summary - BECAN (Balkan Epidemiological Study on Child Abuse and Neglect), 2015 . ( http://www.cordis.europa.eu/result/rcn/58856_en.html .)
Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: a neglected component in child victimization. Child Abuse Negl 2007; 31 :7–26.
Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA 1999; 282 :1652–8.
Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation 2004; 110 :1761–6.
Anda RF, Brown DW, Dube SR, Bremner JD, Felitti VJ, Giles WH. Adverse childhood experiences and chronic obstructive pulmonary disease in adults. Am J Prev Med 2008; 34 :396–403.
Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med 2009; 71 :243–50.
Felitti VJ, Anda RF. The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders, and sexual behavior: implications for healthcare. In: Lanius R, Vermetten E, eds. The Hidden Epidemic: The Impact of Early Life Trauma on Health and Disease . Cambridge University Press, 2010:77–87.
Chapter Google Scholar
Pilowsky DJ, Keyes KM, Hasin DS. Adverse childhood events and lifetime alcohol dependence. Am J Public Health 2009; 99 :258–63.
Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse Negl 2013; 37 :917–25.
Schilling EA, Aseltine RH Jr, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health 2007; 7 :30.
Hillis SD, Anda RF, Felitti VJ, Nordenberg D, Marchbanks PA. Adverse childhood experiences and sexually transmitted diseases in men and women: a retrospective study. Pediatrics 2000; 106 :E11.
Dube SR, Cook ML, Edwards VJ. Health-related outcomes of adverse childhood experiences in Texas, 2002. Prev Chronic Dis 2010; 7 :1–9.
Brown DW, Anda RF, Tiemeier H, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med 2009; 37 :389–96.
Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache 2010; 50 :1473–81.
Bader K, Schäfer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. J Sleep Res 2007; 16 :285–96.
Danese A, Moffitt TE, Harrington H, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med 2009; 163 :1135–43.
Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics 2010; 125 :e778–86.
Flaherty EG, Thompson R, Litrownik AJ, et al. Adverse childhood exposures and reported child health at age 12. Acad Pediatr 2009; 9 :150–6.
Maaranen P, Tanskanen A, Haatainen K, Koivumaa-Honkanen H, Hintikka J, Viinamäki H. Somatoform dissociation and adverse childhood experiences in the general population. J Nerv Ment Dis 2004; 192 :337–42.
Briggs ES, Price IR. The relationship between adverse childhood experience and obsessive-compulsive symptoms and beliefs: the role of anxiety, depression, and experiential avoidance. J Anxiety Disord 2009; 23 :1037–46.
Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse Negl 2010; 34 :454–64.
Mc Elroy S, Hevey D. Relationship between adverse early experiences, stressors, psychosocial resources and wellbeing. Child Abuse Negl 2014; 38 :65–75.
Anda RF, Dong M, Brown DW, et al. The relationship of adverse childhood experiences to a history of premature death of family members. BMC Public Health 2009; 9 :106.
Bentovim A, Davenport M. Resolving the trauma organized system of sexual abuse by confronting the abuser. J Fam Therapy 1992; 14 :29–50.
Burns EE, Jackson JL, Harding HG. Child maltreatment, emotion regulation, and posttraumatic stress: the impact of emotional abuse. J Aggress Maltreatment Trauma 2010; 19 :801.
Powers A, Cross D, Fani N, Bradley B. PTSD, emotional dysregulation, and dissociative symptoms in a highly traumatized sample. J Psychiatr Res 2015: 61 ;144–179.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 . Washington, D.C: American Psychiatric Association, 2013.
Klimova A, Bryant RA, Williams LM, Felmingham KL. Dysregulation in cortical reactivity to emotional faces in PTSD patients with high dissociation symptoms. Eur J Psychotraumatol 2013; 4 .
Dahlberg LL, Krug EG. Violence-a global public health problem. In: Krug E, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, eds. World Report on Violence and Health . Geneva, Switzerland: World Health Organization, 2002:1–56.
DeCandia C, Guarino K, Clervil R. Trauma-informed care and trauma-specific services: a comprehensive approach to trauma intervention, 2015. ( http://www.air.org/sites/default/files/downloads/report/Trauma-Informed%20Care%20White%20Paper_October%202014.pdf .)
Poole MK, Seal DW, Taylor CA. A systematic review of universal campaigns targeting child physical abuse prevention. Health Educ Res 2014; 29 :388–432.
Prinz RJ, Sanders MR, Shapiro CJ, Whitaker DJ, Lutzker JR. Population-based prevention of child maltreatment: the U.S. Triple p system population trial. Prev Sci 2009; 10 :1–12.
Cassidy J, Woodhouse SS, Sherman LJ, Stupica B, Lejuez CW. Enhancing infant attachment security: an examination of treatment efficacy and differential susceptibility. Dev Psychopathol 2011; 23 :131–48.
Barr RG, Rivara FP, Barr M, et al. Effectiveness of educational materials designed to change knowledge and behaviors regarding crying and shaken-baby syndrome in mothers of newborns: a randomized, controlled trial. Pediatrics 2009; 123 :972–80.
Garner AS. Home visiting and the biology of toxic stress: opportunities to address early childhood adversity. Pediatrics 2013; 132 :Suppl 2:S65–73.
National Research Council. Preparing for the Psychological Consequences of Terrorism: A Public Health Strategy . Washington, DC: The National Academies Press, 2003:99–135.
Berger R, Pat-Horenczyk R, Gelkopf M. School-based intervention for prevention and treatment of elementary-students’ terror-related distress in Israel: a quasi-randomized controlled trial. J Trauma Stress 2007; 20 :541–51.
Ramirez M, Harland K, Frederick M, Shepherd R, Wong M, Cavanaugh JE. Listen protect connect for traumatized schoolchildren: a pilot study of psychological first aid. BMC Psychol 2013; 1 :26.
World Health Organization, War Trauma Foundation and World Vision International. Psychological First Aid: Guide for Field Workers . Geneva, Switzerland: World Health Organization, 2011. ( http://whqlibdoc.who.int/publications/2011/9789241548205_eng.pdf?ua=1 .)
Kelly CM, Mithen JM, Fischer JA, et al. Youth mental health first aid: a description of the program and an initial evaluation. Int J Ment Health Syst 2011; 5 :4.
Jorm AF, Kitchener BA, Sawyer MG, Scales H, Cvetkovski S. Mental health first aid training for high school teachers: a cluster randomized trial. BMC Psychiatry 2010; 10 :51.
The National Child Traumatic Stress Network. Treatments for Children and Families, 2015 . ( http://www.nctsn.org/content/treatments-children-and-families .)
American Academy of Pediatrics (AAP). Conference on Violence, Abuse and Toxic Stress , San Francisco, CA, 30 July 2015–2 August 2015.
Forneris CA, Gartlehner G, Brownley KA, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med 2013; 44 :635–50.
Porto PR, Oliveira L, Mari J, Volchan E, Figueira I, Ventura P. Does cognitive behavioral therapy change the brain? A systematic review of neuroimaging in anxiety disorders. J Neuropsychiatry Clin Neurosci 2009; 21 :114–25.
Cohen JA, Mannarino AP. Trauma-focused cognitive behavior therapy for traumatized children and families. Child Adolesc Psychiatr Clin N Am 2015; 24 :557–70.
Jenkinson E, Williamson H, Byron-Daniel J, Moss TP. Systematic review: psychosocial interventions for children and young people with visible differences resulting from appearance altering conditions, injury, or treatment effects. J Pediatr Psychol ; e-pub ahead of print 25 May 2015.
Green BL, Saunders PA, Power E, et al. Trauma-informed medical care: CME communication training for primary care providers. Fam Med 2015; 47 :7–14.
PubMed PubMed Central Google Scholar
Hanson RF, Lang J. Special focus section: a critical look at trauma informed care (TIC) among agencies and systems serving maltreated youth and their families. Child Maltreat 2014; 19 :275.
Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med 2010; 39 :93–8.
Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach, 2015 . ( http://store.samhsa.gov/shin/content/SMA14-4884/SMA14-4884.pdf .)
Ko SJ, Kassam-Adams N, Wilson C, et al. Creating trauma-informed systems: child welfare, education, first responders, health care, juvenile justices. Prof Psychol-Res Pr 2008; 39 :396–404.
Harris M, Fallot RD. Envisioning a Trauma-Informed Service System: A Vital Paradigm Shift: New Directions for Mental Health Services . San Francisco, CA: Jossey-Bass, 2001:3–22.
Substance Abuse and Mental Health Services Administration. Trauma-Informed Approach and Trauma-Specific Interventions, 2015 . ( http://www.samhsa.gov/nctic/trauma-interventions .)
Childwelfare Information Gateway. Trauma-informed practice, 2015 . ( https://www.childwelfare.gov/topics/responding/trauma/ .)
Suarez E, Jackson DS, Slavin LA, Michels MS, McGeehan KM. Project Kealahou: improving Hawai’i’s system of care for at-risk girls and young women through gender-responsive, trauma-informed care. Hawaii J Med Public Health 2014; 73 :387–92.
Download references
Author information
Authors and affiliations.
Department of Pediatrics, University of Iowa, Iowa City, Iowa
Resmiye Oral & Jenna Benoit
College of Public Health, University of Iowa, Iowa City, Iowa
Marizen Ramirez & Corinne Peek-Asa
School of Social Work, University of Iowa, Iowa City, Iowa
Carol Coohey
Carver College of Medicine, University of Iowa, Iowa City, Iowa
Stephanie Nakada, Amy Walz & Angela Kuntz
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Resmiye Oral .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Oral, R., Ramirez, M., Coohey, C. et al. Adverse childhood experiences and trauma informed care: the future of health care. Pediatr Res 79 , 227–233 (2016). https://doi.org/10.1038/pr.2015.197
Download citation
Received : 17 April 2015
Accepted : 23 August 2015
Published : 13 October 2015
Issue Date : January 2016
DOI : https://doi.org/10.1038/pr.2015.197
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Effect of parental adverse childhood experiences on intergenerational dna methylation signatures from peripheral blood mononuclear cells and buccal mucosa.
- Sahra Mohazzab-Hosseinian
- Erika Garcia
- Carrie V. Breton
Translational Psychiatry (2024)
Mediating Effects of Psychological Resilience and Self-esteem on the Association Between Early Childhood Adversity and Depressive Symptoms Among Adolescents in Nigeria
- Olanrewaju Ibikunle Ibigbami
- Morenike Oluwatoyin Folayan
- Joanne Lusher
Adversity and Resilience Science (2024)
The Direct and Indirect Effects of Adverse Childhood Experiences on Depressive Symptoms and Self-esteem of Children: Does Gender Make a Difference?
- Xinwen Zhang
International Journal of Mental Health and Addiction (2024)
Adverse childhood events and mental health problems in cancer survivors: a systematic review
- Chris Hinnen
- Emma von Haeseler
- Floortje Mols
Supportive Care in Cancer (2024)
Adverse Childhood Experiences and Illegal Drug Use Among College Students: Findings from a French Sample
- Ashlyn Schwartz
- Cédric Galera
- Christophe Tzourio
International Journal of Behavioral Medicine (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Buffalo Center for Social Research >
- Institutes >
- Institute on Trauma and Trauma-Informed Care
The Institute on Trauma and Trauma-Informed Care
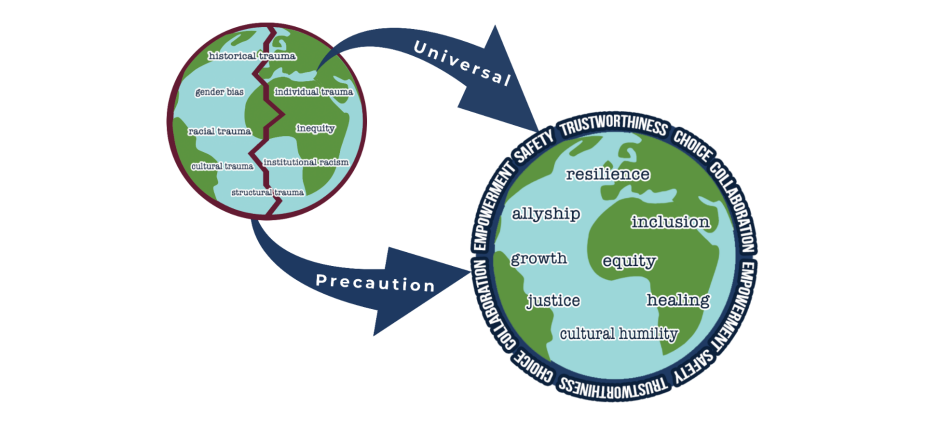
Trauma-informed care provides the framework for individuals, organizations and systems to engage in universal precautions for individual, historical and systemic trauma by using the values and principles of safety, trustworthiness, choice, collaboration and empowerment.

Providing research and training for organizations on trauma and trauma-informed care since 2012.
The UB School of Social Work’s Institute on Trauma and Trauma-Informed Care (ITTIC) helps organizations and individuals understand the effects of trauma and ensure that service systems do not retraumatize vulnerable populations. Through collaborative partnerships and funded research, we work with agencies to provide training, consultation, coaching and evaluation to facilitate trauma-informed culture change and meet your organization’s goals.
Welcome to ITTIC
What is trauma-informed care?
Learn about us
Meet our partners
Make a gift
Work With Us
We collaborate with agencies and organizations to provide education, training, consultation, coaching, and evaluation services on trauma and trauma-informed approaches. Our services are always tailored to your organization's unique needs. Collaborate with us to develop a work plan that meets your goals and aligns with best practices.

The ITTIC team collaborated with the Kenmore-Tonawanda School District to facilitate trauma-informed culture change .
More From ITTIC
Latest news.
5/28/24 - We are happy to share our newly updated What is Trauma-Informed Care page . We have new descriptions, graphics and resources to share. Let us know what you think by sending us an email at [email protected] .
Useful Resources
Request free access to our manual. Use our step-by-step guide to plan, implement and sustain trauma-informed cultural change in your organization.

Improve your understanding of trauma — or train your entire staff on the basics of trauma-informed care — with our online, self-study course.

This online, self-guided training is for all types of supervisors (clinical and non-clinical) who wish to be trauma-informed in their interactions with staff.
- Tools and Resources
- Customer Services
- Addictions and Substance Use
- Administration and Management
- Aging and Older Adults
- Biographies
- Children and Adolescents
- Clinical and Direct Practice
- Couples and Families
- Criminal Justice
- Disabilities
- Ethics and Values
- Gender and Sexuality
- Health Care and Illness
- Human Behavior
- International and Global Issues
- Macro Practice
- Mental and Behavioral Health
- Policy and Advocacy
- Populations and Practice Settings
- Race, Ethnicity, and Culture
- Religion and Spirituality
- Research and Evidence-Based Practice
- Social Justice and Human Rights
- Social Work Profession
- Share This Facebook LinkedIn Twitter
Article contents
Trauma-informed care.
- Charles Wilson , Charles Wilson Chadwick Center for Children and Families, Rady Children Hospital, San Diego
- Donna M. Pence Donna M. Pence San Diego State University
- and Lisa Conradi Lisa Conradi Chadwick Center for Children and Families, Rady Children's Hospital, San Diego
- https://doi.org/10.1093/acrefore/9780199975839.013.1063
- Published online: 04 November 2013
The concepts of trauma and trauma-informed care have evolved greatly over the past 30 years. Following the Vietnam War, professional understanding of post-traumatic stress disorder (PTSD) increased. The greater understanding of trauma and its effects on war veterans has extended to informing our comprehension of trauma in the civilian world and with children and families who have experienced abuse, neglect, and other traumatic events. This elevated insight has led to the development of evidence-based models of trauma treatment along with changes in organizational policies and practices designed to facilitate resilience and recovery. This paper highlights the concept of trauma-informed care by providing an overview of trauma and its effects, then providing a comprehensive description of our understanding of trauma-informed care across child- and family-serving systems.
- post-traumatic stress disorder
- psychological safety
- trauma-informed care
- trauma-informed systems
The concepts of trauma-informed care have evolved over the past 30 years from a variety of streams of thought and innovation. They are now being applied in a wide range of settings, from mental health and substance-abuse treatment providers to child welfare systems and even schools and criminal justice institutions. In the simplest terms, the concept of trauma-informed care is straightforward. If professionals were to pause and consider the role trauma and lingering traumatic stress plays in the lives of the specific client population served by an individual, professional, organization, or an entire system, how would they behave differently? What steps would they take to avoid, or at least minimize, adding new stress or inadvertently reminding their clients of their past traumas? How can they better help their traumatized clients heal? In effect, by looking at how the entire system is organized and services are delivered through a “trauma lens,” what should be done differently? The answer can be used to guide practice, policy, procedures, and even how the physical caregiving environment is structured.
Foundations of Trauma-Informed Care
Long before anyone used the term “trauma-informed,” caring professionals and committed volunteers were instinctively acting in a trauma-informed manner. Much of this was influenced by the emergence of the feminist movement and the increasingly influential voice of survivors of interpersonal trauma, as seen in the rape crisis centers and the domestic violence movements of the 1970s (Burgess & Holmstrom, 1974 ) and the dramatic growth of child-advocacy centers and multidisciplinary teams in child abuse in the 1980s. These natural incubators for trauma-informed innovation and practice were “married” in the 1990s with the growing body of science and trauma-specific empirical research into how human beings respond in the aftermath of traumatic events, and how professionals and concerned activists could help them move toward recovery. That stream of research began with interest in combat-related post-traumatic stress after the Vietnam War. By the mid-1980s, the focus had expanded and was adopted by the wider mental health community as a relevant construct for understanding the cascade of symptoms often noted after rapes, shootings, and other major traumatic life events. In 1985, the International Society for Traumatic Stress was founded in the United States and served as a focal point for professionals searching for answers to support highly traumatized populations. By 1989, the United States Department of Veterans Affairs had created the National Center for Post-Traumatic Stress Disorder ( www.ptsd.va.gov ). In the 1990s, the Substance Abuse and Mental Health Administration (SAMHSA), within the U.S. Department of Health and Human Services, recognized the role of trauma in a significant number of women’s issues and gender-specific treatments. Over the next 20 years, a huge expansion of knowledge about trauma and traumatic stress occurred. This included not only better diagnostic criteria but also the development of empirically tested treatments for PTSD and other related trauma symptoms.

What Is Trauma?
Defining trauma is not without its controversies. Those who approach it from a clinical perspective tend to view trauma as a combination of a terrible event or series of events that involve real or perceived threats of death or serious injury, or threat to the physical integrity of the person or others, and from which that person experiences overwhelming fear, hopelessness, helplessness, or horror. This type of overwhelming stress, especially when it occurs over and over, as is common in many individuals served by the social work community, can create significant long-term impacts, including changes in the physiology of the brains of developing children. Some survivors of trauma, however, favor a definition that places greater emphasis on the subjective experience and the level of stress an individual perceives, independent of an event or series of events that threaten the individual with death, serious injury, or loss of their physical integrity such as a highly emotional argument with a family member (Substance Abuse and Mental Health Services Administration, 2012 ).
Prevalence of Trauma
Most individuals seeking public behavioral health services and other public services, such as homeless and domestic violence services, have histories of physical and sexual abuse, and witnessing or experiencing domestic violence, and they often live in neighborhoods where community violence is ever present. These individuals often present with co-occurring disorders such as chronic health conditions, substance abuse, eating disorders, and HIV/AIDS. In fact, 50% to 70% of women in psychiatric hospitals, 40% to 60% of women receiving outpatient mental health services, and 55% to 90% of women with substance abuse disorders report being physically or sexually abused, or both, in their lives ((Substance Abuse and Mental Health Services Administration, 2007 ). While trauma occurs throughout the lifespan, for many seeking the services of social workers and other helping professionals, the trauma began in childhood. Studies have reported high rates of trauma among children in the United States since the 1950s (Landis, 1956 ). For example, in one study, the authors found that 25% of their sample of nine- to 16-year-olds had recently experienced a potentially traumatic event (Costello, Erkanli, Fairbank, & Angold, 2002 ). Child abuse and neglect is an all-too-common form of trauma. In 2011, there were approximately 3.4 million reports of abuse or neglect that covered 6.2 million children (U.S. Department of Health and Human Services [DHHS], 2011. Another study found that approximately 15.5 million children were estimated to live in homes where they were exposed to at least one incidence of domestic violence in the previous year (McDonald, Jouriles, Ramisetty-Mikler, et al., 2006 .). Anda and Felitti ( 2003 ) found that 21% of a 17,000-person sample drawn from adults enrolled in a San Diego Health Maintenance Organization reported being sexually abused; 26% were physically abused; and 13% lived in a home with domestic violence as a child. These and other studies reveal that a substantial number of children have experienced abuse or exposure to other traumatic events prior to their eighteenth birthday.
Not only are these forms of trauma common, they are among the most emotionally devastating and have been linked to a host of negative outcomes in childhood, from emotional and behavioral problems to impaired school performance (Conradi & Wilson, 2010 ; Ethier, Lemelin, & Lacharite, 2004 ). Without effective intervention, there is compelling evidence of long-term adverse consequences of untreated trauma lasting into adulthood that include substance abuse, suicidality, serious mental illness, and long-term physical health factors associated with early death (Felitti, Anda, Nordenberg, Williamson, et al., 1998 ; Anda, Dong, Brown, et al, 2009 ).
Whether children or adults, those who have experienced a traumatic event are likely to come into contact with multiple systems. Child welfare services alone come into contact with over 6 million children a year (US DHHS, 2011 ), and there are as many as 223,000 children placed in the protective custody of state or local governments at any one time (US DHHS, 2012 ). Youth involved in the juvenile justice system also present with high rates of trauma. In one study of a juvenile justice population, 92.5% of participants had experienced one or more traumatic events in their lifetime, and 11.2% of the sample met criteria for PTSD in the past year (Abram, Teplin, Charles, et al., 2004 ). By virtue of the events that brought the children into contact with these systems, and the additional traumas the system may impose (removal from the home, changes in placement, instability of relationships, use of seclusion and restraint, risk of re-abuse, inconsistent caregivers and caseworkers, separation of siblings, and so forth), virtually all have suffered major trauma.
Unique Response to Highly Stressful Events
Trauma, however, does not affect everyone in the same way. Some people experience a terrible event but suffer no long-term adverse emotional effects, while the same event have a devastating impact on the individual standing next to them. Traumatic response is highly individualized and shaped by a wide range of factors, from genetics, to previous life experiences, to support systems available in the aftermath of the event. How helping professionals respond also influences the long-term impact of traumatic events for the better, when delivered in a trauma-informed environment, or for the worse, if delivered in a trauma-insensitive manner, as has been the case for much of history.
The Emergence of Trauma-Informed Care
In 1994, the Substance Abuse and Mental Health Services Administration (SAMHSA) convened the Dare to Vision conference, which explored the high prevalence of physical and sexual abuse among women served by the public mental health system. This event provided a forum for survivors to discuss their trauma histories and how trauma impacted their physical and mental health. It highlighted the re-victimization many experienced in residential or inpatient settings through the use of such practices as seclusion and restraint. By the late 1990s and early 2000s, a variety of professionals began to articulate the importance of the organizational context in the delivery of services to individuals who have experienced significant traumatic life events (Bloom, 1997 ; Harris & Fallot, 2001 ; Covington, 2002 ; Rivard, Bloom, & Abramovitz, 2003 ; Ko, Ford, Kassam-Adams N., et al., 2008 ; Bloom, 2010 ). The concepts at the core of “trauma-informed care” began to take greater shape and spread with the launch in 1998 of the Women, Co-Occurring Disorders and Violence Study, sponsored by SAMHSA (see www.wcdvs.com for more information), which integrated service system strategies for women with co-occurring mental health and substance abuse disorders who have also been victims of trauma. This study, carried out in 27 sites over five years in two phases (fourteen Phase One women sites, nine Phase Two women sites, and four Phase Two children’s sites), provided recommendations for “trauma-integrated services counseling.” This important study laid out a framework of principles for this population, complete with guidance for providers to be cognizant of their own practices and policies that might put women in danger physically and psychologically, add new traumatic experiences, or unnecessarily trigger memories of past traumatic events. The study highlighted the importance of “all service interventions [being] gender-specific, culturally competent, trauma-informed and trauma-specific, comprehensive, integrated, and [with] consumer/survivor/recovering women involved” (U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, 2007 , p.1). This study and others brought attention to the need for trauma-informed care in the adult world.
In 2001, the U.S. Congress and SAMHSA established the Donald J. Cohen National Child Traumatic Stress Initiative, and, through it, the National Child Traumatic Stress Network (NCTSN, www.nctsn.org ). This national network, under the leadership of the National Center for Child Traumatic Stress at Duke University and the University of California–Los Angeles (UCLA), initially focused on the mission of raising “the standard of care and improve access to services for traumatized children, their families and communities throughout the United States.” Toward that end, the NCTSN concentrated on the identification and spread of empirically supported trauma-specific mental health interventions such as TraumaFocused Cognitive Behavioral Therapy (Deblinger, Lippmann, & Steer, 1996 ; Cohen, Deblinger, Mannarino, & Steer, 2004 ; Cohen, Mannarino, & Staron, 2006 ) Deblinger, Mannarino, Cohen, & Steer ( 2006 ); Cohen, Mannarino & Iyengar ( 2011 ), and Child-Parent Psychotherapy (Lieberman, Weston, & Pawl, 1991 ; Cicchetti, Toth, & Rogosch, 1999 ; Toth, Maughan, Manly, Spagnola, & Cicchetti, 2002 ; Lieberman, Ghosh Ippen, & Van Horn, 2006 ). By 2003, however, the NCTSN increasingly recognized that system issues could support or undermine effective trauma-specific treatments and began to explore the organization and system context in which trauma-specific interventions were being delivered, with the establishment of the Systems Integration Committee (Taylor & Siegfried, 2005 ). In short order, that effort was replaced by system-specific initiatives within the NCTSN designed to facilitate the NCTSN mission within the context of specific systems, including child welfare, juvenile justice, schools, and health care (Ko, Ford, Kassam-Adams, et al., 2008 ). In these efforts, the lessons learned in the Women with Co-Occurring Disorders Study and early adopters of trauma-informed care in the adult trauma world, along with the practical experience implementing trauma-specific interventions in child-serving environments, were integrated to create a trauma-informed perspective to serving traumatized children and their families.
As the term trauma-informed care took root in both adult- and child-serving worlds, distinctions began to be drawn between related, but discrete, perspectives. These ranged from “trauma-informed care” to “trauma-informed practice,” “trauma-informed organizations,” “trauma-specific treatments,” “trauma-informed systems,” and “trauma-informed approaches”; all linked by the concept of “trauma-informed.”
What Does It Mean to Be Trauma-Informed?
Many organizations and authors have offered definitions or a list of elements about what constitutes trauma-informed care or the related concepts of trauma-informed practice, organizations, and systems. In 2005, SAMHSA established the National Center for Trauma- Informed Care (NCTIC). The NCTIC suggested that every part of an organization seeking to be trauma-informed—its organizational structure, its management systems, and its service delivery—be
assessed and potentially modified to include a basic understanding of how trauma affects the life of an individual seeking services. Trauma-informed organizations, programs, and services are based on an understanding of the vulnerabilities or triggers of trauma survivors that traditional service delivery approaches may exacerbate, so that these services and programs can be more supportive and avoid re-traumatization. (National Center for Trauma-Informed Care, 2012 )
Fallot and Harris ( 2009 ) suggest that trauma-informed care is built on five core values: (1) safety, (2) trustworthiness, (3) choice, (4) collaboration, and (5) empowerment. Here safety means both physical and emotional safety, while trustworthiness relates to the clarity of expectations, providing consistent service delivery across the organization, and maintaining boundaries. Fallot and Harris’s view of trauma-informed care emphasizes the active role of the person receiving the services or support. The concept of choice is important because it gives the consumer control over the services they receive. Control is significant because, as a victim of trauma, client control was taken from the during the traumatic event, whether through a rape, physical assault, or even a natural disaster. Collaboration emphasizes the need for client involvement and sharing of power, while empowerment relates to the development and enhancement of consumer skills.
In a working paper, US Department of Health and Human Servicese(USHHS/SAMHSA, 2012 suggests that a trauma-informed approach is guided by 10 principles:
Safety: throughout the organization, staff and the people they serve feel physically and psychologically safe; the physical setting is safe and interpersonal interactions promote a sense of safety.
Trustworthiness and transparency: organizational operations and decisions are conducted with transparency and the goal of building and maintaining trust among staff, clients, and family members of people being served by the organization.
Collaboration and mutuality: there is true partnering and leveling of power differences between staff and clients and among organizational staff from direct care staff to administrators; there is recognition that healing happens in relationships and in the meaningful sharing of power and decision-making.
Empowerment: throughout the organization and among the clients served, individuals’ strengths are recognized, built on, and validated and new skills developed as necessary.
Voice and choice: the organization aims to strengthen the staff’s, clients’, and family members’ experience of choice and recognize that every person’s experience is unique and requires an individualized approach.
Peer support and mutual self-help: are integral to the organizational and service delivery approach and are understood as a key vehicle for building trust, establishing safety, and empowerment.
Resilience and strengths based: a belief in resilience and in the ability of individuals, organizations, and communities to heal and promote recovery from trauma; builds on what clients, staff and communities have to offer rather than responding to their perceived deficits.
Inclusiveness and shared purpose: the organization recognizes that everyone has a role to play in a trauma-informed approach; one does not have to be a therapist to be therapeutic.
Cultural, historical, and gender issues: the organization addresses cultural, historical, and gender issues; the organization actively moves past cultural stereotypes and biases (e.g. based on race, ethnicity, sexual orientation, age, geography, etc.), offers gender responsive services, leverages the healing value of traditional cultural connections, and recognizes and addresses historical trauma.
Change process: is conscious, intentional and ongoing; the organization strives to become a learning community, constantly responding to new knowledge and developments (What are the Key Principles of a Trauma-informed Approach? section)
Meanwhile, the National Child Traumatic Stress Network (NCTSN, 2012 , What is a trauma-informed child- and family-service system? section, para. 1) defines the trauma-informed child-and family-serving system as one in which
all parties involved recognize and respond to the impact of traumatic stress on those who have contact with the system including children, caregivers, and service providers. Programs and agencies within such a system infuse and sustain trauma awareness, knowledge, and skills into their organizational cultures, practices, and policies. They act in collaboration with all those who are involved with the child, using the best available science, to facilitate and support the recovery and resiliency of the child and family.
The NCTSN goes on to suggest that a service system with a trauma-informed perspective is one in which programs, agencies, and service providers (NCTSN, 2012 ):
routinely screen for trauma exposure and related symptoms;
use culturally appropriate evidence-based assessment and treatment for traumatic stress and associated mental health symptoms;
make resources available to children, families, and providers on trauma exposure, its impact, and treatment;
engage in efforts to strengthen the resilience and protective factors of children and families impacted by and vulnerable to trauma;
address parent and caregiver trauma and its impact on the family system;
emphasize continuity of care and collaboration across child-service systems; and
maintain an environment of care for staff that addresses, minimizes, and treats secondary traumatic stress, and that increases staff resilience.
Some organizations, like the National Center for Children in Poverty (NCCP), have outlined a trauma-informed approach into a policy framework (Cooper, Masi, Dababnah, Aratani, & Knitzer, 2007 ). The NCCP advocates that:
All federal, tribal, state, and local policies should reflect a trauma-informed perspective. A trauma-informed response encompasses a fundamental understanding of trauma and how it shapes an individual who has experienced it.
Policies should support delivery systems that identify and implement strategies to prevent trauma, increase capacity for early identification and intervention, and provide comprehensive treatment.
Policies should support and require that strategies are designed to prevent and eliminate treatment practices that cause trauma or re-traumatization.
Policies should reinforce the core components of best practices in trauma-informed care: prevention; developmentally appropriate, effective strategies; cultural and linguistic competence; and family and youth engagement.
Policy and practice should be reflective of trauma-informed principles and be developmentally appropriate, based on a public health framework, and engage children, youth, and their families in healing.
Policies should focus on prevention of trauma and developing strategies to identify and intervene early for children, youth, and their families exposed to trauma or at risk of exposure to trauma.
Policies should focus on enhancing child, youth, and family engagement strategies to support informed trauma care delivery.
Policies should support strategies that encompass family-based approaches to trauma intervention.
Trauma-informed and related policies must include responsive financing, cross-system collaboration and training, accountability, and infrastructure development.
Policies should ensure that funding is supportive of trauma-informed care and based upon sound fiscal strategies.
Policies should make funding contingent upon eliminating harmful practices that cause trauma and re-traumatization across child-serving settings.
Policies should support comprehensive workforce investment strategies. (Cooper et al, 2007 , pp. 1–2)
Emerging Themes
While the actual words vary considerably across definitions and perspectives on trauma-informed care, and the related topics of trauma-informed practice, trauma-informed approach, trauma-informed organizations and systems, some common themes emerge as the essential elements of trauma-informed care (Child Welfare Committee, National Child Traumatic Stress Network, & The California Social Work Education Center, 2012 ; Chadwick Trauma Informed Systems Project, 2013 ).
Maximize Physical and Psychological Safety
At its most fundamental level, recovery from trauma requires a sense of safety, and trauma-informed providers must recognize safety is both physical and psychological. Removing a child from an abusive home, for example, and placing him or her in a physically safe foster home where the child will not be maltreated may achieve physical safety but does not guarantee the child will feel safe. In fact, the very process of securing physical safety may intensify the child’s fears and insecurity and feelings of being out of control, helpless, and inherently unsafe. Without a sense of safety, not only will the client not progress, but the anxiety and stress it creates will add new trauma, amplify old trauma, and impact their behavior, often emerging as unhealthy maladaptive behaviors replayed long after the physical threat is gone.
The term psychological safety means a “sense of safety, or the ability to feel safe, within one’s self and safe from external harm” (Chadwick Trauma-Informed Systems Project, 2013 , p. 13) This type of safety occurs on an emotional level and is not defined by objective observable reality. It has direct implications for physical safety and is critical for optimal functioning as well as physical and emotional growth. A lack of psychological safety can impact an individual’s and family’s interactions with all others, including those trying to help them, and can lead to a variety of maladaptive strategies for coping with the anxiety associated with feeling unsafe. These survival strategies may include high-risk and counterproductive behaviors, such as substance abuse, aggression and violence, high-risk-taking activities, and self-mutilation. The child (and his or her siblings) may continue to feel psychologically unsafe long after the physical threat has been removed or he or she has been relocated to a physically safe environment. In reality, the client may feel psychologically unsafe for a number of reasons. These may include factors the system can control, such as the placement environment and how professionals help the client regulate their emotions. Even after the client gains some degree of security, a trigger, such as a person, place, or event, may unexpectedly remind him or her of the trauma and draw his or her attention back to intense and disturbing memories that overwhelm his or her ability to cope, again creating a sense of fear and anxiety. At other times, a seemingly innocuous event or sensory stimulus like an odor, sound, touch, taste, or particular scene may act as a trigger and be a subconscious reminder of the trauma. In either of these situations, a physiological response is sparked due to the body’s biochemical system reacting as if the trauma were reoccurring. A trauma-informed provider understands that these pressures may help explain a client’s or family member’s behavior and can use this knowledge to help her or him better manage triggers and to feel safe.
As a result, trauma-informed care means considering not only how safe the service delivery environment actually is, but also how safe it is perceived to be by the clients being served; how trauma reminders and trauma triggers are managed; how the physical environment is structured to make the client feel safe; how culturally, developmentally, and linguistically congruent the service delivery system is with the client population served, and what can be done to maximize the sense of safety and security for both clients and service providers.
Partner with Clients
Consumers being served, and often their family members, who have been involved in the service system have a unique perspective. This experience can help the client and family guide their own services, and provide valuable feedback on how the system can better address trauma among those served, as well as others impacted by the experience. As articulated in the foundational work on trauma-informed systems by Fallot and Harris and advanced strongly by SAMHSA and the NCTIC, consumers should be given choices and an active voice in decision-making on both an individual and systemic level ( choice and collaboration ). This can help them reclaim the power ( empowerment ) that was taken away from them during the trauma, enhance their resilience, and provide important information to providers and the system. A sense of control and empowerment also helps build a sense of psychological safety as described above, and facilitates the client’s engagement and active participation in service delivery.
Identify Trauma-Related Needs of Clients
The first step in helping those that have been impacted by abuse, neglect, violence, and other trauma is understanding how trauma impacts them and their families on an individual level. Social workers and other helping professionals should use that knowledge to help educate the clients and their family, when appropriate, about the impact of trauma and how it influences their life and short- and long-term recovery. While much has been written on the subject, the NCTSN has done an excellent job of summarizing this in Core Concepts of Understanding Traumatic Stress Responses in Childhood . While written from a child trauma point of view, many of these concepts apply to adult trauma victims as well.
The 12 core concepts: Concepts for understanding traumatic stress responses in children and families. Core Curriculum on Childhood Trauma 1
Traumatic experiences are inherently complex.
Every traumatic event—even events that are relatively circumscribed—is made up of different traumatic moments. These moments may include varying degrees of objective life threat, physical violation, and witnessing of injury or death. Trauma-exposed children experience subjective reactions to these different moments that include changes in feelings, thoughts, and physiological responses; and concerns for the safety of others. Children may consider a range of possible protective actions during different moments, not all of which they can or do act on. Children’s thoughts and actions (or inaction) during various moments may lead to feelings of conflict at the time, and to feelings of confusion, guilt, regret, and/or anger afterward. The nature of children’s moment-to-moment reactions is strongly influenced by their prior experience and developmental level. Events (both beneficial and adverse) that occur in the aftermath of the traumatic event introduce additional layers of complexity. The degree of complexity often increases in cases of multiple or recurrent trauma exposure, and in situations where a primary caregiver is a perpetrator of the trauma.
Trauma occurs within a broad context that includes children’s personal characteristics, life experiences, and current circumstances.
Childhood trauma occurs within the broad ecology of a child’s life that is composed of both child-intrinsic and child-extrinsic factors. Child- intrinsic factors include temperament, prior exposure to trauma, and prior history of psychopathology. Child- extrinsic factors include the surrounding physical, familial, community, and cultural environments. Both child-intrinsic and child-extrinsic factors influence children’s experience and appraisal of traumatic events; expectations regarding danger, protection, and safety; and course of post-trauma adjustment. For example, both child-intrinsic factors such as prior history of loss; and child-extrinsic factors such as poverty may act as vulnerability factors by exacerbating the adverse effects of trauma on children’s adjustment.
Traumatic events often generate secondary adversities, life changes, and distressing reminders in children’s daily lives.
Traumatic events often generate secondary adversities such as family separations, financial hardship, relocations to a new residence and school, social stigma, ongoing treatment for injuries and/or physical rehabilitation, and legal proceedings. The cascade of changes produced by trauma and loss can tax the coping resources of the child, family, and broader community. These adversities and life changes can be sources of distress in their own right and can create challenges to adjustment and recovery. Children’s exposure to trauma reminders and loss reminders can serve as additional sources of distress. Secondary adversities, trauma reminders, and loss reminders may produce significant fluctuations in trauma survivors’ post-trauma emotional and behavioral functioning.
Children can exhibit a wide range of reactions to trauma and loss.
Trauma-exposed children can exhibit a wide range of post-trauma reactions that vary in their nature, onset, intensity, frequency, and duration. The pattern and course of children’s post-trauma reactions are influenced by the type of traumatic experience and its consequences, child-intrinsic factors including prior trauma or loss, and the post-trauma physical and social environments. Post-traumatic stress and grief reactions can develop over time into psychiatric disorders, including post-traumatic stress disorder (PTSD), separation anxiety, and depression. Post-traumatic stress and grief reactions can also disrupt major domains of child development, including attachment relationships, peer relationships, and emotional regulation, and can reduce children’s level of functioning at home, at school, and in the community. Children’s post-trauma distress reactions can also exacerbate preexisting mental health problems including depression and anxiety. Awareness of the broad range of children’s potential reactions to trauma and loss is essential to competent assessment, accurate diagnosis, and effective intervention.
Danger and safety are core concerns in the lives of traumatized children.
Traumatic experiences can undermine children’s sense of protection and safety, and can magnify their concerns about dangers to themselves and others. Ensuring children’s physical safety is critically important to restoring the sense of a protective shield. However, even placing children in physically safe circumstances may not be sufficient to alleviate their fears or restore their disrupted sense of safety and security. Exposure to trauma can make it more difficult for children to distinguish between safe and unsafe situations, and may lead to significant changes in their own protective and risk-taking behavior. Children who continue to live in dangerous family and/or community circumstances may have greater difficulty recovering from a traumatic experience.
Traumatic experiences affect the family and broader caregiving systems.
Children are embedded within broader caregiving systems, including their families, schools, and communities. Traumatic experiences, losses, and ongoing danger can significantly impact these caregiving systems, leading to serious disruptions in caregiver–child interactions and attachment relationships. Caregivers’ own distress and concerns may impair their ability to support traumatized children. In turn, children’s reduced sense of protection and security may interfere with their ability to respond positively to their parents; and other caregivers’ efforts to provide support. Traumatic events—and their impact on children, parents, and other caregivers—also affect the overall functioning of schools and other community institutions. The ability of caregiving systems to provide the types of support that children and their families need is an important contributor to children’s and families’ post-trauma adjustment. Assessing and enhancing the level of functioning of caregivers and caregiving systems are essential to effective intervention with traumatized youths, families, and communities.
Protective and promotive factors can reduce the adverse impact of trauma.
Protective factors buffer the adverse effects of trauma and its stressful aftermath, whereas promotive factors generally enhance children’s positive adjustment regardless of whether risk factors are present. Promotive and protective factors may include child-intrinsic factors such as high self-esteem, self-efficacy, and possessing a repertoire of adaptive coping skills. Promotive and protective factors may also include child-extrinsic factors such as positive attachment with a primary caregiver, possessing a strong social support network, the presence of reliable adult mentors, and a supportive school and community environment. The presence and strength of promotive and protective factors—both before and after traumatic events—can enhance children’s ability to resist, or to quickly recover (by resiliently “bouncing back”) from the harmful effects of trauma, loss and other adversities.
Trauma and post-trauma adversities can strongly influence development.
Trauma and post-trauma adversities can profoundly influence children’s acquisition of developmental competencies and their capacity to reach important developmental milestones in such domains as cognitive functioning, emotional regulation, and interpersonal relationships. Trauma exposure and its aftermath can lead to developmental disruptions in the form of regressive behavior, reluctance or inability to participate in developmentally appropriate activities, and developmental accelerations such as leaving home at an early age and engagement in precocious sexual behavior. In turn, age, gender, and developmental period are linked to risk for exposure to specific types of trauma (e.g., sexual abuse, motor vehicle accidents, and peer suicide).
Developmental neurobiology underlies children’s reactions to traumatic experiences.
Children’s capacities to appraise and respond to danger are linked to an evolving neurobiology that consists of brain structures, neurophysiological pathways, and neuroendocrine systems. This “danger apparatus” underlies appraisals of dangerous situations, emotional and physical reactions, and protective actions. Traumatic experiences evoke strong biological responses that can persist and that can alter the normal course of neurobiological maturation. The neurobiological impact of traumatic experiences depends in part on the developmental stage in which they occur. Exposure to multiple traumatic experiences carries a greater risk for significant neurobiological disturbances, including impairments in memory, emotional regulation, and behavioral regulation. Conversely, ongoing neurobiological maturation and neural plasticity also create continuing opportunities for recovery and adaptive developmental progression.
Culture is closely interwoven with traumatic experiences, response, and recovery.
Culture can profoundly affect the meaning that a child or family attributes to specific types of traumatic events such as sexual abuse, physical abuse, and suicide. Culture may also powerfully influence the ways in which children and their families respond to traumatic events, including the ways in which they experience and express distress, disclose personal information to others, exchange support, and seek help. A cultural group’s experiences with historical or multigenerational trauma can also affect their responses to trauma and loss, their world view, and their expectations regarding the self, others, and social institutions. Culture also strongly influences the rituals and other ways through which children and families grieve over and mourn their losses.
Challenges to the social contract, including legal and ethical issues, affect trauma response and recovery.
Traumatic experiences often constitute a major violation of the expectations of the child, family, community, and society regarding the primary social roles and responsibilities of influential figures in the child’s life. These life figures may include family members, teachers, peers, adult mentors, and agents of social institutions such as judges, police officers, and child welfare workers. Children and their caregivers frequently content with issues involving justice, obtaining legal redress, and seeking protection against further harm. They are often acutely aware of whether justice is properly served and the social contract is upheld. The ways in which social institutions respond to breaches of the social contract may vary widely and often take months or years to carry out. The perceived success or failure of these institutional responses may exert a profound influence on the course of children’s post-trauma adjustment, and on their evolving beliefs, and attitudes and values regarding family, work, and civic life.
Working with trauma-exposed children can evoke distress in providers that makes it more difficult for them to provide good care.
Mental healthcare providers must deal with many personal and professional challenges as they confront details of children’s traumatic experiences and life adversities, witness children’s and caregivers’ distress, and attempt to strengthen children’s and families’ belief in the social contract. Engaging in clinical work may also evoke strong memories of personal trauma- and loss-related experiences. Proper self-care is an important part of providing quality care and of sustaining personal and professional resources and capacities over time.
A key to trauma-informed care is recognizing many, but not all, clients have trauma-related needs and would benefit from a trauma-specific intervention. To identify who would benefit from a trauma-specific intervention and to guide future interactions with those with a trauma history in a way that does not exacerbate past traumas or unnecessarily trigger trauma memories, a broad trauma-screening system is indicated. Where possible, a trauma-informed approach suggests the use of a reliable and valid screening tool for identifying the client’s trauma history and traumatic stress responses, and to make direct referrals for assessment and treatment when indicated (Conradi, Wherry, & Kisiel, 2011 ).
Enhance Client Well-Being and Resilience
Some individuals who have experienced maltreatment and subsequent trauma are more resilient than others; most often, these individuals have both internal and external resources, such as strong relationships; success in school, work, or other activities; and a temperament that helps them manage stress more readily. It is important for the social worker or other helping professional to recognize and build on the client’s existing strengths, while linking them to trauma-informed services when needed. Trauma-informed care seeks to support positive relationships in the client’s life and minimize disruptions of what is familiar, and to make sure that positive figures, including parents, children, teachers, neighbors, siblings, and other relatives, remain involved in client’s lives.
For many clients, recovery requires the support of specially trained mental health professionals who are schooled in evidence-based treatment models that are tailored to meet the needs of the clients. Any decision to treat a client with a history of significant trauma should be based on a thorough assessment that yields a clear picture of their unique strengths and needs. For children, this type of multidimensional assessment algorithm is exemplified by the Trauma Assessment Pathway (Chadwick Center for Children and Families, 2009 ; Taylor, Gilbert, Mann, & Ryan, 2005 ; Igelman, Taylor, & Gilbert, 2007 ) developed at the Chadwick Center for Children and Families at Rady Children’s Hospital in San Diego ( www.chadwickcenter.org ) with support from SAMHSA. The assessment should be designed to match the client to the evidence-based or evidence-informed treatment model best suited for their unique needs. It is important to remember that trauma often co-occurs with other major behavioral health disorders. In some cases, trauma serves as a precursor for another disorder like substance abuse. In other cases, another disorder, such as some forms of serious mental illness, may precede the trauma events or develop independently of the trauma history, and the assessment must explore those connections.
Recovery from trauma often requires the right evidence-based or evidence-informed mental health treatment, delivered by a skilled therapist, that helps the client reduce the overwhelming emotions related to the trauma, manage the behavioral and emotional symptoms of traumatic stress, address any traumatic grief issues the traumas produced, cope with trauma triggers, and make new meaning of his or her trauma history. The treatment also may need to address a second co-occurring disorder first, or a treatment model should be selected that addresses the co-occurring disorder in a trauma context, such as how Seeking Safety addresses substance abuse (Najavits, Weissbecker & Clark, 2007 ; Najavits, 2009 ).
There are numerous evidence-based treatment models now available that have been empirically tested with highly traumatized children and adults and fit well in a trauma-informed environment. Seeking out the empirical evidence on each possible model can be overwhelming for those actively involved in service delivery. Fortunately, there are multiple Internet-based clearinghouses that contain trauma-specific interventions in which the research reviews have already been conducted (see www.nrepp.samhsa.gov ; www.cebc4cw.org ; www.colorado.edu/cspv ; and www.samhsa.gov/nctic ).
Enhance Family Well-Being and Resilience
When it comes to child trauma victims and many adults, especially transition-age youths, families are a critical part of their recovery and enhance their natural resilience. However, families may find it difficult to be protective if they have been affected by trauma themselves, and they may need help and support in order to draw on their natural strengths.
Asking parents and other caregivers about their history of trauma provides critical information to social workers or other helping professionals about their behavior and needs, as well as helping inform service planning for all family members. It is common for the parents of traumatized children and young adults to share a significant trauma history. Sometimes that history is based in childhood experiences such as physical or sexual abuse, or it may be contemporary, such as ongoing intimate-partner violence.
Providing effective trauma-informed education and professionally delivered trauma-informed services to parents enhances their protective capacities, thereby increasing their children’s resilience and feelings of safety, permanency, and well-being. Additionally, educating other caregivers, foster parents, members of the child’s safety network and the parent’s support system enhances their protective capacities, thereby reducing the risk that the child will be inadvertently exposed to trauma triggers or have their behaviors, which may be trauma-related, misidentified as “bad” and subject the child to inappropriate and trauma-insensitive discipline or punishment.
Those working with these families must recognize that caregivers may also experience secondary traumatic stress related to their children’s trauma, and provide them with appropriate training and supports.
Enhance the Well-Being and Resilience of Those Working in the System
While the origins of trauma-informed care are clearly centered on the clients served, it is apparent that the professionals working with highly traumatized populations are also profoundly affected by the experience. Those experiences can influence their judgments on the job, invade their private lives, and shape their worldview at home as well as at work. Those working in a trauma-informed environment must be aware of this sometimes-insidious side effect of serving this population. Trauma-informed organizations must consider their staff’s physical and psychological safety. Actively working to increase staff resilience to secondary traumatic stress (STS) involves seeking ways to reduce the risk of STS among all personnel—from the receptionists, to transcriptionists, to the frontline professionals and their supervisors; identifying the early signs of STS among personnel; minimizing the impact of STS; and promoting effective interventions for secondary traumatic stress. Helping staff manage professional and personal stress and addressing the impact of secondary traumatic stress on both individuals and on the system as a whole is beneficial for all levels, from client to community.
Partner with Agencies and Systems that Interact with Clients
Because trauma can impact many aspects of an individual’s life, it is important that those aspiring to provide trauma-informed care partner with others in parallel service systems in identifying and addressing trauma. Working with allied professionals who know the clients and family can help in developing an appropriate service plan and prevent potentially competing priorities.
Failure to work together can not only undermine all the efforts to provide trauma-informed care, but actually can inadvertently add new traumas. Well-meaning agencies or professionals pursuing their own mission and goals independently can work at cross-purposes and trigger traumatic reactions, causing more harm. In fact, this was the genesis of the child-advocacy center movement (see www.nationalcac.org and www.nationalchildrensallaince.org ) which began when the grandmother of an abused child in Huntsville, Alabama, protested to the district attorney how uncoordinated agencies in child protection, law enforcement, health care, and prosecution were not only operating independently, but were making things worse for her grandchild. The result was a national movement starting in the 1980s to create a multidisciplinary investigative team response to child-abuse allegations. This model was designed so that all aspects of the forensic investigation process were reconfigured to be child-centered, with tasks focused on providing all services in a single location, reducing unnecessary duplication of interviews, and having representatives from all involved agencies co-located. All this was done to enhance the possibility the system did not re-traumatize the child through lack of coordination and communication among the professionals.
A truly trauma-informed system is one in which all the disparate elements understand trauma, and, as articulated by the NCTSN, “infuse and sustain trauma awareness, knowledge, and skills into their organizational cultures, practices, and policie” (NCTSN, 2012 , What is a trauma-informed child- and family-service system? section, para. 1). To achieve this lofty goal, those aspiring to deliver true trauma-informed care need to establish strong partnerships with others serving the same clients and families. Service providers should develop common protocols and frameworks where possible for documenting trauma history, exchanging information, coordinating assessments, and planning and delivering services.
Moving to Trauma-Informed Care
Several organizations have developed formal self-assessment tools to help organizations and systems assess the degree to which they have become trauma-informed or are ready to move in that direction. Among the stronger assessments are Community Connections’ Creating Cultures of Trauma-Informed Care: a Self-Assessment and Planning Protocol (Fallot & Harris, 2009 ); the Chadwick Center’s Community Trauma-Informed Assessment Protocol (Hendricks, Conradi, & Wilson, 2011 ) and Trauma System Readiness Tool (Hendricks, Conradi, & Wilson, 2011 ); the National Center on Family Homelessness’s Trauma-Informed Organizational Toolkit (Guarino et al., 2009 ); and Western Michigan University’s Trauma-Informed System Change Instrument (Richardson, Coryn, Henry, Black-Pond, & Unrau, 2010 ). The NCTSN has developed training resources to support transformation efforts at the system level, with Caring for Children Who Have Experienced Trauma: A Resource Parent Curriculum , and Child Welfare Trauma Training Tookit (Child Welfare Committee, National Child Traumatic Stress Network, & The California Social Work Education Center, 2013 ). Early studies show these type resources show promise in practice change efforts (Kramer, Sigel, Conners-Burrow, Savary, & Tempel, 2013 ).
Trauma-informed care is not so much a new model of service delivery as it is an approach to service delivery. It weaves trauma knowledge and sensitivity into existing actions and models in a way that avoids or minimizes negative side-effects of intervention and increases the likelihood of meaningful engagement and effective implementation of other models. Effective trauma-informed care does rely on the capacity to deliver evidence-based and evidence-informed trauma-specific interventions when needed, but it goes further in viewing the whole service-delivery experience through a trauma lens. Trauma-informed care engages the customers and clients as partners, empowering them to help guide their intervention and seeking out the unique path to safety and resilience that will give the clients the capacity to face and overcome trauma triggers and new adversities in the future.
- Abram, K. M. , Teplin, L. A. , Charles, D. R. , et al. (2004). Posttraumatic stress disorder and psychiatric comorbidity among detained youths. Archives of General Psychiatry , 61 , 403–410.
- Anda, R. F. , Dong, M. , Brown, D. W. , et al. (2009). The relationship of adverse childhood experiences to a history of premature death of family members. BMC Public Health , 1 , 106–115.
- Anda, R. A. , & Felitti, V. J. (2003). Origins and essence of the study. ACE Reporter , 1 (1), 1–3.
- Bloom, S. (1997). Creating sanctuary: Toward the evolution of sane societies . London: Taylor & Francis.
- Bloom, S. (2010). Organizational stress as a barrier to trauma-informed service delivery. In M. Becker & B. Levin , A public health perspective of women’s mental health (pp. 295–311). New York: Springer.
- Burgess, A. W. , & Holmstrom, L. L. (1974). Rape trauma syndrome. American Journal of Psychiatry , 131 , 981–986.
- Chadwick Center for Children and Families . (2009). Assessment-based treatment for traumatized children: A trauma assessment pathway (TAP). San Diego, CA: Author.
- Chadwick Trauma-Informed Systems Project . (2013). Creating trauma-informed child welfare systems: A guide for administrators (2nd ed.). San Diego, CA: Chadwick Center for Children and Families.
- Child Welfare Committee, National Child Traumatic Stress Network, & The California Social Work Education Center . (2012). Child welfare trauma training toolkit: Comprehensive guide (3rd ed.). Los Angeles, CA, and Durham, NC: National Center for Child Traumatic Stress.
- Child Welfare Committee, National Child Traumatic Stress Network, & The California Social Work Education Center . (2013). Child welfare trauma training toolkit (2nd ed.). Los Angeles, CA, and Durham, NC: National Center for Child Traumatic Stress.
- Cicchetti, D. , Toth, S. L. , & Rogosch, F. A. (1999). The efficacy of toddler-parent psychotherapy to increase attachment security in offspring of depressed mothers. Attachment & Human Development , 1 (1), 34–66.
- Cohen, J. A. , Deblinger, E. , Mannarino, A. P. , & Steer, R. (2004). A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry , 43 , 393–402.
- Cohen, J. A. , Mannarino, A. P. , & Iyengar, S. (2011). Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence. Archives of Pediatrics & Adolescent Medicine , 165 (1), 16–21.
- Cohen, J. A. , Mannarino, A. P. , & Knudsen, K. (2004) Treating childhood traumatic grief: a pilot study. Journal of the American Academy of Child & Adolescent Psychiatry , 43 , 1225–1233.
- Cohen, J. A. , Mannarino, A. P. , & Staron, V. (2006). A pilot study of modified cognitive behavioral therapy for childhood traumatic grief (CBT-CTG). Journal of the American Academy of Child & Adolescent Psychiatry , 45 (12), 1465–1473.
- Conradi, L. , Wherry, J. , & Kisiel, C. (2011). Linking child welfare and mental health using trauma-informed screening and assessment practices. Child Welfare , 90 (6), 129–148.
- Conradi, L. , & Wilson, C. (2010). Managing traumatized children: a trauma systems perspective. Current Opinion in Pediatrics , 22 , 621–625.
- Cooper, J. L. , Masi, R. , Dababnah, S. , Aratani, Y. , & Knitzer, J. (2007). Unclaimed children revisited working paper no. 2, Strengthening policies to support children, youth, and families who experience trauma . New York: National Center for Children in Poverty.
- Costello, E. J. , Erkanli, A. , Fairbank, J. A. , & Angold, A. (2002). The prevalence of potentially traumatic events in childhood and adolescence. Journal of Traumatic Stress , 15 , 99–112.
- Covington, S. S. (2002). Helping women recover: creating gender-responsive treatment. In S. Straussner and S. Brown (Eds.), Handbook of women’s addictions treatment (pp. 52–72). San Francisco: Jossey-Bass.
- Deblinger, E. , Lippmann, J. , & Steer, R. (1996). Sexually abused children suffering posttraumatic stress symptoms: initial treatment outcome findings. Child Maltreatment , 1 (4), 310–321.
- Deblinger, E. , Mannarino, A. P. , Cohen, J. A. , & Steer, R. A. (2006). A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms: examining predictors of treatment response. Journal of the American Academy of Child and Adolescent Psychiatry , 45 , 1474–1484.
- Ethier, L. S. , Lemelin, J. , & Lacharite, C. A. (2004). A longitudinal study of the effects of chronic maltreatment on children’s behavioral and emotional problems. Child Abuse and Neglect , 28 , 1265–1278.
- Fallot, R. D. , & Harris, M. (2009). Creating cultures of trauma-informed care (CCTIC): A self-assessment and planning protocol . Washington, DC: Community Connections.
- Felitti, V. J. , Anda, R. F. , Nordenberg, D. , Williamson, D. F. , et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine , 14 , 245–258.
- Guarino, K. , Soares, P. , Konnath, K. , Clervil, R. , & Bassuk, E. (2009). Trauma-informed organizational toolkit . Rockville MD: Center for Mental Health Services, SAMHSA.
- Harris, M. , & Fallot, R. (2001). Using trauma theory to design service systems . San Francisco: Jossey-Bass.
- Hendricks, A. , Conradi, L. , & Wilson, C. (2011). Creating trauma-informed child welfare systems using a community assessment process. Child Welfare , 90 (6), 187–206.
- Igelman, R. , Taylor, N. , Gilbert, A. , et al. (2007). Creating more trauma-informed services for children using assessment-focused tools. Child Welfare , 86 , 15–33.
- Ko, S. J. , Ford, J. D. , Kassam-Adams N. , et al. (2008). Creating trauma-informed systems: child welfare, education, first responders, health care, juvenile justice. Professional Psychology: Research & Practice , 39 , 396–404.
- Kramer, T. , Sigel, B. , Conners-Burrow, N. , Savary, P. , & Tempel, A. (2013). A statewide introduction of trauma-informed care in child welfare. Children & Youth Services Review , 35 , 19–24.
- Landis, J. T. (1956). Experiences of 500 children with adult sexual deviation. Psychiatric Quarterly Supplement , 30 (1), 91–109.
- Lieberman, A. F. , Ghosh Ippen, C. , & Van Horn, P. (2006). Child-parent psychotherapy: Six- month follow-up of a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 45 (8), 913–918.
- Lieberman, A. F. , Weston, D. R. , & Pawl, J. H. (1991). Preventive interaction and outcome with anxiously attached dyads. Child Development , 62 , 199–209.
- McDonald, R. , Jouriles, E. , Ramisetty-Mikler, S. , et al. (2006). Estimating the number of American children living in partner violent families. Journal of Family Psychology , 30 , 137–142.
- Najavits, L. M. (2009). Seeking Safety: An implementation guide. In A. Rubin & D. W. Springer (Eds.), Substance Abuse Treatment for Youth and Adults: he clinician’s guide to evidence-based practice (311-348). Hoboken, NJ: John Wiley.
- Najavits, L. M. , Weissbecker I. , & Clark, C. (2007). The impact of violence and abuse on women’s physical health: can trauma-informed treatment make a difference? Journal of Community Psychology , 35 , 909–923.
- National Center for Trauma-Informed Care . (2012). Retrieved November 18, 2012, from www.mentalhealth.samhsa.gov/nctic/trauma.asp
- National Child Traumatic Stress Network . (2012). Creating trauma-informed child- and family-serving systems: A definition. Retrieved January 15, 2013, from http://www.nctsn.org/resources/topics/creating-trauma-informed-systems
- NCTSN Core Curriculum on Childhood Trauma Task Force . (2012). The 12 core concepts: Concepts for understanding traumatic stress responses in children and families. Core Curriculum on Childhood Trauma. Los Angeles, CA, and Durham, NC: UCLA-Duke University National Center for Child Traumatic Stress.
- Richardson, C. , Henry, B.-P. , & Unrau , (2010). Trauma-informed system change instrument. Western Michigan University, unpublished manuscript.
- Rivard, J. C. , Bloom, S. L. , Abramovitz, R. , et al. (2003). Assessing the implementation and effects of a trauma-focused intervention for youths in residential treatment. Psychiatric Quarterly ; 74 , 137–154.
- Taylor, N. , Gilbert, A. , Mann, G. , & Ryan, B. E. (2005). Unpublished manuscript. San Diego: Chadwick Center for Children & Families, Rady Children’s Hospital.
- Taylor, N. , & Siegfried, C. (2005). Helping children in child welfare system heal from trauma: A systems integration approach . Los Angeles, CA & Durham, NC: National Center for Child Traumatic Stress (NCTSN).
- Toth, S. L. , Maughan, A. , Manly, J. T. , Spagnola, M. , & Cicchetti, D. (2002). The relative efficacy of two interventions in altering maltreated preschool children’s representational models: implications for attachment theory. Development & Psychopathology , 14 , 877–908.
- U.S. Department of Health and Human Services, Administration on Children, Youth and Families . (n.d.). General findings from the federal child and family services review [document on the Internet]. Washington DC: Government Printing Office; Retrieved May 3, 2010, from http://www.acf.hhs.gov/sites/default/files/cb/summary_of_the_results_of_the_2001_2004_cfsr.pdf
- U.S. Department of Health and Human Services 2011, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau . Child maltreatment. Available from http://www.acf.hhs.gov/programs/cb/resource/child-maltreatment-2011
- U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration . (2007). Lessons Learned From the Women, Co-Occurring Disorders, and Violence Study: Exploring How to Best Serve Women Survivors of Violence and Trauma Who Have Substance Abuse and Mental Health Disorders . Rockville, Maryland: Author.
- U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration . (2012). Trauma definition. Part two: A trauma-informed approach . Retrieved December 2, 2012, from http://www.samhsa.gov/traumajustice/traumadefinition/approach.aspx
Further Reading
- California Evidence-Based Clearinghouse for Child Welfare (CEBC): http://www.cebc4cw.org
- Center for the Study and Prevention of Violence: http://www.colorado.edu/cspv/ .
- Chadwick Center for Children and Families at Rady Children’s Hospital in San Diego: http://www.chadwickcenter.org .
- National Center for Post-Traumatic Stress Disorder: http://www.ptsd.va.gov .
- National Center for Trauma-Informed Care: http://www.samhsa.gov/nctic/ .
- National Child Traumatic Stress Network: http://www.nctsn.org
- National Children’s Advocacy Center: http://www.nationalcac.org .
- National Children’s Alliance: http://www.nationalchildrensalliance.org .
- National Registry of Evidence-based Programs and Practices: http://www.nrepp.samhsa.gov/ .
1 NCTSN Core Curriculum on Childhood Trauma Task Force ( 2012 ). The 12 core concepts: Concepts for understanding traumatic stress responses in children and families. Core Curriculum on Childhood Trauma. Los Angeles, CA, and Durham, NC: UCLA–Duke University National Center for Child Traumatic Stress.
Related Articles
- Evidence-Based Practice
- Intimate Partner Violence
- Military Social Work
- Veteran Services
- Community Violence
- Mental Health: Overview
Other Resources
- New & Featured
- Forthcoming Articles
Printed from Encyclopedia of Social Work. Under the terms of the licence agreement, an individual user may print out a single article for personal use (for details see Privacy Policy and Legal Notice).
date: 02 June 2024
- Cookie Policy
- Privacy Policy
- Legal Notice
- Accessibility
- [66.249.64.20|185.147.128.134]
- 185.147.128.134
Character limit 500 /500
- PARTNERSHIP
- GET INVOLVED
- NEWS & UPDATES
UCLA Pritzker Center partners with the Children’s Institute of Los Angeles for the 2023 Trauma-Informed Care Conference
By Christine Lina September 26, 2023

Featured speakers include California Surgeon General, Dr. Diana Ramos, UCLA Professor of Psychiatry, Dr. Eraka Bath, and keynote speaker, Dr. Bessel van der Kolk.
The Children’s Institute of Los Angeles hosted their annual 2023 Trauma-Informed Care Conference in partnership with the UCLA Pritzker Center for Strengthening Children and Families. The conference featured a panel discussion with California Surgeon General, Dr. Diana Ramos, and UCLA Professor of Psychiatry, Dr. Eraka Bath, moderated by LAist Senior Reporter, Mariana Dale, and a keynote from New York Times Best-Selling Author of The Body Keeps the Score and trauma research pioneer, Dr. Bessel van der Kolk.
The annual Trauma-Informed Care Conference brings together professionals working with children and families from the front lines, such as child welfare and mental health professionals, as well as school and juvenile legal system staff. Policymakers, program administrators and organizational leaders from public and private agencies play an equally critical role in conversations around improving trauma-informed care for system-involved families. This year’s theme focuses on Creating a Culture of Wellness & Prevention for Children, Families & Community .
“I’ve witnessed firsthand the profound impact of safe, stable, and nurturing relationships on a child’s health,” said California Surgeon General Diana Ramos, MD . “California is making significant investments to providing more support for communities and families so that all children have an opportunity to lead healthy, thriving lives.”
“The CII conference guided participants to consider the importance of using structural intersectional frameworks to address racism and concentrated poverty as drivers of inequitable health outcomes,” said UCLA Professor of Psychiatry, Eraka Bath, MD . “As a child and adolescent psychiatrist, I am confident that strategic application of these frameworks to operationalize policies, procedures, practices, and programs to address trauma and advance child well-being is critical.”
“Childhood trauma is probably the largest single public health issue facing us as a nation.,” said keynote Bessel van der Kolk, MD , “Learning self-regulation through attuned interactions, play & awareness of self and others are at the core of any effective intervention in any system that deals with children & adolescents.”
“We know that healthy relationships built on consistency and trust can protect families and communities are primary buffers against toxic stress in our communities,” said Martine Singer, CII’s President and CEO , “CII is honored to host this year’s stellar keynote speakers who, like the extraordinary professionals that attend the conference, dedicate their lives to healing and health. CII is committed to equitable access to care and early education. Our teachers and clinicians partner with children and families to achieve educational success and emotional wellbeing, which are foundational to economic mobility and lifelong health.”
“The UCLA Pritzker Center is proud to partner with CII to host this year’s Trauma Informed Care Conference,” said Taylor Dudley, JD, UCLA Pritzker Center Executive Director , “As a bridge from our campus and into neighborhoods across Los Angeles, we team with UCLA researchers and community leaders to challenge and resolve systemic injustices facing children and families. This conference brings that mission to life, and we thank CII for having us take part in its efforts.”
The conference also featured a community panel with individuals who have lived-experience with the system and/or received services and are now able to provide wellness resources to and advocate on behalf of their own community. The Lived Experience panel, moderated by CII’s Vice President of Health Innovation and Training, Jesús Parra, LMFT, included UCLA Pritzker Center Student Researcher and third-year Sociology and African American studies double major with a Community Engagement and Social Change minor, Kahlila Williams , CII’s Community Health Worker for the Enhanced Care Management and Community Services Program, Clarissa Morales Hernandez , and CII’s Project Fatherhood program participant, Terry Hayward .
Breakout workshops were facilitated by experts from CII, UCLA Pritzker Center, the UCLA-UCSF ACEs Aware Family Resilience Network and the Trauma Research Foundation. UCLA Pritzker Center student researcher Kahlila Williams was invited to speak at the “Voices of Resilience: Empowering System Involved Youth through a Trauma-Informed Lens” Breakout Session alongside Evelyn Barycki and Chantel Palmer from the Children’s Institute, moderated by UCLA Pritzker Center Doctoral Researcher and Co-Director of Twinspire, Demontea Thompson.
After the conference, the UCLA Pritzker Center student team assisted Dr. Bessel van der Kolk during the book signing, where conference participants in person received a complimentary copy of The Body Keeps the Score with a personalized message from Dr. Bessel van der Kolk. The Body Keeps the Score is the inspiring story of how a group of therapists and scientists—together with their courageous and memorable patients—have struggled to integrate recent advances in brain science, attachment research, and body awareness into treatments that can tree trauma survivors from the tyranny of the past.
This event gathered over a hundred in-person attendees, and approximately 800 who attended virtually via Zoom. The UCLA Pritzker Center is proud to have played a role in this impactful event in partnership with the Children’s Institute of Los Angeles.
Advancing trauma-informed care in intellectual and developmental disability services: A pilot study of a digital training with direct service providers
Affiliations.
- 1 Indiana University Bloomington School of Social Work, Bloomington, Indiana, USA.
- 2 Indiana University Bloomington School of Public Health, Bloomington, Indiana, USA.
- PMID: 36811269
- DOI: 10.1111/jar.13085
Background: As trauma-informed care advances in the service delivery system for people with intellectual and developmental disabilities, additional resources are needed to foster staff development. This article describes the development and pilot evaluation of a digital training on trauma-informed care among direct service providers (DSPs) in the disability service industry.
Method: Following an AB design, a mixed methods approach was used to analyse the responses of 24 DSPs to an online survey at baseline and at follow-up.
Results: The training was associated with increased staff knowledge in some domains and greater alignment with trauma-informed care. Staff expressed a strong likelihood of using trauma-informed care in practice and identified organisational assets and barriers to implementation.
Conclusions: Digital trainings can facilitate staff development and the advancement of trauma-informed care. Although additional efforts are warranted, this study fills a gap in the literature regarding staff training and trauma-informed care.
Keywords: direct support; intellectual and developmental disabilities; staff training; trauma; trauma-informed care.
© 2023 The Authors. Journal of Applied Research in Intellectual Disabilities published by John Wiley & Sons Ltd.
- Developmental Disabilities*
- Intellectual Disability*
- Pilot Projects
- Surveys and Questionnaires
- UB Directory
News Center

The move will bolster health, well-being and innovation in Buffalo Niagara and beyond.

This spring, during their spring break, Jacobs School medical students traveled to rural areas in Belize to train 100 farmers and villagers in lifesaving Stop the Bleed techniques.

Four UB faculty researchers will serve as key members of a new initiative to secure the U.S. Department of Defense’s most critical artificial intelligence models, while also accelerating the technology’s commercialization in the private sector.

Last fall, Nathalia Andrade applied for and was awarded a $5,000 seed grant from the UB Office of Curriculum, Assessment and Teaching Transformation to create a new course weaving AI into periodontics.
campus news
Medical students develop course to train peers in trauma-informed care

From left: Michael Lamb, director of surgical education and course instructor; Gaby Cordero, who took the course in her fourth year of medical school; and course developers Katherine Foote, Pia Corujo Avila and Sydney Johnson, all Jacobs School students. Photo: Sandra Kicman
By ELLEN GOLDBAUM
Published May 20, 2024
UB medical students working with community anti-violence groups in Buffalo have developed an elective course on “Trauma surgery and trauma-informed care.”
The purpose is to train medical students, particularly those interested in surgery, in trauma-informed care in Buffalo’s Level 1 Adult Trauma Center at the Erie County Medical Center (ECMC).
Critical partners are Buffalo’s two anti-violence organizations — Buffalo SNUG (Should Never Use Guns) and Buffalo Rising Against Violence (BRAVE) Trauma Recovery Center — housed within ECMC. BRAVE is Western New York’s only Trauma Recovery Center, having attained that distinction from the National Alliance of Trauma Recovery Centers late last year.
Michael Lamb, director of surgical education in the Jacobs School of Medicine and Biomedical Sciences at UB and instructor for the elective, explains how the course works.
“Students spend half their time working on the trauma service at ECMC alongside attendings and residents, and the other half with BRAVE and SNUG,” he says. “The students serve as navigators for trauma patients and their families, offering support and advocacy during their hospital stay, clinical follow-ups and home visits.
“Immersion with BRAVE and SNUG offers these medical students not only longitudinal engagement with this extraordinary team of social workers, psychologists, case managers and credible messengers … but a great deal of time with patients and their families,” Lamb adds.
Bridging two worlds
“The whole goal is to bridge two worlds that usually don’t collide,” says Gaby Cordero, who graduated last month from the Jacobs School and was the first person to take the elective.
The idea to create a trauma-informed curriculum developed from conversations between Jacobs School students Pia Corujo Avila, Katherine Foote and Sydney Johnson, all of whom had been awarded the Department of Surgery’s summer diversity research fellowship for underrepresented students in 2022.
That year, Buffalo was in the midst of a significant rise in the number of shootings; it was also the year that 10 Black people were killed in the May 14 racist massacre at the Jefferson Avenue Tops market.
The purpose of the fellowships is to give underrepresented students interested in surgery early access to the operating room under the guidance of experienced attending physicians while also providing them with opportunities to do research on obstacles to care.
Community-based research
The only requirement for the research component was that it align with the principles of community-based participatory research, where the community collaborates as a full partner in deciding what to study and how.
The students decided their project would involve research into community violence and the resulting trauma experienced by many patients and their families.
“As physicians , we are able to play a part in the medical care of patients who may be victims of violence,” says Cordero, “then we lose touch with what may happen when they go back home. Working with BRAVE/SNUG allows us to connect with our patients beyond the operating room, and the hope is to begin to understand the experiences of the community we are serving.”
The students note their medical school classes do feature patients who share their perspectives.
However, Cordero notes, “With this elective, you see things come full circle that in many ways you didn’t before.”
They began their work by connecting with community organizers, pastors, local leaders and neighborhood residents. They spent time listening to those who had been victims of gun violence. They did this through their close partnerships with BRAVE and SNUG, which provide survivors with the tools and connections to prevent re-victimization or further perpetration of violence.
“We are committed to removing barriers to care and providing services that treat the whole person, not just their physical injuries,” says Paula Kovanic-Spiro, director of the BRAVE Trauma Recovery Center who also serves as SNUG site administrator. She notes this work would not be possible without the support of New York State, ECMC and other local partners.
“We are honored to support the talented Jacobs School students who developed this course and look forward to further advancing the importance of trauma-informed care by tomorrow’s doctors,” she adds.
Voices of victims of violence
“These medical students, having spoken with so many victims and families, and having themselves, I think, too often experienced what it’s like to be discounted, were deeply committed to including the voices of those who have experienced violence,” says Lamb, an environmental psychologist.
Cordero explains how she connected with one patient who had a penetrating wound. “I got to go in to see him with the BRAVE/SNUG team and the surgical residents,” she says. “The patient already knew me because I had just cleaned his wound. I asked him if he felt safe going back home and told him about resources. It changes the trajectory. It’s like finding a middle ground between the social workers and the medical team, to better understand what people need.”
Finding that middle ground is exactly the goal, says Johnson, a founder of the course.
“You want to treat the whole person,” says Johnson, who began working on the elective while recovering from a stroke, an experience that provided her with a unique perspective on the patient experience.
“As the surgeon, the only time you may see the patient is in the OR,” she says. “You need a bit more humanity. When you understand the world the patient comes from, the injury that brought them to the hospital and what they are going home to, you can be more proactive in their care. When you, the provider, are able to take all of this into consideration, the patient will have better outcomes.”
For Corujo Avila, that understanding is critical. Born and raised in Puerto Rico, she says gun violence is a serious problem there, too, especially in urban areas.
“There’s a big Puerto Rican community in Buffalo, too,” she says, “and they are also victims of gun violence who end up in the trauma bay here. Sometimes they don’t speak English. These communities are suffering. I feel like I’m helping my community here.”
Foote’s motivation in developing the course was deeply personal. When she was 7 years old, her father was a victim of gun violence.
“He made it to the hospital, but he didn’t make it out,” she says. “They did everything they could, but they could not save him. As traumatic as it was for my family, I am honored to be part of these survivors’ recovery. It is very important to me. My co-founders and I recognized a need to provide additional support during a difficult time of their lives. I look forward to the positive impact we will have on their journey to recovery.”
UB Faculty Experts

Gino Biondini
Professor of Mathematics
Expertise: mathematical properties of waves, solitons, applied mathematics, mathematical physics, general questions about mathematics
Phone: 716-645-8810
Email: [email protected]

David M. Holmes
Clinical Associate Professor of Family Medicine
Expertise: global health, health care for underserved communities and human trafficking victims, spirituality in health, religious exemptions for vaccines, addiction medicine, wilderness medicine, travel medicine
Email: [email protected]
Contact: David M. Holmes can be reached through Ellen Goldbaum in University Communications at 716-645-4605 or [email protected] , or Douglas Sitler in University Communications at 716-645-9069 or [email protected] .

Negar Elhami-Khorasani
Associate Professor of Civil, Structural and Environmental Engineering
Expertise: structural fire engineering, wildfires in wildland-urban interface communities, fire following earthquake, multi-hazard engineering, disaster resilience
Phone: 716-645-3019
Email: [email protected]

Elizabeth K. Thomas
Associate Professor of Geology
Expertise: climate change, Arctic ice sheets, precipitation, lake effect snow, sea level rise, monsoons
Phone: 716-645-4329
Email: [email protected]

Ciprian N. Ionita
Assistant Professor of Biomedical Engineering
Expertise: 3-D medical imaging, 3-D printing in medicine, neuroimaging, cardiovascular imaging, endovascular disease
Phone: 716-829-5413
Email: [email protected]

Associate Professor of Restorative Dentistry
Expertise: forensic dentistry, bite mark analysis, victim identification
Phone: 716-829-2862
Email: [email protected]

Timothy Hellwig
Professor of Political Science
Expertise: politics of European nations, the European Union, immigration and trade in Europe, the US, and globally, public support for presidents and governments around the world.
Phone: 716-645-8440
Email: [email protected]

Mark H. Karwan
Praxair Professor of Operations Research
Expertise: sports scheduling, especially in the NFL
Phone: 716-645-2422
Email: [email protected]

Annette Wysocki
Dean of the School of Nursing
Expertise: wound care, delayed healing in chronic wounds, federal funding of nursing programs, media representation of nurses, ethical guidelines.
Phone: 716-829-3308
Email: [email protected]

Panayotis (Peter) K. Thanos
Senior Research Scientist of Pharmacology and Toxicology
Expertise: ADHD treatment, addiction; brain imaging; alcohol and drug abuse, obesity, binge eating disorder, bariatric surgery, prenatal nicotine use, prenatal cannabis
Phone: 716-881-7520
Email: [email protected]

Hua (Helen) Wang
Professor of Communication
Expertise: communication strategies for health promotion and social change; entertainment-education; communication technology; social networks; digital media literacy; health interventions
Phone: 716-645-1501
Email: [email protected]

Ghazala Saleem
Assistant Professor of Rehabilitation Science
Expertise: concussions (especially in children), traumatic brain injury, brain injury and intimate partner violence
Phone: 716-829-2589
Email: [email protected]

Mark Daniel Hicar
Associate Professor of Pediatrics
Expertise: pediatric infectious diseases, viral infections, antibody responses against HIV, Kawasaki disease
Phone: 716-323-0150
Email: [email protected]

Michael LaMonte
Research Professor of Epidemiology and Environmental Health
Expertise: healthy aging, cardiovascular disease, physical activity, women’s health, menopause, cancer, the microbiome, periodontal disease
Phone: 716-829-5379
Email: [email protected]

Jason Benedict
Associate Professor of Chemistry
Expertise: chemistry, chemical reactions, chemical crystallography, photochemistry, nanomaterials, synchrotron light sources, science of snowflakes
Phone: 716-645-4276
Email: [email protected]

Catherine Cook-Cottone
Professor of Counseling, School and Educational Psychology
Expertise: yoga, mindfulness, embodied self-regulation, eating disorders, anxiety-based disorders
Phone: 716-645-1128
Email: [email protected]

Greg A. Valentine
UB Distinguished Professor of Geology
Expertise: volcanoes, volcanic eruptions, disaster preparedness, supervolcanoes
Phone: 716-645-4295
Email: [email protected]

Amy Reynolds
Expertise: multicultural issues, college student mental health
Phone: 716-645-1112
Email: [email protected]

Andrew Talal, MD
Professor of Medicine
Expertise: diagnosing and treating hepatitis C virus, developing and evaluating new therapies for liver disease
Phone: 716-829-6208
Email: [email protected]

Joann Sands
Clinical Assistant Professor of Nursing
Expertise: disaster response education and training; emergency preparedness and management; the role of nurses in disasters
Phone: 716-829-2342
Email: [email protected]

Ndubueze L. Mbah
Associate Professor of History
Expertise: African history; the Atlantic World; colonialism; gender in West Africa; history of slavery and emancipation; Boko Haram
Phone: 716-645-8415
Email: [email protected]

Corrie Stone-Johnson
Professor of Educational Leadership and Policy
Expertise: school leadership, school reform, schools and communities, organizational culture of schools
Phone: 716-645-2471
Email: [email protected]

Lucinda M. Finley
Frank G. Raichle Professor of Trial and Appellate Advocacy
Expertise: abortion, reproductive rights, women and the law, Supreme Court, employment discrimination, equal protection law, tort law and reform
Phone: 716-645-6152
Email: [email protected]
Contact: Finley can also be contacted through Doug Sitler in UB Media Relations at 716-645-9069 or [email protected] .

Machiko R. Tomita
Clinical Professor of Rehabilitation Science
Expertise: aging, falls and frailty prevention in older adults, caregiving for older adults, smart home technology, virtual group exercise
Phone: 716-829-6740
Email: [email protected]

Margaret Rhee
Assistant Professor of Media Study
Expertise: digital storytelling; participatory art; new media, ethnic, cultural, Asian American, queer and feminist studies
Phone: 716-645-0923
Email: [email protected]

Luis A. Colón
A. Conger Goodyear Professor of Chemistry
Expertise: analytical chemistry, separation science, liquid chromatography, diversity in STEM, mentoring students of color
Phone: 716-645-4213
Email: [email protected]

Matilde Sanchez-Pena
Assistant Professor of Engineering Education
Expertise: engineering education, cultures of wellbeing, institutional diversity, faculty advancement, equity in the engineering field, women in STEM, intersectionality
Phone: 716-645-5861
Email: [email protected]

Oscar G. Gómez-Duarte
Chief of the Division of Pediatric Infectious Diseases in the Department of Pediatrics
Expertise: pediatric infectious diseases, vaccines, childhood diarrhea, health disparities, COVID-19 community interventions
Phone: 716-323-0150. Gómez-Duarte can also be reached through Ellen Goldbaum in University Communications at 716-645-4605 or [email protected] , or Douglas Sitler in University Communications at 716-645-9069 or [email protected]
Email: [email protected]

Helen A. “Nellie” Drew
Director of the Center for the Advancement of Sport
Expertise: sports law, including student-athletes’ name, image and likeness (NIL), antitrust laws, collective bargaining, discipline of athletes, drug testing, NCAA compliance and Title IX; diversity in sport
Phone: 716-645-2071
Email: [email protected]

Amanda Nickerson
Director of the Alberti Center for Bullying Abuse Prevention
Expertise: school violence, bullying prevention and intervention, parent and peer relationships, assessment and treatment of emotional and behavioral disorders
Phone: 716-645-1532
Email: [email protected]

Sarah A. Robert
Associate Professor of Learning and Instruction
Expertise: teaching as an occupation; teachers’ unions; labor issues in education; global education reform; gender and equity in education; school food
Phone: 716-645-4046
Email: [email protected]

Peter Pfordresher
Professor of Psychology
Expertise: singing accuracy, relationship between music and language, cognitive bases of music performance, psychology of music
Phone: 716-645-0234
Email: [email protected]

Eun-Hye “Enki” Yoo
Associate Professor of Geography
Expertise: GIScience, human mobility, spatial statistics (including in relation to public health, air pollution and the environment)
Phone: 716-645-0476
Email: [email protected]

David Schmid
Associate Professor of English
Expertise: popular culture, cultural studies, celebrity, crime, manhood, the monstrous, contemporary British and American fiction, American literary and cultural treatments of the city
Phone: 716-645-0679
Email: [email protected]

Sunyee Yoon
Assistant Professor of Marketing
Expertise: social status and mobility; socially responsible consumption; products that promote animal welfare; consumer behavior
Contact: Sunyee Yoon can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

X. Christine Wang
Director of the Fisher-Price Early Childhood Research Center
Expertise: early childhood development and learning, technology in early childhood, early literacy and science, early education in international contexts
Phone: 716-645-2379
Email: [email protected]

Derek Daniels
Professor and Chair of Biological Sciences
Expertise: science of thirst; science of food, water and salt intake; ingestive/eating behaviors
Phone: 716-645-0264
Email: [email protected]

Assistant Professor of Civil, Structural and Environmental Engineering
Expertise: surveillance and disinfection of pathogens in wastewater and the environment; wastewater-based disease monitoring; environmental microbiology; proteomics
Phone: 716-645-4002
Email: [email protected]

Mickey Sperlich
Associate Professor of Social Work
Expertise: trauma and mental health challenges in pregnancy, childbirth and the postpartum period; women’s health; midwifery
Phone: 716-645-9087
Email: [email protected]

Peter Winkelstein
Executive Director of the Institute for Healthcare Informatics
Expertise: electronic health/medical records; medical informatics; ethics and informatics; computer modeling
Phone: 716-881-7546. Winkelstein can also be reached through Ellen Goldbaum in University Communications at 716-645-4605 or [email protected] , or Douglas Sitler in University Communications at 716-645-9069 or [email protected] .
Email: [email protected]

Ryan Muldoon
Associate Professor of Philosophy
Expertise: social and political philosophy, diversity, international development policy, social norms, behavior change, ethics
Phone: 716-645-0140
Email: [email protected]

Lucia A. Leone
Associate Professor of Community Health and Health Behavior
Expertise: food access, mobile produce markets, WIC, obesity prevention, physical activity
Phone: 716-829-6953
Email: [email protected]

S. Todd Brown
Dean of the School of Law
Expertise: business bankruptcy, bankruptcy trusts, complex litigation/mass torts, corporate governance, and corporate fraud
Phone: 716-645-2052
Email: [email protected]

Expertise: filmmaking; cinematography; narrative, documentary, experimental and hybrid films; storytelling
Phone: 716-645-0954
Email: [email protected]

Thomas Murdock
Clinical Assistant Professor of Entrepreneurship
Expertise: emerging entrepreneurship, business incubation, economic development (particularly technology-based), startups as economic drivers, startup business plans/business models, customer discovery, social entrepreneurship
Contact: Thomas Murdock can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

Elizabeth Mazzolini
Expertise: Mountaineering deaths, climbing technology, consumerism, material culture, garbage, culture of waste
Phone: 716-645-0691
Email: [email protected]

Amy Hequembourg
Associate Professor of Nursing
Expertise: health disparities affecting sexual minorities
Phone: 716-829-2608
Email: [email protected]

Richard Salvi
SUNY Distinguished Professor Emeritus of Communicative Disorders and Sciences
Expertise: tinnitus, hearing, noise-induced hearing loss, hyperacusis, central auditory system
Phone: 716-829-5310
Email: [email protected]

Mike Mingcheng Wei
Associate Professor of Operations Management and Strategy
Expertise: supply chain management; dynamic pricing; revenue management; strategic consumer behavior; online learning and decision-making; online recommendation systems; assortment optimization; high-dimensional machine learning
Contact: Mike Mingcheng Wei can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

Robert Adelman
Chair and Professor of Sociology
Expertise: urban sociology, segregation, race, immigration, U.S. Census
Phone: 716-645-8478
Email: [email protected]

Professor of Environment and Sustainability
Expertise: environmental movement in the U.S., environmental history, Earth Day, sustainable business, suburban sprawl
Phone: 716-645-8665
Email: [email protected]

Annahita Ball
Expertise: family engagement in schools; educational justice and reform; school-based mental health services; school-community partnerships
Phone: 716-645-8951
Email: [email protected]

John J. Leddy
Director of the Concussion Management Clinic
Expertise: concussions, post-concussion syndrome, sports medicine
Phone: 716-829-5501
Email: [email protected]

Sophie Nowicki
SUNY Empire Innovation Professor of Geology
Expertise: climate change, ice sheet modeling, Greenland and Antarctic ice sheets, glaciers, sea level rise
Phone: 716-645-4335
Email: [email protected]

Clayton Masterman
Associate Professor of Law
Expertise: Health law, tort law, benefit-cost analysis, damages and other remedies, law and economics
Phone: 716-645-2480
Email: [email protected]

Beata Csatho
Professor of Geology
Expertise: climate change, sea level rise, Greenland Ice Sheet, Antarctic ice loss, glaciers, remote sensing, using satellite data and laser altimetry to measure the Earth
Phone: 716-645-4325
Email: [email protected]

G. James Lemoine
Associate Professor of Organization and Human Resources
Expertise: servant leadership; gender and leadership; ethics and moral leadership; leadership and motivation; entrepreneurial leaders; creativity and innovation; managing under volatility, uncertainty, complexity and ambiguity (VUCA)
Contact: G. James Lemoine can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

Lynn Shanahan
Associate Professor of of Learning and Instruction
Expertise: childhood literacy; literacy, technology and multimodality; STEM and urban education
Phone: 716-645-4028
Email: [email protected]

Thomas Ulbrich
Executive in Residence for Entrepreneurship in the UB School of Management
Expertise: entrepreneurship and startups, entrepreneurial skills and attributes, entrepreneurial education, small business, family business, customer loyalty, social entrepreneurship
Contact: Thomas Ulbrich can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

Expertise: history of Chinese medicine, food and spices; history of epidemics; history of the senses; comparative historical perspectives in medicine
Phone: 716-645-8404
Email: [email protected]

Laura Rusche
Professor of Biological Sciences
Expertise: yeast, genomics, genetics, gene expression, chromosomes, DNA, RNA, chromatin, sirtuins
Phone: 716-645-5198
Email: [email protected]

Victor Albert
Empire Innovation Professor of Biological Sciences
Expertise: plant evolutionary biology; evolution of carnivorous plants; genomes of Amborella, avocado, birch, coffee and gardenia; comparative genomics; junk DNA
Phone: 716-645-4983
Email: [email protected]

Professor of Chemical and Biological Engineering
Expertise: materials science, electrochemical energy storage, batteries, hydrogen fuel cells, supercapacitators, catalysts, electrochemistry
Phone: 716-645-8618
Email: [email protected]

Michael Dambra
Associate Professor of Accounting and Law
Expertise: economic consequences of regulatory changes; initial public offerings (IPOs); pension accounting; valuation of privately held equity
Contact: Michael Dambra can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

Susan Green
Co-director of the Institute on Trauma and Trauma-Informed Care
Expertise: trauma, trauma-informed care in organizations and service delivery systems
Phone: 716-645-1249
Email: [email protected]

Stephanie A. Poindexter
Assistant Professor of Anthropology
Expertise: biological anthropology, primate evolution, primate conservation
Phone: 716-645-0427
Email: [email protected]

Antoine Yoshinaka
Associate Professor of Political Science
Expertise: American politics, U.S. political parties, polarization, party switching, legislatures, political lobbying, redistricting
Phone: 716-645-8435
Email: [email protected]

Sanjay Sethi
Chief of the Division of Pulmonary, Critical Care and Sleep Medicine in the Department of Medicine
Expertise: respiratory infections and lung disease, especially in chronic obstructive pulmonary disease (COPD) and lung infections, such as bronchitis and pneumonia
Phone: Sanjay Sethi can be reached through Ellen Goldbaum in University Communications at 716-645-4605 or [email protected] , or Douglas Sitler in University Communications at 716-645-9069 or [email protected] .
Email: [email protected]

Margaret Sallee
Associate Professor of Educational Leadership and Policy
Expertise: university work environment, work/family policies, work/life balance, faculty diversity, gender on college campuses, graduate student experience
Phone: 716-645-1091
Email: [email protected]

Ekin Atilla-Gokcumen
Dr. Marjorie E. Winkler Distinguished Professor of Chemistry
Expertise: chemical biology, lipids; cellular aging and senescence; cell death (apoptosis and necroptosis); omics approaches to research
Phone: 716-645-4130
Email: [email protected]

Trina Hamilton
Associate Professor of Geography
Expertise: corporate responsibility, social and environmental activism, diamond trade, gentrification
Phone: 716-645-0482
Email: [email protected]

Dejan Stojkovic
Professor of Physics
Expertise: cosmology, gravity, black holes, particle physics, exotic physics, origins of the universe, extra dimensions
Phone: 716-645-5014
Email: [email protected]

Jennifer A. Surtees
Professor of Biochemistry
Expertise: genomes, genetic diversity, DNA, science communication, COVID-19 genomic surveillance and genetic variants
Phone: 716-829-6083
Email: [email protected]

Susan K. Cahn
Emerita Professor of History
Expertise: gender and sexuality in sports, homophobia in sports, women’s history, feminist theory, history of chronic illness, history of mental illness
Phone: 716-645-8418
Email: [email protected]

Sayanti Mukherjee
Assistant Professor of Industrial and Systems Engineering
Expertise: resilient sociotechnical systems, predictive analytics, risk-informed decision-making, public health and health care, electrical grid and energy, climate change impact assessment
Phone: 716-645-4699
Email: [email protected]

Expertise: science, health, environmental and risk communication
Phone: 716-645-1169
Email: [email protected]

Haiqing Lin
Expertise: separation science, carbon capture, water purification, polymers, materials science
Phone: 716-645-1856
Email: [email protected]

Irus Braverman
Professor of Law
Expertise: laws governing animals, zoos, wildlife, coral reefs, extinction and climate change law, law and society, law and conservation, law and the environment, environmental justice in Israel/Palestine
Phone: 716-645-3030
Email: [email protected]

Riana R. Pryor
Assistant Professor of Exercise and Nutrition Sciences
Expertise: heat and exercise; heat illness, including heat stroke; hydration; high school sports and athlete safety; occupational safety; exercise physiology
Phone: 716-829-5456
Email: [email protected]

Samantha Barbas
Expertise: Mass media law, libel, privacy, freedom of the press
Phone: 716-645-6216
Email: [email protected]

Joanne Song McLaughlin
Associate Professor of Economics
Expertise: labor economics; health insurance mandates; age discrimination; older workers; AI and the future of work
Phone: 716-645-8685
Email: [email protected]

Xiaozhong Wen
Assistant Professor of Pediatrics
Expertise: diet and health in infants and young children, origins of obesity, smoking cessation during pregnancy
Phone: 716-829-6811
Email: [email protected]

Jacob Kathman
Professor and Chair of Political Science
Expertise: civil wars, United Nations, peacekeeping, conflict resolution
Phone: 716-645-8445
Email: [email protected]

Expertise: air pollution, greenhouse gases, climate change, remote sensing, molecular spectroscopy
Phone: 716-645-6167
Email: [email protected]

Robert Silverman
Professor of Urban and Regional Planning
Expertise: shrinking cities, fair housing, affordable housing, licensing and siting of cannabis dispensaries, gentrification, community development, nonprofit organizations, community-based organizations in urban neighborhoods
Phone: 716-829-5882
Email: [email protected]

Despina Stratigakos
Professor of Architecture
Expertise: diversity in architecture; gender and modernity in European cities; German architecture; Nazi propaganda and architecture
Phone: 716-829-3486
Email: [email protected]

Brandon Szerwo
Assistant Professor of Accounting and Law
Expertise: financial reporting and audit quality, corporate governance, financial regulation, management disclosures, auditor disclosures, financial accounting
Contact: Brandon Szerwo can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

Howard Lasker
Professor Emeritus of Environment and Sustainability
Expertise: coral reefs; coral bleaching; climate change and oceans
Phone: 716-645-4870
Email: [email protected]

Timothy F. Murphy
SUNY Distinguished Professor of Medicine
Expertise: infectious diseases, chronic obstructive pulmonary disease (COPD), vaccine development, children’s ear infections, health disparities, clinical and translational science
Phone: 716-881-8911
Email: [email protected]

Lindsay Hahn
Assistant Professor of Communication
Expertise: media psychology, morality, media effects, children and media, media and radicalization
Phone: 716-645-1172
Email: [email protected]

Henry-Louis Taylor Jr.
Director of the Center for Urban Studies
Expertise: urban development, housing, gentrification, underdeveloped neighborhoods, shrinking cities, race and class, U.S.-Cuba relations
Phone: 716-829-5458
Email: [email protected]

Ryan M. Rish
Assistant Professor of Learning and Instruction
Expertise: adolescent literacy practices; culture and identity in learning; teaching social issues
Phone: 716-645-4042
Email: [email protected]

Kemper E. Lewis
Dean of the School of Engineering and Applied Sciences
Expertise: advanced manufacturing, mass customization, engineering design
Phone: 716-645-2682
Email: [email protected]

Jamie Ostrov
Expertise: subtypes of aggression and victimization, developmental psychopathology, media effects on children, peer relationships, applied developmental psychology
Phone: 716-645-3680
Email: [email protected]

James Campbell
UB Distinguished Professor of Political Science
Expertise: U.S. politics, political parties, political polarization, campaigns, public opinion, political participation, congressional elections, election forecasting, elections and the economy, presidential approval, electoral systems (including redistricting and ranked choice voting)
Phone: 716-645-8452
Email: [email protected]

Pauline Mendola
Professor and Chair of Epidemiology and Environmental Health
Expertise: chronic diseases in pregnancy; environmental factors impacting reproductive and pediatric health; health effects of air pollution and extreme temperatures
Phone: 716-829-5356
Email: [email protected]

Elizabeth Bowen
Expertise: homelessness, health issues affecting homeless populations, recovery from alcohol and other drug problems
Phone: 716-645-1258
Email: [email protected]

Cody Mejeur
Expertise: game studies; trans, queer and feminist studies; narrative; storytelling; social justice and inclusion in video games and new media; games pedagogy
Phone: 716-645-0932
Email: [email protected]

Natalie Simpson
Chair of Operations Management and Strategy
Expertise: emergency services and disaster response; supply chain risk and resilience; creative and temporary operations; complex networks
Contact: Natalie Simpson can be reached most quickly through Jackie Ghosen in the School of Management Communications Office at 716-645-2833 or [email protected] .

Annette Semanchin Jones
Associate Professor and Director, PhD in Social Welfare program
Expertise: child welfare, foster care, child protection services
Phone: 716-645-1862
Email: [email protected]
UB on Futurity.org

- 4/17/24 Genome unveils coffee’s prehistoric origins
- 3/5/19 Unique vibrations lead to protein ‘fingerprints’
- 3/1/19 Maps: These states get less federal money for fires
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Center for Substance Abuse Treatment (US). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. (Treatment Improvement Protocol (TIP) Series, No. 57.)

Trauma-Informed Care in Behavioral Health Services.
- Order print copy from SAMHSA
Chapter 3 Understanding the Impact of Trauma
Trauma-informed care (TIC) involves a broad understanding of traumatic stress reactions and common responses to trauma. Providers need to understand how trauma can affect treatment presentation, engagement, and the outcome of behavioral health services. This chapter examines common experiences survivors may encounter immediately following or long after a traumatic experience.
Trauma, including one-time, multiple, or long-lasting repetitive events, affects everyone differently. Some individuals may clearly display criteria associated with posttraumatic stress disorder (PTSD), but many more individuals will exhibit resilient responses or brief subclinical symptoms or consequences that fall outside of diagnostic criteria. The impact of trauma can be subtle, insidious, or outright destructive. How an event affects an individual depends on many factors, including characteristics of the individual, the type and characteristics of the event(s), developmental processes, the meaning of the trauma, and sociocultural factors.
This chapter begins with an overview of common responses, emphasizing that traumatic stress reactions are normal reactions to abnormal circumstances. It highlights common short- and long-term responses to traumatic experiences in the context of individuals who may seek behavioral health services. This chapter discusses psychological symptoms not represented in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; American Psychiatric Association [APA], 2013a ), and responses associated with trauma that either fall below the threshold of mental disorders or reflect resilience. It also addresses common disorders associated with traumatic stress. This chapter explores the role of culture in defining mental illness, particularly PTSD, and ends by addressing co-occurring mental and substance-related disorders.

TIC Framework in Behavioral Health Services—The Impact of Trauma
- Sequence of Trauma Reactions
Survivors’ immediate reactions in the aftermath of trauma are quite complicated and are affected by their own experiences, the accessibility of natural supports and healers, their coping and life skills and those of immediate family, and the responses of the larger community in which they live. Although reactions range in severity, even the most acute responses are natural responses to manage trauma— they are not a sign of psychopathology. Coping styles vary from action oriented to reflective and from emotionally expressive to reticent. Clinically, a response style is less important than the degree to which coping efforts successfully allow one to continue necessary activities, regulate emotions, sustain self-esteem, and maintain and enjoy interpersonal contacts. Indeed, a past error in traumatic stress psychology, particularly regarding group or mass traumas, was the assumption that all survivors need to express emotions associated with trauma and talk about the trauma; more recent research indicates that survivors who choose not to process their trauma are just as psychologically healthy as those who do. The most recent psychological debriefing approaches emphasize respecting the individual’s style of coping and not valuing one type over another.
Foreshortened future: Trauma can affect one’s beliefs about the future via loss of hope, limited expectations about life, fear that life will end abruptly or early, or anticipation that normal life events won’t occur (e.g., access to education, ability to have a significant and committed relationship, good opportunities for work).
Initial reactions to trauma can include exhaustion, confusion, sadness, anxiety, agitation, numbness, dissociation, confusion, physical arousal, and blunted affect. Most responses are normal in that they affect most survivors and are socially acceptable, psychologically effective, and self-limited. Indicators of more severe responses include continuous distress without periods of relative calm or rest, severe dissociation symptoms, and intense intrusive recollections that continue despite a return to safety. Delayed responses to trauma can include persistent fatigue, sleep disorders, nightmares, fear of recurrence, anxiety focused on flashbacks, depression, and avoidance of emotions, sensations, or activities that are associated with the trauma, even remotely. Exhibit 1.3-1 outlines some common reactions.
Exhibit 1.3-1
Immediate and Delayed Reactions to Trauma.
- Common Experiences and Responses to Trauma
A variety of reactions are often reported and/or observed after trauma. Most survivors exhibit immediate reactions, yet these typically resolve without severe long-term consequences. This is because most trauma survivors are highly resilient and develop appropriate coping strategies, including the use of social supports, to deal with the aftermath and effects of trauma. Most recover with time, show minimal distress, and function effectively across major life areas and developmental stages. Even so, clients who show little impairment may still have subclinical symptoms or symptoms that do not fit diagnostic criteria for acute stress disorder (ASD) or PTSD. Only a small percentage of people with a history of trauma show impairment and symptoms that meet criteria for trauma-related stress disorders, including mood and anxiety disorders.
The following sections focus on some common reactions across domains (emotional, physical, cognitive, behavioral, social, and developmental) associated with singular, multiple, and enduring traumatic events. These reactions are often normal responses to trauma but can still be distressing to experience. Such responses are not signs of mental illness, nor do they indicate a mental disorder. Traumatic stress-related disorders comprise a specific constellation of symptoms and criteria.
Emotional reactions to trauma can vary greatly and are significantly influenced by the individual’s sociocultural history. Beyond the initial emotional reactions during the event, those most likely to surface include anger, fear, sadness, and shame. However, individuals may encounter difficulty in identifying any of these feelings for various reasons. They might lack experience with or prior exposure to emotional expression in their family or community. They may associate strong feelings with the past trauma, thus believing that emotional expression is too dangerous or will lead to feeling out of control (e.g., a sense of “losing it” or going crazy). Still others might deny that they have any feelings associated with their traumatic experiences and define their reactions as numbness or lack of emotions.
Emotional dysregulation
Some trauma survivors have difficulty regulating emotions such as anger, anxiety, sadness, and shame—this is more so when the trauma occurred at a young age ( van der Kolk, Roth, Pelcovitz, & Mandel, 1993 ). In individuals who are older and functioning well prior to the trauma, such emotional dysregulation is usually short lived and represents an immediate reaction to the trauma, rather than an ongoing pattern. Self-medication—namely, substance abuse—is one of the methods that traumatized people use in an attempt to regain emotional control, although ultimately it causes even further emotional dysregulation (e.g., substance-induced changes in affect during and after use). Other efforts toward emotional regulation can include engagement in high-risk or self-injurious behaviors, disordered eating, compulsive behaviors such as gambling or overworking, and repression or denial of emotions; however, not all behaviors associated with self-regulation are considered negative. In fact, some individuals find creative, healthy, and industrious ways to manage strong affect generated by trauma, such as through renewed commitment to physical activity or by creating an organization to support survivors of a particular trauma.
Traumatic stress tends to evoke two emotional extremes: feeling either too much (overwhelmed) or too little (numb) emotion. Treatment can help the client find the optimal level of emotion and assist him or her with appropriately experiencing and regulating difficult emotions. In treatment, the goal is to help clients learn to regulate their emotions without the use of substances or other unsafe behavior. This will likely require learning new coping skills and how to tolerate distressing emotions; some clients may benefit from mindfulness practices, cognitive restructuring, and trauma-specific desensitization approaches, such as exposure therapy and eye movement desensitization and reprocessing (EMDR; refer to Part 1, Chapter 6 , for more information on trauma-specific therapies).
Numbing is a biological process whereby emotions are detached from thoughts, behaviors, and memories. In the following case illustration, Sadhanna’s numbing is evidenced by her limited range of emotions associated with interpersonal interactions and her inability to associate any emotion with her history of abuse. She also possesses a belief in a foreshortened future. A prospective longitudinal study ( Malta, Levitt, Martin, Davis, & Cloitre, 2009 ) that followed the development of PTSD in disaster workers highlighted the importance of understanding and appreciating numbing as a traumatic stress reaction. Because numbing symptoms hide what is going on inside emotionally, there can be a tendency for family members, counselors, and other behavioral health staff to assess levels of traumatic stress symptoms and the impact of trauma as less severe than they actually are.
Case Illustration: Sadhanna
Sadhanna is a 22-year-old woman mandated to outpatient mental health and substance abuse treatment as the alternative to incarceration. She was arrested and charged with assault after arguing and fighting with another woman on the street. At intake, Sadhanna reported a 7-year history of alcohol abuse and one depressive episode at age 18. She was surprised that she got into a fight but admitted that she was drinking at the time of the incident. She also reported severe physical abuse at the hands of her mother’s boyfriend between ages 4 and 15. Of particular note to the intake worker was Sadhanna’s matter-of-fact way of presenting the abuse history. During the interview, she clearly indicated that she did not want to attend group therapy and hear other people talk about their feelings, saying, “I learned long ago not to wear emotions on my sleeve.”
Sadhanna reported dropping out of 10th grade, saying she never liked school. She didn’t expect much from life. In Sadhanna’s first weeks in treatment, she reported feeling disconnected from other group members and questioned the purpose of the group. When asked about her own history, she denied that she had any difficulties and did not understand why she was mandated to treatment. She further denied having feelings about her abuse and did not believe that it affected her life now. Group members often commented that she did not show much empathy and maintained a flat affect, even when group discussions were emotionally charged.
Diagnostic criteria for PTSD place considerable emphasis on psychological symptoms, but some people who have experienced traumatic stress may present initially with physical symptoms. Thus, primary care may be the first and only door through which these individuals seek assistance for trauma-related symptoms. Moreover, there is a significant connection between trauma, including adverse childhood experiences (ACEs), and chronic health conditions. Common physical disorders and symptoms include somatic complaints; sleep disturbances; gastrointestinal, cardiovascular, neurological, musculoskeletal, respiratory, and dermatological disorders; urological problems; and substance use disorders.
Somatization
Somatization indicates a focus on bodily symptoms or dysfunctions to express emotional distress. Somatic symptoms are more likely to occur with individuals who have traumatic stress reactions, including PTSD. People from certain ethnic and cultural backgrounds may initially or solely present emotional distress via physical ailments or concerns. Many individuals who present with somatization are likely unaware of the connection between their emotions and the physical symptoms that they’re experiencing. At times, clients may remain resistant to exploring emotional content and remain focused on bodily complaints as a means of avoidance. Some clients may insist that their primary problems are physical even when medical evaluations and tests fail to confirm ailments. In these situations, somatization may be a sign of a mental illness. However, various cultures approach emotional distress through the physical realm or view emotional and physical symptoms and well-being as one. It is important not to assume that clients with physical complaints are using somatization as a means to express emotional pain; they may have specific conditions or disorders that require medical attention. Foremost, counselors need to refer for medical evaluation.
Advice to Counselors: Using Information About Biology and Trauma
Frame reexperiencing the event(s), hyperarousal, sleep disturbances, and other physical symptoms as physiological reactions to extreme stress.
Communicate that treatment and other wellness activities can improve both psychological and physiological symptoms (e.g., therapy, meditation, exercise, yoga). You may need to refer certain clients to a psychiatrist who can evaluate them and, if warranted, prescribe psycho-tropic medication to address severe symptoms.
Discuss traumatic stress symptoms and their physiological components.
Explain links between traumatic stress symptoms and substance use disorders, if appropriate.
Normalize trauma symptoms. For example, explain to clients that their symptoms are not a sign of weakness, a character flaw, being damaged, or going crazy.
- Support your clients and provide a message of hope—that they are not alone, they are not at fault, and recovery is possible and anticipated.
Biology of trauma
Trauma biology is an area of burgeoning research, with the promise of more complex and explanatory findings yet to come. Although a thorough presentation on the biological aspects of trauma is beyond the scope of this publication, what is currently known is that exposure to trauma leads to a cascade of biological changes and stress responses. These biological alterations are highly associated with PTSD, other mental illnesses, and substance use disorders. These include:
- Changes in limbic system functioning.
- Hypothalamic–pituitary–adrenal axis activity changes with variable cortisol levels.
- Neurotransmitter-related dysregulation of arousal and endogenous opioid systems.
As a clear example, early ACEs such as abuse, neglect, and other traumas affect brain development and increase a person’s vulnerability to encountering interpersonal violence as an adult and to developing chronic diseases and other physical illnesses, mental illnesses, substance-related disorders, and impairment in other life areas ( Centers for Disease Control and Prevention, 2012 ).
Hyperarousal and sleep disturbances
A common symptom that arises from traumatic experiences is hyperarousal (also called hypervigilance). Hyperarousal is the body’s way of remaining prepared. It is characterized by sleep disturbances, muscle tension, and a lower threshold for startle responses and can persist years after trauma occurs. It is also one of the primary diagnostic criteria for PTSD.
Hyperarousal is a consequence of biological changes initiated by trauma. Although it serves as a means of self-protection after trauma, it can be detrimental. Hyperarousal can interfere with an individual’s ability to take the necessary time to assess and appropriately respond to specific input, such as loud noises or sudden movements. Sometimes, hyperarousal can produce overreactions to situations perceived as dangerous when, in fact, the circumstances are safe.
Case Illustration: Kimi
Kimi is a 35-year-old Native American woman who was group raped at the age of 16 on her walk home from a suburban high school. She recounts how her whole life changed on that day. “I never felt safe being alone after the rape. I used to enjoy walking everywhere. Afterward, I couldn’t tolerate the fear that would arise when I walked in the neighborhood. It didn’t matter whether I was alone or with friends—every sound that I heard would throw me into a state of fear. I felt like the same thing was going to happen again. It’s gotten better with time, but I often feel as if I’m sitting on a tree limb waiting for it to break. I have a hard time relaxing. I can easily get startled if a leaf blows across my path or if my children scream while playing in the yard. The best way I can describe how I experience life is by comparing it to watching a scary, suspenseful movie—anxiously waiting for something to happen, palms sweating, heart pounding, on the edge of your chair.”
Along with hyperarousal, sleep disturbances are very common in individuals who have experienced trauma. They can come in the form of early awakening, restless sleep, difficulty falling asleep, and nightmares. Sleep disturbances are most persistent among individuals who have trauma-related stress; the disturbances sometimes remain resistant to intervention long after other traumatic stress symptoms have been successfully treated. Numerous strategies are available beyond medication, including good sleep hygiene practices, cognitive rehearsals of nightmares, relaxation strategies, and nutrition.
Traumatic experiences can affect and alter cognitions. From the outset, trauma challenges the just-world or core life assumptions that help individuals navigate daily life ( Janoff-Bulman, 1992 ). For example, it would be difficult to leave the house in the morning if you believed that the world was not safe, that all people are dangerous, or that life holds no promise. Belief that one’s efforts and intentions can protect oneself from bad things makes it less likely for an individual to perceive personal vulnerability. However, traumatic events—particularly if they are unexpected—can challenge such beliefs.
Cognitions and Trauma
The following examples reflect some of the types of cognitive or thought-process changes that can occur in response to traumatic stress.
Cognitive errors: Misinterpreting a current situation as dangerous because it resembles, even remotely, a previous trauma (e.g., a client overreacting to an overturned canoe in 8 inches of water, as if she and her paddle companion would drown, due to her previous experience of nearly drowning in a rip current 5 years earlier).
Excessive or inappropriate guilt: Attempting to make sense cognitively and gain control over a traumatic experience by assuming responsibility or possessing survivor’s guilt, because others who experienced the same trauma did not survive.
Idealization: Demonstrating inaccurate rationalizations, idealizations, or justifications of the perpetrator’s behavior, particularly if the perpetrator is or was a caregiver. Other similar reactions mirror idealization; traumatic bonding is an emotional attachment that develops (in part to secure survival) between perpetrators who engage in interpersonal trauma and their victims, and Stockholm syndrome involves compassion and loyalty toward hostage takers ( de Fabrique, Van Hasselt, Vecchi, & Romano, 2007 ).
Trauma-induced hallucinations or delusions: Experiencing hallucinations and delusions that, although they are biological in origin, contain cognitions that are congruent with trauma content (e.g., a woman believes that a person stepping onto her bus is her father, who had sexually abused her repeatedly as child, because he wore shoes similar to those her father once wore).
Intrusive thoughts and memories: Experiencing, without warning or desire, thoughts and memories associated with the trauma. These intrusive thoughts and memories can easily trigger strong emotional and behavioral reactions, as if the trauma was recurring in the present. The intrusive thoughts and memories can come rapidly, referred to as flooding, and can be disruptive at the time of their occurrence. If an individual experiences a trigger, he or she may have an increase in intrusive thoughts and memories for a while. For instance, individuals who inadvertently are retraumatized due to program or clinical practices may have a surge of intrusive thoughts of past trauma, thus making it difficult for them to discern what is happening now versus what happened then. Whenever counseling focuses on trauma, it is likely that the client will experience some intrusive thoughts and memories. It is important to develop coping strategies before, as much as possible, and during the delivery of trauma-informed and trauma-specific treatment.
Let’s say you always considered your driving time as “your time”—and your car as a safe place to spend that time. Then someone hits you from behind at a highway entrance. Almost immediately, the accident affects how you perceive the world, and from that moment onward, for months following the crash, you feel unsafe in any car. You become hypervigilant about other drivers and perceive that other cars are drifting into your lane or failing to stop at a safe distance behind you. For a time, your perception of safety is eroded, often leading to compensating behaviors (e.g., excessive glancing into the rearview mirror to see whether the vehicles behind you are stopping) until the belief is restored or reworked. Some individuals never return to their previous belief systems after a trauma, nor do they find a way to rework them—thus leading to a worldview that life is unsafe. Still, many other individuals are able to return to organizing core beliefs that support their perception of safety.
Many factors contribute to cognitive patterns prior to, during, and after a trauma. Adopting Beck and colleagues’ cognitive triad model ( 1979 ), trauma can alter three main cognitive patterns: thoughts about self, the world (others/environment), and the future. To clarify, trauma can lead individuals to see themselves as incompetent or damaged, to see others and the world as unsafe and unpredictable, and to see the future as hopeless—believing that personal suffering will continue, or negative outcomes will preside for the foreseeable future (see Exhibit 1.3-2 ). Subsequently, this set of cognitions can greatly influence clients’ belief in their ability to use internal resources and external support effectively. From a cognitive– behavioral perspective, these cognitions have a bidirectional relationship in sustaining or contributing to the development of depressive and anxiety symptoms after trauma. However, it is possible for cognitive patterns to help protect against debilitating psychological symptoms as well. Many factors contribute to cognitive patterns prior to, during, and after a trauma.
Exhibit 1.3-2
Cognitive Triad of Traumatic Stress.
Feeling different
An integral part of experiencing trauma is feeling different from others, whether or not the trauma was an individual or group experience. Traumatic experiences typically feel surreal and challenge the necessity and value of mundane activities of daily life. Survivors often believe that others will not fully understand their experiences, and they may think that sharing their feelings, thoughts, and reactions related to the trauma will fall short of expectations. However horrid the trauma may be, the experience of the trauma is typically profound.
The type of trauma can dictate how an individual feels different or believes that they are different from others. Traumas that generate shame will often lead survivors to feel more alienated from others—believing that they are “damaged goods.” When individuals believe that their experiences are unique and incomprehensible, they are more likely to seek support, if they seek support at all, only with others who have experienced a similar trauma.
Triggers and flashbacks
A trigger is a stimulus that sets off a memory of a trauma or a specific portion of a traumatic experience. Imagine you were trapped briefly in a car after an accident. Then, several years later, you were unable to unlatch a lock after using a restroom stall; you might have begun to feel a surge of panic reminiscent of the accident, even though there were other avenues of escape from the stall. Some triggers can be identified and anticipated easily, but many are subtle and inconspicuous, often surprising the individual or catching him or her off guard. In treatment, it is important to help clients identify potential triggers, draw a connection between strong emotional reactions and triggers, and develop coping strategies to manage those moments when a trigger occurs. A trigger is any sensory reminder of the traumatic event: a noise, smell, temperature, other physical sensation, or visual scene. Triggers can generalize to any characteristic, no matter how remote, that resembles or represents a previous trauma, such as revisiting the location where the trauma occurred, being alone, having your children reach the same age that you were when you experienced the trauma, seeing the same breed of dog that bit you, or hearing loud voices. Triggers are often associated with the time of day, season, holiday, or anniversary of the event.
A flashback is reexperiencing a previous traumatic experience as if it were actually happening in that moment. It includes reactions that often resemble the client’s reactions during the trauma. Flashback experiences are very brief and typically last only a few seconds, but the emotional aftereffects linger for hours or longer. Flashbacks are commonly initiated by a trigger, but not necessarily. Sometimes, they occur out of the blue. Other times, specific physical states increase a person’s vulnerability to reexperiencing a trauma, (e.g., fatigue, high stress levels). Flashbacks can feel like a brief movie scene that intrudes on the client. For example, hearing a car backfire on a hot, sunny day may be enough to cause a veteran to respond as if he or she were back on military patrol. Other ways people reexperience trauma, besides flashbacks, are via nightmares and intrusive thoughts of the trauma.
Advice to Counselors: Helping Clients Manage Flashbacks and Triggers
If a client is triggered in a session or during some aspect of treatment, help the client focus on what is happening in the here and now; that is, use grounding techniques. Behavioral health service providers should be prepared to help the client get regrounded so that they can distinguish between what is happening now versus what had happened in the past (see Covington, 2008 , and Najavits, 2002b , 2007b , for more grounding techniques). Offer education about the experience of triggers and flashbacks, and then normalize these events as common traumatic stress reactions. Afterward, some clients need to discuss the experience and understand why the flashback or trigger occurred. It often helps for the client to draw a connection between the trigger and the traumatic event(s). This can be a preventive strategy whereby the client can anticipate that a given situation places him or her at higher risk for retraumatization and requires use of coping strategies, including seeking support.
Source: Green Cross Academy of Traumatology, 2010 .
Dissociation, depersonalization, and derealization
Dissociation is a mental process that severs connections among a person’s thoughts, memories, feelings, actions, and/or sense of identity. Most of us have experienced dissociation—losing the ability to recall or track a particular action (e.g., arriving at work but not remembering the last minutes of the drive). Dissociation happens because the person is engaged in an automatic activity and is not paying attention to his or her immediate environment. Dissociation can also occur during severe stress or trauma as a protective element whereby the individual incurs distortion of time, space, or identity. This is a common symptom in traumatic stress reactions.
Dissociation helps distance the experience from the individual. People who have experienced severe or developmental trauma may have learned to separate themselves from distress to survive. At times, dissociation can be very pervasive and symptomatic of a mental disorder, such as dissociative identity disorder (DID; formerly known as multiple personality disorder). According to the DSM-5, “dissociative disorders are characterized by a disruption of and/or discontinuity in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behavior” ( APA, 2013a , p. 291). Dissociative disorder diagnoses are closely associated with histories of severe childhood trauma or pervasive, human-caused, intentional trauma, such as that experienced by concentration camp survivors or victims of ongoing political imprisonment, torture, or long-term isolation. A mental health professional, preferably with significant training in working with dissociative disorders and with trauma, should be consulted when a dissociative disorder diagnosis is suspected.
Potential Signs of Dissociation
- Fixed or “glazed” eyes
- Sudden flattening of affect
- Long periods of silence
- Monotonous voice
- Stereotyped movements
- Responses not congruent with the present context or situation
- Excessive intellectualization
( Briere, 1996a )
The characteristics of DID can be commonly accepted experiences in other cultures, rather than being viewed as symptomatic of a traumatic experience. For example, in non-Western cultures, a sense of alternate beings within oneself may be interpreted as being inhabited by spirits or ancestors ( Kirmayer, 1996 ). Other experiences associated with dissociation include depersonalization—psychologically “leaving one’s body,” as if watching oneself from a distance as an observer or through derealization, leading to a sense that what is taking place is unfamiliar or is not real.
If clients exhibit signs of dissociation, behavioral health service providers can use grounding techniques to help them reduce this defense strategy. One major long-term consequence of dissociation is the difficulty it causes in connecting strong emotional or physical reactions with an event. Often, individuals may believe that they are going crazy because they are not in touch with the nature of their reactions. By educating clients on the resilient qualities of dissociation while also emphasizing that it prevents them from addressing or validating the trauma, individuals can begin to understand the role of dissociation. All in all, it is important when working with trauma survivors that the intensity level is not so great that it triggers a dissociative reaction and prevents the person from engaging in the process.
Traumatic stress reactions vary widely; often, people engage in behaviors to manage the aftereffects, the intensity of emotions, or the distressing aspects of the traumatic experience. Some people reduce tension or stress through avoidant, self-medicating (e.g., alcohol abuse), compulsive (e.g., overeating), impulsive (e.g., high-risk behaviors), and/or self-injurious behaviors. Others may try to gain control over their experiences by being aggressive or subconsciously reenacting aspects of the trauma.
Behavioral reactions are also the consequences of, or learned from, traumatic experiences. For example, some people act like they can’t control their current environment, thus failing to take action or make decisions long after the trauma (learned helplessness). Other associate elements of the trauma with current activities, such as by reacting to an intimate moment in a significant relationship as dangerous or unsafe years after a date rape. The following sections discuss behavioral consequences of trauma and traumatic stress reactions.
Reenactments
A hallmark symptom of trauma is reexperiencing the trauma in various ways. Reexperiencing can occur through reenactments (literally, to “redo”), by which trauma survivors repetitively relive and recreate a past trauma in their present lives. This is very apparent in children, who play by mimicking what occurred during the trauma, such as by pretending to crash a toy airplane into a toy building after seeing televised images of the terrorist attacks on the World Trade Center on September 11, 2001. Attempts to understand reenactments are very complicated, as reenactments occur for a variety of reasons. Sometimes, individuals reenact past traumas to master them. Examples of reenactments include a variety of behaviors: self-injurious behaviors, hypersexuality, walking alone in unsafe areas or other high-risk behaviors, driving recklessly, or involvement in repetitive destructive relationships (e.g., repeatedly getting into romantic relationships with people who are abusive or violent), to name a few.
Self-harm and self-destructive behaviors
Self-harm is any type of intentionally self-inflicted harm, regardless of the severity of injury or whether suicide is intended. Often, self-harm is an attempt to cope with emotional or physical distress that seems overwhelming or to cope with a profound sense of dissociation or being trapped, helpless, and “damaged” ( Herman, 1997 ; Santa Mina & Gallop, 1998 ). Self-harm is associated with past childhood sexual abuse and other forms of trauma as well as substance abuse. Thus, addressing self-harm requires attention to the client’s reasons for self-harm. More than likely, the client needs help recognizing and coping with emotional or physical distress in manageable amounts and ways.
Resilient Responses to Trauma
Many people find healthy ways to cope with, respond to, and heal from trauma. Often, people automatically reevaluate their values and redefine what is important after a trauma. Such resilient responses include:
- Increased bonding with family and community.
- Redefined or increased sense of purpose and meaning.
- Increased commitment to a personal mission.
- Revised priorities.
- Increased charitable giving and volunteerism.
Case Illustration: Marco
Marco, a 30-year-old man, sought treatment at a local mental health center after a 2-year bout of anxiety symptoms. He was an active member of his church for 12 years, but although he sought help from his pastor about a year ago, he reports that he has had no contact with his pastor or his church since that time. Approximately 3 years ago, his wife took her own life. He describes her as his soul-mate and has had a difficult time understanding her actions or how he could have prevented them.
In the initial intake, he mentioned that he was the first person to find his wife after the suicide and reported feelings of betrayal, hurt, anger, and devastation since her death. He claimed that everyone leaves him or dies. He also talked about his difficulty sleeping, having repetitive dreams of his wife, and avoiding relationships. In his first session with the counselor, he initially rejected the counselor before the counselor had an opportunity to begin reviewing and talking about the events and discomfort that led him to treatment.
In this scenario, Marco is likely reenacting his feelings of abandonment by attempting to reject others before he experiences another rejection or abandonment. In this situation, the counselor will need to recognize the reenactment, explore the behavior, and examine how reenactments appear in other situations in Marco’s life.
Among the self-harm behaviors reported in the literature are cutting, burning skin by heat (e.g., cigarettes) or caustic liquids, punching hard enough to self-bruise, head banging, hair pulling, self-poisoning, inserting foreign objects into bodily orifices, excessive nail biting, excessive scratching, bone breaking, gnawing at flesh, interfering with wound healing, tying off body parts to stop breathing or blood flow, swallowing sharp objects, and suicide. Cutting and burning are among the most common forms of self-harm.
Self-harm tends to occur most in people who have experienced repeated and/or early trauma (e.g., childhood sexual abuse) rather than in those who have undergone a single adult trauma (e.g., a community-wide disaster or a serious car accident). There are strong associations between eating disorders, self-harm, and substance abuse ( Claes & Vandereycken, 2007 ; for discussion, see Harned, Najavits, & Weiss, 2006 ). Self-mutilation is also associated with (and part of the diagnostic criteria for) a number of personality disorders, including borderline and histrionic, as well as DID, depression, and some forms of schizophrenia; these disorders can co-occur with traumatic stress reactions and disorders.
It is important to distinguish self-harm that is suicidal from self-harm that is not suicidal and to assess and manage both of these very serious dangers carefully. Most people who engage in self-harm are not doing so with the intent to kill themselves ( Noll, Horowitz, Bonanno, Trickett, & Putnam, 2003 )—although self-harm can be life threatening and can escalate into suicidality if not managed therapeutically. Self-harm can be a way of getting attention or manipulating others, but most often it is not. Self-destructive behaviors such as substance abuse, restrictive or binge eating, reckless automobile driving, or high-risk impulsive behavior are different from self-harming behaviors but are also seen in clients with a history of trauma. Self-destructive behaviors differ from self-harming behaviors in that there may be no immediate negative impact of the behavior on the individual; they differ from suicidal behavior in that there is no intent to cause death in the short term.
Advice to Counselors: Working With Clients Who Are Self-Injurious
Counselors who are unqualified or uncomfortable working with clients who demonstrate self-harming, self-destructive, or suicidal or homicidal ideation, intent, or behavior should work with their agencies and supervisors to refer such clients to other counselors. They should consider seeking specialized supervision on how to manage such clients effectively and safely and how to manage their feelings about these issues. The following suggestions assume that the counselor has had sufficient training and experience to work with clients who are self-injurious. To respond appropriately to a client who engages in self-harm, counselors should:
- Screen the client for self-harm and suicide risk at the initial evaluation and throughout treatment.
- Learn the client’s perspective on self-harm and how it “helps.”
- Understand that self-harm is often a coping strategy to manage the intensity of emotional and/or physical distress.
- Teach the client coping skills that improve his or her management of emotions without self-harm.
- Help the client obtain the level of care needed to manage genuine risk of suicide or severe self-injury. This might include hospitalization, more intensive programming (e.g., intensive outpatient, partial hospitalization, residential treatment), or more frequent treatment sessions. The goal is to stabilize the client as quickly as possible, and then, if possible, begin to focus treatment on developing coping strategies to manage self-injurious and other harmful impulses.
- Consult with other team members, supervisors, and, if necessary, legal experts to determine whether one’s efforts with and conceptualization of the self-harming client fit best practice guidelines. See, for example, Treatment Improvement Protocol (TIP) 42, Substance Abuse Treatment for Persons With Co-Occurring Disorders ( Center for Substance Abuse Treatment [CSAT], 2005c ). Document such consultations and the decisions made as a result of them thoroughly and frequently.
- Help the client identify how substance use affects self-harm. In some cases, it can increase the behavior (e.g., alcohol disinhibits the client, who is then more likely to self-harm). In other cases, it can decrease the behavior (e.g., heroin evokes relaxation and, thus, can lessen the urge to self-harm). In either case, continue to help the client understand how abstinence from substances is necessary so that he or she can learn more adaptive coping.
- Work collaboratively with the client to develop a plan to create a sense of safety. Individuals are affected by trauma in different ways; therefore, safety or a safe environment may mean something entirely different from one person to the next. Allow the client to define what safety means to him or her.
Counselors can also help the client prepare a safety card that the client can carry at all times. The card might include the counselor’s contact information, a 24-hour crisis number to call in emergencies, contact information for supportive individuals who can be contacted when needed, and, if appropriate, telephone numbers for emergency medical services. The counselor can discuss with the client the types of signs or crises that might warrant using the numbers on the card. Additionally, the counselor might check with the client from time to time to confirm that the information on the card is current.
TIP 50, Addressing Suicidal Thoughts and Behaviors in Substance Abuse Treatment ( CSAT, 2009a ), has examples of safety agreements specifically for suicidal clients and discusses their uses in more detail. There is no credible evidence that a safety agreement is effective in preventing a suicide attempt or death. Safety agreements for clients with suicidal thoughts and behaviors should only be used as an adjunct support accompanying professional screening, assessment, and treatment for people with suicidal thoughts and behaviors. Keep in mind that safety plans or agreements may be perceived by the trauma survivor as a means of controlling behavior, subsequently replicating or triggering previous traumatic experiences.
All professionals—and in some States, anyone—could have ethical and legal responsibilities to those clients who pose an imminent danger to themselves or others. Clinicians should be aware of the pertinent State laws where they practice and the relevant Federal and professional regulations.
However, as with self-harming behavior, self-destructive behavior needs to be recognized and addressed and may persist—or worsen—without intervention.
Consumption of substances
Substance use often is initiated or increased after trauma. Clients in early recovery— especially those who develop PTSD or have it reactivated—have a higher relapse risk if they experience a trauma. In the first 2 months after September 11, 2001, more than a quarter of New Yorker residents who smoked cigarettes, drank alcohol, or used marijuana (about 265,000 people) increased their consumption. The increases continued 6 months after the attacks ( Vlahov, Galea, Ahern, Resnick, & Kilpatrick, 2004 ). A study by the Substance Abuse and Mental Health Services Administration ( SAMHSA, Office of Applied Studies, 2002 ) used National Survey on Drug Use and Health data to compare the first three quarters of 2001 with the last quarter and reported an increase in the prevalence rate for alcohol use among people 18 or older in the New York metropolitan area during the fourth quarter.
Interviews with New York City residents who were current or former cocaine or heroin users indicated that many who had been clean for 6 months or less relapsed after September 11, 2001. Others, who lost their income and could no longer support their habit, enrolled in methadone programs ( Weiss et al., 2002 ). After the Oklahoma City bombing in 1995, Oklahomans reported double the normal rate of alcohol use, smoking more cigarettes, and a higher incidence of initiating smoking months and even years after the bombing ( Smith, Christiansen, Vincent, & Hann, 1999 ).
Self-medication
Khantzian’s self-medication theory ( 1985 ) suggests that drugs of abuse are selected for their specific effects. However, no definitive pattern has yet emerged of the use of particular substances in relation to PTSD or trauma symptoms. Use of substances can vary based on a variety of factors, including which trauma symptoms are most prominent for an individual and the individual’s access to particular substances. Unresolved traumas sometimes lurk behind the emotions that clients cannot allow themselves to experience. Substance use and abuse in trauma survivors can be a way to self-medicate and thereby avoid or displace difficult emotions associated with traumatic experiences. When the substances are withdrawn, the survivor may use other behaviors to self-soothe, self-medicate, or avoid emotions. As likely, emotions can appear after abstinence in the form of anxiety and depression.
Avoidance often coincides with anxiety and the promotion of anxiety symptoms. Individuals begin to avoid people, places, or situations to alleviate unpleasant emotions, memories, or circumstances. Initially, the avoidance works, but over time, anxiety increases and the perception that the situation is unbearable or dangerous increases as well, leading to a greater need to avoid. Avoidance can be adaptive, but it is also a behavioral pattern that reinforces perceived danger without testing its validity, and it typically leads to greater problems across major life areas (e.g., avoiding emotionally oriented conversations in an intimate relationship). For many individuals who have traumatic stress reactions, avoidance is commonplace. A person may drive 5 miles longer to avoid the road where he or she had an accident. Another individual may avoid crowded places in fear of an assault or to circumvent strong emotional memories about an earlier assault that took place in a crowded area. Avoidance can come in many forms. When people can’t tolerate strong affects associated with traumatic memories, they avoid, project, deny, or distort their trauma-related emotional and cognitive experiences. A key ingredient in trauma recovery is learning to manage triggers, memories, and emotions without avoidance—in essence, becoming desensitized to traumatic memories and associated symptoms.
Social/Interpersonal
A key ingredient in the early stage of TIC is to establish, confirm, or reestablish a support system, including culturally appropriate activities, as soon as possible. Social supports and relationships can be protective factors against traumatic stress. However, trauma typically affects relationships significantly, regardless of whether the trauma is interpersonal or is of some other type. Relationships require emotional exchanges, which means that others who have close relationships or friendships with the individual who survived the trauma(s) are often affected as well—either through secondary traumatization or by directly experiencing the survivor’s traumatic stress reactions. In natural disasters, social and community supports can be abruptly eroded and difficult to rebuild after the initial disaster relief efforts have waned.
Survivors may readily rely on family members, friends, or other social supports—or they may avoid support, either because they believe that no one will be understanding or trustworthy or because they perceive their own needs as a burden to others. Survivors who have strong emotional or physical reactions, including outbursts during nightmares, may pull away further in fear of being unable to predict their own reactions or to protect their own safety and that of others. Often, trauma survivors feel ashamed of their stress reactions, which further hampers their ability to use their support systems and resources adequately.
Many survivors of childhood abuse and interpersonal violence have experienced a significant sense of betrayal. They have often encountered trauma at the hands of trusted caregivers and family members or through significant relationships. This history of betrayal can disrupt forming or relying on supportive relationships in recovery, such as peer supports and counseling. Although this fear of trusting others is protective, it can lead to difficulty in connecting with others and greater vigilance in observing the behaviors of others, including behavioral health service providers. It is exceptionally difficult to override the feeling that someone is going to hurt you, take advantage of you, or, minimally, disappoint you. Early betrayal can affect one’s ability to develop attachments, yet the formation of supportive relationships is an important antidote in the recovery from traumatic stress.
Developmental
Each age group is vulnerable in unique ways to the stresses of a disaster, with children and the elderly at greatest risk. Young children may display generalized fear, nightmares, heightened arousal and confusion, and physical symptoms, (e.g., stomachaches, headaches). School-age children may exhibit symptoms such as aggressive behavior and anger, regression to behavior seen at younger ages, repetitious traumatic play, loss of ability to concentrate, and worse school performance. Adolescents may display depression and social withdrawal, rebellion, increased risky activities such as sexual acting out, wish for revenge and action-oriented responses to trauma, and sleep and eating disturbances ( Hamblen, 2001 ). Adults may display sleep problems, increased agitation, hypervigilance, isolation or withdrawal, and increased use of alcohol or drugs. Older adults may exhibit increased withdrawal and isolation, reluctance to leave home, worsening of chronic illnesses, confusion, depression, and fear (DeWolfe & Nordboe, 2000b).
Neurobiological Development: Consequences of Early Childhood Trauma
Findings in developmental psychobiology suggest that the consequences of early maltreatment produce enduring negative effects on brain development ( De Bellis, 2002 ; Liu, Diorio, Day, Francis, & Meaney, 2000 ; Teicher, 2002 ). Research suggests that the first stage in a cascade of events produced by early trauma and/or maltreatment involves the disruption of chemicals that function as neurotransmitters (e.g., cortisol, norepinephrine, dopamine), causing escalation of the stress response ( Heim, Mletzko, Purselle, Musselman, & Nemeroff, 2008 ; Heim, Newport, Mletzko, Miller, & Nemeroff, 2008 ; Teicher, 2002 ). These chemical responses can then negatively affect critical neural growth during specific sensitive periods of childhood development and can even lead to cell death.
Adverse brain development can also result from elevated levels of cortisol and catecholamines by contributing to maturational failures in other brain regions, such as the prefrontal cortex ( Meaney, Brake, & Gratton, 2002 ). Heim, Mletzko et al. (2008) found that the neuropeptide oxytocin— important for social affiliation and support, attachment, trust, and management of stress and anxiety—was markedly decreased in the cerebrospinal fluid of women who had been exposed to childhood maltreatment, particularly those who had experienced emotional abuse. The more childhood traumas a person had experienced, and the longer their duration, the lower that person’s current level of oxytocin was likely to be and the higher her rating of current anxiety was likely to be.
Using data from the Adverse Childhood Experiences Study, an analysis by Anda, Felitti, Brown et al. (2006) confirmed that the risk of negative outcomes in affective, somatic, substance abuse, memory, sexual, and aggression-related domains increased as scores on a measure of eight ACEs increased. The researchers concluded that the association of study scores with these outcomes can serve as a theoretical parallel for the effects of cumulative exposure to stress on the developing brain and for the resulting impairment seen in multiple brain structures and functions.
The National Child Traumatic Stress Network ( http://www.nctsn.org ) offers information about childhood abuse, stress, and physiological responses of children who are traumatized. Materials are available for counselors, educators, parents, and caregivers. There are special sections on the needs of children in military families and on the impact of natural disasters on children’s mental health.
- Subthreshold Trauma-Related Symptoms
Many trauma survivors experience symptoms that, although they do not meet the diagnostic criteria for ASD or PTSD, nonetheless limit their ability to function normally (e.g., regulate emotional states, maintain steady and rewarding social and family relationships, function competently at a job, maintain a steady pattern of abstinence in recovery). These symptoms can be transient, only arising in a specific context; intermittent, appearing for several weeks or months and then receding; or a part of the individual’s regular pattern of functioning (but not to the level of DSM-5 diagnostic criteria). Often, these patterns are termed “subthreshold” trauma symptoms. Like PTSD, the symptoms can be misdiagnosed as depression, anxiety, oran other mental illness. Likewise, clients who have experienced trauma may link some of their symptoms to their trauma and diagnose themselves as having PTSD, even though they do not meet all criteria for that disorder.
Combat Stress Reaction
A phenomenon unique to war, and one that counselors need to understand well, is combat stress reaction (CSR). CSR is an acute anxiety reaction occurring during or shortly after participating in military conflicts and wars as well as other operations within the war zone, known as the theater. CSR is not a formal diagnosis, nor is it included in the DSM-5 ( APA, 2013a ). It is similar to acute stress reaction, except that the precipitating event or events affect military personnel (and civilians exposed to the events) in an armed conflict situation. The terms “combat stress reaction” and “posttraumatic stress injury” are relatively new, and the intent of using these new terms is to call attention to the unique experiences of combat-related stress as well as to decrease the shame that can be associated with seeking behavioral health services for PTSD (for more information on veterans and combat stress reactions, see the planned TIP, Reintegration-Related Behavioral Health Issues for Veterans and Military Families ; SAMHSA, planned f).
Case Illustration: Frank
Frank is a 36-year-old man who was severely beaten in a fight outside a bar. He had multiple injuries, including broken bones, a concussion, and a stab wound in his lower abdomen. He was hospitalized for 3.5 weeks and was unable to return to work, thus losing his job as a warehouse forklift operator. For several years, when faced with situations in which he perceived himself as helpless and overwhelmed, Frank reacted with violent anger that, to others, appeared grossly out of proportion to the situation. He has not had a drink in almost 3 years, but the bouts of anger persist and occur three to five times a year. They leave Frank feeling even more isolated from others and alienated from those who love him. He reports that he cannot watch certain television shows that depict violent anger; he has to stop watching when such scenes occur. He sometimes daydreams about getting revenge on the people who assaulted him.
Psychiatric and neurological evaluations do not reveal a cause for Frank’s anger attacks. Other than these symptoms, Frank has progressed well in his abstinence from alcohol. He attends a support group regularly, has acquired friends who are also abstinent, and has reconciled with his family of origin. His marriage is more stable, although the episodes of rage limit his wife’s willingness to commit fully to the relationship. In recounting the traumatic event in counseling, Frank acknowledges that he thought he was going to die as a result of the fight, especially when he realized he had been stabbed. As he described his experience, he began to become very anxious, and the counselor observed the rage beginning to appear.
After his initial evaluation, Frank was referred to an outpatient program that provided trauma-specific interventions to address his subthreshold trauma symptoms. With a combination of cognitive– behavioral counseling, EMDR, and anger management techniques, he saw a gradual decrease in symptoms when he recalled the assault. He started having more control of his anger when memories of the trauma emerged. Today, when feeling trapped, helpless, or overwhelmed, Frank has resources for coping and does not allow his anger to interfere with his marriage or other relationships.
Although stress mobilizes an individual’s physical and psychological resources to perform more effectively in combat, reactions to the stress may persist long after the actual danger has ended. As with other traumas, the nature of the event(s), the reactions of others, and the survivor’s psychological history and resources affect the likelihood and severity of CSR. With combat veterans, this translates to the number, intensity, and duration of threat factors; the social support of peers in the veterans’ unit; the emotional and cognitive resilience of the service members; and the quality of military leadership. CSR can vary from manageable and mild to debilitating and severe. Common, less severe symptoms of CSR include tension, hypervigilance, sleep problems, anger, and difficulty concentrating. If left untreated, CSR can lead to PTSD.
Common causes of CSR are events such as a direct attack from insurgent small arms fire or a military convoy being hit by an improvised explosive device, but combat stressors encompass a diverse array of traumatizing events, such as seeing grave injuries, watching others die, and making on-the-spot decisions in ambiguous conditions (e.g., having to determine whether a vehicle speeding toward a military checkpoint contains insurgents with explosives or a family traveling to another area). Such circumstances can lead to combat stress. Military personnel also serve in noncombat positions (e.g., healthcare and administrative roles), and personnel filling these supportive roles can be exposed to combat situations by proximity or by witnessing their results.
Advice to Counselors: Understanding the Nature of Combat Stress
Several sources of information are available to help counselors deepen their understanding of combat stress and postdeployment adjustment. Friedman (2006) explains how a prolonged combat-ready stance, which is adaptive in a war zone, becomes hypervigilance and overprotectiveness at home. He makes the point that the “mutual interdependence, trust, and affection” (p. 587) that are so necessarily a part of a combat unit are different from relationships with family members and colleagues in a civilian workplace. This complicates the transition to civilian life. Wheels Down: Adjusting to Life After Deployment ( Moore & Kennedy, 2011 ) provides practical advice for military service members, including inactive or active duty personnel and veterans, in transitioning from the theater to home.
The following are just a few of the many resources and reports focused on combat-related psychological and stress issues:
- Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery ( Tanielian & Jaycox, 2008 )
- On Killing ( Grossman, 1995 ), an indepth analysis of the psychological dynamics of combat
- Haunted by Combat ( Paulson & Krippner, 2007 ), which contains specific chapters on Reserve and National Guard troops and female veterans
- Treating Young Veterans: Promoting Resilience Through Practice and Advocacy ( Kelly, Howe-Barksdale, & Gitelson, 2011 )
- Specific Trauma-Related Psychological Disorders
Part of the definition of trauma is that the individual responds with intense fear, helplessness, or horror. Beyond that, in both the short term and the long term, trauma comprises a range of reactions from normal (e.g., being unable to concentrate, feeling sad, having trouble sleeping) to warranting a diagnosis of a trauma-related mental disorder. Most people who experience trauma have no long-lasting disabling effects; their coping skills and the support of those around them are sufficient to help them overcome their difficulties, and their ability to function on a daily basis over time is unimpaired. For others, though, the symptoms of trauma are more severe and last longer. The most common diagnoses associated with trauma are PTSD and ASD, but trauma is also associated with the onset of other mental disorders—particularly substance use disorders, mood disorders, various anxiety disorders, and personality disorders. Trauma also typically exacerbates symptoms of preexisting disorders, and, for people who are predisposed to a mental disorder, trauma can precipitate its onset. Mental disorders can occur almost simultaneously with trauma exposure or manifest sometime thereafter.
Acute Stress Disorder
ASD represents a normal response to stress. Symptoms develop within 4 weeks of the trauma and can cause significant levels of distress. Most individuals who have acute stress reactions never develop further impairment or PTSD. Acute stress disorder is highly associated with the experience of one specific trauma rather than the experience of long-term exposure to chronic traumatic stress. Diagnostic criteria are presented in Exhibit 1.3-3 .
Exhibit 1.3-3
DSM-5 Diagnostic Criteria for ASD. Exposure to actual or threatened death, serious injury, or sexual violation in one (or more) of the following ways: Directly experiencing the traumatic event(s).
The primary presentation of an individual with an acute stress reaction is often that of someone who appears overwhelmed by the traumatic experience. The need to talk about the experience can lead the client to seem self-centered and unconcerned about the needs of others. He or she may need to describe, in repetitive detail, what happened, or may seem obsessed with trying to understand what happened in an effort to make sense of the experience. The client is often hypervigilant and avoids circumstances that are reminders of the trauma. For instance, someone who was in a serious car crash in heavy traffic can become anxious and avoid riding in a car or driving in traffic for a finite time afterward. Partial amnesia for the trauma often accompanies ASD, and the individual may repetitively question others to fill in details. People with ASD symptoms sometimes seek assurance from others that the event happened in the way they remember, that they are not “going crazy” or “losing it,” and that they could not have prevented the event. The next case illustration demonstrates the time-limited nature of ASD.
Differences between ASD and PTSD
It is important to consider the differences between ASD and PTSD when forming a diagnostic impression. The primary difference is the amount of time the symptoms have been present. ASD resolves 2 days to 4 weeks after an event, whereas PTSD continues beyond the 4-week period. The diagnosis of ASD can change to a diagnosis of PTSD if the condition is noted within the first 4 weeks after the event, but the symptoms persist past 4 weeks.
ASD also differs from PTSD in that the ASD diagnosis requires 9 out of 14 symptoms from five categories, including intrusion, negative mood, dissociation, avoidance, and arousal. These symptoms can occur at the time of the trauma or in the following month. Studies indicate that dissociation at the time of trauma is a good predictor of subsequent PTSD, so the inclusion of dissociative symptoms makes it more likely that those who develop ASD will later be diagnosed with PTSD ( Bryant & Harvey, 2000 ). Additionally, ASD is a transient disorder, meaning that it is present in a person’s life for a relatively short time and then passes. In contrast, PTSD typically becomes a primary feature of an individual’s life. Over a lengthy period, PTSD can have profound effects on clients’ perceptions of safety, their sense of hope for the future, their relationships with others, their physical health, the appearance of psychiatric symptoms, and their patterns of substance use and abuse.
There are common symptoms between PTSD and ASD, and untreated ASD is a possible predisposing factor to PTSD, but it is unknown whether most people with ASD are likely to develop PTSD. There is some suggestion that, as with PTSD, ASD is more prevalent in women than in men ( Bryant & Harvey, 2003 ). However, many people with PTSD do not have a diagnosis or recall a history of acute stress symptoms before seeking treatment for or receiving a diagnosis of PTSD.
Case Illustration: Sheila
Two months ago, Sheila, a 55-year-old married woman, experienced a tornado in her home town. In the previous year, she had addressed a long-time marijuana use problem with the help of a treatment program and had been abstinent for about 6 months. Sheila was proud of her abstinence; it was something she wanted to continue. She regarded it as a mark of personal maturity; it improved her relationship with her husband, and their business had flourished as a result of her abstinence.
During the tornado, an employee reported that Sheila had become very agitated and had grabbed her assistant to drag him under a large table for cover. Sheila repeatedly yelled to her assistant that they were going to die. Following the storm, Sheila could not remember certain details of her behavior during the event. Furthermore, Sheila said that after the storm, she felt numb, as if she was floating out of her body and could watch herself from the outside. She stated that nothing felt real and it was all like a dream.
Following the tornado, Sheila experienced emotional numbness and detachment, even from people close to her, for about 2 weeks. The symptoms slowly decreased in intensity but still disrupted her life. Sheila reported experiencing disjointed or unconnected images and dreams of the storm that made no real sense to her. She was unwilling to return to the building where she had been during the storm, despite having maintained a business at this location for 15 years. In addition, she began smoking marijuana again because it helped her sleep. She had been very irritable and had uncharacteristic angry outbursts toward her husband, children, and other family members.
As a result of her earlier contact with a treatment program, Sheila returned to that program and engaged in psychoeducational, supportive counseling focused on her acute stress reaction. She regained abstinence from marijuana and returned shortly to a normal level of functioning. Her symptoms slowly diminished over a period of 3 weeks. With the help of her counselor, she came to understand the link between the trauma and her relapse, regained support from her spouse, and again felt in control of her life.
Effective interventions for ASD can significantly reduce the possibility of the subsequent development of PTSD. Effective treatment of ASD can also reduce the incidence of other co-occurring problems, such as depression, anxiety, dissociative disorders, and compulsive behaviors ( Bryant & Harvey, 2000 ). Intervention for ASD also helps the individual develop coping skills that can effectively prevent the recurrence of ASD after later traumas.
Although predictive science for ASD and PTSD will continue to evolve, both disorders are associated with increased substance use and mental disorders and increased risk of relapse; therefore, effective screening for ASD and PTSD is important for all clients with these disorders. Individuals in early recovery—lacking well-practiced coping skills, lacking environmental supports, and already operating at high levels of anxiety—are particularly susceptible to ASD. Events that would not normally be disabling can produce symptoms of intense helplessness and fear, numbing and depersonalization, disabling anxiety, and an inability to handle normal life events. Counselors should be able to recognize ASD and treat it rather than attributing the symptoms to a client’s lack of motivation to change, being “dry drunk” (for those in substance abuse recovery), or being manipulative.
Posttraumatic Stress Disorder
The trauma-related disorder that receives the greatest attention is PTSD; it is the most commonly diagnosed trauma-related disorder, and its symptoms can be quite debilitating over time. Nonetheless, it is important to remember that PTSD symptoms are represented in a number of other mental illnesses, including major depressive disorder (MDD), anxiety disorders, and psychotic disorders ( Foa et al., 2006 ). The DSM-5 ( APA, 2013a ) identifies four symptom clusters for PTSD: presence of intrusion symptoms, persistent avoidance of stimuli, negative alterations in cognitions and mood, and marked alterations in arousal and reactivity. Individuals must have been exposed to actual or threatened death, serious injury, or sexual violence, and the symptoms must produce significant distress and impairment for more than 4 weeks ( Exhibit 1.3-4 ).
Exhibit 1.3-4
DSM-5 Diagnostic Criteria for PTSD. Note: The following criteria apply to adults, adolescents, and children older than 6 years. For children 6 years and younger, see the DSM-5 section titled “Posttraumatic Stress Disorder for Children 6 Years (more...)
Case Illustration: Michael
Michael is a 62-year-old Vietnam veteran. He is a divorced father of two children and has four grandchildren. Both of his parents were dependent on alcohol. He describes his childhood as isolated. His father physically and psychologically abused him (e.g., he was beaten with a switch until he had welts on his legs, back, and buttocks). By age 10, his parents regarded him as incorrigible and sent him to a reformatory school for 6 months. By age 15, he was using marijuana, hallucinogens, and alcohol and was frequently truant from school.
At age 19, Michael was drafted and sent to Vietnam, where he witnessed the deaths of six American military personnel. In one incident, the soldier he was next to in a bunker was shot. Michael felt helpless as he talked to this soldier, who was still conscious. In Vietnam, Michael increased his use of both alcohol and marijuana. On his return to the United States, Michael continued to drink and use marijuana. He reenlisted in the military for another tour of duty.
His life stabilized in his early 30s, as he had a steady job, supportive friends, and a relatively stable family life. However, he divorced in his late 30s. Shortly thereafter, he married a second time, but that marriage ended in divorce as well. He was chronically anxious and depressed and had insomnia and frequent nightmares. He periodically binged on alcohol. He complained of feeling empty, had suicidal ideation, and frequently stated that he lacked purpose in his life.
In the 1980s, Michael received several years of mental health treatment for dysthymia. He was hospitalized twice and received 1 year of outpatient psychotherapy. In the mid-1990s, he returned to outpatient treatment for similar symptoms and was diagnosed with PTSD and dysthymia. He no longer used marijuana and rarely drank. He reported that he didn’t like how alcohol or other substances made him feel anymore—he felt out of control with his emotions when he used them. Michael reported symptoms of hyperarousal, intrusion (intrusive memories, nightmares, and preoccupying thoughts about Vietnam), and avoidance (isolating himself from others and feeling “numb”). He reported that these symptoms seemed to relate to his childhood abuse and his experiences in Vietnam. In treatment, he expressed relief that he now understood the connection between his symptoms and his history.
Certain characteristics make people more susceptible to PTSD, including one’s unique personal vulnerabilities at the time of the traumatic exposure, the support (or lack of support) received from others at the time of the trauma and at the onset of trauma-related symptoms, and the way others in the person’s environment gauge the nature of the traumatic event ( Brewin, Andrews, & Valentine, 2000 ).
People with PTSD often present varying clinical profiles and histories. They can experience symptoms that are activated by environmental triggers and then recede for a period of time. Some people with PTSD who show mostly psychiatric symptoms (particularly depression and anxiety) are misdiagnosed and go untreated for their primary condition. For many people, the trauma experience and diagnosis are obscured by co-occurring substance use disorder symptoms. The important feature of PTSD is that the disorder becomes an orienting feature of the individual’s life. How well the person can work, with whom he or she associates, the nature of close and intimate relationships, the ability to have fun and rejuvenate, and the way in which an individual goes about confronting and solving problems in life are all affected by the client’s trauma experiences and his or her struggle to recover.
Posttraumatic stress disorder: Timing of symptoms
Although symptoms of PTSD usually begin within 3 months of a trauma in adulthood, there can be a delay of months or even years before symptoms appear for some people. Some people may have minimal symptoms after a trauma but then experience a crisis later in life. Trauma symptoms can appear suddenly, even without conscious memory of the original trauma or without any overt provocation. Survivors of abuse in childhood can have a delayed response triggered by something that happens to them as adults. For example, seeing a movie about child abuse can trigger symptoms related to the trauma. Other triggers include returning to the scene of the trauma, being reminded of it in some other way, or noting the anniversary of an event. Likewise, combat veterans and survivors of community-wide disasters may seem to be coping well shortly after a trauma, only to have symptoms emerge later when their life situations seem to have stabilized. Some clients in substance abuse recovery only begin to experience trauma symptoms when they maintain abstinence for some time. As individuals decrease tension-reducing or self-medicating behaviors, trauma memories and symptoms can emerge.
Advice to Counselors: Helping Clients With Delayed Trauma Responses
Clients who are experiencing a delayed trauma response can benefit if you help them to:
- Create an environment that allows acknowledgment of the traumatic event(s).
- Discuss their initial recall or first suspicion that they were having a traumatic response.
- Become educated on delayed trauma responses.
- Draw a connection between the trauma and presenting trauma-related symptoms.
- Create a safe environment.
- Explore their support systems and fortify them as needed.
- Understand that triggers can precede traumatic stress reactions, including delayed responses to trauma.
- Identify their triggers.
- Develop coping strategies to navigate and manage symptoms.
Culture and posttraumatic stress
Although research is limited across cultures, PTSD has been observed in Southeast Asian, South American, Middle Eastern, and Native American survivors ( Osterman & de Jong, 2007 ; Wilson & Tang, 2007 ). As Stamm and Friedman (2000) point out, however, simply observing PTSD does not mean that it is the “best conceptual tool for characterizing post-traumatic distress among non-Western individuals” (p. 73). In fact, many trauma-related symptoms from other cultures do not fit the DSM-5 criteria. These include somatic and psychological symptoms and beliefs about the origins and nature of traumatic events. Moreover, religious and spiritual beliefs can affect how a survivor experiences a traumatic event and whether he or she reports the distress. For example, in societies where attitudes toward karma and the glorification of war veterans are predominant, it is harder for war veterans to come forward and disclose that they are emotionally overwhelmed or struggling. It would be perceived as inappropriate and possibly demoralizing to focus on the emotional distress that he or she still bears. (For a review of cultural competence in treating trauma, refer to Brown, 2008 .)
Methods for measuring PTSD are also culturally specific. As part of a project begun in 1972, the World Health Organization (WHO) and the National Institutes of Health (NIH) embarked on a joint study to test the cross-cultural applicability of classification systems for various diagnoses. WHO and NIH identified apparently universal factors of psychological disorders and developed specific instruments to measure them. These instruments, the Composite International Diagnostic Interview and the Schedules for Clinical Assessment in Neuropsychiatry, include certain criteria from the DSM (Fourth Edition, Text Revision; APA, 2000a ) as well as criteria from the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10; Exhibit 1.3-5 ).
Exhibit 1.3-5
ICD-10 Diagnostic Criteria for PTSD. The patient must have been exposed to a stressful event or situation (either brief or long-lasting) of exceptionally threatening or catastrophic nature, which would be likely to cause pervasive distress in almost anyone. (more...)
Complex trauma and complex traumatic stress
When individuals experience multiple traumas, prolonged and repeated trauma during childhood, or repetitive trauma in the context of significant interpersonal relationships, their reactions to trauma have unique characteristics ( Herman, 1992 ). This unique constellation of reactions, called complex traumatic stress, is not recognized diagnostically in the DSM-5, but theoretical discussions and research have begun to highlight the similarities and differences in symptoms of posttraumatic stress versus complex traumatic stress ( Courtois & Ford, 2009 ). Often, the symptoms generated from complex trauma do not fully match PTSD criteria and exceed the severity of PTSD. Overall, literature reflects that PTSD criteria or subthreshold symptoms do not fully account for the persistent and more impairing clinical presentation of complex trauma. Even though current research in the study of traumatology is prolific, it is still in the early stages of development. The idea that there may be more diagnostic variations or subtypes is forthcoming, and this will likely pave the way for more client-matching interventions to better serve those individuals who have been repeatedly exposed to multiple, early childhood, and/or interpersonal traumas.
- Other Trauma-Related and Co-Occurring Disorders
The symptoms of PTSD and other mental disorders overlap considerably; these disorders often coexist and in clude mood, anxiety, substance use, and personality disorders. Thus, it’s common for trauma survivors to be underdiagnosed or misdiagnosed. If they have not been identified as trauma survivors, their psychological distress is often not associated with previous trauma, and/or they are diagnosed with a disorder that marginally matches their presenting symptoms and psychological sequelae of trauma. The following sections present a brief overview of some mental disorders that can result from (or be worsened by) traumatic stress. PTSD is not the only diagnosis related to trauma nor its only psychological consequence; trauma can broadly influence mental and physical health in clients who already have behavioral health disorders.
The term “ co-occurring disorders ” refers to cases when a person has one or more mental disorders as well as one or more substance use disorders (including substance abuse). Co-occurring disorders are common among individuals who have a history of trauma and are seeking help.
Advice to Counselors: Universal Screening and Assessment
Only people specifically trained and licensed in mental health assessment should make diagnoses; trauma can result in complicated cases, and many symptoms can be present, whether or not they meet full diagnostic criteria for a specific disorder. Only a trained assessor can distinguish accurately among various symptoms and in the presence of co-occurring disorders. However, behavioral health professionals without specific assessment training can still serve an important role in screening for possible mental disorders using established screening tools ( CSAT, 2005c ; see also Chapter 4 of this TIP). In agencies and clinics, it is critical to provide such screenings systematically—for each client—as PTSD and other co-occurring disorders are typically under diagnosed or misdiagnosed.
People With Mental Disorders
MDD is the most common co-occurring disorder in people who have experienced trauma and are diagnosed with PTSD. A well-established causal relationship exists between stressful events and depression, and a prior history of MDD is predictive of PTSD after exposure to major trauma ( Foa et al., 2006 ).
Many survivors with severe mental disorders function fairly well following trauma, including disasters, as long as essential services aren’t interrupted. For others, additional mental health supports may be necessary. For more information, see Responding to the Needs of People With Serious and Persistent Mental Illness in Times of Major Disaster ( Center for Mental Health Services, 1996 ).
Co-occurrence is also linked with greater impairment and more severe symptoms of both disorders, and the person is less likely to experience remission of symptoms within 6 months.
Generalized anxiety, obsessive–compulsive, and other anxiety disorders are also associated with PTSD. PTSD may exacerbate anxiety disorder symptoms, but it is also likely that preexisting anxiety symptoms and anxiety disorders increase vulnerability to PTSD. Preexisting anxiety primes survivors for greater hyperarousal and distress. Other disorders, such as personality and somatization disorders, are also associated with trauma, but the history of trauma is often overlooked as a significant factor or necessary target in treatment.
The relationship between PTSD and other disorders is complex. More research is now examining the multiple potential pathways among PTSD and other disorders and how various sequences affect clinical presentation. TIP 42, Substance Abuse Treatment for Persons With Co-Occurring Disorders ( CSAT, 2005c ), is valuable in understanding the relationship of substance use to other mental disorders.
People With Substance Use Disorders
There is clearly a correlation between trauma (including individual, group, or mass trauma) and substance use as well as the presence of posttraumatic stress (and other trauma-related disorders) and substance use disorders. Alcohol and drug use can be, for some, an effort to manage traumatic stress and specific PTSD symptoms. Likewise, people with substance use disorders are at higher risk of developing PTSD than people who do not abuse substances. Counselors working with trauma survivors or clients who have substance use disorders have to be particularly aware of the possibility of the other disorder arising.
Co-Occurring PTSD and Other Mental Disorders
- Individuals with PTSD often have at least one additional diagnosis of a mental disorder.
- The presence of other disorders typically worsens and prolongs the course of PTSD and complicates clinical assessment, diagnosis, and treatment.
- The most common co-occurring disorders, in addition to substance use disorders, include mood disorders, various anxiety disorders, eating disorders, and personality disorders.
- Exposure to early, severe, and chronic trauma is linked to more complex symptoms, including impulse control deficits, greater difficulty in emotional regulation and establishing stable relationships, and disruptions in consciousness, memory, identity, and/or perception of the environment ( Dom, De, Hulstijn, & Sabbe, 2007 ; Waldrop, Back, Verduin, & Brady, 2007 ).
- Certain diagnostic groups and at-risk populations (e.g., people with developmental disabilities, people who are homeless or incarcerated) are more susceptible to trauma exposure and to developing PTSD if exposed but less likely to receive appropriate diagnosis and treatment.
- Given the prevalence of traumatic events in clients who present for substance abuse treatment, counselors should assess all clients for possible trauma-related disorders.
Timeframe: PTSD and the onset of substance use disorders
Knowing whether substance abuse or PTSD came first informs whether a causal relationship exists, but learning this requires thorough assessment of clients and access to complete data on PTSD; substance use, abuse, and dependence; and the onset of each. Much current research focuses solely on the age of onset of substance use (not abuse), so determining causal relationships can be difficult. The relationship between PTSD and substance use disorders is thought to be bidirectional and cyclical: substance use increases trauma risk, and exposure to trauma escalates substance use to manage trauma-related symptoms. Three other causal pathways described by Chilcoat and Breslau’s seminal work ( 1998 ) further explain the relationship between PTSD and substance use disorders:
- The “self-medication” hypothesis suggests that clients with PTSD use substances to manage PTSD symptoms (e.g., intrusive memories, physical arousal). Substances such as alcohol, cocaine, barbiturates, opioids, and amphetamines are frequently abused in attempts to relieve or numb emotional pain or to forget the event.
- The “high-risk” hypothesis states that drug and alcohol use places people who use substances in high-risk situations that increase their chances of being exposed to events that lead to PTSD.
- The “susceptibility” hypothesis suggests that people who use substances are more susceptible to developing PTSD after exposure to trauma than people who do not. Increased vulnerability may result from failure to develop effective stress management strategies, changes in brain chemistry, or damage to neurophysiological systems due to extensive substance use.
PTSD and substance abuse treatment
PTSD can limit progress in substance abuse recovery, increase the potential for relapse, and complicate a client’s ability to achieve success in various life areas. Each disorder can mask or hide the symptoms of the other, and both need to be assessed and treated if the individual is to have a full recovery. There is a risk of misinterpreting trauma-related symptoms in substance abuse treatment settings. For example, avoidance symptoms in an individual with PTSD can be misinterpreted as lack of motivation or unwillingness to engage in substance abuse treatment; a counselor’s efforts to address substance abuse–related behaviors in early recovery can likewise provoke an exaggerated response from a trauma survivor who has profound traumatic experiences of being trapped and controlled. Exhibit 1.3-6 lists important facts about PTSD and substance use disorders for counselors.
Exhibit 1.3-6
PTSD and Substance Use Disorders: Important Treatment Facts. PTSD is one of the most common co-occurring mental disorders found in clients in substance abuse treatment (CSAT, 2005c). People in treatment for PTSD tend to abuse a wide range of substances, (more...)
Case Illustration: Maria
Maria is a 31-year-old woman diagnosed with PTSD and alcohol dependence. From ages 8 to 12, she was sexually abused by an uncle. Maria never told anyone about the abuse for fear that she would not be believed. Her uncle remains close to the family, and Maria still sees him on certain holidays. When she came in for treatment, she described her emotions and thoughts as out of control. Maria often experiences intrusive memories of the abuse, which at times can be vivid and unrelenting. She cannot predict when the thoughts will come; efforts to distract herself from them do not always work. She often drinks in response to these thoughts or his presence, as she has found that alcohol can dull her level of distress. Maria also has difficulty falling asleep and is often awakened by nightmares. She does not usually remember the dreams, but she wakes up feeling frightened and alert and cannot go back to sleep.
Maria tries to avoid family gatherings but often feels pressured to go. Whenever she sees her uncle, she feels intense panic and anger but says she can usually “hold it together” if she avoids him. Afterward, however, she describes being overtaken by these feelings and unable to calm down. She also describes feeling physically ill and shaky. At these times, she often isolates herself, stays in her apartment, and drinks steadily for several days. Maria also reports distress pertaining to her relationship with her boyfriend. In the beginning of their relationship, she found him comforting and enjoyed his affection, but more recently, she has begun to feel anxious and unsettled around him. Maria tries to avoid sex with him, but she sometimes gives in for fear of losing the relationship. She finds it easier to have sex with him when she is drunk, but she often experiences strong feelings of dread and disgust reminiscent of her abuse. Maria feels guilty and confused about these feelings.
Sleep, PTSD, and substance use
Many people have trouble getting to sleep and/or staying asleep after a traumatic event; consequently, some have a drink or two to help them fall asleep. Unfortunately, any initially helpful effects are likely not only to wane quickly, but also to incur a negative rebound effect. When someone uses a substance before going to bed, “sleep becomes lighter and more easily disrupted,” and rapid eye movement sleep (REM) “increases, with an associated increase in dreams and nightmares,” as the effects wear off ( Auerbach, 2003 , p. 1185).
People with alcohol dependence report multiple types of sleep disturbances over time, and it is not unusual for clients to report that they cannot fall asleep without first having a drink. Both REM and slow wave sleep are reduced in clients with alcohol dependence, which is also associated with an increase in the amount of time it takes before sleep occurs, decreased overall sleep time, more nightmares, and reduced sleep efficiency. Sleep during withdrawal is “frequently marked by severe insomnia and sleep fragmentation…a loss of restful sleep and feelings of daytime fatigue. Nightmares and vivid dreams are not uncommon” ( Auerbach, 2003 , pp. 1185–1186).
Confounding changes in the biology of sleep that occur in clients with PTSD and substance use disorders often add to the problems of recovery. Sleep can fail to return to normal for months or even years after abstinence, and the persistence of sleep disruptions appears related to the likelihood of relapse. Of particular clinical importance is the vicious cycle that can also begin during “slips”; relapse initially improves sleep, but continued drinking leads to sleep disruption. This cycle of initial reduction of an unpleasant symptom, which only ends up exacerbating the process as a whole, can take place for clients with PTSD as well as for clients with substance use disorders. There are effective cognitive–behavioral therapies and nonaddictive pharmacological interventions for sleep difficulties.
- Cite this Page Center for Substance Abuse Treatment (US). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. (Treatment Improvement Protocol (TIP) Series, No. 57.) Chapter 3, Understanding the Impact of Trauma.
- PDF version of this title (5.2M)
In this Page
Other titles in these collections.
- SAMHSA/CSAT Treatment Improvement Protocols
- Health Services/Technology Assessment Texts (HSTAT)
Recent Activity
- Understanding the Impact of Trauma - Trauma-Informed Care in Behavioral Health S... Understanding the Impact of Trauma - Trauma-Informed Care in Behavioral Health Services
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Trauma-informed and resilience-informed approaches to care may help address these concerns across health and social care research. These approaches take an empowerment-based response to adversity, and are suitable for integration and extension as Trauma and Resilience Informed Research Principles and Practice (TRIRPP) for studies beyond the ...
Trauma is often viewed as an individual or interpersonal issue. This paper expands the definition of trauma to include the impact collective and structural elements on health and well-being. The need for a trauma-informed response is demonstrated, with instruction as to how to implement this type of care in order to resist re-traumatization.
While there is a growing body of the literature on trauma-informed care, no prior review has systematically addressed trauma-informed interventions; one published review of literature ... Psychological Trauma: Theory, Research, Practice, and Policy. 2011; 3 (1):84-93.
In 2018, SAMHSA's Interagency Task Force on Trauma-Informed Care was established to collate existing evidence, develop best practices, and make recommendations for ways federal agencies can better support and coordinate their response to families impacted by trauma. 42 Future research should continue to evaluate the critical elements of TIC ...
There is a growing body of the literature on trauma informed and culturally competent care as essential elements of promoting health equity, yet no prior review has systematically addressed trauma informed interventions. ... and physiological activity in complex trauma. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(4):438 ...
The trauma-informed care approach seeks to enhance patient engagement and promote more effective recovery for those with a history of psychological trauma. This qualitative systematic review aims to synthesize evidence related to the experiences of women receiving trauma-informed care using Sandelowski and Barroso's two-step approach for ...
How services are provided can have important impacts on health and well-being (Lee & Lin, 2010; Rathert et al., 2013).When serving survivors of trauma and violence, a lack of understanding of the complex and lasting impacts of these experiences may lead to harm and to missed opportunities to provide effective care.
Trauma-informed (TI) approach is a framework for a system change intervention that transforms the organizational culture and practices to address the high prevalence and impact of trauma on patients and healthcare professionals, and prevents re-traumatization in healthcare services. Review of TI approaches in primary and community mental healthcare identified limited evidence for its ...
The Trauma-Informed Care team at AIR takes a comprehensive, collaborative, and reflective approach in our work with agencies, organizations and systems across service sectors and of all sizes. Comprehensive: Our expertise spans a wide range of systems—from schools and justice settings to human service organizations and government entities.;
In 2005, the National Center for Trauma Informed Care was created by SAMHSA to provide training and technical assistance to support communities and organizations interested in becoming trauma ...
Trauma-Informed Care. Trauma-Informed Care (TIC) is an organizational change process that requires all individuals, practices and protocols, and environments to engage in universal precaution for trauma. Similar to how healthcare professionals put on gloves when needing to touch patients as universal precautions for pathogens, being trauma ...
Trauma-informed care provides the framework for individuals, organizations and systems to engage in universal precautions for individual, historical and systemic trauma by using the values and principles of safety, trustworthiness, choice, collaboration and empowerment. ... Through collaborative partnerships and funded research, we work with ...
The brief is a product of Advancing Trauma-Informed Care, a multi-site demonstration project supported by the Robert Wood Johnson Foundation and led by the Center for Health ... study. 1,2,3 Because of the ACE study, and other subsequent research, health care policymakers and providers increasingly recognize that exposure to traumatic events ...
Trauma-Informed Care. The concepts of trauma-informed care have evolved over the past 30 years from a variety of streams of thought and innovation. They are now being applied in a wide range of settings, from mental health and substance-abuse treatment providers to child welfare systems and even schools and criminal justice institutions.
Trauma-Informed Care. Central to a TIC approach is the consideration of trauma and traumatic responses from an ecological lens with an emphasis on the historical, gendered, and cultural context that envelop the affected individual (Piotrowski, 2020). ... The groundbreaking ACEs Study research has informed policy and practice across multiple ...
Since the inception of trauma-informed care in the medical field in the late 1980s , the practice has evolved and permeated peripheral fields, including behavioral health, advocacy, and, in the past 20 years, research.The Centers for Disease Control and Prevention recently partnered with the Substance Abuse and Mental Health Services Administration to create guiding principles of trauma ...
Providing a comprehensive literature review on trauma, traumatic stress, trauma-informed care (TIC), and trauma-related interventions is a daunting task when considering the quantity and prolific production of research in this area in the past 20 years. To manage the volume of information, this literature review mainly focuses on reviews and meta-analyses rather than seminal work to address ...
Life trauma is highly correlated with an increased risk of mortality from chronic disease. Trauma-informed care (TIC) is an evidence-based approach to deliver healthcare in a way that recognizes and responds to the long-term health effects of the experience of trauma in patients' lives. Four essential features and six defining concepts delineate a TIC approach to healthcare.
for research purposes Trauma-informed approaches to care and research Trauma-informed (TI) approaches respond to the knowl-edge that inattention to the impact of trauma may deter people from accessing or maintaining contact with ser-vices.16 Trauma-informed approaches aim to improve en-gagement by realising the widespread impact of trauma,
Trauma has been repeatedly linked to increased risk of mental health (MH) difficulties along with poor prognosis (McKay et al., Citation 2021).Trauma may be the outcome of "an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual's functioning and ...
Trauma-informed care (TIC) or Trauma-and violence-informed care ... Professionals might reflect on their own understanding of current research about safety and danger. The offer of relatively comprehensive support for trauma and safety plan options may ease and promote discussions. Particularly if the discussion about trauma is extensive, a ...
The annual Trauma-Informed Care Conference brings together professionals working with children and families from the front lines, such as child welfare and mental health professionals, as well as school and juvenile legal system staff. ... UCLA Pritzker Center, the UCLA-UCSF ACEs Aware Family Resilience Network and the Trauma Research ...
Background: As trauma-informed care advances in the service delivery system for people with intellectual and developmental disabilities, additional resources are needed to foster staff development. This article describes the development and pilot evaluation of a digital training on trauma-informed care among direct service providers (DSPs) in the disability service industry.
Trauma-informed Care. May 2024. Seminars in Pediatric Neurology. May 2024. DOI: 10.1016/j.spen.2024.101139. Authors: Heather N. Williams. Brenna Farley. To read the full-text of this research, you ...
Trauma-informed care: Developing fieldwork competence. Tamerill Faison and Barbara Demchick, Volume 29 • Issue 6 • June 2024, pp. 12-15 06/01/2024. Trauma is a widespread, harmful, and costly public health problem (Substance Abuse and Mental Health Services Administration [SAMHSA], 2014). It has no boundaries with regard to age, gender ...
The social work profession recognises the value of trauma-informed care for women with multiple disadvantage. For women involved in street-based prostitution this is mostly descriptive in nature with limited practice-based investigation. ... Guided by the principles of qualitative feminist research, this article explores the enablers and ...
UB medical students working with community anti-violence groups in Buffalo have developed an elective course on "Trauma surgery and trauma-informed care.". The purpose is to train medical students, particularly those interested in surgery, in trauma-informed care in Buffalo's Level 1 Adult Trauma Center at the Erie County Medical Center (ECMC).
The phrase 'trauma-informed' is appearing with increasingly regularity in health and social care, referring not to physical injury but to the psychological and neurological impact of adverse events and circumstances. 1 Trauma-informed practice (TIP) is a growing phenomenon, for example, it is now integral to the NHS Long Term Plan. 2 The concept of TIP gained traction first in the US ...
Trauma-informed care (TIC) involves a broad understanding of traumatic stress reactions and common responses to trauma. Providers need to understand how trauma can affect treatment presentation, engagement, and the outcome of behavioral health services. This chapter examines common experiences survivors may encounter immediately following or long after a traumatic experience.
Introduction: Trauma is a major problem which has a significant health, social, and economic impact. Particularly, pediatric trauma carries substantial mortality and morbidity. This is a great concern for subspecialized general and pediatric surgeons. Therefore, a global initiative for pediatric trauma care is warranted and should be initiated. Aim: The international association "Global ...