- Login / FREE TRIAL

‘Nursing Times wants to ensure that the voices of nurses and midwives are heard’
STEVE FORD, EDITOR
- You are here: COPD

Diagnosis and management of COPD: a case study
04 May, 2020
This case study explains the symptoms, causes, pathophysiology, diagnosis and management of chronic obstructive pulmonary disease
This article uses a case study to discuss the symptoms, causes and management of chronic obstructive pulmonary disease, describing the patient’s associated pathophysiology. Diagnosis involves spirometry testing to measure the volume of air that can be exhaled; it is often performed after administering a short-acting beta-agonist. Management of chronic obstructive pulmonary disease involves lifestyle interventions – vaccinations, smoking cessation and pulmonary rehabilitation – pharmacological interventions and self-management.
Citation: Price D, Williams N (2020) Diagnosis and management of COPD: a case study. Nursing Times [online]; 116: 6, 36-38.
Authors: Debbie Price is lead practice nurse, Llandrindod Wells Medical Practice; Nikki Williams is associate professor of respiratory and sleep physiology, Swansea University.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
Introduction
The term chronic obstructive pulmonary disease (COPD) is used to describe a number of conditions, including chronic bronchitis and emphysema. Although common, preventable and treatable, COPD was projected to become the third leading cause of death globally by 2020 (Lozano et al, 2012). In the UK in 2012, approximately 30,000 people died of COPD – 5.3% of the total number of deaths. By 2016, information published by the World Health Organization indicated that Lozano et al (2012)’s projection had already come true.
People with COPD experience persistent respiratory symptoms and airflow limitation that can be due to airway or alveolar abnormalities, caused by significant exposure to noxious particles or gases, commonly from tobacco smoking. The projected level of disease burden poses a major public-health challenge and primary care nurses can be pivotal in the early identification, assessment and management of COPD (Hooper et al, 2012).
Grace Parker (the patient’s name has been changed) attends a nurse-led COPD clinic for routine reviews. A widowed, 60-year-old, retired post office clerk, her main complaint is breathlessness after moderate exertion. She scored 3 on the modified Medical Research Council (mMRC) scale (Fletcher et al, 1959), indicating she is unable to walk more than 100 yards without stopping due to breathlessness. Ms Parker also has a cough that produces yellow sputum (particularly in the mornings) and an intermittent wheeze. Her symptoms have worsened over the last six months. She feels anxious leaving the house alone because of her breathlessness and reduced exercise tolerance, and scored 26 on the COPD Assessment Test (CAT, catestonline.org), indicating a high level of impact.
Ms Parker smokes 10 cigarettes a day and has a pack-year score of 29. She has not experienced any haemoptysis (coughing up blood) or chest pain, and her weight is stable; a body mass index of 40kg/m 2 means she is classified as obese. She has had three exacerbations of COPD in the previous 12 months, each managed in the community with antibiotics, steroids and salbutamol.
Ms Parker was diagnosed with COPD five years ago. Using Epstein et al’s (2008) guidelines, a nurse took a history from her, which provided 80% of the information needed for a COPD diagnosis; it was then confirmed following spirometry testing as per National Institute for Health and Care Excellence (2018) guidance.
The nurse used the Calgary-Cambridge consultation model, as it combines the pathological description of COPD with the patient’s subjective experience of the illness (Silverman et al, 2013). Effective communication skills are essential in building a trusting therapeutic relationship, as the quality of the relationship between Ms Parker and the nurse will have a direct impact on the effectiveness of clinical outcomes (Fawcett and Rhynas, 2012).
In a national clinical audit report, Baxter et al (2016) identified inaccurate history taking and inadequately performed spirometry as important factors in the inaccurate diagnosis of COPD on general practice COPD registers; only 52.1% of patients included in the report had received quality-assured spirometry.
Pathophysiology of COPD
Knowing the pathophysiology of COPD allowed the nurse to recognise and understand the physical symptoms and provide effective care (Mitchell, 2015). Continued exposure to tobacco smoke is the likely cause of the damage to Ms Parker’s small airways, causing her cough and increased sputum production. She could also have chronic inflammation, resulting in airway smooth-muscle contraction, sluggish ciliary movement, hypertrophy and hyperplasia of mucus-secreting goblet cells, as well as release of inflammatory mediators (Mitchell, 2015).
Ms Parker may also have emphysema, which leads to damaged parenchyma (alveoli and structures involved in gas exchange) and loss of alveolar attachments (elastic connective fibres). This causes gas trapping, dynamic hyperinflation, decreased expiratory flow rates and airway collapse, particularly during expiration (Kaufman, 2013). Ms Parker also displayed pursed-lip breathing; this is a technique used to lengthen the expiratory time and improve gaseous exchange, and is a sign of dynamic hyperinflation (Douglas et al, 2013).
In a healthy lung, the destruction and repair of alveolar tissue depends on proteases and antiproteases, mainly released by neutrophils and macrophages. Inhaling cigarette smoke disrupts the usually delicately balanced activity of these enzymes, resulting in the parenchymal damage and small airways (with a lumen of <2mm in diameter) airways disease that is characteristic of emphysema. The severity of parenchymal damage or small airways disease varies, with no pattern related to disease progression (Global Initiative for Chronic Obstructive Lung Disease, 2018).
Ms Parker also had a wheeze, heard through a stethoscope as a continuous whistling sound, which arises from turbulent airflow through constricted airway smooth muscle, a process noted by Mitchell (2015). The wheeze, her 29 pack-year score, exertional breathlessness, cough, sputum production and tiredness, and the findings from her physical examination, were consistent with a diagnosis of COPD (GOLD, 2018; NICE, 2018).
Spirometry is a tool used to identify airflow obstruction but does not identify the cause. Commonly measured parameters are:
- Forced expiratory volume – the volume of air that can be exhaled – in one second (FEV1), starting from a maximal inspiration (in litres);
- Forced vital capacity (FVC) – the total volume of air that can be forcibly exhaled – at timed intervals, starting from a maximal inspiration (in litres).
Calculating the FEV1 as a percentage of the FVC gives the forced expiratory ratio (FEV1/FVC). This provides an index of airflow obstruction; the lower the ratio, the greater the degree of obstruction. In the absence of respiratory disease, FEV1 should be ≥70% of FVC. An FEV1/FVC of <70% is commonly used to denote airflow obstruction (Moore, 2012).
As they are time dependent, FEV1 and FEV1/FVC are reduced in diseases that cause airways to narrow and expiration to slow. FVC, however, is not time dependent: with enough expiratory time, a person can usually exhale to their full FVC. Lung function parameters vary depending on age, height, gender and ethnicity, so the degree of FEV1 and FVC impairment is calculated by comparing a person’s recorded values with predicted values. A recorded value of >80% of the predicted value has been considered ‘normal’ for spirometry parameters but the lower limit of normal – equal to the fifth percentile of a healthy, non-smoking population – based on more robust statistical models is increasingly being used (Cooper et al, 2017).
A reversibility test involves performing spirometry before and after administering a short-acting beta-agonist (SABA) such as salbutamol; the test is used to distinguish between reversible and fixed airflow obstruction. For symptomatic asthma, airflow obstruction due to airway smooth-muscle contraction is reversible: administering a SABA results in smooth-muscle relaxation and improved airflow (Lumb, 2016). However, COPD is associated with fixed airflow obstruction, resulting from neutrophil-driven inflammatory changes, excess mucus secretion and disrupted alveolar attachments, as opposed to airway smooth-muscle contraction.
Administering a SABA for COPD does not usually produce bronchodilation to the extent seen in someone with asthma: a person with asthma may demonstrate significant improvement in FEV1 (of >400ml) after having a SABA, but this may not change in someone with COPD (NICE, 2018). However, a negative response does not rule out therapeutic benefit from long-term SABA use (Marín et al, 2014).
NICE (2018) and GOLD (2018) guidelines advocate performing spirometry after administering a bronchodilator to diagnose COPD. Both suggest a FEV1/FVC of <70% in a person with respiratory symptoms supports a diagnosis of COPD, and both grade the severity of the condition using the predicted FEV1. Ms Parker’s spirometry results showed an FEV1/FVC of 56% and a predicted FEV1 of 57%, with no significant improvement in these values with a reversibility test.
GOLD (2018) guidance is widely accepted and used internationally. However, it was developed by medical practitioners with a medicalised approach, so there is potential for a bias towards pharmacological management of COPD. NICE (2018) guidance may be more useful for practice nurses, as it was developed by a multidisciplinary team using evidence from systematic reviews or meta-analyses of randomised controlled trials, providing a holistic approach. NICE guidance may be outdated on publication, but regular reviews are performed and published online.
NHS England (2016) holds a national register of all health professionals certified in spirometry. It was set up to raise spirometry standards across the country.
Assessment and management
The goals of assessing and managing Ms Parker’s COPD are to:
- Review and determine the level of airflow obstruction;
- Assess the disease’s impact on her life;
- Risk assess future disease progression and exacerbations;
- Recommend pharmacological and therapeutic management.
GOLD’s (2018) ABCD assessment tool (Fig 1) grades COPD severity using spirometry results, number of exacerbations, CAT score and mMRC score, and can be used to support evidence-based pharmacological management of COPD.

When Ms Parker was diagnosed, her predicted FEV1 of 57% categorised her as GOLD grade 2, and her mMRC score, CAT score and exacerbation history placed her in group D. The mMRC scale only measures breathlessness, but the CAT also assesses the impact COPD has on her life, meaning consecutive CAT scores can be compared, providing valuable information for follow-up and management (Zhao, et al, 2014).
After assessing the level of disease burden, Ms Parker was then provided with education for self-management and lifestyle interventions.
Lifestyle interventions
Smoking cessation.
Cessation of smoking alongside support and pharmacotherapy is the second-most cost-effective intervention for COPD, when compared with most other pharmacological interventions (BTS and PCRS UK, 2012). Smoking cessation:
- Slows the progression of COPD;
- Improves lung function;
- Improves survival rates;
- Reduces the risk of lung cancer;
- Reduces the risk of coronary heart disease risk (Qureshi et al, 2014).
Ms Parker accepted a referral to an All Wales Smoking Cessation Service adviser based at her GP surgery. The adviser used the internationally accepted ‘five As’ approach:
- Ask – record the number of cigarettes the individual smokes per day or week, and the year they started smoking;
- Advise – urge them to quit. Advice should be clear and personalised;
- Assess – determine their willingness and confidence to attempt to quit. Note the state of change;
- Assist – help them to quit. Provide behavioural support and recommend or prescribe pharmacological aids. If they are not ready to quit, promote motivation for a future attempt;
- Arrange – book a follow-up appointment within one week or, if appropriate, refer them to a specialist cessation service for intensive support. Document the intervention.
NICE (2013) guidance recommends that this be used at every opportunity. Stead et al (2016) suggested that a combination of counselling and pharmacotherapy have proven to be the most effective strategy.
Pulmonary rehabilitation
Ms Parker’s positive response to smoking cessation provided an ideal opportunity to offer her pulmonary rehabilitation (PR) – as indicated by Johnson et al (2014), changing one behaviour significantly increases a person’s chance of changing another.
PR – a supervised programme including exercise training, health education and breathing techniques – is an evidence-based, comprehensive, multidisciplinary intervention that:
- Improves exercise tolerance;
- Reduces dyspnoea;
- Promotes weight loss (Bolton et al, 2013).
These improvements often lead to an improved quality of life (Sciriha et al, 2015).
Most relevant for Ms Parker, PR has been shown to reduce anxiety and depression, which are linked to an increased risk of exacerbations and poorer health status (Miller and Davenport, 2015). People most at risk of future exacerbations are those who already experience them (Agusti et al, 2010), as in Ms Parker’s case. Patients who have frequent exacerbations have a lower quality of life, quicker progression of disease, reduced mobility and more-rapid decline in lung function than those who do not (Donaldson et al, 2002).
“COPD is a major public-health challenge; nurses can be pivotal in early identification, assessment and management”
Pharmacological interventions
Ms Parker has been prescribed inhaled salbutamol as required; this is a SABA that mediates the increase of cyclic adenosine monophosphate in airway smooth-muscle cells, leading to muscle relaxation and bronchodilation. SABAs facilitate lung emptying by dilatating the small airways, reversing dynamic hyperinflation of the lungs (Thomas et al, 2013). Ms Parker also uses a long-acting muscarinic antagonist (LAMA) inhaler, which works by blocking the bronchoconstrictor effects of acetylcholine on M3 muscarinic receptors in airway smooth muscle; release of acetylcholine by the parasympathetic nerves in the airways results in increased airway tone with reduced diameter.
At a routine review, Ms Parker admitted to only using the SABA and LAMA inhalers, despite also being prescribed a combined inhaled corticosteroid and long-acting beta 2 -agonist (ICS/LABA) inhaler. She was unaware that ICS/LABA inhalers are preferred over SABA inhalers, as they:
- Last for 12 hours;
- Improve the symptoms of breathlessness;
- Increase exercise tolerance;
- Can reduce the frequency of exacerbations (Agusti et al, 2010).
However, moderate-quality evidence shows that ICS/LABA combinations, particularly fluticasone, cause an increased risk of pneumonia (Suissa et al, 2013; Nannini et al, 2007). Inhaler choice should, therefore, be individualised, based on symptoms, delivery technique, patient education and compliance.
It is essential to teach and assess inhaler technique at every review (NICE, 2011). Ms Parker uses both a metered-dose inhaler and a dry-powder inhaler; an in-check device is used to assess her inspiratory effort, as different inhaler types require different inhalation speeds. Braido et al (2016) estimated that 50% of patients have poor inhaler technique, which may be due to health professionals lacking the confidence and capability to teach and assess their use.
Patients may also not have the dexterity, capacity to learn or vision required to use the inhaler. Online resources are available from, for example, RightBreathe (rightbreathe.com), British Lung Foundation (blf.org.uk). Ms Parker’s adherence could be improved through once-daily inhalers, as indicated by results from a study by Lipson et al (2017). Any change in her inhaler would be monitored as per local policy.
Vaccinations
Ms Parker keeps up to date with her seasonal influenza and pneumococcus vaccinations. This is in line with the low-cost, highest-benefit strategy identified by the British Thoracic Society and Primary Care Respiratory Society UK’s (2012) study, which was conducted to inform interventions for patients with COPD and their relative quality-adjusted life years. Influenza vaccinations have been shown to decrease the risk of lower respiratory tract infections and concurrent COPD exacerbations (Walters et al, 2017; Department of Health, 2011; Poole et al, 2006).
Self-management
Ms Parker was given a self-management plan that included:
- Information on how to monitor her symptoms;
- A rescue pack of antibiotics, steroids and salbutamol;
- A traffic-light system demonstrating when, and how, to commence treatment or seek medical help.
Self-management plans and rescue packs have been shown to reduce symptoms of an exacerbation (Baxter et al, 2016), allowing patients to be cared for in the community rather than in a hospital setting and increasing patient satisfaction (Fletcher and Dahl, 2013).
Improving Ms Parker’s adherence to once-daily inhalers and supporting her to self-manage and make the necessary lifestyle changes, should improve her symptoms and result in fewer exacerbations.
The earlier a diagnosis of COPD is made, the greater the chances of reducing lung damage through interventions such as smoking cessation, lifestyle modifications and treatment, if required (Price et al, 2011).
- Chronic obstructive pulmonary disease is a progressive respiratory condition, projected to become the third leading cause of death globally
- Diagnosis involves taking a patient history and performing spirometry testing
- Spirometry identifies airflow obstruction by measuring the volume of air that can be exhaled
- Chronic obstructive pulmonary disease is managed with lifestyle and pharmacological interventions, as well as self-management
Related files
200506 diagnosis and management of copd – a case study.
- Add to Bookmarks
Related articles

Nurse-led cognitive behavioural therapy for respiratory patients
Anxiety and depression are common comorbidities of chronic obstructive pulmonary disease. This…

Issues of home-based non-invasive ventilation
Non-invasive ventilation is increasingly used to manage patients with COPD at home,…

Improving outcomes with online COPD self-care
An innovative approach to the self-management of chronic obstructive pulmonary disease is…

An audit of care provided to patients with COPD
Nationwide audit of COPD care reveals many aspects of provision have improved,…
Have your say
Sign in or Register a new account to join the discussion.

COPD Case Study: Patient Diagnosis and Treatment (2024)
by John Landry, BS, RRT | Updated: May 16, 2024
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that affects millions of people around the world. It is primarily caused by smoking and is characterized by a persistent obstruction of airflow that worsens over time.
COPD can lead to a range of symptoms, including coughing, wheezing, shortness of breath, and chest tightness, which can significantly impact a person’s quality of life.
This case study will review the diagnosis and treatment of an adult patient who presented with signs and symptoms of this condition.
25+ RRT Cheat Sheets and Quizzes
Get access to 25+ premium quizzes, mini-courses, and downloadable cheat sheets for FREE.
COPD Clinical Scenario
A 56-year-old male patient is in the ER with increased work of breathing. He felt mildly short of breath after waking this morning but became extremely dyspneic after climbing a few flights of stairs. He is even too short of breath to finish full sentences. His wife is present in the room and revealed that the patient has a history of liver failure, is allergic to penicillin, and has a 15-pack-year smoking history. She also stated that he builds cabinets for a living and is constantly required to work around a lot of fine dust and debris.

Physical Findings
On physical examination, the patient showed the following signs and symptoms:
- His pupils are equal and reactive to light.
- He is alert and oriented.
- He is breathing through pursed lips.
- His trachea is positioned in the midline, and no jugular venous distention is present.
Vital Signs
- Heart rate: 92 beats/min
- Respiratory rate: 22 breaths/min
Chest Assessment
- He has a larger-than-normal anterior-posterior chest diameter.
- He demonstrates bilateral chest expansion.
- He demonstrates a prolonged expiratory phase and diminished breath sounds during auscultation.
- He is showing signs of subcostal retractions.
- Chest palpation reveals no tactile fremitus.
- Chest percussion reveals increased resonance.
- His abdomen is soft and tender.
- No distention is present.
Extremities
- His capillary refill time is two seconds.
- Digital clubbing is present in his fingertips.
- There are no signs of pedal edema.
- His skin appears to have a yellow tint.
Lab and Radiology Results
- ABG results: pH 7.35 mmHg, PaCO2 59 mmHg, HCO3 30 mEq/L, and PaO2 64 mmHg.
- Chest x-ray: Flat diaphragm, increased retrosternal space, dark lung fields, slight hypertrophy of the right ventricle, and a narrow heart.
- Blood work: RBC 6.5 mill/m3, Hb 19 g/100 mL, and Hct 57%.
Based on the information given, the patient likely has chronic obstructive pulmonary disease (COPD) .
The key findings that point to this diagnosis include:
- Barrel chest
- A long expiratory time
- Diminished breath sounds
- Use of accessory muscles while breathing
- Digital clubbing
- Pursed lip breathing
- History of smoking
- Exposure to dust from work
What Findings are Relevant to the Patient’s COPD Diagnosis?
The patient’s chest x-ray showed classic signs of chronic COPD, which include hyperexpansion, dark lung fields, and a narrow heart.
This patient does not have a history of cor pulmonale ; however, the findings revealed hypertrophy of the right ventricle. This is something that should be further investigated as right-sided heart failure is common in patients with COPD.
The lab values that suggest the patient has COPD include increased RBC, Hct, and Hb levels, which are signs of chronic hypoxemia.
Furthermore, the patient’s ABG results indicate COPD is present because the interpretation reveals compensated respiratory acidosis with mild hypoxemia. Compensated blood gases indicate an issue that has been present for an extended period of time.
What Tests Could Further Support This Diagnosis?
A series of pulmonary function tests (PFT) would be useful for assessing the patient’s lung volumes and capacities. This would help confirm the diagnosis of COPD and inform you of the severity.
Note: COPD patients typically have an FEV1/FVC ratio of < 70%, with an FEV1 that is < 80%.
The initial treatment for this patient should involve the administration of low-flow oxygen to treat or prevent hypoxemia .
It’s acceptable to start with a nasal cannula at 1-2 L/min. However, it’s often recommended to use an air-entrainment mask on COPD patients in order to provide an exact FiO2.
Either way, you should start with the lowest possible FiO2 that can maintain adequate oxygenation and titrate based on the patient’s response.
Example: Let’s say you start the patient with an FiO2 of 28% via air-entrainment mask but increase it to 32% due to no improvement. The SpO2 originally was 84% but now has decreased to 80%, and his retractions are worsening. This patient is sitting in the tripod position and continues to demonstrate pursed-lip breathing. Another blood gas was collected, and the results show a PaCO2 of 65 mmHg and a PaO2 of 59 mmHg.
What Do You Recommend?
The patient has an increased work of breathing, and their condition is clearly getting worse. The latest ABG results confirmed this with an increased PaCO2 and a PaO2 that is decreasing.
This indicates that the patient needs further assistance with both ventilation and oxygenation .
Note: In general, mechanical ventilation should be avoided in patients with COPD (if possible) because they are often difficult to wean from the machine.
Therefore, at this time, the most appropriate treatment method is noninvasive ventilation (e.g., BiPAP).
Initial BiPAP Settings
In general, the most commonly recommended initial BiPAP settings for an adult patient include this following:
- IPAP: 8–12 cmH2O
- EPAP: 5–8 cmH2O
- Rate: 10–12 breaths/min
- FiO2: Whatever they were previously on
For example, let’s say you initiate BiPAP with an IPAP of 10 cmH20, an EPAP of 5 cmH2O, a rate of 12, and an FiO2 of 32% (since that is what he was previously getting).
After 30 minutes on the machine, the physician requested another ABG to be drawn, which revealed acute respiratory acidosis with mild hypoxemia.
What Adjustments to BiPAP Settings Would You Recommend?
The latest ABG results indicate that two parameters must be corrected:
- Increased PaCO2
- Decreased PaO2
You can address the PaO2 by increasing either the FiO2 or EPAP setting. EPAP functions as PEEP, which is effective in increasing oxygenation.
The PaCO2 can be lowered by increasing the IPAP setting. By doing so, it helps to increase the patient’s tidal volume, which increased their expired CO2.
Note: In general, when making adjustments to a patient’s BiPAP settings, it’s acceptable to increase the pressure in increments of 2 cmH2O and the FiO2 setting in 5% increments.
Oxygenation
To improve the patient’s oxygenation , you can increase the EPAP setting to 7 cmH2O. This would decrease the pressure support by 2 cmH2O because it’s essentially the difference between the IPAP and EPAP.
Therefore, if you increase the EPAP, you must also increase the IPAP by the same amount to maintain the same pressure support level.
Ventilation
However, this patient also has an increased PaCO2 , which means that you must increase the IPAP setting to blow off more CO2. Therefore, you can adjust the pressure settings on the machine as follows:
- IPAP: 14 cmH2O
- EPAP: 7 cmH2O
After making these changes and performing an assessment , you can see that the patient’s condition is improving.
Two days later, the patient has been successfully weaned off the BiPAP machine and no longer needs oxygen support. He is now ready to be discharged.
The doctor wants you to recommend home therapy and treatment modalities that could benefit this patient.
What Home Therapy Would You Recommend?
You can recommend home oxygen therapy if the patient’s PaO2 drops below 55 mmHg or their SpO2 drops below 88% more than twice in a three-week period.
Remember: You must use a conservative approach when administering oxygen to a patient with COPD.
Pharmacology
You may also consider the following pharmacological agents:
- Short-acting bronchodilators (e.g., Albuterol)
- Long-acting bronchodilators (e.g., Formoterol)
- Anticholinergic agents (e.g., Ipratropium bromide)
- Inhaled corticosteroids (e.g., Budesonide)
- Methylxanthine agents (e.g., Theophylline)
In addition, education on smoking cessation is also important for patients who smoke. Nicotine replacement therapy may also be indicated.
In some cases, bronchial hygiene therapy should be recommended to help with secretion clearance (e.g., positive expiratory pressure (PEP) therapy).
It’s also important to instruct the patient to stay active, maintain a healthy diet, avoid infections, and get an annual flu vaccine. Lastly, some COPD patients may benefit from cardiopulmonary rehabilitation .
By taking all of these factors into consideration, you can better manage this patient’s COPD and improve their quality of life.

Final Thoughts
There are two key points to remember when treating a patient with COPD. First, you must always be mindful of the amount of oxygen being delivered to keep the FiO2 as low as possible.
Second, you should use noninvasive ventilation, if possible, before performing intubation and conventional mechanical ventilation . Too much oxygen can knock out the patient’s drive to breathe, and once intubated, these patients can be difficult to wean from the ventilator .
Furthermore, once the patient is ready to be discharged, you must ensure that you are sending them home with the proper medications and home treatments to avoid readmission.

Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
- Faarc, Kacmarek Robert PhD Rrt, et al. Egan’s Fundamentals of Respiratory Care. 12th ed., Mosby, 2020.
- Chang, David. Clinical Application of Mechanical Ventilation . 4th ed., Cengage Learning, 2013.
- Rrt, Cairo J. PhD. Pilbeam’s Mechanical Ventilation: Physiological and Clinical Applications. 7th ed., Mosby, 2019.
- Faarc, Gardenhire Douglas EdD Rrt-Nps. Rau’s Respiratory Care Pharmacology. 10th ed., Mosby, 2019.
- Faarc, Heuer Al PhD Mba Rrt Rpft. Wilkins’ Clinical Assessment in Respiratory Care. 8th ed., Mosby, 2017.
- Rrt, Des Terry Jardins MEd, and Burton George Md Facp Fccp Faarc. Clinical Manifestations and Assessment of Respiratory Disease. 8th ed., Mosby, 2019.
Recommended Reading
How to prepare for the clinical simulations exam (cse), faqs about the clinical simulation exam (cse), 7+ mistakes to avoid on the clinical simulation exam (cse), copd exacerbation: chronic obstructive pulmonary disease, epiglottitis scenario: clinical simulation exam (practice problem), guillain barré syndrome case study: clinical simulation scenario, drugs and medications to avoid if you have copd, the pros and cons of the zephyr valve procedure, the 50+ diseases to learn for the clinical sims exam (cse).
- Open access
- Published: 13 December 2023
The patient journey in Chronic Obstructive Pulmonary Disease (COPD): a human factors qualitative international study to understand the needs of people living with COPD
- Nicola Scichilone 1 ,
- Andrew Whittamore 2 ,
- Chris White 3 ,
- Elena Nudo 4 ,
- Massimo Savella 4 &
- Marta Lombardini 4
BMC Pulmonary Medicine volume 23 , Article number: 506 ( 2023 ) Cite this article
2887 Accesses
1 Altmetric
Metrics details
Chronic obstructive pulmonary disease (COPD) is a common condition that causes irreversible airway obstruction. Fatigue and exertional dyspnoea, for example, have a detrimental impact on the patient’s daily life. Current research has revealed the need to empower the patient, which can result in not only educated and effective decision-making, but also a considerable improvement in patient satisfaction and treatment compliance.
The current study aimed to investigate the perspectives and requirements of people living with COPD to possibly explore new ways to manage their disease.
Adults with COPD from 8 European countries were interviewed by human factor experts to evaluate their disease journey through the gathering of information on the age, performance, length, and impact of diagnosis, symptoms progression, and family and friends' reactions. The assessment of present symptoms, services, and challenges was performed through a 90-min semi-structured interview. To identify possible unmet needs of participants, a generic thematic method was used to explore patterns, themes, linkages, and sequences within the data collected. Flow charts and diagrams were created to communicate the primary findings. Following analysis, the data was consolidated into cohesive insights and conversation themes relevant to determining the patient's unmet needs.
The 62, who voluntarily accepted to be interviewed, were patients (61% females, aged 32–70 years) with a COPD diagnosis for at least 6 months with stable symptoms of different severity. The main challenges expressed by the patients were the impact on their lifestyle, reduced physical activity, and issues with their mobility. About one-fourth had challenges with their symptoms or medication including difficulty in breathing. Beyond finding a cure for COPD was the primary goal for patients, their main needs were to receive adequate information on the disease and treatments, and to have adequate support to improve physical activity and mobility, helpful both for patients and their families.
Conclusions
These results could aid in the creation of new ideas and concepts to improve our patient’s quality of life, encouraging a holistic approach to people living with COPD and reinforcing the commitment to understanding their needs.
Peer Review reports
Introduction
Chronic obstructive pulmonary disease (COPD) is defined by irreversible airway obstruction linked with comorbidities or systemic effects [ 1 ]. COPD is a worldwide epidemic that contributes significantly to healthcare expenses due to high morbidity and mortality rates [ 2 , 3 ]. The clinical assessment of fixed airflow limitation and symptoms such as coughing and wheezing determine a COPD diagnosis; nevertheless, COPD symptoms negatively impact the patient's daily activities and lifestyle [ 4 ]. Patients may encounter a variety of debilitating physical symptoms, resulting in functional loss and high degrees of psychosocial anguish [ 5 , 6 , 7 ].
Integrated approaches to disease assessment and management are required to better understand and address the burden of COPD symptoms from a patient's perspective [ 8 ].
According to a recent observational study, regardless of disease severity, more than half of COPD patients experienced symptoms during the whole 24-h day, and almost 80% of patients reported experiencing symptoms at least twice a day. Symptoms are linked to poor health, depression, anxiety, and poor sleep quality [ 9 , 10 ].
Patients with COPD and comorbidities remain particularly challenging to manage because in Europe there is, generally, no guidance at the national level except in the UK, Slovenia, and Germany [ 11 , 12 , 13 ]. In Nordic countries and France, the management of patients with COPD is mainly performed by general practitioners with an inadequate level of assistance [ 14 , 15 , 16 ]. In other countries, patient management is performed at the discretion of the local structures, and the need for a comprehensive, holistic approach is looked forward [ 17 , 18 , 19 , 20 ]. Other chronic conditions increase symptom load, impair functional performance, and negatively impact health status; thus, management strategies must be adjusted accordingly [ 10 ].
Care plans, within the healthcare system, emphasize the importance of addressing these patients' particular physical, psychological, social, and spiritual needs through holistic supportive input offered as person-centered care [ 21 ]. Understanding the patient's perspective on their support requirements (those areas of living with COPD for which they require assistance, such as help controlling symptoms or accessing financial benefits) is critical to facilitating this approach. A recent systematic literature review has identified a whole range of support needs for COPD patients, based on the perspectives of the patients themselves [ 7 ].
Our human factor study aims to explore how COPD has affected the patients’ daily lives and the lives of those around them, through the assessment of symptoms, treatment, and service availability, identifying what challenges the patient faces in living with COPD, and which are the unmet needs in the different stages of the journey of care.
This human factors COPD patient needs study was conducted in November 2022 by an ISO 13485 certified specialist human factors consultant (Rebus Medical Ltd), both in-person or remotely, via video call using the Zoom platform. Remote interviews were needed to enable more severe patients to attend the sessions and to ensure that the intended study sample was achieved. As for other qualitative analyses, a minimum of 48 participants were planned to be interviewed.
Interviews were conducted on a 1–1 basis, with patients who voluntarily accepted to be interviewed from 8 countries: Denmark, France, Germany, Italy, Slovenia, Spain, Sweden, and the UK. Each interview was 90 min long and followed a semi-structured approach allowing for unscripted discussion when the participants’ responses raised new questions. For interviews that took place outside of the UK, a native-speaking moderator conducted the interview, whilst an interpreter translated the conversation live to a data analyst (Fig. 1 ).

Summary of the study methods. Countries involved in the study are indicated in grey
Participants included in the study, aged 18 years or older, with a current COPD diagnosis, were screened for COPD severity according to GOLD criteria-2020-document [ 22 ] and voluntarily provided their informed consent.
Because the objectives were connected to identifying unmet requirements through video conference, the formative interviews were deemed low to minimal risk to participants and, thus, no formal approval to an Ethical Committee was required.
For interviews conducted in a language other than English, a simultaneous translator was recruited to enable a member of Rebus Medical staff to watch the interview listen to the translation, and record notes. Digital video recordings were collected to accurately account for each test session. Notes were verified at the end of each interview, while participant faces recorded on the videos were blurred to anonymize the footage. When all interviews were complete, the raw notes from each interview were collated and verified using the recorded videos in a master data capture spreadsheet.
The interviews were conducted to evaluate the journey of care through the collection of information on the gender, age, performance, length, and impact of diagnosis, symptoms progression, and family and friends’ reactions through questions that were designed on purpose to identify the unmet need and main challenges of each step of the patient’s journey. The evaluation of the current symptoms (fluctuations, flare-ups, alleviations, effect on sleep and daily activities including the use of electronic devices), services (health care providers support, insurance, available information on COPD), and challenges (in lifestyle, daily activities, treatments, symptoms management, emotional and environmental) was included in the semi-structured interview (Table 1 ).
As this was an exploratory insight interview, protocol deviations like alterations to the interviewer’s script to reformulate questions, ad hoc addition of questions and probes to the interviewer’s script to focus on points of interest specific to each participant, and changes to the interviewer’s script as the study progresses to allow for study learnings were permitted and expected.
A generic thematic approach was employed to uncover patterns, themes, links, and sequences within the data collected to identify probable unmet needs of participants through the patient journey of people living with COPD.
To communicate the major findings, flow charts, and diagrams were constructed. Following analysis, the data were synthesized and refined into cohesive insights and discussion themes pertinent to identifying the patient's unmet needs along the different stages of the patient journey.
A total of 62 patients (38—61% females) with COPD aged between 32 and 70 years ( N = 1 aged 25–40 years, N = 42 aged 41–65 years, N = 19 aged > 65 years) were interviewed. Most of the patients (35—56%) had severe COPD (Table 2 ).
Current- or past smokers were 49 (80%) of the 61 respondents. A larger proportion of patients with severe COPD (9/35, 26%) had never smoked compared to the moderate COPD patient group (3/27, 11%); in fact, 26 (74%) severe patients and 24 (89%) moderate were smokers or had smoked in the past (Fig. 2 ).
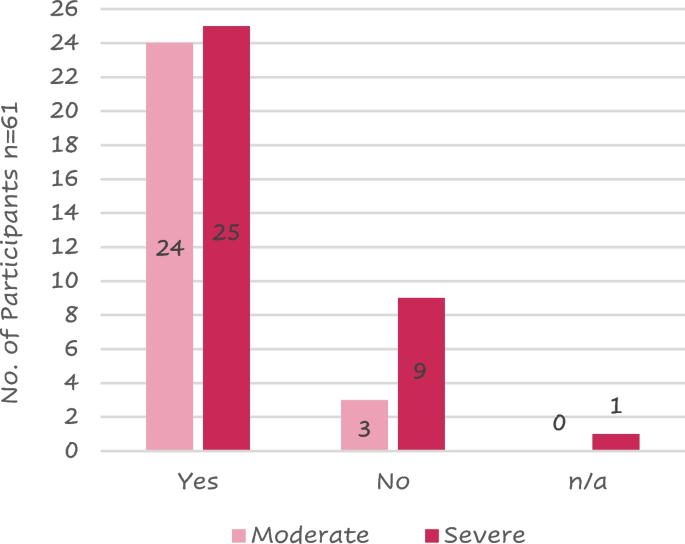
Distribution of patients that have ever been a smoker against COPD severity
Legend: n/a = not available
Patient journey
A total of 113 symptoms of COPD were recorded because most patients reported more than 1 symptom at the onset of the disease; 78 (69%) of these symptoms were related to dyspnoea. The highest reported symptoms were difficulty breathing and coughing (Fig. 3 ).
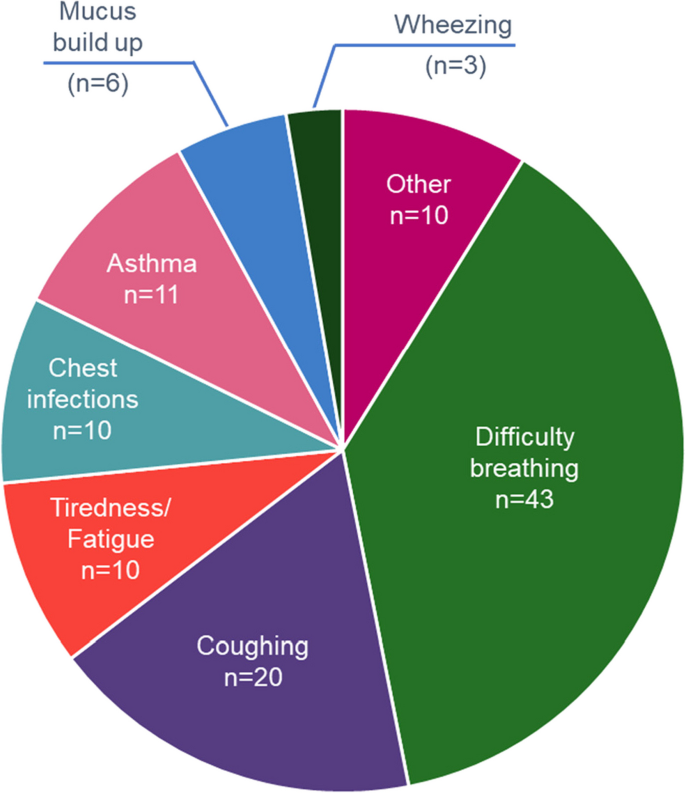
Patient’s reported signs and symptoms leading to COPD diagnosis
Note—Other includes chest tightness, hereditary respiratory issues, persistent flare ups, unable to walk upstairs, difficulty talking, difficulty walking, difficulty swallowing, bronchitis as a child and headaches
Fourteen (30%) of the 46 respondents referred to being diagnosed with COPD more than 1 year after initial symptoms, while 6 (13%) were diagnosed from 7 to 12 months from the onset of symptoms. Ten (64%) of the 14 requiring > 1 year for their diagnosis had severe COPD.
Most of the 56 patients who answered (41 – 73%) were diagnosed by a lung specialist mainly using spirometry (Fig. 4 ).
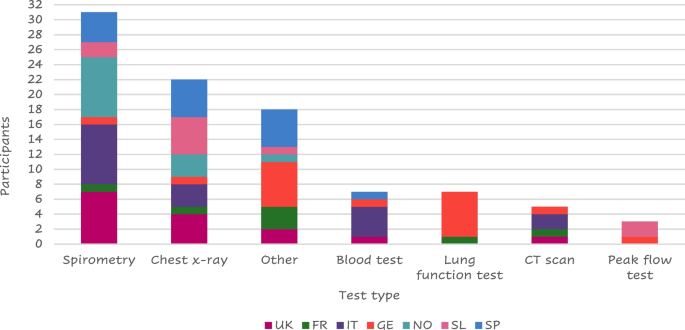
Tests performed at the visit of diagnosis
Legend: FR = France, GE = Germany, IT = Italy, SL = Slovenia, SP = Spain, NO = Northern (Sweden Denmark), UK = United Kingdom. “Other” includes: MRI, pressure cabin test, swabs collected, endoscope to check lungs, chamber, PET scan, Blood taken from the ear, blood gas test, oxygen saturation, walking/ running tests, echocardiogram, pulse oximeter/O 2 saturation, sleep test
About half of the responders (23 of 45 – 51%) felt their symptoms stable from the diagnosis (Fig. 5 ).
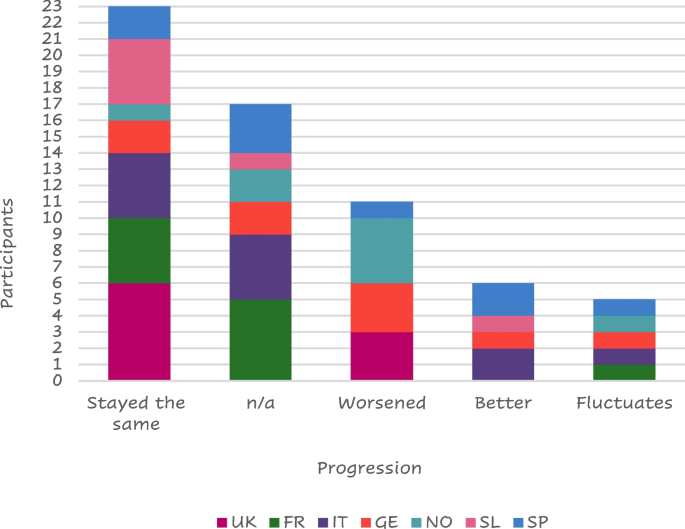
Symptom progression
Legend: FR = France, GE = Germany, IT = Italy, SL = Slovenia, SP = Spain, NO = Northern (Sweden Denmark), UK = United Kingdom, n/a = not available
Thirteen (29%) of those interviewed stated that their family and friends were supportive at the time of COPD diagnosis while 8 (18%) were worried about the diagnosis. Seven of them received no reaction from their family or friends and a further 7 did not tell anyone about their diagnosis. ‘Other’ reactions that were received from family and friends included: acceptance, anger, fear, shock, anguish, and expected, while some patients “prefer not to speak about it”.
The COPD diagnosis hurt 26 (58%) of the responders who described a negative impact of their COPD diagnosis, mainly because of their inability to be active, while 13 of them (29%) felt a positive impact mainly because they stopped or reduced smoking (Table 3 ).
Six (19%) of the 31 patients who provided details on the reason for quitting smoking reported they received more information about how to give up smoking and the risks associated with smoking, 3 patients mentioned some form of medication to support smoking cessation may have helped them give up, and 2 patients reported that they would give up for a family member but would struggle to have the motivation to do it themselves. Three patients reported that nothing would have helped them stop smoking while 8 patients reported that, despite knowing the impact smoking has, they still chose to smoke. Other suggestions to stop smoking reported by participants included: the threat of death, vaping if the smoking affected their fitness, cigarettes stopped being sold, stopping because of asthma and its diagnosis, quitting when they were in the hospital for a week giving it up after then, or because the smell was horrible.
A total of 59 patients answered about their changes in symptoms throughout the day; seventeen (29%) felt no changes while 13 (22%) worsened in the morning, 11 (19%) worsened at night, and 6 (10%) worsened both in the morning and at night.
Twenty-five (41%) of the 61 responders were hospitalized due to a COPD flare-up at least once after their COPD diagnosis; most of them had severe disease (Fig. 6 ).
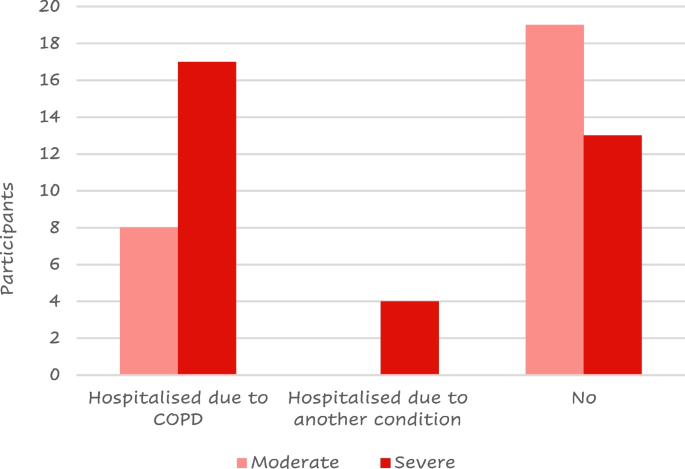
Number of patients that have experienced a COPD flare-up by COPD severity
Seven (30%) of the 23 patients who took any action to alleviate their symptoms, before seeing a doctor and getting a diagnosis, reduced their physical exercise to not trigger symptoms. While others were more vigilant with their health, received help from family and friends, or used inhalers, a rescue pack, or menthol sweets.
Thirty seven out of 58 participants reported sleep disruption. Of these, 12 (32%), reported disruption due to COPD while 10 (17%) had sleep negatively affected by another condition. Other causes for patients’ sleep disruption included coughing, the need to change sleeping positions, and cold weather.
Patients reported needing more support including more information about their condition, financial support for transportation, improved treatment options, accessibility badges, and help in carrying out chores in the house such as cooking, cleaning, and general housekeeping. Some patients also indicated a wish for personal training. Some patients were unaware of what type of support they may require or what type of support could be available to them while others were looking for a different inhaler or treatment to alleviate their cough or a device that assists deep breathing, transplant, a dog or a sport requiring a limited physical effort that would help them be more active, and/or meeting a COPD support group.
About half of the respondents (26/56 – 46%) used electronic devices to monitor their health status including a finger pulse oximeter ( n = 9), smartwatch ( n = 8), or a blood pressure cuff ( n = 5).
A total of 64 responses were collected from the 58 patients who shared their opinion on the treatment they were utilizing; 33 (52%) of the feedback was positive (Table 4 ).
While 20 (31%) of the respondents felt neutral about their current prescribed treatment, 11 (17%) reported either that their medicine had "no therapeutic impact", that they faced "psychological restraint" with their prescribed regime, or that they had issues with treatment compliance.
Six (12%) of the 52 respondents confirmed using digital or analogic reminders to take their dose. Three patients were currently using a dose counter on their device to remind them if their doses had not been taken, and two patients were using a timer on their mobile phones to remind them when their next dose was due. One participant used digital/analogic support but did not indicate which.
The main strategies used to remind them to take their medication include:
leaving the medication in a specific location to prompt them to take their dose at the correct time,
relying on habit or routine to prompt them to take their medication,
taking the COPD medication at the same time as other medications,
feeling unwell to prompt themselves to take their medication.
A total of 32 (56%) of the 57 respondents reported missing a medicine dose; eight of them cited a change in their schedule or routine as its cause. Other reasons for missing a dose reported by patients included: not taking the medication seriously, forgetting to take their dose in the evening, forgetting to bring their medication with them when leaving the house, a change in their environment, a missed medication delivery, and “not taking regular doses”.
The primary reasons why patients appreciate their present treatments were the drug's functionality ( n = 18), the device design ( n = 10), the convenience of use ( n = 8), and the medication's quick and uncomplicated administration ( n = 5). Other patients expressed liking for current medication including feeling comfortable with their present treatment, feeling in charge, and independence.
On the other hand, the device design ( n = 14), the necessity to take their medication ( n = 8), and the side effects of the drug ( n = 5) were the most reported characteristics that patients disliked therapy. Other reported reasons included uncertainty about what the treatment is supposed to do, a sense of guilt when their medication is forgotten, the fact that they are still limited in their activity, and the sensation or taste inside their mouth. Three patients stated that they did not enjoy their current prescribed treatment. "You have to accept what is available," one patient said. Other patients referred detest having to take their medications daily.
About two-thirds ( n = 34 – 67%) of those polled ( n = 51) claimed no involvement with the selection of their present treatment option.
Most of the patients ( n = 42 – 69% of the 61 respondents) reported receiving training for the use of their current treatment. The remaining 31% of the patients did not receive any training, reporting that they “would have liked more formal training, the current device is more complex”, or believed it “could have been useful to receive training and would have loved the explanation, demo training”. Three patients also stated that they did not need training, whether they received it or not.
Twenty-two (52%) of the 42 patients that received training, thought that it was effective and only 5 (12%) did not believe their training to be effective. Fifteen (36%) of patients who received training did not provide feedback on the efficacy of the training they received.
Eight Italian patients reported receiving instruction mostly from a lung specialist, while the majority of British ( n = 5) and Nordic ( n = 4) patients reported receiving training primarily from a nurse (Fig. 7 ); this is probably due to the different structures of the national health systems.
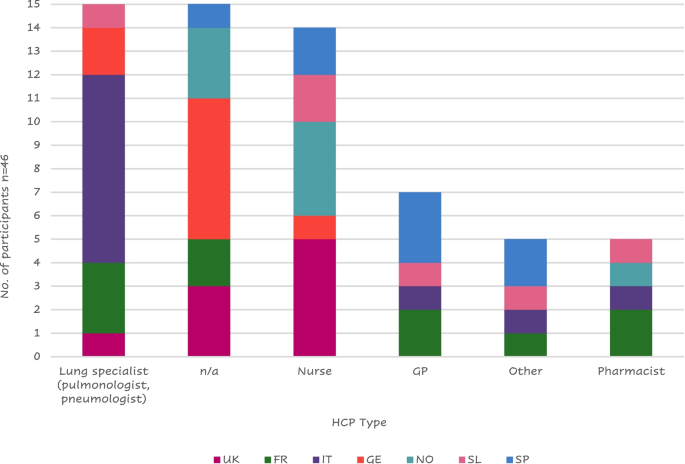
Health care provider (HCP) that administered training to patients by country
Legend: FR = France, GE = Germany, GP = General Practitioner; IT = Italy, SL = Slovenia, SP = Spain, n/a = not applicable; NO = Northern (Sweden Denmark), UK = United Kingdom
One Italian patient stated he received no specific training but was told by his pneumologist to look inside the package and read the instructions; a Frenchman mentioned that his wife was a doctor, so she just showed him how to use the device. Other participants’ training was received at meetings of a lung association from the pharmacists or at a live course organized by the doctor or during rehabilitation.
Six (18% of the 34 respondents) received help from their family or friends to find training materials or treatment information. Most patients received help to find further information and one participant mentioned that he was able to speak to a relative with COPD.
Six (15%) of the 41 respondents had gone online for help with their equipment (looking for tutorials online on forums and finding animated videos on how to use their inhalers). The main reasons for not using the internet for support were a lack of trust in online information ("would rather trust a doctor than go online"), an unwillingness to read more about their condition due to a fear of "reading too much" and becoming "depressed" if they investigated their disease. Other patients did not feel the need for additional support from the internet because their devices were "easy to use" or they wouldn't need further support due to their disease. One patient stated that he looked online and "found it strange that the messages were exclusively for persons with moderate to severe COPD, with only a few messages from people with mild COPD".
Lung specialists were the health care providers (HCPs) who most frequently provided support to patients with COPD ( n = 24/60—40%) followed by general practitioners (23 – 38%) (Fig. 8 ); only 3 patients reported not having received any support.
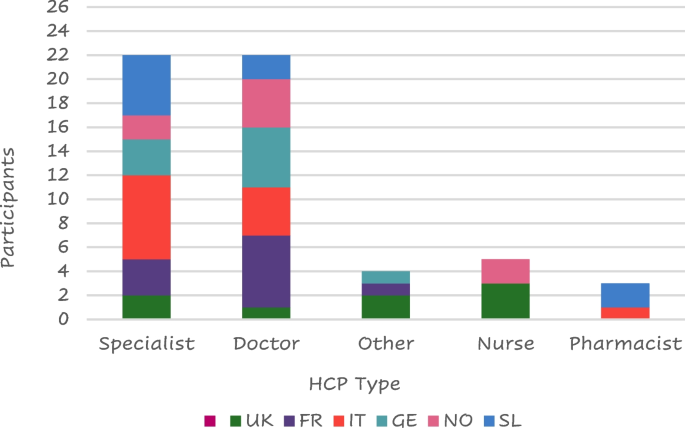
Type of HCP support by country
Legend: FR = France, GE = Germany, IT = Italy, SL = Slovenia, SP = Spain, NO = Northern (Sweden Denmark), UK = United Kingdom
The most frequent answers to the question “If you had a magic wand what would you wish for to improve your life with COPD?” were to find a cure ( n = 18), followed by more regular visits from their doctor/specialist ( n = 11), stop smoking ( n = 5), more information ( n = 4), HCP contact number and COPD support group ( n = 3), and digital monitoring ( n = 2) (Fig. 9 ).
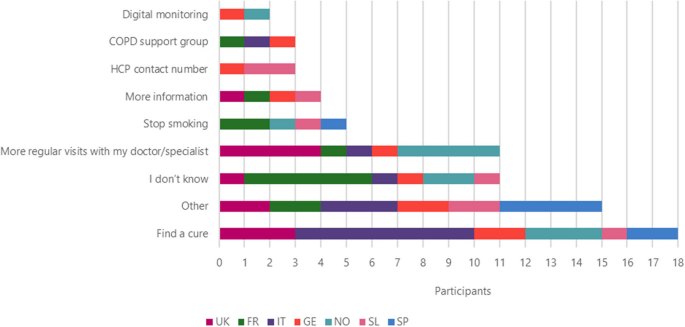
Improvements that patients wish to be made to improve their life by country
Other improvements that patients wish for include: access to new drugs, information about COPD, current and new drugs, reduced side effects, holding COPD workshops, investment in more research, provide cheaper treatment options, new lungs, something to help be more active, to be told that they would not need to take medication anymore, a new type of drug delivery that wouldn’t need to be taken with patient everywhere (like a nicotine patch), instant relief and doctors and nurses to be more humane.
Other services they felt were useful for them included physiotherapy ( n = 12), the use of support groups ( n = 8), exercise classes and psychological assistance ( n = 6), nutrition ( n = 4) while 1 patient from the UK suggested lifestyle (Fig. 10 ).
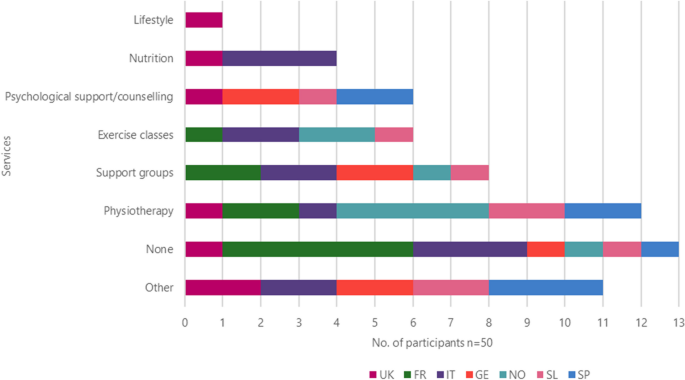
Other services the patient would like to use by country
Other services that patients would like to use included easier access to their HCP, paid, private physiotherapy sessions, smoking cessation support, disability card, training (videos and tutorials) including emergencies, lung transplants, more information about new drugs and the benefits of medication, hear more from doctors and pharmacists, and workshops for families and friends to help them understand what patients are going through.
Even if 3 patients reported having insurance covering additional services, they were generally unaware of the support they could receive through medical insurance. Many had concerns that such services would cost more money.
All the patients included in the study provided a total of 122 daily challenges they must face. 53 (43%) of the responses were related to their lifestyle. Reduced physical activity was referred by more than half ( n = 32) of them and difficulty in mobility was reported by 16; 28 (23%) reported challenges with their symptoms or medication (mainly difficult breathing, n = 15) (Fig. 11 ) while 13 (11%) reported emotional challenges including anxiety, depression, embarrassment due to symptoms or treatment, fear of the conditioning worsening, people recognizing they have a condition, acceptance of the condition and dependence on the medication.
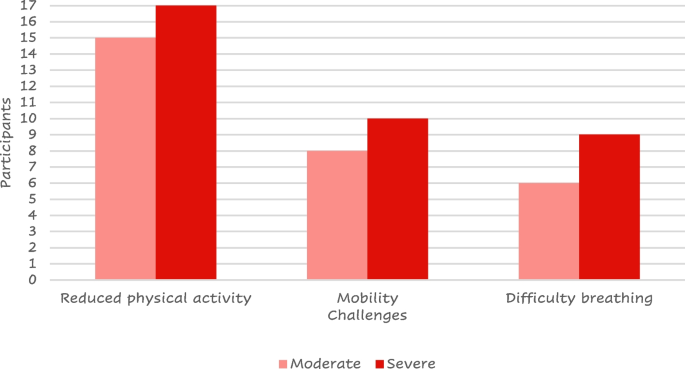
Most reported challenges by COPD severity
The objective of this human factors research was to identify the unmet needs along the different stages of people living with COPD through a one-to-one, semi-structured interview exploring the patient’s feelings and attitudes toward their journeys with the disease.
Differently from other studies exploring similar aspects of the impact of the disease on patient’s daily life where the data belong to medical databases, [ 4 , 6 , 7 , 9 , 10 , 23 ] the current approach is unique, in that it systematically investigates the patient’s feelings in a structured fashion, thus allowing us to better understand the patient’s emotions, which is becoming a relevant aspect of COPD management [ 7 , 24 ]. Furthermore, because of the consistent and wide heterogeneity between the different countries, patients included in this study could have been considered representative of the entire population of European patients with COPD.
The patient reported feelings highlighted that reduced physical activity, mobility challenges, and difficulty breathing resulted as the main challenges in daily life. According to the current international guidelines on COPD management, [ 22 , 25 , 26 ] physical activity is encouraged and monitored to evaluate the prognosis or looked forward to as a target for the evaluation of the treatment efficacy. [ 25 ] Our results confirm that patients perceive COPD as the cause of their reduced physical activity, [ 27 ] having a strong impact on their self-perception. Differently from other studies where increased physical activity was observed independently from patients’ counseling, [ 28 ] general psychological support and accepting their mobility challenges were described as important aims by the patients. Our patients felt reduced mobility as one of their main challenges; aids to improve mobility were described in the available literature as crucial to maintaining the patient’s independence [ 7 ] and have been included in the 2023 GOLD guidelines [ 29 ].
The HCP approach is mainly focused on improving the patient’s breathlessness and exercise intolerance [ 22 , 25 ]; the feeling depicted by the interviewed patients confirms the lack of information about how to manage breathlessness. [ 30 ] The only positive aspect of the COPD diagnosis, reported by 6 of the interviewees, was smoke quitting. Patients frequently feel angry and depressed when they think about the difficulties they have described. Participants discussed a variety of coping mechanisms to deal with these difficulties, including cutting back on physical activity, making sure they stayed active (as much as possible), and utilizing their rescue inhaler as a preventative step.
About one-fourth of the patients did not report having performed spirometry at diagnosis; as spirometry is the landmark of diagnosis; any other method is not gold standard and subjected to criticism [ 22 ]. Because of the qualitative nature of this study, we cannot exclude that this issue was linked to the patient’s reduced memory at the time of diagnosis.
As observed in other studies, [ 31 ] negative behavior has a strong influence on the patient’s quality of life. Patients in the current study generally felt negative emotions before receiving their diagnosis; however, a supportive role of relatives and caregivers was referred by interviewed subjects at the time of diagnosis. About forty percent of patients complained of having waited long before the diagnosis. When asked about the impact of their current treatment, participants gave primarily positive feedback and commonly described their current therapy as “good” and doing its job. Even if most of the patients included in our study felt stable symptoms, some were still looking for a “miraculous” cure. The need for support beyond just pharmacological treatments, such as psychological support and physiotherapy, became clear through the in-depth discussions with patients, confirming the requirement for an integrated and patient-tailored interview to identify the profile of each patient [ 27 , 32 ] to share the most appropriate interventions in the periodic visits, without the need of the patient’s hospitalizations to allow the introduction of new therapies suggested by other research [ 33 ].
As expected, our results show that the information about COPD and the training on both the disease and treatment were provided by different HCPs in various European countries. However, patients often felt that they were not provided with enough information at the point of diagnosis regarding the condition itself or the range of treatment options available. Some felt they did not receive adequate training on how to take their medication correctly, whereas others highlighted that the public should be made more aware of the condition, in general, to help them feel accepted and understood by their family and friends. When asked about the current support they were receiving for their disease, patients reported wanting more information about their clinical condition or treatment options, more regular visits with their HCP, smoking cessation assistance, and support in their day-to-day lives such as housework and improved accessibility, confirming the need of self-management education and skills training highlighted by other authors [ 22 , 25 , 26 ]. However, many patients were unsure or unaware of what support/services were available to them or did not feel they needed any additional support.
This study had a qualitative approach and was, thus, not designed to provide any definitive answer to a study hypothesis. Differently from other studies on general populations of patients with COPD where males and elderly are the most frequent patients [ 34 , 35 ], those who agreed to participate in this study were mostly women and aged between 42 and 65 years. Due to the inclusion of patients that could not be fully representative of the global patients with COPD and the study approach, the outcomes have to be properly generalized. Furthermore, the nature of the study required interviews to be carried out in the participant’s local language with the use of translators to support analysis leading to a potential loss of nuance in meaning.
In conclusion, the current findings show that an apparent discrepancy exists between the traditional lung functional and pharmacological approaches in diagnosing and managing COPD and patient’s needs and challenges in daily activities. In this respect, human factor studies play a relevant role in intercepting gaps in the care of people suffering from COPD, encouraging a novel holistic approach when designing clinical research or shepherding patients along their COPD daily journey.
Availability of data and materials
The data that support the findings of this study are available from Chris White (Rebus Medical), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are not available without permission of Chiesi Farmaceutici.
Decramer M, Janssens W, Miravitlles M. Chronic obstructive pulmonary disease. Lancet. 2012 [cited 2023 May 29];379(9823):1341–51. Available from: https://pubmed.ncbi.nlm.nih.gov/22314182/ .
Roggeri A, Micheletto C, Roggeri DP. Outcomes and costs of treating chronic obstructive pulmonary disease with inhaled fixed combinations: the Italian perspective of the PATHOS study. Int J Chron Obstruct Pulmon Dis. 2014 Jun 5 [cited 2023 May 29];9:569–76. Available from: https://pubmed.ncbi.nlm.nih.gov/24940053/ .
Blasi F, Cesana G, Conti S, Chiodini V, Aliberti S, Fornari C, et al. The clinical and economic impact of exacerbations of chronic obstructive pulmonary disease: a cohort of hospitalized patients. PLoS One. 2014 Jun 27 [cited 2023 May 29];9(6). Available from: https://pubmed.ncbi.nlm.nih.gov/24971791/ .
Rennard S, Decramer M, Calverley PMA, Pride NB, Soriano JB, Vermeire PA, et al. Impact of COPD in North America and Europe in 2000: subjects’ perspective of Confronting COPD International Survey. Eur Respir J. 2002 Oct 1 [cited 2023 May 29];20(4):799–805. Available from: https://pubmed.ncbi.nlm.nih.gov/12412667/ .
Sundh J, Ekström M. Persistent disabling breathlessness in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016 Nov 9 [cited 2023 May 29];11(1):2805–12. Available from: https://pubmed.ncbi.nlm.nih.gov/27877034/ .
Ouellette DR, Lavoie K. Recognition, diagnosis, and treatment of cognitive and psychiatric disorders in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2017 Feb [cited 2023 May 29];12:639–50. Available from: https://pubmed.ncbi.nlm.nih.gov/28243081/ .
Gardener AC, Ewing G, Kuhn I, Farquhar M. Support needs of patients with COPD: a systematic literature search and narrative review. Int J Chron Obstruct Pulmon Dis. 2018 Mar 26 [cited 2023 May 29];13:1021–35. Available from: https://pubmed.ncbi.nlm.nih.gov/29628760/ .
Spruit MA, Singh SJ, Garvey C, Zu Wallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013 Oct 15 [cited 2023 May 29];188(8). Available from: https://pubmed.ncbi.nlm.nih.gov/24127811/ .
Miravitlles M, Worth H, Soler Cataluña JJ, Price D, De Benedetto F, Roche N, et al. Observational study to characterise 24-hour COPD symptoms and their relationship with patient-reported outcomes: results from the ASSESS study. Respir Res. 2014 Oct 21 [cited 2023 May 29];15(1). Available from: https://pubmed.ncbi.nlm.nih.gov/25331383/ .
Jones PW, Watz H, Wouters FM, Cazzola M, COPD: the patient perspective. cited 2023 May 29. Available from: 2016. https://doi.org/10.2147/COPD.S85977 .
Article PubMed Central Google Scholar
Škrgat S, Triller N, Košnik M, Susič TP, Petek D, Jamšek VV, et al. Priporočila za obravnavo bolnika s kronično obstruktivno pljučno boleznijo na primarni in specialistični pulmološki ravni v Sloveniji. Zdravniski Vestnik. 2017;86(1–2):1–12.
Google Scholar
Mehring M, Donnachie E, Fexer J, Hofmann F, Schneider A. Disease management programs for patients with COPD in Germany: a longitudinal evaluation of routinely collected patient records. Respir Care. 2014 [cited 2023 Nov 15];59(7):1123–32. Available from: https://pubmed.ncbi.nlm.nih.gov/24222706/ .
Overview | Chronic obstructive pulmonary disease in over 16s: diagnosis and management | Guidance | NICE. [cited 2023 Nov 15]. Available from: https://www.nice.org.uk/guidance/ng115 .
Molin KR, Søndergaard J, Lange P, Egerod I, Langberg H, Lykkegaard J. Danish general practitioners’ management of patients with COPD: a nationwide survey. Scand J Prim Health Care. 2020 [cited 2023 Nov 15];38(4):391–8. Available from: https://pubmed.ncbi.nlm.nih.gov/33164618/ .
Sandelowsky H, Natalishvili N, Krakau I, Modin S, Ställberg B, Nager A. COPD management by Swedish general practitioners – baseline results of the PRIMAIR study. Scand J Prim Health Care. 2018 Jan 2 [cited 2023 Nov 15];36(1):5. Available from: /pmc/articles/PMC5901441/.
Meeraus W, Wood R, Jakubanis R, Holbrook T, Bizouard G, Despres J, et al. COPD treatment pathways in France: a retrospective analysis of electronic medical record data from general practitioners. Int J Chron Obstruct Pulmon Dis. 2018 Dec 18 [cited 2023 Nov 15];14:51–63. Available from: https://www.dovepress.com/copd-treatment-pathways-in-france-a-retrospective-analysis-of-electron-peer-reviewed-fulltext-article-COPD .
Come migliorare la qualità di vita dei pazienti colpiti da bronco-pneumopatia cronica e dei loro caregiver? | Azienda Ospedaliera Nazionale SS. Antonio e Biagio e Cesare Arrigo Alessandria. [cited 2023 Nov 15]. Available from: https://www.ospedale.al.it/it/comunicazione/notizie/come-migliorare-qualita-vita-pazienti-colpiti-bronco-pneumopatia-cronica-loro-caregiver .
Aiello F, Alunni A, Berardi M, Bordoni F, Calzolari M, Coviello AP, et al. Medicina Pratica L’associazione LABA-LAMA nella gestione del paziente con BPCO-Il punto di vista della Medicina Generale. Rivista Società Italiana di Medicina Generale n 3 • [Internet]. [cited 2023 Nov 15];29:2022. Available from: https://goldcopd.org/ .
ALLEGATOA alla Dgr n. 206 del 24 febbraio 2015.
Miravitlles M, Soler-Cataluña JJ, Calle M, Molina J, Almagro P, Quintano JA, et al. Spanish Guidelines for Management of Chronic Obstructive Pulmonary Disease (GesEPOC) 2017. Pharmacological Treatment of Stable Phase. Arch Bronconeumol. 2017 Jun 1 [cited 2023 Nov 15];53(6):324–35. Available from: https://pubmed.ncbi.nlm.nih.gov/28477954/ .
NHS England » Ambitions for Palliative and End of Life Care: A national framework for local action 2021–2026. [cited 2023 May 29]. Available from: https://www.england.nhs.uk/publication/ambitions-for-palliative-and-end-of-life-care-a-national-framework-for-local-action-2021-2026/ .
POCKET GUIDE TO COPD DIAGNOSIS, MANAGEMENT, AND PREVENTION A Guide for Health Care Professionals. 2020 [cited 2023 May 29]; Available from: www.goldcopd.org .
Rayner J, Khan T, Chan C, Wu C. Illustrating the patient journey through the care continuum: leveraging structured primary care electronic medical record (EMR) data in Ontario, Canada using chronic obstructive pulmonary disease as a case study. Int J Med Inform. 2020 Aug 1 [cited 2023 Jun 3];140. Available from: https://pubmed.ncbi.nlm.nih.gov/32473567/ .
Walker S, Andrew S, Hodson M, Roberts CM. Stage 1 development of a patient-reported experience measure (PREM) for chronic obstructive pulmonary disease (COPD). NPJ Prim Care Respir Med. 2017 Dec 1 [cited 2023 Jun 3];27(1). Available from: https://pubmed.ncbi.nlm.nih.gov/28740181/ .
Agustí A, Celli BR, Criner GJ, Halpin D, Anzueto A, Barnes P, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Eur Respir J. 2023 Apr 1 [cited 2023 May 29];61(4):2300239. Available from: https://erj.ersjournals.com/content/61/4/2300239 .
Reddel HK, Bacharier LB, Bateman ED, Brightling CE, Brusselle GG, Buhl R, et al. Global Initiative for Asthma Strategy 2021 Executive Summary and Rationale for Key Changes. Am J Respir Crit Care Med [Internet]. 2022 Jan 1 [cited 2023 Jun 3];205(1):17–35. Available from: https://pubmed.ncbi.nlm.nih.gov/34658302/ .
Jones PW, Watz H, Wouters EFM, Cazzola M. COPD: the patient perspective. Int J Chron Obstruct Pulmon Dis. 2016 [cited 2023 Jun 3];11 Spec Iss(Spec Iss):13–20. Available from: https://pubmed.ncbi.nlm.nih.gov/26937186/ .
Aggarwal AN, Gupta D, Jindal SK. The relationship between FEV1 and peak expiratory flow in patients with airways obstruction is poor. Chest. 2006 [cited 2023 Jun 3];130(5):1454–61. Available from: https://pubmed.ncbi.nlm.nih.gov/17099024/ .
2023 GOLD guidelines for chronic obstructive pulmonary disease. [cited 2023 Jun 26]. Available from: https://www.jwatch.org/na56004/2023/04/20/2023-gold-guidelines-chronic-obstructive-pulmonary-disease .
Oliver SM. Living with failing lungs: the doctor–patient relationship. Fam Pract. 2001 Aug 1 [cited 2023 Jun 3];18(4):430–9. Available from: https://academic.oup.com/fampra/article/18/4/430/620192 .
JIACI · J Invest Allergol Clin Immunol. [cited 2023 Jun 3]. Available from: https://www.jiaci.org/summary/vol16-issue4-num90 .
Martínez-Guiu J, Arroyo-Fernández I, Rubio R. Impact of patients’ attitudes and dynamics in needs and life experiences during their journey in COPD: an ethnographic study. Expert Rev Respir Med. 2022 [cited 2023 Jun 3];16(1):121–32. Available from: https://pubmed.ncbi.nlm.nih.gov/34238094/ .
Lainscak M, Gosker HR, Schols AMWJ. Chronic obstructive pulmonary disease patient journey: hospitalizations as window of opportunity for extra-pulmonary intervention. Curr Opin Clin Nutr Metab Care. 2013 May [cited 2023 Jun 3];16(3):278–83. Available from: https://pubmed.ncbi.nlm.nih.gov/23507875/ .
Kim-Dorner SJ, Schmidt T, Kuhlmann A, Graf von der Schulenburg JM, Welte T, Lingner H. Age- and gender-based comorbidity categories in general practitioner and pulmonology patients with COPD. NPJ Prim Care Respir Med. 2022 Dec 1 [cited 2023 Nov 15];32(1). Available from: /pmc/articles/PMC9061861/.
Maestri R, Vitacca M, Paneroni M, Zampogna E, Ambrosino N. Gender and age as determinants of success of pulmonary rehabilitation in individuals with chronic obstructive pulmonary disease. Arch Bronconeumol. 2023 Mar 1 [cited 2023 Nov 15];59(3):174–7. Available from: https://www.archbronconeumol.org/en-gender-age-as-determinants-success-articulo-S0300289622005683 .
Download references
Acknowledgements
Rebus Medical (St Nicholas House, 31-34 High St, Bristol BS1 2AW, United Kingdom) was responsible for contacting the patients, data collection, and statistical analyses. The authors thank Andrea Rossi for the medical writing support and the Chiesi and Rebus study team for the management of the Human factors study (Marta Lombardini, Ilaria Milesi, Lorenzo Ventura, Veronica Giminiani, Massimo Savella, Elena Zeni, Elena Nudo, Lisa Forde, Shivani Bhalsod, Elsie Barker, and Chris White).
The authors thank the patients, the interviewers, and the translators who made this study possible.
All the activities were funded by Chiesi Farmaceutici S.p.A. (Parma, Italy).
Author information
Authors and affiliations.
Division of Respiratory Medicine, Department PROMISE, “Giaccone” University Hospital, University of Palermo, Palermo, Italy
Nicola Scichilone
GP, Portsdown Group Practice, Portsmouth, UK
Andrew Whittamore
Rebus Medical LTD, Bristol, UK
Chris White
Chiesi Farmaceutici S.P.A, Via Paradigna 131/A – 43122, Parma, Italy
Elena Nudo, Massimo Savella & Marta Lombardini
You can also search for this author in PubMed Google Scholar
Contributions
NS contributed to the design of the study and critically revised the outcomes according to the clinical needs from a specialistic point of view. AW contributed to the design of the study and critically revised the outcomes according to the clinical needs from a general practitioner’s point of view. CW designed the study, managed and coordinated the study activities. EN, MS, and ML contributed to the design of the study and critically revised the outcomes from a treatment producer’s point of view. All authors critically revised the drafted article and read and approved the final manuscript.
Corresponding author
Correspondence to Nicola Scichilone .
Ethics declarations
Ethics approval and consent to participate.
The DL 20 marzo 2008 specifies that interviews to the patients without any clinical intervention (as the present study) are not considered observational studies and, thus, don't need to be submitted to the revision and approval of an Ethical committee.
All patients provided their informed consent to participate in this study. The informed consent included statements that required participants to agree to maintain confidentiality regarding the information shared during the study session, as well as described the conditions for the collection, use, processing, retention, and transfer of their personal data (including personally identifiable information and personal health information).
Consent for publication
Not applicable.
Competing interests
NS declares no competing interests.
AW declares no competing interests.
CW is a full-time employee of Rebus Medical.
EN, MS, and ML are full-time employees of Chiesi Farmaceutici.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Scichilone, N., Whittamore, A., White, C. et al. The patient journey in Chronic Obstructive Pulmonary Disease (COPD): a human factors qualitative international study to understand the needs of people living with COPD. BMC Pulm Med 23 , 506 (2023). https://doi.org/10.1186/s12890-023-02796-8
Download citation
Received : 18 September 2023
Accepted : 29 November 2023
Published : 13 December 2023
DOI : https://doi.org/10.1186/s12890-023-02796-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chronic obstructive pulmonary disease
- Assessment of healthcare needs
- Qualitative research
- Patient-centered care
- Human-centered design
- Human factors science
- Pharmacologic therapy
- Qualitative evaluation
- Determination of healthcare needs
- Multinational perspective
- Quality of life
- Quality of healthcare
BMC Pulmonary Medicine
ISSN: 1471-2466
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->
| | | |

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
Art & Science Previous Next
Managing a patient with copd and comorbidities: a case study, rachel lucy mitten community matron, peninsula community health community matron service, newquay hospital, newquay, cornwall, england.
This case study provides a critical analysis of the management of a patient with long-term conditions in a community matron service. Particular attention is given to the effect of chronic obstructive pulmonary disease (COPD). The effect of COPD on health and wellbeing, quality of life and hospital admissions is examined, and outcomes are detailed that resulted from the implementation of evidence-based interventions and a case management approach.
Nursing Standard . 30, 13, 46-51. doi: 10.7748/ns.30.13.46.s46
All articles are subject to external double-blind peer review and checked for plagiarism using automated software.
Received: 13 February 2015
Accepted: 29 May 2015
case study - chronic obstructive pulmonary disease - community matron service - comorbidities - complex care - COPD - long-term conditions
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

25 November 2015 / Vol 30 issue 13
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Managing a patient with COPD and comorbidities: a case study
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Case studies
The case studies in this section highlight the need for good practice in the workplace. Simple measures can dramatically reduce the risk of occupational ill health, including COPD .
- High levels of dust in a stonemasonry in Yorkshire
- Silica exposure high in a Welsh quarry
- Company reduces fumes in a Birmingham welders
- Workers concerned about welding fumes
- Segregate workers from the dust source
The Top tips page provides advice for you and your employer on how to achieve a safe working environment.
More guidance and information can be found on the further reading page of this site.
Is this page useful?
Academic Support for Nursing Students
No notifications.
Disclaimer: This essay has been written by a student and not our expert nursing writers. View professional sample essays here.
View full disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this essay are those of the author and do not necessarily reflect the views of NursingAnswers.net. This essay should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
COPD Case Study Essay
Info: 1740 words (7 pages) Nursing Essay Published: 12th Feb 2020
Reference this
Tagged: COPD
If you need assistance with writing your nursing essay, our professional nursing essay writing service is here to help!
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services

- Nursing Essay Writing Service

- Nursing Dissertation Service

- Reflective Writing Service
Related Content
Content relating to: "COPD"
Chronic Obstructive Pulmonary Disease is a group of chronic and progressive respiratory disorders that are characterized by an airway obstruction with little or no reversibility. Damage to the lungs continues to make breathing gradually more difficult over time.
Related Articles

Algorithm to Diagnose Infective COPD Exacerbation
Essay for Algorithm to Diagnose Infective COPD Exacerbation The exacerbation of chronic obstructive pulmonary disease (COPD) is triggered by allergen, air pollution, extreme activities ...
Chronic Obstructive Pulmonary Disease (COPD) Causes
ADEBAYO AINA Contents Explain the physiological origin of Chronic Obstructive Pulmonary Disease Describe the physical effects of the Chronic Obstructive Pulmonary Disease Explain the contributory fa...
Reflective essay relating to a patient with COPD
INTRODUCTION: The purpose of this essay is to adopt Rolfe, Freshwater and Jasper (2001) model of reflection in reflecting upon my experience in practice placement while caring for a patient with a lo...
DMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on the NursingAnswers.net website then please:
Our academic writing and marking services can help you!
- Marking Service
- Samples of our Work
- Full Service Portfolio
Related Lectures
Study for free with our range of nursing lectures!
- Drug Classification
- Emergency Care
- Health Observation
- Palliative Care
- Professional Values

Write for Us
Do you have a 2:1 degree or higher in nursing or healthcare?
Study Resources
Free resources to assist you with your nursing studies!
- APA Citation Tool
- Example Nursing Essays
- Example Nursing Assignments
- Example Nursing Case Studies
- Reflective Nursing Essays
- Nursing Literature Reviews
- Free Resources
- Reflective Model Guides
- Nursing and Healthcare Pay 2021
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Factors Associated with Chronic Obstructive Pulmonary Disease: A Hospital-Based Case-Control Study
Affiliations.
- 1 Department of Internal Medicine, Mbarara University of Science and Technology, Mbarara, Uganda.
- 2 Science Department, Phillips Academy, Andover, MA, USA.
- 3 Department of Public Health, Kabale University, Kabale, Uganda.
- 4 Division of Pulmonary and Critical Care Medicine, Massachusetts General Hospital, Boston, MA, USA.
- 5 Department of Environmental Health, Harvard T.H. Chan School of Public Health, Boston, MA, USA.
- PMID: 38022824
- PMCID: PMC10644879
- DOI: 10.2147/COPD.S426928
Purpose: Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide. In this paper, we determined risk factors for COPD among patients presenting to pulmonology and medical outpatients' clinics of Mbarara Regional Referral Hospital (MRRH).
Methods: In this case-control study, cases were patients with COPD confirmed by spirometry and controls were those with normal spirometry. The two groups were matched by age and gender.
Results: We enrolled 123 participants, of whom 41 were cases and 82 controls. A total of 51 women (41.5%) and 72 men (58.5%), of whom 25 were male cases (61%) and 47 were male controls (57%), were included. The results of our study suggest that the variables associated with the presence of COPD among participants attending MRRH were a history of having ever smoked and a prior history of atopy. This brings to our attention the fact that smoking remains a major risk factor for COPD in this setting, just as it is in developed countries.
Conclusion: Our study has shown that the factors associated with COPD are smoking and a history of atopy. Patients with a history of asthma and tuberculosis are also probably more likely to develop COPD than those without similar disease conditions.
Keywords: asthma; chronic bronchitis; emphysema; smoking.
© 2023 Twinamasiko et al.
PubMed Disclaimer
Conflict of interest statement
The authors declare that they have no competing interests.
Similar articles
- Chronic obstructive pulmonary disease with mild airflow limitation: current knowledge and proposal for future research - a consensus document from six scientific societies. Rossi A, Butorac-Petanjek B, Chilosi M, Cosío BG, Flezar M, Koulouris N, Marin J, Miculinic N, Polese G, Samaržija M, Skrgat S, Vassilakopoulos T, Vukić-Dugac A, Zakynthinos S, Miravitlles M. Rossi A, et al. Int J Chron Obstruct Pulmon Dis. 2017 Aug 29;12:2593-2610. doi: 10.2147/COPD.S132236. eCollection 2017. Int J Chron Obstruct Pulmon Dis. 2017. PMID: 28919728 Free PMC article. Review.
- The objective evaluation of obstructive pulmonary diseases with spirometry. Ozkaya S, Dirican A, Tuna T. Ozkaya S, et al. Int J Chron Obstruct Pulmon Dis. 2016 Aug 25;11:2009-15. doi: 10.2147/COPD.S113774. eCollection 2016. Int J Chron Obstruct Pulmon Dis. 2016. PMID: 27616884 Free PMC article.
- Prevalence of chronic obstructive pulmonary disease among adult male cigarettes smokers: a community-based study in Jordan. Al Omari M, Khassawneh BY, Khader Y, Dauod AS, Bergus G. Al Omari M, et al. Int J Chron Obstruct Pulmon Dis. 2014 Jul 17;9:753-8. doi: 10.2147/COPD.S62898. eCollection 2014. Int J Chron Obstruct Pulmon Dis. 2014. PMID: 25092972 Free PMC article.
- The prevalence of chronic obstructive pulmonary disease in Uppsala, Sweden--the Burden of Obstructive Lung Disease (BOLD) study: cross-sectional population-based study. Danielsson P, Ólafsdóttir IS, Benediktsdóttir B, Gíslason T, Janson C. Danielsson P, et al. Clin Respir J. 2012 Apr;6(2):120-7. doi: 10.1111/j.1752-699X.2011.00257.x. Epub 2011 Jul 6. Clin Respir J. 2012. PMID: 21651748
- Postoperative outcome after coronary artery bypass grafting in chronic obstructive pulmonary disease. Manganas H, Lacasse Y, Bourgeois S, Perron J, Dagenais F, Maltais F. Manganas H, et al. Can Respir J. 2007 Jan-Feb;14(1):19-24. doi: 10.1155/2007/378963. Can Respir J. 2007. PMID: 17315054 Free PMC article.
- Hogea SP, Tudorache E, Fildan AP, Fira-Mladinescu O, Marc M, Oancea C. Risk factors of chronic obstructive pulmonary disease exacerbations. Clin Respir J. 2020;14(3):183–197. PMID: 31814260. doi:10.1111/drj.13129 - DOI - PubMed
- Eisner MD, Anthonisen N, Coultas D, et al. An official American Thoracic Society public policy statement: Novel risk factors and the global burden of chronic obstructive pulmonary disease.Am J Respir Crit Care Med. 2010, 182(5):693–718. doi:10.1164/rccm.200811-1757ST - DOI - PubMed
- Richter DC, Joubert JR, Nell H, Schuurmans MM, Irusen EM. Diagnostic value of post-bronchodilator pulmonary function testing to distinguish between stable, moderate to severe COPD and asthma. Int J Chron Obstruct Pulmon Dis. 2008;3(4):693–699. doi:10.2147/copd.s948 - DOI - PMC - PubMed
- Labaki WW, Rosenberg SR. Chronic obstructive pulmonary disease. Ann Intern Med. 2020;173(3):ITC17–ITC32. PMID:32745458. doi:10.7326/AITC202008040 - DOI - PubMed
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–582. PMID: 28128970. doi:10.1164/rccm.201701-0218PP - DOI - PubMed
- Search in MeSH
Related information
Grants and funding, linkout - more resources, full text sources.
- Dove Medical Press
- Europe PubMed Central
- PubMed Central
- Genetic Alliance
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
VIDEO
COMMENTS
Clinical Case Study on COPD. Danielle McGarry. Introduction. The patient is a 76-year-old female with a history of chronic obstructive pulmonary disease (COPD). The patient is a married housewife with a 1 pack a day smoking history from age 15. The patient states that she, "only smokes a little to calm her nerves" though her husband still ...
COPD Case Study Essay. Chronic obstructive pulmonary disease is a chronic progressive lung disease caused predominantly by smoking National Institute for Health and Clinical Excellence NICE, 2010. It is characterised by airflow obstruction which is not fully reversible. The airflow obstruction does not change markedly over several months and is ...
COPD (GOLD, 2018; NICE, 2018). ation, assessment and management"SpirometrySpirometry is a tool used to identify airfl. w obstruction but does not identi. the cause. Commonly measured parameters are: Forced expiratory volume - the volume of air that can be exhaled - in one second (FEV1), s.
Management of chronic obstructive pulmonary disease involves lifestyle interventions - vaccinations, smoking cessation and pulmonary rehabilitation - pharmacological interventions and self-management. Citation: Price D, Williams N(2020) Diagnosis and management of COPD: a case study. Nursing Times[online]; 116: 6, 36-38.
COPD Exacerbation Case Study. Introduction: A COPD exacerbation can be defined as "an event in the natural course of the disease characterized by a change in the patient's baseline dyspnea, cough, and/or sputum, that is beyond normal day-to-day variations, is acute in onset and may warrant a change in medication in a patient with underlying ...
Each chronic condition comes with a particular set of challenges. This essay will focus on the example of chronic obstructive pulmonary disease (COPD). COPD is presently estimated to affect 3 million people in the UK, two thirds of whom are undiagnosed.3,4 It is currently the
The British Lung Foundation (BLF) COPD Patient Passport is an online tool consisting of 13 questions regarded as core components of COPD care (table 1). It was developed with people with COPD, clinicians in the Northwest England Respiratory Team and the Primary Care Respiratory Society (UK). The intention was to raise awareness among patients ...
Based on the information given, the patient likely has chronic obstructive pulmonary disease (COPD). The key findings that point to this diagnosis include: Barrel chest. Tachypnea. A long expiratory time. Diminished breath sounds. Use of accessory muscles while breathing. Digital clubbing. Pursed lip breathing.
Chronic obstructive pulmonary disease (COPD) is a common condition that causes irreversible airway obstruction. Fatigue and exertional dyspnoea, for example, have a detrimental impact on the patient's daily life. Current research has revealed the need to empower the patient, which can result in not only educated and effective decision-making, but also a considerable improvement in patient ...
Abstract. Chronic obstructive pulmonary disease (COPD) is a very common condition especially. found among those of the older generation who have a history of smoking, a widely accepted. practice where harmful effects were not known in the 1940's, 1950's, and even the early 1960's.
The effect of COPD on health and wellbeing, quality of life and hospital admissions is examined, and outcomes are detailed that resulted from the implementation of evidence-based interventions and a case management approach. Nursing Standard . 30, 13, 46-51. doi: 10.7748/ns.30.13.46.s46. [email protected].
COPD Case Study Essay. Info: 1740 words (7 pages) Nursing Case Study Published: 12th Feb 2020. Reference this ... (GOLD), 2011). In the United Kingdom (UK), chronic respiratory disease, including COPD, is the third most common cause of death, with 30,000 deaths reported annually (NICE, 2010). There are almost one million people diagnosed with ...
The Clinical Case Study Diagnosis. Mike is a 54 year old, self-employed grandfather who smokes 40 cigarettes daily. ... Teenage smoking prevalence is around 15% in developing countries and around 26% in the UK and US. Studies have shown that those who make it past 20 years of age are much less likely to succumb to this addiction (Grimshaw ...
Patients with chronic obstructive pulmonary disease (COPD) can have acute episodes of worsening symptoms, known generically as exacerbations, which are clinically relevant because they involve an acute deterioration of the patient's health status, worsen the patient's prognosis, and are the main cause of economic expenditure associated with COPD.1-5 However, whether these episodes are truly ...
It effect more than three million people in England. (Jones, 2001) In the Western World, the main cause of COPD is smoking, smoking is related with over 90% of this disease, however COPD occurs in merely 10% to 20% of chronic chain smokers. (Beyer et al, 2008)Respiratory illness is also occurred by passive smoking.
Nurse Seema works on a medical-surgical unit and is caring for Richard, a 75-year-old male with a history of smoking, who was admitted for an acute exacerbation of chronic obstructive pulmonary disease, or COPD. After settling Richard in his room, Nurse Seema goes through the steps of the Clinical Judgment Measurement Model to make clinical ...
ISBN. 9781788513586. This document is for healthcare professionals and patients to show how this condition could be best managed from the unscheduled care perspective. Supporting documents. 9. Case Studies. What follows are case studies from three different regions that showcase this best practice through taking a whole system, multi ...
The case studies in this section highlight the need for good practice in the workplace. Simple measures can dramatically reduce the risk of occupational ill health, including COPD. The Top tips page provides advice for you and your employer on how to achieve a safe working environment. More guidance and information can be found on the further ...
Jerry Corners Introduction Chronic Obstructive Pulmonary Disease (COPD) is the fifth leading cause of morbidity and mortality in the UK and fourth in the world (Hurd 2000; Soriano 2000). Though ot UK Essays .com
Pathophysiology of COPD. COPD is a chronic disease in which decreased airflow is related to airway smooth muscle hypereactivity due to an abnormal inflammatory reaction. Inhalation of tobacco products causes airway remodeling, resulting ultimately in emphysema and chronic bronchitis (Srivastava, Dastidar, & Ray 2007).
1) CASE SUMMARY. Mr TLT is a 58 year old taxi driver who was admitted to Hospital Batu Pahat due to newly diagnosed chronic obstructive pulmonary disease. He has had hypertension for the past one year and is taking T Amlodipine 5mg od. He is also a chronic smoker for the past 40 years who smokes about 20 sticks of cigarettes a day.
COPD Case Study Essay. Info: 1740 words (7 pages) Nursing Essay Published: 12th Feb 2020. Reference this ... (GOLD), 2011). In the United Kingdom (UK), chronic respiratory disease, including COPD, is the third most common cause of death, with 30,000 deaths reported annually (NICE, 2010). There are almost one million people diagnosed with COPD ...
Our study has shown that the factors associated with COPD are smoking and a history of atopy. Patients with a history of asthma and tuberculosis are also probably more likely to develop COPD than those without similar disease conditions. ... A Hospital-Based Case-Control Study Int J Chron Obstruct Pulmon Dis. 2023 Nov 10:18:2521-2529. doi: 10. ...
According to Karen & Aidin (2011), Dyspnea causes many patients with COPD to withdraw from day-to-day activities and hobbies. Referral to rehabilitation services was considered to improve her breathing, oxygenation and endurance (NICE, 2006). Home care aide services were considered to assist Elizabeth with her activities of daily living care.