- Follow us on Facebook
- Follow us on Twitter
- Criminal Justice
- Environment
- Politics & Government
- Race & Gender
Expert Commentary

Improving college student mental health: Research on promising campus interventions
Hiring more counselors isn’t enough to improve college student mental health, scholars warn. We look at research on programs and policies schools have tried, with varying results.

Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
by Denise-Marie Ordway, The Journalist's Resource September 13, 2023
This <a target="_blank" href="https://journalistsresource.org/education/college-student-mental-health-research-interventions/">article</a> first appeared on <a target="_blank" href="https://journalistsresource.org">The Journalist's Resource</a> and is republished here under a Creative Commons license.<img src="https://journalistsresource.org/wp-content/uploads/2020/11/cropped-jr-favicon-150x150.png" style="width:1em;height:1em;margin-left:10px;">
If you’re a journalist covering higher education in the U.S., you’ll likely be reporting this fall on what many healthcare professionals and researchers are calling a college student mental health crisis.
An estimated 49% of college students have symptoms of depression or anxiety disorder and 14% seriously considered committing suicide during the past year, according to a national survey of college students conducted during the 2022-23 school year. Nearly one-third of the 76,406 students who participated said they had intentionally injured themselves in recent months.
In December, U.S. Surgeon General Vivek Murthy issued a rare public health advisory calling attention to the rising number of youth attempting suicide , noting the COVID-19 pandemic has “exacerbated the unprecedented stresses young people already faced.”
Meanwhile, colleges and universities of all sizes are struggling to meet the need for mental health care among undergraduate and graduate students. Many schools have hired more counselors and expanded services but continue to fall short.
Hundreds of University of Houston students held a protest earlier this year , demanding the administration increase the number of counselors and make other changes after two students died by suicide during the spring semester, the online publication Chron reported.
In an essay in the student-run newspaper , The Cougar, last week, student journalist Malachi Key blasts the university for having one mental health counselor for every 2,122 students, a ratio higher than recommended by the International Accreditation of Counseling Services , which accredits higher education counseling services.
But adding staff to a campus counseling center won’t be enough to improve college student mental health and well-being, scholars and health care practitioners warn.
“Counseling centers cannot and should not be expected to solve these problems alone, given that the factors and forces affecting student well-being go well beyond the purview and resources that counseling centers can bring to bear,” a committee of the National Academies of Sciences, Engineering, and Medicine writes in a 2021 report examining the issue.
Advice from prominent scholars
The report is the culmination of an 18-month investigation the National Academies launched in 2019, at the request of the federal government, to better understand how campus culture affects college student mental health and well-being. Committee members examined data, studied research articles and met with higher education leaders, mental health practitioners, researchers and students.
The committee’s key recommendation: that schools take a more comprehensive approach to student mental health, implementing a wide range of policies and programs aimed at preventing mental health problems and improving the well-being of all students — in addition to providing services and treatment for students in distress and those with diagnosed mental illnesses.
Everyone on campus, including faculty and staff across departments, needs to pitch in to establish a new campus culture, the committee asserts.
“An ‘all hands’ approach, one that emphasizes shared responsibility and a holistic understanding of what it means in practice to support students, is needed if institutions of higher education are to intervene from anything more than a reactive standpoint,” committee members write. “Creating this systemic change requires that institutions examine the entire culture and environment of the institution and accept more responsibility for creating learning environments where a changing student population can thrive.”
In a more recent analysis , three leading scholars in the field also stress the need for a broader plan of action.
Sara Abelson , a research assistant professor at Temple University’s medical school; Sarah Lipson , an associate professor at the Boston University School of Public Health; and Daniel Eisenberg , a professor of health policy and management at the University of California, Los Angeles’ School of Public Health, have been studying college student mental health for years.
Lipson and Eisenberg also are principal investigators for the Healthy Minds Network , which administers the Healthy Minds Study , a national survey of U.S college students conducted annually to gather information about their mental health, whether and how they receive mental health care and related issues.
Abelson, Lipson and Eisenberg review the research to date on mental health interventions for college students in the 2022 edition of Higher Education: Handbook of Theory and Research . They note that while the evidence indicates a multi-pronged approach is best, it’s unclear which specific strategies are most effective.
Much more research needed
Abelson, Lipson and Eisenberg stress the need for more research. Many interventions in place at colleges and universities today — for instance, schoolwide initiatives aimed at reducing mental health stigma and encouraging students to seek help when in duress – should be evaluated to gauge their effectiveness, they write in their chapter, “ Mental Health in College Populations: A Multidisciplinary Review of What Works, Evidence Gaps, and Paths Forward .”
They add that researchers and higher education leaders also need to look at how campus operations, including hiring practices and budgetary decisions, affect college student mental health. It would be helpful to know, for example, how students are impacted by limits on the number of campus counseling sessions they can have during a given period, Abelson, Lipson and Eisenberg suggest.
Likewise, it would be useful to know whether students are more likely to seek counseling when they must pay for their sessions or when their school charges every member of the student body a mandatory health fee that provides free counseling for all students.
“These financially-based considerations likely influence help-seeking and treatment receipt, but they have not been evaluated within higher education,” they write.
Interventions that show promise
The report from the National Academies of Sciences, Engineering, and Medicine and the chapter by Abelson, Lipson and Eisenberg both spotlight programs and policies shown to prevent mental health problems or improve the mental health and well-being of young people. However, many intervention studies focus on high school students, specific groups of college students or specific institutions. Because of this, it can be tough to predict how well they would work across the higher education landscape.
Scientific evaluations of these types of interventions indicate they are effective:
- Building students’ behavior management skills and having them practice new skills under expert supervision . An example: A class that teaches students how to use mindfulness to improve their mental and physical health that includes instructor-led meditation exercises.
- Training some students to offer support to others , including sharing information and organizing peer counseling groups. “Peers may be ‘the single most potent source of influence’ on student affective and cognitive growth and development during college,” Abelson, Lipson and Eisenberg write.
- Reducing students’ access to things they can use to harm themselves , including guns and lethal doses of over-the-counter medication.
- Creating feelings of belonging through activities that connect students with similar interests or backgrounds.
- Making campuses more inclusive for racial and ethnic minorities, LGBTQ+ students and students who are the first in their families to go to college. One way to do that is by hiring mental health professionals trained to recognize, support and treat students from different backgrounds. “Research has shown that the presentation of [mental health] symptoms can differ based on racial and ethnic backgrounds, as can engaging in help-seeking behaviors that differ from those of cisgender, heteronormative white men,” explain members of National Academies of Sciences, Engineering, and Medicine committee.
Helping journalists sift through the evidence
We encourage journalists to read the full committee report and aforementioned chapter in Higher Education: Handbook of Theory and Research . We realize, though, that many journalists won’t have time to pour over the combined 304 pages of text to better understand this issue and the wide array of interventions colleges and universities have tried, with varying success.
To help, we’ve gathered and summarized meta-analyses that investigate some of the more common interventions. Researchers conduct meta-analyses — a top-tier form of scientific evidence — to systematically analyze all the numerical data that appear in academic studies on a given topic. The findings of a meta-analysis are statistically stronger than those reached in a single study, partly because pooling data from multiple, similar studies creates a larger sample to examine.
Keep reading to learn more. And please check back here occasionally because we’ll add to this list as new research on college student mental health is published.
Peer-led programs
Stigma and Peer-Led Interventions: A Systematic Review and Meta-Analysis Jing Sun; et al. Frontiers in Psychiatry, July 2022.
When people diagnosed with a mental illness received social or emotional support from peers with similar mental health conditions, they experienced less stress about the public stigma of mental illness, this analysis suggests.
The intervention worked for people from various age groups, including college students and middle-aged adults, researchers learned after analyzing seven studies on peer-led mental health programs written or published between 1975 and 2021.
Researchers found that participants also became less likely to identify with negative stereotypes associated with mental illness.
All seven studies they examined are randomized controlled trials conducted in the U.S., Germany or Switzerland. Together, the findings represent the experiences of a total of 763 people, 193 of whom were students at universities in the U.S.
Researchers focused on interventions designed for small groups of people, with the goal of reducing self-stigma and stress associated with the public stigma of mental illness. One or two trained peer counselors led each group for activities spanning three to 10 weeks.
Five of the seven studies tested the Honest, Open, Proud program, which features role-playing exercises, self-reflection and group discussion. It encourages participants to consider disclosing their mental health issues, instead of keeping them a secret, in hopes that will help them feel more confident and empowered. The two other programs studied are PhotoVoice , based in the United Kingdom, and
“By sharing their own experiences or recovery stories, peer moderators may bring a closer relationship, reduce stereotypes, and form a positive sense of identity and group identity, thereby reducing self-stigma,” the authors of the analysis write.
Expert-led instruction
The Effects of Meditation, Yoga, and Mindfulness on Depression, Anxiety, and Stress in Tertiary Education Students: A Meta-Analysis Josefien Breedvelt; et al. Frontiers in Psychiatry, April 2019.
Meditation-based programs help reduce symptoms of depression, anxiety and stress among college students, researchers find after analyzing the results of 24 research studies conducted in various parts of North America, Asia and Europe.
Reductions were “moderate,” researchers write. They warn, however, that the results of their meta-analysis should be interpreted with caution considering studies varied in quality.
A total of 1,373 college students participated in the 24 studies. Students practiced meditation, yoga or mindfulness an average of 153 minutes a week for about seven weeks. Most programs were provided in a group setting.
Although the researchers do not specify which types of mindfulness, yoga or meditation training students received, they note that the most commonly offered mindfulness program is Mindfulness-Based Stress Reduction and that a frequently practiced form of yoga is Hatha Yoga .
Meta-Analytic Evaluation of Stress Reduction Interventions for Undergraduate and Graduate Students Miryam Yusufov; et al. International Journal of Stress Management, May 2019.
After examining six types of stress-reduction programs common on college campuses, researchers determined all were effective at reducing stress or anxiety among students — and some helped with both stress and anxiety.
Programs focusing on cognitive-behavioral therapy , coping skills and building social support networks were more effective in reducing stress. Meanwhile, relaxation training, mindfulness-based stress reduction and psychoeducation were more effective in reducing anxiety.
The authors find that all six program types were equally effective for undergraduate and graduate students.
The findings are based on an analysis of 43 studies dated from 1980 to 2015, 30 of which were conducted in the U.S. The rest were conducted in Australia, China, India, Iran, Japan, Jordan, Kora, Malaysia or Thailand. A total of 4,400 students participated.
Building an inclusive environment
Cultural Adaptations and Therapist Multicultural Competence: Two Meta-Analytic Reviews Alberto Soto; et al. Journal of Clinical Psychology, August 2018.
If racial and ethnic minorities believe their therapist understands their background and culture, their treatment tends to be more successful, this analysis suggests.
“The more a treatment is tailored to match the precise characteristics of a client, the more likely that client will engage in treatment, remain in treatment, and experience improvement as a result of treatment,” the authors write.
Researchers analyzed the results of 15 journal articles and doctoral dissertations that examine therapists’ cultural competence . Nearly three-fourths of those studies were written or published in 2010 or later. Together, the findings represent the experiences of 2,640 therapy clients, many of whom were college students. Just over 40% of participants were African American and 32% were Hispanic or Latino.
The researchers note that they find no link between therapists’ ratings of their own level of cultural competence and client outcomes.
Internet-based interventions
Internet Interventions for Mental Health in University Students: A Systematic Review and Meta-Analysis Mathias Harrer; et al. International Journal of Methods in Psychiatric Research, June 2019.
Internet-based mental health programs can help reduce stress and symptoms of anxiety, depression and eating disorders among college students, according to an analysis of 48 research studies published or written before April 30, 2018 on the topic.
All 48 studies were randomized, controlled trials of mental health interventions that used the internet to engage with students across various platforms and devices, including mobile phones and apps. In total, 10,583 students participated in the trials.
“We found small effects on depression, anxiety, and stress symptoms, as well as moderate‐sized effects on eating disorder symptoms and students’ social and academic functioning,” write the authors, who conducted the meta-analysis as part of the World Mental Health International College Student Initiative .
The analysis indicates programs that focus on cognitive behavioral therapy “were superior to other types of interventions.” Also, programs “of moderate length” — one to two months – were more effective.
The researchers note that studies of programs targeting depression showed better results when students were not compensated for their participation, compared to studies in which no compensation was provided. The researchers do not offer possible explanations for the difference in results or details about the types of compensation offered to students.
About The Author
Denise-Marie Ordway
Center for Collegiate Mental Health 2023 Annual Report
This report from the Center for Collegiate Mental Health (CCMH) presents descriptive data on various domains of mental health and factors related to treatment and care for college students in the United States. The data included in this report was gathered from 195 colleges and universities across the U.S., describing 185,114 de-identified college students seeking mental health treatment. The report examines trends among students seeking mental health services, including prior treatment and “threat-to-self" characteristics, along with trends in various mental health indicators, including depression, anxiety, family distress, and substance use. The report also includes data on appointment statistics, including utilization of mental health services and types of services.
The 2023 report also explores how experiences of discrimination are associated with mental health concerns at college counseling centers, analyzing how discrimination due to race/ethnicity, disability, gender, nationality, religion, or sexuality impact mental health.
Center for Collegiate Mental Health 2023 Annual Report. Center for Collegiate Mental Health 2024. https://ccmh.psu.edu/annual-reports .
Learn more with these Related Resources
This report by The Steve Fund and The JED Foundation provides a framework to help …
This report by The Steve Fund and The JED Foundation provides a framework to help colleges and universities support the mental health of students of color. College students of color are more likely than their white peers to report feeling overwhelmed most or all of the time in their first term, and are less likely than their white peers to seek the help they need. This report proposes ten actionable strategies to tailor or strengthen…
This article uses data from the World Health Organization's World Mental Health Surveys to examine …
This article uses data from the World Health Organization's World Mental Health Surveys to examine whether mental disorders predict college drop-out among over 5,000 college-aged young adults. The survey was conducted in 21 low- and middle-income countries, and found that over 20 percent of respondents had a diagnosable mental illness in the past year. Among those individuals, 80 percent had an onset of illness prior to the start of college, and only 16 percent reported…
This webcast seminar from The Forum at the T.H. Chan School of Public Health examines …
This webcast seminar from The Forum at the T.H. Chan School of Public Health examines the alarming increase in mental health issues among U.S. college students of color and the current gaps in campus responses to these trends. According to recent data, students of color feel both more isolated and overwhelmed than their white classmates, but are simultaneously less likely to seek counseling services on campus. In light of this troubling data, experts will explore…
- Open access
- Published: 20 September 2022
Factors that influence mental health of university and college students in the UK: a systematic review
- Fiona Campbell 1 ,
- Lindsay Blank 1 ,
- Anna Cantrell 1 ,
- Susan Baxter 1 ,
- Christopher Blackmore 1 ,
- Jan Dixon 1 &
- Elizabeth Goyder 1
BMC Public Health volume 22 , Article number: 1778 ( 2022 ) Cite this article
113k Accesses
58 Citations
97 Altmetric
Metrics details
Worsening mental health of students in higher education is a public policy concern and the impact of measures to reduce transmission of COVID-19 has heightened awareness of this issue. Preventing poor mental health and supporting positive mental wellbeing needs to be based on an evidence informed understanding what factors influence the mental health of students.
To identify factors associated with mental health of students in higher education.
We undertook a systematic review of observational studies that measured factors associated with student mental wellbeing and poor mental health. Extensive searches were undertaken across five databases. We included studies undertaken in the UK and published within the last decade (2010–2020). Due to heterogeneity of factors, and diversity of outcomes used to measure wellbeing and poor mental health the findings were analysed and described narratively.
We included 31 studies, most of which were cross sectional in design. Those factors most strongly and consistently associated with increased risk of developing poor mental health included students with experiences of trauma in childhood, those that identify as LGBTQ and students with autism. Factors that promote wellbeing include developing strong and supportive social networks. Students who are prepared and able to adjust to the changes that moving into higher education presents also experience better mental health. Some behaviours that are associated with poor mental health include lack of engagement both with learning and leisure activities and poor mental health literacy.
Improved knowledge of factors associated with poor mental health and also those that increase mental wellbeing can provide a foundation for designing strategies and specific interventions that can prevent poor mental health and ensuring targeted support is available for students at increased risk.
Peer Review reports
Poor mental health of students in further and higher education is an increasing concern for public health and policy [ 1 , 2 , 3 , 4 ]. A 2020 Insight Network survey of students from 10 universities suggests that “1 in 5 students has a current mental health diagnosis” and that “almost half have experienced a serious psychological issue for which they felt they needed professional help”—an increase from 1 in 3 in the same survey conducted in 2018 [ 5 ]. A review of 105 Further Education (FE) colleges in England found that over a three-year period, 85% of colleges reported an increase in mental health difficulties [ 1 ]. Depression and anxiety were both prevalent and widespread in students; all colleges reported students experiencing depression and 99% reported students experiencing severe anxiety [ 5 , 6 ]. A UK cohort study found that levels of psychological distress increase on entering university [ 7 ], and recent evidence suggests that the prevalence of mental health problems among university students, including self-harm and suicide, is rising, [ 3 , 4 ] with increases in demand for services to support student mental health and reports of some universities finding a doubling of the number of students accessing support [ 8 ]. These common mental health difficulties clearly present considerable threat to the mental health and wellbeing of students but their impact also has educational, social and economic consequences such as academic underperformance and increased risk of dropping out of university [ 9 , 10 ].
Policy changes may have had an influence on the student experience, and on the levels of mental health problems seen in the student population; the biggest change has arguably been the move to widen higher education participation and to enable a more diverse demographic to access University education. The trend for widening participation has been continually rising since the late 1960s [ 11 ] but gained impetus in the 2000s through the work of the Higher Education Funding Council for England (HEFCE). Macaskill (2013) [ 12 ] suggests that the increased access to higher education will have resulted in more students attending university from minority groups and less affluent backgrounds, meaning that more students may be vulnerable to mental health problems, and these students may also experience greater challenges in making the transition to higher education.
Another significant change has been the introduction of tuition fees in 1998, which required students to self fund up to £1,000 per academic year. Since then, tuition fees have increased significantly for many students. With the abolition of maintenance grants, around 96% of government support for students now comes in the form of student loans [ 13 ]. It is estimated that in 2017, UK students were graduating with average debts of £50,000, and this figure was even higher for the poorest students [ 13 ]. There is a clear association between a student’s mental health and financial well-being [ 14 ], with “increased financial concern being consistently associated with worse health” [ 15 ].
The extent to which the increase in poor mental health is also being seen amongst non-students of a similar age is not well understood and warrants further study. However, the increase in poor mental health specifically within students in higher education highlights a need to understand what the risk factors are and what might be done within these settings to ensure young people are learning and developing and transitioning into adulthood in environments that promote mental wellbeing.
Commencing higher education represents a key transition point in a young person’s life. It is a stage often accompanied by significant change combined with high expectations of high expectations from students of what university life will be like, and also high expectations from themselves and others around their own academic performance. Relevant factors include moving away from home, learning to live independently, developing new social networks, adjusting to new ways of learning, and now also dealing with the additional greater financial burdens that students now face.
The recent global COVID-19 pandemic has had considerable impact on mental health across society, and there is concern that younger people (ages 18–25) have been particularly affected. Data from Canada [ 16 ] indicate that among survey respondents, “almost two-thirds (64%) of those aged 15 to 24 reported a negative impact on their mental health, while just over one-third (35%) of those aged 65 and older reported a negative impact on their mental health since physical distancing began” (ibid, p.4). This suggests that older adults are more prepared for the kind of social isolation which has been brought about through the response to COVID-19, whereas young adults have found this more difficult to cope with. UK data from the National Union of Students reports that for over half of UK students, their mental health is worse than before the pandemic [ 17 ]. Before COVID-19, students were already reporting increasing levels of mental health problems [ 2 ], but the COVID-19 pandemic has added a layer of “chronic and unpredictable” stress, creating the perfect conditions for a mental health crisis [ 18 ]. An example of this is the referrals (both urgent and routine) of young people with eating disorders for treatment in the NHS which almost doubled in number from 2019 to 2020 [ 19 ]. The travel restrictions enforced during the pandemic have also impacted on student mental health, particularly for international students who may have been unable to commence studies or go home to see friends and family during holidays [ 20 ].
With the increasing awareness and concern in the higher education sector and national bodies regarding student mental health has come increasing focus on how to respond. Various guidelines and best practice have been developed, e.g. ‘Degrees of Disturbance’ [ 21 ], ‘Good Practice Guide on Responding to Student Mental Health Issues: Duty of Care Responsibilities for Student Services in Higher Education’ [ 22 ] and the recent ‘The University Mental Health Charter’ [ 2 ]. Universities UK produced a Good Practice Guide in 2015 called “Student mental wellbeing in higher education” [ 23 ]. An increasing number of initiatives have emerged that are either student-led or jointly developed with students, and which reflect the increasing emphasis students and student bodies place on mental health and well-being and the increased demand for mental health support: Examples include: Nightline— www.nightline.ac.uk , Students Against Depression— www.studentsagainstdepression.org , Student Minds— www.studentminds.org.uk/student-minds-and-mental-wealth.html and The Alliance for Student-Led Wellbeing— www.alliancestudentwellbeing.weebly.com/ .
Although requests for professional support have increased substantially [ 24 ] only a third of students with mental health problems seek support from counselling services in the UK [ 12 ]. Many students encounter barriers to seeking help such as stigma or lack of awareness of services [ 25 ], and without formal support or intervention, there is a risk of deterioration. FE colleges and universities have identified the need to move beyond traditional forms of support and provide alternative, more accessible interventions aimed at improving mental health and well-being. Higher education institutions have a unique opportunity to identify, prevent, and treat mental health problems because they provide support in multiple aspects of students’ lives including academic studies, recreational activities, pastoral and counselling services, and residential accommodation.
In order to develop services that better meet the needs of students and design environments that are supportive of developing mental wellbeing it is necessary to explore and better understand the factors that lead to poor mental health in students.
Research objectives
The overall aim of this review was to identify, appraise and synthesise existing research evidence that explores the aetiology of poor mental health and mental wellbeing amongst students in tertiary level education. We aimed to gain a better understanding of the mechanisms that lead to poor mental health amongst tertiary level students and, in so doing, make evidence-based recommendations for policy, practice and future research priorities. Specific objectives in line with the project brief were to:
To co-produce with stakeholders a conceptual framework for exploring the factors associated with poorer mental health in students in tertiary settings. The factors may be both predictive, identifying students at risk, or causal, explaining why they are at risk. They may also be protective, promoting mental wellbeing.
To conduct a review drawing on qualitative studies, observational studies and surveys to explore the aetiology of poor mental health in students in university and college settings and identify factors which promote mental wellbeing amongst students.
To identify evidence-based recommendations for policy, service provision and future research that focus on prevention and early identification of poor mental health
Methodology
Identification of relevant evidence.
The following inclusion criteria were used to guide the development of the search strategy and the selection of studies.
We included students from a variety of further education settings (16 yrs + or 18 yrs + , including mature students, international students, distance learning students, students at specific transition points).
Universities and colleges in the UK. We were also interested in the context prior to the beginning of tertiary education, including factors during transition from home and secondary education or existing employment to tertiary education.
Any factor shown to be associated with mental health of students in tertiary level education. This included clinical indicators such as diagnosis and treatment and/or referral for depression and anxiety. Self-reported measures of wellbeing, happiness, stress, anxiety and depression were included. We did not include measures of academic achievement or engagement with learning as indicators of mental wellbeing.
Study design
We included cross-sectional and longitudinal studies that looked at factors associated with mental health outcomes in Table 5 .
Data extraction and quality appraisal
We extracted and tabulated key data from the included papers. Data extraction was undertaken by one reviewer, with a 10% sample checked for accuracy and consistency The quality of the included studies were evaluated using the Newcastle-Ottawa Scale [ 26 ] and the findings of the quality appraisal used in weighting the strength of associations and also identifying gaps for future high quality research.
Involvement of stakeholders
We recruited students, ex-students and parents of students to a public involvement group which met on-line three times during the process of the review and following the completion of the review. During a workshop meeting we asked for members of the group to draw on their personal experiences to suggest factors which were not mentioned in the literature.
Methods of synthesis
We undertook a narrative synthesis [ 27 ] due to the heterogeneity in the exposures and outcomes that were measured across the studies. Data showing the direction of effects and the strength of the association (correlation coefficients) were recorded and tabulated to aid comparison between studies.
Search strategy
Searches were conducted in the following electronic databases: Medline, Applied Social Sciences Index and Abstracts (ASSIA), International Bibliography of Social Sciences (IBSS), Science,PsycINFO and Science and Social Sciences Ciatation Indexes. Additional searches of grey literature, and reference lists of included studies were also undertaken.
The search strategy combined a number of terms relating to students and mental health and risk factors. The search terms included both subject (MeSH) and free-text searches. The searches were limited to papers about humans in English, published from 2010 to June 2020. The flow of studies through the review process is summarised in Fig. 1 .
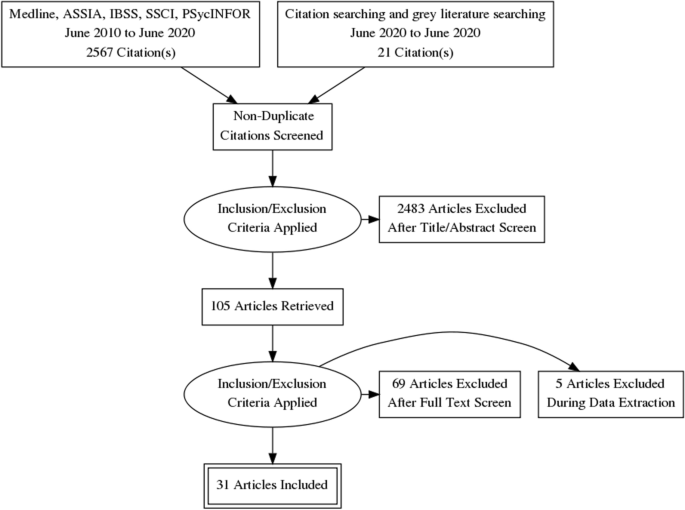
Flow diagram
The full search strategy for Medline is provided in Appendix 1 .
Thirty-one quantitative, observational studies (39 papers) met the inclusion criteria. The total number of students that participated in the quantitative studies was 17,476, with studies ranging in size from 57 to 3706. Eighteen studies recruited student participants from only one university; five studies (10 publications) [ 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ] included seven or more universities. Six studies (7 publications) [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ] only recruited first year students, while the majority of studies recruited students from a range of year groups. Five studies [ 39 , 42 , 43 , 44 , 45 ] recruited only, or mainly, psychology students which may impact on the generalisability of findings. A number of studies focused on students studying particular subjects including: nursing [ 46 ] medicine [ 47 ], business [ 48 ], sports science [ 49 ]. One study [ 50 ] recruited LGBTQ (lesbian, gay, bisexual, transgender, intersex, queer/questioning) students, and one [ 51 ] recruited students who had attended hospital having self-harmed. In 27 of the studies, there were more female than male participants. The mean age of the participants ranged from 19 to 28 years. Ethnicity was not reported in 19 of the studies. Where ethnicity was reported, the proportion that were ‘white British’ ranged from 71 – 90%. See Table 1 for a summary of the characteristics of the included studies and the participants.
Design and quality appraisal of the included studies
The majority of included studies ( n = 22) were cross-sectional surveys. Nine studies (10 publications) [ 35 , 36 , 39 , 41 , 43 , 50 , 51 , 52 , 53 , 62 ] were longitudinal in design, recording survey data at different time points to explore changes in the variables being measured. The duration of time that these studies covered ranged from 19 weeks to 12 years. Most of the studies ( n = 22) only recruited participants from a single university. The use of one university setting and the large number of studies that recruited only psychology students weakens the wider applicability of the included studies.
Quantitative variables
Included studies ( n = 31) measured a wide range of variables and explored their association with poor mental health and wellbeing. These included individual level factors: age, gender, sexual orientation, ethnicity and a range of psychological variables. They also included factors that related to mental health variables (family history, personal history and mental health literacy), pre-university factors (childhood trauma and parenting behaviour. University level factors including social isolation, adjustment and engagement with learning. Their association was measured against different measures of positive mental health and poor mental health.
Measurement of association and the strength of that association has some limitations in addressing our research question. It cannot prove causality, and nor can it capture fully the complexity of the inter-relationship and compounding aspect of the variables. For example, the stress of adjustment may be manageable, until it is combined with feeling isolated and out of place. Measurement itself may also be misleading, only capturing what is measureable, and may miss variables that are important but not known. We included both qualitative and PPI input to identify missed but important variables.
The wide range of variables and different outcomes, with few studies measuring the same variable and outcomes, prevented meta-analyses of findings which are therefore described narratively.
The variables described were categorised during the analyses into the following categories:
Vulnerabilities – factors that are associated with poor mental health
Individual level factors including; age, ethnicity, gender and a range of psychological variables were all measured against different mental health outcomes including depression, anxiety, paranoia, and suicidal behaviour, self-harm, coping and emotional intelligence.
Six studies [ 40 , 42 , 47 , 50 , 60 , 63 ] examined a student’s ages and association with mental health. There was inconsistency in the study findings, with studies finding that age (21 or older) was associated with fewer depressive symptoms, lower likelihood of suicide ideation and attempt, self-harm, and positively associated with better coping skills and mental wellbeing. This finding was not however consistent across studies and the association was weak. Theoretical models that seek to explain this mechanism have suggested that older age groups may cope better due to emotion-regulation strategies improving with age [ 67 ]. However, those over 30 experienced greater financial stress than those aged 17-19 in another study [ 63 ].
Sexual orientation
Four studies [ 33 , 40 , 64 , 68 ] examined the association between poor mental health and sexual orientation status. In all of the studies LGBTQ students were at significantly greater risk of mental health problems including depression [ 40 ], anxiety [ 40 ], suicidal behaviour [ 33 , 40 , 64 ], self harm [ 33 , 40 , 64 ], use of mental health services [ 33 ] and low levels of wellbeing [ 68 ]. The risk of mental health problems in these students compared with heterosexual students, ranged from OR 1.4 to 4.5. This elevated risk may reflect the greater levels of isolation and discrimination commonly experienced by minority groups.
Nine studies [ 33 , 38 , 39 , 40 , 42 , 47 , 50 , 60 , 63 ] examined whether gender was associated mental health variables. Two studies [ 33 , 47 ] found that being female was statistically significantly associated with use of mental health services, having a current mental health problem, suicide risk, self harm [ 33 ] and depression [ 47 ]. The results were not consistent, with another study [ 60 ] finding the association was not significant. Three studies [ 39 , 40 , 42 ] that considered mediating variables such as adaptability and coping found no difference or very weak associations.
Two studies [ 47 , 60 ] examined the extent to which ethnicity was associated with mental health One study [ 47 ] reported that the risks of depression were significantly greater for those who categorised themselves as non-white (OR 8.36 p = 0.004). Non-white ethnicity was also associated with poorer mental health in another cross-sectional study [ 63 ]. There was no significant difference in the McIntyre et al. (2018) study [ 60 ]. The small number of participants from ethnic minority groups represented across the studies means that this data is very limited.
Family factors
Six studies [ 33 , 40 , 42 , 50 , 60 ] explored the association of a concept that related to a student’s experiences in childhood and before going to university. Three studies [ 40 , 50 , 60 ] explored the impact of ACEs (Adverse Childhood Experiences) assessed using the same scale by Feletti (2009) [ 69 ] and another explored the impact of abuse in childhood [ 46 ]. Two studies examined the impact of attachment anxiety and avoidance [ 42 ], and parental acceptance [ 46 , 59 ]. The studies measured different mental health outcomes including; positive and negative affect, coping, suicide risk, suicide attempt, current mental health problem, use of mental health services, psychological adjustment, depression and anxiety.
The three studies that explored the impact of ACE’s all found a significant and positive relationship with poor mental health amongst university students. O’Neill et al. (2018) [ 50 ] in a longitudinal study ( n = 739) showed that there was in increased likelihood in self-harm and suicidal behaviours in those with either moderate or high levels of childhood adversities (OR:5.5 to 8.6) [ 50 ]. McIntyre et al. (2018) [ 60 ] ( n = 1135) also explored other dimensions of adversity including childhood trauma through multiple regression analysis with other predictive variables. They found that childhood trauma was significantly positively correlated with anxiety, depression and paranoia (ß = 0.18, 0.09, 0.18) though the association was not as strong as the correlation seen for loneliness (ß = 0.40) [ 60 ]. McLafferty et al. (2019) [ 40 ] explored the compounding impact of childhood adversity and negative parenting practices (over-control, overprotection and overindulgence) on poor mental health (depression OR 1.8, anxiety OR 2.1 suicidal behaviour OR 2.3, self-harm OR 2.0).
Gaan et al.’s (2019) survey of LGBTQ students ( n = 1567) found in a multivariate analyses that sexual abuse, other abuse from violence from someone close, and being female had the highest odds ratios for poor mental health and were significantly associated with all poor mental health outcomes [ 33 ].
While childhood trauma and past abuse poses a risk to mental health for all young people it may place additional stresses for students at university. Entry to university represents life stage where there is potential exposure to new and additional stressors, and the possibility that these students may become more isolated and find it more difficult to develop a sense of belonging. Students may be separated for the first time from protective friendships. However, the mechanisms that link childhood adversities and negative psychopathology, self-harm and suicidal behaviour are not clear [ 40 ]. McLafferty et al. (2019) also measured the ability to cope and these are not always impacted by childhood adversities [ 40 ]. They suggest that some children learn to cope and build resilience that may be beneficial.
McLafferty et al. (2019) [ 40 ] also studied parenting practices. Parental over-control and over-indulgence was also related to significantly poorer coping (OR -0.075 p < 0.05) and this was related to developing poorer coping scores (OR -0.21 p < 0.001) [ 40 ]. These parenting factors only became risk factors when stress levels were high for students at university. It should be noted that these studies used self-report, and responses regarding views of parenting may be subjective and open to interpretation. Lloyd et al.’s (2014) survey found significant positive correlations between perceived parental acceptance and students’ psychological adjustment, with paternal acceptance being the stronger predictor of adjustment.
Autistic students may display social communication and interaction deficits that can have negative emotional impacts. This may be particularly true during young adulthood, a period of increased social demands and expectations. Two studies [ 56 ] found that those with autism had a low but statistically significant association with poor social problem-solving skills and depression.
Mental health history
Three studies [ 47 , 51 , 68 ] investigated mental health variables and their impact on mental health of students in higher education. These included; a family history of mental illness and a personal history of mental illness.
Students with a family history or a personal history of mental illness appear to have a significantly greater risk of developing problems with mental health at university [ 47 ]. Mahadevan et al. (2010) [ 51 ] found that university students who self-harm have a significantly greater risk (OR 5.33) of having an eating disorder than a comparison group of young adults who self-harm but are not students.
Buffers – factors that are protective of mental wellbeing
Psychological factors.
Twelve studies [ 29 , 39 , 40 , 41 , 42 , 43 , 46 , 49 , 54 , 58 , 64 ] assessed the association of a range of psychological variables and different aspects of mental wellbeing and poor mental health. We categorised these into the following two categories: firstly, psychological variables measuring an individual’s response to change and stressors including adaptability, resilience, grit and emotional regulation [ 39 , 40 , 41 , 42 , 43 , 46 , 49 , 54 , 58 ] and secondly, those that measure self-esteem and body image [ 29 , 64 ].
The evidence from the eight included quantitative studies suggests that students with psychological strengths including; optimism, self-efficacy [ 70 ], resilience, grit [ 58 ], use of positive reappraisal [ 49 ], helpful coping strategies [ 42 ] and emotional intelligence [ 41 , 46 ] are more likely to experience greater mental wellbeing (see Table 2 for a description of the psychological variables measured). The positive association between these psychological strengths and mental well-being had a positive affect with associations ranging from r = 0.2–0.5 and OR1.27 [ 41 , 43 , 46 , 49 , 54 ] (low to moderate strength of association). The negative associations with depressive symptoms are also statistically significant but with a weaker association ( r = -0.2—0.3) [ 43 , 49 , 54 ].
Denovan (2017a) [ 43 ] in a longitudinal study found that the association between psychological strengths and positive mental wellbeing was not static and that not all the strengths remained statistically significant over time. The only factors that remained significant during the transition period were self-efficacy and optimism, remaining statistically significant as they started university and 6 months later.
Parental factors
Only one study [ 59 ] explored family factors associated with the development of psychological strengths that would equip young people as they managed the challenges and stressors encountered during the transition to higher education. Lloyd et al. (2014) [ 59 ] found that perceived maternal and paternal acceptance made significant and unique contributions to students’ psychological adjustment. Their research methods are limited by their reliance on retrospective measures and self-report measures of variables, and these results could be influenced by recall bias.
Two studies [ 29 , 64 ] considered the impact of how individuals view themselves on poor mental health. One study considered the impact of self-esteem and the association with non-accidental self-injury (NSSI) and suicide attempt amongst 734 university students. As rates of suicide and NSSI are higher amongst LGBT (lesbian, gay, bisexual, transgender) students, the prevalence of low self-esteem was compared. There was a low but statistically significant association between low self-esteem and NSSI, though not for suicide attempt. A large survey, including participants from seven universities [ 42 ] compared depressive symptoms in students with marked body image concerns, reporting that the risk of depressive symptoms was greater (OR 2.93) than for those with lower levels of body image concerns.
Mental health literacy and help seeking behaviour
Two studies [ 48 , 68 ] investigated attitudes to mental illness, mental health literacy and help seeking for mental health problems.
University students who lack sufficient mental health literacy skills to be able to recognise problems or where there are attitudes that foster shame at admitting to having mental health problems can result in students not recognising problems and/or failing to seek professional help [ 48 , 68 ]. Gorcyznski et al. (2017) [ 68 ] found that women and those who had a history of previous mental health problems exhibited significantly higher levels of mental health literacy. Greater mental health literacy was associated with an increased likelihood that individuals would seek help for mental health problems. They found that many students find it hard to identify symptoms of mental health problems and that 42% of students are unaware of where to access available resources. Of those who expressed an intention to seek help for mental health problems, most expressed a preference for online resources, and seeking help from family and friends, rather than medical professionals such as GPs.
Kotera et al. (2019) [ 48 ] identified self-compassion as an explanatory variable, reducing social comparison, promoting self-acceptance and recognition that discomfort is an inevitable human experience. The study found a strong, significant correlation between self-compassion and mental health symptoms ( r = -0.6. p < 0.01).
There again appears to be a cycle of reinforcement, where poor mental health symptoms are felt to be a source of shame and become hidden, help is not sought, and further isolation ensues, leading to further deterioration in mental health. Factors that can interrupt the cycle are self-compassion, leading to more readiness to seek help (see Fig. 2 ).
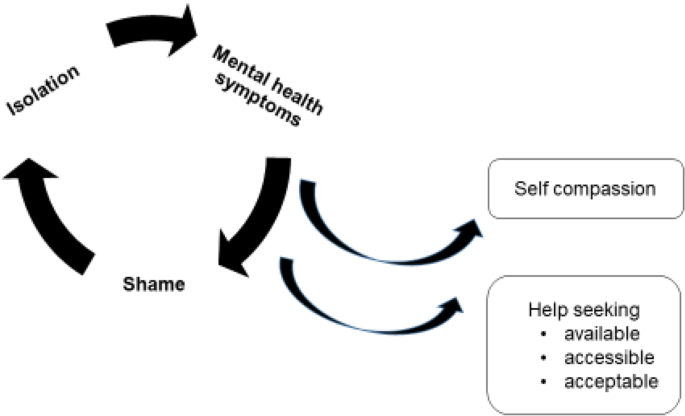
Poor mental health – cycles of reinforcement
Social networks
Nine studies [ 33 , 38 , 41 , 46 , 51 , 54 , 60 , 64 , 65 ] examined the concepts of loneliness and social support and its association with mental health in university students. One study also included students at other Higher Education Institutions [ 46 ]. Eight of the studies were surveys, and one was a retrospective case control study to examine the differences between university students and age-matched young people (non-university students) who attended hospital following deliberate self-harm [ 51 ].
Included studies demonstrated considerable variation in how they measured the concepts of social isolation, loneliness, social support and a sense of belonging. There were also differences in the types of outcomes measured to assess mental wellbeing and poor mental health. Grouping the studies within a broad category of ‘social factors’ therefore represents a limitation of this review given that different aspects of the phenomena may have been being measured. The tools used to measure these variables also differed. Only one scale (The UCLA loneliness scale) was used across multiple studies [ 41 , 60 , 65 ]. Diverse mental health outcomes were measured across the studies including positive affect, flourishing, self-harm, suicide risk, depression, anxiety and paranoia.
Three studies [ 41 , 60 , 62 ] measuring loneliness, two longitudinally [ 41 , 62 ], found a consistently positive association between loneliness and poor mental health in university students. Greater loneliness was linked to greater anxiety, stress, depression, poor general mental health, paranoia, alcohol abuse and eating disorder problems. The strength of the correlations ranged from 0–3-0.4 and were all statistically significant (see Tables 3 and 4 ). Loneliness was the strongest overall predictor of mental distress, of those measured. A strong identification with university friendship groups was most protective against distress relative to other social identities [ 60 ]. Whether poor mental health is the cause, or the result of loneliness was explored further in the studies. The results suggest that for general mental health, stress, depression and anxiety, loneliness induces or exacerbates symptoms of poor mental health over time [ 60 , 62 ]. The feedback cycle is evident, with loneliness leading to poor mental health which leads to withdrawal from social contacts and further exacerbation of loneliness.
Factors associated with protecting against loneliness by fostering supportive friendships and promoting mental wellbeing were also identified. Beliefs about the value of ‘leisure coping’, and attributes of resilience and emotional intelligence had a moderate, positive and significant association with developing mental wellbeing and were explored in three studies [ 46 , 54 , 66 ].
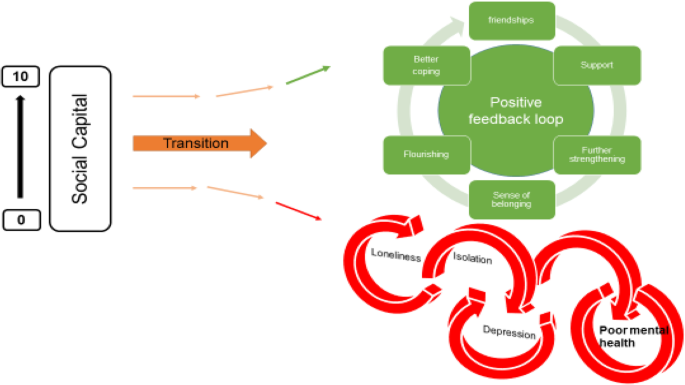
The transition to and first year at university represent critical times when friendships are developed. Thomas et al. (2020) [ 65 ] explored the factors that predict loneliness in the first year of university. A sense of community and higher levels of ‘social capital’ were significantly associated with lower levels of loneliness. ‘Social capital’ scales measure the development of emotionally supportive friendships and the ability to adjust to the disruption of old friendships as students transition to university. Students able to form close relationships within their first year at university are less likely to experience loneliness (r-0.09, r- 0.36, r- 0.34). One study [ 38 ] investigating the relationship between student experience and being the first in the family to attend university found that these students had lower ratings for peer group interactions.
Young adults at university and in higher education are facing multiple adjustments. Their ability to cope with these is influenced by many factors. Supportive friendships and a sense of belonging are factors that strengthen coping. Nightingale et al. (2012) undertook a longitudinal study to explore what factors were associated with university adjustment in a sample of first year students ( n = 331) [ 41 ]. They found that higher skills of emotion management and emotional self-efficacy were predictive of stable adjustment. These students also reported the lowest levels of loneliness and depression. This group had the skills to recognise their emotions and cope with stressors and were confident to access support. Students with poor emotion management and low levels of emotional self-efficacy may benefit from intervention to support the development of adaptive coping strategies and seeking support.
The positive and negative feedback loops
The relationship between the variables described appeared to work in positive and negative feedback loops with high levels of social capital easing the formation of a social network which acts as a critical buffer to stressors (see Fig. 3 ). Social networks and support give further strengthening and reinforcement, stimulating positive affect, engagement and flourishing. These, in turn, widen and deepen social networks for support and enhance a sense of wellbeing. Conversely young people who enter the transition to university/higher education with less social capital are less likely to identify with and locate a social network; isolation may follow, along with loneliness, anxiety, further withdrawal from contact with social networks and learning, and depression.
Triggers – factors that may act in combination with other factors to lead to poor mental health
Stress is seen as playing a key role in the development of poor mental health for students in higher education. Theoretical models and empirical studies have suggested that increases in stress are associated with decreases in student mental health [ 12 , 43 ]. Students at university experience the well-recognised stressors associated with academic study such as exams and course work. However, perhaps less well recognised are the processes of transition, requiring adapting to a new social and academic environment (Fisher 1994 cited by Denovan 2017a) [ 43 ]. Por et al. (2011) [ 46 ] in a small ( n = 130 prospective survey found a statistically significant correlation between higher levels of emotional intelligence and lower levels of perceived stress ( r = 0.40). Higher perceived stress was also associated with negative affect in two studies [ 43 , 46 ], and strongly negatively associated with positive affect (correlation -0.62) [ 54 ].
University variables
Eleven studies [ 35 , 39 , 47 , 51 , 52 , 54 , 60 , 63 , 65 , 83 , 84 ] explored university variables, and their association with mental health outcomes. The range of factors and their impact on mental health variables is limited, and there is little overlap. Knowledge gaps are shown by factors highlighted by our PPI group as potentially important but not identified in the literature (see Table 5 ). It should be noted that these may reflect the focus of our review, and our exclusion of intervention studies which may evaluate university factors.
High levels of perceived stress caused by exam and course work pressure was positively associated with poor mental health and lack of wellbeing [ 51 , 52 , 54 ]. Other potential stressors including financial anxieties and accommodation factors appeared to be less consistently associated with mental health outcomes [ 35 , 38 , 47 , 51 , 60 , 62 ]. Important mediators and buffers to these stressors are coping strategies and supportive networks (see conceptual model Appendix 2 ). One impact of financial pressures was that students who worked longer hours had less interaction with their peers, limiting the opportunities for these students to benefit from the protective effects of social support.
Red flags – behaviours associated with poor mental health and/or wellbeing
Engagement with learning and leisure activities.
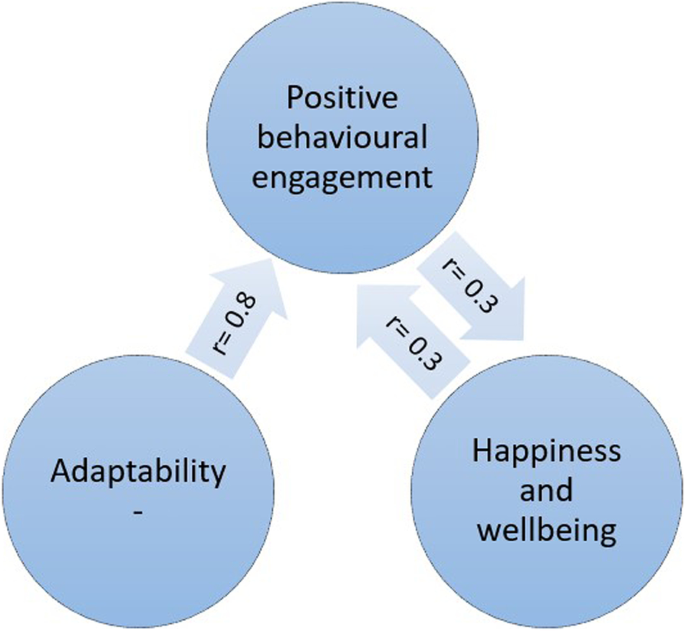
Engagement with learning activities was strongly and positively associated with characteristics of adaptability [ 39 ] and also happiness and wellbeing [ 52 ] (see Fig. 4 ). Boulton et al. (2019) [ 52 ] undertook a longitudinal survey of undergraduate students at a campus-based university. They found that engagement and wellbeing varied during the term but were strongly correlated.
Engagement and wellbeing
Engagement occurred in a wide range of activities and behaviours. The authors suggest that the strong correlation between all forms of engagement with learning has possible instrumental value for the design of systems to monitor student engagement. Monitoring engagement might be used to identify changes in the behaviour of individuals to assist tutors in providing support and pastoral care. Students also were found to benefit from good induction activities provided by the university. Greater induction satisfaction was positively and strongly associated with a sense of community at university and with lower levels of loneliness [ 65 ].
The inte r- related nature of these variables is depicted in Fig. 4 . Greater adaptability is strongly associated with more positive engagement in learning and university life. More engagement is associated with higher mental wellbeing.
Denovan et al. (2017b) [ 54 ] explored leisure coping, its psychosocial functions and its relationship with mental wellbeing. An individual’s beliefs about the benefits of leisure activities to manage stress, facilitate the development of companionship and enhance mood were positively associated with flourishing and were negatively associated with perceived stress. Resilience was also measured. Resilience was strongly and positively associated with leisure coping beliefs and with indicators of mental wellbeing. The authors conclude that resilient individuals are more likely to use constructive means of coping (such as leisure coping) to proactively cultivate positive emotions which counteract the experience of stress and promote wellbeing. Leisure coping is predictive of positive affect which provides a strategy to reduce stress and sustain coping. The belief that friendships acquired through leisure provide social support is an example of leisure coping belief. Strong emotionally attached friendships that develop through participation in shared leisure pursuits are predictive of higher levels of well-being. Friendship bonds formed with fellow students at university are particularly important for maintaining mental health, and opportunities need to be developed and supported to ensure that meaningful social connections are made.
The ‘broaden-and-build theory’ (Fredickson 2004 [ 85 ] cited by [ 54 ]) may offer an explanation for the association seen between resilience, leisure coping and psychological wellbeing. The theory is based upon the role that positive and negative emotions have in shaping human adaptation. Positive emotions broaden thinking, enabling the individual to consider a range of ways of dealing with and adapting to their environment. Conversely, negative emotions narrow thinking and limit options for adapting. The former facilitates flourishing, facilitating future wellbeing. Resilient individuals are more likely to use constructive means of coping which generate positive emotion (Tugade & Fredrickson 2004 [ 86 ], cited by [ 54 ]). Positive emotions therefore lead to growth in coping resources, leading to greater well-being.
Health behaviours at university
Seven studies [ 29 , 31 , 38 , 45 , 51 , 54 , 66 ] examined how lifestyle behaviours might be linked with mental health outcomes. The studies looked at leisure activities [ 63 , 80 ], diet [ 29 ], alcohol use [ 29 , 31 , 38 , 51 ] and sleep [ 45 ].
Depressive symptoms were independently associated with problem drinking and possible alcohol dependence for both genders but were not associated with frequency of drinking and heavy episodic drinking. Students with higher levels of depressive symptoms reported significantly more problem drinking and possible alcohol dependence [ 31 ]. Mahadevan et al. (2010) [ 51 ] compared students and non-students seen in hospital for self-harm and found no difference in harmful use of alcohol and illicit drugs.
Poor sleep quality and increased consumption of unhealthy foods were also positively associated with depressive symptoms and perceived stress [ 29 ]. The correlation with dietary behaviours and poor mental health outcomes was low, but also confirmed by the negative correlation between less perceived stress and depressive symptoms and consumption of a healthier diet.
Physical activity and participation in leisure pursuits were both strongly correlated with mental wellbeing ( r = 0.4) [ 54 ], and negatively correlated with depressive symptoms and anxiety ( r = -0.6, -0.7) [ 66 ].
Thirty studies measuring the association between a wide range of factors and poor mental health and mental wellbeing in university and college students were identified and included in this review. Our purpose was to identify the factors that contribute to the growing prevalence of poor mental health amongst students in tertiary level education within the UK. We also aimed to identify factors that promote mental wellbeing and protect against deteriorating poor mental health.
Loneliness and social isolation were strongly associated with poor mental health and a sense of belonging and a strong support network were strongly associated with mental wellbeing and happiness. These associations were strongly positive in the eight studies that explored them and are consistent with other meta-analyses exploring the link between social support and mental health [ 87 ].
Another factor that appeared to be protective was older age when starting university. A wide range of personal traits and characteristics were also explored. Those associated with resilience, ability to adjust and better coping led to improved mental wellbeing. Better engagement appeared as an important mediator to potentially explain the relationship between these two variables. Engagement led to students being able to then tap into those features that are protective and promoting of mental wellbeing.
Other important risk factors for poor mental wellbeing that emerged were those students with existing or previous mental illness. Students on the autism spectrum and those with poor social problem-solving also were more likely to suffer from poor mental health. Negative self-image was also associated with poor mental health at university. Eating disorders were strongly associated with poor mental wellbeing and were found to be far more of a risk in students at university than in a comparative group of young people not in higher education. Other studies of university students also found that pre-existing poor mental health was a strong predictor of poor mental health in university students [ 88 ].
At a family level, the experience of childhood trauma and adverse experiences including, for example, neglect, household dysfunction or abuse, were strongly associated with poor mental health in young people at university. Students with a greater number of ‘adverse childhood experiences’ were at significantly greater risk of poor mental health than those students without experience of childhood trauma. This was also identified in a review of factors associated with depression and suicide related outcomes amongst university undergraduate students [ 88 ].
Our findings, in contrast to findings from other studies of university students, did not find that female gender associated with poor mental health and wellbeing, and it also found that being a mature student was protective of mental wellbeing.
Exam and course work pressure was associated with perceived stress and poor mental health. A lack of engagement with learning activities was also associated with poor mental health. A number of variables were not consistently shown to be associated with poor mental health including financial concerns and accommodation factors. Very little evidence related to university organisation or support structures was assessed in the evidence. One study found that a good induction programme had benefits for student mental wellbeing and may be a factor that enables students to become a part of a social network positive reinforcement cycle. Involvement in leisure activities was also found to be associated with improved coping strategies and better mental wellbeing. Students with poorer mental health tended to also eat in a less healthy manner, consume more harmful levels of alcohol, and experience poorer sleep.
This evidence review of the factors that influence mental health and wellbeing indicate areas where universities and higher education settings could develop and evaluate innovations in practice. These include:
Interventions before university to improve preparation of young people and their families for the transition to university.
Exploratory work to identify the acceptability and feasibility of identifying students at risk or who many be exhibiting indications of deteriorating mental health
Interventions that set out to foster a sense of belonging and identify
Creating environments that are helpful for building social networks
Improving mental health literacy and access to high quality support services
This review has a number of limitations. Most of the included studies were cross-sectional in design, with a small number being longitudinal ( n = 7), following students over a period of time to observe changes in the outcomes being measured. Two limitations of these sources of data is that they help to understand associations but do not reveal causality; secondly, we can only report the findings for those variables that were measured, and we therefore have to support causation in assuming these are the only factors that are related to mental health.
Furthermore, our approach has segregated and categorised variables in order to better understand the extent to which they impact mental health. This approach does not sufficiently explore or reveal the extent to which variables may compound one another, for example, feeling the stress of new ways of learning may not be a factor that influences mental health until it is combined with a sense of loneliness, anxiety about financial debt and a lack of parental support. We have used our PPI group and the development of vignettes of their experiences to seek to illustrate the compounding nature of the variables identified.
We limited our inclusion criteria to studies undertaken in the UK and published within the last decade (2009–2020), again meaning we may have limited our inclusion of relevant data. We also undertook single data extraction of data which may increase the risk of error in our data.
Understanding factors that influence students’ mental health and wellbeing offers the potential to find ways to identify strategies that enhance the students’ abilities to cope with the challenges of higher education. This review revealed a wide range of variables and the mechanisms that may explain how they impact upon mental wellbeing and increase the risk of poor mental health amongst students. It also identified a need for interventions that are implemented before young people make the transition to higher education. We both identified young people who are particularly vulnerable and the factors that arise that exacerbate poor mental health. We highlight that a sense of belonging and supportive networks are important buffers and that there are indicators including lack of engagement that may enable early intervention to provide targeted and appropriate support.
Availability of data and materials
Further details of the study and the findings can be provided on request to the lead author ([email protected]).
Association of Colleges. Association of Colleges’ survey on students with mental health conditions in further education. London: 2017.
Google Scholar
Hughes G, Spanner L. The University Mental Health Charter. Leeds: Student Minds; 2019.
Sivertsen B, Hysing M, Knapstad M, Harvey AG, Reneflot A, Lønning KJ, et al. Suicide attempts and non-suicidal self-harm among university students: prevalence study. BJPsych Open. 2019;5(2):e26.
Article PubMed PubMed Central Google Scholar
Storrie K, Ahern K, Tuckett A. A systematic review: students with mental health problems—a growing problem. Int J Nurs Pract. 2010;16(1):1–6.
Article PubMed Google Scholar
Pereira S, Reay K, Bottell J, Walker L, Dzikiti C, Platt C, Goodrham C. Student Mental Health Survey 2018: A large scale study into the prevalence of student mental illness within UK universities. 2019.
Bayram N, Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol. 2008;43(8):667–72.
Bewick B, Koutsopoulou G, Miles J, Slaa E, Barkham M. Changes in undergraduate students’ psychological well-being as they progress through university. Stud High Educ. 2010;35(6):633–45.
Article Google Scholar
Thorley C. Not By Degrees: Not by degrees: Improving student mental health in the UK’s universities. London: IPPR; 2017.
Eisenberg D, Golberstein E, Hunt JB. Mental health and academic success in college. BE J Econ Anal Pol. 2009;9(1):1–37.
Hysenbegasi A, Hass SL, Rowland CR. The impact of depression on the academic productivity of university students. J Ment Health Policy Econ. 2005;8(3):145.
PubMed Google Scholar
Chowdry H, Crawford C, Dearden L, Goodman A, Vignoles A. Widening participation in higher education: analysis using linked administrative data. J R Stat Soc A Stat Soc. 2013;176(2):431–57.
Macaskill A. The mental health of university students in the United Kingdom. Br J Guid Couns. 2013;41(4):426–41.
Belfield C, Britton J, van der Erve L. Higher Education finance reform: Raising the repayment threshold to£ 25,000 and freezing the fee cap at £ 9,250: Institute for Fiscal Studies Briefing note. London: Institute for Fiscal Studies; 2017. Available from https://ifs.org.uk/publications/9964 .
Benson-Egglenton J. The financial circumstances associated with high and low wellbeing in undergraduate students: a case study of an English Russell Group institution. J Furth High Educ. 2019;43(7):901–13.
Jessop DC, Herberts C, Solomon L. The impact of financial circumstances on student health. Br J Health Psychol. 2005;10(3):421–39.
(2020) SCSC. Canadians’ mental health during the COVID-19 pandemic. 2020.
(NUS) NUoS. Coronavirus Student Survey phase III November 2020. 2020.
Hellemans K, Abizaid A, Gabrys R, McQuaid R, Patterson Z. For university students, COVID-19 stress creates perfect conditions for mental health crises. The Conversation. 2020. Available from: https://theconversation.com/for-university-students-covid-19-stress-creates-perfect-conditions-for-mental-health-crises-149127 .
England N. Children and Young People with an Eating Disorder Waiting Times: NHS England; 2021 [Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/cyped-waiting-times/
King JA, Cabarkapa S, Leow FH, Ng CH. Addressing international student mental health during COVID-19: an imperative overdue. Australas Psychiatry. 2020;28(4):469.
Rana R, Smith E, Walking J. Degrees of disturbance: the new agenda; the Impact of Increasing Levels of Psychological Disturbance Amongst Students in Higher Education. England: Association for University and College Counselling Rugby; 1999.
AMOSSHE. Responding to student mental health issues: 'Duty of Care' responsibilities for student services in higher education. https://www.amosshe.org.uk/resources/Documents/AMOSSHE_Duty_of_Care_2001.pdf [accessed 24.12.2020]. (2001).
Universities UK. Student mental wellbeing in higher education. Good practice guide. London: Universities UK; 2015.
Williams M, Coare P, Marvell R, Pollard E, Houghton A-M, Anderson J. 2015. Understanding provision for students with mental health problems and intensive support needs: Report to HEFCE by the Institute for Employment Studies (IES) and Researching Equity, Access and Partnership (REAP). Institute for Employment Studies.
Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46(1):3–10.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. In.: Oxford; 2000.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890.
El Ansari W, Adetunji H, Oskrochi R. Food and mental health: relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent Eur J Public Health. 2014a;22(2):90–7.
El Ansari W, Dibba E, Stock C. Body image concerns: levels, correlates and gender differences among students in the United Kingdom. Cent Eur J Public Health. 2014b;22(2):106–17.
Ansari EL, W, Oskrochi R, Stock C. Symptoms and health complaints and their association with perceived stress: Students from seven universities in England, Wales and Northern Ireland. J Public Health. 2013;21(5):413–25.
El Ansari W, Sebena R, Stock C. Do importance of religious faith and healthy lifestyle modify the relationships between depressive symptoms and four indicators of alcohol consumption? A survey of students across seven universities in England, Wales, and Northern Ireland. Subst Use Misuse. 2014c;49(3):211–20.
El Ansari W, Stock C. Is the health and wellbeing of university students associated with their academic performance? Cross sectional findings from the United Kingdom. International Journal of Environmental Research & Public Health [Electronic Resource]. 2010;7(2):509–27.
Gnan GH, Rahman Q, Ussher G, Baker D, West E, Rimes KA. General and LGBTQ-specific factors associated with mental health and suicide risk among LGBTQ students. J Youth Stud. 2019;22(10):1393–408.
Jackson SL, Dritschel B. Modeling the impact of social problem-solving deficits on depressive vulnerability in the broader autism phenotype. Res Aut Spectr Disord. 2016;21:128–38.
Richardson T, Elliott P, Roberts R. The impact of tuition fees amount on mental health over time in British students. J Public Health. 2015;37(3):412–8.
Article CAS Google Scholar
Richardson T, Mma Y, Jansen M, Elliott P, Roberts R. Financial difficulties and psychosis risk in British undergraduate students: a longitudinal analysis. J Public Ment Health. 2018;17(2):61–8.
Thomas L, Briggs P, Hart A, Kerrigan F. Understanding social media and identity work in young people transitioning to university. Comput Hum Behav. 2017;76:541–53.
Hixenbaugh P, Dewart H, Towell T. What enables students to succeed? An investigation of socio-demographic, health and student experience variables. Psychodyn Pract. 2012;18(3):285–301.
Holliman A, Martin A, Collie R. Adaptability, engagement, and degree completion: a longitudinal investigation of university students. Educ Psychol. 2018;38(6):785–99.
McLafferty M, Armour C, Bunting B, Ennis E, Lapsley C, Murray E, et al. Coping, stress, and negative childhood experiences: the link to psychopathology, self-harm, and suicidal behavior. Psychic J. 2019;8(3):293–306.
Nightingale S, Roberts S, Tariq V, Appleby Y, Barnes L, Harris R, et al. Trajectories of university adjustment in the United Kingdom: EMOTION management and emotional self-efficacy protect against initial poor adjustment. Learn Individ Differ. 2013;27:174–81.
Berry K, Kingswell S. An investigation of adult attachment and coping with exam-related stress. Br J Guid Couns. 2012;40(4):315.
Denovan A, Macaskill A. Stress and subjective well-being among first year UK undergraduate students. J Happiness Stud. 2017a;18(2):505–25.
Hassel S, Ridout N. An investigation of first-year students’ and lecturers’ expectations of university education. Front Psychol. 2018;8:2218.
Norbury R, Evans S. Time to think: subjective sleep quality, trait anxiety and university start time. Psychiatry Res. 2019;271:214–9.
Por J, Barriball L, Fitzpatrick J, Roberts J. Emotional intelligence: its relationship to stress, coping, well-being and professional performance in nursing students. Nurse Educ Today. 2011;31(8):855.
Honney K, Buszewicz M, Coppola W, Griffin M. Comparison of levels of depression in medical and non-medical students. Clin Teach. 2010;7(3):180–4.
Kotera Y, Conway E, Van Gordon W. Mental health of UK university business students: Relationship with shame, motivation and self-compassion. Journal of Education for Business. 2019;94(1):11–20.
Oliver EJ, Markland D, Hardy J. Interpretation of self-talk and post-lecture affective states of higher education students: a self-determination theory perspective. Br J Educ Psychol. 2010;80(Pt 2):307–23.
O’Neill S, McLafferty M, Ennis E, Lapsley C, Bjourson T, Armour C, et al. Socio-demographic, mental health and childhood adversity risk factors for self-harm and suicidal behaviour in College students in Northern Ireland. J Affect Disord. 2018;239:58–65.
Mahadevan S, Hawton K, Casey D. Deliberate self-harm in Oxford University students, 1993–2005: a descriptive and case-control study. Soc Psychiatry Psychiatr Epidemiol. 2010;45(2):211–9.
Boulton CA, Hughes E, Kent C, Smith JR, Williams HTP. Student engagement and wellbeing over time at a higher education institution. PLoS One [Electronic Resource]. 2019;14(11): e0225770.
Davies EL, Paltoglou AE. Public self-consciousness, pre-loading and drinking harms among university students. Subst Use Misuse. 2019;54(5):747–57.
Denovan A, Macaskill A. Stress, resilience and leisure coping among university students: Applying the broaden-and-build theory. Leisure Studies. 2017b;36(6):852–65.
El Ansari W, Vallentin-Holbech L, Stock C. Predictors of illicit drug/s use among university students in Northern Ireland, Wales and England. Glob J Health Sci. 2015;7(4):18–29.
Freeth M, Bullock T, Milne E. The distribution of and relationship between autistic traits and social anxiety in a UK student population. Autism. 2013;17(5):571–81.
Jessop DC, Reid M, Solomon L. Financial concern predicts deteriorations in mental and physical health among university students. Psychology Health. 2020;35(2):196–209.
Kannangara CS, Allen RE, Waugh G, Nahar N, Khan SZN, Rogerson S, Carson J. All that glitters is not grit: Three studies of grit in university students. Front Psychol. 2018;9:1539.
Lloyd J, Ward T, Young J. Do parental interpersonal power and prestige moderate the relationship between parental acceptance and psychological adjustment in U.K. Students? Cross-Cultural Research. The Journal of Comparative Social Science. 2014;48(3):326–35.
McIntyre JC, Worsley J, Corcoran R, Harrison Woods P, Bentall RP. Academic and non-academic predictors of student psychological distress: the role of social identity and loneliness. J Ment Health. 2018;27(3):230–9.
Ribchester C, Ross K, Rees EL. Examining the impact of pre-induction social networking on the student transition into higher education. Innov Educ Teach Int. 2014;51(4):355–65.
Richardson T, Elliott P, Roberts R. Relationship between loneliness and mental health in students. J Public Ment Health. 2017a;16(2):48–54.
Richardson T, Elliott P, Roberts R, Jansen M. A Longitudinal Study of Financial Difficulties and Mental Health in a National Sample of British Undergraduate Students. Community Ment Health J. 2017;53(3):344–52.
Taylor PJ, Dhingra K, Dickson JM, McDermott E. Psychological Correlates of Self-Harm within Gay, Lesbian and Bisexual UK University Students. Arch Suicide Res. 2020;24(sup1):41–56.
Thomas L, Orme E, Kerrigan F. Student loneliness: The role of social media through life transitions. Comput Educ. 2020;146:103754.
Tyson P, Wilson K, Crone D, Brailsford R, Laws K. Physical activity and mental health in a student population. J Ment Health. 2010;19(6):492–9.
Folkman S. The Oxford handbook of stress, health, and coping. Oxford: Oxford University Press; 2011.
Gorczynski P, Sims-schouten W, Hill D, Wilson JC. Examining mental health literacy, help seeking behaviours, and mental health outcomes in UK university students. J Ment Health Train Educ Pract. 2017;12(2):111–20.
Felitti VJ. Adverse childhood experiences and adult health. Acad Pediatr. 2009;9(3):131–2.
Denovan A, Macaskill A. An interpretative phenomenological analysis of stress and coping in first year undergraduates. Br Educ Res J. 2013;39(6):1002–24.
Bandura A. Self-efficacy: The foundation of agency. Control of human behavior, mental processes, and consciousness: Essays in honor of the 60th birthday of August Flammer. 2000;16.
Martin AJ, Nejad H, Colmar S, Liem GAD. Adaptability: Conceptual and empirical perspectives on responses to change, novelty and uncertainty. J Psychol Couns Sch. 2012;22(1):58–81.
Lazarus RS, Folkman S. Stress, appraisal, and coping: Springer publishing company; 1984.
Gross JJ. Emotion regulation: Past, present, future. Cogn Emot. 1999;13(5):551–73.
Mayer JD, Salovey P, Caruso DR. TARGET ARTICLES:" Emotional Intelligence: Theory, Findings, and Implications". Psychol Inq. 2004;15(3):197–215.
Duckworth AL, Peterson C, Matthews MD, Kelly DR. Grit: perseverance and passion for long-term goals. J Pers Soc Psychol. 2007;92(6):1087.
Snyder CR, Ilardi SS, Cheavens J, Michael ST, Yamhure L, Sympson S. The role of hope in cognitive-behavior therapies. Cognit Ther Res. 2000;24(6):747–62.
Scheier MF, Carver CS, Bridges MW. Optimism, pessimism, and psychological well-being. 2001.
Seligman ME. Positive psychology in practice: Wiley; 2012.
Masten AS. Ordinary magic: Lessons from research on resilience in human development. Education Canada. 2009;49(3):28–32.
Rosenberg M, Schooler C, Schoenbach C, Rosenberg F. Global self-esteem and specific self-esteem: Different concepts, different outcomes. Am Sociol Rev. 1995:141–56.
Oliver EJ, Markland D, Hardy J. Interpretation of self-talk and post-lecture affective states of higher education students: A self-determination theory perspective. Br J Educ Psychol. 2010;80(2):307–23.
Hofmann W, Friese M, Strack F. Impulse and self-control from a dual-systems perspective. Perspect Psychol Sci. 2009;4(2):162–76.
Aceijas C, Waldhausl S, Lambert N, Cassar S, Bello-Corassa R. Determinants of health-related lifestyles among university students. Perspect Public Health. 2017;137(4):227–36.
Fredrickson BL. The broaden–and–build theory of positive emotions. Philos Trans R Soc Lond B Biol Sci. 2004;359(1449):1367–77.
Tugade MM, Fredrickson BL, Feldman Barrett L. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. J Pers. 2004;72(6):1161–90.
Harandi TF, Taghinasab MM, Nayeri TD. The correlation of social support with mental health: A meta-analysis. Electron physician. 2017;9(9):5212.
Sheldon E, Simmonds-Buckley M, Bone C, Mascarenhas T, Chan N, Wincott M, Gleeson H, Sow K, Hind D, Barkham M. Prevalence and risk factors for mental health problems in university undergraduate students: A systematic review with meta-analysis. J Affect Disord. 2021;287:282–92.
Download references
Acknowledgements
We acknowledge the input from our public advisory group which included current and former students, and family members of students who have struggled with their mental health. The group gave us their extremely valuable insights to assist our understanding of the evidence.
This project was supported by funding from the National Institute for Health Research as part of the NIHR Public Health Research Programme (fuding reference 127659 Public Health Review Team). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
University of Sheffield, Sheffield, UK
Fiona Campbell, Lindsay Blank, Anna Cantrell, Susan Baxter, Christopher Blackmore, Jan Dixon & Elizabeth Goyder
You can also search for this author in PubMed Google Scholar
Contributions
All of the included authors designed the project methods and prepared a protocol. A.C. designed the search strategy. F.C, L.B and C.B screened the identified citations and undertook data extraction. S.B. led the PPI involvement. JD participated as a member of the PPI group. F.C and L.B undertook the analysis. F.C. and L.B wrote the main manuscript text. All authors reviewed the manuscript. F.C designed Figs. 2 , 3 and 4 . The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Fiona Campbell .
Ethics declarations
Ethics approval and consent to participate.
Not applicable as this was secondary research.
Consent for publication
Not applicable.
Competing interests
None of the authors have competing interests or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Campbell, F., Blank, L., Cantrell, A. et al. Factors that influence mental health of university and college students in the UK: a systematic review. BMC Public Health 22 , 1778 (2022). https://doi.org/10.1186/s12889-022-13943-x
Download citation
Received : 03 February 2022
Accepted : 25 July 2022
Published : 20 September 2022
DOI : https://doi.org/10.1186/s12889-022-13943-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student mental health
- Mental wellbeing
- Risk factors
- Rapid review
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

College students' mental health is a higher priority
Colleges and universities are increasing efforts to address student mental health
Vol. 50, No. 11 Print version: page 80

The percentage of U.S. college students with lifetime diagnoses of mental health conditions in 2017, compared with 22% in 2007. The percentage of students who received any mental health treatment , including therapy or medication, rose from 19% to 34% over that 10-year period.
The percentage of college presidents in 2019 who say that student mental health has become a greater priority on their campuses than it was three years earlier.
The percentage of college presidents who say they have reallocated or identified more funds to address student mental health issues, compared with three years earlier.
The percentage of college presidents who said they would hire additional staff , mostly in counseling centers, if they had unlimited resources. Meanwhile, 20% said they would invest in other resources and programs such as early alert systems for at-risk students.
Lipson, S.K., et al. (2019). Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007–2017). Psychiatric Services, 70 , 60–63. DOI: 10.1176/appi.ps.201800332 .
American Council on Education. (2019). Pulse Point presidential survey on student mental health and well-being. Available at www.higheredtoday.org/2019/08/12/college-student-mental-health-well-survey-college-presidents .
Recommended Reading

Contact APA
You may also like.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Stigma and help seeking for mental health among college students
Affiliation.
- 1 Department of Health Policy and Management, University of Michigan, Ann Arbor, MI 48109-2029, USA. [email protected]
- PMID: 19454625
- DOI: 10.1177/1077558709335173
Mental illness stigma has been identified by national policy makers as an important barrier to help seeking for mental health. Using a random sample of 5,555 students from a diverse set of 13 universities, we conducted one of the first empirical studies of the association of help-seeking behavior with both perceived public stigma and people's own stigmatizing attitudes (personal stigma). There were three main findings: (a) Perceived public stigma was considerably higher than personal stigma; (b) personal stigma was higher among students with any of the following characteristics: male, younger, Asian, international, more religious, or from a poor family; and (c) personal stigma was significantly and negatively associated with measures of help seeking (perceived need and use of psychotropic medication, therapy, and nonclinical sources of support), whereas perceived stigma was not significantly associated with help seeking. These findings can help inform efforts to reduce the role of stigma as a barrier to help seeking.
PubMed Disclaimer
Similar articles
- Sociodemographic Correlates of Mental Health Treatment Seeking Among College Students: A Systematic Review and Meta-Analysis. Pei J, Amanvermez Y, Vigo D, Puyat J, Kessler RC, Mortier P, Bruffaerts R, Rankin O, Chua SN, Martínez V, Rapsey C, Fodor LA, David OA, Garcia C, Cuijpers P. Pei J, et al. Psychiatr Serv. 2024 Jun 1;75(6):556-569. doi: 10.1176/appi.ps.20230414. Epub 2024 Jan 31. Psychiatr Serv. 2024. PMID: 38291886 Review.
- Factors that influence Asian American college students use of mental health services: A systematic mixed studies review. Nguyen N, Kim B, Aronowitz T. Nguyen N, et al. J Psychiatr Ment Health Nurs. 2024 Apr;31(2):181-202. doi: 10.1111/jpm.12972. Epub 2023 Sep 4. J Psychiatr Ment Health Nurs. 2024. PMID: 37661752 Review.
- Mental health stigma and professional help-seeking behaviors among Asian American and Asian international students. Maeshima LS, Parent MC. Maeshima LS, et al. J Am Coll Health. 2022 Aug-Sep;70(6):1761-1767. doi: 10.1080/07448481.2020.1819820. Epub 2020 Oct 13. J Am Coll Health. 2022. PMID: 33048652 Free PMC article.
- Comparing perceived public stigma and personal stigma of mental health treatment seeking in a young adult sample. Pedersen ER, Paves AP. Pedersen ER, et al. Psychiatry Res. 2014 Sep 30;219(1):143-50. doi: 10.1016/j.psychres.2014.05.017. Epub 2014 May 20. Psychiatry Res. 2014. PMID: 24889842 Free PMC article.
- Perceived stigma and mental health care seeking. Golberstein E, Eisenberg D, Gollust SE. Golberstein E, et al. Psychiatr Serv. 2008 Apr;59(4):392-9. doi: 10.1176/ps.2008.59.4.392. Psychiatr Serv. 2008. PMID: 18378838
- Mediating roles of perceived stigma and mental health literacy in the relationship between school climate and help-seeking behavior in Indonesian adolescents. Setia Lesmana MH, Chung MH. Setia Lesmana MH, et al. PLoS One. 2024 May 31;19(5):e0298017. doi: 10.1371/journal.pone.0298017. eCollection 2024. PLoS One. 2024. PMID: 38820380 Free PMC article.
- Mental health stigma: a conundrum for healthcare practitioners in conservative communities. Booth WA, Abuhmida M, Anyanwu F. Booth WA, et al. Front Public Health. 2024 May 15;12:1384521. doi: 10.3389/fpubh.2024.1384521. eCollection 2024. Front Public Health. 2024. PMID: 38813403 Free PMC article. Review.
- A modified persian version of the self-stigma of depression scale among the Iranian population: a methodological study in 2023. Jafari A, Moshki M, Naddafi F, Lael-Monfared E, Nejatian M. Jafari A, et al. BMC Psychol. 2024 May 26;12(1):294. doi: 10.1186/s40359-024-01802-w. BMC Psychol. 2024. PMID: 38797822 Free PMC article.
- Visitor characteristics and changes in mental health stigma after attending the Mind Space mental health experience exhibition. Ho GWK, Mui JHC, Wong R, Chien WT, Wong KH, Bressington D. Ho GWK, et al. Front Psychiatry. 2024 Apr 29;15:1302799. doi: 10.3389/fpsyt.2024.1302799. eCollection 2024. Front Psychiatry. 2024. PMID: 38742134 Free PMC article.
- The development and evolution of the research topic on the mental health of college students: A bibliometric review based on CiteSpace and VOSviewer. Chen J, Liu Y, Zhu K, Dai J, Wang C. Chen J, et al. Heliyon. 2024 Apr 9;10(8):e29477. doi: 10.1016/j.heliyon.2024.e29477. eCollection 2024 Apr 30. Heliyon. 2024. PMID: 38638989 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Fostering College Student Mental Health and Resilience
- August 15, 2023
- Healthy living for mental well-being, Patients and Families, Teens and young adults
College student mental health has been the focus of much attention in recent years. Mental health is integral to student success and mental health concerns among college students are an ongoing and systemic problem; not just a consequence of the pandemic.
- 73% of students reported moderate or severe psychological distress in 2021, according to the National College Health Assessment
- 60% of college students reported experiencing one or more mental health challenges in 2021, according to the National Healthy Minds Study(.pdf).
- The percentage of students experiencing mental health problems has increased nearly 50% since 2013 .

Students are affected by a range of stressors and challenges, including academic pressure , balancing obligations, social pressures, and more global/societal concerns. A recent survey found that more than half of Gen Zers (teens and young adults aged 14 to 25) experience mental health impacts related to concerns about gun violence and climate change. Another recent survey of college students finds that more than half (56%) of students have experienced chronic stress (a consistent sense of feeling pressured and overwhelmed over a long period of time) in college. Chronic stress is linked to a range of mental and physical health problems.
Given the extent of the mental health concerns among college students, access to services and use of services is important. A recent national survey of college students found that, among students with a mental health condition, about 50% have not accessed any mental health services. Among all students, about one in four have used on-campus counseling, 12% have used telecounseling, 10% received referrals to off-campus therapists, and 6% have used a mental health hotline and urgent counseling. About two-thirds of students have not accessed any campus resources.
Increasing Student Access to Mental Health Services
Researcher Brett R. Harris, University at Albany School of Public Health, and colleagues offer a set of universal recommendations for increasing college students’ access to and use of mental health services. They note that while each campus is unique, they have developed universal recommendations “based on their experience working with colleges and universities across New York State to help change campus culture and increase uptake and usage of services. Their recommendations include:
- Start the conversation on mental health and increase ommunication. Increasing the conversation around mental health is a first step to reducing stigma.
- Make mental health promotion and puicide prevention a campus‑wide effort.
- Involve students, faculty, and staff in the development and implementation of mental health campaigns, services, resources, and supports.
- Don’t just make training available: Integrate training into academics and student life and follow‑up with resources and support. Mental health or suicide prevention training should become a part of the set of annual trainings required for faculty and staff.
- Make sure information about services and supports Is readily available and communicated to students.
- Assess the needs of students and take a staged approach to meet their needs. For example, screening and assessment can be conducted for all students at the beginning of the semester via online survey or in college health and counseling centers.
- Collaborate with outside organizations and the community. Active collaboration with external organizations and the outside community may help to expand upon limited resources.
The authors also suggest that efforts need to go beyond mental health services in college counseling centers and involve a multipronged, public health approach with buy-in, support, input, and participation of key stakeholders.
Working with Peer Leaders to Promote Wellness and Resilience
A wellness program developed by the Radical Hope Foundation is working to boost student resilience and promote wellness with the help of student leaders. It will be in place in more than 30 college campuses this fall. The RADical Health program works to empower students and equip them with knowledge and coping skills to stay well and stay resilient. During the four-week program students work in small groups with the support of peer leaders or faculty guides to explore themes including
- Staying well, staying resilient (building resilience).
- Connecting with others (strengthening emotional intelligence).
- Empowering yourself (examining principles and priorities).
- Engaging with the world (looking at’ Where do I go from here?’).
Students hear from notable figures in sports, entertainment, and business and participate in group discussions about the program themes, student life experiences and other aspects of their lives. Student Mental Wellness Tips for Thriving on Campus this Fall Students can be proactive in promoting their own mental wellness on a college campus.
- Familiarize yourself with mental health and wellness services offered on campus.
- Check that your health insurance will cover medical and mental healthcare in the area in which you are attending college.
- Look for ways to connect with others on campus. Join a campus organization.
- Communicate with your instructors about your needs.
- Prioritize sleep and a healthy diet. You may be tempted to grab easy not-so-healthy snacks or meals or to forgo sleep to study, but doing so will only make it harder to concentrate, learn and be productive.
More information on college student mental health:
- Jed Foundation
- Higher Education Mental Health Alliance (HEMHA)
- Harris, B. R., Maher, B. M., & Wentworth, L. (2022). Optimizing Efforts to Promote Mental Health on College and University Campuses: Recommendations to Facilitate Usage of Services, Resources, and Supports. The journal of behavioral health services & research, 49(2), 252–258. https://doi.org/10.1007/s11414-021-09780-2
- Flaherty, C. 2023. Student Health and Wellness Survey: The Top 10 Takeaways . Inside Higher Ed.
Medical leadership for mind, brain and body.
Mobile menu.
- Psychiatrists
- Residents & Medical Students
- Patients and Families
- Advocacy & APAPAC
- Diversity & Health Equity
- Research & Registry
- Meetings & Events
- Search Directories & Databases
- International
- Medical Students
- What is Psychiatry?
- Find a Psychiatrist
- Addiction and Substance Use Disorders
- Dementia and Alzheimer's Disease
- Alcohol Use Disorder
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder
- Bipolar Disorders
- Climate Change and Mental Health Connections
- Coping After Disaster
- Disruptive, Impulse-Control and Conduct Disorders
- Dissociative Disorders
- Domestic Violence
- Eating Disorders
- E-Cigarettes and Vaping
- Gambling Disorder
- Gender Dysphoria
- Helping a Loved One Cope with Mental Illness
- Hoarding Disorder
- Integrated Behavioral Healthcare
- Intellectual Disability
- Internet Gaming
- Obsessive-Compulsive Disorder
- Opioid Use Disorder
- Perinatal Depression (formerly Postpartum)
- Personality Disorders
- Posttraumatic Stress Disorder (PTSD)
- Prolonged Grief Disorder
- Schizophrenia
- Seasonal Affective Disorder (SAD)
- Sleep Disorders
- Somatic Symptom Disorder
- Specific Learning Disorders
- Stigma, Prejudice and Discrimination Against People with Mental Illness
- Suicide Prevention
- Technology Addictions: Social Media, Online Gaming, and More
- Warning Signs of Mental Illness
- Electroconvulsive Therapy (ECT)
- What is Mental Illness?
- What is Psychotherapy?
- What is Telepsychiatry?
- La Salud Mental
- Childhood Disorders: Medication Guides for Parents
- Lifestyle to Support Mental Health
- Member Benefits
- Honorary Fellowship (FAPA & DFAPA)
- Awards & Leadership Opportunities
- Get Involved
- Directories, Contact Info & FAQs
- District Branches
- APA's Vision, Mission, Values, and Goals
- Meet Our Organization
- Read APA Organization Documents and Policies
- Work At APA
- About APA's Headquarters
- Policy Finder
- News Releases
- Messages from the APA President
- Reporting on Mental Health Conditions
- Goldwater Rule
- Annual Meeting Press Registration + Guidelines
- APA Public Opinion Polls
- Reporter Toolkit: Recommendations on Covering the AAPI Community
- Comunicados de prensa en español
- APA Annual Meeting
- APA Communities
- APA Foundation
- APA Learning Center
- APA Publishing
- Center for Workplace Mental Health
- Melvin Sabshin, M.D. Library & Archives
- Psychiatric News
- Psychiatry Online
- SMI Adviser
- Annual Meeting
- APA On Demand
- At the APA Educational Series
- Books and Journals
- Certification and Licensure
- Diversity and Health Equity Education Resources
- Meeting Submission and Guidelines
- Mental Health Innovation Zone
- The Mental Health Services Conference
- The Virtual Immersive
- Virtual Paid Courses
- Clinical Practice Guidelines
- Covid-19 / Coronavirus
- Digital Mental Health
- Helping Patients Access Care
- Media and Communications
- Mental Health Apps
- Mental Health Parity
- Practice Management
- Professional Interests
- Quality Improvement
- Risk Management
- Social Media
- Sunshine Act
- Telepsychiatry
- The Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program
- Transition to Practice and Early Career Resources
- Well-being and Burnout
- Mental Health and Faith Community Partnership
- Mental Health Equity Looking Beyond Series
- Minority and Underrepresented (M/UR) Caucuses
- Moore Equity in Mental Health Initiative
- News and Updates
- Striving for Excellence Series
- AMNet: Addiction Medicine Practice Based Research Network
- PsychPRO: APA's Mental Health Registry
- Research Colloquium for Junior Psychiatrist Investigators
- Perinatal Mental Health Toolkit
- Psychiatric Bed Crisis Report
- Advocacy Action Center
- Congressional Advocacy Network
- Federal Affairs
- State Affairs
- Implementing 9-8-8
- Advocacy Update Webinars
- 2025 Annual Meeting
- The 2024 Mental Health Services Conference
- Addressing Structural Racism Town Hall Series
- APA Meetings App
- Governance Meetings
- Mental Health Equity Fireside Chat Series
- Moore Equity in Mental Health 5K
- Policy & Practice Insights Series
- September Component Meetings
- Social Determinants of Mental Health Town Hall Series
- Amicus Briefs
- Assembly Directory
- Component Directory
- Conference Publications
- Library and Archive
- Member Directory
- Member Obituaries
- Practice Guidelines
- Resource Documents
- International Trainees
- International Humanitarian Opportunities
- Global Mental Health
- International Medical Graduates Resources
- Residents' Journal
- Featured Publications
- APA/APAF Fellowships
- External Fellowships and Awards
- Helping Residents Cope with a Patient Suicide
- Vacant Resident Positions
- Leadership Positions
- SET for Success
- Apply for Psychiatric Residency
- Choosing a Career in Psychiatry
- Building a Career in Psychiatry
- Medical Student Programs
- Resident-Fellow Census
- Transitioning to Residency During COVID-19
- What Is a Substance Use Disorder?
- Expert Q&A: Addiction and Substance Use Disorders
- What Are Dementia and Alzheimer’s Disease?
- Expert Q&A: Dementia and Alzheimer's Disease
- What are Anxiety Disorders?
- Expert Q&A: Anxiety Disorders
- What is ADHD?
- Expert Q&A: ADHD
- What Is Autism Spectrum Disorder?
- Expert Q&A: Autism Spectrum Disorder
- What Are Bipolar Disorders?
- Expert Q&A: Bipolar Disorder
- How Extreme Weather Events Affect Mental Health
- Who Is Affected by Climate Change?
- What Is Depression?
- Expert Q&A: Depression
- What are Disruptive, Impulse Control and Conduct Disorders?
- Expert Q&A: Disruptive, Impulse Control and Conduct Disorders
- What Are Dissociative Disorders?
- Expert Q&A: Dissociative Disorders
- What are Eating Disorders?
- Expert Q&A: Eating Disorders
- What is Gambling Disorder?
- Expert Q&A: Gambling Disorder
- What is Gender Dysphoria?
- Expert Q&A: Gender Dysphoria
- What is Hoarding Disorder?
- Expert Q&A: Hoarding Disorder
- What is Intellectual Disability?
- Expert Q&A: Intellectual Disability
- What Is Obsessive-Compulsive Disorder?
- Expert Q&A: Obsessive-Compulsive Disorder
- What is Perinatal Depression (formerly Postpartum)?
- Expert Q&A: Perinatal Depression
- What are Personality Disorders?
- Expert Q&A: Personality Disorders
- What is Posttraumatic Stress Disorder (PTSD)?
- Expert Q&A: Posttraumatic Stress Disorder (PTSD)
- What is Schizophrenia?
- Expert Q&A: Schizophrenia
- What are Sleep Disorders?
- Expert Q&A: Sleep Disorders
- What is Somatic Symptom Disorder?
- Expert Q&A: Somatic Symptom Disorder
- What Are Specific Learning Disorders?
- Expert Q&A: Specific Learning Disorders
- What is Technology Addiction?
- Expert Q&A: Technology Addiction
- Cigarrillos electrónicos y vapeo
- Trastorno del espectro autista
- Trastorno por consumo de alcohol
- Trastorno por consumo de opioides
- Trastorno de estrés postraumático (TEPT)
- Adicción a la tecnología: redes sociales, juegos en línea, y más
- ¿Qué es la psiquiatría?
- Conexiones entre el cambio climático y la salud mental
- General Members
- Early Career Psychiatrists
- Residents and Fellows
- International Resident-Fellows
- Semi-Retired and Retired
- View Your Profile
- Resident-Fellow Members
- Fellow of the APA
- Distinguished Fellow of the APA
- International Fellow of the APA
- International Distinguished Fellow of the APA
- 2024 Class of Honorary Fellows
- 2025 APA National Elections
- Councils, Committees and Components
- Resident-Fellow Leadership Opportunities
- Advocacy and APAPAC
- APA Specialty Interest Caucuses, Listservs & Communities
- Leadership, Equity and Diversity Institute
- Mentorship Program for APA/APAF Fellows
- Research Colloquium
- Contact Your Membership Specialist
- Contact Your District Branch
- Membership FAQs
- Semi-Retired and Retired FAQs
- Lump Sum Dues
- District Branch Resources
- District Branch Dues for General Members
- District Branch Dues for Residents and Fellows
Depression, Anxiety, Loneliness Are Peaking in College Students

Photo by Cydney Scott

Nationwide study, co-led by BU researcher Sarah Ketchen Lipson, reveals a majority of students say mental health has impacted their academic performance
Kat j. mcalpine.
A survey by a Boston University researcher of nearly 33,000 college students across the country reveals the prevalence of depression and anxiety in young people continues to increase, now reaching its highest levels, a sign of the mounting stress factors due to the coronavirus pandemic, political unrest, and systemic racism and inequality.
“Half of students in fall 2020 screened positive for depression and/or anxiety,” says Sarah Ketchen Lipson , a Boston University mental health researcher and a co–principal investigator of the nationwide survey , which was administered online during the fall 2020 semester through the Healthy Minds Network. The survey further reveals that 83 percent of students said their mental health had negatively impacted their academic performance within the past month, and that two-thirds of college students are struggling with loneliness and feeling isolated—an all-time high prevalence that reflects the toll of the pandemic and the social distancing necessary to control it.
Lipson, a BU School of Public Health assistant professor of health law, policy, and management, says the survey’s findings underscore the need for university teaching staff and faculty to put mechanisms in place that can accommodate students’ mental health needs.
“Faculty need to be flexible with deadlines and remind students that their talent is not solely demonstrated by their ability to get a top grade during one challenging semester,” Lipson says.
She adds that instructors can protect students’ mental health by having class assignments due at 5 pm, rather than midnight or 9 am, times that Lipson says can encourage students to go to bed later and lose valuable sleep to meet those deadlines.
Especially in smaller classroom settings, where a student’s absence may be more noticeable than in larger lectures, instructors who notice someone missing classes should reach out to that student directly to ask how they are doing.
“Even in larger classes, where 1:1 outreach is more difficult, instructors can send classwide emails reinforcing the idea that they care about their students not just as learners but as people, and circulating information about campus resources for mental health and wellness,” Lipson says.
And, crucially, she says, instructors must bear in mind that the burden of mental health is not the same across all student demographics. “Students of color and low-income students are more likely to be grieving the loss of a loved one due to COVID,” Lipson says. They are also “more likely to be facing financial stress.” All of these factors can negatively impact mental health and academic performance in “profound ways,” she says.
At a higher level within colleges and universities, Lipson says, administrators should focus on providing students with mental health services that emphasize prevention, coping, and resilience. The fall 2020 survey data revealed a significant “treatment gap,” meaning that many students who screen positive for depression or anxiety are not receiving mental health services.
“Often students will only seek help when they find themselves in a mental health crisis, requiring more urgent resources,” Lipson says. “But how can we create systems to foster wellness before they reach that point?” She has a suggestion: “All students should receive mental health education, ideally as part of the required curriculum.”
It’s also important to note, she says, that rising mental health challenges are not unique to the college setting—instead, the survey findings are consistent with a broader trend of declining mental health in adolescents and young adults. “I think mental health is getting worse [across the US population], and on top of that we are now gathering more data on these trends than ever before,” Lipson says. “We know mental health stigma is going down, and that’s one of the biggest reasons we are able to collect better data. People are being more open, having more dialogue about it, and we’re able to better identify that people are struggling.”
The worsening mental health of Americans, more broadly, Lipson says, could be due to a confluence of factors: the pandemic, the impact of social media, and shifting societal values that are becoming more extrinsically motivated (a successful career, making more money, getting more followers and likes), rather than intrinsically motivated (being a good member of the community).
The crushing weight of historic financial pressures is an added burden. “Student debt is so stressful,” Lipson says. “You’re more predisposed to experiencing anxiety the more debt you have. And research indicates that suicidality is directly connected to financial well-being.”
With more than 22 million young people enrolled in US colleges and universities, “and with the traditional college years of life coinciding with the age of onset for lifetime mental illnesses,” Lipson stresses that higher education is a crucial setting where prevention and treatment can make a difference.
One potential bright spot from the survey was that the stigma around mental health continues to fade. The results reveal that 94 percent of students say that they wouldn’t judge someone for seeking out help for mental health, which Lipson says is an indicator that also correlates with those students being likely to seek out help themselves during a personal crisis (although, paradoxically, almost half of students say they perceive that others may think more poorly of them if they did seek help).
“We’re harsher on ourselves and more critical of ourselves than we are with other people—we call that perceived versus personal stigma,” Lipson says. “Students need to realize, your peers are not judging you.”
Explore Related Topics:
- Community Health Sciences
- Data Sciences
- Gender Studies
- Public Policy
- Share this story
- 25 Comments Add
Former Editor, The Brink Twitter Profile

Kat J. McAlpine Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
There are 25 comments on Depression, Anxiety, Loneliness Are Peaking in College Students
first of all, excellent writing! This report is extremely triggering for a few reasons. Obviously students are NOT okay at the moment, now confirmed by the student. But what does the university do about it? They micro-manage EVERY aspect of students’ life to mitigate Covid risk. Here, tell me why the university took away household table seating in the dining hall? That was one of the ONLY places on campus where students can eat with each other and actually see their friends’ faces. What type of modeling was used to make this decision and its impact on covid spread on campus. Same thing for the green badge, was there a statistical difference in case before and after students have to walk around showing that? The university’s policies are simply incentivizing off-campus, more dangerous gatherings because the university won’t facilitate anything like that on campus. Oh, and the university response? ‘you’re doing great sweetie’ type of deal – absolutely ridiculous. I know BU can’t keep this up much longer, they are losing far too much money because of Covid and less students on campus – there will be a reckoning. Students, stand up.
BU will acknowledge this but then still won’t do anything to actually help.
Great, but this school is doing absolutely nothing to help it
I appreciate this article because I feel that the issue of mental health isn’t talked about enough amongst students and just college culture in general. I don’t see any concerns coming from college faculty, at least clearly. It’s so important to talk about mental health, especially during a pandemic.
This article is definitely going in the right direction. That being said, as the other comments have also mentioned, BU needs to do MUCH more than just publishing an article telling students, “well, at least you aren’t alone.” If 83% of your student body reports their mental health affects their school work, then if not for them, at least change something for the benefit of the school’s name. To put it bluntly, this does not look good. Also referencing BU’s response to sexual harassment, BU now has a track record of acknowledging issues that significantly impact its students in an article or maybe a speech to only do NOTHING about it. Please, I implore the school to act. Act or we will.
We know mental health stigma is going down
Actually, we know support for those taught and teaching that prejudice is diminishing, though that does not mean by any stretch of the imagination it is not still being taught. It continues to be taught (often resolutely) at Boston University. The above sentence is one manner in which it continues to be taught, Passive Reference. It is also actively taught. “Perceived stigma” is another interesting Passive Reference, directed prejudices are intended by their directors to be perceived. “perceived” stigma is an obfuscation of the process whereby it is perceived. It surprises me, that so many women, eschewing “the stigma” of rape, continue to declare “the stigma” of mental illnesses. Sometimes history does not inform us. A few years ago 5 students died by suicide at a Canadian college, blamed was “the stigma” of mental illnesses, not those conveying it. When a young man at U Penn died by suicide it prompted his sister to set up a now national organization protesting “the stigma” of mental illnesses, not those conveying it. National organizations abound conveying “the stigma” of mental illnesses to eagerly awaiting audiences. Publications abound, but to my knowledge not one single publication directly addresses how it is taught or who teaches it. Nor, to my knowledge is there a campus in the US, or any English speaking country, where someone is given guidance on how to address those directing it. Whom to approach. How to resolve it. [email protected] offers no such guidance. I invite each of you to return to 1972, when a small group of personally empowered women said, “Stop directing the term stigma at rape, you have done enough harm” and take that lesson to heart: We stopped.
And I invite [email protected] to take a role in bringing about that change.
Harold A Maio, retired mental health editor
Wow – so what is BU doing about this when we have pleaded with admin and offered so many ideas and solutions to helping here since September 2020?
The silence is deafening BU.
The Well Being Project is stagnate.
The Dean is silent.
The provost says students are happy based on some survey they did just before holidays when students knew they were going home.
The Director of Mental Health says appts for mental health are down – that’s the sign everything is fine?
We are hearing the opposite and many students have just lost their faith in support from BU as well as just returning home for LFA where they have a support system.
Where are the social in person safe activities outside and inside?
Where are the RAs and their weekly activities and support of their residents or are they just there to write students up?
Where are the self-care tips and resources offered daily to students?
Where in the daily MANDATORY self-check survey of their health – are any questions about their emotional well being including their mood, stress levels, sleep and appetite?
Where is the support for faculty who are seeing these issues and trying to reach out?
Where are the therapy dogs from pre-pandemic we asked for weekly or biweekly to come outside and offer unconditional emotional support during this tough time?
Where are some campus wide concerts or comedy relief concert paid for by BU – virtually or outside so students have anything to look forward to? If it’s down to money / the $70,000 Tuition or should cover some of it or funds from housing since many were not reimbursed when they returned home for support.
Where is any work with this amazing wise resource Dr. Lipson to take any of her guidance since last summer instead of just posting it here?
Is anyone listening to the isolation and pain of so many terriers? I have heard troubling stories for months since we began our BU Parent group that is NOT monitored by the Deans office unlike others. I have helped refer and counsel families worried if they speak up there might be some retaliation. There is no retaliation just a deaf ear to making any changes to improve morale and well being of our terriers during a pandemic. And then posting this article is the ultimate hutzpah when no one has listened to Dr.Lipson / your own shining star about these issues.
Why not shine as you have with COVID testing? What if this were your family member feeling isolated and disillusioned with their dreams at BU with no outreach from BU except an occasional ZOOM message.
BU can do so much better and be the example for the rest of the nation. Why test so stringently if you will not allow any safe activities except for favorites like sports teams and band members?
Terriers are ZOOMED OUT. Don’t wait for a suicide or more depression to appear in students. It’s almost too late to be proactive / but you can try and we ask that you try hard. Be an example for other colleges.
We are not giving up on being heard. We are parents who care and love BU and know it can do better.
A lot of good points made – I wanted to touch upon when you mentioned that appointments for mental health are apparently down. As a student actively seeking mental health resources, my experience is that it has been extremely difficult to even schedule any sort of mental health appointments or counseling; we are unable to make an appointment online or in-person anymore, and the only information we are given is a phone number to call (the Behavioral Medicine number). I find this frustrating as many of us need more than just a phone conversation to help – even a zoom meeting would be helpful, but why aren’t there zoom appointments for SHS like there are for almost every other service on campus (e.g., pre-professional advising, financial aid, etc.)? I’ve noticed that the loneliness and isolation is affecting not only me but my roommates as well, who have stronger support systems and more friends on campus than I do – we’ve all been lacking motivation to do any of our work and they’ve mentioned that they feel like they need a break (spring break canceled due to pandemic concerns). Even some of my professors seem burnt out – forgetting class, getting behind on their syllabus, etc. In my opinion, BU should be more proactive in giving students resources instead of making it difficult to find said resources. Lastly, I wanted to add that I understand a lot of services are probably very different now due to the pandemic, but a single “wellness week” and emails about it do not do much to actually help students – I find it comparable to “self care” where the self care is just drinking wine and putting on a skincare mask and pushing all your real problems aside.
I agree with those who are asking for BU to do more to support students. I’m a faculty member who is trying to do my best to support my students. I’m more than willing to give extensions, modify assignments, and lower my expectations this semester. I’m checking in on students who miss class to make sure they’re okay. I’m trying to cut as much material as I can while still meeting my course learning objectives. At the same time, I don’t think it’s fair to expect faculty to do everything when it comes to students’ wellbeing. I’ve been in meetings where faculty were asked (both implicitly and explicitly) to help students make friends and socialize during class. I know faculty who are doing this in their courses (and I applaud them for their efforts), but shouldn’t Res Life and other staff at BU be providing opportunities for students to safely socialize? Sure, it’s cold, but certainly BU can be creative and think of ways to encourage students to get out of their dorms and make friends. Faculty are struggling too, and BU’s administration can help us by helping our students.
This is an excellent article, and though not surprising, it is shocking that the BU administration has not done anything to remedy this mental health crises. This is a mental health pandemic happening and it should be as high of a priority for BU as the trying to control the virus. If BU doesn’t step up and come up with a plan to address this then our students will suffer for years to come. This should have happened months ago. You can’t have a healthy individual/society if you are only concerned with physical health. It has to be a holistic approach.
Nice article I hope all instructors read this article I am one of the students sometimes fell a depression and live in the anxiety that is effectives on my life and do not have the energy to do anything particularly during what we live now
First, I would like to focus on the positive and thank BU mental health staff for being there for my son when he was in urgent need of mental health support back in the Fall semester. My call was answered right away and my son was able to speak with a professional with in 15 minutes. I was very impressed and relieved. They were there when we needed them.
On the other hand, I’m hearing from my son and all of his friends that the academic culture of rigor for the sake of rigor, grade deflation and the purposeful weeding out of students from core classes rather than supporting and helping each student succeed, not only continues but has been increased during COVID. These students have a sense that professors are concerned about online cheating so have ramped the rigor to address this. Not sure if this is real or perceived and I’m sure this is not going on in all classes as I also heard examples of supportive professors, but this is definitely a theme I am hearing from students. This style of academics is known to be outdated and ineffective, yet it continues, even at a higher level, during a pandemic.
I’m hoping this feedback can serve helpful to administration.
THANK YOU!!!! As a college student, who has survived the past year with a 4.0, attending full-time to obtain my degree in IT. I am struggling for the first time. After technology issues that set me behind four days, I really thought my instructors would understand. One of my instructors couldn’t care less. The workload is beyond overwhelming, her curriculum seems almost cruel. I graduate next month and I feel like I am losing my mind. I already suffer from severe anxiety, so the level I’m at now is almost debilitating. I have been obtaining degrees since 1998, and familiar with online learning. I’ve never had issues. This morning I received an email from her reminding me of the due date, in all bold caps, followed by some !!!! … She made it clear she is not available on the weekend, but expects us to be flexible. So my dilemma is this, I am failing my coding class now, but I don’t feel that I should be financially responsible to pay for having to retake it, as well as have it impact my financial aid and scholarships I receive for my academic performance.
Hi. I’m a BU alumna, a college professor, and mom to 4 college-aged sons. WONDERING… Do students feel there is explicit and implicit prejudice against college students as “purveyors of COVID?” I think this adds to the discomfort or enjoyment of being a college student and part of a university community. Thoughts? Thanks!
I notice that the students like to complain on here. One thing that university researchers on mental health have a difficult time assessing is knowing the familial support system (or lack thereof) students come into university life with. Psychologists will affirm that this plays a huge role in the mental health of students, at any age. Just as elementary through high schools today are expected to be the emotional, parental, physical, educational, and social supporter of each student, so too are universities being given this sort of expectation. Don’t get me wrong…I believe in striving for mental health and making resources available on campuses. However, within the communities of students – whether their friends or family – we have to realize that the internal conversation around mental health for many cultures is either non-existent or looked down upon. We can sing mental health from the rooftops all day long and hope that students are listening…..and I hope they do.
ECT/Electroshock use has been on the rise last 5 years or so and not just used for depression nor as a last resort. No FDA testing ever done of devices used or the procedure itself. Increase risk for suicide following as many cannot find help for their repeated brain injuries after consenting to this. Lawsuits taking place in the US and England around these damages covered up. See site ectjustice to learn more. Please speak out on social media so others are made aware of the truth of this practice.
People shouldn’t hesitate to ask for psychological help. I think it’s one of the main problems why people struggle mentally. Maybe, it’s a matter of self-critique, and society says sometimes that we should be strong… But when someone gets in an emotional crisis, only a professional can help. And I also never see when students/educators judge their peers/colleagues if someone contacted mental health support. I looked through the list of different affordable mental health services across English-speaking countries – https://ivypanda.com/blog/mental-health-resources – I was shocked how many problems we can have, and how many professionals exist to help with them. Maybe, it may be helpful to others too. Let’s take care of ourselves.
I tried to find the source for “83 %” of college students say their performance was negatively affected by mental health. Did you just pull that number out of thin air? I tried to go through everything I could and could not find this number anywhere in any actual published writing.
Please see page six of the report, the pie chart listed under Academic Impairment.
I think you just made up certain elements of this article and they actually have 0 foundation whatsoever. It has led me down a rabbit hole of attempting to try to find the published support for some of the claims you make. Including the 83 % figure. If you’re going to write articles that will be heavily referenced (which this is, because other idiots went on to quote this article), you should at least get the facts straight.
Please see page 6 of the report, the pie chart listed under Academic Impairment: https://healthymindsnetwork.org/wp-content/uploads/2021/02/HMS-Fall-2020-National-Data-Report.pdf
That is a misrepresentation of the data, in my opinion. Including students who reported mental health impacting their academic performance 1-2 days out of the week is insufficient to be grouped in with 83% of students. The way it is presented in this article makes it seem much more drastic than that. It should say, “28% of students felt 1-2 days out of the week had been negatively impacted by their mental health in the past month..” and report the other percentages. Not combined into one group and twisted in a sensationalistic way. I was attempting to use this information for a research paper of my own and was sent down a rabbit hole trying to find a source. Other people have cited this article, and that is your responsibility as a researcher.
Reading it because to help a friend with his assignment. He studies in FAST, Islamabad, Pakistan. If anyone of his class fellows are here, good luck to you
It is 3:12 in the morning and I just got off the phone with son. He called because he was riddled with anxiety and suffering with loneliness and a seeming inability to form meaningful connections. This is his first year at BU. He loves the University; However, in addition to the rigorous academic challenges, he is crushed by the seeming inability to form connections with others. This, on so many levels, surprises me. He is intelligent, interesting, friendly, handsome and well rounded. Upon my introduction to the University’s logistical layout, I was immediately aware that it not appear easily conducive to meeting people… As opposed to a smaller private college if you will. Clearly, BU had an obligation to address the many challenges brought about as a result of Covid. Understandable, but perhaps a bit extreme, ie: The students not being allowed to eat or congregate. Regardless, what I also observed is that there are few, if any, common rooms.. areas for students to hang out, play board games, ping pong, darts, tell jokes, b.s. and share common concerns. Or My point being, there should be multiple places (Besides sneaking into local clubs, or drinking Alone in your dorm) where kids can go..day or night. Organized events as well, aside from sports. As aforementioned, my son also found it very challenging and frustrating to contact a counselor through your service. When you do, the schedules are booked…… I have been heartbroken. Nonetheless, the consistent voice if encouragement. I want more from the school. I, like all others noted before me. More social emotional support. More access to social opportunities. More professors understanding and working with the challenges our children are struggling to navigate. In closing, it’s not just a BU crisis. I listen to very similar difficulties from many other University families…. PLEASE be more proactive. PLEASE care PLEASE help It is imperative and essential to a successful college experience and outcome. Thank you. And thank you all aforementioned
very very nice
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Latest from The Brink
Heat waves are scorching boston, but are some neighborhoods hotter than others, six bu researchers win prestigious early-career award to advance their work, new ai program from bu researchers could predict likelihood of alzheimer’s disease, being open about lgbtq+ identities in the classroom creates positive learning environments, should schools struggling with classroom management clamp down with more suspensions or turn to restorative justice, getting police officers to trust implicit bias training, the solar system may have passed through dense interstellar cloud 2 million years ago, altering earth’s climate, air quality sensors could be coming to a bicycle near you, airplane noise may be bad for your health, bu researcher named a 2024 hertz fellow; award honors “innovators with the greatest potential”, is ai biased against some groups and spreading misinformation and extreme views, 3d printing robot uses ai machine learning for us army research, permanent birth control—vasectomies and tubal ligations—up following supreme court abortion ruling, explain this how do planets form, bu’s innovator of the year has pioneered devices to advance astronomy, microscopy, eye exams, bu study shows a correlation between social media use and desire for cosmetic procedures, covid-19 photo contest winners capture moments of joy, sorrow, meaning in crisis, how high-level lawsuits are disrupting climate change policies, the h5n1 bird flu is a growing threat for farm animals and humans—how serious is it, why is a bu researcher so fascinated with the diets of dung beetles.

New study examines social media’s impact on college students’ mental health
By Kim Spurr

The COVID-19 pandemic had an unprecedented effect on college students’ mental health: symptoms like anxiety and major depression in young adults ages 18-25 increased significantly compared to before the pandemic.
A new study from researchers at the University of North Carolina at Chapel Hill looks at a possible contributing factor to the worsening trends in mental health: social media.
We know that college students and adolescents are using social media more. Last May, the US Surgeon General issued an advisory on social media and youth mental health, noting that there are “ample indicators” that social media can “pose a risk of harm to the mental health and well-being of children and adolescents.”
But questions remained: Are more depressed people using social media more? Or is social media contributing to more depression?

To answer this, a team led by economist Jane Cooley Fruehwirth used unique longitudinal survey data from first-year college students at a large public research university which was collected both before and during the pandemic. This data allowed them to compare social media usage before and during the pandemic along with other factors like social isolation, anxiety and depression symptoms, and how much students were sleeping, exercising, and interacting with their friends.
What they found was surprising: increased social media usage at the beginning of the pandemic didn’t have a large effect on college students’ mental health, but increased social media usage 18 months into the pandemic – when colleges had largely reopened and students were back on campus – did have a negative effect on students’ mental health. Students who increased their social media usage by an hour 18 months into the pandemic were much more likely to be depressed and anxious.
Why is this the case?
Fruehwirth and team found some evidence that social media use takes away from time for other activities that are good for mental health, such as exercise, when students were back in dorms, and that social media also seemed to increase stress from peers. Both early and later in the pandemic, the effects of social media usage were worst among socially isolated college students.
“These students who were socially isolated were not using social media to stay connected,” says Fruehwirth. “They were using it in a different way.”
Fruehwirth notes that resilience and social support helps protect students from the negative consequences of social media.
“This is not a “social media is bad” story,” she says. “It’s that some students are using it in a way that isn’t detrimental and some are, and we wanted to tease out those differences.”
The findings suggest that college campuses themselves can play a role in reducing isolation. Approximately 1 in 5 college students currently feels isolated on a college campus. This suggests that there’s more at play than just social media.
“Universities can think about how to build more connections through physical and social spaces, through connections through clubs,” says Fruehwirth. “They can create peer support networks and help build resilience.”
The study was published in Health Economics on June 14, 2024. Jane Fruehwirth is a professor in the department of economics. Coauthors include Alex Xingbang Weng, a Ph.D. candidate in the department of economics and Krista Perreira, a professor in the department of social medicine.
Courtesy of the Carolina Population Center

Study: What is social media’s impact on college students’ mental health?
The Covid-19 pandemic had an unprecedented effect on college students’ mental health: symptoms like anxiety and major depression in young adults ages 18-25 increased significantly compared to before the pandemic.

A new study from researchers at the University of North Carolina at Chapel Hill looks at a possible contributing factor to the worsening trends in mental health: social media.
We know that college students and adolescents are using social media more. Last May, the US Surgeon General issued an advisory on social media and youth mental health, noting that there are “ample indicators” that social media can “pose a risk of harm to the mental health and well-being of children and adolescents.”
But questions remained: Are more depressed people using social media more? Or is social media contributing to more depression?
To answer this, a team led by economist Jane Cooley Fruehwirth used unique longitudinal survey data from first-year college students at a large public research university which was collected both before and during the pandemic. This data allowed them to compare social media usage before and during the pandemic along with other factors like social isolation, anxiety and depression symptoms, and how much students were sleeping, exercising, and interacting with their friends.
What they found was surprising: increased social media usage at the beginning of the pandemic didn’t have a large effect on college students’ mental health, but increased social media usage 18 months into the pandemic – when colleges had largely reopened and students were back on campus – did have a negative effect on students’ mental health. Students who increased their social media usage by an hour 18 months into the pandemic were much more likely to be depressed and anxious.
Why is this the case?

Fruehwirth and team found some evidence that social media use takes away from time for other activities that are good for mental health, such as exercise, when students were back in dorms, and that social media also seemed to increase stress from peers. Both early and later in the pandemic, the effects of social media usage were worst among socially isolated college students.
“These students who were socially isolated were not using social media to stay connected,” says Fruehwirth. “They were using it in a different way.”
Fruehwirth notes that resilience and social support helps protect students from the negative consequences of social media.
“This is not a “social media is bad” story,” she says. “It’s that some students are using it in a way that isn’t detrimental and some are, and we wanted to tease out those differences.”
The findings suggest that college campuses themselves can play a role in reducing isolation. Approximately 1 in 5 college students currently feels isolated on a college campus. This suggests that there’s more at play than just social media.
“Universities can think about how to build more connections through physical and social spaces, through connections through clubs,” says Fruehwirth. “They can create peer support networks and help build resilience.”
The study was published in Health Economics on June 14, 2024. Coauthors include Alex Xingbang Weng and Krista Perreira.
Media Contact
Melody Kramer Director of Communications [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol
Academic Stress and Mental Well-Being in College Students: Correlations, Affected Groups, and COVID-19
Georgia barbayannis.
1 Department of Neurology, Rutgers New Jersey Medical School, Newark, NJ, United States
Mahindra Bandari
Xiang zheng.
2 Rutgers New Jersey Medical School, Newark, NJ, United States
Humberto Baquerizo
3 Office for Diversity and Community Engagement, Rutgers New Jersey Medical School, Newark, NJ, United States
Keith W. Pecor
4 Department of Biology, The College of New Jersey, Ewing, NJ, United States
Associated Data
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Academic stress may be the single most dominant stress factor that affects the mental well-being of college students. Some groups of students may experience more stress than others, and the coronavirus disease 19 (COVID-19) pandemic could further complicate the stress response. We surveyed 843 college students and evaluated whether academic stress levels affected their mental health, and if so, whether there were specific vulnerable groups by gender, race/ethnicity, year of study, and reaction to the pandemic. Using a combination of scores from the Perception of Academic Stress Scale (PAS) and the Short Warwick-Edinburgh Mental Well-Being Scale (SWEMWBS), we found a significant correlation between worse academic stress and poor mental well-being in all the students, who also reported an exacerbation of stress in response to the pandemic. In addition, SWEMWBS scores revealed the lowest mental health and highest academic stress in non-binary individuals, and the opposite trend was observed for both the measures in men. Furthermore, women and non-binary students reported higher academic stress than men, as indicated by PAS scores. The same pattern held as a reaction to COVID-19-related stress. PAS scores and responses to the pandemic varied by the year of study, but no obvious patterns emerged. These results indicate that academic stress in college is significantly correlated to psychological well-being in the students who responded to this survey. In addition, some groups of college students are more affected by stress than others, and additional resources and support should be provided to them.
Introduction
Late adolescence and emerging adulthood are transitional periods marked by major physiological and psychological changes, including elevated stress (Hogan and Astone, 1986 ; Arnett, 2000 ; Shanahan, 2000 ; Spear, 2000 ; Scales et al., 2015 ; Romeo et al., 2016 ; Barbayannis et al., 2017 ; Chiang et al., 2019 ; Lally and Valentine-French, 2019 ; Matud et al., 2020 ). This pattern is particularly true for college students. According to a 2015 American College Health Association-National College Health Assessment survey, three in four college students self-reported feeling stressed, while one in five college students reported stress-related suicidal ideation (Liu, C. H., et al., 2019 ; American Psychological Association, 2020 ). Studies show that a stressor experienced in college may serve as a predictor of mental health diagnoses (Pedrelli et al., 2015 ; Liu, C. H., et al., 2019 ; Karyotaki et al., 2020 ). Indeed, many mental health disorders, including depression, anxiety, and substance abuse disorder, begin during this period (Blanco et al., 2008 ; Pedrelli et al., 2015 ; Saleh et al., 2017 ; Reddy et al., 2018 ; Liu, C. H., et al., 2019 ).
Stress experienced by college students is multi-factorial and can be attributed to a variety of contributing factors (Reddy et al., 2018 ; Karyotaki et al., 2020 ). A growing body of evidence suggests that academic-related stress plays a significant role in college (Misra and McKean, 2000 ; Dusselier et al., 2005 ; Elias et al., 2011 ; Bedewy and Gabriel, 2015 ; Hj Ramli et al., 2018 ; Reddy et al., 2018 ; Pascoe et al., 2020 ). For instance, as many as 87% of college students surveyed across the United States cited education as their primary source of stress (American Psychological Association, 2020 ). College students are exposed to novel academic stressors, such as an extensive academic course load, substantial studying, time management, classroom competition, financial concerns, familial pressures, and adapting to a new environment (Misra and Castillo, 2004 ; Byrd and McKinney, 2012 ; Ekpenyong et al., 2013 ; Bedewy and Gabriel, 2015 ; Ketchen Lipson et al., 2015 ; Pedrelli et al., 2015 ; Reddy et al., 2018 ; Liu, C. H., et al., 2019 ; Freire et al., 2020 ; Karyotaki et al., 2020 ). Academic stress can reduce motivation, hinder academic achievement, and lead to increased college dropout rates (Pascoe et al., 2020 ).
Academic stress has also been shown to negatively impact mental health in students (Li and Lin, 2003 ; Eisenberg et al., 2009 ; Green et al., 2021 ). Mental, or psychological, well-being is one of the components of positive mental health, and it includes happiness, life satisfaction, stress management, and psychological functioning (Ryan and Deci, 2001 ; Tennant et al., 2007 ; Galderisi et al., 2015 ; Trout and Alsandor, 2020 ; Defeyter et al., 2021 ; Green et al., 2021 ). Positive mental health is an understudied but important area that helps paint a more comprehensive picture of overall mental health (Tennant et al., 2007 ; Margraf et al., 2020 ). Moreover, positive mental health has been shown to be predictive of both negative and positive mental health indicators over time (Margraf et al., 2020 ). Further exploring the relationship between academic stress and mental well-being is important because poor mental well-being has been shown to affect academic performance in college (Tennant et al., 2007 ; Eisenberg et al., 2009 ; Freire et al., 2016 ).
Perception of academic stress varies among different groups of college students (Lee et al., 2021 ). For instance, female college students report experiencing increased stress than their male counterparts (Misra et al., 2000 ; Eisenberg et al., 2007 ; Evans et al., 2018 ; Lee et al., 2021 ). Male and female students also respond differently to stressors (Misra et al., 2000 ; Verma et al., 2011 ). Moreover, compared to their cisgender peers, non-binary students report increased stressors and mental health issues (Budge et al., 2020 ). The academic year of study of the college students has also been shown to impact academic stress levels (Misra and McKean, 2000 ; Elias et al., 2011 ; Wyatt et al., 2017 ; Liu, C. H., et al., 2019 ; Defeyter et al., 2021 ). While several studies indicate that racial/ethnic minority groups of students, including Black/African American, Hispanic/Latino, and Asian American students, are more likely to experience anxiety, depression, and suicidality than their white peers (Lesure-Lester and King, 2004 ; Lipson et al., 2018 ; Liu, C. H., et al., 2019 ; Kodish et al., 2022 ), these studies are limited and often report mixed or inconclusive findings (Liu, C. H., et al., 2019 ; Kodish et al., 2022 ). Therefore, more studies should be conducted to address this gap in research to help identify subgroups that may be disproportionately impacted by academic stress and lower well-being.
The coronavirus disease 19 (COVID-19) pandemic is a major stressor that has led to a mental health crisis (American Psychological Association, 2020 ; Dong and Bouey, 2020 ). For college students, the COVID-19 pandemic has resulted in significant changes and disruptions to daily life, elevated stress levels, and mental and physical health deterioration (American Psychological Association, 2020 ; Husky et al., 2020 ; Patsali et al., 2020 ; Son et al., 2020 ; Clabaugh et al., 2021 ; Lee et al., 2021 ; Lopes and Nihei, 2021 ; Yang et al., 2021 ). While any college student is vulnerable to these stressors, these concerns are amplified for members of minority groups (Salerno et al., 2020 ; Clabaugh et al., 2021 ; McQuaid et al., 2021 ; Prowse et al., 2021 ; Kodish et al., 2022 ). Identifying students at greatest risk provides opportunities to offer support, resources, and mental health services to specific subgroups.
The overall aim of this study was to assess academic stress and mental well-being in a sample of college students. Within this umbrella, we had several goals. First, to determine whether a relationship exists between the two constructs of perceived academic stress, measured by the Perception of Academic Stress Scale (PAS), and mental well-being, measured by the Short Warwick-Edinburgh Mental Well-Being Scale (SWEMWBS), in college students. Second, to identify groups that could experience differential levels of academic stress and mental health. Third, to explore how the perception of the ongoing COVID-19 pandemic affected stress levels. We hypothesized that students who experienced more academic stress would have worse psychological well-being and that certain groups of students would be more impacted by academic- and COVID-19-related stress.
Materials and Methods
Survey instrument.
A survey was developed that included all questions from the Short Warwick-Edinburgh Mental Well-Being (Tennant et al., 2007 ; Stewart-Brown and Janmohamed, 2008 ) and from the Perception of Academic Stress Scale (Bedewy and Gabriel, 2015 ). The Short Warwick-Edinburgh Mental Well-Being Scale is a seven-item scale designed to measure mental well-being and positive mental health (Tennant et al., 2007 ; Fung, 2019 ; Shah et al., 2021 ). The Perception of Academic Stress Scale is an 18-item scale designed to assess sources of academic stress perceived by individuals and measures three main academic stressors: academic expectations, workload and examinations, and academic self-perceptions of students (Bedewy and Gabriel, 2015 ). These shorter scales were chosen to increase our response and study completion rates (Kost and de Rosa, 2018 ). Both tools have been shown to be valid and reliable in college students with Likert scale responses (Tennant et al., 2007 ; Bedewy and Gabriel, 2015 ; Ringdal et al., 2018 ; Fung, 2019 ; Koushede et al., 2019 ). Both the SWEMWBS and PAS scores are a summation of responses to the individual questions in the instruments. For the SWEMWBS questions, a higher score indicates better mental health, and scores range from 7 to 35. Similarly, the PAS questions are phrased such that a higher score indicates lower levels of stress, and scores range from 18 to 90. We augmented the survey with demographic questions (e.g., age, gender, and race/ethnicity) at the beginning of the survey and two yes/no questions and one Likert scale question about the impact of the COVID-19 pandemic at the end of our survey.
Participants for the study were self-reported college students between the ages of 18 and 30 years who resided in the United States, were fluent in English, and had Internet access. Participants were solicited through Prolific ( https://prolific.co ) in October 2021. A total of 1,023 individuals enrolled in the survey. Three individuals did not agree to participate after beginning the survey. Two were not fluent in English. Thirteen individuals indicated that they were not college students. Two were not in the 18–30 age range, and one was located outside of the United States. Of the remaining individuals, 906 were full-time students and 96 were part-time students. Given the skew of the data and potential differences in these populations, we removed the part-time students. Of the 906 full-time students, 58 indicated that they were in their fifth year of college or higher. We understand that not every student completes their undergraduate studies in 4 years, but we did not want to have a mixture of undergraduate and graduate students with no way to differentiate them. Finally, one individual reported their age as a non-number, and four individuals did not answer a question about their response to the COVID-19 pandemic. This yielded a final sample of 843 college students.
Data Analyses
After reviewing the dataset, some variables were removed from consideration due to a lack of consistency (e.g., some students reported annual income for themselves and others reported family income) or heterogeneity that prevented easy categorization (e.g., field of study). We settled on four variables of interest: gender, race/ethnicity, year in school, and response to the COVID-19 pandemic ( Table 1 ). Gender was coded as female, male, or non-binary. Race/ethnicity was coded as white or Caucasian; Black or African American; East Asian; Hispanic, Latino, or of Spanish origin; or other. Other was used for groups that were not well-represented in the sample and included individuals who identified themselves as Middle Eastern, Native American or Alaskan Native, and South Asian, as well as individuals who chose “other” or “prefer not to answer” on the survey. The year of study was coded as one through four, and COVID-19 stress was coded as two groups, no change/neutral response/reduced stress or increased stress.
Characteristics of the participants in the study.
| Female | 662 | 78.5% | White or Caucasian | 560 | 66.4% | 1 | 134 | 15.9% | No impact/ neutral response/decreased stress | 165 | 19.6% |
| Male | 141 | 16.7% | Black or African American | 66 | 7.8% | 2 | 233 | 27.6% | |||
| Nonbinary | 40 | 4.7% | East Asian | 78 | 9.3% | 3 | 251 | 29.8% | Increased stress | 678 | 80.4% |
| Hispanic, Latino, or of Spanish origin | 74 | 8.8% | 4 | 225 | 26.7% | ||||||
| Other | 65 | 7.7% | |||||||||
Our first goal was to determine whether there was a relationship between self-reported academic stress and mental health, and we found a significant correlation (see Results section). Given the positive correlation, a multivariate analysis of variance (MANOVA) with a model testing the main effects of gender, race/ethnicity, and year of study was run in SPSS v 26.0. A factorial MANOVA would have been ideal, but our data were drawn from a convenience sample, which did not give equal representation to all groupings, and some combinations of gender, race/ethnicity, and year of study were poorly represented (e.g., a single individual). As such, we determined that it would be better to have a lack of interaction terms as a limitation to the study than to provide potentially spurious results. Finally, we used chi-square analyses to assess the effect of potential differences in the perception of the COVID-19 pandemic on stress levels in general among the groups in each category (gender, race/ethnicity, and year of study).
In terms of internal consistency, Cronbach's alpha was 0.82 for the SMEMWBS and 0.86 for the PAS. A variety of descriptors have been applied to Cronbach's alpha values. That said, 0.7 is often considered a threshold value in terms of acceptable internal consistency, and our values could be considered “high” or “good” (Taber, 2018 ).
The participants in our study were primarily women (78.5% of respondents; Table 1 ). Participants were not equally distributed among races/ethnicities, with the majority of students selecting white or Caucasian (66.4% of responders; Table 1 ), or years of study, with fewer first-year students than other groups ( Table 1 ).
Students who reported higher academic stress also reported worse mental well-being in general, irrespective of age, gender, race/ethnicity, or year of study. PAS and SWEMWBS scores were significantly correlated ( r = 0.53, p < 0.001; Figure 1 ), indicating that a higher level of perceived academic stress is associated with worse mental well-being in college students within the United States.

SWEMWBS and PAS scores for all participants.
Among the subgroups of students, women, non-binary students, and second-year students reported higher academic stress levels and worse mental well-being ( Table 2 ; Figures 2 – 4 ). In addition, the combined measures differed significantly between the groups in each category ( Table 2 ). However, as measured by partial eta squared, the effect sizes were relatively small, given the convention of 0.01 = small, 0.06 = medium, and 0.14 = large differences (Lakens, 2013 ). As such, there were only two instances in which Tukey's post-hoc tests revealed more than one statistical grouping ( Figures 2 – 4 ). For SWEMWBS score by gender, women were intermediate between men (high) and non-binary individuals (low) and not significantly different from either group ( Figure 2 ). Second-year students had the lowest PAS scores for the year of study, and first-year students had the highest scores. Third- and fourth-year students were intermediate and not statistically different from the other two groups ( Figure 4 ). There were no pairwise differences in academic stress levels or mental well-being among racial/ethnic groups.
Results of the MANOVA.
| Gender | 0.018 | 3.86 | 0.004 | 0.009 |
| Race/ethnicity | 0.022 | 2.32 | 0.02 | 0.011 |
| Year of study | 0.016 | 2.24 | 0.04 | 0.008 |

SWEMWBS and PAS scores according to gender (mean ± SEM). Different letters for SWEMWBS scores indicate different statistical groupings ( p < 0.05).

SWEMWBS and PAS scores according to year in college (mean ± SEM). Different letters for PAS scores indicate different statistical groupings ( p < 0.05).

SWEMWBS and PAS scores according to race/ethnicity (mean ± SEM).
The findings varied among categories in terms of stress responses due to the COVID-19 pandemic ( Table 3 ). For gender, men were less likely than women or non-binary individuals to report increased stress from COVID-19 (χ 2 = 27.98, df = 2, p < 0.001). All racial/ethnic groups responded similarly to the pandemic (χ 2 = 3.41, df = 4, p < 0.49). For the year of study, first-year students were less likely than other cohorts to report increased stress from COVID-19 (χ 2 = 9.38, df = 3, p < 0.03).
Impact of COVID-19 on stress level by gender, race/ethnicity, and year of study.
| Female | 118 | 17.8 | 544 | 82.2 |
| Male | 47 | 33.3 | 94 | 66.7 |
| Nonbinary | 0 | 0 | 40 | 100 |
| White or Caucasian | 104 | 18.6 | 456 | 81.4 |
| Black or African American | 16 | 24.2 | 50 | 75.8 |
| East Asian | 20 | 25.6 | 58 | 74.4 |
| Hispanic, Latino, or of Spanish origin | 14 | 18.9 | 60 | 81.1 |
| Middle Eastern, Native American, Alaskan Native, South Asian, other, or prefer not to answer | 11 | 16.9 | 54 | 83.1 |
| 1 | 38 | 28.4 | 96 | 71.6 |
| 2 | 43 | 18.5 | 190 | 81.5 |
| 3 | 39 | 15.5 | 212 | 84.5 |
| 4 | 45 | 20 | 180 | 80 |
Our primary findings showed a positive correlation between perceived academic stress and mental well-being in United States college students, suggesting that academic stressors, including academic expectations, workload and grading, and students' academic self-perceptions, are equally important as psychological well-being. Overall, irrespective of gender, race/ethnicity, or year of study, students who reported higher academic stress levels experienced diminished mental well-being. The utilization of well-established scales and a large sample size are strengths of this study. Our results extend and contribute to the existing literature on stress by confirming findings from past studies that reported higher academic stress and lower psychological well-being in college students utilizing the same two scales (Green et al., 2021 ; Syed, 2021 ). To our knowledge, the majority of other prior studies with similar findings examined different components of stress, studied negative mental health indicators, used different scales or methods, employed smaller sample sizes, or were conducted in different countries (Li and Lin, 2003 ; American Psychological Association, 2020 ; Husky et al., 2020 ; Pascoe et al., 2020 ; Patsali et al., 2020 ; Clabaugh et al., 2021 ; Lee et al., 2021 ; Lopes and Nihei, 2021 ; Yang et al., 2021 ).
This study also demonstrated that college students are not uniformly impacted by academic stress or pandemic-related stress and that there are significant group-level differences in mental well-being. Specifically, non-binary individuals and second-year students were disproportionately impacted by academic stress. When considering the effects of gender, non-binary students, in comparison to gender-conforming students, reported the highest stress levels and worst psychological well-being. Although there is a paucity of research examining the impact of academic stress in non-binary college students, prior studies have indicated that non-binary adults face adverse mental health outcomes when compared to male and female-identifying individuals (Thorne et al., 2018 ; Jones et al., 2019 ; Budge et al., 2020 ). Alarmingly, Lipson et al. ( 2019 ) found that gender non-conforming college students were two to four times more likely to experience mental health struggles than cisgender students (Lipson et al., 2019 ). With a growing number of college students in the United States identifying as as non-binary, additional studies could offer invaluable insight into how academic stress affects this population (Budge et al., 2020 ).
In addition, we found that second-year students reported the most academic-related distress and lowest psychological well-being relative to students in other years of study. We surmise this may be due to this group taking advanced courses, managing heavier academic workloads, and exploring different majors. Other studies support our findings and suggest higher stress levels could be attributed to increased studying and difficulties with time management, as well as having less well-established social support networks and coping mechanisms compared to upperclassmen (Allen and Hiebert, 1991 ; Misra and McKean, 2000 ; Liu, X et al., 2019 ). Benefiting from their additional experience, upperclassmen may have developed more sophisticated studying skills, formed peer support groups, and identified approaches to better manage their academic stress (Allen and Hiebert, 1991 ; Misra and McKean, 2000 ). Our findings suggest that colleges should consider offering tailored mental health resources, such as time management and study skill workshops, based on the year of study to improve students' stress levels and psychological well-being (Liu, X et al., 2019 ).
Although this study reported no significant differences regarding race or ethnicity, this does not indicate that minority groups experienced less academic stress or better mental well-being (Lee et al., 2021 ). Instead, our results may reflect the low sample size of non-white races/ethnicities, which may not have given enough statistical power to corroborate. In addition, since coping and resilience are important mediators of subjective stress experiences (Freire et al., 2020 ), we speculate that the lower ratios of stress reported in non-white participants in our study (75 vs. 81) may be because they are more accustomed to adversity and thereby more resilient (Brown, 2008 ; Acheampong et al., 2019 ). Furthermore, ethnic minority students may face stigma when reporting mental health struggles (Liu, C. H., et al., 2019 ; Lee et al., 2021 ). For instance, studies showed that Black/African American, Hispanic/Latino, and Asian American students disclose fewer mental health issues than white students (Liu, C. H., et al., 2019 ; Lee et al., 2021 ). Moreover, the ability to identify stressors and mental health problems may manifest differently culturally for some minority groups (Huang and Zane, 2016 ; Liu, C. H., et al., 2019 ). Contrary to our findings, other studies cited racial disparities in academic stress levels and mental well-being of students. More specifically, Negga et al. ( 2007 ) concluded that African American college students were more susceptible to higher academic stress levels than their white classmates (Negga et al., 2007 ). Another study reported that minority students experienced greater distress and worse mental health outcomes compared to non-minority students (Smith et al., 2014 ). Since there may be racial disparities in access to mental health services at the college level, universities, professors, and counselors should offer additional resources to support these students while closely monitoring their psychological well-being (Lipson et al., 2018 ; Liu, C. H., et al., 2019 ).
While the COVID-19 pandemic increased stress levels in all the students included in our study, women, non-binary students, and upperclassmen were disproportionately affected. An overwhelming body of evidence suggests that the majority of college students experienced increased stress levels and worsening mental health as a result of the pandemic (Allen and Hiebert, 1991 ; American Psychological Association, 2020 ; Husky et al., 2020 ; Patsali et al., 2020 ; Son et al., 2020 ; Clabaugh et al., 2021 ; Lee et al., 2021 ; Yang et al., 2021 ). Our results also align with prior studies that found similar subgroups of students experience disproportionate pandemic-related distress (Gao et al., 2020 ; Clabaugh et al., 2021 ; Hunt et al., 2021 ; Jarrett et al., 2021 ; Lee et al., 2021 ; Chen and Lucock, 2022 ). In particular, the differences between female students and their male peers may be the result of different psychological and physiological responses to stress reactivity, which in turn may contribute to different coping mechanisms to stress and the higher rates of stress-related disorders experienced by women (Misra et al., 2000 ; Kajantie and Phillips, 2006 ; Verma et al., 2011 ; Gao et al., 2020 ; Graves et al., 2021 ). COVID-19 was a secondary consideration in our study and survey design, so the conclusions drawn here are necessarily limited.
The implications of this study are that college students facing increased stress and struggling with mental health issues should receive personalized and specific mental health services, resources, and support. This is particularly true for groups that have been disproportionately impacted by academic stress and stress due to the pandemic. Many students who experience mental health struggles underutilize college services due to cost, stigma, or lack of information (Cage et al., 2020 ; Lee et al., 2021 ). To raise awareness and destigmatize mental health, colleges can consider distributing confidential validated assessments, such as the PAS and SWEMWBS, in class and teach students to self-score (Lee et al., 2021 ). These results can be used to understand how academic stress and mental well-being change over time and allow for specific and targeted interventions for vulnerable groups. In addition, teaching students healthy stress management techniques has been shown to improve psychological well-being (Alborzkouh et al., 2015 ). Moreover, adaptive coping strategies, including social and emotional support, have been found to improve the mental well-being of students, and stress-reduction peer support groups and workshops on campus could be beneficial in reducing stress and improving the self-efficacy of students (Ruthig et al., 2009 ; Baqutayan, 2011 ; Bedewy and Gabriel, 2015 ; Freire et al., 2020 ; Green et al., 2021 ; Suresh et al., 2021 ). Other interventions that have been effective in improving the coping skills of college students include cognitive-behavioral therapy, mindfulness mediation, and online coping tools (Kang et al., 2009 ; Regehr et al., 2013 ; Molla Jafar et al., 2015 ; Phang et al., 2015 ; Houston et al., 2017 ; Yusufov et al., 2019 ; Freire et al., 2020 ). Given that resilience has also been shown to help mediate stress and improve mental well-being during the COVID-19 pandemic, interventions focusing on enhancing resilience should be considered (Surzykiewicz et al., 2021 ; Skalski et al., 2022 ). Telemental health resources across colleges can also be implemented to reduce stigma and improve at-risk students' access to care (Toscos et al., 2018 ; Hadler et al., 2021 ). University campuses, professors, and counselors should consider focusing on fostering a more equitable and inclusive environment to encourage marginalized students to seek mental health support (Budge et al., 2020 ).
Limitations
While our study has numerous strengths, including using standardized instruments and a large sample size, this study also has several limitations due to both the methodology and sample. First, the correlational study design precludes making any causal relationships (Misra and McKean, 2000 ). Thereby, our findings should be taken in the context of academic stress and mental well-being, and recognize that mental health could be caused by other non-academic factors. Second, the PAS comprised only the perception of responses to academic stress, but stress is a multi-factorial response that encompasses both perceptions and coping mechanisms to different stressors, and the magnitude of stress varies with the perception of the degree of uncontrollability, unpredictability, or threat to self (Miller, 1981 ; Hobfoll and Walfisch, 1984 ; Lazarus and Folkman, 1984 ; Wheaton, 1985 ; Perrewé and Zellars, 1999 ; Schneiderman et al., 2005 ; Bedewy and Gabriel, 2015 ; Schönfeld et al., 2016 ; Reddy et al., 2018 ; Freire et al., 2020 ; Karyotaki et al., 2020 ). Third, the SWEMSBS used in our study and the data only measured positive mental health. Mental health pathways are numerous and complex, and are composed of distinct and interdependent negative and positive indicators that should be considered together (Margraf et al., 2020 ). Fourth, due to the small effect sizes and unequal representation for different combinations of variables, our analysis for both the PAS and SWEMSBS included only summed-up scales and did not examine group differences in response to the type of academic stressors or individual mental health questions.
An additional limitation is that the participants in our study were a convenience sample. The testing service we used, prolific.co, self-reports a sample bias toward young women of high levels of education (i.e., WEIRD bias) (Team Prolific, 2018 ). The skew toward this population was observed in our data, as 80% of our participants were women. While we controlled for these factors, the possibility remains that the conclusions we draw for certain groups, such as nonbinary students, ethnic/racial minorities, and men, may not be as statistically powerful as they should be. Moreover, our pre-screening was designed to recruit undergraduate level, English-speaking, 18–30-year-olds who resided in the United States. This resulted in our participant demographics being skewed toward the WEIRD bias that was already inherent in the testing service we used. Future research will aim to be more inclusive of diverse races/ethnicities, sexual orientations, languages, educational backgrounds, socioeconomic backgrounds, and first-generation college students.
Another limitation of our study is the nature of satisficing. Satisficing is a response strategy in which a participant answers a question to satisfy its condition with little regard to the quality or accuracy of the answer (Roberts et al., 2019 ). Anonymous participants are more likely to satisfice than respondents who answer the question face-to-face (Krosnick et al., 2002 ). We sought to mitigate satisficing by offering financial incentives to increase response rates and decrease straight-lining, item skipping, total missing items, and non-completion (Cole et al., 2015 ). Concerns of poor data quality due to surveys offering financial incentives found little evidence to support that claim and may do the opposite (Cole et al., 2015 ). On the other hand, social desirability bias may have influenced the participant's self-reported responses, although our anonymous survey design aimed to reduce this bias (Joinson, 1999 ; Kecojevic et al., 2020 ).
Future Studies
Future studies should replicate our study to validate our results, conduct longitudinal cohort studies to examine well-being and perceived academic stress over time, and aim for a more representative student sample that includes various groups, including diverse races/ethnicities, sexual orientations, socioeconomic backgrounds, languages, educational levels, and first-generation college students. Additionally, these studies should consider examining other non-academic stressors and students' coping mechanisms, both of which contribute to mental health and well-being (Lazarus and Folkman, 1984 ; Freire et al., 2020 ). Further explorations of negative and other positive indicators of mental health may offer a broader perspective (Margraf et al., 2020 ). Moreover, future research should consider extending our work by exploring group differences in relation to each factor in the PAS (i.e., academic expectations, workload and examinations, and self-perception of students) and SWEMBS to determine which aspects of academic stress and mental health were most affected and allow for the devising of targeted stress-reduction approaches. Ultimately, we hope our research spurs readers into advocating for greater academic support and access to group-specific mental health resources to reduce the stress levels of college students and improve their mental well-being.
Utilizing two well-established scales, our research found a statistically significant correlation between the perceived academic stress of university students and their mental well-being (i.e., the higher the stress, the worse the well-being). This relationship was most apparent among gender and grade levels. More specifically, non-binary and second-year students experienced greater academic burden and lower psychological well-being. Moreover, women, non-binary students, and upper-level students were disproportionately impacted by stress related to the COVID-19 pandemic.
Studies regarding broad concepts of stress and well-being using a questionnaire are limited, but our study adds value to the understanding of academic stress as a contributor to the overall well-being of college students during this specific point in time (i.e., the COVID-19 pandemic). Competition both for admission to college (Bound et al., 2009 ) and during college (Posselt and Lipson, 2016 ) has increased over time. Further, selective American colleges and universities draw applicants from a global pool. As such, it is important to document the dynamics of academic stress with renewed focus. We hope that our study sparks interest in both exploring and funding in-depth and well-designed psychological studies related to stress in colleges in the future.
Data Availability Statement
Ethics statement.
The studies involving human participants were reviewed and approved by Institutional Review Board at Rutgers University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GB and MB contributed to conceptualization, study design, IRB application, manuscript drafting, and revision. XZ participated in the conceptualization and design of the questionnaires. HB participated in subject recruitment and questionnaire collection. KP contributed to data analysis, table and figure preparation, manuscript drafting, and revision. XM contributed to conceptualization, study design, IRB application, supervision of the project, manuscript drafting, and revision. All authors contributed to the article and approved the submitted version.
This study was made possible by a generous donation from the Knights of Columbus East Hanover Chapter in New Jersey.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank Shivani Mehta and Varsha Garla for their assistance with the study. We also thank all the participants for their efforts in the completion of the study.
- Acheampong C., Davis C., Holder D., Averett P., Savitt T., Campbell K. (2019). An exploratory study of stress coping and resiliency of black men at one medical school: a critical race theory perspective . J. Racial Ethnic Health Disparit. 6 , 214–219. 10.1007/s40615-018-0516-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alborzkouh P., Nabati M., Zainali M., Abed Y., Shahgholy Ghahfarokhi F. (2015). A review of the effectiveness of stress management skills training on academic vitality and psychological well-being of college students . J. Med. Life 8 , 39–44. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Allen S., Hiebert B. (1991). Stress and coping in adolescents . Can. J. Counsel. 25 , 19–32. [ Google Scholar ]
- American Psychological Association . (2020). Stress in AmericaTM2020: A National Mental Health Crisis . Washington, DC: American Psychological Association. [ Google Scholar ]
- Arnett J. J.. (2000). Emerging adulthood. A theory of development from the late teens through the twenties . Am. Psychol. 55 , 469–480. 10.1037/0003-066X.55.5.469 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baqutayan S.. (2011). Stress and social support . Indian J. Psychol. Med. 33 , 29–34. 10.4103/0253-7176.85392 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barbayannis G., Franco D., Wong S., Galdamez J., Romeo R. D., Bauer E. P. (2017). Differential effects of stress on fear learning and activation of the amygdala in pre-adolescent and adult male rats . Neuroscience 360 , 210–219. 10.1016/j.neuroscience.2017.07.058 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bedewy D., Gabriel A. (2015). Examining perceptions of academic stress and its sources among university students: the perception of academic stress scale . Health Psychol. Open 2 , 1–9. 10.1177/2055102915596714 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blanco C., Okuda M., Wright C., Hasin D. S., Grant B. F., Liu S. M., et al.. (2008). Mental health of college students and their non-college-attending peers: results from the National Epidemiologic Study on Alcohol and Related Conditions . Arch. Gen. Psychiatry 65 , 1429–1437. 10.1001/archpsyc.65.12.1429 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bound J., Hershbein B., Long B. T. (2009). Playing the admissions game: student reactions to increasing college competition . J. Econ. Perspect. 23 , 119–146. 10.1257/jep.23.4.119 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown D. L.. (2008). African American resiliency: examining racial socialization and social support as protective factors . J. Black Psychol. 34 , 32–48. 10.1177/0095798407310538 [ CrossRef ] [ Google Scholar ]
- Budge S. L., Domínguez S., Jr., Goldberg A. E. (2020). Minority stress in nonbinary students in higher education: the role of campus climate and belongingness . Psychol. Sex. Orient. Gender Divers. 7 , 222–229. 10.1037/sgd0000360 [ CrossRef ] [ Google Scholar ]
- Byrd D. R., McKinney K. J. (2012). Individual, interpersonal, and institutional level factors associated with the mental health of college students . J. Am. Coll. Health 60 , 185–193. 10.1080/07448481.2011.584334 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cage E., Stock M., Sharpington A., Pitman E., Batchelor R. (2020). Barriers to accessing support for mental health issues at university . Stud. High. Educ. 45 , 1637–1649. 10.1080/03075079.2018.1544237 [ CrossRef ] [ Google Scholar ]
- Chen T., Lucock M. (2022). The mental health of university students during the COVID-19 pandemic: an online survey in the UK . PLoS ONE 17 , e0262562. 10.1371/journal.pone.0262562 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chiang J. J., Ko A., Bower J. E., Taylor S. E., Irwin M. R., Fuligni A. J. (2019). Stress, psychological resources, and HPA and inflammatory reactivity during late adolescence . Dev. Psychopathol. 31 , 699–712. 10.1017/S0954579418000287 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clabaugh A., Duque J. F., Fields L. J. (2021). Academic stress and emotional well-being in United States college students following onset of the COVID-19 pandemic . Front. Psychol. 12 , 628787. 10.3389/fpsyg.2021.628787 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cole J. S., Sarraf S. A., Wang X. (2015). Does Use of Survey Incentives Degrade Data Quality? Chicago, IL: Association for Institutional Research Annual Forum. [ Google Scholar ]
- Defeyter M. A., Stretesky P. B., Long M. A., Furey S., Reynolds C., Porteous D., et al.. (2021). Mental well-being in UK higher education during Covid-19: do students trust universities and the government? Front. Public Health 9 , 646916. 10.3389/fpubh.2021.646916 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dong L., Bouey J. (2020). Public mental health crisis during COVID-19 Pandemic, China . Emerging Infect. Dis. 26 , 1616–1618. 10.3201/eid2607.200407 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dusselier L., Dunn B., Yongyi W., Shelley M., II, Whalen D. (2005). Personal, health, academic, and environmental predictors of stress in residence halls . J. Am. Coll. Health 54 , 15–24. 10.3200/JACH.54.1.15-24 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eisenberg D., Golberstein E., Hunt J. B. (2009). Mental health and academic success in college . B.E. J Econ Anal Policy 9 , 1–35. 10.2202/1935-1682.2191 [ CrossRef ] [ Google Scholar ]
- Eisenberg D., Gollust S. E., Golberstein E., Hefner J. L. (2007). Prevalence and correlates of depression, anxiety, and suicidality among university students . Am. J. Orthopsychiatry 77 , 534–542. 10.1037/0002-9432.77.4.534 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ekpenyong C. E., Daniel N. E., Aribo E. O. (2013). Associations between academic stressors, reaction to stress, coping strategies and musculoskeletal disorders among college students . Ethiop. J. Health Sci. 23 , 98–112. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Elias H., Ping W. S., Abdullah M. C. (2011). Stress and academic achievement among undergraduate students in Universiti Putra Malaysia . Proc. Soc. Behav. Sci. 29 , 646–655. 10.1016/j.sbspro.2011.11.288 [ CrossRef ] [ Google Scholar ]
- Evans T. M., Bira L., Gastelum J. B., Weiss L. T., Vanderford N. L. (2018). Evidence for a mental health crisis in graduate education . Nat. Biotechnol . 36 , 282–284. 10.1038/nbt.4089 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Freire C., Ferradás M., Regueiro B., Rodríguez S., Valle A., Núñez J. C. (2020). Coping strategies and self-efficacy in university students: a person-centered approach . Front. Psychol. 11 , 841. 10.3389/fpsyg.2020.00841 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Freire C., Ferradás M. D., Valle A., Núñez J. C., Vallejo G. (2016). Profiles of psychological well-being and coping strategies among university students . Front. Psychol. 7 , 1554. 10.3389/fpsyg.2016.01554 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fung S.. (2019). Psychometric evaluation of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) with Chinese University Students . Health Qual. Life Outcomes 17 , 46. 10.1186/s12955-019-1113-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Galderisi S., Heinz A., Kastrup M., Beezhold J., Sartorius N. (2015). Toward a new definition of mental health . World Psychiatry 14 , 231–233. 10.1002/wps.20231 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gao W., Ping S., Liu X. (2020). Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China . J. Affect. Disord. 263 , 292–300. 10.1016/j.jad.2019.11.121 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Graves B. S., Hall M. E., Dias-Karch C., Haischer M. H., Apter C. (2021). Gender differences in perceived stress and coping among college students . PLoS ONE 16 , e0255634. 10.1371/journal.pone.0255634 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Green Z. A., Faizi F., Jalal R., Zadran Z. (2021). Emotional support received moderates academic stress and mental well-being in a sample of Afghan university students amid COVID-19 . Int. J. Soc. Psychiatry . 207640211057729. 10.1177/00207640211057729. [Epub ahead of print]. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hadler N. L., Bu P., Winkler A., Alexander A. W. (2021). College student perspectives of telemental health: a review of the recent literature . Curr. Psychiatry Rep. 23 , 6. 10.1007/s11920-020-01215-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hj Ramli N. H., Alavi M., Mehrinezhad S. A., Ahmadi A. (2018). Academic stress and self-regulation among university students in Malaysia: mediator role of mindfulness . Behav. Sci. 8 , 12. 10.3390/bs8010012 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hobfoll S. E., Walfisch S. (1984). Coping with a threat to life: a longitudinal study of self-concept, social support, and psychological distress . Am. J. Community Psychol. 12 , 87–100. 10.1007/BF00896930 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hogan D. P., Astone N. M. (1986). The transition to adulthood . Annu. Rev. Sociol. 12 , 109–130. 10.1146/annurev.so.12.080186.000545 [ CrossRef ] [ Google Scholar ]
- Houston J. B., First J., Spialek M. L., Sorenson M. E., Mills-Sandoval T., Lockett, et al.. (2017). Randomized controlled trial of the Resilience and Coping Intervention (RCI) with undergraduate university students . J Am. Coll. Health 65 , 1–9. 10.1080/07448481.2016.1227826 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang C. Y., Zane N. (2016). Cultural influences in mental health treatment . Curr. Opin. Psychol. 8 , 131–136. 10.1016/j.copsyc.2015.10.009 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hunt C., Gibson G. C., Vander Horst A., Cleveland K. A., Wawrosch C., Granot M., et al.. (2021). Gender diverse college students exhibit higher psychological distress than male and female peers during the novel coronavirus (COVID-19) pandemic . Psychol. Sex. Orient. Gender Divers. 8 , 238–244. 10.1037/sgd0000461 [ CrossRef ] [ Google Scholar ]
- Husky M. M., Kovess-Masfety V., Swendsen J. D. (2020). Stress and anxiety among university students in France during Covid-19 mandatory confinement . Compr. Psychiatry 102 :152191. 10.1016/j.comppsych.2020.152191 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jarrett B. A., Peitzmeier S. M., Restar A., Adamson T., Howell S., Baral S., et al.. (2021). Gender-affirming care, mental health, and economic stability in the time of COVID-19: a multi-national, cross-sectional study of transgender and nonbinary people . PLoS ONE 16 , e0254215. 10.1371/journal.pone.0254215 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Joinson A.. (1999). Social desirability, anonymity, and Internet-based questionnaires . Behav. Res. Methods Instrum. Comput. 31 , 433–438. 10.3758/BF03200723 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jones B. A., Pierre Bouman W., Haycraft E., Arcelus J. (2019). Mental health and quality of life in non-binary transgender adults: a case control study . Int. J. Transgender. 20 , 251–262. 10.1080/15532739.2019.1630346 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kajantie E., Phillips D. I. (2006). The effects of sex and hormonal status on the physiological response to acute psychosocial stress . Psychoneuroendocrinology 31 , 151–178. 10.1016/j.psyneuen.2005.07.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kang Y. S., Choi S. Y., Ryu E. (2009). The effectiveness of a stress coping program based on mindfulness meditation on the stress, anxiety, and depression experienced by nursing students in Korea . Nurse Educ. Today 29 , 538–543. 10.1016/j.nedt.2008.12.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karyotaki E., Cuijpers P., Albor Y., Alonso J., Auerbach R. P., Bantjes J., et al.. (2020). Sources of stress and their associations with mental disorders among college students: results of the World Health Organization World Mental Health Surveys International College Student Initiative . Front. Psychol. 11 , 1759. 10.3389/fpsyg.2020.01759 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kecojevic A., Basch C. H., Sullivan M., Davi N. K. (2020). The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study . PLoS ONE 15 , e0239696. 10.1371/journal.pone.0239696 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ketchen Lipson S., Gaddis S. M., Heinze J., Beck K., Eisenberg D. (2015). Variations in student mental health and treatment utilization across US Colleges and Universities . J Am. Coll. Health 63 , 388–396. 10.1080/07448481.2015.1040411 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kodish T., Lau A. S., Gong-Guy E., Congdon E., Arnaudova I., Schmidt M., et al.. (2022). Enhancing racial/ethnic equity in college student mental health through innovative screening and treatment . Adm. Policy Ment. Health 49 , 267–282. 10.1007/s10488-021-01163-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kost R. G., de Rosa J. C. (2018). Impact of survey length and compensation on validity, reliability, and sample characteristics for ultrashort-, short-, and long-research participant perception surveys . J. Clin. Transl. Sci. 2 , 31–37. 10.1017/cts.2018.18 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koushede V., Lasgaard M., Hinrichsen C., Meilstrup C., Nielsen L., Rayce S. B., et al.. (2019). Measuring mental well-being in Denmark: validation of the original and short version of the Warwick-Edinburgh mental well-being scale (WEMWBS and SWEMWBS) and cross-cultural comparison across four European settings . Psychiatry Res. 271 , 502–509. 10.1016/j.psychres.2018.12.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krosnick J. A., Holbrook A. L., Berent M. K., Carson R. T., Michael Hanemann W., Kopp R. J., et al.. (2002). The impact of “no opinion” response options on data quality: non-attitude reduction or an invitation to satisfice? Public Opin. Q. 66 , 371–403. 10.1086/341394 [ CrossRef ] [ Google Scholar ]
- Lakens D.. (2013). Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs . Front. Psychol. 4 , 863. 10.3389/fpsyg.2013.00863 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lally M., Valentine-French S. (2019). Chapter 7: Emerging and Early Adulthood. Lifespan Development: A Psychological Perspective. 2nd Edn. p.246-306). [E-book] San Francisco: Creative Commons . Available online at: http://dept.clcillinois.edu/psy/LifespanDevelopment.pdf (accessed February 6, 2022).
- Lazarus R. S., Folkman S. (1984). Stress, Appraisal, and Coping . New York, NY: Springer. [ Google Scholar ]
- Lee J., Jeong H. J., Kim S. (2021). Stress, anxiety, and depression among undergraduate students during the COVID-19 pandemic and their use of mental health services . Innovat. High. Educ. 1–20. 10.1007/s10755-021-09552-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lesure-Lester G. E., King N. (2004). Racial-ethnic differences in social anxiety among college students . J. Coll. Stud. Retent. Res. Theory Pract. 6 , 359–367. 10.2190/P5FR-CGAH-YHA4-1DYC [ CrossRef ] [ Google Scholar ]
- Li H., Lin C. (2003). College stress and psychological well-being of Chinese college students . Acta Psychol. Sinca 25 , 222–230. [ Google Scholar ]
- Lipson S. K., Kern A., Eisenberg D., Breland-Noble A. M. (2018). Mental health disparities among college students of color . J. Adolesc. Health 63 , 348–356. 10.1016/j.jadohealth.2018.04.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lipson S. K., Raifman J., Abelson S., Reisner S. L. (2019). Gender minority mental health in the U.S.: results of a National Survey on College Campuses . Am. J. Prev. Med. 57 , 293–301. 10.1016/j.amepre.2019.04.025 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu C. H., Stevens C., Wong S., Yasui M., Chen J. A. (2019). The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use . Depress. Anxiety 36 , 8–17. 10.1002/da.22830 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu X., Ping S., Gao W. (2019). Changes in undergraduate students' psychological well-being as they experience University Life . Int. J. Environ. Res. Public Health 16 , 2864. 10.3390/ijerph16162864 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lopes A. R., Nihei O. K. (2021). Depression, anxiety and stress symptoms in Brazilian university students during the COVID-19 pandemic: predictors and association with life satisfaction, psychological well-being and coping strategies . PLoS ONE 16 , e0258493. 10.1371/journal.pone.0258493 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Margraf J., Zhang X. C., Lavallee K. L., Schneider S. (2020). Longitudinal prediction of positive and negative mental health in Germany, Russia, and China . PLoS ONE 15 , e0234997. 10.1371/journal.pone.0234997 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Matud M. P., Díaz A., Bethencourt J. M., Ibáñez I. (2020). Stress and psychological distress in emerging adulthood: a gender analysis . J. Clin. Med. 9 , 2859. 10.3390/jcm9092859 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McQuaid R. J., Cox S., Ogunlana A., Jaworska N. (2021). The burden of loneliness: implications of the social determinants of health during COVID-19 . Psychiatry Res. 296 , 113648. 10.1016/j.psychres.2020.113648 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller S. M.. (1981). Predictability and human stress: toward a clarification of evidence and theory . Adv. Exp. Soc. Psychol. 14 , 203–256. 10.1016/S0065-2601(08)60373-1 [ CrossRef ] [ Google Scholar ]
- Misra R., Castillo L. G. (2004). Academic stress among college students: comparison of American and International Students . Int. J. Stress Manag. 11 , 132–148. 10.1037/1072-5245.11.2.132 [ CrossRef ] [ Google Scholar ]
- Misra R., McKean M. (2000). College students' academic stress and its relation to their anxiety, time management, and leisure satisfaction . Am. J. Health Stud. 16 , 41–51. [ Google Scholar ]
- Misra R., McKean M., West S., Russo T. (2000). Academic stress of college students: Comparison of student and faculty perceptions . Coll. Stud. J. 34 , 236–245. [ Google Scholar ]
- Molla Jafar H., Salabifard S., Mousavi S. M., Sobhani Z. (2015). The effectiveness of group training of CBT-based stress management on anxiety, psychological hardiness and general self-efficacy among university students . Glob. J. Health Sci. 8 , 47–54. 10.5539/gjhs.v8n6p47 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Negga F., Applewhite S., Livingston I. (2007). African American college students and stress: school racial composition, self-esteem and social support . Coll. Stud. J. 41 , 823. [ Google Scholar ]
- Pascoe M. C., Hetrick S. E., Parker A. G. (2020). The impact of stress on students in secondary school and higher education . Int. J. Adolesc. Youth 25 , 104–112. 10.1080/02673843.2019.1596823 [ CrossRef ] [ Google Scholar ]
- Patsali M. E., Mousa D. V., Papadopoulou E., Papadopoulou K., Kaparounaki C. K., Diakogiannis I., et al.. (2020). University students' changes in mental health status and determinants of behavior during the COVID-19 lockdown in Greece . Psychiatry Res. 292 , 113298. 10.1016/j.psychres.2020.113298 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pedrelli P., Nyer M., Yeung A., Zulauf C., Wilens T. (2015). College students: mental health problems and treatment considerations . Acad. Psychiatry 39 , 503–511. 10.1007/s40596-014-0205-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Perrewé P. L., Zellars K. L. (1999). An examination of attributions and emotions in the transactional approach to the organizational stress process . J. Org. Behav. 20 , 739–752. 10.1002/(SICI)1099-1379(199909)20:5<739::AID-JOB1949>3.0.CO;2-C [ CrossRef ] [ Google Scholar ]
- Phang C. K., Mukhtar F., Ibrahim N., Keng S. L., Mohd Sidik S. (2015). Effects of a brief mindfulness-based intervention program for stress management among medical students: the Mindful-Gym randomized controlled study . Adv. Health Sci. Educ. Theory Pract. 20 , 1115–1134. 10.1007/s10459-015-9591-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Posselt J. R., Lipson S. K. (2016). Competition, anxiety, and depression in the college classroom: variations by student identity and field of study . J. Coll. Stud. Dev. 57 , 973–989. 10.1353/csd.2016.0094 [ CrossRef ] [ Google Scholar ]
- Prowse R., Sherratt F., Abizaid A., Gabrys R. L., Hellemans K., Patterson Z. R., et al.. (2021). Coping with the COVID-19 pandemic: examining gender differences in stress and mental health among university students . Front. Psychiatry 12 , 650759. 10.3389/fpsyt.2021.650759 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reddy K. J., Menon K. R., Thattil A. (2018). Academic stress and its sources among university students . Biomed Pharmacol J 11 , 1. 10.13005/bpj/1404 [ CrossRef ] [ Google Scholar ]
- Regehr C., Glancy D., Pitts A. (2013). Interventions to reduce stress in university students: a review and meta-analysis . J. Affect. Disord. 148 , 1–11. 10.1016/j.jad.2012.11.026 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ringdal R., Bradley Eilertsen M. E., Bjørnsen H. N., Espnes G. A., Moksnes U. K. (2018). Validation of two versions of the Warwick-Edinburgh Mental Well-Being Scale among Norwegian adolescents . Scand. J. Public Health 46 , 718–725. 10.1177/1403494817735391 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts C., Gilbert E., Allum N., Eisner L. (2019). Research synthesis: Satisficing in surveys: a systematic review of the literature . Public Opin. Q. 83 , 598–626. 10.1093/poq/nfz035 [ CrossRef ] [ Google Scholar ]
- Romeo R. D., Patel R., Pham L., So V. M. (2016). Adolescence and the ontogeny of the hormonal stress response in male and female rats and mice . Neurosci. Biobehav. Rev. 70 , 206–216. 10.1016/j.neubiorev.2016.05.020 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ruthig J. C., Haynes T. L., Stupnisky R. H., Perry R. P. (2009). Perceived Academic Control: mediating the effects of optimism and social support on college students' psychological health . Soc. Psychol. Educ. 12 , 233–249. 10.1007/s11218-008-9079-6 [ CrossRef ] [ Google Scholar ]
- Ryan R. M., Deci E. L. (2001). On happiness and human potentials: a review of research on hedonic and eudaimonic well-being . Annu. Rev. Psychol. 52 , 141–166. 10.1146/annurev.psych.52.1.141 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Saleh D., Camart N., Romo L. (2017). Predictors of stress in college students . Front. Psychol. 8 , 19. 10.3389/fpsyg.2017.00019 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Salerno J. P., Williams N. D., Gattamorta K. A. (2020). LGBTQ populations: psychologically vulnerable communities in the COVID-19 pandemic . Psychol. Trauma 12 , S239–S242. 10.1037/tra0000837 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Scales P. C., Benson P. L., Oesterle S., Hill K. G., Hawkins J. D., Pashak T. J. (2015). The dimensions of successful young adult development: a conceptual and measurement framework . Appl. Dev. Sci. 20 , 150–174. 10.1080/10888691.2015.1082429 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schneiderman N., Ironson G., Siegel S. D. (2005). Stress and health: psychological, behavioral, and biological determinants . Annu. Rev. Clin. Psychol. 1 , 607–628. 10.1146/annurev.clinpsy.1.102803.144141 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schönfeld P., Brailovskaia J., Bieda A., Zhang X. C., Margraf J. (2016). The effects of daily stress on positive and negative mental health: mediation through self-efficacy . Int. J. Clin. Health Psychol. 16 , 1–10. 10.1016/j.ijchp.2015.08.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shah N., Cader M., Andrews B., McCabe R., Stewart-Brown S. L. (2021). Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS): performance in a clinical sample in relation to PHQ-9 and GAD-7 . Health Qual. Life Outcomes 19 , 260. 10.1186/s12955-021-01882-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shanahan M. J.. (2000). Pathways to adulthood in changing societies: variability and mechanisms in life course perspective . Annu. Rev. Sociol. 26 , 667–692. 10.1146/annurev.soc.26.1.667 [ CrossRef ] [ Google Scholar ]
- Skalski S. B., Konaszewski K., Büssing A., Surzykiewicz J. (2022). Resilience and mental well-being during the COVID-19 pandemic: serial mediation by persistent thinking and anxiety about coronavirus . Front. Psychiatry 12 , 810274. 10.3389/fpsyt.2021.810274 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith K. M., Chesin M. S., Jeglic E. L. (2014). Minority college student mental health: does majority status matter? Implications for college counseling services . J. Multicult. Counsel. Dev. 42 , 77–92. 10.1002/j.2161-1912.2014.00046.x [ CrossRef ] [ Google Scholar ]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. (2020). Effects of COVID-19 on college students' mental health in the United States: interview survey study . J. Med. Internet Res. 22 , e21279. 10.2196/21279 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spear L. P.. (2000). The adolescent brain and age-related behavioral manifestations . Neurosci. Biobehav. Rev. 24 , 417–463. 10.1016/S0149-7634(00)00014-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stewart-Brown S., Janmohamed K. (2008). Warwick-Edinburgh mental well-being scale. User guide. Version, 1 . 10.1037/t80221-000 [ CrossRef ] [ Google Scholar ]
- Suresh R., Karkossa Z., Richard J., Karia M. (2021). Program evaluation of a student-led peer support service at a Canadian university . Int. J. Ment. Health Syst. 15 , 54. 10.1186/s13033-021-00479-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Surzykiewicz J., Konaszewski K., Skalski S., Dobrakowski P. P., Muszyńska J. (2021). Resilience and mental health in the polish population during the COVID-19 lockdown: a mediation analysis . J. Clin. Med. 10 , 4974. 10.3390/jcm10214974 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Syed N. B.. (2021). Impact of levels of education on perceived academic stress and mental wellbeing: an investigation into online mode of learning during pandemic . J. Psychol. Res. 3 , 12–18. 10.30564/jpr.v3i2.3032 [ CrossRef ] [ Google Scholar ]
- Taber K. S.. (2018). The use of Cronbach's alpha when developing and reporting research instruments in science education . Res. High. Educ. 48 , 1273–1296. 10.1007/s11165-016-9602-2 [ CrossRef ] [ Google Scholar ]
- Team Prolific (2018). What Are the Advantages and Limitations of an Online Sample? Prolific Researcher Help Centre . Available online at: https://researcher-help.prolific.co/hc/en-gb/articles/360009501473-What-are-the-advantages-and-limitations-of-an-online-sample-#:~:text=Limitations%20Rapid-responder%20bias.%20Prolific%20predominantly%20uses%20convenience%20sampling%2C,and%20fairly%20distribute%20study%20places%20among%20active%20participants (accessed February 22, 2022).
- Tennant R., Hiller L., Fishwick R., Platt S., Joseph S., Weich S., et al.. (2007). The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation . Health Qual. Life Outcomes 5 , 63. 10.1186/1477-7525-5-63 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thorne N., Witcomb G. L., Nieder T., Nixon E., Yip A., Arcelus J. (2018). A comparison of mental health symptomatology and levels of social support in young treatment seeking transgender individuals who identify as binary and non-binary . Int. J. Transgender. 20 , 241–250. 10.1080/15532739.2018.1452660 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Toscos T., Carpenter M., Drouin M., Roebuck A., Kerrigan C., Mirro M. (2018). College students' experiences with, and willingness to use, different types of telemental health resources: do gender, depression/anxiety, or stress levels matter? Telemed. J. E Health 24 , 998–1005. 10.1089/tmj.2017.0243 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Trout I. Y., Alsandor D. J. (2020). Graduate student well-being: learning and living in the US during the COVID-19 pandemic . Int. J. Multidiscipl. Perspect. High. Educ. 5 , 150–155 10.32674/jimphe.v5i1.2576 [ CrossRef ] [ Google Scholar ]
- Verma R., Balhara Y. P., Gupta C. S. (2011). Gender differences in stress response: role of developmental and biological determinants . Ind. Psychiatry J. 20 , 4–10. 10.4103/0972-6748.98407 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wheaton B.. (1985). Models for the stress-buffering functions of coping resources . J. Health Soc. Behav. 26 , 352–364. 10.2307/2136658 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wyatt T. J., Oswalt S. B., Ochoa Y. (2017). Mental health and academic performance of first-year college students . Int. J. High. Educ. 6,178–187. 10.5430/ijhe.v6n3p178 [ CrossRef ] [ Google Scholar ]
- Yang C., Chen A., Chen Y. (2021). College students' stress and health in the COVID-19 pandemic: the role of academic workload, separation from school, and fears of contagion . PLoS ONE 16 , e0246676. 10.1371/journal.pone.0246676 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yusufov M., Nicoloro-SantaBarbara J., Grey N. E., Moyer A., Lobel M. (2019). Meta-analytic evaluation of stress reduction interventions for undergraduate and graduate students . Int. J. Stress Mang . 26 , 132–145. 10.1037/str0000099 [ CrossRef ] [ Google Scholar ]
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
July 1, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Researchers disclose the effect of social media use on the mental health of college students during the pandemic
by University of North Carolina at Chapel Hill

The COVID-19 pandemic had an unprecedented effect on college students' mental health. Symptoms like anxiety and major depression in young adults ages 18-25 increased significantly compared to before the pandemic.
A new study from researchers at the University of North Carolina at Chapel Hill looks at a possible contributing factor to the worsening trends in mental health: social media. The findings are published in the journal Health Economics .
We know that college students and adolescents are using social media more. Last May, the US Surgeon General issued an advisory on social media and youth mental health, noting that there are "ample indicators" that social media can "pose a risk of harm to the mental health and well-being of children and adolescents."
But questions remained: Are more depressed people using social media more? Or is social media contributing to more depression?
To answer this, a team led by economist Jane Cooley Fruehwirth used unique longitudinal survey data from first-year college students at a large public research university. The data was collected both before and during the pandemic . This information allowed the researchers to compare social media usage before and during the pandemic along with other factors like social isolation , anxiety and depression symptoms, and how much students were sleeping, exercising, and interacting with their friends.
What they found was surprising: Increased social media usage at the beginning of the pandemic didn't have a large effect on college students' mental health, but increased social media usage 18 months into the pandemic—when colleges had largely reopened and students were back on campus—did have a negative effect on students' mental health. Students who increased their social media usage by an hour 18 months into the pandemic were much more likely to be depressed and anxious.
Why is this the case?
Fruehwirth and team found some evidence that social media use took away from time for other activities that are good for mental health --such as exercise--when students were back in dorms, and that social media also seemed to increase stress from peers. Both early and later in the pandemic, the effects of social media usage were worst among socially isolated college students.
"These students who were socially isolated were not using social media to stay connected," says Fruehwirth. "They were using it in a different way."
Fruehwirth notes that resilience and social support helps protect students from the negative consequences of social media.
"This is not a 'social media is bad' story," she says. "It's that some students are using it in a way that isn't detrimental and some are, and we wanted to tease out those differences."
The findings suggest that college campuses themselves can play a role in reducing isolation. Approximately 1 in 5 college students currently feels isolated on a college campus. This suggests that there's more at play than just social media.
"Universities can think about how to build more connections through physical and social spaces, through connections through clubs," says Fruehwirth. "They can create peer support networks and help build resilience."
Co-authors include Alex Xingbang Weng and Krista Perreira.
Explore further
Feedback to editors

Scientists may have discovered how to diagnose elusive neuro disorder
3 minutes ago

Study finds poor health, stress in 20s takes toll in 40s with lower cognition

30-minute exercise session found to increase proportion of tumor-killing white blood cells in the bloodstream
11 minutes ago

Study finds brain stores motor memories differently based on decision uncertainty

Cracking the code for cerebellar movement disorders

What is language for? Researchers make the case that it's a tool for communication, not for thought

Study finds smokers are on average more extraverted, but less conscientious and agreeable
2 hours ago

Fighting COVID-19 with a cancer drug: A new approach to preventing irreversible organ damage in infectious diseases

Dengue linked to heightened short- and long-term risk of depression in Taiwan

Scientists discover PVP-037, a potent vaccine adjuvant
Related stories.

Which adolescents are at risk of depression following early social media use?
Jun 26, 2024

College drinking declined during the pandemic
Aug 13, 2021

Depression and anxiety among first-year college students worsen during pandemic
Mar 3, 2021

Social media-related nightmares: Study explores links between social media use, mental health and sleep quality
May 20, 2024

Need to vent? Turn to real-life support, not social media
May 3, 2021

Study shows more than just social media use may be causing depression in young adults
May 29, 2024
Recommended for you

Why most people are right handed but left eyed
4 hours ago

Mobile phone data helps track pathogen spread and evolution of superbugs
5 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Higher Education Today
- American Council On Education
- Carnegie Classifications
- Race and Ethnicity In Higher Education
College Student Mental Health and Well-Being

According to the latest research on college students and mental health, three out of 10 students have struggled with depression in the last two weeks, and over one in four have expressed issues with anxiety. Even more distressing is the one in 20 college students who had created a suicide plan in the past year.
College student mental health and well-being is a major source of concern for higher education administrators, faculty, and staff. College counseling centers report being overwhelmed with requests for services. Other faculty and staff report working with campus and local resources to assist students with their mental health concerns.
This blog series aims to explore the various dimensions associated with college student mental health and well-being. Scholars, administrators, analysts, and practitioners will address the challenges faced by different populations of students and offer resources and ideas for support. The series, which will be updated throughout 2019, will serve as a resource for those interested in learning more about the issues surrounding college students and their mental health and the quest for well-being.
Centering Equity in Student Mental Health Task Forces: Lessons Learned From the University of Michigan by Sara R. Abelson, Janelle R. Goodwill, and Meghan A. Duffy Sept. 21, 2020 Based on their work with the University of Michigan’s Rackham Graduate School Task Force on Graduate Student Mental Health, Sara Abelson, Meghan Duffy, and Janelle Goodwill identify eight ways that university mental health task forces can center equity in their work.
Supporting College Students Through a Public Health Crisis: Lessons Learned from Hurricane Harvey by Ruth M. López and Vincent D. Carales April 20, 2020 In the fall of 2017, Hurricane Harvey struck the Gulf Coast, significantly affecting 13 million people in states throughout the region. Ruth M. López and Vincent D. Carales of the University of Houston look at what colleges can learn from Hurricane Harvey to address student mental health and well-being during the COVID-19 pandemic.
Involuntary Withdrawal Policies: No Room for Mental Health Stereotypes in a Fair Process b y Amy C. Foerster Nov. 4, 2019 Recent developments have highlighted the importance of comprehensive, transparent involuntary withdrawal policies for students who pose a risk of self-harm. Attorney Amy C. Foerster discusses what higher education institutions should consider and how to incorporate principles established by the Education Department’s Office for Civil Rights.
Helping Students at Risk of Self-Harm: Considerations for the New Academic Year by Peter McDonough Sept. 4, 2019 ACE General Counsel Peter McDonough outlines a series of principles gleaned from past Department of Education documents that campuses can use as they design policies and practices to help at-risk students.
College Student Mental Health and Well-Being: A Survey of College Presidents by Hollie M. Chessman and Morgan Taylor August 12, 2019 To better understand how campuses are navigating the challenge of student mental health and well-being, ACE conducted a survey of 400 college and university presidents at the end of April. Read what they had to say.
Mental Health and Post-traditional Learners by Gail Bruce-Sanford and Louis Soares April 22, 2019 Post-traditional learners are often expected to adjust their own lives and schedules to campus life and services, including in the area of mental health. But it is equally important that campus services and culture are adjusted to better serve this growing group of students and their unique needs.
Non-Suicidal Self-Injury on College Campuses by Janis Whitlock, Stephen P. Lewis, Imke Baetens, and Penelope Hasking Feb. 6, 2019 Conversations about the mental health and well-being of college students often underestimate the prevalence and impact of non-suicidal self-injury in college settings. Four scholars from institutions in the United States, Canada, Belgium, and Australia look at the problem—and how institutions can respond.
The Rise of Mental Health on College Campuses: Protecting the Emotional Health of Our Nation’s College Students by Nance Roy Dec. 17, 2018 Nance Roy, chief clinical officer of the Jed Foundation, provides action steps to support emotional well-being and reduce suicide and substance abuse among college students.
Cannabis and the College Campus: Considering the Impact on Students in a Changing Legal Climate by Jason Kilmer Nov. 13, 2018 On Nov. 6, 2012, voters in Washington State joined voters in Colorado in passing legislation that legalized marijuana. Since then, eight other states and Washington, DC have passed similar bills. Jason R. Kilmer of the University of Washington looks at what legalization means for college campuses.
When College Feels Like the End Rather Than the Beginning by Kelly Davis Oct. 24, 2018 Students are leading the way to change campus mental health, says Kelly Davis, director of peer advocacy at Mental Health America.
The Mental and Physical Well-Being of Incoming Freshmen: Three Decades of Research by Ellen Bara Stolzenberg Sept. 6, 2018 How have the health concerns of freshman college students have changed in recent decades?
Why We Should Partner with Students to Address Campus Mental Health by Laura Horne July 16, 2018 Students know students, says Laura Horne of Active Minds. Engaging them as equal partners in improving mental health on campus can make all the difference.
It Doesn’t Always Get Better for Queer-Spectrum and Trans-Spectrum College Students by Maren Greathouse June 6, 2018 Many queer-spectrum and trans-spectrum students continue to navigate stigma, peer aggression, and exclusion well into their college years. Researchers are beginning to capture their experiences, which could help lead the way to change.
College on the Autism Spectrum by Connie Anderson May 9, 2018 Most first-time college students face challenges adjusting to new academic demands and campus life. For students on the autism spectrum, these challenges can be overwhelming—but with the proper support, they don’t have to be.
College Students of Color: Confronting the Complexities of Diversity, Culture, and Mental Health by Annelle B. Primm April 2, 2018 Annelle Primm of The Steve Fund discusses the need for the higher education community to institute policies and procedures to support the mental health and emotional well-being of students of color. This post is the first in a series on college student mental health and well-being.
- Student Success
- Health & Wellness
Student Wellness Tip: First-Year Workshops Promote Health and Wellness
Champlain College launched a 10-week curricular program to build students’ skills in transition, teaching healthy habits and campus resources.
By Ashley Mowreader
You have / 5 articles left. Sign up for a free account or log in.

Incoming students at Champlain College complete a 10-week course on health, wellness and academic preparation to promote a seamless transition into higher education.
Champlain College
For many students, balancing academics and other responsibilities is their top stressor and what they believe to be the driver of the collegiate mental health crisis, according to a recent Student Voice survey by Inside Higher Ed and the Generation Lab.
To ease student anxieties and stressors in the transition to college, Champlain College in Vermont developed a first-year program that facilitates peer connection, successful habit building and proactive resource connection.
Champ 101 , first launched in fall 2022, has proven successful in promoting healthy living and wellness among students, prompting campus leaders to integrate the program as part of a required wellness curriculum.
What’s the need: Two-thirds of college students report being lonely, and an additional three in 10 students experience severe psychological distress, according to May data from TimelyCare and Active Minds. While there is no one cause for the increase in mental health concerns, isolation during the COVID-19 pandemic and subsequent lockdowns and heightened political tensions have impacted how learners engage with one another.
Leaders at Champlain recognized the difficulties first-year students were facing integrating into campus life and “saw this as an opportunity to redefine student support and meet these changing student needs,” says Danelle Berube, vice president for student affairs and institutional emergency management coordinator.
How it works: Champ 101 is a required 10-week program for first-year students to help them adjust to their new lives on campus and set them up to thrive.
Each week, students participate in one or two workshops, co-led by a student and a staff or faculty facilitator, meeting regularly with the same small group (20 students or so) throughout the duration of the program.
“This dynamic helps new students build early friendships within their group and creates trust between the students and facilitators,” Berube explains. “It makes it ‘OK not to be OK’ within a peer group that gives students an intrinsic level of comfort and encourages openness.”
Workshop content varies from academic, well-being and social topics such as identity development in the college years, managing homesickness and how to prepare for advising appointments. Students don’t complete assignments or homework as part of the initiative but instead are graded on attendance.
The curriculum was developed by the director of student success and advising and the coordinator of first-year transitions and well-being initiatives, with input from campus stakeholders.
The peer facilitator is also crucial to the program’s success, adding a near peer who can empathize with students’ experiences moving away from home. Student peers are paid for their work.
Faculty and staff facilitators represent various disciplines, academic divisions and departments. Facilitators help mold content through feedback and insights, ensuring the program is relevant and responsive to student needs.
Editors’ Picks
- DEI Ban Prompts Utah Colleges to Close Cultural Centers, Too
- Supreme Court Decision Weakens Education Department
- The Only Certainty Is Uncertainty
The impact: The program was piloted in fall 2022 and last year became a requirement for all incoming students.
A wide majority of students participated in the program regularly this past fall (92 percent) and achieved a satisfactory completion rate (99.8 percent). A 2023 post-survey found:
- Eighty-six percent of students said the program made them feel knowledgeable about campus resources,
- Sixty-seven percent said the program helped them set personal, social and academic goals,
- Sixty percent increased their focus on their own personal health and well-being, and
- Ninety-one percent felt welcomed and included by their peer facilitator.
“Student resources are only helpful if the students needing support understand that they are available and know how to access them, and Champ 101 was extremely successful at creating awareness,” Berube says.
Fall-to-spring retention for the 2023 cohort was 94 percent, compared to the fall 2022 cohort, which had an 88 percent retention rate.
“While not directly tied to Champ 101, this six-percentage-point increase from 2022 to 2023 corresponds with the shift to making Champ 101 a required part of the curriculum in the fall of 2023,” Berube says.
A bigger picture: Champ 101 is now the first step to students’ meeting a l arger graduation requirement focused on wellness and life skills, InSight . The program teaches students career competencies, personal finances and, more recently, wellness.
Each year, students are assigned a list of milestones to complete outside of the classroom in person or online, tracked through the college’s LMS, Canvas. As they work through InSight, students are paired with peer coaches who provide mentorship, encouragement and advice, further developing connections from the learner to the institution.
If your student success program has a unique feature or twist, we’d like to know about it. Click here to submit.
This article has been updated to correct the spelling of Danelle Berube's name.

The Dangers of Distractions in Post–Affirmative Action Admissions
Shaun Harper and Julie Posselt write that many other issues have competed for attention in the year since the Supreme
Share This Article
More from health & wellness.

Today’s Students Expect More. Are You Listening?
Students today are more willing to take a stand and advocate for each other than their predecessors, so higher ed lea

Student Health and Wellness Tip: Recognizing the Red Zone
The start of the fall semester is infamous for high reports of sexual assaults on college campuses

Student Wellness Tip: Making Counseling Centers More Inviting
To promote help-seeking behaviors and encourage students to utilize mental health resources, physical spaces in colle
- Become a Member
- Sign up for Newsletters
- Learning & Assessment
- Diversity & Equity
- Career Development
- Labor & Unionization
- Shared Governance
- Academic Freedom
- Books & Publishing
- Financial Aid
- Residential Life
- Free Speech
- Physical & Mental Health
- Race & Ethnicity
- Sex & Gender
- Socioeconomics
- Traditional-Age
- Adult & Post-Traditional
- Teaching & Learning
- Artificial Intelligence
- Digital Publishing
- Data Analytics
- Administrative Tech
- Alternative Credentials
- Financial Health
- Cost-Cutting
- Revenue Strategies
- Academic Programs
- Physical Campuses
- Mergers & Collaboration
- Fundraising
- Research Universities
- Regional Public Universities
- Community Colleges
- Private Nonprofit Colleges
- Minority-Serving Institutions
- Religious Colleges
- Women's Colleges
- Specialized Colleges
- For-Profit Colleges
- Executive Leadership
- Trustees & Regents
- State Oversight
- Accreditation
- Politics & Elections
- Supreme Court
- Student Aid Policy
- Science & Research Policy
- State Policy
- Colleges & Localities
- Employee Satisfaction
- Remote & Flexible Work
- Staff Issues
- Study Abroad
- International Students in U.S.
- U.S. Colleges in the World
- Intellectual Affairs
- Seeking a Faculty Job
- Advancing in the Faculty
- Seeking an Administrative Job
- Advancing as an Administrator
- Beyond Transfer
- Call to Action
- Confessions of a Community College Dean
- Higher Ed Gamma
- Higher Ed Policy
- Just Explain It to Me!
- Just Visiting
- Law, Policy—and IT?
- Leadership & StratEDgy
- Leadership in Higher Education
- Learning Innovation
- Online: Trending Now
- Resident Scholar
- University of Venus
- Student Voice
- Academic Life
- The College Experience
- Life After College
- Academic Minute
- Weekly Wisdom
- Reports & Data
- Quick Takes
- Advertising & Marketing
- Consulting Services
- Data & Insights
- Hiring & Jobs
- Event Partnerships
4 /5 Articles remaining this month.
Sign up for a free account or log in.
- Sign Up, It’s FREE
June 25, 2024
Teens’ Mental Health May Improve When They Help Others
Volunteering in community programs can reduce youth depression and anxiety, researchers are beginning to learn
By Lydia Denworth

In college my oldest son volunteered as a Big Brother and taught computer science at local elementary and middle schools. After graduating, he said his time with those young students was one of the most rewarding parts of his college experience. According to emerging research, it might also have improved his mental health. There is already considerable evidence from studies with adults that volunteering—doing something for someone else or for one’s community—benefits a person’s physical and mental health and improves overall well-being. Researchers have found that the sense of mattering to those around you that volunteering provides is one important reason it is associated with psychological well-being.
Now scientists are finding similar links to both physical and mental health in children and adolescents. An early experiment found that 10th graders who volunteered in an elementary school for two months showed fewer signs of harmful inflammation and lower levels of obesity compared with students who didn’t volunteer. A 2023 analysis found that among more than 50,000 children and adolescents in the National Survey of Children’s Health, young people who had participated in community service or had volunteered over the previous 12 months were more likely to be in very good or excellent health and stayed calm and in control when faced with challenges, and the adolescents were less likely to be anxious, among other benefits. This improvement was in comparison with young people who did not volunteer.
Granted, those findings are only correlations. “It could be that the children who were volunteering were already in great health,” says study co-leader Kevin Lanza, who is an environmental health scientist at UTHealth Houston School of Public Health.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
But because of an alarming rise in mental health issues among young people, Lanza and others believe this early evidence is promising enough to pursue. A 2021 advisory from U.S. Surgeon General Vivek Murthy warned that the proportion of young people reporting persistent feelings of sadness or hopelessness had increased by 40 percent over the previous decade, starting even before the pandemic. The number of high school students seriously considering a suicide attempt rose by 36 percent. In the first years of the pandemic, the percentage of young people with depressive and anxiety symptoms doubled. There are multiple possible causes in addition to the pandemic, experts say, including the polarized political environment, anxiety over climate change, the effects of social media use and adverse personal circumstances.
When looking for ways to counter these problems, researchers point to the importance of “contribution”—providing support or resources to others or helping to achieve a shared goal—as an essential piece of social and emotional development for adolescents. Young people have a developmental need to connect and belong. “Part of the exploration of adolescence and young adulthood is figuring out where you can be needed and useful—arguably core aspects of our mental health,” says developmental psychologist Andrew Fuligni, co-executive director of the Center for the Developing Adolescent at the University of California, Los Angeles.
Volunteering is one good way young people can contribute. The importance of mattering to others and to the larger world “translates really well to the needs of adolescents to have a meaningful role to play in their community,” says developmental psychologist Parissa Ballard of the Wake Forest University School of Medicine. In a small 2022 pilot study, Ballard and her colleagues tested volunteering as an intervention for nine 14- to 20-year-olds who had been recently diagnosed with mild to moderate depression or anxiety and were recruited through their clinicians. After 30 hours of volunteer work at animal shelters, food banks, and other community organizations, the average reduction in depressive symptoms among participants was 19 percent.
Everyone in the study enjoyed the work and reported a sense of pride and accomplishment. “Young people who were struggling with anxiety said that they were pretty anxious before doing it but then felt so much better after,” Ballard says. Although volunteering should not replace mental health treatment, she says, it could help in conjunction with other forms of therapy. She is pursuing that hypothesis in a larger study.
What accounts for the benefits? Helping others improves mood and raises self-esteem. It provides fertile ground for building social connections. It also shifts people’s focus away from negative things and can change how they see themselves. Many teens say they don’t feel important, Ballard says. “Volunteering can give people a different sense of themselves, a sense of confidence and efficacy.” Lanza thinks of it as “a health pipeline.” He adds that “it equips you with certain types of skills that better control anxiety.”
There may be a potential downside to volunteering, however. Fuligni and his colleagues have found that young people’s mental health can suffer if they feel their contributions are devalued because of their gender, racial or ethnic identity. And if they feel like they are being forced to participate or are not doing much, the experience can be harmful, Ballard says. One report found that people who were required to volunteer when they were young were less likely to do such work when they were older. “Young people have to choose something that feels meaningful to them,” Ballard says. Adults can help by offering choices and by vetting volunteer opportunities to be sure that organizations are well run and equipped to offer a good experience.
When these situations are carefully thought out, volunteering doesn’t just help the volunteers. It also helps the people and communities on the receiving end. “Volunteering could be a win-win,” Lanza says.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.

Centre for Behaviour Change
- Consultancy
- CBC Conference
- Related Organisations

Optimising the involvement of young people in mental health research
Understanding the barriers and enablers of involving young people of different identities in mental health research.

2 July 2024
PhD project
Title: Optimising the involvement of young people in mental health research
Funder: This PhD is funded through a UCL Demonstratorship
CBC Doctoral Student: Rachel Perowne
CBC Supervisors: Professor Leslie Gutman , Dr Sarah Rowe
Why this research is important
Young people’s mental health is a growing concern in the UK, but not all young people experience mental health issues in the same way. For example, lower household income is associated with worse adolescent mental health. So that services and treaments can best support young people, they need to be designed to meet the needs of young people of all backgrounds and identities. Involving a diverse range of young people in a meaningful way in all stages of mental health research can help achieve this. We will use a behaviour change approach to understand the barriers and enablers of involving young people of different identities in mental health research. We will identify behaviour change strategies and techniques to optimise involvement.
Find out more
Read the team's latest paper, which provides a practical resource for researchers considering involving young people in the research process, and suggests what data should be collected to improve reporting on the diversity of the young people involved:
- Paper on 'Understanding and Defining Young People's Involvement and Under-Representation in Mental Health Research: A Delphi Study'
Email Rachel: [email protected]

IMAGES
COMMENTS
The intervention worked for people from various age groups, including college students and middle-aged adults, researchers learned after analyzing seven studies on peer-led mental health programs written or published between 1975 and 2021. Researchers found that participants also became less likely to identify with negative stereotypes ...
The number of students seeking help at campus counseling centers increased almost 40% between 2009 and 2015 and continued to rise until the pandemic began, according to data from Penn State University's Center for Collegiate Mental Health (CCMH), a research-practice network of more than 700 college and university counseling centers (CCMH Annual Report, 2015).
COVID-19 and Student Mental Health. Empirical studies reported a high prevalence of college mental health issues during the early phase of COVID-19 around the world (Cao et al., 2020; Chang et al., 2020; Liu et al., 2020, Rajkumar, 2020; Saddik et al., 2020).In the U.S. a few, but a growing number of empirical surveys and studies were conducted to assess college students' mental health ...
Another common mental health problem among college students is depression, with prevalence rates in college students of 7 to 9 % [ 1, 9 ]. Zisook et al. [ 10] found that over half of all cases of depression had a first onset during childhood, adolescence, or young adulthood.
College Student Mental Health During the COVID-19 Pandemic. Studies from the U.S., Asia, ... The samples were recruited via an undergraduate research pool in which students complete research studies for partial course credit. Notably, the largest course that uses this research pool is a general education credit, so students across many majors ...
Center for Collegiate Mental Health 2023 Annual Report. 2024. This report from the Center for Collegiate Mental Health (CCMH) presents descriptive data on various domains of mental health and factors related to treatment and care for college students in the United States. The data included in this report was gathered from 195 colleges and ...
Poor mental health of students in further and higher education is an increasing concern for public health and policy [1,2,3,4].A 2020 Insight Network survey of students from 10 universities suggests that "1 in 5 students has a current mental health diagnosis" and that "almost half have experienced a serious psychological issue for which they felt they needed professional help"—an ...
infrastructure on students. Brown's chapter works tirelessly to provide advocacy support to mentally ill and neurodivergent students who are navigating the. ableism prevalent at Brown. For example, the Peer Mental Health Advocacy (PMHA) program trains over 100 students every year to be peer supporters to studen.
As with youth mental health (Wilson, 2020 ), research into student mental health (and well-being) is influenced by the differing priorities of individual research teams, as well as cultural context, and policy. Moving forward, research should also represent the priorities of students and universities, including a pragmatic focus on factors ...
Objective: This paper surveys the mental health status and severity of depression and anxiety of college students in a large university system in the United States during the COVID-19 pandemic. Methods: An online survey was conducted among undergraduate and graduate students recruited from Texas A&M University via email. The survey consisted of ...
The percentage of U.S. college students with lifetime diagnoses of mental health conditions in 2017, compared with 22% in 2007. The percentage of students who received any mental health treatment, including therapy or medication, rose from 19% to 34% over that 10-year period.
Mental Health and Mental Health Services Research, 42 (6), 682-694. doi: 10.1007/s10488- ... College student mental health has been a concern on U.S. college campuses for decades. The COVID-19 ...
Abstract. Mental illness stigma has been identified by national policy makers as an important barrier to help seeking for mental health. Using a random sample of 5,555 students from a diverse set of 13 universities, we conducted one of the first empirical studies of the association of help-seeking behavior with both perceived public stigma and ...
60% of college students reported experiencing one or more mental health challenges in 2021, according to the National Healthy Minds Study (.pdf). The percentage of students experiencing mental health problems has increased nearly 50% since 2013. Students are affected by a range of stressors and challenges, including academic pressure, balancing ...
The Gallup/Lumina study found that 44% of associate degree students and 36% of bachelor's degree students are considering stopping their coursework for at least one term. Of those students, 55% ...
In a new study, Lipson and her colleagues reveal just how common depression, anxiety, and other mental health issues are, and how these issues take a toll on students of color unequally. The paper looks at survey data collected by the Healthy Minds Network between 2013 and 2021 from 350,000 students at over 300 campuses.
February 17, 2021. 25. Kat J. McAlpine. A survey by a Boston University researcher of nearly 33,000 college students across the country reveals the prevalence of depression and anxiety in young people continues to increase, now reaching its highest levels, a sign of the mounting stress factors due to the coronavirus pandemic, political unrest ...
(courtesy of AdobeStock) The COVID-19 pandemic had an unprecedented effect on college students' mental health: symptoms like anxiety and major depression in young adults ages 18-25 increased significantly compared to before the pandemic.. A new study from researchers at the University of North Carolina at Chapel Hill looks at a possible contributing factor to the worsening trends in mental ...
What they found was surprising: increased social media usage at the beginning of the pandemic didn't have a large effect on college students' mental health, but increased social media usage 18 months into the pandemic - when colleges had largely reopened and students were back on campus - did have a negative effect on students' mental health.
Title Digital Mental Health Interventions at Colleges & Universities. Authors: Sara Abelson, Daniel Eisenberg, Ashley Johnston, Sarah Ketchen Lipson, Michelle Liu, Shannon N. Ogden, and Stephen M. Schueller Source: Ruderman Family Foundation In the last decade, the number of college students reporting clinically significant mental health symptoms has doubled, causing higher education ...
Although there is a paucity of research examining the impact of academic stress in non-binary college students, prior studies have indicated that non-binary adults face adverse mental health outcomes when compared to male and female-identifying individuals (Thorne et al., 2018; Jones et al., 2019; Budge et al., 2020).
The COVID-19 pandemic had an unprecedented effect on college students' mental health. Symptoms like anxiety and major depression in young adults ages 18-25 increased significantly compared to ...
College Student Mental Health and Well-Being . According to the latest research on college students and mental health, three out of 10 students have struggled with depression in the last two weeks, and over one in four have expressed issues with anxiety. Even more distressing is the one in 20 college students who had created a suicide plan in ...
However, a US based research estimated that the death toll from the pandemic to be in the several millions and 10 times the official count as reported by the Union Health Ministry (Shan, 2021). ... Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet Res., 22 (9) (2020 ...
Champlain College launched a 10-week curricular program to build students' skills in transition, teaching healthy habits and campus resources. For many students, balancing academics and other responsibilities is their top stressor and what they believe to be the driver of the collegiate mental health crisis, according to a recent Student Voice survey by Inside Higher Ed and the Generation Lab.
This paper provides a practical resource for researchers considering involving young people in the research process, and suggests what data should be collected to improve reporting on the diversity of the young people involved. The mental health of young people (aged 16-25 years) is a growing ...
The resilience of students minimized the negative effects of academic stress on their hospitality career intentions while enhancing their well-being. The theoretical and empirical contributions of the study were highlighted and directions for future research were also indicated.
This article was originally published with the title " Rx for Teen Mental Health: Volunteering " in Scientific American Magazine Vol. 331 No. 1 (July/August 2024), p. 85 doi:10.1038 ...
Tryan L. McMickens, Ed.D., is lead co-editor of the first issue of Black College Men's Mental Health. "Today, more college students are coming to campus with mental health challenges, and the COVID-19 pandemic, which occurred from 2020-2022 and whose effects still linger, has exacerbated the mental health conditions of college students," said McMickens, an associate professor of higher ...
Young people's mental health is a growing concern in the UK, but not all young people experience mental health issues in the same way. For example, lower household income is associated with worse adolescent mental health. So that services and treaments can best support young people, they need to ...