Loading metrics
Open Access
Collection Review
Collection Review articles synthesize in narrative form the best available evidence on a topic. Submission of Collection Review articles is by invitation only, and they are only published as part of a PLOS Collection as agreed in advance by the PLOS Medicine Editors.
See all article types »

Progress in the HIV epidemic: Identifying goals and measuring success
* E-mail: [email protected]
Affiliation Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia, United States of America
- Jeb Jones,
- Patrick S. Sullivan,
- James W. Curran

Published: January 18, 2019
- https://doi.org/10.1371/journal.pmed.1002729
- Reader Comments
Substantial progress has been made towards the goal of ending the HIV/AIDS epidemic due to advancements in both prevention and treatment of HIV. However, major challenges still remain. We describe basic principles of epidemic control in the context of HIV and identify a number of attainable goals in terms of control and elimination of HIV in specific populations and risk groups, given currently available HIV prevention and treatment methods. Currently available HIV prevention methods make it a feasible goal to eliminate HIV transmission attributable to mother-to-child transmission and blood transfusions. Reductions in transmission attributable to sexual behavior and injection drug use are feasible, but elimination of these modes of transmission will require further advancements in behavioral and biomedical HIV prevention. With regard to HIV-related mortality, we argue that elimination of death due to HIV-related causes is a feasible goal. HIV-related deaths should be treated as sentinel events triggering epidemiological investigation into the breakdowns in the HIV care continuum that led to them. We briefly discuss additional considerations that will affect the success of HIV prevention programs.
Citation: Jones J, Sullivan PS, Curran JW (2019) Progress in the HIV epidemic: Identifying goals and measuring success. PLoS Med 16(1): e1002729. https://doi.org/10.1371/journal.pmed.1002729
Copyright: © 2019 Jones et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: An earlier version of this paper was commissioned by UNAIDS for a meeting convened in October 2017. JJ received compensation for producing the earlier version of the paper. UNAIDS reviewed and provided feedback on earlier drafts of the paper; however, final editorial decisions were made by coauthors.
Competing interests: I have read the journal's policy and the authors of this manuscript have the following competing interests: PSS reports research funding from NIH, research grants and personal fees from Centers for Disease Control and Prevention, research fees from Gilead Sciences, and research fees from MAC AIDS Fund.
Abbreviations: ARV, antiretroviral; MSM, men who have sex with men; PLWH, persons living with HIV; PrEP, pre-exposure prophylaxis; UNAIDS, Joint United Nations Programme on HIV/AIDS; VMMC, voluntary medical male circumcision
Provenance: Not commissioned; externally peer reviewed
Introduction
The United Nations has declared a goal of ending the AIDS epidemic by 2030 [ 1 ], an aspiration echoed by many individual countries. To achieve this goal, targets have been set for each step in the HIV diagnosis and care continuum. Specifically, besides primary prevention targets for voluntary medical male circumcision (VMMC) [ 2 , 3 ], pre-exposure prophylaxis (PrEP) [ 4 , 5 ], use of condoms [ 6 ], harm reduction [ 7 ], and opioid substitution treatment [ 8 ], the 90-90-90 goals aim for 90% of individuals infected with HIV to be aware of their status, 90% of those diagnosed to initiate antiretroviral (ARV) treatment, and 90% of those on ARVs to have viral loads suppressed below levels of detection, by 2020 [ 9 , 10 ]. These aspirational goals are laudable and, to the degree that they can be achieved, will have a meaningful impact on HIV incidence as well as mortality globally. However, the heterogeneity of the HIV epidemic globally raises challenges in terms of measuring success along the way. In a recently published article, Peter Ghys and colleagues have proposed six different metrics to measure transitions in different aspects (e.g., incidence, mortality) of the HIV epidemic [ 11 ].
Differing definitions of what it means for the epidemic to be “over” or “under control” can lead to confusion among stakeholders and the public. It is crucial to define quantifiable goals that will be clearly understood and can be used to measure progress toward vanquishing HIV/AIDS as a major public health problem. This will bring focus and provide benchmarks to measure success of HIV prevention and care programs globally. The purpose of this paper is to review concepts of epidemic control and apply them to the case of HIV. We identify aspirational but feasible goals for control and elimination of HIV transmission and HIV-related mortality. Finally, we will briefly discuss additional challenges and considerations that play an important role in controlling the HIV epidemic.
Epidemiological principles
Disease occurrence is typically measured in terms of incidence (all new cases of a disease during a given period of time) and prevalence (all existing cases of disease at a given point in time). Incidence and prevalence represent measures that we aspire to accurately count or estimate to characterize a certain disease at the population level. However, there are practical considerations, particularly with respect to HIV, that make estimating these measures difficult.
HIV incidence is difficult to measure because HIV infections are initially asymptomatic or cause minimal nonspecific symptoms. Therefore, most newly infected persons do not immediately seek HIV testing and are often diagnosed many months or years after infection. In addition, HIV infection is associated with a window period of one to three months, during which antibody tests cannot detect infection, meaning that early infection may be missed, even when people with very recent HIV infections are tested for antibodies to HIV. Because of these challenges, new infections are frequently measured in terms of new HIV diagnoses. Although this is a pragmatic approach, reporting diagnoses instead of incidence can be problematic in terms of understanding prevailing disease dynamics. For example, increases in diagnoses might be due to more effective HIV testing campaigns that identify previously undiagnosed individuals. The proportion of new diagnoses that occur among individuals with CD4 cell counts <350 (i.e., late-stage diagnosis) highlight the fact that many new diagnoses are not new cases of HIV. For example, a 2015 Dutch study found that 28% of men who have sex with men (MSM) had a CD4 count <350 at the time of diagnosis [ 12 ]. Similarly, the proportion of late-stage diagnoses in a 2013 South African study was 34% [ 13 ]. It is a goal to reduce the time between HIV infection and HIV diagnosis in order for persons to access ARV treatment and to reduce incident infections. As an alternative to using new HIV diagnoses as a proxy for HIV incidence, statistical modeling methods can be used to obtain estimates of HIV incidence in general and within specific populations [ 14 , 15 ].
In the absence of curative therapy, HIV is a lifelong infection. Thus, prevalence measures alone cannot provide a meaningful indication of changes in the epidemic in the short or near term; changes in prevalence must be interpreted in the context of HIV incidence, treatment outcomes, and mortality. Reducing HIV transmission and incidence requires identifying and counselling persons with HIV infection and providing lifelong ARV treatment in order to decrease the probability of transmission of the virus and reduce HIV-associated mortality, in addition to increasing coverage of primary HIV prevention methods among those at risk of infection. Programmatically, these are costly endeavors; estimates suggest that the cost of mounting a comprehensive AIDS response will be US$26–$36 billion annually [ 1 , 10 , 16 ].
Standard measures of epidemic control include control, elimination, eradication, and extinction ( Box 1 ) [ 17 , 18 ]. These measures represent increasing levels of success with respect to ending disease incidence. The language surrounding epidemic control can be confusing, because the terms describing each level of control have common and imprecise meanings in colloquial language. In this paper, we use the words control, elimination, eradication, and extinction only in accord with their technical definitions.
Box 1. Relationship between incidence, prevalence, and duration of disease under steady state
Prevalence = Incidence * Average duration of disease
This equation demonstrates that reductions in prevalence can be achieved by reducing incidence of a disease or the average duration of a disease. Conversely, increases in incidence or duration will increase prevalence. This is why public health successes, such as increasing coverage of ARV therapy, which increases the average duration of HIV infection by extending the life span, leads to increases in HIV prevalence.
Measures of disease control
Control : reduction of disease incidence, prevalence, or mortality in a geographically defined area to a locally acceptable level via effective interventions.
Elimination : complete cessation of incidence in a geographically defined area. Because the disease-causing agent persists, elimination requires ongoing intervention to be maintained.
Eradication : complete removal of the disease-causing agent from the natural environment. The disease-causing agent might persist in controlled laboratory environments. Prevention interventions are no longer needed.
Extinction : complete removal of the disease-causing agent from all natural and laboratory environments.
Formulating goals for controlling the HIV epidemic
HIV has unique characteristics that affect the interpretation and utility of standard measures of epidemic control. Any measurable goals that are put forward in terms of reducing incidence of HIV must take into account the biological and sociological characteristics of the epidemic. Because eradication requires that a disease-causing agent is entirely removed from the natural environment on a global scale, eradication of HIV will not be an attainable goal until a vaccine and cure are developed and uniformly utilized. Table 1 presents aspirational epidemic control goals in terms of HIV transmission and HIV mortality that are attainable using current prevention methods. Control of the HIV epidemic includes both primary prevention of HIV among those at risk of infection and treatment of persons living with HIV (PLWH) to prevent HIV-related mortality and reduce the risk of onward transmission. Although these are distinct processes, there are some overlapping approaches that contribute to both.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1002729.t001
HIV transmission
Elimination achieved within a given geographic region by mode of transmission is defined as a reduction of incidence to zero. Unlike with eradication, the disease-causing agent continues to persist in the population, and prevention efforts are necessary to ensure that elimination persists. Elimination of incident infections could thus theoretically be achieved even as HIV prevalence persists, using existing prevention methods like treatment as prevention [ 19 ], PrEP [ 4 , 5 ], condoms [ 6 ], VMMC [ 2 , 3 ], harm reduction [ 7 ], and opioid substitution programs [ 8 ], but only if these interventions are universally and continually utilized over time. Thus, goals related to transmission differ by risk populations.
The aspirational goal of elimination of transmission is more feasible for transmission attributable to blood transfusions and mother-to-child transmission because prevention methods are currently available that are very effective [ 20 , 21 ], and because these modes of transmission largely occur within medical settings, in which interventions can be scaled up universally. HIV infections caused by blood transfusions can be eliminated by testing all donated blood. Mother-to-child transmission can be eliminated by HIV testing all pregnant women, by providing lifelong ARV therapy to mothers who are diagnosed, by providing appropriate prophylaxis at the time of birth, and by following the breastfeeding guidelines established by the World Health Organization [ 22 ]. Transmission events due to these causes should be investigated to understand where the breakdown in systems to identify mothers living with HIV and systems to protect infants occurred, so that necessary systems and policies can be put in place to ensure universal coverage of these prevention methods. Of note, new HIV infections among children had reduced 35% to 180,000 in 2017 compared to 270,000 in 2010 [ 23 ].
HIV transmission due to sexual behavior and injection drug use can be controlled, but elimination is not currently realistic in that the number of transmissions is considerably higher and the structural opportunities for intervention (such as in the context of perinatal care) do not exist. A realistic goal will therefore be epidemic control (e.g., to reduce HIV incidence to locally acceptable low levels, which should be defined clearly and represent considerable improvement over the status quo). Many prevention tools, both old and new, are available to reduce the transmission of HIV due to these risk behaviors. The effectiveness of ARV therapy [ 19 ] and PrEP [ 4 , 24 ]—in addition to condom use [ 25 , 26 ], needle and syringe exchange programs [ 27 ], and VMMC [ 2 , 3 ]—in reducing the risk of HIV transmission following strong adherence by HIV + and HIV − individuals, respectively, demonstrates that existing methods have the potential to greatly reduce HIV transmission. Delivering these tools in combinations and in appropriate service settings, monitoring the uptake in target populations, and monitoring for inequities in uptake will be important to maximize impact. Current ARV-based prevention strategies require substantial levels of adherence for prevention efficacy; these tools can be improved by considering long-acting formulations or shorter, on-demand approaches. A safe and effective vaccine and curative therapy, neither of which are currently available, would change the HIV prevention and treatment landscape. These types of future advancements in biomedical and behavioral prevention research are needed to achieve a goal of elimination of sexual and injection drug use transmission.
HIV mortality
Given current treatment options, elimination of HIV mortality should be an aspirational yet feasible goal. Combination ARV therapy with substantial adherence has been shown to be effective in reducing viral loads and extending the life span of PLWH [ 28 ]. Expanding testing programs to identify all PLWH followed by treatment initiation and adherence support for those persons who are diagnosed could lead to the elimination of mortality due to AIDS-related complications. Deaths from HIV-related causes should be treated as sentinel events, instigating a public health investigation to understand the factors leading to treatment failure. In 2017 there were approximately 940,000 AIDS-related deaths globally [ 23 ]. Appropriate resources will need to be made available to investigate the complex, multilevel failures that likely contribute to HIV-related mortality, including limited healthcare access, poverty, substance use, and mental health problems.
Current progress in controlling the HIV epidemic
Since the 90-90-90 targets were announced in 2014, substantial progress has been made. Compiling country-level data from around the world, the Joint United Nations Programme on HIV/AIDS (UNAIDS) has summarized progress through the end of 2017 [ 29 ]. Although progress—in some countries, substantial progress—has been made, a number of gaps and challenges remain. It is beyond the scope of this paper to fully review global progress, but there are some conspicuous trends. Gains in epidemic control have been notably slower among men and young people, highlighting that existing interventions and programs are not equally effective across demographic groups. This is evident in the faster declines in mortality from AIDS-related causes among women compared with men since 2000. This suggests that additional work will be necessary to increase uptake of HIV testing and treatment among groups that lag behind in the current environment. Additional marginal gains towards the 90-90-90 targets will require engaging these harder-to-reach groups.
There have also been consistent increases in HIV infections and AIDS-related deaths in Eastern Europe and Central Asia since 2000. This is in contrast to generally stable or declining rates of HIV infections and AIDS-related deaths in other regions globally. This suggests additional dynamics that need to be understood and managed in Eastern Europe and Central Asia, in order to halt the growing epidemic in this region.
Varying definitions of control: Defining feasibility
Control of the HIV epidemic should be measured at the local, national, and global levels. To achieve control of the HIV epidemic will mean identifying local goals that result in forward progress but are achievable for a given epidemiological context, as well as identifying and implementing the means to achieve those goals. In the 2016 Prevention Gap Report, UNAIDS identified a target of fewer than 500,000 new HIV infections globally by 2020 [ 30 ]. To achieve this goal, the report recommends implementing the Fast-Track strategy, including achieving the 90-90-90 targets in combination with primary prevention programs. Substantial progress will be required to achieve the 90-90-90 targets globally by 2020, and, under this aspirational goal, a substantial proportion, that is 27% of PLWH, will continue to have unsuppressed viral loads (i.e., if the goals are met, about 73% of PLWH will have a suppressed viral load [90% * 90% * 90% = 73%]).
Beyond identifying methods most appropriate to measure successes and identify challenges in HIV prevention, defining epidemic control also requires identifying aspirational yet feasible goals for a given geographical region and epidemiological context. Because control is achieved within a specific geographic region, the local dynamics and epidemic characteristics must be considered in order to identify appropriate goals. Thus, although benchmarks such as the 90-90-90 goals are helpful in planning at a global level, the target epidemiologic measures of incidence, prevalence, transmission rate, or mortality might need to be different depending on local epidemic characteristics. Goals must be identified in terms of what is aspirational, feasible, and measurable at the local, national, and global levels.
Additional considerations
Any discussion of epidemic control must acknowledge the sociocultural context in which HIV exists. It will be difficult, if not impossible, to achieve control of the HIV epidemic without addressing other factors that contribute to the epidemic, such as stigma and criminalization associated with HIV infection and the need for ancillary health services.
Stigma associated with HIV infection and HIV risk behaviors continues to pose a challenge to public health programs designed to reduce HIV incidence [ 31 ]. Stigma can reduce the likelihood that an individual is aware of their status and seeking treatment or effective prevention tools owing to fear of testing and disclosure. Joseph Amon and colleagues [ 32 ] have described the importance of measuring stigma in addition to other disease-specific indicators (e.g., HIV incidence, AIDS-related mortality) in order to track changes in the epidemic over time.
HIV prevention and treatment programs exist within larger healthcare and economic systems and PLWH, and those at risk of HIV seroconversion, have health needs beyond HIV treatment and prevention services. Mental health services, drug treatment programs, and programs ensuring continuity of care for incarcerated populations are all necessary components of a holistic approach to HIV prevention. Furthermore, these issues serve as a reminder that the populations of PLWH without a diagnosis and those at high risk of HIV infection are very heterogeneous, and there are additional challenges that can be barriers to reaching them. As programs approach the 90-90-90 goals, continued progress might be increasingly challenging because certain key populations have not been reached in individual settings, or different strategies might be required to make further progress.
Conclusions
In this paper, we have reviewed concepts related to epidemiological control in the context of the biology and epidemiology of HIV infection and considered sociobehavioral factors that contribute to the HIV epidemic. Substantial progress has been made in the past 35 years with regard to HIV prevention, treatment, and surveillance methods; however, significant challenges remain. The global commitment to ending the HIV epidemic, exemplified through the United Nations’ Political Declaration On HIV and AIDS [ 1 ], indicates a high degree of motivation from countries around the world to reduce morbidity and mortality due to HIV/AIDS. Existing strategies to measure and evaluate progress of HIV prevention interventions should be examined, and additional new measures should be considered in order to most effectively characterize current and future progress in stemming the epidemic. Targets related to controlling HIV incidence and AIDS-related mortality should reflect realistic capabilities of currently available interventions.
In addition to reliable data to track progress in controlling the HIV epidemic, continued research, including implementation science, will be needed to further our understanding of the most effective HIV prevention interventions and how to most effectively deploy these interventions. As outlined above, we identified elimination of HIV transmission due to mother-to-child transmission and blood transfusions as currently attainable. In order to meet this goal, however, resources will need to be allocated appropriately to ensure that appropriate interventions are broadly available, and studies will need to be conducted to understand barriers to implementation when those interventions are underutilized or ineffective. A holistic approach including surveillance, appropriate measures to track epidemic transition, and implementation science is key to continued progress in meeting global targets for control of the HIV epidemic.
- View Article
- Google Scholar
- PubMed/NCBI
- 9. UNAIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic 2014 [cited 2018 Mar 1]. Available from: http://www.unaids.org/en/resources/documents/2017/90-90-90 .
- 14. UNAIDS. Methods for estimating HIV incidence 2010 [cited 2018 Mar 1]. Available from: http://www.unaids.org/sites/default/files/media_asset/epi_alert_1stqtr2010_en_0.pdf .
- 18. Miller M, Barrett S, Henderson DA. Chapter 62. Control and Eradication. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al., editors. Disease Control Priorities in Developing Countries. 2nd ed. New York: Oxford University Press; 2006.
- 20. World Health Organization. Screening donated blood for transfusion-transmissible infections: recommendations. Geneva: 2009.
- 21. World Health Organization. PMTCT Strategic Vision 2010–2015: Preventing mother-to-child transmission of HIV to reach the UNGASS and Millennium Development Goals. Geneva: 2010.
- 22. World Health Organization, United Nations Children's Fund. Guideline: updates on HIV and infant feeding: the duration of breastfeeding and support from health services to improve feeding practices among mothers living with HIV. Geneva: 2016.
- 23. UNAIDS. Global HIV & AIDS statistics—2018 fact sheet 2018 [cited 2019 Jan 2]. Available from: http://www.unaids.org/en/resources/fact-sheet .
- 27. Organization WH. Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. Geneva: 2004.
- 29. UNAIDS. UNAIDS Data 2017. 2017.
- 30. UNAIDS. Prevention Gap Report 2016 [cited 2018 Mar 1]. Available from: http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf .
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
- Submit your manuscript
Secondary Logo
Journal logo, current issue.

July 01, 2024 - Volume 38 - Issue 8
- Editor-in-Chief: Michael S. Saag Editors: Roel A. Coutinho Mathias D. Lichterfeld Sarah L. Rowland-Jones
- ISSN: 0269-9370
- Online ISSN: 1473-5571
- Frequency: 15 / year
- Ranking: 21 of 41 Virology 47 of 132 Infectious Diseases 93 of 181 Immunology
- Impact Factor: 3.4
Featured Supplement

Open Access Special Issue

December 15, 2021 - Volume 35 - Supplement 2
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Current Issue Highlights
- NOTES & QUOTES
Liver health matters: targeting modifiable factors to reduce the risk of advanced liver disease in people with HIV
AIDS. 38(8):N15-N16, July 01, 2024.
- Permissions
- BASIC SCIENCE

HIV-1 drug resistance and genetic diversity in people with HIV-1 in Cape Verde
AIDS. 38(8):1101-1110, July 01, 2024.
- Abstract Abstract
- CLINICAL SCIENCE

Effects of COVID-19 mRNA vaccination on HIV viremia and reservoir size
AIDS. 38(8):1120-1130, July 01, 2024.
Go to Full Text of this Article
CONCISE COMMUNICATION

Outcomes of discordant HIV screening test results at a southern academic medical center
AIDS. 38(8):1181-1185, July 01, 2024.
- Epidemiology and Social

Age-associated dementia among older people aging with HIV in the United States: a modeling study
AIDS. 38(8):1186-1197, July 01, 2024.

Negative impact of a health insurer-mandated de-simplification from a single-tablet regimen to a two-tablet regimen
AIDS. 38(8):1257-1262, July 01, 2024.
- Editorial Comments
Is early initiation of antiretroviral therapy important?
AIDS. 38(8):1263-1264, July 01, 2024.
- Research Letters

Low cabotegravir trough concentrations without oral lead-in in patients with HIV-1 switching to long-acting cabotegravir and rilpivirine
AIDS. 38(8):1267-1269, July 01, 2024.
- Correspondence
Concerns and clarifications regarding the article ‘Virological, weight, and drug resistance outcomes among patients initiating a dolutegravir-based first line ART regimen in Zimbabwe’
AIDS. 38(8):1273, July 01, 2024.
Decay of coronavirus disease 2019 mRNA vaccine-induced immunity in people with HIV: Erratum
AIDS. 38(8):1279, July 01, 2024.
- CLINICAL SCIENCE: CONCISE COMMUNICATION
- Epidemiology and Social: CONCISE COMMUNICATION
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplement Archive
- Editorial Commentaries
- Perspectives
- Cover Archive
- IDSA Journals
- Clinical Infectious Diseases
- Open Forum Infectious Diseases
- Author Guidelines
- Open Access
- Why Publish
- IDSA Journals Calls for Papers
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- Journals Career Network
- About The Journal of Infectious Diseases
- About the Infectious Diseases Society of America
- About the HIV Medicine Association
- IDSA COI Policy
- Editorial Board
- Self-Archiving Policy
- For Reviewers
- For Press Offices
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Conclusions.
- < Previous
The Extended Impact of Human Immunodeficiency Virus/AIDS Research
- Article contents
- Figures & tables
- Supplementary Data
Tara A Schwetz, Anthony S Fauci, The Extended Impact of Human Immunodeficiency Virus/AIDS Research, The Journal of Infectious Diseases , Volume 219, Issue 1, 1 January 2019, Pages 6–9, https://doi.org/10.1093/infdis/jiy441
- Permissions Icon Permissions
Human immunodeficiency virus (HIV) is one of the most extensively studied viruses in history, and numerous extraordinary scientific advances, including an in-depth understanding of viral biology, pathogenesis, and life-saving antiretroviral therapies, have resulted from investments in HIV/AIDS research. While the substantial investments in HIV/AIDS research are validated solely on these advances, the collateral broader scientific progress resulting from the support of HIV/AIDS research over the past 30 years is extraordinary as well. The positive impact has ranged from innovations in basic immunology and structural biology to treatments for immune-mediated diseases and cancer and has had an enormous effect on the research and public and global health communities well beyond the field of HIV/AIDS. This article highlights a few select examples of the unanticipated and substantial positive spin-offs of HIV/AIDS research on other scientific areas.
The first cases of AIDS were reported in the United States 37 years ago. Since then, >77 million people have been infected worldwide, resulting in over 35 million deaths. Currently, there are 36.9 million people living with human immunodeficiency virus (HIV), 1.8 million new infections, and nearly 1 million AIDS-related deaths annually [ 1 ]. Billions of research dollars have been invested toward understanding, treating, and preventing HIV infection. The largest funder of HIV/AIDS research is the National Institutes of Health (NIH), investing nearly $69 billion in AIDS research from fiscal years 1982–2018. Despite the staggering disease burden, the scientific advances directly resulting from investments in AIDS research have been extraordinary. HIV is one of the most intensively studied viruses in history, leading to an in-depth understanding of viral biology and pathogenesis. However, the most impressive advances in HIV/AIDS research have come in the arena of antiretroviral therapy. Before the development of these life-saving drugs, AIDS was an almost universally fatal disease. Since the demonstration in 1987 that a single drug, zidovudine, better known as azidothymidine or AZT, could partially and temporarily suppress virus replication [ 2 ], the lives of people living with HIV have been transformed by the current availability of >30 antiretroviral drugs that, when administered in combinations of 3 drugs, now in a single daily pill, suppress the virus to undetectable levels. Today, if a person in their 20s is infected and given a combination of antiretroviral drugs that almost invariably will durably suppress virus to below detectable levels, they can anticipate living an additional 50 years, allowing them almost a normal life expectancy [ 3 ]. In addition, a person receiving antiretroviral therapy with an undetectable viral load will not transmit virus to their uninfected sexual partner. This strategy is referred to as “treatment as prevention” [ 4 ]. Also, administration of a single pill containing 2 antiretroviral drugs taken daily by an at-risk uninfected person decreases the chance of acquiring HIV by >95%. Finally, major strides are being made in the quest for a safe and effective HIV vaccine [ 5 ].
The enormous investment in HIV research is clearly justified and validated purely on the basis of advances specifically related to HIV/AIDS. However, the collateral advantages of this investment above and beyond HIV/AIDS have been profound, leading to insights and concrete advances in separate, diverse, and unrelated fields of biomedical research and medicine. In the current Perspective, we discuss a few select examples of the positive spin-offs of HIV/AIDS research on other scientific areas ( Table 1 ).
Positive Spin-offs of Human Immuno deficiency Virus/AIDS Research on Other Areas of Medicine
| Regulation of the human immune system |
| Targeted antiviral drug development |
| Probing the B-cell repertoire |
| Structure-based vaccine design |
| Advances in HIV/AIDS-related technologies |
| Role of immune activation in disease pathogenesis |
| Comorbidities in HIV disease |
| Regulation of the human immune system |
| Targeted antiviral drug development |
| Probing the B-cell repertoire |
| Structure-based vaccine design |
| Advances in HIV/AIDS-related technologies |
| Role of immune activation in disease pathogenesis |
| Comorbidities in HIV disease |
Abbreviation: HIV, human immunodeficiency virus.
Regulation of the Human Immune System
Congenital immunodeficiencies have been described as “experiments of nature,” whereby a specific defect in a single component of the complex immune system sheds light on the entire system. Such is the case with AIDS, an acquired defect in the immune system whereby HIV specifically and selectively infects and destroys the CD4 + subset of T lymphocytes [ 6 ]. In this respect, HIV infection functions as a natural experiment that elucidates the complexity of the human immune system. The selectivity of this defect and its resulting catastrophic effect on host defense mechanisms, as manifested by the wide range of opportunistic infections and neoplasms, underscore the critical role this cell type plays in the overall regulation of the human immune system. This has provided substantial insights into the pathogenesis of an array of other diseases characterized by aberrancies of immune regulation. Additionally, the in-depth study of immune dysfunction in HIV disease has shed light on the role of the immune system in surveillance against a variety of neoplastic diseases, such as non-Hodgkin lymphoma and Kaposi sarcoma. As a result of its association with HIV/AIDS, Kaposi sarcoma was discovered to be caused by human herpesvirus 8 [ 7 ].
Targeted Antiviral Drug Development
Targeted antiviral drug development did not begin with HIV infection. However, the enormous investments in biomedical research supported by the NIH and in drug development supported by pharmaceutical companies led to highly effective antiretroviral drugs targeting the enzymes reverse transcriptase, protease, and integrase, among other vulnerable points in the HIV replication cycle, and have transformed the field of targeted drug development, bringing it to an unprecedented level of sophistication. Building on 3 decades of experience, this HIV model has been applied in the successful development of antiviral drugs for other viral diseases, including the highly effective and curative direct-acting antivirals for hepatitis C [ 8 ].
Probing the B-Cell Repertoire
The past decade has witnessed extraordinary advances in probing the human B-cell lineage resulting from the availability of highly sophisticated technologies in cellular cloning and genomic sequencing [ 9 ]. AIDS research aimed at developing broadly reactive neutralizing antibodies against HIV and an HIV vaccine that could induce broadly neutralizing antibodies has greatly advanced the field of interrogation of human B-cell lineages, leading to greater insights into the humoral response to other infectious diseases, including Ebola [ 10 ], Zika [ 11 ], and influenza [ 12 ], as well as a range of autoimmune, neoplastic, and other noncommunicable diseases [ 13 ].
Structure-Based Vaccine Design
Although a safe and effective HIV vaccine has not yet been developed, the discipline of structure-based vaccine design using protein X-ray crystallography and cryoelectron microscopy has matured greatly in the context of HIV vaccine research. The design of immunogens based on the precise conformation of epitopes in the viral envelope as they bind to neutralizing antibodies has been perfected within the arena of HIV vaccine immunogen design. This has had immediate positive spinoffs in the design of vaccines for other viruses, such as respiratory syncytial virus, in which the prefusion glycoprotein was identified as the important immunogen for a vaccine using structure-based approaches [ 14 ].
Advances in HIV/AIDS-Related Technologies
Insights into the basic immunology of HIV drove the development and optimization of several broadly applicable technologies. Using inactivated HIV as a means of altering T lymphocytes to modulate the immune response, safe lentiviral gene therapy vectors are now US Food and Drug Administration–approved to treat certain cancers (eg, acute lymphoblastic leukemia) [ 15 ]. Additionally, it was discovered early in the epidemic that HIV is associated with the loss of CD4 + T lymphocytes [ 16 ]. While much of the initial research on CD4 + T lymphocytes was possible due to existing flow cytometry technologies, probing the complexities of immune dysregulation in HIV infection spurred the development of multicolor cytofluorometric technologies that have proven extremely useful for studying a variety of other diseases characterized by immune dysfunction [ 17 ]. The reality of utilizing these technologies in resource-poor areas accelerated the advancement of new simplified, automated, affordable, and portable point-of-care devices with broader implications for clinical medicine [ 18 ].
Role of Immune Activation in Disease Pathogenesis
Studying the pathogenesis of HIV disease has clearly demonstrated that aberrant immune activation stimulated by virus replication is the driving force of HIV replication [ 19 ]. In essence, the somewhat paradoxical situation exists whereby the very immune activation triggered by the virus in an attempt to control virus replication creates the microenvironment where the virus efficiently replicates. Even when the virus is effectively suppressed by antiretroviral drugs, a low degree of immune activation persists [ 20 ]. In this regard, the flagrant immune activation associated with uncontrolled virus replication, as well as the subtle immune activation associated with control of virus replication, are important pathogenic triggers of the increased cardiovascular and other organ system diseases associated with HIV infection. This direct association of even subtle levels of immune activation seen in HIV infection with a variety of systemic diseases has led to considerable insight into the role of immune activation and inflammation in human disease [ 21 ]. For example, recognition of the increased incidence of heart disease in the HIV population that is associated with chronic inflammation has stimulated interdisciplinary advances in understanding and treating coronary heart disease apart from HIV infection [ 22 ].
Comorbidities in HIV Disease
Antiretroviral therapy, which has transformed HIV treatment, is shifting the incidence of certain diseases in people living with HIV. Even when well-controlled by antiretrovirals, HIV disease is associated with an increased incidence of diseases, such as cardiovascular disease, kidney and liver disease, the premature appearance of pathophysiologic processes associated with aging, and several cancers [ 21–24 ]. This is especially true for non-AIDS-defining cancers, whose incidence rates are increasing while AIDS-defining cancer rates are decreasing [ 24 ]. In lower-income countries, tuberculosis is a common coinfection with HIV, and HIV coinfection was shown to be a key risk factor for progression of latent Mycobacterium tuberculosis infection to active disease [ 25 ]. There are a variety of ongoing studies [ 21 ] investigating the pathogenic bases of these conditions to shed greater insight into their causes and potential interventions that might impact these diseases apart from HIV infection and immunodeficiency.
The collateral advantages resulting from the substantial resources devoted to HIV/AIDS research over the past 30 years are extraordinary. From innovations in basic immunology and structural biology to treatments for immune-mediated diseases and cancer, the conceptual and technological advances resulting from HIV/AIDS research have had an enormous impact on the research and public and global health communities over and above the field of HIV/AIDS. The HIV/AIDS research model has proven that cross-fertilization of ideas, innovation, and research progress can lead to unforeseen and substantial advantages for a variety of other diseases.
Acknowledgments. The authors thank Carl Dieffenbach, Daniel Rotrosen, Charles Hackett, and Robert Eisinger for their helpful input in preparation of the manuscript.
Potential conflicts of interest. Both authors: No reported conflicts of interest. Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Joint United Nations Progamme on HIV/AIDS . Fact sheet: latest statistics on the status of the AIDS epidemic . http://www.unaids.org/en/resources/fact-sheet . Accessed 23 July 2018.
Fischl MA , Richman DD , Grieco MH , et al. The efficacy of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. A double-blind, placebo-controlled trial . N Engl J Med 1987 ; 317 : 185 – 91 .
Google Scholar
Samji H , Cescon A , Hogg RS , et al. North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEA . Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada . PLoS One 2013 ; 8 : e81355 .
Lundgren JD , Babiker AG , Gordin F , et al. INSIGHT START Study Group . Initiation of antiretroviral therapy in early asymptomatic HIV infection . N Engl J Med 2015 ; 373 : 795 – 807 .
Trovato M , D’Apice L , Prisco A , De Berardinis P . HIV vaccination: a roadmap among advancements and concerns . Int J Mol Sci 2018 ; 19 . doi: 10.3390/ijms19041241 .
Dalgleish AG , Beverley PC , Clapham PR , Crawford DH , Greaves MF , Weiss RA . The CD4 (T4) antigen is an essential component of the receptor for the AIDS retrovirus . Nature 1984 ; 312 : 763 – 7 .
Schulz TF , Boshoff CH , Weiss RA . HIV infection and neoplasia . Lancet 1996 ; 348 : 587 – 91 .
Wyles DL . Antiviral resistance and the future landscape of hepatitis C virus infection therapy . J Infect Dis 2013 ; 207 ( Suppl 1 ): S33 – 9 .
Boyd SD , Crowe JE Jr . Deep sequencing and human antibody repertoire analysis . Curr Opin Immunol 2016 ; 40 : 103 – 9 .
Flyak AI , Kuzmina N , Murin CD , et al. Broadly neutralizing antibodies from human survivors target a conserved site in the Ebola virus glycoprotein HR2-MPER region . Nat Microbiol 2018 ; 3 : 670 – 7 .
Sapparapu G , Fernandez E , Kose N , et al. Neutralizing human antibodies prevent Zika virus replication and fetal disease in mice . Nature 2016 ; 540 : 443 – 7 .
Raymond DD , Bajic G , Ferdman J , et al. Conserved epitope on influenza-virus hemagglutinin head defined by a vaccine-induced antibody . Proc Natl Acad Sci U S A 2018 ; 115 : 168 – 73 .
Röhn TA , Bachmann MF . Vaccines against non-communicable diseases . Curr Opin Immunol 2010 ; 22 : 391 – 6 .
Tian D , Battles MB , Moin SM , et al. Structural basis of respiratory syncytial virus subtype-dependent neutralization by an antibody targeting the fusion glycoprotein . Nat Commun 2017 ; 8 : 1877 .
US Food and Drug Administration . FDA approval brings first gene therapy to the United States . Silver Spring, MD : FDA , 2017 .
Google Preview
Gottlieb MS , Schroff R , Schanker HM , et al. Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency . N Engl J Med 1981 ; 305 : 1425 – 31 .
Chattopadhyay PK , Roederer M . Cytometry: today’s technology and tomorrow’s horizons . Methods 2012 ; 57 : 251 – 8 .
Kestens L , Mandy F . Thirty-five years of CD4 T-cell counting in HIV infection: from flow cytometry in the lab to point-of-care testing in the field . Cytometry B Clin Cytom 2017 ; 92 : 437 – 44 .
Moir S , Fauci AS . B-cell exhaustion in HIV infection: the role of immune activation . Curr Opin HIV AIDS 2014 ; 9 : 472 – 7 .
Paiardini M , Müller-Trutwin M . HIV-associated chronic immune activation . Immunol Rev 2013 ; 254 : 78 – 101 .
Lucas S , Nelson AM . HIV and the spectrum of human disease . J Pathol 2015 ; 235 : 229 – 41 .
Boccara F , Lang S , Meuleman C , et al. HIV and coronary heart disease: time for a better understanding . J Am Coll Cardiol 2013 ; 61 : 511 – 23 .
Torres RA , Lewis W . Aging and HIV/AIDS: pathogenetic role of therapeutic side effects . Lab Invest 2014 ; 94 : 120 – 8 .
Thrift AP , Chiao EY . Are non-HIV malignancies increased in the HIV-infected population ? Curr Infect Dis Rep 2018 ; 20 : 22 .
Getahun H , Gunneberg C , Granich R , Nunn P . HIV infection-associated tuberculosis: the epidemiology and the response . Clin Infect Dis 2010 ; 50 ( Suppl 3 ): S201 – 7 .
- acquired immunodeficiency syndrome
| Month: | Total Views: |
|---|---|
| August 2018 | 1,097 |
| September 2018 | 845 |
| October 2018 | 315 |
| November 2018 | 223 |
| December 2018 | 585 |
| January 2019 | 291 |
| February 2019 | 202 |
| March 2019 | 191 |
| April 2019 | 177 |
| May 2019 | 189 |
| June 2019 | 63 |
| July 2019 | 49 |
| August 2019 | 61 |
| September 2019 | 131 |
| October 2019 | 342 |
| November 2019 | 393 |
| December 2019 | 260 |
| January 2020 | 253 |
| February 2020 | 472 |
| March 2020 | 453 |
| April 2020 | 371 |
| May 2020 | 342 |
| June 2020 | 442 |
| July 2020 | 318 |
| August 2020 | 247 |
| September 2020 | 402 |
| October 2020 | 453 |
| November 2020 | 505 |
| December 2020 | 403 |
| January 2021 | 307 |
| February 2021 | 371 |
| March 2021 | 541 |
| April 2021 | 639 |
| May 2021 | 570 |
| June 2021 | 419 |
| July 2021 | 311 |
| August 2021 | 418 |
| September 2021 | 650 |
| October 2021 | 827 |
| November 2021 | 859 |
| December 2021 | 635 |
| January 2022 | 477 |
| February 2022 | 535 |
| March 2022 | 692 |
| April 2022 | 685 |
| May 2022 | 518 |
| June 2022 | 334 |
| July 2022 | 214 |
| August 2022 | 254 |
| September 2022 | 452 |
| October 2022 | 522 |
| November 2022 | 533 |
| December 2022 | 402 |
| January 2023 | 417 |
| February 2023 | 469 |
| March 2023 | 587 |
| April 2023 | 560 |
| May 2023 | 488 |
| June 2023 | 325 |
| July 2023 | 471 |
| August 2023 | 290 |
| September 2023 | 381 |
| October 2023 | 442 |
| November 2023 | 427 |
| December 2023 | 337 |
| January 2024 | 287 |
| February 2024 | 411 |
| March 2024 | 399 |
| April 2024 | 464 |
| May 2024 | 355 |
| June 2024 | 145 |
Email alerts
Related articles in pubmed, citing articles via, looking for your next opportunity.
- Recommend to your Library
Affiliations
- Online ISSN 1537-6613
- Print ISSN 0022-1899
- Copyright © 2024 Infectious Diseases Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Volume 27, Number 6—June 2021
Perspective
Reflections on 40 years of aids.
Cite This Article
June 2021 marks the 40th anniversary of the first description of AIDS. On the 30th anniversary, we defined priorities as improving use of existing interventions, clarifying optimal use of HIV testing and antiretroviral therapy for prevention and treatment, continuing research, and ensuring sustainability of the response. Despite scientific and programmatic progress, the end of AIDS is not in sight. Other major epidemics over the past decade have included Ebola, arbovirus infections, and coronavirus disease (COVID-19). A benchmark against which to compare other global interventions is the HIV/AIDS response in terms of funding, coordination, and solidarity. Lessons from Ebola and HIV/AIDS are pertinent to the COVID-19 response. The fifth decade of AIDS will have to position HIV/AIDS in the context of enhanced preparedness and capacity to respond to other potential pandemics and transnational health threats.
“When the history of AIDS and the global response is written, our most precious contribution may well be that, at a time of plague, we did not flee, we did not hide, we did not separate ourselves.”
—Jonathan Mann, Founding Director of Project SIDA and the World Health Organization Global Programme on AIDS, 1998
Forty years ago, on June 5, 1981, the Centers for Disease Control’s Morbidity and Mortality Weekly Report described 5 cases of Pneumocystis pneumonia in gay men ( 1 ). That report heralded the HIV/AIDS pandemic, which has resulted in over 75 million HIV infections and 32 million deaths. In 2011, we reviewed 30 years of AIDS and commented that the HIV/AIDS response would be a benchmark against which responses to other health threats would be compared ( 2 ). After 40 years of AIDS, we present our personal reflections on scientific and global health evolution over the fourth decade of AIDS in a world that has recently suffered other major epidemics. We focus on biomedical advances because these have had the greatest effect on HIV transmission and disease; advances in structural and behavioral interventions are reviewed in the CDC Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention ( 3 ).
After the initial MMWR report was published, it took 2–3 years for the cause of AIDS, the novel retrovirus designated HIV, to be identified ( 4 , 5 ), and many more years to uncover its simian origin ( 6 ). Because of the asymptomatic spread of HIV, the long incubation period before disease, and transmission through sex and blood, millions of persons around the world, including several hundred thousand in the United States, were infected by the time the first AIDS cases were reported. The epidemiology and natural history of HIV infection, combining elements of acute and chronic diseases, ensured a diverse and long-lasting pandemic.
The history of HIV/AIDS and the struggle to contain it have seen the best and worst of human nature. Frequent examples of discrimination and exclusion are contrasted by leadership, illustrated by community activists ( 7 ), Jonathan Mann molding the first global response ( 8 ), Kofi Annan rallying the United Nations behind the search for a global fund ( 9 ), and President George W. Bush committing United States generosity to a war on HIV/AIDS of uncertain duration ( 10 ). Despite continued instances of injustice, the story has overall been a positive one, providing lessons for how to respond to other epidemic and pandemic threats.
Evolving Epidemiology
The Joint United Nations Programme on HIV/AIDS (UNAIDS) estimates that in 2019, 38 million persons worldwide were living with HIV, 1.7 million became newly infected, and 690,000 died with HIV disease ( 11 ). Compared with 2010 estimates, overall HIV incidence in 2019 decreased by 23% and mortality by 37%. However, age stratification shows that new infections have decreased by 52% among children but by only 13% among adults. With reduced mortality rates yet continued HIV incidence and population growth, the overall number of persons living with HIV was 24% greater in 2019 than in 2010.
Global summaries hide regional differences. The epicenter of the pandemic remains in East and southern Africa, which account for 54% of all HIV-infected persons and 43% of incident HIV infections and deaths ( 11 ). High prevalence of HIV-infected persons with unsuppressed viremia predicts high incidence and maintenance of community infection, an observation that applies to regions and countries, as well as specific populations such as men who have sex with men (MSM).
The next greatest HIV burden is in the Asia and Pacific region, where the population is vastly greater than that of East and southern Africa but there are 3.5 times fewer HIV-infected persons ( 11 ). Despite overall prevention progress, HIV incidence has not declined equally everywhere; little success has been seen in eastern Europe, the Middle East, and Central Asia.
Ever clearer is the global burden of HIV in key populations: MSM, transgender persons, people who inject drugs, sex workers and their clients, and incarcerated persons. In 2019, an estimated 62% of all new HIV infections were in members of those key populations ( 11 ). In 7 of the 8 UNAIDS regions, key populations accounted for 60%–99% of incident HIV infections; only in East and southern Africa, where the proportion was 28%, were new infections predominant in general populations ( 11 ).
Among high-income nations, the most heavily affected country is still the United States. In 2018, a total of 37,881 HIV infections were newly reported, with regional differences ( 12 ). In the South, the rate of new infections was more than twice that for the Midwest, where the rate was the lowest. Major disparities by race/ethnicity persist; the rate among Black/African American persons is 2 times that among Hispanic and 8 times that among White persons. Also associated with higher rates are factors indicating social deprivation and poverty, even allowing for racial and ethnic disparities. Among new HIV infections, 70% resulted from male-to-male sex. A cause for concern is potential overlap between the HIV/AIDS and opioid epidemics through increased drug injection and needle sharing, which has resulted in explosive HIV outbreaks ( 13 ).
Evolving Science and Program
In our 2011 commentary ( 2 ), we considered the following as priorities: improving use of existing interventions, defining how best to use HIV testing and antiretroviral therapy (ART) for prevention as well as treatment, continuing the quest for new knowledge and interventions, and ensuring sustainability of the global response. By and large, progress has been made on all fronts.
After the CAPRISA 004 trial of precoital and postcoital use of tenofovir gel was published in 2010 ( 14 ), the Ring ( 15 ) and Aspire ( 16 ) studies (randomized, placebo-controlled trials in South Africa) examined the protective efficacy of a self-inserted vaginal ring impregnated with slow-release dapivirine, a nonnucleoside reverse transcription inhibitor. The overall efficacy rates for reducing HIV incidence were 31% (Ring) and 27% (Aspire); many questions about overall efficacy, adherence, and differences by age remained. This collective experience provided proof of concept for woman-controlled prevention but did not provide the definitive public health solution to high HIV incidence among young women in Africa.
Four pivotal randomized trials ( 17 – 20 ) of oral preexposure prophylaxis (PrEP) with Truvada (combination of tenofovir and emtricitabine) were pivotal for international licensing of the compound. The relevant trials studied MSM, transgender women having sex with men, and at-risk heterosexual persons. A review of evidence considered another 9 studies, some of tenofovir alone, in different populations including people who inject drugs ( 21 ). The pivotal trials showed reduced HIV incidence (44%–86%) with Truvada use. However, a consistent observation has been a strong association between efficacy and adherence; PrEP is effective, but the drugs need to be taken.
Subsequent research focused on differential tissue penetration of drugs to relevant anatomic sites in men and women and on modes of drug delivery. HIV Prevention Trials Network (HPTN) studies compared the prevention efficacy of the long-acting injectable drug cabotegravir with Truvada in men and transgender women who have sex with men (study 083 [ 22 ]) and in heterosexual women (study 084 [ 23 ]). Interim results showed that cabotegravir, delivered every 8 weeks by injection, was associated with 66% lower incidence than oral Truvada in study 083 and 89% less in study 084. The long half-life of cabotegravir enables intermittent dosing, but waning drug levels over time may become subtherapeutic, thus requiring additional interventions to prevent infection and preclude development of drug resistance.
In its 2016 guidelines, the World Health Organization (WHO) recommended public health use of PrEP, as have other national and international regulatory or advisory bodies. However, the enthusiasm engendered by PreP science needs to be tempered by consideration of cost, need for rigorous adherence, rising rates of other sexually transmitted infections and thus need for continued condom use, and contraception for women. Long-acting injectables could be a major advance, but accessibility and logistics for their delivery need to be considered.
Mathematical modeling and ecologic studies suggested that greatly increased delivery of ART could reduce HIV transmission at the community level. The definitive study showing that ART provided prevention benefits was the landmark HPTN 052 study ( 24 ), published in interim form in 2011. This trial among discordant couples found a 96% reduction in HIV transmission among those who started ART early versus those for whom it was deferred. Combined with an influential modeling study ( 25 ) that suggested that regular HIV testing and immediate use of ART could suppress and perhaps ultimately eliminate HIV transmission, the results of HPTN 052 led to studies in East and southern Africa of the so-called test and treat intervention ( 26 – 29 ). These studies were community randomized evaluations of widespread HIV testing and immediate ART compared with standard care; the primary endpoint was HIV incidence. These large, expensive implementation science studies yielded rich information but did not lead to local HIV elimination. Of the 4 studies, 2 showed no significant incidence reduction and the other 2 showed 20%–30% reduction.
One of the reasons for the unexpectedly modest differences in HIV incidence between intervention and control communities in the test and treat study was changing global practice with regard to when to start ART. In 2015, results of the START ( 30 ) and TEMPRANO ( 31 ) trials showed unequivocally that immediate ART, irrespective of CD4+ lymphocyte count, resulted in reduced HIV-associated disease and death, ending more than 2 decades of argument about when to start treatment. WHO rapidly changed global recommendations to immediately start ART, one result of which was erosion of differences between intervention and control communities in the test and treat trials.
Although test and treat did not reduce HIV incidence to the extent hoped for, the accumulated evidence supports the notion of early, universal ART for extending the lives of HIV-positive persons as well as reducing the prevalence of unsuppressed viremia, the driver of HIV transmission. Large observational studies ( 32 ) showed that persons with suppressed viremia do not transmit the virus sexually, leading to the slogan “U = U”—undetectable equals untransmittable. This experience provides a much more compelling argument for active HIV case finding through increased HIV testing and partner notification, to enhance individual and public health through early treatment.
Although none of the approaches described provides a unique solution, the combination of widespread HIV testing, early ART for those infected, and PrEP for those at risk offers opportunity for substantially limiting the epidemic. Such approaches have been associated with reductions in new HIV infections among MSM in London, UK ( 33 ), and in New South Wales, Australia ( 34 ). In the United States, these advances—testing, case finding including through partner notification, universal treatment, PrEP, and rapid molecular investigation of clusters for service provision—have been incorporated into a revised national strategy for HIV elimination ( 35 ).
Progress toward an HIV vaccine remains discouraging. The only report of protective efficacy, published in 2009, has been the RV-144 study in Thailand ( 36 ), which investigated use of a recombinant canarypox vector vaccine (ALVAC-HIV) delivered in 4 monthly priming injections followed by a recombinant glycoprotein 120 subunit vaccine (AIDSVAX B/E) given in 2 additional injections. Reported efficacy was 26%–31%, but statistical and technical interpretation of these results was controversial ( 37 ). In 2016, the HVTN 702 study was launched in South Africa and used the same product as in the Thailand trial but modified for the dominant subtype C. After interim analysis, the study was halted for futility in early 2020 ( 38 ). Other efficacy studies of vaccines based on so-called mosaic immunogens from diverse HIV subtypes are in progress.
There has been great interest in broadly neutralizing antibodies to HIV, which some infected persons produce naturally and which might protect against a wide variety of strains. Two international trials of infusions with a broadly neutralizing antibody, VRC01, every 8 weeks showed relative protection against sensitive strains but no significantly reduced HIV incidence overall ( 39 ).
In 2014, UNAIDS launched its 90:90:90 initiative, aiming for 90% of persons with HIV infection to be diagnosed, 90% of those with an HIV diagnosis to receive ART, and 90% of those receiving treatment to show viral suppression by 2020. Globally, the respective proportions in 2019 were 81%, 82%, and 88%, so that an estimated 59% of persons living with HIV were showing viral suppression. Initially, 90:90:90 (with a goal of these numbers being 95s by 2030) was an advocacy proposal rather than an evidence-based initiative, but these targets have become adopted as policy promising “epidemic control,” itself a concept requiring precise definition ( 40 ).
ART scale-up, increased male circumcision, and prevention of mother-to-child transmission have all contributed to encouraging advances in the most heavily affected regions of Africa ( 11 , 41 , 42 ). Successful program implementation and declines in new HIV infections and deaths, combined with scientific progress, have led to a certain complacency that “AIDS is over.” Former US Secretary of State Hillary Clinton and staff promoted the idea that current tools could abruptly halt the epidemic. We largely agree with the 2018 judgment of the International AIDS Society–Lancet Commission on AIDS: “The HIV/AIDS community made a serious error by pursuing ‘the end of AIDS’ message” ( 43 ). Key populations, hiding in obscurity as well as in plain sight, will probably remain as reservoirs, even with highly performing programs. Experience in East and southern Africa has highlighted the challenge of adequate service provision to youth and men. Stigma and discrimination remain barriers in many parts of the world, and lack of an HIV cure (a priority research area) and vaccine remain scientific obstacles ( 44 ).
Evolving Global Health
The HIV/AIDS pandemic has evolved in parallel with other global health events that necessarily influence how HIV/AIDS is perceived and prioritized. In a 2012 paper, author K.D.C. suggested that global health trends could best be analyzed through the lenses of development, public health, and health security ( 45 ). The fourth decade of AIDS started in the aftermath of the global financial crisis and the influenza (H1N1) pandemic and is finishing amid the coronavirus disease (COVID-19) pandemic. Although substantial progress has been made toward reducing maternal deaths, improving child survival rates, and scaling up programs for HIV/AIDS, malaria, and tuberculosis, the past decade has seen major disease outbreaks and a consequent focus on health security. Because of its sociodemographic effects, AIDS was portrayed as a security issue in United Nations discussions early in this century. With massive scale-up of treatment and prevention, HIV/AIDS is now perceived as another public health priority rather than a security emergency.
In 2014, Ebola was reported in Guinea, Liberia, and Sierra Leone, far west of previously recognized outbreaks. The epidemic lasted until mid-2016 and ultimately resulted in 28,646 reported cases and 11,323 deaths ( 46 ). Infections were exported to 3 other countries in Africa, several countries in Europe, and the United States. This health crisis resulted in widespread fear of possible global spread, unparalleled global mobilization of emergency health assistance including use of armed forces of the different high-income countries, and political involvement at the highest levels of governments and the United Nations. Subsequent outbreaks of Ebola have occurred in Uganda and the Democratic Republic of the Congo (DRC), including a large epidemic in conflict-ridden eastern DRC in 2018–2020 that resulted in 3,481 reported cases and 2,299 deaths ( 47 ). Underemphasized aspects of these Ebola epidemics were that cases over the past 6 years represent more than 90% of all cases reported cumulatively since recognition of Ebola in 1976; that vast geographic distances were involved; and that these outbreaks were largely urban, sometimes involving capital and other major cities. Ebola epidemiology has changed from that of an exotic, remote infection in Africa to one capable of causing extensive urban outbreaks threatening global health ( 48 ). Also of note was that field research conducted during the outbreaks under the most difficult conditions showed efficacy of a vaccine and therapeutics, both now considered the standard of care for Ebola ( 49 , 50 ).
Over the past decade, arboviral epidemic activity has been diverse. The epidemics of yellow fever in Angola and the DRC in 2015–2016 were the world’s largest over the past 30 years. A total of 965 cases and 400 deaths were reported, but true numbers were far greater. Over 30 million persons were vaccinated, and shortage of yellow fever vaccine required healthcare providers to resort to the untested practice of fractionating vaccine doses ( 51 ). Huge epidemics of chikungunya and dengue occurred internationally; virus was transmitted to areas previously considered at low risk, such as Europe ( 52 ). In 2015, the Zika epidemic raised global concern when infection with this virus was shown to be associated with microcephaly in infants and with Guillain-Barré syndrome and to be sexually transmissible. The outbreak resulted in at least 3,700 cases of birth defects in the Americas ( 53 ).
In 2005, after the outbreak of severe acute respiratory syndrome (SARS), WHO revised its International Health Regulations ( 54 ). A key change was authority to declare a Public Health Emergency of International Concern, a health emergency that could result in international spread or required coordinated action. WHO has implemented this authority only 6 times, 5 of them during the fourth decade of AIDS: for polio (2014), Ebola (2014 and 2019), Zika (2015), and COVID-19 (2019).
Related to health security are the interrelated challenges of global warming, demographic change, and migration. Climate change affects social and environmental determinants of health, such as access to clean air, water, shelter, and arable lands, but also exerts direct health effects. The United Nations High Commissioner for Refugees characterized 2010–2019 as “a decade of displacement,” during which 100 million persons were forced to flee their homes, many because of conflict such as that in the Middle East. During 2014–2020, some 20,000 migrants crossing the Mediterranean Sea to Europe drowned, and another 12,000 or more were unaccounted for.
Broad themes that have dominated global health discourse include the transition from the era of the Millennium Development Goals (MDGs; 2000–2015) to that of the broader Sustainable Development Goals (SDGs; 2015–2030) ( 55 ) and the issue of universal health coverage. Other disease-specific programs require continued support, such as the unfinished efforts to eradicate polio and Guinea worm disease. The MDGs had 3 specific health goals relating to child survival; maternal health; and HIV/AIDS, tuberculosis, and malaria. Only 1 of the 17 SDGs is devoted to health, SDG3, which has 13 targets and 28 indicators. Specifically, SDG3 calls for: “By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.” Another target and WHO priority is provision of universal health coverage, global access to decent healthcare, and protection against penury from out-of-pocket health expenditures. HIV/AIDS exists in a crowded and complex global health space.
Preparing for the Fifth Decade of AIDS
As the world emerged from the financial crisis a decade ago, there was concern that HIV/AIDS funding might be constrained. Development assistance for health reached $40.6 billion in 2019, an increase of 15% over the amount in 2010 ( 56 ). Approximately half of this assistance goes to HIV/AIDS, especially for treatment, and to newborn, maternal, and child health. Thus, although health security has eclipsed health development and global public health in this fourth decade of AIDS, financial commitments have been largely maintained.
The overall annual spending on HIV/AIDS by low- and middle-income countries is ≈$20.2 billion, of which ≈$9.5 billion represents donor funding. UNAIDS consistently communicates that to meet SDG targets, overall spending on HIV/AIDS needs to increase by ≈40%. Nonetheless, this HIV-specific spending is privileged compared with funding for other high-impact diseases in low-income settings, such as malaria and tuberculosis. AIDS is no longer among the 10 leading causes of death globally and is now widely viewed as a medically manageable disease. HIV/AIDS prioritization and funding may be justified by the youthful groups affected and its lifelong nature, but this view may be increasingly challenged. Expecting the United States to pay indefinitely for most of the world’s HIV/AIDS response is unrealistic. The end of the SDG era in 2030 will probably come with reappraisal of global commitments, including those for global health funding, disease-specific focus, and maintenance of single-disease organizations such as UNAIDS. Over the coming years, HIV/AIDS programs need to show good fiscal management and epidemiologic results, and affected countries need to shoulder an increased share of their disease burdens.
Lessons from HIV/AIDS and Other Epidemics
The most dramatic epidemics in recent time (COVID-19 [ 57 ], Ebola, and HIV/AIDS) involve quite different biological agents and challenges yet also raise common themes and questions. Especially needed are global responses to challenges that transcend national borders. Pathogen emergence is enhanced by globalization, but globalized systems are needed to address an interconnected worldwide emergency. The slogan “no one is safe until everyone is safe” has been heard in relation to COVID-19, but it was said years ago about HIV. And global health needs global funding.
Individual leaders and organizations have performed valiant work on COVID-19, yet countries have isolated themselves in all senses, resulting in global fragmentation. Major powers look inward yet are reluctant to cede space, and the influence of multilateral agencies is limited. WHO was heavily criticized after the Ebola epidemic in West Africa but is constrained by restricted authority, inadequate funding, and unrealistic expectations from member states. Repeated calls for WHO reform are unclear about what is really wanted.
Honesty is required concerning preparedness and surveillance. The Ebola epidemic in West Africa became as severe as it did because the 3 affected countries had been neglected for years and had no functioning surveillance and public health infrastructure. We cannot say that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was completely unexpected; the literature on pandemic threats is voluminous. SARS in 2002–2003 was severe but not widespread; the 2009 influenza (H1N1) pandemic was widespread but not severe. It is hubristic to assume that pathogen severity and spread would always segregate, yet we were not prepared. Preparedness metrics can give false reassurance, witnessed by the lamentable response to COVID-19 in the United States in 2020. “Never again” was the mood after the Ebola epidemic in West Africa, but preparedness just seems too hard and costly. Perhaps true preparedness exists only in the military, where personnel train continuously for wars they hope will never happen.
As a result of technologic advances such as whole-genome sequencing, scientific progress on COVID-19 has been breathtakingly rapid compared with early laboratory research on HIV. We hope to not see a replay of the early history of ART, with scientific advances relating to COVID-19, and specifically vaccines, not being rapidly or equitably accessible everywhere. “Vaccine nationalism” is a new term raising the specter of lower risk groups in high-income countries receiving vaccine before, for example, frontline healthcare workers in low-income settings. Healthcare workers have been disproportionately affected by Ebola and COVID-19, highlighting the need for much greater investment in infection prevention and control in healthcare settings worldwide. Attention and innovation are required to ensure maintenance of HIV and other essential public health services amid other outbreaks such as COVID-19.
Although initially slow, the HIV/AIDS response over the years has been a beacon in global health for respect for individuals and their rights and for health equity. More reflection is required with regard to what the responses to HIV and Ebola have taught us and how they might be relevant to COVID-19 and other future epidemics.
Conclusions
Although great need remains, the past decade has seen scientific and programmatic successes with regard to the HIV/AIDS priorities we defined after 30 years of AIDS. Existing interventions have been scaled up, and new tools such as PrEP and long-lasting drug preparations have been introduced. The roles of HIV testing and ART for treatment and prevention have been clarified, and the need for immediate ART for all HIV-infected persons has been proven. The global HIV/AIDS response has been sustained, financing has been maintained, and the world has kept focus on the SDGs. Mann’s judgment that “we did not separate ourselves” remains justified. We must also accept that political promises of “the end of AIDS” were hyperbole that current epidemiology does not support.
The COVID-19 pandemic has exploited the fault lines of global systems and existing inequalities in a way that HIV did early on. Regrettably, the solidarity that HIV/AIDS engendered has not yet been carried over. In retrospect, the recent epidemics of Ebola in West Africa and DRC were preparation for the COVID-19 pandemic, but follow-through was lacking. The fifth decade of AIDS will take us to the SDG target date and reassessment of global health and development priorities. HIV/AIDS may not be central to global health discourse as it was earlier, but it will remain a yardstick by which to judge commitment and efforts, including, and especially in relation to, health security.
On February 7, 2021, the Ministry of Health of DRC reported a laboratory-confirmed case of Ebola in North Kivu Province, the most heavily affected province during the 2018–2020 outbreak in eastern Congo. The case-patient experienced symptom onset on January 25, 2021, and died in Butembo, a city of ≈1 million persons, on February 4, 2021. She was reportedly linked epidemiologically to an Ebola survivor, and genetic sequencing reportedly showed phylogenetic association with the earlier outbreak rather than a new spillover event. As of February 8, 2021, a total of 118 contacts were being investigated ( https://www.who.int/emergencies/diseases/ebola/ebola-2021-north-kivu , https://www.who.int/csr/don/10-february-2021-ebola-drc/en ).
Separately, on February 14, 2021, the Ministry of Health of the Republic of Guinea reported an outbreak of Ebola in the subprefecture of Gouécké, Nzérékoré Region, the first report of Ebola in Guinea since the 2014–2016 epidemic. The index case-patient, a nurse, experienced symptoms on January 18, 2021, and died on January 28, 2021. A total of 6 secondary Ebola cases were reported, 1 in a traditional practitioner who cared for the index case-patient and 5 in family members attending her subsequent funeral. Of the 7 case-patients, 5 died. As of February 15, 2021, a total of 192 contacts were being investigated, including in the capital city, Conakry ( https://www.who.int/emergencies/diseases/ebola/ebola-2021-nzerekore-guinea , https://www.who.int/csr/don/17-february-2021-ebola-gin/en ).
Dr. De Cock retired from CDC in December 2020. He had previously served as founding director of Projet RETRO-CI, Abidjan, Côte d’Ivoire; director of the CDC Division of HIV/AIDS Prevention, Surveillance and Epidemiology; director of the WHO Department of HIV/AIDS; founding director of the CDC Center for Global Health; and director, CDC Kenya.
- Centers for Disease Control (CDC) . Pneumocystis pneumonia—Los Angeles. MMWR Morb Mortal Wkly Rep . 1981 ; 30 : 250 – 2 . PubMed Google Scholar
- De Cock KM , Jaffe HW , Curran JW . Reflections on 30 years of AIDS. Emerg Infect Dis . 2011 ; 17 : 1044 – 8 . DOI PubMed Google Scholar
- Centers for Disease Control and Prevention . Compendium of evidence-based interventions and best practices for HIV prevention [ cited 2021 Apr 18 ]. https://www.cdc.gov/hiv/research/interventionresearch/compendium/index.html
- Barré-Sinoussi F , Chermann J-C , Rey F , Nugeyre MT , Chamaret S , Gruest J , et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science . 1983 ; 220 : 868 – 71 . DOI PubMed Google Scholar
- Popovic M , Sarngadharan MG , Read E , Gallo RC . Detection, isolation, and continuous production of cytopathic retroviruses (HTLV-III) from patients with AIDS and pre-AIDS. Science . 1984 ; 224 : 497 – 500 . DOI PubMed Google Scholar
- Hahn BH , Shaw GM , De Cock KM , Sharp PM . AIDS as a zoonosis: scientific and public health implications. Science . 2000 ; 287 : 607 – 14 . DOI PubMed Google Scholar
- France D . How to survive a plague: the inside story of how citizens and science tamed AIDS. New York: Alfred Knopf; 2016 .
- Merson M , Inrig S . The AIDS pandemic. Searching for a global response. 2018 . Cham (Switzerland); Springer International Publishing; 2018. p. 25–113.
- Piot P . No time to lose. A life in pursuit of deadly viruses. New York: W.W. Norton & Co.; 2012 . p. 316–34.
- Fauci AS , Eisinger RW . PEPFAR—15 years and counting the lives saved. N Engl J Med . 2018 ; 378 : 314 – 6 . DOI PubMed Google Scholar
- Joint United Nations Programme on HIV/AIDS . UNAIDS data 2020 [ cited 2021 Apr 18 ]. https://www.unaids.org/sites/default/files/media_asset/2020_aids-data-book_en.pdf
- Centers for Disease Control and Prevention . HIV surveillance report, 2018 (Preliminary); vol. 30 [ cited 2021 Mar 14 ]. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- Peters PJ , Pontones P , Hoover KW , Patel MR , Galang RR , Shields J , et al. ; Indiana HIV Outbreak Investigation Team . HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med . 2016 ; 375 : 229 – 39 . DOI PubMed Google Scholar
- Abdool Karim Q , Abdool Karim SS , Frohlich JA , Grobler AC , Baxter C , Mansoor LE , et al. ; CAPRISA 004 Trial Group . Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science . 2010 ; 329 : 1168 – 74 . DOI PubMed Google Scholar
- Nel A , van Niekerk N , Kapiga S , Bekker L-G , Gama C , Gill K , et al. ; Ring Study Team . Safety and efficacy of a dapivirine vaginal ring for HIV prevention in women. N Engl J Med . 2016 ; 375 : 2133 – 43 . DOI PubMed Google Scholar
- Baeten JM , Palanee-Phillips T , Brown ER , Schwartz K , Soto-Torres LE , Govender V , et al. ; MTN-020–ASPIRE Study Team . Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med . 2016 ; 375 : 2121 – 32 . DOI PubMed Google Scholar
- Grant RM , Lama JR , Anderson PL , McMahan V , Liu AY , Vargas L , et al. ; iPrEx Study Team . Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med . 2010 ; 363 : 2587 – 99 . DOI PubMed Google Scholar
- Baeten JM , Donnell D , Ndase P , Mugo NR , Campbell JD , Wangisi J , et al. ; Partners PrEP Study Team . Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med . 2012 ; 367 : 399 – 410 . DOI PubMed Google Scholar
- McCormack S , Dunn DT , Desai M , Dolling DI , Gafos M , Gilson R , et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet . 2016 ; 387 : 53 – 60 . DOI PubMed Google Scholar
- Molina J-M , Capitant C , Spire B , Pialoux G , Cotte L , Charreau I , et al. ; ANRS IPERGAY Study Group . On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med . 2015 ; 373 : 2237 – 46 . DOI PubMed Google Scholar
- National Institute for Health and Care Excellence . Pre-exposure prophylaxis of HIV in adults at high risk: Truvada (emtricitabine/tenofovir disoproxil). Evidence summary. [ESNM78] [ cited 2021 Mar 14 ]. https://www.nice.org.uk/advice/esnm78/chapter/full-evidence-summary
- National Institutes of Health . Long-acting injectable form of HIV prevention outperforms daily pill in NIH study [ cited 2021 Apr 18 ]. https://www.nih.gov/news-events/news-releases/long-acting-injectable-form-hiv-prevention-outperforms-daily-pill-nih-study
- National Institutes of Health . NIH study finds long-acting injectable drug prevents HIV acquisition in cisgender women [ cited 2021 Apr 18 ]. https://www.nih.gov/news-events/news-releases/nih-study-finds-long-acting-injectable-drug-prevents-hiv-acquisition-cisgender-women
- Cohen MS , Chen YQ , McCauley M , Gamble T , Hosseinipour MC , Kumarasamy N , et al. ; HPTN 052 Study Team . Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med . 2011 ; 365 : 493 – 505 . DOI PubMed Google Scholar
- Granich RM , Gilks CF , Dye C , De Cock KM , Williams BG . Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet . 2009 ; 373 : 48 – 57 . DOI PubMed Google Scholar
- Iwuji CC , Orne-Gliemann J , Larmarange J , Balestre E , Thiebaut R , Tanser F , et al. ; ANRS 12249 TasP Study Group . Universal test and treat and the HIV epidemic in rural South Africa: a phase 4, open-label, community cluster randomised trial. Lancet HIV . 2018 ; 5 : e116 – 25 . DOI PubMed Google Scholar
- Havlir DV , Balzer LB , Charlebois ED , Clark TD , Kwarisiima D , Ayieko J , et al. HIV testing and treatment with the use of a community health approach in rural Africa. N Engl J Med . 2019 ; 381 : 219 – 29 . DOI PubMed Google Scholar
- Makhema J , Wirth KE , Pretorius Holme M , Gaolathe T , Mmalane M , Kadima E , et al. Universal testing, expanded treatment, and incidence of HIV infection in Botswana. N Engl J Med . 2019 ; 381 : 230 – 42 . DOI PubMed Google Scholar
- Hayes RJ , Donnell D , Floyd S , Mandla N , Bwalya J , Sabapathy K , et al. ; HPTN 071 (PopART) Study Team . HPTN 071 (PopART) Study Team. Effect of universal testing and treatment on HIV incidence—HPTN 071 (PopART). N Engl J Med . 2019 ; 381 : 207 – 18 . DOI PubMed Google Scholar
- Lundgren JD , Babiker AG , Gordin F , Emery S , Grund B , Sharma S , et al. ; INSIGHT START Study Group . Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med . 2015 ; 373 : 795 – 807 . DOI PubMed Google Scholar
- Danel C , Moh R , Gabillard D , Badje A , Le Carrou J , Ouassa T , et al. ; TEMPRANO ANRS 12136 Study Group . TEMPRANO ANRS 12136 Study Group. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med . 2015 ; 373 : 808 – 22 . DOI PubMed Google Scholar
- Rodger AJ , Cambiano V , Bruun T , Vernazza P , Collins S , van Lunzen J , et al. ; PARTNER Study Group . Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA . 2016 ; 316 : 171 – 81 . DOI PubMed Google Scholar
- Nwokolo N , Hill A , McOwan A , Pozniak A . Rapidly declining HIV infection in MSM in central London. Lancet HIV . 2017 ; 4 : e482 – 3 . DOI PubMed Google Scholar
- Grulich AE , Guy R , Amin J , Jin F , Selvey C , Holden J , et al. ; Expanded PrEP Implementation in Communities New South Wales (EPIC-NSW) research group . Population-level effectiveness of rapid, targeted, high-coverage roll-out of HIV pre-exposure prophylaxis in men who have sex with men: the EPIC-NSW prospective cohort study. Lancet HIV . 2018 ; 5 : e629 – 37 . DOI PubMed Google Scholar
- Fauci AS , Redfield RR , Sigounas G , Weahkee MD , Giroir BP . Ending the HIV epidemic: a plan for the United States. JAMA . 2019 ; 321 : 844 – 5 . DOI PubMed Google Scholar
- Rerks-Ngarm S , Pitisuttithum P , Nitayaphan S , Kaewkungwal J , Chiu J , Paris R , et al. ; MOPH-TAVEG Investigators . Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med . 2009 ; 361 : 2209 – 20 . DOI PubMed Google Scholar
- Desrosiers RC . Protection against HIV acquisition in the RV144 trial. J Virol . 2017 ; 91 : e00905 – 17 . DOI PubMed Google Scholar
- National Institutes of Health . Experimental HIV vaccine regimen ineffective in preventing HIV [ cited 2021 Apr 18 ]. https://www.niaid.nih.gov/news-events/experimental-hiv-vaccine-regimen-ineffective-preventing-hiv
- National Institutes of Health . Antibody infusions prevent acquisition of some HIV strains, NIH studies find [ cited 2021 Apr 18 ]. https://www.niaid.nih.gov/news-events/antibody-infusions-prevent-acquisition-some-hiv-strains-nih-studies-find
- Ghys PD , Williams BG , Over M , Hallett TB , Godfrey-Faussett P . Epidemiological metrics and benchmarks for a transition in the HIV epidemic. PLoS Med . 2018 ; 15 : e1002678 . DOI PubMed Google Scholar
- Grabowski MK , Serwadda DM , Gray RH , Nakigozi G , Kigozi G , Kagaayi J , et al. ; Rakai Health Sciences Program . HIV prevention efforts and incidence of HIV in Uganda. N Engl J Med . 2017 ; 377 : 2154 – 66 . DOI PubMed Google Scholar
- Borgdorff MW , Kwaro D , Obor D , Otieno G , Kamire V , Odongo F , et al. HIV incidence in western Kenya during scale-up of antiretroviral therapy and voluntary medical male circumcision: a population-based cohort analysis. Lancet HIV . 2018 ; 5 : e241 – 9 . DOI PubMed Google Scholar
- Das P , Horton R . Beyond the silos: integrating HIV and global health. Lancet . 2018 ; 392 : 260 – 1 . DOI PubMed Google Scholar
- Eisinger RW , Fauci AS . Ending the HIV/AIDS Pandemic. Emerg Infect Dis . 2018 ; 24 : 413 – 6 . DOI PubMed Google Scholar
- De Cock KM , Simone PM , Davison V , Slutsker L . The new global health. Emerg Infect Dis . 2013 ; 19 : 1192 – 7 . DOI PubMed Google Scholar
- Lo TQ , Marston BJ , Dahl BA , De Cock KM . Ebola: Anatomy of an Epidemic. Annu Rev Med . 2017 ; 68 : 359 – 70 . DOI PubMed Google Scholar
- World Health Organization . Ending an Ebola outbreak in a conflict zone [ cited 2021 Apr 18 ]. https://storymaps.arcgis.com/stories/813561c780d44af38c57730418cd96cd
- Arwady MA , Bawo L , Hunter JC , Massaquoi M , Matanock A , Dahn B , et al. Evolution of ebola virus disease from exotic infection to global health priority, Liberia, mid-2014. Emerg Infect Dis . 2015 ; 21 : 578 – 84 . DOI PubMed Google Scholar
- Mulangu S , Dodd LE , Davey RT Jr , Tshiani Mbaya O , Proschan M , Mukadi D , et al. ; PALM Writing Group ; PALM Consortium Study Team . PALM Consortium Study Team. A randomized, controlled trial of Ebola virus disease therapeutics. N Engl J Med . 2019 ; 381 : 2293 – 303 . DOI PubMed Google Scholar
- Henao-Restrepo AM , Camacho A , Longini IM , Watson CH , Edmunds WJ , Egger M , et al. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet . 2017 ; 389 : 505 – 18 . DOI PubMed Google Scholar
- World Health Organization . Yellow fever outbreak Angola, Democratic Republic of the Congo and Uganda 2016–2017 [ cited 2021 Mar 14 ]. https://www.who.int/emergencies/yellow-fever/en
- Paixão ES , Teixeira MG , Rodrigues LC . Zika, chikungunya and dengue: the causes and threats of new and re-emerging arboviral diseases. BMJ Glob Health . 2018 ; 3 ( Suppl 1 ): e000530 . DOI PubMed Google Scholar
- Musso D , Ko AI , Baud D . Zika virus infection—after the pandemic. N Engl J Med . 2019 ; 381 : 1444 – 57 . DOI PubMed Google Scholar
- World Health Organization . International Health Regulations (2005). 2nd ed. Geneva: The Organization; 2008 .
- United Nations . The 17 goals [ cited 2021 Apr 18 ]. https://sdgs.un.org/goals
- Institute for Health Metrics and Evaluation . Financing global health 2019 . Tracking health spending in a time of crisis [ cited 2021 Mar 14 ]. http://www.healthdata.org/policy-report/financing-global-health-2019-tracking-health-spending-time-crisis
- World Health Organization . Weekly epidemiological update on COVID-19—13 April 2021 [ cited 2021 Apr 27 ]. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---13-april-2021
DOI: 10.3201/eid2706.210284
Original Publication Date: April 29, 2021
Table of Contents – Volume 27, Number 6—June 2021
| EID Search Options |
|---|
| – Search articles by author and/or keyword. |
| – Search articles by the topic country. |
| – Search articles by article type and issue. |
Please use the form below to submit correspondence to the authors or contact them at the following address:
Kevin M. De Cock, c/o Miriam McNally, 669 Palmetto Ave, Suites H–I, Chico, CA 95926, USA, and PO Box 25705-00603, Lavington, Nairobi, Kenya
Comment submitted successfully, thank you for your feedback.
There was an unexpected error. Message not sent.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Article Citations
Highlight and copy the desired format.
| EID | De Cock KM, Jaffe HW, Curran JW. Reflections on 40 Years of AIDS. Emerg Infect Dis. 2021;27(6):1553-1560. https://doi.org/10.3201/eid2706.210284 |
|---|---|
| AMA | De Cock KM, Jaffe HW, Curran JW. Reflections on 40 Years of AIDS. . 2021;27(6):1553-1560. doi:10.3201/eid2706.210284. |
| APA | De Cock, K. M., Jaffe, H. W., & Curran, J. W. (2021). Reflections on 40 Years of AIDS. , (6), 1553-1560. https://doi.org/10.3201/eid2706.210284. |
Metric Details
Article views: 9267.
Data is collected weekly and does not include downloads and attachments. View data is from .
What is the Altmetric Attention Score?
The Altmetric Attention Score for a research output provides an indicator of the amount of attention that it has received. The score is derived from an automated algorithm, and represents a weighted count of the amount of attention Altmetric picked up for a research output.
- What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medicine as Prescribed
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Nutrition and People with HIV
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- Ready, Set, PrEP Resources
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 27
- National African Immigrant and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
NIH HIV Research – Highlights at AIDS 2022
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
Cross-posted from NIH Office of AIDS Research, Director’s Corner

The 24th International AIDS Conference (AIDS 2022), held July 29 to August 2 in Montreal, Canada, and online, brought together researchers, policymakers, health practitioners, civil society leaders, advocates, and other partners working to end the HIV/AIDS pandemic. This conference marked the first time that the international HIV research and advocacy communities have gathered in person since 2019.
The conference had a significant global presence in concert with strong representation from the U.S. government, including the White House Office of National AIDS Policy (ONAP), the U.S. Department of Health and Human Services (HHS) Office of Infectious Disease and HIV/AIDS Policy (OIDP), the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), and the National Institutes of Health (NIH). Federal officials shared progress in the Ending the HIV Epidemic in the U.S. (EHE) initiative and implementation of the National HIV/AIDS Strategy .
NIH at AIDS 2022
NIH-sponsored HIV/AIDS research was an integral aspect of formal presentations and informal discussions throughout the conference. More than 100 presentations highlighted NIH-funded research fueling advances in implementation science, HIV-related stigma and discrimination, cure, vaccine development, and more.
Examples of sessions involving NIH staff include:
- A workshop Exit Disclaimer , organized by National Institute of Mental Health (NIMH) staff, on advancing HIV health communication science to improve messaging among key populations, with remarks by NIH OAR staff;
- A satellite session, co-organized by NIMH and NIH OAR staff, to launch a special issue of the American Journal of Public Health Exit Disclaimer highlighting innovative theory and research on HIV-related intersectional stigma and discrimination;
- A satellite session on implementation science tied to a special issue of the Journal of Acquired Immune Deficiency Syndromes Exit Disclaimer ;
- A satellite session, organized by NIMH, on the role of behavioral economics and conditional incentives in strengthening HIV treatment and prevention;
- A workshop on infants, children, and adolescents with perinatal HIV exposure, moderated by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD);
- A session on current approaches to HIV vaccine and cure research, co-moderated by the National Institute of Allergy and Infectious Diseases (NIAID); and
- A satellite session on ethical considerations and community engagement for experimental medicine trials in Africa, with a panelist from NIAID.
Anthony S. Fauci, M.D., Director of NIAID, delivered a plenary address, where he discussed approaches for HIV cure and vaccine research. In comments to HIV.gov , Dr. Fauci charted the history Exit Disclaimer of HIV vaccine development efforts, pointing out the difficulty in eradicating the virus from reservoirs even after the virus has been suppressed to undetectable levels.
The NIH OAR, as the coordinator of the NIH HIV/AIDS research program, collaborated with colleagues across the NIH to collect highlights during the conference that may inform the NIH HIV/AIDS research agenda. Scientists from eight NIH Institutes, Centers, and Offices (ICOs) shared insights from conference sessions on topics such as innovations in diagnostics, prevention, and treatment; community engagement; and inclusion of all people affected by HIV when implementing programs. 1
Community Engagement and Global Learning
AIDS 2022 underscored the value of NIH-sponsored HIV/AIDS research and its overall impact on public health for those with, or affected by, HIV. Central to this discussion was the importance of community engagement in HIV prevention and treatment. Recent research has led to breakthroughs in HIV testing, prevention, and treatment; however, these innovations must be tailored to meet the needs of diverse communities affected by HIV. Among other venues and opportunities, this was especially highlighted during my tour through the AIDS 2022 Global Village Exit Disclaimer .
The focus on community engagement and global learning was underscored by a site visit to two co-located community-based HIV clinics in Montreal. ONAP coordinated the visit for the U.S. delegation, which was led by Admiral Rachel L. Levine, M.D., HHS Assistant Secretary for Health. The clinics demonstrated how community engagement can remove barriers to HIV services. Their innovative models leverage technology to enable clients to complete screenings and schedule appointments online, self-test on-site, and learn results via telehealth appointments. These innovations, along with flexible hours and a status-neutral model that provides HIV and STI testing, prevention, and treatment services all in one place, make it more convenient for clients to access interventions. As ONAP Director Harold Phillips said in our joint interview with HIV.gov Exit Disclaimer , “The clinic was really patient- and person-centered. … I would love to see that kind of ease and access to STI testing in the United States.”
AIDS 2022 presented opportunities to learn from other countries that have reached HIV/AIDS epidemic control. While the United States has not yet achieved this goal, at least 20 countries have done so or have met the 90-90-90 HIV treatment targets, in part through PEPFAR support. 2 PEPFAR successes in HIV service delivery and programs that meet the needs of diverse communities abroad can inform research and public health efforts in the United States. In an HIV.gov interview Exit Disclaimer I gave with Ambassador John Nkengasong, Ph.D., the U.S. Global AIDS Coordinator, we stressed the importance of research in making these success stories possible and the critical need for more research in the areas of behavioral and social science, implementation science, and communication science.
Prominent Discussions About U=U, PrEP, Vaccine, and Cure
Other AIDS 2022 highlights spanned health communication science and advances in HIV prevention, testing, and vaccine research, including:
- The health communication campaign U=U, which promotes the message that undetectable is untransmittable;
- The applicability of lessons from HIV in responses to COVID-19 and monkeypox, including pandemic preparedness, surveillance and contact tracking, program implementation, and the need to address stigma and discrimination;
- Efforts to ensure equitable access to pre-exposure prophylaxis (PrEP), both within the United States and globally, as well as advances in PrEP formulations and implementation;
- Advances in diagnostics, such as multiplex technologies that test for both HIV and other infections like hepatitis and STIs, as well as creative distribution, through pharmacies, vending machines, and mobile services, that facilitates private self-testing and has the potential to expand access to health care and reduce stigma;
- Vaccine development, including the acceleration of early Phase 1 trials of candidates using mRNA technology, compared with previously tested platforms;
- Vaccine candidates that produce broadly neutralizing antibodies (bNAbs), which can combat a wide range of genetic variants of HIV hidden within the body, driving research toward a potential cure; and
- HIV management throughout the lifespan, with presentations on pediatrics, adolescence, pregnancy and breastfeeding, and aging.
AIDS 2022 was a welcome moment for the global HIV/AIDS community to come together, in a hybrid format, to share insights and affirm the commitment to end the HIV/AIDS pandemic. To learn more about NIH participation, visit the NIH OAR website . To learn more about the conference generally, visit the AIDS 2022 website Exit Disclaimer .
1 - ICOs participating in the data call included the Fogarty International Center, the National Institute of Allergy and Infectious Diseases, the National Cancer Institute, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Mental Health, the Office of AIDS Research, and the Office of Research on Women’s Health.
2 - PEPFAR, PEPFAR 2022 Country and Regional Operational Plan (COP/ROP) Guidance for all PEPFAR-Supported Countries , January 2022.
Related HIV.gov Blogs
- AIDS 2022 International AIDS Conference 2022
- Conferences
- NIH National Institutes of Health
- OAR NIH Office of AIDS Research
- Fact sheets
Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment case
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
- HIV remains a major global public health issue, having claimed 40.4 million [32.9–51.3 million] lives so far with ongoing transmission in all countries globally; with some countries reporting increasing trends in new infections when previously on the decline.
- There were an estimated 39.0 million [33.1–45.7 million] people living with HIV at the end of 2022, two thirds of whom (25.6 million) are in the WHO African Region.
- In 2022, 630 000 [480 000–880 000] people died from HIV-related causes and 1.3 million [1.0–1.7 million] people acquired HIV.
- There is no cure for HIV infection. However, with access to effective HIV prevention, diagnosis, treatment and care, including for opportunistic infections, HIV infection has become a manageable chronic health condition, enabling people living with HIV to lead long and healthy lives.
- WHO, the Global Fund and UNAIDS all have global HIV strategies that are aligned with the SDG target 3.3 of ending the HIV epidemic by 2030.
- By 2025, 95% of all people living with HIV (PLHIV) should have a diagnosis, 95% of those should be taking lifesaving antiretroviral treatment (ART) and 95% of PLHIV on treatment should achieve a suppressed viral load for the benefit of the person’s health and for reducing onward HIV transmission. In 2022, these percentages were 86% [73–>98%], 89% 75–>98%] and 93% [79–>98%], respectively.
- When considering all people living with HIV, 86% [73–>98%] knew their status, 76% [65–89%] were receiving antiretroviral therapy and 71% [60–83%] had suppressed viral loads.
Human immunodeficiency virus (HIV) is an infection that attacks the body’s immune system. Acquired immunodeficiency syndrome (AIDS) is the most advanced stage of the disease.
HIV targets the body’s white blood cells, weakening the immune system. This makes it easier to get sick with diseases like tuberculosis, infections and some cancers.
HIV is spread from the body fluids of an infected person, including blood, breast milk, semen and vaginal fluids. It is not spread by kisses, hugs or sharing food. It can also spread from a mother to her baby.
HIV can be treated and prevented with antiretroviral therapy (ART). Untreated HIV can progress to AIDS, often after many years.
WHO now defines Advanced HIV Disease (AHD) as CD4 cell count less than 200cells/mm3 or WHO stage 3 or 4 in adults and adolescents. All children with HIV younger than 5 years of age are considered to have advanced HIV disease.
Signs and symptoms
The symptoms of HIV vary depending on the stage of infection.
The disease spreads more easily in the first few months after a person is infected, but many are unaware of their status until the later stages. In the first few weeks after being infected people may not experience symptoms. Others may have an influenza-like illness including:
- sore throat.
The infection progressively weakens the immune system. This can cause other signs and symptoms:
- swollen lymph nodes
- weight loss
Without treatment, people with HIV infection can also develop severe illnesses:
- tuberculosis (TB)
- cryptococcal meningitis
- severe bacterial infections
- cancers such as lymphomas and Kaposi's sarcoma.
HIV causes other infections to get worse, such as hepatitis C, hepatitis B and mpox.
Transmission
HIV can be transmitted via the exchange of a variety of body fluids from people living with HIV, such as blood, breast milk, semen and vaginal secretions. HIV can also be transmitted during pregnancy and delivery to the child. People cannot become infected through ordinary day-to-day contact such as kissing, hugging, shaking hands, or sharing personal objects, food or water.
It is important to note that people with HIV who are taking ART and have an undetectable viral load do not transmit HIV to their sexual partners. Early access to ART and support to remain on treatment is therefore critical not only to improve the health of people with HIV but also to prevent HIV transmission.
Risk factors
Behaviours and conditions that put people at greater risk of contracting HIV include:
- having condomless anal or vaginal sex;
- having another sexually transmitted infection (STI) such as syphilis, herpes, chlamydia, gonorrhoea and bacterial vaginosis;
- engaging in harmful use of alcohol and drugs in the context of sexual behaviour;
- sharing contaminated needles, syringes and other injecting equipment and drug solutions when injecting drugs;
- receiving unsafe injections, blood transfusions and tissue transplantation, and medical procedures that involve unsterile cutting or piercing; and
- experiencing accidental needle stick injuries, including among health workers.
HIV can be diagnosed through rapid diagnostic tests that provide same-day results. This greatly facilitates early diagnosis and linkage with treatment and prevention. People can also use HIV self-tests to test themselves. However, no single test can provide a full HIV positive diagnosis; confirmatory testing is required, conducted by a qualified and trained health or community worker at a community centre or clinic. HIV infection can be detected with great accuracy using WHO prequalified tests within a nationally approved testing strategy and algorithm.
Most widely used HIV diagnostic tests detect antibodies produced by the person as part of their immune response to fight HIV. In most cases, people develop antibodies to HIV within 28 days of infection. During this time, people are in the so-called window period when they have low levels of antibodies which cannot be detected by many rapid tests, but may transmit HIV to others. People who have had a recent high-risk exposure and test negative can have a further test after 28 days.
Following a positive diagnosis, people should be retested before they are enrolled in treatment and care to rule out any potential testing or reporting error. While testing for adolescents and adults has been made simple and efficient, this is not the case for babies born to HIV-positive mothers. For children less than 18 months of age, rapid antibody testing is not sufficient to identify HIV infection – virological testing must be provided as early as birth or at 6 weeks of age. New technologies are now available to perform this test at the point of care and enable same-day results, which will accelerate appropriate linkage with treatment and care.
HIV is a preventable disease.
Reduce the risk of HIV infection by:
- using a male or female condom during sex
- being tested for HIV and sexually transmitted infections
- having a voluntary medical male circumcision
- using harm reduction services for people who inject and use drugs.
Doctors may suggest medicines and medical devices to help prevent HIV, including:
- antiretroviral drugs (ARVs), including oral PrEP and long acting products
- dapivirine vaginal rings
- injectable long acting cabotegravir.
ARVs can also be used to prevent mothers from passing HIV to their children.
People taking antiretroviral therapy (ART) and who have no evidence of virus in the blood will not pass HIV to their sexual partners. Access to testing and ART is an important part of preventing HIV.
There is no cure for HIV infection. It is treated with antiretroviral drugs, which stop the virus from replicating in the body.
Current antiretroviral therapy (ART) does not cure HIV infection but allows a person’s immune system to get stronger. This helps them to fight other infections.
Currently, ART must be taken every day for the rest of a person’s life.
ART lowers the amount of the virus in a person’s body. This stops symptoms and allows people to live a full and healthy life. People living with HIV who are taking ART and who have no evidence of virus in the blood will not spread the virus to their sexual partners.
Pregnant women with HIV should have access to and take ART as soon as possible. This protects the health of the mother and will help prevent HIV from passing to the fetus before birth, or to the baby through breast milk.
Antiretroviral drugs given to people without HIV can prevent the disease.
When given before possible exposures to HIV it is called pre-exposure prophylaxis (PrEP) and when given after an exposure it is called post-exposure prophylaxis (PEP). People can use PrEP or PEP when the risk of contracting HIV is high; people should seek advice from a clinician when thinking about using PrEP or PEP.
Advanced HIV disease remains a persistent problem in the HIV response. WHO is supporting countries to implement the advanced HIV disease package of care to reduce illness and death. Newer HIV medicines and short course treatments for opportunistic infections like cryptococcal meningitis are being developed that may change the way people take ART and prevention medicines, including access to injectable formulations, in the future.
More information on HIV treatments
WHO response
Global health sector strategies on, respectively, HIV, viral hepatitis, and sexually transmitted infections for the period 2022–2030 (GHSSs) guide the health sector in implementing strategically focused responses to achieve the goals of ending AIDS, viral hepatitis B and C and sexually transmitted infections by 2030.
The GHSS recommend shared and disease-specific country actions supported by actions by WHO and partners. They consider the epidemiological, technological, and contextual shifts of previous years, foster learnings across the disease areas, and create opportunities to leverage innovations and new knowledge for effective responses to the diseases. They call for a precise focus to reach the people most affected and at risk for each disease that addresses inequities. They promote synergies under a universal health coverage and primary health care framework and contribute to achieving the goals of the 2030 Agenda for Sustainable Development.
Global HIV Programme
HIV country profiles
Global Health Sector Strategies on, respectively, HIV, viral hepatitis and sexually transmitted infections for the period 2022–2030 (GHSS)
- History Classics
- Your Profile
- Find History on Facebook (Opens in a new window)
- Find History on Twitter (Opens in a new window)
- Find History on YouTube (Opens in a new window)
- Find History on Instagram (Opens in a new window)
- Find History on TikTok (Opens in a new window)
- This Day In History
- History Podcasts
- History Vault
History of AIDS
By: History.com Editors
Updated: February 21, 2021 | Original: July 13, 2017

In the 1980s and early 1990s, the outbreak of HIV and AIDS swept across the United States and rest of the world, though the disease originated decades earlier. Today, more than 70 million people have been infected with HIV and about 35 million have died from AIDS since the start of the pandemic, according to the World Health Organization (WHO).
READ MORE: AIDS Crisis Timeline
What is HIV?
The human immunodeficiency virus, or HIV, is a virus that attacks the immune system, specifically CD4 cells (or T cells).
The virus is transmitted through bodily fluids such as blood, semen, vaginal fluids, anal fluids, and breast milk. Historically, HIV has most often been spread through unprotected sex, the sharing of needles for drug use, and through birth.
Over time, HIV can destroy so many CD4 cells that the body can’t fight infections and diseases, eventually leading to the most severe form of an HIV infection: acquired immunodeficiency syndrome, or AIDS. A person with AIDS is very vulnerable to cancer and to life-threatening infections, such as pneumonia.
Though there is no cure for HIV or AIDS, a person with HIV who receives treatment early can live nearly as long as someone without the virus. And a study in 2019 in the medical journal, Lancet , showed that an anti-viral treatment effectively halted the spread of HIV.
Where Did AIDS Come From?
Scientists have traced the origin of HIV back to chimpanzees and simian immunodeficiency virus (SIV), an HIV-like virus that attacks the immune system of monkeys and apes.
In 1999, researchers identified a strain of chimpanzee SIV called SIVcpz, which was nearly identical to HIV. Chimps, the scientist later discovered, hunt and eat two smaller species of monkeys—red-capped mangabeys and greater spot-nosed monkeys—that carry and infect the chimps with two strains of SIV. These two strains likely combined to form SIVcpz, which can spread between chimpanzees and humans.
SIVcpz likely jumped to humans when hunters in Africa ate infected chimps, or the chimps’ infected blood got into the cuts or wounds of hunters. Researchers believe the first transmission of SIV to HIV in humans that then led to the global pandemic occurred in 1920 in Kinshasa, the capital and largest city in the Democratic Republic of Congo.
The virus spread may have spread from Kinshasa along infrastructure routes (roads, railways, and rivers) via migrants and the sex trade.
In the 1960s, HIV spread from Africa to Haiti and the Caribbean when Haitian professionals in the colonial Democratic Republic of Congo returned home. The virus then moved from the Caribbean to New York City around 1970 and then to San Francisco later in the decade.
International travel from the United States helped the virus spread across the rest of the globe.
READ MORE: Pandemics That Changed History: A Timeline
The AIDS Epidemic Arises
Though HIV arrived in the United States around 1970, it didn’t come to the public’s attention until the early 1980s.
In 1981, the Centers for Disease Control and Prevention (CDC) published a report about five previously healthy homosexual men becoming infected with Pneumocystis pneumonia , which is caused by the normally harmless fungus Pneumocystis jirovecii. This type of pneumonia, the CDC noted, almost never affects people with uncompromised immune systems.
The following year, The New York Times published an alarming article about the new immune system disorder, which, by that time, had affected 335 people, killing 136 of them. Because the disease appeared to affect mostly homosexual men, officials initially called it gay-related immune deficiency, or GRID.
Though the CDC discovered all major routes of the disease’s transmission—as well as that female partners of AIDS-positive men could be infected—in 1983, the public considered AIDS a gay disease. It was even called the “gay plague” for many years after.
In September of 1982, the CDC used the term AIDS to describe the disease for the first time. By the end of the year, AIDS cases were also reported in a number of European countries.
READ MORE: Pandemics that Changed History

The HIV Test Arrives
In 1984, researchers finally identified the cause of AIDS—the HIV virus—and the Food and Drug Administration (FDA) licensed the first commercial blood test for HIV in 1985.
Today, numerous tests can detect HIV, most of which work by detecting HIV antibodies. The tests can be done on blood, saliva, or urine, though the blood tests detect HIV sooner after exposure due to higher levels of antibodies.
In 1985, actor Rock Hudson became the first high-profile fatality from AIDS. In fear of HIV making it into blood banks, the FDA also enacted regulations that ban gay men from donating blood. The FDA would revise its rules in 2015 to allow gay men to give blood if they’ve been celibate for a year, though blood banks routinely test blood for HIV.
By the end of 1985, there were more than 20,000 reported cases of AIDS, with at least one case in every region of the world.
AZT is Developed
In 1987, the first antiretroviral medication for HIV, azidothymidine (AZT), became available.
Numerous other medications for HIV are now available, and are typically used together in what’s known as antiretroviral therapy (ART) or highly active antiretroviral treatment (HAART).
The regimes work by preventing the virus from multiplying, giving the immune system a chance to recover and fight off infections and HIV-related cancers. The therapy also helps reduce the risk of HIV transmission, including between an infected mother and her unborn child.
The World Health Organization (WHO), in 1988, declared December 1st to be World AIDS Day. By the end of the decade, there were at least 100,000 reported cases of AIDS in the United States and WHO estimated 400,000 AIDS cases worldwide.
HIV/AIDS in the 1990s and 2000s
In 1991, the red ribbon became an international symbol of AIDS awareness.
In that year, basketball player Magic Johnson announced he had HIV, helping to further bring awareness to the issue and dispel the stereotype of it being a gay disease. Soon after, Freddie Mercury —lead singer of the band Queen—announced he had AIDS and died a day later.
In 1994, the FDA approved the first oral (and non-blood) HIV test. Two years later, it approved the first home testing kit and the first urine test.
AIDS-related deaths and hospitalizations in developed countries began to decline sharply in 1995 thanks to new medications and the introduction of HAART. Still, by 1999, AIDS was the fourth biggest cause of death in the world and the leading cause of death in Africa.

HIV Treatment Progresses
WATCH: 30 Years of AIDs Research
In 2001, generic drug manufacturers began selling discounted copies of patented HIV drugs to developing countries, leading to several major pharmaceutical manufacturers slashing prices on their HIV drugs. The following year, the Joint United Nations Programme on HIV/AIDS (UNAIDS) reported that AIDS was by far the leading cause of death in sub-Saharan Africa.
In 2009, President Barack Obama lifted a 1987 U.S. ban that prevented HIV-positive people from entering the country.
The FDA approved pre-exposure prophylaxis, or PrEP, for HIV-negative people in 2012. When taken daily, PrEP can reduce the risk of HIV from sex by more than 90 percent and from intravenous drug use by 70 percent, according to the CDC. A major study completed in 2019 showed that over 750 gay men on an anti-viral treatment did not transmit the virus to their partners. "Our findings provide conclusive evidence that the risk of HIV transmission through anal sex when HIV viral load is suppressed is effectively zero," the paper, published in Lancet, stated .
At the end of 2019, some 38 million people were living with HIV/AIDS worldwide, and 940,000 people died from AIDS-related illnesses that year, according to WHO . Sub-Saharan Africa remains the most severely affected region, accounting for nearly two-thirds of the world’s current HIV cases.
Origin of HIV and AIDS: AVERT . HIV Originated With Monkeys, Not Chimps, Study Finds: National Geographic . HIV pandemic originated in Kinshasa in the 1920s, say scientists: The Guardian . America’s HIV outbreak started in this city, 10 years before anyone noticed: PBS . HIV Testing: CDC . About HIV/AIDS: CDC . How HIV spread across the West: CNN . Obama Lifts a Ban on Entry Into U.S. by H.I.V.-Positive People: The New York Times . Global Health Observatory (GHO) data: World Health Organization .

Sign up for Inside History
Get HISTORY’s most fascinating stories delivered to your inbox three times a week.
By submitting your information, you agree to receive emails from HISTORY and A+E Networks. You can opt out at any time. You must be 16 years or older and a resident of the United States.
More details : Privacy Notice | Terms of Use | Contact Us
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 November 2021
A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data
- Shobhit Srivastava ORCID: orcid.org/0000-0002-7138-4916 1 ,
- Shekhar Chauhan ORCID: orcid.org/0000-0002-6926-7649 2 ,
- Ratna Patel ORCID: orcid.org/0000-0002-5371-7369 3 &
- Pradeep Kumar ORCID: orcid.org/0000-0003-4259-820X 1
Scientific Reports volume 11 , Article number: 22841 ( 2021 ) Cite this article
11k Accesses
8 Citations
11 Altmetric
Metrics details
- Health care
- Health services
- Public health
Acquired Immunodeficiency Syndrome caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. This study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with the change in awareness level on HIV-related information among adolescents over the period. Data used for this study were drawn from Understanding the lives of adolescents and young adults, a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh. The present study utilized a sample of 4421 and 7587 unmarried adolescent boys and girls, respectively aged 10–19 years in wave-1 and wave-2. Descriptive analysis and t-test and proportion test were done to observe changes in certain selected variables from wave-1 (2015–2016) to wave-2 (2018–2019). Moreover, random effect regression analysis was used to estimate the association of change in HIV awareness among unmarried adolescents with household and individual factors. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2 to 39.1% between wave-1 & wave-2. With the increase in age and years of schooling, the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV. Adolescent boys' paid work status was inversely associated with HIV awareness [Coef: − 0.01; p < 0.10]. Use of internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness with reference to their counterparts. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups, as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents.
Similar content being viewed by others

Investigating child sexual abuse material availability, searches, and users on the anonymous Tor network for a public health intervention strategy

Long COVID: major findings, mechanisms and recommendations
Psychiatric adverse events following COVID-19 vaccination: a population-based cohort study in Seoul, South Korea
Introduction.
Acquired Immunodeficiency Syndrome (AIDS) caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. So far, HIV has claimed almost 33 million lives; however, off lately, increasing access to HIV prevention, diagnosis, treatment, and care has enabled people living with HIV to lead a long and healthy life 1 . By the end of 2019, an estimated 38 million people were living with HIV 1 . More so, new infections fell by 39 percent, and HIV-related deaths fell by almost 51 percent between 2000 and 2019 1 . Despite all the positive news related to HIV, the success story is not the same everywhere; HIV varies between region, country, and population, where not everyone is able to access HIV testing and treatment and care 1 . HIV/AIDS holds back economic growth by destroying human capital by predominantly affecting adolescents and young adults 2 .
There are nearly 1.2 billion adolescents (10–19 years) worldwide, which constitute 18 percent of the world’s population, and in some countries, adolescents make up as much as one-fourth of the population 3 . In India, adolescents comprise more than one-fifth (21.8%) of the total population 4 . Despite a decline projection for the adolescent population in India 5 , there is a critical need to hold adolescents as adolescence is characterized as a period when peer victimization/pressure on psychosocial development is noteworthy 6 . Peer victimization/pressure is further linked to risky sexual behaviours among adolescents 7 , 8 . A higher proportion of low literacy in the Indian population leads to a low level of awareness of HIV/AIDS 9 . Furthermore, the awareness of HIV among adolescents is quite alarming 10 , 11 , 12 .
Unfortunately, there is a shortage of evidence on what predicts awareness of HIV among adolescents. Almost all the research in India is based on beliefs, attitudes, and awareness of HIV among adolescents 2 , 12 . However, few other studies worldwide have examined mass media as a strong predictor of HIV awareness among adolescents 13 . Mass media is an effective channel to increase an individuals’ knowledge about sexual health and improve understanding of facilities related to HIV prevention 14 , 15 . Various studies have outlined other factors associated with the increasing awareness of HIV among adolescents, including; age 16 , 17 , 18 , occupation 18 , education 16 , 17 , 18 , 19 , sex 16 , place of residence 16 , marital status 16 , and household wealth index 16 .
Several community-based studies have examined awareness of HIV among Indian adolescents 2 , 10 , 12 , 20 , 21 , 22 . However, studies investigating awareness of HIV among adolescents in a larger sample size remained elusive to date, courtesy of the unavailability of relevant data. Furthermore, no study in India had ever examined awareness of HIV among adolescents utilizing information on longitudinal data. To the author’s best knowledge, this is the first study in the Indian context with a large sample size that examines awareness of HIV among adolescents and combines information from a longitudinal survey. Therefore, this study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with a change in awareness level on HIV-related information among adolescents over the period.
Data and methods
Data used for this study were drawn from Understanding the lives of adolescents and young adults (UDAYA), a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh 23 . The first wave was conducted in 2015–2016, and the follow-up survey was conducted after three years in 2018–2019 23 . The survey provides the estimates for state and the sample of unmarried boys and girls aged 10–19 and married girls aged 15–19. The study adopted a systematic, multi-stage stratified sampling design to draw sample areas independently for rural and urban areas. 150 primary sampling units (PSUs)—villages in rural areas and census wards in urban areas—were selected in each state, using the 2011 census list of villages and wards as the sampling frame. In each primary sampling unit (PSU), households to be interviewed were selected by systematic sampling. More details about the study design and sampling procedure have been published elsewhere 23 . Written consent was obtained from the respondents in both waves. In wave 1 (2015–2016), 20,594 adolescents were interviewed using the structured questionnaire with a response rate of 92%.
Moreover, in wave 2 (2018–2019), the study interviewed the participants who were successfully interviewed in 2015–2016 and who consented to be re-interviewed 23 . Of the 20,594 eligible for the re-interview, the survey re-interviewed 4567 boys and 12,251 girls (married and unmarried). After excluding the respondents who gave an inconsistent response to age and education at the follow-up survey (3%), the final follow-up sample covered 4428 boys and 11,864 girls with the follow-up rate of 74% for boys and 81% for girls. The effective sample size for the present study was 4421 unmarried adolescent boys aged 10–19 years in wave-1 and wave-2. Additionally, 7587 unmarried adolescent girls aged 10–19 years were interviewed in wave-1 and wave-2 23 . The cases whose follow-up was lost were excluded from the sample to strongly balance the dataset and set it for longitudinal analysis using xtset command in STATA 15. The survey questionnaire is available at https://dataverse.harvard.edu/file.xhtml?fileId=4163718&version=2.0 & https://dataverse.harvard.edu/file.xhtml?fileId=4163720&version=2.0 .
Outcome variable
HIV awareness was the outcome variable for this study, which is dichotomous. The question was asked to the adolescents ‘Have you heard of HIV/AIDS?’ The response was recorded as yes and no.
Exposure variables
The predictors for this study were selected based on previous literature. These were age (10–19 years at wave 1, continuous variable), schooling (continuous), any mass media exposure (no and yes), paid work in the last 12 months (no and yes), internet use (no and yes), wealth index (poorest, poorer, middle, richer, and richest), religion (Hindu and Non-Hindu), caste (Scheduled Caste/Scheduled Tribe, Other Backward Class, and others), place of residence (urban and rural), and states (Uttar Pradesh and Bihar).
Exposure to mass media (how often they read newspapers, listened to the radio, and watched television; responses on the frequencies were: almost every day, at least once a week, at least once a month, rarely or not at all; adolescents were considered to have any exposure to mass media if they had exposure to any of these sources and as having no exposure if they responded with ‘not at all’ for all three sources of media) 24 . Household wealth index based on ownership of selected durable goods and amenities with possible scores ranging from 0 to 57; households were then divided into quintiles, with the first quintile representing households of the poorest wealth status and the fifth quintile representing households with the wealthiest status 25 .
Statistical analysis
Descriptive analysis was done to observe the characteristics of unmarried adolescent boys and girls at wave-1 (2015–2016). In addition, the changes in certain selected variables were observed from wave-1 (2015–2016) to wave-2 (2018–2019), and the significance was tested using t-test and proportion test 26 , 27 . Moreover, random effect regression analysis 28 , 29 was used to estimate the association of change in HIV awareness among unmarried adolescents with household factors and individual factors. The random effect model has a specific benefit for the present paper's analysis: its ability to estimate the effect of any variable that does not vary within clusters, which holds for household variables, e.g., wealth status, which is assumed to be constant for wave-1 and wave-2 30 .
Table 1 represents the socio-economic profile of adolescent boys and girls. The estimates are from the baseline dataset, and it was assumed that none of the household characteristics changed over time among adolescent boys and girls.
Figure 1 represents the change in HIV awareness among adolescent boys and girls. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2% in wave-1 to 39.1% in wave-2.
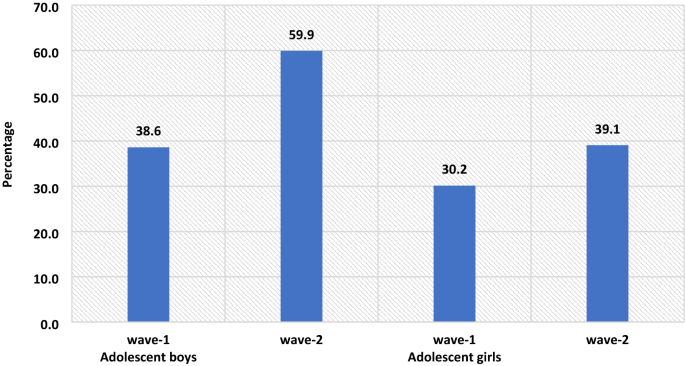
The percenate of HIV awareness among adolescent boys and girls, wave-1 (2015–2016) and wave-2 (2018–2019).
Table 2 represents the summary statistics for explanatory variables used in the analysis of UDAYA wave-1 and wave-2. The exposure to mass media is almost universal for adolescent boys, while for adolescent girls, it increases to 93% in wave-2 from 89.8% in wave-1. About 35.3% of adolescent boys were engaged in paid work during wave-1, whereas in wave-II, the share dropped to 33.5%, while in the case of adolescent girls, the estimates are almost unchanged. In wave-1, about 27.8% of adolescent boys were using the internet, while in wave-2, there is a steep increase of nearly 46.2%. Similarly, in adolescent girls, the use of the internet increased from 7.6% in wave-1 to 39.3% in wave-2.
Table 3 represents the estimates from random effects for awareness of HIV among adolescent boys and girls. It was found that with the increases in age and years of schooling the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV in comparison to those who had no exposure to mass media. Adolescent boys' paid work status was inversely associated with HIV awareness about adolescent boys who did not do paid work [Coef: − 0.01; p < 0.10]. Use of the internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness in reference to their counterparts.
The awareness regarding HIV increases with the increase in household wealth index among both adolescent boys and girls. The adolescent girls from the non-Hindu household had a lower likelihood to be aware of HIV in reference to adolescent girls from Hindu households [Coef: − 0.09; p < 0.01]. Adolescent girls from non-SC/ST households had a higher likelihood of being aware of HIV in reference to adolescent girls from other caste households [Coef: 0.04; p < 0.01]. Adolescent boys [Coef: − 0.03; p < 0.01] and girls [Coef: − 0.09; p < 0.01] from a rural place of residence had a lower likelihood to be aware about HIV in reference to those from the urban place of residence. Adolescent boys [Coef: 0.04; p < 0.01] and girls [Coef: 0.02; p < 0.01] from Bihar had a higher likelihood to be aware about HIV in reference to those from Uttar Pradesh.
This is the first study of its kind to address awareness of HIV among adolescents utilizing longitudinal data in two indian states. Our study demonstrated that the awareness of HIV has increased over the period; however, it was more prominent among adolescent boys than in adolescent girls. Overall, the knowledge on HIV was relatively low, even during wave-II. Almost three-fifths (59.9%) of the boys and two-fifths (39.1%) of the girls were aware of HIV. The prevalence of awareness on HIV among adolescents in this study was lower than almost all of the community-based studies conducted in India 10 , 11 , 22 . A study conducted in slums in Delhi has found almost similar prevalence (40% compared to 39.1% during wave-II in this study) of awareness of HIV among adolescent girls 31 . The difference in prevalence could be attributed to the difference in methodology, study population, and study area.
The study found that the awareness of HIV among adolescent boys has increased from 38.6 percent in wave-I to 59.9 percent in wave-II; similarly, only 30.2 percent of the girls had an awareness of HIV during wave-I, which had increased to 39.1 percent. Several previous studies corroborated the finding and noticed a higher prevalence of awareness on HIV among adolescent boys than in adolescent girls 16 , 32 , 33 , 34 . However, a study conducted in a different setting noticed a higher awareness among girls than in boys 35 . Also, a study in the Indian context failed to notice any statistical differences in HIV knowledge between boys and girls 18 . Gender seems to be one of the significant determinants of comprehensive knowledge of HIV among adolescents. There is a wide gap in educational attainment among male and female adolescents, which could be attributed to lower awareness of HIV among girls in this study. Higher peer victimization among adolescent boys could be another reason for higher awareness of HIV among them 36 . Also, cultural double standards placed on males and females that encourage males to discuss HIV/AIDS and related sexual matters more openly and discourage or even restrict females from discussing sexual-related issues could be another pertinent factor of higher awareness among male adolescents 33 . Behavioural interventions among girls could be an effective way to improving knowledge HIV related information, as seen in previous study 37 . Furthermore, strengthening school-community accountability for girls' education would augment school retention among girls and deliver HIV awareness to girls 38 .
Similar to other studies 2 , 10 , 17 , 18 , 39 , 40 , 41 , age was another significant determinant observed in this study. Increasing age could be attributed to higher education which could explain better awareness with increasing age. As in other studies 18 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , education was noted as a significant driver of awareness of HIV among adolescents in this study. Higher education might be associated with increased probability of mass media and internet exposure leading to higher awareness of HIV among adolescents. A study noted that school is one of the important factors in raising the awareness of HIV among adolescents, which could be linked to higher awareness among those with higher education 47 , 48 . Also, schooling provides adolescents an opportunity to improve their social capital, leading to increased awareness of HIV.
Following previous studies 18 , 40 , 46 , the current study also outlines a higher awareness among urban adolescents than their rural counterparts. One plausible reason for lower awareness among adolescents in rural areas could be limited access to HIV prevention information 16 . Moreover, rural–urban differences in awareness of HIV could also be due to differences in schooling, exposure to mass media, and wealth 44 , 45 . The household's wealth status was also noted as a significant predictor of awareness of HIV among adolescents. Corroborating with previous findings 16 , 33 , 42 , 49 , this study reported a higher awareness among adolescents from richer households than their counterparts from poor households. This could be because wealthier families can afford mass-media items like televisions and radios for their children, which, in turn, improves awareness of HIV among adolescents 33 .
Exposure to mass media and internet access were also significant predictors of higher awareness of HIV among adolescents. This finding agrees with several previous research, and almost all the research found a positive relationship between mass-media exposure and awareness of HIV among adolescents 10 . Mass media addresses such topics more openly and in a way that could attract adolescents’ attention is the plausible reason for higher awareness of HIV among those having access to mass media and the internet 33 . Improving mass media and internet usage, specifically among rural and uneducated masses, would bring required changes. Integrating sexual education into school curricula would be an important means of imparting awareness on HIV among adolescents; however, this is debatable as to which standard to include the required sexual education in the Indian schooling system. Glick (2009) thinks that the syllabus on sexual education might be included during secondary schooling 44 . Another study in the Indian context confirms the need for sex education for adolescents 50 , 51 .
Limitations and strengths of the study
The study has several limitations. At first, the awareness of HIV was measured with one question only. Given that no study has examined awareness of HIV among adolescents using longitudinal data, this limitation is not a concern. Second, the study findings cannot be generalized to the whole Indian population as the study was conducted in only two states of India. However, the two states selected in this study (Uttar Pradesh and Bihar) constitute almost one-fourth of India’s total population. Thirdly, the estimates were provided separately for boys and girls and could not be presented combined. However, the data is designed to provide estimates separately for girls and boys. The data had information on unmarried boys and girls and married girls; however, data did not collect information on married boys. Fourthly, the study estimates might have been affected by the recall bias. Since HIV is a sensitive topic, the possibility of respondents modifying their responses could not be ruled out. Hawthorne effect, respondents, modifying aspect of their behaviour in response, has a role to play in HIV related study 52 . Despite several limitations, the study has specific strengths too. This is the first study examining awareness of HIV among adolescent boys and girls utilizing longitudinal data. The study was conducted with a large sample size as several previous studies were conducted in a community setting with a minimal sample size 10 , 12 , 18 , 20 , 53 .
The study noted a higher awareness among adolescent boys than in adolescent girls. Specific predictors of high awareness were also noted in the study, including; higher age, higher education, exposure to mass media, internet use, household wealth, and urban residence. Based on the study findings, this study has specific suggestions to improve awareness of HIV among adolescents. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents. Investment in education will help, but it would be a long-term solution; therefore, public information campaigns could be more useful in the short term.
WHO. HIV/AIDS . https://www.who.int/news-room/fact-sheets/detail/hiv-aids (2020).
Singh, A. & Jain, S. Awareness of HIV/AIDS among school adolescents in Banaskantha district of Gujarat. Health Popul.: Perspect. Issues 32 , 59–65 (2009).
Google Scholar
WHO & UNICEF. adolescents Health: The Missing Population in Universal Health Coverage . 1–31 https://www.google.com/search?q=adolescents+population+WHO+report&rlz=1C1CHBF_enIN904IN904&oq=adolescents+population+WHO+report&aqs=chrome..69i57.7888j1j7&sourceid=chrome&ie=UTF-8 (2018).
Chauhan, S. & Arokiasamy, P. India’s demographic dividend: state-wise perspective. J. Soc. Econ. Dev. 20 , 1–23 (2018).
Tiwari, A. K., Singh, B. P. & Patel, V. Population projection of India: an application of dynamic demographic projection model. JCR 7 , 547–555 (2020).
Troop-Gordon, W. Peer victimization in adolescence: the nature, progression, and consequences of being bullied within a developmental context. J. Adolesc. 55 , 116–128 (2017).
PubMed Google Scholar
Dermody, S. S., Friedman, M., Chisolm, D. J., Burton, C. M. & Marshal, M. P. Elevated risky sexual behaviors among sexual minority girls: indirect risk pathways through peer victimization and heavy drinking. J. Interpers. Violence 35 , 2236–2253 (2020).
Lee, R. L. T., Loke, A. Y., Hung, T. T. M. & Sobel, H. A systematic review on identifying risk factors associated with early sexual debut and coerced sex among adolescents and young people in communities. J. Clin. Nurs. 27 , 478–501 (2018).
Gurram, S. & Bollampalli, B. A study on awareness of human immunodeficiency virus among adolescent girls in urban and rural field practice areas of Osmania Medical College, Hyderabad, Telangana, India. (2020).
Jain, R., Anand, P., Dhyani, A. & Bansal, D. Knowledge and awareness regarding menstruation and HIV/AIDS among schoolgoing adolescent girls. J. Fam. Med. Prim Care 6 , 47–51 (2017).
Kawale, S., Sharma, V., Thaware, P. & Mohankar, A. A study to assess awareness about HIV/AIDS among rural population of central India. Int. J. Commun. Med. Public Health 5 , 373–376 (2017).
Lal, P., Nath, A., Badhan, S. & Ingle, G. K. A study of awareness about HIV/AIDS among senior secondary school Children of Delhi. Indian J. Commun. Med. 33 , 190–192 (2008).
CAS Google Scholar
Bago, J.-L. & Lompo, M. L. Exploring the linkage between exposure to mass media and HIV awareness among adolescents in Uganda. Sex. Reprod. Healthcare 21 , 1–8 (2019).
McCombie, S., Hornik, R. C. & Anarfi, J. K. Effects of a mass media campaign to prevent AIDS among young people in Ghana . Public Health Commun. 163–178 (Routledge, 2002). https://doi.org/10.4324/9781410603029-17 .
Sano, Y. et al. Exploring the linkage between exposure to mass media and HIV testing among married women and men in Ghana. AIDS Care 28 , 684–688 (2016).
Oginni, A. B., Adebajo, S. B. & Ahonsi, B. A. Trends and determinants of comprehensive knowledge of HIV among adolescents and young adults in Nigeria: 2003–2013. Afr. J. Reprod. Health 21 , 26–34 (2017).
Rahman, M. M., Kabir, M. & Shahidullah, M. Adolescent knowledge and awareness about AIDS/HIV and factors affecting them in Bangladesh. J. Ayub. Med. Coll. Abbottabad 21 , 3–6 (2009).
Yadav, S. B., Makwana, N. R., Vadera, B. N., Dhaduk, K. M. & Gandha, K. M. Awareness of HIV/AIDS among rural youth in India: a community based cross-sectional study. J. Infect. Dev. Countries 5 , 711–716 (2011).
Alhasawi, A. et al. Assessing HIV/AIDS knowledge, awareness, and attitudes among senior high school students in Kuwait. MPP 28 , 470–476 (2019).
Chakrovarty, A. et al. A study of awareness on HIV/AIDS among higher secondary school students in Central Kolkata. Indian J. Commun. Med. 32 , 228 (2007).
Katoch, D. K. S. & Kumar, A. HIV/AIDS awareness among students of tribal and non-tribal area of Himachal Pradesh. J. Educ. 5 , 1–9 (2017).
Shinde, M., Trivedi, A., Shinde, A. & Mishra, S. A study of awareness regarding HIV/AIDS among secondary school students. Int. J. Commun. Med. Public Health https://doi.org/10.18203/2394-6040.ijcmph20161611 (2016).
Article Google Scholar
Council, P. UDAYA, adolescent survey, Bihar and Uttar Pradesh, 2015–16. Harvard Dataverse https://doi.org/10.7910/DVN/RRXQNT (2018).
Kumar, P. & Dhillon, P. Household- and community-level determinants of low-risk Caesarean deliveries among women in India. J. Biosoc. Sci. 53 , 55–70 (2021).
Patel, S. K., Santhya, K. G. & Haberland, N. What shapes gender attitudes among adolescent girls and boys? Evidence from the UDAYA Longitudinal Study in India. PLoS ONE 16 , e0248766 (2021).
CAS PubMed PubMed Central Google Scholar
Fan, C., Wang, L. & Wei, L. Comparing two tests for two rates. Am. Stat. 71 , 275–281 (2017).
MathSciNet Google Scholar
Kim, T. K. T test as a parametric statistic. Korean J. Anesthesiol. 68 , 540–546 (2015).
PubMed PubMed Central Google Scholar
Bell, A., Fairbrother, M. & Jones, K. Fixed and random effects models: making an informed choice. Qual. Quant. 53 , 1051–1074 (2019).
Jarrett, R., Farewell, V. & Herzberg, A. Random effects models for complex designs. Stat. Methods Med. Res. 29 , 3695–3706 (2020).
MathSciNet CAS PubMed PubMed Central Google Scholar
Neuhaus, J. M. & Kalbfleisch, J. D. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 54 , 638–645 (1998).
CAS PubMed MATH Google Scholar
Kaur, G. Factors influencing HIV awareness amongst adolescent women: a study of slums in Delhi. Demogr. India 47 , 100–111 (2018).
Alene, G. D., Wheeler, J. G. & Grosskurth, H. Adolescent reproductive health and awareness of HIV among rural high school students, North Western Ethiopia. AIDS Care 16 , 57–68 (2004).
CAS PubMed Google Scholar
Oljira, L., Berhane, Y. & Worku, A. Assessment of comprehensive HIV/AIDS knowledge level among in-school adolescents in eastern Ethiopia. J. Int. AIDS Soc. 16 , 17349 (2013).
Samkange-Zeeb, F. N., Spallek, L. & Zeeb, H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: a systematic review of published literature. BMC Public Health 11 , 727 (2011).
Laguna, E. P. Knowledge of HIV/AIDS and unsafe sex practices among Filipino youth. in 15 (PAA, 2004).
Teitelman, A. M. et al. Partner violence, power, and gender differences in South African adolescents’ HIV/sexually transmitted infections risk behaviors. Health Psychol. 35 , 751–760 (2016).
Oberth, G. et al. Effectiveness of the Sista2Sista programme in improving HIV and other sexual and reproductive health outcomes among vulnerable adolescent girls and young women in Zimbabwe. Afr. J. AIDS Res. 20 , 158–164 (2021).
DeSoto, J. et al. Using school-based early warning systems as a social and behavioral approach for HIV prevention among adolescent girls. Preventing HIV Among Young People in Southern and Eastern Africa 280 (2020).
Ochako, R., Ulwodi, D., Njagi, P., Kimetu, S. & Onyango, A. Trends and determinants of Comprehensive HIV and AIDS knowledge among urban young women in Kenya. AIDS Res. Ther. 8 , 11 (2011).
Peltzer, K. & Supa, P. HIV/AIDS knowledge and sexual behavior among junior secondary school students in South Africa. J. Soc. Sci. 1 , 1–8 (2005).
Shweta, C., Mundkur, S. & Chaitanya, V. Knowledge and beliefs about HIV/AIDS among adolescents. WebMed Cent. 2 , 1–9 (2011).
Anwar, M., Sulaiman, S. A. S., Ahmadi, K. & Khan, T. M. Awareness of school students on sexually transmitted infections (STIs) and their sexual behavior: a cross-sectional study conducted in Pulau Pinang, Malaysia. BMC Public Health 10 , 47 (2010).
Cicciò, L. & Sera, D. Assessing the knowledge and behavior towards HIV/AIDS among youth in Northern Uganda: a cross-sectional survey. Giornale Italiano di Medicina Tropicale 15 , 29–34 (2010).
Glick, P., Randriamamonjy, J. & Sahn, D. E. Determinants of HIV knowledge and condom use among women in madagascar: an analysis using matched household and community data. Afr. Dev. Rev. 21 , 147–179 (2009).
Rahman, M. Determinants of knowledge and awareness about AIDS: Urban-rural differentials in Bangladesh. JPHE 1 , 014–021 (2009).
Siziya, S., Muula, A. S. & Rudatsikira, E. HIV and AIDS-related knowledge among women in Iraq. BMC. Res. Notes 1 , 123 (2008).
Gao, X. et al. Effectiveness of school-based education on HIV/AIDS knowledge, attitude, and behavior among secondary school students in Wuhan, China. PLoS ONE 7 , e44881 (2012).
ADS CAS PubMed PubMed Central Google Scholar
Kotecha, P. V. et al. Reproductive health awareness among urban school going adolescents in Vadodara city. Indian J. Psychiatry 54 , 344–348 (2012).
Dimbuene, T. Z. & Defo, K. B. Fostering accurate HIV/AIDS knowledge among unmarried youths in Cameroon: do family environment and peers matter?. BMC Public Health 11 , 348 (2011).
Kumar, R. et al. Knowledge attitude and perception of sex education among school going adolescents in Ambala District, Haryana, India: a cross-sectional study. J. Clin. Diagn. Res. 11 , LC01–LC04 (2017).
ADS PubMed PubMed Central Google Scholar
Tripathi, N. & Sekher, T. V. Youth in India ready for sex education? Emerging evidence from national surveys. PLoS ONE 8 , e71584 (2013).
Rosenberg, M. et al. Evidence for sample selection effect and Hawthorne effect in behavioural HIV prevention trial among young women in a rural South African community. BMJ Open 8 , e019167 (2018).
Gupta, P., Anjum, F., Bhardwaj, P., Srivastav, J. & Zaidi, Z. H. Knowledge about HIV/AIDS among secondary school students. N. Am. J. Med. Sci. 5 , 119–123 (2013).
Download references
This paper was written using data collected as part of Population Council’s UDAYA study, which is funded by the Bill and Melinda Gates Foundation and the David and Lucile Packard Foundation. No additional funds were received for the preparation of the paper.
Author information
Authors and affiliations.
Ph.D. Research Scholar, Department of Survey Research & Data Analytics, International Institute for Population Sciences, Mumbai, India
Shobhit Srivastava & Pradeep Kumar
Ph.D. Research Scholar, Department of Family and Generations, International Institute for Population Sciences, Mumbai, India
Shekhar Chauhan
Ph.D. Research Scholar, Department of Public Health and Mortality Studies, International Institute for Population Sciences, Mumbai, India
Ratna Patel
You can also search for this author in PubMed Google Scholar
Contributions
Conception and design of the study: S.S. and P.K.; analysis and/or interpretation of data: P.K. and S.S.; drafting the manuscript: S.C., and R.P.; reading and approving the manuscript: S.S., P.K., S.C. and R.P.
Corresponding author
Correspondence to Pradeep Kumar .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Srivastava, S., Chauhan, S., Patel, R. et al. A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data. Sci Rep 11 , 22841 (2021). https://doi.org/10.1038/s41598-021-02090-9
Download citation
Received : 05 June 2021
Accepted : 29 September 2021
Published : 24 November 2021
DOI : https://doi.org/10.1038/s41598-021-02090-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- General Assembly
Highlighting Significant Gains against HIV/AIDS, Top UN Officials Tell General Assembly Global Goal of Ending Deadly Disease as Public Health Threat by 2030 Is within Reach
The global response to HIV/AIDS has been “a success story”, senior United Nations officials told the General Assembly today, as delegates spotlighted significant gains in the fight against the widespread disease as well as the remaining challenges to ending the public health scare by 2030.
“We have an inspirational story to tell,” said United Nations Deputy Secretary-General Amina J. Mohammed, noting that more than three quarters of those living with HIV are receiving life-saving treatment — almost 30 million people globally.
Citing expanded and rapid access to therapy across sub-Saharan Africa, Asia and the Pacific — home to almost 80 per cent of people living with HIV, she stressed that “this is the most outstanding public health achievement of recent times”. If this progress is maintained, the international community is on track to reach the global goal of ending AIDS as a public health threat by 2030, she said, underscoring: “This is a cause of celebration at a time when many of the other Sustainable Development Goals (SDGs) are widely off-track.”
Agreeing, Jörundur Valtýsson (Iceland), Vice President of the General Assembly, said: “The global response to the HIV/AIDS epidemic stands as a multilateral success story — having made remarkable gains.” Since peaking in 2004, the number of HIV/AIDS-related deaths has significantly declined, he added.
However, challenges remain, he emphasized. “Despite these gains, more work is needed to completely end the HIV/AIDS epidemic by 2030, as outlined in Sustainable Development Goal 3.3.,” he said, reporting that millions still lack access to HIV/AIDS prevention and treatment — and gender inequalities, stigma, and discrimination persist as major barriers to those services.
In the ensuing discussion, delegates exchanged views on the Secretary-General’s latest report on “the path to ending AIDS — progress report on 2025 targets and solutions for the future” (document A/78/883 ). Several Member States with high infection rates among their populations shared their “success stories” and donor countries highlighted their financial and technical support.
Cuba is the first country in the world to eliminate mother-to-child transmission, said its representative, adding that the goal is to reach the 95-95-95 target — 95 per cent of people living with HIV know their status, 95 per cent of people who know that they are living with HIV to be on life-saving antiretroviral treatment, and 95 per cent of people on such treatment to be virally suppressed. “We must join our efforts to eradicate this disease once and for all”, he stated, underscoring the need to promote South-South cooperation for the benefit of other countries — mainly on the African continent — with technology transfer projects.
Namibia prides itself in recently becoming the first African country — and the first high-burden country in the world — to reach a significant milestone on the path towards eliminating vertical mother-to-child transmission of both HIV and viral hepatitis B, said its representative. Currently, 99 per cent of all children born to HIV-positive mothers are born HIV-free. “This achievement is anchored in an approach that prioritized the decentralization of services to support community-based antiretroviral therapy and improve access to treatment,” she said.
While a reduction in new HIV/AIDS infection in sub-Saharan Africa is “encouraging”, this progress “must not be cause for complacency”, said the representative of Zimbabwe. In his country, community health workers have played a pivotal role in reaching underserved populations, improving HIV testing rates and ensuring better follow-up and care for people living with HIV. The Government instituted a novel 3 per cent tax on corporate profits and personal incomes to bridge donor resource gaps and finance programmes. Educating youth about HIV/AIDS has proven effective with schools and universities incorporating this subject into their curriculum, he said.
HIV infection is increasing rapidly in the western Pacific region, warned the representative of the Philippines. Stressing that “sustainable and equitable funding is needed to stem the rising numbers”, he echoed the Secretary-General’s call for increased domestic and international donor allocations for the HIV response in middle-income countries.
“Japan has been at the forefront of developing and providing child-friendly HIV treatments and effective HIV testing and treatments for low- and middle-income countries,” its delegate stressed, noting that Tokyo’s firm commitment to the global HIV agenda aligns with its broader focus on universal health coverage and preparedness for future pandemics, based on human security.
Poland was among the first Central European countries to offer wide and free access to diagnostics, antiretroviral treatment and care for people living with HIV/AIDS, including those at risk of marginalization, its representative said, noting that each year, the Ministry of Health and the National Health Fund allocate funds to implement its antiretroviral treatment programme.
Elaborating on the gender aspect of the endemic, the representative of the Netherlands, also speaking for Belgium and Luxembourg, said that 4,000 young women and girls become infected with HIV/AIDS every week globally. Sex workers are seven times more likely to live with HIV compared to adults who are not sex workers. “It is urgent to reach sex workers with condoms, HIV testing and treatment,” she stressed, declaring: “The path to end AIDS is a path in line with the Universal Declaration of Human Rights and rights to health for all”.
The representative of the Russian Federation pointed out that the Secretary-General’s report contains controversial and non-consensual concepts, such as “comprehensive sexuality education”, “vulnerable populations” and “gender-responsive and human rights-based HIV prevention and treatment programmes”. Rejecting the report’s arbitrary interpretation of criminal liability for same-sex relations, drug use and sex-industry work as “harmful”, he underscored the importance of respecting national priorities, development strategies and ways of life. “We regret that the authors of this document once more turned a blind eye to this key principle — a principle pivotal to the achievement of global solidarity in the combat against HIV infections,” he asserted.
In other business, the Assembly adopted — without a vote — a resolution (document A/78/L.71) proclaiming 2025 the International Year of Cooperatives. The representative of Mongolia, who introduced the text, highlighted the role of cooperatives in achieving the 2030 Agenda for Sustainable Development, noting that there are about 3 million cooperatives, with 12 per cent of people on the planet being members of these cooperatives. A soft launch of the Year will take place in New York on 9 July 2024. It will be officially launched in New Delhi during the week of 25-30 November 2024.
Opening Remarks
JÖRUNDUR VALTÝSSON (Iceland), Vice President of the General Assembly , delivered opening remarks on behalf of Dennis Francis (Trinidad and Tobago), President of the General Assembly. “The global response to the HIV/AIDS epidemic stands as a multilateral success story — having made remarkable gains,” he said, noting that since peaking in 2004, the number of HIV/AIDS-related deaths has significantly declined. Moreover, easier accessibility to HIV/AIDS treatment, increased equity in health systems and improved access to education and health care — including improved prevention, testing and treatment services — have averted almost 20.8 million HIV/AIDS-related deaths over the past three decades. “Despite these gains, more work is needed to completely end the HIV/AIDS epidemic by 2030, as outlined in Sustainable Development Goal 3.3,” he stressed.
He reported that millions still lack access to HIV/AIDS prevention and treatment — and gender inequalities, stigma, and discrimination persist as major barriers to those services. Additionally, there is untapped potential for HIV/AIDS prevention programmes, and the funding gap for national responses — especially in developing countries — is widening and concerning. “Therefore, we must scale up national and regional interventions and responses — and forge strong multistakeholder partnerships to end the HIV/AIDS epidemic by 2030,” he said, urging: “To achieve our goals, we must keep HIV/AIDS high on the multilateral agenda” and close the financing gaps, address technology transfer, and improve access to medicines, diagnostics, and other health products in developing countries. It is also imperative to significantly scale up research and development and capacity-building, including for local pharmaceutical production.
Given that the HIV/AIDS challenge extends beyond the public health sector, a comprehensive response — with a human rights perspective and a development lens — is crucial, he went on to say, underscoring the need to build on the commitments made in the Political Declaration on Universal Health Coverage — to improve the capacity of national health systems to deliver quality, affordable and accessible health-care for all, including HIV/AIDS interventions. Proposing the full use of upcoming events, especially the next High-level Meeting on HIV/AIDS in 2026, he said it is vital to streamline and accelerate efforts and ensure that “we are on track to end the HIV/AIDS epidemic by 2030”. The path ahead is, indeed, challenging. “But with our collective will to fully implement the commitments made in the latest Political Declaration on HIV and AIDS: Ending Inequalities and Getting on Track to End AIDS by 2030, we can accelerate our efforts to overcome the obstacles and end this epidemic once and for all, leaving no one behind,” he stressed.
AMINA J. MOHAMMED, Deputy Secretary-General of the United Nations , speaking on behalf of Secretary-General António Guterres, highlighted progress on the vital issue of HIV/AIDS: “We have an inspirational story to tell — globally, more than three quarters of those living with HIV are receiving life-saving treatment — almost 30 million people.” Access to therapy has expanded rapidly across sub-Saharan Africa, Asia and the Pacific — together, home to almost 80 per cent of people living with HIV. This is the most outstanding public health achievement of recent times, she observed, adding that “if this progress is maintained, we are on course to reach a key global milestone — 34 million people receiving HIV treatment”. That puts the international community on track to reach the global goal of ending AIDS as a public health threat by 2030.
“This is a cause of celebration at a time when many of the other Sustainable Development Goals (SDGs) are widely off-track,” she pointed out, stressing that the progress made in AIDS response is a demonstration of what can be achieved when decision-makers collaborate, follow the science, invest adequately, tackle inequality, protect human rights and let communities lead the way. However, AIDS still claims lives every minute and the progress made is under threat as resources are declining, she cautioned, declaring: “Let’s build on the immense progress we have made and finish the job together.”
The representative of Australia , also speaking for Canada and New Zealand , welcomed the progress made in tackling HIV/AIDS, including the achievement of targets in Botswana, Eswatini, Rwanda, the United Republic of Tanzania and Zimbabwe, as well as the increased access to antiviral therapy. Noting that this demonstrates the value of “collective efforts, global solidarity and a whole of society approach”, he said it must not cause complacency. 9.2 million people living with HIV did not have access to antiretroviral treatment in 2024, he noted also noting the large number of adolescent girls and young women who become infected with HIV globally.
Stressing the importance of a human-rights-based approach, he said this is a necessity to achieve progress in the fight against HIV and AIDS. “Countries that have seen the biggest progress have met their obligations under international human rights law to remove societal and structural barriers that put people in harm’s way and prevent them from accessing health and other services,” he pointed out. Health and other services must be open to all, particularly key populations, including transgender people, who must remain free from stigma and discrimination, arrest and imprisonment, he said, also stressing the importance of a multisectoral approach.
The representative of Brazil expressed concern that, despite remarkable progress made, HIV infections and AIDS-related deaths are not declining fast enough to reach the global goal and targets set. For its part, his country established an Inter-ministerial Committee for the Elimination of Tuberculosis and Other Socially Determined Diseases in 2023. In 2024, the Committee developed the Healthy Brazil Programme to eliminate HIV/AIDS as a public health issue by 2030. Brazil has consistently advanced in the prevention and care of HIV/AIDS thanks to its unified health system, which guarantees universal and free-of-charge access to prevention, treatment and diagnosis. Through the national health system, 800,000 people are assisted with free antiretroviral drugs — a steady increase from 2022. To ensure early detection among key populations, no-cost HIV self-tests are distributed, he added.
The representative of Cuba reaffirmed his country’s commitment to combating HIV/AIDS, “a battle we have been fighting for more than two decades”. Despite the progress made, inequalities in access to health persist, and “we must join our efforts to eradicate this disease once and for all”, he stated, underscoring the need to promote South-South cooperation for the benefit of other countries in the region and the rest of the world — mainly the African continent — with technology transfer projects. Spotlighting Cuba’s significant progress in combating HIV/AIDS, he said it is the first country to eliminate mother-to-child transmission and is striving to reach the 95-95-95 goal. Nevertheless, he said that the economic blockade imposed by the United States has hindered Cuba’s efforts, causing million-dollar losses in the health sector.
The representative of the Philippines , stressing the importance of multilateralism, human rights and “community and country leadership”, said his country is facing one of the fastest-growing HIV epidemics in the western Pacific region. Its strategic plan to tackle this ensures early diagnosis and treatment, ample testing sites and medications. “Sustainable and equitable funding is needed to stem the rising numbers,” he said, reiterating the Secretary-General’s call for increased domestic and international donor allocations for the HIV response in middle-income countries. Stressing the need for equitable access to medicines and health technologies, he said the Philippines has modernized its approach to HIV prevention and treatment and is tackling discrimination against people living with the disease, utilizing a lifecycle approach and expanding coverage of young key populations.
The representative of the Netherlands , also speaking for Belgium and Luxembourg , said that 40 years since the HIV/AIDS pandemic began, it is still not over. AIDS claimed a life every minute in 2022, and around 9.2 million people still miss out on treatment. Women and girls are still disproportionately affected, particularly in sub-Saharan Africa. Globally, 4,000 young women and girls become infected with HIV/AIDS every week. “Too often, women and girls are denied economic autonomy, deprived of control over their physical and mental health, including sexual reproductive health and rights,” she pointed out, noting that the Secretary-General’s report emphasizes the need for comprehensive sexuality education. It also highlights the need to close the gender inequalities for adolescent girls and young women.
Some women are at greater risk than others, she said, citing global epidemiological evidence, which demonstrates that sex workers are seven times more likely to live with HIV compared to adults who are not sex workers. “It is urgent to reach sex workers with condoms, HIV testing and treatment,” she stressed. Community-led services are also key on the path to end AIDS. “However, community-led responses are under-recognized, under-resourced, and in some places, even under attack,” she warned. The Joint United Nations Programme on HIV/AIDS (UNAIDS) must be fully funded. Welcoming the recommendations of the Secretary-General’s report, she declared: “The path to end AIDS is a path in line with the Universal Declaration of Human Rights and rights to health for all”.
The representative of Haiti recognized that despite the progress reached in combating HIV, the scourge remains a major global crisis. In 2021, Governments took on the commitment of eradicating this epidemic, he said, noting that, according to the data provided by UNAIDS, since the peak achieved in 1995, the number of new HIV infections has dropped by 60 per cent and HIV-related deaths by 70 per cent. Also, over 30 million people have access to HIV treatment. Haiti has made enormous strides in the struggle to stabilize the epidemic — from 2017 to 2022, HIV/AIDS incidents dropped by 25 per cent; between 2018 and 2023, the number of AIDS-related deaths fell by 50 per cent; and the number of new infections dropped by 25 per cent. However, despite the progress made, Haiti continues to face numerous challenges linked to mounting insecurity, he added.
The representative of Thailand said it is very crucial to integrate HIV prevention, testing and treatment services into primary health care and universal health coverage. “Doing so increases access to such services for all those at risk,” he said, adding that his country has expanded its health benefit package to increase access to cost-effective self-tests to encourage early detection while also addressing stigmatization. Also underscoring the importance of a community-led and key-population-driven response, he highlighted Thailand’s national community health worker certification programme on HIV/AIDS for and by people living with that condition. Stigma and discrimination continue to be societal barriers to HIV response, he said, noting that his country is promoting an understanding of HIV human rights and gender diversity in this regard.
The representative of Zimbabwe reaffirmed his country’s unwavering commitment to eradicating HIV/AIDS and fulfilling the pledges made in 2021 to end the epidemic by 2030. Citing a reduction in new HIV/AIDS infection in sub-Saharan Africa as “encouraging,” he said this progress “must not be cause for complacency, as there is much still to be done towards the attainment of our goal of ending AIDS as a public health threat by 2030”. His country has successfully implemented programmes to prevent mother-to-child transmission of HIV. Community health workers in the local organizations have played a pivotal role in reaching underserved populations, improving HIV testing rates and ensuring better follow-up and care for people living with HIV. The Government instituted a novel 3 per cent tax on corporate profits and personal incomes to bridge donor resource gaps and finance programmes. Educating youth about HIV/AIDS has proven effective with schools and universities incorporating this subject into their curriculum, he said.
The representative of Mexico underscored that multilateralism and international cooperation can generate tangible results for the most vulnerable populations. “Without a doubt, combating HIV is a success story for multilateralism and the principle of putting the individual at the heart of our global efforts,” she said. In 2022, 1.3 million people suffered an HIV infection, compared to 3.2 million in 1995. And since 2010, global infections have decreased by 38 per cent, while 76 per cent of infected people receive treatment. However, “much remains to be done”, she observed, noting barriers such as gender inequality, stigma, discrimination and access to health services. The Summit of the Future represents an additional opportunity to strengthen States’ collective work in the fight against HIV. In Mexico, at the end of 2021, there were an estimated 1.5 million new HIV infections, compared to 3.2 million people in 1996 — a reduction of 54 per cent, she said, adding that her Government has applied an HIV prevention and care model.
The representative of South Africa , applauding the progress made in African countries, said his country too has made remarkable strides, with a positive decline in overall HIV prevalence amongst adults — 90 per cent of whom are aware of their HIV status. Ninety-nine per cent of those diagnosed with HIV are on antiretroviral treatment. Highlighting the launch of the South African chapter of the Global Alliance to End Aids in Children, he said it helps parents protect their children from vertical transmission of HIV. Stressing the need to mobilize political leadership for an equitable response to end AIDS by 2030, he called for a strong multilateral system and a multisectoral approach that promotes human rights. It is vital to combat stigma, discrimination and other negative social determinants such as harmful gender norms, gender-based violence and unequal economic opportunities. Stressing the importance of universal health coverage and international solidarity in issues of global concern, he said the decline of funding is deeply concerning.
The representative of the Russian Federation detailed the implementation of his country’s 2030 strategy to combat the spread of HIV infection, underscoring that, compared to 2021, the number of tests performed in the Russian Federation increased by more than 23 per cent to 51 million. Thanks to these actions, “we’ve seen a high rate of detection of HIV infections at early stages, as well as a sustained decrease in new cases”. He said that the Secretary-General’s report contains controversial and non-consensual concepts, such as “comprehensive sexuality education”, “vulnerable populations” and “gender-responsive and human rights-based HIV prevention and treatment programmes”. Statements that the principle of “undetectable” equals “untransmissible” are unacceptable, so is the report’s arbitrary interpretation of criminal liability for same-sex relations, drug use and work in the sex industry as “harmful”, he said, underscoring the importance of respecting national priorities, development strategies and ways of life. “We regret that the authors of this document once more turned a blind eye to this key principle — a principle pivotal to the achievement of global solidarity in the combat against HIV infections,” he said.
The representative of Poland underscored that despite the unquestionable progress achieved at the global level in combating HIV/AIDS, the epidemic remains a significant threat to global public health. Noting that his country was among the first Central European countries to offer wide and free access to diagnostics, antiretroviral treatment and care for people living with HIV/AIDS — including those at risk of marginalization — he said that each year, the Ministry of Health and the National Health Fund allocate funds that ensure the implementation of the antiretroviral treatment programme. Ukrainian refugees account for approximately 20 per cent of all HIV patients in Poland, he said, adding that his Government provides them with treatment and care, as well as comprehensive social, psychological, economic and medical assistance. He further emphasized that to accelerate global efforts, the international community must increase efficiency in early diagnosis of HIV and improve the ability to respond quickly to crisis scenarios entailing HIV outbreaks.
The representative of India highlighted community initiatives and projects in her country, including targeted interventions and schemes that focus on providing services to high-risk groups and bridge populations. “The biggest breakthrough came with the expansion of antiretroviral therapy,” she said, adding that as of December 2022, 1.5 million people living with HIV in her country were receiving this life-saving treatment. The National AIDS Control Organization has been instrumental in scaling up services and ensuring that these treatments are accessible and affordable, she said, pointing to concerted efforts to tackle the stigma and discrimination associated with HIV/AIDS. The country has put in place a “rights-based and equity-driven approach”, she said, adding that prevention efforts extend to priority populations such as people in prisons and young key populations in hard-to-reach areas.
The representative of Japan said that his country has been a steadfast member of the UNAIDS Programme Coordinating Board since its establishment in 1996. Tokyo’s firm commitment to the global HIV agenda aligns with its broader focus on universal health coverage and preparedness for future pandemics. Outlining key measures to end AIDS as a public health threat by 2030, he said that health services must reach the most vulnerable populations and that strategic collaboration between finance and health authorities is essential to securing sustainable funding for HIV/AIDS responses. “Japan has been at the forefront of developing and providing child-friendly HIV treatments and effective HIV testing and treatments for low- and middle-income countries,” he stressed, pledging the country’s unwavering dedication to achieving universal health coverage, based on human security. “Let this UN General Assembly be a catalyst for action, solidarity, and hope for a future free from AIDS,” he said.
The representative of the United Kingdom said that the Secretary-General’s report presents causes for celebration, such as data showing that more than three quarters of people living with HIV globally are receiving life-saving treatment. However, it also presents causes for concern, he observed, noting that HIV remains more likely to affect young women and girls in sub-Saharan Africa and key populations, including lesbian, gay, bisexual, transgender+ people, elsewhere in the world. Accordingly, he underlined the need for community-led responses and greater attention to HIV prevention. As a significant funder of the HIV response, London remains committed to seeing this ambition achieved, and to ending AIDS-related deaths and preventing new HIV infections. It also recognizes the benefit of multilateralism in bringing nations together to confront complex global challenges through a universal approach. “Without action on the barriers stopping us from tackling the AIDS epidemic, we risk sliding backwards and losing our hard-won gains,” he cautioned.
The representative of China , noting that global epidemics such as AIDS and COVID-19 show that no country is immune to infectious diseases, said “our destiny is intertwined.” Stressing the need to put people first, he said his Government has actively fulfilled its commitments under SDG 3. After many years of efforts, bloodborne transmission of the disease has been virtually halted, while rates of diagnosis and treatment have increased, he said, also noting the improved coverage of antiretroviral treatment, among other achievements. China’s national AIDS prevention strategy combines prevention and treatment, he said, reaffirming commitment to global AIDS prevention programmes, technical exchanges with Global South countries as well as active engagement with UNAIDS and the World Health Organization (WHO).
The representative of Namibia said that her country is home to more than 200,000 people living with HIV, acknowledging the great importance of the work carried out by UNAIDS. Its commitment to the 95-95-95 targets is prioritized in its strategic health targets. Namibia has achieved 94-97-95 by 2023 and prides itself in recently becoming the first African country — and the first high-burden country in the world — to reach a significant milestone on the path towards eliminating vertical mother-to-child transmission of both HIV and viral hepatitis B. Currently, 99 per cent of all children born to HIV-positive mothers are born HIV-free. “This achievement is anchored in an approach that prioritized the decentralization of services to support community-based antiretroviral therapy and improve access to treatment,” she said, adding that partnerships remain an important component of its national response, coupled with a political commitment that prioritizes access to resources, especially domestic resources.
The representative of the United States said that “as a global community, we have made enormous progress in preventing and treating HIV”. Despite these achievements, 39 million people continue to live with HIV, including more than 1 million in the United States. HIV remains a serious health, security and development threat and ending the HIV/AIDS pandemic remains Washington, D.C.’s priority, he said, adding: “We must sustain the gains we have made” and ensure that essential lessons are not ignored. Highlighting the importance and effectiveness of ensuring access to health services for members of vulnerable populations, including those facing intersecting forms of discrimination, he stated: “We have to act as if our lives depended on getting this right”. Also, ensuring that the response is adequately resourced and framed by resilient national systems is pivotal, he added.
The representative of Uganda , reaffirming commitment to ending inequalities and getting back on track to end AIDS by 2030, highlighted his country’s ambitious targets in its third national development plan. Over the last four decades, the national campaigns aiming to tackle this problem have resulted in a decline in HIV/AIDS prevalence, he said, noting numerous milestones. Pointing to a 35 per cent reduction in new infections from 97,000 in 2010 to 38,000 in 2023 and a 54 per cent reduction in annual AIDS-related deaths from 37,000 in 2010 to 17,000 in 2023, he also highlighted a decline in stigma and discrimination. These gains were made possible by support from development partners, the private sector, religious and cultural leaders and people living with HIV. Uganda prioritizes primary interventions, expanding HIV testing services and promoting behavioral change, including through condom promotion and safe male circumcision, he said.
Facebook Twitter Email Print LinkedIn
STORY REMOVED: US-MED--HIV-Latinos-Localize It

Nurse practitioner Eliza Otero, left, talks with Fernando Hermida at Pineapple Healthcare in Orlando, Fla., on May 28, 2024. Credit: AP/Phelan M. Ebenhack
CHARLOTTE, N.C. — Please disregard US-MED--HIV-Latinos-Localize It, published on Jun. 24, 2024, and datelined in CHARLOTTE, N.C. It is meant for member newsrooms, not the general public.

Nassau approves transgender ban ... BOCES hit-and-run ... Plane emergency landing ... Make your own charm bracelet
Get more on these and other NewsdayTV stories
Most Popular
Latest videos.
Unlimited Digital Access Only 25¢ for 5 months
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
June 24, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Exploitation of supply chain monitoring loopholes fueled US opioid epidemic, study finds
by Indiana University

New research from the Indiana University Kelley School of Business explains how pharmaceutical companies were able to saturate the country with massive quantities of opioids, despite efforts by the Drug Enforcement Administration to regulate their supply.
The research identifies a loophole in the DEA's monitoring system exploited by some pharmaceutical companies , leading to an oversupply of opioid drugs in communities. The hallmark of this activity was high supply chain complexity, such as pharmacies with dozens of distributors across the country.
The paper , "Hiding Behind Complexity: Supply Chain, Oversight, Race, and the Opioid Crisis," appears in the journal Production and Operations Management.
The same research also documents how the opioid epidemic—commonly regarded as a national public health crisis among white Americans—had a much deeper impact in Black communities, where overdose deaths tripled from 2014 to 2020.
"We believe we are the first to uncover insights into the supply chain mechanisms that were used to evade the DEA and fuel the opioid crisis ," said Jonathan Helm, professor of operations and decision technologies and the W.W. Grainger Inc. Faculty Fellow at the Kelley School. "Up until now, the focus has been on each of the pharmaceutical companies individually, ignoring the huge impact of the broader supply chain."
"No one was looking at it from a supply chain perspective," added Iman Attari, a Kelley School doctoral candidate in operations and decision technologies and the paper's corresponding author.
Attari, Helm and Jorge Mejia, an associate professor in the Kelley School, analyzed information in the 2019 release of the DEA's Automation of Reports and Consolidated Orders System—commonly known as the ARCOS database—which tracked each shipment in the U.S. opioid supply chain from 2006 to 2014.
The researchers uncovered how supply chain complexity may have facilitated the influx of large qualities of opioids into the market, undetected by the DEA. Their research combined ARCOS data about pharmacies' opioid dispensing and supply chain structures with county-level demographics and socioeconomic factors.
Using a fixed-effect model, they found that a one-unit increase across three dimensions of supply chain complexity was associated with a 16% increase in opioid dispensing.
DEA monitoring involves using ARCOS to collect data on all shipments of controlled substances, and requiring manufacturers and distributors to report suspicious orders of unusual size and frequency.
"The issue was that pharmacies wanting to have large shipments were very smart about it," Attari said. "Instead of placing an order for a large shipment from one single distributor, they broke down that large order across multiple distributors. They got smaller shipments from different distributors; when added up, it was a huge order. Each distributor is only going to see the data from the pharmacy that links themselves to it, and not to shipments from other distributors."
As a result, the DEA monitoring system failed. By using more suppliers, pharmacies were able to evade detection.
Another factor they studied was the location of distributors. Because of the DEA's structure, with 23 often independently operated field divisions spread across the U.S., the researchers found that a lack of coordination and aggregation of information among them was another factor in overlooking potentially suspicious activity.
"Even if a supplier reports a suspicious order in one division, other divisions that the pharmacy orders from are unlikely to be informed," they wrote.
"It cannot be just 'business,' because when you look at it from a business standpoint, it makes more sense to work with one distributor because you benefit from economy of scale," Attari said. "It is expected for a pharmacy to have one or two distributors, or at most three distributors of opioid drugs.
"When we saw pharmacies in the data set with 25 distributors—all over the U.S.—that was a strong indication that they were trying to mess with the monitoring system."
The research found that supply chain complexity had a stronger association with the increase in opioid dispensing in non-white communities. A 10% increase in the non-white proportion of the population yielded a 3.39% increase in the overall dispensing by pharmacies with high supply chain complexity.
"Communities of color have been historically under-resourced and neglected by many government and social services," the researchers wrote. "In the context of the opioid crisis, it appears that the DEA has spent more effort arresting non-White drug users than on regulating the flow of opioids from pharmaceutical companies into non-White communities."
To be certain that their analysis was distinguishing between legitimate medical use and non-medical, recreational demand, they compared statistics for the reformulated OxyContin, which was redesigned to prevent abuse.
"In a novel approach, we leverage the fact that different pharmacies received their first shipment of reformulated OxyContin at different times and use a difference-in-differences model to estimate the heterogeneous effect of the shock on dispensing," they wrote.
"As the reformulated OxyContin stifled (non-medical) demand, high-complexity pharmacies experienced a 15.31% greater reduction in dispensing compared to lower-complexity pharmacies, suggesting that their excess dispensing was indeed satisfying non-medical/recreational demand."
As a follow-up to this paper, the researchers are investigating the dynamics between major chain pharmacies and their distributors, and how they may facilitate the oversupply by pharmacies.
Their initial findings suggest that the pharmacies' practice of self-distribution, where they distribute opioids from their own distribution centers, combined with their close ties to large distributors, also may have led to excessive opioid dispensing without adequate oversight by the DEA.
Explore further
Feedback to editors

Chronic loneliness may increase stroke risk among older adults
2 hours ago

Scientists can now detect antibiotics in fingerprints, aiding the fight against drug-resistant TB

Children born underweight found to be at increased risk of disease if they develop obesity
3 hours ago

Wearable sweat monitor uses machine learning to protect workers from dehydration
6 hours ago

Signaling pathway in brain helps maintain balance in microglia, prevent cognitive deficit

New research points to possibility for testing to explore early-stage Alzheimer's disease

Study elucidates crucial role of G900 gene enhancers in asthma-associated inflammation

Texas's 2021 abortion ban tied to rise in infant deaths
7 hours ago

Study reveals same genes that can drive cancer also guide neural-circuit growth
9 hours ago

New evidence shows that higher oxygen concentrations may help prevent deaths of preterm babies
Related stories.

Baltimore City wins $45 million settlement with Allergan, seeks billions in suits vs. other opioid distributors
Jun 10, 2024

Study reveals pharmacy-level barriers to treatment for opioid use disorder in Appalachian Kentucky
Apr 28, 2020

Pressures within supply chains paved the way to an oversupply of prescription opioids, researcher finds
Jun 7, 2022

Availability of recreational cannabis reduced demand for prescription codeine
Jan 19, 2023
US sues top drug firm over opioid distribution
Dec 29, 2022

Investigating the role of retail pharmacies in the US opioid epidemic
Aug 29, 2022
Recommended for you

New study finds medication abortion without ultrasound to be safe
10 hours ago

Trial offers hope for cheaper, more tolerable, ketamine treatment

Q&A: How future medications could be personalized on a 3D printer
11 hours ago

New approach accurately identifies medications most toxic to the liver

Common blood pressure drug may increase risk of bleeding
Jun 21, 2024

Study identifies first drug therapy for sleep apnea
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

The emergence and evolution of the research fronts in HIV/AIDS research
David fajardo-ortiz.
1 Facultad de Medicina, Universidad Nacional Autónoma de México, Mexico City, Mexico
Malaquias Lopez-Cervantes
Michel dumontier.
2 Institute of Data Science, Maastricht University, Maastricht, The Netherlands
Miguel Lara
3 Instituto de Biología, Universidad Nacional Autónoma de México, Mexico City, Mexico
Hector Ochoa
4 Colegio de la Frontera Sur, Chiapas, Mexico
Victor M. Castano
5 Centro de Física Aplicada y Tecnología Avanzada, Universidad Nacional Autónoma de México, Queretaro, Mexico
- Conceptualization: DF-O VMC.
- Data curation: DF-O.
- Formal analysis: DF-O.
- Investigation: DF-O.
- Methodology: DF-O.
- Project administration: DF-O.
- Resources: DF-O.
- Supervision: DF-O VMC.
- Validation: DF-O.
- Visualization: DF-O.
- Writing – original draft: DF-O VMC ML-C LD MD ML HO.
- Writing – review & editing: DF-O MD.
Associated Data
All relevant data are within the paper and its Supporting Information files.
In this paper, we have identified and analyzed the emergence, structure and dynamics of the paradigmatic research fronts that established the fundamentals of the biomedical knowledge on HIV/AIDS. A search of papers with the identifiers "HIV/AIDS", "Human Immunodeficiency Virus", “HIV-1” and "Acquired Immunodeficiency Syndrome" in the Web of Science (Thomson Reuters), was carried out. A citation network of those papers was constructed. Then, a sub-network of the papers with the highest number of inter-citations (with a minimal in-degree of 28) was selected to perform a combination of network clustering and text mining to identify the paradigmatic research fronts and analyze their dynamics. Thirteen research fronts were identified in this sub-network. The biggest and oldest front is related to the clinical knowledge on the disease in the patient. Nine of the fronts are related to the study of specific molecular structures and mechanisms and two of these fronts are related to the development of drugs. The rest of the fronts are related to the study of the disease at the cellular level. Interestingly, the emergence of these fronts occurred in successive "waves" over the time which suggest a transition in the paradigmatic focus. The emergence and evolution of the biomedical fronts in HIV/AIDS research is explained not just by the partition of the problem in elements and interactions leading to increasingly specialized communities, but also by changes in the technological context of this health problem and the dramatic changes in the epidemiological reality of HIV/AIDS that occurred between 1993 and 1995.
Introduction
The Human Immunodeficiency Virus/ Acquired Immunodeficiency Syndrome (HIV/AIDS) is a global health problem: over 70 million people have been infected with HIV, 35 million have died and 36.7 million people currently live with the disease [ 1 ]. HIV/AIDS is one of the most studied infection diseases with more than 260,000 papers (mentioning the topic) listed in GOPubMed [ 2 ] and more than 42,000 papers (mentioning HIV/AIDS in the title) in the Web of Science [ 3 ] spanning over thirty year of scientific research. HIV/AIDS is studied by a plurality of biomedical disciplines like epidemiology [ 4 ], virology [ 5 ], immunology [ 6 ] or drug development [ 7 ] and non-biomedical disciplines like social sciences [ 8 ] and humanities [ 9 ]. All the biomedical disciplines working on HIV/AIDS strongly rely on a solid scientific consensus, which explains the clinical manifestation of HIV/AIDS in terms of the virus interactions with the immune system cells; the behavior and demography of the immune system cells, and, most importantly, the virus interaction with the biomolecular machinery of the host cells [ 10 – 12 ]. Two features are believed to be at the core of the scientific consensus on HIV/AIDS: the natural history of the HIV infection (the number of CD4+ cells and HIV RNA copies plotted over the time) [ 11 ] and the virus replication cycle (from the virus entry to the virus assembly, budding and maturation) [ 10 , 12 ].
Paradigms are the keystone of research communities [ 13 , 14 ], for they provide a foundation for members of the community; they also define the questions, the standards, the rules and the expected results that drive research efforts [ 13 , 14 ]. Paradigms of HIV/AIDS research are often presented in a timeline format [ 12 , 15 ]. However, while such a historical perspective is informative, they present two disadvantages: the first is that the selection of the most relevant discoveries is arbitrary, i.e., not supported by scientometric evidence, while the second disadvantage is that the paradigms are not presented as the key elements of the organizing process of the research communities.
The study of the emerging research fronts offers the possibility of analyzing the relationship between the paradigms and the organizational process of the scientific communities [ 14 , 16 , 17 ]. Research fronts can be considered as modules or clusters in a citation network of papers, i.e., sparse sub-networks of papers that exhibit dense connections [ 18 ].
It must be pointed out that research fronts are the footprint of the scientific communities. That is, citation patterns of scientists exhibit homophily [ 14 , 19 ], which is caused by the scientists trend to cite those papers that focus in similar topics with a similar approach -and very often they cite those papers that strengthen the papers argumentation [ 14 , 19 , 20 ]. Citations tend to point toward those discoveries that the research (sub)communities consider the most relevant ones. i.e., the paradigms [ 13 , 14 , 21 – 23 ]. Therefore, paradigms occupy the most central location in the citation networks; they are the seeds that organize the emergence of the research fronts [ 14 , 17 ]. To explain the emergence of the biomedical consensus on HIV/AIDS requires a study of the structure and dynamics of the research fronts.
Previous studies using the research fronts analysis approach were mainly focused in topics from engineering [ 24 , 25 ], biotechnologies [ 18 ] and scientometrics [ 26 ]. There are some studies that focused in the structure of the biomedical knowledge on specific diseases [ 14 , 16 , 17 , 27 , 28 ]. Our previous research has been particularly focused in the core region of the literature networks [ 14 , 17 , 27 ]. By doing this we have discovered the key feature of the organization of the knowledge on cervical cancer [ 27 ] and Ebola fever [ 17 ]. Others have reported the evolution of research fronts in anthrax research [ 16 ], cancer research [ 28 ] and cardiovascular medicine [ 28 ]. By analyzing the structure and evolution of HIV/AIDS knowledge we further our understanding of the nature of the biomedical knowledge discovery.
Through a combination of text mining and network analysis, we sought to understand the emergence and evolution of the research fronts (the footprints of the research communities) that produced the paradigmatic explanation of this disease.
Methodology
- A search of papers on HIV/AIDS was performed in the Web of Science [ 3 ] during March, 2017. The search criteria were the following: TITLE: ("HIV AIDS") OR TITLE: ("Human immunodeficiency virus") OR TITLE: ("acquired immune deficiency syndrome") OR TITLE: (hiv-1). Refined by: DOCUMENT TYPES: (ARTICLE). Timespan: All years. Indexes: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI. 60,464 papers were found.
- A network model was built with the papers found in the Web of Science by using the software HistCite [ 29 ]. Then, the network model was analyzed and visualized with Cytoscape [ 30 ]. The indegree distribution of the network was evaluated to determine if it fitted to a power law function (y = ax^b).
- A core sub-network of papers with an indegree ≥ 28 was then closely examined. Normally, the indegree distribution in citation networks follows a power law function such that only a few papers are very well cited, while most papers are not [ 31 ]. This applies to the case of HIV/AIDS research as we report. We selected the papers with an indegree ≥ 28 because they are a small and workable quantity of papers that account for nearly half of the communication process through the citations network as it is reported in the results section (The selected papers received 42,8911 out of 679,497 citations from the HIV/AIDS literature). Top cited papers appear related to the paradigmatic milestones of a particular research topic.
- A cluster analysis based in the Newman modularity [ 32 ] was performed on the core sub-network using Clust&see, a Cystoscape plug-in [ 33 ]. This analysis divided the sub-network of citation in several research fronts (clusters or modules of papers). This clusters are defined by Newman as “groups of vertices within which connections are dense but between which they are sparse” [ 32 ].
- The sub-network was displayed by using the “yFiles organic” algorithm, which is based on the force-directed layout [ 30 ]. This algorithm considers the nodes as charged particles that exhibit repulsive forces and the vertices as springs. In this layout, the papers that cite the same papers tend to stick together making easier the visualization of the research fronts.
- The number of papers of each research front was plotted over the years in order to track the dynamics of the research fronts.
- The content of the identified research fronts -the abstract of their papers- was analyzed with KH Coder [ 34 ], a software for quantitative content analysis (Text mining). KH Coder delivered several outputs. However, we considered that the most informative output was the list of the most distinctive words which provided key information about what was the main focus of the papers of each front. Additionally, the five papers with the highest indegree within each of the research fronts were identified. in order to provide a context to the reading of the text mining results.
- Because front 1 “patient” is the largest and most central front according to our results, a cluster analysis was then performed on it by using Clust&see. The sub-modules that form front 1 were identified.
The network model
60,464 published articles on HIV/AIDS were identified by keyword search over the Thomson Reuters Web of Science. 57,485 of these papers form a single network of 679,497 inter-citations. The structural network analysis performed by Cytoscape showed that the distribution of the indegree in this network fitted a power law function (y = ax^b, a = 51,954, b = -1.79, correlation = 0.827, R-squared = 0.909). This means that a very small number of papers receive the overwhelming majority of citations while most papers receive few if any citations [ 31 , 35 ].
We selected papers with an indegree ≥ 28, that is, 5,933 documents. Together, these papers receive 63% of the inter-citations that form the whole network (42,8911 of 679,497), and would represent a relevant part of the historical core of the HIV/AIDS research as it was explained in the methodology section. These 5,933 highly cited papers formed a network of 86,963 inter-citations ( Fig 1 ). The cluster network analysis identified fourteen clusters (or modules as defined by Newman). However, one cluster were too small to be considered relevant research fronts. The thirteen clusters were formed by 12,303, 9,115, 7,407, 6,746, 5,680, 4,763, 4,696, 3507, 2,861, 2,768, 2,597, 2,053, and 1,662 inter-citations.

The model is displayed by using the “yFiles organic” algorithm. The color of nodes (representing the papers) and vertices indicates which research front they belong to.
The organization and dynamics of the research fronts
The main interaction among the seven research fronts is shown in Fig 2 . In this figure, each of the research fronts is represented by a single node, and the edges represent the sum of the inter-citations among the fronts ( Fig 2 ). Therefore, this graphical synthesis allows us to understand how the paradigmatic core of HIV/AIDS research was organized. However, the complete panorama can be only understood when Fig 2 is simultaneously read with Fig 3 and with Table 1 and S1 Table . Fig 3 shows the dynamics of the research fronts by plotting the number of citation papers per year of each research. In Fig 3 , the fronts are shown in different plots according to the period of time in which the fronts reached their maximum number of papers per year: between 1990 and 1991 ( Fig 3A ), between 1996 and 1999 ( Fig 3B ), and between 2004 and 2007 ( Fig 3C ). S1 Table provides the detailed description of each research front, including its structural features; the main topics of each research fronts according to the text mining analysis, and the list of the papers with the highest indegree within each research front. Table 1 groups the fronts according to the organization level (Individual, cellular-tissular and molecular) and the period in which the number of papers of each front peaked. The figures and the tables together offer an interesting view of the evolution and organization of HIV/AIDS research in the three first decades:

Each node represents one of the seven research fronts. The edges represent the sum of the inter-citations between two clusters. Only the interactions formed by a minimal of 500 inter-citations or the largest interaction (If the front have none interaction ≥ 500 inter-citations) of each front are shown.

A: Research fronts whose number of papers peaked between 1990 and 1991, B: peaked between 1996 and 1999 and C: peaked between 2004 and 2007.
| Level/peak | 1990–1991 | 1996–1998 | 2004–2007 |
|---|---|---|---|
| Individual | F1 Patient | ||
| Cellular-tissular | F10 Brain | F3 isolate | F9 Cytotoxic T lymphocyte |
| Molecular | F2 gp120, F4 Tat-tar, F5 Reverse transcriptase | F8 Integrase, F11 Replication/Nef, F12 Nucleocapsid | F6 Gag/assembly, F7 protease, F13 Infectivity/Vif |
HIV/AIDS research is reductionistly-organized, following a hierarchy of biological structures and systems ( Fig 2 , Table 1 ). That is, at the core of the network is located the front 1 “patient” (Figs (Figs1 1 and and2) 2 ) which focus on the study of the HIV/AIDS phenomenon at individual-systemic level. Surrounding front 1, there are research fronts (Front 3 “isolate,” front 9 “Cytotoxic T lymphocyte” and front 10 “brain” in Fgs 1 and 2) that are related to the study of specific events of the disease at cellular level ( Table 1 and S1 Table ). In the most external part of the network model there are most of the fronts related to the study of molecular structures and mechanisms (Front 5 “reverse transcriptase inhibitor” front 6 “assembly,” front 7 “protease inhibitor” front 8 “integration,” front 11 “replication,” front 12 “nucleocapsid” front and 13 “infectivity”; see Figs Figs1 1 and and2 2 and Table 1 and S1 Table ). On the other hand, Front 2 “glycoprotein 120” and front 5 “reverse transcriptase inhibitor” are strongly connected to front 1 “patient” (Figs (Figs1 1 and and2) 2 ) However, the research in these fronts (2 and 5) is oriented to the development of treatments (immuno-therapies and small molecules drugs, respectively), which may explain their strong connection to front 1. Notice that fronts 3 and 2 function as transition zones in HIV/AIDS research connecting the different levels of observation (systemic, tissular-to-cellular and molecular) (Figs (Figs1 1 and and2 2 ).
On the other hand, the research fronts clearly can be grouped in three different periods of time in which the fronts reach their maximum number of papers per year: 1990–1991, 1996–1999 and 2004–2007 ( Fig 3 ). In order to properly read Fig 3 it is important to keep in mind the dramatic changes in the epidemiology of HIV/AIDS in the United States (USA) that happened between 1993 and 1995 [ 36 ]. In that period, the number of AIDS diagnosis and deaths reached their maximum and then declined[ 36 ]. Simultaneously, in 1995, the number of persons living with HIV began to rise[ 36 ]. Therefore, we can consider the existence of two stages in the history of HIV/AIDS: before 1995 in which AIDS was the main concern and after 1995 when HIV infection is at the center of HIV/AIDS research. A second important consideration to understand Fig 3 is that the phase of expansion or growth in science (the “normal” science of Thomas Kuhn) follows the publication of those scientific achievements that organize the subsequent research[ 13 ]. This would explain that the peaks in Fig 3 generally occurred years after the publication of the papers with the highest degree ( Fig 3 and S1 Table ). The peaks in figure can be considered a delayed response to fundamental events and discoveries in the history of HIV/AIDS research. A third consideration is that the network model is made from the ten percent of papers with the highest indegree. Therefore, the succession of research fronts observed in Fig 3 does not mean the end of the research on specific topics but that these topics are not longer in the core of HIV/AIDS research.
Fronts 2 “glycoprotein 120,” 4 “tat-tar,” 5 “reverse transcriptase inhibitor” and 10 “brain” emerged immediately after front 1 and peaked in the 1990 and 1991 years. The expansion of these fronts in this early stage in the history of HIV/AIDS research suggests that these fronts are relevant to the description, explanation or intervention of AIDS. For example, it has been pointed out that tat (Trans-activator of transcription) protein, which is essential for virus replication, could be involved in the progression to AIDS and in the development of Kaposi's sarcoma lesions.[ 37 , 38 ] Along the same line, the interaction between glycoprotein 120 and CD4 is the first event in the replication cycle and is considered fundamental to virus entry.[ 39 ] It is important to keep in mind that the depletion of lymphocytes expressing CD4 is considered the most severe hematological feature of AIDS.[ 39 ] Similarly, encephalopathy is one of the most dominant feature of AIDS.[ 40 ] Finally, a reverse transcriptase inhibitor, zidovudine (AZT) was the first drug approved by the United States Food and Drug Administration (FDA) to treat AIDS.[ 41 ]
Research fronts 1 “patient,”and 3 “isolate,” reached their maximum number of papers per year between 1996 and 1999 ( Fig 3 ). The peaks of these fronts follow the changes in the epidemiology of HIV/AIDS in the USA. Therefore, these fronts are possibly related to a collective response from the scientific community to the new reality of the disease. The research in front 1 is the largest, central and most clinical among the fronts (Figs (Figs1 1 and and2, 2 , and S1 Table ). This front connects the clinical and epidemiological manifestations of HIV/AIDS with their explanation at a cellular level. Because of the size, the centrality and clinical relevance, we decided to perform a second round of cluster analysis to identify the sub-modules that may conform front 1. We plotted the contribution of each sub-module to the evolution of front 1 in Fig 4 . Sub-module 1A, 1D and 1E are the key components of the 1999's peak ( Fig 4 ). The papers with the highest indegree in sub-modules 1A, 1D and 1E are, respectively, “Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment,”[ 42 ] “Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection”[ 43 ] and “Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy”.[ 44 ] These papers report and explain fundamental changes in the clinical reality of HIV/AIDS produced by the implementation of anti-retroviral therapies. Front 3 “isolate,” to the study of HIV tropism, i.e., the differential capacity of the HIV strains to infect and replicates in different cell types ( Table 1 ). Importantly, the availability of screening tools that allowed the identification of asymptomatic individuals infected with HIV and the use of anti-retroviral therapies make extensively available the blood and tissue samples from the patients that were fundamental to the emergence of front 3.

On the other hand, most of the research fronts specialized in the study of specific molecular mechanisms and structures (fronts 6 to 9 and fronts 11 to 13) peaked either in the 1996–1999 or 2004–2007 periods ( Fig 3 ). It is important to notice that all these fronts emerged at the end of the first decade of HIV/AIDS research. The difference between fronts peaking in the second and the third periods is that the former decline earlier. In order to understand the evolution of these fronts is important to keep in mind that the scientific specialization is a continuous process of solving problems that follows the establishment of a paradigm (HIV-1 as the etiological agent of HIV/AIDS).[ 13 ] In that sense, the decline of fronts 8, 11 and 12 ( Fig 3B ) may be so because the scientific problem is either essentially solved or the changes in the HIV/AIDS epidemiology made less relevant the topics related to these fronts.
According to the Cytoscape analysis, the network of HIV/AIDS papers displays a power law distribution of their citations, which has important methodological implications. The first implication is that a research front (a citation network module) could be formed by other research fronts, which in turn can be partioned into sub-modules [ 44 ]. The second implication is that the nodes (papers) with the highest indegree tend to be more “cosmopolitan” i.e., they have the lowest clustering coefficient values [ 44 ]. That is, they could belong simultaneously to several fronts or any of them. Therefore, there are not clearly defined frontiers dividing the research fronts. However, the standard in the scientometrics study of research fronts seems to be to use clustering methods that define frontiers between the modules [ 14 , 17 , 18 , 24 , 25 , 27 , 28 ], probably because this is make much more understandable the community structure in a literature network. Moreover, our analysis reveals the front that is most relevant to each paper. Finally, the most important implication is that in a hierarchical literature network the most the papers with the highest indegree are related with the paradigms that organize a research field or topic [ 14 ]. Top cited papers have been extensively used to identify the scientific achievements that establish the standards of research practice of a particular community [ 14 , 17 , 22 , 23 , 27 , 28 , 45 , 46 ]. There are no set guidelines on the proportion of top cited papers that should be selected. However, there is a trade off between selecting the most informative papers and maintaining diversity of the information [ 14 , 17 ]. In this work, we used a minimal indegree of 30 to select the top cited papers, and in turn obtaining a considerable percentage of the citations. The selected papers consist of only ten percent of the network but they effectively account for two thirds of the citations. The selected papers are a reasonable representation of the paradigmatic core of HIV/AIDS research.
Once the HIV was recognized as the etiological factor HIV/AIDS research entered in normal science mode that is characterized by a high productivity and for a specialization of the researchers. By specialization we refer to “concentrate exclusively upon the subtlest and most esoteric aspects of the natural phenomena that concern his group” [ 12 ]. Once the paradigms are established, researchers focus on the details, the smaller range problems and solutions that the current paradigm provide [ 13 ]. Our results suggest that the emergence of several of the specialized research fronts was caused by the partition of the general problem in interacting elements. That is, HIV/AIDS research could be understood to some extent as a particular instance of part-whole science in which paradigms determine the abstraction of the parts that are considered the most relevant to explain the whole phenomenon [ 47 , 48 ].
The general structure and evolution of the research fronts in HIV/AIDS research shares similarities to that of anthrax and Ebola. The evolution of anthrax investigation began with a preliminary on the immunology of the disease [ 16 ]. From this, four research fronts emerged: “anthrax gene sequencing”, “vaccine research”, secondary research on PA (protective antigen) and LF (lethal factor), and “making and purifiying toxin” [ 16 ]. Subsequently, the research front on PA and LF split in three fronts: “specific PA research”, PA mediated delivery of other substances” and specific “LF research” [ 16 ]. Similarly, the evolution of the fronts in Ebola research are marked by a front related to the report of the epidemiology and the clinical manifestation of the disease [ 17 ]. A second front provide an explanation of the disease at tissue-cellular level [ 17 ]. Then, research on Ebola split into four research fronts, each one specialized in one different virus protein [ 17 ]. There is also a front aimed to the development of vaccines and other immunotherapies [ 17 ]. Similarly, the emergence of the fronts in HIV/AIDS research started with a general research front that provided the pathology of the disease and subsequently split into specialized fronts focused on the study of specific molecular mechanism of the virus replication cycle. In all three cases, the specialization of the research led to the emergence of research fronts focused in the study of the parts that are thought to be key in explaining the diseases. A report on the emergence of the research fronts in cancer and cardiovascular diseases showed that the specialization process in these types of diseases is complex [ 28 ]. Jones et al. reported fronts specialized on microarrays, targeted therapies, clinical trials, epidemiology and molecular etiology in cancer research [ 28 ], while in cardiovascular diseases the fronts are organized around drug-eluting stents, anti-platelet agents, pacemakers, hypertension and atrial fibrillation [ 28 ]. The difference between these two groups of diseases is that HIV/AIDS, anthrax and Ebola are infectious diseases with a clearly identified etiological agent while cancer and cardiovascular diseases are both complex multifactorial diseases [ 49 ].
This is the first time that the complex organization (and the evolution) of HIV/AIDS research is reported. Our research provides fundamental knowledge concerning the emergence of the paradigmatic explanation for HIV/AIDS and therefore makes a contribution to the understanding of the nature of biomedical knowledge. In addition, our work suggests that the development of the paradigmatic knowledge on HIV/AIDS in terms of the emergence and evolution of the research fronts followed two different routes. First, the emergence of the specialized fronts (molecular mechanism and structures and cellular process) was caused by the division of the general problem in their key process, element and interactions, which is related to the concept of part-whole science. Second, the dynamics of the fronts, particularly the evolution of front 1 “patient” and 2 “isolate”, appears to represent an adaptive and collective response from the scientific community to changes in the epidemiological (the decline in the morbidity and mortality of AIDS in the USA) and technological (the availability of treatments and screening tools) context of this health problem.
Supporting information
Structural properties; top 10 distinctive worlds, and list of the five papers with the highest indegree within each of the research fronts.
Funding Statement
The authors received no specific funding for this work.
Data Availability

IMAGES
VIDEO
COMMENTS
HIV/AIDS is an exceptional epidemic that demands an exceptional response. Much progress has been made in a short space of time, despite many scientific and programmatic challenges ( figure 6 ). In the absence of a protective vaccine or a cure, prevention and access to antiretroviral treatments are the best options to slow down the HIV-1 pandemic.
Interview with Dr. Anthony Fauci on progress made during the past four decades of the HIV/AIDS pandemic and ongoing efforts to end this threat. 18m 44s Download. The dramatic saga of the acquired ...
HIV/AIDS is a pandemic condition—an epidemic of diseases that spreads across large areas like multiple continents or ... Research studies suggest that the termination of forming ds-DNA chains is a crucial factor that leads to an inhibitory effect. ... The authors listed in this paper wish to express their appreciation to the RSST trust ...
Abstract. Substantial progress has been made towards the goal of ending the HIV/AIDS epidemic due to advancements in both prevention and treatment of HIV. However, major challenges still remain. We describe basic principles of epidemic control in the context of HIV and identify a number of attainable goals in terms of control and elimination of ...
The global burden of HIV/AIDS was 36.9 million cases in 2019, corresponding to 0.5% of the world's population, with a prevalence rate of 476 cases per 100,000. Global HIV prevalence showed a peak in 2005, decreasing for 5 years and then regaining a rising trend since 2010 (possibly due to increased survival with ART).
nities in the research agenda and in the process of drug availability Progress against the HIV/AIDS Epidemic. 1980s 1990s 2000s 2010s 1981:˘AIDS epidemic first recognized; cases reported in New York
Future focus. Investing in innovative strategies that meet the needs of individuals won't just be key to ending the HIV/AIDS pandemic by 2030. It will also help to ensure that global health ...
Center for Clinical AIDS Research and Education, David Geffen School of Medicine, University of California, Los Angeles, CA, USA Raphael J. Landovitz Bridge HIV, San Francisco Department of Public ...
Africa, has the highest global burden of HIV (70·8%; fi gure 1). The global epidemiology of HIV infection has changed markedly as a result of the expanding access to antiretroviral therapy; by 2012, 9·7 million people in low-income and middle-income countries had started antiretroviral therapy.4 The global prevalence of HIV has increased from ...
The HIV-1 pandemic is a complex mix of diverse epidemics within and between countries and regions of the world, and is undoubtedly the defining public-health crisis of our time. Research has deepened our understanding of how the virus replicates, manipulates, and hides in an infected person. Although our understanding of pathogenesis and transmission dynamics has become more nuanced and ...
Publishing the very latest ground breaking research on HIV and AIDS. Read by all the top clinicians and researchers, AIDS has the highest impact of all AIDS-related journals. With 18 issues per year, AIDS guarantees the authoritative presentation of significant advances. The Editors, themselves noted international experts who know the demands of your work, are committed to making AIDS the most ...
The threat of epidemic resurgence in HIV is absolute, and the incidence reported from recent prevention trials should be seen as a crucial indicator that the HIV and AIDS pandemic is not over. Persistence in funding primary prevention research for a vaccine and in implementation of all available biomedical interventions is needed for policy ...
The collective output of the HIV and AIDS research community has been prodigious: more than 125,000 papers related to HIV and AIDS are catalogued in the PubMed database of the National Library of ...
The largest funder of HIV/AIDS research is the National Institutes of Health (NIH), investing nearly $69 billion in AIDS research from fiscal years 1982-2018. Despite the staggering disease burden, the scientific advances directly resulting from investments in AIDS research have been extraordinary.
Approximately 1.2 million people in the United States are currently living with HIV, and an estimated 14% are infected, yet unaware of their status (Office of Infectious Disease and HIV/AIDS Policy, 2020).HIV and AIDS continue to have a disproportionate impact on certain populations, including youth—gay, bisexual, and other men who have sex with men (MSM)—racial and ethnic minorities ...
In a 2012 paper, author K.D.C. suggested that global health trends could best be analyzed through the lenses of development, public health, and health security . The fourth decade of AIDS started in the aftermath of the global financial crisis and the influenza (H1N1) pandemic and is finishing amid the coronavirus disease (COVID-19) pandemic.
AIDS 2022 underscored the value of NIH-sponsored HIV/AIDS research and its overall impact on public health for those with, or affected by, HIV. Central to this discussion was the importance of community engagement in HIV prevention and treatment. Recent research has led to breakthroughs in HIV testing, prevention, and treatment; however, these ...
Human immunodeficiency virus (HIV) is an infection that attacks the body's immune system. Acquired immunodeficiency syndrome (AIDS) is the most advanced stage of the disease. HIV targets the body's white blood cells, weakening the immune system. This makes it easier to get sick with diseases like tuberculosis, infections and some cancers.
AIDS is a. condition in humans in which p rogressive failure of the immune s ystem allows life-threatening. infections and cancers to thrive. Infection with HIV occurs by t he transfer of blood ...
The AIDS Epidemic Arises . ... 30 Years of AIDs Research. ... evidence that the risk of HIV transmission through anal sex when HIV viral load is suppressed is effectively zero," the paper ...
Almost all the research in India is based on beliefs, attitudes, and awareness of HIV among adolescents 2,12. However, few other studies worldwide have examined mass media as a strong predictor of ...
In this paper, we systematically review the scientific literature on HIV/AIDS related stigma to document the current state of research, identify gaps in the available evidence, and highlight promising strategies to address stigma. ... and diminish the phenomenon. In this systematic review of stigma and the HIV/AIDS epidemic, we examined the ...
"The global response to the HIV/AIDS epidemic stands as a multilateral success story — having made remarkable gains," he said, noting that since peaking in 2004, the number of HIV/AIDS-related deaths has significantly declined. ... It is also imperative to significantly scale up research and development and capacity-building, including ...
COVID-19 was—and to a large extent remains—the most meaningful health event in recent global history ().Unlike the 2003 Severe Acute Respiratory Syndrome (SARS) epidemic, it spread globally; unlike Zika, everyone is at risk of infection with COVID-19; and unlike recent swine flu pandemics, the disease severity and mortality from COVID-19 were so high it led to life expectancy reversals in ...
A federal initiative called Ending the HIV Epidemic, which launched in 2019, has doled out more than $2.2 billion. The extra money goes to 57 jurisdictions with the highest rates of new HIV diagnoses.
Ever since HIV-1 was first discovered, the reasons for its sudden emergence, epidemic spread, and unique pathogenicity have been a subject of intense study. A first clue came in 1986 when a morphologically similar but antigenically distinct virus was found to cause AIDS in patients in western Africa (Clavel et al. 1986).
The same research also documents how the opioid epidemic—commonly regarded as a national public health crisis among white Americans—had a much deeper impact in Black communities, where ...
HIV/AIDS is one of the most studied infection diseases with more than 260,000 papers (mentioning the topic) listed in GOPubMed and more than 42,000 papers (mentioning HIV/AIDS in the title) in the Web of Science spanning over thirty year of scientific research. HIV/AIDS is studied by a plurality of biomedical disciplines like epidemiology ...